User login
Childhood abuse linked with tripled adult SLE incidence
CHICAGO – , in a study of more than 67,000 American nurses.
The results also suggested that development of depression and post-traumatic stress disorder (PTSD) may have been intermediary steps between episodes of childhood abuse and later development of systemic lupus erythematosus (SLE), Candace H. Feldman, MD, said at the annual meeting of the American College of Rheumatology.
These findings suggest the “importance of screening for childhood abuse exposures as well as for depression and PTSD in routine practice,” although Dr. Feldman acknowledged that interventions aimed at treating depression and PTSD have as of now no proven role for mitigating SLE.
The analysis Dr. Feldman and her associates ran on data collected in the Nurses Health Study II also documented a “striking” number of the enrolled women who completed the survey in 2001 and reported a history of abuse when they were 11 years old or younger: 30% of the 67,516 respondents reported a moderate level of abuse, and 24% reported a high level of abuse. An additional 22% reported either no or a very low level of abuse. These numbers suggest that abuse of girls “is very common and probably underreported,” she said in a video interview.
The Nurses Health Study II enrolled more than 116,429 U.S. women in 1989 who were 25-42 years old and had no history of SLE. Recording of incident SLE cases began in 1991 and for this analysis continued for 24 years, through 2015, during which time 94 women developed SLE that was confirmed in a review by two rheumatologists applying the 1997 SLE classification criteria (Arthritis Rheum. 1997 Sept;40[9]:1725. The incidence of SLE was 2.57-fold more common among women who reported a high level of abuse, compared with those who had no or very low abuse, after adjustment for several demographic and clinical confounders, reported Dr. Feldman, a rheumatologist at Brigham and Women’s Hospital in Boston.
“To our knowledge this is the first study to prospectively look at exposure to different forms of childhood abuse and SLE incidence in a general population of women,” she said.
To make the analysis more prospective the researchers also ran a calculation that considered only SLE cases that appeared after completion of the 2001 abuse survey. Using this criterion the incidence was 3.11-fold higher among women who reported a high level of childhood abuse. Further analyses showed that statistically a diagnosis of PTSD accounted for about 23% of the risk for developing SLE, and depression appeared responsible for about 17% of the risk. The analysis also showed no statistically significant link between sexual abuse in childhood or as a teenager and later onset of SLE.
The findings are consistent with prior reports that linked stress to development of various autoimmune diseases, Dr. Feldman noted. She speculated that high childhood stress could cause changes in inflammation, immune function, epigenetics, the autonomic nervous system, and endocrine pathways that could play a role in triggering depression or PTSD, and eventually SLE.
[email protected]
On Twitter @mitchelzoler
SOURCE:Feldman C et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract 2807.
CHICAGO – , in a study of more than 67,000 American nurses.
The results also suggested that development of depression and post-traumatic stress disorder (PTSD) may have been intermediary steps between episodes of childhood abuse and later development of systemic lupus erythematosus (SLE), Candace H. Feldman, MD, said at the annual meeting of the American College of Rheumatology.
These findings suggest the “importance of screening for childhood abuse exposures as well as for depression and PTSD in routine practice,” although Dr. Feldman acknowledged that interventions aimed at treating depression and PTSD have as of now no proven role for mitigating SLE.
The analysis Dr. Feldman and her associates ran on data collected in the Nurses Health Study II also documented a “striking” number of the enrolled women who completed the survey in 2001 and reported a history of abuse when they were 11 years old or younger: 30% of the 67,516 respondents reported a moderate level of abuse, and 24% reported a high level of abuse. An additional 22% reported either no or a very low level of abuse. These numbers suggest that abuse of girls “is very common and probably underreported,” she said in a video interview.
The Nurses Health Study II enrolled more than 116,429 U.S. women in 1989 who were 25-42 years old and had no history of SLE. Recording of incident SLE cases began in 1991 and for this analysis continued for 24 years, through 2015, during which time 94 women developed SLE that was confirmed in a review by two rheumatologists applying the 1997 SLE classification criteria (Arthritis Rheum. 1997 Sept;40[9]:1725. The incidence of SLE was 2.57-fold more common among women who reported a high level of abuse, compared with those who had no or very low abuse, after adjustment for several demographic and clinical confounders, reported Dr. Feldman, a rheumatologist at Brigham and Women’s Hospital in Boston.
“To our knowledge this is the first study to prospectively look at exposure to different forms of childhood abuse and SLE incidence in a general population of women,” she said.
To make the analysis more prospective the researchers also ran a calculation that considered only SLE cases that appeared after completion of the 2001 abuse survey. Using this criterion the incidence was 3.11-fold higher among women who reported a high level of childhood abuse. Further analyses showed that statistically a diagnosis of PTSD accounted for about 23% of the risk for developing SLE, and depression appeared responsible for about 17% of the risk. The analysis also showed no statistically significant link between sexual abuse in childhood or as a teenager and later onset of SLE.
The findings are consistent with prior reports that linked stress to development of various autoimmune diseases, Dr. Feldman noted. She speculated that high childhood stress could cause changes in inflammation, immune function, epigenetics, the autonomic nervous system, and endocrine pathways that could play a role in triggering depression or PTSD, and eventually SLE.
[email protected]
On Twitter @mitchelzoler
SOURCE:Feldman C et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract 2807.
CHICAGO – , in a study of more than 67,000 American nurses.
The results also suggested that development of depression and post-traumatic stress disorder (PTSD) may have been intermediary steps between episodes of childhood abuse and later development of systemic lupus erythematosus (SLE), Candace H. Feldman, MD, said at the annual meeting of the American College of Rheumatology.
These findings suggest the “importance of screening for childhood abuse exposures as well as for depression and PTSD in routine practice,” although Dr. Feldman acknowledged that interventions aimed at treating depression and PTSD have as of now no proven role for mitigating SLE.
The analysis Dr. Feldman and her associates ran on data collected in the Nurses Health Study II also documented a “striking” number of the enrolled women who completed the survey in 2001 and reported a history of abuse when they were 11 years old or younger: 30% of the 67,516 respondents reported a moderate level of abuse, and 24% reported a high level of abuse. An additional 22% reported either no or a very low level of abuse. These numbers suggest that abuse of girls “is very common and probably underreported,” she said in a video interview.
The Nurses Health Study II enrolled more than 116,429 U.S. women in 1989 who were 25-42 years old and had no history of SLE. Recording of incident SLE cases began in 1991 and for this analysis continued for 24 years, through 2015, during which time 94 women developed SLE that was confirmed in a review by two rheumatologists applying the 1997 SLE classification criteria (Arthritis Rheum. 1997 Sept;40[9]:1725. The incidence of SLE was 2.57-fold more common among women who reported a high level of abuse, compared with those who had no or very low abuse, after adjustment for several demographic and clinical confounders, reported Dr. Feldman, a rheumatologist at Brigham and Women’s Hospital in Boston.
“To our knowledge this is the first study to prospectively look at exposure to different forms of childhood abuse and SLE incidence in a general population of women,” she said.
To make the analysis more prospective the researchers also ran a calculation that considered only SLE cases that appeared after completion of the 2001 abuse survey. Using this criterion the incidence was 3.11-fold higher among women who reported a high level of childhood abuse. Further analyses showed that statistically a diagnosis of PTSD accounted for about 23% of the risk for developing SLE, and depression appeared responsible for about 17% of the risk. The analysis also showed no statistically significant link between sexual abuse in childhood or as a teenager and later onset of SLE.
The findings are consistent with prior reports that linked stress to development of various autoimmune diseases, Dr. Feldman noted. She speculated that high childhood stress could cause changes in inflammation, immune function, epigenetics, the autonomic nervous system, and endocrine pathways that could play a role in triggering depression or PTSD, and eventually SLE.
[email protected]
On Twitter @mitchelzoler
SOURCE:Feldman C et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract 2807.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: A history of high childhood abuse linked with a nearly three-fold higher incidence of systemic lupus erythematosus during adulthood.
Major finding: The incidence of systemic lupus erythematosus was 2.57-fold higher among women with high childhood abuse compared with unabused women.
Study details: Data from 67,516 women enrolled in the Nurses Health Study II.
Disclosures: Dr. Feldman had no disclosures.
Source: Feldman C et al. Arthritis Rheumatol. 2018;70(suppl 10) Abstract 2807.
Breakthrough designation for pathogen-reduced cryoprecipitate
The U.S. Food and Drug Administration (FDA) has granted breakthrough device designation for pathogen-reduced cryoprecipitate manufactured from plasma treated with the INTERCEPT Blood System.
Cerus Corporation aims to seek FDA approval for this pathogen-reduced cryoprecipitate to treat massive hemorrhage.
“The proposed label indication for pathogen-reduced cryoprecipitate would be to control massive bleeding associated with fibrinogen deficiency,” said Laurence Corash, chief scientific officer of Cerus.
The proposed shelf life for pathogen-reduced cyroprecipitate is 5 days at room temperature.
The INTERCEPT Blood System is already FDA-approved for the inactivation of pathogens in platelets and plasma.
“Cryo[precipitate] is a natural extension to our current FDA-approved INTERCEPT Blood System for plasma,” said William “Obi” Greenman, president and chief executive officer of Cerus.
If the FDA granted approval, INTERCEPT-treated plasma could be manufactured into pathogen-reduced cryoprecipitate.
About breakthrough device designation
The FDA says it grants breakthrough designation to devices “that provide more effective treatment or diagnosis of life-threatening or irreversibly debilitating human diseases or conditions.”
Breakthrough designation is intended to expedite the development, assessment, and review of medical devices. The breakthrough devices program supersedes the FDA’s expedited access pathway and priority review programs.
The U.S. Food and Drug Administration (FDA) has granted breakthrough device designation for pathogen-reduced cryoprecipitate manufactured from plasma treated with the INTERCEPT Blood System.
Cerus Corporation aims to seek FDA approval for this pathogen-reduced cryoprecipitate to treat massive hemorrhage.
“The proposed label indication for pathogen-reduced cryoprecipitate would be to control massive bleeding associated with fibrinogen deficiency,” said Laurence Corash, chief scientific officer of Cerus.
The proposed shelf life for pathogen-reduced cyroprecipitate is 5 days at room temperature.
The INTERCEPT Blood System is already FDA-approved for the inactivation of pathogens in platelets and plasma.
“Cryo[precipitate] is a natural extension to our current FDA-approved INTERCEPT Blood System for plasma,” said William “Obi” Greenman, president and chief executive officer of Cerus.
If the FDA granted approval, INTERCEPT-treated plasma could be manufactured into pathogen-reduced cryoprecipitate.
About breakthrough device designation
The FDA says it grants breakthrough designation to devices “that provide more effective treatment or diagnosis of life-threatening or irreversibly debilitating human diseases or conditions.”
Breakthrough designation is intended to expedite the development, assessment, and review of medical devices. The breakthrough devices program supersedes the FDA’s expedited access pathway and priority review programs.
The U.S. Food and Drug Administration (FDA) has granted breakthrough device designation for pathogen-reduced cryoprecipitate manufactured from plasma treated with the INTERCEPT Blood System.
Cerus Corporation aims to seek FDA approval for this pathogen-reduced cryoprecipitate to treat massive hemorrhage.
“The proposed label indication for pathogen-reduced cryoprecipitate would be to control massive bleeding associated with fibrinogen deficiency,” said Laurence Corash, chief scientific officer of Cerus.
The proposed shelf life for pathogen-reduced cyroprecipitate is 5 days at room temperature.
The INTERCEPT Blood System is already FDA-approved for the inactivation of pathogens in platelets and plasma.
“Cryo[precipitate] is a natural extension to our current FDA-approved INTERCEPT Blood System for plasma,” said William “Obi” Greenman, president and chief executive officer of Cerus.
If the FDA granted approval, INTERCEPT-treated plasma could be manufactured into pathogen-reduced cryoprecipitate.
About breakthrough device designation
The FDA says it grants breakthrough designation to devices “that provide more effective treatment or diagnosis of life-threatening or irreversibly debilitating human diseases or conditions.”
Breakthrough designation is intended to expedite the development, assessment, and review of medical devices. The breakthrough devices program supersedes the FDA’s expedited access pathway and priority review programs.
FDA panels back brexanolone infusion for postpartum depression
A joint panel of the Food and Drug Administration voted Nov. 2 in support of brexanolone infusion as a treatment for postpartum depression.
The 17-1 vote by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based primarily on data from three studies, including 247 women aged 18-44 years with postpartum depression; 140 received brexanolone and 107 received placebo. Effectiveness was assessed based on the Hamilton Depression Scale (HAM-D) at the end of the infusion (hour 60).
In all three studies, patients given brexanolone showed significantly improved HAM-D scores, compared with placebo. The patients experienced significant differences at hour 24, which illustrated the rapid response. “The individual item scores of the HAM-D consistently favored brexanolone IV over placebo, confirming an overall antidepressant effect of the drug,” according to the briefing document of Sage Therapeutics, developer of the drug. In addition, more than 80% of the patients in the treatment and placebo groups sustained their improvement in symptoms at 30 days after the end of the infusion.
“[Postpartum depression] is symptomatically indistinguishable from an episode of major depression,” the FDA briefing document said. “However, the timing of its onset has led to its recognition as a potentially unique illness. There are no drugs specifically approved to treat [postpartum depression].”
Some clinicians use drugs approved for major depression to treat postpartum depression, but the effectiveness of these drugs is limited, the agency said. Other interventions, such as electroconvulsive therapy, repetitive transcranial magnetic stimulation, and psychotherapy also are used, but they can take several weeks to show results.
Recent estimates of postpartum depression in the United States range from about 8% to 20%, according to the FDA document. and both the FDA and Sage Therapeutics agreed on the need for additional treatment options for women with postpartum depression. , according to Sage.
The treatment protocol for brexanolone involves a single 60-hour continuous infusion with a recommended maximum dose of 90 µg/kg/h, referred to as a “90 dose regimen.” The patient receives a single infusion per episode of postpartum depression. The infusion includes three dosing phases: titration at 30 μg/kg/h for 4 hours followed by 60 μg/kg/h for 20 hours (hour 0-24), maintenance at 90 μg/kg/h for 28 hours (hour 24-52), and taper at 60 μg/kg/h for 4 hours – followed by 30 μg/kg/h for 4 hours (hour 52-60).
Brexanolone is an allosteric modulator of GABAA receptors and “a new molecular entity not currently marketed anywhere in the world for any indication,” according to the FDA document. The drug originally was studied as a treatment for seizure patients before its antidepressant properties were discovered.
Adverse reactions observed in 3% or more of the brexanolone patients during the 60-hour treatment and 4-week follow-up included dry mouth, infusion site pain, fatigue, headache, sedation/somnolence, dizziness/vertigo, and loss of consciousness.
Of those reactions, loss of consciousness was the issue of greatest concern to the committee members and informed their discussion of the strict Risk Evaluation and Mitigation Strategy protocol that would be needed to accompany approval of the drug. The details of the REMS will be determined, but the basics of the FDA’s proposed REMS to mitigate the risk of loss of consciousness include administration of the drug only in medically supervised settings by an authorized representative.
In addition, the proposed REMS states that the authorized representative must “establish policies and procedures to ensure that 1) all staff are trained on the risks and 2) the product is not dispensed for use outside the health care setting.”
The proposed REMS also stated that, “Patients must be continuously monitored for the duration of the infusion and 12 hours after, by health care provider who can intervene if the patient experiences excessive sedation or loss of consciousness.”
Despite those concerns, which most committee members thought could be addressed by the REMS, the overall impression of the committees’ members was that brexanolone could have a significant impact on postpartum depression. According to one member, brexanolone is mechanistically “groundbreaking” and “could be a tremendous help in changing the trajectory of postpartum depression.”
The FDA usually follows its panels’ recommendations, which are not binding.
A joint panel of the Food and Drug Administration voted Nov. 2 in support of brexanolone infusion as a treatment for postpartum depression.
The 17-1 vote by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based primarily on data from three studies, including 247 women aged 18-44 years with postpartum depression; 140 received brexanolone and 107 received placebo. Effectiveness was assessed based on the Hamilton Depression Scale (HAM-D) at the end of the infusion (hour 60).
In all three studies, patients given brexanolone showed significantly improved HAM-D scores, compared with placebo. The patients experienced significant differences at hour 24, which illustrated the rapid response. “The individual item scores of the HAM-D consistently favored brexanolone IV over placebo, confirming an overall antidepressant effect of the drug,” according to the briefing document of Sage Therapeutics, developer of the drug. In addition, more than 80% of the patients in the treatment and placebo groups sustained their improvement in symptoms at 30 days after the end of the infusion.
“[Postpartum depression] is symptomatically indistinguishable from an episode of major depression,” the FDA briefing document said. “However, the timing of its onset has led to its recognition as a potentially unique illness. There are no drugs specifically approved to treat [postpartum depression].”
Some clinicians use drugs approved for major depression to treat postpartum depression, but the effectiveness of these drugs is limited, the agency said. Other interventions, such as electroconvulsive therapy, repetitive transcranial magnetic stimulation, and psychotherapy also are used, but they can take several weeks to show results.
Recent estimates of postpartum depression in the United States range from about 8% to 20%, according to the FDA document. and both the FDA and Sage Therapeutics agreed on the need for additional treatment options for women with postpartum depression. , according to Sage.
The treatment protocol for brexanolone involves a single 60-hour continuous infusion with a recommended maximum dose of 90 µg/kg/h, referred to as a “90 dose regimen.” The patient receives a single infusion per episode of postpartum depression. The infusion includes three dosing phases: titration at 30 μg/kg/h for 4 hours followed by 60 μg/kg/h for 20 hours (hour 0-24), maintenance at 90 μg/kg/h for 28 hours (hour 24-52), and taper at 60 μg/kg/h for 4 hours – followed by 30 μg/kg/h for 4 hours (hour 52-60).
Brexanolone is an allosteric modulator of GABAA receptors and “a new molecular entity not currently marketed anywhere in the world for any indication,” according to the FDA document. The drug originally was studied as a treatment for seizure patients before its antidepressant properties were discovered.
Adverse reactions observed in 3% or more of the brexanolone patients during the 60-hour treatment and 4-week follow-up included dry mouth, infusion site pain, fatigue, headache, sedation/somnolence, dizziness/vertigo, and loss of consciousness.
Of those reactions, loss of consciousness was the issue of greatest concern to the committee members and informed their discussion of the strict Risk Evaluation and Mitigation Strategy protocol that would be needed to accompany approval of the drug. The details of the REMS will be determined, but the basics of the FDA’s proposed REMS to mitigate the risk of loss of consciousness include administration of the drug only in medically supervised settings by an authorized representative.
In addition, the proposed REMS states that the authorized representative must “establish policies and procedures to ensure that 1) all staff are trained on the risks and 2) the product is not dispensed for use outside the health care setting.”
The proposed REMS also stated that, “Patients must be continuously monitored for the duration of the infusion and 12 hours after, by health care provider who can intervene if the patient experiences excessive sedation or loss of consciousness.”
Despite those concerns, which most committee members thought could be addressed by the REMS, the overall impression of the committees’ members was that brexanolone could have a significant impact on postpartum depression. According to one member, brexanolone is mechanistically “groundbreaking” and “could be a tremendous help in changing the trajectory of postpartum depression.”
The FDA usually follows its panels’ recommendations, which are not binding.
A joint panel of the Food and Drug Administration voted Nov. 2 in support of brexanolone infusion as a treatment for postpartum depression.
The 17-1 vote by members of the Psychopharmacologic Drugs Advisory Committee and the Drug Safety and Risk Management Advisory Committee was based primarily on data from three studies, including 247 women aged 18-44 years with postpartum depression; 140 received brexanolone and 107 received placebo. Effectiveness was assessed based on the Hamilton Depression Scale (HAM-D) at the end of the infusion (hour 60).
In all three studies, patients given brexanolone showed significantly improved HAM-D scores, compared with placebo. The patients experienced significant differences at hour 24, which illustrated the rapid response. “The individual item scores of the HAM-D consistently favored brexanolone IV over placebo, confirming an overall antidepressant effect of the drug,” according to the briefing document of Sage Therapeutics, developer of the drug. In addition, more than 80% of the patients in the treatment and placebo groups sustained their improvement in symptoms at 30 days after the end of the infusion.
“[Postpartum depression] is symptomatically indistinguishable from an episode of major depression,” the FDA briefing document said. “However, the timing of its onset has led to its recognition as a potentially unique illness. There are no drugs specifically approved to treat [postpartum depression].”
Some clinicians use drugs approved for major depression to treat postpartum depression, but the effectiveness of these drugs is limited, the agency said. Other interventions, such as electroconvulsive therapy, repetitive transcranial magnetic stimulation, and psychotherapy also are used, but they can take several weeks to show results.
Recent estimates of postpartum depression in the United States range from about 8% to 20%, according to the FDA document. and both the FDA and Sage Therapeutics agreed on the need for additional treatment options for women with postpartum depression. , according to Sage.
The treatment protocol for brexanolone involves a single 60-hour continuous infusion with a recommended maximum dose of 90 µg/kg/h, referred to as a “90 dose regimen.” The patient receives a single infusion per episode of postpartum depression. The infusion includes three dosing phases: titration at 30 μg/kg/h for 4 hours followed by 60 μg/kg/h for 20 hours (hour 0-24), maintenance at 90 μg/kg/h for 28 hours (hour 24-52), and taper at 60 μg/kg/h for 4 hours – followed by 30 μg/kg/h for 4 hours (hour 52-60).
Brexanolone is an allosteric modulator of GABAA receptors and “a new molecular entity not currently marketed anywhere in the world for any indication,” according to the FDA document. The drug originally was studied as a treatment for seizure patients before its antidepressant properties were discovered.
Adverse reactions observed in 3% or more of the brexanolone patients during the 60-hour treatment and 4-week follow-up included dry mouth, infusion site pain, fatigue, headache, sedation/somnolence, dizziness/vertigo, and loss of consciousness.
Of those reactions, loss of consciousness was the issue of greatest concern to the committee members and informed their discussion of the strict Risk Evaluation and Mitigation Strategy protocol that would be needed to accompany approval of the drug. The details of the REMS will be determined, but the basics of the FDA’s proposed REMS to mitigate the risk of loss of consciousness include administration of the drug only in medically supervised settings by an authorized representative.
In addition, the proposed REMS states that the authorized representative must “establish policies and procedures to ensure that 1) all staff are trained on the risks and 2) the product is not dispensed for use outside the health care setting.”
The proposed REMS also stated that, “Patients must be continuously monitored for the duration of the infusion and 12 hours after, by health care provider who can intervene if the patient experiences excessive sedation or loss of consciousness.”
Despite those concerns, which most committee members thought could be addressed by the REMS, the overall impression of the committees’ members was that brexanolone could have a significant impact on postpartum depression. According to one member, brexanolone is mechanistically “groundbreaking” and “could be a tremendous help in changing the trajectory of postpartum depression.”
The FDA usually follows its panels’ recommendations, which are not binding.
FDA approves second pegfilgrastim biosimilar
The Food and Drug Administration has approved a second biosimilar to pegfilgrastim (Neulasta) to decrease the chance of infection in patients with nonmyeloid cancer who are receiving myelosuppressive chemotherapy and are at risk of febrile neutropenia.
Approval of pegfilgrastim-cbqv, previously known as CHS-1701, was based on analyses establishing biosimilarity, including pharmacokinetic, pharmacodynamic, and immunogenicity studies. Clinical trial results were presented at the 2017 ASCO Annual Meeting.
The most common adverse reactions with pegfilgrastim-cbqv are bone pain and pain in extremities.
The FDA approved the first pegfilgrastim biosimilar, pegfilgrastim-jmdb (Fulphila) in June.
Pegfilgrastim-cbqv will be marketed as Udenyca by Coherus BioSciences.
“Udenyca’s robust clinical package includes a dedicated immunogenicity similarity study in over 300 healthy subjects,” Barbara Finck, MD, chief medical officer of Coherus BioSciences, said in a press release.
“In support of that study, and as part of our commitment to ensuring patient safety, we deployed a battery of sensitive immunogenicity assays. This effort not only supported the biosimilarity of Udenyca but also advanced the understanding of the immunogenic response of pegfilgrastim products.”
Coherus BioSciences plans to provide details about pricing and the launch of pegfilgrastim-cbqv during an earnings call on Nov. 8.
The Food and Drug Administration has approved a second biosimilar to pegfilgrastim (Neulasta) to decrease the chance of infection in patients with nonmyeloid cancer who are receiving myelosuppressive chemotherapy and are at risk of febrile neutropenia.
Approval of pegfilgrastim-cbqv, previously known as CHS-1701, was based on analyses establishing biosimilarity, including pharmacokinetic, pharmacodynamic, and immunogenicity studies. Clinical trial results were presented at the 2017 ASCO Annual Meeting.
The most common adverse reactions with pegfilgrastim-cbqv are bone pain and pain in extremities.
The FDA approved the first pegfilgrastim biosimilar, pegfilgrastim-jmdb (Fulphila) in June.
Pegfilgrastim-cbqv will be marketed as Udenyca by Coherus BioSciences.
“Udenyca’s robust clinical package includes a dedicated immunogenicity similarity study in over 300 healthy subjects,” Barbara Finck, MD, chief medical officer of Coherus BioSciences, said in a press release.
“In support of that study, and as part of our commitment to ensuring patient safety, we deployed a battery of sensitive immunogenicity assays. This effort not only supported the biosimilarity of Udenyca but also advanced the understanding of the immunogenic response of pegfilgrastim products.”
Coherus BioSciences plans to provide details about pricing and the launch of pegfilgrastim-cbqv during an earnings call on Nov. 8.
The Food and Drug Administration has approved a second biosimilar to pegfilgrastim (Neulasta) to decrease the chance of infection in patients with nonmyeloid cancer who are receiving myelosuppressive chemotherapy and are at risk of febrile neutropenia.
Approval of pegfilgrastim-cbqv, previously known as CHS-1701, was based on analyses establishing biosimilarity, including pharmacokinetic, pharmacodynamic, and immunogenicity studies. Clinical trial results were presented at the 2017 ASCO Annual Meeting.
The most common adverse reactions with pegfilgrastim-cbqv are bone pain and pain in extremities.
The FDA approved the first pegfilgrastim biosimilar, pegfilgrastim-jmdb (Fulphila) in June.
Pegfilgrastim-cbqv will be marketed as Udenyca by Coherus BioSciences.
“Udenyca’s robust clinical package includes a dedicated immunogenicity similarity study in over 300 healthy subjects,” Barbara Finck, MD, chief medical officer of Coherus BioSciences, said in a press release.
“In support of that study, and as part of our commitment to ensuring patient safety, we deployed a battery of sensitive immunogenicity assays. This effort not only supported the biosimilarity of Udenyca but also advanced the understanding of the immunogenic response of pegfilgrastim products.”
Coherus BioSciences plans to provide details about pricing and the launch of pegfilgrastim-cbqv during an earnings call on Nov. 8.
CMS delays controversial E/M changes in final rule
After a torrent of criticism from the physician community, .
The agency’s final 2019 Physician Fee Schedule, announced Nov. 1, rescinds a proposal that would have blended payments for new and established patients for office/outpatient E/M levels 2 through 5 into single payments. Instead, the agency will continue to hear perspective on the proposal with plans to collapse E/M code levels 2 through 4 into single payments beginning in 2021, while maintaining level 5.
CMS also pulled back its proposal to apply a multiple procedure payment reduction to E/M visits furnished on the same day as a procedure. Payment rates for the less expensive of the two will be maintained, rather than cut in half as initially proposed.
The American Academy of Dermatology Association (AADA) expressed appreciation that CMS took feedback from the physician community seriously and that the agency took steps to eliminate some of its proposals.
“The AADA appreciates the effort and willingness of key decision makers at CMS, at HHS, and on Capitol Hill to hear the concerns of dermatologists and other physicians, and to take them into consideration in developing this final rule,” George J. Hruza, MD, president-elect of the AADA said in an interview. “We appreciate that CMS decided against moving forward with the proposal to make aggressive changes to payment associated with modifier 25 – when an office visit and one or more procedures are provided to a patient on the same day. We are also pleased that CMS made the decision to delay its larger proposal to collapse E/M codes for two years to 2021; this delay gives physicians of different perspectives the opportunity to come together, through the RUC/CPT Workgroup, and work toward developing a solution and a path forward in payment reform.”
Dr. Hruza noted that the AADA worked closely with the American Medical Association and other medical specialty groups to convey their concerns to CMS about the proposed rule, and that they look forward to working with policymakers on further refinements.
The final rule released is much different than the one proposed, which shows that CMS heeded concerns by physicians and took time to craft a more realistic fee schedule, said Orly Avitzur, MD, chair of the American Academy of Neurology’s Medical Economics and Management Committee. The proposed collapsed E/M levels would have likely led to shorter visit times, negatively impacting the doctor-patient relationship and patient care, she said.
“Overall, the American Academy of Neurology was extremely pleased that CMS made several reversals to the proposed rule that indicated that they really listened to our concerns and tried to address them,” Dr. Avitzur said in an interview. “We are very pleased they are giving us an additional 2 years to help us and other stakeholders to give them feedback about how to refine their decision to collapse levels 2, 3, and 4 codes.”
As part of its final rule, CMS moved forward with several other changes to coding and documentation, including eliminating the need to document the medical necessity of a home visit in lieu of an office visit, and allowing physicians to skip documentation of changes since a prior patient visit when relevant information is already contained in the record.
Additionally, the final rule clarifies that for E/M office/outpatient visits physicians do not need to re-enter information on the patient’s chief complaint and history that has already been entered by ancillary staff or the patient. The physician may just indicate in the medical record that he or she has reviewed and verified the information.
In a statement, CMS administrator Seema Verma said the final rule cements dramatic improvements for clinicians and patients and reflects extensive input from the medical community.
“Addressing clinician burnout is critical to keeping doctors in the workforce to meet the growing needs of America’s seniors,” Ms. Verma said in the statement. “[The] rule offers immediate relief from onerous requirements that contribute to burnout in the medical profession and detract from patient care. It also delays even more significant changes to give clinicians the time they need for implementation and provides time for us to continue to work with the medical community on this effort.”
With physicians facing excessive documentation requirements in their practices, it is a relief to see that the administration not only understands the problem of regulatory burden but is taking concrete steps to address it, said Barbara L. McAneny, MD, president of the American Medical Association.
“Patients are likely to see the effect as their physicians will have more time to spend with them and be able to more quickly locate relevant information in medical records,” Dr. McAneny said in a statement. “Implementation of these policies will streamline documentation requirements, reducing paperwork burdens that interfere with a meaningful patient-physician relationship.”
CMS finalized a number of proposals to pay doctors separately for communication technology services. This includes HCPCS code G2012 for brief communication technology-based services, such as virtual check-ins and HCPCS code G2010 for remote evaluation of a recorded video and/or images submitted by an established patient, also known as store and forward.
Additionally, CMS will pay separately for new codes that describe chronic care remote physiologic monitoring (CPT codes 99453, 99454, and 99457) and interprofessional Internet consultation (CPT codes 99451, 99452, 99446, 99447, 99448, and 99449). Also new to the list of reimbursable telehealth services are HCPCS codes G0513 and G0514 for prolonged preventive services.
Telehealth physicians who treat opioid use disorder received more flexibility under the CMS 2019 fee schedule through the agency’s removal of originating site geographic requirements. CMS will now allow a patient’s home to be an originating site for telehealth services for substance use disorder treatment or co-occurring mental health disorder. The agency is also accepting comments on a new Medicare benefit category for opioid use disorder treatment furnished by opioid treatment programs under Part B beginning on or after Jan. 1, 2020.
CMS also approved updates to its Medicare Shared Savings Program, including finalizing time-sensitive program policy changes for currently participating Accountable Care Organizations (ACOs). These changes include:
- A voluntary 6-month extension for existing ACOs whose participation agreements expire on Dec. 31, 2018, and the methodology for determining financial and quality performance for the 6-month performance year from Jan. 1 to June 30, 2019.
- Revising the definition of primary care services used in beneficiary assignment.
- Providing relief for ACOs and their clinicians impacted by extreme and uncontrollable circumstances in 2018 and subsequent years.
After a torrent of criticism from the physician community, .
The agency’s final 2019 Physician Fee Schedule, announced Nov. 1, rescinds a proposal that would have blended payments for new and established patients for office/outpatient E/M levels 2 through 5 into single payments. Instead, the agency will continue to hear perspective on the proposal with plans to collapse E/M code levels 2 through 4 into single payments beginning in 2021, while maintaining level 5.
CMS also pulled back its proposal to apply a multiple procedure payment reduction to E/M visits furnished on the same day as a procedure. Payment rates for the less expensive of the two will be maintained, rather than cut in half as initially proposed.
The American Academy of Dermatology Association (AADA) expressed appreciation that CMS took feedback from the physician community seriously and that the agency took steps to eliminate some of its proposals.
“The AADA appreciates the effort and willingness of key decision makers at CMS, at HHS, and on Capitol Hill to hear the concerns of dermatologists and other physicians, and to take them into consideration in developing this final rule,” George J. Hruza, MD, president-elect of the AADA said in an interview. “We appreciate that CMS decided against moving forward with the proposal to make aggressive changes to payment associated with modifier 25 – when an office visit and one or more procedures are provided to a patient on the same day. We are also pleased that CMS made the decision to delay its larger proposal to collapse E/M codes for two years to 2021; this delay gives physicians of different perspectives the opportunity to come together, through the RUC/CPT Workgroup, and work toward developing a solution and a path forward in payment reform.”
Dr. Hruza noted that the AADA worked closely with the American Medical Association and other medical specialty groups to convey their concerns to CMS about the proposed rule, and that they look forward to working with policymakers on further refinements.
The final rule released is much different than the one proposed, which shows that CMS heeded concerns by physicians and took time to craft a more realistic fee schedule, said Orly Avitzur, MD, chair of the American Academy of Neurology’s Medical Economics and Management Committee. The proposed collapsed E/M levels would have likely led to shorter visit times, negatively impacting the doctor-patient relationship and patient care, she said.
“Overall, the American Academy of Neurology was extremely pleased that CMS made several reversals to the proposed rule that indicated that they really listened to our concerns and tried to address them,” Dr. Avitzur said in an interview. “We are very pleased they are giving us an additional 2 years to help us and other stakeholders to give them feedback about how to refine their decision to collapse levels 2, 3, and 4 codes.”
As part of its final rule, CMS moved forward with several other changes to coding and documentation, including eliminating the need to document the medical necessity of a home visit in lieu of an office visit, and allowing physicians to skip documentation of changes since a prior patient visit when relevant information is already contained in the record.
Additionally, the final rule clarifies that for E/M office/outpatient visits physicians do not need to re-enter information on the patient’s chief complaint and history that has already been entered by ancillary staff or the patient. The physician may just indicate in the medical record that he or she has reviewed and verified the information.
In a statement, CMS administrator Seema Verma said the final rule cements dramatic improvements for clinicians and patients and reflects extensive input from the medical community.
“Addressing clinician burnout is critical to keeping doctors in the workforce to meet the growing needs of America’s seniors,” Ms. Verma said in the statement. “[The] rule offers immediate relief from onerous requirements that contribute to burnout in the medical profession and detract from patient care. It also delays even more significant changes to give clinicians the time they need for implementation and provides time for us to continue to work with the medical community on this effort.”
With physicians facing excessive documentation requirements in their practices, it is a relief to see that the administration not only understands the problem of regulatory burden but is taking concrete steps to address it, said Barbara L. McAneny, MD, president of the American Medical Association.
“Patients are likely to see the effect as their physicians will have more time to spend with them and be able to more quickly locate relevant information in medical records,” Dr. McAneny said in a statement. “Implementation of these policies will streamline documentation requirements, reducing paperwork burdens that interfere with a meaningful patient-physician relationship.”
CMS finalized a number of proposals to pay doctors separately for communication technology services. This includes HCPCS code G2012 for brief communication technology-based services, such as virtual check-ins and HCPCS code G2010 for remote evaluation of a recorded video and/or images submitted by an established patient, also known as store and forward.
Additionally, CMS will pay separately for new codes that describe chronic care remote physiologic monitoring (CPT codes 99453, 99454, and 99457) and interprofessional Internet consultation (CPT codes 99451, 99452, 99446, 99447, 99448, and 99449). Also new to the list of reimbursable telehealth services are HCPCS codes G0513 and G0514 for prolonged preventive services.
Telehealth physicians who treat opioid use disorder received more flexibility under the CMS 2019 fee schedule through the agency’s removal of originating site geographic requirements. CMS will now allow a patient’s home to be an originating site for telehealth services for substance use disorder treatment or co-occurring mental health disorder. The agency is also accepting comments on a new Medicare benefit category for opioid use disorder treatment furnished by opioid treatment programs under Part B beginning on or after Jan. 1, 2020.
CMS also approved updates to its Medicare Shared Savings Program, including finalizing time-sensitive program policy changes for currently participating Accountable Care Organizations (ACOs). These changes include:
- A voluntary 6-month extension for existing ACOs whose participation agreements expire on Dec. 31, 2018, and the methodology for determining financial and quality performance for the 6-month performance year from Jan. 1 to June 30, 2019.
- Revising the definition of primary care services used in beneficiary assignment.
- Providing relief for ACOs and their clinicians impacted by extreme and uncontrollable circumstances in 2018 and subsequent years.
After a torrent of criticism from the physician community, .
The agency’s final 2019 Physician Fee Schedule, announced Nov. 1, rescinds a proposal that would have blended payments for new and established patients for office/outpatient E/M levels 2 through 5 into single payments. Instead, the agency will continue to hear perspective on the proposal with plans to collapse E/M code levels 2 through 4 into single payments beginning in 2021, while maintaining level 5.
CMS also pulled back its proposal to apply a multiple procedure payment reduction to E/M visits furnished on the same day as a procedure. Payment rates for the less expensive of the two will be maintained, rather than cut in half as initially proposed.
The American Academy of Dermatology Association (AADA) expressed appreciation that CMS took feedback from the physician community seriously and that the agency took steps to eliminate some of its proposals.
“The AADA appreciates the effort and willingness of key decision makers at CMS, at HHS, and on Capitol Hill to hear the concerns of dermatologists and other physicians, and to take them into consideration in developing this final rule,” George J. Hruza, MD, president-elect of the AADA said in an interview. “We appreciate that CMS decided against moving forward with the proposal to make aggressive changes to payment associated with modifier 25 – when an office visit and one or more procedures are provided to a patient on the same day. We are also pleased that CMS made the decision to delay its larger proposal to collapse E/M codes for two years to 2021; this delay gives physicians of different perspectives the opportunity to come together, through the RUC/CPT Workgroup, and work toward developing a solution and a path forward in payment reform.”
Dr. Hruza noted that the AADA worked closely with the American Medical Association and other medical specialty groups to convey their concerns to CMS about the proposed rule, and that they look forward to working with policymakers on further refinements.
The final rule released is much different than the one proposed, which shows that CMS heeded concerns by physicians and took time to craft a more realistic fee schedule, said Orly Avitzur, MD, chair of the American Academy of Neurology’s Medical Economics and Management Committee. The proposed collapsed E/M levels would have likely led to shorter visit times, negatively impacting the doctor-patient relationship and patient care, she said.
“Overall, the American Academy of Neurology was extremely pleased that CMS made several reversals to the proposed rule that indicated that they really listened to our concerns and tried to address them,” Dr. Avitzur said in an interview. “We are very pleased they are giving us an additional 2 years to help us and other stakeholders to give them feedback about how to refine their decision to collapse levels 2, 3, and 4 codes.”
As part of its final rule, CMS moved forward with several other changes to coding and documentation, including eliminating the need to document the medical necessity of a home visit in lieu of an office visit, and allowing physicians to skip documentation of changes since a prior patient visit when relevant information is already contained in the record.
Additionally, the final rule clarifies that for E/M office/outpatient visits physicians do not need to re-enter information on the patient’s chief complaint and history that has already been entered by ancillary staff or the patient. The physician may just indicate in the medical record that he or she has reviewed and verified the information.
In a statement, CMS administrator Seema Verma said the final rule cements dramatic improvements for clinicians and patients and reflects extensive input from the medical community.
“Addressing clinician burnout is critical to keeping doctors in the workforce to meet the growing needs of America’s seniors,” Ms. Verma said in the statement. “[The] rule offers immediate relief from onerous requirements that contribute to burnout in the medical profession and detract from patient care. It also delays even more significant changes to give clinicians the time they need for implementation and provides time for us to continue to work with the medical community on this effort.”
With physicians facing excessive documentation requirements in their practices, it is a relief to see that the administration not only understands the problem of regulatory burden but is taking concrete steps to address it, said Barbara L. McAneny, MD, president of the American Medical Association.
“Patients are likely to see the effect as their physicians will have more time to spend with them and be able to more quickly locate relevant information in medical records,” Dr. McAneny said in a statement. “Implementation of these policies will streamline documentation requirements, reducing paperwork burdens that interfere with a meaningful patient-physician relationship.”
CMS finalized a number of proposals to pay doctors separately for communication technology services. This includes HCPCS code G2012 for brief communication technology-based services, such as virtual check-ins and HCPCS code G2010 for remote evaluation of a recorded video and/or images submitted by an established patient, also known as store and forward.
Additionally, CMS will pay separately for new codes that describe chronic care remote physiologic monitoring (CPT codes 99453, 99454, and 99457) and interprofessional Internet consultation (CPT codes 99451, 99452, 99446, 99447, 99448, and 99449). Also new to the list of reimbursable telehealth services are HCPCS codes G0513 and G0514 for prolonged preventive services.
Telehealth physicians who treat opioid use disorder received more flexibility under the CMS 2019 fee schedule through the agency’s removal of originating site geographic requirements. CMS will now allow a patient’s home to be an originating site for telehealth services for substance use disorder treatment or co-occurring mental health disorder. The agency is also accepting comments on a new Medicare benefit category for opioid use disorder treatment furnished by opioid treatment programs under Part B beginning on or after Jan. 1, 2020.
CMS also approved updates to its Medicare Shared Savings Program, including finalizing time-sensitive program policy changes for currently participating Accountable Care Organizations (ACOs). These changes include:
- A voluntary 6-month extension for existing ACOs whose participation agreements expire on Dec. 31, 2018, and the methodology for determining financial and quality performance for the 6-month performance year from Jan. 1 to June 30, 2019.
- Revising the definition of primary care services used in beneficiary assignment.
- Providing relief for ACOs and their clinicians impacted by extreme and uncontrollable circumstances in 2018 and subsequent years.
FDA approves sufentanil for adults with acute pain
The Food and Drug Administration on Nov. 2 approved sufentanil (Dsuvia) for managing acute pain in adult patients in certified, medically supervised health care settings.
Sufentanil, an opioid analgesic manufactured by AcelRx Pharmaceuticals, was approved as a 30-mcg sublingual tablet. The efficacy of Dsuvia was shown in a randomized, clinical trial where patients who received the drug demonstrated significantly greater pain relief after both 15 minutes and 12 hours, compared with placebo.
“As a single-dose, noninvasive medication with a rapid reduction in pain intensity, Dsuvia represents an important alternative for health care providers to offer patients for acute pain management,” David Leiman, MD, of the department of surgery at the University of Texas, Houston, said in the AcelRx press statement.
FDA Commissioner Scott Gottlieb, MD, commented on the approval amid concerns expressed by some, such as the advocacy group Public Citizen, that the drug is “more than 1,000 times more potent than morphine,” and that approval could lead to diversion and abuse – particularly in light of the U.S. opioid epidemic.
In his statement, Dr. Gottlieb identified one broad, significant issue. “Why do we need an oral formulation of sufentanil – a more potent form of fentanyl that’s been approved for intravenous and epidural use in the U.S. since 1984 – on the market?”
In particular, he focused on the needs of the military. The Department of Defense has taken interest in sufentanil as it fulfills a small but specific battlefield need, namely as a means of pain relief in battlefield situations where soldiers cannot swallow oral medication and access to intravenous medication is limited.
Dr. Gottlieb made clear that sufentanil was meant only to be taken in controlled settings and will have strong limitations on its use. It cannot be prescribed for home use, and treatment should be limited to 72 hours. It can only be delivered by health care professionals using a single-dose applicator and will not be available in pharmacies. It is only to be used in patients who have not tolerated or are expected not to tolerate alternative methods of pain management.
“The FDA has implemented a REMS [Risk Evaluation and Mitigation Strategy] that reflects the potential risks associated with this product and mandates that Dsuvia will only be made available for use in a certified medically supervised heath care setting, including its use on the battlefield,” Dr. Gottlieb said.
However, he recognized that the debate runs deeper than how the FDA should mitigate risk over a new drug, and “as a public health agency, we have an obligation to address this question openly and directly. As a physician and regulator, I won’t bypass legitimate questions and concerns related to our role in addressing the opioid crisis,” he said.
Find Dr. Gottlieb’s full statement on the FDA website.
The Food and Drug Administration on Nov. 2 approved sufentanil (Dsuvia) for managing acute pain in adult patients in certified, medically supervised health care settings.
Sufentanil, an opioid analgesic manufactured by AcelRx Pharmaceuticals, was approved as a 30-mcg sublingual tablet. The efficacy of Dsuvia was shown in a randomized, clinical trial where patients who received the drug demonstrated significantly greater pain relief after both 15 minutes and 12 hours, compared with placebo.
“As a single-dose, noninvasive medication with a rapid reduction in pain intensity, Dsuvia represents an important alternative for health care providers to offer patients for acute pain management,” David Leiman, MD, of the department of surgery at the University of Texas, Houston, said in the AcelRx press statement.
FDA Commissioner Scott Gottlieb, MD, commented on the approval amid concerns expressed by some, such as the advocacy group Public Citizen, that the drug is “more than 1,000 times more potent than morphine,” and that approval could lead to diversion and abuse – particularly in light of the U.S. opioid epidemic.
In his statement, Dr. Gottlieb identified one broad, significant issue. “Why do we need an oral formulation of sufentanil – a more potent form of fentanyl that’s been approved for intravenous and epidural use in the U.S. since 1984 – on the market?”
In particular, he focused on the needs of the military. The Department of Defense has taken interest in sufentanil as it fulfills a small but specific battlefield need, namely as a means of pain relief in battlefield situations where soldiers cannot swallow oral medication and access to intravenous medication is limited.
Dr. Gottlieb made clear that sufentanil was meant only to be taken in controlled settings and will have strong limitations on its use. It cannot be prescribed for home use, and treatment should be limited to 72 hours. It can only be delivered by health care professionals using a single-dose applicator and will not be available in pharmacies. It is only to be used in patients who have not tolerated or are expected not to tolerate alternative methods of pain management.
“The FDA has implemented a REMS [Risk Evaluation and Mitigation Strategy] that reflects the potential risks associated with this product and mandates that Dsuvia will only be made available for use in a certified medically supervised heath care setting, including its use on the battlefield,” Dr. Gottlieb said.
However, he recognized that the debate runs deeper than how the FDA should mitigate risk over a new drug, and “as a public health agency, we have an obligation to address this question openly and directly. As a physician and regulator, I won’t bypass legitimate questions and concerns related to our role in addressing the opioid crisis,” he said.
Find Dr. Gottlieb’s full statement on the FDA website.
The Food and Drug Administration on Nov. 2 approved sufentanil (Dsuvia) for managing acute pain in adult patients in certified, medically supervised health care settings.
Sufentanil, an opioid analgesic manufactured by AcelRx Pharmaceuticals, was approved as a 30-mcg sublingual tablet. The efficacy of Dsuvia was shown in a randomized, clinical trial where patients who received the drug demonstrated significantly greater pain relief after both 15 minutes and 12 hours, compared with placebo.
“As a single-dose, noninvasive medication with a rapid reduction in pain intensity, Dsuvia represents an important alternative for health care providers to offer patients for acute pain management,” David Leiman, MD, of the department of surgery at the University of Texas, Houston, said in the AcelRx press statement.
FDA Commissioner Scott Gottlieb, MD, commented on the approval amid concerns expressed by some, such as the advocacy group Public Citizen, that the drug is “more than 1,000 times more potent than morphine,” and that approval could lead to diversion and abuse – particularly in light of the U.S. opioid epidemic.
In his statement, Dr. Gottlieb identified one broad, significant issue. “Why do we need an oral formulation of sufentanil – a more potent form of fentanyl that’s been approved for intravenous and epidural use in the U.S. since 1984 – on the market?”
In particular, he focused on the needs of the military. The Department of Defense has taken interest in sufentanil as it fulfills a small but specific battlefield need, namely as a means of pain relief in battlefield situations where soldiers cannot swallow oral medication and access to intravenous medication is limited.
Dr. Gottlieb made clear that sufentanil was meant only to be taken in controlled settings and will have strong limitations on its use. It cannot be prescribed for home use, and treatment should be limited to 72 hours. It can only be delivered by health care professionals using a single-dose applicator and will not be available in pharmacies. It is only to be used in patients who have not tolerated or are expected not to tolerate alternative methods of pain management.
“The FDA has implemented a REMS [Risk Evaluation and Mitigation Strategy] that reflects the potential risks associated with this product and mandates that Dsuvia will only be made available for use in a certified medically supervised heath care setting, including its use on the battlefield,” Dr. Gottlieb said.
However, he recognized that the debate runs deeper than how the FDA should mitigate risk over a new drug, and “as a public health agency, we have an obligation to address this question openly and directly. As a physician and regulator, I won’t bypass legitimate questions and concerns related to our role in addressing the opioid crisis,” he said.
Find Dr. Gottlieb’s full statement on the FDA website.
Mood Disorders May Worsen Multiple Sclerosis Disability
Patients with depression are more likely to reach EDSS scores of 3.0, 4.0, and 6.0.
BERLIN—Depression and bipolar disorder are major risk factors for worsening disability in people with multiple sclerosis (MS), according to t
Depression increased the risk of having a sustained Expanded Disability Status Scale (EDSS) score of 3.0 by 54%. Depression increased the risk of having a sustained EDSS score of 4.0 by 87%. Depression also doubled the risk of having an EDSS of 6.0.
SSRI treatment also increased the risk of greater disability, with patients exposed to SSRIs having a 40% increased risk of a sustained EDSS of 3.0, a 97% increased risk of having a sustained EDSS of 4.0, and a 2.2-fold increased risk of a sustained EDSS of 6.0.
Prevalent Comorbidities
“We know that mood disorders are highly prevalent in people with MS,” said Stefanie Binzer, MD, at ECTRIMS 2018.
Mood disorders are associated with reduced quality of life, said Dr. Binzer, of the Department of Clinical Neuroscience at the Karolinska Institute in Stockholm. Furthermore, depression is a major risk factor for suicidality in patients with MS. However, prior studies have not established the effect of having a comorbid mood disorder on disability levels of patients with MS.
Dr. Binzer and her coinvestigators analyzed data from 5,875 patients in the Swedish MS registry between 2001 and 2014. By matching these patients to records in the Swedish National Patient Registry and the Swedish National Prescribed Drug Registry, they found that 8.5% of the patients with MS (n = 502) had an International Classification of Diseases, 10th revision (ICD-10) code for depression. Of these patients, 261 had received a diagnosis of depression before their diagnosis of MS.
Of 3,817 patients with MS onset between 2005 and 2014, 27.4% (n = 1,048) had collected at least one prescription for an SSRI.
Patients with MS who had an ICD code for depression or who had received SSRIs “had a significantly increased risk of reaching EDSS 3.0,” Dr. Binzer reported. The age at which patients reached these milestones were younger in both groups when compared with MS patients without depression, she said.
“The difference between the groups [with and without depression] seemed to increase with EDSS,” Dr. Binzer said.
Patients with depression tended to be more likely to convert to secondary progressive MS, with a hazard ratio (HR) of 1.38.
Disability at Younger Ages
A sensitivity analysis found that among those who had depression before their first MS symptom, “the median age when they reached EDSS 3.0 and 4.0 was reduced by three and seven years, respectively,” Dr. Binzer said.
In addition, 1.5% (n = 200) of 13,125 patients with MS diagnosed between 1973 and 2014 were identified with bipolar disorder. It significantly increased the risk of reaching an EDSS score of 4.0 by 58%, but not did not affect the risk of reaching EDSS 3.0 (HR = 1.34) or 6.0 (HR = 1.16).
The investigators’ analysis of the results stratified by sex, conducted because men tend to fare worse than women with MS and progress faster, showed that for depression and bipolar disorder, men were at significantly higher risk of reaching sustained disability milestones. Indeed, compared with women, men with depression had a 61% increased risk, and those with bipolar disorder a 31% increased risk, of reaching an EDSS score of 6.0. They also had 51% and 32% increased risks of conversion to secondary progressive MS, respectively.
“We do not know the mechanisms that underlie these associations,” Dr. Binzer said. “Irrespective of the underlying mechanisms, [the study] clearly shows that it is imperative that we recognize early mood disorders in MS patients and manage them effectively to provide better care and hopefully reduce MS disability worsening.”
The research was funded by the Swedish Research Council and the Swedish Brain Foundation. Dr. Binzer has received speaker fees and travel grants from Biogen.
—Sara Freeman
Patients with depression are more likely to reach EDSS scores of 3.0, 4.0, and 6.0.
Patients with depression are more likely to reach EDSS scores of 3.0, 4.0, and 6.0.
BERLIN—Depression and bipolar disorder are major risk factors for worsening disability in people with multiple sclerosis (MS), according to t
Depression increased the risk of having a sustained Expanded Disability Status Scale (EDSS) score of 3.0 by 54%. Depression increased the risk of having a sustained EDSS score of 4.0 by 87%. Depression also doubled the risk of having an EDSS of 6.0.
SSRI treatment also increased the risk of greater disability, with patients exposed to SSRIs having a 40% increased risk of a sustained EDSS of 3.0, a 97% increased risk of having a sustained EDSS of 4.0, and a 2.2-fold increased risk of a sustained EDSS of 6.0.
Prevalent Comorbidities
“We know that mood disorders are highly prevalent in people with MS,” said Stefanie Binzer, MD, at ECTRIMS 2018.
Mood disorders are associated with reduced quality of life, said Dr. Binzer, of the Department of Clinical Neuroscience at the Karolinska Institute in Stockholm. Furthermore, depression is a major risk factor for suicidality in patients with MS. However, prior studies have not established the effect of having a comorbid mood disorder on disability levels of patients with MS.
Dr. Binzer and her coinvestigators analyzed data from 5,875 patients in the Swedish MS registry between 2001 and 2014. By matching these patients to records in the Swedish National Patient Registry and the Swedish National Prescribed Drug Registry, they found that 8.5% of the patients with MS (n = 502) had an International Classification of Diseases, 10th revision (ICD-10) code for depression. Of these patients, 261 had received a diagnosis of depression before their diagnosis of MS.
Of 3,817 patients with MS onset between 2005 and 2014, 27.4% (n = 1,048) had collected at least one prescription for an SSRI.
Patients with MS who had an ICD code for depression or who had received SSRIs “had a significantly increased risk of reaching EDSS 3.0,” Dr. Binzer reported. The age at which patients reached these milestones were younger in both groups when compared with MS patients without depression, she said.
“The difference between the groups [with and without depression] seemed to increase with EDSS,” Dr. Binzer said.
Patients with depression tended to be more likely to convert to secondary progressive MS, with a hazard ratio (HR) of 1.38.
Disability at Younger Ages
A sensitivity analysis found that among those who had depression before their first MS symptom, “the median age when they reached EDSS 3.0 and 4.0 was reduced by three and seven years, respectively,” Dr. Binzer said.
In addition, 1.5% (n = 200) of 13,125 patients with MS diagnosed between 1973 and 2014 were identified with bipolar disorder. It significantly increased the risk of reaching an EDSS score of 4.0 by 58%, but not did not affect the risk of reaching EDSS 3.0 (HR = 1.34) or 6.0 (HR = 1.16).
The investigators’ analysis of the results stratified by sex, conducted because men tend to fare worse than women with MS and progress faster, showed that for depression and bipolar disorder, men were at significantly higher risk of reaching sustained disability milestones. Indeed, compared with women, men with depression had a 61% increased risk, and those with bipolar disorder a 31% increased risk, of reaching an EDSS score of 6.0. They also had 51% and 32% increased risks of conversion to secondary progressive MS, respectively.
“We do not know the mechanisms that underlie these associations,” Dr. Binzer said. “Irrespective of the underlying mechanisms, [the study] clearly shows that it is imperative that we recognize early mood disorders in MS patients and manage them effectively to provide better care and hopefully reduce MS disability worsening.”
The research was funded by the Swedish Research Council and the Swedish Brain Foundation. Dr. Binzer has received speaker fees and travel grants from Biogen.
—Sara Freeman
BERLIN—Depression and bipolar disorder are major risk factors for worsening disability in people with multiple sclerosis (MS), according to t
Depression increased the risk of having a sustained Expanded Disability Status Scale (EDSS) score of 3.0 by 54%. Depression increased the risk of having a sustained EDSS score of 4.0 by 87%. Depression also doubled the risk of having an EDSS of 6.0.
SSRI treatment also increased the risk of greater disability, with patients exposed to SSRIs having a 40% increased risk of a sustained EDSS of 3.0, a 97% increased risk of having a sustained EDSS of 4.0, and a 2.2-fold increased risk of a sustained EDSS of 6.0.
Prevalent Comorbidities
“We know that mood disorders are highly prevalent in people with MS,” said Stefanie Binzer, MD, at ECTRIMS 2018.
Mood disorders are associated with reduced quality of life, said Dr. Binzer, of the Department of Clinical Neuroscience at the Karolinska Institute in Stockholm. Furthermore, depression is a major risk factor for suicidality in patients with MS. However, prior studies have not established the effect of having a comorbid mood disorder on disability levels of patients with MS.
Dr. Binzer and her coinvestigators analyzed data from 5,875 patients in the Swedish MS registry between 2001 and 2014. By matching these patients to records in the Swedish National Patient Registry and the Swedish National Prescribed Drug Registry, they found that 8.5% of the patients with MS (n = 502) had an International Classification of Diseases, 10th revision (ICD-10) code for depression. Of these patients, 261 had received a diagnosis of depression before their diagnosis of MS.
Of 3,817 patients with MS onset between 2005 and 2014, 27.4% (n = 1,048) had collected at least one prescription for an SSRI.
Patients with MS who had an ICD code for depression or who had received SSRIs “had a significantly increased risk of reaching EDSS 3.0,” Dr. Binzer reported. The age at which patients reached these milestones were younger in both groups when compared with MS patients without depression, she said.
“The difference between the groups [with and without depression] seemed to increase with EDSS,” Dr. Binzer said.
Patients with depression tended to be more likely to convert to secondary progressive MS, with a hazard ratio (HR) of 1.38.
Disability at Younger Ages
A sensitivity analysis found that among those who had depression before their first MS symptom, “the median age when they reached EDSS 3.0 and 4.0 was reduced by three and seven years, respectively,” Dr. Binzer said.
In addition, 1.5% (n = 200) of 13,125 patients with MS diagnosed between 1973 and 2014 were identified with bipolar disorder. It significantly increased the risk of reaching an EDSS score of 4.0 by 58%, but not did not affect the risk of reaching EDSS 3.0 (HR = 1.34) or 6.0 (HR = 1.16).
The investigators’ analysis of the results stratified by sex, conducted because men tend to fare worse than women with MS and progress faster, showed that for depression and bipolar disorder, men were at significantly higher risk of reaching sustained disability milestones. Indeed, compared with women, men with depression had a 61% increased risk, and those with bipolar disorder a 31% increased risk, of reaching an EDSS score of 6.0. They also had 51% and 32% increased risks of conversion to secondary progressive MS, respectively.
“We do not know the mechanisms that underlie these associations,” Dr. Binzer said. “Irrespective of the underlying mechanisms, [the study] clearly shows that it is imperative that we recognize early mood disorders in MS patients and manage them effectively to provide better care and hopefully reduce MS disability worsening.”
The research was funded by the Swedish Research Council and the Swedish Brain Foundation. Dr. Binzer has received speaker fees and travel grants from Biogen.
—Sara Freeman
TIA and Stroke May Affect Risk of Subsequent Events Differently in Patients With Atrial Fibrillation
A history of TIA appears not to increase the risks of stroke and mortality significantly in this population.
MONTREAL—Neurologists usually consider stroke and transient ischemic attack (TIA) to indicate a similar need for anticoagulation, but these events may not entail equivalent risks, according to a presentation given at the 11th World Stroke Congress.
An analysis of two-year follow-up data from the Global Anticoagulant Registry in the Field (GARFIELD-AF), which included more than 52,000 patients with newly diagnosed atrial fibrillation, showed that while patients with a history of stroke had significantly elevated rates of all-cause mortality and stroke, those with a history of TIA alone had rates of mortality and stroke that were virtually identical to those of patients with atrial fibrillation with no history of a cerebrovascular event.
Should Risk Calculators Be Revised?
“A history of TIA [alone] is not a reliable predictor of an increased risk for events,” said Werner Hacke, MD, Professor and Chair of Neurology at the University of Heidelberg in Germany. “A history of TIA should be removed from scores estimating the risk for stroke and systemic embolism in patients with atrial fibrillation.
“The weak predictive power of a history of TIA is probably caused by the relatively low reliability of establishing the diagnosis of TIA,” especially when the diagnosis is made by someone who is not a neurologist. “It is a fuzzy diagnosis,” even for a neurologist, and it consistently confounds other clinicians, he said. “I would be careful about deciding to anticoagulate a patient [with atrial fibrillation] based on a history of TIA. I am convinced that most people with a history of TIA [in the GARFIELD-AF registry] actually never had a TIA.”
Dr. Hacke has been unable to find the reason that TIA began to be considered to entail similar risks as stroke. “I asked all the old atrial fibrillation guys, ‘When did TIA start coming in and why?’ And none of them could remember,” he said. “At first, they talked about a history of cerebrovascular events, but then that became stroke and TIA, and it was as if it was one word” always said in the same breath. The CHADS2 score and the CHA2DS2-VASc score make a history of stroke or TIA, as well as thromboembolism, coequal risk factors that count for 2 points when calculating the thrombotic risk score for a patient with atrial fibrillation.
An Examination of Registry Data
To test whether this convention was appropriate, Dr. Hacke and his associates examined the consequences of a history of stroke alone, compared with those of a history of a TIA alone. They used data collected in GARFIELD-AF, a multinational registry with 51,670 patients newly diagnosed with atrial fibrillation who were followed for two years. All participants had complete information on their stroke and TIA history. This information included 5,617 patients with a history of at least one diagnosed cerebrovascular event, including 3,362 diagnosed with stroke alone, 1,788 diagnosed with TIA alone, and the remaining patients diagnosed with both events.
When compared with patients with atrial fibrillation without a history of any type of cerebrovascular event, those with a history of a stroke alone had a statistically significant 29% increased rate of all-cause death and a 2.3-fold higher rate of stroke after adjustment for baseline demographic and clinical differences. In contrast, the patients with a history of TIA alone had mortality and stroke rates during follow-up that did not differ significantly from the comparator group.
—Mitchel L. Zoler
A history of TIA appears not to increase the risks of stroke and mortality significantly in this population.
A history of TIA appears not to increase the risks of stroke and mortality significantly in this population.
MONTREAL—Neurologists usually consider stroke and transient ischemic attack (TIA) to indicate a similar need for anticoagulation, but these events may not entail equivalent risks, according to a presentation given at the 11th World Stroke Congress.
An analysis of two-year follow-up data from the Global Anticoagulant Registry in the Field (GARFIELD-AF), which included more than 52,000 patients with newly diagnosed atrial fibrillation, showed that while patients with a history of stroke had significantly elevated rates of all-cause mortality and stroke, those with a history of TIA alone had rates of mortality and stroke that were virtually identical to those of patients with atrial fibrillation with no history of a cerebrovascular event.
Should Risk Calculators Be Revised?
“A history of TIA [alone] is not a reliable predictor of an increased risk for events,” said Werner Hacke, MD, Professor and Chair of Neurology at the University of Heidelberg in Germany. “A history of TIA should be removed from scores estimating the risk for stroke and systemic embolism in patients with atrial fibrillation.
“The weak predictive power of a history of TIA is probably caused by the relatively low reliability of establishing the diagnosis of TIA,” especially when the diagnosis is made by someone who is not a neurologist. “It is a fuzzy diagnosis,” even for a neurologist, and it consistently confounds other clinicians, he said. “I would be careful about deciding to anticoagulate a patient [with atrial fibrillation] based on a history of TIA. I am convinced that most people with a history of TIA [in the GARFIELD-AF registry] actually never had a TIA.”
Dr. Hacke has been unable to find the reason that TIA began to be considered to entail similar risks as stroke. “I asked all the old atrial fibrillation guys, ‘When did TIA start coming in and why?’ And none of them could remember,” he said. “At first, they talked about a history of cerebrovascular events, but then that became stroke and TIA, and it was as if it was one word” always said in the same breath. The CHADS2 score and the CHA2DS2-VASc score make a history of stroke or TIA, as well as thromboembolism, coequal risk factors that count for 2 points when calculating the thrombotic risk score for a patient with atrial fibrillation.
An Examination of Registry Data
To test whether this convention was appropriate, Dr. Hacke and his associates examined the consequences of a history of stroke alone, compared with those of a history of a TIA alone. They used data collected in GARFIELD-AF, a multinational registry with 51,670 patients newly diagnosed with atrial fibrillation who were followed for two years. All participants had complete information on their stroke and TIA history. This information included 5,617 patients with a history of at least one diagnosed cerebrovascular event, including 3,362 diagnosed with stroke alone, 1,788 diagnosed with TIA alone, and the remaining patients diagnosed with both events.
When compared with patients with atrial fibrillation without a history of any type of cerebrovascular event, those with a history of a stroke alone had a statistically significant 29% increased rate of all-cause death and a 2.3-fold higher rate of stroke after adjustment for baseline demographic and clinical differences. In contrast, the patients with a history of TIA alone had mortality and stroke rates during follow-up that did not differ significantly from the comparator group.
—Mitchel L. Zoler
MONTREAL—Neurologists usually consider stroke and transient ischemic attack (TIA) to indicate a similar need for anticoagulation, but these events may not entail equivalent risks, according to a presentation given at the 11th World Stroke Congress.
An analysis of two-year follow-up data from the Global Anticoagulant Registry in the Field (GARFIELD-AF), which included more than 52,000 patients with newly diagnosed atrial fibrillation, showed that while patients with a history of stroke had significantly elevated rates of all-cause mortality and stroke, those with a history of TIA alone had rates of mortality and stroke that were virtually identical to those of patients with atrial fibrillation with no history of a cerebrovascular event.
Should Risk Calculators Be Revised?
“A history of TIA [alone] is not a reliable predictor of an increased risk for events,” said Werner Hacke, MD, Professor and Chair of Neurology at the University of Heidelberg in Germany. “A history of TIA should be removed from scores estimating the risk for stroke and systemic embolism in patients with atrial fibrillation.
“The weak predictive power of a history of TIA is probably caused by the relatively low reliability of establishing the diagnosis of TIA,” especially when the diagnosis is made by someone who is not a neurologist. “It is a fuzzy diagnosis,” even for a neurologist, and it consistently confounds other clinicians, he said. “I would be careful about deciding to anticoagulate a patient [with atrial fibrillation] based on a history of TIA. I am convinced that most people with a history of TIA [in the GARFIELD-AF registry] actually never had a TIA.”
Dr. Hacke has been unable to find the reason that TIA began to be considered to entail similar risks as stroke. “I asked all the old atrial fibrillation guys, ‘When did TIA start coming in and why?’ And none of them could remember,” he said. “At first, they talked about a history of cerebrovascular events, but then that became stroke and TIA, and it was as if it was one word” always said in the same breath. The CHADS2 score and the CHA2DS2-VASc score make a history of stroke or TIA, as well as thromboembolism, coequal risk factors that count for 2 points when calculating the thrombotic risk score for a patient with atrial fibrillation.
An Examination of Registry Data
To test whether this convention was appropriate, Dr. Hacke and his associates examined the consequences of a history of stroke alone, compared with those of a history of a TIA alone. They used data collected in GARFIELD-AF, a multinational registry with 51,670 patients newly diagnosed with atrial fibrillation who were followed for two years. All participants had complete information on their stroke and TIA history. This information included 5,617 patients with a history of at least one diagnosed cerebrovascular event, including 3,362 diagnosed with stroke alone, 1,788 diagnosed with TIA alone, and the remaining patients diagnosed with both events.
When compared with patients with atrial fibrillation without a history of any type of cerebrovascular event, those with a history of a stroke alone had a statistically significant 29% increased rate of all-cause death and a 2.3-fold higher rate of stroke after adjustment for baseline demographic and clinical differences. In contrast, the patients with a history of TIA alone had mortality and stroke rates during follow-up that did not differ significantly from the comparator group.
—Mitchel L. Zoler
Comorbidities are important in psoriasis care
LAS VEGAS – Pay attention to comorbidities in your psoriasis patients because there may not be anyone else doing so.
“Many of our patients don’t have primary care physicians; many are untreated for psoriasis. They come to a clinical trial to get treated – some of them may not have insurance – so it is important for us to watch for these comorbidities,” Kristina C. Duffin, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Yet, that does not seem to be happening consistently, according to Dr. Duffin, of the department of dermatology at the University of Utah, Salt Lake City. One in five dermatologists admitted to never screening or referring their psoriasis patients for management of cardiovascular risks in a 2015 survey (J Am Acad Dermatol. 2015 doi: 10.1016/j.jaad.2015.07.029).
Often patients at the start of biologic therapy are counseled about the risk for developing tuberculosis, yet the lifetime risk for doing so in the United States is 0.3%. Similarly, patients are often counseled on the risk for developing lymphoma, even though the excess risk for developing lymphoma that can be attributed to psoriasis treatment is 7.9 per 100,000 psoriasis patients per year. That screening seems to be driven by warnings issued in direct-to-consumer advertising, Dr. Duffin suggested.
“Although psoriasis patients have an increased relative risk of lymphoma, the absolute risk attributable to psoriasis is low,” Dr. Duffin pointed out.
Some of the comorbidities she advised dermatologists to watch for are described below.
Psoriatic arthritis
Psoriatic arthritis is the most important psoriasis comorbidity, Dr. Duffin said. Between 20% and 30% of psoriasis patients will develop psoriatic arthritis.
In a study of 1,511 patients in 48 centers in Germany, 21% of psoriasis patients were diagnosed with psoriatic arthritis and of those, more than 95% had active arthritis and 53% had five or more affected joints (Br J Dermatol. 2009;160[5]:1040-7).
The GRAPPA app is an easy, free screening tool for psoriatic arthritis; patients who score 3 or more out of 5 items on the psoriasis epidemiology screening tool (PEST) are deemed positive for psoriatic arthritis, Dr. Duffin noted.
Cardiovascular disease
Psoriasis patients are at increased risk of myocardial infarction, stroke, cardiovascular death, diabetes, and chronic kidney disease, Dr. Duffin said. In fact, CV risk from severe psoriasis is similar to the risk conferred by diabetes.
She added that there is epidemiologic evidence for CV risk modification with several of the biologics approved for psoriasis.
Hypertension
Hypertension is prevalent and more severe in psoriasis patients, Dr. Duffin said, citing a 2011 case-control study of electronic medical records at the University of California, Davis. Psoriasis patients with hypertension were 5 times more likely than patients without psoriasis to be on one antihypertensive medication, 9.5 times more likely to be on two, and almost 20 times more likely to be on four antihypertensive medications (PLoS One. 2011 Mar 29;6[3]:e18227. doi: 10.1371/journal.pone.0018227).
Importantly, few primary care physicians and cardiologists are aware of the increased risk for hypertension in psoriasis patients.
Less than half (45%) of primary care physicians and 57% of cardiologists reported they were aware that psoriasis was associated with worse cardiovascular outcome, and only 43% of physicians reported screening psoriasis patients for hypertension starting at age 20 years, according to a 2012 survey of 251 physicians (J Am Acad Dermatol. 2012 Sep;67[3]:357-62).
Dr. Duffin called on dermatologists to ensure that the primary care physicians they work with understand these increased risks.
“Commit to including a comment in consultation letters or letters back to primary care physicians that talks about the cardiovascular risks of the disease,” she said.
Dr. Duffin reported that she is a consultant and has received grant or contracted research support for many companies that manufacture dermatologic therapies.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Pay attention to comorbidities in your psoriasis patients because there may not be anyone else doing so.
“Many of our patients don’t have primary care physicians; many are untreated for psoriasis. They come to a clinical trial to get treated – some of them may not have insurance – so it is important for us to watch for these comorbidities,” Kristina C. Duffin, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Yet, that does not seem to be happening consistently, according to Dr. Duffin, of the department of dermatology at the University of Utah, Salt Lake City. One in five dermatologists admitted to never screening or referring their psoriasis patients for management of cardiovascular risks in a 2015 survey (J Am Acad Dermatol. 2015 doi: 10.1016/j.jaad.2015.07.029).
Often patients at the start of biologic therapy are counseled about the risk for developing tuberculosis, yet the lifetime risk for doing so in the United States is 0.3%. Similarly, patients are often counseled on the risk for developing lymphoma, even though the excess risk for developing lymphoma that can be attributed to psoriasis treatment is 7.9 per 100,000 psoriasis patients per year. That screening seems to be driven by warnings issued in direct-to-consumer advertising, Dr. Duffin suggested.
“Although psoriasis patients have an increased relative risk of lymphoma, the absolute risk attributable to psoriasis is low,” Dr. Duffin pointed out.
Some of the comorbidities she advised dermatologists to watch for are described below.
Psoriatic arthritis
Psoriatic arthritis is the most important psoriasis comorbidity, Dr. Duffin said. Between 20% and 30% of psoriasis patients will develop psoriatic arthritis.
In a study of 1,511 patients in 48 centers in Germany, 21% of psoriasis patients were diagnosed with psoriatic arthritis and of those, more than 95% had active arthritis and 53% had five or more affected joints (Br J Dermatol. 2009;160[5]:1040-7).
The GRAPPA app is an easy, free screening tool for psoriatic arthritis; patients who score 3 or more out of 5 items on the psoriasis epidemiology screening tool (PEST) are deemed positive for psoriatic arthritis, Dr. Duffin noted.
Cardiovascular disease
Psoriasis patients are at increased risk of myocardial infarction, stroke, cardiovascular death, diabetes, and chronic kidney disease, Dr. Duffin said. In fact, CV risk from severe psoriasis is similar to the risk conferred by diabetes.
She added that there is epidemiologic evidence for CV risk modification with several of the biologics approved for psoriasis.
Hypertension
Hypertension is prevalent and more severe in psoriasis patients, Dr. Duffin said, citing a 2011 case-control study of electronic medical records at the University of California, Davis. Psoriasis patients with hypertension were 5 times more likely than patients without psoriasis to be on one antihypertensive medication, 9.5 times more likely to be on two, and almost 20 times more likely to be on four antihypertensive medications (PLoS One. 2011 Mar 29;6[3]:e18227. doi: 10.1371/journal.pone.0018227).
Importantly, few primary care physicians and cardiologists are aware of the increased risk for hypertension in psoriasis patients.
Less than half (45%) of primary care physicians and 57% of cardiologists reported they were aware that psoriasis was associated with worse cardiovascular outcome, and only 43% of physicians reported screening psoriasis patients for hypertension starting at age 20 years, according to a 2012 survey of 251 physicians (J Am Acad Dermatol. 2012 Sep;67[3]:357-62).
Dr. Duffin called on dermatologists to ensure that the primary care physicians they work with understand these increased risks.
“Commit to including a comment in consultation letters or letters back to primary care physicians that talks about the cardiovascular risks of the disease,” she said.
Dr. Duffin reported that she is a consultant and has received grant or contracted research support for many companies that manufacture dermatologic therapies.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Pay attention to comorbidities in your psoriasis patients because there may not be anyone else doing so.
“Many of our patients don’t have primary care physicians; many are untreated for psoriasis. They come to a clinical trial to get treated – some of them may not have insurance – so it is important for us to watch for these comorbidities,” Kristina C. Duffin, MD, said at Skin Disease Education Foundation’s annual Las Vegas Dermatology Seminar.
Yet, that does not seem to be happening consistently, according to Dr. Duffin, of the department of dermatology at the University of Utah, Salt Lake City. One in five dermatologists admitted to never screening or referring their psoriasis patients for management of cardiovascular risks in a 2015 survey (J Am Acad Dermatol. 2015 doi: 10.1016/j.jaad.2015.07.029).
Often patients at the start of biologic therapy are counseled about the risk for developing tuberculosis, yet the lifetime risk for doing so in the United States is 0.3%. Similarly, patients are often counseled on the risk for developing lymphoma, even though the excess risk for developing lymphoma that can be attributed to psoriasis treatment is 7.9 per 100,000 psoriasis patients per year. That screening seems to be driven by warnings issued in direct-to-consumer advertising, Dr. Duffin suggested.
“Although psoriasis patients have an increased relative risk of lymphoma, the absolute risk attributable to psoriasis is low,” Dr. Duffin pointed out.
Some of the comorbidities she advised dermatologists to watch for are described below.
Psoriatic arthritis
Psoriatic arthritis is the most important psoriasis comorbidity, Dr. Duffin said. Between 20% and 30% of psoriasis patients will develop psoriatic arthritis.
In a study of 1,511 patients in 48 centers in Germany, 21% of psoriasis patients were diagnosed with psoriatic arthritis and of those, more than 95% had active arthritis and 53% had five or more affected joints (Br J Dermatol. 2009;160[5]:1040-7).
The GRAPPA app is an easy, free screening tool for psoriatic arthritis; patients who score 3 or more out of 5 items on the psoriasis epidemiology screening tool (PEST) are deemed positive for psoriatic arthritis, Dr. Duffin noted.
Cardiovascular disease
Psoriasis patients are at increased risk of myocardial infarction, stroke, cardiovascular death, diabetes, and chronic kidney disease, Dr. Duffin said. In fact, CV risk from severe psoriasis is similar to the risk conferred by diabetes.
She added that there is epidemiologic evidence for CV risk modification with several of the biologics approved for psoriasis.
Hypertension
Hypertension is prevalent and more severe in psoriasis patients, Dr. Duffin said, citing a 2011 case-control study of electronic medical records at the University of California, Davis. Psoriasis patients with hypertension were 5 times more likely than patients without psoriasis to be on one antihypertensive medication, 9.5 times more likely to be on two, and almost 20 times more likely to be on four antihypertensive medications (PLoS One. 2011 Mar 29;6[3]:e18227. doi: 10.1371/journal.pone.0018227).
Importantly, few primary care physicians and cardiologists are aware of the increased risk for hypertension in psoriasis patients.
Less than half (45%) of primary care physicians and 57% of cardiologists reported they were aware that psoriasis was associated with worse cardiovascular outcome, and only 43% of physicians reported screening psoriasis patients for hypertension starting at age 20 years, according to a 2012 survey of 251 physicians (J Am Acad Dermatol. 2012 Sep;67[3]:357-62).
Dr. Duffin called on dermatologists to ensure that the primary care physicians they work with understand these increased risks.
“Commit to including a comment in consultation letters or letters back to primary care physicians that talks about the cardiovascular risks of the disease,” she said.
Dr. Duffin reported that she is a consultant and has received grant or contracted research support for many companies that manufacture dermatologic therapies.
SDEF and this news organization are owned by the same parent company.
REPORTING FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Concomitant Fibrofolliculoma and Trichodiscoma on the Abdomen
Fibrofolliculomas and trichodiscomas typically present on the head or neck as smooth, flesh-colored, dome-shaped papules. These two entities are considered to constitute two separate time points on a spectrum of histopathologic changes in mantleoma differentiation.1 Histologically, both are benign hamartomas of the pilosebaceous subunit and collectively are known as mantleomas. We present an unusual case of a concomitant fibrofolliculoma and trichodiscoma on the abdomen.
Case Report
An asymptomatic 54-year-old man presented for a routine full-body skin examination. A solitary, 2×1-cm, subcutaneous, doughy, mobile nodule was found on the left side of the abdomen with an overlying 2-mm yellow fleshy papule. The patient declined excision of the lesion, and it was recommended that he return for follow-up 3 months later.
The patient did not present for follow-up until 4.5 years later, at which point the lesion had grown to 3.0×2.5 cm in size. An excision was performed, at which time the lesion was noted to be cystic, extruding an oily, yellow-white liquid. Bacterial culture was negative. Histopathologic sections showed a dome-shaped papule with connection to the overlying epidermis. Epithelial extensions from the infundibular epithelium formed a fenestrated pattern surrounding a fibrous and mucinous stroma (Figure, A and B). The differential diagnosis at this time included an epidermal inclusion cyst, fibroma, intradermal nevus, verruca, hemangioma, angiofibroma, and lipoma.2-4
The same lesion cut in a different plane of sectioning showed an expansile dermal nodule comprising clusters of sebaceous lobules surrounding a fibrous and mucinous stroma. Within the second lesion, fibrous and stromal components predominated over epithelial components (Figure, C). A diagnosis of fibrofolliculoma showing features of a trichodiscoma arising in the unusual location of the abdomen was made.
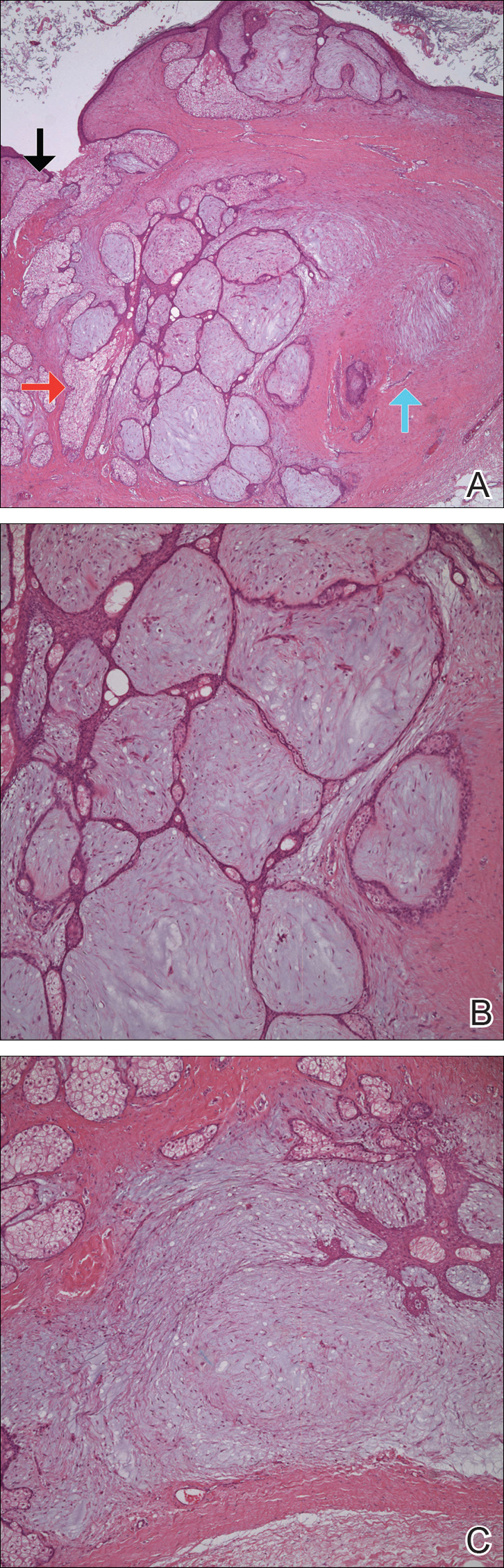
Comment
Solitary fibrofolliculomas and trichodiscomas are flesh-colored, dome-shaped papules that generally present on the face, specifically on the chin, nose, cheeks, ears, and eyebrows without considerable symptoms.2,4,5 Clinically, fibrofolliculomas are indistinguishable from trichodiscomas but demonstrate different features on biopsy.1,5
Fibrofolliculomas and trichodiscomas are well known for their association with Birt-Hogg-Dubé (BHD) syndrome when they present concomitantly and typically arise earlier in the third decade of life than solitary fibrofolliculomas; however, there have been reports of solitary fibrofolliculomas in patients aged 1 to 36 years.4,6 The triad of BHD syndrome consists of multiple fibrofolliculomas, trichodiscomas, and acrochordons, and it is acquired in an autosomal-dominant manner, unlike solitary fibrofolliculomas, which typically are not inherited. Birt-Hogg-Dubé syndrome is caused by a mutation in the FLCN gene that codes for the tumor-suppressor protein folliculin, which when mutated can cause unregulated proliferation of cells.7 Solitary fibrofolliculomas and the multiple fibrofolliculomas seen in BHD syndrome are histologically similar.
Fibrofolliculoma can be clinically indistinguishable from fibroepithelioma of Pinkus, perifollicular fibroma, trichilemmoma, trichodiscoma, trichoepithelioma, and trichofolliculoma. All typically present clinically as flesh-colored papules,1 although histologic distinction can be made (Table).5,8-13
Fibrofolliculoma is a benign hamartoma that arises from the pilosebaceous follicle and consists of an expansion of the fibrous root sheath, which typically surrounds the hair follicle along with proliferating bands or ribbons of perifollicular connective tissue. As such, the hair follicle may be dilated and filled with keratin in the expanded infundibulum.8 Follicles also may be surrounded by a myxoid stroma.2 In contrast, trichodiscoma is characterized by connective tissue with mature sebaceous lobules in the periphery. It has a myxoid stroma, as opposed to the more fibrous stroma seen in fibrofolliculomas.
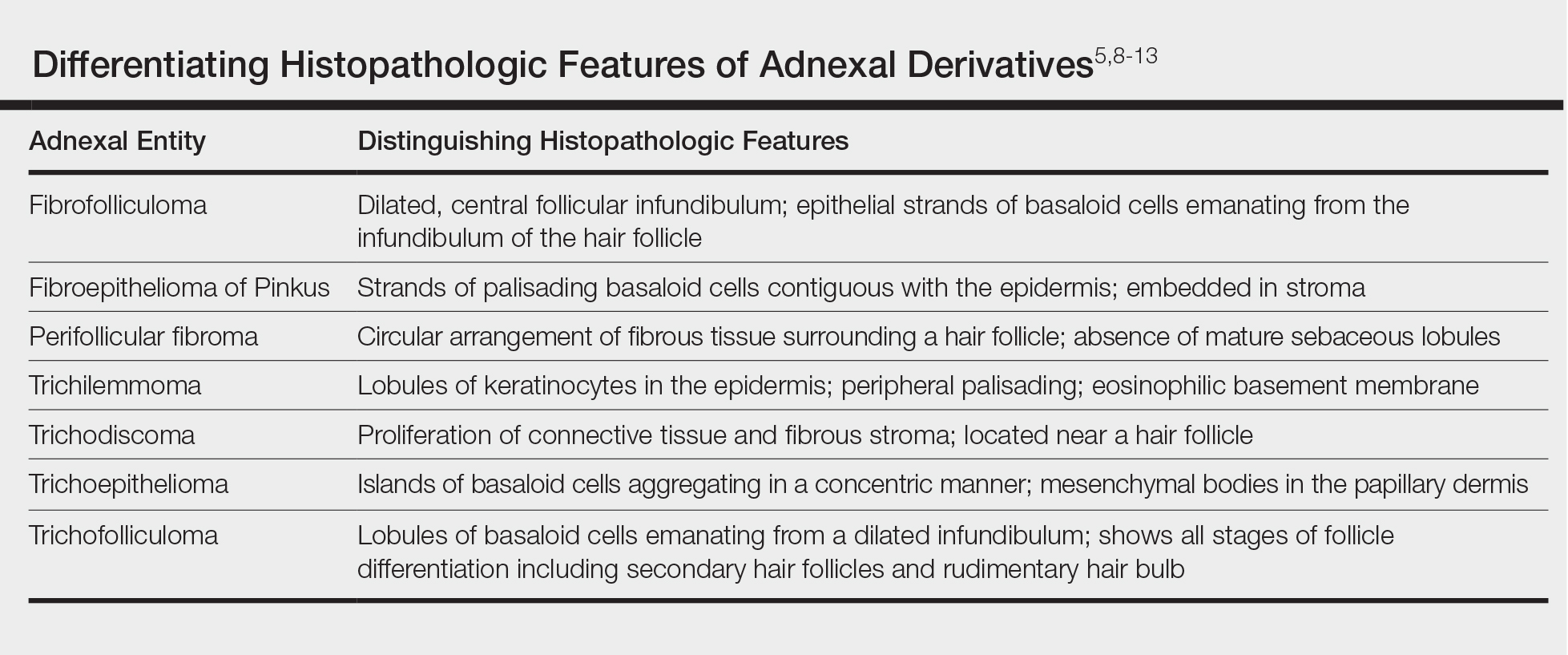
Reports have examined the staining patterns of fibrofolliculomas, which show characteristics similar to those of other hair follicle hamartomas, including trichodiscomas.10 The connective tissue and epithelial components that constitute a fibrofolliculoma show different staining patterns. The connective tissue component stains positive for CD34 spindle cells, factor XIIIa, and nestin (a marker of angiogenesis). CD117 (c-kit) expression in the stroma, a marker of fibrocytes, is a feature of both fibrofolliculoma and perifollicular fibromas. The epithelial component, consisting of the hair follicle itself, stains positive for CK15. CK15 expression has been reported in undifferentiated sebocytes of the mantle and in the hair follicle.10 Immunohistochemical staining supports the notion that fibrofolliculomas contain connective tissue and epithelial components and helps to compare and contrast them to those of other hair follicle hamartomas.
Ackerman et al1 considered both fibrofolliculomas and trichodiscomas to be hamartomas of the epithelial hair follicle. The exact etiology of each of these hamartomas is unknown, but the undifferentiated epithelial strands protruding from the hair follicle in a fibrofolliculoma lie in close proximity to sebaceous glands. Furthermore, the authors postulated that fibrofolliculomas and trichodiscomas constitute a spectrum that encompasses the differentiation process of a mantleoma, with fibrofolliculoma representing the beginning of mantleoma differentiation and trichodiscoma representing the end. This end stage of follicular differentiation is one in which there is a predominant stroma and the previously undifferentiated epithelium has formed into sebaceous ducts and lobules in the stroma.1
Most cases of fibrofolliculoma and/or trichodiscoma arise in areas of dense sebaceous follicle concentration (eg, face), further supporting the hypothesis that sebaceous gland proliferation contributes to fibrofolliculoma.14 The case described here, with the fibrofolliculoma arising on the abdomen in conjunction with a trichodiscoma, is therefore worth noting because its location differs from what has been observed in previously reported cases.4
There are both surgical and medical options for treatment of fibrofolliculoma. Although surgical excision is an option for a single lesion, patients with multiple fibrofolliculomas or BHD may prefer removal with the combined CO2 laser and erbium-doped YAG laser.15
Conclusion
We present a rare case of concomitant fibrofolliculoma and trichodiscoma arising on the unusual location of the abdomen. This report highlights the histopathologic features of multiple adnexal tumors and emphasizes the importance of biopsy for differentiating fibrofolliculoma and trichodiscoma.
- Ackerman AB, Chongchitnant N, DeViragh P. Neoplasms with Follicular Differentiation. Philadelphia, PA: Lea & Febiger; 1993.
- Scully K, Bargman H, Assaad D. Solitary fibrofolliculoma. J Am Acad Dermatol. 1984;11:361-363.
- Chang JK, Lee DC, Chang MH. A solitary fibrofolliculoma in the eyelid. Korean J Ophthalmol. 2007;21:169-171.
- Starink TM, Brownstein MH. Fibrofolliculoma: solitary and multiple types. J Am Acad Dermatol. 1987;17:493-496.
- Cho EU, Lee JD, Cho SH. A solitary fibrofolliculoma on the concha of the ear. Int J Dermatol. 2012;51:616-628.
- Mo HJ, Park CK, Yi JY. A case of solitary fibrofolliculoma. Korean J Dermatol. 2001;39:602-604.
- Nickerson ML, Warren MB, Toro JR, et al. Mutations in a novel gene lead to kidney tumors, lung wall defects, and benign tumors of the hair follicle in patients with the Birt-Hogg-Dubé syndrome. Cancer Cell. 2002;2:157-164.
- Birt AR, Hogg GR, Dubé WJ. Hereditary multiple fibrofolliculomas with trichodiscomas and acrochordons. Arch Dermatol. 1977;113:1674-1677.
- Foucar K, Rosen TH, Foucar E, et al. Fibrofolliculoma: a clinicopathologic study. Cutis. 1981;28:429-432.
- Misago NO, Kimura TE, Narisawa YU. Fibrofolliculoma/trichodiscoma and fibrous papule (perifollicular fibroma/angiofibroma): a revaluation of the histopathological and immunohistochemical features. J Cutan Pathol. 2009;36:943-951.
- Schaffer JV, Gohara MA, McNiff JM, et al. Multiple facial angiofibromas: a cutaneous manifestation of Birt-Hogg-Dubé syndrome. J Am Acad Dermatol. 2005;53(2 suppl 1):S108-S111.
- Lee Y, Su H, Chen H. Fibroepithelioma of Pinkus. a case report. Dermatologica Sinica. 2002;20:142-146.
- Nam JH, Min JH, Lee GY, et al. A case of perifollicular fibroma. Ann Dermatol. 2011:23:236-238.
- Vernooij M, Claessens T, Luijten M, et al. Birt-Hogg-Dubé syndrome and the skin. Fam Cancer. 2013;12:381-385.
- Jacob CI, Dover JS. Birt-Hogg-Dubé syndrome: treatment of cutaneous manifestations with laser skin resurfacing. Arch Dermatol. 2001;137:98-99.
Fibrofolliculomas and trichodiscomas typically present on the head or neck as smooth, flesh-colored, dome-shaped papules. These two entities are considered to constitute two separate time points on a spectrum of histopathologic changes in mantleoma differentiation.1 Histologically, both are benign hamartomas of the pilosebaceous subunit and collectively are known as mantleomas. We present an unusual case of a concomitant fibrofolliculoma and trichodiscoma on the abdomen.
Case Report
An asymptomatic 54-year-old man presented for a routine full-body skin examination. A solitary, 2×1-cm, subcutaneous, doughy, mobile nodule was found on the left side of the abdomen with an overlying 2-mm yellow fleshy papule. The patient declined excision of the lesion, and it was recommended that he return for follow-up 3 months later.
The patient did not present for follow-up until 4.5 years later, at which point the lesion had grown to 3.0×2.5 cm in size. An excision was performed, at which time the lesion was noted to be cystic, extruding an oily, yellow-white liquid. Bacterial culture was negative. Histopathologic sections showed a dome-shaped papule with connection to the overlying epidermis. Epithelial extensions from the infundibular epithelium formed a fenestrated pattern surrounding a fibrous and mucinous stroma (Figure, A and B). The differential diagnosis at this time included an epidermal inclusion cyst, fibroma, intradermal nevus, verruca, hemangioma, angiofibroma, and lipoma.2-4
The same lesion cut in a different plane of sectioning showed an expansile dermal nodule comprising clusters of sebaceous lobules surrounding a fibrous and mucinous stroma. Within the second lesion, fibrous and stromal components predominated over epithelial components (Figure, C). A diagnosis of fibrofolliculoma showing features of a trichodiscoma arising in the unusual location of the abdomen was made.
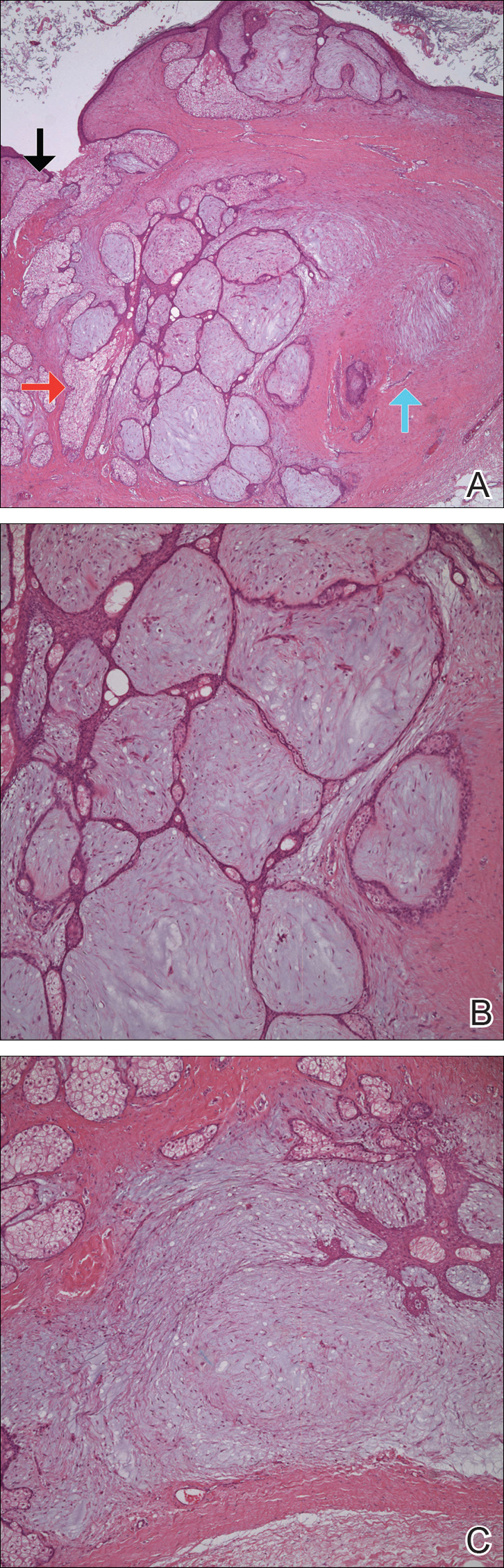
Comment
Solitary fibrofolliculomas and trichodiscomas are flesh-colored, dome-shaped papules that generally present on the face, specifically on the chin, nose, cheeks, ears, and eyebrows without considerable symptoms.2,4,5 Clinically, fibrofolliculomas are indistinguishable from trichodiscomas but demonstrate different features on biopsy.1,5
Fibrofolliculomas and trichodiscomas are well known for their association with Birt-Hogg-Dubé (BHD) syndrome when they present concomitantly and typically arise earlier in the third decade of life than solitary fibrofolliculomas; however, there have been reports of solitary fibrofolliculomas in patients aged 1 to 36 years.4,6 The triad of BHD syndrome consists of multiple fibrofolliculomas, trichodiscomas, and acrochordons, and it is acquired in an autosomal-dominant manner, unlike solitary fibrofolliculomas, which typically are not inherited. Birt-Hogg-Dubé syndrome is caused by a mutation in the FLCN gene that codes for the tumor-suppressor protein folliculin, which when mutated can cause unregulated proliferation of cells.7 Solitary fibrofolliculomas and the multiple fibrofolliculomas seen in BHD syndrome are histologically similar.
Fibrofolliculoma can be clinically indistinguishable from fibroepithelioma of Pinkus, perifollicular fibroma, trichilemmoma, trichodiscoma, trichoepithelioma, and trichofolliculoma. All typically present clinically as flesh-colored papules,1 although histologic distinction can be made (Table).5,8-13
Fibrofolliculoma is a benign hamartoma that arises from the pilosebaceous follicle and consists of an expansion of the fibrous root sheath, which typically surrounds the hair follicle along with proliferating bands or ribbons of perifollicular connective tissue. As such, the hair follicle may be dilated and filled with keratin in the expanded infundibulum.8 Follicles also may be surrounded by a myxoid stroma.2 In contrast, trichodiscoma is characterized by connective tissue with mature sebaceous lobules in the periphery. It has a myxoid stroma, as opposed to the more fibrous stroma seen in fibrofolliculomas.
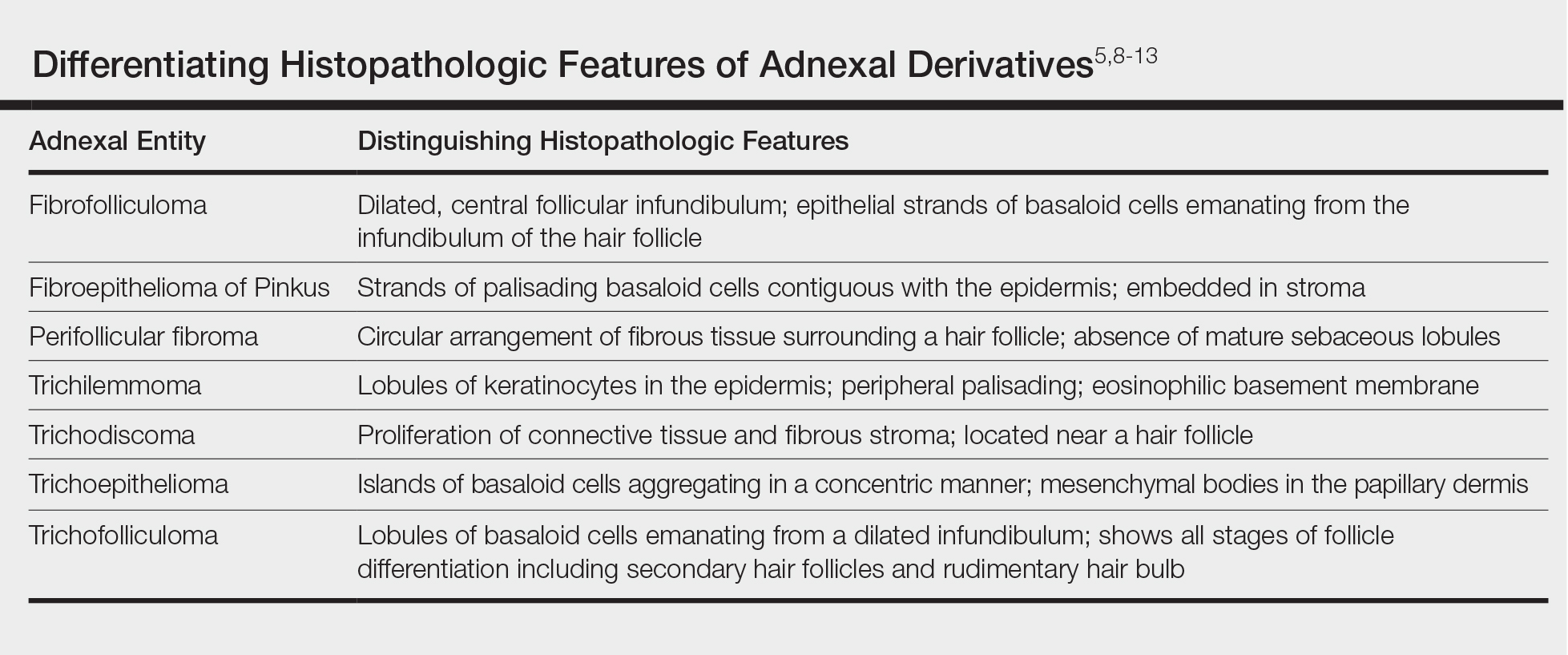
Reports have examined the staining patterns of fibrofolliculomas, which show characteristics similar to those of other hair follicle hamartomas, including trichodiscomas.10 The connective tissue and epithelial components that constitute a fibrofolliculoma show different staining patterns. The connective tissue component stains positive for CD34 spindle cells, factor XIIIa, and nestin (a marker of angiogenesis). CD117 (c-kit) expression in the stroma, a marker of fibrocytes, is a feature of both fibrofolliculoma and perifollicular fibromas. The epithelial component, consisting of the hair follicle itself, stains positive for CK15. CK15 expression has been reported in undifferentiated sebocytes of the mantle and in the hair follicle.10 Immunohistochemical staining supports the notion that fibrofolliculomas contain connective tissue and epithelial components and helps to compare and contrast them to those of other hair follicle hamartomas.
Ackerman et al1 considered both fibrofolliculomas and trichodiscomas to be hamartomas of the epithelial hair follicle. The exact etiology of each of these hamartomas is unknown, but the undifferentiated epithelial strands protruding from the hair follicle in a fibrofolliculoma lie in close proximity to sebaceous glands. Furthermore, the authors postulated that fibrofolliculomas and trichodiscomas constitute a spectrum that encompasses the differentiation process of a mantleoma, with fibrofolliculoma representing the beginning of mantleoma differentiation and trichodiscoma representing the end. This end stage of follicular differentiation is one in which there is a predominant stroma and the previously undifferentiated epithelium has formed into sebaceous ducts and lobules in the stroma.1
Most cases of fibrofolliculoma and/or trichodiscoma arise in areas of dense sebaceous follicle concentration (eg, face), further supporting the hypothesis that sebaceous gland proliferation contributes to fibrofolliculoma.14 The case described here, with the fibrofolliculoma arising on the abdomen in conjunction with a trichodiscoma, is therefore worth noting because its location differs from what has been observed in previously reported cases.4
There are both surgical and medical options for treatment of fibrofolliculoma. Although surgical excision is an option for a single lesion, patients with multiple fibrofolliculomas or BHD may prefer removal with the combined CO2 laser and erbium-doped YAG laser.15
Conclusion
We present a rare case of concomitant fibrofolliculoma and trichodiscoma arising on the unusual location of the abdomen. This report highlights the histopathologic features of multiple adnexal tumors and emphasizes the importance of biopsy for differentiating fibrofolliculoma and trichodiscoma.
Fibrofolliculomas and trichodiscomas typically present on the head or neck as smooth, flesh-colored, dome-shaped papules. These two entities are considered to constitute two separate time points on a spectrum of histopathologic changes in mantleoma differentiation.1 Histologically, both are benign hamartomas of the pilosebaceous subunit and collectively are known as mantleomas. We present an unusual case of a concomitant fibrofolliculoma and trichodiscoma on the abdomen.
Case Report
An asymptomatic 54-year-old man presented for a routine full-body skin examination. A solitary, 2×1-cm, subcutaneous, doughy, mobile nodule was found on the left side of the abdomen with an overlying 2-mm yellow fleshy papule. The patient declined excision of the lesion, and it was recommended that he return for follow-up 3 months later.
The patient did not present for follow-up until 4.5 years later, at which point the lesion had grown to 3.0×2.5 cm in size. An excision was performed, at which time the lesion was noted to be cystic, extruding an oily, yellow-white liquid. Bacterial culture was negative. Histopathologic sections showed a dome-shaped papule with connection to the overlying epidermis. Epithelial extensions from the infundibular epithelium formed a fenestrated pattern surrounding a fibrous and mucinous stroma (Figure, A and B). The differential diagnosis at this time included an epidermal inclusion cyst, fibroma, intradermal nevus, verruca, hemangioma, angiofibroma, and lipoma.2-4
The same lesion cut in a different plane of sectioning showed an expansile dermal nodule comprising clusters of sebaceous lobules surrounding a fibrous and mucinous stroma. Within the second lesion, fibrous and stromal components predominated over epithelial components (Figure, C). A diagnosis of fibrofolliculoma showing features of a trichodiscoma arising in the unusual location of the abdomen was made.
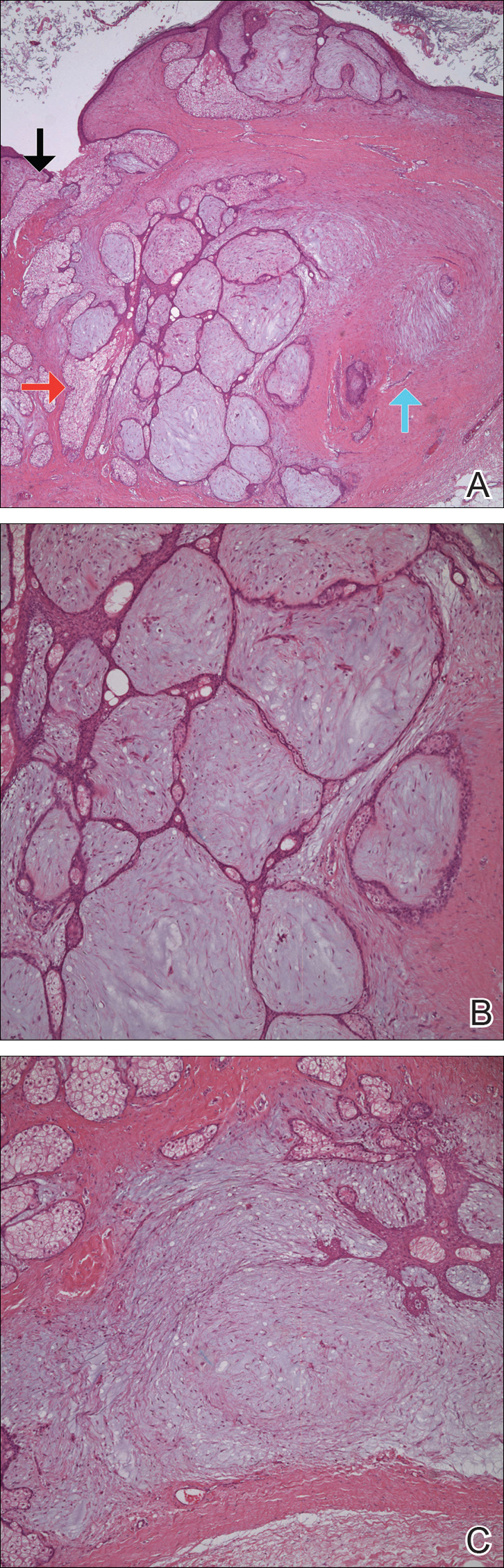
Comment
Solitary fibrofolliculomas and trichodiscomas are flesh-colored, dome-shaped papules that generally present on the face, specifically on the chin, nose, cheeks, ears, and eyebrows without considerable symptoms.2,4,5 Clinically, fibrofolliculomas are indistinguishable from trichodiscomas but demonstrate different features on biopsy.1,5
Fibrofolliculomas and trichodiscomas are well known for their association with Birt-Hogg-Dubé (BHD) syndrome when they present concomitantly and typically arise earlier in the third decade of life than solitary fibrofolliculomas; however, there have been reports of solitary fibrofolliculomas in patients aged 1 to 36 years.4,6 The triad of BHD syndrome consists of multiple fibrofolliculomas, trichodiscomas, and acrochordons, and it is acquired in an autosomal-dominant manner, unlike solitary fibrofolliculomas, which typically are not inherited. Birt-Hogg-Dubé syndrome is caused by a mutation in the FLCN gene that codes for the tumor-suppressor protein folliculin, which when mutated can cause unregulated proliferation of cells.7 Solitary fibrofolliculomas and the multiple fibrofolliculomas seen in BHD syndrome are histologically similar.
Fibrofolliculoma can be clinically indistinguishable from fibroepithelioma of Pinkus, perifollicular fibroma, trichilemmoma, trichodiscoma, trichoepithelioma, and trichofolliculoma. All typically present clinically as flesh-colored papules,1 although histologic distinction can be made (Table).5,8-13
Fibrofolliculoma is a benign hamartoma that arises from the pilosebaceous follicle and consists of an expansion of the fibrous root sheath, which typically surrounds the hair follicle along with proliferating bands or ribbons of perifollicular connective tissue. As such, the hair follicle may be dilated and filled with keratin in the expanded infundibulum.8 Follicles also may be surrounded by a myxoid stroma.2 In contrast, trichodiscoma is characterized by connective tissue with mature sebaceous lobules in the periphery. It has a myxoid stroma, as opposed to the more fibrous stroma seen in fibrofolliculomas.
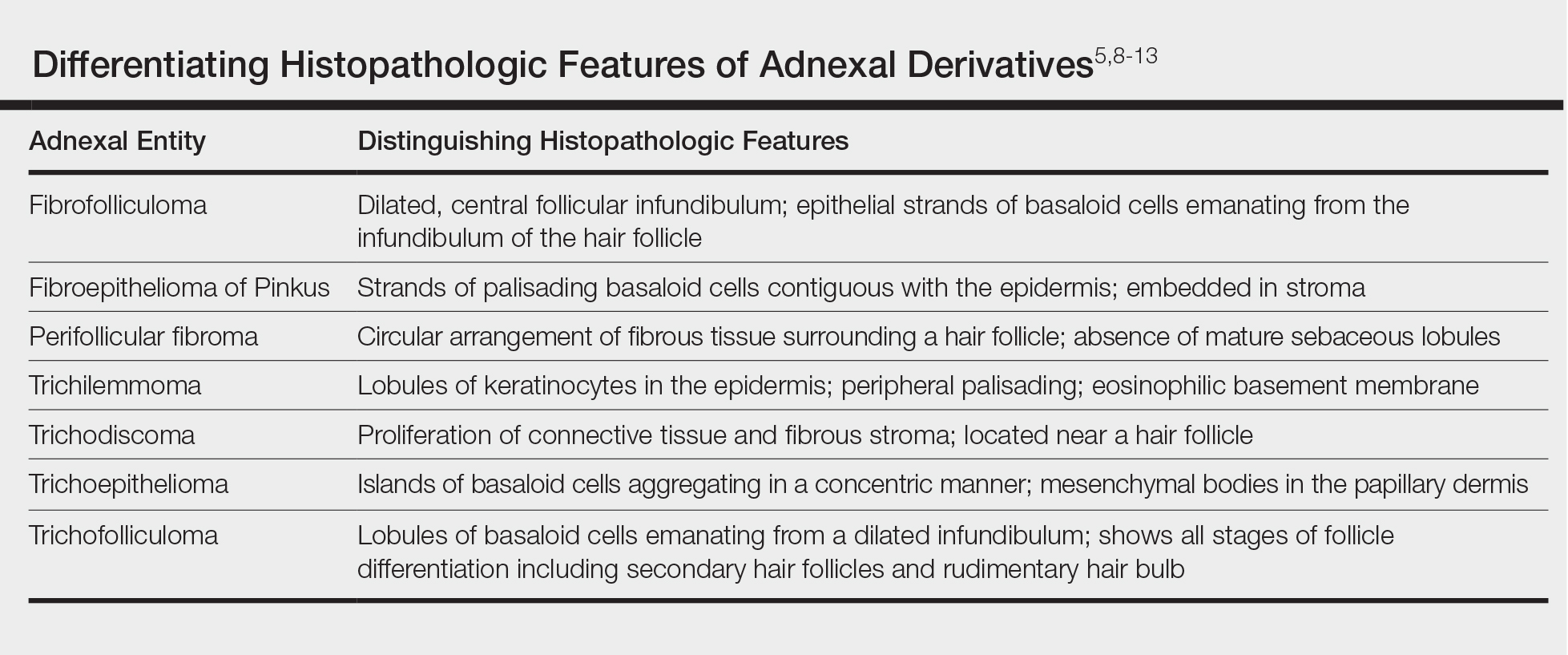
Reports have examined the staining patterns of fibrofolliculomas, which show characteristics similar to those of other hair follicle hamartomas, including trichodiscomas.10 The connective tissue and epithelial components that constitute a fibrofolliculoma show different staining patterns. The connective tissue component stains positive for CD34 spindle cells, factor XIIIa, and nestin (a marker of angiogenesis). CD117 (c-kit) expression in the stroma, a marker of fibrocytes, is a feature of both fibrofolliculoma and perifollicular fibromas. The epithelial component, consisting of the hair follicle itself, stains positive for CK15. CK15 expression has been reported in undifferentiated sebocytes of the mantle and in the hair follicle.10 Immunohistochemical staining supports the notion that fibrofolliculomas contain connective tissue and epithelial components and helps to compare and contrast them to those of other hair follicle hamartomas.
Ackerman et al1 considered both fibrofolliculomas and trichodiscomas to be hamartomas of the epithelial hair follicle. The exact etiology of each of these hamartomas is unknown, but the undifferentiated epithelial strands protruding from the hair follicle in a fibrofolliculoma lie in close proximity to sebaceous glands. Furthermore, the authors postulated that fibrofolliculomas and trichodiscomas constitute a spectrum that encompasses the differentiation process of a mantleoma, with fibrofolliculoma representing the beginning of mantleoma differentiation and trichodiscoma representing the end. This end stage of follicular differentiation is one in which there is a predominant stroma and the previously undifferentiated epithelium has formed into sebaceous ducts and lobules in the stroma.1
Most cases of fibrofolliculoma and/or trichodiscoma arise in areas of dense sebaceous follicle concentration (eg, face), further supporting the hypothesis that sebaceous gland proliferation contributes to fibrofolliculoma.14 The case described here, with the fibrofolliculoma arising on the abdomen in conjunction with a trichodiscoma, is therefore worth noting because its location differs from what has been observed in previously reported cases.4
There are both surgical and medical options for treatment of fibrofolliculoma. Although surgical excision is an option for a single lesion, patients with multiple fibrofolliculomas or BHD may prefer removal with the combined CO2 laser and erbium-doped YAG laser.15
Conclusion
We present a rare case of concomitant fibrofolliculoma and trichodiscoma arising on the unusual location of the abdomen. This report highlights the histopathologic features of multiple adnexal tumors and emphasizes the importance of biopsy for differentiating fibrofolliculoma and trichodiscoma.
- Ackerman AB, Chongchitnant N, DeViragh P. Neoplasms with Follicular Differentiation. Philadelphia, PA: Lea & Febiger; 1993.
- Scully K, Bargman H, Assaad D. Solitary fibrofolliculoma. J Am Acad Dermatol. 1984;11:361-363.
- Chang JK, Lee DC, Chang MH. A solitary fibrofolliculoma in the eyelid. Korean J Ophthalmol. 2007;21:169-171.
- Starink TM, Brownstein MH. Fibrofolliculoma: solitary and multiple types. J Am Acad Dermatol. 1987;17:493-496.
- Cho EU, Lee JD, Cho SH. A solitary fibrofolliculoma on the concha of the ear. Int J Dermatol. 2012;51:616-628.
- Mo HJ, Park CK, Yi JY. A case of solitary fibrofolliculoma. Korean J Dermatol. 2001;39:602-604.
- Nickerson ML, Warren MB, Toro JR, et al. Mutations in a novel gene lead to kidney tumors, lung wall defects, and benign tumors of the hair follicle in patients with the Birt-Hogg-Dubé syndrome. Cancer Cell. 2002;2:157-164.
- Birt AR, Hogg GR, Dubé WJ. Hereditary multiple fibrofolliculomas with trichodiscomas and acrochordons. Arch Dermatol. 1977;113:1674-1677.
- Foucar K, Rosen TH, Foucar E, et al. Fibrofolliculoma: a clinicopathologic study. Cutis. 1981;28:429-432.
- Misago NO, Kimura TE, Narisawa YU. Fibrofolliculoma/trichodiscoma and fibrous papule (perifollicular fibroma/angiofibroma): a revaluation of the histopathological and immunohistochemical features. J Cutan Pathol. 2009;36:943-951.
- Schaffer JV, Gohara MA, McNiff JM, et al. Multiple facial angiofibromas: a cutaneous manifestation of Birt-Hogg-Dubé syndrome. J Am Acad Dermatol. 2005;53(2 suppl 1):S108-S111.
- Lee Y, Su H, Chen H. Fibroepithelioma of Pinkus. a case report. Dermatologica Sinica. 2002;20:142-146.
- Nam JH, Min JH, Lee GY, et al. A case of perifollicular fibroma. Ann Dermatol. 2011:23:236-238.
- Vernooij M, Claessens T, Luijten M, et al. Birt-Hogg-Dubé syndrome and the skin. Fam Cancer. 2013;12:381-385.
- Jacob CI, Dover JS. Birt-Hogg-Dubé syndrome: treatment of cutaneous manifestations with laser skin resurfacing. Arch Dermatol. 2001;137:98-99.
- Ackerman AB, Chongchitnant N, DeViragh P. Neoplasms with Follicular Differentiation. Philadelphia, PA: Lea & Febiger; 1993.
- Scully K, Bargman H, Assaad D. Solitary fibrofolliculoma. J Am Acad Dermatol. 1984;11:361-363.
- Chang JK, Lee DC, Chang MH. A solitary fibrofolliculoma in the eyelid. Korean J Ophthalmol. 2007;21:169-171.
- Starink TM, Brownstein MH. Fibrofolliculoma: solitary and multiple types. J Am Acad Dermatol. 1987;17:493-496.
- Cho EU, Lee JD, Cho SH. A solitary fibrofolliculoma on the concha of the ear. Int J Dermatol. 2012;51:616-628.
- Mo HJ, Park CK, Yi JY. A case of solitary fibrofolliculoma. Korean J Dermatol. 2001;39:602-604.
- Nickerson ML, Warren MB, Toro JR, et al. Mutations in a novel gene lead to kidney tumors, lung wall defects, and benign tumors of the hair follicle in patients with the Birt-Hogg-Dubé syndrome. Cancer Cell. 2002;2:157-164.
- Birt AR, Hogg GR, Dubé WJ. Hereditary multiple fibrofolliculomas with trichodiscomas and acrochordons. Arch Dermatol. 1977;113:1674-1677.
- Foucar K, Rosen TH, Foucar E, et al. Fibrofolliculoma: a clinicopathologic study. Cutis. 1981;28:429-432.
- Misago NO, Kimura TE, Narisawa YU. Fibrofolliculoma/trichodiscoma and fibrous papule (perifollicular fibroma/angiofibroma): a revaluation of the histopathological and immunohistochemical features. J Cutan Pathol. 2009;36:943-951.
- Schaffer JV, Gohara MA, McNiff JM, et al. Multiple facial angiofibromas: a cutaneous manifestation of Birt-Hogg-Dubé syndrome. J Am Acad Dermatol. 2005;53(2 suppl 1):S108-S111.
- Lee Y, Su H, Chen H. Fibroepithelioma of Pinkus. a case report. Dermatologica Sinica. 2002;20:142-146.
- Nam JH, Min JH, Lee GY, et al. A case of perifollicular fibroma. Ann Dermatol. 2011:23:236-238.
- Vernooij M, Claessens T, Luijten M, et al. Birt-Hogg-Dubé syndrome and the skin. Fam Cancer. 2013;12:381-385.
- Jacob CI, Dover JS. Birt-Hogg-Dubé syndrome: treatment of cutaneous manifestations with laser skin resurfacing. Arch Dermatol. 2001;137:98-99.
Practice Points
- Fibrofolliculoma and trichodiscoma are flesh-colored adnexal tumors that arise from or around hair follicles.
- It is important to recognize these entities, as they can be related to Birt-Hogg-Dubé syndrome.