User login
Early estrogen loss increases cardiovascular risk in women
The relationship between estrogen levels and heart health makes it particularly important for clinicians to be aware of those patients who might be at risk for cardiovascular disease despite not having other traditional risk factors, according to a presentation Oct. 12 at the North American Menopause Society annual meeting in Atlanta.
”Endogenous estrogens are protective for cardiovascular disease in premenopausal women,” Chrisandra L. Shufelt, MD, chair of the division of general internal medicine and associate director of the Women’s Health Research Center at Mayo Clinic in Jacksonville, Fla., told attendees. Yet, “a substantial population of young women are dying prematurely from cardiovascular disease,” with rates of cardiovascular death increasing in women aged 35-44 even as rates have decreased in postmenopausal women and in men. One potential reason may be premature estrogen loss.
Dr. Shufelt reminded attendees of four major causes of premature estrogen loss: Natural premature menopause, surgical menopause, chemotherapy-induced menopause, and premature ovarian insufficiency. But she would go on to discuss a less widely recognized condition, functional hypothalamic amenorrhea, that also may be contributing to increased cardiovascular risk.
First, Dr. Shufelt reviewed the evidence supporting the relationship between estrogen and cardiovascular health, starting with the Framingham study’s findings that cardiovascular disease is approximately two to four times more common in postmenopausal women than in premenopausal women, depending on the age range.
“Menopause at an early age, particularly under the age of 40, matters,” Dr. Shufelt said. “So we should be discussing this with our patients.”
Surgical menopause makes a difference to cardiovascular health as well, she said. In women under age 35, for example, the risk of a nonfatal heart attack in those with a bilateral oophorectomy was 7.7 times greater than in women who retained both ovaries and their uterus, and 1.5 times greater in women who had a hysterectomy without bilateral oophorectomy.
In a 2019 study, surgical premature menopause was associated with an 87% increased risk of heart disease even after researchers accounted for age, cardiovascular risk factors, and some forms of hormone therapy. The increased risk from natural premature menopause, on the other hand, was lower – a 36% increased risk of heart disease – compared with those producing endogenous hormones. Although randomized controlled trials are unavailable and unlikely to be done, the Nurses’ Health Study and the Danish Nurses Cohort Study, both observational studies, found that heart disease risk was diminished in those taking hormone therapy after surgical premature menopause.
Recommendations for premature or early menopause, from a wide range of different medical societies including NAMS, are that women without contraindications be given estrogen-based hormone therapy until the average age of natural menopause. Though not included in the same guidance, research has also shown that estrogen after oophorectomy does not increase the risk of breast cancer in women with a BRCA1 mutation, Dr. Shufelt said. Hormone therapy for premature or early menopause should adequately replace the levels women have lost and that means younger menopausal women often need higher doses than what older women receive, such as 2 mg/day of oral estradiol rather than the standard doses of 0.5 or 1 mg/day.
Functional hypothalamic amenorrhea and cardiovascular risk
Dr. Shufelt then discussed functional hypothalamic amenorrhea (hypogonadotropic hypogonadism), a common type of secondary amenorrhea that affects at least 1.4 million U.S. women. Diagnosis includes lack of a period for at least 3 months in someone who previously menstruated plus lab values below 50 pg/mL for estradiol, below 10 mIU/L for follicle stimulating hormone, and below 10 mIU/L for luteinizing hormone. Causes of this reversible form of infertility can include stress, overexercising, undereating, or some combination of these, plus an underlying genetic predisposition.
“After ruling out polycystic ovary syndrome, prolactinoma, and thyroid dysfunction, clinicians need to consider the diagnosis of hypothalamic amenorrhea,” Dr. Shufelt said. This condition goes beyond low estrogen levels: Women have elevated cortisol, low thyroid levels, low leptin levels, and increased ghrelin.
”This is not going away,” Dr. Shufelt said, sharing data on stress levels among U.S. adults, particularly Gen Z and millennial adults, noting that the ongoing “national mental health crisis” may be contributing to functional hypothalamic amenorrhea.
A 2020 substudy from the Nurses’ Health Study II found an increased risk of premature death in those who didn’t have a period or always had irregular periods starting as early as 14-17 years old. The increased risk of premature death rose with age in those with irregular or absent cycles – a 37% higher risk in 18- to 22-year-olds and a 39% increased risk in 29- to 46-year-olds.
But clinicians aren’t adequately identifying the “phenotype of the hypothalamic women,” Dr. Shufelt said, despite research showing overlap between hypothalamic amenorrhea and a higher risk of cardiovascular disease. Hypothalamic amenorrhea is so understudied that the last original research on the topic was in 2008, Dr. Shufelt said in an interview. ”No research except mine has been done to evaluate heart health in these young women,” she said.
Dr. Shufelt described a study she led involving 30 women with functional hypothalamic amenorrhea, 29 women with normal menstrual cycles, and 30 women who were recently menopausal and not on hormone therapy. The women with hypothalamic amenorrhea had average stress levels but their depression scores were higher than those of the other two groups.
The results showed that women with hypothalamic amenorrhea had lower estradiol and leptin levels and higher testosterone levels compared with the control group, and they had higher cortisol levels than those of both groups. Despite having similar body mass indexes as the control and menopausal groups, women with hypothalamic amenorrhea had lower blood pressure than that of the other two groups, yet they had higher cholesterol levels than those of the control group. EndoPAT© (Itamar Medical) testing showed that they had poor vascular function.
“In fact, one-third of the women [with hypothalamic amenorrhea] entered the trial with a diagnosis of what would be considered endothelial dysfunction,” Dr. Shufelt said. “Our results demonstrated significantly higher circulating levels of serum proinflammatory cytokines in the women with hypothalamic amenorrhea compared to eumenorrheic controls.”
Dr. Shufelt’s team then tested whether giving estradiol to the women with hypothalamic amenorrhea for 12 weeks would improve their vascular health, but they saw no significant differences between the women who received estrogen and those who received placebo.
“Endothelial function is partly mediated by estrogen, and it was expected that giving back estrogen would ‘fix’ the endothelium, but that is not what happened,” Nanette Santoro, MD, professor and chair of obstetrics and gynecology at the University of Colorado at Denver, Aurora, said in interview. “The mechanisms that maintain vascular function in women are not limited to hormones,” said Dr. Santoro, who was not involved in Dr. Shufelt’s study but attended her lecture. “We need to think beyond the simple model of estrogen-good, no-estrogen-bad.”
Dr. Santoro noted how easy it is to overlook the women who may have cardiovascular risk because of hypothalamic amenorrhea.
“Because many women with functional hypothalamic amenorrhea are super athletic and do not have the typical features of people with cardiometabolic disease – such as glucose intolerance, obesity, abnormal cholesterol or triglycerides, or high blood pressure – clinicians tend to think of them as healthy and to think that simply giving back hormones will fix the problems with bone density and vascular function, but that is not enough,” Dr. Santoro said. “The cognitive-behavioral therapy model for treatment of women with functional hypothalamic amenorrhea addresses the stress-related factors that drive the disorder, and this needs to be considered the standard of care for treatment.”
Stephanie S. Faubion, MD, professor of medicine and director of Mayo Clinic’s Center for Women’s Health in Jacksonville, Fla., who was not involved in Dr. Shufelt’s presentation, also emphasized the importance of recognizing functional hypothalamic amenorrhea.
“This is an underrecognized entity to begin with, and the fact that these women appear to be at increased risk for vascular dysfunction and potentially increased risk for cardiovascular disease down the road makes it even more important for clinicians to identify them and provide interventions early on,” Dr. Faubion said in an interview. “These women need to be identified and the etiology of the amenorrhea addressed, whether it relates to overexercising, being underweight, or experiencing significant stressors that have led to the loss of menstrual cycles.”
Dr. Shufelt’s research was funded by the National Institutes of Health. She had no disclosures. Dr. Santoro is a member of the scientific advisory board for Astellas, Menogenix, Amazon Ember, and Que Oncology, and she consults for Ansh Labs. Dr. Faubion had no disclosures.
The relationship between estrogen levels and heart health makes it particularly important for clinicians to be aware of those patients who might be at risk for cardiovascular disease despite not having other traditional risk factors, according to a presentation Oct. 12 at the North American Menopause Society annual meeting in Atlanta.
”Endogenous estrogens are protective for cardiovascular disease in premenopausal women,” Chrisandra L. Shufelt, MD, chair of the division of general internal medicine and associate director of the Women’s Health Research Center at Mayo Clinic in Jacksonville, Fla., told attendees. Yet, “a substantial population of young women are dying prematurely from cardiovascular disease,” with rates of cardiovascular death increasing in women aged 35-44 even as rates have decreased in postmenopausal women and in men. One potential reason may be premature estrogen loss.
Dr. Shufelt reminded attendees of four major causes of premature estrogen loss: Natural premature menopause, surgical menopause, chemotherapy-induced menopause, and premature ovarian insufficiency. But she would go on to discuss a less widely recognized condition, functional hypothalamic amenorrhea, that also may be contributing to increased cardiovascular risk.
First, Dr. Shufelt reviewed the evidence supporting the relationship between estrogen and cardiovascular health, starting with the Framingham study’s findings that cardiovascular disease is approximately two to four times more common in postmenopausal women than in premenopausal women, depending on the age range.
“Menopause at an early age, particularly under the age of 40, matters,” Dr. Shufelt said. “So we should be discussing this with our patients.”
Surgical menopause makes a difference to cardiovascular health as well, she said. In women under age 35, for example, the risk of a nonfatal heart attack in those with a bilateral oophorectomy was 7.7 times greater than in women who retained both ovaries and their uterus, and 1.5 times greater in women who had a hysterectomy without bilateral oophorectomy.
In a 2019 study, surgical premature menopause was associated with an 87% increased risk of heart disease even after researchers accounted for age, cardiovascular risk factors, and some forms of hormone therapy. The increased risk from natural premature menopause, on the other hand, was lower – a 36% increased risk of heart disease – compared with those producing endogenous hormones. Although randomized controlled trials are unavailable and unlikely to be done, the Nurses’ Health Study and the Danish Nurses Cohort Study, both observational studies, found that heart disease risk was diminished in those taking hormone therapy after surgical premature menopause.
Recommendations for premature or early menopause, from a wide range of different medical societies including NAMS, are that women without contraindications be given estrogen-based hormone therapy until the average age of natural menopause. Though not included in the same guidance, research has also shown that estrogen after oophorectomy does not increase the risk of breast cancer in women with a BRCA1 mutation, Dr. Shufelt said. Hormone therapy for premature or early menopause should adequately replace the levels women have lost and that means younger menopausal women often need higher doses than what older women receive, such as 2 mg/day of oral estradiol rather than the standard doses of 0.5 or 1 mg/day.
Functional hypothalamic amenorrhea and cardiovascular risk
Dr. Shufelt then discussed functional hypothalamic amenorrhea (hypogonadotropic hypogonadism), a common type of secondary amenorrhea that affects at least 1.4 million U.S. women. Diagnosis includes lack of a period for at least 3 months in someone who previously menstruated plus lab values below 50 pg/mL for estradiol, below 10 mIU/L for follicle stimulating hormone, and below 10 mIU/L for luteinizing hormone. Causes of this reversible form of infertility can include stress, overexercising, undereating, or some combination of these, plus an underlying genetic predisposition.
“After ruling out polycystic ovary syndrome, prolactinoma, and thyroid dysfunction, clinicians need to consider the diagnosis of hypothalamic amenorrhea,” Dr. Shufelt said. This condition goes beyond low estrogen levels: Women have elevated cortisol, low thyroid levels, low leptin levels, and increased ghrelin.
”This is not going away,” Dr. Shufelt said, sharing data on stress levels among U.S. adults, particularly Gen Z and millennial adults, noting that the ongoing “national mental health crisis” may be contributing to functional hypothalamic amenorrhea.
A 2020 substudy from the Nurses’ Health Study II found an increased risk of premature death in those who didn’t have a period or always had irregular periods starting as early as 14-17 years old. The increased risk of premature death rose with age in those with irregular or absent cycles – a 37% higher risk in 18- to 22-year-olds and a 39% increased risk in 29- to 46-year-olds.
But clinicians aren’t adequately identifying the “phenotype of the hypothalamic women,” Dr. Shufelt said, despite research showing overlap between hypothalamic amenorrhea and a higher risk of cardiovascular disease. Hypothalamic amenorrhea is so understudied that the last original research on the topic was in 2008, Dr. Shufelt said in an interview. ”No research except mine has been done to evaluate heart health in these young women,” she said.
Dr. Shufelt described a study she led involving 30 women with functional hypothalamic amenorrhea, 29 women with normal menstrual cycles, and 30 women who were recently menopausal and not on hormone therapy. The women with hypothalamic amenorrhea had average stress levels but their depression scores were higher than those of the other two groups.
The results showed that women with hypothalamic amenorrhea had lower estradiol and leptin levels and higher testosterone levels compared with the control group, and they had higher cortisol levels than those of both groups. Despite having similar body mass indexes as the control and menopausal groups, women with hypothalamic amenorrhea had lower blood pressure than that of the other two groups, yet they had higher cholesterol levels than those of the control group. EndoPAT© (Itamar Medical) testing showed that they had poor vascular function.
“In fact, one-third of the women [with hypothalamic amenorrhea] entered the trial with a diagnosis of what would be considered endothelial dysfunction,” Dr. Shufelt said. “Our results demonstrated significantly higher circulating levels of serum proinflammatory cytokines in the women with hypothalamic amenorrhea compared to eumenorrheic controls.”
Dr. Shufelt’s team then tested whether giving estradiol to the women with hypothalamic amenorrhea for 12 weeks would improve their vascular health, but they saw no significant differences between the women who received estrogen and those who received placebo.
“Endothelial function is partly mediated by estrogen, and it was expected that giving back estrogen would ‘fix’ the endothelium, but that is not what happened,” Nanette Santoro, MD, professor and chair of obstetrics and gynecology at the University of Colorado at Denver, Aurora, said in interview. “The mechanisms that maintain vascular function in women are not limited to hormones,” said Dr. Santoro, who was not involved in Dr. Shufelt’s study but attended her lecture. “We need to think beyond the simple model of estrogen-good, no-estrogen-bad.”
Dr. Santoro noted how easy it is to overlook the women who may have cardiovascular risk because of hypothalamic amenorrhea.
“Because many women with functional hypothalamic amenorrhea are super athletic and do not have the typical features of people with cardiometabolic disease – such as glucose intolerance, obesity, abnormal cholesterol or triglycerides, or high blood pressure – clinicians tend to think of them as healthy and to think that simply giving back hormones will fix the problems with bone density and vascular function, but that is not enough,” Dr. Santoro said. “The cognitive-behavioral therapy model for treatment of women with functional hypothalamic amenorrhea addresses the stress-related factors that drive the disorder, and this needs to be considered the standard of care for treatment.”
Stephanie S. Faubion, MD, professor of medicine and director of Mayo Clinic’s Center for Women’s Health in Jacksonville, Fla., who was not involved in Dr. Shufelt’s presentation, also emphasized the importance of recognizing functional hypothalamic amenorrhea.
“This is an underrecognized entity to begin with, and the fact that these women appear to be at increased risk for vascular dysfunction and potentially increased risk for cardiovascular disease down the road makes it even more important for clinicians to identify them and provide interventions early on,” Dr. Faubion said in an interview. “These women need to be identified and the etiology of the amenorrhea addressed, whether it relates to overexercising, being underweight, or experiencing significant stressors that have led to the loss of menstrual cycles.”
Dr. Shufelt’s research was funded by the National Institutes of Health. She had no disclosures. Dr. Santoro is a member of the scientific advisory board for Astellas, Menogenix, Amazon Ember, and Que Oncology, and she consults for Ansh Labs. Dr. Faubion had no disclosures.
The relationship between estrogen levels and heart health makes it particularly important for clinicians to be aware of those patients who might be at risk for cardiovascular disease despite not having other traditional risk factors, according to a presentation Oct. 12 at the North American Menopause Society annual meeting in Atlanta.
”Endogenous estrogens are protective for cardiovascular disease in premenopausal women,” Chrisandra L. Shufelt, MD, chair of the division of general internal medicine and associate director of the Women’s Health Research Center at Mayo Clinic in Jacksonville, Fla., told attendees. Yet, “a substantial population of young women are dying prematurely from cardiovascular disease,” with rates of cardiovascular death increasing in women aged 35-44 even as rates have decreased in postmenopausal women and in men. One potential reason may be premature estrogen loss.
Dr. Shufelt reminded attendees of four major causes of premature estrogen loss: Natural premature menopause, surgical menopause, chemotherapy-induced menopause, and premature ovarian insufficiency. But she would go on to discuss a less widely recognized condition, functional hypothalamic amenorrhea, that also may be contributing to increased cardiovascular risk.
First, Dr. Shufelt reviewed the evidence supporting the relationship between estrogen and cardiovascular health, starting with the Framingham study’s findings that cardiovascular disease is approximately two to four times more common in postmenopausal women than in premenopausal women, depending on the age range.
“Menopause at an early age, particularly under the age of 40, matters,” Dr. Shufelt said. “So we should be discussing this with our patients.”
Surgical menopause makes a difference to cardiovascular health as well, she said. In women under age 35, for example, the risk of a nonfatal heart attack in those with a bilateral oophorectomy was 7.7 times greater than in women who retained both ovaries and their uterus, and 1.5 times greater in women who had a hysterectomy without bilateral oophorectomy.
In a 2019 study, surgical premature menopause was associated with an 87% increased risk of heart disease even after researchers accounted for age, cardiovascular risk factors, and some forms of hormone therapy. The increased risk from natural premature menopause, on the other hand, was lower – a 36% increased risk of heart disease – compared with those producing endogenous hormones. Although randomized controlled trials are unavailable and unlikely to be done, the Nurses’ Health Study and the Danish Nurses Cohort Study, both observational studies, found that heart disease risk was diminished in those taking hormone therapy after surgical premature menopause.
Recommendations for premature or early menopause, from a wide range of different medical societies including NAMS, are that women without contraindications be given estrogen-based hormone therapy until the average age of natural menopause. Though not included in the same guidance, research has also shown that estrogen after oophorectomy does not increase the risk of breast cancer in women with a BRCA1 mutation, Dr. Shufelt said. Hormone therapy for premature or early menopause should adequately replace the levels women have lost and that means younger menopausal women often need higher doses than what older women receive, such as 2 mg/day of oral estradiol rather than the standard doses of 0.5 or 1 mg/day.
Functional hypothalamic amenorrhea and cardiovascular risk
Dr. Shufelt then discussed functional hypothalamic amenorrhea (hypogonadotropic hypogonadism), a common type of secondary amenorrhea that affects at least 1.4 million U.S. women. Diagnosis includes lack of a period for at least 3 months in someone who previously menstruated plus lab values below 50 pg/mL for estradiol, below 10 mIU/L for follicle stimulating hormone, and below 10 mIU/L for luteinizing hormone. Causes of this reversible form of infertility can include stress, overexercising, undereating, or some combination of these, plus an underlying genetic predisposition.
“After ruling out polycystic ovary syndrome, prolactinoma, and thyroid dysfunction, clinicians need to consider the diagnosis of hypothalamic amenorrhea,” Dr. Shufelt said. This condition goes beyond low estrogen levels: Women have elevated cortisol, low thyroid levels, low leptin levels, and increased ghrelin.
”This is not going away,” Dr. Shufelt said, sharing data on stress levels among U.S. adults, particularly Gen Z and millennial adults, noting that the ongoing “national mental health crisis” may be contributing to functional hypothalamic amenorrhea.
A 2020 substudy from the Nurses’ Health Study II found an increased risk of premature death in those who didn’t have a period or always had irregular periods starting as early as 14-17 years old. The increased risk of premature death rose with age in those with irregular or absent cycles – a 37% higher risk in 18- to 22-year-olds and a 39% increased risk in 29- to 46-year-olds.
But clinicians aren’t adequately identifying the “phenotype of the hypothalamic women,” Dr. Shufelt said, despite research showing overlap between hypothalamic amenorrhea and a higher risk of cardiovascular disease. Hypothalamic amenorrhea is so understudied that the last original research on the topic was in 2008, Dr. Shufelt said in an interview. ”No research except mine has been done to evaluate heart health in these young women,” she said.
Dr. Shufelt described a study she led involving 30 women with functional hypothalamic amenorrhea, 29 women with normal menstrual cycles, and 30 women who were recently menopausal and not on hormone therapy. The women with hypothalamic amenorrhea had average stress levels but their depression scores were higher than those of the other two groups.
The results showed that women with hypothalamic amenorrhea had lower estradiol and leptin levels and higher testosterone levels compared with the control group, and they had higher cortisol levels than those of both groups. Despite having similar body mass indexes as the control and menopausal groups, women with hypothalamic amenorrhea had lower blood pressure than that of the other two groups, yet they had higher cholesterol levels than those of the control group. EndoPAT© (Itamar Medical) testing showed that they had poor vascular function.
“In fact, one-third of the women [with hypothalamic amenorrhea] entered the trial with a diagnosis of what would be considered endothelial dysfunction,” Dr. Shufelt said. “Our results demonstrated significantly higher circulating levels of serum proinflammatory cytokines in the women with hypothalamic amenorrhea compared to eumenorrheic controls.”
Dr. Shufelt’s team then tested whether giving estradiol to the women with hypothalamic amenorrhea for 12 weeks would improve their vascular health, but they saw no significant differences between the women who received estrogen and those who received placebo.
“Endothelial function is partly mediated by estrogen, and it was expected that giving back estrogen would ‘fix’ the endothelium, but that is not what happened,” Nanette Santoro, MD, professor and chair of obstetrics and gynecology at the University of Colorado at Denver, Aurora, said in interview. “The mechanisms that maintain vascular function in women are not limited to hormones,” said Dr. Santoro, who was not involved in Dr. Shufelt’s study but attended her lecture. “We need to think beyond the simple model of estrogen-good, no-estrogen-bad.”
Dr. Santoro noted how easy it is to overlook the women who may have cardiovascular risk because of hypothalamic amenorrhea.
“Because many women with functional hypothalamic amenorrhea are super athletic and do not have the typical features of people with cardiometabolic disease – such as glucose intolerance, obesity, abnormal cholesterol or triglycerides, or high blood pressure – clinicians tend to think of them as healthy and to think that simply giving back hormones will fix the problems with bone density and vascular function, but that is not enough,” Dr. Santoro said. “The cognitive-behavioral therapy model for treatment of women with functional hypothalamic amenorrhea addresses the stress-related factors that drive the disorder, and this needs to be considered the standard of care for treatment.”
Stephanie S. Faubion, MD, professor of medicine and director of Mayo Clinic’s Center for Women’s Health in Jacksonville, Fla., who was not involved in Dr. Shufelt’s presentation, also emphasized the importance of recognizing functional hypothalamic amenorrhea.
“This is an underrecognized entity to begin with, and the fact that these women appear to be at increased risk for vascular dysfunction and potentially increased risk for cardiovascular disease down the road makes it even more important for clinicians to identify them and provide interventions early on,” Dr. Faubion said in an interview. “These women need to be identified and the etiology of the amenorrhea addressed, whether it relates to overexercising, being underweight, or experiencing significant stressors that have led to the loss of menstrual cycles.”
Dr. Shufelt’s research was funded by the National Institutes of Health. She had no disclosures. Dr. Santoro is a member of the scientific advisory board for Astellas, Menogenix, Amazon Ember, and Que Oncology, and she consults for Ansh Labs. Dr. Faubion had no disclosures.
FROM NAMS 2022
Remote assessment of atopic dermatitis is feasible with patient-provided images: Study
MONTREAL – , as well as the possibility of conducting remote clinical trials that would be less expensive and less burdensome for participants, according to investigators, who presented the study at the annual meeting of the International Society of Atopic Dermatitis.
Still, practical barriers need to be addressed, particularly the problem of image quality, noted study investigator Aviël Ragamin, MD, from the department of dermatology, Erasmus MC, University Medical Center, Rotterdam, the Netherlands.
“Good-quality images are crucial, [and] in our study, patients didn’t have any incentive to provide images because they had already received their medical consultation,” he explained. He suggested that this problem could be overcome by providing technical support for patients and compensation for trial participants.
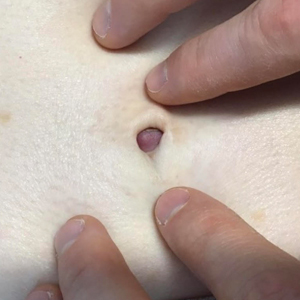
The study included 87 children (median age, 7 years), who were assessed for AD severity at an academic outpatient clinic. The in-person visit included assessment with the Eczema Area and Severity Index (EASI) score, as well as the collection of whole-body clinical images. Parents were then asked to return home and to provide their own clinical images and self-administered EASI assessments of their child for comparison. Four raters were asked to rate all images twice and to compare in-clinic and self-administered EASI scores based on the images.
At the in-clinic visit, the median EASI score of the group was 8.8. The majority of patients had moderate (46.6%) or severe (14.8%) AD. Roughly 40% of the patients had darker skin (Fitzpatrick skin types IV–VI).
Using Spearman rank correlation of 1,534 in-clinic and 425 patient-provided images, the study found good inter- and intra-rater reliability for clinical image assessment and strong agreement between images and the in-clinic EASI scores. The top outliers in the assessment were individuals with either darker skin or significant postinflammatory hyperpigmentation, which are “the most difficult cases to rate, based on images,” Dr. Ragamin noted.
There was only moderate correlation between the in-clinic and self-administered EASI scores, with a significant number of patients either underestimating or overestimating their AD severity, he added.
Overall, the main problem with remote assessment seems to be the feasibility of patients providing images, said Dr. Ragamin. Only 36.8% of parents provided any images at all, and of these, 1 of 5 were deemed too blurry, leaving just 13 for final assessment, he explained.
“Pragmatically, it’s tricky,” said Aaron Drucker, MD, a dermatologist at Women’s College Hospital and associate professor at the University of Toronto, who was asked to comment on the study. “It takes long enough to do an EASI score in person, let alone looking through blurry pictures that take too long to load into your electronic medical record. We know it works, but when our hospital went virtual [during the COVID pandemic] ... most of my patients with chronic eczema weren’t even sending me pictures.”
Regarding the utility of remote, full-body photography in clinical practice, he said, “There’s too many feasibility hoops to jump through at this point. The most promise I see is for clinical trials, where it’s hard to get people to come in.”
Dr. Ragamin and Dr. Drucker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – , as well as the possibility of conducting remote clinical trials that would be less expensive and less burdensome for participants, according to investigators, who presented the study at the annual meeting of the International Society of Atopic Dermatitis.
Still, practical barriers need to be addressed, particularly the problem of image quality, noted study investigator Aviël Ragamin, MD, from the department of dermatology, Erasmus MC, University Medical Center, Rotterdam, the Netherlands.
“Good-quality images are crucial, [and] in our study, patients didn’t have any incentive to provide images because they had already received their medical consultation,” he explained. He suggested that this problem could be overcome by providing technical support for patients and compensation for trial participants.
The study included 87 children (median age, 7 years), who were assessed for AD severity at an academic outpatient clinic. The in-person visit included assessment with the Eczema Area and Severity Index (EASI) score, as well as the collection of whole-body clinical images. Parents were then asked to return home and to provide their own clinical images and self-administered EASI assessments of their child for comparison. Four raters were asked to rate all images twice and to compare in-clinic and self-administered EASI scores based on the images.
At the in-clinic visit, the median EASI score of the group was 8.8. The majority of patients had moderate (46.6%) or severe (14.8%) AD. Roughly 40% of the patients had darker skin (Fitzpatrick skin types IV–VI).
Using Spearman rank correlation of 1,534 in-clinic and 425 patient-provided images, the study found good inter- and intra-rater reliability for clinical image assessment and strong agreement between images and the in-clinic EASI scores. The top outliers in the assessment were individuals with either darker skin or significant postinflammatory hyperpigmentation, which are “the most difficult cases to rate, based on images,” Dr. Ragamin noted.
There was only moderate correlation between the in-clinic and self-administered EASI scores, with a significant number of patients either underestimating or overestimating their AD severity, he added.
Overall, the main problem with remote assessment seems to be the feasibility of patients providing images, said Dr. Ragamin. Only 36.8% of parents provided any images at all, and of these, 1 of 5 were deemed too blurry, leaving just 13 for final assessment, he explained.
“Pragmatically, it’s tricky,” said Aaron Drucker, MD, a dermatologist at Women’s College Hospital and associate professor at the University of Toronto, who was asked to comment on the study. “It takes long enough to do an EASI score in person, let alone looking through blurry pictures that take too long to load into your electronic medical record. We know it works, but when our hospital went virtual [during the COVID pandemic] ... most of my patients with chronic eczema weren’t even sending me pictures.”
Regarding the utility of remote, full-body photography in clinical practice, he said, “There’s too many feasibility hoops to jump through at this point. The most promise I see is for clinical trials, where it’s hard to get people to come in.”
Dr. Ragamin and Dr. Drucker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – , as well as the possibility of conducting remote clinical trials that would be less expensive and less burdensome for participants, according to investigators, who presented the study at the annual meeting of the International Society of Atopic Dermatitis.
Still, practical barriers need to be addressed, particularly the problem of image quality, noted study investigator Aviël Ragamin, MD, from the department of dermatology, Erasmus MC, University Medical Center, Rotterdam, the Netherlands.
“Good-quality images are crucial, [and] in our study, patients didn’t have any incentive to provide images because they had already received their medical consultation,” he explained. He suggested that this problem could be overcome by providing technical support for patients and compensation for trial participants.
The study included 87 children (median age, 7 years), who were assessed for AD severity at an academic outpatient clinic. The in-person visit included assessment with the Eczema Area and Severity Index (EASI) score, as well as the collection of whole-body clinical images. Parents were then asked to return home and to provide their own clinical images and self-administered EASI assessments of their child for comparison. Four raters were asked to rate all images twice and to compare in-clinic and self-administered EASI scores based on the images.
At the in-clinic visit, the median EASI score of the group was 8.8. The majority of patients had moderate (46.6%) or severe (14.8%) AD. Roughly 40% of the patients had darker skin (Fitzpatrick skin types IV–VI).
Using Spearman rank correlation of 1,534 in-clinic and 425 patient-provided images, the study found good inter- and intra-rater reliability for clinical image assessment and strong agreement between images and the in-clinic EASI scores. The top outliers in the assessment were individuals with either darker skin or significant postinflammatory hyperpigmentation, which are “the most difficult cases to rate, based on images,” Dr. Ragamin noted.
There was only moderate correlation between the in-clinic and self-administered EASI scores, with a significant number of patients either underestimating or overestimating their AD severity, he added.
Overall, the main problem with remote assessment seems to be the feasibility of patients providing images, said Dr. Ragamin. Only 36.8% of parents provided any images at all, and of these, 1 of 5 were deemed too blurry, leaving just 13 for final assessment, he explained.
“Pragmatically, it’s tricky,” said Aaron Drucker, MD, a dermatologist at Women’s College Hospital and associate professor at the University of Toronto, who was asked to comment on the study. “It takes long enough to do an EASI score in person, let alone looking through blurry pictures that take too long to load into your electronic medical record. We know it works, but when our hospital went virtual [during the COVID pandemic] ... most of my patients with chronic eczema weren’t even sending me pictures.”
Regarding the utility of remote, full-body photography in clinical practice, he said, “There’s too many feasibility hoops to jump through at this point. The most promise I see is for clinical trials, where it’s hard to get people to come in.”
Dr. Ragamin and Dr. Drucker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Study reveals racial disparities in advanced HF therapies
A new study shows that Black Americans received ventricular assist devices (VADs) and heart transplants about half as often as White Americans, even when receiving care at an advanced heart failure (HF) center.
The analysis, drawn from 377 patients treated at one of 21 VAD centers in the United States as part of the RIVIVAL study, found that 22.3% of White adults received a heart transplant or VAD, compared with 11% of Black adults.
“That’s what is so concerning to us, that we’re seeing this pattern within this select population. I think it would be too reasonable to hypothesize that it very well could be worse in the general population,” study author Thomas Cascino, MD, MSc, University of Michigan, Ann Arbor, commented.
The study was published online in Circulation: Heart Failure, and it builds on previous work by the researchers, showing that patient preference for early VAD therapy is associated with higher New York Heart Association (NYHA) class and lower income level but not race.
In the present analysis, the number of Black and White participants who said they “definitely or probably” wanted VAD therapy was similar (27% vs. 29%), as was the number wanting “any and all life-sustaining therapies” (74% vs. 65%).
Two-thirds of the cohort was NYHA class III, the average EuroQoL visual analog scale (EQ-VAS) score was 64.6 among the 100 participants who identified as Black and 62.1 in the 277 White participants, and the average age was 58 and 61 years, respectively.
Death rates were also similar during the 2-year follow-up: 18% of Black patients and 13% of White patients.
After controlling for multiple clinical and social determinants of health, including age, Interagency Registry for Mechanically Assisted Circulator Support (INTERMACS) patient profile, EQ-VAS score, and level of education, Black participants had a 55% lower rate of VAD or transplant, compared with White participants (hazard ratio, 0.45; 95% confidence interval, 0.23-0.85). Adding VAD preference to the model did not affect the association.
“Our study suggests that we as providers may be making decisions differently,” Dr. Cascino said. “We can’t say for sure what the reasons are but certainly structural racism, discrimination, and provider biases are the things I worry about.”
“There’s an absolute need for us to look inwards, reflect, and acknowledge that we are likely playing a role in this and then start to be part of the change,” he added.
“The lives disabled or lost are simply too many,” coauthor Wendy Taddei-Peters, PhD, a clinical trials project official at the National Heart, Lung, and Blood Institute, said in an NIH statement. “An immediate step could be to require implicit bias training, particularly for transplant and VAD team members.”
Other suggestions are better tracking of underserved patients and the reasons why they do not receive VAD or become listed for transplant; inclusion of psychosocial components into decision-making about advanced therapy candidacy; and having “disparity experts” join in heart team meetings to help identify biases in real time.
Commenting on the study, Khadijah Breathett, MD, HF/transplant cardiologist and tenured associate professor of medicine, Indiana University Bloomington, said, “I’m glad there’s more push for awareness, because there’s still a population of people that don’t believe this is a real problem.”
Dr. Breathett, who is also a racial equity researcher, noted that the findings are similar to those of multiple studies suggesting racial disparities in HF care. In her own 2019 study of 400 providers shown identical clinical vignettes except for race, survey results and think-aloud interviews showed that decisions about advanced HF therapies are hierarchal and not democratic, social history and adherence are the most influential factors, and Black men are seen as not trustworthy and adherent, despite identical social histories, which ultimately led to White men being offered transplantation and Black men VAD implantation. The bias was particularly evident among older providers.
“This problem is real,” Dr. Breathett said. “The process of allocating life-saving therapies is not fair, and there is some level of discrimination that’s taking place towards persons of color, particularly Black patients. It’s time that we consider how we fix these issues.”
To see whether centers can move the needle and put systemic level changes into practice, Dr. Breathett and colleagues are launching the Seeking Objectivity in Allocation of Advanced Heart Failure (SOCIAL HF) Therapies Trial at 14 sites in the United States. It will measure the number of minority and female patients receiving advanced HF therapies at centers randomized to usual care or HF training, including evidence-based bias reduction training, use of objective measures of social support, and changes to facilitate group dynamics. The trial is set to start in January and be completed in September 2026.
“The main takeaway from this study is that it highlights and re-highlights the fact that racial disparities do exist in access to advanced therapy care,” Jaimin Trivedi, MD, MPH, associate professor of cardiothoracic surgery and director of clinical research and bioinformatics, University of Louisville, Ky., said in an interview.
He also called for education and training for all professionals, not just during residency or fellowship, to specifically identify issues with Black patients and encourage Black patients and their family members to get more involved in their HF care.
Dr. Trivedi said that further studies should examine why death rates were similar in the study despite the observed disparities in VAD implantation and transplantation.
He also pointed out that while patients in the study were treated from July 2015 to June 2016, a recent analysis by his team of the United Network for Organ Sharing (UNOS) database showed that 26% of transplants in 2019 were among Black patients, up from just 5% in 1987. “So, there are some encouraging signs as well.”
The study was funded by the National Institutes of Health/National Heart, Lung, and Blood Institute (NHLBI) and the National Center for Advancing Translational Sciences. Dr. Cascino reports having no relevant financial relationships. Four coauthors report financial relationships, including David Lanfear, who serves on the advisory board at Medscape. Dr. Breathett reported funding from multiple NHLBI grants.
A version of this article first appeared on Medscape.com.
A new study shows that Black Americans received ventricular assist devices (VADs) and heart transplants about half as often as White Americans, even when receiving care at an advanced heart failure (HF) center.
The analysis, drawn from 377 patients treated at one of 21 VAD centers in the United States as part of the RIVIVAL study, found that 22.3% of White adults received a heart transplant or VAD, compared with 11% of Black adults.
“That’s what is so concerning to us, that we’re seeing this pattern within this select population. I think it would be too reasonable to hypothesize that it very well could be worse in the general population,” study author Thomas Cascino, MD, MSc, University of Michigan, Ann Arbor, commented.
The study was published online in Circulation: Heart Failure, and it builds on previous work by the researchers, showing that patient preference for early VAD therapy is associated with higher New York Heart Association (NYHA) class and lower income level but not race.
In the present analysis, the number of Black and White participants who said they “definitely or probably” wanted VAD therapy was similar (27% vs. 29%), as was the number wanting “any and all life-sustaining therapies” (74% vs. 65%).
Two-thirds of the cohort was NYHA class III, the average EuroQoL visual analog scale (EQ-VAS) score was 64.6 among the 100 participants who identified as Black and 62.1 in the 277 White participants, and the average age was 58 and 61 years, respectively.
Death rates were also similar during the 2-year follow-up: 18% of Black patients and 13% of White patients.
After controlling for multiple clinical and social determinants of health, including age, Interagency Registry for Mechanically Assisted Circulator Support (INTERMACS) patient profile, EQ-VAS score, and level of education, Black participants had a 55% lower rate of VAD or transplant, compared with White participants (hazard ratio, 0.45; 95% confidence interval, 0.23-0.85). Adding VAD preference to the model did not affect the association.
“Our study suggests that we as providers may be making decisions differently,” Dr. Cascino said. “We can’t say for sure what the reasons are but certainly structural racism, discrimination, and provider biases are the things I worry about.”
“There’s an absolute need for us to look inwards, reflect, and acknowledge that we are likely playing a role in this and then start to be part of the change,” he added.
“The lives disabled or lost are simply too many,” coauthor Wendy Taddei-Peters, PhD, a clinical trials project official at the National Heart, Lung, and Blood Institute, said in an NIH statement. “An immediate step could be to require implicit bias training, particularly for transplant and VAD team members.”
Other suggestions are better tracking of underserved patients and the reasons why they do not receive VAD or become listed for transplant; inclusion of psychosocial components into decision-making about advanced therapy candidacy; and having “disparity experts” join in heart team meetings to help identify biases in real time.
Commenting on the study, Khadijah Breathett, MD, HF/transplant cardiologist and tenured associate professor of medicine, Indiana University Bloomington, said, “I’m glad there’s more push for awareness, because there’s still a population of people that don’t believe this is a real problem.”
Dr. Breathett, who is also a racial equity researcher, noted that the findings are similar to those of multiple studies suggesting racial disparities in HF care. In her own 2019 study of 400 providers shown identical clinical vignettes except for race, survey results and think-aloud interviews showed that decisions about advanced HF therapies are hierarchal and not democratic, social history and adherence are the most influential factors, and Black men are seen as not trustworthy and adherent, despite identical social histories, which ultimately led to White men being offered transplantation and Black men VAD implantation. The bias was particularly evident among older providers.
“This problem is real,” Dr. Breathett said. “The process of allocating life-saving therapies is not fair, and there is some level of discrimination that’s taking place towards persons of color, particularly Black patients. It’s time that we consider how we fix these issues.”
To see whether centers can move the needle and put systemic level changes into practice, Dr. Breathett and colleagues are launching the Seeking Objectivity in Allocation of Advanced Heart Failure (SOCIAL HF) Therapies Trial at 14 sites in the United States. It will measure the number of minority and female patients receiving advanced HF therapies at centers randomized to usual care or HF training, including evidence-based bias reduction training, use of objective measures of social support, and changes to facilitate group dynamics. The trial is set to start in January and be completed in September 2026.
“The main takeaway from this study is that it highlights and re-highlights the fact that racial disparities do exist in access to advanced therapy care,” Jaimin Trivedi, MD, MPH, associate professor of cardiothoracic surgery and director of clinical research and bioinformatics, University of Louisville, Ky., said in an interview.
He also called for education and training for all professionals, not just during residency or fellowship, to specifically identify issues with Black patients and encourage Black patients and their family members to get more involved in their HF care.
Dr. Trivedi said that further studies should examine why death rates were similar in the study despite the observed disparities in VAD implantation and transplantation.
He also pointed out that while patients in the study were treated from July 2015 to June 2016, a recent analysis by his team of the United Network for Organ Sharing (UNOS) database showed that 26% of transplants in 2019 were among Black patients, up from just 5% in 1987. “So, there are some encouraging signs as well.”
The study was funded by the National Institutes of Health/National Heart, Lung, and Blood Institute (NHLBI) and the National Center for Advancing Translational Sciences. Dr. Cascino reports having no relevant financial relationships. Four coauthors report financial relationships, including David Lanfear, who serves on the advisory board at Medscape. Dr. Breathett reported funding from multiple NHLBI grants.
A version of this article first appeared on Medscape.com.
A new study shows that Black Americans received ventricular assist devices (VADs) and heart transplants about half as often as White Americans, even when receiving care at an advanced heart failure (HF) center.
The analysis, drawn from 377 patients treated at one of 21 VAD centers in the United States as part of the RIVIVAL study, found that 22.3% of White adults received a heart transplant or VAD, compared with 11% of Black adults.
“That’s what is so concerning to us, that we’re seeing this pattern within this select population. I think it would be too reasonable to hypothesize that it very well could be worse in the general population,” study author Thomas Cascino, MD, MSc, University of Michigan, Ann Arbor, commented.
The study was published online in Circulation: Heart Failure, and it builds on previous work by the researchers, showing that patient preference for early VAD therapy is associated with higher New York Heart Association (NYHA) class and lower income level but not race.
In the present analysis, the number of Black and White participants who said they “definitely or probably” wanted VAD therapy was similar (27% vs. 29%), as was the number wanting “any and all life-sustaining therapies” (74% vs. 65%).
Two-thirds of the cohort was NYHA class III, the average EuroQoL visual analog scale (EQ-VAS) score was 64.6 among the 100 participants who identified as Black and 62.1 in the 277 White participants, and the average age was 58 and 61 years, respectively.
Death rates were also similar during the 2-year follow-up: 18% of Black patients and 13% of White patients.
After controlling for multiple clinical and social determinants of health, including age, Interagency Registry for Mechanically Assisted Circulator Support (INTERMACS) patient profile, EQ-VAS score, and level of education, Black participants had a 55% lower rate of VAD or transplant, compared with White participants (hazard ratio, 0.45; 95% confidence interval, 0.23-0.85). Adding VAD preference to the model did not affect the association.
“Our study suggests that we as providers may be making decisions differently,” Dr. Cascino said. “We can’t say for sure what the reasons are but certainly structural racism, discrimination, and provider biases are the things I worry about.”
“There’s an absolute need for us to look inwards, reflect, and acknowledge that we are likely playing a role in this and then start to be part of the change,” he added.
“The lives disabled or lost are simply too many,” coauthor Wendy Taddei-Peters, PhD, a clinical trials project official at the National Heart, Lung, and Blood Institute, said in an NIH statement. “An immediate step could be to require implicit bias training, particularly for transplant and VAD team members.”
Other suggestions are better tracking of underserved patients and the reasons why they do not receive VAD or become listed for transplant; inclusion of psychosocial components into decision-making about advanced therapy candidacy; and having “disparity experts” join in heart team meetings to help identify biases in real time.
Commenting on the study, Khadijah Breathett, MD, HF/transplant cardiologist and tenured associate professor of medicine, Indiana University Bloomington, said, “I’m glad there’s more push for awareness, because there’s still a population of people that don’t believe this is a real problem.”
Dr. Breathett, who is also a racial equity researcher, noted that the findings are similar to those of multiple studies suggesting racial disparities in HF care. In her own 2019 study of 400 providers shown identical clinical vignettes except for race, survey results and think-aloud interviews showed that decisions about advanced HF therapies are hierarchal and not democratic, social history and adherence are the most influential factors, and Black men are seen as not trustworthy and adherent, despite identical social histories, which ultimately led to White men being offered transplantation and Black men VAD implantation. The bias was particularly evident among older providers.
“This problem is real,” Dr. Breathett said. “The process of allocating life-saving therapies is not fair, and there is some level of discrimination that’s taking place towards persons of color, particularly Black patients. It’s time that we consider how we fix these issues.”
To see whether centers can move the needle and put systemic level changes into practice, Dr. Breathett and colleagues are launching the Seeking Objectivity in Allocation of Advanced Heart Failure (SOCIAL HF) Therapies Trial at 14 sites in the United States. It will measure the number of minority and female patients receiving advanced HF therapies at centers randomized to usual care or HF training, including evidence-based bias reduction training, use of objective measures of social support, and changes to facilitate group dynamics. The trial is set to start in January and be completed in September 2026.
“The main takeaway from this study is that it highlights and re-highlights the fact that racial disparities do exist in access to advanced therapy care,” Jaimin Trivedi, MD, MPH, associate professor of cardiothoracic surgery and director of clinical research and bioinformatics, University of Louisville, Ky., said in an interview.
He also called for education and training for all professionals, not just during residency or fellowship, to specifically identify issues with Black patients and encourage Black patients and their family members to get more involved in their HF care.
Dr. Trivedi said that further studies should examine why death rates were similar in the study despite the observed disparities in VAD implantation and transplantation.
He also pointed out that while patients in the study were treated from July 2015 to June 2016, a recent analysis by his team of the United Network for Organ Sharing (UNOS) database showed that 26% of transplants in 2019 were among Black patients, up from just 5% in 1987. “So, there are some encouraging signs as well.”
The study was funded by the National Institutes of Health/National Heart, Lung, and Blood Institute (NHLBI) and the National Center for Advancing Translational Sciences. Dr. Cascino reports having no relevant financial relationships. Four coauthors report financial relationships, including David Lanfear, who serves on the advisory board at Medscape. Dr. Breathett reported funding from multiple NHLBI grants.
A version of this article first appeared on Medscape.com.
How can I keep from losing my mind?
A) Thiamine
B) Vitamin E
C) Multivitamin (MV)
D) Keto diet
E) Red wine
FDA-approved therapies for dementia
To date the actual therapies for dementia have been disappointing. Donepezil, the most prescribed medication for the treatment of dementia has a number-needed-to treat (NNT) over 17, and causes frequent side effects. Aducanumab was recently approved by the Food and Drug Administration for the treatment of Alzheimer’s disease (AD), but controversy has arisen, as the clinical results were modest, and the price tag will be large – estimated at $30,000-$50,000/year.
Preventive options that may decrease the likelihood of dementia
Patients often ask the question stated above. Regarding how to respond to that question, choice C, MV, has some recent evidence of benefit. Baker and colleagues studied the effect of cocoa extract and multivitamins on cognitive function in the COSMOS-Mind trial.1 A total of 2,262 people were enrolled, and over 90% completed baseline and at least one annual cognitive assessment. Cocoa extract had no impact on global cognition (confidence interval [CI], –.02-.08, P = .28), but MV supplementation did have a statistically significant impact on global cognition (CI, .02-.12, P less than .007).
Vitamin E has been enthusiastically endorsed in the past as a treatment to prevent cognitive decline. The most recent Cochrane review on vitamin E concluded there was no evidence that the alpha-tocopherol form of vitamin E given to people with MCI prevents progression to dementia, or that it improves cognitive function in people with MCI or dementia due to AD.2
Exercise has long been a mainstay of our advice to patients as something they can do to help prevent dementia. Yu and colleagues did a meta-analysis of almost 400 randomized controlled trials and observational studies to grade the evidence on different interventions.3 They gave exercise a grade B for evidence of benefit.
A recent study addressed this issue, and I think it is helpful on quantifying how much exercise is needed. Del Pozo Cruz and colleagues did a prospective population-based cohort study of 78,000 adults aged 40-79, with an average of 6.9 years of follow up.4 The optimal step count was 9,826 steps (hazard ratio [HR], 0.49; 95% CI, 0.39-0.62) and the minimal step count for benefit was 3,826 steps (HR, 0.75; 95% CI, 0.67-0.83).
Modifiable factors
The other major modifiable factors to consider are problems with special senses. Both vision loss and hearing loss have been associated with cognitive impairment.
Shang and colleagues published a meta-analysis of 14 cohort studies addressing vision impairment and cognitive function involving more than 6 million individuals.5 They concluded that vision impairment is associated with an increased risk of both dementia and cognitive impairment in older adults.
Loughrey and colleagues performed a meta-analysis of 36 studies addressing hearing loss and cognitive decline.6 They reported that, among cross-sectional studies, a significant association was found for cognitive impairment (odds ratio [OR], 2.00; 95% CI, 1.39-2.89) and dementia (OR, 2.42; 95% CI, 1.24-4.72). A similar finding was present in prospective cohort studies with a significant association being found for cognitive impairment (OR, 1.22; 95% CI, 1.09-1.36) and dementia (OR, 1.28; 95% CI, 1.02-1.59).
A 25-year prospective, population-based study of patients with hearing loss revealed a difference in the rate of change in MMSE score over the 25-year follow-up between participants with hearing loss not using hearing aids matched with controls who didn’t have hearing loss. Those with untreated hearing loss had more cognitive decline than that of patients without hearing loss.7 The subjects with hearing loss using a hearing aid had no difference in cognitive decline from controls.
Pearl
Several simple and safe interventions may protect our patients from cognitive decline. These include taking a daily multivitamin, walking more than 4,000 steps a day, and optimizing vision and hearing.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Baker LD et al. Effects of cocoa extract and a multivitamin on cognitive function: A randomized clinical trial. Alzheimer’s Dement. 2022 Sep 14. doi: 10.1002/alz.12767.
2. Farina N et al. Vitamin E for Alzheimer’s dementia and mild cognitive impairment. Cochrane Database Syst Rev. 2017 Apr 18;4(4):CD002854. doi: 10.1002/14651858.CD002854.pub5.
3. Yu JT et al. Evidence-based prevention of Alzheimer’s disease: Systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020 Nov;91(11):1201-9.
4. Del Pozo Cruz B et al. Association of daily step count and intensity with incident dementia in 78,430 adults living in the UK. JAMA Neurol. 2022 Oct 1;79(10):1059-63.
5. Shang X et al. The association between vision impairment and incidence of dementia and cognitive impairment: A systematic review and meta-analysis. Ophthalmology. 2021 Aug;128(8):1135-49.
6. Loughrey DG et al. Association of age-related hearing loss with cognitive function, cognitive impairment, and dementia: A systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2018 Feb 1;144(2):115-26.
7. Amieva H et al. Self-reported hearing loss, hearing aids, and cognitive decline in elderly adults: A 25-year study. J Am Geriatr Soc. 2015 Oct;63(10):2099-104.
A) Thiamine
B) Vitamin E
C) Multivitamin (MV)
D) Keto diet
E) Red wine
FDA-approved therapies for dementia
To date the actual therapies for dementia have been disappointing. Donepezil, the most prescribed medication for the treatment of dementia has a number-needed-to treat (NNT) over 17, and causes frequent side effects. Aducanumab was recently approved by the Food and Drug Administration for the treatment of Alzheimer’s disease (AD), but controversy has arisen, as the clinical results were modest, and the price tag will be large – estimated at $30,000-$50,000/year.
Preventive options that may decrease the likelihood of dementia
Patients often ask the question stated above. Regarding how to respond to that question, choice C, MV, has some recent evidence of benefit. Baker and colleagues studied the effect of cocoa extract and multivitamins on cognitive function in the COSMOS-Mind trial.1 A total of 2,262 people were enrolled, and over 90% completed baseline and at least one annual cognitive assessment. Cocoa extract had no impact on global cognition (confidence interval [CI], –.02-.08, P = .28), but MV supplementation did have a statistically significant impact on global cognition (CI, .02-.12, P less than .007).
Vitamin E has been enthusiastically endorsed in the past as a treatment to prevent cognitive decline. The most recent Cochrane review on vitamin E concluded there was no evidence that the alpha-tocopherol form of vitamin E given to people with MCI prevents progression to dementia, or that it improves cognitive function in people with MCI or dementia due to AD.2
Exercise has long been a mainstay of our advice to patients as something they can do to help prevent dementia. Yu and colleagues did a meta-analysis of almost 400 randomized controlled trials and observational studies to grade the evidence on different interventions.3 They gave exercise a grade B for evidence of benefit.
A recent study addressed this issue, and I think it is helpful on quantifying how much exercise is needed. Del Pozo Cruz and colleagues did a prospective population-based cohort study of 78,000 adults aged 40-79, with an average of 6.9 years of follow up.4 The optimal step count was 9,826 steps (hazard ratio [HR], 0.49; 95% CI, 0.39-0.62) and the minimal step count for benefit was 3,826 steps (HR, 0.75; 95% CI, 0.67-0.83).
Modifiable factors
The other major modifiable factors to consider are problems with special senses. Both vision loss and hearing loss have been associated with cognitive impairment.
Shang and colleagues published a meta-analysis of 14 cohort studies addressing vision impairment and cognitive function involving more than 6 million individuals.5 They concluded that vision impairment is associated with an increased risk of both dementia and cognitive impairment in older adults.
Loughrey and colleagues performed a meta-analysis of 36 studies addressing hearing loss and cognitive decline.6 They reported that, among cross-sectional studies, a significant association was found for cognitive impairment (odds ratio [OR], 2.00; 95% CI, 1.39-2.89) and dementia (OR, 2.42; 95% CI, 1.24-4.72). A similar finding was present in prospective cohort studies with a significant association being found for cognitive impairment (OR, 1.22; 95% CI, 1.09-1.36) and dementia (OR, 1.28; 95% CI, 1.02-1.59).
A 25-year prospective, population-based study of patients with hearing loss revealed a difference in the rate of change in MMSE score over the 25-year follow-up between participants with hearing loss not using hearing aids matched with controls who didn’t have hearing loss. Those with untreated hearing loss had more cognitive decline than that of patients without hearing loss.7 The subjects with hearing loss using a hearing aid had no difference in cognitive decline from controls.
Pearl
Several simple and safe interventions may protect our patients from cognitive decline. These include taking a daily multivitamin, walking more than 4,000 steps a day, and optimizing vision and hearing.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Baker LD et al. Effects of cocoa extract and a multivitamin on cognitive function: A randomized clinical trial. Alzheimer’s Dement. 2022 Sep 14. doi: 10.1002/alz.12767.
2. Farina N et al. Vitamin E for Alzheimer’s dementia and mild cognitive impairment. Cochrane Database Syst Rev. 2017 Apr 18;4(4):CD002854. doi: 10.1002/14651858.CD002854.pub5.
3. Yu JT et al. Evidence-based prevention of Alzheimer’s disease: Systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020 Nov;91(11):1201-9.
4. Del Pozo Cruz B et al. Association of daily step count and intensity with incident dementia in 78,430 adults living in the UK. JAMA Neurol. 2022 Oct 1;79(10):1059-63.
5. Shang X et al. The association between vision impairment and incidence of dementia and cognitive impairment: A systematic review and meta-analysis. Ophthalmology. 2021 Aug;128(8):1135-49.
6. Loughrey DG et al. Association of age-related hearing loss with cognitive function, cognitive impairment, and dementia: A systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2018 Feb 1;144(2):115-26.
7. Amieva H et al. Self-reported hearing loss, hearing aids, and cognitive decline in elderly adults: A 25-year study. J Am Geriatr Soc. 2015 Oct;63(10):2099-104.
A) Thiamine
B) Vitamin E
C) Multivitamin (MV)
D) Keto diet
E) Red wine
FDA-approved therapies for dementia
To date the actual therapies for dementia have been disappointing. Donepezil, the most prescribed medication for the treatment of dementia has a number-needed-to treat (NNT) over 17, and causes frequent side effects. Aducanumab was recently approved by the Food and Drug Administration for the treatment of Alzheimer’s disease (AD), but controversy has arisen, as the clinical results were modest, and the price tag will be large – estimated at $30,000-$50,000/year.
Preventive options that may decrease the likelihood of dementia
Patients often ask the question stated above. Regarding how to respond to that question, choice C, MV, has some recent evidence of benefit. Baker and colleagues studied the effect of cocoa extract and multivitamins on cognitive function in the COSMOS-Mind trial.1 A total of 2,262 people were enrolled, and over 90% completed baseline and at least one annual cognitive assessment. Cocoa extract had no impact on global cognition (confidence interval [CI], –.02-.08, P = .28), but MV supplementation did have a statistically significant impact on global cognition (CI, .02-.12, P less than .007).
Vitamin E has been enthusiastically endorsed in the past as a treatment to prevent cognitive decline. The most recent Cochrane review on vitamin E concluded there was no evidence that the alpha-tocopherol form of vitamin E given to people with MCI prevents progression to dementia, or that it improves cognitive function in people with MCI or dementia due to AD.2
Exercise has long been a mainstay of our advice to patients as something they can do to help prevent dementia. Yu and colleagues did a meta-analysis of almost 400 randomized controlled trials and observational studies to grade the evidence on different interventions.3 They gave exercise a grade B for evidence of benefit.
A recent study addressed this issue, and I think it is helpful on quantifying how much exercise is needed. Del Pozo Cruz and colleagues did a prospective population-based cohort study of 78,000 adults aged 40-79, with an average of 6.9 years of follow up.4 The optimal step count was 9,826 steps (hazard ratio [HR], 0.49; 95% CI, 0.39-0.62) and the minimal step count for benefit was 3,826 steps (HR, 0.75; 95% CI, 0.67-0.83).
Modifiable factors
The other major modifiable factors to consider are problems with special senses. Both vision loss and hearing loss have been associated with cognitive impairment.
Shang and colleagues published a meta-analysis of 14 cohort studies addressing vision impairment and cognitive function involving more than 6 million individuals.5 They concluded that vision impairment is associated with an increased risk of both dementia and cognitive impairment in older adults.
Loughrey and colleagues performed a meta-analysis of 36 studies addressing hearing loss and cognitive decline.6 They reported that, among cross-sectional studies, a significant association was found for cognitive impairment (odds ratio [OR], 2.00; 95% CI, 1.39-2.89) and dementia (OR, 2.42; 95% CI, 1.24-4.72). A similar finding was present in prospective cohort studies with a significant association being found for cognitive impairment (OR, 1.22; 95% CI, 1.09-1.36) and dementia (OR, 1.28; 95% CI, 1.02-1.59).
A 25-year prospective, population-based study of patients with hearing loss revealed a difference in the rate of change in MMSE score over the 25-year follow-up between participants with hearing loss not using hearing aids matched with controls who didn’t have hearing loss. Those with untreated hearing loss had more cognitive decline than that of patients without hearing loss.7 The subjects with hearing loss using a hearing aid had no difference in cognitive decline from controls.
Pearl
Several simple and safe interventions may protect our patients from cognitive decline. These include taking a daily multivitamin, walking more than 4,000 steps a day, and optimizing vision and hearing.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Baker LD et al. Effects of cocoa extract and a multivitamin on cognitive function: A randomized clinical trial. Alzheimer’s Dement. 2022 Sep 14. doi: 10.1002/alz.12767.
2. Farina N et al. Vitamin E for Alzheimer’s dementia and mild cognitive impairment. Cochrane Database Syst Rev. 2017 Apr 18;4(4):CD002854. doi: 10.1002/14651858.CD002854.pub5.
3. Yu JT et al. Evidence-based prevention of Alzheimer’s disease: Systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020 Nov;91(11):1201-9.
4. Del Pozo Cruz B et al. Association of daily step count and intensity with incident dementia in 78,430 adults living in the UK. JAMA Neurol. 2022 Oct 1;79(10):1059-63.
5. Shang X et al. The association between vision impairment and incidence of dementia and cognitive impairment: A systematic review and meta-analysis. Ophthalmology. 2021 Aug;128(8):1135-49.
6. Loughrey DG et al. Association of age-related hearing loss with cognitive function, cognitive impairment, and dementia: A systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg. 2018 Feb 1;144(2):115-26.
7. Amieva H et al. Self-reported hearing loss, hearing aids, and cognitive decline in elderly adults: A 25-year study. J Am Geriatr Soc. 2015 Oct;63(10):2099-104.
Four commonly abused drugs linked with atrial fibrillation
Cocaine, methamphetamine, opioids, and cannabis may independently increase risk of atrial fibrillation (AFib), based on data from almost 24 million people.
While more work is needed to uncover causal links, physicians should be aware that these commonly abused substances could be driving new cases of AFib, reported investigators from the University of California, San Francisco.
“Though alcohol and tobacco smoking have each been associated with a heightened risk of [AFib], relationships between other drug use and [AFib] are poorly understood,” they wrote in European Heart Journal.
Some previous studies have ventured into this terrain, but most focused on fatal arrhythmias, or offered anecdotal evidence. This knowledge gap is particularly concerning for cannabis, the researchers noted, as medical and recreational use are on the rise.
The present analysis included data from 23.5 million adults in California who received care through a hospital, emergency department, or outpatient surgery center during 2005-2015. Based on ICD-9 diagnostic codes, 132,834 of these patients used cannabis, 98,271 used methamphetamines, 48,701 used cocaine, and 10,032 used opiates. Inclusion required lack of AFib at baseline.
Reliance on ICD-9 codes makes the data “quite specific,” but lacking sensitivity, according to principal author Gregory M. Marcus, MD, cardiologist and professor of medicine at UCSF.
“If they were designated as using these drugs, that is very likely true,” Dr. Marcus said in an interview. “But certainly, the absence of any mention of use of these drugs does not exclude the possibility that some people were still using them. That would not create spurious false-positive relationships; if anything, it attenuates existing relationships.”
In other words, using ICD-9 codes reduced the power to detect an association between each drug and AFib, meaning any relationship needed to be sufficiently strong enough to generate a significant result.
At the end of the decade-long study period, 998,747 patients (4.2%) had developed incident AFib. After adjusting for potential confounders and mediators, all four drugs showed significant, independent associations with AFib. Methamphetamines presented the greatest risk (hazard ratio, 1.86%), followed by opiates (HR, 1.74), cocaine (HR, 1.61), and cannabis (HR, 1.35).
“Our findings provide the first evidence utilizing a longitudinal cohort to demonstrate that cannabis use predicts the future onset of AFib,” Dr. Marcus and colleagues wrote.
Dose-response relationships were not detected for any of the substances; however, usage levels were also derived from ICD-9 codes, which may have been insufficient for this purpose, according to the investigators.
Causal mechanisms deserve a closer look
Causal links between AFib and each of the drugs remain unclear. Citing prior research, Dr. Marcus and colleagues explained how methamphetamines are capable of “significant cardiac electrical remodeling,” while cocaine may cause sodium channel dysregulation, and opioids can render atrial myocytes more susceptible to oxidative damage. Although cannabis has previously been linked with hospitalization for arrhythmia, a pharmacologic driver of this phenomenon remains largely unexamined.
“We don’t know for sure precisely what the constituents are that are responsible for our findings,” Dr. Marcus said. “It’s possible that there are some effects that are much more generic, such as inhaling a burned substance. There is good evidence that if you inhale pretty much any sort of particulate matter, that increases inflammation in the body. Inflammation is known to be a trigger for atrial fibrillation.”
Alternatively, all four drugs – whether stimulants or depressants – cause “quite dramatic and often rapid effects on the autonomic nervous system,” Dr. Marcus said, noting that these rapid swings are a known trigger for AFib.
Brian Olshansky, MD, emeritus professor of internal medicine-cardiovascular medicine at the University of Iowa, Iowa City, suggested that nonpharmacologic factors are likely also playing a role.
“All these drugs have slightly different mechanisms of action, so there’s not one mechanism that would explain why all of them would cause atrial fibrillation,” Dr. Olshansky said in an interview. “That does suggest that there’s something else going on, besides just the drug itself. It would be potentially concerning if we were to lay the blame totally on these drugs.”
Dr. Olshansky, who recently coauthored a review of stimulant drugs and arrhythmias, suggested that lifestyle, comorbidities, and drug impurities may have added to the risk of AF.
“[The investigators] did try to correct for that kind of stuff, but it’s very hard to correct for a lot of the issues that may be ongoing with individuals who partake in these drugs,” Dr. Olshansky said in an interview. “They may not be a healthy lot, in general.”
Still, considering previous data linking drugs of abuse with arrhythmias, he said the detected risks were “intriguing,” and deserved a closer look.
“It’s a nice groundbreaking study, with regard to the fact that they showed unique relationships that we don’t completely understand,” Dr. Olshansky said. “It opens up a new opportunity for further investigation.”
The investigators disclosed relationships with InCarda, Baylis Medical, Johnson & Johnson, and others. Dr. Olshansky disclosed no relevant competing interests.
Cocaine, methamphetamine, opioids, and cannabis may independently increase risk of atrial fibrillation (AFib), based on data from almost 24 million people.
While more work is needed to uncover causal links, physicians should be aware that these commonly abused substances could be driving new cases of AFib, reported investigators from the University of California, San Francisco.
“Though alcohol and tobacco smoking have each been associated with a heightened risk of [AFib], relationships between other drug use and [AFib] are poorly understood,” they wrote in European Heart Journal.
Some previous studies have ventured into this terrain, but most focused on fatal arrhythmias, or offered anecdotal evidence. This knowledge gap is particularly concerning for cannabis, the researchers noted, as medical and recreational use are on the rise.
The present analysis included data from 23.5 million adults in California who received care through a hospital, emergency department, or outpatient surgery center during 2005-2015. Based on ICD-9 diagnostic codes, 132,834 of these patients used cannabis, 98,271 used methamphetamines, 48,701 used cocaine, and 10,032 used opiates. Inclusion required lack of AFib at baseline.
Reliance on ICD-9 codes makes the data “quite specific,” but lacking sensitivity, according to principal author Gregory M. Marcus, MD, cardiologist and professor of medicine at UCSF.
“If they were designated as using these drugs, that is very likely true,” Dr. Marcus said in an interview. “But certainly, the absence of any mention of use of these drugs does not exclude the possibility that some people were still using them. That would not create spurious false-positive relationships; if anything, it attenuates existing relationships.”
In other words, using ICD-9 codes reduced the power to detect an association between each drug and AFib, meaning any relationship needed to be sufficiently strong enough to generate a significant result.
At the end of the decade-long study period, 998,747 patients (4.2%) had developed incident AFib. After adjusting for potential confounders and mediators, all four drugs showed significant, independent associations with AFib. Methamphetamines presented the greatest risk (hazard ratio, 1.86%), followed by opiates (HR, 1.74), cocaine (HR, 1.61), and cannabis (HR, 1.35).
“Our findings provide the first evidence utilizing a longitudinal cohort to demonstrate that cannabis use predicts the future onset of AFib,” Dr. Marcus and colleagues wrote.
Dose-response relationships were not detected for any of the substances; however, usage levels were also derived from ICD-9 codes, which may have been insufficient for this purpose, according to the investigators.
Causal mechanisms deserve a closer look
Causal links between AFib and each of the drugs remain unclear. Citing prior research, Dr. Marcus and colleagues explained how methamphetamines are capable of “significant cardiac electrical remodeling,” while cocaine may cause sodium channel dysregulation, and opioids can render atrial myocytes more susceptible to oxidative damage. Although cannabis has previously been linked with hospitalization for arrhythmia, a pharmacologic driver of this phenomenon remains largely unexamined.
“We don’t know for sure precisely what the constituents are that are responsible for our findings,” Dr. Marcus said. “It’s possible that there are some effects that are much more generic, such as inhaling a burned substance. There is good evidence that if you inhale pretty much any sort of particulate matter, that increases inflammation in the body. Inflammation is known to be a trigger for atrial fibrillation.”
Alternatively, all four drugs – whether stimulants or depressants – cause “quite dramatic and often rapid effects on the autonomic nervous system,” Dr. Marcus said, noting that these rapid swings are a known trigger for AFib.
Brian Olshansky, MD, emeritus professor of internal medicine-cardiovascular medicine at the University of Iowa, Iowa City, suggested that nonpharmacologic factors are likely also playing a role.
“All these drugs have slightly different mechanisms of action, so there’s not one mechanism that would explain why all of them would cause atrial fibrillation,” Dr. Olshansky said in an interview. “That does suggest that there’s something else going on, besides just the drug itself. It would be potentially concerning if we were to lay the blame totally on these drugs.”
Dr. Olshansky, who recently coauthored a review of stimulant drugs and arrhythmias, suggested that lifestyle, comorbidities, and drug impurities may have added to the risk of AF.
“[The investigators] did try to correct for that kind of stuff, but it’s very hard to correct for a lot of the issues that may be ongoing with individuals who partake in these drugs,” Dr. Olshansky said in an interview. “They may not be a healthy lot, in general.”
Still, considering previous data linking drugs of abuse with arrhythmias, he said the detected risks were “intriguing,” and deserved a closer look.
“It’s a nice groundbreaking study, with regard to the fact that they showed unique relationships that we don’t completely understand,” Dr. Olshansky said. “It opens up a new opportunity for further investigation.”
The investigators disclosed relationships with InCarda, Baylis Medical, Johnson & Johnson, and others. Dr. Olshansky disclosed no relevant competing interests.
Cocaine, methamphetamine, opioids, and cannabis may independently increase risk of atrial fibrillation (AFib), based on data from almost 24 million people.
While more work is needed to uncover causal links, physicians should be aware that these commonly abused substances could be driving new cases of AFib, reported investigators from the University of California, San Francisco.
“Though alcohol and tobacco smoking have each been associated with a heightened risk of [AFib], relationships between other drug use and [AFib] are poorly understood,” they wrote in European Heart Journal.
Some previous studies have ventured into this terrain, but most focused on fatal arrhythmias, or offered anecdotal evidence. This knowledge gap is particularly concerning for cannabis, the researchers noted, as medical and recreational use are on the rise.
The present analysis included data from 23.5 million adults in California who received care through a hospital, emergency department, or outpatient surgery center during 2005-2015. Based on ICD-9 diagnostic codes, 132,834 of these patients used cannabis, 98,271 used methamphetamines, 48,701 used cocaine, and 10,032 used opiates. Inclusion required lack of AFib at baseline.
Reliance on ICD-9 codes makes the data “quite specific,” but lacking sensitivity, according to principal author Gregory M. Marcus, MD, cardiologist and professor of medicine at UCSF.
“If they were designated as using these drugs, that is very likely true,” Dr. Marcus said in an interview. “But certainly, the absence of any mention of use of these drugs does not exclude the possibility that some people were still using them. That would not create spurious false-positive relationships; if anything, it attenuates existing relationships.”
In other words, using ICD-9 codes reduced the power to detect an association between each drug and AFib, meaning any relationship needed to be sufficiently strong enough to generate a significant result.
At the end of the decade-long study period, 998,747 patients (4.2%) had developed incident AFib. After adjusting for potential confounders and mediators, all four drugs showed significant, independent associations with AFib. Methamphetamines presented the greatest risk (hazard ratio, 1.86%), followed by opiates (HR, 1.74), cocaine (HR, 1.61), and cannabis (HR, 1.35).
“Our findings provide the first evidence utilizing a longitudinal cohort to demonstrate that cannabis use predicts the future onset of AFib,” Dr. Marcus and colleagues wrote.
Dose-response relationships were not detected for any of the substances; however, usage levels were also derived from ICD-9 codes, which may have been insufficient for this purpose, according to the investigators.
Causal mechanisms deserve a closer look
Causal links between AFib and each of the drugs remain unclear. Citing prior research, Dr. Marcus and colleagues explained how methamphetamines are capable of “significant cardiac electrical remodeling,” while cocaine may cause sodium channel dysregulation, and opioids can render atrial myocytes more susceptible to oxidative damage. Although cannabis has previously been linked with hospitalization for arrhythmia, a pharmacologic driver of this phenomenon remains largely unexamined.
“We don’t know for sure precisely what the constituents are that are responsible for our findings,” Dr. Marcus said. “It’s possible that there are some effects that are much more generic, such as inhaling a burned substance. There is good evidence that if you inhale pretty much any sort of particulate matter, that increases inflammation in the body. Inflammation is known to be a trigger for atrial fibrillation.”
Alternatively, all four drugs – whether stimulants or depressants – cause “quite dramatic and often rapid effects on the autonomic nervous system,” Dr. Marcus said, noting that these rapid swings are a known trigger for AFib.
Brian Olshansky, MD, emeritus professor of internal medicine-cardiovascular medicine at the University of Iowa, Iowa City, suggested that nonpharmacologic factors are likely also playing a role.
“All these drugs have slightly different mechanisms of action, so there’s not one mechanism that would explain why all of them would cause atrial fibrillation,” Dr. Olshansky said in an interview. “That does suggest that there’s something else going on, besides just the drug itself. It would be potentially concerning if we were to lay the blame totally on these drugs.”
Dr. Olshansky, who recently coauthored a review of stimulant drugs and arrhythmias, suggested that lifestyle, comorbidities, and drug impurities may have added to the risk of AF.
“[The investigators] did try to correct for that kind of stuff, but it’s very hard to correct for a lot of the issues that may be ongoing with individuals who partake in these drugs,” Dr. Olshansky said in an interview. “They may not be a healthy lot, in general.”
Still, considering previous data linking drugs of abuse with arrhythmias, he said the detected risks were “intriguing,” and deserved a closer look.
“It’s a nice groundbreaking study, with regard to the fact that they showed unique relationships that we don’t completely understand,” Dr. Olshansky said. “It opens up a new opportunity for further investigation.”
The investigators disclosed relationships with InCarda, Baylis Medical, Johnson & Johnson, and others. Dr. Olshansky disclosed no relevant competing interests.
FROM EUROPEAN HEART JOURNAL
Asymptomatic Umbilical Nodule
The Diagnosis: Sister Mary Joseph Nodule
Histopathologic analysis of the biopsy specimen revealed a dense infiltrate of large, hyperchromatic, mucin-producing cells exhibiting varying degrees of nuclear pleomorphism (Figure 1). Immunohistochemical (IHC) staining was negative for cytokeratin (CK) 20; however, CK7 was found positive (Figure 2), which confirmed the presence of a metastatic adenocarcinoma, consistent with the clinical diagnosis of a Sister Mary Joseph nodule (SMJN). Subsequent IHC workup to determine the site of origin revealed densely positive expression of both cancer antigen 125 and paired homeobox gene 8 (PAX-8)(Figure 3), consistent with primary ovarian disease. Furthermore, expression of estrogen receptor and p53 both were positive within the nuclei, illustrating an aberrant expression pattern. On the other hand, cancer antigen 19-9, caudal-type homeobox 2, gross cystic disease fluid protein 15, and mammaglobin were all determined negative, thus leading to the pathologic diagnosis of a metastatic ovarian adenocarcinoma. Additional workup with computed tomography of the abdomen and pelvis highlighted a large left ovarian mass with multiple omental nodules as well as enlarged retroperitoneal and pelvic lymph nodes.

The SMJN is a rare presentation of internal malignancy that appears as a nodule that metastasizes to the umbilicus. It may be ulcerated or necrotic and is seen in up to 10% of patients with cutaneous metastases from internal malignancy.1 These nodules are named after Sister Mary Joseph, the surgical assistant of Dr. William Mayo who first described the relationship between umbilical nodules seen in patients with gastrointestinal and genitourinary cancer. The most common underlying malignancies include primary gastrointestinal and gynecologic adenocarcinomas. In a retrospective study of 34 patients by Chalya et al,2 the stomach was found to be the most common primary site (41.1%). The presence of an SMJN affords a poor prognosis, with a mean overall survival of 11 months from the time of diagnosis.3 The mechanism of disease dissemination remains unknown but is thought to occur through lymphovascular invasion of tumor cells and spread via the umbilical ligament.1,4
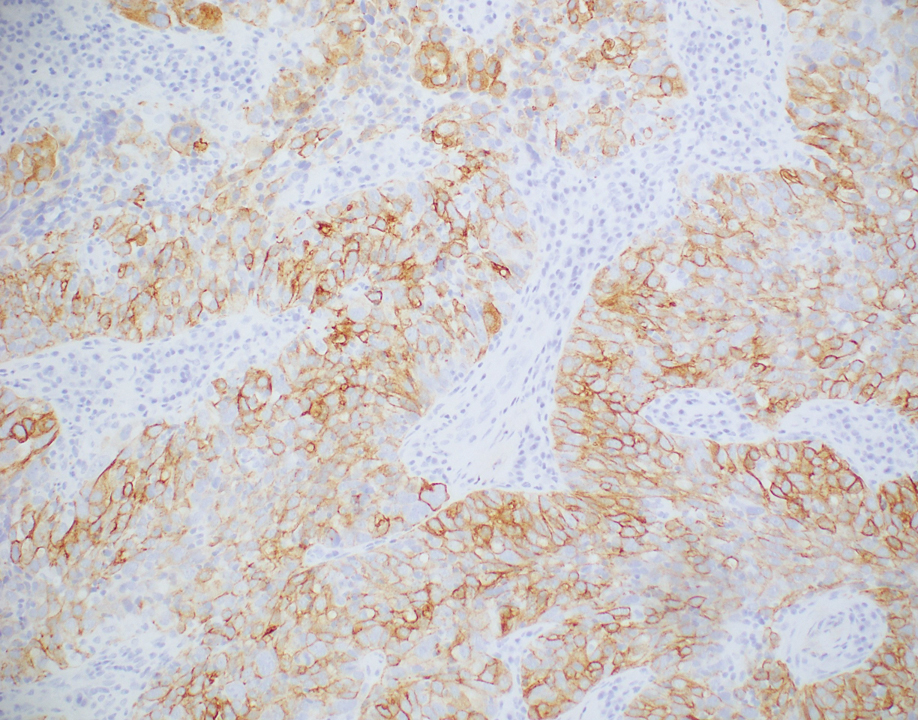
Merkel cell carcinoma is a cutaneous neuroendocrine tumor that most commonly presents in elderly patients as red-violet nodules or plaques. Although Merkel cell carcinoma most frequently is encountered on sun-exposed skin, they also can arise on the trunk and abdomen. Positive IHC staining for CK20 would be expected; however, it was negative in our case.5
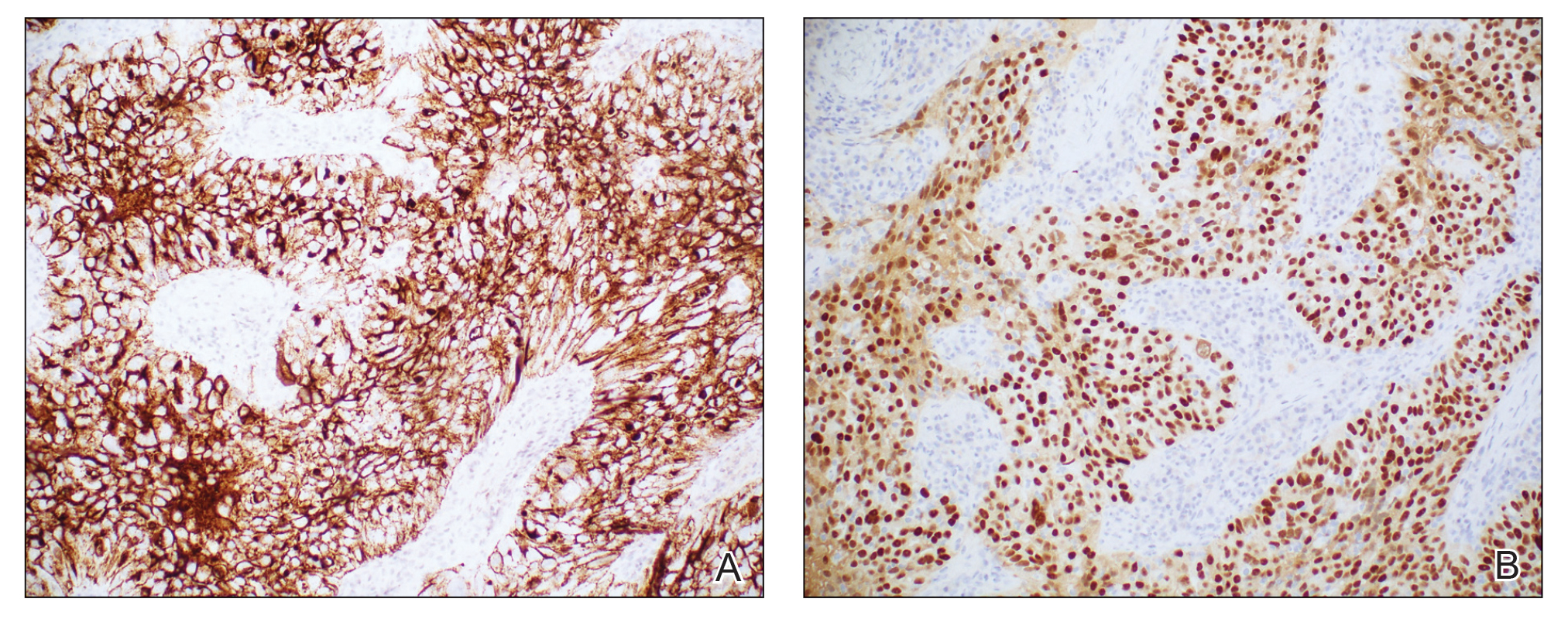
Cutaneous endometriosis is a rare disease presentation and most commonly occurs as a secondary process due to surgical inoculation of the abdominal wall. Primary cutaneous endometriosis in which there is no history of abdominal surgery less frequently is encountered. Patients typically will report pain and cyclical bleeding with menses. Pathology demonstrates ectopic endometrial tissue with glands and uterine myxoid stroma.6
Amelanotic melanoma is an uncommon subtype of malignant melanoma that presents as nonpigmented nodules that have a propensity to ulcerate and bleed. Furthermore, the umbilicus is an exceedingly rare location for primary melanoma. However, one report does exist, and amelanotic melanoma should be considered in the differential for patients with umbilical nodules.7
Dermoid cysts are benign congenital lesions that typically present as a painless, slow-growing, and wellcircumscribed nodule, as similarly experienced by our patient. They most commonly are found on the testicles and ovaries but also are known to arise in embryologic fusion planes, and reports of umbilical lesions exist.8 Dermoid cysts are diagnosed based on histopathology, supporting the need for a biopsy to distinguish a malignant process from benign lesions.9
- Gabriele R, Conte M, Egidi F, et al. Umbilical metastases: current viewpoint. World J Surg Oncol. 2005;3:13.
- Chalya PL, Mabula JB, Rambau PF, et al. Sister Mary Joseph’s nodule at a university teaching hospital in northwestern Tanzania: a retrospective review of 34 cases. World J Surg Oncol. 2013;11:151.
- Leyrat B, Bernadach M, Ginzac A, et al. Sister Mary Joseph nodules: a case report about a rare location of skin metastasis. Case Rep Oncol. 2021;14:664-670.
- Yendluri V, Centeno B, Springett GM. Pancreatic cancer presenting as a Sister Mary Joseph’s nodule: case report and update of the literature. Pancreas. 2007;34:161-164.
- Uchi H. Merkel cell carcinoma: an update and immunotherapy. Front Oncol. 2018;8:48.
- Bittar PG, Hryneewycz KT, Bryant EA. Primary cutaneous endometriosis presenting as an umbilical nodule. JAMA Dermatol. 2021;157:1227.
- Kovitwanichkanont T, Joseph S, Yip L. Hidden in plain sight: umbilical melanoma [published online January 28, 2020]. Med J Aust. 2020;212:154-155.e1.
- Prior A, Anania P, Pacetti M, et al. Dermoid and epidermoid cysts of scalp: case series of 234 consecutive patients. World Neurosurg. 2018;120:119-124.
- Akinci O, Turker C, Erturk MS, et al. Umbilical dermoid cyst: a rare case. Cerrahpasa Med J. 2020;44:51-53.
The Diagnosis: Sister Mary Joseph Nodule
Histopathologic analysis of the biopsy specimen revealed a dense infiltrate of large, hyperchromatic, mucin-producing cells exhibiting varying degrees of nuclear pleomorphism (Figure 1). Immunohistochemical (IHC) staining was negative for cytokeratin (CK) 20; however, CK7 was found positive (Figure 2), which confirmed the presence of a metastatic adenocarcinoma, consistent with the clinical diagnosis of a Sister Mary Joseph nodule (SMJN). Subsequent IHC workup to determine the site of origin revealed densely positive expression of both cancer antigen 125 and paired homeobox gene 8 (PAX-8)(Figure 3), consistent with primary ovarian disease. Furthermore, expression of estrogen receptor and p53 both were positive within the nuclei, illustrating an aberrant expression pattern. On the other hand, cancer antigen 19-9, caudal-type homeobox 2, gross cystic disease fluid protein 15, and mammaglobin were all determined negative, thus leading to the pathologic diagnosis of a metastatic ovarian adenocarcinoma. Additional workup with computed tomography of the abdomen and pelvis highlighted a large left ovarian mass with multiple omental nodules as well as enlarged retroperitoneal and pelvic lymph nodes.

The SMJN is a rare presentation of internal malignancy that appears as a nodule that metastasizes to the umbilicus. It may be ulcerated or necrotic and is seen in up to 10% of patients with cutaneous metastases from internal malignancy.1 These nodules are named after Sister Mary Joseph, the surgical assistant of Dr. William Mayo who first described the relationship between umbilical nodules seen in patients with gastrointestinal and genitourinary cancer. The most common underlying malignancies include primary gastrointestinal and gynecologic adenocarcinomas. In a retrospective study of 34 patients by Chalya et al,2 the stomach was found to be the most common primary site (41.1%). The presence of an SMJN affords a poor prognosis, with a mean overall survival of 11 months from the time of diagnosis.3 The mechanism of disease dissemination remains unknown but is thought to occur through lymphovascular invasion of tumor cells and spread via the umbilical ligament.1,4
Merkel cell carcinoma is a cutaneous neuroendocrine tumor that most commonly presents in elderly patients as red-violet nodules or plaques. Although Merkel cell carcinoma most frequently is encountered on sun-exposed skin, they also can arise on the trunk and abdomen. Positive IHC staining for CK20 would be expected; however, it was negative in our case.5
Cutaneous endometriosis is a rare disease presentation and most commonly occurs as a secondary process due to surgical inoculation of the abdominal wall. Primary cutaneous endometriosis in which there is no history of abdominal surgery less frequently is encountered. Patients typically will report pain and cyclical bleeding with menses. Pathology demonstrates ectopic endometrial tissue with glands and uterine myxoid stroma.6
Amelanotic melanoma is an uncommon subtype of malignant melanoma that presents as nonpigmented nodules that have a propensity to ulcerate and bleed. Furthermore, the umbilicus is an exceedingly rare location for primary melanoma. However, one report does exist, and amelanotic melanoma should be considered in the differential for patients with umbilical nodules.7
Dermoid cysts are benign congenital lesions that typically present as a painless, slow-growing, and wellcircumscribed nodule, as similarly experienced by our patient. They most commonly are found on the testicles and ovaries but also are known to arise in embryologic fusion planes, and reports of umbilical lesions exist.8 Dermoid cysts are diagnosed based on histopathology, supporting the need for a biopsy to distinguish a malignant process from benign lesions.9
The Diagnosis: Sister Mary Joseph Nodule
Histopathologic analysis of the biopsy specimen revealed a dense infiltrate of large, hyperchromatic, mucin-producing cells exhibiting varying degrees of nuclear pleomorphism (Figure 1). Immunohistochemical (IHC) staining was negative for cytokeratin (CK) 20; however, CK7 was found positive (Figure 2), which confirmed the presence of a metastatic adenocarcinoma, consistent with the clinical diagnosis of a Sister Mary Joseph nodule (SMJN). Subsequent IHC workup to determine the site of origin revealed densely positive expression of both cancer antigen 125 and paired homeobox gene 8 (PAX-8)(Figure 3), consistent with primary ovarian disease. Furthermore, expression of estrogen receptor and p53 both were positive within the nuclei, illustrating an aberrant expression pattern. On the other hand, cancer antigen 19-9, caudal-type homeobox 2, gross cystic disease fluid protein 15, and mammaglobin were all determined negative, thus leading to the pathologic diagnosis of a metastatic ovarian adenocarcinoma. Additional workup with computed tomography of the abdomen and pelvis highlighted a large left ovarian mass with multiple omental nodules as well as enlarged retroperitoneal and pelvic lymph nodes.

The SMJN is a rare presentation of internal malignancy that appears as a nodule that metastasizes to the umbilicus. It may be ulcerated or necrotic and is seen in up to 10% of patients with cutaneous metastases from internal malignancy.1 These nodules are named after Sister Mary Joseph, the surgical assistant of Dr. William Mayo who first described the relationship between umbilical nodules seen in patients with gastrointestinal and genitourinary cancer. The most common underlying malignancies include primary gastrointestinal and gynecologic adenocarcinomas. In a retrospective study of 34 patients by Chalya et al,2 the stomach was found to be the most common primary site (41.1%). The presence of an SMJN affords a poor prognosis, with a mean overall survival of 11 months from the time of diagnosis.3 The mechanism of disease dissemination remains unknown but is thought to occur through lymphovascular invasion of tumor cells and spread via the umbilical ligament.1,4
Merkel cell carcinoma is a cutaneous neuroendocrine tumor that most commonly presents in elderly patients as red-violet nodules or plaques. Although Merkel cell carcinoma most frequently is encountered on sun-exposed skin, they also can arise on the trunk and abdomen. Positive IHC staining for CK20 would be expected; however, it was negative in our case.5
Cutaneous endometriosis is a rare disease presentation and most commonly occurs as a secondary process due to surgical inoculation of the abdominal wall. Primary cutaneous endometriosis in which there is no history of abdominal surgery less frequently is encountered. Patients typically will report pain and cyclical bleeding with menses. Pathology demonstrates ectopic endometrial tissue with glands and uterine myxoid stroma.6
Amelanotic melanoma is an uncommon subtype of malignant melanoma that presents as nonpigmented nodules that have a propensity to ulcerate and bleed. Furthermore, the umbilicus is an exceedingly rare location for primary melanoma. However, one report does exist, and amelanotic melanoma should be considered in the differential for patients with umbilical nodules.7
Dermoid cysts are benign congenital lesions that typically present as a painless, slow-growing, and wellcircumscribed nodule, as similarly experienced by our patient. They most commonly are found on the testicles and ovaries but also are known to arise in embryologic fusion planes, and reports of umbilical lesions exist.8 Dermoid cysts are diagnosed based on histopathology, supporting the need for a biopsy to distinguish a malignant process from benign lesions.9
- Gabriele R, Conte M, Egidi F, et al. Umbilical metastases: current viewpoint. World J Surg Oncol. 2005;3:13.
- Chalya PL, Mabula JB, Rambau PF, et al. Sister Mary Joseph’s nodule at a university teaching hospital in northwestern Tanzania: a retrospective review of 34 cases. World J Surg Oncol. 2013;11:151.
- Leyrat B, Bernadach M, Ginzac A, et al. Sister Mary Joseph nodules: a case report about a rare location of skin metastasis. Case Rep Oncol. 2021;14:664-670.
- Yendluri V, Centeno B, Springett GM. Pancreatic cancer presenting as a Sister Mary Joseph’s nodule: case report and update of the literature. Pancreas. 2007;34:161-164.
- Uchi H. Merkel cell carcinoma: an update and immunotherapy. Front Oncol. 2018;8:48.
- Bittar PG, Hryneewycz KT, Bryant EA. Primary cutaneous endometriosis presenting as an umbilical nodule. JAMA Dermatol. 2021;157:1227.
- Kovitwanichkanont T, Joseph S, Yip L. Hidden in plain sight: umbilical melanoma [published online January 28, 2020]. Med J Aust. 2020;212:154-155.e1.
- Prior A, Anania P, Pacetti M, et al. Dermoid and epidermoid cysts of scalp: case series of 234 consecutive patients. World Neurosurg. 2018;120:119-124.
- Akinci O, Turker C, Erturk MS, et al. Umbilical dermoid cyst: a rare case. Cerrahpasa Med J. 2020;44:51-53.
- Gabriele R, Conte M, Egidi F, et al. Umbilical metastases: current viewpoint. World J Surg Oncol. 2005;3:13.
- Chalya PL, Mabula JB, Rambau PF, et al. Sister Mary Joseph’s nodule at a university teaching hospital in northwestern Tanzania: a retrospective review of 34 cases. World J Surg Oncol. 2013;11:151.
- Leyrat B, Bernadach M, Ginzac A, et al. Sister Mary Joseph nodules: a case report about a rare location of skin metastasis. Case Rep Oncol. 2021;14:664-670.
- Yendluri V, Centeno B, Springett GM. Pancreatic cancer presenting as a Sister Mary Joseph’s nodule: case report and update of the literature. Pancreas. 2007;34:161-164.
- Uchi H. Merkel cell carcinoma: an update and immunotherapy. Front Oncol. 2018;8:48.
- Bittar PG, Hryneewycz KT, Bryant EA. Primary cutaneous endometriosis presenting as an umbilical nodule. JAMA Dermatol. 2021;157:1227.
- Kovitwanichkanont T, Joseph S, Yip L. Hidden in plain sight: umbilical melanoma [published online January 28, 2020]. Med J Aust. 2020;212:154-155.e1.
- Prior A, Anania P, Pacetti M, et al. Dermoid and epidermoid cysts of scalp: case series of 234 consecutive patients. World Neurosurg. 2018;120:119-124.
- Akinci O, Turker C, Erturk MS, et al. Umbilical dermoid cyst: a rare case. Cerrahpasa Med J. 2020;44:51-53.
A 64-year-old woman with no notable medical history was referred to our dermatology clinic with an intermittent eczematous rash around the eyelids of 3 months’ duration. While performing a total-body skin examination, a firm pink nodule with a smooth surface incidentally was discovered on the umbilicus. The patient was uncertain when the lesion first appeared and denied any associated symptoms including pain and bleeding. Additionally, a lymph node examination revealed right inguinal lymphadenopathy. Upon further questioning, she reported worsening muscle weakness, fatigue, night sweats, and an unintentional weight loss of 10 pounds. A 6-mm punch biopsy of the umbilical lesion was obtained for routine histopathology.

Preoperative D-dimer level is an independent prognostic factor for gastric cancer after radical resection
Key clinical point: Preoperative elevated plasma D-dimer levels serve as an independent risk factor for poorer long-term survival outcomes in patients who have undergone curative surgery for gastric cancer.
Major finding: Multivariate analysis revealed elevated D-dimer levels to be independently associated with shorter overall survival (adjusted hazard ratio [aHR] 1.633; P = .003) and disease-free survival (aHR 1.58; P = .005).
Study details: Findings are from a retrospective study that included 903 patients with gastric cancer who underwent radical gastrectomy.
Disclosures: This study was sponsored by the National Natural Science Foundation of China, among others. The authors declared no conflicts of interest.
Source: Zhang X et al. D-dimer, a predictor of bad outcome in gastric cancer patients undergoing radical resection. Sci Rep. 2022;12:16432 (Sep 30). Doi: 10.1038/s41598-022-16582-9
Key clinical point: Preoperative elevated plasma D-dimer levels serve as an independent risk factor for poorer long-term survival outcomes in patients who have undergone curative surgery for gastric cancer.
Major finding: Multivariate analysis revealed elevated D-dimer levels to be independently associated with shorter overall survival (adjusted hazard ratio [aHR] 1.633; P = .003) and disease-free survival (aHR 1.58; P = .005).
Study details: Findings are from a retrospective study that included 903 patients with gastric cancer who underwent radical gastrectomy.
Disclosures: This study was sponsored by the National Natural Science Foundation of China, among others. The authors declared no conflicts of interest.
Source: Zhang X et al. D-dimer, a predictor of bad outcome in gastric cancer patients undergoing radical resection. Sci Rep. 2022;12:16432 (Sep 30). Doi: 10.1038/s41598-022-16582-9
Key clinical point: Preoperative elevated plasma D-dimer levels serve as an independent risk factor for poorer long-term survival outcomes in patients who have undergone curative surgery for gastric cancer.
Major finding: Multivariate analysis revealed elevated D-dimer levels to be independently associated with shorter overall survival (adjusted hazard ratio [aHR] 1.633; P = .003) and disease-free survival (aHR 1.58; P = .005).
Study details: Findings are from a retrospective study that included 903 patients with gastric cancer who underwent radical gastrectomy.
Disclosures: This study was sponsored by the National Natural Science Foundation of China, among others. The authors declared no conflicts of interest.
Source: Zhang X et al. D-dimer, a predictor of bad outcome in gastric cancer patients undergoing radical resection. Sci Rep. 2022;12:16432 (Sep 30). Doi: 10.1038/s41598-022-16582-9
Helicobacter pylori infection may predict a good response to immunotherapy in gastric cancer
Key clinical point: Helicobacter pylori (HP) infection is associated with the tumor expression of programmed death ligand-1 (PD-L1) in patients with gastric cancer.
Major finding: HP infection was significantly associated with the tumor expression of PD-L1 in patients with gastric cancer (odds ratio 1.90; P < .001), with the association not being significantly affected by the sample size, evaluation methods for PD-L1 expression, or quality score (all P > .05).
Study details: This meta-analysis of 10 observational studies investigated the association between HP infection and the tumor expression of PD-L1 in 1870 patients with gastric cancer.
Disclosures: This study was sponsored by the Natural Science Foundation of the Anhui Higher Education Institutions of China and others. The authors declared no conflicts of interest.
Source: Zhu Y et al. Helicobacter pylori infection and PD-L1 expression in gastric cancer: A meta-analysis. Eur J Clin Invest. 2022:e13880 (Sep 27). Doi: 10.1111/eci.13880
Key clinical point: Helicobacter pylori (HP) infection is associated with the tumor expression of programmed death ligand-1 (PD-L1) in patients with gastric cancer.
Major finding: HP infection was significantly associated with the tumor expression of PD-L1 in patients with gastric cancer (odds ratio 1.90; P < .001), with the association not being significantly affected by the sample size, evaluation methods for PD-L1 expression, or quality score (all P > .05).
Study details: This meta-analysis of 10 observational studies investigated the association between HP infection and the tumor expression of PD-L1 in 1870 patients with gastric cancer.
Disclosures: This study was sponsored by the Natural Science Foundation of the Anhui Higher Education Institutions of China and others. The authors declared no conflicts of interest.
Source: Zhu Y et al. Helicobacter pylori infection and PD-L1 expression in gastric cancer: A meta-analysis. Eur J Clin Invest. 2022:e13880 (Sep 27). Doi: 10.1111/eci.13880
Key clinical point: Helicobacter pylori (HP) infection is associated with the tumor expression of programmed death ligand-1 (PD-L1) in patients with gastric cancer.
Major finding: HP infection was significantly associated with the tumor expression of PD-L1 in patients with gastric cancer (odds ratio 1.90; P < .001), with the association not being significantly affected by the sample size, evaluation methods for PD-L1 expression, or quality score (all P > .05).
Study details: This meta-analysis of 10 observational studies investigated the association between HP infection and the tumor expression of PD-L1 in 1870 patients with gastric cancer.
Disclosures: This study was sponsored by the Natural Science Foundation of the Anhui Higher Education Institutions of China and others. The authors declared no conflicts of interest.
Source: Zhu Y et al. Helicobacter pylori infection and PD-L1 expression in gastric cancer: A meta-analysis. Eur J Clin Invest. 2022:e13880 (Sep 27). Doi: 10.1111/eci.13880
Early gastric cancer: Outcomes of pylorus-preserving vs conventional distal gastrectomy
Key clinical point: In patients with early gastric cancer (EGC), pylorus-preserving gastrectomy (PPG) vs conventional distal gastrectomy (CDG) results in the harvest of fewer lymph nodes at stations 5, 6, 9, and 11p but similar survival outcomes.
Major finding: Patients who underwent PPG vs CDG had significantly lower numbers of lymph nodes harvested at stations 5, 6, 9, and 11p (weighted mean difference, −3.09; P < .001) but similar overall survival (hazard ratio [HR] 0.63; P = .852) and recurrence-free survival (HR 0.29; P = .900).
Study details: This was a meta-analysis of 16 studies including 4500 patients with EGC who had undergone PPG or CDG with lymph node dissection.
Disclosures: This study was sponsored by the Peking University People’s Hospital Research and Development Fund. The authors declared no conflicts of interest.
Source: Hou S et al. Pathological and oncological outcomes of pylorus-preserving versus conventional distal gastrectomy in early gastric cancer: A systematic review and meta-analysis. World J Surg Oncol. 2022;20:308 (Sep 24). Doi: 10.1186/s12957-022-02766-0
Key clinical point: In patients with early gastric cancer (EGC), pylorus-preserving gastrectomy (PPG) vs conventional distal gastrectomy (CDG) results in the harvest of fewer lymph nodes at stations 5, 6, 9, and 11p but similar survival outcomes.
Major finding: Patients who underwent PPG vs CDG had significantly lower numbers of lymph nodes harvested at stations 5, 6, 9, and 11p (weighted mean difference, −3.09; P < .001) but similar overall survival (hazard ratio [HR] 0.63; P = .852) and recurrence-free survival (HR 0.29; P = .900).
Study details: This was a meta-analysis of 16 studies including 4500 patients with EGC who had undergone PPG or CDG with lymph node dissection.
Disclosures: This study was sponsored by the Peking University People’s Hospital Research and Development Fund. The authors declared no conflicts of interest.
Source: Hou S et al. Pathological and oncological outcomes of pylorus-preserving versus conventional distal gastrectomy in early gastric cancer: A systematic review and meta-analysis. World J Surg Oncol. 2022;20:308 (Sep 24). Doi: 10.1186/s12957-022-02766-0
Key clinical point: In patients with early gastric cancer (EGC), pylorus-preserving gastrectomy (PPG) vs conventional distal gastrectomy (CDG) results in the harvest of fewer lymph nodes at stations 5, 6, 9, and 11p but similar survival outcomes.
Major finding: Patients who underwent PPG vs CDG had significantly lower numbers of lymph nodes harvested at stations 5, 6, 9, and 11p (weighted mean difference, −3.09; P < .001) but similar overall survival (hazard ratio [HR] 0.63; P = .852) and recurrence-free survival (HR 0.29; P = .900).
Study details: This was a meta-analysis of 16 studies including 4500 patients with EGC who had undergone PPG or CDG with lymph node dissection.
Disclosures: This study was sponsored by the Peking University People’s Hospital Research and Development Fund. The authors declared no conflicts of interest.
Source: Hou S et al. Pathological and oncological outcomes of pylorus-preserving versus conventional distal gastrectomy in early gastric cancer: A systematic review and meta-analysis. World J Surg Oncol. 2022;20:308 (Sep 24). Doi: 10.1186/s12957-022-02766-0
Risk factors for delayed gastric emptying following gastrectomy for gastric cancer
Key clinical point: The female sex, distal gastric tumors, and diabetes are risk factors for delayed gastric emptying (DGE) in patients who have undergone gastrectomy for gastric cancer.
Major finding: Multivariate analysis revealed female sex (adjusted odds ratio [aOR] 2.47; P = .037), diabetes (aOR 2.44; P = .041), and distal gastric tumors (aOR 2.59; P = .033) as independent risk factors for DGE.
Study details: This retrospective study included 412 patients with gastric cancer who underwent distal gastrectomy and thereafter did (n = 27) or did not (n = 385) experience DGE.
Disclosures: No information on funding sources was provided. The author declared no conflicts of interest.
Source: Mukoyama T et al. Assessment of risk factors for delayed gastric emptying after distal gastrectomy for gastric cancer. Sci Rep. 2022;12:15903 (Sep 23). Doi: 10.1038/s41598-022-20151-5
Key clinical point: The female sex, distal gastric tumors, and diabetes are risk factors for delayed gastric emptying (DGE) in patients who have undergone gastrectomy for gastric cancer.
Major finding: Multivariate analysis revealed female sex (adjusted odds ratio [aOR] 2.47; P = .037), diabetes (aOR 2.44; P = .041), and distal gastric tumors (aOR 2.59; P = .033) as independent risk factors for DGE.
Study details: This retrospective study included 412 patients with gastric cancer who underwent distal gastrectomy and thereafter did (n = 27) or did not (n = 385) experience DGE.
Disclosures: No information on funding sources was provided. The author declared no conflicts of interest.
Source: Mukoyama T et al. Assessment of risk factors for delayed gastric emptying after distal gastrectomy for gastric cancer. Sci Rep. 2022;12:15903 (Sep 23). Doi: 10.1038/s41598-022-20151-5
Key clinical point: The female sex, distal gastric tumors, and diabetes are risk factors for delayed gastric emptying (DGE) in patients who have undergone gastrectomy for gastric cancer.
Major finding: Multivariate analysis revealed female sex (adjusted odds ratio [aOR] 2.47; P = .037), diabetes (aOR 2.44; P = .041), and distal gastric tumors (aOR 2.59; P = .033) as independent risk factors for DGE.
Study details: This retrospective study included 412 patients with gastric cancer who underwent distal gastrectomy and thereafter did (n = 27) or did not (n = 385) experience DGE.
Disclosures: No information on funding sources was provided. The author declared no conflicts of interest.
Source: Mukoyama T et al. Assessment of risk factors for delayed gastric emptying after distal gastrectomy for gastric cancer. Sci Rep. 2022;12:15903 (Sep 23). Doi: 10.1038/s41598-022-20151-5