User login
‘Fascinating’ link between Alzheimer’s and COVID-19
The findings could lead to new treatment targets to slow progression and severity of both diseases.
Investigators found that a single genetic variant in the oligoadenylate synthetase 1 (OAS1) gene increases the risk for AD and that related variants in the same gene increase the likelihood of severe COVID-19 outcomes.
“These findings may allow us to identify new drug targets to slow progression of both diseases and reduce their severity,” Dervis Salih, PhD, senior research associate, UK Dementia Research Institute, University College London, said in an interview.
“Our work also suggests new approaches to treat both diseases with the same drugs,” Dr. Salih added.
The study was published online Oct. 7 in Brain.
Shared genetic network
The OAS1 gene is expressed in microglia, a type of immune cell that makes up around 10% of all cells in the brain.
In earlier work, investigators found evidence suggesting a link between the OAS1 gene and AD, but the function of the gene in microglia was unknown.
To further investigate the gene’s link to AD, they sequenced genetic data from 2,547 people – half with AD, and half without.
The genotyping analysis confirmed that the single-nucleotide polymorphism (SNP) rs1131454 within OAS1 is significantly associated with AD.
Given that the same OAS1 locus has recently been linked with severe COVID-19 outcomes, the researchers investigated four variants on the OAS1 gene.
Results indicate that SNPs within OAS1 associated with AD also show linkage to SNP variants associated with critical illness in COVID-19.
The rs1131454 (risk allele A) and rs4766676 (risk allele T) are associated with AD, and rs10735079 (risk allele A) and rs6489867 (risk allele T) are associated with critical illness with COVID-19, the investigators reported. All of these risk alleles dampen expression of OAS1.
“This study also provides strong new evidence that interferon signaling by the innate immune system plays a substantial role in the progression of Alzheimer’s,” said Dr. Salih.
“Identifying this shared genetic network in innate immune cells will allow us with future work to identify new biomarkers to track disease progression and also predict disease risk better for both disorders,” he added.
‘Fascinating’ link
In a statement from the UK nonprofit organization, Science Media Center, Kenneth Baillie, MBChB, with the University of Edinburgh, said this study builds on a discovery he and his colleagues made last year that OAS1 variants are associated with severe COVID-19.
“In the ISARIC4C study, we recently found that this is probably due to a change in the way cell membranes detect viruses, but this mechanism doesn’t explain the fascinating association with Alzheimer’s disease reported in this new work,” Dr. Baillie said.
“It is often the case that the same gene can have different roles in different parts of the body. Importantly, it doesn’t mean that having COVID-19 has any effect on your risk of Alzheimer’s,” he added.
Also weighing in on the new study, Jonathan Schott, MD, professor of neurology, University College London, noted that dementia is the “main preexisting health condition associated with COVID-19 mortality, accounting for about one in four deaths from COVID-19 between March and June 2020.
“While some of this excessive mortality may relate to people with dementia being overrepresented in care homes, which were particularly hard hit by the pandemic, or due to general increased vulnerability to infections, there have been questions as to whether there are common factors that might increase susceptibility both to developing dementia and to dying from COVID-19,” Dr. Schott explained.
This “elegant paper” provides evidence for the latter, “suggesting a common genetic mechanism both for Alzheimer’s disease and for severe COVID-19 infection,” Dr. Schott said.
“The identification of a genetic risk factor and elucidation of inflammatory pathways through which it may increase risk has important implications for our understanding of both diseases, with potential implications for novel treatments,” he added.
The study was funded by the UK Dementia Research Institute. The authors have disclosed no relevant financial relationships. Dr. Schott serves as chief medical officer for Alzheimer’s Research UK and is clinical adviser to the UK Dementia Research Institute. Dr. Baillie has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The findings could lead to new treatment targets to slow progression and severity of both diseases.
Investigators found that a single genetic variant in the oligoadenylate synthetase 1 (OAS1) gene increases the risk for AD and that related variants in the same gene increase the likelihood of severe COVID-19 outcomes.
“These findings may allow us to identify new drug targets to slow progression of both diseases and reduce their severity,” Dervis Salih, PhD, senior research associate, UK Dementia Research Institute, University College London, said in an interview.
“Our work also suggests new approaches to treat both diseases with the same drugs,” Dr. Salih added.
The study was published online Oct. 7 in Brain.
Shared genetic network
The OAS1 gene is expressed in microglia, a type of immune cell that makes up around 10% of all cells in the brain.
In earlier work, investigators found evidence suggesting a link between the OAS1 gene and AD, but the function of the gene in microglia was unknown.
To further investigate the gene’s link to AD, they sequenced genetic data from 2,547 people – half with AD, and half without.
The genotyping analysis confirmed that the single-nucleotide polymorphism (SNP) rs1131454 within OAS1 is significantly associated with AD.
Given that the same OAS1 locus has recently been linked with severe COVID-19 outcomes, the researchers investigated four variants on the OAS1 gene.
Results indicate that SNPs within OAS1 associated with AD also show linkage to SNP variants associated with critical illness in COVID-19.
The rs1131454 (risk allele A) and rs4766676 (risk allele T) are associated with AD, and rs10735079 (risk allele A) and rs6489867 (risk allele T) are associated with critical illness with COVID-19, the investigators reported. All of these risk alleles dampen expression of OAS1.
“This study also provides strong new evidence that interferon signaling by the innate immune system plays a substantial role in the progression of Alzheimer’s,” said Dr. Salih.
“Identifying this shared genetic network in innate immune cells will allow us with future work to identify new biomarkers to track disease progression and also predict disease risk better for both disorders,” he added.
‘Fascinating’ link
In a statement from the UK nonprofit organization, Science Media Center, Kenneth Baillie, MBChB, with the University of Edinburgh, said this study builds on a discovery he and his colleagues made last year that OAS1 variants are associated with severe COVID-19.
“In the ISARIC4C study, we recently found that this is probably due to a change in the way cell membranes detect viruses, but this mechanism doesn’t explain the fascinating association with Alzheimer’s disease reported in this new work,” Dr. Baillie said.
“It is often the case that the same gene can have different roles in different parts of the body. Importantly, it doesn’t mean that having COVID-19 has any effect on your risk of Alzheimer’s,” he added.
Also weighing in on the new study, Jonathan Schott, MD, professor of neurology, University College London, noted that dementia is the “main preexisting health condition associated with COVID-19 mortality, accounting for about one in four deaths from COVID-19 between March and June 2020.
“While some of this excessive mortality may relate to people with dementia being overrepresented in care homes, which were particularly hard hit by the pandemic, or due to general increased vulnerability to infections, there have been questions as to whether there are common factors that might increase susceptibility both to developing dementia and to dying from COVID-19,” Dr. Schott explained.
This “elegant paper” provides evidence for the latter, “suggesting a common genetic mechanism both for Alzheimer’s disease and for severe COVID-19 infection,” Dr. Schott said.
“The identification of a genetic risk factor and elucidation of inflammatory pathways through which it may increase risk has important implications for our understanding of both diseases, with potential implications for novel treatments,” he added.
The study was funded by the UK Dementia Research Institute. The authors have disclosed no relevant financial relationships. Dr. Schott serves as chief medical officer for Alzheimer’s Research UK and is clinical adviser to the UK Dementia Research Institute. Dr. Baillie has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The findings could lead to new treatment targets to slow progression and severity of both diseases.
Investigators found that a single genetic variant in the oligoadenylate synthetase 1 (OAS1) gene increases the risk for AD and that related variants in the same gene increase the likelihood of severe COVID-19 outcomes.
“These findings may allow us to identify new drug targets to slow progression of both diseases and reduce their severity,” Dervis Salih, PhD, senior research associate, UK Dementia Research Institute, University College London, said in an interview.
“Our work also suggests new approaches to treat both diseases with the same drugs,” Dr. Salih added.
The study was published online Oct. 7 in Brain.
Shared genetic network
The OAS1 gene is expressed in microglia, a type of immune cell that makes up around 10% of all cells in the brain.
In earlier work, investigators found evidence suggesting a link between the OAS1 gene and AD, but the function of the gene in microglia was unknown.
To further investigate the gene’s link to AD, they sequenced genetic data from 2,547 people – half with AD, and half without.
The genotyping analysis confirmed that the single-nucleotide polymorphism (SNP) rs1131454 within OAS1 is significantly associated with AD.
Given that the same OAS1 locus has recently been linked with severe COVID-19 outcomes, the researchers investigated four variants on the OAS1 gene.
Results indicate that SNPs within OAS1 associated with AD also show linkage to SNP variants associated with critical illness in COVID-19.
The rs1131454 (risk allele A) and rs4766676 (risk allele T) are associated with AD, and rs10735079 (risk allele A) and rs6489867 (risk allele T) are associated with critical illness with COVID-19, the investigators reported. All of these risk alleles dampen expression of OAS1.
“This study also provides strong new evidence that interferon signaling by the innate immune system plays a substantial role in the progression of Alzheimer’s,” said Dr. Salih.
“Identifying this shared genetic network in innate immune cells will allow us with future work to identify new biomarkers to track disease progression and also predict disease risk better for both disorders,” he added.
‘Fascinating’ link
In a statement from the UK nonprofit organization, Science Media Center, Kenneth Baillie, MBChB, with the University of Edinburgh, said this study builds on a discovery he and his colleagues made last year that OAS1 variants are associated with severe COVID-19.
“In the ISARIC4C study, we recently found that this is probably due to a change in the way cell membranes detect viruses, but this mechanism doesn’t explain the fascinating association with Alzheimer’s disease reported in this new work,” Dr. Baillie said.
“It is often the case that the same gene can have different roles in different parts of the body. Importantly, it doesn’t mean that having COVID-19 has any effect on your risk of Alzheimer’s,” he added.
Also weighing in on the new study, Jonathan Schott, MD, professor of neurology, University College London, noted that dementia is the “main preexisting health condition associated with COVID-19 mortality, accounting for about one in four deaths from COVID-19 between March and June 2020.
“While some of this excessive mortality may relate to people with dementia being overrepresented in care homes, which were particularly hard hit by the pandemic, or due to general increased vulnerability to infections, there have been questions as to whether there are common factors that might increase susceptibility both to developing dementia and to dying from COVID-19,” Dr. Schott explained.
This “elegant paper” provides evidence for the latter, “suggesting a common genetic mechanism both for Alzheimer’s disease and for severe COVID-19 infection,” Dr. Schott said.
“The identification of a genetic risk factor and elucidation of inflammatory pathways through which it may increase risk has important implications for our understanding of both diseases, with potential implications for novel treatments,” he added.
The study was funded by the UK Dementia Research Institute. The authors have disclosed no relevant financial relationships. Dr. Schott serves as chief medical officer for Alzheimer’s Research UK and is clinical adviser to the UK Dementia Research Institute. Dr. Baillie has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Even one vaccinated member can cut family’s COVID risk
The chances are reduced even further with each additional vaccinated or otherwise immune family member, according to new data.
Lead author Peter Nordström, MD, PhD, with the unit of geriatric medicine, Umeå (Sweden) University, said in an interview the message is important for public health: “When you vaccinate, you do not just protect yourself but also your relatives.”
The findings were published online on Oct. 11, 2021, in JAMA Internal Medicine.
Researchers analyzed data from 1,789,728 individuals from 814,806 families from nationwide registries in Sweden. All individuals had acquired immunity either from previously being infected with SARS-CoV-2 or by being fully vaccinated (that is, having received two doses of the Moderna, Pfizer, or Oxford/AstraZeneca vaccines). Persons were considered for inclusion until May 26, 2021.
Each person with immunity was matched in a 1:1 ratio to a person without immunity from a cohort of individuals with families that had from two to five members. Families with more than five members were excluded because of small sample sizes.
Primarily nonimmune families in which there was one immune family member had a 45%-61% lower risk of contracting COVID-19 (hazard ratio, 0.39-0.55; 95% confidence interval, 0.37-0.61; P < .001).
The risk reduction increased to 75%-86% when two family members were immune (HR, 0.14-0.25; 95% CI, 0.11-0.27; P < .001).
It increased to 91%-94% when three family members were immune (HR, 0.06-0.09; 95% CI, 0.04-0.10; P < .001) and to 97% with four immune family members (HR, 0.03; 95% CI, 0.02-0.05; P < .001).
“The results were similar for the outcome of COVID-19 infection that was severe enough to warrant a hospital stay,” the authors wrote. They listed as an example that, in three-member families in which two members were immune, the remaining nonimmune family member had an 80% lower risk for hospitalization (HR, 0.20; 95% CI, 0.10-0.43; P < .001).
Global implications
Dr. Nordström said the team used the family setting because it was more easily identifiable as a cohort with the national registries and because COVID-19 is spread among people in close contact with each other. The findings have implications for other groups that spend large amounts of time together and for herd immunity, he added.
The findings may be particularly welcome in regions of the world where vaccination rates are very low. The authors noted that most of the global population has not yet been vaccinated and that “it is anticipated that most of the population in low-income countries will be unable to receive a vaccine in 2021, with current vaccination rates suggesting that completely inoculating 70%-85% of the global population may take up to 5 years.”
Jill Foster, MD, a pediatric infectious disease specialist at the University of Minnesota, Minneapolis, said in an interview she agrees that the news could encourage countries that have very low vaccination rates.
This study may help motivate areas with few resources to start small, she said: “Even one is better than zero.”
She added that this news could also help ease the minds of families that have immunocompromised members or in which there are children who are too young to be vaccinated.
With these data, she said, people can see there’s something they can do to help protect a family member.
Dr. Foster said that although it’s intuitive to think that the more vaccinated people there are in a family, the safer people are, “it’s really nice to see the data coming out of such a large dataset.”
The authors acknowledged that a limitation of the study is that, at the time the study was conducted, the Delta variant was uncommon in Sweden. It is therefore unclear whether the findings regarding immunity are still relevant in Sweden and elsewhere now that the Delta strain is dominant.
The authors reported no relevant financial relationships. Dr. Foster has received grant support from Moderna.
A version of this article first appeared on Medscape.com.
The chances are reduced even further with each additional vaccinated or otherwise immune family member, according to new data.
Lead author Peter Nordström, MD, PhD, with the unit of geriatric medicine, Umeå (Sweden) University, said in an interview the message is important for public health: “When you vaccinate, you do not just protect yourself but also your relatives.”
The findings were published online on Oct. 11, 2021, in JAMA Internal Medicine.
Researchers analyzed data from 1,789,728 individuals from 814,806 families from nationwide registries in Sweden. All individuals had acquired immunity either from previously being infected with SARS-CoV-2 or by being fully vaccinated (that is, having received two doses of the Moderna, Pfizer, or Oxford/AstraZeneca vaccines). Persons were considered for inclusion until May 26, 2021.
Each person with immunity was matched in a 1:1 ratio to a person without immunity from a cohort of individuals with families that had from two to five members. Families with more than five members were excluded because of small sample sizes.
Primarily nonimmune families in which there was one immune family member had a 45%-61% lower risk of contracting COVID-19 (hazard ratio, 0.39-0.55; 95% confidence interval, 0.37-0.61; P < .001).
The risk reduction increased to 75%-86% when two family members were immune (HR, 0.14-0.25; 95% CI, 0.11-0.27; P < .001).
It increased to 91%-94% when three family members were immune (HR, 0.06-0.09; 95% CI, 0.04-0.10; P < .001) and to 97% with four immune family members (HR, 0.03; 95% CI, 0.02-0.05; P < .001).
“The results were similar for the outcome of COVID-19 infection that was severe enough to warrant a hospital stay,” the authors wrote. They listed as an example that, in three-member families in which two members were immune, the remaining nonimmune family member had an 80% lower risk for hospitalization (HR, 0.20; 95% CI, 0.10-0.43; P < .001).
Global implications
Dr. Nordström said the team used the family setting because it was more easily identifiable as a cohort with the national registries and because COVID-19 is spread among people in close contact with each other. The findings have implications for other groups that spend large amounts of time together and for herd immunity, he added.
The findings may be particularly welcome in regions of the world where vaccination rates are very low. The authors noted that most of the global population has not yet been vaccinated and that “it is anticipated that most of the population in low-income countries will be unable to receive a vaccine in 2021, with current vaccination rates suggesting that completely inoculating 70%-85% of the global population may take up to 5 years.”
Jill Foster, MD, a pediatric infectious disease specialist at the University of Minnesota, Minneapolis, said in an interview she agrees that the news could encourage countries that have very low vaccination rates.
This study may help motivate areas with few resources to start small, she said: “Even one is better than zero.”
She added that this news could also help ease the minds of families that have immunocompromised members or in which there are children who are too young to be vaccinated.
With these data, she said, people can see there’s something they can do to help protect a family member.
Dr. Foster said that although it’s intuitive to think that the more vaccinated people there are in a family, the safer people are, “it’s really nice to see the data coming out of such a large dataset.”
The authors acknowledged that a limitation of the study is that, at the time the study was conducted, the Delta variant was uncommon in Sweden. It is therefore unclear whether the findings regarding immunity are still relevant in Sweden and elsewhere now that the Delta strain is dominant.
The authors reported no relevant financial relationships. Dr. Foster has received grant support from Moderna.
A version of this article first appeared on Medscape.com.
The chances are reduced even further with each additional vaccinated or otherwise immune family member, according to new data.
Lead author Peter Nordström, MD, PhD, with the unit of geriatric medicine, Umeå (Sweden) University, said in an interview the message is important for public health: “When you vaccinate, you do not just protect yourself but also your relatives.”
The findings were published online on Oct. 11, 2021, in JAMA Internal Medicine.
Researchers analyzed data from 1,789,728 individuals from 814,806 families from nationwide registries in Sweden. All individuals had acquired immunity either from previously being infected with SARS-CoV-2 or by being fully vaccinated (that is, having received two doses of the Moderna, Pfizer, or Oxford/AstraZeneca vaccines). Persons were considered for inclusion until May 26, 2021.
Each person with immunity was matched in a 1:1 ratio to a person without immunity from a cohort of individuals with families that had from two to five members. Families with more than five members were excluded because of small sample sizes.
Primarily nonimmune families in which there was one immune family member had a 45%-61% lower risk of contracting COVID-19 (hazard ratio, 0.39-0.55; 95% confidence interval, 0.37-0.61; P < .001).
The risk reduction increased to 75%-86% when two family members were immune (HR, 0.14-0.25; 95% CI, 0.11-0.27; P < .001).
It increased to 91%-94% when three family members were immune (HR, 0.06-0.09; 95% CI, 0.04-0.10; P < .001) and to 97% with four immune family members (HR, 0.03; 95% CI, 0.02-0.05; P < .001).
“The results were similar for the outcome of COVID-19 infection that was severe enough to warrant a hospital stay,” the authors wrote. They listed as an example that, in three-member families in which two members were immune, the remaining nonimmune family member had an 80% lower risk for hospitalization (HR, 0.20; 95% CI, 0.10-0.43; P < .001).
Global implications
Dr. Nordström said the team used the family setting because it was more easily identifiable as a cohort with the national registries and because COVID-19 is spread among people in close contact with each other. The findings have implications for other groups that spend large amounts of time together and for herd immunity, he added.
The findings may be particularly welcome in regions of the world where vaccination rates are very low. The authors noted that most of the global population has not yet been vaccinated and that “it is anticipated that most of the population in low-income countries will be unable to receive a vaccine in 2021, with current vaccination rates suggesting that completely inoculating 70%-85% of the global population may take up to 5 years.”
Jill Foster, MD, a pediatric infectious disease specialist at the University of Minnesota, Minneapolis, said in an interview she agrees that the news could encourage countries that have very low vaccination rates.
This study may help motivate areas with few resources to start small, she said: “Even one is better than zero.”
She added that this news could also help ease the minds of families that have immunocompromised members or in which there are children who are too young to be vaccinated.
With these data, she said, people can see there’s something they can do to help protect a family member.
Dr. Foster said that although it’s intuitive to think that the more vaccinated people there are in a family, the safer people are, “it’s really nice to see the data coming out of such a large dataset.”
The authors acknowledged that a limitation of the study is that, at the time the study was conducted, the Delta variant was uncommon in Sweden. It is therefore unclear whether the findings regarding immunity are still relevant in Sweden and elsewhere now that the Delta strain is dominant.
The authors reported no relevant financial relationships. Dr. Foster has received grant support from Moderna.
A version of this article first appeared on Medscape.com.
CDC: Children just as vulnerable to COVID as adults
The study, which focused on 1,000 schools in Arizona’s Maricopa and Pima counties, found that there were 113 COVID-19 outbreaks in schools without mask requirements in the first month of in-person learning. There were 16 outbreaks in schools with mask requirements.
“Masks in schools work to protect our children, to keep them and their school communities safe, and to keep them in school for in-person learning,” CDC Director Rochelle Walensky, MD, said at an Oct. 13 White House briefing.
But, she said, more than 95% of schools across the country had remained open through the end of September, despite 1,800 school closures affecting nearly 1 million students.
Protection for children in school is just one piece of the puzzle, Dr. Walensky said – there must also be COVID-safe practices at home to limit transmission. A CDC study published in October found that children had similar infection rates, compared with adults, confirming there is risk to people of all ages.
“For those children not yet eligible for vaccination, the best protection we can provide them is to make sure everyone around them in the household is vaccinated and to make sure they’re wearing a mask in school and during indoor extracurricular activities,” Dr. Walensky said.
Meanwhile, Pfizer’s vaccine for children ages 5-11 may be approved by early November. The Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee will meet Oct. 26 to discuss available data, and the CDC’s Advisory Committee on Immunization Practices will meet Nov. 2. A decision is expected soon after.
A version of this article first appeared on WebMD.com.
The study, which focused on 1,000 schools in Arizona’s Maricopa and Pima counties, found that there were 113 COVID-19 outbreaks in schools without mask requirements in the first month of in-person learning. There were 16 outbreaks in schools with mask requirements.
“Masks in schools work to protect our children, to keep them and their school communities safe, and to keep them in school for in-person learning,” CDC Director Rochelle Walensky, MD, said at an Oct. 13 White House briefing.
But, she said, more than 95% of schools across the country had remained open through the end of September, despite 1,800 school closures affecting nearly 1 million students.
Protection for children in school is just one piece of the puzzle, Dr. Walensky said – there must also be COVID-safe practices at home to limit transmission. A CDC study published in October found that children had similar infection rates, compared with adults, confirming there is risk to people of all ages.
“For those children not yet eligible for vaccination, the best protection we can provide them is to make sure everyone around them in the household is vaccinated and to make sure they’re wearing a mask in school and during indoor extracurricular activities,” Dr. Walensky said.
Meanwhile, Pfizer’s vaccine for children ages 5-11 may be approved by early November. The Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee will meet Oct. 26 to discuss available data, and the CDC’s Advisory Committee on Immunization Practices will meet Nov. 2. A decision is expected soon after.
A version of this article first appeared on WebMD.com.
The study, which focused on 1,000 schools in Arizona’s Maricopa and Pima counties, found that there were 113 COVID-19 outbreaks in schools without mask requirements in the first month of in-person learning. There were 16 outbreaks in schools with mask requirements.
“Masks in schools work to protect our children, to keep them and their school communities safe, and to keep them in school for in-person learning,” CDC Director Rochelle Walensky, MD, said at an Oct. 13 White House briefing.
But, she said, more than 95% of schools across the country had remained open through the end of September, despite 1,800 school closures affecting nearly 1 million students.
Protection for children in school is just one piece of the puzzle, Dr. Walensky said – there must also be COVID-safe practices at home to limit transmission. A CDC study published in October found that children had similar infection rates, compared with adults, confirming there is risk to people of all ages.
“For those children not yet eligible for vaccination, the best protection we can provide them is to make sure everyone around them in the household is vaccinated and to make sure they’re wearing a mask in school and during indoor extracurricular activities,” Dr. Walensky said.
Meanwhile, Pfizer’s vaccine for children ages 5-11 may be approved by early November. The Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee will meet Oct. 26 to discuss available data, and the CDC’s Advisory Committee on Immunization Practices will meet Nov. 2. A decision is expected soon after.
A version of this article first appeared on WebMD.com.
WHO unveils global roadmap to defeat meningitis by 2030
The World Health Organization and its partners recently released an ambitious plan, Defeating meningitis by 2030: A global road map. The goal is to reduce deaths and disabilities from bacterial meningitis, which kills about 250,000 people annually of the 1.2 million estimated to be infected.
This type of infection around the brain and spinal cord also causes long-term disabilities – deafness, learning problems, seizures, loss of limbs – in about one-quarter of survivors.
The leading causes of bacterial meningitis are Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and group B streptococcus. As with malaria, about half of the cases are in children under age 5 years. The most severely affected area for both infections is sub-Saharan Africa.
The main goal of the roadmap is to reduce vaccine-preventable cases of bacterial meningitis by 50% and deaths by 70% by 2030. WHO’s partners included the Centers for Disease Control and Prevention, the London School of Hygiene and Tropical Medicine, Médecins Sans Frontières (Doctors Without Borders), the Meningitis Research Foundation, PATH, UNICEF, and numerous global consultants.
For primary prevention and epidemic control, a major goal is to achieve higher vaccine coverage. Another goal is developing and deploying rapid diagnostic tests to guide treatment and prevention activities and measure the impact of vaccination. The lack of laboratory capacity to confirm the bacteria is a significant challenge. Also, patients often receive antibiotics before appropriate tests are conducted, and lumbar punctures are frequently not done.
The commitment to this project emerged in 2017. It was followed by a baseline analysis in 2018 and a draft roadmap the following year. Consultations with experts and with more than 600 patient groups in more than 90 countries followed.
Prevention through greater vaccine uptake was the top priority. Vaccination is considered the first line of defense against antibiotic resistance among the targeted bacteria.
Another goal is to quantify the decrease in antibiotic use for invasive infections or prophylaxis and the subsequent reduction in antimicrobial resistance in relation to increased vaccination.
Surveillance is weak in many regions, limiting the ability to detect epidemics and to respond appropriately. Similarly, there are limited data on the burden of sequelae, such as deafness, on meningitis survivors.
There is an inadequate supply of affordable vaccines to respond to epidemics. Currently, routine vaccination against Neisseria meningitidis is occurring in 18 of 26 countries in the meningitis belt. Epidemics of meningococcus occur every few years in the driest time of the year and abate with the rains. Epidemics of pneumococcal meningitis are much rarer but follow a similar pattern; they have also been associated with crowding and alcohol use.
Care for those affected by meningitis is another focus, as is affirming the right to prevention and care. There’s a need for earlier recognition of the complications of meningitis and an increase in efforts to treat those complications.
WHO’s final goal in its roadmap is to boost awareness of meningitis and make it a priority for policymakers. Similarly, there is a need to educate communities about the disease, including how to access vaccines. If someone becomes ill, they need to be aware of the symptoms, the need for early treatment, and what aftercare is available.
Marie-Pierre Préziosi, MD, the core secretariat of WHO’s Technical Taskforce, told this news organization that while the roadmap looks aspirational, “it is feasible … you have strategic goals – each has milestones with time limits and who will do it.”
Regarding vaccinations, Dr. Préziosi said that “the strategy was a victim of its success. The mass campaign knocked down transmission completely.” Some countries are now waiting for multivalent vaccines. She said that vaccine hesitancy is not a significant problem in Africa “because the disease is so feared.”
Major obstacles to implementing the roadmap include the complacency of public health leaders and the COVID-19 lockdowns, which decreased vaccination coverage rates. “The second thing is also sufficient funding to do the research and innovation so that we get the affordable tools that we need globally,” Dr. Préziosi said.
Marilyn Felkner, DrPH, School of Human Ecology, University of Texas at Austin, said in an interview, “It’s very cliché, but we have often said that communicable diseases do not respect political boundaries. So to expect a country to be able to control that by themselves is a false hope.”
Regarding the roadmap, Dr. Felkner said, “I think that organizing ideas and having them in writing is always a good first step. And it can help people move forward if they’re feeling overwhelmed ... Having a written plan can certainly provide that fundamental basis. So, the important thing is not to say, ‘Oh, we have this great plan done; hope somebody picks up the plan.’ There’s got to be some momentum behind it, and hopefully some funding.”
Dr. Préziosi and Dr. Felkner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The World Health Organization and its partners recently released an ambitious plan, Defeating meningitis by 2030: A global road map. The goal is to reduce deaths and disabilities from bacterial meningitis, which kills about 250,000 people annually of the 1.2 million estimated to be infected.
This type of infection around the brain and spinal cord also causes long-term disabilities – deafness, learning problems, seizures, loss of limbs – in about one-quarter of survivors.
The leading causes of bacterial meningitis are Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and group B streptococcus. As with malaria, about half of the cases are in children under age 5 years. The most severely affected area for both infections is sub-Saharan Africa.
The main goal of the roadmap is to reduce vaccine-preventable cases of bacterial meningitis by 50% and deaths by 70% by 2030. WHO’s partners included the Centers for Disease Control and Prevention, the London School of Hygiene and Tropical Medicine, Médecins Sans Frontières (Doctors Without Borders), the Meningitis Research Foundation, PATH, UNICEF, and numerous global consultants.
For primary prevention and epidemic control, a major goal is to achieve higher vaccine coverage. Another goal is developing and deploying rapid diagnostic tests to guide treatment and prevention activities and measure the impact of vaccination. The lack of laboratory capacity to confirm the bacteria is a significant challenge. Also, patients often receive antibiotics before appropriate tests are conducted, and lumbar punctures are frequently not done.
The commitment to this project emerged in 2017. It was followed by a baseline analysis in 2018 and a draft roadmap the following year. Consultations with experts and with more than 600 patient groups in more than 90 countries followed.
Prevention through greater vaccine uptake was the top priority. Vaccination is considered the first line of defense against antibiotic resistance among the targeted bacteria.
Another goal is to quantify the decrease in antibiotic use for invasive infections or prophylaxis and the subsequent reduction in antimicrobial resistance in relation to increased vaccination.
Surveillance is weak in many regions, limiting the ability to detect epidemics and to respond appropriately. Similarly, there are limited data on the burden of sequelae, such as deafness, on meningitis survivors.
There is an inadequate supply of affordable vaccines to respond to epidemics. Currently, routine vaccination against Neisseria meningitidis is occurring in 18 of 26 countries in the meningitis belt. Epidemics of meningococcus occur every few years in the driest time of the year and abate with the rains. Epidemics of pneumococcal meningitis are much rarer but follow a similar pattern; they have also been associated with crowding and alcohol use.
Care for those affected by meningitis is another focus, as is affirming the right to prevention and care. There’s a need for earlier recognition of the complications of meningitis and an increase in efforts to treat those complications.
WHO’s final goal in its roadmap is to boost awareness of meningitis and make it a priority for policymakers. Similarly, there is a need to educate communities about the disease, including how to access vaccines. If someone becomes ill, they need to be aware of the symptoms, the need for early treatment, and what aftercare is available.
Marie-Pierre Préziosi, MD, the core secretariat of WHO’s Technical Taskforce, told this news organization that while the roadmap looks aspirational, “it is feasible … you have strategic goals – each has milestones with time limits and who will do it.”
Regarding vaccinations, Dr. Préziosi said that “the strategy was a victim of its success. The mass campaign knocked down transmission completely.” Some countries are now waiting for multivalent vaccines. She said that vaccine hesitancy is not a significant problem in Africa “because the disease is so feared.”
Major obstacles to implementing the roadmap include the complacency of public health leaders and the COVID-19 lockdowns, which decreased vaccination coverage rates. “The second thing is also sufficient funding to do the research and innovation so that we get the affordable tools that we need globally,” Dr. Préziosi said.
Marilyn Felkner, DrPH, School of Human Ecology, University of Texas at Austin, said in an interview, “It’s very cliché, but we have often said that communicable diseases do not respect political boundaries. So to expect a country to be able to control that by themselves is a false hope.”
Regarding the roadmap, Dr. Felkner said, “I think that organizing ideas and having them in writing is always a good first step. And it can help people move forward if they’re feeling overwhelmed ... Having a written plan can certainly provide that fundamental basis. So, the important thing is not to say, ‘Oh, we have this great plan done; hope somebody picks up the plan.’ There’s got to be some momentum behind it, and hopefully some funding.”
Dr. Préziosi and Dr. Felkner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The World Health Organization and its partners recently released an ambitious plan, Defeating meningitis by 2030: A global road map. The goal is to reduce deaths and disabilities from bacterial meningitis, which kills about 250,000 people annually of the 1.2 million estimated to be infected.
This type of infection around the brain and spinal cord also causes long-term disabilities – deafness, learning problems, seizures, loss of limbs – in about one-quarter of survivors.
The leading causes of bacterial meningitis are Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), Haemophilus influenzae, and group B streptococcus. As with malaria, about half of the cases are in children under age 5 years. The most severely affected area for both infections is sub-Saharan Africa.
The main goal of the roadmap is to reduce vaccine-preventable cases of bacterial meningitis by 50% and deaths by 70% by 2030. WHO’s partners included the Centers for Disease Control and Prevention, the London School of Hygiene and Tropical Medicine, Médecins Sans Frontières (Doctors Without Borders), the Meningitis Research Foundation, PATH, UNICEF, and numerous global consultants.
For primary prevention and epidemic control, a major goal is to achieve higher vaccine coverage. Another goal is developing and deploying rapid diagnostic tests to guide treatment and prevention activities and measure the impact of vaccination. The lack of laboratory capacity to confirm the bacteria is a significant challenge. Also, patients often receive antibiotics before appropriate tests are conducted, and lumbar punctures are frequently not done.
The commitment to this project emerged in 2017. It was followed by a baseline analysis in 2018 and a draft roadmap the following year. Consultations with experts and with more than 600 patient groups in more than 90 countries followed.
Prevention through greater vaccine uptake was the top priority. Vaccination is considered the first line of defense against antibiotic resistance among the targeted bacteria.
Another goal is to quantify the decrease in antibiotic use for invasive infections or prophylaxis and the subsequent reduction in antimicrobial resistance in relation to increased vaccination.
Surveillance is weak in many regions, limiting the ability to detect epidemics and to respond appropriately. Similarly, there are limited data on the burden of sequelae, such as deafness, on meningitis survivors.
There is an inadequate supply of affordable vaccines to respond to epidemics. Currently, routine vaccination against Neisseria meningitidis is occurring in 18 of 26 countries in the meningitis belt. Epidemics of meningococcus occur every few years in the driest time of the year and abate with the rains. Epidemics of pneumococcal meningitis are much rarer but follow a similar pattern; they have also been associated with crowding and alcohol use.
Care for those affected by meningitis is another focus, as is affirming the right to prevention and care. There’s a need for earlier recognition of the complications of meningitis and an increase in efforts to treat those complications.
WHO’s final goal in its roadmap is to boost awareness of meningitis and make it a priority for policymakers. Similarly, there is a need to educate communities about the disease, including how to access vaccines. If someone becomes ill, they need to be aware of the symptoms, the need for early treatment, and what aftercare is available.
Marie-Pierre Préziosi, MD, the core secretariat of WHO’s Technical Taskforce, told this news organization that while the roadmap looks aspirational, “it is feasible … you have strategic goals – each has milestones with time limits and who will do it.”
Regarding vaccinations, Dr. Préziosi said that “the strategy was a victim of its success. The mass campaign knocked down transmission completely.” Some countries are now waiting for multivalent vaccines. She said that vaccine hesitancy is not a significant problem in Africa “because the disease is so feared.”
Major obstacles to implementing the roadmap include the complacency of public health leaders and the COVID-19 lockdowns, which decreased vaccination coverage rates. “The second thing is also sufficient funding to do the research and innovation so that we get the affordable tools that we need globally,” Dr. Préziosi said.
Marilyn Felkner, DrPH, School of Human Ecology, University of Texas at Austin, said in an interview, “It’s very cliché, but we have often said that communicable diseases do not respect political boundaries. So to expect a country to be able to control that by themselves is a false hope.”
Regarding the roadmap, Dr. Felkner said, “I think that organizing ideas and having them in writing is always a good first step. And it can help people move forward if they’re feeling overwhelmed ... Having a written plan can certainly provide that fundamental basis. So, the important thing is not to say, ‘Oh, we have this great plan done; hope somebody picks up the plan.’ There’s got to be some momentum behind it, and hopefully some funding.”
Dr. Préziosi and Dr. Felkner have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Wearable sensors pick up infection before symptoms occur
A simple wristband containing biometric monitoring sensors is able to pick up early infection from both influenza and the common cold before symptoms develop. Moreover, it can predict the severity of the illness once it becomes symptomatic, new research shows.
“Prior to the development of symptoms, people are still infectious and can potentially infect others,” senior author Jessilyn Dunn, PhD, Duke University, Durham, N.C., told this news organization.
“That’s why it’s so important to be able to detect infection even when a person doesn’t feel symptomatic, as this would help prevent the spread of pathogens that occur before somebody knows they are sick – and which is why it is important from a public health perspective,” she added.
The study was published online Sept. 29, 2021, in JAMA Network Open.
Two challenge studies
The study involved 31 participants who were inoculated with the H1N1 influenza virus and 18 others who were inoculated with rhinovirus. The rhinovirus challenge study was conducted in 2015, and the H1N1 challenge study was carried out in 2018. Both groups of patients were inoculated via intranasal drops of either the diluted H1N1 virus or the diluted rhinovirus strain type 16.
Participants in both challenge studies wore the E4 wristband (Empatica). Those in the influenza study wore the wristband 1 day before and 11 days after being inoculated, and those in the rhinovirus study wore the wristband for 4 days before and 5 days after inoculation. The E4 wristband measures heart rate, skin temperature, electrodermal activity, and movement.
Symptoms were typical of each infection and were classified as both observable events, such as runny nose, cough, and wheezy chest, or unobservable events, such as muscle soreness and fatigue. Infection status was classified as asymptomatic or noninfectious (AON), mild, or moderate.
The biosensors contained within the wristband were able to detect the presence or absence of H1N1 infection with an accuracy of 79% within 12 hours after participants had been inoculated and an accuracy of 92% within 24 hours of being inoculated, the authors report. Thus, “we could assess whether or not a participant was infected with H1N1 between 24 and 36 hours before symptom onset,” the investigators noted.
The median time for symptom onset following the rhinovirus challenge was 36 hours after inoculation. The biosensors predicted the presence or absence of rhinovirus infection with an accuracy of 88%, the authors wrote. And when both viral challenges were combined, models predicting infection had an accuracy of 76% at 24 hours after participants being inoculated.
Prediction of severity
Twelve hours after participants had been inoculated, the technology was also able to predict the development of either AON or moderate H1N1 infection with 83% accuracy. For rhinovirus, the predictive accuracy of distinguishing AON versus moderate infection was slightly higher at 92% whereas for both viruses combined, the technology predicted the future development of AON versus moderate infection with an 84% accuracy rate.
As the authors pointed out, the ability to identify individuals during the early critical stage of viral infection could have wide-ranging effects. “In the midst of the global SARS-CoV-2 pandemic, the need for novel approaches like this has never been more apparent,” they suggested.
And in point of fact, in a not-yet peer-reviewed study using a real-time smartwatch-based alerting system again designed to detect aberrant physiologic and activity signals associated with early infection, Stanford (Calif.) University investigators found that alerts were generated for presymptomatic and asymptomatic COVID-19 infections in 78% of cases in over 3200 participants tested at a median of 3 days prior to symptom onset.
The authors also noted that their system is scalable to millions of users, thus offering a personal health monitoring system that can operate in real time.
In a comment, Steven Steinhubl, MD, a research scientist and formerly the director of digital medicine at Scripps Research’s Translational Institute, La Jolla, Calif., told this news organization that he personally has a lot of faith in this type of technology.
“Unfortunately, COVID-19 has changed our perspective about respiratory infections but if you think of the bad flu seasons we’ve had in the past, people do die from influenza, so I think there is a lot of value [in this technology], although the degree of value depends on the severity of the infection,” he said.
For example, if people actually ever go back into work together, early recognition that an employee might have influenza or another highly contagious infection could alert them to the necessity to stay home and self-isolate.
“We have a bit to go before we get there,” Dr. Steinhubl acknowledged, “but you could have a really big impact on the spread of any infectious disease that would be better for everybody.”
Dr. Dunn has disclosed no relevant financial relationships. Dr. Steinhubl is chief medical officer at physIQ, a company involved in the development of personalized analytics.
A version of this article first appeared on Medscape.com.
A simple wristband containing biometric monitoring sensors is able to pick up early infection from both influenza and the common cold before symptoms develop. Moreover, it can predict the severity of the illness once it becomes symptomatic, new research shows.
“Prior to the development of symptoms, people are still infectious and can potentially infect others,” senior author Jessilyn Dunn, PhD, Duke University, Durham, N.C., told this news organization.
“That’s why it’s so important to be able to detect infection even when a person doesn’t feel symptomatic, as this would help prevent the spread of pathogens that occur before somebody knows they are sick – and which is why it is important from a public health perspective,” she added.
The study was published online Sept. 29, 2021, in JAMA Network Open.
Two challenge studies
The study involved 31 participants who were inoculated with the H1N1 influenza virus and 18 others who were inoculated with rhinovirus. The rhinovirus challenge study was conducted in 2015, and the H1N1 challenge study was carried out in 2018. Both groups of patients were inoculated via intranasal drops of either the diluted H1N1 virus or the diluted rhinovirus strain type 16.
Participants in both challenge studies wore the E4 wristband (Empatica). Those in the influenza study wore the wristband 1 day before and 11 days after being inoculated, and those in the rhinovirus study wore the wristband for 4 days before and 5 days after inoculation. The E4 wristband measures heart rate, skin temperature, electrodermal activity, and movement.
Symptoms were typical of each infection and were classified as both observable events, such as runny nose, cough, and wheezy chest, or unobservable events, such as muscle soreness and fatigue. Infection status was classified as asymptomatic or noninfectious (AON), mild, or moderate.
The biosensors contained within the wristband were able to detect the presence or absence of H1N1 infection with an accuracy of 79% within 12 hours after participants had been inoculated and an accuracy of 92% within 24 hours of being inoculated, the authors report. Thus, “we could assess whether or not a participant was infected with H1N1 between 24 and 36 hours before symptom onset,” the investigators noted.
The median time for symptom onset following the rhinovirus challenge was 36 hours after inoculation. The biosensors predicted the presence or absence of rhinovirus infection with an accuracy of 88%, the authors wrote. And when both viral challenges were combined, models predicting infection had an accuracy of 76% at 24 hours after participants being inoculated.
Prediction of severity
Twelve hours after participants had been inoculated, the technology was also able to predict the development of either AON or moderate H1N1 infection with 83% accuracy. For rhinovirus, the predictive accuracy of distinguishing AON versus moderate infection was slightly higher at 92% whereas for both viruses combined, the technology predicted the future development of AON versus moderate infection with an 84% accuracy rate.
As the authors pointed out, the ability to identify individuals during the early critical stage of viral infection could have wide-ranging effects. “In the midst of the global SARS-CoV-2 pandemic, the need for novel approaches like this has never been more apparent,” they suggested.
And in point of fact, in a not-yet peer-reviewed study using a real-time smartwatch-based alerting system again designed to detect aberrant physiologic and activity signals associated with early infection, Stanford (Calif.) University investigators found that alerts were generated for presymptomatic and asymptomatic COVID-19 infections in 78% of cases in over 3200 participants tested at a median of 3 days prior to symptom onset.
The authors also noted that their system is scalable to millions of users, thus offering a personal health monitoring system that can operate in real time.
In a comment, Steven Steinhubl, MD, a research scientist and formerly the director of digital medicine at Scripps Research’s Translational Institute, La Jolla, Calif., told this news organization that he personally has a lot of faith in this type of technology.
“Unfortunately, COVID-19 has changed our perspective about respiratory infections but if you think of the bad flu seasons we’ve had in the past, people do die from influenza, so I think there is a lot of value [in this technology], although the degree of value depends on the severity of the infection,” he said.
For example, if people actually ever go back into work together, early recognition that an employee might have influenza or another highly contagious infection could alert them to the necessity to stay home and self-isolate.
“We have a bit to go before we get there,” Dr. Steinhubl acknowledged, “but you could have a really big impact on the spread of any infectious disease that would be better for everybody.”
Dr. Dunn has disclosed no relevant financial relationships. Dr. Steinhubl is chief medical officer at physIQ, a company involved in the development of personalized analytics.
A version of this article first appeared on Medscape.com.
A simple wristband containing biometric monitoring sensors is able to pick up early infection from both influenza and the common cold before symptoms develop. Moreover, it can predict the severity of the illness once it becomes symptomatic, new research shows.
“Prior to the development of symptoms, people are still infectious and can potentially infect others,” senior author Jessilyn Dunn, PhD, Duke University, Durham, N.C., told this news organization.
“That’s why it’s so important to be able to detect infection even when a person doesn’t feel symptomatic, as this would help prevent the spread of pathogens that occur before somebody knows they are sick – and which is why it is important from a public health perspective,” she added.
The study was published online Sept. 29, 2021, in JAMA Network Open.
Two challenge studies
The study involved 31 participants who were inoculated with the H1N1 influenza virus and 18 others who were inoculated with rhinovirus. The rhinovirus challenge study was conducted in 2015, and the H1N1 challenge study was carried out in 2018. Both groups of patients were inoculated via intranasal drops of either the diluted H1N1 virus or the diluted rhinovirus strain type 16.
Participants in both challenge studies wore the E4 wristband (Empatica). Those in the influenza study wore the wristband 1 day before and 11 days after being inoculated, and those in the rhinovirus study wore the wristband for 4 days before and 5 days after inoculation. The E4 wristband measures heart rate, skin temperature, electrodermal activity, and movement.
Symptoms were typical of each infection and were classified as both observable events, such as runny nose, cough, and wheezy chest, or unobservable events, such as muscle soreness and fatigue. Infection status was classified as asymptomatic or noninfectious (AON), mild, or moderate.
The biosensors contained within the wristband were able to detect the presence or absence of H1N1 infection with an accuracy of 79% within 12 hours after participants had been inoculated and an accuracy of 92% within 24 hours of being inoculated, the authors report. Thus, “we could assess whether or not a participant was infected with H1N1 between 24 and 36 hours before symptom onset,” the investigators noted.
The median time for symptom onset following the rhinovirus challenge was 36 hours after inoculation. The biosensors predicted the presence or absence of rhinovirus infection with an accuracy of 88%, the authors wrote. And when both viral challenges were combined, models predicting infection had an accuracy of 76% at 24 hours after participants being inoculated.
Prediction of severity
Twelve hours after participants had been inoculated, the technology was also able to predict the development of either AON or moderate H1N1 infection with 83% accuracy. For rhinovirus, the predictive accuracy of distinguishing AON versus moderate infection was slightly higher at 92% whereas for both viruses combined, the technology predicted the future development of AON versus moderate infection with an 84% accuracy rate.
As the authors pointed out, the ability to identify individuals during the early critical stage of viral infection could have wide-ranging effects. “In the midst of the global SARS-CoV-2 pandemic, the need for novel approaches like this has never been more apparent,” they suggested.
And in point of fact, in a not-yet peer-reviewed study using a real-time smartwatch-based alerting system again designed to detect aberrant physiologic and activity signals associated with early infection, Stanford (Calif.) University investigators found that alerts were generated for presymptomatic and asymptomatic COVID-19 infections in 78% of cases in over 3200 participants tested at a median of 3 days prior to symptom onset.
The authors also noted that their system is scalable to millions of users, thus offering a personal health monitoring system that can operate in real time.
In a comment, Steven Steinhubl, MD, a research scientist and formerly the director of digital medicine at Scripps Research’s Translational Institute, La Jolla, Calif., told this news organization that he personally has a lot of faith in this type of technology.
“Unfortunately, COVID-19 has changed our perspective about respiratory infections but if you think of the bad flu seasons we’ve had in the past, people do die from influenza, so I think there is a lot of value [in this technology], although the degree of value depends on the severity of the infection,” he said.
For example, if people actually ever go back into work together, early recognition that an employee might have influenza or another highly contagious infection could alert them to the necessity to stay home and self-isolate.
“We have a bit to go before we get there,” Dr. Steinhubl acknowledged, “but you could have a really big impact on the spread of any infectious disease that would be better for everybody.”
Dr. Dunn has disclosed no relevant financial relationships. Dr. Steinhubl is chief medical officer at physIQ, a company involved in the development of personalized analytics.
A version of this article first appeared on Medscape.com.
No short-term death risk in elderly after COVID-19 vaccines
and launched an investigation into the safety of the BNT162b2 vaccine (Comirnaty; Pfizer-BioNTech).
Now, the results of that investigation and of a subsequent larger study of nursing home residents in Norway have shown no increased risk for short-term mortality following COVID-19 vaccination in the overall population of elderly patients. The new research also showed clear evidence of a survival benefit compared with the unvaccinated population, Anette Hylen Ranhoff, MD, PhD, said at the annual meeting of the European Geriatric Medicine Society, held in a hybrid format in Athens, Greece, and online.
“We found no evidence of increased short-term mortality among vaccinated older individuals, and particularly not among the nursing home patients,” said Dr. Ranhoff, a senior researcher at the Norwegian Institute of Public Health and professor at University of Bergen, Norway. “But we think that this [lower] mortality risk was most likely a sort of ‘healthy-vaccinee’ effect, which means that people who were a bit more healthy were vaccinated, and not those who were the very, very most frail.”
“We have more or less the same data in France about events, with very high rates of vaccination,” said session moderator Athanase Benetos MD, PhD, professor and chairman of geriatric medicine at the University Hospital of Nancy in France, who was not involved in the study.
“In my department, a month after the end of the vaccination and at the same time while the pandemic in the city was going up, we had a 90% decrease in mortality from COVID in the nursing homes,” he told Dr. Ranhoff.
Potential risks
Frail elderly patients were not included in clinical trials of COVID-19 vaccines, and although previous studies have shown a low incidence of local or systemic reactions to vaccination among older people, “we think that quite mild adverse events following vaccination could trigger and destabilize a frail person,” Dr. Ranhoff said.
As reported Jan. 15, 2021, in BMJ, investigation by the Norwegian Medicines Agency (NOMA) into 13 of the 23 reported cases concluded that common adverse reactions associated with mRNA vaccines could have contributed to the deaths of some of the frail elderly patients
Steinar Madsen, MD, NOMA medical director, told BMJ “we are not alarmed or worried about this, because these are very rare occurrences and they occurred in very frail patients with very serious disease.”
Health authorities investigate
In response to the report and at the request of the Norwegian Public Health Institute and NOMA, Dr. Ranhoff and colleagues investigated the first 100 deaths among nursing-home residents who received the vaccine. The team consisted of three geriatricians and an infectious disease specialist who sees patients in nursing homes.
They looked at each patient’s clinical course before and after vaccination, their health trajectory and life expectancy at the time of vaccination, new symptoms following vaccination, and the time from vaccination to new symptoms and to death.
In addition, the investigators evaluated Clinical Frailty Scale (CFS) scores for each patient. CFS scores range from 1 (very fit) to 9 (terminally ill, with a life expectancy of less than 6 months who are otherwise evidently frail).
The initial investigation found that among 95 evaluable patients, the association between vaccination and death was “probable” in 10, “possible” in 26, and “unlikely” in 59.
The mean time from vaccination to symptoms was 1.4 days in the probable cases, 2.5 days in the possible cases, and 4.7 days in the unlikely cases.
The mean time from vaccination to death was 3.1, 8.3, and 8.2 days, respectively.
In all three categories, the patients had mean CFS scores ranging from 7.6 to 7.9, putting them in the “severely frail” category, defined as people who are completely dependent for personal care but seem stable and not at high risk for dying.
“We have quite many nursing home residents in Norway, 35,000; more than 80% have dementia, and the mean age is 85 years. We know that approximately 45 people die every day in these nursing homes, and their mean age of death is 87.5 years,” Dr. Ranhoff said.
Population-wide study
Dr. Ranhoff and colleagues also looked more broadly into the question of potential vaccine-related mortality in the total population of older people in Norway from the day of vaccination to follow-up at 3 weeks.
They conducted a matched cohort study to investigate the relationship between the mRNA SARS-CoV-2 vaccine and overall death among persons aged 65 and older in the general population, and across four groups: patients receiving home-based care, long-term nursing home patients, short-term nursing home patients, and those not receiving health services.
The researchers identified a total of 967,786 residents of Norway aged 65 and over at the start of the country’s vaccination campaign at the end of December, 2020, and they matched vaccinated individuals with unvaccinated persons based on demographic, geographic, and clinical risk group factors.
Dr. Ranhoff showed Kaplan-Meier survival curves for the total population and for each of the health-service states. In all cases there was a clear survival benefit for vaccinated vs. unvaccinated patients. She did not, however, provide specific numbers or hazard ratios for the differences between vaccinated and unvaccinated individuals in each of the comparisons.
The study was supported by the Norwegian Institute of Public Health. Dr. Ranhoff and Dr. Benetos reported no conflicts of interest.
and launched an investigation into the safety of the BNT162b2 vaccine (Comirnaty; Pfizer-BioNTech).
Now, the results of that investigation and of a subsequent larger study of nursing home residents in Norway have shown no increased risk for short-term mortality following COVID-19 vaccination in the overall population of elderly patients. The new research also showed clear evidence of a survival benefit compared with the unvaccinated population, Anette Hylen Ranhoff, MD, PhD, said at the annual meeting of the European Geriatric Medicine Society, held in a hybrid format in Athens, Greece, and online.
“We found no evidence of increased short-term mortality among vaccinated older individuals, and particularly not among the nursing home patients,” said Dr. Ranhoff, a senior researcher at the Norwegian Institute of Public Health and professor at University of Bergen, Norway. “But we think that this [lower] mortality risk was most likely a sort of ‘healthy-vaccinee’ effect, which means that people who were a bit more healthy were vaccinated, and not those who were the very, very most frail.”
“We have more or less the same data in France about events, with very high rates of vaccination,” said session moderator Athanase Benetos MD, PhD, professor and chairman of geriatric medicine at the University Hospital of Nancy in France, who was not involved in the study.
“In my department, a month after the end of the vaccination and at the same time while the pandemic in the city was going up, we had a 90% decrease in mortality from COVID in the nursing homes,” he told Dr. Ranhoff.
Potential risks
Frail elderly patients were not included in clinical trials of COVID-19 vaccines, and although previous studies have shown a low incidence of local or systemic reactions to vaccination among older people, “we think that quite mild adverse events following vaccination could trigger and destabilize a frail person,” Dr. Ranhoff said.
As reported Jan. 15, 2021, in BMJ, investigation by the Norwegian Medicines Agency (NOMA) into 13 of the 23 reported cases concluded that common adverse reactions associated with mRNA vaccines could have contributed to the deaths of some of the frail elderly patients
Steinar Madsen, MD, NOMA medical director, told BMJ “we are not alarmed or worried about this, because these are very rare occurrences and they occurred in very frail patients with very serious disease.”
Health authorities investigate
In response to the report and at the request of the Norwegian Public Health Institute and NOMA, Dr. Ranhoff and colleagues investigated the first 100 deaths among nursing-home residents who received the vaccine. The team consisted of three geriatricians and an infectious disease specialist who sees patients in nursing homes.
They looked at each patient’s clinical course before and after vaccination, their health trajectory and life expectancy at the time of vaccination, new symptoms following vaccination, and the time from vaccination to new symptoms and to death.
In addition, the investigators evaluated Clinical Frailty Scale (CFS) scores for each patient. CFS scores range from 1 (very fit) to 9 (terminally ill, with a life expectancy of less than 6 months who are otherwise evidently frail).
The initial investigation found that among 95 evaluable patients, the association between vaccination and death was “probable” in 10, “possible” in 26, and “unlikely” in 59.
The mean time from vaccination to symptoms was 1.4 days in the probable cases, 2.5 days in the possible cases, and 4.7 days in the unlikely cases.
The mean time from vaccination to death was 3.1, 8.3, and 8.2 days, respectively.
In all three categories, the patients had mean CFS scores ranging from 7.6 to 7.9, putting them in the “severely frail” category, defined as people who are completely dependent for personal care but seem stable and not at high risk for dying.
“We have quite many nursing home residents in Norway, 35,000; more than 80% have dementia, and the mean age is 85 years. We know that approximately 45 people die every day in these nursing homes, and their mean age of death is 87.5 years,” Dr. Ranhoff said.
Population-wide study
Dr. Ranhoff and colleagues also looked more broadly into the question of potential vaccine-related mortality in the total population of older people in Norway from the day of vaccination to follow-up at 3 weeks.
They conducted a matched cohort study to investigate the relationship between the mRNA SARS-CoV-2 vaccine and overall death among persons aged 65 and older in the general population, and across four groups: patients receiving home-based care, long-term nursing home patients, short-term nursing home patients, and those not receiving health services.
The researchers identified a total of 967,786 residents of Norway aged 65 and over at the start of the country’s vaccination campaign at the end of December, 2020, and they matched vaccinated individuals with unvaccinated persons based on demographic, geographic, and clinical risk group factors.
Dr. Ranhoff showed Kaplan-Meier survival curves for the total population and for each of the health-service states. In all cases there was a clear survival benefit for vaccinated vs. unvaccinated patients. She did not, however, provide specific numbers or hazard ratios for the differences between vaccinated and unvaccinated individuals in each of the comparisons.
The study was supported by the Norwegian Institute of Public Health. Dr. Ranhoff and Dr. Benetos reported no conflicts of interest.
and launched an investigation into the safety of the BNT162b2 vaccine (Comirnaty; Pfizer-BioNTech).
Now, the results of that investigation and of a subsequent larger study of nursing home residents in Norway have shown no increased risk for short-term mortality following COVID-19 vaccination in the overall population of elderly patients. The new research also showed clear evidence of a survival benefit compared with the unvaccinated population, Anette Hylen Ranhoff, MD, PhD, said at the annual meeting of the European Geriatric Medicine Society, held in a hybrid format in Athens, Greece, and online.
“We found no evidence of increased short-term mortality among vaccinated older individuals, and particularly not among the nursing home patients,” said Dr. Ranhoff, a senior researcher at the Norwegian Institute of Public Health and professor at University of Bergen, Norway. “But we think that this [lower] mortality risk was most likely a sort of ‘healthy-vaccinee’ effect, which means that people who were a bit more healthy were vaccinated, and not those who were the very, very most frail.”
“We have more or less the same data in France about events, with very high rates of vaccination,” said session moderator Athanase Benetos MD, PhD, professor and chairman of geriatric medicine at the University Hospital of Nancy in France, who was not involved in the study.
“In my department, a month after the end of the vaccination and at the same time while the pandemic in the city was going up, we had a 90% decrease in mortality from COVID in the nursing homes,” he told Dr. Ranhoff.
Potential risks
Frail elderly patients were not included in clinical trials of COVID-19 vaccines, and although previous studies have shown a low incidence of local or systemic reactions to vaccination among older people, “we think that quite mild adverse events following vaccination could trigger and destabilize a frail person,” Dr. Ranhoff said.
As reported Jan. 15, 2021, in BMJ, investigation by the Norwegian Medicines Agency (NOMA) into 13 of the 23 reported cases concluded that common adverse reactions associated with mRNA vaccines could have contributed to the deaths of some of the frail elderly patients
Steinar Madsen, MD, NOMA medical director, told BMJ “we are not alarmed or worried about this, because these are very rare occurrences and they occurred in very frail patients with very serious disease.”
Health authorities investigate
In response to the report and at the request of the Norwegian Public Health Institute and NOMA, Dr. Ranhoff and colleagues investigated the first 100 deaths among nursing-home residents who received the vaccine. The team consisted of three geriatricians and an infectious disease specialist who sees patients in nursing homes.
They looked at each patient’s clinical course before and after vaccination, their health trajectory and life expectancy at the time of vaccination, new symptoms following vaccination, and the time from vaccination to new symptoms and to death.
In addition, the investigators evaluated Clinical Frailty Scale (CFS) scores for each patient. CFS scores range from 1 (very fit) to 9 (terminally ill, with a life expectancy of less than 6 months who are otherwise evidently frail).
The initial investigation found that among 95 evaluable patients, the association between vaccination and death was “probable” in 10, “possible” in 26, and “unlikely” in 59.
The mean time from vaccination to symptoms was 1.4 days in the probable cases, 2.5 days in the possible cases, and 4.7 days in the unlikely cases.
The mean time from vaccination to death was 3.1, 8.3, and 8.2 days, respectively.
In all three categories, the patients had mean CFS scores ranging from 7.6 to 7.9, putting them in the “severely frail” category, defined as people who are completely dependent for personal care but seem stable and not at high risk for dying.
“We have quite many nursing home residents in Norway, 35,000; more than 80% have dementia, and the mean age is 85 years. We know that approximately 45 people die every day in these nursing homes, and their mean age of death is 87.5 years,” Dr. Ranhoff said.
Population-wide study
Dr. Ranhoff and colleagues also looked more broadly into the question of potential vaccine-related mortality in the total population of older people in Norway from the day of vaccination to follow-up at 3 weeks.
They conducted a matched cohort study to investigate the relationship between the mRNA SARS-CoV-2 vaccine and overall death among persons aged 65 and older in the general population, and across four groups: patients receiving home-based care, long-term nursing home patients, short-term nursing home patients, and those not receiving health services.
The researchers identified a total of 967,786 residents of Norway aged 65 and over at the start of the country’s vaccination campaign at the end of December, 2020, and they matched vaccinated individuals with unvaccinated persons based on demographic, geographic, and clinical risk group factors.
Dr. Ranhoff showed Kaplan-Meier survival curves for the total population and for each of the health-service states. In all cases there was a clear survival benefit for vaccinated vs. unvaccinated patients. She did not, however, provide specific numbers or hazard ratios for the differences between vaccinated and unvaccinated individuals in each of the comparisons.
The study was supported by the Norwegian Institute of Public Health. Dr. Ranhoff and Dr. Benetos reported no conflicts of interest.
FROM EUGMS 2021
Uncomplicated pediatric chest infection: Antibiotics don’t help
Unless pneumonia is suspected, clinicians should not prescribe antibiotics for most children with chest infections, according to findings of the ARTIC-PC randomized controlled trial, published in The Lancet.
“Prescribing for children with uncomplicated chest infections is still common in most countries,” said lead author Paul Little, MD, professor of primary care research at the University of Southampton, England, in an interview.
But there are barriers to stopping this practice, he said. “If you prescribe an antibiotic and the child gets better, even if the antibiotic was not doing that much, the parents then think that it was the antibiotic that was responsible for the recovery and so expect antibiotics the next time. So, physician prescribing of antibiotics in effect medicalizes illness and keeps the cycle of expectations, reconsultations, and prescriptions going.”
The study included 432 children aged 6 months to 12 years (median age, 3.2 years) who presented at 56 general practices in England with acute, uncomplicated lower respiratory tract infection (LRTI) of less than 21 days’ duration and in whom pneumonia was not suspected clinically. The children were randomly assigned to undergo 7 days of treatment with either amoxicillin 50 mg/kg or placebo. The primary outcome was duration of symptoms rated moderately bad or worse.
For up to 4 weeks, parents scored symptoms – including cough, phlegm, shortness of breath, wheeze, blocked or runny nose, disturbed sleep, feeling generally unwell, fever, and interference with normal activities – in a daily diary. The secondary outcome was symptom severity. Prespecified analyses were made for key clinical subgroups of patients for whom clinicians commonly prescribe (those with chest signs, fever, physician rating of unwell, sputum or chest rattle, and shortness of breath).
There was no significant difference in outcome between children treated with antibiotics and those treated with placebo. The median duration of moderately bad or worse symptoms was similar between the antibiotics group and the placebo group (5 vs. 6 days; hazard ratio, 1.13), as was the median time until symptoms were rated absent or as causing very little problem (7 vs. 8 days; HR, 1.09). There was a small significant difference between the groups in symptom severity score on days 2-4 after seeing the doctor (1.8 in the antibiotics group vs. 2.1 in the placebo group), “which was equivalent to less than one child in three rating symptoms a slight problem rather than very little problem,” the study authors report. “The treatment effects for all outcomes were similar for most subgroups ... but the effect of antibiotics was slightly, but not significantly, greater among those with fever or those who were unwell,” they add.
The investigators conclude that “similar to adults, antibiotics are unlikely to make a clinically important difference to the symptom burden for uncomplicated lower respiratory tract infections in children – both overall, and for the key clinical subgroups where antibiotic prescribing is most common.” They recommend that clinicians provide “safety-netting advice” to parents, such as explaining what illness course to expect and when a return visit would be necessary.
The findings provide “more evidence to do less,” wrote Rianne Oostenbrink, MD, PhD, from Erasmus MC-Sophia, in Rotterdam, the Netherlands, and Lina Jankauskaite, MD, PhD, from Lithuanian University of Health Sciences, Kaunas, in an accompanying comment.
“Overtesting and overtreatment of children are especially prominent in infectious diseases, when fever or other symptoms such as cough can be unspecific and can be of viral or bacterial origin,” they write.
The commenters note that despite antibiotics, most children did have moderately bad or worse symptoms on day 3, and symptoms had improved in about 75% of children in both groups at day 14. “A notable finding of this study is that only a few children had moderately bad or worse symptoms by day 14, and antibiotics did not alleviate the symptoms compared with placebo. Additionally, this trial aligns with other studies that have shown that reducing antibiotic treatment for LRTI is not associated with prolonged morbidity or higher incidence of complications.”
The study was funded by the UK National Institute for Health Research. Dr. Little, Dr. Jankauskaite, and Dr. Oostenbrink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unless pneumonia is suspected, clinicians should not prescribe antibiotics for most children with chest infections, according to findings of the ARTIC-PC randomized controlled trial, published in The Lancet.
“Prescribing for children with uncomplicated chest infections is still common in most countries,” said lead author Paul Little, MD, professor of primary care research at the University of Southampton, England, in an interview.
But there are barriers to stopping this practice, he said. “If you prescribe an antibiotic and the child gets better, even if the antibiotic was not doing that much, the parents then think that it was the antibiotic that was responsible for the recovery and so expect antibiotics the next time. So, physician prescribing of antibiotics in effect medicalizes illness and keeps the cycle of expectations, reconsultations, and prescriptions going.”
The study included 432 children aged 6 months to 12 years (median age, 3.2 years) who presented at 56 general practices in England with acute, uncomplicated lower respiratory tract infection (LRTI) of less than 21 days’ duration and in whom pneumonia was not suspected clinically. The children were randomly assigned to undergo 7 days of treatment with either amoxicillin 50 mg/kg or placebo. The primary outcome was duration of symptoms rated moderately bad or worse.
For up to 4 weeks, parents scored symptoms – including cough, phlegm, shortness of breath, wheeze, blocked or runny nose, disturbed sleep, feeling generally unwell, fever, and interference with normal activities – in a daily diary. The secondary outcome was symptom severity. Prespecified analyses were made for key clinical subgroups of patients for whom clinicians commonly prescribe (those with chest signs, fever, physician rating of unwell, sputum or chest rattle, and shortness of breath).
There was no significant difference in outcome between children treated with antibiotics and those treated with placebo. The median duration of moderately bad or worse symptoms was similar between the antibiotics group and the placebo group (5 vs. 6 days; hazard ratio, 1.13), as was the median time until symptoms were rated absent or as causing very little problem (7 vs. 8 days; HR, 1.09). There was a small significant difference between the groups in symptom severity score on days 2-4 after seeing the doctor (1.8 in the antibiotics group vs. 2.1 in the placebo group), “which was equivalent to less than one child in three rating symptoms a slight problem rather than very little problem,” the study authors report. “The treatment effects for all outcomes were similar for most subgroups ... but the effect of antibiotics was slightly, but not significantly, greater among those with fever or those who were unwell,” they add.
The investigators conclude that “similar to adults, antibiotics are unlikely to make a clinically important difference to the symptom burden for uncomplicated lower respiratory tract infections in children – both overall, and for the key clinical subgroups where antibiotic prescribing is most common.” They recommend that clinicians provide “safety-netting advice” to parents, such as explaining what illness course to expect and when a return visit would be necessary.
The findings provide “more evidence to do less,” wrote Rianne Oostenbrink, MD, PhD, from Erasmus MC-Sophia, in Rotterdam, the Netherlands, and Lina Jankauskaite, MD, PhD, from Lithuanian University of Health Sciences, Kaunas, in an accompanying comment.
“Overtesting and overtreatment of children are especially prominent in infectious diseases, when fever or other symptoms such as cough can be unspecific and can be of viral or bacterial origin,” they write.
The commenters note that despite antibiotics, most children did have moderately bad or worse symptoms on day 3, and symptoms had improved in about 75% of children in both groups at day 14. “A notable finding of this study is that only a few children had moderately bad or worse symptoms by day 14, and antibiotics did not alleviate the symptoms compared with placebo. Additionally, this trial aligns with other studies that have shown that reducing antibiotic treatment for LRTI is not associated with prolonged morbidity or higher incidence of complications.”
The study was funded by the UK National Institute for Health Research. Dr. Little, Dr. Jankauskaite, and Dr. Oostenbrink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Unless pneumonia is suspected, clinicians should not prescribe antibiotics for most children with chest infections, according to findings of the ARTIC-PC randomized controlled trial, published in The Lancet.
“Prescribing for children with uncomplicated chest infections is still common in most countries,” said lead author Paul Little, MD, professor of primary care research at the University of Southampton, England, in an interview.
But there are barriers to stopping this practice, he said. “If you prescribe an antibiotic and the child gets better, even if the antibiotic was not doing that much, the parents then think that it was the antibiotic that was responsible for the recovery and so expect antibiotics the next time. So, physician prescribing of antibiotics in effect medicalizes illness and keeps the cycle of expectations, reconsultations, and prescriptions going.”
The study included 432 children aged 6 months to 12 years (median age, 3.2 years) who presented at 56 general practices in England with acute, uncomplicated lower respiratory tract infection (LRTI) of less than 21 days’ duration and in whom pneumonia was not suspected clinically. The children were randomly assigned to undergo 7 days of treatment with either amoxicillin 50 mg/kg or placebo. The primary outcome was duration of symptoms rated moderately bad or worse.
For up to 4 weeks, parents scored symptoms – including cough, phlegm, shortness of breath, wheeze, blocked or runny nose, disturbed sleep, feeling generally unwell, fever, and interference with normal activities – in a daily diary. The secondary outcome was symptom severity. Prespecified analyses were made for key clinical subgroups of patients for whom clinicians commonly prescribe (those with chest signs, fever, physician rating of unwell, sputum or chest rattle, and shortness of breath).
There was no significant difference in outcome between children treated with antibiotics and those treated with placebo. The median duration of moderately bad or worse symptoms was similar between the antibiotics group and the placebo group (5 vs. 6 days; hazard ratio, 1.13), as was the median time until symptoms were rated absent or as causing very little problem (7 vs. 8 days; HR, 1.09). There was a small significant difference between the groups in symptom severity score on days 2-4 after seeing the doctor (1.8 in the antibiotics group vs. 2.1 in the placebo group), “which was equivalent to less than one child in three rating symptoms a slight problem rather than very little problem,” the study authors report. “The treatment effects for all outcomes were similar for most subgroups ... but the effect of antibiotics was slightly, but not significantly, greater among those with fever or those who were unwell,” they add.
The investigators conclude that “similar to adults, antibiotics are unlikely to make a clinically important difference to the symptom burden for uncomplicated lower respiratory tract infections in children – both overall, and for the key clinical subgroups where antibiotic prescribing is most common.” They recommend that clinicians provide “safety-netting advice” to parents, such as explaining what illness course to expect and when a return visit would be necessary.
The findings provide “more evidence to do less,” wrote Rianne Oostenbrink, MD, PhD, from Erasmus MC-Sophia, in Rotterdam, the Netherlands, and Lina Jankauskaite, MD, PhD, from Lithuanian University of Health Sciences, Kaunas, in an accompanying comment.
“Overtesting and overtreatment of children are especially prominent in infectious diseases, when fever or other symptoms such as cough can be unspecific and can be of viral or bacterial origin,” they write.
The commenters note that despite antibiotics, most children did have moderately bad or worse symptoms on day 3, and symptoms had improved in about 75% of children in both groups at day 14. “A notable finding of this study is that only a few children had moderately bad or worse symptoms by day 14, and antibiotics did not alleviate the symptoms compared with placebo. Additionally, this trial aligns with other studies that have shown that reducing antibiotic treatment for LRTI is not associated with prolonged morbidity or higher incidence of complications.”
The study was funded by the UK National Institute for Health Research. Dr. Little, Dr. Jankauskaite, and Dr. Oostenbrink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Omega-3s tame inflammation in elderly COVID-19 patients
results of a small randomized controlled trial suggest.
Results of the study, which included 22 patients with multiple comorbidities, were presented at the European Geriatric Medicine Society annual congress, a hybrid live and online meeting.
The patients, who had a median age of 81 years, were randomized to receive an intravenous infusion of an omega-3 polyunsaturated fatty acid (PUFA) emulsion containing 10 g of fish oil per 100 mL or a saline placebo.
Those who received the intravenous infusion had significant decreases from baseline to end of treatment in the neutrophil-to-lymphocyte ratio (NLR), indicating marked reductions in systemic inflammation.
In contrast, patients randomized to a saline placebo had no significant improvements in NLR, Magnus Bäck, MD, PhD, from the Karolinska Institute in Stockholm reported at the meeting.
“Our lipidomic analysis also showed that omega-3 treatment skewed the lipid response, with reduced levels of proinflammatory lipid mediators, and increased levels of proresolving mediators,” according to a late-breaking abstract, which Dr. Bäck presented during the session.
Omega-3 treatment was not significantly associated with reduction in either C-reactive protein (CRP) or the proinflammatory cytokine interleukin-6, however.
‘Eicosanoid storm’
In a review article published in January 2021 in the open-access journal Frontiers in Physiology, Dr. Bäck and colleagues outlined the rationale for their randomized trial.
“Excessive inflammation has been reported in severe cases with respiratory failure and cardiovascular complications,” they wrote. “In addition to the release of cytokines, referred to as cytokine release syndrome or ‘cytokine storm,’ increased proinflammatory lipid mediators derived from the omega-6 polyunsaturated fatty acid (PUFA) arachidonic acid may cause an ‘eicosanoid storm,’ which contributes to the uncontrolled systemic inflammation.”
Omega-3 PUFA contains proresolving mediators that can limit inflammatory reactions, suggesting the possibility of an inflammation-resolving benefit in patients with COVID-19 without concerns about immunosuppression, the authors hypothesized.
Trial details
In the trial, COVID-Omega-F, they enrolled patients with a COVID-19 diagnosis requiring hospitalization. Patients with an allergy to fish oil or who had contraindications to intravenous PUFA administration (for example, risk for bleeding, shock, or emboli) were excluded.
Ten patients were randomly assigned to receive infusions of the omega-3 PUFA and 12 were assigned to receive infusions of the placebo, once daily for 5 days. The primary outcome measure was change in inflammatory biomarkers, including white blood cell counts, CRP, cytokines, and lipid mediators.
Baseline demographic and clinical characteristics were similar between the two study arms, with a median of about 7 days since the onset of symptoms, and 3.5 days since a diagnosis of COVID-19.
All patients had low lymphocyte responses reflected by a high NLR, a prognostic measure for worse outcomes in patients with COVID-19 infections, Dr. Bäck said.
Inflammation was moderate, with a CRP of 65 mg/L in the placebo group and 62 mg/L in the omega-3 group.
Seven patients in each study arm received concomitant corticoid treatment. Two patients in each arm died in hospital, but there were no serious treatment-related adverse events.
Inflammatory markers improve
As noted before, there was a significant decline in NLR from baseline among patients randomized to omega-3 (P = .02) but no corresponding decrease in patients assigned to placebo infusions.
“The significant decrease was largely driven by an increase in the lymphocyte count in the omega-3 treated group (P = .004), whereas lymphocytes did not significantly change,” Dr. Bäck said.
As expected, patients in the omega-3 group had pronounced increases in omega-3 fatty acids, including eicosapentaenoic acid and docosahexaenoic acid.
The metabolism of fatty acids also differed markedly between the groups, with a significant decrease in the omega-3 group but not the placebo group in proinflammatory mediators, and an increase in precursors to proresolving mediators, Dr. Bäck noted.
AFib concerns
In a question-and-answer part of the session, a physician who identified herself as “Senya from Russia” questioned the safety of omega-3 treatment in this population, “because recently there was a meta-analysis which showed that omega-3 fatty acids will increase the risk of atrial fibrillation in older adults especially.”
The systematic review and meta-analysis she referred to, published in Circulation and reported on by this news organization, showed that, among 81,210 patients with a mean age of 65 enrolled in seven randomized controlled trials, omega-3 fatty acid supplementation was associated with a 25% increase in risk for atrial fibrillation. This risk appeared to be higher in trials testing doses greater than 1 g/day, according to the paper.
“This was not monitored in this study,” Dr. Bäck replied. “It is true that the meta-analysis showed an increased incidence of atrial fibrillation, so it would be something to monitor in case this trial would be expanded to a larger population.”
The study was supported by the Karolinska Institute. Dr. Bäck disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
results of a small randomized controlled trial suggest.
Results of the study, which included 22 patients with multiple comorbidities, were presented at the European Geriatric Medicine Society annual congress, a hybrid live and online meeting.
The patients, who had a median age of 81 years, were randomized to receive an intravenous infusion of an omega-3 polyunsaturated fatty acid (PUFA) emulsion containing 10 g of fish oil per 100 mL or a saline placebo.
Those who received the intravenous infusion had significant decreases from baseline to end of treatment in the neutrophil-to-lymphocyte ratio (NLR), indicating marked reductions in systemic inflammation.
In contrast, patients randomized to a saline placebo had no significant improvements in NLR, Magnus Bäck, MD, PhD, from the Karolinska Institute in Stockholm reported at the meeting.
“Our lipidomic analysis also showed that omega-3 treatment skewed the lipid response, with reduced levels of proinflammatory lipid mediators, and increased levels of proresolving mediators,” according to a late-breaking abstract, which Dr. Bäck presented during the session.
Omega-3 treatment was not significantly associated with reduction in either C-reactive protein (CRP) or the proinflammatory cytokine interleukin-6, however.
‘Eicosanoid storm’
In a review article published in January 2021 in the open-access journal Frontiers in Physiology, Dr. Bäck and colleagues outlined the rationale for their randomized trial.
“Excessive inflammation has been reported in severe cases with respiratory failure and cardiovascular complications,” they wrote. “In addition to the release of cytokines, referred to as cytokine release syndrome or ‘cytokine storm,’ increased proinflammatory lipid mediators derived from the omega-6 polyunsaturated fatty acid (PUFA) arachidonic acid may cause an ‘eicosanoid storm,’ which contributes to the uncontrolled systemic inflammation.”
Omega-3 PUFA contains proresolving mediators that can limit inflammatory reactions, suggesting the possibility of an inflammation-resolving benefit in patients with COVID-19 without concerns about immunosuppression, the authors hypothesized.
Trial details
In the trial, COVID-Omega-F, they enrolled patients with a COVID-19 diagnosis requiring hospitalization. Patients with an allergy to fish oil or who had contraindications to intravenous PUFA administration (for example, risk for bleeding, shock, or emboli) were excluded.
Ten patients were randomly assigned to receive infusions of the omega-3 PUFA and 12 were assigned to receive infusions of the placebo, once daily for 5 days. The primary outcome measure was change in inflammatory biomarkers, including white blood cell counts, CRP, cytokines, and lipid mediators.
Baseline demographic and clinical characteristics were similar between the two study arms, with a median of about 7 days since the onset of symptoms, and 3.5 days since a diagnosis of COVID-19.
All patients had low lymphocyte responses reflected by a high NLR, a prognostic measure for worse outcomes in patients with COVID-19 infections, Dr. Bäck said.
Inflammation was moderate, with a CRP of 65 mg/L in the placebo group and 62 mg/L in the omega-3 group.
Seven patients in each study arm received concomitant corticoid treatment. Two patients in each arm died in hospital, but there were no serious treatment-related adverse events.
Inflammatory markers improve
As noted before, there was a significant decline in NLR from baseline among patients randomized to omega-3 (P = .02) but no corresponding decrease in patients assigned to placebo infusions.
“The significant decrease was largely driven by an increase in the lymphocyte count in the omega-3 treated group (P = .004), whereas lymphocytes did not significantly change,” Dr. Bäck said.
As expected, patients in the omega-3 group had pronounced increases in omega-3 fatty acids, including eicosapentaenoic acid and docosahexaenoic acid.
The metabolism of fatty acids also differed markedly between the groups, with a significant decrease in the omega-3 group but not the placebo group in proinflammatory mediators, and an increase in precursors to proresolving mediators, Dr. Bäck noted.
AFib concerns
In a question-and-answer part of the session, a physician who identified herself as “Senya from Russia” questioned the safety of omega-3 treatment in this population, “because recently there was a meta-analysis which showed that omega-3 fatty acids will increase the risk of atrial fibrillation in older adults especially.”
The systematic review and meta-analysis she referred to, published in Circulation and reported on by this news organization, showed that, among 81,210 patients with a mean age of 65 enrolled in seven randomized controlled trials, omega-3 fatty acid supplementation was associated with a 25% increase in risk for atrial fibrillation. This risk appeared to be higher in trials testing doses greater than 1 g/day, according to the paper.
“This was not monitored in this study,” Dr. Bäck replied. “It is true that the meta-analysis showed an increased incidence of atrial fibrillation, so it would be something to monitor in case this trial would be expanded to a larger population.”
The study was supported by the Karolinska Institute. Dr. Bäck disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
results of a small randomized controlled trial suggest.
Results of the study, which included 22 patients with multiple comorbidities, were presented at the European Geriatric Medicine Society annual congress, a hybrid live and online meeting.
The patients, who had a median age of 81 years, were randomized to receive an intravenous infusion of an omega-3 polyunsaturated fatty acid (PUFA) emulsion containing 10 g of fish oil per 100 mL or a saline placebo.
Those who received the intravenous infusion had significant decreases from baseline to end of treatment in the neutrophil-to-lymphocyte ratio (NLR), indicating marked reductions in systemic inflammation.
In contrast, patients randomized to a saline placebo had no significant improvements in NLR, Magnus Bäck, MD, PhD, from the Karolinska Institute in Stockholm reported at the meeting.
“Our lipidomic analysis also showed that omega-3 treatment skewed the lipid response, with reduced levels of proinflammatory lipid mediators, and increased levels of proresolving mediators,” according to a late-breaking abstract, which Dr. Bäck presented during the session.
Omega-3 treatment was not significantly associated with reduction in either C-reactive protein (CRP) or the proinflammatory cytokine interleukin-6, however.
‘Eicosanoid storm’
In a review article published in January 2021 in the open-access journal Frontiers in Physiology, Dr. Bäck and colleagues outlined the rationale for their randomized trial.
“Excessive inflammation has been reported in severe cases with respiratory failure and cardiovascular complications,” they wrote. “In addition to the release of cytokines, referred to as cytokine release syndrome or ‘cytokine storm,’ increased proinflammatory lipid mediators derived from the omega-6 polyunsaturated fatty acid (PUFA) arachidonic acid may cause an ‘eicosanoid storm,’ which contributes to the uncontrolled systemic inflammation.”
Omega-3 PUFA contains proresolving mediators that can limit inflammatory reactions, suggesting the possibility of an inflammation-resolving benefit in patients with COVID-19 without concerns about immunosuppression, the authors hypothesized.
Trial details
In the trial, COVID-Omega-F, they enrolled patients with a COVID-19 diagnosis requiring hospitalization. Patients with an allergy to fish oil or who had contraindications to intravenous PUFA administration (for example, risk for bleeding, shock, or emboli) were excluded.
Ten patients were randomly assigned to receive infusions of the omega-3 PUFA and 12 were assigned to receive infusions of the placebo, once daily for 5 days. The primary outcome measure was change in inflammatory biomarkers, including white blood cell counts, CRP, cytokines, and lipid mediators.
Baseline demographic and clinical characteristics were similar between the two study arms, with a median of about 7 days since the onset of symptoms, and 3.5 days since a diagnosis of COVID-19.
All patients had low lymphocyte responses reflected by a high NLR, a prognostic measure for worse outcomes in patients with COVID-19 infections, Dr. Bäck said.
Inflammation was moderate, with a CRP of 65 mg/L in the placebo group and 62 mg/L in the omega-3 group.
Seven patients in each study arm received concomitant corticoid treatment. Two patients in each arm died in hospital, but there were no serious treatment-related adverse events.
Inflammatory markers improve
As noted before, there was a significant decline in NLR from baseline among patients randomized to omega-3 (P = .02) but no corresponding decrease in patients assigned to placebo infusions.
“The significant decrease was largely driven by an increase in the lymphocyte count in the omega-3 treated group (P = .004), whereas lymphocytes did not significantly change,” Dr. Bäck said.
As expected, patients in the omega-3 group had pronounced increases in omega-3 fatty acids, including eicosapentaenoic acid and docosahexaenoic acid.
The metabolism of fatty acids also differed markedly between the groups, with a significant decrease in the omega-3 group but not the placebo group in proinflammatory mediators, and an increase in precursors to proresolving mediators, Dr. Bäck noted.
AFib concerns
In a question-and-answer part of the session, a physician who identified herself as “Senya from Russia” questioned the safety of omega-3 treatment in this population, “because recently there was a meta-analysis which showed that omega-3 fatty acids will increase the risk of atrial fibrillation in older adults especially.”
The systematic review and meta-analysis she referred to, published in Circulation and reported on by this news organization, showed that, among 81,210 patients with a mean age of 65 enrolled in seven randomized controlled trials, omega-3 fatty acid supplementation was associated with a 25% increase in risk for atrial fibrillation. This risk appeared to be higher in trials testing doses greater than 1 g/day, according to the paper.
“This was not monitored in this study,” Dr. Bäck replied. “It is true that the meta-analysis showed an increased incidence of atrial fibrillation, so it would be something to monitor in case this trial would be expanded to a larger population.”
The study was supported by the Karolinska Institute. Dr. Bäck disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EUGMS
Children and COVID-19: U.S. adds latest million cases in record time
The United States just passed the 6-million mark in COVID-19 cases among children, with the last million cases taking less time to record than any of the first five, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
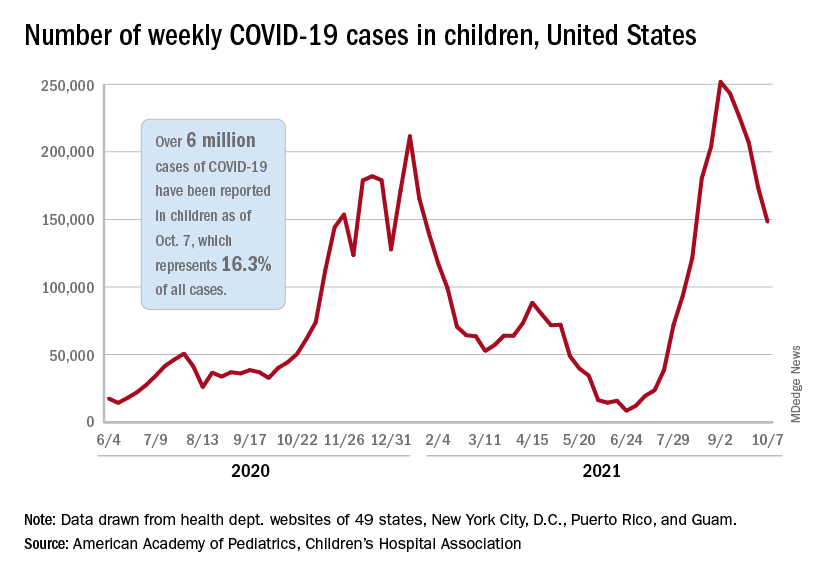
The five-millionth case was reported during the week of Aug. 27 to Sept. 2, and case number 6 million came during the week of Oct. 1-7, just 5 weeks later, compared with the 6 weeks it took to go from 1 million to 2 million last November and December, the AAP and CHA said in their weekly COVID-19 report.
New cases continued to drop, however, and that weekly count was down by 14.6% from the previous week and by 41.1% from the peak of almost 252,000 reached in early September, the two groups said while also noting limitations to the data, such as three states (Alabama, Nebraska, and Texas) that are no longer updating their COVID-19 dashboards.
Other metrics show similar drops in recent weeks. Among children aged 0-11 years, emergency department visits involving a COVID-19 diagnosis dropped from 4.1% of all ED visits in late August to 1.4% of ED visits on Oct. 6. ED visits with a COVID-19 diagnosis fell from a peak of 8.5% on Aug. 22 to 1.5% on Oct. 6 for 12- to 15-year-olds and from 8.5% to 1.5% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
The rate of new hospital admissions for children aged 0-17 years was down to 0.26 per 100,000 population on Oct. 9 after reaching 0.51 per 100,000 on Sept. 4. Hospitalizations in children totaled just over 64,000 from Aug. 1, 2020, to Oct. 9, 2021, which is just over 2% of all COVID-19–related admissions over that time period, the CDC said on its COVID Data Tracker.
That pattern, unfortunately, also applies to vaccinations. “The number of children receiving their first COVID-19 vaccine this week [Sept. 30 to Oct. 6], about 156,000, was the lowest number since vaccines were available,” the AAP said in a separate report on vaccination trends, adding that “the number of children receiving their first dose has steadily declined from 8 weeks ago when 586,000 children received their initial dose the week ending Aug. 11.”
The United States just passed the 6-million mark in COVID-19 cases among children, with the last million cases taking less time to record than any of the first five, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
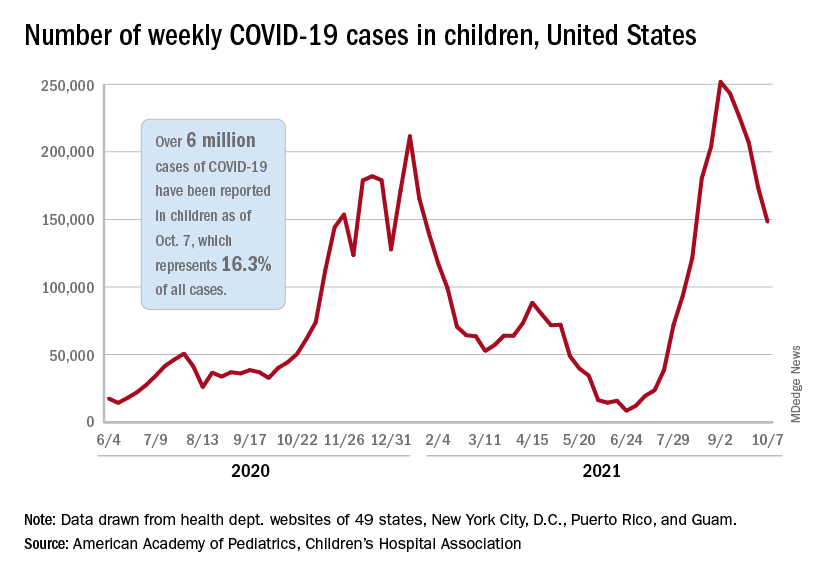
The five-millionth case was reported during the week of Aug. 27 to Sept. 2, and case number 6 million came during the week of Oct. 1-7, just 5 weeks later, compared with the 6 weeks it took to go from 1 million to 2 million last November and December, the AAP and CHA said in their weekly COVID-19 report.
New cases continued to drop, however, and that weekly count was down by 14.6% from the previous week and by 41.1% from the peak of almost 252,000 reached in early September, the two groups said while also noting limitations to the data, such as three states (Alabama, Nebraska, and Texas) that are no longer updating their COVID-19 dashboards.
Other metrics show similar drops in recent weeks. Among children aged 0-11 years, emergency department visits involving a COVID-19 diagnosis dropped from 4.1% of all ED visits in late August to 1.4% of ED visits on Oct. 6. ED visits with a COVID-19 diagnosis fell from a peak of 8.5% on Aug. 22 to 1.5% on Oct. 6 for 12- to 15-year-olds and from 8.5% to 1.5% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
The rate of new hospital admissions for children aged 0-17 years was down to 0.26 per 100,000 population on Oct. 9 after reaching 0.51 per 100,000 on Sept. 4. Hospitalizations in children totaled just over 64,000 from Aug. 1, 2020, to Oct. 9, 2021, which is just over 2% of all COVID-19–related admissions over that time period, the CDC said on its COVID Data Tracker.
That pattern, unfortunately, also applies to vaccinations. “The number of children receiving their first COVID-19 vaccine this week [Sept. 30 to Oct. 6], about 156,000, was the lowest number since vaccines were available,” the AAP said in a separate report on vaccination trends, adding that “the number of children receiving their first dose has steadily declined from 8 weeks ago when 586,000 children received their initial dose the week ending Aug. 11.”
The United States just passed the 6-million mark in COVID-19 cases among children, with the last million cases taking less time to record than any of the first five, according to new data from the American Academy of Pediatrics and the Children’s Hospital Association.
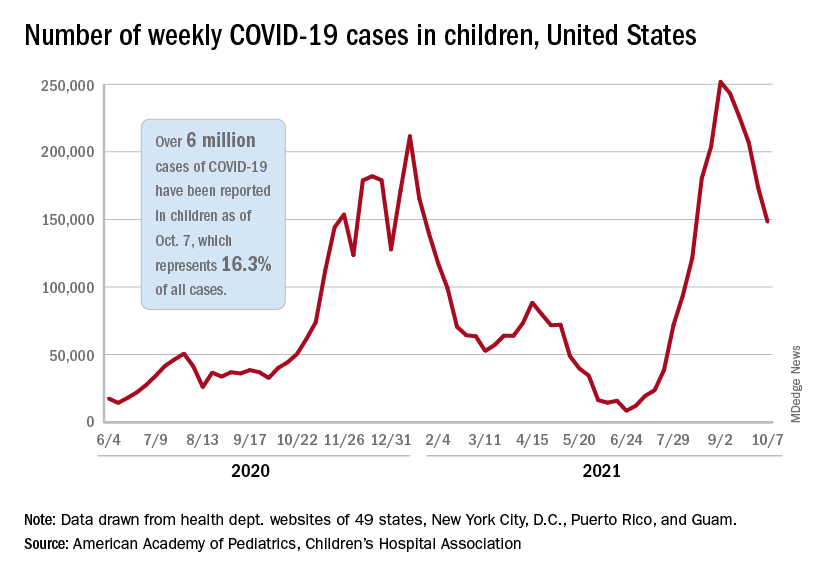
The five-millionth case was reported during the week of Aug. 27 to Sept. 2, and case number 6 million came during the week of Oct. 1-7, just 5 weeks later, compared with the 6 weeks it took to go from 1 million to 2 million last November and December, the AAP and CHA said in their weekly COVID-19 report.
New cases continued to drop, however, and that weekly count was down by 14.6% from the previous week and by 41.1% from the peak of almost 252,000 reached in early September, the two groups said while also noting limitations to the data, such as three states (Alabama, Nebraska, and Texas) that are no longer updating their COVID-19 dashboards.
Other metrics show similar drops in recent weeks. Among children aged 0-11 years, emergency department visits involving a COVID-19 diagnosis dropped from 4.1% of all ED visits in late August to 1.4% of ED visits on Oct. 6. ED visits with a COVID-19 diagnosis fell from a peak of 8.5% on Aug. 22 to 1.5% on Oct. 6 for 12- to 15-year-olds and from 8.5% to 1.5% in those aged 16-17 years, according to data from the Centers for Disease Control and Prevention.
The rate of new hospital admissions for children aged 0-17 years was down to 0.26 per 100,000 population on Oct. 9 after reaching 0.51 per 100,000 on Sept. 4. Hospitalizations in children totaled just over 64,000 from Aug. 1, 2020, to Oct. 9, 2021, which is just over 2% of all COVID-19–related admissions over that time period, the CDC said on its COVID Data Tracker.
That pattern, unfortunately, also applies to vaccinations. “The number of children receiving their first COVID-19 vaccine this week [Sept. 30 to Oct. 6], about 156,000, was the lowest number since vaccines were available,” the AAP said in a separate report on vaccination trends, adding that “the number of children receiving their first dose has steadily declined from 8 weeks ago when 586,000 children received their initial dose the week ending Aug. 11.”
Mineral Oil Scabies Preparation From Under the Fingernail
Practice Gap
The Sarcoptes scabiei mite is a microscopic organism that causes scabies in the human host. The scabies mite is highly transmissible, making scabies a common disease in heavily populated areas. The mite survives by burrowing into the epidermis, where it feeds, lays eggs, and defecates.1
The rash in the host represents an allergic reaction to the body of the scabies mite, producing symptoms such as intense itching, rash, and erosions of the skin. The scabies rash tends to occur in warm and occluded areas of the body such as the hands, axillae, groin, buttocks, and feet.1,2
Delaying treatment of scabies can be hazardous because of the risk of rapid spread from one person to another. This rapid spread can be debilitating in specific populations, such as the immunocompromised, elderly, and disabled.
Mineral oil preparation is the classic method used to identify scabies (Figure 1). This method relies on obtaining mites by applying mineral oil to the skin and using a 15-mm blade to scrape off layers of the affected skin. The scraped material is spread onto a microscope slide with mineral oil, a coverslip is applied, and the specimen is analyzed by direct microscopy. This method proves only as effective as knowing where the few mites are located.

At any time, only 10 to 12 mites live on a human host.3 Therefore, it can be challenging to obtain a mite for diagnosis because the location of the skin mites may be unknown. Dermoscopy can be used to locate burrows and other signs of S scabiei. With a dermatoscope, the scabies mite can be identified by the so-called delta-wing jet sign.4
However, dermoscopy is not always successful because extensive hemorrhagic crusting and erosions of the skin secondary to constant scratching can obscure the appearance of burrows and mites. Because patients are constantly scratching areas of irritation, it is possible that S scabiei can be located under the fingernail of the dominant hand.
The Technique
To address this practice gap, a mineral oil scabies preparation can be performed by scraping under the fingernail plate at the level of the hyponychium. Mites might accumulate underneath the fingernails of the dominant hand when patients scratch the area of the skin where S scabiei mites are burrowing and reproducing.
A convenient and painless way to obtain a mineral oil scabies preparation from under the fingernail is to use the tip of a disposable hyfrecator, readily available in most dermatology practices for use in electrosurgery (Figure 2). Using the blunt end of the hyfrecator tip for the mineral oil preparation would be done without attachment to the full apparatus.
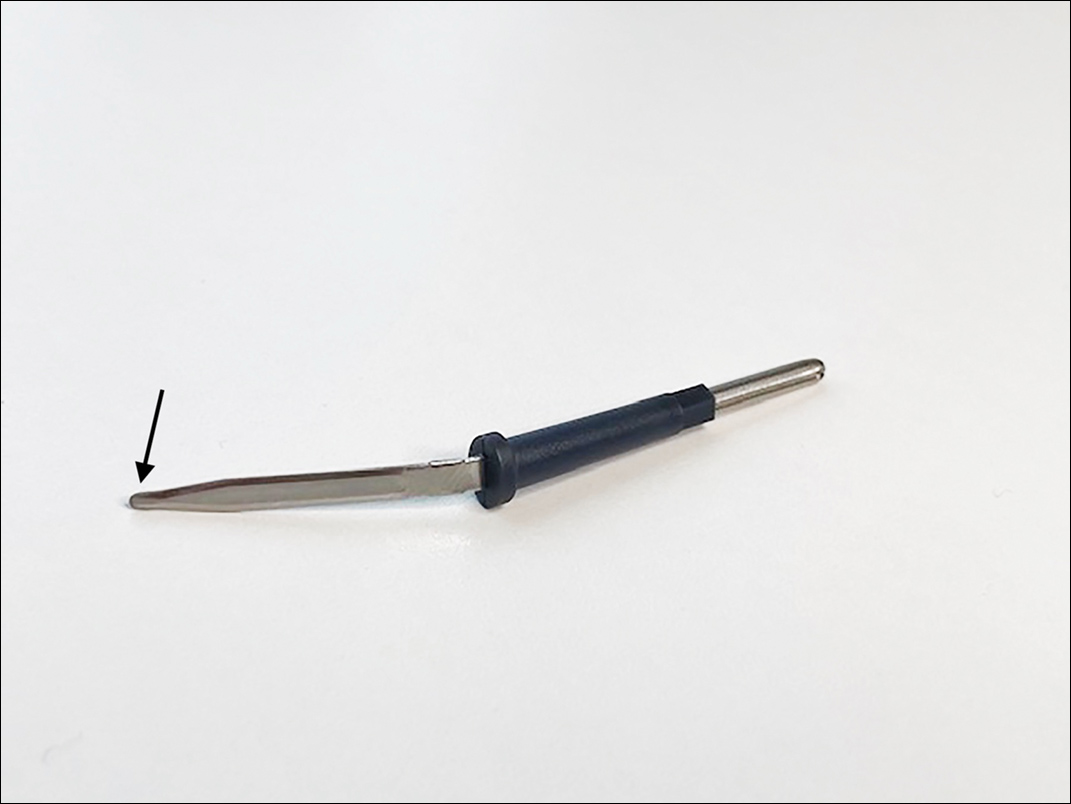
The hyponychium of the fingernail is prepared with mineral oil, which aids in collecting and suspending the material obtained from under the nail plate. Using the blunt end of the hyfrecator tip, material from underneath the fingernail is removed using a gentle sweeping motion (Figure 3). The specimen is then analyzed under the microscope similar to a routine mineral oil scabies preparation. This method can be utilized by health care providers for easy and painless diagnosis of scabies.

Practice Implications
Use of a blunt hyfrecator tip to extract S scabiei from underneath the fingernail plate can be used for efficient diagnosis of scabies. This technique can be implemented in any clinic where blunt-tip hyfrecator electrodes are available. Using a gentle sweeping motion, the blunt-tip hyfrecator allows the provider to extract material from under the fingernail for diagnosis. The material obtained is used to prepare a mineral oil scabies preparation for direct microscopic analysis.
This technique can diagnose scabies efficiently, and treatment can be initiated promptly. Use of a disposable blunt-tip hyfrecator for scabies extraction is a novel technique that can be added to the armamentarium of tools to diagnose scabies, which includes traditional mineral oil preparation and dermoscopy.
- Banerji A; Canadian Paediatric Society, First Nations, Inuit and Métis Health Committee. Scabies. Paediatr Child Health. 2015;20:395-402. doi:10.1093/pch/20.7.395
- Johnston G, Sladden M. Scabies: diagnosis and treatment. BMJ. 2005;331:619-622. doi:10.1136/bmj.331.7517.619
- Mellanby K. The development of symptoms, parasitic infection and immunity in human scabies. Parasitology. 1944;35:197-206. doi:10.1017/S0031182000021612
- Fox G. Diagnosis of scabies by dermoscopy [published online February 2, 2009]. BMJ Case Rep. 2009;2009:bcr06.2008.0279. doi:10.1136/bcr.06.2008.0279
Practice Gap
The Sarcoptes scabiei mite is a microscopic organism that causes scabies in the human host. The scabies mite is highly transmissible, making scabies a common disease in heavily populated areas. The mite survives by burrowing into the epidermis, where it feeds, lays eggs, and defecates.1
The rash in the host represents an allergic reaction to the body of the scabies mite, producing symptoms such as intense itching, rash, and erosions of the skin. The scabies rash tends to occur in warm and occluded areas of the body such as the hands, axillae, groin, buttocks, and feet.1,2
Delaying treatment of scabies can be hazardous because of the risk of rapid spread from one person to another. This rapid spread can be debilitating in specific populations, such as the immunocompromised, elderly, and disabled.
Mineral oil preparation is the classic method used to identify scabies (Figure 1). This method relies on obtaining mites by applying mineral oil to the skin and using a 15-mm blade to scrape off layers of the affected skin. The scraped material is spread onto a microscope slide with mineral oil, a coverslip is applied, and the specimen is analyzed by direct microscopy. This method proves only as effective as knowing where the few mites are located.

At any time, only 10 to 12 mites live on a human host.3 Therefore, it can be challenging to obtain a mite for diagnosis because the location of the skin mites may be unknown. Dermoscopy can be used to locate burrows and other signs of S scabiei. With a dermatoscope, the scabies mite can be identified by the so-called delta-wing jet sign.4
However, dermoscopy is not always successful because extensive hemorrhagic crusting and erosions of the skin secondary to constant scratching can obscure the appearance of burrows and mites. Because patients are constantly scratching areas of irritation, it is possible that S scabiei can be located under the fingernail of the dominant hand.
The Technique
To address this practice gap, a mineral oil scabies preparation can be performed by scraping under the fingernail plate at the level of the hyponychium. Mites might accumulate underneath the fingernails of the dominant hand when patients scratch the area of the skin where S scabiei mites are burrowing and reproducing.
A convenient and painless way to obtain a mineral oil scabies preparation from under the fingernail is to use the tip of a disposable hyfrecator, readily available in most dermatology practices for use in electrosurgery (Figure 2). Using the blunt end of the hyfrecator tip for the mineral oil preparation would be done without attachment to the full apparatus.
The hyponychium of the fingernail is prepared with mineral oil, which aids in collecting and suspending the material obtained from under the nail plate. Using the blunt end of the hyfrecator tip, material from underneath the fingernail is removed using a gentle sweeping motion (Figure 3). The specimen is then analyzed under the microscope similar to a routine mineral oil scabies preparation. This method can be utilized by health care providers for easy and painless diagnosis of scabies.

Practice Implications
Use of a blunt hyfrecator tip to extract S scabiei from underneath the fingernail plate can be used for efficient diagnosis of scabies. This technique can be implemented in any clinic where blunt-tip hyfrecator electrodes are available. Using a gentle sweeping motion, the blunt-tip hyfrecator allows the provider to extract material from under the fingernail for diagnosis. The material obtained is used to prepare a mineral oil scabies preparation for direct microscopic analysis.
This technique can diagnose scabies efficiently, and treatment can be initiated promptly. Use of a disposable blunt-tip hyfrecator for scabies extraction is a novel technique that can be added to the armamentarium of tools to diagnose scabies, which includes traditional mineral oil preparation and dermoscopy.
Practice Gap
The Sarcoptes scabiei mite is a microscopic organism that causes scabies in the human host. The scabies mite is highly transmissible, making scabies a common disease in heavily populated areas. The mite survives by burrowing into the epidermis, where it feeds, lays eggs, and defecates.1
The rash in the host represents an allergic reaction to the body of the scabies mite, producing symptoms such as intense itching, rash, and erosions of the skin. The scabies rash tends to occur in warm and occluded areas of the body such as the hands, axillae, groin, buttocks, and feet.1,2
Delaying treatment of scabies can be hazardous because of the risk of rapid spread from one person to another. This rapid spread can be debilitating in specific populations, such as the immunocompromised, elderly, and disabled.
Mineral oil preparation is the classic method used to identify scabies (Figure 1). This method relies on obtaining mites by applying mineral oil to the skin and using a 15-mm blade to scrape off layers of the affected skin. The scraped material is spread onto a microscope slide with mineral oil, a coverslip is applied, and the specimen is analyzed by direct microscopy. This method proves only as effective as knowing where the few mites are located.

At any time, only 10 to 12 mites live on a human host.3 Therefore, it can be challenging to obtain a mite for diagnosis because the location of the skin mites may be unknown. Dermoscopy can be used to locate burrows and other signs of S scabiei. With a dermatoscope, the scabies mite can be identified by the so-called delta-wing jet sign.4
However, dermoscopy is not always successful because extensive hemorrhagic crusting and erosions of the skin secondary to constant scratching can obscure the appearance of burrows and mites. Because patients are constantly scratching areas of irritation, it is possible that S scabiei can be located under the fingernail of the dominant hand.
The Technique
To address this practice gap, a mineral oil scabies preparation can be performed by scraping under the fingernail plate at the level of the hyponychium. Mites might accumulate underneath the fingernails of the dominant hand when patients scratch the area of the skin where S scabiei mites are burrowing and reproducing.
A convenient and painless way to obtain a mineral oil scabies preparation from under the fingernail is to use the tip of a disposable hyfrecator, readily available in most dermatology practices for use in electrosurgery (Figure 2). Using the blunt end of the hyfrecator tip for the mineral oil preparation would be done without attachment to the full apparatus.
The hyponychium of the fingernail is prepared with mineral oil, which aids in collecting and suspending the material obtained from under the nail plate. Using the blunt end of the hyfrecator tip, material from underneath the fingernail is removed using a gentle sweeping motion (Figure 3). The specimen is then analyzed under the microscope similar to a routine mineral oil scabies preparation. This method can be utilized by health care providers for easy and painless diagnosis of scabies.

Practice Implications
Use of a blunt hyfrecator tip to extract S scabiei from underneath the fingernail plate can be used for efficient diagnosis of scabies. This technique can be implemented in any clinic where blunt-tip hyfrecator electrodes are available. Using a gentle sweeping motion, the blunt-tip hyfrecator allows the provider to extract material from under the fingernail for diagnosis. The material obtained is used to prepare a mineral oil scabies preparation for direct microscopic analysis.
This technique can diagnose scabies efficiently, and treatment can be initiated promptly. Use of a disposable blunt-tip hyfrecator for scabies extraction is a novel technique that can be added to the armamentarium of tools to diagnose scabies, which includes traditional mineral oil preparation and dermoscopy.
- Banerji A; Canadian Paediatric Society, First Nations, Inuit and Métis Health Committee. Scabies. Paediatr Child Health. 2015;20:395-402. doi:10.1093/pch/20.7.395
- Johnston G, Sladden M. Scabies: diagnosis and treatment. BMJ. 2005;331:619-622. doi:10.1136/bmj.331.7517.619
- Mellanby K. The development of symptoms, parasitic infection and immunity in human scabies. Parasitology. 1944;35:197-206. doi:10.1017/S0031182000021612
- Fox G. Diagnosis of scabies by dermoscopy [published online February 2, 2009]. BMJ Case Rep. 2009;2009:bcr06.2008.0279. doi:10.1136/bcr.06.2008.0279
- Banerji A; Canadian Paediatric Society, First Nations, Inuit and Métis Health Committee. Scabies. Paediatr Child Health. 2015;20:395-402. doi:10.1093/pch/20.7.395
- Johnston G, Sladden M. Scabies: diagnosis and treatment. BMJ. 2005;331:619-622. doi:10.1136/bmj.331.7517.619
- Mellanby K. The development of symptoms, parasitic infection and immunity in human scabies. Parasitology. 1944;35:197-206. doi:10.1017/S0031182000021612
- Fox G. Diagnosis of scabies by dermoscopy [published online February 2, 2009]. BMJ Case Rep. 2009;2009:bcr06.2008.0279. doi:10.1136/bcr.06.2008.0279
