User login
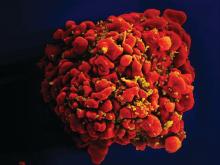
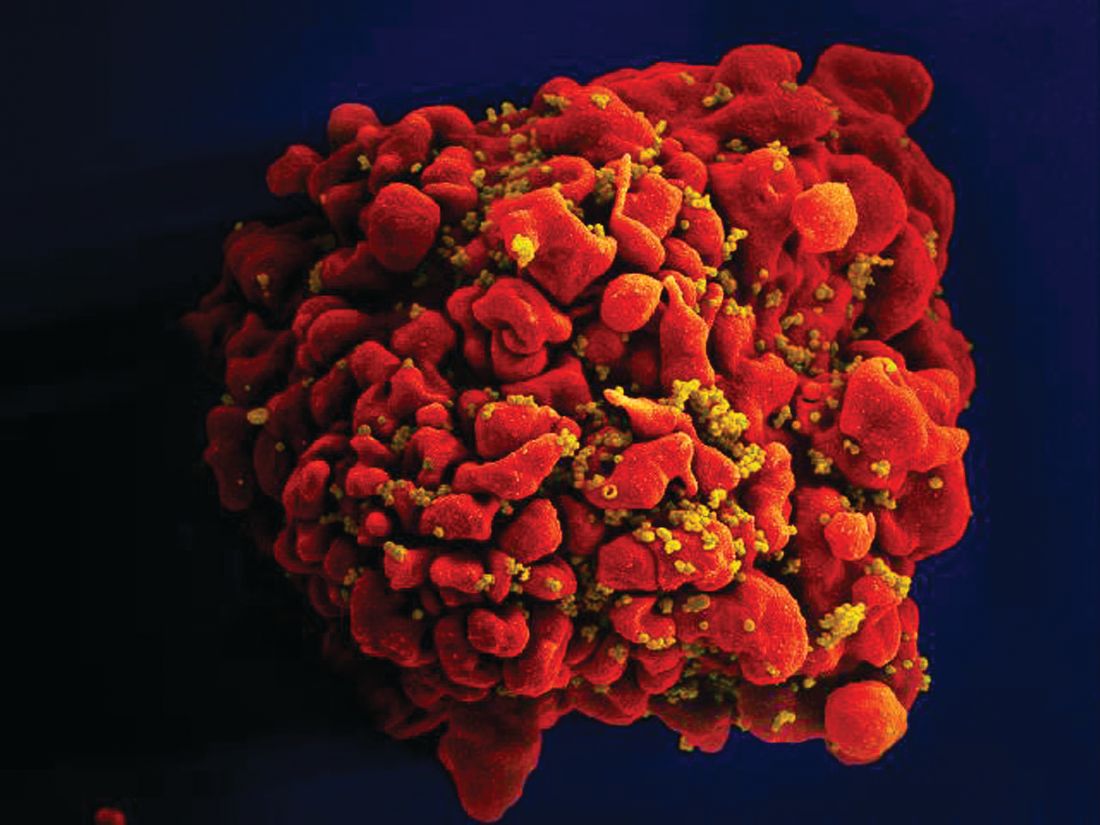
Apremilast and Phototherapy for Treatment of Psoriasis in a Patient With Human Immunodeficiency Virus
To the Editor:
A 50-year old man with Fitzpatrick skin type IV, human immunodeficiency virus (HIV), fatty liver disease, and moderate psoriasis (10% body surface area [BSA] affected) currently treated with clobetasol spray and calcitriol ointment presented with persistent psoriatic lesions on the trunk, arms, legs, and buttocks. His CD4 count was 460 and his HIV RNA count was 48 copies/mL on polymerase chain reaction 2 months prior to the current presentation. He had been undergoing phototherapy 3 times weekly for the last 5 months for treatment of psoriasis.
At the current presentation, he was started on an apremilast starter pack with the dosage titrated from 10 mg to 30 mg over the course of 1 week. He was maintained on a dose of 30 mg twice daily after 1 week and continued clobetasol spray, calcitriol ointment, and phototherapy 3 times weekly with the intent to reduce the frequency after adequate control of psoriasis was achieved. After 3 months of treatment, the affected BSA was 0%. He continued apremilast, and phototherapy was reduced to once weekly. Phototherapy was discontinued after 7 months of concomitant treatment with apremilast after clearance was maintained. It was reinitiated twice weekly after a mild flare (3% BSA affected). After 20 total months of treatment, the patient was no longer able to afford apremilast treatment and presented with a severe psoriasis flare (40% BSA affected). He was switched to acitretin with a plan to apply for apremilast financial assistance programs.
Psoriasis treatment in the HIV population poses a challenge given the immunosuppressed state of these patients, the risk of reactivation of latent infections, and the refractory nature of psoriasis in the setting of HIV. Two of the authors (S.P.R. and J.J.W.) previously reported a case of moderate to severe psoriasis in a patient with HIV and hepatitis C who demonstrated treatment success with apremilast until it was discontinued due to financial implications.1 Currently, apremilast is not widely used to treat psoriasis in the HIV population. The National Psoriasis Foundation 2010 guidelines recommended UV light therapy for treatment of moderate to severe psoriasis in HIV-positive patients, with oral retinoids as the second-line treatment.2 There remains a need for updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population.
Apremilast, a phosphodiesterase 4 inhibitor, is an oral therapy that restores the balance of proinflammatory and anti-inflammatory cytokines by inhibiting inflammatory cytokine (eg, tumor necrosis factor α, IFN-γ, IL-2, IL-12, IL-23) secretion and stimulating anti-inflammatory cytokine (eg, IL-6, IL-10) production. In 2015, the phase 3 ESTEEM 13 and ESTEEM 24 trials demonstrated the efficacy of apremilast 30 mg twice daily for treatment of psoriasis. In both trials, the psoriasis area and severity index 75 response rate at week 16 was significantly
Use of other systemic agents such as tumor necrosis factor α inhibitors and ustekinumab has been reported in HIV-positive patients.5-7 There is no current data on IL-17 and IL-23 inhibitors. Acitretin generally is recommended as a second-line agent in HIV patients given its lack of immunosuppression2; however, methotrexate and cyclosporine should be avoided given the risk of opportunistic infections.8
Apremilast is a promising therapy with a favorable safety profile that should be considered as an adjuvant treatment to first-line agents such as phototherapy in HIV-positive patients. Apremilast has been successfully used in an HIV patient with a concomitant chronic hepatitis C infection.1 Systemic medications such as apremilast should be managed in coordination with infectious disease specialists with close monitoring of CD4 levels and viral loads as well as prophylactic agents.
- Reddy SP, Shah VV, Wu JJ. Apremilast for a psoriasis patient with HIV and hepatitis C. J Eur Acad Dermatol Venereol. 2017;31:e481-e482.
- Menon K, Van Voorhees AS, Bebo BF Jr, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation [published online July 31, 2009]. J Am Acad Dermatol. 2010;62:291-299.
- Papp K, Reich K, Leonardi CL, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol. 2015;73:37-49.
- Paul C, Cather J, Gooderham M, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol. 2015;173:1387-1399.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV-positive patient. J Drugs Dermatol. 2014;13:869-871.
- Saeki H, Ito T, Hayashi M, et al. Successful treatment of ustekinumab in a severe psoriasis patient with human immunodeficiency virus infection. J Eur Acad Dermatol Venereol. 2015;29:1653-1655.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatolog Treat. 2012;23:398-399.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections [published online July 11, 2018]. J Am Acad Dermatol. 2019;80:43-53.
To the Editor:
A 50-year old man with Fitzpatrick skin type IV, human immunodeficiency virus (HIV), fatty liver disease, and moderate psoriasis (10% body surface area [BSA] affected) currently treated with clobetasol spray and calcitriol ointment presented with persistent psoriatic lesions on the trunk, arms, legs, and buttocks. His CD4 count was 460 and his HIV RNA count was 48 copies/mL on polymerase chain reaction 2 months prior to the current presentation. He had been undergoing phototherapy 3 times weekly for the last 5 months for treatment of psoriasis.
At the current presentation, he was started on an apremilast starter pack with the dosage titrated from 10 mg to 30 mg over the course of 1 week. He was maintained on a dose of 30 mg twice daily after 1 week and continued clobetasol spray, calcitriol ointment, and phototherapy 3 times weekly with the intent to reduce the frequency after adequate control of psoriasis was achieved. After 3 months of treatment, the affected BSA was 0%. He continued apremilast, and phototherapy was reduced to once weekly. Phototherapy was discontinued after 7 months of concomitant treatment with apremilast after clearance was maintained. It was reinitiated twice weekly after a mild flare (3% BSA affected). After 20 total months of treatment, the patient was no longer able to afford apremilast treatment and presented with a severe psoriasis flare (40% BSA affected). He was switched to acitretin with a plan to apply for apremilast financial assistance programs.
Psoriasis treatment in the HIV population poses a challenge given the immunosuppressed state of these patients, the risk of reactivation of latent infections, and the refractory nature of psoriasis in the setting of HIV. Two of the authors (S.P.R. and J.J.W.) previously reported a case of moderate to severe psoriasis in a patient with HIV and hepatitis C who demonstrated treatment success with apremilast until it was discontinued due to financial implications.1 Currently, apremilast is not widely used to treat psoriasis in the HIV population. The National Psoriasis Foundation 2010 guidelines recommended UV light therapy for treatment of moderate to severe psoriasis in HIV-positive patients, with oral retinoids as the second-line treatment.2 There remains a need for updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population.
Apremilast, a phosphodiesterase 4 inhibitor, is an oral therapy that restores the balance of proinflammatory and anti-inflammatory cytokines by inhibiting inflammatory cytokine (eg, tumor necrosis factor α, IFN-γ, IL-2, IL-12, IL-23) secretion and stimulating anti-inflammatory cytokine (eg, IL-6, IL-10) production. In 2015, the phase 3 ESTEEM 13 and ESTEEM 24 trials demonstrated the efficacy of apremilast 30 mg twice daily for treatment of psoriasis. In both trials, the psoriasis area and severity index 75 response rate at week 16 was significantly
Use of other systemic agents such as tumor necrosis factor α inhibitors and ustekinumab has been reported in HIV-positive patients.5-7 There is no current data on IL-17 and IL-23 inhibitors. Acitretin generally is recommended as a second-line agent in HIV patients given its lack of immunosuppression2; however, methotrexate and cyclosporine should be avoided given the risk of opportunistic infections.8
Apremilast is a promising therapy with a favorable safety profile that should be considered as an adjuvant treatment to first-line agents such as phototherapy in HIV-positive patients. Apremilast has been successfully used in an HIV patient with a concomitant chronic hepatitis C infection.1 Systemic medications such as apremilast should be managed in coordination with infectious disease specialists with close monitoring of CD4 levels and viral loads as well as prophylactic agents.
To the Editor:
A 50-year old man with Fitzpatrick skin type IV, human immunodeficiency virus (HIV), fatty liver disease, and moderate psoriasis (10% body surface area [BSA] affected) currently treated with clobetasol spray and calcitriol ointment presented with persistent psoriatic lesions on the trunk, arms, legs, and buttocks. His CD4 count was 460 and his HIV RNA count was 48 copies/mL on polymerase chain reaction 2 months prior to the current presentation. He had been undergoing phototherapy 3 times weekly for the last 5 months for treatment of psoriasis.
At the current presentation, he was started on an apremilast starter pack with the dosage titrated from 10 mg to 30 mg over the course of 1 week. He was maintained on a dose of 30 mg twice daily after 1 week and continued clobetasol spray, calcitriol ointment, and phototherapy 3 times weekly with the intent to reduce the frequency after adequate control of psoriasis was achieved. After 3 months of treatment, the affected BSA was 0%. He continued apremilast, and phototherapy was reduced to once weekly. Phototherapy was discontinued after 7 months of concomitant treatment with apremilast after clearance was maintained. It was reinitiated twice weekly after a mild flare (3% BSA affected). After 20 total months of treatment, the patient was no longer able to afford apremilast treatment and presented with a severe psoriasis flare (40% BSA affected). He was switched to acitretin with a plan to apply for apremilast financial assistance programs.
Psoriasis treatment in the HIV population poses a challenge given the immunosuppressed state of these patients, the risk of reactivation of latent infections, and the refractory nature of psoriasis in the setting of HIV. Two of the authors (S.P.R. and J.J.W.) previously reported a case of moderate to severe psoriasis in a patient with HIV and hepatitis C who demonstrated treatment success with apremilast until it was discontinued due to financial implications.1 Currently, apremilast is not widely used to treat psoriasis in the HIV population. The National Psoriasis Foundation 2010 guidelines recommended UV light therapy for treatment of moderate to severe psoriasis in HIV-positive patients, with oral retinoids as the second-line treatment.2 There remains a need for updated guidelines on the use of systemic agents for psoriasis treatment in the HIV population.
Apremilast, a phosphodiesterase 4 inhibitor, is an oral therapy that restores the balance of proinflammatory and anti-inflammatory cytokines by inhibiting inflammatory cytokine (eg, tumor necrosis factor α, IFN-γ, IL-2, IL-12, IL-23) secretion and stimulating anti-inflammatory cytokine (eg, IL-6, IL-10) production. In 2015, the phase 3 ESTEEM 13 and ESTEEM 24 trials demonstrated the efficacy of apremilast 30 mg twice daily for treatment of psoriasis. In both trials, the psoriasis area and severity index 75 response rate at week 16 was significantly
Use of other systemic agents such as tumor necrosis factor α inhibitors and ustekinumab has been reported in HIV-positive patients.5-7 There is no current data on IL-17 and IL-23 inhibitors. Acitretin generally is recommended as a second-line agent in HIV patients given its lack of immunosuppression2; however, methotrexate and cyclosporine should be avoided given the risk of opportunistic infections.8
Apremilast is a promising therapy with a favorable safety profile that should be considered as an adjuvant treatment to first-line agents such as phototherapy in HIV-positive patients. Apremilast has been successfully used in an HIV patient with a concomitant chronic hepatitis C infection.1 Systemic medications such as apremilast should be managed in coordination with infectious disease specialists with close monitoring of CD4 levels and viral loads as well as prophylactic agents.
- Reddy SP, Shah VV, Wu JJ. Apremilast for a psoriasis patient with HIV and hepatitis C. J Eur Acad Dermatol Venereol. 2017;31:e481-e482.
- Menon K, Van Voorhees AS, Bebo BF Jr, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation [published online July 31, 2009]. J Am Acad Dermatol. 2010;62:291-299.
- Papp K, Reich K, Leonardi CL, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol. 2015;73:37-49.
- Paul C, Cather J, Gooderham M, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol. 2015;173:1387-1399.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV-positive patient. J Drugs Dermatol. 2014;13:869-871.
- Saeki H, Ito T, Hayashi M, et al. Successful treatment of ustekinumab in a severe psoriasis patient with human immunodeficiency virus infection. J Eur Acad Dermatol Venereol. 2015;29:1653-1655.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatolog Treat. 2012;23:398-399.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections [published online July 11, 2018]. J Am Acad Dermatol. 2019;80:43-53.
- Reddy SP, Shah VV, Wu JJ. Apremilast for a psoriasis patient with HIV and hepatitis C. J Eur Acad Dermatol Venereol. 2017;31:e481-e482.
- Menon K, Van Voorhees AS, Bebo BF Jr, et al. Psoriasis in patients with HIV infection: from the medical board of the National Psoriasis Foundation [published online July 31, 2009]. J Am Acad Dermatol. 2010;62:291-299.
- Papp K, Reich K, Leonardi CL, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol. 2015;73:37-49.
- Paul C, Cather J, Gooderham M, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol. 2015;173:1387-1399.
- Lindsey SF, Weiss J, Lee ES, et al. Treatment of severe psoriasis and psoriatic arthritis with adalimumab in an HIV-positive patient. J Drugs Dermatol. 2014;13:869-871.
- Saeki H, Ito T, Hayashi M, et al. Successful treatment of ustekinumab in a severe psoriasis patient with human immunodeficiency virus infection. J Eur Acad Dermatol Venereol. 2015;29:1653-1655.
- Paparizos V, Rallis E, Kirsten L, et al. Ustekinumab for the treatment of HIV psoriasis. J Dermatolog Treat. 2012;23:398-399.
- Kaushik SB, Lebwohl MG. Psoriasis: which therapy for which patient: focus on special populations and chronic infections [published online July 11, 2018]. J Am Acad Dermatol. 2019;80:43-53.
Practice Point
- Apremilast may be considered as a first-line therapy in the human immunodeficiency virus population due to decreased immunosuppression.
Is routine induction of labor in a healthy pregnancy at 39 weeks reasonable?
NASHVILLE, TENN. – Aaron B. Caughey, MD, PhD, discussed this in a video at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
In a healthy pregnancy, with no medical indications for induction of labor, 39-40 weeks’ gestation is a time when there is a relatively low risk of stillbirth, although the risk is not zero, Dr. Caughey explained. The same is true for neonatal death. This gestational age is a time when there is a low risk for respiratory complications and a low risk for meconium.
“This might be a nice time to have a baby,” said Dr. Caughey, professor and chair of the department of obstetrics and gynecology at Oregon Health & Science University, Portland. “The trade-off is intervention. Don’t you increase the risk of C-sections?”
Actually, numerous retrospective studies have shown that there is either no difference or a decreased rate of C-sections with induction of labor at 39-40 weeks’ gestation, compared with expectant management.
These findings led to a prospective, randomized study by William A. Grobman, MD, and associates for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network called the ARRIVE trial (N Engl J Med. 2018;379:513-23). In that trial, the investigators randomized 3,062 women to induction of labor and 3,044 to expectant management. A significantly lower percentage of women in the induction of labor group underwent C-section than did women randomized to expectant management: 19% vs. 22% (relative risk, 0.84; P less than .001) – that is, 16% fewer C-sections. Also, 36% fewer women in the induction of labor group experienced preeclampsia. No significant differences were found between the two groups in terms of neonatal outcomes.
However, this is just one study, Dr. Caughey noted. What does is mean for a local community hospital? What does it mean for a busy private obstetrics practice?
Watch this video for his answer.
NASHVILLE, TENN. – Aaron B. Caughey, MD, PhD, discussed this in a video at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
In a healthy pregnancy, with no medical indications for induction of labor, 39-40 weeks’ gestation is a time when there is a relatively low risk of stillbirth, although the risk is not zero, Dr. Caughey explained. The same is true for neonatal death. This gestational age is a time when there is a low risk for respiratory complications and a low risk for meconium.
“This might be a nice time to have a baby,” said Dr. Caughey, professor and chair of the department of obstetrics and gynecology at Oregon Health & Science University, Portland. “The trade-off is intervention. Don’t you increase the risk of C-sections?”
Actually, numerous retrospective studies have shown that there is either no difference or a decreased rate of C-sections with induction of labor at 39-40 weeks’ gestation, compared with expectant management.
These findings led to a prospective, randomized study by William A. Grobman, MD, and associates for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network called the ARRIVE trial (N Engl J Med. 2018;379:513-23). In that trial, the investigators randomized 3,062 women to induction of labor and 3,044 to expectant management. A significantly lower percentage of women in the induction of labor group underwent C-section than did women randomized to expectant management: 19% vs. 22% (relative risk, 0.84; P less than .001) – that is, 16% fewer C-sections. Also, 36% fewer women in the induction of labor group experienced preeclampsia. No significant differences were found between the two groups in terms of neonatal outcomes.
However, this is just one study, Dr. Caughey noted. What does is mean for a local community hospital? What does it mean for a busy private obstetrics practice?
Watch this video for his answer.
NASHVILLE, TENN. – Aaron B. Caughey, MD, PhD, discussed this in a video at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists.
In a healthy pregnancy, with no medical indications for induction of labor, 39-40 weeks’ gestation is a time when there is a relatively low risk of stillbirth, although the risk is not zero, Dr. Caughey explained. The same is true for neonatal death. This gestational age is a time when there is a low risk for respiratory complications and a low risk for meconium.
“This might be a nice time to have a baby,” said Dr. Caughey, professor and chair of the department of obstetrics and gynecology at Oregon Health & Science University, Portland. “The trade-off is intervention. Don’t you increase the risk of C-sections?”
Actually, numerous retrospective studies have shown that there is either no difference or a decreased rate of C-sections with induction of labor at 39-40 weeks’ gestation, compared with expectant management.
These findings led to a prospective, randomized study by William A. Grobman, MD, and associates for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network called the ARRIVE trial (N Engl J Med. 2018;379:513-23). In that trial, the investigators randomized 3,062 women to induction of labor and 3,044 to expectant management. A significantly lower percentage of women in the induction of labor group underwent C-section than did women randomized to expectant management: 19% vs. 22% (relative risk, 0.84; P less than .001) – that is, 16% fewer C-sections. Also, 36% fewer women in the induction of labor group experienced preeclampsia. No significant differences were found between the two groups in terms of neonatal outcomes.
However, this is just one study, Dr. Caughey noted. What does is mean for a local community hospital? What does it mean for a busy private obstetrics practice?
Watch this video for his answer.
REPORTING FROM ACOG 2019
Ultrasound offers advantages for long-term lymph node surveillance in high-grade SCC patients
BALTIMORE – Ultrasound can be a very effective way to track early nodal metastasis in patients with high-stage cutaneous squamous cell carcinomas, and at a fraction of the cost of other imaging modalities.
The technique shows not only abnormal variations in the shape of nodes, but changes in the core and outer density, and vascular patterns, Emily Ruiz, MD, said at the annual meeting of the American College of Mohs Surgery. And over a 2-year surveillance period, this costs thousands less than radiation-based imaging.
Dr. Ruiz, director of the High-Risk Skin Cancer Clinic at Dana-Farber/Brigham and Women’s Cancer Center, Boston, said the standard imaging technique at that center used to be serial CT scans performed at diagnosis and every 6 months thereafter, for 2 years. But recently, the protocol changed: Ultrasound is now the preferred technique.
“The big problem with CT in this earlier disease, is that it can only identify the nodes that are enlarged, and doesn’t tell us anything about the etiology. Ultrasound, on the other hand, looks at a number of different features of the node.”
Tracking high-risk squamous cell carcinoma patients is a must, she said. “About 4% of people diagnosed with high-risk SCC will develop nodal metastases, and 1.5% of those will die from disease-specific death,” most often from locoregional disease. “So it’s critical to identify nodal diseases early as possible. Earlier identification leads to better outcomes.” Ultrasound simply provides more information about nodal metastasis, Dr. Ruiz added.
“The first thing we look at is the general architecture of the node. Resting and reactive nodes have a hypoechoic hilus and a hyperechoic cortex. As they become infiltrated with tumor, the hilus becomes more hyperechoic, and areas of metastasis stand out as much more hyperechoic than the surrounding node.”
Another tip-off is overall shape. If the ratio of the long axis to short axis diameter is less than 2, the lymph node is more likely to be malignant, she said.
“One more important factor that can’t be seen on CT is the node’s vascular pattern. Both resting and reactive nodes tend to have a centralized vascular pattern in the hilus. With tumor infiltration you start to see an asymmetrical vascularization as the nodes are replaced by tumor. The perfusion becomes much more peripheral.”
Cost is another consideration, Dr. Ruiz said. Five CT scans conducted over the recommended 2 years of follow-up will run about $5,000. Five scans with magnetic resonance imaging come in at about $6,500. PET CT is, of course, the most expensive, racking up a national average cost of $28,500 for five scans.
Ultrasound is amazingly inexpensive, Dr. Ruiz said. The national average cost of one scan is around $180, bringing the 2-year cost of five surveillance scans to $900.
Finally, clinicians and patients should consider the potential impact of repeated radiation exposure. “This can really add up over the follow-up period. Because there’s a 10-year latency period for these cancers, this might not be an issue for our older patients, but it really is something to consider in younger ones. “
However, she acknowledged that it’s not a completely rosy picture.
“Ultrasound is very user dependent, but we do think that by putting this in the hands of dermatologists with special training, we can solve this issue. In Europe, ultrasound’s very high sensitivity and specificity, combined with clinical exams, really improves disease detection.”
Unfortunately, at this point, anyone who wants to learn the technique has to go to Europe. “I trained in Germany, where I took a standard 3-day course, did 250 supervised scans, and completed an exam. I realize that’s unrealistic for most people,” she said. But a training protocol is being developed at Brigham and Women’s, under the auspices of the institution’s imaging experts, who felt that 3 days and 250 supervised scans was excessive. The Brigham and Women’s program comprises 8 hours of didactic training and at least 30 supervised scans with at least three abnormalities correctly identified, and will be put into place soon, Dr. Ruiz said.
The biggest obstacle to large-scale adoption of this protocol is data – there are not a lot, at least now.
“We are working on that, too. In conjunction with the Skin Cancer Foundation, we’re launching a prospective study. We want to recruit 80 patients with T2B/T3 cutaneous SCCs. They get both and ultrasound and a CT scan at diagnosis and every 6 months for 2 years,” she said.
BALTIMORE – Ultrasound can be a very effective way to track early nodal metastasis in patients with high-stage cutaneous squamous cell carcinomas, and at a fraction of the cost of other imaging modalities.
The technique shows not only abnormal variations in the shape of nodes, but changes in the core and outer density, and vascular patterns, Emily Ruiz, MD, said at the annual meeting of the American College of Mohs Surgery. And over a 2-year surveillance period, this costs thousands less than radiation-based imaging.
Dr. Ruiz, director of the High-Risk Skin Cancer Clinic at Dana-Farber/Brigham and Women’s Cancer Center, Boston, said the standard imaging technique at that center used to be serial CT scans performed at diagnosis and every 6 months thereafter, for 2 years. But recently, the protocol changed: Ultrasound is now the preferred technique.
“The big problem with CT in this earlier disease, is that it can only identify the nodes that are enlarged, and doesn’t tell us anything about the etiology. Ultrasound, on the other hand, looks at a number of different features of the node.”
Tracking high-risk squamous cell carcinoma patients is a must, she said. “About 4% of people diagnosed with high-risk SCC will develop nodal metastases, and 1.5% of those will die from disease-specific death,” most often from locoregional disease. “So it’s critical to identify nodal diseases early as possible. Earlier identification leads to better outcomes.” Ultrasound simply provides more information about nodal metastasis, Dr. Ruiz added.
“The first thing we look at is the general architecture of the node. Resting and reactive nodes have a hypoechoic hilus and a hyperechoic cortex. As they become infiltrated with tumor, the hilus becomes more hyperechoic, and areas of metastasis stand out as much more hyperechoic than the surrounding node.”
Another tip-off is overall shape. If the ratio of the long axis to short axis diameter is less than 2, the lymph node is more likely to be malignant, she said.
“One more important factor that can’t be seen on CT is the node’s vascular pattern. Both resting and reactive nodes tend to have a centralized vascular pattern in the hilus. With tumor infiltration you start to see an asymmetrical vascularization as the nodes are replaced by tumor. The perfusion becomes much more peripheral.”
Cost is another consideration, Dr. Ruiz said. Five CT scans conducted over the recommended 2 years of follow-up will run about $5,000. Five scans with magnetic resonance imaging come in at about $6,500. PET CT is, of course, the most expensive, racking up a national average cost of $28,500 for five scans.
Ultrasound is amazingly inexpensive, Dr. Ruiz said. The national average cost of one scan is around $180, bringing the 2-year cost of five surveillance scans to $900.
Finally, clinicians and patients should consider the potential impact of repeated radiation exposure. “This can really add up over the follow-up period. Because there’s a 10-year latency period for these cancers, this might not be an issue for our older patients, but it really is something to consider in younger ones. “
However, she acknowledged that it’s not a completely rosy picture.
“Ultrasound is very user dependent, but we do think that by putting this in the hands of dermatologists with special training, we can solve this issue. In Europe, ultrasound’s very high sensitivity and specificity, combined with clinical exams, really improves disease detection.”
Unfortunately, at this point, anyone who wants to learn the technique has to go to Europe. “I trained in Germany, where I took a standard 3-day course, did 250 supervised scans, and completed an exam. I realize that’s unrealistic for most people,” she said. But a training protocol is being developed at Brigham and Women’s, under the auspices of the institution’s imaging experts, who felt that 3 days and 250 supervised scans was excessive. The Brigham and Women’s program comprises 8 hours of didactic training and at least 30 supervised scans with at least three abnormalities correctly identified, and will be put into place soon, Dr. Ruiz said.
The biggest obstacle to large-scale adoption of this protocol is data – there are not a lot, at least now.
“We are working on that, too. In conjunction with the Skin Cancer Foundation, we’re launching a prospective study. We want to recruit 80 patients with T2B/T3 cutaneous SCCs. They get both and ultrasound and a CT scan at diagnosis and every 6 months for 2 years,” she said.
BALTIMORE – Ultrasound can be a very effective way to track early nodal metastasis in patients with high-stage cutaneous squamous cell carcinomas, and at a fraction of the cost of other imaging modalities.
The technique shows not only abnormal variations in the shape of nodes, but changes in the core and outer density, and vascular patterns, Emily Ruiz, MD, said at the annual meeting of the American College of Mohs Surgery. And over a 2-year surveillance period, this costs thousands less than radiation-based imaging.
Dr. Ruiz, director of the High-Risk Skin Cancer Clinic at Dana-Farber/Brigham and Women’s Cancer Center, Boston, said the standard imaging technique at that center used to be serial CT scans performed at diagnosis and every 6 months thereafter, for 2 years. But recently, the protocol changed: Ultrasound is now the preferred technique.
“The big problem with CT in this earlier disease, is that it can only identify the nodes that are enlarged, and doesn’t tell us anything about the etiology. Ultrasound, on the other hand, looks at a number of different features of the node.”
Tracking high-risk squamous cell carcinoma patients is a must, she said. “About 4% of people diagnosed with high-risk SCC will develop nodal metastases, and 1.5% of those will die from disease-specific death,” most often from locoregional disease. “So it’s critical to identify nodal diseases early as possible. Earlier identification leads to better outcomes.” Ultrasound simply provides more information about nodal metastasis, Dr. Ruiz added.
“The first thing we look at is the general architecture of the node. Resting and reactive nodes have a hypoechoic hilus and a hyperechoic cortex. As they become infiltrated with tumor, the hilus becomes more hyperechoic, and areas of metastasis stand out as much more hyperechoic than the surrounding node.”
Another tip-off is overall shape. If the ratio of the long axis to short axis diameter is less than 2, the lymph node is more likely to be malignant, she said.
“One more important factor that can’t be seen on CT is the node’s vascular pattern. Both resting and reactive nodes tend to have a centralized vascular pattern in the hilus. With tumor infiltration you start to see an asymmetrical vascularization as the nodes are replaced by tumor. The perfusion becomes much more peripheral.”
Cost is another consideration, Dr. Ruiz said. Five CT scans conducted over the recommended 2 years of follow-up will run about $5,000. Five scans with magnetic resonance imaging come in at about $6,500. PET CT is, of course, the most expensive, racking up a national average cost of $28,500 for five scans.
Ultrasound is amazingly inexpensive, Dr. Ruiz said. The national average cost of one scan is around $180, bringing the 2-year cost of five surveillance scans to $900.
Finally, clinicians and patients should consider the potential impact of repeated radiation exposure. “This can really add up over the follow-up period. Because there’s a 10-year latency period for these cancers, this might not be an issue for our older patients, but it really is something to consider in younger ones. “
However, she acknowledged that it’s not a completely rosy picture.
“Ultrasound is very user dependent, but we do think that by putting this in the hands of dermatologists with special training, we can solve this issue. In Europe, ultrasound’s very high sensitivity and specificity, combined with clinical exams, really improves disease detection.”
Unfortunately, at this point, anyone who wants to learn the technique has to go to Europe. “I trained in Germany, where I took a standard 3-day course, did 250 supervised scans, and completed an exam. I realize that’s unrealistic for most people,” she said. But a training protocol is being developed at Brigham and Women’s, under the auspices of the institution’s imaging experts, who felt that 3 days and 250 supervised scans was excessive. The Brigham and Women’s program comprises 8 hours of didactic training and at least 30 supervised scans with at least three abnormalities correctly identified, and will be put into place soon, Dr. Ruiz said.
The biggest obstacle to large-scale adoption of this protocol is data – there are not a lot, at least now.
“We are working on that, too. In conjunction with the Skin Cancer Foundation, we’re launching a prospective study. We want to recruit 80 patients with T2B/T3 cutaneous SCCs. They get both and ultrasound and a CT scan at diagnosis and every 6 months for 2 years,” she said.
EXPERT ANALYSIS FROM the ACMS Annual Meeting
Rotavirus vaccine had strong protective effect in routine U.K. practice
Oral rotavirus vaccination had a strong protective effect against laboratory-confirmed rotavirus infection in the first 2 years of the U.K. infant immunization program, investigators are reporting.
The estimated effectiveness was 77% for all infants with confirmed infection, and greater than 80% for those under 12 months of age, according to the report. The vaccine did not demonstrate efficacy against all-cause acute gastroenteritis, although this was likely because of high, sustained vaccine coverage coupled with the “substantial impact” of the rotavirus vaccine, wrote investigators led by Sara L. Thomas, MB BS, PhD, of the London School of Hygiene & Tropical Medicine.
Taken together, these findings provide “reassurance” that rotavirus vaccine is effective in a real-world setting and set the stage for future analyses of cost effectiveness, Dr. Thomas and coauthors said in a report on the study appearing in Vaccine: X, the open access mirror journal of Vaccine.
“As data accumulate in the post-vaccination era, more detailed assessment of waning of effectiveness over time can be undertaken, and investigation of rotavirus strain-specific protection,” they wrote.
Oral live-attenuated rotavirus vaccine (Rotarix) was introduced in the U.K. in 2013 as a two-dose schedule at 2 and 3 months of age. Vaccine uptake by the age of 25 weeks was rapid and sustained, exceeding 90%, according to previous reports. Declines in hospital admissions and primary care for all-cause acute gastroenteritis were substantial, associated with an estimated reduction of £12.5 million in health care costs in the first year of the program for children 5 years of age and younger.
To assess rotavirus vaccine effectiveness in the public health setting, Dr. Thomas and colleagues conducted a pair of studies: one designed to evaluate vaccine effectiveness against laboratory-confirmed rotavirus infections using laboratory surveillance data for 1,869 children and 1,032 controls and another to estimate vaccine effectiveness against all-cause acute gastroenteritis using electronic health data on 40,723 children.
Stratified by age, the data showed that vaccine effectiveness was 85% in those younger than 12 months, and 54% for older children.
By contrast, they found no evidence that the rotavirus vaccine protected against all-cause acute gastroenteritis in an analysis that adjusted for age and other factors. Analysis also suggested a lack of effectiveness against hospitalized acute gastroenteritis, according to the study authors.
In prelicensure trials, oral live-attenuated rotavirus vaccine in middle- and high-income settings had efficacy against severe rotavirus-confirmed gastroenteritis of greater than 85% and efficacy against severe all-cause gastroenteritis up to 40%, investigators noted.
The lack of vaccine efficacy on all-cause acute gastroenteritis is likely because of “highly effective implementation” of the vaccine program and rapid attainment of coverage, plus high vaccine effectiveness against rotavirus-specific acute gastroenteritis, the investigators said.
“As a result, almost all AGE in the study population in the post-vaccine era was likely to have been due to nonrotavirus organisms or non-infectious causes,” said Dr. Thomas and coauthors.
This highlights the importance of choosing “specific outcomes” to study when vaccine coverage and effectiveness are both high, they concluded.
Funding for this research came from the National Institute for Health Research Health Protection Research Unit in Immunisation at the London School of Hygiene and Tropical Medicine in partnership with Public Health England. The Immunisation and Countermeasures Division of Public Health England provided vaccine manufacturers with postmarketing surveillance reports, according to the article’s disclosure section.
SOURCE: Walker JL et al. Vaccine: X. 2019 Apr 11. doi: 10.1016/j.jvacx.2019.100005.
Oral rotavirus vaccination had a strong protective effect against laboratory-confirmed rotavirus infection in the first 2 years of the U.K. infant immunization program, investigators are reporting.
The estimated effectiveness was 77% for all infants with confirmed infection, and greater than 80% for those under 12 months of age, according to the report. The vaccine did not demonstrate efficacy against all-cause acute gastroenteritis, although this was likely because of high, sustained vaccine coverage coupled with the “substantial impact” of the rotavirus vaccine, wrote investigators led by Sara L. Thomas, MB BS, PhD, of the London School of Hygiene & Tropical Medicine.
Taken together, these findings provide “reassurance” that rotavirus vaccine is effective in a real-world setting and set the stage for future analyses of cost effectiveness, Dr. Thomas and coauthors said in a report on the study appearing in Vaccine: X, the open access mirror journal of Vaccine.
“As data accumulate in the post-vaccination era, more detailed assessment of waning of effectiveness over time can be undertaken, and investigation of rotavirus strain-specific protection,” they wrote.
Oral live-attenuated rotavirus vaccine (Rotarix) was introduced in the U.K. in 2013 as a two-dose schedule at 2 and 3 months of age. Vaccine uptake by the age of 25 weeks was rapid and sustained, exceeding 90%, according to previous reports. Declines in hospital admissions and primary care for all-cause acute gastroenteritis were substantial, associated with an estimated reduction of £12.5 million in health care costs in the first year of the program for children 5 years of age and younger.
To assess rotavirus vaccine effectiveness in the public health setting, Dr. Thomas and colleagues conducted a pair of studies: one designed to evaluate vaccine effectiveness against laboratory-confirmed rotavirus infections using laboratory surveillance data for 1,869 children and 1,032 controls and another to estimate vaccine effectiveness against all-cause acute gastroenteritis using electronic health data on 40,723 children.
Stratified by age, the data showed that vaccine effectiveness was 85% in those younger than 12 months, and 54% for older children.
By contrast, they found no evidence that the rotavirus vaccine protected against all-cause acute gastroenteritis in an analysis that adjusted for age and other factors. Analysis also suggested a lack of effectiveness against hospitalized acute gastroenteritis, according to the study authors.
In prelicensure trials, oral live-attenuated rotavirus vaccine in middle- and high-income settings had efficacy against severe rotavirus-confirmed gastroenteritis of greater than 85% and efficacy against severe all-cause gastroenteritis up to 40%, investigators noted.
The lack of vaccine efficacy on all-cause acute gastroenteritis is likely because of “highly effective implementation” of the vaccine program and rapid attainment of coverage, plus high vaccine effectiveness against rotavirus-specific acute gastroenteritis, the investigators said.
“As a result, almost all AGE in the study population in the post-vaccine era was likely to have been due to nonrotavirus organisms or non-infectious causes,” said Dr. Thomas and coauthors.
This highlights the importance of choosing “specific outcomes” to study when vaccine coverage and effectiveness are both high, they concluded.
Funding for this research came from the National Institute for Health Research Health Protection Research Unit in Immunisation at the London School of Hygiene and Tropical Medicine in partnership with Public Health England. The Immunisation and Countermeasures Division of Public Health England provided vaccine manufacturers with postmarketing surveillance reports, according to the article’s disclosure section.
SOURCE: Walker JL et al. Vaccine: X. 2019 Apr 11. doi: 10.1016/j.jvacx.2019.100005.
Oral rotavirus vaccination had a strong protective effect against laboratory-confirmed rotavirus infection in the first 2 years of the U.K. infant immunization program, investigators are reporting.
The estimated effectiveness was 77% for all infants with confirmed infection, and greater than 80% for those under 12 months of age, according to the report. The vaccine did not demonstrate efficacy against all-cause acute gastroenteritis, although this was likely because of high, sustained vaccine coverage coupled with the “substantial impact” of the rotavirus vaccine, wrote investigators led by Sara L. Thomas, MB BS, PhD, of the London School of Hygiene & Tropical Medicine.
Taken together, these findings provide “reassurance” that rotavirus vaccine is effective in a real-world setting and set the stage for future analyses of cost effectiveness, Dr. Thomas and coauthors said in a report on the study appearing in Vaccine: X, the open access mirror journal of Vaccine.
“As data accumulate in the post-vaccination era, more detailed assessment of waning of effectiveness over time can be undertaken, and investigation of rotavirus strain-specific protection,” they wrote.
Oral live-attenuated rotavirus vaccine (Rotarix) was introduced in the U.K. in 2013 as a two-dose schedule at 2 and 3 months of age. Vaccine uptake by the age of 25 weeks was rapid and sustained, exceeding 90%, according to previous reports. Declines in hospital admissions and primary care for all-cause acute gastroenteritis were substantial, associated with an estimated reduction of £12.5 million in health care costs in the first year of the program for children 5 years of age and younger.
To assess rotavirus vaccine effectiveness in the public health setting, Dr. Thomas and colleagues conducted a pair of studies: one designed to evaluate vaccine effectiveness against laboratory-confirmed rotavirus infections using laboratory surveillance data for 1,869 children and 1,032 controls and another to estimate vaccine effectiveness against all-cause acute gastroenteritis using electronic health data on 40,723 children.
Stratified by age, the data showed that vaccine effectiveness was 85% in those younger than 12 months, and 54% for older children.
By contrast, they found no evidence that the rotavirus vaccine protected against all-cause acute gastroenteritis in an analysis that adjusted for age and other factors. Analysis also suggested a lack of effectiveness against hospitalized acute gastroenteritis, according to the study authors.
In prelicensure trials, oral live-attenuated rotavirus vaccine in middle- and high-income settings had efficacy against severe rotavirus-confirmed gastroenteritis of greater than 85% and efficacy against severe all-cause gastroenteritis up to 40%, investigators noted.
The lack of vaccine efficacy on all-cause acute gastroenteritis is likely because of “highly effective implementation” of the vaccine program and rapid attainment of coverage, plus high vaccine effectiveness against rotavirus-specific acute gastroenteritis, the investigators said.
“As a result, almost all AGE in the study population in the post-vaccine era was likely to have been due to nonrotavirus organisms or non-infectious causes,” said Dr. Thomas and coauthors.
This highlights the importance of choosing “specific outcomes” to study when vaccine coverage and effectiveness are both high, they concluded.
Funding for this research came from the National Institute for Health Research Health Protection Research Unit in Immunisation at the London School of Hygiene and Tropical Medicine in partnership with Public Health England. The Immunisation and Countermeasures Division of Public Health England provided vaccine manufacturers with postmarketing surveillance reports, according to the article’s disclosure section.
SOURCE: Walker JL et al. Vaccine: X. 2019 Apr 11. doi: 10.1016/j.jvacx.2019.100005.
FROM VACCINE
New recommendations on immune tolerance induction in hemophilia A
New treatment recommendations, released by a panel of nine experts, offer consensus advice on the use of immune tolerance induction (ITI) therapy in patients with hemophilia A with inhibitors.
The recommendations from the Future of Immunotolerance Treatment (FIT) group were authored by a nine-member committee with expertise in the treatment of hemophilia. The authors attended three meetings from 2017-2018 to form a consensus on the use of nonfactor therapies with current inhibitor management strategies.
“The treatment of hemophilia A has evolved and a number of molecules that potentially can be used in the setting of patients with inhibitors have been developed, or are in various phases of development,” wrote Manuel Carcao, MD, of the University of Toronto and colleagues. The report is published in Haemophilia.
The current body of literature is lacking high-quality evidence on the concomitant use of nonfactor treatments, such as emicizumab, and current inhibitor therapies. The recommendations included the panel’s consensus opinions on treatment of inhibitors, with and without the use of nonreplacement therapies. The concurrent use of factor VIII replacement therapy and emicizumab could inhibit bleeding with lower dose immunotolerance strategies, according to the recommendations.
The group hypothesized that increased uptake of lower dose and lower frequency factor VIII ITI treatment strategies could reduce the likelihood of requiring central venous access while retaining a high probability of treatment success.
“In our new algorithm, we have indicated that one option might be to start patients on low-dose ITI with emicizumab regardless of their historical peak inhibitor titre. Patients could then escalate their ITI regimen should their response to low-dose ITI be deemed insufficient,” they wrote.
The experts provided a novel treatment algorithm for immune tolerance induction without emicizumab in addition to a new theoretical strategy with emicizumab.
Other recommendations included that patients with inhibitors should be offered at least one attempt at ITI and that monthly monitoring should be done and ITI dose and frequency should be adjusted based on changes in bleeding phenotype and inhibitor titer.
The authors acknowledged a current limitation is the lack of published evidence pertaining to the concurrent use of emicizumab and factor VIII replacement therapy.
“The FIT group sees the need for properly conducted prospective studies to evaluate the impact of adding emicizumab, and in the future, other nonfactor therapies, into the management of patients with inhibitors,” the experts wrote.
The manuscript was supported by Grifols. The authors reported financial disclosures related to Grifols and other companies.
SOURCE: Carcao M et al. Haemophilia. 2019 Apr 29. doi: 10.1111/hae.13762.
New treatment recommendations, released by a panel of nine experts, offer consensus advice on the use of immune tolerance induction (ITI) therapy in patients with hemophilia A with inhibitors.
The recommendations from the Future of Immunotolerance Treatment (FIT) group were authored by a nine-member committee with expertise in the treatment of hemophilia. The authors attended three meetings from 2017-2018 to form a consensus on the use of nonfactor therapies with current inhibitor management strategies.
“The treatment of hemophilia A has evolved and a number of molecules that potentially can be used in the setting of patients with inhibitors have been developed, or are in various phases of development,” wrote Manuel Carcao, MD, of the University of Toronto and colleagues. The report is published in Haemophilia.
The current body of literature is lacking high-quality evidence on the concomitant use of nonfactor treatments, such as emicizumab, and current inhibitor therapies. The recommendations included the panel’s consensus opinions on treatment of inhibitors, with and without the use of nonreplacement therapies. The concurrent use of factor VIII replacement therapy and emicizumab could inhibit bleeding with lower dose immunotolerance strategies, according to the recommendations.
The group hypothesized that increased uptake of lower dose and lower frequency factor VIII ITI treatment strategies could reduce the likelihood of requiring central venous access while retaining a high probability of treatment success.
“In our new algorithm, we have indicated that one option might be to start patients on low-dose ITI with emicizumab regardless of their historical peak inhibitor titre. Patients could then escalate their ITI regimen should their response to low-dose ITI be deemed insufficient,” they wrote.
The experts provided a novel treatment algorithm for immune tolerance induction without emicizumab in addition to a new theoretical strategy with emicizumab.
Other recommendations included that patients with inhibitors should be offered at least one attempt at ITI and that monthly monitoring should be done and ITI dose and frequency should be adjusted based on changes in bleeding phenotype and inhibitor titer.
The authors acknowledged a current limitation is the lack of published evidence pertaining to the concurrent use of emicizumab and factor VIII replacement therapy.
“The FIT group sees the need for properly conducted prospective studies to evaluate the impact of adding emicizumab, and in the future, other nonfactor therapies, into the management of patients with inhibitors,” the experts wrote.
The manuscript was supported by Grifols. The authors reported financial disclosures related to Grifols and other companies.
SOURCE: Carcao M et al. Haemophilia. 2019 Apr 29. doi: 10.1111/hae.13762.
New treatment recommendations, released by a panel of nine experts, offer consensus advice on the use of immune tolerance induction (ITI) therapy in patients with hemophilia A with inhibitors.
The recommendations from the Future of Immunotolerance Treatment (FIT) group were authored by a nine-member committee with expertise in the treatment of hemophilia. The authors attended three meetings from 2017-2018 to form a consensus on the use of nonfactor therapies with current inhibitor management strategies.
“The treatment of hemophilia A has evolved and a number of molecules that potentially can be used in the setting of patients with inhibitors have been developed, or are in various phases of development,” wrote Manuel Carcao, MD, of the University of Toronto and colleagues. The report is published in Haemophilia.
The current body of literature is lacking high-quality evidence on the concomitant use of nonfactor treatments, such as emicizumab, and current inhibitor therapies. The recommendations included the panel’s consensus opinions on treatment of inhibitors, with and without the use of nonreplacement therapies. The concurrent use of factor VIII replacement therapy and emicizumab could inhibit bleeding with lower dose immunotolerance strategies, according to the recommendations.
The group hypothesized that increased uptake of lower dose and lower frequency factor VIII ITI treatment strategies could reduce the likelihood of requiring central venous access while retaining a high probability of treatment success.
“In our new algorithm, we have indicated that one option might be to start patients on low-dose ITI with emicizumab regardless of their historical peak inhibitor titre. Patients could then escalate their ITI regimen should their response to low-dose ITI be deemed insufficient,” they wrote.
The experts provided a novel treatment algorithm for immune tolerance induction without emicizumab in addition to a new theoretical strategy with emicizumab.
Other recommendations included that patients with inhibitors should be offered at least one attempt at ITI and that monthly monitoring should be done and ITI dose and frequency should be adjusted based on changes in bleeding phenotype and inhibitor titer.
The authors acknowledged a current limitation is the lack of published evidence pertaining to the concurrent use of emicizumab and factor VIII replacement therapy.
“The FIT group sees the need for properly conducted prospective studies to evaluate the impact of adding emicizumab, and in the future, other nonfactor therapies, into the management of patients with inhibitors,” the experts wrote.
The manuscript was supported by Grifols. The authors reported financial disclosures related to Grifols and other companies.
SOURCE: Carcao M et al. Haemophilia. 2019 Apr 29. doi: 10.1111/hae.13762.
FROM HAEMOPHILIA
Machine learning tool may predict LSG outcomes
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
BALTIMORE – Neural networks are the building blocks of machine learning and artificial intelligence, and researchers from the University of Minnesota have identified a panel of “simple, readily known” preoperative patient factors that they fed into an artificial neural network model that can be predictive of 30-day outcomes after laparoscopic sleeve gastrectomy, one of the researchers reported at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons.
“The biggest limitation to using neural networks clinically is the fact that they’re algorithmic complex,” said Eric S. Wise, MD, of the University of Minnesota, Minneapolis, in presenting the research. “There is an underlying algorithm that’s developed, but it’s very difficult to understand.” He called it “a black box problem.”
Nonetheless, the researchers drew upon 101,721 laparoscopic sleeve gastrectomy cases from the 2016 Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program national database to extract factors that were associated with postoperative complications. “More pertinently, we wanted to optimize predictability of a panel of readily obtainable, easily qualifiable preoperative factors and maximize the variants that are contained within those variables to predict the outcome of 30-day morbidity and mortality,” Dr. Wise said.
Essentially, neural networks recognize patterns through a machine-learning process in a manner modeled on the human brain. As Dr. Wise explained, they first emerged in the 1960s to simulate the human brain’s psychological-neurologic systems.
Through bivariate and multivariate analyses, the research identified eight preoperative variables strongly associated with the 30-day endpoints. After univariate analysis, seven of those variables were statistically significant: older age (P = .03), nonwhite race, higher initial body mass index, severe hypertension, history of diabetes, nonindependent functional status, and previous foregut/bariatric surgery (all P less than .001). “Gender was the only factor that was not predictive,” Dr. Wise said.
The factors held up under logistic regression modeling. “We were able to use a traditional logistic regression model that came up with a reasonable area under the curve of 0.572,” he said. Using artificial neural network analysis, the training set, which comprised 80% of patients, was more accurate than logistic regression, with an area under the curve of 0.582.
One limitation was that this was a “small study,” Dr. Wise said, influenced by selection bias inherent in any retrospective data selection. Other major factors that may exist were not considered.
However, he noted, “in the past we’ve had some success translating neural networks into something that’s clinically useful.” His group at Vanderbilt University published a report of artificial neural network modeling to identify five factors predictive of weight loss after Roux-en-Y gastric bypass 2 years ago (Surg Endosc. 2016;30:480-8). “There are ways to translate neural networks clinically,” Dr. Wise said.
Dr. Wise had no financial relationships to disclose.
SOURCE: Wise ES et al. SAGES 2019, Abstract S053.
REPORTING FROM SAGES 2019
Zero HIV transmission rate when viral load suppressed
according to a new paper published in the Lancet.
The prospective observational PARTNER2 study (Lancet 2019 May 2. doi: 10.1016/S0140-6736[19]304018-0) followed 782 serodiscordant gay couples from 14 European countries, where the HIV-positive partner had to be virally suppressed to below 200 copies of HIV-1 RNA per milliliter, and the couple was engaging in condomless sex without using pre- or postexposure prophylaxis.
After a median follow-up of 2 years, there was not a single case of HIV transmission between couples, representing a transmission rate of zero. The study did record 15 new HIV infections during follow-up but these were all phylogenetically linked to sources other than the HIV-positive partner.
The HIV-positive partners had been on antiretroviral therapy for a median of 4.3 years – most on regimens of three or more drugs – with high levels of adherence. During the follow-up period, 37 HIV-positive partners (5%) reported missing their antiretroviral therapy for more than 4 consecutive days.
“Our results give equivalence of evidence for gay men as for heterosexual couples and indicate that the risk of HIV transmission when HIV viral load is suppressed is effectively zero for both anal and vaginal sex,” wrote Dr. Alison J. Rodger of the Institute for Global Health at University College London, and coauthors. “These findings emphasize the importance of regular monitoring to ensure HIV viral load remains suppressed and supporting HIV-positive people with long-term adherence.”
Around one-quarter of the HIV-negative men and 27% of the HIV-positive men reported a sexually-transmitted infection during follow-up; the most common infections were syphilis, gonorrhea, and chlamydia.
The study noted six additional cases of seroconversion of HIV-negative partners. However, these occurred outside the eligible couple-years of the follow-up period. They were ineligible due to no questionnaire about sexual behavior having been completed by either partner in the couple, a lack of condomless sex between the couple, use of postexposure prophylaxis, or a lack of viral load measurement for the HIV-positive partner in the past year.
The authors did note that the study population was predominantly white and with a median age of 38 years, while most HIV transmission occurs in young people aged under 25 years.
“The results from the PARTNER studies support wider dissemination of the message of the U=U [Undetectable equals Untransmittable] campaign that risk of transmission of HIV in the context of virally suppressive ART is zero,” they wrote.
The study was supported by the National Institute for Health Research, the British HIV Association, the Danish National Research Foundation, ViiV Healthcare, Gilead Sciences, Augustinus Fonden, and A P Møller Fonden. Fourteen authors declared grants, personal fees and other support from the pharmaceutical sector.
SOURCE: Rodger A et al. Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]304018-0.
The results of the PARTNER and PARTNER2 trials show that timely diagnosis and effective treatment can virtually eliminate the risk of HIV transmission. However, access to HIV testing and care is not always easy, and fear, stigma, homophobia, and other forces continue to limit access to HIV treatment. This study also highlights the impact of sexual relations outside the bounds of a couple’s relationship.
While the use of preexposure prophylaxis was a criterion for exclusion from this study, this intervention should also be recognized as an important part of HIV prevention. A recent survey found that men who have sex with men are more likely to trust preexposure prophylaxis for HIV prevention than antiretroviral therapy.
Dr. Myron S Cohen is from the departments of medicine, microbiology, immunology, and epidemiology, University of North Carolina at Chapel Hill, and the UNC Institute for Global Health and Infectious Diseases in Chapel Hill. These comments are adapted from an editorial (Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]30701-9). Dr. Cohen reported advisory board travel fees from Merck and Gilead unrelated to this work.
The results of the PARTNER and PARTNER2 trials show that timely diagnosis and effective treatment can virtually eliminate the risk of HIV transmission. However, access to HIV testing and care is not always easy, and fear, stigma, homophobia, and other forces continue to limit access to HIV treatment. This study also highlights the impact of sexual relations outside the bounds of a couple’s relationship.
While the use of preexposure prophylaxis was a criterion for exclusion from this study, this intervention should also be recognized as an important part of HIV prevention. A recent survey found that men who have sex with men are more likely to trust preexposure prophylaxis for HIV prevention than antiretroviral therapy.
Dr. Myron S Cohen is from the departments of medicine, microbiology, immunology, and epidemiology, University of North Carolina at Chapel Hill, and the UNC Institute for Global Health and Infectious Diseases in Chapel Hill. These comments are adapted from an editorial (Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]30701-9). Dr. Cohen reported advisory board travel fees from Merck and Gilead unrelated to this work.
The results of the PARTNER and PARTNER2 trials show that timely diagnosis and effective treatment can virtually eliminate the risk of HIV transmission. However, access to HIV testing and care is not always easy, and fear, stigma, homophobia, and other forces continue to limit access to HIV treatment. This study also highlights the impact of sexual relations outside the bounds of a couple’s relationship.
While the use of preexposure prophylaxis was a criterion for exclusion from this study, this intervention should also be recognized as an important part of HIV prevention. A recent survey found that men who have sex with men are more likely to trust preexposure prophylaxis for HIV prevention than antiretroviral therapy.
Dr. Myron S Cohen is from the departments of medicine, microbiology, immunology, and epidemiology, University of North Carolina at Chapel Hill, and the UNC Institute for Global Health and Infectious Diseases in Chapel Hill. These comments are adapted from an editorial (Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]30701-9). Dr. Cohen reported advisory board travel fees from Merck and Gilead unrelated to this work.
according to a new paper published in the Lancet.
The prospective observational PARTNER2 study (Lancet 2019 May 2. doi: 10.1016/S0140-6736[19]304018-0) followed 782 serodiscordant gay couples from 14 European countries, where the HIV-positive partner had to be virally suppressed to below 200 copies of HIV-1 RNA per milliliter, and the couple was engaging in condomless sex without using pre- or postexposure prophylaxis.
After a median follow-up of 2 years, there was not a single case of HIV transmission between couples, representing a transmission rate of zero. The study did record 15 new HIV infections during follow-up but these were all phylogenetically linked to sources other than the HIV-positive partner.
The HIV-positive partners had been on antiretroviral therapy for a median of 4.3 years – most on regimens of three or more drugs – with high levels of adherence. During the follow-up period, 37 HIV-positive partners (5%) reported missing their antiretroviral therapy for more than 4 consecutive days.
“Our results give equivalence of evidence for gay men as for heterosexual couples and indicate that the risk of HIV transmission when HIV viral load is suppressed is effectively zero for both anal and vaginal sex,” wrote Dr. Alison J. Rodger of the Institute for Global Health at University College London, and coauthors. “These findings emphasize the importance of regular monitoring to ensure HIV viral load remains suppressed and supporting HIV-positive people with long-term adherence.”
Around one-quarter of the HIV-negative men and 27% of the HIV-positive men reported a sexually-transmitted infection during follow-up; the most common infections were syphilis, gonorrhea, and chlamydia.
The study noted six additional cases of seroconversion of HIV-negative partners. However, these occurred outside the eligible couple-years of the follow-up period. They were ineligible due to no questionnaire about sexual behavior having been completed by either partner in the couple, a lack of condomless sex between the couple, use of postexposure prophylaxis, or a lack of viral load measurement for the HIV-positive partner in the past year.
The authors did note that the study population was predominantly white and with a median age of 38 years, while most HIV transmission occurs in young people aged under 25 years.
“The results from the PARTNER studies support wider dissemination of the message of the U=U [Undetectable equals Untransmittable] campaign that risk of transmission of HIV in the context of virally suppressive ART is zero,” they wrote.
The study was supported by the National Institute for Health Research, the British HIV Association, the Danish National Research Foundation, ViiV Healthcare, Gilead Sciences, Augustinus Fonden, and A P Møller Fonden. Fourteen authors declared grants, personal fees and other support from the pharmaceutical sector.
SOURCE: Rodger A et al. Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]304018-0.
according to a new paper published in the Lancet.
The prospective observational PARTNER2 study (Lancet 2019 May 2. doi: 10.1016/S0140-6736[19]304018-0) followed 782 serodiscordant gay couples from 14 European countries, where the HIV-positive partner had to be virally suppressed to below 200 copies of HIV-1 RNA per milliliter, and the couple was engaging in condomless sex without using pre- or postexposure prophylaxis.
After a median follow-up of 2 years, there was not a single case of HIV transmission between couples, representing a transmission rate of zero. The study did record 15 new HIV infections during follow-up but these were all phylogenetically linked to sources other than the HIV-positive partner.
The HIV-positive partners had been on antiretroviral therapy for a median of 4.3 years – most on regimens of three or more drugs – with high levels of adherence. During the follow-up period, 37 HIV-positive partners (5%) reported missing their antiretroviral therapy for more than 4 consecutive days.
“Our results give equivalence of evidence for gay men as for heterosexual couples and indicate that the risk of HIV transmission when HIV viral load is suppressed is effectively zero for both anal and vaginal sex,” wrote Dr. Alison J. Rodger of the Institute for Global Health at University College London, and coauthors. “These findings emphasize the importance of regular monitoring to ensure HIV viral load remains suppressed and supporting HIV-positive people with long-term adherence.”
Around one-quarter of the HIV-negative men and 27% of the HIV-positive men reported a sexually-transmitted infection during follow-up; the most common infections were syphilis, gonorrhea, and chlamydia.
The study noted six additional cases of seroconversion of HIV-negative partners. However, these occurred outside the eligible couple-years of the follow-up period. They were ineligible due to no questionnaire about sexual behavior having been completed by either partner in the couple, a lack of condomless sex between the couple, use of postexposure prophylaxis, or a lack of viral load measurement for the HIV-positive partner in the past year.
The authors did note that the study population was predominantly white and with a median age of 38 years, while most HIV transmission occurs in young people aged under 25 years.
“The results from the PARTNER studies support wider dissemination of the message of the U=U [Undetectable equals Untransmittable] campaign that risk of transmission of HIV in the context of virally suppressive ART is zero,” they wrote.
The study was supported by the National Institute for Health Research, the British HIV Association, the Danish National Research Foundation, ViiV Healthcare, Gilead Sciences, Augustinus Fonden, and A P Møller Fonden. Fourteen authors declared grants, personal fees and other support from the pharmaceutical sector.
SOURCE: Rodger A et al. Lancet 2019, May 2. doi: 10.1016/S0140-6736[19]304018-0.
FROM THE LANCET
Study identifies GI bleed risk factors in von Willebrand disease
Researchers have identified several risk factors associated with gastrointestinal (GI) bleeding in adult patients with von Willebrand disease (VWD), based on findings from a retrospective analysis.
“[We] evaluated prevalence and risk factors of GIB among individuals with and without VWD, using a large national database,” wrote Anastasia Tsagianni, MD, of the University of Pittsburgh, and colleagues. The findings were published in Thrombosis Research.
The researchers retrospectively reviewed discharge data from the National Inpatient Sample database. The team analyzed correlates of GI bleeding among patients with VWD and estimated prevalence rates using measures in the database. Risk factors for GI bleeding in VWD were correlated via multivariable logistic regression.
Between Jan. 1, 2009, and Dec. 31, 2014, there were 16,640 admissions with VWD and 618 were admitted with GI bleeding, the researchers reported. After analysis, the researchers found that the prevalence of GI bleeding was 3.7% and 1.49% in VWD and non-VWD patients, respectively – a 2.5-fold greater rate in VWD patients.
“Comorbidities associated with greater [GI bleeding] risk in individuals with VWD include past surgery, hypertension, hyperlipidemia, smoking, renal disease, hepatitis C, thrombocytopenia, or liver disease,” the researchers wrote.
In the multivariable analysis, the factors associated with GI bleeding were smoking status (odds ratio, 1.40), African American race (OR, 1.80), male gender (OR, 1.61), angiodysplasia (OR, 104.06), colonic diverticulitis (OR, 16.66), and hepatitis C (OR 2.17). These variables were similar to risk factors identified in the non-VWD group, the researchers noted.
“Although significant, age did not appear to be a strong risk factor for either group,” they wrote. “Steroids were not associated with increased risk for [GI bleeding] in either group.”
A key limitation of the study was the use of discharge diagnosis codes as an inclusion method, the researchers noted. As a result, misclassification bias could be present, they added.
The Pennsylvania Department of Health and the Health Resources and Services Administration funded the study. The authors reported having no conflicts of interest.
SOURCE: Tsagianni A et al. Thromb Res. 2019 Apr 17. doi: 10.1016/j.thromres.2019.04.017.
Researchers have identified several risk factors associated with gastrointestinal (GI) bleeding in adult patients with von Willebrand disease (VWD), based on findings from a retrospective analysis.
“[We] evaluated prevalence and risk factors of GIB among individuals with and without VWD, using a large national database,” wrote Anastasia Tsagianni, MD, of the University of Pittsburgh, and colleagues. The findings were published in Thrombosis Research.
The researchers retrospectively reviewed discharge data from the National Inpatient Sample database. The team analyzed correlates of GI bleeding among patients with VWD and estimated prevalence rates using measures in the database. Risk factors for GI bleeding in VWD were correlated via multivariable logistic regression.
Between Jan. 1, 2009, and Dec. 31, 2014, there were 16,640 admissions with VWD and 618 were admitted with GI bleeding, the researchers reported. After analysis, the researchers found that the prevalence of GI bleeding was 3.7% and 1.49% in VWD and non-VWD patients, respectively – a 2.5-fold greater rate in VWD patients.
“Comorbidities associated with greater [GI bleeding] risk in individuals with VWD include past surgery, hypertension, hyperlipidemia, smoking, renal disease, hepatitis C, thrombocytopenia, or liver disease,” the researchers wrote.
In the multivariable analysis, the factors associated with GI bleeding were smoking status (odds ratio, 1.40), African American race (OR, 1.80), male gender (OR, 1.61), angiodysplasia (OR, 104.06), colonic diverticulitis (OR, 16.66), and hepatitis C (OR 2.17). These variables were similar to risk factors identified in the non-VWD group, the researchers noted.
“Although significant, age did not appear to be a strong risk factor for either group,” they wrote. “Steroids were not associated with increased risk for [GI bleeding] in either group.”
A key limitation of the study was the use of discharge diagnosis codes as an inclusion method, the researchers noted. As a result, misclassification bias could be present, they added.
The Pennsylvania Department of Health and the Health Resources and Services Administration funded the study. The authors reported having no conflicts of interest.
SOURCE: Tsagianni A et al. Thromb Res. 2019 Apr 17. doi: 10.1016/j.thromres.2019.04.017.
Researchers have identified several risk factors associated with gastrointestinal (GI) bleeding in adult patients with von Willebrand disease (VWD), based on findings from a retrospective analysis.
“[We] evaluated prevalence and risk factors of GIB among individuals with and without VWD, using a large national database,” wrote Anastasia Tsagianni, MD, of the University of Pittsburgh, and colleagues. The findings were published in Thrombosis Research.
The researchers retrospectively reviewed discharge data from the National Inpatient Sample database. The team analyzed correlates of GI bleeding among patients with VWD and estimated prevalence rates using measures in the database. Risk factors for GI bleeding in VWD were correlated via multivariable logistic regression.
Between Jan. 1, 2009, and Dec. 31, 2014, there were 16,640 admissions with VWD and 618 were admitted with GI bleeding, the researchers reported. After analysis, the researchers found that the prevalence of GI bleeding was 3.7% and 1.49% in VWD and non-VWD patients, respectively – a 2.5-fold greater rate in VWD patients.
“Comorbidities associated with greater [GI bleeding] risk in individuals with VWD include past surgery, hypertension, hyperlipidemia, smoking, renal disease, hepatitis C, thrombocytopenia, or liver disease,” the researchers wrote.
In the multivariable analysis, the factors associated with GI bleeding were smoking status (odds ratio, 1.40), African American race (OR, 1.80), male gender (OR, 1.61), angiodysplasia (OR, 104.06), colonic diverticulitis (OR, 16.66), and hepatitis C (OR 2.17). These variables were similar to risk factors identified in the non-VWD group, the researchers noted.
“Although significant, age did not appear to be a strong risk factor for either group,” they wrote. “Steroids were not associated with increased risk for [GI bleeding] in either group.”
A key limitation of the study was the use of discharge diagnosis codes as an inclusion method, the researchers noted. As a result, misclassification bias could be present, they added.
The Pennsylvania Department of Health and the Health Resources and Services Administration funded the study. The authors reported having no conflicts of interest.
SOURCE: Tsagianni A et al. Thromb Res. 2019 Apr 17. doi: 10.1016/j.thromres.2019.04.017.
FROM THROMBOSIS RESEARCH
Key clinical point: Researchers identified several risk factors associated for gastrointestinal bleeding in adult patients with von Willebrand disease.
Major finding: In a multivariate analysis, the most significant factors associated with gastrointestinal bleeding in von Willebrand disease were smoking status, African American race, male gender, angiodysplasia, diverticulitis, and hepatitis C.
Study details: A retrospective analysis of 16,640 patients with the disease.
Disclosures: The Pennsylvania Department of Health and the Health Resources and Services Administration funded the study. The authors reported having no conflicts of interest.
Source: Tsagianni A et al. Thromb Res. 2019 Apr 17. doi: 10.1016/j.thromres.2019.04.017.
Insomnia meds get boxed warning from FDA
The Food and Drug Administration will now require that certain
Complex sleep behaviors have been seen with these medications in patients with and without a history of them, at low doses, and even after one dose of the medication. They’ve also been observed with and without concomitant use of alcohol or other CNS depressants.
Health care professionals should advise patients about these risks, even though they are rare. Patients should contact health care professionals if they either experience a complex sleep behavior while not fully awake on one of these medicines or have performed activities they don’t remember while taking the medicine.
More information about these risks and the safety warnings can be found in the FDA’s safety announcement. Other information is also available in a press announcement from the agency.
The Food and Drug Administration will now require that certain
Complex sleep behaviors have been seen with these medications in patients with and without a history of them, at low doses, and even after one dose of the medication. They’ve also been observed with and without concomitant use of alcohol or other CNS depressants.
Health care professionals should advise patients about these risks, even though they are rare. Patients should contact health care professionals if they either experience a complex sleep behavior while not fully awake on one of these medicines or have performed activities they don’t remember while taking the medicine.
More information about these risks and the safety warnings can be found in the FDA’s safety announcement. Other information is also available in a press announcement from the agency.
The Food and Drug Administration will now require that certain
Complex sleep behaviors have been seen with these medications in patients with and without a history of them, at low doses, and even after one dose of the medication. They’ve also been observed with and without concomitant use of alcohol or other CNS depressants.
Health care professionals should advise patients about these risks, even though they are rare. Patients should contact health care professionals if they either experience a complex sleep behavior while not fully awake on one of these medicines or have performed activities they don’t remember while taking the medicine.
More information about these risks and the safety warnings can be found in the FDA’s safety announcement. Other information is also available in a press announcement from the agency.
Time to embrace minimally invasive colorectal surgery?
LAS VEGAS – Two-thirds of colon resections in the United States are open procedures, but a colorectal surgeon told colleagues that evidence shows minimally invasive surgery deserves a wider place in his field.
Why? Because minimally invasive surgery – despite its limited utilization – is linked to multiple improved outcomes in colorectal surgery, said Matthew G. Mutch, MD, chief of colon and rectal surgery at Washington University, St. Louis, in a presentation at the Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
“Our goal should be to offer minimally invasive surgery to as many patients as possible by as many different methods as needed,” Dr. Mutch said. “If you’re willing to take this on and do this over a regular basis, you’ll get over that learning curve and expand the number of patients you can offer laparoscopy to.”
According to Dr. Mutch, benefits of minimally invasive colorectal surgery include:
- Improved short-term outcomes – length of stay and return of bowel function, and morbidity and mortality. A 2012 retrospective study of 85,712 colon resections that found laparoscopic resections, when feasible, “had better outcomes than open colectomy in the immediate perioperative period.” (Ann Surg. 2012 Sep;256[3]462-8).
- Improved long-term outcomes: faster recovery, fewer hernias, and fewer bowel obstructions.
- Lower overall costs.
- Fewer complications in the elderly.
When it comes to laparoscopic colorectal surgery, Dr. Mutch cautioned that the robotic technology has unclear benefit in rectal cancer, and the cost in colorectal cancer is unclear.
Another alternative is to perform laparoscopic colorectal surgery through alternative extraction sites such as the rectum, vagina, stomach, and even a stoma site or perineal wound. Both transanal and transvaginal extraction are feasible and safe, he said, adding that transvaginal procedures are best performed in conjunction with a hysterectomy. One benefit of these procedures is that they avoid abdominal wall trauma. However, he cautioned that colorectal surgery is unique because a cancerous specimen cannot be morcellated and must instead be removed whole.
Dr. Mutch also discussed laparoendoscopic resection of colon polyps. Benefits include shorter length of stay and faster recovery, he said, but complications can include perforation and bleeding. And, he said, there’s currently no code for the procedure.
Global Academy for Medical Education and this news organization are owned by the same parent company. Dr. Mutch has no relevant disclosures.
LAS VEGAS – Two-thirds of colon resections in the United States are open procedures, but a colorectal surgeon told colleagues that evidence shows minimally invasive surgery deserves a wider place in his field.
Why? Because minimally invasive surgery – despite its limited utilization – is linked to multiple improved outcomes in colorectal surgery, said Matthew G. Mutch, MD, chief of colon and rectal surgery at Washington University, St. Louis, in a presentation at the Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
“Our goal should be to offer minimally invasive surgery to as many patients as possible by as many different methods as needed,” Dr. Mutch said. “If you’re willing to take this on and do this over a regular basis, you’ll get over that learning curve and expand the number of patients you can offer laparoscopy to.”
According to Dr. Mutch, benefits of minimally invasive colorectal surgery include:
- Improved short-term outcomes – length of stay and return of bowel function, and morbidity and mortality. A 2012 retrospective study of 85,712 colon resections that found laparoscopic resections, when feasible, “had better outcomes than open colectomy in the immediate perioperative period.” (Ann Surg. 2012 Sep;256[3]462-8).
- Improved long-term outcomes: faster recovery, fewer hernias, and fewer bowel obstructions.
- Lower overall costs.
- Fewer complications in the elderly.
When it comes to laparoscopic colorectal surgery, Dr. Mutch cautioned that the robotic technology has unclear benefit in rectal cancer, and the cost in colorectal cancer is unclear.
Another alternative is to perform laparoscopic colorectal surgery through alternative extraction sites such as the rectum, vagina, stomach, and even a stoma site or perineal wound. Both transanal and transvaginal extraction are feasible and safe, he said, adding that transvaginal procedures are best performed in conjunction with a hysterectomy. One benefit of these procedures is that they avoid abdominal wall trauma. However, he cautioned that colorectal surgery is unique because a cancerous specimen cannot be morcellated and must instead be removed whole.
Dr. Mutch also discussed laparoendoscopic resection of colon polyps. Benefits include shorter length of stay and faster recovery, he said, but complications can include perforation and bleeding. And, he said, there’s currently no code for the procedure.
Global Academy for Medical Education and this news organization are owned by the same parent company. Dr. Mutch has no relevant disclosures.
LAS VEGAS – Two-thirds of colon resections in the United States are open procedures, but a colorectal surgeon told colleagues that evidence shows minimally invasive surgery deserves a wider place in his field.
Why? Because minimally invasive surgery – despite its limited utilization – is linked to multiple improved outcomes in colorectal surgery, said Matthew G. Mutch, MD, chief of colon and rectal surgery at Washington University, St. Louis, in a presentation at the Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
“Our goal should be to offer minimally invasive surgery to as many patients as possible by as many different methods as needed,” Dr. Mutch said. “If you’re willing to take this on and do this over a regular basis, you’ll get over that learning curve and expand the number of patients you can offer laparoscopy to.”
According to Dr. Mutch, benefits of minimally invasive colorectal surgery include:
- Improved short-term outcomes – length of stay and return of bowel function, and morbidity and mortality. A 2012 retrospective study of 85,712 colon resections that found laparoscopic resections, when feasible, “had better outcomes than open colectomy in the immediate perioperative period.” (Ann Surg. 2012 Sep;256[3]462-8).
- Improved long-term outcomes: faster recovery, fewer hernias, and fewer bowel obstructions.
- Lower overall costs.
- Fewer complications in the elderly.
When it comes to laparoscopic colorectal surgery, Dr. Mutch cautioned that the robotic technology has unclear benefit in rectal cancer, and the cost in colorectal cancer is unclear.
Another alternative is to perform laparoscopic colorectal surgery through alternative extraction sites such as the rectum, vagina, stomach, and even a stoma site or perineal wound. Both transanal and transvaginal extraction are feasible and safe, he said, adding that transvaginal procedures are best performed in conjunction with a hysterectomy. One benefit of these procedures is that they avoid abdominal wall trauma. However, he cautioned that colorectal surgery is unique because a cancerous specimen cannot be morcellated and must instead be removed whole.
Dr. Mutch also discussed laparoendoscopic resection of colon polyps. Benefits include shorter length of stay and faster recovery, he said, but complications can include perforation and bleeding. And, he said, there’s currently no code for the procedure.
Global Academy for Medical Education and this news organization are owned by the same parent company. Dr. Mutch has no relevant disclosures.
EXPERT ANALYSIS FROM MISS