User login
Study: Problems persist with APMs
Physicians continue to support advanced alternative payment models despite the fact that operational issues have not improved over the last 4 years and new ones have cropped up, according to a follow-up survey conducted by the RAND Corporation for the American Medical Association.
“All the things we heard in 2014 were still present in 2018. Both the challenges that practices had experienced back in 2014 having to do with data timeliness, data completeness and accuracy, payment model execution, all those challenges persisted,” Mark W. Friedberg, MD, senior physician policy researcher at RAND, said in an interview.
RAND surveyed 31 practices of varying practice size and specialty across six geographic regions, some of which participated in the 2014 survey. Supplemental information was provided by interviews with 32 market observers, 8 health plan leaders, 10 hospital and hospital system leaders, 10 state and local medical society leaders, and 4 chapter leaders with MGMA (formerly the Medical Group Management Association).
“We had thought we would hear that the problem had gotten a little bit better since there has been some investment in trying to tamp down the wide range of measures that are involved in these alternative payment models,” Dr. Friedberg said. “We did not see any evidence of that having any effect on the practices that participated in this study this time around.”
Indeed, concerns reported in 2014 were again reported in 2018, along with a new set of concerns, including the perceived pace of change in alternative payment models (APMs), the complexity of APMs, and physician concerns over two-sided risk models.
“Practices, especially those that participated both times, said in 2014 we had these challenges [of rapid changes in APM models] and since then, things have just gotten a lot faster,” he said, noting that doctors are complaining of models that are going through changes, sometimes without much warning. “They are changing quite rapidly from year to year. If you look at the MACRA QPP [Quality Payment Program] for example, that model changes every year to some extent and those things are hard for them to keep up with.”
Running hand in hand with the change is the complexity of the changes, a result of expanding performance measures and uncertainty with thresholds for penalties and rewards and in some ways has had little impact on improving care.
Dr. Friedberg noted that some practices are hiring people to examine APMs to devise strategic ways to choose and report data for maximum return.
“In a practice, for example, if their quality of care was already very good, what these folks ended up doing was help them choose measures and work the attribution algorithms in a strategic way to either guarantee a bonus or minimize the risk of incurring a penalty,” he said.
He also noted that practices appear to becoming more risk averse.
“We heard a lot more of the following thing, which is that if [practices] were in a two-sided risk model, several of them reported trying and succeeding in some cases offloading the downside risk to partners,” Dr. Friedberg reported. “And what this resulted in was that the practice, even though from the payer’s perspective they are in a two-sided model, the practice was actually in a one-sided model with a partner who is taking all of the downside risk and a portion of the upside risk, leaving a small upside risk proposition that remained for the practice.”
He said the range of partners that were absorbing the downside risk included hospitals, device manufacturers, consulting companies, or private equity firms.
Despite the concerns surrounding APMs, Dr. Friedberg said that “we did not hear practices broadly saying that they just weren’t interested in alternative payment models. In general, practices still remained pretty enthusiastic about these alternative payment models in theory. If they could be made simpler, if the pace of change weren’t quite so fast, that they would have a chance to really do some important care improvements in alternative payment models.”
He noted some of the surveyed practices were able to make investments in care as a direct result of participating in APMs, such as in behavioral health capabilities in primary care, for example, leading to quality of care improvements.
However, these issues could reveal a future unwillingness to participate in APMs, especially two-sided risk models, something at least the Centers for Medicare & Medicaid Services are pushing for as a stated goal of the QPP is to get practices to participate in APMs and take on more risk.
The growing aversion to taking on downside risk could lead practices to simply stay in fee for service and simply take the payment penalty because it is a fixed amount that can be planned for, as opposed to the fluctuations of bonuses and penalties that comes with a rapidly changing APM environment, Dr. Friedberg said.
Going forward, the report makes a number of recommendations to help create an environment that would potentially make APMs more successful, including simplifying the models; creating stable, predictable, and moderately paced pathways to APM participation; making data available in a more timely fashion; minimizing downside risk or helping practices better manage it; and designing APMs that will encourage clinical changes to help improve the effectiveness of care delivered.
Physicians continue to support advanced alternative payment models despite the fact that operational issues have not improved over the last 4 years and new ones have cropped up, according to a follow-up survey conducted by the RAND Corporation for the American Medical Association.
“All the things we heard in 2014 were still present in 2018. Both the challenges that practices had experienced back in 2014 having to do with data timeliness, data completeness and accuracy, payment model execution, all those challenges persisted,” Mark W. Friedberg, MD, senior physician policy researcher at RAND, said in an interview.
RAND surveyed 31 practices of varying practice size and specialty across six geographic regions, some of which participated in the 2014 survey. Supplemental information was provided by interviews with 32 market observers, 8 health plan leaders, 10 hospital and hospital system leaders, 10 state and local medical society leaders, and 4 chapter leaders with MGMA (formerly the Medical Group Management Association).
“We had thought we would hear that the problem had gotten a little bit better since there has been some investment in trying to tamp down the wide range of measures that are involved in these alternative payment models,” Dr. Friedberg said. “We did not see any evidence of that having any effect on the practices that participated in this study this time around.”
Indeed, concerns reported in 2014 were again reported in 2018, along with a new set of concerns, including the perceived pace of change in alternative payment models (APMs), the complexity of APMs, and physician concerns over two-sided risk models.
“Practices, especially those that participated both times, said in 2014 we had these challenges [of rapid changes in APM models] and since then, things have just gotten a lot faster,” he said, noting that doctors are complaining of models that are going through changes, sometimes without much warning. “They are changing quite rapidly from year to year. If you look at the MACRA QPP [Quality Payment Program] for example, that model changes every year to some extent and those things are hard for them to keep up with.”
Running hand in hand with the change is the complexity of the changes, a result of expanding performance measures and uncertainty with thresholds for penalties and rewards and in some ways has had little impact on improving care.
Dr. Friedberg noted that some practices are hiring people to examine APMs to devise strategic ways to choose and report data for maximum return.
“In a practice, for example, if their quality of care was already very good, what these folks ended up doing was help them choose measures and work the attribution algorithms in a strategic way to either guarantee a bonus or minimize the risk of incurring a penalty,” he said.
He also noted that practices appear to becoming more risk averse.
“We heard a lot more of the following thing, which is that if [practices] were in a two-sided risk model, several of them reported trying and succeeding in some cases offloading the downside risk to partners,” Dr. Friedberg reported. “And what this resulted in was that the practice, even though from the payer’s perspective they are in a two-sided model, the practice was actually in a one-sided model with a partner who is taking all of the downside risk and a portion of the upside risk, leaving a small upside risk proposition that remained for the practice.”
He said the range of partners that were absorbing the downside risk included hospitals, device manufacturers, consulting companies, or private equity firms.
Despite the concerns surrounding APMs, Dr. Friedberg said that “we did not hear practices broadly saying that they just weren’t interested in alternative payment models. In general, practices still remained pretty enthusiastic about these alternative payment models in theory. If they could be made simpler, if the pace of change weren’t quite so fast, that they would have a chance to really do some important care improvements in alternative payment models.”
He noted some of the surveyed practices were able to make investments in care as a direct result of participating in APMs, such as in behavioral health capabilities in primary care, for example, leading to quality of care improvements.
However, these issues could reveal a future unwillingness to participate in APMs, especially two-sided risk models, something at least the Centers for Medicare & Medicaid Services are pushing for as a stated goal of the QPP is to get practices to participate in APMs and take on more risk.
The growing aversion to taking on downside risk could lead practices to simply stay in fee for service and simply take the payment penalty because it is a fixed amount that can be planned for, as opposed to the fluctuations of bonuses and penalties that comes with a rapidly changing APM environment, Dr. Friedberg said.
Going forward, the report makes a number of recommendations to help create an environment that would potentially make APMs more successful, including simplifying the models; creating stable, predictable, and moderately paced pathways to APM participation; making data available in a more timely fashion; minimizing downside risk or helping practices better manage it; and designing APMs that will encourage clinical changes to help improve the effectiveness of care delivered.
Physicians continue to support advanced alternative payment models despite the fact that operational issues have not improved over the last 4 years and new ones have cropped up, according to a follow-up survey conducted by the RAND Corporation for the American Medical Association.
“All the things we heard in 2014 were still present in 2018. Both the challenges that practices had experienced back in 2014 having to do with data timeliness, data completeness and accuracy, payment model execution, all those challenges persisted,” Mark W. Friedberg, MD, senior physician policy researcher at RAND, said in an interview.
RAND surveyed 31 practices of varying practice size and specialty across six geographic regions, some of which participated in the 2014 survey. Supplemental information was provided by interviews with 32 market observers, 8 health plan leaders, 10 hospital and hospital system leaders, 10 state and local medical society leaders, and 4 chapter leaders with MGMA (formerly the Medical Group Management Association).
“We had thought we would hear that the problem had gotten a little bit better since there has been some investment in trying to tamp down the wide range of measures that are involved in these alternative payment models,” Dr. Friedberg said. “We did not see any evidence of that having any effect on the practices that participated in this study this time around.”
Indeed, concerns reported in 2014 were again reported in 2018, along with a new set of concerns, including the perceived pace of change in alternative payment models (APMs), the complexity of APMs, and physician concerns over two-sided risk models.
“Practices, especially those that participated both times, said in 2014 we had these challenges [of rapid changes in APM models] and since then, things have just gotten a lot faster,” he said, noting that doctors are complaining of models that are going through changes, sometimes without much warning. “They are changing quite rapidly from year to year. If you look at the MACRA QPP [Quality Payment Program] for example, that model changes every year to some extent and those things are hard for them to keep up with.”
Running hand in hand with the change is the complexity of the changes, a result of expanding performance measures and uncertainty with thresholds for penalties and rewards and in some ways has had little impact on improving care.
Dr. Friedberg noted that some practices are hiring people to examine APMs to devise strategic ways to choose and report data for maximum return.
“In a practice, for example, if their quality of care was already very good, what these folks ended up doing was help them choose measures and work the attribution algorithms in a strategic way to either guarantee a bonus or minimize the risk of incurring a penalty,” he said.
He also noted that practices appear to becoming more risk averse.
“We heard a lot more of the following thing, which is that if [practices] were in a two-sided risk model, several of them reported trying and succeeding in some cases offloading the downside risk to partners,” Dr. Friedberg reported. “And what this resulted in was that the practice, even though from the payer’s perspective they are in a two-sided model, the practice was actually in a one-sided model with a partner who is taking all of the downside risk and a portion of the upside risk, leaving a small upside risk proposition that remained for the practice.”
He said the range of partners that were absorbing the downside risk included hospitals, device manufacturers, consulting companies, or private equity firms.
Despite the concerns surrounding APMs, Dr. Friedberg said that “we did not hear practices broadly saying that they just weren’t interested in alternative payment models. In general, practices still remained pretty enthusiastic about these alternative payment models in theory. If they could be made simpler, if the pace of change weren’t quite so fast, that they would have a chance to really do some important care improvements in alternative payment models.”
He noted some of the surveyed practices were able to make investments in care as a direct result of participating in APMs, such as in behavioral health capabilities in primary care, for example, leading to quality of care improvements.
However, these issues could reveal a future unwillingness to participate in APMs, especially two-sided risk models, something at least the Centers for Medicare & Medicaid Services are pushing for as a stated goal of the QPP is to get practices to participate in APMs and take on more risk.
The growing aversion to taking on downside risk could lead practices to simply stay in fee for service and simply take the payment penalty because it is a fixed amount that can be planned for, as opposed to the fluctuations of bonuses and penalties that comes with a rapidly changing APM environment, Dr. Friedberg said.
Going forward, the report makes a number of recommendations to help create an environment that would potentially make APMs more successful, including simplifying the models; creating stable, predictable, and moderately paced pathways to APM participation; making data available in a more timely fashion; minimizing downside risk or helping practices better manage it; and designing APMs that will encourage clinical changes to help improve the effectiveness of care delivered.
Case review: Posttransplant lupus nephritis recurrence rates declining
CHICAGO – Lupus nephritis recurrence rates in kidney transplant recipients declined over the past decade, compared with rates seen in earlier studies, according to a review of cases at the University of Tennessee Health Science Center (UTHSC).
The findings are likely related to improvements in posttransplant immunosuppressive regimens, and may have implications for the timing of transplant going forward, Debendra N. Pattanaik, MD, said at the annual meeting of the American College of Rheumatology.
The biopsy-proven recurrence rate in 38 transplant recipients who received standard immunosuppression with prednisone, tacrolimus, and mycophenolate mofetil was 11%, and graft loss or death occurred in 26% at a median follow-up of 1,230 days, said Dr. Pattanaik, a rheumatologist at UTHSC, Memphis.
Patients with recurrence showed a trend for increased risk for graft loss or death, compared with recipients without recurrence (hazard ratio = 3.14), he noted during a press briefing at the meeting.
Lupus nephritis is a severe complication occurring in more than half of all patients with systemic lupus erythematosus (SLE), and despite a great deal of progress over the years, 10%-30% develop end-stage renal disease and require dialysis and/or transplant, he said, noting that studies have shown that transplant recipients do better over time than do those who remain on dialysis.
“So renal transplant is an important modality of treatment for end-stage renal disease from lupus nephritis,” he added.
However, recurrence of lupus nephritis in the graft is a concern, he said.
In previous eras – prior to improvements in immunosuppressive regimens for transplant recipients – studies showed variable rates of lupus nephritis recurrence, with some reporting rates up to 50% depending on the patient populations and protocols, he noted.
The rates in recent years at UTHSC seemed lower than that, so he and his colleagues looked more closely at the outcomes.
Case patients included all those with end-stage renal disease secondary to lupus nephritis who were transplanted between 2006 and 2017 at the center. Medical records of all 38 were reviewed along with information from the United Network for Organ Sharing Network. The mean age of the patients at baseline was 42 years, 89% were women, 89% were African American, and previous time on dialysis was a median of 4 years. Most (80%) received hemodialysis, and nearly one-third (31%) received living donor transplantation, Dr. Pattanaik said.
The main difference in the past decade compared with those previous eras is the use of posttransplant immunosuppressive regimens consisting of tacrolimus and mycophenolate mofetil rather than cyclosporine and azathioprine in addition to prednisone, he explained.
Previous reports showing higher recurrence rates were from studies in which patients received cyclosporine and azathioprine as part of the posttransplant regimen, he said.
“Our next question is whether patients can be transplanted early,” he said, explaining that transplant is often delayed for many months or years until SLE is in remission, but if the new regimens are reducing recurrence risk, early transplant may be feasible.
Dr. Pattanaik reported having no disclosures.
SOURCE: Pattanaik D et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 711.
CHICAGO – Lupus nephritis recurrence rates in kidney transplant recipients declined over the past decade, compared with rates seen in earlier studies, according to a review of cases at the University of Tennessee Health Science Center (UTHSC).
The findings are likely related to improvements in posttransplant immunosuppressive regimens, and may have implications for the timing of transplant going forward, Debendra N. Pattanaik, MD, said at the annual meeting of the American College of Rheumatology.
The biopsy-proven recurrence rate in 38 transplant recipients who received standard immunosuppression with prednisone, tacrolimus, and mycophenolate mofetil was 11%, and graft loss or death occurred in 26% at a median follow-up of 1,230 days, said Dr. Pattanaik, a rheumatologist at UTHSC, Memphis.
Patients with recurrence showed a trend for increased risk for graft loss or death, compared with recipients without recurrence (hazard ratio = 3.14), he noted during a press briefing at the meeting.
Lupus nephritis is a severe complication occurring in more than half of all patients with systemic lupus erythematosus (SLE), and despite a great deal of progress over the years, 10%-30% develop end-stage renal disease and require dialysis and/or transplant, he said, noting that studies have shown that transplant recipients do better over time than do those who remain on dialysis.
“So renal transplant is an important modality of treatment for end-stage renal disease from lupus nephritis,” he added.
However, recurrence of lupus nephritis in the graft is a concern, he said.
In previous eras – prior to improvements in immunosuppressive regimens for transplant recipients – studies showed variable rates of lupus nephritis recurrence, with some reporting rates up to 50% depending on the patient populations and protocols, he noted.
The rates in recent years at UTHSC seemed lower than that, so he and his colleagues looked more closely at the outcomes.
Case patients included all those with end-stage renal disease secondary to lupus nephritis who were transplanted between 2006 and 2017 at the center. Medical records of all 38 were reviewed along with information from the United Network for Organ Sharing Network. The mean age of the patients at baseline was 42 years, 89% were women, 89% were African American, and previous time on dialysis was a median of 4 years. Most (80%) received hemodialysis, and nearly one-third (31%) received living donor transplantation, Dr. Pattanaik said.
The main difference in the past decade compared with those previous eras is the use of posttransplant immunosuppressive regimens consisting of tacrolimus and mycophenolate mofetil rather than cyclosporine and azathioprine in addition to prednisone, he explained.
Previous reports showing higher recurrence rates were from studies in which patients received cyclosporine and azathioprine as part of the posttransplant regimen, he said.
“Our next question is whether patients can be transplanted early,” he said, explaining that transplant is often delayed for many months or years until SLE is in remission, but if the new regimens are reducing recurrence risk, early transplant may be feasible.
Dr. Pattanaik reported having no disclosures.
SOURCE: Pattanaik D et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 711.
CHICAGO – Lupus nephritis recurrence rates in kidney transplant recipients declined over the past decade, compared with rates seen in earlier studies, according to a review of cases at the University of Tennessee Health Science Center (UTHSC).
The findings are likely related to improvements in posttransplant immunosuppressive regimens, and may have implications for the timing of transplant going forward, Debendra N. Pattanaik, MD, said at the annual meeting of the American College of Rheumatology.
The biopsy-proven recurrence rate in 38 transplant recipients who received standard immunosuppression with prednisone, tacrolimus, and mycophenolate mofetil was 11%, and graft loss or death occurred in 26% at a median follow-up of 1,230 days, said Dr. Pattanaik, a rheumatologist at UTHSC, Memphis.
Patients with recurrence showed a trend for increased risk for graft loss or death, compared with recipients without recurrence (hazard ratio = 3.14), he noted during a press briefing at the meeting.
Lupus nephritis is a severe complication occurring in more than half of all patients with systemic lupus erythematosus (SLE), and despite a great deal of progress over the years, 10%-30% develop end-stage renal disease and require dialysis and/or transplant, he said, noting that studies have shown that transplant recipients do better over time than do those who remain on dialysis.
“So renal transplant is an important modality of treatment for end-stage renal disease from lupus nephritis,” he added.
However, recurrence of lupus nephritis in the graft is a concern, he said.
In previous eras – prior to improvements in immunosuppressive regimens for transplant recipients – studies showed variable rates of lupus nephritis recurrence, with some reporting rates up to 50% depending on the patient populations and protocols, he noted.
The rates in recent years at UTHSC seemed lower than that, so he and his colleagues looked more closely at the outcomes.
Case patients included all those with end-stage renal disease secondary to lupus nephritis who were transplanted between 2006 and 2017 at the center. Medical records of all 38 were reviewed along with information from the United Network for Organ Sharing Network. The mean age of the patients at baseline was 42 years, 89% were women, 89% were African American, and previous time on dialysis was a median of 4 years. Most (80%) received hemodialysis, and nearly one-third (31%) received living donor transplantation, Dr. Pattanaik said.
The main difference in the past decade compared with those previous eras is the use of posttransplant immunosuppressive regimens consisting of tacrolimus and mycophenolate mofetil rather than cyclosporine and azathioprine in addition to prednisone, he explained.
Previous reports showing higher recurrence rates were from studies in which patients received cyclosporine and azathioprine as part of the posttransplant regimen, he said.
“Our next question is whether patients can be transplanted early,” he said, explaining that transplant is often delayed for many months or years until SLE is in remission, but if the new regimens are reducing recurrence risk, early transplant may be feasible.
Dr. Pattanaik reported having no disclosures.
SOURCE: Pattanaik D et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 711.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point:
Major finding: The biopsy-proven recurrence rate was 11%.
Study details: A review of 38 cases at one center.
Disclosures: Dr. Pattanaik reported having no disclosures.
Source: Pattanaik D et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 711.
Stroke risk in elderly following AMI extends to 12 weeks
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
ATLANTA – Acute myocardial infarction is associated with a risk of stroke that extends beyond the 1-month time window currently considered the at-risk period, according to an analysis of Medicare data.
“The results of our study may allow clinicians to more accurately counsel patients regarding their stroke etiology and may allow refinement of stroke etiology classification systems and clinical trial selection criteria,” lead study author Alexander E. Merkler, MD, said in an interview in advance of the annual meeting of the American Neurological Association.
In an effort to better understand the duration of heightened stroke risk after acute myocardial infarction, Dr. Merkler, a neurologist at New York–based Weill Cornell Medicine, and his colleagues conducted a retrospective cohort study using inpatient and outpatient claims during 2008-2015 from a nationally representative 5% sample of Medicare beneficiaries who were at least 66 years old. They used previously validated ICD-9-CM diagnosis codes to ascertain the exposure variable of acute MI and the outcome of ischemic stroke but excluded strokes that occurred during an acute MI hospitalization.
Patients were censored at the time of ischemic stroke, death, end of Medicare coverage, or by Sept. 30, 2015. The researchers fit Cox regression models separately for the groups with and without acute MI to examine its association with ischemic stroke after adjusting for demographics, stroke risk factors, and Charlson comorbidities. Next, they used the corresponding survival probabilities to compute the hazard ratio (HR) in each 4-week interval after discharge, up to week 12. They also conducted a subgroup analysis to evaluate the duration of heightened ischemic stroke risk by MI type: ST-segment elevation MI (STEMI) versus non-STEMI (NSTEMI).
Dr. Merkler and his colleagues drew from data on 1.7 million eligible beneficiaries. Of these, 46,182 were hospitalized for acute MI and 80,466 for ischemic stroke. After they adjusted for demographics, stroke risk factors, and Charlson comorbidities, the researchers found that the risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6). It was no longer significantly elevated afterward. The prolonged period of heightened ischemic stroke risk was evident in patients with both STEMI and NSTEMI.
“We were surprised by how long the risk of stroke lasts after MI,” Dr. Merkler said. He acknowledged certain limitations of the analysis, including the fact that patients were all over the age of 65 years. “In addition, we lack granular detail such as severity of MI [and] the extent of stroke work-up,” he said.
Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
[email protected]
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
AT ANA 2018
Key clinical point: .
Major finding: The risk of ischemic stroke was highest in the first 4 weeks after discharge from the MI hospitalization (HR, 2.7), yet remained elevated during weeks 5-8 (HR, 2.0) and weeks 9-12 (HR, 1.6).
Study details: An analysis of 46,182 Medicare beneficiaries who were hospitalized for acute MI and 80,466 who were hospitalized for ischemic stroke.
Disclosures: Dr. Merkler disclosed that he is supported by a grant from the National Institutes of Health and by the Leon Levy Foundation in Neuroscience. Most of his coauthors are also supported by NIH grants.
Source: Ann Neurol. 2018;84[S22]:S146-7, Abstract M122.
Intervention may improve genetic testing for HBOC
Researchers from general obstetrics and gynecology (ob.gyn.) practices in New York and Connecticut have shown that (HBOC).
Genetic screening and testing can reduce the morbidity and mortality from breast, ovarian, and endometrial cancers through prevention and early detection. Mark S. DeFrancesco, MD, of Westwood Women’s Health, Waterbury, Conn., and his colleagues reported that, in spite of the American College of Obstetricians and Gynecologists’ recommendation for ob.gyns. to regularly screen, counsel, and refer accordingly for HBOC (Obstet Gynecol. 2015;125:153843), the “incorporation of hereditary cancer risk assessment and testing remains underutilized in the [ob.gyn.] setting.” The authors have addressed this issue in their own practice with promising results and important caveats (Obstet Gynecol 2018;132:1121-9).
The intervention included a process evaluation, improvements to patient work flow, and training of providers by genetic counselors and engineering personnel from the testing laboratory (Myriad Genetics), which provided support for the study. Patients in the study completed a family history questionnaire and, those meeting National Comprehensive Cancer Center Network criteria for genetic testing, were given pretest counseling and offered testing on the same day or referral for testing within 2 weeks.
Of the 3,811 women who completed the questionnaire, 24% (906) met NCCN criteria, 90% of whom were offered testing. However, only 52% (165) of patients who agreed to testing underwent genetic evaluation. This included 70% of patients who were offered same-day testing and 35% of patients who were offered a referral appointment for testing.
Conversations about HBOC and genetic testing can be complicated and may not be a patient’s initial priority. The authors should be commended for identifying the vast majority of high-risk patients. However, only half of patients meeting criteria completed testing and 10% who should have been offered testing were not – numbers still well below target.
Incorporation of family history questionnaires should become commonplace in the generalist’s office and optimizing EHRs may be an opportunity for rapid risk interpretation. As the success of same-day genetic testing was striking, opportunities for partnerships with insurance companies and private laboratories are likely needed to make this a more feasible option. Lastly, assessing women’s knowledge and attitudes around genetic testing could help to more specifically address barriers to testing in future interventions.
Improving genetic screening and testing completion rates requires a coordinated effort. Using tools and applications to optimize convenience (same-day testing, telemedicine) and simplification (electronic screening platforms), we can strive to appropriately detect all women at high risk for hereditary breast and ovarian cancers.
Michelle Lightfoot is a gynecologic oncology fellow at the Ohio State University in Columbus. She has no relevant financial disclosures. Email her at [email protected].
Researchers from general obstetrics and gynecology (ob.gyn.) practices in New York and Connecticut have shown that (HBOC).
Genetic screening and testing can reduce the morbidity and mortality from breast, ovarian, and endometrial cancers through prevention and early detection. Mark S. DeFrancesco, MD, of Westwood Women’s Health, Waterbury, Conn., and his colleagues reported that, in spite of the American College of Obstetricians and Gynecologists’ recommendation for ob.gyns. to regularly screen, counsel, and refer accordingly for HBOC (Obstet Gynecol. 2015;125:153843), the “incorporation of hereditary cancer risk assessment and testing remains underutilized in the [ob.gyn.] setting.” The authors have addressed this issue in their own practice with promising results and important caveats (Obstet Gynecol 2018;132:1121-9).
The intervention included a process evaluation, improvements to patient work flow, and training of providers by genetic counselors and engineering personnel from the testing laboratory (Myriad Genetics), which provided support for the study. Patients in the study completed a family history questionnaire and, those meeting National Comprehensive Cancer Center Network criteria for genetic testing, were given pretest counseling and offered testing on the same day or referral for testing within 2 weeks.
Of the 3,811 women who completed the questionnaire, 24% (906) met NCCN criteria, 90% of whom were offered testing. However, only 52% (165) of patients who agreed to testing underwent genetic evaluation. This included 70% of patients who were offered same-day testing and 35% of patients who were offered a referral appointment for testing.
Conversations about HBOC and genetic testing can be complicated and may not be a patient’s initial priority. The authors should be commended for identifying the vast majority of high-risk patients. However, only half of patients meeting criteria completed testing and 10% who should have been offered testing were not – numbers still well below target.
Incorporation of family history questionnaires should become commonplace in the generalist’s office and optimizing EHRs may be an opportunity for rapid risk interpretation. As the success of same-day genetic testing was striking, opportunities for partnerships with insurance companies and private laboratories are likely needed to make this a more feasible option. Lastly, assessing women’s knowledge and attitudes around genetic testing could help to more specifically address barriers to testing in future interventions.
Improving genetic screening and testing completion rates requires a coordinated effort. Using tools and applications to optimize convenience (same-day testing, telemedicine) and simplification (electronic screening platforms), we can strive to appropriately detect all women at high risk for hereditary breast and ovarian cancers.
Michelle Lightfoot is a gynecologic oncology fellow at the Ohio State University in Columbus. She has no relevant financial disclosures. Email her at [email protected].
Researchers from general obstetrics and gynecology (ob.gyn.) practices in New York and Connecticut have shown that (HBOC).
Genetic screening and testing can reduce the morbidity and mortality from breast, ovarian, and endometrial cancers through prevention and early detection. Mark S. DeFrancesco, MD, of Westwood Women’s Health, Waterbury, Conn., and his colleagues reported that, in spite of the American College of Obstetricians and Gynecologists’ recommendation for ob.gyns. to regularly screen, counsel, and refer accordingly for HBOC (Obstet Gynecol. 2015;125:153843), the “incorporation of hereditary cancer risk assessment and testing remains underutilized in the [ob.gyn.] setting.” The authors have addressed this issue in their own practice with promising results and important caveats (Obstet Gynecol 2018;132:1121-9).
The intervention included a process evaluation, improvements to patient work flow, and training of providers by genetic counselors and engineering personnel from the testing laboratory (Myriad Genetics), which provided support for the study. Patients in the study completed a family history questionnaire and, those meeting National Comprehensive Cancer Center Network criteria for genetic testing, were given pretest counseling and offered testing on the same day or referral for testing within 2 weeks.
Of the 3,811 women who completed the questionnaire, 24% (906) met NCCN criteria, 90% of whom were offered testing. However, only 52% (165) of patients who agreed to testing underwent genetic evaluation. This included 70% of patients who were offered same-day testing and 35% of patients who were offered a referral appointment for testing.
Conversations about HBOC and genetic testing can be complicated and may not be a patient’s initial priority. The authors should be commended for identifying the vast majority of high-risk patients. However, only half of patients meeting criteria completed testing and 10% who should have been offered testing were not – numbers still well below target.
Incorporation of family history questionnaires should become commonplace in the generalist’s office and optimizing EHRs may be an opportunity for rapid risk interpretation. As the success of same-day genetic testing was striking, opportunities for partnerships with insurance companies and private laboratories are likely needed to make this a more feasible option. Lastly, assessing women’s knowledge and attitudes around genetic testing could help to more specifically address barriers to testing in future interventions.
Improving genetic screening and testing completion rates requires a coordinated effort. Using tools and applications to optimize convenience (same-day testing, telemedicine) and simplification (electronic screening platforms), we can strive to appropriately detect all women at high risk for hereditary breast and ovarian cancers.
Michelle Lightfoot is a gynecologic oncology fellow at the Ohio State University in Columbus. She has no relevant financial disclosures. Email her at [email protected].
Endocuff decreases withdrawal time but not detection rate during colonoscopy
PHILADELPHIA – Use of a device on the distal end of a colonoscope to expand the view of the colon lowered the mean inspection time during colonoscopy without significantly reducing adenoma or sessile serrated polyp detection rate, according to a presentation at the annual meeting of the American College of Gastroenterology.
“The finger projections on the tip of the Endocuff can engage the colonic folds, and that allows us to see the proximal sides of these folds,” Seth A. Gross, MD, chief of gastroenterology at NYU Langone Health Tisch Hospital in New York, said in his presentation. “It also changes topography and temporarily stretches different segments of the colon depending on where you are to help expose more surface area and ultimately identify more polyps.”
Dr. Gross and his colleagues analyzed the withdrawal time of colonoscopy with the Endocuff Vision (Olympus, Center Valley, Penn.) in 101 patients, compared with withdrawal time during a standard colonoscopy in 99 patients as measured by stopwatch. Other endpoints in the study included insertion time, adenoma detection rate (ADR), sessile serrated polyp detection (SSPD), and number of adenomas and sessile serrated polyps per colonoscopy. Patients were included if they were at least 40 years old with a screening, surveillance, or diagnostic indication for colonoscopy; they were excluded if they had inflammatory bowel disease, polyposis syndrome, prior colon resection, prior colorectal polyp or cancer, previous incomplete colonoscopy or severe diverticular disease.
Inspection time in the Endocuff group was 6.3 minutes, compared with 8.2 minutes in the standard colonoscopy group (P less than .001), and insertion time was 9.9 minutes in the Endocuff group, compared with 11.3 minutes in the standard colonoscopy group. A multivariate analysis showed the shorter inspection times in the Endocuff group remained significant (P less than .0001).
In the Endocuff group, ADR was 61.4% with 1.43 adenomas per colonoscopy, while the standard colonoscopy group had an ADR of 52.5% with an adenoma detection rate of 1.07 per colonoscopy. SSPD was 19.8% in the Endocuff group and 11.1% in the standard group with a SSPD per colonoscopy of 0.27 and 0.21, respectively.
The study was unblinded and there were two endoscopists performing the procedures, which raises the question of whether the results could be generalized to other gastroenterologists, Dr. Gross noted.
“We recommend that future studies that are meant to be powered for adenoma detection rate and sessile serrated lesions be done to sort of validate this, and probably have more endoscopists involved in a study like this,” Dr. Gross said. “But this is the start of an interesting conversation where one could be more efficient without sacrificing our detection rate for both adenomas and sessile serrated lesions.”
Dr. Gross reports a consultancy with Olympus.
SOURCE: Gross SA et al. ACG 2018, Presentation 37.
PHILADELPHIA – Use of a device on the distal end of a colonoscope to expand the view of the colon lowered the mean inspection time during colonoscopy without significantly reducing adenoma or sessile serrated polyp detection rate, according to a presentation at the annual meeting of the American College of Gastroenterology.
“The finger projections on the tip of the Endocuff can engage the colonic folds, and that allows us to see the proximal sides of these folds,” Seth A. Gross, MD, chief of gastroenterology at NYU Langone Health Tisch Hospital in New York, said in his presentation. “It also changes topography and temporarily stretches different segments of the colon depending on where you are to help expose more surface area and ultimately identify more polyps.”
Dr. Gross and his colleagues analyzed the withdrawal time of colonoscopy with the Endocuff Vision (Olympus, Center Valley, Penn.) in 101 patients, compared with withdrawal time during a standard colonoscopy in 99 patients as measured by stopwatch. Other endpoints in the study included insertion time, adenoma detection rate (ADR), sessile serrated polyp detection (SSPD), and number of adenomas and sessile serrated polyps per colonoscopy. Patients were included if they were at least 40 years old with a screening, surveillance, or diagnostic indication for colonoscopy; they were excluded if they had inflammatory bowel disease, polyposis syndrome, prior colon resection, prior colorectal polyp or cancer, previous incomplete colonoscopy or severe diverticular disease.
Inspection time in the Endocuff group was 6.3 minutes, compared with 8.2 minutes in the standard colonoscopy group (P less than .001), and insertion time was 9.9 minutes in the Endocuff group, compared with 11.3 minutes in the standard colonoscopy group. A multivariate analysis showed the shorter inspection times in the Endocuff group remained significant (P less than .0001).
In the Endocuff group, ADR was 61.4% with 1.43 adenomas per colonoscopy, while the standard colonoscopy group had an ADR of 52.5% with an adenoma detection rate of 1.07 per colonoscopy. SSPD was 19.8% in the Endocuff group and 11.1% in the standard group with a SSPD per colonoscopy of 0.27 and 0.21, respectively.
The study was unblinded and there were two endoscopists performing the procedures, which raises the question of whether the results could be generalized to other gastroenterologists, Dr. Gross noted.
“We recommend that future studies that are meant to be powered for adenoma detection rate and sessile serrated lesions be done to sort of validate this, and probably have more endoscopists involved in a study like this,” Dr. Gross said. “But this is the start of an interesting conversation where one could be more efficient without sacrificing our detection rate for both adenomas and sessile serrated lesions.”
Dr. Gross reports a consultancy with Olympus.
SOURCE: Gross SA et al. ACG 2018, Presentation 37.
PHILADELPHIA – Use of a device on the distal end of a colonoscope to expand the view of the colon lowered the mean inspection time during colonoscopy without significantly reducing adenoma or sessile serrated polyp detection rate, according to a presentation at the annual meeting of the American College of Gastroenterology.
“The finger projections on the tip of the Endocuff can engage the colonic folds, and that allows us to see the proximal sides of these folds,” Seth A. Gross, MD, chief of gastroenterology at NYU Langone Health Tisch Hospital in New York, said in his presentation. “It also changes topography and temporarily stretches different segments of the colon depending on where you are to help expose more surface area and ultimately identify more polyps.”
Dr. Gross and his colleagues analyzed the withdrawal time of colonoscopy with the Endocuff Vision (Olympus, Center Valley, Penn.) in 101 patients, compared with withdrawal time during a standard colonoscopy in 99 patients as measured by stopwatch. Other endpoints in the study included insertion time, adenoma detection rate (ADR), sessile serrated polyp detection (SSPD), and number of adenomas and sessile serrated polyps per colonoscopy. Patients were included if they were at least 40 years old with a screening, surveillance, or diagnostic indication for colonoscopy; they were excluded if they had inflammatory bowel disease, polyposis syndrome, prior colon resection, prior colorectal polyp or cancer, previous incomplete colonoscopy or severe diverticular disease.
Inspection time in the Endocuff group was 6.3 minutes, compared with 8.2 minutes in the standard colonoscopy group (P less than .001), and insertion time was 9.9 minutes in the Endocuff group, compared with 11.3 minutes in the standard colonoscopy group. A multivariate analysis showed the shorter inspection times in the Endocuff group remained significant (P less than .0001).
In the Endocuff group, ADR was 61.4% with 1.43 adenomas per colonoscopy, while the standard colonoscopy group had an ADR of 52.5% with an adenoma detection rate of 1.07 per colonoscopy. SSPD was 19.8% in the Endocuff group and 11.1% in the standard group with a SSPD per colonoscopy of 0.27 and 0.21, respectively.
The study was unblinded and there were two endoscopists performing the procedures, which raises the question of whether the results could be generalized to other gastroenterologists, Dr. Gross noted.
“We recommend that future studies that are meant to be powered for adenoma detection rate and sessile serrated lesions be done to sort of validate this, and probably have more endoscopists involved in a study like this,” Dr. Gross said. “But this is the start of an interesting conversation where one could be more efficient without sacrificing our detection rate for both adenomas and sessile serrated lesions.”
Dr. Gross reports a consultancy with Olympus.
SOURCE: Gross SA et al. ACG 2018, Presentation 37.
REPORTING FROM ACG 2018
Key clinical point: Inspection times were lower during colonoscopy for patients who underwent the procedure using Endocuff, but there was no significant decrease in adenoma or sessile serrated polyp detection rate.
Major finding: Endocuff reduced inspection time to 6.3 minutes, compared with 8.2 minutes in the standard colonoscopy group.
Study details: An analysis of 200 patients who underwent standard colonoscopy or colonoscopy with Endocuff Vision.
Disclosures: Dr. Gross reports a consultancy with Olympus.
Source: Gross SA et al. ACG 2018, Presentation 37.
Carol Bernstein: Physician burnout
Diabetes Programs Aren’t Reaching Their Targets
The CDC’s lifestyle change program (LCP), part of the National Diabetes Prevention Program, teaches people with prediabetes practical, real-life changes. Those changes can be enough to reduce the risk of type 2 diabetes by as much as 58%—or even 71% for people aged > 60 years. But are enough people getting the opportunity to participate?
CDC researchers assessed the availability of in-person LCP classes by diabetes incidence and socioeconomic status at the county level. They mapped 1,558 LCP class locations. They found classes in 711 (23%) US counties as of March 2017 (there may be more now, the researchers say).
But the classes were not necessarily located where they could do the most good, the researchers found. Only 17% of the counties with the highest diabetes incidence and 10% of counties with the most socioeconomic disadvantage had a publicly available class location. By contrast, 26.8% of counties in the lowest tertile of incidence had class locations.
The researchers say policy makers, program planners, and others engaged in expanding the availability of the classes can use the information to prioritize locations, especially for underrepresented populations.
The CDC’s lifestyle change program (LCP), part of the National Diabetes Prevention Program, teaches people with prediabetes practical, real-life changes. Those changes can be enough to reduce the risk of type 2 diabetes by as much as 58%—or even 71% for people aged > 60 years. But are enough people getting the opportunity to participate?
CDC researchers assessed the availability of in-person LCP classes by diabetes incidence and socioeconomic status at the county level. They mapped 1,558 LCP class locations. They found classes in 711 (23%) US counties as of March 2017 (there may be more now, the researchers say).
But the classes were not necessarily located where they could do the most good, the researchers found. Only 17% of the counties with the highest diabetes incidence and 10% of counties with the most socioeconomic disadvantage had a publicly available class location. By contrast, 26.8% of counties in the lowest tertile of incidence had class locations.
The researchers say policy makers, program planners, and others engaged in expanding the availability of the classes can use the information to prioritize locations, especially for underrepresented populations.
The CDC’s lifestyle change program (LCP), part of the National Diabetes Prevention Program, teaches people with prediabetes practical, real-life changes. Those changes can be enough to reduce the risk of type 2 diabetes by as much as 58%—or even 71% for people aged > 60 years. But are enough people getting the opportunity to participate?
CDC researchers assessed the availability of in-person LCP classes by diabetes incidence and socioeconomic status at the county level. They mapped 1,558 LCP class locations. They found classes in 711 (23%) US counties as of March 2017 (there may be more now, the researchers say).
But the classes were not necessarily located where they could do the most good, the researchers found. Only 17% of the counties with the highest diabetes incidence and 10% of counties with the most socioeconomic disadvantage had a publicly available class location. By contrast, 26.8% of counties in the lowest tertile of incidence had class locations.
The researchers say policy makers, program planners, and others engaged in expanding the availability of the classes can use the information to prioritize locations, especially for underrepresented populations.
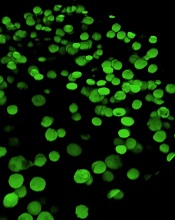
MDM2 inhibitors could treat resistant AML
Preclinical research has revealed a potential treatment for chemotherapy-resistant acute myeloid leukemia (AML).
Researchers characterized a mechanism of chemotherapy resistance in AML and found that MDM2 is a key player in this dysregulated signaling pathway.
They tested MDM2 inhibitors and found these drugs could sensitize resistant AML to chemotherapy in vitro and in vivo.
In fact, mice with refractory AML responded to standard induction therapy when combined with an MDM2 inhibitor, showing no signs of disease and prolonged survival.
These results were published in Cancer Discovery.
“We were blown away when we saw the results,” said study author William Stanford, PhD, of Ottawa Hospital Research Institute in Ontario, Canada.
“If these findings hold up in clinical trials, we could have a new treatment for people who would almost certainly die of their disease today.”
Mechanism of resistance
Dr. Stanford’s research began with the protein MTF2. He and his colleagues previously found that MTF2 plays a role in erythropoiesis, and the team wanted to determine if MTF2 also plays a role in AML.
Using AML samples from patients treated at The Ottawa Hospital, the researchers found the mean survival was three times longer in patients with normal MTF2 activity than in patients with low MTF2 activity.
“Initially, we thought that MTF2 could be an important biomarker to identify patients who might benefit from experimental therapies,” Dr. Stanford said. “But then we started thinking that if we could understand what MTF2 was doing, maybe we could use this information to develop a new treatment.”
Dr. Stanford and his colleagues discovered that MTF2 represses MDM2, a protein that helps cells resist chemotherapy.
The team found that MTF2-deficient cells overexpress MDM2, which inhibits p53, and this leads to defects in cell-cycle regulation and apoptosis that enable resistance to chemotherapy.
Testing MDM2 inhibitors
Since MDM2 inhibitors are already being tested in clinical trials for other cancers, Dr. Stanford and his colleagues tested these inhibitors in vitro and in mouse models of chemotherapy-resistant AML.
The in vitro experiments included two MDM2 inhibitors—Nutlin3A and MI-773—combined with daunorubicin or cytarabine.
The researchers found that refractory, MTF2-deficient AML cells underwent apoptosis when treated with either daunorubicin or cytarabine in combination with Nutlin3A or MI-773. The effect was comparable to that observed in AML cells with normal MTF2.
The team found that Nutlin3A was more efficient at sensitizing refractory, MTF2-deficient AML cells to daunorubicin, so they used Nutlin3A in the in vivo experiments.
For these experiments, the researchers tested Nutlin3A in mice injected with either chemotherapy-responsive AML cells (with normal MTF2) or refractory, MTF2-deficient AML cells.
Once the mice had “a substantial leukemic burden” (≥ 20% CD45+CD33+ leukemic blasts in their peripheral blood), they were randomized to receive vehicle control, Nutlin3A, standard induction therapy, or induction plus Nutlin3A.
The mice engrafted with chemotherapy-responsive AML cells did not respond to vehicle control or Nutlin3A alone. However, they did respond to standard induction and induction plus Nutlin3A, surviving until the end of the experiment at 16 weeks.
Among the mice engrafted with refractory, MTF2-deficient AML cells, only those animals treated with induction plus Nutlin3A survived until the end of the experiment.
The researchers also noted a “dramatic loss” in the blast-containing CD45+CD33+ and CD34+CD38− populations in mice treated with induction plus Nutlin3A.
To assess residual disease, the researchers performed secondary transplants with cells from mice that had engrafted with refractory, MTF2-deficient AML cells but responded to induction plus Nutlin3A.
The recipient mice had no evidence of AML at 16 weeks after transplant when the experiment ended.
Dr. Stanford and his colleagues are now trying to obtain pharmaceutical-grade MDM2 inhibitors to conduct trials in AML patients at The Ottawa Hospital.
The researchers are also screening libraries of approved drugs to see if any of these can block MDM2, and they are working with a biotech company to develop a test to identify chemotherapy-resistant AML patients who would respond to MDM2 inhibitors.
The current research was supported by grants from the Canadian Cancer Society Research Institute, Canadian Institutes of Health Research, Cancer Research Society, National Institutes of Health, and a Tier 1 Canada Research Chair in Integrative Stem Cell Biology. One study author reported a relationship with Epicypher, Inc. No other conflicts of interest were reported.
Preclinical research has revealed a potential treatment for chemotherapy-resistant acute myeloid leukemia (AML).
Researchers characterized a mechanism of chemotherapy resistance in AML and found that MDM2 is a key player in this dysregulated signaling pathway.
They tested MDM2 inhibitors and found these drugs could sensitize resistant AML to chemotherapy in vitro and in vivo.
In fact, mice with refractory AML responded to standard induction therapy when combined with an MDM2 inhibitor, showing no signs of disease and prolonged survival.
These results were published in Cancer Discovery.
“We were blown away when we saw the results,” said study author William Stanford, PhD, of Ottawa Hospital Research Institute in Ontario, Canada.
“If these findings hold up in clinical trials, we could have a new treatment for people who would almost certainly die of their disease today.”
Mechanism of resistance
Dr. Stanford’s research began with the protein MTF2. He and his colleagues previously found that MTF2 plays a role in erythropoiesis, and the team wanted to determine if MTF2 also plays a role in AML.
Using AML samples from patients treated at The Ottawa Hospital, the researchers found the mean survival was three times longer in patients with normal MTF2 activity than in patients with low MTF2 activity.
“Initially, we thought that MTF2 could be an important biomarker to identify patients who might benefit from experimental therapies,” Dr. Stanford said. “But then we started thinking that if we could understand what MTF2 was doing, maybe we could use this information to develop a new treatment.”
Dr. Stanford and his colleagues discovered that MTF2 represses MDM2, a protein that helps cells resist chemotherapy.
The team found that MTF2-deficient cells overexpress MDM2, which inhibits p53, and this leads to defects in cell-cycle regulation and apoptosis that enable resistance to chemotherapy.
Testing MDM2 inhibitors
Since MDM2 inhibitors are already being tested in clinical trials for other cancers, Dr. Stanford and his colleagues tested these inhibitors in vitro and in mouse models of chemotherapy-resistant AML.
The in vitro experiments included two MDM2 inhibitors—Nutlin3A and MI-773—combined with daunorubicin or cytarabine.
The researchers found that refractory, MTF2-deficient AML cells underwent apoptosis when treated with either daunorubicin or cytarabine in combination with Nutlin3A or MI-773. The effect was comparable to that observed in AML cells with normal MTF2.
The team found that Nutlin3A was more efficient at sensitizing refractory, MTF2-deficient AML cells to daunorubicin, so they used Nutlin3A in the in vivo experiments.
For these experiments, the researchers tested Nutlin3A in mice injected with either chemotherapy-responsive AML cells (with normal MTF2) or refractory, MTF2-deficient AML cells.
Once the mice had “a substantial leukemic burden” (≥ 20% CD45+CD33+ leukemic blasts in their peripheral blood), they were randomized to receive vehicle control, Nutlin3A, standard induction therapy, or induction plus Nutlin3A.
The mice engrafted with chemotherapy-responsive AML cells did not respond to vehicle control or Nutlin3A alone. However, they did respond to standard induction and induction plus Nutlin3A, surviving until the end of the experiment at 16 weeks.
Among the mice engrafted with refractory, MTF2-deficient AML cells, only those animals treated with induction plus Nutlin3A survived until the end of the experiment.
The researchers also noted a “dramatic loss” in the blast-containing CD45+CD33+ and CD34+CD38− populations in mice treated with induction plus Nutlin3A.
To assess residual disease, the researchers performed secondary transplants with cells from mice that had engrafted with refractory, MTF2-deficient AML cells but responded to induction plus Nutlin3A.
The recipient mice had no evidence of AML at 16 weeks after transplant when the experiment ended.
Dr. Stanford and his colleagues are now trying to obtain pharmaceutical-grade MDM2 inhibitors to conduct trials in AML patients at The Ottawa Hospital.
The researchers are also screening libraries of approved drugs to see if any of these can block MDM2, and they are working with a biotech company to develop a test to identify chemotherapy-resistant AML patients who would respond to MDM2 inhibitors.
The current research was supported by grants from the Canadian Cancer Society Research Institute, Canadian Institutes of Health Research, Cancer Research Society, National Institutes of Health, and a Tier 1 Canada Research Chair in Integrative Stem Cell Biology. One study author reported a relationship with Epicypher, Inc. No other conflicts of interest were reported.
Preclinical research has revealed a potential treatment for chemotherapy-resistant acute myeloid leukemia (AML).
Researchers characterized a mechanism of chemotherapy resistance in AML and found that MDM2 is a key player in this dysregulated signaling pathway.
They tested MDM2 inhibitors and found these drugs could sensitize resistant AML to chemotherapy in vitro and in vivo.
In fact, mice with refractory AML responded to standard induction therapy when combined with an MDM2 inhibitor, showing no signs of disease and prolonged survival.
These results were published in Cancer Discovery.
“We were blown away when we saw the results,” said study author William Stanford, PhD, of Ottawa Hospital Research Institute in Ontario, Canada.
“If these findings hold up in clinical trials, we could have a new treatment for people who would almost certainly die of their disease today.”
Mechanism of resistance
Dr. Stanford’s research began with the protein MTF2. He and his colleagues previously found that MTF2 plays a role in erythropoiesis, and the team wanted to determine if MTF2 also plays a role in AML.
Using AML samples from patients treated at The Ottawa Hospital, the researchers found the mean survival was three times longer in patients with normal MTF2 activity than in patients with low MTF2 activity.
“Initially, we thought that MTF2 could be an important biomarker to identify patients who might benefit from experimental therapies,” Dr. Stanford said. “But then we started thinking that if we could understand what MTF2 was doing, maybe we could use this information to develop a new treatment.”
Dr. Stanford and his colleagues discovered that MTF2 represses MDM2, a protein that helps cells resist chemotherapy.
The team found that MTF2-deficient cells overexpress MDM2, which inhibits p53, and this leads to defects in cell-cycle regulation and apoptosis that enable resistance to chemotherapy.
Testing MDM2 inhibitors
Since MDM2 inhibitors are already being tested in clinical trials for other cancers, Dr. Stanford and his colleagues tested these inhibitors in vitro and in mouse models of chemotherapy-resistant AML.
The in vitro experiments included two MDM2 inhibitors—Nutlin3A and MI-773—combined with daunorubicin or cytarabine.
The researchers found that refractory, MTF2-deficient AML cells underwent apoptosis when treated with either daunorubicin or cytarabine in combination with Nutlin3A or MI-773. The effect was comparable to that observed in AML cells with normal MTF2.
The team found that Nutlin3A was more efficient at sensitizing refractory, MTF2-deficient AML cells to daunorubicin, so they used Nutlin3A in the in vivo experiments.
For these experiments, the researchers tested Nutlin3A in mice injected with either chemotherapy-responsive AML cells (with normal MTF2) or refractory, MTF2-deficient AML cells.
Once the mice had “a substantial leukemic burden” (≥ 20% CD45+CD33+ leukemic blasts in their peripheral blood), they were randomized to receive vehicle control, Nutlin3A, standard induction therapy, or induction plus Nutlin3A.
The mice engrafted with chemotherapy-responsive AML cells did not respond to vehicle control or Nutlin3A alone. However, they did respond to standard induction and induction plus Nutlin3A, surviving until the end of the experiment at 16 weeks.
Among the mice engrafted with refractory, MTF2-deficient AML cells, only those animals treated with induction plus Nutlin3A survived until the end of the experiment.
The researchers also noted a “dramatic loss” in the blast-containing CD45+CD33+ and CD34+CD38− populations in mice treated with induction plus Nutlin3A.
To assess residual disease, the researchers performed secondary transplants with cells from mice that had engrafted with refractory, MTF2-deficient AML cells but responded to induction plus Nutlin3A.
The recipient mice had no evidence of AML at 16 weeks after transplant when the experiment ended.
Dr. Stanford and his colleagues are now trying to obtain pharmaceutical-grade MDM2 inhibitors to conduct trials in AML patients at The Ottawa Hospital.
The researchers are also screening libraries of approved drugs to see if any of these can block MDM2, and they are working with a biotech company to develop a test to identify chemotherapy-resistant AML patients who would respond to MDM2 inhibitors.
The current research was supported by grants from the Canadian Cancer Society Research Institute, Canadian Institutes of Health Research, Cancer Research Society, National Institutes of Health, and a Tier 1 Canada Research Chair in Integrative Stem Cell Biology. One study author reported a relationship with Epicypher, Inc. No other conflicts of interest were reported.
SNPs linked to bleeding in African Americans on warfarin
Researchers say they have identified single-nucleotide polymorphisms (SNPs) that are associated with increased bleeding risk in African-American patients on warfarin.
A retrospective study revealed four SNPs associated with increased bleeding risk in African Americans with an international normalized ratio (INR) of less than 4.
One of these SNPs was seen in more than a third of bleeding cases and less than 5% of controls.
These preliminary findings could have implications for patients of African descent, but independent validation of the study results are needed, according to Minoli A. Perera, PharmD, PhD, of Northwestern University in Chicago, and her coauthors.
The researchers reported their findings in JAMA.
The report covered findings in a discovery cohort of African-American patients from a genome-wide study conducted at the University of Chicago and a replication cohort of patients who self-identified as African American and had routinely received care at University of Chicago hospitals.
The discovery cohort included 31 patients with major bleeding that occurred at an INR less than 4 and 184 controls with no documented history of bleeding related to warfarin.
In that cohort, Dr. Perera and her colleagues found four SNPs in linkage disequilibrium on chromosome 6 associated with warfarin-related bleeding:
- rs115112393
- rs16871327
- rs78132896
- rs114504854.
In particular, rs78132896 was found in 35.5% of cases (11/31) and 4.9% of controls (9/184), with an odds ratio of 8.31 (95% confidence interval [CI], 3.2-21.5).
The replication cohort, including 40 cases and 148 warfarin-treated controls, was genotyped specifically for rs78132896. The SNP was similarly found in 35.0% of cases (14/40) and 4.8% of controls (7/148), with an odds ratio of 8.24 (95% CI, 3.1-25.3).
“Genome-wide significance of this cohort was achieved when the cohorts were combined via meta-analysis,” the researchers wrote. They reported an odds ratio of 8.27 for that analysis (95% CI, 4.18-16.38).
Further analysis showed that, compared with wild-type alleles, the rs16871327 and rs78132896 risk alleles increased EPHA7 gene transcription.
Expression of the EPHA7 gene on vascular endothelial cells and peripheral lymphocytes is increased during inflammation, according to Dr. Perera and her coauthors. Increased EPHA7 expression might lead to bleeding in patients who are taking warfarin.
“This haplotype might also have potential implications for bleeding risk with direct oral anticoagulants,” the researchers wrote.
Dr. Perera and her coauthors reported no conflicts of interest related to their work on this study, which was funded by grants from the National Heart, Lung, and Blood Institute; the National Institute of General Medicine; the National Institutes of Health; and the American Heart Association Midwest Affiliate; as well as a research award from the University of Illinois at Chicago College of Pharmacy.
Researchers say they have identified single-nucleotide polymorphisms (SNPs) that are associated with increased bleeding risk in African-American patients on warfarin.
A retrospective study revealed four SNPs associated with increased bleeding risk in African Americans with an international normalized ratio (INR) of less than 4.
One of these SNPs was seen in more than a third of bleeding cases and less than 5% of controls.
These preliminary findings could have implications for patients of African descent, but independent validation of the study results are needed, according to Minoli A. Perera, PharmD, PhD, of Northwestern University in Chicago, and her coauthors.
The researchers reported their findings in JAMA.
The report covered findings in a discovery cohort of African-American patients from a genome-wide study conducted at the University of Chicago and a replication cohort of patients who self-identified as African American and had routinely received care at University of Chicago hospitals.
The discovery cohort included 31 patients with major bleeding that occurred at an INR less than 4 and 184 controls with no documented history of bleeding related to warfarin.
In that cohort, Dr. Perera and her colleagues found four SNPs in linkage disequilibrium on chromosome 6 associated with warfarin-related bleeding:
- rs115112393
- rs16871327
- rs78132896
- rs114504854.
In particular, rs78132896 was found in 35.5% of cases (11/31) and 4.9% of controls (9/184), with an odds ratio of 8.31 (95% confidence interval [CI], 3.2-21.5).
The replication cohort, including 40 cases and 148 warfarin-treated controls, was genotyped specifically for rs78132896. The SNP was similarly found in 35.0% of cases (14/40) and 4.8% of controls (7/148), with an odds ratio of 8.24 (95% CI, 3.1-25.3).
“Genome-wide significance of this cohort was achieved when the cohorts were combined via meta-analysis,” the researchers wrote. They reported an odds ratio of 8.27 for that analysis (95% CI, 4.18-16.38).
Further analysis showed that, compared with wild-type alleles, the rs16871327 and rs78132896 risk alleles increased EPHA7 gene transcription.
Expression of the EPHA7 gene on vascular endothelial cells and peripheral lymphocytes is increased during inflammation, according to Dr. Perera and her coauthors. Increased EPHA7 expression might lead to bleeding in patients who are taking warfarin.
“This haplotype might also have potential implications for bleeding risk with direct oral anticoagulants,” the researchers wrote.
Dr. Perera and her coauthors reported no conflicts of interest related to their work on this study, which was funded by grants from the National Heart, Lung, and Blood Institute; the National Institute of General Medicine; the National Institutes of Health; and the American Heart Association Midwest Affiliate; as well as a research award from the University of Illinois at Chicago College of Pharmacy.
Researchers say they have identified single-nucleotide polymorphisms (SNPs) that are associated with increased bleeding risk in African-American patients on warfarin.
A retrospective study revealed four SNPs associated with increased bleeding risk in African Americans with an international normalized ratio (INR) of less than 4.
One of these SNPs was seen in more than a third of bleeding cases and less than 5% of controls.
These preliminary findings could have implications for patients of African descent, but independent validation of the study results are needed, according to Minoli A. Perera, PharmD, PhD, of Northwestern University in Chicago, and her coauthors.
The researchers reported their findings in JAMA.
The report covered findings in a discovery cohort of African-American patients from a genome-wide study conducted at the University of Chicago and a replication cohort of patients who self-identified as African American and had routinely received care at University of Chicago hospitals.
The discovery cohort included 31 patients with major bleeding that occurred at an INR less than 4 and 184 controls with no documented history of bleeding related to warfarin.
In that cohort, Dr. Perera and her colleagues found four SNPs in linkage disequilibrium on chromosome 6 associated with warfarin-related bleeding:
- rs115112393
- rs16871327
- rs78132896
- rs114504854.
In particular, rs78132896 was found in 35.5% of cases (11/31) and 4.9% of controls (9/184), with an odds ratio of 8.31 (95% confidence interval [CI], 3.2-21.5).
The replication cohort, including 40 cases and 148 warfarin-treated controls, was genotyped specifically for rs78132896. The SNP was similarly found in 35.0% of cases (14/40) and 4.8% of controls (7/148), with an odds ratio of 8.24 (95% CI, 3.1-25.3).
“Genome-wide significance of this cohort was achieved when the cohorts were combined via meta-analysis,” the researchers wrote. They reported an odds ratio of 8.27 for that analysis (95% CI, 4.18-16.38).
Further analysis showed that, compared with wild-type alleles, the rs16871327 and rs78132896 risk alleles increased EPHA7 gene transcription.
Expression of the EPHA7 gene on vascular endothelial cells and peripheral lymphocytes is increased during inflammation, according to Dr. Perera and her coauthors. Increased EPHA7 expression might lead to bleeding in patients who are taking warfarin.
“This haplotype might also have potential implications for bleeding risk with direct oral anticoagulants,” the researchers wrote.
Dr. Perera and her coauthors reported no conflicts of interest related to their work on this study, which was funded by grants from the National Heart, Lung, and Blood Institute; the National Institute of General Medicine; the National Institutes of Health; and the American Heart Association Midwest Affiliate; as well as a research award from the University of Illinois at Chicago College of Pharmacy.
Engineered MSCs could treat GVHD
LAUSANNE, SWITZERLAND—A mesenchymal stem cell (MSC) product could treat acute graft-versus-host disease (GVHD), according to preclinical research.
The product, apceth-201, improved symptoms of GVHD and prolonged survival in two mouse models.
Researchers described results with apceth-201 in a poster presentation at the Annual Congress of the European Society of Gene and Cell Therapy.
Most of the researchers involved in this study work for apceth Biopharma, the company developing apceth-201.
Apceth-201 consists of allogeneic human MSCs that have been genetically modified to express alpha-1 antitrypsin, a protease inhibitor exerting anti-inflammatory and tissue-protective functions.
In vitro assays showed that apceth-201 suppresses T-cell proliferation, polarizes macrophages to an anti-inflammatory M2 type, converts dendritic cells to a tolerogenic phenotype, and increases induction of regulatory T cells.
Apeceth-201 also demonstrated activity in vivo.
In a humanized GVHD model, treatment with apceth-201 improved bone marrow cellularity and reduced levels of inflammatory markers.
Additionally, mice treated with apceth-201 had double the median survival of mice treated with native MSCs.
Researchers also tested the effects of apceth-201 against GVHD in a model of haploidentical hematopoietic stem cell transplant.
All control mice succumbed to GVHD within 22 days, but more than half of mice treated with apceth-201 survived until the end of the experiment, which was 100 days.
All of the survivors had complete resolution of GVHD symptoms.
The researchers also said apceth-201 was safe. It did not impair T-cell-dependent antibody responses, and host resistance was similar in treated mice and controls.
“We are very excited with these results that clearly show the transformative therapeutic potential of apceth-201 in an immune-mediated disease with high unmet medical need and few treatment options,” said Christine Guenther, CEO of apceth Biopharma.
“Based on these promising and impressive data, we are currently preparing to initiate a phase 1/2 clinical study assessing the safety and efficacy of apceth-201 in adult steroid-refractory GVHD patients.”
LAUSANNE, SWITZERLAND—A mesenchymal stem cell (MSC) product could treat acute graft-versus-host disease (GVHD), according to preclinical research.
The product, apceth-201, improved symptoms of GVHD and prolonged survival in two mouse models.
Researchers described results with apceth-201 in a poster presentation at the Annual Congress of the European Society of Gene and Cell Therapy.
Most of the researchers involved in this study work for apceth Biopharma, the company developing apceth-201.
Apceth-201 consists of allogeneic human MSCs that have been genetically modified to express alpha-1 antitrypsin, a protease inhibitor exerting anti-inflammatory and tissue-protective functions.
In vitro assays showed that apceth-201 suppresses T-cell proliferation, polarizes macrophages to an anti-inflammatory M2 type, converts dendritic cells to a tolerogenic phenotype, and increases induction of regulatory T cells.
Apeceth-201 also demonstrated activity in vivo.
In a humanized GVHD model, treatment with apceth-201 improved bone marrow cellularity and reduced levels of inflammatory markers.
Additionally, mice treated with apceth-201 had double the median survival of mice treated with native MSCs.
Researchers also tested the effects of apceth-201 against GVHD in a model of haploidentical hematopoietic stem cell transplant.
All control mice succumbed to GVHD within 22 days, but more than half of mice treated with apceth-201 survived until the end of the experiment, which was 100 days.
All of the survivors had complete resolution of GVHD symptoms.
The researchers also said apceth-201 was safe. It did not impair T-cell-dependent antibody responses, and host resistance was similar in treated mice and controls.
“We are very excited with these results that clearly show the transformative therapeutic potential of apceth-201 in an immune-mediated disease with high unmet medical need and few treatment options,” said Christine Guenther, CEO of apceth Biopharma.
“Based on these promising and impressive data, we are currently preparing to initiate a phase 1/2 clinical study assessing the safety and efficacy of apceth-201 in adult steroid-refractory GVHD patients.”
LAUSANNE, SWITZERLAND—A mesenchymal stem cell (MSC) product could treat acute graft-versus-host disease (GVHD), according to preclinical research.
The product, apceth-201, improved symptoms of GVHD and prolonged survival in two mouse models.
Researchers described results with apceth-201 in a poster presentation at the Annual Congress of the European Society of Gene and Cell Therapy.
Most of the researchers involved in this study work for apceth Biopharma, the company developing apceth-201.
Apceth-201 consists of allogeneic human MSCs that have been genetically modified to express alpha-1 antitrypsin, a protease inhibitor exerting anti-inflammatory and tissue-protective functions.
In vitro assays showed that apceth-201 suppresses T-cell proliferation, polarizes macrophages to an anti-inflammatory M2 type, converts dendritic cells to a tolerogenic phenotype, and increases induction of regulatory T cells.
Apeceth-201 also demonstrated activity in vivo.
In a humanized GVHD model, treatment with apceth-201 improved bone marrow cellularity and reduced levels of inflammatory markers.
Additionally, mice treated with apceth-201 had double the median survival of mice treated with native MSCs.
Researchers also tested the effects of apceth-201 against GVHD in a model of haploidentical hematopoietic stem cell transplant.
All control mice succumbed to GVHD within 22 days, but more than half of mice treated with apceth-201 survived until the end of the experiment, which was 100 days.
All of the survivors had complete resolution of GVHD symptoms.
The researchers also said apceth-201 was safe. It did not impair T-cell-dependent antibody responses, and host resistance was similar in treated mice and controls.
“We are very excited with these results that clearly show the transformative therapeutic potential of apceth-201 in an immune-mediated disease with high unmet medical need and few treatment options,” said Christine Guenther, CEO of apceth Biopharma.
“Based on these promising and impressive data, we are currently preparing to initiate a phase 1/2 clinical study assessing the safety and efficacy of apceth-201 in adult steroid-refractory GVHD patients.”