User login
Optimal management of dysplastic nevi continues to evolve
San Diego – The way Benjamin Kelley, MD, sees it,
“There’s a confusion in the terminology, a term the late A. Bernard Ackerman, MD, called ‘patho-babel,’ ” Dr. Kelley, a Mohs micrographic surgeon and dermatopathologist in La Jolla, Calif., said at the annual Cutaneous Malignancy Update. “The idea of DN was originally used to describe a clinical melanoma syndrome. Now we use it for individual lesions, not just clinically but histologically. Some dermatologists refer to DN as ‘pre-melanoma,’ which is a negative framing,” he noted.
“We also refer to common nevi as ‘benign,’ which implies that DN are not benign,” he added. “The good news is that regardless of what they are called, the histologic criteria is generally agreed upon. The names can be used interchangeably.”
The bad news, he continued, is that there is less-than-perfect interobserver variability for grading DN lesions and significant variability in the treatment recommendations that pathologists give to clinicians. In one study, a group of pathology experts was asked to review 48 photomicrographs of melanocytic lesions and provide their diagnosis and treatment recommendations based on the Melanocytic Pathology Assessment Tool and Hierarchy for Diagnosis scheme. For one, which showed a broad lesion with irregular epidermal thinning and thickening, the diagnoses ranged from solar lentigo to melanoma in situ. Treatment recommendations ranged from no treatment to re-excise with appropriate margins.
“This is an extreme example, but it shows you how difficult [establishing a diagnosis] can be,” Dr. Kelley said.
In a more recent study, researchers analyzed interobserver reproducibility in grading 179 DN cases among three observers who applied the 2018 World Health Organization grading criteria. The observers showed moderate to good agreement for most of the architectural features, except for criteria regarding focal continuous basal proliferation of melanocytes, density of non-nested junctional melanocytes, and presence of dyscohesive nests of intraepidermal melanocytes, whereas fair agreement was achieved for the cytological criteria. “So, it sounds to me like there was not a whole lot of agreement,” Dr. Kelley said.
An earlier single-center study titled “Clinicians Are From Mars and Pathologists Are From Venus” found that surgeons misunderstood the pathologist’s report 30% of the time.
In Dr. Kelly’s opinion, management of DNs will be successful if clinicians have a good working relationship with their dermatopathologists, if they biopsy to ensure an adequate, representative specimen, and if that they know what the terminology on the pathology report means and what actions to take. “The biopsy method matters,” he emphasized.
In a 14-year follow-up survey, investigators assessed DN management trends among 703 U.S. dermatologists. One key finding was that 69% of dermatologists in 2015 performed total removals when biopsying DN to achieve clear margins, compared with 86% in 2001.
A subsequent survey of 213 New England–based dermatologists found that the degree of clinical suspicion for melanoma was important in DN biopsy technique, with more respondents favoring shave biopsies for lesions with low suspicion and full-thickness biopsies for highly suspicious lesions.
“Misdiagnosis is more common for melanomas that have been assessed with punch and shave biopsies than with an excisional biopsy,” Dr. Kelley said. “I’m not too much of a stickler. I don’t require everyone to send me a giant excision, but I do want a representative sample.”
What about re-excision of DN considered to be mild or moderate? In 2015, members of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group published a consensus statement on DN management recommendations for clinically atypical nevi/DN based on a review of published evidence. The subcommittee members concluded that mildly and moderately DN with clear margins do not need to be re-excised, and that mildly DN biopsied with positive histologic margins without clinical residual pigmentation may be safely observed rather than re-excised.
For moderately DN with positive histologic margins without clinically apparent residual pigmentation, the subcommittee members concluded that observation may be reasonable.
In his own informal analysis, Dr. Kelley compiled data from published studies he could find on DN management and divided them into two groups: the observation group, in which researchers from eight studies biopsied the DN lesion and watched the patients over time to see what happened, and the re-excision group, in which researchers from seven studies biopsied the DN lesion and subsequently re-excised it. There were about 1,500 patients in both groups. No deaths occurred in either group, he said, but 15 patients in the re-excision group developed a melanoma at the site of the original biopsy (1%), compared with 7 in the observation group (0.5%).
Six of seven melanomas in the observation group came from one article conducted at a VA clinic. In the study, 6 of 304 observed DN subsequently developed melanoma at the site of the lesion. “However, five of six that developed melanoma had an original biopsy that was a partial biopsy with grossly positive margins; I think that’s where the problem lies,” Dr. Kelley said at the meeting, which was hosted by Scripps MD Anderson Cancer Center. “All five grew lentigo maligna type melanoma, which we know can extend multiple millimeters beyond the clinically apparent lesion.”
The findings support mounting evidence that re-excising mild and moderate DN, regardless of border involvement, may not be necessary. “Currently, most clinicians still re-excise moderate and severe DN involving margins, especially if there is residual pigment,” Dr. Kelley said. “Most re-excise severe DN regardless of margin involvement, but beware if your biopsy was a partial sample of a larger lesion.”
He acknowledged limitations to pathologic studies of DN, including the potential for diagnostic uncertainty. “That doesn’t necessarily mean that the pathologist got the diagnosis wrong. It could be, what is the risk that the portion of tissue not visualized contains melanoma? If you give me a 5 mm sample of a DN, and I cut it into 4-micrometer sections, I’m only looking at less than 1% of the actual nevus. That’s compounded if the pathologist only receives a partial sample.”
Dr. Kelley reported having no relevant disclosures.
San Diego – The way Benjamin Kelley, MD, sees it,
“There’s a confusion in the terminology, a term the late A. Bernard Ackerman, MD, called ‘patho-babel,’ ” Dr. Kelley, a Mohs micrographic surgeon and dermatopathologist in La Jolla, Calif., said at the annual Cutaneous Malignancy Update. “The idea of DN was originally used to describe a clinical melanoma syndrome. Now we use it for individual lesions, not just clinically but histologically. Some dermatologists refer to DN as ‘pre-melanoma,’ which is a negative framing,” he noted.
“We also refer to common nevi as ‘benign,’ which implies that DN are not benign,” he added. “The good news is that regardless of what they are called, the histologic criteria is generally agreed upon. The names can be used interchangeably.”
The bad news, he continued, is that there is less-than-perfect interobserver variability for grading DN lesions and significant variability in the treatment recommendations that pathologists give to clinicians. In one study, a group of pathology experts was asked to review 48 photomicrographs of melanocytic lesions and provide their diagnosis and treatment recommendations based on the Melanocytic Pathology Assessment Tool and Hierarchy for Diagnosis scheme. For one, which showed a broad lesion with irregular epidermal thinning and thickening, the diagnoses ranged from solar lentigo to melanoma in situ. Treatment recommendations ranged from no treatment to re-excise with appropriate margins.
“This is an extreme example, but it shows you how difficult [establishing a diagnosis] can be,” Dr. Kelley said.
In a more recent study, researchers analyzed interobserver reproducibility in grading 179 DN cases among three observers who applied the 2018 World Health Organization grading criteria. The observers showed moderate to good agreement for most of the architectural features, except for criteria regarding focal continuous basal proliferation of melanocytes, density of non-nested junctional melanocytes, and presence of dyscohesive nests of intraepidermal melanocytes, whereas fair agreement was achieved for the cytological criteria. “So, it sounds to me like there was not a whole lot of agreement,” Dr. Kelley said.
An earlier single-center study titled “Clinicians Are From Mars and Pathologists Are From Venus” found that surgeons misunderstood the pathologist’s report 30% of the time.
In Dr. Kelly’s opinion, management of DNs will be successful if clinicians have a good working relationship with their dermatopathologists, if they biopsy to ensure an adequate, representative specimen, and if that they know what the terminology on the pathology report means and what actions to take. “The biopsy method matters,” he emphasized.
In a 14-year follow-up survey, investigators assessed DN management trends among 703 U.S. dermatologists. One key finding was that 69% of dermatologists in 2015 performed total removals when biopsying DN to achieve clear margins, compared with 86% in 2001.
A subsequent survey of 213 New England–based dermatologists found that the degree of clinical suspicion for melanoma was important in DN biopsy technique, with more respondents favoring shave biopsies for lesions with low suspicion and full-thickness biopsies for highly suspicious lesions.
“Misdiagnosis is more common for melanomas that have been assessed with punch and shave biopsies than with an excisional biopsy,” Dr. Kelley said. “I’m not too much of a stickler. I don’t require everyone to send me a giant excision, but I do want a representative sample.”
What about re-excision of DN considered to be mild or moderate? In 2015, members of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group published a consensus statement on DN management recommendations for clinically atypical nevi/DN based on a review of published evidence. The subcommittee members concluded that mildly and moderately DN with clear margins do not need to be re-excised, and that mildly DN biopsied with positive histologic margins without clinical residual pigmentation may be safely observed rather than re-excised.
For moderately DN with positive histologic margins without clinically apparent residual pigmentation, the subcommittee members concluded that observation may be reasonable.
In his own informal analysis, Dr. Kelley compiled data from published studies he could find on DN management and divided them into two groups: the observation group, in which researchers from eight studies biopsied the DN lesion and watched the patients over time to see what happened, and the re-excision group, in which researchers from seven studies biopsied the DN lesion and subsequently re-excised it. There were about 1,500 patients in both groups. No deaths occurred in either group, he said, but 15 patients in the re-excision group developed a melanoma at the site of the original biopsy (1%), compared with 7 in the observation group (0.5%).
Six of seven melanomas in the observation group came from one article conducted at a VA clinic. In the study, 6 of 304 observed DN subsequently developed melanoma at the site of the lesion. “However, five of six that developed melanoma had an original biopsy that was a partial biopsy with grossly positive margins; I think that’s where the problem lies,” Dr. Kelley said at the meeting, which was hosted by Scripps MD Anderson Cancer Center. “All five grew lentigo maligna type melanoma, which we know can extend multiple millimeters beyond the clinically apparent lesion.”
The findings support mounting evidence that re-excising mild and moderate DN, regardless of border involvement, may not be necessary. “Currently, most clinicians still re-excise moderate and severe DN involving margins, especially if there is residual pigment,” Dr. Kelley said. “Most re-excise severe DN regardless of margin involvement, but beware if your biopsy was a partial sample of a larger lesion.”
He acknowledged limitations to pathologic studies of DN, including the potential for diagnostic uncertainty. “That doesn’t necessarily mean that the pathologist got the diagnosis wrong. It could be, what is the risk that the portion of tissue not visualized contains melanoma? If you give me a 5 mm sample of a DN, and I cut it into 4-micrometer sections, I’m only looking at less than 1% of the actual nevus. That’s compounded if the pathologist only receives a partial sample.”
Dr. Kelley reported having no relevant disclosures.
San Diego – The way Benjamin Kelley, MD, sees it,
“There’s a confusion in the terminology, a term the late A. Bernard Ackerman, MD, called ‘patho-babel,’ ” Dr. Kelley, a Mohs micrographic surgeon and dermatopathologist in La Jolla, Calif., said at the annual Cutaneous Malignancy Update. “The idea of DN was originally used to describe a clinical melanoma syndrome. Now we use it for individual lesions, not just clinically but histologically. Some dermatologists refer to DN as ‘pre-melanoma,’ which is a negative framing,” he noted.
“We also refer to common nevi as ‘benign,’ which implies that DN are not benign,” he added. “The good news is that regardless of what they are called, the histologic criteria is generally agreed upon. The names can be used interchangeably.”
The bad news, he continued, is that there is less-than-perfect interobserver variability for grading DN lesions and significant variability in the treatment recommendations that pathologists give to clinicians. In one study, a group of pathology experts was asked to review 48 photomicrographs of melanocytic lesions and provide their diagnosis and treatment recommendations based on the Melanocytic Pathology Assessment Tool and Hierarchy for Diagnosis scheme. For one, which showed a broad lesion with irregular epidermal thinning and thickening, the diagnoses ranged from solar lentigo to melanoma in situ. Treatment recommendations ranged from no treatment to re-excise with appropriate margins.
“This is an extreme example, but it shows you how difficult [establishing a diagnosis] can be,” Dr. Kelley said.
In a more recent study, researchers analyzed interobserver reproducibility in grading 179 DN cases among three observers who applied the 2018 World Health Organization grading criteria. The observers showed moderate to good agreement for most of the architectural features, except for criteria regarding focal continuous basal proliferation of melanocytes, density of non-nested junctional melanocytes, and presence of dyscohesive nests of intraepidermal melanocytes, whereas fair agreement was achieved for the cytological criteria. “So, it sounds to me like there was not a whole lot of agreement,” Dr. Kelley said.
An earlier single-center study titled “Clinicians Are From Mars and Pathologists Are From Venus” found that surgeons misunderstood the pathologist’s report 30% of the time.
In Dr. Kelly’s opinion, management of DNs will be successful if clinicians have a good working relationship with their dermatopathologists, if they biopsy to ensure an adequate, representative specimen, and if that they know what the terminology on the pathology report means and what actions to take. “The biopsy method matters,” he emphasized.
In a 14-year follow-up survey, investigators assessed DN management trends among 703 U.S. dermatologists. One key finding was that 69% of dermatologists in 2015 performed total removals when biopsying DN to achieve clear margins, compared with 86% in 2001.
A subsequent survey of 213 New England–based dermatologists found that the degree of clinical suspicion for melanoma was important in DN biopsy technique, with more respondents favoring shave biopsies for lesions with low suspicion and full-thickness biopsies for highly suspicious lesions.
“Misdiagnosis is more common for melanomas that have been assessed with punch and shave biopsies than with an excisional biopsy,” Dr. Kelley said. “I’m not too much of a stickler. I don’t require everyone to send me a giant excision, but I do want a representative sample.”
What about re-excision of DN considered to be mild or moderate? In 2015, members of the Pigmented Lesion Subcommittee of the Melanoma Prevention Working Group published a consensus statement on DN management recommendations for clinically atypical nevi/DN based on a review of published evidence. The subcommittee members concluded that mildly and moderately DN with clear margins do not need to be re-excised, and that mildly DN biopsied with positive histologic margins without clinical residual pigmentation may be safely observed rather than re-excised.
For moderately DN with positive histologic margins without clinically apparent residual pigmentation, the subcommittee members concluded that observation may be reasonable.
In his own informal analysis, Dr. Kelley compiled data from published studies he could find on DN management and divided them into two groups: the observation group, in which researchers from eight studies biopsied the DN lesion and watched the patients over time to see what happened, and the re-excision group, in which researchers from seven studies biopsied the DN lesion and subsequently re-excised it. There were about 1,500 patients in both groups. No deaths occurred in either group, he said, but 15 patients in the re-excision group developed a melanoma at the site of the original biopsy (1%), compared with 7 in the observation group (0.5%).
Six of seven melanomas in the observation group came from one article conducted at a VA clinic. In the study, 6 of 304 observed DN subsequently developed melanoma at the site of the lesion. “However, five of six that developed melanoma had an original biopsy that was a partial biopsy with grossly positive margins; I think that’s where the problem lies,” Dr. Kelley said at the meeting, which was hosted by Scripps MD Anderson Cancer Center. “All five grew lentigo maligna type melanoma, which we know can extend multiple millimeters beyond the clinically apparent lesion.”
The findings support mounting evidence that re-excising mild and moderate DN, regardless of border involvement, may not be necessary. “Currently, most clinicians still re-excise moderate and severe DN involving margins, especially if there is residual pigment,” Dr. Kelley said. “Most re-excise severe DN regardless of margin involvement, but beware if your biopsy was a partial sample of a larger lesion.”
He acknowledged limitations to pathologic studies of DN, including the potential for diagnostic uncertainty. “That doesn’t necessarily mean that the pathologist got the diagnosis wrong. It could be, what is the risk that the portion of tissue not visualized contains melanoma? If you give me a 5 mm sample of a DN, and I cut it into 4-micrometer sections, I’m only looking at less than 1% of the actual nevus. That’s compounded if the pathologist only receives a partial sample.”
Dr. Kelley reported having no relevant disclosures.
AT MELANOMA 2023
Are repeat radiographs necessary in rheumatoid and psoriatic arthritis?
Follow-up radiographs after an initial baseline reading in patients with rheumatoid arthritis or psoriatic arthritis may still show radiographic progression despite treatment with current therapies, but it’s unclear if they will affect treatment decisions between patients and doctors that may take place regardless of the radiographic information, according to arguments made for and against their usefulness in a point-counterpoint session at the 2023 Rheumatology Winter Clinical Symposium.
Alvin Wells, MD, PhD, director of the department of rheumatology at Advocate Aurora Health in Franklin, Wisc., said that x-rays “reflect the history of joint pathology” and can get worse over time, correlating with disease activity and severity.
While RA does not yet have the “holy grail” of complete or true remission, Dr. Wells argued, the combination of clinical remission, laboratory remission, and imaging remission gets patients with RA close to the ideal when measured over time. “You need to continue to monitor these patients as you follow them along,” he said.
The BARFOT study, which evaluated 1,938 patients with early RA in two cohorts during 1992-1999 and again between 2000 and 2006, showed that more active treatments in the 2000s did not result in improvements in Health Assessment Questionnaire (HAQ) and pain scores, compared with patients treated in the 1990s. “You can see in some of those patients those scores do increase, and that even despite aggressive therapies that we had in 2006, you can still see some of those patients still have progression of the disease,” Dr. Wells explained. “How did they know? Because they looked.”
He also cited a study from researchers at the Mayo Clinic who examined 586 patients with RA that showed a higher prevalence of functional disability in patients with RA who also had radiographic changes, compared with patients without RA. “Radiographic changes correlate with disease severity and functional disability as well,” Dr. Wells said.
Just as prostate-specific antigen levels are used in prostate cancer screening and hemoglobin A1c is measured in diabetes management, radiographs should be used to track progression of disease in RA and PsA, Dr. Wells argued. “[I]f you don’t know, you can’t treat,” he said.
Some patients near remission may have radiographic progression even though disease activity measurements such as C-reactive protein (CRP) values do not show presence of active disease. In a study analyzing 1,184 patients with RA in the ASPIRE, ERA, Leflunomide, PREMIER and TEMPO trials, swollen joint count (SJC) was a better predictor of radiographic progression than CRP in patients near remission.
“[E]ven where you don’t see smoke, there still could be fire,” Dr. Wells said. “Some of these patients still progress and these are outliers, and the way they saw that [was] because they followed those patients along. If you don’t look, you don’t know.”
Radiographic progression can also be seen among nonswollen joints in patients with RA and PsA. In a study of 1,207 joints in 55 patients with RA and 352 joints in 18 patients with PsA, researchers in Austria found tenderness in nonswollen joints was associated with radiographic progression.
Despite having effective treatments in RA and PsA, “none of our therapies show that they’re able to prevent progression,” Dr. Wells said.
When it comes to hitting the treatment target in RA, some rheumatologists may think they can accomplish it without use of repeated radiographs. “I have a different perspective on that – that you really do indeed need to do the x-rays today and follow those x-rays along, especially if it’s going to change your treatment paradigm and what your treatment decision would be for the patient,” he said.
Counterpoint: Repeat radiographs aren’t helpful
Almost all rheumatologists would likely order an initial radiograph for their patients with RA or PsA, Roy M. Fleischmann, MD, clinical professor of medicine at the University of Texas and codirector of the Metroplex Clinical Research Center, both in Dallas, said in his presentation.
“If you see erosions when you start, chances are you’re going to be much more aggressive,” Dr. Fleischmann said. “So it is justification for early, more aggressive treatment of disease.”
In recent decades, radiographic progression in RA has decreased as more effective antirheumatic treatments have come into use, Dr. Fleischmann argued.
“We had x-ray progression in virtually everybody, and it was consistent no matter what we treated with, which was gold or penicillamine or any of the NSAIDs or sulfasalazine,” he said. “With methotrexate ... about 60% of patients actually have no x-ray progression, and that was a major change, and that’s one of the reasons why methotrexate has become the keystone of therapy. But even with methotrexate, [we] still had many patients who progressed.”
After the introduction of tumor necrosis factor inhibitors and other mechanisms in the late 1990s, “all of a sudden, you don’t see x-ray progression – mean x-ray progression – in a group of patients,” he noted.
Many rheumatologists now use a treat-to-target strategy, and if the patient achieves true clinical remission or sustained very low disease activity as measured by Boolean remission, Simple Disease Activity Index, or Clinical Disease Activity Index, they have “very little chance of radiographic progression and functional decline,” he said.
“If a patient doesn’t achieve remission or very low disease activity, obtaining a radiograph doesn’t change what you do because the patient’s not where they want to be, where you want them to be; you’re going to make a change anyway,” Dr. Fleischmann explained. “The radiograph isn’t going to help you do that.”
If a patient is in sustained remission but a radiograph is ordered and shows disease progression, he questioned what the rheumatologist would do in that situation.
“Now the patient’s in, let’s say, a Boolean remission. They have no tender joints. They have no swollen joints ... their pain assessment is zero, their CRP is zero, and they do have some x-ray progression. Where are you going to change?” Dr. Fleischmann asked. “There’s no data that anything else would work. I don’t know what you would do. So, in conclusion, I would say you really don’t need to repeat an x-ray.”
AI reading x-rays?
Commenting on the point-counterpoint session, Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, and director of RWCS, asked Dr. Fleischmann and Dr. Wells how they address the issue of how many radiologists seem to be unfamiliar with reading hand radiographs and RA progression.
Dr. Fleischmann said he was trained in how to read hand radiographs in medical school, but that training no longer appears to be occurring. “If you have a good bone radiologist, of which there are not a lot, you’re great. But if you don’t have a really good bone radiologist, it’s difficult,” he said.
Dr. Kavanaugh alluded to the advancement of artificial intelligence (AI) in radiology and posed the question of how both rheumatologists felt about AI reading and interpreting their radiographs. “If you could reliably submit x-rays and they would say what the Sharp score was and where the differences were, would that change anything?” he asked.
“I think having artificial intelligence read the x-ray or an MRI is really, really good. It’ll be better than the radiologists,” Dr. Fleischmann responded. “But I don’t think that you really need to repeat the x-ray. I mean, I really don’t think you need to repeat it. You need to treat the patient.”
Dr. Wells reported having financial relationships with numerous pharmaceutical companies. Dr. Fleischmann reported no relevant financial relationships.
Follow-up radiographs after an initial baseline reading in patients with rheumatoid arthritis or psoriatic arthritis may still show radiographic progression despite treatment with current therapies, but it’s unclear if they will affect treatment decisions between patients and doctors that may take place regardless of the radiographic information, according to arguments made for and against their usefulness in a point-counterpoint session at the 2023 Rheumatology Winter Clinical Symposium.
Alvin Wells, MD, PhD, director of the department of rheumatology at Advocate Aurora Health in Franklin, Wisc., said that x-rays “reflect the history of joint pathology” and can get worse over time, correlating with disease activity and severity.
While RA does not yet have the “holy grail” of complete or true remission, Dr. Wells argued, the combination of clinical remission, laboratory remission, and imaging remission gets patients with RA close to the ideal when measured over time. “You need to continue to monitor these patients as you follow them along,” he said.
The BARFOT study, which evaluated 1,938 patients with early RA in two cohorts during 1992-1999 and again between 2000 and 2006, showed that more active treatments in the 2000s did not result in improvements in Health Assessment Questionnaire (HAQ) and pain scores, compared with patients treated in the 1990s. “You can see in some of those patients those scores do increase, and that even despite aggressive therapies that we had in 2006, you can still see some of those patients still have progression of the disease,” Dr. Wells explained. “How did they know? Because they looked.”
He also cited a study from researchers at the Mayo Clinic who examined 586 patients with RA that showed a higher prevalence of functional disability in patients with RA who also had radiographic changes, compared with patients without RA. “Radiographic changes correlate with disease severity and functional disability as well,” Dr. Wells said.
Just as prostate-specific antigen levels are used in prostate cancer screening and hemoglobin A1c is measured in diabetes management, radiographs should be used to track progression of disease in RA and PsA, Dr. Wells argued. “[I]f you don’t know, you can’t treat,” he said.
Some patients near remission may have radiographic progression even though disease activity measurements such as C-reactive protein (CRP) values do not show presence of active disease. In a study analyzing 1,184 patients with RA in the ASPIRE, ERA, Leflunomide, PREMIER and TEMPO trials, swollen joint count (SJC) was a better predictor of radiographic progression than CRP in patients near remission.
“[E]ven where you don’t see smoke, there still could be fire,” Dr. Wells said. “Some of these patients still progress and these are outliers, and the way they saw that [was] because they followed those patients along. If you don’t look, you don’t know.”
Radiographic progression can also be seen among nonswollen joints in patients with RA and PsA. In a study of 1,207 joints in 55 patients with RA and 352 joints in 18 patients with PsA, researchers in Austria found tenderness in nonswollen joints was associated with radiographic progression.
Despite having effective treatments in RA and PsA, “none of our therapies show that they’re able to prevent progression,” Dr. Wells said.
When it comes to hitting the treatment target in RA, some rheumatologists may think they can accomplish it without use of repeated radiographs. “I have a different perspective on that – that you really do indeed need to do the x-rays today and follow those x-rays along, especially if it’s going to change your treatment paradigm and what your treatment decision would be for the patient,” he said.
Counterpoint: Repeat radiographs aren’t helpful
Almost all rheumatologists would likely order an initial radiograph for their patients with RA or PsA, Roy M. Fleischmann, MD, clinical professor of medicine at the University of Texas and codirector of the Metroplex Clinical Research Center, both in Dallas, said in his presentation.
“If you see erosions when you start, chances are you’re going to be much more aggressive,” Dr. Fleischmann said. “So it is justification for early, more aggressive treatment of disease.”
In recent decades, radiographic progression in RA has decreased as more effective antirheumatic treatments have come into use, Dr. Fleischmann argued.
“We had x-ray progression in virtually everybody, and it was consistent no matter what we treated with, which was gold or penicillamine or any of the NSAIDs or sulfasalazine,” he said. “With methotrexate ... about 60% of patients actually have no x-ray progression, and that was a major change, and that’s one of the reasons why methotrexate has become the keystone of therapy. But even with methotrexate, [we] still had many patients who progressed.”
After the introduction of tumor necrosis factor inhibitors and other mechanisms in the late 1990s, “all of a sudden, you don’t see x-ray progression – mean x-ray progression – in a group of patients,” he noted.
Many rheumatologists now use a treat-to-target strategy, and if the patient achieves true clinical remission or sustained very low disease activity as measured by Boolean remission, Simple Disease Activity Index, or Clinical Disease Activity Index, they have “very little chance of radiographic progression and functional decline,” he said.
“If a patient doesn’t achieve remission or very low disease activity, obtaining a radiograph doesn’t change what you do because the patient’s not where they want to be, where you want them to be; you’re going to make a change anyway,” Dr. Fleischmann explained. “The radiograph isn’t going to help you do that.”
If a patient is in sustained remission but a radiograph is ordered and shows disease progression, he questioned what the rheumatologist would do in that situation.
“Now the patient’s in, let’s say, a Boolean remission. They have no tender joints. They have no swollen joints ... their pain assessment is zero, their CRP is zero, and they do have some x-ray progression. Where are you going to change?” Dr. Fleischmann asked. “There’s no data that anything else would work. I don’t know what you would do. So, in conclusion, I would say you really don’t need to repeat an x-ray.”
AI reading x-rays?
Commenting on the point-counterpoint session, Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, and director of RWCS, asked Dr. Fleischmann and Dr. Wells how they address the issue of how many radiologists seem to be unfamiliar with reading hand radiographs and RA progression.
Dr. Fleischmann said he was trained in how to read hand radiographs in medical school, but that training no longer appears to be occurring. “If you have a good bone radiologist, of which there are not a lot, you’re great. But if you don’t have a really good bone radiologist, it’s difficult,” he said.
Dr. Kavanaugh alluded to the advancement of artificial intelligence (AI) in radiology and posed the question of how both rheumatologists felt about AI reading and interpreting their radiographs. “If you could reliably submit x-rays and they would say what the Sharp score was and where the differences were, would that change anything?” he asked.
“I think having artificial intelligence read the x-ray or an MRI is really, really good. It’ll be better than the radiologists,” Dr. Fleischmann responded. “But I don’t think that you really need to repeat the x-ray. I mean, I really don’t think you need to repeat it. You need to treat the patient.”
Dr. Wells reported having financial relationships with numerous pharmaceutical companies. Dr. Fleischmann reported no relevant financial relationships.
Follow-up radiographs after an initial baseline reading in patients with rheumatoid arthritis or psoriatic arthritis may still show radiographic progression despite treatment with current therapies, but it’s unclear if they will affect treatment decisions between patients and doctors that may take place regardless of the radiographic information, according to arguments made for and against their usefulness in a point-counterpoint session at the 2023 Rheumatology Winter Clinical Symposium.
Alvin Wells, MD, PhD, director of the department of rheumatology at Advocate Aurora Health in Franklin, Wisc., said that x-rays “reflect the history of joint pathology” and can get worse over time, correlating with disease activity and severity.
While RA does not yet have the “holy grail” of complete or true remission, Dr. Wells argued, the combination of clinical remission, laboratory remission, and imaging remission gets patients with RA close to the ideal when measured over time. “You need to continue to monitor these patients as you follow them along,” he said.
The BARFOT study, which evaluated 1,938 patients with early RA in two cohorts during 1992-1999 and again between 2000 and 2006, showed that more active treatments in the 2000s did not result in improvements in Health Assessment Questionnaire (HAQ) and pain scores, compared with patients treated in the 1990s. “You can see in some of those patients those scores do increase, and that even despite aggressive therapies that we had in 2006, you can still see some of those patients still have progression of the disease,” Dr. Wells explained. “How did they know? Because they looked.”
He also cited a study from researchers at the Mayo Clinic who examined 586 patients with RA that showed a higher prevalence of functional disability in patients with RA who also had radiographic changes, compared with patients without RA. “Radiographic changes correlate with disease severity and functional disability as well,” Dr. Wells said.
Just as prostate-specific antigen levels are used in prostate cancer screening and hemoglobin A1c is measured in diabetes management, radiographs should be used to track progression of disease in RA and PsA, Dr. Wells argued. “[I]f you don’t know, you can’t treat,” he said.
Some patients near remission may have radiographic progression even though disease activity measurements such as C-reactive protein (CRP) values do not show presence of active disease. In a study analyzing 1,184 patients with RA in the ASPIRE, ERA, Leflunomide, PREMIER and TEMPO trials, swollen joint count (SJC) was a better predictor of radiographic progression than CRP in patients near remission.
“[E]ven where you don’t see smoke, there still could be fire,” Dr. Wells said. “Some of these patients still progress and these are outliers, and the way they saw that [was] because they followed those patients along. If you don’t look, you don’t know.”
Radiographic progression can also be seen among nonswollen joints in patients with RA and PsA. In a study of 1,207 joints in 55 patients with RA and 352 joints in 18 patients with PsA, researchers in Austria found tenderness in nonswollen joints was associated with radiographic progression.
Despite having effective treatments in RA and PsA, “none of our therapies show that they’re able to prevent progression,” Dr. Wells said.
When it comes to hitting the treatment target in RA, some rheumatologists may think they can accomplish it without use of repeated radiographs. “I have a different perspective on that – that you really do indeed need to do the x-rays today and follow those x-rays along, especially if it’s going to change your treatment paradigm and what your treatment decision would be for the patient,” he said.
Counterpoint: Repeat radiographs aren’t helpful
Almost all rheumatologists would likely order an initial radiograph for their patients with RA or PsA, Roy M. Fleischmann, MD, clinical professor of medicine at the University of Texas and codirector of the Metroplex Clinical Research Center, both in Dallas, said in his presentation.
“If you see erosions when you start, chances are you’re going to be much more aggressive,” Dr. Fleischmann said. “So it is justification for early, more aggressive treatment of disease.”
In recent decades, radiographic progression in RA has decreased as more effective antirheumatic treatments have come into use, Dr. Fleischmann argued.
“We had x-ray progression in virtually everybody, and it was consistent no matter what we treated with, which was gold or penicillamine or any of the NSAIDs or sulfasalazine,” he said. “With methotrexate ... about 60% of patients actually have no x-ray progression, and that was a major change, and that’s one of the reasons why methotrexate has become the keystone of therapy. But even with methotrexate, [we] still had many patients who progressed.”
After the introduction of tumor necrosis factor inhibitors and other mechanisms in the late 1990s, “all of a sudden, you don’t see x-ray progression – mean x-ray progression – in a group of patients,” he noted.
Many rheumatologists now use a treat-to-target strategy, and if the patient achieves true clinical remission or sustained very low disease activity as measured by Boolean remission, Simple Disease Activity Index, or Clinical Disease Activity Index, they have “very little chance of radiographic progression and functional decline,” he said.
“If a patient doesn’t achieve remission or very low disease activity, obtaining a radiograph doesn’t change what you do because the patient’s not where they want to be, where you want them to be; you’re going to make a change anyway,” Dr. Fleischmann explained. “The radiograph isn’t going to help you do that.”
If a patient is in sustained remission but a radiograph is ordered and shows disease progression, he questioned what the rheumatologist would do in that situation.
“Now the patient’s in, let’s say, a Boolean remission. They have no tender joints. They have no swollen joints ... their pain assessment is zero, their CRP is zero, and they do have some x-ray progression. Where are you going to change?” Dr. Fleischmann asked. “There’s no data that anything else would work. I don’t know what you would do. So, in conclusion, I would say you really don’t need to repeat an x-ray.”
AI reading x-rays?
Commenting on the point-counterpoint session, Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego, and director of RWCS, asked Dr. Fleischmann and Dr. Wells how they address the issue of how many radiologists seem to be unfamiliar with reading hand radiographs and RA progression.
Dr. Fleischmann said he was trained in how to read hand radiographs in medical school, but that training no longer appears to be occurring. “If you have a good bone radiologist, of which there are not a lot, you’re great. But if you don’t have a really good bone radiologist, it’s difficult,” he said.
Dr. Kavanaugh alluded to the advancement of artificial intelligence (AI) in radiology and posed the question of how both rheumatologists felt about AI reading and interpreting their radiographs. “If you could reliably submit x-rays and they would say what the Sharp score was and where the differences were, would that change anything?” he asked.
“I think having artificial intelligence read the x-ray or an MRI is really, really good. It’ll be better than the radiologists,” Dr. Fleischmann responded. “But I don’t think that you really need to repeat the x-ray. I mean, I really don’t think you need to repeat it. You need to treat the patient.”
Dr. Wells reported having financial relationships with numerous pharmaceutical companies. Dr. Fleischmann reported no relevant financial relationships.
FROM RWCS 2023
Immunodeficiencies tied to psychiatric disorders in offspring
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.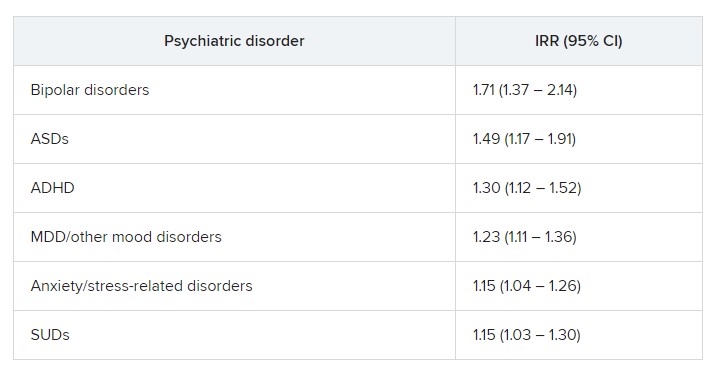
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.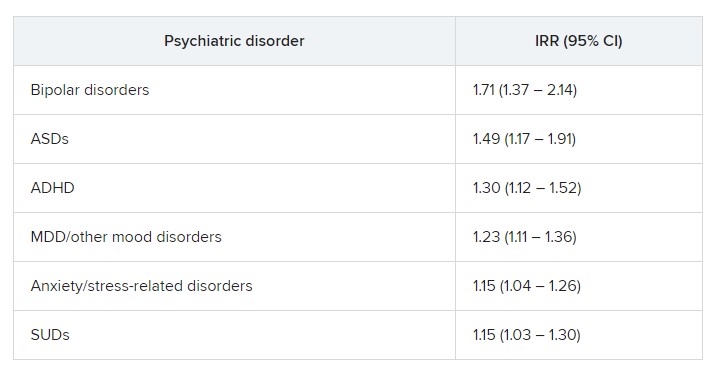
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research suggests.
Results from a cohort study of more than 4.2 million individuals showed that offspring of mothers with PIDs had a 17% increased risk for a psychiatric disorder and a 20% increased risk for suicidal behavior, compared with their peers with mothers who did not have PIDs.
The risk was more pronounced in offspring of mothers with both PIDs and autoimmune diseases. These risks remained after strictly controlling for different covariates, such as the parents’ psychiatric history, offspring PIDs, and offspring autoimmune diseases.
The investigators, led by Josef Isung, MD, PhD, Centre for Psychiatry Research, department of clinical neuroscience, Karolinska Institutet, Stockholm, noted that they could not “pinpoint a precise causal mechanism” underlying these findings.
Still, “the results add to the existing literature suggesting that the intrauterine immune environment may have implications for fetal neurodevelopment and that a compromised maternal immune system during pregnancy may be a risk factor for psychiatric disorders and suicidal behavior in their offspring in the long term,” they wrote.
The findings were published online in JAMA Psychiatry.
‘Natural experiment’
Maternal immune activation (MIA) is “an overarching term for aberrant and disrupted immune activity in the mother during gestation [and] has long been of interest in relation to adverse health outcomes in the offspring,” Dr. Isung noted.
“In relation to negative psychiatric outcomes, there is an abundance of preclinical evidence that has shown a negative impact on offspring secondary to MIA. And in humans, there are several observational studies supporting this link,” he said in an interview.
Dr. Isung added that PIDs are “rare conditions” known to be associated with repeated infections and high rates of autoimmune diseases, causing substantial disability.
“PIDs represent an interesting ‘natural experiment’ for researchers to understand more about the association between immune system dysfunctions and mental health,” he said.
Dr. Isung’s group previously showed that individuals with PIDs have increased odds of psychiatric disorders and suicidal behavior. The link was more pronounced in women with PIDs – and was even more pronounced in those with both PIDs and autoimmune diseases.
In the current study, “we wanted to see whether offspring of individuals were differentially at risk of psychiatric disorders and suicidal behavior, depending on being offspring of mothers or fathers with PIDs,” Dr. Isung said.
“Our hypothesis was that mothers with PIDs would have an increased risk of having offspring with neuropsychiatric outcomes, and that this risk could be due to MIA,” he added.
The researchers turned to Swedish nationwide health and administrative registers. They analyzed data on all individuals with diagnoses of PIDs identified between 1973 and 2013. Offspring born prior to 2003 were included, and parent-offspring pairs in which both parents had a history of PIDs were excluded.
The final study sample consisted of 4,294,169 offspring (51.4% boys). Of these participants, 7,270 (0.17%) had a parent with PIDs.
The researchers identified lifetime records of 10 psychiatric disorders: obsessive-compulsive disorder, ADHD, autism spectrum disorders, schizophrenia and other psychotic disorders, bipolar disorders, major depressive disorder and other mood disorders, anxiety and stress-related disorders, eating disorders, substance use disorders, and Tourette syndrome and chronic tic disorders.
The investigators included parental birth year, psychopathology, suicide attempts, suicide deaths, and autoimmune diseases as covariates, as well as offsprings’ birth year and gender.
Elucidation needed
Results showed that, of the 4,676 offspring of mothers with PID, 17.1% had a psychiatric disorder versus 12.7% of offspring of mothers without PIDs. This translated “into a 17% increased risk for offspring of mothers with PIDs in the fully adjusted model,” the investigators reported.
The risk was even higher for offspring of mothers who had not only PIDs but also one of six of the individual psychiatric disorders, with incident rate ratios ranging from 1.15 to 1.71.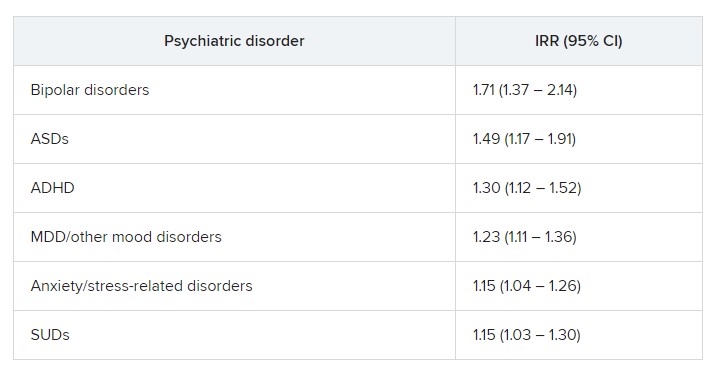
“In fully adjusted models, offspring of mothers with PIDs had an increased risk of any psychiatric disorder, while no such risks were observed in offspring of fathers with PIDs” (IRR, 1.17 vs. 1.03; P < .001), the researchers reported.
A higher risk for suicidal behavior was also observed among offspring of mothers with PIDS, in contrast to those of fathers with PIDs (IRR, 1.2 vs. 1.1; P = .01).
The greatest risk for any psychiatric disorder, as well as suicidal behavior, was found in offspring of mothers who had both PIDs and autoimmune diseases (IRRs, 1.24 and 1.44, respectively).
“The results could be seen as substantiating the hypothesis that immune disruption may be important in the pathophysiology of psychiatric disorders and suicidal behavior,” Dr. Isung said.
“Furthermore, the fact that only offspring of mothers and not offspring of fathers with PIDs had this association would align with our hypothesis that MIA is of importance,” he added.
However, he noted that “the specific mechanisms are most likely multifactorial and remain to be elucidated.”
Important piece of the puzzle?
In a comment, Michael Eriksen Benros, MD, PhD, professor of immunopsychiatry, department of immunology and microbiology, health, and medical sciences, University of Copenhagen, said this was a “high-quality study” that used a “rich data source.”
Dr. Benros, who is also head of research (biological and precision psychiatry) at the Copenhagen Research Centre for Mental Health, Copenhagen University Hospital, was not involved with the current study.
He noted that prior studies, including some conducted by his own group, have shown that maternal infections overall did not seem to be “specifically linked to mental disorders in the offspring.”
However, “specific maternal infections or specific brain-reactive antibodies during the pregnancy period have been shown to be associated with neurodevelopmental outcomes among the children,” such as intellectual disability, he said.
Regarding direct clinical implications of the study, “it is important to note that the increased risk of psychiatric disorders and suicidality in the offspring of mothers with PID were small,” Dr. Benros said.
“However, it adds an important part to the scientific puzzle regarding the role of maternal immune activation during pregnancy and the risk of mental disorders,” he added.
The study was funded by the Söderström König Foundation and the Fredrik and Ingrid Thuring Foundation. Neither Dr. Isung nor Dr. Benros reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Not testing VO2 max in your older patients? Here’s why you should
Once the focus of cyclists and other elite athletes, VO2 max has in recent years caught the attention of geriatricians, who have linked the measure to maximum functional capacity – an umbrella term for the body’s ability to perform aerobic exercise.
“Function is prognostic of mortality,” said Daniel E. Forman, MD, FAHA, FACC, professor of medicine and chair of the section of geriatric cardiology at the University of Pittsburgh Medical Center. “If you aren’t looking at that, you’re missing the boat.”
Although cardiopulmonary exercise testing (CPET) remains the gold standard for assessing VO2 max, Dr. Forman said clinicians often overlook CPET because it is old.
Getting precise
As a person ages, the amount of physical activity needed to stay fit varies, depending on genes, health, and fitness history. Measuring VO2 max can help doctors better prescribe physical activity, both with regard to specific exercises and for how long, Claudio Gil Araújo, MD, PhD, dean of research and education at the Exercise Medicine Clinic at CLINIMEX in Rio de Janeiro, Brazil, told this news organization. The test can also measure progress.
“Guidelines talk about how much exercise you should do every week, but it’s somewhat misleading because the health outcomes are much more linked to physical fitness than the amount of exercise you do,” Dr. Araújo said. Treating a patient with hypertension requires an individualized approach. “The same thing is true with exercise,” he said.
A person with high aerobic fitness, either because of favorable genetics or because he or she has maintained good fitness by exercising, may need less activity, but 200 minutes per week may not be enough for someone else.
In his own lab, Dr. Araújo is following “dozens” of men and women who have been able to increase their ability to exercise – especially high-intensity activity – over time. And their VO2 max readings have risen, he said.
Getting patients moving and collecting data on VO2 max is the most precise way to measure aerobic fitness. But the test is far from a staple in primary care.
Dr. Araújo said a growing body of research has long shown VO2 max to be a significant determinant of health and one that physicians should be paying closer attention to, especially for aging patients.
“If someone has a low VO2 max, the treatment to correct this unfavorable health profile is to increase exercise levels,” Dr. Araújo said. “This is a very relevant public health message.”
Investigators have found that inactivity increases a person’s risk of dying from an atherosclerotic cardiovascular disease event by about the same amount as smoking, and that a sedentary lifestyle increases with age . A patient’s fitness is crucial to his or her overall health, and VO2 max can play a key role. Poor performance on CPET could be a warning regarding a number of conditions, particularly cardiovascular and lung disease, Dr. Araújo said.
Indeed, acing the CPET is not easy.
“Your joints have to be normal, you can’t have low potassium, low sodium, or high blood sugar, your heart has to pump well, your blood vessels have to be healthy,” said Thomas Allison, PhD, MPH, director of the Integrated Stress Testing Center and the Sports Cardiology Clinic at Mayo Clinic, in Rochester, Minn. “All of those things can show up on the treadmill in terms of your VO2 max.”
Low VO2 max can be a physician’s first indication to investigate further. A review published in November 2022 in the International Journal of Cardiology Cardiovascular Risk and Prevention outlined what cross-sectional and longitudinal studies have documented regarding how VO2 max changes as people age. From ages 18 to 35, VO2 max remains fairly consistent. Between 35 and 55, it drops slightly but inexorably before falling sharply, if inconsistently. This inconsistency is where the important data lie.
“That lower level of physical activity may just be a behavioral change that needs to be reversed, or it could be a change that has been forced by underlying occult disease,” Dr. Allison said. That older people can’t run as fast as young people or are more likely to die in a given period than young people is not surprising. “The question is, at any given age, does your fitness level predict good health outcomes?” he said. “And the answer is yes.”
Fitness should be treated as any other data point, he added.
“If I want to know your blood pressure, I’m going to check your blood pressure; I’m not going to just ask you what it is,” Dr. Allison said. “If I ask if you have any limitations or symptoms with exercise or how physically active you are, if possible, I want to check that.”
Culture shift
Dr. Forman acknowledged that VO2 max tests can be difficult and expensive to administer in offices that aren’t already equipped with CPET machines. He said conducting other assessments, such as observing the patient performing a short walk, won’t provide as accurate data but is better than not assessing function at all.
“Specialists all have different things they measure, but function is the common denominator. For an aging population, it is the number one thing we should be looking at,” Dr. Forman said. “It’s a skill set, it’s an investment, it’s a change in culture at a time when cardiologists are obsessed with getting the latest imaging machines.”
Dr. Allison said all cardiologists should assess their patients’ VO2 max and that family medicine doctors should use the test for certain patients, such as those who have gained an unusual amount of weight or report being out of breath more than usual.
“We have all sorts of things that can go wrong with us as we get older, but if we’re sitting in a doctor’s office, it may not be apparent what they are,” Dr. Allison said. “We have to get patients up and moving.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Once the focus of cyclists and other elite athletes, VO2 max has in recent years caught the attention of geriatricians, who have linked the measure to maximum functional capacity – an umbrella term for the body’s ability to perform aerobic exercise.
“Function is prognostic of mortality,” said Daniel E. Forman, MD, FAHA, FACC, professor of medicine and chair of the section of geriatric cardiology at the University of Pittsburgh Medical Center. “If you aren’t looking at that, you’re missing the boat.”
Although cardiopulmonary exercise testing (CPET) remains the gold standard for assessing VO2 max, Dr. Forman said clinicians often overlook CPET because it is old.
Getting precise
As a person ages, the amount of physical activity needed to stay fit varies, depending on genes, health, and fitness history. Measuring VO2 max can help doctors better prescribe physical activity, both with regard to specific exercises and for how long, Claudio Gil Araújo, MD, PhD, dean of research and education at the Exercise Medicine Clinic at CLINIMEX in Rio de Janeiro, Brazil, told this news organization. The test can also measure progress.
“Guidelines talk about how much exercise you should do every week, but it’s somewhat misleading because the health outcomes are much more linked to physical fitness than the amount of exercise you do,” Dr. Araújo said. Treating a patient with hypertension requires an individualized approach. “The same thing is true with exercise,” he said.
A person with high aerobic fitness, either because of favorable genetics or because he or she has maintained good fitness by exercising, may need less activity, but 200 minutes per week may not be enough for someone else.
In his own lab, Dr. Araújo is following “dozens” of men and women who have been able to increase their ability to exercise – especially high-intensity activity – over time. And their VO2 max readings have risen, he said.
Getting patients moving and collecting data on VO2 max is the most precise way to measure aerobic fitness. But the test is far from a staple in primary care.
Dr. Araújo said a growing body of research has long shown VO2 max to be a significant determinant of health and one that physicians should be paying closer attention to, especially for aging patients.
“If someone has a low VO2 max, the treatment to correct this unfavorable health profile is to increase exercise levels,” Dr. Araújo said. “This is a very relevant public health message.”
Investigators have found that inactivity increases a person’s risk of dying from an atherosclerotic cardiovascular disease event by about the same amount as smoking, and that a sedentary lifestyle increases with age . A patient’s fitness is crucial to his or her overall health, and VO2 max can play a key role. Poor performance on CPET could be a warning regarding a number of conditions, particularly cardiovascular and lung disease, Dr. Araújo said.
Indeed, acing the CPET is not easy.
“Your joints have to be normal, you can’t have low potassium, low sodium, or high blood sugar, your heart has to pump well, your blood vessels have to be healthy,” said Thomas Allison, PhD, MPH, director of the Integrated Stress Testing Center and the Sports Cardiology Clinic at Mayo Clinic, in Rochester, Minn. “All of those things can show up on the treadmill in terms of your VO2 max.”
Low VO2 max can be a physician’s first indication to investigate further. A review published in November 2022 in the International Journal of Cardiology Cardiovascular Risk and Prevention outlined what cross-sectional and longitudinal studies have documented regarding how VO2 max changes as people age. From ages 18 to 35, VO2 max remains fairly consistent. Between 35 and 55, it drops slightly but inexorably before falling sharply, if inconsistently. This inconsistency is where the important data lie.
“That lower level of physical activity may just be a behavioral change that needs to be reversed, or it could be a change that has been forced by underlying occult disease,” Dr. Allison said. That older people can’t run as fast as young people or are more likely to die in a given period than young people is not surprising. “The question is, at any given age, does your fitness level predict good health outcomes?” he said. “And the answer is yes.”
Fitness should be treated as any other data point, he added.
“If I want to know your blood pressure, I’m going to check your blood pressure; I’m not going to just ask you what it is,” Dr. Allison said. “If I ask if you have any limitations or symptoms with exercise or how physically active you are, if possible, I want to check that.”
Culture shift
Dr. Forman acknowledged that VO2 max tests can be difficult and expensive to administer in offices that aren’t already equipped with CPET machines. He said conducting other assessments, such as observing the patient performing a short walk, won’t provide as accurate data but is better than not assessing function at all.
“Specialists all have different things they measure, but function is the common denominator. For an aging population, it is the number one thing we should be looking at,” Dr. Forman said. “It’s a skill set, it’s an investment, it’s a change in culture at a time when cardiologists are obsessed with getting the latest imaging machines.”
Dr. Allison said all cardiologists should assess their patients’ VO2 max and that family medicine doctors should use the test for certain patients, such as those who have gained an unusual amount of weight or report being out of breath more than usual.
“We have all sorts of things that can go wrong with us as we get older, but if we’re sitting in a doctor’s office, it may not be apparent what they are,” Dr. Allison said. “We have to get patients up and moving.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Once the focus of cyclists and other elite athletes, VO2 max has in recent years caught the attention of geriatricians, who have linked the measure to maximum functional capacity – an umbrella term for the body’s ability to perform aerobic exercise.
“Function is prognostic of mortality,” said Daniel E. Forman, MD, FAHA, FACC, professor of medicine and chair of the section of geriatric cardiology at the University of Pittsburgh Medical Center. “If you aren’t looking at that, you’re missing the boat.”
Although cardiopulmonary exercise testing (CPET) remains the gold standard for assessing VO2 max, Dr. Forman said clinicians often overlook CPET because it is old.
Getting precise
As a person ages, the amount of physical activity needed to stay fit varies, depending on genes, health, and fitness history. Measuring VO2 max can help doctors better prescribe physical activity, both with regard to specific exercises and for how long, Claudio Gil Araújo, MD, PhD, dean of research and education at the Exercise Medicine Clinic at CLINIMEX in Rio de Janeiro, Brazil, told this news organization. The test can also measure progress.
“Guidelines talk about how much exercise you should do every week, but it’s somewhat misleading because the health outcomes are much more linked to physical fitness than the amount of exercise you do,” Dr. Araújo said. Treating a patient with hypertension requires an individualized approach. “The same thing is true with exercise,” he said.
A person with high aerobic fitness, either because of favorable genetics or because he or she has maintained good fitness by exercising, may need less activity, but 200 minutes per week may not be enough for someone else.
In his own lab, Dr. Araújo is following “dozens” of men and women who have been able to increase their ability to exercise – especially high-intensity activity – over time. And their VO2 max readings have risen, he said.
Getting patients moving and collecting data on VO2 max is the most precise way to measure aerobic fitness. But the test is far from a staple in primary care.
Dr. Araújo said a growing body of research has long shown VO2 max to be a significant determinant of health and one that physicians should be paying closer attention to, especially for aging patients.
“If someone has a low VO2 max, the treatment to correct this unfavorable health profile is to increase exercise levels,” Dr. Araújo said. “This is a very relevant public health message.”
Investigators have found that inactivity increases a person’s risk of dying from an atherosclerotic cardiovascular disease event by about the same amount as smoking, and that a sedentary lifestyle increases with age . A patient’s fitness is crucial to his or her overall health, and VO2 max can play a key role. Poor performance on CPET could be a warning regarding a number of conditions, particularly cardiovascular and lung disease, Dr. Araújo said.
Indeed, acing the CPET is not easy.
“Your joints have to be normal, you can’t have low potassium, low sodium, or high blood sugar, your heart has to pump well, your blood vessels have to be healthy,” said Thomas Allison, PhD, MPH, director of the Integrated Stress Testing Center and the Sports Cardiology Clinic at Mayo Clinic, in Rochester, Minn. “All of those things can show up on the treadmill in terms of your VO2 max.”
Low VO2 max can be a physician’s first indication to investigate further. A review published in November 2022 in the International Journal of Cardiology Cardiovascular Risk and Prevention outlined what cross-sectional and longitudinal studies have documented regarding how VO2 max changes as people age. From ages 18 to 35, VO2 max remains fairly consistent. Between 35 and 55, it drops slightly but inexorably before falling sharply, if inconsistently. This inconsistency is where the important data lie.
“That lower level of physical activity may just be a behavioral change that needs to be reversed, or it could be a change that has been forced by underlying occult disease,” Dr. Allison said. That older people can’t run as fast as young people or are more likely to die in a given period than young people is not surprising. “The question is, at any given age, does your fitness level predict good health outcomes?” he said. “And the answer is yes.”
Fitness should be treated as any other data point, he added.
“If I want to know your blood pressure, I’m going to check your blood pressure; I’m not going to just ask you what it is,” Dr. Allison said. “If I ask if you have any limitations or symptoms with exercise or how physically active you are, if possible, I want to check that.”
Culture shift
Dr. Forman acknowledged that VO2 max tests can be difficult and expensive to administer in offices that aren’t already equipped with CPET machines. He said conducting other assessments, such as observing the patient performing a short walk, won’t provide as accurate data but is better than not assessing function at all.
“Specialists all have different things they measure, but function is the common denominator. For an aging population, it is the number one thing we should be looking at,” Dr. Forman said. “It’s a skill set, it’s an investment, it’s a change in culture at a time when cardiologists are obsessed with getting the latest imaging machines.”
Dr. Allison said all cardiologists should assess their patients’ VO2 max and that family medicine doctors should use the test for certain patients, such as those who have gained an unusual amount of weight or report being out of breath more than usual.
“We have all sorts of things that can go wrong with us as we get older, but if we’re sitting in a doctor’s office, it may not be apparent what they are,” Dr. Allison said. “We have to get patients up and moving.”
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Breast cancer exacts high financial toll worldwide
but in low- and middle-income countries as well, a meta-analysis found.
Although the rate of financial toxicity was much higher in low- and middle-income countries – affecting 79% of patients – more than 35% of patients in high-income countries also incurred financial hardship, the study team found.
The findings highlight the need for policies to offset the burden of direct and indirect costs for breast cancer care and improve the financial health of vulnerable patients, said the study authors, led by Kavitha Ranganathan, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston.
The study was published online in JAMA Network Open.
The most expensive malignancy?
Patients with breast cancer may be particularly burdened by costs of care, with one study showing substantially higher out-of-pocket costs for patients with breast cancer than colorectal, lung, and prostate cancer combined.
A Lancet Oncology Commission report revealed that breast cancer was the most expensive cancer in the United States in 2010, accounting for $16.5 billion, or 13% of all cancer-related spending. A separate analysis found that individual direct medical costs of breast cancer care can reach $100,000.
In high-income countries, the financial burden of breast cancer care may be the result of novel and costly cancer therapeutics and interventions, overuse of services, increased willingness to pay, and varying insurance coverage. In low- and middle-income countries, women may experience delayed diagnosis because of limited access to screening and high-quality diagnostic services, leading to more later-stage diagnoses requiring more extensive treatments. Lower baseline income, limited insurance coverage, and greater distance to treatment centers may also be factors.
“Establishing the global extent of financial toxicity and comparing the economic burden of disease in different populations is imperative to help policy makers prioritize funding of breast cancer care infrastructure,” Dr. Ranganathan and colleagues write.
In their meta-analysis of 18 studies – 14 from high-income countries and 4 from low – published from 2008 to 2021, the authors found that the definition of financial toxicity varied widely across studies.
For example, some used specific numerical criteria for defining financial toxicity, such as medical cost exceeding 40% of household capacity to pay or potential income or out-of-pocket costs exceeding 30% of annual household income.
Others used patient-reported outcome measures instruments evaluating subjective statements of financial difficulty, such as an affirmative answer to having financial difficulty or trouble paying medical bills, or paying more for medical care than is affordable.
In other studies, financial toxicity was defined according to a patient’s report of specific, objective financial consequences of care, including losing income or a job; having to borrow money or go into debt; having trouble paying for food, rent, or transportation; or having to forgo any type of medical care because of cost.
In their analysis, the pooled rate of financial toxicity among patients with breast cancer was 35.3% in high-income countries and 78.8% in low/middle-income countries, both demonstrating high heterogeneity or variability (P for heterogeneity < .001). In contrast, typical financial toxicity rates across all health conditions in low-income countries ranged from 6% to 12%, the investigators noted.
One study assessing quality of life measures in Egypt found that 47.5% of patients were food insecure, 66% needed financial assistance, 34% used savings to pay for treatment, and 41.2% lacked savings altogether.
Burden reduction
Given the high rates of financial toxicity associated with breast cancer, what strategies might reduce this cost burden?
When exploring potential factors associated with financial toxicity, the researchers found no clear association between financial toxicity and race, employment status, and age, and could draw no firm conclusions about the impact of comorbidities and urban vs. rural place of residence. In addition, cancer stage and treatments were “extremely” heterogeneous across studies and the authors found no clear association between either factor and financial toxicity.
But the authors noted that the highest-priority patients are typically those who have low education, have low socioeconomic status, lack health insurance, and live in low-resource areas.
To reduce financial toxicity and improve outcomes among patients with breast cancer, the study team recommended four potential strategies:
- Use targeted educational campaigns to raise awareness about the signs and symptoms of breast cancer and the importance of early diagnosis and treatment.
- Expand health care coverage to minimize direct medical out-of-pocket costs.
- Develop programs to assist with direct nonmedical and indirect costs, such as transportation to and lodging near treatment centers and childcare.
- Improve screening, referral, and treatment infrastructure for breast cancer care.
The researchers also noted that their data highlight the value of universal health care coverage as a policy strategy, with evidence of lower financial toxicity rates in countries with universal health coverage.
Support for the study was provided in part by the National Cancer Institute, United Nations Institute for Training and Research and the Global Surgery Foundation, Harvard Global Health Institute, Connors Center for Women’s Health and Gender Biology, the Center for Surgery and Public Health, and the National Endowment for Plastic Surgery. Dr. Ranganathan reports no relevant financial relationships. Several coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
but in low- and middle-income countries as well, a meta-analysis found.
Although the rate of financial toxicity was much higher in low- and middle-income countries – affecting 79% of patients – more than 35% of patients in high-income countries also incurred financial hardship, the study team found.
The findings highlight the need for policies to offset the burden of direct and indirect costs for breast cancer care and improve the financial health of vulnerable patients, said the study authors, led by Kavitha Ranganathan, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston.
The study was published online in JAMA Network Open.
The most expensive malignancy?
Patients with breast cancer may be particularly burdened by costs of care, with one study showing substantially higher out-of-pocket costs for patients with breast cancer than colorectal, lung, and prostate cancer combined.
A Lancet Oncology Commission report revealed that breast cancer was the most expensive cancer in the United States in 2010, accounting for $16.5 billion, or 13% of all cancer-related spending. A separate analysis found that individual direct medical costs of breast cancer care can reach $100,000.
In high-income countries, the financial burden of breast cancer care may be the result of novel and costly cancer therapeutics and interventions, overuse of services, increased willingness to pay, and varying insurance coverage. In low- and middle-income countries, women may experience delayed diagnosis because of limited access to screening and high-quality diagnostic services, leading to more later-stage diagnoses requiring more extensive treatments. Lower baseline income, limited insurance coverage, and greater distance to treatment centers may also be factors.
“Establishing the global extent of financial toxicity and comparing the economic burden of disease in different populations is imperative to help policy makers prioritize funding of breast cancer care infrastructure,” Dr. Ranganathan and colleagues write.
In their meta-analysis of 18 studies – 14 from high-income countries and 4 from low – published from 2008 to 2021, the authors found that the definition of financial toxicity varied widely across studies.
For example, some used specific numerical criteria for defining financial toxicity, such as medical cost exceeding 40% of household capacity to pay or potential income or out-of-pocket costs exceeding 30% of annual household income.
Others used patient-reported outcome measures instruments evaluating subjective statements of financial difficulty, such as an affirmative answer to having financial difficulty or trouble paying medical bills, or paying more for medical care than is affordable.
In other studies, financial toxicity was defined according to a patient’s report of specific, objective financial consequences of care, including losing income or a job; having to borrow money or go into debt; having trouble paying for food, rent, or transportation; or having to forgo any type of medical care because of cost.
In their analysis, the pooled rate of financial toxicity among patients with breast cancer was 35.3% in high-income countries and 78.8% in low/middle-income countries, both demonstrating high heterogeneity or variability (P for heterogeneity < .001). In contrast, typical financial toxicity rates across all health conditions in low-income countries ranged from 6% to 12%, the investigators noted.
One study assessing quality of life measures in Egypt found that 47.5% of patients were food insecure, 66% needed financial assistance, 34% used savings to pay for treatment, and 41.2% lacked savings altogether.
Burden reduction
Given the high rates of financial toxicity associated with breast cancer, what strategies might reduce this cost burden?
When exploring potential factors associated with financial toxicity, the researchers found no clear association between financial toxicity and race, employment status, and age, and could draw no firm conclusions about the impact of comorbidities and urban vs. rural place of residence. In addition, cancer stage and treatments were “extremely” heterogeneous across studies and the authors found no clear association between either factor and financial toxicity.
But the authors noted that the highest-priority patients are typically those who have low education, have low socioeconomic status, lack health insurance, and live in low-resource areas.
To reduce financial toxicity and improve outcomes among patients with breast cancer, the study team recommended four potential strategies:
- Use targeted educational campaigns to raise awareness about the signs and symptoms of breast cancer and the importance of early diagnosis and treatment.
- Expand health care coverage to minimize direct medical out-of-pocket costs.
- Develop programs to assist with direct nonmedical and indirect costs, such as transportation to and lodging near treatment centers and childcare.
- Improve screening, referral, and treatment infrastructure for breast cancer care.
The researchers also noted that their data highlight the value of universal health care coverage as a policy strategy, with evidence of lower financial toxicity rates in countries with universal health coverage.
Support for the study was provided in part by the National Cancer Institute, United Nations Institute for Training and Research and the Global Surgery Foundation, Harvard Global Health Institute, Connors Center for Women’s Health and Gender Biology, the Center for Surgery and Public Health, and the National Endowment for Plastic Surgery. Dr. Ranganathan reports no relevant financial relationships. Several coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
but in low- and middle-income countries as well, a meta-analysis found.
Although the rate of financial toxicity was much higher in low- and middle-income countries – affecting 79% of patients – more than 35% of patients in high-income countries also incurred financial hardship, the study team found.
The findings highlight the need for policies to offset the burden of direct and indirect costs for breast cancer care and improve the financial health of vulnerable patients, said the study authors, led by Kavitha Ranganathan, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston.
The study was published online in JAMA Network Open.
The most expensive malignancy?
Patients with breast cancer may be particularly burdened by costs of care, with one study showing substantially higher out-of-pocket costs for patients with breast cancer than colorectal, lung, and prostate cancer combined.
A Lancet Oncology Commission report revealed that breast cancer was the most expensive cancer in the United States in 2010, accounting for $16.5 billion, or 13% of all cancer-related spending. A separate analysis found that individual direct medical costs of breast cancer care can reach $100,000.
In high-income countries, the financial burden of breast cancer care may be the result of novel and costly cancer therapeutics and interventions, overuse of services, increased willingness to pay, and varying insurance coverage. In low- and middle-income countries, women may experience delayed diagnosis because of limited access to screening and high-quality diagnostic services, leading to more later-stage diagnoses requiring more extensive treatments. Lower baseline income, limited insurance coverage, and greater distance to treatment centers may also be factors.
“Establishing the global extent of financial toxicity and comparing the economic burden of disease in different populations is imperative to help policy makers prioritize funding of breast cancer care infrastructure,” Dr. Ranganathan and colleagues write.
In their meta-analysis of 18 studies – 14 from high-income countries and 4 from low – published from 2008 to 2021, the authors found that the definition of financial toxicity varied widely across studies.
For example, some used specific numerical criteria for defining financial toxicity, such as medical cost exceeding 40% of household capacity to pay or potential income or out-of-pocket costs exceeding 30% of annual household income.
Others used patient-reported outcome measures instruments evaluating subjective statements of financial difficulty, such as an affirmative answer to having financial difficulty or trouble paying medical bills, or paying more for medical care than is affordable.
In other studies, financial toxicity was defined according to a patient’s report of specific, objective financial consequences of care, including losing income or a job; having to borrow money or go into debt; having trouble paying for food, rent, or transportation; or having to forgo any type of medical care because of cost.
In their analysis, the pooled rate of financial toxicity among patients with breast cancer was 35.3% in high-income countries and 78.8% in low/middle-income countries, both demonstrating high heterogeneity or variability (P for heterogeneity < .001). In contrast, typical financial toxicity rates across all health conditions in low-income countries ranged from 6% to 12%, the investigators noted.
One study assessing quality of life measures in Egypt found that 47.5% of patients were food insecure, 66% needed financial assistance, 34% used savings to pay for treatment, and 41.2% lacked savings altogether.
Burden reduction
Given the high rates of financial toxicity associated with breast cancer, what strategies might reduce this cost burden?
When exploring potential factors associated with financial toxicity, the researchers found no clear association between financial toxicity and race, employment status, and age, and could draw no firm conclusions about the impact of comorbidities and urban vs. rural place of residence. In addition, cancer stage and treatments were “extremely” heterogeneous across studies and the authors found no clear association between either factor and financial toxicity.
But the authors noted that the highest-priority patients are typically those who have low education, have low socioeconomic status, lack health insurance, and live in low-resource areas.
To reduce financial toxicity and improve outcomes among patients with breast cancer, the study team recommended four potential strategies:
- Use targeted educational campaigns to raise awareness about the signs and symptoms of breast cancer and the importance of early diagnosis and treatment.
- Expand health care coverage to minimize direct medical out-of-pocket costs.
- Develop programs to assist with direct nonmedical and indirect costs, such as transportation to and lodging near treatment centers and childcare.
- Improve screening, referral, and treatment infrastructure for breast cancer care.
The researchers also noted that their data highlight the value of universal health care coverage as a policy strategy, with evidence of lower financial toxicity rates in countries with universal health coverage.
Support for the study was provided in part by the National Cancer Institute, United Nations Institute for Training and Research and the Global Surgery Foundation, Harvard Global Health Institute, Connors Center for Women’s Health and Gender Biology, the Center for Surgery and Public Health, and the National Endowment for Plastic Surgery. Dr. Ranganathan reports no relevant financial relationships. Several coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Slowing, not stopping, Alzheimer’s a better goal for clinical trials?
and may be a more realistic goal for clinical AD drug trials, a new report suggests.
The report is a yearlong undertaking by an expert work group convened by the Alzheimer’s Association and was prompted, in part, by the fallout from the U.S. Food and Drug Administration’s controversial decision to grant aducanumab (Aduhelm) accelerated approval, which came over the objection of an advisory panel that found the drug was ineffective.
The report’s authors call for a “reframing” of how researchers define “clinically meaningful” in randomized controlled trials (RCTs), noting that it’s time to adjust expectations of outcomes from relatively short clinical trials.
“Without lowering the bar, are we expecting too much from a clinical trial by expecting that unless the disease is halted in its tracks and there’s no progression, we failed at treatment?” the report’s lead author and group leader Ronald C. Petersen, MD, PhD, lead author, chair of the work group, and professor of neurology at the Mayo Clinic, Rochester, Minn., told this news organization.
Interpretations of clinical meaningfulness are used in the drug approval process and in decisions about whether an insurer will cover the cost of treatment, the authors note.
While the report doesn’t provide a consensus definition of clinically meaningful benefit, it does offer a starting point for a conversation about how the phrase should be defined in the context of RCTs for disease-modifying therapies (DMTs) in AD, Dr. Petersen said.
“What we tried to do was to put it into some kind of perspective and at least have people reflect on this: If you’re going to design the perfect drug trial in Alzheimer’s disease, what would it be? We wanted to get people to think about it without digging in their heels for or against,” he added.
The report was published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
A proactive measure
The expert group began its work in January 2022, less than a year after the FDA approved aducanumab. Since the panel began its work, the FDA has approved a second AD drug, lecanemab (Leqembi), and denied accelerated approval of a third medication, donanemab.
“At the time we started this group, we had one approved treatment, and we just knew that there were others on the way, and we needed to be prepared to have this conversation and be more proactive than reactive,” Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association and co-author of the report, said in an interview.
The work group suggests that simply slowing disease progression might be a desired goal for drug trials, especially early on, before cognition and memory are affected.
They also note that a benefit identified during an 18-month clinical trial may ultimately lead to even more meaningful changes over coming years, well beyond the trial’s end.
In addition, the report authors call for the development of better research tools to more accurately assess meaningful change. The Clinical Dementia Rating (CDR) scale is currently the key instrument used as a primary outcome measure in RCTs. However, the report’s authors note that it may not be adequate to measure meaningful change in early-stage disease.
“Developing better tools certainly should be on the radar screen for all of us, because I think we can do better,” Dr. Petersen said. “The CDR, as good as it is and as long as it’s been used in the field, is a pretty blunt instrument, and it’s the result of subjective ratings.”
‘Quality of mind’
Jason Karlawish, MD, professor of medicine, medical ethics, health policy, and neurology at the University of Pennsylvania, Philadelphia, said measuring the actual impact of a drug on a patient’s disease and quality of life has been a hot topic in the AD field for some time, but settling on a definition of “clinically meaningful” that everyone agrees upon will be a challenge.
“I think the idea of ‘clinically meaningful’ is truly a socially constructed idea,” said Dr. Karlawish, co-director of Penn’s Memory Center, who did not work on the report.
“You can come up with objective measures of cognition, but a measure to call something ‘clinically meaningful’ ultimately requires some sort of negotiated social order among clinicians and patients and others who have immediate interest in the health and well-being of the patient.”
Dr. Karlawish added that he’s interested in the conversations the report might prompt and the challenges it could highlight, especially when it comes to how meaningful clinical benefit can be measured, regardless of how it’s defined.
“Hidden in this conversation about clinically meaningful treatments in Alzheimer’s disease is, frankly, not quality of life, but quality of mind,” said Dr. Karlawish. “No measure captures acceptably the very thing that everyone actually cares a lot about and why we view this disease as so dreadful, which is damage to our mind.”
More evidence needed
The development of such tools will take time. What does that mean for drugs already in the pipeline? Members of the work group argue that those trials must move forward at the same time new tools are being created.
“We need to continue to refine, develop better instruments, [and] develop tools that are going to assess the disease in its more subtle features early on, even in the so-called ‘pre-symptomatic’ stage of the disease,” said lead author Dr. Petersen. “We shouldn’t wait for the development of that before intervening if we have a drug that seems to work.”
However, not everyone who agrees with the premise of the report agrees with this position, including Joel S. Perlmutter, MD, professor of neurology, Washington University School of Medicine, St. Louis, who also commented on the report.
As reported by this news organization, Dr. Perlmutter was one of three physicians who resigned from the FDA advisory panel that voted against approving aducanumab after the agency moved forward anyway.
“We have to be careful not to recommend DMTs that we hope will help without strong evidence, especially when potential side effects are not trivial,” Dr. Perlmutter said. “We have to have evidence before making these recommendations so we don’t end up harming people more than helping them.”
The report received no specific funding. Dr. Petersen received consulting fees from Roche, Nestle, Merck, Biogen, Eisai, and Genentech. Full disclosures are included in the original article. Dr. Perlmutter and Dr. Karlawish report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
and may be a more realistic goal for clinical AD drug trials, a new report suggests.
The report is a yearlong undertaking by an expert work group convened by the Alzheimer’s Association and was prompted, in part, by the fallout from the U.S. Food and Drug Administration’s controversial decision to grant aducanumab (Aduhelm) accelerated approval, which came over the objection of an advisory panel that found the drug was ineffective.
The report’s authors call for a “reframing” of how researchers define “clinically meaningful” in randomized controlled trials (RCTs), noting that it’s time to adjust expectations of outcomes from relatively short clinical trials.
“Without lowering the bar, are we expecting too much from a clinical trial by expecting that unless the disease is halted in its tracks and there’s no progression, we failed at treatment?” the report’s lead author and group leader Ronald C. Petersen, MD, PhD, lead author, chair of the work group, and professor of neurology at the Mayo Clinic, Rochester, Minn., told this news organization.
Interpretations of clinical meaningfulness are used in the drug approval process and in decisions about whether an insurer will cover the cost of treatment, the authors note.
While the report doesn’t provide a consensus definition of clinically meaningful benefit, it does offer a starting point for a conversation about how the phrase should be defined in the context of RCTs for disease-modifying therapies (DMTs) in AD, Dr. Petersen said.
“What we tried to do was to put it into some kind of perspective and at least have people reflect on this: If you’re going to design the perfect drug trial in Alzheimer’s disease, what would it be? We wanted to get people to think about it without digging in their heels for or against,” he added.
The report was published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
A proactive measure
The expert group began its work in January 2022, less than a year after the FDA approved aducanumab. Since the panel began its work, the FDA has approved a second AD drug, lecanemab (Leqembi), and denied accelerated approval of a third medication, donanemab.
“At the time we started this group, we had one approved treatment, and we just knew that there were others on the way, and we needed to be prepared to have this conversation and be more proactive than reactive,” Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association and co-author of the report, said in an interview.
The work group suggests that simply slowing disease progression might be a desired goal for drug trials, especially early on, before cognition and memory are affected.
They also note that a benefit identified during an 18-month clinical trial may ultimately lead to even more meaningful changes over coming years, well beyond the trial’s end.
In addition, the report authors call for the development of better research tools to more accurately assess meaningful change. The Clinical Dementia Rating (CDR) scale is currently the key instrument used as a primary outcome measure in RCTs. However, the report’s authors note that it may not be adequate to measure meaningful change in early-stage disease.
“Developing better tools certainly should be on the radar screen for all of us, because I think we can do better,” Dr. Petersen said. “The CDR, as good as it is and as long as it’s been used in the field, is a pretty blunt instrument, and it’s the result of subjective ratings.”
‘Quality of mind’
Jason Karlawish, MD, professor of medicine, medical ethics, health policy, and neurology at the University of Pennsylvania, Philadelphia, said measuring the actual impact of a drug on a patient’s disease and quality of life has been a hot topic in the AD field for some time, but settling on a definition of “clinically meaningful” that everyone agrees upon will be a challenge.
“I think the idea of ‘clinically meaningful’ is truly a socially constructed idea,” said Dr. Karlawish, co-director of Penn’s Memory Center, who did not work on the report.
“You can come up with objective measures of cognition, but a measure to call something ‘clinically meaningful’ ultimately requires some sort of negotiated social order among clinicians and patients and others who have immediate interest in the health and well-being of the patient.”
Dr. Karlawish added that he’s interested in the conversations the report might prompt and the challenges it could highlight, especially when it comes to how meaningful clinical benefit can be measured, regardless of how it’s defined.
“Hidden in this conversation about clinically meaningful treatments in Alzheimer’s disease is, frankly, not quality of life, but quality of mind,” said Dr. Karlawish. “No measure captures acceptably the very thing that everyone actually cares a lot about and why we view this disease as so dreadful, which is damage to our mind.”
More evidence needed
The development of such tools will take time. What does that mean for drugs already in the pipeline? Members of the work group argue that those trials must move forward at the same time new tools are being created.
“We need to continue to refine, develop better instruments, [and] develop tools that are going to assess the disease in its more subtle features early on, even in the so-called ‘pre-symptomatic’ stage of the disease,” said lead author Dr. Petersen. “We shouldn’t wait for the development of that before intervening if we have a drug that seems to work.”
However, not everyone who agrees with the premise of the report agrees with this position, including Joel S. Perlmutter, MD, professor of neurology, Washington University School of Medicine, St. Louis, who also commented on the report.
As reported by this news organization, Dr. Perlmutter was one of three physicians who resigned from the FDA advisory panel that voted against approving aducanumab after the agency moved forward anyway.
“We have to be careful not to recommend DMTs that we hope will help without strong evidence, especially when potential side effects are not trivial,” Dr. Perlmutter said. “We have to have evidence before making these recommendations so we don’t end up harming people more than helping them.”
The report received no specific funding. Dr. Petersen received consulting fees from Roche, Nestle, Merck, Biogen, Eisai, and Genentech. Full disclosures are included in the original article. Dr. Perlmutter and Dr. Karlawish report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
and may be a more realistic goal for clinical AD drug trials, a new report suggests.
The report is a yearlong undertaking by an expert work group convened by the Alzheimer’s Association and was prompted, in part, by the fallout from the U.S. Food and Drug Administration’s controversial decision to grant aducanumab (Aduhelm) accelerated approval, which came over the objection of an advisory panel that found the drug was ineffective.
The report’s authors call for a “reframing” of how researchers define “clinically meaningful” in randomized controlled trials (RCTs), noting that it’s time to adjust expectations of outcomes from relatively short clinical trials.
“Without lowering the bar, are we expecting too much from a clinical trial by expecting that unless the disease is halted in its tracks and there’s no progression, we failed at treatment?” the report’s lead author and group leader Ronald C. Petersen, MD, PhD, lead author, chair of the work group, and professor of neurology at the Mayo Clinic, Rochester, Minn., told this news organization.
Interpretations of clinical meaningfulness are used in the drug approval process and in decisions about whether an insurer will cover the cost of treatment, the authors note.
While the report doesn’t provide a consensus definition of clinically meaningful benefit, it does offer a starting point for a conversation about how the phrase should be defined in the context of RCTs for disease-modifying therapies (DMTs) in AD, Dr. Petersen said.
“What we tried to do was to put it into some kind of perspective and at least have people reflect on this: If you’re going to design the perfect drug trial in Alzheimer’s disease, what would it be? We wanted to get people to think about it without digging in their heels for or against,” he added.
The report was published online in Alzheimer’s and Dementia: The Journal of the Alzheimer’s Association.
A proactive measure
The expert group began its work in January 2022, less than a year after the FDA approved aducanumab. Since the panel began its work, the FDA has approved a second AD drug, lecanemab (Leqembi), and denied accelerated approval of a third medication, donanemab.
“At the time we started this group, we had one approved treatment, and we just knew that there were others on the way, and we needed to be prepared to have this conversation and be more proactive than reactive,” Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association and co-author of the report, said in an interview.
The work group suggests that simply slowing disease progression might be a desired goal for drug trials, especially early on, before cognition and memory are affected.
They also note that a benefit identified during an 18-month clinical trial may ultimately lead to even more meaningful changes over coming years, well beyond the trial’s end.
In addition, the report authors call for the development of better research tools to more accurately assess meaningful change. The Clinical Dementia Rating (CDR) scale is currently the key instrument used as a primary outcome measure in RCTs. However, the report’s authors note that it may not be adequate to measure meaningful change in early-stage disease.
“Developing better tools certainly should be on the radar screen for all of us, because I think we can do better,” Dr. Petersen said. “The CDR, as good as it is and as long as it’s been used in the field, is a pretty blunt instrument, and it’s the result of subjective ratings.”
‘Quality of mind’
Jason Karlawish, MD, professor of medicine, medical ethics, health policy, and neurology at the University of Pennsylvania, Philadelphia, said measuring the actual impact of a drug on a patient’s disease and quality of life has been a hot topic in the AD field for some time, but settling on a definition of “clinically meaningful” that everyone agrees upon will be a challenge.
“I think the idea of ‘clinically meaningful’ is truly a socially constructed idea,” said Dr. Karlawish, co-director of Penn’s Memory Center, who did not work on the report.
“You can come up with objective measures of cognition, but a measure to call something ‘clinically meaningful’ ultimately requires some sort of negotiated social order among clinicians and patients and others who have immediate interest in the health and well-being of the patient.”
Dr. Karlawish added that he’s interested in the conversations the report might prompt and the challenges it could highlight, especially when it comes to how meaningful clinical benefit can be measured, regardless of how it’s defined.
“Hidden in this conversation about clinically meaningful treatments in Alzheimer’s disease is, frankly, not quality of life, but quality of mind,” said Dr. Karlawish. “No measure captures acceptably the very thing that everyone actually cares a lot about and why we view this disease as so dreadful, which is damage to our mind.”
More evidence needed
The development of such tools will take time. What does that mean for drugs already in the pipeline? Members of the work group argue that those trials must move forward at the same time new tools are being created.
“We need to continue to refine, develop better instruments, [and] develop tools that are going to assess the disease in its more subtle features early on, even in the so-called ‘pre-symptomatic’ stage of the disease,” said lead author Dr. Petersen. “We shouldn’t wait for the development of that before intervening if we have a drug that seems to work.”
However, not everyone who agrees with the premise of the report agrees with this position, including Joel S. Perlmutter, MD, professor of neurology, Washington University School of Medicine, St. Louis, who also commented on the report.
As reported by this news organization, Dr. Perlmutter was one of three physicians who resigned from the FDA advisory panel that voted against approving aducanumab after the agency moved forward anyway.
“We have to be careful not to recommend DMTs that we hope will help without strong evidence, especially when potential side effects are not trivial,” Dr. Perlmutter said. “We have to have evidence before making these recommendations so we don’t end up harming people more than helping them.”
The report received no specific funding. Dr. Petersen received consulting fees from Roche, Nestle, Merck, Biogen, Eisai, and Genentech. Full disclosures are included in the original article. Dr. Perlmutter and Dr. Karlawish report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ALZHEIMER’S AND DEMENTIA
Novel celery seed–derived drug may improve stroke outcomes
a new report suggests.
Patients treated with butylphthalide had fewer severe neurologic symptoms and better function 90 days after the stroke, compared with those receiving placebo.
Butylphthalide is approved and available for use in China, where the study was conducted. However, the medication hasn’t been approved for use by the U.S. Food and Drug Administration.
“Patients who received butylphthalide had less severe neurological symptoms and a better living status at 90 days post stroke, compared to those who received the placebo,” said coauthor Baixue Jia, MD, an attending physician in interventional neuroradiology at the Beijing Tiantan Hospital of Capital Medical University and a faculty member at the China National Clinical Research Center for Neurological Diseases in Beijing. “If the results are confirmed in other trials, this may lead to more options to treat strokes caused by clots.”
The study was presented at the International Stroke Conference presented by the American Stroke Association, a division of the American Heart Association.
Studying stroke outcomes
The researchers described butylphthalide as a cerebroprotective drug that was originally extracted from seeds of Apium graveolens. In China, previous studies have shown that the drug has cerebroprotective effects in animal models of ischemia-reperfusion, they noted.
In this randomized, double-blind, placebo-controlled trial, Dr. Jia and colleagues evaluated whether treatment with butylphthalide could improve 90-day outcomes for adults with acute ischemic stroke who received intravenous recombinant tissue plasminogen activator (tPA), endovascular treatment, or both.
The participants were treated at one of 59 medical centers in China between July 2018 and February 2022. Those who had minimal stroke symptoms on their initial exam, defined as a score of 0-3 on the National Institutes of Health Stroke Scale, or had severe stroke symptoms, defined as having a score of 26 or higher on the NIHSS, were excluded from the study.
Along with an initial revascularization intervention chosen by their physician, participants were randomly selected to receive either butylphthalide or a placebo daily for 90 days. The drug was administered through daily intravenous injections for the first 14 days, after which patients received oral capsules for 76 days.
The research team defined the outcomes as “favorable” if a patient fell into one of the following categories 90 days after the stroke: an initially mild to moderate stroke (NIHSS, 4-7) and no symptoms after treatment, defined as a score of 0 on the Modified Rankin Scale (mRS), which measures disability and dependence; an initially moderate to serious stroke (NIHSS, 8-14) and no residual symptoms or mild symptoms that don’t impair the ability to perform routine activities of daily living without assistance (mRS, 0-1); or an initially serious to severe stroke (NIHSS, 15-25) and no remaining symptoms or a slight disability that impairs some activities but allows one to conduct daily living without assistance (mRS, 0-2).
Secondary outcomes included symptomatic intracranial hemorrhage, recurrent stroke, and mortality.
Among the 1,216 participants, 607 were assigned to the treatment group, and 609 were assigned to the placebo group. The average age was 66 years, and 68% were men.
Overall, participants in the butylphthalide group were 70% more likely to have a favorable 90-day outcome, compared with the placebo group. Favorable outcomes occurred in 344 patients (56.7%) in the butylphthalide group, compared with 268 patients (44%) in the placebo group (odds ratio, 1.70; 95% confidence interval, 1.35-2.14; P < .001).
In addition, butylphthalide improved function equally well for the patients who initially received tPA, those who received endovascular treatment, and those who received both tPA and endovascular treatment.
Secondary events, such as recurrent stroke and intracranial hemorrhage, weren’t significantly different between the butylphthalide and placebo groups.
Ongoing questions
Dr. Jia and colleagues noted the need to understand how butylphthalide works in the brain. Animal studies have suggested several possible mechanisms, but it remains unclear.
“The next step should be investigating the exact mechanisms of butylphthalide in humans,” Dr. Jia said.
Additional research should assess the medication in other populations, the authors noted, particularly because the study involved participants who received initial treatment with tPA, endovascular treatment, or both. The results may not be generalizable to stroke patients who receive other treatments or to populations outside of China.
“While these are interesting results, this is only one relatively small study on a fairly select population in China. Butylphthalide, a medication initially compounded from celery seed, is not ready for use in standard stroke treatment,” said Daniel Lackland, DrPH, professor of neurology and director of the division of translational neurosciences and population studies at the Medical University of South Carolina, Charleston.
Dr. Lackland, who wasn’t involved with the study, is a member of the American Stroke Association’s Stroke Council. Although butylphthalide was originally extracted from seeds, he noted, it’s not what patients would find commercially available.
“The medication used in this study is not the same as celery seed or celery seed extract supplements,” he said. “Stroke survivors should always consult with their neurologist or healthcare professional regarding diet after a stroke.”
The study was funded by the National Key Technology Research and Development Program of the Ministry of Science and Technology of the People’s Republic of China and Shijiazhuang Pharmaceutical Group dl-3-butylphthalide Pharmaceutical. Several authors are employed with Beijing Tiantan Hospital and the Beijing Institute of Brain Disorders. Dr. Lackland reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new report suggests.
Patients treated with butylphthalide had fewer severe neurologic symptoms and better function 90 days after the stroke, compared with those receiving placebo.
Butylphthalide is approved and available for use in China, where the study was conducted. However, the medication hasn’t been approved for use by the U.S. Food and Drug Administration.
“Patients who received butylphthalide had less severe neurological symptoms and a better living status at 90 days post stroke, compared to those who received the placebo,” said coauthor Baixue Jia, MD, an attending physician in interventional neuroradiology at the Beijing Tiantan Hospital of Capital Medical University and a faculty member at the China National Clinical Research Center for Neurological Diseases in Beijing. “If the results are confirmed in other trials, this may lead to more options to treat strokes caused by clots.”
The study was presented at the International Stroke Conference presented by the American Stroke Association, a division of the American Heart Association.
Studying stroke outcomes
The researchers described butylphthalide as a cerebroprotective drug that was originally extracted from seeds of Apium graveolens. In China, previous studies have shown that the drug has cerebroprotective effects in animal models of ischemia-reperfusion, they noted.
In this randomized, double-blind, placebo-controlled trial, Dr. Jia and colleagues evaluated whether treatment with butylphthalide could improve 90-day outcomes for adults with acute ischemic stroke who received intravenous recombinant tissue plasminogen activator (tPA), endovascular treatment, or both.
The participants were treated at one of 59 medical centers in China between July 2018 and February 2022. Those who had minimal stroke symptoms on their initial exam, defined as a score of 0-3 on the National Institutes of Health Stroke Scale, or had severe stroke symptoms, defined as having a score of 26 or higher on the NIHSS, were excluded from the study.
Along with an initial revascularization intervention chosen by their physician, participants were randomly selected to receive either butylphthalide or a placebo daily for 90 days. The drug was administered through daily intravenous injections for the first 14 days, after which patients received oral capsules for 76 days.
The research team defined the outcomes as “favorable” if a patient fell into one of the following categories 90 days after the stroke: an initially mild to moderate stroke (NIHSS, 4-7) and no symptoms after treatment, defined as a score of 0 on the Modified Rankin Scale (mRS), which measures disability and dependence; an initially moderate to serious stroke (NIHSS, 8-14) and no residual symptoms or mild symptoms that don’t impair the ability to perform routine activities of daily living without assistance (mRS, 0-1); or an initially serious to severe stroke (NIHSS, 15-25) and no remaining symptoms or a slight disability that impairs some activities but allows one to conduct daily living without assistance (mRS, 0-2).
Secondary outcomes included symptomatic intracranial hemorrhage, recurrent stroke, and mortality.
Among the 1,216 participants, 607 were assigned to the treatment group, and 609 were assigned to the placebo group. The average age was 66 years, and 68% were men.
Overall, participants in the butylphthalide group were 70% more likely to have a favorable 90-day outcome, compared with the placebo group. Favorable outcomes occurred in 344 patients (56.7%) in the butylphthalide group, compared with 268 patients (44%) in the placebo group (odds ratio, 1.70; 95% confidence interval, 1.35-2.14; P < .001).
In addition, butylphthalide improved function equally well for the patients who initially received tPA, those who received endovascular treatment, and those who received both tPA and endovascular treatment.
Secondary events, such as recurrent stroke and intracranial hemorrhage, weren’t significantly different between the butylphthalide and placebo groups.
Ongoing questions
Dr. Jia and colleagues noted the need to understand how butylphthalide works in the brain. Animal studies have suggested several possible mechanisms, but it remains unclear.
“The next step should be investigating the exact mechanisms of butylphthalide in humans,” Dr. Jia said.
Additional research should assess the medication in other populations, the authors noted, particularly because the study involved participants who received initial treatment with tPA, endovascular treatment, or both. The results may not be generalizable to stroke patients who receive other treatments or to populations outside of China.
“While these are interesting results, this is only one relatively small study on a fairly select population in China. Butylphthalide, a medication initially compounded from celery seed, is not ready for use in standard stroke treatment,” said Daniel Lackland, DrPH, professor of neurology and director of the division of translational neurosciences and population studies at the Medical University of South Carolina, Charleston.
Dr. Lackland, who wasn’t involved with the study, is a member of the American Stroke Association’s Stroke Council. Although butylphthalide was originally extracted from seeds, he noted, it’s not what patients would find commercially available.
“The medication used in this study is not the same as celery seed or celery seed extract supplements,” he said. “Stroke survivors should always consult with their neurologist or healthcare professional regarding diet after a stroke.”
The study was funded by the National Key Technology Research and Development Program of the Ministry of Science and Technology of the People’s Republic of China and Shijiazhuang Pharmaceutical Group dl-3-butylphthalide Pharmaceutical. Several authors are employed with Beijing Tiantan Hospital and the Beijing Institute of Brain Disorders. Dr. Lackland reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a new report suggests.
Patients treated with butylphthalide had fewer severe neurologic symptoms and better function 90 days after the stroke, compared with those receiving placebo.
Butylphthalide is approved and available for use in China, where the study was conducted. However, the medication hasn’t been approved for use by the U.S. Food and Drug Administration.
“Patients who received butylphthalide had less severe neurological symptoms and a better living status at 90 days post stroke, compared to those who received the placebo,” said coauthor Baixue Jia, MD, an attending physician in interventional neuroradiology at the Beijing Tiantan Hospital of Capital Medical University and a faculty member at the China National Clinical Research Center for Neurological Diseases in Beijing. “If the results are confirmed in other trials, this may lead to more options to treat strokes caused by clots.”
The study was presented at the International Stroke Conference presented by the American Stroke Association, a division of the American Heart Association.
Studying stroke outcomes
The researchers described butylphthalide as a cerebroprotective drug that was originally extracted from seeds of Apium graveolens. In China, previous studies have shown that the drug has cerebroprotective effects in animal models of ischemia-reperfusion, they noted.
In this randomized, double-blind, placebo-controlled trial, Dr. Jia and colleagues evaluated whether treatment with butylphthalide could improve 90-day outcomes for adults with acute ischemic stroke who received intravenous recombinant tissue plasminogen activator (tPA), endovascular treatment, or both.
The participants were treated at one of 59 medical centers in China between July 2018 and February 2022. Those who had minimal stroke symptoms on their initial exam, defined as a score of 0-3 on the National Institutes of Health Stroke Scale, or had severe stroke symptoms, defined as having a score of 26 or higher on the NIHSS, were excluded from the study.
Along with an initial revascularization intervention chosen by their physician, participants were randomly selected to receive either butylphthalide or a placebo daily for 90 days. The drug was administered through daily intravenous injections for the first 14 days, after which patients received oral capsules for 76 days.
The research team defined the outcomes as “favorable” if a patient fell into one of the following categories 90 days after the stroke: an initially mild to moderate stroke (NIHSS, 4-7) and no symptoms after treatment, defined as a score of 0 on the Modified Rankin Scale (mRS), which measures disability and dependence; an initially moderate to serious stroke (NIHSS, 8-14) and no residual symptoms or mild symptoms that don’t impair the ability to perform routine activities of daily living without assistance (mRS, 0-1); or an initially serious to severe stroke (NIHSS, 15-25) and no remaining symptoms or a slight disability that impairs some activities but allows one to conduct daily living without assistance (mRS, 0-2).
Secondary outcomes included symptomatic intracranial hemorrhage, recurrent stroke, and mortality.
Among the 1,216 participants, 607 were assigned to the treatment group, and 609 were assigned to the placebo group. The average age was 66 years, and 68% were men.
Overall, participants in the butylphthalide group were 70% more likely to have a favorable 90-day outcome, compared with the placebo group. Favorable outcomes occurred in 344 patients (56.7%) in the butylphthalide group, compared with 268 patients (44%) in the placebo group (odds ratio, 1.70; 95% confidence interval, 1.35-2.14; P < .001).
In addition, butylphthalide improved function equally well for the patients who initially received tPA, those who received endovascular treatment, and those who received both tPA and endovascular treatment.
Secondary events, such as recurrent stroke and intracranial hemorrhage, weren’t significantly different between the butylphthalide and placebo groups.
Ongoing questions
Dr. Jia and colleagues noted the need to understand how butylphthalide works in the brain. Animal studies have suggested several possible mechanisms, but it remains unclear.
“The next step should be investigating the exact mechanisms of butylphthalide in humans,” Dr. Jia said.
Additional research should assess the medication in other populations, the authors noted, particularly because the study involved participants who received initial treatment with tPA, endovascular treatment, or both. The results may not be generalizable to stroke patients who receive other treatments or to populations outside of China.
“While these are interesting results, this is only one relatively small study on a fairly select population in China. Butylphthalide, a medication initially compounded from celery seed, is not ready for use in standard stroke treatment,” said Daniel Lackland, DrPH, professor of neurology and director of the division of translational neurosciences and population studies at the Medical University of South Carolina, Charleston.
Dr. Lackland, who wasn’t involved with the study, is a member of the American Stroke Association’s Stroke Council. Although butylphthalide was originally extracted from seeds, he noted, it’s not what patients would find commercially available.
“The medication used in this study is not the same as celery seed or celery seed extract supplements,” he said. “Stroke survivors should always consult with their neurologist or healthcare professional regarding diet after a stroke.”
The study was funded by the National Key Technology Research and Development Program of the Ministry of Science and Technology of the People’s Republic of China and Shijiazhuang Pharmaceutical Group dl-3-butylphthalide Pharmaceutical. Several authors are employed with Beijing Tiantan Hospital and the Beijing Institute of Brain Disorders. Dr. Lackland reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ISC 2023
What’s new in brain health?
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
Cutting calories could slow the pace of aging: Study
That may seem like a little benefit for a large cut in calories. But experts say it’s actually a pretty big deal.
“In other studies, that same difference in pace of aging had meaningful consequences for people’s risk of dying,” says senior study author Daniel W. Belsky, PhD, a researcher at the Butler Columbia Aging Center at Columbia University, New York.
Cutting calories by 25% slowed the pace of aging in young and middle-aged adults by a few percentage points, compared with those who continued eating normally, the new research reveals. This first-of-its-kind study in humans adds to evidence from animal studies that the rate of aging can be changed.
Compared with 75 people who ate normally, the 145 people randomly assigned to cut back their calories slowed their pace of aging by 2%-3% over 2 years in the randomized controlled trial.
For example, a similar slowdown in the pace of aging was associated with a 10%-15% lower risk of dying over 10-15 years in previous work, Dr. Belsky says. “So 2%-3% slower aging doesn’t sound like maybe that big of a deal – but 10%-15% reduction in risk of dying seems like a big deal.”
Results of the study were published in the journal Nature Aging.
Even though the pace of aging slowed, the researchers did not find significant changes on two biological aging measures in the study, suggesting more work is needed.
The findings “are intriguing in that caloric restriction seemed to show a slower pace of aging in healthy adults,” says Vandana Sheth, a registered dietitian-nutritionist and owner of a nutrition consulting firm in Los Angeles. “This can have a significant impact on population health. However, larger studies need to be done to follow up on these findings.”
‘Exciting result’
Asked if the findings imply aging could be slowed down in people, Dr. Belsky says. “That is the ... exciting result from the trial. These results suggest it may be possible to slow the pace of biological aging with a behavioral intervention.”
But not everyone is completely convinced.
“This is good suggestive evidence that caloric restriction can modify aspects of biological aging in humans, similar to what has been known in laboratory animals for many decades,” says Matt Kaeberlein, PhD, director of the Healthy Aging and Longevity Research Institute at the University of Washington, Seattle, and senior author of a 2021 review article in Science.
Part of his concern is that cutting your calories by a quarter may not be a sustainable long-term strategy.
“It’s important to keep in mind that these measurements only report on a portion of biological aging and are probably not an accurate overall measurement of biological age or the rate of biological aging,” Dr. Kaeberlein says. The findings might suggest that “at the population level, a 25% reduction in caloric intake is unlikely to have large effects on biological aging unless implemented over many years, which is likely not reasonable for most people.”
Insight into intermittent fasting?
Cutting back on calories is related to other dietary strategies, including intermittent fasting and time-restricted eating, Dr. Belsky says. “Intermittent fasting and time-restricted eating are nutritional interventions that have been developed, in part, because in experiments with animals, they have some of the same biological effects as calorie restriction.”
There remain many unanswered questions.
“There are people who would argue that the reason calorie restriction does what it does is because when people are calorie-restricted, they also tend to restrict the times when they eat,” Dr. Belsky says. “They tend to have these longer fasts during the day.”
A version of this article first appeared on WebMD.com.
That may seem like a little benefit for a large cut in calories. But experts say it’s actually a pretty big deal.
“In other studies, that same difference in pace of aging had meaningful consequences for people’s risk of dying,” says senior study author Daniel W. Belsky, PhD, a researcher at the Butler Columbia Aging Center at Columbia University, New York.
Cutting calories by 25% slowed the pace of aging in young and middle-aged adults by a few percentage points, compared with those who continued eating normally, the new research reveals. This first-of-its-kind study in humans adds to evidence from animal studies that the rate of aging can be changed.
Compared with 75 people who ate normally, the 145 people randomly assigned to cut back their calories slowed their pace of aging by 2%-3% over 2 years in the randomized controlled trial.
For example, a similar slowdown in the pace of aging was associated with a 10%-15% lower risk of dying over 10-15 years in previous work, Dr. Belsky says. “So 2%-3% slower aging doesn’t sound like maybe that big of a deal – but 10%-15% reduction in risk of dying seems like a big deal.”
Results of the study were published in the journal Nature Aging.
Even though the pace of aging slowed, the researchers did not find significant changes on two biological aging measures in the study, suggesting more work is needed.
The findings “are intriguing in that caloric restriction seemed to show a slower pace of aging in healthy adults,” says Vandana Sheth, a registered dietitian-nutritionist and owner of a nutrition consulting firm in Los Angeles. “This can have a significant impact on population health. However, larger studies need to be done to follow up on these findings.”
‘Exciting result’
Asked if the findings imply aging could be slowed down in people, Dr. Belsky says. “That is the ... exciting result from the trial. These results suggest it may be possible to slow the pace of biological aging with a behavioral intervention.”
But not everyone is completely convinced.
“This is good suggestive evidence that caloric restriction can modify aspects of biological aging in humans, similar to what has been known in laboratory animals for many decades,” says Matt Kaeberlein, PhD, director of the Healthy Aging and Longevity Research Institute at the University of Washington, Seattle, and senior author of a 2021 review article in Science.
Part of his concern is that cutting your calories by a quarter may not be a sustainable long-term strategy.
“It’s important to keep in mind that these measurements only report on a portion of biological aging and are probably not an accurate overall measurement of biological age or the rate of biological aging,” Dr. Kaeberlein says. The findings might suggest that “at the population level, a 25% reduction in caloric intake is unlikely to have large effects on biological aging unless implemented over many years, which is likely not reasonable for most people.”
Insight into intermittent fasting?
Cutting back on calories is related to other dietary strategies, including intermittent fasting and time-restricted eating, Dr. Belsky says. “Intermittent fasting and time-restricted eating are nutritional interventions that have been developed, in part, because in experiments with animals, they have some of the same biological effects as calorie restriction.”
There remain many unanswered questions.
“There are people who would argue that the reason calorie restriction does what it does is because when people are calorie-restricted, they also tend to restrict the times when they eat,” Dr. Belsky says. “They tend to have these longer fasts during the day.”
A version of this article first appeared on WebMD.com.
That may seem like a little benefit for a large cut in calories. But experts say it’s actually a pretty big deal.
“In other studies, that same difference in pace of aging had meaningful consequences for people’s risk of dying,” says senior study author Daniel W. Belsky, PhD, a researcher at the Butler Columbia Aging Center at Columbia University, New York.
Cutting calories by 25% slowed the pace of aging in young and middle-aged adults by a few percentage points, compared with those who continued eating normally, the new research reveals. This first-of-its-kind study in humans adds to evidence from animal studies that the rate of aging can be changed.
Compared with 75 people who ate normally, the 145 people randomly assigned to cut back their calories slowed their pace of aging by 2%-3% over 2 years in the randomized controlled trial.
For example, a similar slowdown in the pace of aging was associated with a 10%-15% lower risk of dying over 10-15 years in previous work, Dr. Belsky says. “So 2%-3% slower aging doesn’t sound like maybe that big of a deal – but 10%-15% reduction in risk of dying seems like a big deal.”
Results of the study were published in the journal Nature Aging.
Even though the pace of aging slowed, the researchers did not find significant changes on two biological aging measures in the study, suggesting more work is needed.
The findings “are intriguing in that caloric restriction seemed to show a slower pace of aging in healthy adults,” says Vandana Sheth, a registered dietitian-nutritionist and owner of a nutrition consulting firm in Los Angeles. “This can have a significant impact on population health. However, larger studies need to be done to follow up on these findings.”
‘Exciting result’
Asked if the findings imply aging could be slowed down in people, Dr. Belsky says. “That is the ... exciting result from the trial. These results suggest it may be possible to slow the pace of biological aging with a behavioral intervention.”
But not everyone is completely convinced.
“This is good suggestive evidence that caloric restriction can modify aspects of biological aging in humans, similar to what has been known in laboratory animals for many decades,” says Matt Kaeberlein, PhD, director of the Healthy Aging and Longevity Research Institute at the University of Washington, Seattle, and senior author of a 2021 review article in Science.
Part of his concern is that cutting your calories by a quarter may not be a sustainable long-term strategy.
“It’s important to keep in mind that these measurements only report on a portion of biological aging and are probably not an accurate overall measurement of biological age or the rate of biological aging,” Dr. Kaeberlein says. The findings might suggest that “at the population level, a 25% reduction in caloric intake is unlikely to have large effects on biological aging unless implemented over many years, which is likely not reasonable for most people.”
Insight into intermittent fasting?
Cutting back on calories is related to other dietary strategies, including intermittent fasting and time-restricted eating, Dr. Belsky says. “Intermittent fasting and time-restricted eating are nutritional interventions that have been developed, in part, because in experiments with animals, they have some of the same biological effects as calorie restriction.”
There remain many unanswered questions.
“There are people who would argue that the reason calorie restriction does what it does is because when people are calorie-restricted, they also tend to restrict the times when they eat,” Dr. Belsky says. “They tend to have these longer fasts during the day.”
A version of this article first appeared on WebMD.com.
FROM NATURE AGING
A doctor must go to extremes to save a choking victim
Some time ago I was invited to join a bipartisan congressional task force on valley fever, also known as coccidioidomycosis. A large and diverse crowd attended the task force’s first meeting in Bakersfield, Calif. – a meeting for everyone: the medical profession, the public, it even included veterinarians.
The whole thing was a resounding success. Francis Collins was there, the just-retired director of the NIH. Tom Frieden, then-director of the Centers for Disease Control and Prevention was there, as were several congresspeople and also my college roommate, a retired Navy medical corps captain. I was enjoying it.
Afterward, we had a banquet dinner at a restaurant in downtown Bakersfield. One of the people there was a woman I knew well – her husband was a physician friend. The restaurant served steak and salmon, and this woman made the mistake of ordering the steak.
Not long after the entrees were served, I heard a commotion at the table just behind me. I turned around and saw that woman in distress. A piece of steak had wedged in her trachea and she couldn’t breathe.
Almost immediately, the chef showed up. I don’t know how he got there. The chef at this restaurant was a big guy. I mean, probably 6 feet, 5 inches tall and 275 pounds. He tried the Heimlich maneuver. It didn’t work.
At that point, I jumped up. I thought, “Well, maybe I know how to do this better than him.” Probably not, actually. I tried and couldn’t make it work either. So I knew we were going to have to do something.
Paul Krogstad, my friend and research partner who is a pediatric infectious disease physician, stepped up and tried to put his finger in her throat and dig it out. He couldn’t get it. The patient had lost consciousness.
So, I’m thinking, okay, there’s really only one choice. You have to get an airway surgically.
I said, “We have to put her down on the floor.” And then I said, “Knife!”
I was looking at the steak knives on the table and they weren’t to my liking for doing a procedure. My college roommate – the retired Navy man – whipped out this very good pocketknife.
I had never done this in my life.
While I was making the incision, somebody gave Paul a ballpoint pen and he broke it into pieces to make a tracheostomy tube. Once I’d made the little incision, I put the tube in. She wasn’t breathing, but she still had a pulse.
I leaned forward and blew into the tube and inflated her lungs. I could see her lungs balloon up. It was a nice feeling, because I knew I was clearly in the right place.
I can’t quite explain it, but while I was doing this, I was enormously calm and totally focused. I knew there was a crowd of people around me, all looking at me, but I wasn’t conscious of that.
It was really just the four of us: Paul and Tom and me and our patient. Those were the only people that I was really cognizant of. Paul and Tom were not panic stricken at all. I remember somebody shouting, “We have to start CPR!” and Frieden said, “No. We don’t.”
Moments later, she woke up, sat up, coughed, and shot the piece of steak across the room.
She was breathing on her own, but we still taped that tube into place. Somebody had already summoned an ambulance; they were there not very long after we completed this procedure. I got in the ambulance with her and we rode over to the emergency room at Mercy Truxtun.
She was stable and doing okay. I sat with her until a thoracic surgeon showed up. He checked out the situation and decided we didn’t need that tube and took it out. I didn’t want to take that out until I had a surgeon there who could do a formal tracheostomy.
They kept her in the hospital for 3 or 4 days. Now, this woman had always had difficulties swallowing, so steak may not have been the best choice. She still had trouble swallowing afterward but recovered.
I’ve known her and her husband a long time, so it was certainly rewarding to be able to provide this service. Years later, though, when her husband died, I spoke at his funeral. When she was speaking to the gathering, she said, “And oh, by the way, Royce, thanks for saving my life.”
That surprised me. I didn’t think we were going to go there.
I’d never tried to practice medicine “at the roadside” before. But that’s part of the career.
Royce Johnson, MD, is the chief of the division of infectious disease among other leadership positions at Kern Medical in Bakersfield, Calif., and the medical director of the Valley Fever Institute.
A version of this article first appeared on Medscape.com.
Some time ago I was invited to join a bipartisan congressional task force on valley fever, also known as coccidioidomycosis. A large and diverse crowd attended the task force’s first meeting in Bakersfield, Calif. – a meeting for everyone: the medical profession, the public, it even included veterinarians.
The whole thing was a resounding success. Francis Collins was there, the just-retired director of the NIH. Tom Frieden, then-director of the Centers for Disease Control and Prevention was there, as were several congresspeople and also my college roommate, a retired Navy medical corps captain. I was enjoying it.
Afterward, we had a banquet dinner at a restaurant in downtown Bakersfield. One of the people there was a woman I knew well – her husband was a physician friend. The restaurant served steak and salmon, and this woman made the mistake of ordering the steak.
Not long after the entrees were served, I heard a commotion at the table just behind me. I turned around and saw that woman in distress. A piece of steak had wedged in her trachea and she couldn’t breathe.
Almost immediately, the chef showed up. I don’t know how he got there. The chef at this restaurant was a big guy. I mean, probably 6 feet, 5 inches tall and 275 pounds. He tried the Heimlich maneuver. It didn’t work.
At that point, I jumped up. I thought, “Well, maybe I know how to do this better than him.” Probably not, actually. I tried and couldn’t make it work either. So I knew we were going to have to do something.
Paul Krogstad, my friend and research partner who is a pediatric infectious disease physician, stepped up and tried to put his finger in her throat and dig it out. He couldn’t get it. The patient had lost consciousness.
So, I’m thinking, okay, there’s really only one choice. You have to get an airway surgically.
I said, “We have to put her down on the floor.” And then I said, “Knife!”
I was looking at the steak knives on the table and they weren’t to my liking for doing a procedure. My college roommate – the retired Navy man – whipped out this very good pocketknife.
I had never done this in my life.
While I was making the incision, somebody gave Paul a ballpoint pen and he broke it into pieces to make a tracheostomy tube. Once I’d made the little incision, I put the tube in. She wasn’t breathing, but she still had a pulse.
I leaned forward and blew into the tube and inflated her lungs. I could see her lungs balloon up. It was a nice feeling, because I knew I was clearly in the right place.
I can’t quite explain it, but while I was doing this, I was enormously calm and totally focused. I knew there was a crowd of people around me, all looking at me, but I wasn’t conscious of that.
It was really just the four of us: Paul and Tom and me and our patient. Those were the only people that I was really cognizant of. Paul and Tom were not panic stricken at all. I remember somebody shouting, “We have to start CPR!” and Frieden said, “No. We don’t.”
Moments later, she woke up, sat up, coughed, and shot the piece of steak across the room.
She was breathing on her own, but we still taped that tube into place. Somebody had already summoned an ambulance; they were there not very long after we completed this procedure. I got in the ambulance with her and we rode over to the emergency room at Mercy Truxtun.
She was stable and doing okay. I sat with her until a thoracic surgeon showed up. He checked out the situation and decided we didn’t need that tube and took it out. I didn’t want to take that out until I had a surgeon there who could do a formal tracheostomy.
They kept her in the hospital for 3 or 4 days. Now, this woman had always had difficulties swallowing, so steak may not have been the best choice. She still had trouble swallowing afterward but recovered.
I’ve known her and her husband a long time, so it was certainly rewarding to be able to provide this service. Years later, though, when her husband died, I spoke at his funeral. When she was speaking to the gathering, she said, “And oh, by the way, Royce, thanks for saving my life.”
That surprised me. I didn’t think we were going to go there.
I’d never tried to practice medicine “at the roadside” before. But that’s part of the career.
Royce Johnson, MD, is the chief of the division of infectious disease among other leadership positions at Kern Medical in Bakersfield, Calif., and the medical director of the Valley Fever Institute.
A version of this article first appeared on Medscape.com.
Some time ago I was invited to join a bipartisan congressional task force on valley fever, also known as coccidioidomycosis. A large and diverse crowd attended the task force’s first meeting in Bakersfield, Calif. – a meeting for everyone: the medical profession, the public, it even included veterinarians.
The whole thing was a resounding success. Francis Collins was there, the just-retired director of the NIH. Tom Frieden, then-director of the Centers for Disease Control and Prevention was there, as were several congresspeople and also my college roommate, a retired Navy medical corps captain. I was enjoying it.
Afterward, we had a banquet dinner at a restaurant in downtown Bakersfield. One of the people there was a woman I knew well – her husband was a physician friend. The restaurant served steak and salmon, and this woman made the mistake of ordering the steak.
Not long after the entrees were served, I heard a commotion at the table just behind me. I turned around and saw that woman in distress. A piece of steak had wedged in her trachea and she couldn’t breathe.
Almost immediately, the chef showed up. I don’t know how he got there. The chef at this restaurant was a big guy. I mean, probably 6 feet, 5 inches tall and 275 pounds. He tried the Heimlich maneuver. It didn’t work.
At that point, I jumped up. I thought, “Well, maybe I know how to do this better than him.” Probably not, actually. I tried and couldn’t make it work either. So I knew we were going to have to do something.
Paul Krogstad, my friend and research partner who is a pediatric infectious disease physician, stepped up and tried to put his finger in her throat and dig it out. He couldn’t get it. The patient had lost consciousness.
So, I’m thinking, okay, there’s really only one choice. You have to get an airway surgically.
I said, “We have to put her down on the floor.” And then I said, “Knife!”
I was looking at the steak knives on the table and they weren’t to my liking for doing a procedure. My college roommate – the retired Navy man – whipped out this very good pocketknife.
I had never done this in my life.
While I was making the incision, somebody gave Paul a ballpoint pen and he broke it into pieces to make a tracheostomy tube. Once I’d made the little incision, I put the tube in. She wasn’t breathing, but she still had a pulse.
I leaned forward and blew into the tube and inflated her lungs. I could see her lungs balloon up. It was a nice feeling, because I knew I was clearly in the right place.
I can’t quite explain it, but while I was doing this, I was enormously calm and totally focused. I knew there was a crowd of people around me, all looking at me, but I wasn’t conscious of that.
It was really just the four of us: Paul and Tom and me and our patient. Those were the only people that I was really cognizant of. Paul and Tom were not panic stricken at all. I remember somebody shouting, “We have to start CPR!” and Frieden said, “No. We don’t.”
Moments later, she woke up, sat up, coughed, and shot the piece of steak across the room.
She was breathing on her own, but we still taped that tube into place. Somebody had already summoned an ambulance; they were there not very long after we completed this procedure. I got in the ambulance with her and we rode over to the emergency room at Mercy Truxtun.
She was stable and doing okay. I sat with her until a thoracic surgeon showed up. He checked out the situation and decided we didn’t need that tube and took it out. I didn’t want to take that out until I had a surgeon there who could do a formal tracheostomy.
They kept her in the hospital for 3 or 4 days. Now, this woman had always had difficulties swallowing, so steak may not have been the best choice. She still had trouble swallowing afterward but recovered.
I’ve known her and her husband a long time, so it was certainly rewarding to be able to provide this service. Years later, though, when her husband died, I spoke at his funeral. When she was speaking to the gathering, she said, “And oh, by the way, Royce, thanks for saving my life.”
That surprised me. I didn’t think we were going to go there.
I’d never tried to practice medicine “at the roadside” before. But that’s part of the career.
Royce Johnson, MD, is the chief of the division of infectious disease among other leadership positions at Kern Medical in Bakersfield, Calif., and the medical director of the Valley Fever Institute.
A version of this article first appeared on Medscape.com.





