User login
How to avoid injury to bowel during laparoscopy
The author reports no financial relationships relevant to this article.
CASE Postoperative abdominal pain. Is it gastroenteritis?
R.B., 35 years old, undergoes laparoscopic adhesiolysis for abdominal pain. Previously, she underwent exploratory laparotomy for a ruptured tubal pregnancy and, in separate operations, right oophorectomy via laparotomy for a ruptured corpus luteum cyst and diagnostic laparoscopy.
During the current surgery, extensive adhesions are observed, including interloop intestinal adhesions. The adhesions are lysed using monopolar scissors and a needle electrode, and R.B. is discharged home the same day.
Later that day and the next day, R.B. complains of abdominal pain that does not respond to prescribed analgesics, as well as nausea and vomiting. A nurse practitioner takes her call and prescribes a stronger analgesic, an antiemetic, and an antibiotic.
The following day, the patient’s husband telephones the treating gynecologist to report that his wife is still experiencing severe pain and nausea. He is told to bring her to the office, where she is described as having mild lower abdominal tenderness and mild rebound. An abdominal radiograph shows air-fluid levels and distended bowel. The gynecologist determines that the patient is experiencing gastroenteritis.
On postop day 3, R.B. continues to suffer from severe abdominal pain, nausea, and vomiting, and is unable to get out of bed. Her husband takes her to the emergency room at another hospital, where she is found to have diffuse peritonitis, absent bowel sounds, and:
- temperature, 101.8°F
- heart rate, 130/min
- respiratory rate, 24/min
- blood pressure, 90/60 mm Hg
- white blood cell (WBC) count, 21.5 × 103/μL
- x-ray showing free air.
A general surgeon performs an exploratory laparotomy and finds foul-smelling abdominal fluid, 200 to 300 mL of pus, and a 1-cm perforation of the sigmoid colon. He performs sigmoid colon resection and a left-colon colostomy. A second laparotomy is necessary to drain a subphrenic abscess.
Four months later, the colostomy is taken down and bowel continuity is established.
Subsequently, the patient experiences episodes of gaseous and fecal incontinence, which are thought to be secondary to nerve damage. A ventral hernia is also diagnosed.
Could this outcome have been avoided?
No physician would wish a major complication of surgery upon any patient. Yet, sometimes, preventive efforts fall short of the goal or the physician is slow to suspect injury when the patient experiences postoperative abdominal pain and other symptoms. Intestinal injury may not be common during laparoscopy, but it is certainly not rare. And the longer diagnosis is delayed, the greater the risk of sepsis, even death.
Recognizing the limitations of laparoscopic surgery is a first step toward reducing the complication rate.1,2 The ability to determine when laparotomy would better serve the patient’s interests is also critical, and prompt diagnosis and repair of any complication that does occur will ensure and speed the patient’s recovery.
The most serious complications associated with diagnostic and operative laparoscopy are major vessel and intestinal injuries. Both types of injury significantly raise the risk of mortality, which ranges from 2% to 23%.3,4 The overall risk of injury to the gastrointestinal tract averages 1.6 to 2.0 for every 1,000 cases. The risk of major vessel injury averages 0.5 for every 1,000 cases.5-9
In an earlier article for OBG Management, I reviewed vascular injury during laparoscopy.10 In Part 1 of this article, I focus on ways to avoid intestinal injury.In Part 2 , I outline strategies to identify it in a timely manner when it does occur.
- Avoid laparoscopy when severe adhesions are anticipated—such as when the patient has a history of multiple laparotomies, or when significant adhesions have been documented.
- Be aware that laparoscopy carries additional risks beyond those of the primary surgical procedure, owing to factors peculiar to endoscopic technique and instrumentation.
- Consider open laparoscopy or insert the primary trocar at an alternative location, such as the left upper quadrant, when the patient has a history of laparotomy.
- Avoid blunt dissection for anything other than mild (filmy) adhesions. Sharp dissection associated with hydrodissection is the safest method of adhesiolysis. Clear visualization of the operative site is the sine qua non for precise dissection.
- Avoid monopolar electrosurgical devices for laparoscopic surgery whenever possible. Also remember that bipolar and ultrasonic devices can cause thermal injury by heat conduction as well as by direct application. Laser energy will continue beyond the target unless provision is made to absorb the residual energy.
- At the conclusion of any laparoscopic procedure, especially after adhesiolysis or bowel dissection, inspect the intestines and include the details in the operative report.
- After any laparoscopic procedure, if the patient does not improve steadily, the first presumptive diagnosis to be excluded is injury secondary to the procedure or technique.
- The major symptom of intestinal perforation is abdominal pain, which does not ease without increasing quantities of analgesics.
- Investigate any bowel injury thoroughly to determine viability at the site of injury. Whenever possible, repair all injuries intraoperatively.
- After intestinal perforation, the risk of sepsis is high. Look for early signs such as tachycardia, subnormal body temperature, depressed WBC count, and the appearance of immature white cell elements.
A thorough familiarity with pelvic anatomy is important to avoid injury at trocar entry, but it is even more critical in regard to operative injury. The small intestine spreads diffusely throughout the abdomen beneath the anterior abdominal wall. It lies beneath the umbilicus and anterior midline, whereas the large bowel is located at the periphery. The sigmoid colon swings left to right before joining the rectum anterior to the presacral space. The sigmoid junction with the descending colon lies well to the left of the midline, and the cecum lies at the pelvic brim to the right of midline.
In some women, the intestines droop into the pelvis and cover the adnexa, making adhesions between these structures highly likely following dissection in the vicinity of the tubes and ovaries.
Depending on the degree of redundancy of the mesentery of the cecum or sigmoid colon, these structures may droop into the pelvis and cover the adnexa. Therefore, adhesions are likely to develop between the large or small intestine, or both, and the adnexa following dissection in the vicinity of or immediately over the tubes and ovaries. Knowing the normal anatomic relationships is vital for restorative surgery.
When severe adhesions involve the large intestine, it is critical to know the anatomy of the retroperitoneum and be skilled enough to gain safe entry and to dissect that space to safely separate the adnexa when they are densely adhered to the pelvic sidewall in the area of the obturator fossa.
As laparoscopy evolves, the injury rate rises
Over the past 40 years, laparoscopy has evolved from an uncommonly utilized diagnostic tool to a minimally invasive alternative to laparotomy for even the most difficult and complex operations, reaching a high point with robotic laparoscopy. As this technology has developed, serious complications—to some degree, unique to laparoscopy—have increased. In the future, as less skilled surgeons perform a greater percentage of laparoscopic surgeries, a still greater number of complications will arise.
The frequency of intestinal perforation is not great relative to the total number of laparoscopic procedures performed. The TABLE lists several series totaling more than 380,000 laparoscopic operations. The risk of reported bowel perforation ranged from 0.6 to 6 for every 1,000 procedures, with a mean risk of 2.4 for every 1,000. However, these data are inconclusive because the total number of laparoscopic operations performed in the United States is not accurately known. Nor is the precise number of complications associated with these procedures known—specifically, the number of intestinal perforations—as no law requires them to be reported.
Research surveys are unreliable in many cases. In addition, the relative expertise of the surgeon is impossible to quantify. For example, although a surgeon may have many years of operative experience, it is unclear whether this always translates into skill or comfort with laparoscopic procedures. And, when a resident scrubs in with a faculty surgeon, any data collected fail to reflect which part of the surgery was performed by the resident and which by the fully trained gynecologist.
These unknown variables are important in terms of risk, surgical complications, and outcomes. Surgical skill is the greatest unknown factor in any outcome study of any surgical procedure.
TABLE
Studies of complications reveal: Gastrointestinal injury is no rare event during laparoscopic surgery
| Study (year; country) | Cases | Complications | Deaths | GI injury |
|---|---|---|---|---|
| Brown et al (1978; UK)16 | 50,247 | 345 | 4 | 117 (2.3/1,000) |
| Soderstrom (1993; US)17 | No data | No data | 3 | 66 |
| Bateman et al (1996; US)18 | 1,162 | No data | No data | 3 (2.6/1,000)* |
| Champault et al (1996; France)15 | 103,852 | 337 | 6 | 63 (0.6/1,000)† |
| Saidi et al (1996; US)19 | 452 | 47 | 0 | 0 |
| Jansen et al (1997; Netherlands)5 | 25,764 | 145 | 2 | 29 (1.13/1,000) |
| Harkki-Siren et al (1997; Finland)8 | 70,607 | 96 | 0 | 44 (0.6/1,000) |
| Harkki-Siren et al (1997; Finland)7 | 1,165 | 119 | 0 | 5 (4/1,000)‡ |
| Chapron et al (1998; France)6 | 29,996 | 96 | 1 | 48 (1.6/1,000) |
| Chapron et al (1999; France)9 | No data | No data | No data | 62 (0.6–1.6/1,000) |
| Gordts et al (2001; France)20 | 3,667 | No data | No data | 24 (6/1,000) |
| Bhoyrul et al (2001; US)13 | No data | 629 | 32 | 128§ |
| Wang et al (2001; Taiwan)21 | 6,451 | 42 | 0 | 10 (1.6/1,000) |
| Sharp et al (2002; US)14 | 185 | 84 | 2 | 24** |
| Brosens et al (2003; Belgium)22 | 85,727 | No data | No data | 195 (2.3/1,000) |
| * 80 open laparoscopy procedures; 30 closed laparoscopy procedures | ||||
| † Limited to trocar injuries | ||||
| ‡ Laparoscopic hysterectomy | ||||
| § All trocar injuries obtained through Food and Drug Administration reports | ||||
| ** Limited to optical access trocars | ||||
Classifying intestinal injuries
As in the case of major vessel injury, intestinal injury sustained during laparoscopy can be classified as either:
- Injury secondary to the approach. This category refers to entry complications associated with creation of the pneumoperitoneum and insertion of primary and secondary trocars.
- Injury secondary to the procedure or operation. This type of injury occurs as a result of manipulation with various devices during laparoscopy. The devices may include probes, forceps, scissors, or energy devices such as laser, electrosurgical, and ultrasonic instruments.
How trocar injury happens
Several studies have demonstrated that abdominal adhesions place any patient into a high-risk category for trocar injury to the intestines. Patients who have undergone multiple laparotomies, like the patient in the case that opened this article, are more likely to have severe adhesions and fall into the highest risk category for bowel perforation.11 It is impossible to predict with any degree of accuracy whether the intestine is adherent to the entry site.
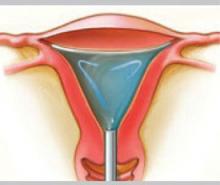
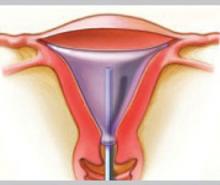
Pneumoperitoneum can be protective
Creation of a pneumoperitoneum creates a cushion of gas between the intestines and the anterior abdominal wall (provided the intestines are not adherent to the abdominal wall). Manufacturers of disposable trocars with a retractable shield recommend creating an adequate pneumoperitoneum so that the “safety shield” deploys quickly and properly, unlike direct insertion, in which no gas is infused and space is insufficient for complete shield activation.
Open laparoscopy techniques, which allow the surgeon to enter the peritoneal cavity by direct vision without a sharp trocar, may diminish but not eliminate the risk of bowel injury.
What the data show
Of the 130 intestinal injuries recently reported by Baggish, 62 of 81 (77%) small bowel injuries were related to trocar insertion, as were 20 of 49 (41%) large intestinal injuries.12 In other words, 82 of 130 intestinal injuries (63%) were the direct result of trocar entry.
Bhoyrul and associates reported 629 trocar injuries, of which 182 were visceral.13 Of the 32 deaths, six were secondary to unrecognized bowel injury. Of 176 nonfatal visceral injuries, 128 (73%) involved the intestines, and 22 were unrecognized.
Optical-access and open laparoscopic systems were designed to prevent such injuries. Sharp and colleagues reported 24 intestinal injuries out of a total of 79 complications (30%) associated with optical-access trocars after reviewing data obtained from the Medical Device Reports (MDR) and Maude databases maintained by the Food and Drug Administration.14 In the Baggish series, 4.6% of injuries were associated with open laparoscopy.12
Champault and colleagues reviewed complications in a survey of 103,852 operations.15 Although they recommended use of open laparoscopy as opposed to blind insertion, they presented no data on the safety of open techniques.
How intraoperative injury happens
Operative injury of the large or small bowel often occurs during sharp or blunt dissection, performed during laparoscopy using accessory mechanical or energy devices. The latter type of device is utilized increasingly because laparoscopic knot tying and suturing are rather awkward and slow, and laparoscopic suturing to control bleeding is difficult. The size of the needle required for laparoscopic suture placement must be small enough to navigate a trocar sleeve.
Avoid blunt dissection when adhesions are present
The separation of dense adhesions between the intestines and neighboring bowel, other viscera, or abdominal wall is risky when blunt dissection is used. The tensile strength of the fibrotic connective tissue may well exceed that of the thin intestinal wall. Tearing the adhesion free may bring with it a portion of the bowel wall. Such injuries are frequently missed or described as serosal injuries and left unexplored and unrepaired.
Hydrodissection is a safer alternative. It involves the infiltration of sterile water or saline under low pressure between the parietal peritoneum and underlying retroperitoneal structures, providing a safe and natural plane for dissection. In addition, when the CO2 laser is used, the liquid acts as a heat sink to absorb any penetrating laser energy.
Energy devices create thermal effects
Energy devices used to cut tissue during operative laparoscopy coagulate blood vessels in a variety of ways, but the common pathway is thermal. Many hypotheses have evolved to explain how vessels are sealed, but none has demonstrated nonthermal activity except for cryocoagulation.
The devices most commonly used for cutting and hemostasis at laparoscopy are:
- electrosurgical (both monopolar and bipolar). Bipolar electrosurgical devices have advantages over monopolar devices when it comes to high-frequency leaks, direct coupling, and capacitive coupling.
- laser (CO2, holmium:YAG, Nd:YAG, KTP-532, argon). As I mentioned, CO2 laser devices are effectively backstopped by water, especially in strategic areas such as over and around intestines, major vessels, and the ureters.
- ultrasonic (Harmonic Scalpel, ultrasonic aspirator [CUSA]).
Laser and ultrasonic devices do not require a flow of electrons to create coagulation, but do produce heat that will spread peripherally by thermal conduction from the zone of impact (target).
The extent of energy-inflicted injury cannot be predicted
Inadvertent injury with energy devices can occur directly through contact with the bowel, indirectly by heat conduction through tissue, through capacitive coupling (monopolar electrical only), and by forward scatter (laser only).
Upon direct contact with the intestine, energy devices cut into the tissue in a manner similar to mechanical scissors or a knife but produce a larger wound. The reason? The transfer of heat to areas adjacent to the primary wound produces additional necrosis. Heat conduction, capacitive coupling, high-frequency leaks, and front scatter coagulate the intestinal wall with subsequent tissue devitalization and necrosis, the extent of which depends on the power density at contact and the duration of energy applied.
It is impossible to predict the depth or area of devitalization in energy-inflicted injury by visualization of the event.
In the Baggish review of 130 intestinal injuries, the number of injuries sustained during the operative procedure was 19 involving the small intestine and 29 involving the large bowel.12 Of this subset, 44% (21 cases) were secondary to the use of energy devices, with monopolar electrosurgical instruments alone accounting for 9 (43%) of the injuries.
Even best-laid plans can go awry
Despite our best intentions and precautions, accidents do sometimes happen, and bowel injury is no exception.In Part 2 of this article, I detail steps you can take to detect injuries in as timely a manner as possible.
1. Mäkinen J, Johansson J, Tomás C, et al. Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod. 2001;16:1473-1478.
2. Fuller J, Ashar BS, Corrado-Carey J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005;12:302-307.
3. Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg. 1997;185:461-465.
4. Baggish MS. Analysis of 31 cases of major-vessel injury associated with gynecologic laparoscopy operations. J Gynecol Surg. 2003;19:63-73.
5. Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB. Complications of laparoscopy: a prospective multicenter observational study. Br J Obstet Gynaecol. 1997;104:595-600.
6. Chapron C, Querleu D, Bruhat MA, et al. Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod. 1998;13:867-872.
7. Härkki-Sirén P, Sjöberg J, Mäkinen J, et al. Finnish National Register of Laparoscopic Hysterectomies: a review and complications of 1165 operations. Am J Obstet Gynecol. 1997;176(1 Pt. 1):118-122.
8. Härkki-Sirén P, Kurki T. A nationwide analysis of laparoscopic complications. Obstet Gynecol. 1997;89:108-112.
9. Chapron C, Pierre F, Harchaoui Y, et al. Gastrointestinal injuries during gynaecological laparoscopy. Hum Reprod. 1999;14:333-337.
10. Baggish MS. Avoiding vascular injury at laparoscopy. OBG Management. 2004;16(10):70-87.
11. Smith ARB. Postoperative complications following minimal access surgery. Baillieres Clin Obstet Gynecol. 2000;14:123.-
12. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
13. Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001;192:677-683.
14. Sharp HT, Dodson MK, Draper ML, Watts DA, Doucette RC, Hurd WW. Complications associated with optical-access laparoscopic trocars. Obstet Gynecol. 2002;99:553-555.
15. Champault G, Cazacu F, Taffi nder N. Serious trocar accidents in laparoscopic surgery: a French survey of 103,852 operations. Surg Laparosc Endosc. 1996;6:367-370.
16. Brown JA, Chamberlain GVP, Jordan JA, et al. Gynaecological laparoscopy. The Report of the Working Party of the Confidential Enquiry into Gynaecological Laparoscopy. Br J Obstet Gynaecol. 1978;85:401-403.
17. Soderstrom RM. Bowel injury ligation after laparoscopy. J Am Assoc Gynecol Laparosc. 1993;1:74-77.
18. Bateman BG, Kolp LA, Hoeger K. Complications of laparoscopy—operative and diagnostic. Fertil Steril. 1996;66:30-35.
19. Saidi MH, Vancaillie TG, White J, Sadler RK, Akright BD, Farhart SA. Complications of major operative laparoscopy. A review of 452 cases. J Reprod Med. 1996;41:471-476.
20. Gordts S, Watrelot A, Camp R, Brosens I. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76:1238-1241.
21. Wang PH, Lee WL, Yuan CC, et al. Major complications of operative and diagnostic laparoscopy for gynecologic disease. J Am Assoc Gynecol Laparosc. 2001;8:68-73.
22. Brosens I, Gordon A, Campo R, Gordts S. Bowel injury in gynecologic laparoscopy. J Am Assoc Gynecol Laparosc. 2003;10:9-13.
The author reports no financial relationships relevant to this article.
CASE Postoperative abdominal pain. Is it gastroenteritis?
R.B., 35 years old, undergoes laparoscopic adhesiolysis for abdominal pain. Previously, she underwent exploratory laparotomy for a ruptured tubal pregnancy and, in separate operations, right oophorectomy via laparotomy for a ruptured corpus luteum cyst and diagnostic laparoscopy.
During the current surgery, extensive adhesions are observed, including interloop intestinal adhesions. The adhesions are lysed using monopolar scissors and a needle electrode, and R.B. is discharged home the same day.
Later that day and the next day, R.B. complains of abdominal pain that does not respond to prescribed analgesics, as well as nausea and vomiting. A nurse practitioner takes her call and prescribes a stronger analgesic, an antiemetic, and an antibiotic.
The following day, the patient’s husband telephones the treating gynecologist to report that his wife is still experiencing severe pain and nausea. He is told to bring her to the office, where she is described as having mild lower abdominal tenderness and mild rebound. An abdominal radiograph shows air-fluid levels and distended bowel. The gynecologist determines that the patient is experiencing gastroenteritis.
On postop day 3, R.B. continues to suffer from severe abdominal pain, nausea, and vomiting, and is unable to get out of bed. Her husband takes her to the emergency room at another hospital, where she is found to have diffuse peritonitis, absent bowel sounds, and:
- temperature, 101.8°F
- heart rate, 130/min
- respiratory rate, 24/min
- blood pressure, 90/60 mm Hg
- white blood cell (WBC) count, 21.5 × 103/μL
- x-ray showing free air.
A general surgeon performs an exploratory laparotomy and finds foul-smelling abdominal fluid, 200 to 300 mL of pus, and a 1-cm perforation of the sigmoid colon. He performs sigmoid colon resection and a left-colon colostomy. A second laparotomy is necessary to drain a subphrenic abscess.
Four months later, the colostomy is taken down and bowel continuity is established.
Subsequently, the patient experiences episodes of gaseous and fecal incontinence, which are thought to be secondary to nerve damage. A ventral hernia is also diagnosed.
Could this outcome have been avoided?
No physician would wish a major complication of surgery upon any patient. Yet, sometimes, preventive efforts fall short of the goal or the physician is slow to suspect injury when the patient experiences postoperative abdominal pain and other symptoms. Intestinal injury may not be common during laparoscopy, but it is certainly not rare. And the longer diagnosis is delayed, the greater the risk of sepsis, even death.
Recognizing the limitations of laparoscopic surgery is a first step toward reducing the complication rate.1,2 The ability to determine when laparotomy would better serve the patient’s interests is also critical, and prompt diagnosis and repair of any complication that does occur will ensure and speed the patient’s recovery.
The most serious complications associated with diagnostic and operative laparoscopy are major vessel and intestinal injuries. Both types of injury significantly raise the risk of mortality, which ranges from 2% to 23%.3,4 The overall risk of injury to the gastrointestinal tract averages 1.6 to 2.0 for every 1,000 cases. The risk of major vessel injury averages 0.5 for every 1,000 cases.5-9
In an earlier article for OBG Management, I reviewed vascular injury during laparoscopy.10 In Part 1 of this article, I focus on ways to avoid intestinal injury.In Part 2 , I outline strategies to identify it in a timely manner when it does occur.
- Avoid laparoscopy when severe adhesions are anticipated—such as when the patient has a history of multiple laparotomies, or when significant adhesions have been documented.
- Be aware that laparoscopy carries additional risks beyond those of the primary surgical procedure, owing to factors peculiar to endoscopic technique and instrumentation.
- Consider open laparoscopy or insert the primary trocar at an alternative location, such as the left upper quadrant, when the patient has a history of laparotomy.
- Avoid blunt dissection for anything other than mild (filmy) adhesions. Sharp dissection associated with hydrodissection is the safest method of adhesiolysis. Clear visualization of the operative site is the sine qua non for precise dissection.
- Avoid monopolar electrosurgical devices for laparoscopic surgery whenever possible. Also remember that bipolar and ultrasonic devices can cause thermal injury by heat conduction as well as by direct application. Laser energy will continue beyond the target unless provision is made to absorb the residual energy.
- At the conclusion of any laparoscopic procedure, especially after adhesiolysis or bowel dissection, inspect the intestines and include the details in the operative report.
- After any laparoscopic procedure, if the patient does not improve steadily, the first presumptive diagnosis to be excluded is injury secondary to the procedure or technique.
- The major symptom of intestinal perforation is abdominal pain, which does not ease without increasing quantities of analgesics.
- Investigate any bowel injury thoroughly to determine viability at the site of injury. Whenever possible, repair all injuries intraoperatively.
- After intestinal perforation, the risk of sepsis is high. Look for early signs such as tachycardia, subnormal body temperature, depressed WBC count, and the appearance of immature white cell elements.
A thorough familiarity with pelvic anatomy is important to avoid injury at trocar entry, but it is even more critical in regard to operative injury. The small intestine spreads diffusely throughout the abdomen beneath the anterior abdominal wall. It lies beneath the umbilicus and anterior midline, whereas the large bowel is located at the periphery. The sigmoid colon swings left to right before joining the rectum anterior to the presacral space. The sigmoid junction with the descending colon lies well to the left of the midline, and the cecum lies at the pelvic brim to the right of midline.
In some women, the intestines droop into the pelvis and cover the adnexa, making adhesions between these structures highly likely following dissection in the vicinity of the tubes and ovaries.
Depending on the degree of redundancy of the mesentery of the cecum or sigmoid colon, these structures may droop into the pelvis and cover the adnexa. Therefore, adhesions are likely to develop between the large or small intestine, or both, and the adnexa following dissection in the vicinity of or immediately over the tubes and ovaries. Knowing the normal anatomic relationships is vital for restorative surgery.
When severe adhesions involve the large intestine, it is critical to know the anatomy of the retroperitoneum and be skilled enough to gain safe entry and to dissect that space to safely separate the adnexa when they are densely adhered to the pelvic sidewall in the area of the obturator fossa.
As laparoscopy evolves, the injury rate rises
Over the past 40 years, laparoscopy has evolved from an uncommonly utilized diagnostic tool to a minimally invasive alternative to laparotomy for even the most difficult and complex operations, reaching a high point with robotic laparoscopy. As this technology has developed, serious complications—to some degree, unique to laparoscopy—have increased. In the future, as less skilled surgeons perform a greater percentage of laparoscopic surgeries, a still greater number of complications will arise.
The frequency of intestinal perforation is not great relative to the total number of laparoscopic procedures performed. The TABLE lists several series totaling more than 380,000 laparoscopic operations. The risk of reported bowel perforation ranged from 0.6 to 6 for every 1,000 procedures, with a mean risk of 2.4 for every 1,000. However, these data are inconclusive because the total number of laparoscopic operations performed in the United States is not accurately known. Nor is the precise number of complications associated with these procedures known—specifically, the number of intestinal perforations—as no law requires them to be reported.
Research surveys are unreliable in many cases. In addition, the relative expertise of the surgeon is impossible to quantify. For example, although a surgeon may have many years of operative experience, it is unclear whether this always translates into skill or comfort with laparoscopic procedures. And, when a resident scrubs in with a faculty surgeon, any data collected fail to reflect which part of the surgery was performed by the resident and which by the fully trained gynecologist.
These unknown variables are important in terms of risk, surgical complications, and outcomes. Surgical skill is the greatest unknown factor in any outcome study of any surgical procedure.
TABLE
Studies of complications reveal: Gastrointestinal injury is no rare event during laparoscopic surgery
| Study (year; country) | Cases | Complications | Deaths | GI injury |
|---|---|---|---|---|
| Brown et al (1978; UK)16 | 50,247 | 345 | 4 | 117 (2.3/1,000) |
| Soderstrom (1993; US)17 | No data | No data | 3 | 66 |
| Bateman et al (1996; US)18 | 1,162 | No data | No data | 3 (2.6/1,000)* |
| Champault et al (1996; France)15 | 103,852 | 337 | 6 | 63 (0.6/1,000)† |
| Saidi et al (1996; US)19 | 452 | 47 | 0 | 0 |
| Jansen et al (1997; Netherlands)5 | 25,764 | 145 | 2 | 29 (1.13/1,000) |
| Harkki-Siren et al (1997; Finland)8 | 70,607 | 96 | 0 | 44 (0.6/1,000) |
| Harkki-Siren et al (1997; Finland)7 | 1,165 | 119 | 0 | 5 (4/1,000)‡ |
| Chapron et al (1998; France)6 | 29,996 | 96 | 1 | 48 (1.6/1,000) |
| Chapron et al (1999; France)9 | No data | No data | No data | 62 (0.6–1.6/1,000) |
| Gordts et al (2001; France)20 | 3,667 | No data | No data | 24 (6/1,000) |
| Bhoyrul et al (2001; US)13 | No data | 629 | 32 | 128§ |
| Wang et al (2001; Taiwan)21 | 6,451 | 42 | 0 | 10 (1.6/1,000) |
| Sharp et al (2002; US)14 | 185 | 84 | 2 | 24** |
| Brosens et al (2003; Belgium)22 | 85,727 | No data | No data | 195 (2.3/1,000) |
| * 80 open laparoscopy procedures; 30 closed laparoscopy procedures | ||||
| † Limited to trocar injuries | ||||
| ‡ Laparoscopic hysterectomy | ||||
| § All trocar injuries obtained through Food and Drug Administration reports | ||||
| ** Limited to optical access trocars | ||||
Classifying intestinal injuries
As in the case of major vessel injury, intestinal injury sustained during laparoscopy can be classified as either:
- Injury secondary to the approach. This category refers to entry complications associated with creation of the pneumoperitoneum and insertion of primary and secondary trocars.
- Injury secondary to the procedure or operation. This type of injury occurs as a result of manipulation with various devices during laparoscopy. The devices may include probes, forceps, scissors, or energy devices such as laser, electrosurgical, and ultrasonic instruments.
How trocar injury happens
Several studies have demonstrated that abdominal adhesions place any patient into a high-risk category for trocar injury to the intestines. Patients who have undergone multiple laparotomies, like the patient in the case that opened this article, are more likely to have severe adhesions and fall into the highest risk category for bowel perforation.11 It is impossible to predict with any degree of accuracy whether the intestine is adherent to the entry site.
Pneumoperitoneum can be protective
Creation of a pneumoperitoneum creates a cushion of gas between the intestines and the anterior abdominal wall (provided the intestines are not adherent to the abdominal wall). Manufacturers of disposable trocars with a retractable shield recommend creating an adequate pneumoperitoneum so that the “safety shield” deploys quickly and properly, unlike direct insertion, in which no gas is infused and space is insufficient for complete shield activation.
Open laparoscopy techniques, which allow the surgeon to enter the peritoneal cavity by direct vision without a sharp trocar, may diminish but not eliminate the risk of bowel injury.
What the data show
Of the 130 intestinal injuries recently reported by Baggish, 62 of 81 (77%) small bowel injuries were related to trocar insertion, as were 20 of 49 (41%) large intestinal injuries.12 In other words, 82 of 130 intestinal injuries (63%) were the direct result of trocar entry.
Bhoyrul and associates reported 629 trocar injuries, of which 182 were visceral.13 Of the 32 deaths, six were secondary to unrecognized bowel injury. Of 176 nonfatal visceral injuries, 128 (73%) involved the intestines, and 22 were unrecognized.
Optical-access and open laparoscopic systems were designed to prevent such injuries. Sharp and colleagues reported 24 intestinal injuries out of a total of 79 complications (30%) associated with optical-access trocars after reviewing data obtained from the Medical Device Reports (MDR) and Maude databases maintained by the Food and Drug Administration.14 In the Baggish series, 4.6% of injuries were associated with open laparoscopy.12
Champault and colleagues reviewed complications in a survey of 103,852 operations.15 Although they recommended use of open laparoscopy as opposed to blind insertion, they presented no data on the safety of open techniques.
How intraoperative injury happens
Operative injury of the large or small bowel often occurs during sharp or blunt dissection, performed during laparoscopy using accessory mechanical or energy devices. The latter type of device is utilized increasingly because laparoscopic knot tying and suturing are rather awkward and slow, and laparoscopic suturing to control bleeding is difficult. The size of the needle required for laparoscopic suture placement must be small enough to navigate a trocar sleeve.
Avoid blunt dissection when adhesions are present
The separation of dense adhesions between the intestines and neighboring bowel, other viscera, or abdominal wall is risky when blunt dissection is used. The tensile strength of the fibrotic connective tissue may well exceed that of the thin intestinal wall. Tearing the adhesion free may bring with it a portion of the bowel wall. Such injuries are frequently missed or described as serosal injuries and left unexplored and unrepaired.
Hydrodissection is a safer alternative. It involves the infiltration of sterile water or saline under low pressure between the parietal peritoneum and underlying retroperitoneal structures, providing a safe and natural plane for dissection. In addition, when the CO2 laser is used, the liquid acts as a heat sink to absorb any penetrating laser energy.
Energy devices create thermal effects
Energy devices used to cut tissue during operative laparoscopy coagulate blood vessels in a variety of ways, but the common pathway is thermal. Many hypotheses have evolved to explain how vessels are sealed, but none has demonstrated nonthermal activity except for cryocoagulation.
The devices most commonly used for cutting and hemostasis at laparoscopy are:
- electrosurgical (both monopolar and bipolar). Bipolar electrosurgical devices have advantages over monopolar devices when it comes to high-frequency leaks, direct coupling, and capacitive coupling.
- laser (CO2, holmium:YAG, Nd:YAG, KTP-532, argon). As I mentioned, CO2 laser devices are effectively backstopped by water, especially in strategic areas such as over and around intestines, major vessels, and the ureters.
- ultrasonic (Harmonic Scalpel, ultrasonic aspirator [CUSA]).
Laser and ultrasonic devices do not require a flow of electrons to create coagulation, but do produce heat that will spread peripherally by thermal conduction from the zone of impact (target).
The extent of energy-inflicted injury cannot be predicted
Inadvertent injury with energy devices can occur directly through contact with the bowel, indirectly by heat conduction through tissue, through capacitive coupling (monopolar electrical only), and by forward scatter (laser only).
Upon direct contact with the intestine, energy devices cut into the tissue in a manner similar to mechanical scissors or a knife but produce a larger wound. The reason? The transfer of heat to areas adjacent to the primary wound produces additional necrosis. Heat conduction, capacitive coupling, high-frequency leaks, and front scatter coagulate the intestinal wall with subsequent tissue devitalization and necrosis, the extent of which depends on the power density at contact and the duration of energy applied.
It is impossible to predict the depth or area of devitalization in energy-inflicted injury by visualization of the event.
In the Baggish review of 130 intestinal injuries, the number of injuries sustained during the operative procedure was 19 involving the small intestine and 29 involving the large bowel.12 Of this subset, 44% (21 cases) were secondary to the use of energy devices, with monopolar electrosurgical instruments alone accounting for 9 (43%) of the injuries.
Even best-laid plans can go awry
Despite our best intentions and precautions, accidents do sometimes happen, and bowel injury is no exception.In Part 2 of this article, I detail steps you can take to detect injuries in as timely a manner as possible.
The author reports no financial relationships relevant to this article.
CASE Postoperative abdominal pain. Is it gastroenteritis?
R.B., 35 years old, undergoes laparoscopic adhesiolysis for abdominal pain. Previously, she underwent exploratory laparotomy for a ruptured tubal pregnancy and, in separate operations, right oophorectomy via laparotomy for a ruptured corpus luteum cyst and diagnostic laparoscopy.
During the current surgery, extensive adhesions are observed, including interloop intestinal adhesions. The adhesions are lysed using monopolar scissors and a needle electrode, and R.B. is discharged home the same day.
Later that day and the next day, R.B. complains of abdominal pain that does not respond to prescribed analgesics, as well as nausea and vomiting. A nurse practitioner takes her call and prescribes a stronger analgesic, an antiemetic, and an antibiotic.
The following day, the patient’s husband telephones the treating gynecologist to report that his wife is still experiencing severe pain and nausea. He is told to bring her to the office, where she is described as having mild lower abdominal tenderness and mild rebound. An abdominal radiograph shows air-fluid levels and distended bowel. The gynecologist determines that the patient is experiencing gastroenteritis.
On postop day 3, R.B. continues to suffer from severe abdominal pain, nausea, and vomiting, and is unable to get out of bed. Her husband takes her to the emergency room at another hospital, where she is found to have diffuse peritonitis, absent bowel sounds, and:
- temperature, 101.8°F
- heart rate, 130/min
- respiratory rate, 24/min
- blood pressure, 90/60 mm Hg
- white blood cell (WBC) count, 21.5 × 103/μL
- x-ray showing free air.
A general surgeon performs an exploratory laparotomy and finds foul-smelling abdominal fluid, 200 to 300 mL of pus, and a 1-cm perforation of the sigmoid colon. He performs sigmoid colon resection and a left-colon colostomy. A second laparotomy is necessary to drain a subphrenic abscess.
Four months later, the colostomy is taken down and bowel continuity is established.
Subsequently, the patient experiences episodes of gaseous and fecal incontinence, which are thought to be secondary to nerve damage. A ventral hernia is also diagnosed.
Could this outcome have been avoided?
No physician would wish a major complication of surgery upon any patient. Yet, sometimes, preventive efforts fall short of the goal or the physician is slow to suspect injury when the patient experiences postoperative abdominal pain and other symptoms. Intestinal injury may not be common during laparoscopy, but it is certainly not rare. And the longer diagnosis is delayed, the greater the risk of sepsis, even death.
Recognizing the limitations of laparoscopic surgery is a first step toward reducing the complication rate.1,2 The ability to determine when laparotomy would better serve the patient’s interests is also critical, and prompt diagnosis and repair of any complication that does occur will ensure and speed the patient’s recovery.
The most serious complications associated with diagnostic and operative laparoscopy are major vessel and intestinal injuries. Both types of injury significantly raise the risk of mortality, which ranges from 2% to 23%.3,4 The overall risk of injury to the gastrointestinal tract averages 1.6 to 2.0 for every 1,000 cases. The risk of major vessel injury averages 0.5 for every 1,000 cases.5-9
In an earlier article for OBG Management, I reviewed vascular injury during laparoscopy.10 In Part 1 of this article, I focus on ways to avoid intestinal injury.In Part 2 , I outline strategies to identify it in a timely manner when it does occur.
- Avoid laparoscopy when severe adhesions are anticipated—such as when the patient has a history of multiple laparotomies, or when significant adhesions have been documented.
- Be aware that laparoscopy carries additional risks beyond those of the primary surgical procedure, owing to factors peculiar to endoscopic technique and instrumentation.
- Consider open laparoscopy or insert the primary trocar at an alternative location, such as the left upper quadrant, when the patient has a history of laparotomy.
- Avoid blunt dissection for anything other than mild (filmy) adhesions. Sharp dissection associated with hydrodissection is the safest method of adhesiolysis. Clear visualization of the operative site is the sine qua non for precise dissection.
- Avoid monopolar electrosurgical devices for laparoscopic surgery whenever possible. Also remember that bipolar and ultrasonic devices can cause thermal injury by heat conduction as well as by direct application. Laser energy will continue beyond the target unless provision is made to absorb the residual energy.
- At the conclusion of any laparoscopic procedure, especially after adhesiolysis or bowel dissection, inspect the intestines and include the details in the operative report.
- After any laparoscopic procedure, if the patient does not improve steadily, the first presumptive diagnosis to be excluded is injury secondary to the procedure or technique.
- The major symptom of intestinal perforation is abdominal pain, which does not ease without increasing quantities of analgesics.
- Investigate any bowel injury thoroughly to determine viability at the site of injury. Whenever possible, repair all injuries intraoperatively.
- After intestinal perforation, the risk of sepsis is high. Look for early signs such as tachycardia, subnormal body temperature, depressed WBC count, and the appearance of immature white cell elements.
A thorough familiarity with pelvic anatomy is important to avoid injury at trocar entry, but it is even more critical in regard to operative injury. The small intestine spreads diffusely throughout the abdomen beneath the anterior abdominal wall. It lies beneath the umbilicus and anterior midline, whereas the large bowel is located at the periphery. The sigmoid colon swings left to right before joining the rectum anterior to the presacral space. The sigmoid junction with the descending colon lies well to the left of the midline, and the cecum lies at the pelvic brim to the right of midline.
In some women, the intestines droop into the pelvis and cover the adnexa, making adhesions between these structures highly likely following dissection in the vicinity of the tubes and ovaries.
Depending on the degree of redundancy of the mesentery of the cecum or sigmoid colon, these structures may droop into the pelvis and cover the adnexa. Therefore, adhesions are likely to develop between the large or small intestine, or both, and the adnexa following dissection in the vicinity of or immediately over the tubes and ovaries. Knowing the normal anatomic relationships is vital for restorative surgery.
When severe adhesions involve the large intestine, it is critical to know the anatomy of the retroperitoneum and be skilled enough to gain safe entry and to dissect that space to safely separate the adnexa when they are densely adhered to the pelvic sidewall in the area of the obturator fossa.
As laparoscopy evolves, the injury rate rises
Over the past 40 years, laparoscopy has evolved from an uncommonly utilized diagnostic tool to a minimally invasive alternative to laparotomy for even the most difficult and complex operations, reaching a high point with robotic laparoscopy. As this technology has developed, serious complications—to some degree, unique to laparoscopy—have increased. In the future, as less skilled surgeons perform a greater percentage of laparoscopic surgeries, a still greater number of complications will arise.
The frequency of intestinal perforation is not great relative to the total number of laparoscopic procedures performed. The TABLE lists several series totaling more than 380,000 laparoscopic operations. The risk of reported bowel perforation ranged from 0.6 to 6 for every 1,000 procedures, with a mean risk of 2.4 for every 1,000. However, these data are inconclusive because the total number of laparoscopic operations performed in the United States is not accurately known. Nor is the precise number of complications associated with these procedures known—specifically, the number of intestinal perforations—as no law requires them to be reported.
Research surveys are unreliable in many cases. In addition, the relative expertise of the surgeon is impossible to quantify. For example, although a surgeon may have many years of operative experience, it is unclear whether this always translates into skill or comfort with laparoscopic procedures. And, when a resident scrubs in with a faculty surgeon, any data collected fail to reflect which part of the surgery was performed by the resident and which by the fully trained gynecologist.
These unknown variables are important in terms of risk, surgical complications, and outcomes. Surgical skill is the greatest unknown factor in any outcome study of any surgical procedure.
TABLE
Studies of complications reveal: Gastrointestinal injury is no rare event during laparoscopic surgery
| Study (year; country) | Cases | Complications | Deaths | GI injury |
|---|---|---|---|---|
| Brown et al (1978; UK)16 | 50,247 | 345 | 4 | 117 (2.3/1,000) |
| Soderstrom (1993; US)17 | No data | No data | 3 | 66 |
| Bateman et al (1996; US)18 | 1,162 | No data | No data | 3 (2.6/1,000)* |
| Champault et al (1996; France)15 | 103,852 | 337 | 6 | 63 (0.6/1,000)† |
| Saidi et al (1996; US)19 | 452 | 47 | 0 | 0 |
| Jansen et al (1997; Netherlands)5 | 25,764 | 145 | 2 | 29 (1.13/1,000) |
| Harkki-Siren et al (1997; Finland)8 | 70,607 | 96 | 0 | 44 (0.6/1,000) |
| Harkki-Siren et al (1997; Finland)7 | 1,165 | 119 | 0 | 5 (4/1,000)‡ |
| Chapron et al (1998; France)6 | 29,996 | 96 | 1 | 48 (1.6/1,000) |
| Chapron et al (1999; France)9 | No data | No data | No data | 62 (0.6–1.6/1,000) |
| Gordts et al (2001; France)20 | 3,667 | No data | No data | 24 (6/1,000) |
| Bhoyrul et al (2001; US)13 | No data | 629 | 32 | 128§ |
| Wang et al (2001; Taiwan)21 | 6,451 | 42 | 0 | 10 (1.6/1,000) |
| Sharp et al (2002; US)14 | 185 | 84 | 2 | 24** |
| Brosens et al (2003; Belgium)22 | 85,727 | No data | No data | 195 (2.3/1,000) |
| * 80 open laparoscopy procedures; 30 closed laparoscopy procedures | ||||
| † Limited to trocar injuries | ||||
| ‡ Laparoscopic hysterectomy | ||||
| § All trocar injuries obtained through Food and Drug Administration reports | ||||
| ** Limited to optical access trocars | ||||
Classifying intestinal injuries
As in the case of major vessel injury, intestinal injury sustained during laparoscopy can be classified as either:
- Injury secondary to the approach. This category refers to entry complications associated with creation of the pneumoperitoneum and insertion of primary and secondary trocars.
- Injury secondary to the procedure or operation. This type of injury occurs as a result of manipulation with various devices during laparoscopy. The devices may include probes, forceps, scissors, or energy devices such as laser, electrosurgical, and ultrasonic instruments.
How trocar injury happens
Several studies have demonstrated that abdominal adhesions place any patient into a high-risk category for trocar injury to the intestines. Patients who have undergone multiple laparotomies, like the patient in the case that opened this article, are more likely to have severe adhesions and fall into the highest risk category for bowel perforation.11 It is impossible to predict with any degree of accuracy whether the intestine is adherent to the entry site.
Pneumoperitoneum can be protective
Creation of a pneumoperitoneum creates a cushion of gas between the intestines and the anterior abdominal wall (provided the intestines are not adherent to the abdominal wall). Manufacturers of disposable trocars with a retractable shield recommend creating an adequate pneumoperitoneum so that the “safety shield” deploys quickly and properly, unlike direct insertion, in which no gas is infused and space is insufficient for complete shield activation.
Open laparoscopy techniques, which allow the surgeon to enter the peritoneal cavity by direct vision without a sharp trocar, may diminish but not eliminate the risk of bowel injury.
What the data show
Of the 130 intestinal injuries recently reported by Baggish, 62 of 81 (77%) small bowel injuries were related to trocar insertion, as were 20 of 49 (41%) large intestinal injuries.12 In other words, 82 of 130 intestinal injuries (63%) were the direct result of trocar entry.
Bhoyrul and associates reported 629 trocar injuries, of which 182 were visceral.13 Of the 32 deaths, six were secondary to unrecognized bowel injury. Of 176 nonfatal visceral injuries, 128 (73%) involved the intestines, and 22 were unrecognized.
Optical-access and open laparoscopic systems were designed to prevent such injuries. Sharp and colleagues reported 24 intestinal injuries out of a total of 79 complications (30%) associated with optical-access trocars after reviewing data obtained from the Medical Device Reports (MDR) and Maude databases maintained by the Food and Drug Administration.14 In the Baggish series, 4.6% of injuries were associated with open laparoscopy.12
Champault and colleagues reviewed complications in a survey of 103,852 operations.15 Although they recommended use of open laparoscopy as opposed to blind insertion, they presented no data on the safety of open techniques.
How intraoperative injury happens
Operative injury of the large or small bowel often occurs during sharp or blunt dissection, performed during laparoscopy using accessory mechanical or energy devices. The latter type of device is utilized increasingly because laparoscopic knot tying and suturing are rather awkward and slow, and laparoscopic suturing to control bleeding is difficult. The size of the needle required for laparoscopic suture placement must be small enough to navigate a trocar sleeve.
Avoid blunt dissection when adhesions are present
The separation of dense adhesions between the intestines and neighboring bowel, other viscera, or abdominal wall is risky when blunt dissection is used. The tensile strength of the fibrotic connective tissue may well exceed that of the thin intestinal wall. Tearing the adhesion free may bring with it a portion of the bowel wall. Such injuries are frequently missed or described as serosal injuries and left unexplored and unrepaired.
Hydrodissection is a safer alternative. It involves the infiltration of sterile water or saline under low pressure between the parietal peritoneum and underlying retroperitoneal structures, providing a safe and natural plane for dissection. In addition, when the CO2 laser is used, the liquid acts as a heat sink to absorb any penetrating laser energy.
Energy devices create thermal effects
Energy devices used to cut tissue during operative laparoscopy coagulate blood vessels in a variety of ways, but the common pathway is thermal. Many hypotheses have evolved to explain how vessels are sealed, but none has demonstrated nonthermal activity except for cryocoagulation.
The devices most commonly used for cutting and hemostasis at laparoscopy are:
- electrosurgical (both monopolar and bipolar). Bipolar electrosurgical devices have advantages over monopolar devices when it comes to high-frequency leaks, direct coupling, and capacitive coupling.
- laser (CO2, holmium:YAG, Nd:YAG, KTP-532, argon). As I mentioned, CO2 laser devices are effectively backstopped by water, especially in strategic areas such as over and around intestines, major vessels, and the ureters.
- ultrasonic (Harmonic Scalpel, ultrasonic aspirator [CUSA]).
Laser and ultrasonic devices do not require a flow of electrons to create coagulation, but do produce heat that will spread peripherally by thermal conduction from the zone of impact (target).
The extent of energy-inflicted injury cannot be predicted
Inadvertent injury with energy devices can occur directly through contact with the bowel, indirectly by heat conduction through tissue, through capacitive coupling (monopolar electrical only), and by forward scatter (laser only).
Upon direct contact with the intestine, energy devices cut into the tissue in a manner similar to mechanical scissors or a knife but produce a larger wound. The reason? The transfer of heat to areas adjacent to the primary wound produces additional necrosis. Heat conduction, capacitive coupling, high-frequency leaks, and front scatter coagulate the intestinal wall with subsequent tissue devitalization and necrosis, the extent of which depends on the power density at contact and the duration of energy applied.
It is impossible to predict the depth or area of devitalization in energy-inflicted injury by visualization of the event.
In the Baggish review of 130 intestinal injuries, the number of injuries sustained during the operative procedure was 19 involving the small intestine and 29 involving the large bowel.12 Of this subset, 44% (21 cases) were secondary to the use of energy devices, with monopolar electrosurgical instruments alone accounting for 9 (43%) of the injuries.
Even best-laid plans can go awry
Despite our best intentions and precautions, accidents do sometimes happen, and bowel injury is no exception.In Part 2 of this article, I detail steps you can take to detect injuries in as timely a manner as possible.
1. Mäkinen J, Johansson J, Tomás C, et al. Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod. 2001;16:1473-1478.
2. Fuller J, Ashar BS, Corrado-Carey J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005;12:302-307.
3. Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg. 1997;185:461-465.
4. Baggish MS. Analysis of 31 cases of major-vessel injury associated with gynecologic laparoscopy operations. J Gynecol Surg. 2003;19:63-73.
5. Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB. Complications of laparoscopy: a prospective multicenter observational study. Br J Obstet Gynaecol. 1997;104:595-600.
6. Chapron C, Querleu D, Bruhat MA, et al. Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod. 1998;13:867-872.
7. Härkki-Sirén P, Sjöberg J, Mäkinen J, et al. Finnish National Register of Laparoscopic Hysterectomies: a review and complications of 1165 operations. Am J Obstet Gynecol. 1997;176(1 Pt. 1):118-122.
8. Härkki-Sirén P, Kurki T. A nationwide analysis of laparoscopic complications. Obstet Gynecol. 1997;89:108-112.
9. Chapron C, Pierre F, Harchaoui Y, et al. Gastrointestinal injuries during gynaecological laparoscopy. Hum Reprod. 1999;14:333-337.
10. Baggish MS. Avoiding vascular injury at laparoscopy. OBG Management. 2004;16(10):70-87.
11. Smith ARB. Postoperative complications following minimal access surgery. Baillieres Clin Obstet Gynecol. 2000;14:123.-
12. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
13. Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001;192:677-683.
14. Sharp HT, Dodson MK, Draper ML, Watts DA, Doucette RC, Hurd WW. Complications associated with optical-access laparoscopic trocars. Obstet Gynecol. 2002;99:553-555.
15. Champault G, Cazacu F, Taffi nder N. Serious trocar accidents in laparoscopic surgery: a French survey of 103,852 operations. Surg Laparosc Endosc. 1996;6:367-370.
16. Brown JA, Chamberlain GVP, Jordan JA, et al. Gynaecological laparoscopy. The Report of the Working Party of the Confidential Enquiry into Gynaecological Laparoscopy. Br J Obstet Gynaecol. 1978;85:401-403.
17. Soderstrom RM. Bowel injury ligation after laparoscopy. J Am Assoc Gynecol Laparosc. 1993;1:74-77.
18. Bateman BG, Kolp LA, Hoeger K. Complications of laparoscopy—operative and diagnostic. Fertil Steril. 1996;66:30-35.
19. Saidi MH, Vancaillie TG, White J, Sadler RK, Akright BD, Farhart SA. Complications of major operative laparoscopy. A review of 452 cases. J Reprod Med. 1996;41:471-476.
20. Gordts S, Watrelot A, Camp R, Brosens I. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76:1238-1241.
21. Wang PH, Lee WL, Yuan CC, et al. Major complications of operative and diagnostic laparoscopy for gynecologic disease. J Am Assoc Gynecol Laparosc. 2001;8:68-73.
22. Brosens I, Gordon A, Campo R, Gordts S. Bowel injury in gynecologic laparoscopy. J Am Assoc Gynecol Laparosc. 2003;10:9-13.
1. Mäkinen J, Johansson J, Tomás C, et al. Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod. 2001;16:1473-1478.
2. Fuller J, Ashar BS, Corrado-Carey J. Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol. 2005;12:302-307.
3. Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg. 1997;185:461-465.
4. Baggish MS. Analysis of 31 cases of major-vessel injury associated with gynecologic laparoscopy operations. J Gynecol Surg. 2003;19:63-73.
5. Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB. Complications of laparoscopy: a prospective multicenter observational study. Br J Obstet Gynaecol. 1997;104:595-600.
6. Chapron C, Querleu D, Bruhat MA, et al. Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod. 1998;13:867-872.
7. Härkki-Sirén P, Sjöberg J, Mäkinen J, et al. Finnish National Register of Laparoscopic Hysterectomies: a review and complications of 1165 operations. Am J Obstet Gynecol. 1997;176(1 Pt. 1):118-122.
8. Härkki-Sirén P, Kurki T. A nationwide analysis of laparoscopic complications. Obstet Gynecol. 1997;89:108-112.
9. Chapron C, Pierre F, Harchaoui Y, et al. Gastrointestinal injuries during gynaecological laparoscopy. Hum Reprod. 1999;14:333-337.
10. Baggish MS. Avoiding vascular injury at laparoscopy. OBG Management. 2004;16(10):70-87.
11. Smith ARB. Postoperative complications following minimal access surgery. Baillieres Clin Obstet Gynecol. 2000;14:123.-
12. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
13. Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001;192:677-683.
14. Sharp HT, Dodson MK, Draper ML, Watts DA, Doucette RC, Hurd WW. Complications associated with optical-access laparoscopic trocars. Obstet Gynecol. 2002;99:553-555.
15. Champault G, Cazacu F, Taffi nder N. Serious trocar accidents in laparoscopic surgery: a French survey of 103,852 operations. Surg Laparosc Endosc. 1996;6:367-370.
16. Brown JA, Chamberlain GVP, Jordan JA, et al. Gynaecological laparoscopy. The Report of the Working Party of the Confidential Enquiry into Gynaecological Laparoscopy. Br J Obstet Gynaecol. 1978;85:401-403.
17. Soderstrom RM. Bowel injury ligation after laparoscopy. J Am Assoc Gynecol Laparosc. 1993;1:74-77.
18. Bateman BG, Kolp LA, Hoeger K. Complications of laparoscopy—operative and diagnostic. Fertil Steril. 1996;66:30-35.
19. Saidi MH, Vancaillie TG, White J, Sadler RK, Akright BD, Farhart SA. Complications of major operative laparoscopy. A review of 452 cases. J Reprod Med. 1996;41:471-476.
20. Gordts S, Watrelot A, Camp R, Brosens I. Risk and outcome of bowel injury during transvaginal pelvic endoscopy. Fertil Steril. 2001;76:1238-1241.
21. Wang PH, Lee WL, Yuan CC, et al. Major complications of operative and diagnostic laparoscopy for gynecologic disease. J Am Assoc Gynecol Laparosc. 2001;8:68-73.
22. Brosens I, Gordon A, Campo R, Gordts S. Bowel injury in gynecologic laparoscopy. J Am Assoc Gynecol Laparosc. 2003;10:9-13.
Lessons in timely recognition of laparoscopy-related bowel injury
In Part 1 of this article, I outlined circumstances in which abdominal adhesions should be anticipated and described strategies to prevent intestinal injury during operative procedures. Here, I describe ways to identify intestinal injury as soon as possible after it occurs, which is vital to prevent serious sequelae such as sepsis and even death.
During operative laparoscopy, a quick search for injury through the laparoscope cannot assure any surgeon that the intestinal wall has not been seriously denuded. A damaged muscularis—even if it is not recognized as transmural injury—may subsequently rupture if it is not appropriately repaired intraoperatively.
Following dissection of adhesions, irrigate the neighboring intestine with sterile saline, and perform a detailed inspection of the intestine to ascertain integrity of the bowel wall. The color of the intestine is important, as it can indicate whether the abundant vascular supply has been compromised. Include a detailed description of the intestines in the operative note.
Avoid stapling or vascular clips when repairing any wound; careful suturing is preferred.
Why early diagnosis is critical
The most favorable time to diagnose an iatrogenic intestinal perforation is within the intraoperative period. Prompt recognition and repair of bowel perforation offers several advantages:
- A second or third operation is less likely (
- The risk of abdominal sepsis is decreased.
- The volume of peripheral injury to the intestine is reduced.
- The patient can be followed for subsequent complications more precisely, permitting earlier diagnosis, more timely and effective treatment, and lower morbidity.
The 130 intestinal injuries reported by Baggish reflect the clinical significance of timely diagnosis.1 Seventy percent of small bowel and 51% of large bowel perforations were correctly diagnosed more than 48 hours postoperatively. Sepsis was present in a majority of these cases at the time of diagnosis.
Infection, fluid-electrolyte imbalance, sepsis syndrome
The principal derangements that arise as a result of bowel perforation are infection and fluid-electrolyte imbalance and their sequelae. Intestinal fluid and feces contain a variety of bacteria, such as Escherichia coli, Enterococcus, Klebsiella, Proteus, Pseudomonas, and Clostridium, to name a few. These bacteria produce toxins that facilitate entry of bacteria into the circulation and contribute to a downward spiral of events, referred to as sepsis syndrome, as well as intra-abdominal abscess:
- Contamination of the abdominal cavity leads to inflammation of the peritoneum
- In turn, subperitoneal blood vessels become porous, causing interstitial fluid to leak into the third space
- Paralytic ileus and an accumulation of intra-abdominal fluid push the diaphragm upward, lowering the capacity for lung expansion within the thorax and contributing to partial lung collapse
- Fluid of inflammatory origin may accumulate in the chest as pleural cavity effusion.
A number of progressive complications are predictable, but may occur at variable intervals after the initial perforation. The most frequent complications associated with colonic injuries are:
- peritonitis (98% of cases)
- ileus (92%)
- pleural effusion (84%)
- colostomy (80%)
- intra-abdominal abscess (78%).
The most common sequelae after small-bowel perforation are:
- peritonitis (100% of cases)
- ileus (89%)
- intra-abdominal abscess (63%)
- pleural effusion (59%).1
Reasons for diagnostic delay
- The gynecologic surgeon fails to place intestinal injury at the top of the differential diagnosis.
- A surgical consultant is delayed in making a correct diagnosis. Surgeons have less experience with perforation than do gynecologists, and invariably consider the postoperative abdominal problem to be ileus or intestinal obstruction. The presence of postoperative pneumoperitoneum is incorrectly thought to be lingering CO2 gas from the initial laparoscopy rather than air from a perforated viscus.
- Ancillary diagnosis confuses the primary physician. Pleural effusion, chest pain, and tachypnea are usually thought to indicate pulmonary embolism; as a result, the gynecologist and consulting pulmonologist focus on pulmonary embolus and deep-vein thrombosis. Only a spiral computed tomography (CT) scan, a ventilation perfusion (VQ) scan, or arteriogram quickly rules pulmonary embolus in or out. Peritonitis associated with ileus or third-space fluid leakage resulting in diaphragmatic elevation also creates pleural effusion, tachypnea, and dyspnea.
Presumptive diagnosis is critical
Definitive diagnosis of intestinal perforation happens at the operating table under direct vision and is corroborated by the pathology laboratory if bowel resection is performed. However, presumptive diagnosis helps overcome inertia and gets the patient to the operating room sooner.
The process by which the presumptive diagnosis is made is the most important issue in this article. The shorter the process, the lower the patient’s morbidity, and vice versa.
Look for steady improvement. Worry when it is absent
After any laparoscopic operation, the postoperative course should be one of steady clinical improvement. When a patient deviates from this model, the foremost presumptive diagnosis should be laparoscopy-associated injury, and the intestine should top the list of organs that may be injured. Other diagnoses should be subordinate to the principal presumptive diagnosis; these include ileus, bowel obstruction, pulmonary embolus, gastroenteritis, and hematoma, to name a few.
I do not mean to imply that a potentially life-threatening complication such as pulmonary embolus should not be ruled in or out, but that the necessary imaging should be performed in a timely fashion. The abdominal-pelvic CT scan will offer clues to the presence of free air, free fluid, air-fluid levels, and foreign bodies. It also is useful in detecting intra-abdominal—specifically, subphrenic—abscess. If necessary, a VQ scan or spiral CT scan can then be performed without delaying the diagnosis of the primary intra-abdominal catastrophe responsible for the pulmonary symptoms.
In the opening case, before making an improbable presumptive diagnosis, the surgeon should have questioned why an otherwise healthy woman would coincidentally develop gastroenteritis after laparoscopic surgery. The same can be said for diagnoses of intestinal obstruction or vascular thrombosis involving the intestinal blood supply.
Typical presentation of the injured patient
An injured patient does not experience daily improvement and a return to normal activity. Instead, the postoperative period is marked by persistent and worsening pain, often compounded by nausea or vomiting, or both. The patient may complain of fever, chills, weakness, or simply not feeling normal. Breathing may be labored. As time elapses, the symptoms become worse.
Reports of more than one visit to an emergency care facility are not uncommon. When examined, the patient exhibits direct or rebound tenderness, or both. The abdomen may or may not be distended, but usually is increased in girth. Bowel sounds are diminished or absent.
Vital signs initially reveal normal, low-grade, or subnormal temperature, and tachycardia, tachypnea, and normal blood pressure are typical. As time and sepsis progress, however, fever and hypotension develop. Most other symptoms and signs become progressively more abnormal in direct proportion to the length of time the diagnosis is delayed.
Seminal laboratory values for sepsis include a lower than normal white blood cell (WBC) count, elevated immature white-cell elements (e.g., “bandemia”), elevated liver chemistries, and an elevated serum creatinine level.
Mortality is most often the result of overwhelming and prolonged sepsis, leading to multiorgan failure, bleeding diathesis, and adult respiratory distress syndrome.
Among 130 laparoscopic surgical cases complicated by bowel injury and reported by Baggish, sepsis was diagnosed in 100% of colonic perforations and 50% of small-bowel perforations when the diagnosis was delayed more than 48 hours after surgery.1
TABLE 1 lists the signs and frequency of sepsis in these 100 cases, and TABLE 2 collates the signs and symptoms that were observed. Peritoneal cultures obtained at the time of exploratory laparotomy revealed multiple organisms (polymicrobial) in 60% of cases.
TABLE 1
Frequency of signs of sepsis among 130 patients with colon or small-bowel injury
| Sign | Colon (49 patients) | Small bowel (81 patients) |
|---|---|---|
| Normal or subnormal temperature | 30* | 41* |
| Fever | 19 | 40 |
| Tachycardia | 31 | 44 |
| Tachypnea | 30 | 40 |
| Hypotension | 21 | 15 |
| Anemia | 38 | 51 |
| Depressed WBC count | 20 | 18 |
| Elevated WBC count | 24 | 32 |
| Bandemia | 25 | 30 |
| Elevated creatinine and blood urea nitrogen levels | 12 | 5 |
| *Number of patients. | ||
| Source: Baggish1 | ||
Watch for signs and symptoms of intestinal injury
| Symptom | Sign |
|---|---|
| Abdominal pain | Direct or rebound tenderness |
| Bloating | Abdominal distension |
| Nausea, vomiting | Diminished bowel sounds |
| Fever, chills | Elevated or subnormal temperature |
| Difficulty breathing | Tachypnea, tachycardia |
| Weakness | Pallor, hypotension, diminished consciousness |
| Source: Baggish1 | |
Concurrent injuries to neighboring structures
A number of collateral injuries may occur in conjunction with intestinal perforation, depending on the location of the trauma. The most dangerous combination includes indirect laceration of one of the major retroperitoneal vessels. A through-and-through perforation of the cecum can also involve one or more of the right iliac vessels. A trocar perforation of the ileum may continue directly into the presacral space or pass above it and penetrate the left common iliac vein or aorta. Similarly, perforation of the sigmoid colon may penetrate the left iliac vessels.
Careful inspection of the posterior peritoneum for tears and evidence of retroperitoneal hematoma is required to avoid missing a serious collateral injury. More likely, however, is a penetrating injury to the small bowel presenting with collateral mesenteric damage and compromise of the blood supply of an entire segment of bowel. The ureter and bladder may also be injured when dissection along the pelvic sidewall, or a trocar thrust, deviates to the right or left of midline. In thin patients, the stomach may be perforated as well as the small intestine or transverse colon.
In one memorable case, a primary trocar penetrated the omentum, injuring several underlying structures. In its transit, the trocar passed through both the anterior and posterior walls of the duodenum and finally entered the superior mesenteric artery. The gynecologic surgeon performing the laparoscopic tubal ligation failed to recognize any of these injuries. The patient went into shock in the recovery room and was returned to the operating room. Fortunately, a transplant surgeon from a neighboring theater was immediately available to consult and repair the damage.
Another danger: intestinal ischemic necrosis
Abnormalities in splanchnic blood flow are sometimes caused by elevations in intra-abdominal pressure. Caldwell and Ricotta inflated the abdomens of nine dogs and reported a significant reduction of blood flow to omentum, stomach, duodenum, jejunum, ileum, colon, pancreas, liver, and spleen, but not to the adrenal glands.2 The splanchnic flow reductions essentially shunted blood away from abdominal viscera with auto-transfusion to the heart, lungs, and systemic circulation.
Eleftheriadis and colleagues studied 16 women randomized to laparoscopic versus open cholecystectomy.3 Significant depression of the hepatic microcirculation during the period of CO2 gas insufflation was noted in the laparoscopy cohort but not in the control group. Gastric mucosal ischemia also was observed in the laparoscopy group.
Several case reports of catastrophic intestinal ischemia have appeared in the literature (1994–1995).4-7 These articles have mainly involved laparoscopic upper abdominal operations in elderly people.
Recently, however, Hasson and colleagues reported a case of possible ischemic necrosis of the small intestine following laparoscopic adhesiolysis and bipolar myolysis.8 The authors emphasized that CO2 pneumoperitoneum reduces splanchnic blood flow, predisposing the patient to ischemia, but that ischemia with infarction requires an underlying vasculopathy or inciting factors such as traction on a short mesentery, atherosclerosis, or thrombosis.
A high index of suspicion for bowel ischemia following laparoscopic surgery should occur when, postoperatively, a patient experiences inordinately severe abdominal pain associated with tachypnea, tachycardia, and alterations in the WBC count. A paucity of physical abdominal signs in the early phases of this disorder should alert the clinician to the possibility of bowel ischemia.
Diagnosing and treating ischemia
A CT scan with contrast can suggest ischemia, but angiography is usually required for definitive diagnosis.
Treatment begins with infusion of papaverine into the intestinal vasculature via angiography cannula. In some cases, anticoagulation may be indicated. Surgery by laparotomy is clearly indicated for patients who fail to respond to vasodilatation measures.
This condition can be ameliorated by intermittent intraoperative decompression of the abdomen. Avoiding prolonged CO2 pneumoperitoneum and a lengthy laparoscopic operation also may diminish the risk of intestinal ischemia.
1. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
2. Caldwell CB, Ricotta JJ. Changes in visceral blood flow with elevated intra-abdominal pressure. J Surg Res. 1987;43:14-20.
3. Eleftheriadis E, Kotzampassi K, Botsios D, Tzartinoglu E, Farmakis H, Dadoukis J. Splanchnic ischemia during laparoscopic cholecystectomy. Surg Endosc. 1996;10:324-326.
4. Schorr RT. Laparoscopic upper abdominal operations and mesenteric infarction. J Laparoendosc Surg. 1995;5:389-392.
5. Mitchell PC, Jamieson GG. Coeliac axis and mesenteric arterial thrombosis following laparoscopic Nissen fundoplication. Aust N Z J Surg. 1994;64:728-730.
6. Dwerryhouse SJ, Melsom DS, Burton PA, Thompson MH. Acute intestinal ischaemia after laparoscopic cholecystectomy. Br J Surg. 1995;82:1413.-
7. Jaffe V, Russell RCG. Fatal intestinal ischaemia following laparoscopic cholecystectomy. Br J Surg. 1994;81:1827-1828.
8. Hasson HM, Galanopoulos C, Lanferman A. Ischemic necrosis of small bowel following laparoscopic surgery. JSLS. 2004;8:159-163.
In Part 1 of this article, I outlined circumstances in which abdominal adhesions should be anticipated and described strategies to prevent intestinal injury during operative procedures. Here, I describe ways to identify intestinal injury as soon as possible after it occurs, which is vital to prevent serious sequelae such as sepsis and even death.
During operative laparoscopy, a quick search for injury through the laparoscope cannot assure any surgeon that the intestinal wall has not been seriously denuded. A damaged muscularis—even if it is not recognized as transmural injury—may subsequently rupture if it is not appropriately repaired intraoperatively.
Following dissection of adhesions, irrigate the neighboring intestine with sterile saline, and perform a detailed inspection of the intestine to ascertain integrity of the bowel wall. The color of the intestine is important, as it can indicate whether the abundant vascular supply has been compromised. Include a detailed description of the intestines in the operative note.
Avoid stapling or vascular clips when repairing any wound; careful suturing is preferred.
Why early diagnosis is critical
The most favorable time to diagnose an iatrogenic intestinal perforation is within the intraoperative period. Prompt recognition and repair of bowel perforation offers several advantages:
- A second or third operation is less likely (
- The risk of abdominal sepsis is decreased.
- The volume of peripheral injury to the intestine is reduced.
- The patient can be followed for subsequent complications more precisely, permitting earlier diagnosis, more timely and effective treatment, and lower morbidity.
The 130 intestinal injuries reported by Baggish reflect the clinical significance of timely diagnosis.1 Seventy percent of small bowel and 51% of large bowel perforations were correctly diagnosed more than 48 hours postoperatively. Sepsis was present in a majority of these cases at the time of diagnosis.
Infection, fluid-electrolyte imbalance, sepsis syndrome
The principal derangements that arise as a result of bowel perforation are infection and fluid-electrolyte imbalance and their sequelae. Intestinal fluid and feces contain a variety of bacteria, such as Escherichia coli, Enterococcus, Klebsiella, Proteus, Pseudomonas, and Clostridium, to name a few. These bacteria produce toxins that facilitate entry of bacteria into the circulation and contribute to a downward spiral of events, referred to as sepsis syndrome, as well as intra-abdominal abscess:
- Contamination of the abdominal cavity leads to inflammation of the peritoneum
- In turn, subperitoneal blood vessels become porous, causing interstitial fluid to leak into the third space
- Paralytic ileus and an accumulation of intra-abdominal fluid push the diaphragm upward, lowering the capacity for lung expansion within the thorax and contributing to partial lung collapse
- Fluid of inflammatory origin may accumulate in the chest as pleural cavity effusion.
A number of progressive complications are predictable, but may occur at variable intervals after the initial perforation. The most frequent complications associated with colonic injuries are:
- peritonitis (98% of cases)
- ileus (92%)
- pleural effusion (84%)
- colostomy (80%)
- intra-abdominal abscess (78%).
The most common sequelae after small-bowel perforation are:
- peritonitis (100% of cases)
- ileus (89%)
- intra-abdominal abscess (63%)
- pleural effusion (59%).1
Reasons for diagnostic delay
- The gynecologic surgeon fails to place intestinal injury at the top of the differential diagnosis.
- A surgical consultant is delayed in making a correct diagnosis. Surgeons have less experience with perforation than do gynecologists, and invariably consider the postoperative abdominal problem to be ileus or intestinal obstruction. The presence of postoperative pneumoperitoneum is incorrectly thought to be lingering CO2 gas from the initial laparoscopy rather than air from a perforated viscus.
- Ancillary diagnosis confuses the primary physician. Pleural effusion, chest pain, and tachypnea are usually thought to indicate pulmonary embolism; as a result, the gynecologist and consulting pulmonologist focus on pulmonary embolus and deep-vein thrombosis. Only a spiral computed tomography (CT) scan, a ventilation perfusion (VQ) scan, or arteriogram quickly rules pulmonary embolus in or out. Peritonitis associated with ileus or third-space fluid leakage resulting in diaphragmatic elevation also creates pleural effusion, tachypnea, and dyspnea.
Presumptive diagnosis is critical
Definitive diagnosis of intestinal perforation happens at the operating table under direct vision and is corroborated by the pathology laboratory if bowel resection is performed. However, presumptive diagnosis helps overcome inertia and gets the patient to the operating room sooner.
The process by which the presumptive diagnosis is made is the most important issue in this article. The shorter the process, the lower the patient’s morbidity, and vice versa.
Look for steady improvement. Worry when it is absent
After any laparoscopic operation, the postoperative course should be one of steady clinical improvement. When a patient deviates from this model, the foremost presumptive diagnosis should be laparoscopy-associated injury, and the intestine should top the list of organs that may be injured. Other diagnoses should be subordinate to the principal presumptive diagnosis; these include ileus, bowel obstruction, pulmonary embolus, gastroenteritis, and hematoma, to name a few.
I do not mean to imply that a potentially life-threatening complication such as pulmonary embolus should not be ruled in or out, but that the necessary imaging should be performed in a timely fashion. The abdominal-pelvic CT scan will offer clues to the presence of free air, free fluid, air-fluid levels, and foreign bodies. It also is useful in detecting intra-abdominal—specifically, subphrenic—abscess. If necessary, a VQ scan or spiral CT scan can then be performed without delaying the diagnosis of the primary intra-abdominal catastrophe responsible for the pulmonary symptoms.
In the opening case, before making an improbable presumptive diagnosis, the surgeon should have questioned why an otherwise healthy woman would coincidentally develop gastroenteritis after laparoscopic surgery. The same can be said for diagnoses of intestinal obstruction or vascular thrombosis involving the intestinal blood supply.
Typical presentation of the injured patient
An injured patient does not experience daily improvement and a return to normal activity. Instead, the postoperative period is marked by persistent and worsening pain, often compounded by nausea or vomiting, or both. The patient may complain of fever, chills, weakness, or simply not feeling normal. Breathing may be labored. As time elapses, the symptoms become worse.
Reports of more than one visit to an emergency care facility are not uncommon. When examined, the patient exhibits direct or rebound tenderness, or both. The abdomen may or may not be distended, but usually is increased in girth. Bowel sounds are diminished or absent.
Vital signs initially reveal normal, low-grade, or subnormal temperature, and tachycardia, tachypnea, and normal blood pressure are typical. As time and sepsis progress, however, fever and hypotension develop. Most other symptoms and signs become progressively more abnormal in direct proportion to the length of time the diagnosis is delayed.
Seminal laboratory values for sepsis include a lower than normal white blood cell (WBC) count, elevated immature white-cell elements (e.g., “bandemia”), elevated liver chemistries, and an elevated serum creatinine level.
Mortality is most often the result of overwhelming and prolonged sepsis, leading to multiorgan failure, bleeding diathesis, and adult respiratory distress syndrome.
Among 130 laparoscopic surgical cases complicated by bowel injury and reported by Baggish, sepsis was diagnosed in 100% of colonic perforations and 50% of small-bowel perforations when the diagnosis was delayed more than 48 hours after surgery.1
TABLE 1 lists the signs and frequency of sepsis in these 100 cases, and TABLE 2 collates the signs and symptoms that were observed. Peritoneal cultures obtained at the time of exploratory laparotomy revealed multiple organisms (polymicrobial) in 60% of cases.
TABLE 1
Frequency of signs of sepsis among 130 patients with colon or small-bowel injury
| Sign | Colon (49 patients) | Small bowel (81 patients) |
|---|---|---|
| Normal or subnormal temperature | 30* | 41* |
| Fever | 19 | 40 |
| Tachycardia | 31 | 44 |
| Tachypnea | 30 | 40 |
| Hypotension | 21 | 15 |
| Anemia | 38 | 51 |
| Depressed WBC count | 20 | 18 |
| Elevated WBC count | 24 | 32 |
| Bandemia | 25 | 30 |
| Elevated creatinine and blood urea nitrogen levels | 12 | 5 |
| *Number of patients. | ||
| Source: Baggish1 | ||
Watch for signs and symptoms of intestinal injury
| Symptom | Sign |
|---|---|
| Abdominal pain | Direct or rebound tenderness |
| Bloating | Abdominal distension |
| Nausea, vomiting | Diminished bowel sounds |
| Fever, chills | Elevated or subnormal temperature |
| Difficulty breathing | Tachypnea, tachycardia |
| Weakness | Pallor, hypotension, diminished consciousness |
| Source: Baggish1 | |
Concurrent injuries to neighboring structures
A number of collateral injuries may occur in conjunction with intestinal perforation, depending on the location of the trauma. The most dangerous combination includes indirect laceration of one of the major retroperitoneal vessels. A through-and-through perforation of the cecum can also involve one or more of the right iliac vessels. A trocar perforation of the ileum may continue directly into the presacral space or pass above it and penetrate the left common iliac vein or aorta. Similarly, perforation of the sigmoid colon may penetrate the left iliac vessels.
Careful inspection of the posterior peritoneum for tears and evidence of retroperitoneal hematoma is required to avoid missing a serious collateral injury. More likely, however, is a penetrating injury to the small bowel presenting with collateral mesenteric damage and compromise of the blood supply of an entire segment of bowel. The ureter and bladder may also be injured when dissection along the pelvic sidewall, or a trocar thrust, deviates to the right or left of midline. In thin patients, the stomach may be perforated as well as the small intestine or transverse colon.
In one memorable case, a primary trocar penetrated the omentum, injuring several underlying structures. In its transit, the trocar passed through both the anterior and posterior walls of the duodenum and finally entered the superior mesenteric artery. The gynecologic surgeon performing the laparoscopic tubal ligation failed to recognize any of these injuries. The patient went into shock in the recovery room and was returned to the operating room. Fortunately, a transplant surgeon from a neighboring theater was immediately available to consult and repair the damage.
Another danger: intestinal ischemic necrosis
Abnormalities in splanchnic blood flow are sometimes caused by elevations in intra-abdominal pressure. Caldwell and Ricotta inflated the abdomens of nine dogs and reported a significant reduction of blood flow to omentum, stomach, duodenum, jejunum, ileum, colon, pancreas, liver, and spleen, but not to the adrenal glands.2 The splanchnic flow reductions essentially shunted blood away from abdominal viscera with auto-transfusion to the heart, lungs, and systemic circulation.
Eleftheriadis and colleagues studied 16 women randomized to laparoscopic versus open cholecystectomy.3 Significant depression of the hepatic microcirculation during the period of CO2 gas insufflation was noted in the laparoscopy cohort but not in the control group. Gastric mucosal ischemia also was observed in the laparoscopy group.
Several case reports of catastrophic intestinal ischemia have appeared in the literature (1994–1995).4-7 These articles have mainly involved laparoscopic upper abdominal operations in elderly people.
Recently, however, Hasson and colleagues reported a case of possible ischemic necrosis of the small intestine following laparoscopic adhesiolysis and bipolar myolysis.8 The authors emphasized that CO2 pneumoperitoneum reduces splanchnic blood flow, predisposing the patient to ischemia, but that ischemia with infarction requires an underlying vasculopathy or inciting factors such as traction on a short mesentery, atherosclerosis, or thrombosis.
A high index of suspicion for bowel ischemia following laparoscopic surgery should occur when, postoperatively, a patient experiences inordinately severe abdominal pain associated with tachypnea, tachycardia, and alterations in the WBC count. A paucity of physical abdominal signs in the early phases of this disorder should alert the clinician to the possibility of bowel ischemia.
Diagnosing and treating ischemia
A CT scan with contrast can suggest ischemia, but angiography is usually required for definitive diagnosis.
Treatment begins with infusion of papaverine into the intestinal vasculature via angiography cannula. In some cases, anticoagulation may be indicated. Surgery by laparotomy is clearly indicated for patients who fail to respond to vasodilatation measures.
This condition can be ameliorated by intermittent intraoperative decompression of the abdomen. Avoiding prolonged CO2 pneumoperitoneum and a lengthy laparoscopic operation also may diminish the risk of intestinal ischemia.
In Part 1 of this article, I outlined circumstances in which abdominal adhesions should be anticipated and described strategies to prevent intestinal injury during operative procedures. Here, I describe ways to identify intestinal injury as soon as possible after it occurs, which is vital to prevent serious sequelae such as sepsis and even death.
During operative laparoscopy, a quick search for injury through the laparoscope cannot assure any surgeon that the intestinal wall has not been seriously denuded. A damaged muscularis—even if it is not recognized as transmural injury—may subsequently rupture if it is not appropriately repaired intraoperatively.
Following dissection of adhesions, irrigate the neighboring intestine with sterile saline, and perform a detailed inspection of the intestine to ascertain integrity of the bowel wall. The color of the intestine is important, as it can indicate whether the abundant vascular supply has been compromised. Include a detailed description of the intestines in the operative note.
Avoid stapling or vascular clips when repairing any wound; careful suturing is preferred.
Why early diagnosis is critical
The most favorable time to diagnose an iatrogenic intestinal perforation is within the intraoperative period. Prompt recognition and repair of bowel perforation offers several advantages:
- A second or third operation is less likely (
- The risk of abdominal sepsis is decreased.
- The volume of peripheral injury to the intestine is reduced.
- The patient can be followed for subsequent complications more precisely, permitting earlier diagnosis, more timely and effective treatment, and lower morbidity.
The 130 intestinal injuries reported by Baggish reflect the clinical significance of timely diagnosis.1 Seventy percent of small bowel and 51% of large bowel perforations were correctly diagnosed more than 48 hours postoperatively. Sepsis was present in a majority of these cases at the time of diagnosis.
Infection, fluid-electrolyte imbalance, sepsis syndrome
The principal derangements that arise as a result of bowel perforation are infection and fluid-electrolyte imbalance and their sequelae. Intestinal fluid and feces contain a variety of bacteria, such as Escherichia coli, Enterococcus, Klebsiella, Proteus, Pseudomonas, and Clostridium, to name a few. These bacteria produce toxins that facilitate entry of bacteria into the circulation and contribute to a downward spiral of events, referred to as sepsis syndrome, as well as intra-abdominal abscess:
- Contamination of the abdominal cavity leads to inflammation of the peritoneum
- In turn, subperitoneal blood vessels become porous, causing interstitial fluid to leak into the third space
- Paralytic ileus and an accumulation of intra-abdominal fluid push the diaphragm upward, lowering the capacity for lung expansion within the thorax and contributing to partial lung collapse
- Fluid of inflammatory origin may accumulate in the chest as pleural cavity effusion.
A number of progressive complications are predictable, but may occur at variable intervals after the initial perforation. The most frequent complications associated with colonic injuries are:
- peritonitis (98% of cases)
- ileus (92%)
- pleural effusion (84%)
- colostomy (80%)
- intra-abdominal abscess (78%).
The most common sequelae after small-bowel perforation are:
- peritonitis (100% of cases)
- ileus (89%)
- intra-abdominal abscess (63%)
- pleural effusion (59%).1
Reasons for diagnostic delay
- The gynecologic surgeon fails to place intestinal injury at the top of the differential diagnosis.
- A surgical consultant is delayed in making a correct diagnosis. Surgeons have less experience with perforation than do gynecologists, and invariably consider the postoperative abdominal problem to be ileus or intestinal obstruction. The presence of postoperative pneumoperitoneum is incorrectly thought to be lingering CO2 gas from the initial laparoscopy rather than air from a perforated viscus.
- Ancillary diagnosis confuses the primary physician. Pleural effusion, chest pain, and tachypnea are usually thought to indicate pulmonary embolism; as a result, the gynecologist and consulting pulmonologist focus on pulmonary embolus and deep-vein thrombosis. Only a spiral computed tomography (CT) scan, a ventilation perfusion (VQ) scan, or arteriogram quickly rules pulmonary embolus in or out. Peritonitis associated with ileus or third-space fluid leakage resulting in diaphragmatic elevation also creates pleural effusion, tachypnea, and dyspnea.
Presumptive diagnosis is critical
Definitive diagnosis of intestinal perforation happens at the operating table under direct vision and is corroborated by the pathology laboratory if bowel resection is performed. However, presumptive diagnosis helps overcome inertia and gets the patient to the operating room sooner.
The process by which the presumptive diagnosis is made is the most important issue in this article. The shorter the process, the lower the patient’s morbidity, and vice versa.
Look for steady improvement. Worry when it is absent
After any laparoscopic operation, the postoperative course should be one of steady clinical improvement. When a patient deviates from this model, the foremost presumptive diagnosis should be laparoscopy-associated injury, and the intestine should top the list of organs that may be injured. Other diagnoses should be subordinate to the principal presumptive diagnosis; these include ileus, bowel obstruction, pulmonary embolus, gastroenteritis, and hematoma, to name a few.
I do not mean to imply that a potentially life-threatening complication such as pulmonary embolus should not be ruled in or out, but that the necessary imaging should be performed in a timely fashion. The abdominal-pelvic CT scan will offer clues to the presence of free air, free fluid, air-fluid levels, and foreign bodies. It also is useful in detecting intra-abdominal—specifically, subphrenic—abscess. If necessary, a VQ scan or spiral CT scan can then be performed without delaying the diagnosis of the primary intra-abdominal catastrophe responsible for the pulmonary symptoms.
In the opening case, before making an improbable presumptive diagnosis, the surgeon should have questioned why an otherwise healthy woman would coincidentally develop gastroenteritis after laparoscopic surgery. The same can be said for diagnoses of intestinal obstruction or vascular thrombosis involving the intestinal blood supply.
Typical presentation of the injured patient
An injured patient does not experience daily improvement and a return to normal activity. Instead, the postoperative period is marked by persistent and worsening pain, often compounded by nausea or vomiting, or both. The patient may complain of fever, chills, weakness, or simply not feeling normal. Breathing may be labored. As time elapses, the symptoms become worse.
Reports of more than one visit to an emergency care facility are not uncommon. When examined, the patient exhibits direct or rebound tenderness, or both. The abdomen may or may not be distended, but usually is increased in girth. Bowel sounds are diminished or absent.
Vital signs initially reveal normal, low-grade, or subnormal temperature, and tachycardia, tachypnea, and normal blood pressure are typical. As time and sepsis progress, however, fever and hypotension develop. Most other symptoms and signs become progressively more abnormal in direct proportion to the length of time the diagnosis is delayed.
Seminal laboratory values for sepsis include a lower than normal white blood cell (WBC) count, elevated immature white-cell elements (e.g., “bandemia”), elevated liver chemistries, and an elevated serum creatinine level.
Mortality is most often the result of overwhelming and prolonged sepsis, leading to multiorgan failure, bleeding diathesis, and adult respiratory distress syndrome.
Among 130 laparoscopic surgical cases complicated by bowel injury and reported by Baggish, sepsis was diagnosed in 100% of colonic perforations and 50% of small-bowel perforations when the diagnosis was delayed more than 48 hours after surgery.1
TABLE 1 lists the signs and frequency of sepsis in these 100 cases, and TABLE 2 collates the signs and symptoms that were observed. Peritoneal cultures obtained at the time of exploratory laparotomy revealed multiple organisms (polymicrobial) in 60% of cases.
TABLE 1
Frequency of signs of sepsis among 130 patients with colon or small-bowel injury
| Sign | Colon (49 patients) | Small bowel (81 patients) |
|---|---|---|
| Normal or subnormal temperature | 30* | 41* |
| Fever | 19 | 40 |
| Tachycardia | 31 | 44 |
| Tachypnea | 30 | 40 |
| Hypotension | 21 | 15 |
| Anemia | 38 | 51 |
| Depressed WBC count | 20 | 18 |
| Elevated WBC count | 24 | 32 |
| Bandemia | 25 | 30 |
| Elevated creatinine and blood urea nitrogen levels | 12 | 5 |
| *Number of patients. | ||
| Source: Baggish1 | ||
Watch for signs and symptoms of intestinal injury
| Symptom | Sign |
|---|---|
| Abdominal pain | Direct or rebound tenderness |
| Bloating | Abdominal distension |
| Nausea, vomiting | Diminished bowel sounds |
| Fever, chills | Elevated or subnormal temperature |
| Difficulty breathing | Tachypnea, tachycardia |
| Weakness | Pallor, hypotension, diminished consciousness |
| Source: Baggish1 | |
Concurrent injuries to neighboring structures
A number of collateral injuries may occur in conjunction with intestinal perforation, depending on the location of the trauma. The most dangerous combination includes indirect laceration of one of the major retroperitoneal vessels. A through-and-through perforation of the cecum can also involve one or more of the right iliac vessels. A trocar perforation of the ileum may continue directly into the presacral space or pass above it and penetrate the left common iliac vein or aorta. Similarly, perforation of the sigmoid colon may penetrate the left iliac vessels.
Careful inspection of the posterior peritoneum for tears and evidence of retroperitoneal hematoma is required to avoid missing a serious collateral injury. More likely, however, is a penetrating injury to the small bowel presenting with collateral mesenteric damage and compromise of the blood supply of an entire segment of bowel. The ureter and bladder may also be injured when dissection along the pelvic sidewall, or a trocar thrust, deviates to the right or left of midline. In thin patients, the stomach may be perforated as well as the small intestine or transverse colon.
In one memorable case, a primary trocar penetrated the omentum, injuring several underlying structures. In its transit, the trocar passed through both the anterior and posterior walls of the duodenum and finally entered the superior mesenteric artery. The gynecologic surgeon performing the laparoscopic tubal ligation failed to recognize any of these injuries. The patient went into shock in the recovery room and was returned to the operating room. Fortunately, a transplant surgeon from a neighboring theater was immediately available to consult and repair the damage.
Another danger: intestinal ischemic necrosis
Abnormalities in splanchnic blood flow are sometimes caused by elevations in intra-abdominal pressure. Caldwell and Ricotta inflated the abdomens of nine dogs and reported a significant reduction of blood flow to omentum, stomach, duodenum, jejunum, ileum, colon, pancreas, liver, and spleen, but not to the adrenal glands.2 The splanchnic flow reductions essentially shunted blood away from abdominal viscera with auto-transfusion to the heart, lungs, and systemic circulation.
Eleftheriadis and colleagues studied 16 women randomized to laparoscopic versus open cholecystectomy.3 Significant depression of the hepatic microcirculation during the period of CO2 gas insufflation was noted in the laparoscopy cohort but not in the control group. Gastric mucosal ischemia also was observed in the laparoscopy group.
Several case reports of catastrophic intestinal ischemia have appeared in the literature (1994–1995).4-7 These articles have mainly involved laparoscopic upper abdominal operations in elderly people.
Recently, however, Hasson and colleagues reported a case of possible ischemic necrosis of the small intestine following laparoscopic adhesiolysis and bipolar myolysis.8 The authors emphasized that CO2 pneumoperitoneum reduces splanchnic blood flow, predisposing the patient to ischemia, but that ischemia with infarction requires an underlying vasculopathy or inciting factors such as traction on a short mesentery, atherosclerosis, or thrombosis.
A high index of suspicion for bowel ischemia following laparoscopic surgery should occur when, postoperatively, a patient experiences inordinately severe abdominal pain associated with tachypnea, tachycardia, and alterations in the WBC count. A paucity of physical abdominal signs in the early phases of this disorder should alert the clinician to the possibility of bowel ischemia.
Diagnosing and treating ischemia
A CT scan with contrast can suggest ischemia, but angiography is usually required for definitive diagnosis.
Treatment begins with infusion of papaverine into the intestinal vasculature via angiography cannula. In some cases, anticoagulation may be indicated. Surgery by laparotomy is clearly indicated for patients who fail to respond to vasodilatation measures.
This condition can be ameliorated by intermittent intraoperative decompression of the abdomen. Avoiding prolonged CO2 pneumoperitoneum and a lengthy laparoscopic operation also may diminish the risk of intestinal ischemia.
1. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
2. Caldwell CB, Ricotta JJ. Changes in visceral blood flow with elevated intra-abdominal pressure. J Surg Res. 1987;43:14-20.
3. Eleftheriadis E, Kotzampassi K, Botsios D, Tzartinoglu E, Farmakis H, Dadoukis J. Splanchnic ischemia during laparoscopic cholecystectomy. Surg Endosc. 1996;10:324-326.
4. Schorr RT. Laparoscopic upper abdominal operations and mesenteric infarction. J Laparoendosc Surg. 1995;5:389-392.
5. Mitchell PC, Jamieson GG. Coeliac axis and mesenteric arterial thrombosis following laparoscopic Nissen fundoplication. Aust N Z J Surg. 1994;64:728-730.
6. Dwerryhouse SJ, Melsom DS, Burton PA, Thompson MH. Acute intestinal ischaemia after laparoscopic cholecystectomy. Br J Surg. 1995;82:1413.-
7. Jaffe V, Russell RCG. Fatal intestinal ischaemia following laparoscopic cholecystectomy. Br J Surg. 1994;81:1827-1828.
8. Hasson HM, Galanopoulos C, Lanferman A. Ischemic necrosis of small bowel following laparoscopic surgery. JSLS. 2004;8:159-163.
1. Baggish MS. One hundred and thirty small and large bowel injuries associated with gynecologic laparoscopic operations. J Gynecol Surg. 2007;23:83-95.
2. Caldwell CB, Ricotta JJ. Changes in visceral blood flow with elevated intra-abdominal pressure. J Surg Res. 1987;43:14-20.
3. Eleftheriadis E, Kotzampassi K, Botsios D, Tzartinoglu E, Farmakis H, Dadoukis J. Splanchnic ischemia during laparoscopic cholecystectomy. Surg Endosc. 1996;10:324-326.
4. Schorr RT. Laparoscopic upper abdominal operations and mesenteric infarction. J Laparoendosc Surg. 1995;5:389-392.
5. Mitchell PC, Jamieson GG. Coeliac axis and mesenteric arterial thrombosis following laparoscopic Nissen fundoplication. Aust N Z J Surg. 1994;64:728-730.
6. Dwerryhouse SJ, Melsom DS, Burton PA, Thompson MH. Acute intestinal ischaemia after laparoscopic cholecystectomy. Br J Surg. 1995;82:1413.-
7. Jaffe V, Russell RCG. Fatal intestinal ischaemia following laparoscopic cholecystectomy. Br J Surg. 1994;81:1827-1828.
8. Hasson HM, Galanopoulos C, Lanferman A. Ischemic necrosis of small bowel following laparoscopic surgery. JSLS. 2004;8:159-163.
Endometrial ablation devices: How to make them truly safe
CASE: Leaking fluid causes intraoperative burns
G.S. is a 45-year-old mother of three who is admitted for surgery for persistent menorrhagia. She has experienced at least two menstrual periods every month for several months, each of them associated with heavy bleeding. She has a history of hypothyroidism and hypertension, but no serious disease or surgery, and considers herself to be in good physical and mental health.
G.S. undergoes endometrial hydrothermablation (HTA) under general inhalation anesthesia. After the HTA mechanism is primed, the heating cycle is started, with a good seal and no fluid leaking from the cervix.
Approximately 8 minutes into the procedure, a 5-mL fluid deficit is noted, and a small amount of hot fluid is observed to be leaking from the cervical os. Examination reveals a thermal injury to the cervix and anterior vaginal wall. The wound is irrigated with cool, sterile saline, and silver sulfadiazine cream is applied. The patient is discharged.
Could this injury have been avoided? Is further treatment warranted?
A minimally invasive operation does not necessarily translate to minimal risk of serious complications. Although few studies of nonhysteroscopic endometrial ablation techniques report any complications,1,2 Baggish and Savells3 found a number of injuries when they searched hospital records and the Food and Drug Administration (FDA) database (TABLE). They identified serious complications associated with the following devices:
- HydroThermablator (Boston Scientific), which utilizes a modified operating hysteroscope to deliver 10 to 12 mL of preheated saline into the uterus under low pressure.4 Complications: 16 adverse events were reported to the FDA, 13 of which involved the retrograde leakage of hot water, causing burns to the cervix, vagina, and vulva. Six additional injuries not reported to the FDA were identified at a single institution.
- Novasure (Cytyc), which employs bipolar electrodes that cover a porous bag.5,6 Complications: 32 injuries, 26 of them uterine perforations.
- Thermachoice (Gynecare), a fluid-distended balloon ablator.7 Complications: 22 injuries included retrograde leakage of hot water after balloon failure and transmural thermal injury, with spread to, and injury of, proximal structures. One death was reported.
- Microsulis (MEA), which uses microwave energy to ablate the endometrium.8-10 Complications: 19 injuries, including 13 thermal injuries to the intestines.
Baggish and Savells3 initiated this study after discovering six adverse events within their own hospital system utilizing a single device (HTA). Because these injuries were not reported to the FDA, the overall number of complications is likely higher than the figures given here.
This article describes the proper use of nonhysteroscopic endometrial ablation devices, the best ways to avert serious injury, and optimal treatment when complication occurs.
TABLE
Complications associated with 4 endometrial ablation devices
| COMPLICATION | HYDRO THERMABLATOR* | THERMACHOICE | NOVASURE | MICROSULIS |
|---|---|---|---|---|
| Uterine perforation | 2 | 3 | 26 | 19 |
| Intestinal injury | 1† | 1† | – | 13† |
| Retrograde leakage burn | 19 | 6 | – | – |
| Infection/sepsis | – | 1† | 2 | 1 |
| Fistula/sinus | – | 1† | 1 | – |
| Transmural uterine burn | – | 1 | – | – |
| Cervical stenosis | – | 8 | 1 | – |
| Cardiac arrest | 1 | – | 1 | – |
| Death | – | 1 | – | – |
| Other major | – | 3 | 1 | 4† |
| Total | 22 | 22 | 32 | 20 |
| * Includes author’s data; 6 retrograde leaks | ||||
| † Collateral injury | ||||
CASE continued: Patient opts for hysterectomy
In the case just described, G.S. was examined 1 week after surgery and found to have an exophytic burn over the entire right half of the cervix, extending into the vagina. She was readmitted for 3 days of intravenous (IV) antibiotic treatment and wound care. Computed tomography imaging showed gas formation within the damaged cervix.
Six weeks after surgery, the patient was still menstruating heavily, but her cervix and vagina had healed. Six months later, she underwent total abdominal hysterectomy for continued menorrhagia.
When is endometrial ablation an option?
Indications for endometrial ablation using a nonhysteroscopic, minimally invasive technique are no different from those for hysteroscopic ablation.11 Abnormal, or dysfunctional, uterine bleeding is the principal reason for this operation. Dysfunctional bleeding is heavy or prolonged menses over 6 months or longer that fail to respond to conservative measures and occur in the absence of tumor, pregnancy, or inflammation (ie, infection).
A woman who meets these criteria should have a desire to retain her uterus if she is to be a candidate for a nonhysteroscopic, minimally invasive technique. She also should understand that ablation can render pregnancy unlikely and even pathologic. Her understanding of this consequence should be documented in the chart! Last, she should be informed that ablation will not necessarily render her sterile, so contraception or sterilization will be required to avoid pregnancy. This should also be clearly documented in the medical record.
Endometrial ablation may also be an alternative to hysterectomy for a mentally retarded woman who is unable to manage menses. Abnormal uterine bleeding in conjunction with bleeding diathesis, significant obesity, or serious medical disorders can also be treated by endometrial ablation.
Avoid endometrial ablation in certain circumstances
These circumstances include the presence of endometrial hyperplasia, endometrial cancer, endocervical neoplasia, cervical stenosis, an undiagnosed adnexal mass, moderate to severe dysmenorrhea, adenomyosis, or a uterine cavity larger than 10 cm.12-15
Valle and Baggish15 reported eight cases in which women developed endometrial carcinoma following ablation, and identified the following major risk factors for postablation cancer:
- endometrial hyperplasia unresponsive to progesterone or progestin therapy
- complex endometrial hyperplasia
- atypical hyperplasia.
These conditions are contraindications to endometrial ablation.
Avoid a rush to ablation
The growing popularity of office-based, minimally invasive, nonhysteroscopic techniques, coupled with an increasing desire for and acceptance of elective cessation of menses, may stretch the indications listed above and cut short the discovery of contraindications. Clearly, thorough endometrial sampling and precise histopathologic interpretation are required before embarking on any type of endometrial ablation, to minimize the risk of complications.
How to prevent injury
Reduce the risk of perforation
Uterine perforation occurs for a variety of reasons:
- position of the uterus is unknown
- uterus has not been gently and carefully sounded
- cervix is insufficiently dilated to permit passage of the probe
- device is too long (large) to be accommodated in an individual patient’s uterus
- uterine cavity is distorted by pathology, such as adhesions, myomas, etc.
Attention to these details before surgery can prevent perforation.
When uterine injury occurs, the bowel is also at risk
The intestines can be injured following perforation or transmural injury of the uterus. Bowel injury has been reported with hysteroscopic ablation and resection as well as with Nd-YAG laser ablation.16-18
Do not activate hot water or electrosurgical energy unless you are 100% certain that the device is within the uterine cavity.
Ideally, manufacturers’ safety studies should guarantee no risk of transtubal spillage of hot liquid.
Hot fluid adds to risk of burns
Devices that permit retrograde leakage of hot fluid, such as the HTA, should be modified to ensure sealing at the level of the external and internal cervical os. The Enable device (Innerdyne), no longer marketed in the United States, had such a sealing mechanism, which minimized retrograde leakage of hot water.
Balloon failure may be an unavoidable injury, but pretesting of the device and careful attention to pressure readings—particularly in a small uterus—may mitigate the risk.
Be alert for electrical leakage
The microwave device operates at the megahertz range of frequency. At this high frequency, the risk of leakage is much greater than with devices that operate in the kilohertz range. Therefore, it is important to pay close attention to grounding sites, such as cardiovascular-monitoring electrodes.
High-power monopolar devices, prolonged application of energy to tissue, and high generator frequency are all associated with leakage and subsequent burns.
- Keep the success rate above 90%
- Minimize complications by proper technique and instrument selection
- Press the market to develop a range of device sizes that will individualize the procedure
- Keep the price of a procedure under $1,000
- Establish and adhere to careful patient selection criteria
Early recognition and treatment are vital to ensure the patient’s safety and reduce the risk of medicolegal liability. I recommend the following steps:
- Stop the procedure immediately if perforation is suspected. If you suspect that hot water has been dispersed within the abdominal cavity, switch to laparotomy and consult a general surgeon to inspect the entire intestine for injury. If perforation occurs during the use of electrosurgical energy, the same action is warranted. If uterine perforation occurs in isolation (ie, there is no thermal energy compounding the problem), admit the patient for careful observation, appropriate blood chemistries and hematologic studies, and radiologic examination.
- When hot liquids are spilled, switch to retrograde flow immediately and generously flush the vulva, vagina, and cervix with cold water. Cleanse the entire area with a soapless detergent, and apply clindamycin cream to the vagina and silver sulfadiazine cream to the vulva. Admit the patient for application of cold compresses, ice packs, and burn therapy, and obtain baseline cultures and hematologic studies and a plastic surgery consult. If third-degree (full thickness) burns are suspected, treat any suspected wound infection aggressively after obtaining cultures. Severe and inordinate pain should be investigated as a possible sign of necrotizing fasciitis. After discharge, follow the patient’s progress at weekly intervals.
- Talk to the patient and her family. It is a good idea to explain the complication in very clear terms. I believe it is reasonable to explain how the complication occurred, without speculation or theatrical explanations. Also be sure to document this conversation, including date and time. It may be useful to have a neutral witness present during the conversation. By and large, the patient and her family are likely to appreciate an honest account of how the complication occurred. Hiding data or attempting to cover up the injury may motivate the patient to seek legal representation.
The long-term success of endometrial ablation devices as a whole depends on several conditions. Foremost, the entire class of devices should demonstrate efficacy on par with hysteroscopic ablation. Currently, efficacy ranges from 80% to 95% (short-term follow-up).11 The goal of minimally invasive procedures should be a sustainable 92% rate of amenorrhea, hypomenorrhea, or light, periodic menses. A long-term failure rate of 25% is unacceptable.22-24 If the devices can, by their simplicity, be adapted to more or less universal office application and attain a 5-year success rate of 90% or higher, they will become the standard of care.
One size does not really fit all
Serious complications from endometrial ablation devices occur with regular frequency and must be eliminated or greatly reduced. Perforation is a significant problem and may be related to the “one-size-fits-all” design of the device. Perhaps a range of sizes needs to be produced and fitted to the individual uterine cavity.
If such complications as perforation and burns to the bowel, cervix, vagina, and vulva can be eliminated or relegated to rarity, then a happy future for these procedures lies beyond the horizon.
Price ceiling should be set at $1,000
If an operation can consistently be performed for less than $1,000 total cost—the cost of in-hospital endometrial ablation—it will gain mass appeal. In hospitals and so-called surgicenters, ablations are expensive and, therefore, less attractive to self- or third-party payers. If fees are based on the volume of cases, then a procedure may be price-efficient.
Outcome depends on patient selection
Poorly screened patients who have underlying hyperplasia may develop postablation carcinoma. Women who have dysmenorrhea before the procedure can be predicted to suffer from it afterward. Older women (ie, 40 years or older) will have better long-term success than younger women. And women with a large uterus or myomas will have a higher failure rate than women with smaller cavities (ie, less than 10 cm in length).
What this means for the individual surgeon
Although minimally invasive techniques are relatively easy to perform and simple to learn, each part of the procedure requires careful application and great attention to detail. Perforation of the uterus and leakage of scalding hot liquid must be avoided. If these complications occur, prompt diagnosis and appropriate treatment are critical. The removal of these procedures from the operating room to the office as well as competitive pricing of instrumentation will make nonhysteroscopic, minimally invasive endometrial ablation more cost-effective.
The modern era of practical endometrial ablation began in 1981, when Goldrath and colleagues19 reported Nd-YAG laser photovaporization of the endometrium via hysteroscopy for treatment of excessive uterine bleeding. Two years later, DeCherney and Polan20 reported hysteroscopic control of abnormal uterine bleeding using the urologic resectoscope.
Over succeeding years, Baggish and Baltoyannis21 and Baggish and Sze22 reported extensive experience with hysteroscopic endometrial ablation in both high- and average-risk patients, including long-term follow-up of 568 cases over 11 years. Garry and colleagues23 reported a large series of 600 cases from the United Kingdom. Not only did these laser techniques prove to be effective, achieving amenorrhea rates ranging from 30% to 60%, but overall control of abnormal bleeding exceeded 90%. In the large series involving approximately 1,200 cases, no uterine perforations were reported.21-23 The major complication: Fluid overload secondary to vascular uptake of distension medium.
In Europe and the United Kingdom, most hysteroscopic treatment of abnormal bleeding involved endometrial resection using the cutting loop of the resectoscope. In the United States, ablation with the ball electrode of the resectoscope largely replaced the Nd-YAG laser because the resectoscopic trigger mechanism required less skill and hand–eye coordination than the hand–finger-controlled movement of the 600- to 1,000-micron laser fiber.24-26
A search for more benign techniques
A 1997 UK survey analyzed 10,686 cases of hysteroscopic endometrial destruction and identified 474 complications.27 Resection alone had a complication rate of 10.9% and an emergency hysterectomy rate of 13 for every 1,000 patients. Laser ablation had a complication rate of 5.5% and an emergency hysterectomy rate of 2 for every 1,000 patients, and the corresponding figures for rollerball ablation were a 4.5% complication rate and 3 emergency hysterectomies for every 1,000 patients. Two deaths occurred (in 10,000 cases) and were associated with loop excision.
Published data indicated that:
- Successful outcomes after endometrial ablation or resection were directly proportional to the skill of the surgeon
- Complications, particularly serious complications, were related to the experience and skill of the surgeon
- Infusion of uterine distension medium, particularly hypo-osmolar solutions, was associated with serious complications when fluid deficits exceeded approximately 500 to 1,000 mL.
As a result, a number of investigators sought to develop new surgical techniques to control abnormal uterine bleeding that would minimize the skill required by the surgeon (requiring only insertion of a cannula into the uterus and a “cookbook” ablation procedure), eliminate the need for distension medium and general anesthesia, and attain efficacy equivalent to earlier techniques.
A quartet of options
Among the devices that resulted were:
- A microwave technique, described by several investigators.8-10 Its chief drawback: High-frequency electrical leakage with the potential to cause thermal burns.
- An intrauterine balloon device distended with sterile water or saline is heated in situ to 85° to 90° Celsius, thereby cooking the endometrium.
- An electrode-bearing device that features an array of monopolar electrodes over the endometrium-facing aspect of a balloon or bipolar electrodes over a porous bag.
- Devices that circulate a small volume of hot saline freely within the uterine cavity. Hydrothermablation delivers 10 to 12 mL of preheated saline into the uterus under low pressure. A similar technique delivers 10 to 12 mL of cool water or saline into the uterus through a sealed cannula, followed by in situ heating and circulation of the fluid at low pressure via a computer-controlled device.
Safety studies were required by the FDA and were performed on all these devices, and the risk of complications appeared to be negligible.1,2 As this article illustrates, that is not the case.
Four devices, four ways of achieving ablation
Since the advent of nonhysteroscopic, minimally invasive endometrial ablation devices, four distinct techniques have gained widespread use
Hydrothermablation
The closed-loop system (HTA) ablates the lining of the endometrium under hysteroscopic visualization by recirculating heated saline within the uterus. The modified hysteroscope allows the operator to view the ablation as it occurs within the uterine cavity.
Balloon ablation
Balloon ablation (Thermachoice) features a double-dip balloon construction that conforms to the contours of the uterine cavity. The saline or water in the balloon is heated in situ. This device requires an undistorted uterine cavity, relies on the integrity of the balloon to prevent forward or retrograde spillage of scalding water, and is time-controlled.
Radiofrequency technology
The three-dimensional gold-plated bipolar mesh electrode (NovaSure) is inserted into the uterine cavity and advanced toward the fundus. Once it is properly positioned (above, left), the system is activated to produce 180 W of bipolar power. A moisture-transport vacuum system draws the endometrium into contact with the mesh to enhance tissue vaporization and evacuate debris.
Microwave energy
Microwave energy is emitted from the tip of the device (Microsulis), which is moved back and forth in a sweeping manner, from the fundus to the lower uterine segment. The device directly heats tissue to a depth of 3 mm, with conductive heating of adjacent tissue for an additional 2 to 3 mm. The total 5- to 6-mm depth ensures coagulation and destruction of the basal layer. Microwave energy does not require direct contact with the tissue, as it will “fill the gap” caused by cornual and fibroid distortions.
1. Bustos-Lopez H, Baggish MS, Valle RF, et al. Assessment of the safety of intrauterine instillation of heated saline for endometrial ablation. Fertil Steril. 1998;69:155-160.
2. Baggish MS, Paraiso M, Breznock EM, et al. A computer-controlled, continuously circulating, hot irrigating system for endometrial ablation. Am J Obstet Gynecol. 1995;173:1842-1848.
3. Baggish MS, Savells A. Complications associated with minimally invasive non-hysteroscopic endometrial ablation techniques. J Gynecol Surg. 2007;23:7-12.
4. Goldrath MH. Evaluation of HydroThermablator and rollerball endometrial ablation for menorrhagia: 3 years after treatment. J Am Assoc Gynecol Laparosc. 2003;10:505-511.
5. Abbott J, Hawe J, Hunter D, et al. A double-blind randomized trial comparing the cavaterm and the Novasure endometrial ablation systems for the treatment of dysfunctional uterine bleeding. Fertil Steril. 2003;80:203-208.
6. Cooper J, Gimpelson R, Laberge P, et al. A randomized, multi-center trial of safety and efficacy of the Novasure system in the treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2002;9:418-428.
7. Loffer FD, Grainger D. Five-year follow-up of patients participating in a randomized trial of uterine balloon therapy versus rollerball ablation for treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2002;9:429-435.
8. Phipps JH, Lewis BV, Roberts T, et al. Treatment of functional menorrhagia with radiofrequency endometrial ablation. Lancet. 1990;335:374-376.
9. Sharp N, Cronin N, Feldberg I, et al. Microwaves for menorrhagia: a new fast technique for endometrial ablation. Lancet. 1995;346:1003-1004.
10. Thijssen RFA. Radiofrequency-induced endometrial ablation: an update. Br J Obstet Gynaecol. 1997;104:608-613.
11. Baggish MS. Minimally invasive non-hysteroscopic methods for endometrial ablation. In: Baggish MS, Valle RF, Guedj H, eds. Hysteroscopy: Visual Perspectives of Uterine Anatomy, Physiology, and Pathology. 3rd ed. Philadelphia: Lippincott, Williams and Wilkins; 2007:405-415.
12. Dwyer N, Hutton J, Stirrat GM. Randomized controlled trial comparing endometrial resection with abdominal hysterectomy for the surgical treatment of menorrhagia. Br J Obstet Gynaecol. 1993;100:237-243.
13. Raiga J, Mage G, Glowaczower E, et al. Factors affecting risk of failure after endometrial resection. J Gynecol Surg. 1995;11:1-5.
14. Shelly-Jones D, Mooney P, Garry R. Factors influencing the outcome of endometrial laser ablation. J Gynecol Surg. 1994;10:211-215.
15. Valle RF, Baggish MS. Endometrial carcinoma after endometrial ablation: high-risk factors predicting its occurrence. Am J Obstet Gynecol. 1998;176:569-572.
16. Kanter MH, Kivnick S. Bowel injury from rollerball ablation of the endometrium. Obstet Gynecol. 1992;79:833-835.
17. Perry CP, Daniell JF, Gimpelson RJ. Bowel injury from Nd-YAG endometrial ablation. J Gynecol Surg. 1990;6:1999-2003.
18. Scottish Hysteroscopy Audit Group. A Scottish audit of hysteroscopic surgery for menorrhagia: complications and follow-up. Br J Obstet Gynaecol. 1995;102:239-254.
19. Goldrath MH, Fuller TA, Segal S. Laser photovaporization of the endometrium for the treatment of menorrhagia. Am J Obstet Gynecol. 1981;40:14-19.
20. DeCherney A, Polan ML. Hysteroscopic management of intrauterine lesions and intractable uterine bleeding. Obstet Gynecol. 1983;61:392-396.
21. Baggish MS, Baltoyannis P. New techniques for laser ablation of the endometrium in high-risk patients. Am J Obstet Gynecol. 1988;159:287-292.
22. Baggish MS, Sze EHM. Endometrial ablation: a series of 568 patients treated over an 11-year period. Am J Obstet Gynecol. 1996;174:908-913.
23. Garry R, Shelly-Jones D, Mooney P, et al. Six hundred endometrial laser ablations. Obstet Gynecol. 1995;85:24-29.
24. Magos AL, Bauman R, Lockwood GM, et al. Experience with the first 250 endometrial resections for menorrhagia. Lancet. 1991;337:1074-1078.
25. Wortman M, Daggett A. Hysteroscopic endometrial resection: a new technique for the treatment of menorrhagia. Obstet Gynecol. 1994;83:295-298.
26. Townsend DE, Richart RM, Paskowitz, et al. Rollerball coagulation of the endometrium. Obstet Gynecol. 1990;76:310-313.
27. Overton C, Hargreaves J, Maresh M. A national survey of the complications of endometrial destruction for menstrual disorders: the mistletoe study. Br J Obstet Gynaecol. 1997;104:1351-1359.
CASE: Leaking fluid causes intraoperative burns
G.S. is a 45-year-old mother of three who is admitted for surgery for persistent menorrhagia. She has experienced at least two menstrual periods every month for several months, each of them associated with heavy bleeding. She has a history of hypothyroidism and hypertension, but no serious disease or surgery, and considers herself to be in good physical and mental health.
G.S. undergoes endometrial hydrothermablation (HTA) under general inhalation anesthesia. After the HTA mechanism is primed, the heating cycle is started, with a good seal and no fluid leaking from the cervix.
Approximately 8 minutes into the procedure, a 5-mL fluid deficit is noted, and a small amount of hot fluid is observed to be leaking from the cervical os. Examination reveals a thermal injury to the cervix and anterior vaginal wall. The wound is irrigated with cool, sterile saline, and silver sulfadiazine cream is applied. The patient is discharged.
Could this injury have been avoided? Is further treatment warranted?
A minimally invasive operation does not necessarily translate to minimal risk of serious complications. Although few studies of nonhysteroscopic endometrial ablation techniques report any complications,1,2 Baggish and Savells3 found a number of injuries when they searched hospital records and the Food and Drug Administration (FDA) database (TABLE). They identified serious complications associated with the following devices:
- HydroThermablator (Boston Scientific), which utilizes a modified operating hysteroscope to deliver 10 to 12 mL of preheated saline into the uterus under low pressure.4 Complications: 16 adverse events were reported to the FDA, 13 of which involved the retrograde leakage of hot water, causing burns to the cervix, vagina, and vulva. Six additional injuries not reported to the FDA were identified at a single institution.
- Novasure (Cytyc), which employs bipolar electrodes that cover a porous bag.5,6 Complications: 32 injuries, 26 of them uterine perforations.
- Thermachoice (Gynecare), a fluid-distended balloon ablator.7 Complications: 22 injuries included retrograde leakage of hot water after balloon failure and transmural thermal injury, with spread to, and injury of, proximal structures. One death was reported.
- Microsulis (MEA), which uses microwave energy to ablate the endometrium.8-10 Complications: 19 injuries, including 13 thermal injuries to the intestines.
Baggish and Savells3 initiated this study after discovering six adverse events within their own hospital system utilizing a single device (HTA). Because these injuries were not reported to the FDA, the overall number of complications is likely higher than the figures given here.
This article describes the proper use of nonhysteroscopic endometrial ablation devices, the best ways to avert serious injury, and optimal treatment when complication occurs.
TABLE
Complications associated with 4 endometrial ablation devices
| COMPLICATION | HYDRO THERMABLATOR* | THERMACHOICE | NOVASURE | MICROSULIS |
|---|---|---|---|---|
| Uterine perforation | 2 | 3 | 26 | 19 |
| Intestinal injury | 1† | 1† | – | 13† |
| Retrograde leakage burn | 19 | 6 | – | – |
| Infection/sepsis | – | 1† | 2 | 1 |
| Fistula/sinus | – | 1† | 1 | – |
| Transmural uterine burn | – | 1 | – | – |
| Cervical stenosis | – | 8 | 1 | – |
| Cardiac arrest | 1 | – | 1 | – |
| Death | – | 1 | – | – |
| Other major | – | 3 | 1 | 4† |
| Total | 22 | 22 | 32 | 20 |
| * Includes author’s data; 6 retrograde leaks | ||||
| † Collateral injury | ||||
CASE continued: Patient opts for hysterectomy
In the case just described, G.S. was examined 1 week after surgery and found to have an exophytic burn over the entire right half of the cervix, extending into the vagina. She was readmitted for 3 days of intravenous (IV) antibiotic treatment and wound care. Computed tomography imaging showed gas formation within the damaged cervix.
Six weeks after surgery, the patient was still menstruating heavily, but her cervix and vagina had healed. Six months later, she underwent total abdominal hysterectomy for continued menorrhagia.
When is endometrial ablation an option?
Indications for endometrial ablation using a nonhysteroscopic, minimally invasive technique are no different from those for hysteroscopic ablation.11 Abnormal, or dysfunctional, uterine bleeding is the principal reason for this operation. Dysfunctional bleeding is heavy or prolonged menses over 6 months or longer that fail to respond to conservative measures and occur in the absence of tumor, pregnancy, or inflammation (ie, infection).
A woman who meets these criteria should have a desire to retain her uterus if she is to be a candidate for a nonhysteroscopic, minimally invasive technique. She also should understand that ablation can render pregnancy unlikely and even pathologic. Her understanding of this consequence should be documented in the chart! Last, she should be informed that ablation will not necessarily render her sterile, so contraception or sterilization will be required to avoid pregnancy. This should also be clearly documented in the medical record.
Endometrial ablation may also be an alternative to hysterectomy for a mentally retarded woman who is unable to manage menses. Abnormal uterine bleeding in conjunction with bleeding diathesis, significant obesity, or serious medical disorders can also be treated by endometrial ablation.
Avoid endometrial ablation in certain circumstances
These circumstances include the presence of endometrial hyperplasia, endometrial cancer, endocervical neoplasia, cervical stenosis, an undiagnosed adnexal mass, moderate to severe dysmenorrhea, adenomyosis, or a uterine cavity larger than 10 cm.12-15
Valle and Baggish15 reported eight cases in which women developed endometrial carcinoma following ablation, and identified the following major risk factors for postablation cancer:
- endometrial hyperplasia unresponsive to progesterone or progestin therapy
- complex endometrial hyperplasia
- atypical hyperplasia.
These conditions are contraindications to endometrial ablation.
Avoid a rush to ablation
The growing popularity of office-based, minimally invasive, nonhysteroscopic techniques, coupled with an increasing desire for and acceptance of elective cessation of menses, may stretch the indications listed above and cut short the discovery of contraindications. Clearly, thorough endometrial sampling and precise histopathologic interpretation are required before embarking on any type of endometrial ablation, to minimize the risk of complications.
How to prevent injury
Reduce the risk of perforation
Uterine perforation occurs for a variety of reasons:
- position of the uterus is unknown
- uterus has not been gently and carefully sounded
- cervix is insufficiently dilated to permit passage of the probe
- device is too long (large) to be accommodated in an individual patient’s uterus
- uterine cavity is distorted by pathology, such as adhesions, myomas, etc.
Attention to these details before surgery can prevent perforation.
When uterine injury occurs, the bowel is also at risk
The intestines can be injured following perforation or transmural injury of the uterus. Bowel injury has been reported with hysteroscopic ablation and resection as well as with Nd-YAG laser ablation.16-18
Do not activate hot water or electrosurgical energy unless you are 100% certain that the device is within the uterine cavity.
Ideally, manufacturers’ safety studies should guarantee no risk of transtubal spillage of hot liquid.
Hot fluid adds to risk of burns
Devices that permit retrograde leakage of hot fluid, such as the HTA, should be modified to ensure sealing at the level of the external and internal cervical os. The Enable device (Innerdyne), no longer marketed in the United States, had such a sealing mechanism, which minimized retrograde leakage of hot water.
Balloon failure may be an unavoidable injury, but pretesting of the device and careful attention to pressure readings—particularly in a small uterus—may mitigate the risk.
Be alert for electrical leakage
The microwave device operates at the megahertz range of frequency. At this high frequency, the risk of leakage is much greater than with devices that operate in the kilohertz range. Therefore, it is important to pay close attention to grounding sites, such as cardiovascular-monitoring electrodes.
High-power monopolar devices, prolonged application of energy to tissue, and high generator frequency are all associated with leakage and subsequent burns.
- Keep the success rate above 90%
- Minimize complications by proper technique and instrument selection
- Press the market to develop a range of device sizes that will individualize the procedure
- Keep the price of a procedure under $1,000
- Establish and adhere to careful patient selection criteria
Early recognition and treatment are vital to ensure the patient’s safety and reduce the risk of medicolegal liability. I recommend the following steps:
- Stop the procedure immediately if perforation is suspected. If you suspect that hot water has been dispersed within the abdominal cavity, switch to laparotomy and consult a general surgeon to inspect the entire intestine for injury. If perforation occurs during the use of electrosurgical energy, the same action is warranted. If uterine perforation occurs in isolation (ie, there is no thermal energy compounding the problem), admit the patient for careful observation, appropriate blood chemistries and hematologic studies, and radiologic examination.
- When hot liquids are spilled, switch to retrograde flow immediately and generously flush the vulva, vagina, and cervix with cold water. Cleanse the entire area with a soapless detergent, and apply clindamycin cream to the vagina and silver sulfadiazine cream to the vulva. Admit the patient for application of cold compresses, ice packs, and burn therapy, and obtain baseline cultures and hematologic studies and a plastic surgery consult. If third-degree (full thickness) burns are suspected, treat any suspected wound infection aggressively after obtaining cultures. Severe and inordinate pain should be investigated as a possible sign of necrotizing fasciitis. After discharge, follow the patient’s progress at weekly intervals.
- Talk to the patient and her family. It is a good idea to explain the complication in very clear terms. I believe it is reasonable to explain how the complication occurred, without speculation or theatrical explanations. Also be sure to document this conversation, including date and time. It may be useful to have a neutral witness present during the conversation. By and large, the patient and her family are likely to appreciate an honest account of how the complication occurred. Hiding data or attempting to cover up the injury may motivate the patient to seek legal representation.
The long-term success of endometrial ablation devices as a whole depends on several conditions. Foremost, the entire class of devices should demonstrate efficacy on par with hysteroscopic ablation. Currently, efficacy ranges from 80% to 95% (short-term follow-up).11 The goal of minimally invasive procedures should be a sustainable 92% rate of amenorrhea, hypomenorrhea, or light, periodic menses. A long-term failure rate of 25% is unacceptable.22-24 If the devices can, by their simplicity, be adapted to more or less universal office application and attain a 5-year success rate of 90% or higher, they will become the standard of care.
One size does not really fit all
Serious complications from endometrial ablation devices occur with regular frequency and must be eliminated or greatly reduced. Perforation is a significant problem and may be related to the “one-size-fits-all” design of the device. Perhaps a range of sizes needs to be produced and fitted to the individual uterine cavity.
If such complications as perforation and burns to the bowel, cervix, vagina, and vulva can be eliminated or relegated to rarity, then a happy future for these procedures lies beyond the horizon.
Price ceiling should be set at $1,000
If an operation can consistently be performed for less than $1,000 total cost—the cost of in-hospital endometrial ablation—it will gain mass appeal. In hospitals and so-called surgicenters, ablations are expensive and, therefore, less attractive to self- or third-party payers. If fees are based on the volume of cases, then a procedure may be price-efficient.
Outcome depends on patient selection
Poorly screened patients who have underlying hyperplasia may develop postablation carcinoma. Women who have dysmenorrhea before the procedure can be predicted to suffer from it afterward. Older women (ie, 40 years or older) will have better long-term success than younger women. And women with a large uterus or myomas will have a higher failure rate than women with smaller cavities (ie, less than 10 cm in length).
What this means for the individual surgeon
Although minimally invasive techniques are relatively easy to perform and simple to learn, each part of the procedure requires careful application and great attention to detail. Perforation of the uterus and leakage of scalding hot liquid must be avoided. If these complications occur, prompt diagnosis and appropriate treatment are critical. The removal of these procedures from the operating room to the office as well as competitive pricing of instrumentation will make nonhysteroscopic, minimally invasive endometrial ablation more cost-effective.
The modern era of practical endometrial ablation began in 1981, when Goldrath and colleagues19 reported Nd-YAG laser photovaporization of the endometrium via hysteroscopy for treatment of excessive uterine bleeding. Two years later, DeCherney and Polan20 reported hysteroscopic control of abnormal uterine bleeding using the urologic resectoscope.
Over succeeding years, Baggish and Baltoyannis21 and Baggish and Sze22 reported extensive experience with hysteroscopic endometrial ablation in both high- and average-risk patients, including long-term follow-up of 568 cases over 11 years. Garry and colleagues23 reported a large series of 600 cases from the United Kingdom. Not only did these laser techniques prove to be effective, achieving amenorrhea rates ranging from 30% to 60%, but overall control of abnormal bleeding exceeded 90%. In the large series involving approximately 1,200 cases, no uterine perforations were reported.21-23 The major complication: Fluid overload secondary to vascular uptake of distension medium.
In Europe and the United Kingdom, most hysteroscopic treatment of abnormal bleeding involved endometrial resection using the cutting loop of the resectoscope. In the United States, ablation with the ball electrode of the resectoscope largely replaced the Nd-YAG laser because the resectoscopic trigger mechanism required less skill and hand–eye coordination than the hand–finger-controlled movement of the 600- to 1,000-micron laser fiber.24-26
A search for more benign techniques
A 1997 UK survey analyzed 10,686 cases of hysteroscopic endometrial destruction and identified 474 complications.27 Resection alone had a complication rate of 10.9% and an emergency hysterectomy rate of 13 for every 1,000 patients. Laser ablation had a complication rate of 5.5% and an emergency hysterectomy rate of 2 for every 1,000 patients, and the corresponding figures for rollerball ablation were a 4.5% complication rate and 3 emergency hysterectomies for every 1,000 patients. Two deaths occurred (in 10,000 cases) and were associated with loop excision.
Published data indicated that:
- Successful outcomes after endometrial ablation or resection were directly proportional to the skill of the surgeon
- Complications, particularly serious complications, were related to the experience and skill of the surgeon
- Infusion of uterine distension medium, particularly hypo-osmolar solutions, was associated with serious complications when fluid deficits exceeded approximately 500 to 1,000 mL.
As a result, a number of investigators sought to develop new surgical techniques to control abnormal uterine bleeding that would minimize the skill required by the surgeon (requiring only insertion of a cannula into the uterus and a “cookbook” ablation procedure), eliminate the need for distension medium and general anesthesia, and attain efficacy equivalent to earlier techniques.
A quartet of options
Among the devices that resulted were:
- A microwave technique, described by several investigators.8-10 Its chief drawback: High-frequency electrical leakage with the potential to cause thermal burns.
- An intrauterine balloon device distended with sterile water or saline is heated in situ to 85° to 90° Celsius, thereby cooking the endometrium.
- An electrode-bearing device that features an array of monopolar electrodes over the endometrium-facing aspect of a balloon or bipolar electrodes over a porous bag.
- Devices that circulate a small volume of hot saline freely within the uterine cavity. Hydrothermablation delivers 10 to 12 mL of preheated saline into the uterus under low pressure. A similar technique delivers 10 to 12 mL of cool water or saline into the uterus through a sealed cannula, followed by in situ heating and circulation of the fluid at low pressure via a computer-controlled device.
Safety studies were required by the FDA and were performed on all these devices, and the risk of complications appeared to be negligible.1,2 As this article illustrates, that is not the case.
Four devices, four ways of achieving ablation
Since the advent of nonhysteroscopic, minimally invasive endometrial ablation devices, four distinct techniques have gained widespread use
Hydrothermablation
The closed-loop system (HTA) ablates the lining of the endometrium under hysteroscopic visualization by recirculating heated saline within the uterus. The modified hysteroscope allows the operator to view the ablation as it occurs within the uterine cavity.
Balloon ablation
Balloon ablation (Thermachoice) features a double-dip balloon construction that conforms to the contours of the uterine cavity. The saline or water in the balloon is heated in situ. This device requires an undistorted uterine cavity, relies on the integrity of the balloon to prevent forward or retrograde spillage of scalding water, and is time-controlled.
Radiofrequency technology
The three-dimensional gold-plated bipolar mesh electrode (NovaSure) is inserted into the uterine cavity and advanced toward the fundus. Once it is properly positioned (above, left), the system is activated to produce 180 W of bipolar power. A moisture-transport vacuum system draws the endometrium into contact with the mesh to enhance tissue vaporization and evacuate debris.
Microwave energy
Microwave energy is emitted from the tip of the device (Microsulis), which is moved back and forth in a sweeping manner, from the fundus to the lower uterine segment. The device directly heats tissue to a depth of 3 mm, with conductive heating of adjacent tissue for an additional 2 to 3 mm. The total 5- to 6-mm depth ensures coagulation and destruction of the basal layer. Microwave energy does not require direct contact with the tissue, as it will “fill the gap” caused by cornual and fibroid distortions.
CASE: Leaking fluid causes intraoperative burns
G.S. is a 45-year-old mother of three who is admitted for surgery for persistent menorrhagia. She has experienced at least two menstrual periods every month for several months, each of them associated with heavy bleeding. She has a history of hypothyroidism and hypertension, but no serious disease or surgery, and considers herself to be in good physical and mental health.
G.S. undergoes endometrial hydrothermablation (HTA) under general inhalation anesthesia. After the HTA mechanism is primed, the heating cycle is started, with a good seal and no fluid leaking from the cervix.
Approximately 8 minutes into the procedure, a 5-mL fluid deficit is noted, and a small amount of hot fluid is observed to be leaking from the cervical os. Examination reveals a thermal injury to the cervix and anterior vaginal wall. The wound is irrigated with cool, sterile saline, and silver sulfadiazine cream is applied. The patient is discharged.
Could this injury have been avoided? Is further treatment warranted?
A minimally invasive operation does not necessarily translate to minimal risk of serious complications. Although few studies of nonhysteroscopic endometrial ablation techniques report any complications,1,2 Baggish and Savells3 found a number of injuries when they searched hospital records and the Food and Drug Administration (FDA) database (TABLE). They identified serious complications associated with the following devices:
- HydroThermablator (Boston Scientific), which utilizes a modified operating hysteroscope to deliver 10 to 12 mL of preheated saline into the uterus under low pressure.4 Complications: 16 adverse events were reported to the FDA, 13 of which involved the retrograde leakage of hot water, causing burns to the cervix, vagina, and vulva. Six additional injuries not reported to the FDA were identified at a single institution.
- Novasure (Cytyc), which employs bipolar electrodes that cover a porous bag.5,6 Complications: 32 injuries, 26 of them uterine perforations.
- Thermachoice (Gynecare), a fluid-distended balloon ablator.7 Complications: 22 injuries included retrograde leakage of hot water after balloon failure and transmural thermal injury, with spread to, and injury of, proximal structures. One death was reported.
- Microsulis (MEA), which uses microwave energy to ablate the endometrium.8-10 Complications: 19 injuries, including 13 thermal injuries to the intestines.
Baggish and Savells3 initiated this study after discovering six adverse events within their own hospital system utilizing a single device (HTA). Because these injuries were not reported to the FDA, the overall number of complications is likely higher than the figures given here.
This article describes the proper use of nonhysteroscopic endometrial ablation devices, the best ways to avert serious injury, and optimal treatment when complication occurs.
TABLE
Complications associated with 4 endometrial ablation devices
| COMPLICATION | HYDRO THERMABLATOR* | THERMACHOICE | NOVASURE | MICROSULIS |
|---|---|---|---|---|
| Uterine perforation | 2 | 3 | 26 | 19 |
| Intestinal injury | 1† | 1† | – | 13† |
| Retrograde leakage burn | 19 | 6 | – | – |
| Infection/sepsis | – | 1† | 2 | 1 |
| Fistula/sinus | – | 1† | 1 | – |
| Transmural uterine burn | – | 1 | – | – |
| Cervical stenosis | – | 8 | 1 | – |
| Cardiac arrest | 1 | – | 1 | – |
| Death | – | 1 | – | – |
| Other major | – | 3 | 1 | 4† |
| Total | 22 | 22 | 32 | 20 |
| * Includes author’s data; 6 retrograde leaks | ||||
| † Collateral injury | ||||
CASE continued: Patient opts for hysterectomy
In the case just described, G.S. was examined 1 week after surgery and found to have an exophytic burn over the entire right half of the cervix, extending into the vagina. She was readmitted for 3 days of intravenous (IV) antibiotic treatment and wound care. Computed tomography imaging showed gas formation within the damaged cervix.
Six weeks after surgery, the patient was still menstruating heavily, but her cervix and vagina had healed. Six months later, she underwent total abdominal hysterectomy for continued menorrhagia.
When is endometrial ablation an option?
Indications for endometrial ablation using a nonhysteroscopic, minimally invasive technique are no different from those for hysteroscopic ablation.11 Abnormal, or dysfunctional, uterine bleeding is the principal reason for this operation. Dysfunctional bleeding is heavy or prolonged menses over 6 months or longer that fail to respond to conservative measures and occur in the absence of tumor, pregnancy, or inflammation (ie, infection).
A woman who meets these criteria should have a desire to retain her uterus if she is to be a candidate for a nonhysteroscopic, minimally invasive technique. She also should understand that ablation can render pregnancy unlikely and even pathologic. Her understanding of this consequence should be documented in the chart! Last, she should be informed that ablation will not necessarily render her sterile, so contraception or sterilization will be required to avoid pregnancy. This should also be clearly documented in the medical record.
Endometrial ablation may also be an alternative to hysterectomy for a mentally retarded woman who is unable to manage menses. Abnormal uterine bleeding in conjunction with bleeding diathesis, significant obesity, or serious medical disorders can also be treated by endometrial ablation.
Avoid endometrial ablation in certain circumstances
These circumstances include the presence of endometrial hyperplasia, endometrial cancer, endocervical neoplasia, cervical stenosis, an undiagnosed adnexal mass, moderate to severe dysmenorrhea, adenomyosis, or a uterine cavity larger than 10 cm.12-15
Valle and Baggish15 reported eight cases in which women developed endometrial carcinoma following ablation, and identified the following major risk factors for postablation cancer:
- endometrial hyperplasia unresponsive to progesterone or progestin therapy
- complex endometrial hyperplasia
- atypical hyperplasia.
These conditions are contraindications to endometrial ablation.
Avoid a rush to ablation
The growing popularity of office-based, minimally invasive, nonhysteroscopic techniques, coupled with an increasing desire for and acceptance of elective cessation of menses, may stretch the indications listed above and cut short the discovery of contraindications. Clearly, thorough endometrial sampling and precise histopathologic interpretation are required before embarking on any type of endometrial ablation, to minimize the risk of complications.
How to prevent injury
Reduce the risk of perforation
Uterine perforation occurs for a variety of reasons:
- position of the uterus is unknown
- uterus has not been gently and carefully sounded
- cervix is insufficiently dilated to permit passage of the probe
- device is too long (large) to be accommodated in an individual patient’s uterus
- uterine cavity is distorted by pathology, such as adhesions, myomas, etc.
Attention to these details before surgery can prevent perforation.
When uterine injury occurs, the bowel is also at risk
The intestines can be injured following perforation or transmural injury of the uterus. Bowel injury has been reported with hysteroscopic ablation and resection as well as with Nd-YAG laser ablation.16-18
Do not activate hot water or electrosurgical energy unless you are 100% certain that the device is within the uterine cavity.
Ideally, manufacturers’ safety studies should guarantee no risk of transtubal spillage of hot liquid.
Hot fluid adds to risk of burns
Devices that permit retrograde leakage of hot fluid, such as the HTA, should be modified to ensure sealing at the level of the external and internal cervical os. The Enable device (Innerdyne), no longer marketed in the United States, had such a sealing mechanism, which minimized retrograde leakage of hot water.
Balloon failure may be an unavoidable injury, but pretesting of the device and careful attention to pressure readings—particularly in a small uterus—may mitigate the risk.
Be alert for electrical leakage
The microwave device operates at the megahertz range of frequency. At this high frequency, the risk of leakage is much greater than with devices that operate in the kilohertz range. Therefore, it is important to pay close attention to grounding sites, such as cardiovascular-monitoring electrodes.
High-power monopolar devices, prolonged application of energy to tissue, and high generator frequency are all associated with leakage and subsequent burns.
- Keep the success rate above 90%
- Minimize complications by proper technique and instrument selection
- Press the market to develop a range of device sizes that will individualize the procedure
- Keep the price of a procedure under $1,000
- Establish and adhere to careful patient selection criteria
Early recognition and treatment are vital to ensure the patient’s safety and reduce the risk of medicolegal liability. I recommend the following steps:
- Stop the procedure immediately if perforation is suspected. If you suspect that hot water has been dispersed within the abdominal cavity, switch to laparotomy and consult a general surgeon to inspect the entire intestine for injury. If perforation occurs during the use of electrosurgical energy, the same action is warranted. If uterine perforation occurs in isolation (ie, there is no thermal energy compounding the problem), admit the patient for careful observation, appropriate blood chemistries and hematologic studies, and radiologic examination.
- When hot liquids are spilled, switch to retrograde flow immediately and generously flush the vulva, vagina, and cervix with cold water. Cleanse the entire area with a soapless detergent, and apply clindamycin cream to the vagina and silver sulfadiazine cream to the vulva. Admit the patient for application of cold compresses, ice packs, and burn therapy, and obtain baseline cultures and hematologic studies and a plastic surgery consult. If third-degree (full thickness) burns are suspected, treat any suspected wound infection aggressively after obtaining cultures. Severe and inordinate pain should be investigated as a possible sign of necrotizing fasciitis. After discharge, follow the patient’s progress at weekly intervals.
- Talk to the patient and her family. It is a good idea to explain the complication in very clear terms. I believe it is reasonable to explain how the complication occurred, without speculation or theatrical explanations. Also be sure to document this conversation, including date and time. It may be useful to have a neutral witness present during the conversation. By and large, the patient and her family are likely to appreciate an honest account of how the complication occurred. Hiding data or attempting to cover up the injury may motivate the patient to seek legal representation.
The long-term success of endometrial ablation devices as a whole depends on several conditions. Foremost, the entire class of devices should demonstrate efficacy on par with hysteroscopic ablation. Currently, efficacy ranges from 80% to 95% (short-term follow-up).11 The goal of minimally invasive procedures should be a sustainable 92% rate of amenorrhea, hypomenorrhea, or light, periodic menses. A long-term failure rate of 25% is unacceptable.22-24 If the devices can, by their simplicity, be adapted to more or less universal office application and attain a 5-year success rate of 90% or higher, they will become the standard of care.
One size does not really fit all
Serious complications from endometrial ablation devices occur with regular frequency and must be eliminated or greatly reduced. Perforation is a significant problem and may be related to the “one-size-fits-all” design of the device. Perhaps a range of sizes needs to be produced and fitted to the individual uterine cavity.
If such complications as perforation and burns to the bowel, cervix, vagina, and vulva can be eliminated or relegated to rarity, then a happy future for these procedures lies beyond the horizon.
Price ceiling should be set at $1,000
If an operation can consistently be performed for less than $1,000 total cost—the cost of in-hospital endometrial ablation—it will gain mass appeal. In hospitals and so-called surgicenters, ablations are expensive and, therefore, less attractive to self- or third-party payers. If fees are based on the volume of cases, then a procedure may be price-efficient.
Outcome depends on patient selection
Poorly screened patients who have underlying hyperplasia may develop postablation carcinoma. Women who have dysmenorrhea before the procedure can be predicted to suffer from it afterward. Older women (ie, 40 years or older) will have better long-term success than younger women. And women with a large uterus or myomas will have a higher failure rate than women with smaller cavities (ie, less than 10 cm in length).
What this means for the individual surgeon
Although minimally invasive techniques are relatively easy to perform and simple to learn, each part of the procedure requires careful application and great attention to detail. Perforation of the uterus and leakage of scalding hot liquid must be avoided. If these complications occur, prompt diagnosis and appropriate treatment are critical. The removal of these procedures from the operating room to the office as well as competitive pricing of instrumentation will make nonhysteroscopic, minimally invasive endometrial ablation more cost-effective.
The modern era of practical endometrial ablation began in 1981, when Goldrath and colleagues19 reported Nd-YAG laser photovaporization of the endometrium via hysteroscopy for treatment of excessive uterine bleeding. Two years later, DeCherney and Polan20 reported hysteroscopic control of abnormal uterine bleeding using the urologic resectoscope.
Over succeeding years, Baggish and Baltoyannis21 and Baggish and Sze22 reported extensive experience with hysteroscopic endometrial ablation in both high- and average-risk patients, including long-term follow-up of 568 cases over 11 years. Garry and colleagues23 reported a large series of 600 cases from the United Kingdom. Not only did these laser techniques prove to be effective, achieving amenorrhea rates ranging from 30% to 60%, but overall control of abnormal bleeding exceeded 90%. In the large series involving approximately 1,200 cases, no uterine perforations were reported.21-23 The major complication: Fluid overload secondary to vascular uptake of distension medium.
In Europe and the United Kingdom, most hysteroscopic treatment of abnormal bleeding involved endometrial resection using the cutting loop of the resectoscope. In the United States, ablation with the ball electrode of the resectoscope largely replaced the Nd-YAG laser because the resectoscopic trigger mechanism required less skill and hand–eye coordination than the hand–finger-controlled movement of the 600- to 1,000-micron laser fiber.24-26
A search for more benign techniques
A 1997 UK survey analyzed 10,686 cases of hysteroscopic endometrial destruction and identified 474 complications.27 Resection alone had a complication rate of 10.9% and an emergency hysterectomy rate of 13 for every 1,000 patients. Laser ablation had a complication rate of 5.5% and an emergency hysterectomy rate of 2 for every 1,000 patients, and the corresponding figures for rollerball ablation were a 4.5% complication rate and 3 emergency hysterectomies for every 1,000 patients. Two deaths occurred (in 10,000 cases) and were associated with loop excision.
Published data indicated that:
- Successful outcomes after endometrial ablation or resection were directly proportional to the skill of the surgeon
- Complications, particularly serious complications, were related to the experience and skill of the surgeon
- Infusion of uterine distension medium, particularly hypo-osmolar solutions, was associated with serious complications when fluid deficits exceeded approximately 500 to 1,000 mL.
As a result, a number of investigators sought to develop new surgical techniques to control abnormal uterine bleeding that would minimize the skill required by the surgeon (requiring only insertion of a cannula into the uterus and a “cookbook” ablation procedure), eliminate the need for distension medium and general anesthesia, and attain efficacy equivalent to earlier techniques.
A quartet of options
Among the devices that resulted were:
- A microwave technique, described by several investigators.8-10 Its chief drawback: High-frequency electrical leakage with the potential to cause thermal burns.
- An intrauterine balloon device distended with sterile water or saline is heated in situ to 85° to 90° Celsius, thereby cooking the endometrium.
- An electrode-bearing device that features an array of monopolar electrodes over the endometrium-facing aspect of a balloon or bipolar electrodes over a porous bag.
- Devices that circulate a small volume of hot saline freely within the uterine cavity. Hydrothermablation delivers 10 to 12 mL of preheated saline into the uterus under low pressure. A similar technique delivers 10 to 12 mL of cool water or saline into the uterus through a sealed cannula, followed by in situ heating and circulation of the fluid at low pressure via a computer-controlled device.
Safety studies were required by the FDA and were performed on all these devices, and the risk of complications appeared to be negligible.1,2 As this article illustrates, that is not the case.
Four devices, four ways of achieving ablation
Since the advent of nonhysteroscopic, minimally invasive endometrial ablation devices, four distinct techniques have gained widespread use
Hydrothermablation
The closed-loop system (HTA) ablates the lining of the endometrium under hysteroscopic visualization by recirculating heated saline within the uterus. The modified hysteroscope allows the operator to view the ablation as it occurs within the uterine cavity.
Balloon ablation
Balloon ablation (Thermachoice) features a double-dip balloon construction that conforms to the contours of the uterine cavity. The saline or water in the balloon is heated in situ. This device requires an undistorted uterine cavity, relies on the integrity of the balloon to prevent forward or retrograde spillage of scalding water, and is time-controlled.
Radiofrequency technology
The three-dimensional gold-plated bipolar mesh electrode (NovaSure) is inserted into the uterine cavity and advanced toward the fundus. Once it is properly positioned (above, left), the system is activated to produce 180 W of bipolar power. A moisture-transport vacuum system draws the endometrium into contact with the mesh to enhance tissue vaporization and evacuate debris.
Microwave energy
Microwave energy is emitted from the tip of the device (Microsulis), which is moved back and forth in a sweeping manner, from the fundus to the lower uterine segment. The device directly heats tissue to a depth of 3 mm, with conductive heating of adjacent tissue for an additional 2 to 3 mm. The total 5- to 6-mm depth ensures coagulation and destruction of the basal layer. Microwave energy does not require direct contact with the tissue, as it will “fill the gap” caused by cornual and fibroid distortions.
1. Bustos-Lopez H, Baggish MS, Valle RF, et al. Assessment of the safety of intrauterine instillation of heated saline for endometrial ablation. Fertil Steril. 1998;69:155-160.
2. Baggish MS, Paraiso M, Breznock EM, et al. A computer-controlled, continuously circulating, hot irrigating system for endometrial ablation. Am J Obstet Gynecol. 1995;173:1842-1848.
3. Baggish MS, Savells A. Complications associated with minimally invasive non-hysteroscopic endometrial ablation techniques. J Gynecol Surg. 2007;23:7-12.
4. Goldrath MH. Evaluation of HydroThermablator and rollerball endometrial ablation for menorrhagia: 3 years after treatment. J Am Assoc Gynecol Laparosc. 2003;10:505-511.
5. Abbott J, Hawe J, Hunter D, et al. A double-blind randomized trial comparing the cavaterm and the Novasure endometrial ablation systems for the treatment of dysfunctional uterine bleeding. Fertil Steril. 2003;80:203-208.
6. Cooper J, Gimpelson R, Laberge P, et al. A randomized, multi-center trial of safety and efficacy of the Novasure system in the treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2002;9:418-428.
7. Loffer FD, Grainger D. Five-year follow-up of patients participating in a randomized trial of uterine balloon therapy versus rollerball ablation for treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2002;9:429-435.
8. Phipps JH, Lewis BV, Roberts T, et al. Treatment of functional menorrhagia with radiofrequency endometrial ablation. Lancet. 1990;335:374-376.
9. Sharp N, Cronin N, Feldberg I, et al. Microwaves for menorrhagia: a new fast technique for endometrial ablation. Lancet. 1995;346:1003-1004.
10. Thijssen RFA. Radiofrequency-induced endometrial ablation: an update. Br J Obstet Gynaecol. 1997;104:608-613.
11. Baggish MS. Minimally invasive non-hysteroscopic methods for endometrial ablation. In: Baggish MS, Valle RF, Guedj H, eds. Hysteroscopy: Visual Perspectives of Uterine Anatomy, Physiology, and Pathology. 3rd ed. Philadelphia: Lippincott, Williams and Wilkins; 2007:405-415.
12. Dwyer N, Hutton J, Stirrat GM. Randomized controlled trial comparing endometrial resection with abdominal hysterectomy for the surgical treatment of menorrhagia. Br J Obstet Gynaecol. 1993;100:237-243.
13. Raiga J, Mage G, Glowaczower E, et al. Factors affecting risk of failure after endometrial resection. J Gynecol Surg. 1995;11:1-5.
14. Shelly-Jones D, Mooney P, Garry R. Factors influencing the outcome of endometrial laser ablation. J Gynecol Surg. 1994;10:211-215.
15. Valle RF, Baggish MS. Endometrial carcinoma after endometrial ablation: high-risk factors predicting its occurrence. Am J Obstet Gynecol. 1998;176:569-572.
16. Kanter MH, Kivnick S. Bowel injury from rollerball ablation of the endometrium. Obstet Gynecol. 1992;79:833-835.
17. Perry CP, Daniell JF, Gimpelson RJ. Bowel injury from Nd-YAG endometrial ablation. J Gynecol Surg. 1990;6:1999-2003.
18. Scottish Hysteroscopy Audit Group. A Scottish audit of hysteroscopic surgery for menorrhagia: complications and follow-up. Br J Obstet Gynaecol. 1995;102:239-254.
19. Goldrath MH, Fuller TA, Segal S. Laser photovaporization of the endometrium for the treatment of menorrhagia. Am J Obstet Gynecol. 1981;40:14-19.
20. DeCherney A, Polan ML. Hysteroscopic management of intrauterine lesions and intractable uterine bleeding. Obstet Gynecol. 1983;61:392-396.
21. Baggish MS, Baltoyannis P. New techniques for laser ablation of the endometrium in high-risk patients. Am J Obstet Gynecol. 1988;159:287-292.
22. Baggish MS, Sze EHM. Endometrial ablation: a series of 568 patients treated over an 11-year period. Am J Obstet Gynecol. 1996;174:908-913.
23. Garry R, Shelly-Jones D, Mooney P, et al. Six hundred endometrial laser ablations. Obstet Gynecol. 1995;85:24-29.
24. Magos AL, Bauman R, Lockwood GM, et al. Experience with the first 250 endometrial resections for menorrhagia. Lancet. 1991;337:1074-1078.
25. Wortman M, Daggett A. Hysteroscopic endometrial resection: a new technique for the treatment of menorrhagia. Obstet Gynecol. 1994;83:295-298.
26. Townsend DE, Richart RM, Paskowitz, et al. Rollerball coagulation of the endometrium. Obstet Gynecol. 1990;76:310-313.
27. Overton C, Hargreaves J, Maresh M. A national survey of the complications of endometrial destruction for menstrual disorders: the mistletoe study. Br J Obstet Gynaecol. 1997;104:1351-1359.
1. Bustos-Lopez H, Baggish MS, Valle RF, et al. Assessment of the safety of intrauterine instillation of heated saline for endometrial ablation. Fertil Steril. 1998;69:155-160.
2. Baggish MS, Paraiso M, Breznock EM, et al. A computer-controlled, continuously circulating, hot irrigating system for endometrial ablation. Am J Obstet Gynecol. 1995;173:1842-1848.
3. Baggish MS, Savells A. Complications associated with minimally invasive non-hysteroscopic endometrial ablation techniques. J Gynecol Surg. 2007;23:7-12.
4. Goldrath MH. Evaluation of HydroThermablator and rollerball endometrial ablation for menorrhagia: 3 years after treatment. J Am Assoc Gynecol Laparosc. 2003;10:505-511.
5. Abbott J, Hawe J, Hunter D, et al. A double-blind randomized trial comparing the cavaterm and the Novasure endometrial ablation systems for the treatment of dysfunctional uterine bleeding. Fertil Steril. 2003;80:203-208.
6. Cooper J, Gimpelson R, Laberge P, et al. A randomized, multi-center trial of safety and efficacy of the Novasure system in the treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2002;9:418-428.
7. Loffer FD, Grainger D. Five-year follow-up of patients participating in a randomized trial of uterine balloon therapy versus rollerball ablation for treatment of menorrhagia. J Am Assoc Gynecol Laparosc. 2002;9:429-435.
8. Phipps JH, Lewis BV, Roberts T, et al. Treatment of functional menorrhagia with radiofrequency endometrial ablation. Lancet. 1990;335:374-376.
9. Sharp N, Cronin N, Feldberg I, et al. Microwaves for menorrhagia: a new fast technique for endometrial ablation. Lancet. 1995;346:1003-1004.
10. Thijssen RFA. Radiofrequency-induced endometrial ablation: an update. Br J Obstet Gynaecol. 1997;104:608-613.
11. Baggish MS. Minimally invasive non-hysteroscopic methods for endometrial ablation. In: Baggish MS, Valle RF, Guedj H, eds. Hysteroscopy: Visual Perspectives of Uterine Anatomy, Physiology, and Pathology. 3rd ed. Philadelphia: Lippincott, Williams and Wilkins; 2007:405-415.
12. Dwyer N, Hutton J, Stirrat GM. Randomized controlled trial comparing endometrial resection with abdominal hysterectomy for the surgical treatment of menorrhagia. Br J Obstet Gynaecol. 1993;100:237-243.
13. Raiga J, Mage G, Glowaczower E, et al. Factors affecting risk of failure after endometrial resection. J Gynecol Surg. 1995;11:1-5.
14. Shelly-Jones D, Mooney P, Garry R. Factors influencing the outcome of endometrial laser ablation. J Gynecol Surg. 1994;10:211-215.
15. Valle RF, Baggish MS. Endometrial carcinoma after endometrial ablation: high-risk factors predicting its occurrence. Am J Obstet Gynecol. 1998;176:569-572.
16. Kanter MH, Kivnick S. Bowel injury from rollerball ablation of the endometrium. Obstet Gynecol. 1992;79:833-835.
17. Perry CP, Daniell JF, Gimpelson RJ. Bowel injury from Nd-YAG endometrial ablation. J Gynecol Surg. 1990;6:1999-2003.
18. Scottish Hysteroscopy Audit Group. A Scottish audit of hysteroscopic surgery for menorrhagia: complications and follow-up. Br J Obstet Gynaecol. 1995;102:239-254.
19. Goldrath MH, Fuller TA, Segal S. Laser photovaporization of the endometrium for the treatment of menorrhagia. Am J Obstet Gynecol. 1981;40:14-19.
20. DeCherney A, Polan ML. Hysteroscopic management of intrauterine lesions and intractable uterine bleeding. Obstet Gynecol. 1983;61:392-396.
21. Baggish MS, Baltoyannis P. New techniques for laser ablation of the endometrium in high-risk patients. Am J Obstet Gynecol. 1988;159:287-292.
22. Baggish MS, Sze EHM. Endometrial ablation: a series of 568 patients treated over an 11-year period. Am J Obstet Gynecol. 1996;174:908-913.
23. Garry R, Shelly-Jones D, Mooney P, et al. Six hundred endometrial laser ablations. Obstet Gynecol. 1995;85:24-29.
24. Magos AL, Bauman R, Lockwood GM, et al. Experience with the first 250 endometrial resections for menorrhagia. Lancet. 1991;337:1074-1078.
25. Wortman M, Daggett A. Hysteroscopic endometrial resection: a new technique for the treatment of menorrhagia. Obstet Gynecol. 1994;83:295-298.
26. Townsend DE, Richart RM, Paskowitz, et al. Rollerball coagulation of the endometrium. Obstet Gynecol. 1990;76:310-313.
27. Overton C, Hargreaves J, Maresh M. A national survey of the complications of endometrial destruction for menstrual disorders: the mistletoe study. Br J Obstet Gynaecol. 1997;104:1351-1359.