User login
Prognostic model has clinical utility in mCRPC
Researchers have developed what they say is a clinically useful prognostic model for overall survival in chemotherapy-naive men with metastatic castration-resistant prostate cancer (mCRPC) treated with the second-generation androgen receptor inhibitor enzalutamide.
Knowledge of prognosis gained by the model, which includes 11 variables routinely collected from patients, may help clinicians make decisions on the aggressiveness with which to pursue active therapy and could also help shape trial designs that utilize combinations with androgen receptor–directed therapies, the research team wrote in Annals of Oncology.
Led by Andrew J. Armstrong, MD, of Duke University, Durham, N.C., the researchers randomly split patients from the PREVAIL trial database (enzalutamide vs. placebo) 2:1 into training (n = 1,159) and testing (n = 550) sets.
They noted that, in the PREVAIL trial, enzalutamide significantly reduced the risk of death by 29% (hazard ratio, 0.71; P less than .001), compared with placebo.
Using the training set, the research team analyzed 23 predefined variables based on previous work demonstrating their potential importance in mCRPC outcomes. A multivariable model predicting overall survival (OS) was then developed and the HR and 95% confidence interval were established for each potentially prognostic variable.
The final validated multivariable model included 11 independent prognostic variables: albumin, alkaline phosphatase, hemoglobin, lactate dehydrogenase, neutrophil-lymphocyte ratio, number of bone metastases, presence of pain, pattern of spread, prostate specific antigen, time from diagnosis to randomization, and treatment.
The 11-variable model provided a significant separation between low-risk and high-risk patients (HR, 0.35; 95% CI, 0.27-0.46) and between low-risk (HR, 0.20; 95% CI, 0.14-0.29) and intermediate-risk (HR, 0.40; 95% CI, 0.30-0.53) versus high-risk patients.
Median OS for low-risk, intermediate-risk, and high-risk groups (testing set) defined by prognostic risk tertiles were not yet reached, 34.2 months, and 21.1 months, respectively.
“This model has potential clinical utility for individual and trial-level survival, potential outcomes prognostication, and clinical trial design of novel treatment approaches in this population,” the research team concluded.
The researchers said their model had several advantages over others because it was developed and validated in a contemporary treatment setting that reflected current practice. However, they cautioned that while the variables in their model had “strong biologic rationale” outcomes for individuals in contemporary practice may differ from those in clinical trial populations.
“External validation is recommended in a broader, nontrial population of men with mCRPC. Accordingly, the prognostic model presented in this paper and in general, should not displace the well-informed clinical judgment of health care professionals treating individual patients,” they wrote.
The research was supported by Medivation and Astellas Pharma (the codevelopers of enzalutamide).
SOURCE: Armstrong AJ et al. Ann Oncol. 2018 Sept 10. doi: 10.1093/annonc/mdy406.
Researchers have developed what they say is a clinically useful prognostic model for overall survival in chemotherapy-naive men with metastatic castration-resistant prostate cancer (mCRPC) treated with the second-generation androgen receptor inhibitor enzalutamide.
Knowledge of prognosis gained by the model, which includes 11 variables routinely collected from patients, may help clinicians make decisions on the aggressiveness with which to pursue active therapy and could also help shape trial designs that utilize combinations with androgen receptor–directed therapies, the research team wrote in Annals of Oncology.
Led by Andrew J. Armstrong, MD, of Duke University, Durham, N.C., the researchers randomly split patients from the PREVAIL trial database (enzalutamide vs. placebo) 2:1 into training (n = 1,159) and testing (n = 550) sets.
They noted that, in the PREVAIL trial, enzalutamide significantly reduced the risk of death by 29% (hazard ratio, 0.71; P less than .001), compared with placebo.
Using the training set, the research team analyzed 23 predefined variables based on previous work demonstrating their potential importance in mCRPC outcomes. A multivariable model predicting overall survival (OS) was then developed and the HR and 95% confidence interval were established for each potentially prognostic variable.
The final validated multivariable model included 11 independent prognostic variables: albumin, alkaline phosphatase, hemoglobin, lactate dehydrogenase, neutrophil-lymphocyte ratio, number of bone metastases, presence of pain, pattern of spread, prostate specific antigen, time from diagnosis to randomization, and treatment.
The 11-variable model provided a significant separation between low-risk and high-risk patients (HR, 0.35; 95% CI, 0.27-0.46) and between low-risk (HR, 0.20; 95% CI, 0.14-0.29) and intermediate-risk (HR, 0.40; 95% CI, 0.30-0.53) versus high-risk patients.
Median OS for low-risk, intermediate-risk, and high-risk groups (testing set) defined by prognostic risk tertiles were not yet reached, 34.2 months, and 21.1 months, respectively.
“This model has potential clinical utility for individual and trial-level survival, potential outcomes prognostication, and clinical trial design of novel treatment approaches in this population,” the research team concluded.
The researchers said their model had several advantages over others because it was developed and validated in a contemporary treatment setting that reflected current practice. However, they cautioned that while the variables in their model had “strong biologic rationale” outcomes for individuals in contemporary practice may differ from those in clinical trial populations.
“External validation is recommended in a broader, nontrial population of men with mCRPC. Accordingly, the prognostic model presented in this paper and in general, should not displace the well-informed clinical judgment of health care professionals treating individual patients,” they wrote.
The research was supported by Medivation and Astellas Pharma (the codevelopers of enzalutamide).
SOURCE: Armstrong AJ et al. Ann Oncol. 2018 Sept 10. doi: 10.1093/annonc/mdy406.
Researchers have developed what they say is a clinically useful prognostic model for overall survival in chemotherapy-naive men with metastatic castration-resistant prostate cancer (mCRPC) treated with the second-generation androgen receptor inhibitor enzalutamide.
Knowledge of prognosis gained by the model, which includes 11 variables routinely collected from patients, may help clinicians make decisions on the aggressiveness with which to pursue active therapy and could also help shape trial designs that utilize combinations with androgen receptor–directed therapies, the research team wrote in Annals of Oncology.
Led by Andrew J. Armstrong, MD, of Duke University, Durham, N.C., the researchers randomly split patients from the PREVAIL trial database (enzalutamide vs. placebo) 2:1 into training (n = 1,159) and testing (n = 550) sets.
They noted that, in the PREVAIL trial, enzalutamide significantly reduced the risk of death by 29% (hazard ratio, 0.71; P less than .001), compared with placebo.
Using the training set, the research team analyzed 23 predefined variables based on previous work demonstrating their potential importance in mCRPC outcomes. A multivariable model predicting overall survival (OS) was then developed and the HR and 95% confidence interval were established for each potentially prognostic variable.
The final validated multivariable model included 11 independent prognostic variables: albumin, alkaline phosphatase, hemoglobin, lactate dehydrogenase, neutrophil-lymphocyte ratio, number of bone metastases, presence of pain, pattern of spread, prostate specific antigen, time from diagnosis to randomization, and treatment.
The 11-variable model provided a significant separation between low-risk and high-risk patients (HR, 0.35; 95% CI, 0.27-0.46) and between low-risk (HR, 0.20; 95% CI, 0.14-0.29) and intermediate-risk (HR, 0.40; 95% CI, 0.30-0.53) versus high-risk patients.
Median OS for low-risk, intermediate-risk, and high-risk groups (testing set) defined by prognostic risk tertiles were not yet reached, 34.2 months, and 21.1 months, respectively.
“This model has potential clinical utility for individual and trial-level survival, potential outcomes prognostication, and clinical trial design of novel treatment approaches in this population,” the research team concluded.
The researchers said their model had several advantages over others because it was developed and validated in a contemporary treatment setting that reflected current practice. However, they cautioned that while the variables in their model had “strong biologic rationale” outcomes for individuals in contemporary practice may differ from those in clinical trial populations.
“External validation is recommended in a broader, nontrial population of men with mCRPC. Accordingly, the prognostic model presented in this paper and in general, should not displace the well-informed clinical judgment of health care professionals treating individual patients,” they wrote.
The research was supported by Medivation and Astellas Pharma (the codevelopers of enzalutamide).
SOURCE: Armstrong AJ et al. Ann Oncol. 2018 Sept 10. doi: 10.1093/annonc/mdy406.
FROM ANNALS OF ONCOLOGY
Key clinical point: A new prognosis model which includes routinely collected variables could help guide treatment decisions in patients with metastatic castration-resistant prostate cancer.
Major finding: The 11-variable model provided a significant separation between low-risk and high-risk patients (HR, 0.35; 95% confidence interval, 0.27-0.46) and between low-risk (HR, 0.20; 95% CI, 0.14-0.29) and intermediate-risk (HR, 0.40; 95% CI, 0.30-0.53) versus high-risk patients.
Study details: An analysis of data sets from the randomized, double-blind, placebo-controlled, phase 3 PREVAIL trial
Disclosures: The research was supported by Medivation and Astellas Pharma (the codevelopers of enzalutamide).
Source: Armstrong AJ et al. Ann Oncol. 2018 Sep 10. doi: 10.1093/annonc/mdy406.
Huntington’s progression tracks with levels of mutant huntingtin, neurofilament light
Concentrations of mutant huntingtin protein and neurofilament light proteins in cerebrospinal fluid and blood may be the first signs of progression in Huntington’s disease, according to a paper published online Sept. 12 in Science Translational Medicine.
In a cohort of 40 Huntington’s mutation carriers with manifest disease, 20 carriers without clinical symptoms, and 20 healthy controls, researchers examined levels of mutant huntingtin (mHTT) and neurofilament light (NfL) protein in biofluids, in parallel with clinical evaluations and MRI imaging.
They found that concentrations of mHTT in the cerebrospinal fluid (CSF) and concentrations of NfL proteins in the CSF and plasma were significantly higher in participants with manifest Huntington’s disease (HD) than in those without manifest disease or in controls.
Researchers also saw that CSF concentrations of mHTT showed the earliest detectable change in progression of the disease, followed by plasma and CSF levels of NfL. After that came changes in caudate and global brain volume, motor score, word reading, and other clinical measures.
“These results suggest that as our understanding grows further, analysis of mHTT and NfL might be useful for developing HD therapeutics and for clinical management,” wrote Lauren M. Byrne of the Huntington’s Disease Centre at the University College London Institute of Neurology and her coauthors.
Plasma concentrations of NfL showed the strongest association with clinical severity, even after adjusting for the number of CAG (or cytosine, adenine, and guanine) repeats – a measure of disease severity – and age.
“Our previous work suggests that NfL is a dynamic marker of ongoing neuronal damage in HD that predicts subsequent progression,” the authors wrote. “This perhaps reflects that NfL, as a marker of axonal damage, has a more direct relationship with the development of clinical manifestations and brain atrophy.”
NfL concentrations in CSF more closely predicted brain volume than did plasma NfL or CSF concentrations of mHTT.
In participants who carried the Huntington’s mutation, CSF concentrations of mHTT and NfL were strongly correlated. Researchers also noted that mutation carriers had a significantly higher CSF-to-plasma ratio of NfL than did controls.
The study also showed that mHTT in the CSF and NfL in the cerebrospinal fluid and plasma, were very stable within individuals over 4-8 weeks.
“The very high intraclass correlation values of the three markers revealed them to be highly stable, suggesting that intraindividual variation in these analytes is likely to be a minimal source of noise in natural history and therapeutic studies,” the authors wrote.
This work was supported by the Medical Research Council U.K., the CHDI Foundation, the Wellcome Trust, the U.K. Department of Health’s National Institute for Health Research Biomedical Research Centres funding scheme, the U.K. Dementia Research Institute, F. Hoffmann-La Roche, the Horizon 2020 Framework Programme, and the Engineering and Physical Sciences Research Council. A number of authors disclosed consulting or serving on advisory boards for F. Hoffmann-La Roche and/or other companies. Three authors are full-time employees of F. Hoffmann-La Roche.
SOURCE: Byrne L et al. Sci Transl Med. 2018;10:eaat7108. doi: 10.1126/scitranslmed.aat7108.
Concentrations of mutant huntingtin protein and neurofilament light proteins in cerebrospinal fluid and blood may be the first signs of progression in Huntington’s disease, according to a paper published online Sept. 12 in Science Translational Medicine.
In a cohort of 40 Huntington’s mutation carriers with manifest disease, 20 carriers without clinical symptoms, and 20 healthy controls, researchers examined levels of mutant huntingtin (mHTT) and neurofilament light (NfL) protein in biofluids, in parallel with clinical evaluations and MRI imaging.
They found that concentrations of mHTT in the cerebrospinal fluid (CSF) and concentrations of NfL proteins in the CSF and plasma were significantly higher in participants with manifest Huntington’s disease (HD) than in those without manifest disease or in controls.
Researchers also saw that CSF concentrations of mHTT showed the earliest detectable change in progression of the disease, followed by plasma and CSF levels of NfL. After that came changes in caudate and global brain volume, motor score, word reading, and other clinical measures.
“These results suggest that as our understanding grows further, analysis of mHTT and NfL might be useful for developing HD therapeutics and for clinical management,” wrote Lauren M. Byrne of the Huntington’s Disease Centre at the University College London Institute of Neurology and her coauthors.
Plasma concentrations of NfL showed the strongest association with clinical severity, even after adjusting for the number of CAG (or cytosine, adenine, and guanine) repeats – a measure of disease severity – and age.
“Our previous work suggests that NfL is a dynamic marker of ongoing neuronal damage in HD that predicts subsequent progression,” the authors wrote. “This perhaps reflects that NfL, as a marker of axonal damage, has a more direct relationship with the development of clinical manifestations and brain atrophy.”
NfL concentrations in CSF more closely predicted brain volume than did plasma NfL or CSF concentrations of mHTT.
In participants who carried the Huntington’s mutation, CSF concentrations of mHTT and NfL were strongly correlated. Researchers also noted that mutation carriers had a significantly higher CSF-to-plasma ratio of NfL than did controls.
The study also showed that mHTT in the CSF and NfL in the cerebrospinal fluid and plasma, were very stable within individuals over 4-8 weeks.
“The very high intraclass correlation values of the three markers revealed them to be highly stable, suggesting that intraindividual variation in these analytes is likely to be a minimal source of noise in natural history and therapeutic studies,” the authors wrote.
This work was supported by the Medical Research Council U.K., the CHDI Foundation, the Wellcome Trust, the U.K. Department of Health’s National Institute for Health Research Biomedical Research Centres funding scheme, the U.K. Dementia Research Institute, F. Hoffmann-La Roche, the Horizon 2020 Framework Programme, and the Engineering and Physical Sciences Research Council. A number of authors disclosed consulting or serving on advisory boards for F. Hoffmann-La Roche and/or other companies. Three authors are full-time employees of F. Hoffmann-La Roche.
SOURCE: Byrne L et al. Sci Transl Med. 2018;10:eaat7108. doi: 10.1126/scitranslmed.aat7108.
Concentrations of mutant huntingtin protein and neurofilament light proteins in cerebrospinal fluid and blood may be the first signs of progression in Huntington’s disease, according to a paper published online Sept. 12 in Science Translational Medicine.
In a cohort of 40 Huntington’s mutation carriers with manifest disease, 20 carriers without clinical symptoms, and 20 healthy controls, researchers examined levels of mutant huntingtin (mHTT) and neurofilament light (NfL) protein in biofluids, in parallel with clinical evaluations and MRI imaging.
They found that concentrations of mHTT in the cerebrospinal fluid (CSF) and concentrations of NfL proteins in the CSF and plasma were significantly higher in participants with manifest Huntington’s disease (HD) than in those without manifest disease or in controls.
Researchers also saw that CSF concentrations of mHTT showed the earliest detectable change in progression of the disease, followed by plasma and CSF levels of NfL. After that came changes in caudate and global brain volume, motor score, word reading, and other clinical measures.
“These results suggest that as our understanding grows further, analysis of mHTT and NfL might be useful for developing HD therapeutics and for clinical management,” wrote Lauren M. Byrne of the Huntington’s Disease Centre at the University College London Institute of Neurology and her coauthors.
Plasma concentrations of NfL showed the strongest association with clinical severity, even after adjusting for the number of CAG (or cytosine, adenine, and guanine) repeats – a measure of disease severity – and age.
“Our previous work suggests that NfL is a dynamic marker of ongoing neuronal damage in HD that predicts subsequent progression,” the authors wrote. “This perhaps reflects that NfL, as a marker of axonal damage, has a more direct relationship with the development of clinical manifestations and brain atrophy.”
NfL concentrations in CSF more closely predicted brain volume than did plasma NfL or CSF concentrations of mHTT.
In participants who carried the Huntington’s mutation, CSF concentrations of mHTT and NfL were strongly correlated. Researchers also noted that mutation carriers had a significantly higher CSF-to-plasma ratio of NfL than did controls.
The study also showed that mHTT in the CSF and NfL in the cerebrospinal fluid and plasma, were very stable within individuals over 4-8 weeks.
“The very high intraclass correlation values of the three markers revealed them to be highly stable, suggesting that intraindividual variation in these analytes is likely to be a minimal source of noise in natural history and therapeutic studies,” the authors wrote.
This work was supported by the Medical Research Council U.K., the CHDI Foundation, the Wellcome Trust, the U.K. Department of Health’s National Institute for Health Research Biomedical Research Centres funding scheme, the U.K. Dementia Research Institute, F. Hoffmann-La Roche, the Horizon 2020 Framework Programme, and the Engineering and Physical Sciences Research Council. A number of authors disclosed consulting or serving on advisory boards for F. Hoffmann-La Roche and/or other companies. Three authors are full-time employees of F. Hoffmann-La Roche.
SOURCE: Byrne L et al. Sci Transl Med. 2018;10:eaat7108. doi: 10.1126/scitranslmed.aat7108.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: Cerebrospinal levels of mutant huntingtin could be earliest sign of Huntington’s disease progression.
Major finding: Changing levels of mutant huntingtin in the cerebrospinal fluid are the first sign of disease progression.
Study details: Cohort study in 60 Huntington’s disease mutation carriers and 20 controls.
Disclosures: This work was supported by the Medical Research Council U.K., the CHDI Foundation, the Wellcome Trust, the U.K. Department of Health’s National Institute for Health Research Biomedical Research Centres funding scheme, the U.K. Dementia Research Institute, F. Hoffmann-La Roche, the Horizon 2020 Framework Programme, and the Engineering and Physical Sciences Research Council. A number of authors disclosed consulting or serving on advisory boards for F. Hoffmann-La Roche and/or other companies. Three authors are full-time employees of F. Hoffmann-La Roche.
Source: Byrne L et al. Sci Transl Med. 2018;10:eaat7108. doi: 10.1126/scitranslmed.aat7108.
New stroke intervention guidelines stress volume
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
FROM THE JOURNAL OF NEUROINTERVENTIONAL SURGERY
Guidelines released for perimenopausal depression
and affect women with no previous symptoms of depression, according to recent guidelines on perimenopausal depression copublished in the Journal of Women’s Health and Menopause.
“Epidemiologic findings, animal data, and clinical observations have shed some light into plausible mechanistic hypotheses on why some, but not all, women may be particularly sensitive to changes in the hormonal milieu experienced premenstrually, during the postpartum period or during the menopause transition,” Pauline M. Maki, PhD, past president of the North American Menopause Society (NAMS) and professor of psychiatry and psychology at the University of Illinois at Chicago, and her colleagues wrote. “The notion of a menopause-associated depression, however, has been the focus of clinical and scientific debate for years. The lack of consensus on this issue has also led to a lack of clarity in how to evaluate and treat depression in women during the menopausal transition and postmenopausal period.”
The guidelines were developed on behalf of the NAMS Board of Trustees and the Women and Mood Disorders Task Force of the National Network of Depression Centers. Dr. Maki and her colleagues convened an 11-person expert panel on perimenopausal depression, which looked at the effects of factors such as epidemiology; clinical presentation; antidepressants; hormone therapy; and other therapies such as exercise, natural health products, and psychotherapy.
Most women who experience perimenopausal depression have previously undergone a major depressive episode (MDE), while major depressive disorder (MDD) onset at midlife is less common. However, even among women with no previous history of depression, the risk of perimenopausal depression – both depressive symptoms and MDE – is elevated for women at midlife. Studies suggest that 45%-68% of perimenopausal women have elevated depression symptoms.
Dr. Maki and her associates cited studies that showed women who underwent surgical menopause in the form of hysterectomy with and without oophorectomy and women with ovarian insufficiency also showed an elevated rate of depression.
Other risk factors for perimenopausal depression included sociodemographic (black race, financial difficulties) and psychosocial factors (adverse life events, low social support), anxiety, and menopausal symptoms such as interrupted sleep and vasomotor symptoms. Risk factors for MDD include use of antidepressants, premenstrual depressive symptoms, anxiety, menopausal sleep disturbance, sociodemographic factors such as high body mass index and black race, and psychosocial factors such as social isolation and upsetting life events.
Depressive symptoms in perimenopause present as classic depressive symptoms but may also be in combination with perimenopausal symptoms such as changes in weight, cognitive shifts, night sweats, hot flashes, and sexual and sleep disturbances. In addition, the stressors of life for women in midlife can further complicate depressive symptoms.
“Many women face a series of stressors including, but not exclusive to, caring for aging parents, death of parents, medical illness in self and family, adjusting to emotional and physical sequelae of surgical menopause and other health issues that are common to this stage of life, children leaving the home, and changes in marital status. With the onset of childbirth at an increasingly later age, women are often faced with the dual responsibility of raising young children amid caring for aging parents while navigating their careers and ensuing challenges,” Dr. Maki and her colleagues wrote. “These multiple demands are often faced without supports in place to identify or address the ensuing distress placed on a woman during this stage.”
Assessment and diagnosis should include factoring all these symptoms in and disentangling menopausal and psychiatric symptoms, evaluating women with past MDEs and MDD for a mood disorder, and use of differential diagnosis for psychiatric symptoms.
There is no menopause-specific mood disorder scale, Dr. Maki and her associates emphasized, but the Patient Health Questionnaire-9 can be used to categorize mood disorder diagnoses. There are “validated menopause symptom and health-related quality of life scales [that] include mood items” such as the Menopause Rating Scale, and the Menopause-Specific Quality of Life Scale.
Frontline treatment of MDE with traditional therapies such as antidepressants, cognitive behavioral therapy, and other psychotherapies is appropriate, while previous antidepressant trial and responses should be followed to find the best efficacy and tolerability for a women with a history of MDD. There is data on some SSRIs and serotonin norepinephrine reuptake inhibitors suggesting efficacy and tolerability at usual doses. Of note, Dr. Maki and her colleagues found estrogen therapy has some evidence for use as an antidepressant, but most studies on hormone therapy examined unopposed estrogen instead of estrogen plus progestogen, which has limited data.
The authors recommended exercise as a complement to psychotherapy and pharmacotherapies for perimenopausal women with depression, but said there is no available evidence to recommend “botanical or complementary/alternative approaches for treating depression related to the perimenopause.”
Several authors have reported honoraria, research support, consulting fees, and grants from numerous pharmaceutical companies, the National Pregnancy Registry for Atypical Antipsychotics; the Brain & Behavior Research Foundation; the Ontario Brain Institute; and the Ontario Ministry of Technology, Innovation, and Science. Six of the authors reported no relevant conflicts of interest.
SOURCE: Maki PM et al. J Womens Health. 2018 Sep 5. doi: 10.1089/jwh.2018.27099.mensocrec.
I think the authors of this paper did a beautiful job summarizing a decade or more of very good observational research and even some randomized, controlled trials on a complex topic. This paper is really important because it takes a large body of evidence on the topic and pulls it together in a coherent way by asking specific questions and then looking to the literature to address those questions. The team of 11 experts in the field – led by Dr. Maki, who is a past president of the North American Menopause Society and began this paper as her presidential project – deserves a lot of credit for doing a beautiful job addressing some important questions with the research that is already available.
There are many clinical implications in these guidelines for any provider who cares for women in their 40s and 50s, whether they are gynecologists, family physicians, internists, psychiatrists, or psychologists. These health care practitioners need to be aware that this is a high-risk period for both depressive symptoms and major depression. The authors reported about one-third of premenopausal women complain of depressive symptoms, and yet, in those women experiencing perimenopause, that percentage is between 45% and 68%. Health care practitioners caring for women in this age group need to be aware of, and looking for, these symptoms so they can identify them, address them, let women know that they’re common at this time, and help them get appropriate treatment.
The authors also looked at the literature on the impact of the menopausal transition on sleep and how that can affect depressive symptoms and major depression; it is important for health care providers to think about sleep disruption in women at this age. The domino hypothesis, the theory that hot flashes can lead to sleep disruption that then leads to depressive symptoms of the menopause transition, was examined in a literature review. The authors found some of the literature shows that these symptoms are separate from hot flashes.
Menopausal transition and the association with symptoms of depression is not only looking at hormonal fluctuations but also recognizing this is a time of extraordinary psychosocial and physical change for women. They may have responsibilities for their partners and children as well as for aging parents. They may have their own health problems and the health problems of their partner to handle. Career changes may be happening at this time. This is a very complex psychosocial time in women’s lives that may be complicated by other health issues occurring at the same time.
Jan Leslie Shifren, MD , is director of the Midlife Women’s Health Center in the department of obstetrics and gynecology at Massachusetts General Hospital, Boston. She also is an Ob.Gyn. News editorial board member. Dr. Shifren reported no relevant conflicts of interest.
I think the authors of this paper did a beautiful job summarizing a decade or more of very good observational research and even some randomized, controlled trials on a complex topic. This paper is really important because it takes a large body of evidence on the topic and pulls it together in a coherent way by asking specific questions and then looking to the literature to address those questions. The team of 11 experts in the field – led by Dr. Maki, who is a past president of the North American Menopause Society and began this paper as her presidential project – deserves a lot of credit for doing a beautiful job addressing some important questions with the research that is already available.
There are many clinical implications in these guidelines for any provider who cares for women in their 40s and 50s, whether they are gynecologists, family physicians, internists, psychiatrists, or psychologists. These health care practitioners need to be aware that this is a high-risk period for both depressive symptoms and major depression. The authors reported about one-third of premenopausal women complain of depressive symptoms, and yet, in those women experiencing perimenopause, that percentage is between 45% and 68%. Health care practitioners caring for women in this age group need to be aware of, and looking for, these symptoms so they can identify them, address them, let women know that they’re common at this time, and help them get appropriate treatment.
The authors also looked at the literature on the impact of the menopausal transition on sleep and how that can affect depressive symptoms and major depression; it is important for health care providers to think about sleep disruption in women at this age. The domino hypothesis, the theory that hot flashes can lead to sleep disruption that then leads to depressive symptoms of the menopause transition, was examined in a literature review. The authors found some of the literature shows that these symptoms are separate from hot flashes.
Menopausal transition and the association with symptoms of depression is not only looking at hormonal fluctuations but also recognizing this is a time of extraordinary psychosocial and physical change for women. They may have responsibilities for their partners and children as well as for aging parents. They may have their own health problems and the health problems of their partner to handle. Career changes may be happening at this time. This is a very complex psychosocial time in women’s lives that may be complicated by other health issues occurring at the same time.
Jan Leslie Shifren, MD , is director of the Midlife Women’s Health Center in the department of obstetrics and gynecology at Massachusetts General Hospital, Boston. She also is an Ob.Gyn. News editorial board member. Dr. Shifren reported no relevant conflicts of interest.
I think the authors of this paper did a beautiful job summarizing a decade or more of very good observational research and even some randomized, controlled trials on a complex topic. This paper is really important because it takes a large body of evidence on the topic and pulls it together in a coherent way by asking specific questions and then looking to the literature to address those questions. The team of 11 experts in the field – led by Dr. Maki, who is a past president of the North American Menopause Society and began this paper as her presidential project – deserves a lot of credit for doing a beautiful job addressing some important questions with the research that is already available.
There are many clinical implications in these guidelines for any provider who cares for women in their 40s and 50s, whether they are gynecologists, family physicians, internists, psychiatrists, or psychologists. These health care practitioners need to be aware that this is a high-risk period for both depressive symptoms and major depression. The authors reported about one-third of premenopausal women complain of depressive symptoms, and yet, in those women experiencing perimenopause, that percentage is between 45% and 68%. Health care practitioners caring for women in this age group need to be aware of, and looking for, these symptoms so they can identify them, address them, let women know that they’re common at this time, and help them get appropriate treatment.
The authors also looked at the literature on the impact of the menopausal transition on sleep and how that can affect depressive symptoms and major depression; it is important for health care providers to think about sleep disruption in women at this age. The domino hypothesis, the theory that hot flashes can lead to sleep disruption that then leads to depressive symptoms of the menopause transition, was examined in a literature review. The authors found some of the literature shows that these symptoms are separate from hot flashes.
Menopausal transition and the association with symptoms of depression is not only looking at hormonal fluctuations but also recognizing this is a time of extraordinary psychosocial and physical change for women. They may have responsibilities for their partners and children as well as for aging parents. They may have their own health problems and the health problems of their partner to handle. Career changes may be happening at this time. This is a very complex psychosocial time in women’s lives that may be complicated by other health issues occurring at the same time.
Jan Leslie Shifren, MD , is director of the Midlife Women’s Health Center in the department of obstetrics and gynecology at Massachusetts General Hospital, Boston. She also is an Ob.Gyn. News editorial board member. Dr. Shifren reported no relevant conflicts of interest.
and affect women with no previous symptoms of depression, according to recent guidelines on perimenopausal depression copublished in the Journal of Women’s Health and Menopause.
“Epidemiologic findings, animal data, and clinical observations have shed some light into plausible mechanistic hypotheses on why some, but not all, women may be particularly sensitive to changes in the hormonal milieu experienced premenstrually, during the postpartum period or during the menopause transition,” Pauline M. Maki, PhD, past president of the North American Menopause Society (NAMS) and professor of psychiatry and psychology at the University of Illinois at Chicago, and her colleagues wrote. “The notion of a menopause-associated depression, however, has been the focus of clinical and scientific debate for years. The lack of consensus on this issue has also led to a lack of clarity in how to evaluate and treat depression in women during the menopausal transition and postmenopausal period.”
The guidelines were developed on behalf of the NAMS Board of Trustees and the Women and Mood Disorders Task Force of the National Network of Depression Centers. Dr. Maki and her colleagues convened an 11-person expert panel on perimenopausal depression, which looked at the effects of factors such as epidemiology; clinical presentation; antidepressants; hormone therapy; and other therapies such as exercise, natural health products, and psychotherapy.
Most women who experience perimenopausal depression have previously undergone a major depressive episode (MDE), while major depressive disorder (MDD) onset at midlife is less common. However, even among women with no previous history of depression, the risk of perimenopausal depression – both depressive symptoms and MDE – is elevated for women at midlife. Studies suggest that 45%-68% of perimenopausal women have elevated depression symptoms.
Dr. Maki and her associates cited studies that showed women who underwent surgical menopause in the form of hysterectomy with and without oophorectomy and women with ovarian insufficiency also showed an elevated rate of depression.
Other risk factors for perimenopausal depression included sociodemographic (black race, financial difficulties) and psychosocial factors (adverse life events, low social support), anxiety, and menopausal symptoms such as interrupted sleep and vasomotor symptoms. Risk factors for MDD include use of antidepressants, premenstrual depressive symptoms, anxiety, menopausal sleep disturbance, sociodemographic factors such as high body mass index and black race, and psychosocial factors such as social isolation and upsetting life events.
Depressive symptoms in perimenopause present as classic depressive symptoms but may also be in combination with perimenopausal symptoms such as changes in weight, cognitive shifts, night sweats, hot flashes, and sexual and sleep disturbances. In addition, the stressors of life for women in midlife can further complicate depressive symptoms.
“Many women face a series of stressors including, but not exclusive to, caring for aging parents, death of parents, medical illness in self and family, adjusting to emotional and physical sequelae of surgical menopause and other health issues that are common to this stage of life, children leaving the home, and changes in marital status. With the onset of childbirth at an increasingly later age, women are often faced with the dual responsibility of raising young children amid caring for aging parents while navigating their careers and ensuing challenges,” Dr. Maki and her colleagues wrote. “These multiple demands are often faced without supports in place to identify or address the ensuing distress placed on a woman during this stage.”
Assessment and diagnosis should include factoring all these symptoms in and disentangling menopausal and psychiatric symptoms, evaluating women with past MDEs and MDD for a mood disorder, and use of differential diagnosis for psychiatric symptoms.
There is no menopause-specific mood disorder scale, Dr. Maki and her associates emphasized, but the Patient Health Questionnaire-9 can be used to categorize mood disorder diagnoses. There are “validated menopause symptom and health-related quality of life scales [that] include mood items” such as the Menopause Rating Scale, and the Menopause-Specific Quality of Life Scale.
Frontline treatment of MDE with traditional therapies such as antidepressants, cognitive behavioral therapy, and other psychotherapies is appropriate, while previous antidepressant trial and responses should be followed to find the best efficacy and tolerability for a women with a history of MDD. There is data on some SSRIs and serotonin norepinephrine reuptake inhibitors suggesting efficacy and tolerability at usual doses. Of note, Dr. Maki and her colleagues found estrogen therapy has some evidence for use as an antidepressant, but most studies on hormone therapy examined unopposed estrogen instead of estrogen plus progestogen, which has limited data.
The authors recommended exercise as a complement to psychotherapy and pharmacotherapies for perimenopausal women with depression, but said there is no available evidence to recommend “botanical or complementary/alternative approaches for treating depression related to the perimenopause.”
Several authors have reported honoraria, research support, consulting fees, and grants from numerous pharmaceutical companies, the National Pregnancy Registry for Atypical Antipsychotics; the Brain & Behavior Research Foundation; the Ontario Brain Institute; and the Ontario Ministry of Technology, Innovation, and Science. Six of the authors reported no relevant conflicts of interest.
SOURCE: Maki PM et al. J Womens Health. 2018 Sep 5. doi: 10.1089/jwh.2018.27099.mensocrec.
and affect women with no previous symptoms of depression, according to recent guidelines on perimenopausal depression copublished in the Journal of Women’s Health and Menopause.
“Epidemiologic findings, animal data, and clinical observations have shed some light into plausible mechanistic hypotheses on why some, but not all, women may be particularly sensitive to changes in the hormonal milieu experienced premenstrually, during the postpartum period or during the menopause transition,” Pauline M. Maki, PhD, past president of the North American Menopause Society (NAMS) and professor of psychiatry and psychology at the University of Illinois at Chicago, and her colleagues wrote. “The notion of a menopause-associated depression, however, has been the focus of clinical and scientific debate for years. The lack of consensus on this issue has also led to a lack of clarity in how to evaluate and treat depression in women during the menopausal transition and postmenopausal period.”
The guidelines were developed on behalf of the NAMS Board of Trustees and the Women and Mood Disorders Task Force of the National Network of Depression Centers. Dr. Maki and her colleagues convened an 11-person expert panel on perimenopausal depression, which looked at the effects of factors such as epidemiology; clinical presentation; antidepressants; hormone therapy; and other therapies such as exercise, natural health products, and psychotherapy.
Most women who experience perimenopausal depression have previously undergone a major depressive episode (MDE), while major depressive disorder (MDD) onset at midlife is less common. However, even among women with no previous history of depression, the risk of perimenopausal depression – both depressive symptoms and MDE – is elevated for women at midlife. Studies suggest that 45%-68% of perimenopausal women have elevated depression symptoms.
Dr. Maki and her associates cited studies that showed women who underwent surgical menopause in the form of hysterectomy with and without oophorectomy and women with ovarian insufficiency also showed an elevated rate of depression.
Other risk factors for perimenopausal depression included sociodemographic (black race, financial difficulties) and psychosocial factors (adverse life events, low social support), anxiety, and menopausal symptoms such as interrupted sleep and vasomotor symptoms. Risk factors for MDD include use of antidepressants, premenstrual depressive symptoms, anxiety, menopausal sleep disturbance, sociodemographic factors such as high body mass index and black race, and psychosocial factors such as social isolation and upsetting life events.
Depressive symptoms in perimenopause present as classic depressive symptoms but may also be in combination with perimenopausal symptoms such as changes in weight, cognitive shifts, night sweats, hot flashes, and sexual and sleep disturbances. In addition, the stressors of life for women in midlife can further complicate depressive symptoms.
“Many women face a series of stressors including, but not exclusive to, caring for aging parents, death of parents, medical illness in self and family, adjusting to emotional and physical sequelae of surgical menopause and other health issues that are common to this stage of life, children leaving the home, and changes in marital status. With the onset of childbirth at an increasingly later age, women are often faced with the dual responsibility of raising young children amid caring for aging parents while navigating their careers and ensuing challenges,” Dr. Maki and her colleagues wrote. “These multiple demands are often faced without supports in place to identify or address the ensuing distress placed on a woman during this stage.”
Assessment and diagnosis should include factoring all these symptoms in and disentangling menopausal and psychiatric symptoms, evaluating women with past MDEs and MDD for a mood disorder, and use of differential diagnosis for psychiatric symptoms.
There is no menopause-specific mood disorder scale, Dr. Maki and her associates emphasized, but the Patient Health Questionnaire-9 can be used to categorize mood disorder diagnoses. There are “validated menopause symptom and health-related quality of life scales [that] include mood items” such as the Menopause Rating Scale, and the Menopause-Specific Quality of Life Scale.
Frontline treatment of MDE with traditional therapies such as antidepressants, cognitive behavioral therapy, and other psychotherapies is appropriate, while previous antidepressant trial and responses should be followed to find the best efficacy and tolerability for a women with a history of MDD. There is data on some SSRIs and serotonin norepinephrine reuptake inhibitors suggesting efficacy and tolerability at usual doses. Of note, Dr. Maki and her colleagues found estrogen therapy has some evidence for use as an antidepressant, but most studies on hormone therapy examined unopposed estrogen instead of estrogen plus progestogen, which has limited data.
The authors recommended exercise as a complement to psychotherapy and pharmacotherapies for perimenopausal women with depression, but said there is no available evidence to recommend “botanical or complementary/alternative approaches for treating depression related to the perimenopause.”
Several authors have reported honoraria, research support, consulting fees, and grants from numerous pharmaceutical companies, the National Pregnancy Registry for Atypical Antipsychotics; the Brain & Behavior Research Foundation; the Ontario Brain Institute; and the Ontario Ministry of Technology, Innovation, and Science. Six of the authors reported no relevant conflicts of interest.
SOURCE: Maki PM et al. J Womens Health. 2018 Sep 5. doi: 10.1089/jwh.2018.27099.mensocrec.
FROM THE JOURNAL OF WOMEN’S HEALTH
NYC outbreak of Candida auris linked to 45% mortality
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
FROM EMERGING INFECTIOUS DISEASES
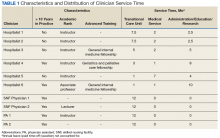
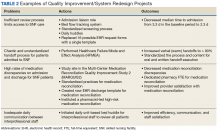
Orthopedics in the Age of Accountable Care Organizations and Population Health: From Profit-Center to Cost-Center
The way we are paid as doctors is changing. In some cases, the delivery of orthopedic care could change from healthcare institutions’ most significant financial asset to one of their most detrimental liabilities. These changes provide a chance to improve both the quality and efficiency of the care we deliver, but we are unlikely to capitalize on this opportunity unless we understand this shifting paradigm. This change requires us to first appreciate the recent history of our reimbursement environment.
Traditionally, healthcare has been a relatively lucrative field, especially for those providing surgical care: doctors are paid “physician fees” by insurance companies (including Medicare), and institutions where procedures are performed are paid “facility fees.” Profits are measured as revenue (ie, reimbursement) minus costs of providing care, and while there has always been the potential to make more money by lowering costs, providers have historically had much more to gain by increasing their revenue. This fact has been exacerbated by the “fee-for-service” (FFS) payment model, which unintentionally encourages physicians to provide high volumes of care by “paying more for doing more.” For example, rather than being paid a fixed sum to care for a patient’s knee arthritis, each provider involved in the patient’s care is paid for each intervention. Clearly, this system encourages providers to maximize their interventions (ie, earning revenue) rather than search for ways to cut costs.
The Centers for Medicare and Medicaid Services (CMS) partially addressed this issue during the 1980s by introducing the Diagnosis Related Group (DRG).1,2 Under this classification scheme, hospitals would be paid a pre-specified amount for a particular type of admission, often based on a specific procedure. For example, there is a DRG with a set payment for total knee arthroplasty (TKA).3 When reimbursement for the condition is set at a fixed amount, facilities are motivated to decrease their expenses since this is the only way to maximize the financial return for a given patient. This change, theoretically, encourages providers to cut their costs for providing a TKA as much as possible, potentially even to the point of sacrificing quality of care. As usual, when CMS makes a sweeping change, private insurers followed suit, and as a result, both government and corporate insurance is now structured around DRGs.
However, this was not a complete departure from FFS payment. We were still not paid to manage a patient’s knee arthritis as cheaply as possible; we were paid for each steroid injection, preoperative clinic visit, TKA (with numerous coding modifiers for complexity or comorbidities) as well as post-discharge admissions to skilled nursing and acute rehabilitation facilities. However, it was a start: for example, hospitals were no longer incentivized to keep TKA patients in house with a growing bill for each administered drug or therapy session. Yet, it is noteworthy that hospitals and physicians were still paid separately. This is important because doctors have historically made almost all treatment decisions and thereby determined the cost of care, yet hospitals have borne most of those costs, such as expensive implants or unplanned admissions, without a commensurate increase in reimbursement. As long as physicians are guaranteed their “fee,” they have little motivation to reduce those costs. Unsurprisingly, and as we well know, the advent of DRGs did not successfully curb our growing healthcare budget.
Recently, TKA and total hip arthroplasty reimbursement changed more dramatically. After experimenting with several pilots, CMS rolled out the Comprehensive Care for Joint Replacement (CJR) bundled payment program in 2015.1,4 Participation in CJR is mandatory for most arthroplasty providers in approximately half of all “metropolitan” areas. In this scheme, hospital and physician pay is intertwined. Specifically, hospitals are held accountable for costs, so if the total Medicare bill for a patient’s TKA exceeds the “target price,” the hospital faces a penalty. Conversely, a charge below the target can earn a bonus payment.4 The hospital and surgeons must decide how they will share the bonus (or penalty), which creates an incentive to work together to lower costs.
Continue to: While bundled payments like CJR shift some...
While bundled payments like CJR shift some of the risk for high costs to the hospital and surgeon, a much more extreme example of this type of shift is capitation (ie, paying a healthcare institution a set amount per patient to care for whatever maladies arise). Insurers have experimented with various forms of capitation in the past, which led to the expansion of health management organizations (HMOs) during the 1990s. In theory, capitation should encourage providers to invest in disease prevention to minimize the need for costly interventions. However, more nefarious incentives developed, resulting in “cherry picking” healthy patients, which restricts access to care for sicker patients, and even withholds care from patients in need. The most infamous example was arguably “drive-through deliveries,” where newborns and their mothers were prematurely discharged following birth.5 As a result, the “HMO backlash” occurred, and capitation temporarily fell out of favor. The heart of the problem was a strong incentive to reduce the cost of care without a counterbalancing incentive to maintain quality. CJR and other modern programs attempt to avoid similar adverse incentives by requiring participants to meet certain quality criteria.6
Since the passage of the Affordable Care Act in 2010, capitation has reemerged under a new name: Accountable Care Organizations (ACOs). Numerous forms of ACO’s exist with differing payment schemes7, but the most comprehensive version, named Next Generation (Next Gen), allows providers to choose full capitation.8 While early ACOs focused on individual patients, Next Gen ACOs are also focused on “population health.” That is, they must demonstrate outcomes for individuals and the patient population as a whole, while simultaneously assuming all financial risk via capitation. Specifically, these ACO’s are paid an “all-inclusive population-based payment” for each patient based on how much that type of patient’s care is expected to cost for the year.9 The ACO then provides all necessary treatment and, if the ACO cannot provide a necessary intervention, it is responsible for funding that care at another institution. Appropriately, there has been an increased focus on quality to avoid unintentional incentives to withhold care. Specifically, CMS has introduced mandatory quality metrics in the domains of patient experience, care coordination, preventive care, and management of at-risk populations.10 At present, unfortunately, these metrics are not nearly comprehensive enough nor adequately validated to assess the quality of care,11 especially for subspecialized fields like orthopedics where functional outcome scores are needed.
To date, very limited attention in the media or academic literature has been dedicated to subspecialty surgical care in the setting of ACOs even though implications for specialized surgeons could be immense. While ACOs bring numerous reporting requirements, the most essential first step for orthopedists in transition to this new reimbursement scheme will be a change in mindset. As explained above, orthopedics and other forms of specialized surgical care have traditionally been extremely profitable for healthcare institutions through relatively high revenue. However, within a capitated ACO all revenue has been paid upfront for each patient, and every orthopedic surgery performed represents a substantial cost to the institution rather than a large profit. For example, it has been reported that the average contribution margin earned by a hospital for an episode of care to provide a TKA (which includes postoperative care such as clinic visits, unplanned readmissions, and reoperations for complications) based on Medicare reimbursement is $11,726.12 This figure consists of reimbursement (median, $24,149) less variable costs (median, $10,190). Additionally, the surgeon currently receives $1400 in physician fees.13 These earnings represent a significant financial benefit for both the facility and doctor in the current FFS environment. However, a capitated ACO caring for a TKA patient would already have received full payment for his care for the year. As a result, providing a TKA would not afford any further financial benefit and would, instead, mean a loss of $10,190 (the aforementioned variable cost for the episode of care) directly from the bottom line. The orthopedic department within that ACO, along with other departments, can be expected to share that loss. This implies that upon becoming an ACO, an institution’s orthopedics department will change from a major profit-center to a major cost-center.
Continue to: CMS must establish adequate quality assurance...
CMS must establish adequate quality assurance measures to ensure that ACOs do not withhold cost-effective care, like TKAs,14,15 from their patients. Hopefully, for both professional and ethical reasons, providers will be active partners in this process. Groups like the International Consortium for Health Outcome Measurement, which has convened international expert panels to agree on comprehensive outcome sets for total joint arthroplasty and the management of low back pain, among other non-orthopedic conditions, may be useful examples in this process.16-18
At the provider level, surgeons will be more likely to be salaried employees, contracting directly with the ACO rather than primarily working to earn physician fees from insurance providers. Surgeons will likely be judged (and rewarded financially) on their ability to direct nonoperative care, to find non-surgical solutions to problems that may currently be treated operatively, and to reduce costs for patients that require surgery. Additionally, with an increased focus on quality assurance, there will likely be more pressure from ACOs and CMS to demonstrate results of both operative and nonoperative care, likely in the forms of patient-reported metrics and objective measures of physical function. Surgeons will have a strong incentive to be leaders in the process of collecting such data.
It is also worth considering the position of orthopedic practices that are not part of an ACO. Some ACOs will not have the capacity to provide all (or possibly any) of the orthopedic care their patients require. When necessary, they will contract with outside orthopedic practices. Compared with CMS, ACOs are much smaller purchasers and can be expected to be more sensitive to price, likely negotiating intensely between local orthopedic providers. As a result, even orthopedists outside of ACOs may feel the cost pressure created by this new reimbursement model and may be driven to implement cost-reduction measures such as standardized implant choices and discharge pathways.
ACOs are in an active growth phase,19,20 and recent updates to ACO policies make it clear that CMS intends for this trend to continue.8 Since ACOs are still a nascent reimbursement model, orthopedists will still do better financially, in almost all markets, by continuing to expend their energy and resources pursuing revenue, rather than cutting costs or demonstrating outcomes. However, as ACOs and population health gain traction, those orthopedists who recognize this shift and plan accordingly will have a definite strategic advantage, whether their practice is within an ACO, interacting with external ACOs, or both.
1. Carter Clement R, Bhat SB, Clement ME, Krieg JC. Medicare reimbursement and orthopedic surgery: past, present, and future. Curr Rev Musculoskelet Med. 2017;10(2):224-232. doi:10.1007/s12178-017-9406-7.
2. Centers for Medicare & Medicaid Services. Acute Inpatient PPS. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. Published August 2, 2017. Accessed September 8, 2018.
3. Centers for Medicare & Medicaid Services. Draft ICD-10-CM/PCS MS-DRGv28 Definitions Manual. https://www.cms.gov/icd10manual/fullcode_cms/P0185.html. Accessed September 8, 2018.
4. Centers for Medicare & Medicaid Services. Comprehensive Care for Joint Replacement Model. https://innovation.cms.gov/initiatives/cjr. Accessed September 8, 2018.
5. Volpp KG, Bundorf MK. Consumer protection and the HMO backlash: are HMOs to blame for drive-through deliveries? Inquiry. 1999;36(1):101-109.
6. Centers for Medicare & Medicaid Services. Quality Measures and Performance Standards. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Quality_Measures_Standards.html. Published March 2, 2015. Accessed November 3, 2015.
7. Centers for Medicare & Medicaid Services. Accountable Care Organizations (ACOs): General Information. https://innovation.cms.gov/initiatives/aco/. Accessed September 8, 2018.
8. Centers for Medicare & Medicaid Services. Next Generation ACO Model. https://innovation.cms.gov/initiatives/Next-Generation-ACO-Model/. Accessed September 8, 2018.
9. Centers for Medicare & Medicaid Services. Next Generation Accountable Care Organization (ACO) Model: Frequently Asked Questions. https://innovation.cms.gov/Files/x/nextgenacofaq.pdf. Accessed September 8, 2018.
10. Centers for Medicare & Medicaid Services. Quality Measure Benchmarks for the 2018 and 2019 Reporting Years. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/2018-and-2019-quality-benchmarks-guidance.pdf. Published December 2017. Accessed September 8, 2018.
11. Toussaint J, Krueger D, Shortell SM, Milstein A, Cutler DM. ACO model should encourage efficient care delivery. Healthc (Amst). 2015;3(3):150-152. doi:10.1016/j.hjdsi.2015.06.003.
12. Clement RC, Kheir MM, Derman PB, et al. What are the economic consequences of unplanned readmissions after TKA? Clin Orthop Relat Res. 2014;472(10):3134-3141. doi:10.1007/s11999-014-3795-3.
13. Centers for Medicare & Medicaid Services. Physician Fee Schedule Search Results. http://www.cms.gov/apps/physician-fee-schedule/search/search-results.aspx?Y=0&T=0&HT=0&CT=0&H1=27447&M=1. Accessed June 4, 2015.
14. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113-1121; discussion 1121-1122. doi:10.1001/archinternmed.2009.136.
15. Mather RC 3rd, Hug KT, Orlando LA, et al. Economic evaluation of access to musculoskeletal care: the case of waiting for total knee arthroplasty. BMC Musculoskelet Disord. 2014;15:22. doi:10.1186/1471-2474-15-22.
16. International Consortium for Health Outcomes Measurement. ICHOM web site. https://www.ichom.org/. Accessed November 3, 2015.
17. Rolfson O, Wissig S, van Maasakkers L, et al. Defining an international standard set of outcome measures for patients with hip or knee osteoarthritis: consensus of the International Consortium for Health Outcomes Measurement Hip and Knee Osteoarthritis Working Group. Arthritis Care Res (Hoboken). 2016;68(11):1631-1639. doi:10.1002/acr.22868.
18. Clement RC, Welander A, Stowell C, et al. A proposed set of metrics for standardized outcome reporting in the management of low back pain. Acta Orthop. 2015;86(5):523-533. doi:10.3109/17453674.2015.1036696.
19. Shortell SM, Colla CH, Lewis VA, Fisher E, Kessell E, Ramsay P. Accountable care organizations: the national landscape. J Health Polit Policy Law. 2015;40(4):647-668. doi:10.1215/03616878-3149976.
20. Centers for Medicare & Medicaid Services. CMS Proposes “Pathways to Success,” an Overhaul of Medicare’s ACO Program https://www.cms.gov/newsroom/press-releases/cms-proposes-pathways-success-overhaul-medicares-aco-program. Published August 9, 2018. Accessed September 10, 2018.
The way we are paid as doctors is changing. In some cases, the delivery of orthopedic care could change from healthcare institutions’ most significant financial asset to one of their most detrimental liabilities. These changes provide a chance to improve both the quality and efficiency of the care we deliver, but we are unlikely to capitalize on this opportunity unless we understand this shifting paradigm. This change requires us to first appreciate the recent history of our reimbursement environment.
Traditionally, healthcare has been a relatively lucrative field, especially for those providing surgical care: doctors are paid “physician fees” by insurance companies (including Medicare), and institutions where procedures are performed are paid “facility fees.” Profits are measured as revenue (ie, reimbursement) minus costs of providing care, and while there has always been the potential to make more money by lowering costs, providers have historically had much more to gain by increasing their revenue. This fact has been exacerbated by the “fee-for-service” (FFS) payment model, which unintentionally encourages physicians to provide high volumes of care by “paying more for doing more.” For example, rather than being paid a fixed sum to care for a patient’s knee arthritis, each provider involved in the patient’s care is paid for each intervention. Clearly, this system encourages providers to maximize their interventions (ie, earning revenue) rather than search for ways to cut costs.
The Centers for Medicare and Medicaid Services (CMS) partially addressed this issue during the 1980s by introducing the Diagnosis Related Group (DRG).1,2 Under this classification scheme, hospitals would be paid a pre-specified amount for a particular type of admission, often based on a specific procedure. For example, there is a DRG with a set payment for total knee arthroplasty (TKA).3 When reimbursement for the condition is set at a fixed amount, facilities are motivated to decrease their expenses since this is the only way to maximize the financial return for a given patient. This change, theoretically, encourages providers to cut their costs for providing a TKA as much as possible, potentially even to the point of sacrificing quality of care. As usual, when CMS makes a sweeping change, private insurers followed suit, and as a result, both government and corporate insurance is now structured around DRGs.
However, this was not a complete departure from FFS payment. We were still not paid to manage a patient’s knee arthritis as cheaply as possible; we were paid for each steroid injection, preoperative clinic visit, TKA (with numerous coding modifiers for complexity or comorbidities) as well as post-discharge admissions to skilled nursing and acute rehabilitation facilities. However, it was a start: for example, hospitals were no longer incentivized to keep TKA patients in house with a growing bill for each administered drug or therapy session. Yet, it is noteworthy that hospitals and physicians were still paid separately. This is important because doctors have historically made almost all treatment decisions and thereby determined the cost of care, yet hospitals have borne most of those costs, such as expensive implants or unplanned admissions, without a commensurate increase in reimbursement. As long as physicians are guaranteed their “fee,” they have little motivation to reduce those costs. Unsurprisingly, and as we well know, the advent of DRGs did not successfully curb our growing healthcare budget.
Recently, TKA and total hip arthroplasty reimbursement changed more dramatically. After experimenting with several pilots, CMS rolled out the Comprehensive Care for Joint Replacement (CJR) bundled payment program in 2015.1,4 Participation in CJR is mandatory for most arthroplasty providers in approximately half of all “metropolitan” areas. In this scheme, hospital and physician pay is intertwined. Specifically, hospitals are held accountable for costs, so if the total Medicare bill for a patient’s TKA exceeds the “target price,” the hospital faces a penalty. Conversely, a charge below the target can earn a bonus payment.4 The hospital and surgeons must decide how they will share the bonus (or penalty), which creates an incentive to work together to lower costs.
Continue to: While bundled payments like CJR shift some...
While bundled payments like CJR shift some of the risk for high costs to the hospital and surgeon, a much more extreme example of this type of shift is capitation (ie, paying a healthcare institution a set amount per patient to care for whatever maladies arise). Insurers have experimented with various forms of capitation in the past, which led to the expansion of health management organizations (HMOs) during the 1990s. In theory, capitation should encourage providers to invest in disease prevention to minimize the need for costly interventions. However, more nefarious incentives developed, resulting in “cherry picking” healthy patients, which restricts access to care for sicker patients, and even withholds care from patients in need. The most infamous example was arguably “drive-through deliveries,” where newborns and their mothers were prematurely discharged following birth.5 As a result, the “HMO backlash” occurred, and capitation temporarily fell out of favor. The heart of the problem was a strong incentive to reduce the cost of care without a counterbalancing incentive to maintain quality. CJR and other modern programs attempt to avoid similar adverse incentives by requiring participants to meet certain quality criteria.6
Since the passage of the Affordable Care Act in 2010, capitation has reemerged under a new name: Accountable Care Organizations (ACOs). Numerous forms of ACO’s exist with differing payment schemes7, but the most comprehensive version, named Next Generation (Next Gen), allows providers to choose full capitation.8 While early ACOs focused on individual patients, Next Gen ACOs are also focused on “population health.” That is, they must demonstrate outcomes for individuals and the patient population as a whole, while simultaneously assuming all financial risk via capitation. Specifically, these ACO’s are paid an “all-inclusive population-based payment” for each patient based on how much that type of patient’s care is expected to cost for the year.9 The ACO then provides all necessary treatment and, if the ACO cannot provide a necessary intervention, it is responsible for funding that care at another institution. Appropriately, there has been an increased focus on quality to avoid unintentional incentives to withhold care. Specifically, CMS has introduced mandatory quality metrics in the domains of patient experience, care coordination, preventive care, and management of at-risk populations.10 At present, unfortunately, these metrics are not nearly comprehensive enough nor adequately validated to assess the quality of care,11 especially for subspecialized fields like orthopedics where functional outcome scores are needed.
To date, very limited attention in the media or academic literature has been dedicated to subspecialty surgical care in the setting of ACOs even though implications for specialized surgeons could be immense. While ACOs bring numerous reporting requirements, the most essential first step for orthopedists in transition to this new reimbursement scheme will be a change in mindset. As explained above, orthopedics and other forms of specialized surgical care have traditionally been extremely profitable for healthcare institutions through relatively high revenue. However, within a capitated ACO all revenue has been paid upfront for each patient, and every orthopedic surgery performed represents a substantial cost to the institution rather than a large profit. For example, it has been reported that the average contribution margin earned by a hospital for an episode of care to provide a TKA (which includes postoperative care such as clinic visits, unplanned readmissions, and reoperations for complications) based on Medicare reimbursement is $11,726.12 This figure consists of reimbursement (median, $24,149) less variable costs (median, $10,190). Additionally, the surgeon currently receives $1400 in physician fees.13 These earnings represent a significant financial benefit for both the facility and doctor in the current FFS environment. However, a capitated ACO caring for a TKA patient would already have received full payment for his care for the year. As a result, providing a TKA would not afford any further financial benefit and would, instead, mean a loss of $10,190 (the aforementioned variable cost for the episode of care) directly from the bottom line. The orthopedic department within that ACO, along with other departments, can be expected to share that loss. This implies that upon becoming an ACO, an institution’s orthopedics department will change from a major profit-center to a major cost-center.
Continue to: CMS must establish adequate quality assurance...
CMS must establish adequate quality assurance measures to ensure that ACOs do not withhold cost-effective care, like TKAs,14,15 from their patients. Hopefully, for both professional and ethical reasons, providers will be active partners in this process. Groups like the International Consortium for Health Outcome Measurement, which has convened international expert panels to agree on comprehensive outcome sets for total joint arthroplasty and the management of low back pain, among other non-orthopedic conditions, may be useful examples in this process.16-18
At the provider level, surgeons will be more likely to be salaried employees, contracting directly with the ACO rather than primarily working to earn physician fees from insurance providers. Surgeons will likely be judged (and rewarded financially) on their ability to direct nonoperative care, to find non-surgical solutions to problems that may currently be treated operatively, and to reduce costs for patients that require surgery. Additionally, with an increased focus on quality assurance, there will likely be more pressure from ACOs and CMS to demonstrate results of both operative and nonoperative care, likely in the forms of patient-reported metrics and objective measures of physical function. Surgeons will have a strong incentive to be leaders in the process of collecting such data.
It is also worth considering the position of orthopedic practices that are not part of an ACO. Some ACOs will not have the capacity to provide all (or possibly any) of the orthopedic care their patients require. When necessary, they will contract with outside orthopedic practices. Compared with CMS, ACOs are much smaller purchasers and can be expected to be more sensitive to price, likely negotiating intensely between local orthopedic providers. As a result, even orthopedists outside of ACOs may feel the cost pressure created by this new reimbursement model and may be driven to implement cost-reduction measures such as standardized implant choices and discharge pathways.
ACOs are in an active growth phase,19,20 and recent updates to ACO policies make it clear that CMS intends for this trend to continue.8 Since ACOs are still a nascent reimbursement model, orthopedists will still do better financially, in almost all markets, by continuing to expend their energy and resources pursuing revenue, rather than cutting costs or demonstrating outcomes. However, as ACOs and population health gain traction, those orthopedists who recognize this shift and plan accordingly will have a definite strategic advantage, whether their practice is within an ACO, interacting with external ACOs, or both.
The way we are paid as doctors is changing. In some cases, the delivery of orthopedic care could change from healthcare institutions’ most significant financial asset to one of their most detrimental liabilities. These changes provide a chance to improve both the quality and efficiency of the care we deliver, but we are unlikely to capitalize on this opportunity unless we understand this shifting paradigm. This change requires us to first appreciate the recent history of our reimbursement environment.
Traditionally, healthcare has been a relatively lucrative field, especially for those providing surgical care: doctors are paid “physician fees” by insurance companies (including Medicare), and institutions where procedures are performed are paid “facility fees.” Profits are measured as revenue (ie, reimbursement) minus costs of providing care, and while there has always been the potential to make more money by lowering costs, providers have historically had much more to gain by increasing their revenue. This fact has been exacerbated by the “fee-for-service” (FFS) payment model, which unintentionally encourages physicians to provide high volumes of care by “paying more for doing more.” For example, rather than being paid a fixed sum to care for a patient’s knee arthritis, each provider involved in the patient’s care is paid for each intervention. Clearly, this system encourages providers to maximize their interventions (ie, earning revenue) rather than search for ways to cut costs.
The Centers for Medicare and Medicaid Services (CMS) partially addressed this issue during the 1980s by introducing the Diagnosis Related Group (DRG).1,2 Under this classification scheme, hospitals would be paid a pre-specified amount for a particular type of admission, often based on a specific procedure. For example, there is a DRG with a set payment for total knee arthroplasty (TKA).3 When reimbursement for the condition is set at a fixed amount, facilities are motivated to decrease their expenses since this is the only way to maximize the financial return for a given patient. This change, theoretically, encourages providers to cut their costs for providing a TKA as much as possible, potentially even to the point of sacrificing quality of care. As usual, when CMS makes a sweeping change, private insurers followed suit, and as a result, both government and corporate insurance is now structured around DRGs.
However, this was not a complete departure from FFS payment. We were still not paid to manage a patient’s knee arthritis as cheaply as possible; we were paid for each steroid injection, preoperative clinic visit, TKA (with numerous coding modifiers for complexity or comorbidities) as well as post-discharge admissions to skilled nursing and acute rehabilitation facilities. However, it was a start: for example, hospitals were no longer incentivized to keep TKA patients in house with a growing bill for each administered drug or therapy session. Yet, it is noteworthy that hospitals and physicians were still paid separately. This is important because doctors have historically made almost all treatment decisions and thereby determined the cost of care, yet hospitals have borne most of those costs, such as expensive implants or unplanned admissions, without a commensurate increase in reimbursement. As long as physicians are guaranteed their “fee,” they have little motivation to reduce those costs. Unsurprisingly, and as we well know, the advent of DRGs did not successfully curb our growing healthcare budget.
Recently, TKA and total hip arthroplasty reimbursement changed more dramatically. After experimenting with several pilots, CMS rolled out the Comprehensive Care for Joint Replacement (CJR) bundled payment program in 2015.1,4 Participation in CJR is mandatory for most arthroplasty providers in approximately half of all “metropolitan” areas. In this scheme, hospital and physician pay is intertwined. Specifically, hospitals are held accountable for costs, so if the total Medicare bill for a patient’s TKA exceeds the “target price,” the hospital faces a penalty. Conversely, a charge below the target can earn a bonus payment.4 The hospital and surgeons must decide how they will share the bonus (or penalty), which creates an incentive to work together to lower costs.
Continue to: While bundled payments like CJR shift some...
While bundled payments like CJR shift some of the risk for high costs to the hospital and surgeon, a much more extreme example of this type of shift is capitation (ie, paying a healthcare institution a set amount per patient to care for whatever maladies arise). Insurers have experimented with various forms of capitation in the past, which led to the expansion of health management organizations (HMOs) during the 1990s. In theory, capitation should encourage providers to invest in disease prevention to minimize the need for costly interventions. However, more nefarious incentives developed, resulting in “cherry picking” healthy patients, which restricts access to care for sicker patients, and even withholds care from patients in need. The most infamous example was arguably “drive-through deliveries,” where newborns and their mothers were prematurely discharged following birth.5 As a result, the “HMO backlash” occurred, and capitation temporarily fell out of favor. The heart of the problem was a strong incentive to reduce the cost of care without a counterbalancing incentive to maintain quality. CJR and other modern programs attempt to avoid similar adverse incentives by requiring participants to meet certain quality criteria.6
Since the passage of the Affordable Care Act in 2010, capitation has reemerged under a new name: Accountable Care Organizations (ACOs). Numerous forms of ACO’s exist with differing payment schemes7, but the most comprehensive version, named Next Generation (Next Gen), allows providers to choose full capitation.8 While early ACOs focused on individual patients, Next Gen ACOs are also focused on “population health.” That is, they must demonstrate outcomes for individuals and the patient population as a whole, while simultaneously assuming all financial risk via capitation. Specifically, these ACO’s are paid an “all-inclusive population-based payment” for each patient based on how much that type of patient’s care is expected to cost for the year.9 The ACO then provides all necessary treatment and, if the ACO cannot provide a necessary intervention, it is responsible for funding that care at another institution. Appropriately, there has been an increased focus on quality to avoid unintentional incentives to withhold care. Specifically, CMS has introduced mandatory quality metrics in the domains of patient experience, care coordination, preventive care, and management of at-risk populations.10 At present, unfortunately, these metrics are not nearly comprehensive enough nor adequately validated to assess the quality of care,11 especially for subspecialized fields like orthopedics where functional outcome scores are needed.
To date, very limited attention in the media or academic literature has been dedicated to subspecialty surgical care in the setting of ACOs even though implications for specialized surgeons could be immense. While ACOs bring numerous reporting requirements, the most essential first step for orthopedists in transition to this new reimbursement scheme will be a change in mindset. As explained above, orthopedics and other forms of specialized surgical care have traditionally been extremely profitable for healthcare institutions through relatively high revenue. However, within a capitated ACO all revenue has been paid upfront for each patient, and every orthopedic surgery performed represents a substantial cost to the institution rather than a large profit. For example, it has been reported that the average contribution margin earned by a hospital for an episode of care to provide a TKA (which includes postoperative care such as clinic visits, unplanned readmissions, and reoperations for complications) based on Medicare reimbursement is $11,726.12 This figure consists of reimbursement (median, $24,149) less variable costs (median, $10,190). Additionally, the surgeon currently receives $1400 in physician fees.13 These earnings represent a significant financial benefit for both the facility and doctor in the current FFS environment. However, a capitated ACO caring for a TKA patient would already have received full payment for his care for the year. As a result, providing a TKA would not afford any further financial benefit and would, instead, mean a loss of $10,190 (the aforementioned variable cost for the episode of care) directly from the bottom line. The orthopedic department within that ACO, along with other departments, can be expected to share that loss. This implies that upon becoming an ACO, an institution’s orthopedics department will change from a major profit-center to a major cost-center.
Continue to: CMS must establish adequate quality assurance...
CMS must establish adequate quality assurance measures to ensure that ACOs do not withhold cost-effective care, like TKAs,14,15 from their patients. Hopefully, for both professional and ethical reasons, providers will be active partners in this process. Groups like the International Consortium for Health Outcome Measurement, which has convened international expert panels to agree on comprehensive outcome sets for total joint arthroplasty and the management of low back pain, among other non-orthopedic conditions, may be useful examples in this process.16-18
At the provider level, surgeons will be more likely to be salaried employees, contracting directly with the ACO rather than primarily working to earn physician fees from insurance providers. Surgeons will likely be judged (and rewarded financially) on their ability to direct nonoperative care, to find non-surgical solutions to problems that may currently be treated operatively, and to reduce costs for patients that require surgery. Additionally, with an increased focus on quality assurance, there will likely be more pressure from ACOs and CMS to demonstrate results of both operative and nonoperative care, likely in the forms of patient-reported metrics and objective measures of physical function. Surgeons will have a strong incentive to be leaders in the process of collecting such data.
It is also worth considering the position of orthopedic practices that are not part of an ACO. Some ACOs will not have the capacity to provide all (or possibly any) of the orthopedic care their patients require. When necessary, they will contract with outside orthopedic practices. Compared with CMS, ACOs are much smaller purchasers and can be expected to be more sensitive to price, likely negotiating intensely between local orthopedic providers. As a result, even orthopedists outside of ACOs may feel the cost pressure created by this new reimbursement model and may be driven to implement cost-reduction measures such as standardized implant choices and discharge pathways.
ACOs are in an active growth phase,19,20 and recent updates to ACO policies make it clear that CMS intends for this trend to continue.8 Since ACOs are still a nascent reimbursement model, orthopedists will still do better financially, in almost all markets, by continuing to expend their energy and resources pursuing revenue, rather than cutting costs or demonstrating outcomes. However, as ACOs and population health gain traction, those orthopedists who recognize this shift and plan accordingly will have a definite strategic advantage, whether their practice is within an ACO, interacting with external ACOs, or both.
1. Carter Clement R, Bhat SB, Clement ME, Krieg JC. Medicare reimbursement and orthopedic surgery: past, present, and future. Curr Rev Musculoskelet Med. 2017;10(2):224-232. doi:10.1007/s12178-017-9406-7.
2. Centers for Medicare & Medicaid Services. Acute Inpatient PPS. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. Published August 2, 2017. Accessed September 8, 2018.
3. Centers for Medicare & Medicaid Services. Draft ICD-10-CM/PCS MS-DRGv28 Definitions Manual. https://www.cms.gov/icd10manual/fullcode_cms/P0185.html. Accessed September 8, 2018.
4. Centers for Medicare & Medicaid Services. Comprehensive Care for Joint Replacement Model. https://innovation.cms.gov/initiatives/cjr. Accessed September 8, 2018.
5. Volpp KG, Bundorf MK. Consumer protection and the HMO backlash: are HMOs to blame for drive-through deliveries? Inquiry. 1999;36(1):101-109.
6. Centers for Medicare & Medicaid Services. Quality Measures and Performance Standards. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Quality_Measures_Standards.html. Published March 2, 2015. Accessed November 3, 2015.
7. Centers for Medicare & Medicaid Services. Accountable Care Organizations (ACOs): General Information. https://innovation.cms.gov/initiatives/aco/. Accessed September 8, 2018.
8. Centers for Medicare & Medicaid Services. Next Generation ACO Model. https://innovation.cms.gov/initiatives/Next-Generation-ACO-Model/. Accessed September 8, 2018.
9. Centers for Medicare & Medicaid Services. Next Generation Accountable Care Organization (ACO) Model: Frequently Asked Questions. https://innovation.cms.gov/Files/x/nextgenacofaq.pdf. Accessed September 8, 2018.
10. Centers for Medicare & Medicaid Services. Quality Measure Benchmarks for the 2018 and 2019 Reporting Years. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/2018-and-2019-quality-benchmarks-guidance.pdf. Published December 2017. Accessed September 8, 2018.
11. Toussaint J, Krueger D, Shortell SM, Milstein A, Cutler DM. ACO model should encourage efficient care delivery. Healthc (Amst). 2015;3(3):150-152. doi:10.1016/j.hjdsi.2015.06.003.
12. Clement RC, Kheir MM, Derman PB, et al. What are the economic consequences of unplanned readmissions after TKA? Clin Orthop Relat Res. 2014;472(10):3134-3141. doi:10.1007/s11999-014-3795-3.
13. Centers for Medicare & Medicaid Services. Physician Fee Schedule Search Results. http://www.cms.gov/apps/physician-fee-schedule/search/search-results.aspx?Y=0&T=0&HT=0&CT=0&H1=27447&M=1. Accessed June 4, 2015.
14. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113-1121; discussion 1121-1122. doi:10.1001/archinternmed.2009.136.
15. Mather RC 3rd, Hug KT, Orlando LA, et al. Economic evaluation of access to musculoskeletal care: the case of waiting for total knee arthroplasty. BMC Musculoskelet Disord. 2014;15:22. doi:10.1186/1471-2474-15-22.
16. International Consortium for Health Outcomes Measurement. ICHOM web site. https://www.ichom.org/. Accessed November 3, 2015.
17. Rolfson O, Wissig S, van Maasakkers L, et al. Defining an international standard set of outcome measures for patients with hip or knee osteoarthritis: consensus of the International Consortium for Health Outcomes Measurement Hip and Knee Osteoarthritis Working Group. Arthritis Care Res (Hoboken). 2016;68(11):1631-1639. doi:10.1002/acr.22868.
18. Clement RC, Welander A, Stowell C, et al. A proposed set of metrics for standardized outcome reporting in the management of low back pain. Acta Orthop. 2015;86(5):523-533. doi:10.3109/17453674.2015.1036696.
19. Shortell SM, Colla CH, Lewis VA, Fisher E, Kessell E, Ramsay P. Accountable care organizations: the national landscape. J Health Polit Policy Law. 2015;40(4):647-668. doi:10.1215/03616878-3149976.
20. Centers for Medicare & Medicaid Services. CMS Proposes “Pathways to Success,” an Overhaul of Medicare’s ACO Program https://www.cms.gov/newsroom/press-releases/cms-proposes-pathways-success-overhaul-medicares-aco-program. Published August 9, 2018. Accessed September 10, 2018.
1. Carter Clement R, Bhat SB, Clement ME, Krieg JC. Medicare reimbursement and orthopedic surgery: past, present, and future. Curr Rev Musculoskelet Med. 2017;10(2):224-232. doi:10.1007/s12178-017-9406-7.
2. Centers for Medicare & Medicaid Services. Acute Inpatient PPS. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/index.html. Published August 2, 2017. Accessed September 8, 2018.
3. Centers for Medicare & Medicaid Services. Draft ICD-10-CM/PCS MS-DRGv28 Definitions Manual. https://www.cms.gov/icd10manual/fullcode_cms/P0185.html. Accessed September 8, 2018.
4. Centers for Medicare & Medicaid Services. Comprehensive Care for Joint Replacement Model. https://innovation.cms.gov/initiatives/cjr. Accessed September 8, 2018.
5. Volpp KG, Bundorf MK. Consumer protection and the HMO backlash: are HMOs to blame for drive-through deliveries? Inquiry. 1999;36(1):101-109.
6. Centers for Medicare & Medicaid Services. Quality Measures and Performance Standards. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Quality_Measures_Standards.html. Published March 2, 2015. Accessed November 3, 2015.
7. Centers for Medicare & Medicaid Services. Accountable Care Organizations (ACOs): General Information. https://innovation.cms.gov/initiatives/aco/. Accessed September 8, 2018.
8. Centers for Medicare & Medicaid Services. Next Generation ACO Model. https://innovation.cms.gov/initiatives/Next-Generation-ACO-Model/. Accessed September 8, 2018.
9. Centers for Medicare & Medicaid Services. Next Generation Accountable Care Organization (ACO) Model: Frequently Asked Questions. https://innovation.cms.gov/Files/x/nextgenacofaq.pdf. Accessed September 8, 2018.
10. Centers for Medicare & Medicaid Services. Quality Measure Benchmarks for the 2018 and 2019 Reporting Years. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/2018-and-2019-quality-benchmarks-guidance.pdf. Published December 2017. Accessed September 8, 2018.
11. Toussaint J, Krueger D, Shortell SM, Milstein A, Cutler DM. ACO model should encourage efficient care delivery. Healthc (Amst). 2015;3(3):150-152. doi:10.1016/j.hjdsi.2015.06.003.
12. Clement RC, Kheir MM, Derman PB, et al. What are the economic consequences of unplanned readmissions after TKA? Clin Orthop Relat Res. 2014;472(10):3134-3141. doi:10.1007/s11999-014-3795-3.
13. Centers for Medicare & Medicaid Services. Physician Fee Schedule Search Results. http://www.cms.gov/apps/physician-fee-schedule/search/search-results.aspx?Y=0&T=0&HT=0&CT=0&H1=27447&M=1. Accessed June 4, 2015.
14. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113-1121; discussion 1121-1122. doi:10.1001/archinternmed.2009.136.
15. Mather RC 3rd, Hug KT, Orlando LA, et al. Economic evaluation of access to musculoskeletal care: the case of waiting for total knee arthroplasty. BMC Musculoskelet Disord. 2014;15:22. doi:10.1186/1471-2474-15-22.
16. International Consortium for Health Outcomes Measurement. ICHOM web site. https://www.ichom.org/. Accessed November 3, 2015.
17. Rolfson O, Wissig S, van Maasakkers L, et al. Defining an international standard set of outcome measures for patients with hip or knee osteoarthritis: consensus of the International Consortium for Health Outcomes Measurement Hip and Knee Osteoarthritis Working Group. Arthritis Care Res (Hoboken). 2016;68(11):1631-1639. doi:10.1002/acr.22868.
18. Clement RC, Welander A, Stowell C, et al. A proposed set of metrics for standardized outcome reporting in the management of low back pain. Acta Orthop. 2015;86(5):523-533. doi:10.3109/17453674.2015.1036696.
19. Shortell SM, Colla CH, Lewis VA, Fisher E, Kessell E, Ramsay P. Accountable care organizations: the national landscape. J Health Polit Policy Law. 2015;40(4):647-668. doi:10.1215/03616878-3149976.
20. Centers for Medicare & Medicaid Services. CMS Proposes “Pathways to Success,” an Overhaul of Medicare’s ACO Program https://www.cms.gov/newsroom/press-releases/cms-proposes-pathways-success-overhaul-medicares-aco-program. Published August 9, 2018. Accessed September 10, 2018.
Difficult-to-treat RA remains difficult to define
Active disease, failure of disease-modifying antirheumatic drug therapy, and an inability to taper glucocorticoid treatment are the main characteristics of difficult-to-treat RA, according to results of a survey of mostly European rheumatologists that also revealed a wide variation in views on the factors that contribute to the concept.
Some of the issues that survey respondents considered clinically relevant in difficult-to-treat RA are not covered by current EULAR management recommendations, Nadia M.T. Roodenrijs, of University Medical Center Utrecht, the Netherlands, and her colleagues noted in a study published online in Annals of the Rheumatic Diseases.
The investigators set out to determine what a range of rheumatologists from different countries considered to be the key characteristics of difficult-to-treat RA, which has an estimated prevalence of 5%-20%, depending on the criteria used. They also sought to identify the issues relating to work-up and management that were not covered by the current EULAR recommendations.
The online survey contained four multiple choice questions that asked about the necessity of incorporating disease activity level, fatigue, number of disease-modifying antirheumatic drugs (DMARDs) that failed, and the inability to taper glucocorticoids into the concept of difficult-to-treat RA. The survey also asked three open questions seeking additional clinically relevant views on difficult-to-treat RA.
A total of 410 respondents from 33 countries (96% European) completed the survey, which was sent to rheumatologists through the Emerging EULAR Network. Overall, half of the respondents selected “disease activity score assessing 28 joints using erythrocyte sedimentation rate [DAS28-ESR] greater than 3.2 or the presence of signs suggestive of active inflammatory disease activity with a DAS28-ESR of 3.2 or less” as characteristics of difficult-to-treat RA. About 42% of respondents included fatigue as a characteristic and 48% selected failure to two or more conventional DMARDs and two or more biological/targeted synthetic DMARDs. Furthermore, 89% of respondents identified the inability to taper glucocorticoids below 5 mg or 10 mg prednisone equivalent daily to be a characteristic of difficult-to-treat RA.
Other clinically important issues identified by the respondents as currently missing from EULAR management recommendations included interfering comorbidities, especially cardiovascular disease, infection, and malignancy; extra-articular manifestations; and polypharmacy.
“The results of this survey underscore the difficulty in establishing an unambiguous concept of difficult-to-treat RA, which is seen as a heterogeneous condition not fully covered by EULAR recommendations,” the authors wrote.
The authors noted that their findings would help fuel discussion on the issues to include in the management recommendations for difficult-to-treat RA currently under consideration by a recently established EULAR task force.
The study was not funded with a specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Some of the authors reported receiving fees from several pharmaceutical countries.
SOURCE: Roodenrijs NMT et al. Ann Rheum Dis. 2018 Sep 7. doi: 10.1136/annrheumdis-2018-213687.
Active disease, failure of disease-modifying antirheumatic drug therapy, and an inability to taper glucocorticoid treatment are the main characteristics of difficult-to-treat RA, according to results of a survey of mostly European rheumatologists that also revealed a wide variation in views on the factors that contribute to the concept.
Some of the issues that survey respondents considered clinically relevant in difficult-to-treat RA are not covered by current EULAR management recommendations, Nadia M.T. Roodenrijs, of University Medical Center Utrecht, the Netherlands, and her colleagues noted in a study published online in Annals of the Rheumatic Diseases.
The investigators set out to determine what a range of rheumatologists from different countries considered to be the key characteristics of difficult-to-treat RA, which has an estimated prevalence of 5%-20%, depending on the criteria used. They also sought to identify the issues relating to work-up and management that were not covered by the current EULAR recommendations.
The online survey contained four multiple choice questions that asked about the necessity of incorporating disease activity level, fatigue, number of disease-modifying antirheumatic drugs (DMARDs) that failed, and the inability to taper glucocorticoids into the concept of difficult-to-treat RA. The survey also asked three open questions seeking additional clinically relevant views on difficult-to-treat RA.
A total of 410 respondents from 33 countries (96% European) completed the survey, which was sent to rheumatologists through the Emerging EULAR Network. Overall, half of the respondents selected “disease activity score assessing 28 joints using erythrocyte sedimentation rate [DAS28-ESR] greater than 3.2 or the presence of signs suggestive of active inflammatory disease activity with a DAS28-ESR of 3.2 or less” as characteristics of difficult-to-treat RA. About 42% of respondents included fatigue as a characteristic and 48% selected failure to two or more conventional DMARDs and two or more biological/targeted synthetic DMARDs. Furthermore, 89% of respondents identified the inability to taper glucocorticoids below 5 mg or 10 mg prednisone equivalent daily to be a characteristic of difficult-to-treat RA.
Other clinically important issues identified by the respondents as currently missing from EULAR management recommendations included interfering comorbidities, especially cardiovascular disease, infection, and malignancy; extra-articular manifestations; and polypharmacy.
“The results of this survey underscore the difficulty in establishing an unambiguous concept of difficult-to-treat RA, which is seen as a heterogeneous condition not fully covered by EULAR recommendations,” the authors wrote.
The authors noted that their findings would help fuel discussion on the issues to include in the management recommendations for difficult-to-treat RA currently under consideration by a recently established EULAR task force.
The study was not funded with a specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Some of the authors reported receiving fees from several pharmaceutical countries.
SOURCE: Roodenrijs NMT et al. Ann Rheum Dis. 2018 Sep 7. doi: 10.1136/annrheumdis-2018-213687.
Active disease, failure of disease-modifying antirheumatic drug therapy, and an inability to taper glucocorticoid treatment are the main characteristics of difficult-to-treat RA, according to results of a survey of mostly European rheumatologists that also revealed a wide variation in views on the factors that contribute to the concept.
Some of the issues that survey respondents considered clinically relevant in difficult-to-treat RA are not covered by current EULAR management recommendations, Nadia M.T. Roodenrijs, of University Medical Center Utrecht, the Netherlands, and her colleagues noted in a study published online in Annals of the Rheumatic Diseases.
The investigators set out to determine what a range of rheumatologists from different countries considered to be the key characteristics of difficult-to-treat RA, which has an estimated prevalence of 5%-20%, depending on the criteria used. They also sought to identify the issues relating to work-up and management that were not covered by the current EULAR recommendations.
The online survey contained four multiple choice questions that asked about the necessity of incorporating disease activity level, fatigue, number of disease-modifying antirheumatic drugs (DMARDs) that failed, and the inability to taper glucocorticoids into the concept of difficult-to-treat RA. The survey also asked three open questions seeking additional clinically relevant views on difficult-to-treat RA.
A total of 410 respondents from 33 countries (96% European) completed the survey, which was sent to rheumatologists through the Emerging EULAR Network. Overall, half of the respondents selected “disease activity score assessing 28 joints using erythrocyte sedimentation rate [DAS28-ESR] greater than 3.2 or the presence of signs suggestive of active inflammatory disease activity with a DAS28-ESR of 3.2 or less” as characteristics of difficult-to-treat RA. About 42% of respondents included fatigue as a characteristic and 48% selected failure to two or more conventional DMARDs and two or more biological/targeted synthetic DMARDs. Furthermore, 89% of respondents identified the inability to taper glucocorticoids below 5 mg or 10 mg prednisone equivalent daily to be a characteristic of difficult-to-treat RA.
Other clinically important issues identified by the respondents as currently missing from EULAR management recommendations included interfering comorbidities, especially cardiovascular disease, infection, and malignancy; extra-articular manifestations; and polypharmacy.
“The results of this survey underscore the difficulty in establishing an unambiguous concept of difficult-to-treat RA, which is seen as a heterogeneous condition not fully covered by EULAR recommendations,” the authors wrote.
The authors noted that their findings would help fuel discussion on the issues to include in the management recommendations for difficult-to-treat RA currently under consideration by a recently established EULAR task force.
The study was not funded with a specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Some of the authors reported receiving fees from several pharmaceutical countries.
SOURCE: Roodenrijs NMT et al. Ann Rheum Dis. 2018 Sep 7. doi: 10.1136/annrheumdis-2018-213687.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: There is wide variation in the views of rheumatologists across Europe on the key characteristics of difficult-to-treat RA. Some issues that rheumatologists consider to be clinically relevant are not covered by current EULAR recommendations.
Major finding:
Study details: An online survey completed by 410 rheumatologists from 33 countries.
Disclosures: The study was not funded with a specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Some of the authors reported receiving fees from several pharmaceutical countries.
Source: Roodenrijs NMT et al. Ann Rheum Dis. 2018 Sep 7. doi: 10.1136/annrheumdis-2018-213687.
Pregnancy boosts cardiac disease mortality nearly 100-fold
MUNICH – Women with cardiac disease who became pregnant had a nearly 100-fold higher mortality rate, compared with pregnant women without cardiac disease, according to the outcomes of more than 5,700 pregnancies in an international registry of women with cardiac disease.
In addition to increased mortality, women with cardiac disease who become pregnant also had a greater than 100-fold higher rate of developing heart failure, compared with pregnant women without cardiac disease.
Despite these highly elevated relative risks, the absolute rate of serious complications from pregnancy for most women with heart disease was relatively modest. The worst prognosis by far was for the 1% of women in the registry who had pulmonary arterial hypertension at the time their pregnancy began. For these women, mortality during pregnancy was about 9%, and new-onset heart failure occurred in about one third. Another subgroup showing particularly poor outcomes were women classified with WHO IV maternal cardiovascular risk by the modified World Health Organization criteria, which corresponds to having an “extremely high risk of maternal mortality or severe morbidity,” according to guidelines published in the European Heart Journal (2011 Dec 1;32[24]:3147-97).These women, constituting 7% of the registry cohort, had a 2.5% mortality rate during pregnancy and a 33% incidence of heart failure.
Across all women with cardiac disease enrolled in the registry, the incidence of death during pregnancy was 0.6% and the incidence of heart failure was 11%. Women without cardiac disease have rates of 0.007% and less than 0.1%, respectively, Jolien Roos-Hesselink, MD, said at the annual congress of the European Society of Cardiology.
“The most important message of my talk is that all patients should be counseled, not just the women at high risk, for whom pregnancy is contraindicated, but also the women at low risk,” who can have a child with relative safety, she said. “Many women [with cardiac disease] can go through pregnancy at low risk.” Counseling is the key so that women know their risk before becoming pregnant, stressed Dr. Roos-Hesselink, a cardiologist at Erasmus Medical Center in Rotterdam, the Netherlands.
Based on the observed rates of mortality and other complications, pulmonary arterial hypertension and the other cardiac conditions that define a WHO IV maternal risk classification remain contraindications for pregnancy, she said. According to the 2011 guidelines from the European Society of Cardiology for managing cardiovascular disease during pregnancy, the full list of conditions that define a WHO IV classification are the following:
- Pulmonary arterial hypertension of any cause.
- Severe systemic ventricular dysfunction (a left ventricular ejection fraction of less than 30%) or New York Heart Association functional class III or IV.
- Previous peripartum cardiomyopathy with any residual impairment of left ventricular function.
- Severe mitral stenosis or severe symptomatic aortic stenosis.
- Marfan syndrome with the aorta dilated to more than 45 mm.
- Aortic dilatation greater than 50 mm in aortic disease associated with a bicuspid aortic valve.
- Native severe coarctation.
The registry data, collected during 2007-2018, showed a clear increase in the percentage of women with WHO class IV cardiovascular disease who became pregnant and entered the registry despite the contraindication designation for that classification, rising from about 1% of enrolled women in 2008 and 2009 to more than 10% of women in 2013, 2016, and 2017. “Individualization is necessary, but all these women are at very high risk and should be counseled against pregnancy,” Dr. Roos-Hesselink said.
The Registry of Pregnancy and Cardiac Disease (ROPAC) enrolled 5,739 pregnant women at any of 138 participating centers in 53 countries including the United States. Clinicians submitted WHO classification of cardiovascular risk for 5,711 of these women. The most common risk was congenital heart disease in 57% of enrolled women, followed by valvular heart disease in 29% and cardiomyopathy in 7%. Nearly 1,200 women in the registry – about 21% of the total – had a WHO I classification, which meant that they would be expected to have no detectable increase in mortality rate during pregnancy, compared with women without cardiac disease, and either no rise in morbidity or a mild effect.
Delivery was by cesarean section in 44% of the pregnancies, roughly twice the rate in women without diagnosed cardiac disease, even though published guidelines don’t advise cesarean delivery because of cardiac disease, Dr. Roos-Hesselink said. “Cesarean sections are used too often, in my opinion,” she commented, but added that many of these women require delivery at a tertiary, specialized center.
Overall fetal mortality was 1%, nearly threefold higher than in pregnancies in women without cardiac disease, and the overall incidence of fetal and neonatal complications was especially high, at 53%, in women with pulmonary arterial hypertension. The incidence of obstetrical complications was roughly similar across the range of cardiac disease type, ranging from 16% to 24%. Premature delivery occurred in 28% of women in the high-risk WHO IV class, compared with a 13% rate among women in the WHO I class. The mortality rate was 0.2% among the WHO class I women, and their heart failure incidence was 5%.
The ROPAC registry is sponsored by the European Society of Cardiology. Dr. Roos-Hesselink had no disclosures.
MUNICH – Women with cardiac disease who became pregnant had a nearly 100-fold higher mortality rate, compared with pregnant women without cardiac disease, according to the outcomes of more than 5,700 pregnancies in an international registry of women with cardiac disease.
In addition to increased mortality, women with cardiac disease who become pregnant also had a greater than 100-fold higher rate of developing heart failure, compared with pregnant women without cardiac disease.
Despite these highly elevated relative risks, the absolute rate of serious complications from pregnancy for most women with heart disease was relatively modest. The worst prognosis by far was for the 1% of women in the registry who had pulmonary arterial hypertension at the time their pregnancy began. For these women, mortality during pregnancy was about 9%, and new-onset heart failure occurred in about one third. Another subgroup showing particularly poor outcomes were women classified with WHO IV maternal cardiovascular risk by the modified World Health Organization criteria, which corresponds to having an “extremely high risk of maternal mortality or severe morbidity,” according to guidelines published in the European Heart Journal (2011 Dec 1;32[24]:3147-97).These women, constituting 7% of the registry cohort, had a 2.5% mortality rate during pregnancy and a 33% incidence of heart failure.
Across all women with cardiac disease enrolled in the registry, the incidence of death during pregnancy was 0.6% and the incidence of heart failure was 11%. Women without cardiac disease have rates of 0.007% and less than 0.1%, respectively, Jolien Roos-Hesselink, MD, said at the annual congress of the European Society of Cardiology.
“The most important message of my talk is that all patients should be counseled, not just the women at high risk, for whom pregnancy is contraindicated, but also the women at low risk,” who can have a child with relative safety, she said. “Many women [with cardiac disease] can go through pregnancy at low risk.” Counseling is the key so that women know their risk before becoming pregnant, stressed Dr. Roos-Hesselink, a cardiologist at Erasmus Medical Center in Rotterdam, the Netherlands.
Based on the observed rates of mortality and other complications, pulmonary arterial hypertension and the other cardiac conditions that define a WHO IV maternal risk classification remain contraindications for pregnancy, she said. According to the 2011 guidelines from the European Society of Cardiology for managing cardiovascular disease during pregnancy, the full list of conditions that define a WHO IV classification are the following:
- Pulmonary arterial hypertension of any cause.
- Severe systemic ventricular dysfunction (a left ventricular ejection fraction of less than 30%) or New York Heart Association functional class III or IV.
- Previous peripartum cardiomyopathy with any residual impairment of left ventricular function.
- Severe mitral stenosis or severe symptomatic aortic stenosis.
- Marfan syndrome with the aorta dilated to more than 45 mm.
- Aortic dilatation greater than 50 mm in aortic disease associated with a bicuspid aortic valve.
- Native severe coarctation.
The registry data, collected during 2007-2018, showed a clear increase in the percentage of women with WHO class IV cardiovascular disease who became pregnant and entered the registry despite the contraindication designation for that classification, rising from about 1% of enrolled women in 2008 and 2009 to more than 10% of women in 2013, 2016, and 2017. “Individualization is necessary, but all these women are at very high risk and should be counseled against pregnancy,” Dr. Roos-Hesselink said.
The Registry of Pregnancy and Cardiac Disease (ROPAC) enrolled 5,739 pregnant women at any of 138 participating centers in 53 countries including the United States. Clinicians submitted WHO classification of cardiovascular risk for 5,711 of these women. The most common risk was congenital heart disease in 57% of enrolled women, followed by valvular heart disease in 29% and cardiomyopathy in 7%. Nearly 1,200 women in the registry – about 21% of the total – had a WHO I classification, which meant that they would be expected to have no detectable increase in mortality rate during pregnancy, compared with women without cardiac disease, and either no rise in morbidity or a mild effect.
Delivery was by cesarean section in 44% of the pregnancies, roughly twice the rate in women without diagnosed cardiac disease, even though published guidelines don’t advise cesarean delivery because of cardiac disease, Dr. Roos-Hesselink said. “Cesarean sections are used too often, in my opinion,” she commented, but added that many of these women require delivery at a tertiary, specialized center.
Overall fetal mortality was 1%, nearly threefold higher than in pregnancies in women without cardiac disease, and the overall incidence of fetal and neonatal complications was especially high, at 53%, in women with pulmonary arterial hypertension. The incidence of obstetrical complications was roughly similar across the range of cardiac disease type, ranging from 16% to 24%. Premature delivery occurred in 28% of women in the high-risk WHO IV class, compared with a 13% rate among women in the WHO I class. The mortality rate was 0.2% among the WHO class I women, and their heart failure incidence was 5%.
The ROPAC registry is sponsored by the European Society of Cardiology. Dr. Roos-Hesselink had no disclosures.
MUNICH – Women with cardiac disease who became pregnant had a nearly 100-fold higher mortality rate, compared with pregnant women without cardiac disease, according to the outcomes of more than 5,700 pregnancies in an international registry of women with cardiac disease.
In addition to increased mortality, women with cardiac disease who become pregnant also had a greater than 100-fold higher rate of developing heart failure, compared with pregnant women without cardiac disease.
Despite these highly elevated relative risks, the absolute rate of serious complications from pregnancy for most women with heart disease was relatively modest. The worst prognosis by far was for the 1% of women in the registry who had pulmonary arterial hypertension at the time their pregnancy began. For these women, mortality during pregnancy was about 9%, and new-onset heart failure occurred in about one third. Another subgroup showing particularly poor outcomes were women classified with WHO IV maternal cardiovascular risk by the modified World Health Organization criteria, which corresponds to having an “extremely high risk of maternal mortality or severe morbidity,” according to guidelines published in the European Heart Journal (2011 Dec 1;32[24]:3147-97).These women, constituting 7% of the registry cohort, had a 2.5% mortality rate during pregnancy and a 33% incidence of heart failure.
Across all women with cardiac disease enrolled in the registry, the incidence of death during pregnancy was 0.6% and the incidence of heart failure was 11%. Women without cardiac disease have rates of 0.007% and less than 0.1%, respectively, Jolien Roos-Hesselink, MD, said at the annual congress of the European Society of Cardiology.
“The most important message of my talk is that all patients should be counseled, not just the women at high risk, for whom pregnancy is contraindicated, but also the women at low risk,” who can have a child with relative safety, she said. “Many women [with cardiac disease] can go through pregnancy at low risk.” Counseling is the key so that women know their risk before becoming pregnant, stressed Dr. Roos-Hesselink, a cardiologist at Erasmus Medical Center in Rotterdam, the Netherlands.
Based on the observed rates of mortality and other complications, pulmonary arterial hypertension and the other cardiac conditions that define a WHO IV maternal risk classification remain contraindications for pregnancy, she said. According to the 2011 guidelines from the European Society of Cardiology for managing cardiovascular disease during pregnancy, the full list of conditions that define a WHO IV classification are the following:
- Pulmonary arterial hypertension of any cause.
- Severe systemic ventricular dysfunction (a left ventricular ejection fraction of less than 30%) or New York Heart Association functional class III or IV.
- Previous peripartum cardiomyopathy with any residual impairment of left ventricular function.
- Severe mitral stenosis or severe symptomatic aortic stenosis.
- Marfan syndrome with the aorta dilated to more than 45 mm.
- Aortic dilatation greater than 50 mm in aortic disease associated with a bicuspid aortic valve.
- Native severe coarctation.
The registry data, collected during 2007-2018, showed a clear increase in the percentage of women with WHO class IV cardiovascular disease who became pregnant and entered the registry despite the contraindication designation for that classification, rising from about 1% of enrolled women in 2008 and 2009 to more than 10% of women in 2013, 2016, and 2017. “Individualization is necessary, but all these women are at very high risk and should be counseled against pregnancy,” Dr. Roos-Hesselink said.
The Registry of Pregnancy and Cardiac Disease (ROPAC) enrolled 5,739 pregnant women at any of 138 participating centers in 53 countries including the United States. Clinicians submitted WHO classification of cardiovascular risk for 5,711 of these women. The most common risk was congenital heart disease in 57% of enrolled women, followed by valvular heart disease in 29% and cardiomyopathy in 7%. Nearly 1,200 women in the registry – about 21% of the total – had a WHO I classification, which meant that they would be expected to have no detectable increase in mortality rate during pregnancy, compared with women without cardiac disease, and either no rise in morbidity or a mild effect.
Delivery was by cesarean section in 44% of the pregnancies, roughly twice the rate in women without diagnosed cardiac disease, even though published guidelines don’t advise cesarean delivery because of cardiac disease, Dr. Roos-Hesselink said. “Cesarean sections are used too often, in my opinion,” she commented, but added that many of these women require delivery at a tertiary, specialized center.
Overall fetal mortality was 1%, nearly threefold higher than in pregnancies in women without cardiac disease, and the overall incidence of fetal and neonatal complications was especially high, at 53%, in women with pulmonary arterial hypertension. The incidence of obstetrical complications was roughly similar across the range of cardiac disease type, ranging from 16% to 24%. Premature delivery occurred in 28% of women in the high-risk WHO IV class, compared with a 13% rate among women in the WHO I class. The mortality rate was 0.2% among the WHO class I women, and their heart failure incidence was 5%.
The ROPAC registry is sponsored by the European Society of Cardiology. Dr. Roos-Hesselink had no disclosures.
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point: Women with cardiac disease who became pregnant had substantially increased mortality and morbidity.
Major finding: Pregnancy mortality was 0.6% in women with cardiac disease versus 0.007% in women without cardiac disorders.
Study details: The ROPAC registry, which enrolled 5,739 pregnant women at any of 138 centers in 53 countries during 2007-2018.
Disclosures: The ROPAC registry is sponsored by the European Society of Cardiology. Dr. Roos-Hesselink had no disclosures.
Improved Transitional Care Through an Innovative Hospitalist Model: Expanding Clinician Practice From Acute to Subacute Care
Hospitalist physician rotations between acute inpatient hospitals and subacute care facilities with dedicated time in each environment may foster quality improvement and educational opportunities.
Care transitions between hospitals and skilled nursing facilities (SNFs) are a vulnerable time for patients. The current health care climate of decreasing hospital length of stay, readmission penalties, and increasing patient complexity has made hospital care transitions an important safety concern. Suboptimal transitions across clinical settings can result in adverse events, inadequately controlled comorbidities, deficient patient and caregiver preparation for discharge, medication errors, relocation stress, and overall increased morbidity and mortality.1,2 Such care transitions also may generate unnecessary spending, including avoidable readmissions, emergency department utilization, and duplicative laboratory and imaging studies. Approximately 23% of patients admitted to SNFs are readmitted to acute care hospitals within 30 days, and these patients have increased mortality rates in risk-adjusted analyses. 3,4
Compounding the magnitude of this risk and vulnerability is the significant growth in the number of patients discharged to SNFs over the past 30 years. In 2013, more than 20% of Medicare patients discharged from acute care hospitals were destined for SNFs.5,6 Paradoxically, despite the increasing need for SNF providers, there is a shortage of clinicians with training in geriatrics or nursing home care.7 The result is a growing need to identify organizational systems to optimize physician practice in these settings, enhance quality of care, especially around transitions, and increase educational training opportunities in SNFs for future practitioners.
Many SNFs today are staffed by physicians and other licensed clinicians whose exclusive practice location is the nursing facility or possibly several such facilities. This prevailing model of care can isolate the physicians, depriving them of interaction with clinicians in other specialties, and can contribute to burnout.8 This model does not lend itself to academic scholarship, quality improvement (QI), and student or resident training, as each of these endeavors depends on interprofessional collaboration as well as access to an academic medical center with additional resources.9
Few studies have described innovative hospitalist rotation models from acute to subacute care. The Cleveland Clinic implemented the Connected Care model where hospital-employed physicians and advanced practice professionals integrated into postacute care and reduced the 30-day hospital readmission rate from SNFs from 28% to 22%.10 Goth and colleagues performed a comparative effectiveness trial between a postacute care hospitalist (PACH) model and a community-based physician model of nursing home care. They found that the institution of a PACH model in a nursing home was associated with a significant increase in laboratory costs, nonsignificant reduction in medication errors and pharmacy costs, and no improvement in fall rates.11 The conclusion was that the PACH model may lead to greater clinician involvement and that the potential decrease in pharmacy costs and medications errors may offset the costs associated with additional laboratory testing. Overall, there has been a lack of studies on the impact of these hospitalist rotation models from acute to subacute care on educational programs, QI activities, and the interprofessional environment.
To achieve a system in which physicians in a SNF can excel in these areas, Veterans Affairs Boston Healthcare System (VABHS) adopted a staffing model in which academic hospitalist physicians rotate between the inpatient hospital and subacute settings. This report describes the model structure, the varying roles of the physicians, and early indicators of its positive effects on educational programs, QI activities, and the interprofessional environment.
Methods
The VABHS consists of a 159-bed acute care hospital in West Roxbury, Massachusetts; and a 110-bed SNF in Brockton, Massachusetts, with 3 units: a 65-bed transitional care unit (TCU), a 30-bed long-term care unit, and a 15-bed palliative care/hospice unit. The majority of patients admitted to the SNF are transferred from the acute care hospital in West Roxbury and other regional hospitals. Prior to 2015, the TCU was staffed with full-time clinicians who exclusively practiced in the SNF.
In the new staffing model, 6 hospitalist physicians divide their clinical time between the acute care hospital’s inpatient medical service and the TCU. The hospitalists come from varied backgrounds in terms of years in practice and advanced training (Table 1).
The amount of nonclinical (protected) time and clinical time on the acute inpatient service and the TCU varies for each physician. For example, a physician serves as principal investigator for several major research grants and has a hospital-wide administrative leadership role; as a result, the principal investigator has fewer months of clinical responsibility. Physicians are expected to use the protected time for scholarship, educational program development and teaching, QI, and administrative responsibilities. The VABHS leadership determines the amount of protected time based on individualized benchmarks for research, education, and administrative responsibilities that follow VA national and local institutional guidelines. These metrics and time allocations are negotiated at the time of recruitment and then are reviewed annually.
The TCU also is staffed with 4 full-time clinicians (2 physicians and 2 physician assistants) who provide additional continuity of care. The new hospitalist staffing model only required an approximate 10% increase in TCU clinical staffing full-time equivalents. Patients and admissions are divided equally among clinicians on service (census per clinician 12-15 patients), with redistribution of patients at times of transition from clinical to nonclinical time. Blocks of clinical time are scheduled for greater than 2 weeks at a time to preserve continuity. In addition, the new staffing model allocates assignment of clinical responsibilities that allows for clinicians to take leave without resultant shortages in clinical coverage.
To facilitate communication among physicians serving in the acute inpatient facility and the TCU, leaders of both of these programs meet monthly and ad hoc to review the transitions of care between the 2 settings. The description of this model and its assessment have been reviewed and deemed exempt from oversight by the VA Boston Healthcare System Research and Development Committee.
Results
Since the implementation of this staffing model in 2015, the system has grown considerably in the breadth and depth of educational programming, QI, and systems redesign in the TCU and, more broadly, in the SNF. The TCU, which previously had limited training opportunities, has experienced marked expansion of educational offerings. It is now a site for core general medicine rotations for first-year psychiatry residents and physician assistant students. The TCU also has expanded as a clinical site for transitions-in-care internal medicine resident curricula and electives, as well as a clinical site for a geriatrics fellowship.
A hospitalist developed and implemented a 4-week interprofessional curriculum for all clinical trainees and students, which occurs continuously. The curriculum includes a monthly academic conference and 12 didactic lectures and is taught by 16 interprofessional faculty from the TCU and the Palliative Care/Hospice Unit, including medicine, geriatric and palliative care physicians, physician assistants, social workers, physical and occupational therapists, pharmacists, and a geriatric psychologist. The goal of the curriculum is to provide learners the knowledge, attitudes, and skills necessary to perform effective, efficient, and safe transfers between clinical settings as well as education in transitional care. In addition, using a team of interprofessional faculty, the curriculum develops the interprofessional competencies of teamwork and communication. The curriculum also has provided a significant opportunity for interprofessional collaboration among faculty who have volunteered their teaching time in the development and teaching of the curriculum, with potential for improved clinical staff knowledge of other disciplines.
Quality improvement and system redesign projects in care transitions also have expanded (Table 2).
Early assessment indicates that the new staffing model is having positive effects on the clinical environment of the TCU. A survey was conducted of a convenience sample of all physicians, nurse managers, social workers, and other members of the clinical team in the TCU (N=24)(Table 3), with response categories ranging on a Likert scale from 1 (very negative) to 5 (very positive).
Although not rigorously analyzed using qualitative research methods, comments from respondents have consistently indicated that this staffing model increases the transfer of clinical and logistical knowledge among staff members working in the acute inpatient facility and the TCU.
Discussion
With greater numbers of increasingly complex patients transitioning from the hospital to SNF, health care systems need to expand the capacity of their skilled nursing systems, not only to provide clinical care, but also to support QI and medical education. The VABHS developed a physician staffing model with the goal of enriching physician practice and enhancing QI and educational opportunities in its SNF. The model offers an opportunity to improve transitions in care as physicians gain a greater knowledge of both the hospital and subacute clinical settings. This hospitalist rotation model may improve the knowledge necessary for caring for patients moving across care settings, as well as improve communication between settings. It also has served as a foundation for systematic innovation in QI and education at this institution. Clinical staff in the transitional care setting have reported positive effects of this model on clinical skills and patient care, educational opportunities, as well as a desire for replication in other health care systems.
The potential generalizability of this model requires careful consideration. The VABHS is a tertiary care integrated health care system, enabling physicians to work in multiple clinical settings. Other settings may not have the staffing or clinical volume to sustain such a model. In addition, this model may increase discontinuity in patient care as hospitalists move between acute and subacute settings and nonclinical roles. This loss of continuity may be a greater concern in the SNF setting, as the inpatient hospitalist model generally involves high provider turnover as shift work. Our survey included nurse managers, and not floor nurses due to survey administration limitations, and feedback may not have captured a comprehensive view from CLC staff. Moreover, some of the perceived positive impacts also may be related to professional and personal attributes of the physicians rather than the actual model of care. In addition, the survey response rate was 86%. However, the nature of the improvement work (focused on care transitions) and educational opportunities (interprofessional care) would likely not occur had the physicians been based in one clinical setting.
Other new physician staffing models have been designed to improve the continuity between the hospital, subacute, and outpatient settings. For example, the University of Chicago Comprehensive Care model pairs patients with trained hospitalists who provide both inpatient and outpatient care, thereby optimizing continuity between these settings.14 At CareMore Health System, high-risk patients also are paired with hospitalists, referred to as “extensivists,” who lead care teams that follow patients between settings and provide acute, postacute, and outpatient care.15 In these models, a single physician takes responsibility for the patient throughout transitions of care and through various care settings. Both models have shown reduction in hospital readmissions. One concern with such models is that the treatment teams need to coexist in the various settings of care, and the ability to impact and create systematic change within each environment is limited. This may limit QI, educational opportunities, and system level impact within each environment of care.
In comparison, the “transitionalist” model proposed here features hospitalist physicians rotating between the acute inpatient hospital and subacute care with dedicated time in each environment. This innovative organizational structure may enhance physician practice and enrich QI and educational opportunities in SNFs. Further evaluation will include the impact on quality metrics of patient care and patient satisfaction, as this model has the potential to influence quality, cost, and overall health outcomes.
Acknowledgments
We would like to thank Shivani Jindal, Matthew Russell, Matthew Ronan, Juman Hijab, Wei Shen, Sandra Vilbrun-Bruno, and Jack Earnshaw for their significant contributions to this staffing model. We would also like to thank Paul Conlin, Jay Orlander, and the leadership team of Veterans Affairs Boston Healthcare System for supporting this staffing model.
1. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20(4):317-323.
2. Murtaugh CM, Litke A. Transitions through postacute and long-term care settings: patterns of use and outcomes for a national cohort of elders. Med Care. 2002;40(3):227-236.
3. Burke RE, Whitfield EA, Hittle D, et al. Hospital readmission from post-acute care facilities: risk factors, timing, and outcomes. J Am Med Dir Assoc. 2016;17(3):249-255.
4. Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood). 2010;29(1):57-64.
5. Tian W. An all-payer view of hospital discharge to postacute care, 2013: Statistical Brief #205. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb205-Hospital-Discharge-Postacute-Care.jsp. Published May 2016. Accessed August 13, 2018.
6. Barnett ML, Grabowski DC, Mehrotra A. Home-to-home time–measuring what matters to patients and payers. N Engl J Med. 2017;377(1):4-6.
7. Golden AG, Silverman MA, Mintzer MJ. Is geriatric medicine terminally ill? Ann Intern Med. 2012;156(9):654-656.
8. Nazir A, Smalbrugge M, Moser A, et al. The prevalence of burnout among nursing home physicians: an international perspective. J Am Med Dir Assoc. 2018;19(1):86-88.
9. Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141(7):533-536.
10. Kim LD, Kou L, Hu B, Gorodeski EZ, Rothberg MB. Impact of a connected care model on 30-day readmission rates from skilled nursing facilities. J Hosp Med. 2017;12(4):238-244.
11. Gloth MF, Gloth MJ. A comparative effectiveness trial between a post-acute care hospitalist model and a community-based physician model of nursing home care. J Am Med Dir Assoc. 2011;12(5):384-386.
12. Baughman AW, Cain G, Ruopp MD, et al. Improving access to care by admission process redesign in a veterans affairs skilled nursing facility. Jt Comm J Qual Patient Saf. 2018;44(8):454-462.
13. Mixon A, Smith GR, Dalal A et al. The Multi-Center Medication Reconciliation Quality Improvement Study 2 (MARQUIS2): methods and implementation. Abstract 248. Present at: Society of Hospital Medicine Annual Meeting; 2018 Apr 8 – 11, 2018; Orlando, FL. https://www.shmabstracts.com/abstract/the-multi-center-medication-reconciliation-quality-improvement-study-2-marquis2-methods-and-implementation. Accessed August 13, 2018.
14. Meltzer DO, Ruhnke GW. Redesigning care for patients at increased hospitalization risk: the comprehensive care physician model. Health Aff (Millwood). 2014;33(5):770-777.
15. Powers BW, Milstein A, Jain SH. Delivery models for high-risk older patients: back to the future? JAMA. 2016;315(1):23-24.
Hospitalist physician rotations between acute inpatient hospitals and subacute care facilities with dedicated time in each environment may foster quality improvement and educational opportunities.
Hospitalist physician rotations between acute inpatient hospitals and subacute care facilities with dedicated time in each environment may foster quality improvement and educational opportunities.
Care transitions between hospitals and skilled nursing facilities (SNFs) are a vulnerable time for patients. The current health care climate of decreasing hospital length of stay, readmission penalties, and increasing patient complexity has made hospital care transitions an important safety concern. Suboptimal transitions across clinical settings can result in adverse events, inadequately controlled comorbidities, deficient patient and caregiver preparation for discharge, medication errors, relocation stress, and overall increased morbidity and mortality.1,2 Such care transitions also may generate unnecessary spending, including avoidable readmissions, emergency department utilization, and duplicative laboratory and imaging studies. Approximately 23% of patients admitted to SNFs are readmitted to acute care hospitals within 30 days, and these patients have increased mortality rates in risk-adjusted analyses. 3,4
Compounding the magnitude of this risk and vulnerability is the significant growth in the number of patients discharged to SNFs over the past 30 years. In 2013, more than 20% of Medicare patients discharged from acute care hospitals were destined for SNFs.5,6 Paradoxically, despite the increasing need for SNF providers, there is a shortage of clinicians with training in geriatrics or nursing home care.7 The result is a growing need to identify organizational systems to optimize physician practice in these settings, enhance quality of care, especially around transitions, and increase educational training opportunities in SNFs for future practitioners.
Many SNFs today are staffed by physicians and other licensed clinicians whose exclusive practice location is the nursing facility or possibly several such facilities. This prevailing model of care can isolate the physicians, depriving them of interaction with clinicians in other specialties, and can contribute to burnout.8 This model does not lend itself to academic scholarship, quality improvement (QI), and student or resident training, as each of these endeavors depends on interprofessional collaboration as well as access to an academic medical center with additional resources.9
Few studies have described innovative hospitalist rotation models from acute to subacute care. The Cleveland Clinic implemented the Connected Care model where hospital-employed physicians and advanced practice professionals integrated into postacute care and reduced the 30-day hospital readmission rate from SNFs from 28% to 22%.10 Goth and colleagues performed a comparative effectiveness trial between a postacute care hospitalist (PACH) model and a community-based physician model of nursing home care. They found that the institution of a PACH model in a nursing home was associated with a significant increase in laboratory costs, nonsignificant reduction in medication errors and pharmacy costs, and no improvement in fall rates.11 The conclusion was that the PACH model may lead to greater clinician involvement and that the potential decrease in pharmacy costs and medications errors may offset the costs associated with additional laboratory testing. Overall, there has been a lack of studies on the impact of these hospitalist rotation models from acute to subacute care on educational programs, QI activities, and the interprofessional environment.
To achieve a system in which physicians in a SNF can excel in these areas, Veterans Affairs Boston Healthcare System (VABHS) adopted a staffing model in which academic hospitalist physicians rotate between the inpatient hospital and subacute settings. This report describes the model structure, the varying roles of the physicians, and early indicators of its positive effects on educational programs, QI activities, and the interprofessional environment.
Methods
The VABHS consists of a 159-bed acute care hospital in West Roxbury, Massachusetts; and a 110-bed SNF in Brockton, Massachusetts, with 3 units: a 65-bed transitional care unit (TCU), a 30-bed long-term care unit, and a 15-bed palliative care/hospice unit. The majority of patients admitted to the SNF are transferred from the acute care hospital in West Roxbury and other regional hospitals. Prior to 2015, the TCU was staffed with full-time clinicians who exclusively practiced in the SNF.
In the new staffing model, 6 hospitalist physicians divide their clinical time between the acute care hospital’s inpatient medical service and the TCU. The hospitalists come from varied backgrounds in terms of years in practice and advanced training (Table 1).
The amount of nonclinical (protected) time and clinical time on the acute inpatient service and the TCU varies for each physician. For example, a physician serves as principal investigator for several major research grants and has a hospital-wide administrative leadership role; as a result, the principal investigator has fewer months of clinical responsibility. Physicians are expected to use the protected time for scholarship, educational program development and teaching, QI, and administrative responsibilities. The VABHS leadership determines the amount of protected time based on individualized benchmarks for research, education, and administrative responsibilities that follow VA national and local institutional guidelines. These metrics and time allocations are negotiated at the time of recruitment and then are reviewed annually.
The TCU also is staffed with 4 full-time clinicians (2 physicians and 2 physician assistants) who provide additional continuity of care. The new hospitalist staffing model only required an approximate 10% increase in TCU clinical staffing full-time equivalents. Patients and admissions are divided equally among clinicians on service (census per clinician 12-15 patients), with redistribution of patients at times of transition from clinical to nonclinical time. Blocks of clinical time are scheduled for greater than 2 weeks at a time to preserve continuity. In addition, the new staffing model allocates assignment of clinical responsibilities that allows for clinicians to take leave without resultant shortages in clinical coverage.
To facilitate communication among physicians serving in the acute inpatient facility and the TCU, leaders of both of these programs meet monthly and ad hoc to review the transitions of care between the 2 settings. The description of this model and its assessment have been reviewed and deemed exempt from oversight by the VA Boston Healthcare System Research and Development Committee.
Results
Since the implementation of this staffing model in 2015, the system has grown considerably in the breadth and depth of educational programming, QI, and systems redesign in the TCU and, more broadly, in the SNF. The TCU, which previously had limited training opportunities, has experienced marked expansion of educational offerings. It is now a site for core general medicine rotations for first-year psychiatry residents and physician assistant students. The TCU also has expanded as a clinical site for transitions-in-care internal medicine resident curricula and electives, as well as a clinical site for a geriatrics fellowship.
A hospitalist developed and implemented a 4-week interprofessional curriculum for all clinical trainees and students, which occurs continuously. The curriculum includes a monthly academic conference and 12 didactic lectures and is taught by 16 interprofessional faculty from the TCU and the Palliative Care/Hospice Unit, including medicine, geriatric and palliative care physicians, physician assistants, social workers, physical and occupational therapists, pharmacists, and a geriatric psychologist. The goal of the curriculum is to provide learners the knowledge, attitudes, and skills necessary to perform effective, efficient, and safe transfers between clinical settings as well as education in transitional care. In addition, using a team of interprofessional faculty, the curriculum develops the interprofessional competencies of teamwork and communication. The curriculum also has provided a significant opportunity for interprofessional collaboration among faculty who have volunteered their teaching time in the development and teaching of the curriculum, with potential for improved clinical staff knowledge of other disciplines.
Quality improvement and system redesign projects in care transitions also have expanded (Table 2).
Early assessment indicates that the new staffing model is having positive effects on the clinical environment of the TCU. A survey was conducted of a convenience sample of all physicians, nurse managers, social workers, and other members of the clinical team in the TCU (N=24)(Table 3), with response categories ranging on a Likert scale from 1 (very negative) to 5 (very positive).
Although not rigorously analyzed using qualitative research methods, comments from respondents have consistently indicated that this staffing model increases the transfer of clinical and logistical knowledge among staff members working in the acute inpatient facility and the TCU.
Discussion
With greater numbers of increasingly complex patients transitioning from the hospital to SNF, health care systems need to expand the capacity of their skilled nursing systems, not only to provide clinical care, but also to support QI and medical education. The VABHS developed a physician staffing model with the goal of enriching physician practice and enhancing QI and educational opportunities in its SNF. The model offers an opportunity to improve transitions in care as physicians gain a greater knowledge of both the hospital and subacute clinical settings. This hospitalist rotation model may improve the knowledge necessary for caring for patients moving across care settings, as well as improve communication between settings. It also has served as a foundation for systematic innovation in QI and education at this institution. Clinical staff in the transitional care setting have reported positive effects of this model on clinical skills and patient care, educational opportunities, as well as a desire for replication in other health care systems.
The potential generalizability of this model requires careful consideration. The VABHS is a tertiary care integrated health care system, enabling physicians to work in multiple clinical settings. Other settings may not have the staffing or clinical volume to sustain such a model. In addition, this model may increase discontinuity in patient care as hospitalists move between acute and subacute settings and nonclinical roles. This loss of continuity may be a greater concern in the SNF setting, as the inpatient hospitalist model generally involves high provider turnover as shift work. Our survey included nurse managers, and not floor nurses due to survey administration limitations, and feedback may not have captured a comprehensive view from CLC staff. Moreover, some of the perceived positive impacts also may be related to professional and personal attributes of the physicians rather than the actual model of care. In addition, the survey response rate was 86%. However, the nature of the improvement work (focused on care transitions) and educational opportunities (interprofessional care) would likely not occur had the physicians been based in one clinical setting.
Other new physician staffing models have been designed to improve the continuity between the hospital, subacute, and outpatient settings. For example, the University of Chicago Comprehensive Care model pairs patients with trained hospitalists who provide both inpatient and outpatient care, thereby optimizing continuity between these settings.14 At CareMore Health System, high-risk patients also are paired with hospitalists, referred to as “extensivists,” who lead care teams that follow patients between settings and provide acute, postacute, and outpatient care.15 In these models, a single physician takes responsibility for the patient throughout transitions of care and through various care settings. Both models have shown reduction in hospital readmissions. One concern with such models is that the treatment teams need to coexist in the various settings of care, and the ability to impact and create systematic change within each environment is limited. This may limit QI, educational opportunities, and system level impact within each environment of care.
In comparison, the “transitionalist” model proposed here features hospitalist physicians rotating between the acute inpatient hospital and subacute care with dedicated time in each environment. This innovative organizational structure may enhance physician practice and enrich QI and educational opportunities in SNFs. Further evaluation will include the impact on quality metrics of patient care and patient satisfaction, as this model has the potential to influence quality, cost, and overall health outcomes.
Acknowledgments
We would like to thank Shivani Jindal, Matthew Russell, Matthew Ronan, Juman Hijab, Wei Shen, Sandra Vilbrun-Bruno, and Jack Earnshaw for their significant contributions to this staffing model. We would also like to thank Paul Conlin, Jay Orlander, and the leadership team of Veterans Affairs Boston Healthcare System for supporting this staffing model.
Care transitions between hospitals and skilled nursing facilities (SNFs) are a vulnerable time for patients. The current health care climate of decreasing hospital length of stay, readmission penalties, and increasing patient complexity has made hospital care transitions an important safety concern. Suboptimal transitions across clinical settings can result in adverse events, inadequately controlled comorbidities, deficient patient and caregiver preparation for discharge, medication errors, relocation stress, and overall increased morbidity and mortality.1,2 Such care transitions also may generate unnecessary spending, including avoidable readmissions, emergency department utilization, and duplicative laboratory and imaging studies. Approximately 23% of patients admitted to SNFs are readmitted to acute care hospitals within 30 days, and these patients have increased mortality rates in risk-adjusted analyses. 3,4
Compounding the magnitude of this risk and vulnerability is the significant growth in the number of patients discharged to SNFs over the past 30 years. In 2013, more than 20% of Medicare patients discharged from acute care hospitals were destined for SNFs.5,6 Paradoxically, despite the increasing need for SNF providers, there is a shortage of clinicians with training in geriatrics or nursing home care.7 The result is a growing need to identify organizational systems to optimize physician practice in these settings, enhance quality of care, especially around transitions, and increase educational training opportunities in SNFs for future practitioners.
Many SNFs today are staffed by physicians and other licensed clinicians whose exclusive practice location is the nursing facility or possibly several such facilities. This prevailing model of care can isolate the physicians, depriving them of interaction with clinicians in other specialties, and can contribute to burnout.8 This model does not lend itself to academic scholarship, quality improvement (QI), and student or resident training, as each of these endeavors depends on interprofessional collaboration as well as access to an academic medical center with additional resources.9
Few studies have described innovative hospitalist rotation models from acute to subacute care. The Cleveland Clinic implemented the Connected Care model where hospital-employed physicians and advanced practice professionals integrated into postacute care and reduced the 30-day hospital readmission rate from SNFs from 28% to 22%.10 Goth and colleagues performed a comparative effectiveness trial between a postacute care hospitalist (PACH) model and a community-based physician model of nursing home care. They found that the institution of a PACH model in a nursing home was associated with a significant increase in laboratory costs, nonsignificant reduction in medication errors and pharmacy costs, and no improvement in fall rates.11 The conclusion was that the PACH model may lead to greater clinician involvement and that the potential decrease in pharmacy costs and medications errors may offset the costs associated with additional laboratory testing. Overall, there has been a lack of studies on the impact of these hospitalist rotation models from acute to subacute care on educational programs, QI activities, and the interprofessional environment.
To achieve a system in which physicians in a SNF can excel in these areas, Veterans Affairs Boston Healthcare System (VABHS) adopted a staffing model in which academic hospitalist physicians rotate between the inpatient hospital and subacute settings. This report describes the model structure, the varying roles of the physicians, and early indicators of its positive effects on educational programs, QI activities, and the interprofessional environment.
Methods
The VABHS consists of a 159-bed acute care hospital in West Roxbury, Massachusetts; and a 110-bed SNF in Brockton, Massachusetts, with 3 units: a 65-bed transitional care unit (TCU), a 30-bed long-term care unit, and a 15-bed palliative care/hospice unit. The majority of patients admitted to the SNF are transferred from the acute care hospital in West Roxbury and other regional hospitals. Prior to 2015, the TCU was staffed with full-time clinicians who exclusively practiced in the SNF.
In the new staffing model, 6 hospitalist physicians divide their clinical time between the acute care hospital’s inpatient medical service and the TCU. The hospitalists come from varied backgrounds in terms of years in practice and advanced training (Table 1).
The amount of nonclinical (protected) time and clinical time on the acute inpatient service and the TCU varies for each physician. For example, a physician serves as principal investigator for several major research grants and has a hospital-wide administrative leadership role; as a result, the principal investigator has fewer months of clinical responsibility. Physicians are expected to use the protected time for scholarship, educational program development and teaching, QI, and administrative responsibilities. The VABHS leadership determines the amount of protected time based on individualized benchmarks for research, education, and administrative responsibilities that follow VA national and local institutional guidelines. These metrics and time allocations are negotiated at the time of recruitment and then are reviewed annually.
The TCU also is staffed with 4 full-time clinicians (2 physicians and 2 physician assistants) who provide additional continuity of care. The new hospitalist staffing model only required an approximate 10% increase in TCU clinical staffing full-time equivalents. Patients and admissions are divided equally among clinicians on service (census per clinician 12-15 patients), with redistribution of patients at times of transition from clinical to nonclinical time. Blocks of clinical time are scheduled for greater than 2 weeks at a time to preserve continuity. In addition, the new staffing model allocates assignment of clinical responsibilities that allows for clinicians to take leave without resultant shortages in clinical coverage.
To facilitate communication among physicians serving in the acute inpatient facility and the TCU, leaders of both of these programs meet monthly and ad hoc to review the transitions of care between the 2 settings. The description of this model and its assessment have been reviewed and deemed exempt from oversight by the VA Boston Healthcare System Research and Development Committee.
Results
Since the implementation of this staffing model in 2015, the system has grown considerably in the breadth and depth of educational programming, QI, and systems redesign in the TCU and, more broadly, in the SNF. The TCU, which previously had limited training opportunities, has experienced marked expansion of educational offerings. It is now a site for core general medicine rotations for first-year psychiatry residents and physician assistant students. The TCU also has expanded as a clinical site for transitions-in-care internal medicine resident curricula and electives, as well as a clinical site for a geriatrics fellowship.
A hospitalist developed and implemented a 4-week interprofessional curriculum for all clinical trainees and students, which occurs continuously. The curriculum includes a monthly academic conference and 12 didactic lectures and is taught by 16 interprofessional faculty from the TCU and the Palliative Care/Hospice Unit, including medicine, geriatric and palliative care physicians, physician assistants, social workers, physical and occupational therapists, pharmacists, and a geriatric psychologist. The goal of the curriculum is to provide learners the knowledge, attitudes, and skills necessary to perform effective, efficient, and safe transfers between clinical settings as well as education in transitional care. In addition, using a team of interprofessional faculty, the curriculum develops the interprofessional competencies of teamwork and communication. The curriculum also has provided a significant opportunity for interprofessional collaboration among faculty who have volunteered their teaching time in the development and teaching of the curriculum, with potential for improved clinical staff knowledge of other disciplines.
Quality improvement and system redesign projects in care transitions also have expanded (Table 2).
Early assessment indicates that the new staffing model is having positive effects on the clinical environment of the TCU. A survey was conducted of a convenience sample of all physicians, nurse managers, social workers, and other members of the clinical team in the TCU (N=24)(Table 3), with response categories ranging on a Likert scale from 1 (very negative) to 5 (very positive).
Although not rigorously analyzed using qualitative research methods, comments from respondents have consistently indicated that this staffing model increases the transfer of clinical and logistical knowledge among staff members working in the acute inpatient facility and the TCU.
Discussion
With greater numbers of increasingly complex patients transitioning from the hospital to SNF, health care systems need to expand the capacity of their skilled nursing systems, not only to provide clinical care, but also to support QI and medical education. The VABHS developed a physician staffing model with the goal of enriching physician practice and enhancing QI and educational opportunities in its SNF. The model offers an opportunity to improve transitions in care as physicians gain a greater knowledge of both the hospital and subacute clinical settings. This hospitalist rotation model may improve the knowledge necessary for caring for patients moving across care settings, as well as improve communication between settings. It also has served as a foundation for systematic innovation in QI and education at this institution. Clinical staff in the transitional care setting have reported positive effects of this model on clinical skills and patient care, educational opportunities, as well as a desire for replication in other health care systems.
The potential generalizability of this model requires careful consideration. The VABHS is a tertiary care integrated health care system, enabling physicians to work in multiple clinical settings. Other settings may not have the staffing or clinical volume to sustain such a model. In addition, this model may increase discontinuity in patient care as hospitalists move between acute and subacute settings and nonclinical roles. This loss of continuity may be a greater concern in the SNF setting, as the inpatient hospitalist model generally involves high provider turnover as shift work. Our survey included nurse managers, and not floor nurses due to survey administration limitations, and feedback may not have captured a comprehensive view from CLC staff. Moreover, some of the perceived positive impacts also may be related to professional and personal attributes of the physicians rather than the actual model of care. In addition, the survey response rate was 86%. However, the nature of the improvement work (focused on care transitions) and educational opportunities (interprofessional care) would likely not occur had the physicians been based in one clinical setting.
Other new physician staffing models have been designed to improve the continuity between the hospital, subacute, and outpatient settings. For example, the University of Chicago Comprehensive Care model pairs patients with trained hospitalists who provide both inpatient and outpatient care, thereby optimizing continuity between these settings.14 At CareMore Health System, high-risk patients also are paired with hospitalists, referred to as “extensivists,” who lead care teams that follow patients between settings and provide acute, postacute, and outpatient care.15 In these models, a single physician takes responsibility for the patient throughout transitions of care and through various care settings. Both models have shown reduction in hospital readmissions. One concern with such models is that the treatment teams need to coexist in the various settings of care, and the ability to impact and create systematic change within each environment is limited. This may limit QI, educational opportunities, and system level impact within each environment of care.
In comparison, the “transitionalist” model proposed here features hospitalist physicians rotating between the acute inpatient hospital and subacute care with dedicated time in each environment. This innovative organizational structure may enhance physician practice and enrich QI and educational opportunities in SNFs. Further evaluation will include the impact on quality metrics of patient care and patient satisfaction, as this model has the potential to influence quality, cost, and overall health outcomes.
Acknowledgments
We would like to thank Shivani Jindal, Matthew Russell, Matthew Ronan, Juman Hijab, Wei Shen, Sandra Vilbrun-Bruno, and Jack Earnshaw for their significant contributions to this staffing model. We would also like to thank Paul Conlin, Jay Orlander, and the leadership team of Veterans Affairs Boston Healthcare System for supporting this staffing model.
1. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20(4):317-323.
2. Murtaugh CM, Litke A. Transitions through postacute and long-term care settings: patterns of use and outcomes for a national cohort of elders. Med Care. 2002;40(3):227-236.
3. Burke RE, Whitfield EA, Hittle D, et al. Hospital readmission from post-acute care facilities: risk factors, timing, and outcomes. J Am Med Dir Assoc. 2016;17(3):249-255.
4. Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood). 2010;29(1):57-64.
5. Tian W. An all-payer view of hospital discharge to postacute care, 2013: Statistical Brief #205. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb205-Hospital-Discharge-Postacute-Care.jsp. Published May 2016. Accessed August 13, 2018.
6. Barnett ML, Grabowski DC, Mehrotra A. Home-to-home time–measuring what matters to patients and payers. N Engl J Med. 2017;377(1):4-6.
7. Golden AG, Silverman MA, Mintzer MJ. Is geriatric medicine terminally ill? Ann Intern Med. 2012;156(9):654-656.
8. Nazir A, Smalbrugge M, Moser A, et al. The prevalence of burnout among nursing home physicians: an international perspective. J Am Med Dir Assoc. 2018;19(1):86-88.
9. Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141(7):533-536.
10. Kim LD, Kou L, Hu B, Gorodeski EZ, Rothberg MB. Impact of a connected care model on 30-day readmission rates from skilled nursing facilities. J Hosp Med. 2017;12(4):238-244.
11. Gloth MF, Gloth MJ. A comparative effectiveness trial between a post-acute care hospitalist model and a community-based physician model of nursing home care. J Am Med Dir Assoc. 2011;12(5):384-386.
12. Baughman AW, Cain G, Ruopp MD, et al. Improving access to care by admission process redesign in a veterans affairs skilled nursing facility. Jt Comm J Qual Patient Saf. 2018;44(8):454-462.
13. Mixon A, Smith GR, Dalal A et al. The Multi-Center Medication Reconciliation Quality Improvement Study 2 (MARQUIS2): methods and implementation. Abstract 248. Present at: Society of Hospital Medicine Annual Meeting; 2018 Apr 8 – 11, 2018; Orlando, FL. https://www.shmabstracts.com/abstract/the-multi-center-medication-reconciliation-quality-improvement-study-2-marquis2-methods-and-implementation. Accessed August 13, 2018.
14. Meltzer DO, Ruhnke GW. Redesigning care for patients at increased hospitalization risk: the comprehensive care physician model. Health Aff (Millwood). 2014;33(5):770-777.
15. Powers BW, Milstein A, Jain SH. Delivery models for high-risk older patients: back to the future? JAMA. 2016;315(1):23-24.
1. Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20(4):317-323.
2. Murtaugh CM, Litke A. Transitions through postacute and long-term care settings: patterns of use and outcomes for a national cohort of elders. Med Care. 2002;40(3):227-236.
3. Burke RE, Whitfield EA, Hittle D, et al. Hospital readmission from post-acute care facilities: risk factors, timing, and outcomes. J Am Med Dir Assoc. 2016;17(3):249-255.
4. Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood). 2010;29(1):57-64.
5. Tian W. An all-payer view of hospital discharge to postacute care, 2013: Statistical Brief #205. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb205-Hospital-Discharge-Postacute-Care.jsp. Published May 2016. Accessed August 13, 2018.
6. Barnett ML, Grabowski DC, Mehrotra A. Home-to-home time–measuring what matters to patients and payers. N Engl J Med. 2017;377(1):4-6.
7. Golden AG, Silverman MA, Mintzer MJ. Is geriatric medicine terminally ill? Ann Intern Med. 2012;156(9):654-656.
8. Nazir A, Smalbrugge M, Moser A, et al. The prevalence of burnout among nursing home physicians: an international perspective. J Am Med Dir Assoc. 2018;19(1):86-88.
9. Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141(7):533-536.
10. Kim LD, Kou L, Hu B, Gorodeski EZ, Rothberg MB. Impact of a connected care model on 30-day readmission rates from skilled nursing facilities. J Hosp Med. 2017;12(4):238-244.
11. Gloth MF, Gloth MJ. A comparative effectiveness trial between a post-acute care hospitalist model and a community-based physician model of nursing home care. J Am Med Dir Assoc. 2011;12(5):384-386.
12. Baughman AW, Cain G, Ruopp MD, et al. Improving access to care by admission process redesign in a veterans affairs skilled nursing facility. Jt Comm J Qual Patient Saf. 2018;44(8):454-462.
13. Mixon A, Smith GR, Dalal A et al. The Multi-Center Medication Reconciliation Quality Improvement Study 2 (MARQUIS2): methods and implementation. Abstract 248. Present at: Society of Hospital Medicine Annual Meeting; 2018 Apr 8 – 11, 2018; Orlando, FL. https://www.shmabstracts.com/abstract/the-multi-center-medication-reconciliation-quality-improvement-study-2-marquis2-methods-and-implementation. Accessed August 13, 2018.
14. Meltzer DO, Ruhnke GW. Redesigning care for patients at increased hospitalization risk: the comprehensive care physician model. Health Aff (Millwood). 2014;33(5):770-777.
15. Powers BW, Milstein A, Jain SH. Delivery models for high-risk older patients: back to the future? JAMA. 2016;315(1):23-24.
AACR: New cancer cases predicted to rise above 2.3 million by 2035
during the last 12 months.
Among the advances outlined in the AACR Cancer Progress Report 2018 are “revolutionary new immunotherapeutics called CAR T–cell therapies, exciting new targeted radiotherapeutics, and numerous new targeted therapeutics that are expanding the scope of precision medicine,” the AACR said in a written statement.
Despite this progress, however, cancer continues to pose immense public health challenges.
The number of new cancer cases in the United States is predicted to increase from more than 1.7 million in 2018 to almost 2.4 million in 2035, due in large part to the rising number of people age 65 and older, according to the report.
AACR calls on elected officials to:
- Maintain “robust, sustained, and predictable growth” of the National Institutes of Health budget, increasing it at least $2 billion in fiscal year (FY) 2019, for a total funding level of at least $39.1 billion.
- Make sure that the $711 million in funding provided through the 21st Century Cures Act for targeted initiatives – including the National Cancer Moonshot – “is fully appropriated in FY 2019 and is supplemental to the healthy increase for the NIH’s base budget.”
- Raise the Food and Drug Administration’s base budget in FY 2019 to $3.1 billion – a $308 million increase above its FY 2018 level – to secure support for regulatory science and speed the development of medical products, ones that are safe and effective. Particularly, in FY 2019, the AACR backs a funding level of $20 million for the FDA Oncology Center of Excellence.
- Provide the Centers for Disease Control and Prevention Cancer Prevention and Control Programs with total funding of at least $517 million. This would include funding for “comprehensive cancer control, cancer registries, and screening and awareness programs for specific cancers.”
Read the full report and watch video stories from patients here.
during the last 12 months.
Among the advances outlined in the AACR Cancer Progress Report 2018 are “revolutionary new immunotherapeutics called CAR T–cell therapies, exciting new targeted radiotherapeutics, and numerous new targeted therapeutics that are expanding the scope of precision medicine,” the AACR said in a written statement.
Despite this progress, however, cancer continues to pose immense public health challenges.
The number of new cancer cases in the United States is predicted to increase from more than 1.7 million in 2018 to almost 2.4 million in 2035, due in large part to the rising number of people age 65 and older, according to the report.
AACR calls on elected officials to:
- Maintain “robust, sustained, and predictable growth” of the National Institutes of Health budget, increasing it at least $2 billion in fiscal year (FY) 2019, for a total funding level of at least $39.1 billion.
- Make sure that the $711 million in funding provided through the 21st Century Cures Act for targeted initiatives – including the National Cancer Moonshot – “is fully appropriated in FY 2019 and is supplemental to the healthy increase for the NIH’s base budget.”
- Raise the Food and Drug Administration’s base budget in FY 2019 to $3.1 billion – a $308 million increase above its FY 2018 level – to secure support for regulatory science and speed the development of medical products, ones that are safe and effective. Particularly, in FY 2019, the AACR backs a funding level of $20 million for the FDA Oncology Center of Excellence.
- Provide the Centers for Disease Control and Prevention Cancer Prevention and Control Programs with total funding of at least $517 million. This would include funding for “comprehensive cancer control, cancer registries, and screening and awareness programs for specific cancers.”
Read the full report and watch video stories from patients here.
during the last 12 months.
Among the advances outlined in the AACR Cancer Progress Report 2018 are “revolutionary new immunotherapeutics called CAR T–cell therapies, exciting new targeted radiotherapeutics, and numerous new targeted therapeutics that are expanding the scope of precision medicine,” the AACR said in a written statement.
Despite this progress, however, cancer continues to pose immense public health challenges.
The number of new cancer cases in the United States is predicted to increase from more than 1.7 million in 2018 to almost 2.4 million in 2035, due in large part to the rising number of people age 65 and older, according to the report.
AACR calls on elected officials to:
- Maintain “robust, sustained, and predictable growth” of the National Institutes of Health budget, increasing it at least $2 billion in fiscal year (FY) 2019, for a total funding level of at least $39.1 billion.
- Make sure that the $711 million in funding provided through the 21st Century Cures Act for targeted initiatives – including the National Cancer Moonshot – “is fully appropriated in FY 2019 and is supplemental to the healthy increase for the NIH’s base budget.”
- Raise the Food and Drug Administration’s base budget in FY 2019 to $3.1 billion – a $308 million increase above its FY 2018 level – to secure support for regulatory science and speed the development of medical products, ones that are safe and effective. Particularly, in FY 2019, the AACR backs a funding level of $20 million for the FDA Oncology Center of Excellence.
- Provide the Centers for Disease Control and Prevention Cancer Prevention and Control Programs with total funding of at least $517 million. This would include funding for “comprehensive cancer control, cancer registries, and screening and awareness programs for specific cancers.”
Read the full report and watch video stories from patients here.