User login
Society of Hospital Medicine Nearing 15,000 Members
More than 14,000 hospitalists are now members of SHM, and we expect to welcome the 15,000th member early in 2016. SHM will celebrate this milestone for the hospital medicine movement at Hospital Medicine 2016, so stay tuned to learn the identity of the 15,000th member!
More than 14,000 hospitalists are now members of SHM, and we expect to welcome the 15,000th member early in 2016. SHM will celebrate this milestone for the hospital medicine movement at Hospital Medicine 2016, so stay tuned to learn the identity of the 15,000th member!
More than 14,000 hospitalists are now members of SHM, and we expect to welcome the 15,000th member early in 2016. SHM will celebrate this milestone for the hospital medicine movement at Hospital Medicine 2016, so stay tuned to learn the identity of the 15,000th member!
Holiday Discounts for SHM Merchandise
Looking for the perfect holiday gift for a hospitalist friend or colleague? Think about a stainless steel SHM coffee tumbler or a cozy SHM hoodie. All SHM merchandise is currently 10% off. To start your SHM shopping, click “eStore”.
Looking for the perfect holiday gift for a hospitalist friend or colleague? Think about a stainless steel SHM coffee tumbler or a cozy SHM hoodie. All SHM merchandise is currently 10% off. To start your SHM shopping, click “eStore”.
Looking for the perfect holiday gift for a hospitalist friend or colleague? Think about a stainless steel SHM coffee tumbler or a cozy SHM hoodie. All SHM merchandise is currently 10% off. To start your SHM shopping, click “eStore”.
Maintenance of Certification Process Should Ensure Physicians Deliver Quality Care
When the American Board of Internal Medicine (ABIM) announced changes to its Maintenance of Certification (MOC) process in early 2014, the response was overwhelmingly negative. Individual physicians and medical societies criticized ABIM for adding significant time and expense to MOC, and loudly challenged the program’s effectiveness, relevance, and value.
After months of backlash, ABIM issued an apology in February and rolled back or delayed some of the MOC changes. In a letter to diplomates, ABIM President and Chief Executive Officer Richard J. Baron, MD, acknowledged that some of the criticism of ABIM was legitimate and that “some believe ABIM has turned a deaf ear to practicing physicians.” He said, “We got it wrong and sincerely apologize. We are sorry.”
Despite ABIM’s apology, the conversation about MOC continues to rage—and for good reason.
Though the medical community needs a formal process like MOC to ensure that physicians at all stages of their careers are knowledgeable, qualified, and capable of handling their patients’ care, it’s not clear that the current MOC process delivers those outcomes. I’m certain there are individuals who, over the course of seven or 10 years, complete their training modules, pass an exam, and still do not practice according to the most current, evidence-based guidelines. Just because we know the information needed to pass an exam doesn’t mean we actively use that knowledge to deliver quality care to patients.
To bridge this gap, certifying organizations like ABIM and the American Board of Family Medicine (ABFM) should consider how to better integrate the MOC process into physicians’ daily practice of medicine, so that actual patient care and outcomes are used to determine whether or not an individual is recertified.
Done well, this integration would solve multiple problems.
New Approach Required
Instead of measuring our test-taking ability, it would tie certification directly to how we care for patients: weighing whether or not we use current, evidence-based practices to achieve optimal outcomes. It also would address the problem of testing physicians’ knowledge on topics that fall outside their normal scope of practice. For example, as I have focused my career in hospital medicine, I no longer practice in pediatrics or OB/GYN, but those topics are still included in my family medicine board examination. When I was recertified in 2013, I spent a lot more time preparing for that section of the exam than for the areas in which I practice daily.
In fact, a better-integrated MOC process could help reduce the significant investment of time and money associated with recertification. Not only do most physicians need to take time off from practicing to prepare for the exam, but we also must bear the direct costs of the test itself, along with the necessary test preparation materials.
According to a study released in July by the University of California at San Francisco and Stanford University, ABIM’s latest MOC requirements will cost individual physicians more than $23,600 over 10 years, with the costs in some subspecialties exceeding $40,000. Of those costs, $9 out of every $10 is associated with the demand the process makes on a physician’s time. In announcing the study, the lead author said, “We estimate that ABIM MOC will cost 33.7 million physician-hours over 10 years. Efforts to reform MOC and lower its costs should focus on making the most efficient use of physician time.”
A Simple SPARK
Until MOC is reformed, physicians seeking recertification have no option but to continue under the current process. To help members with test preparation, SHM has launched SPARK, an online tool to prepare physicians for the ABIM/ABFM Focused Practice in Hospital Medicine (FPHM) exam. It is available to SHM members at a significant discount. SPARK features 175 vignette-style, single best answer, multiple-choice questions, complete with answers, cohort comparison, discussion, references, and quizzing capabilities. This first edition targets gaps in other available tools like palliative care, ethics and decision-making, patient safety, peri-operative care, consultative co-management, quality, cost, and clinical reasoning.
The first iteration of SPARK has launched. From here, we will expand SPARK to include preparation materials for the remainder of the family medicine/internal medicine sections of the MOC exam. As the only FPHM MOC preparation tool created by hospitalists for hospitalists, we believe SPARK provides an effective and more affordable alternative to the test preparation tools offered directly through ABIM and ABFM.
Although the concept of MOC is a valid one, the process should be improved to ensure that physicians maintain the knowledge necessary to deliver high quality care. As we work toward further reforms, we hope SPARK will ease the preparation process for our members.

When the American Board of Internal Medicine (ABIM) announced changes to its Maintenance of Certification (MOC) process in early 2014, the response was overwhelmingly negative. Individual physicians and medical societies criticized ABIM for adding significant time and expense to MOC, and loudly challenged the program’s effectiveness, relevance, and value.
After months of backlash, ABIM issued an apology in February and rolled back or delayed some of the MOC changes. In a letter to diplomates, ABIM President and Chief Executive Officer Richard J. Baron, MD, acknowledged that some of the criticism of ABIM was legitimate and that “some believe ABIM has turned a deaf ear to practicing physicians.” He said, “We got it wrong and sincerely apologize. We are sorry.”
Despite ABIM’s apology, the conversation about MOC continues to rage—and for good reason.
Though the medical community needs a formal process like MOC to ensure that physicians at all stages of their careers are knowledgeable, qualified, and capable of handling their patients’ care, it’s not clear that the current MOC process delivers those outcomes. I’m certain there are individuals who, over the course of seven or 10 years, complete their training modules, pass an exam, and still do not practice according to the most current, evidence-based guidelines. Just because we know the information needed to pass an exam doesn’t mean we actively use that knowledge to deliver quality care to patients.
To bridge this gap, certifying organizations like ABIM and the American Board of Family Medicine (ABFM) should consider how to better integrate the MOC process into physicians’ daily practice of medicine, so that actual patient care and outcomes are used to determine whether or not an individual is recertified.
Done well, this integration would solve multiple problems.
New Approach Required
Instead of measuring our test-taking ability, it would tie certification directly to how we care for patients: weighing whether or not we use current, evidence-based practices to achieve optimal outcomes. It also would address the problem of testing physicians’ knowledge on topics that fall outside their normal scope of practice. For example, as I have focused my career in hospital medicine, I no longer practice in pediatrics or OB/GYN, but those topics are still included in my family medicine board examination. When I was recertified in 2013, I spent a lot more time preparing for that section of the exam than for the areas in which I practice daily.
In fact, a better-integrated MOC process could help reduce the significant investment of time and money associated with recertification. Not only do most physicians need to take time off from practicing to prepare for the exam, but we also must bear the direct costs of the test itself, along with the necessary test preparation materials.
According to a study released in July by the University of California at San Francisco and Stanford University, ABIM’s latest MOC requirements will cost individual physicians more than $23,600 over 10 years, with the costs in some subspecialties exceeding $40,000. Of those costs, $9 out of every $10 is associated with the demand the process makes on a physician’s time. In announcing the study, the lead author said, “We estimate that ABIM MOC will cost 33.7 million physician-hours over 10 years. Efforts to reform MOC and lower its costs should focus on making the most efficient use of physician time.”
A Simple SPARK
Until MOC is reformed, physicians seeking recertification have no option but to continue under the current process. To help members with test preparation, SHM has launched SPARK, an online tool to prepare physicians for the ABIM/ABFM Focused Practice in Hospital Medicine (FPHM) exam. It is available to SHM members at a significant discount. SPARK features 175 vignette-style, single best answer, multiple-choice questions, complete with answers, cohort comparison, discussion, references, and quizzing capabilities. This first edition targets gaps in other available tools like palliative care, ethics and decision-making, patient safety, peri-operative care, consultative co-management, quality, cost, and clinical reasoning.
The first iteration of SPARK has launched. From here, we will expand SPARK to include preparation materials for the remainder of the family medicine/internal medicine sections of the MOC exam. As the only FPHM MOC preparation tool created by hospitalists for hospitalists, we believe SPARK provides an effective and more affordable alternative to the test preparation tools offered directly through ABIM and ABFM.
Although the concept of MOC is a valid one, the process should be improved to ensure that physicians maintain the knowledge necessary to deliver high quality care. As we work toward further reforms, we hope SPARK will ease the preparation process for our members.

When the American Board of Internal Medicine (ABIM) announced changes to its Maintenance of Certification (MOC) process in early 2014, the response was overwhelmingly negative. Individual physicians and medical societies criticized ABIM for adding significant time and expense to MOC, and loudly challenged the program’s effectiveness, relevance, and value.
After months of backlash, ABIM issued an apology in February and rolled back or delayed some of the MOC changes. In a letter to diplomates, ABIM President and Chief Executive Officer Richard J. Baron, MD, acknowledged that some of the criticism of ABIM was legitimate and that “some believe ABIM has turned a deaf ear to practicing physicians.” He said, “We got it wrong and sincerely apologize. We are sorry.”
Despite ABIM’s apology, the conversation about MOC continues to rage—and for good reason.
Though the medical community needs a formal process like MOC to ensure that physicians at all stages of their careers are knowledgeable, qualified, and capable of handling their patients’ care, it’s not clear that the current MOC process delivers those outcomes. I’m certain there are individuals who, over the course of seven or 10 years, complete their training modules, pass an exam, and still do not practice according to the most current, evidence-based guidelines. Just because we know the information needed to pass an exam doesn’t mean we actively use that knowledge to deliver quality care to patients.
To bridge this gap, certifying organizations like ABIM and the American Board of Family Medicine (ABFM) should consider how to better integrate the MOC process into physicians’ daily practice of medicine, so that actual patient care and outcomes are used to determine whether or not an individual is recertified.
Done well, this integration would solve multiple problems.
New Approach Required
Instead of measuring our test-taking ability, it would tie certification directly to how we care for patients: weighing whether or not we use current, evidence-based practices to achieve optimal outcomes. It also would address the problem of testing physicians’ knowledge on topics that fall outside their normal scope of practice. For example, as I have focused my career in hospital medicine, I no longer practice in pediatrics or OB/GYN, but those topics are still included in my family medicine board examination. When I was recertified in 2013, I spent a lot more time preparing for that section of the exam than for the areas in which I practice daily.
In fact, a better-integrated MOC process could help reduce the significant investment of time and money associated with recertification. Not only do most physicians need to take time off from practicing to prepare for the exam, but we also must bear the direct costs of the test itself, along with the necessary test preparation materials.
According to a study released in July by the University of California at San Francisco and Stanford University, ABIM’s latest MOC requirements will cost individual physicians more than $23,600 over 10 years, with the costs in some subspecialties exceeding $40,000. Of those costs, $9 out of every $10 is associated with the demand the process makes on a physician’s time. In announcing the study, the lead author said, “We estimate that ABIM MOC will cost 33.7 million physician-hours over 10 years. Efforts to reform MOC and lower its costs should focus on making the most efficient use of physician time.”
A Simple SPARK
Until MOC is reformed, physicians seeking recertification have no option but to continue under the current process. To help members with test preparation, SHM has launched SPARK, an online tool to prepare physicians for the ABIM/ABFM Focused Practice in Hospital Medicine (FPHM) exam. It is available to SHM members at a significant discount. SPARK features 175 vignette-style, single best answer, multiple-choice questions, complete with answers, cohort comparison, discussion, references, and quizzing capabilities. This first edition targets gaps in other available tools like palliative care, ethics and decision-making, patient safety, peri-operative care, consultative co-management, quality, cost, and clinical reasoning.
The first iteration of SPARK has launched. From here, we will expand SPARK to include preparation materials for the remainder of the family medicine/internal medicine sections of the MOC exam. As the only FPHM MOC preparation tool created by hospitalists for hospitalists, we believe SPARK provides an effective and more affordable alternative to the test preparation tools offered directly through ABIM and ABFM.
Although the concept of MOC is a valid one, the process should be improved to ensure that physicians maintain the knowledge necessary to deliver high quality care. As we work toward further reforms, we hope SPARK will ease the preparation process for our members.

When Should Hospitalists Order Continuous Cardiac Monitoring?
Case
Two patients on continuous cardiac monitoring (CCM) are admitted to the hospital. One is a 56-year-old man with hemodynamically stable sepsis secondary to pneumonia. There is no sign of arrhythmia on initial evaluation. The second patient is a 67-year-old man with a history of coronary artery disease (CAD) admitted with chest pain. Should these patients be admitted with CCM?
Overview
CCM was first introduced in hospitals in the early 1960s for heart rate and rhythm monitoring in coronary ICUs. Since that time, CCM has been widely used in the hospital setting among critically and noncritically ill patients. Some hospitals have a limited capacity for monitoring, which is dictated by bed or technology availability. Other hospitals have the ability to monitor any patient.
Guidelines from the American College of Cardiology (ACC) in 1991 and the American Heart Association (AHA) in 2004 guide inpatient use of CCM. These guidelines make recommendations based on the likelihood of patient benefit—will likely benefit, may benefit, unlikely to benefit—and are primarily based on expert opinion; rigorous clinical trial data is not available.1,2 Based on these guidelines, patients with primary cardiac diagnoses, including acute coronary syndrome (ACS), post-cardiac surgery, and arrhythmia, are the most likely to benefit from monitoring.2,3
In practical use, many hospitalists use CCM to detect signs of hemodynamic instability.3 Currently there is no data to support the idea that CCM is a safe or equivalent method of detecting hemodynamic instability compared to close clinical evaluation and frequent vital sign measurement. In fact, physicians overestimate the utility of CCM in guiding management decisions, and witnessed clinical deterioration is a more frequent factor in the decision to escalate the level of care of a patient.3,4
Guideline Recommendations
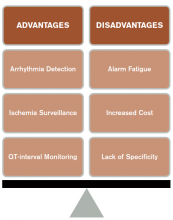
CCM is intended to identify life-threatening arrhythmias, ischemia, and QT prolongation (see Figure 1). The AHA guidelines address which patients will benefit from CCM; the main indications include an acute cardiac diagnosis or critical illness.1
In addition, the AHA guidelines provide recommendations for the duration of monitoring. These recommendations vary from time-limited monitoring (e.g. unexplained syncope) to a therapeutic-based recommendation (e.g. high-grade atrioventricular block requiring pacemaker placement).
The guidelines also identify a subset of patients who are unlikely to benefit from monitoring (Class III), including low-risk post-operative patients, patients with rate-controlled atrial fibrillation, and patients undergoing hemodialysis without other indications for monitoring.
Several studies have examined the frequency of CCM use. In one study of 236 admissions to a community hospital general ward population, approximately 50% of the 745 monitoring days were not indicated by ACC/AHA guidelines.5 In this study, only 5% of telemetry events occurred in patients without indications, and none of these events required any specific therapy.5 Thus, improved adherence to the ACC/AHA guidelines can decrease CCM use in patients who are unlikely to benefit.
Life-threatening arrhythmia detection. Cleverley and colleagues reported that patients who suffered a cardiac arrest on noncritical care units had a higher survival to hospital discharge if they were on CCM during the event.6 However, a similar study recently showed no benefit to cardiac monitoring for in-hospital arrest if patients were monitored remotely.7 Patients who experience a cardiac arrest in a noncritical care area may benefit from direct cardiac monitoring, though larger studies are needed to assess all potential confounding effects, including nurse-to-patient ratios, location of monitoring (remote or unit-based), advanced cardiac life support response times, and whether the event was witnessed.
Bottom line: AHA guidelines recommend use of CCM in patients with a higher likelihood of developing a life-threatening arrhythmia, including those with an ACS, those experiencing post-cardiac arrest, or those who are critically ill. Medical ward patients who should be monitored include those with acute or subacute congestive heart failure, syncope of unknown etiology, and uncontrolled atrial fibrillation.1
Ischemia surveillance. Computerized ST-segment monitoring has been available for high-risk post-operative patients and those with acute cardiac events since the mid-1980s. When properly used, it offers the ability to detect “silent” ischemia, which is associated with increased in-hospital complications and worse patient outcomes.
Computerized ST-segment monitoring is often associated with a high rate of false positive alarms, however, and has not been universally adopted. Recommendations for its use are based on expert opinion, because no randomized trial has shown that increasing the sensitivity of ischemia detection improves patient outcomes.
Bottom line: AHA guidelines recommend ST-segment monitoring in patients with early ACS and post-acute MI as well as in patients at high risk for silent ischemia, including high-risk post-operative patients.1
QT-interval monitoring. A corrected QT-interval (QTc) greater than 0.50 milliseconds correlates with a higher risk for torsades de pointes and is associated with higher mortality. In critically ill patients in a large academic medical center, guideline-based QT-interval monitoring showed poor specificity for predicting the development of QTc prolongation; however, the risk of QTc prolongation increased with the presence of multiple risk factors.8
Bottom line: AHA guidelines recommend QT-interval monitoring in patients with risk factors for QTc-prolongation, including those starting QTc-prolonging drugs, those with overdose of pro-arrhythmic drugs, those with new-onset bradyarrhythmias, those with severe hypokalemia or hypomagnesemia, and those who have experienced acute neurologic events.1
Recommendations Outside of Guidelines
Patients admitted to medical services for noncardiac diagnoses have a high rate of telemetry use and a perceived benefit associated with cardiac monitoring.3 Although guidelines for noncardiac patients to direct hospitalists on when to use this technology are lacking, there may be some utility in monitoring certain subsets of inpatients.
Sepsis. Patients with hemodynamically stable sepsis develop atrial fibrillation at a higher rate than patients without sepsis and have higher in-hospital mortality. Patients at highest risk are those who are elderly or have severe sepsis.7 CCM can identify atrial fibrillation in real time, which may allow for earlier intervention; however, it is important to consider that other modalities, such as patient symptoms, physical exam, and standard EKG, are potentially as effective at detecting atrial fibrillation as CCM.
Bottom line: Our recommendation is to use CCM in patients who are at higher risk, including elderly patients and those with severe sepsis, until sepsis has resolved and/or the patient is hemodynamically stable for 24 hours.
Alcohol withdrawal. Patients with severe alcohol withdrawal have an increased incidence of arrhythmia and ischemia during the detoxification process. Specifically, patients with delirium tremens and seizures are at higher risk for significant QTc prolongation and tachyarrhythmias.9
Bottom line: Our recommendation is to use CCM in patients with severe alcohol withdrawal and to discontinue monitoring once withdrawal has resolved.
COPD. Patients with COPD exacerbations have a high risk of in-hospital and long-term mortality. The highest risk for mortality appears to be in patients presenting with atrial or ventricular arrhythmias and those over 65 years old.10 There is no clear evidence that beta-agonist use in COPD exacerbations increases arrhythmias other than sinus tachycardia or is associated with worse outcomes.11
Bottom line: Our recommendation is to use CCM only in patients with COPD exacerbation who have other indications as described in the AHA guidelines.
CCM Disadvantages
Alarm fatigue. Alarm fatigue is defined as the desensitization of a clinician to an alarm stimulus, resulting from sensory overload and causing the response of an alarm to be delayed or dismissed.12 In 2014, the Emergency Care Research Institute named alarm hazards as the number one health technology hazard, noting that numerous alarms on a daily basis can lead to desensitization and “alarm fatigue.”
CCM, and the overuse of CCM in particular, contribute to alarm fatigue, which can lead to patient safety issues, including delays in treatment, medication errors, and potentially death.
Increased cost. Because telemetry requires specialized equipment and trained monitoring staff, cost can be significant. In addition to equipment, cost includes time spent by providers, nurses, and technicians interpreting the images and discussing findings with consultants, as well as the additional studies obtained as a result of identified arrhythmias.
Studies on CCM cost vary widely, with conservative estimates of approximately $53 to as much as $1,400 per patient per day in some hospitals.13
Lack of specificity. Because of the high sensitivity and low specificity of CCM, use of CCM in low-risk patients without indications increases the risk of misinterpreting false-positive findings as clinically significant. This can lead to errors in management, including overtesting, unnecessary consultation with subspecialists, and the potential for inappropriate invasive procedures.1
High-Value CCM Use
Because of the low value associated with cardiac monitoring in many patients and the high sensitivity of the guidelines to capture patients at high risk for cardiac events, many hospitals have sought to limit the overuse of this technology. The most successful interventions have targeted the electronic ordering system by requiring an indication and hardwiring an order duration based on guideline recommendations. In a recent study, this intervention led to a 70% decrease in usage and reported $4.8 million cost savings without increasing the rate of in-hospital rapid response or cardiac arrest.14
Systems-level interventions to decrease inappropriate initiation and facilitate discontinuation of cardiac monitoring are a proven way to increase compliance with guidelines and decrease the overuse of CCM.
Back to the Case
According to AHA guidelines, the only patient who has an indication for CCM is the 67-year-old man with known CAD and chest pain, and, accordingly, the patient was placed on CCM. The patient underwent evaluation for ACS, and monitoring was discontinued after 24 hours when ACS was ruled out. The 56-year-old man with sepsis responded to treatment of pneumonia and was not placed on CCM.
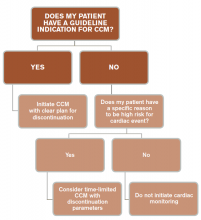
In general, patients admitted with acute cardiac-related diseases should be placed on CCM. Guidelines are lacking with respect to many noncardiac diseases, and we recommend a time-limited duration (typically 24 hours) if CCM is ordered for a patient with a special circumstance outside of guidelines (see Figure 3).
Key Takeaway
Hospitalists should use continuous cardiac monitoring for specific indications and not routinely for all patients.
Drs. Lacy and Rendon are hospitalists in the department of internal medicine at the University of New Mexico School of Medicine in Albuquerque. Dr. Davis is a resident in internal medicine at UNM, and Dr. Tolstrup is a cardiologist at UNM.
References
- Drew BJ, Califf RM, Funk M, et al. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation. 2004;110(17):2721-2746. doi:10.1161/01.CIR.0000145144.56673.59.
- Recommended guidelines for in-hospital cardiac monitoring of adults for detection of arrhythmia. Emergency Cardiac Care Committee members. J Am Coll Cardiol. 1991;18(6):1431-1433.
- Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med. 2012;172(17):1349-1350. doi:10.1001/archinternmed.2012.3163.
- Estrada CA, Rosman HS, Prasad NK, et al. Role of telemetry monitoring in the non-intensive care unit. Am J Cardiol. 1995;76(12):960-965.
- Curry JP, Hanson CW III, Russell MW, Hanna C, Devine G, Ochroch EA. The use and effectiveness of electrocardiographic telemetry monitoring in a community hospital general care setting. Anesth Analg. 2003;97(5):1483-1487.
- Cleverley K, Mousavi N, Stronger L, et al. The impact of telemetry on survival of in-hospital cardiac arrests in non-critical care patients. Resuscitation. 2013;84(7):878-882. doi:10.1016/j.resuscitation.2013.01.038.
- Walkey AJ, Greiner MA, Heckbert SR, et al. Atrial fibrillation among Medicare beneficiaries hospitalized with sepsis: incidence and risk factors. Am Heart J. 2013;165(6):949-955.e3. doi:10.1016/j.ahj.2013.03.020.
- Pickham D, Helfenbein E, Shinn JA, Chan G, Funk M, Drew BJ. How many patients need QT interval monitoring in critical care units? Preliminary report of the QT in Practice study. J Electrocardiol. 2010;43(6):572-576. doi:10.1016/j.jelectrocard.2010.05.016.
- Cuculi F, Kobza R, Ehmann T, Erne P. ECG changes amongst patients with alcohol withdrawal seizures and delirium tremens. Swiss Med Wkly. 2006;136(13-14):223-227. doi:2006/13/smw-11319.
- Fuso L, Incalzi RA, Pistelli R, et al. Predicting mortality of patients hospitalized for acutely exacerbated chronic obstructive pulmonary disease. Am J Med. 1995;98(3):272-277.
- Salpeter SR, Ormiston TM, Salpeter EE. Cardiovascular effects of beta-agonists in patients with asthma and COPD: a meta-analysis. Chest. 2004;125(6):2309-2321.
- McCartney PR. Clinical alarm management. MCN Am J Matern Child Nurs. 2012;37(3):202. doi:10.1097/NMC.0b013e31824c5b4a.
- Benjamin EM, Klugman RA, Luckmann R, Fairchild DG, Abookire SA. Impact of cardiac telemetry on patient safety and cost. Am J Manag Care. 2013;19(6):e225-e232.
- Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174(11):1852-1854. doi:10.1001/jamainternmed.2014.4491.
Case
Two patients on continuous cardiac monitoring (CCM) are admitted to the hospital. One is a 56-year-old man with hemodynamically stable sepsis secondary to pneumonia. There is no sign of arrhythmia on initial evaluation. The second patient is a 67-year-old man with a history of coronary artery disease (CAD) admitted with chest pain. Should these patients be admitted with CCM?
Overview
CCM was first introduced in hospitals in the early 1960s for heart rate and rhythm monitoring in coronary ICUs. Since that time, CCM has been widely used in the hospital setting among critically and noncritically ill patients. Some hospitals have a limited capacity for monitoring, which is dictated by bed or technology availability. Other hospitals have the ability to monitor any patient.
Guidelines from the American College of Cardiology (ACC) in 1991 and the American Heart Association (AHA) in 2004 guide inpatient use of CCM. These guidelines make recommendations based on the likelihood of patient benefit—will likely benefit, may benefit, unlikely to benefit—and are primarily based on expert opinion; rigorous clinical trial data is not available.1,2 Based on these guidelines, patients with primary cardiac diagnoses, including acute coronary syndrome (ACS), post-cardiac surgery, and arrhythmia, are the most likely to benefit from monitoring.2,3
In practical use, many hospitalists use CCM to detect signs of hemodynamic instability.3 Currently there is no data to support the idea that CCM is a safe or equivalent method of detecting hemodynamic instability compared to close clinical evaluation and frequent vital sign measurement. In fact, physicians overestimate the utility of CCM in guiding management decisions, and witnessed clinical deterioration is a more frequent factor in the decision to escalate the level of care of a patient.3,4
Guideline Recommendations
CCM is intended to identify life-threatening arrhythmias, ischemia, and QT prolongation (see Figure 1). The AHA guidelines address which patients will benefit from CCM; the main indications include an acute cardiac diagnosis or critical illness.1
In addition, the AHA guidelines provide recommendations for the duration of monitoring. These recommendations vary from time-limited monitoring (e.g. unexplained syncope) to a therapeutic-based recommendation (e.g. high-grade atrioventricular block requiring pacemaker placement).
The guidelines also identify a subset of patients who are unlikely to benefit from monitoring (Class III), including low-risk post-operative patients, patients with rate-controlled atrial fibrillation, and patients undergoing hemodialysis without other indications for monitoring.
Several studies have examined the frequency of CCM use. In one study of 236 admissions to a community hospital general ward population, approximately 50% of the 745 monitoring days were not indicated by ACC/AHA guidelines.5 In this study, only 5% of telemetry events occurred in patients without indications, and none of these events required any specific therapy.5 Thus, improved adherence to the ACC/AHA guidelines can decrease CCM use in patients who are unlikely to benefit.
Life-threatening arrhythmia detection. Cleverley and colleagues reported that patients who suffered a cardiac arrest on noncritical care units had a higher survival to hospital discharge if they were on CCM during the event.6 However, a similar study recently showed no benefit to cardiac monitoring for in-hospital arrest if patients were monitored remotely.7 Patients who experience a cardiac arrest in a noncritical care area may benefit from direct cardiac monitoring, though larger studies are needed to assess all potential confounding effects, including nurse-to-patient ratios, location of monitoring (remote or unit-based), advanced cardiac life support response times, and whether the event was witnessed.
Bottom line: AHA guidelines recommend use of CCM in patients with a higher likelihood of developing a life-threatening arrhythmia, including those with an ACS, those experiencing post-cardiac arrest, or those who are critically ill. Medical ward patients who should be monitored include those with acute or subacute congestive heart failure, syncope of unknown etiology, and uncontrolled atrial fibrillation.1
Ischemia surveillance. Computerized ST-segment monitoring has been available for high-risk post-operative patients and those with acute cardiac events since the mid-1980s. When properly used, it offers the ability to detect “silent” ischemia, which is associated with increased in-hospital complications and worse patient outcomes.
Computerized ST-segment monitoring is often associated with a high rate of false positive alarms, however, and has not been universally adopted. Recommendations for its use are based on expert opinion, because no randomized trial has shown that increasing the sensitivity of ischemia detection improves patient outcomes.
Bottom line: AHA guidelines recommend ST-segment monitoring in patients with early ACS and post-acute MI as well as in patients at high risk for silent ischemia, including high-risk post-operative patients.1
QT-interval monitoring. A corrected QT-interval (QTc) greater than 0.50 milliseconds correlates with a higher risk for torsades de pointes and is associated with higher mortality. In critically ill patients in a large academic medical center, guideline-based QT-interval monitoring showed poor specificity for predicting the development of QTc prolongation; however, the risk of QTc prolongation increased with the presence of multiple risk factors.8
Bottom line: AHA guidelines recommend QT-interval monitoring in patients with risk factors for QTc-prolongation, including those starting QTc-prolonging drugs, those with overdose of pro-arrhythmic drugs, those with new-onset bradyarrhythmias, those with severe hypokalemia or hypomagnesemia, and those who have experienced acute neurologic events.1
Recommendations Outside of Guidelines
Patients admitted to medical services for noncardiac diagnoses have a high rate of telemetry use and a perceived benefit associated with cardiac monitoring.3 Although guidelines for noncardiac patients to direct hospitalists on when to use this technology are lacking, there may be some utility in monitoring certain subsets of inpatients.
Sepsis. Patients with hemodynamically stable sepsis develop atrial fibrillation at a higher rate than patients without sepsis and have higher in-hospital mortality. Patients at highest risk are those who are elderly or have severe sepsis.7 CCM can identify atrial fibrillation in real time, which may allow for earlier intervention; however, it is important to consider that other modalities, such as patient symptoms, physical exam, and standard EKG, are potentially as effective at detecting atrial fibrillation as CCM.
Bottom line: Our recommendation is to use CCM in patients who are at higher risk, including elderly patients and those with severe sepsis, until sepsis has resolved and/or the patient is hemodynamically stable for 24 hours.
Alcohol withdrawal. Patients with severe alcohol withdrawal have an increased incidence of arrhythmia and ischemia during the detoxification process. Specifically, patients with delirium tremens and seizures are at higher risk for significant QTc prolongation and tachyarrhythmias.9
Bottom line: Our recommendation is to use CCM in patients with severe alcohol withdrawal and to discontinue monitoring once withdrawal has resolved.
COPD. Patients with COPD exacerbations have a high risk of in-hospital and long-term mortality. The highest risk for mortality appears to be in patients presenting with atrial or ventricular arrhythmias and those over 65 years old.10 There is no clear evidence that beta-agonist use in COPD exacerbations increases arrhythmias other than sinus tachycardia or is associated with worse outcomes.11
Bottom line: Our recommendation is to use CCM only in patients with COPD exacerbation who have other indications as described in the AHA guidelines.
CCM Disadvantages
Alarm fatigue. Alarm fatigue is defined as the desensitization of a clinician to an alarm stimulus, resulting from sensory overload and causing the response of an alarm to be delayed or dismissed.12 In 2014, the Emergency Care Research Institute named alarm hazards as the number one health technology hazard, noting that numerous alarms on a daily basis can lead to desensitization and “alarm fatigue.”
CCM, and the overuse of CCM in particular, contribute to alarm fatigue, which can lead to patient safety issues, including delays in treatment, medication errors, and potentially death.
Increased cost. Because telemetry requires specialized equipment and trained monitoring staff, cost can be significant. In addition to equipment, cost includes time spent by providers, nurses, and technicians interpreting the images and discussing findings with consultants, as well as the additional studies obtained as a result of identified arrhythmias.
Studies on CCM cost vary widely, with conservative estimates of approximately $53 to as much as $1,400 per patient per day in some hospitals.13
Lack of specificity. Because of the high sensitivity and low specificity of CCM, use of CCM in low-risk patients without indications increases the risk of misinterpreting false-positive findings as clinically significant. This can lead to errors in management, including overtesting, unnecessary consultation with subspecialists, and the potential for inappropriate invasive procedures.1
High-Value CCM Use
Because of the low value associated with cardiac monitoring in many patients and the high sensitivity of the guidelines to capture patients at high risk for cardiac events, many hospitals have sought to limit the overuse of this technology. The most successful interventions have targeted the electronic ordering system by requiring an indication and hardwiring an order duration based on guideline recommendations. In a recent study, this intervention led to a 70% decrease in usage and reported $4.8 million cost savings without increasing the rate of in-hospital rapid response or cardiac arrest.14
Systems-level interventions to decrease inappropriate initiation and facilitate discontinuation of cardiac monitoring are a proven way to increase compliance with guidelines and decrease the overuse of CCM.
Back to the Case
According to AHA guidelines, the only patient who has an indication for CCM is the 67-year-old man with known CAD and chest pain, and, accordingly, the patient was placed on CCM. The patient underwent evaluation for ACS, and monitoring was discontinued after 24 hours when ACS was ruled out. The 56-year-old man with sepsis responded to treatment of pneumonia and was not placed on CCM.
In general, patients admitted with acute cardiac-related diseases should be placed on CCM. Guidelines are lacking with respect to many noncardiac diseases, and we recommend a time-limited duration (typically 24 hours) if CCM is ordered for a patient with a special circumstance outside of guidelines (see Figure 3).
Key Takeaway
Hospitalists should use continuous cardiac monitoring for specific indications and not routinely for all patients.
Drs. Lacy and Rendon are hospitalists in the department of internal medicine at the University of New Mexico School of Medicine in Albuquerque. Dr. Davis is a resident in internal medicine at UNM, and Dr. Tolstrup is a cardiologist at UNM.
References
- Drew BJ, Califf RM, Funk M, et al. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation. 2004;110(17):2721-2746. doi:10.1161/01.CIR.0000145144.56673.59.
- Recommended guidelines for in-hospital cardiac monitoring of adults for detection of arrhythmia. Emergency Cardiac Care Committee members. J Am Coll Cardiol. 1991;18(6):1431-1433.
- Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med. 2012;172(17):1349-1350. doi:10.1001/archinternmed.2012.3163.
- Estrada CA, Rosman HS, Prasad NK, et al. Role of telemetry monitoring in the non-intensive care unit. Am J Cardiol. 1995;76(12):960-965.
- Curry JP, Hanson CW III, Russell MW, Hanna C, Devine G, Ochroch EA. The use and effectiveness of electrocardiographic telemetry monitoring in a community hospital general care setting. Anesth Analg. 2003;97(5):1483-1487.
- Cleverley K, Mousavi N, Stronger L, et al. The impact of telemetry on survival of in-hospital cardiac arrests in non-critical care patients. Resuscitation. 2013;84(7):878-882. doi:10.1016/j.resuscitation.2013.01.038.
- Walkey AJ, Greiner MA, Heckbert SR, et al. Atrial fibrillation among Medicare beneficiaries hospitalized with sepsis: incidence and risk factors. Am Heart J. 2013;165(6):949-955.e3. doi:10.1016/j.ahj.2013.03.020.
- Pickham D, Helfenbein E, Shinn JA, Chan G, Funk M, Drew BJ. How many patients need QT interval monitoring in critical care units? Preliminary report of the QT in Practice study. J Electrocardiol. 2010;43(6):572-576. doi:10.1016/j.jelectrocard.2010.05.016.
- Cuculi F, Kobza R, Ehmann T, Erne P. ECG changes amongst patients with alcohol withdrawal seizures and delirium tremens. Swiss Med Wkly. 2006;136(13-14):223-227. doi:2006/13/smw-11319.
- Fuso L, Incalzi RA, Pistelli R, et al. Predicting mortality of patients hospitalized for acutely exacerbated chronic obstructive pulmonary disease. Am J Med. 1995;98(3):272-277.
- Salpeter SR, Ormiston TM, Salpeter EE. Cardiovascular effects of beta-agonists in patients with asthma and COPD: a meta-analysis. Chest. 2004;125(6):2309-2321.
- McCartney PR. Clinical alarm management. MCN Am J Matern Child Nurs. 2012;37(3):202. doi:10.1097/NMC.0b013e31824c5b4a.
- Benjamin EM, Klugman RA, Luckmann R, Fairchild DG, Abookire SA. Impact of cardiac telemetry on patient safety and cost. Am J Manag Care. 2013;19(6):e225-e232.
- Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174(11):1852-1854. doi:10.1001/jamainternmed.2014.4491.
Case
Two patients on continuous cardiac monitoring (CCM) are admitted to the hospital. One is a 56-year-old man with hemodynamically stable sepsis secondary to pneumonia. There is no sign of arrhythmia on initial evaluation. The second patient is a 67-year-old man with a history of coronary artery disease (CAD) admitted with chest pain. Should these patients be admitted with CCM?
Overview
CCM was first introduced in hospitals in the early 1960s for heart rate and rhythm monitoring in coronary ICUs. Since that time, CCM has been widely used in the hospital setting among critically and noncritically ill patients. Some hospitals have a limited capacity for monitoring, which is dictated by bed or technology availability. Other hospitals have the ability to monitor any patient.
Guidelines from the American College of Cardiology (ACC) in 1991 and the American Heart Association (AHA) in 2004 guide inpatient use of CCM. These guidelines make recommendations based on the likelihood of patient benefit—will likely benefit, may benefit, unlikely to benefit—and are primarily based on expert opinion; rigorous clinical trial data is not available.1,2 Based on these guidelines, patients with primary cardiac diagnoses, including acute coronary syndrome (ACS), post-cardiac surgery, and arrhythmia, are the most likely to benefit from monitoring.2,3
In practical use, many hospitalists use CCM to detect signs of hemodynamic instability.3 Currently there is no data to support the idea that CCM is a safe or equivalent method of detecting hemodynamic instability compared to close clinical evaluation and frequent vital sign measurement. In fact, physicians overestimate the utility of CCM in guiding management decisions, and witnessed clinical deterioration is a more frequent factor in the decision to escalate the level of care of a patient.3,4
Guideline Recommendations
CCM is intended to identify life-threatening arrhythmias, ischemia, and QT prolongation (see Figure 1). The AHA guidelines address which patients will benefit from CCM; the main indications include an acute cardiac diagnosis or critical illness.1
In addition, the AHA guidelines provide recommendations for the duration of monitoring. These recommendations vary from time-limited monitoring (e.g. unexplained syncope) to a therapeutic-based recommendation (e.g. high-grade atrioventricular block requiring pacemaker placement).
The guidelines also identify a subset of patients who are unlikely to benefit from monitoring (Class III), including low-risk post-operative patients, patients with rate-controlled atrial fibrillation, and patients undergoing hemodialysis without other indications for monitoring.
Several studies have examined the frequency of CCM use. In one study of 236 admissions to a community hospital general ward population, approximately 50% of the 745 monitoring days were not indicated by ACC/AHA guidelines.5 In this study, only 5% of telemetry events occurred in patients without indications, and none of these events required any specific therapy.5 Thus, improved adherence to the ACC/AHA guidelines can decrease CCM use in patients who are unlikely to benefit.
Life-threatening arrhythmia detection. Cleverley and colleagues reported that patients who suffered a cardiac arrest on noncritical care units had a higher survival to hospital discharge if they were on CCM during the event.6 However, a similar study recently showed no benefit to cardiac monitoring for in-hospital arrest if patients were monitored remotely.7 Patients who experience a cardiac arrest in a noncritical care area may benefit from direct cardiac monitoring, though larger studies are needed to assess all potential confounding effects, including nurse-to-patient ratios, location of monitoring (remote or unit-based), advanced cardiac life support response times, and whether the event was witnessed.
Bottom line: AHA guidelines recommend use of CCM in patients with a higher likelihood of developing a life-threatening arrhythmia, including those with an ACS, those experiencing post-cardiac arrest, or those who are critically ill. Medical ward patients who should be monitored include those with acute or subacute congestive heart failure, syncope of unknown etiology, and uncontrolled atrial fibrillation.1
Ischemia surveillance. Computerized ST-segment monitoring has been available for high-risk post-operative patients and those with acute cardiac events since the mid-1980s. When properly used, it offers the ability to detect “silent” ischemia, which is associated with increased in-hospital complications and worse patient outcomes.
Computerized ST-segment monitoring is often associated with a high rate of false positive alarms, however, and has not been universally adopted. Recommendations for its use are based on expert opinion, because no randomized trial has shown that increasing the sensitivity of ischemia detection improves patient outcomes.
Bottom line: AHA guidelines recommend ST-segment monitoring in patients with early ACS and post-acute MI as well as in patients at high risk for silent ischemia, including high-risk post-operative patients.1
QT-interval monitoring. A corrected QT-interval (QTc) greater than 0.50 milliseconds correlates with a higher risk for torsades de pointes and is associated with higher mortality. In critically ill patients in a large academic medical center, guideline-based QT-interval monitoring showed poor specificity for predicting the development of QTc prolongation; however, the risk of QTc prolongation increased with the presence of multiple risk factors.8
Bottom line: AHA guidelines recommend QT-interval monitoring in patients with risk factors for QTc-prolongation, including those starting QTc-prolonging drugs, those with overdose of pro-arrhythmic drugs, those with new-onset bradyarrhythmias, those with severe hypokalemia or hypomagnesemia, and those who have experienced acute neurologic events.1
Recommendations Outside of Guidelines
Patients admitted to medical services for noncardiac diagnoses have a high rate of telemetry use and a perceived benefit associated with cardiac monitoring.3 Although guidelines for noncardiac patients to direct hospitalists on when to use this technology are lacking, there may be some utility in monitoring certain subsets of inpatients.
Sepsis. Patients with hemodynamically stable sepsis develop atrial fibrillation at a higher rate than patients without sepsis and have higher in-hospital mortality. Patients at highest risk are those who are elderly or have severe sepsis.7 CCM can identify atrial fibrillation in real time, which may allow for earlier intervention; however, it is important to consider that other modalities, such as patient symptoms, physical exam, and standard EKG, are potentially as effective at detecting atrial fibrillation as CCM.
Bottom line: Our recommendation is to use CCM in patients who are at higher risk, including elderly patients and those with severe sepsis, until sepsis has resolved and/or the patient is hemodynamically stable for 24 hours.
Alcohol withdrawal. Patients with severe alcohol withdrawal have an increased incidence of arrhythmia and ischemia during the detoxification process. Specifically, patients with delirium tremens and seizures are at higher risk for significant QTc prolongation and tachyarrhythmias.9
Bottom line: Our recommendation is to use CCM in patients with severe alcohol withdrawal and to discontinue monitoring once withdrawal has resolved.
COPD. Patients with COPD exacerbations have a high risk of in-hospital and long-term mortality. The highest risk for mortality appears to be in patients presenting with atrial or ventricular arrhythmias and those over 65 years old.10 There is no clear evidence that beta-agonist use in COPD exacerbations increases arrhythmias other than sinus tachycardia or is associated with worse outcomes.11
Bottom line: Our recommendation is to use CCM only in patients with COPD exacerbation who have other indications as described in the AHA guidelines.
CCM Disadvantages
Alarm fatigue. Alarm fatigue is defined as the desensitization of a clinician to an alarm stimulus, resulting from sensory overload and causing the response of an alarm to be delayed or dismissed.12 In 2014, the Emergency Care Research Institute named alarm hazards as the number one health technology hazard, noting that numerous alarms on a daily basis can lead to desensitization and “alarm fatigue.”
CCM, and the overuse of CCM in particular, contribute to alarm fatigue, which can lead to patient safety issues, including delays in treatment, medication errors, and potentially death.
Increased cost. Because telemetry requires specialized equipment and trained monitoring staff, cost can be significant. In addition to equipment, cost includes time spent by providers, nurses, and technicians interpreting the images and discussing findings with consultants, as well as the additional studies obtained as a result of identified arrhythmias.
Studies on CCM cost vary widely, with conservative estimates of approximately $53 to as much as $1,400 per patient per day in some hospitals.13
Lack of specificity. Because of the high sensitivity and low specificity of CCM, use of CCM in low-risk patients without indications increases the risk of misinterpreting false-positive findings as clinically significant. This can lead to errors in management, including overtesting, unnecessary consultation with subspecialists, and the potential for inappropriate invasive procedures.1
High-Value CCM Use
Because of the low value associated with cardiac monitoring in many patients and the high sensitivity of the guidelines to capture patients at high risk for cardiac events, many hospitals have sought to limit the overuse of this technology. The most successful interventions have targeted the electronic ordering system by requiring an indication and hardwiring an order duration based on guideline recommendations. In a recent study, this intervention led to a 70% decrease in usage and reported $4.8 million cost savings without increasing the rate of in-hospital rapid response or cardiac arrest.14
Systems-level interventions to decrease inappropriate initiation and facilitate discontinuation of cardiac monitoring are a proven way to increase compliance with guidelines and decrease the overuse of CCM.
Back to the Case
According to AHA guidelines, the only patient who has an indication for CCM is the 67-year-old man with known CAD and chest pain, and, accordingly, the patient was placed on CCM. The patient underwent evaluation for ACS, and monitoring was discontinued after 24 hours when ACS was ruled out. The 56-year-old man with sepsis responded to treatment of pneumonia and was not placed on CCM.
In general, patients admitted with acute cardiac-related diseases should be placed on CCM. Guidelines are lacking with respect to many noncardiac diseases, and we recommend a time-limited duration (typically 24 hours) if CCM is ordered for a patient with a special circumstance outside of guidelines (see Figure 3).
Key Takeaway
Hospitalists should use continuous cardiac monitoring for specific indications and not routinely for all patients.
Drs. Lacy and Rendon are hospitalists in the department of internal medicine at the University of New Mexico School of Medicine in Albuquerque. Dr. Davis is a resident in internal medicine at UNM, and Dr. Tolstrup is a cardiologist at UNM.
References
- Drew BJ, Califf RM, Funk M, et al. Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation. 2004;110(17):2721-2746. doi:10.1161/01.CIR.0000145144.56673.59.
- Recommended guidelines for in-hospital cardiac monitoring of adults for detection of arrhythmia. Emergency Cardiac Care Committee members. J Am Coll Cardiol. 1991;18(6):1431-1433.
- Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med. 2012;172(17):1349-1350. doi:10.1001/archinternmed.2012.3163.
- Estrada CA, Rosman HS, Prasad NK, et al. Role of telemetry monitoring in the non-intensive care unit. Am J Cardiol. 1995;76(12):960-965.
- Curry JP, Hanson CW III, Russell MW, Hanna C, Devine G, Ochroch EA. The use and effectiveness of electrocardiographic telemetry monitoring in a community hospital general care setting. Anesth Analg. 2003;97(5):1483-1487.
- Cleverley K, Mousavi N, Stronger L, et al. The impact of telemetry on survival of in-hospital cardiac arrests in non-critical care patients. Resuscitation. 2013;84(7):878-882. doi:10.1016/j.resuscitation.2013.01.038.
- Walkey AJ, Greiner MA, Heckbert SR, et al. Atrial fibrillation among Medicare beneficiaries hospitalized with sepsis: incidence and risk factors. Am Heart J. 2013;165(6):949-955.e3. doi:10.1016/j.ahj.2013.03.020.
- Pickham D, Helfenbein E, Shinn JA, Chan G, Funk M, Drew BJ. How many patients need QT interval monitoring in critical care units? Preliminary report of the QT in Practice study. J Electrocardiol. 2010;43(6):572-576. doi:10.1016/j.jelectrocard.2010.05.016.
- Cuculi F, Kobza R, Ehmann T, Erne P. ECG changes amongst patients with alcohol withdrawal seizures and delirium tremens. Swiss Med Wkly. 2006;136(13-14):223-227. doi:2006/13/smw-11319.
- Fuso L, Incalzi RA, Pistelli R, et al. Predicting mortality of patients hospitalized for acutely exacerbated chronic obstructive pulmonary disease. Am J Med. 1995;98(3):272-277.
- Salpeter SR, Ormiston TM, Salpeter EE. Cardiovascular effects of beta-agonists in patients with asthma and COPD: a meta-analysis. Chest. 2004;125(6):2309-2321.
- McCartney PR. Clinical alarm management. MCN Am J Matern Child Nurs. 2012;37(3):202. doi:10.1097/NMC.0b013e31824c5b4a.
- Benjamin EM, Klugman RA, Luckmann R, Fairchild DG, Abookire SA. Impact of cardiac telemetry on patient safety and cost. Am J Manag Care. 2013;19(6):e225-e232.
- Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174(11):1852-1854. doi:10.1001/jamainternmed.2014.4491.
ED Lung Ultrasound Useful for Differentiating Cardiogenic from Noncardiogenic Dyspnea
Clinical question: Is lung ultrasound a useful tool for helping to diagnose acute decompensated heart failure (ADHF)?
Background: Lung ultrasound is an emerging bedside tool that has been promoted to help evaluate lung water content to help clinicians differentiate ADHF from other causes of dyspnea.
Study design: Prospective, multicenter, observational cohort study.
Setting: Seven EDs in Italy.
Synopsis: A total of 1,005 patients were enrolled in the study. Upon presentation to the ED, patients received a standard workup, including history, physical examination, EKG, and arterial blood gas sampling. Physicians were asked to render a diagnosis of ADHF or noncardiogenic dyspnea. The same physician then performed a lung ultrasound and rendered a revised diagnosis based on the ultrasound findings. A second ED physician and cardiologist, blinded to the ultrasound results, reviewed the medical record and rendered a final diagnosis as to the cause of the patient’s dyspnea.
The ultrasound approach had a higher accuracy than clinical evaluation alone in differentiating ADHF from noncardiac causes of dyspnea (97% vs. 85.3%). The authors also report a higher sensitivity compared to chest X-ray alone (69.5%) and natriuretic peptide testing (85%).
Bottom line: Lung ultrasound combined with clinical evaluation may improve the accuracy of ADHF diagnosis, but its usefulness may be limited by the need for ED physicians to have some degree of expertise in the use of ultrasound.
Citation: Pivetta E, Goffi A, Lupia E, et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: a SIMEU multicenter study. Chest. 2015;148(1):202-210.
Clinical question: Is lung ultrasound a useful tool for helping to diagnose acute decompensated heart failure (ADHF)?
Background: Lung ultrasound is an emerging bedside tool that has been promoted to help evaluate lung water content to help clinicians differentiate ADHF from other causes of dyspnea.
Study design: Prospective, multicenter, observational cohort study.
Setting: Seven EDs in Italy.
Synopsis: A total of 1,005 patients were enrolled in the study. Upon presentation to the ED, patients received a standard workup, including history, physical examination, EKG, and arterial blood gas sampling. Physicians were asked to render a diagnosis of ADHF or noncardiogenic dyspnea. The same physician then performed a lung ultrasound and rendered a revised diagnosis based on the ultrasound findings. A second ED physician and cardiologist, blinded to the ultrasound results, reviewed the medical record and rendered a final diagnosis as to the cause of the patient’s dyspnea.
The ultrasound approach had a higher accuracy than clinical evaluation alone in differentiating ADHF from noncardiac causes of dyspnea (97% vs. 85.3%). The authors also report a higher sensitivity compared to chest X-ray alone (69.5%) and natriuretic peptide testing (85%).
Bottom line: Lung ultrasound combined with clinical evaluation may improve the accuracy of ADHF diagnosis, but its usefulness may be limited by the need for ED physicians to have some degree of expertise in the use of ultrasound.
Citation: Pivetta E, Goffi A, Lupia E, et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: a SIMEU multicenter study. Chest. 2015;148(1):202-210.
Clinical question: Is lung ultrasound a useful tool for helping to diagnose acute decompensated heart failure (ADHF)?
Background: Lung ultrasound is an emerging bedside tool that has been promoted to help evaluate lung water content to help clinicians differentiate ADHF from other causes of dyspnea.
Study design: Prospective, multicenter, observational cohort study.
Setting: Seven EDs in Italy.
Synopsis: A total of 1,005 patients were enrolled in the study. Upon presentation to the ED, patients received a standard workup, including history, physical examination, EKG, and arterial blood gas sampling. Physicians were asked to render a diagnosis of ADHF or noncardiogenic dyspnea. The same physician then performed a lung ultrasound and rendered a revised diagnosis based on the ultrasound findings. A second ED physician and cardiologist, blinded to the ultrasound results, reviewed the medical record and rendered a final diagnosis as to the cause of the patient’s dyspnea.
The ultrasound approach had a higher accuracy than clinical evaluation alone in differentiating ADHF from noncardiac causes of dyspnea (97% vs. 85.3%). The authors also report a higher sensitivity compared to chest X-ray alone (69.5%) and natriuretic peptide testing (85%).
Bottom line: Lung ultrasound combined with clinical evaluation may improve the accuracy of ADHF diagnosis, but its usefulness may be limited by the need for ED physicians to have some degree of expertise in the use of ultrasound.
Citation: Pivetta E, Goffi A, Lupia E, et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: a SIMEU multicenter study. Chest. 2015;148(1):202-210.
Coronary CT Angiography, Perfusion Imaging Effective for Evaluating Patients With Chest Pain
Clinical question: When evaluating the intermediate-risk patient with chest pain, should coronary computed tomography angiography (CCTA) be used instead of myocardial perfusion imaging (MPI)?
Background: CCTA has been shown in prior randomized controlled trials to save time and money compared to other protocols, including stress ECG, echocardiogram, and MPI. Less information is available as to whether CCTA provides a better selection of patients for cardiac catheterization compared to MPI.
Study design: Randomized, controlled, comparative effectiveness trial.
Setting: Telemetry ward of an urban medical center.
Synopsis: Four hundred patients admitted with chest pain and an intermediate, pre-test probability of coronary artery disease were randomized to either CCTA or MPI. Patients were predominantly female, were ethnically varied, and had a mean age of 57 years.
Study results showed no significant difference in rates of cardiac catheterization that did not lead to revascularization at one-year follow-up. Specifically, 7.5% of patients in the CCTA group underwent catheterization not leading to revascularization, compared to 10% in the MPI group.
One limitation of the study is that it was conducted at a single site. Furthermore, the decision to proceed to catheterization was made clinically and not based on a predefined algorithm.
Bottom line: CCTA and MPI are both acceptable choices to determine the need for invasive testing in patients admitted with chest pain.
Citation: Levsky JM, Spevack DM, Travin MI, et al. Coronary computed tomography angiography versus radionuclide myocardial perfusion imaging in patients with chest pain admitted to telemetry: a randomized trial. Ann Intern Med. 2015;163(3):174-183.
Clinical question: When evaluating the intermediate-risk patient with chest pain, should coronary computed tomography angiography (CCTA) be used instead of myocardial perfusion imaging (MPI)?
Background: CCTA has been shown in prior randomized controlled trials to save time and money compared to other protocols, including stress ECG, echocardiogram, and MPI. Less information is available as to whether CCTA provides a better selection of patients for cardiac catheterization compared to MPI.
Study design: Randomized, controlled, comparative effectiveness trial.
Setting: Telemetry ward of an urban medical center.
Synopsis: Four hundred patients admitted with chest pain and an intermediate, pre-test probability of coronary artery disease were randomized to either CCTA or MPI. Patients were predominantly female, were ethnically varied, and had a mean age of 57 years.
Study results showed no significant difference in rates of cardiac catheterization that did not lead to revascularization at one-year follow-up. Specifically, 7.5% of patients in the CCTA group underwent catheterization not leading to revascularization, compared to 10% in the MPI group.
One limitation of the study is that it was conducted at a single site. Furthermore, the decision to proceed to catheterization was made clinically and not based on a predefined algorithm.
Bottom line: CCTA and MPI are both acceptable choices to determine the need for invasive testing in patients admitted with chest pain.
Citation: Levsky JM, Spevack DM, Travin MI, et al. Coronary computed tomography angiography versus radionuclide myocardial perfusion imaging in patients with chest pain admitted to telemetry: a randomized trial. Ann Intern Med. 2015;163(3):174-183.
Clinical question: When evaluating the intermediate-risk patient with chest pain, should coronary computed tomography angiography (CCTA) be used instead of myocardial perfusion imaging (MPI)?
Background: CCTA has been shown in prior randomized controlled trials to save time and money compared to other protocols, including stress ECG, echocardiogram, and MPI. Less information is available as to whether CCTA provides a better selection of patients for cardiac catheterization compared to MPI.
Study design: Randomized, controlled, comparative effectiveness trial.
Setting: Telemetry ward of an urban medical center.
Synopsis: Four hundred patients admitted with chest pain and an intermediate, pre-test probability of coronary artery disease were randomized to either CCTA or MPI. Patients were predominantly female, were ethnically varied, and had a mean age of 57 years.
Study results showed no significant difference in rates of cardiac catheterization that did not lead to revascularization at one-year follow-up. Specifically, 7.5% of patients in the CCTA group underwent catheterization not leading to revascularization, compared to 10% in the MPI group.
One limitation of the study is that it was conducted at a single site. Furthermore, the decision to proceed to catheterization was made clinically and not based on a predefined algorithm.
Bottom line: CCTA and MPI are both acceptable choices to determine the need for invasive testing in patients admitted with chest pain.
Citation: Levsky JM, Spevack DM, Travin MI, et al. Coronary computed tomography angiography versus radionuclide myocardial perfusion imaging in patients with chest pain admitted to telemetry: a randomized trial. Ann Intern Med. 2015;163(3):174-183.
Can Low-Risk Patients with VTE Be Discharged from ED on Rivaroxabon?
Clinical question: Can a low-risk patient newly diagnosed with VTE in the ED be immediately discharged home on a direct factor Xa inhibitor?
Background: Studies have shown that rivaroxaban incurs a risk of 2.1% in VTE recurrence and of 9.4% in clinically relevant major and non-major bleeding (in an average 208 days follow-up). More information is required to determine if similar success can be achieved by discharging low-risk patients from the ED.
Study design: Prospective, observational study.
Setting: EDs at two urban, teaching hospitals.
Synopsis: After fulfilling the criteria for low risk, 106 patients were discharged from the ED with DVT, pulmonary embolism (PE), or both. Most patients were 50 years or younger and had unprovoked VTE. Three of the 106 patients had recurrence of VTE (2.8%, 95% CI=0.6% to 8%) at a mean duration of 389 days. No patient had a major bleeding event.
In this small study, fewer than 80% of patients discharged had at least one clinic follow-up; the majority of these patients (75%) followed up in a clinic staffed by ED physicians. Therefore, ability for close follow-up must be taken into consideration prior to discharge from the ED.
Moreover, one to two days post-discharge, a member of the care team called the patient to confirm their ability to fill the rivaroxaban prescription and to answer other questions related to the new diagnosis.
Bottom line: With close follow-up and confirmation of the ability to fill a rivaroxaban prescription, patients with low-risk VTE may be discharged home from the ED.
Citation: Beam DM, Kahler ZP, Kline JA. Immediate discharge and home treatment with rivaroxaban of low-risk venous thromboembolism diagnosed in two U.S. emergency departments: a one-year preplanned analysis. Acad Emerg Med. 2015;22(7):788-795.
Clinical question: Can a low-risk patient newly diagnosed with VTE in the ED be immediately discharged home on a direct factor Xa inhibitor?
Background: Studies have shown that rivaroxaban incurs a risk of 2.1% in VTE recurrence and of 9.4% in clinically relevant major and non-major bleeding (in an average 208 days follow-up). More information is required to determine if similar success can be achieved by discharging low-risk patients from the ED.
Study design: Prospective, observational study.
Setting: EDs at two urban, teaching hospitals.
Synopsis: After fulfilling the criteria for low risk, 106 patients were discharged from the ED with DVT, pulmonary embolism (PE), or both. Most patients were 50 years or younger and had unprovoked VTE. Three of the 106 patients had recurrence of VTE (2.8%, 95% CI=0.6% to 8%) at a mean duration of 389 days. No patient had a major bleeding event.
In this small study, fewer than 80% of patients discharged had at least one clinic follow-up; the majority of these patients (75%) followed up in a clinic staffed by ED physicians. Therefore, ability for close follow-up must be taken into consideration prior to discharge from the ED.
Moreover, one to two days post-discharge, a member of the care team called the patient to confirm their ability to fill the rivaroxaban prescription and to answer other questions related to the new diagnosis.
Bottom line: With close follow-up and confirmation of the ability to fill a rivaroxaban prescription, patients with low-risk VTE may be discharged home from the ED.
Citation: Beam DM, Kahler ZP, Kline JA. Immediate discharge and home treatment with rivaroxaban of low-risk venous thromboembolism diagnosed in two U.S. emergency departments: a one-year preplanned analysis. Acad Emerg Med. 2015;22(7):788-795.
Clinical question: Can a low-risk patient newly diagnosed with VTE in the ED be immediately discharged home on a direct factor Xa inhibitor?
Background: Studies have shown that rivaroxaban incurs a risk of 2.1% in VTE recurrence and of 9.4% in clinically relevant major and non-major bleeding (in an average 208 days follow-up). More information is required to determine if similar success can be achieved by discharging low-risk patients from the ED.
Study design: Prospective, observational study.
Setting: EDs at two urban, teaching hospitals.
Synopsis: After fulfilling the criteria for low risk, 106 patients were discharged from the ED with DVT, pulmonary embolism (PE), or both. Most patients were 50 years or younger and had unprovoked VTE. Three of the 106 patients had recurrence of VTE (2.8%, 95% CI=0.6% to 8%) at a mean duration of 389 days. No patient had a major bleeding event.
In this small study, fewer than 80% of patients discharged had at least one clinic follow-up; the majority of these patients (75%) followed up in a clinic staffed by ED physicians. Therefore, ability for close follow-up must be taken into consideration prior to discharge from the ED.
Moreover, one to two days post-discharge, a member of the care team called the patient to confirm their ability to fill the rivaroxaban prescription and to answer other questions related to the new diagnosis.
Bottom line: With close follow-up and confirmation of the ability to fill a rivaroxaban prescription, patients with low-risk VTE may be discharged home from the ED.
Citation: Beam DM, Kahler ZP, Kline JA. Immediate discharge and home treatment with rivaroxaban of low-risk venous thromboembolism diagnosed in two U.S. emergency departments: a one-year preplanned analysis. Acad Emerg Med. 2015;22(7):788-795.
Clinical Care Pathway for Cellulitis Can Help Reduce Antibiotic Use, Cost
Clinical question: How would an evidence-based clinical pathway for cellulitis affect process metrics, patient outcomes, and clinical cost?
Background: Cellulitis is a common hospital problem, but its evaluation and treatment vary widely. Specifically, broad-spectrum antibiotics and imaging studies are overutilized when compared to recommended guidelines. A standardized clinical pathway is proposed as a possible solution.
Study design: Retrospective, observational, pre-/post-intervention study.
Setting: University of Utah Health Sciences Center, Salt Lake City.
Synopsis: A multidisciplinary team created a guideline-based care pathway for cellulitis and enrolled 677 adult patients for retrospective analysis during a two-year period. The study showed an overall 59% decrease in the odds of ordering broad-spectrum antibiotics, 23% decrease in pharmacy cost, 44% decrease in laboratory cost, and 13% decrease in overall facility cost, pre-/post-intervention. It also demonstrated no adverse effect on length of stay or 30-day readmission rates.
Given the retrospective, single-center nature of this study, as well as some baseline characteristic differences between enrolled patients, careful conclusions regarding external validity on diverse patient populations must be considered; however, the history of clinical care pathways supports many of the study’s findings. The results make a compelling case for hospitalist groups to implement similar cellulitis pathways and research their effectiveness.
Bottom line: Clinical care pathways for cellulitis provide an opportunity to improve antibiotic stewardship and lower hospital costs without compromising quality of care.
Citation: Yarbrough PM, Kukhareva PV, Spivak ES, Hopkins C, Kawamoto K. Evidence-based care pathway for cellulitis improves process, clinical, and cost outcomes [published online ahead of print July 28, 2015]. J Hosp Med. doi: 10.1002/jhm.2433.
Clinical question: How would an evidence-based clinical pathway for cellulitis affect process metrics, patient outcomes, and clinical cost?
Background: Cellulitis is a common hospital problem, but its evaluation and treatment vary widely. Specifically, broad-spectrum antibiotics and imaging studies are overutilized when compared to recommended guidelines. A standardized clinical pathway is proposed as a possible solution.
Study design: Retrospective, observational, pre-/post-intervention study.
Setting: University of Utah Health Sciences Center, Salt Lake City.
Synopsis: A multidisciplinary team created a guideline-based care pathway for cellulitis and enrolled 677 adult patients for retrospective analysis during a two-year period. The study showed an overall 59% decrease in the odds of ordering broad-spectrum antibiotics, 23% decrease in pharmacy cost, 44% decrease in laboratory cost, and 13% decrease in overall facility cost, pre-/post-intervention. It also demonstrated no adverse effect on length of stay or 30-day readmission rates.
Given the retrospective, single-center nature of this study, as well as some baseline characteristic differences between enrolled patients, careful conclusions regarding external validity on diverse patient populations must be considered; however, the history of clinical care pathways supports many of the study’s findings. The results make a compelling case for hospitalist groups to implement similar cellulitis pathways and research their effectiveness.
Bottom line: Clinical care pathways for cellulitis provide an opportunity to improve antibiotic stewardship and lower hospital costs without compromising quality of care.
Citation: Yarbrough PM, Kukhareva PV, Spivak ES, Hopkins C, Kawamoto K. Evidence-based care pathway for cellulitis improves process, clinical, and cost outcomes [published online ahead of print July 28, 2015]. J Hosp Med. doi: 10.1002/jhm.2433.
Clinical question: How would an evidence-based clinical pathway for cellulitis affect process metrics, patient outcomes, and clinical cost?
Background: Cellulitis is a common hospital problem, but its evaluation and treatment vary widely. Specifically, broad-spectrum antibiotics and imaging studies are overutilized when compared to recommended guidelines. A standardized clinical pathway is proposed as a possible solution.
Study design: Retrospective, observational, pre-/post-intervention study.
Setting: University of Utah Health Sciences Center, Salt Lake City.
Synopsis: A multidisciplinary team created a guideline-based care pathway for cellulitis and enrolled 677 adult patients for retrospective analysis during a two-year period. The study showed an overall 59% decrease in the odds of ordering broad-spectrum antibiotics, 23% decrease in pharmacy cost, 44% decrease in laboratory cost, and 13% decrease in overall facility cost, pre-/post-intervention. It also demonstrated no adverse effect on length of stay or 30-day readmission rates.
Given the retrospective, single-center nature of this study, as well as some baseline characteristic differences between enrolled patients, careful conclusions regarding external validity on diverse patient populations must be considered; however, the history of clinical care pathways supports many of the study’s findings. The results make a compelling case for hospitalist groups to implement similar cellulitis pathways and research their effectiveness.
Bottom line: Clinical care pathways for cellulitis provide an opportunity to improve antibiotic stewardship and lower hospital costs without compromising quality of care.
Citation: Yarbrough PM, Kukhareva PV, Spivak ES, Hopkins C, Kawamoto K. Evidence-based care pathway for cellulitis improves process, clinical, and cost outcomes [published online ahead of print July 28, 2015]. J Hosp Med. doi: 10.1002/jhm.2433.
Practice Administrator Elected Vice President of SHM Maryland Chapter
When you ask Tiffani Panek, division administrator for the division of hospital medicine at Johns Hopkins Bayview Medical Center (BMC) in Baltimore, Md., about her thoughts on the future of hospital medicine, her passion and enthusiasm are immediately apparent. After earning SHM’s Certificate of Leadership in Hospital Medicine, Panek was elected vice president of SHM’s Maryland chapter. She is the only practice administrator currently in chapter leadership.
Her motto? “I’m a hospitalist who happens not to be a clinician.”
The Hospitalist recently spoke with Panek about the future of the HM movement and the roles nonphysician staff play in advancing hospital medicine.
Question: Tell us about your role as division administrator for BMC’s division of hospital medicine.
Answer: As part of the executive leadership team, I serve as the administrative counterpart to site director Flora Kisuule, MD, MPH. I am also the program coordinator for the Academic Hospitalist Fellowship Program and partner with Dr. Kisuule and SHM board member and senior physician advisor Eric Howell, MD, SFHM, on the program’s growing international work to train academic hospitalists and future leaders of hospitalist programs.
Q: What led you to join SHM and get involved in the Practice Administrators Committee?
A: I had never heard of hospital medicine before I started with [my] division, and I really wanted to learn all I could. I was fortunate enough that Dr. Howell was a part of SHM very early, and as my director, he encouraged me to get involved. In the beginning, it was really about educating myself, but after a few years, when I was immersed and truly in love with hospital medicine, I wanted to get more involved and be a part of the change and innovation that SHM and hospital medicine represent. The movement touches so many people in such a direct way. We are in the trenches, taking care of people when they are at their most vulnerable.

Q: How were you able to take what you learned from SHM Leadership Academy and apply it to your professional life and new chapter leader position?
A: I should make a cross-stitch of one of my favorite takeaways: “They won’t care what you know until they know that you care!” The personality and communication lessons have not only helped me develop my own communication skills, but they have helped me become a better supervisor and mentor. I often return to my notes about leading through adversity when faced with challenges at our own facility. I want to bring all of that to the table as the new Maryland chapter vice president, to help us improve the diversity of the chapter and ultimately the hospital medicine movement.
Q: Moving forward, how do you see your role in SHM—and SHM as an organization— impacting positive change for hospitalized patients and the hospitalists who serve them?
A: As an active member, I am excited to leverage SHM, the Practice Administrators Committee, the local chapter, and other meetings to unite talented people working in hospital medicine and work towards the same mission: improving care of hospitalized patients. In addition to bringing our subspecialty colleagues into the fold, we also must improve our inclusivity of nurse practitioners, physician assistants, pharmacists, nurses, and, of course, our administrators. Every single person should feel invested and valued. The diversity of hospital medicine, and of SHM, sets our specialty apart from many others, and we are much stronger for it. There are no healthcare professionals better situated to improve the quality and cost of care than hospitalists.
Brett Radler is SHM’s communications coordinator.
When you ask Tiffani Panek, division administrator for the division of hospital medicine at Johns Hopkins Bayview Medical Center (BMC) in Baltimore, Md., about her thoughts on the future of hospital medicine, her passion and enthusiasm are immediately apparent. After earning SHM’s Certificate of Leadership in Hospital Medicine, Panek was elected vice president of SHM’s Maryland chapter. She is the only practice administrator currently in chapter leadership.
Her motto? “I’m a hospitalist who happens not to be a clinician.”
The Hospitalist recently spoke with Panek about the future of the HM movement and the roles nonphysician staff play in advancing hospital medicine.
Question: Tell us about your role as division administrator for BMC’s division of hospital medicine.
Answer: As part of the executive leadership team, I serve as the administrative counterpart to site director Flora Kisuule, MD, MPH. I am also the program coordinator for the Academic Hospitalist Fellowship Program and partner with Dr. Kisuule and SHM board member and senior physician advisor Eric Howell, MD, SFHM, on the program’s growing international work to train academic hospitalists and future leaders of hospitalist programs.
Q: What led you to join SHM and get involved in the Practice Administrators Committee?
A: I had never heard of hospital medicine before I started with [my] division, and I really wanted to learn all I could. I was fortunate enough that Dr. Howell was a part of SHM very early, and as my director, he encouraged me to get involved. In the beginning, it was really about educating myself, but after a few years, when I was immersed and truly in love with hospital medicine, I wanted to get more involved and be a part of the change and innovation that SHM and hospital medicine represent. The movement touches so many people in such a direct way. We are in the trenches, taking care of people when they are at their most vulnerable.

Q: How were you able to take what you learned from SHM Leadership Academy and apply it to your professional life and new chapter leader position?
A: I should make a cross-stitch of one of my favorite takeaways: “They won’t care what you know until they know that you care!” The personality and communication lessons have not only helped me develop my own communication skills, but they have helped me become a better supervisor and mentor. I often return to my notes about leading through adversity when faced with challenges at our own facility. I want to bring all of that to the table as the new Maryland chapter vice president, to help us improve the diversity of the chapter and ultimately the hospital medicine movement.
Q: Moving forward, how do you see your role in SHM—and SHM as an organization— impacting positive change for hospitalized patients and the hospitalists who serve them?
A: As an active member, I am excited to leverage SHM, the Practice Administrators Committee, the local chapter, and other meetings to unite talented people working in hospital medicine and work towards the same mission: improving care of hospitalized patients. In addition to bringing our subspecialty colleagues into the fold, we also must improve our inclusivity of nurse practitioners, physician assistants, pharmacists, nurses, and, of course, our administrators. Every single person should feel invested and valued. The diversity of hospital medicine, and of SHM, sets our specialty apart from many others, and we are much stronger for it. There are no healthcare professionals better situated to improve the quality and cost of care than hospitalists.
Brett Radler is SHM’s communications coordinator.
When you ask Tiffani Panek, division administrator for the division of hospital medicine at Johns Hopkins Bayview Medical Center (BMC) in Baltimore, Md., about her thoughts on the future of hospital medicine, her passion and enthusiasm are immediately apparent. After earning SHM’s Certificate of Leadership in Hospital Medicine, Panek was elected vice president of SHM’s Maryland chapter. She is the only practice administrator currently in chapter leadership.
Her motto? “I’m a hospitalist who happens not to be a clinician.”
The Hospitalist recently spoke with Panek about the future of the HM movement and the roles nonphysician staff play in advancing hospital medicine.
Question: Tell us about your role as division administrator for BMC’s division of hospital medicine.
Answer: As part of the executive leadership team, I serve as the administrative counterpart to site director Flora Kisuule, MD, MPH. I am also the program coordinator for the Academic Hospitalist Fellowship Program and partner with Dr. Kisuule and SHM board member and senior physician advisor Eric Howell, MD, SFHM, on the program’s growing international work to train academic hospitalists and future leaders of hospitalist programs.
Q: What led you to join SHM and get involved in the Practice Administrators Committee?
A: I had never heard of hospital medicine before I started with [my] division, and I really wanted to learn all I could. I was fortunate enough that Dr. Howell was a part of SHM very early, and as my director, he encouraged me to get involved. In the beginning, it was really about educating myself, but after a few years, when I was immersed and truly in love with hospital medicine, I wanted to get more involved and be a part of the change and innovation that SHM and hospital medicine represent. The movement touches so many people in such a direct way. We are in the trenches, taking care of people when they are at their most vulnerable.

Q: How were you able to take what you learned from SHM Leadership Academy and apply it to your professional life and new chapter leader position?
A: I should make a cross-stitch of one of my favorite takeaways: “They won’t care what you know until they know that you care!” The personality and communication lessons have not only helped me develop my own communication skills, but they have helped me become a better supervisor and mentor. I often return to my notes about leading through adversity when faced with challenges at our own facility. I want to bring all of that to the table as the new Maryland chapter vice president, to help us improve the diversity of the chapter and ultimately the hospital medicine movement.
Q: Moving forward, how do you see your role in SHM—and SHM as an organization— impacting positive change for hospitalized patients and the hospitalists who serve them?
A: As an active member, I am excited to leverage SHM, the Practice Administrators Committee, the local chapter, and other meetings to unite talented people working in hospital medicine and work towards the same mission: improving care of hospitalized patients. In addition to bringing our subspecialty colleagues into the fold, we also must improve our inclusivity of nurse practitioners, physician assistants, pharmacists, nurses, and, of course, our administrators. Every single person should feel invested and valued. The diversity of hospital medicine, and of SHM, sets our specialty apart from many others, and we are much stronger for it. There are no healthcare professionals better situated to improve the quality and cost of care than hospitalists.
Brett Radler is SHM’s communications coordinator.
Revolutionizing Quality Improvement in Hospital Medicine
As the senior physician advisor to SHM’s Center for Hospital Innovation and Improvement, Eric Howell, MD, SFHM, bridges the gap between clinical expertise and project support and development. The Hospitalist recently had a conversation with Dr. Howell, a past president of SHM, to learn more about his role and how the Center for Hospital Innovation and Improvement is revolutionizing quality improvement (QI) in hospital medicine.
Question: What is your role as the senior physician advisor to The Center for Hospital Innovation and Improvement?
Answer: I see my role as the intersection of a Venn diagram; one circle involves my clinical know-how, and the other includes the proposals brought to the Center for Hospital Innovation and Improvement by hospitalists and healthcare professionals. Where those two circles intersect is where I am able to use my experience from the front line of patient care to validate potential projects.
In addition to project assessment, I monitor the pulse of healthcare professionals and hospital leadership to ensure we are meeting their needs, including our efforts of convening a recent summit, where hospitalist clinicians … weighed in on how our team could help them improve. I plan to share this feedback in an upcoming feature, centered on emerging topics in hospital medicine, including care transitions, high-risk medications, advance care planning, and others.
Q: Given your clinical experience and involvement with SHM, how would you say hospitalists are positioned to improve quality, safety, and patient outcomes?

appropriate prescribing practices, which will aid in slowing the emergence of antibiotic-resistant bacteria and prevent the spread of resistant infections.
—Dr. Howell
A: We possess the necessary ingredients to develop a recipe for success in QI from both a clinical and an operational perspective. Hospital medicine is still a young, innovative field that is extremely open to change. Anyone who knows QI knows that it is all about effectively managing and responding to change. Hospitalists also are aware of how to operate in a highly matrixed environment and to collaborate as part of an interdisciplinary team, which are invaluable assets to implementing QI initiatives successfully and proactively monitoring their impact.
Q: What are the biggest assets the Center for Hospital Innovation and Improvement can offer hospitalists in their mission to improve patient care?
A: Our team has resources to help hospitalists improve their skills at whatever stage they are in their careers. If you are just beginning or trying to learn new things independently, you can explore the web-based materials and resource rooms. They are publicly accessible resources that can assist in informing quality improvement efforts in the hospital. For those looking to expand their skills in a more hands-on way, we offer a mentored implementation program, where hospitalists can receive guidance from expert mentors in a number of different clinical areas.
Q: How can the Center for Hospital Innovation and Improvement help hospitalists address emerging challenges in hospital medicine?
A: You cannot talk about the Center for Hospital Innovation and Improvement without mentioning signature mentored implementation programs like Project BOOST, focused on effective care transitions, and glycemic control—they are juggernauts for SHM’s portfolio because of their proven track records and sustainable frameworks for driving positive change. These two alone have already been implemented at over 400 facilities, with more inquiries each day.
With support from The Milbank Foundation, The Hastings Center and SHM have joined forces and will create new skills-based training resources and a QI framework to improve end-of-life care in the hospital. Our goal is to equip hospital clinicians with the requisite tools to provide adequate palliative care, especially given the policy landscape related to advance care planning discussions.
As antibiotic resistance emerges as a global issue, antibiotic stewardship has continued to be a high priority for hospitalists. After attending the related White House forum earlier this year, SHM committed to cultivating initiatives that emphasize appropriate prescribing practices, which will aid in slowing the emergence of antibiotic-resistant bacteria and prevent the spread of resistant infections. SHM looks forward to making noteworthy contributions to this initiative, promoting awareness and behavior change through the “Fight the Resistance” campaign.
Q: What is one major takeaway about The Center for Hospital Innovation and Improvement hospitalists should know?
A: The Center for Hospital Innovation and Improvement is not an exclusive club—rather, it is like an open farmers’ market. Anyone with any amount of expertise can get resources through collaboration and partnership. Whether it is residents trying to improve the house staff or professors at major academic centers looking for research partners, The Center for Hospital Innovation and Improvement will welcome you to collaborate and link you to valuable resources.
Brett Radler is SHM’s communications coordinator.
As the senior physician advisor to SHM’s Center for Hospital Innovation and Improvement, Eric Howell, MD, SFHM, bridges the gap between clinical expertise and project support and development. The Hospitalist recently had a conversation with Dr. Howell, a past president of SHM, to learn more about his role and how the Center for Hospital Innovation and Improvement is revolutionizing quality improvement (QI) in hospital medicine.
Question: What is your role as the senior physician advisor to The Center for Hospital Innovation and Improvement?
Answer: I see my role as the intersection of a Venn diagram; one circle involves my clinical know-how, and the other includes the proposals brought to the Center for Hospital Innovation and Improvement by hospitalists and healthcare professionals. Where those two circles intersect is where I am able to use my experience from the front line of patient care to validate potential projects.
In addition to project assessment, I monitor the pulse of healthcare professionals and hospital leadership to ensure we are meeting their needs, including our efforts of convening a recent summit, where hospitalist clinicians … weighed in on how our team could help them improve. I plan to share this feedback in an upcoming feature, centered on emerging topics in hospital medicine, including care transitions, high-risk medications, advance care planning, and others.
Q: Given your clinical experience and involvement with SHM, how would you say hospitalists are positioned to improve quality, safety, and patient outcomes?

appropriate prescribing practices, which will aid in slowing the emergence of antibiotic-resistant bacteria and prevent the spread of resistant infections.
—Dr. Howell
A: We possess the necessary ingredients to develop a recipe for success in QI from both a clinical and an operational perspective. Hospital medicine is still a young, innovative field that is extremely open to change. Anyone who knows QI knows that it is all about effectively managing and responding to change. Hospitalists also are aware of how to operate in a highly matrixed environment and to collaborate as part of an interdisciplinary team, which are invaluable assets to implementing QI initiatives successfully and proactively monitoring their impact.
Q: What are the biggest assets the Center for Hospital Innovation and Improvement can offer hospitalists in their mission to improve patient care?
A: Our team has resources to help hospitalists improve their skills at whatever stage they are in their careers. If you are just beginning or trying to learn new things independently, you can explore the web-based materials and resource rooms. They are publicly accessible resources that can assist in informing quality improvement efforts in the hospital. For those looking to expand their skills in a more hands-on way, we offer a mentored implementation program, where hospitalists can receive guidance from expert mentors in a number of different clinical areas.
Q: How can the Center for Hospital Innovation and Improvement help hospitalists address emerging challenges in hospital medicine?
A: You cannot talk about the Center for Hospital Innovation and Improvement without mentioning signature mentored implementation programs like Project BOOST, focused on effective care transitions, and glycemic control—they are juggernauts for SHM’s portfolio because of their proven track records and sustainable frameworks for driving positive change. These two alone have already been implemented at over 400 facilities, with more inquiries each day.
With support from The Milbank Foundation, The Hastings Center and SHM have joined forces and will create new skills-based training resources and a QI framework to improve end-of-life care in the hospital. Our goal is to equip hospital clinicians with the requisite tools to provide adequate palliative care, especially given the policy landscape related to advance care planning discussions.
As antibiotic resistance emerges as a global issue, antibiotic stewardship has continued to be a high priority for hospitalists. After attending the related White House forum earlier this year, SHM committed to cultivating initiatives that emphasize appropriate prescribing practices, which will aid in slowing the emergence of antibiotic-resistant bacteria and prevent the spread of resistant infections. SHM looks forward to making noteworthy contributions to this initiative, promoting awareness and behavior change through the “Fight the Resistance” campaign.
Q: What is one major takeaway about The Center for Hospital Innovation and Improvement hospitalists should know?
A: The Center for Hospital Innovation and Improvement is not an exclusive club—rather, it is like an open farmers’ market. Anyone with any amount of expertise can get resources through collaboration and partnership. Whether it is residents trying to improve the house staff or professors at major academic centers looking for research partners, The Center for Hospital Innovation and Improvement will welcome you to collaborate and link you to valuable resources.
Brett Radler is SHM’s communications coordinator.
As the senior physician advisor to SHM’s Center for Hospital Innovation and Improvement, Eric Howell, MD, SFHM, bridges the gap between clinical expertise and project support and development. The Hospitalist recently had a conversation with Dr. Howell, a past president of SHM, to learn more about his role and how the Center for Hospital Innovation and Improvement is revolutionizing quality improvement (QI) in hospital medicine.
Question: What is your role as the senior physician advisor to The Center for Hospital Innovation and Improvement?
Answer: I see my role as the intersection of a Venn diagram; one circle involves my clinical know-how, and the other includes the proposals brought to the Center for Hospital Innovation and Improvement by hospitalists and healthcare professionals. Where those two circles intersect is where I am able to use my experience from the front line of patient care to validate potential projects.
In addition to project assessment, I monitor the pulse of healthcare professionals and hospital leadership to ensure we are meeting their needs, including our efforts of convening a recent summit, where hospitalist clinicians … weighed in on how our team could help them improve. I plan to share this feedback in an upcoming feature, centered on emerging topics in hospital medicine, including care transitions, high-risk medications, advance care planning, and others.
Q: Given your clinical experience and involvement with SHM, how would you say hospitalists are positioned to improve quality, safety, and patient outcomes?

appropriate prescribing practices, which will aid in slowing the emergence of antibiotic-resistant bacteria and prevent the spread of resistant infections.
—Dr. Howell
A: We possess the necessary ingredients to develop a recipe for success in QI from both a clinical and an operational perspective. Hospital medicine is still a young, innovative field that is extremely open to change. Anyone who knows QI knows that it is all about effectively managing and responding to change. Hospitalists also are aware of how to operate in a highly matrixed environment and to collaborate as part of an interdisciplinary team, which are invaluable assets to implementing QI initiatives successfully and proactively monitoring their impact.
Q: What are the biggest assets the Center for Hospital Innovation and Improvement can offer hospitalists in their mission to improve patient care?
A: Our team has resources to help hospitalists improve their skills at whatever stage they are in their careers. If you are just beginning or trying to learn new things independently, you can explore the web-based materials and resource rooms. They are publicly accessible resources that can assist in informing quality improvement efforts in the hospital. For those looking to expand their skills in a more hands-on way, we offer a mentored implementation program, where hospitalists can receive guidance from expert mentors in a number of different clinical areas.
Q: How can the Center for Hospital Innovation and Improvement help hospitalists address emerging challenges in hospital medicine?
A: You cannot talk about the Center for Hospital Innovation and Improvement without mentioning signature mentored implementation programs like Project BOOST, focused on effective care transitions, and glycemic control—they are juggernauts for SHM’s portfolio because of their proven track records and sustainable frameworks for driving positive change. These two alone have already been implemented at over 400 facilities, with more inquiries each day.
With support from The Milbank Foundation, The Hastings Center and SHM have joined forces and will create new skills-based training resources and a QI framework to improve end-of-life care in the hospital. Our goal is to equip hospital clinicians with the requisite tools to provide adequate palliative care, especially given the policy landscape related to advance care planning discussions.
As antibiotic resistance emerges as a global issue, antibiotic stewardship has continued to be a high priority for hospitalists. After attending the related White House forum earlier this year, SHM committed to cultivating initiatives that emphasize appropriate prescribing practices, which will aid in slowing the emergence of antibiotic-resistant bacteria and prevent the spread of resistant infections. SHM looks forward to making noteworthy contributions to this initiative, promoting awareness and behavior change through the “Fight the Resistance” campaign.
Q: What is one major takeaway about The Center for Hospital Innovation and Improvement hospitalists should know?
A: The Center for Hospital Innovation and Improvement is not an exclusive club—rather, it is like an open farmers’ market. Anyone with any amount of expertise can get resources through collaboration and partnership. Whether it is residents trying to improve the house staff or professors at major academic centers looking for research partners, The Center for Hospital Innovation and Improvement will welcome you to collaborate and link you to valuable resources.
Brett Radler is SHM’s communications coordinator.