User login
CAR T-cells induce remissions, avoid GVHD in relapsed B-cell malignancies
In patients with B-cell malignancies who did not obtain remissions after allogeneic hematopoietic stem-cell transplantation (alloHSCT), infusion of anti-CD19 chimeric antigen receptor (CAR19) T-cells induced remissions without causing graft-versus-host disease (GVHD).
Of 20 patients treated, 6 obtained complete remission and 2 obtained partial remissions, while none of the patients experienced new-onset acute GVHD.
“The increased antimalignancy potency of CAR19 T-cells allowed small doses of T-cells to eradicate malignancy without causing GVHD; therefore, this work demonstrates a solution to the central problem of alloHSCT, the separation of [graft-versus-malignancy] from GVHD,” wrote Dr. Jennifer Brudno of the National Cancer Institute, Bethesda, Md., and colleagues (J Clin Onc. 2016 Jan. 25. doi: 10.1200/JCO.2015.64.5929).
In general, CAR19 T-cells did not persist longer than 4 weeks, the median time it takes for GVHD to develop after donor lymphocyte infusion, which may be a factor in avoiding GVHD. Smaller doses may be another contributing factor: CAR19 T-cell doses administered in the trial ranged from 106/kg to 107/kg, which is 10-fold smaller than typical donor lymphocyte infusions.
In contrast to previous CAR T-cell studies, patients did not receive chemotherapy before CAR19 T-cell infusion, so endogenous T-cells and natural killer cells were not depleted. Evidence indicates that lymphocyte depletion enhances antitumor activity of adoptively transferred T-cells, but the current results indicate that prior lymphocyte depletion is not an absolute requirement.
The CAR19 T-cell infusion was especially effective in acute lymphoblastic leukemia (ALL), with four of the five ALL patients obtaining complete remission. Patients with chronic lymphocyte leukemia and lymphoma also obtained remissions.
Toxicities observed were consistent with previous CAR T-cell studies and included fever, tachycardia, and hypotension, indicative of cytokine release syndrome.
Peak levels of CAR19 T-cells were significantly higher in patients with complete or partial responses, and patients who did not obtain a complete or partial response were more likely to have undetectable or very low levels. Increasing peak blood levels of CAR19 T-cells in vivo is an important goal for future research, according to investigators. Since endogenous CD19+ cells may promote proliferation of CAR19 T- cells, CD19+ cellular vaccines might enhance CAR19 T-cell proliferation in patients with low levels, they suggested.
Administration of programmed cell death protein-1 (PD-1) antagonists may also offer improvements. High levels of PD-1 expression on CAR19 T-cells were observed at the time of peak blood CAR19 T-cell levels.
Dr. Brudno reported having no disclosures. Dr. Goy and Dr. Rosenberg reported ties to industry, and Dr. Kochenderfer reported patents pending on CAR T-cell therapy.
In patients with B-cell malignancies who did not obtain remissions after allogeneic hematopoietic stem-cell transplantation (alloHSCT), infusion of anti-CD19 chimeric antigen receptor (CAR19) T-cells induced remissions without causing graft-versus-host disease (GVHD).
Of 20 patients treated, 6 obtained complete remission and 2 obtained partial remissions, while none of the patients experienced new-onset acute GVHD.
“The increased antimalignancy potency of CAR19 T-cells allowed small doses of T-cells to eradicate malignancy without causing GVHD; therefore, this work demonstrates a solution to the central problem of alloHSCT, the separation of [graft-versus-malignancy] from GVHD,” wrote Dr. Jennifer Brudno of the National Cancer Institute, Bethesda, Md., and colleagues (J Clin Onc. 2016 Jan. 25. doi: 10.1200/JCO.2015.64.5929).
In general, CAR19 T-cells did not persist longer than 4 weeks, the median time it takes for GVHD to develop after donor lymphocyte infusion, which may be a factor in avoiding GVHD. Smaller doses may be another contributing factor: CAR19 T-cell doses administered in the trial ranged from 106/kg to 107/kg, which is 10-fold smaller than typical donor lymphocyte infusions.
In contrast to previous CAR T-cell studies, patients did not receive chemotherapy before CAR19 T-cell infusion, so endogenous T-cells and natural killer cells were not depleted. Evidence indicates that lymphocyte depletion enhances antitumor activity of adoptively transferred T-cells, but the current results indicate that prior lymphocyte depletion is not an absolute requirement.
The CAR19 T-cell infusion was especially effective in acute lymphoblastic leukemia (ALL), with four of the five ALL patients obtaining complete remission. Patients with chronic lymphocyte leukemia and lymphoma also obtained remissions.
Toxicities observed were consistent with previous CAR T-cell studies and included fever, tachycardia, and hypotension, indicative of cytokine release syndrome.
Peak levels of CAR19 T-cells were significantly higher in patients with complete or partial responses, and patients who did not obtain a complete or partial response were more likely to have undetectable or very low levels. Increasing peak blood levels of CAR19 T-cells in vivo is an important goal for future research, according to investigators. Since endogenous CD19+ cells may promote proliferation of CAR19 T- cells, CD19+ cellular vaccines might enhance CAR19 T-cell proliferation in patients with low levels, they suggested.
Administration of programmed cell death protein-1 (PD-1) antagonists may also offer improvements. High levels of PD-1 expression on CAR19 T-cells were observed at the time of peak blood CAR19 T-cell levels.
Dr. Brudno reported having no disclosures. Dr. Goy and Dr. Rosenberg reported ties to industry, and Dr. Kochenderfer reported patents pending on CAR T-cell therapy.
In patients with B-cell malignancies who did not obtain remissions after allogeneic hematopoietic stem-cell transplantation (alloHSCT), infusion of anti-CD19 chimeric antigen receptor (CAR19) T-cells induced remissions without causing graft-versus-host disease (GVHD).
Of 20 patients treated, 6 obtained complete remission and 2 obtained partial remissions, while none of the patients experienced new-onset acute GVHD.
“The increased antimalignancy potency of CAR19 T-cells allowed small doses of T-cells to eradicate malignancy without causing GVHD; therefore, this work demonstrates a solution to the central problem of alloHSCT, the separation of [graft-versus-malignancy] from GVHD,” wrote Dr. Jennifer Brudno of the National Cancer Institute, Bethesda, Md., and colleagues (J Clin Onc. 2016 Jan. 25. doi: 10.1200/JCO.2015.64.5929).
In general, CAR19 T-cells did not persist longer than 4 weeks, the median time it takes for GVHD to develop after donor lymphocyte infusion, which may be a factor in avoiding GVHD. Smaller doses may be another contributing factor: CAR19 T-cell doses administered in the trial ranged from 106/kg to 107/kg, which is 10-fold smaller than typical donor lymphocyte infusions.
In contrast to previous CAR T-cell studies, patients did not receive chemotherapy before CAR19 T-cell infusion, so endogenous T-cells and natural killer cells were not depleted. Evidence indicates that lymphocyte depletion enhances antitumor activity of adoptively transferred T-cells, but the current results indicate that prior lymphocyte depletion is not an absolute requirement.
The CAR19 T-cell infusion was especially effective in acute lymphoblastic leukemia (ALL), with four of the five ALL patients obtaining complete remission. Patients with chronic lymphocyte leukemia and lymphoma also obtained remissions.
Toxicities observed were consistent with previous CAR T-cell studies and included fever, tachycardia, and hypotension, indicative of cytokine release syndrome.
Peak levels of CAR19 T-cells were significantly higher in patients with complete or partial responses, and patients who did not obtain a complete or partial response were more likely to have undetectable or very low levels. Increasing peak blood levels of CAR19 T-cells in vivo is an important goal for future research, according to investigators. Since endogenous CD19+ cells may promote proliferation of CAR19 T- cells, CD19+ cellular vaccines might enhance CAR19 T-cell proliferation in patients with low levels, they suggested.
Administration of programmed cell death protein-1 (PD-1) antagonists may also offer improvements. High levels of PD-1 expression on CAR19 T-cells were observed at the time of peak blood CAR19 T-cell levels.
Dr. Brudno reported having no disclosures. Dr. Goy and Dr. Rosenberg reported ties to industry, and Dr. Kochenderfer reported patents pending on CAR T-cell therapy.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: In patients who relapsed after allogeneic hematopoietic stem-cell transplantation, anti-CD19 chimeric antigen receptor (CAR) T-cell therapy induced remissions without causing graft-versus-host disease (GVHD).
Major finding: Of 20 patients treated, 6 obtained complete remission and 2 obtained partial remissions; none experienced new-onset acute GVHD.
Data source: Patients with B-cell malignancies who had progressed after allogeneic hematopoietic stem-cell transplantation.
Disclosures: Dr. Brudno reported having no disclosures. Dr. Goy and Dr. Rosenberg reported ties to industry, and Dr. Kochenderfer reported patents pending on CAR T-cell therapy.
Gemtuzumab ozogamicin boosts overall survival in older AML patients
Older patients with newly diagnosed acute myeloid leukemia who were unsuitable for intensive chemotherapy had significantly longer overall survival with gemtuzumab ozogamicin, compared with best supportive care, according to phase III trial results published Jan. 25.
The phase III EORTC-GIMEMA AML-19 trial randomly assigned 118 patients to receive gemtuzumab ozogamicin and 119 to receive best supportive care, including hydroxyurea. The median age was 77 years. In total, 104 of 118 patients in the gemtuzumab ozogamicin arm received the full induction course, and the median number of gemtuzumab ozogamicin infusions was three (range: 1 to 10).
Median overall survival (OS) for patients who received gemtuzumab ozogamicin was 4.9 months, compared with 3.6 months for those who received best supportive care, including hydroxyurea (hazard ratio, 0.69; 95% confidence interval, 0.53-0.90; P = .005).
One-year survival rates were 24.3% (95% CI, 16.9 to 32.4) for gemtuzumab ozogamicin and 9.7% (5.1 to 15.9) for best supportive care (J Clin Onc. 2016 Jan 25. doi: 10.1200/JCO.2015.64.0060).
The low intensity gemtuzumab ozogamicin regimen was generally well tolerated, with comparable toxicity between arms. Pancytopenia was observed in nearly all patients during gemtuzumab ozogamicin induction, however.
“Of importance, liver toxicity, a hallmark of [gemtuzumab ozogamicin] safety profile, was not increased in [gemtuzumab ozogamicin] recipients. Furthermore, it appeared to be less frequent and severe than previously reported by our group in a first-line trial, in which a more intensive [gemtuzumab ozogamicin] regimen was used in elderly patients with AML unfit for intensive chemotherapy,” wrote Dr. Sergio Amadori of the Tor Vergata University, Rome, and his colleagues.
Gemtuzumab ozogamicin therapy resulted in an overall complete response (CR) rate of 27% (15.3% CR and 11.7% CRi [incomplete recovery of peripheral blood counts]). The overall clinical benefit rate (CR + CRi+ partial response + stable disease for 30 days) was 56.7%.
Gemtuzumab ozogamicin combines a human monoclonal antibody specific for CD33 on myeloid cells with the DNA intercalator calicheamicin.
Patient characteristics that influenced gemtuzumab ozogamicin treatment effect were CD33 expression status, sex, and cytogenic profile. In patients with more than 80% CD33-positive blasts, gemtuzumab ozogamicin resulted in greater improvements over best supportive care (HR, 0.49; 95% CI, 0.32 to 0.76).
In women, OS was significantly improved (HR, 0.53; 95% CI, 0.35 to 0.79), whereas in men the hazard ratio was near 1. Patients with favorable/intermediate cytogenetic risk profiles had significant gemtuzumab ozogamicin benefit (HR, 0.52; 95% CI, 0.34 to 0.77), and those with adverse risk profiles had no treatment difference between arms.
The research was supported by Wyeth (Pfizer) and by the European Organisation for Research and Treatment of Cancer . Dr. Amadori reported having no disclosures. Several of his coauthors reported ties to industry.
Older patients with newly diagnosed acute myeloid leukemia who were unsuitable for intensive chemotherapy had significantly longer overall survival with gemtuzumab ozogamicin, compared with best supportive care, according to phase III trial results published Jan. 25.
The phase III EORTC-GIMEMA AML-19 trial randomly assigned 118 patients to receive gemtuzumab ozogamicin and 119 to receive best supportive care, including hydroxyurea. The median age was 77 years. In total, 104 of 118 patients in the gemtuzumab ozogamicin arm received the full induction course, and the median number of gemtuzumab ozogamicin infusions was three (range: 1 to 10).
Median overall survival (OS) for patients who received gemtuzumab ozogamicin was 4.9 months, compared with 3.6 months for those who received best supportive care, including hydroxyurea (hazard ratio, 0.69; 95% confidence interval, 0.53-0.90; P = .005).
One-year survival rates were 24.3% (95% CI, 16.9 to 32.4) for gemtuzumab ozogamicin and 9.7% (5.1 to 15.9) for best supportive care (J Clin Onc. 2016 Jan 25. doi: 10.1200/JCO.2015.64.0060).
The low intensity gemtuzumab ozogamicin regimen was generally well tolerated, with comparable toxicity between arms. Pancytopenia was observed in nearly all patients during gemtuzumab ozogamicin induction, however.
“Of importance, liver toxicity, a hallmark of [gemtuzumab ozogamicin] safety profile, was not increased in [gemtuzumab ozogamicin] recipients. Furthermore, it appeared to be less frequent and severe than previously reported by our group in a first-line trial, in which a more intensive [gemtuzumab ozogamicin] regimen was used in elderly patients with AML unfit for intensive chemotherapy,” wrote Dr. Sergio Amadori of the Tor Vergata University, Rome, and his colleagues.
Gemtuzumab ozogamicin therapy resulted in an overall complete response (CR) rate of 27% (15.3% CR and 11.7% CRi [incomplete recovery of peripheral blood counts]). The overall clinical benefit rate (CR + CRi+ partial response + stable disease for 30 days) was 56.7%.
Gemtuzumab ozogamicin combines a human monoclonal antibody specific for CD33 on myeloid cells with the DNA intercalator calicheamicin.
Patient characteristics that influenced gemtuzumab ozogamicin treatment effect were CD33 expression status, sex, and cytogenic profile. In patients with more than 80% CD33-positive blasts, gemtuzumab ozogamicin resulted in greater improvements over best supportive care (HR, 0.49; 95% CI, 0.32 to 0.76).
In women, OS was significantly improved (HR, 0.53; 95% CI, 0.35 to 0.79), whereas in men the hazard ratio was near 1. Patients with favorable/intermediate cytogenetic risk profiles had significant gemtuzumab ozogamicin benefit (HR, 0.52; 95% CI, 0.34 to 0.77), and those with adverse risk profiles had no treatment difference between arms.
The research was supported by Wyeth (Pfizer) and by the European Organisation for Research and Treatment of Cancer . Dr. Amadori reported having no disclosures. Several of his coauthors reported ties to industry.
Older patients with newly diagnosed acute myeloid leukemia who were unsuitable for intensive chemotherapy had significantly longer overall survival with gemtuzumab ozogamicin, compared with best supportive care, according to phase III trial results published Jan. 25.
The phase III EORTC-GIMEMA AML-19 trial randomly assigned 118 patients to receive gemtuzumab ozogamicin and 119 to receive best supportive care, including hydroxyurea. The median age was 77 years. In total, 104 of 118 patients in the gemtuzumab ozogamicin arm received the full induction course, and the median number of gemtuzumab ozogamicin infusions was three (range: 1 to 10).
Median overall survival (OS) for patients who received gemtuzumab ozogamicin was 4.9 months, compared with 3.6 months for those who received best supportive care, including hydroxyurea (hazard ratio, 0.69; 95% confidence interval, 0.53-0.90; P = .005).
One-year survival rates were 24.3% (95% CI, 16.9 to 32.4) for gemtuzumab ozogamicin and 9.7% (5.1 to 15.9) for best supportive care (J Clin Onc. 2016 Jan 25. doi: 10.1200/JCO.2015.64.0060).
The low intensity gemtuzumab ozogamicin regimen was generally well tolerated, with comparable toxicity between arms. Pancytopenia was observed in nearly all patients during gemtuzumab ozogamicin induction, however.
“Of importance, liver toxicity, a hallmark of [gemtuzumab ozogamicin] safety profile, was not increased in [gemtuzumab ozogamicin] recipients. Furthermore, it appeared to be less frequent and severe than previously reported by our group in a first-line trial, in which a more intensive [gemtuzumab ozogamicin] regimen was used in elderly patients with AML unfit for intensive chemotherapy,” wrote Dr. Sergio Amadori of the Tor Vergata University, Rome, and his colleagues.
Gemtuzumab ozogamicin therapy resulted in an overall complete response (CR) rate of 27% (15.3% CR and 11.7% CRi [incomplete recovery of peripheral blood counts]). The overall clinical benefit rate (CR + CRi+ partial response + stable disease for 30 days) was 56.7%.
Gemtuzumab ozogamicin combines a human monoclonal antibody specific for CD33 on myeloid cells with the DNA intercalator calicheamicin.
Patient characteristics that influenced gemtuzumab ozogamicin treatment effect were CD33 expression status, sex, and cytogenic profile. In patients with more than 80% CD33-positive blasts, gemtuzumab ozogamicin resulted in greater improvements over best supportive care (HR, 0.49; 95% CI, 0.32 to 0.76).
In women, OS was significantly improved (HR, 0.53; 95% CI, 0.35 to 0.79), whereas in men the hazard ratio was near 1. Patients with favorable/intermediate cytogenetic risk profiles had significant gemtuzumab ozogamicin benefit (HR, 0.52; 95% CI, 0.34 to 0.77), and those with adverse risk profiles had no treatment difference between arms.
The research was supported by Wyeth (Pfizer) and by the European Organisation for Research and Treatment of Cancer . Dr. Amadori reported having no disclosures. Several of his coauthors reported ties to industry.
Key clinical point: First-line, low-dose gemtuzumab ozogamicin significantly improved overall survival, compared with best supportive care in patients aged 61 years or older with AML.
Major finding: Median overall survival for patients who received gemtuzumab ozogamicin was 4.9 months, compared with 3.6 months for best supportive care, including hydroxyurea (hazard ratio, 0.69; 95% confidence interval, 0.53-0.90; P = .005).
Data source: The phase III EORTC-GIMEMA AML-19 trial randomly assigned 118 patients to receive gemtuzumab ozogamicin and 119 to receive best supportive care.
Disclosures: Research was supported by Wyeth (Pfizer) and by the European Organisation for Research and Treatment of Cancer. Dr. Amadori reported having no disclosures. Several of his coauthors reported ties to industry.
Postinflammatory Hyperpigmentation in Patients With Skin of Color
Postinflammatory hyperpigmentation (PIH) develops as darkly pigmented macules that occur after an inflammatory process of the skin such as acne, folliculitis, eczema, or shaving irritation. Patients with Fitzpatrick skin types III to VI usually are most commonly affected, and for many, the remnant pigmentation can be an even greater concern than the original inflammatory process.1,2 Reported treatments of PIH include tretinoin, hydroquinone, azelaic acid, and chemical peels. The ideal combination of therapy has yet to be delineated.
Tretinoin (Vitamin A Derivative)
Bulengo-Ransby et al3 performed one of the first clinical trials testing tretinoin cream 0.1% for PIH in patients with Fitzpatrick skin types IV to VI . The study included 54 patients (24 applied tretinoin and 30 applied a vehicle) with moderate to severe PIH on the face and arms. The patients were divided into therapy and placebo groups and were evaluated for 40 weeks. Changes were evaluated through colorimetry, light microscopy, histology, and photography, with significant clinical improvement in the tretinoin-treated group (P<.001).3 A double-blind, randomized study of 45 photoaged Chinese and Japanese patients using tretinoin cream 0.1% also was conducted for treatment of photoaging-associated hyperpigmented lesions of the face and hands. Assessment was done with clinical, colorimetric, and histological evaluation, with an overall statistical improvement noted in hyperpigmentation.4 Both of the above studies showed mild irritation (ie, retinoid dermatitis) with application of tretinoin, which creates a compliance issue in patients who are recommended to continue therapy with higher-strength tretinoin. This side-effect profile can be circumvented through gradual elevation in the strength of tretinoin.5
Combination Therapies
Combination therapies with tretinoin also have been used to improve PIH. Callender et al6 conducted a study evaluating the efficacy of clindamycin phosphate 1.2%–tretinoin 0.025% gel for the treatment of PIH secondary to mild to moderate acne in patients with Fitzpatrick skin types IV to VI. Thirty patients participated in the randomized, double-blinded, placebo-controlled study, with 15 patients in the clindamycin-tretinoin gel group and 15 in the placebo control group. Based on objective assessment using a chromameter and evaluator global acne severity scale score, clinical efficacy was demonstrated for treating acne and PIH as well as preventing further PIH.6
Hydroquinone Formulation (Tyrosine Inhibitor)
Hydroquinone bleaching cream has been the standard therapy for hyperpigmentation. It works by blocking the conversion of dihydroxyphenylalanine to melanin by inhibiting tyrosinase.7 Topical steroids directly inhibit the synthesis of melanin, and when combined with hydroquinone and tretinoin, they can be effective for short periods of time and may decrease the irritation of application.7,8 The most widely accepted formula consists of a topical steroid (triamcinolone cream 0.1%) in combination with hydroquinone 4% and tretinoin cream 0.05%.8 In a similar 12-week open-label study of 25 patients with darker skin types, Grimes9 used an alternative combination formula of hydroquinone 4% and retinol 0.15%. Overall improvement and tolerance was demonstrated through the use of colorimetry measurement. A combination of hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01% also has been used effectively for the treatment of melasma.10 This formulation has been used more anecdotally for the treatment of PIH and has yet to have a randomized-controlled trial. The concern with repeated long-term use of hydroquinone remains. Permanent leukoderma, exogenous ochronosis, and hyperpigmentation of the surrounding normal skin (halo effect) can occur.
Azelaic Acid (Tyrosinase Inhibitor)
Azelaic acid is a dicarboxylic acid isolated from pityriasis versicolor that acts similar to a tyrosine inhibitor and has an antiproliferative effect toward abnormal melanocytes. Lowe et al11 conducted a randomized, double-blind, vehicle-controlled trial in patients with Fitzpatrick skin types IV through VI with facial hyperpigmentation using azelaic acid cream 20%. Over the course of 24 weeks, patients noted a decrease in overall pigment using both an investigator subjective scale and chromometer analysis.11
Kojic Acid (Tyrosinase Inhibitor)
Kojic acid is a tyrosinase inhibitor found in fungal metabolite species such as Acetobacter, Aspergillus, and Penicillium. It is commonly combined with other skin lightening agents such as hydroquinone or vitamin C to further enhance its efficacy. A randomized, 12-week, split-face study of Chinese women with melasma compared treatment with a glycolic acid 10%–hydroquinone 2% gel versus the combination plus kojic acid 2%. The results showed that 60% (24/40) of patients improved with the use of kojic acid as compared to those using the medication without kojic acid.12 Anecdotal data suggest kojic acid may be effective for PIH13; however, no studies specifically for PIH have been conducted.
Chemical Peels
Chemical peels have been used for a number of years, though their benefits in patients with skin of color is still being elucidated. The ideal chemical peels for Fitzpatrick skin types IV through VI are superficial to medium-depth peeling agents and techniques.14 Glycolic acid is a naturally occurring α-hydroxy acid that causes an increase in collagen synthesis, stimulates epidermolysis, and disperses basal layer melanin. Neutralization of glycolic acid peels can be done with the use of water, sodium bicarbonate, or sodium hydroxide to avoid unnecessary epidermal damage. Multiple clinical trials have been conducted to determine the response of glycolic acid peels in clearing PIH in patients with skin of color. Kessler et al15 compared glycolic acid 30% to salicylic acid 30% in 20 patients with mild to moderate acne and associated PIH. Chemical peels were performed every 2 weeks for 12 weeks. The study showed that salicylic acid was better tolerated than glycolic acid and both were equally effective after the second application (P<.05) for PIH.15 Finally, another study conducted for PIH in patients with Fitzpatrick skin types III and IV utilized glycolic acid peels with 20%, 35%, and 70% concentrations. The results showed overall improvement of PIH and acne from the use of all concentrations of glycolic peels, though faster efficacy was noted at higher concentrations.16
Other self-neutralizing peeling agents include salicylic acid and Jessner solution. Salicylic acid is a β-hydroxy acid that works through keratolysis and disrupting intercellular linkages. Jessner solution is a combination of resorcinol 14%, lactic acid 14%, and salicylic acid 14% in an alcohol base. Salicylic acid is well-tolerated in patients with Fitzpatrick skin types I through VI and has been helpful in treating acne, rosacea, melasma, hyperpigmentation, texturally rough skin, and mild photoaging. Jessner peeling solution has been used for a number of years and works as a keratolytic agent causing intercellular and intracellular edema, and due to its self-neutralizing agent, it is fairly superficial.17 Overall, superficial peeling agents should be used on patients with darker skin types to avoid the risk for worsening dyspigmentation, keloid formation, or deep scarring.18
Conclusion
These treatments are only some of the topical and chemical modalities for PIH in patients with skin of color. The patient history, evaluation, skin type, and underlying medical problems should be considered prior to using any topical or peeling agent. Lastly, photoprotection should be heavily emphasized with both sun protective gear and use of broad-spectrum sunscreens with a high sun protection factor, as UV radiation can cause darkening of PIH areas regardless of skin type and can reverse the progress made by a given therapy.18
- Savory SA, Agim NG, Mao R, et al. Reliability assessment and validation of the postacne hyperpigmentation index (PAHPI), a new instrument to measure postinflammatory hyperpigmentation from acne vulgaris. J Am Acad Dermatol. 2014;70:108-114.
- Halder RM. The role of retinoids in the management of cutaneous conditions in blacks. J Am Acad Dermatol. 1998;39(2, pt 3):S98-S103.
- Bulengo-Ransby SM, Griffiths CE, Kimbrough-Green CK, et al. Topical tretinoin (retinoid acid) therapy for hyperpigmented lesions caused by inflammation of the skin in black patients. N Engl J Med. 1993;328:1438-1443.
- Griffiths CE, Goldfarb MT, Finkel LJ, et al. Topical tretinoin (retinoic acid) treatment of hyperpigmented lesions associated with photoaging in Chinese and Japanese patients: a vehicle-controlled trial. J Am Acad Dermatol. 1994;30:76-84.
- Callendar VD. Acne in ethnic skin: special considerations for therapy. Dermatol Ther. 2004;17:184-195.
- Callender VD, Young CM, Kindred C, et al. Efficacy and safety of clindamycin phosphate 1.2% and tretinoin 0.025% gel for the treatment of acne and acne-induced post-inflammatory hyperpigmentation in patients with skin of color. J Clin Aesthet Dermatol. 2012;5:25-32.
- Badreshia-Bansal S, Draelos ZD. Insight into skin lightening cosmeceuticals for women of color. J Drugs Dermatol. 2007;6:32-39.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Grimes PE. A microsponge formulation of hydroquinone 4% and retinol 0.15% in the treatment of melasma and postinflammatory hyperpigmentation. Cutis. 2004;74:326-328.
- Chan R, Park KC, Lee MH, et al. A randomized controlled trial of the efficacy and safety of a fixed triple combination (fluocinolone acetonide 0.01%, hydroquinone 4%, tretinoin 0.05%) compared with hydroquinone 4% cream in Asian patients with moderate to severe melasma. Br J Dermatol. 2008;159:697-703.
- Lowe NJ, Rizk D, Grimes P. Azelaic acid 20% cream in the treatment of facial hyperpigmentation in darker-skinned patients. Clin Ther. 1998;20:945-959.
- Lim JT. Treatment of melasma using kojic acid in a gel containing hydroquinone and glycolic acid. Dermatol Surg. 1999;25:282-284.
- Alexis AF, Blackcloud P. Natural ingredients for darker skin types: growing options for hyperpigmentation. J Drugs Dermatol. 2013;12:123-127.
- Roberts WE. Chemical peeling in ethnic/dark skin. Dermatol Ther. 2004;17:196-205.
- Kessler E, Flanagan K, Chia C, et al. Comparison of alpha- and beta-hydroxy acid chemical peels in the treatment of mild to moderately severe facial acne vulgaris [published online December 5, 2007]. Dermatol Surg. 2008;34:45-50, discussion 51.
- Erbağci Z, Akçali C. Biweekly serial glycolic acid peels vs. long-term daily use of topical low-strength glycolic acid in the treatment of atrophic acne scars. Int J Dermatol. 2000;39:789-794.
- Jackson A. Chemical peels [published online January 31, 2014]. Facial Plast Surg. 2014;30:26-34.
- Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3:20-31.
Postinflammatory hyperpigmentation (PIH) develops as darkly pigmented macules that occur after an inflammatory process of the skin such as acne, folliculitis, eczema, or shaving irritation. Patients with Fitzpatrick skin types III to VI usually are most commonly affected, and for many, the remnant pigmentation can be an even greater concern than the original inflammatory process.1,2 Reported treatments of PIH include tretinoin, hydroquinone, azelaic acid, and chemical peels. The ideal combination of therapy has yet to be delineated.
Tretinoin (Vitamin A Derivative)
Bulengo-Ransby et al3 performed one of the first clinical trials testing tretinoin cream 0.1% for PIH in patients with Fitzpatrick skin types IV to VI . The study included 54 patients (24 applied tretinoin and 30 applied a vehicle) with moderate to severe PIH on the face and arms. The patients were divided into therapy and placebo groups and were evaluated for 40 weeks. Changes were evaluated through colorimetry, light microscopy, histology, and photography, with significant clinical improvement in the tretinoin-treated group (P<.001).3 A double-blind, randomized study of 45 photoaged Chinese and Japanese patients using tretinoin cream 0.1% also was conducted for treatment of photoaging-associated hyperpigmented lesions of the face and hands. Assessment was done with clinical, colorimetric, and histological evaluation, with an overall statistical improvement noted in hyperpigmentation.4 Both of the above studies showed mild irritation (ie, retinoid dermatitis) with application of tretinoin, which creates a compliance issue in patients who are recommended to continue therapy with higher-strength tretinoin. This side-effect profile can be circumvented through gradual elevation in the strength of tretinoin.5
Combination Therapies
Combination therapies with tretinoin also have been used to improve PIH. Callender et al6 conducted a study evaluating the efficacy of clindamycin phosphate 1.2%–tretinoin 0.025% gel for the treatment of PIH secondary to mild to moderate acne in patients with Fitzpatrick skin types IV to VI. Thirty patients participated in the randomized, double-blinded, placebo-controlled study, with 15 patients in the clindamycin-tretinoin gel group and 15 in the placebo control group. Based on objective assessment using a chromameter and evaluator global acne severity scale score, clinical efficacy was demonstrated for treating acne and PIH as well as preventing further PIH.6
Hydroquinone Formulation (Tyrosine Inhibitor)
Hydroquinone bleaching cream has been the standard therapy for hyperpigmentation. It works by blocking the conversion of dihydroxyphenylalanine to melanin by inhibiting tyrosinase.7 Topical steroids directly inhibit the synthesis of melanin, and when combined with hydroquinone and tretinoin, they can be effective for short periods of time and may decrease the irritation of application.7,8 The most widely accepted formula consists of a topical steroid (triamcinolone cream 0.1%) in combination with hydroquinone 4% and tretinoin cream 0.05%.8 In a similar 12-week open-label study of 25 patients with darker skin types, Grimes9 used an alternative combination formula of hydroquinone 4% and retinol 0.15%. Overall improvement and tolerance was demonstrated through the use of colorimetry measurement. A combination of hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01% also has been used effectively for the treatment of melasma.10 This formulation has been used more anecdotally for the treatment of PIH and has yet to have a randomized-controlled trial. The concern with repeated long-term use of hydroquinone remains. Permanent leukoderma, exogenous ochronosis, and hyperpigmentation of the surrounding normal skin (halo effect) can occur.
Azelaic Acid (Tyrosinase Inhibitor)
Azelaic acid is a dicarboxylic acid isolated from pityriasis versicolor that acts similar to a tyrosine inhibitor and has an antiproliferative effect toward abnormal melanocytes. Lowe et al11 conducted a randomized, double-blind, vehicle-controlled trial in patients with Fitzpatrick skin types IV through VI with facial hyperpigmentation using azelaic acid cream 20%. Over the course of 24 weeks, patients noted a decrease in overall pigment using both an investigator subjective scale and chromometer analysis.11
Kojic Acid (Tyrosinase Inhibitor)
Kojic acid is a tyrosinase inhibitor found in fungal metabolite species such as Acetobacter, Aspergillus, and Penicillium. It is commonly combined with other skin lightening agents such as hydroquinone or vitamin C to further enhance its efficacy. A randomized, 12-week, split-face study of Chinese women with melasma compared treatment with a glycolic acid 10%–hydroquinone 2% gel versus the combination plus kojic acid 2%. The results showed that 60% (24/40) of patients improved with the use of kojic acid as compared to those using the medication without kojic acid.12 Anecdotal data suggest kojic acid may be effective for PIH13; however, no studies specifically for PIH have been conducted.
Chemical Peels
Chemical peels have been used for a number of years, though their benefits in patients with skin of color is still being elucidated. The ideal chemical peels for Fitzpatrick skin types IV through VI are superficial to medium-depth peeling agents and techniques.14 Glycolic acid is a naturally occurring α-hydroxy acid that causes an increase in collagen synthesis, stimulates epidermolysis, and disperses basal layer melanin. Neutralization of glycolic acid peels can be done with the use of water, sodium bicarbonate, or sodium hydroxide to avoid unnecessary epidermal damage. Multiple clinical trials have been conducted to determine the response of glycolic acid peels in clearing PIH in patients with skin of color. Kessler et al15 compared glycolic acid 30% to salicylic acid 30% in 20 patients with mild to moderate acne and associated PIH. Chemical peels were performed every 2 weeks for 12 weeks. The study showed that salicylic acid was better tolerated than glycolic acid and both were equally effective after the second application (P<.05) for PIH.15 Finally, another study conducted for PIH in patients with Fitzpatrick skin types III and IV utilized glycolic acid peels with 20%, 35%, and 70% concentrations. The results showed overall improvement of PIH and acne from the use of all concentrations of glycolic peels, though faster efficacy was noted at higher concentrations.16
Other self-neutralizing peeling agents include salicylic acid and Jessner solution. Salicylic acid is a β-hydroxy acid that works through keratolysis and disrupting intercellular linkages. Jessner solution is a combination of resorcinol 14%, lactic acid 14%, and salicylic acid 14% in an alcohol base. Salicylic acid is well-tolerated in patients with Fitzpatrick skin types I through VI and has been helpful in treating acne, rosacea, melasma, hyperpigmentation, texturally rough skin, and mild photoaging. Jessner peeling solution has been used for a number of years and works as a keratolytic agent causing intercellular and intracellular edema, and due to its self-neutralizing agent, it is fairly superficial.17 Overall, superficial peeling agents should be used on patients with darker skin types to avoid the risk for worsening dyspigmentation, keloid formation, or deep scarring.18
Conclusion
These treatments are only some of the topical and chemical modalities for PIH in patients with skin of color. The patient history, evaluation, skin type, and underlying medical problems should be considered prior to using any topical or peeling agent. Lastly, photoprotection should be heavily emphasized with both sun protective gear and use of broad-spectrum sunscreens with a high sun protection factor, as UV radiation can cause darkening of PIH areas regardless of skin type and can reverse the progress made by a given therapy.18
Postinflammatory hyperpigmentation (PIH) develops as darkly pigmented macules that occur after an inflammatory process of the skin such as acne, folliculitis, eczema, or shaving irritation. Patients with Fitzpatrick skin types III to VI usually are most commonly affected, and for many, the remnant pigmentation can be an even greater concern than the original inflammatory process.1,2 Reported treatments of PIH include tretinoin, hydroquinone, azelaic acid, and chemical peels. The ideal combination of therapy has yet to be delineated.
Tretinoin (Vitamin A Derivative)
Bulengo-Ransby et al3 performed one of the first clinical trials testing tretinoin cream 0.1% for PIH in patients with Fitzpatrick skin types IV to VI . The study included 54 patients (24 applied tretinoin and 30 applied a vehicle) with moderate to severe PIH on the face and arms. The patients were divided into therapy and placebo groups and were evaluated for 40 weeks. Changes were evaluated through colorimetry, light microscopy, histology, and photography, with significant clinical improvement in the tretinoin-treated group (P<.001).3 A double-blind, randomized study of 45 photoaged Chinese and Japanese patients using tretinoin cream 0.1% also was conducted for treatment of photoaging-associated hyperpigmented lesions of the face and hands. Assessment was done with clinical, colorimetric, and histological evaluation, with an overall statistical improvement noted in hyperpigmentation.4 Both of the above studies showed mild irritation (ie, retinoid dermatitis) with application of tretinoin, which creates a compliance issue in patients who are recommended to continue therapy with higher-strength tretinoin. This side-effect profile can be circumvented through gradual elevation in the strength of tretinoin.5
Combination Therapies
Combination therapies with tretinoin also have been used to improve PIH. Callender et al6 conducted a study evaluating the efficacy of clindamycin phosphate 1.2%–tretinoin 0.025% gel for the treatment of PIH secondary to mild to moderate acne in patients with Fitzpatrick skin types IV to VI. Thirty patients participated in the randomized, double-blinded, placebo-controlled study, with 15 patients in the clindamycin-tretinoin gel group and 15 in the placebo control group. Based on objective assessment using a chromameter and evaluator global acne severity scale score, clinical efficacy was demonstrated for treating acne and PIH as well as preventing further PIH.6
Hydroquinone Formulation (Tyrosine Inhibitor)
Hydroquinone bleaching cream has been the standard therapy for hyperpigmentation. It works by blocking the conversion of dihydroxyphenylalanine to melanin by inhibiting tyrosinase.7 Topical steroids directly inhibit the synthesis of melanin, and when combined with hydroquinone and tretinoin, they can be effective for short periods of time and may decrease the irritation of application.7,8 The most widely accepted formula consists of a topical steroid (triamcinolone cream 0.1%) in combination with hydroquinone 4% and tretinoin cream 0.05%.8 In a similar 12-week open-label study of 25 patients with darker skin types, Grimes9 used an alternative combination formula of hydroquinone 4% and retinol 0.15%. Overall improvement and tolerance was demonstrated through the use of colorimetry measurement. A combination of hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01% also has been used effectively for the treatment of melasma.10 This formulation has been used more anecdotally for the treatment of PIH and has yet to have a randomized-controlled trial. The concern with repeated long-term use of hydroquinone remains. Permanent leukoderma, exogenous ochronosis, and hyperpigmentation of the surrounding normal skin (halo effect) can occur.
Azelaic Acid (Tyrosinase Inhibitor)
Azelaic acid is a dicarboxylic acid isolated from pityriasis versicolor that acts similar to a tyrosine inhibitor and has an antiproliferative effect toward abnormal melanocytes. Lowe et al11 conducted a randomized, double-blind, vehicle-controlled trial in patients with Fitzpatrick skin types IV through VI with facial hyperpigmentation using azelaic acid cream 20%. Over the course of 24 weeks, patients noted a decrease in overall pigment using both an investigator subjective scale and chromometer analysis.11
Kojic Acid (Tyrosinase Inhibitor)
Kojic acid is a tyrosinase inhibitor found in fungal metabolite species such as Acetobacter, Aspergillus, and Penicillium. It is commonly combined with other skin lightening agents such as hydroquinone or vitamin C to further enhance its efficacy. A randomized, 12-week, split-face study of Chinese women with melasma compared treatment with a glycolic acid 10%–hydroquinone 2% gel versus the combination plus kojic acid 2%. The results showed that 60% (24/40) of patients improved with the use of kojic acid as compared to those using the medication without kojic acid.12 Anecdotal data suggest kojic acid may be effective for PIH13; however, no studies specifically for PIH have been conducted.
Chemical Peels
Chemical peels have been used for a number of years, though their benefits in patients with skin of color is still being elucidated. The ideal chemical peels for Fitzpatrick skin types IV through VI are superficial to medium-depth peeling agents and techniques.14 Glycolic acid is a naturally occurring α-hydroxy acid that causes an increase in collagen synthesis, stimulates epidermolysis, and disperses basal layer melanin. Neutralization of glycolic acid peels can be done with the use of water, sodium bicarbonate, or sodium hydroxide to avoid unnecessary epidermal damage. Multiple clinical trials have been conducted to determine the response of glycolic acid peels in clearing PIH in patients with skin of color. Kessler et al15 compared glycolic acid 30% to salicylic acid 30% in 20 patients with mild to moderate acne and associated PIH. Chemical peels were performed every 2 weeks for 12 weeks. The study showed that salicylic acid was better tolerated than glycolic acid and both were equally effective after the second application (P<.05) for PIH.15 Finally, another study conducted for PIH in patients with Fitzpatrick skin types III and IV utilized glycolic acid peels with 20%, 35%, and 70% concentrations. The results showed overall improvement of PIH and acne from the use of all concentrations of glycolic peels, though faster efficacy was noted at higher concentrations.16
Other self-neutralizing peeling agents include salicylic acid and Jessner solution. Salicylic acid is a β-hydroxy acid that works through keratolysis and disrupting intercellular linkages. Jessner solution is a combination of resorcinol 14%, lactic acid 14%, and salicylic acid 14% in an alcohol base. Salicylic acid is well-tolerated in patients with Fitzpatrick skin types I through VI and has been helpful in treating acne, rosacea, melasma, hyperpigmentation, texturally rough skin, and mild photoaging. Jessner peeling solution has been used for a number of years and works as a keratolytic agent causing intercellular and intracellular edema, and due to its self-neutralizing agent, it is fairly superficial.17 Overall, superficial peeling agents should be used on patients with darker skin types to avoid the risk for worsening dyspigmentation, keloid formation, or deep scarring.18
Conclusion
These treatments are only some of the topical and chemical modalities for PIH in patients with skin of color. The patient history, evaluation, skin type, and underlying medical problems should be considered prior to using any topical or peeling agent. Lastly, photoprotection should be heavily emphasized with both sun protective gear and use of broad-spectrum sunscreens with a high sun protection factor, as UV radiation can cause darkening of PIH areas regardless of skin type and can reverse the progress made by a given therapy.18
- Savory SA, Agim NG, Mao R, et al. Reliability assessment and validation of the postacne hyperpigmentation index (PAHPI), a new instrument to measure postinflammatory hyperpigmentation from acne vulgaris. J Am Acad Dermatol. 2014;70:108-114.
- Halder RM. The role of retinoids in the management of cutaneous conditions in blacks. J Am Acad Dermatol. 1998;39(2, pt 3):S98-S103.
- Bulengo-Ransby SM, Griffiths CE, Kimbrough-Green CK, et al. Topical tretinoin (retinoid acid) therapy for hyperpigmented lesions caused by inflammation of the skin in black patients. N Engl J Med. 1993;328:1438-1443.
- Griffiths CE, Goldfarb MT, Finkel LJ, et al. Topical tretinoin (retinoic acid) treatment of hyperpigmented lesions associated with photoaging in Chinese and Japanese patients: a vehicle-controlled trial. J Am Acad Dermatol. 1994;30:76-84.
- Callendar VD. Acne in ethnic skin: special considerations for therapy. Dermatol Ther. 2004;17:184-195.
- Callender VD, Young CM, Kindred C, et al. Efficacy and safety of clindamycin phosphate 1.2% and tretinoin 0.025% gel for the treatment of acne and acne-induced post-inflammatory hyperpigmentation in patients with skin of color. J Clin Aesthet Dermatol. 2012;5:25-32.
- Badreshia-Bansal S, Draelos ZD. Insight into skin lightening cosmeceuticals for women of color. J Drugs Dermatol. 2007;6:32-39.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Grimes PE. A microsponge formulation of hydroquinone 4% and retinol 0.15% in the treatment of melasma and postinflammatory hyperpigmentation. Cutis. 2004;74:326-328.
- Chan R, Park KC, Lee MH, et al. A randomized controlled trial of the efficacy and safety of a fixed triple combination (fluocinolone acetonide 0.01%, hydroquinone 4%, tretinoin 0.05%) compared with hydroquinone 4% cream in Asian patients with moderate to severe melasma. Br J Dermatol. 2008;159:697-703.
- Lowe NJ, Rizk D, Grimes P. Azelaic acid 20% cream in the treatment of facial hyperpigmentation in darker-skinned patients. Clin Ther. 1998;20:945-959.
- Lim JT. Treatment of melasma using kojic acid in a gel containing hydroquinone and glycolic acid. Dermatol Surg. 1999;25:282-284.
- Alexis AF, Blackcloud P. Natural ingredients for darker skin types: growing options for hyperpigmentation. J Drugs Dermatol. 2013;12:123-127.
- Roberts WE. Chemical peeling in ethnic/dark skin. Dermatol Ther. 2004;17:196-205.
- Kessler E, Flanagan K, Chia C, et al. Comparison of alpha- and beta-hydroxy acid chemical peels in the treatment of mild to moderately severe facial acne vulgaris [published online December 5, 2007]. Dermatol Surg. 2008;34:45-50, discussion 51.
- Erbağci Z, Akçali C. Biweekly serial glycolic acid peels vs. long-term daily use of topical low-strength glycolic acid in the treatment of atrophic acne scars. Int J Dermatol. 2000;39:789-794.
- Jackson A. Chemical peels [published online January 31, 2014]. Facial Plast Surg. 2014;30:26-34.
- Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3:20-31.
- Savory SA, Agim NG, Mao R, et al. Reliability assessment and validation of the postacne hyperpigmentation index (PAHPI), a new instrument to measure postinflammatory hyperpigmentation from acne vulgaris. J Am Acad Dermatol. 2014;70:108-114.
- Halder RM. The role of retinoids in the management of cutaneous conditions in blacks. J Am Acad Dermatol. 1998;39(2, pt 3):S98-S103.
- Bulengo-Ransby SM, Griffiths CE, Kimbrough-Green CK, et al. Topical tretinoin (retinoid acid) therapy for hyperpigmented lesions caused by inflammation of the skin in black patients. N Engl J Med. 1993;328:1438-1443.
- Griffiths CE, Goldfarb MT, Finkel LJ, et al. Topical tretinoin (retinoic acid) treatment of hyperpigmented lesions associated with photoaging in Chinese and Japanese patients: a vehicle-controlled trial. J Am Acad Dermatol. 1994;30:76-84.
- Callendar VD. Acne in ethnic skin: special considerations for therapy. Dermatol Ther. 2004;17:184-195.
- Callender VD, Young CM, Kindred C, et al. Efficacy and safety of clindamycin phosphate 1.2% and tretinoin 0.025% gel for the treatment of acne and acne-induced post-inflammatory hyperpigmentation in patients with skin of color. J Clin Aesthet Dermatol. 2012;5:25-32.
- Badreshia-Bansal S, Draelos ZD. Insight into skin lightening cosmeceuticals for women of color. J Drugs Dermatol. 2007;6:32-39.
- Kligman AM, Willis I. A new formula for depigmenting human skin. Arch Dermatol. 1975;111:40-48.
- Grimes PE. A microsponge formulation of hydroquinone 4% and retinol 0.15% in the treatment of melasma and postinflammatory hyperpigmentation. Cutis. 2004;74:326-328.
- Chan R, Park KC, Lee MH, et al. A randomized controlled trial of the efficacy and safety of a fixed triple combination (fluocinolone acetonide 0.01%, hydroquinone 4%, tretinoin 0.05%) compared with hydroquinone 4% cream in Asian patients with moderate to severe melasma. Br J Dermatol. 2008;159:697-703.
- Lowe NJ, Rizk D, Grimes P. Azelaic acid 20% cream in the treatment of facial hyperpigmentation in darker-skinned patients. Clin Ther. 1998;20:945-959.
- Lim JT. Treatment of melasma using kojic acid in a gel containing hydroquinone and glycolic acid. Dermatol Surg. 1999;25:282-284.
- Alexis AF, Blackcloud P. Natural ingredients for darker skin types: growing options for hyperpigmentation. J Drugs Dermatol. 2013;12:123-127.
- Roberts WE. Chemical peeling in ethnic/dark skin. Dermatol Ther. 2004;17:196-205.
- Kessler E, Flanagan K, Chia C, et al. Comparison of alpha- and beta-hydroxy acid chemical peels in the treatment of mild to moderately severe facial acne vulgaris [published online December 5, 2007]. Dermatol Surg. 2008;34:45-50, discussion 51.
- Erbağci Z, Akçali C. Biweekly serial glycolic acid peels vs. long-term daily use of topical low-strength glycolic acid in the treatment of atrophic acne scars. Int J Dermatol. 2000;39:789-794.
- Jackson A. Chemical peels [published online January 31, 2014]. Facial Plast Surg. 2014;30:26-34.
- Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3:20-31.
STS: BMI impacts risk for complications after lung resection
PHOENIX – Being underweight is associated with a substantially increased risk of complications following lung resection for cancer, results from a large database study found.
“This is not generally known among surgeons or their patients,” Dr. Trevor Williams said in an interview before the annual meeting of the Society of Thoracic Surgeons. “Studies are conflicting about the relationship of BMI [body mass index] to surgical outcomes. Most of the previous studies simply categorize BMI as overweight or not. We’ve stratified based on World Health Organization categories to get a more precise look at BMI.”
Dr. Williams, a surgeon at the University of Chicago Medical Center, and his associates evaluated 41,446 patients in the STS General Thoracic Surgery Database who underwent elective anatomic lung resection for cancer between 2009 and 2014. Their mean age was 68 years, and 53% were female. The researchers performed multivariable analysis after adjusting for validated STS risk model covariates, including gender and spirometry.
According to WHO criteria for BMI, 3% were underweight (less than 18.5 kg/m2); 33.5% were normal weight (18.5-24.9 kg/m2); 35.4% were overweight (25-29.9 kg/m2); 18.1% were obese I (30-34.9 kg/m2); 6.4% were obese II (35-39.9 kg/m2), and 3.6% were obese III (40 kg/m2 or greater). Dr. Williams and his associates observed that women were more often underweight, compared with men (4.1% vs. 1.8%, respectively; P less than .001), and underweight patients more often had chronic obstructive pulmonary disease (51.7% vs. 35.2%; P less than .001). Pulmonary complication rates were higher among underweight and obese III patients (P less than .001), while being underweight was also associated with higher rates of infections and any surgical complications.
Multivariable analysis revealed that pulmonary and any postoperative complications were more common among underweight patients (odds ratio, 1.44 and OR, 1.41, respectively), while any major complication was more common among obese III patients (OR, 1.18). Overweight and obese I-II patients were less likely to have any postoperative and pulmonary complications, compared with patients who had a normal BMI. “The finding of underweight patients being such a high-risk patient population is suggested in the literature but not demonstrated as clearly as in this study,” Dr. Williams said. “A truly surprising finding was that obese patients actually have a lower risk of pulmonary and overall complications than ‘normal’-BMI patients.”
He concluded that according to the current analysis, “careful risk assessment is appropriate when considering operating on underweight patients. Whether there are interventions that could be instituted to improve an individual’s risk profile has not been determined. Any preconceived notions about not operating on obese patients due to elevated risk appear to be unfounded.”
Dr. Williams reported having no financial disclosures.
PHOENIX – Being underweight is associated with a substantially increased risk of complications following lung resection for cancer, results from a large database study found.
“This is not generally known among surgeons or their patients,” Dr. Trevor Williams said in an interview before the annual meeting of the Society of Thoracic Surgeons. “Studies are conflicting about the relationship of BMI [body mass index] to surgical outcomes. Most of the previous studies simply categorize BMI as overweight or not. We’ve stratified based on World Health Organization categories to get a more precise look at BMI.”
Dr. Williams, a surgeon at the University of Chicago Medical Center, and his associates evaluated 41,446 patients in the STS General Thoracic Surgery Database who underwent elective anatomic lung resection for cancer between 2009 and 2014. Their mean age was 68 years, and 53% were female. The researchers performed multivariable analysis after adjusting for validated STS risk model covariates, including gender and spirometry.
According to WHO criteria for BMI, 3% were underweight (less than 18.5 kg/m2); 33.5% were normal weight (18.5-24.9 kg/m2); 35.4% were overweight (25-29.9 kg/m2); 18.1% were obese I (30-34.9 kg/m2); 6.4% were obese II (35-39.9 kg/m2), and 3.6% were obese III (40 kg/m2 or greater). Dr. Williams and his associates observed that women were more often underweight, compared with men (4.1% vs. 1.8%, respectively; P less than .001), and underweight patients more often had chronic obstructive pulmonary disease (51.7% vs. 35.2%; P less than .001). Pulmonary complication rates were higher among underweight and obese III patients (P less than .001), while being underweight was also associated with higher rates of infections and any surgical complications.
Multivariable analysis revealed that pulmonary and any postoperative complications were more common among underweight patients (odds ratio, 1.44 and OR, 1.41, respectively), while any major complication was more common among obese III patients (OR, 1.18). Overweight and obese I-II patients were less likely to have any postoperative and pulmonary complications, compared with patients who had a normal BMI. “The finding of underweight patients being such a high-risk patient population is suggested in the literature but not demonstrated as clearly as in this study,” Dr. Williams said. “A truly surprising finding was that obese patients actually have a lower risk of pulmonary and overall complications than ‘normal’-BMI patients.”
He concluded that according to the current analysis, “careful risk assessment is appropriate when considering operating on underweight patients. Whether there are interventions that could be instituted to improve an individual’s risk profile has not been determined. Any preconceived notions about not operating on obese patients due to elevated risk appear to be unfounded.”
Dr. Williams reported having no financial disclosures.
PHOENIX – Being underweight is associated with a substantially increased risk of complications following lung resection for cancer, results from a large database study found.
“This is not generally known among surgeons or their patients,” Dr. Trevor Williams said in an interview before the annual meeting of the Society of Thoracic Surgeons. “Studies are conflicting about the relationship of BMI [body mass index] to surgical outcomes. Most of the previous studies simply categorize BMI as overweight or not. We’ve stratified based on World Health Organization categories to get a more precise look at BMI.”
Dr. Williams, a surgeon at the University of Chicago Medical Center, and his associates evaluated 41,446 patients in the STS General Thoracic Surgery Database who underwent elective anatomic lung resection for cancer between 2009 and 2014. Their mean age was 68 years, and 53% were female. The researchers performed multivariable analysis after adjusting for validated STS risk model covariates, including gender and spirometry.
According to WHO criteria for BMI, 3% were underweight (less than 18.5 kg/m2); 33.5% were normal weight (18.5-24.9 kg/m2); 35.4% were overweight (25-29.9 kg/m2); 18.1% were obese I (30-34.9 kg/m2); 6.4% were obese II (35-39.9 kg/m2), and 3.6% were obese III (40 kg/m2 or greater). Dr. Williams and his associates observed that women were more often underweight, compared with men (4.1% vs. 1.8%, respectively; P less than .001), and underweight patients more often had chronic obstructive pulmonary disease (51.7% vs. 35.2%; P less than .001). Pulmonary complication rates were higher among underweight and obese III patients (P less than .001), while being underweight was also associated with higher rates of infections and any surgical complications.
Multivariable analysis revealed that pulmonary and any postoperative complications were more common among underweight patients (odds ratio, 1.44 and OR, 1.41, respectively), while any major complication was more common among obese III patients (OR, 1.18). Overweight and obese I-II patients were less likely to have any postoperative and pulmonary complications, compared with patients who had a normal BMI. “The finding of underweight patients being such a high-risk patient population is suggested in the literature but not demonstrated as clearly as in this study,” Dr. Williams said. “A truly surprising finding was that obese patients actually have a lower risk of pulmonary and overall complications than ‘normal’-BMI patients.”
He concluded that according to the current analysis, “careful risk assessment is appropriate when considering operating on underweight patients. Whether there are interventions that could be instituted to improve an individual’s risk profile has not been determined. Any preconceived notions about not operating on obese patients due to elevated risk appear to be unfounded.”
Dr. Williams reported having no financial disclosures.
AT THE STS ANNUAL MEETING
Key clinical point: Careful risk assessment is appropriate when considering performing lung resection on underweight patients.
Major finding: Multivariable analysis revealed that pulmonary and any postoperative complications were more common among underweight patients (OR, 1.44 and OR, 1.41, respectively), while any major complication was more common among obese III patients (OR, 1.18).
Data source: An analysis of 41,446 patients in the STS General Thoracic Surgery Database who underwent elective lung resection for cancer between 2009 and 2014.
Disclosures: Dr. Williams reported having no financial disclosures.
VIDEO: Novel imaging technique helps hunt for pulmonary lesions
PHOENIX – Each year more than 250,000 patients present with ground-glass opacities and other solitary pulmonary nodules, and they are difficult to locate.
“There’s been a need for our field to develop new technologies to find these nodules in the OR,” Dr. Sunil Singhal said in a video interview at the annual meeting of the Society of Thoracic Surgeons. “The fallback plan has always been that we can make a thoracotomy. Some studies have shown that in about one out of every two cases you end up opening a patient just to find a tiny little nodule.”
Dr. Singhal of the division of cardiothoracic surgery at the University of Pennsylvania School of Medicine, Philadelphia, discussed preoperative and intraoperative localization methods, including an investigational technology in which patients receive an intravascular dye that localizes the pulmonary tumor. “When we put our video-assisted thoracoscopic surgery camera in, the tumors are glowing,” he said. “We can then do a localized wedge excision and confirm margins of the staple line. We’ve done this [in] about 80 patients, and it’s been non-toxic, very safe, and very effective. Our biggest limitation has been our depth of penetration.”
Dr. Singhal reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – Each year more than 250,000 patients present with ground-glass opacities and other solitary pulmonary nodules, and they are difficult to locate.
“There’s been a need for our field to develop new technologies to find these nodules in the OR,” Dr. Sunil Singhal said in a video interview at the annual meeting of the Society of Thoracic Surgeons. “The fallback plan has always been that we can make a thoracotomy. Some studies have shown that in about one out of every two cases you end up opening a patient just to find a tiny little nodule.”
Dr. Singhal of the division of cardiothoracic surgery at the University of Pennsylvania School of Medicine, Philadelphia, discussed preoperative and intraoperative localization methods, including an investigational technology in which patients receive an intravascular dye that localizes the pulmonary tumor. “When we put our video-assisted thoracoscopic surgery camera in, the tumors are glowing,” he said. “We can then do a localized wedge excision and confirm margins of the staple line. We’ve done this [in] about 80 patients, and it’s been non-toxic, very safe, and very effective. Our biggest limitation has been our depth of penetration.”
Dr. Singhal reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
PHOENIX – Each year more than 250,000 patients present with ground-glass opacities and other solitary pulmonary nodules, and they are difficult to locate.
“There’s been a need for our field to develop new technologies to find these nodules in the OR,” Dr. Sunil Singhal said in a video interview at the annual meeting of the Society of Thoracic Surgeons. “The fallback plan has always been that we can make a thoracotomy. Some studies have shown that in about one out of every two cases you end up opening a patient just to find a tiny little nodule.”
Dr. Singhal of the division of cardiothoracic surgery at the University of Pennsylvania School of Medicine, Philadelphia, discussed preoperative and intraoperative localization methods, including an investigational technology in which patients receive an intravascular dye that localizes the pulmonary tumor. “When we put our video-assisted thoracoscopic surgery camera in, the tumors are glowing,” he said. “We can then do a localized wedge excision and confirm margins of the staple line. We’ve done this [in] about 80 patients, and it’s been non-toxic, very safe, and very effective. Our biggest limitation has been our depth of penetration.”
Dr. Singhal reported having no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
EXPERT ANALYSIS FROM THE STS ANNUAL MEETING
Viruses, Part 2: RNA Viruses
Review the PDF of the fact sheet on RNA viruses with board-relevant, easy-to-review material. This fact sheet will review the spectrum of RNA viruses that cause or are associated with cutaneous manifestations. RNA virus classification, clinical findings, potential treatments, and other board-relevant facts will be discussed.
Practice Questions
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus
c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
Review the PDF of the fact sheet on RNA viruses with board-relevant, easy-to-review material. This fact sheet will review the spectrum of RNA viruses that cause or are associated with cutaneous manifestations. RNA virus classification, clinical findings, potential treatments, and other board-relevant facts will be discussed.
Practice Questions
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus
c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
Review the PDF of the fact sheet on RNA viruses with board-relevant, easy-to-review material. This fact sheet will review the spectrum of RNA viruses that cause or are associated with cutaneous manifestations. RNA virus classification, clinical findings, potential treatments, and other board-relevant facts will be discussed.
Practice Questions
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus
c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
1. Which virus is transmitted by Culex mosquitos?
a. chikungunya virus
b. coxsackievirus A16
c. dengue virus
d. human T-lymphotropic virus
e. West Nile virus
2. Which virus causes an illness associated with an enanthem of grey papules on the buccal mucosa?
a. Paramyxoviridae
b. Parvoviridae
c. Picornaviridae
d. Retroviridae
e. Togaviridae
3. Illness associated with which viral infection may be prevented via vaccination?
a. coxsackievirus
b. dengue virus c. enterovirus
d. hepatitis C virus
e. togavirus
4. Which virus is classically associated with retro-orbital pain and a morbilliform eruption with areas of sparing?
a. chikungunya virus
b. dengue virus
c. human immunodeficiency virus
d. West Nile virus
e. yellow fever virus
5. Which of the following may be included in the treatment of hepatitis C virus (HCV) infection?
a. doxorubicin
b. HCV vaccine
c. ribavirin
d. tenofovir
e. vitamin A
STS: Score stratifies risks for isolated tricuspid valve surgery patients
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
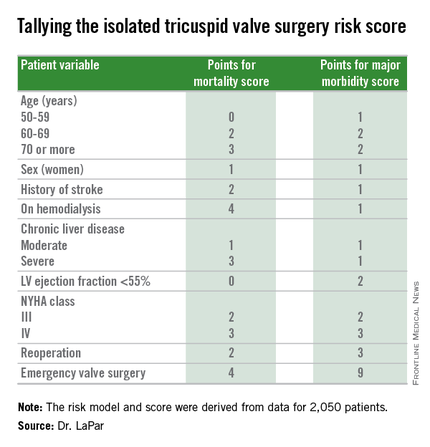
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
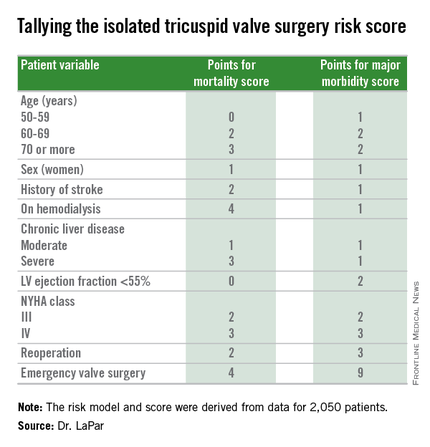
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
PHOENIX – A team of cardiac surgeons has developed the first clinical risk score for predicting the risk that patients face for operative mortality and postsurgical major morbidity when undergoing isolated tricuspid valve repair or replacement.
The risk score uses nine easily collected variables, and the derived model discriminates outcomes based on patients who score from 0-10 or more points on both a mortality and a morbidity risk scale, Dr. Damien J. LaPar said at the annual meeting of the Society of Thoracic Surgeons.
The risk scores allow surgeons to better describe and quantify to patients considering isolated tricuspid valve surgery the risks they face from the operation, and they have already been incorporated into practice at the University of Virginia, in Charlottesville, where Dr. LaPar practices.
“Patients love to better understand their risks. We can provide them with empirical data from a large, heterogeneous population that are better than a surgeon’s gut feeling” about the risks they face, said Dr. LaPar, a cardiothoracic surgeon at the University.
Another consequence of having the new risk model and score is that it identified certain key risk factors that are controllable, and thereby, “makes the case for early referrals” for isolated tricuspid valve surgery, Dr. LaPar said in an interview. For example, the risk score shows that patients who are older, on hemodialysis, have a reduced left ventricular ejection fraction, or require emergency intervention all contribute to worse outcomes, compared with patients who are younger, have better renal function, better cardiac output, or can be treated on a more routine basis.
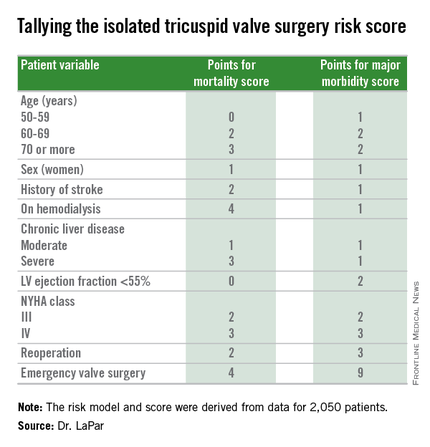
Many physicians have viewed isolated tricuspid valve surgery as posing similar risks to all patients, with an overall average operative mortality rate of about 10%, he noted. The new risk score model shows that some patients who are younger and healthier have operative mortality rates below 5%, while older and sicker patients have rates that can surpass 20%.
“Our data show a spectrum of risk, and that it is better to operate sooner than later. That is the huge clinical message of these data,” Dr. LaPar said.
Designated discussant Dr. Michael A. Acker noted that the risk score for tricuspid-valve surgery “is a first of its kind and a major contribution.” Dr. Acker is professor of surgery and chief of cardiovascular surgery at the University of Pennsylvania in Philadelphia. He is a consultant to Thoratec and HeartWare.
Dr. LaPar and his associates derived the risk model and score from data collected on 2,050 patients who underwent isolated tricuspid valve repair or replacement at 49 hospitals in Virginia or Michigan during 2002-2014. The data came from databases maintained by the Virginia Cardiac Surgery Quality Initiative and by the Michigan Society of Thoracic & Cardiovascular Surgeons, and reported to the Adult Cardiac Surgery Database of the Society of Thoracic Surgeons. The model they developed showed operative mortality rates that ranged from 2%, for patients with a mortality score of zero, to 34% for patients with a score of 10 or more. It further showed major morbidity rates of 13%, for patients with a morbidity score of zero, to 71% for those with a score of 10 or more. Scoring for mortality uses a slightly different system than the scoring for morbidity, so the scores must be calculated individually, and the score totals for a patient can differ for each endpoint. The maximum score is 22 for mortality and 23 for morbidity.
Only 5%-15% of patients undergoing tricuspid valve surgery have an isolated procedure, so a relatively limited number of patients fall into this category, a fact that has in the past limited collection of data from large numbers of patients. The dataset used for this analysis, with 2,050 patients “is one of the largest series collected,” and made possible derivation of a robust risk model and scoring system. Future analysis of even more patients should further improve the model and scoring system.
“These data set the stage for looking at national-level data to further refine the model and make it even more generalizable,” Dr. LaPar said.
On Twitter @mitchelzoler
AT THE STS ANNUAL MEETING
Key clinical point: A risk-scoring system estimates a patient’s mortality and morbidity risk when undergoing isolated tricuspid valve surgery.
Major finding: The scoring system discriminated mortality risk from 2% to 34%, and major morbidity risk from 13% to 71%.
Data source: Analysis of 2,050 patients who underwent isolated tricuspid valve surgery in the STS Adult Cardiac Surgery Database.
Disclosures: Dr. LaPar had no disclosures.
Workplace Interactions for Rosacea Patients
A new survey from the National Rosacea Society of 794 rosacea patients revealed that the majority of respondents indicated the disease had affected interactions with others in the workplace. More than 82% of respondents said they would notice people staring when they were experiencing a flare-up, and nearly 54% reported hearing rude or inappropriate comments about their facial appearance. More than 66% of the survey respondents said rosacea had negatively impacted interactions with customers or coworkers. Twenty-nine percent of patients with mild symptoms and 43% of those with severe symptoms reported they had missed work because of the condition.
Although rosacea may impact workplace interactions, 76.5% of respondents did not feel their appearance had cost them a promotion or new responsibilities, and 77.5% indicated that it had not kept them from landing a new job. Most respondents indicated that workplace problems were resolved when medical therapy was started, with nearly 67% reporting that effective treatment had improved their interactions with others at work.
In a January 2015 Cutis article, “The Rosacea Patient Journey: A Novel Approach to Conceptualizing Patient Experiences,” Kuo and colleagues discussed how patients can be educated to prepare for the rosacea patient experience. “Rosacea patients are faced with confusing and aggravating symptoms that can cause anxiety and may lead them to seek treatment from a physician,” the authors said. Rosacea can be a socially stigmatizing disease because the facial flushing and phymatous changes may be mistaken for alcohol abuse. It can also disrupt social and professional interactions, leading to quality-of-life effects such as difficulty functioning on a day-to-day basis.
Because there is no cure for rosacea, the patient and dermatologist must work together to devise a treatment plan that will help control the symptoms of rosacea. “Ultimately, with the alleviation of visible symptoms, the patient’s quality of life also can improve,” Kuo and colleagues reported. “Better understanding of the rosacea patient perspective can lead to a more efficient health care system, improved patient care, and better patient satisfaction.”
Share a copy of the Cutis rosacea patient journey guide with your patients today.
A new survey from the National Rosacea Society of 794 rosacea patients revealed that the majority of respondents indicated the disease had affected interactions with others in the workplace. More than 82% of respondents said they would notice people staring when they were experiencing a flare-up, and nearly 54% reported hearing rude or inappropriate comments about their facial appearance. More than 66% of the survey respondents said rosacea had negatively impacted interactions with customers or coworkers. Twenty-nine percent of patients with mild symptoms and 43% of those with severe symptoms reported they had missed work because of the condition.
Although rosacea may impact workplace interactions, 76.5% of respondents did not feel their appearance had cost them a promotion or new responsibilities, and 77.5% indicated that it had not kept them from landing a new job. Most respondents indicated that workplace problems were resolved when medical therapy was started, with nearly 67% reporting that effective treatment had improved their interactions with others at work.
In a January 2015 Cutis article, “The Rosacea Patient Journey: A Novel Approach to Conceptualizing Patient Experiences,” Kuo and colleagues discussed how patients can be educated to prepare for the rosacea patient experience. “Rosacea patients are faced with confusing and aggravating symptoms that can cause anxiety and may lead them to seek treatment from a physician,” the authors said. Rosacea can be a socially stigmatizing disease because the facial flushing and phymatous changes may be mistaken for alcohol abuse. It can also disrupt social and professional interactions, leading to quality-of-life effects such as difficulty functioning on a day-to-day basis.
Because there is no cure for rosacea, the patient and dermatologist must work together to devise a treatment plan that will help control the symptoms of rosacea. “Ultimately, with the alleviation of visible symptoms, the patient’s quality of life also can improve,” Kuo and colleagues reported. “Better understanding of the rosacea patient perspective can lead to a more efficient health care system, improved patient care, and better patient satisfaction.”
Share a copy of the Cutis rosacea patient journey guide with your patients today.
A new survey from the National Rosacea Society of 794 rosacea patients revealed that the majority of respondents indicated the disease had affected interactions with others in the workplace. More than 82% of respondents said they would notice people staring when they were experiencing a flare-up, and nearly 54% reported hearing rude or inappropriate comments about their facial appearance. More than 66% of the survey respondents said rosacea had negatively impacted interactions with customers or coworkers. Twenty-nine percent of patients with mild symptoms and 43% of those with severe symptoms reported they had missed work because of the condition.
Although rosacea may impact workplace interactions, 76.5% of respondents did not feel their appearance had cost them a promotion or new responsibilities, and 77.5% indicated that it had not kept them from landing a new job. Most respondents indicated that workplace problems were resolved when medical therapy was started, with nearly 67% reporting that effective treatment had improved their interactions with others at work.
In a January 2015 Cutis article, “The Rosacea Patient Journey: A Novel Approach to Conceptualizing Patient Experiences,” Kuo and colleagues discussed how patients can be educated to prepare for the rosacea patient experience. “Rosacea patients are faced with confusing and aggravating symptoms that can cause anxiety and may lead them to seek treatment from a physician,” the authors said. Rosacea can be a socially stigmatizing disease because the facial flushing and phymatous changes may be mistaken for alcohol abuse. It can also disrupt social and professional interactions, leading to quality-of-life effects such as difficulty functioning on a day-to-day basis.
Because there is no cure for rosacea, the patient and dermatologist must work together to devise a treatment plan that will help control the symptoms of rosacea. “Ultimately, with the alleviation of visible symptoms, the patient’s quality of life also can improve,” Kuo and colleagues reported. “Better understanding of the rosacea patient perspective can lead to a more efficient health care system, improved patient care, and better patient satisfaction.”
Share a copy of the Cutis rosacea patient journey guide with your patients today.
Dealing with adversity in vascular surgery
Adversity is part of life and everyone must deal with it. How one manages adversity matters, separates the winners from the losers, and is a major determinant of success.
Adverse challenges may be minor, intermediate or major. Although everyone is faced with such challenges, they are particularly relevant in a vascular surgery career. This is because of the serious nature and consequences of vascular diseases which can threaten loss of life, limb, and neurological function, and because of the complicated administrative world in which vascular surgery functions.
Minor frustrations are almost daily occurrences in a busy vascular surgeon’s life. They occur in and out of the operating room or angio suite, and many of them relate to other coworkers and associates making errors that interfere with smooth work flow or even good patient care. An angry response to these minor frustrations can exacerbate the problem and lead to strained, unpleasant working relationships and further errors. In contrast, a calm, measured response to these minor frustrations can minimize the damage caused and lead to a tranquil and effective work place.
Moreover, the individuals who control their responses are destined to be more effective and well liked. Equanimity when things go wrong during a stressful procedure in the operating room or angio suite is an even more valuable asset. Such composed responses will usually yield a better outcome than will loud and angry expressions of blame. The more serious the situation, the greater will be the value of composure.
Intermediate adversity in a work environment can take the form of rejection of a paper, denial of a grant request, or failure to get a sought promotion or assignment to a particular area of one’s interest. The latter two failures can best be managed by quietly continuing to work and strive. Success should only be regarded as delayed not denied. Rejection of grants and articles is almost routine despite the amount of time and hard work required to prepare them. Calm persistence can overcome many of these adverse events. Rewriting the paper or grant to correct the deficiencies detected by the reviewers followed by resubmission, even re-resubmission or submission to another journal, will ultimately result in publication of the work. To paraphrase Winston Churchill’s credo: Never, never, never, never, never, never give up.
A particularly challenging case can also be stressful and disheartening. It can appear at first to be an adverse event to the person faced with it. By staying calm and thinking clearly, it is sometimes possible to devise a new solution to the problem – one never described before. Thus, by meeting the challenge of this adversity, the vascular surgeon serendipitously turns adversity to his or her advantage and becomes an innovator. The seeming adversity becomes a creative opportunity. Many new developments and progress in vascular surgery have begun this way. No problem should be viewed as unsolvable despite so-called current wisdom.
More major adversity in a job setting can take the form of firing or termination. Such termination may be warranted or not. Often it is totally unjustified and based on personality differences or ego issues. Jealousy or negative bias are often involved. Such firings may take the form of a witch hunt based on a clinical or administrative superior highlighting selective and unrepresentative bad outcomes in a few difficult cases – something every good vascular surgeon has because of the difficult nature of the diseases we treat.
How should one deal with such a termination – unfair or not? Do not seek revenge. Get over it. Get another job and move on. Fortunately other jobs are abundant in the United States. Moreover, the new job often turns out to be better than the one left behind. The termination actually becomes a blessing in disguise, although it may take time for this to become apparent. Interestingly, many first-line leaders or biggest names in vascular surgery have profited in this way from the apparent major adversity of a termination. As one door closes, another may open if one is alert to the possibilities that may arise from change. Furthermore, the best revenge for an unfair termination is gained by achieving great success in one’s next position.
Although the discussion about dealing with adversity has thus far dealt largely with professional issues, the same principles can be applied to dealing with other aspects of life in general. Vigorous and excessive responses to adversity often result in greater pain and enhancing the wealth of lawyers. Equanimity, minimizing reactivity, and succeeding in the new venture one is forced into – even if unfairly – usually produce the best long-term outcome. It is an imperfect world, and how one deals with the many adversities that are part of it can make it less imperfect.
Adversity is part of life and everyone must deal with it. How one manages adversity matters, separates the winners from the losers, and is a major determinant of success.
Adverse challenges may be minor, intermediate or major. Although everyone is faced with such challenges, they are particularly relevant in a vascular surgery career. This is because of the serious nature and consequences of vascular diseases which can threaten loss of life, limb, and neurological function, and because of the complicated administrative world in which vascular surgery functions.
Minor frustrations are almost daily occurrences in a busy vascular surgeon’s life. They occur in and out of the operating room or angio suite, and many of them relate to other coworkers and associates making errors that interfere with smooth work flow or even good patient care. An angry response to these minor frustrations can exacerbate the problem and lead to strained, unpleasant working relationships and further errors. In contrast, a calm, measured response to these minor frustrations can minimize the damage caused and lead to a tranquil and effective work place.
Moreover, the individuals who control their responses are destined to be more effective and well liked. Equanimity when things go wrong during a stressful procedure in the operating room or angio suite is an even more valuable asset. Such composed responses will usually yield a better outcome than will loud and angry expressions of blame. The more serious the situation, the greater will be the value of composure.
Intermediate adversity in a work environment can take the form of rejection of a paper, denial of a grant request, or failure to get a sought promotion or assignment to a particular area of one’s interest. The latter two failures can best be managed by quietly continuing to work and strive. Success should only be regarded as delayed not denied. Rejection of grants and articles is almost routine despite the amount of time and hard work required to prepare them. Calm persistence can overcome many of these adverse events. Rewriting the paper or grant to correct the deficiencies detected by the reviewers followed by resubmission, even re-resubmission or submission to another journal, will ultimately result in publication of the work. To paraphrase Winston Churchill’s credo: Never, never, never, never, never, never give up.
A particularly challenging case can also be stressful and disheartening. It can appear at first to be an adverse event to the person faced with it. By staying calm and thinking clearly, it is sometimes possible to devise a new solution to the problem – one never described before. Thus, by meeting the challenge of this adversity, the vascular surgeon serendipitously turns adversity to his or her advantage and becomes an innovator. The seeming adversity becomes a creative opportunity. Many new developments and progress in vascular surgery have begun this way. No problem should be viewed as unsolvable despite so-called current wisdom.
More major adversity in a job setting can take the form of firing or termination. Such termination may be warranted or not. Often it is totally unjustified and based on personality differences or ego issues. Jealousy or negative bias are often involved. Such firings may take the form of a witch hunt based on a clinical or administrative superior highlighting selective and unrepresentative bad outcomes in a few difficult cases – something every good vascular surgeon has because of the difficult nature of the diseases we treat.
How should one deal with such a termination – unfair or not? Do not seek revenge. Get over it. Get another job and move on. Fortunately other jobs are abundant in the United States. Moreover, the new job often turns out to be better than the one left behind. The termination actually becomes a blessing in disguise, although it may take time for this to become apparent. Interestingly, many first-line leaders or biggest names in vascular surgery have profited in this way from the apparent major adversity of a termination. As one door closes, another may open if one is alert to the possibilities that may arise from change. Furthermore, the best revenge for an unfair termination is gained by achieving great success in one’s next position.
Although the discussion about dealing with adversity has thus far dealt largely with professional issues, the same principles can be applied to dealing with other aspects of life in general. Vigorous and excessive responses to adversity often result in greater pain and enhancing the wealth of lawyers. Equanimity, minimizing reactivity, and succeeding in the new venture one is forced into – even if unfairly – usually produce the best long-term outcome. It is an imperfect world, and how one deals with the many adversities that are part of it can make it less imperfect.
Adversity is part of life and everyone must deal with it. How one manages adversity matters, separates the winners from the losers, and is a major determinant of success.
Adverse challenges may be minor, intermediate or major. Although everyone is faced with such challenges, they are particularly relevant in a vascular surgery career. This is because of the serious nature and consequences of vascular diseases which can threaten loss of life, limb, and neurological function, and because of the complicated administrative world in which vascular surgery functions.
Minor frustrations are almost daily occurrences in a busy vascular surgeon’s life. They occur in and out of the operating room or angio suite, and many of them relate to other coworkers and associates making errors that interfere with smooth work flow or even good patient care. An angry response to these minor frustrations can exacerbate the problem and lead to strained, unpleasant working relationships and further errors. In contrast, a calm, measured response to these minor frustrations can minimize the damage caused and lead to a tranquil and effective work place.
Moreover, the individuals who control their responses are destined to be more effective and well liked. Equanimity when things go wrong during a stressful procedure in the operating room or angio suite is an even more valuable asset. Such composed responses will usually yield a better outcome than will loud and angry expressions of blame. The more serious the situation, the greater will be the value of composure.
Intermediate adversity in a work environment can take the form of rejection of a paper, denial of a grant request, or failure to get a sought promotion or assignment to a particular area of one’s interest. The latter two failures can best be managed by quietly continuing to work and strive. Success should only be regarded as delayed not denied. Rejection of grants and articles is almost routine despite the amount of time and hard work required to prepare them. Calm persistence can overcome many of these adverse events. Rewriting the paper or grant to correct the deficiencies detected by the reviewers followed by resubmission, even re-resubmission or submission to another journal, will ultimately result in publication of the work. To paraphrase Winston Churchill’s credo: Never, never, never, never, never, never give up.
A particularly challenging case can also be stressful and disheartening. It can appear at first to be an adverse event to the person faced with it. By staying calm and thinking clearly, it is sometimes possible to devise a new solution to the problem – one never described before. Thus, by meeting the challenge of this adversity, the vascular surgeon serendipitously turns adversity to his or her advantage and becomes an innovator. The seeming adversity becomes a creative opportunity. Many new developments and progress in vascular surgery have begun this way. No problem should be viewed as unsolvable despite so-called current wisdom.
More major adversity in a job setting can take the form of firing or termination. Such termination may be warranted or not. Often it is totally unjustified and based on personality differences or ego issues. Jealousy or negative bias are often involved. Such firings may take the form of a witch hunt based on a clinical or administrative superior highlighting selective and unrepresentative bad outcomes in a few difficult cases – something every good vascular surgeon has because of the difficult nature of the diseases we treat.
How should one deal with such a termination – unfair or not? Do not seek revenge. Get over it. Get another job and move on. Fortunately other jobs are abundant in the United States. Moreover, the new job often turns out to be better than the one left behind. The termination actually becomes a blessing in disguise, although it may take time for this to become apparent. Interestingly, many first-line leaders or biggest names in vascular surgery have profited in this way from the apparent major adversity of a termination. As one door closes, another may open if one is alert to the possibilities that may arise from change. Furthermore, the best revenge for an unfair termination is gained by achieving great success in one’s next position.
Although the discussion about dealing with adversity has thus far dealt largely with professional issues, the same principles can be applied to dealing with other aspects of life in general. Vigorous and excessive responses to adversity often result in greater pain and enhancing the wealth of lawyers. Equanimity, minimizing reactivity, and succeeding in the new venture one is forced into – even if unfairly – usually produce the best long-term outcome. It is an imperfect world, and how one deals with the many adversities that are part of it can make it less imperfect.
Overall Patient Satisfaction Better on Hospitalist Teams Compared with Teaching Teams
Clinical question: Is there a difference in patient experience on hospitalist teams compared with teaching teams?
Background: Hospitalist-intensive hospitals tend to perform better on patient-satisfaction measures on HCAHPS survey; however, little is known about the difference in patient experience between patients cared for by hospitalist and trainee teams.
Study design: Retrospective cohort analysis.
Setting: University of Chicago Medical Center.
Synopsis: A 30-day post-discharge survey was sent to 14,855 patients cared for by hospitalist and teaching teams, with 57% of teaching and 31% of hospitalist team patients returning fully completed surveys. A higher percentage of hospitalist team patients reported satisfaction with their overall care (73% vs. 67%; P<0.001; regression model odds ratio = 1.33; 95% CI, 1.15–1.47). There was no statistically significant difference in patient satisfaction with the teamwork of their providers, confidence in identifying their provider, or ability to understand the role of their provider.
Other than the inability to mitigate response-selection bias, the main limitation of this study is the single-center setting, which impacts the generalizability of the findings. Hospital-specific factors like different services and structures (hospitalists at their institution care for renal and lung transplant and oncology patients) could influence patients’ perception of their care. More research needs to be done to determine the specific factors that lead to a better patient experience.
Bottom line: At a single academic center, overall patient satisfaction was higher on a hospitalist service compared with teaching teams.
Citation: Wray CM, Flores A, Padula WV, Prochaska MT, Meltzer DO, Arora VM. Measuring patient experiences on hospitalist and teaching services: patient responses to a 30-day postdischarge questionnaire [published online ahead of print September 18, 2015]. J Hosp Med. doi:10.1002/jhm.2485.
Clinical question: Is there a difference in patient experience on hospitalist teams compared with teaching teams?
Background: Hospitalist-intensive hospitals tend to perform better on patient-satisfaction measures on HCAHPS survey; however, little is known about the difference in patient experience between patients cared for by hospitalist and trainee teams.
Study design: Retrospective cohort analysis.
Setting: University of Chicago Medical Center.
Synopsis: A 30-day post-discharge survey was sent to 14,855 patients cared for by hospitalist and teaching teams, with 57% of teaching and 31% of hospitalist team patients returning fully completed surveys. A higher percentage of hospitalist team patients reported satisfaction with their overall care (73% vs. 67%; P<0.001; regression model odds ratio = 1.33; 95% CI, 1.15–1.47). There was no statistically significant difference in patient satisfaction with the teamwork of their providers, confidence in identifying their provider, or ability to understand the role of their provider.
Other than the inability to mitigate response-selection bias, the main limitation of this study is the single-center setting, which impacts the generalizability of the findings. Hospital-specific factors like different services and structures (hospitalists at their institution care for renal and lung transplant and oncology patients) could influence patients’ perception of their care. More research needs to be done to determine the specific factors that lead to a better patient experience.
Bottom line: At a single academic center, overall patient satisfaction was higher on a hospitalist service compared with teaching teams.
Citation: Wray CM, Flores A, Padula WV, Prochaska MT, Meltzer DO, Arora VM. Measuring patient experiences on hospitalist and teaching services: patient responses to a 30-day postdischarge questionnaire [published online ahead of print September 18, 2015]. J Hosp Med. doi:10.1002/jhm.2485.
Clinical question: Is there a difference in patient experience on hospitalist teams compared with teaching teams?
Background: Hospitalist-intensive hospitals tend to perform better on patient-satisfaction measures on HCAHPS survey; however, little is known about the difference in patient experience between patients cared for by hospitalist and trainee teams.
Study design: Retrospective cohort analysis.
Setting: University of Chicago Medical Center.
Synopsis: A 30-day post-discharge survey was sent to 14,855 patients cared for by hospitalist and teaching teams, with 57% of teaching and 31% of hospitalist team patients returning fully completed surveys. A higher percentage of hospitalist team patients reported satisfaction with their overall care (73% vs. 67%; P<0.001; regression model odds ratio = 1.33; 95% CI, 1.15–1.47). There was no statistically significant difference in patient satisfaction with the teamwork of their providers, confidence in identifying their provider, or ability to understand the role of their provider.
Other than the inability to mitigate response-selection bias, the main limitation of this study is the single-center setting, which impacts the generalizability of the findings. Hospital-specific factors like different services and structures (hospitalists at their institution care for renal and lung transplant and oncology patients) could influence patients’ perception of their care. More research needs to be done to determine the specific factors that lead to a better patient experience.
Bottom line: At a single academic center, overall patient satisfaction was higher on a hospitalist service compared with teaching teams.
Citation: Wray CM, Flores A, Padula WV, Prochaska MT, Meltzer DO, Arora VM. Measuring patient experiences on hospitalist and teaching services: patient responses to a 30-day postdischarge questionnaire [published online ahead of print September 18, 2015]. J Hosp Med. doi:10.1002/jhm.2485.










