User login
CBO predicts more Medicare spending with drug rebate proposal
Medicare spending on pharmaceuticals is projected to increase if the Centers for Medicare & Medicaid Services finalizes changes to drug rebates in the Medicare program.
The Congressional Budget Office is estimating that Medicare spending would increase by $170 billion from 2020-2029 if the rebate rule goes into effect, according to a report released May 2.
The proposed rule, issued Jan. 31, would make it illegal for drug manufacturers to pay rebates to health plans and pharmacy benefit managers in return for better formulary placement. Instead of rebates, manufacturers could offer discounts directly to beneficiaries by lowering list prices or making a payment to the pharmacy for the full amount of the negotiated discount – a chargeback. Under the proposal, a beneficiary’s cost sharing would be based on the lower list price or the price after the chargeback.
The CBO’s projected spending increases are based on the assumption that manufacturers will withhold 15% of current-law rebates, as well as increases in federal subsidies for premiums, changes in annual thresholds to beneficiary cost sharing, and the cost of implementing the chargeback system.
The agency expects premiums to rise, as many plans currently use the rebates they receive from drug companies to lower premiums across the board.
However, some beneficiaries “would pay lower prices on their prescription drugs, and for some beneficiaries, those reductions would be greater than their premium increases,” the CBO stated in its report. For beneficiaries who use few drugs or who use drugs that have no significant rebates, “the premium increase would outweigh the price reduction.”
Another reason federal spending would increase under this proposal is an expected increase in utilization that would come with the lowering of prices.
“In CBO’s estimate, the additional Part D utilization stemming from implementing the proposed rule would increase federal spending for beneficiaries who are not enrolled in the low-income subsidy program over the 2020-2029 period by a total of about 2% or $10 billion,” the report noted.
But the increase in utilization would have a net positive effect on Medicare spending for this population, as more beneficiaries followed their drug regimens resulting in lower spending for physician and hospital services under Medicare Part A and Part B by an estimated $20 billion over the same period, according to the CBO.
“On net, those effects are projected to reduce Medicare spending by $10 billion over the 2020-2029 period,” according to the report.
Medicare spending on pharmaceuticals is projected to increase if the Centers for Medicare & Medicaid Services finalizes changes to drug rebates in the Medicare program.
The Congressional Budget Office is estimating that Medicare spending would increase by $170 billion from 2020-2029 if the rebate rule goes into effect, according to a report released May 2.
The proposed rule, issued Jan. 31, would make it illegal for drug manufacturers to pay rebates to health plans and pharmacy benefit managers in return for better formulary placement. Instead of rebates, manufacturers could offer discounts directly to beneficiaries by lowering list prices or making a payment to the pharmacy for the full amount of the negotiated discount – a chargeback. Under the proposal, a beneficiary’s cost sharing would be based on the lower list price or the price after the chargeback.
The CBO’s projected spending increases are based on the assumption that manufacturers will withhold 15% of current-law rebates, as well as increases in federal subsidies for premiums, changes in annual thresholds to beneficiary cost sharing, and the cost of implementing the chargeback system.
The agency expects premiums to rise, as many plans currently use the rebates they receive from drug companies to lower premiums across the board.
However, some beneficiaries “would pay lower prices on their prescription drugs, and for some beneficiaries, those reductions would be greater than their premium increases,” the CBO stated in its report. For beneficiaries who use few drugs or who use drugs that have no significant rebates, “the premium increase would outweigh the price reduction.”
Another reason federal spending would increase under this proposal is an expected increase in utilization that would come with the lowering of prices.
“In CBO’s estimate, the additional Part D utilization stemming from implementing the proposed rule would increase federal spending for beneficiaries who are not enrolled in the low-income subsidy program over the 2020-2029 period by a total of about 2% or $10 billion,” the report noted.
But the increase in utilization would have a net positive effect on Medicare spending for this population, as more beneficiaries followed their drug regimens resulting in lower spending for physician and hospital services under Medicare Part A and Part B by an estimated $20 billion over the same period, according to the CBO.
“On net, those effects are projected to reduce Medicare spending by $10 billion over the 2020-2029 period,” according to the report.
Medicare spending on pharmaceuticals is projected to increase if the Centers for Medicare & Medicaid Services finalizes changes to drug rebates in the Medicare program.
The Congressional Budget Office is estimating that Medicare spending would increase by $170 billion from 2020-2029 if the rebate rule goes into effect, according to a report released May 2.
The proposed rule, issued Jan. 31, would make it illegal for drug manufacturers to pay rebates to health plans and pharmacy benefit managers in return for better formulary placement. Instead of rebates, manufacturers could offer discounts directly to beneficiaries by lowering list prices or making a payment to the pharmacy for the full amount of the negotiated discount – a chargeback. Under the proposal, a beneficiary’s cost sharing would be based on the lower list price or the price after the chargeback.
The CBO’s projected spending increases are based on the assumption that manufacturers will withhold 15% of current-law rebates, as well as increases in federal subsidies for premiums, changes in annual thresholds to beneficiary cost sharing, and the cost of implementing the chargeback system.
The agency expects premiums to rise, as many plans currently use the rebates they receive from drug companies to lower premiums across the board.
However, some beneficiaries “would pay lower prices on their prescription drugs, and for some beneficiaries, those reductions would be greater than their premium increases,” the CBO stated in its report. For beneficiaries who use few drugs or who use drugs that have no significant rebates, “the premium increase would outweigh the price reduction.”
Another reason federal spending would increase under this proposal is an expected increase in utilization that would come with the lowering of prices.
“In CBO’s estimate, the additional Part D utilization stemming from implementing the proposed rule would increase federal spending for beneficiaries who are not enrolled in the low-income subsidy program over the 2020-2029 period by a total of about 2% or $10 billion,” the report noted.
But the increase in utilization would have a net positive effect on Medicare spending for this population, as more beneficiaries followed their drug regimens resulting in lower spending for physician and hospital services under Medicare Part A and Part B by an estimated $20 billion over the same period, according to the CBO.
“On net, those effects are projected to reduce Medicare spending by $10 billion over the 2020-2029 period,” according to the report.
In a tight vote, FDA panel backs mannitol for CF
A Food and Drug Administration Advisory Committee voted that the benefit-risk profile of an inhaled treatment for cystic fibrosis merits approval of the drug – dry powder mannitol (DPM).
Mannitol is a naturally occurring sugar alcohol that is used as a low-calorie sweetener; it is generally recognized as safe when taken enterically. Inhaled DPM, marketed as Aridol, is currently approved as a bronchoprovocation agent. For the current indication, DPM is given as 10x40-mg capsules twice daily.
In a 9-7 vote, the FDA’s Pulmonary-Allergy Drugs Advisory Committee (PADAC) decided that DPM’s modest potential to improve pulmonary function in adults with cystic fibrosis (CF) outweighed a potential signal for increased exacerbations seen in clinical trials.
Chiesi USA Inc. is seeking approval of DPM for the management of cystic fibrosis to improve pulmonary function in patients 18 years of age and older in conjunction with standard therapies. It plans to market DPM as Bronchitol.
Some committee members who voted against approval, including PADAC chair David H. Au, MD, worried that DPM’s ease of use might prompt patients and caregivers to substitute it for inhaled hypertonic saline, a medication that’s more burdensome to use but has a longer track record for efficacy and safety. While hypertonic saline requires cumbersome equipment and cleaning regimens and takes 20-30 minutes to administer, DPM is administered over about 5 minutes via a series of capsules inserted into a small inhaler device.
“I was very impressed by conversations that we heard from the community that this will be viewed as a substitute drug [for hypertonic saline],” said Dr. Au, professor of medicine at the University of Washington, Seattle. “Before we make that leap of faith ... we have to better understand how it has to be used.” He also acknowledged that making the call for DPM was “challenging.”
Other committee members were reassured by the fact that DPM is approved for adult use in 35 countries; it’s been in use since 2011 in Australia for adults and children.
Some members also noted an unmet need in CF therapies and placed confidence in those treating CF patients to find ways to use DPM safely and effectively. “I’m really counting on the cystic fibrosis clinicians who do this for a living to figure out where to use this in their armamentarium,” said John M. Kelso, MD, an allergist at Scripps Clinic, San Diego.
In 2012, the initial new drug application submitted by Pharmaxis, which then held marketing rights to DPM, resulted in a “no” vote for approval from PADAC, and eventual FDA denial of approval. The initial submission was supported by two phase 3 clinical trials, 301 and 302, that included pediatric patients. In the pediatric population, there was concern for increased hemoptysis with DPM, so the FDA advised the drug’s marketers to consider seeking approval for an adult population only in its reapplication. The current submission followed a new double-blind, randomized, placebo-controlled trial, study 303, that included adults with CF aged 18 or over.
All three studies had similar designs, tracking change from baseline in forced expiratory volume in one second (FEV1) from baseline to the end of the 26-week study period. In addition to this primary endpoint, secondary endpoints included other pulmonary function measures, as well as the number of protocol-defined pulmonary exacerbations (PDPEs). Participants also reported quality of life and symptom measures on the Cystic Fibrosis Questionnaire–Revised (CFQ-R).
In study 301, the dropout rate approached one in three participants with higher discontinuation in the intervention than the control arm, causing significant statistical problems in dealing with missing data. Thus, said the FDA’s Robert Lim, MD, though this study had positive results for FEV1, it was not “statistically robust.”
The second study, 302, did not meet its primary endpoint, and there was “no support from secondary endpoints” for efficacy, said Dr. Lim, a clinical team leader in the FDA’s Division of Pulmonary, Allergy, and Rheumatology Products.
The current submission was also supported by a new post hoc subgroup analysis of adults in studies 301 and 302. A total of 414 patients receiving DPM and 347 receiving placebo (DPM at a nontherapeutic level) were included in the integrated analysis of patients from all three studies. Studies 301 and 302 both had open-label extension arms, allowing more patients to be included in safety data.
The problems caused by the missing data from study 301 were addressed in the design of study 303 by encouraging patients who discontinued the study drug to continue data collection efforts for the study. Dropout rates were lower overall in study 303 and balanced between arms.
Over the 26-week duration of study 303, investigators saw a statistically significant improvement in FEV1 of about 50 mL, according to the FDA’s analysis. Post hoc analyses of studies 301 and 302 showed point estimate increases of approximately 80 mL, according to Dr. Lim.
In its presentations, Chiesi USA presented its integrated analysis of adult data from the three clinical trials. The analysis showed an increase in FEV1 from baseline of 73 mL for the DPM group, compared with an increase of 7 mL for the control group, using an intention-to-treat population (P less than .001). The committee heard evidence that in adults with CF, pulmonary function typically decreases by 1%-3% annually.
The PDPE rate was slightly higher in the DPM group than in the control group in studies 302 and 303, but the differences were not statistically significant. These findings have a backdrop of an overall low rate of PDPEs ranging from 0.221 to 0.995 per year, according to Chiesi presenter Scott Donaldson, MD, a pulmonologist who directs the adult cystic fibrosis center at the University of North Carolina at Chapel Hill.
When looking at the subgroup of United States study participants, the DPM integrated cohort included more patients with a history of prior pulmonary exacerbations. In the DPM group, 45% of U.S. participants had at least one exacerbation in the prior year, and 20% had two or more exacerbations, compared with 38% and 14%, respectively, in the control group. Chiesi argued that this imbalance was likely responsible for the increased exacerbation rate.
The sponsor and the FDA used different imputation methods to account for missing data from the earlier studies, complicating interpretation of the potential signal for increased exacerbations.
Quality of life data were similar between groups across the studies.
In the end, the view of the “yes” voters was encapsulated by James M. Tracy, DO, an allergist in private practice in Omaha, Neb. “This is not a drug for everybody; but absolutely, it’s a drug for somebody. Ultimately we have to make that decision – I do think that we study populations, but we really take care of people.”
The FDA usually follows the recommendations of its advisory panels.
A Food and Drug Administration Advisory Committee voted that the benefit-risk profile of an inhaled treatment for cystic fibrosis merits approval of the drug – dry powder mannitol (DPM).
Mannitol is a naturally occurring sugar alcohol that is used as a low-calorie sweetener; it is generally recognized as safe when taken enterically. Inhaled DPM, marketed as Aridol, is currently approved as a bronchoprovocation agent. For the current indication, DPM is given as 10x40-mg capsules twice daily.
In a 9-7 vote, the FDA’s Pulmonary-Allergy Drugs Advisory Committee (PADAC) decided that DPM’s modest potential to improve pulmonary function in adults with cystic fibrosis (CF) outweighed a potential signal for increased exacerbations seen in clinical trials.
Chiesi USA Inc. is seeking approval of DPM for the management of cystic fibrosis to improve pulmonary function in patients 18 years of age and older in conjunction with standard therapies. It plans to market DPM as Bronchitol.
Some committee members who voted against approval, including PADAC chair David H. Au, MD, worried that DPM’s ease of use might prompt patients and caregivers to substitute it for inhaled hypertonic saline, a medication that’s more burdensome to use but has a longer track record for efficacy and safety. While hypertonic saline requires cumbersome equipment and cleaning regimens and takes 20-30 minutes to administer, DPM is administered over about 5 minutes via a series of capsules inserted into a small inhaler device.
“I was very impressed by conversations that we heard from the community that this will be viewed as a substitute drug [for hypertonic saline],” said Dr. Au, professor of medicine at the University of Washington, Seattle. “Before we make that leap of faith ... we have to better understand how it has to be used.” He also acknowledged that making the call for DPM was “challenging.”
Other committee members were reassured by the fact that DPM is approved for adult use in 35 countries; it’s been in use since 2011 in Australia for adults and children.
Some members also noted an unmet need in CF therapies and placed confidence in those treating CF patients to find ways to use DPM safely and effectively. “I’m really counting on the cystic fibrosis clinicians who do this for a living to figure out where to use this in their armamentarium,” said John M. Kelso, MD, an allergist at Scripps Clinic, San Diego.
In 2012, the initial new drug application submitted by Pharmaxis, which then held marketing rights to DPM, resulted in a “no” vote for approval from PADAC, and eventual FDA denial of approval. The initial submission was supported by two phase 3 clinical trials, 301 and 302, that included pediatric patients. In the pediatric population, there was concern for increased hemoptysis with DPM, so the FDA advised the drug’s marketers to consider seeking approval for an adult population only in its reapplication. The current submission followed a new double-blind, randomized, placebo-controlled trial, study 303, that included adults with CF aged 18 or over.
All three studies had similar designs, tracking change from baseline in forced expiratory volume in one second (FEV1) from baseline to the end of the 26-week study period. In addition to this primary endpoint, secondary endpoints included other pulmonary function measures, as well as the number of protocol-defined pulmonary exacerbations (PDPEs). Participants also reported quality of life and symptom measures on the Cystic Fibrosis Questionnaire–Revised (CFQ-R).
In study 301, the dropout rate approached one in three participants with higher discontinuation in the intervention than the control arm, causing significant statistical problems in dealing with missing data. Thus, said the FDA’s Robert Lim, MD, though this study had positive results for FEV1, it was not “statistically robust.”
The second study, 302, did not meet its primary endpoint, and there was “no support from secondary endpoints” for efficacy, said Dr. Lim, a clinical team leader in the FDA’s Division of Pulmonary, Allergy, and Rheumatology Products.
The current submission was also supported by a new post hoc subgroup analysis of adults in studies 301 and 302. A total of 414 patients receiving DPM and 347 receiving placebo (DPM at a nontherapeutic level) were included in the integrated analysis of patients from all three studies. Studies 301 and 302 both had open-label extension arms, allowing more patients to be included in safety data.
The problems caused by the missing data from study 301 were addressed in the design of study 303 by encouraging patients who discontinued the study drug to continue data collection efforts for the study. Dropout rates were lower overall in study 303 and balanced between arms.
Over the 26-week duration of study 303, investigators saw a statistically significant improvement in FEV1 of about 50 mL, according to the FDA’s analysis. Post hoc analyses of studies 301 and 302 showed point estimate increases of approximately 80 mL, according to Dr. Lim.
In its presentations, Chiesi USA presented its integrated analysis of adult data from the three clinical trials. The analysis showed an increase in FEV1 from baseline of 73 mL for the DPM group, compared with an increase of 7 mL for the control group, using an intention-to-treat population (P less than .001). The committee heard evidence that in adults with CF, pulmonary function typically decreases by 1%-3% annually.
The PDPE rate was slightly higher in the DPM group than in the control group in studies 302 and 303, but the differences were not statistically significant. These findings have a backdrop of an overall low rate of PDPEs ranging from 0.221 to 0.995 per year, according to Chiesi presenter Scott Donaldson, MD, a pulmonologist who directs the adult cystic fibrosis center at the University of North Carolina at Chapel Hill.
When looking at the subgroup of United States study participants, the DPM integrated cohort included more patients with a history of prior pulmonary exacerbations. In the DPM group, 45% of U.S. participants had at least one exacerbation in the prior year, and 20% had two or more exacerbations, compared with 38% and 14%, respectively, in the control group. Chiesi argued that this imbalance was likely responsible for the increased exacerbation rate.
The sponsor and the FDA used different imputation methods to account for missing data from the earlier studies, complicating interpretation of the potential signal for increased exacerbations.
Quality of life data were similar between groups across the studies.
In the end, the view of the “yes” voters was encapsulated by James M. Tracy, DO, an allergist in private practice in Omaha, Neb. “This is not a drug for everybody; but absolutely, it’s a drug for somebody. Ultimately we have to make that decision – I do think that we study populations, but we really take care of people.”
The FDA usually follows the recommendations of its advisory panels.
A Food and Drug Administration Advisory Committee voted that the benefit-risk profile of an inhaled treatment for cystic fibrosis merits approval of the drug – dry powder mannitol (DPM).
Mannitol is a naturally occurring sugar alcohol that is used as a low-calorie sweetener; it is generally recognized as safe when taken enterically. Inhaled DPM, marketed as Aridol, is currently approved as a bronchoprovocation agent. For the current indication, DPM is given as 10x40-mg capsules twice daily.
In a 9-7 vote, the FDA’s Pulmonary-Allergy Drugs Advisory Committee (PADAC) decided that DPM’s modest potential to improve pulmonary function in adults with cystic fibrosis (CF) outweighed a potential signal for increased exacerbations seen in clinical trials.
Chiesi USA Inc. is seeking approval of DPM for the management of cystic fibrosis to improve pulmonary function in patients 18 years of age and older in conjunction with standard therapies. It plans to market DPM as Bronchitol.
Some committee members who voted against approval, including PADAC chair David H. Au, MD, worried that DPM’s ease of use might prompt patients and caregivers to substitute it for inhaled hypertonic saline, a medication that’s more burdensome to use but has a longer track record for efficacy and safety. While hypertonic saline requires cumbersome equipment and cleaning regimens and takes 20-30 minutes to administer, DPM is administered over about 5 minutes via a series of capsules inserted into a small inhaler device.
“I was very impressed by conversations that we heard from the community that this will be viewed as a substitute drug [for hypertonic saline],” said Dr. Au, professor of medicine at the University of Washington, Seattle. “Before we make that leap of faith ... we have to better understand how it has to be used.” He also acknowledged that making the call for DPM was “challenging.”
Other committee members were reassured by the fact that DPM is approved for adult use in 35 countries; it’s been in use since 2011 in Australia for adults and children.
Some members also noted an unmet need in CF therapies and placed confidence in those treating CF patients to find ways to use DPM safely and effectively. “I’m really counting on the cystic fibrosis clinicians who do this for a living to figure out where to use this in their armamentarium,” said John M. Kelso, MD, an allergist at Scripps Clinic, San Diego.
In 2012, the initial new drug application submitted by Pharmaxis, which then held marketing rights to DPM, resulted in a “no” vote for approval from PADAC, and eventual FDA denial of approval. The initial submission was supported by two phase 3 clinical trials, 301 and 302, that included pediatric patients. In the pediatric population, there was concern for increased hemoptysis with DPM, so the FDA advised the drug’s marketers to consider seeking approval for an adult population only in its reapplication. The current submission followed a new double-blind, randomized, placebo-controlled trial, study 303, that included adults with CF aged 18 or over.
All three studies had similar designs, tracking change from baseline in forced expiratory volume in one second (FEV1) from baseline to the end of the 26-week study period. In addition to this primary endpoint, secondary endpoints included other pulmonary function measures, as well as the number of protocol-defined pulmonary exacerbations (PDPEs). Participants also reported quality of life and symptom measures on the Cystic Fibrosis Questionnaire–Revised (CFQ-R).
In study 301, the dropout rate approached one in three participants with higher discontinuation in the intervention than the control arm, causing significant statistical problems in dealing with missing data. Thus, said the FDA’s Robert Lim, MD, though this study had positive results for FEV1, it was not “statistically robust.”
The second study, 302, did not meet its primary endpoint, and there was “no support from secondary endpoints” for efficacy, said Dr. Lim, a clinical team leader in the FDA’s Division of Pulmonary, Allergy, and Rheumatology Products.
The current submission was also supported by a new post hoc subgroup analysis of adults in studies 301 and 302. A total of 414 patients receiving DPM and 347 receiving placebo (DPM at a nontherapeutic level) were included in the integrated analysis of patients from all three studies. Studies 301 and 302 both had open-label extension arms, allowing more patients to be included in safety data.
The problems caused by the missing data from study 301 were addressed in the design of study 303 by encouraging patients who discontinued the study drug to continue data collection efforts for the study. Dropout rates were lower overall in study 303 and balanced between arms.
Over the 26-week duration of study 303, investigators saw a statistically significant improvement in FEV1 of about 50 mL, according to the FDA’s analysis. Post hoc analyses of studies 301 and 302 showed point estimate increases of approximately 80 mL, according to Dr. Lim.
In its presentations, Chiesi USA presented its integrated analysis of adult data from the three clinical trials. The analysis showed an increase in FEV1 from baseline of 73 mL for the DPM group, compared with an increase of 7 mL for the control group, using an intention-to-treat population (P less than .001). The committee heard evidence that in adults with CF, pulmonary function typically decreases by 1%-3% annually.
The PDPE rate was slightly higher in the DPM group than in the control group in studies 302 and 303, but the differences were not statistically significant. These findings have a backdrop of an overall low rate of PDPEs ranging from 0.221 to 0.995 per year, according to Chiesi presenter Scott Donaldson, MD, a pulmonologist who directs the adult cystic fibrosis center at the University of North Carolina at Chapel Hill.
When looking at the subgroup of United States study participants, the DPM integrated cohort included more patients with a history of prior pulmonary exacerbations. In the DPM group, 45% of U.S. participants had at least one exacerbation in the prior year, and 20% had two or more exacerbations, compared with 38% and 14%, respectively, in the control group. Chiesi argued that this imbalance was likely responsible for the increased exacerbation rate.
The sponsor and the FDA used different imputation methods to account for missing data from the earlier studies, complicating interpretation of the potential signal for increased exacerbations.
Quality of life data were similar between groups across the studies.
In the end, the view of the “yes” voters was encapsulated by James M. Tracy, DO, an allergist in private practice in Omaha, Neb. “This is not a drug for everybody; but absolutely, it’s a drug for somebody. Ultimately we have to make that decision – I do think that we study populations, but we really take care of people.”
The FDA usually follows the recommendations of its advisory panels.
FROM AN FDA ADVISORY COMMITTEE HEARING
SGLT2 inhibitors prevent HF hospitalization regardless of baseline LVEF
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.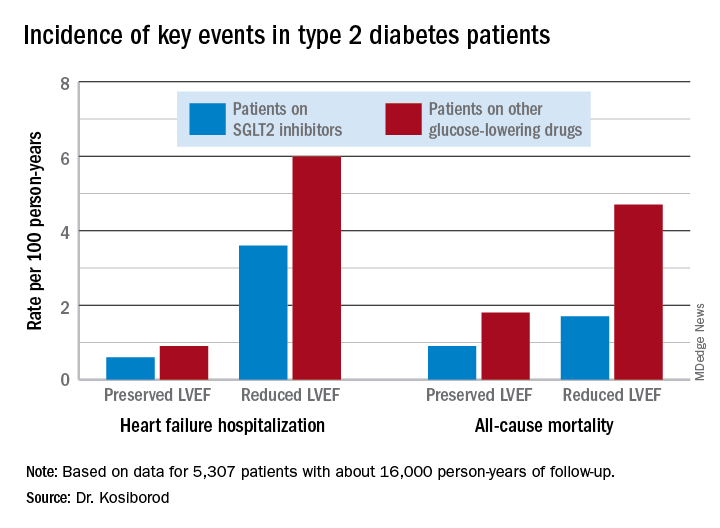
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.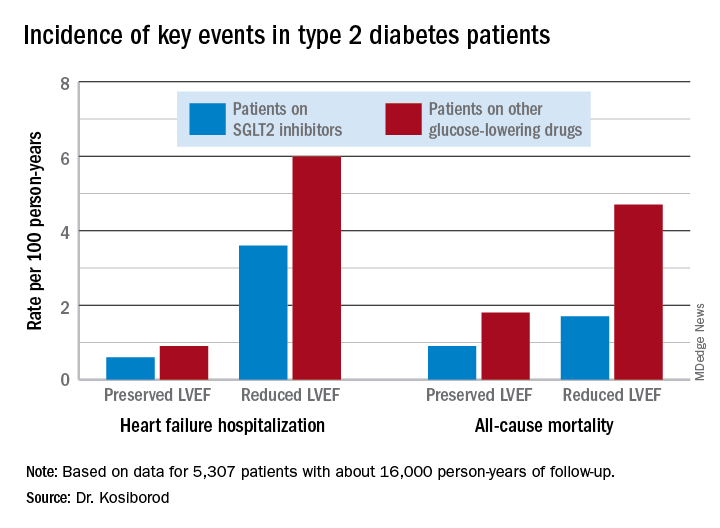
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.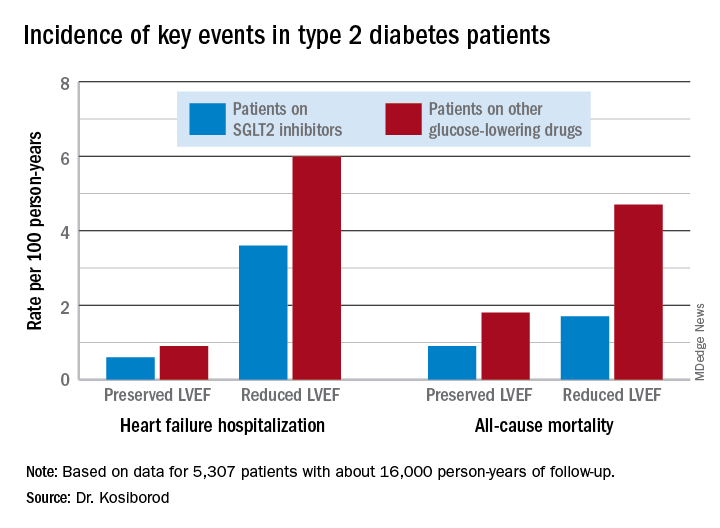
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
REPORTING FROM ACC 19
Short-term use of CGMs can deliver life-changing data for patients with type 2 diabetes
LOS ANGELES – Cardiology patients can strap on a Holter monitor for a day or two to track their heart activity and get a brief but helpful glimpse at their cardiac health. Could patients with type 2 diabetes benefit by monitoring their blood sugar for a short period? Absolutely, according to an endocrinologist who says he’s had tremendous success with the temporary use of continuous glucose monitors (CGMs) in appropriate patients.
“There’s an actionable surprise with almost every patient,” said Daniel Einhorn, MD, FACP, FACE, medical director of Scripps Whittier Diabetes Institute and clinical professor of medicine at the University of California, San Diego.
The key is to use CGM data to pinpoint glucose spikes and then quickly make adjustments, typically over a period of 2 weeks. “This is about pattern recognition. We can do [CGM] over a week, see what the pattern is, and then try to fix something. Then they come back after the second week or send [the monitor] in, and they have the problem fixed. You have a happy patient and a happy family,” said Dr. Einhorn, who spoke in a presentation at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
He highlighted how CGM data allow patients to track their blood sugar over extended periods of time and detect patterns. The data can uncover hidden hypoglycemia and hyperglycemia, he said, and is much more useful to patients than the self-monitoring of glucose levels or hemoglobin A1c (HbA1c) data.
Reading the patterns, adjusting behavior
Dr. Einhorn discussed several specific cases of patients who had changed their behavior in regard to food or medicine after CGM data disclosed certain blood sugar patterns.
Often, he said, patients say they’re surprised to find their well-being improves after they make adjustments, saying something along the lines of “I didn’t feel badly, but I feel better now.” According to Dr. Einhorn, “You hear that all the time.”
For example, he said, one patient knew his blood sugar occasionally topped 200 mg/dL, but he felt all right and didn’t want to take insulin. CGM monitoring over 6 days showed the patient had continuous glucose levels well over 200 mg/dL, especially at night. The patient accepted insulin, and a few months later his HbA1c dropped from 10.4% to 6.6%, and his blood sugar level stayed near or below the target range of 154 mg/dL.
Dr. Einhorn said the CGM data can reveal a range of problems, including:
- The “breakfast bump” after carbohydrate-heavy breakfasts of cereal, toast, and juice. “Breakfast cereal is diabolical,” he said.
- Hypoglycemia hours after exercise.
- Nocturnal hypoglycemia.
- Hypoglycemia unawareness.
Insurance coverage of the CGM device varies widely, he said, and insurers may not cover it at all in type 2 diabetes or only pay if the patient takes insulin. Fortunately, he said, the devices can be inexpensive.
Temporary use is not for everyone
Dr. Einhorn cautioned that temporary use of CGM is not appropriate for every patient with type 2 diabetes. “There’s absolutely a place for [permanent] monitoring for those people who have to make decisions throughout the day, especially if they are taking insulin,” he said.
And anyone with type 1 diabetes should use CGM on an ongoing basis, he emphasized. “Type 1 is a different world, a different universe,” he said.
He also noted that some patients don’t fare well on CGM, even on a temporary basis. That would include patients who hate to wear devices (possibly out of embarrassment), those who can’t manage to switch over from self-monitoring, and those who can’t manage to understand the data.
Dr. Einhorn disclosed various types of relationships with a number of drug makers, including Abbott, Boehringer Ingelheim, Novo, Sanofi, Janssen, and others.
LOS ANGELES – Cardiology patients can strap on a Holter monitor for a day or two to track their heart activity and get a brief but helpful glimpse at their cardiac health. Could patients with type 2 diabetes benefit by monitoring their blood sugar for a short period? Absolutely, according to an endocrinologist who says he’s had tremendous success with the temporary use of continuous glucose monitors (CGMs) in appropriate patients.
“There’s an actionable surprise with almost every patient,” said Daniel Einhorn, MD, FACP, FACE, medical director of Scripps Whittier Diabetes Institute and clinical professor of medicine at the University of California, San Diego.
The key is to use CGM data to pinpoint glucose spikes and then quickly make adjustments, typically over a period of 2 weeks. “This is about pattern recognition. We can do [CGM] over a week, see what the pattern is, and then try to fix something. Then they come back after the second week or send [the monitor] in, and they have the problem fixed. You have a happy patient and a happy family,” said Dr. Einhorn, who spoke in a presentation at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
He highlighted how CGM data allow patients to track their blood sugar over extended periods of time and detect patterns. The data can uncover hidden hypoglycemia and hyperglycemia, he said, and is much more useful to patients than the self-monitoring of glucose levels or hemoglobin A1c (HbA1c) data.
Reading the patterns, adjusting behavior
Dr. Einhorn discussed several specific cases of patients who had changed their behavior in regard to food or medicine after CGM data disclosed certain blood sugar patterns.
Often, he said, patients say they’re surprised to find their well-being improves after they make adjustments, saying something along the lines of “I didn’t feel badly, but I feel better now.” According to Dr. Einhorn, “You hear that all the time.”
For example, he said, one patient knew his blood sugar occasionally topped 200 mg/dL, but he felt all right and didn’t want to take insulin. CGM monitoring over 6 days showed the patient had continuous glucose levels well over 200 mg/dL, especially at night. The patient accepted insulin, and a few months later his HbA1c dropped from 10.4% to 6.6%, and his blood sugar level stayed near or below the target range of 154 mg/dL.
Dr. Einhorn said the CGM data can reveal a range of problems, including:
- The “breakfast bump” after carbohydrate-heavy breakfasts of cereal, toast, and juice. “Breakfast cereal is diabolical,” he said.
- Hypoglycemia hours after exercise.
- Nocturnal hypoglycemia.
- Hypoglycemia unawareness.
Insurance coverage of the CGM device varies widely, he said, and insurers may not cover it at all in type 2 diabetes or only pay if the patient takes insulin. Fortunately, he said, the devices can be inexpensive.
Temporary use is not for everyone
Dr. Einhorn cautioned that temporary use of CGM is not appropriate for every patient with type 2 diabetes. “There’s absolutely a place for [permanent] monitoring for those people who have to make decisions throughout the day, especially if they are taking insulin,” he said.
And anyone with type 1 diabetes should use CGM on an ongoing basis, he emphasized. “Type 1 is a different world, a different universe,” he said.
He also noted that some patients don’t fare well on CGM, even on a temporary basis. That would include patients who hate to wear devices (possibly out of embarrassment), those who can’t manage to switch over from self-monitoring, and those who can’t manage to understand the data.
Dr. Einhorn disclosed various types of relationships with a number of drug makers, including Abbott, Boehringer Ingelheim, Novo, Sanofi, Janssen, and others.
LOS ANGELES – Cardiology patients can strap on a Holter monitor for a day or two to track their heart activity and get a brief but helpful glimpse at their cardiac health. Could patients with type 2 diabetes benefit by monitoring their blood sugar for a short period? Absolutely, according to an endocrinologist who says he’s had tremendous success with the temporary use of continuous glucose monitors (CGMs) in appropriate patients.
“There’s an actionable surprise with almost every patient,” said Daniel Einhorn, MD, FACP, FACE, medical director of Scripps Whittier Diabetes Institute and clinical professor of medicine at the University of California, San Diego.
The key is to use CGM data to pinpoint glucose spikes and then quickly make adjustments, typically over a period of 2 weeks. “This is about pattern recognition. We can do [CGM] over a week, see what the pattern is, and then try to fix something. Then they come back after the second week or send [the monitor] in, and they have the problem fixed. You have a happy patient and a happy family,” said Dr. Einhorn, who spoke in a presentation at the annual scientific and clinical congress of the American Association of Clinical Endocrinologists.
He highlighted how CGM data allow patients to track their blood sugar over extended periods of time and detect patterns. The data can uncover hidden hypoglycemia and hyperglycemia, he said, and is much more useful to patients than the self-monitoring of glucose levels or hemoglobin A1c (HbA1c) data.
Reading the patterns, adjusting behavior
Dr. Einhorn discussed several specific cases of patients who had changed their behavior in regard to food or medicine after CGM data disclosed certain blood sugar patterns.
Often, he said, patients say they’re surprised to find their well-being improves after they make adjustments, saying something along the lines of “I didn’t feel badly, but I feel better now.” According to Dr. Einhorn, “You hear that all the time.”
For example, he said, one patient knew his blood sugar occasionally topped 200 mg/dL, but he felt all right and didn’t want to take insulin. CGM monitoring over 6 days showed the patient had continuous glucose levels well over 200 mg/dL, especially at night. The patient accepted insulin, and a few months later his HbA1c dropped from 10.4% to 6.6%, and his blood sugar level stayed near or below the target range of 154 mg/dL.
Dr. Einhorn said the CGM data can reveal a range of problems, including:
- The “breakfast bump” after carbohydrate-heavy breakfasts of cereal, toast, and juice. “Breakfast cereal is diabolical,” he said.
- Hypoglycemia hours after exercise.
- Nocturnal hypoglycemia.
- Hypoglycemia unawareness.
Insurance coverage of the CGM device varies widely, he said, and insurers may not cover it at all in type 2 diabetes or only pay if the patient takes insulin. Fortunately, he said, the devices can be inexpensive.
Temporary use is not for everyone
Dr. Einhorn cautioned that temporary use of CGM is not appropriate for every patient with type 2 diabetes. “There’s absolutely a place for [permanent] monitoring for those people who have to make decisions throughout the day, especially if they are taking insulin,” he said.
And anyone with type 1 diabetes should use CGM on an ongoing basis, he emphasized. “Type 1 is a different world, a different universe,” he said.
He also noted that some patients don’t fare well on CGM, even on a temporary basis. That would include patients who hate to wear devices (possibly out of embarrassment), those who can’t manage to switch over from self-monitoring, and those who can’t manage to understand the data.
Dr. Einhorn disclosed various types of relationships with a number of drug makers, including Abbott, Boehringer Ingelheim, Novo, Sanofi, Janssen, and others.
REPORTING FROM AACE 2019
HM19: Pediatric clinical conundrums
Atypical symptoms and diagnoses
Presenters
Yemisi Jones, MD; Mirna Giordano, MD
Session title
Pediatric Clinical Conundrums
Session summary
Dr. Mirna Giordano of Columbia University Irving Medical Center, New York, and Dr. Yemisi Jones of Cincinnati Children’s Hospital Medical Center, moderated the Pediatric Clinical Conundrums session at HM19. After reviewing multiple submissions, they invited four trainees to present their interesting cases.
Malignancy or infection? Dr. Jeremy Brown, a resident at the University of Louisville, presented a case of a 15-year-old male with right upper quadrant abdominal pain with associated weight loss and intermittent fevers, over the course of several weeks. CT revealed multiple liver lesions, providing concern for possible malignancy, although liver biopsy proved otherwise, with mostly liquefactive tissue and benign liver parenchyma. After a large infectious work-up ensued, the patient was diagnosed with disseminated Bartonella. He was treated with a 10-day course of azithromycin, and his symptoms resolved.
Leg blisters as an uncommon manifestation of a common childhood disease. Dr. Stefan Mammele, a resident at Kapi’olani Medical Center in Honolulu, and the University of Hawaii, presented a case of an 11-year-old boy with a painful and pruritic rash associated with multiple 5- to 10-mm tense bullae located on the patient’s bilateral lower extremities with extension to the trunk. The patient was also found to have hematuria and proteinuria. The bullae drained both serosanguinous and purulent material. Fluid culture grew group A Streptococcus and skin biopsy confirmed IgA vasculitis. Bullae are a rare characteristic of Henoch Schönlein pupura in children, but are more commonly seen as a disease manifestation in adults. The patient was treated with cefazolin, and his lesions improved over the course of several weeks with resolution of his hematuria by 6 months.
Is she crying blood? Dr. Joshua Price, a resident at Baystate Children’s Hospital in Springfield, Mass., described a 12-year-old female who presented with 7 days of left-sided hemolacria with acute vision loss and unilateral eye pain. This patient did not respond to outpatient topical steroids and antibiotics, as prescribed by ophthalmology. For this reason, she underwent further work-up and imaging. MRI of the head and orbits revealed left maxillary sinus disease. She was treated with antibiotics for acute left maxillary sinusitis and her hemolacria resolved within 24 hours. While the differential diagnosis for hemolacria is broad, rarely acute sinusitis has been reported as a cause in medical literature.
Recurrent bronchiolitis or something more? Dr. Moira Black, a resident at Children’s Memorial Hermann in Houston, presented a case of a 7-month-old female with a history of recurrent admissions for increased work of breathing believed to be secondary to viral bronchiolitis. Her first hospitalization occurred at 7 weeks of age and was complicated by spontaneous pneumothorax requiring chest tube placement. She was again hospitalized at 5 months of age with resolution of her increased work of breathing with high-flow nasal cannula. She presented again at 7 months of age with presumed bronchiolitis, however, she decompensated and required intubation on the 5th day of hospitalization. A bronchoscopy was performed and revealed a significantly narrowed left bronchus at the carina and a blind pouch on the right with notable pulsation of the walls. She underwent further imaging and was ultimately diagnosed with a left pulmonary artery sling. Left pulmonary artery slings are a rare, but potentially fatal anomaly that can present with wheezing, stridor, and recurrent respiratory infections. Patient underwent correction by cardiovascular surgery and has since been doing well.
Key takeaways for HM
• Bartonella is a common cause of fever of unknown origin, and should be considered in unusual presentations of febrile illnesses.
• Bullae in IgA vasculitis are rare in children and do not have prognostic value, but streptococcal infection may be a trigger for IgA vasculitis.
• Hemolacria is an atypical presentation of rare and common diagnoses that should prompt further work-up.
• Acute respiratory distress can be caused by underlying cardiac or vascular anomalies and can be mistaken for common viral illnesses.
Dr. Marsicek is a pediatric hospital medicine fellow at Johns Hopkins All Children’s Hospital, St. Petersburg, Fla. Dr. Wysocka is a pediatric resident at Johns Hopkins All Children’s Hospital.
Atypical symptoms and diagnoses
Atypical symptoms and diagnoses
Presenters
Yemisi Jones, MD; Mirna Giordano, MD
Session title
Pediatric Clinical Conundrums
Session summary
Dr. Mirna Giordano of Columbia University Irving Medical Center, New York, and Dr. Yemisi Jones of Cincinnati Children’s Hospital Medical Center, moderated the Pediatric Clinical Conundrums session at HM19. After reviewing multiple submissions, they invited four trainees to present their interesting cases.
Malignancy or infection? Dr. Jeremy Brown, a resident at the University of Louisville, presented a case of a 15-year-old male with right upper quadrant abdominal pain with associated weight loss and intermittent fevers, over the course of several weeks. CT revealed multiple liver lesions, providing concern for possible malignancy, although liver biopsy proved otherwise, with mostly liquefactive tissue and benign liver parenchyma. After a large infectious work-up ensued, the patient was diagnosed with disseminated Bartonella. He was treated with a 10-day course of azithromycin, and his symptoms resolved.
Leg blisters as an uncommon manifestation of a common childhood disease. Dr. Stefan Mammele, a resident at Kapi’olani Medical Center in Honolulu, and the University of Hawaii, presented a case of an 11-year-old boy with a painful and pruritic rash associated with multiple 5- to 10-mm tense bullae located on the patient’s bilateral lower extremities with extension to the trunk. The patient was also found to have hematuria and proteinuria. The bullae drained both serosanguinous and purulent material. Fluid culture grew group A Streptococcus and skin biopsy confirmed IgA vasculitis. Bullae are a rare characteristic of Henoch Schönlein pupura in children, but are more commonly seen as a disease manifestation in adults. The patient was treated with cefazolin, and his lesions improved over the course of several weeks with resolution of his hematuria by 6 months.
Is she crying blood? Dr. Joshua Price, a resident at Baystate Children’s Hospital in Springfield, Mass., described a 12-year-old female who presented with 7 days of left-sided hemolacria with acute vision loss and unilateral eye pain. This patient did not respond to outpatient topical steroids and antibiotics, as prescribed by ophthalmology. For this reason, she underwent further work-up and imaging. MRI of the head and orbits revealed left maxillary sinus disease. She was treated with antibiotics for acute left maxillary sinusitis and her hemolacria resolved within 24 hours. While the differential diagnosis for hemolacria is broad, rarely acute sinusitis has been reported as a cause in medical literature.
Recurrent bronchiolitis or something more? Dr. Moira Black, a resident at Children’s Memorial Hermann in Houston, presented a case of a 7-month-old female with a history of recurrent admissions for increased work of breathing believed to be secondary to viral bronchiolitis. Her first hospitalization occurred at 7 weeks of age and was complicated by spontaneous pneumothorax requiring chest tube placement. She was again hospitalized at 5 months of age with resolution of her increased work of breathing with high-flow nasal cannula. She presented again at 7 months of age with presumed bronchiolitis, however, she decompensated and required intubation on the 5th day of hospitalization. A bronchoscopy was performed and revealed a significantly narrowed left bronchus at the carina and a blind pouch on the right with notable pulsation of the walls. She underwent further imaging and was ultimately diagnosed with a left pulmonary artery sling. Left pulmonary artery slings are a rare, but potentially fatal anomaly that can present with wheezing, stridor, and recurrent respiratory infections. Patient underwent correction by cardiovascular surgery and has since been doing well.
Key takeaways for HM
• Bartonella is a common cause of fever of unknown origin, and should be considered in unusual presentations of febrile illnesses.
• Bullae in IgA vasculitis are rare in children and do not have prognostic value, but streptococcal infection may be a trigger for IgA vasculitis.
• Hemolacria is an atypical presentation of rare and common diagnoses that should prompt further work-up.
• Acute respiratory distress can be caused by underlying cardiac or vascular anomalies and can be mistaken for common viral illnesses.
Dr. Marsicek is a pediatric hospital medicine fellow at Johns Hopkins All Children’s Hospital, St. Petersburg, Fla. Dr. Wysocka is a pediatric resident at Johns Hopkins All Children’s Hospital.
Presenters
Yemisi Jones, MD; Mirna Giordano, MD
Session title
Pediatric Clinical Conundrums
Session summary
Dr. Mirna Giordano of Columbia University Irving Medical Center, New York, and Dr. Yemisi Jones of Cincinnati Children’s Hospital Medical Center, moderated the Pediatric Clinical Conundrums session at HM19. After reviewing multiple submissions, they invited four trainees to present their interesting cases.
Malignancy or infection? Dr. Jeremy Brown, a resident at the University of Louisville, presented a case of a 15-year-old male with right upper quadrant abdominal pain with associated weight loss and intermittent fevers, over the course of several weeks. CT revealed multiple liver lesions, providing concern for possible malignancy, although liver biopsy proved otherwise, with mostly liquefactive tissue and benign liver parenchyma. After a large infectious work-up ensued, the patient was diagnosed with disseminated Bartonella. He was treated with a 10-day course of azithromycin, and his symptoms resolved.
Leg blisters as an uncommon manifestation of a common childhood disease. Dr. Stefan Mammele, a resident at Kapi’olani Medical Center in Honolulu, and the University of Hawaii, presented a case of an 11-year-old boy with a painful and pruritic rash associated with multiple 5- to 10-mm tense bullae located on the patient’s bilateral lower extremities with extension to the trunk. The patient was also found to have hematuria and proteinuria. The bullae drained both serosanguinous and purulent material. Fluid culture grew group A Streptococcus and skin biopsy confirmed IgA vasculitis. Bullae are a rare characteristic of Henoch Schönlein pupura in children, but are more commonly seen as a disease manifestation in adults. The patient was treated with cefazolin, and his lesions improved over the course of several weeks with resolution of his hematuria by 6 months.
Is she crying blood? Dr. Joshua Price, a resident at Baystate Children’s Hospital in Springfield, Mass., described a 12-year-old female who presented with 7 days of left-sided hemolacria with acute vision loss and unilateral eye pain. This patient did not respond to outpatient topical steroids and antibiotics, as prescribed by ophthalmology. For this reason, she underwent further work-up and imaging. MRI of the head and orbits revealed left maxillary sinus disease. She was treated with antibiotics for acute left maxillary sinusitis and her hemolacria resolved within 24 hours. While the differential diagnosis for hemolacria is broad, rarely acute sinusitis has been reported as a cause in medical literature.
Recurrent bronchiolitis or something more? Dr. Moira Black, a resident at Children’s Memorial Hermann in Houston, presented a case of a 7-month-old female with a history of recurrent admissions for increased work of breathing believed to be secondary to viral bronchiolitis. Her first hospitalization occurred at 7 weeks of age and was complicated by spontaneous pneumothorax requiring chest tube placement. She was again hospitalized at 5 months of age with resolution of her increased work of breathing with high-flow nasal cannula. She presented again at 7 months of age with presumed bronchiolitis, however, she decompensated and required intubation on the 5th day of hospitalization. A bronchoscopy was performed and revealed a significantly narrowed left bronchus at the carina and a blind pouch on the right with notable pulsation of the walls. She underwent further imaging and was ultimately diagnosed with a left pulmonary artery sling. Left pulmonary artery slings are a rare, but potentially fatal anomaly that can present with wheezing, stridor, and recurrent respiratory infections. Patient underwent correction by cardiovascular surgery and has since been doing well.
Key takeaways for HM
• Bartonella is a common cause of fever of unknown origin, and should be considered in unusual presentations of febrile illnesses.
• Bullae in IgA vasculitis are rare in children and do not have prognostic value, but streptococcal infection may be a trigger for IgA vasculitis.
• Hemolacria is an atypical presentation of rare and common diagnoses that should prompt further work-up.
• Acute respiratory distress can be caused by underlying cardiac or vascular anomalies and can be mistaken for common viral illnesses.
Dr. Marsicek is a pediatric hospital medicine fellow at Johns Hopkins All Children’s Hospital, St. Petersburg, Fla. Dr. Wysocka is a pediatric resident at Johns Hopkins All Children’s Hospital.
ctDNA predicts recurrence in nonmetastatic colorectal cancer
Circulating tumor DNA (ctDNA) could be used to predict disease recurrence in patients with nonmetastatic colorectal cancer (CRC), according to investigators following an observational study.
About three out of four patients with a positive ctDNA test went on to have disease recurrence, reported lead author Yuxuan Wang, MD, PhD, of Johns Hopkins University School of Medicine in Baltimore, and her colleagues. On average, positive tests preceded clinical and radiologic evidence of recurrence by 3 months.
“[T]he optimal protocol for surveillance of resected colorectal cancer remains uncertain,” the investigators wrote in JAMA Oncology.
“The only recommended blood marker for CRC surveillance is serum [carcinoembryonic antigen (CEA)], an oncofetal protein that is elevated in the serum of patients with a variety of disease conditions, including CRC. Unfortunately, its utility is limited by the lack of sensitivity and specificity.” Although computed tomography and magnetic resonance imaging can improve disease detection, these techniques also have their own shortcomings, the investigators noted, setting the stage for the present study.
The investigators recruited 63 patients with stage I, II, or III CRC who underwent surgical resection in Sweden between 2007 and 2013. Blood samples for ctDNA testing were collected 1 month after surgery, then every 3-6 months. CT was performed every 6-12 months. During this process, 5 patients were excluded, leaving 58 patients in the final dataset, 18 (31%) of whom received adjuvant chemotherapy. Patients were followed until metastasis or a median of 49 months.
Among all patients, 13 tested positive for ctDNA, and 10 of these relapsed (77%), with a median time of 3 months between ctDNA positivity and CT or clinical evidence of recurrence. Three of the 48 patients (6%) who did not relapse had a positive ctDNA result that later dropped to an undetectable level. Of the 45 patients who tested negative for ctDNA, none had recurrence, although 1 was positive for CEA.
Results were also divided into patients who received or did not receive adjuvant chemotherapy. Among the 40 patients who did not receive chemotherapy, 8 had disease recurrence after a positive ctDNA test, although only 5 tested positive for CEA. Among the 18 patients who did receive chemotherapy, 2 tested positive for ctDNA and later relapsed, although only 1 tested positive for CEA. These figures translated to a ctDNA sensitivity for recurrence of 100%, compared with 60% for CEA testing.
“Serial ctDNA levels during follow-up can precede disease recurrence prior to routine radiographic imaging,” the investigators concluded. “Because ctDNA measurements can be obtained from blood samples collected during routine follow-up, they may be easily incorporated into routine follow-up to complement a CEA test, radiographic imaging, and other conventional modalities to help stratify patients on the basis of the risk of disease recurrence. Such a personalized surveillance strategy may allow for earlier detection of relapse and minimize unnecessary testing.”
The study was funded by the Virginia and D.K. Ludwig Fund for Cancer Research, the Commonwealth Foundation, the John Templeton Foundation, and others. The investigators reported financial relationships with PapGene, Sysmex, Eisai, and others.
SOURCE: Wang et al. JAMA Onc. 2019 May 9. doi: 10.1001/jamaoncol.2019.0512.
Based on recent findings of a study conducted by Wang et al. and an increasing amount of research, circulating tumor DNA (ctDNA) testing “will likely revolutionize” postoperative management for patients with early-stage colorectal cancer (CRC), according to Van Morris, MD; Arvind Dasari, MD; and Scott Kopetz, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“The ability to optimize adjuvant chemotherapy recommendations for patients with resected CRC has been historically limited by the use of clinicopathologic characteristics, which imperfectly prognosticate the risk for recurrence,” the doctors wrote in a JAMA Oncology editorial accompanying the article by Wang et al.
In the study by Dr. Wang and associates, “clinical recurrence was strongly linked with ctDNA detection at the time of recurrence,” the doctors wrote, adding that “the absence of ctDNA was highly associated with excellent oncologic outcomes.” These associations translated to predictive advantages, as “[ctDNA] status outperformed traditional risk factors, including the pathological stage, in stratifying patients’ risk for recurrence.”
“With the implications of ctDNA status for recurrence risk, the question remains regarding how this exciting technology can be used to improve the standard practices for CRC,” the authors of the editorial wrote, noting that the National Comprehensive Cancer Network currently recommends monitoring with imaging studies, carcinoembryonic antigen (CEA) tests, and endoscopies. “ctDNA positivity may eventually serve as a biomarker for high-risk patients for whom a more aggressive systemic treatment against residual micrometastatic disease may be advantageous,” they wrote.
They also highlighted how, in the Wang et al. study, chemotherapy was associated with conversion from ctDNA positivity to negativity in one patient, a phenomenon that has been observed in other trials. “Interpretation of these data is limited by a small sample size of patients,” the doctors wrote, “but these findings nonetheless begin to provide important insight into the ability of chemotherapy to clear minimal residual disease, as tracked by serial changes in ctDNA status over time, which is associated with favorable prognostic implications for patients with early-stage CRC. Future trials in CRC and other solid cancers should assess ctDNA clearance more robustly as a surrogate marker for disease-free survival in patients undergoing definitive therapies for their solid tumors.”
“At present, payers in the United States have not yet approved the routine use of ctDNA technologies in patients with early-stage CRC after resection,” the doctors wrote. “However, compelling data on ctDNA as a robust prognostic marker should be a reason to reassess coverage.”
“[With payer support and improved techniques], then this exciting ctDNA technology will likely revolutionize the routine postoperative management of early-stage CRC by providing a reliable, objective tool for oncologists,” they concluded.
Dr. Morris, Dr. Dasari, and Dr. Kopetz are affiliated with the University of Texas MD Anderson Cancer Center in Houston. Dr. Morris reported financial relationships with GuardantHealth and Array Biopharma. Dr. Kopetz reported relationships with Symphogen, Amgen, Merck, and Holy Stone.
Based on recent findings of a study conducted by Wang et al. and an increasing amount of research, circulating tumor DNA (ctDNA) testing “will likely revolutionize” postoperative management for patients with early-stage colorectal cancer (CRC), according to Van Morris, MD; Arvind Dasari, MD; and Scott Kopetz, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“The ability to optimize adjuvant chemotherapy recommendations for patients with resected CRC has been historically limited by the use of clinicopathologic characteristics, which imperfectly prognosticate the risk for recurrence,” the doctors wrote in a JAMA Oncology editorial accompanying the article by Wang et al.
In the study by Dr. Wang and associates, “clinical recurrence was strongly linked with ctDNA detection at the time of recurrence,” the doctors wrote, adding that “the absence of ctDNA was highly associated with excellent oncologic outcomes.” These associations translated to predictive advantages, as “[ctDNA] status outperformed traditional risk factors, including the pathological stage, in stratifying patients’ risk for recurrence.”
“With the implications of ctDNA status for recurrence risk, the question remains regarding how this exciting technology can be used to improve the standard practices for CRC,” the authors of the editorial wrote, noting that the National Comprehensive Cancer Network currently recommends monitoring with imaging studies, carcinoembryonic antigen (CEA) tests, and endoscopies. “ctDNA positivity may eventually serve as a biomarker for high-risk patients for whom a more aggressive systemic treatment against residual micrometastatic disease may be advantageous,” they wrote.
They also highlighted how, in the Wang et al. study, chemotherapy was associated with conversion from ctDNA positivity to negativity in one patient, a phenomenon that has been observed in other trials. “Interpretation of these data is limited by a small sample size of patients,” the doctors wrote, “but these findings nonetheless begin to provide important insight into the ability of chemotherapy to clear minimal residual disease, as tracked by serial changes in ctDNA status over time, which is associated with favorable prognostic implications for patients with early-stage CRC. Future trials in CRC and other solid cancers should assess ctDNA clearance more robustly as a surrogate marker for disease-free survival in patients undergoing definitive therapies for their solid tumors.”
“At present, payers in the United States have not yet approved the routine use of ctDNA technologies in patients with early-stage CRC after resection,” the doctors wrote. “However, compelling data on ctDNA as a robust prognostic marker should be a reason to reassess coverage.”
“[With payer support and improved techniques], then this exciting ctDNA technology will likely revolutionize the routine postoperative management of early-stage CRC by providing a reliable, objective tool for oncologists,” they concluded.
Dr. Morris, Dr. Dasari, and Dr. Kopetz are affiliated with the University of Texas MD Anderson Cancer Center in Houston. Dr. Morris reported financial relationships with GuardantHealth and Array Biopharma. Dr. Kopetz reported relationships with Symphogen, Amgen, Merck, and Holy Stone.
Based on recent findings of a study conducted by Wang et al. and an increasing amount of research, circulating tumor DNA (ctDNA) testing “will likely revolutionize” postoperative management for patients with early-stage colorectal cancer (CRC), according to Van Morris, MD; Arvind Dasari, MD; and Scott Kopetz, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“The ability to optimize adjuvant chemotherapy recommendations for patients with resected CRC has been historically limited by the use of clinicopathologic characteristics, which imperfectly prognosticate the risk for recurrence,” the doctors wrote in a JAMA Oncology editorial accompanying the article by Wang et al.
In the study by Dr. Wang and associates, “clinical recurrence was strongly linked with ctDNA detection at the time of recurrence,” the doctors wrote, adding that “the absence of ctDNA was highly associated with excellent oncologic outcomes.” These associations translated to predictive advantages, as “[ctDNA] status outperformed traditional risk factors, including the pathological stage, in stratifying patients’ risk for recurrence.”
“With the implications of ctDNA status for recurrence risk, the question remains regarding how this exciting technology can be used to improve the standard practices for CRC,” the authors of the editorial wrote, noting that the National Comprehensive Cancer Network currently recommends monitoring with imaging studies, carcinoembryonic antigen (CEA) tests, and endoscopies. “ctDNA positivity may eventually serve as a biomarker for high-risk patients for whom a more aggressive systemic treatment against residual micrometastatic disease may be advantageous,” they wrote.
They also highlighted how, in the Wang et al. study, chemotherapy was associated with conversion from ctDNA positivity to negativity in one patient, a phenomenon that has been observed in other trials. “Interpretation of these data is limited by a small sample size of patients,” the doctors wrote, “but these findings nonetheless begin to provide important insight into the ability of chemotherapy to clear minimal residual disease, as tracked by serial changes in ctDNA status over time, which is associated with favorable prognostic implications for patients with early-stage CRC. Future trials in CRC and other solid cancers should assess ctDNA clearance more robustly as a surrogate marker for disease-free survival in patients undergoing definitive therapies for their solid tumors.”
“At present, payers in the United States have not yet approved the routine use of ctDNA technologies in patients with early-stage CRC after resection,” the doctors wrote. “However, compelling data on ctDNA as a robust prognostic marker should be a reason to reassess coverage.”
“[With payer support and improved techniques], then this exciting ctDNA technology will likely revolutionize the routine postoperative management of early-stage CRC by providing a reliable, objective tool for oncologists,” they concluded.
Dr. Morris, Dr. Dasari, and Dr. Kopetz are affiliated with the University of Texas MD Anderson Cancer Center in Houston. Dr. Morris reported financial relationships with GuardantHealth and Array Biopharma. Dr. Kopetz reported relationships with Symphogen, Amgen, Merck, and Holy Stone.
Circulating tumor DNA (ctDNA) could be used to predict disease recurrence in patients with nonmetastatic colorectal cancer (CRC), according to investigators following an observational study.
About three out of four patients with a positive ctDNA test went on to have disease recurrence, reported lead author Yuxuan Wang, MD, PhD, of Johns Hopkins University School of Medicine in Baltimore, and her colleagues. On average, positive tests preceded clinical and radiologic evidence of recurrence by 3 months.
“[T]he optimal protocol for surveillance of resected colorectal cancer remains uncertain,” the investigators wrote in JAMA Oncology.
“The only recommended blood marker for CRC surveillance is serum [carcinoembryonic antigen (CEA)], an oncofetal protein that is elevated in the serum of patients with a variety of disease conditions, including CRC. Unfortunately, its utility is limited by the lack of sensitivity and specificity.” Although computed tomography and magnetic resonance imaging can improve disease detection, these techniques also have their own shortcomings, the investigators noted, setting the stage for the present study.
The investigators recruited 63 patients with stage I, II, or III CRC who underwent surgical resection in Sweden between 2007 and 2013. Blood samples for ctDNA testing were collected 1 month after surgery, then every 3-6 months. CT was performed every 6-12 months. During this process, 5 patients were excluded, leaving 58 patients in the final dataset, 18 (31%) of whom received adjuvant chemotherapy. Patients were followed until metastasis or a median of 49 months.
Among all patients, 13 tested positive for ctDNA, and 10 of these relapsed (77%), with a median time of 3 months between ctDNA positivity and CT or clinical evidence of recurrence. Three of the 48 patients (6%) who did not relapse had a positive ctDNA result that later dropped to an undetectable level. Of the 45 patients who tested negative for ctDNA, none had recurrence, although 1 was positive for CEA.
Results were also divided into patients who received or did not receive adjuvant chemotherapy. Among the 40 patients who did not receive chemotherapy, 8 had disease recurrence after a positive ctDNA test, although only 5 tested positive for CEA. Among the 18 patients who did receive chemotherapy, 2 tested positive for ctDNA and later relapsed, although only 1 tested positive for CEA. These figures translated to a ctDNA sensitivity for recurrence of 100%, compared with 60% for CEA testing.
“Serial ctDNA levels during follow-up can precede disease recurrence prior to routine radiographic imaging,” the investigators concluded. “Because ctDNA measurements can be obtained from blood samples collected during routine follow-up, they may be easily incorporated into routine follow-up to complement a CEA test, radiographic imaging, and other conventional modalities to help stratify patients on the basis of the risk of disease recurrence. Such a personalized surveillance strategy may allow for earlier detection of relapse and minimize unnecessary testing.”
The study was funded by the Virginia and D.K. Ludwig Fund for Cancer Research, the Commonwealth Foundation, the John Templeton Foundation, and others. The investigators reported financial relationships with PapGene, Sysmex, Eisai, and others.
SOURCE: Wang et al. JAMA Onc. 2019 May 9. doi: 10.1001/jamaoncol.2019.0512.
Circulating tumor DNA (ctDNA) could be used to predict disease recurrence in patients with nonmetastatic colorectal cancer (CRC), according to investigators following an observational study.
About three out of four patients with a positive ctDNA test went on to have disease recurrence, reported lead author Yuxuan Wang, MD, PhD, of Johns Hopkins University School of Medicine in Baltimore, and her colleagues. On average, positive tests preceded clinical and radiologic evidence of recurrence by 3 months.
“[T]he optimal protocol for surveillance of resected colorectal cancer remains uncertain,” the investigators wrote in JAMA Oncology.
“The only recommended blood marker for CRC surveillance is serum [carcinoembryonic antigen (CEA)], an oncofetal protein that is elevated in the serum of patients with a variety of disease conditions, including CRC. Unfortunately, its utility is limited by the lack of sensitivity and specificity.” Although computed tomography and magnetic resonance imaging can improve disease detection, these techniques also have their own shortcomings, the investigators noted, setting the stage for the present study.
The investigators recruited 63 patients with stage I, II, or III CRC who underwent surgical resection in Sweden between 2007 and 2013. Blood samples for ctDNA testing were collected 1 month after surgery, then every 3-6 months. CT was performed every 6-12 months. During this process, 5 patients were excluded, leaving 58 patients in the final dataset, 18 (31%) of whom received adjuvant chemotherapy. Patients were followed until metastasis or a median of 49 months.
Among all patients, 13 tested positive for ctDNA, and 10 of these relapsed (77%), with a median time of 3 months between ctDNA positivity and CT or clinical evidence of recurrence. Three of the 48 patients (6%) who did not relapse had a positive ctDNA result that later dropped to an undetectable level. Of the 45 patients who tested negative for ctDNA, none had recurrence, although 1 was positive for CEA.
Results were also divided into patients who received or did not receive adjuvant chemotherapy. Among the 40 patients who did not receive chemotherapy, 8 had disease recurrence after a positive ctDNA test, although only 5 tested positive for CEA. Among the 18 patients who did receive chemotherapy, 2 tested positive for ctDNA and later relapsed, although only 1 tested positive for CEA. These figures translated to a ctDNA sensitivity for recurrence of 100%, compared with 60% for CEA testing.
“Serial ctDNA levels during follow-up can precede disease recurrence prior to routine radiographic imaging,” the investigators concluded. “Because ctDNA measurements can be obtained from blood samples collected during routine follow-up, they may be easily incorporated into routine follow-up to complement a CEA test, radiographic imaging, and other conventional modalities to help stratify patients on the basis of the risk of disease recurrence. Such a personalized surveillance strategy may allow for earlier detection of relapse and minimize unnecessary testing.”
The study was funded by the Virginia and D.K. Ludwig Fund for Cancer Research, the Commonwealth Foundation, the John Templeton Foundation, and others. The investigators reported financial relationships with PapGene, Sysmex, Eisai, and others.
SOURCE: Wang et al. JAMA Onc. 2019 May 9. doi: 10.1001/jamaoncol.2019.0512.
FROM JAMA ONCOLOGY
Hospitalist movers and shakers – May 2019
Christina L. Andrew, DO, a medical director on the hospitalist team at McLeod Regional Medical Center in Florence, S.C., and Zeshan Anwar, MD, medical director of Evangelical Community Hospital’s hospitalist group in Lewisburg, Pa., recently were named Senior Fellows in Hospital Medicine (SFHM) by the Society of Hospital Medicine. SFHMs are dedicated to promoting excellence, innovation and improving the quality of patient care.
Dr. Andrew has been with McLeod since 2008. The board-certified internist received her medical degree from Des Moines (Iowa) University Osteopathic Medical Center and did her residency at the Cleveland Clinic. To earn SFHM status, physicians must have worked as a hospitalist for at least 5 years and be a member of SHM for 5 years, as well.
Dr. Anwar has been in his current position since 2015. He coordinates staff resources and inpatient care for the facility where he has worked since 2013. He has his medical degree from King Edward Medical University, Lahore, Pakistan, and did his residency at Bronx-Lebanon Hospital Center in New York.
Tiffany Egbe, MD, has been named to the board of directors of Refuge International, an organization that builds relationships in Guatemala that allow for medical services to be provided to an underserved population.
Dr. Egbe is a hospitalist in internal medicine at Christus Good Shepherd in Longview and Marshall, Tex. She also serves as program director of internal medicine residency for the University of Texas Health Science Center in Tyler, Tex.
Dr. Egbe earned her medical degree from the University of Alabama at Birmingham.
Il Jun Chon, MD, has been named vice president of medical affairs with WellSpan Ephrata (Pa.) Community Hospital. Dr. Chon, a hospitalist, had previously been the medical director of WellSpan Ephrata’s hospitalist services and president of the facility’s medical staff.
Dr. Chon earned his medical degree from the Medical College of Pennsylvania (now Drexel College of Medicine) and completed his residency at Thomas Jefferson University Hospital, both in Philadelphia.
Megan Hamreus, DO, recently was named chief of staff at Scripps Mercy Hospital in San Diego, Calif. Dr. Hamreus will oversee 1,000 doctors at two facilities.
Dr. Hamreus has been with Scripps Mercy for 10 years, serving as a hospitalist and a faculty member of the family medicine residence training program of Family Health Centers of San Diego.
Chief of staff is a 2-year, elected term. Among her duties, Dr. Hamreus will be Scripps Mercy’s liaison to the facilities’ administrative staff and Scripps Health’s board of trustees.
Jade Brice Roshell, MD, recently was named chief medical officer at Shelby Baptist Medical Center in Alabaster, Ala. Dr. Brice Roshell was promoted from director of the center’s hospitalist program.
In addition to her new position, Dr. Brice Roshell was named as one of 68 honorees on Becker’s 2019 list of African-American Leaders in Health.
Dr. Brice Roshell has been with Shelby Baptist since 2015. Previously, she was an internist at centers in Louisiana, Georgia, and Nebraska. Her medical degree is from Howard University in Washington, and she completed her residency at Tulane University in New Orleans.
Anju Manral, MD, recently was appointed as medical director for the University of New Mexico Student Health and Counseling Center in Albuquerque. The internist has experience as a hospitalist focused on palliative care and most recently has worked at UNM’s Family Health Clinic, providing care to patients of all ages and conditions.
Dr. Manral also serves as an assistant professor in the UNM General Internal Medicine Department and mentors UNM medical students in the health science learning community.
The Hiawatha (Kan.) Community Hospital unveiled its new hospitalist program on Feb. 12.
The program will be led by Dustin Williams, DNP. Dr. Williams will provide hospitalist and emergency medical services to patients every Tuesday through Friday, while an on-call specialist will serve as hospitalist on Saturday, Sunday, and Monday.
Christina L. Andrew, DO, a medical director on the hospitalist team at McLeod Regional Medical Center in Florence, S.C., and Zeshan Anwar, MD, medical director of Evangelical Community Hospital’s hospitalist group in Lewisburg, Pa., recently were named Senior Fellows in Hospital Medicine (SFHM) by the Society of Hospital Medicine. SFHMs are dedicated to promoting excellence, innovation and improving the quality of patient care.
Dr. Andrew has been with McLeod since 2008. The board-certified internist received her medical degree from Des Moines (Iowa) University Osteopathic Medical Center and did her residency at the Cleveland Clinic. To earn SFHM status, physicians must have worked as a hospitalist for at least 5 years and be a member of SHM for 5 years, as well.
Dr. Anwar has been in his current position since 2015. He coordinates staff resources and inpatient care for the facility where he has worked since 2013. He has his medical degree from King Edward Medical University, Lahore, Pakistan, and did his residency at Bronx-Lebanon Hospital Center in New York.
Tiffany Egbe, MD, has been named to the board of directors of Refuge International, an organization that builds relationships in Guatemala that allow for medical services to be provided to an underserved population.
Dr. Egbe is a hospitalist in internal medicine at Christus Good Shepherd in Longview and Marshall, Tex. She also serves as program director of internal medicine residency for the University of Texas Health Science Center in Tyler, Tex.
Dr. Egbe earned her medical degree from the University of Alabama at Birmingham.
Il Jun Chon, MD, has been named vice president of medical affairs with WellSpan Ephrata (Pa.) Community Hospital. Dr. Chon, a hospitalist, had previously been the medical director of WellSpan Ephrata’s hospitalist services and president of the facility’s medical staff.
Dr. Chon earned his medical degree from the Medical College of Pennsylvania (now Drexel College of Medicine) and completed his residency at Thomas Jefferson University Hospital, both in Philadelphia.
Megan Hamreus, DO, recently was named chief of staff at Scripps Mercy Hospital in San Diego, Calif. Dr. Hamreus will oversee 1,000 doctors at two facilities.
Dr. Hamreus has been with Scripps Mercy for 10 years, serving as a hospitalist and a faculty member of the family medicine residence training program of Family Health Centers of San Diego.
Chief of staff is a 2-year, elected term. Among her duties, Dr. Hamreus will be Scripps Mercy’s liaison to the facilities’ administrative staff and Scripps Health’s board of trustees.
Jade Brice Roshell, MD, recently was named chief medical officer at Shelby Baptist Medical Center in Alabaster, Ala. Dr. Brice Roshell was promoted from director of the center’s hospitalist program.
In addition to her new position, Dr. Brice Roshell was named as one of 68 honorees on Becker’s 2019 list of African-American Leaders in Health.
Dr. Brice Roshell has been with Shelby Baptist since 2015. Previously, she was an internist at centers in Louisiana, Georgia, and Nebraska. Her medical degree is from Howard University in Washington, and she completed her residency at Tulane University in New Orleans.
Anju Manral, MD, recently was appointed as medical director for the University of New Mexico Student Health and Counseling Center in Albuquerque. The internist has experience as a hospitalist focused on palliative care and most recently has worked at UNM’s Family Health Clinic, providing care to patients of all ages and conditions.
Dr. Manral also serves as an assistant professor in the UNM General Internal Medicine Department and mentors UNM medical students in the health science learning community.
The Hiawatha (Kan.) Community Hospital unveiled its new hospitalist program on Feb. 12.
The program will be led by Dustin Williams, DNP. Dr. Williams will provide hospitalist and emergency medical services to patients every Tuesday through Friday, while an on-call specialist will serve as hospitalist on Saturday, Sunday, and Monday.
Christina L. Andrew, DO, a medical director on the hospitalist team at McLeod Regional Medical Center in Florence, S.C., and Zeshan Anwar, MD, medical director of Evangelical Community Hospital’s hospitalist group in Lewisburg, Pa., recently were named Senior Fellows in Hospital Medicine (SFHM) by the Society of Hospital Medicine. SFHMs are dedicated to promoting excellence, innovation and improving the quality of patient care.
Dr. Andrew has been with McLeod since 2008. The board-certified internist received her medical degree from Des Moines (Iowa) University Osteopathic Medical Center and did her residency at the Cleveland Clinic. To earn SFHM status, physicians must have worked as a hospitalist for at least 5 years and be a member of SHM for 5 years, as well.
Dr. Anwar has been in his current position since 2015. He coordinates staff resources and inpatient care for the facility where he has worked since 2013. He has his medical degree from King Edward Medical University, Lahore, Pakistan, and did his residency at Bronx-Lebanon Hospital Center in New York.
Tiffany Egbe, MD, has been named to the board of directors of Refuge International, an organization that builds relationships in Guatemala that allow for medical services to be provided to an underserved population.
Dr. Egbe is a hospitalist in internal medicine at Christus Good Shepherd in Longview and Marshall, Tex. She also serves as program director of internal medicine residency for the University of Texas Health Science Center in Tyler, Tex.
Dr. Egbe earned her medical degree from the University of Alabama at Birmingham.
Il Jun Chon, MD, has been named vice president of medical affairs with WellSpan Ephrata (Pa.) Community Hospital. Dr. Chon, a hospitalist, had previously been the medical director of WellSpan Ephrata’s hospitalist services and president of the facility’s medical staff.
Dr. Chon earned his medical degree from the Medical College of Pennsylvania (now Drexel College of Medicine) and completed his residency at Thomas Jefferson University Hospital, both in Philadelphia.
Megan Hamreus, DO, recently was named chief of staff at Scripps Mercy Hospital in San Diego, Calif. Dr. Hamreus will oversee 1,000 doctors at two facilities.
Dr. Hamreus has been with Scripps Mercy for 10 years, serving as a hospitalist and a faculty member of the family medicine residence training program of Family Health Centers of San Diego.
Chief of staff is a 2-year, elected term. Among her duties, Dr. Hamreus will be Scripps Mercy’s liaison to the facilities’ administrative staff and Scripps Health’s board of trustees.
Jade Brice Roshell, MD, recently was named chief medical officer at Shelby Baptist Medical Center in Alabaster, Ala. Dr. Brice Roshell was promoted from director of the center’s hospitalist program.
In addition to her new position, Dr. Brice Roshell was named as one of 68 honorees on Becker’s 2019 list of African-American Leaders in Health.
Dr. Brice Roshell has been with Shelby Baptist since 2015. Previously, she was an internist at centers in Louisiana, Georgia, and Nebraska. Her medical degree is from Howard University in Washington, and she completed her residency at Tulane University in New Orleans.
Anju Manral, MD, recently was appointed as medical director for the University of New Mexico Student Health and Counseling Center in Albuquerque. The internist has experience as a hospitalist focused on palliative care and most recently has worked at UNM’s Family Health Clinic, providing care to patients of all ages and conditions.
Dr. Manral also serves as an assistant professor in the UNM General Internal Medicine Department and mentors UNM medical students in the health science learning community.
The Hiawatha (Kan.) Community Hospital unveiled its new hospitalist program on Feb. 12.
The program will be led by Dustin Williams, DNP. Dr. Williams will provide hospitalist and emergency medical services to patients every Tuesday through Friday, while an on-call specialist will serve as hospitalist on Saturday, Sunday, and Monday.
Higher AFib ablation volumes linked with better outcomes
SAN FRANCISCO – The number of atrial fibrillation (Afib) catheter ablations a hospital did a year had a substantial, independent effect on patient outcomes in a study of more than 54,000 U.S. catheter ablations performed during 2010-2014.
The results showed that the roughly one-third of studied hospitals with the lowest annual volume of catheter ablations performed, 20 or fewer, had twice the acute complication rate and twice the 30-day in-hospital mortality rate, compared with the hospitals that did 53 or more such procedures annually in patients with atrial fibrillation, Jim W. Cheung, MD, said while presenting a poster at the annual scientific sessions of the Heart Rhythm Society.
The data, taken from 1,738 U.S. hospitals during 2010-2014 and captured in the Nationwide Readmissions Database, also showed that 79% of these hospitals performed 20 or fewer catheter ablations for atrial fibrillation (AFib) annually, with 63% doing 10 or fewer cases per year during the 5 years studied.
The findings raise the question of whether U.S. guidelines for catheter ablation of AFib should specify a minimum case volume for hospital programs, and if so, how high the minimum should be. Volume thresholds are “something to think about,” or a system to designate centers of excellence, Dr. Cheung suggested in a video interview. But interest in setting volume thresholds to better insure competence is often counterbalanced by concerns about patient access, he noted.
The prevailing U.S. guidelines for catheter ablation of AFib are in a 2017 statement from the Heart Rhythm Society and several collaborating groups (J Arrhythm. 2017 Oct;33[5]:369-409). The statement focused on operator volume rather than hospital volume and said that each operator should perform “several” AFib ablation procedures each month, which is generally understood to mean at least 2 per month or at least about 25 annually, commented Hugh Calkins, MD, chair of the panel that wrote the statement and professor of medicine at Johns Hopkins Medicine in Baltimore. The major rationale for setting a suggested minimum of about 25 cases/year came largely from a 2013 report that is cited as the first study to document a volume-outcome relationship for catheter ablation of AFib (Circulation. 2013 Nov 5;128[19]:2104-12), Dr. Calkins noted. “Volume does matter,” he agreed in an interview, but no society or organization monitors hospital or operator volumes, nor takes any steps when volumes are low.
The Nationwide Readmissions Database included 54,599 patients who underwent AFib catheter ablation during 2010-2014. Dr. Cheung and his associates divided these patients into rough tertiles based on the annual procedure volumes of the hospitals that performed these ablations. The 36% of patients treated at hospitals that did 20 or fewer procedures annually were on average older and had more comorbidities than the 31% treated at hospitals in the highest-volume tertile, which performed at least 53 ablations annually. In an analysis that adjusted for these demographic and clinical differences, patients ablated at the lower-volume hospitals had a statistically significant 2.06-fold higher rate of any complication and a 2.24-fold increased rate of in-hospital mortality, either during the index hospitalization or during a 30-day hospital readmission, reported Dr. Cheung, director of clinical electrophysiology research at Weill Cornell Medical College in New York. The increased rate of complications was driven by a fivefold increased rate of cardiac perforations, a greater than doubled periprocedural stroke rate, and a roughly 50% increased rate of vascular complications, compared with the highest-volume hospitals and after adjustment for baseline differences.
Dr. Cheung has been a consultant to Abbott and Biotronik, and has received fellowship support from Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. Dr. Calkins disclosed ties to Abbott, Altathera, AtriCure, Boehringer Ingelheim, Boston Scientific, Medtronic, St. Jude, and MRI Interventions.
SOURCE: Cheung JW. HRS 2019, Abstract S-P001-123.
SAN FRANCISCO – The number of atrial fibrillation (Afib) catheter ablations a hospital did a year had a substantial, independent effect on patient outcomes in a study of more than 54,000 U.S. catheter ablations performed during 2010-2014.
The results showed that the roughly one-third of studied hospitals with the lowest annual volume of catheter ablations performed, 20 or fewer, had twice the acute complication rate and twice the 30-day in-hospital mortality rate, compared with the hospitals that did 53 or more such procedures annually in patients with atrial fibrillation, Jim W. Cheung, MD, said while presenting a poster at the annual scientific sessions of the Heart Rhythm Society.
The data, taken from 1,738 U.S. hospitals during 2010-2014 and captured in the Nationwide Readmissions Database, also showed that 79% of these hospitals performed 20 or fewer catheter ablations for atrial fibrillation (AFib) annually, with 63% doing 10 or fewer cases per year during the 5 years studied.
The findings raise the question of whether U.S. guidelines for catheter ablation of AFib should specify a minimum case volume for hospital programs, and if so, how high the minimum should be. Volume thresholds are “something to think about,” or a system to designate centers of excellence, Dr. Cheung suggested in a video interview. But interest in setting volume thresholds to better insure competence is often counterbalanced by concerns about patient access, he noted.
The prevailing U.S. guidelines for catheter ablation of AFib are in a 2017 statement from the Heart Rhythm Society and several collaborating groups (J Arrhythm. 2017 Oct;33[5]:369-409). The statement focused on operator volume rather than hospital volume and said that each operator should perform “several” AFib ablation procedures each month, which is generally understood to mean at least 2 per month or at least about 25 annually, commented Hugh Calkins, MD, chair of the panel that wrote the statement and professor of medicine at Johns Hopkins Medicine in Baltimore. The major rationale for setting a suggested minimum of about 25 cases/year came largely from a 2013 report that is cited as the first study to document a volume-outcome relationship for catheter ablation of AFib (Circulation. 2013 Nov 5;128[19]:2104-12), Dr. Calkins noted. “Volume does matter,” he agreed in an interview, but no society or organization monitors hospital or operator volumes, nor takes any steps when volumes are low.
The Nationwide Readmissions Database included 54,599 patients who underwent AFib catheter ablation during 2010-2014. Dr. Cheung and his associates divided these patients into rough tertiles based on the annual procedure volumes of the hospitals that performed these ablations. The 36% of patients treated at hospitals that did 20 or fewer procedures annually were on average older and had more comorbidities than the 31% treated at hospitals in the highest-volume tertile, which performed at least 53 ablations annually. In an analysis that adjusted for these demographic and clinical differences, patients ablated at the lower-volume hospitals had a statistically significant 2.06-fold higher rate of any complication and a 2.24-fold increased rate of in-hospital mortality, either during the index hospitalization or during a 30-day hospital readmission, reported Dr. Cheung, director of clinical electrophysiology research at Weill Cornell Medical College in New York. The increased rate of complications was driven by a fivefold increased rate of cardiac perforations, a greater than doubled periprocedural stroke rate, and a roughly 50% increased rate of vascular complications, compared with the highest-volume hospitals and after adjustment for baseline differences.
Dr. Cheung has been a consultant to Abbott and Biotronik, and has received fellowship support from Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. Dr. Calkins disclosed ties to Abbott, Altathera, AtriCure, Boehringer Ingelheim, Boston Scientific, Medtronic, St. Jude, and MRI Interventions.
SOURCE: Cheung JW. HRS 2019, Abstract S-P001-123.
SAN FRANCISCO – The number of atrial fibrillation (Afib) catheter ablations a hospital did a year had a substantial, independent effect on patient outcomes in a study of more than 54,000 U.S. catheter ablations performed during 2010-2014.
The results showed that the roughly one-third of studied hospitals with the lowest annual volume of catheter ablations performed, 20 or fewer, had twice the acute complication rate and twice the 30-day in-hospital mortality rate, compared with the hospitals that did 53 or more such procedures annually in patients with atrial fibrillation, Jim W. Cheung, MD, said while presenting a poster at the annual scientific sessions of the Heart Rhythm Society.
The data, taken from 1,738 U.S. hospitals during 2010-2014 and captured in the Nationwide Readmissions Database, also showed that 79% of these hospitals performed 20 or fewer catheter ablations for atrial fibrillation (AFib) annually, with 63% doing 10 or fewer cases per year during the 5 years studied.
The findings raise the question of whether U.S. guidelines for catheter ablation of AFib should specify a minimum case volume for hospital programs, and if so, how high the minimum should be. Volume thresholds are “something to think about,” or a system to designate centers of excellence, Dr. Cheung suggested in a video interview. But interest in setting volume thresholds to better insure competence is often counterbalanced by concerns about patient access, he noted.
The prevailing U.S. guidelines for catheter ablation of AFib are in a 2017 statement from the Heart Rhythm Society and several collaborating groups (J Arrhythm. 2017 Oct;33[5]:369-409). The statement focused on operator volume rather than hospital volume and said that each operator should perform “several” AFib ablation procedures each month, which is generally understood to mean at least 2 per month or at least about 25 annually, commented Hugh Calkins, MD, chair of the panel that wrote the statement and professor of medicine at Johns Hopkins Medicine in Baltimore. The major rationale for setting a suggested minimum of about 25 cases/year came largely from a 2013 report that is cited as the first study to document a volume-outcome relationship for catheter ablation of AFib (Circulation. 2013 Nov 5;128[19]:2104-12), Dr. Calkins noted. “Volume does matter,” he agreed in an interview, but no society or organization monitors hospital or operator volumes, nor takes any steps when volumes are low.
The Nationwide Readmissions Database included 54,599 patients who underwent AFib catheter ablation during 2010-2014. Dr. Cheung and his associates divided these patients into rough tertiles based on the annual procedure volumes of the hospitals that performed these ablations. The 36% of patients treated at hospitals that did 20 or fewer procedures annually were on average older and had more comorbidities than the 31% treated at hospitals in the highest-volume tertile, which performed at least 53 ablations annually. In an analysis that adjusted for these demographic and clinical differences, patients ablated at the lower-volume hospitals had a statistically significant 2.06-fold higher rate of any complication and a 2.24-fold increased rate of in-hospital mortality, either during the index hospitalization or during a 30-day hospital readmission, reported Dr. Cheung, director of clinical electrophysiology research at Weill Cornell Medical College in New York. The increased rate of complications was driven by a fivefold increased rate of cardiac perforations, a greater than doubled periprocedural stroke rate, and a roughly 50% increased rate of vascular complications, compared with the highest-volume hospitals and after adjustment for baseline differences.
Dr. Cheung has been a consultant to Abbott and Biotronik, and has received fellowship support from Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude. Dr. Calkins disclosed ties to Abbott, Altathera, AtriCure, Boehringer Ingelheim, Boston Scientific, Medtronic, St. Jude, and MRI Interventions.
SOURCE: Cheung JW. HRS 2019, Abstract S-P001-123.
REPORTING FROM HEART RHYTHM 2019
Key clinical point: .
Major finding: Hospitals performing 20 or fewer catheter ablations annually had twice as many acute complications as hospitals doing at least 53.
Study details: Analysis of 54,599 atrial fibrillation patients who underwent catheter ablation in the Nationwide Readmissions Database.
Disclosures: Dr. Cheung has been a consultant to Abbott and Biotronik, and has received fellowship support from Biosense Webster, Biotronik, Boston Scientific, Medtronic, and St. Jude.
Source: Cheung JW et al. Heart Rhythm 2019, Abstract S-P001-123.
No exudates or fever? Age over 11? Skip strep test
BALTIMORE – In children with pharyngitis, it’s safe to skip group A Streptococcus testing if there are no exudates, children are 11 years or older, and there is either no cervical adenopathy or adenopathy without fever, according to a Boston Children’s Hospital investigation.
The prevalence of group A Streptococcus among children who meet those criteria is 13%, less than the estimated asymptomatic carriage rate of about 15%. Among 67,127 children tested for strep and treated for sore throats in a network of retail health clinics across the United States, 35% fit the profile.
Investigators led by Daniel Shapiro, MD, a pediatrics fellow at Boston Children’s, concluded that “laboratory testing for GAS [group A Streptococcus] might be safely avoided in a large proportion of patients with sore throats. In doing so, we may avoid some of the downstream effects of unnecessary antibiotic use.” Incorporating the rules into EHRs “might help physicians identify patients who are at low risk of GAS pharyngitis.”
The study team tackled a long-standing and vexing problem in general pediatrics: how to distinguish viral from GAS pharyngitis. They often present the same way, so it’s difficult to tell them apart, but important to do so to prevent misuse of antibiotics. Health care providers generally rely on rapid strep tests and other assays to make the call, but they have to be used cautiously, because asymptomatic carriers also will test positive and be at risk for unnecessary treatment, Dr. Shapiro said at the Pediatric Academic Societies annual meeting.
To try to prevent that, the Infectious Disease Society of America (IDSA) recommends against strep testing in children who present with overt viral signs, including cough, rhinorrhea, oral ulcers, and hoarseness (Clin Infect Dis. 2012 Nov 15;55[10]:1279-82).
In a previous study at Boston Children’s ED, however, Dr. Shapiro and his colleagues found that 29% of children with overt viral features were positive for GAS, suggesting that the IDSA guidelines probably go too far (Pediatrics. 2017 May;139[5]. pii: e20163403).
“One might conclude that while it’s a good rule of thumb to avoid testing patients with viral features, some of the patients with viral features really do have GAS pharyngitis, so the recommendation to forgo testing in all these kids needs a little bit of refinement,” he said.
That was the goal of the new study; the team sought to identify viral features that signaled a low risk of GAS pharyngitis and, therefore, no need for testing. Low risk was defined as less than 15%, in keeping with the asymptomatic carriage rate.
The 67,127 patients were aged 3-21 years. Their signs and symptoms were collected at the retail clinics in a standardized form. The subjects had rapid strep tests, with negative results confirmed by DNA probe or culture.
Fifty-four percent had viral features, defined in the study as cough, runny nose, or hoarseness (oral ulcers weren’t collected on the form). The overall prevalence of GAS was 35%, similar to previous studies; 39% of children with no viral features tested positive for GAS versus 26% of children with all three. Exudates and age below 11 years were strongly associated with GAS among patients with viral features.
It turned out that just 23% of children without exudates were GAS positive; the number fell to 15% when limited to children 11 years or older, and to 13% when either no cervical adenopathy or adenopathy without fever were added to the mix.
There was no industry funding, and Dr. Shapiro didn’t have any disclosures.
BALTIMORE – In children with pharyngitis, it’s safe to skip group A Streptococcus testing if there are no exudates, children are 11 years or older, and there is either no cervical adenopathy or adenopathy without fever, according to a Boston Children’s Hospital investigation.
The prevalence of group A Streptococcus among children who meet those criteria is 13%, less than the estimated asymptomatic carriage rate of about 15%. Among 67,127 children tested for strep and treated for sore throats in a network of retail health clinics across the United States, 35% fit the profile.
Investigators led by Daniel Shapiro, MD, a pediatrics fellow at Boston Children’s, concluded that “laboratory testing for GAS [group A Streptococcus] might be safely avoided in a large proportion of patients with sore throats. In doing so, we may avoid some of the downstream effects of unnecessary antibiotic use.” Incorporating the rules into EHRs “might help physicians identify patients who are at low risk of GAS pharyngitis.”
The study team tackled a long-standing and vexing problem in general pediatrics: how to distinguish viral from GAS pharyngitis. They often present the same way, so it’s difficult to tell them apart, but important to do so to prevent misuse of antibiotics. Health care providers generally rely on rapid strep tests and other assays to make the call, but they have to be used cautiously, because asymptomatic carriers also will test positive and be at risk for unnecessary treatment, Dr. Shapiro said at the Pediatric Academic Societies annual meeting.
To try to prevent that, the Infectious Disease Society of America (IDSA) recommends against strep testing in children who present with overt viral signs, including cough, rhinorrhea, oral ulcers, and hoarseness (Clin Infect Dis. 2012 Nov 15;55[10]:1279-82).
In a previous study at Boston Children’s ED, however, Dr. Shapiro and his colleagues found that 29% of children with overt viral features were positive for GAS, suggesting that the IDSA guidelines probably go too far (Pediatrics. 2017 May;139[5]. pii: e20163403).
“One might conclude that while it’s a good rule of thumb to avoid testing patients with viral features, some of the patients with viral features really do have GAS pharyngitis, so the recommendation to forgo testing in all these kids needs a little bit of refinement,” he said.
That was the goal of the new study; the team sought to identify viral features that signaled a low risk of GAS pharyngitis and, therefore, no need for testing. Low risk was defined as less than 15%, in keeping with the asymptomatic carriage rate.
The 67,127 patients were aged 3-21 years. Their signs and symptoms were collected at the retail clinics in a standardized form. The subjects had rapid strep tests, with negative results confirmed by DNA probe or culture.
Fifty-four percent had viral features, defined in the study as cough, runny nose, or hoarseness (oral ulcers weren’t collected on the form). The overall prevalence of GAS was 35%, similar to previous studies; 39% of children with no viral features tested positive for GAS versus 26% of children with all three. Exudates and age below 11 years were strongly associated with GAS among patients with viral features.
It turned out that just 23% of children without exudates were GAS positive; the number fell to 15% when limited to children 11 years or older, and to 13% when either no cervical adenopathy or adenopathy without fever were added to the mix.
There was no industry funding, and Dr. Shapiro didn’t have any disclosures.
BALTIMORE – In children with pharyngitis, it’s safe to skip group A Streptococcus testing if there are no exudates, children are 11 years or older, and there is either no cervical adenopathy or adenopathy without fever, according to a Boston Children’s Hospital investigation.
The prevalence of group A Streptococcus among children who meet those criteria is 13%, less than the estimated asymptomatic carriage rate of about 15%. Among 67,127 children tested for strep and treated for sore throats in a network of retail health clinics across the United States, 35% fit the profile.
Investigators led by Daniel Shapiro, MD, a pediatrics fellow at Boston Children’s, concluded that “laboratory testing for GAS [group A Streptococcus] might be safely avoided in a large proportion of patients with sore throats. In doing so, we may avoid some of the downstream effects of unnecessary antibiotic use.” Incorporating the rules into EHRs “might help physicians identify patients who are at low risk of GAS pharyngitis.”
The study team tackled a long-standing and vexing problem in general pediatrics: how to distinguish viral from GAS pharyngitis. They often present the same way, so it’s difficult to tell them apart, but important to do so to prevent misuse of antibiotics. Health care providers generally rely on rapid strep tests and other assays to make the call, but they have to be used cautiously, because asymptomatic carriers also will test positive and be at risk for unnecessary treatment, Dr. Shapiro said at the Pediatric Academic Societies annual meeting.
To try to prevent that, the Infectious Disease Society of America (IDSA) recommends against strep testing in children who present with overt viral signs, including cough, rhinorrhea, oral ulcers, and hoarseness (Clin Infect Dis. 2012 Nov 15;55[10]:1279-82).
In a previous study at Boston Children’s ED, however, Dr. Shapiro and his colleagues found that 29% of children with overt viral features were positive for GAS, suggesting that the IDSA guidelines probably go too far (Pediatrics. 2017 May;139[5]. pii: e20163403).
“One might conclude that while it’s a good rule of thumb to avoid testing patients with viral features, some of the patients with viral features really do have GAS pharyngitis, so the recommendation to forgo testing in all these kids needs a little bit of refinement,” he said.
That was the goal of the new study; the team sought to identify viral features that signaled a low risk of GAS pharyngitis and, therefore, no need for testing. Low risk was defined as less than 15%, in keeping with the asymptomatic carriage rate.
The 67,127 patients were aged 3-21 years. Their signs and symptoms were collected at the retail clinics in a standardized form. The subjects had rapid strep tests, with negative results confirmed by DNA probe or culture.
Fifty-four percent had viral features, defined in the study as cough, runny nose, or hoarseness (oral ulcers weren’t collected on the form). The overall prevalence of GAS was 35%, similar to previous studies; 39% of children with no viral features tested positive for GAS versus 26% of children with all three. Exudates and age below 11 years were strongly associated with GAS among patients with viral features.
It turned out that just 23% of children without exudates were GAS positive; the number fell to 15% when limited to children 11 years or older, and to 13% when either no cervical adenopathy or adenopathy without fever were added to the mix.
There was no industry funding, and Dr. Shapiro didn’t have any disclosures.
REPORTING FROM PAS 2019
Rimegepant dissolving tablets treat acute migraine in phase 3 trial
PHILADELPHIA – according to phase 3 trial results presented at the annual meeting of the American Academy of Neurology. The treatment’s efficacy is sustained for 2-48 hours, researchers reported.
Rimegepant is a small molecule calcitonin gene–related peptide receptor antagonist. A 75-mg oral tablet formulation was effective in phase 3 trials. The present study evaluated a novel, orally dissolving tablet formulation that is intended to speed the drug’s onset. The tablet’s time to peak concentration is 1.50 hours, compared with 1.99 hours for the oral tablet.
Formulation preferences
“People with migraine prefer orally dissolving tablets to oral tablets, mainly for their convenience, onset of action, and ability to be taken without drinking liquids,” said first author Richard B. Lipton, MD, of Albert Einstein College of Medicine, New York, and colleagues.
To assess the formulation’s efficacy and safety, the investigators conducted a double-blind, randomized, placebo-controlled, multicenter trial. Participants were aged at least 18 years and had migraine for at least 1 year. They had 2-8 moderate or severe migraine attacks and fewer than 15 headache days per month during the 3 months before the trial. Their preventive migraine medication doses, if any, had been stable for at least 3 months.
Coprimary efficacy endpoints were pain freedom 2 hours post dose and freedom from the most bothersome symptom at 2 hours post dose. The efficacy analyses included randomized subjects who had a qualifying migraine attack, took the study medication, and provided at least one postbaseline efficacy data point.
The investigators included 1,351 patients in their efficacy analysis – 669 who received rimegepant and 682 who received placebo. About 85% were female, and patients’ mean age was 40.2 years. They averaged 4.6 migraine attacks per month, and their most bothersome symptoms included photophobia (57%), nausea (23.5%), and phonophobia (19.3%). About 14% used preventive treatment.
Within 45 days of randomization, patients treated a migraine attack of moderate to severe intensity and completed an electronic diary predose to 48 hours post dose.
Less use of rescue medication
At 2 hours post dose, patients who received 75 mg rimegepant were more likely than patients who received placebo to achieve pain freedom (21.2% vs. 10.9%) and freedom from the most bothersome symptom (35.1% vs. 26.8%).
Numerical differences in the likelihood of pain relief between group began 15 minutes post dose, and the difference was statistically significant at 60 minutes (36.8% vs. 31.2%).
Various secondary endpoints, including ability to function normally at 2 hours post dose (38.1% vs. 25.8%), sustained pain relief from 2-48 hours (42.2% vs. 25.2%), and use of rescue medications within 24 hours (14.2% vs. 29.2%), also were statistically significant.
In the safety analysis, the most common adverse events were nausea (1.6% in the rimegepant group and 0.4% in the placebo group) and urinary tract infection (1.5% in the rimegepant group and 0.6% in the placebo group). There were no serious adverse events. “Safety and tolerability were similar to placebo,” Dr. Lipton and colleagues said.
Biohaven Pharmaceuticals, the developer of the drug, sponsored the study. Dr. Lipton has received honoraria and research support from Biohaven and holds stock in the company. Coauthors are employees of Biohaven.
PHILADELPHIA – according to phase 3 trial results presented at the annual meeting of the American Academy of Neurology. The treatment’s efficacy is sustained for 2-48 hours, researchers reported.
Rimegepant is a small molecule calcitonin gene–related peptide receptor antagonist. A 75-mg oral tablet formulation was effective in phase 3 trials. The present study evaluated a novel, orally dissolving tablet formulation that is intended to speed the drug’s onset. The tablet’s time to peak concentration is 1.50 hours, compared with 1.99 hours for the oral tablet.
Formulation preferences
“People with migraine prefer orally dissolving tablets to oral tablets, mainly for their convenience, onset of action, and ability to be taken without drinking liquids,” said first author Richard B. Lipton, MD, of Albert Einstein College of Medicine, New York, and colleagues.
To assess the formulation’s efficacy and safety, the investigators conducted a double-blind, randomized, placebo-controlled, multicenter trial. Participants were aged at least 18 years and had migraine for at least 1 year. They had 2-8 moderate or severe migraine attacks and fewer than 15 headache days per month during the 3 months before the trial. Their preventive migraine medication doses, if any, had been stable for at least 3 months.
Coprimary efficacy endpoints were pain freedom 2 hours post dose and freedom from the most bothersome symptom at 2 hours post dose. The efficacy analyses included randomized subjects who had a qualifying migraine attack, took the study medication, and provided at least one postbaseline efficacy data point.
The investigators included 1,351 patients in their efficacy analysis – 669 who received rimegepant and 682 who received placebo. About 85% were female, and patients’ mean age was 40.2 years. They averaged 4.6 migraine attacks per month, and their most bothersome symptoms included photophobia (57%), nausea (23.5%), and phonophobia (19.3%). About 14% used preventive treatment.
Within 45 days of randomization, patients treated a migraine attack of moderate to severe intensity and completed an electronic diary predose to 48 hours post dose.
Less use of rescue medication
At 2 hours post dose, patients who received 75 mg rimegepant were more likely than patients who received placebo to achieve pain freedom (21.2% vs. 10.9%) and freedom from the most bothersome symptom (35.1% vs. 26.8%).
Numerical differences in the likelihood of pain relief between group began 15 minutes post dose, and the difference was statistically significant at 60 minutes (36.8% vs. 31.2%).
Various secondary endpoints, including ability to function normally at 2 hours post dose (38.1% vs. 25.8%), sustained pain relief from 2-48 hours (42.2% vs. 25.2%), and use of rescue medications within 24 hours (14.2% vs. 29.2%), also were statistically significant.
In the safety analysis, the most common adverse events were nausea (1.6% in the rimegepant group and 0.4% in the placebo group) and urinary tract infection (1.5% in the rimegepant group and 0.6% in the placebo group). There were no serious adverse events. “Safety and tolerability were similar to placebo,” Dr. Lipton and colleagues said.
Biohaven Pharmaceuticals, the developer of the drug, sponsored the study. Dr. Lipton has received honoraria and research support from Biohaven and holds stock in the company. Coauthors are employees of Biohaven.
PHILADELPHIA – according to phase 3 trial results presented at the annual meeting of the American Academy of Neurology. The treatment’s efficacy is sustained for 2-48 hours, researchers reported.
Rimegepant is a small molecule calcitonin gene–related peptide receptor antagonist. A 75-mg oral tablet formulation was effective in phase 3 trials. The present study evaluated a novel, orally dissolving tablet formulation that is intended to speed the drug’s onset. The tablet’s time to peak concentration is 1.50 hours, compared with 1.99 hours for the oral tablet.
Formulation preferences
“People with migraine prefer orally dissolving tablets to oral tablets, mainly for their convenience, onset of action, and ability to be taken without drinking liquids,” said first author Richard B. Lipton, MD, of Albert Einstein College of Medicine, New York, and colleagues.
To assess the formulation’s efficacy and safety, the investigators conducted a double-blind, randomized, placebo-controlled, multicenter trial. Participants were aged at least 18 years and had migraine for at least 1 year. They had 2-8 moderate or severe migraine attacks and fewer than 15 headache days per month during the 3 months before the trial. Their preventive migraine medication doses, if any, had been stable for at least 3 months.
Coprimary efficacy endpoints were pain freedom 2 hours post dose and freedom from the most bothersome symptom at 2 hours post dose. The efficacy analyses included randomized subjects who had a qualifying migraine attack, took the study medication, and provided at least one postbaseline efficacy data point.
The investigators included 1,351 patients in their efficacy analysis – 669 who received rimegepant and 682 who received placebo. About 85% were female, and patients’ mean age was 40.2 years. They averaged 4.6 migraine attacks per month, and their most bothersome symptoms included photophobia (57%), nausea (23.5%), and phonophobia (19.3%). About 14% used preventive treatment.
Within 45 days of randomization, patients treated a migraine attack of moderate to severe intensity and completed an electronic diary predose to 48 hours post dose.
Less use of rescue medication
At 2 hours post dose, patients who received 75 mg rimegepant were more likely than patients who received placebo to achieve pain freedom (21.2% vs. 10.9%) and freedom from the most bothersome symptom (35.1% vs. 26.8%).
Numerical differences in the likelihood of pain relief between group began 15 minutes post dose, and the difference was statistically significant at 60 minutes (36.8% vs. 31.2%).
Various secondary endpoints, including ability to function normally at 2 hours post dose (38.1% vs. 25.8%), sustained pain relief from 2-48 hours (42.2% vs. 25.2%), and use of rescue medications within 24 hours (14.2% vs. 29.2%), also were statistically significant.
In the safety analysis, the most common adverse events were nausea (1.6% in the rimegepant group and 0.4% in the placebo group) and urinary tract infection (1.5% in the rimegepant group and 0.6% in the placebo group). There were no serious adverse events. “Safety and tolerability were similar to placebo,” Dr. Lipton and colleagues said.
Biohaven Pharmaceuticals, the developer of the drug, sponsored the study. Dr. Lipton has received honoraria and research support from Biohaven and holds stock in the company. Coauthors are employees of Biohaven.
REPORTING FROM AAN 2019