User login
Netflix addiction, COPD blues, waistline-busting memes
The hottest new drug? Netflix
We all knew this was coming eventually. The first case of “Netflix addiction” has emerged, as a 26-year-old man in India has reportedly sought help at an addiction treatment center in Bangalore. Symptoms included 7-10 hours of TV watching per day and increasing isolation from others. Honestly, sounds like an ideal weekend. A clinical psychology professor at the treatment center warns that this instance is very similar to cases where patients are addicted to video games or social media, wherein the virtual world takes precedence over the real one. No reports yet about exactly what he was bingeing on, but our money’s on “The Great British Baking Show.” And can you blame him? The things they make on that show! This is the first case of Netflix addiction but undoubtedly will not be the last. It’s just so easy to watch 19 episodes of “Law & Order” in a row! I’m not an addict, I’m just a dedicated fan. Please don’t take my computer away from me.
Losin’ the COPD blues
The pursuit of improved therapies for chronic obstructive pulmonary disease has produced a wealth of treatment options. But one new approach sounds better than them all. In a pilot study, an inexpensive, handheld device improved breathing control and self-confidence in people with COPD. And it boosted their quality of life. In fact, 3 months of use for only about a half hour a day most days of the week improved several pulmonary outcome measures, including maximal inspiratory pressure, maximal expiratory pressure, and distance on the 6-minute walk test. The 14 patients, all ex-smokers, even posted significant improvements in performance of “Happy Birthday,” “You Are My Sunshine,” and the respiratorily challenging Johnny Cash’s “Ring of Fire.” Technically called a “free reed wind instrument,” the pulmonary rehab device is also known as a “harmonica.” Can a mouth organ really counter emphysema? Well, neither of the two hard-blowing blues harmonica legends named Sonny Boy Williamson succumbed to COPD.
This is why you’re fat
Apparently, the real reason for rising levels of obesity is not sugar or lack of exercise – it’s memes. Researchers from England’s Loughborough University sent a memo to Parliament displaying evidence that Internet memes are contributing to unhealthy eating habits and sending damaging messages to today’s Internet-loving youth. Researchers blamed such memes as a picture of an obese child with the words “Free food? Count me in!” and a series of toned bodies next to a body made of hot dogs and pizza captioned “me.” Clearly, researchers have never experienced the pure joy of eating too much pizza and truly feeling like you are one with the pie. The report didn’t mention whether more-fit countries meme less or just work out more. We’re inclined to believe a healthy lifestyle includes eating in moderation, staying fit, and meme-ing to your heart’s content.
Mad for vittles
You may not think you need to warn patients about eating rodent brains, but a Rochester, N.Y., man landed in a local hospital after his cognitive abilities took a plunge and his grip on everyday reality had loosened considerably. He’d also misplaced the ability to ambulate on his own. An MRI of his brain revealed a strange, tragic condition: The images bore a striking similarity to the brains of victims suffering from variant Creutzfeldt-Jakob disease, the prion-fueled fatal brain condition known more colloquially as “mad cow disease.” Yet most of the few hundred cases ever encountered were the result of eating bad beef in the United Kingdom more than a quarter century ago. How did this Empire State citizen succumb to a notorious English affliction? The culprits: squirrels. Seems the victim was an avid hunter who’d enjoyed his share of bushy-tailed acorn eaters, and who’d on occasion ensured that no part of his twitchy prey had gone to culinary waste. Including their brains.
The hottest new drug? Netflix
We all knew this was coming eventually. The first case of “Netflix addiction” has emerged, as a 26-year-old man in India has reportedly sought help at an addiction treatment center in Bangalore. Symptoms included 7-10 hours of TV watching per day and increasing isolation from others. Honestly, sounds like an ideal weekend. A clinical psychology professor at the treatment center warns that this instance is very similar to cases where patients are addicted to video games or social media, wherein the virtual world takes precedence over the real one. No reports yet about exactly what he was bingeing on, but our money’s on “The Great British Baking Show.” And can you blame him? The things they make on that show! This is the first case of Netflix addiction but undoubtedly will not be the last. It’s just so easy to watch 19 episodes of “Law & Order” in a row! I’m not an addict, I’m just a dedicated fan. Please don’t take my computer away from me.
Losin’ the COPD blues
The pursuit of improved therapies for chronic obstructive pulmonary disease has produced a wealth of treatment options. But one new approach sounds better than them all. In a pilot study, an inexpensive, handheld device improved breathing control and self-confidence in people with COPD. And it boosted their quality of life. In fact, 3 months of use for only about a half hour a day most days of the week improved several pulmonary outcome measures, including maximal inspiratory pressure, maximal expiratory pressure, and distance on the 6-minute walk test. The 14 patients, all ex-smokers, even posted significant improvements in performance of “Happy Birthday,” “You Are My Sunshine,” and the respiratorily challenging Johnny Cash’s “Ring of Fire.” Technically called a “free reed wind instrument,” the pulmonary rehab device is also known as a “harmonica.” Can a mouth organ really counter emphysema? Well, neither of the two hard-blowing blues harmonica legends named Sonny Boy Williamson succumbed to COPD.
This is why you’re fat
Apparently, the real reason for rising levels of obesity is not sugar or lack of exercise – it’s memes. Researchers from England’s Loughborough University sent a memo to Parliament displaying evidence that Internet memes are contributing to unhealthy eating habits and sending damaging messages to today’s Internet-loving youth. Researchers blamed such memes as a picture of an obese child with the words “Free food? Count me in!” and a series of toned bodies next to a body made of hot dogs and pizza captioned “me.” Clearly, researchers have never experienced the pure joy of eating too much pizza and truly feeling like you are one with the pie. The report didn’t mention whether more-fit countries meme less or just work out more. We’re inclined to believe a healthy lifestyle includes eating in moderation, staying fit, and meme-ing to your heart’s content.
Mad for vittles
You may not think you need to warn patients about eating rodent brains, but a Rochester, N.Y., man landed in a local hospital after his cognitive abilities took a plunge and his grip on everyday reality had loosened considerably. He’d also misplaced the ability to ambulate on his own. An MRI of his brain revealed a strange, tragic condition: The images bore a striking similarity to the brains of victims suffering from variant Creutzfeldt-Jakob disease, the prion-fueled fatal brain condition known more colloquially as “mad cow disease.” Yet most of the few hundred cases ever encountered were the result of eating bad beef in the United Kingdom more than a quarter century ago. How did this Empire State citizen succumb to a notorious English affliction? The culprits: squirrels. Seems the victim was an avid hunter who’d enjoyed his share of bushy-tailed acorn eaters, and who’d on occasion ensured that no part of his twitchy prey had gone to culinary waste. Including their brains.
The hottest new drug? Netflix
We all knew this was coming eventually. The first case of “Netflix addiction” has emerged, as a 26-year-old man in India has reportedly sought help at an addiction treatment center in Bangalore. Symptoms included 7-10 hours of TV watching per day and increasing isolation from others. Honestly, sounds like an ideal weekend. A clinical psychology professor at the treatment center warns that this instance is very similar to cases where patients are addicted to video games or social media, wherein the virtual world takes precedence over the real one. No reports yet about exactly what he was bingeing on, but our money’s on “The Great British Baking Show.” And can you blame him? The things they make on that show! This is the first case of Netflix addiction but undoubtedly will not be the last. It’s just so easy to watch 19 episodes of “Law & Order” in a row! I’m not an addict, I’m just a dedicated fan. Please don’t take my computer away from me.
Losin’ the COPD blues
The pursuit of improved therapies for chronic obstructive pulmonary disease has produced a wealth of treatment options. But one new approach sounds better than them all. In a pilot study, an inexpensive, handheld device improved breathing control and self-confidence in people with COPD. And it boosted their quality of life. In fact, 3 months of use for only about a half hour a day most days of the week improved several pulmonary outcome measures, including maximal inspiratory pressure, maximal expiratory pressure, and distance on the 6-minute walk test. The 14 patients, all ex-smokers, even posted significant improvements in performance of “Happy Birthday,” “You Are My Sunshine,” and the respiratorily challenging Johnny Cash’s “Ring of Fire.” Technically called a “free reed wind instrument,” the pulmonary rehab device is also known as a “harmonica.” Can a mouth organ really counter emphysema? Well, neither of the two hard-blowing blues harmonica legends named Sonny Boy Williamson succumbed to COPD.
This is why you’re fat
Apparently, the real reason for rising levels of obesity is not sugar or lack of exercise – it’s memes. Researchers from England’s Loughborough University sent a memo to Parliament displaying evidence that Internet memes are contributing to unhealthy eating habits and sending damaging messages to today’s Internet-loving youth. Researchers blamed such memes as a picture of an obese child with the words “Free food? Count me in!” and a series of toned bodies next to a body made of hot dogs and pizza captioned “me.” Clearly, researchers have never experienced the pure joy of eating too much pizza and truly feeling like you are one with the pie. The report didn’t mention whether more-fit countries meme less or just work out more. We’re inclined to believe a healthy lifestyle includes eating in moderation, staying fit, and meme-ing to your heart’s content.
Mad for vittles
You may not think you need to warn patients about eating rodent brains, but a Rochester, N.Y., man landed in a local hospital after his cognitive abilities took a plunge and his grip on everyday reality had loosened considerably. He’d also misplaced the ability to ambulate on his own. An MRI of his brain revealed a strange, tragic condition: The images bore a striking similarity to the brains of victims suffering from variant Creutzfeldt-Jakob disease, the prion-fueled fatal brain condition known more colloquially as “mad cow disease.” Yet most of the few hundred cases ever encountered were the result of eating bad beef in the United Kingdom more than a quarter century ago. How did this Empire State citizen succumb to a notorious English affliction? The culprits: squirrels. Seems the victim was an avid hunter who’d enjoyed his share of bushy-tailed acorn eaters, and who’d on occasion ensured that no part of his twitchy prey had gone to culinary waste. Including their brains.
Diagnosis of Epilepsy with Myoclonic-Atonic Seizures Often Changes
Pediatric patients who have been initially diagnosed with epilepsy with myoclonic-atonic seizures (EMAS) are likely to be switched to another diagnosis over time, according to a retrospective chart analysis of 77 children at Children’s Hospital of Colorado.
- Over 50% of patients in this study were switched from suspected EMAS to another epilepsy diagnosis.
- Among the 77 patients, 30 had an initial diagnosis of EMAS and 57 had a final diagnosis of EMAS.
- Among 65% of patients who had more than one diagnosis over time, the first, second, and third diagnoses were provided within 1 year, 3 years, and 10 years after the onset of the disease.
- Signs of Lennox-Gastaut syndrome (LGS), including paroxysmal fast activity, slow spike-and-wave, and tonic seizure, were detected in 50% of the 77 patients but only a minority received a final diagnosis of LGS.
Eschbach K., Moss A, Joshi C, et al. Diagnosis switching and outcomes in a cohort of patients with potential epilepsy with myoclonic-atonic seizures. Epilepsy Res. 2018; 147:95-101. https://doi.org/10.1016/j.eplepsyres.2018.09.011
Pediatric patients who have been initially diagnosed with epilepsy with myoclonic-atonic seizures (EMAS) are likely to be switched to another diagnosis over time, according to a retrospective chart analysis of 77 children at Children’s Hospital of Colorado.
- Over 50% of patients in this study were switched from suspected EMAS to another epilepsy diagnosis.
- Among the 77 patients, 30 had an initial diagnosis of EMAS and 57 had a final diagnosis of EMAS.
- Among 65% of patients who had more than one diagnosis over time, the first, second, and third diagnoses were provided within 1 year, 3 years, and 10 years after the onset of the disease.
- Signs of Lennox-Gastaut syndrome (LGS), including paroxysmal fast activity, slow spike-and-wave, and tonic seizure, were detected in 50% of the 77 patients but only a minority received a final diagnosis of LGS.
Eschbach K., Moss A, Joshi C, et al. Diagnosis switching and outcomes in a cohort of patients with potential epilepsy with myoclonic-atonic seizures. Epilepsy Res. 2018; 147:95-101. https://doi.org/10.1016/j.eplepsyres.2018.09.011
Pediatric patients who have been initially diagnosed with epilepsy with myoclonic-atonic seizures (EMAS) are likely to be switched to another diagnosis over time, according to a retrospective chart analysis of 77 children at Children’s Hospital of Colorado.
- Over 50% of patients in this study were switched from suspected EMAS to another epilepsy diagnosis.
- Among the 77 patients, 30 had an initial diagnosis of EMAS and 57 had a final diagnosis of EMAS.
- Among 65% of patients who had more than one diagnosis over time, the first, second, and third diagnoses were provided within 1 year, 3 years, and 10 years after the onset of the disease.
- Signs of Lennox-Gastaut syndrome (LGS), including paroxysmal fast activity, slow spike-and-wave, and tonic seizure, were detected in 50% of the 77 patients but only a minority received a final diagnosis of LGS.
Eschbach K., Moss A, Joshi C, et al. Diagnosis switching and outcomes in a cohort of patients with potential epilepsy with myoclonic-atonic seizures. Epilepsy Res. 2018; 147:95-101. https://doi.org/10.1016/j.eplepsyres.2018.09.011
Finding Better Way to Pinpoint Seizure Onset Zone
Researchers have found that using 256-channel high-density EEG and high-resolution head models of individual patients can help establish precise electrical source imaging of oscillatory features of the onset of a seizure, which in turn improves presurgical planning. Precisely localizing the seizure onset zone in the cortex is important for the best surgical outcomes.
- Using noninvasive electrical source imaging to plan surgery has proven problematic to date because of the interference of noise artifacts and non-seizure activity, which can be superimposed over the seizure signal.
- In this study, high density EEG was combined with exact sensor positioning and individual electrical head models, which were derived from T1 MRI results.
- Among 84 seizures, investigators were able to localize the onset of 56.
- High density EEG with interictal spikes was more accurate than international 10-20 EEG for interictal spikes and ictal onset.
Kuo C-C, Tucker DM, Luu P, et al. EEG source imaging of epileptic activity at seizure onset. Epilepsy Res. 2018;146:160-171. https://doi.org/10.1016/j.eplepsyres.2018.07.006
Researchers have found that using 256-channel high-density EEG and high-resolution head models of individual patients can help establish precise electrical source imaging of oscillatory features of the onset of a seizure, which in turn improves presurgical planning. Precisely localizing the seizure onset zone in the cortex is important for the best surgical outcomes.
- Using noninvasive electrical source imaging to plan surgery has proven problematic to date because of the interference of noise artifacts and non-seizure activity, which can be superimposed over the seizure signal.
- In this study, high density EEG was combined with exact sensor positioning and individual electrical head models, which were derived from T1 MRI results.
- Among 84 seizures, investigators were able to localize the onset of 56.
- High density EEG with interictal spikes was more accurate than international 10-20 EEG for interictal spikes and ictal onset.
Kuo C-C, Tucker DM, Luu P, et al. EEG source imaging of epileptic activity at seizure onset. Epilepsy Res. 2018;146:160-171. https://doi.org/10.1016/j.eplepsyres.2018.07.006
Researchers have found that using 256-channel high-density EEG and high-resolution head models of individual patients can help establish precise electrical source imaging of oscillatory features of the onset of a seizure, which in turn improves presurgical planning. Precisely localizing the seizure onset zone in the cortex is important for the best surgical outcomes.
- Using noninvasive electrical source imaging to plan surgery has proven problematic to date because of the interference of noise artifacts and non-seizure activity, which can be superimposed over the seizure signal.
- In this study, high density EEG was combined with exact sensor positioning and individual electrical head models, which were derived from T1 MRI results.
- Among 84 seizures, investigators were able to localize the onset of 56.
- High density EEG with interictal spikes was more accurate than international 10-20 EEG for interictal spikes and ictal onset.
Kuo C-C, Tucker DM, Luu P, et al. EEG source imaging of epileptic activity at seizure onset. Epilepsy Res. 2018;146:160-171. https://doi.org/10.1016/j.eplepsyres.2018.07.006
Unique MRI Findings in Juvenile Myoclonic Epilepsy
The cortical regions of the brains of patients with juvenile myoclonic epilepsy (JME) are more likely to be disassociated from subcortical structures, according to a recent study that compared the MRI readings of JME patients to those of normal children.
- Investigators from the University of Wisconsin School of Medicine compared 21 children with JME to 22 healthy controls over a 2 year period.
- Normal children had modular cortical development and network integration between cortical and subcortical regions.
- Patients with epilepsy had a less modular cortical network that was disassociated from subcortical structures.
- Children with JME were also found to have weaker modules or communities, as indicated by higher clustering and lower modularity indices.
Garcia-Ramos C, Dabbs K, Lin JJ, et al. Progressive dissociation of cortical and subcortical network development in children with new‐onset juvenile myoclonic epilepsy [Published online ahead of print Oct 3, 2018]. Epilepsia. https://doi.org/10.1111/epi.14560
The cortical regions of the brains of patients with juvenile myoclonic epilepsy (JME) are more likely to be disassociated from subcortical structures, according to a recent study that compared the MRI readings of JME patients to those of normal children.
- Investigators from the University of Wisconsin School of Medicine compared 21 children with JME to 22 healthy controls over a 2 year period.
- Normal children had modular cortical development and network integration between cortical and subcortical regions.
- Patients with epilepsy had a less modular cortical network that was disassociated from subcortical structures.
- Children with JME were also found to have weaker modules or communities, as indicated by higher clustering and lower modularity indices.
Garcia-Ramos C, Dabbs K, Lin JJ, et al. Progressive dissociation of cortical and subcortical network development in children with new‐onset juvenile myoclonic epilepsy [Published online ahead of print Oct 3, 2018]. Epilepsia. https://doi.org/10.1111/epi.14560
The cortical regions of the brains of patients with juvenile myoclonic epilepsy (JME) are more likely to be disassociated from subcortical structures, according to a recent study that compared the MRI readings of JME patients to those of normal children.
- Investigators from the University of Wisconsin School of Medicine compared 21 children with JME to 22 healthy controls over a 2 year period.
- Normal children had modular cortical development and network integration between cortical and subcortical regions.
- Patients with epilepsy had a less modular cortical network that was disassociated from subcortical structures.
- Children with JME were also found to have weaker modules or communities, as indicated by higher clustering and lower modularity indices.
Garcia-Ramos C, Dabbs K, Lin JJ, et al. Progressive dissociation of cortical and subcortical network development in children with new‐onset juvenile myoclonic epilepsy [Published online ahead of print Oct 3, 2018]. Epilepsia. https://doi.org/10.1111/epi.14560
Platelet-rich patch helps heal difficult diabetic foot ulcers
BERLIN –
With the LeucoPatch – which contained study participants’ own cells (platelets, fibrin, and leukocytes) – 34.1% of ulcers healed within 20 weeks versus 21.6% of ulcers that were treated using the best standard care (unadjusted odds ratio, 1.58; 95% confidence interval, 1.06-2.25; P = .02). Healing was defined as complete epithelialization maintained for 4 weeks, as confirmed by an observer blinded to the treatment group.
Results remained significant after adjusting for baseline wound size (adjusted OR 1.89; P = .02) and following a per-protocol analysis (aOR, 1.75; P = .048).
Furthermore, time to healing was shorter in the intervention group (P = .02), lead study investigator Frances Game, MD, of the Derby (England) Teaching Hospitals National Health Service Foundation Trust, reported at the annual meeting of the European Association for the Study of Diabetes.
“Successive systematic reviews from the International Working Group of the Diabetic Foot have shown that there’s very poor evidence for many of the things that we do in day-to-day practice,” she said.
“Having said that, there have been some positive studies using platelets or platelet-rich plasma to improve healing of the diabetic foot,” Dr. Game noted, although results have been inconsistent. From this the idea of the LeucoPatch was born. This is an autologous active cell therapy, which according to the Danish company Reapplix that markets it, helps patients “heal themselves.”
The LeucoPatch system is made by taking 18 mL of a patient’s blood and spinning the collection tube in a centrifuge for 20 minutes to generate a three-layered disc that contains fibrin, platelets, and leukocytes. This can then be applied to the surface of the diabetic foot ulcer. Dr. Game noted that 18 mL of blood will make a 5-cm patch and more than one patch can be made from the blood sample.
“It looks like a bit of wet skin when it comes out of the centrifuge and you just put it on sole side down. It’s taking the patient’s own cells, that often aren’t getting to the ulcer because of the morbidity of the patient and vascular disease, and actually putting them where they need to be,” she explained. The patch usually becomes absorbed within a week; depending on the ulcer, reapplication may be required.
“It’s quite a straightforward procedure that’s performed the bedside,” Dr. Game observed. “That’s how we were able to recruit so many patients, as it’s quite simple.” Indeed, almost 600 people with diabetic foot ulcers agreed to participate in the study, but only those with difficult-to-treat ulcers were included after a 4-week run-in period. The 269 patients who were finally randomized were treated at 32 specialist diabetic foot clinics in the United Kingdom, Denmark, and Sweden.
The majority of participants were male (82%) and had type 2 diabetes mellitus (83%). The mean age was 62 years and the median duration of diabetes was 16 years. The mean ulcer area was 240 mm2, with 87% being superficial, 10% reaching down to the tendon, and 3% down to the bone. In 78% of cases, the total forefoot was affected, with the plantar forefoot and hind foot affected in a respective 42% and 22% of cases.
The LeucoPatch system is already being used in several European countries, including Germany and Belgium, Dr. Game noted. However, this is the first randomized, controlled trial to demonstrate a clinical and statistically significant benefit. The data show that the weekly application of LeucoPatch is clearly of benefit in a population of patients with hard-to-heal diabetic foot ulcers.
“The low drop-out numbers suggest a good patient acceptability,” she noted, and “the treatment was without apparent increase in adverse events, particularly without evidence of new onset anemia.”
Cost-effectiveness data were collected throughout the study and will be available at a future date when these have been analyzed, Dr. Game said.
The LeucoPatch system received Food and Drug Administration approval in April 2017.
The research was published online in the Lancet Diabetes & Endocrinology ahead of the presentation.
The trial was funded by Reapplix. Dr. Game reported receiving research funding from the company.
SOURCES: Game F et al. EASD 2018, Abstract 9.
BERLIN –
With the LeucoPatch – which contained study participants’ own cells (platelets, fibrin, and leukocytes) – 34.1% of ulcers healed within 20 weeks versus 21.6% of ulcers that were treated using the best standard care (unadjusted odds ratio, 1.58; 95% confidence interval, 1.06-2.25; P = .02). Healing was defined as complete epithelialization maintained for 4 weeks, as confirmed by an observer blinded to the treatment group.
Results remained significant after adjusting for baseline wound size (adjusted OR 1.89; P = .02) and following a per-protocol analysis (aOR, 1.75; P = .048).
Furthermore, time to healing was shorter in the intervention group (P = .02), lead study investigator Frances Game, MD, of the Derby (England) Teaching Hospitals National Health Service Foundation Trust, reported at the annual meeting of the European Association for the Study of Diabetes.
“Successive systematic reviews from the International Working Group of the Diabetic Foot have shown that there’s very poor evidence for many of the things that we do in day-to-day practice,” she said.
“Having said that, there have been some positive studies using platelets or platelet-rich plasma to improve healing of the diabetic foot,” Dr. Game noted, although results have been inconsistent. From this the idea of the LeucoPatch was born. This is an autologous active cell therapy, which according to the Danish company Reapplix that markets it, helps patients “heal themselves.”
The LeucoPatch system is made by taking 18 mL of a patient’s blood and spinning the collection tube in a centrifuge for 20 minutes to generate a three-layered disc that contains fibrin, platelets, and leukocytes. This can then be applied to the surface of the diabetic foot ulcer. Dr. Game noted that 18 mL of blood will make a 5-cm patch and more than one patch can be made from the blood sample.
“It looks like a bit of wet skin when it comes out of the centrifuge and you just put it on sole side down. It’s taking the patient’s own cells, that often aren’t getting to the ulcer because of the morbidity of the patient and vascular disease, and actually putting them where they need to be,” she explained. The patch usually becomes absorbed within a week; depending on the ulcer, reapplication may be required.
“It’s quite a straightforward procedure that’s performed the bedside,” Dr. Game observed. “That’s how we were able to recruit so many patients, as it’s quite simple.” Indeed, almost 600 people with diabetic foot ulcers agreed to participate in the study, but only those with difficult-to-treat ulcers were included after a 4-week run-in period. The 269 patients who were finally randomized were treated at 32 specialist diabetic foot clinics in the United Kingdom, Denmark, and Sweden.
The majority of participants were male (82%) and had type 2 diabetes mellitus (83%). The mean age was 62 years and the median duration of diabetes was 16 years. The mean ulcer area was 240 mm2, with 87% being superficial, 10% reaching down to the tendon, and 3% down to the bone. In 78% of cases, the total forefoot was affected, with the plantar forefoot and hind foot affected in a respective 42% and 22% of cases.
The LeucoPatch system is already being used in several European countries, including Germany and Belgium, Dr. Game noted. However, this is the first randomized, controlled trial to demonstrate a clinical and statistically significant benefit. The data show that the weekly application of LeucoPatch is clearly of benefit in a population of patients with hard-to-heal diabetic foot ulcers.
“The low drop-out numbers suggest a good patient acceptability,” she noted, and “the treatment was without apparent increase in adverse events, particularly without evidence of new onset anemia.”
Cost-effectiveness data were collected throughout the study and will be available at a future date when these have been analyzed, Dr. Game said.
The LeucoPatch system received Food and Drug Administration approval in April 2017.
The research was published online in the Lancet Diabetes & Endocrinology ahead of the presentation.
The trial was funded by Reapplix. Dr. Game reported receiving research funding from the company.
SOURCES: Game F et al. EASD 2018, Abstract 9.
BERLIN –
With the LeucoPatch – which contained study participants’ own cells (platelets, fibrin, and leukocytes) – 34.1% of ulcers healed within 20 weeks versus 21.6% of ulcers that were treated using the best standard care (unadjusted odds ratio, 1.58; 95% confidence interval, 1.06-2.25; P = .02). Healing was defined as complete epithelialization maintained for 4 weeks, as confirmed by an observer blinded to the treatment group.
Results remained significant after adjusting for baseline wound size (adjusted OR 1.89; P = .02) and following a per-protocol analysis (aOR, 1.75; P = .048).
Furthermore, time to healing was shorter in the intervention group (P = .02), lead study investigator Frances Game, MD, of the Derby (England) Teaching Hospitals National Health Service Foundation Trust, reported at the annual meeting of the European Association for the Study of Diabetes.
“Successive systematic reviews from the International Working Group of the Diabetic Foot have shown that there’s very poor evidence for many of the things that we do in day-to-day practice,” she said.
“Having said that, there have been some positive studies using platelets or platelet-rich plasma to improve healing of the diabetic foot,” Dr. Game noted, although results have been inconsistent. From this the idea of the LeucoPatch was born. This is an autologous active cell therapy, which according to the Danish company Reapplix that markets it, helps patients “heal themselves.”
The LeucoPatch system is made by taking 18 mL of a patient’s blood and spinning the collection tube in a centrifuge for 20 minutes to generate a three-layered disc that contains fibrin, platelets, and leukocytes. This can then be applied to the surface of the diabetic foot ulcer. Dr. Game noted that 18 mL of blood will make a 5-cm patch and more than one patch can be made from the blood sample.
“It looks like a bit of wet skin when it comes out of the centrifuge and you just put it on sole side down. It’s taking the patient’s own cells, that often aren’t getting to the ulcer because of the morbidity of the patient and vascular disease, and actually putting them where they need to be,” she explained. The patch usually becomes absorbed within a week; depending on the ulcer, reapplication may be required.
“It’s quite a straightforward procedure that’s performed the bedside,” Dr. Game observed. “That’s how we were able to recruit so many patients, as it’s quite simple.” Indeed, almost 600 people with diabetic foot ulcers agreed to participate in the study, but only those with difficult-to-treat ulcers were included after a 4-week run-in period. The 269 patients who were finally randomized were treated at 32 specialist diabetic foot clinics in the United Kingdom, Denmark, and Sweden.
The majority of participants were male (82%) and had type 2 diabetes mellitus (83%). The mean age was 62 years and the median duration of diabetes was 16 years. The mean ulcer area was 240 mm2, with 87% being superficial, 10% reaching down to the tendon, and 3% down to the bone. In 78% of cases, the total forefoot was affected, with the plantar forefoot and hind foot affected in a respective 42% and 22% of cases.
The LeucoPatch system is already being used in several European countries, including Germany and Belgium, Dr. Game noted. However, this is the first randomized, controlled trial to demonstrate a clinical and statistically significant benefit. The data show that the weekly application of LeucoPatch is clearly of benefit in a population of patients with hard-to-heal diabetic foot ulcers.
“The low drop-out numbers suggest a good patient acceptability,” she noted, and “the treatment was without apparent increase in adverse events, particularly without evidence of new onset anemia.”
Cost-effectiveness data were collected throughout the study and will be available at a future date when these have been analyzed, Dr. Game said.
The LeucoPatch system received Food and Drug Administration approval in April 2017.
The research was published online in the Lancet Diabetes & Endocrinology ahead of the presentation.
The trial was funded by Reapplix. Dr. Game reported receiving research funding from the company.
SOURCES: Game F et al. EASD 2018, Abstract 9.
REPORTING FROM EASD 2018
Key clinical point: Weekly application of LeucoPatch enabled greater healing in a shorter time frame than standard care.
Major finding: Within 20 weeks, 34.1% versus 21.6% of diabetic foot ulcers had healed (unadjusted odds ratio, 1.58; 95% confidence interval, 1.06-2.25; P = .02).
Study details: A multicenter, multinational, observer-blinded, randomized, controlled trial of 269 patients with hard-to-heal diabetic foot ulcers.
Disclosures: The trial was funded by Reapplix. Dr. Game reported receiving research funding from the company.
Sources: Game F et al. EASD 2018, Abstract 9.
Claudication, CLI differ significantly in hospital readmission, costs, mortality
Patients treated for claudication vs. critical limb ischemia (CLI) differed significantly in their initial cost of admission, readmission costs, length of stay (LOS), days to readmission, and mortality (during initial admission, as well as any admission), according to the results of a database analysis of more than 90,000 patients in the Nationwide Readmission Database.
Readmissions were influenced not only by the admission diagnosis and intervention performed “but more importantly and significantly by the patient’s characteristics such as age, sex, CCI [Charlson Comorbidity Index], and various other demographic factors,” wrote Rennier A. Martinez, MD, of JFK Medical Center, Atlantis, Fla., and his colleagues. The report was published in the October issue of Annals of Vascular Surgery.
The study used the International Classification of Diseases, Ninth Revision (ICD-9) codes and queried the Nationwide Readmission Database for 2013 and 2014 for all 92,769 adult patients admitted with the principal diagnosis of claudication (ICD-9 code 440.21; n = 33,055 patients) or CLI (ICD-9 code 440.22e440.24; n = 59,714 patients) who underwent percutaneous angioplasty (ICD-9 code 39.50, 39.90), peripheral bypass (ICD-9 code 39.29), or aortofemoral bypass (ICD-9 code 39.25).
The 30-day readmission rates were 9.0% for claudication and 19.3% for CLI. Similarly, the any readmission rates were 21.5% and 40.4% for claudication vs. CLI.
Significant differences were found for claudication and CLI, respectively, on initial cost of admission ($18,548 vs. $29,148), readmission costs ($14,726 vs. $17,681), LOS (4 days vs. 9 days), days to readmission (73 days vs. 59 days), mortality during initial admission (256 vs. 1,363), and mortality during any admission (538 vs. 3,838), all P less than .001.
Univariate and multivariate logistic regression analysis found that claudication, CLI, angioplasty, peripheral bypass, aortofemoral bypass, female sex, age younger than 65, Charlson Comorbidity Index, LOS, and primary expected payer status were all significant predictors of 30-day and overall readmissions at varying degrees.
The researchers also found that the five most common disease readmission groups were other vascular procedures (12.6%), amputation of lower limb except toes (6.3%), sepsis (5.4%), heart failure (4.9%), and postoperative or other device infections (4.8%) (Ann Vasc Surg. 2018;52:96-107).
The increased costs and higher levels of morbidity and mortality seen with CLI vs. claudication are not surprising given previous research showing that there are higher rates of complications in patients with CLI. A previous review showed there was a threefold higher risk of myocardial infarction, stroke, and vascular death in patients with CLI compared with patients with claudication, according Dr. Martinez and his colleagues.
“Readmissions after lower extremity procedures for patients admitted for claudication or CLI are influenced not only by the admission diagnosis and intervention performed but more importantly and significantly by the patient’s characteristics such as age, sex, CCI, and various other demographic factors,” the researchers wrote. “It is paramount to continue to perform this kind of study to better identify patients at risk for readmission and work toward prevention,” they concluded.
Dr. Martinez and his colleagues did not report disclosures, but indicated that the study did not receive any outside funding.
SOURCE: Martinez RA et al. Ann Vasc Surg. 2018;52:96-107.
Patients treated for claudication vs. critical limb ischemia (CLI) differed significantly in their initial cost of admission, readmission costs, length of stay (LOS), days to readmission, and mortality (during initial admission, as well as any admission), according to the results of a database analysis of more than 90,000 patients in the Nationwide Readmission Database.
Readmissions were influenced not only by the admission diagnosis and intervention performed “but more importantly and significantly by the patient’s characteristics such as age, sex, CCI [Charlson Comorbidity Index], and various other demographic factors,” wrote Rennier A. Martinez, MD, of JFK Medical Center, Atlantis, Fla., and his colleagues. The report was published in the October issue of Annals of Vascular Surgery.
The study used the International Classification of Diseases, Ninth Revision (ICD-9) codes and queried the Nationwide Readmission Database for 2013 and 2014 for all 92,769 adult patients admitted with the principal diagnosis of claudication (ICD-9 code 440.21; n = 33,055 patients) or CLI (ICD-9 code 440.22e440.24; n = 59,714 patients) who underwent percutaneous angioplasty (ICD-9 code 39.50, 39.90), peripheral bypass (ICD-9 code 39.29), or aortofemoral bypass (ICD-9 code 39.25).
The 30-day readmission rates were 9.0% for claudication and 19.3% for CLI. Similarly, the any readmission rates were 21.5% and 40.4% for claudication vs. CLI.
Significant differences were found for claudication and CLI, respectively, on initial cost of admission ($18,548 vs. $29,148), readmission costs ($14,726 vs. $17,681), LOS (4 days vs. 9 days), days to readmission (73 days vs. 59 days), mortality during initial admission (256 vs. 1,363), and mortality during any admission (538 vs. 3,838), all P less than .001.
Univariate and multivariate logistic regression analysis found that claudication, CLI, angioplasty, peripheral bypass, aortofemoral bypass, female sex, age younger than 65, Charlson Comorbidity Index, LOS, and primary expected payer status were all significant predictors of 30-day and overall readmissions at varying degrees.
The researchers also found that the five most common disease readmission groups were other vascular procedures (12.6%), amputation of lower limb except toes (6.3%), sepsis (5.4%), heart failure (4.9%), and postoperative or other device infections (4.8%) (Ann Vasc Surg. 2018;52:96-107).
The increased costs and higher levels of morbidity and mortality seen with CLI vs. claudication are not surprising given previous research showing that there are higher rates of complications in patients with CLI. A previous review showed there was a threefold higher risk of myocardial infarction, stroke, and vascular death in patients with CLI compared with patients with claudication, according Dr. Martinez and his colleagues.
“Readmissions after lower extremity procedures for patients admitted for claudication or CLI are influenced not only by the admission diagnosis and intervention performed but more importantly and significantly by the patient’s characteristics such as age, sex, CCI, and various other demographic factors,” the researchers wrote. “It is paramount to continue to perform this kind of study to better identify patients at risk for readmission and work toward prevention,” they concluded.
Dr. Martinez and his colleagues did not report disclosures, but indicated that the study did not receive any outside funding.
SOURCE: Martinez RA et al. Ann Vasc Surg. 2018;52:96-107.
Patients treated for claudication vs. critical limb ischemia (CLI) differed significantly in their initial cost of admission, readmission costs, length of stay (LOS), days to readmission, and mortality (during initial admission, as well as any admission), according to the results of a database analysis of more than 90,000 patients in the Nationwide Readmission Database.
Readmissions were influenced not only by the admission diagnosis and intervention performed “but more importantly and significantly by the patient’s characteristics such as age, sex, CCI [Charlson Comorbidity Index], and various other demographic factors,” wrote Rennier A. Martinez, MD, of JFK Medical Center, Atlantis, Fla., and his colleagues. The report was published in the October issue of Annals of Vascular Surgery.
The study used the International Classification of Diseases, Ninth Revision (ICD-9) codes and queried the Nationwide Readmission Database for 2013 and 2014 for all 92,769 adult patients admitted with the principal diagnosis of claudication (ICD-9 code 440.21; n = 33,055 patients) or CLI (ICD-9 code 440.22e440.24; n = 59,714 patients) who underwent percutaneous angioplasty (ICD-9 code 39.50, 39.90), peripheral bypass (ICD-9 code 39.29), or aortofemoral bypass (ICD-9 code 39.25).
The 30-day readmission rates were 9.0% for claudication and 19.3% for CLI. Similarly, the any readmission rates were 21.5% and 40.4% for claudication vs. CLI.
Significant differences were found for claudication and CLI, respectively, on initial cost of admission ($18,548 vs. $29,148), readmission costs ($14,726 vs. $17,681), LOS (4 days vs. 9 days), days to readmission (73 days vs. 59 days), mortality during initial admission (256 vs. 1,363), and mortality during any admission (538 vs. 3,838), all P less than .001.
Univariate and multivariate logistic regression analysis found that claudication, CLI, angioplasty, peripheral bypass, aortofemoral bypass, female sex, age younger than 65, Charlson Comorbidity Index, LOS, and primary expected payer status were all significant predictors of 30-day and overall readmissions at varying degrees.
The researchers also found that the five most common disease readmission groups were other vascular procedures (12.6%), amputation of lower limb except toes (6.3%), sepsis (5.4%), heart failure (4.9%), and postoperative or other device infections (4.8%) (Ann Vasc Surg. 2018;52:96-107).
The increased costs and higher levels of morbidity and mortality seen with CLI vs. claudication are not surprising given previous research showing that there are higher rates of complications in patients with CLI. A previous review showed there was a threefold higher risk of myocardial infarction, stroke, and vascular death in patients with CLI compared with patients with claudication, according Dr. Martinez and his colleagues.
“Readmissions after lower extremity procedures for patients admitted for claudication or CLI are influenced not only by the admission diagnosis and intervention performed but more importantly and significantly by the patient’s characteristics such as age, sex, CCI, and various other demographic factors,” the researchers wrote. “It is paramount to continue to perform this kind of study to better identify patients at risk for readmission and work toward prevention,” they concluded.
Dr. Martinez and his colleagues did not report disclosures, but indicated that the study did not receive any outside funding.
SOURCE: Martinez RA et al. Ann Vasc Surg. 2018;52:96-107.
FROM ANNALS OF VASCULAR SURGERY
Key clinical point: CLI was significantly more expensive and showed higher mortality rates compared with claudication.
Major finding: The 30-day readmission/any readmission rate was 9.0%/21.5% and 19.3%/40.4%, for claudication and CLI, respectively.
Study details: An analysis of more than 90,000 patients in the Nationwide Readmission Database in 2013 and 2014.
Disclosures: The authors did not report disclosures but indicated that the study did not receive any outside funding.
Source: Martinez RA et al. Ann Vasc Surg. 2018;52:96-107.
Helping alleviate hospitalist burnout
Focus on systemic factors
For hospitalists, burnout is a widespread and ongoing problem. In 2011, a Mayo Clinic study found that 45% of U.S. physicians had at least one symptom of professional burnout; by 2014, that number had risen to 54%.

“Burnout among physicians has been shown to be linked to quality of care, impacting medical errors, mortality ratios in hospitalized patients, and lower patient satisfaction,” said Ingrid T. Katz, MD, MHS, assistant professor of medicine at Harvard Medical School, Boston, and coauthor of a recent column on the subject published in the New England Journal of Medicine.
Widespread burnout is caused by systemic factors, not individual failures. “These systemic factors range from excessive clerical burden to ‘work beyond work,’ where people end up taking work home at night and are often found interfacing with the EHR well after their normal work day,” Dr. Katz said. “Many also express their disdain for the model of practice that no longer values autonomy, which was seen as inherent in the profession prior to the current model of care.”
Moving towards a better framework would require an inherent trust in physicians, limiting unnecessary intrusions into a physician’s practice that do not impact medical care. “It would remove the burden of excessive documentation and allow for physicians to get reinspired by the practice of medicine, an inherently altruistic profession,” Dr. Katz said.
Changes might include eliminating excessive clerical demands and improving EHRs to allow physicians to return to the bedside. Workloads would be geared towards quality in care and not focused on improving the bottom line of a health care system. One health system Dr. Katz wrote about instituted a team-based model; under this system medical assistants gather data and reconcile medications, allowing physicians to focus on performing physical exams and making medical decisions.
“Burnout will diminish when physicians are empowered to be part of the solution and hospital systems make changes that recognize the totality of the challenges that physicians face,” Dr. Katz said, adding that hospitalists are in a unique position to promote such changes on a systemic level. “Leadership needs to be willing to inform and engage their physicians, monitor well-being of physicians as closely as they monitor quality in care, and implement changes when needed.”
Reference
1. Katz IT et al. Beyond Burnout – Redesigning Care to Restore Meaning and Sanity for Physicians. N Engl J Med. 2018 Jan 25. doi: 10.1056/NEJMp1716845.
Focus on systemic factors
Focus on systemic factors
For hospitalists, burnout is a widespread and ongoing problem. In 2011, a Mayo Clinic study found that 45% of U.S. physicians had at least one symptom of professional burnout; by 2014, that number had risen to 54%.

“Burnout among physicians has been shown to be linked to quality of care, impacting medical errors, mortality ratios in hospitalized patients, and lower patient satisfaction,” said Ingrid T. Katz, MD, MHS, assistant professor of medicine at Harvard Medical School, Boston, and coauthor of a recent column on the subject published in the New England Journal of Medicine.
Widespread burnout is caused by systemic factors, not individual failures. “These systemic factors range from excessive clerical burden to ‘work beyond work,’ where people end up taking work home at night and are often found interfacing with the EHR well after their normal work day,” Dr. Katz said. “Many also express their disdain for the model of practice that no longer values autonomy, which was seen as inherent in the profession prior to the current model of care.”
Moving towards a better framework would require an inherent trust in physicians, limiting unnecessary intrusions into a physician’s practice that do not impact medical care. “It would remove the burden of excessive documentation and allow for physicians to get reinspired by the practice of medicine, an inherently altruistic profession,” Dr. Katz said.
Changes might include eliminating excessive clerical demands and improving EHRs to allow physicians to return to the bedside. Workloads would be geared towards quality in care and not focused on improving the bottom line of a health care system. One health system Dr. Katz wrote about instituted a team-based model; under this system medical assistants gather data and reconcile medications, allowing physicians to focus on performing physical exams and making medical decisions.
“Burnout will diminish when physicians are empowered to be part of the solution and hospital systems make changes that recognize the totality of the challenges that physicians face,” Dr. Katz said, adding that hospitalists are in a unique position to promote such changes on a systemic level. “Leadership needs to be willing to inform and engage their physicians, monitor well-being of physicians as closely as they monitor quality in care, and implement changes when needed.”
Reference
1. Katz IT et al. Beyond Burnout – Redesigning Care to Restore Meaning and Sanity for Physicians. N Engl J Med. 2018 Jan 25. doi: 10.1056/NEJMp1716845.
For hospitalists, burnout is a widespread and ongoing problem. In 2011, a Mayo Clinic study found that 45% of U.S. physicians had at least one symptom of professional burnout; by 2014, that number had risen to 54%.

“Burnout among physicians has been shown to be linked to quality of care, impacting medical errors, mortality ratios in hospitalized patients, and lower patient satisfaction,” said Ingrid T. Katz, MD, MHS, assistant professor of medicine at Harvard Medical School, Boston, and coauthor of a recent column on the subject published in the New England Journal of Medicine.
Widespread burnout is caused by systemic factors, not individual failures. “These systemic factors range from excessive clerical burden to ‘work beyond work,’ where people end up taking work home at night and are often found interfacing with the EHR well after their normal work day,” Dr. Katz said. “Many also express their disdain for the model of practice that no longer values autonomy, which was seen as inherent in the profession prior to the current model of care.”
Moving towards a better framework would require an inherent trust in physicians, limiting unnecessary intrusions into a physician’s practice that do not impact medical care. “It would remove the burden of excessive documentation and allow for physicians to get reinspired by the practice of medicine, an inherently altruistic profession,” Dr. Katz said.
Changes might include eliminating excessive clerical demands and improving EHRs to allow physicians to return to the bedside. Workloads would be geared towards quality in care and not focused on improving the bottom line of a health care system. One health system Dr. Katz wrote about instituted a team-based model; under this system medical assistants gather data and reconcile medications, allowing physicians to focus on performing physical exams and making medical decisions.
“Burnout will diminish when physicians are empowered to be part of the solution and hospital systems make changes that recognize the totality of the challenges that physicians face,” Dr. Katz said, adding that hospitalists are in a unique position to promote such changes on a systemic level. “Leadership needs to be willing to inform and engage their physicians, monitor well-being of physicians as closely as they monitor quality in care, and implement changes when needed.”
Reference
1. Katz IT et al. Beyond Burnout – Redesigning Care to Restore Meaning and Sanity for Physicians. N Engl J Med. 2018 Jan 25. doi: 10.1056/NEJMp1716845.
ACIP supports hepatitis A vaccine for homeless individuals
Homeless individuals aged 1 year and older should be vaccinated against hepatitis A, based on a unanimous vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
“It is important that we take a national approach to vaccinating homeless” people, Noele Nelson, MD, PhD, MPH, of the CDC’s Division of Viral Hepatitis, said in a presentation prior to the vote, in which all 11 committee members voted in favor of hepatitis A vaccination for the homeless population.
Even limited vaccination will increase the herd immunity of the homeless population over time, she said.
Dr. Nelson presented data on the pros and cons of routine hepatitis A vaccination for homeless individuals aged 1 year and older. The Hepatitis Vaccines Work Group convened four meetings in advance of the October ACIP meeting and reached a consensus that homelessness is an independent indication for hepatitis A vaccination, she said.
If the hepatitis A vaccine is included as an ACIP recommendation, “it is more likely to be considered by homeless service providers,” noted Dr. Nelson. She also cited a low quality of evidence for adverse events associated with hepatitis A vaccination.
The work group considerations in the wake of a nationwide hepatitis A outbreak earlier in 2018 included the challenges of controlling outbreaks, which can spread quickly among the homeless population because of poor personal hygiene, limited sanitation, and tight living quarters. These factors make the homeless population more reliant on a vaccine for protection. An outbreak in San Diego, Calif., in particular, occurred largely in the homeless population.
“Routine vaccination is a more feasible approach to reach the homeless over time through regular homeless care providers,” Dr. Nelson said. As for costs, integrating vaccination into routine care for the homeless is cheaper and much less disruptive than the cost of responding to an outbreak.
The “cons” of recommending routine hepatitis A vaccination for the homeless population included the challenges of administrative record keeping. However, during the public comment period, Mae Morgan, MD, an internist who is medical director of Mercy Care Decatur Street & City of Refuge in Atlanta, emphasized that local homeless care organizations have procedures to manage routine vaccination. “If anyone is concerned that there is not a network in place, there are health centers to do this [that] would implement the vaccine.”
The ACIP committee members had no financial conflicts to disclose.
Homeless individuals aged 1 year and older should be vaccinated against hepatitis A, based on a unanimous vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
“It is important that we take a national approach to vaccinating homeless” people, Noele Nelson, MD, PhD, MPH, of the CDC’s Division of Viral Hepatitis, said in a presentation prior to the vote, in which all 11 committee members voted in favor of hepatitis A vaccination for the homeless population.
Even limited vaccination will increase the herd immunity of the homeless population over time, she said.
Dr. Nelson presented data on the pros and cons of routine hepatitis A vaccination for homeless individuals aged 1 year and older. The Hepatitis Vaccines Work Group convened four meetings in advance of the October ACIP meeting and reached a consensus that homelessness is an independent indication for hepatitis A vaccination, she said.
If the hepatitis A vaccine is included as an ACIP recommendation, “it is more likely to be considered by homeless service providers,” noted Dr. Nelson. She also cited a low quality of evidence for adverse events associated with hepatitis A vaccination.
The work group considerations in the wake of a nationwide hepatitis A outbreak earlier in 2018 included the challenges of controlling outbreaks, which can spread quickly among the homeless population because of poor personal hygiene, limited sanitation, and tight living quarters. These factors make the homeless population more reliant on a vaccine for protection. An outbreak in San Diego, Calif., in particular, occurred largely in the homeless population.
“Routine vaccination is a more feasible approach to reach the homeless over time through regular homeless care providers,” Dr. Nelson said. As for costs, integrating vaccination into routine care for the homeless is cheaper and much less disruptive than the cost of responding to an outbreak.
The “cons” of recommending routine hepatitis A vaccination for the homeless population included the challenges of administrative record keeping. However, during the public comment period, Mae Morgan, MD, an internist who is medical director of Mercy Care Decatur Street & City of Refuge in Atlanta, emphasized that local homeless care organizations have procedures to manage routine vaccination. “If anyone is concerned that there is not a network in place, there are health centers to do this [that] would implement the vaccine.”
The ACIP committee members had no financial conflicts to disclose.
Homeless individuals aged 1 year and older should be vaccinated against hepatitis A, based on a unanimous vote at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices.
“It is important that we take a national approach to vaccinating homeless” people, Noele Nelson, MD, PhD, MPH, of the CDC’s Division of Viral Hepatitis, said in a presentation prior to the vote, in which all 11 committee members voted in favor of hepatitis A vaccination for the homeless population.
Even limited vaccination will increase the herd immunity of the homeless population over time, she said.
Dr. Nelson presented data on the pros and cons of routine hepatitis A vaccination for homeless individuals aged 1 year and older. The Hepatitis Vaccines Work Group convened four meetings in advance of the October ACIP meeting and reached a consensus that homelessness is an independent indication for hepatitis A vaccination, she said.
If the hepatitis A vaccine is included as an ACIP recommendation, “it is more likely to be considered by homeless service providers,” noted Dr. Nelson. She also cited a low quality of evidence for adverse events associated with hepatitis A vaccination.
The work group considerations in the wake of a nationwide hepatitis A outbreak earlier in 2018 included the challenges of controlling outbreaks, which can spread quickly among the homeless population because of poor personal hygiene, limited sanitation, and tight living quarters. These factors make the homeless population more reliant on a vaccine for protection. An outbreak in San Diego, Calif., in particular, occurred largely in the homeless population.
“Routine vaccination is a more feasible approach to reach the homeless over time through regular homeless care providers,” Dr. Nelson said. As for costs, integrating vaccination into routine care for the homeless is cheaper and much less disruptive than the cost of responding to an outbreak.
The “cons” of recommending routine hepatitis A vaccination for the homeless population included the challenges of administrative record keeping. However, during the public comment period, Mae Morgan, MD, an internist who is medical director of Mercy Care Decatur Street & City of Refuge in Atlanta, emphasized that local homeless care organizations have procedures to manage routine vaccination. “If anyone is concerned that there is not a network in place, there are health centers to do this [that] would implement the vaccine.”
The ACIP committee members had no financial conflicts to disclose.
FROM AN ACIP MEETING
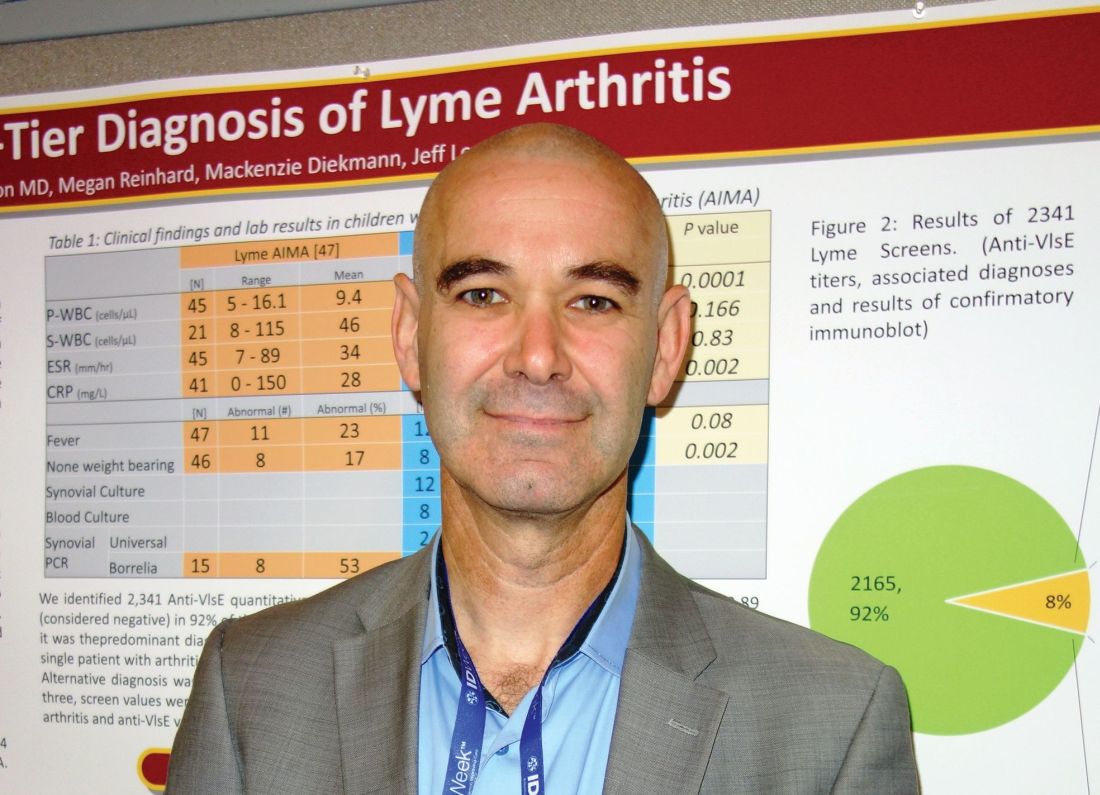
Swollen knee in a kid? Above 9, treat for Lyme
SAN FRANCISCO – There’s no need to wait for western blot results to differentiate Lyme arthritis from septic arthritis in children, as long as your lab, like many, uses the Liaison Borrelia burgdorferi assay, according to investigators at the University of Minnesota, Minneapolis.
Acute, isolated monoarthritis presents with a single swollen joint and pain whether it’s due to Lyme disease or infection, so it’s hard to tell them apart. Current guidelines recommend a two-tier approach to diagnose Lyme arthritis, an initial blood screen followed by western blot confirmation. Screening results come back in a few hours, but western blot confirmation can take days.
In the meantime, children are treated presumptively for the more concerning diagnosis – septic arthritis – which means hospitalization, surgical drainage, and IV antibiotics. Those who turn out to have Lyme are exposed to the risks and costs of unnecessary treatment and delays to proper diagnosis and doxycycline.
When “kids come in with a swollen knee, maybe 10% or 15% end up in the hospital being treated for septic arthritis that they never had. I wanted to see if we can diagnose Lyme arthritis more quickly,” said lead investigator Bazak Sharon, MD, a pediatric infectious disease specialist at the university’s Masonic Children’s Hospital.
Masonic and its affiliated health system use the Liaison Borrelia burgdorferi assay (DiaSorin) to screen for Lyme, and a careful parsing of the results seems to solve the problem.
Liaison is a chemiluminescence immunoassay that uses light to measure IgM and IgG antibodies to a B. burgdorferi surface protein in serum samples. Results are reported as relative light units (RLUs); below 0.9 RLUs is negative; 0.9-1.1 is equivocal, and over 1.1 is positive.
It’s where patients fall in the range of positivity that matters when it comes to differentiating Lyme from septic arthritis, Dr. Sharon said at ID Week, an annual scientific meeting on infectious diseases (Clin Vaccine Immunol. 2008 Dec;15[12]:1796-804).
He and his team reviewed 60 cases of acute, isolated monoarthritis culled from more than 700 children who presented with joint complaints from 2011 to 2016; 47 had Lyme arthritis confirmed by western blot; 13 had septic arthritis.
It turned out that “every single patient with a” Liaison value of 9 RLUs or higher was confirmed on western blot for Lyme. “Under 9, there was not a single case of Lyme arthritis,” Dr. Sharon said. Three other patients with acute arthritis also tested positive on the screen, but their RLU values were below 4; two turned out to be trauma related and one was ultimately diagnosed with juvenile idiopathic arthritis. Western blots were negative in all three.
The RLU number reported on the screening test “appears to correlate very well with Lyme arthritis. In an otherwise healthy child presenting with acute joint swelling, utilizing this screening test can confirm clinical suspicion of Lyme arthritis within hours, and prevent the potential harmful interventions accompanying a misdiagnosis of septic arthritis. Just do the screening. If it comes up above 9, you’ve got Lyme arthritis,” and don’t need to wait for western blot results to treat, Dr. Sharon said.
In other words, above 9, treat for Lyme.
The investigators plan to delve further into their results with sensitivity/specificity and other analyses before publishing. Ultimately, “my goal is to have a better diagnosis algorithm for kids who present with acute, isolated monoarthritis,” Dr. Sharon said.
There was no industry funding for the work, and the investigators didn’t have any disclosures.
SOURCE: Sharon B et al. 2018 ID Week abstract 286.
SAN FRANCISCO – There’s no need to wait for western blot results to differentiate Lyme arthritis from septic arthritis in children, as long as your lab, like many, uses the Liaison Borrelia burgdorferi assay, according to investigators at the University of Minnesota, Minneapolis.
Acute, isolated monoarthritis presents with a single swollen joint and pain whether it’s due to Lyme disease or infection, so it’s hard to tell them apart. Current guidelines recommend a two-tier approach to diagnose Lyme arthritis, an initial blood screen followed by western blot confirmation. Screening results come back in a few hours, but western blot confirmation can take days.
In the meantime, children are treated presumptively for the more concerning diagnosis – septic arthritis – which means hospitalization, surgical drainage, and IV antibiotics. Those who turn out to have Lyme are exposed to the risks and costs of unnecessary treatment and delays to proper diagnosis and doxycycline.
When “kids come in with a swollen knee, maybe 10% or 15% end up in the hospital being treated for septic arthritis that they never had. I wanted to see if we can diagnose Lyme arthritis more quickly,” said lead investigator Bazak Sharon, MD, a pediatric infectious disease specialist at the university’s Masonic Children’s Hospital.
Masonic and its affiliated health system use the Liaison Borrelia burgdorferi assay (DiaSorin) to screen for Lyme, and a careful parsing of the results seems to solve the problem.
Liaison is a chemiluminescence immunoassay that uses light to measure IgM and IgG antibodies to a B. burgdorferi surface protein in serum samples. Results are reported as relative light units (RLUs); below 0.9 RLUs is negative; 0.9-1.1 is equivocal, and over 1.1 is positive.
It’s where patients fall in the range of positivity that matters when it comes to differentiating Lyme from septic arthritis, Dr. Sharon said at ID Week, an annual scientific meeting on infectious diseases (Clin Vaccine Immunol. 2008 Dec;15[12]:1796-804).
He and his team reviewed 60 cases of acute, isolated monoarthritis culled from more than 700 children who presented with joint complaints from 2011 to 2016; 47 had Lyme arthritis confirmed by western blot; 13 had septic arthritis.
It turned out that “every single patient with a” Liaison value of 9 RLUs or higher was confirmed on western blot for Lyme. “Under 9, there was not a single case of Lyme arthritis,” Dr. Sharon said. Three other patients with acute arthritis also tested positive on the screen, but their RLU values were below 4; two turned out to be trauma related and one was ultimately diagnosed with juvenile idiopathic arthritis. Western blots were negative in all three.
The RLU number reported on the screening test “appears to correlate very well with Lyme arthritis. In an otherwise healthy child presenting with acute joint swelling, utilizing this screening test can confirm clinical suspicion of Lyme arthritis within hours, and prevent the potential harmful interventions accompanying a misdiagnosis of septic arthritis. Just do the screening. If it comes up above 9, you’ve got Lyme arthritis,” and don’t need to wait for western blot results to treat, Dr. Sharon said.
In other words, above 9, treat for Lyme.
The investigators plan to delve further into their results with sensitivity/specificity and other analyses before publishing. Ultimately, “my goal is to have a better diagnosis algorithm for kids who present with acute, isolated monoarthritis,” Dr. Sharon said.
There was no industry funding for the work, and the investigators didn’t have any disclosures.
SOURCE: Sharon B et al. 2018 ID Week abstract 286.
SAN FRANCISCO – There’s no need to wait for western blot results to differentiate Lyme arthritis from septic arthritis in children, as long as your lab, like many, uses the Liaison Borrelia burgdorferi assay, according to investigators at the University of Minnesota, Minneapolis.
Acute, isolated monoarthritis presents with a single swollen joint and pain whether it’s due to Lyme disease or infection, so it’s hard to tell them apart. Current guidelines recommend a two-tier approach to diagnose Lyme arthritis, an initial blood screen followed by western blot confirmation. Screening results come back in a few hours, but western blot confirmation can take days.
In the meantime, children are treated presumptively for the more concerning diagnosis – septic arthritis – which means hospitalization, surgical drainage, and IV antibiotics. Those who turn out to have Lyme are exposed to the risks and costs of unnecessary treatment and delays to proper diagnosis and doxycycline.
When “kids come in with a swollen knee, maybe 10% or 15% end up in the hospital being treated for septic arthritis that they never had. I wanted to see if we can diagnose Lyme arthritis more quickly,” said lead investigator Bazak Sharon, MD, a pediatric infectious disease specialist at the university’s Masonic Children’s Hospital.
Masonic and its affiliated health system use the Liaison Borrelia burgdorferi assay (DiaSorin) to screen for Lyme, and a careful parsing of the results seems to solve the problem.
Liaison is a chemiluminescence immunoassay that uses light to measure IgM and IgG antibodies to a B. burgdorferi surface protein in serum samples. Results are reported as relative light units (RLUs); below 0.9 RLUs is negative; 0.9-1.1 is equivocal, and over 1.1 is positive.
It’s where patients fall in the range of positivity that matters when it comes to differentiating Lyme from septic arthritis, Dr. Sharon said at ID Week, an annual scientific meeting on infectious diseases (Clin Vaccine Immunol. 2008 Dec;15[12]:1796-804).
He and his team reviewed 60 cases of acute, isolated monoarthritis culled from more than 700 children who presented with joint complaints from 2011 to 2016; 47 had Lyme arthritis confirmed by western blot; 13 had septic arthritis.
It turned out that “every single patient with a” Liaison value of 9 RLUs or higher was confirmed on western blot for Lyme. “Under 9, there was not a single case of Lyme arthritis,” Dr. Sharon said. Three other patients with acute arthritis also tested positive on the screen, but their RLU values were below 4; two turned out to be trauma related and one was ultimately diagnosed with juvenile idiopathic arthritis. Western blots were negative in all three.
The RLU number reported on the screening test “appears to correlate very well with Lyme arthritis. In an otherwise healthy child presenting with acute joint swelling, utilizing this screening test can confirm clinical suspicion of Lyme arthritis within hours, and prevent the potential harmful interventions accompanying a misdiagnosis of septic arthritis. Just do the screening. If it comes up above 9, you’ve got Lyme arthritis,” and don’t need to wait for western blot results to treat, Dr. Sharon said.
In other words, above 9, treat for Lyme.
The investigators plan to delve further into their results with sensitivity/specificity and other analyses before publishing. Ultimately, “my goal is to have a better diagnosis algorithm for kids who present with acute, isolated monoarthritis,” Dr. Sharon said.
There was no industry funding for the work, and the investigators didn’t have any disclosures.
SOURCE: Sharon B et al. 2018 ID Week abstract 286.
REPORTING FROM IDWEEK 2018
Key clinical point:
Major finding: There was not a single case of Lyme arthritis under 9 RLUs on the screening test.
Study details: Review of 60 children with acute, isolated monoarthritis, culled from more than 700 with joint complaints.
Disclosures: There was no industry funding for the work, and the investigators didn’t have any disclosures.
Source: Sharon B et al. 2018 ID Week abstract 286.
FDA approves Xofluza for treatment of influenza
The Food and Drug Administration has approved Xofluza (baloxavir marboxil) for the treatment of acute uncomplicated influenza in people aged 12 years or older who have been symptomatic for 48 hours or less.
The FDA approval is based on results from two randomized, clinical trials. In both trials, patients who received Xofluza experienced a shorter duration until alleviation of symptoms, compared with patients who received a placebo. In the second trial, patients who received Xofluza and patients who received another approved antiviral influenza medication experienced similar durations until symptom alleviation.
“When treatment is started within 48 hours of becoming sick with flu symptoms, antiviral drugs can lessen symptoms and shorten the time patients feel sick. Having more treatment options that work in different ways to attack the virus is important because flu viruses can become resistant to antiviral drugs,” Debra Birnkrant, MD, director of the Division of Antiviral Products in the FDA’s Center for Drug Evaluation and Research, said in a press release.
The most common adverse events associated with Xofluza were diarrhea and bronchitis.
“This is the first new antiviral flu treatment with a novel mechanism of action approved by the FDA in nearly 20 years,” FDA Commissioner Scott Gottlieb, MD, added. “With thousands of people getting the flu every year, and many people becoming seriously ill, having safe and effective treatment alternatives is critical. This novel drug provides an important, additional treatment option.”
Find the full press release on the FDA website.
The Food and Drug Administration has approved Xofluza (baloxavir marboxil) for the treatment of acute uncomplicated influenza in people aged 12 years or older who have been symptomatic for 48 hours or less.
The FDA approval is based on results from two randomized, clinical trials. In both trials, patients who received Xofluza experienced a shorter duration until alleviation of symptoms, compared with patients who received a placebo. In the second trial, patients who received Xofluza and patients who received another approved antiviral influenza medication experienced similar durations until symptom alleviation.
“When treatment is started within 48 hours of becoming sick with flu symptoms, antiviral drugs can lessen symptoms and shorten the time patients feel sick. Having more treatment options that work in different ways to attack the virus is important because flu viruses can become resistant to antiviral drugs,” Debra Birnkrant, MD, director of the Division of Antiviral Products in the FDA’s Center for Drug Evaluation and Research, said in a press release.
The most common adverse events associated with Xofluza were diarrhea and bronchitis.
“This is the first new antiviral flu treatment with a novel mechanism of action approved by the FDA in nearly 20 years,” FDA Commissioner Scott Gottlieb, MD, added. “With thousands of people getting the flu every year, and many people becoming seriously ill, having safe and effective treatment alternatives is critical. This novel drug provides an important, additional treatment option.”
Find the full press release on the FDA website.
The Food and Drug Administration has approved Xofluza (baloxavir marboxil) for the treatment of acute uncomplicated influenza in people aged 12 years or older who have been symptomatic for 48 hours or less.
The FDA approval is based on results from two randomized, clinical trials. In both trials, patients who received Xofluza experienced a shorter duration until alleviation of symptoms, compared with patients who received a placebo. In the second trial, patients who received Xofluza and patients who received another approved antiviral influenza medication experienced similar durations until symptom alleviation.
“When treatment is started within 48 hours of becoming sick with flu symptoms, antiviral drugs can lessen symptoms and shorten the time patients feel sick. Having more treatment options that work in different ways to attack the virus is important because flu viruses can become resistant to antiviral drugs,” Debra Birnkrant, MD, director of the Division of Antiviral Products in the FDA’s Center for Drug Evaluation and Research, said in a press release.
The most common adverse events associated with Xofluza were diarrhea and bronchitis.
“This is the first new antiviral flu treatment with a novel mechanism of action approved by the FDA in nearly 20 years,” FDA Commissioner Scott Gottlieb, MD, added. “With thousands of people getting the flu every year, and many people becoming seriously ill, having safe and effective treatment alternatives is critical. This novel drug provides an important, additional treatment option.”
Find the full press release on the FDA website.