User login
EC approves venetoclax in combo with rituximab
The European Commission (EC) has approved a new indication for venetoclax (Venclyxto®).
The drug is now approved for use in combination with rituximab to treat patients with relapsed/refractory chronic lymphocytic leukemia (CLL) who have received at least one prior therapy.
The approval is valid in all member states of the European Union as well as Iceland, Liechtenstein, and Norway.
The EC’s approval is based on results from the phase 3 MURANO trial, which were published in The New England Journal of Medicine in March.
The trial included 389 CLL patients who were randomized to receive venetoclax plus rituximab (VEN+R) or bendamustine plus rituximab (B+R). The median follow-up was 23.8 months.
According to an independent review committee, the overall response rate was 92.3% in the VEN+R arm and 72.3% in the B+R arm. The investigator-assessed overall response rates were 93.3% and 67.7%, respectively.
According to investigators, the median progression-free survival (PFS) was not reached in the VEN+R arm and was 17.0 months in the B+R arm (hazard ratio [HR]=0.17; P<0.0001).
According to the independent review committee, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (HR=0.20; P<0.0001).
Investigators said the 2-year PFS rate was 84.9% in the VEN+R arm and 36.3% in the B+R arm.
They said the 2-year overall survival rates were 91.9% and 86.6%, respectively (HR=0.48; P<0.0001). The median overall survival was not reached in either arm.
Grade 3/4 adverse events (AEs) with at least a 2% difference in incidence between the treatment arms (in the VEN+R and B+R arms, respectively) included:
- Neutropenia (57.7% and 38.8%)
- Infections and infestations (17.5% and 21.8%)
- Anemia (10.8% and 13.8%)
- Thrombocytopenia (5.7% and 10.1%)
- Febrile neutropenia (3.6% and 9.6%)
- Pneumonia (5.2% and 8.0%)
- Infusion-related reactions (1.5% and 5.3%)
- Tumor lysis syndrome (3.1% and 1.1%)
- Hypotension (0% and 2.7%)
- Hyperglycemia (2.1% and 0%)
- Hypogammaglobulinemia (2.1% and 0%).
Serious AEs with at least a 2% difference in incidence between the arms (in the VEN+R and B+R arms, respectively) were:
- Pneumonia (8.2% and 8.0%)
- Febrile neutropenia (3.6% and 8.5%)
- Pyrexia (2.6% and 6.9%)
- Anemia (1.5% and 2.7%)
- Infusion-related reactions (0.5% and 3.2%)
- Sepsis (0.5% and 2.1%)
- Tumor lysis syndrome (2.1% and 0.5%)
- Hypotension (0% and 2.7%).
Fatal AEs occurred in 5.2% of patients in the VEN+R arm and 5.9% in the B+R arm.
Fatal AEs in the VEN+R arm included pneumonia (n=3), sepsis (n=1), thrombocytopenia (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1). Two cases of pneumonia occurred in the setting of progression/Richter’s transformation.
The European Commission (EC) has approved a new indication for venetoclax (Venclyxto®).
The drug is now approved for use in combination with rituximab to treat patients with relapsed/refractory chronic lymphocytic leukemia (CLL) who have received at least one prior therapy.
The approval is valid in all member states of the European Union as well as Iceland, Liechtenstein, and Norway.
The EC’s approval is based on results from the phase 3 MURANO trial, which were published in The New England Journal of Medicine in March.
The trial included 389 CLL patients who were randomized to receive venetoclax plus rituximab (VEN+R) or bendamustine plus rituximab (B+R). The median follow-up was 23.8 months.
According to an independent review committee, the overall response rate was 92.3% in the VEN+R arm and 72.3% in the B+R arm. The investigator-assessed overall response rates were 93.3% and 67.7%, respectively.
According to investigators, the median progression-free survival (PFS) was not reached in the VEN+R arm and was 17.0 months in the B+R arm (hazard ratio [HR]=0.17; P<0.0001).
According to the independent review committee, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (HR=0.20; P<0.0001).
Investigators said the 2-year PFS rate was 84.9% in the VEN+R arm and 36.3% in the B+R arm.
They said the 2-year overall survival rates were 91.9% and 86.6%, respectively (HR=0.48; P<0.0001). The median overall survival was not reached in either arm.
Grade 3/4 adverse events (AEs) with at least a 2% difference in incidence between the treatment arms (in the VEN+R and B+R arms, respectively) included:
- Neutropenia (57.7% and 38.8%)
- Infections and infestations (17.5% and 21.8%)
- Anemia (10.8% and 13.8%)
- Thrombocytopenia (5.7% and 10.1%)
- Febrile neutropenia (3.6% and 9.6%)
- Pneumonia (5.2% and 8.0%)
- Infusion-related reactions (1.5% and 5.3%)
- Tumor lysis syndrome (3.1% and 1.1%)
- Hypotension (0% and 2.7%)
- Hyperglycemia (2.1% and 0%)
- Hypogammaglobulinemia (2.1% and 0%).
Serious AEs with at least a 2% difference in incidence between the arms (in the VEN+R and B+R arms, respectively) were:
- Pneumonia (8.2% and 8.0%)
- Febrile neutropenia (3.6% and 8.5%)
- Pyrexia (2.6% and 6.9%)
- Anemia (1.5% and 2.7%)
- Infusion-related reactions (0.5% and 3.2%)
- Sepsis (0.5% and 2.1%)
- Tumor lysis syndrome (2.1% and 0.5%)
- Hypotension (0% and 2.7%).
Fatal AEs occurred in 5.2% of patients in the VEN+R arm and 5.9% in the B+R arm.
Fatal AEs in the VEN+R arm included pneumonia (n=3), sepsis (n=1), thrombocytopenia (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1). Two cases of pneumonia occurred in the setting of progression/Richter’s transformation.
The European Commission (EC) has approved a new indication for venetoclax (Venclyxto®).
The drug is now approved for use in combination with rituximab to treat patients with relapsed/refractory chronic lymphocytic leukemia (CLL) who have received at least one prior therapy.
The approval is valid in all member states of the European Union as well as Iceland, Liechtenstein, and Norway.
The EC’s approval is based on results from the phase 3 MURANO trial, which were published in The New England Journal of Medicine in March.
The trial included 389 CLL patients who were randomized to receive venetoclax plus rituximab (VEN+R) or bendamustine plus rituximab (B+R). The median follow-up was 23.8 months.
According to an independent review committee, the overall response rate was 92.3% in the VEN+R arm and 72.3% in the B+R arm. The investigator-assessed overall response rates were 93.3% and 67.7%, respectively.
According to investigators, the median progression-free survival (PFS) was not reached in the VEN+R arm and was 17.0 months in the B+R arm (hazard ratio [HR]=0.17; P<0.0001).
According to the independent review committee, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (HR=0.20; P<0.0001).
Investigators said the 2-year PFS rate was 84.9% in the VEN+R arm and 36.3% in the B+R arm.
They said the 2-year overall survival rates were 91.9% and 86.6%, respectively (HR=0.48; P<0.0001). The median overall survival was not reached in either arm.
Grade 3/4 adverse events (AEs) with at least a 2% difference in incidence between the treatment arms (in the VEN+R and B+R arms, respectively) included:
- Neutropenia (57.7% and 38.8%)
- Infections and infestations (17.5% and 21.8%)
- Anemia (10.8% and 13.8%)
- Thrombocytopenia (5.7% and 10.1%)
- Febrile neutropenia (3.6% and 9.6%)
- Pneumonia (5.2% and 8.0%)
- Infusion-related reactions (1.5% and 5.3%)
- Tumor lysis syndrome (3.1% and 1.1%)
- Hypotension (0% and 2.7%)
- Hyperglycemia (2.1% and 0%)
- Hypogammaglobulinemia (2.1% and 0%).
Serious AEs with at least a 2% difference in incidence between the arms (in the VEN+R and B+R arms, respectively) were:
- Pneumonia (8.2% and 8.0%)
- Febrile neutropenia (3.6% and 8.5%)
- Pyrexia (2.6% and 6.9%)
- Anemia (1.5% and 2.7%)
- Infusion-related reactions (0.5% and 3.2%)
- Sepsis (0.5% and 2.1%)
- Tumor lysis syndrome (2.1% and 0.5%)
- Hypotension (0% and 2.7%).
Fatal AEs occurred in 5.2% of patients in the VEN+R arm and 5.9% in the B+R arm.
Fatal AEs in the VEN+R arm included pneumonia (n=3), sepsis (n=1), thrombocytopenia (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1). Two cases of pneumonia occurred in the setting of progression/Richter’s transformation.
Test strips for warfarin monitoring recalled due to serious risks
The U.S. Food and Drug Administration (FDA) announced a Class I recall of test strips used with medical devices that monitor warfarin levels, which means use of these strips may cause serious injuries or death.
Roche Diagnostics has recalled certain test strip lots used with its CoaguChek test meter devices.
The recall involves more than 1.1 million packages of CoaguChek XS PT Test Strips that were distributed nationwide from January 12, 2018, to October 29, 2018.
The test strips are used with the CoaguChek XS plus, CoaguChek XS Pro, CoaguChek XS professional, CoaguChek XS PST, and CoaguChek Vantus test meter devices.
The FDA said patients and healthcare professionals should not rely on these test meter devices to monitor warfarin levels if they’re using test strips affected by the recall. Instead, patients should have blood drawn from a vein and have their levels measured by a laboratory test or use an alternative meter device.
“These strips are widely used, and we are working diligently to warn healthcare providers and the public about the dangers associated with this recall,” said Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health.
“Using faulty strips can lead to serious errors in medication dosage that could cause serious harm or death in some patients. We are also working with the company on the swift removal of the recalled strips and to ensure the new corrected strips are distributed to patients and healthcare providers as quickly as possible.”
The FDA’s warning concerning the CoaguChek XS PT Test Strips is based on medical device reports submitted by Roche Diagnostics indicating that the test strips may provide results that are higher than the actual international normalized ratio (INR).
As a result of incorrect INR results, some patients may be prescribed an insufficient warfarin dose or instructed to interrupt warfarin use, which may increase the risk of thrombosis.
Approximately 90 medical device reports and two serious patient injuries involving strokes were reported to the FDA.
Roche Diagnostics attributes the cause of the problem to a recent recalibration of the test strips to a different international standard.
The company plans to provide new batches of recalibrated test strips, based on the previous international standard, to their customers by the end of November.
The FDA reviewed validation data submitted by the company for these recalibrated strips.
Patients who are using CoaguChek meters should contact their healthcare provider to get information about alternative test methods and to address questions regarding their individual testing schedule. Patients should also contact their self-testing service providers to find out when they will be getting their corrected test strips.
For questions about the recall or to report adverse reactions or quality problems, contact Roche Diagnostics Point of Care Technical Service at 1-800-428-4674.
Adverse reactions can also be reported to the FDA through MedWatch, the agency’s voluntary reporting program.
The U.S. Food and Drug Administration (FDA) announced a Class I recall of test strips used with medical devices that monitor warfarin levels, which means use of these strips may cause serious injuries or death.
Roche Diagnostics has recalled certain test strip lots used with its CoaguChek test meter devices.
The recall involves more than 1.1 million packages of CoaguChek XS PT Test Strips that were distributed nationwide from January 12, 2018, to October 29, 2018.
The test strips are used with the CoaguChek XS plus, CoaguChek XS Pro, CoaguChek XS professional, CoaguChek XS PST, and CoaguChek Vantus test meter devices.
The FDA said patients and healthcare professionals should not rely on these test meter devices to monitor warfarin levels if they’re using test strips affected by the recall. Instead, patients should have blood drawn from a vein and have their levels measured by a laboratory test or use an alternative meter device.
“These strips are widely used, and we are working diligently to warn healthcare providers and the public about the dangers associated with this recall,” said Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health.
“Using faulty strips can lead to serious errors in medication dosage that could cause serious harm or death in some patients. We are also working with the company on the swift removal of the recalled strips and to ensure the new corrected strips are distributed to patients and healthcare providers as quickly as possible.”
The FDA’s warning concerning the CoaguChek XS PT Test Strips is based on medical device reports submitted by Roche Diagnostics indicating that the test strips may provide results that are higher than the actual international normalized ratio (INR).
As a result of incorrect INR results, some patients may be prescribed an insufficient warfarin dose or instructed to interrupt warfarin use, which may increase the risk of thrombosis.
Approximately 90 medical device reports and two serious patient injuries involving strokes were reported to the FDA.
Roche Diagnostics attributes the cause of the problem to a recent recalibration of the test strips to a different international standard.
The company plans to provide new batches of recalibrated test strips, based on the previous international standard, to their customers by the end of November.
The FDA reviewed validation data submitted by the company for these recalibrated strips.
Patients who are using CoaguChek meters should contact their healthcare provider to get information about alternative test methods and to address questions regarding their individual testing schedule. Patients should also contact their self-testing service providers to find out when they will be getting their corrected test strips.
For questions about the recall or to report adverse reactions or quality problems, contact Roche Diagnostics Point of Care Technical Service at 1-800-428-4674.
Adverse reactions can also be reported to the FDA through MedWatch, the agency’s voluntary reporting program.
The U.S. Food and Drug Administration (FDA) announced a Class I recall of test strips used with medical devices that monitor warfarin levels, which means use of these strips may cause serious injuries or death.
Roche Diagnostics has recalled certain test strip lots used with its CoaguChek test meter devices.
The recall involves more than 1.1 million packages of CoaguChek XS PT Test Strips that were distributed nationwide from January 12, 2018, to October 29, 2018.
The test strips are used with the CoaguChek XS plus, CoaguChek XS Pro, CoaguChek XS professional, CoaguChek XS PST, and CoaguChek Vantus test meter devices.
The FDA said patients and healthcare professionals should not rely on these test meter devices to monitor warfarin levels if they’re using test strips affected by the recall. Instead, patients should have blood drawn from a vein and have their levels measured by a laboratory test or use an alternative meter device.
“These strips are widely used, and we are working diligently to warn healthcare providers and the public about the dangers associated with this recall,” said Jeffrey Shuren, MD, director of the FDA’s Center for Devices and Radiological Health.
“Using faulty strips can lead to serious errors in medication dosage that could cause serious harm or death in some patients. We are also working with the company on the swift removal of the recalled strips and to ensure the new corrected strips are distributed to patients and healthcare providers as quickly as possible.”
The FDA’s warning concerning the CoaguChek XS PT Test Strips is based on medical device reports submitted by Roche Diagnostics indicating that the test strips may provide results that are higher than the actual international normalized ratio (INR).
As a result of incorrect INR results, some patients may be prescribed an insufficient warfarin dose or instructed to interrupt warfarin use, which may increase the risk of thrombosis.
Approximately 90 medical device reports and two serious patient injuries involving strokes were reported to the FDA.
Roche Diagnostics attributes the cause of the problem to a recent recalibration of the test strips to a different international standard.
The company plans to provide new batches of recalibrated test strips, based on the previous international standard, to their customers by the end of November.
The FDA reviewed validation data submitted by the company for these recalibrated strips.
Patients who are using CoaguChek meters should contact their healthcare provider to get information about alternative test methods and to address questions regarding their individual testing schedule. Patients should also contact their self-testing service providers to find out when they will be getting their corrected test strips.
For questions about the recall or to report adverse reactions or quality problems, contact Roche Diagnostics Point of Care Technical Service at 1-800-428-4674.
Adverse reactions can also be reported to the FDA through MedWatch, the agency’s voluntary reporting program.
FDA panels vote no on opioid-containing drug for MDD
A joint panel of the Food and Drug Administration voted Nov. 1 against approving a new opioid-containing drug as an adjunctive treatment for major depressive disorder.
The 21-2 vote against approval by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based on concerns that the drug’s benefit-risk profile was not strong enough to warrant approval, according to a press release from Alkermes, developer of the drug, which is a combination of buprenorphine and samidorphan known as ALKS 5461.
“We were disappointed and surprised by the FDA’s characterization of the safety and efficacy data for ALKS 5461 and the resulting outcome of the advisory committee vote, particularly for the patients, their families and treatment providers who need and deserve access to novel therapies that work differently than currently available antidepressants, Richard Pops, chief executive officer of Alkermes, said in the release. “We remain steadfast in our commitment to make a meaningful difference in the lives of people suffering with serious mental health conditions, and will continue to work with the FDA as it completes its review of the ALKS 5461 regulatory submission.”
At the meeting, Sanjay J. Mathew, MD, a psychiatrist affiliated with the Baylor College of Medicine in Houston and a consultant for Alkermes who was paid for his time and travel to the meeting, discussed which patients might be good candidates for the new drug. He used an example of a patient who had failed on several monotherapies and would consider augmentation with a second drug. “In my view, this drug has a positive benefit-risk profile with a comparable efficacy” to currently available drugs, but with a new distinct mechanism that appears not to have certain undesirable side effects such as weight gain and sleepiness, he said.
Meanwhile, representatives from Alkermes discussed phase 3 studies, in which adults with treatment-resistant major depressive disorder were randomized to BUP/SAM in doses of 1mg/1mg or 2mg/2mg, or a placebo. In the trial, known as Study 207, changes in the MADRAS-10 total scores were significantly higher in the 2mg/2mg treatment groups, compared with placebo when data from 5 weeks and 6 weeks of treatment were combined.
However, in the FDA’s review of the data, it was noted that the efficacy was based on the MADRAS-10 average vs. the MADRAS-10 end of treatment, and the average “tends to obscure a possible drop-off in drug efficacy after the first few weeks of treatment.”
The FDA usually follows its panels’ recommendations, which are not binding.
A joint panel of the Food and Drug Administration voted Nov. 1 against approving a new opioid-containing drug as an adjunctive treatment for major depressive disorder.
The 21-2 vote against approval by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based on concerns that the drug’s benefit-risk profile was not strong enough to warrant approval, according to a press release from Alkermes, developer of the drug, which is a combination of buprenorphine and samidorphan known as ALKS 5461.
“We were disappointed and surprised by the FDA’s characterization of the safety and efficacy data for ALKS 5461 and the resulting outcome of the advisory committee vote, particularly for the patients, their families and treatment providers who need and deserve access to novel therapies that work differently than currently available antidepressants, Richard Pops, chief executive officer of Alkermes, said in the release. “We remain steadfast in our commitment to make a meaningful difference in the lives of people suffering with serious mental health conditions, and will continue to work with the FDA as it completes its review of the ALKS 5461 regulatory submission.”
At the meeting, Sanjay J. Mathew, MD, a psychiatrist affiliated with the Baylor College of Medicine in Houston and a consultant for Alkermes who was paid for his time and travel to the meeting, discussed which patients might be good candidates for the new drug. He used an example of a patient who had failed on several monotherapies and would consider augmentation with a second drug. “In my view, this drug has a positive benefit-risk profile with a comparable efficacy” to currently available drugs, but with a new distinct mechanism that appears not to have certain undesirable side effects such as weight gain and sleepiness, he said.
Meanwhile, representatives from Alkermes discussed phase 3 studies, in which adults with treatment-resistant major depressive disorder were randomized to BUP/SAM in doses of 1mg/1mg or 2mg/2mg, or a placebo. In the trial, known as Study 207, changes in the MADRAS-10 total scores were significantly higher in the 2mg/2mg treatment groups, compared with placebo when data from 5 weeks and 6 weeks of treatment were combined.
However, in the FDA’s review of the data, it was noted that the efficacy was based on the MADRAS-10 average vs. the MADRAS-10 end of treatment, and the average “tends to obscure a possible drop-off in drug efficacy after the first few weeks of treatment.”
The FDA usually follows its panels’ recommendations, which are not binding.
A joint panel of the Food and Drug Administration voted Nov. 1 against approving a new opioid-containing drug as an adjunctive treatment for major depressive disorder.
The 21-2 vote against approval by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based on concerns that the drug’s benefit-risk profile was not strong enough to warrant approval, according to a press release from Alkermes, developer of the drug, which is a combination of buprenorphine and samidorphan known as ALKS 5461.
“We were disappointed and surprised by the FDA’s characterization of the safety and efficacy data for ALKS 5461 and the resulting outcome of the advisory committee vote, particularly for the patients, their families and treatment providers who need and deserve access to novel therapies that work differently than currently available antidepressants, Richard Pops, chief executive officer of Alkermes, said in the release. “We remain steadfast in our commitment to make a meaningful difference in the lives of people suffering with serious mental health conditions, and will continue to work with the FDA as it completes its review of the ALKS 5461 regulatory submission.”
At the meeting, Sanjay J. Mathew, MD, a psychiatrist affiliated with the Baylor College of Medicine in Houston and a consultant for Alkermes who was paid for his time and travel to the meeting, discussed which patients might be good candidates for the new drug. He used an example of a patient who had failed on several monotherapies and would consider augmentation with a second drug. “In my view, this drug has a positive benefit-risk profile with a comparable efficacy” to currently available drugs, but with a new distinct mechanism that appears not to have certain undesirable side effects such as weight gain and sleepiness, he said.
Meanwhile, representatives from Alkermes discussed phase 3 studies, in which adults with treatment-resistant major depressive disorder were randomized to BUP/SAM in doses of 1mg/1mg or 2mg/2mg, or a placebo. In the trial, known as Study 207, changes in the MADRAS-10 total scores were significantly higher in the 2mg/2mg treatment groups, compared with placebo when data from 5 weeks and 6 weeks of treatment were combined.
However, in the FDA’s review of the data, it was noted that the efficacy was based on the MADRAS-10 average vs. the MADRAS-10 end of treatment, and the average “tends to obscure a possible drop-off in drug efficacy after the first few weeks of treatment.”
The FDA usually follows its panels’ recommendations, which are not binding.
Investigational agent VT-1161 looks promising for onychomycosis
LAS VEGAS – An investigational oral therapy for onychomycosis could be on the horizon as a new treatment option.
VT-1161 is a cytochrome P51 (CYP51) inhibitor with potent in vitro activity against several species of tinea and yeast, David M. Pariser, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. It is highly selective for fungal CYP51 over human cytochrome P enzymes.
Dr. Pariser served as an . Patients enrolled were aged 18-70 years, with a mean age of 49. Most were men (80%) and white (85%), as is typical in trials for onychomycosis drugs, noted Dr. Pariser, professor of dermatology at Eastern Virginia Medical School in Norfolk.
Distal subungual onychomycosis was evident in 25%-75% of the nail, and patients needed 2 mm of clear nail to be included in the trial. Disease was confirmed by positive KOH staining and culture.
Patients were randomized into four active treatment groups; a fifth received placebo. All active treatment groups were started on 14 days of a daily loading dose of VT-1161, with one arm getting 300 mg per day and one getting 600 mg per day.
After the loading dose, two groups were treated for 12 weeks with VT-1161 (weekly doses of 300 mg and 600 mg); two other groups had treatment extended out to 24 weeks.
Few patients, roughly 20% in each treatment arm, had achieved the primary endpoint, a complete cure (0% nail involvement and negative KOH stain and culture) at the end of active treatment, Dr. Pariser said.
“I personally think that all of these onychomycosis studies should be carried out for longer than a year, up to 2 years, even if you were able to get rid of all the fungus, because that’s how long it’s going to take for the nail to grow out, especially in older patients with slower nail growth,” Dr. Pariser said.
At 48 weeks, approximately 40% of patients in each active treatment arm achieved complete cure, Dr. Pariser noted. “The results indicated that there was not a lot of difference in outcomes based on the dose the patient received.”
About 60%-70% of treated patients sustained mycologic cure of onychomycosis at 60 weeks.
No serious drug-related adverse events were seen in the study, and no patients dropped out because of lab abnormalities, including liver function tests. Other adverse events were rare and occurred equally in the treatment and placebo arms and consisted of dermatitis, headache, and cough. Nausea, cough, and dysgeusia each occurred in 2% of patients and could have been related to the study drug, Dr. Pariser said.
Looking at both mycologic and complete cure rates of available onychomycosis treatments, the results from the RENOVATE trial are comparable to approved systemic therapies, and superior to topicals, he said.
Dr. Pariser disclosed serving as an investigator for pharmaceutical manufactures Viamet (maker of VT-1161), Valeant, and Ancor/Pharmaderm.
SDEF and this news organization are owned by the same parent company.
[email protected]
LAS VEGAS – An investigational oral therapy for onychomycosis could be on the horizon as a new treatment option.
VT-1161 is a cytochrome P51 (CYP51) inhibitor with potent in vitro activity against several species of tinea and yeast, David M. Pariser, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. It is highly selective for fungal CYP51 over human cytochrome P enzymes.
Dr. Pariser served as an . Patients enrolled were aged 18-70 years, with a mean age of 49. Most were men (80%) and white (85%), as is typical in trials for onychomycosis drugs, noted Dr. Pariser, professor of dermatology at Eastern Virginia Medical School in Norfolk.
Distal subungual onychomycosis was evident in 25%-75% of the nail, and patients needed 2 mm of clear nail to be included in the trial. Disease was confirmed by positive KOH staining and culture.
Patients were randomized into four active treatment groups; a fifth received placebo. All active treatment groups were started on 14 days of a daily loading dose of VT-1161, with one arm getting 300 mg per day and one getting 600 mg per day.
After the loading dose, two groups were treated for 12 weeks with VT-1161 (weekly doses of 300 mg and 600 mg); two other groups had treatment extended out to 24 weeks.
Few patients, roughly 20% in each treatment arm, had achieved the primary endpoint, a complete cure (0% nail involvement and negative KOH stain and culture) at the end of active treatment, Dr. Pariser said.
“I personally think that all of these onychomycosis studies should be carried out for longer than a year, up to 2 years, even if you were able to get rid of all the fungus, because that’s how long it’s going to take for the nail to grow out, especially in older patients with slower nail growth,” Dr. Pariser said.
At 48 weeks, approximately 40% of patients in each active treatment arm achieved complete cure, Dr. Pariser noted. “The results indicated that there was not a lot of difference in outcomes based on the dose the patient received.”
About 60%-70% of treated patients sustained mycologic cure of onychomycosis at 60 weeks.
No serious drug-related adverse events were seen in the study, and no patients dropped out because of lab abnormalities, including liver function tests. Other adverse events were rare and occurred equally in the treatment and placebo arms and consisted of dermatitis, headache, and cough. Nausea, cough, and dysgeusia each occurred in 2% of patients and could have been related to the study drug, Dr. Pariser said.
Looking at both mycologic and complete cure rates of available onychomycosis treatments, the results from the RENOVATE trial are comparable to approved systemic therapies, and superior to topicals, he said.
Dr. Pariser disclosed serving as an investigator for pharmaceutical manufactures Viamet (maker of VT-1161), Valeant, and Ancor/Pharmaderm.
SDEF and this news organization are owned by the same parent company.
[email protected]
LAS VEGAS – An investigational oral therapy for onychomycosis could be on the horizon as a new treatment option.
VT-1161 is a cytochrome P51 (CYP51) inhibitor with potent in vitro activity against several species of tinea and yeast, David M. Pariser, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar. It is highly selective for fungal CYP51 over human cytochrome P enzymes.
Dr. Pariser served as an . Patients enrolled were aged 18-70 years, with a mean age of 49. Most were men (80%) and white (85%), as is typical in trials for onychomycosis drugs, noted Dr. Pariser, professor of dermatology at Eastern Virginia Medical School in Norfolk.
Distal subungual onychomycosis was evident in 25%-75% of the nail, and patients needed 2 mm of clear nail to be included in the trial. Disease was confirmed by positive KOH staining and culture.
Patients were randomized into four active treatment groups; a fifth received placebo. All active treatment groups were started on 14 days of a daily loading dose of VT-1161, with one arm getting 300 mg per day and one getting 600 mg per day.
After the loading dose, two groups were treated for 12 weeks with VT-1161 (weekly doses of 300 mg and 600 mg); two other groups had treatment extended out to 24 weeks.
Few patients, roughly 20% in each treatment arm, had achieved the primary endpoint, a complete cure (0% nail involvement and negative KOH stain and culture) at the end of active treatment, Dr. Pariser said.
“I personally think that all of these onychomycosis studies should be carried out for longer than a year, up to 2 years, even if you were able to get rid of all the fungus, because that’s how long it’s going to take for the nail to grow out, especially in older patients with slower nail growth,” Dr. Pariser said.
At 48 weeks, approximately 40% of patients in each active treatment arm achieved complete cure, Dr. Pariser noted. “The results indicated that there was not a lot of difference in outcomes based on the dose the patient received.”
About 60%-70% of treated patients sustained mycologic cure of onychomycosis at 60 weeks.
No serious drug-related adverse events were seen in the study, and no patients dropped out because of lab abnormalities, including liver function tests. Other adverse events were rare and occurred equally in the treatment and placebo arms and consisted of dermatitis, headache, and cough. Nausea, cough, and dysgeusia each occurred in 2% of patients and could have been related to the study drug, Dr. Pariser said.
Looking at both mycologic and complete cure rates of available onychomycosis treatments, the results from the RENOVATE trial are comparable to approved systemic therapies, and superior to topicals, he said.
Dr. Pariser disclosed serving as an investigator for pharmaceutical manufactures Viamet (maker of VT-1161), Valeant, and Ancor/Pharmaderm.
SDEF and this news organization are owned by the same parent company.
[email protected]
REPORTING FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Did I really say that?
Unless you decide to start a second career as an expert witness, giving a deposition is a challenge you should avoid at all costs. I have given a few depositions myself, as both a defendant and a witness, and I have reviewed a dozen or more as a consultant for a local law firm. It is an unnatural and artificial format for transferring information. You will survive the depositions rigid and arbitrary rules only by listening to and following your lawyer’s coaching both before and during the deposition. Hopefully you never will be deposed. However,
First, in a deposition every word you utter is recorded. There are no second chances to edit or clarify what you have said. Your words must be carefully chosen. Several times each year I encounter the parent of a former patient in the grocery store who quotes to me some advice they claim I gave them 2 or 3 decades ago. Although I can imagine that I might have voiced the message they are remembering, sometimes I have to cringe at the bluntness and the crude choice of words they are attributing to me. Obviously, I got away with my fast and loose handling of the English language most of the time and am flattered that it was memorable. But I wonder how often I offended a family with my shoot-from-the-hip advice.
In a similar vein, I found that one of the benefits of having medical students shadow me around the office was that their presence forced me to listen to myself. Did I really say that? How sloppy had I gotten in my explanations to parents and patients? Having another pair of ears in the office can be like having a court stenographer at your deposition.
The situation can be particularly insidious when a parent asks what you take to be a rhetorical question or more likely makes a statement that is incorrect, but you fail to correct it because it is off topic and you are in a hurry to get to the next exam room. If in a deposition the plaintiff’s lawyer prefaces a question with “We all know that sugar makes children hyper,” before you leap over his preface and give your answer you should respond that you are unaware of any scientific evidence that supports his assertion. But if a parent offhandedly mentions that his child was on a “sugar high” you might not take the time to disagree because the parent’s observation had no significance to the history he was relating. However, the parent could interpret from your silence that you believe sugar causes hyperactivity.
Of course the volume of old wives tales, urban legends, and chat room myths that float by you in the office every day makes it impractical to counter every bit of misinformation we hear. But the rules of deposition should remind us that our failure to disagree might sometimes be interpreted as an agreement.
One of the more difficult concepts challenging the deposed physician is avoiding the too much information trap. Your answers in a deposition should be simple and to the point. Physicians are trained to teach. How often are we clouding the answers the patients want by trying to impress them with our breadth of knowledge and command of scientific language?
Although you may have a scribe helping you craft your electronic medical records, hopefully he or she won’t be a court stenographer. And even more fortunately, most patients and parents aren’t listening to every word you say. But from time to time, it helps to pretend you are being deposed. Or at least take a moment to listen to what you have been saying.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Unless you decide to start a second career as an expert witness, giving a deposition is a challenge you should avoid at all costs. I have given a few depositions myself, as both a defendant and a witness, and I have reviewed a dozen or more as a consultant for a local law firm. It is an unnatural and artificial format for transferring information. You will survive the depositions rigid and arbitrary rules only by listening to and following your lawyer’s coaching both before and during the deposition. Hopefully you never will be deposed. However,
First, in a deposition every word you utter is recorded. There are no second chances to edit or clarify what you have said. Your words must be carefully chosen. Several times each year I encounter the parent of a former patient in the grocery store who quotes to me some advice they claim I gave them 2 or 3 decades ago. Although I can imagine that I might have voiced the message they are remembering, sometimes I have to cringe at the bluntness and the crude choice of words they are attributing to me. Obviously, I got away with my fast and loose handling of the English language most of the time and am flattered that it was memorable. But I wonder how often I offended a family with my shoot-from-the-hip advice.
In a similar vein, I found that one of the benefits of having medical students shadow me around the office was that their presence forced me to listen to myself. Did I really say that? How sloppy had I gotten in my explanations to parents and patients? Having another pair of ears in the office can be like having a court stenographer at your deposition.
The situation can be particularly insidious when a parent asks what you take to be a rhetorical question or more likely makes a statement that is incorrect, but you fail to correct it because it is off topic and you are in a hurry to get to the next exam room. If in a deposition the plaintiff’s lawyer prefaces a question with “We all know that sugar makes children hyper,” before you leap over his preface and give your answer you should respond that you are unaware of any scientific evidence that supports his assertion. But if a parent offhandedly mentions that his child was on a “sugar high” you might not take the time to disagree because the parent’s observation had no significance to the history he was relating. However, the parent could interpret from your silence that you believe sugar causes hyperactivity.
Of course the volume of old wives tales, urban legends, and chat room myths that float by you in the office every day makes it impractical to counter every bit of misinformation we hear. But the rules of deposition should remind us that our failure to disagree might sometimes be interpreted as an agreement.
One of the more difficult concepts challenging the deposed physician is avoiding the too much information trap. Your answers in a deposition should be simple and to the point. Physicians are trained to teach. How often are we clouding the answers the patients want by trying to impress them with our breadth of knowledge and command of scientific language?
Although you may have a scribe helping you craft your electronic medical records, hopefully he or she won’t be a court stenographer. And even more fortunately, most patients and parents aren’t listening to every word you say. But from time to time, it helps to pretend you are being deposed. Or at least take a moment to listen to what you have been saying.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Unless you decide to start a second career as an expert witness, giving a deposition is a challenge you should avoid at all costs. I have given a few depositions myself, as both a defendant and a witness, and I have reviewed a dozen or more as a consultant for a local law firm. It is an unnatural and artificial format for transferring information. You will survive the depositions rigid and arbitrary rules only by listening to and following your lawyer’s coaching both before and during the deposition. Hopefully you never will be deposed. However,
First, in a deposition every word you utter is recorded. There are no second chances to edit or clarify what you have said. Your words must be carefully chosen. Several times each year I encounter the parent of a former patient in the grocery store who quotes to me some advice they claim I gave them 2 or 3 decades ago. Although I can imagine that I might have voiced the message they are remembering, sometimes I have to cringe at the bluntness and the crude choice of words they are attributing to me. Obviously, I got away with my fast and loose handling of the English language most of the time and am flattered that it was memorable. But I wonder how often I offended a family with my shoot-from-the-hip advice.
In a similar vein, I found that one of the benefits of having medical students shadow me around the office was that their presence forced me to listen to myself. Did I really say that? How sloppy had I gotten in my explanations to parents and patients? Having another pair of ears in the office can be like having a court stenographer at your deposition.
The situation can be particularly insidious when a parent asks what you take to be a rhetorical question or more likely makes a statement that is incorrect, but you fail to correct it because it is off topic and you are in a hurry to get to the next exam room. If in a deposition the plaintiff’s lawyer prefaces a question with “We all know that sugar makes children hyper,” before you leap over his preface and give your answer you should respond that you are unaware of any scientific evidence that supports his assertion. But if a parent offhandedly mentions that his child was on a “sugar high” you might not take the time to disagree because the parent’s observation had no significance to the history he was relating. However, the parent could interpret from your silence that you believe sugar causes hyperactivity.
Of course the volume of old wives tales, urban legends, and chat room myths that float by you in the office every day makes it impractical to counter every bit of misinformation we hear. But the rules of deposition should remind us that our failure to disagree might sometimes be interpreted as an agreement.
One of the more difficult concepts challenging the deposed physician is avoiding the too much information trap. Your answers in a deposition should be simple and to the point. Physicians are trained to teach. How often are we clouding the answers the patients want by trying to impress them with our breadth of knowledge and command of scientific language?
Although you may have a scribe helping you craft your electronic medical records, hopefully he or she won’t be a court stenographer. And even more fortunately, most patients and parents aren’t listening to every word you say. But from time to time, it helps to pretend you are being deposed. Or at least take a moment to listen to what you have been saying.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Ultrasound denervation tops RF ablation for resistant hypertension
SAN DIEGO – Denervation of the main renal arteries with ultrasound is more effective than radiofrequency (RF) ablation at lowering blood pressure in patients with resistant hypertension, according to a single-center, randomized trial from Germany.
Dubbed RADIOSOUND–HTN, it was the first time the two emerging technologies have been pitted against each other. At 3-month follow-up, the 42 patients randomized to ultrasound ablation with the Paradise catheter (ReCor Medical) had a mean systolic daytime blood pressure reduction of 13.2 mm Hg on ambulatory monitoring, vs. 6.5 mm Hg among 39 patients randomized to RF ablation with Medtronic’s Symplicity Spyral catheter (P = .043).
Meanwhile, 39 patients randomized to both main artery and side branch ablation with the Spyral had a mean reduction of 8.3 mm Hg, slightly better than RF ablation of the main renal arteries alone, but the difference was not statistically significant, and “no definite conclusion on the value of an additional side branch ablation can be drawn,” said senior investigator Philipp Lurz , MD, PhD, a cardiologist at the University of Leipzig, Germany, and his colleagues (Circulation. 2018 Sep 25. doi: 10.1161/circulationaha.118.037654).
Denervation was probably more complete with the Paradise catheter, which might explain the results. Ultrasound energy penetrates about 6-7 mm from the lumen, reaching up to 90% of sympathetic nerve fibers, while RF energy penetrates 3-4 mm; indeed, the idea of going into the branches with RF ablation is because nerve fibers are closer to the lumen surface, Dr. Lurz said at the Transcatheter Cardiovascular Therapeutics (TCT) annual meeting, where he presented the study, which was simultaneously published in Circulation.
Also, the Paradise catheter – an endovascular balloon device inflated to fit the lumen – delivers fully circumferential, ringlike ablations with each application, while the Spyral catheter delivers four ablations simultaneously in a spiral pattern, and requires more ablations to create a similar effect, according to Dr. Lurz.
About two-thirds of patients in all three arms responded to treatment, meaning at least a 5 mm Hg drop in systolic blood pressure. Among the nonresponders, it’s possible that their hypertension wasn’t caused by sympathetic overdrive. “Future trials should focus on identifying these patients to avoid futile” procedures, and define “specific anatomic predictors associated with a more effective” renal denervation, Dr. Lurz and his team said in their study report.
The researchers noted that “the present study included patients with larger renal arteries” – at least one renal artery 5.5 mm or greater in diameter – “based on the assumption that sympathetic fibers are in greater distance from the lumen than in smaller arteries, and therefore ... higher penetration depth would be more relevant ... Results might have differed in a cohort of patients with smaller renal artery diameters.”
Both Paradise and Spyral are in pivotal trials for Food and Drug Administration approval.
The subjects were an average of 64 years. The majority were men, and there were no significant differences in baseline characteristics between the arms. The mean baseline daytime blood pressure was 153/86 mm Hg despite treatment with three or more classes of antihypertensives dosed to at least 50% of their maximum. There was no drug testing to confirm patients were taking their medications, but their general practitioners vouched for their adherence.
One patient in the ultrasound arm group developed a pseudoaneurysm treated successfully by compression. One of the RF subjects developed a postprocedural intracapsular and retroperitoneal hematoma that resolved spontaneously. No renal vascular complications or stenoses were detected at follow-up.
There was no industry funding for the work. Dr. Lurz is a speaker and consultant for both ReCor Medical and Medtronic.
SOURCE: Fengler K et al. TCT 2018, Abstract.
SAN DIEGO – Denervation of the main renal arteries with ultrasound is more effective than radiofrequency (RF) ablation at lowering blood pressure in patients with resistant hypertension, according to a single-center, randomized trial from Germany.
Dubbed RADIOSOUND–HTN, it was the first time the two emerging technologies have been pitted against each other. At 3-month follow-up, the 42 patients randomized to ultrasound ablation with the Paradise catheter (ReCor Medical) had a mean systolic daytime blood pressure reduction of 13.2 mm Hg on ambulatory monitoring, vs. 6.5 mm Hg among 39 patients randomized to RF ablation with Medtronic’s Symplicity Spyral catheter (P = .043).
Meanwhile, 39 patients randomized to both main artery and side branch ablation with the Spyral had a mean reduction of 8.3 mm Hg, slightly better than RF ablation of the main renal arteries alone, but the difference was not statistically significant, and “no definite conclusion on the value of an additional side branch ablation can be drawn,” said senior investigator Philipp Lurz , MD, PhD, a cardiologist at the University of Leipzig, Germany, and his colleagues (Circulation. 2018 Sep 25. doi: 10.1161/circulationaha.118.037654).
Denervation was probably more complete with the Paradise catheter, which might explain the results. Ultrasound energy penetrates about 6-7 mm from the lumen, reaching up to 90% of sympathetic nerve fibers, while RF energy penetrates 3-4 mm; indeed, the idea of going into the branches with RF ablation is because nerve fibers are closer to the lumen surface, Dr. Lurz said at the Transcatheter Cardiovascular Therapeutics (TCT) annual meeting, where he presented the study, which was simultaneously published in Circulation.
Also, the Paradise catheter – an endovascular balloon device inflated to fit the lumen – delivers fully circumferential, ringlike ablations with each application, while the Spyral catheter delivers four ablations simultaneously in a spiral pattern, and requires more ablations to create a similar effect, according to Dr. Lurz.
About two-thirds of patients in all three arms responded to treatment, meaning at least a 5 mm Hg drop in systolic blood pressure. Among the nonresponders, it’s possible that their hypertension wasn’t caused by sympathetic overdrive. “Future trials should focus on identifying these patients to avoid futile” procedures, and define “specific anatomic predictors associated with a more effective” renal denervation, Dr. Lurz and his team said in their study report.
The researchers noted that “the present study included patients with larger renal arteries” – at least one renal artery 5.5 mm or greater in diameter – “based on the assumption that sympathetic fibers are in greater distance from the lumen than in smaller arteries, and therefore ... higher penetration depth would be more relevant ... Results might have differed in a cohort of patients with smaller renal artery diameters.”
Both Paradise and Spyral are in pivotal trials for Food and Drug Administration approval.
The subjects were an average of 64 years. The majority were men, and there were no significant differences in baseline characteristics between the arms. The mean baseline daytime blood pressure was 153/86 mm Hg despite treatment with three or more classes of antihypertensives dosed to at least 50% of their maximum. There was no drug testing to confirm patients were taking their medications, but their general practitioners vouched for their adherence.
One patient in the ultrasound arm group developed a pseudoaneurysm treated successfully by compression. One of the RF subjects developed a postprocedural intracapsular and retroperitoneal hematoma that resolved spontaneously. No renal vascular complications or stenoses were detected at follow-up.
There was no industry funding for the work. Dr. Lurz is a speaker and consultant for both ReCor Medical and Medtronic.
SOURCE: Fengler K et al. TCT 2018, Abstract.
SAN DIEGO – Denervation of the main renal arteries with ultrasound is more effective than radiofrequency (RF) ablation at lowering blood pressure in patients with resistant hypertension, according to a single-center, randomized trial from Germany.
Dubbed RADIOSOUND–HTN, it was the first time the two emerging technologies have been pitted against each other. At 3-month follow-up, the 42 patients randomized to ultrasound ablation with the Paradise catheter (ReCor Medical) had a mean systolic daytime blood pressure reduction of 13.2 mm Hg on ambulatory monitoring, vs. 6.5 mm Hg among 39 patients randomized to RF ablation with Medtronic’s Symplicity Spyral catheter (P = .043).
Meanwhile, 39 patients randomized to both main artery and side branch ablation with the Spyral had a mean reduction of 8.3 mm Hg, slightly better than RF ablation of the main renal arteries alone, but the difference was not statistically significant, and “no definite conclusion on the value of an additional side branch ablation can be drawn,” said senior investigator Philipp Lurz , MD, PhD, a cardiologist at the University of Leipzig, Germany, and his colleagues (Circulation. 2018 Sep 25. doi: 10.1161/circulationaha.118.037654).
Denervation was probably more complete with the Paradise catheter, which might explain the results. Ultrasound energy penetrates about 6-7 mm from the lumen, reaching up to 90% of sympathetic nerve fibers, while RF energy penetrates 3-4 mm; indeed, the idea of going into the branches with RF ablation is because nerve fibers are closer to the lumen surface, Dr. Lurz said at the Transcatheter Cardiovascular Therapeutics (TCT) annual meeting, where he presented the study, which was simultaneously published in Circulation.
Also, the Paradise catheter – an endovascular balloon device inflated to fit the lumen – delivers fully circumferential, ringlike ablations with each application, while the Spyral catheter delivers four ablations simultaneously in a spiral pattern, and requires more ablations to create a similar effect, according to Dr. Lurz.
About two-thirds of patients in all three arms responded to treatment, meaning at least a 5 mm Hg drop in systolic blood pressure. Among the nonresponders, it’s possible that their hypertension wasn’t caused by sympathetic overdrive. “Future trials should focus on identifying these patients to avoid futile” procedures, and define “specific anatomic predictors associated with a more effective” renal denervation, Dr. Lurz and his team said in their study report.
The researchers noted that “the present study included patients with larger renal arteries” – at least one renal artery 5.5 mm or greater in diameter – “based on the assumption that sympathetic fibers are in greater distance from the lumen than in smaller arteries, and therefore ... higher penetration depth would be more relevant ... Results might have differed in a cohort of patients with smaller renal artery diameters.”
Both Paradise and Spyral are in pivotal trials for Food and Drug Administration approval.
The subjects were an average of 64 years. The majority were men, and there were no significant differences in baseline characteristics between the arms. The mean baseline daytime blood pressure was 153/86 mm Hg despite treatment with three or more classes of antihypertensives dosed to at least 50% of their maximum. There was no drug testing to confirm patients were taking their medications, but their general practitioners vouched for their adherence.
One patient in the ultrasound arm group developed a pseudoaneurysm treated successfully by compression. One of the RF subjects developed a postprocedural intracapsular and retroperitoneal hematoma that resolved spontaneously. No renal vascular complications or stenoses were detected at follow-up.
There was no industry funding for the work. Dr. Lurz is a speaker and consultant for both ReCor Medical and Medtronic.
SOURCE: Fengler K et al. TCT 2018, Abstract.
REPORTING FROM TCT 2018
Key clinical point: Denervation might be more complete with ultrasound.
Major finding: Patients randomized to ultrasound ablation had a mean systolic blood pressure reduction of 13.2 mm Hg, vs. 6.5 mm Hg among patients randomized to RF ablation (P = .043).
Study details: Randomized trial with 120 subjects
Disclosures: There was no industry funding for the work. The senior investigator is a speaker and consultant for both ReCor Medical and Medtronic.
Source: Fengler K et al. TCT 2018, Abstract.
Primary care needs pile up for sickle cell patients
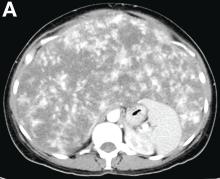
BETHESDA, MD. – With many people surviving well into adulthood with sickle cell disease (SCD) because of advances in treatment, there’s a strong need for more primary care to address chronic conditions, such as obesity and the complications of the blood disorder, researchers said.
People who have lived for decades with SCD may be at higher risk for renal disease while still needing the same routine vaccinations and screening for colon, prostate, and lung cancer that the general population receives, Sophie Lanzkron, MD, of Johns Hopkins University, Baltimore, said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
And obesity is an additional a concern in treating people with SCD, Dr. Lanzkron said.
“It is really hard to have a conversation for 20 minutes with a patient about pain, talk about what you’re going to do about their sickle cell disease, and then address all of” their routine health needs, she said.
People with SCD seem less likely to get renal transplants, but those with end-stage kidney disease should be encouraged to be evaluated for them, Dr. Lanzkron advised.
Older data had suggested that patients with SCD who underwent renal transplant didn’t do as well as everyone else who underwent the procedure, but new data have changed that approach. “There’s some additional data in the modern era suggesting that the outcomes for people who undergo transplant with sickle cell disease are the same as for those who undergo it with diabetes,” Dr. Lanzkron said.
She highlighted one newer study in which the kidney transplant survival rate was 73.1% among individuals with SCD, compared with 74.1% for those with diabetes (Nephrol Dial Transplant. 2013 Apr;28[4]:1039-46).
It’s unclear what the average life expectancy is at this time for someone with SCD, Dr. Lanzkron said. Research looking at death certificate data suggests a median age of death in the mid-40s, but there are limitations to this work given it may exclude many older people with SCD, she said.
“We’re hopeful that people are living into their 50s and 60s, but we don’t have a lot of great data,” she said.
One of the organizers of the NIH conference said she hoped that Dr. Lanzkron’s presentation would draw attention to the need for primary care for people with SCD. Maintaining a healthy lifestyle is particularly important for this group because they likely have had complications from the disease, as well as issues seen with normal aging, Swee Lay Thein, MBBS, of the National Heart, Lung, and Blood Institute, said in an interview.
“This is a key message for many patients with sickle cell disease,” Dr. Thein said. “It’s important to hook up with a primary care physician.”
Dr. Thein cited a recent paper, which reported on four people who had lived into their 80s with sickle cell disease. The paper said their longevity was aided by factors such as being nonsmokers, abstaining from alcohol or drinking it only on occasionally, and maintaining a normal body mass index (Blood. 2016 Nov 10;128[19]:2367-9).
Additionally, the patients had close ties with relatives. The paper said that one patient was married with a helpful husband. Others in this octogenarian set had maintained close ties with their children.
“A common factor for all of the four patients in their 80s was that they had a healthy lifestyle and very strong family support,” Dr. Thein said.
Dr. Lanzkron has been an investigator for trials sponsored by Pfizer, Global Blood Therapeutics, and Ironwood.
BETHESDA, MD. – With many people surviving well into adulthood with sickle cell disease (SCD) because of advances in treatment, there’s a strong need for more primary care to address chronic conditions, such as obesity and the complications of the blood disorder, researchers said.
People who have lived for decades with SCD may be at higher risk for renal disease while still needing the same routine vaccinations and screening for colon, prostate, and lung cancer that the general population receives, Sophie Lanzkron, MD, of Johns Hopkins University, Baltimore, said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
And obesity is an additional a concern in treating people with SCD, Dr. Lanzkron said.
“It is really hard to have a conversation for 20 minutes with a patient about pain, talk about what you’re going to do about their sickle cell disease, and then address all of” their routine health needs, she said.
People with SCD seem less likely to get renal transplants, but those with end-stage kidney disease should be encouraged to be evaluated for them, Dr. Lanzkron advised.
Older data had suggested that patients with SCD who underwent renal transplant didn’t do as well as everyone else who underwent the procedure, but new data have changed that approach. “There’s some additional data in the modern era suggesting that the outcomes for people who undergo transplant with sickle cell disease are the same as for those who undergo it with diabetes,” Dr. Lanzkron said.
She highlighted one newer study in which the kidney transplant survival rate was 73.1% among individuals with SCD, compared with 74.1% for those with diabetes (Nephrol Dial Transplant. 2013 Apr;28[4]:1039-46).
It’s unclear what the average life expectancy is at this time for someone with SCD, Dr. Lanzkron said. Research looking at death certificate data suggests a median age of death in the mid-40s, but there are limitations to this work given it may exclude many older people with SCD, she said.
“We’re hopeful that people are living into their 50s and 60s, but we don’t have a lot of great data,” she said.
One of the organizers of the NIH conference said she hoped that Dr. Lanzkron’s presentation would draw attention to the need for primary care for people with SCD. Maintaining a healthy lifestyle is particularly important for this group because they likely have had complications from the disease, as well as issues seen with normal aging, Swee Lay Thein, MBBS, of the National Heart, Lung, and Blood Institute, said in an interview.
“This is a key message for many patients with sickle cell disease,” Dr. Thein said. “It’s important to hook up with a primary care physician.”
Dr. Thein cited a recent paper, which reported on four people who had lived into their 80s with sickle cell disease. The paper said their longevity was aided by factors such as being nonsmokers, abstaining from alcohol or drinking it only on occasionally, and maintaining a normal body mass index (Blood. 2016 Nov 10;128[19]:2367-9).
Additionally, the patients had close ties with relatives. The paper said that one patient was married with a helpful husband. Others in this octogenarian set had maintained close ties with their children.
“A common factor for all of the four patients in their 80s was that they had a healthy lifestyle and very strong family support,” Dr. Thein said.
Dr. Lanzkron has been an investigator for trials sponsored by Pfizer, Global Blood Therapeutics, and Ironwood.
BETHESDA, MD. – With many people surviving well into adulthood with sickle cell disease (SCD) because of advances in treatment, there’s a strong need for more primary care to address chronic conditions, such as obesity and the complications of the blood disorder, researchers said.
People who have lived for decades with SCD may be at higher risk for renal disease while still needing the same routine vaccinations and screening for colon, prostate, and lung cancer that the general population receives, Sophie Lanzkron, MD, of Johns Hopkins University, Baltimore, said at Sickle Cell in Focus, a conference held by the National Institutes of Health.
And obesity is an additional a concern in treating people with SCD, Dr. Lanzkron said.
“It is really hard to have a conversation for 20 minutes with a patient about pain, talk about what you’re going to do about their sickle cell disease, and then address all of” their routine health needs, she said.
People with SCD seem less likely to get renal transplants, but those with end-stage kidney disease should be encouraged to be evaluated for them, Dr. Lanzkron advised.
Older data had suggested that patients with SCD who underwent renal transplant didn’t do as well as everyone else who underwent the procedure, but new data have changed that approach. “There’s some additional data in the modern era suggesting that the outcomes for people who undergo transplant with sickle cell disease are the same as for those who undergo it with diabetes,” Dr. Lanzkron said.
She highlighted one newer study in which the kidney transplant survival rate was 73.1% among individuals with SCD, compared with 74.1% for those with diabetes (Nephrol Dial Transplant. 2013 Apr;28[4]:1039-46).
It’s unclear what the average life expectancy is at this time for someone with SCD, Dr. Lanzkron said. Research looking at death certificate data suggests a median age of death in the mid-40s, but there are limitations to this work given it may exclude many older people with SCD, she said.
“We’re hopeful that people are living into their 50s and 60s, but we don’t have a lot of great data,” she said.
One of the organizers of the NIH conference said she hoped that Dr. Lanzkron’s presentation would draw attention to the need for primary care for people with SCD. Maintaining a healthy lifestyle is particularly important for this group because they likely have had complications from the disease, as well as issues seen with normal aging, Swee Lay Thein, MBBS, of the National Heart, Lung, and Blood Institute, said in an interview.
“This is a key message for many patients with sickle cell disease,” Dr. Thein said. “It’s important to hook up with a primary care physician.”
Dr. Thein cited a recent paper, which reported on four people who had lived into their 80s with sickle cell disease. The paper said their longevity was aided by factors such as being nonsmokers, abstaining from alcohol or drinking it only on occasionally, and maintaining a normal body mass index (Blood. 2016 Nov 10;128[19]:2367-9).
Additionally, the patients had close ties with relatives. The paper said that one patient was married with a helpful husband. Others in this octogenarian set had maintained close ties with their children.
“A common factor for all of the four patients in their 80s was that they had a healthy lifestyle and very strong family support,” Dr. Thein said.
Dr. Lanzkron has been an investigator for trials sponsored by Pfizer, Global Blood Therapeutics, and Ironwood.
EXPERT ANALYSIS FROM SICKLE CELL IN FOCUS
Yoga feasible, provides modest benefits for women with urinary incontinence
according to Alison J. Huang, MD, of the University of California, San Francisco, and her associates.
In a small study published in the American Journal of Obstetrics and Gynecology, 28 women enrolled in a 3-month yoga intervention program and 28 were enrolled in a control program consisting of nonspecific muscle stretching and strengthening. The mean age was 65 years, baseline urinary incontinence was 3.5 episodes/day, and 37 women had urgency-predominant incontinence.
Of those who completed the study, 89% of 27 patients in the yoga group attended at least 80% of classes, compared with 87% in the control group; over 90% of women in the yoga group completed at least 9 home practice hours.
Overall incontinence frequency was reduced by 76% in the yoga group and by 56% in the control group. Incontinence caused by stress was significantly reduced in the yoga group, compared with the control group (61% vs. 35%; P = .045), but the rate of incontinence caused by urgency did not noticeably differ. A total of 48 nonserious adverse events were reported over the 3-month period (23 in the yoga and 25 in the control group), but none were associated with either yoga or control treatment.
“Yoga may be useful for incontinent women in the community who lack access to incontinence specialists, are unable to use clinical therapies, or wish to enhance conventional care. Since yoga can be practiced in a group setting without continuous supervision by health care specialists, it offers a potentially cost-effective, community-based self-management strategy for incontinence, provided that it can be taught with appropriate attention to safety and to patients’ clinical needs,” the authors noted.
The study was supported with grants from the National Center for Complementary and Integrative Medicine and the UCSF Osher Center for Integrative Medicine’s Bradley fund. One of the authors received a grant from the National Institute of Diabetes and Digestive and Kidney Disorders. Two study authors reported receiving funding from Pfizer and Astellas to conduct research unrelated to the current study.
SOURCE: Huang AJ et al. Am J Obstet Gynecol. 2018 Oct 26. doi: 10.1016/j.ajog.2018.10.031.
according to Alison J. Huang, MD, of the University of California, San Francisco, and her associates.
In a small study published in the American Journal of Obstetrics and Gynecology, 28 women enrolled in a 3-month yoga intervention program and 28 were enrolled in a control program consisting of nonspecific muscle stretching and strengthening. The mean age was 65 years, baseline urinary incontinence was 3.5 episodes/day, and 37 women had urgency-predominant incontinence.
Of those who completed the study, 89% of 27 patients in the yoga group attended at least 80% of classes, compared with 87% in the control group; over 90% of women in the yoga group completed at least 9 home practice hours.
Overall incontinence frequency was reduced by 76% in the yoga group and by 56% in the control group. Incontinence caused by stress was significantly reduced in the yoga group, compared with the control group (61% vs. 35%; P = .045), but the rate of incontinence caused by urgency did not noticeably differ. A total of 48 nonserious adverse events were reported over the 3-month period (23 in the yoga and 25 in the control group), but none were associated with either yoga or control treatment.
“Yoga may be useful for incontinent women in the community who lack access to incontinence specialists, are unable to use clinical therapies, or wish to enhance conventional care. Since yoga can be practiced in a group setting without continuous supervision by health care specialists, it offers a potentially cost-effective, community-based self-management strategy for incontinence, provided that it can be taught with appropriate attention to safety and to patients’ clinical needs,” the authors noted.
The study was supported with grants from the National Center for Complementary and Integrative Medicine and the UCSF Osher Center for Integrative Medicine’s Bradley fund. One of the authors received a grant from the National Institute of Diabetes and Digestive and Kidney Disorders. Two study authors reported receiving funding from Pfizer and Astellas to conduct research unrelated to the current study.
SOURCE: Huang AJ et al. Am J Obstet Gynecol. 2018 Oct 26. doi: 10.1016/j.ajog.2018.10.031.
according to Alison J. Huang, MD, of the University of California, San Francisco, and her associates.
In a small study published in the American Journal of Obstetrics and Gynecology, 28 women enrolled in a 3-month yoga intervention program and 28 were enrolled in a control program consisting of nonspecific muscle stretching and strengthening. The mean age was 65 years, baseline urinary incontinence was 3.5 episodes/day, and 37 women had urgency-predominant incontinence.
Of those who completed the study, 89% of 27 patients in the yoga group attended at least 80% of classes, compared with 87% in the control group; over 90% of women in the yoga group completed at least 9 home practice hours.
Overall incontinence frequency was reduced by 76% in the yoga group and by 56% in the control group. Incontinence caused by stress was significantly reduced in the yoga group, compared with the control group (61% vs. 35%; P = .045), but the rate of incontinence caused by urgency did not noticeably differ. A total of 48 nonserious adverse events were reported over the 3-month period (23 in the yoga and 25 in the control group), but none were associated with either yoga or control treatment.
“Yoga may be useful for incontinent women in the community who lack access to incontinence specialists, are unable to use clinical therapies, or wish to enhance conventional care. Since yoga can be practiced in a group setting without continuous supervision by health care specialists, it offers a potentially cost-effective, community-based self-management strategy for incontinence, provided that it can be taught with appropriate attention to safety and to patients’ clinical needs,” the authors noted.
The study was supported with grants from the National Center for Complementary and Integrative Medicine and the UCSF Osher Center for Integrative Medicine’s Bradley fund. One of the authors received a grant from the National Institute of Diabetes and Digestive and Kidney Disorders. Two study authors reported receiving funding from Pfizer and Astellas to conduct research unrelated to the current study.
SOURCE: Huang AJ et al. Am J Obstet Gynecol. 2018 Oct 26. doi: 10.1016/j.ajog.2018.10.031.
FROM THE AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY
Delusional infestation: not so rare
PARIS – Ever wonder, when encountering an occasional patient afflicted with delusional infestation, just how common this mental disorder is?
John J. Kohorst, MD, and his coinvestigators at the Mayo Clinic in Rochester, Minn., have the evidence-based answer.
The age- and sex-adjusted point prevalence of delusional infestation among Olmsted County, Minn., residents on the final day of 2010 was 27.3 cases per 100,000 person-years, he reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is the than previously suspected,” according to the dermatologist.
He and his coinvestigators retrospectively analyzed data from the Rochester Epidemiology Project. They identified 22 female and 13 male county residents with a firm diagnosis of delusional infestation, also known as delusional parasitosis. This disorder is marked by a patient’s fixed false belief that they are infested with insects, worms, or other pathogens.
The prevalence was similar in men and women. The most striking study finding was how heavily age-dependent delusional infestation was. Before age 40, the prevalence was a mere 1.2 cases per 100,000 person-years. Among 40- to 59-year-old Olmsted County residents, it was 35/100,000, jumping to 64.5/100,000 in the 60- to 79-year-old age bracket, then doubling to 130.1 cases per 100,000 person-years in individuals aged 80 or older.
Dr. Kohorst reported having no financial conflicts regarding his study, conducted free of commercial support.
PARIS – Ever wonder, when encountering an occasional patient afflicted with delusional infestation, just how common this mental disorder is?
John J. Kohorst, MD, and his coinvestigators at the Mayo Clinic in Rochester, Minn., have the evidence-based answer.
The age- and sex-adjusted point prevalence of delusional infestation among Olmsted County, Minn., residents on the final day of 2010 was 27.3 cases per 100,000 person-years, he reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is the than previously suspected,” according to the dermatologist.
He and his coinvestigators retrospectively analyzed data from the Rochester Epidemiology Project. They identified 22 female and 13 male county residents with a firm diagnosis of delusional infestation, also known as delusional parasitosis. This disorder is marked by a patient’s fixed false belief that they are infested with insects, worms, or other pathogens.
The prevalence was similar in men and women. The most striking study finding was how heavily age-dependent delusional infestation was. Before age 40, the prevalence was a mere 1.2 cases per 100,000 person-years. Among 40- to 59-year-old Olmsted County residents, it was 35/100,000, jumping to 64.5/100,000 in the 60- to 79-year-old age bracket, then doubling to 130.1 cases per 100,000 person-years in individuals aged 80 or older.
Dr. Kohorst reported having no financial conflicts regarding his study, conducted free of commercial support.
PARIS – Ever wonder, when encountering an occasional patient afflicted with delusional infestation, just how common this mental disorder is?
John J. Kohorst, MD, and his coinvestigators at the Mayo Clinic in Rochester, Minn., have the evidence-based answer.
The age- and sex-adjusted point prevalence of delusional infestation among Olmsted County, Minn., residents on the final day of 2010 was 27.3 cases per 100,000 person-years, he reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is the than previously suspected,” according to the dermatologist.
He and his coinvestigators retrospectively analyzed data from the Rochester Epidemiology Project. They identified 22 female and 13 male county residents with a firm diagnosis of delusional infestation, also known as delusional parasitosis. This disorder is marked by a patient’s fixed false belief that they are infested with insects, worms, or other pathogens.
The prevalence was similar in men and women. The most striking study finding was how heavily age-dependent delusional infestation was. Before age 40, the prevalence was a mere 1.2 cases per 100,000 person-years. Among 40- to 59-year-old Olmsted County residents, it was 35/100,000, jumping to 64.5/100,000 in the 60- to 79-year-old age bracket, then doubling to 130.1 cases per 100,000 person-years in individuals aged 80 or older.
Dr. Kohorst reported having no financial conflicts regarding his study, conducted free of commercial support.
REPORTING FROM THE EADV CONGRESS
Key clinical point: Delusional infestation may be more common than previously suspected, particularly among older age groups.
Major finding: The age- and sex-adjusted point prevalence of delusional infestation among residents of one county in southeastern Minnesota is 27.3 cases per 100,000 person-years.
Study details: This was a retrospective analysis of data from the Rochester (Minn.) Epidemiology Project.
Disclosures: The presenter reported having no financial conflicts regarding his study, conducted free of commercial support.
What is Your Diagnosis? - November 2018
Over the next 6 months she developed progressive liver failure (Model for End-stage Liver Disease score 34), and required several hospitalizations for worsening abdominal pain and debility. Despite the high risk of complications, she agreed to pursue a liver transplant. During the course of surgery, there was significant hemorrhage from tearing of the portal vein (PV) anastomosis and surrounding areas; despite all resuscitative efforts, she went into cardiac arrest and died. The sections of explanted liver revealed soft, spongy parenchyma with blood-filled cyst-like cavities measuring 1-6 mm in diameter (Figure F). The entire liver was affected by vascular malformations (VMs) and there was no evidence of malignancy. On elastin stain, the elastic lamina of the vascular wall appeared thin and disrupted; D2-40 and GLUT1 antibody stains were negative. The hilar PV wall thickness was variable with areas of intramural loose connective tissue separating smooth muscle bundles. This made the PV very friable, which, along with coagulopathy, was the likely cause of uncontrollable intraoperative bleeding. These findings indicate that the vascular spaces were derived from malformation of PV branches.
VMs are rare liver lesions that can be idiopathic or associated with cirrhosis, traumatic injuries, and syndromes such as hereditary hemorrhagic telangiectasia. Although not always apparent, VMs are present at birth and grow proportionally with the patient’s age.1 They are usually solitary or multifocal, but rare cases of diffuse hepatic involvement have been reported.2 To our knowledge, this is the first reported case of diffuse hepatic VM in an adult with no evidence of extrahepatic involvement. Diffuse hepatic VM may be confused with diffuse hepatic hemangiomatosis, another rare condition in adults characterized by replacement of the hepatic parenchyma with hemangiomatous lesions, but differs in that it is a vascular tumor and not VM. While vascular tumors, such as hemangioma, are characterized by abnormal endothelial proliferation, VMs develop from abnormal vascular morphogenesis, and are named after the vascular element they closely resemble, namely, capillary, venous, or arterial malformations. Although these are 2 distinct entities, the terms hemangioma and VM have been used indiscriminately and interchangeably in the literature to describe vascular anomalies.1 Most hepatic VMs are asymptomatic, but depending on the extent of involvement, patients may develop high-output heart failure, portal hypertension, and biliary disease.3 Despite extensive liver involvement, our patient did not manifest shunt physiology. The radiographic findings were nonspecific but indicative of diffuse vascular lesions in the liver. Histologic characteristics include dilated, irregular vascular channels, lined by a flat endothelium, separated by liver parenchyma and fibrovascular tissue.2 Histochemical stains for collagen, elastin, and smooth muscle are often used to further characterize VMs. Therapeutic options in focal VMs include sclerotherapy, embolization, and surgical resection. In severe cases with progressive hepatic failure, liver transplantation may be the only feasible option. A case of successful living donor liver transplant in a 14-year-old with VMs involving liver and colon has been described in literature.3 Unfortunately, our patient did not survive the surgery. More reports using accurate terminology to describe hepatic vascular anomalies are needed for further understanding of this rare yet fatal disease.
References
1. George A., Mani V., Noufal A. Update on the classification of hemangioma. J Oral Maxillofac Pathol. 2014;18:S117-20.
2. Sato K., Amanuma M., Fukusato T., et al. Diffuse hepatic vascular malformations with right aortic arch. J Hepatol. 2005;43:1094-5.
3. Hatanaka M., Nakazawa A., Nakano N., et al. Successful living donor liver transplantation for giant extensive venous malformation. Pediatr Transplant. 2014;18:E152-6.
Over the next 6 months she developed progressive liver failure (Model for End-stage Liver Disease score 34), and required several hospitalizations for worsening abdominal pain and debility. Despite the high risk of complications, she agreed to pursue a liver transplant. During the course of surgery, there was significant hemorrhage from tearing of the portal vein (PV) anastomosis and surrounding areas; despite all resuscitative efforts, she went into cardiac arrest and died. The sections of explanted liver revealed soft, spongy parenchyma with blood-filled cyst-like cavities measuring 1-6 mm in diameter (Figure F). The entire liver was affected by vascular malformations (VMs) and there was no evidence of malignancy. On elastin stain, the elastic lamina of the vascular wall appeared thin and disrupted; D2-40 and GLUT1 antibody stains were negative. The hilar PV wall thickness was variable with areas of intramural loose connective tissue separating smooth muscle bundles. This made the PV very friable, which, along with coagulopathy, was the likely cause of uncontrollable intraoperative bleeding. These findings indicate that the vascular spaces were derived from malformation of PV branches.
VMs are rare liver lesions that can be idiopathic or associated with cirrhosis, traumatic injuries, and syndromes such as hereditary hemorrhagic telangiectasia. Although not always apparent, VMs are present at birth and grow proportionally with the patient’s age.1 They are usually solitary or multifocal, but rare cases of diffuse hepatic involvement have been reported.2 To our knowledge, this is the first reported case of diffuse hepatic VM in an adult with no evidence of extrahepatic involvement. Diffuse hepatic VM may be confused with diffuse hepatic hemangiomatosis, another rare condition in adults characterized by replacement of the hepatic parenchyma with hemangiomatous lesions, but differs in that it is a vascular tumor and not VM. While vascular tumors, such as hemangioma, are characterized by abnormal endothelial proliferation, VMs develop from abnormal vascular morphogenesis, and are named after the vascular element they closely resemble, namely, capillary, venous, or arterial malformations. Although these are 2 distinct entities, the terms hemangioma and VM have been used indiscriminately and interchangeably in the literature to describe vascular anomalies.1 Most hepatic VMs are asymptomatic, but depending on the extent of involvement, patients may develop high-output heart failure, portal hypertension, and biliary disease.3 Despite extensive liver involvement, our patient did not manifest shunt physiology. The radiographic findings were nonspecific but indicative of diffuse vascular lesions in the liver. Histologic characteristics include dilated, irregular vascular channels, lined by a flat endothelium, separated by liver parenchyma and fibrovascular tissue.2 Histochemical stains for collagen, elastin, and smooth muscle are often used to further characterize VMs. Therapeutic options in focal VMs include sclerotherapy, embolization, and surgical resection. In severe cases with progressive hepatic failure, liver transplantation may be the only feasible option. A case of successful living donor liver transplant in a 14-year-old with VMs involving liver and colon has been described in literature.3 Unfortunately, our patient did not survive the surgery. More reports using accurate terminology to describe hepatic vascular anomalies are needed for further understanding of this rare yet fatal disease.
References
1. George A., Mani V., Noufal A. Update on the classification of hemangioma. J Oral Maxillofac Pathol. 2014;18:S117-20.
2. Sato K., Amanuma M., Fukusato T., et al. Diffuse hepatic vascular malformations with right aortic arch. J Hepatol. 2005;43:1094-5.
3. Hatanaka M., Nakazawa A., Nakano N., et al. Successful living donor liver transplantation for giant extensive venous malformation. Pediatr Transplant. 2014;18:E152-6.
Over the next 6 months she developed progressive liver failure (Model for End-stage Liver Disease score 34), and required several hospitalizations for worsening abdominal pain and debility. Despite the high risk of complications, she agreed to pursue a liver transplant. During the course of surgery, there was significant hemorrhage from tearing of the portal vein (PV) anastomosis and surrounding areas; despite all resuscitative efforts, she went into cardiac arrest and died. The sections of explanted liver revealed soft, spongy parenchyma with blood-filled cyst-like cavities measuring 1-6 mm in diameter (Figure F). The entire liver was affected by vascular malformations (VMs) and there was no evidence of malignancy. On elastin stain, the elastic lamina of the vascular wall appeared thin and disrupted; D2-40 and GLUT1 antibody stains were negative. The hilar PV wall thickness was variable with areas of intramural loose connective tissue separating smooth muscle bundles. This made the PV very friable, which, along with coagulopathy, was the likely cause of uncontrollable intraoperative bleeding. These findings indicate that the vascular spaces were derived from malformation of PV branches.
VMs are rare liver lesions that can be idiopathic or associated with cirrhosis, traumatic injuries, and syndromes such as hereditary hemorrhagic telangiectasia. Although not always apparent, VMs are present at birth and grow proportionally with the patient’s age.1 They are usually solitary or multifocal, but rare cases of diffuse hepatic involvement have been reported.2 To our knowledge, this is the first reported case of diffuse hepatic VM in an adult with no evidence of extrahepatic involvement. Diffuse hepatic VM may be confused with diffuse hepatic hemangiomatosis, another rare condition in adults characterized by replacement of the hepatic parenchyma with hemangiomatous lesions, but differs in that it is a vascular tumor and not VM. While vascular tumors, such as hemangioma, are characterized by abnormal endothelial proliferation, VMs develop from abnormal vascular morphogenesis, and are named after the vascular element they closely resemble, namely, capillary, venous, or arterial malformations. Although these are 2 distinct entities, the terms hemangioma and VM have been used indiscriminately and interchangeably in the literature to describe vascular anomalies.1 Most hepatic VMs are asymptomatic, but depending on the extent of involvement, patients may develop high-output heart failure, portal hypertension, and biliary disease.3 Despite extensive liver involvement, our patient did not manifest shunt physiology. The radiographic findings were nonspecific but indicative of diffuse vascular lesions in the liver. Histologic characteristics include dilated, irregular vascular channels, lined by a flat endothelium, separated by liver parenchyma and fibrovascular tissue.2 Histochemical stains for collagen, elastin, and smooth muscle are often used to further characterize VMs. Therapeutic options in focal VMs include sclerotherapy, embolization, and surgical resection. In severe cases with progressive hepatic failure, liver transplantation may be the only feasible option. A case of successful living donor liver transplant in a 14-year-old with VMs involving liver and colon has been described in literature.3 Unfortunately, our patient did not survive the surgery. More reports using accurate terminology to describe hepatic vascular anomalies are needed for further understanding of this rare yet fatal disease.
References
1. George A., Mani V., Noufal A. Update on the classification of hemangioma. J Oral Maxillofac Pathol. 2014;18:S117-20.
2. Sato K., Amanuma M., Fukusato T., et al. Diffuse hepatic vascular malformations with right aortic arch. J Hepatol. 2005;43:1094-5.
3. Hatanaka M., Nakazawa A., Nakano N., et al. Successful living donor liver transplantation for giant extensive venous malformation. Pediatr Transplant. 2014;18:E152-6.
A 50-year-old Guyanese woman was found to have abnormal liver tests on routine testing with total bilirubin, 1.8 mg/dL (normal, 0.2–1.2); alkaline phosphatase, 189 U/L (normal, 47–154); aspartate transaminase, 57 U/L (normal, 11–42); and alanine transaminase, 33 U/L (normal, 0–20).
Published previously in Gastroenterology (2016;151[6]:1081-2).