User login
Research highlights the use of neurofilament light chain as a biomarker
Several papers presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis in Berlin will describe new developments on the topic.
A highlighted session on the congress’s last day explores recent development in progressive MS. While much of the research on using Nf-L as a biomarker focuses on relapsing remitting MS, researchers from University Hospital, Basel, Switzerland, and Novartis used data from placebo-controlled, phase 3 trials of fingolimod (INFORMS) and siponimod (EXPAND) to learn how to use biomarkers to track brain atrophy in patients with primary and secondary progressive MS. Hear the results from lead researcher Jens Kuhle, MD, in Hall A at 10:30 a.m. (local time) on Friday, Oct. 12.
Nf-L also is being looked at as a way to suss out treatment failure. Researchers with the Swiss MS Cohort Study will present their study of Nf-L as a biomarker of suboptimal treatment response in patients with relapsing remitting MS on established disease-modifying therapy. Their findings will be presented by Özguer Yaldizli, MD, also of University Hospital, also in Hall A, at 8:30 a.m. (local time) on Friday, Oct. 12.
Follow #ECTRIMS2018 on Twitter to see live highlights and perspective from researchers and meeting attendees.
Several papers presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis in Berlin will describe new developments on the topic.
A highlighted session on the congress’s last day explores recent development in progressive MS. While much of the research on using Nf-L as a biomarker focuses on relapsing remitting MS, researchers from University Hospital, Basel, Switzerland, and Novartis used data from placebo-controlled, phase 3 trials of fingolimod (INFORMS) and siponimod (EXPAND) to learn how to use biomarkers to track brain atrophy in patients with primary and secondary progressive MS. Hear the results from lead researcher Jens Kuhle, MD, in Hall A at 10:30 a.m. (local time) on Friday, Oct. 12.
Nf-L also is being looked at as a way to suss out treatment failure. Researchers with the Swiss MS Cohort Study will present their study of Nf-L as a biomarker of suboptimal treatment response in patients with relapsing remitting MS on established disease-modifying therapy. Their findings will be presented by Özguer Yaldizli, MD, also of University Hospital, also in Hall A, at 8:30 a.m. (local time) on Friday, Oct. 12.
Follow #ECTRIMS2018 on Twitter to see live highlights and perspective from researchers and meeting attendees.
Several papers presented at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis in Berlin will describe new developments on the topic.
A highlighted session on the congress’s last day explores recent development in progressive MS. While much of the research on using Nf-L as a biomarker focuses on relapsing remitting MS, researchers from University Hospital, Basel, Switzerland, and Novartis used data from placebo-controlled, phase 3 trials of fingolimod (INFORMS) and siponimod (EXPAND) to learn how to use biomarkers to track brain atrophy in patients with primary and secondary progressive MS. Hear the results from lead researcher Jens Kuhle, MD, in Hall A at 10:30 a.m. (local time) on Friday, Oct. 12.
Nf-L also is being looked at as a way to suss out treatment failure. Researchers with the Swiss MS Cohort Study will present their study of Nf-L as a biomarker of suboptimal treatment response in patients with relapsing remitting MS on established disease-modifying therapy. Their findings will be presented by Özguer Yaldizli, MD, also of University Hospital, also in Hall A, at 8:30 a.m. (local time) on Friday, Oct. 12.
Follow #ECTRIMS2018 on Twitter to see live highlights and perspective from researchers and meeting attendees.
REPORTING FROM ECTRIMS 2018
In the battle to control drug costs, old patent laws get new life
In the drug-pricing battle, progressive lawmakers such as Sen. Bernie Sanders (I-Vt.) and patients’ rights activists rarely find themselves in step with the health industry’s big players.
But in a twist, these usually at-odds actors are championing similar tactics to tame prescription drug prices.
The strategies involve repurposing two obscure and rarely deployed workarounds in patent law that, in different ways, empower the federal government to take back patents and license them to other companies. The first is known as “march-in rights.” The second is generally referred to as Section 1498 because of its location in the U.S. Code.
Sanders has in recent years pointed to these steps as useful tools in the drug-pricing debate.
As an indicator of how high the stakes have become, these ideas also are finding traction among some major health industry players – most notably, two large trade groups that represent health plans and the “middlemen” companies that negotiate drug coverage.
“It used to be the case that everyone played nicely with one another, and now as prices have gone up, the knives have come out,” said Jacob S. Sherkow, a law professor at New York University who focuses on intellectual property and the pharmaceutical industry.
The push for march-in rights gained momentum this past summer, when activists launched a campaign challenging the patent for Truvada (emtricitabine/tenofovir), the HIV treatment by Gilead Sciences that has been shown to reduce the risks of contracting HIV when taken daily as a preventive.
Initially, patient advocates focused mainly on shaming insurance companies into providing better coverage of that pill, also known as pre-exposure prophylaxis, or PrEP, because it is taken before someone is exposed to the virus. But they soon found themselves targeting a frustration that insurance companies happened to share: the drug’s list price.
James Krellenstein, cofounder of the PrEP4All Collaboration, an advocacy group, was part of that campaign. Health plans had put barriers in place to limit access to the drug, he said. But they, too, were worried about Truvada’s escalating price.
“You can’t scale up to a level you need to unless we deal with the pricing problem,” he said.
Now, as insurers signal they might adopt an approach similar to that of the campaign, he voiced skepticism. On the one hand, the support could benefit their cause. At the same time, “they have their interests, and that’s not the interests of public health,” Mr. Krellenstein said.
Still, in Washington, the influence of groups like America’s Health Insurance Plans (AHIP), which is the largest trade association for health insurers, and the Pharmaceutical Care Management Association (PCMA), which represents those middlemen companies known as pharmacy benefit managers (PBMs), could add political credibility to these long-shot ideas.
President Trump has said curbing prescription drug costs is a high priority. But, as congressional action seems increasingly unlikely, these two approaches offer another possible path forward.
They are “already part of a law that is intact. ... An option the administration can take now,” said Walid Gellad, MD, MPH, director of the Center for Pharmaceutical Policy and Prescribing at the University of Pittsburgh.
AHIP says the Department of Health & Human Services should lean on a federal statute that lets the government take over drug patents and grant them to other manufacturers, as long as it adequately compensates the original patent holder.
Meanwhile, PCMA is pressing the administration to use the march-in rights championed by HIV activists. Provided under the 1980 Bayh-Dole Act, they empower the government to rescind a drug’s patent and let other companies develop versions of it. This applies only if government funding helped develop the drug, and it can be invoked only in specific circumstances, including a threat to public health or safety.
“Everybody is feeling the heat, and I think that is the reason you’re seeing this interest in using the tools that exist,” said Amy Kapczynski, a professor at Yale Law School who has written extensively about drug patents.
But opposition is strong among drugmakers.
“Policies should spur competition and new innovations to meet patient needs not disincentivize them such as the use of 1498 and march-in could do,” said Priscilla VanderVeer, a spokeswoman for the Pharmaceutical Researchers and Manufacturers of America, or PhRMA, a trade and lobbying group.
Gilead, which manufactures Truvada, has a similar stance.
“We believe that there is no rationale or precedent for the government to exercise march-in or other [intellectual property] rights related to Truvada for PrEP,” said Ryan McKeel, a spokesman for Gilead. The company’s other efforts to make the drug “available for health and safety needs,” he added, “clearly satisfy” the company’s legal requirements.
And the potential for march-in authority is still theoretical. It has never been used, despite at least five petitions to the National Institutes of Health, three of which cited high drug prices.
Section 1498 was used to negotiate lower drug prices in the 1960s and 1970s, but has since faded. In 2001, during the nation’s anthrax scare, HHS threatened to invoke it to procure more of the antibiotic used to treat the deadly bacterial disease, according to contemporaneous reports. Last year, Louisiana’s health secretary unsuccessfully tried to use it to ease the toll pricey hepatitis C medications exerted on the state’s Medicaid program.
NIH Director Francis Collins, MD, PhD, remains skeptical, repeatedly saying that a drug’s price doesn’t constitute a health or safety concern within the agency’s jurisdiction.
HHS Secretary Alex M. Azar II, speaking at a June Senate hearing, described march-in, also known as “compulsory licensing,” as a “socialist” approach.
But health plans and other payers, increasingly squeezed by fast-climbing prices, are undeterred – touting this kind of intervention as a “market-based solution.”
“The trends of drug prices in this country suggest that we all collectively need to find new approaches – including new approaches that are available under existing law – to try to change this trend,” said Mark Hamelburg, AHIP’s senior vice president of federal programs.
Kaiser Permanente, the health system and insurance provider, called for leveraging Section 1498 in a public comment submitted to HHS about its strategy to bring down drug prices. In a similar filing, Humana, a major insurer, pointed to “existing law [that] allows for actions around patents,” singling out march-in rights.
Humana did not respond to requests for comment. Both PCMA and Kaiser Permanente declined to comment beyond their statements. (Kaiser Health News is not affiliated with Kaiser Permanente.)
Nonetheless, experts say there are serious sticking points.
Neither of these legal provisions would be a sweeping solution. And both require administration buy-in.
“They’re only as effective as the government’s willingness to pursue them,” said Robin Feldman, a law professor at the University of California-Hastings.
Simply taking a patent doesn’t bring down prices, either. There are other ways manufacturers gain favorable market positioning for specific drugs, said Rachel Sachs, an associate law professor at Washington University in St. Louis who tracks drug-pricing laws.
And creating an opening for generics is only one step. Another drugmaker would still need to create a competing product, gain approval, and make it available. Then, theoretically, market competition can kick in.
Finally, there’s no guarantee such savings would benefit consumers, argued Nicholson Price, an assistant professor at the University of Michigan Law School. Insurance plans or PBMs could simply bargain greater discounts on drugs and pocket the money. (AHIP says any savings should be passed on.)
That’s the fundamental question, Mr. Krellenstein said.
“Is this going to be more armor in the fighting [between payers and drug companies]?” he said. “Or is it actually going to be a dramatic reform that actually results in real changes, that actually makes it easier for Americans to access the medications they need?”
KHN’s coverage of prescription drug development, costs, and pricing is supported in part by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
In the drug-pricing battle, progressive lawmakers such as Sen. Bernie Sanders (I-Vt.) and patients’ rights activists rarely find themselves in step with the health industry’s big players.
But in a twist, these usually at-odds actors are championing similar tactics to tame prescription drug prices.
The strategies involve repurposing two obscure and rarely deployed workarounds in patent law that, in different ways, empower the federal government to take back patents and license them to other companies. The first is known as “march-in rights.” The second is generally referred to as Section 1498 because of its location in the U.S. Code.
Sanders has in recent years pointed to these steps as useful tools in the drug-pricing debate.
As an indicator of how high the stakes have become, these ideas also are finding traction among some major health industry players – most notably, two large trade groups that represent health plans and the “middlemen” companies that negotiate drug coverage.
“It used to be the case that everyone played nicely with one another, and now as prices have gone up, the knives have come out,” said Jacob S. Sherkow, a law professor at New York University who focuses on intellectual property and the pharmaceutical industry.
The push for march-in rights gained momentum this past summer, when activists launched a campaign challenging the patent for Truvada (emtricitabine/tenofovir), the HIV treatment by Gilead Sciences that has been shown to reduce the risks of contracting HIV when taken daily as a preventive.
Initially, patient advocates focused mainly on shaming insurance companies into providing better coverage of that pill, also known as pre-exposure prophylaxis, or PrEP, because it is taken before someone is exposed to the virus. But they soon found themselves targeting a frustration that insurance companies happened to share: the drug’s list price.
James Krellenstein, cofounder of the PrEP4All Collaboration, an advocacy group, was part of that campaign. Health plans had put barriers in place to limit access to the drug, he said. But they, too, were worried about Truvada’s escalating price.
“You can’t scale up to a level you need to unless we deal with the pricing problem,” he said.
Now, as insurers signal they might adopt an approach similar to that of the campaign, he voiced skepticism. On the one hand, the support could benefit their cause. At the same time, “they have their interests, and that’s not the interests of public health,” Mr. Krellenstein said.
Still, in Washington, the influence of groups like America’s Health Insurance Plans (AHIP), which is the largest trade association for health insurers, and the Pharmaceutical Care Management Association (PCMA), which represents those middlemen companies known as pharmacy benefit managers (PBMs), could add political credibility to these long-shot ideas.
President Trump has said curbing prescription drug costs is a high priority. But, as congressional action seems increasingly unlikely, these two approaches offer another possible path forward.
They are “already part of a law that is intact. ... An option the administration can take now,” said Walid Gellad, MD, MPH, director of the Center for Pharmaceutical Policy and Prescribing at the University of Pittsburgh.
AHIP says the Department of Health & Human Services should lean on a federal statute that lets the government take over drug patents and grant them to other manufacturers, as long as it adequately compensates the original patent holder.
Meanwhile, PCMA is pressing the administration to use the march-in rights championed by HIV activists. Provided under the 1980 Bayh-Dole Act, they empower the government to rescind a drug’s patent and let other companies develop versions of it. This applies only if government funding helped develop the drug, and it can be invoked only in specific circumstances, including a threat to public health or safety.
“Everybody is feeling the heat, and I think that is the reason you’re seeing this interest in using the tools that exist,” said Amy Kapczynski, a professor at Yale Law School who has written extensively about drug patents.
But opposition is strong among drugmakers.
“Policies should spur competition and new innovations to meet patient needs not disincentivize them such as the use of 1498 and march-in could do,” said Priscilla VanderVeer, a spokeswoman for the Pharmaceutical Researchers and Manufacturers of America, or PhRMA, a trade and lobbying group.
Gilead, which manufactures Truvada, has a similar stance.
“We believe that there is no rationale or precedent for the government to exercise march-in or other [intellectual property] rights related to Truvada for PrEP,” said Ryan McKeel, a spokesman for Gilead. The company’s other efforts to make the drug “available for health and safety needs,” he added, “clearly satisfy” the company’s legal requirements.
And the potential for march-in authority is still theoretical. It has never been used, despite at least five petitions to the National Institutes of Health, three of which cited high drug prices.
Section 1498 was used to negotiate lower drug prices in the 1960s and 1970s, but has since faded. In 2001, during the nation’s anthrax scare, HHS threatened to invoke it to procure more of the antibiotic used to treat the deadly bacterial disease, according to contemporaneous reports. Last year, Louisiana’s health secretary unsuccessfully tried to use it to ease the toll pricey hepatitis C medications exerted on the state’s Medicaid program.
NIH Director Francis Collins, MD, PhD, remains skeptical, repeatedly saying that a drug’s price doesn’t constitute a health or safety concern within the agency’s jurisdiction.
HHS Secretary Alex M. Azar II, speaking at a June Senate hearing, described march-in, also known as “compulsory licensing,” as a “socialist” approach.
But health plans and other payers, increasingly squeezed by fast-climbing prices, are undeterred – touting this kind of intervention as a “market-based solution.”
“The trends of drug prices in this country suggest that we all collectively need to find new approaches – including new approaches that are available under existing law – to try to change this trend,” said Mark Hamelburg, AHIP’s senior vice president of federal programs.
Kaiser Permanente, the health system and insurance provider, called for leveraging Section 1498 in a public comment submitted to HHS about its strategy to bring down drug prices. In a similar filing, Humana, a major insurer, pointed to “existing law [that] allows for actions around patents,” singling out march-in rights.
Humana did not respond to requests for comment. Both PCMA and Kaiser Permanente declined to comment beyond their statements. (Kaiser Health News is not affiliated with Kaiser Permanente.)
Nonetheless, experts say there are serious sticking points.
Neither of these legal provisions would be a sweeping solution. And both require administration buy-in.
“They’re only as effective as the government’s willingness to pursue them,” said Robin Feldman, a law professor at the University of California-Hastings.
Simply taking a patent doesn’t bring down prices, either. There are other ways manufacturers gain favorable market positioning for specific drugs, said Rachel Sachs, an associate law professor at Washington University in St. Louis who tracks drug-pricing laws.
And creating an opening for generics is only one step. Another drugmaker would still need to create a competing product, gain approval, and make it available. Then, theoretically, market competition can kick in.
Finally, there’s no guarantee such savings would benefit consumers, argued Nicholson Price, an assistant professor at the University of Michigan Law School. Insurance plans or PBMs could simply bargain greater discounts on drugs and pocket the money. (AHIP says any savings should be passed on.)
That’s the fundamental question, Mr. Krellenstein said.
“Is this going to be more armor in the fighting [between payers and drug companies]?” he said. “Or is it actually going to be a dramatic reform that actually results in real changes, that actually makes it easier for Americans to access the medications they need?”
KHN’s coverage of prescription drug development, costs, and pricing is supported in part by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
In the drug-pricing battle, progressive lawmakers such as Sen. Bernie Sanders (I-Vt.) and patients’ rights activists rarely find themselves in step with the health industry’s big players.
But in a twist, these usually at-odds actors are championing similar tactics to tame prescription drug prices.
The strategies involve repurposing two obscure and rarely deployed workarounds in patent law that, in different ways, empower the federal government to take back patents and license them to other companies. The first is known as “march-in rights.” The second is generally referred to as Section 1498 because of its location in the U.S. Code.
Sanders has in recent years pointed to these steps as useful tools in the drug-pricing debate.
As an indicator of how high the stakes have become, these ideas also are finding traction among some major health industry players – most notably, two large trade groups that represent health plans and the “middlemen” companies that negotiate drug coverage.
“It used to be the case that everyone played nicely with one another, and now as prices have gone up, the knives have come out,” said Jacob S. Sherkow, a law professor at New York University who focuses on intellectual property and the pharmaceutical industry.
The push for march-in rights gained momentum this past summer, when activists launched a campaign challenging the patent for Truvada (emtricitabine/tenofovir), the HIV treatment by Gilead Sciences that has been shown to reduce the risks of contracting HIV when taken daily as a preventive.
Initially, patient advocates focused mainly on shaming insurance companies into providing better coverage of that pill, also known as pre-exposure prophylaxis, or PrEP, because it is taken before someone is exposed to the virus. But they soon found themselves targeting a frustration that insurance companies happened to share: the drug’s list price.
James Krellenstein, cofounder of the PrEP4All Collaboration, an advocacy group, was part of that campaign. Health plans had put barriers in place to limit access to the drug, he said. But they, too, were worried about Truvada’s escalating price.
“You can’t scale up to a level you need to unless we deal with the pricing problem,” he said.
Now, as insurers signal they might adopt an approach similar to that of the campaign, he voiced skepticism. On the one hand, the support could benefit their cause. At the same time, “they have their interests, and that’s not the interests of public health,” Mr. Krellenstein said.
Still, in Washington, the influence of groups like America’s Health Insurance Plans (AHIP), which is the largest trade association for health insurers, and the Pharmaceutical Care Management Association (PCMA), which represents those middlemen companies known as pharmacy benefit managers (PBMs), could add political credibility to these long-shot ideas.
President Trump has said curbing prescription drug costs is a high priority. But, as congressional action seems increasingly unlikely, these two approaches offer another possible path forward.
They are “already part of a law that is intact. ... An option the administration can take now,” said Walid Gellad, MD, MPH, director of the Center for Pharmaceutical Policy and Prescribing at the University of Pittsburgh.
AHIP says the Department of Health & Human Services should lean on a federal statute that lets the government take over drug patents and grant them to other manufacturers, as long as it adequately compensates the original patent holder.
Meanwhile, PCMA is pressing the administration to use the march-in rights championed by HIV activists. Provided under the 1980 Bayh-Dole Act, they empower the government to rescind a drug’s patent and let other companies develop versions of it. This applies only if government funding helped develop the drug, and it can be invoked only in specific circumstances, including a threat to public health or safety.
“Everybody is feeling the heat, and I think that is the reason you’re seeing this interest in using the tools that exist,” said Amy Kapczynski, a professor at Yale Law School who has written extensively about drug patents.
But opposition is strong among drugmakers.
“Policies should spur competition and new innovations to meet patient needs not disincentivize them such as the use of 1498 and march-in could do,” said Priscilla VanderVeer, a spokeswoman for the Pharmaceutical Researchers and Manufacturers of America, or PhRMA, a trade and lobbying group.
Gilead, which manufactures Truvada, has a similar stance.
“We believe that there is no rationale or precedent for the government to exercise march-in or other [intellectual property] rights related to Truvada for PrEP,” said Ryan McKeel, a spokesman for Gilead. The company’s other efforts to make the drug “available for health and safety needs,” he added, “clearly satisfy” the company’s legal requirements.
And the potential for march-in authority is still theoretical. It has never been used, despite at least five petitions to the National Institutes of Health, three of which cited high drug prices.
Section 1498 was used to negotiate lower drug prices in the 1960s and 1970s, but has since faded. In 2001, during the nation’s anthrax scare, HHS threatened to invoke it to procure more of the antibiotic used to treat the deadly bacterial disease, according to contemporaneous reports. Last year, Louisiana’s health secretary unsuccessfully tried to use it to ease the toll pricey hepatitis C medications exerted on the state’s Medicaid program.
NIH Director Francis Collins, MD, PhD, remains skeptical, repeatedly saying that a drug’s price doesn’t constitute a health or safety concern within the agency’s jurisdiction.
HHS Secretary Alex M. Azar II, speaking at a June Senate hearing, described march-in, also known as “compulsory licensing,” as a “socialist” approach.
But health plans and other payers, increasingly squeezed by fast-climbing prices, are undeterred – touting this kind of intervention as a “market-based solution.”
“The trends of drug prices in this country suggest that we all collectively need to find new approaches – including new approaches that are available under existing law – to try to change this trend,” said Mark Hamelburg, AHIP’s senior vice president of federal programs.
Kaiser Permanente, the health system and insurance provider, called for leveraging Section 1498 in a public comment submitted to HHS about its strategy to bring down drug prices. In a similar filing, Humana, a major insurer, pointed to “existing law [that] allows for actions around patents,” singling out march-in rights.
Humana did not respond to requests for comment. Both PCMA and Kaiser Permanente declined to comment beyond their statements. (Kaiser Health News is not affiliated with Kaiser Permanente.)
Nonetheless, experts say there are serious sticking points.
Neither of these legal provisions would be a sweeping solution. And both require administration buy-in.
“They’re only as effective as the government’s willingness to pursue them,” said Robin Feldman, a law professor at the University of California-Hastings.
Simply taking a patent doesn’t bring down prices, either. There are other ways manufacturers gain favorable market positioning for specific drugs, said Rachel Sachs, an associate law professor at Washington University in St. Louis who tracks drug-pricing laws.
And creating an opening for generics is only one step. Another drugmaker would still need to create a competing product, gain approval, and make it available. Then, theoretically, market competition can kick in.
Finally, there’s no guarantee such savings would benefit consumers, argued Nicholson Price, an assistant professor at the University of Michigan Law School. Insurance plans or PBMs could simply bargain greater discounts on drugs and pocket the money. (AHIP says any savings should be passed on.)
That’s the fundamental question, Mr. Krellenstein said.
“Is this going to be more armor in the fighting [between payers and drug companies]?” he said. “Or is it actually going to be a dramatic reform that actually results in real changes, that actually makes it easier for Americans to access the medications they need?”
KHN’s coverage of prescription drug development, costs, and pricing is supported in part by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Opioid use cut nearly 50% for urologic oncology surgery patients
PHOENIX – Opioid use in urologic oncology patients dropped by 46% after one high-volume surgical center introduced changes to order sets and adopted new patient communication strategies, a researcher has reported.
The changes, which promoted opioid-sparing pain regimens, led to a substantial drop in postoperative opioid use with no compromise in pain control, according to Kerri Stevenson, a nurse practitioner with Stanford Health Care.
“Patients can be successfully managed with minimal opioid medication,” Ms. Stevenson said at a symposium on quality care sponsored by the American Society of Clinical Oncology.
However, “it takes a multidisciplinary team for effective change to occur – this cannot be done in silos,” she told attendees at the meeting.
Seeking to reduce their reliance on opioids to manage postoperative pain, Ms. Stevenson and her colleagues set out to reduce opioid use by 50%, from a baseline morphine equivalent daily dose (MEDD) of 95.1 in June to September 2017 to a target of 47.5 by March 2018.
The actual MEDD at the end of the quality improvement project was 51.5, a 46% reduction that was just shy of that goal, she reported.
Factors fueling opioid use included patient expectations that they would be used and the belief that adjunct medications were not as effective as opioids, Dr. Stevenson found in a team survey.
“We decided to target those,” she said. “Our key drivers were really focused on appropriate prescriptions, increasing patient and provider awareness, standardizing our pathways, and setting expectations.”
To tackle the problem, they revised EMR order sets to default to selection of adjunct medications, educated providers, and introduced new patient communication strategies.
Instead of asking “Would you like me to bring you some oxycodone?” providers would instead start by asking about the patient’s current pain control medications and whether they were working well. When prescribed, opioids should be started at lower doses and escalated only if needed.
“Once we started our interventions, we noticed an immediate effect,” Ms. Stevenson.
The decreases were consistent across a range of surgery types. For example, the MEDD dropped to 55.1 with robotic prostatectomy, a procedure with a 1-day admission and very small incisions, and to 50.6 for open radical cystectomy, which involves a large incision and a stay of approximately 4 days, she said.
To address concerns that they might just be undertreating patients, investigators looked retrospectively at pain scores. They saw no differences pre- and post intervention in pain or anxiety scores within the first 24-48 hours post procedure, Ms. Stevenson reported.
Ms. Stevenson had no disclosures related to the presentation. Coauthor Jay Bakul Shah, MD of Stanford Health Care reported a consulting or advisory role with Pacira Pharmaceuticals.
SOURCE: Stevenson K et al. Quality Care Symposium, Abstract 269.
PHOENIX – Opioid use in urologic oncology patients dropped by 46% after one high-volume surgical center introduced changes to order sets and adopted new patient communication strategies, a researcher has reported.
The changes, which promoted opioid-sparing pain regimens, led to a substantial drop in postoperative opioid use with no compromise in pain control, according to Kerri Stevenson, a nurse practitioner with Stanford Health Care.
“Patients can be successfully managed with minimal opioid medication,” Ms. Stevenson said at a symposium on quality care sponsored by the American Society of Clinical Oncology.
However, “it takes a multidisciplinary team for effective change to occur – this cannot be done in silos,” she told attendees at the meeting.
Seeking to reduce their reliance on opioids to manage postoperative pain, Ms. Stevenson and her colleagues set out to reduce opioid use by 50%, from a baseline morphine equivalent daily dose (MEDD) of 95.1 in June to September 2017 to a target of 47.5 by March 2018.
The actual MEDD at the end of the quality improvement project was 51.5, a 46% reduction that was just shy of that goal, she reported.
Factors fueling opioid use included patient expectations that they would be used and the belief that adjunct medications were not as effective as opioids, Dr. Stevenson found in a team survey.
“We decided to target those,” she said. “Our key drivers were really focused on appropriate prescriptions, increasing patient and provider awareness, standardizing our pathways, and setting expectations.”
To tackle the problem, they revised EMR order sets to default to selection of adjunct medications, educated providers, and introduced new patient communication strategies.
Instead of asking “Would you like me to bring you some oxycodone?” providers would instead start by asking about the patient’s current pain control medications and whether they were working well. When prescribed, opioids should be started at lower doses and escalated only if needed.
“Once we started our interventions, we noticed an immediate effect,” Ms. Stevenson.
The decreases were consistent across a range of surgery types. For example, the MEDD dropped to 55.1 with robotic prostatectomy, a procedure with a 1-day admission and very small incisions, and to 50.6 for open radical cystectomy, which involves a large incision and a stay of approximately 4 days, she said.
To address concerns that they might just be undertreating patients, investigators looked retrospectively at pain scores. They saw no differences pre- and post intervention in pain or anxiety scores within the first 24-48 hours post procedure, Ms. Stevenson reported.
Ms. Stevenson had no disclosures related to the presentation. Coauthor Jay Bakul Shah, MD of Stanford Health Care reported a consulting or advisory role with Pacira Pharmaceuticals.
SOURCE: Stevenson K et al. Quality Care Symposium, Abstract 269.
PHOENIX – Opioid use in urologic oncology patients dropped by 46% after one high-volume surgical center introduced changes to order sets and adopted new patient communication strategies, a researcher has reported.
The changes, which promoted opioid-sparing pain regimens, led to a substantial drop in postoperative opioid use with no compromise in pain control, according to Kerri Stevenson, a nurse practitioner with Stanford Health Care.
“Patients can be successfully managed with minimal opioid medication,” Ms. Stevenson said at a symposium on quality care sponsored by the American Society of Clinical Oncology.
However, “it takes a multidisciplinary team for effective change to occur – this cannot be done in silos,” she told attendees at the meeting.
Seeking to reduce their reliance on opioids to manage postoperative pain, Ms. Stevenson and her colleagues set out to reduce opioid use by 50%, from a baseline morphine equivalent daily dose (MEDD) of 95.1 in June to September 2017 to a target of 47.5 by March 2018.
The actual MEDD at the end of the quality improvement project was 51.5, a 46% reduction that was just shy of that goal, she reported.
Factors fueling opioid use included patient expectations that they would be used and the belief that adjunct medications were not as effective as opioids, Dr. Stevenson found in a team survey.
“We decided to target those,” she said. “Our key drivers were really focused on appropriate prescriptions, increasing patient and provider awareness, standardizing our pathways, and setting expectations.”
To tackle the problem, they revised EMR order sets to default to selection of adjunct medications, educated providers, and introduced new patient communication strategies.
Instead of asking “Would you like me to bring you some oxycodone?” providers would instead start by asking about the patient’s current pain control medications and whether they were working well. When prescribed, opioids should be started at lower doses and escalated only if needed.
“Once we started our interventions, we noticed an immediate effect,” Ms. Stevenson.
The decreases were consistent across a range of surgery types. For example, the MEDD dropped to 55.1 with robotic prostatectomy, a procedure with a 1-day admission and very small incisions, and to 50.6 for open radical cystectomy, which involves a large incision and a stay of approximately 4 days, she said.
To address concerns that they might just be undertreating patients, investigators looked retrospectively at pain scores. They saw no differences pre- and post intervention in pain or anxiety scores within the first 24-48 hours post procedure, Ms. Stevenson reported.
Ms. Stevenson had no disclosures related to the presentation. Coauthor Jay Bakul Shah, MD of Stanford Health Care reported a consulting or advisory role with Pacira Pharmaceuticals.
SOURCE: Stevenson K et al. Quality Care Symposium, Abstract 269.
REPORTING FROM THE QUALITY CARE SYMPOSIUM
Key clinical point: Substantial reductions in postoperative opioid use might be achievable through strategies that promote opioid-sparing pain regimens.
Major finding: Postoperative opioid use dropped 46% for urologic oncology patients after changing default order sets, introducing new patient communication strategies, and educating providers.
Study details: An analysis of opioid prescribing before and after introduction of a quality improvement project at one high-volume surgical center.
Disclosures: One study coauthor reported a consulting or advisory role with Pacira Pharmaceuticals.
Source: Stevenson K et al. Quality Care Symposium, Abstract 269.
The Three H’s: Head, Heart, and Heat Considerations in Soccer
ABSTRACT
Soccer requires significant physical conditioning and endurance, as well as the physicality required for contact play. In order to keep athletes safe, it is important that coaches, medical staff, and the players themselves are educated on the most common dangers to their health that they may encounter on a soccer pitch. This article aims to review the current literature and recommendations on concussion, cardiovascular considerations, and heat-related illness as they relate to competitive soccer, with a goal of educating all those who help to keep athletes healthy and competing to their full potential.
Continue to: Soccer is one of the most popular sports...
Soccer is one of the most popular sports in the modern world and requires significant physical conditioning and endurance, as well as the physicality required for contact play. This article covers the topics of concussion, cardiovascular considerations, and heat-related illness as they relate to competitive soccer players. We provide a review of the prevention, recognition, and management required to keep athletes safe on the soccer pitch, both in practice and in competitive play.
HEAD
With an estimated 1.6 to 3.8 million sports-related mild traumatic brain injuries (ie, concussions) occurring annually in the United States,1 there has been an appropriate increase in the focus on prevention and treatment of these injuries. For more than a decade the spotlight has been on concussions that occur in American football, but other sports have also had to examine the prevalence of concussions in their sport. This is certainly true for soccer.
There has been a steady increase in soccer participation in the United States. From 1973 to 2014 there was a 4-fold increase in high school boys and a 35-fold increase in high school girls playing soccer.2 Currently, there are more than 3.7 million youth who play on teams under the supervision of the US Soccer Federation, the sport’s national governing body.3 With the growth of the sport, there has also been an intensified focus on injury prevention in soccer players, including concussive brain injuries.
A recent study examined injury rates in high school soccer players and noted that concussion is the second most common injury (17.9%), after ligament sprains (29.7%).4 The overall injury rate was 2.06 per 1000 athletic exposures (AEs [defined as participation in practice or game play]), but higher in games (4.42 per 1000 AEs) than during practices (1.05 per 1000 AEs). The overall concussion rate was 0.36 per 1000 AEs.4
Most concussions (54.8%) resulted in missing play between 1 to 3 weeks, but a sizeable portion of the athletes (14.9%) were out of play for more than 3 weeks. Additionally, 10.7% of all medical disqualifications were due to concussive injuries. Khodaee and colleagues4 found no statistically significant difference in concussion rates between male and female soccer players over the 9-year period of time that they examined, however previous studies have found higher rates in female athletes.5
In soccer, as in other sports, there is a concern about both the adequate recognition of concussions during practice and play and the underreporting of concussions by athletes. The US Soccer Federation has taken a proactive stance on addressing concussion in youth soccer by developing the “Recognize to Recover” program.6 Recognize to Recover is the US Soccer Federation’s “comprehensive player health and safety program aimed at promoting safe play and reducing injuries in soccer players of all ages.” The website provides an educational video geared toward players, along with links to concussion assessment tools, the US Soccer Federation Concussion Protocol, and US Soccer Federation-Centers for Disease Control fact sheets for athletes, parents, and coaches.6
Continue to: A challenge for all sports...
A challenge for all sports is allowing adequate evaluation of a suspected concussion by properly trained healthcare professionals. The 2017 Berlin Concussion in Sport Group position paper stated, “when a concussion is suspected, the athlete should be removed from the sporting environment and a multimodal assessment should be conducted in standardized fashion (eg, Sport Concussion Assessment Tool- 5th edition). Sporting bodies should allow adequate time to conduct this evaluation.”7 However, the International Federation of Football Association (FIFA) rules limit substitutions to 3 over the course of the game, which can make a thorough evaluation of players difficult as trainers and coaches are under increased pressure to quickly determine whether to use one of their valuable substitutions. Fortunately, the National Collegiate Athletic Association (NCAA) soccer has mitigated this issue by allowing unlimited substitutions during matches, and high school teams generally follow similar rules.
One of the goals of any safety education program is not only to raise the awareness of the signs and symptoms of concussion by all those involved in the sport, but also to increase the number of athletes who self-report their symptoms and decrease those who hide any possible concussions. A study found that a majority (58.6%) of middle school soccer players continued to play while experiencing concussion symptoms.5 However, in a very recent (not yet published) study, 92% of US Soccer Federation players reported that they did seek out a medical evaluation for their concussion.8 This is certainly a positive sign and further research needs to clarify what methods of education or training will maintain this level of self-reporting in soccer players.
There has also been an increased focus on understanding the mechanism of injury of concussions. In soccer, concussions can occur from player-to-player contact, contact with the player surface, contact with playing apparatus (eg, goal posts) and non-contact mechanisms. While there has been a focus on concussions from heading the ball, player-to-player contact is the most common cause of concussions. A 2017 study of 7- to 12-year-old soccer players in 4 European countries found that about 1 out of 10 concussions were caused by heading the ball.9 Comstock and colleageues10 found slightly higher numbers, roughly 25% to 30% (depending on gender), but 70% to 78% (again depending on gender) of those were caused by player-to-player contact rather than contact with the ball.
To date there has not been any meta-analytic review evaluating the cognitive and physical symptoms associated with heading in soccer. A recent review paper stated that the “current evidence seems insufficient to support a ban of heading in children’s football (soccer).”10 However, in December 2015 the US Soccer Federation included age-specific heading limitations. Players ages 10 years and under “shall not engage in heading, either in practices or in games” and players age 11 years and 12 years should have “limited heading in practice; maximum of 30 minutes of heading training per week, with no more than 15-20 headers per player, per week.”11 US Soccer Federation officials acknowledged the limitations in the current science regarding heading in young soccer players but chose to err on the side of caution until further empirical evidence regarding the risks associated with repetitive heading is available.
The US Soccer Federation is also exploring other ways to reduce the incidence rate of concussions, including ensuring that the age-appropriate sized ball is used in practice and play, possible rule changes, evaluation of different playing surfaces, and equipment usage. To date, there is no strong evidence to support the use of mouth guards or helmets to reduce concussions in soccer. Additionally, the current data about the value of head impact sensors in soccer has not supported its widespread use.
Continue to: Finally, the issue of the prevalence...
Finally, the issue of the prevalence of chronic traumatic encephalopathy (CTE) in soccer players is beyond the scope of this article. The expert opinion from the 2017 US Soccer Federation, Major League Soccer (MLS), and National Women’s Soccer League (NWSL) conference concluded, “At present, no data exist that support that soccer participation is a risk factor for the development of neurodegenerative disease. Similarly, at this time, consistent with evidence discussed in the Berlin Concussion in Sport Group (CISG) Consensus Conference, our review suggests no causal relationship has been demonstrated between soccer and CTE pathology.”12
The more we know about concussions, both in general and those sustained during soccer play, the better we are able to diagnose and manage these injuries in our athletes. An important step is creating evidence-based protocols that evolve as our knowledge of concussions does as well. In April 2017, the US Soccer Federation, MLS, and the NWSL held a joint summit entitled, “Head Injury in Soccer: From Science to the Field” to address the current evidence-based science of concussions in soccer.8 An article discussing the findings of this meeting is forthcoming and will undoubtedly guide further development of concussion protocols for soccer players of all ages.
HEART
The physiologic demands of soccer place considerable stress on the cardiovascular system. Participation in training and competition is characterized by a combination of aerobic and anaerobic physiology with the typical athlete covering approximately 10 km over the course of the 90-minute match. The primary role of the heart and blood vessels is to supply the exercising skeletal muscle with oxygen and energy substrate and to clear the byproducts of metabolism. Among healthy athletes without cardiovascular disease, these processes are typically well tolerated and may be associated with beneficial cardiovascular adaptations over time. However, competitive soccer players are not completely immune to cardiovascular disease. Athletes across the age and competition spectrum may develop symptoms suggestive of underlying cardiovascular disease during play including exertional chest pain, inappropriate shortness of breath, palpitations, and syncope. These athletes require timely clinical evaluation. In extremely rare but high visibility cases, competitive soccer players may succumb to cardiac arrest on the pitch, underscoring the need for comprehensive emergency action plans (EAPs). We provide the practicing clinician with an overview of cardiovascular issues relevant to the competitive soccer athlete.
CARDIOVASCULAR ADAPTATIONS TO SPORT
The pressure (ie, repetitive surges in systemic blood pressure) and volume (ie, sustained increases in high cardiac output) challenges inherent in soccer participation place stress on the cardiovascular system. Healthy athletes across the age spectrum typically tolerate the hemodynamic stressors of participation without issues. Athletes that engage in training and competition over months to years often develop beneficial adaptations of the cardiovascular system that enhance on-field performance and contribute to optimal long-term health. Detailed discussion of how the heart and blood vessels respond to exercise training is beyond the scope of this article, but the interested reader is referred to several prior publications.13,14 In brief, the heart of the healthy soccer athlete demonstrates the balanced mild chamber dilation and wall thickening characteristic of left ventricular eccentric remodeling. This form of exercise-induced cardiac remodeling facilitates maintenance of high stroke volume during exercise with minimal increases in cardiac work. In parallel, routine aerobic exercise training confers favorable changes in the systemic arterial system, which leads to reductions in age-associated ventricular stiffening and maintenance of healthy low blood pressure. It must be emphasized that the healthy heart muscle dilation and thickening that develop in response to sports participation, regardless of age, ethnicity, or gender, are relatively mild and should not be confused with common forms of heart muscle disease that may be seen in athletes at risk for adverse outcomes. In some situations, consultation with an extreme sports cardiologist may be required to differentiate exercise-induced remodeling from over heart muscle pathology.15
Continue to: THE SYMPTOMATIC ATHLETE...
THE SYMPTOMATIC ATHLETE
Any athlete presenting with symptoms suggestive of underlying cardiovascular disease should be withheld from training and competition until a comprehensive clinical evaluation has been completed. Common manifestations of underlying heart disease that occur in soccer players include exertional chest pain/pressure/tightness, shortness of breath that is out of proportion to workload, palpitations or the perception of irregular cardiac activity, and syncope. Chest discomfort, inappropriate shortness of breath, and palpitations that occur during training or competition should be managed with immediate removal from the playing field and prompt medical assessment. In many cases, thorough evaluation will involve collaboration between sports medicine and sports cardiology providers. Evaluations must be individualized on a case-by-case basis as tailored to the athlete’s presenting chief complaint and prior medical history. Most of these assessments will include a detailed medical history and physical examination, a 12-lead electrocardiogram (ECG), provocative exercise testing in a controlled environment, noninvasive cardiac imaging, and in some cases ambulatory rhythm monitoring. Uniformly, the athlete should be withheld from further training and competition until high-risk cardiovascular disease has been excluded. We refer the interested reader to a comprehensive discussion of symptom-based assessment of the athlete with suspected cardiovascular disease.16
Syncope (sudden and abrupt loss of consciousness with spontaneous neurologic recovery) is common among trained athletes. The vast majority of syncope is caused by “neurocardiogenic” mechanisms and carries a benign prognosis. Benign neurally-mediated syncope most often occurs outside of training and competition among athletes with heightened vagal tone and a predisposed susceptibility to triggers including pain, anxiety, emotional stimulation, and sudden postural change. Athletes who experience neurally-mediated syncope outside of training and competition routinely report a pre-event prodrome or aura that permits them to lower themselves to the ground, thereby avoiding injury. A distinct, but similarly benign and common, form of neurally-mediated fainting is post-exertional syncope. Here, fainting occurs within seconds of abrupt termination of exercise due to a rapid reduction cardiac preload and corollary cerebral blood supply. When either form of neurally-mediated syncope is suggested by a comprehensive medical history, normal physical examination, and a normal 12- lead ECG, further evaluation is unnecessary. However, the athlete and their coaching staff should be educated about avoidance tactics including hydration, dietary sodium supplementation, and avoidance of abrupt exercise termination as neutrally-mediated syncope tends to be recurrent without such measures. Fainting episodes that occur during training or competition that are not clearly post-exertional should be considered a medical emergency and should prompt comprehensive evaluation by a qualified cardiovascular specialist. Working closely with team physicians and athletic training staff, it is the responsibility of sports cardiologists to exclude potentially life-threatening forms of electrical, muscular, coronary, and valvular heart disease. Ideally, this evaluation should be conducted rapidly to avoid unnecessary delays in return to play.
CARDIAC ARREST AND SUDDEN DEATH
Numerous high-visibility cases of cardiac arrest on the soccer pitch have alerted the sporting community to the potential for these rare and potentially tragic events. Definitive incidence statistics defining the risk of cardiac arrest among soccer players are lacking. Data from the NCAA database suggest a sudden death incidence rate among collegiate male soccer athletes of approximately 1:24,000 athlete years.8 Similar data documenting incidence among female athletes and among those at lower (ie, youth level and high school) and higher (ie, professional) levels of play are unavailable. Underlying cardiovascular disease in the forms of heart muscle abnormalities (ie, genetic and acquired cardiomyopathy), coronary artery abnormalities (ie, genetic coronary anomalies and atherosclerotic coronary disease), valvular heart problems (ie, congenitally malformed aortic valves), and primary disturbances of the cardiac electrical system (ie, Wolf-Parkinson-White syndrome, long QT syndrome, etc.) explain a substantial percentage of on-pitch cardiac arrest. However, it is increasingly recognized that a significant minority of sudden cardiac deaths among athletes occur in the absence of attributable cardiovascular abnormality.17 Such cases, often referred to as “sudden unexplained death,” present unique challenges in the context of pre-participation screening, as they are undetectable and thus unpredictable.
Reduction of cardiac arrest and sudden death may best be accomplished through a combination of focused pre-participation screening and the development and implementation of a comprehensive EAP. Pre-participation involves the performance of a battery of tests prior to training and competition that are geared toward the detection of occult high-risk cardiovascular disease. Recommendations regarding pre-participation screening vary both across and within countries. Current US recommendations call for a focused medical history and physical examination prior to training and competition with consideration of the addition of a 12-lead ECG on a local level based on expertise and available resources.18 Conversely, current European guidelines including those endorsed by FIFA, suggest routine inclusion of a 12-lead ECG and in some cases, a transthoracic ECG.19 It must be emphasized that no screening approach has been confirmed to reduce the incidence of sudden death, and the decision to extend screening beyond the medical history and physical examination to include a 12-lead ECG or echocardiogram may come at the cost of increased false positive testing. In practice, decisions about how and when to screen are ideally made at a local level after consideration of medical and financial resources.20
Continue to: Even the most comprehensive approach...
Even the most comprehensive approach to screening and evaluation of symptomatic athletes will not completely eliminate on-pitch cardiac arrest. Thus, all stakeholders that engage in the oversight of organized soccer must be committed to the development and implementation of an EAP.21 Key components of an effective EAP include the training of coaching staff, athletic trainers, and players in basic cardiopulmonary resuscitation, access to and training in the use of automated external defibrillators, and a triage/transport protocol that ensures timely access to advanced cardiac life support. Much like screening, emergency action planning involving these key core components must be developed and tailored locally. In the era of contemporary organized athletics, the absence of an EAP at any level of competition, from youth to professional leagues, is unacceptable. Effective EAPs must be developed, documented, and rehearsed at regular intervals. For the health and safety of competitive soccer players, as well as coaching staff and spectators, these steps are of critical importance.
HEAT
Heat-related illnesses can be serious and, at times, even life threatening. It is important for athletic staff and athletes to be well versed in the prevention, signs and symptoms, and treatment of heat-related illnesses in order to prevent serious and lasting injury. We aim to educate physicians about the prevention, recognition, and management of heat-related injury, and stress the importance of similarly educating athletes and coaching staff.
Exertional heat illnesses most often occur at temperatures >86°F, however they can occur at any temperature with heavy exertion.22 Signs and symptoms can be nonspecific early on, including weakness, fatigue, headache, nausea, and dizziness. Later signs can include imbalance, altered mentation, confusion, and behavior that is out of character such as irritability or aggression.23 It is easy to see how the later signs can be confused for concussion in the right context. We cover the recognition and treatment of two common and serious heat-related illnesses: heat exhaustion and exertional heat stroke (EHS).
HEAT EXHAUSTION
Heat exhaustion occurs when an athlete cannot continue to exercise due to weakness and fatigue. While the exact mechanism is not well understood, it has been established that the combined effect of heat and dehydration have been proven to decrease exercise capacity and performance to a greater degree than either alone. The heat created by the body during exercise is 15 to 20 times greater than when at rest, and can increase core body temperature by 1°C every 5 minutes if no heat is lost, such as through sweating.24 Additionally, when fluid deficits reach >3% to 5% of total body water, sweat production and skin blood flow decline, blunting the ability for the body to cool itself and causing progressive elevation of core body temperature if the athlete continues exerting him or herself. When fluid deficits reach 6% to 10%, cardiac output, sweat, and muscle blood flow decrease, likely leading to the symptoms seen with heat exhaustion: weakness, profound fatigue, and occasionally confusion and disorientation. Athletes with suspected heat exhaustion should be moved to a cooler area, laid down with legs elevated, and orally rehydrated. If they do not improve with oral rehydration, they may require intravenous fluids. The diagnosis of heat exhaustion hinges on a rectal temperature of <104°F; if >104°F the athlete should be presumed to have heat stroke, which will be addressed in the following paragraphs. Players can be cleared to return to play in mild cases within 24 to 48 hours with gradual increases in exercise intensity.24
EXERTIONAL HEAT STROKE
EHS occurs when the body can no longer regulate the core body temperature and it rises to upwards of 104°F. In EHS, elevated core body temperature is associated with evidence of end organ dysfunction. The most easily identified on the playing field is likely central nervous system dysfunction, including irritability, confusion, irrational behavior, lethargy, dizziness, confusion, and even loss of consciousness. Temperature should be measured with rectal temperature only, as other methods of measurement have been shown to be consistently inaccurate.22 Heat stroke can be confused with exertional hyponatremia, heat exhaustion, or concussion, especially when core body temperature cannot be determined. However, EHS should always be the presumed cause of altered mentation when no rectal temperature is available because rapid cooling is critical to minimizing lasting effects. Morbidity and mortality are directly related to the length of time required to cool the athlete under 40°C (104°F).24 Cooling should be completed on site prior to transport to a medical facility and is best achieved with submersion in an ice bath (ie, a kiddie pool or soaking tub full of ice and water).22,25 If an ice bath is not available, ice bags should be applied to the neck axilla and groin and exchanged for fresh bags every 2 to 3 minutes.22 Ice bags have been shown to be inferior to whole body cooling, only cooling the athlete .04°C to .08°C/min compared to .15°C to .24°C/min with the ice bath.24 All other tests should be delayed until cooling is achieved, unless they can be completed while cooling the athlete. The athlete can be removed from the ice bath once rectal temperatures reach <101°F to 102°F.23 If the athlete returns to baseline after cooling, transportation to a medical facility may not be necessary. However, they should refrain from physical activity and heat exposure for at least 7 days and should be evaluated by a physician at that time. If all labs are normal and the athlete is asymptomatic, they can start progressive return to play under the direction of an athletic trainer or a sports medicine physician.23
Continue to: HEAT-RELATED ILLNESS...
HEAT-RELATED ILLNESS
It is impossible to predict exactly which athletes will be most at risk for heat-related illness, so it is important to have a high degree of suspicion when environmental conditions are right. Athletes with recent illness, fever, or lack of sleep are at higher risk. Additional intrinsic risk factors include low fitness level, obesity, and inadequate hydration. Athletes who are highly competitive or motivated can be more likely to push through the early signs of illness or be reluctant to report symptoms.23 Those with a history of exertional heat illness are more at risk for developing it again in the future.23
The extrinsic risk factors for the development of heat-related illness are much easier to identify and modify in order to keep athletes safe. High temperature and high humidity conditions, heavy sun exposure, and exposure to similar conditions the preceding day put athletes at risk for exertional heat illness. Risks are even greater when the exercise is prolonged or intense with few breaks and access to hydration is limited.23 Therefore, prevention of exertional heat illness is centered on these external risk factors.
Each team should have a heat policy as part of their EAP aimed at prevention and early recognition of heat-related illness. This policy should be shared with all athletes and coaches. The plan should be centered on acclimatization, activity modification, and early recognition and management as previously discussed. The US Soccer Federation “Recognize to Recover” Heat Guidelines suggest a 3-step process for appropriate activity modification:22
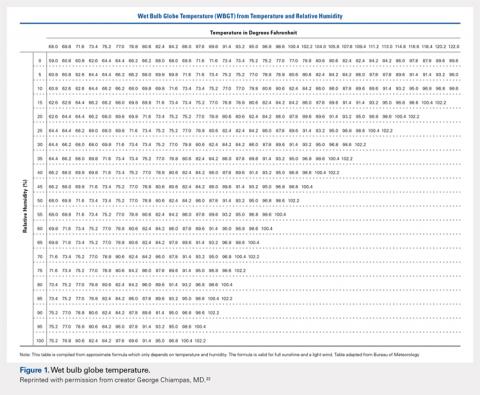
1. Find the wet bulb globe temperature, either using a wet bulb globe thermometer or the temperature and humidity (Figure 1).
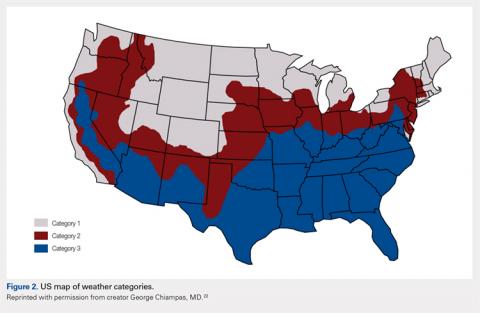
2. Find your regional weather category on the map (Figure 2).
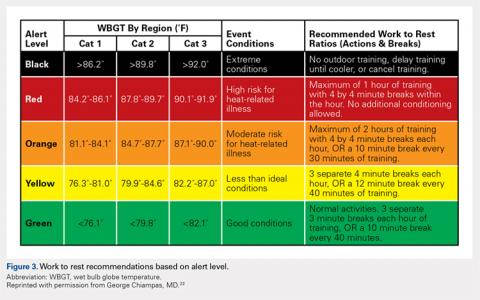
3. Find your alert level and work to rest ratio recommendations (Figure 3).
Scheduled hydration breaks should be given as listed in Figure 3. Breaks of 4 minutes should be given for each 30 minutes of continuous practice or play. In a regulation 90-minute match, a hydration break should be given at 30 and 75 minutes (with half time at 45 minutes) at minimum. Athletes should be educated about where hydration can be accessed, and given unlimited access to hydration even outside of planned breaks.22
Acclimatization to conditions is another integral part of preventing heat-related illness. It allows the body time to adapt to exercising in heat gradually, with a measured progression of exertion over the course of 10 to 14 days. The “Recognize to Recover” Heat Guidelines also provide guidance on acclimatization, and specifics can be found on the website.1 Generally speaking, the warmest part of the day, usually between 11 AM and 4 PM, should be avoided for all training sessions, and length of practice and exertion should be gradually increased over 2 weeks.22
In summary, appropriate acclimatization, hydration, activity modification, and education of athletes and staff are essential for the prevention of heat-related illness. Athletes and staff should understand the signs and symptoms of heat-related illness so that it can be recognized early and treated appropriately. If an athlete is altered in the heat and rectal temperature is >104°F or rectal temperature cannot be obtained, rapid cooling using an ice bath or ice bags is essential to prevent the morbidity and mortality associated with EHS. Above all, teams should have an explicit plan that includes protocols for acclimatization, activity modification, and all necessary equipment to prevent and treat heat-related illnesses should they occur, and ultimately keep athletes safe and healthy.
1. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain Injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375-378.
2. The National Federation of State High School Associations. 2013-14 high school athletics participation survey. http://www.nfhs.org/ParticipationStatics/PDF/2013-14_Participation_Survey_PDF.pdf. Accessed August 6, 2018.
3. Youth Council. US Soccer Federation Web site. https://www.ussoccer.com/about/affiliates/youth-council. Accessed July 31, 2018.
4. Khodaee M, Currie DW, Asif IM, Comstock RD. Nine-year study of US high school soccer injuries: data from a national sports injury surveillance programme. Br J Sports Med. 2017;51(3):185-193. doi:10.1136/bjsports-2015-095946.
5. Schallmo MS, Weiner JA, Hsu WK. Sport and sex-specific trends in the epidemiology of concussions sustained by high school athletes. J Bone Joint Surg Am. 2017;99(15):1314-1320. doi:10.2106/JBJS.16.01573.
6. US Soccer Federation. U.S. Soccer’s comprehensive player health and safety program. Recognize to Recover Web site. http://www.recognizetorecover.org/#us-soccers-comprehensive-player-health-and-safety-program. Accessed July 31, 2018.
7. McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847. doi:10.1136/bjsports-2017-097699.
8. Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123(15):1594-1600. doi:10.1161/CIRCULATIONAHA.110.004622.
9. Faude O, Rössler R, Junge A, et al. Head injuries in children’s football-results from two prospective cohort studies in four European countries. Scand J Med Sci Sports. 2017;27(12):1986-1992. doi:10.1111/sms.12839.
10. Comstock RD, Currie DW, Pierpoint LA, Grubenhoff JA, Fields SK. An evidence-based discussion of heading the ball and concussions in high school soccer. JAMA Pediatr. 2015;169(9):830-837. doi:10.1001/jamapediatrics.2015.1062.
11. Tarnutzer AA. Should heading be forbidden in children’s football? Sci Med Football. 2018;2(1):75-79.
12. US Soccer Federation. US Soccer, NWSL and MLS to host “head injury in soccer; science to field”. https://www.ussoccer.com/stories/2017/04/18/17/35/20170418-news-us-soccer-nwsl-mls-host-head-injury-in-soccer-science-to-field. Published April 18, 2017. Accessed August 6, 2018.
13. Weiner RB, Baggish AL. Exercise-induced cardiac remodeling. Prog Cardiovasc Dis. 2012;54(5):380-386. doi:10.1016/j.pcad.2012.01.006.
14. Baggish AL, Wood MJ. Athlete's heart and cardiovascular care of the athlete: scientific and clinical update. Circulation. 2011;123(23):2723-2735. doi:10.1161/CIRCULATIONAHA.110.981571.
15. Kim JH, Baggish AL. Differentiating exercise-induced cardiac adaptations from cardiac pathology: the "Grey Zone" of clinical uncertainty. Can J Cardiol. 2016;32(4):429-437. doi:10.1016/j.cjca.2015.11.025.
16. Baggish AL, Battle RW, Beckerman JG, et al; ACC’s Sports and Exercise Council Leadership Group. Sports cardiology: core curriculum for providing cardiovascular care to competitive athletes and highly active people. J Am Coll Cardiol. 2017;70(15):1902-1918. doi:10.1016/j.jacc.2017.08.055.
17. Harmon KG, Asif IM, Maleszewski JJ, et al. Incidence, cause, and comparative frequency of sudden cardiac death in National Collegiate Athletic Association athletes: a decade in review. Circulation. 2015;132(1):10-19. doi:10.1161/CIRCULATIONAHA.115.015431.
18. Maron BJ, Levine BD, Washington RL, Baggish AL, Kovacs RJ, Maron MS. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 2: preparticipation screening for cardiovascular disease in competitive athletes: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2015;66(21):2356-2361. doi:10.1016/j.jacc.2015.09.034.
19. Corrado D, Pelliccia A, Bjørnstad HH, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26(5):516-524.
20. Baggish AL, Kovacs RJ. Preparticipation cardiovascular screening: clinical partnership is the only certainty. Br J Sports Med. 2017;51(3):150-151. doi:10.1136/bjsports-2016-096954.
21. Hainline B, Drezner J, Baggish A, et al. Interassociation consensus statement on cardiovascular care of college student-athletes. J Athl Train. 2016;51(4):344-357. doi:10.4085/j.jacc.2016.03.527.
22. US Soccer Federation. Environmental conditions. Recognize to Recover Web site. http://www.recognizetorecover.org/environmental/#environmental-conditions. Accessed April 15, 2018.
23. Korey Stringer Institute. Emergency conditions: heat illnesses. University of Connecticut Web site. https://ksi.uconn.edu/. Accessed April 15, 2018.
24. American College of Sports Medicine, Armstrong LE, Casa DJ, et al. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556-572.
25. Belval LN, Casa DJ, Adams WM, et al. Consensus statement- prehospital care of exertional heat stroke. Prehosp Emerg Care. 2018;22(3):392-397. doi:10.1080/10903127.2017.1392666.
ABSTRACT
Soccer requires significant physical conditioning and endurance, as well as the physicality required for contact play. In order to keep athletes safe, it is important that coaches, medical staff, and the players themselves are educated on the most common dangers to their health that they may encounter on a soccer pitch. This article aims to review the current literature and recommendations on concussion, cardiovascular considerations, and heat-related illness as they relate to competitive soccer, with a goal of educating all those who help to keep athletes healthy and competing to their full potential.
Continue to: Soccer is one of the most popular sports...
Soccer is one of the most popular sports in the modern world and requires significant physical conditioning and endurance, as well as the physicality required for contact play. This article covers the topics of concussion, cardiovascular considerations, and heat-related illness as they relate to competitive soccer players. We provide a review of the prevention, recognition, and management required to keep athletes safe on the soccer pitch, both in practice and in competitive play.
HEAD
With an estimated 1.6 to 3.8 million sports-related mild traumatic brain injuries (ie, concussions) occurring annually in the United States,1 there has been an appropriate increase in the focus on prevention and treatment of these injuries. For more than a decade the spotlight has been on concussions that occur in American football, but other sports have also had to examine the prevalence of concussions in their sport. This is certainly true for soccer.
There has been a steady increase in soccer participation in the United States. From 1973 to 2014 there was a 4-fold increase in high school boys and a 35-fold increase in high school girls playing soccer.2 Currently, there are more than 3.7 million youth who play on teams under the supervision of the US Soccer Federation, the sport’s national governing body.3 With the growth of the sport, there has also been an intensified focus on injury prevention in soccer players, including concussive brain injuries.
A recent study examined injury rates in high school soccer players and noted that concussion is the second most common injury (17.9%), after ligament sprains (29.7%).4 The overall injury rate was 2.06 per 1000 athletic exposures (AEs [defined as participation in practice or game play]), but higher in games (4.42 per 1000 AEs) than during practices (1.05 per 1000 AEs). The overall concussion rate was 0.36 per 1000 AEs.4
Most concussions (54.8%) resulted in missing play between 1 to 3 weeks, but a sizeable portion of the athletes (14.9%) were out of play for more than 3 weeks. Additionally, 10.7% of all medical disqualifications were due to concussive injuries. Khodaee and colleagues4 found no statistically significant difference in concussion rates between male and female soccer players over the 9-year period of time that they examined, however previous studies have found higher rates in female athletes.5
In soccer, as in other sports, there is a concern about both the adequate recognition of concussions during practice and play and the underreporting of concussions by athletes. The US Soccer Federation has taken a proactive stance on addressing concussion in youth soccer by developing the “Recognize to Recover” program.6 Recognize to Recover is the US Soccer Federation’s “comprehensive player health and safety program aimed at promoting safe play and reducing injuries in soccer players of all ages.” The website provides an educational video geared toward players, along with links to concussion assessment tools, the US Soccer Federation Concussion Protocol, and US Soccer Federation-Centers for Disease Control fact sheets for athletes, parents, and coaches.6
Continue to: A challenge for all sports...
A challenge for all sports is allowing adequate evaluation of a suspected concussion by properly trained healthcare professionals. The 2017 Berlin Concussion in Sport Group position paper stated, “when a concussion is suspected, the athlete should be removed from the sporting environment and a multimodal assessment should be conducted in standardized fashion (eg, Sport Concussion Assessment Tool- 5th edition). Sporting bodies should allow adequate time to conduct this evaluation.”7 However, the International Federation of Football Association (FIFA) rules limit substitutions to 3 over the course of the game, which can make a thorough evaluation of players difficult as trainers and coaches are under increased pressure to quickly determine whether to use one of their valuable substitutions. Fortunately, the National Collegiate Athletic Association (NCAA) soccer has mitigated this issue by allowing unlimited substitutions during matches, and high school teams generally follow similar rules.
One of the goals of any safety education program is not only to raise the awareness of the signs and symptoms of concussion by all those involved in the sport, but also to increase the number of athletes who self-report their symptoms and decrease those who hide any possible concussions. A study found that a majority (58.6%) of middle school soccer players continued to play while experiencing concussion symptoms.5 However, in a very recent (not yet published) study, 92% of US Soccer Federation players reported that they did seek out a medical evaluation for their concussion.8 This is certainly a positive sign and further research needs to clarify what methods of education or training will maintain this level of self-reporting in soccer players.
There has also been an increased focus on understanding the mechanism of injury of concussions. In soccer, concussions can occur from player-to-player contact, contact with the player surface, contact with playing apparatus (eg, goal posts) and non-contact mechanisms. While there has been a focus on concussions from heading the ball, player-to-player contact is the most common cause of concussions. A 2017 study of 7- to 12-year-old soccer players in 4 European countries found that about 1 out of 10 concussions were caused by heading the ball.9 Comstock and colleageues10 found slightly higher numbers, roughly 25% to 30% (depending on gender), but 70% to 78% (again depending on gender) of those were caused by player-to-player contact rather than contact with the ball.
To date there has not been any meta-analytic review evaluating the cognitive and physical symptoms associated with heading in soccer. A recent review paper stated that the “current evidence seems insufficient to support a ban of heading in children’s football (soccer).”10 However, in December 2015 the US Soccer Federation included age-specific heading limitations. Players ages 10 years and under “shall not engage in heading, either in practices or in games” and players age 11 years and 12 years should have “limited heading in practice; maximum of 30 minutes of heading training per week, with no more than 15-20 headers per player, per week.”11 US Soccer Federation officials acknowledged the limitations in the current science regarding heading in young soccer players but chose to err on the side of caution until further empirical evidence regarding the risks associated with repetitive heading is available.
The US Soccer Federation is also exploring other ways to reduce the incidence rate of concussions, including ensuring that the age-appropriate sized ball is used in practice and play, possible rule changes, evaluation of different playing surfaces, and equipment usage. To date, there is no strong evidence to support the use of mouth guards or helmets to reduce concussions in soccer. Additionally, the current data about the value of head impact sensors in soccer has not supported its widespread use.
Continue to: Finally, the issue of the prevalence...
Finally, the issue of the prevalence of chronic traumatic encephalopathy (CTE) in soccer players is beyond the scope of this article. The expert opinion from the 2017 US Soccer Federation, Major League Soccer (MLS), and National Women’s Soccer League (NWSL) conference concluded, “At present, no data exist that support that soccer participation is a risk factor for the development of neurodegenerative disease. Similarly, at this time, consistent with evidence discussed in the Berlin Concussion in Sport Group (CISG) Consensus Conference, our review suggests no causal relationship has been demonstrated between soccer and CTE pathology.”12
The more we know about concussions, both in general and those sustained during soccer play, the better we are able to diagnose and manage these injuries in our athletes. An important step is creating evidence-based protocols that evolve as our knowledge of concussions does as well. In April 2017, the US Soccer Federation, MLS, and the NWSL held a joint summit entitled, “Head Injury in Soccer: From Science to the Field” to address the current evidence-based science of concussions in soccer.8 An article discussing the findings of this meeting is forthcoming and will undoubtedly guide further development of concussion protocols for soccer players of all ages.
HEART
The physiologic demands of soccer place considerable stress on the cardiovascular system. Participation in training and competition is characterized by a combination of aerobic and anaerobic physiology with the typical athlete covering approximately 10 km over the course of the 90-minute match. The primary role of the heart and blood vessels is to supply the exercising skeletal muscle with oxygen and energy substrate and to clear the byproducts of metabolism. Among healthy athletes without cardiovascular disease, these processes are typically well tolerated and may be associated with beneficial cardiovascular adaptations over time. However, competitive soccer players are not completely immune to cardiovascular disease. Athletes across the age and competition spectrum may develop symptoms suggestive of underlying cardiovascular disease during play including exertional chest pain, inappropriate shortness of breath, palpitations, and syncope. These athletes require timely clinical evaluation. In extremely rare but high visibility cases, competitive soccer players may succumb to cardiac arrest on the pitch, underscoring the need for comprehensive emergency action plans (EAPs). We provide the practicing clinician with an overview of cardiovascular issues relevant to the competitive soccer athlete.
CARDIOVASCULAR ADAPTATIONS TO SPORT
The pressure (ie, repetitive surges in systemic blood pressure) and volume (ie, sustained increases in high cardiac output) challenges inherent in soccer participation place stress on the cardiovascular system. Healthy athletes across the age spectrum typically tolerate the hemodynamic stressors of participation without issues. Athletes that engage in training and competition over months to years often develop beneficial adaptations of the cardiovascular system that enhance on-field performance and contribute to optimal long-term health. Detailed discussion of how the heart and blood vessels respond to exercise training is beyond the scope of this article, but the interested reader is referred to several prior publications.13,14 In brief, the heart of the healthy soccer athlete demonstrates the balanced mild chamber dilation and wall thickening characteristic of left ventricular eccentric remodeling. This form of exercise-induced cardiac remodeling facilitates maintenance of high stroke volume during exercise with minimal increases in cardiac work. In parallel, routine aerobic exercise training confers favorable changes in the systemic arterial system, which leads to reductions in age-associated ventricular stiffening and maintenance of healthy low blood pressure. It must be emphasized that the healthy heart muscle dilation and thickening that develop in response to sports participation, regardless of age, ethnicity, or gender, are relatively mild and should not be confused with common forms of heart muscle disease that may be seen in athletes at risk for adverse outcomes. In some situations, consultation with an extreme sports cardiologist may be required to differentiate exercise-induced remodeling from over heart muscle pathology.15
Continue to: THE SYMPTOMATIC ATHLETE...
THE SYMPTOMATIC ATHLETE
Any athlete presenting with symptoms suggestive of underlying cardiovascular disease should be withheld from training and competition until a comprehensive clinical evaluation has been completed. Common manifestations of underlying heart disease that occur in soccer players include exertional chest pain/pressure/tightness, shortness of breath that is out of proportion to workload, palpitations or the perception of irregular cardiac activity, and syncope. Chest discomfort, inappropriate shortness of breath, and palpitations that occur during training or competition should be managed with immediate removal from the playing field and prompt medical assessment. In many cases, thorough evaluation will involve collaboration between sports medicine and sports cardiology providers. Evaluations must be individualized on a case-by-case basis as tailored to the athlete’s presenting chief complaint and prior medical history. Most of these assessments will include a detailed medical history and physical examination, a 12-lead electrocardiogram (ECG), provocative exercise testing in a controlled environment, noninvasive cardiac imaging, and in some cases ambulatory rhythm monitoring. Uniformly, the athlete should be withheld from further training and competition until high-risk cardiovascular disease has been excluded. We refer the interested reader to a comprehensive discussion of symptom-based assessment of the athlete with suspected cardiovascular disease.16
Syncope (sudden and abrupt loss of consciousness with spontaneous neurologic recovery) is common among trained athletes. The vast majority of syncope is caused by “neurocardiogenic” mechanisms and carries a benign prognosis. Benign neurally-mediated syncope most often occurs outside of training and competition among athletes with heightened vagal tone and a predisposed susceptibility to triggers including pain, anxiety, emotional stimulation, and sudden postural change. Athletes who experience neurally-mediated syncope outside of training and competition routinely report a pre-event prodrome or aura that permits them to lower themselves to the ground, thereby avoiding injury. A distinct, but similarly benign and common, form of neurally-mediated fainting is post-exertional syncope. Here, fainting occurs within seconds of abrupt termination of exercise due to a rapid reduction cardiac preload and corollary cerebral blood supply. When either form of neurally-mediated syncope is suggested by a comprehensive medical history, normal physical examination, and a normal 12- lead ECG, further evaluation is unnecessary. However, the athlete and their coaching staff should be educated about avoidance tactics including hydration, dietary sodium supplementation, and avoidance of abrupt exercise termination as neutrally-mediated syncope tends to be recurrent without such measures. Fainting episodes that occur during training or competition that are not clearly post-exertional should be considered a medical emergency and should prompt comprehensive evaluation by a qualified cardiovascular specialist. Working closely with team physicians and athletic training staff, it is the responsibility of sports cardiologists to exclude potentially life-threatening forms of electrical, muscular, coronary, and valvular heart disease. Ideally, this evaluation should be conducted rapidly to avoid unnecessary delays in return to play.
CARDIAC ARREST AND SUDDEN DEATH
Numerous high-visibility cases of cardiac arrest on the soccer pitch have alerted the sporting community to the potential for these rare and potentially tragic events. Definitive incidence statistics defining the risk of cardiac arrest among soccer players are lacking. Data from the NCAA database suggest a sudden death incidence rate among collegiate male soccer athletes of approximately 1:24,000 athlete years.8 Similar data documenting incidence among female athletes and among those at lower (ie, youth level and high school) and higher (ie, professional) levels of play are unavailable. Underlying cardiovascular disease in the forms of heart muscle abnormalities (ie, genetic and acquired cardiomyopathy), coronary artery abnormalities (ie, genetic coronary anomalies and atherosclerotic coronary disease), valvular heart problems (ie, congenitally malformed aortic valves), and primary disturbances of the cardiac electrical system (ie, Wolf-Parkinson-White syndrome, long QT syndrome, etc.) explain a substantial percentage of on-pitch cardiac arrest. However, it is increasingly recognized that a significant minority of sudden cardiac deaths among athletes occur in the absence of attributable cardiovascular abnormality.17 Such cases, often referred to as “sudden unexplained death,” present unique challenges in the context of pre-participation screening, as they are undetectable and thus unpredictable.
Reduction of cardiac arrest and sudden death may best be accomplished through a combination of focused pre-participation screening and the development and implementation of a comprehensive EAP. Pre-participation involves the performance of a battery of tests prior to training and competition that are geared toward the detection of occult high-risk cardiovascular disease. Recommendations regarding pre-participation screening vary both across and within countries. Current US recommendations call for a focused medical history and physical examination prior to training and competition with consideration of the addition of a 12-lead ECG on a local level based on expertise and available resources.18 Conversely, current European guidelines including those endorsed by FIFA, suggest routine inclusion of a 12-lead ECG and in some cases, a transthoracic ECG.19 It must be emphasized that no screening approach has been confirmed to reduce the incidence of sudden death, and the decision to extend screening beyond the medical history and physical examination to include a 12-lead ECG or echocardiogram may come at the cost of increased false positive testing. In practice, decisions about how and when to screen are ideally made at a local level after consideration of medical and financial resources.20
Continue to: Even the most comprehensive approach...
Even the most comprehensive approach to screening and evaluation of symptomatic athletes will not completely eliminate on-pitch cardiac arrest. Thus, all stakeholders that engage in the oversight of organized soccer must be committed to the development and implementation of an EAP.21 Key components of an effective EAP include the training of coaching staff, athletic trainers, and players in basic cardiopulmonary resuscitation, access to and training in the use of automated external defibrillators, and a triage/transport protocol that ensures timely access to advanced cardiac life support. Much like screening, emergency action planning involving these key core components must be developed and tailored locally. In the era of contemporary organized athletics, the absence of an EAP at any level of competition, from youth to professional leagues, is unacceptable. Effective EAPs must be developed, documented, and rehearsed at regular intervals. For the health and safety of competitive soccer players, as well as coaching staff and spectators, these steps are of critical importance.
HEAT
Heat-related illnesses can be serious and, at times, even life threatening. It is important for athletic staff and athletes to be well versed in the prevention, signs and symptoms, and treatment of heat-related illnesses in order to prevent serious and lasting injury. We aim to educate physicians about the prevention, recognition, and management of heat-related injury, and stress the importance of similarly educating athletes and coaching staff.
Exertional heat illnesses most often occur at temperatures >86°F, however they can occur at any temperature with heavy exertion.22 Signs and symptoms can be nonspecific early on, including weakness, fatigue, headache, nausea, and dizziness. Later signs can include imbalance, altered mentation, confusion, and behavior that is out of character such as irritability or aggression.23 It is easy to see how the later signs can be confused for concussion in the right context. We cover the recognition and treatment of two common and serious heat-related illnesses: heat exhaustion and exertional heat stroke (EHS).
HEAT EXHAUSTION
Heat exhaustion occurs when an athlete cannot continue to exercise due to weakness and fatigue. While the exact mechanism is not well understood, it has been established that the combined effect of heat and dehydration have been proven to decrease exercise capacity and performance to a greater degree than either alone. The heat created by the body during exercise is 15 to 20 times greater than when at rest, and can increase core body temperature by 1°C every 5 minutes if no heat is lost, such as through sweating.24 Additionally, when fluid deficits reach >3% to 5% of total body water, sweat production and skin blood flow decline, blunting the ability for the body to cool itself and causing progressive elevation of core body temperature if the athlete continues exerting him or herself. When fluid deficits reach 6% to 10%, cardiac output, sweat, and muscle blood flow decrease, likely leading to the symptoms seen with heat exhaustion: weakness, profound fatigue, and occasionally confusion and disorientation. Athletes with suspected heat exhaustion should be moved to a cooler area, laid down with legs elevated, and orally rehydrated. If they do not improve with oral rehydration, they may require intravenous fluids. The diagnosis of heat exhaustion hinges on a rectal temperature of <104°F; if >104°F the athlete should be presumed to have heat stroke, which will be addressed in the following paragraphs. Players can be cleared to return to play in mild cases within 24 to 48 hours with gradual increases in exercise intensity.24
EXERTIONAL HEAT STROKE
EHS occurs when the body can no longer regulate the core body temperature and it rises to upwards of 104°F. In EHS, elevated core body temperature is associated with evidence of end organ dysfunction. The most easily identified on the playing field is likely central nervous system dysfunction, including irritability, confusion, irrational behavior, lethargy, dizziness, confusion, and even loss of consciousness. Temperature should be measured with rectal temperature only, as other methods of measurement have been shown to be consistently inaccurate.22 Heat stroke can be confused with exertional hyponatremia, heat exhaustion, or concussion, especially when core body temperature cannot be determined. However, EHS should always be the presumed cause of altered mentation when no rectal temperature is available because rapid cooling is critical to minimizing lasting effects. Morbidity and mortality are directly related to the length of time required to cool the athlete under 40°C (104°F).24 Cooling should be completed on site prior to transport to a medical facility and is best achieved with submersion in an ice bath (ie, a kiddie pool or soaking tub full of ice and water).22,25 If an ice bath is not available, ice bags should be applied to the neck axilla and groin and exchanged for fresh bags every 2 to 3 minutes.22 Ice bags have been shown to be inferior to whole body cooling, only cooling the athlete .04°C to .08°C/min compared to .15°C to .24°C/min with the ice bath.24 All other tests should be delayed until cooling is achieved, unless they can be completed while cooling the athlete. The athlete can be removed from the ice bath once rectal temperatures reach <101°F to 102°F.23 If the athlete returns to baseline after cooling, transportation to a medical facility may not be necessary. However, they should refrain from physical activity and heat exposure for at least 7 days and should be evaluated by a physician at that time. If all labs are normal and the athlete is asymptomatic, they can start progressive return to play under the direction of an athletic trainer or a sports medicine physician.23
Continue to: HEAT-RELATED ILLNESS...
HEAT-RELATED ILLNESS
It is impossible to predict exactly which athletes will be most at risk for heat-related illness, so it is important to have a high degree of suspicion when environmental conditions are right. Athletes with recent illness, fever, or lack of sleep are at higher risk. Additional intrinsic risk factors include low fitness level, obesity, and inadequate hydration. Athletes who are highly competitive or motivated can be more likely to push through the early signs of illness or be reluctant to report symptoms.23 Those with a history of exertional heat illness are more at risk for developing it again in the future.23
The extrinsic risk factors for the development of heat-related illness are much easier to identify and modify in order to keep athletes safe. High temperature and high humidity conditions, heavy sun exposure, and exposure to similar conditions the preceding day put athletes at risk for exertional heat illness. Risks are even greater when the exercise is prolonged or intense with few breaks and access to hydration is limited.23 Therefore, prevention of exertional heat illness is centered on these external risk factors.
Each team should have a heat policy as part of their EAP aimed at prevention and early recognition of heat-related illness. This policy should be shared with all athletes and coaches. The plan should be centered on acclimatization, activity modification, and early recognition and management as previously discussed. The US Soccer Federation “Recognize to Recover” Heat Guidelines suggest a 3-step process for appropriate activity modification:22
1. Find the wet bulb globe temperature, either using a wet bulb globe thermometer or the temperature and humidity (Figure 1).
2. Find your regional weather category on the map (Figure 2).
3. Find your alert level and work to rest ratio recommendations (Figure 3).
Scheduled hydration breaks should be given as listed in Figure 3. Breaks of 4 minutes should be given for each 30 minutes of continuous practice or play. In a regulation 90-minute match, a hydration break should be given at 30 and 75 minutes (with half time at 45 minutes) at minimum. Athletes should be educated about where hydration can be accessed, and given unlimited access to hydration even outside of planned breaks.22
Acclimatization to conditions is another integral part of preventing heat-related illness. It allows the body time to adapt to exercising in heat gradually, with a measured progression of exertion over the course of 10 to 14 days. The “Recognize to Recover” Heat Guidelines also provide guidance on acclimatization, and specifics can be found on the website.1 Generally speaking, the warmest part of the day, usually between 11 AM and 4 PM, should be avoided for all training sessions, and length of practice and exertion should be gradually increased over 2 weeks.22
In summary, appropriate acclimatization, hydration, activity modification, and education of athletes and staff are essential for the prevention of heat-related illness. Athletes and staff should understand the signs and symptoms of heat-related illness so that it can be recognized early and treated appropriately. If an athlete is altered in the heat and rectal temperature is >104°F or rectal temperature cannot be obtained, rapid cooling using an ice bath or ice bags is essential to prevent the morbidity and mortality associated with EHS. Above all, teams should have an explicit plan that includes protocols for acclimatization, activity modification, and all necessary equipment to prevent and treat heat-related illnesses should they occur, and ultimately keep athletes safe and healthy.
ABSTRACT
Soccer requires significant physical conditioning and endurance, as well as the physicality required for contact play. In order to keep athletes safe, it is important that coaches, medical staff, and the players themselves are educated on the most common dangers to their health that they may encounter on a soccer pitch. This article aims to review the current literature and recommendations on concussion, cardiovascular considerations, and heat-related illness as they relate to competitive soccer, with a goal of educating all those who help to keep athletes healthy and competing to their full potential.
Continue to: Soccer is one of the most popular sports...
Soccer is one of the most popular sports in the modern world and requires significant physical conditioning and endurance, as well as the physicality required for contact play. This article covers the topics of concussion, cardiovascular considerations, and heat-related illness as they relate to competitive soccer players. We provide a review of the prevention, recognition, and management required to keep athletes safe on the soccer pitch, both in practice and in competitive play.
HEAD
With an estimated 1.6 to 3.8 million sports-related mild traumatic brain injuries (ie, concussions) occurring annually in the United States,1 there has been an appropriate increase in the focus on prevention and treatment of these injuries. For more than a decade the spotlight has been on concussions that occur in American football, but other sports have also had to examine the prevalence of concussions in their sport. This is certainly true for soccer.
There has been a steady increase in soccer participation in the United States. From 1973 to 2014 there was a 4-fold increase in high school boys and a 35-fold increase in high school girls playing soccer.2 Currently, there are more than 3.7 million youth who play on teams under the supervision of the US Soccer Federation, the sport’s national governing body.3 With the growth of the sport, there has also been an intensified focus on injury prevention in soccer players, including concussive brain injuries.
A recent study examined injury rates in high school soccer players and noted that concussion is the second most common injury (17.9%), after ligament sprains (29.7%).4 The overall injury rate was 2.06 per 1000 athletic exposures (AEs [defined as participation in practice or game play]), but higher in games (4.42 per 1000 AEs) than during practices (1.05 per 1000 AEs). The overall concussion rate was 0.36 per 1000 AEs.4
Most concussions (54.8%) resulted in missing play between 1 to 3 weeks, but a sizeable portion of the athletes (14.9%) were out of play for more than 3 weeks. Additionally, 10.7% of all medical disqualifications were due to concussive injuries. Khodaee and colleagues4 found no statistically significant difference in concussion rates between male and female soccer players over the 9-year period of time that they examined, however previous studies have found higher rates in female athletes.5
In soccer, as in other sports, there is a concern about both the adequate recognition of concussions during practice and play and the underreporting of concussions by athletes. The US Soccer Federation has taken a proactive stance on addressing concussion in youth soccer by developing the “Recognize to Recover” program.6 Recognize to Recover is the US Soccer Federation’s “comprehensive player health and safety program aimed at promoting safe play and reducing injuries in soccer players of all ages.” The website provides an educational video geared toward players, along with links to concussion assessment tools, the US Soccer Federation Concussion Protocol, and US Soccer Federation-Centers for Disease Control fact sheets for athletes, parents, and coaches.6
Continue to: A challenge for all sports...
A challenge for all sports is allowing adequate evaluation of a suspected concussion by properly trained healthcare professionals. The 2017 Berlin Concussion in Sport Group position paper stated, “when a concussion is suspected, the athlete should be removed from the sporting environment and a multimodal assessment should be conducted in standardized fashion (eg, Sport Concussion Assessment Tool- 5th edition). Sporting bodies should allow adequate time to conduct this evaluation.”7 However, the International Federation of Football Association (FIFA) rules limit substitutions to 3 over the course of the game, which can make a thorough evaluation of players difficult as trainers and coaches are under increased pressure to quickly determine whether to use one of their valuable substitutions. Fortunately, the National Collegiate Athletic Association (NCAA) soccer has mitigated this issue by allowing unlimited substitutions during matches, and high school teams generally follow similar rules.
One of the goals of any safety education program is not only to raise the awareness of the signs and symptoms of concussion by all those involved in the sport, but also to increase the number of athletes who self-report their symptoms and decrease those who hide any possible concussions. A study found that a majority (58.6%) of middle school soccer players continued to play while experiencing concussion symptoms.5 However, in a very recent (not yet published) study, 92% of US Soccer Federation players reported that they did seek out a medical evaluation for their concussion.8 This is certainly a positive sign and further research needs to clarify what methods of education or training will maintain this level of self-reporting in soccer players.
There has also been an increased focus on understanding the mechanism of injury of concussions. In soccer, concussions can occur from player-to-player contact, contact with the player surface, contact with playing apparatus (eg, goal posts) and non-contact mechanisms. While there has been a focus on concussions from heading the ball, player-to-player contact is the most common cause of concussions. A 2017 study of 7- to 12-year-old soccer players in 4 European countries found that about 1 out of 10 concussions were caused by heading the ball.9 Comstock and colleageues10 found slightly higher numbers, roughly 25% to 30% (depending on gender), but 70% to 78% (again depending on gender) of those were caused by player-to-player contact rather than contact with the ball.
To date there has not been any meta-analytic review evaluating the cognitive and physical symptoms associated with heading in soccer. A recent review paper stated that the “current evidence seems insufficient to support a ban of heading in children’s football (soccer).”10 However, in December 2015 the US Soccer Federation included age-specific heading limitations. Players ages 10 years and under “shall not engage in heading, either in practices or in games” and players age 11 years and 12 years should have “limited heading in practice; maximum of 30 minutes of heading training per week, with no more than 15-20 headers per player, per week.”11 US Soccer Federation officials acknowledged the limitations in the current science regarding heading in young soccer players but chose to err on the side of caution until further empirical evidence regarding the risks associated with repetitive heading is available.
The US Soccer Federation is also exploring other ways to reduce the incidence rate of concussions, including ensuring that the age-appropriate sized ball is used in practice and play, possible rule changes, evaluation of different playing surfaces, and equipment usage. To date, there is no strong evidence to support the use of mouth guards or helmets to reduce concussions in soccer. Additionally, the current data about the value of head impact sensors in soccer has not supported its widespread use.
Continue to: Finally, the issue of the prevalence...
Finally, the issue of the prevalence of chronic traumatic encephalopathy (CTE) in soccer players is beyond the scope of this article. The expert opinion from the 2017 US Soccer Federation, Major League Soccer (MLS), and National Women’s Soccer League (NWSL) conference concluded, “At present, no data exist that support that soccer participation is a risk factor for the development of neurodegenerative disease. Similarly, at this time, consistent with evidence discussed in the Berlin Concussion in Sport Group (CISG) Consensus Conference, our review suggests no causal relationship has been demonstrated between soccer and CTE pathology.”12
The more we know about concussions, both in general and those sustained during soccer play, the better we are able to diagnose and manage these injuries in our athletes. An important step is creating evidence-based protocols that evolve as our knowledge of concussions does as well. In April 2017, the US Soccer Federation, MLS, and the NWSL held a joint summit entitled, “Head Injury in Soccer: From Science to the Field” to address the current evidence-based science of concussions in soccer.8 An article discussing the findings of this meeting is forthcoming and will undoubtedly guide further development of concussion protocols for soccer players of all ages.
HEART
The physiologic demands of soccer place considerable stress on the cardiovascular system. Participation in training and competition is characterized by a combination of aerobic and anaerobic physiology with the typical athlete covering approximately 10 km over the course of the 90-minute match. The primary role of the heart and blood vessels is to supply the exercising skeletal muscle with oxygen and energy substrate and to clear the byproducts of metabolism. Among healthy athletes without cardiovascular disease, these processes are typically well tolerated and may be associated with beneficial cardiovascular adaptations over time. However, competitive soccer players are not completely immune to cardiovascular disease. Athletes across the age and competition spectrum may develop symptoms suggestive of underlying cardiovascular disease during play including exertional chest pain, inappropriate shortness of breath, palpitations, and syncope. These athletes require timely clinical evaluation. In extremely rare but high visibility cases, competitive soccer players may succumb to cardiac arrest on the pitch, underscoring the need for comprehensive emergency action plans (EAPs). We provide the practicing clinician with an overview of cardiovascular issues relevant to the competitive soccer athlete.
CARDIOVASCULAR ADAPTATIONS TO SPORT
The pressure (ie, repetitive surges in systemic blood pressure) and volume (ie, sustained increases in high cardiac output) challenges inherent in soccer participation place stress on the cardiovascular system. Healthy athletes across the age spectrum typically tolerate the hemodynamic stressors of participation without issues. Athletes that engage in training and competition over months to years often develop beneficial adaptations of the cardiovascular system that enhance on-field performance and contribute to optimal long-term health. Detailed discussion of how the heart and blood vessels respond to exercise training is beyond the scope of this article, but the interested reader is referred to several prior publications.13,14 In brief, the heart of the healthy soccer athlete demonstrates the balanced mild chamber dilation and wall thickening characteristic of left ventricular eccentric remodeling. This form of exercise-induced cardiac remodeling facilitates maintenance of high stroke volume during exercise with minimal increases in cardiac work. In parallel, routine aerobic exercise training confers favorable changes in the systemic arterial system, which leads to reductions in age-associated ventricular stiffening and maintenance of healthy low blood pressure. It must be emphasized that the healthy heart muscle dilation and thickening that develop in response to sports participation, regardless of age, ethnicity, or gender, are relatively mild and should not be confused with common forms of heart muscle disease that may be seen in athletes at risk for adverse outcomes. In some situations, consultation with an extreme sports cardiologist may be required to differentiate exercise-induced remodeling from over heart muscle pathology.15
Continue to: THE SYMPTOMATIC ATHLETE...
THE SYMPTOMATIC ATHLETE
Any athlete presenting with symptoms suggestive of underlying cardiovascular disease should be withheld from training and competition until a comprehensive clinical evaluation has been completed. Common manifestations of underlying heart disease that occur in soccer players include exertional chest pain/pressure/tightness, shortness of breath that is out of proportion to workload, palpitations or the perception of irregular cardiac activity, and syncope. Chest discomfort, inappropriate shortness of breath, and palpitations that occur during training or competition should be managed with immediate removal from the playing field and prompt medical assessment. In many cases, thorough evaluation will involve collaboration between sports medicine and sports cardiology providers. Evaluations must be individualized on a case-by-case basis as tailored to the athlete’s presenting chief complaint and prior medical history. Most of these assessments will include a detailed medical history and physical examination, a 12-lead electrocardiogram (ECG), provocative exercise testing in a controlled environment, noninvasive cardiac imaging, and in some cases ambulatory rhythm monitoring. Uniformly, the athlete should be withheld from further training and competition until high-risk cardiovascular disease has been excluded. We refer the interested reader to a comprehensive discussion of symptom-based assessment of the athlete with suspected cardiovascular disease.16
Syncope (sudden and abrupt loss of consciousness with spontaneous neurologic recovery) is common among trained athletes. The vast majority of syncope is caused by “neurocardiogenic” mechanisms and carries a benign prognosis. Benign neurally-mediated syncope most often occurs outside of training and competition among athletes with heightened vagal tone and a predisposed susceptibility to triggers including pain, anxiety, emotional stimulation, and sudden postural change. Athletes who experience neurally-mediated syncope outside of training and competition routinely report a pre-event prodrome or aura that permits them to lower themselves to the ground, thereby avoiding injury. A distinct, but similarly benign and common, form of neurally-mediated fainting is post-exertional syncope. Here, fainting occurs within seconds of abrupt termination of exercise due to a rapid reduction cardiac preload and corollary cerebral blood supply. When either form of neurally-mediated syncope is suggested by a comprehensive medical history, normal physical examination, and a normal 12- lead ECG, further evaluation is unnecessary. However, the athlete and their coaching staff should be educated about avoidance tactics including hydration, dietary sodium supplementation, and avoidance of abrupt exercise termination as neutrally-mediated syncope tends to be recurrent without such measures. Fainting episodes that occur during training or competition that are not clearly post-exertional should be considered a medical emergency and should prompt comprehensive evaluation by a qualified cardiovascular specialist. Working closely with team physicians and athletic training staff, it is the responsibility of sports cardiologists to exclude potentially life-threatening forms of electrical, muscular, coronary, and valvular heart disease. Ideally, this evaluation should be conducted rapidly to avoid unnecessary delays in return to play.
CARDIAC ARREST AND SUDDEN DEATH
Numerous high-visibility cases of cardiac arrest on the soccer pitch have alerted the sporting community to the potential for these rare and potentially tragic events. Definitive incidence statistics defining the risk of cardiac arrest among soccer players are lacking. Data from the NCAA database suggest a sudden death incidence rate among collegiate male soccer athletes of approximately 1:24,000 athlete years.8 Similar data documenting incidence among female athletes and among those at lower (ie, youth level and high school) and higher (ie, professional) levels of play are unavailable. Underlying cardiovascular disease in the forms of heart muscle abnormalities (ie, genetic and acquired cardiomyopathy), coronary artery abnormalities (ie, genetic coronary anomalies and atherosclerotic coronary disease), valvular heart problems (ie, congenitally malformed aortic valves), and primary disturbances of the cardiac electrical system (ie, Wolf-Parkinson-White syndrome, long QT syndrome, etc.) explain a substantial percentage of on-pitch cardiac arrest. However, it is increasingly recognized that a significant minority of sudden cardiac deaths among athletes occur in the absence of attributable cardiovascular abnormality.17 Such cases, often referred to as “sudden unexplained death,” present unique challenges in the context of pre-participation screening, as they are undetectable and thus unpredictable.
Reduction of cardiac arrest and sudden death may best be accomplished through a combination of focused pre-participation screening and the development and implementation of a comprehensive EAP. Pre-participation involves the performance of a battery of tests prior to training and competition that are geared toward the detection of occult high-risk cardiovascular disease. Recommendations regarding pre-participation screening vary both across and within countries. Current US recommendations call for a focused medical history and physical examination prior to training and competition with consideration of the addition of a 12-lead ECG on a local level based on expertise and available resources.18 Conversely, current European guidelines including those endorsed by FIFA, suggest routine inclusion of a 12-lead ECG and in some cases, a transthoracic ECG.19 It must be emphasized that no screening approach has been confirmed to reduce the incidence of sudden death, and the decision to extend screening beyond the medical history and physical examination to include a 12-lead ECG or echocardiogram may come at the cost of increased false positive testing. In practice, decisions about how and when to screen are ideally made at a local level after consideration of medical and financial resources.20
Continue to: Even the most comprehensive approach...
Even the most comprehensive approach to screening and evaluation of symptomatic athletes will not completely eliminate on-pitch cardiac arrest. Thus, all stakeholders that engage in the oversight of organized soccer must be committed to the development and implementation of an EAP.21 Key components of an effective EAP include the training of coaching staff, athletic trainers, and players in basic cardiopulmonary resuscitation, access to and training in the use of automated external defibrillators, and a triage/transport protocol that ensures timely access to advanced cardiac life support. Much like screening, emergency action planning involving these key core components must be developed and tailored locally. In the era of contemporary organized athletics, the absence of an EAP at any level of competition, from youth to professional leagues, is unacceptable. Effective EAPs must be developed, documented, and rehearsed at regular intervals. For the health and safety of competitive soccer players, as well as coaching staff and spectators, these steps are of critical importance.
HEAT
Heat-related illnesses can be serious and, at times, even life threatening. It is important for athletic staff and athletes to be well versed in the prevention, signs and symptoms, and treatment of heat-related illnesses in order to prevent serious and lasting injury. We aim to educate physicians about the prevention, recognition, and management of heat-related injury, and stress the importance of similarly educating athletes and coaching staff.
Exertional heat illnesses most often occur at temperatures >86°F, however they can occur at any temperature with heavy exertion.22 Signs and symptoms can be nonspecific early on, including weakness, fatigue, headache, nausea, and dizziness. Later signs can include imbalance, altered mentation, confusion, and behavior that is out of character such as irritability or aggression.23 It is easy to see how the later signs can be confused for concussion in the right context. We cover the recognition and treatment of two common and serious heat-related illnesses: heat exhaustion and exertional heat stroke (EHS).
HEAT EXHAUSTION
Heat exhaustion occurs when an athlete cannot continue to exercise due to weakness and fatigue. While the exact mechanism is not well understood, it has been established that the combined effect of heat and dehydration have been proven to decrease exercise capacity and performance to a greater degree than either alone. The heat created by the body during exercise is 15 to 20 times greater than when at rest, and can increase core body temperature by 1°C every 5 minutes if no heat is lost, such as through sweating.24 Additionally, when fluid deficits reach >3% to 5% of total body water, sweat production and skin blood flow decline, blunting the ability for the body to cool itself and causing progressive elevation of core body temperature if the athlete continues exerting him or herself. When fluid deficits reach 6% to 10%, cardiac output, sweat, and muscle blood flow decrease, likely leading to the symptoms seen with heat exhaustion: weakness, profound fatigue, and occasionally confusion and disorientation. Athletes with suspected heat exhaustion should be moved to a cooler area, laid down with legs elevated, and orally rehydrated. If they do not improve with oral rehydration, they may require intravenous fluids. The diagnosis of heat exhaustion hinges on a rectal temperature of <104°F; if >104°F the athlete should be presumed to have heat stroke, which will be addressed in the following paragraphs. Players can be cleared to return to play in mild cases within 24 to 48 hours with gradual increases in exercise intensity.24
EXERTIONAL HEAT STROKE
EHS occurs when the body can no longer regulate the core body temperature and it rises to upwards of 104°F. In EHS, elevated core body temperature is associated with evidence of end organ dysfunction. The most easily identified on the playing field is likely central nervous system dysfunction, including irritability, confusion, irrational behavior, lethargy, dizziness, confusion, and even loss of consciousness. Temperature should be measured with rectal temperature only, as other methods of measurement have been shown to be consistently inaccurate.22 Heat stroke can be confused with exertional hyponatremia, heat exhaustion, or concussion, especially when core body temperature cannot be determined. However, EHS should always be the presumed cause of altered mentation when no rectal temperature is available because rapid cooling is critical to minimizing lasting effects. Morbidity and mortality are directly related to the length of time required to cool the athlete under 40°C (104°F).24 Cooling should be completed on site prior to transport to a medical facility and is best achieved with submersion in an ice bath (ie, a kiddie pool or soaking tub full of ice and water).22,25 If an ice bath is not available, ice bags should be applied to the neck axilla and groin and exchanged for fresh bags every 2 to 3 minutes.22 Ice bags have been shown to be inferior to whole body cooling, only cooling the athlete .04°C to .08°C/min compared to .15°C to .24°C/min with the ice bath.24 All other tests should be delayed until cooling is achieved, unless they can be completed while cooling the athlete. The athlete can be removed from the ice bath once rectal temperatures reach <101°F to 102°F.23 If the athlete returns to baseline after cooling, transportation to a medical facility may not be necessary. However, they should refrain from physical activity and heat exposure for at least 7 days and should be evaluated by a physician at that time. If all labs are normal and the athlete is asymptomatic, they can start progressive return to play under the direction of an athletic trainer or a sports medicine physician.23
Continue to: HEAT-RELATED ILLNESS...
HEAT-RELATED ILLNESS
It is impossible to predict exactly which athletes will be most at risk for heat-related illness, so it is important to have a high degree of suspicion when environmental conditions are right. Athletes with recent illness, fever, or lack of sleep are at higher risk. Additional intrinsic risk factors include low fitness level, obesity, and inadequate hydration. Athletes who are highly competitive or motivated can be more likely to push through the early signs of illness or be reluctant to report symptoms.23 Those with a history of exertional heat illness are more at risk for developing it again in the future.23
The extrinsic risk factors for the development of heat-related illness are much easier to identify and modify in order to keep athletes safe. High temperature and high humidity conditions, heavy sun exposure, and exposure to similar conditions the preceding day put athletes at risk for exertional heat illness. Risks are even greater when the exercise is prolonged or intense with few breaks and access to hydration is limited.23 Therefore, prevention of exertional heat illness is centered on these external risk factors.
Each team should have a heat policy as part of their EAP aimed at prevention and early recognition of heat-related illness. This policy should be shared with all athletes and coaches. The plan should be centered on acclimatization, activity modification, and early recognition and management as previously discussed. The US Soccer Federation “Recognize to Recover” Heat Guidelines suggest a 3-step process for appropriate activity modification:22
1. Find the wet bulb globe temperature, either using a wet bulb globe thermometer or the temperature and humidity (Figure 1).
2. Find your regional weather category on the map (Figure 2).
3. Find your alert level and work to rest ratio recommendations (Figure 3).
Scheduled hydration breaks should be given as listed in Figure 3. Breaks of 4 minutes should be given for each 30 minutes of continuous practice or play. In a regulation 90-minute match, a hydration break should be given at 30 and 75 minutes (with half time at 45 minutes) at minimum. Athletes should be educated about where hydration can be accessed, and given unlimited access to hydration even outside of planned breaks.22
Acclimatization to conditions is another integral part of preventing heat-related illness. It allows the body time to adapt to exercising in heat gradually, with a measured progression of exertion over the course of 10 to 14 days. The “Recognize to Recover” Heat Guidelines also provide guidance on acclimatization, and specifics can be found on the website.1 Generally speaking, the warmest part of the day, usually between 11 AM and 4 PM, should be avoided for all training sessions, and length of practice and exertion should be gradually increased over 2 weeks.22
In summary, appropriate acclimatization, hydration, activity modification, and education of athletes and staff are essential for the prevention of heat-related illness. Athletes and staff should understand the signs and symptoms of heat-related illness so that it can be recognized early and treated appropriately. If an athlete is altered in the heat and rectal temperature is >104°F or rectal temperature cannot be obtained, rapid cooling using an ice bath or ice bags is essential to prevent the morbidity and mortality associated with EHS. Above all, teams should have an explicit plan that includes protocols for acclimatization, activity modification, and all necessary equipment to prevent and treat heat-related illnesses should they occur, and ultimately keep athletes safe and healthy.
1. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain Injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375-378.
2. The National Federation of State High School Associations. 2013-14 high school athletics participation survey. http://www.nfhs.org/ParticipationStatics/PDF/2013-14_Participation_Survey_PDF.pdf. Accessed August 6, 2018.
3. Youth Council. US Soccer Federation Web site. https://www.ussoccer.com/about/affiliates/youth-council. Accessed July 31, 2018.
4. Khodaee M, Currie DW, Asif IM, Comstock RD. Nine-year study of US high school soccer injuries: data from a national sports injury surveillance programme. Br J Sports Med. 2017;51(3):185-193. doi:10.1136/bjsports-2015-095946.
5. Schallmo MS, Weiner JA, Hsu WK. Sport and sex-specific trends in the epidemiology of concussions sustained by high school athletes. J Bone Joint Surg Am. 2017;99(15):1314-1320. doi:10.2106/JBJS.16.01573.
6. US Soccer Federation. U.S. Soccer’s comprehensive player health and safety program. Recognize to Recover Web site. http://www.recognizetorecover.org/#us-soccers-comprehensive-player-health-and-safety-program. Accessed July 31, 2018.
7. McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847. doi:10.1136/bjsports-2017-097699.
8. Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123(15):1594-1600. doi:10.1161/CIRCULATIONAHA.110.004622.
9. Faude O, Rössler R, Junge A, et al. Head injuries in children’s football-results from two prospective cohort studies in four European countries. Scand J Med Sci Sports. 2017;27(12):1986-1992. doi:10.1111/sms.12839.
10. Comstock RD, Currie DW, Pierpoint LA, Grubenhoff JA, Fields SK. An evidence-based discussion of heading the ball and concussions in high school soccer. JAMA Pediatr. 2015;169(9):830-837. doi:10.1001/jamapediatrics.2015.1062.
11. Tarnutzer AA. Should heading be forbidden in children’s football? Sci Med Football. 2018;2(1):75-79.
12. US Soccer Federation. US Soccer, NWSL and MLS to host “head injury in soccer; science to field”. https://www.ussoccer.com/stories/2017/04/18/17/35/20170418-news-us-soccer-nwsl-mls-host-head-injury-in-soccer-science-to-field. Published April 18, 2017. Accessed August 6, 2018.
13. Weiner RB, Baggish AL. Exercise-induced cardiac remodeling. Prog Cardiovasc Dis. 2012;54(5):380-386. doi:10.1016/j.pcad.2012.01.006.
14. Baggish AL, Wood MJ. Athlete's heart and cardiovascular care of the athlete: scientific and clinical update. Circulation. 2011;123(23):2723-2735. doi:10.1161/CIRCULATIONAHA.110.981571.
15. Kim JH, Baggish AL. Differentiating exercise-induced cardiac adaptations from cardiac pathology: the "Grey Zone" of clinical uncertainty. Can J Cardiol. 2016;32(4):429-437. doi:10.1016/j.cjca.2015.11.025.
16. Baggish AL, Battle RW, Beckerman JG, et al; ACC’s Sports and Exercise Council Leadership Group. Sports cardiology: core curriculum for providing cardiovascular care to competitive athletes and highly active people. J Am Coll Cardiol. 2017;70(15):1902-1918. doi:10.1016/j.jacc.2017.08.055.
17. Harmon KG, Asif IM, Maleszewski JJ, et al. Incidence, cause, and comparative frequency of sudden cardiac death in National Collegiate Athletic Association athletes: a decade in review. Circulation. 2015;132(1):10-19. doi:10.1161/CIRCULATIONAHA.115.015431.
18. Maron BJ, Levine BD, Washington RL, Baggish AL, Kovacs RJ, Maron MS. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 2: preparticipation screening for cardiovascular disease in competitive athletes: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2015;66(21):2356-2361. doi:10.1016/j.jacc.2015.09.034.
19. Corrado D, Pelliccia A, Bjørnstad HH, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26(5):516-524.
20. Baggish AL, Kovacs RJ. Preparticipation cardiovascular screening: clinical partnership is the only certainty. Br J Sports Med. 2017;51(3):150-151. doi:10.1136/bjsports-2016-096954.
21. Hainline B, Drezner J, Baggish A, et al. Interassociation consensus statement on cardiovascular care of college student-athletes. J Athl Train. 2016;51(4):344-357. doi:10.4085/j.jacc.2016.03.527.
22. US Soccer Federation. Environmental conditions. Recognize to Recover Web site. http://www.recognizetorecover.org/environmental/#environmental-conditions. Accessed April 15, 2018.
23. Korey Stringer Institute. Emergency conditions: heat illnesses. University of Connecticut Web site. https://ksi.uconn.edu/. Accessed April 15, 2018.
24. American College of Sports Medicine, Armstrong LE, Casa DJ, et al. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556-572.
25. Belval LN, Casa DJ, Adams WM, et al. Consensus statement- prehospital care of exertional heat stroke. Prehosp Emerg Care. 2018;22(3):392-397. doi:10.1080/10903127.2017.1392666.
1. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain Injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375-378.
2. The National Federation of State High School Associations. 2013-14 high school athletics participation survey. http://www.nfhs.org/ParticipationStatics/PDF/2013-14_Participation_Survey_PDF.pdf. Accessed August 6, 2018.
3. Youth Council. US Soccer Federation Web site. https://www.ussoccer.com/about/affiliates/youth-council. Accessed July 31, 2018.
4. Khodaee M, Currie DW, Asif IM, Comstock RD. Nine-year study of US high school soccer injuries: data from a national sports injury surveillance programme. Br J Sports Med. 2017;51(3):185-193. doi:10.1136/bjsports-2015-095946.
5. Schallmo MS, Weiner JA, Hsu WK. Sport and sex-specific trends in the epidemiology of concussions sustained by high school athletes. J Bone Joint Surg Am. 2017;99(15):1314-1320. doi:10.2106/JBJS.16.01573.
6. US Soccer Federation. U.S. Soccer’s comprehensive player health and safety program. Recognize to Recover Web site. http://www.recognizetorecover.org/#us-soccers-comprehensive-player-health-and-safety-program. Accessed July 31, 2018.
7. McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport-the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838-847. doi:10.1136/bjsports-2017-097699.
8. Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123(15):1594-1600. doi:10.1161/CIRCULATIONAHA.110.004622.
9. Faude O, Rössler R, Junge A, et al. Head injuries in children’s football-results from two prospective cohort studies in four European countries. Scand J Med Sci Sports. 2017;27(12):1986-1992. doi:10.1111/sms.12839.
10. Comstock RD, Currie DW, Pierpoint LA, Grubenhoff JA, Fields SK. An evidence-based discussion of heading the ball and concussions in high school soccer. JAMA Pediatr. 2015;169(9):830-837. doi:10.1001/jamapediatrics.2015.1062.
11. Tarnutzer AA. Should heading be forbidden in children’s football? Sci Med Football. 2018;2(1):75-79.
12. US Soccer Federation. US Soccer, NWSL and MLS to host “head injury in soccer; science to field”. https://www.ussoccer.com/stories/2017/04/18/17/35/20170418-news-us-soccer-nwsl-mls-host-head-injury-in-soccer-science-to-field. Published April 18, 2017. Accessed August 6, 2018.
13. Weiner RB, Baggish AL. Exercise-induced cardiac remodeling. Prog Cardiovasc Dis. 2012;54(5):380-386. doi:10.1016/j.pcad.2012.01.006.
14. Baggish AL, Wood MJ. Athlete's heart and cardiovascular care of the athlete: scientific and clinical update. Circulation. 2011;123(23):2723-2735. doi:10.1161/CIRCULATIONAHA.110.981571.
15. Kim JH, Baggish AL. Differentiating exercise-induced cardiac adaptations from cardiac pathology: the "Grey Zone" of clinical uncertainty. Can J Cardiol. 2016;32(4):429-437. doi:10.1016/j.cjca.2015.11.025.
16. Baggish AL, Battle RW, Beckerman JG, et al; ACC’s Sports and Exercise Council Leadership Group. Sports cardiology: core curriculum for providing cardiovascular care to competitive athletes and highly active people. J Am Coll Cardiol. 2017;70(15):1902-1918. doi:10.1016/j.jacc.2017.08.055.
17. Harmon KG, Asif IM, Maleszewski JJ, et al. Incidence, cause, and comparative frequency of sudden cardiac death in National Collegiate Athletic Association athletes: a decade in review. Circulation. 2015;132(1):10-19. doi:10.1161/CIRCULATIONAHA.115.015431.
18. Maron BJ, Levine BD, Washington RL, Baggish AL, Kovacs RJ, Maron MS. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 2: preparticipation screening for cardiovascular disease in competitive athletes: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2015;66(21):2356-2361. doi:10.1016/j.jacc.2015.09.034.
19. Corrado D, Pelliccia A, Bjørnstad HH, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26(5):516-524.
20. Baggish AL, Kovacs RJ. Preparticipation cardiovascular screening: clinical partnership is the only certainty. Br J Sports Med. 2017;51(3):150-151. doi:10.1136/bjsports-2016-096954.
21. Hainline B, Drezner J, Baggish A, et al. Interassociation consensus statement on cardiovascular care of college student-athletes. J Athl Train. 2016;51(4):344-357. doi:10.4085/j.jacc.2016.03.527.
22. US Soccer Federation. Environmental conditions. Recognize to Recover Web site. http://www.recognizetorecover.org/environmental/#environmental-conditions. Accessed April 15, 2018.
23. Korey Stringer Institute. Emergency conditions: heat illnesses. University of Connecticut Web site. https://ksi.uconn.edu/. Accessed April 15, 2018.
24. American College of Sports Medicine, Armstrong LE, Casa DJ, et al. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556-572.
25. Belval LN, Casa DJ, Adams WM, et al. Consensus statement- prehospital care of exertional heat stroke. Prehosp Emerg Care. 2018;22(3):392-397. doi:10.1080/10903127.2017.1392666.
TAKE-HOME POINTS
- Current concussion education programs such as “Recognize to Recover” aim to increase self-reporting of concussion symptoms by players, and recognition and appropriate evaluation by medical and coaching staff.
- Athletes who develop symptoms suggestive of underlying cardiovascular disease during play, including exertional chest pain, inappropriate shortness of breath, palpitations, and syncope should be withheld from play until they can be evaluated by a qualified medical professional.
- Key components of an effective EAP include the training of coaching staff, athletic trainers, and players in basic cardiopulmonary resuscitation, access to and training in the use of automated external defibrillators, and a triage/transport protocol that ensures timely access to advanced cardiac life support.
- Exertional heat stroke should always be the presumed cause of altered mentation when no rectal temperature is available because rapid cooling is critical to minimizing lasting effects.
- Prevention of exertional heat illness should center around appropriate acclimatization, access to adequate hydration and scheduled hydration breaks, and avoiding exertion all together when conditions are too dangerous.
Epacadostat plus pembrolizumab shows promise in advanced solid tumors
Epacadostat, a highly selective oral inhibitor of the indoleamine 2,3-dioxygenase 1 (IDO1) enzyme, was well tolerated when combined with pembrolizumab and demonstrated encouraging antitumor activity in multiple types of advanced solid tumors, according to the results of a phase l/ll trial.
Tumors may evade immunosurveillance through upregulation of the IDO1 enzyme, and thus there is a great interest in developing combination therapies that can target various immune evasion pathways to improve therapeutic response and outcomes. In this study, the authors evaluated the investigational agent epacadostat combined with pembrolizumab in 62 patients with advanced solid tumors.
In the dose escalation phase, patents received increasing doses of oral epacadostat (25, 50, 100, or 300 mg) twice per day plus intravenous pembrolizumab 2 mg/kg or 200 mg every 3 weeks. During the safety expansion, epacadostat at 50, 100, or 300 mg was given twice per day, plus pembrolizumab 200 mg every 3 weeks. The maximum tolerated dose of epacadostat in combination with pembrolizumab was not reached.
Objective responses (per Response Evaluation Criteria in Solid Tumors [RECIST] version 1.1) occurred in 12 (55%) of 22 patients with melanoma and in patients with non–small-cell lung cancer, renal cell carcinoma, endometrial adenocarcinoma, urothelial carcinoma, and squamous cell carcinoma of the head and neck, reported Tara C. Mitchell, MD, of the Abramson Cancer Center, University of Pennsylvania, Philadelphia, and her colleagues. The report is in the Journal of Clinical Oncology.
The authors observed that there was antitumor activity at all epacadostat doses and in several tumor types. A complete response was achieved by 8 patients (treatment naive melanoma [5 patients] and previously treated for advanced/ metastatic melanoma, endometrial adenocarcinoma [EA], or urothelial carcinoma [UC] [1 patient each]), while 17 patients achieved a partial response (treatment-naive melanoma [6 patients], non–small cell lung cancer [NSCLC] [5 patients], renal cell carcinoma [RCC] and UC [2 patients each], and EA and squamous cell carcinoma of the head and neck [1 patient each]).
Most patients (n = 52, 84%) experienced treatment-related adverse events (TRAEs), the most frequently observed being fatigue (36%), rash (36%), arthralgia (24%), pruritus (23%), and nausea (21%). Grade 3/4 TRAEs occurred in 24% of patients, and 7 patients (11%) discontinued their treatment because of TRAEs. There were no deaths associated with TRAEs.
“The safety profile observed with epacadostat plus pembrolizumab compares favorably with studies of other combination immunotherapies,” wrote Dr. Mitchell and her colleagues. “Although not powered to evaluate efficacy, the phase I portion of this study showed that epacadostat plus pembrolizumab had encouraging and durable antitumor activity,” they said.
SOURCE: Mitchell TC et al. J Clin Oncol. 2018 Sep 28. doi: 10.1200/JCO.2018.78.9602.
Epacadostat, a highly selective oral inhibitor of the indoleamine 2,3-dioxygenase 1 (IDO1) enzyme, was well tolerated when combined with pembrolizumab and demonstrated encouraging antitumor activity in multiple types of advanced solid tumors, according to the results of a phase l/ll trial.
Tumors may evade immunosurveillance through upregulation of the IDO1 enzyme, and thus there is a great interest in developing combination therapies that can target various immune evasion pathways to improve therapeutic response and outcomes. In this study, the authors evaluated the investigational agent epacadostat combined with pembrolizumab in 62 patients with advanced solid tumors.
In the dose escalation phase, patents received increasing doses of oral epacadostat (25, 50, 100, or 300 mg) twice per day plus intravenous pembrolizumab 2 mg/kg or 200 mg every 3 weeks. During the safety expansion, epacadostat at 50, 100, or 300 mg was given twice per day, plus pembrolizumab 200 mg every 3 weeks. The maximum tolerated dose of epacadostat in combination with pembrolizumab was not reached.
Objective responses (per Response Evaluation Criteria in Solid Tumors [RECIST] version 1.1) occurred in 12 (55%) of 22 patients with melanoma and in patients with non–small-cell lung cancer, renal cell carcinoma, endometrial adenocarcinoma, urothelial carcinoma, and squamous cell carcinoma of the head and neck, reported Tara C. Mitchell, MD, of the Abramson Cancer Center, University of Pennsylvania, Philadelphia, and her colleagues. The report is in the Journal of Clinical Oncology.
The authors observed that there was antitumor activity at all epacadostat doses and in several tumor types. A complete response was achieved by 8 patients (treatment naive melanoma [5 patients] and previously treated for advanced/ metastatic melanoma, endometrial adenocarcinoma [EA], or urothelial carcinoma [UC] [1 patient each]), while 17 patients achieved a partial response (treatment-naive melanoma [6 patients], non–small cell lung cancer [NSCLC] [5 patients], renal cell carcinoma [RCC] and UC [2 patients each], and EA and squamous cell carcinoma of the head and neck [1 patient each]).
Most patients (n = 52, 84%) experienced treatment-related adverse events (TRAEs), the most frequently observed being fatigue (36%), rash (36%), arthralgia (24%), pruritus (23%), and nausea (21%). Grade 3/4 TRAEs occurred in 24% of patients, and 7 patients (11%) discontinued their treatment because of TRAEs. There were no deaths associated with TRAEs.
“The safety profile observed with epacadostat plus pembrolizumab compares favorably with studies of other combination immunotherapies,” wrote Dr. Mitchell and her colleagues. “Although not powered to evaluate efficacy, the phase I portion of this study showed that epacadostat plus pembrolizumab had encouraging and durable antitumor activity,” they said.
SOURCE: Mitchell TC et al. J Clin Oncol. 2018 Sep 28. doi: 10.1200/JCO.2018.78.9602.
Epacadostat, a highly selective oral inhibitor of the indoleamine 2,3-dioxygenase 1 (IDO1) enzyme, was well tolerated when combined with pembrolizumab and demonstrated encouraging antitumor activity in multiple types of advanced solid tumors, according to the results of a phase l/ll trial.
Tumors may evade immunosurveillance through upregulation of the IDO1 enzyme, and thus there is a great interest in developing combination therapies that can target various immune evasion pathways to improve therapeutic response and outcomes. In this study, the authors evaluated the investigational agent epacadostat combined with pembrolizumab in 62 patients with advanced solid tumors.
In the dose escalation phase, patents received increasing doses of oral epacadostat (25, 50, 100, or 300 mg) twice per day plus intravenous pembrolizumab 2 mg/kg or 200 mg every 3 weeks. During the safety expansion, epacadostat at 50, 100, or 300 mg was given twice per day, plus pembrolizumab 200 mg every 3 weeks. The maximum tolerated dose of epacadostat in combination with pembrolizumab was not reached.
Objective responses (per Response Evaluation Criteria in Solid Tumors [RECIST] version 1.1) occurred in 12 (55%) of 22 patients with melanoma and in patients with non–small-cell lung cancer, renal cell carcinoma, endometrial adenocarcinoma, urothelial carcinoma, and squamous cell carcinoma of the head and neck, reported Tara C. Mitchell, MD, of the Abramson Cancer Center, University of Pennsylvania, Philadelphia, and her colleagues. The report is in the Journal of Clinical Oncology.
The authors observed that there was antitumor activity at all epacadostat doses and in several tumor types. A complete response was achieved by 8 patients (treatment naive melanoma [5 patients] and previously treated for advanced/ metastatic melanoma, endometrial adenocarcinoma [EA], or urothelial carcinoma [UC] [1 patient each]), while 17 patients achieved a partial response (treatment-naive melanoma [6 patients], non–small cell lung cancer [NSCLC] [5 patients], renal cell carcinoma [RCC] and UC [2 patients each], and EA and squamous cell carcinoma of the head and neck [1 patient each]).
Most patients (n = 52, 84%) experienced treatment-related adverse events (TRAEs), the most frequently observed being fatigue (36%), rash (36%), arthralgia (24%), pruritus (23%), and nausea (21%). Grade 3/4 TRAEs occurred in 24% of patients, and 7 patients (11%) discontinued their treatment because of TRAEs. There were no deaths associated with TRAEs.
“The safety profile observed with epacadostat plus pembrolizumab compares favorably with studies of other combination immunotherapies,” wrote Dr. Mitchell and her colleagues. “Although not powered to evaluate efficacy, the phase I portion of this study showed that epacadostat plus pembrolizumab had encouraging and durable antitumor activity,” they said.
SOURCE: Mitchell TC et al. J Clin Oncol. 2018 Sep 28. doi: 10.1200/JCO.2018.78.9602.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Epacadostat plus pembrolizumab showed antitumor activity and tolerability in patients with advanced solid tumors.
Major finding: Among 62 patients, 25 achieved an objective response.
Study details: Phase l/ll clinical trial of 62 patients with advanced solid tumors.
Disclosures: Incyte and Merck funded the study. All of the authors have disclosed relationships with industry, including the study sponsor.
Source: Mitchell TC et al. J Clin Oncol. 2018 Sep 28. doi: 10.1200/JCO.2018.78.9602.
Encourage influenza vaccination in pregnant women
They are at greater risk for more severe illness, and influenza can lead to adverse outcomes in infants. The good news is that recent studies have shown that flu vaccines are safe and effective in pregnant women.
The bad news is that many women are hesitant to be vaccinated out of concerns over safety, in a trend that reflects broader societal worries over vaccination, said Dr. Chu, of the University of Washington, Seattle. In a video interview at an annual scientific meeting on infectious diseases, Dr. Chu advised steps to ensure that pregnant women are aware of the safety and efficacy of flu vaccines, and the benefits to the infant who acquires immunity through the mother. It’s also a good idea to have vaccine on hand to be able to offer it immediately during an office visit.
They are at greater risk for more severe illness, and influenza can lead to adverse outcomes in infants. The good news is that recent studies have shown that flu vaccines are safe and effective in pregnant women.
The bad news is that many women are hesitant to be vaccinated out of concerns over safety, in a trend that reflects broader societal worries over vaccination, said Dr. Chu, of the University of Washington, Seattle. In a video interview at an annual scientific meeting on infectious diseases, Dr. Chu advised steps to ensure that pregnant women are aware of the safety and efficacy of flu vaccines, and the benefits to the infant who acquires immunity through the mother. It’s also a good idea to have vaccine on hand to be able to offer it immediately during an office visit.
They are at greater risk for more severe illness, and influenza can lead to adverse outcomes in infants. The good news is that recent studies have shown that flu vaccines are safe and effective in pregnant women.
The bad news is that many women are hesitant to be vaccinated out of concerns over safety, in a trend that reflects broader societal worries over vaccination, said Dr. Chu, of the University of Washington, Seattle. In a video interview at an annual scientific meeting on infectious diseases, Dr. Chu advised steps to ensure that pregnant women are aware of the safety and efficacy of flu vaccines, and the benefits to the infant who acquires immunity through the mother. It’s also a good idea to have vaccine on hand to be able to offer it immediately during an office visit.
REPORTING FROM ID WEEK 2018
Bilateral Brown Plaques Behind the Ears
The Diagnosis: Terra Firma-Forme Dermatosis
Terra firma-forme dermatosis (TFFD), also known as Duncan dirty dermatosis, is an idiopathic benign cutaneous condition that is easily misdiagnosed or mismanaged. In 1987, Duncan et al1 first described the condition in children who had mothers that lamented over dirty skin spots that could not be washed off. The term terra firma translates in Latin to solid ground, which describes the characteristic dirtlike appearance of these lesions.
Terra firma-forme dermatosis most commonly affects children and young adults, though it can present in patients of any age without any known predisposing risk factors.1-4 The lesions have a predilection for the face, neck, shoulders, trunk, and ankles. Terra firma-forme dermatosis has no association with bathing and hygiene habits, and most patients describe unsuccessful removal of the lesions, even after vigorous scrubbing with soaps and detergents at home. The lesions are asymptomatic, and many patients present to dermatology for cosmetic concerns.1-8
The etiology of TFFD is not well understood and is considered a retention hyperkeratosis. Duncan et al1 postulated that TFFD is the result of partial or improper maturation of keratinocytes leading to keratinocyte and melanin retention. Hematoxylin and eosin stains demonstrate lamellar hyperkeratosis of the stratum corneum without parakeratosis as well as keratin pearls scattered throughout. Mild acanthosis and papillomatosis also have been reported.1,5-7 Fontana-Masson stain shows excess melanin in these lesions, extending from the basal layer to the stratum corneum. Fungal and bacterial stains as well as cultures often have no notable findings.1,7 Similarly, histopathologic examination of our patient's biopsy with hematoxylin and eosin stain revealed hyperorthokeratosis with scattered naked vellus hair shafts and incidental yeast forms (Figure 1).
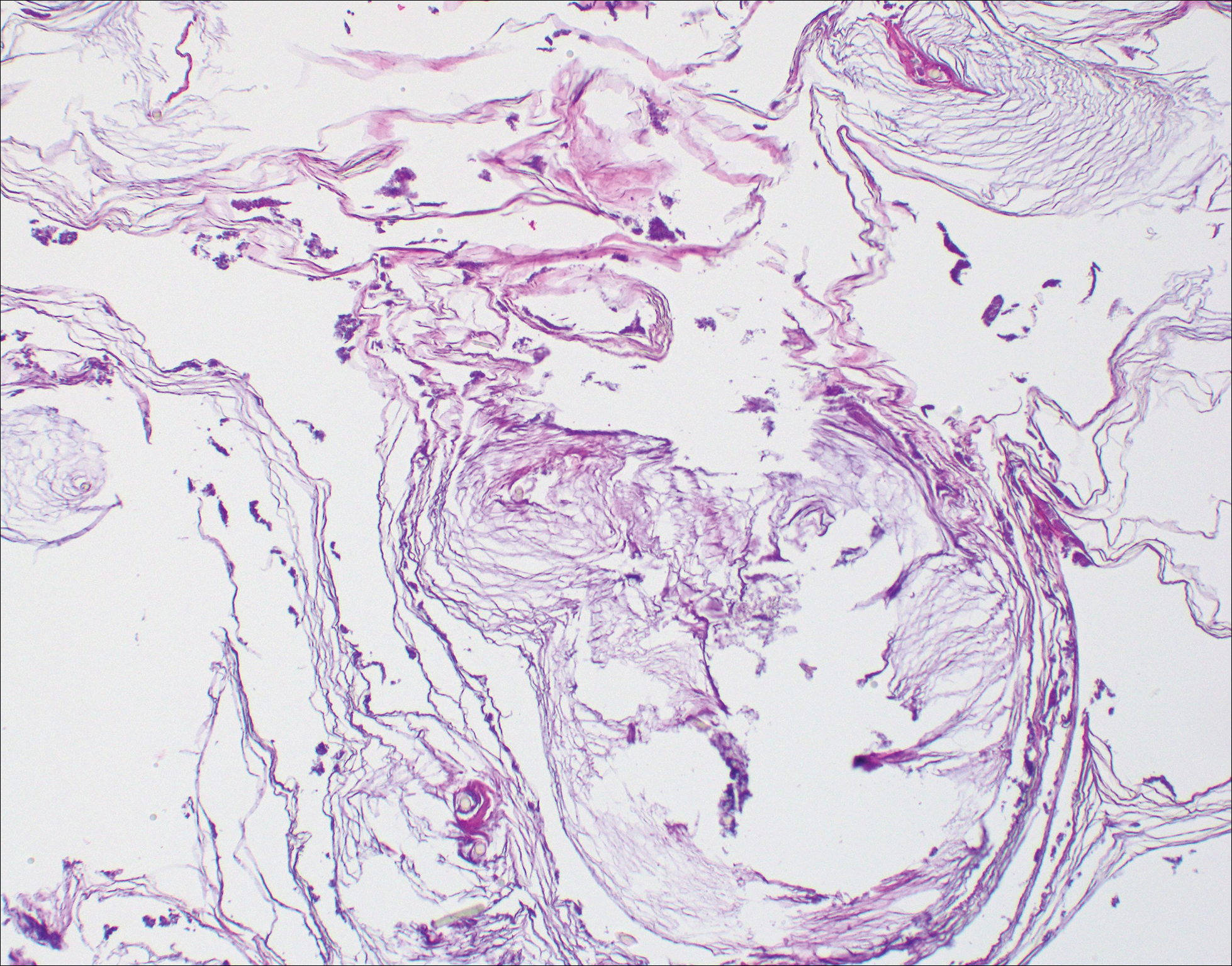
The differential diagnosis for TFFD may include pityriasis versicolor, confluent and reticulated papillomatosis, acanthosis nigricans, ichthyosis, malignant melanoma, and seborrheic keratosis. All of these diagnoses can be ruled out by the easy removal of the lesions with isopropyl alcohol 70%, which was performed on our patient by scrubbing the lesions with soaked gauze (Figure 2). Indeed, removal with isopropyl alcohol 70% is both the therapeutic and diagnostic procedure for TFFD.1-8 Of note, dermatitis neglecta is histologically and clinically identical to TFFD, albeit with a history of uncleanly habits or exposure to dirty environments.

The diagnosis of TFFD often is discovered incidentally as physicians wipe the area with alcohol to prepare for biopsy.1 Occasionally, vigorous scrubbing is needed to completely remove the lesions, and without this effort the lesions may be easily mistaken for another cutaneous process.3 Failure to consider TFFD as a diagnosis has led to unnecessary endocrine workups and invasive biopsies.4 Therefore, physicians should have early clinical suspicion of TFFD and be aware of the bedside diagnostic procedure using isopropyl alcohol.
- Duncan WC, Tschen JA, Knox JM. Terra firma-forme dermatosis. Arch Dermatol. 1987;123:567-569.
- Greywal T, Cohen PR. Terra firma-forme dermatosis: a report of ten individuals with Duncan's dirty dermatosis and literature review. Dermatol Pract Concept. 2015;5:29-33.
- Moon J, Kim MW, Yoon HS, et al. A case of terra firma-forme dermatosis: differentiation from other dirty-appearing diseases. Ann Dermatol. 2016;28:413-415.
- Berk DR. Terra firma-forme dermatosis: a retrospective review of 31 patients. Pediatr Dermatol. 2012;29:297-300.
- Akkash L, Badran D, Al-Omari AQ. Terra firma forme dermatosis. case series and review of the literature. J Dtsch Dermatol Ges. 2009;7:102-107.
- Ashique KT, Kaliyadan F, Goyal T. Terra firma-forme dermatosis: report of a series of 11 cases and a brief review of the literature. Int J Dermatol. 2016;55:769-774.
- Chun SW, Lee SY, Kim JB, et al. A case of terra firma-forme dermatosis treated with salicylic acid alcohol peeling. Ann Dermatol. 2017;29:83-85.
- Aslan NC, Guler S, Demirci K, et al. Features of terra firma-forme dermatosis. Ann Fam Med. 2018;16:52-54.
The Diagnosis: Terra Firma-Forme Dermatosis
Terra firma-forme dermatosis (TFFD), also known as Duncan dirty dermatosis, is an idiopathic benign cutaneous condition that is easily misdiagnosed or mismanaged. In 1987, Duncan et al1 first described the condition in children who had mothers that lamented over dirty skin spots that could not be washed off. The term terra firma translates in Latin to solid ground, which describes the characteristic dirtlike appearance of these lesions.
Terra firma-forme dermatosis most commonly affects children and young adults, though it can present in patients of any age without any known predisposing risk factors.1-4 The lesions have a predilection for the face, neck, shoulders, trunk, and ankles. Terra firma-forme dermatosis has no association with bathing and hygiene habits, and most patients describe unsuccessful removal of the lesions, even after vigorous scrubbing with soaps and detergents at home. The lesions are asymptomatic, and many patients present to dermatology for cosmetic concerns.1-8
The etiology of TFFD is not well understood and is considered a retention hyperkeratosis. Duncan et al1 postulated that TFFD is the result of partial or improper maturation of keratinocytes leading to keratinocyte and melanin retention. Hematoxylin and eosin stains demonstrate lamellar hyperkeratosis of the stratum corneum without parakeratosis as well as keratin pearls scattered throughout. Mild acanthosis and papillomatosis also have been reported.1,5-7 Fontana-Masson stain shows excess melanin in these lesions, extending from the basal layer to the stratum corneum. Fungal and bacterial stains as well as cultures often have no notable findings.1,7 Similarly, histopathologic examination of our patient's biopsy with hematoxylin and eosin stain revealed hyperorthokeratosis with scattered naked vellus hair shafts and incidental yeast forms (Figure 1).
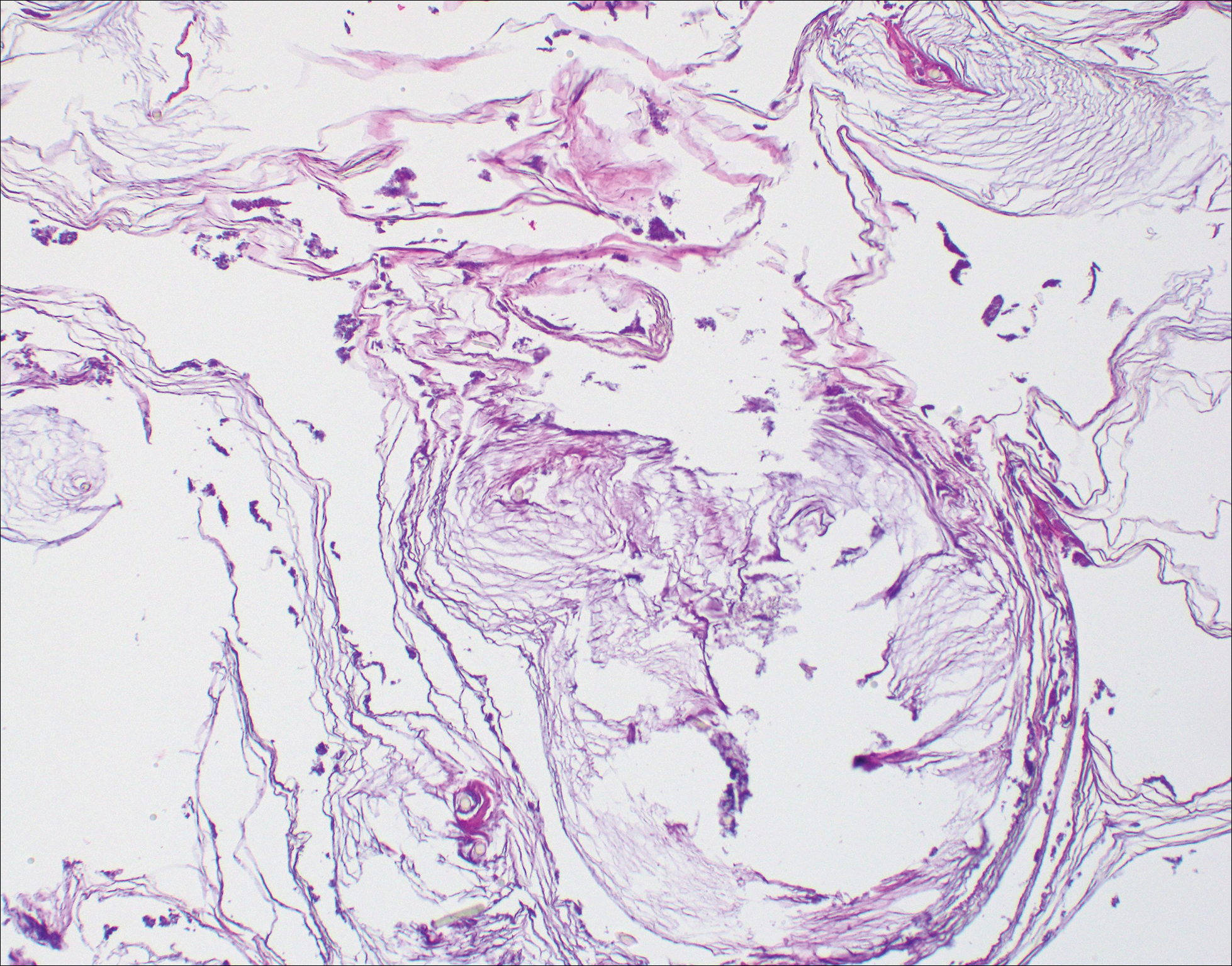
The differential diagnosis for TFFD may include pityriasis versicolor, confluent and reticulated papillomatosis, acanthosis nigricans, ichthyosis, malignant melanoma, and seborrheic keratosis. All of these diagnoses can be ruled out by the easy removal of the lesions with isopropyl alcohol 70%, which was performed on our patient by scrubbing the lesions with soaked gauze (Figure 2). Indeed, removal with isopropyl alcohol 70% is both the therapeutic and diagnostic procedure for TFFD.1-8 Of note, dermatitis neglecta is histologically and clinically identical to TFFD, albeit with a history of uncleanly habits or exposure to dirty environments.

The diagnosis of TFFD often is discovered incidentally as physicians wipe the area with alcohol to prepare for biopsy.1 Occasionally, vigorous scrubbing is needed to completely remove the lesions, and without this effort the lesions may be easily mistaken for another cutaneous process.3 Failure to consider TFFD as a diagnosis has led to unnecessary endocrine workups and invasive biopsies.4 Therefore, physicians should have early clinical suspicion of TFFD and be aware of the bedside diagnostic procedure using isopropyl alcohol.
The Diagnosis: Terra Firma-Forme Dermatosis
Terra firma-forme dermatosis (TFFD), also known as Duncan dirty dermatosis, is an idiopathic benign cutaneous condition that is easily misdiagnosed or mismanaged. In 1987, Duncan et al1 first described the condition in children who had mothers that lamented over dirty skin spots that could not be washed off. The term terra firma translates in Latin to solid ground, which describes the characteristic dirtlike appearance of these lesions.
Terra firma-forme dermatosis most commonly affects children and young adults, though it can present in patients of any age without any known predisposing risk factors.1-4 The lesions have a predilection for the face, neck, shoulders, trunk, and ankles. Terra firma-forme dermatosis has no association with bathing and hygiene habits, and most patients describe unsuccessful removal of the lesions, even after vigorous scrubbing with soaps and detergents at home. The lesions are asymptomatic, and many patients present to dermatology for cosmetic concerns.1-8
The etiology of TFFD is not well understood and is considered a retention hyperkeratosis. Duncan et al1 postulated that TFFD is the result of partial or improper maturation of keratinocytes leading to keratinocyte and melanin retention. Hematoxylin and eosin stains demonstrate lamellar hyperkeratosis of the stratum corneum without parakeratosis as well as keratin pearls scattered throughout. Mild acanthosis and papillomatosis also have been reported.1,5-7 Fontana-Masson stain shows excess melanin in these lesions, extending from the basal layer to the stratum corneum. Fungal and bacterial stains as well as cultures often have no notable findings.1,7 Similarly, histopathologic examination of our patient's biopsy with hematoxylin and eosin stain revealed hyperorthokeratosis with scattered naked vellus hair shafts and incidental yeast forms (Figure 1).
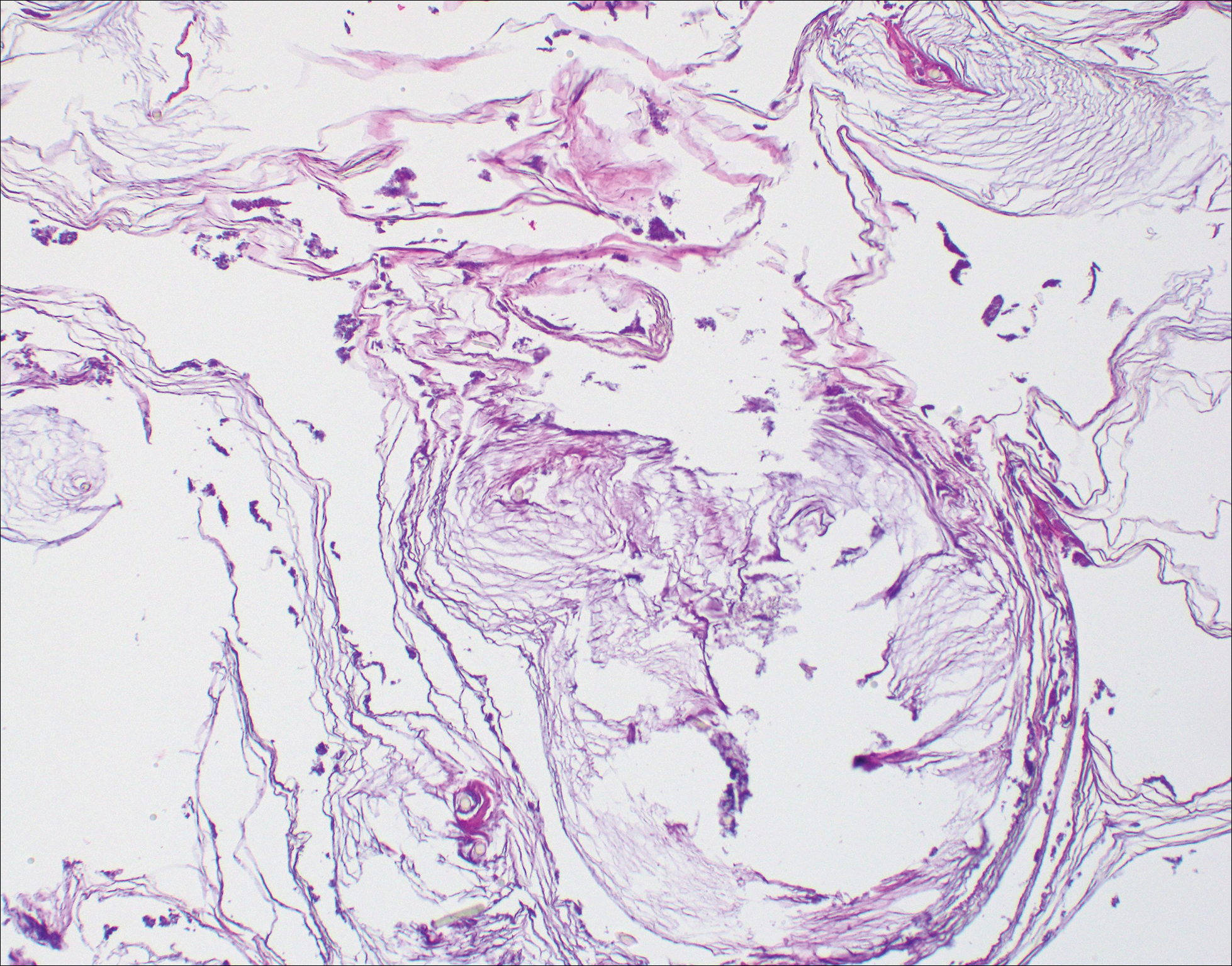
The differential diagnosis for TFFD may include pityriasis versicolor, confluent and reticulated papillomatosis, acanthosis nigricans, ichthyosis, malignant melanoma, and seborrheic keratosis. All of these diagnoses can be ruled out by the easy removal of the lesions with isopropyl alcohol 70%, which was performed on our patient by scrubbing the lesions with soaked gauze (Figure 2). Indeed, removal with isopropyl alcohol 70% is both the therapeutic and diagnostic procedure for TFFD.1-8 Of note, dermatitis neglecta is histologically and clinically identical to TFFD, albeit with a history of uncleanly habits or exposure to dirty environments.

The diagnosis of TFFD often is discovered incidentally as physicians wipe the area with alcohol to prepare for biopsy.1 Occasionally, vigorous scrubbing is needed to completely remove the lesions, and without this effort the lesions may be easily mistaken for another cutaneous process.3 Failure to consider TFFD as a diagnosis has led to unnecessary endocrine workups and invasive biopsies.4 Therefore, physicians should have early clinical suspicion of TFFD and be aware of the bedside diagnostic procedure using isopropyl alcohol.
- Duncan WC, Tschen JA, Knox JM. Terra firma-forme dermatosis. Arch Dermatol. 1987;123:567-569.
- Greywal T, Cohen PR. Terra firma-forme dermatosis: a report of ten individuals with Duncan's dirty dermatosis and literature review. Dermatol Pract Concept. 2015;5:29-33.
- Moon J, Kim MW, Yoon HS, et al. A case of terra firma-forme dermatosis: differentiation from other dirty-appearing diseases. Ann Dermatol. 2016;28:413-415.
- Berk DR. Terra firma-forme dermatosis: a retrospective review of 31 patients. Pediatr Dermatol. 2012;29:297-300.
- Akkash L, Badran D, Al-Omari AQ. Terra firma forme dermatosis. case series and review of the literature. J Dtsch Dermatol Ges. 2009;7:102-107.
- Ashique KT, Kaliyadan F, Goyal T. Terra firma-forme dermatosis: report of a series of 11 cases and a brief review of the literature. Int J Dermatol. 2016;55:769-774.
- Chun SW, Lee SY, Kim JB, et al. A case of terra firma-forme dermatosis treated with salicylic acid alcohol peeling. Ann Dermatol. 2017;29:83-85.
- Aslan NC, Guler S, Demirci K, et al. Features of terra firma-forme dermatosis. Ann Fam Med. 2018;16:52-54.
- Duncan WC, Tschen JA, Knox JM. Terra firma-forme dermatosis. Arch Dermatol. 1987;123:567-569.
- Greywal T, Cohen PR. Terra firma-forme dermatosis: a report of ten individuals with Duncan's dirty dermatosis and literature review. Dermatol Pract Concept. 2015;5:29-33.
- Moon J, Kim MW, Yoon HS, et al. A case of terra firma-forme dermatosis: differentiation from other dirty-appearing diseases. Ann Dermatol. 2016;28:413-415.
- Berk DR. Terra firma-forme dermatosis: a retrospective review of 31 patients. Pediatr Dermatol. 2012;29:297-300.
- Akkash L, Badran D, Al-Omari AQ. Terra firma forme dermatosis. case series and review of the literature. J Dtsch Dermatol Ges. 2009;7:102-107.
- Ashique KT, Kaliyadan F, Goyal T. Terra firma-forme dermatosis: report of a series of 11 cases and a brief review of the literature. Int J Dermatol. 2016;55:769-774.
- Chun SW, Lee SY, Kim JB, et al. A case of terra firma-forme dermatosis treated with salicylic acid alcohol peeling. Ann Dermatol. 2017;29:83-85.
- Aslan NC, Guler S, Demirci K, et al. Features of terra firma-forme dermatosis. Ann Fam Med. 2018;16:52-54.

A 94-year-old woman was referred to the dermatology department for biopsy of pigmented tumors behind the ears of unknown duration. The growths were asymptomatic. Her medical history included the early stages of Alzheimer disease. On physical examination dark brown, smooth, coalescing papules and plaques were noted extending from the posterior neck to the conchal bowls and ear folds bilaterally. The nodules were removed by scrubbing with isopropyl alcohol 70%. A nodule was submitted for histopathologic review.
AITL responds to 5-azacytidine in small series
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
Older patients with refractory angioimmunoblastic T cell lymphoma (AITL) appear to respond well to treatment with 5-azacytidine, regardless of mutations.
Francois Lemonnier, MD, of Henri Mondor University Hospitals in Créteil, France, and his colleagues, reported on a retrospective series of 12 AITL patients who received 5-azacytidine for concomitant myeloid neoplasm or as compassionate therapy for relapsed or refractory AITL. The findings were published in Blood.
Patients were given 5-azacytidine subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days. The treatment was given every 28 days until progression or unacceptable toxicity for a median of 5.5 cycles. Along with 5-azacytidine, half of the patients received rituximab due to the presence of EBV replication or EBV B-blasts in the lymph node biopsy.
The patients were assessed via CT scan and responses were evaluated by investigators following the Cheson criteria.
This was a heavily pretreated patient population. The median age was 70 years and 11 of the patients had relapsed or refractory disease and had received a median of two lines of therapy. There was only one treatment-naive patient in the series.
Treatment with 5-azacytidine produced an overall response rate of 75%, with six patients achieving a complete response and three patients achieving a partial response. The median progression-free survival was 15 months and median overall survival was 21 months at a median follow-up of 27 months.
The researchers noted that some elderly patients with poor performance status achieved a sustained response after treatment with an acceptable tolerance.
Treatment was well tolerated overall. There were no treatment-related deaths and no patients developed neutropenia. Three patients required transfusion and another had grade 3 diarrhea.
The researchers also performed molecular studies using targeted deep sequencing. They detected TET2 mutations in all 12 patients, with seven patients having two mutations. Four patients had DNMT3A mutations, five patients had RHOA mutations, and four patients had p.G17V substitution. One patient had an IDH2R172 mutation.
Since all patients had a TET2 mutation, the researchers were unable to assess its impact on treatment response. However, they saw no association between the number of TET2 mutations and treatment response, or mutations in DNMT3A, IDH2, and RHOA and treatment response.
The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
SOURCE: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
FROM BLOOD
Key clinical point:
Major finding: The overall response rate was 75% among the 12 patients, with 6 patients achieving complete response.
Study details: A retrospective case series of 12 patients with angioimmunoblastic T cell lymphoma.
Disclosures: The study was funded by a grant from the Leukemia & Lymphoma Society. Three of the coauthors received honoraria from Celgene.
Source: Lemonnier F et al. Blood. 2018 Oct 2. doi: 10.1182/blood-2018-04-840538.
Suicide prevention in rheumatology: Engagement is key
Fibromyalgia patients with no documented suicide attempt spent far more hours in face-to-face meetings with providers than did those who made a suicide attempt over a 20-year period at a single academic medical center. The results, based on a machine-learning analysis of electronic health records, shed more light on the heavy burden of suicidality among patients with rheumatologic illnesses.
“People who didn’t have suicide attempts were present at the doctor 50 hours in a year, compared to less than an hour in a year for those who did attempt suicide. It’s a staggering difference,” said study author Lindsey McKernan, PhD, of the department of psychiatry and behavioral sciences at Vanderbilt University, Nashville, Tenn. What’s more, patients who did not have suicidal thoughts averaged about 6 office hours per year, compared with less than 2 hours for those with suicidal ideation (Arthritis Care Res. 2018 Sep 7. doi: 10.1002/acr.23748).
Fibromyalgia patients are at about ten times the risk of suicide as the general population, and rates of depression and anxiety are higher in patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic disease as well.
Still, mental health issues often go unaddressed. “Many times rheumatologists focus on the patient’s joints and their rheumatologic illness, and they don’t focus on their mental health, and as a result depression in a suicidal patient is, I think, more often missed in a rheumatologic practice than it should be,” said Rakesh Jain, MD, of the department of psychiatry at Texas Tech University, Odessa.

But that gap isn’t for lack of awareness, says Barton Wise, MD, of the departments of orthopedic surgery and internal medicine at the University of California, Davis. “In general, people recognize that depression is a major problem in their patients,” he said. He was the lead author of a study that found that rheumatologists often lack the time, confidence, and connections to properly address a patient’s mental health needs (J Clin Rheumatol. 2016 Sep;22[6]:307-11).
Together, the two studies underscore the pressing need for better mental health care among rheumatology patients. Such issues often take a back seat to a rheumatologist’s primary concern about joint and overall health, but studies have shown that mental health issues are tied to worse rheumatologic disease outcomes. “Addressing comorbid depression will just make the rheumatological outcome be better. So why not do it?” Dr. Jain said.
Screening is a key consideration, according to Dr. Jain, who recommends the Patient Health Questionnaire-9. But even when a problem arises, rheumatologists may lack the confidence to tackle mental health issues. This can be addressed through various resources, such as courses at professional meetings, but another challenge awaits. Rheumatologists may also be unsure of who should be responsible for handling mental health concerns. Even though the rheumatologist may see the patient more often than his or her other providers, “you often feel that you can’t manage everything,” Dr. Wise said.
One way to address that is to establish relationships with mental health providers who can receive referrals for patients who require it. In academic medical centers or other large institutions, relationships can be formalized, so that a patient could see a psychiatrist on the same day as the rheumatologist visit. He even suggests group sessions for patients with similar comorbidities, such as depression related to fibromyalgia or lupus.
Special challenges
Rheumatologic conditions are well documented to have heightened rates of suicide and mental health issues, and this may be related to some of the additional challenges such patients face. Many have chronic pain, which in itself is a risk factor for suicide.
Fibromyalgia can be particularly difficult because patients struggle to communicate about their condition with their clinician and even with loved ones. “Patients report feeling stigmatized and often struggle to communicate about what’s happening in their bodies. The pain can change location and intensity, and it doesn’t show up on medical tests,” Dr. McKernan said.
Another burden is that rheumatologic patients typically have high levels of inflammation, a characteristic that has been linked to lower responses to some antidepressants, according to Dr. Jain.
Antidepressants should still be considered for these patients, but they should be combined with other treatments or management techniques, he says. He emphasizes the importance of a low-inflammatory diet, exercise, and other lifestyle factors. He has also created the free Wild 5 Wellness program, which seeks to broadly improve wellness in patients with chronic pain and mental health challenges.
Physician response
The results of the study on fibromyalgia patients suggests another avenue toward improving mental health. The researchers examined data on 8,879 patients with fibromyalgia, using data collected between 1998 and 2017. There were 34 suicide attempts and 96 cases of suicidal ideation. A machine-learning algorithm spat out some factors associated with heightened suicide risk, such as fatigue, dizziness, and weakness, as well as obesity and drug dependence.
But it also generated some associations that weren’t obviously related, such as receiving a flu shot or taking vitamin supplements. “There were a lot of things associated with routine medical care in the patients who didn’t have thoughts about suicide and didn’t attempt suicide. So we looked at how much time people spent with their doctor. I think we might have found an important signal that requires further investigation in bigger samples, and also in other populations. If we can look at people who are at risk [of suicide] but who aren’t engaged with their doctors, that gives us a potential avenue to do something about it, where we can get them connected with a provider, or reconnected if they’ve fallen off, or give them a call to see how they’re doing,” Dr. McKernan said.
In fact, the research suggests that such an effort alone might be enough to reduce suicidality, since patient-provider contact appears to be so important.
“I know in the past that physicians have expressed feeling frustrated – like they don’t have some sort of [mental health] intervention to provide patients who have fibromyalgia. This might show that continuing to see the patient, to stay engaged, may have intrinsic benefit that serves almost like an intervention in itself,” Dr. McKernan said.
Dr. McKernan, Dr. Jain, and Dr. Wise had no financial conflicts of interest.
Fibromyalgia patients with no documented suicide attempt spent far more hours in face-to-face meetings with providers than did those who made a suicide attempt over a 20-year period at a single academic medical center. The results, based on a machine-learning analysis of electronic health records, shed more light on the heavy burden of suicidality among patients with rheumatologic illnesses.
“People who didn’t have suicide attempts were present at the doctor 50 hours in a year, compared to less than an hour in a year for those who did attempt suicide. It’s a staggering difference,” said study author Lindsey McKernan, PhD, of the department of psychiatry and behavioral sciences at Vanderbilt University, Nashville, Tenn. What’s more, patients who did not have suicidal thoughts averaged about 6 office hours per year, compared with less than 2 hours for those with suicidal ideation (Arthritis Care Res. 2018 Sep 7. doi: 10.1002/acr.23748).
Fibromyalgia patients are at about ten times the risk of suicide as the general population, and rates of depression and anxiety are higher in patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic disease as well.
Still, mental health issues often go unaddressed. “Many times rheumatologists focus on the patient’s joints and their rheumatologic illness, and they don’t focus on their mental health, and as a result depression in a suicidal patient is, I think, more often missed in a rheumatologic practice than it should be,” said Rakesh Jain, MD, of the department of psychiatry at Texas Tech University, Odessa.

But that gap isn’t for lack of awareness, says Barton Wise, MD, of the departments of orthopedic surgery and internal medicine at the University of California, Davis. “In general, people recognize that depression is a major problem in their patients,” he said. He was the lead author of a study that found that rheumatologists often lack the time, confidence, and connections to properly address a patient’s mental health needs (J Clin Rheumatol. 2016 Sep;22[6]:307-11).
Together, the two studies underscore the pressing need for better mental health care among rheumatology patients. Such issues often take a back seat to a rheumatologist’s primary concern about joint and overall health, but studies have shown that mental health issues are tied to worse rheumatologic disease outcomes. “Addressing comorbid depression will just make the rheumatological outcome be better. So why not do it?” Dr. Jain said.
Screening is a key consideration, according to Dr. Jain, who recommends the Patient Health Questionnaire-9. But even when a problem arises, rheumatologists may lack the confidence to tackle mental health issues. This can be addressed through various resources, such as courses at professional meetings, but another challenge awaits. Rheumatologists may also be unsure of who should be responsible for handling mental health concerns. Even though the rheumatologist may see the patient more often than his or her other providers, “you often feel that you can’t manage everything,” Dr. Wise said.
One way to address that is to establish relationships with mental health providers who can receive referrals for patients who require it. In academic medical centers or other large institutions, relationships can be formalized, so that a patient could see a psychiatrist on the same day as the rheumatologist visit. He even suggests group sessions for patients with similar comorbidities, such as depression related to fibromyalgia or lupus.
Special challenges
Rheumatologic conditions are well documented to have heightened rates of suicide and mental health issues, and this may be related to some of the additional challenges such patients face. Many have chronic pain, which in itself is a risk factor for suicide.
Fibromyalgia can be particularly difficult because patients struggle to communicate about their condition with their clinician and even with loved ones. “Patients report feeling stigmatized and often struggle to communicate about what’s happening in their bodies. The pain can change location and intensity, and it doesn’t show up on medical tests,” Dr. McKernan said.
Another burden is that rheumatologic patients typically have high levels of inflammation, a characteristic that has been linked to lower responses to some antidepressants, according to Dr. Jain.
Antidepressants should still be considered for these patients, but they should be combined with other treatments or management techniques, he says. He emphasizes the importance of a low-inflammatory diet, exercise, and other lifestyle factors. He has also created the free Wild 5 Wellness program, which seeks to broadly improve wellness in patients with chronic pain and mental health challenges.
Physician response
The results of the study on fibromyalgia patients suggests another avenue toward improving mental health. The researchers examined data on 8,879 patients with fibromyalgia, using data collected between 1998 and 2017. There were 34 suicide attempts and 96 cases of suicidal ideation. A machine-learning algorithm spat out some factors associated with heightened suicide risk, such as fatigue, dizziness, and weakness, as well as obesity and drug dependence.
But it also generated some associations that weren’t obviously related, such as receiving a flu shot or taking vitamin supplements. “There were a lot of things associated with routine medical care in the patients who didn’t have thoughts about suicide and didn’t attempt suicide. So we looked at how much time people spent with their doctor. I think we might have found an important signal that requires further investigation in bigger samples, and also in other populations. If we can look at people who are at risk [of suicide] but who aren’t engaged with their doctors, that gives us a potential avenue to do something about it, where we can get them connected with a provider, or reconnected if they’ve fallen off, or give them a call to see how they’re doing,” Dr. McKernan said.
In fact, the research suggests that such an effort alone might be enough to reduce suicidality, since patient-provider contact appears to be so important.
“I know in the past that physicians have expressed feeling frustrated – like they don’t have some sort of [mental health] intervention to provide patients who have fibromyalgia. This might show that continuing to see the patient, to stay engaged, may have intrinsic benefit that serves almost like an intervention in itself,” Dr. McKernan said.
Dr. McKernan, Dr. Jain, and Dr. Wise had no financial conflicts of interest.
Fibromyalgia patients with no documented suicide attempt spent far more hours in face-to-face meetings with providers than did those who made a suicide attempt over a 20-year period at a single academic medical center. The results, based on a machine-learning analysis of electronic health records, shed more light on the heavy burden of suicidality among patients with rheumatologic illnesses.
“People who didn’t have suicide attempts were present at the doctor 50 hours in a year, compared to less than an hour in a year for those who did attempt suicide. It’s a staggering difference,” said study author Lindsey McKernan, PhD, of the department of psychiatry and behavioral sciences at Vanderbilt University, Nashville, Tenn. What’s more, patients who did not have suicidal thoughts averaged about 6 office hours per year, compared with less than 2 hours for those with suicidal ideation (Arthritis Care Res. 2018 Sep 7. doi: 10.1002/acr.23748).
Fibromyalgia patients are at about ten times the risk of suicide as the general population, and rates of depression and anxiety are higher in patients with rheumatoid arthritis, ankylosing spondylitis, and psoriatic disease as well.
Still, mental health issues often go unaddressed. “Many times rheumatologists focus on the patient’s joints and their rheumatologic illness, and they don’t focus on their mental health, and as a result depression in a suicidal patient is, I think, more often missed in a rheumatologic practice than it should be,” said Rakesh Jain, MD, of the department of psychiatry at Texas Tech University, Odessa.

But that gap isn’t for lack of awareness, says Barton Wise, MD, of the departments of orthopedic surgery and internal medicine at the University of California, Davis. “In general, people recognize that depression is a major problem in their patients,” he said. He was the lead author of a study that found that rheumatologists often lack the time, confidence, and connections to properly address a patient’s mental health needs (J Clin Rheumatol. 2016 Sep;22[6]:307-11).
Together, the two studies underscore the pressing need for better mental health care among rheumatology patients. Such issues often take a back seat to a rheumatologist’s primary concern about joint and overall health, but studies have shown that mental health issues are tied to worse rheumatologic disease outcomes. “Addressing comorbid depression will just make the rheumatological outcome be better. So why not do it?” Dr. Jain said.
Screening is a key consideration, according to Dr. Jain, who recommends the Patient Health Questionnaire-9. But even when a problem arises, rheumatologists may lack the confidence to tackle mental health issues. This can be addressed through various resources, such as courses at professional meetings, but another challenge awaits. Rheumatologists may also be unsure of who should be responsible for handling mental health concerns. Even though the rheumatologist may see the patient more often than his or her other providers, “you often feel that you can’t manage everything,” Dr. Wise said.
One way to address that is to establish relationships with mental health providers who can receive referrals for patients who require it. In academic medical centers or other large institutions, relationships can be formalized, so that a patient could see a psychiatrist on the same day as the rheumatologist visit. He even suggests group sessions for patients with similar comorbidities, such as depression related to fibromyalgia or lupus.
Special challenges
Rheumatologic conditions are well documented to have heightened rates of suicide and mental health issues, and this may be related to some of the additional challenges such patients face. Many have chronic pain, which in itself is a risk factor for suicide.
Fibromyalgia can be particularly difficult because patients struggle to communicate about their condition with their clinician and even with loved ones. “Patients report feeling stigmatized and often struggle to communicate about what’s happening in their bodies. The pain can change location and intensity, and it doesn’t show up on medical tests,” Dr. McKernan said.
Another burden is that rheumatologic patients typically have high levels of inflammation, a characteristic that has been linked to lower responses to some antidepressants, according to Dr. Jain.
Antidepressants should still be considered for these patients, but they should be combined with other treatments or management techniques, he says. He emphasizes the importance of a low-inflammatory diet, exercise, and other lifestyle factors. He has also created the free Wild 5 Wellness program, which seeks to broadly improve wellness in patients with chronic pain and mental health challenges.
Physician response
The results of the study on fibromyalgia patients suggests another avenue toward improving mental health. The researchers examined data on 8,879 patients with fibromyalgia, using data collected between 1998 and 2017. There were 34 suicide attempts and 96 cases of suicidal ideation. A machine-learning algorithm spat out some factors associated with heightened suicide risk, such as fatigue, dizziness, and weakness, as well as obesity and drug dependence.
But it also generated some associations that weren’t obviously related, such as receiving a flu shot or taking vitamin supplements. “There were a lot of things associated with routine medical care in the patients who didn’t have thoughts about suicide and didn’t attempt suicide. So we looked at how much time people spent with their doctor. I think we might have found an important signal that requires further investigation in bigger samples, and also in other populations. If we can look at people who are at risk [of suicide] but who aren’t engaged with their doctors, that gives us a potential avenue to do something about it, where we can get them connected with a provider, or reconnected if they’ve fallen off, or give them a call to see how they’re doing,” Dr. McKernan said.
In fact, the research suggests that such an effort alone might be enough to reduce suicidality, since patient-provider contact appears to be so important.
“I know in the past that physicians have expressed feeling frustrated – like they don’t have some sort of [mental health] intervention to provide patients who have fibromyalgia. This might show that continuing to see the patient, to stay engaged, may have intrinsic benefit that serves almost like an intervention in itself,” Dr. McKernan said.
Dr. McKernan, Dr. Jain, and Dr. Wise had no financial conflicts of interest.
Procalcitonin not helpful in critically ill COPD
Clinical question: Can a procalcitonin (PCT)–guided strategy safely reduce antibiotic exposure in patients admitted to the ICU with severe acute exacerbations of chronic obstructive pulmonary disease (COPD) with or without pneumonia?
Background: Studies have demonstrated PCT-based strategies can safely reduce antibiotic use in patients without severe lower respiratory tract infections, community-acquired pneumonia, or acute exacerbations of COPD. The data on safety of PCT-based strategies in critically ill patients is limited.
Study design: Prospective, multicenter, randomized, controlled trial.
Setting: ICUs of 11 hospitals in France, including 7 tertiary care hospitals.
Synopsis: In this study 302 patients admitted to the ICU with severe exacerbations of COPD with or without pneumonia were randomly assigned to groups with antibiotic therapy guided by a PCT protocol or standard guidelines. Overall, the study failed to demonstrate noninferiority of a PCT-based strategy to reduce exposure to antibiotics. Specifically, the adjusted difference in mortality was 6.6% higher (90% confidence interval, 0.3%-13.5%) in the intervention group with no significant reduction in antibiotic exposure.
One limitation of this study was that it was an open trial in which clinicians were aware that their management was being observed.
Bottom line: A PCT-based algorithm was not effective in safely reducing antibiotic exposure in patients with acute exacerbations of COPD admitted to the ICU.
Citation: Daubin C et al. Procalcitonin algorithm to guide initial antibiotic therapy in acute exacerbations of COPD admitted to the ICU: A randomized multicenter study. Intensive Care Med. 2018 Apr;44(4):428-37.
Dr. Agith is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: Can a procalcitonin (PCT)–guided strategy safely reduce antibiotic exposure in patients admitted to the ICU with severe acute exacerbations of chronic obstructive pulmonary disease (COPD) with or without pneumonia?
Background: Studies have demonstrated PCT-based strategies can safely reduce antibiotic use in patients without severe lower respiratory tract infections, community-acquired pneumonia, or acute exacerbations of COPD. The data on safety of PCT-based strategies in critically ill patients is limited.
Study design: Prospective, multicenter, randomized, controlled trial.
Setting: ICUs of 11 hospitals in France, including 7 tertiary care hospitals.
Synopsis: In this study 302 patients admitted to the ICU with severe exacerbations of COPD with or without pneumonia were randomly assigned to groups with antibiotic therapy guided by a PCT protocol or standard guidelines. Overall, the study failed to demonstrate noninferiority of a PCT-based strategy to reduce exposure to antibiotics. Specifically, the adjusted difference in mortality was 6.6% higher (90% confidence interval, 0.3%-13.5%) in the intervention group with no significant reduction in antibiotic exposure.
One limitation of this study was that it was an open trial in which clinicians were aware that their management was being observed.
Bottom line: A PCT-based algorithm was not effective in safely reducing antibiotic exposure in patients with acute exacerbations of COPD admitted to the ICU.
Citation: Daubin C et al. Procalcitonin algorithm to guide initial antibiotic therapy in acute exacerbations of COPD admitted to the ICU: A randomized multicenter study. Intensive Care Med. 2018 Apr;44(4):428-37.
Dr. Agith is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: Can a procalcitonin (PCT)–guided strategy safely reduce antibiotic exposure in patients admitted to the ICU with severe acute exacerbations of chronic obstructive pulmonary disease (COPD) with or without pneumonia?
Background: Studies have demonstrated PCT-based strategies can safely reduce antibiotic use in patients without severe lower respiratory tract infections, community-acquired pneumonia, or acute exacerbations of COPD. The data on safety of PCT-based strategies in critically ill patients is limited.
Study design: Prospective, multicenter, randomized, controlled trial.
Setting: ICUs of 11 hospitals in France, including 7 tertiary care hospitals.
Synopsis: In this study 302 patients admitted to the ICU with severe exacerbations of COPD with or without pneumonia were randomly assigned to groups with antibiotic therapy guided by a PCT protocol or standard guidelines. Overall, the study failed to demonstrate noninferiority of a PCT-based strategy to reduce exposure to antibiotics. Specifically, the adjusted difference in mortality was 6.6% higher (90% confidence interval, 0.3%-13.5%) in the intervention group with no significant reduction in antibiotic exposure.
One limitation of this study was that it was an open trial in which clinicians were aware that their management was being observed.
Bottom line: A PCT-based algorithm was not effective in safely reducing antibiotic exposure in patients with acute exacerbations of COPD admitted to the ICU.
Citation: Daubin C et al. Procalcitonin algorithm to guide initial antibiotic therapy in acute exacerbations of COPD admitted to the ICU: A randomized multicenter study. Intensive Care Med. 2018 Apr;44(4):428-37.
Dr. Agith is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.