User login
Yellow Nodule on the Scalp
The Diagnosis: Solitary Sclerotic Fibroma
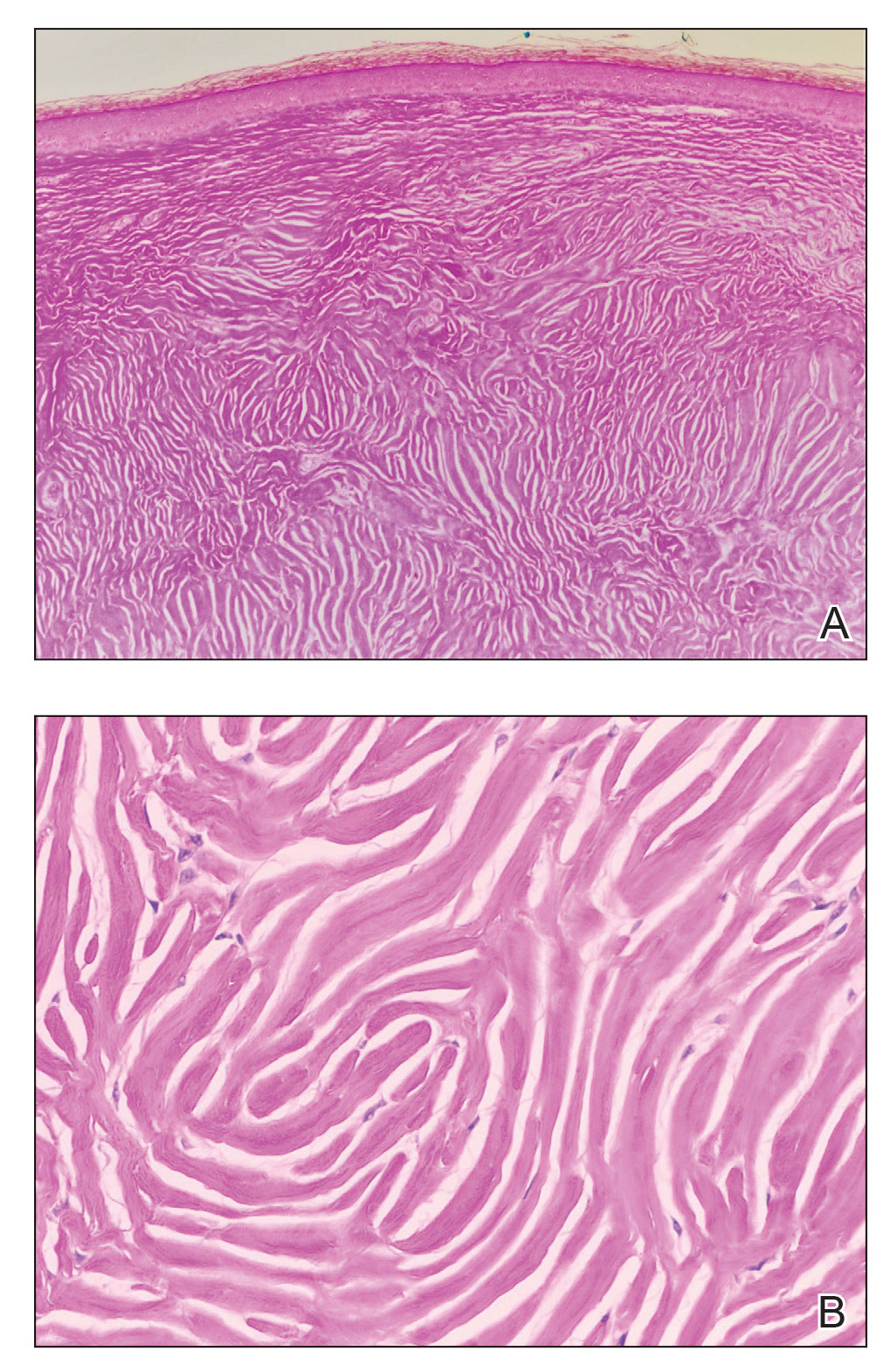
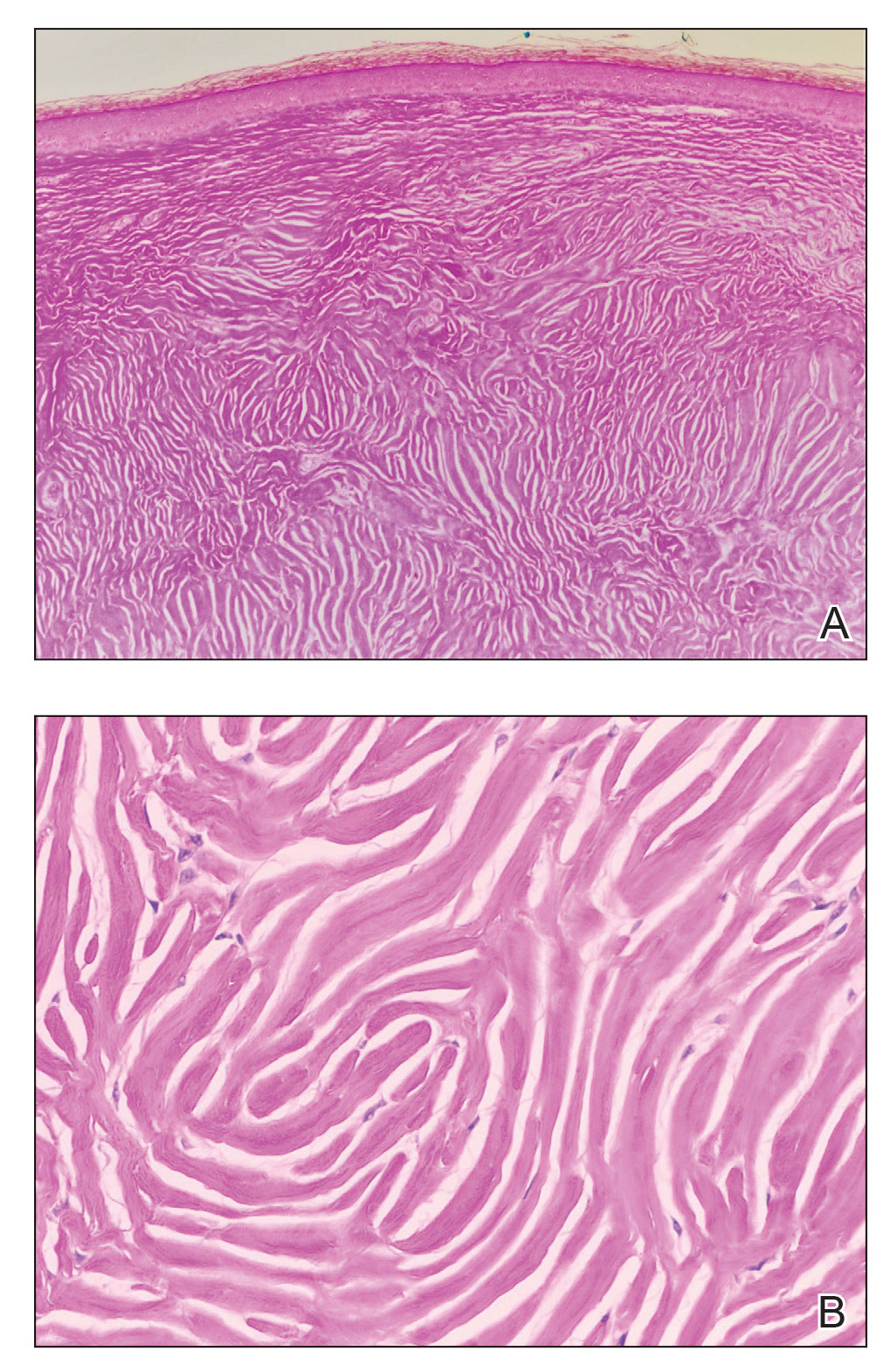
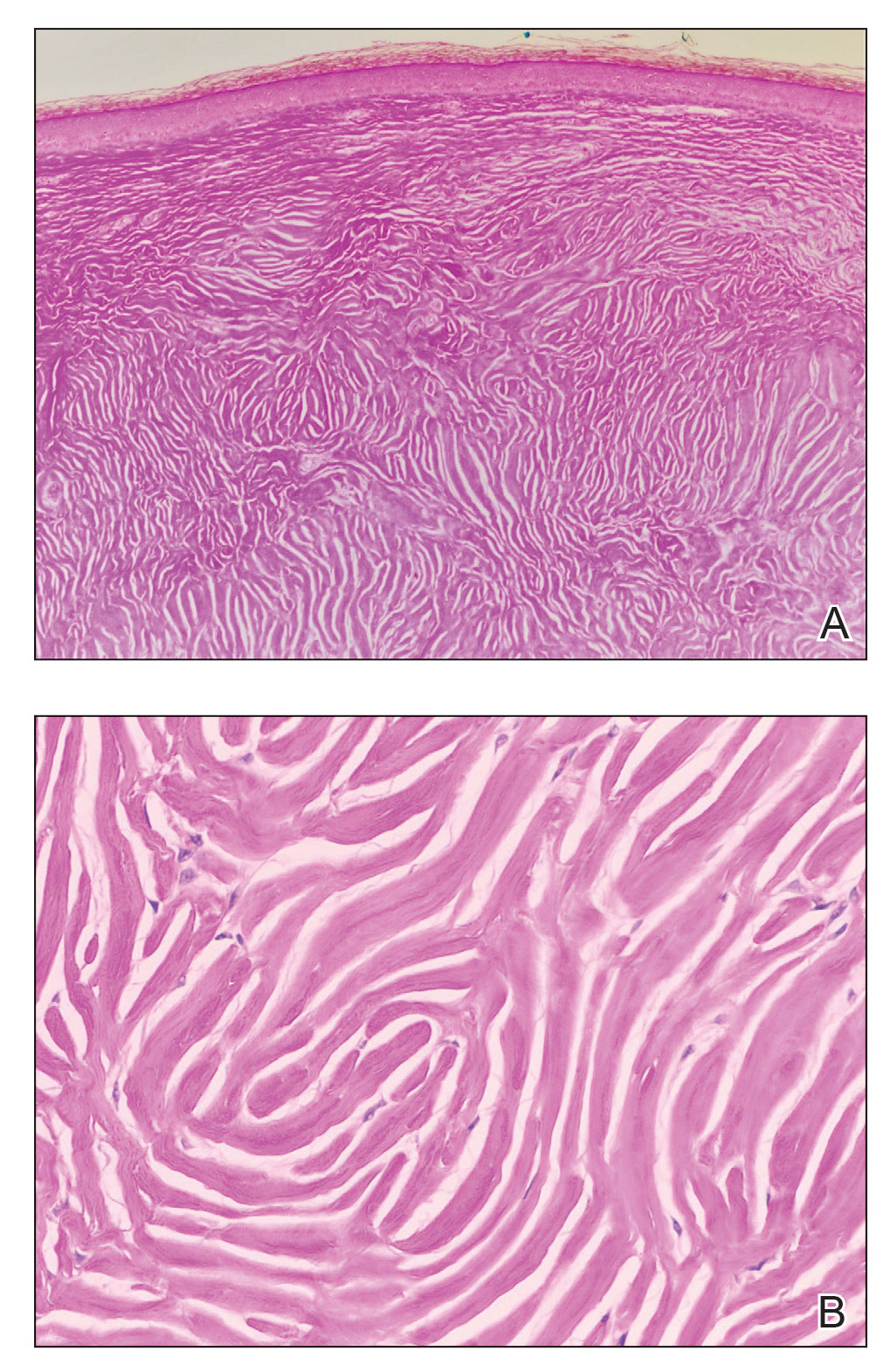
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
The Diagnosis: Solitary Sclerotic Fibroma
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
The Diagnosis: Solitary Sclerotic Fibroma
Based on the clinical and histologic findings, the patient was diagnosed with solitary sclerotic fibroma (SF). Sclerotic fibroma is a rare benign tumor that first was described in 1972 by Weary et al1 in the oral mucosa of a patient with Cowden syndrome, a genodermatosis associated with multiple benign and malignant tumors. Rapini and Golitz2 reported solitary SF in 11 otherwise-healthy individuals with no signs of multiple hamartoma syndrome. Solitary SF is a sporadic benign condition, whereas multiple lesions are suggestive of Cowden syndrome. Solitary SF most commonly appears as an asymptomatic white-yellow papule or nodule on the head or neck, though larger tumors have been reported on the trunk and extremities.3 Histologic features of solitary SF include a well-circumscribed dermal nodule composed of eosinophilic dense collagen bundles arranged in a plywoodlike pattern (Figure). Immunohistochemistry is positive for CD34 and vimentin but negative for S-100, epithelial membrane antigen, and neuron-specific enolase.4
The differential diagnosis of solitary SF of the head and neck includes sebaceous adenoma, pilar cyst, nodular basal cell carcinoma, and giant molluscum contagiosum. Sebaceous adenomas usually are solitary yellow nodules less than 1 cm in diameter and located on the head and neck. They are the most common sebaceous neoplasm associated with Muir-Torre syndrome, an autosomal-dominant disorder characterized by sebaceous adenoma or carcinoma and colorectal cancer. Histopathology demonstrates well-circumscribed, round aggregations of mature lipid-filled sebocytes with a rim of basaloid germinative cells at the periphery. Pilar cysts typically are flesh-colored subcutaneous nodules on the scalp that are freely mobile over underlying tissue. Histopathology shows stratified squamous epithelium lining and trichilemmal keratinization. Nodular basal cell carcinoma has a pearly translucent appearance and arborizing telangiectases. Histopathology demonstrates nests of basaloid cells with palisading of the cells at the periphery. Giant solitary molluscum contagiosum is a dome-shaped, flesh-colored nodule with central umbilication. Histopathology reveals hyperplastic squamous epithelium with characteristic eosinophilic inclusion bodies above the basal layer.
Solitary SF can be difficult to diagnose based solely on the clinical presentation; thus biopsy with histologic evaluation is recommended. If SF is confirmed, the clinician should inquire about a family history of Cowden syndrome and then perform a total-body skin examination to check for multiple SF and other clinical hamartomas of Cowden syndrome such as trichilemmomas, acral keratosis, and oral papillomas.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
- Weary PE, Gorlin RJ, Gentry Jr WC, et al. Multiple hamartoma syndrome (Cowden’s disease). Arch Dermatol. 1972;106:682-690.
- Rapini RP, Golitz LE. Sclerotic fibromas of the skin. J Am Acad Dermatol. 1989;20(2 pt 1):266-271.
- Tosa M, Ansai S, Kuwahara H, et al. Two cases of sclerotic fibroma of the skin that mimicked keloids clinically. J Nippon Med Sch. 2018;85:283-286.
- High WA, Stewart D, Essary LR, et al. Sclerotic fibroma-like changes in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? J Cutan Pathol. 2004;31:373-378.
A 45-year-old woman was referred to dermatology by a primary care physician for evaluation of a raised skin lesion on the scalp. She was otherwise healthy. The lesion had been present for many years but recently grew in size. The patient reported that the lesion was subject to recurrent physical trauma and she wanted it removed. Physical examination revealed a 6×6-mm, domeshaped, yellow nodule on the left inferior parietal scalp. There were no similar lesions located elsewhere on the body. A shave removal was performed and sent for histopathologic evaluation.

DEI advances in dermatology unremarkable to date, studies find
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
suggest.
To evaluate diversity and career goals of graduating allopathic medical students pursuing careers in dermatology, corresponding author Matthew Mansh, MD, of the department of dermatology at the University of Minnesota, Minneapolis, and colleagues drew from the 2016-2019 Association of American Medical Colleges Graduation Questionnaire for their study. The main outcome measures were the proportion of female students, students from racial and ethnic groups underrepresented in medicine (URM), and sexual minority (SM) students pursuing dermatology versus those pursuing other specialties, as well as the proportions and multivariable adjusted odds of intended career goals between students pursuing dermatology and those pursuing other specialties, and by sex, race, and ethnicity, and sexual orientation among students pursuing dermatology.
Of the 58,077 graduating students, 49% were women, 15% were URM, and 6% were SM. The researchers found that women pursuing dermatology were significantly less likely than women pursuing other specialties to identify as URM (11.6% vs. 17.2%; P < .001) or SM (1.9% vs. 5.7%; P < .001).
In multivariable-adjusted analyses of all students, those pursuing dermatology compared with other specialties had decreased odds of intending to care for underserved populations (18.3% vs. 34%; adjusted odd ratio, 0.40; P < .001), practice in underserved areas (12.7% vs. 25.9%; aOR, 0.40; P < .001), and practice public health (17% vs. 30.2%; aOR, 0.44; P < .001). The odds for pursuing research in their careers was greater among those pursuing dermatology (64.7% vs. 51.7%; aOR, 1.76; P < .001).
“Addressing health inequities and improving care for underserved patients is the responsibility of all dermatologists, and efforts are needed to increase diversity and interest in careers focused on underserved care among trainees in the dermatology workforce pipeline,” the authors concluded. They acknowledged certain limitations of the analysis, including lack of data delineating sex, sex assigned at birth, and gender identity, and lack of intersectional analyses between multiple minority identities and multiple career goals. “Importantly, diversity factors and their relationship to underserved care is likely multidimensional, and many students pursuing dermatology identified with multiple minority identities, highlighting the need for future studies focused on intersectionality,” they wrote.
Trends over 15 years
In a separate study, Jazzmin C. Williams, a medical student at the University of California, San Francisco, and coauthors drew from an Association of American Medical Colleges report of trainees’ and applicants’ self-reported race and ethnicity by specialty from 2005 to 2020 to evaluate diversity trends over the 15-year period. They found that Black and Latinx trainees were underrepresented in all specialties, but even more so in dermatology (mean annual rate ratios of 0.32 and 0.14, respectively), compared with those in primary care (mean annual RRs of 0.54 and 0.23) and those in specialty care (mean annual RRs of 0.39 and 0.18).
In other findings, the annual representation of Black trainees remained unchanged in dermatology between 2005 and 2020, but down-trended for primary (P < .001) and specialty care (P = .001). At the same time, representation of Latinx trainees remained unchanged in dermatology and specialty care but increased in primary care (P < .001). Finally, Black and Latinx race and ethnicity comprised a lower mean proportion of matriculating dermatology trainees (postgraduate year-2s) compared with annual dermatology applicants (4.01% vs. 5.97%, respectively, and 2.06% vs. 6.37% among Latinx; P < .001 for all associations).
“Much of these disparities can be attributed to the leaky pipeline – the disproportionate, stepwise reduction in racial and ethnic minority representation along the path to medicine,” the authors wrote. “This leaky pipeline is the direct result of structural racism, which includes, but is not limited to, historical and contemporary economic disinvestment from majority-minority schools, kindergarten through grade 12.” They concluded by stating that “dermatologists must intervene throughout the educational pipeline, including residency selection and mentorship, to effectively increase diversity.”
Solutions to address diversity
In an editorial accompanying the two studies published in the same issue of JAMA Dermatology, Ellen N. Pritchett, MD, MPH, of the department of dermatology at Howard University, Washington, and Andrew J. Park, MD, MBA, and Rebecca Vasquez, MD, of the department of dermatology at the University of Texas Southwestern Medical Center, Dallas, offered several solutions to address diversity in the dermatology work force. They include:
Go beyond individual bias in recruitment. “A residency selection framework that meaningfully incorporates diversity, equity, and inclusion (DEI) will require more than strategies that address individual bias,” they wrote. “Departmental recruitment committees must become familiar with systems that serve to perpetuate individual bias, like institutional racism or practices that disproportionately favor non-URM versus URM individuals.”
Challenge the myth of meritocracy. “The inaccurate notion of meritocracy – that success purely derives from individual effort has become the foundation of residency selection,” the authors wrote. “Unfortunately, this view ignores the inequitably distributed sociostructural resources that limit the rewards of individual effort.”
Avoid tokenism in retention strategies. Tokenism, which they defined as “a symbolic addition of members from a marginalized group to give the impression of social inclusiveness and diversity without meaningful incorporation of DEI in the policies, processes, and culture,” can lead to depression, burnout, and attrition, they wrote. They advise leaders of dermatology departments to “review their residency selection framework to ensure that it allows for meaningful representation, inclusion, and equity among trainees and faculty to better support URM individuals at all levels.”
Omar N. Qutub, MD, a Portland, Ore.–based dermatologist who was asked to comment on the studies, characterized the findings by Dr. Mansh and colleagues as sobering. “It appears that there is work to do as far as improving diversity in the dermatology workforce that will likely benefit greatly from an honest and steadfast approach to equitable application standards as well as mentorship during all stages of the application process,” such as medical school and residency, said Dr. Qutub, who is the director of equity, diversity, and inclusion of the ODAC Dermatology, Aesthetic & Surgical Conference. “With a focused attempt, we are likely to matriculate more racial minorities into our residency programs, maximizing patient outcomes.”
As for the study by Ms. Williams and colleagues, he told this news organization that efforts toward recruiting URM students as well as sexual minority students “is likely to not only improve health inequities in underserved areas, but will also enrich the specialty as a whole, allowing for better understanding of our diverse patient population and [for us to] to deliver quality care more readily for people and in areas where the focus has often been limited.”
In an interview, Chesahna Kindred, MD, a Columbia, Md.–based dermatologist and immediate past chair of the National Medical Association dermatology section, pointed out that the number of Black physicians in the United States has increased by only 4% in the last 120 years. The study by Dr. Mansh and colleagues, she commented, “underscores what I’ve recognized in the last couple of years: Where are the Black male dermatologists? NMA Derm started recruiting this demographic aggressively about a year ago and started the Black Men in Derm events. Black male members of NMA Derm travel to the Student National Medical Association and NMA conference and hold a panel to expose Black male students into dermatology. This article provides the numbers needed to measure how successful this and other programs are to closing the equity gap.”
Ms. Williams reported having no financial disclosures. Dr. Mansh reported receiving grants from National Institute of Environmental Health Sciences outside the submitted work. Dr. Pritchett and colleagues reported having no relevant financial disclosures, as did Dr. Qutub and Dr. Kindred.
FROM JAMA DERMATOLOGY
Advancing health equity in neurology is essential to patient care
Black and Latinx older adults are up to three times as likely to develop Alzheimer’s disease than non-Latinx White adults and tend to experience onset at a younger age with more severe symptoms, according to Monica Rivera-Mindt, PhD, a professor of psychology at Fordham University and the Icahn School of Medicine at Mount Sinai, New York. Looking ahead, that means by 2030, nearly 40% of the 8.4 million Americans affected by Alzheimer’s disease will be Black and/or Latinx, she said. These facts were among the stark disparities in health care outcomes Dr. Rivera-Mindt discussed in her presentation on brain health equity at the 2022 annual meeting of the American Neurological Association.
Dr. Rivera-Mindt’s presentation opened the ANA’s plenary session on health disparities and inequities. The plenary, “Advancing Neurologic Equity: Challenges and Paths Forward,” did not simply enumerate racial and ethnic disparities that exist with various neurological conditions. Rather it went beyond the discussion of what disparities exist into understanding the roots of them as well as tips, tools, and resources that can aid clinicians in addressing or ameliorating them.
Roy Hamilton, MD, an associate professor of neurology and physical medicine and rehabilitation at the University of Pennsylvania, Philadelphia, said. “If clinicians are unaware of these disparities or don’t have any sense of how to start to address or think about them, then they’re really missing out on an important component of their education as persons who take care of patients with brain disorders.”
Dr. Hamilton, who organized the plenary, noted that awareness of these disparities is crucial to comprehensively caring for patients.
Missed opportunities
“We’re talking about disadvantages that are structural and large scale, but those disadvantages play themselves out in the individual encounter,” Dr. Hamilton said. “When physicians see patients, they have to treat the whole patient in front of them,” which means being aware of the risks and factors that could affect a patient’s clinical presentation. “Being aware of disparities has practical impacts on physician judgment,” he said.
For example, recent research in multiple sclerosis (MS) has highlighted how clinicians may be missing diagnosis of this condition in non-White populations because the condition has been regarded for so long as a “White person’s” disease, Dr. Hamilton said. In non-White patients exhibiting MS symptoms, then, clinicians may have been less likely to consider MS as a possibility, thereby delaying diagnosis and treatment.
Those patterns may partly explain why the mortality rate for MS is greater in Black patients, who also show more rapid neurodegeneration than White patients with MS, Lilyana Amezcua, MD, an associate professor of neurology at the University of Southern California, Los Angeles, reported in the plenary’s second presentation.
Transgender issues
The third session, presented by Nicole Rosendale, MD, an assistant professor of neurology at the University of California, San Francisco, and director of the San Francisco General Hospital neurology inpatient services, examined disparities in neurology within the LGBTQ+ community through representative case studies and then offered specific ways that neurologists could make their practices more inclusive and equitable for sexual and gender minorities.
Her first case study was a 52-year-old man who presented with new-onset seizures, right hemiparesis, and aphasia. A brain biopsy consistent with adenocarcinoma eventually led his physician to discover he had metastatic breast cancer. It turned out the man was transgender and, despite a family history of breast cancer, hadn’t been advised to get breast cancer screenings.
“Breast cancer was not initially on the differential as no one had identified that the patient was transmasculine,” Dr. Rosendale said. A major challenge to providing care to transgender patients is a dearth of data on risks and screening recommendations. Another barrier is low knowledge of LGBTQ+ health among neurologists, Dr. Rosendale said while sharing findings from her 2019 study on the topic and calling for more research in LGBTQ+ populations.
Dr. Rosendale’s second case study dealt with a nonbinary patient who suffered from debilitating headaches for decades, first because they lacked access to health insurance and then because negative experiences with providers dissuaded them from seeking care. In data from the Center for American Progress she shared, 8% of LGB respondents and 22% of transgender respondents said they had avoided or delayed care because of fear of discrimination or mistreatment.
“So it’s not only access but also what experiences people are having when they go in and whether they’re actually even getting access to care or being taken care of,” Dr. Rosendale said. Other findings from the CAP found that:
- 8% of LGB patients and 29% of transgender patients reported having a clinician refuse to see them.
- 6% of LGB patients and 12% of transgender patients reported that a clinician refused to give them health care.
- 9% of LGB patients and 21% of transgender patients experienced harsh or abusive language during a health care experience.
- 7% of LGB patients and nearly a third (29%) of transgender patients experienced unwanted physical contact, such as fondling or sexual assault.
Reducing the disparities
Adys Mendizabal, MD, an assistant professor of neurology at the Institute of Society and Genetics at the University of California, Los Angeles, who attended the presentation, was grateful to see how the various lectures enriched the discussion beyond stating the fact of racial/ethnic disparities and dug into the nuances on how to think about and address these disparities. She particularly appreciated discussion about the need to go out of the way to recruit diverse patient populations for clinical trials while also providing them care.
“It is definitely complicated, but it’s not impossible for an individual neurologist or an individual department to do something to reduce some of the disparities,” Dr. Mendizabal said. “It starts with just knowing that they exist and being aware of some of the things that may be impacting care for a particular patient.”
Tools to counter disparity
In the final presentation, Amy Kind, MD, PhD, the associate dean for social health sciences and programs at the University of Wisconsin–Madison, rounded out the discussion by exploring social determinants of health and their influence on outcomes.
“Social determinants impact brain health, and brain health is not distributed equally,” Dr. Kind told attendees. “We have known this for decades, yet disparities persist.”
Dr. Kind described the “exposome,” a “measure of all the exposures of an individual in a lifetime and how those exposures relate to health,” according to the CDC, and then introduced a tool clinicians can use to better understand social determinants of health in specific geographic areas. The Neighborhood Atlas, which Dr. Kind described in the New England Journal of Medicine in 2018, measures 17 social determinants across small population-sensitive areas and provides an area deprivation index. A high area deprivation index is linked to a range of negative outcomes, including reshopitalization, later diagnoses, less comprehensive diagnostic evaluation, increased risk of postsurgical complications, and decreased life expectancy.
“One of the things that really stood out to me about Dr. Kind’s discussion of the use of the area deprivation index was the fact that understanding and quantifying these kinds of risks and exposures is the vehicle for creating the kinds of social changes, including policy changes, that will actually lead to addressing and mitigating some of these lifelong risks and exposures,” Dr. Hamilton said. “It is implausible to think that a specific group of people would be genetically more susceptible to basically every disease that we know,” he added. “It makes much more sense to think that groups of individuals have been subjected systematically to conditions that impair health in a variety of ways.”
Not just race, ethnicity, sex, and gender
Following the four presentations from researchers in health inequities was an Emerging Scholar presentation in which Jay B. Lusk, an MD/MBA candidate at Duke University, Durham, N.C., shared new research findings on the role of neighborhood disadvantage in predicting mortality from coma, stroke, and other neurologic conditions. His findings revealed that living in a neighborhood with greater deprivation substantially increased risk of mortality even after accounting for individual wealth and demographics.
Maria Eugenia Diaz-Ortiz, PhD, of the department of neurology, University of Pennsylvania, Philadelphia, said she found the five presentations to be an excellent introduction to people like herself who are in the earlier stages of learning about health equity research.
“I think they introduced various important concepts and frameworks and provided tools for people who don’t know about them,” Dr. Diaz-Ortiz said. “Then they asked important questions and provided some solutions to them.”
Dr. Diaz-Ortiz also appreciated seemingly minor but actually important details in how the speakers presented themselves, such as Dr. Rivera-Mindt opening with a land acknowledgment and her disclosures of “positionality.” The former recognized the traditional Native American custodians of the land on which she lives and works, and the latter revealed details about her as an individual – such as being the Afro-Latinx daughter of immigrants yet being cisgender, able-bodied, and U.S.-born – that show where she falls on the axis of adversity and axis of privilege.
Implications for research
The biggest takeaway for Dr. Diaz-Ortiz, however, came from the first Q&A session when someone asked how to increase underrepresented populations in dementia research. Dr. Rivera-Mindt described her experience engaging these communities by employing “community-based participatory research practices, which involves making yourself a part of the community and making the community active participants in the research,” Dr. Diaz-Ortiz said. “It’s an evidence-based approach that has been shown to increase participation in research not only in her work but in the work of others.”
Preaching to the choir
Dr. Diaz-Ortiz was pleased overall with the plenary but disappointed in its placement at the end of the meeting, when attendance is always lower as attendees head home.
“The people who stayed were people who already know and recognize the value of health equity work, so I think that was a missed opportunity where the session could have been included on day one or two to boost attendance and also to educate like a broader group of neurologists,” Dr. Diaz-Ortiz said in an interview.
Dr. Mendizabal felt similarly, appreciating the plenary but noting it was “definitely overdue” and that it should not be the last session. Instead, sessions on health equity should be as easy as possible to attend to bring in larger audiences. “Perhaps having that session on a Saturday or Sunday would have a higher likelihood of greater attendance than on a Tuesday,” she said. That said, Dr. Mendizabal also noticed that greater attention to health care disparities was woven into many other sessions throughout the conference, which is “the best way of addressing health equity instead of trying to just designate a session,” she said.
Dr. Mendizabal hopes that plenaries like this one and the weaving of health equity issues into presentations throughout neurology conferences continue.
“After the racial reckoning in 2020, there was a big impetus and a big wave of energy in addressing health disparities in the field, and I hope that that momentum is not starting to wane,” Dr. Mendizabal said. “It’s important because not talking about is not going to make this issue go away.”
Dr. Hamilton agreed that it is important that the conversation continue and that physicians recognize the importance of understanding health care disparities and determinants of health, regardless of where they fall on the political spectrum or whether they choose to get involved in policy or advocacy.
“Irrespective of whether you think race or ethnicity or socioeconomic status are political issues or not, it is the case that you’re obligated to have an objective understanding of the factors that contribute to your patient’s health and as points of intervention,” Dr. Hamilton said. “So even if you don’t want to sit down and jot off that email to your senator, you still have to take these factors into account when you’re treating the person who’s sitting right in front of you, and that’s not political. That’s the promise of being a physician.”
Dr. Amezcua has received personal compensation for consulting, speaking, or serving on steering committees or advisory boards for Biogen Idec, Novartis, Genentech, and EMD Serono, and she has received research support from Biogen Idec and Bristol Myers Squibb Foundation. Dr. Kind reported support from the Alzheimer’s Association. Dr. Diaz-Ortiz is coinventor of a provisional patent submitted by the University of Pennsylvania that relates to a potential therapeutic in Parkinson’s disease. Mr. Lusk reported fellowship support from American Heart Association and travel support from the American Neurological Association. No other speakers or sources had relevant disclosures.
Black and Latinx older adults are up to three times as likely to develop Alzheimer’s disease than non-Latinx White adults and tend to experience onset at a younger age with more severe symptoms, according to Monica Rivera-Mindt, PhD, a professor of psychology at Fordham University and the Icahn School of Medicine at Mount Sinai, New York. Looking ahead, that means by 2030, nearly 40% of the 8.4 million Americans affected by Alzheimer’s disease will be Black and/or Latinx, she said. These facts were among the stark disparities in health care outcomes Dr. Rivera-Mindt discussed in her presentation on brain health equity at the 2022 annual meeting of the American Neurological Association.
Dr. Rivera-Mindt’s presentation opened the ANA’s plenary session on health disparities and inequities. The plenary, “Advancing Neurologic Equity: Challenges and Paths Forward,” did not simply enumerate racial and ethnic disparities that exist with various neurological conditions. Rather it went beyond the discussion of what disparities exist into understanding the roots of them as well as tips, tools, and resources that can aid clinicians in addressing or ameliorating them.
Roy Hamilton, MD, an associate professor of neurology and physical medicine and rehabilitation at the University of Pennsylvania, Philadelphia, said. “If clinicians are unaware of these disparities or don’t have any sense of how to start to address or think about them, then they’re really missing out on an important component of their education as persons who take care of patients with brain disorders.”
Dr. Hamilton, who organized the plenary, noted that awareness of these disparities is crucial to comprehensively caring for patients.
Missed opportunities
“We’re talking about disadvantages that are structural and large scale, but those disadvantages play themselves out in the individual encounter,” Dr. Hamilton said. “When physicians see patients, they have to treat the whole patient in front of them,” which means being aware of the risks and factors that could affect a patient’s clinical presentation. “Being aware of disparities has practical impacts on physician judgment,” he said.
For example, recent research in multiple sclerosis (MS) has highlighted how clinicians may be missing diagnosis of this condition in non-White populations because the condition has been regarded for so long as a “White person’s” disease, Dr. Hamilton said. In non-White patients exhibiting MS symptoms, then, clinicians may have been less likely to consider MS as a possibility, thereby delaying diagnosis and treatment.
Those patterns may partly explain why the mortality rate for MS is greater in Black patients, who also show more rapid neurodegeneration than White patients with MS, Lilyana Amezcua, MD, an associate professor of neurology at the University of Southern California, Los Angeles, reported in the plenary’s second presentation.
Transgender issues
The third session, presented by Nicole Rosendale, MD, an assistant professor of neurology at the University of California, San Francisco, and director of the San Francisco General Hospital neurology inpatient services, examined disparities in neurology within the LGBTQ+ community through representative case studies and then offered specific ways that neurologists could make their practices more inclusive and equitable for sexual and gender minorities.
Her first case study was a 52-year-old man who presented with new-onset seizures, right hemiparesis, and aphasia. A brain biopsy consistent with adenocarcinoma eventually led his physician to discover he had metastatic breast cancer. It turned out the man was transgender and, despite a family history of breast cancer, hadn’t been advised to get breast cancer screenings.
“Breast cancer was not initially on the differential as no one had identified that the patient was transmasculine,” Dr. Rosendale said. A major challenge to providing care to transgender patients is a dearth of data on risks and screening recommendations. Another barrier is low knowledge of LGBTQ+ health among neurologists, Dr. Rosendale said while sharing findings from her 2019 study on the topic and calling for more research in LGBTQ+ populations.
Dr. Rosendale’s second case study dealt with a nonbinary patient who suffered from debilitating headaches for decades, first because they lacked access to health insurance and then because negative experiences with providers dissuaded them from seeking care. In data from the Center for American Progress she shared, 8% of LGB respondents and 22% of transgender respondents said they had avoided or delayed care because of fear of discrimination or mistreatment.
“So it’s not only access but also what experiences people are having when they go in and whether they’re actually even getting access to care or being taken care of,” Dr. Rosendale said. Other findings from the CAP found that:
- 8% of LGB patients and 29% of transgender patients reported having a clinician refuse to see them.
- 6% of LGB patients and 12% of transgender patients reported that a clinician refused to give them health care.
- 9% of LGB patients and 21% of transgender patients experienced harsh or abusive language during a health care experience.
- 7% of LGB patients and nearly a third (29%) of transgender patients experienced unwanted physical contact, such as fondling or sexual assault.
Reducing the disparities
Adys Mendizabal, MD, an assistant professor of neurology at the Institute of Society and Genetics at the University of California, Los Angeles, who attended the presentation, was grateful to see how the various lectures enriched the discussion beyond stating the fact of racial/ethnic disparities and dug into the nuances on how to think about and address these disparities. She particularly appreciated discussion about the need to go out of the way to recruit diverse patient populations for clinical trials while also providing them care.
“It is definitely complicated, but it’s not impossible for an individual neurologist or an individual department to do something to reduce some of the disparities,” Dr. Mendizabal said. “It starts with just knowing that they exist and being aware of some of the things that may be impacting care for a particular patient.”
Tools to counter disparity
In the final presentation, Amy Kind, MD, PhD, the associate dean for social health sciences and programs at the University of Wisconsin–Madison, rounded out the discussion by exploring social determinants of health and their influence on outcomes.
“Social determinants impact brain health, and brain health is not distributed equally,” Dr. Kind told attendees. “We have known this for decades, yet disparities persist.”
Dr. Kind described the “exposome,” a “measure of all the exposures of an individual in a lifetime and how those exposures relate to health,” according to the CDC, and then introduced a tool clinicians can use to better understand social determinants of health in specific geographic areas. The Neighborhood Atlas, which Dr. Kind described in the New England Journal of Medicine in 2018, measures 17 social determinants across small population-sensitive areas and provides an area deprivation index. A high area deprivation index is linked to a range of negative outcomes, including reshopitalization, later diagnoses, less comprehensive diagnostic evaluation, increased risk of postsurgical complications, and decreased life expectancy.
“One of the things that really stood out to me about Dr. Kind’s discussion of the use of the area deprivation index was the fact that understanding and quantifying these kinds of risks and exposures is the vehicle for creating the kinds of social changes, including policy changes, that will actually lead to addressing and mitigating some of these lifelong risks and exposures,” Dr. Hamilton said. “It is implausible to think that a specific group of people would be genetically more susceptible to basically every disease that we know,” he added. “It makes much more sense to think that groups of individuals have been subjected systematically to conditions that impair health in a variety of ways.”
Not just race, ethnicity, sex, and gender
Following the four presentations from researchers in health inequities was an Emerging Scholar presentation in which Jay B. Lusk, an MD/MBA candidate at Duke University, Durham, N.C., shared new research findings on the role of neighborhood disadvantage in predicting mortality from coma, stroke, and other neurologic conditions. His findings revealed that living in a neighborhood with greater deprivation substantially increased risk of mortality even after accounting for individual wealth and demographics.
Maria Eugenia Diaz-Ortiz, PhD, of the department of neurology, University of Pennsylvania, Philadelphia, said she found the five presentations to be an excellent introduction to people like herself who are in the earlier stages of learning about health equity research.
“I think they introduced various important concepts and frameworks and provided tools for people who don’t know about them,” Dr. Diaz-Ortiz said. “Then they asked important questions and provided some solutions to them.”
Dr. Diaz-Ortiz also appreciated seemingly minor but actually important details in how the speakers presented themselves, such as Dr. Rivera-Mindt opening with a land acknowledgment and her disclosures of “positionality.” The former recognized the traditional Native American custodians of the land on which she lives and works, and the latter revealed details about her as an individual – such as being the Afro-Latinx daughter of immigrants yet being cisgender, able-bodied, and U.S.-born – that show where she falls on the axis of adversity and axis of privilege.
Implications for research
The biggest takeaway for Dr. Diaz-Ortiz, however, came from the first Q&A session when someone asked how to increase underrepresented populations in dementia research. Dr. Rivera-Mindt described her experience engaging these communities by employing “community-based participatory research practices, which involves making yourself a part of the community and making the community active participants in the research,” Dr. Diaz-Ortiz said. “It’s an evidence-based approach that has been shown to increase participation in research not only in her work but in the work of others.”
Preaching to the choir
Dr. Diaz-Ortiz was pleased overall with the plenary but disappointed in its placement at the end of the meeting, when attendance is always lower as attendees head home.
“The people who stayed were people who already know and recognize the value of health equity work, so I think that was a missed opportunity where the session could have been included on day one or two to boost attendance and also to educate like a broader group of neurologists,” Dr. Diaz-Ortiz said in an interview.
Dr. Mendizabal felt similarly, appreciating the plenary but noting it was “definitely overdue” and that it should not be the last session. Instead, sessions on health equity should be as easy as possible to attend to bring in larger audiences. “Perhaps having that session on a Saturday or Sunday would have a higher likelihood of greater attendance than on a Tuesday,” she said. That said, Dr. Mendizabal also noticed that greater attention to health care disparities was woven into many other sessions throughout the conference, which is “the best way of addressing health equity instead of trying to just designate a session,” she said.
Dr. Mendizabal hopes that plenaries like this one and the weaving of health equity issues into presentations throughout neurology conferences continue.
“After the racial reckoning in 2020, there was a big impetus and a big wave of energy in addressing health disparities in the field, and I hope that that momentum is not starting to wane,” Dr. Mendizabal said. “It’s important because not talking about is not going to make this issue go away.”
Dr. Hamilton agreed that it is important that the conversation continue and that physicians recognize the importance of understanding health care disparities and determinants of health, regardless of where they fall on the political spectrum or whether they choose to get involved in policy or advocacy.
“Irrespective of whether you think race or ethnicity or socioeconomic status are political issues or not, it is the case that you’re obligated to have an objective understanding of the factors that contribute to your patient’s health and as points of intervention,” Dr. Hamilton said. “So even if you don’t want to sit down and jot off that email to your senator, you still have to take these factors into account when you’re treating the person who’s sitting right in front of you, and that’s not political. That’s the promise of being a physician.”
Dr. Amezcua has received personal compensation for consulting, speaking, or serving on steering committees or advisory boards for Biogen Idec, Novartis, Genentech, and EMD Serono, and she has received research support from Biogen Idec and Bristol Myers Squibb Foundation. Dr. Kind reported support from the Alzheimer’s Association. Dr. Diaz-Ortiz is coinventor of a provisional patent submitted by the University of Pennsylvania that relates to a potential therapeutic in Parkinson’s disease. Mr. Lusk reported fellowship support from American Heart Association and travel support from the American Neurological Association. No other speakers or sources had relevant disclosures.
Black and Latinx older adults are up to three times as likely to develop Alzheimer’s disease than non-Latinx White adults and tend to experience onset at a younger age with more severe symptoms, according to Monica Rivera-Mindt, PhD, a professor of psychology at Fordham University and the Icahn School of Medicine at Mount Sinai, New York. Looking ahead, that means by 2030, nearly 40% of the 8.4 million Americans affected by Alzheimer’s disease will be Black and/or Latinx, she said. These facts were among the stark disparities in health care outcomes Dr. Rivera-Mindt discussed in her presentation on brain health equity at the 2022 annual meeting of the American Neurological Association.
Dr. Rivera-Mindt’s presentation opened the ANA’s plenary session on health disparities and inequities. The plenary, “Advancing Neurologic Equity: Challenges and Paths Forward,” did not simply enumerate racial and ethnic disparities that exist with various neurological conditions. Rather it went beyond the discussion of what disparities exist into understanding the roots of them as well as tips, tools, and resources that can aid clinicians in addressing or ameliorating them.
Roy Hamilton, MD, an associate professor of neurology and physical medicine and rehabilitation at the University of Pennsylvania, Philadelphia, said. “If clinicians are unaware of these disparities or don’t have any sense of how to start to address or think about them, then they’re really missing out on an important component of their education as persons who take care of patients with brain disorders.”
Dr. Hamilton, who organized the plenary, noted that awareness of these disparities is crucial to comprehensively caring for patients.
Missed opportunities
“We’re talking about disadvantages that are structural and large scale, but those disadvantages play themselves out in the individual encounter,” Dr. Hamilton said. “When physicians see patients, they have to treat the whole patient in front of them,” which means being aware of the risks and factors that could affect a patient’s clinical presentation. “Being aware of disparities has practical impacts on physician judgment,” he said.
For example, recent research in multiple sclerosis (MS) has highlighted how clinicians may be missing diagnosis of this condition in non-White populations because the condition has been regarded for so long as a “White person’s” disease, Dr. Hamilton said. In non-White patients exhibiting MS symptoms, then, clinicians may have been less likely to consider MS as a possibility, thereby delaying diagnosis and treatment.
Those patterns may partly explain why the mortality rate for MS is greater in Black patients, who also show more rapid neurodegeneration than White patients with MS, Lilyana Amezcua, MD, an associate professor of neurology at the University of Southern California, Los Angeles, reported in the plenary’s second presentation.
Transgender issues
The third session, presented by Nicole Rosendale, MD, an assistant professor of neurology at the University of California, San Francisco, and director of the San Francisco General Hospital neurology inpatient services, examined disparities in neurology within the LGBTQ+ community through representative case studies and then offered specific ways that neurologists could make their practices more inclusive and equitable for sexual and gender minorities.
Her first case study was a 52-year-old man who presented with new-onset seizures, right hemiparesis, and aphasia. A brain biopsy consistent with adenocarcinoma eventually led his physician to discover he had metastatic breast cancer. It turned out the man was transgender and, despite a family history of breast cancer, hadn’t been advised to get breast cancer screenings.
“Breast cancer was not initially on the differential as no one had identified that the patient was transmasculine,” Dr. Rosendale said. A major challenge to providing care to transgender patients is a dearth of data on risks and screening recommendations. Another barrier is low knowledge of LGBTQ+ health among neurologists, Dr. Rosendale said while sharing findings from her 2019 study on the topic and calling for more research in LGBTQ+ populations.
Dr. Rosendale’s second case study dealt with a nonbinary patient who suffered from debilitating headaches for decades, first because they lacked access to health insurance and then because negative experiences with providers dissuaded them from seeking care. In data from the Center for American Progress she shared, 8% of LGB respondents and 22% of transgender respondents said they had avoided or delayed care because of fear of discrimination or mistreatment.
“So it’s not only access but also what experiences people are having when they go in and whether they’re actually even getting access to care or being taken care of,” Dr. Rosendale said. Other findings from the CAP found that:
- 8% of LGB patients and 29% of transgender patients reported having a clinician refuse to see them.
- 6% of LGB patients and 12% of transgender patients reported that a clinician refused to give them health care.
- 9% of LGB patients and 21% of transgender patients experienced harsh or abusive language during a health care experience.
- 7% of LGB patients and nearly a third (29%) of transgender patients experienced unwanted physical contact, such as fondling or sexual assault.
Reducing the disparities
Adys Mendizabal, MD, an assistant professor of neurology at the Institute of Society and Genetics at the University of California, Los Angeles, who attended the presentation, was grateful to see how the various lectures enriched the discussion beyond stating the fact of racial/ethnic disparities and dug into the nuances on how to think about and address these disparities. She particularly appreciated discussion about the need to go out of the way to recruit diverse patient populations for clinical trials while also providing them care.
“It is definitely complicated, but it’s not impossible for an individual neurologist or an individual department to do something to reduce some of the disparities,” Dr. Mendizabal said. “It starts with just knowing that they exist and being aware of some of the things that may be impacting care for a particular patient.”
Tools to counter disparity
In the final presentation, Amy Kind, MD, PhD, the associate dean for social health sciences and programs at the University of Wisconsin–Madison, rounded out the discussion by exploring social determinants of health and their influence on outcomes.
“Social determinants impact brain health, and brain health is not distributed equally,” Dr. Kind told attendees. “We have known this for decades, yet disparities persist.”
Dr. Kind described the “exposome,” a “measure of all the exposures of an individual in a lifetime and how those exposures relate to health,” according to the CDC, and then introduced a tool clinicians can use to better understand social determinants of health in specific geographic areas. The Neighborhood Atlas, which Dr. Kind described in the New England Journal of Medicine in 2018, measures 17 social determinants across small population-sensitive areas and provides an area deprivation index. A high area deprivation index is linked to a range of negative outcomes, including reshopitalization, later diagnoses, less comprehensive diagnostic evaluation, increased risk of postsurgical complications, and decreased life expectancy.
“One of the things that really stood out to me about Dr. Kind’s discussion of the use of the area deprivation index was the fact that understanding and quantifying these kinds of risks and exposures is the vehicle for creating the kinds of social changes, including policy changes, that will actually lead to addressing and mitigating some of these lifelong risks and exposures,” Dr. Hamilton said. “It is implausible to think that a specific group of people would be genetically more susceptible to basically every disease that we know,” he added. “It makes much more sense to think that groups of individuals have been subjected systematically to conditions that impair health in a variety of ways.”
Not just race, ethnicity, sex, and gender
Following the four presentations from researchers in health inequities was an Emerging Scholar presentation in which Jay B. Lusk, an MD/MBA candidate at Duke University, Durham, N.C., shared new research findings on the role of neighborhood disadvantage in predicting mortality from coma, stroke, and other neurologic conditions. His findings revealed that living in a neighborhood with greater deprivation substantially increased risk of mortality even after accounting for individual wealth and demographics.
Maria Eugenia Diaz-Ortiz, PhD, of the department of neurology, University of Pennsylvania, Philadelphia, said she found the five presentations to be an excellent introduction to people like herself who are in the earlier stages of learning about health equity research.
“I think they introduced various important concepts and frameworks and provided tools for people who don’t know about them,” Dr. Diaz-Ortiz said. “Then they asked important questions and provided some solutions to them.”
Dr. Diaz-Ortiz also appreciated seemingly minor but actually important details in how the speakers presented themselves, such as Dr. Rivera-Mindt opening with a land acknowledgment and her disclosures of “positionality.” The former recognized the traditional Native American custodians of the land on which she lives and works, and the latter revealed details about her as an individual – such as being the Afro-Latinx daughter of immigrants yet being cisgender, able-bodied, and U.S.-born – that show where she falls on the axis of adversity and axis of privilege.
Implications for research
The biggest takeaway for Dr. Diaz-Ortiz, however, came from the first Q&A session when someone asked how to increase underrepresented populations in dementia research. Dr. Rivera-Mindt described her experience engaging these communities by employing “community-based participatory research practices, which involves making yourself a part of the community and making the community active participants in the research,” Dr. Diaz-Ortiz said. “It’s an evidence-based approach that has been shown to increase participation in research not only in her work but in the work of others.”
Preaching to the choir
Dr. Diaz-Ortiz was pleased overall with the plenary but disappointed in its placement at the end of the meeting, when attendance is always lower as attendees head home.
“The people who stayed were people who already know and recognize the value of health equity work, so I think that was a missed opportunity where the session could have been included on day one or two to boost attendance and also to educate like a broader group of neurologists,” Dr. Diaz-Ortiz said in an interview.
Dr. Mendizabal felt similarly, appreciating the plenary but noting it was “definitely overdue” and that it should not be the last session. Instead, sessions on health equity should be as easy as possible to attend to bring in larger audiences. “Perhaps having that session on a Saturday or Sunday would have a higher likelihood of greater attendance than on a Tuesday,” she said. That said, Dr. Mendizabal also noticed that greater attention to health care disparities was woven into many other sessions throughout the conference, which is “the best way of addressing health equity instead of trying to just designate a session,” she said.
Dr. Mendizabal hopes that plenaries like this one and the weaving of health equity issues into presentations throughout neurology conferences continue.
“After the racial reckoning in 2020, there was a big impetus and a big wave of energy in addressing health disparities in the field, and I hope that that momentum is not starting to wane,” Dr. Mendizabal said. “It’s important because not talking about is not going to make this issue go away.”
Dr. Hamilton agreed that it is important that the conversation continue and that physicians recognize the importance of understanding health care disparities and determinants of health, regardless of where they fall on the political spectrum or whether they choose to get involved in policy or advocacy.
“Irrespective of whether you think race or ethnicity or socioeconomic status are political issues or not, it is the case that you’re obligated to have an objective understanding of the factors that contribute to your patient’s health and as points of intervention,” Dr. Hamilton said. “So even if you don’t want to sit down and jot off that email to your senator, you still have to take these factors into account when you’re treating the person who’s sitting right in front of you, and that’s not political. That’s the promise of being a physician.”
Dr. Amezcua has received personal compensation for consulting, speaking, or serving on steering committees or advisory boards for Biogen Idec, Novartis, Genentech, and EMD Serono, and she has received research support from Biogen Idec and Bristol Myers Squibb Foundation. Dr. Kind reported support from the Alzheimer’s Association. Dr. Diaz-Ortiz is coinventor of a provisional patent submitted by the University of Pennsylvania that relates to a potential therapeutic in Parkinson’s disease. Mr. Lusk reported fellowship support from American Heart Association and travel support from the American Neurological Association. No other speakers or sources had relevant disclosures.
FROM ANA 2022
Cardiovascular societies less apt to recognize women, minorities
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Major cardiovascular societies are more apt to give out awards to men and White individuals than to women and minorities, according to a look at 2 decades’ worth of data.
“Women received significantly fewer awards than men in all societies, countries, and award categories,” author Martha Gulati, MD, director of preventive cardiology at Smidt Heart Institute at Cedars-Sinai, Los Angeles, said in a news release. “This bias may be responsible for preventing underrepresented groups from ascending the academic ladder and receiving senior awards like lifetime achievement awards.”
The study was published online in the Journal of the American College of Cardiology.
A slow climb
The findings are based on a review of honors given from 2000 to 2021 by the ACC, the American Heart Association, the American Society of Echocardiography, the Society for Cardiovascular Angiography and Interventions, the Heart Rhythm Society, the European Society of Cardiology, and the Canadian Cardiovascular Society.
Among the 173 unique awards, 94 were given by the AHA, 27 by the HRS, 17 by the ACC, 16 by the CCS, 8 by the ASE, 7 by the ESC, and 4 by the SCAI. There were 3,044 recipients of these awards, including 2,830 unique awardees.
The vast majority of the awardees were White (75.2%), with Asian, Hispanic/Latino, and Black awardees representing just 18.9%, 4.5%, and 1.4% of the total awardees, respectively.
In a gender analysis, the researchers looked at 169 awards after excluding female-specific awards. These 169 awards were distributed to 2,995 recipients. More than three-quarters of these awardees (76.2%) were men, with women making up less than one-quarter (23.8%).
Encouragingly, there was an increasing trend in recognition of women over time, with 7.7% of female awardees in 2000 and climbing to 31.2% in 2021 (average annual percentage change, 6.6%; P < .05).
The distribution of awards also became more racially/ethnically diverse over time; in 2000, 92.3% of awardees were White versus 62.8% in 2021 (AAPC, –1.4%; P < .001).
There was also a significant increase in Asian (AAPC, 5.7%; P < .001), Hispanic/Latino (AAPC, 4.8%; P = .040), and Black (AAPC, 7.8%; P < .05) honorees.
Core influencers
By award type, women received fewer leadership awards than men, “which can be attributed to fewer leadership opportunities for women and a lack of acknowledgment of leadership responsibilities fulfilled by women,” the researchers said.
Award recipients with a PhD degree were nearly gender balanced (48.2% women), whereas men formed an overwhelming majority of awardees with an MD (84.7%).
Awards with male eponyms had fewer women recipients than did noneponymous awards (20.9% vs. 23.2%; P < .01).
“Male-eponymous awards can deter women applicants and give a subtle hint to selection committees to favor men as winners, creating an implicit bias,” the researchers said.
“Given the increased emphasis on redesigning cardiovascular health care delivery by incorporating the tenets of diversity, equity, and inclusion (DEI), cardiovascular societies have a significant role as core influencers,” Dr. Gulati and colleagues wrote.
They said that equitable award distribution can be a “key strategy to celebrate women and diverse members of the cardiovascular workforce and promulgate DEI.”
“Recognition of their contributions is pivotal to enhancing their self-perception. In addition to boosting confidence, receiving an award can also catalyze their career trajectory,” the authors added.
The study had no specific funding. The authors have declared no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Consider gaps in access and knowledge in diagnosis and treatment in skin of color
LAS VEGAS – and patients, Susan C. Taylor, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
Additionally, some disparities occur because of gaps in access to health care, said Dr. Taylor, vice chair, diversity, equity and inclusion, in the department of dermatology at the University of Pennsylvania, Philadelphia, who moderated an expert panel discussion of treatment tips for several common dermatologic conditions in skin of color patients.
Atopic dermatitis angles
Atopic dermatitis (AD) is the fourth most common dermatologic complaint in Black patients, based on data from the United States National Ambulatory Medical Care Survey. Also, data from the National Health and Nutrition Examination Survey show that Black children are nearly twice as likely as White children to develop AD after controlling for socioeconomic factors, Dr. Taylor said.
When Black patients present with AD, “you may not see the erythema,” said Valerie D. Callender, MD, of Howard University, Washington, who presented on AD. Instead, “you may see more follicular and papular presentations.” Erythema and erythroderma can present as shades of violet, gray, or dark brown in patients with rich skin tones, added Dr. Callender, who practices in Glenn Dale, Md.
Consequently, disease severity can be misinterpreted, she said, noting that data suggest that scoring systems such as the Eczema Area and Severity Index and Scoring Atopic Dermatitis underestimate AD severity in dark skin.
As for treatment, skin of color patients with AD are often as bothered by postinflammatory hyperpigmentation (PIH) as by active lesions, so treatment should take these concerns into account, Dr. Callender said. Studies evaluating the effectiveness of AD treatments in diverse populations are limited by lack of representation of racial groups in clinical trials and lack of subset analyses by race.
Acne awareness
An important consideration of acne in skin of color patients is that the acne “might not be red, it might just be darker,” said Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology, and professor of clinical dermatology at Weill Cornell Medicine, New York. A study published in JAMA Dermatology of nearly 30,000 patients with acne from 2007 to 2017 found that non-Hispanic Black patients were more likely than non-Hispanic White patients to see a dermatologist for acne, but Black patients received fewer prescriptions for acne medications than White patients.
The study also showed that Black patients who received prescriptions for acne were more likely to receive topical retinoids and topical antibiotics, and less likely to receive oral antibiotics, spironolactone, or isotretinoin, compared with White patients. Similarly, Asian patients were more likely to receive topical antibiotics and less likely to receive oral antibiotics, compared with White patients.
Other panelists shared some of their best practices for acne in patients with skin of color, including treatment with topical retinoids (for inflammation) and spironolactone, and therapies that address both inflammation and pigmentation, such as salicylic acid and azelaic acid. Dr. Callender also advised asking patients about makeup, as they may not know that many types of makeup used to cover acne are in fact comedogenic.
Melanoma misconceptions
One of the most common misperceptions about melanoma among skin of color patients is that they don’t think they can get it, Dr. Taylor said. Many health care providers don’t think about melanoma in skin of color patients because of the dramatically lower incidence in this population, but as a result, cases may go undiagnosed, and as studies have shown, the mortality rate from melanoma is higher in Black patients.
Consider the palms, soles, nails, and web spaces as possible melanoma sites, Dr. Taylor added.
Educating skin of color patients about melanoma is important, although the incidence is 20 to 30 times lower than in non-Hispanic Whites, said Nada Elbuluk, MD, the founder and director of the University of Southern California Skin of Color Center and Pigmentary Disorders Clinic, Los Angeles. A 2020 editorial published in Cancer Cytopathology pointed out that 1 in 3 Black men or women with a melanoma diagnosis in the United States dies of the disease, compared with 1 in 7 non-Hispanic White men and 1 in 11 non-Hispanic White women with melanoma.
Don’t skip the total body skin exam in these patients, Dr. Elbuluk emphasized. Many patients will only partially undress, and areas such as toes can be missed.
Rosacea review
For patients with skin of color, clinicians need to look for different signs of rosacea than those typically seen in White patients, Dr. Elbuluk said. “The most common presentation of rosacea in skin of color is papulopustular,” and the granulomatous variant.
“These patients will often give you a history of sensitivity to products,” Dr. Elbuluk noted. They may not always have the flushing, but they may report warmth or itching, in addition to product sensitivity.
When considering rosacea in skin of color patients, be sure to have good lighting for close examination, as skin thickening is another subtle sign of rosacea in these patients, she said. Skin thickening “is a very early sign that will present in skin of color with no erythema, so keep that in mind.”
Stinging and burning sensations may be reported by skin of color patients with rosacea. Use patient history to confirm the diagnosis of rosacea, which is often delayed in skin of color patients because of a low index of suspicion, she said.
Psoriasis pointers
Psoriasis in skin of color patients used to be considered rare, “but that is far from true,” Dr. Alexis said. In fact, many cases of psoriasis are undiagnosed or the diagnosis is delayed in these patients.
The panelists noted that current guidelines for psoriasis treatment are based on clinical trials composed mainly of White patients, and do not contain specific recommendations for skin of color patients.
Notably, the morphology, location, and color of psoriasis lesions may be different for patients with darker skin, such as thicker plaques and more scaling over larger areas, they said. Also, skin of color patients may experience long-lasting dyspigmentation from psoriasis lesions that have resolved.
When developing a strategy for psoriasis in skin of color patients, consider not only disease severity, but also comorbidities and medications, response (if any) to prior therapies, patient preferences, and quality of life, the panelists said.
Dr. Callender, Dr. Elbuluk, Dr. Taylor, and Dr. Alexis reported conflicts of interest from numerous sources in industry. MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – and patients, Susan C. Taylor, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
Additionally, some disparities occur because of gaps in access to health care, said Dr. Taylor, vice chair, diversity, equity and inclusion, in the department of dermatology at the University of Pennsylvania, Philadelphia, who moderated an expert panel discussion of treatment tips for several common dermatologic conditions in skin of color patients.
Atopic dermatitis angles
Atopic dermatitis (AD) is the fourth most common dermatologic complaint in Black patients, based on data from the United States National Ambulatory Medical Care Survey. Also, data from the National Health and Nutrition Examination Survey show that Black children are nearly twice as likely as White children to develop AD after controlling for socioeconomic factors, Dr. Taylor said.
When Black patients present with AD, “you may not see the erythema,” said Valerie D. Callender, MD, of Howard University, Washington, who presented on AD. Instead, “you may see more follicular and papular presentations.” Erythema and erythroderma can present as shades of violet, gray, or dark brown in patients with rich skin tones, added Dr. Callender, who practices in Glenn Dale, Md.
Consequently, disease severity can be misinterpreted, she said, noting that data suggest that scoring systems such as the Eczema Area and Severity Index and Scoring Atopic Dermatitis underestimate AD severity in dark skin.
As for treatment, skin of color patients with AD are often as bothered by postinflammatory hyperpigmentation (PIH) as by active lesions, so treatment should take these concerns into account, Dr. Callender said. Studies evaluating the effectiveness of AD treatments in diverse populations are limited by lack of representation of racial groups in clinical trials and lack of subset analyses by race.
Acne awareness
An important consideration of acne in skin of color patients is that the acne “might not be red, it might just be darker,” said Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology, and professor of clinical dermatology at Weill Cornell Medicine, New York. A study published in JAMA Dermatology of nearly 30,000 patients with acne from 2007 to 2017 found that non-Hispanic Black patients were more likely than non-Hispanic White patients to see a dermatologist for acne, but Black patients received fewer prescriptions for acne medications than White patients.
The study also showed that Black patients who received prescriptions for acne were more likely to receive topical retinoids and topical antibiotics, and less likely to receive oral antibiotics, spironolactone, or isotretinoin, compared with White patients. Similarly, Asian patients were more likely to receive topical antibiotics and less likely to receive oral antibiotics, compared with White patients.
Other panelists shared some of their best practices for acne in patients with skin of color, including treatment with topical retinoids (for inflammation) and spironolactone, and therapies that address both inflammation and pigmentation, such as salicylic acid and azelaic acid. Dr. Callender also advised asking patients about makeup, as they may not know that many types of makeup used to cover acne are in fact comedogenic.
Melanoma misconceptions
One of the most common misperceptions about melanoma among skin of color patients is that they don’t think they can get it, Dr. Taylor said. Many health care providers don’t think about melanoma in skin of color patients because of the dramatically lower incidence in this population, but as a result, cases may go undiagnosed, and as studies have shown, the mortality rate from melanoma is higher in Black patients.
Consider the palms, soles, nails, and web spaces as possible melanoma sites, Dr. Taylor added.
Educating skin of color patients about melanoma is important, although the incidence is 20 to 30 times lower than in non-Hispanic Whites, said Nada Elbuluk, MD, the founder and director of the University of Southern California Skin of Color Center and Pigmentary Disorders Clinic, Los Angeles. A 2020 editorial published in Cancer Cytopathology pointed out that 1 in 3 Black men or women with a melanoma diagnosis in the United States dies of the disease, compared with 1 in 7 non-Hispanic White men and 1 in 11 non-Hispanic White women with melanoma.
Don’t skip the total body skin exam in these patients, Dr. Elbuluk emphasized. Many patients will only partially undress, and areas such as toes can be missed.
Rosacea review
For patients with skin of color, clinicians need to look for different signs of rosacea than those typically seen in White patients, Dr. Elbuluk said. “The most common presentation of rosacea in skin of color is papulopustular,” and the granulomatous variant.
“These patients will often give you a history of sensitivity to products,” Dr. Elbuluk noted. They may not always have the flushing, but they may report warmth or itching, in addition to product sensitivity.
When considering rosacea in skin of color patients, be sure to have good lighting for close examination, as skin thickening is another subtle sign of rosacea in these patients, she said. Skin thickening “is a very early sign that will present in skin of color with no erythema, so keep that in mind.”
Stinging and burning sensations may be reported by skin of color patients with rosacea. Use patient history to confirm the diagnosis of rosacea, which is often delayed in skin of color patients because of a low index of suspicion, she said.
Psoriasis pointers
Psoriasis in skin of color patients used to be considered rare, “but that is far from true,” Dr. Alexis said. In fact, many cases of psoriasis are undiagnosed or the diagnosis is delayed in these patients.
The panelists noted that current guidelines for psoriasis treatment are based on clinical trials composed mainly of White patients, and do not contain specific recommendations for skin of color patients.
Notably, the morphology, location, and color of psoriasis lesions may be different for patients with darker skin, such as thicker plaques and more scaling over larger areas, they said. Also, skin of color patients may experience long-lasting dyspigmentation from psoriasis lesions that have resolved.
When developing a strategy for psoriasis in skin of color patients, consider not only disease severity, but also comorbidities and medications, response (if any) to prior therapies, patient preferences, and quality of life, the panelists said.
Dr. Callender, Dr. Elbuluk, Dr. Taylor, and Dr. Alexis reported conflicts of interest from numerous sources in industry. MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – and patients, Susan C. Taylor, MD, said in a presentation at MedscapeLive’s annual Las Vegas Dermatology Seminar.
Additionally, some disparities occur because of gaps in access to health care, said Dr. Taylor, vice chair, diversity, equity and inclusion, in the department of dermatology at the University of Pennsylvania, Philadelphia, who moderated an expert panel discussion of treatment tips for several common dermatologic conditions in skin of color patients.
Atopic dermatitis angles
Atopic dermatitis (AD) is the fourth most common dermatologic complaint in Black patients, based on data from the United States National Ambulatory Medical Care Survey. Also, data from the National Health and Nutrition Examination Survey show that Black children are nearly twice as likely as White children to develop AD after controlling for socioeconomic factors, Dr. Taylor said.
When Black patients present with AD, “you may not see the erythema,” said Valerie D. Callender, MD, of Howard University, Washington, who presented on AD. Instead, “you may see more follicular and papular presentations.” Erythema and erythroderma can present as shades of violet, gray, or dark brown in patients with rich skin tones, added Dr. Callender, who practices in Glenn Dale, Md.
Consequently, disease severity can be misinterpreted, she said, noting that data suggest that scoring systems such as the Eczema Area and Severity Index and Scoring Atopic Dermatitis underestimate AD severity in dark skin.
As for treatment, skin of color patients with AD are often as bothered by postinflammatory hyperpigmentation (PIH) as by active lesions, so treatment should take these concerns into account, Dr. Callender said. Studies evaluating the effectiveness of AD treatments in diverse populations are limited by lack of representation of racial groups in clinical trials and lack of subset analyses by race.
Acne awareness
An important consideration of acne in skin of color patients is that the acne “might not be red, it might just be darker,” said Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology, and professor of clinical dermatology at Weill Cornell Medicine, New York. A study published in JAMA Dermatology of nearly 30,000 patients with acne from 2007 to 2017 found that non-Hispanic Black patients were more likely than non-Hispanic White patients to see a dermatologist for acne, but Black patients received fewer prescriptions for acne medications than White patients.
The study also showed that Black patients who received prescriptions for acne were more likely to receive topical retinoids and topical antibiotics, and less likely to receive oral antibiotics, spironolactone, or isotretinoin, compared with White patients. Similarly, Asian patients were more likely to receive topical antibiotics and less likely to receive oral antibiotics, compared with White patients.
Other panelists shared some of their best practices for acne in patients with skin of color, including treatment with topical retinoids (for inflammation) and spironolactone, and therapies that address both inflammation and pigmentation, such as salicylic acid and azelaic acid. Dr. Callender also advised asking patients about makeup, as they may not know that many types of makeup used to cover acne are in fact comedogenic.
Melanoma misconceptions
One of the most common misperceptions about melanoma among skin of color patients is that they don’t think they can get it, Dr. Taylor said. Many health care providers don’t think about melanoma in skin of color patients because of the dramatically lower incidence in this population, but as a result, cases may go undiagnosed, and as studies have shown, the mortality rate from melanoma is higher in Black patients.
Consider the palms, soles, nails, and web spaces as possible melanoma sites, Dr. Taylor added.
Educating skin of color patients about melanoma is important, although the incidence is 20 to 30 times lower than in non-Hispanic Whites, said Nada Elbuluk, MD, the founder and director of the University of Southern California Skin of Color Center and Pigmentary Disorders Clinic, Los Angeles. A 2020 editorial published in Cancer Cytopathology pointed out that 1 in 3 Black men or women with a melanoma diagnosis in the United States dies of the disease, compared with 1 in 7 non-Hispanic White men and 1 in 11 non-Hispanic White women with melanoma.
Don’t skip the total body skin exam in these patients, Dr. Elbuluk emphasized. Many patients will only partially undress, and areas such as toes can be missed.
Rosacea review
For patients with skin of color, clinicians need to look for different signs of rosacea than those typically seen in White patients, Dr. Elbuluk said. “The most common presentation of rosacea in skin of color is papulopustular,” and the granulomatous variant.
“These patients will often give you a history of sensitivity to products,” Dr. Elbuluk noted. They may not always have the flushing, but they may report warmth or itching, in addition to product sensitivity.
When considering rosacea in skin of color patients, be sure to have good lighting for close examination, as skin thickening is another subtle sign of rosacea in these patients, she said. Skin thickening “is a very early sign that will present in skin of color with no erythema, so keep that in mind.”
Stinging and burning sensations may be reported by skin of color patients with rosacea. Use patient history to confirm the diagnosis of rosacea, which is often delayed in skin of color patients because of a low index of suspicion, she said.
Psoriasis pointers
Psoriasis in skin of color patients used to be considered rare, “but that is far from true,” Dr. Alexis said. In fact, many cases of psoriasis are undiagnosed or the diagnosis is delayed in these patients.
The panelists noted that current guidelines for psoriasis treatment are based on clinical trials composed mainly of White patients, and do not contain specific recommendations for skin of color patients.
Notably, the morphology, location, and color of psoriasis lesions may be different for patients with darker skin, such as thicker plaques and more scaling over larger areas, they said. Also, skin of color patients may experience long-lasting dyspigmentation from psoriasis lesions that have resolved.
When developing a strategy for psoriasis in skin of color patients, consider not only disease severity, but also comorbidities and medications, response (if any) to prior therapies, patient preferences, and quality of life, the panelists said.
Dr. Callender, Dr. Elbuluk, Dr. Taylor, and Dr. Alexis reported conflicts of interest from numerous sources in industry. MedscapeLive and this news organization are owned by the same parent company.
AT INNOVATIONS IN DERMATOLOGY
Chronic stress, especially race related, may hasten cancer death
The American folk hero John Henry pitted his hammer against a mechanical steam drill, only to die of exhaustion after winning the battle. In the legend, John Henry was African American, and it’s a fitting metaphor, according to Justin Xavier Moore, PhD.
It’s a metaphor for accumulated stress over a lifetime, also known as allostatic load. Though it affects everyone, Black, Indigenous, and people of color experience it in excess. “It serves as a symbolism for the plight of African Americans within the United States, that regardless of all the triumph and trying to overcompensate and work just as hard as your counterpart, it oftentimes leads to this overtaxing or exhaustion because your competitor has an unfair advantage. You have Jim Crow laws in the South. We have the history of slavery. We have individuals of racial subgroups that are exposed daily to microaggressions, racial discrimination, stereotypes, redlining, all of these different issues that basically reduce to systemic racism,” said Dr. Moore, who is an assistant professor of medicine at the Medical College of Georgia, Augusta.
Dr. Moore is also a coauthor of a new study published online in SSM–Population Health, which examined the association between increased allostatic load and cancer outcomes among participants in the National Health and Nutrition Examination Survey (NHANES) and the National Death Index. They found that both non-Hispanic Black and non-Hispanic White adults with high allostatic load had about a doubled risk of cancer death.
To determine allostatic load, the researchers looked at nine factors collected in NHANES: abnormal values of BMI, diastolic blood pressure, glycohemoglobin, systolic blood pressure, total cholesterol, serum triglycerides, serum albumin, serum creatinine, and C-reactive protein. “The fact that we’re looking at cardiovascular, metabolic and immune function, all in one gives us a better risk assessment for morbidity and mortality. Allostatic load has actually been associated with cardiovascular disease. I think we are one of the first studies to actually look at whether allostatic load is associated with cancer mortality,” said Dr. Moore.
Previous research coauthored by Dr. Moore showed 20-year old African Americans have an allostatic load comparable with that seen in 30-year-old non-Hispanic Whites. That can lead to a proinflammatory state that might be causing increased cancer risk. But stress isn’t a simple concept to pin down, Dr. Moore said. “One of the founding fathers of public health research and epidemiology, Paracelsus, [said] ‘the dose makes the poison.’ ”
In this case, it means that not all stress is bad. Exercise is good stress. “Your heart rate goes up, you compete, and then it comes back down. That’s healthy. But then there’s those stressful situations like dealing with a horrible job, and a boss that may just be overdemanding. Deadlines, and not having a work-life balance. Too much stress, in this case, can cause cancer death,” Dr. Moore said.
In the study, both non-Hispanic Black adults and non-Hispanic White adults heightened risk of cancer death when dealing with high allostatic load, even though the cause of stress may be different. “It’s almost like the cause of the stress does not matter as much. There are millions of Americans that live in environments that are not conducive to their health. The fact of the matter is that because of racial discrimination, because all these different biases, African Americans may have higher allostatic load, which they did on an average, but high allostatic load for even White people is associated with dying from cancer,” Dr. Moore said.
After adjustment, the (adjusted subdistributed hazard ratio, 1.14; 95% CI, 1.04-1.26). After stratification by age, high allostatic load was associated with an 80% increased risk of cancer death among adults (SHR, 1.80; 95% CI, 1.35-2.41). Non-Hispanic White adults had a 95% increased risk (SHR, 1.95; 95% CI, 1.22-3.12), non-Hispanic Black adults had a twofold increased risk (SHR, 1.06; 95% CI, 1.27-3.34), and Hispanic adults had a 36% increased risk.
Dr. Moore has no relevant financial disclosures.
The American folk hero John Henry pitted his hammer against a mechanical steam drill, only to die of exhaustion after winning the battle. In the legend, John Henry was African American, and it’s a fitting metaphor, according to Justin Xavier Moore, PhD.
It’s a metaphor for accumulated stress over a lifetime, also known as allostatic load. Though it affects everyone, Black, Indigenous, and people of color experience it in excess. “It serves as a symbolism for the plight of African Americans within the United States, that regardless of all the triumph and trying to overcompensate and work just as hard as your counterpart, it oftentimes leads to this overtaxing or exhaustion because your competitor has an unfair advantage. You have Jim Crow laws in the South. We have the history of slavery. We have individuals of racial subgroups that are exposed daily to microaggressions, racial discrimination, stereotypes, redlining, all of these different issues that basically reduce to systemic racism,” said Dr. Moore, who is an assistant professor of medicine at the Medical College of Georgia, Augusta.
Dr. Moore is also a coauthor of a new study published online in SSM–Population Health, which examined the association between increased allostatic load and cancer outcomes among participants in the National Health and Nutrition Examination Survey (NHANES) and the National Death Index. They found that both non-Hispanic Black and non-Hispanic White adults with high allostatic load had about a doubled risk of cancer death.
To determine allostatic load, the researchers looked at nine factors collected in NHANES: abnormal values of BMI, diastolic blood pressure, glycohemoglobin, systolic blood pressure, total cholesterol, serum triglycerides, serum albumin, serum creatinine, and C-reactive protein. “The fact that we’re looking at cardiovascular, metabolic and immune function, all in one gives us a better risk assessment for morbidity and mortality. Allostatic load has actually been associated with cardiovascular disease. I think we are one of the first studies to actually look at whether allostatic load is associated with cancer mortality,” said Dr. Moore.
Previous research coauthored by Dr. Moore showed 20-year old African Americans have an allostatic load comparable with that seen in 30-year-old non-Hispanic Whites. That can lead to a proinflammatory state that might be causing increased cancer risk. But stress isn’t a simple concept to pin down, Dr. Moore said. “One of the founding fathers of public health research and epidemiology, Paracelsus, [said] ‘the dose makes the poison.’ ”
In this case, it means that not all stress is bad. Exercise is good stress. “Your heart rate goes up, you compete, and then it comes back down. That’s healthy. But then there’s those stressful situations like dealing with a horrible job, and a boss that may just be overdemanding. Deadlines, and not having a work-life balance. Too much stress, in this case, can cause cancer death,” Dr. Moore said.
In the study, both non-Hispanic Black adults and non-Hispanic White adults heightened risk of cancer death when dealing with high allostatic load, even though the cause of stress may be different. “It’s almost like the cause of the stress does not matter as much. There are millions of Americans that live in environments that are not conducive to their health. The fact of the matter is that because of racial discrimination, because all these different biases, African Americans may have higher allostatic load, which they did on an average, but high allostatic load for even White people is associated with dying from cancer,” Dr. Moore said.
After adjustment, the (adjusted subdistributed hazard ratio, 1.14; 95% CI, 1.04-1.26). After stratification by age, high allostatic load was associated with an 80% increased risk of cancer death among adults (SHR, 1.80; 95% CI, 1.35-2.41). Non-Hispanic White adults had a 95% increased risk (SHR, 1.95; 95% CI, 1.22-3.12), non-Hispanic Black adults had a twofold increased risk (SHR, 1.06; 95% CI, 1.27-3.34), and Hispanic adults had a 36% increased risk.
Dr. Moore has no relevant financial disclosures.
The American folk hero John Henry pitted his hammer against a mechanical steam drill, only to die of exhaustion after winning the battle. In the legend, John Henry was African American, and it’s a fitting metaphor, according to Justin Xavier Moore, PhD.
It’s a metaphor for accumulated stress over a lifetime, also known as allostatic load. Though it affects everyone, Black, Indigenous, and people of color experience it in excess. “It serves as a symbolism for the plight of African Americans within the United States, that regardless of all the triumph and trying to overcompensate and work just as hard as your counterpart, it oftentimes leads to this overtaxing or exhaustion because your competitor has an unfair advantage. You have Jim Crow laws in the South. We have the history of slavery. We have individuals of racial subgroups that are exposed daily to microaggressions, racial discrimination, stereotypes, redlining, all of these different issues that basically reduce to systemic racism,” said Dr. Moore, who is an assistant professor of medicine at the Medical College of Georgia, Augusta.
Dr. Moore is also a coauthor of a new study published online in SSM–Population Health, which examined the association between increased allostatic load and cancer outcomes among participants in the National Health and Nutrition Examination Survey (NHANES) and the National Death Index. They found that both non-Hispanic Black and non-Hispanic White adults with high allostatic load had about a doubled risk of cancer death.
To determine allostatic load, the researchers looked at nine factors collected in NHANES: abnormal values of BMI, diastolic blood pressure, glycohemoglobin, systolic blood pressure, total cholesterol, serum triglycerides, serum albumin, serum creatinine, and C-reactive protein. “The fact that we’re looking at cardiovascular, metabolic and immune function, all in one gives us a better risk assessment for morbidity and mortality. Allostatic load has actually been associated with cardiovascular disease. I think we are one of the first studies to actually look at whether allostatic load is associated with cancer mortality,” said Dr. Moore.
Previous research coauthored by Dr. Moore showed 20-year old African Americans have an allostatic load comparable with that seen in 30-year-old non-Hispanic Whites. That can lead to a proinflammatory state that might be causing increased cancer risk. But stress isn’t a simple concept to pin down, Dr. Moore said. “One of the founding fathers of public health research and epidemiology, Paracelsus, [said] ‘the dose makes the poison.’ ”
In this case, it means that not all stress is bad. Exercise is good stress. “Your heart rate goes up, you compete, and then it comes back down. That’s healthy. But then there’s those stressful situations like dealing with a horrible job, and a boss that may just be overdemanding. Deadlines, and not having a work-life balance. Too much stress, in this case, can cause cancer death,” Dr. Moore said.
In the study, both non-Hispanic Black adults and non-Hispanic White adults heightened risk of cancer death when dealing with high allostatic load, even though the cause of stress may be different. “It’s almost like the cause of the stress does not matter as much. There are millions of Americans that live in environments that are not conducive to their health. The fact of the matter is that because of racial discrimination, because all these different biases, African Americans may have higher allostatic load, which they did on an average, but high allostatic load for even White people is associated with dying from cancer,” Dr. Moore said.
After adjustment, the (adjusted subdistributed hazard ratio, 1.14; 95% CI, 1.04-1.26). After stratification by age, high allostatic load was associated with an 80% increased risk of cancer death among adults (SHR, 1.80; 95% CI, 1.35-2.41). Non-Hispanic White adults had a 95% increased risk (SHR, 1.95; 95% CI, 1.22-3.12), non-Hispanic Black adults had a twofold increased risk (SHR, 1.06; 95% CI, 1.27-3.34), and Hispanic adults had a 36% increased risk.
Dr. Moore has no relevant financial disclosures.
FROM SSM–POPULATION HEALTH
Florida medical boards ban transgender care for minors
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Florida’s two main medical bodies have voted to stop gender-affirming treatment of children, including the use of puberty blockers, cross-sex hormones, and surgery, other than in minors who are already receiving such care.
The move, which is unprecedented, makes Florida one of several U.S. states to restrict gender-affirming care for adolescents, but the first to do so via an administrative process, through the actions of its Board of Medicine and Board of Osteopathic Medicine.
“I appreciate the integrity of the Boards for ruling in the best interest of children in Florida despite facing tremendous pressure to permit these unproven and risky treatments,” Florida Surgeon General Joseph Ladapo, MD, PhD, said in a statement.
In a statement, The Endocrine Society criticizes the decision as “blatantly discriminatory” and not based on medical evidence.
During a meeting on Oct. 28 that involved testimonies from doctors, parents of transgender children, detransitioners, and patients, board members referred to similar changes in Europe, where some countries have pushed psychotherapy instead of surgery or hormone treatment.
Then, on Nov. 4, the boards each set slightly different instructions, with the Board of Osteopathic Medicine voting to restrict care for new patients but allowing an exception for children enrolled in clinical studies, which “must include long-term longitudinal assessments of the patients’ physiologic and psychologic outcomes,” according to the Florida Department of Health.
The Board of Medicine did not allow the latter.
The proposed rules are open to public comment before finalization.
Arkansas was the first state to enact such a ban on gender-affirming care, with Republican lawmakers in 2021 overriding GOP Gov. Asa Hutchinson’s veto of the legislation. Alabama Republicans in 2022 approved legislation to outlaw gender-affirming medications for transgender youths. Both laws have been paused amid unfolding legal battles, according to Associated Press.
Oklahoma Gov. Kevin Stitt, a Republican, signed a bill in October that bars federal funds earmarked for the University of Oklahoma Medical Center from being used for gender reassignment treatments for minors. Gov. Stitt also called for the legislature to ban some of those gender reassignment treatments statewide when it returns in February.
Top Tennessee Republicans also have vowed to push for strict antitransgender policies. The state already bans doctors from providing gender-confirming hormone treatment to prepubescent minors. To date, no one has legally challenged the law as medical experts maintain no doctor in Tennessee does so.
A version of this article first appeared on Medscape.com.
Physicians react: Climate change and other social issues
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
Around half of them rated climate change among their five most important issues. Slightly lower percentages of doctors prioritized domestic violence and immigration/refugee policies that highly, and about 40% did so regarding reproductive rights in the United States.
Survey responses and comments left on the Physicians’ Views on Today’s Divisive Social Issues 2022 report provide insights into doctors’ attitudes and thinking about these four social challenges.
Relevance of climate change to health care
In the Medscape report, 61% of physicians described themselves as “very concerned” or “concerned” about climate change, and about 7 in 10 agreed with the statement that it should be a top worldwide priority. “Climate change is the most pressing issue of this century,” a psychiatrist respondent wrote.
What about direct effects on patients’ health? An internist worried that rising temperatures will cause “pathogens to spread and infect disadvantaged people who do not have health access and have immunocompromised conditions.” A family medicine physician predicted “more weather disasters, more asthma, more hormonal changes, and more obesity.”
However, physician viewpoints ran the gamut with an issue that has become politically and emotionally charged. Descriptions such as “overblown,” “hysteria,” “hoax,” and “farce” were used. “Climate change is a natural phenomenon under God’s purview,” an emergency medicine physician said.
And there was some middle-ground thinking. “It’s overstated but quite real,” a pediatrician respondent wrote. Added an ophthalmologist: “It has gone on for ages. We must work to decrease man-made conditions that affect climate change, but it must be done in an intelligent fashion.”
Domestic violence: What physicians can do
About 7 in 10 physicians surveyed by Medscape said they don’t think the United States is adequately tackling domestic violence. “It is underrecognized and ignored,” a psychiatrist respondent argued. The problem is “rampant and unacceptable, pushed into a closet and normalized, with associated shame,” an emergency medicine doctor wrote.
Many respondents noted that physicians are under a mandate to report abuse of or a suspicious injury to a patient. Some shared anecdotes about how they reported action they had taken when they suspected it. “I’ve told patients who may be in dangerous situations that I’m a safe person and provide a safe space,” a radiologist added. An internist said, “I’ve recently started to ask about safety at home during triage on every patient.”
Other doctors bemoaned a lack of adequate education on detecting and managing domestic violence and abuse. “Domestic violence is often not recognized by health care providers,” a psychiatrist respondent observed.
Expanding legal immigration
In the Medscape report, 34% of physicians felt U.S. immigration/refugee policies need to be tougher, while 28% said they are too restrictive, and about a fifth saw them as appropriate.
“As an immigrant, I can tell you that the system is flawed and needs a complete overhaul, which will take a bipartisan effort,” an endocrinologist respondent wrote.
A number of respondents argued that it’s critical to simplify the process of obtaining U.S. citizenship so that fewer will feel forced to enter the country illegally. “For a country that relies very heavily on immigrants to sustain our health care system, we behave like idiots in denying safe harbor,” a nephrologist asserted.
A neurologist concurred. “Legal immigration needs to be encouraged. It should be easier to exchange visitor or student visa to immigrant visa in order to retain talent in the health care and technology fields, which would alleviate the shortage of workers in health care.”
Reproductive rights: No easy answers
Medscape’s survey was conducted before the U.S. Supreme Court in June reversed Roe v. Wade. In the report, 71% of physicians described themselves as very to somewhat concerned about women’s reproductive rights, but their viewpoints became nuanced after that. “There is a big disparity among physicians on this topic,” an oncologist respondent wrote.
At one end of the spectrum, 3% of doctors felt that abortions should never be permitted. “The human baby in the womb is an independent person with the right to life,” a pathologist said. At the other end, nearly one-fourth of physicians believed abortion should be accessible under all circumstances, regardless of trimester or reason. “I am just here to support the woman and make her decision a reality,” an internist said.
While saying an abortion should be granted after “fetal viability” only “in extenuating circumstances,” an ob.gyn. respondent said she is “extremely concerned” about attacks on abortion rights. “Some of us are old enough to remember women coming to the ER in extremis after illegal procedures, prior to Roe v. Wade.”
A version of this article first appeared on Medscape.com.
DTC telemedicine expands access to gender-affirming therapy
Direct-to-consumer telemedicine services that provide gender-affirming hormone therapy appear to follow evidence-based guidelines and charge about the same as brick-and-mortar medical centers, according to researchers who reviewed the platforms’ websites.
The findings suggest that virtual care “may be a good option” for transgender, nonbinary, and intersex people, who often report difficulty finding physicians they trust, Erin Jesse, MD, a fifth-year urology resident at University Hospitals Cleveland Medical Center, who is the first author of the study, told this news organization.
Dr. Jesse’s group presented their findings at a joint scientific meeting of the Sexual Medicine Society of North America and the International Society for Sexual Medicine in Miami. The results have not been published in a peer-reviewed journal.
New direct-to-consumer telemedicine companies have emerged with gender-diverse staff and services tailored to the needs of these individuals. They offer “a more inclusive feel” than might be encountered at a physician’s office, Dr. Jesse said.
Confirming that these companies adhere to standards of care and cost-effectiveness “is especially important considering the reduced access to care and potentially increased vulnerability of the gender-diverse population,” she and her colleagues wrote.
From a Google search in March, the team identified six U.S.-based platforms that offer gender-affirming medical therapy: FOLX, True U Clinic, QueerDoc, Queer Med, TransClinique, and Plume.
From information posted on the companies’ websites, the researchers determined that all aligned with the World Professional Association for Transgender Health’s Standards of Care in two areas: use of an informed consent model to ensure that patients have sufficient information and understanding to decide on their own treatment and endorsement of frequent laboratory monitoring of hormone levels in early stages of treatment.
The team also compared the costs listed on the websites for the first year of therapy to the costs of similar care at a tertiary center, as determined using University Hospitals Cleveland Medical Center’s online estimator.
The platforms offered various pricing models, including fee-for-service and monthly membership plans ranging from $59 to $139. For individuals without insurance, estimates ranged from $1,022 to $1,428 for oral estradiol and from $1,184 to $1,668 for intramuscular testosterone from the online companies, compared with $1,184 and $1,216, respectively, at the tertiary center.
Although some platforms accept insurance, the researchers were not able to evaluate the cost of using private insurance or Medicaid, Dr. Jesse said. She noted that transgender individuals are more likely to lack insurance than are cisgender patients.
The team also assessed the scope of services. All companies offered legal help with changes to names and gender markers, such as “M” and “F.” Three or more companies offered preexposure prophylaxis to prevent HIV infection, treatment for erectile dysfunction, referrals for surgery, and medical letters of support for surgery.
Two offered puberty blockers, although the researchers were unable to determine the risk of adolescents obtaining treatment without proper assessments, because details of those services are not disclosed on websites, Dr. Jesse said.
An avenue of further research would be to interview patients to learn how platforms operate in practice and whether patients are properly assessed before treatment. “Those sorts of questions we can’t answer just by looking at the websites,” she said.
However, Charlotte Hoffman, JD, senior policy counsel for the National Center for Transgender Equality, an advocacy group, said she does not harbor concerns about patients being treated inappropriately simply because care is virtual. All clinicians who provide gender-affirming care face potential repercussions, such as malpractice lawsuits or state disciplinary action, if they veer from treatment guidelines, she said.
“I don’t necessarily take the premise that telehealth is inherently worse than in-person care as a given,” Ms. Hoffman said.
During the COVID-19 pandemic, Ms. Hoffman added, direct-to-consumer telemedicine has expanded access for individuals in rural areas, people with disabilities, and those who live in places where in-person providers of transgender care face public hostility, although individuals without the resources to pay may still be left out.
What might happen to that access if telemedicine restrictions that were loosened during the pandemic are reinstated is unclear, she said.
The researchers and Ms. Hoffman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Direct-to-consumer telemedicine services that provide gender-affirming hormone therapy appear to follow evidence-based guidelines and charge about the same as brick-and-mortar medical centers, according to researchers who reviewed the platforms’ websites.
The findings suggest that virtual care “may be a good option” for transgender, nonbinary, and intersex people, who often report difficulty finding physicians they trust, Erin Jesse, MD, a fifth-year urology resident at University Hospitals Cleveland Medical Center, who is the first author of the study, told this news organization.
Dr. Jesse’s group presented their findings at a joint scientific meeting of the Sexual Medicine Society of North America and the International Society for Sexual Medicine in Miami. The results have not been published in a peer-reviewed journal.
New direct-to-consumer telemedicine companies have emerged with gender-diverse staff and services tailored to the needs of these individuals. They offer “a more inclusive feel” than might be encountered at a physician’s office, Dr. Jesse said.
Confirming that these companies adhere to standards of care and cost-effectiveness “is especially important considering the reduced access to care and potentially increased vulnerability of the gender-diverse population,” she and her colleagues wrote.
From a Google search in March, the team identified six U.S.-based platforms that offer gender-affirming medical therapy: FOLX, True U Clinic, QueerDoc, Queer Med, TransClinique, and Plume.
From information posted on the companies’ websites, the researchers determined that all aligned with the World Professional Association for Transgender Health’s Standards of Care in two areas: use of an informed consent model to ensure that patients have sufficient information and understanding to decide on their own treatment and endorsement of frequent laboratory monitoring of hormone levels in early stages of treatment.
The team also compared the costs listed on the websites for the first year of therapy to the costs of similar care at a tertiary center, as determined using University Hospitals Cleveland Medical Center’s online estimator.
The platforms offered various pricing models, including fee-for-service and monthly membership plans ranging from $59 to $139. For individuals without insurance, estimates ranged from $1,022 to $1,428 for oral estradiol and from $1,184 to $1,668 for intramuscular testosterone from the online companies, compared with $1,184 and $1,216, respectively, at the tertiary center.
Although some platforms accept insurance, the researchers were not able to evaluate the cost of using private insurance or Medicaid, Dr. Jesse said. She noted that transgender individuals are more likely to lack insurance than are cisgender patients.
The team also assessed the scope of services. All companies offered legal help with changes to names and gender markers, such as “M” and “F.” Three or more companies offered preexposure prophylaxis to prevent HIV infection, treatment for erectile dysfunction, referrals for surgery, and medical letters of support for surgery.
Two offered puberty blockers, although the researchers were unable to determine the risk of adolescents obtaining treatment without proper assessments, because details of those services are not disclosed on websites, Dr. Jesse said.
An avenue of further research would be to interview patients to learn how platforms operate in practice and whether patients are properly assessed before treatment. “Those sorts of questions we can’t answer just by looking at the websites,” she said.
However, Charlotte Hoffman, JD, senior policy counsel for the National Center for Transgender Equality, an advocacy group, said she does not harbor concerns about patients being treated inappropriately simply because care is virtual. All clinicians who provide gender-affirming care face potential repercussions, such as malpractice lawsuits or state disciplinary action, if they veer from treatment guidelines, she said.
“I don’t necessarily take the premise that telehealth is inherently worse than in-person care as a given,” Ms. Hoffman said.
During the COVID-19 pandemic, Ms. Hoffman added, direct-to-consumer telemedicine has expanded access for individuals in rural areas, people with disabilities, and those who live in places where in-person providers of transgender care face public hostility, although individuals without the resources to pay may still be left out.
What might happen to that access if telemedicine restrictions that were loosened during the pandemic are reinstated is unclear, she said.
The researchers and Ms. Hoffman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Direct-to-consumer telemedicine services that provide gender-affirming hormone therapy appear to follow evidence-based guidelines and charge about the same as brick-and-mortar medical centers, according to researchers who reviewed the platforms’ websites.
The findings suggest that virtual care “may be a good option” for transgender, nonbinary, and intersex people, who often report difficulty finding physicians they trust, Erin Jesse, MD, a fifth-year urology resident at University Hospitals Cleveland Medical Center, who is the first author of the study, told this news organization.
Dr. Jesse’s group presented their findings at a joint scientific meeting of the Sexual Medicine Society of North America and the International Society for Sexual Medicine in Miami. The results have not been published in a peer-reviewed journal.
New direct-to-consumer telemedicine companies have emerged with gender-diverse staff and services tailored to the needs of these individuals. They offer “a more inclusive feel” than might be encountered at a physician’s office, Dr. Jesse said.
Confirming that these companies adhere to standards of care and cost-effectiveness “is especially important considering the reduced access to care and potentially increased vulnerability of the gender-diverse population,” she and her colleagues wrote.
From a Google search in March, the team identified six U.S.-based platforms that offer gender-affirming medical therapy: FOLX, True U Clinic, QueerDoc, Queer Med, TransClinique, and Plume.
From information posted on the companies’ websites, the researchers determined that all aligned with the World Professional Association for Transgender Health’s Standards of Care in two areas: use of an informed consent model to ensure that patients have sufficient information and understanding to decide on their own treatment and endorsement of frequent laboratory monitoring of hormone levels in early stages of treatment.
The team also compared the costs listed on the websites for the first year of therapy to the costs of similar care at a tertiary center, as determined using University Hospitals Cleveland Medical Center’s online estimator.
The platforms offered various pricing models, including fee-for-service and monthly membership plans ranging from $59 to $139. For individuals without insurance, estimates ranged from $1,022 to $1,428 for oral estradiol and from $1,184 to $1,668 for intramuscular testosterone from the online companies, compared with $1,184 and $1,216, respectively, at the tertiary center.
Although some platforms accept insurance, the researchers were not able to evaluate the cost of using private insurance or Medicaid, Dr. Jesse said. She noted that transgender individuals are more likely to lack insurance than are cisgender patients.
The team also assessed the scope of services. All companies offered legal help with changes to names and gender markers, such as “M” and “F.” Three or more companies offered preexposure prophylaxis to prevent HIV infection, treatment for erectile dysfunction, referrals for surgery, and medical letters of support for surgery.
Two offered puberty blockers, although the researchers were unable to determine the risk of adolescents obtaining treatment without proper assessments, because details of those services are not disclosed on websites, Dr. Jesse said.
An avenue of further research would be to interview patients to learn how platforms operate in practice and whether patients are properly assessed before treatment. “Those sorts of questions we can’t answer just by looking at the websites,” she said.
However, Charlotte Hoffman, JD, senior policy counsel for the National Center for Transgender Equality, an advocacy group, said she does not harbor concerns about patients being treated inappropriately simply because care is virtual. All clinicians who provide gender-affirming care face potential repercussions, such as malpractice lawsuits or state disciplinary action, if they veer from treatment guidelines, she said.
“I don’t necessarily take the premise that telehealth is inherently worse than in-person care as a given,” Ms. Hoffman said.
During the COVID-19 pandemic, Ms. Hoffman added, direct-to-consumer telemedicine has expanded access for individuals in rural areas, people with disabilities, and those who live in places where in-person providers of transgender care face public hostility, although individuals without the resources to pay may still be left out.
What might happen to that access if telemedicine restrictions that were loosened during the pandemic are reinstated is unclear, she said.
The researchers and Ms. Hoffman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Academic dermatology: Gender diversity advances as some gaps persist
, according to a recent cross-sectional study.
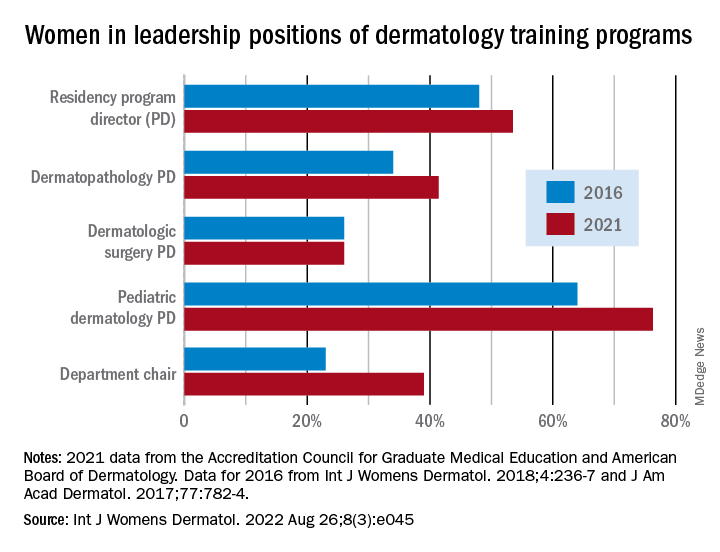
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
, according to a recent cross-sectional study.
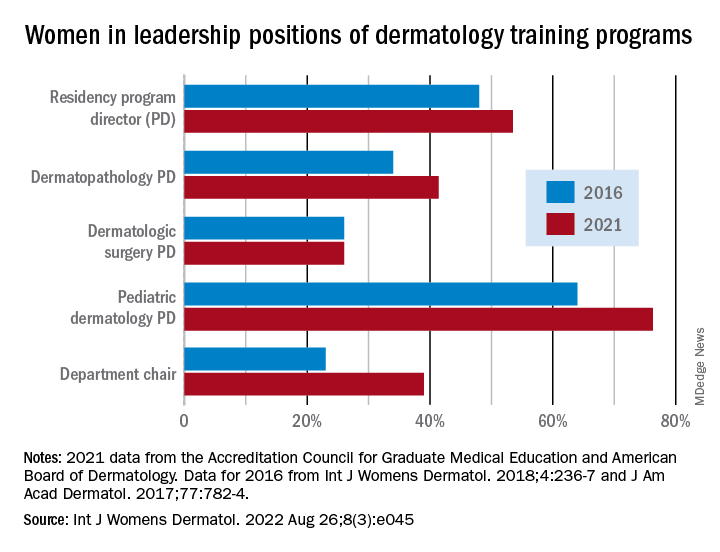
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
, according to a recent cross-sectional study.
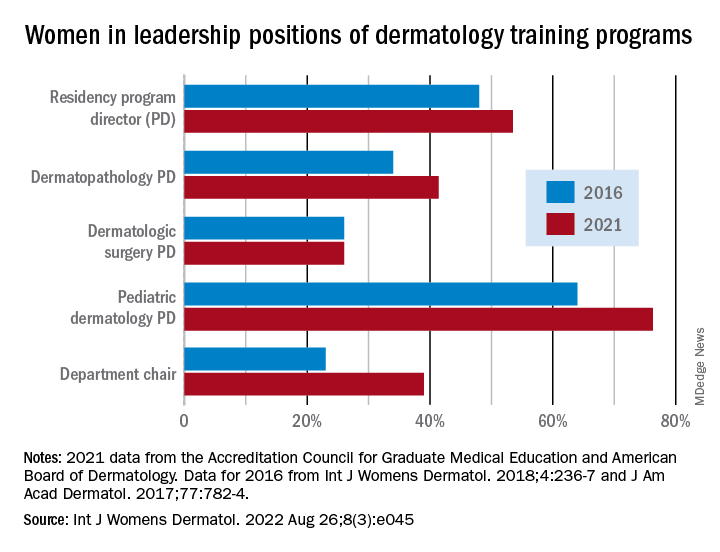
Although women made up more than half of the dermatology residency program directors (53.5%), associate directors (62.6%), and assistant directors (58.3%) in 2021, those numbers fall short of women’s majority (65% in 2018) among the trainees themselves, Yasmine Abushukur of Oakland University in Rochester, Mich., and associates said in a research letter.
Advancements were “made in gender diversity within academic dermatology from 2016 to 2021, [but] women remain underrepresented, particularly in leadership of dermatopathology and dermatologic surgery fellowships,” the investigators wrote.
Data gathered from 142 dermatology residency programs accredited by the Accreditation Council for Graduate Medical Education show that progress has been made since 2016, at least among program directors (PDs), of whom 48% were women, according to a previous study. Data on associate and assistant PDs from 2016 were not available to Ms. Abushukur and associates.
At the fellowship program level, women made gains as PDs in dermatopathology (34% in 2016 and 41% in 2021) and pediatric dermatology (64% in 2016 and 76% in 2021), but not in dermatologic surgery, where the proportion held at 26% over the study period. “This disparity is reflective of the general trend in surgery and pathology leadership nationally,” the researchers noted.
Taking a couple of steps up the ladder of authority shows that 39% of dermatology chairs were women in 2021, compared with 23% in 2016. A study published in 2016 demonstrated decreased diversity among academic faculty members as faculty rank increased, and “our data mirror this sentiment by demonstrating a majority of women in assistant and associate PD positions, with a minority of women chairs,” they wrote.
The investigators said that they had no conflicts of interest and no outside funding. Ms. Abushukur’s coauthors were from the departments of dermatology at the Henry Ford Health System, Detroit, and Wayne State University, Dearborn, Mich.
FROM INTERNATIONAL JOURNAL OF WOMEN’S DERMATOLOGY










