User login
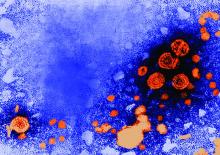
Maintaining virologic response predicted long-term survival in HBV patients with decompensated cirrhosis
according to the results of a multicenter observational study published in the December issue of Clinical Gastroenterology and Hepatology.
Survival times were “excellent” if patients survived the first 6 months of antiviral therapy and did not develop hepatocellular carcinoma, said Jeong Won Jang, MD, of the Catholic University of Korea College of Medicine in Seoul, South Korea, and his associates. Patients who developed hepatocellular carcinoma had persistent declines in survival over time, they said. Predictors of short-term mortality included a baseline Model for End-Stage Liver Disease score above 20 and multiple complications.
Chronic hepatitis B virus (HBV) infection is the most common cause of liver-related disease and death in Asia, and complications such as decompensated cirrhosis affect up to 40% of chronically infected persons. Five-year survival rates are as low as 14% if patients develop decompensated cirrhosis.
To explore whether virologic suppression with oral nucleoside or nucleotide analog therapy improves outcomes in these decompensated patients, the researchers studied 295 such individuals from the Epidemiology and Natural History of Liver Cirrhosis in Korea Study. At baseline, these patients did not have documented chronic hepatitis C virus infection, hepatocellular carcinoma, other cancers, autoimmune hepatitis, or alcohol use disorders. All patients initiated entecavir or lamivudine therapy immediately after their cirrhosis became decompensated. The primary outcome was transplant-free survival.
A total of 60.1% of patients survived 5 years and 45.7% survived 10 years without undergoing transplantation, for a median transplant-free survival time of 7.7 years. The 116 patients (39%) who consistently had undetectable HBV DNA levels (less than 20 IU/mL) throughout treatment had significantly longer transplant-free survival than did patients who did not maintain a virologic response (P less than .001). In addition, a maintained virologic response (MVR) was the strongest predictor of long-term transplant-free survival, the researchers said.
A significantly greater proportion of patients who received entecavir survived 10 years compared with patients who received lamivudine. However, there was no significant difference in long-term survival among patients with MVRs to either drug. “Importantly, it appears that improvement in patient survival is attained by antiviral response, not by the type of nucleos(t)ide analogue per se,” the researchers wrote.
Patients who achieved MVR also showed significant improvements in hepatic function, but “the preventive effects of MVR on the incidence of hepatocellular carcinoma appeared only modest,” the investigators said. “Survival of patients without hepatocellular carcinoma who survived the first 6 months after initiation of antiviral therapy was excellent, with only a 25.3% mortality rate occurring between 6 months and 10 years.”
Based on their findings, Dr. Jang and his associates recommended aiming for an HBV DNA load less than 20 IU/mL in patients with decompensated cirrhosis to significantly improve the chances of long-term survival. Survival curves were similar regardless of whether patients had HBV DNA levels less than 10 IU/mL or between and 10 and 20 IU/mL, they noted.
Funders included Korea Healthcare Technology R&D Project and the Catholic Research Coordinating Center of the Korea Health 21 R&D Project, both of the Ministry of Health and Welfare, Republic of Korea. Dr. Jang disclosed ties to Bristol-Myers Squibb, Gilead, and Merck Sharp & Dohme. Three coinvestigators also disclosed ties to Gilead, MSD, and several other pharmaceutical companies.
SOURCE: Jang JW et al. Clin Gastroenterol Hepatol. 2018 May 18. doi: 10.1016/j.cgh.2018.04.063
according to the results of a multicenter observational study published in the December issue of Clinical Gastroenterology and Hepatology.
Survival times were “excellent” if patients survived the first 6 months of antiviral therapy and did not develop hepatocellular carcinoma, said Jeong Won Jang, MD, of the Catholic University of Korea College of Medicine in Seoul, South Korea, and his associates. Patients who developed hepatocellular carcinoma had persistent declines in survival over time, they said. Predictors of short-term mortality included a baseline Model for End-Stage Liver Disease score above 20 and multiple complications.
Chronic hepatitis B virus (HBV) infection is the most common cause of liver-related disease and death in Asia, and complications such as decompensated cirrhosis affect up to 40% of chronically infected persons. Five-year survival rates are as low as 14% if patients develop decompensated cirrhosis.
To explore whether virologic suppression with oral nucleoside or nucleotide analog therapy improves outcomes in these decompensated patients, the researchers studied 295 such individuals from the Epidemiology and Natural History of Liver Cirrhosis in Korea Study. At baseline, these patients did not have documented chronic hepatitis C virus infection, hepatocellular carcinoma, other cancers, autoimmune hepatitis, or alcohol use disorders. All patients initiated entecavir or lamivudine therapy immediately after their cirrhosis became decompensated. The primary outcome was transplant-free survival.
A total of 60.1% of patients survived 5 years and 45.7% survived 10 years without undergoing transplantation, for a median transplant-free survival time of 7.7 years. The 116 patients (39%) who consistently had undetectable HBV DNA levels (less than 20 IU/mL) throughout treatment had significantly longer transplant-free survival than did patients who did not maintain a virologic response (P less than .001). In addition, a maintained virologic response (MVR) was the strongest predictor of long-term transplant-free survival, the researchers said.
A significantly greater proportion of patients who received entecavir survived 10 years compared with patients who received lamivudine. However, there was no significant difference in long-term survival among patients with MVRs to either drug. “Importantly, it appears that improvement in patient survival is attained by antiviral response, not by the type of nucleos(t)ide analogue per se,” the researchers wrote.
Patients who achieved MVR also showed significant improvements in hepatic function, but “the preventive effects of MVR on the incidence of hepatocellular carcinoma appeared only modest,” the investigators said. “Survival of patients without hepatocellular carcinoma who survived the first 6 months after initiation of antiviral therapy was excellent, with only a 25.3% mortality rate occurring between 6 months and 10 years.”
Based on their findings, Dr. Jang and his associates recommended aiming for an HBV DNA load less than 20 IU/mL in patients with decompensated cirrhosis to significantly improve the chances of long-term survival. Survival curves were similar regardless of whether patients had HBV DNA levels less than 10 IU/mL or between and 10 and 20 IU/mL, they noted.
Funders included Korea Healthcare Technology R&D Project and the Catholic Research Coordinating Center of the Korea Health 21 R&D Project, both of the Ministry of Health and Welfare, Republic of Korea. Dr. Jang disclosed ties to Bristol-Myers Squibb, Gilead, and Merck Sharp & Dohme. Three coinvestigators also disclosed ties to Gilead, MSD, and several other pharmaceutical companies.
SOURCE: Jang JW et al. Clin Gastroenterol Hepatol. 2018 May 18. doi: 10.1016/j.cgh.2018.04.063
according to the results of a multicenter observational study published in the December issue of Clinical Gastroenterology and Hepatology.
Survival times were “excellent” if patients survived the first 6 months of antiviral therapy and did not develop hepatocellular carcinoma, said Jeong Won Jang, MD, of the Catholic University of Korea College of Medicine in Seoul, South Korea, and his associates. Patients who developed hepatocellular carcinoma had persistent declines in survival over time, they said. Predictors of short-term mortality included a baseline Model for End-Stage Liver Disease score above 20 and multiple complications.
Chronic hepatitis B virus (HBV) infection is the most common cause of liver-related disease and death in Asia, and complications such as decompensated cirrhosis affect up to 40% of chronically infected persons. Five-year survival rates are as low as 14% if patients develop decompensated cirrhosis.
To explore whether virologic suppression with oral nucleoside or nucleotide analog therapy improves outcomes in these decompensated patients, the researchers studied 295 such individuals from the Epidemiology and Natural History of Liver Cirrhosis in Korea Study. At baseline, these patients did not have documented chronic hepatitis C virus infection, hepatocellular carcinoma, other cancers, autoimmune hepatitis, or alcohol use disorders. All patients initiated entecavir or lamivudine therapy immediately after their cirrhosis became decompensated. The primary outcome was transplant-free survival.
A total of 60.1% of patients survived 5 years and 45.7% survived 10 years without undergoing transplantation, for a median transplant-free survival time of 7.7 years. The 116 patients (39%) who consistently had undetectable HBV DNA levels (less than 20 IU/mL) throughout treatment had significantly longer transplant-free survival than did patients who did not maintain a virologic response (P less than .001). In addition, a maintained virologic response (MVR) was the strongest predictor of long-term transplant-free survival, the researchers said.
A significantly greater proportion of patients who received entecavir survived 10 years compared with patients who received lamivudine. However, there was no significant difference in long-term survival among patients with MVRs to either drug. “Importantly, it appears that improvement in patient survival is attained by antiviral response, not by the type of nucleos(t)ide analogue per se,” the researchers wrote.
Patients who achieved MVR also showed significant improvements in hepatic function, but “the preventive effects of MVR on the incidence of hepatocellular carcinoma appeared only modest,” the investigators said. “Survival of patients without hepatocellular carcinoma who survived the first 6 months after initiation of antiviral therapy was excellent, with only a 25.3% mortality rate occurring between 6 months and 10 years.”
Based on their findings, Dr. Jang and his associates recommended aiming for an HBV DNA load less than 20 IU/mL in patients with decompensated cirrhosis to significantly improve the chances of long-term survival. Survival curves were similar regardless of whether patients had HBV DNA levels less than 10 IU/mL or between and 10 and 20 IU/mL, they noted.
Funders included Korea Healthcare Technology R&D Project and the Catholic Research Coordinating Center of the Korea Health 21 R&D Project, both of the Ministry of Health and Welfare, Republic of Korea. Dr. Jang disclosed ties to Bristol-Myers Squibb, Gilead, and Merck Sharp & Dohme. Three coinvestigators also disclosed ties to Gilead, MSD, and several other pharmaceutical companies.
SOURCE: Jang JW et al. Clin Gastroenterol Hepatol. 2018 May 18. doi: 10.1016/j.cgh.2018.04.063
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: For patients with decompensated cirrhosis, long-term hepatitis B virus suppression was associated with significantly improved transplant-free survival.
Major finding: Lack of virologic response was associated with a more than twofold increase in hazard of long-term mortality in the multivariate analysis (HR, 2.30; 95% confidence interval, 1.60-3.29; P less than .001).
Study details: Ten-year multicenter observational study of 295 patients who began entecavir or lamivudine therapy immediately after their cirrhosis became decompensated.
Disclosures: Funders included Korea Healthcare Technology R&D Project and the Catholic Research Coordinating Center of the Korea Health 21 R&D Project, both of the Ministry of Health and Welfare, Republic of Korea. Dr. Jang disclosed ties to Bristol-Myers Squibb, Gilead, and Merck Sharp & Dohme. Three coinvestigators also disclosed ties to Gilead, MSD, and several other pharmaceutical companies.
Source: Jang JW et al. Clin Gastroenterol Hepatol. 2018 May 18. doi: 10.1016/j.cgh.2018.04.063
November 2018 Question 1
Rationale
This patient’s symptoms are most concerning for Whipple’s disease in light of the diarrhea, weight loss, arthralgias, and CNS symptoms. This diagnosis requires identification of periodic acid-Schiff staining macrophages in the duodenal lamina propria. Further PCR analysis can also be used to identify RNA of the causative pathogen, Tropheryma whipplei. Congo Red staining is indicated if amyloidosis is suspected. Sudan staining is used to test stool for fat. Birefringence is used to detect crystals, most typically in synovial fluid. Immunohistochemistry has many applications and is commonly employed to evaluate for Helicobacter pylori.
Reference
1. Moos V., Schneider T. Changing paradigms in Whipple’s disease and infection with Tropheryma whipplei. Eur J Clin Microbiol Infect Dis. 2011;30(10):1151-8.
Rationale
This patient’s symptoms are most concerning for Whipple’s disease in light of the diarrhea, weight loss, arthralgias, and CNS symptoms. This diagnosis requires identification of periodic acid-Schiff staining macrophages in the duodenal lamina propria. Further PCR analysis can also be used to identify RNA of the causative pathogen, Tropheryma whipplei. Congo Red staining is indicated if amyloidosis is suspected. Sudan staining is used to test stool for fat. Birefringence is used to detect crystals, most typically in synovial fluid. Immunohistochemistry has many applications and is commonly employed to evaluate for Helicobacter pylori.
Reference
1. Moos V., Schneider T. Changing paradigms in Whipple’s disease and infection with Tropheryma whipplei. Eur J Clin Microbiol Infect Dis. 2011;30(10):1151-8.
Rationale
This patient’s symptoms are most concerning for Whipple’s disease in light of the diarrhea, weight loss, arthralgias, and CNS symptoms. This diagnosis requires identification of periodic acid-Schiff staining macrophages in the duodenal lamina propria. Further PCR analysis can also be used to identify RNA of the causative pathogen, Tropheryma whipplei. Congo Red staining is indicated if amyloidosis is suspected. Sudan staining is used to test stool for fat. Birefringence is used to detect crystals, most typically in synovial fluid. Immunohistochemistry has many applications and is commonly employed to evaluate for Helicobacter pylori.
Reference
1. Moos V., Schneider T. Changing paradigms in Whipple’s disease and infection with Tropheryma whipplei. Eur J Clin Microbiol Infect Dis. 2011;30(10):1151-8.
A 52-year-old man is referred because of diarrhea, with up to 6 loose bowel movements per day for the past 7 months. His stool has been nonbloody. He denies rashes or eye problems, but he has had significant arthralgias. He has lost 15 pounds and also reports having newly developed headaches over this time. A colonoscopy performed 1 year ago for routine screening was unremarkable. Celiac serologies checked last month were negative. Stool cultures, ova and parasite evaluation, and Clostridium difficile toxin assay were all negative.
An upper endoscopy reveals grossly unremarkable mucosa throughout and duodenal biopsies are performed.
Quality programs drive improvements in colorectal surgery outcomes
BOSTON – Rates of (ACS NSQIP), a recent analysis shows.
Reoperation rates have also decreased, while early-discharge rates have steadily increased, according to results of the analysis, presented at the annual clinical congress of the American College of Surgeons.
The findings underline the value of such ACS-led initiatives in improving patient care and surgical quality, said Ahmed M. Al-Mazrou, MD, a general surgery resident at New York-Presbyterian Hospital/Weill Cornell Medical Center in New York.
“Over its first decade of introduction, ACS NSQIP was associated with improved outcomes after colorectal surgery, and also introduction of colectomy-targeted data was also associated with improved outcomes,” Dr. Al-Mazrou said in his presentation describing the results.
Prior to this study, the question of whether the introduction of ACS NSQIP has improved outcomes over time had not been well characterized, according to Dr. Al-Mazrou and his colleagues.
To evaluate the impact, the investigators looked at more than 310,000 nonemergency colorectal resections in ACS NSQIP, of which about 58% were done after the introduction of colectomy-targeted variables in 2013.
They found that, over time, incidence of most complications fell, including surgical site infections, urinary tract infections, sepsis and septic shock, and venous thromboembolism, while rates of early discharge increased.
For example, surgical site infections decreased from 13.7% to 4.7% over the 10-year period, while the number of patients discharged within 5 days or fewer increased from about 8% to 47%.
Introduction of colectomy-targeted data was associated with fewer surgical site infections (odds ratio, 0.78; 95% confidence interval, 0.77-0.80), multivariable analysis showed. Likewise, there were lower rates of systemic infections (OR, 0.94; 95% CI, 0.91-0.98) and urinary tract infections (OR, 0.70; 95% CI, 0.67-0.74) after introduction of the data.
Rates of reoperation also decreased (OR, 0.88; 95% CI, 0.85-0.91) while early-discharge rates increased (OR, 1.60; 95% CI, 1.57-1.63) after colectomy data was introduced, the multivariable analysis further showed.
Principal investigator P. Ravi Kiran, MD, FACS, professor of surgery at Columbia University and chief of the medical center’s division of colorectal surgery, said the improved outcomes were attributable to a few different factors.
First, the NSQIP national data allows participants to benchmark with peer hospitals and find areas for improvement, Dr. Kiran said in an ACS press release.
That benchmarking encourages participating centers to follow evidence-based recommendations, including ACS guidelines for preventing surgical site infections, he added.
The introduction of procedure-targeted datasets in NSQIP was done in response to user requests for more clinically detailed information, according to Clifford Y. Ko, MD, FACS, director of the ACS division of research and optimal patient care.
While the NSQIP data are important in improving surgical outcomes, credit also goes to the organizations that are leading the quality improvement efforts by effectively using the data, Dr. Ko said in the press release.
Dr. Ko was not involved in the study. Dr. Al-Mazrou and Dr. Kiran reported no disclosures relevant to the study.
SOURCE: Al-Mazrou AM et al. ACS Clinical Congress. Abstract SF330.
BOSTON – Rates of (ACS NSQIP), a recent analysis shows.
Reoperation rates have also decreased, while early-discharge rates have steadily increased, according to results of the analysis, presented at the annual clinical congress of the American College of Surgeons.
The findings underline the value of such ACS-led initiatives in improving patient care and surgical quality, said Ahmed M. Al-Mazrou, MD, a general surgery resident at New York-Presbyterian Hospital/Weill Cornell Medical Center in New York.
“Over its first decade of introduction, ACS NSQIP was associated with improved outcomes after colorectal surgery, and also introduction of colectomy-targeted data was also associated with improved outcomes,” Dr. Al-Mazrou said in his presentation describing the results.
Prior to this study, the question of whether the introduction of ACS NSQIP has improved outcomes over time had not been well characterized, according to Dr. Al-Mazrou and his colleagues.
To evaluate the impact, the investigators looked at more than 310,000 nonemergency colorectal resections in ACS NSQIP, of which about 58% were done after the introduction of colectomy-targeted variables in 2013.
They found that, over time, incidence of most complications fell, including surgical site infections, urinary tract infections, sepsis and septic shock, and venous thromboembolism, while rates of early discharge increased.
For example, surgical site infections decreased from 13.7% to 4.7% over the 10-year period, while the number of patients discharged within 5 days or fewer increased from about 8% to 47%.
Introduction of colectomy-targeted data was associated with fewer surgical site infections (odds ratio, 0.78; 95% confidence interval, 0.77-0.80), multivariable analysis showed. Likewise, there were lower rates of systemic infections (OR, 0.94; 95% CI, 0.91-0.98) and urinary tract infections (OR, 0.70; 95% CI, 0.67-0.74) after introduction of the data.
Rates of reoperation also decreased (OR, 0.88; 95% CI, 0.85-0.91) while early-discharge rates increased (OR, 1.60; 95% CI, 1.57-1.63) after colectomy data was introduced, the multivariable analysis further showed.
Principal investigator P. Ravi Kiran, MD, FACS, professor of surgery at Columbia University and chief of the medical center’s division of colorectal surgery, said the improved outcomes were attributable to a few different factors.
First, the NSQIP national data allows participants to benchmark with peer hospitals and find areas for improvement, Dr. Kiran said in an ACS press release.
That benchmarking encourages participating centers to follow evidence-based recommendations, including ACS guidelines for preventing surgical site infections, he added.
The introduction of procedure-targeted datasets in NSQIP was done in response to user requests for more clinically detailed information, according to Clifford Y. Ko, MD, FACS, director of the ACS division of research and optimal patient care.
While the NSQIP data are important in improving surgical outcomes, credit also goes to the organizations that are leading the quality improvement efforts by effectively using the data, Dr. Ko said in the press release.
Dr. Ko was not involved in the study. Dr. Al-Mazrou and Dr. Kiran reported no disclosures relevant to the study.
SOURCE: Al-Mazrou AM et al. ACS Clinical Congress. Abstract SF330.
BOSTON – Rates of (ACS NSQIP), a recent analysis shows.
Reoperation rates have also decreased, while early-discharge rates have steadily increased, according to results of the analysis, presented at the annual clinical congress of the American College of Surgeons.
The findings underline the value of such ACS-led initiatives in improving patient care and surgical quality, said Ahmed M. Al-Mazrou, MD, a general surgery resident at New York-Presbyterian Hospital/Weill Cornell Medical Center in New York.
“Over its first decade of introduction, ACS NSQIP was associated with improved outcomes after colorectal surgery, and also introduction of colectomy-targeted data was also associated with improved outcomes,” Dr. Al-Mazrou said in his presentation describing the results.
Prior to this study, the question of whether the introduction of ACS NSQIP has improved outcomes over time had not been well characterized, according to Dr. Al-Mazrou and his colleagues.
To evaluate the impact, the investigators looked at more than 310,000 nonemergency colorectal resections in ACS NSQIP, of which about 58% were done after the introduction of colectomy-targeted variables in 2013.
They found that, over time, incidence of most complications fell, including surgical site infections, urinary tract infections, sepsis and septic shock, and venous thromboembolism, while rates of early discharge increased.
For example, surgical site infections decreased from 13.7% to 4.7% over the 10-year period, while the number of patients discharged within 5 days or fewer increased from about 8% to 47%.
Introduction of colectomy-targeted data was associated with fewer surgical site infections (odds ratio, 0.78; 95% confidence interval, 0.77-0.80), multivariable analysis showed. Likewise, there were lower rates of systemic infections (OR, 0.94; 95% CI, 0.91-0.98) and urinary tract infections (OR, 0.70; 95% CI, 0.67-0.74) after introduction of the data.
Rates of reoperation also decreased (OR, 0.88; 95% CI, 0.85-0.91) while early-discharge rates increased (OR, 1.60; 95% CI, 1.57-1.63) after colectomy data was introduced, the multivariable analysis further showed.
Principal investigator P. Ravi Kiran, MD, FACS, professor of surgery at Columbia University and chief of the medical center’s division of colorectal surgery, said the improved outcomes were attributable to a few different factors.
First, the NSQIP national data allows participants to benchmark with peer hospitals and find areas for improvement, Dr. Kiran said in an ACS press release.
That benchmarking encourages participating centers to follow evidence-based recommendations, including ACS guidelines for preventing surgical site infections, he added.
The introduction of procedure-targeted datasets in NSQIP was done in response to user requests for more clinically detailed information, according to Clifford Y. Ko, MD, FACS, director of the ACS division of research and optimal patient care.
While the NSQIP data are important in improving surgical outcomes, credit also goes to the organizations that are leading the quality improvement efforts by effectively using the data, Dr. Ko said in the press release.
Dr. Ko was not involved in the study. Dr. Al-Mazrou and Dr. Kiran reported no disclosures relevant to the study.
SOURCE: Al-Mazrou AM et al. ACS Clinical Congress. Abstract SF330.
REPORTING FROM THE ACS CLINICAL CONGRESS
Key clinical point: Rates of colorectal procedure complications have steadily decreased since the introduction of the American College of Surgeons National Surgical Quality Improvement Program.
Major finding: Surgical site infections decreased from 13.7% to 4.7% over the 10-year period, while the number of patients discharged within 5 days or fewer increased from about 8% to 47%.
Study details: Retrospective review of more than 310,000 nonemergency colorectal resections in ACS NSQIP from 2007 to 2016.
Disclosures: Study authors reported no conflicts of interest.
Source: Al-Mazrou AM et al. ACS Clinical Congress, Abstract SF330.
Management of Lewy body dementia remains complex
ATLANTA – In the not-so-distant past, neurologists viewed dementia with Lewy bodies as a disorder primarily of the brain, but it turned out to be far more complex than that.
At the annual meeting of the American Neurological Association, Bradley F. Boeve, MD, described dementia with Lewy bodies (DLB) as a systemic neurologic disorder affecting the brain, including brain stem, spinal cord, and peripheral nervous system, especially the autonomic nervous system. “This leads to the complex array of clinical manifestations, which are quite different from patient to patient cross-sectionally and longitudinally,” said Dr. Boeve, the Little Family Foundation Professor of Lewy Body Dementia in the department of neurology at the Mayo Clinic, Rochester, Minn.
, he said. The four core clinical features are Parkinsonism unrelated to medications; recurrent, fully-formed visual hallucinations; fluctuations in cognition and/or arousal; and rapid eye movement (REM) sleep behavior disorder. “This is the most predictive of all four features,” Dr. Boeve said. He described REM sleep behavior disorder as a parasomnia manifested by the tendency to repeatedly “act out one’s dreams.” The dreams tend to contain a chasing/attacking theme, and behaviors mirror dream content. Injuries to the patient and bed partner can occur.
Typically, patients will present with REM sleep behavior disorder in their 50s and 60s, and sometimes in their 30s and 40s, “decades before cognitive changes begin,” he said. “This is usually followed by Parkinsonism and visual hallucinations. That’s the prototypical DLB [case], but there are many examples where this is not followed. Prominent neuropsychiatric features can also begin before any cognitive changes.”
Neuropsychological features of DLB often include impairment of executive functions and visuospatial functions. “Early in the course of Alzheimer’s disease, typically performance on memory measures – especially delayed recall – are down and the other measures are borderline or mildly impaired,” Dr. Boeve noted. “By contrast, in DLB, attention, executive function, and visuospatial measures are down, but memory is often pretty good. What’s remarkable is that in the office setting, when you take a history the person often says, ‘I’m very forgetful,’ yet in the testing environment people tend to rise to the occasion pretty well.”
Imaging isn’t always helpful in establishing a diagnosis of DLB. MRI scans, for example, “can look pretty normal, including the hippocampi,” he said. “This is really the norm in DLB and it seems to be a disconnect. The person can have significant symptoms yet their MRI scan can be pretty normal.”
In Alzheimer’s disease, 18F-fluorodeoxyglucose-PET (FDG-PET) shows temporal, parietal, and frontal hypometabolism, sparing of the sensory-motor strip and sparing of the primary occipital cortex, while in DLB, FDG-PET shows marked deficits in the occipital regions with relative sparing of the frontal and temporal lobes. Another key neuroimaging sign of DLB is the posterior cingulate island sign, which is characterized by sparing of the posterior cingulate cortex relative to the precuneus plus cuneus on FDG-PET.
In 2017, the Dementia with Lewy Bodies Consortium published updated recommendations on the diagnosis and management of the disease (Neurology. 2017;89[1]:88-100). In its consensus report, the consortium defines probable DLB as dementia plus two or more clinical features or one core clinical feature plus one or more indicative biomarker. These biomarkers include reduced dopamine transport uptake in basal ganglia by SPECT or PET; abnormal (low uptake) meta-iodobenzylguanidine (MIBG) myocardial scintigraphy, and/or polysomnographic confirmation of REM sleep without atonia.
“Neuropathologically, limbic with or without neocortical Lewy bodies and Lewy neurites are the defining characteristics of pathologically-proven DLB,” added Dr. Boeve, a member of the DLB consortium. “The classic DLB phenotype can occur in limbic-predominant DLB. Lewy bodies in the neocortex are not necessary to cause a dementia syndrome.”
He characterized management of DLB as “very complicated. Consider symptoms as they relate to cognitive impairment, neuropsychiatric features, motor features, sleep disorders, and autonomic dysfunction.” He often asks the patient/family to prioritize the three most troublesome issues they seek to change, and develops a plan based on their input.
There is no Food and Drug Administration–approved medication for DLB, but the standard of care is an acetylcholinesterase inhibitor such as donepezil. “There is evidence that memantine can provide a modest benefit,” Dr. Boeve said. “Hypersomnia is quite prominent in DLB and worthy of assessing and treating.” Clinicians must weigh the pros and cons of pharmacotherapy with each patient. “For example, in the atypical neuroleptic class [of drugs], there may be a benefit to the hallucinations and delusions in DLB but hypersomnia can worsen,” he said. “Selecting agents is challenging but worth the effort.”
Survival is lower and more rapid with DLB, compared with Alzheimer’s. Most people pass away from primary DLB-related features or failure to thrive. The second most common is pneumonia or aspiration. Median survival was 4 years after diagnosis in one study, and end-of life discussions occurred in less than half of all patients. “This is a frustrating reminder that we as clinicians are not very good at discussing important topics such as end-of-life care with patients and their families,” Dr. Boeve said. Resources that he recommends for education and support include the Lewy Body Dementia Association and The Lewy Body Society.
At the 2016 Alzheimer’s Disease-Related Dementias Summit, clinicians formed a list of DLB research priorities (Neurology 2017;89[23]:2381-91). Among them were recommendations to “initiate clinical trials in diverse populations using therapies that address symptoms that have the greatest effect on patient function and caregiver burden” and “identify novel common and rare genetic variants, epigenetic changes, and environmental influences that affect the risk for and clinical features of” the disease.
Meanwhile, several research protocols are under way, including the development of a DLB module by the U.S. Alzheimer’s Research Disease Centers and a number of DLB-focused projects from the National Institute of Neurological Disorders and Stroke (NINDS) Parkinson’s Disease Biomarkers Program. In addition, the Lewy Body Dementia Association Research Centers of Excellence program is focused on optimizing clinical care and setting up the infrastructure for clinical trials, while the North American Prodromal Synucleinopathy Consortium is conducting longitudinal studies in those with REM sleep behavior disorder.
Dr. Boeve disclosed that he has been an investigator for clinical trials sponsored by GE Healthcare, Axovant, and Biogen. He is a member of the scientific advisory board for the Tau Consortium and has received research support from the National Institute on Aging, the NINDS, the Mangurian Foundation, and the Little Family Foundation.
ATLANTA – In the not-so-distant past, neurologists viewed dementia with Lewy bodies as a disorder primarily of the brain, but it turned out to be far more complex than that.
At the annual meeting of the American Neurological Association, Bradley F. Boeve, MD, described dementia with Lewy bodies (DLB) as a systemic neurologic disorder affecting the brain, including brain stem, spinal cord, and peripheral nervous system, especially the autonomic nervous system. “This leads to the complex array of clinical manifestations, which are quite different from patient to patient cross-sectionally and longitudinally,” said Dr. Boeve, the Little Family Foundation Professor of Lewy Body Dementia in the department of neurology at the Mayo Clinic, Rochester, Minn.
, he said. The four core clinical features are Parkinsonism unrelated to medications; recurrent, fully-formed visual hallucinations; fluctuations in cognition and/or arousal; and rapid eye movement (REM) sleep behavior disorder. “This is the most predictive of all four features,” Dr. Boeve said. He described REM sleep behavior disorder as a parasomnia manifested by the tendency to repeatedly “act out one’s dreams.” The dreams tend to contain a chasing/attacking theme, and behaviors mirror dream content. Injuries to the patient and bed partner can occur.
Typically, patients will present with REM sleep behavior disorder in their 50s and 60s, and sometimes in their 30s and 40s, “decades before cognitive changes begin,” he said. “This is usually followed by Parkinsonism and visual hallucinations. That’s the prototypical DLB [case], but there are many examples where this is not followed. Prominent neuropsychiatric features can also begin before any cognitive changes.”
Neuropsychological features of DLB often include impairment of executive functions and visuospatial functions. “Early in the course of Alzheimer’s disease, typically performance on memory measures – especially delayed recall – are down and the other measures are borderline or mildly impaired,” Dr. Boeve noted. “By contrast, in DLB, attention, executive function, and visuospatial measures are down, but memory is often pretty good. What’s remarkable is that in the office setting, when you take a history the person often says, ‘I’m very forgetful,’ yet in the testing environment people tend to rise to the occasion pretty well.”
Imaging isn’t always helpful in establishing a diagnosis of DLB. MRI scans, for example, “can look pretty normal, including the hippocampi,” he said. “This is really the norm in DLB and it seems to be a disconnect. The person can have significant symptoms yet their MRI scan can be pretty normal.”
In Alzheimer’s disease, 18F-fluorodeoxyglucose-PET (FDG-PET) shows temporal, parietal, and frontal hypometabolism, sparing of the sensory-motor strip and sparing of the primary occipital cortex, while in DLB, FDG-PET shows marked deficits in the occipital regions with relative sparing of the frontal and temporal lobes. Another key neuroimaging sign of DLB is the posterior cingulate island sign, which is characterized by sparing of the posterior cingulate cortex relative to the precuneus plus cuneus on FDG-PET.
In 2017, the Dementia with Lewy Bodies Consortium published updated recommendations on the diagnosis and management of the disease (Neurology. 2017;89[1]:88-100). In its consensus report, the consortium defines probable DLB as dementia plus two or more clinical features or one core clinical feature plus one or more indicative biomarker. These biomarkers include reduced dopamine transport uptake in basal ganglia by SPECT or PET; abnormal (low uptake) meta-iodobenzylguanidine (MIBG) myocardial scintigraphy, and/or polysomnographic confirmation of REM sleep without atonia.
“Neuropathologically, limbic with or without neocortical Lewy bodies and Lewy neurites are the defining characteristics of pathologically-proven DLB,” added Dr. Boeve, a member of the DLB consortium. “The classic DLB phenotype can occur in limbic-predominant DLB. Lewy bodies in the neocortex are not necessary to cause a dementia syndrome.”
He characterized management of DLB as “very complicated. Consider symptoms as they relate to cognitive impairment, neuropsychiatric features, motor features, sleep disorders, and autonomic dysfunction.” He often asks the patient/family to prioritize the three most troublesome issues they seek to change, and develops a plan based on their input.
There is no Food and Drug Administration–approved medication for DLB, but the standard of care is an acetylcholinesterase inhibitor such as donepezil. “There is evidence that memantine can provide a modest benefit,” Dr. Boeve said. “Hypersomnia is quite prominent in DLB and worthy of assessing and treating.” Clinicians must weigh the pros and cons of pharmacotherapy with each patient. “For example, in the atypical neuroleptic class [of drugs], there may be a benefit to the hallucinations and delusions in DLB but hypersomnia can worsen,” he said. “Selecting agents is challenging but worth the effort.”
Survival is lower and more rapid with DLB, compared with Alzheimer’s. Most people pass away from primary DLB-related features or failure to thrive. The second most common is pneumonia or aspiration. Median survival was 4 years after diagnosis in one study, and end-of life discussions occurred in less than half of all patients. “This is a frustrating reminder that we as clinicians are not very good at discussing important topics such as end-of-life care with patients and their families,” Dr. Boeve said. Resources that he recommends for education and support include the Lewy Body Dementia Association and The Lewy Body Society.
At the 2016 Alzheimer’s Disease-Related Dementias Summit, clinicians formed a list of DLB research priorities (Neurology 2017;89[23]:2381-91). Among them were recommendations to “initiate clinical trials in diverse populations using therapies that address symptoms that have the greatest effect on patient function and caregiver burden” and “identify novel common and rare genetic variants, epigenetic changes, and environmental influences that affect the risk for and clinical features of” the disease.
Meanwhile, several research protocols are under way, including the development of a DLB module by the U.S. Alzheimer’s Research Disease Centers and a number of DLB-focused projects from the National Institute of Neurological Disorders and Stroke (NINDS) Parkinson’s Disease Biomarkers Program. In addition, the Lewy Body Dementia Association Research Centers of Excellence program is focused on optimizing clinical care and setting up the infrastructure for clinical trials, while the North American Prodromal Synucleinopathy Consortium is conducting longitudinal studies in those with REM sleep behavior disorder.
Dr. Boeve disclosed that he has been an investigator for clinical trials sponsored by GE Healthcare, Axovant, and Biogen. He is a member of the scientific advisory board for the Tau Consortium and has received research support from the National Institute on Aging, the NINDS, the Mangurian Foundation, and the Little Family Foundation.
ATLANTA – In the not-so-distant past, neurologists viewed dementia with Lewy bodies as a disorder primarily of the brain, but it turned out to be far more complex than that.
At the annual meeting of the American Neurological Association, Bradley F. Boeve, MD, described dementia with Lewy bodies (DLB) as a systemic neurologic disorder affecting the brain, including brain stem, spinal cord, and peripheral nervous system, especially the autonomic nervous system. “This leads to the complex array of clinical manifestations, which are quite different from patient to patient cross-sectionally and longitudinally,” said Dr. Boeve, the Little Family Foundation Professor of Lewy Body Dementia in the department of neurology at the Mayo Clinic, Rochester, Minn.
, he said. The four core clinical features are Parkinsonism unrelated to medications; recurrent, fully-formed visual hallucinations; fluctuations in cognition and/or arousal; and rapid eye movement (REM) sleep behavior disorder. “This is the most predictive of all four features,” Dr. Boeve said. He described REM sleep behavior disorder as a parasomnia manifested by the tendency to repeatedly “act out one’s dreams.” The dreams tend to contain a chasing/attacking theme, and behaviors mirror dream content. Injuries to the patient and bed partner can occur.
Typically, patients will present with REM sleep behavior disorder in their 50s and 60s, and sometimes in their 30s and 40s, “decades before cognitive changes begin,” he said. “This is usually followed by Parkinsonism and visual hallucinations. That’s the prototypical DLB [case], but there are many examples where this is not followed. Prominent neuropsychiatric features can also begin before any cognitive changes.”
Neuropsychological features of DLB often include impairment of executive functions and visuospatial functions. “Early in the course of Alzheimer’s disease, typically performance on memory measures – especially delayed recall – are down and the other measures are borderline or mildly impaired,” Dr. Boeve noted. “By contrast, in DLB, attention, executive function, and visuospatial measures are down, but memory is often pretty good. What’s remarkable is that in the office setting, when you take a history the person often says, ‘I’m very forgetful,’ yet in the testing environment people tend to rise to the occasion pretty well.”
Imaging isn’t always helpful in establishing a diagnosis of DLB. MRI scans, for example, “can look pretty normal, including the hippocampi,” he said. “This is really the norm in DLB and it seems to be a disconnect. The person can have significant symptoms yet their MRI scan can be pretty normal.”
In Alzheimer’s disease, 18F-fluorodeoxyglucose-PET (FDG-PET) shows temporal, parietal, and frontal hypometabolism, sparing of the sensory-motor strip and sparing of the primary occipital cortex, while in DLB, FDG-PET shows marked deficits in the occipital regions with relative sparing of the frontal and temporal lobes. Another key neuroimaging sign of DLB is the posterior cingulate island sign, which is characterized by sparing of the posterior cingulate cortex relative to the precuneus plus cuneus on FDG-PET.
In 2017, the Dementia with Lewy Bodies Consortium published updated recommendations on the diagnosis and management of the disease (Neurology. 2017;89[1]:88-100). In its consensus report, the consortium defines probable DLB as dementia plus two or more clinical features or one core clinical feature plus one or more indicative biomarker. These biomarkers include reduced dopamine transport uptake in basal ganglia by SPECT or PET; abnormal (low uptake) meta-iodobenzylguanidine (MIBG) myocardial scintigraphy, and/or polysomnographic confirmation of REM sleep without atonia.
“Neuropathologically, limbic with or without neocortical Lewy bodies and Lewy neurites are the defining characteristics of pathologically-proven DLB,” added Dr. Boeve, a member of the DLB consortium. “The classic DLB phenotype can occur in limbic-predominant DLB. Lewy bodies in the neocortex are not necessary to cause a dementia syndrome.”
He characterized management of DLB as “very complicated. Consider symptoms as they relate to cognitive impairment, neuropsychiatric features, motor features, sleep disorders, and autonomic dysfunction.” He often asks the patient/family to prioritize the three most troublesome issues they seek to change, and develops a plan based on their input.
There is no Food and Drug Administration–approved medication for DLB, but the standard of care is an acetylcholinesterase inhibitor such as donepezil. “There is evidence that memantine can provide a modest benefit,” Dr. Boeve said. “Hypersomnia is quite prominent in DLB and worthy of assessing and treating.” Clinicians must weigh the pros and cons of pharmacotherapy with each patient. “For example, in the atypical neuroleptic class [of drugs], there may be a benefit to the hallucinations and delusions in DLB but hypersomnia can worsen,” he said. “Selecting agents is challenging but worth the effort.”
Survival is lower and more rapid with DLB, compared with Alzheimer’s. Most people pass away from primary DLB-related features or failure to thrive. The second most common is pneumonia or aspiration. Median survival was 4 years after diagnosis in one study, and end-of life discussions occurred in less than half of all patients. “This is a frustrating reminder that we as clinicians are not very good at discussing important topics such as end-of-life care with patients and their families,” Dr. Boeve said. Resources that he recommends for education and support include the Lewy Body Dementia Association and The Lewy Body Society.
At the 2016 Alzheimer’s Disease-Related Dementias Summit, clinicians formed a list of DLB research priorities (Neurology 2017;89[23]:2381-91). Among them were recommendations to “initiate clinical trials in diverse populations using therapies that address symptoms that have the greatest effect on patient function and caregiver burden” and “identify novel common and rare genetic variants, epigenetic changes, and environmental influences that affect the risk for and clinical features of” the disease.
Meanwhile, several research protocols are under way, including the development of a DLB module by the U.S. Alzheimer’s Research Disease Centers and a number of DLB-focused projects from the National Institute of Neurological Disorders and Stroke (NINDS) Parkinson’s Disease Biomarkers Program. In addition, the Lewy Body Dementia Association Research Centers of Excellence program is focused on optimizing clinical care and setting up the infrastructure for clinical trials, while the North American Prodromal Synucleinopathy Consortium is conducting longitudinal studies in those with REM sleep behavior disorder.
Dr. Boeve disclosed that he has been an investigator for clinical trials sponsored by GE Healthcare, Axovant, and Biogen. He is a member of the scientific advisory board for the Tau Consortium and has received research support from the National Institute on Aging, the NINDS, the Mangurian Foundation, and the Little Family Foundation.
EXPERT ANALYSIS FROM ANA 2018
Norfloxacin might benefit patients with advanced cirrhosis and low ascites fluid protein levels
Six months of once-daily norfloxacin therapy did not reduce 6-month mortality among patients with Child-Pugh class C cirrhosis who had not recently received fluoroquinolone therapy.
Mortality based on the Kaplan-Meier method was 14.8% in the norfloxacin group versus 19.7% for patients receiving placebo (P = .21). “Norfloxacin, however, appear[ed] to increase survival of patients with low ascites fluid protein concentrations,” wrote Richard Moreau, MD, of Hôpital Beaujon, Paris, and his associates. The results of the multicenter, double-blind trial of 291 patients were published in the December issue of Gastroenterology.
Patients with advanced cirrhosis often develop spontaneous bacterial peritonitis and other severe bacterial infections, with potentially grave outcomes. These are often enteric gram-negative bacteria that cross the intestinal barrier, enter the systemic circulation, and travel to the site of infection.
Long-term fluoroquinolone therapy (typically with norfloxacin) might help prevent these bacterial infections, the translocation of bacterial products, systemic inflammation, and consequent end-organ dysfunction, such as acute kidney disease. However, long-term antibiotic therapy also raises the specter of multidrug resistance, which is especially concerning when it involves a crucial antibiotic class such as fluoroquinolones, the researchers noted. “[In] patients receiving prolonged fluoroquinolone therapy, the development of infections by multidrug resistant bacteria might obscure the beneficial effect of fluoroquinolones on survival,” they added.
Four previous blinded and placebo-controlled trials have investigated fluoroquinolone therapy and mortality patients with cirrhosis, but they were small, usually included mortality only as a secondary outcome, and yielded mixed results. Hence, the researchers enrolled 291 patients with advanced (Child-Pugh class C) cirrhosis from 18 clinical sites in France and randomly assigned them to receive either norfloxacin (400 mg once daily) or placebo for 6 months. Patients were evaluated monthly during treatment and then at 9 months and 12 months. The primary outcome was survival at 6 months.
In a post hoc analysis, the researchers examined cumulative death rates at 6 months after accounting for liver transplantation as a competing risk of death and including survival data for patients who developed spontaneous bacterial peritonitis. Taking this approach, the estimated cumulative rate of death at 6 months was 15.5% (95% confidence interval, 10.1-21.9) in the norfloxacin group and 24.8% (95% CI, 18.1-32.1) in the placebo group, for a hazard ratio of 0.59 (95% CI, 0.35-0.99). Among patients whose ascites fluid levels were less than 15 g/L, the hazard ratio for death at 6 months was 65% lower in the norfloxacin group than in the placebo group (HR, 0.35; 95% CI, 0.13-0.93). Norfloxacin showed no such benefit for patients with ascites fluid protein levels above 15 g/L.
Norfloxacin therapy “could reduce the incidence of death among patients with ascitic fluid protein concentrations of less than 15 g/L but not among those with ascitic fluid protein concentration of 15 g/L or more,” the researchers concluded. “Norfloxacin may prevent some infections, especially gram-negative bacterial infections, but not the development of [spontaneous bacterial peritonitis] and other noninfectious, liver-related complications.”
The study was funded by Programme Hospitalier de Recherche Clinique National 2008 of the French Ministry of Health. Dr. Moreau reported having no conflicts of interest. Two coinvestigators disclosed ties to Gore Norgine, Exalenz, and Conatus.
SOURCE: Moreau R et al. Gastroenterology. 2018 Aug 22. doi: 10.1053/j.gastro.2018.08.026.
Prolonged antimicrobial use in patients with decompensated cirrhosis is an area of unclear mortality benefit and may actually increase risk in some patients given antimicrobial resistance. This randomized double-blind, placebo-controlled trial by Moreau et al. evaluates the mortality associated with long-term fluoroquinolone therapy in patients without indications for primary or secondary prophylaxis. Although the study had limited statistical power to detect clear benefit, the authors found that 6-month mortality was not reduced in patients with Child-Pugh class C cirrhosis who received treatment with daily oral fluoroquinolone therapy for 6 months. Subgroup analysis of individuals with ascites fluid total protein levels lower than 15 g/L showed a survival benefit at 6 months.
Determining quantifiable risk for known factors associated with liver disease mortality is a pressing issue, especially in the pretransplant setting where infectious risk is compounded post transplant with changes in gut flora, addition of potent immunosuppressants, and increased metabolic demands. Biologic measurements that correlate with increased complications and mortality, like low protein ascites, are helpful in complex clinical settings.Studying patients with advanced and decompensated liver disease in a systematic, longitudinal manner with any pharmacologic intervention is a particular challenge given the unpredictable nature of decompensation events and variable outcomes from those events. However, attempts to quantify risk and benefit even in this unpredictable patient population is worthwhile to stratify patients for interventions and minimize risk of liver-related and overall mortality – as well as peritransplant complications and posttransplant survival.
Julia J. Wattacheril, MD, MPH, is a physician- scientist and director of the Nonalcoholic Fatty Liver Disease Program in the Center for Liver Disease and Transplantation at Columbia University Irving Medical Center–New York Presbyterian Hospital, New York; an assistant professor, department of medicine, division of digestive and liver diseases at the Columbia University Vagelos College of Physicians and Surgeons. She has no conflicts.
Prolonged antimicrobial use in patients with decompensated cirrhosis is an area of unclear mortality benefit and may actually increase risk in some patients given antimicrobial resistance. This randomized double-blind, placebo-controlled trial by Moreau et al. evaluates the mortality associated with long-term fluoroquinolone therapy in patients without indications for primary or secondary prophylaxis. Although the study had limited statistical power to detect clear benefit, the authors found that 6-month mortality was not reduced in patients with Child-Pugh class C cirrhosis who received treatment with daily oral fluoroquinolone therapy for 6 months. Subgroup analysis of individuals with ascites fluid total protein levels lower than 15 g/L showed a survival benefit at 6 months.
Determining quantifiable risk for known factors associated with liver disease mortality is a pressing issue, especially in the pretransplant setting where infectious risk is compounded post transplant with changes in gut flora, addition of potent immunosuppressants, and increased metabolic demands. Biologic measurements that correlate with increased complications and mortality, like low protein ascites, are helpful in complex clinical settings.Studying patients with advanced and decompensated liver disease in a systematic, longitudinal manner with any pharmacologic intervention is a particular challenge given the unpredictable nature of decompensation events and variable outcomes from those events. However, attempts to quantify risk and benefit even in this unpredictable patient population is worthwhile to stratify patients for interventions and minimize risk of liver-related and overall mortality – as well as peritransplant complications and posttransplant survival.
Julia J. Wattacheril, MD, MPH, is a physician- scientist and director of the Nonalcoholic Fatty Liver Disease Program in the Center for Liver Disease and Transplantation at Columbia University Irving Medical Center–New York Presbyterian Hospital, New York; an assistant professor, department of medicine, division of digestive and liver diseases at the Columbia University Vagelos College of Physicians and Surgeons. She has no conflicts.
Prolonged antimicrobial use in patients with decompensated cirrhosis is an area of unclear mortality benefit and may actually increase risk in some patients given antimicrobial resistance. This randomized double-blind, placebo-controlled trial by Moreau et al. evaluates the mortality associated with long-term fluoroquinolone therapy in patients without indications for primary or secondary prophylaxis. Although the study had limited statistical power to detect clear benefit, the authors found that 6-month mortality was not reduced in patients with Child-Pugh class C cirrhosis who received treatment with daily oral fluoroquinolone therapy for 6 months. Subgroup analysis of individuals with ascites fluid total protein levels lower than 15 g/L showed a survival benefit at 6 months.
Determining quantifiable risk for known factors associated with liver disease mortality is a pressing issue, especially in the pretransplant setting where infectious risk is compounded post transplant with changes in gut flora, addition of potent immunosuppressants, and increased metabolic demands. Biologic measurements that correlate with increased complications and mortality, like low protein ascites, are helpful in complex clinical settings.Studying patients with advanced and decompensated liver disease in a systematic, longitudinal manner with any pharmacologic intervention is a particular challenge given the unpredictable nature of decompensation events and variable outcomes from those events. However, attempts to quantify risk and benefit even in this unpredictable patient population is worthwhile to stratify patients for interventions and minimize risk of liver-related and overall mortality – as well as peritransplant complications and posttransplant survival.
Julia J. Wattacheril, MD, MPH, is a physician- scientist and director of the Nonalcoholic Fatty Liver Disease Program in the Center for Liver Disease and Transplantation at Columbia University Irving Medical Center–New York Presbyterian Hospital, New York; an assistant professor, department of medicine, division of digestive and liver diseases at the Columbia University Vagelos College of Physicians and Surgeons. She has no conflicts.
Six months of once-daily norfloxacin therapy did not reduce 6-month mortality among patients with Child-Pugh class C cirrhosis who had not recently received fluoroquinolone therapy.
Mortality based on the Kaplan-Meier method was 14.8% in the norfloxacin group versus 19.7% for patients receiving placebo (P = .21). “Norfloxacin, however, appear[ed] to increase survival of patients with low ascites fluid protein concentrations,” wrote Richard Moreau, MD, of Hôpital Beaujon, Paris, and his associates. The results of the multicenter, double-blind trial of 291 patients were published in the December issue of Gastroenterology.
Patients with advanced cirrhosis often develop spontaneous bacterial peritonitis and other severe bacterial infections, with potentially grave outcomes. These are often enteric gram-negative bacteria that cross the intestinal barrier, enter the systemic circulation, and travel to the site of infection.
Long-term fluoroquinolone therapy (typically with norfloxacin) might help prevent these bacterial infections, the translocation of bacterial products, systemic inflammation, and consequent end-organ dysfunction, such as acute kidney disease. However, long-term antibiotic therapy also raises the specter of multidrug resistance, which is especially concerning when it involves a crucial antibiotic class such as fluoroquinolones, the researchers noted. “[In] patients receiving prolonged fluoroquinolone therapy, the development of infections by multidrug resistant bacteria might obscure the beneficial effect of fluoroquinolones on survival,” they added.
Four previous blinded and placebo-controlled trials have investigated fluoroquinolone therapy and mortality patients with cirrhosis, but they were small, usually included mortality only as a secondary outcome, and yielded mixed results. Hence, the researchers enrolled 291 patients with advanced (Child-Pugh class C) cirrhosis from 18 clinical sites in France and randomly assigned them to receive either norfloxacin (400 mg once daily) or placebo for 6 months. Patients were evaluated monthly during treatment and then at 9 months and 12 months. The primary outcome was survival at 6 months.
In a post hoc analysis, the researchers examined cumulative death rates at 6 months after accounting for liver transplantation as a competing risk of death and including survival data for patients who developed spontaneous bacterial peritonitis. Taking this approach, the estimated cumulative rate of death at 6 months was 15.5% (95% confidence interval, 10.1-21.9) in the norfloxacin group and 24.8% (95% CI, 18.1-32.1) in the placebo group, for a hazard ratio of 0.59 (95% CI, 0.35-0.99). Among patients whose ascites fluid levels were less than 15 g/L, the hazard ratio for death at 6 months was 65% lower in the norfloxacin group than in the placebo group (HR, 0.35; 95% CI, 0.13-0.93). Norfloxacin showed no such benefit for patients with ascites fluid protein levels above 15 g/L.
Norfloxacin therapy “could reduce the incidence of death among patients with ascitic fluid protein concentrations of less than 15 g/L but not among those with ascitic fluid protein concentration of 15 g/L or more,” the researchers concluded. “Norfloxacin may prevent some infections, especially gram-negative bacterial infections, but not the development of [spontaneous bacterial peritonitis] and other noninfectious, liver-related complications.”
The study was funded by Programme Hospitalier de Recherche Clinique National 2008 of the French Ministry of Health. Dr. Moreau reported having no conflicts of interest. Two coinvestigators disclosed ties to Gore Norgine, Exalenz, and Conatus.
SOURCE: Moreau R et al. Gastroenterology. 2018 Aug 22. doi: 10.1053/j.gastro.2018.08.026.
Six months of once-daily norfloxacin therapy did not reduce 6-month mortality among patients with Child-Pugh class C cirrhosis who had not recently received fluoroquinolone therapy.
Mortality based on the Kaplan-Meier method was 14.8% in the norfloxacin group versus 19.7% for patients receiving placebo (P = .21). “Norfloxacin, however, appear[ed] to increase survival of patients with low ascites fluid protein concentrations,” wrote Richard Moreau, MD, of Hôpital Beaujon, Paris, and his associates. The results of the multicenter, double-blind trial of 291 patients were published in the December issue of Gastroenterology.
Patients with advanced cirrhosis often develop spontaneous bacterial peritonitis and other severe bacterial infections, with potentially grave outcomes. These are often enteric gram-negative bacteria that cross the intestinal barrier, enter the systemic circulation, and travel to the site of infection.
Long-term fluoroquinolone therapy (typically with norfloxacin) might help prevent these bacterial infections, the translocation of bacterial products, systemic inflammation, and consequent end-organ dysfunction, such as acute kidney disease. However, long-term antibiotic therapy also raises the specter of multidrug resistance, which is especially concerning when it involves a crucial antibiotic class such as fluoroquinolones, the researchers noted. “[In] patients receiving prolonged fluoroquinolone therapy, the development of infections by multidrug resistant bacteria might obscure the beneficial effect of fluoroquinolones on survival,” they added.
Four previous blinded and placebo-controlled trials have investigated fluoroquinolone therapy and mortality patients with cirrhosis, but they were small, usually included mortality only as a secondary outcome, and yielded mixed results. Hence, the researchers enrolled 291 patients with advanced (Child-Pugh class C) cirrhosis from 18 clinical sites in France and randomly assigned them to receive either norfloxacin (400 mg once daily) or placebo for 6 months. Patients were evaluated monthly during treatment and then at 9 months and 12 months. The primary outcome was survival at 6 months.
In a post hoc analysis, the researchers examined cumulative death rates at 6 months after accounting for liver transplantation as a competing risk of death and including survival data for patients who developed spontaneous bacterial peritonitis. Taking this approach, the estimated cumulative rate of death at 6 months was 15.5% (95% confidence interval, 10.1-21.9) in the norfloxacin group and 24.8% (95% CI, 18.1-32.1) in the placebo group, for a hazard ratio of 0.59 (95% CI, 0.35-0.99). Among patients whose ascites fluid levels were less than 15 g/L, the hazard ratio for death at 6 months was 65% lower in the norfloxacin group than in the placebo group (HR, 0.35; 95% CI, 0.13-0.93). Norfloxacin showed no such benefit for patients with ascites fluid protein levels above 15 g/L.
Norfloxacin therapy “could reduce the incidence of death among patients with ascitic fluid protein concentrations of less than 15 g/L but not among those with ascitic fluid protein concentration of 15 g/L or more,” the researchers concluded. “Norfloxacin may prevent some infections, especially gram-negative bacterial infections, but not the development of [spontaneous bacterial peritonitis] and other noninfectious, liver-related complications.”
The study was funded by Programme Hospitalier de Recherche Clinique National 2008 of the French Ministry of Health. Dr. Moreau reported having no conflicts of interest. Two coinvestigators disclosed ties to Gore Norgine, Exalenz, and Conatus.
SOURCE: Moreau R et al. Gastroenterology. 2018 Aug 22. doi: 10.1053/j.gastro.2018.08.026.
FROM GASTROENTEROLOGY
Key clinical point: Six months of once-daily norfloxacin therapy did not reduce 6-month mortality among patients with Child-Pugh class C cirrhosis who had not recently received fluoroquinolone therapy, but norfloxacin did appear to benefit a subgroup of patients with low ascites fluid protein levels.
Major finding: Mortality based on the Kaplan-Meier method was 14.8% in the norfloxacin group versus 19.7% for patients receiving placebo (P = .21). Among patients whose ascites fluid levels were less than 15 g/L, the hazard ratio for death at 6 months was 65% lower in the norfloxacin group than in the placebo group (HR, 0.35; 95% CI, 0.13-0.93).
Study details: Multicenter double-blind trial of 291 patients with Child-Pugh class C cirrhosis who had not received recent fluoroquinolone therapy.
Disclosures: The study was funded by Programme Hospitalier de Recherche Clinique National 2008 of the French Ministry of Health. Dr. Moreau reported having no conflicts of interest. Two coinvestigators disclosed ties to Gore Norgine, Exalenz, and Conatus.
Source: Moreau R et al. Gastroenterology. 2018 Aug 22. doi: 10.1053/j.gastro.2018.08.026.
Ecstasy for PTSD, cockroach-tough C. diff, cardio-friendly queso
Rolling in ecstasy
Treating post-traumatic stress disorder could now be as simple as hitting the club. Not really, but in the longest and largest study of its kind, researchers looked at the effects of MDMA on patients with chronic PTSD.
After three sessions of taking MDMA (in a controlled environment, not in a warehouse in Brooklyn), 76% of study participants no longer met the criteria for PTSD. This is excellent news for those who suffer from PTSD – and the latest breakthrough in a significant shift toward accepting hallucinogenic drugs as possible treatments for mental health issues. Who knows, perhaps medicinal molly cards could soon be appearing.
And what next after that? Ketamine? Oh wait.
Infection is its own reward
Cockroaches are tough. Really tough. Survive compression forces of 300 times their body weight tough. Live without a head for a week tough. Laugh off a nuclear Armageddon tough. Can anything be tougher than that? Researchers at De Montfort University in Leicester, England, have a possible candidate, and it’s not Chuck Norris (Infect Control Hosp Epidemiol. 2018 Oct 16:1-6. doi: 10.1017/ice.2018.255).
They took cotton bed sheets contaminated with Clostridium difficile and put them “through a simulated washer extractor cycle using an industrial bleach detergent with sodium hypochlorite 15% and peracetic acid sour 14%.” Other contaminated sheets went to a commercial laundry service, “where they were washed in a washer extractor (infected linen wash) with industrial detergent, pressed, dried, and finished according to the current National Health Service in the United Kingdom’s health care laundry policy,” they said in a separate written statement. The result of all that effort? The average C. difficile spore load was reduced by 40%. In other words, most of the spores survived.
That not-so-comforting outcome does, however, leave us with a slightly comforting bit of conjecture: Those super tough cockroaches – the ones that survive the apocalypse that wipes out humans – will probably have diarrhea.
More cheese, please
The healing powers of cheese are now backed with science. A study from the University of Eastern Finland examined the incidence of coronary heart disease in men who ate a lot of fermented dairy (cheese, yogurt, kefir) and men who did not.
Researchers divided 2,000 men into four groups based on fermented dairy consumption and found that the men in the highest-consumption group had a 26% lower risk of incident coronary heart disease. Unfortunately for the “Got Milk?” ad campaign, researchers also discovered that men who consumed high levels of non-fermented dairy had a higher risk of coronary heart disease.
Next time your doctor asks about your cheese consumption, you can show them this study as proof that cheese helps the heart and the soul.
The new math, health care edition
You may think that 2 plus 2 always equals 4, but health care billing has taken another route. Here’s a seemingly simple equation, as reported by Kaiser Health News: One patient with a rash that got worse when she used her antifungal cream plus one allergy skin-patch test (okay, so it involved 119 allergens – we’ll give you that) at Stanford (Calif.) Health Care equals one bill … for $48,329.
The patient, Janet Winston of Eureka, Calif., said, “I was grateful I had such wonderful care at Stanford, but I was pretty outraged they could charge that. … No one cut into me. No one gave me anesthesia.” Her insurer paid its negotiated share of $11,376.47, and Ms. Winston’s 20% share of that came to $3,103.73, which she bargained down to $1,561.86.
For insurers, large health systems like Stanford may be too big to fight, suggested Harvard University health care economist Leemore Dafny, who told KHN that “everyone wants to point fingers at the providers, but … a lot of times [insurers] roll over and pay the rates.”
In the end, though, Stanford received less than $13,000 of its original charge, so maybe 2 plus 2 only equals 3. A tough pill to swallow, perhaps, but the whole situation has a kind of chilling Donnie-and-Marie quality to it: a little bit new math, and a little bit “1984.”
Rolling in ecstasy
Treating post-traumatic stress disorder could now be as simple as hitting the club. Not really, but in the longest and largest study of its kind, researchers looked at the effects of MDMA on patients with chronic PTSD.
After three sessions of taking MDMA (in a controlled environment, not in a warehouse in Brooklyn), 76% of study participants no longer met the criteria for PTSD. This is excellent news for those who suffer from PTSD – and the latest breakthrough in a significant shift toward accepting hallucinogenic drugs as possible treatments for mental health issues. Who knows, perhaps medicinal molly cards could soon be appearing.
And what next after that? Ketamine? Oh wait.
Infection is its own reward
Cockroaches are tough. Really tough. Survive compression forces of 300 times their body weight tough. Live without a head for a week tough. Laugh off a nuclear Armageddon tough. Can anything be tougher than that? Researchers at De Montfort University in Leicester, England, have a possible candidate, and it’s not Chuck Norris (Infect Control Hosp Epidemiol. 2018 Oct 16:1-6. doi: 10.1017/ice.2018.255).
They took cotton bed sheets contaminated with Clostridium difficile and put them “through a simulated washer extractor cycle using an industrial bleach detergent with sodium hypochlorite 15% and peracetic acid sour 14%.” Other contaminated sheets went to a commercial laundry service, “where they were washed in a washer extractor (infected linen wash) with industrial detergent, pressed, dried, and finished according to the current National Health Service in the United Kingdom’s health care laundry policy,” they said in a separate written statement. The result of all that effort? The average C. difficile spore load was reduced by 40%. In other words, most of the spores survived.
That not-so-comforting outcome does, however, leave us with a slightly comforting bit of conjecture: Those super tough cockroaches – the ones that survive the apocalypse that wipes out humans – will probably have diarrhea.
More cheese, please
The healing powers of cheese are now backed with science. A study from the University of Eastern Finland examined the incidence of coronary heart disease in men who ate a lot of fermented dairy (cheese, yogurt, kefir) and men who did not.
Researchers divided 2,000 men into four groups based on fermented dairy consumption and found that the men in the highest-consumption group had a 26% lower risk of incident coronary heart disease. Unfortunately for the “Got Milk?” ad campaign, researchers also discovered that men who consumed high levels of non-fermented dairy had a higher risk of coronary heart disease.
Next time your doctor asks about your cheese consumption, you can show them this study as proof that cheese helps the heart and the soul.
The new math, health care edition
You may think that 2 plus 2 always equals 4, but health care billing has taken another route. Here’s a seemingly simple equation, as reported by Kaiser Health News: One patient with a rash that got worse when she used her antifungal cream plus one allergy skin-patch test (okay, so it involved 119 allergens – we’ll give you that) at Stanford (Calif.) Health Care equals one bill … for $48,329.
The patient, Janet Winston of Eureka, Calif., said, “I was grateful I had such wonderful care at Stanford, but I was pretty outraged they could charge that. … No one cut into me. No one gave me anesthesia.” Her insurer paid its negotiated share of $11,376.47, and Ms. Winston’s 20% share of that came to $3,103.73, which she bargained down to $1,561.86.
For insurers, large health systems like Stanford may be too big to fight, suggested Harvard University health care economist Leemore Dafny, who told KHN that “everyone wants to point fingers at the providers, but … a lot of times [insurers] roll over and pay the rates.”
In the end, though, Stanford received less than $13,000 of its original charge, so maybe 2 plus 2 only equals 3. A tough pill to swallow, perhaps, but the whole situation has a kind of chilling Donnie-and-Marie quality to it: a little bit new math, and a little bit “1984.”
Rolling in ecstasy
Treating post-traumatic stress disorder could now be as simple as hitting the club. Not really, but in the longest and largest study of its kind, researchers looked at the effects of MDMA on patients with chronic PTSD.
After three sessions of taking MDMA (in a controlled environment, not in a warehouse in Brooklyn), 76% of study participants no longer met the criteria for PTSD. This is excellent news for those who suffer from PTSD – and the latest breakthrough in a significant shift toward accepting hallucinogenic drugs as possible treatments for mental health issues. Who knows, perhaps medicinal molly cards could soon be appearing.
And what next after that? Ketamine? Oh wait.
Infection is its own reward
Cockroaches are tough. Really tough. Survive compression forces of 300 times their body weight tough. Live without a head for a week tough. Laugh off a nuclear Armageddon tough. Can anything be tougher than that? Researchers at De Montfort University in Leicester, England, have a possible candidate, and it’s not Chuck Norris (Infect Control Hosp Epidemiol. 2018 Oct 16:1-6. doi: 10.1017/ice.2018.255).
They took cotton bed sheets contaminated with Clostridium difficile and put them “through a simulated washer extractor cycle using an industrial bleach detergent with sodium hypochlorite 15% and peracetic acid sour 14%.” Other contaminated sheets went to a commercial laundry service, “where they were washed in a washer extractor (infected linen wash) with industrial detergent, pressed, dried, and finished according to the current National Health Service in the United Kingdom’s health care laundry policy,” they said in a separate written statement. The result of all that effort? The average C. difficile spore load was reduced by 40%. In other words, most of the spores survived.
That not-so-comforting outcome does, however, leave us with a slightly comforting bit of conjecture: Those super tough cockroaches – the ones that survive the apocalypse that wipes out humans – will probably have diarrhea.
More cheese, please
The healing powers of cheese are now backed with science. A study from the University of Eastern Finland examined the incidence of coronary heart disease in men who ate a lot of fermented dairy (cheese, yogurt, kefir) and men who did not.
Researchers divided 2,000 men into four groups based on fermented dairy consumption and found that the men in the highest-consumption group had a 26% lower risk of incident coronary heart disease. Unfortunately for the “Got Milk?” ad campaign, researchers also discovered that men who consumed high levels of non-fermented dairy had a higher risk of coronary heart disease.
Next time your doctor asks about your cheese consumption, you can show them this study as proof that cheese helps the heart and the soul.
The new math, health care edition
You may think that 2 plus 2 always equals 4, but health care billing has taken another route. Here’s a seemingly simple equation, as reported by Kaiser Health News: One patient with a rash that got worse when she used her antifungal cream plus one allergy skin-patch test (okay, so it involved 119 allergens – we’ll give you that) at Stanford (Calif.) Health Care equals one bill … for $48,329.
The patient, Janet Winston of Eureka, Calif., said, “I was grateful I had such wonderful care at Stanford, but I was pretty outraged they could charge that. … No one cut into me. No one gave me anesthesia.” Her insurer paid its negotiated share of $11,376.47, and Ms. Winston’s 20% share of that came to $3,103.73, which she bargained down to $1,561.86.
For insurers, large health systems like Stanford may be too big to fight, suggested Harvard University health care economist Leemore Dafny, who told KHN that “everyone wants to point fingers at the providers, but … a lot of times [insurers] roll over and pay the rates.”
In the end, though, Stanford received less than $13,000 of its original charge, so maybe 2 plus 2 only equals 3. A tough pill to swallow, perhaps, but the whole situation has a kind of chilling Donnie-and-Marie quality to it: a little bit new math, and a little bit “1984.”
Parkinson’s prevalence varies significantly from state to state
ATLANTA – The prevalence of Parkinson’s disease and associated health care spending on the condition vary significantly from state to state, an analysis of Medicare data showed.
“There is a big variation in not only the prevalence of Parkinson’s disease but also in spending and in health care utilization” among Medicare beneficiaries diagnosed with the condition, lead study author Michelle E. Fullard, MD, said in an interview at the annual meeting of the American Neurological Association. “As neurologists, we should be aware of this. We can use this information to identify and target areas in which Parkinson’s patients may have increased need and require more resources. It can also inform planning at the state and federal levels.”
Dr. Fullard, formerly of the department of neurology at the University of Pennsylvania, Philadelphia, and her colleagues evaluated data from Medicare Beneficiary Summary and Medicare Carrier Files for 27,538,023 individuals aged 65 years and older who were continuously enrolled in Medicare parts A and B during 2014. They calculated state-level differences in Parkinson’s disease prevalence, demographic and eligibility characteristics, costs, and health care use, including number of emergency room visits, number of outpatient clinic visits, and inpatient hospitalizations. The researchers used reimbursement data to calculate the mean out-of-pocket and Medicare cost per individual in each state, and compared direct costs and health service utilization for individuals with and without Parkinson’s disease.
Of all Medicare beneficiaries studied, 392,214 (1.42%) had a diagnosis of Parkinson’s disease. Nearly half (46%) were women and 26% were aged 85 years and older. States with the highest prevalence of Parkinson’s disease included New York (1,720/100,000), Illinois (1,566/100,000), Connecticut (1,560/100,000), Florida (1,551/100,000), Pennsylvania (1,549/100,000), Rhode Island (1,543/100,000), New Jersey (1,541/100,000), Texas (1,522/100,000), California (1,520/100,000) and Louisiana (1,519/100,000). Minnesota had the lowest prevalence (803/100,000).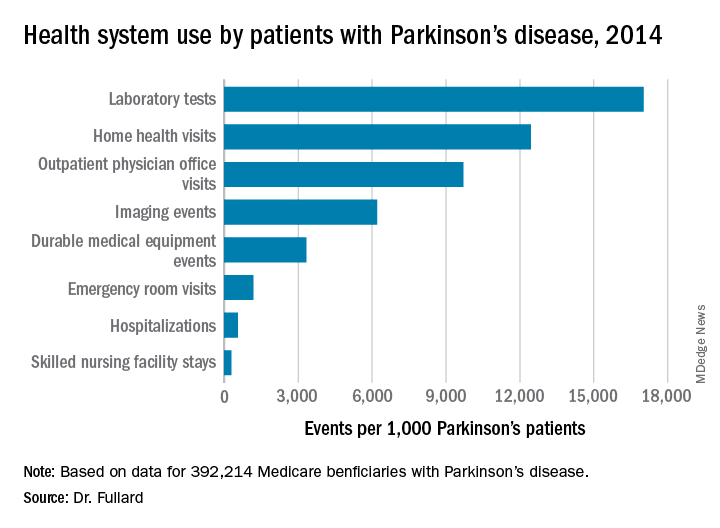
Among the national sample of patients with Parkinson’s disease, there were 219,049 hospitalizations (which represented 558/1,000 Parkinson’s patients), 37,839 readmissions (172/1,000 hospitalizations), 9,740,609 outpatient physician office visits (9,700/1,000 patients), 34,159 hospice stays (87/1,000 patients), 113,027 skilled nursing facility stays (288/1,000 patients), 466,160 emergency room visits (1,188/1,000 patients, 39% of which resulted in hospital admission). In addition, there were 1,308,934 durable medical equipment events (3,337/1,000 patients), 6,676,119 laboratory tests (17,021/1,000 patients), 2,435,654 imaging events (6,210/1,000 patients), and 4,879,538 home health visits (12,441/1,000 patients). The costliest services were inpatient care ($2.1 billion), skilled nursing facility care ($1.4 billion), prescription drugs used by those with prescription coverage ($974.8 million), hospital outpatient care ($881 million), and home health care ($776.5 million).
“States with a higher prevalence of Parkinson’s disease may have a larger proportion of high-risk factor patient groups, a higher concentration of providers who recognize and document Parkinson’s disease, increased public awareness of symptoms, or increased health care–seeking behaviors among people living in the state,” the researchers wrote in their abstract. “Among our top Parkinson’s disease prevalence states, Florida and New York also rank high in terms of absolute number of Medicare beneficiaries and have large supplies of health care providers.”
They also noted that Medicare beneficiaries with Parkinson’s had increased use of health care and spending, compared with their counterparts without the disease. “This was true across all sectors of care (inpatient, outpatient, skilled nursing, and ancillary services) and is in line with data demonstrating that PD, its complications, and the shift away from comorbid disease care and prevention that occurs after a Parkinson’s disease diagnosis drive health care spending and utilization among these individuals,” they wrote.
The study was supported by the Parkinson’s Foundation. Dr. Fullard, who now holds a faculty position at the University of Colorado, Aurora, reported having no financial disclosures.
SOURCE: Ann Neurol. 2018;84[S22]:S89-90, Abstract S215.
ATLANTA – The prevalence of Parkinson’s disease and associated health care spending on the condition vary significantly from state to state, an analysis of Medicare data showed.
“There is a big variation in not only the prevalence of Parkinson’s disease but also in spending and in health care utilization” among Medicare beneficiaries diagnosed with the condition, lead study author Michelle E. Fullard, MD, said in an interview at the annual meeting of the American Neurological Association. “As neurologists, we should be aware of this. We can use this information to identify and target areas in which Parkinson’s patients may have increased need and require more resources. It can also inform planning at the state and federal levels.”
Dr. Fullard, formerly of the department of neurology at the University of Pennsylvania, Philadelphia, and her colleagues evaluated data from Medicare Beneficiary Summary and Medicare Carrier Files for 27,538,023 individuals aged 65 years and older who were continuously enrolled in Medicare parts A and B during 2014. They calculated state-level differences in Parkinson’s disease prevalence, demographic and eligibility characteristics, costs, and health care use, including number of emergency room visits, number of outpatient clinic visits, and inpatient hospitalizations. The researchers used reimbursement data to calculate the mean out-of-pocket and Medicare cost per individual in each state, and compared direct costs and health service utilization for individuals with and without Parkinson’s disease.
Of all Medicare beneficiaries studied, 392,214 (1.42%) had a diagnosis of Parkinson’s disease. Nearly half (46%) were women and 26% were aged 85 years and older. States with the highest prevalence of Parkinson’s disease included New York (1,720/100,000), Illinois (1,566/100,000), Connecticut (1,560/100,000), Florida (1,551/100,000), Pennsylvania (1,549/100,000), Rhode Island (1,543/100,000), New Jersey (1,541/100,000), Texas (1,522/100,000), California (1,520/100,000) and Louisiana (1,519/100,000). Minnesota had the lowest prevalence (803/100,000).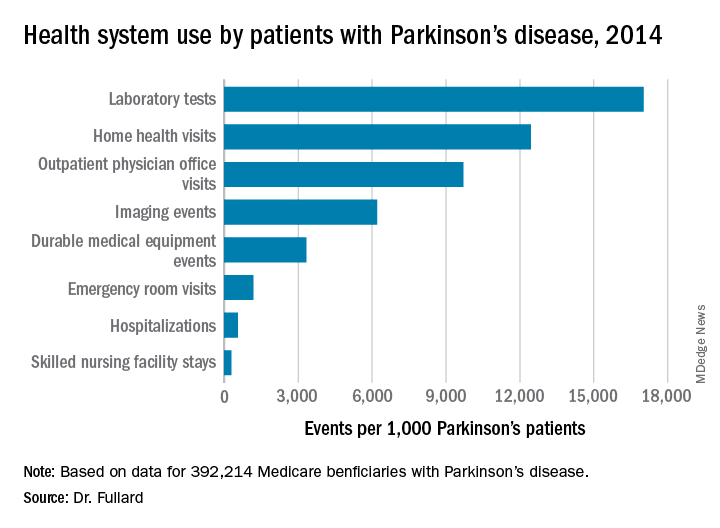
Among the national sample of patients with Parkinson’s disease, there were 219,049 hospitalizations (which represented 558/1,000 Parkinson’s patients), 37,839 readmissions (172/1,000 hospitalizations), 9,740,609 outpatient physician office visits (9,700/1,000 patients), 34,159 hospice stays (87/1,000 patients), 113,027 skilled nursing facility stays (288/1,000 patients), 466,160 emergency room visits (1,188/1,000 patients, 39% of which resulted in hospital admission). In addition, there were 1,308,934 durable medical equipment events (3,337/1,000 patients), 6,676,119 laboratory tests (17,021/1,000 patients), 2,435,654 imaging events (6,210/1,000 patients), and 4,879,538 home health visits (12,441/1,000 patients). The costliest services were inpatient care ($2.1 billion), skilled nursing facility care ($1.4 billion), prescription drugs used by those with prescription coverage ($974.8 million), hospital outpatient care ($881 million), and home health care ($776.5 million).
“States with a higher prevalence of Parkinson’s disease may have a larger proportion of high-risk factor patient groups, a higher concentration of providers who recognize and document Parkinson’s disease, increased public awareness of symptoms, or increased health care–seeking behaviors among people living in the state,” the researchers wrote in their abstract. “Among our top Parkinson’s disease prevalence states, Florida and New York also rank high in terms of absolute number of Medicare beneficiaries and have large supplies of health care providers.”
They also noted that Medicare beneficiaries with Parkinson’s had increased use of health care and spending, compared with their counterparts without the disease. “This was true across all sectors of care (inpatient, outpatient, skilled nursing, and ancillary services) and is in line with data demonstrating that PD, its complications, and the shift away from comorbid disease care and prevention that occurs after a Parkinson’s disease diagnosis drive health care spending and utilization among these individuals,” they wrote.
The study was supported by the Parkinson’s Foundation. Dr. Fullard, who now holds a faculty position at the University of Colorado, Aurora, reported having no financial disclosures.
SOURCE: Ann Neurol. 2018;84[S22]:S89-90, Abstract S215.
ATLANTA – The prevalence of Parkinson’s disease and associated health care spending on the condition vary significantly from state to state, an analysis of Medicare data showed.
“There is a big variation in not only the prevalence of Parkinson’s disease but also in spending and in health care utilization” among Medicare beneficiaries diagnosed with the condition, lead study author Michelle E. Fullard, MD, said in an interview at the annual meeting of the American Neurological Association. “As neurologists, we should be aware of this. We can use this information to identify and target areas in which Parkinson’s patients may have increased need and require more resources. It can also inform planning at the state and federal levels.”
Dr. Fullard, formerly of the department of neurology at the University of Pennsylvania, Philadelphia, and her colleagues evaluated data from Medicare Beneficiary Summary and Medicare Carrier Files for 27,538,023 individuals aged 65 years and older who were continuously enrolled in Medicare parts A and B during 2014. They calculated state-level differences in Parkinson’s disease prevalence, demographic and eligibility characteristics, costs, and health care use, including number of emergency room visits, number of outpatient clinic visits, and inpatient hospitalizations. The researchers used reimbursement data to calculate the mean out-of-pocket and Medicare cost per individual in each state, and compared direct costs and health service utilization for individuals with and without Parkinson’s disease.
Of all Medicare beneficiaries studied, 392,214 (1.42%) had a diagnosis of Parkinson’s disease. Nearly half (46%) were women and 26% were aged 85 years and older. States with the highest prevalence of Parkinson’s disease included New York (1,720/100,000), Illinois (1,566/100,000), Connecticut (1,560/100,000), Florida (1,551/100,000), Pennsylvania (1,549/100,000), Rhode Island (1,543/100,000), New Jersey (1,541/100,000), Texas (1,522/100,000), California (1,520/100,000) and Louisiana (1,519/100,000). Minnesota had the lowest prevalence (803/100,000).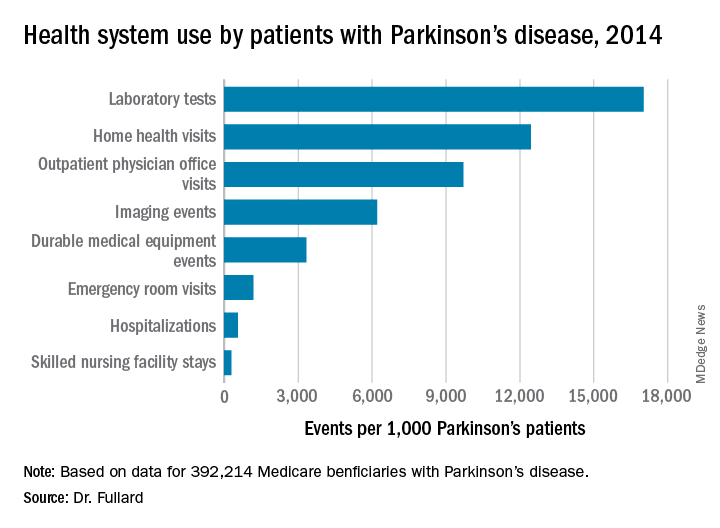
Among the national sample of patients with Parkinson’s disease, there were 219,049 hospitalizations (which represented 558/1,000 Parkinson’s patients), 37,839 readmissions (172/1,000 hospitalizations), 9,740,609 outpatient physician office visits (9,700/1,000 patients), 34,159 hospice stays (87/1,000 patients), 113,027 skilled nursing facility stays (288/1,000 patients), 466,160 emergency room visits (1,188/1,000 patients, 39% of which resulted in hospital admission). In addition, there were 1,308,934 durable medical equipment events (3,337/1,000 patients), 6,676,119 laboratory tests (17,021/1,000 patients), 2,435,654 imaging events (6,210/1,000 patients), and 4,879,538 home health visits (12,441/1,000 patients). The costliest services were inpatient care ($2.1 billion), skilled nursing facility care ($1.4 billion), prescription drugs used by those with prescription coverage ($974.8 million), hospital outpatient care ($881 million), and home health care ($776.5 million).
“States with a higher prevalence of Parkinson’s disease may have a larger proportion of high-risk factor patient groups, a higher concentration of providers who recognize and document Parkinson’s disease, increased public awareness of symptoms, or increased health care–seeking behaviors among people living in the state,” the researchers wrote in their abstract. “Among our top Parkinson’s disease prevalence states, Florida and New York also rank high in terms of absolute number of Medicare beneficiaries and have large supplies of health care providers.”
They also noted that Medicare beneficiaries with Parkinson’s had increased use of health care and spending, compared with their counterparts without the disease. “This was true across all sectors of care (inpatient, outpatient, skilled nursing, and ancillary services) and is in line with data demonstrating that PD, its complications, and the shift away from comorbid disease care and prevention that occurs after a Parkinson’s disease diagnosis drive health care spending and utilization among these individuals,” they wrote.
The study was supported by the Parkinson’s Foundation. Dr. Fullard, who now holds a faculty position at the University of Colorado, Aurora, reported having no financial disclosures.
SOURCE: Ann Neurol. 2018;84[S22]:S89-90, Abstract S215.
REPORTING FROM ANA 2018
Key clinical point:
Major finding: States with the highest prevalence of Parkinson’s disease included New York (1,720/100,000), Illinois (1,566/100,000), and Connecticut (1,560/100,000), while Minnesota had the lowest prevalence (803/100,000).
Study details: An analysis of 392,214 Medicare beneficiaries who carried a diagnosis of Parkinson’s disease.
Disclosures: The study was supported by the Parkinson’s Foundation. Dr. Fullard reported having no financial disclosures.
Source: Ann Neurol. 2018;84[S22]:S89-90. Abstract S215.
Estetrol safely limited menopause symptoms in a phase 2b study
Estetrol (Donesta) relieved vasomotor menopausal symptoms without stimulating breast tenderness or raising triglyceride levels in a dose-finding study of the investigational drug presented at the annual meeting of the North American Menopause Society.
Estetrol (E4), an estrogen produced by the fetal liver, is the first native estrogen acting selectively in tissues. Since it crosses the placenta, estetrol is present in maternal urine at about 9 weeks’ gestation. In fetal plasma, it circulates at concentrations about 12 times higher than maternal estetrol levels. The hormone has a half-life of 28-32 hours, longer than the half-life of most other estrogens.
E4 “has been shown to have a remarkably safe profile and I like to describe it as the first natural oral estrogen with the safety profile of a transdermal estrogen,” said Wulf H. Utian, MD, the Arthur H. Bill Professor of Obstetrics & Gynecology at Case Western Reserve University, Cleveland. Estetrol uniquely activates nuclear estrogen receptor–alpha, while antagonizing membrane estrogen receptor-alpha. These properties give E4 selective tissue action, with low breast stimulation meaning less breast tenderness and “low carcinogenic impact.”
Additionally, triglyceride levels are minimally affected, and serum markers for venous thromboembolism generally remain unchanged with E4 exposure, he said.
In a phase 2b dose-finding study, a variety of estetrol doses were compared with placebo to treat vasomotor symptoms in postmenopausal women aged 40-65 years with at least 7 moderate to severe hot flashes daily, or at least 50 moderate to severe hot flashes in the week before randomization. The multicenter, double-blind randomized controlled trial took place in five European countries, with 200 women overall completing the study. The study design excluded women with personal histories of malignancy, thromboembolism, or coagulopathy, and women with diabetes and poor glycemic control. Women with a uterus who had current or past endometrial hyperplasia, polyps, or an abnormal cervical smear were also excluded.
Women who had an intact uterus were included if transvaginal ultrasound showed endometrial thickness of 5 mm or less. Participants were randomized 1:1:1:1 to receive four different E4 doses: 2.5 mg, 5 mg, 10 mg, or 15 mg.
At the highest dose of 15 mg, E4 significantly reduced the frequency of vasomotor symptoms compared with placebo by study week 4 and throughout the 12-week study period (P less than .05).
This high dose also resulted in a 28% reduction in vasomotor symptom severity, compared with placebo by study week 12, with a significant separation from placebo by week 12.
In terms of the number of women who experienced at least a 50% drop in severe vasomotor symptoms, the 15-mg E4 dose also bested placebo (P less than .01). Among the group taking the 15 mg dose, significantly more also saw at least a 75% drop in frequency of severe vasomotor symptom (P less than .001).
Vaginal cytology showed that by week 12 all doses of E4 significantly increased the vaginal maturation index from baseline, a finding that corresponds with less thinning of vaginal tissues (P less than .001, compared with placebo for all doses).
The safety profile of E4 was good, Dr. Utian said. Coagulation markers were unaffected, and most lipid and blood glucose markers were also unchanged. There were “small but potentially beneficial changes in HDL-C [HDL cholesterol levels] and HbA1c values [hemoglobin A1c]” in groups taking the two highest doses of E4.
Also, C-telopeptide of type 1 collagen and osteocalcin values were reduced, “suggesting reduction in bone resorption,” he said.
According to Dr. Utian, those taking the two highest doses also saw a “slight though significant increase” from baseline in sex hormone–binding globulin levels, “indicating that the E4 estrogenic effect was mild and dose dependent.”
Endometrial biopsies showed no hyperplasia. In those taking the 15-mg E4 dose, mean endometrial thickness did increase from a mean 2 mm at baseline to 6 mm at 12 weeks. However, endometrial thickness returned to baseline after progestin therapy, said Dr. Utian. There were no unexpected adverse events during the study.
Dr. Utian reported consultant relationships with Mithra, the maker of estetrol; AMAG; Pharmavite; and Endoceutics. The study was funded by Mithra.
SOURCE: Utian W. NAMS 2018, Friday concurrent session 1.
Estetrol (Donesta) relieved vasomotor menopausal symptoms without stimulating breast tenderness or raising triglyceride levels in a dose-finding study of the investigational drug presented at the annual meeting of the North American Menopause Society.
Estetrol (E4), an estrogen produced by the fetal liver, is the first native estrogen acting selectively in tissues. Since it crosses the placenta, estetrol is present in maternal urine at about 9 weeks’ gestation. In fetal plasma, it circulates at concentrations about 12 times higher than maternal estetrol levels. The hormone has a half-life of 28-32 hours, longer than the half-life of most other estrogens.
E4 “has been shown to have a remarkably safe profile and I like to describe it as the first natural oral estrogen with the safety profile of a transdermal estrogen,” said Wulf H. Utian, MD, the Arthur H. Bill Professor of Obstetrics & Gynecology at Case Western Reserve University, Cleveland. Estetrol uniquely activates nuclear estrogen receptor–alpha, while antagonizing membrane estrogen receptor-alpha. These properties give E4 selective tissue action, with low breast stimulation meaning less breast tenderness and “low carcinogenic impact.”
Additionally, triglyceride levels are minimally affected, and serum markers for venous thromboembolism generally remain unchanged with E4 exposure, he said.
In a phase 2b dose-finding study, a variety of estetrol doses were compared with placebo to treat vasomotor symptoms in postmenopausal women aged 40-65 years with at least 7 moderate to severe hot flashes daily, or at least 50 moderate to severe hot flashes in the week before randomization. The multicenter, double-blind randomized controlled trial took place in five European countries, with 200 women overall completing the study. The study design excluded women with personal histories of malignancy, thromboembolism, or coagulopathy, and women with diabetes and poor glycemic control. Women with a uterus who had current or past endometrial hyperplasia, polyps, or an abnormal cervical smear were also excluded.
Women who had an intact uterus were included if transvaginal ultrasound showed endometrial thickness of 5 mm or less. Participants were randomized 1:1:1:1 to receive four different E4 doses: 2.5 mg, 5 mg, 10 mg, or 15 mg.
At the highest dose of 15 mg, E4 significantly reduced the frequency of vasomotor symptoms compared with placebo by study week 4 and throughout the 12-week study period (P less than .05).
This high dose also resulted in a 28% reduction in vasomotor symptom severity, compared with placebo by study week 12, with a significant separation from placebo by week 12.
In terms of the number of women who experienced at least a 50% drop in severe vasomotor symptoms, the 15-mg E4 dose also bested placebo (P less than .01). Among the group taking the 15 mg dose, significantly more also saw at least a 75% drop in frequency of severe vasomotor symptom (P less than .001).
Vaginal cytology showed that by week 12 all doses of E4 significantly increased the vaginal maturation index from baseline, a finding that corresponds with less thinning of vaginal tissues (P less than .001, compared with placebo for all doses).
The safety profile of E4 was good, Dr. Utian said. Coagulation markers were unaffected, and most lipid and blood glucose markers were also unchanged. There were “small but potentially beneficial changes in HDL-C [HDL cholesterol levels] and HbA1c values [hemoglobin A1c]” in groups taking the two highest doses of E4.
Also, C-telopeptide of type 1 collagen and osteocalcin values were reduced, “suggesting reduction in bone resorption,” he said.
According to Dr. Utian, those taking the two highest doses also saw a “slight though significant increase” from baseline in sex hormone–binding globulin levels, “indicating that the E4 estrogenic effect was mild and dose dependent.”
Endometrial biopsies showed no hyperplasia. In those taking the 15-mg E4 dose, mean endometrial thickness did increase from a mean 2 mm at baseline to 6 mm at 12 weeks. However, endometrial thickness returned to baseline after progestin therapy, said Dr. Utian. There were no unexpected adverse events during the study.
Dr. Utian reported consultant relationships with Mithra, the maker of estetrol; AMAG; Pharmavite; and Endoceutics. The study was funded by Mithra.
SOURCE: Utian W. NAMS 2018, Friday concurrent session 1.
Estetrol (Donesta) relieved vasomotor menopausal symptoms without stimulating breast tenderness or raising triglyceride levels in a dose-finding study of the investigational drug presented at the annual meeting of the North American Menopause Society.
Estetrol (E4), an estrogen produced by the fetal liver, is the first native estrogen acting selectively in tissues. Since it crosses the placenta, estetrol is present in maternal urine at about 9 weeks’ gestation. In fetal plasma, it circulates at concentrations about 12 times higher than maternal estetrol levels. The hormone has a half-life of 28-32 hours, longer than the half-life of most other estrogens.
E4 “has been shown to have a remarkably safe profile and I like to describe it as the first natural oral estrogen with the safety profile of a transdermal estrogen,” said Wulf H. Utian, MD, the Arthur H. Bill Professor of Obstetrics & Gynecology at Case Western Reserve University, Cleveland. Estetrol uniquely activates nuclear estrogen receptor–alpha, while antagonizing membrane estrogen receptor-alpha. These properties give E4 selective tissue action, with low breast stimulation meaning less breast tenderness and “low carcinogenic impact.”
Additionally, triglyceride levels are minimally affected, and serum markers for venous thromboembolism generally remain unchanged with E4 exposure, he said.
In a phase 2b dose-finding study, a variety of estetrol doses were compared with placebo to treat vasomotor symptoms in postmenopausal women aged 40-65 years with at least 7 moderate to severe hot flashes daily, or at least 50 moderate to severe hot flashes in the week before randomization. The multicenter, double-blind randomized controlled trial took place in five European countries, with 200 women overall completing the study. The study design excluded women with personal histories of malignancy, thromboembolism, or coagulopathy, and women with diabetes and poor glycemic control. Women with a uterus who had current or past endometrial hyperplasia, polyps, or an abnormal cervical smear were also excluded.
Women who had an intact uterus were included if transvaginal ultrasound showed endometrial thickness of 5 mm or less. Participants were randomized 1:1:1:1 to receive four different E4 doses: 2.5 mg, 5 mg, 10 mg, or 15 mg.
At the highest dose of 15 mg, E4 significantly reduced the frequency of vasomotor symptoms compared with placebo by study week 4 and throughout the 12-week study period (P less than .05).
This high dose also resulted in a 28% reduction in vasomotor symptom severity, compared with placebo by study week 12, with a significant separation from placebo by week 12.
In terms of the number of women who experienced at least a 50% drop in severe vasomotor symptoms, the 15-mg E4 dose also bested placebo (P less than .01). Among the group taking the 15 mg dose, significantly more also saw at least a 75% drop in frequency of severe vasomotor symptom (P less than .001).
Vaginal cytology showed that by week 12 all doses of E4 significantly increased the vaginal maturation index from baseline, a finding that corresponds with less thinning of vaginal tissues (P less than .001, compared with placebo for all doses).
The safety profile of E4 was good, Dr. Utian said. Coagulation markers were unaffected, and most lipid and blood glucose markers were also unchanged. There were “small but potentially beneficial changes in HDL-C [HDL cholesterol levels] and HbA1c values [hemoglobin A1c]” in groups taking the two highest doses of E4.
Also, C-telopeptide of type 1 collagen and osteocalcin values were reduced, “suggesting reduction in bone resorption,” he said.
According to Dr. Utian, those taking the two highest doses also saw a “slight though significant increase” from baseline in sex hormone–binding globulin levels, “indicating that the E4 estrogenic effect was mild and dose dependent.”
Endometrial biopsies showed no hyperplasia. In those taking the 15-mg E4 dose, mean endometrial thickness did increase from a mean 2 mm at baseline to 6 mm at 12 weeks. However, endometrial thickness returned to baseline after progestin therapy, said Dr. Utian. There were no unexpected adverse events during the study.
Dr. Utian reported consultant relationships with Mithra, the maker of estetrol; AMAG; Pharmavite; and Endoceutics. The study was funded by Mithra.
SOURCE: Utian W. NAMS 2018, Friday concurrent session 1.
FROM NAMS 2018
Key clinical point: Estetrol relieved hot flashes without adversely affecting lipid markers.
Major finding: Estetrol 15 mg reduced vasomotor symptom severity by 28%.
Study details: Randomized, double-blind, placebo-controlled phase 2b dose-finding study of 200 women.
Disclosures: Dr. Utian reported financial relationships with several pharmaceutical companies, including Mithra, the sponsor of the study.
Source: Utian WH. NAMS 2018, Friday concurrent session 1.
Pricey precision medicine often financially toxic for cancer patients
When Kristen Kilmer was diagnosed with incurable breast cancer at age 38, her first thought was of her 8-year-old daughter. Ms. Kilmer lost her own mother as a teenager and was determined to get more time with her only child.
Ms. Kilmer searched for experimental treatments, opting for an unproven approach in which researchers select drugs based on the genes in patients’ tumors. Doctors have selected her treatments for the past 3 years based on the unique, ever-changing DNA of her cancer cells. Now 41, Ms. Kilmer has responded better than anyone dared to hope. Her cancer has gone into hiding; her tumors are no longer visible on medical scans.
Researchers call the strategy “precision medicine.”
Ms. Kilmer’s insurance company calls it experimental. As a consequence, her insurer has covered only a fraction of her care, forcing Ms. Kilmer to make an agonizing choice: stop taking a drug that costs nearly $17,000 a month or pay out-of-pocket, burdening her family with tremendous debt.
“When you are looking at your daughter, you ask yourself, ‘Do I take a medication that might allow me to see her graduate high school?’ ” asked Ms. Kilmer of Spearfish, S.D. “Or do you stop taking it to avoid causing her financial harm?”
The high cost of cutting-edge tests and treatments is threatening to keep precision medicine – one of the most celebrated areas in cancer research – out of reach for many patients. Patients who pay for these new treatments on their own “could be in debt for decades,” said Scott Ramsey, MD, PhD, director of the Hutchinson Institute for Cancer Outcomes Research in Seattle.
Cancer care already is hugely expensive. A recent study in the American Journal of Medicine found that 42% of patients depleted 100% of their assets – an average loss of $92,000 – within 2 years of diagnosis.
Precision medicine involves running expensive tests called genomic sequencing, which scan the DNA of tumors to find mutations that might be susceptible to available drugs. Although the field is relatively new, hundreds of thousands of cancer patients have had their tumors sequenced to identify cancer-related mutations, according to testing companies.
Medicare, the government insurance plan for people 65 and older, announced in March that it will pay for genomic testing for people with advanced cancers – a decision that could add $2.5 billion to federal health care costs, according to a May analysis in Health Affairs.
Few private insurers cover the tests, leaving some patients with surprise medical bills.
Carrie Wyman, who also has advanced breast cancer, discovered that her insurance plan wouldn’t cover genomic sequencing only after she had received a $5,800 statement.
“I just assumed it would be covered,” said Ms. Wyman, 50, a resident of La Plata, Md., who has six children and stepchildren. “I was blindsided, to be honest with you.”
Looking for financial assistance
Yet paying for that initial test is just the beginning. As Ms. Kilmer learned, finding the money for ongoing treatment is far more challenging, said Gary H. Lyman, MD, who studies way to improve health care quality at Seattle’s Fred Hutchinson Cancer Research Center.
In some cases, genomic tests match patients to experimental drugs available only in clinical trials. Although these trials sometimes provide free medications, many cancer patients can’t afford to travel to participate in them. Ms. Kilmer drives 12 hours round-trip every month to participate in a clinical trial in Sioux Falls, S.D. The expenses add up quickly, she said.
Ms. Kilmer’s genomic tests identified a rearrangement in the PALB2 gene. Preliminary studies suggest that tumors with this genetic rearrangement could be susceptible to the drug olaparib (Lynparza), but those effects haven’t been definitively proven in large-scale studies. The Food and Drug Administration has approved Lynparza only for breast cancer patients with a BRCA mutation.
Legally, doctors can prescribe Lynparza “off label” to anyone with cancer. But insurance programs are reluctant to cover off-label treatments, unless they’re specifically recommended in expert guidelines.
Ms. Kilmer has spent much of the past 3 years battling insurance officials and begging drug companies for financial assistance. The drugmakers have been generous, allowing her to take a rotating cocktail of experimental drugs for free because of her modest income.
In September, however, AstraZeneca decided to end Ms. Kilmer’s financial aid. Ms. Kilmer appealed the drug company’s decision.
Paying thousands of dollars a month is not an option, Ms. Kilmer said. Her family already carries significant credit card debt from earlier cancer treatments. She estimates that she has spent about $80,600 out-of-pocket treating her illness, including $23,600 on her early breast cancer therapy and $57,000 treating metastatic disease.
Ms. Kilmer said she would rather stop taking Lynparza than financially burden her daughter and husband, a truck driver.
“It’s not worth it,” Ms. Kilmer said. “I will not put my family into that kind of debt.”
Uncertain benefits
Insurers say costs aren’t their only concern. Evidence is lacking that the precision medicine approach will work consistently, they argue.
America’s Health Insurance Plans, an industry group, said genetic sequencing remains unproven.
Cathryn Donaldson, the group’s spokeswoman, described recent scientific advances as “remarkable and noteworthy.” But she said insurers “need a more definitive answer” about whether the tests help the average patient live longer.
The South Dakota State Employee Health Plan – which runs Ms. Kilmer’s insurance plan – said it bases its coverage decisions on science and reviews “published, randomized data about the safety and efficacy of the requested drugs.”
Although genetic testing has become the standard of care for melanoma and a common type of lung cancer, no one knows if genomic sequencing will extend the lives of people with other types of cancer, said Carolyn J. Presley, MD, an assistant professor at the Ohio State University Comprehensive Cancer Center, Columbus.
Without insurance coverage, some cancer patients simply give up on treatment.
A study of more than 1,000 women with advanced breast cancer – presented at a September meeting of the American Society of Clinical Oncology – found that 54% had stopped or refused treatment because of costs. The women in the study may have been more vulnerable than most, because 30% were uninsured, about twice the national rate.
In an August study in JAMA, researchers found that relatively few of those who hoped to benefit from precision medicine actually ended up on a medication. Just 15% of those who underwent genomic sequencing ended up taking a targeted therapy, according to the study. The study didn’t ask participants why they failed to get a targeted drug, but Dr. Presley, the lead author, said it’s likely that some patients couldn’t afford them.
“We’re finding the mutations, but patients aren’t getting the drugs,” Dr. Presley said. Without insurance, she said, “you and I would not be able to afford these medications. It’s a huge barrier.”
Within hours of the publication of this story, AstraZeneca called Ms. Kilmer to notify her that it would continue to provide financial aid. Her medication arrived in the mail the next day.
“It’s a huge relief,” Ms. Kilmer said.
KHN’s coverage of these topics is supported by Laura and John Arnold Foundation and Gordon and Betty Moore Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
When Kristen Kilmer was diagnosed with incurable breast cancer at age 38, her first thought was of her 8-year-old daughter. Ms. Kilmer lost her own mother as a teenager and was determined to get more time with her only child.
Ms. Kilmer searched for experimental treatments, opting for an unproven approach in which researchers select drugs based on the genes in patients’ tumors. Doctors have selected her treatments for the past 3 years based on the unique, ever-changing DNA of her cancer cells. Now 41, Ms. Kilmer has responded better than anyone dared to hope. Her cancer has gone into hiding; her tumors are no longer visible on medical scans.
Researchers call the strategy “precision medicine.”
Ms. Kilmer’s insurance company calls it experimental. As a consequence, her insurer has covered only a fraction of her care, forcing Ms. Kilmer to make an agonizing choice: stop taking a drug that costs nearly $17,000 a month or pay out-of-pocket, burdening her family with tremendous debt.
“When you are looking at your daughter, you ask yourself, ‘Do I take a medication that might allow me to see her graduate high school?’ ” asked Ms. Kilmer of Spearfish, S.D. “Or do you stop taking it to avoid causing her financial harm?”
The high cost of cutting-edge tests and treatments is threatening to keep precision medicine – one of the most celebrated areas in cancer research – out of reach for many patients. Patients who pay for these new treatments on their own “could be in debt for decades,” said Scott Ramsey, MD, PhD, director of the Hutchinson Institute for Cancer Outcomes Research in Seattle.
Cancer care already is hugely expensive. A recent study in the American Journal of Medicine found that 42% of patients depleted 100% of their assets – an average loss of $92,000 – within 2 years of diagnosis.
Precision medicine involves running expensive tests called genomic sequencing, which scan the DNA of tumors to find mutations that might be susceptible to available drugs. Although the field is relatively new, hundreds of thousands of cancer patients have had their tumors sequenced to identify cancer-related mutations, according to testing companies.
Medicare, the government insurance plan for people 65 and older, announced in March that it will pay for genomic testing for people with advanced cancers – a decision that could add $2.5 billion to federal health care costs, according to a May analysis in Health Affairs.
Few private insurers cover the tests, leaving some patients with surprise medical bills.
Carrie Wyman, who also has advanced breast cancer, discovered that her insurance plan wouldn’t cover genomic sequencing only after she had received a $5,800 statement.
“I just assumed it would be covered,” said Ms. Wyman, 50, a resident of La Plata, Md., who has six children and stepchildren. “I was blindsided, to be honest with you.”
Looking for financial assistance
Yet paying for that initial test is just the beginning. As Ms. Kilmer learned, finding the money for ongoing treatment is far more challenging, said Gary H. Lyman, MD, who studies way to improve health care quality at Seattle’s Fred Hutchinson Cancer Research Center.
In some cases, genomic tests match patients to experimental drugs available only in clinical trials. Although these trials sometimes provide free medications, many cancer patients can’t afford to travel to participate in them. Ms. Kilmer drives 12 hours round-trip every month to participate in a clinical trial in Sioux Falls, S.D. The expenses add up quickly, she said.
Ms. Kilmer’s genomic tests identified a rearrangement in the PALB2 gene. Preliminary studies suggest that tumors with this genetic rearrangement could be susceptible to the drug olaparib (Lynparza), but those effects haven’t been definitively proven in large-scale studies. The Food and Drug Administration has approved Lynparza only for breast cancer patients with a BRCA mutation.
Legally, doctors can prescribe Lynparza “off label” to anyone with cancer. But insurance programs are reluctant to cover off-label treatments, unless they’re specifically recommended in expert guidelines.
Ms. Kilmer has spent much of the past 3 years battling insurance officials and begging drug companies for financial assistance. The drugmakers have been generous, allowing her to take a rotating cocktail of experimental drugs for free because of her modest income.
In September, however, AstraZeneca decided to end Ms. Kilmer’s financial aid. Ms. Kilmer appealed the drug company’s decision.
Paying thousands of dollars a month is not an option, Ms. Kilmer said. Her family already carries significant credit card debt from earlier cancer treatments. She estimates that she has spent about $80,600 out-of-pocket treating her illness, including $23,600 on her early breast cancer therapy and $57,000 treating metastatic disease.
Ms. Kilmer said she would rather stop taking Lynparza than financially burden her daughter and husband, a truck driver.
“It’s not worth it,” Ms. Kilmer said. “I will not put my family into that kind of debt.”
Uncertain benefits
Insurers say costs aren’t their only concern. Evidence is lacking that the precision medicine approach will work consistently, they argue.
America’s Health Insurance Plans, an industry group, said genetic sequencing remains unproven.
Cathryn Donaldson, the group’s spokeswoman, described recent scientific advances as “remarkable and noteworthy.” But she said insurers “need a more definitive answer” about whether the tests help the average patient live longer.
The South Dakota State Employee Health Plan – which runs Ms. Kilmer’s insurance plan – said it bases its coverage decisions on science and reviews “published, randomized data about the safety and efficacy of the requested drugs.”
Although genetic testing has become the standard of care for melanoma and a common type of lung cancer, no one knows if genomic sequencing will extend the lives of people with other types of cancer, said Carolyn J. Presley, MD, an assistant professor at the Ohio State University Comprehensive Cancer Center, Columbus.
Without insurance coverage, some cancer patients simply give up on treatment.
A study of more than 1,000 women with advanced breast cancer – presented at a September meeting of the American Society of Clinical Oncology – found that 54% had stopped or refused treatment because of costs. The women in the study may have been more vulnerable than most, because 30% were uninsured, about twice the national rate.
In an August study in JAMA, researchers found that relatively few of those who hoped to benefit from precision medicine actually ended up on a medication. Just 15% of those who underwent genomic sequencing ended up taking a targeted therapy, according to the study. The study didn’t ask participants why they failed to get a targeted drug, but Dr. Presley, the lead author, said it’s likely that some patients couldn’t afford them.
“We’re finding the mutations, but patients aren’t getting the drugs,” Dr. Presley said. Without insurance, she said, “you and I would not be able to afford these medications. It’s a huge barrier.”
Within hours of the publication of this story, AstraZeneca called Ms. Kilmer to notify her that it would continue to provide financial aid. Her medication arrived in the mail the next day.
“It’s a huge relief,” Ms. Kilmer said.
KHN’s coverage of these topics is supported by Laura and John Arnold Foundation and Gordon and Betty Moore Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
When Kristen Kilmer was diagnosed with incurable breast cancer at age 38, her first thought was of her 8-year-old daughter. Ms. Kilmer lost her own mother as a teenager and was determined to get more time with her only child.
Ms. Kilmer searched for experimental treatments, opting for an unproven approach in which researchers select drugs based on the genes in patients’ tumors. Doctors have selected her treatments for the past 3 years based on the unique, ever-changing DNA of her cancer cells. Now 41, Ms. Kilmer has responded better than anyone dared to hope. Her cancer has gone into hiding; her tumors are no longer visible on medical scans.
Researchers call the strategy “precision medicine.”
Ms. Kilmer’s insurance company calls it experimental. As a consequence, her insurer has covered only a fraction of her care, forcing Ms. Kilmer to make an agonizing choice: stop taking a drug that costs nearly $17,000 a month or pay out-of-pocket, burdening her family with tremendous debt.
“When you are looking at your daughter, you ask yourself, ‘Do I take a medication that might allow me to see her graduate high school?’ ” asked Ms. Kilmer of Spearfish, S.D. “Or do you stop taking it to avoid causing her financial harm?”
The high cost of cutting-edge tests and treatments is threatening to keep precision medicine – one of the most celebrated areas in cancer research – out of reach for many patients. Patients who pay for these new treatments on their own “could be in debt for decades,” said Scott Ramsey, MD, PhD, director of the Hutchinson Institute for Cancer Outcomes Research in Seattle.
Cancer care already is hugely expensive. A recent study in the American Journal of Medicine found that 42% of patients depleted 100% of their assets – an average loss of $92,000 – within 2 years of diagnosis.
Precision medicine involves running expensive tests called genomic sequencing, which scan the DNA of tumors to find mutations that might be susceptible to available drugs. Although the field is relatively new, hundreds of thousands of cancer patients have had their tumors sequenced to identify cancer-related mutations, according to testing companies.
Medicare, the government insurance plan for people 65 and older, announced in March that it will pay for genomic testing for people with advanced cancers – a decision that could add $2.5 billion to federal health care costs, according to a May analysis in Health Affairs.
Few private insurers cover the tests, leaving some patients with surprise medical bills.
Carrie Wyman, who also has advanced breast cancer, discovered that her insurance plan wouldn’t cover genomic sequencing only after she had received a $5,800 statement.
“I just assumed it would be covered,” said Ms. Wyman, 50, a resident of La Plata, Md., who has six children and stepchildren. “I was blindsided, to be honest with you.”
Looking for financial assistance
Yet paying for that initial test is just the beginning. As Ms. Kilmer learned, finding the money for ongoing treatment is far more challenging, said Gary H. Lyman, MD, who studies way to improve health care quality at Seattle’s Fred Hutchinson Cancer Research Center.
In some cases, genomic tests match patients to experimental drugs available only in clinical trials. Although these trials sometimes provide free medications, many cancer patients can’t afford to travel to participate in them. Ms. Kilmer drives 12 hours round-trip every month to participate in a clinical trial in Sioux Falls, S.D. The expenses add up quickly, she said.
Ms. Kilmer’s genomic tests identified a rearrangement in the PALB2 gene. Preliminary studies suggest that tumors with this genetic rearrangement could be susceptible to the drug olaparib (Lynparza), but those effects haven’t been definitively proven in large-scale studies. The Food and Drug Administration has approved Lynparza only for breast cancer patients with a BRCA mutation.
Legally, doctors can prescribe Lynparza “off label” to anyone with cancer. But insurance programs are reluctant to cover off-label treatments, unless they’re specifically recommended in expert guidelines.
Ms. Kilmer has spent much of the past 3 years battling insurance officials and begging drug companies for financial assistance. The drugmakers have been generous, allowing her to take a rotating cocktail of experimental drugs for free because of her modest income.
In September, however, AstraZeneca decided to end Ms. Kilmer’s financial aid. Ms. Kilmer appealed the drug company’s decision.
Paying thousands of dollars a month is not an option, Ms. Kilmer said. Her family already carries significant credit card debt from earlier cancer treatments. She estimates that she has spent about $80,600 out-of-pocket treating her illness, including $23,600 on her early breast cancer therapy and $57,000 treating metastatic disease.
Ms. Kilmer said she would rather stop taking Lynparza than financially burden her daughter and husband, a truck driver.
“It’s not worth it,” Ms. Kilmer said. “I will not put my family into that kind of debt.”
Uncertain benefits
Insurers say costs aren’t their only concern. Evidence is lacking that the precision medicine approach will work consistently, they argue.
America’s Health Insurance Plans, an industry group, said genetic sequencing remains unproven.
Cathryn Donaldson, the group’s spokeswoman, described recent scientific advances as “remarkable and noteworthy.” But she said insurers “need a more definitive answer” about whether the tests help the average patient live longer.
The South Dakota State Employee Health Plan – which runs Ms. Kilmer’s insurance plan – said it bases its coverage decisions on science and reviews “published, randomized data about the safety and efficacy of the requested drugs.”
Although genetic testing has become the standard of care for melanoma and a common type of lung cancer, no one knows if genomic sequencing will extend the lives of people with other types of cancer, said Carolyn J. Presley, MD, an assistant professor at the Ohio State University Comprehensive Cancer Center, Columbus.
Without insurance coverage, some cancer patients simply give up on treatment.
A study of more than 1,000 women with advanced breast cancer – presented at a September meeting of the American Society of Clinical Oncology – found that 54% had stopped or refused treatment because of costs. The women in the study may have been more vulnerable than most, because 30% were uninsured, about twice the national rate.
In an August study in JAMA, researchers found that relatively few of those who hoped to benefit from precision medicine actually ended up on a medication. Just 15% of those who underwent genomic sequencing ended up taking a targeted therapy, according to the study. The study didn’t ask participants why they failed to get a targeted drug, but Dr. Presley, the lead author, said it’s likely that some patients couldn’t afford them.
“We’re finding the mutations, but patients aren’t getting the drugs,” Dr. Presley said. Without insurance, she said, “you and I would not be able to afford these medications. It’s a huge barrier.”
Within hours of the publication of this story, AstraZeneca called Ms. Kilmer to notify her that it would continue to provide financial aid. Her medication arrived in the mail the next day.
“It’s a huge relief,” Ms. Kilmer said.
KHN’s coverage of these topics is supported by Laura and John Arnold Foundation and Gordon and Betty Moore Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
HIV superinfection: No boost to broadly neutralizing antibodies
Infection by a second HIV strain after established primary infection (HIV superinfection) has been associated with broader antibody production, and such events are analogous to heterologous prime-boost immunizations, according to a report published in Cell Host & Microbe.
This phenomenon offers an opportunity to assess how the human immune system responds to sequential exposure to two distinct HIV envelope (Env) antigens, according to the authors, Daniel J. Sheward, a PhD student and scientific officer at the University of Cape Town, South Africa, and his colleagues.
Mr. Sheward and his colleagues followed 108 women recruited in acute/early infection and screened for superinfection over approximately 2 years in the Centre for the AIDS Programme of Research in South Africa (CAPRISA 002 cohort). In a previous study, they identified five superinfected participants, all of whom were superinfected between 3 and 10 months following primary infection. Only two of these patients developed antibodies capable of neutralizing heterologous viruses at 2 years, and one individual developed extremely potent broadly neutralizing antibodies (bnAbs). However, the contribution of superinfection itself to the development of antibody breadth in these individuals was not clear, prompting the current study (Cell Host Microbe. 2018 Oct 10;24[4]:593-9).
The researchers compared neutralization breadth (defined as the percent of heterologous viruses neutralized) present in plasma sampled 2 years post infection between the previously identified superinfected participants and the remaining CAPRISA 002 cohort participants. Four virus strains accounted for the superinfections. Antibody breadth was compared at 2 years post infection to four of the five of the superinfected participants, as they all had at least 2 years of antiretroviral-naive follow-up.
The researchers compared the peak neutralizing antibody (nAb) titers against all four superinfecting viruses with their matched primary infecting virus, as well as with the nAb titers that increased against early/founder viruses in 22 other participants in the CAPRISA 002 cohort.
They found that titers to the superinfecting virus strains were comparable with those seen in single infections from the rest of the cohort. In contrast, two other superinfecting virus strains developed exceedingly high neutralizing titers against themselves. Also, HIV superinfection did not appear to boost nAb memory responses primed by the initial infection.
Notably, superinfection did not elicit bnAB responses to epitopes conserved in both infecting viruses. The one individual who appeared to have developed a bnAB response, upon analysis, was found to have breadth of response attributable to a single antibody lineage that only affected the superinfecting virus. This indicated that superinfection did not facilitate breadth by directing responses to an Env conserved in both infecting viruses, according to Mr. Sheward and his colleagues.
“HIV superinfection fails to efficiently recruit neutralizing memory B cells and, at best, results in additive nAb responses rather than a synergistic effect leading to cross-neutralization; a distinction that is highly relevant for vaccine design. ... [W]hile sequential immunizations with heterologous Env immunogens may be able to improve the potency of elicited responses, alone, they are unlikely to promote the development of bnAbs,” the researchers concluded.
The study was funded by the Centre for the AIDS Programme of Research in South Africa and the South African Medical Research Council. The authors reported that they had no disclosures.
SOURCE: Sheward DJ et al. Cell Host Microbe. 2018 Oct 10;24[4]:593-9.
Infection by a second HIV strain after established primary infection (HIV superinfection) has been associated with broader antibody production, and such events are analogous to heterologous prime-boost immunizations, according to a report published in Cell Host & Microbe.
This phenomenon offers an opportunity to assess how the human immune system responds to sequential exposure to two distinct HIV envelope (Env) antigens, according to the authors, Daniel J. Sheward, a PhD student and scientific officer at the University of Cape Town, South Africa, and his colleagues.
Mr. Sheward and his colleagues followed 108 women recruited in acute/early infection and screened for superinfection over approximately 2 years in the Centre for the AIDS Programme of Research in South Africa (CAPRISA 002 cohort). In a previous study, they identified five superinfected participants, all of whom were superinfected between 3 and 10 months following primary infection. Only two of these patients developed antibodies capable of neutralizing heterologous viruses at 2 years, and one individual developed extremely potent broadly neutralizing antibodies (bnAbs). However, the contribution of superinfection itself to the development of antibody breadth in these individuals was not clear, prompting the current study (Cell Host Microbe. 2018 Oct 10;24[4]:593-9).
The researchers compared neutralization breadth (defined as the percent of heterologous viruses neutralized) present in plasma sampled 2 years post infection between the previously identified superinfected participants and the remaining CAPRISA 002 cohort participants. Four virus strains accounted for the superinfections. Antibody breadth was compared at 2 years post infection to four of the five of the superinfected participants, as they all had at least 2 years of antiretroviral-naive follow-up.
The researchers compared the peak neutralizing antibody (nAb) titers against all four superinfecting viruses with their matched primary infecting virus, as well as with the nAb titers that increased against early/founder viruses in 22 other participants in the CAPRISA 002 cohort.
They found that titers to the superinfecting virus strains were comparable with those seen in single infections from the rest of the cohort. In contrast, two other superinfecting virus strains developed exceedingly high neutralizing titers against themselves. Also, HIV superinfection did not appear to boost nAb memory responses primed by the initial infection.
Notably, superinfection did not elicit bnAB responses to epitopes conserved in both infecting viruses. The one individual who appeared to have developed a bnAB response, upon analysis, was found to have breadth of response attributable to a single antibody lineage that only affected the superinfecting virus. This indicated that superinfection did not facilitate breadth by directing responses to an Env conserved in both infecting viruses, according to Mr. Sheward and his colleagues.
“HIV superinfection fails to efficiently recruit neutralizing memory B cells and, at best, results in additive nAb responses rather than a synergistic effect leading to cross-neutralization; a distinction that is highly relevant for vaccine design. ... [W]hile sequential immunizations with heterologous Env immunogens may be able to improve the potency of elicited responses, alone, they are unlikely to promote the development of bnAbs,” the researchers concluded.
The study was funded by the Centre for the AIDS Programme of Research in South Africa and the South African Medical Research Council. The authors reported that they had no disclosures.
SOURCE: Sheward DJ et al. Cell Host Microbe. 2018 Oct 10;24[4]:593-9.
Infection by a second HIV strain after established primary infection (HIV superinfection) has been associated with broader antibody production, and such events are analogous to heterologous prime-boost immunizations, according to a report published in Cell Host & Microbe.
This phenomenon offers an opportunity to assess how the human immune system responds to sequential exposure to two distinct HIV envelope (Env) antigens, according to the authors, Daniel J. Sheward, a PhD student and scientific officer at the University of Cape Town, South Africa, and his colleagues.
Mr. Sheward and his colleagues followed 108 women recruited in acute/early infection and screened for superinfection over approximately 2 years in the Centre for the AIDS Programme of Research in South Africa (CAPRISA 002 cohort). In a previous study, they identified five superinfected participants, all of whom were superinfected between 3 and 10 months following primary infection. Only two of these patients developed antibodies capable of neutralizing heterologous viruses at 2 years, and one individual developed extremely potent broadly neutralizing antibodies (bnAbs). However, the contribution of superinfection itself to the development of antibody breadth in these individuals was not clear, prompting the current study (Cell Host Microbe. 2018 Oct 10;24[4]:593-9).
The researchers compared neutralization breadth (defined as the percent of heterologous viruses neutralized) present in plasma sampled 2 years post infection between the previously identified superinfected participants and the remaining CAPRISA 002 cohort participants. Four virus strains accounted for the superinfections. Antibody breadth was compared at 2 years post infection to four of the five of the superinfected participants, as they all had at least 2 years of antiretroviral-naive follow-up.
The researchers compared the peak neutralizing antibody (nAb) titers against all four superinfecting viruses with their matched primary infecting virus, as well as with the nAb titers that increased against early/founder viruses in 22 other participants in the CAPRISA 002 cohort.
They found that titers to the superinfecting virus strains were comparable with those seen in single infections from the rest of the cohort. In contrast, two other superinfecting virus strains developed exceedingly high neutralizing titers against themselves. Also, HIV superinfection did not appear to boost nAb memory responses primed by the initial infection.
Notably, superinfection did not elicit bnAB responses to epitopes conserved in both infecting viruses. The one individual who appeared to have developed a bnAB response, upon analysis, was found to have breadth of response attributable to a single antibody lineage that only affected the superinfecting virus. This indicated that superinfection did not facilitate breadth by directing responses to an Env conserved in both infecting viruses, according to Mr. Sheward and his colleagues.
“HIV superinfection fails to efficiently recruit neutralizing memory B cells and, at best, results in additive nAb responses rather than a synergistic effect leading to cross-neutralization; a distinction that is highly relevant for vaccine design. ... [W]hile sequential immunizations with heterologous Env immunogens may be able to improve the potency of elicited responses, alone, they are unlikely to promote the development of bnAbs,” the researchers concluded.
The study was funded by the Centre for the AIDS Programme of Research in South Africa and the South African Medical Research Council. The authors reported that they had no disclosures.
SOURCE: Sheward DJ et al. Cell Host Microbe. 2018 Oct 10;24[4]:593-9.
FROM CELL HOST & MICROBE
Key clinical point: Sequential immunizations with heterologous HIV Env immunogens are unlikely to promote broadly neutralizing antibodies.
Major finding: HIV superinfection does not efficiently recruit cross-reactive memory B cells.
Study details: Neutralizing antibody responses were compared between 4 superinfected individuals and 22 singly infected individuals in the CAPRISA 002 cohort.
Disclosures: The study was funded by the Centre for the AIDS Programme of Research in South Africa and the South African Medical Research Council. The authors reported that they had no disclosures.
Source: Sheward DJ et al. Cell Host Microbe. 2018 Oct 10;24[4]:593-9.