User login
Burnt Out ? The Phenomenon of Type 2 Diabetes Mellitus in End-Stage Renal Disease
In patients with T2DM and ESRD, insulin is the antidiabetic medication of choice with a hemoglobin A1c target of 6 to 8%, using fructosamine levels or other measures for better assessment of glycemic control.
More than 34 million adults in the US have type 2 diabetes mellitus (T2DM), a chronic progressive disease identified by worsening hyperglycemia and micro- and macrovascular complications.1 Consequently, 12.2% of the US adult population is currently at risk for macrovascular diseases, such as stroke and coronary artery disease (CAD) and microvascular diseases, such as neuropathy and diabetic nephropathy.1
T2DM is the most common comorbid risk factor for chronic kidney disease (CKD) and the leading cause of end-stage renal disease (ESRD). As of 2017, about 750,000 Americans have CKD stage 5 requiring dialysis, and 50% of these patients have preexisting diabetic nephropathy.2 Rates of mortality and morbidity are observed to be higher in patients with both CKD and T2DM compared with patients with CKD without T2DM.2 Previous clinical trials, including the United Kingdom Prospective Diabetes Study of 1998, have proven that optimal glycemic control decreases the risk of complications of T2DM (ie, nephropathy) in the general population.3 Conversely, tight glycemic control that targets hemoglobin A1c (HbA1c) < 7%, in patients with T2DM with ESRD has not shown the same benefits and may lead to worse outcomes. It is postulated that this may be due to the increased incidence of hypoglycemia in this patient population.4
Dialysis has varying effects on patients both with and without T2DM. While patients with ESRD without T2DM have the potential to develop impaired glucose tolerance and T2DM, about 33% of patients with T2DM on dialysis actually have HbA1c < 6%.5 In these patients, glycemic control improves spontaneously as their disease progresses, leading to a decrease or cessation of insulin or other antidiabetic medications. This phenomenon, known as burnt-out diabetes, is characterized by (1) alterations in glucose homeostasis and normoglycemia without antidiabetic treatment; (2) HbA1c levels < 6% despite having established T2DM; (3) decline in insulin requirements or cessation of insulin altogether; and (4) spontaneous hypoglycemia.
There is a misconception that burnt-out diabetes is a favorable condition due to the alteration of the natural course of T2DM. Although this may be true, patients with this condition are prone to develop hypoglycemic episodes and may be linked to poor survival outcomes due to low HbA1c.6,7
Since Kalantar-Zadeh and colleagues presented a 2009 case study, there has been a lack of research regarding this unique condition.8 The purpose of this case study is to shed further light on burnt-out diabetes and present a patient case pertaining to the challenges of glycemic control in ESRD.
Case Presentation
Mr. A is a 49-year-old Hispanic male veteran with a history of ESRD on hemodialysis (HD) for 6 years, anemia of CKD, and T2DM for 22 years. The patient also has an extensive cardiovascular disease history, including hypertension, hyperlipidemia, and CAD status post-4-vessel coronary artery bypass graft in December 2014. The patient receives in-home HD Monday, Wednesday, and Friday and is on the wait list for kidney transplantation. The patient’s T2DM is managed by a primary care clinical pharmacy specialist (CPS) at the
Mr. A’s antidiabetic regimen is 45 units of subcutaneous insulin glargine every morning; insulin aspart sliding scale (about 15-27 units) subcutaneous 3 times daily with meals; and saxagliptin 2.5 mg by mouth once daily.
At a follow-up visit with the CPS, Mr. A stated, “I feel fine except for the occasional low blood sugar episode.” The patient’s most recent HbA1c was 6.1%, and he reported medication adherence and no signs or symptoms of hyperglycemia (ie, polydipsia, polyphagia, nocturia, visual disturbances). Mr. A reported no use of alcohol, tobacco, or illicit drugs. He walks 1 mile every other day and participates in self-monitoring blood glucose (SMBG) about 2 to 3 times daily (Table 1).
Although Mr. A’s most recent HbA1c was well controlled, his estimated fasting blood glucose at the same laboratory draw was 224 mg/dL. His SMBG readings in the past month also were elevated with higher readings in the evening. Mr. A attributed the elevated readings to dietary excursions and a high carbohydrate intake. At this visit, the CPS increased his insulin glargine dose to 50 units subcutaneous every morning and educated him on lifestyle modifications. Follow-up with the CPS was scheduled for 2 months from the day of the visit.
Analysis
Few articles on potential contributors to burnt-out diabetes have been published.6,7 These articles discuss decreased renal and hepatic clearance of insulin (which increases its half-life) hypoglycemia during HD, and low HbA1c due to preexisting anemia. Inappropriately low HbA1c levels may be secondary to, but not limited to, hemolysis, recent blood transfusion, acute blood loss, and medications, such as erythropoietin-stimulating agents (ESAs).9 The conditions that affect red blood cell turnover are common in patients with advanced CKD and may result in discrepancies in HbA1c levels.
Glycated hemoglobin is a series of minor hemoglobin components formed by the adduction of various carbohydrate molecules to hemoglobin. HbA1c is the largest fraction formed and the most consistent index of the concentration of glucose in the blood.10 Hence, HbA1c is the traditional indicator of overall glycemic control. The current HbA1c goals recommended by the American Diabetes Association are derived from landmark trials conducted with patients in the general adult diabetic non-CKD population. However, hemoglobin measurements can be confounded by conditions present in ESRD and tend to underestimate glucose measurements in patients with T2DM on HD. Despite this, HbA1c is still regarded as a reasonable measure of glycemic control even in patients with ESRD; however, alternative markers of glycemia may be preferable.11
Although HbA1c is the gold standard, there are other laboratory measures of average glycemic control available. Fructosamine is a ketoamine formed when glucose binds to serum proteins. When these proteins are exposed to high concentrations of glucose, they experience increased glycation. Fructosamine assays measure the total glycated serum proteins, of which albumin accounts for about 90%.11 Because the half-life of serum proteins is about 20 days, fructosamine levels can reflect glycemic control over a 2- to 3-week period. This is advantageous in conditions that affect the average age of red blood cells, in pregnancy where frequent monitoring and measures of short-term glucose control are especially important, and in the evaluation of a medication adjustment in the management of T2DM. However, this test is not without its limitations. It is less reliable in settings of decreased protein levels (eg, liver disease), there is a lack of availability in routine practice, and reference levels have not been established.11
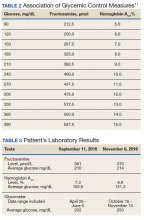
Fructosamine has been shown to be strongly associated with mean blood glucose and HbA1c (Table 2). In 2010, Mittman and colleagues published a study that compared HbA1c with fructosamine and their correlation to glycemic control and morbidity, defined as rates of hospitalization and infection.12 The study included 100 patients with T2DM on HD with a mean age of 63 years, 54% were women, mean HbA1c of 7.2%, and mean dialysis duration of 3 years. Average follow-up was 3 years. At the end of follow-up, Mittman and colleagues found that HbA1c and fructosamine were highly correlated and associated with serum glucose (P < .01). However, fructosamine was found to be more highly correlated with mean glucose levels when those levels were below 150 mg/dL (P = .01). A higher fructosamine level, not HbA1c was a more significant predictor of hospitalization (P = .007) and infection (P = .001). Mittman and colleagues presented evidence for the use of fructosamine over HbA1c in patients with T2DM on HD.12
Hypoglycemic Episodes
At the 2-month follow-up visit with the CPS, Mr. A reported having 5 hypoglycemic episodes in the past 30 days. He also stated he would forget to take his insulin aspart dose before dinner about 3 to 4 times a week but would take it 30 to 60 minutes after the meal. Mr. A did not bring his glucometer or SMBG readings to the visit, but he indicated that his blood glucose levels continued to fluctuate and were elevated when consuming carbohydrates.
Laboratory tests 1 month prior to the 2-month follow-up visit showed HbA1c of 7.3%, which had increased from his previous level of 6.1%. He was counseled on the proper administration of insulin aspart and lifestyle modifications. A fructosamine level was ordered at this visit to further assess his glycemic control. A follow-up appointment and laboratory workup (fructosamine and HbA1c) were scheduled for 2 months from the visit (Table 3).
Mr. A was educated on the unreliability of his HbA1c levels secondary to his condition of ESRD on HD. He was counseled on the purpose of fructosamine and how it may be a better predictor of his glycemic control and morbidity. Mr. A continued to be followed closely by the primary care CPS for T2DM management.
Discussion
Management of T2DM in patients with ESRD presents challenges for clinicians in determining HbA1c goals and selecting appropriate medication options. The 2012 Kidney Disease Outcomes Quality Initiative (KDOQI) diabetes guideline does not recommend treatment for patients with substantially reduced kidney function to a target HbA1c < 7% due to risk of hypoglycemia.13 Although a target HbA1c > 7% is suggested for these patients, little is known about appropriate glycemic control in these patients as there is a paucity of prospective, randomized clinical trials that include patients with advanced CKD.13
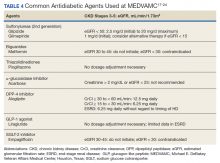
Moreover, many oral antidiabetic medications and their metabolites are cleared by the kidneys and, therefore, pose with potential harm for patients with CKD. Because of this, insulin is the medication of choice for patients with ESRD.7 Although insulin requirements may diminish with worsening kidney function, insulin provides the safest method of glycemic control. Insulin dosing can be individualized according to a patient’s renal status as there is no uniformity in renal dose adjustments. There are some noninsulin antidiabetic agents that can be used in ESRD, but use of these agents requires close monitoring and evaluation of the medication’s pharmacokinetics (Table 4). Overall, medication management can be a difficult task for patients with T2DM and ESRD, but antidiabetic regimens may be reduced or discontinued altogether in burnt-out diabetes.
One of 3 patients with T2DM and ESRD on dialysis has burnt-out diabetes, defined as a phenomenon in which glucose homeostasis is altered to cause normoglycemia, spontaneous hypoglycemia, and decreased insulin requirements in established patients with T2DM.5 Although Mr. A had a normal-to-low HbA1c, he did not meet these criteria. Due to his elevated SMBG readings, he did not have normoglycemia and did require an increase in his basal insulin dose. Therefore, our patient did not have burnt-out diabetes.
Mr. A represents the relevant issue of inappropriately and unreliably low HbA1c levels due to various factors in ESRD. Our patient did not receive a blood transfusion in the past 2 years and was not on ESA therapy; nevertheless, Mr. A was a patient with ESRD on HD with a diagnosis of anemia. These diagnoses are confounders for low HbA1c values. When fructosamine levels were drawn for Mr. A on September 11, 2018 and November 6, 2018, they correlated well with his serum glucose and SMBG readings. This indicated to the CPS that the patient’s glycemic control was poor despite a promising HbA1c level.
This patient’s case and supporting evidence suggests that other measures of glycemic control (eg, fructosamine) can be used to supplement HbA1c, serum glucose, and glucometer readings to provide an accurate assessment of glycemic control in T2DM. Fructosamine also can assist HbA1c with predicting morbidity and potentially mortality, which are of great importance in this patient population.
Kalantar-Zadeh and colleagues conducted a study of 23,618 patients with T2DM on dialysis to observe mortality in association with HbA1c.5 This analysis showed that patients with HbA1c levels < 5% or > 8% had a higher risk of mortality; higher values of HbA1c (> 10%) were associated with increased death risk vs all other values. In the unadjusted analysis, HbA1c levels between 6 and 8% had the lowest death risk (hazard ratios [HR] 0.8 - 0.9, 95% CI) compared with those of higher and lower HbA1c ranges.5 In nonanemic patients, HbA1c > 6% was associated with increased death risk, whereas anemic patients did not show this trend.
Other studies made similar observations. In 2001, Morioka and colleagues published an observational study of 150 patients with DM on intermittent hemodialysis. The study analyzed survival and HbA1c levels at 1, 3, and 5 years. The study found that at 1, 3, and 5 years, patients with HbA1c < 7.5% had better survival than did patients with HbA1c > 7.5% (3.6 years vs 2.0 years, P = .008). Morioka and colleagues also found that there was a 13% increase in death per 1% increase in HbA1c.14 Oomichi and colleagues conducted an observational study of 114 patients with T2DM and ESRD on intermittent hemodialysis. Patients with fair control (HbA1c 6.5 - 8%) and good control (HbA1c < 6.5%) were compared with patients with poor control (HbA1c > 8%); it was found that the poor control group had nearly triple the mortality when compared with the good and fair control groups (HR = 2.89, P = .01).15 Park and colleagues also saw a similar observation in a study of 1,239 patients with ESRD and DM; 70% of these patients were on intermittent hemodialysis. Patients with poor control (HbA1c ≥ 8%) had worse survival outcomes than those with HbA1c < 8% (HR 2.2, P < .001).16
Our patient case forced us to ask the question, “What should our patient’s HbA1c goals be?” In the study by Oomichi and colleagues, a HbA1c level of 8% has usefulness as a “signpost for management of glycemic control.”15 All patients’ goals should be individualized based on various factors (eg, age, comorbidities), but based on the survival studies above, a HbA1c goal range of 6 to 8% may be optimal.
Conclusions
Patients with T2DM and ESRD on dialysis may have higher morbidity and mortality rates than the rates of those without T2DM. It has been shown in various studies that very low HbA1c (< 5%) and high HbA1c (> 8%) are associated with poor survival. Some patients with T2DM on dialysis may experience burnt-out diabetes in which they may have normoglycemia and a HbA1c below goal; despite these facts, this condition is not positive and can be linked to bad outcomes. In patients with T2DM and ESRD, insulin is the antidiabetic medication of choice, and we recommend a HbA1c target of 6 to 8%. In this patient population, consider using fructosamine levels or other measures of glycemic control to supplement HbA1c and glucose values to provide a better assessment of glycemic control, morbidity, and mortality. Larger clinical trials are needed to assist in answering questions regarding mortality and optimal HbA1c targets in burnt-out diabetes.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Updated August 28, 2020. Accessed November 17, 2020.
2. Saran R, Robinson B, et al. US renal data system 2019 annual data report: epidemiology of klidney disease in the United States. Am J Kidney Dis. 2020 Jan;75(1 suppl 1):A6-A7. doi:10.1053/j.ajkd.2019.09.003. Epub 2019 Nov 5.
3. UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):854-865.
4. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545-2559. doi:10.1056/NEJMoa0802743
5. Kalantar-Zadeh K, Kopple JD, Regidor DL, et al. A1c and survival in maintenance hemodialysis patients. Diabetes Care. 2007;30(5):1049-10.55. doi:10.2337/dc06-2127
6. Park J, Lertdumrongluk P, Molnar MZ, Kovesdy CP, Kalantar-Zadeh K. Glycemic control in diabetic dialysis patients and the burnt-out diabetes phenomenon. Curr Diab Rep. 2012;12(4):432-439. doi:10.1007/s11892-012-0286-3
7. Rhee CM, Leung AM, Kovesdy CP, Lynch KE, Brent GA, Kalantar-Zadeh K. Updates on the management of diabetes in dialysis patients. Semin Dial. 2014;27(2):135-145. doi:10.1111/sdi.12198
8. Kalantar-Zadeh K, Derose SF, Nicholas S, Benner D, Sharma K, Kovesdy CP. Burnt-out diabetes: impact of chronic kidney disease progression on the natural course of diabetes mellitus. J Ren Nutr. 2009;19(1):33-37. doi:10.1053/j.jrn.2008.11.012
9. Unnikrishnan R, Anjana RM, Mohan V. Drugs affecting HbA1c levels. Indian J Endocrinol Metab. 2012;16(4):528-531. doi:10.4103/2230-8210.98004
10. Makris K, Spanou L. Is there a relationship between mean blood glucose and glycated hemoglobin? J Diabetes Sci Technol. 2011;5(6):1572-1583. doi:10.1177/193229681100500634
11. Wright LAC, Hirsch IB. The challenge of the use of glycemic biomarkers in diabetes: reflecting on hemoglobin A1c, 1,5-anhydroglucitol, and the glycated proteins fructosamine and glycated albumin. Diabetes Spectr. 2012;25(3):141-148. doi:10.2337/diaspect.25.3.141
12. Mittman N, Desiraju B, Fazil I, et al. Serum fructosamine versus glycosylated hemoglobin as an index of glycemic control, hospitalization, and infection in diabetic hemodialysis patients. Kidney Int. 2010;78 (suppl 117):S41-S45. doi:10.1038/ki.2010.193
13. National Kidney Foundation. KDOQI clinical practice guideline for diabetes and CKD: 2012 update. Am J Kidney Dis. 2012;60(5):850-886. doi:10.1053/j.ajkd.2012.07.005
14. Morioka T, Emoto M, Tabata T, et al. Glycemic control is a predictor of survival for diabetic patients on hemodialysis. Diabetes Care. 2001;24(5):909-913. doi.10.2337/diacare.24.5.909

15. Oomichi T, Emoto M, Tabata T, et al. Impact of glycemic control on survival of diabetic patients on chronic regular hemodialysis: a 7-year observational study. Diabetes Care. 2006;29(7):1496-1500. doi:10.2337/dc05-1887
16. Park JI, Bae E, Kim YL, et al. Glycemic control and mortality in diabetic patients undergoing dialysis focusing on the effects of age and dialysis type: a prospective cohort study in Korea. PLoS ONE. 2015;10(8):e0136085. doi:10.1371/journal.pone.0136085
17. Glucotrol tablets [
18. Amaryl [package insert]. Bridgewater, NJ: Sanofi-Aventis; December 2018.
19. Glucophage [package insert]. Princeton, NJ: Bristol-Myers Squibb; May 2018.
20. Actos [package insert]. Deerfield, IL: Takeda Pharmaceuticals America Inc; December 2017.
21. Precose [package insert]. Whippany, NJ: Bayer HealthCare Pharmaceuticals; March 2015.
22. Nesina [package insert]. Deerfield, IL: Takeda Pharmaceuticals America Inc; June 2019.
23. Victoza [package insert]. Plainsboro, NJ: Novo Nordisk Inc; June 2019.
24. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals Inc; October 2018.
In patients with T2DM and ESRD, insulin is the antidiabetic medication of choice with a hemoglobin A1c target of 6 to 8%, using fructosamine levels or other measures for better assessment of glycemic control.
In patients with T2DM and ESRD, insulin is the antidiabetic medication of choice with a hemoglobin A1c target of 6 to 8%, using fructosamine levels or other measures for better assessment of glycemic control.
More than 34 million adults in the US have type 2 diabetes mellitus (T2DM), a chronic progressive disease identified by worsening hyperglycemia and micro- and macrovascular complications.1 Consequently, 12.2% of the US adult population is currently at risk for macrovascular diseases, such as stroke and coronary artery disease (CAD) and microvascular diseases, such as neuropathy and diabetic nephropathy.1
T2DM is the most common comorbid risk factor for chronic kidney disease (CKD) and the leading cause of end-stage renal disease (ESRD). As of 2017, about 750,000 Americans have CKD stage 5 requiring dialysis, and 50% of these patients have preexisting diabetic nephropathy.2 Rates of mortality and morbidity are observed to be higher in patients with both CKD and T2DM compared with patients with CKD without T2DM.2 Previous clinical trials, including the United Kingdom Prospective Diabetes Study of 1998, have proven that optimal glycemic control decreases the risk of complications of T2DM (ie, nephropathy) in the general population.3 Conversely, tight glycemic control that targets hemoglobin A1c (HbA1c) < 7%, in patients with T2DM with ESRD has not shown the same benefits and may lead to worse outcomes. It is postulated that this may be due to the increased incidence of hypoglycemia in this patient population.4
Dialysis has varying effects on patients both with and without T2DM. While patients with ESRD without T2DM have the potential to develop impaired glucose tolerance and T2DM, about 33% of patients with T2DM on dialysis actually have HbA1c < 6%.5 In these patients, glycemic control improves spontaneously as their disease progresses, leading to a decrease or cessation of insulin or other antidiabetic medications. This phenomenon, known as burnt-out diabetes, is characterized by (1) alterations in glucose homeostasis and normoglycemia without antidiabetic treatment; (2) HbA1c levels < 6% despite having established T2DM; (3) decline in insulin requirements or cessation of insulin altogether; and (4) spontaneous hypoglycemia.
There is a misconception that burnt-out diabetes is a favorable condition due to the alteration of the natural course of T2DM. Although this may be true, patients with this condition are prone to develop hypoglycemic episodes and may be linked to poor survival outcomes due to low HbA1c.6,7
Since Kalantar-Zadeh and colleagues presented a 2009 case study, there has been a lack of research regarding this unique condition.8 The purpose of this case study is to shed further light on burnt-out diabetes and present a patient case pertaining to the challenges of glycemic control in ESRD.
Case Presentation
Mr. A is a 49-year-old Hispanic male veteran with a history of ESRD on hemodialysis (HD) for 6 years, anemia of CKD, and T2DM for 22 years. The patient also has an extensive cardiovascular disease history, including hypertension, hyperlipidemia, and CAD status post-4-vessel coronary artery bypass graft in December 2014. The patient receives in-home HD Monday, Wednesday, and Friday and is on the wait list for kidney transplantation. The patient’s T2DM is managed by a primary care clinical pharmacy specialist (CPS) at the
Mr. A’s antidiabetic regimen is 45 units of subcutaneous insulin glargine every morning; insulin aspart sliding scale (about 15-27 units) subcutaneous 3 times daily with meals; and saxagliptin 2.5 mg by mouth once daily.
At a follow-up visit with the CPS, Mr. A stated, “I feel fine except for the occasional low blood sugar episode.” The patient’s most recent HbA1c was 6.1%, and he reported medication adherence and no signs or symptoms of hyperglycemia (ie, polydipsia, polyphagia, nocturia, visual disturbances). Mr. A reported no use of alcohol, tobacco, or illicit drugs. He walks 1 mile every other day and participates in self-monitoring blood glucose (SMBG) about 2 to 3 times daily (Table 1).
Although Mr. A’s most recent HbA1c was well controlled, his estimated fasting blood glucose at the same laboratory draw was 224 mg/dL. His SMBG readings in the past month also were elevated with higher readings in the evening. Mr. A attributed the elevated readings to dietary excursions and a high carbohydrate intake. At this visit, the CPS increased his insulin glargine dose to 50 units subcutaneous every morning and educated him on lifestyle modifications. Follow-up with the CPS was scheduled for 2 months from the day of the visit.
Analysis
Few articles on potential contributors to burnt-out diabetes have been published.6,7 These articles discuss decreased renal and hepatic clearance of insulin (which increases its half-life) hypoglycemia during HD, and low HbA1c due to preexisting anemia. Inappropriately low HbA1c levels may be secondary to, but not limited to, hemolysis, recent blood transfusion, acute blood loss, and medications, such as erythropoietin-stimulating agents (ESAs).9 The conditions that affect red blood cell turnover are common in patients with advanced CKD and may result in discrepancies in HbA1c levels.
Glycated hemoglobin is a series of minor hemoglobin components formed by the adduction of various carbohydrate molecules to hemoglobin. HbA1c is the largest fraction formed and the most consistent index of the concentration of glucose in the blood.10 Hence, HbA1c is the traditional indicator of overall glycemic control. The current HbA1c goals recommended by the American Diabetes Association are derived from landmark trials conducted with patients in the general adult diabetic non-CKD population. However, hemoglobin measurements can be confounded by conditions present in ESRD and tend to underestimate glucose measurements in patients with T2DM on HD. Despite this, HbA1c is still regarded as a reasonable measure of glycemic control even in patients with ESRD; however, alternative markers of glycemia may be preferable.11
Although HbA1c is the gold standard, there are other laboratory measures of average glycemic control available. Fructosamine is a ketoamine formed when glucose binds to serum proteins. When these proteins are exposed to high concentrations of glucose, they experience increased glycation. Fructosamine assays measure the total glycated serum proteins, of which albumin accounts for about 90%.11 Because the half-life of serum proteins is about 20 days, fructosamine levels can reflect glycemic control over a 2- to 3-week period. This is advantageous in conditions that affect the average age of red blood cells, in pregnancy where frequent monitoring and measures of short-term glucose control are especially important, and in the evaluation of a medication adjustment in the management of T2DM. However, this test is not without its limitations. It is less reliable in settings of decreased protein levels (eg, liver disease), there is a lack of availability in routine practice, and reference levels have not been established.11
Fructosamine has been shown to be strongly associated with mean blood glucose and HbA1c (Table 2). In 2010, Mittman and colleagues published a study that compared HbA1c with fructosamine and their correlation to glycemic control and morbidity, defined as rates of hospitalization and infection.12 The study included 100 patients with T2DM on HD with a mean age of 63 years, 54% were women, mean HbA1c of 7.2%, and mean dialysis duration of 3 years. Average follow-up was 3 years. At the end of follow-up, Mittman and colleagues found that HbA1c and fructosamine were highly correlated and associated with serum glucose (P < .01). However, fructosamine was found to be more highly correlated with mean glucose levels when those levels were below 150 mg/dL (P = .01). A higher fructosamine level, not HbA1c was a more significant predictor of hospitalization (P = .007) and infection (P = .001). Mittman and colleagues presented evidence for the use of fructosamine over HbA1c in patients with T2DM on HD.12
Hypoglycemic Episodes
At the 2-month follow-up visit with the CPS, Mr. A reported having 5 hypoglycemic episodes in the past 30 days. He also stated he would forget to take his insulin aspart dose before dinner about 3 to 4 times a week but would take it 30 to 60 minutes after the meal. Mr. A did not bring his glucometer or SMBG readings to the visit, but he indicated that his blood glucose levels continued to fluctuate and were elevated when consuming carbohydrates.
Laboratory tests 1 month prior to the 2-month follow-up visit showed HbA1c of 7.3%, which had increased from his previous level of 6.1%. He was counseled on the proper administration of insulin aspart and lifestyle modifications. A fructosamine level was ordered at this visit to further assess his glycemic control. A follow-up appointment and laboratory workup (fructosamine and HbA1c) were scheduled for 2 months from the visit (Table 3).
Mr. A was educated on the unreliability of his HbA1c levels secondary to his condition of ESRD on HD. He was counseled on the purpose of fructosamine and how it may be a better predictor of his glycemic control and morbidity. Mr. A continued to be followed closely by the primary care CPS for T2DM management.
Discussion
Management of T2DM in patients with ESRD presents challenges for clinicians in determining HbA1c goals and selecting appropriate medication options. The 2012 Kidney Disease Outcomes Quality Initiative (KDOQI) diabetes guideline does not recommend treatment for patients with substantially reduced kidney function to a target HbA1c < 7% due to risk of hypoglycemia.13 Although a target HbA1c > 7% is suggested for these patients, little is known about appropriate glycemic control in these patients as there is a paucity of prospective, randomized clinical trials that include patients with advanced CKD.13
Moreover, many oral antidiabetic medications and their metabolites are cleared by the kidneys and, therefore, pose with potential harm for patients with CKD. Because of this, insulin is the medication of choice for patients with ESRD.7 Although insulin requirements may diminish with worsening kidney function, insulin provides the safest method of glycemic control. Insulin dosing can be individualized according to a patient’s renal status as there is no uniformity in renal dose adjustments. There are some noninsulin antidiabetic agents that can be used in ESRD, but use of these agents requires close monitoring and evaluation of the medication’s pharmacokinetics (Table 4). Overall, medication management can be a difficult task for patients with T2DM and ESRD, but antidiabetic regimens may be reduced or discontinued altogether in burnt-out diabetes.
One of 3 patients with T2DM and ESRD on dialysis has burnt-out diabetes, defined as a phenomenon in which glucose homeostasis is altered to cause normoglycemia, spontaneous hypoglycemia, and decreased insulin requirements in established patients with T2DM.5 Although Mr. A had a normal-to-low HbA1c, he did not meet these criteria. Due to his elevated SMBG readings, he did not have normoglycemia and did require an increase in his basal insulin dose. Therefore, our patient did not have burnt-out diabetes.
Mr. A represents the relevant issue of inappropriately and unreliably low HbA1c levels due to various factors in ESRD. Our patient did not receive a blood transfusion in the past 2 years and was not on ESA therapy; nevertheless, Mr. A was a patient with ESRD on HD with a diagnosis of anemia. These diagnoses are confounders for low HbA1c values. When fructosamine levels were drawn for Mr. A on September 11, 2018 and November 6, 2018, they correlated well with his serum glucose and SMBG readings. This indicated to the CPS that the patient’s glycemic control was poor despite a promising HbA1c level.
This patient’s case and supporting evidence suggests that other measures of glycemic control (eg, fructosamine) can be used to supplement HbA1c, serum glucose, and glucometer readings to provide an accurate assessment of glycemic control in T2DM. Fructosamine also can assist HbA1c with predicting morbidity and potentially mortality, which are of great importance in this patient population.
Kalantar-Zadeh and colleagues conducted a study of 23,618 patients with T2DM on dialysis to observe mortality in association with HbA1c.5 This analysis showed that patients with HbA1c levels < 5% or > 8% had a higher risk of mortality; higher values of HbA1c (> 10%) were associated with increased death risk vs all other values. In the unadjusted analysis, HbA1c levels between 6 and 8% had the lowest death risk (hazard ratios [HR] 0.8 - 0.9, 95% CI) compared with those of higher and lower HbA1c ranges.5 In nonanemic patients, HbA1c > 6% was associated with increased death risk, whereas anemic patients did not show this trend.
Other studies made similar observations. In 2001, Morioka and colleagues published an observational study of 150 patients with DM on intermittent hemodialysis. The study analyzed survival and HbA1c levels at 1, 3, and 5 years. The study found that at 1, 3, and 5 years, patients with HbA1c < 7.5% had better survival than did patients with HbA1c > 7.5% (3.6 years vs 2.0 years, P = .008). Morioka and colleagues also found that there was a 13% increase in death per 1% increase in HbA1c.14 Oomichi and colleagues conducted an observational study of 114 patients with T2DM and ESRD on intermittent hemodialysis. Patients with fair control (HbA1c 6.5 - 8%) and good control (HbA1c < 6.5%) were compared with patients with poor control (HbA1c > 8%); it was found that the poor control group had nearly triple the mortality when compared with the good and fair control groups (HR = 2.89, P = .01).15 Park and colleagues also saw a similar observation in a study of 1,239 patients with ESRD and DM; 70% of these patients were on intermittent hemodialysis. Patients with poor control (HbA1c ≥ 8%) had worse survival outcomes than those with HbA1c < 8% (HR 2.2, P < .001).16
Our patient case forced us to ask the question, “What should our patient’s HbA1c goals be?” In the study by Oomichi and colleagues, a HbA1c level of 8% has usefulness as a “signpost for management of glycemic control.”15 All patients’ goals should be individualized based on various factors (eg, age, comorbidities), but based on the survival studies above, a HbA1c goal range of 6 to 8% may be optimal.
Conclusions
Patients with T2DM and ESRD on dialysis may have higher morbidity and mortality rates than the rates of those without T2DM. It has been shown in various studies that very low HbA1c (< 5%) and high HbA1c (> 8%) are associated with poor survival. Some patients with T2DM on dialysis may experience burnt-out diabetes in which they may have normoglycemia and a HbA1c below goal; despite these facts, this condition is not positive and can be linked to bad outcomes. In patients with T2DM and ESRD, insulin is the antidiabetic medication of choice, and we recommend a HbA1c target of 6 to 8%. In this patient population, consider using fructosamine levels or other measures of glycemic control to supplement HbA1c and glucose values to provide a better assessment of glycemic control, morbidity, and mortality. Larger clinical trials are needed to assist in answering questions regarding mortality and optimal HbA1c targets in burnt-out diabetes.
More than 34 million adults in the US have type 2 diabetes mellitus (T2DM), a chronic progressive disease identified by worsening hyperglycemia and micro- and macrovascular complications.1 Consequently, 12.2% of the US adult population is currently at risk for macrovascular diseases, such as stroke and coronary artery disease (CAD) and microvascular diseases, such as neuropathy and diabetic nephropathy.1
T2DM is the most common comorbid risk factor for chronic kidney disease (CKD) and the leading cause of end-stage renal disease (ESRD). As of 2017, about 750,000 Americans have CKD stage 5 requiring dialysis, and 50% of these patients have preexisting diabetic nephropathy.2 Rates of mortality and morbidity are observed to be higher in patients with both CKD and T2DM compared with patients with CKD without T2DM.2 Previous clinical trials, including the United Kingdom Prospective Diabetes Study of 1998, have proven that optimal glycemic control decreases the risk of complications of T2DM (ie, nephropathy) in the general population.3 Conversely, tight glycemic control that targets hemoglobin A1c (HbA1c) < 7%, in patients with T2DM with ESRD has not shown the same benefits and may lead to worse outcomes. It is postulated that this may be due to the increased incidence of hypoglycemia in this patient population.4
Dialysis has varying effects on patients both with and without T2DM. While patients with ESRD without T2DM have the potential to develop impaired glucose tolerance and T2DM, about 33% of patients with T2DM on dialysis actually have HbA1c < 6%.5 In these patients, glycemic control improves spontaneously as their disease progresses, leading to a decrease or cessation of insulin or other antidiabetic medications. This phenomenon, known as burnt-out diabetes, is characterized by (1) alterations in glucose homeostasis and normoglycemia without antidiabetic treatment; (2) HbA1c levels < 6% despite having established T2DM; (3) decline in insulin requirements or cessation of insulin altogether; and (4) spontaneous hypoglycemia.
There is a misconception that burnt-out diabetes is a favorable condition due to the alteration of the natural course of T2DM. Although this may be true, patients with this condition are prone to develop hypoglycemic episodes and may be linked to poor survival outcomes due to low HbA1c.6,7
Since Kalantar-Zadeh and colleagues presented a 2009 case study, there has been a lack of research regarding this unique condition.8 The purpose of this case study is to shed further light on burnt-out diabetes and present a patient case pertaining to the challenges of glycemic control in ESRD.
Case Presentation
Mr. A is a 49-year-old Hispanic male veteran with a history of ESRD on hemodialysis (HD) for 6 years, anemia of CKD, and T2DM for 22 years. The patient also has an extensive cardiovascular disease history, including hypertension, hyperlipidemia, and CAD status post-4-vessel coronary artery bypass graft in December 2014. The patient receives in-home HD Monday, Wednesday, and Friday and is on the wait list for kidney transplantation. The patient’s T2DM is managed by a primary care clinical pharmacy specialist (CPS) at the
Mr. A’s antidiabetic regimen is 45 units of subcutaneous insulin glargine every morning; insulin aspart sliding scale (about 15-27 units) subcutaneous 3 times daily with meals; and saxagliptin 2.5 mg by mouth once daily.
At a follow-up visit with the CPS, Mr. A stated, “I feel fine except for the occasional low blood sugar episode.” The patient’s most recent HbA1c was 6.1%, and he reported medication adherence and no signs or symptoms of hyperglycemia (ie, polydipsia, polyphagia, nocturia, visual disturbances). Mr. A reported no use of alcohol, tobacco, or illicit drugs. He walks 1 mile every other day and participates in self-monitoring blood glucose (SMBG) about 2 to 3 times daily (Table 1).
Although Mr. A’s most recent HbA1c was well controlled, his estimated fasting blood glucose at the same laboratory draw was 224 mg/dL. His SMBG readings in the past month also were elevated with higher readings in the evening. Mr. A attributed the elevated readings to dietary excursions and a high carbohydrate intake. At this visit, the CPS increased his insulin glargine dose to 50 units subcutaneous every morning and educated him on lifestyle modifications. Follow-up with the CPS was scheduled for 2 months from the day of the visit.
Analysis
Few articles on potential contributors to burnt-out diabetes have been published.6,7 These articles discuss decreased renal and hepatic clearance of insulin (which increases its half-life) hypoglycemia during HD, and low HbA1c due to preexisting anemia. Inappropriately low HbA1c levels may be secondary to, but not limited to, hemolysis, recent blood transfusion, acute blood loss, and medications, such as erythropoietin-stimulating agents (ESAs).9 The conditions that affect red blood cell turnover are common in patients with advanced CKD and may result in discrepancies in HbA1c levels.
Glycated hemoglobin is a series of minor hemoglobin components formed by the adduction of various carbohydrate molecules to hemoglobin. HbA1c is the largest fraction formed and the most consistent index of the concentration of glucose in the blood.10 Hence, HbA1c is the traditional indicator of overall glycemic control. The current HbA1c goals recommended by the American Diabetes Association are derived from landmark trials conducted with patients in the general adult diabetic non-CKD population. However, hemoglobin measurements can be confounded by conditions present in ESRD and tend to underestimate glucose measurements in patients with T2DM on HD. Despite this, HbA1c is still regarded as a reasonable measure of glycemic control even in patients with ESRD; however, alternative markers of glycemia may be preferable.11
Although HbA1c is the gold standard, there are other laboratory measures of average glycemic control available. Fructosamine is a ketoamine formed when glucose binds to serum proteins. When these proteins are exposed to high concentrations of glucose, they experience increased glycation. Fructosamine assays measure the total glycated serum proteins, of which albumin accounts for about 90%.11 Because the half-life of serum proteins is about 20 days, fructosamine levels can reflect glycemic control over a 2- to 3-week period. This is advantageous in conditions that affect the average age of red blood cells, in pregnancy where frequent monitoring and measures of short-term glucose control are especially important, and in the evaluation of a medication adjustment in the management of T2DM. However, this test is not without its limitations. It is less reliable in settings of decreased protein levels (eg, liver disease), there is a lack of availability in routine practice, and reference levels have not been established.11
Fructosamine has been shown to be strongly associated with mean blood glucose and HbA1c (Table 2). In 2010, Mittman and colleagues published a study that compared HbA1c with fructosamine and their correlation to glycemic control and morbidity, defined as rates of hospitalization and infection.12 The study included 100 patients with T2DM on HD with a mean age of 63 years, 54% were women, mean HbA1c of 7.2%, and mean dialysis duration of 3 years. Average follow-up was 3 years. At the end of follow-up, Mittman and colleagues found that HbA1c and fructosamine were highly correlated and associated with serum glucose (P < .01). However, fructosamine was found to be more highly correlated with mean glucose levels when those levels were below 150 mg/dL (P = .01). A higher fructosamine level, not HbA1c was a more significant predictor of hospitalization (P = .007) and infection (P = .001). Mittman and colleagues presented evidence for the use of fructosamine over HbA1c in patients with T2DM on HD.12
Hypoglycemic Episodes
At the 2-month follow-up visit with the CPS, Mr. A reported having 5 hypoglycemic episodes in the past 30 days. He also stated he would forget to take his insulin aspart dose before dinner about 3 to 4 times a week but would take it 30 to 60 minutes after the meal. Mr. A did not bring his glucometer or SMBG readings to the visit, but he indicated that his blood glucose levels continued to fluctuate and were elevated when consuming carbohydrates.
Laboratory tests 1 month prior to the 2-month follow-up visit showed HbA1c of 7.3%, which had increased from his previous level of 6.1%. He was counseled on the proper administration of insulin aspart and lifestyle modifications. A fructosamine level was ordered at this visit to further assess his glycemic control. A follow-up appointment and laboratory workup (fructosamine and HbA1c) were scheduled for 2 months from the visit (Table 3).
Mr. A was educated on the unreliability of his HbA1c levels secondary to his condition of ESRD on HD. He was counseled on the purpose of fructosamine and how it may be a better predictor of his glycemic control and morbidity. Mr. A continued to be followed closely by the primary care CPS for T2DM management.
Discussion
Management of T2DM in patients with ESRD presents challenges for clinicians in determining HbA1c goals and selecting appropriate medication options. The 2012 Kidney Disease Outcomes Quality Initiative (KDOQI) diabetes guideline does not recommend treatment for patients with substantially reduced kidney function to a target HbA1c < 7% due to risk of hypoglycemia.13 Although a target HbA1c > 7% is suggested for these patients, little is known about appropriate glycemic control in these patients as there is a paucity of prospective, randomized clinical trials that include patients with advanced CKD.13
Moreover, many oral antidiabetic medications and their metabolites are cleared by the kidneys and, therefore, pose with potential harm for patients with CKD. Because of this, insulin is the medication of choice for patients with ESRD.7 Although insulin requirements may diminish with worsening kidney function, insulin provides the safest method of glycemic control. Insulin dosing can be individualized according to a patient’s renal status as there is no uniformity in renal dose adjustments. There are some noninsulin antidiabetic agents that can be used in ESRD, but use of these agents requires close monitoring and evaluation of the medication’s pharmacokinetics (Table 4). Overall, medication management can be a difficult task for patients with T2DM and ESRD, but antidiabetic regimens may be reduced or discontinued altogether in burnt-out diabetes.
One of 3 patients with T2DM and ESRD on dialysis has burnt-out diabetes, defined as a phenomenon in which glucose homeostasis is altered to cause normoglycemia, spontaneous hypoglycemia, and decreased insulin requirements in established patients with T2DM.5 Although Mr. A had a normal-to-low HbA1c, he did not meet these criteria. Due to his elevated SMBG readings, he did not have normoglycemia and did require an increase in his basal insulin dose. Therefore, our patient did not have burnt-out diabetes.
Mr. A represents the relevant issue of inappropriately and unreliably low HbA1c levels due to various factors in ESRD. Our patient did not receive a blood transfusion in the past 2 years and was not on ESA therapy; nevertheless, Mr. A was a patient with ESRD on HD with a diagnosis of anemia. These diagnoses are confounders for low HbA1c values. When fructosamine levels were drawn for Mr. A on September 11, 2018 and November 6, 2018, they correlated well with his serum glucose and SMBG readings. This indicated to the CPS that the patient’s glycemic control was poor despite a promising HbA1c level.
This patient’s case and supporting evidence suggests that other measures of glycemic control (eg, fructosamine) can be used to supplement HbA1c, serum glucose, and glucometer readings to provide an accurate assessment of glycemic control in T2DM. Fructosamine also can assist HbA1c with predicting morbidity and potentially mortality, which are of great importance in this patient population.
Kalantar-Zadeh and colleagues conducted a study of 23,618 patients with T2DM on dialysis to observe mortality in association with HbA1c.5 This analysis showed that patients with HbA1c levels < 5% or > 8% had a higher risk of mortality; higher values of HbA1c (> 10%) were associated with increased death risk vs all other values. In the unadjusted analysis, HbA1c levels between 6 and 8% had the lowest death risk (hazard ratios [HR] 0.8 - 0.9, 95% CI) compared with those of higher and lower HbA1c ranges.5 In nonanemic patients, HbA1c > 6% was associated with increased death risk, whereas anemic patients did not show this trend.
Other studies made similar observations. In 2001, Morioka and colleagues published an observational study of 150 patients with DM on intermittent hemodialysis. The study analyzed survival and HbA1c levels at 1, 3, and 5 years. The study found that at 1, 3, and 5 years, patients with HbA1c < 7.5% had better survival than did patients with HbA1c > 7.5% (3.6 years vs 2.0 years, P = .008). Morioka and colleagues also found that there was a 13% increase in death per 1% increase in HbA1c.14 Oomichi and colleagues conducted an observational study of 114 patients with T2DM and ESRD on intermittent hemodialysis. Patients with fair control (HbA1c 6.5 - 8%) and good control (HbA1c < 6.5%) were compared with patients with poor control (HbA1c > 8%); it was found that the poor control group had nearly triple the mortality when compared with the good and fair control groups (HR = 2.89, P = .01).15 Park and colleagues also saw a similar observation in a study of 1,239 patients with ESRD and DM; 70% of these patients were on intermittent hemodialysis. Patients with poor control (HbA1c ≥ 8%) had worse survival outcomes than those with HbA1c < 8% (HR 2.2, P < .001).16
Our patient case forced us to ask the question, “What should our patient’s HbA1c goals be?” In the study by Oomichi and colleagues, a HbA1c level of 8% has usefulness as a “signpost for management of glycemic control.”15 All patients’ goals should be individualized based on various factors (eg, age, comorbidities), but based on the survival studies above, a HbA1c goal range of 6 to 8% may be optimal.
Conclusions
Patients with T2DM and ESRD on dialysis may have higher morbidity and mortality rates than the rates of those without T2DM. It has been shown in various studies that very low HbA1c (< 5%) and high HbA1c (> 8%) are associated with poor survival. Some patients with T2DM on dialysis may experience burnt-out diabetes in which they may have normoglycemia and a HbA1c below goal; despite these facts, this condition is not positive and can be linked to bad outcomes. In patients with T2DM and ESRD, insulin is the antidiabetic medication of choice, and we recommend a HbA1c target of 6 to 8%. In this patient population, consider using fructosamine levels or other measures of glycemic control to supplement HbA1c and glucose values to provide a better assessment of glycemic control, morbidity, and mortality. Larger clinical trials are needed to assist in answering questions regarding mortality and optimal HbA1c targets in burnt-out diabetes.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Updated August 28, 2020. Accessed November 17, 2020.
2. Saran R, Robinson B, et al. US renal data system 2019 annual data report: epidemiology of klidney disease in the United States. Am J Kidney Dis. 2020 Jan;75(1 suppl 1):A6-A7. doi:10.1053/j.ajkd.2019.09.003. Epub 2019 Nov 5.
3. UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):854-865.
4. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545-2559. doi:10.1056/NEJMoa0802743
5. Kalantar-Zadeh K, Kopple JD, Regidor DL, et al. A1c and survival in maintenance hemodialysis patients. Diabetes Care. 2007;30(5):1049-10.55. doi:10.2337/dc06-2127
6. Park J, Lertdumrongluk P, Molnar MZ, Kovesdy CP, Kalantar-Zadeh K. Glycemic control in diabetic dialysis patients and the burnt-out diabetes phenomenon. Curr Diab Rep. 2012;12(4):432-439. doi:10.1007/s11892-012-0286-3
7. Rhee CM, Leung AM, Kovesdy CP, Lynch KE, Brent GA, Kalantar-Zadeh K. Updates on the management of diabetes in dialysis patients. Semin Dial. 2014;27(2):135-145. doi:10.1111/sdi.12198
8. Kalantar-Zadeh K, Derose SF, Nicholas S, Benner D, Sharma K, Kovesdy CP. Burnt-out diabetes: impact of chronic kidney disease progression on the natural course of diabetes mellitus. J Ren Nutr. 2009;19(1):33-37. doi:10.1053/j.jrn.2008.11.012
9. Unnikrishnan R, Anjana RM, Mohan V. Drugs affecting HbA1c levels. Indian J Endocrinol Metab. 2012;16(4):528-531. doi:10.4103/2230-8210.98004
10. Makris K, Spanou L. Is there a relationship between mean blood glucose and glycated hemoglobin? J Diabetes Sci Technol. 2011;5(6):1572-1583. doi:10.1177/193229681100500634
11. Wright LAC, Hirsch IB. The challenge of the use of glycemic biomarkers in diabetes: reflecting on hemoglobin A1c, 1,5-anhydroglucitol, and the glycated proteins fructosamine and glycated albumin. Diabetes Spectr. 2012;25(3):141-148. doi:10.2337/diaspect.25.3.141
12. Mittman N, Desiraju B, Fazil I, et al. Serum fructosamine versus glycosylated hemoglobin as an index of glycemic control, hospitalization, and infection in diabetic hemodialysis patients. Kidney Int. 2010;78 (suppl 117):S41-S45. doi:10.1038/ki.2010.193
13. National Kidney Foundation. KDOQI clinical practice guideline for diabetes and CKD: 2012 update. Am J Kidney Dis. 2012;60(5):850-886. doi:10.1053/j.ajkd.2012.07.005
14. Morioka T, Emoto M, Tabata T, et al. Glycemic control is a predictor of survival for diabetic patients on hemodialysis. Diabetes Care. 2001;24(5):909-913. doi.10.2337/diacare.24.5.909

15. Oomichi T, Emoto M, Tabata T, et al. Impact of glycemic control on survival of diabetic patients on chronic regular hemodialysis: a 7-year observational study. Diabetes Care. 2006;29(7):1496-1500. doi:10.2337/dc05-1887
16. Park JI, Bae E, Kim YL, et al. Glycemic control and mortality in diabetic patients undergoing dialysis focusing on the effects of age and dialysis type: a prospective cohort study in Korea. PLoS ONE. 2015;10(8):e0136085. doi:10.1371/journal.pone.0136085
17. Glucotrol tablets [
18. Amaryl [package insert]. Bridgewater, NJ: Sanofi-Aventis; December 2018.
19. Glucophage [package insert]. Princeton, NJ: Bristol-Myers Squibb; May 2018.
20. Actos [package insert]. Deerfield, IL: Takeda Pharmaceuticals America Inc; December 2017.
21. Precose [package insert]. Whippany, NJ: Bayer HealthCare Pharmaceuticals; March 2015.
22. Nesina [package insert]. Deerfield, IL: Takeda Pharmaceuticals America Inc; June 2019.
23. Victoza [package insert]. Plainsboro, NJ: Novo Nordisk Inc; June 2019.
24. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals Inc; October 2018.
1. Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Updated August 28, 2020. Accessed November 17, 2020.
2. Saran R, Robinson B, et al. US renal data system 2019 annual data report: epidemiology of klidney disease in the United States. Am J Kidney Dis. 2020 Jan;75(1 suppl 1):A6-A7. doi:10.1053/j.ajkd.2019.09.003. Epub 2019 Nov 5.
3. UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):854-865.
4. Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545-2559. doi:10.1056/NEJMoa0802743
5. Kalantar-Zadeh K, Kopple JD, Regidor DL, et al. A1c and survival in maintenance hemodialysis patients. Diabetes Care. 2007;30(5):1049-10.55. doi:10.2337/dc06-2127
6. Park J, Lertdumrongluk P, Molnar MZ, Kovesdy CP, Kalantar-Zadeh K. Glycemic control in diabetic dialysis patients and the burnt-out diabetes phenomenon. Curr Diab Rep. 2012;12(4):432-439. doi:10.1007/s11892-012-0286-3
7. Rhee CM, Leung AM, Kovesdy CP, Lynch KE, Brent GA, Kalantar-Zadeh K. Updates on the management of diabetes in dialysis patients. Semin Dial. 2014;27(2):135-145. doi:10.1111/sdi.12198
8. Kalantar-Zadeh K, Derose SF, Nicholas S, Benner D, Sharma K, Kovesdy CP. Burnt-out diabetes: impact of chronic kidney disease progression on the natural course of diabetes mellitus. J Ren Nutr. 2009;19(1):33-37. doi:10.1053/j.jrn.2008.11.012
9. Unnikrishnan R, Anjana RM, Mohan V. Drugs affecting HbA1c levels. Indian J Endocrinol Metab. 2012;16(4):528-531. doi:10.4103/2230-8210.98004
10. Makris K, Spanou L. Is there a relationship between mean blood glucose and glycated hemoglobin? J Diabetes Sci Technol. 2011;5(6):1572-1583. doi:10.1177/193229681100500634
11. Wright LAC, Hirsch IB. The challenge of the use of glycemic biomarkers in diabetes: reflecting on hemoglobin A1c, 1,5-anhydroglucitol, and the glycated proteins fructosamine and glycated albumin. Diabetes Spectr. 2012;25(3):141-148. doi:10.2337/diaspect.25.3.141
12. Mittman N, Desiraju B, Fazil I, et al. Serum fructosamine versus glycosylated hemoglobin as an index of glycemic control, hospitalization, and infection in diabetic hemodialysis patients. Kidney Int. 2010;78 (suppl 117):S41-S45. doi:10.1038/ki.2010.193
13. National Kidney Foundation. KDOQI clinical practice guideline for diabetes and CKD: 2012 update. Am J Kidney Dis. 2012;60(5):850-886. doi:10.1053/j.ajkd.2012.07.005
14. Morioka T, Emoto M, Tabata T, et al. Glycemic control is a predictor of survival for diabetic patients on hemodialysis. Diabetes Care. 2001;24(5):909-913. doi.10.2337/diacare.24.5.909

15. Oomichi T, Emoto M, Tabata T, et al. Impact of glycemic control on survival of diabetic patients on chronic regular hemodialysis: a 7-year observational study. Diabetes Care. 2006;29(7):1496-1500. doi:10.2337/dc05-1887
16. Park JI, Bae E, Kim YL, et al. Glycemic control and mortality in diabetic patients undergoing dialysis focusing on the effects of age and dialysis type: a prospective cohort study in Korea. PLoS ONE. 2015;10(8):e0136085. doi:10.1371/journal.pone.0136085
17. Glucotrol tablets [
18. Amaryl [package insert]. Bridgewater, NJ: Sanofi-Aventis; December 2018.
19. Glucophage [package insert]. Princeton, NJ: Bristol-Myers Squibb; May 2018.
20. Actos [package insert]. Deerfield, IL: Takeda Pharmaceuticals America Inc; December 2017.
21. Precose [package insert]. Whippany, NJ: Bayer HealthCare Pharmaceuticals; March 2015.
22. Nesina [package insert]. Deerfield, IL: Takeda Pharmaceuticals America Inc; June 2019.
23. Victoza [package insert]. Plainsboro, NJ: Novo Nordisk Inc; June 2019.
24. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals Inc; October 2018.
Recalled to Life: The Best and Worst of 2020 Is the Year 2020
Some who read Federal Practitioner regularly may recall that since 2017, I have been dedicating the December and January editorials to a more substantive version of the popular best and worst awards that appear in the media this time of year. Everything from the most comfortable slippers to the weirdest lawsuits is scored annually. In an effort to elevate the ranking routine, this column has reviewed and evaluated ethical and unethical events and decisions in the 3 federal health care systems Federal Practitioner primarily serves. In previous years it was a challenge requiring research and deliberation to select the most inspiring and troubling occurrences in the world of federal health care. This year neither great effort or prolonged study was required as the choice was immediate and obvious—the year itself. A year in which our individual identities as health care professionals serving in the US Department of Defense, US Department of Veterans Affairs (VA), and US Public Health Service is subsumed in our realities as citizens of a nation in crisis.
The opening lines of A Tale of Two Cities have become such a literary platitude taken out of the context of the novel that the terror and fascination with which Dickens wrote these oft-quoted lines has been diluted and dulled.1 In citing the entire paragraph as the epigraph, I hope to recapture the moral seriousness of its message, which is so relevant in 2020. While protesting the widespread injustice that fueled the progress of London’s industrial revolution, Dickens also feared such discontent would ignite a bloody uprising as it had done in Paris.1 This passage is a classic example of the literary device of parallelism that so perfectly expressed Dickens’ reflections on the trajectory of the unprecedented historical impact of the French Revolution. A parallelism that also aptly captures the contemporary contrasts and comparisons of the best and worst of 2020.
It is estimated that at least 66% of those eligible to vote did so on November 3, 2020, the highest turnout in more than a century, demonstrating the strength of the United States as a representative democracy.2 It is not about partisan politics, it is that more than 150 million citizens braved the winter, the virus, and potential intimidation to cast a ballot for their values.3 Still, America has never been more divided, and Dickens’ fear of political upheaval has never been more real in our country, or at least since the Civil War.
As I write this editorial, manufacturers for 2 vaccines have submitted phase 3 trial data to the US Food and Drug Administration for Emergency Use Authorizations and a third consortium may follow suit soon. Scientists report that the 2 vaccines, which were developed in less than a year, have high efficacy rates (> 90%) with only modest adverse effects.4 It is an unparalleled, really unimaginable, scientific feat. Americans’ characteristic gift for logistical efficiency and scientific innovation faces daunting administrative and technical barriers to achieve a similar viral victory, yet we may have faced even more formidable odds in World War II.
As of December 4, 2020, Johns Hopkins University reports that more than 275,000 Americans have died of coronavirus.5 The United States is on track to reach 200,000 cases a day with the signature holiday season of family festivities brutally morphed into gatherings of contagion.6 Hospitals across the country are running out of intensive care beds and nurses and doctors to staff them. Unlike the Spring surge in the Northeast, cases are rising in 49 states, and there is nowhere in the land from which respite and reinforcements can come.7
Thousands of health care professionals are exhausted, many with COVID-19 or recovering from it, morally distressed, and emotionally spent. Masks and social distancing are no longer public health essentials but elements of a culture war. Those same nurses, doctors, and public health officers still show up day after night for what is much closer to war than work. They struggle to prevent patients from going on ventilators they may never come off and use the few available therapies to keep as many patients alive as possible—whether those patients believe in COVID-19, wore a mask, no matter who they voted for—because that is what it means to practice health care according to a code of ethics.
In March 2020, I pledged to devote every editorial to COVID-19 for as long as the pandemic lasted, as one small candle for all those who have died of COVID-19, who are suffering as survivors of it, and who take risks and labor to deliver essential services from groceries to intensive care. Prudent public health officials wisely advise that the vaccine(s) are not a miracle cure to revive a depleted country, in part because it may undermine life-saving public health measures.8 And so the columns will continue in 2021 to illuminate the ethical issues of the pandemic as they affect all of us as federal health care professionals and Americans.
The Tale of Two Cities chapter that begins with the “best of times, and the worst of times” is entitled “Recalled to Life.” Let that be our hope and prayer for the coming year.
1. Dickens C. A Tale of Two Cities. Douglas-Fairhust ed. New York: Norton; 2020.
2. Schaul K, Rabinowitz K, Mellnik T. 2020 turnout is the highest in over a century. Washington Post, November 5, 2020. https://www.washingtonpost.com/graphics/2020/elections/voter-turnout. Accessed November 23, 2020.
3. Desilver D. In past elections, U.S. trailed most developed countries in voter turnout. https://www.pewresearch.org/fact-tank/2020/11/03/in-past-elections-u-s-trailed-most-developed-countries-in-voter-turnout. Published November 3, 2020. Accessed November 23, 2020.
4. Herper M, Garde D. Moderna to submit Covid-19 vaccine to FDA as full results show 94% efficacy.https://www.statnews.com/2020/11/30/moderna-covid-19-vaccine-full-results. Published November 30, 2020. Accessed November 30, 2020.
5. Johns Hopkins University and Medicine. Coronavirus research center. https://coronavirus.jhu.edu. Updated November 23, 2020. Accessed December 4, 2020.
6. Hawkins D, Knowles H. As U.S. coronavirus cases soar toward 200,000 a day holiday travel is surging. Washington Post, November 21, 2020. https://www.washingtonpost.com/health/2020/11/21/coronavirus-thanksgiving-travel. Accessed November 23, 2020.
7. Goldhill O. ‘People are going to die’: Hospitals in half the states are facing massive staffing shortages as COVID-19 surges. November 19, 2020. https://www.statnews.com/2020/11/19/covid19-hospitals-in-half-the-states-facing-massive-staffing-shortage. Published November 19, 2020. Accessed November 23, 2020.
8. Lazar K. Is Pfizer’s vaccine a ‘magic bullet?’ Scientists warn masks, distancing may last well into 2021. Boston Globe . November 9, 2020. https://www.bostonglobe.com/2020/11/09/metro/is-pfizer-vaccine-magic-bullet-scientists-warn-public-should-be-prepared-live-with-masks-social-distancing-months. Accessed November 23, 2020.
Some who read Federal Practitioner regularly may recall that since 2017, I have been dedicating the December and January editorials to a more substantive version of the popular best and worst awards that appear in the media this time of year. Everything from the most comfortable slippers to the weirdest lawsuits is scored annually. In an effort to elevate the ranking routine, this column has reviewed and evaluated ethical and unethical events and decisions in the 3 federal health care systems Federal Practitioner primarily serves. In previous years it was a challenge requiring research and deliberation to select the most inspiring and troubling occurrences in the world of federal health care. This year neither great effort or prolonged study was required as the choice was immediate and obvious—the year itself. A year in which our individual identities as health care professionals serving in the US Department of Defense, US Department of Veterans Affairs (VA), and US Public Health Service is subsumed in our realities as citizens of a nation in crisis.
The opening lines of A Tale of Two Cities have become such a literary platitude taken out of the context of the novel that the terror and fascination with which Dickens wrote these oft-quoted lines has been diluted and dulled.1 In citing the entire paragraph as the epigraph, I hope to recapture the moral seriousness of its message, which is so relevant in 2020. While protesting the widespread injustice that fueled the progress of London’s industrial revolution, Dickens also feared such discontent would ignite a bloody uprising as it had done in Paris.1 This passage is a classic example of the literary device of parallelism that so perfectly expressed Dickens’ reflections on the trajectory of the unprecedented historical impact of the French Revolution. A parallelism that also aptly captures the contemporary contrasts and comparisons of the best and worst of 2020.
It is estimated that at least 66% of those eligible to vote did so on November 3, 2020, the highest turnout in more than a century, demonstrating the strength of the United States as a representative democracy.2 It is not about partisan politics, it is that more than 150 million citizens braved the winter, the virus, and potential intimidation to cast a ballot for their values.3 Still, America has never been more divided, and Dickens’ fear of political upheaval has never been more real in our country, or at least since the Civil War.
As I write this editorial, manufacturers for 2 vaccines have submitted phase 3 trial data to the US Food and Drug Administration for Emergency Use Authorizations and a third consortium may follow suit soon. Scientists report that the 2 vaccines, which were developed in less than a year, have high efficacy rates (> 90%) with only modest adverse effects.4 It is an unparalleled, really unimaginable, scientific feat. Americans’ characteristic gift for logistical efficiency and scientific innovation faces daunting administrative and technical barriers to achieve a similar viral victory, yet we may have faced even more formidable odds in World War II.
As of December 4, 2020, Johns Hopkins University reports that more than 275,000 Americans have died of coronavirus.5 The United States is on track to reach 200,000 cases a day with the signature holiday season of family festivities brutally morphed into gatherings of contagion.6 Hospitals across the country are running out of intensive care beds and nurses and doctors to staff them. Unlike the Spring surge in the Northeast, cases are rising in 49 states, and there is nowhere in the land from which respite and reinforcements can come.7
Thousands of health care professionals are exhausted, many with COVID-19 or recovering from it, morally distressed, and emotionally spent. Masks and social distancing are no longer public health essentials but elements of a culture war. Those same nurses, doctors, and public health officers still show up day after night for what is much closer to war than work. They struggle to prevent patients from going on ventilators they may never come off and use the few available therapies to keep as many patients alive as possible—whether those patients believe in COVID-19, wore a mask, no matter who they voted for—because that is what it means to practice health care according to a code of ethics.
In March 2020, I pledged to devote every editorial to COVID-19 for as long as the pandemic lasted, as one small candle for all those who have died of COVID-19, who are suffering as survivors of it, and who take risks and labor to deliver essential services from groceries to intensive care. Prudent public health officials wisely advise that the vaccine(s) are not a miracle cure to revive a depleted country, in part because it may undermine life-saving public health measures.8 And so the columns will continue in 2021 to illuminate the ethical issues of the pandemic as they affect all of us as federal health care professionals and Americans.
The Tale of Two Cities chapter that begins with the “best of times, and the worst of times” is entitled “Recalled to Life.” Let that be our hope and prayer for the coming year.
Some who read Federal Practitioner regularly may recall that since 2017, I have been dedicating the December and January editorials to a more substantive version of the popular best and worst awards that appear in the media this time of year. Everything from the most comfortable slippers to the weirdest lawsuits is scored annually. In an effort to elevate the ranking routine, this column has reviewed and evaluated ethical and unethical events and decisions in the 3 federal health care systems Federal Practitioner primarily serves. In previous years it was a challenge requiring research and deliberation to select the most inspiring and troubling occurrences in the world of federal health care. This year neither great effort or prolonged study was required as the choice was immediate and obvious—the year itself. A year in which our individual identities as health care professionals serving in the US Department of Defense, US Department of Veterans Affairs (VA), and US Public Health Service is subsumed in our realities as citizens of a nation in crisis.
The opening lines of A Tale of Two Cities have become such a literary platitude taken out of the context of the novel that the terror and fascination with which Dickens wrote these oft-quoted lines has been diluted and dulled.1 In citing the entire paragraph as the epigraph, I hope to recapture the moral seriousness of its message, which is so relevant in 2020. While protesting the widespread injustice that fueled the progress of London’s industrial revolution, Dickens also feared such discontent would ignite a bloody uprising as it had done in Paris.1 This passage is a classic example of the literary device of parallelism that so perfectly expressed Dickens’ reflections on the trajectory of the unprecedented historical impact of the French Revolution. A parallelism that also aptly captures the contemporary contrasts and comparisons of the best and worst of 2020.
It is estimated that at least 66% of those eligible to vote did so on November 3, 2020, the highest turnout in more than a century, demonstrating the strength of the United States as a representative democracy.2 It is not about partisan politics, it is that more than 150 million citizens braved the winter, the virus, and potential intimidation to cast a ballot for their values.3 Still, America has never been more divided, and Dickens’ fear of political upheaval has never been more real in our country, or at least since the Civil War.
As I write this editorial, manufacturers for 2 vaccines have submitted phase 3 trial data to the US Food and Drug Administration for Emergency Use Authorizations and a third consortium may follow suit soon. Scientists report that the 2 vaccines, which were developed in less than a year, have high efficacy rates (> 90%) with only modest adverse effects.4 It is an unparalleled, really unimaginable, scientific feat. Americans’ characteristic gift for logistical efficiency and scientific innovation faces daunting administrative and technical barriers to achieve a similar viral victory, yet we may have faced even more formidable odds in World War II.
As of December 4, 2020, Johns Hopkins University reports that more than 275,000 Americans have died of coronavirus.5 The United States is on track to reach 200,000 cases a day with the signature holiday season of family festivities brutally morphed into gatherings of contagion.6 Hospitals across the country are running out of intensive care beds and nurses and doctors to staff them. Unlike the Spring surge in the Northeast, cases are rising in 49 states, and there is nowhere in the land from which respite and reinforcements can come.7
Thousands of health care professionals are exhausted, many with COVID-19 or recovering from it, morally distressed, and emotionally spent. Masks and social distancing are no longer public health essentials but elements of a culture war. Those same nurses, doctors, and public health officers still show up day after night for what is much closer to war than work. They struggle to prevent patients from going on ventilators they may never come off and use the few available therapies to keep as many patients alive as possible—whether those patients believe in COVID-19, wore a mask, no matter who they voted for—because that is what it means to practice health care according to a code of ethics.
In March 2020, I pledged to devote every editorial to COVID-19 for as long as the pandemic lasted, as one small candle for all those who have died of COVID-19, who are suffering as survivors of it, and who take risks and labor to deliver essential services from groceries to intensive care. Prudent public health officials wisely advise that the vaccine(s) are not a miracle cure to revive a depleted country, in part because it may undermine life-saving public health measures.8 And so the columns will continue in 2021 to illuminate the ethical issues of the pandemic as they affect all of us as federal health care professionals and Americans.
The Tale of Two Cities chapter that begins with the “best of times, and the worst of times” is entitled “Recalled to Life.” Let that be our hope and prayer for the coming year.
1. Dickens C. A Tale of Two Cities. Douglas-Fairhust ed. New York: Norton; 2020.
2. Schaul K, Rabinowitz K, Mellnik T. 2020 turnout is the highest in over a century. Washington Post, November 5, 2020. https://www.washingtonpost.com/graphics/2020/elections/voter-turnout. Accessed November 23, 2020.
3. Desilver D. In past elections, U.S. trailed most developed countries in voter turnout. https://www.pewresearch.org/fact-tank/2020/11/03/in-past-elections-u-s-trailed-most-developed-countries-in-voter-turnout. Published November 3, 2020. Accessed November 23, 2020.
4. Herper M, Garde D. Moderna to submit Covid-19 vaccine to FDA as full results show 94% efficacy.https://www.statnews.com/2020/11/30/moderna-covid-19-vaccine-full-results. Published November 30, 2020. Accessed November 30, 2020.
5. Johns Hopkins University and Medicine. Coronavirus research center. https://coronavirus.jhu.edu. Updated November 23, 2020. Accessed December 4, 2020.
6. Hawkins D, Knowles H. As U.S. coronavirus cases soar toward 200,000 a day holiday travel is surging. Washington Post, November 21, 2020. https://www.washingtonpost.com/health/2020/11/21/coronavirus-thanksgiving-travel. Accessed November 23, 2020.
7. Goldhill O. ‘People are going to die’: Hospitals in half the states are facing massive staffing shortages as COVID-19 surges. November 19, 2020. https://www.statnews.com/2020/11/19/covid19-hospitals-in-half-the-states-facing-massive-staffing-shortage. Published November 19, 2020. Accessed November 23, 2020.
8. Lazar K. Is Pfizer’s vaccine a ‘magic bullet?’ Scientists warn masks, distancing may last well into 2021. Boston Globe . November 9, 2020. https://www.bostonglobe.com/2020/11/09/metro/is-pfizer-vaccine-magic-bullet-scientists-warn-public-should-be-prepared-live-with-masks-social-distancing-months. Accessed November 23, 2020.
1. Dickens C. A Tale of Two Cities. Douglas-Fairhust ed. New York: Norton; 2020.
2. Schaul K, Rabinowitz K, Mellnik T. 2020 turnout is the highest in over a century. Washington Post, November 5, 2020. https://www.washingtonpost.com/graphics/2020/elections/voter-turnout. Accessed November 23, 2020.
3. Desilver D. In past elections, U.S. trailed most developed countries in voter turnout. https://www.pewresearch.org/fact-tank/2020/11/03/in-past-elections-u-s-trailed-most-developed-countries-in-voter-turnout. Published November 3, 2020. Accessed November 23, 2020.
4. Herper M, Garde D. Moderna to submit Covid-19 vaccine to FDA as full results show 94% efficacy.https://www.statnews.com/2020/11/30/moderna-covid-19-vaccine-full-results. Published November 30, 2020. Accessed November 30, 2020.
5. Johns Hopkins University and Medicine. Coronavirus research center. https://coronavirus.jhu.edu. Updated November 23, 2020. Accessed December 4, 2020.
6. Hawkins D, Knowles H. As U.S. coronavirus cases soar toward 200,000 a day holiday travel is surging. Washington Post, November 21, 2020. https://www.washingtonpost.com/health/2020/11/21/coronavirus-thanksgiving-travel. Accessed November 23, 2020.
7. Goldhill O. ‘People are going to die’: Hospitals in half the states are facing massive staffing shortages as COVID-19 surges. November 19, 2020. https://www.statnews.com/2020/11/19/covid19-hospitals-in-half-the-states-facing-massive-staffing-shortage. Published November 19, 2020. Accessed November 23, 2020.
8. Lazar K. Is Pfizer’s vaccine a ‘magic bullet?’ Scientists warn masks, distancing may last well into 2021. Boston Globe . November 9, 2020. https://www.bostonglobe.com/2020/11/09/metro/is-pfizer-vaccine-magic-bullet-scientists-warn-public-should-be-prepared-live-with-masks-social-distancing-months. Accessed November 23, 2020.
Prophylactic antibiotics for myomectomy?
In the 1990s, researchers found that patients undergoing any type of surgical procedure were more than twice as likely to die if they developed postsurgical infection.1 Work to reduce surgical site infection (SSI) has and does continue, with perioperative antibiotics representing a good part of that effort. The American College of Obstetricians and Gynecologists currently recommends such antibiotic therapy for women undergoing laparotomy and laparoscopic hysterectomy.2 ACOG does not, however, recommend prophylactic antibiotics for myomectomy procedures.3 Rates of infection for hysterectomy have been reported to be 3.9% for abdominal and 1.4% for minimally invasive approaches.4
To determine the current use of antibiotics during myomectomy and associated rates of SSI at their institutions, Dipti Banerjee, MD, and colleagues conducted a retrospective analysis of women undergoing laparoscopic or abdominal myomectomy between February 2013 and December 2017 at the University of California, Los Angeles and Hoag Memorial Hospital in Orange County, California. They presented their study results at AAGL’s 49th Global Congress on MIGS, held virtually November 6-14, 2020.3
Rate of SSI after myomectomy
A total of 620 women underwent laparoscopic myomectomy and 563 underwent open myomectomy during the study period. Antibiotics were used in 76.9% of cases. SSI developed within 6 weeks of surgery in 34 women (2.9%) overall. The women undergoing abdominal myomectomy without antibiotics were more likely to experience SSI than the women who received antibiotics (odds ratio [OR], 4.89; confidence interval [CI], 1.80–13.27; P = .0006). For laparoscopic myomectomy, antibiotic use did not affect the odds of developing SSI (OR, 1.08; CI, 0.35–3.35).
Antibiotics were more likely to be used in certain cases
Antibiotics were more likely to be administered for patients who:
- were obese (body mass index ≥30 kg/m2) (P = .009)
- underwent previous abdominal surgery (P = .001)
- underwent laparotomy (P <.0001)
- had endometrial cavity entry (P <.0001)
- had >1 fibroid (P = .0004) or an aggregate fibroid weight >500 g (P <.0001).
More data on antibiotics for myomectomy
In a retrospective study conducted at 2 academic hospitals in Boston, Massachusetts, 1,211 women underwent myomectomy from 2009 to 2016. (Exclusions were use of vaginal or hysteroscopic myomectomy, chromopertubation, or conversion to hysterectomy.) More than 92% of the women received perioperative antibiotics at the time of surgery. Although demographics were similar between women receiving and not receiving antibiotics, women who received antibiotics were more likely to have longer operative times (median 140 vs 85 min), a greater myoma burden (7 vs 2 myomas removed and weight 255 vs 53 g), and lose blood during the procedure (137 vs 50 mL). These women also were 4 times less likely to have surgical site infection (adjusted OR, 3.77; 95% CI, 1.30–10.97; P = .015).5,6
Banerjee and colleagues say that their California study demonstrates “that the majority of surgeons elect to use antibiotics prophylactically” during myomectomy, despite current ACOG guidelines, and that their findings of benefit for abdominal myomectomy but not for laparoscopic myomectomy should inform future guidance on antibiotics for myomectomy surgery.3
- Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725-730.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 195: prevention of infection after gynecologic procedures. Obstet Gynecol. 2018;131:e172-e189.
- Banerjee D, Dejbakhsh S, Patel HH, et al. Perioperative antibiotic prophylaxis in myomectomy surgery. Paper presented at 49th Annual Meeting of the AAGL; November 2020.
- Uppal S, Harris J, Al-Niaimi A. Prophylactic antibiotic choice and risk of surgical site infection after hysterectomy. Obstet Gynecol. 2016;127:321-329.
- Kim AJ, Clark NV, Jansen LJ, et al. Perioperative antibiotic use and associated infectious outcomes at the time of myomectomy. Obstet Gynecol. 2019;133:626-635.
- Rebar RW. Should perioperative antibiotics at myomectomy be universal? NEJM J Watch. March 11, 2019.
In the 1990s, researchers found that patients undergoing any type of surgical procedure were more than twice as likely to die if they developed postsurgical infection.1 Work to reduce surgical site infection (SSI) has and does continue, with perioperative antibiotics representing a good part of that effort. The American College of Obstetricians and Gynecologists currently recommends such antibiotic therapy for women undergoing laparotomy and laparoscopic hysterectomy.2 ACOG does not, however, recommend prophylactic antibiotics for myomectomy procedures.3 Rates of infection for hysterectomy have been reported to be 3.9% for abdominal and 1.4% for minimally invasive approaches.4
To determine the current use of antibiotics during myomectomy and associated rates of SSI at their institutions, Dipti Banerjee, MD, and colleagues conducted a retrospective analysis of women undergoing laparoscopic or abdominal myomectomy between February 2013 and December 2017 at the University of California, Los Angeles and Hoag Memorial Hospital in Orange County, California. They presented their study results at AAGL’s 49th Global Congress on MIGS, held virtually November 6-14, 2020.3
Rate of SSI after myomectomy
A total of 620 women underwent laparoscopic myomectomy and 563 underwent open myomectomy during the study period. Antibiotics were used in 76.9% of cases. SSI developed within 6 weeks of surgery in 34 women (2.9%) overall. The women undergoing abdominal myomectomy without antibiotics were more likely to experience SSI than the women who received antibiotics (odds ratio [OR], 4.89; confidence interval [CI], 1.80–13.27; P = .0006). For laparoscopic myomectomy, antibiotic use did not affect the odds of developing SSI (OR, 1.08; CI, 0.35–3.35).
Antibiotics were more likely to be used in certain cases
Antibiotics were more likely to be administered for patients who:
- were obese (body mass index ≥30 kg/m2) (P = .009)
- underwent previous abdominal surgery (P = .001)
- underwent laparotomy (P <.0001)
- had endometrial cavity entry (P <.0001)
- had >1 fibroid (P = .0004) or an aggregate fibroid weight >500 g (P <.0001).
More data on antibiotics for myomectomy
In a retrospective study conducted at 2 academic hospitals in Boston, Massachusetts, 1,211 women underwent myomectomy from 2009 to 2016. (Exclusions were use of vaginal or hysteroscopic myomectomy, chromopertubation, or conversion to hysterectomy.) More than 92% of the women received perioperative antibiotics at the time of surgery. Although demographics were similar between women receiving and not receiving antibiotics, women who received antibiotics were more likely to have longer operative times (median 140 vs 85 min), a greater myoma burden (7 vs 2 myomas removed and weight 255 vs 53 g), and lose blood during the procedure (137 vs 50 mL). These women also were 4 times less likely to have surgical site infection (adjusted OR, 3.77; 95% CI, 1.30–10.97; P = .015).5,6
Banerjee and colleagues say that their California study demonstrates “that the majority of surgeons elect to use antibiotics prophylactically” during myomectomy, despite current ACOG guidelines, and that their findings of benefit for abdominal myomectomy but not for laparoscopic myomectomy should inform future guidance on antibiotics for myomectomy surgery.3
In the 1990s, researchers found that patients undergoing any type of surgical procedure were more than twice as likely to die if they developed postsurgical infection.1 Work to reduce surgical site infection (SSI) has and does continue, with perioperative antibiotics representing a good part of that effort. The American College of Obstetricians and Gynecologists currently recommends such antibiotic therapy for women undergoing laparotomy and laparoscopic hysterectomy.2 ACOG does not, however, recommend prophylactic antibiotics for myomectomy procedures.3 Rates of infection for hysterectomy have been reported to be 3.9% for abdominal and 1.4% for minimally invasive approaches.4
To determine the current use of antibiotics during myomectomy and associated rates of SSI at their institutions, Dipti Banerjee, MD, and colleagues conducted a retrospective analysis of women undergoing laparoscopic or abdominal myomectomy between February 2013 and December 2017 at the University of California, Los Angeles and Hoag Memorial Hospital in Orange County, California. They presented their study results at AAGL’s 49th Global Congress on MIGS, held virtually November 6-14, 2020.3
Rate of SSI after myomectomy
A total of 620 women underwent laparoscopic myomectomy and 563 underwent open myomectomy during the study period. Antibiotics were used in 76.9% of cases. SSI developed within 6 weeks of surgery in 34 women (2.9%) overall. The women undergoing abdominal myomectomy without antibiotics were more likely to experience SSI than the women who received antibiotics (odds ratio [OR], 4.89; confidence interval [CI], 1.80–13.27; P = .0006). For laparoscopic myomectomy, antibiotic use did not affect the odds of developing SSI (OR, 1.08; CI, 0.35–3.35).
Antibiotics were more likely to be used in certain cases
Antibiotics were more likely to be administered for patients who:
- were obese (body mass index ≥30 kg/m2) (P = .009)
- underwent previous abdominal surgery (P = .001)
- underwent laparotomy (P <.0001)
- had endometrial cavity entry (P <.0001)
- had >1 fibroid (P = .0004) or an aggregate fibroid weight >500 g (P <.0001).
More data on antibiotics for myomectomy
In a retrospective study conducted at 2 academic hospitals in Boston, Massachusetts, 1,211 women underwent myomectomy from 2009 to 2016. (Exclusions were use of vaginal or hysteroscopic myomectomy, chromopertubation, or conversion to hysterectomy.) More than 92% of the women received perioperative antibiotics at the time of surgery. Although demographics were similar between women receiving and not receiving antibiotics, women who received antibiotics were more likely to have longer operative times (median 140 vs 85 min), a greater myoma burden (7 vs 2 myomas removed and weight 255 vs 53 g), and lose blood during the procedure (137 vs 50 mL). These women also were 4 times less likely to have surgical site infection (adjusted OR, 3.77; 95% CI, 1.30–10.97; P = .015).5,6
Banerjee and colleagues say that their California study demonstrates “that the majority of surgeons elect to use antibiotics prophylactically” during myomectomy, despite current ACOG guidelines, and that their findings of benefit for abdominal myomectomy but not for laparoscopic myomectomy should inform future guidance on antibiotics for myomectomy surgery.3
- Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725-730.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 195: prevention of infection after gynecologic procedures. Obstet Gynecol. 2018;131:e172-e189.
- Banerjee D, Dejbakhsh S, Patel HH, et al. Perioperative antibiotic prophylaxis in myomectomy surgery. Paper presented at 49th Annual Meeting of the AAGL; November 2020.
- Uppal S, Harris J, Al-Niaimi A. Prophylactic antibiotic choice and risk of surgical site infection after hysterectomy. Obstet Gynecol. 2016;127:321-329.
- Kim AJ, Clark NV, Jansen LJ, et al. Perioperative antibiotic use and associated infectious outcomes at the time of myomectomy. Obstet Gynecol. 2019;133:626-635.
- Rebar RW. Should perioperative antibiotics at myomectomy be universal? NEJM J Watch. March 11, 2019.
- Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725-730.
- American College of Obstetricians and Gynecologists. Practice Bulletin No. 195: prevention of infection after gynecologic procedures. Obstet Gynecol. 2018;131:e172-e189.
- Banerjee D, Dejbakhsh S, Patel HH, et al. Perioperative antibiotic prophylaxis in myomectomy surgery. Paper presented at 49th Annual Meeting of the AAGL; November 2020.
- Uppal S, Harris J, Al-Niaimi A. Prophylactic antibiotic choice and risk of surgical site infection after hysterectomy. Obstet Gynecol. 2016;127:321-329.
- Kim AJ, Clark NV, Jansen LJ, et al. Perioperative antibiotic use and associated infectious outcomes at the time of myomectomy. Obstet Gynecol. 2019;133:626-635.
- Rebar RW. Should perioperative antibiotics at myomectomy be universal? NEJM J Watch. March 11, 2019.
FDA clears first drug for rare genetic causes of severe obesity
The Food and Drug Administration has approved setmelanotide (Imcivree, Rhythm Pharmaceuticals) for weight management in adults and children as young as 6 years with obesity because of proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing.
Individuals with these rare genetic causes of severe obesity have a normal weight at birth but develop persistent severe obesity within months because of insatiable hunger (hyperphagia).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for these disorders.
“Many patients and families who live with these diseases face an often-burdensome stigma associated with severe obesity. To manage this obesity and control disruptive food-seeking behavior, caregivers often lock cabinets and refrigerators and significantly limit social activities,” said Jennifer Miller, MD, a pediatric endocrinologist at University of Florida Health, Gainesville, in a press release issued by the company.
“This FDA approval marks an important turning point, providing a much needed therapy and supporting the use of genetic testing to identify and properly diagnose patients with these rare genetic diseases of obesity,” she noted.
David Meeker, MD, chair, president, and CEO of Rhythm Pharmaceuticals, added: “We are advancing a first-in-class, precision medicine that is designed to directly address the underlying cause of obesities driven by genetic deficits in the MC4R pathway.”
Setmelanotide was evaluated in two phase 3 clinical trials. In one trial, 80% of patients with obesity caused by POMC or PCSK1 deficiency achieved greater than 10% weight loss after 1 year of treatment.
In the other trial, 45.5% of patients with obesity caused by LEPR deficiency achieved greater than 10% weight loss with 1 year of treatment.
Results for the two trials were recently published in The Lancet Diabetes & Endocrinology and discussed at the ObesityWeek Interactive 2020 meeting.
Setmelanotide was generally well tolerated in both trials. The most common adverse events were injection-site reactions, skin hyperpigmentation, and nausea.
The drug label notes that disturbances in sexual arousal, depression, and suicidal ideation; skin pigmentation; and darkening of preexisting nevi may occur with setmelanotide treatment.
The drug label also notes a risk for serious adverse reactions because of benzyl alcohol preservative in neonates and low-birth-weight infants. Setmelanotide is not approved for use in neonates or infants.
The company expects the drug to be commercially available in the United States in the first quarter of 2021.
Setmelanotide for the treatment of obesity associated with rare genetic defects had FDA breakthrough therapy designation as well as orphan drug designation.
The company is also evaluating setmelanotide for reduction in hunger and body weight in a pivotal phase 3 trial in people living with Bardet-Biedl or Alström syndrome, and top-line data are due soon.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has approved setmelanotide (Imcivree, Rhythm Pharmaceuticals) for weight management in adults and children as young as 6 years with obesity because of proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing.
Individuals with these rare genetic causes of severe obesity have a normal weight at birth but develop persistent severe obesity within months because of insatiable hunger (hyperphagia).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for these disorders.
“Many patients and families who live with these diseases face an often-burdensome stigma associated with severe obesity. To manage this obesity and control disruptive food-seeking behavior, caregivers often lock cabinets and refrigerators and significantly limit social activities,” said Jennifer Miller, MD, a pediatric endocrinologist at University of Florida Health, Gainesville, in a press release issued by the company.
“This FDA approval marks an important turning point, providing a much needed therapy and supporting the use of genetic testing to identify and properly diagnose patients with these rare genetic diseases of obesity,” she noted.
David Meeker, MD, chair, president, and CEO of Rhythm Pharmaceuticals, added: “We are advancing a first-in-class, precision medicine that is designed to directly address the underlying cause of obesities driven by genetic deficits in the MC4R pathway.”
Setmelanotide was evaluated in two phase 3 clinical trials. In one trial, 80% of patients with obesity caused by POMC or PCSK1 deficiency achieved greater than 10% weight loss after 1 year of treatment.
In the other trial, 45.5% of patients with obesity caused by LEPR deficiency achieved greater than 10% weight loss with 1 year of treatment.
Results for the two trials were recently published in The Lancet Diabetes & Endocrinology and discussed at the ObesityWeek Interactive 2020 meeting.
Setmelanotide was generally well tolerated in both trials. The most common adverse events were injection-site reactions, skin hyperpigmentation, and nausea.
The drug label notes that disturbances in sexual arousal, depression, and suicidal ideation; skin pigmentation; and darkening of preexisting nevi may occur with setmelanotide treatment.
The drug label also notes a risk for serious adverse reactions because of benzyl alcohol preservative in neonates and low-birth-weight infants. Setmelanotide is not approved for use in neonates or infants.
The company expects the drug to be commercially available in the United States in the first quarter of 2021.
Setmelanotide for the treatment of obesity associated with rare genetic defects had FDA breakthrough therapy designation as well as orphan drug designation.
The company is also evaluating setmelanotide for reduction in hunger and body weight in a pivotal phase 3 trial in people living with Bardet-Biedl or Alström syndrome, and top-line data are due soon.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has approved setmelanotide (Imcivree, Rhythm Pharmaceuticals) for weight management in adults and children as young as 6 years with obesity because of proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing.
Individuals with these rare genetic causes of severe obesity have a normal weight at birth but develop persistent severe obesity within months because of insatiable hunger (hyperphagia).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for these disorders.
“Many patients and families who live with these diseases face an often-burdensome stigma associated with severe obesity. To manage this obesity and control disruptive food-seeking behavior, caregivers often lock cabinets and refrigerators and significantly limit social activities,” said Jennifer Miller, MD, a pediatric endocrinologist at University of Florida Health, Gainesville, in a press release issued by the company.
“This FDA approval marks an important turning point, providing a much needed therapy and supporting the use of genetic testing to identify and properly diagnose patients with these rare genetic diseases of obesity,” she noted.
David Meeker, MD, chair, president, and CEO of Rhythm Pharmaceuticals, added: “We are advancing a first-in-class, precision medicine that is designed to directly address the underlying cause of obesities driven by genetic deficits in the MC4R pathway.”
Setmelanotide was evaluated in two phase 3 clinical trials. In one trial, 80% of patients with obesity caused by POMC or PCSK1 deficiency achieved greater than 10% weight loss after 1 year of treatment.
In the other trial, 45.5% of patients with obesity caused by LEPR deficiency achieved greater than 10% weight loss with 1 year of treatment.
Results for the two trials were recently published in The Lancet Diabetes & Endocrinology and discussed at the ObesityWeek Interactive 2020 meeting.
Setmelanotide was generally well tolerated in both trials. The most common adverse events were injection-site reactions, skin hyperpigmentation, and nausea.
The drug label notes that disturbances in sexual arousal, depression, and suicidal ideation; skin pigmentation; and darkening of preexisting nevi may occur with setmelanotide treatment.
The drug label also notes a risk for serious adverse reactions because of benzyl alcohol preservative in neonates and low-birth-weight infants. Setmelanotide is not approved for use in neonates or infants.
The company expects the drug to be commercially available in the United States in the first quarter of 2021.
Setmelanotide for the treatment of obesity associated with rare genetic defects had FDA breakthrough therapy designation as well as orphan drug designation.
The company is also evaluating setmelanotide for reduction in hunger and body weight in a pivotal phase 3 trial in people living with Bardet-Biedl or Alström syndrome, and top-line data are due soon.
A version of this article originally appeared on Medscape.com.
VTE prophylaxis is feasible, effective in some high-risk cancer patients
Primary thromboprophylaxis is feasible and worth considering for high-risk ambulatory patients with cancer who are initiating systemic chemotherapy, according to Marc Carrier, MD.
Risk scores can identify patients at high risk for venous thromboembolism (VTE), and treatments that are effective and associated with low bleeding risk are available, Dr. Carrier explained at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
However, caution is advised in patients with certain types of cancer, including some gastrointestinal and genitourinary cancers, because of the possibility of increased major and clinically relevant nonmajor bleeding risk, he said.
VTE and cancer
VTE is relatively rare in the general population, occurring in about 1 or 2 per 1,000 people annually. The risk increases 4.1-fold in patients with cancer, and 6.5-fold in patients with cancer receiving chemotherapy.
“So just putting these numbers together, we’re no longer talking about 1 in 1,000, but 1 in 200, so [this is] something that is very common among cancer patients,” said Dr. Carrier, a professor at the University of Ottawa and chief of the division of hematology at The Ottawa Hospital.
The mortality rate associated with cancer-associated thrombosis is about 9%, comparable to that associated with infection in the cancer outpatient setting, which underscores the importance of educating patients about the signs and symptoms of VTE so they can seek medical treatment quickly if necessary, he added.
It may also be useful to discuss prophylaxis or other ways to prevent venous thromboembolic complications with certain patients, he said, noting that in an observational cohort study of nearly 600 patients at the University of Ottawa, 25% of those initiating chemotherapy were identified as intermediate or high risk using the validated Khorana risk score, and thus would likely benefit from thromboprophylaxis.
Risk assessment
The Khorana risk score assesses VTE risk based on cancer site, blood counts, and body mass index. It is simple to use and has been validated in more than 20,000 people in multiple countries, Dr. Carrier said.
In a well-known validation study, Ay et al. showed a VTE complication rate of 10% in patients with a Khorana risk score of 2 or higher who were followed up to 6 months.
“This is huge,” Dr. Carrier stressed. “This is much higher than what we tolerate for all sorts of different populations for which we would recommend anticoagulation or thromboprophylaxis.”
The question is whether the risk score can be helpful in a real-world clinic setting, he said, adding: “I’d like to think the answer to that is yes.”
In the University of Ottawa cohort study, 11% of high-risk patients experienced a VTE complication, compared with 4% of those with lower risk, suggesting that the validation data for the Khorana risk score is not only accurate, it is “actually applicable in real-world practice, and you can use it in your own center,” he said.
Further, recent studies have demonstrated that treatment based on Khorana risk score assessment reduces VTE complications.
Prophylaxis options
Low-molecular-weight heparin (LMWH) has been shown in several studies to be associated with a significant relative VTE risk reduction in patients with cancer initiating chemotherapy – with only a slight, nonsignificant increase in the risk of major bleeding.
However, the absolute benefit was small, and LMWH is “parenteral, relatively costly, and, based on that, although we showed relatively good risk-benefit ratio, it never really got translated to clinical practice,” Dr. Carrier said.
In fact, a 2015 American Society of Clinical Oncology guidelines update recommended against routine thromboprophylaxis in this setting, but stated that it could be considered in select high-risk patients identified using a validated risk-assessment tool.
The guidelines noted that “individual risk factors such as biomarkers and cancer site don’t reliably identify high-risk patients.”
More recent data provide additional support for risk assessment and treatment based on Khorana risk score of 2 or higher.
The AVERT trial, for which Dr. Carrier was the first author, showed that the direct-acting oral anticoagulant (DOAC) apixaban reduced VTE incidence, compared with placebo, in patients with Khorana score of 2 or higher (4.2% vs. 10.2%; hazard ratio, 0.41 overall, and 1.0 vs. 7.3; HR, 0.14 on treatment), and the CASSINI trial showed that another DOAC, rivaroxaban, reduced VTE incidence, compared with placebo, in those with Khorana score of 2 or higher (5.9 vs. 6.7; HR, 0.6 overall, and 2.6 vs. 6.4; HR, 0.40 on treatment). The differences in the on-treatment populations were statistically significant.
The two trials, which included a variety of tumor types, showed similar rates of major bleeding, with an absolute difference of about 1% between treatment and placebo, which was not statistically significant in the on-treatment analyses (HR, 1.89 in AVERT and HR, 1.96 in CASSINI).
A systematic review of these trials showed an overall significant decrease in VTE complication risk with treatment in high-risk patients, and a nonstatistically significant major bleeding risk increase.
Based on these findings, ASCO guidelines were updated in 2020 to state that “routine thromboprophylaxis should not be offered to all patients with cancer. ... However, high-risk outpatients with cancer may be offered thromboprophylaxis with apixaban, rivaroxaban or LMWH, providing there are no significant risk factors for bleeding or drug-drug interactions, and after having a full discussion with patients ... to make sure they understand the risk-benefit ratio and the rationale for that particular recommendation,” he said.
Real-world implementation
Implementing this approach in the clinic setting requires a practical model, such as the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTEPACC) program, a prospective quality improvement research initiative developed in collaboration with the Jeffords Institute for Quality at the University of Vermont Medical Center and described in a recent report, Dr. Carrier said.
The “Vermont model” is “really a comprehensive model that includes identifying patients with the electronic medical records, gathering the formal education and insight from other health care providers like pharmacists and nurses in order to really come up with personalized care for your patients,” he explained.
In 918 outpatients with cancer who were included in the program, VTE awareness increased from less than 5% before VTEPACC to nearly 82% during the implementation phase and 94.7% after 2 years, with nearly 94% of high-risk patients receiving VTE prophylaxis at that time.
“So we can certainly do that in our own center.” he said. “It’s a matter of coming up with the model and making sure that the patients are seen at the right time.”
Given the high frequency of VTE in patients with cancer initiating chemotherapy, the usefulness of risk scores such as the Khorana risk score for identifying those at high risk, and the availability of safe and effective interventions for reducing risk, “we should probably use the data and incorporate them into clinical practice by implementation of programs for primary prevention,” he said.
A word of caution
Caution is warranted, however, when it comes to using DOACs in patients with higher-risk or potentially higher-risk tumor types, he added.
“It’s an important question we are facing as clinicians on a daily basis,” he said, responding to an attendee’s query, as shared by session moderator James Douketis, MD, professor of medicine at McMaster University, Hamilton, Ont., regarding possible bleeding risks in certain genitourinary cancers.
A recent meta-analysis published in Nature, for example, noted that, in the SELECT-D trial, rivaroxaban was associated with significantly higher incidence of clinically relevant nonmajor bleeding, most often in bladder and colorectal cancers, and most often at genitourinary and gastrointestinal sites.
Both Dr. Carrier and fellow panelist Michael Streiff, MD, professor of medicine at Johns Hopkins University and medical director at the Johns Hopkins Hospital Special Coagulation Laboratory, Baltimore, said they approach DOAC use cautiously, but don’t rule it out entirely, in patients with unresected genitourinary tumors that could pose a risk of bleeding.
“It’s worth mentioning and being cautious. In my own personal practice, I’m very careful with unresected urothelial-type tumors or, for example, bladder cancer, for the same reason as [with] unresected luminal GI tumors,” Dr. Carrier said, adding that he’s also mindful that patients with nephropathy were excluded from U.S. DOAC trials because of bleeding risk.
He said he sometimes tries a LMWH challenge first in higher-risk patients, and then might try a DOAC if no bleeding occurs.
“But it certainly is controversial,” he noted.
Dr. Streiff added that he also worries less with genitourinary cancers than with upper GI lesions because “the signals weren’t as big as in GI” cancers, but he noted that “the drugs are going out through the kidneys ... so I’m cautious in those populations.”
“So caution, but not complete exclusion, is the operative management,” Dr. Douketis said, summarizing the panelists’ consensus.
Dr. Carrier reported clinical trial or advisory board participation for Bayer, Pfizer, Servier, Leo Pharma, and/or BMS.
Primary thromboprophylaxis is feasible and worth considering for high-risk ambulatory patients with cancer who are initiating systemic chemotherapy, according to Marc Carrier, MD.
Risk scores can identify patients at high risk for venous thromboembolism (VTE), and treatments that are effective and associated with low bleeding risk are available, Dr. Carrier explained at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
However, caution is advised in patients with certain types of cancer, including some gastrointestinal and genitourinary cancers, because of the possibility of increased major and clinically relevant nonmajor bleeding risk, he said.
VTE and cancer
VTE is relatively rare in the general population, occurring in about 1 or 2 per 1,000 people annually. The risk increases 4.1-fold in patients with cancer, and 6.5-fold in patients with cancer receiving chemotherapy.
“So just putting these numbers together, we’re no longer talking about 1 in 1,000, but 1 in 200, so [this is] something that is very common among cancer patients,” said Dr. Carrier, a professor at the University of Ottawa and chief of the division of hematology at The Ottawa Hospital.
The mortality rate associated with cancer-associated thrombosis is about 9%, comparable to that associated with infection in the cancer outpatient setting, which underscores the importance of educating patients about the signs and symptoms of VTE so they can seek medical treatment quickly if necessary, he added.
It may also be useful to discuss prophylaxis or other ways to prevent venous thromboembolic complications with certain patients, he said, noting that in an observational cohort study of nearly 600 patients at the University of Ottawa, 25% of those initiating chemotherapy were identified as intermediate or high risk using the validated Khorana risk score, and thus would likely benefit from thromboprophylaxis.
Risk assessment
The Khorana risk score assesses VTE risk based on cancer site, blood counts, and body mass index. It is simple to use and has been validated in more than 20,000 people in multiple countries, Dr. Carrier said.
In a well-known validation study, Ay et al. showed a VTE complication rate of 10% in patients with a Khorana risk score of 2 or higher who were followed up to 6 months.
“This is huge,” Dr. Carrier stressed. “This is much higher than what we tolerate for all sorts of different populations for which we would recommend anticoagulation or thromboprophylaxis.”
The question is whether the risk score can be helpful in a real-world clinic setting, he said, adding: “I’d like to think the answer to that is yes.”
In the University of Ottawa cohort study, 11% of high-risk patients experienced a VTE complication, compared with 4% of those with lower risk, suggesting that the validation data for the Khorana risk score is not only accurate, it is “actually applicable in real-world practice, and you can use it in your own center,” he said.
Further, recent studies have demonstrated that treatment based on Khorana risk score assessment reduces VTE complications.
Prophylaxis options
Low-molecular-weight heparin (LMWH) has been shown in several studies to be associated with a significant relative VTE risk reduction in patients with cancer initiating chemotherapy – with only a slight, nonsignificant increase in the risk of major bleeding.
However, the absolute benefit was small, and LMWH is “parenteral, relatively costly, and, based on that, although we showed relatively good risk-benefit ratio, it never really got translated to clinical practice,” Dr. Carrier said.
In fact, a 2015 American Society of Clinical Oncology guidelines update recommended against routine thromboprophylaxis in this setting, but stated that it could be considered in select high-risk patients identified using a validated risk-assessment tool.
The guidelines noted that “individual risk factors such as biomarkers and cancer site don’t reliably identify high-risk patients.”
More recent data provide additional support for risk assessment and treatment based on Khorana risk score of 2 or higher.
The AVERT trial, for which Dr. Carrier was the first author, showed that the direct-acting oral anticoagulant (DOAC) apixaban reduced VTE incidence, compared with placebo, in patients with Khorana score of 2 or higher (4.2% vs. 10.2%; hazard ratio, 0.41 overall, and 1.0 vs. 7.3; HR, 0.14 on treatment), and the CASSINI trial showed that another DOAC, rivaroxaban, reduced VTE incidence, compared with placebo, in those with Khorana score of 2 or higher (5.9 vs. 6.7; HR, 0.6 overall, and 2.6 vs. 6.4; HR, 0.40 on treatment). The differences in the on-treatment populations were statistically significant.
The two trials, which included a variety of tumor types, showed similar rates of major bleeding, with an absolute difference of about 1% between treatment and placebo, which was not statistically significant in the on-treatment analyses (HR, 1.89 in AVERT and HR, 1.96 in CASSINI).
A systematic review of these trials showed an overall significant decrease in VTE complication risk with treatment in high-risk patients, and a nonstatistically significant major bleeding risk increase.
Based on these findings, ASCO guidelines were updated in 2020 to state that “routine thromboprophylaxis should not be offered to all patients with cancer. ... However, high-risk outpatients with cancer may be offered thromboprophylaxis with apixaban, rivaroxaban or LMWH, providing there are no significant risk factors for bleeding or drug-drug interactions, and after having a full discussion with patients ... to make sure they understand the risk-benefit ratio and the rationale for that particular recommendation,” he said.
Real-world implementation
Implementing this approach in the clinic setting requires a practical model, such as the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTEPACC) program, a prospective quality improvement research initiative developed in collaboration with the Jeffords Institute for Quality at the University of Vermont Medical Center and described in a recent report, Dr. Carrier said.
The “Vermont model” is “really a comprehensive model that includes identifying patients with the electronic medical records, gathering the formal education and insight from other health care providers like pharmacists and nurses in order to really come up with personalized care for your patients,” he explained.
In 918 outpatients with cancer who were included in the program, VTE awareness increased from less than 5% before VTEPACC to nearly 82% during the implementation phase and 94.7% after 2 years, with nearly 94% of high-risk patients receiving VTE prophylaxis at that time.
“So we can certainly do that in our own center.” he said. “It’s a matter of coming up with the model and making sure that the patients are seen at the right time.”
Given the high frequency of VTE in patients with cancer initiating chemotherapy, the usefulness of risk scores such as the Khorana risk score for identifying those at high risk, and the availability of safe and effective interventions for reducing risk, “we should probably use the data and incorporate them into clinical practice by implementation of programs for primary prevention,” he said.
A word of caution
Caution is warranted, however, when it comes to using DOACs in patients with higher-risk or potentially higher-risk tumor types, he added.
“It’s an important question we are facing as clinicians on a daily basis,” he said, responding to an attendee’s query, as shared by session moderator James Douketis, MD, professor of medicine at McMaster University, Hamilton, Ont., regarding possible bleeding risks in certain genitourinary cancers.
A recent meta-analysis published in Nature, for example, noted that, in the SELECT-D trial, rivaroxaban was associated with significantly higher incidence of clinically relevant nonmajor bleeding, most often in bladder and colorectal cancers, and most often at genitourinary and gastrointestinal sites.
Both Dr. Carrier and fellow panelist Michael Streiff, MD, professor of medicine at Johns Hopkins University and medical director at the Johns Hopkins Hospital Special Coagulation Laboratory, Baltimore, said they approach DOAC use cautiously, but don’t rule it out entirely, in patients with unresected genitourinary tumors that could pose a risk of bleeding.
“It’s worth mentioning and being cautious. In my own personal practice, I’m very careful with unresected urothelial-type tumors or, for example, bladder cancer, for the same reason as [with] unresected luminal GI tumors,” Dr. Carrier said, adding that he’s also mindful that patients with nephropathy were excluded from U.S. DOAC trials because of bleeding risk.
He said he sometimes tries a LMWH challenge first in higher-risk patients, and then might try a DOAC if no bleeding occurs.
“But it certainly is controversial,” he noted.
Dr. Streiff added that he also worries less with genitourinary cancers than with upper GI lesions because “the signals weren’t as big as in GI” cancers, but he noted that “the drugs are going out through the kidneys ... so I’m cautious in those populations.”
“So caution, but not complete exclusion, is the operative management,” Dr. Douketis said, summarizing the panelists’ consensus.
Dr. Carrier reported clinical trial or advisory board participation for Bayer, Pfizer, Servier, Leo Pharma, and/or BMS.
Primary thromboprophylaxis is feasible and worth considering for high-risk ambulatory patients with cancer who are initiating systemic chemotherapy, according to Marc Carrier, MD.
Risk scores can identify patients at high risk for venous thromboembolism (VTE), and treatments that are effective and associated with low bleeding risk are available, Dr. Carrier explained at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
However, caution is advised in patients with certain types of cancer, including some gastrointestinal and genitourinary cancers, because of the possibility of increased major and clinically relevant nonmajor bleeding risk, he said.
VTE and cancer
VTE is relatively rare in the general population, occurring in about 1 or 2 per 1,000 people annually. The risk increases 4.1-fold in patients with cancer, and 6.5-fold in patients with cancer receiving chemotherapy.
“So just putting these numbers together, we’re no longer talking about 1 in 1,000, but 1 in 200, so [this is] something that is very common among cancer patients,” said Dr. Carrier, a professor at the University of Ottawa and chief of the division of hematology at The Ottawa Hospital.
The mortality rate associated with cancer-associated thrombosis is about 9%, comparable to that associated with infection in the cancer outpatient setting, which underscores the importance of educating patients about the signs and symptoms of VTE so they can seek medical treatment quickly if necessary, he added.
It may also be useful to discuss prophylaxis or other ways to prevent venous thromboembolic complications with certain patients, he said, noting that in an observational cohort study of nearly 600 patients at the University of Ottawa, 25% of those initiating chemotherapy were identified as intermediate or high risk using the validated Khorana risk score, and thus would likely benefit from thromboprophylaxis.
Risk assessment
The Khorana risk score assesses VTE risk based on cancer site, blood counts, and body mass index. It is simple to use and has been validated in more than 20,000 people in multiple countries, Dr. Carrier said.
In a well-known validation study, Ay et al. showed a VTE complication rate of 10% in patients with a Khorana risk score of 2 or higher who were followed up to 6 months.
“This is huge,” Dr. Carrier stressed. “This is much higher than what we tolerate for all sorts of different populations for which we would recommend anticoagulation or thromboprophylaxis.”
The question is whether the risk score can be helpful in a real-world clinic setting, he said, adding: “I’d like to think the answer to that is yes.”
In the University of Ottawa cohort study, 11% of high-risk patients experienced a VTE complication, compared with 4% of those with lower risk, suggesting that the validation data for the Khorana risk score is not only accurate, it is “actually applicable in real-world practice, and you can use it in your own center,” he said.
Further, recent studies have demonstrated that treatment based on Khorana risk score assessment reduces VTE complications.
Prophylaxis options
Low-molecular-weight heparin (LMWH) has been shown in several studies to be associated with a significant relative VTE risk reduction in patients with cancer initiating chemotherapy – with only a slight, nonsignificant increase in the risk of major bleeding.
However, the absolute benefit was small, and LMWH is “parenteral, relatively costly, and, based on that, although we showed relatively good risk-benefit ratio, it never really got translated to clinical practice,” Dr. Carrier said.
In fact, a 2015 American Society of Clinical Oncology guidelines update recommended against routine thromboprophylaxis in this setting, but stated that it could be considered in select high-risk patients identified using a validated risk-assessment tool.
The guidelines noted that “individual risk factors such as biomarkers and cancer site don’t reliably identify high-risk patients.”
More recent data provide additional support for risk assessment and treatment based on Khorana risk score of 2 or higher.
The AVERT trial, for which Dr. Carrier was the first author, showed that the direct-acting oral anticoagulant (DOAC) apixaban reduced VTE incidence, compared with placebo, in patients with Khorana score of 2 or higher (4.2% vs. 10.2%; hazard ratio, 0.41 overall, and 1.0 vs. 7.3; HR, 0.14 on treatment), and the CASSINI trial showed that another DOAC, rivaroxaban, reduced VTE incidence, compared with placebo, in those with Khorana score of 2 or higher (5.9 vs. 6.7; HR, 0.6 overall, and 2.6 vs. 6.4; HR, 0.40 on treatment). The differences in the on-treatment populations were statistically significant.
The two trials, which included a variety of tumor types, showed similar rates of major bleeding, with an absolute difference of about 1% between treatment and placebo, which was not statistically significant in the on-treatment analyses (HR, 1.89 in AVERT and HR, 1.96 in CASSINI).
A systematic review of these trials showed an overall significant decrease in VTE complication risk with treatment in high-risk patients, and a nonstatistically significant major bleeding risk increase.
Based on these findings, ASCO guidelines were updated in 2020 to state that “routine thromboprophylaxis should not be offered to all patients with cancer. ... However, high-risk outpatients with cancer may be offered thromboprophylaxis with apixaban, rivaroxaban or LMWH, providing there are no significant risk factors for bleeding or drug-drug interactions, and after having a full discussion with patients ... to make sure they understand the risk-benefit ratio and the rationale for that particular recommendation,” he said.
Real-world implementation
Implementing this approach in the clinic setting requires a practical model, such as the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTEPACC) program, a prospective quality improvement research initiative developed in collaboration with the Jeffords Institute for Quality at the University of Vermont Medical Center and described in a recent report, Dr. Carrier said.
The “Vermont model” is “really a comprehensive model that includes identifying patients with the electronic medical records, gathering the formal education and insight from other health care providers like pharmacists and nurses in order to really come up with personalized care for your patients,” he explained.
In 918 outpatients with cancer who were included in the program, VTE awareness increased from less than 5% before VTEPACC to nearly 82% during the implementation phase and 94.7% after 2 years, with nearly 94% of high-risk patients receiving VTE prophylaxis at that time.
“So we can certainly do that in our own center.” he said. “It’s a matter of coming up with the model and making sure that the patients are seen at the right time.”
Given the high frequency of VTE in patients with cancer initiating chemotherapy, the usefulness of risk scores such as the Khorana risk score for identifying those at high risk, and the availability of safe and effective interventions for reducing risk, “we should probably use the data and incorporate them into clinical practice by implementation of programs for primary prevention,” he said.
A word of caution
Caution is warranted, however, when it comes to using DOACs in patients with higher-risk or potentially higher-risk tumor types, he added.
“It’s an important question we are facing as clinicians on a daily basis,” he said, responding to an attendee’s query, as shared by session moderator James Douketis, MD, professor of medicine at McMaster University, Hamilton, Ont., regarding possible bleeding risks in certain genitourinary cancers.
A recent meta-analysis published in Nature, for example, noted that, in the SELECT-D trial, rivaroxaban was associated with significantly higher incidence of clinically relevant nonmajor bleeding, most often in bladder and colorectal cancers, and most often at genitourinary and gastrointestinal sites.
Both Dr. Carrier and fellow panelist Michael Streiff, MD, professor of medicine at Johns Hopkins University and medical director at the Johns Hopkins Hospital Special Coagulation Laboratory, Baltimore, said they approach DOAC use cautiously, but don’t rule it out entirely, in patients with unresected genitourinary tumors that could pose a risk of bleeding.
“It’s worth mentioning and being cautious. In my own personal practice, I’m very careful with unresected urothelial-type tumors or, for example, bladder cancer, for the same reason as [with] unresected luminal GI tumors,” Dr. Carrier said, adding that he’s also mindful that patients with nephropathy were excluded from U.S. DOAC trials because of bleeding risk.
He said he sometimes tries a LMWH challenge first in higher-risk patients, and then might try a DOAC if no bleeding occurs.
“But it certainly is controversial,” he noted.
Dr. Streiff added that he also worries less with genitourinary cancers than with upper GI lesions because “the signals weren’t as big as in GI” cancers, but he noted that “the drugs are going out through the kidneys ... so I’m cautious in those populations.”
“So caution, but not complete exclusion, is the operative management,” Dr. Douketis said, summarizing the panelists’ consensus.
Dr. Carrier reported clinical trial or advisory board participation for Bayer, Pfizer, Servier, Leo Pharma, and/or BMS.
FROM THE THSNA BIENNIAL SUMMIT
Vaginal cleansing protocol curbs deep SSIs after cesarean
reported Johanna Quist-Nelson, MD, of the University of North Carolina, Chapel Hill.
“Surgical site infections after a cesarean delivery are more common if the patient is in labor or has ruptured membranes,” she said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists..
Two options to decrease the risk of SSIs after cesarean for those patients in labor or with ruptured membranes are vaginal cleansing and azithromycin, given in addition to preoperative antibiotics, Dr. Quist-Nelson said. She and her colleagues conducted a quality improvement study of the effects of a stepwise implementation of vaginal cleansing and azithromycin to reduce SSIs at cesarean delivery in this high-risk population. The data were collected from 2016 to 2019 at Thomas Jefferson University, Philadelphia.
“We aimed to decrease our SSI rate by 30% by adopting an intervention of cleansing followed by azithromycin,” she said.
The researchers added vaginal cleansing to the SSI prevention protocol in January 2017, with the addition of azithromycin in March 2018. Vaginal cleansing involved 30 seconds of anterior to posterior cleaning prior to urinary catheter placement. Azithromycin was given at a dose of 500 mg intravenously in addition to preoperative antibiotics and within an hour of cesarean delivery.
A total of 1,033 deliveries qualified for the study by being in labor or with ruptured membranes; of these 291 were performed prior to the interventions, 335 received vaginal cleansing only, and 407 received vaginal cleansing and azithromycin. The average age of the participants was 30 years; approximately 42% were Black, and 32% were White.
Cleansing protocol reduces SSIs
Overall, the rate of SSIs was 22% in the standard care group, 17% in the vaginal cleansing group, and 15% in the vaginal cleansing plus azithromycin group. When broken down by infection type, no deep SSI occurred in the vaginal cleansing or cleansing plus azithromycin group, compared with 2% of the standard care group (P = .009). In addition, endometritis, which is an organ-space SSI, was significantly lower in the cleansing group (10%) and the cleansing plus azithromycin group (11%), compared with the standard care group (16%).
The study findings were limited by factors including the use of EMRs for collection of data, and given that it is a quality improvement study, there is a potential lack of generalizability to other institutions. The study focused on patients at high risk for SSI and the use of the Plan-Do-Study-Act (PDSA) method of conducting the research, Dr. Quist-Nelson said. Compared with standard care, the implementation of vaginal cleansing reduced the SSI rate by 33%, with no significantly further change in SSI after the addition of azithromycin, she concluded.
Data sharing boosts compliance
In a question-and-answer session, Dr. Quist-Nelson noted that povidone iodine (Betadine) was chosen for vaginal cleansing because it was easily accessible at her institution, but that patients with allergies were given chlorhexidine. The cleansing itself was “primarily vaginal, not a full vulvar cleansing,” she clarified. The cleansing was performed immediately before catheter placement and included the urethra.
When asked about strategies to increase compliance, Dr. Quist-Nelson noted that sharing data was valuable, namely “reporting to our group the current compliance,” as well as sharing information by email and discussing it during multidisciplinary rounds.
The study was a quality improvement project and not a randomized trial, so the researchers were not able to tease out the impact of vaginal cleansing from the impact of azithromycin, Dr. Quist-Nelson said.
Based on her results, Dr. Quist-Nelson said she would recommend the protocol for use in patients who require cesarean delivery after being in labor or having ruptured membranes, and that “there are trials to support the use of both interventions.”
The results suggest opportunities for further randomized trials, including examination of the use of oral versus IV azithromycin, she added.
The study received no outside funding. Dr. Quist-Nelson had no financial conflicts to disclose.
reported Johanna Quist-Nelson, MD, of the University of North Carolina, Chapel Hill.
“Surgical site infections after a cesarean delivery are more common if the patient is in labor or has ruptured membranes,” she said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists..
Two options to decrease the risk of SSIs after cesarean for those patients in labor or with ruptured membranes are vaginal cleansing and azithromycin, given in addition to preoperative antibiotics, Dr. Quist-Nelson said. She and her colleagues conducted a quality improvement study of the effects of a stepwise implementation of vaginal cleansing and azithromycin to reduce SSIs at cesarean delivery in this high-risk population. The data were collected from 2016 to 2019 at Thomas Jefferson University, Philadelphia.
“We aimed to decrease our SSI rate by 30% by adopting an intervention of cleansing followed by azithromycin,” she said.
The researchers added vaginal cleansing to the SSI prevention protocol in January 2017, with the addition of azithromycin in March 2018. Vaginal cleansing involved 30 seconds of anterior to posterior cleaning prior to urinary catheter placement. Azithromycin was given at a dose of 500 mg intravenously in addition to preoperative antibiotics and within an hour of cesarean delivery.
A total of 1,033 deliveries qualified for the study by being in labor or with ruptured membranes; of these 291 were performed prior to the interventions, 335 received vaginal cleansing only, and 407 received vaginal cleansing and azithromycin. The average age of the participants was 30 years; approximately 42% were Black, and 32% were White.
Cleansing protocol reduces SSIs
Overall, the rate of SSIs was 22% in the standard care group, 17% in the vaginal cleansing group, and 15% in the vaginal cleansing plus azithromycin group. When broken down by infection type, no deep SSI occurred in the vaginal cleansing or cleansing plus azithromycin group, compared with 2% of the standard care group (P = .009). In addition, endometritis, which is an organ-space SSI, was significantly lower in the cleansing group (10%) and the cleansing plus azithromycin group (11%), compared with the standard care group (16%).
The study findings were limited by factors including the use of EMRs for collection of data, and given that it is a quality improvement study, there is a potential lack of generalizability to other institutions. The study focused on patients at high risk for SSI and the use of the Plan-Do-Study-Act (PDSA) method of conducting the research, Dr. Quist-Nelson said. Compared with standard care, the implementation of vaginal cleansing reduced the SSI rate by 33%, with no significantly further change in SSI after the addition of azithromycin, she concluded.
Data sharing boosts compliance
In a question-and-answer session, Dr. Quist-Nelson noted that povidone iodine (Betadine) was chosen for vaginal cleansing because it was easily accessible at her institution, but that patients with allergies were given chlorhexidine. The cleansing itself was “primarily vaginal, not a full vulvar cleansing,” she clarified. The cleansing was performed immediately before catheter placement and included the urethra.
When asked about strategies to increase compliance, Dr. Quist-Nelson noted that sharing data was valuable, namely “reporting to our group the current compliance,” as well as sharing information by email and discussing it during multidisciplinary rounds.
The study was a quality improvement project and not a randomized trial, so the researchers were not able to tease out the impact of vaginal cleansing from the impact of azithromycin, Dr. Quist-Nelson said.
Based on her results, Dr. Quist-Nelson said she would recommend the protocol for use in patients who require cesarean delivery after being in labor or having ruptured membranes, and that “there are trials to support the use of both interventions.”
The results suggest opportunities for further randomized trials, including examination of the use of oral versus IV azithromycin, she added.
The study received no outside funding. Dr. Quist-Nelson had no financial conflicts to disclose.
reported Johanna Quist-Nelson, MD, of the University of North Carolina, Chapel Hill.
“Surgical site infections after a cesarean delivery are more common if the patient is in labor or has ruptured membranes,” she said at the 2020 virtual meeting of the American College of Obstetricians and Gynecologists..
Two options to decrease the risk of SSIs after cesarean for those patients in labor or with ruptured membranes are vaginal cleansing and azithromycin, given in addition to preoperative antibiotics, Dr. Quist-Nelson said. She and her colleagues conducted a quality improvement study of the effects of a stepwise implementation of vaginal cleansing and azithromycin to reduce SSIs at cesarean delivery in this high-risk population. The data were collected from 2016 to 2019 at Thomas Jefferson University, Philadelphia.
“We aimed to decrease our SSI rate by 30% by adopting an intervention of cleansing followed by azithromycin,” she said.
The researchers added vaginal cleansing to the SSI prevention protocol in January 2017, with the addition of azithromycin in March 2018. Vaginal cleansing involved 30 seconds of anterior to posterior cleaning prior to urinary catheter placement. Azithromycin was given at a dose of 500 mg intravenously in addition to preoperative antibiotics and within an hour of cesarean delivery.
A total of 1,033 deliveries qualified for the study by being in labor or with ruptured membranes; of these 291 were performed prior to the interventions, 335 received vaginal cleansing only, and 407 received vaginal cleansing and azithromycin. The average age of the participants was 30 years; approximately 42% were Black, and 32% were White.
Cleansing protocol reduces SSIs
Overall, the rate of SSIs was 22% in the standard care group, 17% in the vaginal cleansing group, and 15% in the vaginal cleansing plus azithromycin group. When broken down by infection type, no deep SSI occurred in the vaginal cleansing or cleansing plus azithromycin group, compared with 2% of the standard care group (P = .009). In addition, endometritis, which is an organ-space SSI, was significantly lower in the cleansing group (10%) and the cleansing plus azithromycin group (11%), compared with the standard care group (16%).
The study findings were limited by factors including the use of EMRs for collection of data, and given that it is a quality improvement study, there is a potential lack of generalizability to other institutions. The study focused on patients at high risk for SSI and the use of the Plan-Do-Study-Act (PDSA) method of conducting the research, Dr. Quist-Nelson said. Compared with standard care, the implementation of vaginal cleansing reduced the SSI rate by 33%, with no significantly further change in SSI after the addition of azithromycin, she concluded.
Data sharing boosts compliance
In a question-and-answer session, Dr. Quist-Nelson noted that povidone iodine (Betadine) was chosen for vaginal cleansing because it was easily accessible at her institution, but that patients with allergies were given chlorhexidine. The cleansing itself was “primarily vaginal, not a full vulvar cleansing,” she clarified. The cleansing was performed immediately before catheter placement and included the urethra.
When asked about strategies to increase compliance, Dr. Quist-Nelson noted that sharing data was valuable, namely “reporting to our group the current compliance,” as well as sharing information by email and discussing it during multidisciplinary rounds.
The study was a quality improvement project and not a randomized trial, so the researchers were not able to tease out the impact of vaginal cleansing from the impact of azithromycin, Dr. Quist-Nelson said.
Based on her results, Dr. Quist-Nelson said she would recommend the protocol for use in patients who require cesarean delivery after being in labor or having ruptured membranes, and that “there are trials to support the use of both interventions.”
The results suggest opportunities for further randomized trials, including examination of the use of oral versus IV azithromycin, she added.
The study received no outside funding. Dr. Quist-Nelson had no financial conflicts to disclose.
FROM ACOG 2020
Patient with CKD: Contrast or no contrast?
A 67-year-old man with stage 3 chronic kidney disease (CKD) develops abdominal pain over 24 hours. He has had low grade fevers and nausea. He has a history of colon cancer and had a resection four years ago. Abdominal exam reveals tenderness to palpation, including rebound tenderness in his right lower quadrant. Labs: hemoglobin: 13; hematocrit: 39; white blood cells: 18,000; platelets: 333; blood urea nitrogen: 28; creatinine: 1.8 (estimated glomerular filtration rate: 37); sodium: 136; potassium: 3.9; bicarbonate: 24; chlorine: 105; and lipase: 10.
What testing would you recommend?
A) Ultrasound
B) Non contrast computed tomography (CT)
C) Contrast CT
D) MRI without gadolinium
The correct answer here is to get a contrast CT scan, as it will give you the most appropriate diagnostic information.
For years, we have hesitated to order contrast studies in our patients with CKD, for fear of causing contrast-induced nephrotoxicity. We might choose less helpful studies that avoid contrast, or might not obtain imaging that is needed. Over the years I have especially seen this in the case of avoiding computed tomography angiography (CTA) for evaluation of pulmonary embolus and choosing the much less useful ventilation/perfusion scan. The problem arises with the fact that patients with CKD are more likely to develop worsening renal function when they get sick.
Lee and colleagues performed an analysis of six retrospective studies involving a total of 55,963 participants. They found that patients with CKD receiving contrast material did not have an increased risk of deteriorating renal function compared with those without CKD (odds ratio, 1.07; 95% confidence interval, 0.98-1.17).1
The early studies reporting contrast-induced renal disease were in patients who received high osmolality contrast agents.2 Most patients now receive low osmolality agents, with less nephrotoxicity.3
Key points of guidelines
This year, the American College of Radiology and the National Kidney Foundation put out joint guidelines that helped clarify why there is a diminished concern for contrast-induced kidney disease in the modern era.4 Below are some of the key points of these guidelines:
- The risk of contrast-induced acute kidney injury (AKI) from intravenous iodinated contrast media is lower than previously thought.
- Necessary contrast material–enhanced CT without a suitable alternative should not be avoided solely on the basis of contrast-induced chronic kidney insufficiency risk.
- Contrast-induced AKI risk should be determined primarily by using CKD stage and AKI.
- Patients at high risk for contrast-induced kidney injury include those with recent AKI and those with estimated glomerular filtration rate (eGFR) less than 30 mL/min per 1.73 m2.
Data supporting guidelines
The data from several studies used to support these recommendations were impressive, showing just how low the risk for contrast-induced AKI is in most patients. In these studies, the risk of contrast-induced AKI has been estimated to be near 0% for patients with an eGFR greater than or equal to 45 and 0%-2% for patients with an eGFR of 30-44.5-7 This information and recommendations make imaging much easier. In most of our patients, we can get contrast studies when we need them. The group to be concerned about are patients with eGFRs less than 30. The guidelines single out this group as the patients where risk/benefit needs to be calculated before proceeding with the study, and to use prophylactic saline hydration in patients not undergoing dialysis.
Myth: Contrast-induced renal disease is common.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Lee YC et al. Contrast-induced acute kidney injury among patients with chronic kidney disease undergoing imaging studies: A meta-analysis. Am J Roentgenol. 2019 Oct;213(4):728-35.
2. Luk L et al. Intravenous contrast-induced nephropathy: The rise and fall of a threatening idea. Adv Chronic Kidney Dis. 2017 May;24(3):169-75.
3. Goldfarb S et al. Low-osmolality contrast media and the risk of contrast-associated nephrotoxicity. Invest Radiol. 1993;28(Suppl 5):7-10.
4. Davenport MS, et al. Use of intravenous iodinated contrast media in patients with kidney disease: Consensus statements from the American College of Radiology and the National Kidney Foundation. Kidney Med. 2020 Jan 22;2(1):85-93.
5. Davenport MS et al. Contrast material–induced nephrotoxicity and intravenous low-osmolality iodinated contrast material. Radiology. 2013;267(1):94-105.
6. McDonald RJ et al. Intravenous contrast material–induced nephropathy: Causal or coincident phenomenon? Radiology. 2013;267(1):106-18.
7. McDonald JS et al. Risk of intravenous contrast material–mediated acute kidney injury: A propensity scorematched study stratified by baseline-estimated glomerular filtration rate. Radiology. 2014;271(1):65-73.
A 67-year-old man with stage 3 chronic kidney disease (CKD) develops abdominal pain over 24 hours. He has had low grade fevers and nausea. He has a history of colon cancer and had a resection four years ago. Abdominal exam reveals tenderness to palpation, including rebound tenderness in his right lower quadrant. Labs: hemoglobin: 13; hematocrit: 39; white blood cells: 18,000; platelets: 333; blood urea nitrogen: 28; creatinine: 1.8 (estimated glomerular filtration rate: 37); sodium: 136; potassium: 3.9; bicarbonate: 24; chlorine: 105; and lipase: 10.
What testing would you recommend?
A) Ultrasound
B) Non contrast computed tomography (CT)
C) Contrast CT
D) MRI without gadolinium
The correct answer here is to get a contrast CT scan, as it will give you the most appropriate diagnostic information.
For years, we have hesitated to order contrast studies in our patients with CKD, for fear of causing contrast-induced nephrotoxicity. We might choose less helpful studies that avoid contrast, or might not obtain imaging that is needed. Over the years I have especially seen this in the case of avoiding computed tomography angiography (CTA) for evaluation of pulmonary embolus and choosing the much less useful ventilation/perfusion scan. The problem arises with the fact that patients with CKD are more likely to develop worsening renal function when they get sick.
Lee and colleagues performed an analysis of six retrospective studies involving a total of 55,963 participants. They found that patients with CKD receiving contrast material did not have an increased risk of deteriorating renal function compared with those without CKD (odds ratio, 1.07; 95% confidence interval, 0.98-1.17).1
The early studies reporting contrast-induced renal disease were in patients who received high osmolality contrast agents.2 Most patients now receive low osmolality agents, with less nephrotoxicity.3
Key points of guidelines
This year, the American College of Radiology and the National Kidney Foundation put out joint guidelines that helped clarify why there is a diminished concern for contrast-induced kidney disease in the modern era.4 Below are some of the key points of these guidelines:
- The risk of contrast-induced acute kidney injury (AKI) from intravenous iodinated contrast media is lower than previously thought.
- Necessary contrast material–enhanced CT without a suitable alternative should not be avoided solely on the basis of contrast-induced chronic kidney insufficiency risk.
- Contrast-induced AKI risk should be determined primarily by using CKD stage and AKI.
- Patients at high risk for contrast-induced kidney injury include those with recent AKI and those with estimated glomerular filtration rate (eGFR) less than 30 mL/min per 1.73 m2.
Data supporting guidelines
The data from several studies used to support these recommendations were impressive, showing just how low the risk for contrast-induced AKI is in most patients. In these studies, the risk of contrast-induced AKI has been estimated to be near 0% for patients with an eGFR greater than or equal to 45 and 0%-2% for patients with an eGFR of 30-44.5-7 This information and recommendations make imaging much easier. In most of our patients, we can get contrast studies when we need them. The group to be concerned about are patients with eGFRs less than 30. The guidelines single out this group as the patients where risk/benefit needs to be calculated before proceeding with the study, and to use prophylactic saline hydration in patients not undergoing dialysis.
Myth: Contrast-induced renal disease is common.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Lee YC et al. Contrast-induced acute kidney injury among patients with chronic kidney disease undergoing imaging studies: A meta-analysis. Am J Roentgenol. 2019 Oct;213(4):728-35.
2. Luk L et al. Intravenous contrast-induced nephropathy: The rise and fall of a threatening idea. Adv Chronic Kidney Dis. 2017 May;24(3):169-75.
3. Goldfarb S et al. Low-osmolality contrast media and the risk of contrast-associated nephrotoxicity. Invest Radiol. 1993;28(Suppl 5):7-10.
4. Davenport MS, et al. Use of intravenous iodinated contrast media in patients with kidney disease: Consensus statements from the American College of Radiology and the National Kidney Foundation. Kidney Med. 2020 Jan 22;2(1):85-93.
5. Davenport MS et al. Contrast material–induced nephrotoxicity and intravenous low-osmolality iodinated contrast material. Radiology. 2013;267(1):94-105.
6. McDonald RJ et al. Intravenous contrast material–induced nephropathy: Causal or coincident phenomenon? Radiology. 2013;267(1):106-18.
7. McDonald JS et al. Risk of intravenous contrast material–mediated acute kidney injury: A propensity scorematched study stratified by baseline-estimated glomerular filtration rate. Radiology. 2014;271(1):65-73.
A 67-year-old man with stage 3 chronic kidney disease (CKD) develops abdominal pain over 24 hours. He has had low grade fevers and nausea. He has a history of colon cancer and had a resection four years ago. Abdominal exam reveals tenderness to palpation, including rebound tenderness in his right lower quadrant. Labs: hemoglobin: 13; hematocrit: 39; white blood cells: 18,000; platelets: 333; blood urea nitrogen: 28; creatinine: 1.8 (estimated glomerular filtration rate: 37); sodium: 136; potassium: 3.9; bicarbonate: 24; chlorine: 105; and lipase: 10.
What testing would you recommend?
A) Ultrasound
B) Non contrast computed tomography (CT)
C) Contrast CT
D) MRI without gadolinium
The correct answer here is to get a contrast CT scan, as it will give you the most appropriate diagnostic information.
For years, we have hesitated to order contrast studies in our patients with CKD, for fear of causing contrast-induced nephrotoxicity. We might choose less helpful studies that avoid contrast, or might not obtain imaging that is needed. Over the years I have especially seen this in the case of avoiding computed tomography angiography (CTA) for evaluation of pulmonary embolus and choosing the much less useful ventilation/perfusion scan. The problem arises with the fact that patients with CKD are more likely to develop worsening renal function when they get sick.
Lee and colleagues performed an analysis of six retrospective studies involving a total of 55,963 participants. They found that patients with CKD receiving contrast material did not have an increased risk of deteriorating renal function compared with those without CKD (odds ratio, 1.07; 95% confidence interval, 0.98-1.17).1
The early studies reporting contrast-induced renal disease were in patients who received high osmolality contrast agents.2 Most patients now receive low osmolality agents, with less nephrotoxicity.3
Key points of guidelines
This year, the American College of Radiology and the National Kidney Foundation put out joint guidelines that helped clarify why there is a diminished concern for contrast-induced kidney disease in the modern era.4 Below are some of the key points of these guidelines:
- The risk of contrast-induced acute kidney injury (AKI) from intravenous iodinated contrast media is lower than previously thought.
- Necessary contrast material–enhanced CT without a suitable alternative should not be avoided solely on the basis of contrast-induced chronic kidney insufficiency risk.
- Contrast-induced AKI risk should be determined primarily by using CKD stage and AKI.
- Patients at high risk for contrast-induced kidney injury include those with recent AKI and those with estimated glomerular filtration rate (eGFR) less than 30 mL/min per 1.73 m2.
Data supporting guidelines
The data from several studies used to support these recommendations were impressive, showing just how low the risk for contrast-induced AKI is in most patients. In these studies, the risk of contrast-induced AKI has been estimated to be near 0% for patients with an eGFR greater than or equal to 45 and 0%-2% for patients with an eGFR of 30-44.5-7 This information and recommendations make imaging much easier. In most of our patients, we can get contrast studies when we need them. The group to be concerned about are patients with eGFRs less than 30. The guidelines single out this group as the patients where risk/benefit needs to be calculated before proceeding with the study, and to use prophylactic saline hydration in patients not undergoing dialysis.
Myth: Contrast-induced renal disease is common.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Lee YC et al. Contrast-induced acute kidney injury among patients with chronic kidney disease undergoing imaging studies: A meta-analysis. Am J Roentgenol. 2019 Oct;213(4):728-35.
2. Luk L et al. Intravenous contrast-induced nephropathy: The rise and fall of a threatening idea. Adv Chronic Kidney Dis. 2017 May;24(3):169-75.
3. Goldfarb S et al. Low-osmolality contrast media and the risk of contrast-associated nephrotoxicity. Invest Radiol. 1993;28(Suppl 5):7-10.
4. Davenport MS, et al. Use of intravenous iodinated contrast media in patients with kidney disease: Consensus statements from the American College of Radiology and the National Kidney Foundation. Kidney Med. 2020 Jan 22;2(1):85-93.
5. Davenport MS et al. Contrast material–induced nephrotoxicity and intravenous low-osmolality iodinated contrast material. Radiology. 2013;267(1):94-105.
6. McDonald RJ et al. Intravenous contrast material–induced nephropathy: Causal or coincident phenomenon? Radiology. 2013;267(1):106-18.
7. McDonald JS et al. Risk of intravenous contrast material–mediated acute kidney injury: A propensity scorematched study stratified by baseline-estimated glomerular filtration rate. Radiology. 2014;271(1):65-73.
Understanding and addressing suicide risk in LGBTQ+ youth
Even as dozens of state legislature bills attempt to limit the rights of sexual-diverse and gender-diverse youth, researchers are learning more and more that can help pediatricians better support this population in their practices, according to David Inwards-Breland, MD, MPH, a professor of clinical pediatrics at the University of California, San Diego.
Dr. Inwards-Breland highlighted two key studies in recent years during the LGBTQ+ section at the annual meeting of the American Academy of Pediatrics, held virtually in 2020.
High suicide rates among sexual minority youth
Past research has found that adolescents who identify as sexual minorities have nearly five times the rate of suicide attempts, compared with their heterosexual peers, Dr. Inwards-Breland said as he introduced a recent study on disparities in adolescent suicide.
“This may be from a disproportionate burden of poor mental health that has been linked to stigma,” he said, adding that an estimated 125 state bills have been introduced in the United States that would restrict the rights of sexual minorities.
The study, published in Pediatrics in March 2020, compiled data from 110,243 adolescents in six states on sexual orientation identity; 25,994 adolescents in four states on same-sex sexual contact and sexual assault; and 20,655 adolescents in three states on sexual orientation identity, the sex of sexual contacts, and sexual assault.
The authors found that heterosexual identity dropped from 93% to 86% between 2009 and 2017, but sexual minority youth accounted for an increasing share of suicide attempts over the same period. A quarter of adolescents who attempted suicide in 2009 were sexual minorities, which increased to 36% in 2017. Similarly, among sexually active teens who attempted suicide, the proportion of those who had same-sex contact nearly doubled, from 16% to 30%.
The good news, Dr. Inwards-Breland said, was that overall suicide attempts declined among sexual minorities, but they remain three times as likely to attempt suicide, compared with their heterosexual counterparts.
“As the number of adolescents increase in our country, there will be increasing numbers of adolescents identifying as sexual minorities or who have had same-sex sexual contact,” Dr. Inwards-Breland said. “Therefore, providing confidential services is even more important to allow youth to feel comfortable with their health care provider.” He also emphasized the importance of consistent universal depression screening and advocacy to eliminate and prevent policies that harm these youth.
Using youths’ chosen names
Transgender and nonbinary youth – those who do not identify as male or female – have a higher risk of poor mental health and higher levels of suicidal ideation and behaviors, compared with their “cis” peers, those who identify with the gender they were assigned at birth, Dr. Inwards-Breland said. However, using the chosen, or assertive, name of transgender and nonbinary youth predicted fewer depressive symptoms and less suicidal ideation and behavior in a study published in the Journal of Adolescent Health in October 2018.
“Choosing a name is an important part of social transition of transgender individuals, yet they’re unable to use their name because of interpersonal or institutional barriers,” he said. In addition, using a name other than their legally given name can subject them to discrimination and victimization.
The study, drawing from a larger cohort of LGBTQ youth, involved 129 transgender and nonbinary adolescents, aged 15-21, of whom 74 had a chosen name. No other differences in personal characteristics were associated with depressive symptoms or suicidal ideation besides increased use of their assertive name in different life contexts.
An increase in one context where chosen name could be used predicted a 5.37-unit decrease in depressive symptoms, a 29% decrease in suicidal ideation, and a 56% decrease in suicidal behavior, the study found. All three outcomes were at their lowest levels when chosen names were used in all four contexts explored in the study.
“The chosen name affirms their gender identity,” Dr. Inwards-Breland said, but “the legal name change process is very onerous.” He highlighted the need for institutions to adjust regulations and information systems, for policies that promote the transition process, and for youths’ names to be affirmed in multiple contexts.
“We as pediatricians, specialists, and primary care doctors can support families as they adjust the transition process by helping them with assertive names and pronouns and giving them resources,” Dr. Inwards-Breland said. He also called for school policies and teacher/staff training that promote the use of assertive names and pronouns, and ensuring that the assertive name and pronouns are in the medical record and used by office staff and other medical professionals.
‘A light in the dark’ for LGBTQ+ youth
Clair Kronk of the University of Cincinnati and Cincinnati Children’s Hospital and Medical Center attended the LGBTQ+ section at the AAP meeting because of concerns about she and her transgender siblings have been treated by the medical community.
“It has always been important to be ‘on the pulse’ of what is happening in the medical community, especially with new, more discriminatory policies being passed seemingly willy-nilly these days, both in the medical realm and outside of it,” Ms. Kronk said in an interview. “I was overjoyed to see how many people seemed to care so much about the transgender community and LGBTQIA+ people generally.”
As an ontologist and bioinformatician, she did not recall many big clinical takeaways for her particular work, but she appreciated how many areas the session covered, especially given the dearth of instruction about LGBTQ+ care in medical training.
“This session was a bit of a light in the dark given the state of LGBTQIA+ health care rights,” she said. “There is a lot at stake in the next year or so, and providers’ and LGBTQIA+ persons’ voices need to be heard right now more than ever.”
Sonia Khan, MD, a pediatrician and the medical director of the substance use disorder counseling program in the department of health and human services in Fremont, Calif., also attended the session and came away feeling invigorated.
“These data make me feel more optimistic than I have been in ages in terms of increasing the safety of young people being able to come out,” Dr. Khan said in the comments during the session. “These last 4 years felt so regressive. [It’s] good to get the big picture.”
The presenters and commentators had no disclosures.
Even as dozens of state legislature bills attempt to limit the rights of sexual-diverse and gender-diverse youth, researchers are learning more and more that can help pediatricians better support this population in their practices, according to David Inwards-Breland, MD, MPH, a professor of clinical pediatrics at the University of California, San Diego.
Dr. Inwards-Breland highlighted two key studies in recent years during the LGBTQ+ section at the annual meeting of the American Academy of Pediatrics, held virtually in 2020.
High suicide rates among sexual minority youth
Past research has found that adolescents who identify as sexual minorities have nearly five times the rate of suicide attempts, compared with their heterosexual peers, Dr. Inwards-Breland said as he introduced a recent study on disparities in adolescent suicide.
“This may be from a disproportionate burden of poor mental health that has been linked to stigma,” he said, adding that an estimated 125 state bills have been introduced in the United States that would restrict the rights of sexual minorities.
The study, published in Pediatrics in March 2020, compiled data from 110,243 adolescents in six states on sexual orientation identity; 25,994 adolescents in four states on same-sex sexual contact and sexual assault; and 20,655 adolescents in three states on sexual orientation identity, the sex of sexual contacts, and sexual assault.
The authors found that heterosexual identity dropped from 93% to 86% between 2009 and 2017, but sexual minority youth accounted for an increasing share of suicide attempts over the same period. A quarter of adolescents who attempted suicide in 2009 were sexual minorities, which increased to 36% in 2017. Similarly, among sexually active teens who attempted suicide, the proportion of those who had same-sex contact nearly doubled, from 16% to 30%.
The good news, Dr. Inwards-Breland said, was that overall suicide attempts declined among sexual minorities, but they remain three times as likely to attempt suicide, compared with their heterosexual counterparts.
“As the number of adolescents increase in our country, there will be increasing numbers of adolescents identifying as sexual minorities or who have had same-sex sexual contact,” Dr. Inwards-Breland said. “Therefore, providing confidential services is even more important to allow youth to feel comfortable with their health care provider.” He also emphasized the importance of consistent universal depression screening and advocacy to eliminate and prevent policies that harm these youth.
Using youths’ chosen names
Transgender and nonbinary youth – those who do not identify as male or female – have a higher risk of poor mental health and higher levels of suicidal ideation and behaviors, compared with their “cis” peers, those who identify with the gender they were assigned at birth, Dr. Inwards-Breland said. However, using the chosen, or assertive, name of transgender and nonbinary youth predicted fewer depressive symptoms and less suicidal ideation and behavior in a study published in the Journal of Adolescent Health in October 2018.
“Choosing a name is an important part of social transition of transgender individuals, yet they’re unable to use their name because of interpersonal or institutional barriers,” he said. In addition, using a name other than their legally given name can subject them to discrimination and victimization.
The study, drawing from a larger cohort of LGBTQ youth, involved 129 transgender and nonbinary adolescents, aged 15-21, of whom 74 had a chosen name. No other differences in personal characteristics were associated with depressive symptoms or suicidal ideation besides increased use of their assertive name in different life contexts.
An increase in one context where chosen name could be used predicted a 5.37-unit decrease in depressive symptoms, a 29% decrease in suicidal ideation, and a 56% decrease in suicidal behavior, the study found. All three outcomes were at their lowest levels when chosen names were used in all four contexts explored in the study.
“The chosen name affirms their gender identity,” Dr. Inwards-Breland said, but “the legal name change process is very onerous.” He highlighted the need for institutions to adjust regulations and information systems, for policies that promote the transition process, and for youths’ names to be affirmed in multiple contexts.
“We as pediatricians, specialists, and primary care doctors can support families as they adjust the transition process by helping them with assertive names and pronouns and giving them resources,” Dr. Inwards-Breland said. He also called for school policies and teacher/staff training that promote the use of assertive names and pronouns, and ensuring that the assertive name and pronouns are in the medical record and used by office staff and other medical professionals.
‘A light in the dark’ for LGBTQ+ youth
Clair Kronk of the University of Cincinnati and Cincinnati Children’s Hospital and Medical Center attended the LGBTQ+ section at the AAP meeting because of concerns about she and her transgender siblings have been treated by the medical community.
“It has always been important to be ‘on the pulse’ of what is happening in the medical community, especially with new, more discriminatory policies being passed seemingly willy-nilly these days, both in the medical realm and outside of it,” Ms. Kronk said in an interview. “I was overjoyed to see how many people seemed to care so much about the transgender community and LGBTQIA+ people generally.”
As an ontologist and bioinformatician, she did not recall many big clinical takeaways for her particular work, but she appreciated how many areas the session covered, especially given the dearth of instruction about LGBTQ+ care in medical training.
“This session was a bit of a light in the dark given the state of LGBTQIA+ health care rights,” she said. “There is a lot at stake in the next year or so, and providers’ and LGBTQIA+ persons’ voices need to be heard right now more than ever.”
Sonia Khan, MD, a pediatrician and the medical director of the substance use disorder counseling program in the department of health and human services in Fremont, Calif., also attended the session and came away feeling invigorated.
“These data make me feel more optimistic than I have been in ages in terms of increasing the safety of young people being able to come out,” Dr. Khan said in the comments during the session. “These last 4 years felt so regressive. [It’s] good to get the big picture.”
The presenters and commentators had no disclosures.
Even as dozens of state legislature bills attempt to limit the rights of sexual-diverse and gender-diverse youth, researchers are learning more and more that can help pediatricians better support this population in their practices, according to David Inwards-Breland, MD, MPH, a professor of clinical pediatrics at the University of California, San Diego.
Dr. Inwards-Breland highlighted two key studies in recent years during the LGBTQ+ section at the annual meeting of the American Academy of Pediatrics, held virtually in 2020.
High suicide rates among sexual minority youth
Past research has found that adolescents who identify as sexual minorities have nearly five times the rate of suicide attempts, compared with their heterosexual peers, Dr. Inwards-Breland said as he introduced a recent study on disparities in adolescent suicide.
“This may be from a disproportionate burden of poor mental health that has been linked to stigma,” he said, adding that an estimated 125 state bills have been introduced in the United States that would restrict the rights of sexual minorities.
The study, published in Pediatrics in March 2020, compiled data from 110,243 adolescents in six states on sexual orientation identity; 25,994 adolescents in four states on same-sex sexual contact and sexual assault; and 20,655 adolescents in three states on sexual orientation identity, the sex of sexual contacts, and sexual assault.
The authors found that heterosexual identity dropped from 93% to 86% between 2009 and 2017, but sexual minority youth accounted for an increasing share of suicide attempts over the same period. A quarter of adolescents who attempted suicide in 2009 were sexual minorities, which increased to 36% in 2017. Similarly, among sexually active teens who attempted suicide, the proportion of those who had same-sex contact nearly doubled, from 16% to 30%.
The good news, Dr. Inwards-Breland said, was that overall suicide attempts declined among sexual minorities, but they remain three times as likely to attempt suicide, compared with their heterosexual counterparts.
“As the number of adolescents increase in our country, there will be increasing numbers of adolescents identifying as sexual minorities or who have had same-sex sexual contact,” Dr. Inwards-Breland said. “Therefore, providing confidential services is even more important to allow youth to feel comfortable with their health care provider.” He also emphasized the importance of consistent universal depression screening and advocacy to eliminate and prevent policies that harm these youth.
Using youths’ chosen names
Transgender and nonbinary youth – those who do not identify as male or female – have a higher risk of poor mental health and higher levels of suicidal ideation and behaviors, compared with their “cis” peers, those who identify with the gender they were assigned at birth, Dr. Inwards-Breland said. However, using the chosen, or assertive, name of transgender and nonbinary youth predicted fewer depressive symptoms and less suicidal ideation and behavior in a study published in the Journal of Adolescent Health in October 2018.
“Choosing a name is an important part of social transition of transgender individuals, yet they’re unable to use their name because of interpersonal or institutional barriers,” he said. In addition, using a name other than their legally given name can subject them to discrimination and victimization.
The study, drawing from a larger cohort of LGBTQ youth, involved 129 transgender and nonbinary adolescents, aged 15-21, of whom 74 had a chosen name. No other differences in personal characteristics were associated with depressive symptoms or suicidal ideation besides increased use of their assertive name in different life contexts.
An increase in one context where chosen name could be used predicted a 5.37-unit decrease in depressive symptoms, a 29% decrease in suicidal ideation, and a 56% decrease in suicidal behavior, the study found. All three outcomes were at their lowest levels when chosen names were used in all four contexts explored in the study.
“The chosen name affirms their gender identity,” Dr. Inwards-Breland said, but “the legal name change process is very onerous.” He highlighted the need for institutions to adjust regulations and information systems, for policies that promote the transition process, and for youths’ names to be affirmed in multiple contexts.
“We as pediatricians, specialists, and primary care doctors can support families as they adjust the transition process by helping them with assertive names and pronouns and giving them resources,” Dr. Inwards-Breland said. He also called for school policies and teacher/staff training that promote the use of assertive names and pronouns, and ensuring that the assertive name and pronouns are in the medical record and used by office staff and other medical professionals.
‘A light in the dark’ for LGBTQ+ youth
Clair Kronk of the University of Cincinnati and Cincinnati Children’s Hospital and Medical Center attended the LGBTQ+ section at the AAP meeting because of concerns about she and her transgender siblings have been treated by the medical community.
“It has always been important to be ‘on the pulse’ of what is happening in the medical community, especially with new, more discriminatory policies being passed seemingly willy-nilly these days, both in the medical realm and outside of it,” Ms. Kronk said in an interview. “I was overjoyed to see how many people seemed to care so much about the transgender community and LGBTQIA+ people generally.”
As an ontologist and bioinformatician, she did not recall many big clinical takeaways for her particular work, but she appreciated how many areas the session covered, especially given the dearth of instruction about LGBTQ+ care in medical training.
“This session was a bit of a light in the dark given the state of LGBTQIA+ health care rights,” she said. “There is a lot at stake in the next year or so, and providers’ and LGBTQIA+ persons’ voices need to be heard right now more than ever.”
Sonia Khan, MD, a pediatrician and the medical director of the substance use disorder counseling program in the department of health and human services in Fremont, Calif., also attended the session and came away feeling invigorated.
“These data make me feel more optimistic than I have been in ages in terms of increasing the safety of young people being able to come out,” Dr. Khan said in the comments during the session. “These last 4 years felt so regressive. [It’s] good to get the big picture.”
The presenters and commentators had no disclosures.
FROM AAP 2020
Watch for cognitive traps that lead diagnostics astray
While it’s important not to think immediately of zebras when hearing hoofbeats, it’s just as important not to assume it’s always a horse. The delicate balance between not jumping to the seemingly obvious diagnosis without overanalyzing and overtesting is familiar to all physicians, and
“When these errors are made, it’s not because physicians lack knowledge, but they go down a wrong path in their thinking process,” Richard Scarfone, MD, a pediatric emergency medicine physician at the Children’s Hospital of Philadelphia, told attendees at the annual meeting of the American Academy of Pediatrics, held virtually this year. “An important point to be made here is that how physicians think seems to be much more important than what physicians know.”
Dr. Scarfone and Joshua Nagler, MD, MHPEd, director, pediatric emergency medicine fellowship program at Children’s Hospital Boston, presented a session on the cognitive biases that can trip up clinicians when making diagnoses and how to avoid them. Research shows that the rate of diagnostic error is approximately 15%. Although those findings come from studies in adults, the rates are likely similar in pediatrics, Dr. Scarfone said.
A wide range of clinical factors contribute to diagnostic errors: limited information, vague or undifferentiated symptoms, incomplete history, multiple transitions of care, diagnostic uncertainty, daily decision density, and reliance on pattern recognition, among others. Personal contributing factors can play a role as well, such as atypical work hours, fatigue, one’s emotional or affective state, a high cognitive load, and others. On top of all that, medical decision-making can be really complex on its own, Dr. Scarfone said. He compared differential diagnosis with a tree where a single leaf is the correct diagnosis.
System 1 thinking: Pros and cons
Dr. Scarfone and Dr. Nagler explained system 1 and system 2 thinking, two different ways of thinking that can influence decision-making that Daniel Kahneman explained in his book “Thinking, Fast and Slow.” System 1 refers to the snap judgments that rely on heuristics while system 2 refers to a more analytic, slower process.
Neither system 1 nor 2 is inherently “right or wrong,” Dr. Scarfone said. “The diagnostic sweet spot is to try to apply the correct system to the correct patient.”
Heuristics are the mental shortcuts people use to make decisions based on past experience. They exist because they’re useful, enabling people to focus only on what they need to accomplish everyday tasks, such as driving or brushing teeth. But heuristics can also lead to predictable cognitive errors.
“The good news about heuristics and system 1 thinking is that it’s efficient and simple, and we desire that in a busy practice or ED setting, but we should recognize that the trade-off is that it may be at the expense of accuracy,” Dr. Scarfone said.
The advantage to system 1 thinking is easy, simple, rapid, and efficient decision-making that rejects ambiguity. It’s also usually accurate, which rewards the approach, and accuracy increases with time based on memory, experience, and pattern recognition. Doctors develop “illness scripts” that help in identifying diagnoses.
“Illness scripts are common patterns of clinical presentations that usually lead us to a diagnostic possibility,” Dr. Scarfone said. “A classic illness script might be a 4-week-old firstborn male with forceful vomiting, and immediately your mind may go to pyloric stenosis as a likely diagnosis.” But the patient may have a different diagnosis than the initial impression your system 1 thinking leads you to believe.
“Generally, the more experience a clinician has, the more accurate they’ll be in using system 1,” he said. “Seasoned physicians are much more likely to employ system 1 than a newer physician or trainee,” which is why heuristics shouldn’t be thought of as hindrances. Dr. Scarfone quoted Kevin Eva in a 2005 review on clinical reasoning: “Successful heuristics should be embraced rather than overcome.”
A drawback to system 1 thinking, however, is thinking that “what you see is all there is,” which can lead to cognitive errors. Feeling wrong feels the same as feeling right, so you may not realize when you’re off target and therefore neglect to consider alternatives.
“When we learn a little about our patient’s complaint, it’s easier to fit everything into a coherent explanation,” Dr. Scarfone said, but “don’t ask, don’t tell doesn’t work in medicine.”
Another challenge with system 1 thinking is that pattern recognition can be unreliable because it’s dependent on context. For example, consider the difference in assessing a patient’s sore throat in a primary care office versus a resuscitation bay. “Clearly our consideration of what may be going on with the patient and what the diagnosis may be is likely to vary in those two settings,” he said.
System 2 thinking: Of zebras and horses
System 2 is the analytic thinking that involves pondering and seek out the optimal answer rather than the “good-enough” answer.
“The good news about system 2 is that it really can monitor system 1,” said Dr. Nagler, who has a master’s degree in health professions education. “If you spend the time to do analytic reasoning, you can actually mitigate some of those errors that may occur from intuitive judgments from system 1 thinking. System 2 spends the time to say ‘let’s make sure we’re doing this right.’ ” In multiple-choice tests, for example, people are twice as likely to change a wrong answer to a right one than a right one to a wrong one.
System 2 thinking allows for the reasoning to assess questions in the gray zone. It’s vigilant, it’s reliable, it’s effective, it acknowledges uncertainty and doubt, it can be safe in terms of providing care, and it has high scientific rigor. But it also has disadvantages, starting with the fact that it’s slower and more time-consuming. System 2 thinking is resource intensive, requiring a higher cognitive demand and more time and effort.
“Sometimes the quick judgment is the best judgment,” Dr. Nagler said. System 2 thinking also is sometimes unnecessary and counter to value-based care. “If you start to think about all the possibilities of what a presentation may be, all of a sudden you might find yourself wanting to do all kinds of tests and all kinds of referrals and other things, which is not necessarily value-based care.” When system 2 thinking goes astray, it makes us think everything we see is a zebra rather than a horse.
Sonia Khan, MD, a pediatrician in Fremont, Calif., found this session particularly worthwhile.
“It really tries to explain the difference between leaping to conclusions and learning how to hold your horses and do a bit more, to double check that you’re not locking everything into a horse stall and missing a zebra, and avoiding go too far with system 2 and thinking that everything’s a zebra,” Dr. Khan said. “It’s a difficult talk to have because you’re asking pediatricians to look in the mirror and own up, to learn to step back and reconsider the picture, and consider the biases that may come into your decision-making; then learn to extrude them, and rethink the case to be sure your knee-jerk diagnostic response is correct.”
Types of cognitive errors
The presenters listed some of the most common cognitive errors, although their list is far from exhaustive.
- Affective error. Avoiding unpleasant but necessary tests or examinations because of sympathy for the patient, such as avoiding blood work to spare a needle stick in a cancer patient with abdominal pain because the mother is convinced it’s constipation from opioids. This is similar to omission bias, which places excessive concern on avoiding a therapy’s adverse effects when the therapy could be highly effective.
- Anchoring. Clinging to an initial impression or salient features of initial presentation, even as conflicting and contradictory data accumulate, such as diagnosing a patient with fever and vomiting with gastroenteritis even when the patient has an oxygen saturation of 94% and tachypnea.
- Attribution errors. Negative stereotypes lead clinicians to ignore or minimize the possibility of serious disease, such as evaluating a confused teen covered in piercings and tattoos for drug ingestion when the actual diagnosis is new-onset diabetic ketoacidosis.
- Availability bias. Overestimating or underestimating the probability of disease because of recent experience, what was most recently “available” to your brain cognitively, such as getting head imaging on several vomiting patients in a row because you recently had one with a new brain tumor diagnosis.
- Bandwagon effect. Accepting the group’s opinion without assessing a clinical situation yourself, such as sending home a crying, vomiting infant with a presumed viral infection only to see the infant return later with intussusception.
- Base rate neglect. Ignoring the true prevalence of disease by either inflating it or reducing it, such as searching for cardiac disease in all pediatric patients with chest pain.
- Commission. A tendency toward action with the belief that harm may only be prevented by action, such as ordering every possible test for a patient with fever to “rule everything out.”
- Confirmation bias. Subconscious cherry-picking: A tendency to look for, notice, and remember information that fits with preexisting expectations while disregarding information that contradicts those expectations.
- Diagnostic momentum. Clinging to that initial diagnostic impression that may have been generated by others, which is particularly common during transitions of care.
- Premature closure. Narrowing down to a diagnosis without thinking about other diagnoses or asking enough questions about other symptoms that may have opened up other diagnostic possibilities.
- Representation bias. Making a decision in the absence of appropriate context by incorrectly comparing two situations because of a perceived similarity between them, or on the flip side, evaluating a situation without comparing it with other situations.
- Overconfidence. Making a decision without enough supportive evidence yet feeling confident about the diagnosis.
- Search satisfying. Stopping the search for additional diagnoses after the anticipated diagnosis has been made.
Cognitive pills for cognitive ills
Being aware of the pitfalls of cognitive errors is the first step to avoiding and mitigating them. “It really does start with preparation and awareness,” Dr. Scarfone said before presenting strategies to build a cognitive “firewall” that can help physicians practice reflectively instead of reflexively.
First, be aware of your cognitive style. People usually have the same thinking pattern in everyday life as in the clinical setting, so determine whether you’re more of a system 1 or system 2 thinker. System 1 thinkers need to watch out for framing (relying too heavily on context), premature closure, diagnostic momentum, anchoring, and confirmation bias. System 2 thinkers need to watch out for commission, availability bias, and base rate neglect.
“Neither system is inherently right or wrong,” Dr. Scarfone reiterated. “In the perfect world, you may use system 1 to form an initial impression, but then system 2 should really act as a check and balance system to cause you to reflect on your initial diagnostic impressions.”
Additional strategies include being a good history taker and performing a meticulous physical exam: be a good listener, clarify unclear aspects of the history, and identify and address the main concern.
“Remember children and families have a story to tell, and if we listen carefully enough, the diagnostic clues are there,” Dr. Scarfone said. “Sometimes they may be quite subtle.” He recommended doctors perform each part of the physical exam as if expecting an abnormality.
Another strategy is using meta-cognition, a forced analysis of the thinking that led to a diagnosis. It involves asking: “If I had to explain my medical decision-making to others, would this make inherent sense?” Dr. Scarfone said. “If you’re testing, try to avoid anchoring and confirmation biases.”
Finally, take a diagnostic time-out with a checklist that asks these questions:
- Does my presumptive diagnosis make sense?
- What evidence supports or refutes it?
- Did I arrive at it via cognitive biases?
- Are there other diagnostic possibilities that should be considered?
One way to do this is creating a table listing the complaint/finding, diagnostic possibilities with system 1 thinking, diagnostic possibilities with system 2 thinking, and then going beyond system 2 – the potential zebras – when even system 2 diagnostic possibilities don’t account for what the patient is saying or what the exam shows.
Enough overlap exists between these cognitive biases and the intrinsic bias related to individual characteristics that Dr. Khan appreciated the talk on another level as well.
“For me, as a brown Muslim immigrant woman of color, I can sometimes see cognitive biases in action with my colleagues and realize that they are oblivious to it,” Dr. Khan said. “It’s really refreshing to see this issue come up and being discussed at the [AAP] National Conference and Exhibition.”
Dr. Scarfone, Dr. Nagler and Dr. Khan have no relevant financial disclosures.
This article was updated 12/8/2020.
While it’s important not to think immediately of zebras when hearing hoofbeats, it’s just as important not to assume it’s always a horse. The delicate balance between not jumping to the seemingly obvious diagnosis without overanalyzing and overtesting is familiar to all physicians, and
“When these errors are made, it’s not because physicians lack knowledge, but they go down a wrong path in their thinking process,” Richard Scarfone, MD, a pediatric emergency medicine physician at the Children’s Hospital of Philadelphia, told attendees at the annual meeting of the American Academy of Pediatrics, held virtually this year. “An important point to be made here is that how physicians think seems to be much more important than what physicians know.”
Dr. Scarfone and Joshua Nagler, MD, MHPEd, director, pediatric emergency medicine fellowship program at Children’s Hospital Boston, presented a session on the cognitive biases that can trip up clinicians when making diagnoses and how to avoid them. Research shows that the rate of diagnostic error is approximately 15%. Although those findings come from studies in adults, the rates are likely similar in pediatrics, Dr. Scarfone said.
A wide range of clinical factors contribute to diagnostic errors: limited information, vague or undifferentiated symptoms, incomplete history, multiple transitions of care, diagnostic uncertainty, daily decision density, and reliance on pattern recognition, among others. Personal contributing factors can play a role as well, such as atypical work hours, fatigue, one’s emotional or affective state, a high cognitive load, and others. On top of all that, medical decision-making can be really complex on its own, Dr. Scarfone said. He compared differential diagnosis with a tree where a single leaf is the correct diagnosis.
System 1 thinking: Pros and cons
Dr. Scarfone and Dr. Nagler explained system 1 and system 2 thinking, two different ways of thinking that can influence decision-making that Daniel Kahneman explained in his book “Thinking, Fast and Slow.” System 1 refers to the snap judgments that rely on heuristics while system 2 refers to a more analytic, slower process.
Neither system 1 nor 2 is inherently “right or wrong,” Dr. Scarfone said. “The diagnostic sweet spot is to try to apply the correct system to the correct patient.”
Heuristics are the mental shortcuts people use to make decisions based on past experience. They exist because they’re useful, enabling people to focus only on what they need to accomplish everyday tasks, such as driving or brushing teeth. But heuristics can also lead to predictable cognitive errors.
“The good news about heuristics and system 1 thinking is that it’s efficient and simple, and we desire that in a busy practice or ED setting, but we should recognize that the trade-off is that it may be at the expense of accuracy,” Dr. Scarfone said.
The advantage to system 1 thinking is easy, simple, rapid, and efficient decision-making that rejects ambiguity. It’s also usually accurate, which rewards the approach, and accuracy increases with time based on memory, experience, and pattern recognition. Doctors develop “illness scripts” that help in identifying diagnoses.
“Illness scripts are common patterns of clinical presentations that usually lead us to a diagnostic possibility,” Dr. Scarfone said. “A classic illness script might be a 4-week-old firstborn male with forceful vomiting, and immediately your mind may go to pyloric stenosis as a likely diagnosis.” But the patient may have a different diagnosis than the initial impression your system 1 thinking leads you to believe.
“Generally, the more experience a clinician has, the more accurate they’ll be in using system 1,” he said. “Seasoned physicians are much more likely to employ system 1 than a newer physician or trainee,” which is why heuristics shouldn’t be thought of as hindrances. Dr. Scarfone quoted Kevin Eva in a 2005 review on clinical reasoning: “Successful heuristics should be embraced rather than overcome.”
A drawback to system 1 thinking, however, is thinking that “what you see is all there is,” which can lead to cognitive errors. Feeling wrong feels the same as feeling right, so you may not realize when you’re off target and therefore neglect to consider alternatives.
“When we learn a little about our patient’s complaint, it’s easier to fit everything into a coherent explanation,” Dr. Scarfone said, but “don’t ask, don’t tell doesn’t work in medicine.”
Another challenge with system 1 thinking is that pattern recognition can be unreliable because it’s dependent on context. For example, consider the difference in assessing a patient’s sore throat in a primary care office versus a resuscitation bay. “Clearly our consideration of what may be going on with the patient and what the diagnosis may be is likely to vary in those two settings,” he said.
System 2 thinking: Of zebras and horses
System 2 is the analytic thinking that involves pondering and seek out the optimal answer rather than the “good-enough” answer.
“The good news about system 2 is that it really can monitor system 1,” said Dr. Nagler, who has a master’s degree in health professions education. “If you spend the time to do analytic reasoning, you can actually mitigate some of those errors that may occur from intuitive judgments from system 1 thinking. System 2 spends the time to say ‘let’s make sure we’re doing this right.’ ” In multiple-choice tests, for example, people are twice as likely to change a wrong answer to a right one than a right one to a wrong one.
System 2 thinking allows for the reasoning to assess questions in the gray zone. It’s vigilant, it’s reliable, it’s effective, it acknowledges uncertainty and doubt, it can be safe in terms of providing care, and it has high scientific rigor. But it also has disadvantages, starting with the fact that it’s slower and more time-consuming. System 2 thinking is resource intensive, requiring a higher cognitive demand and more time and effort.
“Sometimes the quick judgment is the best judgment,” Dr. Nagler said. System 2 thinking also is sometimes unnecessary and counter to value-based care. “If you start to think about all the possibilities of what a presentation may be, all of a sudden you might find yourself wanting to do all kinds of tests and all kinds of referrals and other things, which is not necessarily value-based care.” When system 2 thinking goes astray, it makes us think everything we see is a zebra rather than a horse.
Sonia Khan, MD, a pediatrician in Fremont, Calif., found this session particularly worthwhile.
“It really tries to explain the difference between leaping to conclusions and learning how to hold your horses and do a bit more, to double check that you’re not locking everything into a horse stall and missing a zebra, and avoiding go too far with system 2 and thinking that everything’s a zebra,” Dr. Khan said. “It’s a difficult talk to have because you’re asking pediatricians to look in the mirror and own up, to learn to step back and reconsider the picture, and consider the biases that may come into your decision-making; then learn to extrude them, and rethink the case to be sure your knee-jerk diagnostic response is correct.”
Types of cognitive errors
The presenters listed some of the most common cognitive errors, although their list is far from exhaustive.
- Affective error. Avoiding unpleasant but necessary tests or examinations because of sympathy for the patient, such as avoiding blood work to spare a needle stick in a cancer patient with abdominal pain because the mother is convinced it’s constipation from opioids. This is similar to omission bias, which places excessive concern on avoiding a therapy’s adverse effects when the therapy could be highly effective.
- Anchoring. Clinging to an initial impression or salient features of initial presentation, even as conflicting and contradictory data accumulate, such as diagnosing a patient with fever and vomiting with gastroenteritis even when the patient has an oxygen saturation of 94% and tachypnea.
- Attribution errors. Negative stereotypes lead clinicians to ignore or minimize the possibility of serious disease, such as evaluating a confused teen covered in piercings and tattoos for drug ingestion when the actual diagnosis is new-onset diabetic ketoacidosis.
- Availability bias. Overestimating or underestimating the probability of disease because of recent experience, what was most recently “available” to your brain cognitively, such as getting head imaging on several vomiting patients in a row because you recently had one with a new brain tumor diagnosis.
- Bandwagon effect. Accepting the group’s opinion without assessing a clinical situation yourself, such as sending home a crying, vomiting infant with a presumed viral infection only to see the infant return later with intussusception.
- Base rate neglect. Ignoring the true prevalence of disease by either inflating it or reducing it, such as searching for cardiac disease in all pediatric patients with chest pain.
- Commission. A tendency toward action with the belief that harm may only be prevented by action, such as ordering every possible test for a patient with fever to “rule everything out.”
- Confirmation bias. Subconscious cherry-picking: A tendency to look for, notice, and remember information that fits with preexisting expectations while disregarding information that contradicts those expectations.
- Diagnostic momentum. Clinging to that initial diagnostic impression that may have been generated by others, which is particularly common during transitions of care.
- Premature closure. Narrowing down to a diagnosis without thinking about other diagnoses or asking enough questions about other symptoms that may have opened up other diagnostic possibilities.
- Representation bias. Making a decision in the absence of appropriate context by incorrectly comparing two situations because of a perceived similarity between them, or on the flip side, evaluating a situation without comparing it with other situations.
- Overconfidence. Making a decision without enough supportive evidence yet feeling confident about the diagnosis.
- Search satisfying. Stopping the search for additional diagnoses after the anticipated diagnosis has been made.
Cognitive pills for cognitive ills
Being aware of the pitfalls of cognitive errors is the first step to avoiding and mitigating them. “It really does start with preparation and awareness,” Dr. Scarfone said before presenting strategies to build a cognitive “firewall” that can help physicians practice reflectively instead of reflexively.
First, be aware of your cognitive style. People usually have the same thinking pattern in everyday life as in the clinical setting, so determine whether you’re more of a system 1 or system 2 thinker. System 1 thinkers need to watch out for framing (relying too heavily on context), premature closure, diagnostic momentum, anchoring, and confirmation bias. System 2 thinkers need to watch out for commission, availability bias, and base rate neglect.
“Neither system is inherently right or wrong,” Dr. Scarfone reiterated. “In the perfect world, you may use system 1 to form an initial impression, but then system 2 should really act as a check and balance system to cause you to reflect on your initial diagnostic impressions.”
Additional strategies include being a good history taker and performing a meticulous physical exam: be a good listener, clarify unclear aspects of the history, and identify and address the main concern.
“Remember children and families have a story to tell, and if we listen carefully enough, the diagnostic clues are there,” Dr. Scarfone said. “Sometimes they may be quite subtle.” He recommended doctors perform each part of the physical exam as if expecting an abnormality.
Another strategy is using meta-cognition, a forced analysis of the thinking that led to a diagnosis. It involves asking: “If I had to explain my medical decision-making to others, would this make inherent sense?” Dr. Scarfone said. “If you’re testing, try to avoid anchoring and confirmation biases.”
Finally, take a diagnostic time-out with a checklist that asks these questions:
- Does my presumptive diagnosis make sense?
- What evidence supports or refutes it?
- Did I arrive at it via cognitive biases?
- Are there other diagnostic possibilities that should be considered?
One way to do this is creating a table listing the complaint/finding, diagnostic possibilities with system 1 thinking, diagnostic possibilities with system 2 thinking, and then going beyond system 2 – the potential zebras – when even system 2 diagnostic possibilities don’t account for what the patient is saying or what the exam shows.
Enough overlap exists between these cognitive biases and the intrinsic bias related to individual characteristics that Dr. Khan appreciated the talk on another level as well.
“For me, as a brown Muslim immigrant woman of color, I can sometimes see cognitive biases in action with my colleagues and realize that they are oblivious to it,” Dr. Khan said. “It’s really refreshing to see this issue come up and being discussed at the [AAP] National Conference and Exhibition.”
Dr. Scarfone, Dr. Nagler and Dr. Khan have no relevant financial disclosures.
This article was updated 12/8/2020.
While it’s important not to think immediately of zebras when hearing hoofbeats, it’s just as important not to assume it’s always a horse. The delicate balance between not jumping to the seemingly obvious diagnosis without overanalyzing and overtesting is familiar to all physicians, and
“When these errors are made, it’s not because physicians lack knowledge, but they go down a wrong path in their thinking process,” Richard Scarfone, MD, a pediatric emergency medicine physician at the Children’s Hospital of Philadelphia, told attendees at the annual meeting of the American Academy of Pediatrics, held virtually this year. “An important point to be made here is that how physicians think seems to be much more important than what physicians know.”
Dr. Scarfone and Joshua Nagler, MD, MHPEd, director, pediatric emergency medicine fellowship program at Children’s Hospital Boston, presented a session on the cognitive biases that can trip up clinicians when making diagnoses and how to avoid them. Research shows that the rate of diagnostic error is approximately 15%. Although those findings come from studies in adults, the rates are likely similar in pediatrics, Dr. Scarfone said.
A wide range of clinical factors contribute to diagnostic errors: limited information, vague or undifferentiated symptoms, incomplete history, multiple transitions of care, diagnostic uncertainty, daily decision density, and reliance on pattern recognition, among others. Personal contributing factors can play a role as well, such as atypical work hours, fatigue, one’s emotional or affective state, a high cognitive load, and others. On top of all that, medical decision-making can be really complex on its own, Dr. Scarfone said. He compared differential diagnosis with a tree where a single leaf is the correct diagnosis.
System 1 thinking: Pros and cons
Dr. Scarfone and Dr. Nagler explained system 1 and system 2 thinking, two different ways of thinking that can influence decision-making that Daniel Kahneman explained in his book “Thinking, Fast and Slow.” System 1 refers to the snap judgments that rely on heuristics while system 2 refers to a more analytic, slower process.
Neither system 1 nor 2 is inherently “right or wrong,” Dr. Scarfone said. “The diagnostic sweet spot is to try to apply the correct system to the correct patient.”
Heuristics are the mental shortcuts people use to make decisions based on past experience. They exist because they’re useful, enabling people to focus only on what they need to accomplish everyday tasks, such as driving or brushing teeth. But heuristics can also lead to predictable cognitive errors.
“The good news about heuristics and system 1 thinking is that it’s efficient and simple, and we desire that in a busy practice or ED setting, but we should recognize that the trade-off is that it may be at the expense of accuracy,” Dr. Scarfone said.
The advantage to system 1 thinking is easy, simple, rapid, and efficient decision-making that rejects ambiguity. It’s also usually accurate, which rewards the approach, and accuracy increases with time based on memory, experience, and pattern recognition. Doctors develop “illness scripts” that help in identifying diagnoses.
“Illness scripts are common patterns of clinical presentations that usually lead us to a diagnostic possibility,” Dr. Scarfone said. “A classic illness script might be a 4-week-old firstborn male with forceful vomiting, and immediately your mind may go to pyloric stenosis as a likely diagnosis.” But the patient may have a different diagnosis than the initial impression your system 1 thinking leads you to believe.
“Generally, the more experience a clinician has, the more accurate they’ll be in using system 1,” he said. “Seasoned physicians are much more likely to employ system 1 than a newer physician or trainee,” which is why heuristics shouldn’t be thought of as hindrances. Dr. Scarfone quoted Kevin Eva in a 2005 review on clinical reasoning: “Successful heuristics should be embraced rather than overcome.”
A drawback to system 1 thinking, however, is thinking that “what you see is all there is,” which can lead to cognitive errors. Feeling wrong feels the same as feeling right, so you may not realize when you’re off target and therefore neglect to consider alternatives.
“When we learn a little about our patient’s complaint, it’s easier to fit everything into a coherent explanation,” Dr. Scarfone said, but “don’t ask, don’t tell doesn’t work in medicine.”
Another challenge with system 1 thinking is that pattern recognition can be unreliable because it’s dependent on context. For example, consider the difference in assessing a patient’s sore throat in a primary care office versus a resuscitation bay. “Clearly our consideration of what may be going on with the patient and what the diagnosis may be is likely to vary in those two settings,” he said.
System 2 thinking: Of zebras and horses
System 2 is the analytic thinking that involves pondering and seek out the optimal answer rather than the “good-enough” answer.
“The good news about system 2 is that it really can monitor system 1,” said Dr. Nagler, who has a master’s degree in health professions education. “If you spend the time to do analytic reasoning, you can actually mitigate some of those errors that may occur from intuitive judgments from system 1 thinking. System 2 spends the time to say ‘let’s make sure we’re doing this right.’ ” In multiple-choice tests, for example, people are twice as likely to change a wrong answer to a right one than a right one to a wrong one.
System 2 thinking allows for the reasoning to assess questions in the gray zone. It’s vigilant, it’s reliable, it’s effective, it acknowledges uncertainty and doubt, it can be safe in terms of providing care, and it has high scientific rigor. But it also has disadvantages, starting with the fact that it’s slower and more time-consuming. System 2 thinking is resource intensive, requiring a higher cognitive demand and more time and effort.
“Sometimes the quick judgment is the best judgment,” Dr. Nagler said. System 2 thinking also is sometimes unnecessary and counter to value-based care. “If you start to think about all the possibilities of what a presentation may be, all of a sudden you might find yourself wanting to do all kinds of tests and all kinds of referrals and other things, which is not necessarily value-based care.” When system 2 thinking goes astray, it makes us think everything we see is a zebra rather than a horse.
Sonia Khan, MD, a pediatrician in Fremont, Calif., found this session particularly worthwhile.
“It really tries to explain the difference between leaping to conclusions and learning how to hold your horses and do a bit more, to double check that you’re not locking everything into a horse stall and missing a zebra, and avoiding go too far with system 2 and thinking that everything’s a zebra,” Dr. Khan said. “It’s a difficult talk to have because you’re asking pediatricians to look in the mirror and own up, to learn to step back and reconsider the picture, and consider the biases that may come into your decision-making; then learn to extrude them, and rethink the case to be sure your knee-jerk diagnostic response is correct.”
Types of cognitive errors
The presenters listed some of the most common cognitive errors, although their list is far from exhaustive.
- Affective error. Avoiding unpleasant but necessary tests or examinations because of sympathy for the patient, such as avoiding blood work to spare a needle stick in a cancer patient with abdominal pain because the mother is convinced it’s constipation from opioids. This is similar to omission bias, which places excessive concern on avoiding a therapy’s adverse effects when the therapy could be highly effective.
- Anchoring. Clinging to an initial impression or salient features of initial presentation, even as conflicting and contradictory data accumulate, such as diagnosing a patient with fever and vomiting with gastroenteritis even when the patient has an oxygen saturation of 94% and tachypnea.
- Attribution errors. Negative stereotypes lead clinicians to ignore or minimize the possibility of serious disease, such as evaluating a confused teen covered in piercings and tattoos for drug ingestion when the actual diagnosis is new-onset diabetic ketoacidosis.
- Availability bias. Overestimating or underestimating the probability of disease because of recent experience, what was most recently “available” to your brain cognitively, such as getting head imaging on several vomiting patients in a row because you recently had one with a new brain tumor diagnosis.
- Bandwagon effect. Accepting the group’s opinion without assessing a clinical situation yourself, such as sending home a crying, vomiting infant with a presumed viral infection only to see the infant return later with intussusception.
- Base rate neglect. Ignoring the true prevalence of disease by either inflating it or reducing it, such as searching for cardiac disease in all pediatric patients with chest pain.
- Commission. A tendency toward action with the belief that harm may only be prevented by action, such as ordering every possible test for a patient with fever to “rule everything out.”
- Confirmation bias. Subconscious cherry-picking: A tendency to look for, notice, and remember information that fits with preexisting expectations while disregarding information that contradicts those expectations.
- Diagnostic momentum. Clinging to that initial diagnostic impression that may have been generated by others, which is particularly common during transitions of care.
- Premature closure. Narrowing down to a diagnosis without thinking about other diagnoses or asking enough questions about other symptoms that may have opened up other diagnostic possibilities.
- Representation bias. Making a decision in the absence of appropriate context by incorrectly comparing two situations because of a perceived similarity between them, or on the flip side, evaluating a situation without comparing it with other situations.
- Overconfidence. Making a decision without enough supportive evidence yet feeling confident about the diagnosis.
- Search satisfying. Stopping the search for additional diagnoses after the anticipated diagnosis has been made.
Cognitive pills for cognitive ills
Being aware of the pitfalls of cognitive errors is the first step to avoiding and mitigating them. “It really does start with preparation and awareness,” Dr. Scarfone said before presenting strategies to build a cognitive “firewall” that can help physicians practice reflectively instead of reflexively.
First, be aware of your cognitive style. People usually have the same thinking pattern in everyday life as in the clinical setting, so determine whether you’re more of a system 1 or system 2 thinker. System 1 thinkers need to watch out for framing (relying too heavily on context), premature closure, diagnostic momentum, anchoring, and confirmation bias. System 2 thinkers need to watch out for commission, availability bias, and base rate neglect.
“Neither system is inherently right or wrong,” Dr. Scarfone reiterated. “In the perfect world, you may use system 1 to form an initial impression, but then system 2 should really act as a check and balance system to cause you to reflect on your initial diagnostic impressions.”
Additional strategies include being a good history taker and performing a meticulous physical exam: be a good listener, clarify unclear aspects of the history, and identify and address the main concern.
“Remember children and families have a story to tell, and if we listen carefully enough, the diagnostic clues are there,” Dr. Scarfone said. “Sometimes they may be quite subtle.” He recommended doctors perform each part of the physical exam as if expecting an abnormality.
Another strategy is using meta-cognition, a forced analysis of the thinking that led to a diagnosis. It involves asking: “If I had to explain my medical decision-making to others, would this make inherent sense?” Dr. Scarfone said. “If you’re testing, try to avoid anchoring and confirmation biases.”
Finally, take a diagnostic time-out with a checklist that asks these questions:
- Does my presumptive diagnosis make sense?
- What evidence supports or refutes it?
- Did I arrive at it via cognitive biases?
- Are there other diagnostic possibilities that should be considered?
One way to do this is creating a table listing the complaint/finding, diagnostic possibilities with system 1 thinking, diagnostic possibilities with system 2 thinking, and then going beyond system 2 – the potential zebras – when even system 2 diagnostic possibilities don’t account for what the patient is saying or what the exam shows.
Enough overlap exists between these cognitive biases and the intrinsic bias related to individual characteristics that Dr. Khan appreciated the talk on another level as well.
“For me, as a brown Muslim immigrant woman of color, I can sometimes see cognitive biases in action with my colleagues and realize that they are oblivious to it,” Dr. Khan said. “It’s really refreshing to see this issue come up and being discussed at the [AAP] National Conference and Exhibition.”
Dr. Scarfone, Dr. Nagler and Dr. Khan have no relevant financial disclosures.
This article was updated 12/8/2020.
FROM AAP 2020
Fear of recurrence highly prevalent in RCC survivors
About 55% of survivors surveyed expressed this fear, which is higher than the average prevalence among patients diagnosed with other cancers.
Younger and female RCC survivors appear to be at particular risk, but disease stage and time since diagnosis are not associated with FCR, according to the survey.
The results were published in JCO Oncology Practice.
The majority of existing studies concerning FCR have been of survivors of breast, prostate, and gynecologic cancers. For the first time, researchers examined this issue in RCC survivors in a large trial.
More than 1,000 survivors of localized RCC were asked to participate in a survey through social media by the Kidney Cancer Research Alliance.
A total of 412 survivors were included in the analysis. They had a median age of 54 years (range, 30-80 years), were mostly female (79.4%), were mostly well educated (58.3%), and had a median of 17.5 months’ time since diagnosis.
More than half of patients were diagnosed with stage I disease, and about two-thirds had a clear understanding of their diagnosis.
Results: FCR persists in RCC
Two-thirds of the survivors had a high prevalence of moderate to severe distress, and 54.9% reported FCR.
“This is the first study to assess fear of cancer recurrence in RCC,” said lead study author Cristiane Decat Bergerot, PhD, who conducted the research during a fellowship at City of Hope in Duarte, Calif. She is now director of the department of psycho-oncology at CETTRO Cancer Research Hospital in Brasilia, Brazil.
“RCC patients really experience this emotion,” Dr. Bergerot said. “Other emotional symptoms, even stress, tend to lower over time. This does not happen with FCR in RCC patients. More than 3 years later, they still had the same prevalence of FCR.”
The prevalence of FCR was not associated with race, education level, country, residential area, cancer care facility type, travel time to hospital, or clinical characteristics such as disease stage and time since diagnosis.
However, higher FCR was associated with female gender, younger age, and lack of understanding of diagnosis. For younger and female patients, the social and emotional consequences of RCC may make it hard for them to keep up with daily activities. Younger patients may have multiple social roles and responsibilities, and an RCC diagnosis interrupts their life.
Even though RCC is more prevalent in males, “females traditionally have no fear of saying they are not doing well with diagnosis or treatment. Women appear to be more open to support,” Dr. Bergerot said.
Interventions and support
Psychosocial support with targeted interventions can help address FCR for RCC patients, according to Dr. Bergerot. For example, researchers are developing an app to allow for psychosocial intervention at home to help patients cope with FCR, she said, noting that clinicians in cancer centers more often see metastatic disease, not localized disease.
“Clinicians can teach patients to be more comfortable and feel less anxious about their prognosis and also help them participate in treatment decision-making,” Dr. Bergerot said. “When a RCC patient worries too much about cancer recurrence, refer the patient to a psychosocial team. The patient can receive practical advice to balance emotional symptoms, learn more about their current situation, and find more information through cancer support groups.”
“FCR is a key factor underlying emotional and behavioral difficulties faced by survivors of cancer,” said Daniel L. Hall, PhD, of Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in this study. “Clinicians treating cancer survivors are well positioned to assess and intervene on FCR, distress, and health behaviors.”
Dr. Hall noted that these fears are a near-ubiquitous concern for cancer survivors.
“Inherently, managing FCR requires acknowledging and facing the uncertainty about one’s future health, which, of course, for all of us is unpredictable, ambiguous, and ever-changing. Although many patients who fear recurrence are fortunate to have a low objective risk of recurrence, I believe patients facing cancer, regardless of demographic or medical characteristics, can feel afraid when facing an unknown, possibly dangerous future,” Dr. Hall said.
Calls for interventions targeting FCR have emphasized the need for evidence-based treatments and multimodal interventions that teach a variety of targeted skills. Cognitive behavioral therapy (CBT) and mind-body interventions are being studied to address FCR.
“Our team conducted a meta-analysis of randomized clinical trials of these interventions and found that pooled effects were significant, yet small, suggesting the need for further intervention development,” Dr. Hall said. “Through funding from the NIH’s National Center for Complementary and Integrative Health, we are currently evaluating a multimodal, group-based intervention that integrates many of the most effective FCR management skills: CBT, mindfulness meditation, relaxation response training, and positive psychology.”
Harvard researchers recently published encouraging results from a small pilot study of a group intervention. The next step is to test a remote, synchronous program in a randomized trial, with recruitment anticipated in early 2021.
“In addition to our work, other groups are developing asynchronous interventions that cancer survivors can use by accessing a website, which may appeal to survivors looking for information quickly or who may not be interested in participating in a group intervention,” Dr. Hall said.
The current study did not receive specific funding. The authors disclosed relationships with many companies, which can be found in the paper. Dr. Hall has no disclosures.
SOURCE: Bergerot CD et al. JCO Oncol Pract. 2020 Nov;16(11):e1264-71.
About 55% of survivors surveyed expressed this fear, which is higher than the average prevalence among patients diagnosed with other cancers.
Younger and female RCC survivors appear to be at particular risk, but disease stage and time since diagnosis are not associated with FCR, according to the survey.
The results were published in JCO Oncology Practice.
The majority of existing studies concerning FCR have been of survivors of breast, prostate, and gynecologic cancers. For the first time, researchers examined this issue in RCC survivors in a large trial.
More than 1,000 survivors of localized RCC were asked to participate in a survey through social media by the Kidney Cancer Research Alliance.
A total of 412 survivors were included in the analysis. They had a median age of 54 years (range, 30-80 years), were mostly female (79.4%), were mostly well educated (58.3%), and had a median of 17.5 months’ time since diagnosis.
More than half of patients were diagnosed with stage I disease, and about two-thirds had a clear understanding of their diagnosis.
Results: FCR persists in RCC
Two-thirds of the survivors had a high prevalence of moderate to severe distress, and 54.9% reported FCR.
“This is the first study to assess fear of cancer recurrence in RCC,” said lead study author Cristiane Decat Bergerot, PhD, who conducted the research during a fellowship at City of Hope in Duarte, Calif. She is now director of the department of psycho-oncology at CETTRO Cancer Research Hospital in Brasilia, Brazil.
“RCC patients really experience this emotion,” Dr. Bergerot said. “Other emotional symptoms, even stress, tend to lower over time. This does not happen with FCR in RCC patients. More than 3 years later, they still had the same prevalence of FCR.”
The prevalence of FCR was not associated with race, education level, country, residential area, cancer care facility type, travel time to hospital, or clinical characteristics such as disease stage and time since diagnosis.
However, higher FCR was associated with female gender, younger age, and lack of understanding of diagnosis. For younger and female patients, the social and emotional consequences of RCC may make it hard for them to keep up with daily activities. Younger patients may have multiple social roles and responsibilities, and an RCC diagnosis interrupts their life.
Even though RCC is more prevalent in males, “females traditionally have no fear of saying they are not doing well with diagnosis or treatment. Women appear to be more open to support,” Dr. Bergerot said.
Interventions and support
Psychosocial support with targeted interventions can help address FCR for RCC patients, according to Dr. Bergerot. For example, researchers are developing an app to allow for psychosocial intervention at home to help patients cope with FCR, she said, noting that clinicians in cancer centers more often see metastatic disease, not localized disease.
“Clinicians can teach patients to be more comfortable and feel less anxious about their prognosis and also help them participate in treatment decision-making,” Dr. Bergerot said. “When a RCC patient worries too much about cancer recurrence, refer the patient to a psychosocial team. The patient can receive practical advice to balance emotional symptoms, learn more about their current situation, and find more information through cancer support groups.”
“FCR is a key factor underlying emotional and behavioral difficulties faced by survivors of cancer,” said Daniel L. Hall, PhD, of Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in this study. “Clinicians treating cancer survivors are well positioned to assess and intervene on FCR, distress, and health behaviors.”
Dr. Hall noted that these fears are a near-ubiquitous concern for cancer survivors.
“Inherently, managing FCR requires acknowledging and facing the uncertainty about one’s future health, which, of course, for all of us is unpredictable, ambiguous, and ever-changing. Although many patients who fear recurrence are fortunate to have a low objective risk of recurrence, I believe patients facing cancer, regardless of demographic or medical characteristics, can feel afraid when facing an unknown, possibly dangerous future,” Dr. Hall said.
Calls for interventions targeting FCR have emphasized the need for evidence-based treatments and multimodal interventions that teach a variety of targeted skills. Cognitive behavioral therapy (CBT) and mind-body interventions are being studied to address FCR.
“Our team conducted a meta-analysis of randomized clinical trials of these interventions and found that pooled effects were significant, yet small, suggesting the need for further intervention development,” Dr. Hall said. “Through funding from the NIH’s National Center for Complementary and Integrative Health, we are currently evaluating a multimodal, group-based intervention that integrates many of the most effective FCR management skills: CBT, mindfulness meditation, relaxation response training, and positive psychology.”
Harvard researchers recently published encouraging results from a small pilot study of a group intervention. The next step is to test a remote, synchronous program in a randomized trial, with recruitment anticipated in early 2021.
“In addition to our work, other groups are developing asynchronous interventions that cancer survivors can use by accessing a website, which may appeal to survivors looking for information quickly or who may not be interested in participating in a group intervention,” Dr. Hall said.
The current study did not receive specific funding. The authors disclosed relationships with many companies, which can be found in the paper. Dr. Hall has no disclosures.
SOURCE: Bergerot CD et al. JCO Oncol Pract. 2020 Nov;16(11):e1264-71.
About 55% of survivors surveyed expressed this fear, which is higher than the average prevalence among patients diagnosed with other cancers.
Younger and female RCC survivors appear to be at particular risk, but disease stage and time since diagnosis are not associated with FCR, according to the survey.
The results were published in JCO Oncology Practice.
The majority of existing studies concerning FCR have been of survivors of breast, prostate, and gynecologic cancers. For the first time, researchers examined this issue in RCC survivors in a large trial.
More than 1,000 survivors of localized RCC were asked to participate in a survey through social media by the Kidney Cancer Research Alliance.
A total of 412 survivors were included in the analysis. They had a median age of 54 years (range, 30-80 years), were mostly female (79.4%), were mostly well educated (58.3%), and had a median of 17.5 months’ time since diagnosis.
More than half of patients were diagnosed with stage I disease, and about two-thirds had a clear understanding of their diagnosis.
Results: FCR persists in RCC
Two-thirds of the survivors had a high prevalence of moderate to severe distress, and 54.9% reported FCR.
“This is the first study to assess fear of cancer recurrence in RCC,” said lead study author Cristiane Decat Bergerot, PhD, who conducted the research during a fellowship at City of Hope in Duarte, Calif. She is now director of the department of psycho-oncology at CETTRO Cancer Research Hospital in Brasilia, Brazil.
“RCC patients really experience this emotion,” Dr. Bergerot said. “Other emotional symptoms, even stress, tend to lower over time. This does not happen with FCR in RCC patients. More than 3 years later, they still had the same prevalence of FCR.”
The prevalence of FCR was not associated with race, education level, country, residential area, cancer care facility type, travel time to hospital, or clinical characteristics such as disease stage and time since diagnosis.
However, higher FCR was associated with female gender, younger age, and lack of understanding of diagnosis. For younger and female patients, the social and emotional consequences of RCC may make it hard for them to keep up with daily activities. Younger patients may have multiple social roles and responsibilities, and an RCC diagnosis interrupts their life.
Even though RCC is more prevalent in males, “females traditionally have no fear of saying they are not doing well with diagnosis or treatment. Women appear to be more open to support,” Dr. Bergerot said.
Interventions and support
Psychosocial support with targeted interventions can help address FCR for RCC patients, according to Dr. Bergerot. For example, researchers are developing an app to allow for psychosocial intervention at home to help patients cope with FCR, she said, noting that clinicians in cancer centers more often see metastatic disease, not localized disease.
“Clinicians can teach patients to be more comfortable and feel less anxious about their prognosis and also help them participate in treatment decision-making,” Dr. Bergerot said. “When a RCC patient worries too much about cancer recurrence, refer the patient to a psychosocial team. The patient can receive practical advice to balance emotional symptoms, learn more about their current situation, and find more information through cancer support groups.”
“FCR is a key factor underlying emotional and behavioral difficulties faced by survivors of cancer,” said Daniel L. Hall, PhD, of Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in this study. “Clinicians treating cancer survivors are well positioned to assess and intervene on FCR, distress, and health behaviors.”
Dr. Hall noted that these fears are a near-ubiquitous concern for cancer survivors.
“Inherently, managing FCR requires acknowledging and facing the uncertainty about one’s future health, which, of course, for all of us is unpredictable, ambiguous, and ever-changing. Although many patients who fear recurrence are fortunate to have a low objective risk of recurrence, I believe patients facing cancer, regardless of demographic or medical characteristics, can feel afraid when facing an unknown, possibly dangerous future,” Dr. Hall said.
Calls for interventions targeting FCR have emphasized the need for evidence-based treatments and multimodal interventions that teach a variety of targeted skills. Cognitive behavioral therapy (CBT) and mind-body interventions are being studied to address FCR.
“Our team conducted a meta-analysis of randomized clinical trials of these interventions and found that pooled effects were significant, yet small, suggesting the need for further intervention development,” Dr. Hall said. “Through funding from the NIH’s National Center for Complementary and Integrative Health, we are currently evaluating a multimodal, group-based intervention that integrates many of the most effective FCR management skills: CBT, mindfulness meditation, relaxation response training, and positive psychology.”
Harvard researchers recently published encouraging results from a small pilot study of a group intervention. The next step is to test a remote, synchronous program in a randomized trial, with recruitment anticipated in early 2021.
“In addition to our work, other groups are developing asynchronous interventions that cancer survivors can use by accessing a website, which may appeal to survivors looking for information quickly or who may not be interested in participating in a group intervention,” Dr. Hall said.
The current study did not receive specific funding. The authors disclosed relationships with many companies, which can be found in the paper. Dr. Hall has no disclosures.
SOURCE: Bergerot CD et al. JCO Oncol Pract. 2020 Nov;16(11):e1264-71.
FROM JCO ONCOLOGY PRACTICE