User login
Is ezetimibe/simvastatin no better than simvastatin alone? Lessons learned and clinical implications
The Ezetimibe and Simvastatin in Hypercholesterolemia Enhances Atherosclerosis Regression (ENHANCE) trial1 was probably the most widely publicized clinical study of the past decade. How did a 720-patient imaging trial with a neutral result in patients with severe hypercholesterolemia rise to a level warranting massive media attention, a congressional investigation, and a recommendation to curtail the use of a drug widely used to reduce levels of low-density-lipoprotein cholesterol (LDL-C)?
The reaction to the ENHANCE trial reveals more about the political climate and the relationship between the pharmaceutical industry and the American public than it does about the effects of ezetimibe (available combined with simvastatin as Vytorin and by itself as Zetia) on the progression of atherosclerosis.
SOME SELF-DISCLOSURE
Before I discuss the clinical implications of the ENHANCE trial, I must describe both my financial conflicts and intellectual biases. I am a paid consultant, speaker, and researcher on behalf of Merck/Schering-Plough, the sponsor of the ENHANCE trial. I was a principal investigator in the first phase II trial of ezetimibe and have conducted more than 10 clinical trials of either ezetimibe or ezetimibe/simvastatin. I also have been a strong advocate for imaging trials to assist in the clinical development of novel therapeutic agents and to support regulatory approval.
Therefore, I believe that the thickness of the intima and media layers of the carotid arteries is a useful surrogate to evaluate the potential antiatherosclerotic effects of drugs (more on this topic below). Also, I believe that the LDL-C-lowering hypothesis has been proven: ie, that all drugs that lower LDL-C safely, without off-target adverse effects, should reduce cardiovascular events. I support the goal levels of LDL-C and non-high-density-lipoprotein cholesterol set by the National Cholesterol Education Program’s third Adult Treatment Panel (ATP III) guidelines,2,3 which specify LDL-C targets rather than the use of specific drugs. In spite of these conflicts and potential biases, I believe I have always served the best interests of patient care.
HISTORY OF THE ENHANCE TRIAL
The end point defined as the mean of six measurements
The primary end point was the change in the thickness of the intima and media layers of the carotid arteries over a 2-year period, measured by ultrasonography. A composite measure was used: the mean of the thicknesses in the far walls of the right and left common carotid arteries, the right and left carotid bulbs, and the right and left internal carotid arteries. Secondary end points included the change in the mean maximal carotid artery intima-media thickness (ie, the thickest of the six baseline measurements), the proportion of participants who developed new carotid artery plaque (defined arbitrarily as an intima-media thickness > 1.3 mm), and changes in the mean of the intima-media thickness of the six carotid sites plus the common femoral arteries.
The last participant completed the trial in April 2006. Reading of the almost 30,000 scans was not started until the last participant was finished, so that all scans for each participant could be read in a blinded, randomized order by five separate readers. A significant proportion of the images that the protocol called for could not be obtained or analyzed, particularly in the internal carotid artery and the carotid bulb, which are often difficult to visualize. As a result, 17% of the internal carotid or carotid bulb measurements were discarded.
To change the end point post hoc, or not to change the end point?
The sponsor of the trial was concerned about the missing data points and convened a special advisory board to review the blinded data. This group suggested a solution: changing the primary end point from the six-site composite value to the mean value in just the common carotid arteries. They based this suggestion on the greater success rate in measuring the common carotids (97%) than in measuring all six sites (88%), as well as on recent trials that indicated that the common carotid artery measurement correlates better with clinical outcomes (because the internal carotid and the bulb measurements vary more). On November 26, 2007, Merck/Schering-Plough announced the primary end point would be changed to the mean change in the common carotid arteries.
However, during a separate meeting on November 30, 2007, some members of the Merck/Schering-Plough advisory board objected to the change. On December 11, 2007, the company announced that the original primary end point would not be changed.
Neutral results, negative publicity
On December 31, 2007, the ENHANCE study was unblinded, and on January 14, 2008, Merck/Schering-Plough issued a press release announcing the results. The press release stated that there were no statistically significant differences between the treatment groups in the primary end point or in any of the secondary end points, despite a 16.5% greater reduction in LDL-C (about 50 mg/dL) in the group receiving the ezetimibe/simvastatin combination. The composite intima-media thickness had increased by an average of 0.0111 mm in the combined-therapy group vs 0.0058 mm in the simvastatin-only group (P = .29) over the 24-month treatment period.5
The press release received unprecedented international media attention. One leading cardiologist commented to the media that ENHANCE showed “millions of patients may be taking a drug [ezetimibe] that does not benefit them, raising their risk of heart attacks and exposing them to potential side effects.”6 The perceived message that ezetimibe/simvastatin is harmful resulted in thousands of phone calls from concerned patients to their physicians throughout the United States. The American Heart Association (AHA) and the American College of Cardiology (ACC) issued a joint statement the next day saying that ezetimibe/simvastatin does not appear to be unsafe and that patients should not stop taking the drug on their own. In the following days, Merck/Schering-Plough placed advertisements in newspapers reaffirming the safety of ezetimibe and quoting the AHA/ACC statement.
But the full results of the study were not available at that point. In fact, Senator Charles Grassley (R-Iowa) had launched a congressional investigation into the delays in releasing the results of the ENHANCE trial in December 2007. A focus of the investigation was whether the sponsor was delaying the release either because the data reflected negatively on its product or because it was legitimately concerned about the quality of the measurements of the carotid intima-media thickness. After Merck/Schering-Plough placed the advertisements quoting the AHA/ACC statement, these organizations were criticized for touting the safety of ezetimibe while receiving educational grants and other funds from Merck/Schering-Plough. Senator Grassley sent a letter to the ACC in late March requesting information about the amount of funds the ACC had received.
Full results are published, and the ACC is misquoted
The ENHANCE study was selected for a special presentation at the ACC annual scientific session on March 30, 2008. The full ENHANCE results were presented by Dr. Kastelein, after which an expert panel led by Harlan M. Krumholz, MD, discussed the trial’s implications. The ENHANCE results were simultaneously published in the New England Journal of Medicine,1 accompanied by an editorial by B. Greg Brown, MD, and Allen J. Taylor, MD,7 and another editorial by the editors of that journal, Jeffrey M. Drazen, MD, and colleagues.8 The expert panel and the editorialists concluded that the ENHANCE trial data raised concerns about the cardiovascular benefits of ezetimibe; that statins should be used as initial therapy for hyperlipidemia and titrated to the goal LDL-C level or to the maximally tolerated dose; and that other drugs such as bile acid sequestrants, fibrates, and niacin should be used in combination with statins before considering ezetimibe.9
The next day, stories appeared in the media mistakenly stating that the ACC had recommended that ezetimibe/simvastatin be discontinued. This view was fueled by an article in the ACC’s Scientific Session News, penned by a contract writer and editor, with the headline, “ACC on Vytorin: Go Back to Statins” that said, “After waiting for 18 months for the results of the ENHANCE study, an ACC panel on Sunday encouraged physicians to use statins as a first line and prescribe Vytorin only as a last resort for patients unable to tolerate other cholesterol-lowering agents.”10
The ACC later clarified that this was the opinion of the panelists and not that of the ACC, and they reiterated statements from the AHA/ACC Secondary Prevention Guidelines11 recommending statins in maximally tolerated doses or titrated to a goal LDL-C level for first-line drug treatment of coronary artery disease, and recommending that patients speak with their physicians before discontinuing any therapy.
WHY WERE THE ENHANCE STUDY RESULTS NEUTRAL?
The ACC expert panel concluded that the most likely reason for the neutral ENHANCE results was that ezetimibe lowers LDL-C but does not confer a cardiovascular benefit. In the words of Dr. Krumholz (as quoted by Shannon Pettypiece and Michelle Fay Cortez on bloomberg.com), ezetimibe is “just an expensive placebo.”12
There are at least three potential explanations for the lack of benefit with ezetimibe in the ENHANCE trial. I list them below in order of lowest to highest probability, in my opinion:
Theory 1: Ezetimibe lowers LDL-C but is not antiatherogenic
Since almost all experts agree that lowering LDL-C confers cardiovascular benefits, if ezetimibe does not inhibit atherosclerosis it must have some “off-target” effect that negates its LDL-C-lowering benefit. Critics of ezetimibe point out that oral estrogen and torcetrapib also lower LDL-C but do not improve cardiovascular outcomes.13,14
The lack of benefit with these two other agents can be explained. Oral estrogen does not lower apolipoprotein B (an indication of the number of atherogenic particles), but rather it increases the levels of both triglycerides and C-reactive protein, and it is prothrombotic in some people.15 Torcetrapib increases aldosterone production and substantially raises blood pressure.16 Therefore, both drugs have true off-target effects that could explain their failure to reduce cardiovascular risk despite reductions in LDL-C. (Interestingly, though, oral estrogen has been shown to slow the progression of carotid intima-media thickness in newly postmenopausal women.17
Ezetimibe, however, lowers LDL-C by an ultimate mechanism similar to that of statins and bile acid sequestrants, ie, by up-regulating LDL receptors, although these drugs reach this mechanism via different pathways. Statins inhibit cholesterol synthesis, thereby lowering hepatic intracellular cholesterol and thus up-regulating LDL-receptors and enhancing LDL-C clearance from the plasma. Bile acid sequestrants interrupt bile acid reabsorption in the ileum, thereby decreasing intracellular hepatic cholesterol and up-regulating LDL receptors. Ezetimibe, like bile acid sequestrants, also decreases cholesterol return to the liver, lowering hepatic intracellular levels and thus up-regulating LDL receptors.18
Ezetimibe is unlikely to have an off-target effect because it is only fractionally absorbed systemically, and a recent animal study showed that it enhances macrophage efflux of cholesterol, thereby potentially increasing reverse cholesterol transport.19 Ezetimibe has also been shown to reduce atherosclerosis in animal models.20
In their editorial, Drs. Brown and Taylor7 noted that ezetimibe reduces the expression of adenosine triphosphate binding cassette A1 (ABCA1) in Caco-2 (an intestinal cell line), and this may be an example of an off-target effect. However, statins also reduce ABCA1 expression in macrophages.21 ABCA1 is sensitive to intracellular cholesterol, and when cholesterol levels are decreased, whether by statins or by ezetimibe, ABCA1 expression is down-regulated.22
Theory 2: Intima-media thickness does not reflect the true benefits of lowering LDL-C
The carotid intima-media thickness is a surrogate end point that predicts coronary events and the rate of progression of coronary atherosclerosis.23 In trials of lovastatin (Mevacor),24 pravastatin (Pravachol),25 and rosuvastatin (Crestor),26 the carotid intima-media was thinner at 24 months with the active drug than with placebo. In two relatively small trials—ARBITER 1 (n = 161),27 which was open-label, and ASAP (n = 325)28,29—aggressive lipid-lowering reduced the progression of intima-media thickness better than less-aggressive therapy. However, this measure has been used to evaluate the effects of differing degrees of LDL-C reduction between active treatments in fewer than 500 research participants.
Furthermore, what part or parts of the carotid system are we talking about? In recent trials led by Dr. Kastelein, the intima-media thickness of the common carotid arteries increased with pactimibe (an acyl-coenzyme A:cholesterol O-acyltransferase, or ACAT, inhibitor)30 and torcetrapib,31 but the six-site composite measure (which was the primary end point in these trials, as in ENHANCE) did not increase more than in the control groups. Pactimibe was also shown to increase atheroma volume as measured by intravascular ultrasonography in the ACTIVATE trial.32 Therefore, the thickness of the common carotid arteries has been shown to be a better predictor of harm from a therapy than the composite measurement.
The advantage of measuring the common carotid artery is that it is easier to visualize and measure, and therefore the measurements vary less. In the METEOR trial,26 the six-site measurement increased significantly less with rosuvastatin than with placebo, but the common carotid measurement alone was more strongly associated with a difference in progression. In the ENHANCE trial, the thickness of the common carotid arteries increased by 0.0024 mm with simvastatin alone vs 0.0019 mm with simvastatin/ezetimibe, a difference of 0.005 mm that was not statistically significant (P = .93).1
Although the six-site measurement appears to be good for predicting coronary events and evaluating therapies, the measurement in the common carotid arteries appears to be a more reliable surrogate end point for predicting both benefit and harm from antiatherogenic agents. However, trials of statins and other lipid-lowering therapies that assessed clinical events have shown that the reduction in risk associated with a given reduction in cholesterol is similar regardless of the mechanism by which cholesterol is lowered.33 Therefore, the LDL-C level is far superior as a marker of clinical benefit.
Theory 3: Previous statin treatment affected the ENHANCE results
By far the most likely explanation for the neutral findings in ENHANCE is that the patients were so well treated before entry that it was impossible to detect a difference between the two treatment groups in carotid intima-media thickness at the end of the study. Eighty percent of the patients had received statins previously, and at baseline the mean intima-media thickness of the common carotid arteries was only 0.68 mm.1 In contrast, most other trials required a thickness greater than 0.7 mm for entry.
The two main reasons for selecting a population with familial hypercholesterolemia were the assumptions that these participants would have a greater-than-average carotid intima-media thickness at baseline and that they would show an above-average progression rate, even on high-dose statin therapy.4 Both of these assumptions were incorrect: the baseline thickness was normal and the progression rate was negligible in both groups.
Accordingly, the high prevalence of statin pretreatment and the near-normal carotid intima-media thickness at baseline may have prevented the 16.5% greater reduction in LDL-C due to ezetimibe from producing a difference in progression over 24 months of treatment. This conclusion is supported by the long-term follow-up results from ASAP, RADIANCE 1, and CAPTIVATE, all of which showed that in patients with familial hypercholesterolemia well treated with statins, progression of carotid intima-media thickness is negligible.30,31
Further supporting this view, in a previous trial by Dr. Kastelein’s group in patients with familial hypercholesterolemia,34 giving simvastatin 80 mg for 2 years decreased the intima-medial thickness by .081 mm (P < .001), compared with 0.0058 mm in ENHANCE (a 14-fold difference). In the previous trial, the baseline measurement was 1.07 mm (vs 0.68 mm in ENHANCE), and the extent of the change was significantly associated with the baseline measurement (r = .53, P < .001) but not with the change in LDL-C levels.
This is powerful evidence that, in two similar studies that used the same methodology and the same drug, the thinner arteries in the ENHANCE trial are by far the most likely explanation for the lack of change with the addition of ezetimibe to high-dose simvastatin. The METEOR trial enrolled only patients who had never received statins and whose carotid intima-media was thicker than 1.2 mm. In retrospect, a similar design would have been preferable for ENHANCE.35
LESSONS LEARNED AND CLINICAL IMPLICATIONS
For Merck/Schering-Plough, missed opportunities
Although Dr. Krumholz (the spokesman for the ACC panel discussion) and I disagree on the clinical implications of the ENHANCE trial, we do agree on an important point. Dr. Krumholz posed the question that if the LDL-C-lowering hypothesis was already proven for ezetimibe, why was the ENHANCE trial conducted? After 6 years on the market, the efficacy of ezetimibe on cardiovascular outcomes should already have been established. It should not take this long to determine the clinical outcome benefit for a drug.
Merck/Schering-Plough’s outcome program for ezetimibe was inadequately designed to demonstrate the clinical value of this novel compound. Rather than assuming the LDL-C-lowering hypothesis was already established, they conducted another “lower-is-better” trial with the carotid intima-media thickness as the end point, and they succeeded only in raising doubt about the benefits of ezetimibe rather than showing that dual therapy is at least equivalent to high-dose statin therapy.
A preferable approach would have been to compare the effects of a statin in low doses plus ezetimibe vs high-dose statin monotherapy on either surrogate or hard outcomes. If the low-dose statin/ezetimibe combination, which should lower the LDL-C level as much as high-dose statin monotherapy, could provide similar or better outcomes with fewer side effects, this trial would change our practice.
One had hoped that dual therapy, by reducing both intestinal cholesterol absorption and hepatic synthesis of cholesterol, would improve outcomes by modifying postprandial chylomicron composition or by reducing plant sterol absorption.36 Unfortunately, other outcome trials of ezetimibe/simvastatin will not provide an answer regarding the potential advantages of dual therapy. The SEAS study is comparing the number of clinical events in patients with aortic stenosis who receive ezetimibe/simvastatin or placebo; SHARP is being conducted in patients with chronic kidney disease. Although both groups of patients have high rates of coronary events, these trials will not address whether adding ezetimibe provides additional benefits. In fact, if the results of these trials turn out neutral, as in ENHANCE, then ezetimibe will be blamed for potentially offsetting the benefits of simvastatin, and if the trials show a benefit, the simvastatin component of ezetimibe/simvastatin will be given the credit.
The answer may come in 3 to 4 years with the results of IMPROVE-IT, a study of 18,000 patients with acute coronary syndrome treated with ezetimibe/simvastatin or simvastatin. The simvastatin monotherapy group will have a target LDL-C level of less than 80 mg/dL and the ezetimibe/simvastatin group will have an LDL-C target about 15% less. Although this trial is testing the lower-is-better hypothesis with ezetimibe, if the study does not show a benefit, it may not be because ezetimibe lacks clinical efficacy but rather because the LDL-C effect is curvilinear, and there is minimal further benefit of lowering the LDL-C level past 70 mg/dL. If the results of the IMPROVE-IT trial are negative, it may mean the end of ezetimibe as an LDL-C-lowering drug.
Merck/Schering-Plough has lost valuable time in not demonstrating the benefits of ezetimibe on clinical events. In contrast, consider rosuvastatin, an AstraZeneca product. Rosuvastatin was approved about the same time as ezetimibe/simvastatin, and 6 years later it has already received a label change for the reduction of progression of atherosclerosis, based on positive outcomes in the METEOR trial,35 the ASTEROID intravascular ultrasonography trial,37 and the CORONA trial (an important trial that examined hard clinical end points).38 More importantly, the JUPITER trial was recently stopped early owing to a reduction in cardiovascular deaths. Initially, rosuvastatin received an unfair media portrayal as an unsafe drug. Now, because of its proven benefits in outcome trials, it will receive more widespread consideration for clinical use.
For preventive cardiologists, a painful reminder to focus on LDL-C
For the preventive cardiologist or lipidologist, the ENHANCE trial has been a painful reminder that despite overwhelming evidence, the mantra of “the lower the LDL-C the better” is still not universally accepted. We acknowledge the great benefits of statins, but the lure of “pleiotropic effects” distracts many of us from the necessity of more aggressive LDL-C reduction.
The pleiotropic benefits of statins were first raised as a means of supporting increased clinical use of pravastatin vis-a-vis other, more efficacious statins. It was not until the PROVE-IT study that pravastatin’s pleiotropic effects were found not to translate into a benefit equivalent to that of the more efficacious statin, atorvastatin.39
The success of ezetimibe was its ability to safely and easily lower LDL-C in combination with statins to achieve treatment goals. For many patients, a lower-dose statin and ezetimibe together provide a well-tolerated and efficacious approach to treating hyperlipidemia. The fallout from the ENHANCE trial is that many patients who were well treated or who could be better treated with ezetimibe in combination with a statin will not receive the best tolerated regimen. In fact, preliminary prescription data after the release of the ENHANCE study support our worse fear, ie, that patients at high risk will receive less aggressive LDL-C reduction. Since the ENHANCE data were released, more than 300,000 patients have stopped taking either ezetimibe/simvastatin or ezetimibe, and nearly all have continued on generic simvastatin or on a dose of statin with less overall efficacy.
An example is Senator John McCain, who, according to his recently released medical records, has a Framingham 10-year risk of more than 20% and was on ezetimibe/simvastatin to treat an elevated cholesterol level. After release of the ENHANCE trial, he was switched to generic simvastatin, and his LDL-C increased from 82 mg/dL to 122 mg/dL. He most likely has an LDL-C goal of less than 100 mg/dL according to the ATP III guidelines, and he is therefore no longer at his target.
For physicians in the community, questions from concerned patients
For the physicians who have received hundreds of phone calls and e-mails from concerned patients, the ENHANCE trial results must have been both discouraging and confusing. At present, I think we should remember the following:
- Ezetimibe’s mechanism of action is well understood
- It is safe and well-tolerated
- It still has a role as an add-on to statin therapy (or as monotherapy or combined with other agents in those who cannot tolerate statins) for patients who have not yet achieved their LDL-C target.
For the pharmaceutical industry, enormous challenges
The neutral ENHANCE trial results created an uncomfortable situation for the trial sponsor. A heavily marketed drug failed to achieve its expected result after the study results were delayed for a few months. The pharmaceutical industry ranks 14th out of 17 industries in public trust among the American public, and this study provided an opportunity for its critics to attack what is, in their opinion, an overly marketed drug.
Enormous challenges are on the horizon for the pharmaceutical industry, with a shrinking pipeline of potential new drugs, increasing regulatory hurdles, greater liability risk, political pressure for price controls, enhanced scrutiny of sales practices, and a growing media bias. As a cardiologist and clinical researcher whose father died at age 47 of a myocardial infarction, I am concerned that, unless change occurs, a vibrant pharmaceutical industry with the financial and intellectual capital to find and develop new, more effective treatments will cease to exist.
- Kastelein JJ, Akdim F, Stroes ES, et al ENHANCE Investigators. Simvastatin with or without ezetimibe in familial hypercholesterolemia. N Engl J Med 2008; 358:1431–1443.
- Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106:3143–3421.
- Grundy SM, Cleeman JI, Bairey Merz N, et al for the Coordinating Committee of the National Cholesterol Education Program. Circulation 2004; 110:227–239.
- Kastelein JJ, Sager PT, de Groot E, Veltri E. Comparison of ezetimibe plus simvastatin versus simvastatin monotherapy on atherosclerosis progression in familial hypercholesterolemia. Design and rationale of the Ezetimibe and Simvastatin in Hypercholesterolemia Enhances Atherosclerosis Regression (ENHANCE) trial. Am Heart J 2005; 49:234–239.
- Merck/Schering-Plough Pharmaceutical Press Release, January 14, 2008.
- Berenson A. Study reveals doubt on drug for cholesterol. New York Times January 15, 2008.
- Brown BG, Taylor AJ. Does ENHANCE diminish confidence in lowering LDL or in ezetimibe? N Engl J Med 2008; 358:1504–1507.
- Drazen JM, Jarcho JA, Morrissey S, Curfman GD. Cholesterol lowering and ezetimibe. N Engl J Med 2008; 358:1507–1508.
- American College of Cardiology. ENHANCED analysis of ezetimibe. ACC News, April 2, 2008. www.acc.org/emails/myacc/accnews%5Fapril%5F02%5F08.htm. Accessed 6/2/2008.
- American College of Cardiology. ACC panel on Vytorin: Go back to statins. Scientific Session News 3/31/2008. http://www.acc08.acc.org/SSN/Documents/ACC%20Monday%20v2.pdf. Accessed 6/2/2008.
- Smith SC, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. Endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol 2006; 47:2130–2139.
- Pettypiece S, Cortez MF. Merck, Schering plunge as doctors discourage Vytorin. www.bloomberg.com/apps/news?pid=20601103&refer=news&sid=aV_T9WirgAkI. Accessed 6/2/2008.
- Barter PJ, Caulfield M, Eriksson M, et al ILLUMINATE Investigators. . Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med 2007; 357:2109–2122.
- Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in post-menopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA 1998; 280:605–613.
- Rader DJ. Illuminating HDL—is it still a viable therapeutic target? N Engl J Med 2007; 357:2180–2183.
- Davidson MH, Maki KC, Marx P, et al. Effects of continuous estrogen and estrogen-progestin replacement regimens on cardiovascular risk markers in postmenopausal women. Arch Intern Med 2000; 160:3315–3325.
- Hodis HN, Mack WJ, Lobo RA, et al Estrogen in the Prevention of Atherosclerosis Trial Research Group. . Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 2001; 135:939–953.
- Turley SD. Cholesterol metabolism and therapeutic targets: rationale for targeting multiple metabolic pathways. Clin Cardiol 2004; 27( suppl 3):III16–III21.
- Sehayek E, Hazen SL. Cholesterol absorption from the intestine is a major determinant of reverse cholesterol transport from peripheral tissue macrophages. Arterioscler Thromb Vasc Biol 2008;27 (Epub ahead of print].
- Davis HR, Compton DS, Hoos L, Tetzloff G. Ezetimibe, a potent cholesterol absorption inhibitor, inhibits the development of atherosclerosis in ApoE knockout mice. Arterioscler Thromb Vasc Biol 2001; 21:2032–2038.
- Wong J, Quinn CM, Gelissen IC, Jessup W, Brown AJ. The effect of statins on ABCA1 and ABCG1 expression in human macrophages is influenced by cellular cholesterol levels and extent of differentiation. Atherosclerosis 2008; 196:180–189.
- Wang N, Tall AR. Regulation and mechanisms of ATP-binding cassette transporter A1-mediated cellular cholesterol efflux. Arterioscler Thromb Vasc Biol 2003; 23:1178–1184.
- Bots ML. Carotid intima-media thickness as a surrogate marker for cardiovascular disease in intervention studies. Curr Med Res Opin 2006; 22:2181–2190.
- Byington RP, Evans GW, Espeland MA, et al. Effects of lovastatin and warfarin on early carotid atherosclerosis: sex-specific analyses. Asymptomatic Carotid Artery Progression Study (ACAPS) Research Group. Circulation 1999; 100:e14–e17.
- Byington RP, Furberg CD, Crouse JR, Espeland MA, Bond MG. Pravastatin, Lipids, and Atherosclerosis in the Carotid Arteries (PLAC-II). Am J Cardiol 1995; 76:54C–59C.
- Crouse JR, Raichlen JS, Riley WA, et al METEOR Study Group. . Effect of rosuvastatin on progression of carotid intima-media thickness in low-risk individuals with subclinical atherosclerosis: the METEOR trial. JAMA 2007; 297:1344–1353.
- Taylor AJ, Sullenberger LE, Lee HJ, Lee JK, Grace KA. Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol (ARBITER) 2: a double-blind, placebo-controlled study of extended-release niacin on atherosclerosis progression in secondary prevention patients treated with statins. Circulation 2004; 110:3512–3517.
- Smilde TJ, van Wissen S, Wollersheim H, Trip MD, Kastelein JJ, Stalenhoef AF. Effect of aggressive versus conventional lipid lowering on atherosclerosis progression in familial hypercholesterolaemia (ASAP): a prospective, randomised, double-blind trial. Lancet 2001; 357:577–581.
- van Wissen S, Smilde TJ, Trip MD, Stalenhoef AFH, Kastelein JJP. Long-term safety and efficacy of high-dose atorvastatin treatment in patients with familial hypercholesterolemia. Am J Cardiol 2005; 95:264–266.
- Meuwese MC, Franssen R, Stroes ES, Kastelein JJ. And then there were acyl coenzyme A:cholesterol acyl transferase inhibitors. Curr Opin Lipidol 2006; 17:426–430.
- Kastelein JJ, van Leuven SI, Burgess L, et al RADIANCE 1 Investigators. . Effect of torcetrapib on carotid atherosclerosis in familial hypercholesterolemia. N Engl J Med 2007; 356:1620–1630.
- Nissen SE, Tuzcu EM, Brewer HB, et al ACAT Intravascular Atherosclerosis Treatment Evaluation (ACTIVATE) Investigators. Effect of ACAT inhibition on the progression of coronary atherosclerosis. N Engl J Med 2006; 354:1253–1263.
- Davidson MH. Clinical significance of statin pleiotropic effects: hypotheses versus evidence. Circulation 2005; 111:2280–2281.
- Nolting PR, de Groot E, Zwinderman AH, Buirma RJ, Trip MD, Kastelein JJ. Regression of carotid and femoral artery intima-media thickness in familial hypercholesterolemia. Arch Intern Med 2003; 163:1837–1841.
- Crouse JR, Grobbee DE, O’Leary DH, et al Measuring Effects on intima media Thickness: an Evaluation Of Rosuvastatin Study Group. . Measuring effects on intima media thickness: an evaluation of rosuvastatin in subclinical atherosclerosis—the rationale and methodology of the METEOR study. Cardiovasc Drugs Ther 2004; 18:231–238.
- Toth PP, Davidson MH. Cholesterol absorption blockade with ezetimibe. Curr Drug Targets Cardiovasc Haematol Disord 2005; 5:455–462.
- Nissen SE, Nicholls SJ, Sipahi I, et al ASTEROID Investigators. . Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 2006; 295:1556–1565.
- Kjekshus J, Apetrei E, Barrios V, et al CORONA Group. . Rosuvastatin in older patients with systolic heart failure. N Engl J Med 2007; 357:2248–2261.
- Cannon CP, Braunwald E, McCabe CH, et al Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 Investigators. . Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 2004; 350:1495–1504.
The Ezetimibe and Simvastatin in Hypercholesterolemia Enhances Atherosclerosis Regression (ENHANCE) trial1 was probably the most widely publicized clinical study of the past decade. How did a 720-patient imaging trial with a neutral result in patients with severe hypercholesterolemia rise to a level warranting massive media attention, a congressional investigation, and a recommendation to curtail the use of a drug widely used to reduce levels of low-density-lipoprotein cholesterol (LDL-C)?
The reaction to the ENHANCE trial reveals more about the political climate and the relationship between the pharmaceutical industry and the American public than it does about the effects of ezetimibe (available combined with simvastatin as Vytorin and by itself as Zetia) on the progression of atherosclerosis.
SOME SELF-DISCLOSURE
Before I discuss the clinical implications of the ENHANCE trial, I must describe both my financial conflicts and intellectual biases. I am a paid consultant, speaker, and researcher on behalf of Merck/Schering-Plough, the sponsor of the ENHANCE trial. I was a principal investigator in the first phase II trial of ezetimibe and have conducted more than 10 clinical trials of either ezetimibe or ezetimibe/simvastatin. I also have been a strong advocate for imaging trials to assist in the clinical development of novel therapeutic agents and to support regulatory approval.
Therefore, I believe that the thickness of the intima and media layers of the carotid arteries is a useful surrogate to evaluate the potential antiatherosclerotic effects of drugs (more on this topic below). Also, I believe that the LDL-C-lowering hypothesis has been proven: ie, that all drugs that lower LDL-C safely, without off-target adverse effects, should reduce cardiovascular events. I support the goal levels of LDL-C and non-high-density-lipoprotein cholesterol set by the National Cholesterol Education Program’s third Adult Treatment Panel (ATP III) guidelines,2,3 which specify LDL-C targets rather than the use of specific drugs. In spite of these conflicts and potential biases, I believe I have always served the best interests of patient care.
HISTORY OF THE ENHANCE TRIAL
The end point defined as the mean of six measurements
The primary end point was the change in the thickness of the intima and media layers of the carotid arteries over a 2-year period, measured by ultrasonography. A composite measure was used: the mean of the thicknesses in the far walls of the right and left common carotid arteries, the right and left carotid bulbs, and the right and left internal carotid arteries. Secondary end points included the change in the mean maximal carotid artery intima-media thickness (ie, the thickest of the six baseline measurements), the proportion of participants who developed new carotid artery plaque (defined arbitrarily as an intima-media thickness > 1.3 mm), and changes in the mean of the intima-media thickness of the six carotid sites plus the common femoral arteries.
The last participant completed the trial in April 2006. Reading of the almost 30,000 scans was not started until the last participant was finished, so that all scans for each participant could be read in a blinded, randomized order by five separate readers. A significant proportion of the images that the protocol called for could not be obtained or analyzed, particularly in the internal carotid artery and the carotid bulb, which are often difficult to visualize. As a result, 17% of the internal carotid or carotid bulb measurements were discarded.
To change the end point post hoc, or not to change the end point?
The sponsor of the trial was concerned about the missing data points and convened a special advisory board to review the blinded data. This group suggested a solution: changing the primary end point from the six-site composite value to the mean value in just the common carotid arteries. They based this suggestion on the greater success rate in measuring the common carotids (97%) than in measuring all six sites (88%), as well as on recent trials that indicated that the common carotid artery measurement correlates better with clinical outcomes (because the internal carotid and the bulb measurements vary more). On November 26, 2007, Merck/Schering-Plough announced the primary end point would be changed to the mean change in the common carotid arteries.
However, during a separate meeting on November 30, 2007, some members of the Merck/Schering-Plough advisory board objected to the change. On December 11, 2007, the company announced that the original primary end point would not be changed.
Neutral results, negative publicity
On December 31, 2007, the ENHANCE study was unblinded, and on January 14, 2008, Merck/Schering-Plough issued a press release announcing the results. The press release stated that there were no statistically significant differences between the treatment groups in the primary end point or in any of the secondary end points, despite a 16.5% greater reduction in LDL-C (about 50 mg/dL) in the group receiving the ezetimibe/simvastatin combination. The composite intima-media thickness had increased by an average of 0.0111 mm in the combined-therapy group vs 0.0058 mm in the simvastatin-only group (P = .29) over the 24-month treatment period.5
The press release received unprecedented international media attention. One leading cardiologist commented to the media that ENHANCE showed “millions of patients may be taking a drug [ezetimibe] that does not benefit them, raising their risk of heart attacks and exposing them to potential side effects.”6 The perceived message that ezetimibe/simvastatin is harmful resulted in thousands of phone calls from concerned patients to their physicians throughout the United States. The American Heart Association (AHA) and the American College of Cardiology (ACC) issued a joint statement the next day saying that ezetimibe/simvastatin does not appear to be unsafe and that patients should not stop taking the drug on their own. In the following days, Merck/Schering-Plough placed advertisements in newspapers reaffirming the safety of ezetimibe and quoting the AHA/ACC statement.
But the full results of the study were not available at that point. In fact, Senator Charles Grassley (R-Iowa) had launched a congressional investigation into the delays in releasing the results of the ENHANCE trial in December 2007. A focus of the investigation was whether the sponsor was delaying the release either because the data reflected negatively on its product or because it was legitimately concerned about the quality of the measurements of the carotid intima-media thickness. After Merck/Schering-Plough placed the advertisements quoting the AHA/ACC statement, these organizations were criticized for touting the safety of ezetimibe while receiving educational grants and other funds from Merck/Schering-Plough. Senator Grassley sent a letter to the ACC in late March requesting information about the amount of funds the ACC had received.
Full results are published, and the ACC is misquoted
The ENHANCE study was selected for a special presentation at the ACC annual scientific session on March 30, 2008. The full ENHANCE results were presented by Dr. Kastelein, after which an expert panel led by Harlan M. Krumholz, MD, discussed the trial’s implications. The ENHANCE results were simultaneously published in the New England Journal of Medicine,1 accompanied by an editorial by B. Greg Brown, MD, and Allen J. Taylor, MD,7 and another editorial by the editors of that journal, Jeffrey M. Drazen, MD, and colleagues.8 The expert panel and the editorialists concluded that the ENHANCE trial data raised concerns about the cardiovascular benefits of ezetimibe; that statins should be used as initial therapy for hyperlipidemia and titrated to the goal LDL-C level or to the maximally tolerated dose; and that other drugs such as bile acid sequestrants, fibrates, and niacin should be used in combination with statins before considering ezetimibe.9
The next day, stories appeared in the media mistakenly stating that the ACC had recommended that ezetimibe/simvastatin be discontinued. This view was fueled by an article in the ACC’s Scientific Session News, penned by a contract writer and editor, with the headline, “ACC on Vytorin: Go Back to Statins” that said, “After waiting for 18 months for the results of the ENHANCE study, an ACC panel on Sunday encouraged physicians to use statins as a first line and prescribe Vytorin only as a last resort for patients unable to tolerate other cholesterol-lowering agents.”10
The ACC later clarified that this was the opinion of the panelists and not that of the ACC, and they reiterated statements from the AHA/ACC Secondary Prevention Guidelines11 recommending statins in maximally tolerated doses or titrated to a goal LDL-C level for first-line drug treatment of coronary artery disease, and recommending that patients speak with their physicians before discontinuing any therapy.
WHY WERE THE ENHANCE STUDY RESULTS NEUTRAL?
The ACC expert panel concluded that the most likely reason for the neutral ENHANCE results was that ezetimibe lowers LDL-C but does not confer a cardiovascular benefit. In the words of Dr. Krumholz (as quoted by Shannon Pettypiece and Michelle Fay Cortez on bloomberg.com), ezetimibe is “just an expensive placebo.”12
There are at least three potential explanations for the lack of benefit with ezetimibe in the ENHANCE trial. I list them below in order of lowest to highest probability, in my opinion:
Theory 1: Ezetimibe lowers LDL-C but is not antiatherogenic
Since almost all experts agree that lowering LDL-C confers cardiovascular benefits, if ezetimibe does not inhibit atherosclerosis it must have some “off-target” effect that negates its LDL-C-lowering benefit. Critics of ezetimibe point out that oral estrogen and torcetrapib also lower LDL-C but do not improve cardiovascular outcomes.13,14
The lack of benefit with these two other agents can be explained. Oral estrogen does not lower apolipoprotein B (an indication of the number of atherogenic particles), but rather it increases the levels of both triglycerides and C-reactive protein, and it is prothrombotic in some people.15 Torcetrapib increases aldosterone production and substantially raises blood pressure.16 Therefore, both drugs have true off-target effects that could explain their failure to reduce cardiovascular risk despite reductions in LDL-C. (Interestingly, though, oral estrogen has been shown to slow the progression of carotid intima-media thickness in newly postmenopausal women.17
Ezetimibe, however, lowers LDL-C by an ultimate mechanism similar to that of statins and bile acid sequestrants, ie, by up-regulating LDL receptors, although these drugs reach this mechanism via different pathways. Statins inhibit cholesterol synthesis, thereby lowering hepatic intracellular cholesterol and thus up-regulating LDL-receptors and enhancing LDL-C clearance from the plasma. Bile acid sequestrants interrupt bile acid reabsorption in the ileum, thereby decreasing intracellular hepatic cholesterol and up-regulating LDL receptors. Ezetimibe, like bile acid sequestrants, also decreases cholesterol return to the liver, lowering hepatic intracellular levels and thus up-regulating LDL receptors.18
Ezetimibe is unlikely to have an off-target effect because it is only fractionally absorbed systemically, and a recent animal study showed that it enhances macrophage efflux of cholesterol, thereby potentially increasing reverse cholesterol transport.19 Ezetimibe has also been shown to reduce atherosclerosis in animal models.20
In their editorial, Drs. Brown and Taylor7 noted that ezetimibe reduces the expression of adenosine triphosphate binding cassette A1 (ABCA1) in Caco-2 (an intestinal cell line), and this may be an example of an off-target effect. However, statins also reduce ABCA1 expression in macrophages.21 ABCA1 is sensitive to intracellular cholesterol, and when cholesterol levels are decreased, whether by statins or by ezetimibe, ABCA1 expression is down-regulated.22
Theory 2: Intima-media thickness does not reflect the true benefits of lowering LDL-C
The carotid intima-media thickness is a surrogate end point that predicts coronary events and the rate of progression of coronary atherosclerosis.23 In trials of lovastatin (Mevacor),24 pravastatin (Pravachol),25 and rosuvastatin (Crestor),26 the carotid intima-media was thinner at 24 months with the active drug than with placebo. In two relatively small trials—ARBITER 1 (n = 161),27 which was open-label, and ASAP (n = 325)28,29—aggressive lipid-lowering reduced the progression of intima-media thickness better than less-aggressive therapy. However, this measure has been used to evaluate the effects of differing degrees of LDL-C reduction between active treatments in fewer than 500 research participants.
Furthermore, what part or parts of the carotid system are we talking about? In recent trials led by Dr. Kastelein, the intima-media thickness of the common carotid arteries increased with pactimibe (an acyl-coenzyme A:cholesterol O-acyltransferase, or ACAT, inhibitor)30 and torcetrapib,31 but the six-site composite measure (which was the primary end point in these trials, as in ENHANCE) did not increase more than in the control groups. Pactimibe was also shown to increase atheroma volume as measured by intravascular ultrasonography in the ACTIVATE trial.32 Therefore, the thickness of the common carotid arteries has been shown to be a better predictor of harm from a therapy than the composite measurement.
The advantage of measuring the common carotid artery is that it is easier to visualize and measure, and therefore the measurements vary less. In the METEOR trial,26 the six-site measurement increased significantly less with rosuvastatin than with placebo, but the common carotid measurement alone was more strongly associated with a difference in progression. In the ENHANCE trial, the thickness of the common carotid arteries increased by 0.0024 mm with simvastatin alone vs 0.0019 mm with simvastatin/ezetimibe, a difference of 0.005 mm that was not statistically significant (P = .93).1
Although the six-site measurement appears to be good for predicting coronary events and evaluating therapies, the measurement in the common carotid arteries appears to be a more reliable surrogate end point for predicting both benefit and harm from antiatherogenic agents. However, trials of statins and other lipid-lowering therapies that assessed clinical events have shown that the reduction in risk associated with a given reduction in cholesterol is similar regardless of the mechanism by which cholesterol is lowered.33 Therefore, the LDL-C level is far superior as a marker of clinical benefit.
Theory 3: Previous statin treatment affected the ENHANCE results
By far the most likely explanation for the neutral findings in ENHANCE is that the patients were so well treated before entry that it was impossible to detect a difference between the two treatment groups in carotid intima-media thickness at the end of the study. Eighty percent of the patients had received statins previously, and at baseline the mean intima-media thickness of the common carotid arteries was only 0.68 mm.1 In contrast, most other trials required a thickness greater than 0.7 mm for entry.
The two main reasons for selecting a population with familial hypercholesterolemia were the assumptions that these participants would have a greater-than-average carotid intima-media thickness at baseline and that they would show an above-average progression rate, even on high-dose statin therapy.4 Both of these assumptions were incorrect: the baseline thickness was normal and the progression rate was negligible in both groups.
Accordingly, the high prevalence of statin pretreatment and the near-normal carotid intima-media thickness at baseline may have prevented the 16.5% greater reduction in LDL-C due to ezetimibe from producing a difference in progression over 24 months of treatment. This conclusion is supported by the long-term follow-up results from ASAP, RADIANCE 1, and CAPTIVATE, all of which showed that in patients with familial hypercholesterolemia well treated with statins, progression of carotid intima-media thickness is negligible.30,31
Further supporting this view, in a previous trial by Dr. Kastelein’s group in patients with familial hypercholesterolemia,34 giving simvastatin 80 mg for 2 years decreased the intima-medial thickness by .081 mm (P < .001), compared with 0.0058 mm in ENHANCE (a 14-fold difference). In the previous trial, the baseline measurement was 1.07 mm (vs 0.68 mm in ENHANCE), and the extent of the change was significantly associated with the baseline measurement (r = .53, P < .001) but not with the change in LDL-C levels.
This is powerful evidence that, in two similar studies that used the same methodology and the same drug, the thinner arteries in the ENHANCE trial are by far the most likely explanation for the lack of change with the addition of ezetimibe to high-dose simvastatin. The METEOR trial enrolled only patients who had never received statins and whose carotid intima-media was thicker than 1.2 mm. In retrospect, a similar design would have been preferable for ENHANCE.35
LESSONS LEARNED AND CLINICAL IMPLICATIONS
For Merck/Schering-Plough, missed opportunities
Although Dr. Krumholz (the spokesman for the ACC panel discussion) and I disagree on the clinical implications of the ENHANCE trial, we do agree on an important point. Dr. Krumholz posed the question that if the LDL-C-lowering hypothesis was already proven for ezetimibe, why was the ENHANCE trial conducted? After 6 years on the market, the efficacy of ezetimibe on cardiovascular outcomes should already have been established. It should not take this long to determine the clinical outcome benefit for a drug.
Merck/Schering-Plough’s outcome program for ezetimibe was inadequately designed to demonstrate the clinical value of this novel compound. Rather than assuming the LDL-C-lowering hypothesis was already established, they conducted another “lower-is-better” trial with the carotid intima-media thickness as the end point, and they succeeded only in raising doubt about the benefits of ezetimibe rather than showing that dual therapy is at least equivalent to high-dose statin therapy.
A preferable approach would have been to compare the effects of a statin in low doses plus ezetimibe vs high-dose statin monotherapy on either surrogate or hard outcomes. If the low-dose statin/ezetimibe combination, which should lower the LDL-C level as much as high-dose statin monotherapy, could provide similar or better outcomes with fewer side effects, this trial would change our practice.
One had hoped that dual therapy, by reducing both intestinal cholesterol absorption and hepatic synthesis of cholesterol, would improve outcomes by modifying postprandial chylomicron composition or by reducing plant sterol absorption.36 Unfortunately, other outcome trials of ezetimibe/simvastatin will not provide an answer regarding the potential advantages of dual therapy. The SEAS study is comparing the number of clinical events in patients with aortic stenosis who receive ezetimibe/simvastatin or placebo; SHARP is being conducted in patients with chronic kidney disease. Although both groups of patients have high rates of coronary events, these trials will not address whether adding ezetimibe provides additional benefits. In fact, if the results of these trials turn out neutral, as in ENHANCE, then ezetimibe will be blamed for potentially offsetting the benefits of simvastatin, and if the trials show a benefit, the simvastatin component of ezetimibe/simvastatin will be given the credit.
The answer may come in 3 to 4 years with the results of IMPROVE-IT, a study of 18,000 patients with acute coronary syndrome treated with ezetimibe/simvastatin or simvastatin. The simvastatin monotherapy group will have a target LDL-C level of less than 80 mg/dL and the ezetimibe/simvastatin group will have an LDL-C target about 15% less. Although this trial is testing the lower-is-better hypothesis with ezetimibe, if the study does not show a benefit, it may not be because ezetimibe lacks clinical efficacy but rather because the LDL-C effect is curvilinear, and there is minimal further benefit of lowering the LDL-C level past 70 mg/dL. If the results of the IMPROVE-IT trial are negative, it may mean the end of ezetimibe as an LDL-C-lowering drug.
Merck/Schering-Plough has lost valuable time in not demonstrating the benefits of ezetimibe on clinical events. In contrast, consider rosuvastatin, an AstraZeneca product. Rosuvastatin was approved about the same time as ezetimibe/simvastatin, and 6 years later it has already received a label change for the reduction of progression of atherosclerosis, based on positive outcomes in the METEOR trial,35 the ASTEROID intravascular ultrasonography trial,37 and the CORONA trial (an important trial that examined hard clinical end points).38 More importantly, the JUPITER trial was recently stopped early owing to a reduction in cardiovascular deaths. Initially, rosuvastatin received an unfair media portrayal as an unsafe drug. Now, because of its proven benefits in outcome trials, it will receive more widespread consideration for clinical use.
For preventive cardiologists, a painful reminder to focus on LDL-C
For the preventive cardiologist or lipidologist, the ENHANCE trial has been a painful reminder that despite overwhelming evidence, the mantra of “the lower the LDL-C the better” is still not universally accepted. We acknowledge the great benefits of statins, but the lure of “pleiotropic effects” distracts many of us from the necessity of more aggressive LDL-C reduction.
The pleiotropic benefits of statins were first raised as a means of supporting increased clinical use of pravastatin vis-a-vis other, more efficacious statins. It was not until the PROVE-IT study that pravastatin’s pleiotropic effects were found not to translate into a benefit equivalent to that of the more efficacious statin, atorvastatin.39
The success of ezetimibe was its ability to safely and easily lower LDL-C in combination with statins to achieve treatment goals. For many patients, a lower-dose statin and ezetimibe together provide a well-tolerated and efficacious approach to treating hyperlipidemia. The fallout from the ENHANCE trial is that many patients who were well treated or who could be better treated with ezetimibe in combination with a statin will not receive the best tolerated regimen. In fact, preliminary prescription data after the release of the ENHANCE study support our worse fear, ie, that patients at high risk will receive less aggressive LDL-C reduction. Since the ENHANCE data were released, more than 300,000 patients have stopped taking either ezetimibe/simvastatin or ezetimibe, and nearly all have continued on generic simvastatin or on a dose of statin with less overall efficacy.
An example is Senator John McCain, who, according to his recently released medical records, has a Framingham 10-year risk of more than 20% and was on ezetimibe/simvastatin to treat an elevated cholesterol level. After release of the ENHANCE trial, he was switched to generic simvastatin, and his LDL-C increased from 82 mg/dL to 122 mg/dL. He most likely has an LDL-C goal of less than 100 mg/dL according to the ATP III guidelines, and he is therefore no longer at his target.
For physicians in the community, questions from concerned patients
For the physicians who have received hundreds of phone calls and e-mails from concerned patients, the ENHANCE trial results must have been both discouraging and confusing. At present, I think we should remember the following:
- Ezetimibe’s mechanism of action is well understood
- It is safe and well-tolerated
- It still has a role as an add-on to statin therapy (or as monotherapy or combined with other agents in those who cannot tolerate statins) for patients who have not yet achieved their LDL-C target.
For the pharmaceutical industry, enormous challenges
The neutral ENHANCE trial results created an uncomfortable situation for the trial sponsor. A heavily marketed drug failed to achieve its expected result after the study results were delayed for a few months. The pharmaceutical industry ranks 14th out of 17 industries in public trust among the American public, and this study provided an opportunity for its critics to attack what is, in their opinion, an overly marketed drug.
Enormous challenges are on the horizon for the pharmaceutical industry, with a shrinking pipeline of potential new drugs, increasing regulatory hurdles, greater liability risk, political pressure for price controls, enhanced scrutiny of sales practices, and a growing media bias. As a cardiologist and clinical researcher whose father died at age 47 of a myocardial infarction, I am concerned that, unless change occurs, a vibrant pharmaceutical industry with the financial and intellectual capital to find and develop new, more effective treatments will cease to exist.
The Ezetimibe and Simvastatin in Hypercholesterolemia Enhances Atherosclerosis Regression (ENHANCE) trial1 was probably the most widely publicized clinical study of the past decade. How did a 720-patient imaging trial with a neutral result in patients with severe hypercholesterolemia rise to a level warranting massive media attention, a congressional investigation, and a recommendation to curtail the use of a drug widely used to reduce levels of low-density-lipoprotein cholesterol (LDL-C)?
The reaction to the ENHANCE trial reveals more about the political climate and the relationship between the pharmaceutical industry and the American public than it does about the effects of ezetimibe (available combined with simvastatin as Vytorin and by itself as Zetia) on the progression of atherosclerosis.
SOME SELF-DISCLOSURE
Before I discuss the clinical implications of the ENHANCE trial, I must describe both my financial conflicts and intellectual biases. I am a paid consultant, speaker, and researcher on behalf of Merck/Schering-Plough, the sponsor of the ENHANCE trial. I was a principal investigator in the first phase II trial of ezetimibe and have conducted more than 10 clinical trials of either ezetimibe or ezetimibe/simvastatin. I also have been a strong advocate for imaging trials to assist in the clinical development of novel therapeutic agents and to support regulatory approval.
Therefore, I believe that the thickness of the intima and media layers of the carotid arteries is a useful surrogate to evaluate the potential antiatherosclerotic effects of drugs (more on this topic below). Also, I believe that the LDL-C-lowering hypothesis has been proven: ie, that all drugs that lower LDL-C safely, without off-target adverse effects, should reduce cardiovascular events. I support the goal levels of LDL-C and non-high-density-lipoprotein cholesterol set by the National Cholesterol Education Program’s third Adult Treatment Panel (ATP III) guidelines,2,3 which specify LDL-C targets rather than the use of specific drugs. In spite of these conflicts and potential biases, I believe I have always served the best interests of patient care.
HISTORY OF THE ENHANCE TRIAL
The end point defined as the mean of six measurements
The primary end point was the change in the thickness of the intima and media layers of the carotid arteries over a 2-year period, measured by ultrasonography. A composite measure was used: the mean of the thicknesses in the far walls of the right and left common carotid arteries, the right and left carotid bulbs, and the right and left internal carotid arteries. Secondary end points included the change in the mean maximal carotid artery intima-media thickness (ie, the thickest of the six baseline measurements), the proportion of participants who developed new carotid artery plaque (defined arbitrarily as an intima-media thickness > 1.3 mm), and changes in the mean of the intima-media thickness of the six carotid sites plus the common femoral arteries.
The last participant completed the trial in April 2006. Reading of the almost 30,000 scans was not started until the last participant was finished, so that all scans for each participant could be read in a blinded, randomized order by five separate readers. A significant proportion of the images that the protocol called for could not be obtained or analyzed, particularly in the internal carotid artery and the carotid bulb, which are often difficult to visualize. As a result, 17% of the internal carotid or carotid bulb measurements were discarded.
To change the end point post hoc, or not to change the end point?
The sponsor of the trial was concerned about the missing data points and convened a special advisory board to review the blinded data. This group suggested a solution: changing the primary end point from the six-site composite value to the mean value in just the common carotid arteries. They based this suggestion on the greater success rate in measuring the common carotids (97%) than in measuring all six sites (88%), as well as on recent trials that indicated that the common carotid artery measurement correlates better with clinical outcomes (because the internal carotid and the bulb measurements vary more). On November 26, 2007, Merck/Schering-Plough announced the primary end point would be changed to the mean change in the common carotid arteries.
However, during a separate meeting on November 30, 2007, some members of the Merck/Schering-Plough advisory board objected to the change. On December 11, 2007, the company announced that the original primary end point would not be changed.
Neutral results, negative publicity
On December 31, 2007, the ENHANCE study was unblinded, and on January 14, 2008, Merck/Schering-Plough issued a press release announcing the results. The press release stated that there were no statistically significant differences between the treatment groups in the primary end point or in any of the secondary end points, despite a 16.5% greater reduction in LDL-C (about 50 mg/dL) in the group receiving the ezetimibe/simvastatin combination. The composite intima-media thickness had increased by an average of 0.0111 mm in the combined-therapy group vs 0.0058 mm in the simvastatin-only group (P = .29) over the 24-month treatment period.5
The press release received unprecedented international media attention. One leading cardiologist commented to the media that ENHANCE showed “millions of patients may be taking a drug [ezetimibe] that does not benefit them, raising their risk of heart attacks and exposing them to potential side effects.”6 The perceived message that ezetimibe/simvastatin is harmful resulted in thousands of phone calls from concerned patients to their physicians throughout the United States. The American Heart Association (AHA) and the American College of Cardiology (ACC) issued a joint statement the next day saying that ezetimibe/simvastatin does not appear to be unsafe and that patients should not stop taking the drug on their own. In the following days, Merck/Schering-Plough placed advertisements in newspapers reaffirming the safety of ezetimibe and quoting the AHA/ACC statement.
But the full results of the study were not available at that point. In fact, Senator Charles Grassley (R-Iowa) had launched a congressional investigation into the delays in releasing the results of the ENHANCE trial in December 2007. A focus of the investigation was whether the sponsor was delaying the release either because the data reflected negatively on its product or because it was legitimately concerned about the quality of the measurements of the carotid intima-media thickness. After Merck/Schering-Plough placed the advertisements quoting the AHA/ACC statement, these organizations were criticized for touting the safety of ezetimibe while receiving educational grants and other funds from Merck/Schering-Plough. Senator Grassley sent a letter to the ACC in late March requesting information about the amount of funds the ACC had received.
Full results are published, and the ACC is misquoted
The ENHANCE study was selected for a special presentation at the ACC annual scientific session on March 30, 2008. The full ENHANCE results were presented by Dr. Kastelein, after which an expert panel led by Harlan M. Krumholz, MD, discussed the trial’s implications. The ENHANCE results were simultaneously published in the New England Journal of Medicine,1 accompanied by an editorial by B. Greg Brown, MD, and Allen J. Taylor, MD,7 and another editorial by the editors of that journal, Jeffrey M. Drazen, MD, and colleagues.8 The expert panel and the editorialists concluded that the ENHANCE trial data raised concerns about the cardiovascular benefits of ezetimibe; that statins should be used as initial therapy for hyperlipidemia and titrated to the goal LDL-C level or to the maximally tolerated dose; and that other drugs such as bile acid sequestrants, fibrates, and niacin should be used in combination with statins before considering ezetimibe.9
The next day, stories appeared in the media mistakenly stating that the ACC had recommended that ezetimibe/simvastatin be discontinued. This view was fueled by an article in the ACC’s Scientific Session News, penned by a contract writer and editor, with the headline, “ACC on Vytorin: Go Back to Statins” that said, “After waiting for 18 months for the results of the ENHANCE study, an ACC panel on Sunday encouraged physicians to use statins as a first line and prescribe Vytorin only as a last resort for patients unable to tolerate other cholesterol-lowering agents.”10
The ACC later clarified that this was the opinion of the panelists and not that of the ACC, and they reiterated statements from the AHA/ACC Secondary Prevention Guidelines11 recommending statins in maximally tolerated doses or titrated to a goal LDL-C level for first-line drug treatment of coronary artery disease, and recommending that patients speak with their physicians before discontinuing any therapy.
WHY WERE THE ENHANCE STUDY RESULTS NEUTRAL?
The ACC expert panel concluded that the most likely reason for the neutral ENHANCE results was that ezetimibe lowers LDL-C but does not confer a cardiovascular benefit. In the words of Dr. Krumholz (as quoted by Shannon Pettypiece and Michelle Fay Cortez on bloomberg.com), ezetimibe is “just an expensive placebo.”12
There are at least three potential explanations for the lack of benefit with ezetimibe in the ENHANCE trial. I list them below in order of lowest to highest probability, in my opinion:
Theory 1: Ezetimibe lowers LDL-C but is not antiatherogenic
Since almost all experts agree that lowering LDL-C confers cardiovascular benefits, if ezetimibe does not inhibit atherosclerosis it must have some “off-target” effect that negates its LDL-C-lowering benefit. Critics of ezetimibe point out that oral estrogen and torcetrapib also lower LDL-C but do not improve cardiovascular outcomes.13,14
The lack of benefit with these two other agents can be explained. Oral estrogen does not lower apolipoprotein B (an indication of the number of atherogenic particles), but rather it increases the levels of both triglycerides and C-reactive protein, and it is prothrombotic in some people.15 Torcetrapib increases aldosterone production and substantially raises blood pressure.16 Therefore, both drugs have true off-target effects that could explain their failure to reduce cardiovascular risk despite reductions in LDL-C. (Interestingly, though, oral estrogen has been shown to slow the progression of carotid intima-media thickness in newly postmenopausal women.17
Ezetimibe, however, lowers LDL-C by an ultimate mechanism similar to that of statins and bile acid sequestrants, ie, by up-regulating LDL receptors, although these drugs reach this mechanism via different pathways. Statins inhibit cholesterol synthesis, thereby lowering hepatic intracellular cholesterol and thus up-regulating LDL-receptors and enhancing LDL-C clearance from the plasma. Bile acid sequestrants interrupt bile acid reabsorption in the ileum, thereby decreasing intracellular hepatic cholesterol and up-regulating LDL receptors. Ezetimibe, like bile acid sequestrants, also decreases cholesterol return to the liver, lowering hepatic intracellular levels and thus up-regulating LDL receptors.18
Ezetimibe is unlikely to have an off-target effect because it is only fractionally absorbed systemically, and a recent animal study showed that it enhances macrophage efflux of cholesterol, thereby potentially increasing reverse cholesterol transport.19 Ezetimibe has also been shown to reduce atherosclerosis in animal models.20
In their editorial, Drs. Brown and Taylor7 noted that ezetimibe reduces the expression of adenosine triphosphate binding cassette A1 (ABCA1) in Caco-2 (an intestinal cell line), and this may be an example of an off-target effect. However, statins also reduce ABCA1 expression in macrophages.21 ABCA1 is sensitive to intracellular cholesterol, and when cholesterol levels are decreased, whether by statins or by ezetimibe, ABCA1 expression is down-regulated.22
Theory 2: Intima-media thickness does not reflect the true benefits of lowering LDL-C
The carotid intima-media thickness is a surrogate end point that predicts coronary events and the rate of progression of coronary atherosclerosis.23 In trials of lovastatin (Mevacor),24 pravastatin (Pravachol),25 and rosuvastatin (Crestor),26 the carotid intima-media was thinner at 24 months with the active drug than with placebo. In two relatively small trials—ARBITER 1 (n = 161),27 which was open-label, and ASAP (n = 325)28,29—aggressive lipid-lowering reduced the progression of intima-media thickness better than less-aggressive therapy. However, this measure has been used to evaluate the effects of differing degrees of LDL-C reduction between active treatments in fewer than 500 research participants.
Furthermore, what part or parts of the carotid system are we talking about? In recent trials led by Dr. Kastelein, the intima-media thickness of the common carotid arteries increased with pactimibe (an acyl-coenzyme A:cholesterol O-acyltransferase, or ACAT, inhibitor)30 and torcetrapib,31 but the six-site composite measure (which was the primary end point in these trials, as in ENHANCE) did not increase more than in the control groups. Pactimibe was also shown to increase atheroma volume as measured by intravascular ultrasonography in the ACTIVATE trial.32 Therefore, the thickness of the common carotid arteries has been shown to be a better predictor of harm from a therapy than the composite measurement.
The advantage of measuring the common carotid artery is that it is easier to visualize and measure, and therefore the measurements vary less. In the METEOR trial,26 the six-site measurement increased significantly less with rosuvastatin than with placebo, but the common carotid measurement alone was more strongly associated with a difference in progression. In the ENHANCE trial, the thickness of the common carotid arteries increased by 0.0024 mm with simvastatin alone vs 0.0019 mm with simvastatin/ezetimibe, a difference of 0.005 mm that was not statistically significant (P = .93).1
Although the six-site measurement appears to be good for predicting coronary events and evaluating therapies, the measurement in the common carotid arteries appears to be a more reliable surrogate end point for predicting both benefit and harm from antiatherogenic agents. However, trials of statins and other lipid-lowering therapies that assessed clinical events have shown that the reduction in risk associated with a given reduction in cholesterol is similar regardless of the mechanism by which cholesterol is lowered.33 Therefore, the LDL-C level is far superior as a marker of clinical benefit.
Theory 3: Previous statin treatment affected the ENHANCE results
By far the most likely explanation for the neutral findings in ENHANCE is that the patients were so well treated before entry that it was impossible to detect a difference between the two treatment groups in carotid intima-media thickness at the end of the study. Eighty percent of the patients had received statins previously, and at baseline the mean intima-media thickness of the common carotid arteries was only 0.68 mm.1 In contrast, most other trials required a thickness greater than 0.7 mm for entry.
The two main reasons for selecting a population with familial hypercholesterolemia were the assumptions that these participants would have a greater-than-average carotid intima-media thickness at baseline and that they would show an above-average progression rate, even on high-dose statin therapy.4 Both of these assumptions were incorrect: the baseline thickness was normal and the progression rate was negligible in both groups.
Accordingly, the high prevalence of statin pretreatment and the near-normal carotid intima-media thickness at baseline may have prevented the 16.5% greater reduction in LDL-C due to ezetimibe from producing a difference in progression over 24 months of treatment. This conclusion is supported by the long-term follow-up results from ASAP, RADIANCE 1, and CAPTIVATE, all of which showed that in patients with familial hypercholesterolemia well treated with statins, progression of carotid intima-media thickness is negligible.30,31
Further supporting this view, in a previous trial by Dr. Kastelein’s group in patients with familial hypercholesterolemia,34 giving simvastatin 80 mg for 2 years decreased the intima-medial thickness by .081 mm (P < .001), compared with 0.0058 mm in ENHANCE (a 14-fold difference). In the previous trial, the baseline measurement was 1.07 mm (vs 0.68 mm in ENHANCE), and the extent of the change was significantly associated with the baseline measurement (r = .53, P < .001) but not with the change in LDL-C levels.
This is powerful evidence that, in two similar studies that used the same methodology and the same drug, the thinner arteries in the ENHANCE trial are by far the most likely explanation for the lack of change with the addition of ezetimibe to high-dose simvastatin. The METEOR trial enrolled only patients who had never received statins and whose carotid intima-media was thicker than 1.2 mm. In retrospect, a similar design would have been preferable for ENHANCE.35
LESSONS LEARNED AND CLINICAL IMPLICATIONS
For Merck/Schering-Plough, missed opportunities
Although Dr. Krumholz (the spokesman for the ACC panel discussion) and I disagree on the clinical implications of the ENHANCE trial, we do agree on an important point. Dr. Krumholz posed the question that if the LDL-C-lowering hypothesis was already proven for ezetimibe, why was the ENHANCE trial conducted? After 6 years on the market, the efficacy of ezetimibe on cardiovascular outcomes should already have been established. It should not take this long to determine the clinical outcome benefit for a drug.
Merck/Schering-Plough’s outcome program for ezetimibe was inadequately designed to demonstrate the clinical value of this novel compound. Rather than assuming the LDL-C-lowering hypothesis was already established, they conducted another “lower-is-better” trial with the carotid intima-media thickness as the end point, and they succeeded only in raising doubt about the benefits of ezetimibe rather than showing that dual therapy is at least equivalent to high-dose statin therapy.
A preferable approach would have been to compare the effects of a statin in low doses plus ezetimibe vs high-dose statin monotherapy on either surrogate or hard outcomes. If the low-dose statin/ezetimibe combination, which should lower the LDL-C level as much as high-dose statin monotherapy, could provide similar or better outcomes with fewer side effects, this trial would change our practice.
One had hoped that dual therapy, by reducing both intestinal cholesterol absorption and hepatic synthesis of cholesterol, would improve outcomes by modifying postprandial chylomicron composition or by reducing plant sterol absorption.36 Unfortunately, other outcome trials of ezetimibe/simvastatin will not provide an answer regarding the potential advantages of dual therapy. The SEAS study is comparing the number of clinical events in patients with aortic stenosis who receive ezetimibe/simvastatin or placebo; SHARP is being conducted in patients with chronic kidney disease. Although both groups of patients have high rates of coronary events, these trials will not address whether adding ezetimibe provides additional benefits. In fact, if the results of these trials turn out neutral, as in ENHANCE, then ezetimibe will be blamed for potentially offsetting the benefits of simvastatin, and if the trials show a benefit, the simvastatin component of ezetimibe/simvastatin will be given the credit.
The answer may come in 3 to 4 years with the results of IMPROVE-IT, a study of 18,000 patients with acute coronary syndrome treated with ezetimibe/simvastatin or simvastatin. The simvastatin monotherapy group will have a target LDL-C level of less than 80 mg/dL and the ezetimibe/simvastatin group will have an LDL-C target about 15% less. Although this trial is testing the lower-is-better hypothesis with ezetimibe, if the study does not show a benefit, it may not be because ezetimibe lacks clinical efficacy but rather because the LDL-C effect is curvilinear, and there is minimal further benefit of lowering the LDL-C level past 70 mg/dL. If the results of the IMPROVE-IT trial are negative, it may mean the end of ezetimibe as an LDL-C-lowering drug.
Merck/Schering-Plough has lost valuable time in not demonstrating the benefits of ezetimibe on clinical events. In contrast, consider rosuvastatin, an AstraZeneca product. Rosuvastatin was approved about the same time as ezetimibe/simvastatin, and 6 years later it has already received a label change for the reduction of progression of atherosclerosis, based on positive outcomes in the METEOR trial,35 the ASTEROID intravascular ultrasonography trial,37 and the CORONA trial (an important trial that examined hard clinical end points).38 More importantly, the JUPITER trial was recently stopped early owing to a reduction in cardiovascular deaths. Initially, rosuvastatin received an unfair media portrayal as an unsafe drug. Now, because of its proven benefits in outcome trials, it will receive more widespread consideration for clinical use.
For preventive cardiologists, a painful reminder to focus on LDL-C
For the preventive cardiologist or lipidologist, the ENHANCE trial has been a painful reminder that despite overwhelming evidence, the mantra of “the lower the LDL-C the better” is still not universally accepted. We acknowledge the great benefits of statins, but the lure of “pleiotropic effects” distracts many of us from the necessity of more aggressive LDL-C reduction.
The pleiotropic benefits of statins were first raised as a means of supporting increased clinical use of pravastatin vis-a-vis other, more efficacious statins. It was not until the PROVE-IT study that pravastatin’s pleiotropic effects were found not to translate into a benefit equivalent to that of the more efficacious statin, atorvastatin.39
The success of ezetimibe was its ability to safely and easily lower LDL-C in combination with statins to achieve treatment goals. For many patients, a lower-dose statin and ezetimibe together provide a well-tolerated and efficacious approach to treating hyperlipidemia. The fallout from the ENHANCE trial is that many patients who were well treated or who could be better treated with ezetimibe in combination with a statin will not receive the best tolerated regimen. In fact, preliminary prescription data after the release of the ENHANCE study support our worse fear, ie, that patients at high risk will receive less aggressive LDL-C reduction. Since the ENHANCE data were released, more than 300,000 patients have stopped taking either ezetimibe/simvastatin or ezetimibe, and nearly all have continued on generic simvastatin or on a dose of statin with less overall efficacy.
An example is Senator John McCain, who, according to his recently released medical records, has a Framingham 10-year risk of more than 20% and was on ezetimibe/simvastatin to treat an elevated cholesterol level. After release of the ENHANCE trial, he was switched to generic simvastatin, and his LDL-C increased from 82 mg/dL to 122 mg/dL. He most likely has an LDL-C goal of less than 100 mg/dL according to the ATP III guidelines, and he is therefore no longer at his target.
For physicians in the community, questions from concerned patients
For the physicians who have received hundreds of phone calls and e-mails from concerned patients, the ENHANCE trial results must have been both discouraging and confusing. At present, I think we should remember the following:
- Ezetimibe’s mechanism of action is well understood
- It is safe and well-tolerated
- It still has a role as an add-on to statin therapy (or as monotherapy or combined with other agents in those who cannot tolerate statins) for patients who have not yet achieved their LDL-C target.
For the pharmaceutical industry, enormous challenges
The neutral ENHANCE trial results created an uncomfortable situation for the trial sponsor. A heavily marketed drug failed to achieve its expected result after the study results were delayed for a few months. The pharmaceutical industry ranks 14th out of 17 industries in public trust among the American public, and this study provided an opportunity for its critics to attack what is, in their opinion, an overly marketed drug.
Enormous challenges are on the horizon for the pharmaceutical industry, with a shrinking pipeline of potential new drugs, increasing regulatory hurdles, greater liability risk, political pressure for price controls, enhanced scrutiny of sales practices, and a growing media bias. As a cardiologist and clinical researcher whose father died at age 47 of a myocardial infarction, I am concerned that, unless change occurs, a vibrant pharmaceutical industry with the financial and intellectual capital to find and develop new, more effective treatments will cease to exist.
- Kastelein JJ, Akdim F, Stroes ES, et al ENHANCE Investigators. Simvastatin with or without ezetimibe in familial hypercholesterolemia. N Engl J Med 2008; 358:1431–1443.
- Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106:3143–3421.
- Grundy SM, Cleeman JI, Bairey Merz N, et al for the Coordinating Committee of the National Cholesterol Education Program. Circulation 2004; 110:227–239.
- Kastelein JJ, Sager PT, de Groot E, Veltri E. Comparison of ezetimibe plus simvastatin versus simvastatin monotherapy on atherosclerosis progression in familial hypercholesterolemia. Design and rationale of the Ezetimibe and Simvastatin in Hypercholesterolemia Enhances Atherosclerosis Regression (ENHANCE) trial. Am Heart J 2005; 49:234–239.
- Merck/Schering-Plough Pharmaceutical Press Release, January 14, 2008.
- Berenson A. Study reveals doubt on drug for cholesterol. New York Times January 15, 2008.
- Brown BG, Taylor AJ. Does ENHANCE diminish confidence in lowering LDL or in ezetimibe? N Engl J Med 2008; 358:1504–1507.
- Drazen JM, Jarcho JA, Morrissey S, Curfman GD. Cholesterol lowering and ezetimibe. N Engl J Med 2008; 358:1507–1508.
- American College of Cardiology. ENHANCED analysis of ezetimibe. ACC News, April 2, 2008. www.acc.org/emails/myacc/accnews%5Fapril%5F02%5F08.htm. Accessed 6/2/2008.
- American College of Cardiology. ACC panel on Vytorin: Go back to statins. Scientific Session News 3/31/2008. http://www.acc08.acc.org/SSN/Documents/ACC%20Monday%20v2.pdf. Accessed 6/2/2008.
- Smith SC, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. Endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol 2006; 47:2130–2139.
- Pettypiece S, Cortez MF. Merck, Schering plunge as doctors discourage Vytorin. www.bloomberg.com/apps/news?pid=20601103&refer=news&sid=aV_T9WirgAkI. Accessed 6/2/2008.
- Barter PJ, Caulfield M, Eriksson M, et al ILLUMINATE Investigators. . Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med 2007; 357:2109–2122.
- Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in post-menopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA 1998; 280:605–613.
- Rader DJ. Illuminating HDL—is it still a viable therapeutic target? N Engl J Med 2007; 357:2180–2183.
- Davidson MH, Maki KC, Marx P, et al. Effects of continuous estrogen and estrogen-progestin replacement regimens on cardiovascular risk markers in postmenopausal women. Arch Intern Med 2000; 160:3315–3325.
- Hodis HN, Mack WJ, Lobo RA, et al Estrogen in the Prevention of Atherosclerosis Trial Research Group. . Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 2001; 135:939–953.
- Turley SD. Cholesterol metabolism and therapeutic targets: rationale for targeting multiple metabolic pathways. Clin Cardiol 2004; 27( suppl 3):III16–III21.
- Sehayek E, Hazen SL. Cholesterol absorption from the intestine is a major determinant of reverse cholesterol transport from peripheral tissue macrophages. Arterioscler Thromb Vasc Biol 2008;27 (Epub ahead of print].
- Davis HR, Compton DS, Hoos L, Tetzloff G. Ezetimibe, a potent cholesterol absorption inhibitor, inhibits the development of atherosclerosis in ApoE knockout mice. Arterioscler Thromb Vasc Biol 2001; 21:2032–2038.
- Wong J, Quinn CM, Gelissen IC, Jessup W, Brown AJ. The effect of statins on ABCA1 and ABCG1 expression in human macrophages is influenced by cellular cholesterol levels and extent of differentiation. Atherosclerosis 2008; 196:180–189.
- Wang N, Tall AR. Regulation and mechanisms of ATP-binding cassette transporter A1-mediated cellular cholesterol efflux. Arterioscler Thromb Vasc Biol 2003; 23:1178–1184.
- Bots ML. Carotid intima-media thickness as a surrogate marker for cardiovascular disease in intervention studies. Curr Med Res Opin 2006; 22:2181–2190.
- Byington RP, Evans GW, Espeland MA, et al. Effects of lovastatin and warfarin on early carotid atherosclerosis: sex-specific analyses. Asymptomatic Carotid Artery Progression Study (ACAPS) Research Group. Circulation 1999; 100:e14–e17.
- Byington RP, Furberg CD, Crouse JR, Espeland MA, Bond MG. Pravastatin, Lipids, and Atherosclerosis in the Carotid Arteries (PLAC-II). Am J Cardiol 1995; 76:54C–59C.
- Crouse JR, Raichlen JS, Riley WA, et al METEOR Study Group. . Effect of rosuvastatin on progression of carotid intima-media thickness in low-risk individuals with subclinical atherosclerosis: the METEOR trial. JAMA 2007; 297:1344–1353.
- Taylor AJ, Sullenberger LE, Lee HJ, Lee JK, Grace KA. Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol (ARBITER) 2: a double-blind, placebo-controlled study of extended-release niacin on atherosclerosis progression in secondary prevention patients treated with statins. Circulation 2004; 110:3512–3517.
- Smilde TJ, van Wissen S, Wollersheim H, Trip MD, Kastelein JJ, Stalenhoef AF. Effect of aggressive versus conventional lipid lowering on atherosclerosis progression in familial hypercholesterolaemia (ASAP): a prospective, randomised, double-blind trial. Lancet 2001; 357:577–581.
- van Wissen S, Smilde TJ, Trip MD, Stalenhoef AFH, Kastelein JJP. Long-term safety and efficacy of high-dose atorvastatin treatment in patients with familial hypercholesterolemia. Am J Cardiol 2005; 95:264–266.
- Meuwese MC, Franssen R, Stroes ES, Kastelein JJ. And then there were acyl coenzyme A:cholesterol acyl transferase inhibitors. Curr Opin Lipidol 2006; 17:426–430.
- Kastelein JJ, van Leuven SI, Burgess L, et al RADIANCE 1 Investigators. . Effect of torcetrapib on carotid atherosclerosis in familial hypercholesterolemia. N Engl J Med 2007; 356:1620–1630.
- Nissen SE, Tuzcu EM, Brewer HB, et al ACAT Intravascular Atherosclerosis Treatment Evaluation (ACTIVATE) Investigators. Effect of ACAT inhibition on the progression of coronary atherosclerosis. N Engl J Med 2006; 354:1253–1263.
- Davidson MH. Clinical significance of statin pleiotropic effects: hypotheses versus evidence. Circulation 2005; 111:2280–2281.
- Nolting PR, de Groot E, Zwinderman AH, Buirma RJ, Trip MD, Kastelein JJ. Regression of carotid and femoral artery intima-media thickness in familial hypercholesterolemia. Arch Intern Med 2003; 163:1837–1841.
- Crouse JR, Grobbee DE, O’Leary DH, et al Measuring Effects on intima media Thickness: an Evaluation Of Rosuvastatin Study Group. . Measuring effects on intima media thickness: an evaluation of rosuvastatin in subclinical atherosclerosis—the rationale and methodology of the METEOR study. Cardiovasc Drugs Ther 2004; 18:231–238.
- Toth PP, Davidson MH. Cholesterol absorption blockade with ezetimibe. Curr Drug Targets Cardiovasc Haematol Disord 2005; 5:455–462.
- Nissen SE, Nicholls SJ, Sipahi I, et al ASTEROID Investigators. . Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 2006; 295:1556–1565.
- Kjekshus J, Apetrei E, Barrios V, et al CORONA Group. . Rosuvastatin in older patients with systolic heart failure. N Engl J Med 2007; 357:2248–2261.
- Cannon CP, Braunwald E, McCabe CH, et al Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 Investigators. . Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 2004; 350:1495–1504.
- Kastelein JJ, Akdim F, Stroes ES, et al ENHANCE Investigators. Simvastatin with or without ezetimibe in familial hypercholesterolemia. N Engl J Med 2008; 358:1431–1443.
- Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106:3143–3421.
- Grundy SM, Cleeman JI, Bairey Merz N, et al for the Coordinating Committee of the National Cholesterol Education Program. Circulation 2004; 110:227–239.
- Kastelein JJ, Sager PT, de Groot E, Veltri E. Comparison of ezetimibe plus simvastatin versus simvastatin monotherapy on atherosclerosis progression in familial hypercholesterolemia. Design and rationale of the Ezetimibe and Simvastatin in Hypercholesterolemia Enhances Atherosclerosis Regression (ENHANCE) trial. Am Heart J 2005; 49:234–239.
- Merck/Schering-Plough Pharmaceutical Press Release, January 14, 2008.
- Berenson A. Study reveals doubt on drug for cholesterol. New York Times January 15, 2008.
- Brown BG, Taylor AJ. Does ENHANCE diminish confidence in lowering LDL or in ezetimibe? N Engl J Med 2008; 358:1504–1507.
- Drazen JM, Jarcho JA, Morrissey S, Curfman GD. Cholesterol lowering and ezetimibe. N Engl J Med 2008; 358:1507–1508.
- American College of Cardiology. ENHANCED analysis of ezetimibe. ACC News, April 2, 2008. www.acc.org/emails/myacc/accnews%5Fapril%5F02%5F08.htm. Accessed 6/2/2008.
- American College of Cardiology. ACC panel on Vytorin: Go back to statins. Scientific Session News 3/31/2008. http://www.acc08.acc.org/SSN/Documents/ACC%20Monday%20v2.pdf. Accessed 6/2/2008.
- Smith SC, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. Endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol 2006; 47:2130–2139.
- Pettypiece S, Cortez MF. Merck, Schering plunge as doctors discourage Vytorin. www.bloomberg.com/apps/news?pid=20601103&refer=news&sid=aV_T9WirgAkI. Accessed 6/2/2008.
- Barter PJ, Caulfield M, Eriksson M, et al ILLUMINATE Investigators. . Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med 2007; 357:2109–2122.
- Hulley S, Grady D, Bush T, et al. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in post-menopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group. JAMA 1998; 280:605–613.
- Rader DJ. Illuminating HDL—is it still a viable therapeutic target? N Engl J Med 2007; 357:2180–2183.
- Davidson MH, Maki KC, Marx P, et al. Effects of continuous estrogen and estrogen-progestin replacement regimens on cardiovascular risk markers in postmenopausal women. Arch Intern Med 2000; 160:3315–3325.
- Hodis HN, Mack WJ, Lobo RA, et al Estrogen in the Prevention of Atherosclerosis Trial Research Group. . Estrogen in the prevention of atherosclerosis. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 2001; 135:939–953.
- Turley SD. Cholesterol metabolism and therapeutic targets: rationale for targeting multiple metabolic pathways. Clin Cardiol 2004; 27( suppl 3):III16–III21.
- Sehayek E, Hazen SL. Cholesterol absorption from the intestine is a major determinant of reverse cholesterol transport from peripheral tissue macrophages. Arterioscler Thromb Vasc Biol 2008;27 (Epub ahead of print].
- Davis HR, Compton DS, Hoos L, Tetzloff G. Ezetimibe, a potent cholesterol absorption inhibitor, inhibits the development of atherosclerosis in ApoE knockout mice. Arterioscler Thromb Vasc Biol 2001; 21:2032–2038.
- Wong J, Quinn CM, Gelissen IC, Jessup W, Brown AJ. The effect of statins on ABCA1 and ABCG1 expression in human macrophages is influenced by cellular cholesterol levels and extent of differentiation. Atherosclerosis 2008; 196:180–189.
- Wang N, Tall AR. Regulation and mechanisms of ATP-binding cassette transporter A1-mediated cellular cholesterol efflux. Arterioscler Thromb Vasc Biol 2003; 23:1178–1184.
- Bots ML. Carotid intima-media thickness as a surrogate marker for cardiovascular disease in intervention studies. Curr Med Res Opin 2006; 22:2181–2190.
- Byington RP, Evans GW, Espeland MA, et al. Effects of lovastatin and warfarin on early carotid atherosclerosis: sex-specific analyses. Asymptomatic Carotid Artery Progression Study (ACAPS) Research Group. Circulation 1999; 100:e14–e17.
- Byington RP, Furberg CD, Crouse JR, Espeland MA, Bond MG. Pravastatin, Lipids, and Atherosclerosis in the Carotid Arteries (PLAC-II). Am J Cardiol 1995; 76:54C–59C.
- Crouse JR, Raichlen JS, Riley WA, et al METEOR Study Group. . Effect of rosuvastatin on progression of carotid intima-media thickness in low-risk individuals with subclinical atherosclerosis: the METEOR trial. JAMA 2007; 297:1344–1353.
- Taylor AJ, Sullenberger LE, Lee HJ, Lee JK, Grace KA. Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol (ARBITER) 2: a double-blind, placebo-controlled study of extended-release niacin on atherosclerosis progression in secondary prevention patients treated with statins. Circulation 2004; 110:3512–3517.
- Smilde TJ, van Wissen S, Wollersheim H, Trip MD, Kastelein JJ, Stalenhoef AF. Effect of aggressive versus conventional lipid lowering on atherosclerosis progression in familial hypercholesterolaemia (ASAP): a prospective, randomised, double-blind trial. Lancet 2001; 357:577–581.
- van Wissen S, Smilde TJ, Trip MD, Stalenhoef AFH, Kastelein JJP. Long-term safety and efficacy of high-dose atorvastatin treatment in patients with familial hypercholesterolemia. Am J Cardiol 2005; 95:264–266.
- Meuwese MC, Franssen R, Stroes ES, Kastelein JJ. And then there were acyl coenzyme A:cholesterol acyl transferase inhibitors. Curr Opin Lipidol 2006; 17:426–430.
- Kastelein JJ, van Leuven SI, Burgess L, et al RADIANCE 1 Investigators. . Effect of torcetrapib on carotid atherosclerosis in familial hypercholesterolemia. N Engl J Med 2007; 356:1620–1630.
- Nissen SE, Tuzcu EM, Brewer HB, et al ACAT Intravascular Atherosclerosis Treatment Evaluation (ACTIVATE) Investigators. Effect of ACAT inhibition on the progression of coronary atherosclerosis. N Engl J Med 2006; 354:1253–1263.
- Davidson MH. Clinical significance of statin pleiotropic effects: hypotheses versus evidence. Circulation 2005; 111:2280–2281.
- Nolting PR, de Groot E, Zwinderman AH, Buirma RJ, Trip MD, Kastelein JJ. Regression of carotid and femoral artery intima-media thickness in familial hypercholesterolemia. Arch Intern Med 2003; 163:1837–1841.
- Crouse JR, Grobbee DE, O’Leary DH, et al Measuring Effects on intima media Thickness: an Evaluation Of Rosuvastatin Study Group. . Measuring effects on intima media thickness: an evaluation of rosuvastatin in subclinical atherosclerosis—the rationale and methodology of the METEOR study. Cardiovasc Drugs Ther 2004; 18:231–238.
- Toth PP, Davidson MH. Cholesterol absorption blockade with ezetimibe. Curr Drug Targets Cardiovasc Haematol Disord 2005; 5:455–462.
- Nissen SE, Nicholls SJ, Sipahi I, et al ASTEROID Investigators. . Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 2006; 295:1556–1565.
- Kjekshus J, Apetrei E, Barrios V, et al CORONA Group. . Rosuvastatin in older patients with systolic heart failure. N Engl J Med 2007; 357:2248–2261.
- Cannon CP, Braunwald E, McCabe CH, et al Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 Investigators. . Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 2004; 350:1495–1504.
What's Eating You? Io Moth (Automeris io)
How to avoid injury to bowel during laparoscopy
The author reports no financial relationships relevant to this article.
CASE Postoperative abdominal pain. Is it gastroenteritis?
R.B., 35 years old, undergoes laparoscopic adhesiolysis for abdominal pain. Previously, she underwent exploratory laparotomy for a ruptured tubal pregnancy and, in separate operations, right oophorectomy via laparotomy for a ruptured corpus luteum cyst and diagnostic laparoscopy.
During the current surgery, extensive adhesions are observed, including interloop intestinal adhesions. The adhesions are lysed using monopolar scissors and a needle electrode, and R.B. is discharged home the same day.
Later that day and the next day, R.B. complains of abdominal pain that does not respond to prescribed analgesics, as well as nausea and vomiting. A nurse practitioner takes her call and prescribes a stronger analgesic, an antiemetic, and an antibiotic.
The following day, the patient’s husband telephones the treating gynecologist to report that his wife is still experiencing severe pain and nausea. He is told to bring her to the office, where she is described as having mild lower abdominal tenderness and mild rebound. An abdominal radiograph shows air-fluid levels and distended bowel. The gynecologist determines that the patient is experiencing gastroenteritis.
On postop day 3, R.B. continues to suffer from severe abdominal pain, nausea, and vomiting, and is unable to get out of bed. Her husband takes her to the emergency room at another hospital, where she is found to have diffuse peritonitis, absent bowel sounds, and:
- temperature, 101.8°F
- heart rate, 130/min
- respiratory rate, 24/min
- blood pressure, 90/60 mm Hg
- white blood cell (WBC) count, 21.5 × 103/μL
- x-ray showing free air.
A general surgeon performs an exploratory laparotomy and finds foul-smelling abdominal fluid, 200 to 300 mL of pus, and a 1-cm perforation of the sigmoid colon. He performs sigmoid colon resection and a left-colon colostomy. A second laparotomy is necessary to drain a subphrenic abscess.
Four months later, the colostomy is taken down and bowel continuity is established.
Subsequently, the patient experiences episodes of gaseous and fecal incontinence, which are thought to be secondary to nerve damage. A ventral hernia is also diagnosed.
Could this outcome have been avoided?
No physician would wish a major complication of surgery upon any patient. Yet, sometimes, preventive efforts fall short of the goal or the physician is slow to suspect injury when the patient experiences postoperative abdominal pain and other symptoms. Intestinal injury may not be common during laparoscopy, but it is certainly not rare. And the longer diagnosis is delayed, the greater the risk of sepsis, even death.
Recognizing the limitations of laparoscopic surgery is a first step toward reducing the complication rate.1,2 The ability to determine when laparotomy would better serve the patient’s interests is also critical, and prompt diagnosis and repair of any complication that does occur will ensure and speed the patient’s recovery.
The most serious complications associated with diagnostic and operative laparoscopy are major vessel and intestinal injuries. Both types of injury significantly raise the risk of mortality, which ranges from 2% to 23%.3,4 The overall risk of injury to the gastrointestinal tract averages 1.6 to 2.0 for every 1,000 cases. The risk of major vessel injury averages 0.5 for every 1,000 cases.5-9
In an earlier article for OBG Management, I reviewed vascular injury during laparoscopy.10 In Part 1 of this article, I focus on ways to avoid intestinal injury.In Part 2 , I outline strategies to identify it in a timely manner when it does occur.
- Avoid laparoscopy when severe adhesions are anticipated—such as when the patient has a history of multiple laparotomies, or when significant adhesions have been documented.
- Be aware that laparoscopy carries additional risks beyond those of the primary surgical procedure, owing to factors peculiar to endoscopic technique and instrumentation.
- Consider open laparoscopy or insert the primary trocar at an alternative location, such as the left upper quadrant, when the patient has a history of laparotomy.
- Avoid blunt dissection for anything other than mild (filmy) adhesions. Sharp dissection associated with hydrodissection is the safest method of adhesiolysis. Clear visualization of the operative site is the sine qua non for precise dissection.
- Avoid monopolar electrosurgical devices for laparoscopic surgery whenever possible. Also remember that bipolar and ultrasonic devices can cause thermal injury by heat conduction as well as by direct application. Laser energy will continue beyond the target unless provision is made to absorb the residual energy.
- At the conclusion of any laparoscopic procedure, especially after adhesiolysis or bowel dissection, inspect the intestines and include the details in the operative report.
- After any laparoscopic procedure, if the patient does not improve steadily, the first presumptive diagnosis to be excluded is injury secondary to the procedure or technique.
- The major symptom of intestinal perforation is abdominal pain, which does not ease without increasing quantities of analgesics.
- Investigate any bowel injury thoroughly to determine viability at the site of injury. Whenever possible, repair all injuries intraoperatively.
- After intestinal perforation, the risk of sepsis is high. Look for early signs such as tachycardia, subnormal body temperature, depressed WBC count, and the appearance of immature white cell elements.
A thorough familiarity with pelvic anatomy is important to avoid injury at trocar entry, but it is even more critical in regard to operative injury. The small intestine spreads diffusely throughout the abdomen beneath the anterior abdominal wall. It lies beneath the umbilicus and anterior midline, whereas the large bowel is located at the periphery. The sigmoid colon swings left to right before joining the rectum anterior to the presacral space. The sigmoid junction with the descending colon lies well to the left of the midline, and the cecum lies at the pelvic brim to the right of midline.
In some women, the intestines droop into the pelvis and cover the adnexa, making adhesions between these structures highly likely following dissection in the vicinity of the tubes and ovaries.
Depending on the degree of redundancy of the mesentery of the cecum or sigmoid colon, these structures may droop into the pelvis and cover the adnexa. Therefore, adhesions are likely to develop between the large or small intestine, or both, and the adnexa following dissection in the vicinity of or immediately over the tubes and ovaries. Knowing the normal anatomic relationships is vital for restorative surgery.
When severe adhesions involve the large intestine, it is critical to know the anatomy of the retroperitoneum and be skilled enough to gain safe entry and to dissect that space to safely separate the adnexa when they are densely adhered to the pelvic sidewall in the area of the obturator fossa.
As laparoscopy evolves, the injury rate rises
Over the past 40 years, laparoscopy has evolved from an uncommonly utilized diagnostic tool to a minimally invasive alternative to laparotomy for even the most difficult and complex operations, reaching a high point with robotic laparoscopy. As this technology has developed, serious complications—to some degree, unique to laparoscopy—have increased. In the future, as less skilled surgeons perform a greater percentage of laparoscopic surgeries, a still greater number of complications will arise.
The frequency of intestinal perforation is not great relative to the total number of laparoscopic procedures performed. The TABLE lists several series totaling more than 380,000 laparoscopic operations. The risk of reported bowel perforation ranged from 0.6 to 6 for every 1,000 procedures, with a mean risk of 2.4 for every 1,000. However, these data are inconclusive because the total number of laparoscopic operations performed in the United States is not accurately known. Nor is the precise number of complications associated with these procedures known—specifically, the number of intestinal perforations—as no law requires them to be reported.
Research surveys are unreliable in many cases. In addition, the relative expertise of the surgeon is impossible to quantify. For example, although a surgeon may have many years of operative experience, it is unclear whether this always translates into skill or comfort with laparoscopic procedures. And, when a resident scrubs in with a faculty surgeon, any data collected fail to reflect which part of the surgery was performed by the resident and which by the fully trained gynecologist.
These unknown variables are important in terms of risk, surgical complications, and outcomes. Surgical skill is the greatest unknown factor in any outcome study of any surgical procedure.
TABLE
Studies of complications reveal: Gastrointestinal injury is no rare event during laparoscopic surgery
| Study (year; country) | Cases | Complications | Deaths | GI injury |
|---|---|---|---|---|
| Brown et al (1978; UK)16 | 50,247 | 345 | 4 | 117 (2.3/1,000) |
| Soderstrom (1993; US)17 | No data | No data | 3 | 66 |
| Bateman et al (1996; US)18 | 1,162 | No data | No data | 3 (2.6/1,000)* |
| Champault et al (1996; France)15 | 103,852 | 337 | 6 | 63 (0.6/1,000)† |
| Saidi et al (1996; US)19 | 452 | 47 | 0 | 0 |
| Jansen et al (1997; Netherlands)5 | 25,764 | 145 | 2 | 29 (1.13/1,000) |
| Harkki-Siren et al (1997; Finland)8 | 70,607 | 96 | 0 | 44 (0.6/1,000) |
| Harkki-Siren et al (1997; Finland)7 | 1,165 | 119 | 0 | 5 (4/1,000)‡ |
| Chapron et al (1998; France)6 | 29,996 | 96 | 1 | 48 (1.6/1,000) |
| Chapron et al (1999; France)9 | No data | No data | No data | 62 (0.6–1.6/1,000) |
| Gordts et al (2001; France)20 | 3,667 | No data | No data | 24 (6/1,000) |
| Bhoyrul et al (2001; US)13 | No data | 629 | 32 | 128§ |
| Wang et al (2001; Taiwan)21 | 6,451 | 42 | 0 | 10 (1.6/1,000) |
| Sharp et al (2002; US)14 | 185 | 84 | 2 | 24** |
| Brosens et al (2003; Belgium)22 | 85,727 | No data | No data | 195 (2.3/1,000) |
| * 80 open laparoscopy procedures; 30 closed laparoscopy procedures | ||||
| † Limited to trocar injuries | ||||
| ‡ Laparoscopic hysterectomy | ||||
| § All trocar injuries obtained through Food and Drug Administration reports | ||||
| ** Limited to optical access trocars | ||||
Classifying intestinal injuries
As in the case of major vessel injury, intestinal injury sustained during laparoscopy can be classified as either:
- Injury secondary to the approach. This category refers to entry complications associated with creation of the pneumoperitoneum and insertion of primary and secondary trocars.
- Injury secondary to the procedure or operation. This type of injury occurs as a result of manipulation with various devices during laparoscopy. The devices may include probes, forceps, scissors, or energy devices such as laser, electrosurgical, and ultrasonic instruments.
How trocar injury happens
Several studies have demonstrated that abdominal adhesions place any patient into a high-risk category for trocar injury to the intestines. Patients who have undergone multiple laparotomies, like the patient in the case that opened this article, are more likely to have severe adhesions and fall into the highest risk category for bowel perforation.11 It is impossible to predict with any degree of accuracy whether the intestine is adherent to the entry site.
Pneumoperitoneum can be protective
Creation of a pneumoperitoneum creates a cushion of gas between the intestines and the anterior abdominal wall (provided the intestines are not adherent to the abdominal wall). Manufacturers of disposable trocars with a retractable shield recommend creating an adequate pneumoperitoneum so that the “safety shield” deploys quickly and properly, unlike direct insertion, in which no gas is infused and space is insufficient for complete shield activation.
Open laparoscopy techniques, which allow the surgeon to enter the peritoneal cavity by direct vision without a sharp trocar, may diminish but not eliminate the risk of bowel injury.
What the data show
Of the 130 intestinal injuries recently reported by Baggish, 62 of 81 (77%) small bowel injuries were related to trocar insertion, as were 20 of 49 (41%) large intestinal injuries.12 In other words, 82 of 130 intestinal injuries (63%) were the direct result of trocar entry.
Bhoyrul and associates reported 629 trocar injuries, of which 182 were visceral.13 Of the 32 deaths, six were secondary to unrecognized bowel injury. Of 176 nonfatal visceral injuries, 128 (73%) involved the intestines, and 22 were unrecognized.
Optical-access and open laparoscopic systems were designed to prevent such injuries. Sharp and colleagues reported 24 intestinal injuries out of a total of 79 complications (30%) associated with optical-access trocars after reviewing data obtained from the Medical Device Reports (MDR) and Maude databases maintained by the Food and Drug Administration.14 In the Baggish series, 4.6% of injuries were associated with open laparoscopy.12
Champault and colleagues reviewed complications in a survey of 103,852 operations.15 Although they recommended use of open laparoscopy as opposed to blind insertion, they presented no data on the safety of open techniques.
How intraoperative injury happens
Operative injury of the large or small bowel often occurs during sharp or blunt dissection, performed during laparoscopy using accessory mechanical or energy devices. The latter type of device is utilized increasingly because laparoscopic knot tying and suturing are rather awkward and slow, and laparoscopic suturing to control bleeding is difficult. The size of the needle required for laparoscopic suture placement must be small enough to navigate a trocar sleeve.
Avoid blunt dissection when adhesions are present
The separation of dense adhesions between the intestines and neighboring bowel, other viscera, or abdominal wall is risky when blunt dissection is used. The tensile strength of the fibrotic connective tissue may well exceed that of the thin intestinal wall. Tearing the adhesion free may bring with it a portion of the bowel wall. Such injuries are frequently missed or described as serosal injuries and left unexplored and unrepaired.
Hydrodissection is a safer alternative. It involves the infiltration of sterile water or saline under low pressure between the parietal peritoneum and underlying retroperitoneal structures, providing a safe and natural plane for dissection. In addition, when the CO2 laser is used, the liquid acts as a heat sink to absorb any penetrating laser energy.
Energy devices create thermal effects
Energy devices used to cut tissue during operative laparoscopy coagulate blood vessels in a variety of ways, but the common pathway is thermal. Many hypotheses have evolved to explain how vessels are sealed, but none has demonstrated nonthermal activity except for cryocoagulation.
The devices most commonly used for cutting and hemostasis at laparoscopy are:
- electrosurgical (both monopolar and bipolar). Bipolar electrosurgical devices have advantages over monopolar devices when it comes to high-frequency leaks, direct coupling, and capacitive coupling.
- laser (CO2, holmium:YAG, Nd:YAG, KTP-532, argon). As I mentioned, CO2 laser devices are effectively backstopped by water, especially in strategic areas such as over and around intestines, major vessels, and the ureters.
- ultrasonic (Harmonic Scalpel, ultrasonic aspirator [CUSA]).
Laser and ultrasonic devices do not require a flow of electrons to create coagulation, but do produce heat that will spread peripherally by thermal conduction from the zone of impact (target).
The extent of energy-inflicted injury cannot be predicted
Inadvertent injury with energy devices can occur directly through contact with the bowel, indirectly by heat conduction through tissue, through capacitive coupling (monopolar electrical only), and by forward scatter (laser only).
Upon direct contact with the intestine, energy devices cut into the tissue in a manner similar to mechanical scissors or a knife but produce a larger wound. The reason? The transfer of heat to areas adjacent to the primary wound produces additional necrosis. Heat conduction, capacitive coupling, high-frequency leaks, and front scatter coagulate the intestinal wall with subsequent tissue devitalization and necrosis, the extent of which depends on the power density at contact and the duration of energy applied.
It is impossible to predict the depth or area of devitalization in energy-inflicted injury by visualization of the event.
In the Baggish review of 130 intestinal injuries, the number of injuries sustained during the operative procedure was 19 involving the small intestine and 29 involving the large bowel.12 Of this subset, 44% (21 cases) were secondary to the use of energy devices, with monopolar electrosurgical instruments alone accounting for 9 (43%) of the injuries.
Even best-laid plans can go awry
Despite our best intentions and precautions, accidents do sometimes happen, and bowel injury is no exception.In Part 2 of this article, I detail steps you can take to detect injuries in as timely a manner as possible.
1. Mäkinen J, Johansson J, Tomás C, et al. Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod. 2001;16:1473-1478.
2. Fuller J, Ashar BS, Corrado-Carey J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005;12:302-307.
3. Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg. 1997;185:461-465.
4. Baggish MS. Analysis of 31 cases of major-vessel injury associated with gynecologic laparoscopy operations. J Gynecol Surg. 2003;19:63-73.
5. Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB. Complications of laparoscopy: a prospective multicenter observational study. Br J Obstet Gynaecol. 1997;104:595-600.
6. Chapron C, Querleu D, Bruhat MA, et al. Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod. 1998;13:867-872.
7. Härkki-Sirén P, Sjöberg J, Mäkinen J, et al. Finnish National Register of Laparoscopic Hysterectomies: a review and complications of 1165 operations. Am J Obstet Gynecol. 1997;176(1 Pt. 1):118-122.
8. Härkki-Sirén P, Kurki T. A nationwide analysis of laparoscopic complications. Obstet Gynecol. 1997;89:108-112.
9. Chapron C, Pierre F, Harchaoui Y, et al. Gastrointestinal injuries during gynaecological laparoscopy. Hum Reprod. 1999;14:333-337.
10. Baggish MS. Avoiding vascular injury at laparoscopy. OBG Management. 2004;16(10):70-87.
11. Smith ARB. Postoperative complications following minimal access surgery. Baillieres Clin Obstet Gynecol. 2000;14:123.-
12. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
13. Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001;192:677-683.
14. Sharp HT, Dodson MK, Draper ML, Watts DA, Doucette RC, Hurd WW. Complications associated with optical-access laparoscopic trocars. Obstet Gynecol. 2002;99:553-555.
15. Champault G, Cazacu F, Taffi nder N. Serious trocar accidents in laparoscopic surgery: a French survey of 103,852 operations. Surg Laparosc Endosc. 1996;6:367-370.
16. Brown JA, Chamberlain GVP, Jordan JA, et al. Gynaecological laparoscopy. The Report of the Working Party of the Confidential Enquiry into Gynaecological Laparoscopy. Br J Obstet Gynaecol. 1978;85:401-403.
17. Soderstrom RM. Bowel injury ligation after laparoscopy. J Am Assoc Gynecol Laparosc. 1993;1:74-77.
18. Bateman BG, Kolp LA, Hoeger K. Complications of laparoscopy—operative and diagnostic. Fertil Steril. 1996;66:30-35.
19. Saidi MH, Vancaillie TG, White J, Sadler RK, Akright BD, Farhart SA. Complications of major operative laparoscopy. A review of 452 cases. J Reprod Med. 1996;41:471-476.
20. Gordts S, Watrelot A, Camp R, Brosens I. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76:1238-1241.
21. Wang PH, Lee WL, Yuan CC, et al. Major complications of operative and diagnostic laparoscopy for gynecologic disease. J Am Assoc Gynecol Laparosc. 2001;8:68-73.
22. Brosens I, Gordon A, Campo R, Gordts S. Bowel injury in gynecologic laparoscopy. J Am Assoc Gynecol Laparosc. 2003;10:9-13.
The author reports no financial relationships relevant to this article.
CASE Postoperative abdominal pain. Is it gastroenteritis?
R.B., 35 years old, undergoes laparoscopic adhesiolysis for abdominal pain. Previously, she underwent exploratory laparotomy for a ruptured tubal pregnancy and, in separate operations, right oophorectomy via laparotomy for a ruptured corpus luteum cyst and diagnostic laparoscopy.
During the current surgery, extensive adhesions are observed, including interloop intestinal adhesions. The adhesions are lysed using monopolar scissors and a needle electrode, and R.B. is discharged home the same day.
Later that day and the next day, R.B. complains of abdominal pain that does not respond to prescribed analgesics, as well as nausea and vomiting. A nurse practitioner takes her call and prescribes a stronger analgesic, an antiemetic, and an antibiotic.
The following day, the patient’s husband telephones the treating gynecologist to report that his wife is still experiencing severe pain and nausea. He is told to bring her to the office, where she is described as having mild lower abdominal tenderness and mild rebound. An abdominal radiograph shows air-fluid levels and distended bowel. The gynecologist determines that the patient is experiencing gastroenteritis.
On postop day 3, R.B. continues to suffer from severe abdominal pain, nausea, and vomiting, and is unable to get out of bed. Her husband takes her to the emergency room at another hospital, where she is found to have diffuse peritonitis, absent bowel sounds, and:
- temperature, 101.8°F
- heart rate, 130/min
- respiratory rate, 24/min
- blood pressure, 90/60 mm Hg
- white blood cell (WBC) count, 21.5 × 103/μL
- x-ray showing free air.
A general surgeon performs an exploratory laparotomy and finds foul-smelling abdominal fluid, 200 to 300 mL of pus, and a 1-cm perforation of the sigmoid colon. He performs sigmoid colon resection and a left-colon colostomy. A second laparotomy is necessary to drain a subphrenic abscess.
Four months later, the colostomy is taken down and bowel continuity is established.
Subsequently, the patient experiences episodes of gaseous and fecal incontinence, which are thought to be secondary to nerve damage. A ventral hernia is also diagnosed.
Could this outcome have been avoided?
No physician would wish a major complication of surgery upon any patient. Yet, sometimes, preventive efforts fall short of the goal or the physician is slow to suspect injury when the patient experiences postoperative abdominal pain and other symptoms. Intestinal injury may not be common during laparoscopy, but it is certainly not rare. And the longer diagnosis is delayed, the greater the risk of sepsis, even death.
Recognizing the limitations of laparoscopic surgery is a first step toward reducing the complication rate.1,2 The ability to determine when laparotomy would better serve the patient’s interests is also critical, and prompt diagnosis and repair of any complication that does occur will ensure and speed the patient’s recovery.
The most serious complications associated with diagnostic and operative laparoscopy are major vessel and intestinal injuries. Both types of injury significantly raise the risk of mortality, which ranges from 2% to 23%.3,4 The overall risk of injury to the gastrointestinal tract averages 1.6 to 2.0 for every 1,000 cases. The risk of major vessel injury averages 0.5 for every 1,000 cases.5-9
In an earlier article for OBG Management, I reviewed vascular injury during laparoscopy.10 In Part 1 of this article, I focus on ways to avoid intestinal injury.In Part 2 , I outline strategies to identify it in a timely manner when it does occur.
- Avoid laparoscopy when severe adhesions are anticipated—such as when the patient has a history of multiple laparotomies, or when significant adhesions have been documented.
- Be aware that laparoscopy carries additional risks beyond those of the primary surgical procedure, owing to factors peculiar to endoscopic technique and instrumentation.
- Consider open laparoscopy or insert the primary trocar at an alternative location, such as the left upper quadrant, when the patient has a history of laparotomy.
- Avoid blunt dissection for anything other than mild (filmy) adhesions. Sharp dissection associated with hydrodissection is the safest method of adhesiolysis. Clear visualization of the operative site is the sine qua non for precise dissection.
- Avoid monopolar electrosurgical devices for laparoscopic surgery whenever possible. Also remember that bipolar and ultrasonic devices can cause thermal injury by heat conduction as well as by direct application. Laser energy will continue beyond the target unless provision is made to absorb the residual energy.
- At the conclusion of any laparoscopic procedure, especially after adhesiolysis or bowel dissection, inspect the intestines and include the details in the operative report.
- After any laparoscopic procedure, if the patient does not improve steadily, the first presumptive diagnosis to be excluded is injury secondary to the procedure or technique.
- The major symptom of intestinal perforation is abdominal pain, which does not ease without increasing quantities of analgesics.
- Investigate any bowel injury thoroughly to determine viability at the site of injury. Whenever possible, repair all injuries intraoperatively.
- After intestinal perforation, the risk of sepsis is high. Look for early signs such as tachycardia, subnormal body temperature, depressed WBC count, and the appearance of immature white cell elements.
A thorough familiarity with pelvic anatomy is important to avoid injury at trocar entry, but it is even more critical in regard to operative injury. The small intestine spreads diffusely throughout the abdomen beneath the anterior abdominal wall. It lies beneath the umbilicus and anterior midline, whereas the large bowel is located at the periphery. The sigmoid colon swings left to right before joining the rectum anterior to the presacral space. The sigmoid junction with the descending colon lies well to the left of the midline, and the cecum lies at the pelvic brim to the right of midline.
In some women, the intestines droop into the pelvis and cover the adnexa, making adhesions between these structures highly likely following dissection in the vicinity of the tubes and ovaries.
Depending on the degree of redundancy of the mesentery of the cecum or sigmoid colon, these structures may droop into the pelvis and cover the adnexa. Therefore, adhesions are likely to develop between the large or small intestine, or both, and the adnexa following dissection in the vicinity of or immediately over the tubes and ovaries. Knowing the normal anatomic relationships is vital for restorative surgery.
When severe adhesions involve the large intestine, it is critical to know the anatomy of the retroperitoneum and be skilled enough to gain safe entry and to dissect that space to safely separate the adnexa when they are densely adhered to the pelvic sidewall in the area of the obturator fossa.
As laparoscopy evolves, the injury rate rises
Over the past 40 years, laparoscopy has evolved from an uncommonly utilized diagnostic tool to a minimally invasive alternative to laparotomy for even the most difficult and complex operations, reaching a high point with robotic laparoscopy. As this technology has developed, serious complications—to some degree, unique to laparoscopy—have increased. In the future, as less skilled surgeons perform a greater percentage of laparoscopic surgeries, a still greater number of complications will arise.
The frequency of intestinal perforation is not great relative to the total number of laparoscopic procedures performed. The TABLE lists several series totaling more than 380,000 laparoscopic operations. The risk of reported bowel perforation ranged from 0.6 to 6 for every 1,000 procedures, with a mean risk of 2.4 for every 1,000. However, these data are inconclusive because the total number of laparoscopic operations performed in the United States is not accurately known. Nor is the precise number of complications associated with these procedures known—specifically, the number of intestinal perforations—as no law requires them to be reported.
Research surveys are unreliable in many cases. In addition, the relative expertise of the surgeon is impossible to quantify. For example, although a surgeon may have many years of operative experience, it is unclear whether this always translates into skill or comfort with laparoscopic procedures. And, when a resident scrubs in with a faculty surgeon, any data collected fail to reflect which part of the surgery was performed by the resident and which by the fully trained gynecologist.
These unknown variables are important in terms of risk, surgical complications, and outcomes. Surgical skill is the greatest unknown factor in any outcome study of any surgical procedure.
TABLE
Studies of complications reveal: Gastrointestinal injury is no rare event during laparoscopic surgery
| Study (year; country) | Cases | Complications | Deaths | GI injury |
|---|---|---|---|---|
| Brown et al (1978; UK)16 | 50,247 | 345 | 4 | 117 (2.3/1,000) |
| Soderstrom (1993; US)17 | No data | No data | 3 | 66 |
| Bateman et al (1996; US)18 | 1,162 | No data | No data | 3 (2.6/1,000)* |
| Champault et al (1996; France)15 | 103,852 | 337 | 6 | 63 (0.6/1,000)† |
| Saidi et al (1996; US)19 | 452 | 47 | 0 | 0 |
| Jansen et al (1997; Netherlands)5 | 25,764 | 145 | 2 | 29 (1.13/1,000) |
| Harkki-Siren et al (1997; Finland)8 | 70,607 | 96 | 0 | 44 (0.6/1,000) |
| Harkki-Siren et al (1997; Finland)7 | 1,165 | 119 | 0 | 5 (4/1,000)‡ |
| Chapron et al (1998; France)6 | 29,996 | 96 | 1 | 48 (1.6/1,000) |
| Chapron et al (1999; France)9 | No data | No data | No data | 62 (0.6–1.6/1,000) |
| Gordts et al (2001; France)20 | 3,667 | No data | No data | 24 (6/1,000) |
| Bhoyrul et al (2001; US)13 | No data | 629 | 32 | 128§ |
| Wang et al (2001; Taiwan)21 | 6,451 | 42 | 0 | 10 (1.6/1,000) |
| Sharp et al (2002; US)14 | 185 | 84 | 2 | 24** |
| Brosens et al (2003; Belgium)22 | 85,727 | No data | No data | 195 (2.3/1,000) |
| * 80 open laparoscopy procedures; 30 closed laparoscopy procedures | ||||
| † Limited to trocar injuries | ||||
| ‡ Laparoscopic hysterectomy | ||||
| § All trocar injuries obtained through Food and Drug Administration reports | ||||
| ** Limited to optical access trocars | ||||
Classifying intestinal injuries
As in the case of major vessel injury, intestinal injury sustained during laparoscopy can be classified as either:
- Injury secondary to the approach. This category refers to entry complications associated with creation of the pneumoperitoneum and insertion of primary and secondary trocars.
- Injury secondary to the procedure or operation. This type of injury occurs as a result of manipulation with various devices during laparoscopy. The devices may include probes, forceps, scissors, or energy devices such as laser, electrosurgical, and ultrasonic instruments.
How trocar injury happens
Several studies have demonstrated that abdominal adhesions place any patient into a high-risk category for trocar injury to the intestines. Patients who have undergone multiple laparotomies, like the patient in the case that opened this article, are more likely to have severe adhesions and fall into the highest risk category for bowel perforation.11 It is impossible to predict with any degree of accuracy whether the intestine is adherent to the entry site.
Pneumoperitoneum can be protective
Creation of a pneumoperitoneum creates a cushion of gas between the intestines and the anterior abdominal wall (provided the intestines are not adherent to the abdominal wall). Manufacturers of disposable trocars with a retractable shield recommend creating an adequate pneumoperitoneum so that the “safety shield” deploys quickly and properly, unlike direct insertion, in which no gas is infused and space is insufficient for complete shield activation.
Open laparoscopy techniques, which allow the surgeon to enter the peritoneal cavity by direct vision without a sharp trocar, may diminish but not eliminate the risk of bowel injury.
What the data show
Of the 130 intestinal injuries recently reported by Baggish, 62 of 81 (77%) small bowel injuries were related to trocar insertion, as were 20 of 49 (41%) large intestinal injuries.12 In other words, 82 of 130 intestinal injuries (63%) were the direct result of trocar entry.
Bhoyrul and associates reported 629 trocar injuries, of which 182 were visceral.13 Of the 32 deaths, six were secondary to unrecognized bowel injury. Of 176 nonfatal visceral injuries, 128 (73%) involved the intestines, and 22 were unrecognized.
Optical-access and open laparoscopic systems were designed to prevent such injuries. Sharp and colleagues reported 24 intestinal injuries out of a total of 79 complications (30%) associated with optical-access trocars after reviewing data obtained from the Medical Device Reports (MDR) and Maude databases maintained by the Food and Drug Administration.14 In the Baggish series, 4.6% of injuries were associated with open laparoscopy.12
Champault and colleagues reviewed complications in a survey of 103,852 operations.15 Although they recommended use of open laparoscopy as opposed to blind insertion, they presented no data on the safety of open techniques.
How intraoperative injury happens
Operative injury of the large or small bowel often occurs during sharp or blunt dissection, performed during laparoscopy using accessory mechanical or energy devices. The latter type of device is utilized increasingly because laparoscopic knot tying and suturing are rather awkward and slow, and laparoscopic suturing to control bleeding is difficult. The size of the needle required for laparoscopic suture placement must be small enough to navigate a trocar sleeve.
Avoid blunt dissection when adhesions are present
The separation of dense adhesions between the intestines and neighboring bowel, other viscera, or abdominal wall is risky when blunt dissection is used. The tensile strength of the fibrotic connective tissue may well exceed that of the thin intestinal wall. Tearing the adhesion free may bring with it a portion of the bowel wall. Such injuries are frequently missed or described as serosal injuries and left unexplored and unrepaired.
Hydrodissection is a safer alternative. It involves the infiltration of sterile water or saline under low pressure between the parietal peritoneum and underlying retroperitoneal structures, providing a safe and natural plane for dissection. In addition, when the CO2 laser is used, the liquid acts as a heat sink to absorb any penetrating laser energy.
Energy devices create thermal effects
Energy devices used to cut tissue during operative laparoscopy coagulate blood vessels in a variety of ways, but the common pathway is thermal. Many hypotheses have evolved to explain how vessels are sealed, but none has demonstrated nonthermal activity except for cryocoagulation.
The devices most commonly used for cutting and hemostasis at laparoscopy are:
- electrosurgical (both monopolar and bipolar). Bipolar electrosurgical devices have advantages over monopolar devices when it comes to high-frequency leaks, direct coupling, and capacitive coupling.
- laser (CO2, holmium:YAG, Nd:YAG, KTP-532, argon). As I mentioned, CO2 laser devices are effectively backstopped by water, especially in strategic areas such as over and around intestines, major vessels, and the ureters.
- ultrasonic (Harmonic Scalpel, ultrasonic aspirator [CUSA]).
Laser and ultrasonic devices do not require a flow of electrons to create coagulation, but do produce heat that will spread peripherally by thermal conduction from the zone of impact (target).
The extent of energy-inflicted injury cannot be predicted
Inadvertent injury with energy devices can occur directly through contact with the bowel, indirectly by heat conduction through tissue, through capacitive coupling (monopolar electrical only), and by forward scatter (laser only).
Upon direct contact with the intestine, energy devices cut into the tissue in a manner similar to mechanical scissors or a knife but produce a larger wound. The reason? The transfer of heat to areas adjacent to the primary wound produces additional necrosis. Heat conduction, capacitive coupling, high-frequency leaks, and front scatter coagulate the intestinal wall with subsequent tissue devitalization and necrosis, the extent of which depends on the power density at contact and the duration of energy applied.
It is impossible to predict the depth or area of devitalization in energy-inflicted injury by visualization of the event.
In the Baggish review of 130 intestinal injuries, the number of injuries sustained during the operative procedure was 19 involving the small intestine and 29 involving the large bowel.12 Of this subset, 44% (21 cases) were secondary to the use of energy devices, with monopolar electrosurgical instruments alone accounting for 9 (43%) of the injuries.
Even best-laid plans can go awry
Despite our best intentions and precautions, accidents do sometimes happen, and bowel injury is no exception.In Part 2 of this article, I detail steps you can take to detect injuries in as timely a manner as possible.
The author reports no financial relationships relevant to this article.
CASE Postoperative abdominal pain. Is it gastroenteritis?
R.B., 35 years old, undergoes laparoscopic adhesiolysis for abdominal pain. Previously, she underwent exploratory laparotomy for a ruptured tubal pregnancy and, in separate operations, right oophorectomy via laparotomy for a ruptured corpus luteum cyst and diagnostic laparoscopy.
During the current surgery, extensive adhesions are observed, including interloop intestinal adhesions. The adhesions are lysed using monopolar scissors and a needle electrode, and R.B. is discharged home the same day.
Later that day and the next day, R.B. complains of abdominal pain that does not respond to prescribed analgesics, as well as nausea and vomiting. A nurse practitioner takes her call and prescribes a stronger analgesic, an antiemetic, and an antibiotic.
The following day, the patient’s husband telephones the treating gynecologist to report that his wife is still experiencing severe pain and nausea. He is told to bring her to the office, where she is described as having mild lower abdominal tenderness and mild rebound. An abdominal radiograph shows air-fluid levels and distended bowel. The gynecologist determines that the patient is experiencing gastroenteritis.
On postop day 3, R.B. continues to suffer from severe abdominal pain, nausea, and vomiting, and is unable to get out of bed. Her husband takes her to the emergency room at another hospital, where she is found to have diffuse peritonitis, absent bowel sounds, and:
- temperature, 101.8°F
- heart rate, 130/min
- respiratory rate, 24/min
- blood pressure, 90/60 mm Hg
- white blood cell (WBC) count, 21.5 × 103/μL
- x-ray showing free air.
A general surgeon performs an exploratory laparotomy and finds foul-smelling abdominal fluid, 200 to 300 mL of pus, and a 1-cm perforation of the sigmoid colon. He performs sigmoid colon resection and a left-colon colostomy. A second laparotomy is necessary to drain a subphrenic abscess.
Four months later, the colostomy is taken down and bowel continuity is established.
Subsequently, the patient experiences episodes of gaseous and fecal incontinence, which are thought to be secondary to nerve damage. A ventral hernia is also diagnosed.
Could this outcome have been avoided?
No physician would wish a major complication of surgery upon any patient. Yet, sometimes, preventive efforts fall short of the goal or the physician is slow to suspect injury when the patient experiences postoperative abdominal pain and other symptoms. Intestinal injury may not be common during laparoscopy, but it is certainly not rare. And the longer diagnosis is delayed, the greater the risk of sepsis, even death.
Recognizing the limitations of laparoscopic surgery is a first step toward reducing the complication rate.1,2 The ability to determine when laparotomy would better serve the patient’s interests is also critical, and prompt diagnosis and repair of any complication that does occur will ensure and speed the patient’s recovery.
The most serious complications associated with diagnostic and operative laparoscopy are major vessel and intestinal injuries. Both types of injury significantly raise the risk of mortality, which ranges from 2% to 23%.3,4 The overall risk of injury to the gastrointestinal tract averages 1.6 to 2.0 for every 1,000 cases. The risk of major vessel injury averages 0.5 for every 1,000 cases.5-9
In an earlier article for OBG Management, I reviewed vascular injury during laparoscopy.10 In Part 1 of this article, I focus on ways to avoid intestinal injury.In Part 2 , I outline strategies to identify it in a timely manner when it does occur.
- Avoid laparoscopy when severe adhesions are anticipated—such as when the patient has a history of multiple laparotomies, or when significant adhesions have been documented.
- Be aware that laparoscopy carries additional risks beyond those of the primary surgical procedure, owing to factors peculiar to endoscopic technique and instrumentation.
- Consider open laparoscopy or insert the primary trocar at an alternative location, such as the left upper quadrant, when the patient has a history of laparotomy.
- Avoid blunt dissection for anything other than mild (filmy) adhesions. Sharp dissection associated with hydrodissection is the safest method of adhesiolysis. Clear visualization of the operative site is the sine qua non for precise dissection.
- Avoid monopolar electrosurgical devices for laparoscopic surgery whenever possible. Also remember that bipolar and ultrasonic devices can cause thermal injury by heat conduction as well as by direct application. Laser energy will continue beyond the target unless provision is made to absorb the residual energy.
- At the conclusion of any laparoscopic procedure, especially after adhesiolysis or bowel dissection, inspect the intestines and include the details in the operative report.
- After any laparoscopic procedure, if the patient does not improve steadily, the first presumptive diagnosis to be excluded is injury secondary to the procedure or technique.
- The major symptom of intestinal perforation is abdominal pain, which does not ease without increasing quantities of analgesics.
- Investigate any bowel injury thoroughly to determine viability at the site of injury. Whenever possible, repair all injuries intraoperatively.
- After intestinal perforation, the risk of sepsis is high. Look for early signs such as tachycardia, subnormal body temperature, depressed WBC count, and the appearance of immature white cell elements.
A thorough familiarity with pelvic anatomy is important to avoid injury at trocar entry, but it is even more critical in regard to operative injury. The small intestine spreads diffusely throughout the abdomen beneath the anterior abdominal wall. It lies beneath the umbilicus and anterior midline, whereas the large bowel is located at the periphery. The sigmoid colon swings left to right before joining the rectum anterior to the presacral space. The sigmoid junction with the descending colon lies well to the left of the midline, and the cecum lies at the pelvic brim to the right of midline.
In some women, the intestines droop into the pelvis and cover the adnexa, making adhesions between these structures highly likely following dissection in the vicinity of the tubes and ovaries.
Depending on the degree of redundancy of the mesentery of the cecum or sigmoid colon, these structures may droop into the pelvis and cover the adnexa. Therefore, adhesions are likely to develop between the large or small intestine, or both, and the adnexa following dissection in the vicinity of or immediately over the tubes and ovaries. Knowing the normal anatomic relationships is vital for restorative surgery.
When severe adhesions involve the large intestine, it is critical to know the anatomy of the retroperitoneum and be skilled enough to gain safe entry and to dissect that space to safely separate the adnexa when they are densely adhered to the pelvic sidewall in the area of the obturator fossa.
As laparoscopy evolves, the injury rate rises
Over the past 40 years, laparoscopy has evolved from an uncommonly utilized diagnostic tool to a minimally invasive alternative to laparotomy for even the most difficult and complex operations, reaching a high point with robotic laparoscopy. As this technology has developed, serious complications—to some degree, unique to laparoscopy—have increased. In the future, as less skilled surgeons perform a greater percentage of laparoscopic surgeries, a still greater number of complications will arise.
The frequency of intestinal perforation is not great relative to the total number of laparoscopic procedures performed. The TABLE lists several series totaling more than 380,000 laparoscopic operations. The risk of reported bowel perforation ranged from 0.6 to 6 for every 1,000 procedures, with a mean risk of 2.4 for every 1,000. However, these data are inconclusive because the total number of laparoscopic operations performed in the United States is not accurately known. Nor is the precise number of complications associated with these procedures known—specifically, the number of intestinal perforations—as no law requires them to be reported.
Research surveys are unreliable in many cases. In addition, the relative expertise of the surgeon is impossible to quantify. For example, although a surgeon may have many years of operative experience, it is unclear whether this always translates into skill or comfort with laparoscopic procedures. And, when a resident scrubs in with a faculty surgeon, any data collected fail to reflect which part of the surgery was performed by the resident and which by the fully trained gynecologist.
These unknown variables are important in terms of risk, surgical complications, and outcomes. Surgical skill is the greatest unknown factor in any outcome study of any surgical procedure.
TABLE
Studies of complications reveal: Gastrointestinal injury is no rare event during laparoscopic surgery
| Study (year; country) | Cases | Complications | Deaths | GI injury |
|---|---|---|---|---|
| Brown et al (1978; UK)16 | 50,247 | 345 | 4 | 117 (2.3/1,000) |
| Soderstrom (1993; US)17 | No data | No data | 3 | 66 |
| Bateman et al (1996; US)18 | 1,162 | No data | No data | 3 (2.6/1,000)* |
| Champault et al (1996; France)15 | 103,852 | 337 | 6 | 63 (0.6/1,000)† |
| Saidi et al (1996; US)19 | 452 | 47 | 0 | 0 |
| Jansen et al (1997; Netherlands)5 | 25,764 | 145 | 2 | 29 (1.13/1,000) |
| Harkki-Siren et al (1997; Finland)8 | 70,607 | 96 | 0 | 44 (0.6/1,000) |
| Harkki-Siren et al (1997; Finland)7 | 1,165 | 119 | 0 | 5 (4/1,000)‡ |
| Chapron et al (1998; France)6 | 29,996 | 96 | 1 | 48 (1.6/1,000) |
| Chapron et al (1999; France)9 | No data | No data | No data | 62 (0.6–1.6/1,000) |
| Gordts et al (2001; France)20 | 3,667 | No data | No data | 24 (6/1,000) |
| Bhoyrul et al (2001; US)13 | No data | 629 | 32 | 128§ |
| Wang et al (2001; Taiwan)21 | 6,451 | 42 | 0 | 10 (1.6/1,000) |
| Sharp et al (2002; US)14 | 185 | 84 | 2 | 24** |
| Brosens et al (2003; Belgium)22 | 85,727 | No data | No data | 195 (2.3/1,000) |
| * 80 open laparoscopy procedures; 30 closed laparoscopy procedures | ||||
| † Limited to trocar injuries | ||||
| ‡ Laparoscopic hysterectomy | ||||
| § All trocar injuries obtained through Food and Drug Administration reports | ||||
| ** Limited to optical access trocars | ||||
Classifying intestinal injuries
As in the case of major vessel injury, intestinal injury sustained during laparoscopy can be classified as either:
- Injury secondary to the approach. This category refers to entry complications associated with creation of the pneumoperitoneum and insertion of primary and secondary trocars.
- Injury secondary to the procedure or operation. This type of injury occurs as a result of manipulation with various devices during laparoscopy. The devices may include probes, forceps, scissors, or energy devices such as laser, electrosurgical, and ultrasonic instruments.
How trocar injury happens
Several studies have demonstrated that abdominal adhesions place any patient into a high-risk category for trocar injury to the intestines. Patients who have undergone multiple laparotomies, like the patient in the case that opened this article, are more likely to have severe adhesions and fall into the highest risk category for bowel perforation.11 It is impossible to predict with any degree of accuracy whether the intestine is adherent to the entry site.
Pneumoperitoneum can be protective
Creation of a pneumoperitoneum creates a cushion of gas between the intestines and the anterior abdominal wall (provided the intestines are not adherent to the abdominal wall). Manufacturers of disposable trocars with a retractable shield recommend creating an adequate pneumoperitoneum so that the “safety shield” deploys quickly and properly, unlike direct insertion, in which no gas is infused and space is insufficient for complete shield activation.
Open laparoscopy techniques, which allow the surgeon to enter the peritoneal cavity by direct vision without a sharp trocar, may diminish but not eliminate the risk of bowel injury.
What the data show
Of the 130 intestinal injuries recently reported by Baggish, 62 of 81 (77%) small bowel injuries were related to trocar insertion, as were 20 of 49 (41%) large intestinal injuries.12 In other words, 82 of 130 intestinal injuries (63%) were the direct result of trocar entry.
Bhoyrul and associates reported 629 trocar injuries, of which 182 were visceral.13 Of the 32 deaths, six were secondary to unrecognized bowel injury. Of 176 nonfatal visceral injuries, 128 (73%) involved the intestines, and 22 were unrecognized.
Optical-access and open laparoscopic systems were designed to prevent such injuries. Sharp and colleagues reported 24 intestinal injuries out of a total of 79 complications (30%) associated with optical-access trocars after reviewing data obtained from the Medical Device Reports (MDR) and Maude databases maintained by the Food and Drug Administration.14 In the Baggish series, 4.6% of injuries were associated with open laparoscopy.12
Champault and colleagues reviewed complications in a survey of 103,852 operations.15 Although they recommended use of open laparoscopy as opposed to blind insertion, they presented no data on the safety of open techniques.
How intraoperative injury happens
Operative injury of the large or small bowel often occurs during sharp or blunt dissection, performed during laparoscopy using accessory mechanical or energy devices. The latter type of device is utilized increasingly because laparoscopic knot tying and suturing are rather awkward and slow, and laparoscopic suturing to control bleeding is difficult. The size of the needle required for laparoscopic suture placement must be small enough to navigate a trocar sleeve.
Avoid blunt dissection when adhesions are present
The separation of dense adhesions between the intestines and neighboring bowel, other viscera, or abdominal wall is risky when blunt dissection is used. The tensile strength of the fibrotic connective tissue may well exceed that of the thin intestinal wall. Tearing the adhesion free may bring with it a portion of the bowel wall. Such injuries are frequently missed or described as serosal injuries and left unexplored and unrepaired.
Hydrodissection is a safer alternative. It involves the infiltration of sterile water or saline under low pressure between the parietal peritoneum and underlying retroperitoneal structures, providing a safe and natural plane for dissection. In addition, when the CO2 laser is used, the liquid acts as a heat sink to absorb any penetrating laser energy.
Energy devices create thermal effects
Energy devices used to cut tissue during operative laparoscopy coagulate blood vessels in a variety of ways, but the common pathway is thermal. Many hypotheses have evolved to explain how vessels are sealed, but none has demonstrated nonthermal activity except for cryocoagulation.
The devices most commonly used for cutting and hemostasis at laparoscopy are:
- electrosurgical (both monopolar and bipolar). Bipolar electrosurgical devices have advantages over monopolar devices when it comes to high-frequency leaks, direct coupling, and capacitive coupling.
- laser (CO2, holmium:YAG, Nd:YAG, KTP-532, argon). As I mentioned, CO2 laser devices are effectively backstopped by water, especially in strategic areas such as over and around intestines, major vessels, and the ureters.
- ultrasonic (Harmonic Scalpel, ultrasonic aspirator [CUSA]).
Laser and ultrasonic devices do not require a flow of electrons to create coagulation, but do produce heat that will spread peripherally by thermal conduction from the zone of impact (target).
The extent of energy-inflicted injury cannot be predicted
Inadvertent injury with energy devices can occur directly through contact with the bowel, indirectly by heat conduction through tissue, through capacitive coupling (monopolar electrical only), and by forward scatter (laser only).
Upon direct contact with the intestine, energy devices cut into the tissue in a manner similar to mechanical scissors or a knife but produce a larger wound. The reason? The transfer of heat to areas adjacent to the primary wound produces additional necrosis. Heat conduction, capacitive coupling, high-frequency leaks, and front scatter coagulate the intestinal wall with subsequent tissue devitalization and necrosis, the extent of which depends on the power density at contact and the duration of energy applied.
It is impossible to predict the depth or area of devitalization in energy-inflicted injury by visualization of the event.
In the Baggish review of 130 intestinal injuries, the number of injuries sustained during the operative procedure was 19 involving the small intestine and 29 involving the large bowel.12 Of this subset, 44% (21 cases) were secondary to the use of energy devices, with monopolar electrosurgical instruments alone accounting for 9 (43%) of the injuries.
Even best-laid plans can go awry
Despite our best intentions and precautions, accidents do sometimes happen, and bowel injury is no exception.In Part 2 of this article, I detail steps you can take to detect injuries in as timely a manner as possible.
1. Mäkinen J, Johansson J, Tomás C, et al. Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod. 2001;16:1473-1478.
2. Fuller J, Ashar BS, Corrado-Carey J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005;12:302-307.
3. Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg. 1997;185:461-465.
4. Baggish MS. Analysis of 31 cases of major-vessel injury associated with gynecologic laparoscopy operations. J Gynecol Surg. 2003;19:63-73.
5. Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB. Complications of laparoscopy: a prospective multicenter observational study. Br J Obstet Gynaecol. 1997;104:595-600.
6. Chapron C, Querleu D, Bruhat MA, et al. Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod. 1998;13:867-872.
7. Härkki-Sirén P, Sjöberg J, Mäkinen J, et al. Finnish National Register of Laparoscopic Hysterectomies: a review and complications of 1165 operations. Am J Obstet Gynecol. 1997;176(1 Pt. 1):118-122.
8. Härkki-Sirén P, Kurki T. A nationwide analysis of laparoscopic complications. Obstet Gynecol. 1997;89:108-112.
9. Chapron C, Pierre F, Harchaoui Y, et al. Gastrointestinal injuries during gynaecological laparoscopy. Hum Reprod. 1999;14:333-337.
10. Baggish MS. Avoiding vascular injury at laparoscopy. OBG Management. 2004;16(10):70-87.
11. Smith ARB. Postoperative complications following minimal access surgery. Baillieres Clin Obstet Gynecol. 2000;14:123.-
12. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
13. Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001;192:677-683.
14. Sharp HT, Dodson MK, Draper ML, Watts DA, Doucette RC, Hurd WW. Complications associated with optical-access laparoscopic trocars. Obstet Gynecol. 2002;99:553-555.
15. Champault G, Cazacu F, Taffi nder N. Serious trocar accidents in laparoscopic surgery: a French survey of 103,852 operations. Surg Laparosc Endosc. 1996;6:367-370.
16. Brown JA, Chamberlain GVP, Jordan JA, et al. Gynaecological laparoscopy. The Report of the Working Party of the Confidential Enquiry into Gynaecological Laparoscopy. Br J Obstet Gynaecol. 1978;85:401-403.
17. Soderstrom RM. Bowel injury ligation after laparoscopy. J Am Assoc Gynecol Laparosc. 1993;1:74-77.
18. Bateman BG, Kolp LA, Hoeger K. Complications of laparoscopy—operative and diagnostic. Fertil Steril. 1996;66:30-35.
19. Saidi MH, Vancaillie TG, White J, Sadler RK, Akright BD, Farhart SA. Complications of major operative laparoscopy. A review of 452 cases. J Reprod Med. 1996;41:471-476.
20. Gordts S, Watrelot A, Camp R, Brosens I. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76:1238-1241.
21. Wang PH, Lee WL, Yuan CC, et al. Major complications of operative and diagnostic laparoscopy for gynecologic disease. J Am Assoc Gynecol Laparosc. 2001;8:68-73.
22. Brosens I, Gordon A, Campo R, Gordts S. Bowel injury in gynecologic laparoscopy. J Am Assoc Gynecol Laparosc. 2003;10:9-13.
1. Mäkinen J, Johansson J, Tomás C, et al. Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod. 2001;16:1473-1478.
2. Fuller J, Ashar BS, Corrado-Carey J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005;12:302-307.
3. Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg. 1997;185:461-465.
4. Baggish MS. Analysis of 31 cases of major-vessel injury associated with gynecologic laparoscopy operations. J Gynecol Surg. 2003;19:63-73.
5. Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB. Complications of laparoscopy: a prospective multicenter observational study. Br J Obstet Gynaecol. 1997;104:595-600.
6. Chapron C, Querleu D, Bruhat MA, et al. Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod. 1998;13:867-872.
7. Härkki-Sirén P, Sjöberg J, Mäkinen J, et al. Finnish National Register of Laparoscopic Hysterectomies: a review and complications of 1165 operations. Am J Obstet Gynecol. 1997;176(1 Pt. 1):118-122.
8. Härkki-Sirén P, Kurki T. A nationwide analysis of laparoscopic complications. Obstet Gynecol. 1997;89:108-112.
9. Chapron C, Pierre F, Harchaoui Y, et al. Gastrointestinal injuries during gynaecological laparoscopy. Hum Reprod. 1999;14:333-337.
10. Baggish MS. Avoiding vascular injury at laparoscopy. OBG Management. 2004;16(10):70-87.
11. Smith ARB. Postoperative complications following minimal access surgery. Baillieres Clin Obstet Gynecol. 2000;14:123.-
12. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
13. Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001;192:677-683.
14. Sharp HT, Dodson MK, Draper ML, Watts DA, Doucette RC, Hurd WW. Complications associated with optical-access laparoscopic trocars. Obstet Gynecol. 2002;99:553-555.
15. Champault G, Cazacu F, Taffi nder N. Serious trocar accidents in laparoscopic surgery: a French survey of 103,852 operations. Surg Laparosc Endosc. 1996;6:367-370.
16. Brown JA, Chamberlain GVP, Jordan JA, et al. Gynaecological laparoscopy. The Report of the Working Party of the Confidential Enquiry into Gynaecological Laparoscopy. Br J Obstet Gynaecol. 1978;85:401-403.
17. Soderstrom RM. Bowel injury ligation after laparoscopy. J Am Assoc Gynecol Laparosc. 1993;1:74-77.
18. Bateman BG, Kolp LA, Hoeger K. Complications of laparoscopy—operative and diagnostic. Fertil Steril. 1996;66:30-35.
19. Saidi MH, Vancaillie TG, White J, Sadler RK, Akright BD, Farhart SA. Complications of major operative laparoscopy. A review of 452 cases. J Reprod Med. 1996;41:471-476.
20. Gordts S, Watrelot A, Camp R, Brosens I. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76:1238-1241.
21. Wang PH, Lee WL, Yuan CC, et al. Major complications of operative and diagnostic laparoscopy for gynecologic disease. J Am Assoc Gynecol Laparosc. 2001;8:68-73.
22. Brosens I, Gordon A, Campo R, Gordts S. Bowel injury in gynecologic laparoscopy. J Am Assoc Gynecol Laparosc. 2003;10:9-13.
Lessons in timely recognition of laparoscopy-related bowel injury
In Part 1 of this article, I outlined circumstances in which abdominal adhesions should be anticipated and described strategies to prevent intestinal injury during operative procedures. Here, I describe ways to identify intestinal injury as soon as possible after it occurs, which is vital to prevent serious sequelae such as sepsis and even death.
During operative laparoscopy, a quick search for injury through the laparoscope cannot assure any surgeon that the intestinal wall has not been seriously denuded. A damaged muscularis—even if it is not recognized as transmural injury—may subsequently rupture if it is not appropriately repaired intraoperatively.
Following dissection of adhesions, irrigate the neighboring intestine with sterile saline, and perform a detailed inspection of the intestine to ascertain integrity of the bowel wall. The color of the intestine is important, as it can indicate whether the abundant vascular supply has been compromised. Include a detailed description of the intestines in the operative note.
Avoid stapling or vascular clips when repairing any wound; careful suturing is preferred.
Why early diagnosis is critical
The most favorable time to diagnose an iatrogenic intestinal perforation is within the intraoperative period. Prompt recognition and repair of bowel perforation offers several advantages:
- A second or third operation is less likely (
- The risk of abdominal sepsis is decreased.
- The volume of peripheral injury to the intestine is reduced.
- The patient can be followed for subsequent complications more precisely, permitting earlier diagnosis, more timely and effective treatment, and lower morbidity.
The 130 intestinal injuries reported by Baggish reflect the clinical significance of timely diagnosis.1 Seventy percent of small bowel and 51% of large bowel perforations were correctly diagnosed more than 48 hours postoperatively. Sepsis was present in a majority of these cases at the time of diagnosis.
Infection, fluid-electrolyte imbalance, sepsis syndrome
The principal derangements that arise as a result of bowel perforation are infection and fluid-electrolyte imbalance and their sequelae. Intestinal fluid and feces contain a variety of bacteria, such as Escherichia coli, Enterococcus, Klebsiella, Proteus, Pseudomonas, and Clostridium, to name a few. These bacteria produce toxins that facilitate entry of bacteria into the circulation and contribute to a downward spiral of events, referred to as sepsis syndrome, as well as intra-abdominal abscess:
- Contamination of the abdominal cavity leads to inflammation of the peritoneum
- In turn, subperitoneal blood vessels become porous, causing interstitial fluid to leak into the third space
- Paralytic ileus and an accumulation of intra-abdominal fluid push the diaphragm upward, lowering the capacity for lung expansion within the thorax and contributing to partial lung collapse
- Fluid of inflammatory origin may accumulate in the chest as pleural cavity effusion.
A number of progressive complications are predictable, but may occur at variable intervals after the initial perforation. The most frequent complications associated with colonic injuries are:
- peritonitis (98% of cases)
- ileus (92%)
- pleural effusion (84%)
- colostomy (80%)
- intra-abdominal abscess (78%).
The most common sequelae after small-bowel perforation are:
- peritonitis (100% of cases)
- ileus (89%)
- intra-abdominal abscess (63%)
- pleural effusion (59%).1
Reasons for diagnostic delay
- The gynecologic surgeon fails to place intestinal injury at the top of the differential diagnosis.
- A surgical consultant is delayed in making a correct diagnosis. Surgeons have less experience with perforation than do gynecologists, and invariably consider the postoperative abdominal problem to be ileus or intestinal obstruction. The presence of postoperative pneumoperitoneum is incorrectly thought to be lingering CO2 gas from the initial laparoscopy rather than air from a perforated viscus.
- Ancillary diagnosis confuses the primary physician. Pleural effusion, chest pain, and tachypnea are usually thought to indicate pulmonary embolism; as a result, the gynecologist and consulting pulmonologist focus on pulmonary embolus and deep-vein thrombosis. Only a spiral computed tomography (CT) scan, a ventilation perfusion (VQ) scan, or arteriogram quickly rules pulmonary embolus in or out. Peritonitis associated with ileus or third-space fluid leakage resulting in diaphragmatic elevation also creates pleural effusion, tachypnea, and dyspnea.
Presumptive diagnosis is critical
Definitive diagnosis of intestinal perforation happens at the operating table under direct vision and is corroborated by the pathology laboratory if bowel resection is performed. However, presumptive diagnosis helps overcome inertia and gets the patient to the operating room sooner.
The process by which the presumptive diagnosis is made is the most important issue in this article. The shorter the process, the lower the patient’s morbidity, and vice versa.
Look for steady improvement. Worry when it is absent
After any laparoscopic operation, the postoperative course should be one of steady clinical improvement. When a patient deviates from this model, the foremost presumptive diagnosis should be laparoscopy-associated injury, and the intestine should top the list of organs that may be injured. Other diagnoses should be subordinate to the principal presumptive diagnosis; these include ileus, bowel obstruction, pulmonary embolus, gastroenteritis, and hematoma, to name a few.
I do not mean to imply that a potentially life-threatening complication such as pulmonary embolus should not be ruled in or out, but that the necessary imaging should be performed in a timely fashion. The abdominal-pelvic CT scan will offer clues to the presence of free air, free fluid, air-fluid levels, and foreign bodies. It also is useful in detecting intra-abdominal—specifically, subphrenic—abscess. If necessary, a VQ scan or spiral CT scan can then be performed without delaying the diagnosis of the primary intra-abdominal catastrophe responsible for the pulmonary symptoms.
In the opening case, before making an improbable presumptive diagnosis, the surgeon should have questioned why an otherwise healthy woman would coincidentally develop gastroenteritis after laparoscopic surgery. The same can be said for diagnoses of intestinal obstruction or vascular thrombosis involving the intestinal blood supply.
Typical presentation of the injured patient
An injured patient does not experience daily improvement and a return to normal activity. Instead, the postoperative period is marked by persistent and worsening pain, often compounded by nausea or vomiting, or both. The patient may complain of fever, chills, weakness, or simply not feeling normal. Breathing may be labored. As time elapses, the symptoms become worse.
Reports of more than one visit to an emergency care facility are not uncommon. When examined, the patient exhibits direct or rebound tenderness, or both. The abdomen may or may not be distended, but usually is increased in girth. Bowel sounds are diminished or absent.
Vital signs initially reveal normal, low-grade, or subnormal temperature, and tachycardia, tachypnea, and normal blood pressure are typical. As time and sepsis progress, however, fever and hypotension develop. Most other symptoms and signs become progressively more abnormal in direct proportion to the length of time the diagnosis is delayed.
Seminal laboratory values for sepsis include a lower than normal white blood cell (WBC) count, elevated immature white-cell elements (e.g., “bandemia”), elevated liver chemistries, and an elevated serum creatinine level.
Mortality is most often the result of overwhelming and prolonged sepsis, leading to multiorgan failure, bleeding diathesis, and adult respiratory distress syndrome.
Among 130 laparoscopic surgical cases complicated by bowel injury and reported by Baggish, sepsis was diagnosed in 100% of colonic perforations and 50% of small-bowel perforations when the diagnosis was delayed more than 48 hours after surgery.1
TABLE 1 lists the signs and frequency of sepsis in these 100 cases, and TABLE 2 collates the signs and symptoms that were observed. Peritoneal cultures obtained at the time of exploratory laparotomy revealed multiple organisms (polymicrobial) in 60% of cases.
TABLE 1
Frequency of signs of sepsis among 130 patients with colon or small-bowel injury
| Sign | Colon (49 patients) | Small bowel (81 patients) |
|---|---|---|
| Normal or subnormal temperature | 30* | 41* |
| Fever | 19 | 40 |
| Tachycardia | 31 | 44 |
| Tachypnea | 30 | 40 |
| Hypotension | 21 | 15 |
| Anemia | 38 | 51 |
| Depressed WBC count | 20 | 18 |
| Elevated WBC count | 24 | 32 |
| Bandemia | 25 | 30 |
| Elevated creatinine and blood urea nitrogen levels | 12 | 5 |
| *Number of patients. | ||
| Source: Baggish1 | ||
Watch for signs and symptoms of intestinal injury
| Symptom | Sign |
|---|---|
| Abdominal pain | Direct or rebound tenderness |
| Bloating | Abdominal distension |
| Nausea, vomiting | Diminished bowel sounds |
| Fever, chills | Elevated or subnormal temperature |
| Difficulty breathing | Tachypnea, tachycardia |
| Weakness | Pallor, hypotension, diminished consciousness |
| Source: Baggish1 | |
Concurrent injuries to neighboring structures
A number of collateral injuries may occur in conjunction with intestinal perforation, depending on the location of the trauma. The most dangerous combination includes indirect laceration of one of the major retroperitoneal vessels. A through-and-through perforation of the cecum can also involve one or more of the right iliac vessels. A trocar perforation of the ileum may continue directly into the presacral space or pass above it and penetrate the left common iliac vein or aorta. Similarly, perforation of the sigmoid colon may penetrate the left iliac vessels.
Careful inspection of the posterior peritoneum for tears and evidence of retroperitoneal hematoma is required to avoid missing a serious collateral injury. More likely, however, is a penetrating injury to the small bowel presenting with collateral mesenteric damage and compromise of the blood supply of an entire segment of bowel. The ureter and bladder may also be injured when dissection along the pelvic sidewall, or a trocar thrust, deviates to the right or left of midline. In thin patients, the stomach may be perforated as well as the small intestine or transverse colon.
In one memorable case, a primary trocar penetrated the omentum, injuring several underlying structures. In its transit, the trocar passed through both the anterior and posterior walls of the duodenum and finally entered the superior mesenteric artery. The gynecologic surgeon performing the laparoscopic tubal ligation failed to recognize any of these injuries. The patient went into shock in the recovery room and was returned to the operating room. Fortunately, a transplant surgeon from a neighboring theater was immediately available to consult and repair the damage.
Another danger: intestinal ischemic necrosis
Abnormalities in splanchnic blood flow are sometimes caused by elevations in intra-abdominal pressure. Caldwell and Ricotta inflated the abdomens of nine dogs and reported a significant reduction of blood flow to omentum, stomach, duodenum, jejunum, ileum, colon, pancreas, liver, and spleen, but not to the adrenal glands.2 The splanchnic flow reductions essentially shunted blood away from abdominal viscera with auto-transfusion to the heart, lungs, and systemic circulation.
Eleftheriadis and colleagues studied 16 women randomized to laparoscopic versus open cholecystectomy.3 Significant depression of the hepatic microcirculation during the period of CO2 gas insufflation was noted in the laparoscopy cohort but not in the control group. Gastric mucosal ischemia also was observed in the laparoscopy group.
Several case reports of catastrophic intestinal ischemia have appeared in the literature (1994–1995).4-7 These articles have mainly involved laparoscopic upper abdominal operations in elderly people.
Recently, however, Hasson and colleagues reported a case of possible ischemic necrosis of the small intestine following laparoscopic adhesiolysis and bipolar myolysis.8 The authors emphasized that CO2 pneumoperitoneum reduces splanchnic blood flow, predisposing the patient to ischemia, but that ischemia with infarction requires an underlying vasculopathy or inciting factors such as traction on a short mesentery, atherosclerosis, or thrombosis.
A high index of suspicion for bowel ischemia following laparoscopic surgery should occur when, postoperatively, a patient experiences inordinately severe abdominal pain associated with tachypnea, tachycardia, and alterations in the WBC count. A paucity of physical abdominal signs in the early phases of this disorder should alert the clinician to the possibility of bowel ischemia.
Diagnosing and treating ischemia
A CT scan with contrast can suggest ischemia, but angiography is usually required for definitive diagnosis.
Treatment begins with infusion of papaverine into the intestinal vasculature via angiography cannula. In some cases, anticoagulation may be indicated. Surgery by laparotomy is clearly indicated for patients who fail to respond to vasodilatation measures.
This condition can be ameliorated by intermittent intraoperative decompression of the abdomen. Avoiding prolonged CO2 pneumoperitoneum and a lengthy laparoscopic operation also may diminish the risk of intestinal ischemia.
1. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
2. Caldwell CB, Ricotta JJ. Changes in visceral blood flow with elevated intra-abdominal pressure. J Surg Res. 1987;43:14-20.
3. Eleftheriadis E, Kotzampassi K, Botsios D, Tzartinoglu E, Farmakis H, Dadoukis J. Splanchnic ischemia during laparoscopic cholecystectomy. Surg Endosc. 1996;10:324-326.
4. Schorr RT. Laparoscopic upper abdominal operations and mesenteric infarction. J Laparoendosc Surg. 1995;5:389-392.
5. Mitchell PC, Jamieson GG. Coeliac axis and mesenteric arterial thrombosis following laparoscopic Nissen fundoplication. Aust N Z J Surg. 1994;64:728-730.
6. Dwerryhouse SJ, Melsom DS, Burton PA, Thompson MH. Acute intestinal ischaemia after laparoscopic cholecystectomy. Br J Surg. 1995;82:1413.-
7. Jaffe V, Russell RCG. Fatal intestinal ischaemia following laparoscopic cholecystectomy. Br J Surg. 1994;81:1827-1828.
8. Hasson HM, Galanopoulos C, Lanferman A. Ischemic necrosis of small bowel following laparoscopic surgery. JSLS. 2004;8:159-163.
In Part 1 of this article, I outlined circumstances in which abdominal adhesions should be anticipated and described strategies to prevent intestinal injury during operative procedures. Here, I describe ways to identify intestinal injury as soon as possible after it occurs, which is vital to prevent serious sequelae such as sepsis and even death.
During operative laparoscopy, a quick search for injury through the laparoscope cannot assure any surgeon that the intestinal wall has not been seriously denuded. A damaged muscularis—even if it is not recognized as transmural injury—may subsequently rupture if it is not appropriately repaired intraoperatively.
Following dissection of adhesions, irrigate the neighboring intestine with sterile saline, and perform a detailed inspection of the intestine to ascertain integrity of the bowel wall. The color of the intestine is important, as it can indicate whether the abundant vascular supply has been compromised. Include a detailed description of the intestines in the operative note.
Avoid stapling or vascular clips when repairing any wound; careful suturing is preferred.
Why early diagnosis is critical
The most favorable time to diagnose an iatrogenic intestinal perforation is within the intraoperative period. Prompt recognition and repair of bowel perforation offers several advantages:
- A second or third operation is less likely (
- The risk of abdominal sepsis is decreased.
- The volume of peripheral injury to the intestine is reduced.
- The patient can be followed for subsequent complications more precisely, permitting earlier diagnosis, more timely and effective treatment, and lower morbidity.
The 130 intestinal injuries reported by Baggish reflect the clinical significance of timely diagnosis.1 Seventy percent of small bowel and 51% of large bowel perforations were correctly diagnosed more than 48 hours postoperatively. Sepsis was present in a majority of these cases at the time of diagnosis.
Infection, fluid-electrolyte imbalance, sepsis syndrome
The principal derangements that arise as a result of bowel perforation are infection and fluid-electrolyte imbalance and their sequelae. Intestinal fluid and feces contain a variety of bacteria, such as Escherichia coli, Enterococcus, Klebsiella, Proteus, Pseudomonas, and Clostridium, to name a few. These bacteria produce toxins that facilitate entry of bacteria into the circulation and contribute to a downward spiral of events, referred to as sepsis syndrome, as well as intra-abdominal abscess:
- Contamination of the abdominal cavity leads to inflammation of the peritoneum
- In turn, subperitoneal blood vessels become porous, causing interstitial fluid to leak into the third space
- Paralytic ileus and an accumulation of intra-abdominal fluid push the diaphragm upward, lowering the capacity for lung expansion within the thorax and contributing to partial lung collapse
- Fluid of inflammatory origin may accumulate in the chest as pleural cavity effusion.
A number of progressive complications are predictable, but may occur at variable intervals after the initial perforation. The most frequent complications associated with colonic injuries are:
- peritonitis (98% of cases)
- ileus (92%)
- pleural effusion (84%)
- colostomy (80%)
- intra-abdominal abscess (78%).
The most common sequelae after small-bowel perforation are:
- peritonitis (100% of cases)
- ileus (89%)
- intra-abdominal abscess (63%)
- pleural effusion (59%).1
Reasons for diagnostic delay
- The gynecologic surgeon fails to place intestinal injury at the top of the differential diagnosis.
- A surgical consultant is delayed in making a correct diagnosis. Surgeons have less experience with perforation than do gynecologists, and invariably consider the postoperative abdominal problem to be ileus or intestinal obstruction. The presence of postoperative pneumoperitoneum is incorrectly thought to be lingering CO2 gas from the initial laparoscopy rather than air from a perforated viscus.
- Ancillary diagnosis confuses the primary physician. Pleural effusion, chest pain, and tachypnea are usually thought to indicate pulmonary embolism; as a result, the gynecologist and consulting pulmonologist focus on pulmonary embolus and deep-vein thrombosis. Only a spiral computed tomography (CT) scan, a ventilation perfusion (VQ) scan, or arteriogram quickly rules pulmonary embolus in or out. Peritonitis associated with ileus or third-space fluid leakage resulting in diaphragmatic elevation also creates pleural effusion, tachypnea, and dyspnea.
Presumptive diagnosis is critical
Definitive diagnosis of intestinal perforation happens at the operating table under direct vision and is corroborated by the pathology laboratory if bowel resection is performed. However, presumptive diagnosis helps overcome inertia and gets the patient to the operating room sooner.
The process by which the presumptive diagnosis is made is the most important issue in this article. The shorter the process, the lower the patient’s morbidity, and vice versa.
Look for steady improvement. Worry when it is absent
After any laparoscopic operation, the postoperative course should be one of steady clinical improvement. When a patient deviates from this model, the foremost presumptive diagnosis should be laparoscopy-associated injury, and the intestine should top the list of organs that may be injured. Other diagnoses should be subordinate to the principal presumptive diagnosis; these include ileus, bowel obstruction, pulmonary embolus, gastroenteritis, and hematoma, to name a few.
I do not mean to imply that a potentially life-threatening complication such as pulmonary embolus should not be ruled in or out, but that the necessary imaging should be performed in a timely fashion. The abdominal-pelvic CT scan will offer clues to the presence of free air, free fluid, air-fluid levels, and foreign bodies. It also is useful in detecting intra-abdominal—specifically, subphrenic—abscess. If necessary, a VQ scan or spiral CT scan can then be performed without delaying the diagnosis of the primary intra-abdominal catastrophe responsible for the pulmonary symptoms.
In the opening case, before making an improbable presumptive diagnosis, the surgeon should have questioned why an otherwise healthy woman would coincidentally develop gastroenteritis after laparoscopic surgery. The same can be said for diagnoses of intestinal obstruction or vascular thrombosis involving the intestinal blood supply.
Typical presentation of the injured patient
An injured patient does not experience daily improvement and a return to normal activity. Instead, the postoperative period is marked by persistent and worsening pain, often compounded by nausea or vomiting, or both. The patient may complain of fever, chills, weakness, or simply not feeling normal. Breathing may be labored. As time elapses, the symptoms become worse.
Reports of more than one visit to an emergency care facility are not uncommon. When examined, the patient exhibits direct or rebound tenderness, or both. The abdomen may or may not be distended, but usually is increased in girth. Bowel sounds are diminished or absent.
Vital signs initially reveal normal, low-grade, or subnormal temperature, and tachycardia, tachypnea, and normal blood pressure are typical. As time and sepsis progress, however, fever and hypotension develop. Most other symptoms and signs become progressively more abnormal in direct proportion to the length of time the diagnosis is delayed.
Seminal laboratory values for sepsis include a lower than normal white blood cell (WBC) count, elevated immature white-cell elements (e.g., “bandemia”), elevated liver chemistries, and an elevated serum creatinine level.
Mortality is most often the result of overwhelming and prolonged sepsis, leading to multiorgan failure, bleeding diathesis, and adult respiratory distress syndrome.
Among 130 laparoscopic surgical cases complicated by bowel injury and reported by Baggish, sepsis was diagnosed in 100% of colonic perforations and 50% of small-bowel perforations when the diagnosis was delayed more than 48 hours after surgery.1
TABLE 1 lists the signs and frequency of sepsis in these 100 cases, and TABLE 2 collates the signs and symptoms that were observed. Peritoneal cultures obtained at the time of exploratory laparotomy revealed multiple organisms (polymicrobial) in 60% of cases.
TABLE 1
Frequency of signs of sepsis among 130 patients with colon or small-bowel injury
| Sign | Colon (49 patients) | Small bowel (81 patients) |
|---|---|---|
| Normal or subnormal temperature | 30* | 41* |
| Fever | 19 | 40 |
| Tachycardia | 31 | 44 |
| Tachypnea | 30 | 40 |
| Hypotension | 21 | 15 |
| Anemia | 38 | 51 |
| Depressed WBC count | 20 | 18 |
| Elevated WBC count | 24 | 32 |
| Bandemia | 25 | 30 |
| Elevated creatinine and blood urea nitrogen levels | 12 | 5 |
| *Number of patients. | ||
| Source: Baggish1 | ||
Watch for signs and symptoms of intestinal injury
| Symptom | Sign |
|---|---|
| Abdominal pain | Direct or rebound tenderness |
| Bloating | Abdominal distension |
| Nausea, vomiting | Diminished bowel sounds |
| Fever, chills | Elevated or subnormal temperature |
| Difficulty breathing | Tachypnea, tachycardia |
| Weakness | Pallor, hypotension, diminished consciousness |
| Source: Baggish1 | |
Concurrent injuries to neighboring structures
A number of collateral injuries may occur in conjunction with intestinal perforation, depending on the location of the trauma. The most dangerous combination includes indirect laceration of one of the major retroperitoneal vessels. A through-and-through perforation of the cecum can also involve one or more of the right iliac vessels. A trocar perforation of the ileum may continue directly into the presacral space or pass above it and penetrate the left common iliac vein or aorta. Similarly, perforation of the sigmoid colon may penetrate the left iliac vessels.
Careful inspection of the posterior peritoneum for tears and evidence of retroperitoneal hematoma is required to avoid missing a serious collateral injury. More likely, however, is a penetrating injury to the small bowel presenting with collateral mesenteric damage and compromise of the blood supply of an entire segment of bowel. The ureter and bladder may also be injured when dissection along the pelvic sidewall, or a trocar thrust, deviates to the right or left of midline. In thin patients, the stomach may be perforated as well as the small intestine or transverse colon.
In one memorable case, a primary trocar penetrated the omentum, injuring several underlying structures. In its transit, the trocar passed through both the anterior and posterior walls of the duodenum and finally entered the superior mesenteric artery. The gynecologic surgeon performing the laparoscopic tubal ligation failed to recognize any of these injuries. The patient went into shock in the recovery room and was returned to the operating room. Fortunately, a transplant surgeon from a neighboring theater was immediately available to consult and repair the damage.
Another danger: intestinal ischemic necrosis
Abnormalities in splanchnic blood flow are sometimes caused by elevations in intra-abdominal pressure. Caldwell and Ricotta inflated the abdomens of nine dogs and reported a significant reduction of blood flow to omentum, stomach, duodenum, jejunum, ileum, colon, pancreas, liver, and spleen, but not to the adrenal glands.2 The splanchnic flow reductions essentially shunted blood away from abdominal viscera with auto-transfusion to the heart, lungs, and systemic circulation.
Eleftheriadis and colleagues studied 16 women randomized to laparoscopic versus open cholecystectomy.3 Significant depression of the hepatic microcirculation during the period of CO2 gas insufflation was noted in the laparoscopy cohort but not in the control group. Gastric mucosal ischemia also was observed in the laparoscopy group.
Several case reports of catastrophic intestinal ischemia have appeared in the literature (1994–1995).4-7 These articles have mainly involved laparoscopic upper abdominal operations in elderly people.
Recently, however, Hasson and colleagues reported a case of possible ischemic necrosis of the small intestine following laparoscopic adhesiolysis and bipolar myolysis.8 The authors emphasized that CO2 pneumoperitoneum reduces splanchnic blood flow, predisposing the patient to ischemia, but that ischemia with infarction requires an underlying vasculopathy or inciting factors such as traction on a short mesentery, atherosclerosis, or thrombosis.
A high index of suspicion for bowel ischemia following laparoscopic surgery should occur when, postoperatively, a patient experiences inordinately severe abdominal pain associated with tachypnea, tachycardia, and alterations in the WBC count. A paucity of physical abdominal signs in the early phases of this disorder should alert the clinician to the possibility of bowel ischemia.
Diagnosing and treating ischemia
A CT scan with contrast can suggest ischemia, but angiography is usually required for definitive diagnosis.
Treatment begins with infusion of papaverine into the intestinal vasculature via angiography cannula. In some cases, anticoagulation may be indicated. Surgery by laparotomy is clearly indicated for patients who fail to respond to vasodilatation measures.
This condition can be ameliorated by intermittent intraoperative decompression of the abdomen. Avoiding prolonged CO2 pneumoperitoneum and a lengthy laparoscopic operation also may diminish the risk of intestinal ischemia.
In Part 1 of this article, I outlined circumstances in which abdominal adhesions should be anticipated and described strategies to prevent intestinal injury during operative procedures. Here, I describe ways to identify intestinal injury as soon as possible after it occurs, which is vital to prevent serious sequelae such as sepsis and even death.
During operative laparoscopy, a quick search for injury through the laparoscope cannot assure any surgeon that the intestinal wall has not been seriously denuded. A damaged muscularis—even if it is not recognized as transmural injury—may subsequently rupture if it is not appropriately repaired intraoperatively.
Following dissection of adhesions, irrigate the neighboring intestine with sterile saline, and perform a detailed inspection of the intestine to ascertain integrity of the bowel wall. The color of the intestine is important, as it can indicate whether the abundant vascular supply has been compromised. Include a detailed description of the intestines in the operative note.
Avoid stapling or vascular clips when repairing any wound; careful suturing is preferred.
Why early diagnosis is critical
The most favorable time to diagnose an iatrogenic intestinal perforation is within the intraoperative period. Prompt recognition and repair of bowel perforation offers several advantages:
- A second or third operation is less likely (
- The risk of abdominal sepsis is decreased.
- The volume of peripheral injury to the intestine is reduced.
- The patient can be followed for subsequent complications more precisely, permitting earlier diagnosis, more timely and effective treatment, and lower morbidity.
The 130 intestinal injuries reported by Baggish reflect the clinical significance of timely diagnosis.1 Seventy percent of small bowel and 51% of large bowel perforations were correctly diagnosed more than 48 hours postoperatively. Sepsis was present in a majority of these cases at the time of diagnosis.
Infection, fluid-electrolyte imbalance, sepsis syndrome
The principal derangements that arise as a result of bowel perforation are infection and fluid-electrolyte imbalance and their sequelae. Intestinal fluid and feces contain a variety of bacteria, such as Escherichia coli, Enterococcus, Klebsiella, Proteus, Pseudomonas, and Clostridium, to name a few. These bacteria produce toxins that facilitate entry of bacteria into the circulation and contribute to a downward spiral of events, referred to as sepsis syndrome, as well as intra-abdominal abscess:
- Contamination of the abdominal cavity leads to inflammation of the peritoneum
- In turn, subperitoneal blood vessels become porous, causing interstitial fluid to leak into the third space
- Paralytic ileus and an accumulation of intra-abdominal fluid push the diaphragm upward, lowering the capacity for lung expansion within the thorax and contributing to partial lung collapse
- Fluid of inflammatory origin may accumulate in the chest as pleural cavity effusion.
A number of progressive complications are predictable, but may occur at variable intervals after the initial perforation. The most frequent complications associated with colonic injuries are:
- peritonitis (98% of cases)
- ileus (92%)
- pleural effusion (84%)
- colostomy (80%)
- intra-abdominal abscess (78%).
The most common sequelae after small-bowel perforation are:
- peritonitis (100% of cases)
- ileus (89%)
- intra-abdominal abscess (63%)
- pleural effusion (59%).1
Reasons for diagnostic delay
- The gynecologic surgeon fails to place intestinal injury at the top of the differential diagnosis.
- A surgical consultant is delayed in making a correct diagnosis. Surgeons have less experience with perforation than do gynecologists, and invariably consider the postoperative abdominal problem to be ileus or intestinal obstruction. The presence of postoperative pneumoperitoneum is incorrectly thought to be lingering CO2 gas from the initial laparoscopy rather than air from a perforated viscus.
- Ancillary diagnosis confuses the primary physician. Pleural effusion, chest pain, and tachypnea are usually thought to indicate pulmonary embolism; as a result, the gynecologist and consulting pulmonologist focus on pulmonary embolus and deep-vein thrombosis. Only a spiral computed tomography (CT) scan, a ventilation perfusion (VQ) scan, or arteriogram quickly rules pulmonary embolus in or out. Peritonitis associated with ileus or third-space fluid leakage resulting in diaphragmatic elevation also creates pleural effusion, tachypnea, and dyspnea.
Presumptive diagnosis is critical
Definitive diagnosis of intestinal perforation happens at the operating table under direct vision and is corroborated by the pathology laboratory if bowel resection is performed. However, presumptive diagnosis helps overcome inertia and gets the patient to the operating room sooner.
The process by which the presumptive diagnosis is made is the most important issue in this article. The shorter the process, the lower the patient’s morbidity, and vice versa.
Look for steady improvement. Worry when it is absent
After any laparoscopic operation, the postoperative course should be one of steady clinical improvement. When a patient deviates from this model, the foremost presumptive diagnosis should be laparoscopy-associated injury, and the intestine should top the list of organs that may be injured. Other diagnoses should be subordinate to the principal presumptive diagnosis; these include ileus, bowel obstruction, pulmonary embolus, gastroenteritis, and hematoma, to name a few.
I do not mean to imply that a potentially life-threatening complication such as pulmonary embolus should not be ruled in or out, but that the necessary imaging should be performed in a timely fashion. The abdominal-pelvic CT scan will offer clues to the presence of free air, free fluid, air-fluid levels, and foreign bodies. It also is useful in detecting intra-abdominal—specifically, subphrenic—abscess. If necessary, a VQ scan or spiral CT scan can then be performed without delaying the diagnosis of the primary intra-abdominal catastrophe responsible for the pulmonary symptoms.
In the opening case, before making an improbable presumptive diagnosis, the surgeon should have questioned why an otherwise healthy woman would coincidentally develop gastroenteritis after laparoscopic surgery. The same can be said for diagnoses of intestinal obstruction or vascular thrombosis involving the intestinal blood supply.
Typical presentation of the injured patient
An injured patient does not experience daily improvement and a return to normal activity. Instead, the postoperative period is marked by persistent and worsening pain, often compounded by nausea or vomiting, or both. The patient may complain of fever, chills, weakness, or simply not feeling normal. Breathing may be labored. As time elapses, the symptoms become worse.
Reports of more than one visit to an emergency care facility are not uncommon. When examined, the patient exhibits direct or rebound tenderness, or both. The abdomen may or may not be distended, but usually is increased in girth. Bowel sounds are diminished or absent.
Vital signs initially reveal normal, low-grade, or subnormal temperature, and tachycardia, tachypnea, and normal blood pressure are typical. As time and sepsis progress, however, fever and hypotension develop. Most other symptoms and signs become progressively more abnormal in direct proportion to the length of time the diagnosis is delayed.
Seminal laboratory values for sepsis include a lower than normal white blood cell (WBC) count, elevated immature white-cell elements (e.g., “bandemia”), elevated liver chemistries, and an elevated serum creatinine level.
Mortality is most often the result of overwhelming and prolonged sepsis, leading to multiorgan failure, bleeding diathesis, and adult respiratory distress syndrome.
Among 130 laparoscopic surgical cases complicated by bowel injury and reported by Baggish, sepsis was diagnosed in 100% of colonic perforations and 50% of small-bowel perforations when the diagnosis was delayed more than 48 hours after surgery.1
TABLE 1 lists the signs and frequency of sepsis in these 100 cases, and TABLE 2 collates the signs and symptoms that were observed. Peritoneal cultures obtained at the time of exploratory laparotomy revealed multiple organisms (polymicrobial) in 60% of cases.
TABLE 1
Frequency of signs of sepsis among 130 patients with colon or small-bowel injury
| Sign | Colon (49 patients) | Small bowel (81 patients) |
|---|---|---|
| Normal or subnormal temperature | 30* | 41* |
| Fever | 19 | 40 |
| Tachycardia | 31 | 44 |
| Tachypnea | 30 | 40 |
| Hypotension | 21 | 15 |
| Anemia | 38 | 51 |
| Depressed WBC count | 20 | 18 |
| Elevated WBC count | 24 | 32 |
| Bandemia | 25 | 30 |
| Elevated creatinine and blood urea nitrogen levels | 12 | 5 |
| *Number of patients. | ||
| Source: Baggish1 | ||
Watch for signs and symptoms of intestinal injury
| Symptom | Sign |
|---|---|
| Abdominal pain | Direct or rebound tenderness |
| Bloating | Abdominal distension |
| Nausea, vomiting | Diminished bowel sounds |
| Fever, chills | Elevated or subnormal temperature |
| Difficulty breathing | Tachypnea, tachycardia |
| Weakness | Pallor, hypotension, diminished consciousness |
| Source: Baggish1 | |
Concurrent injuries to neighboring structures
A number of collateral injuries may occur in conjunction with intestinal perforation, depending on the location of the trauma. The most dangerous combination includes indirect laceration of one of the major retroperitoneal vessels. A through-and-through perforation of the cecum can also involve one or more of the right iliac vessels. A trocar perforation of the ileum may continue directly into the presacral space or pass above it and penetrate the left common iliac vein or aorta. Similarly, perforation of the sigmoid colon may penetrate the left iliac vessels.
Careful inspection of the posterior peritoneum for tears and evidence of retroperitoneal hematoma is required to avoid missing a serious collateral injury. More likely, however, is a penetrating injury to the small bowel presenting with collateral mesenteric damage and compromise of the blood supply of an entire segment of bowel. The ureter and bladder may also be injured when dissection along the pelvic sidewall, or a trocar thrust, deviates to the right or left of midline. In thin patients, the stomach may be perforated as well as the small intestine or transverse colon.
In one memorable case, a primary trocar penetrated the omentum, injuring several underlying structures. In its transit, the trocar passed through both the anterior and posterior walls of the duodenum and finally entered the superior mesenteric artery. The gynecologic surgeon performing the laparoscopic tubal ligation failed to recognize any of these injuries. The patient went into shock in the recovery room and was returned to the operating room. Fortunately, a transplant surgeon from a neighboring theater was immediately available to consult and repair the damage.
Another danger: intestinal ischemic necrosis
Abnormalities in splanchnic blood flow are sometimes caused by elevations in intra-abdominal pressure. Caldwell and Ricotta inflated the abdomens of nine dogs and reported a significant reduction of blood flow to omentum, stomach, duodenum, jejunum, ileum, colon, pancreas, liver, and spleen, but not to the adrenal glands.2 The splanchnic flow reductions essentially shunted blood away from abdominal viscera with auto-transfusion to the heart, lungs, and systemic circulation.
Eleftheriadis and colleagues studied 16 women randomized to laparoscopic versus open cholecystectomy.3 Significant depression of the hepatic microcirculation during the period of CO2 gas insufflation was noted in the laparoscopy cohort but not in the control group. Gastric mucosal ischemia also was observed in the laparoscopy group.
Several case reports of catastrophic intestinal ischemia have appeared in the literature (1994–1995).4-7 These articles have mainly involved laparoscopic upper abdominal operations in elderly people.
Recently, however, Hasson and colleagues reported a case of possible ischemic necrosis of the small intestine following laparoscopic adhesiolysis and bipolar myolysis.8 The authors emphasized that CO2 pneumoperitoneum reduces splanchnic blood flow, predisposing the patient to ischemia, but that ischemia with infarction requires an underlying vasculopathy or inciting factors such as traction on a short mesentery, atherosclerosis, or thrombosis.
A high index of suspicion for bowel ischemia following laparoscopic surgery should occur when, postoperatively, a patient experiences inordinately severe abdominal pain associated with tachypnea, tachycardia, and alterations in the WBC count. A paucity of physical abdominal signs in the early phases of this disorder should alert the clinician to the possibility of bowel ischemia.
Diagnosing and treating ischemia
A CT scan with contrast can suggest ischemia, but angiography is usually required for definitive diagnosis.
Treatment begins with infusion of papaverine into the intestinal vasculature via angiography cannula. In some cases, anticoagulation may be indicated. Surgery by laparotomy is clearly indicated for patients who fail to respond to vasodilatation measures.
This condition can be ameliorated by intermittent intraoperative decompression of the abdomen. Avoiding prolonged CO2 pneumoperitoneum and a lengthy laparoscopic operation also may diminish the risk of intestinal ischemia.
1. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
2. Caldwell CB, Ricotta JJ. Changes in visceral blood flow with elevated intra-abdominal pressure. J Surg Res. 1987;43:14-20.
3. Eleftheriadis E, Kotzampassi K, Botsios D, Tzartinoglu E, Farmakis H, Dadoukis J. Splanchnic ischemia during laparoscopic cholecystectomy. Surg Endosc. 1996;10:324-326.
4. Schorr RT. Laparoscopic upper abdominal operations and mesenteric infarction. J Laparoendosc Surg. 1995;5:389-392.
5. Mitchell PC, Jamieson GG. Coeliac axis and mesenteric arterial thrombosis following laparoscopic Nissen fundoplication. Aust N Z J Surg. 1994;64:728-730.
6. Dwerryhouse SJ, Melsom DS, Burton PA, Thompson MH. Acute intestinal ischaemia after laparoscopic cholecystectomy. Br J Surg. 1995;82:1413.-
7. Jaffe V, Russell RCG. Fatal intestinal ischaemia following laparoscopic cholecystectomy. Br J Surg. 1994;81:1827-1828.
8. Hasson HM, Galanopoulos C, Lanferman A. Ischemic necrosis of small bowel following laparoscopic surgery. JSLS. 2004;8:159-163.
1. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
2. Caldwell CB, Ricotta JJ. Changes in visceral blood flow with elevated intra-abdominal pressure. J Surg Res. 1987;43:14-20.
3. Eleftheriadis E, Kotzampassi K, Botsios D, Tzartinoglu E, Farmakis H, Dadoukis J. Splanchnic ischemia during laparoscopic cholecystectomy. Surg Endosc. 1996;10:324-326.
4. Schorr RT. Laparoscopic upper abdominal operations and mesenteric infarction. J Laparoendosc Surg. 1995;5:389-392.
5. Mitchell PC, Jamieson GG. Coeliac axis and mesenteric arterial thrombosis following laparoscopic Nissen fundoplication. Aust N Z J Surg. 1994;64:728-730.
6. Dwerryhouse SJ, Melsom DS, Burton PA, Thompson MH. Acute intestinal ischaemia after laparoscopic cholecystectomy. Br J Surg. 1995;82:1413.-
7. Jaffe V, Russell RCG. Fatal intestinal ischaemia following laparoscopic cholecystectomy. Br J Surg. 1994;81:1827-1828.
8. Hasson HM, Galanopoulos C, Lanferman A. Ischemic necrosis of small bowel following laparoscopic surgery. JSLS. 2004;8:159-163.
Colorectal cancer screening: How to help patients comply
- Be more assertive about the need for screening with patients at risk, and do not rely solely on patient-education materials to communicate the message.
- Address key issues such as fear of pain from colonoscopy, costs and comparative benefits of different tests, and safety of procedures—even if patients don’t raise these issues.
Purpose: We elicited patient opinions about how physicians can improve communications about colorectal cancer (CRC) screening.
Methods: We recruited 15 patients, ages 50 years and older, from an urban family medicine teaching clinic. All patients in the initial pool of candidates had been seen at the university of Arkansas for Medical Sciences Family Medical Center within the past 12 months. The recruits participated in 1 of 3 focus groups to discuss how to enhance the rate of CRC screening.
Participants watched a videotape that described the different approaches to CRC screening. We then asked them to comment on how patients could be encouraged to undergo CRC screening.
Results: using a qualitative analysis of focus group data, we determined the most common reasons participants had not undergone CRC screening: fear, lack of information, and failure of the physician to strongly recommend CRC screening. Participants offered 7 recommendations for how physicians could address their concerns. Participants emphasized the importance of strong physician endorsement of screening, of frank and informative dialogue about patient’s concerns, and of using educational materials to supplement personal advice.
Conclusion: A physician’s recommendation for screening is the most powerful motivator in patients’ decisions. However, other sources of information such as videotapes, written materials, and even endorsement of CRC screening by the clinic’s office staff can help patients decide to undergo screening.
It’s well known that patients may avoid colorectal cancer (CRC) screening for fear of pain, embarrassment, lack of awareness of the importance of CRC screening, misperceptions about screening effectiveness, or lack of resources.1-5 But how well do physicians address these concerns and misgivings to help patients make a different choice? Equipped with an understanding of patients’ perspectives, physicians could reframe their counsel and likely increase the rate of CRC screening in their practices.
We conducted 3 in-depth focus group sessions to draw out details of patients’ concerns regarding CRC screening and to solicit their thoughts on how physicians could address and even resolve these issues.
Methods
Patients randomly selected for focus groups
Our initial pool of candidates was approximately 500 patients who were at least 50 years old and had been seen at our Family Medicine Center during the prior 12 months. We stratified this population into 4 ethnic/gender groups: African American males, African American females, Caucasian males, and Caucasian females. Sixty percent of the patients were female; 50% were African American, 48% were Caucasian, and 2% were Latino.
After creating a database that listed these patients by number and concealed their identities except for race and gender, we sequentially selected participants for groups of 8 patients (2 drawn from each of the ethnic/gender groups). Our random selection process avoided such biases as choosing patients by name or age or whether they had been seen more recently.
The first group of 8 patients received a letter asking them to participate in the project. The invitation included the offer of an honorarium. Invitations were mailed every 10 days until we had recruited 4 to 6 volunteers from each ethnic/gender group. After enlisting 20 participants, we were finally able to assemble 15 of them into 3 groups roughly balanced by gender and race. We also had 4 stand-by groups of 8 patients, in case any of the original participants chose to leave the study. All patients who volunteered were assured that if they chose not to participate, their continuing care would be unaffected.
Sessions thoroughly explored patients’ issues
The same experienced focus group leader (Caucasian, female) led all 3 sessions, adhering to a widely accepted structure for focus groups.6 This facilitator was familiar with the common barriers to CRC screening, as cited in the medical literature.1,7-9 She first asked an open-ended question and then probed specifically to determine why some participants or their family members had not received CRC screening. She solicited input from all attendees, sought clarification on points of view, and polled participants about their reactions to statements made by other members of the group. Participants were encouraged to discuss their experiences and their talks with family physicians about CRC screening.
How the sessions unfolded
After receiving instruction about the purpose of the session, participants viewed 2 patient-education videotapes that discussed CRC screening in an average-risk population. They also read a brief patient-education booklet about CRC screening before the facilitator engaged them in dialogue.
The videotapes—”Colon Cancer Screening: What You Need to Know,” produced by Harris and Pignone10; and “Screening for Colorectal Cancer: An Easy Step to Save Your Life,” produced by the Foundation for Digestive Health and Nutrition11—gave all focus group members a common understanding of the rationale and importance of CRC screening. We chose these 2 tapes because of their widespread use in clinical practice, complementary messages, easy-to-read graphics, content aimed at a lay audience, good sound quality, and recommendations that followed the American Cancer Society guidelines for average-risk patients.12
After participants contemplated the information they had viewed and read, the facilitator asked, “What suggestions would you give to a doctor to encourage a patient to be screened for colorectal cancer?” This began approximately 1 hour of feedback from the focus group members.
All 3 sessions were videotaped, but due to technical problems, video was available for only 2 groups. All 3 sessions were audiotaped.
Data analyzed promptly and rigorously
We systematically gathered and analyzed the qualitative data. The focus group leader and Dr. Goldsmith (principle investigator) together categorized the data by themes, which were structured so as to reduce overlapping. Disagreements on categorization were resolved by referring to transcripts and videos. We reassembled this information using an axial coding approach.
Though body language, gestures, and voice tone are important indicators of intent in communication, we did not classify data according to these non-verbal cues. However, we did note such cues during review of the videotapes, and also took into account the frequency and extensiveness of remarks (eg, how many people made a similar comment). Rapid transcription of the sessions and prompt review of the transcripts minimized the inaccurate interpretation of data that can occur when review is delayed.
We used 2 means of assessing the educational level of attendees. Patients in the first 2 focus groups were given the Rapid Estimate of Adult Literacy in Medicine (REALM) test,13 and members of the third group were asked for the highest grade level they completed in school.
Results
The average age of participants was 56 years. Few men volunteered to begin with. So to replace patients who dropped out on short notice, only women were immediately available from the standby groups. Thus, 13 participants were women and 2 were men. Two were covered by Medicaid, 6 by Medicare, 5 had private insurance, and 2 had no insurance. Eleven of the insured participants reported their insurance would pay for CRC screening.
Seven participants were African American, 7 were Caucasian, and 1 was Latino. Each focus group had approximately an equal mix of subjects by ethnic group, but only 2 groups had an uninsured subject. One man was part of each of the first 2 groups.
Reasons for low screening rate
Of the 15 subjects, 5 (at least 1 in each group) had undergone some type of CRC screening: colonoscopy (3), flexible sigmoidoscopy (1), or fecal occult blood testing (1).
Of the 10 subjects not screened, medical records lacked evidence that their family physicians had discussed CRC screening. The facilitator asked them why they had not been screened. The primary reason given was failure of their physicians to recommend screening; although on further inquiry, 1 patient said, “If the doctor did mention it [CRC screening], it was done in a fashion that didn’t impress me enough to remember.” Several other unscreened patients nodded in agreement. Other reasons given were costs, psychological issues (fear and embarrassment), belief that screening was unnecessary, and difficult logistics (time off and transportation) (TABLE).
Patients offered 7 suggestions for physicians
Our focus-group participants offered 7 recommendations for addressing issues that can hinder patients’ decisions to be screened.
- Do not rely on educational materials alone. Though participants thought videotapes and written information were important, all of them strongly stated that the primary endorsement for CRC screening must come from their physicians. All 3 groups agreed that videos and written materials were helpful supplements to a physician’s advice.
- Address fear of pain. Anticipate patients’ fear of pain from colonoscopy, and explain what is done to minimize discomfort.
- Cite costs of tests. A common theme was the lack of knowledge about the costs of the CRC screening options. Let patients know they can opt for less expensive screening.
- Discuss pros and cons of each test. A strongly held belief was that colonoscopy is the best, if not the only, test to have. If a physician had frankly discussed both costs and benefits of the options, patients might have been reassured enough to proceed with a screening procedure, even if it was not colonoscopy.
- Challenge the “worst case” mindset. Focus group participants feared that if cancer is found, it may not be curable. They urged physicians to expect this apprehension and to counter it with a realistic assessment.
- Emphasize safety of testing. Several participants who had not been screened feared being disabled by the test itself and said physicians should spend time to counter this belief.
- Elicit concerns about logistics. Some group members had avoided colonoscopy because it required taking time off from work, which they could not afford to do. The solution is to match the screening test to a patient’s needs and preferences.
Find a way to address the above concerns. Participants suggested that if a doctor’s time is limited, then someone else in the office (a nurse or even a clinic staff member) ought to speak with patients—preferably someone who has undergone endoscopy screening and can talk about what it was like in “real terms we can understand.”
TABLE
How to improve CRC screening rates—focus group recommendations by theme
| Strategies, other than physician communications, that could improve CRC screening rates |
Most common responses in order of frequency:
|
| Family physician communications that could improve CRC screening |
Most common responses in order of frequency (and typical comments):
|
| Preferred communication strategy for learning about the importance of CRC screening |
Most common responses based on frequency (and typical comments):
|
Discussion
Many factors keep the CRC screening rate lower than it ought to be. Physicians do not uniformly follow screening guidelines.7,14 Limited practice time, difficulty in identifying patients needing preventive services, and little financial incentive to provide preventive care in the ambulatory setting all hinder the effort to increase screening. And even when CRC screening is advised, patients are often reluctant to comply because of the reasons already discussed.
Effective communication between patients and physicians therefore becomes ever more important.15 Informed decision making about cancer screening is difficult for many patients to grasp, as evidenced by inaccuracies, distortions, and oversimplification of cancer-related beliefs.16 Patient-centered communications can give the physician a clearer understanding of the patient’s perspective and influence health-seeking behavior.17
The suggestions offered by this study’s participants can help family physicians improve communication about CRC screening, which should encourage more patients to opt for screening.
Participants unanimously recommended that physicians speak directly to well-known patient concerns about endoscopy, even if the patient does not bring them up during a visit.
Though participants spoke mainly about ways physicians could improve doctor/patient communications about CRC screening, they also expressed high regard for videotapes in patient education. The videos they watched taught them that CRC could be prevented or cured if discovered early, and they felt this message was not conveyed by their physicians. The value of video-based patient education observed in our study is consistent with the results of other studies.18,19 Given that primary care physicians often have insufficient time to educate patients fully, using a videotape may be well received by patients and prove an efficient way to augment advice about CRC screening.
Shared decision making has many advocates these days, but the focus group population in this context preferred that physicians be more assertive in promoting CRC screening. Patients may more readily comply with screening recommendations if physicians convey a message that is persuasive rather than factual but emotionally neutral.
This study confirmed the findings of others: fear, lack of information, cost of testing, and the physician’s failure to recommend CRC screening are all potential barriers to increasing screening rates.1,2,20,21 The study also showed the importance of physicians asking patients to clarify the origin of their fears about CRC testing.
Of the 10 focus group members who had not been screened for CRC, fully half said they would now consider screening given what they learned in the focus group. This encouraging finding implies that giving patients accurate information can improve screening rates. The remaining members of the focus group were still uncertain as to whether they would accept CRC screening if offered, and they did not give reasons for their indecision.
Limitations
The focus group participants may have been more assertive than most of the general population, given their willingness to freely express their feelings in front of others.
A sample of convenience was selected and most participants were women, despite efforts to recruit an equal number of men and women. Thus, our findings should be interpreted with caution for the male population.
The education level was higher than that of our urban, family practice clinic population. Thirteen of the 15 attendees had some type of insurance (Medicare, Medicaid, or private insurance). Of the insured, 11 had insurance coverage for CRC screening. Lack of availability of insurance coverage for CRC screening undoubtedly affects purchasing behavior for CRC screening, but we did not specifically separate comments of the insured from the uninsured. We do not have data on response of the subjects by ethnic group or sex.
Although the sample size was small, comments about the inadequacy of doctor/patient communications that emerged in each of the focus groups were remarkably similar.
Acknowledgements
This study is part of ongoing research at the university of Arkansas for Medical Sciences (UAMS), Department of Family and Preventive Medicine, and the uAMS, Arkansas Cancer Research Center, Division of Cancer Control. We thank the Division of Cancer Control for its technical support. We are also grateful for the assistance of Diane Metzler, university of Arkansas at little Rock, Institute for Economic Advancement, Division of Survey Research, who led the focus groups.
Correspondence
Geoffrey Goldsmith, MD, MPH, uAMS Department of Family and Preventive Medicine, 4301 W. Markham St., #530, little Rock, AR 72205-7199; [email protected]
1. Myers RE, Ross EA, Wolf FA, et al. Behavioral interventions to increase adherence in colorectal cancer screening. Med Care. 1991;29:1039-1050.
2. Weitzman ER, Zapka J, Estabrook B, et al. Risk and reluctance: understanding impediments to colorectal cancer screening. Prev Med. 2001;32:502-513.
3. Codori AM, Petersen GM, Miglioretti DL, et al. Health beliefs and endoscopic screening for colorectal cancer: potential for cancer prevention. Prev Med. 2001;33:128-136.
4. Coronado G, Thompson B. Rural Mexican American men’s attitudes and beliefs about cancer screening. J Cancer Educ. 2000;15:41-45.
5. Borum ML. Childhood sexual trauma as a potential factor for noncompliance with endoscopic procedures. Gen Hosp Psychiatry. 1998;20:381-382.
6. Morgan DL, Krueger RA. The Focus Group Kit. Thousand Oaks, CA: Sage Press; 1998.
7. Resnicow KA, Schorow M, Bloom HG, et al. Obstacles to family practitioners’ use of screening tests: determinants of practice? Prev Med. 1989-18:101-112.
8. Baier M, Calonge N, Cutter G, et al. Validity of self-reported colorectal cancer screening behavior. Cancer Epidemiol Biomarkers Prev. 2000;9:229-232.
9. Leider HL. Influencing physicians: the three critical elements of a successful strategy. Am J Manag Care. 1998;4:583-588.
10. Harris R, Pignone M. Colorectal Cancer Screening videotape. University of North Carolina, 1998.
11. Screening for Colon Cancer: An Easy Step to Save Your Life. Bethesda, Md: Foundation for Digestive Health and Nutrition; 1999.
12. American Cancer Society. Screening Guidelines for Colorectal Cancer Screening, ACS. 2005.
13. Davis TC, Crouch MA, Long SW, et al. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433-435.
14. Leider HL. Influencing physicians: the three critical elements of a successful strategy. Am J Manag Care. 1998;4:583-588.
15. Clark N, Becker MH. Theoretical models and strategies for improving adherence and disease management. In Shumaker SA, Schron EB, Ockene JK, McBee WL, eds. The Handbook of Health Behavior Change. New York, NY: Springer Publishing Co; 1998:5-32.
16. Denberg TD, Wong S, Beattie A. Women’s misconceptions about cancer screening: implications for informed decision making. Patient Educ Counsel. 2005;57:280-285.
17. Stewart M. What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med. 1984;19:167-175.
18. Meade CD, McKinney WP, Barnas GP. Educating patients with limited literacy skills: the effectiveness of printed and videotaped materials about colon cancer. Am J Public Health. 1994;84:119-121.
19. Pignone M, Harris R, Kinsinger L. Videotape-based decision aid for colon cancer screening. A randomized, controlled trial. Ann Intern Med. 2000;;133:761-769.
20. Green LW, Eriksen MP, Schor EL. Preventive practices by physicians: behavioral determinants and potential interventions. Am J Prev Med. 1988;4(suppl):101-107.
21. Brenes GA, Paskett ED. Predictors of stage of adoption for colorectal cancer screening. Prev Med. 2000;31:410-416.
- Be more assertive about the need for screening with patients at risk, and do not rely solely on patient-education materials to communicate the message.
- Address key issues such as fear of pain from colonoscopy, costs and comparative benefits of different tests, and safety of procedures—even if patients don’t raise these issues.
Purpose: We elicited patient opinions about how physicians can improve communications about colorectal cancer (CRC) screening.
Methods: We recruited 15 patients, ages 50 years and older, from an urban family medicine teaching clinic. All patients in the initial pool of candidates had been seen at the university of Arkansas for Medical Sciences Family Medical Center within the past 12 months. The recruits participated in 1 of 3 focus groups to discuss how to enhance the rate of CRC screening.
Participants watched a videotape that described the different approaches to CRC screening. We then asked them to comment on how patients could be encouraged to undergo CRC screening.
Results: using a qualitative analysis of focus group data, we determined the most common reasons participants had not undergone CRC screening: fear, lack of information, and failure of the physician to strongly recommend CRC screening. Participants offered 7 recommendations for how physicians could address their concerns. Participants emphasized the importance of strong physician endorsement of screening, of frank and informative dialogue about patient’s concerns, and of using educational materials to supplement personal advice.
Conclusion: A physician’s recommendation for screening is the most powerful motivator in patients’ decisions. However, other sources of information such as videotapes, written materials, and even endorsement of CRC screening by the clinic’s office staff can help patients decide to undergo screening.
It’s well known that patients may avoid colorectal cancer (CRC) screening for fear of pain, embarrassment, lack of awareness of the importance of CRC screening, misperceptions about screening effectiveness, or lack of resources.1-5 But how well do physicians address these concerns and misgivings to help patients make a different choice? Equipped with an understanding of patients’ perspectives, physicians could reframe their counsel and likely increase the rate of CRC screening in their practices.
We conducted 3 in-depth focus group sessions to draw out details of patients’ concerns regarding CRC screening and to solicit their thoughts on how physicians could address and even resolve these issues.
Methods
Patients randomly selected for focus groups
Our initial pool of candidates was approximately 500 patients who were at least 50 years old and had been seen at our Family Medicine Center during the prior 12 months. We stratified this population into 4 ethnic/gender groups: African American males, African American females, Caucasian males, and Caucasian females. Sixty percent of the patients were female; 50% were African American, 48% were Caucasian, and 2% were Latino.
After creating a database that listed these patients by number and concealed their identities except for race and gender, we sequentially selected participants for groups of 8 patients (2 drawn from each of the ethnic/gender groups). Our random selection process avoided such biases as choosing patients by name or age or whether they had been seen more recently.
The first group of 8 patients received a letter asking them to participate in the project. The invitation included the offer of an honorarium. Invitations were mailed every 10 days until we had recruited 4 to 6 volunteers from each ethnic/gender group. After enlisting 20 participants, we were finally able to assemble 15 of them into 3 groups roughly balanced by gender and race. We also had 4 stand-by groups of 8 patients, in case any of the original participants chose to leave the study. All patients who volunteered were assured that if they chose not to participate, their continuing care would be unaffected.
Sessions thoroughly explored patients’ issues
The same experienced focus group leader (Caucasian, female) led all 3 sessions, adhering to a widely accepted structure for focus groups.6 This facilitator was familiar with the common barriers to CRC screening, as cited in the medical literature.1,7-9 She first asked an open-ended question and then probed specifically to determine why some participants or their family members had not received CRC screening. She solicited input from all attendees, sought clarification on points of view, and polled participants about their reactions to statements made by other members of the group. Participants were encouraged to discuss their experiences and their talks with family physicians about CRC screening.
How the sessions unfolded
After receiving instruction about the purpose of the session, participants viewed 2 patient-education videotapes that discussed CRC screening in an average-risk population. They also read a brief patient-education booklet about CRC screening before the facilitator engaged them in dialogue.
The videotapes—”Colon Cancer Screening: What You Need to Know,” produced by Harris and Pignone10; and “Screening for Colorectal Cancer: An Easy Step to Save Your Life,” produced by the Foundation for Digestive Health and Nutrition11—gave all focus group members a common understanding of the rationale and importance of CRC screening. We chose these 2 tapes because of their widespread use in clinical practice, complementary messages, easy-to-read graphics, content aimed at a lay audience, good sound quality, and recommendations that followed the American Cancer Society guidelines for average-risk patients.12
After participants contemplated the information they had viewed and read, the facilitator asked, “What suggestions would you give to a doctor to encourage a patient to be screened for colorectal cancer?” This began approximately 1 hour of feedback from the focus group members.
All 3 sessions were videotaped, but due to technical problems, video was available for only 2 groups. All 3 sessions were audiotaped.
Data analyzed promptly and rigorously
We systematically gathered and analyzed the qualitative data. The focus group leader and Dr. Goldsmith (principle investigator) together categorized the data by themes, which were structured so as to reduce overlapping. Disagreements on categorization were resolved by referring to transcripts and videos. We reassembled this information using an axial coding approach.
Though body language, gestures, and voice tone are important indicators of intent in communication, we did not classify data according to these non-verbal cues. However, we did note such cues during review of the videotapes, and also took into account the frequency and extensiveness of remarks (eg, how many people made a similar comment). Rapid transcription of the sessions and prompt review of the transcripts minimized the inaccurate interpretation of data that can occur when review is delayed.
We used 2 means of assessing the educational level of attendees. Patients in the first 2 focus groups were given the Rapid Estimate of Adult Literacy in Medicine (REALM) test,13 and members of the third group were asked for the highest grade level they completed in school.
Results
The average age of participants was 56 years. Few men volunteered to begin with. So to replace patients who dropped out on short notice, only women were immediately available from the standby groups. Thus, 13 participants were women and 2 were men. Two were covered by Medicaid, 6 by Medicare, 5 had private insurance, and 2 had no insurance. Eleven of the insured participants reported their insurance would pay for CRC screening.
Seven participants were African American, 7 were Caucasian, and 1 was Latino. Each focus group had approximately an equal mix of subjects by ethnic group, but only 2 groups had an uninsured subject. One man was part of each of the first 2 groups.
Reasons for low screening rate
Of the 15 subjects, 5 (at least 1 in each group) had undergone some type of CRC screening: colonoscopy (3), flexible sigmoidoscopy (1), or fecal occult blood testing (1).
Of the 10 subjects not screened, medical records lacked evidence that their family physicians had discussed CRC screening. The facilitator asked them why they had not been screened. The primary reason given was failure of their physicians to recommend screening; although on further inquiry, 1 patient said, “If the doctor did mention it [CRC screening], it was done in a fashion that didn’t impress me enough to remember.” Several other unscreened patients nodded in agreement. Other reasons given were costs, psychological issues (fear and embarrassment), belief that screening was unnecessary, and difficult logistics (time off and transportation) (TABLE).
Patients offered 7 suggestions for physicians
Our focus-group participants offered 7 recommendations for addressing issues that can hinder patients’ decisions to be screened.
- Do not rely on educational materials alone. Though participants thought videotapes and written information were important, all of them strongly stated that the primary endorsement for CRC screening must come from their physicians. All 3 groups agreed that videos and written materials were helpful supplements to a physician’s advice.
- Address fear of pain. Anticipate patients’ fear of pain from colonoscopy, and explain what is done to minimize discomfort.
- Cite costs of tests. A common theme was the lack of knowledge about the costs of the CRC screening options. Let patients know they can opt for less expensive screening.
- Discuss pros and cons of each test. A strongly held belief was that colonoscopy is the best, if not the only, test to have. If a physician had frankly discussed both costs and benefits of the options, patients might have been reassured enough to proceed with a screening procedure, even if it was not colonoscopy.
- Challenge the “worst case” mindset. Focus group participants feared that if cancer is found, it may not be curable. They urged physicians to expect this apprehension and to counter it with a realistic assessment.
- Emphasize safety of testing. Several participants who had not been screened feared being disabled by the test itself and said physicians should spend time to counter this belief.
- Elicit concerns about logistics. Some group members had avoided colonoscopy because it required taking time off from work, which they could not afford to do. The solution is to match the screening test to a patient’s needs and preferences.
Find a way to address the above concerns. Participants suggested that if a doctor’s time is limited, then someone else in the office (a nurse or even a clinic staff member) ought to speak with patients—preferably someone who has undergone endoscopy screening and can talk about what it was like in “real terms we can understand.”
TABLE
How to improve CRC screening rates—focus group recommendations by theme
| Strategies, other than physician communications, that could improve CRC screening rates |
Most common responses in order of frequency:
|
| Family physician communications that could improve CRC screening |
Most common responses in order of frequency (and typical comments):
|
| Preferred communication strategy for learning about the importance of CRC screening |
Most common responses based on frequency (and typical comments):
|
Discussion
Many factors keep the CRC screening rate lower than it ought to be. Physicians do not uniformly follow screening guidelines.7,14 Limited practice time, difficulty in identifying patients needing preventive services, and little financial incentive to provide preventive care in the ambulatory setting all hinder the effort to increase screening. And even when CRC screening is advised, patients are often reluctant to comply because of the reasons already discussed.
Effective communication between patients and physicians therefore becomes ever more important.15 Informed decision making about cancer screening is difficult for many patients to grasp, as evidenced by inaccuracies, distortions, and oversimplification of cancer-related beliefs.16 Patient-centered communications can give the physician a clearer understanding of the patient’s perspective and influence health-seeking behavior.17
The suggestions offered by this study’s participants can help family physicians improve communication about CRC screening, which should encourage more patients to opt for screening.
Participants unanimously recommended that physicians speak directly to well-known patient concerns about endoscopy, even if the patient does not bring them up during a visit.
Though participants spoke mainly about ways physicians could improve doctor/patient communications about CRC screening, they also expressed high regard for videotapes in patient education. The videos they watched taught them that CRC could be prevented or cured if discovered early, and they felt this message was not conveyed by their physicians. The value of video-based patient education observed in our study is consistent with the results of other studies.18,19 Given that primary care physicians often have insufficient time to educate patients fully, using a videotape may be well received by patients and prove an efficient way to augment advice about CRC screening.
Shared decision making has many advocates these days, but the focus group population in this context preferred that physicians be more assertive in promoting CRC screening. Patients may more readily comply with screening recommendations if physicians convey a message that is persuasive rather than factual but emotionally neutral.
This study confirmed the findings of others: fear, lack of information, cost of testing, and the physician’s failure to recommend CRC screening are all potential barriers to increasing screening rates.1,2,20,21 The study also showed the importance of physicians asking patients to clarify the origin of their fears about CRC testing.
Of the 10 focus group members who had not been screened for CRC, fully half said they would now consider screening given what they learned in the focus group. This encouraging finding implies that giving patients accurate information can improve screening rates. The remaining members of the focus group were still uncertain as to whether they would accept CRC screening if offered, and they did not give reasons for their indecision.
Limitations
The focus group participants may have been more assertive than most of the general population, given their willingness to freely express their feelings in front of others.
A sample of convenience was selected and most participants were women, despite efforts to recruit an equal number of men and women. Thus, our findings should be interpreted with caution for the male population.
The education level was higher than that of our urban, family practice clinic population. Thirteen of the 15 attendees had some type of insurance (Medicare, Medicaid, or private insurance). Of the insured, 11 had insurance coverage for CRC screening. Lack of availability of insurance coverage for CRC screening undoubtedly affects purchasing behavior for CRC screening, but we did not specifically separate comments of the insured from the uninsured. We do not have data on response of the subjects by ethnic group or sex.
Although the sample size was small, comments about the inadequacy of doctor/patient communications that emerged in each of the focus groups were remarkably similar.
Acknowledgements
This study is part of ongoing research at the university of Arkansas for Medical Sciences (UAMS), Department of Family and Preventive Medicine, and the uAMS, Arkansas Cancer Research Center, Division of Cancer Control. We thank the Division of Cancer Control for its technical support. We are also grateful for the assistance of Diane Metzler, university of Arkansas at little Rock, Institute for Economic Advancement, Division of Survey Research, who led the focus groups.
Correspondence
Geoffrey Goldsmith, MD, MPH, uAMS Department of Family and Preventive Medicine, 4301 W. Markham St., #530, little Rock, AR 72205-7199; [email protected]
- Be more assertive about the need for screening with patients at risk, and do not rely solely on patient-education materials to communicate the message.
- Address key issues such as fear of pain from colonoscopy, costs and comparative benefits of different tests, and safety of procedures—even if patients don’t raise these issues.
Purpose: We elicited patient opinions about how physicians can improve communications about colorectal cancer (CRC) screening.
Methods: We recruited 15 patients, ages 50 years and older, from an urban family medicine teaching clinic. All patients in the initial pool of candidates had been seen at the university of Arkansas for Medical Sciences Family Medical Center within the past 12 months. The recruits participated in 1 of 3 focus groups to discuss how to enhance the rate of CRC screening.
Participants watched a videotape that described the different approaches to CRC screening. We then asked them to comment on how patients could be encouraged to undergo CRC screening.
Results: using a qualitative analysis of focus group data, we determined the most common reasons participants had not undergone CRC screening: fear, lack of information, and failure of the physician to strongly recommend CRC screening. Participants offered 7 recommendations for how physicians could address their concerns. Participants emphasized the importance of strong physician endorsement of screening, of frank and informative dialogue about patient’s concerns, and of using educational materials to supplement personal advice.
Conclusion: A physician’s recommendation for screening is the most powerful motivator in patients’ decisions. However, other sources of information such as videotapes, written materials, and even endorsement of CRC screening by the clinic’s office staff can help patients decide to undergo screening.
It’s well known that patients may avoid colorectal cancer (CRC) screening for fear of pain, embarrassment, lack of awareness of the importance of CRC screening, misperceptions about screening effectiveness, or lack of resources.1-5 But how well do physicians address these concerns and misgivings to help patients make a different choice? Equipped with an understanding of patients’ perspectives, physicians could reframe their counsel and likely increase the rate of CRC screening in their practices.
We conducted 3 in-depth focus group sessions to draw out details of patients’ concerns regarding CRC screening and to solicit their thoughts on how physicians could address and even resolve these issues.
Methods
Patients randomly selected for focus groups
Our initial pool of candidates was approximately 500 patients who were at least 50 years old and had been seen at our Family Medicine Center during the prior 12 months. We stratified this population into 4 ethnic/gender groups: African American males, African American females, Caucasian males, and Caucasian females. Sixty percent of the patients were female; 50% were African American, 48% were Caucasian, and 2% were Latino.
After creating a database that listed these patients by number and concealed their identities except for race and gender, we sequentially selected participants for groups of 8 patients (2 drawn from each of the ethnic/gender groups). Our random selection process avoided such biases as choosing patients by name or age or whether they had been seen more recently.
The first group of 8 patients received a letter asking them to participate in the project. The invitation included the offer of an honorarium. Invitations were mailed every 10 days until we had recruited 4 to 6 volunteers from each ethnic/gender group. After enlisting 20 participants, we were finally able to assemble 15 of them into 3 groups roughly balanced by gender and race. We also had 4 stand-by groups of 8 patients, in case any of the original participants chose to leave the study. All patients who volunteered were assured that if they chose not to participate, their continuing care would be unaffected.
Sessions thoroughly explored patients’ issues
The same experienced focus group leader (Caucasian, female) led all 3 sessions, adhering to a widely accepted structure for focus groups.6 This facilitator was familiar with the common barriers to CRC screening, as cited in the medical literature.1,7-9 She first asked an open-ended question and then probed specifically to determine why some participants or their family members had not received CRC screening. She solicited input from all attendees, sought clarification on points of view, and polled participants about their reactions to statements made by other members of the group. Participants were encouraged to discuss their experiences and their talks with family physicians about CRC screening.
How the sessions unfolded
After receiving instruction about the purpose of the session, participants viewed 2 patient-education videotapes that discussed CRC screening in an average-risk population. They also read a brief patient-education booklet about CRC screening before the facilitator engaged them in dialogue.
The videotapes—”Colon Cancer Screening: What You Need to Know,” produced by Harris and Pignone10; and “Screening for Colorectal Cancer: An Easy Step to Save Your Life,” produced by the Foundation for Digestive Health and Nutrition11—gave all focus group members a common understanding of the rationale and importance of CRC screening. We chose these 2 tapes because of their widespread use in clinical practice, complementary messages, easy-to-read graphics, content aimed at a lay audience, good sound quality, and recommendations that followed the American Cancer Society guidelines for average-risk patients.12
After participants contemplated the information they had viewed and read, the facilitator asked, “What suggestions would you give to a doctor to encourage a patient to be screened for colorectal cancer?” This began approximately 1 hour of feedback from the focus group members.
All 3 sessions were videotaped, but due to technical problems, video was available for only 2 groups. All 3 sessions were audiotaped.
Data analyzed promptly and rigorously
We systematically gathered and analyzed the qualitative data. The focus group leader and Dr. Goldsmith (principle investigator) together categorized the data by themes, which were structured so as to reduce overlapping. Disagreements on categorization were resolved by referring to transcripts and videos. We reassembled this information using an axial coding approach.
Though body language, gestures, and voice tone are important indicators of intent in communication, we did not classify data according to these non-verbal cues. However, we did note such cues during review of the videotapes, and also took into account the frequency and extensiveness of remarks (eg, how many people made a similar comment). Rapid transcription of the sessions and prompt review of the transcripts minimized the inaccurate interpretation of data that can occur when review is delayed.
We used 2 means of assessing the educational level of attendees. Patients in the first 2 focus groups were given the Rapid Estimate of Adult Literacy in Medicine (REALM) test,13 and members of the third group were asked for the highest grade level they completed in school.
Results
The average age of participants was 56 years. Few men volunteered to begin with. So to replace patients who dropped out on short notice, only women were immediately available from the standby groups. Thus, 13 participants were women and 2 were men. Two were covered by Medicaid, 6 by Medicare, 5 had private insurance, and 2 had no insurance. Eleven of the insured participants reported their insurance would pay for CRC screening.
Seven participants were African American, 7 were Caucasian, and 1 was Latino. Each focus group had approximately an equal mix of subjects by ethnic group, but only 2 groups had an uninsured subject. One man was part of each of the first 2 groups.
Reasons for low screening rate
Of the 15 subjects, 5 (at least 1 in each group) had undergone some type of CRC screening: colonoscopy (3), flexible sigmoidoscopy (1), or fecal occult blood testing (1).
Of the 10 subjects not screened, medical records lacked evidence that their family physicians had discussed CRC screening. The facilitator asked them why they had not been screened. The primary reason given was failure of their physicians to recommend screening; although on further inquiry, 1 patient said, “If the doctor did mention it [CRC screening], it was done in a fashion that didn’t impress me enough to remember.” Several other unscreened patients nodded in agreement. Other reasons given were costs, psychological issues (fear and embarrassment), belief that screening was unnecessary, and difficult logistics (time off and transportation) (TABLE).
Patients offered 7 suggestions for physicians
Our focus-group participants offered 7 recommendations for addressing issues that can hinder patients’ decisions to be screened.
- Do not rely on educational materials alone. Though participants thought videotapes and written information were important, all of them strongly stated that the primary endorsement for CRC screening must come from their physicians. All 3 groups agreed that videos and written materials were helpful supplements to a physician’s advice.
- Address fear of pain. Anticipate patients’ fear of pain from colonoscopy, and explain what is done to minimize discomfort.
- Cite costs of tests. A common theme was the lack of knowledge about the costs of the CRC screening options. Let patients know they can opt for less expensive screening.
- Discuss pros and cons of each test. A strongly held belief was that colonoscopy is the best, if not the only, test to have. If a physician had frankly discussed both costs and benefits of the options, patients might have been reassured enough to proceed with a screening procedure, even if it was not colonoscopy.
- Challenge the “worst case” mindset. Focus group participants feared that if cancer is found, it may not be curable. They urged physicians to expect this apprehension and to counter it with a realistic assessment.
- Emphasize safety of testing. Several participants who had not been screened feared being disabled by the test itself and said physicians should spend time to counter this belief.
- Elicit concerns about logistics. Some group members had avoided colonoscopy because it required taking time off from work, which they could not afford to do. The solution is to match the screening test to a patient’s needs and preferences.
Find a way to address the above concerns. Participants suggested that if a doctor’s time is limited, then someone else in the office (a nurse or even a clinic staff member) ought to speak with patients—preferably someone who has undergone endoscopy screening and can talk about what it was like in “real terms we can understand.”
TABLE
How to improve CRC screening rates—focus group recommendations by theme
| Strategies, other than physician communications, that could improve CRC screening rates |
Most common responses in order of frequency:
|
| Family physician communications that could improve CRC screening |
Most common responses in order of frequency (and typical comments):
|
| Preferred communication strategy for learning about the importance of CRC screening |
Most common responses based on frequency (and typical comments):
|
Discussion
Many factors keep the CRC screening rate lower than it ought to be. Physicians do not uniformly follow screening guidelines.7,14 Limited practice time, difficulty in identifying patients needing preventive services, and little financial incentive to provide preventive care in the ambulatory setting all hinder the effort to increase screening. And even when CRC screening is advised, patients are often reluctant to comply because of the reasons already discussed.
Effective communication between patients and physicians therefore becomes ever more important.15 Informed decision making about cancer screening is difficult for many patients to grasp, as evidenced by inaccuracies, distortions, and oversimplification of cancer-related beliefs.16 Patient-centered communications can give the physician a clearer understanding of the patient’s perspective and influence health-seeking behavior.17
The suggestions offered by this study’s participants can help family physicians improve communication about CRC screening, which should encourage more patients to opt for screening.
Participants unanimously recommended that physicians speak directly to well-known patient concerns about endoscopy, even if the patient does not bring them up during a visit.
Though participants spoke mainly about ways physicians could improve doctor/patient communications about CRC screening, they also expressed high regard for videotapes in patient education. The videos they watched taught them that CRC could be prevented or cured if discovered early, and they felt this message was not conveyed by their physicians. The value of video-based patient education observed in our study is consistent with the results of other studies.18,19 Given that primary care physicians often have insufficient time to educate patients fully, using a videotape may be well received by patients and prove an efficient way to augment advice about CRC screening.
Shared decision making has many advocates these days, but the focus group population in this context preferred that physicians be more assertive in promoting CRC screening. Patients may more readily comply with screening recommendations if physicians convey a message that is persuasive rather than factual but emotionally neutral.
This study confirmed the findings of others: fear, lack of information, cost of testing, and the physician’s failure to recommend CRC screening are all potential barriers to increasing screening rates.1,2,20,21 The study also showed the importance of physicians asking patients to clarify the origin of their fears about CRC testing.
Of the 10 focus group members who had not been screened for CRC, fully half said they would now consider screening given what they learned in the focus group. This encouraging finding implies that giving patients accurate information can improve screening rates. The remaining members of the focus group were still uncertain as to whether they would accept CRC screening if offered, and they did not give reasons for their indecision.
Limitations
The focus group participants may have been more assertive than most of the general population, given their willingness to freely express their feelings in front of others.
A sample of convenience was selected and most participants were women, despite efforts to recruit an equal number of men and women. Thus, our findings should be interpreted with caution for the male population.
The education level was higher than that of our urban, family practice clinic population. Thirteen of the 15 attendees had some type of insurance (Medicare, Medicaid, or private insurance). Of the insured, 11 had insurance coverage for CRC screening. Lack of availability of insurance coverage for CRC screening undoubtedly affects purchasing behavior for CRC screening, but we did not specifically separate comments of the insured from the uninsured. We do not have data on response of the subjects by ethnic group or sex.
Although the sample size was small, comments about the inadequacy of doctor/patient communications that emerged in each of the focus groups were remarkably similar.
Acknowledgements
This study is part of ongoing research at the university of Arkansas for Medical Sciences (UAMS), Department of Family and Preventive Medicine, and the uAMS, Arkansas Cancer Research Center, Division of Cancer Control. We thank the Division of Cancer Control for its technical support. We are also grateful for the assistance of Diane Metzler, university of Arkansas at little Rock, Institute for Economic Advancement, Division of Survey Research, who led the focus groups.
Correspondence
Geoffrey Goldsmith, MD, MPH, uAMS Department of Family and Preventive Medicine, 4301 W. Markham St., #530, little Rock, AR 72205-7199; [email protected]
1. Myers RE, Ross EA, Wolf FA, et al. Behavioral interventions to increase adherence in colorectal cancer screening. Med Care. 1991;29:1039-1050.
2. Weitzman ER, Zapka J, Estabrook B, et al. Risk and reluctance: understanding impediments to colorectal cancer screening. Prev Med. 2001;32:502-513.
3. Codori AM, Petersen GM, Miglioretti DL, et al. Health beliefs and endoscopic screening for colorectal cancer: potential for cancer prevention. Prev Med. 2001;33:128-136.
4. Coronado G, Thompson B. Rural Mexican American men’s attitudes and beliefs about cancer screening. J Cancer Educ. 2000;15:41-45.
5. Borum ML. Childhood sexual trauma as a potential factor for noncompliance with endoscopic procedures. Gen Hosp Psychiatry. 1998;20:381-382.
6. Morgan DL, Krueger RA. The Focus Group Kit. Thousand Oaks, CA: Sage Press; 1998.
7. Resnicow KA, Schorow M, Bloom HG, et al. Obstacles to family practitioners’ use of screening tests: determinants of practice? Prev Med. 1989-18:101-112.
8. Baier M, Calonge N, Cutter G, et al. Validity of self-reported colorectal cancer screening behavior. Cancer Epidemiol Biomarkers Prev. 2000;9:229-232.
9. Leider HL. Influencing physicians: the three critical elements of a successful strategy. Am J Manag Care. 1998;4:583-588.
10. Harris R, Pignone M. Colorectal Cancer Screening videotape. University of North Carolina, 1998.
11. Screening for Colon Cancer: An Easy Step to Save Your Life. Bethesda, Md: Foundation for Digestive Health and Nutrition; 1999.
12. American Cancer Society. Screening Guidelines for Colorectal Cancer Screening, ACS. 2005.
13. Davis TC, Crouch MA, Long SW, et al. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433-435.
14. Leider HL. Influencing physicians: the three critical elements of a successful strategy. Am J Manag Care. 1998;4:583-588.
15. Clark N, Becker MH. Theoretical models and strategies for improving adherence and disease management. In Shumaker SA, Schron EB, Ockene JK, McBee WL, eds. The Handbook of Health Behavior Change. New York, NY: Springer Publishing Co; 1998:5-32.
16. Denberg TD, Wong S, Beattie A. Women’s misconceptions about cancer screening: implications for informed decision making. Patient Educ Counsel. 2005;57:280-285.
17. Stewart M. What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med. 1984;19:167-175.
18. Meade CD, McKinney WP, Barnas GP. Educating patients with limited literacy skills: the effectiveness of printed and videotaped materials about colon cancer. Am J Public Health. 1994;84:119-121.
19. Pignone M, Harris R, Kinsinger L. Videotape-based decision aid for colon cancer screening. A randomized, controlled trial. Ann Intern Med. 2000;;133:761-769.
20. Green LW, Eriksen MP, Schor EL. Preventive practices by physicians: behavioral determinants and potential interventions. Am J Prev Med. 1988;4(suppl):101-107.
21. Brenes GA, Paskett ED. Predictors of stage of adoption for colorectal cancer screening. Prev Med. 2000;31:410-416.
1. Myers RE, Ross EA, Wolf FA, et al. Behavioral interventions to increase adherence in colorectal cancer screening. Med Care. 1991;29:1039-1050.
2. Weitzman ER, Zapka J, Estabrook B, et al. Risk and reluctance: understanding impediments to colorectal cancer screening. Prev Med. 2001;32:502-513.
3. Codori AM, Petersen GM, Miglioretti DL, et al. Health beliefs and endoscopic screening for colorectal cancer: potential for cancer prevention. Prev Med. 2001;33:128-136.
4. Coronado G, Thompson B. Rural Mexican American men’s attitudes and beliefs about cancer screening. J Cancer Educ. 2000;15:41-45.
5. Borum ML. Childhood sexual trauma as a potential factor for noncompliance with endoscopic procedures. Gen Hosp Psychiatry. 1998;20:381-382.
6. Morgan DL, Krueger RA. The Focus Group Kit. Thousand Oaks, CA: Sage Press; 1998.
7. Resnicow KA, Schorow M, Bloom HG, et al. Obstacles to family practitioners’ use of screening tests: determinants of practice? Prev Med. 1989-18:101-112.
8. Baier M, Calonge N, Cutter G, et al. Validity of self-reported colorectal cancer screening behavior. Cancer Epidemiol Biomarkers Prev. 2000;9:229-232.
9. Leider HL. Influencing physicians: the three critical elements of a successful strategy. Am J Manag Care. 1998;4:583-588.
10. Harris R, Pignone M. Colorectal Cancer Screening videotape. University of North Carolina, 1998.
11. Screening for Colon Cancer: An Easy Step to Save Your Life. Bethesda, Md: Foundation for Digestive Health and Nutrition; 1999.
12. American Cancer Society. Screening Guidelines for Colorectal Cancer Screening, ACS. 2005.
13. Davis TC, Crouch MA, Long SW, et al. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433-435.
14. Leider HL. Influencing physicians: the three critical elements of a successful strategy. Am J Manag Care. 1998;4:583-588.
15. Clark N, Becker MH. Theoretical models and strategies for improving adherence and disease management. In Shumaker SA, Schron EB, Ockene JK, McBee WL, eds. The Handbook of Health Behavior Change. New York, NY: Springer Publishing Co; 1998:5-32.
16. Denberg TD, Wong S, Beattie A. Women’s misconceptions about cancer screening: implications for informed decision making. Patient Educ Counsel. 2005;57:280-285.
17. Stewart M. What is a successful doctor-patient interview? A study of interactions and outcomes. Soc Sci Med. 1984;19:167-175.
18. Meade CD, McKinney WP, Barnas GP. Educating patients with limited literacy skills: the effectiveness of printed and videotaped materials about colon cancer. Am J Public Health. 1994;84:119-121.
19. Pignone M, Harris R, Kinsinger L. Videotape-based decision aid for colon cancer screening. A randomized, controlled trial. Ann Intern Med. 2000;;133:761-769.
20. Green LW, Eriksen MP, Schor EL. Preventive practices by physicians: behavioral determinants and potential interventions. Am J Prev Med. 1988;4(suppl):101-107.
21. Brenes GA, Paskett ED. Predictors of stage of adoption for colorectal cancer screening. Prev Med. 2000;31:410-416.
Should you screen—or not? The latest recommendations
Not enough time and too many potential tests to do. This is the problem faced daily by family physicians. We want to practice up-to-date preventive medicine, but there’s little time to analyze the latest studies. Thankfully, we can rely on the United States Preventive Services Task Force, the organization with the most rigorous evidence-based approach, to do the legwork for us.1
Last year, and in the early part of this year, the Task Force issued a number of recommendations on topics ranging from hypertension screening to screening for illicit drug use. (See TABLE 1 for a breakdown of the 5 categories of recommendations.)
While some of these recommendations (TABLE 2) were reaffirmations of past recommendations, others included some changes.
The Task Force has:
- dropped the age for routine screening for Chlamydia in sexually active women from 25 years and younger to 24 and younger.
- added a recommendation against the use of aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) to prevent colorectal cancer (CRC).
- changed its recommendation on screening for carotid artery stenosis. In 1996, the Task Force noted that the evidence was insufficient to make a recommendation; in 2007 it recommended against such routine screening.
- added recommendations on counseling patients about drinking and driving, as well as on screening for illicit drug use. In both cases, the Task Force says the evidence is insufficient to recommend for or against.
TABLE 1
USPSTF recommendation categories
| A Recommendation: The Task Force recommends the service. There is a high certainty that the net benefit is substantial. |
| B Recommendation: The Task Force recommends the service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial. |
| C Recommendation: The Task Force recommends against routinely providing the service. There may be considerations that support providing the service in an individual patient. There is at least moderate certainty that the net benefit is small. |
| D Recommendation: The Task Force recommends against the service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. |
| I Recommendation: The Task Force concludes that the current evidence is insufficient to assess the balance of benefits and harms of the service. Evidence is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined. |
TABLE 2
Summary of new USPSTF recommendations
| A RECOMMENDATIONS |
The USPSTF recommends routinely:
|
| B RECOMMENDATIONS |
The USPSTF recommends routinely:
|
| C RECOMMENDATIONS |
The USPSTF recommends against routine:
|
| D RECOMMENDATIONS |
The USPSTF recommends against routine:
|
| I RECOMMENDATIONS |
The USPSTF concludes that the current evidence is insufficient to recommend for or against routine:
|
Continue to screen for HTN, sickle cell, Chlamydia
The latest A and B recommendations from the Task Force largely reaffirm previous recommendations. These recommendations cover hypertension, sickle cell disease, and Chlamydia.
Hypertension. Screening and treatment of hypertension in adults leads to lower morbidity and mortality from cardiovascular disease and is still recommended.2
Sickle cell disease. Screening newborns for sickle cell disease and treating those affected with oral prophylactic penicillin prevents serious bacterial infections. It also remains a recommended service.3
Chlamydia. Following a review of the evidence, the Task Force reconfirms the benefits of screening for Chlamydia in sexually active young women, but it has changed the age cutoff. In 2001, the Task Force indicated that sexually active women who were 25 years of age and younger should be screened. In 2007, the Task Force dropped the age to 24 and younger.
The latest recommendation reaffirms the need to screen women (above the cutoff) who are at risk—that is, women who have previously had a sexually transmitted infection (STI), those who have a new or multiple sex partners, and those who exchange sex for money or drugs.4 Screening is recommended annually; nucleic acid amplification tests are acceptable, allowing testing of urine or vaginal swabs.
Screening during pregnancy is recommended for the same groups—women who are 24 and younger and older women at risk—at the first prenatal visit and again in the third trimester if risk continues. Chlamydia is the most common bacterial STI, and screening and treatment prevents pelvic inflammatory disease in women and leads to improved pregnancy outcomes.
Interventions that are not recommended
Chemopreventon of colorectal cancer. For the first time, the Task Force issued a recommendation on the use of aspirin or other NSAIDs to prevent CRC. The Task Force does not recommend the routine use of these agents.5 The dosage needed to prevent CRC is higher than that which prevents cardiovascular disease and can cause significant harm.
Aspirin use is associated with gastrointestinal bleeding and hemorrhagic stroke; NSAID use is associated with gastrointestinal bleeding and renal impairment. The Task Force concludes that in the general adult population, potential harms exceed potential benefits.
Screening for carotid artery stenosis. In 1996, the Task Force found insufficient evidence to recommend for or against routine screening for carotid artery stenosis. In 2007, the Task Force made a recommendation against routine screening for carotid artery stenosis.6 Screening with duplex ultrasonography results in frequent false positives. Confirmatory testing with angiography is associated with a 1% rate of stroke. Endarterectomy itself has a death or stroke rate of about 3%.
In the general population, close to 8700 adults would need to be screened to prevent 1 disabling stroke. The Task Force indicates that primary care physicians would have better outcomes by concentrating on optimal management of risk factors for cerebral artery disease.
Screening for bacterial vaginosis among low-risk pregnant women. The final D recommendation pertains to screening for bacterial vaginosis during pregnancy to prevent preterm delivery.7 Pregnant women who have not had a previous preterm delivery are considered at low risk for preterm delivery and there is good evidence that this group does not benefit from screening for, or treatment of, asymptomatic bacterial vaginosis. (A similar recommendation was made in 2001, but it referred to women of “average” risk.)
Insufficient evidence to make a recommendation
Routinely screening men for Chlamydia. While it makes clinical sense to test and treat male partners of women with Chlamydia infection, the Task Force could not find evidence of the effectiveness of routinely screening men as a way to prevent infection in women.4 That said, the Task Force points out that screening men is relatively inexpensive and has negligible harms.
Screening for hyperlipidemia in children. While 50% of children with hyperlipidemia continue to have this disorder as adults, the long-term benefits and harms of early detection and treatment with medications and lipid-lowering diets have not been studied.8 This echoes the position the Task Force took in 1996, when it commented on children as part of an adult hyperlipidemia recommendation.
Physician counseling on drinking and driving. Motor vehicle crashes result in significant morbidity and mortality—especially among adolescents and young adults. Improved car and road design, as well as public health safety efforts, have led to significant improvements in motor vehicle safety. While avoidance of driving under the influence and proper use of occupant restraints are important public health goals, the Task Force, in this first recommendation on the subject, could find no evidence that physician counseling added benefit above those provided by community-wide efforts.9
Screening for bacterial vaginosis in pregnant women at high risk for preterm birth. As mentioned previously, screening low-risk pregnant women for bacterial vaginosis results in no benefit. The issue is less clear cut among women at high risk for a preterm delivery—that is, those who have had one previously.
The evidence regarding screening and treating asymptomatic bacterial vaginosis as a means of preventing preterm delivery in these women is mixed and the Task Force was unable to recommend for or against this practice.7 This reaffirms the Task Force’s 2001 recommendation.
Screening for illicit drug use. The Task Force recognizes that illicit drug use is a major cause of illness and social problems. It would appear to have great potential for early detection and intervention. However, the Task Force, in this first-time recommendation, found that screening tools have not been well studied, nor have the long-term effects of different treatment strategies.10 These are high priority areas for future research.
Correspondence
Doug Campos-Outcalt, MD, MPA, 550 E. Van Buren, Phoenix, AZ 85004; [email protected]
1. Agency for Healthcare Quality and Research. USPSTF. Available at: http://www.ahrq.gov/clinic/uspstfix.htm. Accessed May 5, 2008.
2. USPSTF. Screening for High Blood Pressure. Available at: http://www.ahrq.gov/clinic/uspstf/uspshype.htm. Accessed May 5, 2008.
3. USPSTF. Screening for Sickle Cell Disease in Newborns. Available at: http://www.ahrq.gov/clinic/uspstf/uspshemo.htm. Accessed May 5, 2008.
4. USPSTF. Screening for Chlamydia Infection. Available at: http://www.ahrq.gov/clinic/uspstf/uspschlm.htm. Accessed May 5, 2008.
5. USPSTF. Aspirin or Nonsteroidal Anti-inflamatory Drugs for the Primary Prevention of Colorectal Cancer. Available at: http://www.ahrq.gov/clinic/uspstf/uspsasco.htm. Accessed May 5, 2008.
6. USPSTF. Screening for Carotid Artery Stenosis. Available at: http://www.ahrq.gov/clinic/uspstf/uspsacas.htm. Accessed May 5, 2008.
7. USPSTF. Screening for Bacterial Vaginosis in Pregnancy. Available at: http://www.ahrq.gov/clinic/uspstf/uspsbvag.htm. Accessed May 5, 2008.
8. USPSTF. Screening for Lipid Disorders in Children. Available at: http://www.ahrq.gov/clinic/uspstf/uspschlip.htm. Accessed May 5, 2008.
9. USPSTF. Counseling About Proper Use of Motor Vehicle Occupant Restraints and Avoidance of Alcohol Use While Driving. Available at: http://www.ahrq.gov/clinic/uspstf/uspsmvin.htm. Accessed May 5, 2008.
10. USPSTF. Screening for Illicit Drug Use. Available at: http://www.ahrq.gov/clinic/uspstf/uspsdrug.htm. Accessed May 5, 2008.
Not enough time and too many potential tests to do. This is the problem faced daily by family physicians. We want to practice up-to-date preventive medicine, but there’s little time to analyze the latest studies. Thankfully, we can rely on the United States Preventive Services Task Force, the organization with the most rigorous evidence-based approach, to do the legwork for us.1
Last year, and in the early part of this year, the Task Force issued a number of recommendations on topics ranging from hypertension screening to screening for illicit drug use. (See TABLE 1 for a breakdown of the 5 categories of recommendations.)
While some of these recommendations (TABLE 2) were reaffirmations of past recommendations, others included some changes.
The Task Force has:
- dropped the age for routine screening for Chlamydia in sexually active women from 25 years and younger to 24 and younger.
- added a recommendation against the use of aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) to prevent colorectal cancer (CRC).
- changed its recommendation on screening for carotid artery stenosis. In 1996, the Task Force noted that the evidence was insufficient to make a recommendation; in 2007 it recommended against such routine screening.
- added recommendations on counseling patients about drinking and driving, as well as on screening for illicit drug use. In both cases, the Task Force says the evidence is insufficient to recommend for or against.
TABLE 1
USPSTF recommendation categories
| A Recommendation: The Task Force recommends the service. There is a high certainty that the net benefit is substantial. |
| B Recommendation: The Task Force recommends the service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial. |
| C Recommendation: The Task Force recommends against routinely providing the service. There may be considerations that support providing the service in an individual patient. There is at least moderate certainty that the net benefit is small. |
| D Recommendation: The Task Force recommends against the service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. |
| I Recommendation: The Task Force concludes that the current evidence is insufficient to assess the balance of benefits and harms of the service. Evidence is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined. |
TABLE 2
Summary of new USPSTF recommendations
| A RECOMMENDATIONS |
The USPSTF recommends routinely:
|
| B RECOMMENDATIONS |
The USPSTF recommends routinely:
|
| C RECOMMENDATIONS |
The USPSTF recommends against routine:
|
| D RECOMMENDATIONS |
The USPSTF recommends against routine:
|
| I RECOMMENDATIONS |
The USPSTF concludes that the current evidence is insufficient to recommend for or against routine:
|
Continue to screen for HTN, sickle cell, Chlamydia
The latest A and B recommendations from the Task Force largely reaffirm previous recommendations. These recommendations cover hypertension, sickle cell disease, and Chlamydia.
Hypertension. Screening and treatment of hypertension in adults leads to lower morbidity and mortality from cardiovascular disease and is still recommended.2
Sickle cell disease. Screening newborns for sickle cell disease and treating those affected with oral prophylactic penicillin prevents serious bacterial infections. It also remains a recommended service.3
Chlamydia. Following a review of the evidence, the Task Force reconfirms the benefits of screening for Chlamydia in sexually active young women, but it has changed the age cutoff. In 2001, the Task Force indicated that sexually active women who were 25 years of age and younger should be screened. In 2007, the Task Force dropped the age to 24 and younger.
The latest recommendation reaffirms the need to screen women (above the cutoff) who are at risk—that is, women who have previously had a sexually transmitted infection (STI), those who have a new or multiple sex partners, and those who exchange sex for money or drugs.4 Screening is recommended annually; nucleic acid amplification tests are acceptable, allowing testing of urine or vaginal swabs.
Screening during pregnancy is recommended for the same groups—women who are 24 and younger and older women at risk—at the first prenatal visit and again in the third trimester if risk continues. Chlamydia is the most common bacterial STI, and screening and treatment prevents pelvic inflammatory disease in women and leads to improved pregnancy outcomes.
Interventions that are not recommended
Chemopreventon of colorectal cancer. For the first time, the Task Force issued a recommendation on the use of aspirin or other NSAIDs to prevent CRC. The Task Force does not recommend the routine use of these agents.5 The dosage needed to prevent CRC is higher than that which prevents cardiovascular disease and can cause significant harm.
Aspirin use is associated with gastrointestinal bleeding and hemorrhagic stroke; NSAID use is associated with gastrointestinal bleeding and renal impairment. The Task Force concludes that in the general adult population, potential harms exceed potential benefits.
Screening for carotid artery stenosis. In 1996, the Task Force found insufficient evidence to recommend for or against routine screening for carotid artery stenosis. In 2007, the Task Force made a recommendation against routine screening for carotid artery stenosis.6 Screening with duplex ultrasonography results in frequent false positives. Confirmatory testing with angiography is associated with a 1% rate of stroke. Endarterectomy itself has a death or stroke rate of about 3%.
In the general population, close to 8700 adults would need to be screened to prevent 1 disabling stroke. The Task Force indicates that primary care physicians would have better outcomes by concentrating on optimal management of risk factors for cerebral artery disease.
Screening for bacterial vaginosis among low-risk pregnant women. The final D recommendation pertains to screening for bacterial vaginosis during pregnancy to prevent preterm delivery.7 Pregnant women who have not had a previous preterm delivery are considered at low risk for preterm delivery and there is good evidence that this group does not benefit from screening for, or treatment of, asymptomatic bacterial vaginosis. (A similar recommendation was made in 2001, but it referred to women of “average” risk.)
Insufficient evidence to make a recommendation
Routinely screening men for Chlamydia. While it makes clinical sense to test and treat male partners of women with Chlamydia infection, the Task Force could not find evidence of the effectiveness of routinely screening men as a way to prevent infection in women.4 That said, the Task Force points out that screening men is relatively inexpensive and has negligible harms.
Screening for hyperlipidemia in children. While 50% of children with hyperlipidemia continue to have this disorder as adults, the long-term benefits and harms of early detection and treatment with medications and lipid-lowering diets have not been studied.8 This echoes the position the Task Force took in 1996, when it commented on children as part of an adult hyperlipidemia recommendation.
Physician counseling on drinking and driving. Motor vehicle crashes result in significant morbidity and mortality—especially among adolescents and young adults. Improved car and road design, as well as public health safety efforts, have led to significant improvements in motor vehicle safety. While avoidance of driving under the influence and proper use of occupant restraints are important public health goals, the Task Force, in this first recommendation on the subject, could find no evidence that physician counseling added benefit above those provided by community-wide efforts.9
Screening for bacterial vaginosis in pregnant women at high risk for preterm birth. As mentioned previously, screening low-risk pregnant women for bacterial vaginosis results in no benefit. The issue is less clear cut among women at high risk for a preterm delivery—that is, those who have had one previously.
The evidence regarding screening and treating asymptomatic bacterial vaginosis as a means of preventing preterm delivery in these women is mixed and the Task Force was unable to recommend for or against this practice.7 This reaffirms the Task Force’s 2001 recommendation.
Screening for illicit drug use. The Task Force recognizes that illicit drug use is a major cause of illness and social problems. It would appear to have great potential for early detection and intervention. However, the Task Force, in this first-time recommendation, found that screening tools have not been well studied, nor have the long-term effects of different treatment strategies.10 These are high priority areas for future research.
Correspondence
Doug Campos-Outcalt, MD, MPA, 550 E. Van Buren, Phoenix, AZ 85004; [email protected]
Not enough time and too many potential tests to do. This is the problem faced daily by family physicians. We want to practice up-to-date preventive medicine, but there’s little time to analyze the latest studies. Thankfully, we can rely on the United States Preventive Services Task Force, the organization with the most rigorous evidence-based approach, to do the legwork for us.1
Last year, and in the early part of this year, the Task Force issued a number of recommendations on topics ranging from hypertension screening to screening for illicit drug use. (See TABLE 1 for a breakdown of the 5 categories of recommendations.)
While some of these recommendations (TABLE 2) were reaffirmations of past recommendations, others included some changes.
The Task Force has:
- dropped the age for routine screening for Chlamydia in sexually active women from 25 years and younger to 24 and younger.
- added a recommendation against the use of aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) to prevent colorectal cancer (CRC).
- changed its recommendation on screening for carotid artery stenosis. In 1996, the Task Force noted that the evidence was insufficient to make a recommendation; in 2007 it recommended against such routine screening.
- added recommendations on counseling patients about drinking and driving, as well as on screening for illicit drug use. In both cases, the Task Force says the evidence is insufficient to recommend for or against.
TABLE 1
USPSTF recommendation categories
| A Recommendation: The Task Force recommends the service. There is a high certainty that the net benefit is substantial. |
| B Recommendation: The Task Force recommends the service. There is high certainty that the net benefit is moderate or there is moderate certainty that the net benefit is moderate to substantial. |
| C Recommendation: The Task Force recommends against routinely providing the service. There may be considerations that support providing the service in an individual patient. There is at least moderate certainty that the net benefit is small. |
| D Recommendation: The Task Force recommends against the service. There is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits. |
| I Recommendation: The Task Force concludes that the current evidence is insufficient to assess the balance of benefits and harms of the service. Evidence is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined. |
TABLE 2
Summary of new USPSTF recommendations
| A RECOMMENDATIONS |
The USPSTF recommends routinely:
|
| B RECOMMENDATIONS |
The USPSTF recommends routinely:
|
| C RECOMMENDATIONS |
The USPSTF recommends against routine:
|
| D RECOMMENDATIONS |
The USPSTF recommends against routine:
|
| I RECOMMENDATIONS |
The USPSTF concludes that the current evidence is insufficient to recommend for or against routine:
|
Continue to screen for HTN, sickle cell, Chlamydia
The latest A and B recommendations from the Task Force largely reaffirm previous recommendations. These recommendations cover hypertension, sickle cell disease, and Chlamydia.
Hypertension. Screening and treatment of hypertension in adults leads to lower morbidity and mortality from cardiovascular disease and is still recommended.2
Sickle cell disease. Screening newborns for sickle cell disease and treating those affected with oral prophylactic penicillin prevents serious bacterial infections. It also remains a recommended service.3
Chlamydia. Following a review of the evidence, the Task Force reconfirms the benefits of screening for Chlamydia in sexually active young women, but it has changed the age cutoff. In 2001, the Task Force indicated that sexually active women who were 25 years of age and younger should be screened. In 2007, the Task Force dropped the age to 24 and younger.
The latest recommendation reaffirms the need to screen women (above the cutoff) who are at risk—that is, women who have previously had a sexually transmitted infection (STI), those who have a new or multiple sex partners, and those who exchange sex for money or drugs.4 Screening is recommended annually; nucleic acid amplification tests are acceptable, allowing testing of urine or vaginal swabs.
Screening during pregnancy is recommended for the same groups—women who are 24 and younger and older women at risk—at the first prenatal visit and again in the third trimester if risk continues. Chlamydia is the most common bacterial STI, and screening and treatment prevents pelvic inflammatory disease in women and leads to improved pregnancy outcomes.
Interventions that are not recommended
Chemopreventon of colorectal cancer. For the first time, the Task Force issued a recommendation on the use of aspirin or other NSAIDs to prevent CRC. The Task Force does not recommend the routine use of these agents.5 The dosage needed to prevent CRC is higher than that which prevents cardiovascular disease and can cause significant harm.
Aspirin use is associated with gastrointestinal bleeding and hemorrhagic stroke; NSAID use is associated with gastrointestinal bleeding and renal impairment. The Task Force concludes that in the general adult population, potential harms exceed potential benefits.
Screening for carotid artery stenosis. In 1996, the Task Force found insufficient evidence to recommend for or against routine screening for carotid artery stenosis. In 2007, the Task Force made a recommendation against routine screening for carotid artery stenosis.6 Screening with duplex ultrasonography results in frequent false positives. Confirmatory testing with angiography is associated with a 1% rate of stroke. Endarterectomy itself has a death or stroke rate of about 3%.
In the general population, close to 8700 adults would need to be screened to prevent 1 disabling stroke. The Task Force indicates that primary care physicians would have better outcomes by concentrating on optimal management of risk factors for cerebral artery disease.
Screening for bacterial vaginosis among low-risk pregnant women. The final D recommendation pertains to screening for bacterial vaginosis during pregnancy to prevent preterm delivery.7 Pregnant women who have not had a previous preterm delivery are considered at low risk for preterm delivery and there is good evidence that this group does not benefit from screening for, or treatment of, asymptomatic bacterial vaginosis. (A similar recommendation was made in 2001, but it referred to women of “average” risk.)
Insufficient evidence to make a recommendation
Routinely screening men for Chlamydia. While it makes clinical sense to test and treat male partners of women with Chlamydia infection, the Task Force could not find evidence of the effectiveness of routinely screening men as a way to prevent infection in women.4 That said, the Task Force points out that screening men is relatively inexpensive and has negligible harms.
Screening for hyperlipidemia in children. While 50% of children with hyperlipidemia continue to have this disorder as adults, the long-term benefits and harms of early detection and treatment with medications and lipid-lowering diets have not been studied.8 This echoes the position the Task Force took in 1996, when it commented on children as part of an adult hyperlipidemia recommendation.
Physician counseling on drinking and driving. Motor vehicle crashes result in significant morbidity and mortality—especially among adolescents and young adults. Improved car and road design, as well as public health safety efforts, have led to significant improvements in motor vehicle safety. While avoidance of driving under the influence and proper use of occupant restraints are important public health goals, the Task Force, in this first recommendation on the subject, could find no evidence that physician counseling added benefit above those provided by community-wide efforts.9
Screening for bacterial vaginosis in pregnant women at high risk for preterm birth. As mentioned previously, screening low-risk pregnant women for bacterial vaginosis results in no benefit. The issue is less clear cut among women at high risk for a preterm delivery—that is, those who have had one previously.
The evidence regarding screening and treating asymptomatic bacterial vaginosis as a means of preventing preterm delivery in these women is mixed and the Task Force was unable to recommend for or against this practice.7 This reaffirms the Task Force’s 2001 recommendation.
Screening for illicit drug use. The Task Force recognizes that illicit drug use is a major cause of illness and social problems. It would appear to have great potential for early detection and intervention. However, the Task Force, in this first-time recommendation, found that screening tools have not been well studied, nor have the long-term effects of different treatment strategies.10 These are high priority areas for future research.
Correspondence
Doug Campos-Outcalt, MD, MPA, 550 E. Van Buren, Phoenix, AZ 85004; [email protected]
1. Agency for Healthcare Quality and Research. USPSTF. Available at: http://www.ahrq.gov/clinic/uspstfix.htm. Accessed May 5, 2008.
2. USPSTF. Screening for High Blood Pressure. Available at: http://www.ahrq.gov/clinic/uspstf/uspshype.htm. Accessed May 5, 2008.
3. USPSTF. Screening for Sickle Cell Disease in Newborns. Available at: http://www.ahrq.gov/clinic/uspstf/uspshemo.htm. Accessed May 5, 2008.
4. USPSTF. Screening for Chlamydia Infection. Available at: http://www.ahrq.gov/clinic/uspstf/uspschlm.htm. Accessed May 5, 2008.
5. USPSTF. Aspirin or Nonsteroidal Anti-inflamatory Drugs for the Primary Prevention of Colorectal Cancer. Available at: http://www.ahrq.gov/clinic/uspstf/uspsasco.htm. Accessed May 5, 2008.
6. USPSTF. Screening for Carotid Artery Stenosis. Available at: http://www.ahrq.gov/clinic/uspstf/uspsacas.htm. Accessed May 5, 2008.
7. USPSTF. Screening for Bacterial Vaginosis in Pregnancy. Available at: http://www.ahrq.gov/clinic/uspstf/uspsbvag.htm. Accessed May 5, 2008.
8. USPSTF. Screening for Lipid Disorders in Children. Available at: http://www.ahrq.gov/clinic/uspstf/uspschlip.htm. Accessed May 5, 2008.
9. USPSTF. Counseling About Proper Use of Motor Vehicle Occupant Restraints and Avoidance of Alcohol Use While Driving. Available at: http://www.ahrq.gov/clinic/uspstf/uspsmvin.htm. Accessed May 5, 2008.
10. USPSTF. Screening for Illicit Drug Use. Available at: http://www.ahrq.gov/clinic/uspstf/uspsdrug.htm. Accessed May 5, 2008.
1. Agency for Healthcare Quality and Research. USPSTF. Available at: http://www.ahrq.gov/clinic/uspstfix.htm. Accessed May 5, 2008.
2. USPSTF. Screening for High Blood Pressure. Available at: http://www.ahrq.gov/clinic/uspstf/uspshype.htm. Accessed May 5, 2008.
3. USPSTF. Screening for Sickle Cell Disease in Newborns. Available at: http://www.ahrq.gov/clinic/uspstf/uspshemo.htm. Accessed May 5, 2008.
4. USPSTF. Screening for Chlamydia Infection. Available at: http://www.ahrq.gov/clinic/uspstf/uspschlm.htm. Accessed May 5, 2008.
5. USPSTF. Aspirin or Nonsteroidal Anti-inflamatory Drugs for the Primary Prevention of Colorectal Cancer. Available at: http://www.ahrq.gov/clinic/uspstf/uspsasco.htm. Accessed May 5, 2008.
6. USPSTF. Screening for Carotid Artery Stenosis. Available at: http://www.ahrq.gov/clinic/uspstf/uspsacas.htm. Accessed May 5, 2008.
7. USPSTF. Screening for Bacterial Vaginosis in Pregnancy. Available at: http://www.ahrq.gov/clinic/uspstf/uspsbvag.htm. Accessed May 5, 2008.
8. USPSTF. Screening for Lipid Disorders in Children. Available at: http://www.ahrq.gov/clinic/uspstf/uspschlip.htm. Accessed May 5, 2008.
9. USPSTF. Counseling About Proper Use of Motor Vehicle Occupant Restraints and Avoidance of Alcohol Use While Driving. Available at: http://www.ahrq.gov/clinic/uspstf/uspsmvin.htm. Accessed May 5, 2008.
10. USPSTF. Screening for Illicit Drug Use. Available at: http://www.ahrq.gov/clinic/uspstf/uspsdrug.htm. Accessed May 5, 2008.
Extended-release fluvoxamine for social anxiety disorder and OCD
Fluvoxamine extended-release formulation was FDA-approved to treat generalized social anxiety disorder (GSAD) and obsessive-compulsive disorder (OCD) because it demonstrated efficacy in reducing anxiety symptoms of these disorders in 3 clinical trials. The new formulation may benefit patients unable to tolerate the existing immediate-release form.
Clinical implications
Like other selective serotonin reuptake inhibitors (SSRIs), fluvoxamine alleviates symptoms of GSAD and OCD. The extended-release formulation allows the medication to be administered once daily (Table 1) and, according to the manufacturer, may reduce side effects and improve tolerability.
Many clinicians have prescribed immediate-release fluvoxamine once daily, and the efficacy and tolerability of the immediate- and extended-release formulations have not been compared in head-to-head trials. In addition, no studies have examined the efficacy of extended-release fluvoxamine in treating other psychiatric conditions.
Table 1
Extended-release fluvoxamine: Fast facts
| Brand name: Luvox CR |
| Class: Selective serotonin reuptake inhibitor |
| Indication: Generalized social anxiety disorder and obsessive-compulsive disorder |
| Approval date: February 29, 2008 |
| Availability date: March 2008 |
| Manufacturer: Jazz Pharmaceuticals |
| Dosing forms: 100 mg and 150 mg extended-release capsules |
| Recommended dose: Starting dose: 100 mg/d. Titrate in 50-mg/week increments until maximum therapeutic benefit is achieved. Maximum recommended dose: 300 mg/d |
How it works
Decreased serotonin levels are associated with GSAD and OCD. Fluvoxamine’s therapeutic effect is thought to be mediated through its specific serotonin reuptake inhibition in the CNS.1
The drug acts primarily on serotonin 2C receptors, with no reported significant affinity for histaminergic, adrenergic, muscarinic, or dopaminergic receptors.1 Fluvoxamine’s 1-sigma receptor antagonism is unique among SSRIs, and researchers have suggested that this may make fluvoxamine more effective than other SSRIs in treating anxious or delusional depression.2
The extended-release formulation uses a spheroidal oral drug absorption system, a proprietary technology that limits peak-to-trough variance for 24 hours.1 The manufacturer postulates that decreased plasma concentration variability will improve fluvoxamine’s tolerability.1
Pharmacokinetics
In a single-dose crossover study of 28 healthy subjects, the mean maximum concentration of drug (Cmax) for extended-release fluvoxamine was 38% lower than that of the immediate-release formulation, which may reduce the risk of adverse effects.1 Its relative bioavailability was 84%, and mean plasma half-life was 16.3 hours in male and female volunteers.1
Fluvoxamine is extensively metabolized in the liver, primarily through oxidative demethylation and deamination.1 Nine metabolites constitute 85% of the urinary excretion product; the main metabolite is fluvoxamine acid.1 Approximately 2% of fluvoxamine is excreted unchanged in urine. Administering extended-release fluvoxamine capsules with food does not appear to affect the drug’s absorption.1
Fluvoxamine is a potent inhibitor of the cytochrome P450 (CYP) 1A2 isoenzyme and also is believed to significantly inhibit CYP3A4, CYP2C9, CYP3A4, and CYP2C19. It is a relatively weak inhibitor of CYP2D6.1
Efficacy
The FDA based its approval of extended-release fluvoxamine on data from 3 clinical trials with positive outcomes: 2 for GSAD and 1 for OCD (Table 2).1,3-6
GSAD trials. In the first GSAD study—a randomized, double-blind, placebo-controlled, multicenter trial of 300 subjects with GSAD—participants were randomly assigned to receive extended-release fluvoxamine or placebo for 12 weeks.3 The extended-release fluvoxamine group started at 100 mg administered at night, with dosages titrated at 50 mg/week based on efficacy and tolerability to a maximum of 300 mg/d.1 Subjects in the extended-release fluvoxamine group demonstrated a statistically significant change in Liebowitz Social Anxiety Scale (LSAS) scores from baseline compared with those receiving placebo (P=0.02). Researchers observed similar results in secondary measures.
In an extension of this study, 112 subjects who demonstrated at least minimal improvement from extended-release fluvoxamine by week 12 continued the same dosing regimen for an additional 12 weeks. Investigators found the drug’s beneficial effects persisted to 24 weeks, although the magnitude of the effect decreased.4
A separate study using the same dosing regimen enrolled 279 adult patients in a 12-week, multicenter, randomized, placebo-controlled trial.5 The fluvoxamine-treated group showed statistically and clinically significant improvement:
- by week 4 on the LSAS and the Clinical Global Impression-Improvement (CGI-I) scale
- by week 6 on the Sheehan Disability Scale, Clinical Global Impression-Severity scale (CGI-S) and Patient Global Impression of Improvement (PGI) scale.5
OCD trial. Hollander et al6 conducted a 12-week, double-blind, placebo-controlled, flexible-dose, parallel multicenter trial of 253 adult patients with OCD.6 Compared with those receiving placebo, subjects treated with extended-release fluvoxamine, 100 to 300 mg/d, showed a statistically significant decrease in score on the Yale-Brown Obsessive Compulsive Scale (P=0.001).6 Analysis of the CGIS and CGI-I also revealed statistically significant improvement compared with placebo. The effect appeared to begin at week 2.
As did the GSAD studies, this study compared extended-release fluvoxamine with placebo and not with the immediate-release formulation. Although no additional studies have examined the efficacy of extended-release fluvoxamine in treating OCD and the drug has not been evaluated in pediatric patients, the manufacturer notes that the immediate-release formulation has been evaluated in 2 studies with adult OCD patients and 1 pediatric OCD study, all of which had positive results.1
Table 2
Fluvoxamine extended-release: What the evidence says
| Study | Measures used | Results |
|---|---|---|
| Generalized social anxiety disorder | ||
| Westenberg et al (2004)3 | LSAS, CGI-S, CGI-I, SDS, PGI | Fluvoxamine was significantly more effective than placebo in decreasing LSAS total score (primary measure) starting at week 4 and in improving SDS, CGI-S, and CGI-I (secondary measures) |
| Stein et al (2003)4 | LSAS, CGI-S, CGI-I, SDS, PGI | Severity of illness on the CGI-S scale and disability on the SDS were significantly lower in the fluvoxamine group than in the placebo group; fluvoxamine-treated subjects had a numerically greater decrease in LSAS total scores than subjects treated with placebo |
| Davidson et al (2004)5 | LSAS, CGI-G, SDS, CGI-S, PGI | Fluvoxamine produced statistically and clinically significant improvements in symptoms starting at week 4 on the LSAS and CGI-I and at week 6 on the SDS, CGI-S, and PGI |
| Obsessive-compulsive disorder | ||
| Hollander et al (2003)6 | YBOCS, CGI-S, CGI-I | Fluvoxamine was significantly more effective than placebo in decreasing YBOCS total score beginning at week 2 and in improving CGI-S and CGI-I scores |
| LSAS: Liebowitz Social Anxiety Scale; SDS: Sheehan Disability Scale; CGI-S: Clinical Global Impression-Severity of illness; CGI-I: Clinical Global Impression-Improvement; PGI: Patient Global Impression of Improvement; YBOCS: Yale-Brown Obsessive Compulsive Scale | ||
Tolerability
In the 3 published trials of extended-release fluvoxamine, adverse event rates were similar and consistent with earlier studies of the immediate-release formulation. 1 The manufacturer considered adverse events likely to be drug-related if they had an incidence ≥5% and at least twice that of placebo (Table 3). 1, 3- 6
Adverse events caused 26% of patients in the GSAD studies and 19% in the OCD trial to discontinue treatment. No deaths, life-threatening adverse events, or suicide attempts were reported.3-6 No statistically significant differences in weight gain or loss, vital signs, laboratory findings, or ECG changes were found between patients treated with extended-release fluvoxamine and those receiving placebo.1
Table 3
Extended-release fluvoxamine: Adverse events*
| Study | Adverse events |
|---|---|
| Both GSAD and OCD studies | Abnormal ejaculation, anorexia, anorgasmia, asthenia, diarrhea, nausea, somnolence, sweating, tremor |
| GSAD studies only | Dyspepsia, dizziness, insomnia, yawning |
| OCD study only | Accidental injury, anxiety, decreased libido, myalgia, pharyngitis, emesis |
| * Includes events with an incidence ≥5% and at least twice that of placebo GSAD: generalized social anxiety disorder; OCD: obsessive-compulsive disorder | |
| Source: References 3-6 | |
Contraindications
Immediate- and extended-release fluvoxamine have the same active ingredient and therefore the same contraindications. Coadministration of alosetron, pimozide, thioridazine, or tizanidine, is contraindicated, as is using monoamine oxidase (MAO) inhibitors with extended-release fluvoxamine or within 14 days of discontinuing fluvoxamine treatment. Extended-release fluvoxamine has the same warnings that all SSRIs share regarding clinical worsening and suicide risk, administration to bipolar patients, neuroleptic malignant syndrome, serotonin syndrome, and possible increases in coagulation.1,2
The FDA classifies extended-release fluvoxamine as pregnancy category C.1 The drug is not contraindicated for lactating mothers, but because fluvoxamine is secreted in breast milk discuss with breast-feeding patients the benefits and risks of continuing fluvoxamine therapy.1 Infants exposed to immediate-release fluvoxamine in late pregnancy have developed serious adverse reactions, including respiratory distress, cyanosis, apnea, and seizures.1
Dosing
The recommended starting dose of extended-release fluvoxamine is 100 mg once daily, with or without food.1 The dose can be titrated in 50-mg/week increments as tolerated to achieve maximum therapeutic benefit, to the maximum recommended dose of 300 mg/d. Unlike immediate-release fluvoxamine, which is occasionally split into twice-daily doses, extended-release fluvoxamine must be administered only once daily, even at high doses.1,2
Related resource
- Luvox CR prescribing information. www.jazzpharmaceuticals.com/content/news/documents/LUVOX_CR.pdf.
Drug brand names
- Alosetron • Lotronex
- Fluvoxamine • Luvox
- Fluvoxamine extended-release • Luvox CR
- Pimozide • Orap
- Thioridazine • Mellaril
- Tizanidine • Zanaflex
Disclosures
Dr. Kuzma reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
1. Luvox CR [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2008.
2. Stahl SM. Essential psychopharmacology: the prescriber’s guide. Revised and updated edition. New York, NY: Cambridge University Press; 2006.
3. Westenberg HG, Stein DJ, Yang H, et al. A double-blind placebo-controlled study of controlled release fluvoxamine for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(1):49-55.
4. Stein DJ, Westenberg HG, Yang H, et al. Fluvoxamine CR in the long-term treatment of social anxiety disorder: the 12- to 24-week extension phase of a multicentre, randomized, placebo-controlled trial. Int J Neuropsychopharmacol 2003;6(4):317-23.
5. Davidson J, Yaryura-Tobias J, DuPont R, et al. Fluvoxamine-controlled release formulation for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(2):118-25.
6. Hollander E, Koran LM, Goodman WK, et al. A double-blind, placebo-controlled study of the efficacy and safety of controlled-release fluvoxamine in patients with obsessive-compulsive disorder. J Clin Psychiatry 2003;64(6):640-7.
Fluvoxamine extended-release formulation was FDA-approved to treat generalized social anxiety disorder (GSAD) and obsessive-compulsive disorder (OCD) because it demonstrated efficacy in reducing anxiety symptoms of these disorders in 3 clinical trials. The new formulation may benefit patients unable to tolerate the existing immediate-release form.
Clinical implications
Like other selective serotonin reuptake inhibitors (SSRIs), fluvoxamine alleviates symptoms of GSAD and OCD. The extended-release formulation allows the medication to be administered once daily (Table 1) and, according to the manufacturer, may reduce side effects and improve tolerability.
Many clinicians have prescribed immediate-release fluvoxamine once daily, and the efficacy and tolerability of the immediate- and extended-release formulations have not been compared in head-to-head trials. In addition, no studies have examined the efficacy of extended-release fluvoxamine in treating other psychiatric conditions.
Table 1
Extended-release fluvoxamine: Fast facts
| Brand name: Luvox CR |
| Class: Selective serotonin reuptake inhibitor |
| Indication: Generalized social anxiety disorder and obsessive-compulsive disorder |
| Approval date: February 29, 2008 |
| Availability date: March 2008 |
| Manufacturer: Jazz Pharmaceuticals |
| Dosing forms: 100 mg and 150 mg extended-release capsules |
| Recommended dose: Starting dose: 100 mg/d. Titrate in 50-mg/week increments until maximum therapeutic benefit is achieved. Maximum recommended dose: 300 mg/d |
How it works
Decreased serotonin levels are associated with GSAD and OCD. Fluvoxamine’s therapeutic effect is thought to be mediated through its specific serotonin reuptake inhibition in the CNS.1
The drug acts primarily on serotonin 2C receptors, with no reported significant affinity for histaminergic, adrenergic, muscarinic, or dopaminergic receptors.1 Fluvoxamine’s 1-sigma receptor antagonism is unique among SSRIs, and researchers have suggested that this may make fluvoxamine more effective than other SSRIs in treating anxious or delusional depression.2
The extended-release formulation uses a spheroidal oral drug absorption system, a proprietary technology that limits peak-to-trough variance for 24 hours.1 The manufacturer postulates that decreased plasma concentration variability will improve fluvoxamine’s tolerability.1
Pharmacokinetics
In a single-dose crossover study of 28 healthy subjects, the mean maximum concentration of drug (Cmax) for extended-release fluvoxamine was 38% lower than that of the immediate-release formulation, which may reduce the risk of adverse effects.1 Its relative bioavailability was 84%, and mean plasma half-life was 16.3 hours in male and female volunteers.1
Fluvoxamine is extensively metabolized in the liver, primarily through oxidative demethylation and deamination.1 Nine metabolites constitute 85% of the urinary excretion product; the main metabolite is fluvoxamine acid.1 Approximately 2% of fluvoxamine is excreted unchanged in urine. Administering extended-release fluvoxamine capsules with food does not appear to affect the drug’s absorption.1
Fluvoxamine is a potent inhibitor of the cytochrome P450 (CYP) 1A2 isoenzyme and also is believed to significantly inhibit CYP3A4, CYP2C9, CYP3A4, and CYP2C19. It is a relatively weak inhibitor of CYP2D6.1
Efficacy
The FDA based its approval of extended-release fluvoxamine on data from 3 clinical trials with positive outcomes: 2 for GSAD and 1 for OCD (Table 2).1,3-6
GSAD trials. In the first GSAD study—a randomized, double-blind, placebo-controlled, multicenter trial of 300 subjects with GSAD—participants were randomly assigned to receive extended-release fluvoxamine or placebo for 12 weeks.3 The extended-release fluvoxamine group started at 100 mg administered at night, with dosages titrated at 50 mg/week based on efficacy and tolerability to a maximum of 300 mg/d.1 Subjects in the extended-release fluvoxamine group demonstrated a statistically significant change in Liebowitz Social Anxiety Scale (LSAS) scores from baseline compared with those receiving placebo (P=0.02). Researchers observed similar results in secondary measures.
In an extension of this study, 112 subjects who demonstrated at least minimal improvement from extended-release fluvoxamine by week 12 continued the same dosing regimen for an additional 12 weeks. Investigators found the drug’s beneficial effects persisted to 24 weeks, although the magnitude of the effect decreased.4
A separate study using the same dosing regimen enrolled 279 adult patients in a 12-week, multicenter, randomized, placebo-controlled trial.5 The fluvoxamine-treated group showed statistically and clinically significant improvement:
- by week 4 on the LSAS and the Clinical Global Impression-Improvement (CGI-I) scale
- by week 6 on the Sheehan Disability Scale, Clinical Global Impression-Severity scale (CGI-S) and Patient Global Impression of Improvement (PGI) scale.5
OCD trial. Hollander et al6 conducted a 12-week, double-blind, placebo-controlled, flexible-dose, parallel multicenter trial of 253 adult patients with OCD.6 Compared with those receiving placebo, subjects treated with extended-release fluvoxamine, 100 to 300 mg/d, showed a statistically significant decrease in score on the Yale-Brown Obsessive Compulsive Scale (P=0.001).6 Analysis of the CGIS and CGI-I also revealed statistically significant improvement compared with placebo. The effect appeared to begin at week 2.
As did the GSAD studies, this study compared extended-release fluvoxamine with placebo and not with the immediate-release formulation. Although no additional studies have examined the efficacy of extended-release fluvoxamine in treating OCD and the drug has not been evaluated in pediatric patients, the manufacturer notes that the immediate-release formulation has been evaluated in 2 studies with adult OCD patients and 1 pediatric OCD study, all of which had positive results.1
Table 2
Fluvoxamine extended-release: What the evidence says
| Study | Measures used | Results |
|---|---|---|
| Generalized social anxiety disorder | ||
| Westenberg et al (2004)3 | LSAS, CGI-S, CGI-I, SDS, PGI | Fluvoxamine was significantly more effective than placebo in decreasing LSAS total score (primary measure) starting at week 4 and in improving SDS, CGI-S, and CGI-I (secondary measures) |
| Stein et al (2003)4 | LSAS, CGI-S, CGI-I, SDS, PGI | Severity of illness on the CGI-S scale and disability on the SDS were significantly lower in the fluvoxamine group than in the placebo group; fluvoxamine-treated subjects had a numerically greater decrease in LSAS total scores than subjects treated with placebo |
| Davidson et al (2004)5 | LSAS, CGI-G, SDS, CGI-S, PGI | Fluvoxamine produced statistically and clinically significant improvements in symptoms starting at week 4 on the LSAS and CGI-I and at week 6 on the SDS, CGI-S, and PGI |
| Obsessive-compulsive disorder | ||
| Hollander et al (2003)6 | YBOCS, CGI-S, CGI-I | Fluvoxamine was significantly more effective than placebo in decreasing YBOCS total score beginning at week 2 and in improving CGI-S and CGI-I scores |
| LSAS: Liebowitz Social Anxiety Scale; SDS: Sheehan Disability Scale; CGI-S: Clinical Global Impression-Severity of illness; CGI-I: Clinical Global Impression-Improvement; PGI: Patient Global Impression of Improvement; YBOCS: Yale-Brown Obsessive Compulsive Scale | ||
Tolerability
In the 3 published trials of extended-release fluvoxamine, adverse event rates were similar and consistent with earlier studies of the immediate-release formulation. 1 The manufacturer considered adverse events likely to be drug-related if they had an incidence ≥5% and at least twice that of placebo (Table 3). 1, 3- 6
Adverse events caused 26% of patients in the GSAD studies and 19% in the OCD trial to discontinue treatment. No deaths, life-threatening adverse events, or suicide attempts were reported.3-6 No statistically significant differences in weight gain or loss, vital signs, laboratory findings, or ECG changes were found between patients treated with extended-release fluvoxamine and those receiving placebo.1
Table 3
Extended-release fluvoxamine: Adverse events*
| Study | Adverse events |
|---|---|
| Both GSAD and OCD studies | Abnormal ejaculation, anorexia, anorgasmia, asthenia, diarrhea, nausea, somnolence, sweating, tremor |
| GSAD studies only | Dyspepsia, dizziness, insomnia, yawning |
| OCD study only | Accidental injury, anxiety, decreased libido, myalgia, pharyngitis, emesis |
| * Includes events with an incidence ≥5% and at least twice that of placebo GSAD: generalized social anxiety disorder; OCD: obsessive-compulsive disorder | |
| Source: References 3-6 | |
Contraindications
Immediate- and extended-release fluvoxamine have the same active ingredient and therefore the same contraindications. Coadministration of alosetron, pimozide, thioridazine, or tizanidine, is contraindicated, as is using monoamine oxidase (MAO) inhibitors with extended-release fluvoxamine or within 14 days of discontinuing fluvoxamine treatment. Extended-release fluvoxamine has the same warnings that all SSRIs share regarding clinical worsening and suicide risk, administration to bipolar patients, neuroleptic malignant syndrome, serotonin syndrome, and possible increases in coagulation.1,2
The FDA classifies extended-release fluvoxamine as pregnancy category C.1 The drug is not contraindicated for lactating mothers, but because fluvoxamine is secreted in breast milk discuss with breast-feeding patients the benefits and risks of continuing fluvoxamine therapy.1 Infants exposed to immediate-release fluvoxamine in late pregnancy have developed serious adverse reactions, including respiratory distress, cyanosis, apnea, and seizures.1
Dosing
The recommended starting dose of extended-release fluvoxamine is 100 mg once daily, with or without food.1 The dose can be titrated in 50-mg/week increments as tolerated to achieve maximum therapeutic benefit, to the maximum recommended dose of 300 mg/d. Unlike immediate-release fluvoxamine, which is occasionally split into twice-daily doses, extended-release fluvoxamine must be administered only once daily, even at high doses.1,2
Related resource
- Luvox CR prescribing information. www.jazzpharmaceuticals.com/content/news/documents/LUVOX_CR.pdf.
Drug brand names
- Alosetron • Lotronex
- Fluvoxamine • Luvox
- Fluvoxamine extended-release • Luvox CR
- Pimozide • Orap
- Thioridazine • Mellaril
- Tizanidine • Zanaflex
Disclosures
Dr. Kuzma reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
Fluvoxamine extended-release formulation was FDA-approved to treat generalized social anxiety disorder (GSAD) and obsessive-compulsive disorder (OCD) because it demonstrated efficacy in reducing anxiety symptoms of these disorders in 3 clinical trials. The new formulation may benefit patients unable to tolerate the existing immediate-release form.
Clinical implications
Like other selective serotonin reuptake inhibitors (SSRIs), fluvoxamine alleviates symptoms of GSAD and OCD. The extended-release formulation allows the medication to be administered once daily (Table 1) and, according to the manufacturer, may reduce side effects and improve tolerability.
Many clinicians have prescribed immediate-release fluvoxamine once daily, and the efficacy and tolerability of the immediate- and extended-release formulations have not been compared in head-to-head trials. In addition, no studies have examined the efficacy of extended-release fluvoxamine in treating other psychiatric conditions.
Table 1
Extended-release fluvoxamine: Fast facts
| Brand name: Luvox CR |
| Class: Selective serotonin reuptake inhibitor |
| Indication: Generalized social anxiety disorder and obsessive-compulsive disorder |
| Approval date: February 29, 2008 |
| Availability date: March 2008 |
| Manufacturer: Jazz Pharmaceuticals |
| Dosing forms: 100 mg and 150 mg extended-release capsules |
| Recommended dose: Starting dose: 100 mg/d. Titrate in 50-mg/week increments until maximum therapeutic benefit is achieved. Maximum recommended dose: 300 mg/d |
How it works
Decreased serotonin levels are associated with GSAD and OCD. Fluvoxamine’s therapeutic effect is thought to be mediated through its specific serotonin reuptake inhibition in the CNS.1
The drug acts primarily on serotonin 2C receptors, with no reported significant affinity for histaminergic, adrenergic, muscarinic, or dopaminergic receptors.1 Fluvoxamine’s 1-sigma receptor antagonism is unique among SSRIs, and researchers have suggested that this may make fluvoxamine more effective than other SSRIs in treating anxious or delusional depression.2
The extended-release formulation uses a spheroidal oral drug absorption system, a proprietary technology that limits peak-to-trough variance for 24 hours.1 The manufacturer postulates that decreased plasma concentration variability will improve fluvoxamine’s tolerability.1
Pharmacokinetics
In a single-dose crossover study of 28 healthy subjects, the mean maximum concentration of drug (Cmax) for extended-release fluvoxamine was 38% lower than that of the immediate-release formulation, which may reduce the risk of adverse effects.1 Its relative bioavailability was 84%, and mean plasma half-life was 16.3 hours in male and female volunteers.1
Fluvoxamine is extensively metabolized in the liver, primarily through oxidative demethylation and deamination.1 Nine metabolites constitute 85% of the urinary excretion product; the main metabolite is fluvoxamine acid.1 Approximately 2% of fluvoxamine is excreted unchanged in urine. Administering extended-release fluvoxamine capsules with food does not appear to affect the drug’s absorption.1
Fluvoxamine is a potent inhibitor of the cytochrome P450 (CYP) 1A2 isoenzyme and also is believed to significantly inhibit CYP3A4, CYP2C9, CYP3A4, and CYP2C19. It is a relatively weak inhibitor of CYP2D6.1
Efficacy
The FDA based its approval of extended-release fluvoxamine on data from 3 clinical trials with positive outcomes: 2 for GSAD and 1 for OCD (Table 2).1,3-6
GSAD trials. In the first GSAD study—a randomized, double-blind, placebo-controlled, multicenter trial of 300 subjects with GSAD—participants were randomly assigned to receive extended-release fluvoxamine or placebo for 12 weeks.3 The extended-release fluvoxamine group started at 100 mg administered at night, with dosages titrated at 50 mg/week based on efficacy and tolerability to a maximum of 300 mg/d.1 Subjects in the extended-release fluvoxamine group demonstrated a statistically significant change in Liebowitz Social Anxiety Scale (LSAS) scores from baseline compared with those receiving placebo (P=0.02). Researchers observed similar results in secondary measures.
In an extension of this study, 112 subjects who demonstrated at least minimal improvement from extended-release fluvoxamine by week 12 continued the same dosing regimen for an additional 12 weeks. Investigators found the drug’s beneficial effects persisted to 24 weeks, although the magnitude of the effect decreased.4
A separate study using the same dosing regimen enrolled 279 adult patients in a 12-week, multicenter, randomized, placebo-controlled trial.5 The fluvoxamine-treated group showed statistically and clinically significant improvement:
- by week 4 on the LSAS and the Clinical Global Impression-Improvement (CGI-I) scale
- by week 6 on the Sheehan Disability Scale, Clinical Global Impression-Severity scale (CGI-S) and Patient Global Impression of Improvement (PGI) scale.5
OCD trial. Hollander et al6 conducted a 12-week, double-blind, placebo-controlled, flexible-dose, parallel multicenter trial of 253 adult patients with OCD.6 Compared with those receiving placebo, subjects treated with extended-release fluvoxamine, 100 to 300 mg/d, showed a statistically significant decrease in score on the Yale-Brown Obsessive Compulsive Scale (P=0.001).6 Analysis of the CGIS and CGI-I also revealed statistically significant improvement compared with placebo. The effect appeared to begin at week 2.
As did the GSAD studies, this study compared extended-release fluvoxamine with placebo and not with the immediate-release formulation. Although no additional studies have examined the efficacy of extended-release fluvoxamine in treating OCD and the drug has not been evaluated in pediatric patients, the manufacturer notes that the immediate-release formulation has been evaluated in 2 studies with adult OCD patients and 1 pediatric OCD study, all of which had positive results.1
Table 2
Fluvoxamine extended-release: What the evidence says
| Study | Measures used | Results |
|---|---|---|
| Generalized social anxiety disorder | ||
| Westenberg et al (2004)3 | LSAS, CGI-S, CGI-I, SDS, PGI | Fluvoxamine was significantly more effective than placebo in decreasing LSAS total score (primary measure) starting at week 4 and in improving SDS, CGI-S, and CGI-I (secondary measures) |
| Stein et al (2003)4 | LSAS, CGI-S, CGI-I, SDS, PGI | Severity of illness on the CGI-S scale and disability on the SDS were significantly lower in the fluvoxamine group than in the placebo group; fluvoxamine-treated subjects had a numerically greater decrease in LSAS total scores than subjects treated with placebo |
| Davidson et al (2004)5 | LSAS, CGI-G, SDS, CGI-S, PGI | Fluvoxamine produced statistically and clinically significant improvements in symptoms starting at week 4 on the LSAS and CGI-I and at week 6 on the SDS, CGI-S, and PGI |
| Obsessive-compulsive disorder | ||
| Hollander et al (2003)6 | YBOCS, CGI-S, CGI-I | Fluvoxamine was significantly more effective than placebo in decreasing YBOCS total score beginning at week 2 and in improving CGI-S and CGI-I scores |
| LSAS: Liebowitz Social Anxiety Scale; SDS: Sheehan Disability Scale; CGI-S: Clinical Global Impression-Severity of illness; CGI-I: Clinical Global Impression-Improvement; PGI: Patient Global Impression of Improvement; YBOCS: Yale-Brown Obsessive Compulsive Scale | ||
Tolerability
In the 3 published trials of extended-release fluvoxamine, adverse event rates were similar and consistent with earlier studies of the immediate-release formulation. 1 The manufacturer considered adverse events likely to be drug-related if they had an incidence ≥5% and at least twice that of placebo (Table 3). 1, 3- 6
Adverse events caused 26% of patients in the GSAD studies and 19% in the OCD trial to discontinue treatment. No deaths, life-threatening adverse events, or suicide attempts were reported.3-6 No statistically significant differences in weight gain or loss, vital signs, laboratory findings, or ECG changes were found between patients treated with extended-release fluvoxamine and those receiving placebo.1
Table 3
Extended-release fluvoxamine: Adverse events*
| Study | Adverse events |
|---|---|
| Both GSAD and OCD studies | Abnormal ejaculation, anorexia, anorgasmia, asthenia, diarrhea, nausea, somnolence, sweating, tremor |
| GSAD studies only | Dyspepsia, dizziness, insomnia, yawning |
| OCD study only | Accidental injury, anxiety, decreased libido, myalgia, pharyngitis, emesis |
| * Includes events with an incidence ≥5% and at least twice that of placebo GSAD: generalized social anxiety disorder; OCD: obsessive-compulsive disorder | |
| Source: References 3-6 | |
Contraindications
Immediate- and extended-release fluvoxamine have the same active ingredient and therefore the same contraindications. Coadministration of alosetron, pimozide, thioridazine, or tizanidine, is contraindicated, as is using monoamine oxidase (MAO) inhibitors with extended-release fluvoxamine or within 14 days of discontinuing fluvoxamine treatment. Extended-release fluvoxamine has the same warnings that all SSRIs share regarding clinical worsening and suicide risk, administration to bipolar patients, neuroleptic malignant syndrome, serotonin syndrome, and possible increases in coagulation.1,2
The FDA classifies extended-release fluvoxamine as pregnancy category C.1 The drug is not contraindicated for lactating mothers, but because fluvoxamine is secreted in breast milk discuss with breast-feeding patients the benefits and risks of continuing fluvoxamine therapy.1 Infants exposed to immediate-release fluvoxamine in late pregnancy have developed serious adverse reactions, including respiratory distress, cyanosis, apnea, and seizures.1
Dosing
The recommended starting dose of extended-release fluvoxamine is 100 mg once daily, with or without food.1 The dose can be titrated in 50-mg/week increments as tolerated to achieve maximum therapeutic benefit, to the maximum recommended dose of 300 mg/d. Unlike immediate-release fluvoxamine, which is occasionally split into twice-daily doses, extended-release fluvoxamine must be administered only once daily, even at high doses.1,2
Related resource
- Luvox CR prescribing information. www.jazzpharmaceuticals.com/content/news/documents/LUVOX_CR.pdf.
Drug brand names
- Alosetron • Lotronex
- Fluvoxamine • Luvox
- Fluvoxamine extended-release • Luvox CR
- Pimozide • Orap
- Thioridazine • Mellaril
- Tizanidine • Zanaflex
Disclosures
Dr. Kuzma reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Black receives research/grant support from Forest Laboratories and is a consultant to Jazz Pharmaceuticals.
1. Luvox CR [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2008.
2. Stahl SM. Essential psychopharmacology: the prescriber’s guide. Revised and updated edition. New York, NY: Cambridge University Press; 2006.
3. Westenberg HG, Stein DJ, Yang H, et al. A double-blind placebo-controlled study of controlled release fluvoxamine for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(1):49-55.
4. Stein DJ, Westenberg HG, Yang H, et al. Fluvoxamine CR in the long-term treatment of social anxiety disorder: the 12- to 24-week extension phase of a multicentre, randomized, placebo-controlled trial. Int J Neuropsychopharmacol 2003;6(4):317-23.
5. Davidson J, Yaryura-Tobias J, DuPont R, et al. Fluvoxamine-controlled release formulation for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(2):118-25.
6. Hollander E, Koran LM, Goodman WK, et al. A double-blind, placebo-controlled study of the efficacy and safety of controlled-release fluvoxamine in patients with obsessive-compulsive disorder. J Clin Psychiatry 2003;64(6):640-7.
1. Luvox CR [package insert]. Palo Alto, CA: Jazz Pharmaceuticals; 2008.
2. Stahl SM. Essential psychopharmacology: the prescriber’s guide. Revised and updated edition. New York, NY: Cambridge University Press; 2006.
3. Westenberg HG, Stein DJ, Yang H, et al. A double-blind placebo-controlled study of controlled release fluvoxamine for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(1):49-55.
4. Stein DJ, Westenberg HG, Yang H, et al. Fluvoxamine CR in the long-term treatment of social anxiety disorder: the 12- to 24-week extension phase of a multicentre, randomized, placebo-controlled trial. Int J Neuropsychopharmacol 2003;6(4):317-23.
5. Davidson J, Yaryura-Tobias J, DuPont R, et al. Fluvoxamine-controlled release formulation for the treatment of generalized social anxiety disorder. J Clin Psychopharmacol 2004;24(2):118-25.
6. Hollander E, Koran LM, Goodman WK, et al. A double-blind, placebo-controlled study of the efficacy and safety of controlled-release fluvoxamine in patients with obsessive-compulsive disorder. J Clin Psychiatry 2003;64(6):640-7.
Newly identified NHP2 biallelic mutation can cause dyskeratosis congenita

Copenhagen— Researchers have identified a new biallelic mutation in the telomerase component NHP2, which can cause the premature aging syndrome dyskeratosis congenita.
Thomas J. Vulliamy, PhD, MRCPath, from Barts and the London School of Medicine and Dentistry, presented this finding at the 13th Congress of the European Hematology Association.
Dyskeratosis congenita is a genetically heterogeneous, multisystem disorder. The unifying feature of dyskeratosis congenita is that all mutations identified thus far affect molecules involved in telomere maintenance. Defective telomerase leads to premature aging, bone marrow failure, and a predisposition to 32 cancers.
Investigators analyzed the proteins NHP2 and GAR1 using high performance liquid chromatography screening followed by direct DNA sequencing. NHP2 and GAR1 are key components of telomerase, along with dyskerin and NOP10, and small nucleolar ribonucleoprotein (snoRNP) complexes.
Investigators measured telomere lengths by Southern blot analysis and assessed TERC levels and the effects of siRNA knockdown of gene transcripts using quantitative real-time PCR.
Dr Vulliamy and colleagues found that mutations in NHP2 can cause autosomal recessive dyskeratosis congenita. Patients with NHP2, dyskerin, and NOP10 mutations have short telomeres and low TERC levels.
Investigators concluded that this provided direct evidence of their role in telomere maintenance in humans. They did not find any GAR1 mutations, suggesting that GAR1 has a different impact on the accumulation of TERC.
This abstract was chosen as one of the 5 best of the Congress. ![]()

Copenhagen— Researchers have identified a new biallelic mutation in the telomerase component NHP2, which can cause the premature aging syndrome dyskeratosis congenita.
Thomas J. Vulliamy, PhD, MRCPath, from Barts and the London School of Medicine and Dentistry, presented this finding at the 13th Congress of the European Hematology Association.
Dyskeratosis congenita is a genetically heterogeneous, multisystem disorder. The unifying feature of dyskeratosis congenita is that all mutations identified thus far affect molecules involved in telomere maintenance. Defective telomerase leads to premature aging, bone marrow failure, and a predisposition to 32 cancers.
Investigators analyzed the proteins NHP2 and GAR1 using high performance liquid chromatography screening followed by direct DNA sequencing. NHP2 and GAR1 are key components of telomerase, along with dyskerin and NOP10, and small nucleolar ribonucleoprotein (snoRNP) complexes.
Investigators measured telomere lengths by Southern blot analysis and assessed TERC levels and the effects of siRNA knockdown of gene transcripts using quantitative real-time PCR.
Dr Vulliamy and colleagues found that mutations in NHP2 can cause autosomal recessive dyskeratosis congenita. Patients with NHP2, dyskerin, and NOP10 mutations have short telomeres and low TERC levels.
Investigators concluded that this provided direct evidence of their role in telomere maintenance in humans. They did not find any GAR1 mutations, suggesting that GAR1 has a different impact on the accumulation of TERC.
This abstract was chosen as one of the 5 best of the Congress. ![]()

Copenhagen— Researchers have identified a new biallelic mutation in the telomerase component NHP2, which can cause the premature aging syndrome dyskeratosis congenita.
Thomas J. Vulliamy, PhD, MRCPath, from Barts and the London School of Medicine and Dentistry, presented this finding at the 13th Congress of the European Hematology Association.
Dyskeratosis congenita is a genetically heterogeneous, multisystem disorder. The unifying feature of dyskeratosis congenita is that all mutations identified thus far affect molecules involved in telomere maintenance. Defective telomerase leads to premature aging, bone marrow failure, and a predisposition to 32 cancers.
Investigators analyzed the proteins NHP2 and GAR1 using high performance liquid chromatography screening followed by direct DNA sequencing. NHP2 and GAR1 are key components of telomerase, along with dyskerin and NOP10, and small nucleolar ribonucleoprotein (snoRNP) complexes.
Investigators measured telomere lengths by Southern blot analysis and assessed TERC levels and the effects of siRNA knockdown of gene transcripts using quantitative real-time PCR.
Dr Vulliamy and colleagues found that mutations in NHP2 can cause autosomal recessive dyskeratosis congenita. Patients with NHP2, dyskerin, and NOP10 mutations have short telomeres and low TERC levels.
Investigators concluded that this provided direct evidence of their role in telomere maintenance in humans. They did not find any GAR1 mutations, suggesting that GAR1 has a different impact on the accumulation of TERC.
This abstract was chosen as one of the 5 best of the Congress. ![]()
Acute paraplegia in a patient with AIDS and a normal CSF examination
A 35‐year‐old Zimbabwean woman living in London, England, presented to the local accident and emergency department with a history of cough, shortness of breath, nausea, vomiting, diarrhea, and weight loss of 3 months' duration. Her chest X‐ray showed miliary shadowing. She was admitted to the hospital and commenced on antituberculous medications and offered an HIV test. Two weeks later, her sputum grew acid‐fast bacilli (AFB) and her HIV‐1 test came back positive. Her baseline T‐lymphocyte CD4 cell count was 6 cells/mm3 (reference range 4551320), and her HIV‐1 RNA viral load (VL) was 4,760,000 copies/mL. However, because of her multiple symptoms, her antiretroviral therapy was postponed. Four weeks later the patient's general condition improved, but she started to experience pain in her right thigh, followed by progressive right leg weakness without sensory loss. This new change affected her mobility, and she fell while walking. Within a week the patient developed progressive flaccid paraparesis with radicular sensory disturbance. This was followed by acute onset of flaccid paraplegia, extensor plantars, sensory loss to T10, and urinary incontinence. Her cerebrospinal fluid (CSF) examination revealed normal protein, glucose, and white cell count and no AFB or malignant cells, A second CSF after 3 weeks was abnormal, with protein of 0.79 g/L, normal glucose, 7 white cells (no malignant cells), and positive oligoclonal bands. The CSF screening for AFB‐PCR, treponemes, toxoplasma, cryptococcal antigen Epstein‐Barr virus, cytomegalovirus (CMV), herpes simplex virus, human T‐lymphotropic virus, and JC virus was negative. Neurophysiological studies confirmed the presence of severe multilevel radiculopathy. The MRI scan of her head and spine showed multiple intraparenchymal cerebral tuberculomata and cavitation at T 911 that enhanced postgadolinium (see Fig. 1). She was commenced on highly active antiretroviral therapy (HAART) and steroids. Ten weeks later her HIV‐1 RNA VL became undetectable in the ultrasensitive assay (cutoff 50 copies/mL), and she regained sensation in both legs and was able to stand with support. Posttreatment MRI appearances demonstrated improvement, and 14 months after treatment the MRI brain was normal (see Fig. 1).
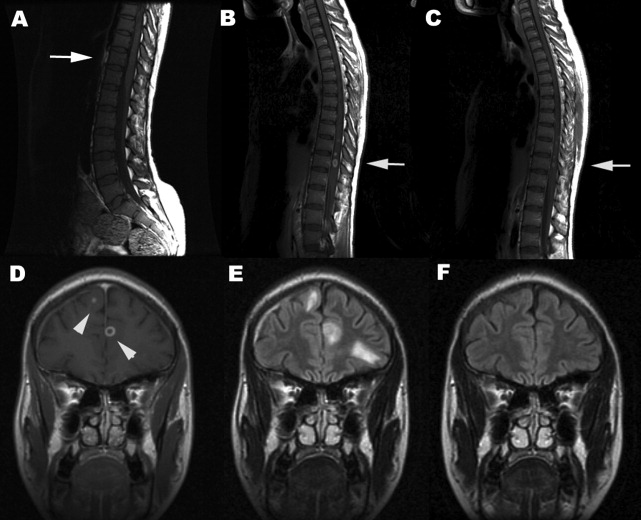
DISCUSSION
Tuberculous myeloradiculitis is a rarely reported manifestation of tuberculosis, and there are no accurate figures for its incidence.13 It may arise as a primary manifestation of the infection, by downward extension of tuberculous meningitis, or by spread from a vertebral osteomyelitis.3 It is not uncommon for it to develop during treatment for a primary infection elsewhere.4 The clinical features of this patient were those of radiculitis followed by rapid flaccid paraparesis. The acute onset of the paraplegia with a normal CSF could be mistakenly interpreted as purely peripheral HIV‐related conditions such as CMV or PML. The extensor plantars and acute development of a paraplegia and sensory level (a combination of radiculopathy, myelopathy, and spinal shock) betrayed the central involvement of the thoracolumbar region.2 In many cases there is a copious leptomeningeal exudate, which helps to explain the fairly typical clinical presentation. This case was unusual in that there was no visible imaging evidence of exudate. The presentation should be differentiated from the vacuolar myelopathy seen with HIV infection alone.1, 5 A further unusual and unique feature was the normality of the CSF examination. Although in cases of tuberculous abscess, the CSF may be normal until rupture occurs into the subarachnoid space, a lymhocytosis, raised protein and possibly hypoglycorrachia would have been expected even in a treated and sterile CSF.3 A normal CSF examination was reported in a previous study.6 This case strongly emphasizes that the diagnosis of opportunistic tuberculosis in the setting of HIV infection can be elusive. Immune reconstruction inflammatory syndrome is an unlikely cause of her neurological symptoms, as she developed these symptoms before HAART. Antituberculous medications and antimycobacterial treatment must be modified to take into account the altered pharmacokinetics as a result of HAART and steroids. There are no published guidelines on how long steroids should be maintained despite their efficacy as an adjunct in TB meningitis.7 There is no evidence to guide their use in patients with coexistent HIV. Treatment until significant improvement or a 6‐month tailed trial of steroids (in the absence of other contraindications) is probably acceptable. Even though the consequences of a well‐placed mycobacterial lesion may be devastating, appropriate treatment may lead to partial and clinically important reversal of disability.
- ,,, et al.Spectrum of myelopathies in HIV seropositive South African patients.Neurology.2001;57:348–351.
- ,.Diagnosis and management of tuberculous paraplegia with special reference to tuberculous radiculomyelitis.J Neurol Neurosurg Psychiatry.1979;42:12–18.
- ,,, et al.Tuberculous radiculomyelitis complicating tuberculous meningitis: case report and review.Clin Infect Dis.2000;30:915–921.
- ,,.Symptomatic intracranial tuberculoma developing during treatment of tuberculosis: a report of 10 patients and review of the literature.Q J Med.1987;63:449–460.
- ,.Infectious myelopathies.Semin Neurol.2002;22:133–141.
- ,,,,,, et al.Tuberculous meningitis in patients infected with the human immunodeficiency virus.New Engl J Med.1992;326:668–672.
- ,,, et al.Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults.N Engl J Med.2004;351:1741–1751.
A 35‐year‐old Zimbabwean woman living in London, England, presented to the local accident and emergency department with a history of cough, shortness of breath, nausea, vomiting, diarrhea, and weight loss of 3 months' duration. Her chest X‐ray showed miliary shadowing. She was admitted to the hospital and commenced on antituberculous medications and offered an HIV test. Two weeks later, her sputum grew acid‐fast bacilli (AFB) and her HIV‐1 test came back positive. Her baseline T‐lymphocyte CD4 cell count was 6 cells/mm3 (reference range 4551320), and her HIV‐1 RNA viral load (VL) was 4,760,000 copies/mL. However, because of her multiple symptoms, her antiretroviral therapy was postponed. Four weeks later the patient's general condition improved, but she started to experience pain in her right thigh, followed by progressive right leg weakness without sensory loss. This new change affected her mobility, and she fell while walking. Within a week the patient developed progressive flaccid paraparesis with radicular sensory disturbance. This was followed by acute onset of flaccid paraplegia, extensor plantars, sensory loss to T10, and urinary incontinence. Her cerebrospinal fluid (CSF) examination revealed normal protein, glucose, and white cell count and no AFB or malignant cells, A second CSF after 3 weeks was abnormal, with protein of 0.79 g/L, normal glucose, 7 white cells (no malignant cells), and positive oligoclonal bands. The CSF screening for AFB‐PCR, treponemes, toxoplasma, cryptococcal antigen Epstein‐Barr virus, cytomegalovirus (CMV), herpes simplex virus, human T‐lymphotropic virus, and JC virus was negative. Neurophysiological studies confirmed the presence of severe multilevel radiculopathy. The MRI scan of her head and spine showed multiple intraparenchymal cerebral tuberculomata and cavitation at T 911 that enhanced postgadolinium (see Fig. 1). She was commenced on highly active antiretroviral therapy (HAART) and steroids. Ten weeks later her HIV‐1 RNA VL became undetectable in the ultrasensitive assay (cutoff 50 copies/mL), and she regained sensation in both legs and was able to stand with support. Posttreatment MRI appearances demonstrated improvement, and 14 months after treatment the MRI brain was normal (see Fig. 1).
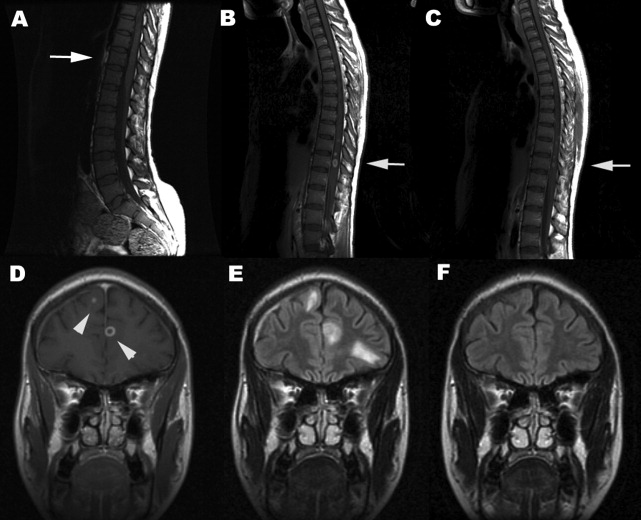
DISCUSSION
Tuberculous myeloradiculitis is a rarely reported manifestation of tuberculosis, and there are no accurate figures for its incidence.13 It may arise as a primary manifestation of the infection, by downward extension of tuberculous meningitis, or by spread from a vertebral osteomyelitis.3 It is not uncommon for it to develop during treatment for a primary infection elsewhere.4 The clinical features of this patient were those of radiculitis followed by rapid flaccid paraparesis. The acute onset of the paraplegia with a normal CSF could be mistakenly interpreted as purely peripheral HIV‐related conditions such as CMV or PML. The extensor plantars and acute development of a paraplegia and sensory level (a combination of radiculopathy, myelopathy, and spinal shock) betrayed the central involvement of the thoracolumbar region.2 In many cases there is a copious leptomeningeal exudate, which helps to explain the fairly typical clinical presentation. This case was unusual in that there was no visible imaging evidence of exudate. The presentation should be differentiated from the vacuolar myelopathy seen with HIV infection alone.1, 5 A further unusual and unique feature was the normality of the CSF examination. Although in cases of tuberculous abscess, the CSF may be normal until rupture occurs into the subarachnoid space, a lymhocytosis, raised protein and possibly hypoglycorrachia would have been expected even in a treated and sterile CSF.3 A normal CSF examination was reported in a previous study.6 This case strongly emphasizes that the diagnosis of opportunistic tuberculosis in the setting of HIV infection can be elusive. Immune reconstruction inflammatory syndrome is an unlikely cause of her neurological symptoms, as she developed these symptoms before HAART. Antituberculous medications and antimycobacterial treatment must be modified to take into account the altered pharmacokinetics as a result of HAART and steroids. There are no published guidelines on how long steroids should be maintained despite their efficacy as an adjunct in TB meningitis.7 There is no evidence to guide their use in patients with coexistent HIV. Treatment until significant improvement or a 6‐month tailed trial of steroids (in the absence of other contraindications) is probably acceptable. Even though the consequences of a well‐placed mycobacterial lesion may be devastating, appropriate treatment may lead to partial and clinically important reversal of disability.
A 35‐year‐old Zimbabwean woman living in London, England, presented to the local accident and emergency department with a history of cough, shortness of breath, nausea, vomiting, diarrhea, and weight loss of 3 months' duration. Her chest X‐ray showed miliary shadowing. She was admitted to the hospital and commenced on antituberculous medications and offered an HIV test. Two weeks later, her sputum grew acid‐fast bacilli (AFB) and her HIV‐1 test came back positive. Her baseline T‐lymphocyte CD4 cell count was 6 cells/mm3 (reference range 4551320), and her HIV‐1 RNA viral load (VL) was 4,760,000 copies/mL. However, because of her multiple symptoms, her antiretroviral therapy was postponed. Four weeks later the patient's general condition improved, but she started to experience pain in her right thigh, followed by progressive right leg weakness without sensory loss. This new change affected her mobility, and she fell while walking. Within a week the patient developed progressive flaccid paraparesis with radicular sensory disturbance. This was followed by acute onset of flaccid paraplegia, extensor plantars, sensory loss to T10, and urinary incontinence. Her cerebrospinal fluid (CSF) examination revealed normal protein, glucose, and white cell count and no AFB or malignant cells, A second CSF after 3 weeks was abnormal, with protein of 0.79 g/L, normal glucose, 7 white cells (no malignant cells), and positive oligoclonal bands. The CSF screening for AFB‐PCR, treponemes, toxoplasma, cryptococcal antigen Epstein‐Barr virus, cytomegalovirus (CMV), herpes simplex virus, human T‐lymphotropic virus, and JC virus was negative. Neurophysiological studies confirmed the presence of severe multilevel radiculopathy. The MRI scan of her head and spine showed multiple intraparenchymal cerebral tuberculomata and cavitation at T 911 that enhanced postgadolinium (see Fig. 1). She was commenced on highly active antiretroviral therapy (HAART) and steroids. Ten weeks later her HIV‐1 RNA VL became undetectable in the ultrasensitive assay (cutoff 50 copies/mL), and she regained sensation in both legs and was able to stand with support. Posttreatment MRI appearances demonstrated improvement, and 14 months after treatment the MRI brain was normal (see Fig. 1).
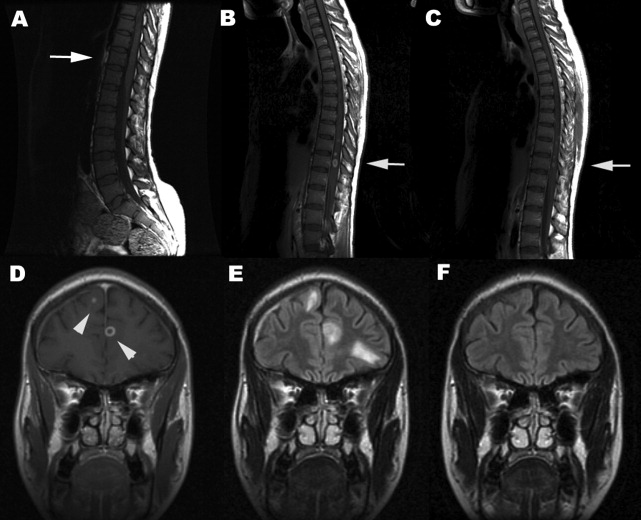
DISCUSSION
Tuberculous myeloradiculitis is a rarely reported manifestation of tuberculosis, and there are no accurate figures for its incidence.13 It may arise as a primary manifestation of the infection, by downward extension of tuberculous meningitis, or by spread from a vertebral osteomyelitis.3 It is not uncommon for it to develop during treatment for a primary infection elsewhere.4 The clinical features of this patient were those of radiculitis followed by rapid flaccid paraparesis. The acute onset of the paraplegia with a normal CSF could be mistakenly interpreted as purely peripheral HIV‐related conditions such as CMV or PML. The extensor plantars and acute development of a paraplegia and sensory level (a combination of radiculopathy, myelopathy, and spinal shock) betrayed the central involvement of the thoracolumbar region.2 In many cases there is a copious leptomeningeal exudate, which helps to explain the fairly typical clinical presentation. This case was unusual in that there was no visible imaging evidence of exudate. The presentation should be differentiated from the vacuolar myelopathy seen with HIV infection alone.1, 5 A further unusual and unique feature was the normality of the CSF examination. Although in cases of tuberculous abscess, the CSF may be normal until rupture occurs into the subarachnoid space, a lymhocytosis, raised protein and possibly hypoglycorrachia would have been expected even in a treated and sterile CSF.3 A normal CSF examination was reported in a previous study.6 This case strongly emphasizes that the diagnosis of opportunistic tuberculosis in the setting of HIV infection can be elusive. Immune reconstruction inflammatory syndrome is an unlikely cause of her neurological symptoms, as she developed these symptoms before HAART. Antituberculous medications and antimycobacterial treatment must be modified to take into account the altered pharmacokinetics as a result of HAART and steroids. There are no published guidelines on how long steroids should be maintained despite their efficacy as an adjunct in TB meningitis.7 There is no evidence to guide their use in patients with coexistent HIV. Treatment until significant improvement or a 6‐month tailed trial of steroids (in the absence of other contraindications) is probably acceptable. Even though the consequences of a well‐placed mycobacterial lesion may be devastating, appropriate treatment may lead to partial and clinically important reversal of disability.
- ,,, et al.Spectrum of myelopathies in HIV seropositive South African patients.Neurology.2001;57:348–351.
- ,.Diagnosis and management of tuberculous paraplegia with special reference to tuberculous radiculomyelitis.J Neurol Neurosurg Psychiatry.1979;42:12–18.
- ,,, et al.Tuberculous radiculomyelitis complicating tuberculous meningitis: case report and review.Clin Infect Dis.2000;30:915–921.
- ,,.Symptomatic intracranial tuberculoma developing during treatment of tuberculosis: a report of 10 patients and review of the literature.Q J Med.1987;63:449–460.
- ,.Infectious myelopathies.Semin Neurol.2002;22:133–141.
- ,,,,,, et al.Tuberculous meningitis in patients infected with the human immunodeficiency virus.New Engl J Med.1992;326:668–672.
- ,,, et al.Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults.N Engl J Med.2004;351:1741–1751.
- ,,, et al.Spectrum of myelopathies in HIV seropositive South African patients.Neurology.2001;57:348–351.
- ,.Diagnosis and management of tuberculous paraplegia with special reference to tuberculous radiculomyelitis.J Neurol Neurosurg Psychiatry.1979;42:12–18.
- ,,, et al.Tuberculous radiculomyelitis complicating tuberculous meningitis: case report and review.Clin Infect Dis.2000;30:915–921.
- ,,.Symptomatic intracranial tuberculoma developing during treatment of tuberculosis: a report of 10 patients and review of the literature.Q J Med.1987;63:449–460.
- ,.Infectious myelopathies.Semin Neurol.2002;22:133–141.
- ,,,,,, et al.Tuberculous meningitis in patients infected with the human immunodeficiency virus.New Engl J Med.1992;326:668–672.
- ,,, et al.Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults.N Engl J Med.2004;351:1741–1751.
Cullen's sign associated with metastatic esophageal carcinoma
Examination of the abdomen is an important element of the physical examination, especially in patients with known or suspected cancer. Patients with intraabdominal malignancy occasionally manifest unusual ominous findings on abdominal examination that may portend a poor prognosis: periumbilical adenopathy (Sister Mary Joseph sign),1 hepatic pulsations,2 or a hepatic friction rub or bruit.3 An uncommonly reported, and likely under‐appreciated, sign of intraabdominal cancer is periumbilical ecchymosis, also known as Cullen's sign.4 Reported below is a case of Cullen's sign associated with metastatic esophageal carcinoma.
CASE REPORT
An 80‐year‐old man with recently diagnosed esophageal adenocarcinoma presented with fever, cough, lassitude, and abdominal distention. Several weeks earlier, the patient underwent esophagogastroduodenoscopy for dysphagia and weight loss and was found to have a partially obstructing, ulcerated distal esophageal mass. Biopsy revealed poorly differentiated adenocarcinoma. At that time, computed tomography showed mediastinal adenopathy Subsequently, the patient developed increasing dysphagia with a cough, painful abdominal distention, and profound weight loss and was admitted to the hospital for further evaluation.
The patient was tachycardic and hypotensive. Physical examination revealed muscle wasting, anasarca, and abdominal distention with diffuse tenderness. An area of periumbilical ecchymosis measuring approximately 10 cm in diameter was noted. The patient had not sustained any obvious abdominal trauma or received any injections in the periumbilical area. There were no other significant ecchymoses on the abdominal wall, including the flanks. Computed tomography revealed pulmonary infiltrates compatible with pneumonia, mediastinal adenopathy, thickening of the distal esophagus, and ascites; there were no obvious liver lesions, pancreatic or retroperitoneal hemorrhage, or evidence of pancreatitis. Liver enzymes, bilirubin, and alkaline phosphatase were normal, but anemia and leukocytosis were noted. Prothombin time and partial thromboplastin time were 20 and 28 seconds, respectively. Platelet count was normal. Broad‐spectrum antimicrobials were administered for pneumonia. Because of abdominal discomfort, paracentesis was performed. Approximately 2000 cc of opaque yellow fluid was removed. The ascitic fluid was positive for erythrocytes and adenocarcinoma cells, consistent with his known diagnosis of esophageal carcinoma. The patient developed acute renal failure, and his condition continue to decline. He subsequently was discharged to hospice care and died several days later; an autopsy was not performed.
DISCUSSION
Cullen's signecchymosis surrounding the umbilicusis classically associated with hemorrhagic pancreatitis, often occurring in conjunction with ecchymosis of the flank (Grey‐Turner sign).4 Cullen's sign, however, has been reported with other abdominal pathologies such as ruptured ectopic pregnancy, leaking aortic aneurysm, splenic rupture, and retroperitoneal hemorrhage.4, 5 Hemoperitoneum from any of these processes leads to diffusion of blood along fascial planes, resulting in flank staining (Grey‐Turner sign) or periumbilical staining (Cullen's sign). Cullen's sign, however, is traditionally not attributed to malignant disease in standard medical and surgical texts.6, 7 However, the results of a Medline literature search, which revealed only a handful of case reports, suggests an association between advanced malignancy and Cullen's sign (Table 1). All previous reports oc‐curred in patients with advanced terminal malignancy, although no firm conclusions regarding specific malignancies or other risk factors can be surmised from such a small number of cases.5, 8, 9
| Reference | Sex | Age | Cancer | Outcome |
|---|---|---|---|---|
| Present study | M | 80 | Esophageal | Died |
| 5 | M | 55 | Thyroid | Died |
| 8 | M | 62 | Lymphoma | Died |
| 9 | M | 32 | Hepatoma | Died |
| 9 | M | 64 | Hepatoma | Died |
Our patient had stage IV esophageal carcinoma with malignant ascites associated with periumbilical ecchymosis. Unfortunately, serum amylase and lipase were not obtained, but acute pancreatitis‐induced Cullen's sign is unlikely because the patient did not have symptoms of pancreatitis and computed tomography did not reveal pancreatic inflammation or hemorrhage. It is well known that patients with disseminated visceral adenocarcinoma can develop coagulopathy, and that cannot be excluded in our patient. The likely mechanism of periumbilical blood collection is unclear but could relate to subclinical hemoperitoneum from mesenteric and peritoneal carcinomatosus, abdominal wall trauma, or coagulopathy from cancer and acute renal failure. Nonetheless, it is evident from this and previously reported cases that Cullen's sign complicating cancer has a dismal prognosis and is a premorbid sign. Clinicians should consider occult or metastatic visceral malignancy in patients with unexplained abdominal wall ecchymosis.
- ,.Gastric cancer. In:Clinical Hematology and Oncology: Presentation, Diagnosis, and Treatment.Philadelphia:Churchill‐Livingstone,2003;887–898.
- ,.Hepatic pulsations in a patient with cholangiocarcinoma.Arch Intern Med.1996;157:133–134.
- The Abdomen. In:.The Art and Science of Bedside Diagnosis.Baltimore, MD:Williams and Wilkins,1990;371–390.
- .Cullen's sign.Hosp Physician.1999;35:35–36.
- .Cullen's sign associated with metastatic thyroid cancer.N Engl J Med.1999;340:149–150.
- Acute Pancreatitis. In:.Cope's Early Diagnosis of the Acute Abdomen.18th ed.New York:Oxford University Press;1991:123–131.
- ,.Acute and chronic pancreatitis. In:Braunwald E,Fauci AS,Kasper EL, et al., eds.Harrison's Principles of Internal Medicine.15th ed.New York:McGraw‐Hill;2001:1792–1804.
- ,,, et al.Cullen's sign secondary to intraabdominal non‐Hodgkin's lymphoma.Am J Gastroenterol.1996;91:1040–1041.
- ,.Cullen's sign, a feature in liver disease.BMJ.1974;1:493–494.
Examination of the abdomen is an important element of the physical examination, especially in patients with known or suspected cancer. Patients with intraabdominal malignancy occasionally manifest unusual ominous findings on abdominal examination that may portend a poor prognosis: periumbilical adenopathy (Sister Mary Joseph sign),1 hepatic pulsations,2 or a hepatic friction rub or bruit.3 An uncommonly reported, and likely under‐appreciated, sign of intraabdominal cancer is periumbilical ecchymosis, also known as Cullen's sign.4 Reported below is a case of Cullen's sign associated with metastatic esophageal carcinoma.
CASE REPORT
An 80‐year‐old man with recently diagnosed esophageal adenocarcinoma presented with fever, cough, lassitude, and abdominal distention. Several weeks earlier, the patient underwent esophagogastroduodenoscopy for dysphagia and weight loss and was found to have a partially obstructing, ulcerated distal esophageal mass. Biopsy revealed poorly differentiated adenocarcinoma. At that time, computed tomography showed mediastinal adenopathy Subsequently, the patient developed increasing dysphagia with a cough, painful abdominal distention, and profound weight loss and was admitted to the hospital for further evaluation.
The patient was tachycardic and hypotensive. Physical examination revealed muscle wasting, anasarca, and abdominal distention with diffuse tenderness. An area of periumbilical ecchymosis measuring approximately 10 cm in diameter was noted. The patient had not sustained any obvious abdominal trauma or received any injections in the periumbilical area. There were no other significant ecchymoses on the abdominal wall, including the flanks. Computed tomography revealed pulmonary infiltrates compatible with pneumonia, mediastinal adenopathy, thickening of the distal esophagus, and ascites; there were no obvious liver lesions, pancreatic or retroperitoneal hemorrhage, or evidence of pancreatitis. Liver enzymes, bilirubin, and alkaline phosphatase were normal, but anemia and leukocytosis were noted. Prothombin time and partial thromboplastin time were 20 and 28 seconds, respectively. Platelet count was normal. Broad‐spectrum antimicrobials were administered for pneumonia. Because of abdominal discomfort, paracentesis was performed. Approximately 2000 cc of opaque yellow fluid was removed. The ascitic fluid was positive for erythrocytes and adenocarcinoma cells, consistent with his known diagnosis of esophageal carcinoma. The patient developed acute renal failure, and his condition continue to decline. He subsequently was discharged to hospice care and died several days later; an autopsy was not performed.
DISCUSSION
Cullen's signecchymosis surrounding the umbilicusis classically associated with hemorrhagic pancreatitis, often occurring in conjunction with ecchymosis of the flank (Grey‐Turner sign).4 Cullen's sign, however, has been reported with other abdominal pathologies such as ruptured ectopic pregnancy, leaking aortic aneurysm, splenic rupture, and retroperitoneal hemorrhage.4, 5 Hemoperitoneum from any of these processes leads to diffusion of blood along fascial planes, resulting in flank staining (Grey‐Turner sign) or periumbilical staining (Cullen's sign). Cullen's sign, however, is traditionally not attributed to malignant disease in standard medical and surgical texts.6, 7 However, the results of a Medline literature search, which revealed only a handful of case reports, suggests an association between advanced malignancy and Cullen's sign (Table 1). All previous reports oc‐curred in patients with advanced terminal malignancy, although no firm conclusions regarding specific malignancies or other risk factors can be surmised from such a small number of cases.5, 8, 9
| Reference | Sex | Age | Cancer | Outcome |
|---|---|---|---|---|
| Present study | M | 80 | Esophageal | Died |
| 5 | M | 55 | Thyroid | Died |
| 8 | M | 62 | Lymphoma | Died |
| 9 | M | 32 | Hepatoma | Died |
| 9 | M | 64 | Hepatoma | Died |
Our patient had stage IV esophageal carcinoma with malignant ascites associated with periumbilical ecchymosis. Unfortunately, serum amylase and lipase were not obtained, but acute pancreatitis‐induced Cullen's sign is unlikely because the patient did not have symptoms of pancreatitis and computed tomography did not reveal pancreatic inflammation or hemorrhage. It is well known that patients with disseminated visceral adenocarcinoma can develop coagulopathy, and that cannot be excluded in our patient. The likely mechanism of periumbilical blood collection is unclear but could relate to subclinical hemoperitoneum from mesenteric and peritoneal carcinomatosus, abdominal wall trauma, or coagulopathy from cancer and acute renal failure. Nonetheless, it is evident from this and previously reported cases that Cullen's sign complicating cancer has a dismal prognosis and is a premorbid sign. Clinicians should consider occult or metastatic visceral malignancy in patients with unexplained abdominal wall ecchymosis.
Examination of the abdomen is an important element of the physical examination, especially in patients with known or suspected cancer. Patients with intraabdominal malignancy occasionally manifest unusual ominous findings on abdominal examination that may portend a poor prognosis: periumbilical adenopathy (Sister Mary Joseph sign),1 hepatic pulsations,2 or a hepatic friction rub or bruit.3 An uncommonly reported, and likely under‐appreciated, sign of intraabdominal cancer is periumbilical ecchymosis, also known as Cullen's sign.4 Reported below is a case of Cullen's sign associated with metastatic esophageal carcinoma.
CASE REPORT
An 80‐year‐old man with recently diagnosed esophageal adenocarcinoma presented with fever, cough, lassitude, and abdominal distention. Several weeks earlier, the patient underwent esophagogastroduodenoscopy for dysphagia and weight loss and was found to have a partially obstructing, ulcerated distal esophageal mass. Biopsy revealed poorly differentiated adenocarcinoma. At that time, computed tomography showed mediastinal adenopathy Subsequently, the patient developed increasing dysphagia with a cough, painful abdominal distention, and profound weight loss and was admitted to the hospital for further evaluation.
The patient was tachycardic and hypotensive. Physical examination revealed muscle wasting, anasarca, and abdominal distention with diffuse tenderness. An area of periumbilical ecchymosis measuring approximately 10 cm in diameter was noted. The patient had not sustained any obvious abdominal trauma or received any injections in the periumbilical area. There were no other significant ecchymoses on the abdominal wall, including the flanks. Computed tomography revealed pulmonary infiltrates compatible with pneumonia, mediastinal adenopathy, thickening of the distal esophagus, and ascites; there were no obvious liver lesions, pancreatic or retroperitoneal hemorrhage, or evidence of pancreatitis. Liver enzymes, bilirubin, and alkaline phosphatase were normal, but anemia and leukocytosis were noted. Prothombin time and partial thromboplastin time were 20 and 28 seconds, respectively. Platelet count was normal. Broad‐spectrum antimicrobials were administered for pneumonia. Because of abdominal discomfort, paracentesis was performed. Approximately 2000 cc of opaque yellow fluid was removed. The ascitic fluid was positive for erythrocytes and adenocarcinoma cells, consistent with his known diagnosis of esophageal carcinoma. The patient developed acute renal failure, and his condition continue to decline. He subsequently was discharged to hospice care and died several days later; an autopsy was not performed.
DISCUSSION
Cullen's signecchymosis surrounding the umbilicusis classically associated with hemorrhagic pancreatitis, often occurring in conjunction with ecchymosis of the flank (Grey‐Turner sign).4 Cullen's sign, however, has been reported with other abdominal pathologies such as ruptured ectopic pregnancy, leaking aortic aneurysm, splenic rupture, and retroperitoneal hemorrhage.4, 5 Hemoperitoneum from any of these processes leads to diffusion of blood along fascial planes, resulting in flank staining (Grey‐Turner sign) or periumbilical staining (Cullen's sign). Cullen's sign, however, is traditionally not attributed to malignant disease in standard medical and surgical texts.6, 7 However, the results of a Medline literature search, which revealed only a handful of case reports, suggests an association between advanced malignancy and Cullen's sign (Table 1). All previous reports oc‐curred in patients with advanced terminal malignancy, although no firm conclusions regarding specific malignancies or other risk factors can be surmised from such a small number of cases.5, 8, 9
| Reference | Sex | Age | Cancer | Outcome |
|---|---|---|---|---|
| Present study | M | 80 | Esophageal | Died |
| 5 | M | 55 | Thyroid | Died |
| 8 | M | 62 | Lymphoma | Died |
| 9 | M | 32 | Hepatoma | Died |
| 9 | M | 64 | Hepatoma | Died |
Our patient had stage IV esophageal carcinoma with malignant ascites associated with periumbilical ecchymosis. Unfortunately, serum amylase and lipase were not obtained, but acute pancreatitis‐induced Cullen's sign is unlikely because the patient did not have symptoms of pancreatitis and computed tomography did not reveal pancreatic inflammation or hemorrhage. It is well known that patients with disseminated visceral adenocarcinoma can develop coagulopathy, and that cannot be excluded in our patient. The likely mechanism of periumbilical blood collection is unclear but could relate to subclinical hemoperitoneum from mesenteric and peritoneal carcinomatosus, abdominal wall trauma, or coagulopathy from cancer and acute renal failure. Nonetheless, it is evident from this and previously reported cases that Cullen's sign complicating cancer has a dismal prognosis and is a premorbid sign. Clinicians should consider occult or metastatic visceral malignancy in patients with unexplained abdominal wall ecchymosis.
- ,.Gastric cancer. In:Clinical Hematology and Oncology: Presentation, Diagnosis, and Treatment.Philadelphia:Churchill‐Livingstone,2003;887–898.
- ,.Hepatic pulsations in a patient with cholangiocarcinoma.Arch Intern Med.1996;157:133–134.
- The Abdomen. In:.The Art and Science of Bedside Diagnosis.Baltimore, MD:Williams and Wilkins,1990;371–390.
- .Cullen's sign.Hosp Physician.1999;35:35–36.
- .Cullen's sign associated with metastatic thyroid cancer.N Engl J Med.1999;340:149–150.
- Acute Pancreatitis. In:.Cope's Early Diagnosis of the Acute Abdomen.18th ed.New York:Oxford University Press;1991:123–131.
- ,.Acute and chronic pancreatitis. In:Braunwald E,Fauci AS,Kasper EL, et al., eds.Harrison's Principles of Internal Medicine.15th ed.New York:McGraw‐Hill;2001:1792–1804.
- ,,, et al.Cullen's sign secondary to intraabdominal non‐Hodgkin's lymphoma.Am J Gastroenterol.1996;91:1040–1041.
- ,.Cullen's sign, a feature in liver disease.BMJ.1974;1:493–494.
- ,.Gastric cancer. In:Clinical Hematology and Oncology: Presentation, Diagnosis, and Treatment.Philadelphia:Churchill‐Livingstone,2003;887–898.
- ,.Hepatic pulsations in a patient with cholangiocarcinoma.Arch Intern Med.1996;157:133–134.
- The Abdomen. In:.The Art and Science of Bedside Diagnosis.Baltimore, MD:Williams and Wilkins,1990;371–390.
- .Cullen's sign.Hosp Physician.1999;35:35–36.
- .Cullen's sign associated with metastatic thyroid cancer.N Engl J Med.1999;340:149–150.
- Acute Pancreatitis. In:.Cope's Early Diagnosis of the Acute Abdomen.18th ed.New York:Oxford University Press;1991:123–131.
- ,.Acute and chronic pancreatitis. In:Braunwald E,Fauci AS,Kasper EL, et al., eds.Harrison's Principles of Internal Medicine.15th ed.New York:McGraw‐Hill;2001:1792–1804.
- ,,, et al.Cullen's sign secondary to intraabdominal non‐Hodgkin's lymphoma.Am J Gastroenterol.1996;91:1040–1041.
- ,.Cullen's sign, a feature in liver disease.BMJ.1974;1:493–494.