User login
Geography and behaviors linked to early-onset colorectal cancer survival in U.S. women
An analysis of nearly 29,000 U.S. women with early-onset colorectal cancer (CRC) showed that physical inactivity and fertility correlated modestly with living in “hot spots,” or counties with high early-onset CRC mortality rates among women.
Approximately one-third of the variation in early-onset CRC survival among women was accounted for by differences in individual- or community-level features.
Andreana N. Holowatyj, PhD, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues reported these findings in Clinical and Translational Gastroenterology.
Dr. Holowatyj and colleagues noted that prior studies have linked health behaviors with an increased risk of early-onset CRC among women. However, the impact of health behaviors on outcomes of early-onset CRC is unknown.
The researchers hypothesized that biological-, individual-, and community-level factors may be contributing to known sex-specific differences in CRC outcomes and geographic variations in survival by sex.
Hot spot counties with high mortality
The researchers identified geographic hot spots using three geospatial autocorrelation approaches with Centers for Disease Control and Prevention national
mortality data. The team also analyzed data from the Surveillance, Epidemiology, and End Results program on 28,790 women (aged 15-49 years) diagnosed with CRC during 1999-2016.
Of the 3,108 counties in the contiguous United States, 191 were identified as hot spots. Among these, 101 (52.9%) were located in the South.
Earlier research had shown a predominance of hot spots for early-onset CRC mortality among both men and women in the South.
However, the current study of women showed that almost half of these counties were located in the Midwest and the Northeast as well as the South.
Also in the current analysis, about one in every seven women (13.7%) with early-onset CRC resided in hot spot counties.
Race/ethnicity, stage at diagnosis, histopathology, and receipt of first-course therapies also differed significantly (P ≤ .0001) between women residing in hot spot versus non–hot spot counties.
Non-Hispanic Black patients, for example, accounted for 23.7% of early-onset CRC cases in hot spot counties, as compared with 14.3% in non–hot spot counties (P < .0001). The county-level proportion of non-Hispanic Black patients also modestly correlated with hot spot residence (rs = .26; P < .0001).
Race and ethnicity accounted for less than 0.5% of the variation in early-onset CRC survival among women in non–hot spot counties. In hot spot counties, however, this factor explained 1.4% of the variation in early-onset CRC-specific survival among women.
Inactivity correlates with hot spot residence
Dr. Holowatyj and colleagues also identified physical inactivity and lower fertility as county-level factors modestly correlated with hot spot residence (rs = .21, rs = –.23: P < .01).
Nearly a quarter of adults living in hot spot counties reported no physical activity during their leisure time (24.1% vs. 21.7% in non–hot spot counties; P < .01).
The rate of live births in the last year among women aged 15-50 years was lower in hot spot counties than in non–hot spot counties (4.9% vs. 5.4%; P < .01).
Individual- and community-level features overall accounted for different proportions of variance in early-onset CRC survival among women residing in hot spot counties (33.8%) versus non–hot spot counties (34.1%).
In addition to race and ethnicity, age at diagnosis, tumor histology, county-level proportions of the non-Hispanic Black population, women with a live birth in the last year, and annual household income of less than $20,000 all explained greater variance in CRC survival in young women in hot spot counties versus non–hot spot counties.
Keep CRC in differential diagnosis
“These individual- and community-level feature differences between hot spot and non–hot spot counties illustrate the importance of understanding how these factors may be contributing to early-onset CRC mortality among women – particularly in hot spot counties,” Dr. Holowatyj said in an interview. “They may provide us with key clues for developing effective strategies to reduce the burden of CRC in young women across the United States.
“Every primary care physician and gastroenterologist, particularly in hot spot counties, should keep CRC in their differential diagnosis, particularly if a patient is presenting with typical signs and symptoms, even if they are not yet of screening age. Early-stage diagnosis increases survival odds because the cancer may be easier to treat.”
Health professionals can also encourage physical activity and a healthy lifestyle, she added.
The authors declared no competing interests. Their research was funded by grants from the federal government and foundations.
SOURCE: Holowatyj AN et al. Clin and Transl Gastroenterol. 2020;11:e00266.
An analysis of nearly 29,000 U.S. women with early-onset colorectal cancer (CRC) showed that physical inactivity and fertility correlated modestly with living in “hot spots,” or counties with high early-onset CRC mortality rates among women.
Approximately one-third of the variation in early-onset CRC survival among women was accounted for by differences in individual- or community-level features.
Andreana N. Holowatyj, PhD, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues reported these findings in Clinical and Translational Gastroenterology.
Dr. Holowatyj and colleagues noted that prior studies have linked health behaviors with an increased risk of early-onset CRC among women. However, the impact of health behaviors on outcomes of early-onset CRC is unknown.
The researchers hypothesized that biological-, individual-, and community-level factors may be contributing to known sex-specific differences in CRC outcomes and geographic variations in survival by sex.
Hot spot counties with high mortality
The researchers identified geographic hot spots using three geospatial autocorrelation approaches with Centers for Disease Control and Prevention national
mortality data. The team also analyzed data from the Surveillance, Epidemiology, and End Results program on 28,790 women (aged 15-49 years) diagnosed with CRC during 1999-2016.
Of the 3,108 counties in the contiguous United States, 191 were identified as hot spots. Among these, 101 (52.9%) were located in the South.
Earlier research had shown a predominance of hot spots for early-onset CRC mortality among both men and women in the South.
However, the current study of women showed that almost half of these counties were located in the Midwest and the Northeast as well as the South.
Also in the current analysis, about one in every seven women (13.7%) with early-onset CRC resided in hot spot counties.
Race/ethnicity, stage at diagnosis, histopathology, and receipt of first-course therapies also differed significantly (P ≤ .0001) between women residing in hot spot versus non–hot spot counties.
Non-Hispanic Black patients, for example, accounted for 23.7% of early-onset CRC cases in hot spot counties, as compared with 14.3% in non–hot spot counties (P < .0001). The county-level proportion of non-Hispanic Black patients also modestly correlated with hot spot residence (rs = .26; P < .0001).
Race and ethnicity accounted for less than 0.5% of the variation in early-onset CRC survival among women in non–hot spot counties. In hot spot counties, however, this factor explained 1.4% of the variation in early-onset CRC-specific survival among women.
Inactivity correlates with hot spot residence
Dr. Holowatyj and colleagues also identified physical inactivity and lower fertility as county-level factors modestly correlated with hot spot residence (rs = .21, rs = –.23: P < .01).
Nearly a quarter of adults living in hot spot counties reported no physical activity during their leisure time (24.1% vs. 21.7% in non–hot spot counties; P < .01).
The rate of live births in the last year among women aged 15-50 years was lower in hot spot counties than in non–hot spot counties (4.9% vs. 5.4%; P < .01).
Individual- and community-level features overall accounted for different proportions of variance in early-onset CRC survival among women residing in hot spot counties (33.8%) versus non–hot spot counties (34.1%).
In addition to race and ethnicity, age at diagnosis, tumor histology, county-level proportions of the non-Hispanic Black population, women with a live birth in the last year, and annual household income of less than $20,000 all explained greater variance in CRC survival in young women in hot spot counties versus non–hot spot counties.
Keep CRC in differential diagnosis
“These individual- and community-level feature differences between hot spot and non–hot spot counties illustrate the importance of understanding how these factors may be contributing to early-onset CRC mortality among women – particularly in hot spot counties,” Dr. Holowatyj said in an interview. “They may provide us with key clues for developing effective strategies to reduce the burden of CRC in young women across the United States.
“Every primary care physician and gastroenterologist, particularly in hot spot counties, should keep CRC in their differential diagnosis, particularly if a patient is presenting with typical signs and symptoms, even if they are not yet of screening age. Early-stage diagnosis increases survival odds because the cancer may be easier to treat.”
Health professionals can also encourage physical activity and a healthy lifestyle, she added.
The authors declared no competing interests. Their research was funded by grants from the federal government and foundations.
SOURCE: Holowatyj AN et al. Clin and Transl Gastroenterol. 2020;11:e00266.
An analysis of nearly 29,000 U.S. women with early-onset colorectal cancer (CRC) showed that physical inactivity and fertility correlated modestly with living in “hot spots,” or counties with high early-onset CRC mortality rates among women.
Approximately one-third of the variation in early-onset CRC survival among women was accounted for by differences in individual- or community-level features.
Andreana N. Holowatyj, PhD, of Vanderbilt University Medical Center in Nashville, Tenn., and colleagues reported these findings in Clinical and Translational Gastroenterology.
Dr. Holowatyj and colleagues noted that prior studies have linked health behaviors with an increased risk of early-onset CRC among women. However, the impact of health behaviors on outcomes of early-onset CRC is unknown.
The researchers hypothesized that biological-, individual-, and community-level factors may be contributing to known sex-specific differences in CRC outcomes and geographic variations in survival by sex.
Hot spot counties with high mortality
The researchers identified geographic hot spots using three geospatial autocorrelation approaches with Centers for Disease Control and Prevention national
mortality data. The team also analyzed data from the Surveillance, Epidemiology, and End Results program on 28,790 women (aged 15-49 years) diagnosed with CRC during 1999-2016.
Of the 3,108 counties in the contiguous United States, 191 were identified as hot spots. Among these, 101 (52.9%) were located in the South.
Earlier research had shown a predominance of hot spots for early-onset CRC mortality among both men and women in the South.
However, the current study of women showed that almost half of these counties were located in the Midwest and the Northeast as well as the South.
Also in the current analysis, about one in every seven women (13.7%) with early-onset CRC resided in hot spot counties.
Race/ethnicity, stage at diagnosis, histopathology, and receipt of first-course therapies also differed significantly (P ≤ .0001) between women residing in hot spot versus non–hot spot counties.
Non-Hispanic Black patients, for example, accounted for 23.7% of early-onset CRC cases in hot spot counties, as compared with 14.3% in non–hot spot counties (P < .0001). The county-level proportion of non-Hispanic Black patients also modestly correlated with hot spot residence (rs = .26; P < .0001).
Race and ethnicity accounted for less than 0.5% of the variation in early-onset CRC survival among women in non–hot spot counties. In hot spot counties, however, this factor explained 1.4% of the variation in early-onset CRC-specific survival among women.
Inactivity correlates with hot spot residence
Dr. Holowatyj and colleagues also identified physical inactivity and lower fertility as county-level factors modestly correlated with hot spot residence (rs = .21, rs = –.23: P < .01).
Nearly a quarter of adults living in hot spot counties reported no physical activity during their leisure time (24.1% vs. 21.7% in non–hot spot counties; P < .01).
The rate of live births in the last year among women aged 15-50 years was lower in hot spot counties than in non–hot spot counties (4.9% vs. 5.4%; P < .01).
Individual- and community-level features overall accounted for different proportions of variance in early-onset CRC survival among women residing in hot spot counties (33.8%) versus non–hot spot counties (34.1%).
In addition to race and ethnicity, age at diagnosis, tumor histology, county-level proportions of the non-Hispanic Black population, women with a live birth in the last year, and annual household income of less than $20,000 all explained greater variance in CRC survival in young women in hot spot counties versus non–hot spot counties.
Keep CRC in differential diagnosis
“These individual- and community-level feature differences between hot spot and non–hot spot counties illustrate the importance of understanding how these factors may be contributing to early-onset CRC mortality among women – particularly in hot spot counties,” Dr. Holowatyj said in an interview. “They may provide us with key clues for developing effective strategies to reduce the burden of CRC in young women across the United States.
“Every primary care physician and gastroenterologist, particularly in hot spot counties, should keep CRC in their differential diagnosis, particularly if a patient is presenting with typical signs and symptoms, even if they are not yet of screening age. Early-stage diagnosis increases survival odds because the cancer may be easier to treat.”
Health professionals can also encourage physical activity and a healthy lifestyle, she added.
The authors declared no competing interests. Their research was funded by grants from the federal government and foundations.
SOURCE: Holowatyj AN et al. Clin and Transl Gastroenterol. 2020;11:e00266.
FROM CLINICAL AND TRANSLATIONAL GASTROENTEROLOGY
Medical societies waive fees, weigh other options during pandemic
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
COVID-19’s toll on member facilities pushed the American Academy of Sleep Medicine (AASM) recently to take a sizable gamble.
AASM announced in September that it would waive facility fees at all 2,648 AASM-accredited sleep facilities for 2021.
At $1,800-$2,600 for each facility, that will mean lost revenue of between $4.8 million and $6.9 million, but it’s a risk the academy felt it had to take.
AASM President Kannan Ramar, MBBS, MD, said in an interview that they are betting on the future of the field.
An internal survey of members, he said, found that nearly half (46%) of the 551 respondents thought they might have to close by the end of the year.
In addition, 66% reported a lower patient volume in the past month, and 36% reported that their practice or facility had to apply for loans or other financial assistance because of COVID-19, AASM said in its press release.
“We are hoping that if we help our members through this, they will be there for our patients,” Dr. Ramar said.
Other medical societies also are weighing options, straddling the line between needing income to provide resources for members but being acutely aware of the financial toll the pandemic is taking, according to one sampling.
As previously reported, primary care practices are projected to lose more than $68,000 in revenue per full-time physician in 2020, after steep drops in office visits and the collection of fees from March to May, according to a study led by researchers in the Blavatnik Institute at Harvard Medical School, Boston.
Those losses were calculated without considering a potential second wave of COVID-19 this year, the authors noted.
‘We can survive this’
Although AASM waived fees for its member facilities, individual physician fees have not been reduced so far. But the group is looking for more ways to help lower the economic burden on members, Dr. Ramar said.
“I don’t think we’ve ever been in this situation in the 45 years of the academy. This is a once-in-a-lifetime event for challenges we’re going through,” he said. “The board and the leadership realized that, if we’re going to do something, this is the time to do it.”
In addition to waiving the fees, AASM and the AASM Foundation are offering relief funding to state and regional sleep societies and research award recipients through programs created in response to COVID-19.
Some societies said they are not making changes to their dues or fees, some are forgoing cost-of-living fee increases, and some are waiving registration fees for annual meetings.
The American College of Allergy, Asthma and Immunology (ACAAI) waived most members’ registration fees for its annual meeting in November. Typically, that fee would be $500-$800 per member, plus charges for some premium sessions, Michael Blaiss, MD, ACAAI executive medical director, said.
Dr. Blaiss said in an interview that the college thought offering its 6,000 members essentially 25 free hours of CME would benefit them more than waiving annual membership dues, which are about $425 for physicians in the United States.
If the pandemic stretches through 2021, Dr. Blaiss said, “We can survive this. I’m not worried about that at all.”
But he acknowledged the painful effect on medical societies.
“I don’t think any organization would tell you it’s not having an effect on their income,” he said. “I know it is for us and for virtually any medical organization. A high percentage of income comes from the annual meeting.”
Waiving dues has not been a high priority among members in communications so far, Blaiss said.
American Academy of Dermatology President Bruce H. Thiers, MD, said in an interview that there will be no cost-of-living increase for 2021 dues, and AAD members can request a reduction in dues, which will be considered on a case-by-case basis.
“We understand that many members will have to make tough financial decisions,” he said.
In addition, AAD, which has more than 20,000 members, is exploring payment options to help members spread out the cost of membership.
ACP extends membership
The American College of Physicians, whose membership cycle starts in July, did not reduce dues but extended membership at no cost for 3 months through September to its 163,000 members, Phil Masters, MD, ACP’s vice president of membership, said in an interview.
It also expanded its educational offerings related to the pandemic, including webinars on physician wellness and issues regarding telemedicine.
He said expanding educational resources rather than waiving dues was an intentional decision after much discussion because “we’re primarily a services resource organization.”
Membership data are still being calculated, but early indications are that membership is not increasing this year, after seeing annual growth of about 2%-2.5%, Dr. Masters said. He noted that income is down “by several percent.” Annual membership dues average about $500 for physicians who have been practicing for 10 years.
“We’re well positioned to tolerate the ups and downs,” he said, but he acknowledged that “there’s no question the financial impact has been devastating on some practices.”
Like some other associations, ACP decided to cancel this year’s annual meeting, which had been planned for April. The 2021 annual meeting will be conducted online from April 29 to May 1.
Smaller organizations that rely heavily on income from the annual meeting will be severely challenged the longer the pandemic continues, Dr. Masters said.
The decision is not as simple as whether to reduce or eliminate dues, he noted. Organizations will have to reexamine their missions and structure their fees and offerings according to the needs of members.
“It’s a balance in doing things for the community at large and balancing the need to be sensitive to financial implications,” Dr. Masters said.
This article first appeared on Medscape.com.
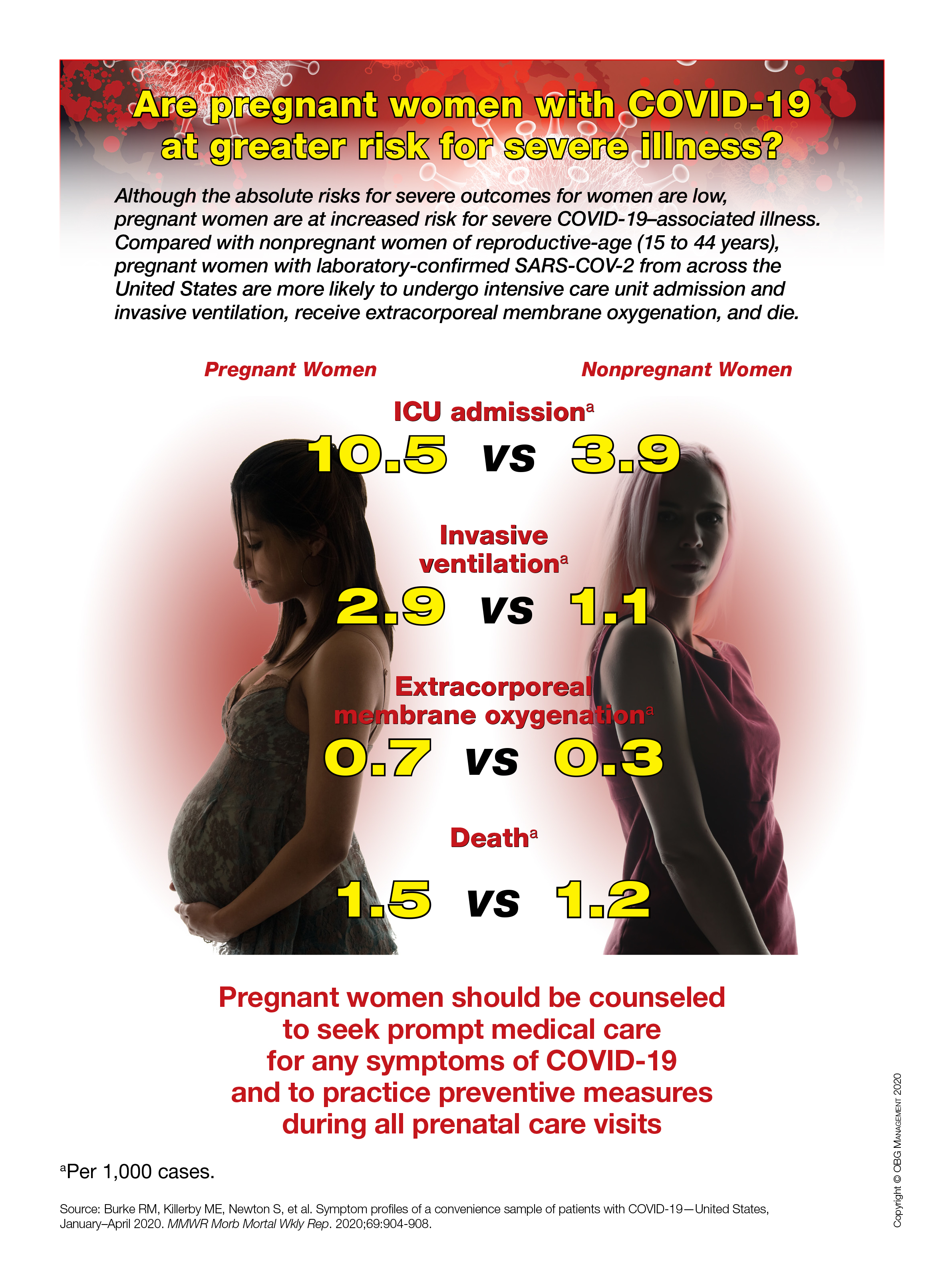
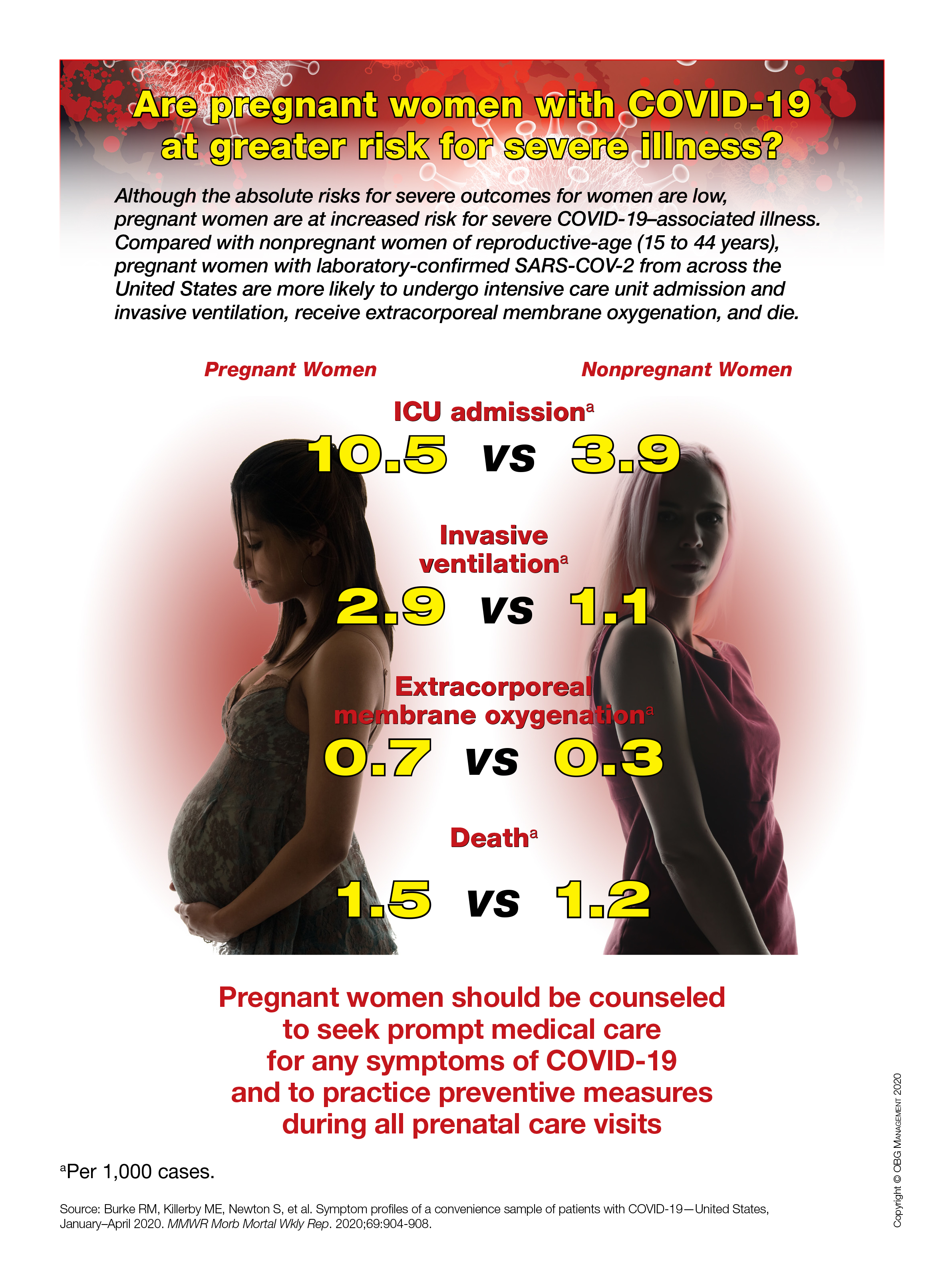
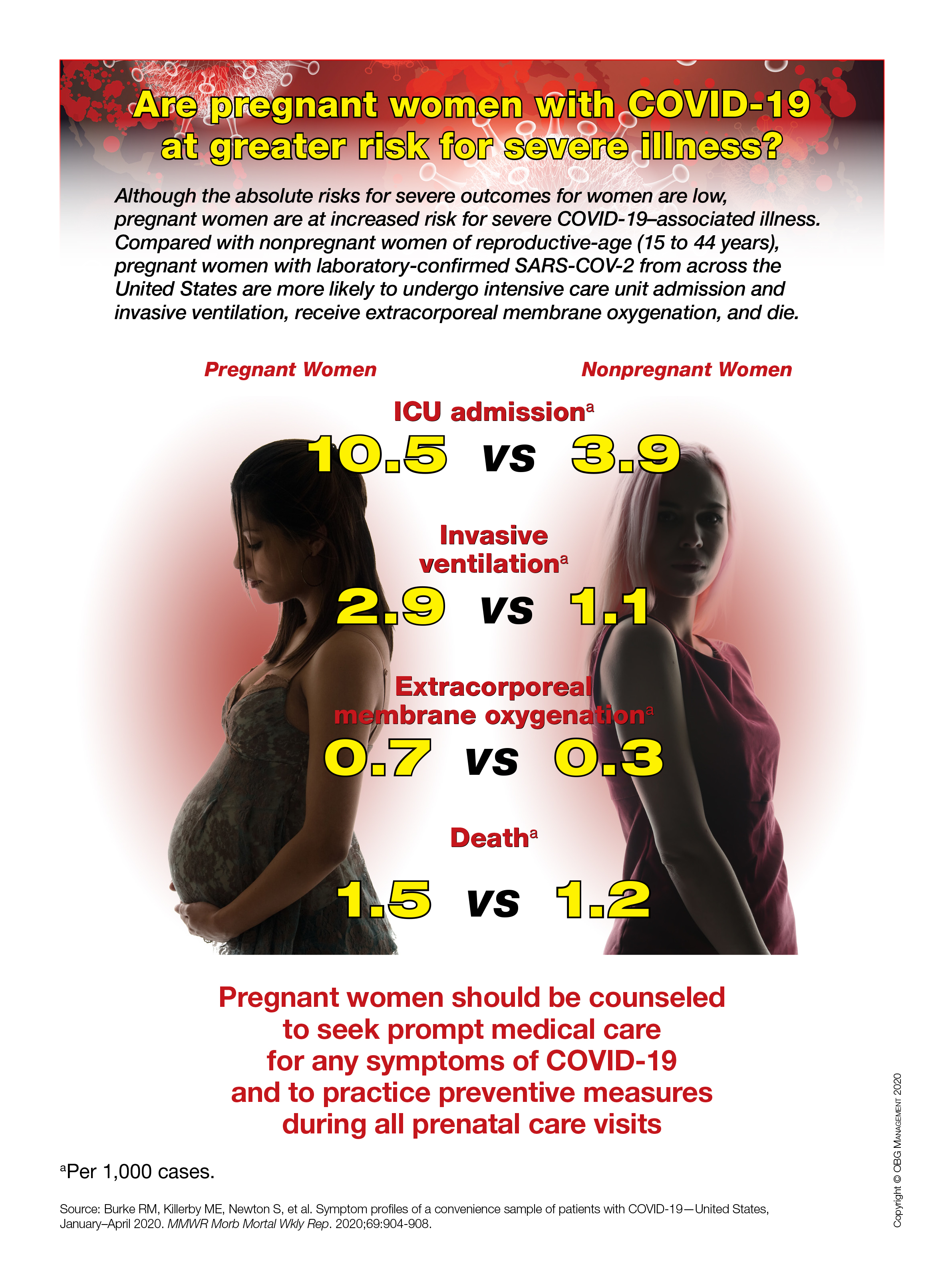
Are pregnant women with COVID-19 at greater risk for severe illness?
Meningococcal transmission risk appears low among pediatric health care professionals
at a university – lower than expected for all age groups, Lisa-Maria Steurer, MD, said regarding study findings reported at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
“This implicates that the risk of horizontal meningococcal transmission via this health care professional cohort seems to be low,” said Dr. Steurer, of the Medical University of Vienna.
Her data were based on a survey conducted between April and October 2018 at the department of paediatrics and adolescent medicine at the tertiary university pediatric hospital. The study aimed to determine colonization rates of Neisseria meningitidis and the serogroup distribution of carried meningococcal isolates in asymptomatic health care professionals employed there, reported Dr. Steurer. Her research team also sought to identify what factors increased risk of N. meningitidis carriage.
“We who work in pediatrics and adolescent medicine are exposed to those patient cohorts with the highest risk for meningococcal carriage, but also to those patients who have the highest risk for serious, invasive meningococcal disease, which peaks at the extremities of age,” declared Dr. Steurer. “But currently, there is no surveillance of asymptomatic carriers in this health care professional cohort.”
A total of 437 oropharyngeal swabs were collected from enrolled nurses, pediatricians, and medical students working in the department and immediately plated onto selective agar plates. Conventional culture was used to identify bacteria, and meningococcal isolates were characterized further through whole-genome sequencing. Sociodemographic data and information on participants’ vaccination status were collected via questionnaire.
The main finding was an overall meningococcal prevalence of 1.14%. Among the participants, the median age was 33 years, and the highest rate of carriage, 4.4%, was observed in those aged 18-25 years. None of the carriers were older than 35 years. There was a negative association found between carriage and participants’ age and time employed in the field, Dr. Steurer said.
“Risk-factor analysis found an inverse correlation with meningococcal carriage for age and timespan working in pediatrics. On the contrary, no correlations with carriage could be found for all other factors evaluated,” she said. These factors included recent contact with an immunodeficient patient, respiratory tract infection, smoking, vaccination against any meningococcal serogroup, different professions, main work settings, month of swab collection, and living with children or adolescents in the same household.
Of the study population, 29% reported that they had been vaccinated against at least one meningococcal serogroup. “Interestingly, while more than 50% of doctors and medical students had a vaccination against at least one meningococcal serogroup, only 17% of nurses were vaccinated,” Dr. Steurer remarked.
The study was financially supported by Pfizer. Dr. Steurer had no other relevant financial disclosures.
at a university – lower than expected for all age groups, Lisa-Maria Steurer, MD, said regarding study findings reported at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
“This implicates that the risk of horizontal meningococcal transmission via this health care professional cohort seems to be low,” said Dr. Steurer, of the Medical University of Vienna.
Her data were based on a survey conducted between April and October 2018 at the department of paediatrics and adolescent medicine at the tertiary university pediatric hospital. The study aimed to determine colonization rates of Neisseria meningitidis and the serogroup distribution of carried meningococcal isolates in asymptomatic health care professionals employed there, reported Dr. Steurer. Her research team also sought to identify what factors increased risk of N. meningitidis carriage.
“We who work in pediatrics and adolescent medicine are exposed to those patient cohorts with the highest risk for meningococcal carriage, but also to those patients who have the highest risk for serious, invasive meningococcal disease, which peaks at the extremities of age,” declared Dr. Steurer. “But currently, there is no surveillance of asymptomatic carriers in this health care professional cohort.”
A total of 437 oropharyngeal swabs were collected from enrolled nurses, pediatricians, and medical students working in the department and immediately plated onto selective agar plates. Conventional culture was used to identify bacteria, and meningococcal isolates were characterized further through whole-genome sequencing. Sociodemographic data and information on participants’ vaccination status were collected via questionnaire.
The main finding was an overall meningococcal prevalence of 1.14%. Among the participants, the median age was 33 years, and the highest rate of carriage, 4.4%, was observed in those aged 18-25 years. None of the carriers were older than 35 years. There was a negative association found between carriage and participants’ age and time employed in the field, Dr. Steurer said.
“Risk-factor analysis found an inverse correlation with meningococcal carriage for age and timespan working in pediatrics. On the contrary, no correlations with carriage could be found for all other factors evaluated,” she said. These factors included recent contact with an immunodeficient patient, respiratory tract infection, smoking, vaccination against any meningococcal serogroup, different professions, main work settings, month of swab collection, and living with children or adolescents in the same household.
Of the study population, 29% reported that they had been vaccinated against at least one meningococcal serogroup. “Interestingly, while more than 50% of doctors and medical students had a vaccination against at least one meningococcal serogroup, only 17% of nurses were vaccinated,” Dr. Steurer remarked.
The study was financially supported by Pfizer. Dr. Steurer had no other relevant financial disclosures.
at a university – lower than expected for all age groups, Lisa-Maria Steurer, MD, said regarding study findings reported at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
“This implicates that the risk of horizontal meningococcal transmission via this health care professional cohort seems to be low,” said Dr. Steurer, of the Medical University of Vienna.
Her data were based on a survey conducted between April and October 2018 at the department of paediatrics and adolescent medicine at the tertiary university pediatric hospital. The study aimed to determine colonization rates of Neisseria meningitidis and the serogroup distribution of carried meningococcal isolates in asymptomatic health care professionals employed there, reported Dr. Steurer. Her research team also sought to identify what factors increased risk of N. meningitidis carriage.
“We who work in pediatrics and adolescent medicine are exposed to those patient cohorts with the highest risk for meningococcal carriage, but also to those patients who have the highest risk for serious, invasive meningococcal disease, which peaks at the extremities of age,” declared Dr. Steurer. “But currently, there is no surveillance of asymptomatic carriers in this health care professional cohort.”
A total of 437 oropharyngeal swabs were collected from enrolled nurses, pediatricians, and medical students working in the department and immediately plated onto selective agar plates. Conventional culture was used to identify bacteria, and meningococcal isolates were characterized further through whole-genome sequencing. Sociodemographic data and information on participants’ vaccination status were collected via questionnaire.
The main finding was an overall meningococcal prevalence of 1.14%. Among the participants, the median age was 33 years, and the highest rate of carriage, 4.4%, was observed in those aged 18-25 years. None of the carriers were older than 35 years. There was a negative association found between carriage and participants’ age and time employed in the field, Dr. Steurer said.
“Risk-factor analysis found an inverse correlation with meningococcal carriage for age and timespan working in pediatrics. On the contrary, no correlations with carriage could be found for all other factors evaluated,” she said. These factors included recent contact with an immunodeficient patient, respiratory tract infection, smoking, vaccination against any meningococcal serogroup, different professions, main work settings, month of swab collection, and living with children or adolescents in the same household.
Of the study population, 29% reported that they had been vaccinated against at least one meningococcal serogroup. “Interestingly, while more than 50% of doctors and medical students had a vaccination against at least one meningococcal serogroup, only 17% of nurses were vaccinated,” Dr. Steurer remarked.
The study was financially supported by Pfizer. Dr. Steurer had no other relevant financial disclosures.
FROM ESPID 2020
Major depression linked to insulin resistance
Individuals experiencing a current episode of major depressive disorder (MDD) are significantly more likely to have insulin resistance (IR), research shows.
Investigators found patients with MDD were 51% more likely to have IR, compared with their counterparts without depressive disorder. In addition, in individuals experiencing current depression, IR was also associated with depression severity and depression chronicity.
“We learned two things from this study – first, that insulin resistance was associated with being in a depressive episode and with the severity of that episode,” Kathleen Watson, PhD, a postdoctoral research fellow in the department of psychiatry, Stanford (Calif.) University, told this news organization. “Second, we learned that we can estimate insulin resistance using a surrogate measure that is clinically accessible – the triglyceride/HDL ratio.”
The study was published online Dec. 2 in JAMA Psychiatry.
Targeted approach
Many studies have linked MDD and IR. However, said Dr. Watson, “We did not have much description of the nature of this relationship.” She added that her team wanted to gain a better understanding of how IR relates to depression characteristics, such as remission status, severity, and chronicity.
Characterizing these associations will “represent a critical step at better phenotyping, a prelude to longitudinal studies, and a more targeted approach to the treatment of MDD,” the authors note.
For the study, the researchers drew on data from the Netherlands Study of Depression and Anxiety, a longitudinal Dutch study of adults that “describes the course and consequences of depressive and anxiety disorders.”
The study included 1,269 study participants with current MDD (n = 536), remitted MDD (n = 394), and control participants without a history of MDD (n = 339).
In addition to investigating the association between MDD and IR, the researchers also wanted to understand “whether using different surrogate IR measures has consistent association with MDD.” IR was determined using two surrogate markers – the quantitative insulin sensitivity check index (QUICKI) and the triglyceride to high-density lipoprotein ratio. Participants in the bottom quartile of the QUICKI were categorized as IR, while all other participants were categorized as being “insulin sensitive.”
The second surrogate IR measure – the triglyceride-HDL ratio – is an index based on fasting blood sample measurements, in which the determination of IR was based on sex-specific cut points (female ratio, IR > 1.9; male ratio, IR > 2.8).
Depression was determined based on the Composite International Diagnostic Interview (version 2.1), while depression severity was based on the Inventory of Depression Symptomatology. “Chronicity” was defined as depression during the preceding 4 years and was measured using the life chart review.
State vs. trait
Insulin resistance was associated with current, but not with remitted, MDD (odds ratio, 1.51; 95% confidence interval, 1.08-2.12 and OR, 1.14; 95% CI, 0.79-1.64, respectively).
In a model adjusted for age, sex, education, partner status, smoking status, and alcohol consumption, IR, as assessed by both measures, was linked to depression severity – but only the triglyceride-HDL ratio yielded an association between IR and depression chronicity.
IR was not associated with depression severity or chronicity in remitted MDD on either measure.
The findings – specifically the association between current, but not remitted, MDD – suggest that “IR is a state, rather than a trait, biomarker of depression,” the authors note.
“There are many plausible mechanisms between IR and MDD,” said Dr. Watson. “Some hypotheses for the link include inflammations, alterations to the hypothalamic-pituitary-adrenal axis, and changes in health behavior.
“Understanding these nuances helped us to lay the foundation for future research, including asking whether IR can lead to the development of MDD,” she added.
Finally, and ways to target them with potential treatments or interventions.
Shared biological mechanisms?
Commenting on the study in an interview, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto and head of the Mood Disorders Psychopharmacology Unit, said the results “suggest that a subpopulation of people with depression have what might be referred to as ‘metabolic syndrome type II’ – the depression is a consequence of abnormal metabolic processes.”
The results also suggest “maybe metabolic markers can be used as biomarkers of disease presence vs. absence,” said Dr. McIntyre, who is also the chairman and executive director of the Brain and Cognition Discovery Foundation, Toronto, and was not involved with the study.
Also commenting on the study, Andrea Fagiolini, MD, professor of psychiatry, University of Siena (Italy), said depression, metabolic, and inflammatory diseases “likely share some common biological mechanism, as they share risk factors such as unhealthy diet, unhealthy lifestyles, and frequent exposure to physical and psychological distress.”
It is “possible that treatment of depression improves IR; conversely, it is possible that lifestyle programs or medications that are able to improve IR may improve depressive symptoms,” suggested Dr. Fagiolini, who was not involved with the study. “It remains to be established which symptoms of depression are most involved in this correlation and whether their improvement precedes or follows the improvement in IR,” he noted.
The Netherlands Study of Depression and Anxiety is funded through the Geestkracht program of the Netherlands Organisation for Health Research and Development and is supported by several participating universities and mental health care organizations. Dr. Watson has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reported research grant support from CIHR/GACD/Chinese National Natural Research Foundation and speaker/consultation fees from multiple pharmaceutical companies. Dr. McIntyre is also CEO of AltMed. Dr. Fagiolini has served or is currently serving as consultant or speaker for or is a research grant recipient from multiple pharmaceutical companies.
A version of this article originally appeared on Medscape.com.
Individuals experiencing a current episode of major depressive disorder (MDD) are significantly more likely to have insulin resistance (IR), research shows.
Investigators found patients with MDD were 51% more likely to have IR, compared with their counterparts without depressive disorder. In addition, in individuals experiencing current depression, IR was also associated with depression severity and depression chronicity.
“We learned two things from this study – first, that insulin resistance was associated with being in a depressive episode and with the severity of that episode,” Kathleen Watson, PhD, a postdoctoral research fellow in the department of psychiatry, Stanford (Calif.) University, told this news organization. “Second, we learned that we can estimate insulin resistance using a surrogate measure that is clinically accessible – the triglyceride/HDL ratio.”
The study was published online Dec. 2 in JAMA Psychiatry.
Targeted approach
Many studies have linked MDD and IR. However, said Dr. Watson, “We did not have much description of the nature of this relationship.” She added that her team wanted to gain a better understanding of how IR relates to depression characteristics, such as remission status, severity, and chronicity.
Characterizing these associations will “represent a critical step at better phenotyping, a prelude to longitudinal studies, and a more targeted approach to the treatment of MDD,” the authors note.
For the study, the researchers drew on data from the Netherlands Study of Depression and Anxiety, a longitudinal Dutch study of adults that “describes the course and consequences of depressive and anxiety disorders.”
The study included 1,269 study participants with current MDD (n = 536), remitted MDD (n = 394), and control participants without a history of MDD (n = 339).
In addition to investigating the association between MDD and IR, the researchers also wanted to understand “whether using different surrogate IR measures has consistent association with MDD.” IR was determined using two surrogate markers – the quantitative insulin sensitivity check index (QUICKI) and the triglyceride to high-density lipoprotein ratio. Participants in the bottom quartile of the QUICKI were categorized as IR, while all other participants were categorized as being “insulin sensitive.”
The second surrogate IR measure – the triglyceride-HDL ratio – is an index based on fasting blood sample measurements, in which the determination of IR was based on sex-specific cut points (female ratio, IR > 1.9; male ratio, IR > 2.8).
Depression was determined based on the Composite International Diagnostic Interview (version 2.1), while depression severity was based on the Inventory of Depression Symptomatology. “Chronicity” was defined as depression during the preceding 4 years and was measured using the life chart review.
State vs. trait
Insulin resistance was associated with current, but not with remitted, MDD (odds ratio, 1.51; 95% confidence interval, 1.08-2.12 and OR, 1.14; 95% CI, 0.79-1.64, respectively).
In a model adjusted for age, sex, education, partner status, smoking status, and alcohol consumption, IR, as assessed by both measures, was linked to depression severity – but only the triglyceride-HDL ratio yielded an association between IR and depression chronicity.
IR was not associated with depression severity or chronicity in remitted MDD on either measure.
The findings – specifically the association between current, but not remitted, MDD – suggest that “IR is a state, rather than a trait, biomarker of depression,” the authors note.
“There are many plausible mechanisms between IR and MDD,” said Dr. Watson. “Some hypotheses for the link include inflammations, alterations to the hypothalamic-pituitary-adrenal axis, and changes in health behavior.
“Understanding these nuances helped us to lay the foundation for future research, including asking whether IR can lead to the development of MDD,” she added.
Finally, and ways to target them with potential treatments or interventions.
Shared biological mechanisms?
Commenting on the study in an interview, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto and head of the Mood Disorders Psychopharmacology Unit, said the results “suggest that a subpopulation of people with depression have what might be referred to as ‘metabolic syndrome type II’ – the depression is a consequence of abnormal metabolic processes.”
The results also suggest “maybe metabolic markers can be used as biomarkers of disease presence vs. absence,” said Dr. McIntyre, who is also the chairman and executive director of the Brain and Cognition Discovery Foundation, Toronto, and was not involved with the study.
Also commenting on the study, Andrea Fagiolini, MD, professor of psychiatry, University of Siena (Italy), said depression, metabolic, and inflammatory diseases “likely share some common biological mechanism, as they share risk factors such as unhealthy diet, unhealthy lifestyles, and frequent exposure to physical and psychological distress.”
It is “possible that treatment of depression improves IR; conversely, it is possible that lifestyle programs or medications that are able to improve IR may improve depressive symptoms,” suggested Dr. Fagiolini, who was not involved with the study. “It remains to be established which symptoms of depression are most involved in this correlation and whether their improvement precedes or follows the improvement in IR,” he noted.
The Netherlands Study of Depression and Anxiety is funded through the Geestkracht program of the Netherlands Organisation for Health Research and Development and is supported by several participating universities and mental health care organizations. Dr. Watson has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reported research grant support from CIHR/GACD/Chinese National Natural Research Foundation and speaker/consultation fees from multiple pharmaceutical companies. Dr. McIntyre is also CEO of AltMed. Dr. Fagiolini has served or is currently serving as consultant or speaker for or is a research grant recipient from multiple pharmaceutical companies.
A version of this article originally appeared on Medscape.com.
Individuals experiencing a current episode of major depressive disorder (MDD) are significantly more likely to have insulin resistance (IR), research shows.
Investigators found patients with MDD were 51% more likely to have IR, compared with their counterparts without depressive disorder. In addition, in individuals experiencing current depression, IR was also associated with depression severity and depression chronicity.
“We learned two things from this study – first, that insulin resistance was associated with being in a depressive episode and with the severity of that episode,” Kathleen Watson, PhD, a postdoctoral research fellow in the department of psychiatry, Stanford (Calif.) University, told this news organization. “Second, we learned that we can estimate insulin resistance using a surrogate measure that is clinically accessible – the triglyceride/HDL ratio.”
The study was published online Dec. 2 in JAMA Psychiatry.
Targeted approach
Many studies have linked MDD and IR. However, said Dr. Watson, “We did not have much description of the nature of this relationship.” She added that her team wanted to gain a better understanding of how IR relates to depression characteristics, such as remission status, severity, and chronicity.
Characterizing these associations will “represent a critical step at better phenotyping, a prelude to longitudinal studies, and a more targeted approach to the treatment of MDD,” the authors note.
For the study, the researchers drew on data from the Netherlands Study of Depression and Anxiety, a longitudinal Dutch study of adults that “describes the course and consequences of depressive and anxiety disorders.”
The study included 1,269 study participants with current MDD (n = 536), remitted MDD (n = 394), and control participants without a history of MDD (n = 339).
In addition to investigating the association between MDD and IR, the researchers also wanted to understand “whether using different surrogate IR measures has consistent association with MDD.” IR was determined using two surrogate markers – the quantitative insulin sensitivity check index (QUICKI) and the triglyceride to high-density lipoprotein ratio. Participants in the bottom quartile of the QUICKI were categorized as IR, while all other participants were categorized as being “insulin sensitive.”
The second surrogate IR measure – the triglyceride-HDL ratio – is an index based on fasting blood sample measurements, in which the determination of IR was based on sex-specific cut points (female ratio, IR > 1.9; male ratio, IR > 2.8).
Depression was determined based on the Composite International Diagnostic Interview (version 2.1), while depression severity was based on the Inventory of Depression Symptomatology. “Chronicity” was defined as depression during the preceding 4 years and was measured using the life chart review.
State vs. trait
Insulin resistance was associated with current, but not with remitted, MDD (odds ratio, 1.51; 95% confidence interval, 1.08-2.12 and OR, 1.14; 95% CI, 0.79-1.64, respectively).
In a model adjusted for age, sex, education, partner status, smoking status, and alcohol consumption, IR, as assessed by both measures, was linked to depression severity – but only the triglyceride-HDL ratio yielded an association between IR and depression chronicity.
IR was not associated with depression severity or chronicity in remitted MDD on either measure.
The findings – specifically the association between current, but not remitted, MDD – suggest that “IR is a state, rather than a trait, biomarker of depression,” the authors note.
“There are many plausible mechanisms between IR and MDD,” said Dr. Watson. “Some hypotheses for the link include inflammations, alterations to the hypothalamic-pituitary-adrenal axis, and changes in health behavior.
“Understanding these nuances helped us to lay the foundation for future research, including asking whether IR can lead to the development of MDD,” she added.
Finally, and ways to target them with potential treatments or interventions.
Shared biological mechanisms?
Commenting on the study in an interview, Roger McIntyre, MD, professor of psychiatry and pharmacology, University of Toronto and head of the Mood Disorders Psychopharmacology Unit, said the results “suggest that a subpopulation of people with depression have what might be referred to as ‘metabolic syndrome type II’ – the depression is a consequence of abnormal metabolic processes.”
The results also suggest “maybe metabolic markers can be used as biomarkers of disease presence vs. absence,” said Dr. McIntyre, who is also the chairman and executive director of the Brain and Cognition Discovery Foundation, Toronto, and was not involved with the study.
Also commenting on the study, Andrea Fagiolini, MD, professor of psychiatry, University of Siena (Italy), said depression, metabolic, and inflammatory diseases “likely share some common biological mechanism, as they share risk factors such as unhealthy diet, unhealthy lifestyles, and frequent exposure to physical and psychological distress.”
It is “possible that treatment of depression improves IR; conversely, it is possible that lifestyle programs or medications that are able to improve IR may improve depressive symptoms,” suggested Dr. Fagiolini, who was not involved with the study. “It remains to be established which symptoms of depression are most involved in this correlation and whether their improvement precedes or follows the improvement in IR,” he noted.
The Netherlands Study of Depression and Anxiety is funded through the Geestkracht program of the Netherlands Organisation for Health Research and Development and is supported by several participating universities and mental health care organizations. Dr. Watson has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reported research grant support from CIHR/GACD/Chinese National Natural Research Foundation and speaker/consultation fees from multiple pharmaceutical companies. Dr. McIntyre is also CEO of AltMed. Dr. Fagiolini has served or is currently serving as consultant or speaker for or is a research grant recipient from multiple pharmaceutical companies.
A version of this article originally appeared on Medscape.com.
Children and school during the pandemic: What’s the answer?
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
Countries across the world are in the process of closing and reopening schools to contain the spread of COVID-19. Should there be universal testing and quarantining of sick school children and their classmates?
In a lively debate at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year, Andreea M. Panciu, MD, from the National Institute of Infectious Diseases in Bucharest, argued for routine testing and quarantining of all school children. Her opposite number, Danilo Buonsenso, MD, from the Centre for Global Health Research and Studies, Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricovero e Cura a Carattere Scientifico, Rome, made the case for a more selective approach.
Should children be sent to school?
stated Dr. Panciu as she started the debate by explaining the challenges faced by schools in adhering to key mitigation strategies. The U.S. Centers for Disease Control and Prevention recommends that students keep 1.8 m (6 feet) distance from one another. “In many school settings this is not feasible without drastically limiting the number of students,” she explained. “This is a massive challenge for many schools that are already overcrowded.”
The use of facemasks also is a challenge in classrooms. Children have a lower tolerance or may not be able to use the mask properly. There also are concerns regarding impaired learning, speech development, social development, and facial recognition. “We need to look at the evidence; preventive measures work,” responded Dr. Buonsenso. If distance can be implemented, the more distance the lower the transmission of infection, with 1.5-2 meters having the best effects. “Distance can be difficult when school buildings do not allow it, however, governments have had time to plan, and this should not be a limitation to education for kids.”
A recent review clearly showed that children and adolescents aged under 20 years have a much lower risk of susceptibility to COVID-19 infection, compared with adults. This is especially the case for children younger than 14 years. “There is no excuse, let’s bring the children back to school,” argued Dr. Buonsenso.
Dr. Panciu responded with several studies that have tried to quantify the amount of SARS-CoV-2 virus that is carried by infected children. Viral load in the nasopharynx in children under 5 years with mild to moderate COVID-19 symptoms was higher than that of both children over 5 as well as adults. The viral load in young children did not seem to differ by age or symptom severity. “There doesn’t appear to be a significant difference in viral load between symptomatic children and symptomatic adults,” she stated.
“But the question is: ‘How infectious are children?’ ” reacted Dr. Buonsenso. Data from South Korea showed that, for children, particularly those under 10 years, the number of secondary cases of contacts was very low, suggesting that children are rarely spreading the virus.
Dr. Buonsenso and colleagues assessed 30 households containing children aged under 18 years where an adult had been infected with COVID-19 in Rome during the peak of the pandemic. In no cases was it found that a child was the index case. This was supported by data from China, also obtained during the peak of the pandemic, which showed that the number of children infected was very low, but more importantly the number of secondary attacks from contact with children was also very low.
What about children who are sick at school?
The debate moved to discussing what should be done when a child is sick at school. Dr. Panciu clarified recommendations by the CDC regarding what steps to take if a student displays signs of infection consistent with COVID-19: Should they test positive, they are to stay at home for 10 days from the time signs and symptoms first appeared. Further, any teachers or students identified as close contacts are advised to stay at home for 14 days. (Since the ESPID meeting, the CDC has made changes in quarantine times for COVID-19. People can now quarantine for 10 days without a COVID-19 test if they have no symptoms. Alternatively, a quarantine can end after 7 days for someone with a negative test and no symptoms. The agency recommends a polymerase chain reaction test or an antigen assay within 48 hours before the end of a quarantine.)
A significant problem is the overlap between COVID-19 symptoms and those associated with other common illnesses because of a range of viruses. This is particularly true in younger children who often suffer from viral infections. “It is common for children to have up to eight respiratory illnesses a year,” explained Dr. Panciu, “and some may have symptoms so mild that they don’t notice them.”
“We need to be a little bit more children focused, otherwise we are going to be isolating children all the time,” said Dr. Buonsenso. The Royal College of Paediatrics and Child Health state that a child with a simple runny nose or sporadic cough without a fever, who would have attended school in other times, should not be tested for COVID-19. He moved on to then cite several studies that show little or no evidence of COVID-19 transmission between school children. This included a prospective cohort study in Australia showing that child-to-child transmission occurred in 0.3%. “To date, the advantages from routine quarantine and over testing seem too low to balance the social consequences on children and families,” he concluded.
As the debate drew to a close, Dr. Panciu reported several studies that did demonstrate transmission between school-age children. Data from an overnight camp in Georgia where the median age was 12 years showed the attack rate was 44% for ages 11-17 years and 51% for ages 6-10 years. Similar conclusions were reached in an Israeli study looking at a large COVID-19 outbreak in a school. This occurred 10 days after reopening, in spite of preventive measures being in place. “Opening safely isn’t just about the adjustments a school makes,” she said, “it’s also about how much of the virus is circulating in the community, which affects the likelihood that students and staff will bring COVID-19 into their classrooms.”
Damian Roland, consultant and honorary associate professor in pediatric emergency medicine at the University of Leicester (England), commented: “Maximizing educational potential while reducing the spread of COVID19 is a challenge laden with scientific equipoise while simultaneously infused with emotion. The evidence of transmission between, and infectivity from, children is not complete, as this debate has demonstrated. It is important scientists, clinicians, educators, and policy makers make collaborative decisions, aware there is not one perfect answer, and willing to understand and incorporate others views and objectives rather than holding onto single beliefs or approaches.”
No financial conflicts of interest were declared.
FROM ESPID 2020
Breast surgery may be a gateway to addictive medication use
After their surgery, 13.1% of opioid-naive patients become new persistent opioid users, and 6.6% of sedative-hypnotic–naive patients become new persistent users of sedative-hypnotics. Risk factors for persistent substance use included younger age, a breast cancer diagnosis, and chemotherapy.
“As the opioid epidemic in the United States continues, the rate of opioid dependence in the cancer population continues to increase as well,” study investigator Jacob Cogan, MD, of NewYork-Presbyterian/Columbia University Irving Medical Center in New York, said during a press conference.
“The perioperative period is one of high risk for cancer patients, with up to 10% becoming new persistent opioid users after cancer-related surgery. The rates surrounding mastectomy and reconstruction, however, are unknown. Another class of controlled substances worth our attention are the sedative-hypnotics. Despite the high rates of psychiatric disorders in the cancer population, there is little research into the rates of persistent sedative-hypnotic use in these patients.”
With this in mind, Dr. Cogan and colleagues analyzed MarketScan health care claims data for patients who underwent mastectomy and reconstruction (whether therapeutic or prophylactic) between 2008 and 2017.
The researchers then identified prescription claims for opioids and sedative-hypnotics during three periods:
- Preoperative period – 365 days to 31 days before surgery.
- Perioperative period – 31 days before to 90 days after surgery.
- Postoperative period – 90 days to 365 days after surgery.
‘Striking’ results
Analyses were based on 25,270 women who were not prior users of opioids and 27,651 women who were not prior users of sedative-hypnotics.
Women were considered new persistent substance users if they had no use in the preoperative period but filled at least one prescription in the perioperative period and at least two in the postoperative period.
Overall, 13.1% of opioid-naive patients became persistent opioid users, and 6.6% of sedative-hypnotic-naive patients became persistent sedative-hypnotic users after their mastectomy and reconstruction.
Proportions of substance use were even higher, 17.5% for opioids and 17.0% for sedative-hypnotics, after excluding women who did not receive or fill a perioperative prescription.
In multivariate analysis, patients were significantly more likely to become new persistent opioid users if they had Medicaid insurance (odds ratio, 2.31), had a breast cancer diagnosis vs a prophylactic indication (OR, 1.44), received chemotherapy (OR, 1.33), and were 50-64 years of age (OR, 1.29) or 49 years or younger (OR, 1.27), compared with 65 years or older.
Similarly, patients were significantly more likely to become new persistent sedative-hypnotic users if they received chemotherapy (OR, 2.24), had Medicaid insurance (OR, 1.85), had a breast cancer diagnosis (OR, 1.79), and were 50 to 64 years (OR, 1.65) or 49 years or younger (OR, 1.79).
Finally, patients’ likelihood of new persistent use increased with their number of risk factors. For persistent opioid use, the odds ratio rose from 2.27 in patients with two risk factors to 6.34 in those with five risk factors. For persistent sedative-hypnotic use, the odds ratio rose from 2.55 to 7.71, respectively.
The observed incidences of new persistent substance use in this patient population are “striking,” according to Dr. Cogan. Although the identified risk factors can help providers spot patients who should be monitored more closely, a proactive, systematic approach to postoperative follow-up for all patients is likely needed.
“When you are seeing patients in follow-up, this is something that you might want to explicitly ask about, for example, and not just assume that the postoperative opioids were taken and then disposed of,” Dr. Cogan recommended. “Ask them, ‘Are you still taking opioids, are you still taking your Ambien or whatever medication you were prescribed?’ That’s something to diligently follow up on and make sure the drug is disposed of, or if it somebody is still taking it, refer them for the appropriate services.”
In addition, patients should be encouraged to use over-the-counter medications as much as possible, he advised.
Prescribing: It’s complicated
“I wonder if perhaps we should not be giving opioids at all to certain patients. For example, a mastectomy and implant reconstruction, oftentimes, surprisingly, that’s not a terribly painful procedure. But a TRAM [transverse rectus abdominis] flap or abdominal flap, that really is,” commented press conference comoderator C. Kent Osborne, MD, of Baylor College of Medicine in Houston.
“I’ve been surprised that a lot of my patients get the prescription, but they don’t even use the pills, and I wonder if the prescription is given just so that we’re not bothered at nighttime by somebody calling with pain,” Dr. Osbourne added.
Prescribing opioids for postoperative pain is complicated, Dr. Cogan said, noting that the study did not assess the specific type of reconstruction patients had.
“You don’t want people in pain. Even if they need just one or two pills, it’s still reasonable for them to have it, and we certainly don’t want to imply from our study that people shouldn’t be getting these prescriptions if they need them,” Dr. Cogan elaborated. “But once patients have them, don’t just leave them there in their home because other studies have shown that that’s when people really get addicted to these medications, when they use them later on for other reasons, or they keep using them just because they have them around.”
The risk for persistent use of controlled substances “is something that all physicians need to be aware of for their patients. This is something that we are missing,” maintained press conference comoderator Virginia Kaklamani, MD, DSc, of UT Health San Antonio.
“It’s easy to just give a prescription instead of arguing with a patient about why you are not going to give them a prescription,” Dr. Kaklamani said. “And ultimately ... pain is subjective. If a patient tells you they are in pain, you are, quote-endquote, a bad physician if you tell them they should not be in pain.”
“We need to focus on other ways to deal with the pain, like physical therapy, sending patients to physical medicine and rehab physicians who are trained to help with symptoms from the surgery, with range of motion and all that; that can help with pain,” she recommended. “It’s much harder to do that, right, than to send a prescription in for a narcotic? But that easy answer is always the worst answer.”
This study was funded by the Breast Cancer Research Foundation and the National Institutes of Health. Dr. Cogan declared no conflicts of interest. Dr. Osborne disclosed relationships with Wolters Kluwer, Lilly, Tolmar, and GeneTex. Dr. Kaklamani disclosed relationships with Amgen, AstraZeneca, Athenex, Celgene, Celldex, Daiichi, Eisai, Genentech, Genomic Health, Immunomedics, Novartis, Pfizer, Puma, and Seattle Genetics.
SOURCE: Cogan JC et al. SABCS 2020, Abstract GS3-08.
After their surgery, 13.1% of opioid-naive patients become new persistent opioid users, and 6.6% of sedative-hypnotic–naive patients become new persistent users of sedative-hypnotics. Risk factors for persistent substance use included younger age, a breast cancer diagnosis, and chemotherapy.
“As the opioid epidemic in the United States continues, the rate of opioid dependence in the cancer population continues to increase as well,” study investigator Jacob Cogan, MD, of NewYork-Presbyterian/Columbia University Irving Medical Center in New York, said during a press conference.
“The perioperative period is one of high risk for cancer patients, with up to 10% becoming new persistent opioid users after cancer-related surgery. The rates surrounding mastectomy and reconstruction, however, are unknown. Another class of controlled substances worth our attention are the sedative-hypnotics. Despite the high rates of psychiatric disorders in the cancer population, there is little research into the rates of persistent sedative-hypnotic use in these patients.”
With this in mind, Dr. Cogan and colleagues analyzed MarketScan health care claims data for patients who underwent mastectomy and reconstruction (whether therapeutic or prophylactic) between 2008 and 2017.
The researchers then identified prescription claims for opioids and sedative-hypnotics during three periods:
- Preoperative period – 365 days to 31 days before surgery.
- Perioperative period – 31 days before to 90 days after surgery.
- Postoperative period – 90 days to 365 days after surgery.
‘Striking’ results
Analyses were based on 25,270 women who were not prior users of opioids and 27,651 women who were not prior users of sedative-hypnotics.
Women were considered new persistent substance users if they had no use in the preoperative period but filled at least one prescription in the perioperative period and at least two in the postoperative period.
Overall, 13.1% of opioid-naive patients became persistent opioid users, and 6.6% of sedative-hypnotic-naive patients became persistent sedative-hypnotic users after their mastectomy and reconstruction.
Proportions of substance use were even higher, 17.5% for opioids and 17.0% for sedative-hypnotics, after excluding women who did not receive or fill a perioperative prescription.
In multivariate analysis, patients were significantly more likely to become new persistent opioid users if they had Medicaid insurance (odds ratio, 2.31), had a breast cancer diagnosis vs a prophylactic indication (OR, 1.44), received chemotherapy (OR, 1.33), and were 50-64 years of age (OR, 1.29) or 49 years or younger (OR, 1.27), compared with 65 years or older.
Similarly, patients were significantly more likely to become new persistent sedative-hypnotic users if they received chemotherapy (OR, 2.24), had Medicaid insurance (OR, 1.85), had a breast cancer diagnosis (OR, 1.79), and were 50 to 64 years (OR, 1.65) or 49 years or younger (OR, 1.79).
Finally, patients’ likelihood of new persistent use increased with their number of risk factors. For persistent opioid use, the odds ratio rose from 2.27 in patients with two risk factors to 6.34 in those with five risk factors. For persistent sedative-hypnotic use, the odds ratio rose from 2.55 to 7.71, respectively.
The observed incidences of new persistent substance use in this patient population are “striking,” according to Dr. Cogan. Although the identified risk factors can help providers spot patients who should be monitored more closely, a proactive, systematic approach to postoperative follow-up for all patients is likely needed.
“When you are seeing patients in follow-up, this is something that you might want to explicitly ask about, for example, and not just assume that the postoperative opioids were taken and then disposed of,” Dr. Cogan recommended. “Ask them, ‘Are you still taking opioids, are you still taking your Ambien or whatever medication you were prescribed?’ That’s something to diligently follow up on and make sure the drug is disposed of, or if it somebody is still taking it, refer them for the appropriate services.”
In addition, patients should be encouraged to use over-the-counter medications as much as possible, he advised.
Prescribing: It’s complicated
“I wonder if perhaps we should not be giving opioids at all to certain patients. For example, a mastectomy and implant reconstruction, oftentimes, surprisingly, that’s not a terribly painful procedure. But a TRAM [transverse rectus abdominis] flap or abdominal flap, that really is,” commented press conference comoderator C. Kent Osborne, MD, of Baylor College of Medicine in Houston.
“I’ve been surprised that a lot of my patients get the prescription, but they don’t even use the pills, and I wonder if the prescription is given just so that we’re not bothered at nighttime by somebody calling with pain,” Dr. Osbourne added.
Prescribing opioids for postoperative pain is complicated, Dr. Cogan said, noting that the study did not assess the specific type of reconstruction patients had.
“You don’t want people in pain. Even if they need just one or two pills, it’s still reasonable for them to have it, and we certainly don’t want to imply from our study that people shouldn’t be getting these prescriptions if they need them,” Dr. Cogan elaborated. “But once patients have them, don’t just leave them there in their home because other studies have shown that that’s when people really get addicted to these medications, when they use them later on for other reasons, or they keep using them just because they have them around.”
The risk for persistent use of controlled substances “is something that all physicians need to be aware of for their patients. This is something that we are missing,” maintained press conference comoderator Virginia Kaklamani, MD, DSc, of UT Health San Antonio.
“It’s easy to just give a prescription instead of arguing with a patient about why you are not going to give them a prescription,” Dr. Kaklamani said. “And ultimately ... pain is subjective. If a patient tells you they are in pain, you are, quote-endquote, a bad physician if you tell them they should not be in pain.”
“We need to focus on other ways to deal with the pain, like physical therapy, sending patients to physical medicine and rehab physicians who are trained to help with symptoms from the surgery, with range of motion and all that; that can help with pain,” she recommended. “It’s much harder to do that, right, than to send a prescription in for a narcotic? But that easy answer is always the worst answer.”
This study was funded by the Breast Cancer Research Foundation and the National Institutes of Health. Dr. Cogan declared no conflicts of interest. Dr. Osborne disclosed relationships with Wolters Kluwer, Lilly, Tolmar, and GeneTex. Dr. Kaklamani disclosed relationships with Amgen, AstraZeneca, Athenex, Celgene, Celldex, Daiichi, Eisai, Genentech, Genomic Health, Immunomedics, Novartis, Pfizer, Puma, and Seattle Genetics.
SOURCE: Cogan JC et al. SABCS 2020, Abstract GS3-08.
After their surgery, 13.1% of opioid-naive patients become new persistent opioid users, and 6.6% of sedative-hypnotic–naive patients become new persistent users of sedative-hypnotics. Risk factors for persistent substance use included younger age, a breast cancer diagnosis, and chemotherapy.
“As the opioid epidemic in the United States continues, the rate of opioid dependence in the cancer population continues to increase as well,” study investigator Jacob Cogan, MD, of NewYork-Presbyterian/Columbia University Irving Medical Center in New York, said during a press conference.
“The perioperative period is one of high risk for cancer patients, with up to 10% becoming new persistent opioid users after cancer-related surgery. The rates surrounding mastectomy and reconstruction, however, are unknown. Another class of controlled substances worth our attention are the sedative-hypnotics. Despite the high rates of psychiatric disorders in the cancer population, there is little research into the rates of persistent sedative-hypnotic use in these patients.”
With this in mind, Dr. Cogan and colleagues analyzed MarketScan health care claims data for patients who underwent mastectomy and reconstruction (whether therapeutic or prophylactic) between 2008 and 2017.
The researchers then identified prescription claims for opioids and sedative-hypnotics during three periods:
- Preoperative period – 365 days to 31 days before surgery.
- Perioperative period – 31 days before to 90 days after surgery.
- Postoperative period – 90 days to 365 days after surgery.
‘Striking’ results
Analyses were based on 25,270 women who were not prior users of opioids and 27,651 women who were not prior users of sedative-hypnotics.
Women were considered new persistent substance users if they had no use in the preoperative period but filled at least one prescription in the perioperative period and at least two in the postoperative period.
Overall, 13.1% of opioid-naive patients became persistent opioid users, and 6.6% of sedative-hypnotic-naive patients became persistent sedative-hypnotic users after their mastectomy and reconstruction.
Proportions of substance use were even higher, 17.5% for opioids and 17.0% for sedative-hypnotics, after excluding women who did not receive or fill a perioperative prescription.
In multivariate analysis, patients were significantly more likely to become new persistent opioid users if they had Medicaid insurance (odds ratio, 2.31), had a breast cancer diagnosis vs a prophylactic indication (OR, 1.44), received chemotherapy (OR, 1.33), and were 50-64 years of age (OR, 1.29) or 49 years or younger (OR, 1.27), compared with 65 years or older.
Similarly, patients were significantly more likely to become new persistent sedative-hypnotic users if they received chemotherapy (OR, 2.24), had Medicaid insurance (OR, 1.85), had a breast cancer diagnosis (OR, 1.79), and were 50 to 64 years (OR, 1.65) or 49 years or younger (OR, 1.79).
Finally, patients’ likelihood of new persistent use increased with their number of risk factors. For persistent opioid use, the odds ratio rose from 2.27 in patients with two risk factors to 6.34 in those with five risk factors. For persistent sedative-hypnotic use, the odds ratio rose from 2.55 to 7.71, respectively.
The observed incidences of new persistent substance use in this patient population are “striking,” according to Dr. Cogan. Although the identified risk factors can help providers spot patients who should be monitored more closely, a proactive, systematic approach to postoperative follow-up for all patients is likely needed.
“When you are seeing patients in follow-up, this is something that you might want to explicitly ask about, for example, and not just assume that the postoperative opioids were taken and then disposed of,” Dr. Cogan recommended. “Ask them, ‘Are you still taking opioids, are you still taking your Ambien or whatever medication you were prescribed?’ That’s something to diligently follow up on and make sure the drug is disposed of, or if it somebody is still taking it, refer them for the appropriate services.”
In addition, patients should be encouraged to use over-the-counter medications as much as possible, he advised.
Prescribing: It’s complicated
“I wonder if perhaps we should not be giving opioids at all to certain patients. For example, a mastectomy and implant reconstruction, oftentimes, surprisingly, that’s not a terribly painful procedure. But a TRAM [transverse rectus abdominis] flap or abdominal flap, that really is,” commented press conference comoderator C. Kent Osborne, MD, of Baylor College of Medicine in Houston.
“I’ve been surprised that a lot of my patients get the prescription, but they don’t even use the pills, and I wonder if the prescription is given just so that we’re not bothered at nighttime by somebody calling with pain,” Dr. Osbourne added.
Prescribing opioids for postoperative pain is complicated, Dr. Cogan said, noting that the study did not assess the specific type of reconstruction patients had.
“You don’t want people in pain. Even if they need just one or two pills, it’s still reasonable for them to have it, and we certainly don’t want to imply from our study that people shouldn’t be getting these prescriptions if they need them,” Dr. Cogan elaborated. “But once patients have them, don’t just leave them there in their home because other studies have shown that that’s when people really get addicted to these medications, when they use them later on for other reasons, or they keep using them just because they have them around.”
The risk for persistent use of controlled substances “is something that all physicians need to be aware of for their patients. This is something that we are missing,” maintained press conference comoderator Virginia Kaklamani, MD, DSc, of UT Health San Antonio.
“It’s easy to just give a prescription instead of arguing with a patient about why you are not going to give them a prescription,” Dr. Kaklamani said. “And ultimately ... pain is subjective. If a patient tells you they are in pain, you are, quote-endquote, a bad physician if you tell them they should not be in pain.”
“We need to focus on other ways to deal with the pain, like physical therapy, sending patients to physical medicine and rehab physicians who are trained to help with symptoms from the surgery, with range of motion and all that; that can help with pain,” she recommended. “It’s much harder to do that, right, than to send a prescription in for a narcotic? But that easy answer is always the worst answer.”
This study was funded by the Breast Cancer Research Foundation and the National Institutes of Health. Dr. Cogan declared no conflicts of interest. Dr. Osborne disclosed relationships with Wolters Kluwer, Lilly, Tolmar, and GeneTex. Dr. Kaklamani disclosed relationships with Amgen, AstraZeneca, Athenex, Celgene, Celldex, Daiichi, Eisai, Genentech, Genomic Health, Immunomedics, Novartis, Pfizer, Puma, and Seattle Genetics.
SOURCE: Cogan JC et al. SABCS 2020, Abstract GS3-08.
FROM SABCS 2020
CTCs predict overall survival in metastatic breast cancer
The CTC results are available about 4 weeks after start of therapy. Conventional imaging is carried out after about 3 months.
But an expert is not convinced that this approach is currently ready for clinical use and suggests that, for now, it should remain a tool for use in research.
The new meta-analysis, which involved data on more than 4000 patients, showed that the presence or the absence of CTCs “strongly” predicts overall survival (OS).
Median OS was greatest (47 months) for patients who had no CTCs at baseline and at follow-up. In contrast, the median OS was shortest (17.8 months) for patients who had CTCs at both time points.
The risk for death was more than 200% greater for patients in the latter group than in the former group.
The results “suggest the potential for clinical utility” of CTC monitoring as an early response marker in metastatic breast cancer, said lead author Wolfgang Janni, MD, PhD, of the Ulm University Hospital, Ulm, Germany. He was speaking at an online press conference for the virtual San Antonio Breast Cancer Symposium (SABCS) 2020, where the new study will be presented this week.
The investigators say the findings from this meta-analysis add to literature in which “several studies suggest clinical utility” of measuring CTC levels as a means of assessing response status for patients with metastatic breast cancer.
Unfortunately, the new study does not show that assessing CTCs over time improves clinical outcomes, which is an ongoing problem in the literature, said Virginia Kaklamani, MD, University of Texas Health Sciences Center, San Antonio, Texas, who is also a meeting co-director.
“Previous randomized clinical trial data have shown that assessing CTCs does not benefit patients (vs not assessing),” Kaklamani told Medscape Medical News.
Kaklamani explained how CTC assessments have worked in practice. “You do these circulating tumor cell tests and you find, for example, that the number increases. The assumption is the treatment’s not working. So you switch treatments around,” she explained. That pattern can be repeated every 3 to 4 weeks, resulting in more toxicity, which, in turn, may nullify any treatment benefit.
However, she noted that, so far, key data have come from the era of chemotherapy and do not reflect targeted therapies, which may make a difference. In addition, the more recent ability to assess and identify circulating tumor DNA may allow clinicians to match drugs to mutations, which may have greater impact on cancer outcomes.
Currently, CTCs are best used by researchers, Kaklamani said during the press conference, because they have not been definitively proven to improve patient results.
Investigator Janni did not object to that description.
But in a press statement, he suggested that CTCs can be used currently by clinicians.
“These data indicate that CTC dynamics can predict the trajectory of the disease a little more than four weeks after initiating treatment,” Janni said in the press statement. “This provides an advantage over conventional imaging methods and can help physicians determine very early on whether a treatment should be continued.”
But, to Kaklamani’s point, an article published in November in JAMA Oncology showed that use of CTCs did not yield significant clinical benefit in comparison with use of other clinical factors in determining whether to choose endocrine therapy or chemotherapy. In that randomized trial, which was conducted in Europe and included women with HR-positive, HER2-negative breast cancer, progression-free survival was similar in both arms, as reported by Medscape Medical News. However, use of chemotherapy (and attendant toxicity) was greater among women in the CTC arm, which was considered an undesirable outcome by experts not involved with the trial.
Details of the study results
For their study, Janni and colleagues conducted a comprehensive pooled analysis of globally available data. They identified 4079 metastatic breast cancer patients who had undergone baseline and follow-up CTC measurements (at least one, at a median of 29 days later) in previous clinical trials.
The investigators analyzed changes in CTC levels between baseline and follow-up to determine whether they were associated with OS.
Of the 2961 patients who were CTC-positive at baseline, 1855 remained CTC-positive after treatment was initiated (positive/positive), and 1106 patients had converted to CTC-negative status (positive/negative).
Of the 1118 patients who were CTC-negative at baseline, 813 remained CTC-negative (negative/negative), and 305 had become CTC-positive (negative/positive).
As noted above, median OS was greatest for patients who were negative/negative (47 months), followed by patients who were positive/negative (32.2 months), negative/positive (29.6 months), and positive/positive (17.8 months).
Hazard ratios in which the reference group was negative/negative were 1.52 for the positive/negative group, 1.74 for the negative/positive group, and 3.15 for the positive/positive group (P < .0001 for all groups).
These CTC dynamics were found across all breast cancer subtypes, said Janni.
“These data indicate that CTC dynamics can predict the trajectory of the disease a little more than four weeks after initiating treatment,” said Janni in the press statement. “This provides an advantage over conventional imaging methods and can help physicians determine very early on whether a treatment should be continued. It is also very reassuring that CTC dynamics predicted outcomes for all breast cancer subtypes.”
The study was supported by Menarini Silicon Biosystems, the makers of CellSearch, the CTC test used for all of the patients and studies in the meta-analysis. Janni received a research grant from Menarini Silicon Biosystems. Other study authors have financial ties to healthcare industries. Kaklamani has received consulting fees from Amgen, Eisai, Puma, Celldex, AstraZeneca, and Athenex; fees for non-CME services received directly from commercial interest or their agents from Pfizer, Celgene, Genentech, Genomic Health, Puma, Eisai, and Novartis; and has contracted research with Eisai.
This article first appeared on Medscape.com.
The CTC results are available about 4 weeks after start of therapy. Conventional imaging is carried out after about 3 months.
But an expert is not convinced that this approach is currently ready for clinical use and suggests that, for now, it should remain a tool for use in research.
The new meta-analysis, which involved data on more than 4000 patients, showed that the presence or the absence of CTCs “strongly” predicts overall survival (OS).
Median OS was greatest (47 months) for patients who had no CTCs at baseline and at follow-up. In contrast, the median OS was shortest (17.8 months) for patients who had CTCs at both time points.
The risk for death was more than 200% greater for patients in the latter group than in the former group.
The results “suggest the potential for clinical utility” of CTC monitoring as an early response marker in metastatic breast cancer, said lead author Wolfgang Janni, MD, PhD, of the Ulm University Hospital, Ulm, Germany. He was speaking at an online press conference for the virtual San Antonio Breast Cancer Symposium (SABCS) 2020, where the new study will be presented this week.
The investigators say the findings from this meta-analysis add to literature in which “several studies suggest clinical utility” of measuring CTC levels as a means of assessing response status for patients with metastatic breast cancer.
Unfortunately, the new study does not show that assessing CTCs over time improves clinical outcomes, which is an ongoing problem in the literature, said Virginia Kaklamani, MD, University of Texas Health Sciences Center, San Antonio, Texas, who is also a meeting co-director.
“Previous randomized clinical trial data have shown that assessing CTCs does not benefit patients (vs not assessing),” Kaklamani told Medscape Medical News.
Kaklamani explained how CTC assessments have worked in practice. “You do these circulating tumor cell tests and you find, for example, that the number increases. The assumption is the treatment’s not working. So you switch treatments around,” she explained. That pattern can be repeated every 3 to 4 weeks, resulting in more toxicity, which, in turn, may nullify any treatment benefit.
However, she noted that, so far, key data have come from the era of chemotherapy and do not reflect targeted therapies, which may make a difference. In addition, the more recent ability to assess and identify circulating tumor DNA may allow clinicians to match drugs to mutations, which may have greater impact on cancer outcomes.
Currently, CTCs are best used by researchers, Kaklamani said during the press conference, because they have not been definitively proven to improve patient results.
Investigator Janni did not object to that description.
But in a press statement, he suggested that CTCs can be used currently by clinicians.
“These data indicate that CTC dynamics can predict the trajectory of the disease a little more than four weeks after initiating treatment,” Janni said in the press statement. “This provides an advantage over conventional imaging methods and can help physicians determine very early on whether a treatment should be continued.”
But, to Kaklamani’s point, an article published in November in JAMA Oncology showed that use of CTCs did not yield significant clinical benefit in comparison with use of other clinical factors in determining whether to choose endocrine therapy or chemotherapy. In that randomized trial, which was conducted in Europe and included women with HR-positive, HER2-negative breast cancer, progression-free survival was similar in both arms, as reported by Medscape Medical News. However, use of chemotherapy (and attendant toxicity) was greater among women in the CTC arm, which was considered an undesirable outcome by experts not involved with the trial.
Details of the study results
For their study, Janni and colleagues conducted a comprehensive pooled analysis of globally available data. They identified 4079 metastatic breast cancer patients who had undergone baseline and follow-up CTC measurements (at least one, at a median of 29 days later) in previous clinical trials.
The investigators analyzed changes in CTC levels between baseline and follow-up to determine whether they were associated with OS.
Of the 2961 patients who were CTC-positive at baseline, 1855 remained CTC-positive after treatment was initiated (positive/positive), and 1106 patients had converted to CTC-negative status (positive/negative).
Of the 1118 patients who were CTC-negative at baseline, 813 remained CTC-negative (negative/negative), and 305 had become CTC-positive (negative/positive).
As noted above, median OS was greatest for patients who were negative/negative (47 months), followed by patients who were positive/negative (32.2 months), negative/positive (29.6 months), and positive/positive (17.8 months).
Hazard ratios in which the reference group was negative/negative were 1.52 for the positive/negative group, 1.74 for the negative/positive group, and 3.15 for the positive/positive group (P < .0001 for all groups).
These CTC dynamics were found across all breast cancer subtypes, said Janni.
“These data indicate that CTC dynamics can predict the trajectory of the disease a little more than four weeks after initiating treatment,” said Janni in the press statement. “This provides an advantage over conventional imaging methods and can help physicians determine very early on whether a treatment should be continued. It is also very reassuring that CTC dynamics predicted outcomes for all breast cancer subtypes.”
The study was supported by Menarini Silicon Biosystems, the makers of CellSearch, the CTC test used for all of the patients and studies in the meta-analysis. Janni received a research grant from Menarini Silicon Biosystems. Other study authors have financial ties to healthcare industries. Kaklamani has received consulting fees from Amgen, Eisai, Puma, Celldex, AstraZeneca, and Athenex; fees for non-CME services received directly from commercial interest or their agents from Pfizer, Celgene, Genentech, Genomic Health, Puma, Eisai, and Novartis; and has contracted research with Eisai.
This article first appeared on Medscape.com.
The CTC results are available about 4 weeks after start of therapy. Conventional imaging is carried out after about 3 months.
But an expert is not convinced that this approach is currently ready for clinical use and suggests that, for now, it should remain a tool for use in research.
The new meta-analysis, which involved data on more than 4000 patients, showed that the presence or the absence of CTCs “strongly” predicts overall survival (OS).
Median OS was greatest (47 months) for patients who had no CTCs at baseline and at follow-up. In contrast, the median OS was shortest (17.8 months) for patients who had CTCs at both time points.
The risk for death was more than 200% greater for patients in the latter group than in the former group.
The results “suggest the potential for clinical utility” of CTC monitoring as an early response marker in metastatic breast cancer, said lead author Wolfgang Janni, MD, PhD, of the Ulm University Hospital, Ulm, Germany. He was speaking at an online press conference for the virtual San Antonio Breast Cancer Symposium (SABCS) 2020, where the new study will be presented this week.
The investigators say the findings from this meta-analysis add to literature in which “several studies suggest clinical utility” of measuring CTC levels as a means of assessing response status for patients with metastatic breast cancer.
Unfortunately, the new study does not show that assessing CTCs over time improves clinical outcomes, which is an ongoing problem in the literature, said Virginia Kaklamani, MD, University of Texas Health Sciences Center, San Antonio, Texas, who is also a meeting co-director.
“Previous randomized clinical trial data have shown that assessing CTCs does not benefit patients (vs not assessing),” Kaklamani told Medscape Medical News.
Kaklamani explained how CTC assessments have worked in practice. “You do these circulating tumor cell tests and you find, for example, that the number increases. The assumption is the treatment’s not working. So you switch treatments around,” she explained. That pattern can be repeated every 3 to 4 weeks, resulting in more toxicity, which, in turn, may nullify any treatment benefit.
However, she noted that, so far, key data have come from the era of chemotherapy and do not reflect targeted therapies, which may make a difference. In addition, the more recent ability to assess and identify circulating tumor DNA may allow clinicians to match drugs to mutations, which may have greater impact on cancer outcomes.
Currently, CTCs are best used by researchers, Kaklamani said during the press conference, because they have not been definitively proven to improve patient results.
Investigator Janni did not object to that description.
But in a press statement, he suggested that CTCs can be used currently by clinicians.
“These data indicate that CTC dynamics can predict the trajectory of the disease a little more than four weeks after initiating treatment,” Janni said in the press statement. “This provides an advantage over conventional imaging methods and can help physicians determine very early on whether a treatment should be continued.”
But, to Kaklamani’s point, an article published in November in JAMA Oncology showed that use of CTCs did not yield significant clinical benefit in comparison with use of other clinical factors in determining whether to choose endocrine therapy or chemotherapy. In that randomized trial, which was conducted in Europe and included women with HR-positive, HER2-negative breast cancer, progression-free survival was similar in both arms, as reported by Medscape Medical News. However, use of chemotherapy (and attendant toxicity) was greater among women in the CTC arm, which was considered an undesirable outcome by experts not involved with the trial.
Details of the study results
For their study, Janni and colleagues conducted a comprehensive pooled analysis of globally available data. They identified 4079 metastatic breast cancer patients who had undergone baseline and follow-up CTC measurements (at least one, at a median of 29 days later) in previous clinical trials.
The investigators analyzed changes in CTC levels between baseline and follow-up to determine whether they were associated with OS.
Of the 2961 patients who were CTC-positive at baseline, 1855 remained CTC-positive after treatment was initiated (positive/positive), and 1106 patients had converted to CTC-negative status (positive/negative).
Of the 1118 patients who were CTC-negative at baseline, 813 remained CTC-negative (negative/negative), and 305 had become CTC-positive (negative/positive).
As noted above, median OS was greatest for patients who were negative/negative (47 months), followed by patients who were positive/negative (32.2 months), negative/positive (29.6 months), and positive/positive (17.8 months).
Hazard ratios in which the reference group was negative/negative were 1.52 for the positive/negative group, 1.74 for the negative/positive group, and 3.15 for the positive/positive group (P < .0001 for all groups).
These CTC dynamics were found across all breast cancer subtypes, said Janni.
“These data indicate that CTC dynamics can predict the trajectory of the disease a little more than four weeks after initiating treatment,” said Janni in the press statement. “This provides an advantage over conventional imaging methods and can help physicians determine very early on whether a treatment should be continued. It is also very reassuring that CTC dynamics predicted outcomes for all breast cancer subtypes.”
The study was supported by Menarini Silicon Biosystems, the makers of CellSearch, the CTC test used for all of the patients and studies in the meta-analysis. Janni received a research grant from Menarini Silicon Biosystems. Other study authors have financial ties to healthcare industries. Kaklamani has received consulting fees from Amgen, Eisai, Puma, Celldex, AstraZeneca, and Athenex; fees for non-CME services received directly from commercial interest or their agents from Pfizer, Celgene, Genentech, Genomic Health, Puma, Eisai, and Novartis; and has contracted research with Eisai.
This article first appeared on Medscape.com.
FROM SABCS 2020
Getting closer to an accurate early Alzheimer’s test
Researchers have created the most sensitive test yet
Scientists at Washington University in St. Louis have developed the most sensitive blood test yet for Alzheimer’s. In studies, the test identified patients with amyloid deposits, using mass spectrometry, before brain scans did.
Of course, amyloid is a normal brain protein; most people with amyloid deposits will not develop dementia, but it’s a significant risk factor. When blood amyloid levels are low, it may indicate it is clumping in the brain.
Researchers used mass spectrometry to test volunteers’ stored blood for beta amyloid, then checked if the levels predicted the results of PET scans. Mass spectrometry identified asymptomatic people accumulating beta amyloid in their brains when PET scans were still negative. The scans only showed beta amyloid in the brain years later. The blood test predicted the presence of plaque even in mostly asymptomatic people with 94% accuracy.
The test will not be available for clinical use for years, but prior to that it will be helpful to scientists conducting trials of drugs to prevent Alzheimer’s, seeking participants in the earliest stages of the disease.
Reference
1. Kolata G. A Blood Test for Alzheimer’s? It’s Coming, Scientists Report. New York Times. Aug. 1, 2019. https://www.nytimes.com/2019/08/01/health/alzheimers-blood-test.html.
Researchers have created the most sensitive test yet
Researchers have created the most sensitive test yet
Scientists at Washington University in St. Louis have developed the most sensitive blood test yet for Alzheimer’s. In studies, the test identified patients with amyloid deposits, using mass spectrometry, before brain scans did.
Of course, amyloid is a normal brain protein; most people with amyloid deposits will not develop dementia, but it’s a significant risk factor. When blood amyloid levels are low, it may indicate it is clumping in the brain.
Researchers used mass spectrometry to test volunteers’ stored blood for beta amyloid, then checked if the levels predicted the results of PET scans. Mass spectrometry identified asymptomatic people accumulating beta amyloid in their brains when PET scans were still negative. The scans only showed beta amyloid in the brain years later. The blood test predicted the presence of plaque even in mostly asymptomatic people with 94% accuracy.
The test will not be available for clinical use for years, but prior to that it will be helpful to scientists conducting trials of drugs to prevent Alzheimer’s, seeking participants in the earliest stages of the disease.
Reference
1. Kolata G. A Blood Test for Alzheimer’s? It’s Coming, Scientists Report. New York Times. Aug. 1, 2019. https://www.nytimes.com/2019/08/01/health/alzheimers-blood-test.html.
Scientists at Washington University in St. Louis have developed the most sensitive blood test yet for Alzheimer’s. In studies, the test identified patients with amyloid deposits, using mass spectrometry, before brain scans did.
Of course, amyloid is a normal brain protein; most people with amyloid deposits will not develop dementia, but it’s a significant risk factor. When blood amyloid levels are low, it may indicate it is clumping in the brain.
Researchers used mass spectrometry to test volunteers’ stored blood for beta amyloid, then checked if the levels predicted the results of PET scans. Mass spectrometry identified asymptomatic people accumulating beta amyloid in their brains when PET scans were still negative. The scans only showed beta amyloid in the brain years later. The blood test predicted the presence of plaque even in mostly asymptomatic people with 94% accuracy.
The test will not be available for clinical use for years, but prior to that it will be helpful to scientists conducting trials of drugs to prevent Alzheimer’s, seeking participants in the earliest stages of the disease.
Reference
1. Kolata G. A Blood Test for Alzheimer’s? It’s Coming, Scientists Report. New York Times. Aug. 1, 2019. https://www.nytimes.com/2019/08/01/health/alzheimers-blood-test.html.
Endoscopic intragastric balloon improved NASH parameters
Endoscopically placed intragastric balloons were safe and effective for managing nonalcoholic fatty liver disease (NAFLD), according to the findings of an open-label, prospective study of 21 patients.
Six months after balloon placement, nonalcoholic fatty liver disease activity scores (NAS) had improved in 18 of 20 biopsied patients (90%), with a median decrease of 3 points (range, 1-4 points). Magnetic resonance elastography showed that fibrosis had improved by 1.5 stages in half of patients (10 of 20). “Other than postprocedural pain (in 5% of patients), no serious adverse events were reported,” Fateh Bazerbachi, MD, of Massachusetts General Hospital in Boston, and associates wrote in Clinical Gastroenterology and Hepatology.
Nonalcoholic fatty liver disease affects approximately 70% of obese adults and half of obese children, meaning that tens of millions of individuals are affected in the United States alone. Lifestyle changes rarely induce more than 10% body weight loss, the threshold for “meaningful improvement in NASH,” and bariatric surgery is not recommended for managing mild or moderate obesity and often is not desired by patients who do qualify, the researchers noted. “Endoscopic bariatric therapies are garnering more attention as potential strategies to address these shortcomings in obesity care and its comorbidities [, but] their influences on the driving and prognostic parameters of NAFLD remain unclear.”
In all, 81% of the study participants were women, with a mean age of 54 years and an average body mass index (BMI) of 44 kg/m2. At baseline, more than half had NAS scores of 4 or 5 and histologic fibrosis scores of 2 or 3. Baseline hemoglobin A1c levels averaged 7.4% (range, 5.1%-11.1%) and 29% of patients had impaired glucose tolerance. After receiving endoscopic ultrasound (EUS)–guided core liver biopsies, patients received an endoscopically placed fluid-filled intragastric balloon (Orbera, Apollo Endosurgery, Austin, Tex.). The balloon was removed 6 months later and magnetic resonance elastography and a second core biopsy were performed. One patient did not receive an exit biopsy (because of starting antithrombotic therapy) and thus was excluded from the final analysis.
Of 20 patients, 16 (80%) had at least a two-point improvement in NAS at 6 months, and half had NAS scores of less than 2, indicating remission of NASH. Three of 20 patients (15%) showed improvements in mild fibrosis, 12 showed no change, and 5 showed worsening. Patients lost an average of 11.7% of body weight (standard deviation, 7.7%; P = .01), BMI dropped by a mean of 5.2 (SD, 0.75; P = .01) and A1c fell by an average of 1.3% (SD, 0.5%; P = .02). Waist circumference also decreased significantly (mean, –14.4 cm; SD, –2.2 cm; P = .001), as did hip circumference, fasting glucose, AST, ALT, and AST-to-platelet ratio index. “Percent total body weight loss did not correlate with reductions in NAS or fibrosis,” the researchers noted.
Together, these findings suggest that intragastric balloon placement “may allow a reversal in the natural history of NAFLD and NASH, despite the short duration of the intervention,” they concluded. “The logistics of IGB [intragastric balloon] placement will enable accurate risk stratification of these patients in a safe and reproducible manner, obviating the need for additional investigations, and clarifying the real risk of patients afflicted with NAFLD.”
Apollo Endosurgery provided intragastric balloons, and Medtronic provided SharkCore needles. The senior author and two coinvestigators disclosed ties to Apollo Endosurgery, Medtronic, Metamodix, Boston Scientific, Cairn Diagnostics, Aspire Bariatrics, Johnson and Johnson, AstraZeneca, Genfit, Gila Therapeutics, and several other companies. The other investigators reported having no conflicts of interest.
SOURCE: Bazerbachi F et al. Clin Gastroenterol Hepatol. 2020 Apr 30. doi: 10.1016/j.cgh.2020.04.068.
Obesity a well-known risk factor for the development of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis, the latter of which is expected to become the leading indication for liver transplantation. As such addressing the steatosis in these patients is critical. A drop of even 5%-10% of total body weight with diet and exercise can result in significant improvement in liver disease.
In this article, Dr. Bazerbachi and colleagues work to advance the case for intragastric balloons as a successful treatment option for NAFLD. They performed a prospective, open-label study on 21 patients treated with an intragastric balloon for 6 months. Using gold-standard histology and noninvasive magnetic resonance elastography before and after therapy, they show significant improvement in NAFLD activity score (median change, 3 points; range, 1-4) over a short duration of treatment. Interestingly, the collection of the liver biopsy sample is done via endoscopic ultrasound, which can be easily performed during placement and removal of this intragastric balloon. While promising, follow-up studies are needed to show sustained improvement in NAFLD after the balloon is removed.
Wasif M. Abidi, MD, PhD, is assistant professor of medicine, gastroenterology, Baylor College of Medicine, Houston.
Obesity a well-known risk factor for the development of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis, the latter of which is expected to become the leading indication for liver transplantation. As such addressing the steatosis in these patients is critical. A drop of even 5%-10% of total body weight with diet and exercise can result in significant improvement in liver disease.
In this article, Dr. Bazerbachi and colleagues work to advance the case for intragastric balloons as a successful treatment option for NAFLD. They performed a prospective, open-label study on 21 patients treated with an intragastric balloon for 6 months. Using gold-standard histology and noninvasive magnetic resonance elastography before and after therapy, they show significant improvement in NAFLD activity score (median change, 3 points; range, 1-4) over a short duration of treatment. Interestingly, the collection of the liver biopsy sample is done via endoscopic ultrasound, which can be easily performed during placement and removal of this intragastric balloon. While promising, follow-up studies are needed to show sustained improvement in NAFLD after the balloon is removed.
Wasif M. Abidi, MD, PhD, is assistant professor of medicine, gastroenterology, Baylor College of Medicine, Houston.
Obesity a well-known risk factor for the development of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis, the latter of which is expected to become the leading indication for liver transplantation. As such addressing the steatosis in these patients is critical. A drop of even 5%-10% of total body weight with diet and exercise can result in significant improvement in liver disease.
In this article, Dr. Bazerbachi and colleagues work to advance the case for intragastric balloons as a successful treatment option for NAFLD. They performed a prospective, open-label study on 21 patients treated with an intragastric balloon for 6 months. Using gold-standard histology and noninvasive magnetic resonance elastography before and after therapy, they show significant improvement in NAFLD activity score (median change, 3 points; range, 1-4) over a short duration of treatment. Interestingly, the collection of the liver biopsy sample is done via endoscopic ultrasound, which can be easily performed during placement and removal of this intragastric balloon. While promising, follow-up studies are needed to show sustained improvement in NAFLD after the balloon is removed.
Wasif M. Abidi, MD, PhD, is assistant professor of medicine, gastroenterology, Baylor College of Medicine, Houston.
Endoscopically placed intragastric balloons were safe and effective for managing nonalcoholic fatty liver disease (NAFLD), according to the findings of an open-label, prospective study of 21 patients.
Six months after balloon placement, nonalcoholic fatty liver disease activity scores (NAS) had improved in 18 of 20 biopsied patients (90%), with a median decrease of 3 points (range, 1-4 points). Magnetic resonance elastography showed that fibrosis had improved by 1.5 stages in half of patients (10 of 20). “Other than postprocedural pain (in 5% of patients), no serious adverse events were reported,” Fateh Bazerbachi, MD, of Massachusetts General Hospital in Boston, and associates wrote in Clinical Gastroenterology and Hepatology.
Nonalcoholic fatty liver disease affects approximately 70% of obese adults and half of obese children, meaning that tens of millions of individuals are affected in the United States alone. Lifestyle changes rarely induce more than 10% body weight loss, the threshold for “meaningful improvement in NASH,” and bariatric surgery is not recommended for managing mild or moderate obesity and often is not desired by patients who do qualify, the researchers noted. “Endoscopic bariatric therapies are garnering more attention as potential strategies to address these shortcomings in obesity care and its comorbidities [, but] their influences on the driving and prognostic parameters of NAFLD remain unclear.”
In all, 81% of the study participants were women, with a mean age of 54 years and an average body mass index (BMI) of 44 kg/m2. At baseline, more than half had NAS scores of 4 or 5 and histologic fibrosis scores of 2 or 3. Baseline hemoglobin A1c levels averaged 7.4% (range, 5.1%-11.1%) and 29% of patients had impaired glucose tolerance. After receiving endoscopic ultrasound (EUS)–guided core liver biopsies, patients received an endoscopically placed fluid-filled intragastric balloon (Orbera, Apollo Endosurgery, Austin, Tex.). The balloon was removed 6 months later and magnetic resonance elastography and a second core biopsy were performed. One patient did not receive an exit biopsy (because of starting antithrombotic therapy) and thus was excluded from the final analysis.
Of 20 patients, 16 (80%) had at least a two-point improvement in NAS at 6 months, and half had NAS scores of less than 2, indicating remission of NASH. Three of 20 patients (15%) showed improvements in mild fibrosis, 12 showed no change, and 5 showed worsening. Patients lost an average of 11.7% of body weight (standard deviation, 7.7%; P = .01), BMI dropped by a mean of 5.2 (SD, 0.75; P = .01) and A1c fell by an average of 1.3% (SD, 0.5%; P = .02). Waist circumference also decreased significantly (mean, –14.4 cm; SD, –2.2 cm; P = .001), as did hip circumference, fasting glucose, AST, ALT, and AST-to-platelet ratio index. “Percent total body weight loss did not correlate with reductions in NAS or fibrosis,” the researchers noted.
Together, these findings suggest that intragastric balloon placement “may allow a reversal in the natural history of NAFLD and NASH, despite the short duration of the intervention,” they concluded. “The logistics of IGB [intragastric balloon] placement will enable accurate risk stratification of these patients in a safe and reproducible manner, obviating the need for additional investigations, and clarifying the real risk of patients afflicted with NAFLD.”
Apollo Endosurgery provided intragastric balloons, and Medtronic provided SharkCore needles. The senior author and two coinvestigators disclosed ties to Apollo Endosurgery, Medtronic, Metamodix, Boston Scientific, Cairn Diagnostics, Aspire Bariatrics, Johnson and Johnson, AstraZeneca, Genfit, Gila Therapeutics, and several other companies. The other investigators reported having no conflicts of interest.
SOURCE: Bazerbachi F et al. Clin Gastroenterol Hepatol. 2020 Apr 30. doi: 10.1016/j.cgh.2020.04.068.
Endoscopically placed intragastric balloons were safe and effective for managing nonalcoholic fatty liver disease (NAFLD), according to the findings of an open-label, prospective study of 21 patients.
Six months after balloon placement, nonalcoholic fatty liver disease activity scores (NAS) had improved in 18 of 20 biopsied patients (90%), with a median decrease of 3 points (range, 1-4 points). Magnetic resonance elastography showed that fibrosis had improved by 1.5 stages in half of patients (10 of 20). “Other than postprocedural pain (in 5% of patients), no serious adverse events were reported,” Fateh Bazerbachi, MD, of Massachusetts General Hospital in Boston, and associates wrote in Clinical Gastroenterology and Hepatology.
Nonalcoholic fatty liver disease affects approximately 70% of obese adults and half of obese children, meaning that tens of millions of individuals are affected in the United States alone. Lifestyle changes rarely induce more than 10% body weight loss, the threshold for “meaningful improvement in NASH,” and bariatric surgery is not recommended for managing mild or moderate obesity and often is not desired by patients who do qualify, the researchers noted. “Endoscopic bariatric therapies are garnering more attention as potential strategies to address these shortcomings in obesity care and its comorbidities [, but] their influences on the driving and prognostic parameters of NAFLD remain unclear.”
In all, 81% of the study participants were women, with a mean age of 54 years and an average body mass index (BMI) of 44 kg/m2. At baseline, more than half had NAS scores of 4 or 5 and histologic fibrosis scores of 2 or 3. Baseline hemoglobin A1c levels averaged 7.4% (range, 5.1%-11.1%) and 29% of patients had impaired glucose tolerance. After receiving endoscopic ultrasound (EUS)–guided core liver biopsies, patients received an endoscopically placed fluid-filled intragastric balloon (Orbera, Apollo Endosurgery, Austin, Tex.). The balloon was removed 6 months later and magnetic resonance elastography and a second core biopsy were performed. One patient did not receive an exit biopsy (because of starting antithrombotic therapy) and thus was excluded from the final analysis.
Of 20 patients, 16 (80%) had at least a two-point improvement in NAS at 6 months, and half had NAS scores of less than 2, indicating remission of NASH. Three of 20 patients (15%) showed improvements in mild fibrosis, 12 showed no change, and 5 showed worsening. Patients lost an average of 11.7% of body weight (standard deviation, 7.7%; P = .01), BMI dropped by a mean of 5.2 (SD, 0.75; P = .01) and A1c fell by an average of 1.3% (SD, 0.5%; P = .02). Waist circumference also decreased significantly (mean, –14.4 cm; SD, –2.2 cm; P = .001), as did hip circumference, fasting glucose, AST, ALT, and AST-to-platelet ratio index. “Percent total body weight loss did not correlate with reductions in NAS or fibrosis,” the researchers noted.
Together, these findings suggest that intragastric balloon placement “may allow a reversal in the natural history of NAFLD and NASH, despite the short duration of the intervention,” they concluded. “The logistics of IGB [intragastric balloon] placement will enable accurate risk stratification of these patients in a safe and reproducible manner, obviating the need for additional investigations, and clarifying the real risk of patients afflicted with NAFLD.”
Apollo Endosurgery provided intragastric balloons, and Medtronic provided SharkCore needles. The senior author and two coinvestigators disclosed ties to Apollo Endosurgery, Medtronic, Metamodix, Boston Scientific, Cairn Diagnostics, Aspire Bariatrics, Johnson and Johnson, AstraZeneca, Genfit, Gila Therapeutics, and several other companies. The other investigators reported having no conflicts of interest.
SOURCE: Bazerbachi F et al. Clin Gastroenterol Hepatol. 2020 Apr 30. doi: 10.1016/j.cgh.2020.04.068.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY