User login
Syncope alone after age 60 does not require admission
SAN DIEGO – Unless the cause of syncope has been identified after a thorough workup in the emergency department, there is no advantage to admitting patients aged 60 years and older who complain of syncope, an ED-based study has found.
Almost 2,500 patients aged 60 or older with unexplained syncope after a thorough workup had similar 30-day outcomes whether they were admitted to the hospital or sent home from the ED, based on the results of a retrospective study presented at the annual meeting of the American College of Emergency Physicians.
Dr. Marc A. Probst of the Icahn School of Medicine at Mount Sinai, New York, who presented the data, reported that many centers admit older patients with syncope, although the benefit of this practice has not been well established.
In a video interview, Dr. Probst points out how the findings may be useful in guiding clinical decisions or counseling patients when admission is being considered.
SAN DIEGO – Unless the cause of syncope has been identified after a thorough workup in the emergency department, there is no advantage to admitting patients aged 60 years and older who complain of syncope, an ED-based study has found.
Almost 2,500 patients aged 60 or older with unexplained syncope after a thorough workup had similar 30-day outcomes whether they were admitted to the hospital or sent home from the ED, based on the results of a retrospective study presented at the annual meeting of the American College of Emergency Physicians.
Dr. Marc A. Probst of the Icahn School of Medicine at Mount Sinai, New York, who presented the data, reported that many centers admit older patients with syncope, although the benefit of this practice has not been well established.
In a video interview, Dr. Probst points out how the findings may be useful in guiding clinical decisions or counseling patients when admission is being considered.
SAN DIEGO – Unless the cause of syncope has been identified after a thorough workup in the emergency department, there is no advantage to admitting patients aged 60 years and older who complain of syncope, an ED-based study has found.
Almost 2,500 patients aged 60 or older with unexplained syncope after a thorough workup had similar 30-day outcomes whether they were admitted to the hospital or sent home from the ED, based on the results of a retrospective study presented at the annual meeting of the American College of Emergency Physicians.
Dr. Marc A. Probst of the Icahn School of Medicine at Mount Sinai, New York, who presented the data, reported that many centers admit older patients with syncope, although the benefit of this practice has not been well established.
In a video interview, Dr. Probst points out how the findings may be useful in guiding clinical decisions or counseling patients when admission is being considered.
REPORTING FROM ACEP18
Early supportive care cuts costs and admissions in cancer patients undergoing curative treatment
PHOENIX – By starting supportive measures early in the care of cancer patients undergoing curative treatment, a cancer center cut costs, emergency department visits, and admissions, a researcher said at symposium on quality care sponsored by the American Society of Clinical Oncology.
The supportive care pathway resulted in double-digit decreases in admissions and an opportunity cost savings of $1,500 per patient, reported Christopher D. Koprowski, MD, MBA, of Helen F. Graham Cancer Center & Research Institute, Christiana Care Health System, Newark, Del.
Although satisfaction hasn’t been measured yet, anecdotal reports suggest the patient experience has improved because of the multidisciplinary program, which included mandatory supportive care screening and enhancements to computer systems, said Dr. Koprowski, who is director of quality and safety at the cancer center.
“From all outward signs, the patients are extraordinarily grateful in this program,” Dr. Koprowski said in an interview. “I just had one who said that being seen at the same time by all these people just makes things so much easier.”
The Supportive Care of Oncology Patients (SCOOP) clinical pathway, introduced in November 2016, includes palliative and supportive care service screening that occurs during the multidisciplinary visit. The pathway incorporates a checklist integrated into a nurse navigator information system to support care standardization, according to Dr. Koprowski.
Also added were “flags” in the inpatient information system that trigger alerts to navigators, oncologists, and the supportive care service whenever a patient in the SCOOP pathway is admitted, discharged, or seen in the emergency room, he said.
Enrollment in SCOOP was limited to lung, esophageal, head and neck, and colorectal cancer patients receiving concurrent radiation and chemotherapy. Out of approximately 200 eligible patients in the first year, about half entered the clinical pathway, according to Dr. Koprowski.
For that first year, 32% of SCOOP patients had ED visits, compared with 54% of combined modality patients who did not enter the pathway, Dr. Koprowski reported.
Similarly, admissions were 25% for the SCOOP patients and 34% of non-SCOOP patients, and readmissions were seen in 20% versus 32% of those groups, respectively.
These findings are much like what has been seen when early supportive care is introduced in patients with more advanced disease, according to Dr. Koprowski.
He said the SCOOP program was partly inspired by a study in the New England Journal of Medicine showing that patients with advanced non–small cell lung cancer who received early palliative care had longer survival despite less-aggressive care, including reduced use of chemotherapy, at the end of life.
“Early-stage patients aren’t that much different if they are being treated very aggressively with combined modality chemotherapy and radiation,” he said. “The treatment is very, very tough on people.”
Dr. Koprowski and his coinvestigators had no relationships to disclose relevant to the research presented at the ASCO symposium.
SOURCE: Koprowski CD et al. 2018 ASCO Quality Care Symposium, Abstract 142.
PHOENIX – By starting supportive measures early in the care of cancer patients undergoing curative treatment, a cancer center cut costs, emergency department visits, and admissions, a researcher said at symposium on quality care sponsored by the American Society of Clinical Oncology.
The supportive care pathway resulted in double-digit decreases in admissions and an opportunity cost savings of $1,500 per patient, reported Christopher D. Koprowski, MD, MBA, of Helen F. Graham Cancer Center & Research Institute, Christiana Care Health System, Newark, Del.
Although satisfaction hasn’t been measured yet, anecdotal reports suggest the patient experience has improved because of the multidisciplinary program, which included mandatory supportive care screening and enhancements to computer systems, said Dr. Koprowski, who is director of quality and safety at the cancer center.
“From all outward signs, the patients are extraordinarily grateful in this program,” Dr. Koprowski said in an interview. “I just had one who said that being seen at the same time by all these people just makes things so much easier.”
The Supportive Care of Oncology Patients (SCOOP) clinical pathway, introduced in November 2016, includes palliative and supportive care service screening that occurs during the multidisciplinary visit. The pathway incorporates a checklist integrated into a nurse navigator information system to support care standardization, according to Dr. Koprowski.
Also added were “flags” in the inpatient information system that trigger alerts to navigators, oncologists, and the supportive care service whenever a patient in the SCOOP pathway is admitted, discharged, or seen in the emergency room, he said.
Enrollment in SCOOP was limited to lung, esophageal, head and neck, and colorectal cancer patients receiving concurrent radiation and chemotherapy. Out of approximately 200 eligible patients in the first year, about half entered the clinical pathway, according to Dr. Koprowski.
For that first year, 32% of SCOOP patients had ED visits, compared with 54% of combined modality patients who did not enter the pathway, Dr. Koprowski reported.
Similarly, admissions were 25% for the SCOOP patients and 34% of non-SCOOP patients, and readmissions were seen in 20% versus 32% of those groups, respectively.
These findings are much like what has been seen when early supportive care is introduced in patients with more advanced disease, according to Dr. Koprowski.
He said the SCOOP program was partly inspired by a study in the New England Journal of Medicine showing that patients with advanced non–small cell lung cancer who received early palliative care had longer survival despite less-aggressive care, including reduced use of chemotherapy, at the end of life.
“Early-stage patients aren’t that much different if they are being treated very aggressively with combined modality chemotherapy and radiation,” he said. “The treatment is very, very tough on people.”
Dr. Koprowski and his coinvestigators had no relationships to disclose relevant to the research presented at the ASCO symposium.
SOURCE: Koprowski CD et al. 2018 ASCO Quality Care Symposium, Abstract 142.
PHOENIX – By starting supportive measures early in the care of cancer patients undergoing curative treatment, a cancer center cut costs, emergency department visits, and admissions, a researcher said at symposium on quality care sponsored by the American Society of Clinical Oncology.
The supportive care pathway resulted in double-digit decreases in admissions and an opportunity cost savings of $1,500 per patient, reported Christopher D. Koprowski, MD, MBA, of Helen F. Graham Cancer Center & Research Institute, Christiana Care Health System, Newark, Del.
Although satisfaction hasn’t been measured yet, anecdotal reports suggest the patient experience has improved because of the multidisciplinary program, which included mandatory supportive care screening and enhancements to computer systems, said Dr. Koprowski, who is director of quality and safety at the cancer center.
“From all outward signs, the patients are extraordinarily grateful in this program,” Dr. Koprowski said in an interview. “I just had one who said that being seen at the same time by all these people just makes things so much easier.”
The Supportive Care of Oncology Patients (SCOOP) clinical pathway, introduced in November 2016, includes palliative and supportive care service screening that occurs during the multidisciplinary visit. The pathway incorporates a checklist integrated into a nurse navigator information system to support care standardization, according to Dr. Koprowski.
Also added were “flags” in the inpatient information system that trigger alerts to navigators, oncologists, and the supportive care service whenever a patient in the SCOOP pathway is admitted, discharged, or seen in the emergency room, he said.
Enrollment in SCOOP was limited to lung, esophageal, head and neck, and colorectal cancer patients receiving concurrent radiation and chemotherapy. Out of approximately 200 eligible patients in the first year, about half entered the clinical pathway, according to Dr. Koprowski.
For that first year, 32% of SCOOP patients had ED visits, compared with 54% of combined modality patients who did not enter the pathway, Dr. Koprowski reported.
Similarly, admissions were 25% for the SCOOP patients and 34% of non-SCOOP patients, and readmissions were seen in 20% versus 32% of those groups, respectively.
These findings are much like what has been seen when early supportive care is introduced in patients with more advanced disease, according to Dr. Koprowski.
He said the SCOOP program was partly inspired by a study in the New England Journal of Medicine showing that patients with advanced non–small cell lung cancer who received early palliative care had longer survival despite less-aggressive care, including reduced use of chemotherapy, at the end of life.
“Early-stage patients aren’t that much different if they are being treated very aggressively with combined modality chemotherapy and radiation,” he said. “The treatment is very, very tough on people.”
Dr. Koprowski and his coinvestigators had no relationships to disclose relevant to the research presented at the ASCO symposium.
SOURCE: Koprowski CD et al. 2018 ASCO Quality Care Symposium, Abstract 142.
REPORTING FROM THE QUALITY CARE SYMPOSIUM
Key clinical point: Early supportive care measures reduced costs, ED visits, and admissions in cancer patients who underwent combined modality therapy.
Major finding: 32% of patients had ED visits, compared with 54% of patients who did not enter the early supportive care pathway.
Study details: Analysis of cost and health care utilization for approximately 200 patients who underwent concurrent radiation and chemotherapy.
Disclosures: Authors had no relationships to disclose.
Source: Koprowski CD et al. 2018 ASCO Quality Care Symposium, Abstract 142.
PCV13 for older adults
Also today, ED visits that are related to psychiatric complaints are up 20 among elderly, nonobstructive angina should trigger functional testing, and antibiotics trigger proteolytic activity that leads to chronic colitis.
Amazon Alexa
Apple Podcasts
Spotify
Also today, ED visits that are related to psychiatric complaints are up 20 among elderly, nonobstructive angina should trigger functional testing, and antibiotics trigger proteolytic activity that leads to chronic colitis.
Amazon Alexa
Apple Podcasts
Spotify
Also today, ED visits that are related to psychiatric complaints are up 20 among elderly, nonobstructive angina should trigger functional testing, and antibiotics trigger proteolytic activity that leads to chronic colitis.
Amazon Alexa
Apple Podcasts
Spotify
Adding a Cream May Enhance Flu Vaccine Effectiveness
Can a cream help a flu vaccine work better? In a phase 1 clinical trial, researchers from Baylor College of Medicine in Houston, Texas, are testing whether imiquimod cream—commonly used to treat genital warts and some skin cancers—can boost the immune response to an H5N1 flu vaccine. Studies have shown imiquimod generates significantly more robust immune responses.
Participants in the Vaccine and Treatment Evaluation Units trial will be given 2 intradermal doses of an H5N1 vaccine, 21 days apart. In one group, participants will have Aldara (imiquimod cream) applied to their upper arm before each vaccination; in the control group, a placebo cream will be applied.
Participants will return at regular intervals over 7 months to have blood drawn; they also will keep diaries to record symptoms.
The first participant was vaccinated in June. Early results are expected by the end of the year.
Can a cream help a flu vaccine work better? In a phase 1 clinical trial, researchers from Baylor College of Medicine in Houston, Texas, are testing whether imiquimod cream—commonly used to treat genital warts and some skin cancers—can boost the immune response to an H5N1 flu vaccine. Studies have shown imiquimod generates significantly more robust immune responses.
Participants in the Vaccine and Treatment Evaluation Units trial will be given 2 intradermal doses of an H5N1 vaccine, 21 days apart. In one group, participants will have Aldara (imiquimod cream) applied to their upper arm before each vaccination; in the control group, a placebo cream will be applied.
Participants will return at regular intervals over 7 months to have blood drawn; they also will keep diaries to record symptoms.
The first participant was vaccinated in June. Early results are expected by the end of the year.
Can a cream help a flu vaccine work better? In a phase 1 clinical trial, researchers from Baylor College of Medicine in Houston, Texas, are testing whether imiquimod cream—commonly used to treat genital warts and some skin cancers—can boost the immune response to an H5N1 flu vaccine. Studies have shown imiquimod generates significantly more robust immune responses.
Participants in the Vaccine and Treatment Evaluation Units trial will be given 2 intradermal doses of an H5N1 vaccine, 21 days apart. In one group, participants will have Aldara (imiquimod cream) applied to their upper arm before each vaccination; in the control group, a placebo cream will be applied.
Participants will return at regular intervals over 7 months to have blood drawn; they also will keep diaries to record symptoms.
The first participant was vaccinated in June. Early results are expected by the end of the year.
Quadruplet therapy could be the future in MM
New York—Four-drug combinations are holding promise for the treatment of multiple myeloma (MM), although data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center.
The efficacy of multiple triplet regimens has been well documented, and data are now emerging on the potential of 4-drug combinations.
“Triplet therapy is the standard,” she said during a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies, “and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, she said, is SWOG 0777, an open label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable. The trial was recently reported in The Lancet.
The median progression free survival (PFS) was 43 months for the triplet, versus 30 months for the two-drug regimen (P=0.0018).
Likewise, median overall survival (OS) was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P=0.025).
“Very convincingly, just receiving that short exposure to bortezomib,” she said, “ended up causing a substantial increase of progression-free and overall survival.”
Effective triplet regimens include the combination of carfilzomib, lenalidomide, and dexamethasone (KRd), cyclophosphamide, bortezomib, and dexamethasone (CyBorD), and more recently, ixazomib, lenalidomide, and dexamethasone (IRd).
These regimens have “excellent” response rates and survival data, Dr. Callander noted.
Quadruplet data
The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at ASCO 2017 (abstract 8002).
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data also presented at ASCO 2017 (abstract 8000), with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr Callander conjectured.
Four versus three drug strategies are being evaluated in ongoing randomized clinical trials including patients with previously untreated myeloma, she said.
These studies include Cassiopeia (NCT02541383), which is evaluating bortezomib, thalidomide, and dexamethasone with or without daratumumab, and GRIFFIN (NCT02874742), which is looking at VRd with or without daratumumab.
Daratumumab received an additional indication in myeloma, this time as part of a 4-drug regimen, several months ago, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The U.S. Food and Drug Administration (FDA) approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE (MMY3007) study, published in The New England Journal of Medicine, showing an 18-month PFS of 71.6% for the 4-drug combination versus 50.2% for VMP alone (P<0.001).
New York—Four-drug combinations are holding promise for the treatment of multiple myeloma (MM), although data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center.
The efficacy of multiple triplet regimens has been well documented, and data are now emerging on the potential of 4-drug combinations.
“Triplet therapy is the standard,” she said during a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies, “and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, she said, is SWOG 0777, an open label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable. The trial was recently reported in The Lancet.
The median progression free survival (PFS) was 43 months for the triplet, versus 30 months for the two-drug regimen (P=0.0018).
Likewise, median overall survival (OS) was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P=0.025).
“Very convincingly, just receiving that short exposure to bortezomib,” she said, “ended up causing a substantial increase of progression-free and overall survival.”
Effective triplet regimens include the combination of carfilzomib, lenalidomide, and dexamethasone (KRd), cyclophosphamide, bortezomib, and dexamethasone (CyBorD), and more recently, ixazomib, lenalidomide, and dexamethasone (IRd).
These regimens have “excellent” response rates and survival data, Dr. Callander noted.
Quadruplet data
The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at ASCO 2017 (abstract 8002).
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data also presented at ASCO 2017 (abstract 8000), with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr Callander conjectured.
Four versus three drug strategies are being evaluated in ongoing randomized clinical trials including patients with previously untreated myeloma, she said.
These studies include Cassiopeia (NCT02541383), which is evaluating bortezomib, thalidomide, and dexamethasone with or without daratumumab, and GRIFFIN (NCT02874742), which is looking at VRd with or without daratumumab.
Daratumumab received an additional indication in myeloma, this time as part of a 4-drug regimen, several months ago, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The U.S. Food and Drug Administration (FDA) approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE (MMY3007) study, published in The New England Journal of Medicine, showing an 18-month PFS of 71.6% for the 4-drug combination versus 50.2% for VMP alone (P<0.001).
New York—Four-drug combinations are holding promise for the treatment of multiple myeloma (MM), although data from additional randomized trials are needed to define their role in clinical practice, according to Natalie S. Callander, MD, of the University of Wisconsin Carbone Cancer Center.
The efficacy of multiple triplet regimens has been well documented, and data are now emerging on the potential of 4-drug combinations.
“Triplet therapy is the standard,” she said during a presentation at the NCCN 13th Annual Congress: Hematologic Malignancies, “and quad therapy may be in the future.”
The study that set the standard for triplets in myeloma, she said, is SWOG 0777, an open label, phase 3 trial that compared bortezomib with lenalidomide and dexamethasone (VRd) to lenalidomide and dexamethasone alone in patients with newly diagnosed myeloma.
Adding bortezomib to lenalidomide and dexamethasone significantly improved both progression-free and overall survival in the 525-patient trial, with a risk-benefit profile that was acceptable. The trial was recently reported in The Lancet.
The median progression free survival (PFS) was 43 months for the triplet, versus 30 months for the two-drug regimen (P=0.0018).
Likewise, median overall survival (OS) was significantly improved, at 75 months versus 64 months for triplet versus doublet therapy (P=0.025).
“Very convincingly, just receiving that short exposure to bortezomib,” she said, “ended up causing a substantial increase of progression-free and overall survival.”
Effective triplet regimens include the combination of carfilzomib, lenalidomide, and dexamethasone (KRd), cyclophosphamide, bortezomib, and dexamethasone (CyBorD), and more recently, ixazomib, lenalidomide, and dexamethasone (IRd).
These regimens have “excellent” response rates and survival data, Dr. Callander noted.
Quadruplet data
The combination of elotuzumab plus VRd produced high response rates that were even higher after transplant, with reasonable toxicity, Dr. Callander said of phase 2 trial data presented at ASCO 2017 (abstract 8002).
Similarly, the combination of daratumumab plus KRd had a 100% rate of partial response or better in phase 2 data also presented at ASCO 2017 (abstract 8000), with rates of very good partial response and complete response that improved with successive cycles of therapy, she said.
Even so, “it remains to be seen whether four drugs will be the new standard,” Dr Callander conjectured.
Four versus three drug strategies are being evaluated in ongoing randomized clinical trials including patients with previously untreated myeloma, she said.
These studies include Cassiopeia (NCT02541383), which is evaluating bortezomib, thalidomide, and dexamethasone with or without daratumumab, and GRIFFIN (NCT02874742), which is looking at VRd with or without daratumumab.
Daratumumab received an additional indication in myeloma, this time as part of a 4-drug regimen, several months ago, Dr. Callander added in a discussion on treatment options for elderly myeloma patients.
The U.S. Food and Drug Administration (FDA) approved the monoclonal antibody in combination with bortezomib, melphalan, and prednisone (VMP) for treatment of newly diagnosed myeloma patients who are transplant ineligible.
That approval was based on results of the multicenter phase 3 ALCYONE (MMY3007) study, published in The New England Journal of Medicine, showing an 18-month PFS of 71.6% for the 4-drug combination versus 50.2% for VMP alone (P<0.001).
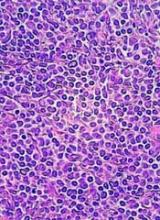
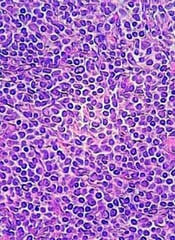
5-year remission rates with combo prove durable in MCL
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Communication and consent
We knew that the case would be a difficult one. The patient was a man in his mid-40s who had several serious chronic conditions and was on high-dose steroids. He had been operated on 10 days earlier by one of my partners for a bowel obstruction and had required a resection of a small portion of the terminal ileum. Unfortunately, on the day after surgery, it became obvious that the patient needed a reexploration for bleeding. He had developed clear evidence of a significant anastomotic leak and had to be taken emergently back to the operating room.
His condition had been worsening during the day. We had booked the case in the OR but had been put off by a trauma emergency and a neurosurgical emergency. During the 3 hours of waiting to take him to the OR, the patient’s sister and mother came to the hospital and were now waiting with him in the preop area. I was on my way up to see him when my resident called. Despite the patient having signed an operative consent form a few hours earlier when we booked the case, he was now “declining” an operation. I was surprised. This man had undergone several operations in the last few years and two in the last 2 weeks. I arrived to find the patient stating that he did not want surgery. Lying in bed, he was adamant that he should not have surgery. The surgical resident who had spoken with the patient several times over the last few hours was also surprised. The patient’s family members were yelling that, of course, he wanted surgery and why would he change his mind.
This is a difficult situation since one of the central tenets of the ethical practice of surgery is to allow patients to make decisions about their own care. The right to make autonomous choices even extends to circumstances in which patients make what we might consider “bad” decisions. As long as the patient has the capacity to make an autonomous choice, he or she should have that choice respected.
This patient, who just a few hours ago had agreed to surgery, now seemed to have changed his mind. Although it can be frustrating, we do allow patients to change their minds. On the one hand, this was a straightforward case. The patient was refusing a potentially life-saving operation. Such a situation is never pleasant for a surgeon, but as long as the patient understands the risks, we respect such choices.
However, my resident made an astute observation. She pointed out that, when asked why he now did not want surgery, he replied that “this is all a movie – it’s not really happening.” The patient appeared to be oriented to person and place, but nevertheless, his reasoning seemed to have been altered. It appeared that this patient was no longer making sense because his underlying medical condition had deteriorated. We considered whether he was becoming septic and that this change in medical condition had rendered him unable to make an informed decision. My resident, who had discussed the operation with the patient several times, stated that the patient’s decision making seemed very different than even an hour ago. His family members agreed, stating that, up until a few minutes before, he was in favor of surgery. They pleaded with us to just take him into the operating room.
We considered our options. We could delay surgery and consult psychiatry to ask them to assess his competency. However, on a weekend night, this would likely take several hours. We considered the option of waiting in the preop area for the patient’s medical condition to further worsen. If he became overtly septic and lost consciousness, then we could readily turn to the family members – his surrogate decision makers – and ask them to consent to the procedure. Although this “by the book” approach might take away any worry that we were overriding an autonomous patient’s choice, we knew that it would unnecessarily expose him to greater operative risks. This option was not in his best interest and therefore not much of an option.
Ultimately, the surgical resident, the attending anesthesiologist, the family, and I decided that his decision to not have surgery at this moment was not consistent with his prior decisions, and he could provide no reason for changing his mind. We brought the patient into the operating room and explored him. He did have a large anastomotic leak with a large volume of enteric contents in the peritoneal cavity. He survived the operation and, not unexpectedly, required a long postoperative stay in the hospital. Once he was a few days out, I inquired about whether he was glad that he had surgery. He was quick to state his confidence that it had been the right choice for him. He did not even remember having ever refused the surgery.
Although this case raised many concerns for all of us involved in the patient’s care, one overriding lesson that came through to me. Informed consent should not be viewed as a solitary event, but a conversation. This patient had expressed his desire to have surgery multiple times to my surgical resident and to his family. Even though we should never take the position that patients cannot change their minds, we should carefully question those choices that are inconsistent with the prior discussions that have been undertaken. Good communication skills – including listening to the patient, understanding the patient’s reasoning, and reflecting on the entire conversation – are essential in obtaining informed consent.
Dr. Angelos is the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
We knew that the case would be a difficult one. The patient was a man in his mid-40s who had several serious chronic conditions and was on high-dose steroids. He had been operated on 10 days earlier by one of my partners for a bowel obstruction and had required a resection of a small portion of the terminal ileum. Unfortunately, on the day after surgery, it became obvious that the patient needed a reexploration for bleeding. He had developed clear evidence of a significant anastomotic leak and had to be taken emergently back to the operating room.
His condition had been worsening during the day. We had booked the case in the OR but had been put off by a trauma emergency and a neurosurgical emergency. During the 3 hours of waiting to take him to the OR, the patient’s sister and mother came to the hospital and were now waiting with him in the preop area. I was on my way up to see him when my resident called. Despite the patient having signed an operative consent form a few hours earlier when we booked the case, he was now “declining” an operation. I was surprised. This man had undergone several operations in the last few years and two in the last 2 weeks. I arrived to find the patient stating that he did not want surgery. Lying in bed, he was adamant that he should not have surgery. The surgical resident who had spoken with the patient several times over the last few hours was also surprised. The patient’s family members were yelling that, of course, he wanted surgery and why would he change his mind.
This is a difficult situation since one of the central tenets of the ethical practice of surgery is to allow patients to make decisions about their own care. The right to make autonomous choices even extends to circumstances in which patients make what we might consider “bad” decisions. As long as the patient has the capacity to make an autonomous choice, he or she should have that choice respected.
This patient, who just a few hours ago had agreed to surgery, now seemed to have changed his mind. Although it can be frustrating, we do allow patients to change their minds. On the one hand, this was a straightforward case. The patient was refusing a potentially life-saving operation. Such a situation is never pleasant for a surgeon, but as long as the patient understands the risks, we respect such choices.
However, my resident made an astute observation. She pointed out that, when asked why he now did not want surgery, he replied that “this is all a movie – it’s not really happening.” The patient appeared to be oriented to person and place, but nevertheless, his reasoning seemed to have been altered. It appeared that this patient was no longer making sense because his underlying medical condition had deteriorated. We considered whether he was becoming septic and that this change in medical condition had rendered him unable to make an informed decision. My resident, who had discussed the operation with the patient several times, stated that the patient’s decision making seemed very different than even an hour ago. His family members agreed, stating that, up until a few minutes before, he was in favor of surgery. They pleaded with us to just take him into the operating room.
We considered our options. We could delay surgery and consult psychiatry to ask them to assess his competency. However, on a weekend night, this would likely take several hours. We considered the option of waiting in the preop area for the patient’s medical condition to further worsen. If he became overtly septic and lost consciousness, then we could readily turn to the family members – his surrogate decision makers – and ask them to consent to the procedure. Although this “by the book” approach might take away any worry that we were overriding an autonomous patient’s choice, we knew that it would unnecessarily expose him to greater operative risks. This option was not in his best interest and therefore not much of an option.
Ultimately, the surgical resident, the attending anesthesiologist, the family, and I decided that his decision to not have surgery at this moment was not consistent with his prior decisions, and he could provide no reason for changing his mind. We brought the patient into the operating room and explored him. He did have a large anastomotic leak with a large volume of enteric contents in the peritoneal cavity. He survived the operation and, not unexpectedly, required a long postoperative stay in the hospital. Once he was a few days out, I inquired about whether he was glad that he had surgery. He was quick to state his confidence that it had been the right choice for him. He did not even remember having ever refused the surgery.
Although this case raised many concerns for all of us involved in the patient’s care, one overriding lesson that came through to me. Informed consent should not be viewed as a solitary event, but a conversation. This patient had expressed his desire to have surgery multiple times to my surgical resident and to his family. Even though we should never take the position that patients cannot change their minds, we should carefully question those choices that are inconsistent with the prior discussions that have been undertaken. Good communication skills – including listening to the patient, understanding the patient’s reasoning, and reflecting on the entire conversation – are essential in obtaining informed consent.
Dr. Angelos is the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
We knew that the case would be a difficult one. The patient was a man in his mid-40s who had several serious chronic conditions and was on high-dose steroids. He had been operated on 10 days earlier by one of my partners for a bowel obstruction and had required a resection of a small portion of the terminal ileum. Unfortunately, on the day after surgery, it became obvious that the patient needed a reexploration for bleeding. He had developed clear evidence of a significant anastomotic leak and had to be taken emergently back to the operating room.
His condition had been worsening during the day. We had booked the case in the OR but had been put off by a trauma emergency and a neurosurgical emergency. During the 3 hours of waiting to take him to the OR, the patient’s sister and mother came to the hospital and were now waiting with him in the preop area. I was on my way up to see him when my resident called. Despite the patient having signed an operative consent form a few hours earlier when we booked the case, he was now “declining” an operation. I was surprised. This man had undergone several operations in the last few years and two in the last 2 weeks. I arrived to find the patient stating that he did not want surgery. Lying in bed, he was adamant that he should not have surgery. The surgical resident who had spoken with the patient several times over the last few hours was also surprised. The patient’s family members were yelling that, of course, he wanted surgery and why would he change his mind.
This is a difficult situation since one of the central tenets of the ethical practice of surgery is to allow patients to make decisions about their own care. The right to make autonomous choices even extends to circumstances in which patients make what we might consider “bad” decisions. As long as the patient has the capacity to make an autonomous choice, he or she should have that choice respected.
This patient, who just a few hours ago had agreed to surgery, now seemed to have changed his mind. Although it can be frustrating, we do allow patients to change their minds. On the one hand, this was a straightforward case. The patient was refusing a potentially life-saving operation. Such a situation is never pleasant for a surgeon, but as long as the patient understands the risks, we respect such choices.
However, my resident made an astute observation. She pointed out that, when asked why he now did not want surgery, he replied that “this is all a movie – it’s not really happening.” The patient appeared to be oriented to person and place, but nevertheless, his reasoning seemed to have been altered. It appeared that this patient was no longer making sense because his underlying medical condition had deteriorated. We considered whether he was becoming septic and that this change in medical condition had rendered him unable to make an informed decision. My resident, who had discussed the operation with the patient several times, stated that the patient’s decision making seemed very different than even an hour ago. His family members agreed, stating that, up until a few minutes before, he was in favor of surgery. They pleaded with us to just take him into the operating room.
We considered our options. We could delay surgery and consult psychiatry to ask them to assess his competency. However, on a weekend night, this would likely take several hours. We considered the option of waiting in the preop area for the patient’s medical condition to further worsen. If he became overtly septic and lost consciousness, then we could readily turn to the family members – his surrogate decision makers – and ask them to consent to the procedure. Although this “by the book” approach might take away any worry that we were overriding an autonomous patient’s choice, we knew that it would unnecessarily expose him to greater operative risks. This option was not in his best interest and therefore not much of an option.
Ultimately, the surgical resident, the attending anesthesiologist, the family, and I decided that his decision to not have surgery at this moment was not consistent with his prior decisions, and he could provide no reason for changing his mind. We brought the patient into the operating room and explored him. He did have a large anastomotic leak with a large volume of enteric contents in the peritoneal cavity. He survived the operation and, not unexpectedly, required a long postoperative stay in the hospital. Once he was a few days out, I inquired about whether he was glad that he had surgery. He was quick to state his confidence that it had been the right choice for him. He did not even remember having ever refused the surgery.
Although this case raised many concerns for all of us involved in the patient’s care, one overriding lesson that came through to me. Informed consent should not be viewed as a solitary event, but a conversation. This patient had expressed his desire to have surgery multiple times to my surgical resident and to his family. Even though we should never take the position that patients cannot change their minds, we should carefully question those choices that are inconsistent with the prior discussions that have been undertaken. Good communication skills – including listening to the patient, understanding the patient’s reasoning, and reflecting on the entire conversation – are essential in obtaining informed consent.
Dr. Angelos is the Linda Kohler Anderson Professor of Surgery and Surgical Ethics, chief of endocrine surgery, and associate director of the MacLean Center for Clinical Medical Ethics at the University of Chicago.
Upcoming CPT® Changes
Pulmonary, critical care, and sleep physicians often provide services to patients, as well as consultative services to other health-care professionals, without a patient being present. This can be done via telephone or electronic (internet or electronic health record) communications. Many are not aware that Current Procedural Terminology (CPT®) codes were published to describe and define the work involved in these services. In 2019, there will be additional CPT codes available for health-care workers to use for these non-face-to-face services.
Telephone services are reported using CPT codes 99441-99443 and may be used for evaluation and management (E/M) services provided by telephone for an established patient that do not result in a patient visit within the next 24 hours or are associated with an E/M visit from the last 7 days.
99441 Telephone evaluation and management service by a physician or other qualified health-care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M serv ice provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion
99442 11-20 minutes of medical discussion
99443 21-30 minutes of medical discussion
These codes may not be reported by a provider more frequently than every 7 days. The details of the service should be documented in the medical record.
If the E/M service is prompted by an online patient request, then CPT code 99444 can be used.
99444 Online evaluation and management service provided by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient or guardian, not originating from a related E/M service provided within the previous 7 days, using the internet or similar electronic communications network.
This code may be reported only every 7 days and can not be related to a previous E/M evaluation in the last 7 days or to a previous surgical procedure. The service includes all of the communication (eg, related telephone calls, prescription provision, laboratory orders) pertaining to the online patient encounter.
There are also CPT codes for Interprofessional Telephone/Internet/Electronic Health Record Consultations. These codes are used when one health-care provider requests the opinion and/or treatment advice of another provider (consultant) for either a new or established patient without face-to-face contact between the patient and the consultant.
99446 Interprofessional telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a verbal and written report to the patient’s treating/requesting physician or other qualified health care professional; 5-10 minutes of medical consultative discussion and review.
99447 11-20 minutes of medical consultative discussion and review
99448 21-30 minutes of medical consultative discussion and review
99449 31 minutes or more of medical consultative discussion and review
These codes are not used if the consultant has seen the patient in a face-to-face encounter within the last 14 days or the consultation results in a transfer of care or other face-to-face service with the consultant within the next 14 days. In addition, greater than 50% of the service time reported must be devoted to the medical consultative verbal or internet discussion. The request and reason for telephone/internet/electronic health record consultation by the requesting health-care professional should be documented in the patient’s medical record. After an oral report from the consultant is provided to the treating/requesting physician, a written report should be documented in the medical record. Consultations of less than 5 minutes should not be reported.
As noted, CPT codes 99446-49 require an oral and written report. A new code is added for 2019.
99451 Interprofessional telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a written report to the patient’s treating/requesting physician or other qualified health care professional, 5 minutes or more of medical consultative time.
CPT code 99451 describes a consultative service lasting more than 5 minutes and requires only a written report to the requesting physician. This was added recognizing that oral communications do not always occur between healthcare professionals and may facilitate consultative services in geographic areas with no specialists available.
99452 Interprofessional telephone/Internet/electronic health record referral service(s) provided by a treating/requesting physician or other qualified health care professional, 30 minutes.
CPT code 99452 is reported for 16-30 minutes preparing for the referral and/or communicating with a consultant. If more than 30 minutes is spent by the treating/requesting healthcare provider, then one would use a prolonged services code (99358-59).
As with all coding and billing issues, review the CPT manual for parentheticals that describe coding rules not included in the code description. In addition, not all CPT codes are paid by all providers. Knowledge of payer policies is, therefore, important for appropriate reimbursement.
Pulmonary, critical care, and sleep physicians often provide services to patients, as well as consultative services to other health-care professionals, without a patient being present. This can be done via telephone or electronic (internet or electronic health record) communications. Many are not aware that Current Procedural Terminology (CPT®) codes were published to describe and define the work involved in these services. In 2019, there will be additional CPT codes available for health-care workers to use for these non-face-to-face services.
Telephone services are reported using CPT codes 99441-99443 and may be used for evaluation and management (E/M) services provided by telephone for an established patient that do not result in a patient visit within the next 24 hours or are associated with an E/M visit from the last 7 days.
99441 Telephone evaluation and management service by a physician or other qualified health-care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M serv ice provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion
99442 11-20 minutes of medical discussion
99443 21-30 minutes of medical discussion
These codes may not be reported by a provider more frequently than every 7 days. The details of the service should be documented in the medical record.
If the E/M service is prompted by an online patient request, then CPT code 99444 can be used.
99444 Online evaluation and management service provided by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient or guardian, not originating from a related E/M service provided within the previous 7 days, using the internet or similar electronic communications network.
This code may be reported only every 7 days and can not be related to a previous E/M evaluation in the last 7 days or to a previous surgical procedure. The service includes all of the communication (eg, related telephone calls, prescription provision, laboratory orders) pertaining to the online patient encounter.
There are also CPT codes for Interprofessional Telephone/Internet/Electronic Health Record Consultations. These codes are used when one health-care provider requests the opinion and/or treatment advice of another provider (consultant) for either a new or established patient without face-to-face contact between the patient and the consultant.
99446 Interprofessional telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a verbal and written report to the patient’s treating/requesting physician or other qualified health care professional; 5-10 minutes of medical consultative discussion and review.
99447 11-20 minutes of medical consultative discussion and review
99448 21-30 minutes of medical consultative discussion and review
99449 31 minutes or more of medical consultative discussion and review
These codes are not used if the consultant has seen the patient in a face-to-face encounter within the last 14 days or the consultation results in a transfer of care or other face-to-face service with the consultant within the next 14 days. In addition, greater than 50% of the service time reported must be devoted to the medical consultative verbal or internet discussion. The request and reason for telephone/internet/electronic health record consultation by the requesting health-care professional should be documented in the patient’s medical record. After an oral report from the consultant is provided to the treating/requesting physician, a written report should be documented in the medical record. Consultations of less than 5 minutes should not be reported.
As noted, CPT codes 99446-49 require an oral and written report. A new code is added for 2019.
99451 Interprofessional telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a written report to the patient’s treating/requesting physician or other qualified health care professional, 5 minutes or more of medical consultative time.
CPT code 99451 describes a consultative service lasting more than 5 minutes and requires only a written report to the requesting physician. This was added recognizing that oral communications do not always occur between healthcare professionals and may facilitate consultative services in geographic areas with no specialists available.
99452 Interprofessional telephone/Internet/electronic health record referral service(s) provided by a treating/requesting physician or other qualified health care professional, 30 minutes.
CPT code 99452 is reported for 16-30 minutes preparing for the referral and/or communicating with a consultant. If more than 30 minutes is spent by the treating/requesting healthcare provider, then one would use a prolonged services code (99358-59).
As with all coding and billing issues, review the CPT manual for parentheticals that describe coding rules not included in the code description. In addition, not all CPT codes are paid by all providers. Knowledge of payer policies is, therefore, important for appropriate reimbursement.
Pulmonary, critical care, and sleep physicians often provide services to patients, as well as consultative services to other health-care professionals, without a patient being present. This can be done via telephone or electronic (internet or electronic health record) communications. Many are not aware that Current Procedural Terminology (CPT®) codes were published to describe and define the work involved in these services. In 2019, there will be additional CPT codes available for health-care workers to use for these non-face-to-face services.
Telephone services are reported using CPT codes 99441-99443 and may be used for evaluation and management (E/M) services provided by telephone for an established patient that do not result in a patient visit within the next 24 hours or are associated with an E/M visit from the last 7 days.
99441 Telephone evaluation and management service by a physician or other qualified health-care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M serv ice provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion
99442 11-20 minutes of medical discussion
99443 21-30 minutes of medical discussion
These codes may not be reported by a provider more frequently than every 7 days. The details of the service should be documented in the medical record.
If the E/M service is prompted by an online patient request, then CPT code 99444 can be used.
99444 Online evaluation and management service provided by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient or guardian, not originating from a related E/M service provided within the previous 7 days, using the internet or similar electronic communications network.
This code may be reported only every 7 days and can not be related to a previous E/M evaluation in the last 7 days or to a previous surgical procedure. The service includes all of the communication (eg, related telephone calls, prescription provision, laboratory orders) pertaining to the online patient encounter.
There are also CPT codes for Interprofessional Telephone/Internet/Electronic Health Record Consultations. These codes are used when one health-care provider requests the opinion and/or treatment advice of another provider (consultant) for either a new or established patient without face-to-face contact between the patient and the consultant.
99446 Interprofessional telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a verbal and written report to the patient’s treating/requesting physician or other qualified health care professional; 5-10 minutes of medical consultative discussion and review.
99447 11-20 minutes of medical consultative discussion and review
99448 21-30 minutes of medical consultative discussion and review
99449 31 minutes or more of medical consultative discussion and review
These codes are not used if the consultant has seen the patient in a face-to-face encounter within the last 14 days or the consultation results in a transfer of care or other face-to-face service with the consultant within the next 14 days. In addition, greater than 50% of the service time reported must be devoted to the medical consultative verbal or internet discussion. The request and reason for telephone/internet/electronic health record consultation by the requesting health-care professional should be documented in the patient’s medical record. After an oral report from the consultant is provided to the treating/requesting physician, a written report should be documented in the medical record. Consultations of less than 5 minutes should not be reported.
As noted, CPT codes 99446-49 require an oral and written report. A new code is added for 2019.
99451 Interprofessional telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a written report to the patient’s treating/requesting physician or other qualified health care professional, 5 minutes or more of medical consultative time.
CPT code 99451 describes a consultative service lasting more than 5 minutes and requires only a written report to the requesting physician. This was added recognizing that oral communications do not always occur between healthcare professionals and may facilitate consultative services in geographic areas with no specialists available.
99452 Interprofessional telephone/Internet/electronic health record referral service(s) provided by a treating/requesting physician or other qualified health care professional, 30 minutes.
CPT code 99452 is reported for 16-30 minutes preparing for the referral and/or communicating with a consultant. If more than 30 minutes is spent by the treating/requesting healthcare provider, then one would use a prolonged services code (99358-59).
As with all coding and billing issues, review the CPT manual for parentheticals that describe coding rules not included in the code description. In addition, not all CPT codes are paid by all providers. Knowledge of payer policies is, therefore, important for appropriate reimbursement.
Welcome Dr. Cowl!
As we greet our new CHEST President, Clayton T. Cowl, MD, MS, FCCP, we asked him for a few thoughts about his upcoming presidential year. He kindly offered these responses:
What would be one of the many things you would like to accomplish as President of CHEST?
We plan to increase the engagement of our membership, and, in do so, allow for more opportunities to serve in leadership roles, educate as faculty, or to participate in more of the wide array of educational opportunities within CHEST – whether the member is a long-tenured physician, a trainee, an earlier career researcher or educator, or a colleague in the care team, such as a respiratory therapist, advanced practice provider, or a pharmacist. CHEST has been and will continue to be a leader in delivery of education, and will further advance opportunities to present breaking research. Ultimately, the reason we are in medicine is to improve the care that we deliver to our patients, so it is incumbent upon us to keep the mission aimed toward “patient-centric” goals.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
Our greatest strength is our members, who bring a diversity of experience, expertise, and passion for what they do at the forefront. Together, with our incredibly talented and dedicated support staff at CHEST, as well as our industry and publishing partners, our organization is poised to bring medical education in pulmonary, critical care, and sleep medicine globally to the next level. The CHEST Foundation has stimulated important opportunities for research, increased the ability for younger members to attend meetings and actively engage in CHEST activities, and provided valuable information to patients in a language they can understand. Thanks to advances in technology, there are improved platforms for communicating with our membership and for delivering education in novel and more effective ways than ever before. We plan to double down on our strategic focus of utilizing innovation and new technologies to lead trends in education, influence health-care improvements for our patients and their families, and to deliver the latest in medical education to clinicians and investigators worldwide.
What are some challenges facing CHEST, and how will you address these challenges?
Many of our members are facing challenges in their practices – both domestically and internationally. Industry and employer-based sponsorship to attend meetings has declined, travel remains expensive, and time away from the practice has become more and more difficult for a variety of reasons. Our members are being challenged with greater regulatory and administrative burdens and are bombarded with the demands of work overload. In addition to working with other organizations to identify workplace burnout and, more importantly, to offer better solutions, we are focused on leveraging a variety of new technologies to bring our CHEST brand of quality education to all of our members, regardless of location, and to do so in a way that best suits individual needs. The traditional model of attending a large meeting comprised solely of didactic presentations is, frankly, becoming outdated. CHEST will continue to “tip the apple cart” of worn out educational delivery methods and look toward innovating courses that are more accessible, more effective and relevant, more affordable, and more fun.
And finally, what is your charge to the members and new Fellows of CHEST?
We have each been blessed with the opportunity to serve patients and their families in their times of need. Let’s not forget that privilege as we deliver care each and every day. The word “doctor” comes from an agentive noun of the Latin verb docēre (“to teach”). Regardless of where you practice, what your role is in the health-care paradigm, or whether your contribution is directly with patients or indirectly through research, education, or administration, we are all teachers in various ways to various people. That’s why the American College of Chest Physicians (CHEST) needs to listen to your needs, cultivate your collective wisdom, and continue to be the leading organization within our specialties for delivering medical education and, ultimately, for providing outstanding care and compassion to our patients.
As we greet our new CHEST President, Clayton T. Cowl, MD, MS, FCCP, we asked him for a few thoughts about his upcoming presidential year. He kindly offered these responses:
What would be one of the many things you would like to accomplish as President of CHEST?
We plan to increase the engagement of our membership, and, in do so, allow for more opportunities to serve in leadership roles, educate as faculty, or to participate in more of the wide array of educational opportunities within CHEST – whether the member is a long-tenured physician, a trainee, an earlier career researcher or educator, or a colleague in the care team, such as a respiratory therapist, advanced practice provider, or a pharmacist. CHEST has been and will continue to be a leader in delivery of education, and will further advance opportunities to present breaking research. Ultimately, the reason we are in medicine is to improve the care that we deliver to our patients, so it is incumbent upon us to keep the mission aimed toward “patient-centric” goals.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
Our greatest strength is our members, who bring a diversity of experience, expertise, and passion for what they do at the forefront. Together, with our incredibly talented and dedicated support staff at CHEST, as well as our industry and publishing partners, our organization is poised to bring medical education in pulmonary, critical care, and sleep medicine globally to the next level. The CHEST Foundation has stimulated important opportunities for research, increased the ability for younger members to attend meetings and actively engage in CHEST activities, and provided valuable information to patients in a language they can understand. Thanks to advances in technology, there are improved platforms for communicating with our membership and for delivering education in novel and more effective ways than ever before. We plan to double down on our strategic focus of utilizing innovation and new technologies to lead trends in education, influence health-care improvements for our patients and their families, and to deliver the latest in medical education to clinicians and investigators worldwide.
What are some challenges facing CHEST, and how will you address these challenges?
Many of our members are facing challenges in their practices – both domestically and internationally. Industry and employer-based sponsorship to attend meetings has declined, travel remains expensive, and time away from the practice has become more and more difficult for a variety of reasons. Our members are being challenged with greater regulatory and administrative burdens and are bombarded with the demands of work overload. In addition to working with other organizations to identify workplace burnout and, more importantly, to offer better solutions, we are focused on leveraging a variety of new technologies to bring our CHEST brand of quality education to all of our members, regardless of location, and to do so in a way that best suits individual needs. The traditional model of attending a large meeting comprised solely of didactic presentations is, frankly, becoming outdated. CHEST will continue to “tip the apple cart” of worn out educational delivery methods and look toward innovating courses that are more accessible, more effective and relevant, more affordable, and more fun.
And finally, what is your charge to the members and new Fellows of CHEST?
We have each been blessed with the opportunity to serve patients and their families in their times of need. Let’s not forget that privilege as we deliver care each and every day. The word “doctor” comes from an agentive noun of the Latin verb docēre (“to teach”). Regardless of where you practice, what your role is in the health-care paradigm, or whether your contribution is directly with patients or indirectly through research, education, or administration, we are all teachers in various ways to various people. That’s why the American College of Chest Physicians (CHEST) needs to listen to your needs, cultivate your collective wisdom, and continue to be the leading organization within our specialties for delivering medical education and, ultimately, for providing outstanding care and compassion to our patients.
As we greet our new CHEST President, Clayton T. Cowl, MD, MS, FCCP, we asked him for a few thoughts about his upcoming presidential year. He kindly offered these responses:
What would be one of the many things you would like to accomplish as President of CHEST?
We plan to increase the engagement of our membership, and, in do so, allow for more opportunities to serve in leadership roles, educate as faculty, or to participate in more of the wide array of educational opportunities within CHEST – whether the member is a long-tenured physician, a trainee, an earlier career researcher or educator, or a colleague in the care team, such as a respiratory therapist, advanced practice provider, or a pharmacist. CHEST has been and will continue to be a leader in delivery of education, and will further advance opportunities to present breaking research. Ultimately, the reason we are in medicine is to improve the care that we deliver to our patients, so it is incumbent upon us to keep the mission aimed toward “patient-centric” goals.
What do you consider to be the greatest strength of CHEST, and how will you build upon this during your Presidency?
Our greatest strength is our members, who bring a diversity of experience, expertise, and passion for what they do at the forefront. Together, with our incredibly talented and dedicated support staff at CHEST, as well as our industry and publishing partners, our organization is poised to bring medical education in pulmonary, critical care, and sleep medicine globally to the next level. The CHEST Foundation has stimulated important opportunities for research, increased the ability for younger members to attend meetings and actively engage in CHEST activities, and provided valuable information to patients in a language they can understand. Thanks to advances in technology, there are improved platforms for communicating with our membership and for delivering education in novel and more effective ways than ever before. We plan to double down on our strategic focus of utilizing innovation and new technologies to lead trends in education, influence health-care improvements for our patients and their families, and to deliver the latest in medical education to clinicians and investigators worldwide.
What are some challenges facing CHEST, and how will you address these challenges?
Many of our members are facing challenges in their practices – both domestically and internationally. Industry and employer-based sponsorship to attend meetings has declined, travel remains expensive, and time away from the practice has become more and more difficult for a variety of reasons. Our members are being challenged with greater regulatory and administrative burdens and are bombarded with the demands of work overload. In addition to working with other organizations to identify workplace burnout and, more importantly, to offer better solutions, we are focused on leveraging a variety of new technologies to bring our CHEST brand of quality education to all of our members, regardless of location, and to do so in a way that best suits individual needs. The traditional model of attending a large meeting comprised solely of didactic presentations is, frankly, becoming outdated. CHEST will continue to “tip the apple cart” of worn out educational delivery methods and look toward innovating courses that are more accessible, more effective and relevant, more affordable, and more fun.
And finally, what is your charge to the members and new Fellows of CHEST?
We have each been blessed with the opportunity to serve patients and their families in their times of need. Let’s not forget that privilege as we deliver care each and every day. The word “doctor” comes from an agentive noun of the Latin verb docēre (“to teach”). Regardless of where you practice, what your role is in the health-care paradigm, or whether your contribution is directly with patients or indirectly through research, education, or administration, we are all teachers in various ways to various people. That’s why the American College of Chest Physicians (CHEST) needs to listen to your needs, cultivate your collective wisdom, and continue to be the leading organization within our specialties for delivering medical education and, ultimately, for providing outstanding care and compassion to our patients.
The importance of diversity and inclusion in medicine
Diversity
There is growing appreciation for diversity and inclusion (DI) as drivers of excellence in medicine. CHEST also promotes excellence in medicine. Therefore, it is intuitive that CHEST promote DI. Diversity encompasses differences in gender, race/ethnicity, vocational training, age, sexual orientation, thought processes, etc.
Academic medicine is rich with examples of how diversity is critical to the health of our nation:
– Diverse student populations have been shown to improve our learners’ satisfaction with their educational experience.
– Diverse teams have been shown to be more capable of solving complex problems than homogenous teams.
– Health care is moving toward a team-based, interprofessional model that values the contributions of a range of providers’ perspectives in improving patient outcomes.
– In biomedical research, investigators ask different research questions based on their own background and experiences. This implies that finding solutions to diseases that affect specific populations will require a diverse pool of biomedical researchers.
– Faculty diversity as a key component of excellence for medical education and research has been documented.
Diversity alone doesn’t drive inclusion. Noted diversity advocate, Verna Myers, stated, “Diversity is being invited to the party. Inclusion is being asked to dance.” In my opinion, diversity is the commencement of work, but inclusion helps complete the task.
Inclusion
An inclusive environment values the unique contributions all members bring. Teams with diversity of thought are more innovative as individual members with different backgrounds and points of view bring an extensive range of ideas and creativity to scientific discovery and decision-making processes. Inclusion leverages the power of our unique differences to accomplish our mutual goals. By valuing everyone’s perspective, we demonstrate excellence.
I recommend an article from the Harvard Business Review (HBR Feb 2017). The authors suggest several ways to promote inclusiveness: (1) ensuring team members speak up and are heard; (2) making it safe to propose novel ideas; (3) empowering team members to make decisions; (4) taking advice and implementing feedback; (5) giving actionable feedback; and ( 6) sharing credit for team success. If the team leader possesses at least three of these traits, 87% of team members say they feel welcome and included in their team; 87% say they feel free to express their views and opinions; and 74% say they feel that their ideas are heard and recognized. If the team leader possessed none of these traits, those percentages dropped to 51%, 46%, and 37%, respectively. I believe this concept is applicable in medicine also.
Sponsors
What can we do to advance diversity and inclusion individually and in our individual institutions? A sponsor is a senior level leader who advocates for key assignments, promotes for and puts his or her reputation on the line for the protégé’s advancement. This invigorates and drives engagement. One key to rising above the playing field for women and people of color is sponsorship. Being a sponsor does not mean one would recommend someone who is not qualified. It means one recommends or supports those who are capable of doing the job but would not otherwise be given the opportunity.
Ask yourself: Have I served as a sponsor? What would prevent me from being a sponsor? Do I believe in this concept?
Cause for Alarm
Numerous publications have recently discussed the crisis of the decline of black men entering medicine. In 1978, there were 1,410 black male applicants to medical school, and in 2014, there were 1,337. Additionally, the number of black male matriculants to medical school over more than 35 years has not surpassed the 1978 numbers. In 1978, there were 542 black male matriculants, and in 2014, there were 515 (J of Racial and Ethnic Health Disparities. 2017, 4:317-321). This report is thorough and insightful and illustrates the work that we must do to help improve this situation.
Dr. Marc Nivet, Association of American Medical Colleges (AAMC) Chief Diversity Officer, stated “No other minority group has experienced such declines. The inability to find, engage, and develop candidates for careers in medicine from all members of our society limits our ability to improve health care for all.” I recommend you read the 2015 AAMC publication entitled: Altering the Course: Black Males in Medicine.
Health-care Disparities
Research suggests that the overall health of Americans has improved; however, disparities continue to persist among many populations within the United States. Racial and ethnic minority populations have poorer access to care and worse outcomes than their white counterparts. Approximately 20% of the nation living in rural areas is less likely than those living in urban areas to receive preventive care and more likely to experience language barriers.
Individuals identifying as lesbian, gay, bisexual, or transgender are likely to experience discrimination in health-care settings. These individuals often face insurance-based barriers and are less likely to have a usual source of care than patients who identify as straight.
A 2002 report by the Institute of Medicine entitled: Unequal Treatment: What Healthcare Providers Need to Know about Racial and Ethnic Disparities in Healthcare is revealing. Salient information reported is: It is generally accepted that a diverse workforce is a key component in the delivery of quality, competent care throughout the nation. Physicians from racial and ethnic backgrounds typically underrepresented in medicine are significantly more likely to practice primary care than white physicians and are more likely to practice in impoverished and medically underserved areas. Diversity in the physician workforce impacts the quality of care received by patients. Race concordance between patient and physician results in longer visits and increased patient satisfaction, and language concordance is positively associated with adherence to treatment among certain racial or ethnic groups.
Improving the patient experience or quality of care received also requires attention to education and training on cultural competence. By weaving together a diverse and culturally responsive pool of physicians working collaboratively with other health-care professionals, access and quality of care can improve throughout the nation.
CHEST cannot attain more racial diversity in our organization if we don’t have this diversity in medical education and training. This is why CHEST must be actively involved in addressing these issues.
Unconscious Bias
Despite many examples of how diversity enriches the quality of health care and health research, there is still much work to be done to address the human biases that impede our ability to benefit from diversity in medicine. While academic medicine has made progress toward addressing overt discrimination, unconscious bias (implicit bias) represents another threat. Unconscious bias describes the prejudices we don’t know we have. While unconscious biases vary from person to person, we all possess them. The existence of unconscious bias in academic medicine, while uncomfortable and unsettling, is a reality. The AAMC developed an unconscious bias learning lab for the health professions and produced an oft-cited video about addressing unconscious bias in the faculty advancement, promotion, and tenure process. We must consider this and other ways in which we can help promote the acknowledgment of unconscious bias. The CHEST staff have undergone unconscious bias training, and I recommend it for all faculty in academic medicine.
Summary
Diversity and inclusion in medicine is of paramount importance. It leads to better patient care and better trainee education and will decrease health-care disparities. Progress has been made, but there is more work to be done.
CHEST is supportive of these efforts and has worked on this previously and with a renewed push in the past 2 years with the DI Task Force initially and, now, the DI Roundtable, which has representatives from each of the standing committees, including the Board of Regents. This roundtable group will help advance the DI initiatives of the organization. I ask that each person reading this article consider what we as individuals can do in helping make DI in medicine a priority.
Dr. Haynes is Professor of Medicine at The University of Mississippi Medical Center in Jackson, MS. He is also the Executive Vice Chair of the Department of Medicine. At CHEST, he is a member of the training and transitions committee, executive scientific program committee, former chair of the diversity and inclusion task force, and is the current chair of the diversity and inclusion roundtable.
Diversity
There is growing appreciation for diversity and inclusion (DI) as drivers of excellence in medicine. CHEST also promotes excellence in medicine. Therefore, it is intuitive that CHEST promote DI. Diversity encompasses differences in gender, race/ethnicity, vocational training, age, sexual orientation, thought processes, etc.
Academic medicine is rich with examples of how diversity is critical to the health of our nation:
– Diverse student populations have been shown to improve our learners’ satisfaction with their educational experience.
– Diverse teams have been shown to be more capable of solving complex problems than homogenous teams.
– Health care is moving toward a team-based, interprofessional model that values the contributions of a range of providers’ perspectives in improving patient outcomes.
– In biomedical research, investigators ask different research questions based on their own background and experiences. This implies that finding solutions to diseases that affect specific populations will require a diverse pool of biomedical researchers.
– Faculty diversity as a key component of excellence for medical education and research has been documented.
Diversity alone doesn’t drive inclusion. Noted diversity advocate, Verna Myers, stated, “Diversity is being invited to the party. Inclusion is being asked to dance.” In my opinion, diversity is the commencement of work, but inclusion helps complete the task.
Inclusion
An inclusive environment values the unique contributions all members bring. Teams with diversity of thought are more innovative as individual members with different backgrounds and points of view bring an extensive range of ideas and creativity to scientific discovery and decision-making processes. Inclusion leverages the power of our unique differences to accomplish our mutual goals. By valuing everyone’s perspective, we demonstrate excellence.
I recommend an article from the Harvard Business Review (HBR Feb 2017). The authors suggest several ways to promote inclusiveness: (1) ensuring team members speak up and are heard; (2) making it safe to propose novel ideas; (3) empowering team members to make decisions; (4) taking advice and implementing feedback; (5) giving actionable feedback; and ( 6) sharing credit for team success. If the team leader possesses at least three of these traits, 87% of team members say they feel welcome and included in their team; 87% say they feel free to express their views and opinions; and 74% say they feel that their ideas are heard and recognized. If the team leader possessed none of these traits, those percentages dropped to 51%, 46%, and 37%, respectively. I believe this concept is applicable in medicine also.
Sponsors
What can we do to advance diversity and inclusion individually and in our individual institutions? A sponsor is a senior level leader who advocates for key assignments, promotes for and puts his or her reputation on the line for the protégé’s advancement. This invigorates and drives engagement. One key to rising above the playing field for women and people of color is sponsorship. Being a sponsor does not mean one would recommend someone who is not qualified. It means one recommends or supports those who are capable of doing the job but would not otherwise be given the opportunity.
Ask yourself: Have I served as a sponsor? What would prevent me from being a sponsor? Do I believe in this concept?
Cause for Alarm
Numerous publications have recently discussed the crisis of the decline of black men entering medicine. In 1978, there were 1,410 black male applicants to medical school, and in 2014, there were 1,337. Additionally, the number of black male matriculants to medical school over more than 35 years has not surpassed the 1978 numbers. In 1978, there were 542 black male matriculants, and in 2014, there were 515 (J of Racial and Ethnic Health Disparities. 2017, 4:317-321). This report is thorough and insightful and illustrates the work that we must do to help improve this situation.
Dr. Marc Nivet, Association of American Medical Colleges (AAMC) Chief Diversity Officer, stated “No other minority group has experienced such declines. The inability to find, engage, and develop candidates for careers in medicine from all members of our society limits our ability to improve health care for all.” I recommend you read the 2015 AAMC publication entitled: Altering the Course: Black Males in Medicine.
Health-care Disparities
Research suggests that the overall health of Americans has improved; however, disparities continue to persist among many populations within the United States. Racial and ethnic minority populations have poorer access to care and worse outcomes than their white counterparts. Approximately 20% of the nation living in rural areas is less likely than those living in urban areas to receive preventive care and more likely to experience language barriers.
Individuals identifying as lesbian, gay, bisexual, or transgender are likely to experience discrimination in health-care settings. These individuals often face insurance-based barriers and are less likely to have a usual source of care than patients who identify as straight.
A 2002 report by the Institute of Medicine entitled: Unequal Treatment: What Healthcare Providers Need to Know about Racial and Ethnic Disparities in Healthcare is revealing. Salient information reported is: It is generally accepted that a diverse workforce is a key component in the delivery of quality, competent care throughout the nation. Physicians from racial and ethnic backgrounds typically underrepresented in medicine are significantly more likely to practice primary care than white physicians and are more likely to practice in impoverished and medically underserved areas. Diversity in the physician workforce impacts the quality of care received by patients. Race concordance between patient and physician results in longer visits and increased patient satisfaction, and language concordance is positively associated with adherence to treatment among certain racial or ethnic groups.
Improving the patient experience or quality of care received also requires attention to education and training on cultural competence. By weaving together a diverse and culturally responsive pool of physicians working collaboratively with other health-care professionals, access and quality of care can improve throughout the nation.
CHEST cannot attain more racial diversity in our organization if we don’t have this diversity in medical education and training. This is why CHEST must be actively involved in addressing these issues.
Unconscious Bias
Despite many examples of how diversity enriches the quality of health care and health research, there is still much work to be done to address the human biases that impede our ability to benefit from diversity in medicine. While academic medicine has made progress toward addressing overt discrimination, unconscious bias (implicit bias) represents another threat. Unconscious bias describes the prejudices we don’t know we have. While unconscious biases vary from person to person, we all possess them. The existence of unconscious bias in academic medicine, while uncomfortable and unsettling, is a reality. The AAMC developed an unconscious bias learning lab for the health professions and produced an oft-cited video about addressing unconscious bias in the faculty advancement, promotion, and tenure process. We must consider this and other ways in which we can help promote the acknowledgment of unconscious bias. The CHEST staff have undergone unconscious bias training, and I recommend it for all faculty in academic medicine.
Summary
Diversity and inclusion in medicine is of paramount importance. It leads to better patient care and better trainee education and will decrease health-care disparities. Progress has been made, but there is more work to be done.
CHEST is supportive of these efforts and has worked on this previously and with a renewed push in the past 2 years with the DI Task Force initially and, now, the DI Roundtable, which has representatives from each of the standing committees, including the Board of Regents. This roundtable group will help advance the DI initiatives of the organization. I ask that each person reading this article consider what we as individuals can do in helping make DI in medicine a priority.
Dr. Haynes is Professor of Medicine at The University of Mississippi Medical Center in Jackson, MS. He is also the Executive Vice Chair of the Department of Medicine. At CHEST, he is a member of the training and transitions committee, executive scientific program committee, former chair of the diversity and inclusion task force, and is the current chair of the diversity and inclusion roundtable.
Diversity
There is growing appreciation for diversity and inclusion (DI) as drivers of excellence in medicine. CHEST also promotes excellence in medicine. Therefore, it is intuitive that CHEST promote DI. Diversity encompasses differences in gender, race/ethnicity, vocational training, age, sexual orientation, thought processes, etc.
Academic medicine is rich with examples of how diversity is critical to the health of our nation:
– Diverse student populations have been shown to improve our learners’ satisfaction with their educational experience.
– Diverse teams have been shown to be more capable of solving complex problems than homogenous teams.
– Health care is moving toward a team-based, interprofessional model that values the contributions of a range of providers’ perspectives in improving patient outcomes.
– In biomedical research, investigators ask different research questions based on their own background and experiences. This implies that finding solutions to diseases that affect specific populations will require a diverse pool of biomedical researchers.
– Faculty diversity as a key component of excellence for medical education and research has been documented.
Diversity alone doesn’t drive inclusion. Noted diversity advocate, Verna Myers, stated, “Diversity is being invited to the party. Inclusion is being asked to dance.” In my opinion, diversity is the commencement of work, but inclusion helps complete the task.
Inclusion
An inclusive environment values the unique contributions all members bring. Teams with diversity of thought are more innovative as individual members with different backgrounds and points of view bring an extensive range of ideas and creativity to scientific discovery and decision-making processes. Inclusion leverages the power of our unique differences to accomplish our mutual goals. By valuing everyone’s perspective, we demonstrate excellence.
I recommend an article from the Harvard Business Review (HBR Feb 2017). The authors suggest several ways to promote inclusiveness: (1) ensuring team members speak up and are heard; (2) making it safe to propose novel ideas; (3) empowering team members to make decisions; (4) taking advice and implementing feedback; (5) giving actionable feedback; and ( 6) sharing credit for team success. If the team leader possesses at least three of these traits, 87% of team members say they feel welcome and included in their team; 87% say they feel free to express their views and opinions; and 74% say they feel that their ideas are heard and recognized. If the team leader possessed none of these traits, those percentages dropped to 51%, 46%, and 37%, respectively. I believe this concept is applicable in medicine also.
Sponsors
What can we do to advance diversity and inclusion individually and in our individual institutions? A sponsor is a senior level leader who advocates for key assignments, promotes for and puts his or her reputation on the line for the protégé’s advancement. This invigorates and drives engagement. One key to rising above the playing field for women and people of color is sponsorship. Being a sponsor does not mean one would recommend someone who is not qualified. It means one recommends or supports those who are capable of doing the job but would not otherwise be given the opportunity.
Ask yourself: Have I served as a sponsor? What would prevent me from being a sponsor? Do I believe in this concept?
Cause for Alarm
Numerous publications have recently discussed the crisis of the decline of black men entering medicine. In 1978, there were 1,410 black male applicants to medical school, and in 2014, there were 1,337. Additionally, the number of black male matriculants to medical school over more than 35 years has not surpassed the 1978 numbers. In 1978, there were 542 black male matriculants, and in 2014, there were 515 (J of Racial and Ethnic Health Disparities. 2017, 4:317-321). This report is thorough and insightful and illustrates the work that we must do to help improve this situation.
Dr. Marc Nivet, Association of American Medical Colleges (AAMC) Chief Diversity Officer, stated “No other minority group has experienced such declines. The inability to find, engage, and develop candidates for careers in medicine from all members of our society limits our ability to improve health care for all.” I recommend you read the 2015 AAMC publication entitled: Altering the Course: Black Males in Medicine.
Health-care Disparities
Research suggests that the overall health of Americans has improved; however, disparities continue to persist among many populations within the United States. Racial and ethnic minority populations have poorer access to care and worse outcomes than their white counterparts. Approximately 20% of the nation living in rural areas is less likely than those living in urban areas to receive preventive care and more likely to experience language barriers.
Individuals identifying as lesbian, gay, bisexual, or transgender are likely to experience discrimination in health-care settings. These individuals often face insurance-based barriers and are less likely to have a usual source of care than patients who identify as straight.
A 2002 report by the Institute of Medicine entitled: Unequal Treatment: What Healthcare Providers Need to Know about Racial and Ethnic Disparities in Healthcare is revealing. Salient information reported is: It is generally accepted that a diverse workforce is a key component in the delivery of quality, competent care throughout the nation. Physicians from racial and ethnic backgrounds typically underrepresented in medicine are significantly more likely to practice primary care than white physicians and are more likely to practice in impoverished and medically underserved areas. Diversity in the physician workforce impacts the quality of care received by patients. Race concordance between patient and physician results in longer visits and increased patient satisfaction, and language concordance is positively associated with adherence to treatment among certain racial or ethnic groups.
Improving the patient experience or quality of care received also requires attention to education and training on cultural competence. By weaving together a diverse and culturally responsive pool of physicians working collaboratively with other health-care professionals, access and quality of care can improve throughout the nation.
CHEST cannot attain more racial diversity in our organization if we don’t have this diversity in medical education and training. This is why CHEST must be actively involved in addressing these issues.
Unconscious Bias
Despite many examples of how diversity enriches the quality of health care and health research, there is still much work to be done to address the human biases that impede our ability to benefit from diversity in medicine. While academic medicine has made progress toward addressing overt discrimination, unconscious bias (implicit bias) represents another threat. Unconscious bias describes the prejudices we don’t know we have. While unconscious biases vary from person to person, we all possess them. The existence of unconscious bias in academic medicine, while uncomfortable and unsettling, is a reality. The AAMC developed an unconscious bias learning lab for the health professions and produced an oft-cited video about addressing unconscious bias in the faculty advancement, promotion, and tenure process. We must consider this and other ways in which we can help promote the acknowledgment of unconscious bias. The CHEST staff have undergone unconscious bias training, and I recommend it for all faculty in academic medicine.
Summary
Diversity and inclusion in medicine is of paramount importance. It leads to better patient care and better trainee education and will decrease health-care disparities. Progress has been made, but there is more work to be done.
CHEST is supportive of these efforts and has worked on this previously and with a renewed push in the past 2 years with the DI Task Force initially and, now, the DI Roundtable, which has representatives from each of the standing committees, including the Board of Regents. This roundtable group will help advance the DI initiatives of the organization. I ask that each person reading this article consider what we as individuals can do in helping make DI in medicine a priority.
Dr. Haynes is Professor of Medicine at The University of Mississippi Medical Center in Jackson, MS. He is also the Executive Vice Chair of the Department of Medicine. At CHEST, he is a member of the training and transitions committee, executive scientific program committee, former chair of the diversity and inclusion task force, and is the current chair of the diversity and inclusion roundtable.