User login
Guidelines needed for outpatient opioid use after vaginal delivery
A new study of pregnant Medicaid patients in Pennsylvania found that 12% filled prescriptions for opioids within 5 days of vaginal delivery, even though fewer than one-third of the women had pain-inducing conditions.
“Our study raises the question: Why is outpatient opioid use not rare after vaginal delivery?” lead author Marian Jarlenski, PhD, MPH, said in an interview. “Outpatient opioid prescriptions after a hospitalization may be one potential pathway to opioid use disorder. I hope the study will prompt some thought about why opioids are being prescribed for women after vaginal delivery and how to best manage postdelivery pain. This is especially important in areas of the country that have extraordinarily high rates of opioid use disorder.”
A total of 12% of the women (18,131) filled an outpatient prescription for an opioid with 5 days of giving birth. Of those, just 28.2% (5,110) had one or more conditions that cause an increased level of pain after delivery, such as bilateral tubal ligation, certain kinds of lacerations, and episiotomy.
During the first 5 days after birth, the most commonly prescribed opioid was oxycodone-acetaminophen (53.3%), followed by acetaminophen-codeine (20.5%), and hydrocodone-acetaminophen (19.6%).
Of the 18,131 women with an early postdelivery opioid prescription, 14% (2,592) filled at least one other opioid prescription within 6-60 days – that’s 1.6% of all the women in the study.
“On a positive note, we saw the supply of opioid prescriptions was generally short at 3-7 days,” Dr. Jarlenski said.
The researchers linked tobacco use and a mental health condition (both adjusted odds ratio 1.3; 95% confidence interval, 1.2-1.4) to a higher risk of filling a prescription without being diagnosed with a pain-causing disorder. They also found an association between substance use disorder (not related to opioids) and a higher risk of these types of prescriptions, but only for filling a second opioid prescription in the 6-60 day period (aOR 1.4; 95% CI, 1.2-1.6).
The researchers called for national guidelines regarding the use of opioids after birth.
“Several organizations have developed opioid prescribing guidelines for chronic and acute pain,” Dr. Jarlenski said. “These guidelines are necessary because the risk of opioid use disorder and subsequent overdose events is well established. Although delivery is the most common reason for hospitalization in the United States, there are no national guidelines for outpatient opioid use after vaginal delivery.”
The study was partially supported by the University of Pittsburgh, the Pennsylvania Department of Human Services, the Building Interdisciplinary Research Careers in Women’s Health Program, and the National Institute on Drug Abuse. The researchers reported having no relevant financial disclosures.
A new study of pregnant Medicaid patients in Pennsylvania found that 12% filled prescriptions for opioids within 5 days of vaginal delivery, even though fewer than one-third of the women had pain-inducing conditions.
“Our study raises the question: Why is outpatient opioid use not rare after vaginal delivery?” lead author Marian Jarlenski, PhD, MPH, said in an interview. “Outpatient opioid prescriptions after a hospitalization may be one potential pathway to opioid use disorder. I hope the study will prompt some thought about why opioids are being prescribed for women after vaginal delivery and how to best manage postdelivery pain. This is especially important in areas of the country that have extraordinarily high rates of opioid use disorder.”
A total of 12% of the women (18,131) filled an outpatient prescription for an opioid with 5 days of giving birth. Of those, just 28.2% (5,110) had one or more conditions that cause an increased level of pain after delivery, such as bilateral tubal ligation, certain kinds of lacerations, and episiotomy.
During the first 5 days after birth, the most commonly prescribed opioid was oxycodone-acetaminophen (53.3%), followed by acetaminophen-codeine (20.5%), and hydrocodone-acetaminophen (19.6%).
Of the 18,131 women with an early postdelivery opioid prescription, 14% (2,592) filled at least one other opioid prescription within 6-60 days – that’s 1.6% of all the women in the study.
“On a positive note, we saw the supply of opioid prescriptions was generally short at 3-7 days,” Dr. Jarlenski said.
The researchers linked tobacco use and a mental health condition (both adjusted odds ratio 1.3; 95% confidence interval, 1.2-1.4) to a higher risk of filling a prescription without being diagnosed with a pain-causing disorder. They also found an association between substance use disorder (not related to opioids) and a higher risk of these types of prescriptions, but only for filling a second opioid prescription in the 6-60 day period (aOR 1.4; 95% CI, 1.2-1.6).
The researchers called for national guidelines regarding the use of opioids after birth.
“Several organizations have developed opioid prescribing guidelines for chronic and acute pain,” Dr. Jarlenski said. “These guidelines are necessary because the risk of opioid use disorder and subsequent overdose events is well established. Although delivery is the most common reason for hospitalization in the United States, there are no national guidelines for outpatient opioid use after vaginal delivery.”
The study was partially supported by the University of Pittsburgh, the Pennsylvania Department of Human Services, the Building Interdisciplinary Research Careers in Women’s Health Program, and the National Institute on Drug Abuse. The researchers reported having no relevant financial disclosures.
A new study of pregnant Medicaid patients in Pennsylvania found that 12% filled prescriptions for opioids within 5 days of vaginal delivery, even though fewer than one-third of the women had pain-inducing conditions.
“Our study raises the question: Why is outpatient opioid use not rare after vaginal delivery?” lead author Marian Jarlenski, PhD, MPH, said in an interview. “Outpatient opioid prescriptions after a hospitalization may be one potential pathway to opioid use disorder. I hope the study will prompt some thought about why opioids are being prescribed for women after vaginal delivery and how to best manage postdelivery pain. This is especially important in areas of the country that have extraordinarily high rates of opioid use disorder.”
A total of 12% of the women (18,131) filled an outpatient prescription for an opioid with 5 days of giving birth. Of those, just 28.2% (5,110) had one or more conditions that cause an increased level of pain after delivery, such as bilateral tubal ligation, certain kinds of lacerations, and episiotomy.
During the first 5 days after birth, the most commonly prescribed opioid was oxycodone-acetaminophen (53.3%), followed by acetaminophen-codeine (20.5%), and hydrocodone-acetaminophen (19.6%).
Of the 18,131 women with an early postdelivery opioid prescription, 14% (2,592) filled at least one other opioid prescription within 6-60 days – that’s 1.6% of all the women in the study.
“On a positive note, we saw the supply of opioid prescriptions was generally short at 3-7 days,” Dr. Jarlenski said.
The researchers linked tobacco use and a mental health condition (both adjusted odds ratio 1.3; 95% confidence interval, 1.2-1.4) to a higher risk of filling a prescription without being diagnosed with a pain-causing disorder. They also found an association between substance use disorder (not related to opioids) and a higher risk of these types of prescriptions, but only for filling a second opioid prescription in the 6-60 day period (aOR 1.4; 95% CI, 1.2-1.6).
The researchers called for national guidelines regarding the use of opioids after birth.
“Several organizations have developed opioid prescribing guidelines for chronic and acute pain,” Dr. Jarlenski said. “These guidelines are necessary because the risk of opioid use disorder and subsequent overdose events is well established. Although delivery is the most common reason for hospitalization in the United States, there are no national guidelines for outpatient opioid use after vaginal delivery.”
The study was partially supported by the University of Pittsburgh, the Pennsylvania Department of Human Services, the Building Interdisciplinary Research Careers in Women’s Health Program, and the National Institute on Drug Abuse. The researchers reported having no relevant financial disclosures.
FROM OBSTETRICS AND GYNECOLOGY
Key clinical point:
Major finding: A total of 12% of women on Medicaid filled opioid prescriptions within 5 days of delivery; just 28.2% of those patients had a pain-inducing condition.
Data source: A retrospective cohort study of 164,720 women enrolled in Medicaid in Pennsylvania who delivered live-born babies vaginally from 2008 to 2013.
Disclosures: The study is partially supported by the University of Pittsburgh, the Pennsylvania Department of Human Services, the Building Interdisciplinary Research Careers in Women’s Health Program, and the National Institute on Drug Abuse. The researchers reported having no relevant financial disclosures.
Review offers reassurance on prenatal Tdap vaccination safety
Combined tetanus, diphtheria, and pertussis (Tdap) vaccination during the second or third trimester of pregnancy does not appear to be associated with clinically significant harm to the fetus or neonate, according to findings from a systematic review of the literature.
However, the findings are limited by a dearth of randomized, placebo-controlled trials.
Point estimates for all anomalies after Tdap vaccination ranged from 1.20 to 1.60, Mark McMillan of the University of Adelaide, North Adelaide, Australia and his colleagues reported (Obstet Gynecol. 2017;129:560-73).
“Statistical imprecision for combined ‘all anomalies’ outcomes meant that upper 95% [confidence intervals] were 2.0 or above,” the researchers wrote. “Statistical imprecision was even greater in the individual congenital anomaly outcomes and little confidence can be placed in these estimates.”
Additionally, one of three studies assessing chorioamnionitis showed a small but significant increase in risk (relative risk, 1.19) after vaccination.
Among the studies examining medically attended adverse events, no association was seen between vaccination and such events or reactions, including neurologic events, gestational diabetes, preeclampsia or eclampsia, and cardiac events. Maternal effects included fever in 1%-3% of subjects, and headache, malaise, and myalgia, which were more common.
“Overall, despite the limitations described, the review offers reassurance for antenatal Tdap or Tdap-IPV [diphtheria, tetanus, pertussis, and polio] vaccination administered during the second or third trimester of pregnancy,” the researchers wrote. “These findings need to be interpreted in the context of the evidence of effectiveness of antenatal vaccination programs at preventing serious morbidity and mortality from pertussis in young infants.”
Mr. McMillan received travel support from GlaxoSmithKline, and institutional research grants from GSK and Sanofi Pasteur. Other researchers also reported receiving research funding and/or travel support from these companies.
Combined tetanus, diphtheria, and pertussis (Tdap) vaccination during the second or third trimester of pregnancy does not appear to be associated with clinically significant harm to the fetus or neonate, according to findings from a systematic review of the literature.
However, the findings are limited by a dearth of randomized, placebo-controlled trials.
Point estimates for all anomalies after Tdap vaccination ranged from 1.20 to 1.60, Mark McMillan of the University of Adelaide, North Adelaide, Australia and his colleagues reported (Obstet Gynecol. 2017;129:560-73).
“Statistical imprecision for combined ‘all anomalies’ outcomes meant that upper 95% [confidence intervals] were 2.0 or above,” the researchers wrote. “Statistical imprecision was even greater in the individual congenital anomaly outcomes and little confidence can be placed in these estimates.”
Additionally, one of three studies assessing chorioamnionitis showed a small but significant increase in risk (relative risk, 1.19) after vaccination.
Among the studies examining medically attended adverse events, no association was seen between vaccination and such events or reactions, including neurologic events, gestational diabetes, preeclampsia or eclampsia, and cardiac events. Maternal effects included fever in 1%-3% of subjects, and headache, malaise, and myalgia, which were more common.
“Overall, despite the limitations described, the review offers reassurance for antenatal Tdap or Tdap-IPV [diphtheria, tetanus, pertussis, and polio] vaccination administered during the second or third trimester of pregnancy,” the researchers wrote. “These findings need to be interpreted in the context of the evidence of effectiveness of antenatal vaccination programs at preventing serious morbidity and mortality from pertussis in young infants.”
Mr. McMillan received travel support from GlaxoSmithKline, and institutional research grants from GSK and Sanofi Pasteur. Other researchers also reported receiving research funding and/or travel support from these companies.
Combined tetanus, diphtheria, and pertussis (Tdap) vaccination during the second or third trimester of pregnancy does not appear to be associated with clinically significant harm to the fetus or neonate, according to findings from a systematic review of the literature.
However, the findings are limited by a dearth of randomized, placebo-controlled trials.
Point estimates for all anomalies after Tdap vaccination ranged from 1.20 to 1.60, Mark McMillan of the University of Adelaide, North Adelaide, Australia and his colleagues reported (Obstet Gynecol. 2017;129:560-73).
“Statistical imprecision for combined ‘all anomalies’ outcomes meant that upper 95% [confidence intervals] were 2.0 or above,” the researchers wrote. “Statistical imprecision was even greater in the individual congenital anomaly outcomes and little confidence can be placed in these estimates.”
Additionally, one of three studies assessing chorioamnionitis showed a small but significant increase in risk (relative risk, 1.19) after vaccination.
Among the studies examining medically attended adverse events, no association was seen between vaccination and such events or reactions, including neurologic events, gestational diabetes, preeclampsia or eclampsia, and cardiac events. Maternal effects included fever in 1%-3% of subjects, and headache, malaise, and myalgia, which were more common.
“Overall, despite the limitations described, the review offers reassurance for antenatal Tdap or Tdap-IPV [diphtheria, tetanus, pertussis, and polio] vaccination administered during the second or third trimester of pregnancy,” the researchers wrote. “These findings need to be interpreted in the context of the evidence of effectiveness of antenatal vaccination programs at preventing serious morbidity and mortality from pertussis in young infants.”
Mr. McMillan received travel support from GlaxoSmithKline, and institutional research grants from GSK and Sanofi Pasteur. Other researchers also reported receiving research funding and/or travel support from these companies.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: Point estimates for all anomalies after Tdap vaccination ranged from 1.20 to 1.60.
Data source: A systematic review of 21 studies.
Disclosures: Mr. McMillan received travel support from GlaxoSmithKline, and institutional research grants from GSK and Sanofi Pasteur. Other researchers also reported receiving research funding and/or travel support from these companies.
Crusted scabies outbreak: How much prophylaxis?
, a small case series suggests.
What remains a matter of debate is how widely to use prophylaxis, according to authors of a study of two approaches published in Infection, Disease & Health.
The case series, coauthored by Dr. Nikki R. Adler and her colleagues at Alfred Hospital in Melbourne, compares and contrasts two approaches to a scabies outbreak in a tertiary care setting (Infect Dis Health. 2017. doi: 10.1016/j.idh.2017.01.001).
One scenario involved an elderly woman who had been transferred from a rehabilitation facility for hip replacement surgery. Although upon admission the patient reported a pruritic truncal rash of 2 weeks’ duration, it was associated by the care team with either a cutaneous adverse drug reaction or with paraneoplastic syndrome, as she had recently been diagnosed with multiple myeloma. As a result, it wasn’t until after the patient’s emergent care needs were met 4 weeks later that she was given a formal dermatology consult, at which time several punch biopsies confirmed crusted scabies; she was treated with 5% permethrin cream for a week, weekly oral ivermectin 200 mcg/kg for 1 month, as well as with topical keratolytics.
Meanwhile, because the delayed diagnosis meant the patient – who had been treated across several wards – had potentially exposed multiple health care workers and patients to Sarcoptes scabiei, the hospital immediately instituted contact precautions and implemented its outbreak protocols: communication statements, prophylactic treatment of asymptomatic staff and close patients, and treatment and quarantine for those with clinical symptoms.
The second case involved an elderly man admitted through the emergency department after presenting with fever, hypotension, and a 3-week history of a progressive, hyperkeratotic, pruritic rash on his trunk and arms. A recent heart transplant recipient, he was taking cyclosporine, mycophenolate, and prednisolone, and he had hemodialysis-dependent end-stage kidney disease. After an ED dermatologic review, he was diagnosed with S. scabiei, immediately triggering contact precautions in the ED and elsewhere. He was treated with ivermectin, 5% permethrin, and topical keratolytics. All staff thought to have been exposed to the patient were treated prophylactically with 5% permethrin single-dose therapy.
Because thickened skin flakes that slough off in crusted scabies may house hundreds of mites for longer than 48 hours, environmental cleaning was enhanced in both cases.
The latter case did not feature a prolonged outbreak thanks to early diagnosis and quick preventive action. The outbreak in the first case lasted 7 weeks and 5 days. The hospital in that case opted not to employ a mass prophylaxis strategy, instead treating 306 persons identified to have been in contact with the patient. In all, 54 symptomatic patients and health care workers were identified.
The authors cited data that, across 19 nosocomial outbreaks between 1990 and 2003, the mean number of infested patients was 18; the mean number for health care workers was 39. The attack rate, defined as the number of new cases divided by the total number of persons at risk, was 13% for patients and 35% in health care workers. The median duration of outbreak was 14.5 weeks (range, 4-52 weeks).
“The variation of outbreak size and duration in the reported literature suggests that there may be important differences in the efficacy of various infection control strategies,” Dr. Adler and her colleagues wrote, noting that while some institutions might prefer simultaneous mass prophylaxis to rapidly and efficiently control a scabies outbreak, the cost of doing so can be prohibitive, and might not be more effective than the information-centered management model used in Case 1 that relied on close tracking of all patient contacts, and use of the hospital intranet and internal memos.
This strategy does run the risk of overreaction, however: “The communication strategy may have contributed to heightened levels of concern among staff and arguably, excessive prophylaxis and/or overdiagnosis,” the authors wrote.
To help diagnose potential cases of crusted scabies quickly, Dr. Adler and her colleagues suggested clinicians consider that various dermatoses can mimic a scabies infestation and that care teams have a high index of suspicion in patients most at risk for scabies: the elderly and those who are immunocompromised, such as the heart transplant patient in Case 2, and also those with altered T-cell function.
[email protected]
On Twitter @whitneymcknight
, a small case series suggests.
What remains a matter of debate is how widely to use prophylaxis, according to authors of a study of two approaches published in Infection, Disease & Health.
The case series, coauthored by Dr. Nikki R. Adler and her colleagues at Alfred Hospital in Melbourne, compares and contrasts two approaches to a scabies outbreak in a tertiary care setting (Infect Dis Health. 2017. doi: 10.1016/j.idh.2017.01.001).
One scenario involved an elderly woman who had been transferred from a rehabilitation facility for hip replacement surgery. Although upon admission the patient reported a pruritic truncal rash of 2 weeks’ duration, it was associated by the care team with either a cutaneous adverse drug reaction or with paraneoplastic syndrome, as she had recently been diagnosed with multiple myeloma. As a result, it wasn’t until after the patient’s emergent care needs were met 4 weeks later that she was given a formal dermatology consult, at which time several punch biopsies confirmed crusted scabies; she was treated with 5% permethrin cream for a week, weekly oral ivermectin 200 mcg/kg for 1 month, as well as with topical keratolytics.
Meanwhile, because the delayed diagnosis meant the patient – who had been treated across several wards – had potentially exposed multiple health care workers and patients to Sarcoptes scabiei, the hospital immediately instituted contact precautions and implemented its outbreak protocols: communication statements, prophylactic treatment of asymptomatic staff and close patients, and treatment and quarantine for those with clinical symptoms.
The second case involved an elderly man admitted through the emergency department after presenting with fever, hypotension, and a 3-week history of a progressive, hyperkeratotic, pruritic rash on his trunk and arms. A recent heart transplant recipient, he was taking cyclosporine, mycophenolate, and prednisolone, and he had hemodialysis-dependent end-stage kidney disease. After an ED dermatologic review, he was diagnosed with S. scabiei, immediately triggering contact precautions in the ED and elsewhere. He was treated with ivermectin, 5% permethrin, and topical keratolytics. All staff thought to have been exposed to the patient were treated prophylactically with 5% permethrin single-dose therapy.
Because thickened skin flakes that slough off in crusted scabies may house hundreds of mites for longer than 48 hours, environmental cleaning was enhanced in both cases.
The latter case did not feature a prolonged outbreak thanks to early diagnosis and quick preventive action. The outbreak in the first case lasted 7 weeks and 5 days. The hospital in that case opted not to employ a mass prophylaxis strategy, instead treating 306 persons identified to have been in contact with the patient. In all, 54 symptomatic patients and health care workers were identified.
The authors cited data that, across 19 nosocomial outbreaks between 1990 and 2003, the mean number of infested patients was 18; the mean number for health care workers was 39. The attack rate, defined as the number of new cases divided by the total number of persons at risk, was 13% for patients and 35% in health care workers. The median duration of outbreak was 14.5 weeks (range, 4-52 weeks).
“The variation of outbreak size and duration in the reported literature suggests that there may be important differences in the efficacy of various infection control strategies,” Dr. Adler and her colleagues wrote, noting that while some institutions might prefer simultaneous mass prophylaxis to rapidly and efficiently control a scabies outbreak, the cost of doing so can be prohibitive, and might not be more effective than the information-centered management model used in Case 1 that relied on close tracking of all patient contacts, and use of the hospital intranet and internal memos.
This strategy does run the risk of overreaction, however: “The communication strategy may have contributed to heightened levels of concern among staff and arguably, excessive prophylaxis and/or overdiagnosis,” the authors wrote.
To help diagnose potential cases of crusted scabies quickly, Dr. Adler and her colleagues suggested clinicians consider that various dermatoses can mimic a scabies infestation and that care teams have a high index of suspicion in patients most at risk for scabies: the elderly and those who are immunocompromised, such as the heart transplant patient in Case 2, and also those with altered T-cell function.
[email protected]
On Twitter @whitneymcknight
, a small case series suggests.
What remains a matter of debate is how widely to use prophylaxis, according to authors of a study of two approaches published in Infection, Disease & Health.
The case series, coauthored by Dr. Nikki R. Adler and her colleagues at Alfred Hospital in Melbourne, compares and contrasts two approaches to a scabies outbreak in a tertiary care setting (Infect Dis Health. 2017. doi: 10.1016/j.idh.2017.01.001).
One scenario involved an elderly woman who had been transferred from a rehabilitation facility for hip replacement surgery. Although upon admission the patient reported a pruritic truncal rash of 2 weeks’ duration, it was associated by the care team with either a cutaneous adverse drug reaction or with paraneoplastic syndrome, as she had recently been diagnosed with multiple myeloma. As a result, it wasn’t until after the patient’s emergent care needs were met 4 weeks later that she was given a formal dermatology consult, at which time several punch biopsies confirmed crusted scabies; she was treated with 5% permethrin cream for a week, weekly oral ivermectin 200 mcg/kg for 1 month, as well as with topical keratolytics.
Meanwhile, because the delayed diagnosis meant the patient – who had been treated across several wards – had potentially exposed multiple health care workers and patients to Sarcoptes scabiei, the hospital immediately instituted contact precautions and implemented its outbreak protocols: communication statements, prophylactic treatment of asymptomatic staff and close patients, and treatment and quarantine for those with clinical symptoms.
The second case involved an elderly man admitted through the emergency department after presenting with fever, hypotension, and a 3-week history of a progressive, hyperkeratotic, pruritic rash on his trunk and arms. A recent heart transplant recipient, he was taking cyclosporine, mycophenolate, and prednisolone, and he had hemodialysis-dependent end-stage kidney disease. After an ED dermatologic review, he was diagnosed with S. scabiei, immediately triggering contact precautions in the ED and elsewhere. He was treated with ivermectin, 5% permethrin, and topical keratolytics. All staff thought to have been exposed to the patient were treated prophylactically with 5% permethrin single-dose therapy.
Because thickened skin flakes that slough off in crusted scabies may house hundreds of mites for longer than 48 hours, environmental cleaning was enhanced in both cases.
The latter case did not feature a prolonged outbreak thanks to early diagnosis and quick preventive action. The outbreak in the first case lasted 7 weeks and 5 days. The hospital in that case opted not to employ a mass prophylaxis strategy, instead treating 306 persons identified to have been in contact with the patient. In all, 54 symptomatic patients and health care workers were identified.
The authors cited data that, across 19 nosocomial outbreaks between 1990 and 2003, the mean number of infested patients was 18; the mean number for health care workers was 39. The attack rate, defined as the number of new cases divided by the total number of persons at risk, was 13% for patients and 35% in health care workers. The median duration of outbreak was 14.5 weeks (range, 4-52 weeks).
“The variation of outbreak size and duration in the reported literature suggests that there may be important differences in the efficacy of various infection control strategies,” Dr. Adler and her colleagues wrote, noting that while some institutions might prefer simultaneous mass prophylaxis to rapidly and efficiently control a scabies outbreak, the cost of doing so can be prohibitive, and might not be more effective than the information-centered management model used in Case 1 that relied on close tracking of all patient contacts, and use of the hospital intranet and internal memos.
This strategy does run the risk of overreaction, however: “The communication strategy may have contributed to heightened levels of concern among staff and arguably, excessive prophylaxis and/or overdiagnosis,” the authors wrote.
To help diagnose potential cases of crusted scabies quickly, Dr. Adler and her colleagues suggested clinicians consider that various dermatoses can mimic a scabies infestation and that care teams have a high index of suspicion in patients most at risk for scabies: the elderly and those who are immunocompromised, such as the heart transplant patient in Case 2, and also those with altered T-cell function.
[email protected]
On Twitter @whitneymcknight
FROM INFECTION, DISEASE, & HEALTH
Verrucous Carcinoma of the Buccal Mucosa With Extension to the Cheek
To the Editor:
Verrucous carcinoma is an uncommon type of squamous cell carcinoma (SCC) and was first described by Ackerman1 in 1948. Rock and Fisher2 called this condition oral florid papillomatosis. The distinctive features of this tumor are low-grade malignancy, slow growth, local invasiveness, and rarely intraoral and extraoral metastasis. Extraorally, it can occur in any part of the body,3 a common site being the anogenital region. Depending on the area of occurrence, the condition also is known as Buschke-Lowenstein tumor4 or giant condyloma acuminatum (anogenital region) and carcinoma cuniculatum5 (plantar region). The exact etiology of the condition is unknown, though it is associated with human papillomavirus infection, traumatic scars, chronic infection, tobacco, and chemical carcinogens.3 We report a rare case of verrucous carcinoma originating from the buccal mucosa that subsequently spread to involve the lip and cheek as a large cauliflowerlike growth, which is an unusual presentation.
A 65-year-old man presented to the dermatology department with a painless growth inside the left side of the oral cavity that had developed 5 years prior as a growth on the left buccal mucosa. The lesion gradually increased in size to involve the left oral commissure including the upper and lower lips and the skin of the left cheek; it extended beyond the nasolabial fold in a cauliflowerlike pattern. The lesion was insidious in onset and was not associated with pain, itching, or bleeding. The patient chewed tobacco for the last 40 years, with no similar lesions on any part of the body. On physical examination a warty papilliform lesion was seen on the left buccal mucosa with extension to 2 cm of the upper and lower lip on the left side including the left oral commissure and the skin of the left cheek beyond the nasolabial fold where it appeared as a cauliflowerlike growth measuring 4×5 cm in size (Figure 1). No notable lymphadenopathy was present.

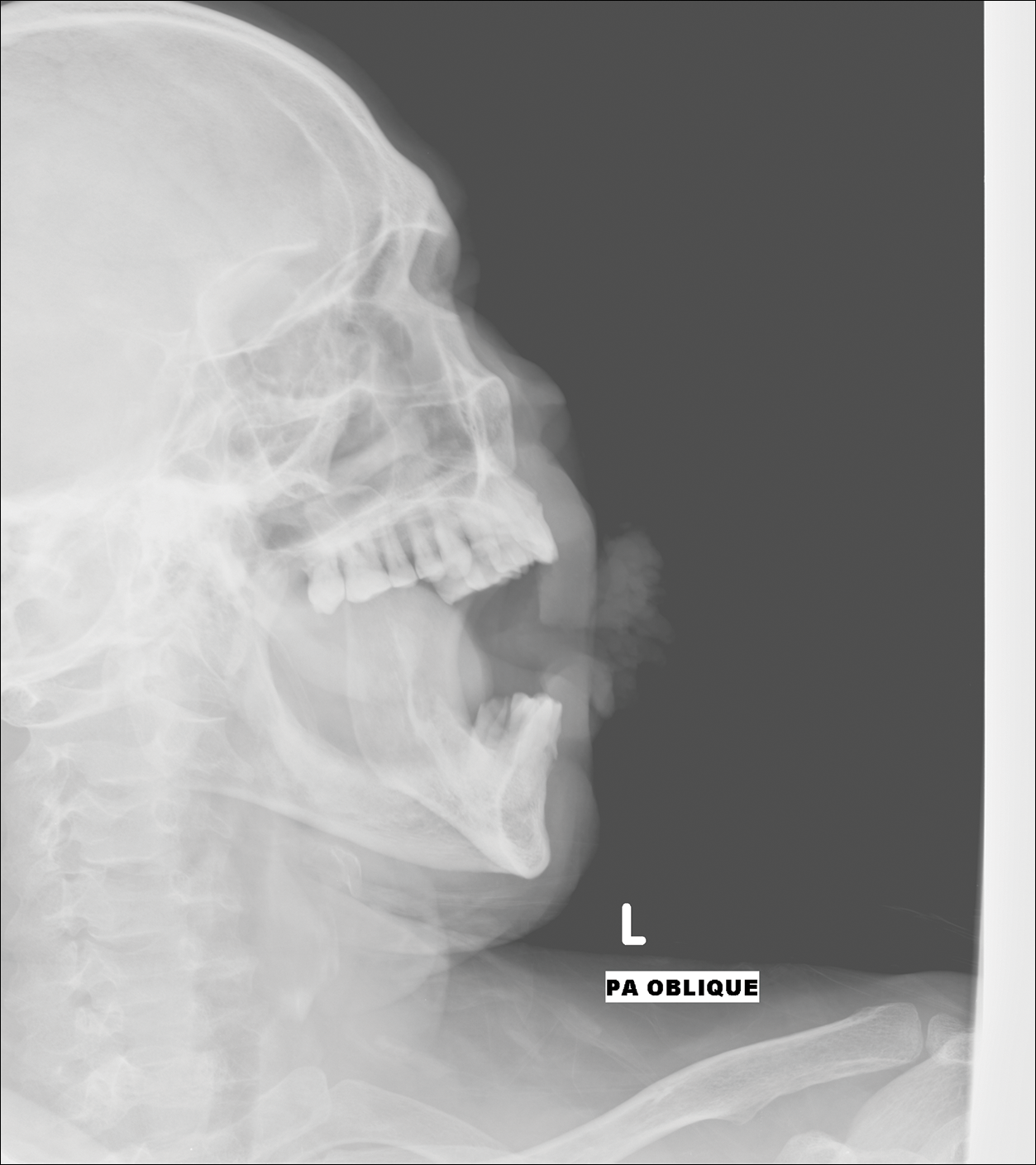
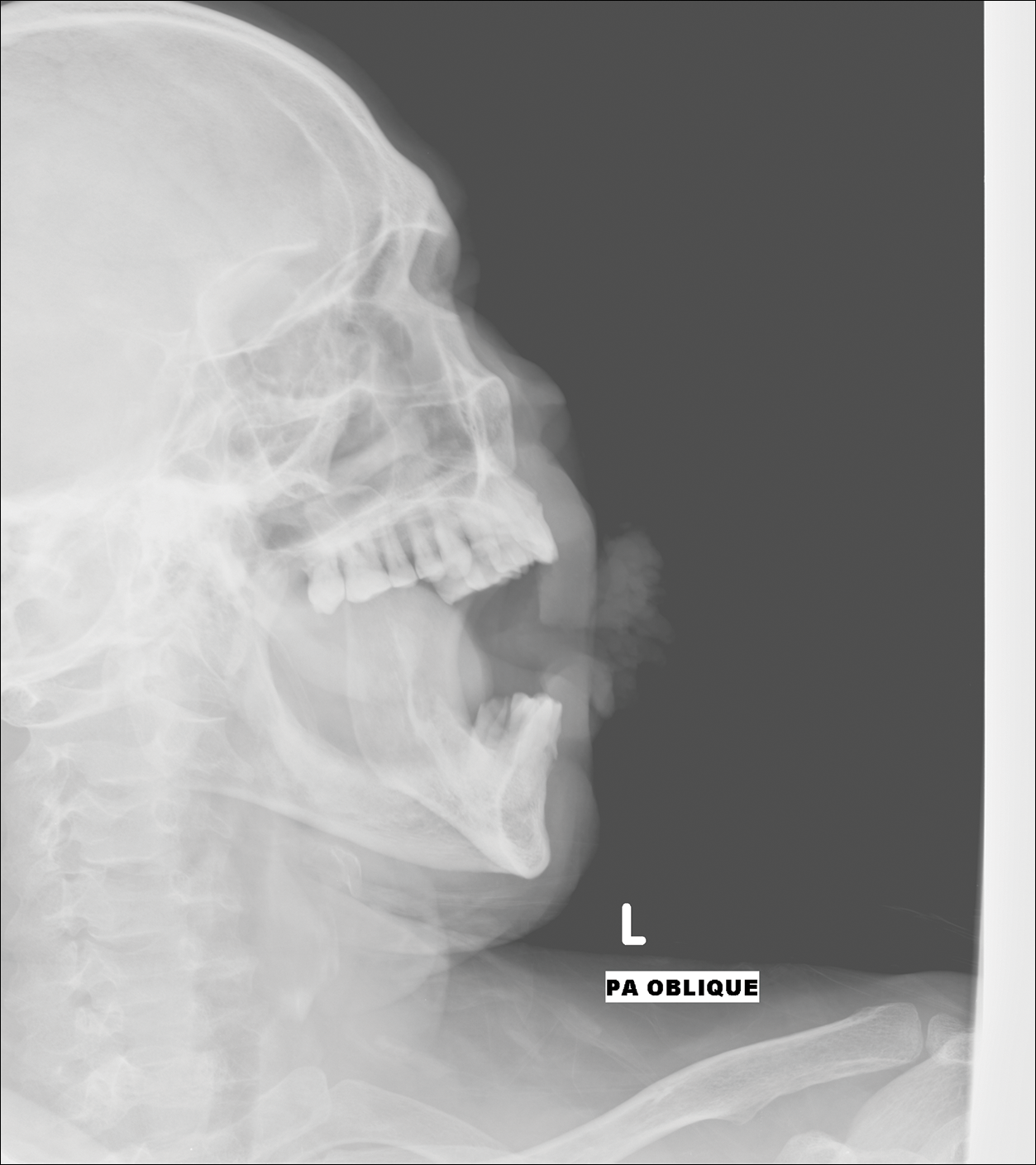
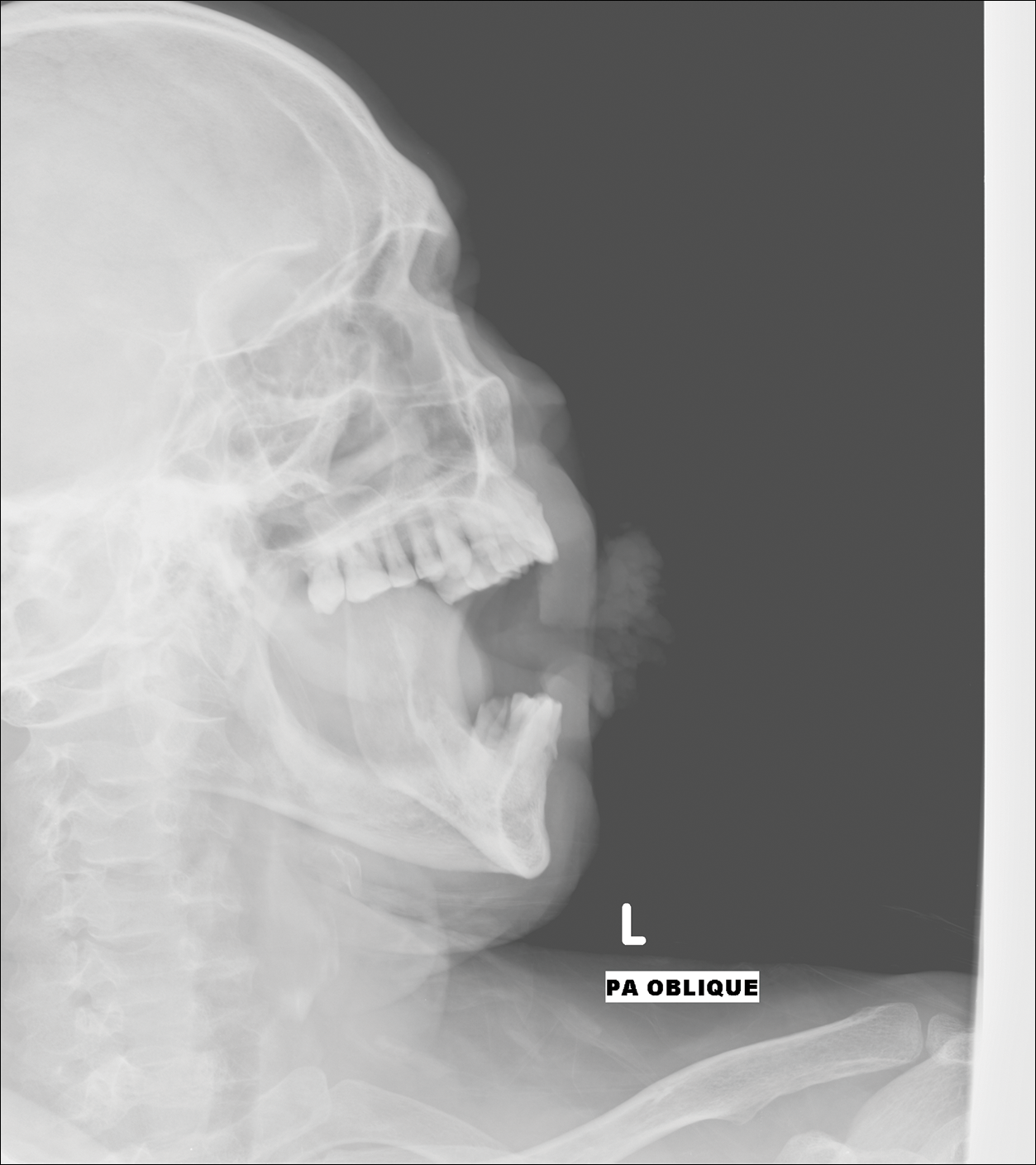
Digital radiographs of the skull (posteroanterior oblique view)(Figure 2) and mandible (left oblique view) showed a lobulated soft-tissue density lesion overlying the left half of the mandible (near the mandibular angle) with involvement of both the upper and lower lips on the left side. However, no obvious underlying bony erosion was noted.
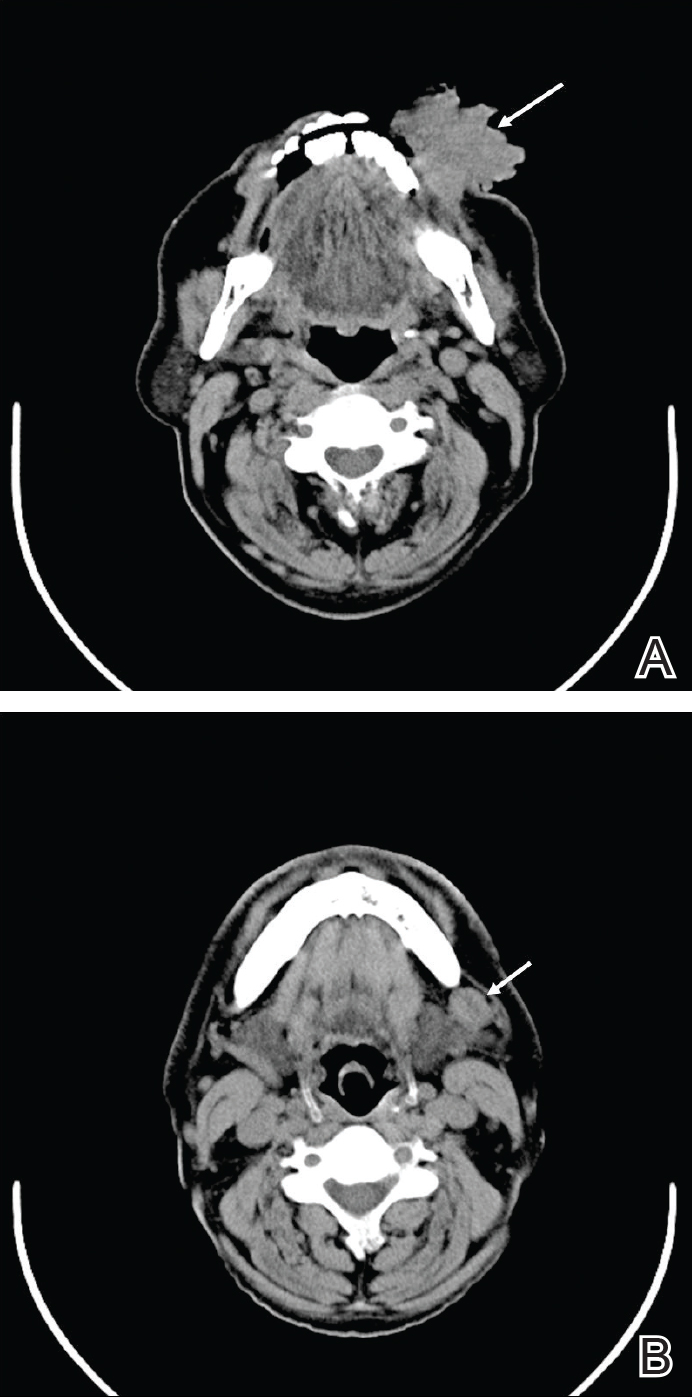
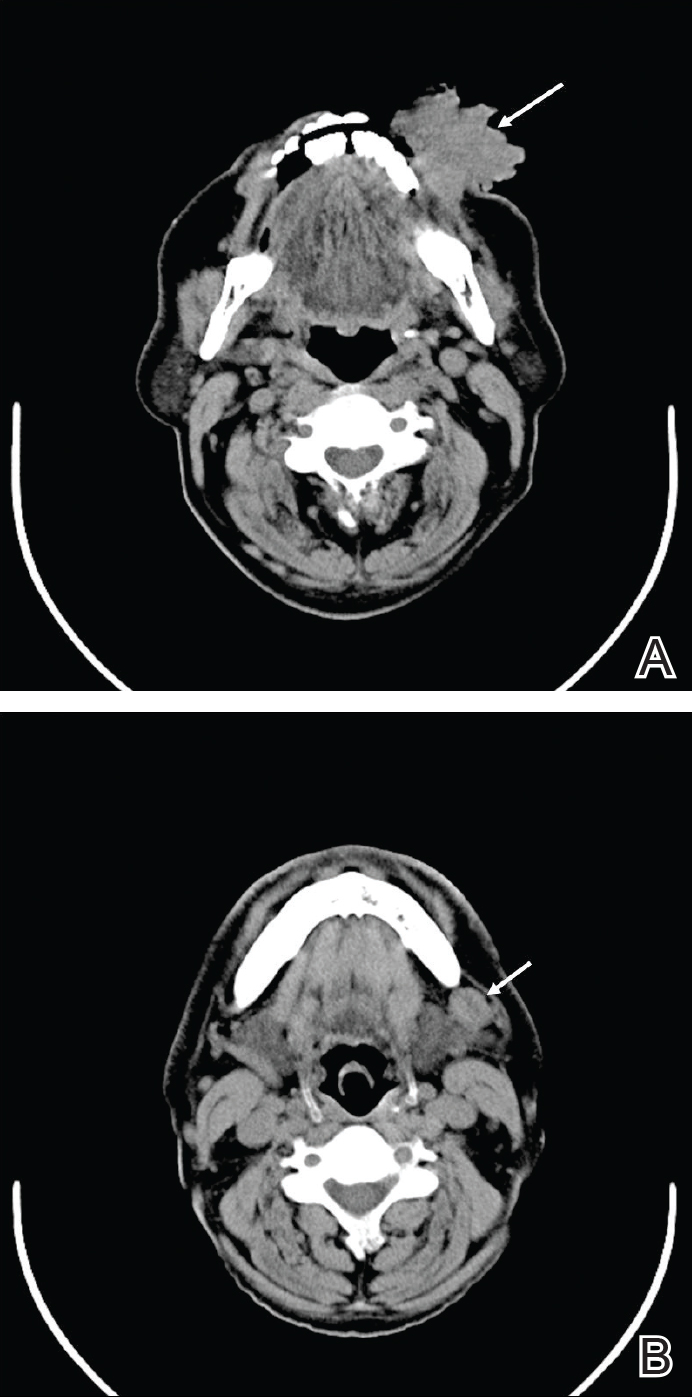
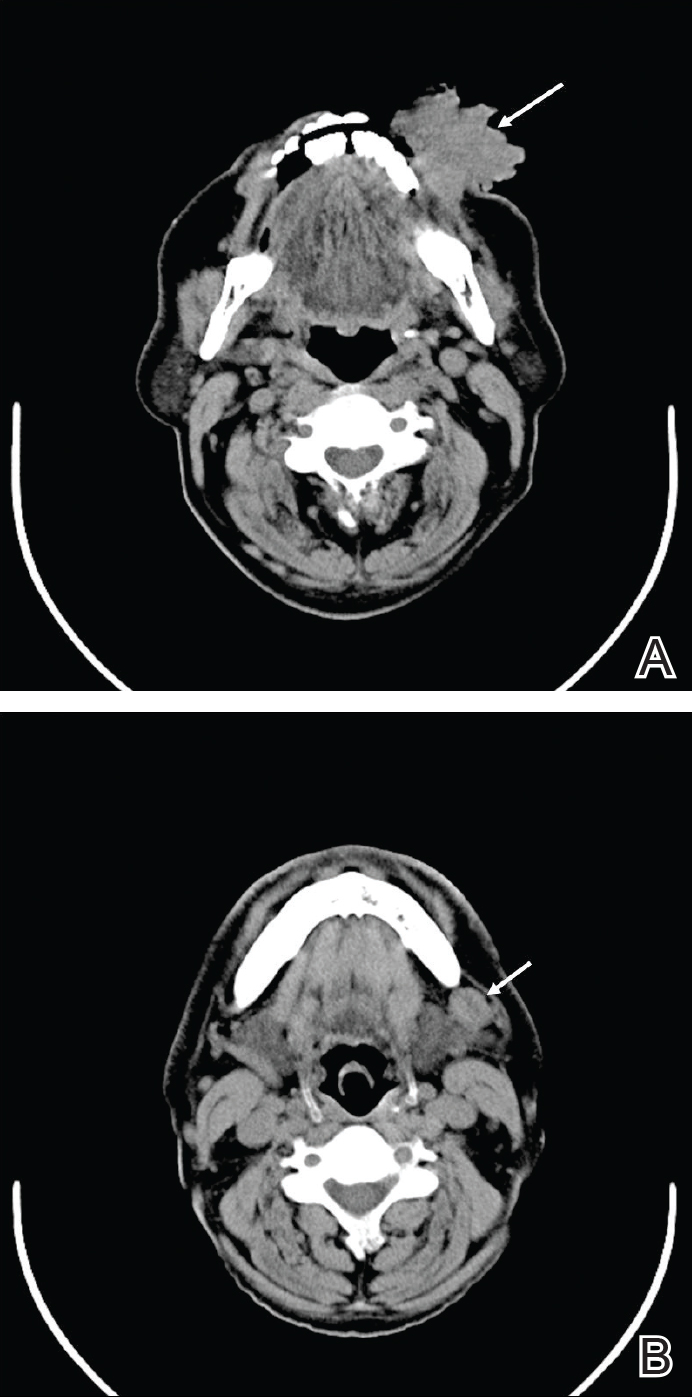
Computed tomography revealed a large soft-tissue mass (41.3×35.3 mm)(Figure 3A) involving the left buccal mucosa with extension into overlying muscle, subcutaneous tissue, and skin. Externally, the lesion was exophytic, irregular, and polypoidal with surface ulceration. Medially, the lesion involved the left oral commissure and parts of the adjoining upper and lower lips. No underlying bony erosion was seen. An enlarged lymph node measuring 20×15 mm was noted in the left upper deep cervical group in the submandibular region (Figure 3B).
Our clinical differential diagnosis included verrucous carcinoma and hypertrophic variety of lupus vulgaris. A 1×2-cm diagnostic incisional biopsy was performed from the cauliflowerlike growth and ultrasound-guided fine-needle aspiration was done from the lymph node. Histopathology revealed a hyperplastic stratified squamous epithelium with upward extension of verrucous projections, which was largely superficial to the adjacent epithelium (Figure 4A). In addition to the surface verrucous projections, there was lesion extension into the subepithelial zone in the form of round club-shaped protrusions (Figure 4B). There was no loss of polarity in these downward proliferations. No horn pearl formation was present. Fine-needle aspiration revealed reactive lymphadenitis.

The final diagnosis of verrucous carcinoma was made and the patient was referred to the oncosurgery department for further management.
Verrucous carcinoma is a rare, low-grade, well-differentiated SCC of the skin or mucosa presenting with a verrucoid or cauliflowerlike appearance. It shows locally aggressive behavior and has low metastatic potential,6 a low degree of dysplasia, and a good prognosis. Because it is a tumor with predominantly horizontal growth, it tends to erode more than infiltrate. It does not present with remote metastasis.7 It has been known by several different names, usually related to anatomic sites (eg, Ackerman tumor, oral florid papillomatosis, carcinoma cuniculatum).
In the oral cavity, verrucous carcinoma constitutes 2% to 4.5% of all forms of SCC seen mainly in men older than 50 years and also is associated with a high incidence (37.7%) of a second primary tumor mainly in the oral mucosa (eg, tongue, lips, palate, salivary gland).8 Indudharan et al9 reported a case of verrucous carcinoma of the maxillary antrum in a young male patient, which also was a rare entity. Verrucous carcinoma is thought to predominantly affect elderly men. Walvekar et al10 reported a male to female ratio of 3.6 to 1 in patients with verrucous carcinoma, with a mean age of 53.9 years. According to Varshney et al,11 patients may range in age from the fourth to eighth decades of life, with a mean age of 60 years; 80% are male. The etiopathogenesis of verrucous carcinoma is related to the following carcinogens: biologic (eg, human papillomavirus), chemical (eg, smoking), and physical (eg, constant trauma).
Verrucous carcinoma should be considered in the differential diagnosis of slow-growing, locally spreading tumors. Oral tumors, especially in tobacco chewers, should raise suspicion of verrucous carcinoma, which will enable prompt management of the tumor.
- Ackerman LV. Verrucous carcinoma of the oral cavity. Surgery. 1948;23:670-678.
- Rock JA, Fisher ER. Florid papillomatosis of the oral cavity and larynx. Arch Otolaryngol. 1960;72:593-598.
- Pattee SF, Bordeaux J, Mahalingam M, et al. Verrucous carcinoma of the scalp. J Am Acad Dermatol. 2007;56:506-507.
- Buschke A, Lowenstein L. Uber carcinomahnliche condylomata acuminata despenis. Klin Wochenschr. 1925;4:1726-1728.
- Aird I, Johnson HD, Lennox B, et al. Epithelioma cuniculatum: a variety of squamous carcinoma peculiar to the foot. Br J Surg. 1954;42:245-250.
- Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-21.
- Zanini M, Wulkan C, Paschoal FM, et al. Verrucous carcinoma: a clinical histopathologic variant of squamous cell carcinoma. An Bras Dermatol. 2004;79:619-621.
- Kalsotra P, Manhas M, Sood R. Verrucous carcinoma of hard palate. JK Science. 2000;2:52-54.
- Indudharan R, Das PK, Thida T. Verrucous carcinoma of maxillary antrum. Singapore Med J. 1996;37:559-561.
- Walvekar RR, Chaukar DA, Deshpande MS, et al. Verrucous carcinoma of the oral cavity: a clinical and pathological study of 101 cases. Oral Oncol. 2009;45:47-51.
- Varshney S, Singh J, Saxena RK, et al. Verrucous carcinoma of larynx. Indian J Otolaryngol Head Neck Surg. 2004;56:54-56.
To the Editor:
Verrucous carcinoma is an uncommon type of squamous cell carcinoma (SCC) and was first described by Ackerman1 in 1948. Rock and Fisher2 called this condition oral florid papillomatosis. The distinctive features of this tumor are low-grade malignancy, slow growth, local invasiveness, and rarely intraoral and extraoral metastasis. Extraorally, it can occur in any part of the body,3 a common site being the anogenital region. Depending on the area of occurrence, the condition also is known as Buschke-Lowenstein tumor4 or giant condyloma acuminatum (anogenital region) and carcinoma cuniculatum5 (plantar region). The exact etiology of the condition is unknown, though it is associated with human papillomavirus infection, traumatic scars, chronic infection, tobacco, and chemical carcinogens.3 We report a rare case of verrucous carcinoma originating from the buccal mucosa that subsequently spread to involve the lip and cheek as a large cauliflowerlike growth, which is an unusual presentation.
A 65-year-old man presented to the dermatology department with a painless growth inside the left side of the oral cavity that had developed 5 years prior as a growth on the left buccal mucosa. The lesion gradually increased in size to involve the left oral commissure including the upper and lower lips and the skin of the left cheek; it extended beyond the nasolabial fold in a cauliflowerlike pattern. The lesion was insidious in onset and was not associated with pain, itching, or bleeding. The patient chewed tobacco for the last 40 years, with no similar lesions on any part of the body. On physical examination a warty papilliform lesion was seen on the left buccal mucosa with extension to 2 cm of the upper and lower lip on the left side including the left oral commissure and the skin of the left cheek beyond the nasolabial fold where it appeared as a cauliflowerlike growth measuring 4×5 cm in size (Figure 1). No notable lymphadenopathy was present.

Digital radiographs of the skull (posteroanterior oblique view)(Figure 2) and mandible (left oblique view) showed a lobulated soft-tissue density lesion overlying the left half of the mandible (near the mandibular angle) with involvement of both the upper and lower lips on the left side. However, no obvious underlying bony erosion was noted.
Computed tomography revealed a large soft-tissue mass (41.3×35.3 mm)(Figure 3A) involving the left buccal mucosa with extension into overlying muscle, subcutaneous tissue, and skin. Externally, the lesion was exophytic, irregular, and polypoidal with surface ulceration. Medially, the lesion involved the left oral commissure and parts of the adjoining upper and lower lips. No underlying bony erosion was seen. An enlarged lymph node measuring 20×15 mm was noted in the left upper deep cervical group in the submandibular region (Figure 3B).
Our clinical differential diagnosis included verrucous carcinoma and hypertrophic variety of lupus vulgaris. A 1×2-cm diagnostic incisional biopsy was performed from the cauliflowerlike growth and ultrasound-guided fine-needle aspiration was done from the lymph node. Histopathology revealed a hyperplastic stratified squamous epithelium with upward extension of verrucous projections, which was largely superficial to the adjacent epithelium (Figure 4A). In addition to the surface verrucous projections, there was lesion extension into the subepithelial zone in the form of round club-shaped protrusions (Figure 4B). There was no loss of polarity in these downward proliferations. No horn pearl formation was present. Fine-needle aspiration revealed reactive lymphadenitis.

The final diagnosis of verrucous carcinoma was made and the patient was referred to the oncosurgery department for further management.
Verrucous carcinoma is a rare, low-grade, well-differentiated SCC of the skin or mucosa presenting with a verrucoid or cauliflowerlike appearance. It shows locally aggressive behavior and has low metastatic potential,6 a low degree of dysplasia, and a good prognosis. Because it is a tumor with predominantly horizontal growth, it tends to erode more than infiltrate. It does not present with remote metastasis.7 It has been known by several different names, usually related to anatomic sites (eg, Ackerman tumor, oral florid papillomatosis, carcinoma cuniculatum).
In the oral cavity, verrucous carcinoma constitutes 2% to 4.5% of all forms of SCC seen mainly in men older than 50 years and also is associated with a high incidence (37.7%) of a second primary tumor mainly in the oral mucosa (eg, tongue, lips, palate, salivary gland).8 Indudharan et al9 reported a case of verrucous carcinoma of the maxillary antrum in a young male patient, which also was a rare entity. Verrucous carcinoma is thought to predominantly affect elderly men. Walvekar et al10 reported a male to female ratio of 3.6 to 1 in patients with verrucous carcinoma, with a mean age of 53.9 years. According to Varshney et al,11 patients may range in age from the fourth to eighth decades of life, with a mean age of 60 years; 80% are male. The etiopathogenesis of verrucous carcinoma is related to the following carcinogens: biologic (eg, human papillomavirus), chemical (eg, smoking), and physical (eg, constant trauma).
Verrucous carcinoma should be considered in the differential diagnosis of slow-growing, locally spreading tumors. Oral tumors, especially in tobacco chewers, should raise suspicion of verrucous carcinoma, which will enable prompt management of the tumor.
To the Editor:
Verrucous carcinoma is an uncommon type of squamous cell carcinoma (SCC) and was first described by Ackerman1 in 1948. Rock and Fisher2 called this condition oral florid papillomatosis. The distinctive features of this tumor are low-grade malignancy, slow growth, local invasiveness, and rarely intraoral and extraoral metastasis. Extraorally, it can occur in any part of the body,3 a common site being the anogenital region. Depending on the area of occurrence, the condition also is known as Buschke-Lowenstein tumor4 or giant condyloma acuminatum (anogenital region) and carcinoma cuniculatum5 (plantar region). The exact etiology of the condition is unknown, though it is associated with human papillomavirus infection, traumatic scars, chronic infection, tobacco, and chemical carcinogens.3 We report a rare case of verrucous carcinoma originating from the buccal mucosa that subsequently spread to involve the lip and cheek as a large cauliflowerlike growth, which is an unusual presentation.
A 65-year-old man presented to the dermatology department with a painless growth inside the left side of the oral cavity that had developed 5 years prior as a growth on the left buccal mucosa. The lesion gradually increased in size to involve the left oral commissure including the upper and lower lips and the skin of the left cheek; it extended beyond the nasolabial fold in a cauliflowerlike pattern. The lesion was insidious in onset and was not associated with pain, itching, or bleeding. The patient chewed tobacco for the last 40 years, with no similar lesions on any part of the body. On physical examination a warty papilliform lesion was seen on the left buccal mucosa with extension to 2 cm of the upper and lower lip on the left side including the left oral commissure and the skin of the left cheek beyond the nasolabial fold where it appeared as a cauliflowerlike growth measuring 4×5 cm in size (Figure 1). No notable lymphadenopathy was present.

Digital radiographs of the skull (posteroanterior oblique view)(Figure 2) and mandible (left oblique view) showed a lobulated soft-tissue density lesion overlying the left half of the mandible (near the mandibular angle) with involvement of both the upper and lower lips on the left side. However, no obvious underlying bony erosion was noted.
Computed tomography revealed a large soft-tissue mass (41.3×35.3 mm)(Figure 3A) involving the left buccal mucosa with extension into overlying muscle, subcutaneous tissue, and skin. Externally, the lesion was exophytic, irregular, and polypoidal with surface ulceration. Medially, the lesion involved the left oral commissure and parts of the adjoining upper and lower lips. No underlying bony erosion was seen. An enlarged lymph node measuring 20×15 mm was noted in the left upper deep cervical group in the submandibular region (Figure 3B).
Our clinical differential diagnosis included verrucous carcinoma and hypertrophic variety of lupus vulgaris. A 1×2-cm diagnostic incisional biopsy was performed from the cauliflowerlike growth and ultrasound-guided fine-needle aspiration was done from the lymph node. Histopathology revealed a hyperplastic stratified squamous epithelium with upward extension of verrucous projections, which was largely superficial to the adjacent epithelium (Figure 4A). In addition to the surface verrucous projections, there was lesion extension into the subepithelial zone in the form of round club-shaped protrusions (Figure 4B). There was no loss of polarity in these downward proliferations. No horn pearl formation was present. Fine-needle aspiration revealed reactive lymphadenitis.

The final diagnosis of verrucous carcinoma was made and the patient was referred to the oncosurgery department for further management.
Verrucous carcinoma is a rare, low-grade, well-differentiated SCC of the skin or mucosa presenting with a verrucoid or cauliflowerlike appearance. It shows locally aggressive behavior and has low metastatic potential,6 a low degree of dysplasia, and a good prognosis. Because it is a tumor with predominantly horizontal growth, it tends to erode more than infiltrate. It does not present with remote metastasis.7 It has been known by several different names, usually related to anatomic sites (eg, Ackerman tumor, oral florid papillomatosis, carcinoma cuniculatum).
In the oral cavity, verrucous carcinoma constitutes 2% to 4.5% of all forms of SCC seen mainly in men older than 50 years and also is associated with a high incidence (37.7%) of a second primary tumor mainly in the oral mucosa (eg, tongue, lips, palate, salivary gland).8 Indudharan et al9 reported a case of verrucous carcinoma of the maxillary antrum in a young male patient, which also was a rare entity. Verrucous carcinoma is thought to predominantly affect elderly men. Walvekar et al10 reported a male to female ratio of 3.6 to 1 in patients with verrucous carcinoma, with a mean age of 53.9 years. According to Varshney et al,11 patients may range in age from the fourth to eighth decades of life, with a mean age of 60 years; 80% are male. The etiopathogenesis of verrucous carcinoma is related to the following carcinogens: biologic (eg, human papillomavirus), chemical (eg, smoking), and physical (eg, constant trauma).
Verrucous carcinoma should be considered in the differential diagnosis of slow-growing, locally spreading tumors. Oral tumors, especially in tobacco chewers, should raise suspicion of verrucous carcinoma, which will enable prompt management of the tumor.
- Ackerman LV. Verrucous carcinoma of the oral cavity. Surgery. 1948;23:670-678.
- Rock JA, Fisher ER. Florid papillomatosis of the oral cavity and larynx. Arch Otolaryngol. 1960;72:593-598.
- Pattee SF, Bordeaux J, Mahalingam M, et al. Verrucous carcinoma of the scalp. J Am Acad Dermatol. 2007;56:506-507.
- Buschke A, Lowenstein L. Uber carcinomahnliche condylomata acuminata despenis. Klin Wochenschr. 1925;4:1726-1728.
- Aird I, Johnson HD, Lennox B, et al. Epithelioma cuniculatum: a variety of squamous carcinoma peculiar to the foot. Br J Surg. 1954;42:245-250.
- Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-21.
- Zanini M, Wulkan C, Paschoal FM, et al. Verrucous carcinoma: a clinical histopathologic variant of squamous cell carcinoma. An Bras Dermatol. 2004;79:619-621.
- Kalsotra P, Manhas M, Sood R. Verrucous carcinoma of hard palate. JK Science. 2000;2:52-54.
- Indudharan R, Das PK, Thida T. Verrucous carcinoma of maxillary antrum. Singapore Med J. 1996;37:559-561.
- Walvekar RR, Chaukar DA, Deshpande MS, et al. Verrucous carcinoma of the oral cavity: a clinical and pathological study of 101 cases. Oral Oncol. 2009;45:47-51.
- Varshney S, Singh J, Saxena RK, et al. Verrucous carcinoma of larynx. Indian J Otolaryngol Head Neck Surg. 2004;56:54-56.
- Ackerman LV. Verrucous carcinoma of the oral cavity. Surgery. 1948;23:670-678.
- Rock JA, Fisher ER. Florid papillomatosis of the oral cavity and larynx. Arch Otolaryngol. 1960;72:593-598.
- Pattee SF, Bordeaux J, Mahalingam M, et al. Verrucous carcinoma of the scalp. J Am Acad Dermatol. 2007;56:506-507.
- Buschke A, Lowenstein L. Uber carcinomahnliche condylomata acuminata despenis. Klin Wochenschr. 1925;4:1726-1728.
- Aird I, Johnson HD, Lennox B, et al. Epithelioma cuniculatum: a variety of squamous carcinoma peculiar to the foot. Br J Surg. 1954;42:245-250.
- Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-21.
- Zanini M, Wulkan C, Paschoal FM, et al. Verrucous carcinoma: a clinical histopathologic variant of squamous cell carcinoma. An Bras Dermatol. 2004;79:619-621.
- Kalsotra P, Manhas M, Sood R. Verrucous carcinoma of hard palate. JK Science. 2000;2:52-54.
- Indudharan R, Das PK, Thida T. Verrucous carcinoma of maxillary antrum. Singapore Med J. 1996;37:559-561.
- Walvekar RR, Chaukar DA, Deshpande MS, et al. Verrucous carcinoma of the oral cavity: a clinical and pathological study of 101 cases. Oral Oncol. 2009;45:47-51.
- Varshney S, Singh J, Saxena RK, et al. Verrucous carcinoma of larynx. Indian J Otolaryngol Head Neck Surg. 2004;56:54-56.
Practice Points
- Verrucous carcinoma is a slow-growing tumor that often presents in advanced clinical stages because it is poorly understood and underrecognized, especially in developing countries.
- Good clinicopathological correlation is required in cases of verrucous carcinoma to avoid misdiagnosis and provide appropriate treatment.
- Case-specific management should be considered, as presentation of verrucous carcinoma varies.
- Radiography should be considered to assess for lymph node involvement.
Atherosclerosis severity in diabetes can be predicted by select biomarkers
in patient with type 2 diabetes, results from a long-term analysis of VA patients suggest.
Advanced glycation end products (AGEs) and oxidation products (OxPs) “can damage vascular cells by different mechanisms,” wrote researchers led by corresponding authors Aramesh Saremi, MD, and Peter D. Reaven, MD, and colleagues. The report appeared online Feb. 1 in Diabetes Care.
“One frequently reported pathway is AGE binding to their purported (and relatively promiscuous) receptors on cells, such as macrophages, vascular endothelial cells, and vascular smooth muscle cells, although this has not been consistent for all AGEs. Other mechanisms include, among others, binding to and altering the function of intracellular proteins, the activation of vascular NADPH [nicotinamide adenine dinucleotide phosphate] oxidase, and the uncoupling of endothelial nitric oxide synthase.”
Noting that data in the current medical literature are lacking with respect to long-term longitudinal associations between plasma levels of AGEs and OxPs on the extent of subclinical atherosclerosis in T2D patients, the researchers set out to determine whether baseline plasma levels of AGEs and OxPs are associated with the extent of carotid intima-media thickness (CIMT), coronary artery calcification (CAC), and abdominal aortic artery calcification (AAC) over an average of 10 years of follow-up in the VA Diabetes Trial (VADT). They also examined whether this relationship was altered by intervening improved glucose control (Diabetes Care 2017 Feb. 1. doi: 10.2337/dc16-1875]).
At baseline of the VADT, 411 study participants underwent plasma measurements of methylglyoxal hydroimidazolone, N epsilon–carboxymethyl lysine (CML), N epsilon–carboxyethyl lysine (CEL), 3-deoxyglucosone hydroimidazolone and glyoxal hydroimidazolone (G-H1), 2-aminoadipic acid (2-AAA), and methionine sulfoxide. The mean age of the study subjects was 58 years, 64% were non-Hispanic white, 96% were male, 69% had a history of hypertension, and they had diabetes for a mean of 11 years.
After a mean follow-up of 10 years, the 411 patients underwent ultrasound assessment of CIMT, and computed tomography scanning of CAC and AAC.
In risk factor–adjusted multivariable regression models, G-H1was associated with the extent of CIMT as well as with the extent of CAC (P = .01 for both associations). In addition, 2-AAA was strongly associated with the extent of CAC (P = .03 for continuous variables and P less than .01 for dichotomous variables), and CEL was strongly associated with the extent of AAC (P less than .01).
“These findings suggest that the effect of hyperglycemia and subsequent increased levels of AGEs and OxPs in patients with long-standing T2D may have long-lasting adverse effects on the development of macrovascular complications,” the researchers concluded. They acknowledged certain limitations of the analysis, including the fact that it was conducted in an older, primarily male population. Therefore, “extrapolation of the study findings to other populations must be done with caution,” they wrote. “This study also does not allow us to make a definite claim of causation between AGEs and OxPs with the extent of atherosclerosis.”
The Veterans Affairs Cooperative Studies Program of the U.S. Department of Veterans Affairs Office of Research and Development funded the study. Additional support was received from National Institutes of Health, the American Diabetes Association, and the National Institute of Diabetes and Digestive and Kidney Diseases. Two study authors, Scott Howell, MS, and Paul J. Beisswenger, MD, disclosed that they are affiliated with PreventAGE Healthcare. The other researchers reported having no financial disclosures.
[email protected]
For a long time the question about how glucose control relates to macrovascular disease has not been easy to answer. There are reports suggesting that glucose control correlates with macrovascular disease later in life, and others that do not make the association so convincing. This paper provides an important link between glucose control and the subsequent development of macrovascular disease. The link is by way of advanced glycation end products as well as oxidative byproducts and how they set the stage for macrovascular disease later on in life. It’s something that clinicians have postulated as being important, but to my knowledge this is one of the only studies to actually show the association.
The investigators used important endpoints like coronary artery calcification and carotid intima-media thickness. I was surprised at how well the relationship between glycosylated end products and oxidative products correlated, but there’s biologic plausibility; it makes sense. Glucose not only glycosates hemoglobin, but glycosates proteins throughout. This provides a logical, stepwise pathway for how the initial glycosylated protein will result years later in macrovascular disease as evidenced by the parameters that were used.
It was interesting to learn from this study that glycosylated end products and oxidative products interact with each other. That’s important, because as blood sugars rise acutely, both oxidative products and glycosylated products are produced. As a result of the oxidative stress that’s created by the sharp rise in blood sugar, endothelial function is affected and more glycosylated proteins are being formed.
Clinically, this study shows the importance of early, aggressive control of diabetes to not allow accumulation of both glycosylated end products and oxidative end products. It demonstrates that accumulation of these byproducts years later seems to relate strongly to macrovascular disease.
The study should be reproduced in younger, less sick patients. That may or may not further clarify the findings, but these findings need to be demonstrated in patients at a much earlier stage as well. We’ve been saying for a long time that early control of diabetes is so important because years later it makes a difference. This is a link to that rationale.
Paul S. Jellinger, MD, MACE, is professor of clinical medicine at the University of Miami Miller School of Medicine, Ft. Lauderdale. He is past president of the American Association of Clinical Endocrinologists (AACE) and past president of the American College of Endocrinology. Dr. Jellinger provided these comments in an interview.
For a long time the question about how glucose control relates to macrovascular disease has not been easy to answer. There are reports suggesting that glucose control correlates with macrovascular disease later in life, and others that do not make the association so convincing. This paper provides an important link between glucose control and the subsequent development of macrovascular disease. The link is by way of advanced glycation end products as well as oxidative byproducts and how they set the stage for macrovascular disease later on in life. It’s something that clinicians have postulated as being important, but to my knowledge this is one of the only studies to actually show the association.
The investigators used important endpoints like coronary artery calcification and carotid intima-media thickness. I was surprised at how well the relationship between glycosylated end products and oxidative products correlated, but there’s biologic plausibility; it makes sense. Glucose not only glycosates hemoglobin, but glycosates proteins throughout. This provides a logical, stepwise pathway for how the initial glycosylated protein will result years later in macrovascular disease as evidenced by the parameters that were used.
It was interesting to learn from this study that glycosylated end products and oxidative products interact with each other. That’s important, because as blood sugars rise acutely, both oxidative products and glycosylated products are produced. As a result of the oxidative stress that’s created by the sharp rise in blood sugar, endothelial function is affected and more glycosylated proteins are being formed.
Clinically, this study shows the importance of early, aggressive control of diabetes to not allow accumulation of both glycosylated end products and oxidative end products. It demonstrates that accumulation of these byproducts years later seems to relate strongly to macrovascular disease.
The study should be reproduced in younger, less sick patients. That may or may not further clarify the findings, but these findings need to be demonstrated in patients at a much earlier stage as well. We’ve been saying for a long time that early control of diabetes is so important because years later it makes a difference. This is a link to that rationale.
Paul S. Jellinger, MD, MACE, is professor of clinical medicine at the University of Miami Miller School of Medicine, Ft. Lauderdale. He is past president of the American Association of Clinical Endocrinologists (AACE) and past president of the American College of Endocrinology. Dr. Jellinger provided these comments in an interview.
For a long time the question about how glucose control relates to macrovascular disease has not been easy to answer. There are reports suggesting that glucose control correlates with macrovascular disease later in life, and others that do not make the association so convincing. This paper provides an important link between glucose control and the subsequent development of macrovascular disease. The link is by way of advanced glycation end products as well as oxidative byproducts and how they set the stage for macrovascular disease later on in life. It’s something that clinicians have postulated as being important, but to my knowledge this is one of the only studies to actually show the association.
The investigators used important endpoints like coronary artery calcification and carotid intima-media thickness. I was surprised at how well the relationship between glycosylated end products and oxidative products correlated, but there’s biologic plausibility; it makes sense. Glucose not only glycosates hemoglobin, but glycosates proteins throughout. This provides a logical, stepwise pathway for how the initial glycosylated protein will result years later in macrovascular disease as evidenced by the parameters that were used.
It was interesting to learn from this study that glycosylated end products and oxidative products interact with each other. That’s important, because as blood sugars rise acutely, both oxidative products and glycosylated products are produced. As a result of the oxidative stress that’s created by the sharp rise in blood sugar, endothelial function is affected and more glycosylated proteins are being formed.
Clinically, this study shows the importance of early, aggressive control of diabetes to not allow accumulation of both glycosylated end products and oxidative end products. It demonstrates that accumulation of these byproducts years later seems to relate strongly to macrovascular disease.
The study should be reproduced in younger, less sick patients. That may or may not further clarify the findings, but these findings need to be demonstrated in patients at a much earlier stage as well. We’ve been saying for a long time that early control of diabetes is so important because years later it makes a difference. This is a link to that rationale.
Paul S. Jellinger, MD, MACE, is professor of clinical medicine at the University of Miami Miller School of Medicine, Ft. Lauderdale. He is past president of the American Association of Clinical Endocrinologists (AACE) and past president of the American College of Endocrinology. Dr. Jellinger provided these comments in an interview.
in patient with type 2 diabetes, results from a long-term analysis of VA patients suggest.
Advanced glycation end products (AGEs) and oxidation products (OxPs) “can damage vascular cells by different mechanisms,” wrote researchers led by corresponding authors Aramesh Saremi, MD, and Peter D. Reaven, MD, and colleagues. The report appeared online Feb. 1 in Diabetes Care.
“One frequently reported pathway is AGE binding to their purported (and relatively promiscuous) receptors on cells, such as macrophages, vascular endothelial cells, and vascular smooth muscle cells, although this has not been consistent for all AGEs. Other mechanisms include, among others, binding to and altering the function of intracellular proteins, the activation of vascular NADPH [nicotinamide adenine dinucleotide phosphate] oxidase, and the uncoupling of endothelial nitric oxide synthase.”
Noting that data in the current medical literature are lacking with respect to long-term longitudinal associations between plasma levels of AGEs and OxPs on the extent of subclinical atherosclerosis in T2D patients, the researchers set out to determine whether baseline plasma levels of AGEs and OxPs are associated with the extent of carotid intima-media thickness (CIMT), coronary artery calcification (CAC), and abdominal aortic artery calcification (AAC) over an average of 10 years of follow-up in the VA Diabetes Trial (VADT). They also examined whether this relationship was altered by intervening improved glucose control (Diabetes Care 2017 Feb. 1. doi: 10.2337/dc16-1875]).
At baseline of the VADT, 411 study participants underwent plasma measurements of methylglyoxal hydroimidazolone, N epsilon–carboxymethyl lysine (CML), N epsilon–carboxyethyl lysine (CEL), 3-deoxyglucosone hydroimidazolone and glyoxal hydroimidazolone (G-H1), 2-aminoadipic acid (2-AAA), and methionine sulfoxide. The mean age of the study subjects was 58 years, 64% were non-Hispanic white, 96% were male, 69% had a history of hypertension, and they had diabetes for a mean of 11 years.
After a mean follow-up of 10 years, the 411 patients underwent ultrasound assessment of CIMT, and computed tomography scanning of CAC and AAC.
In risk factor–adjusted multivariable regression models, G-H1was associated with the extent of CIMT as well as with the extent of CAC (P = .01 for both associations). In addition, 2-AAA was strongly associated with the extent of CAC (P = .03 for continuous variables and P less than .01 for dichotomous variables), and CEL was strongly associated with the extent of AAC (P less than .01).
“These findings suggest that the effect of hyperglycemia and subsequent increased levels of AGEs and OxPs in patients with long-standing T2D may have long-lasting adverse effects on the development of macrovascular complications,” the researchers concluded. They acknowledged certain limitations of the analysis, including the fact that it was conducted in an older, primarily male population. Therefore, “extrapolation of the study findings to other populations must be done with caution,” they wrote. “This study also does not allow us to make a definite claim of causation between AGEs and OxPs with the extent of atherosclerosis.”
The Veterans Affairs Cooperative Studies Program of the U.S. Department of Veterans Affairs Office of Research and Development funded the study. Additional support was received from National Institutes of Health, the American Diabetes Association, and the National Institute of Diabetes and Digestive and Kidney Diseases. Two study authors, Scott Howell, MS, and Paul J. Beisswenger, MD, disclosed that they are affiliated with PreventAGE Healthcare. The other researchers reported having no financial disclosures.
[email protected]
in patient with type 2 diabetes, results from a long-term analysis of VA patients suggest.
Advanced glycation end products (AGEs) and oxidation products (OxPs) “can damage vascular cells by different mechanisms,” wrote researchers led by corresponding authors Aramesh Saremi, MD, and Peter D. Reaven, MD, and colleagues. The report appeared online Feb. 1 in Diabetes Care.
“One frequently reported pathway is AGE binding to their purported (and relatively promiscuous) receptors on cells, such as macrophages, vascular endothelial cells, and vascular smooth muscle cells, although this has not been consistent for all AGEs. Other mechanisms include, among others, binding to and altering the function of intracellular proteins, the activation of vascular NADPH [nicotinamide adenine dinucleotide phosphate] oxidase, and the uncoupling of endothelial nitric oxide synthase.”
Noting that data in the current medical literature are lacking with respect to long-term longitudinal associations between plasma levels of AGEs and OxPs on the extent of subclinical atherosclerosis in T2D patients, the researchers set out to determine whether baseline plasma levels of AGEs and OxPs are associated with the extent of carotid intima-media thickness (CIMT), coronary artery calcification (CAC), and abdominal aortic artery calcification (AAC) over an average of 10 years of follow-up in the VA Diabetes Trial (VADT). They also examined whether this relationship was altered by intervening improved glucose control (Diabetes Care 2017 Feb. 1. doi: 10.2337/dc16-1875]).
At baseline of the VADT, 411 study participants underwent plasma measurements of methylglyoxal hydroimidazolone, N epsilon–carboxymethyl lysine (CML), N epsilon–carboxyethyl lysine (CEL), 3-deoxyglucosone hydroimidazolone and glyoxal hydroimidazolone (G-H1), 2-aminoadipic acid (2-AAA), and methionine sulfoxide. The mean age of the study subjects was 58 years, 64% were non-Hispanic white, 96% were male, 69% had a history of hypertension, and they had diabetes for a mean of 11 years.
After a mean follow-up of 10 years, the 411 patients underwent ultrasound assessment of CIMT, and computed tomography scanning of CAC and AAC.
In risk factor–adjusted multivariable regression models, G-H1was associated with the extent of CIMT as well as with the extent of CAC (P = .01 for both associations). In addition, 2-AAA was strongly associated with the extent of CAC (P = .03 for continuous variables and P less than .01 for dichotomous variables), and CEL was strongly associated with the extent of AAC (P less than .01).
“These findings suggest that the effect of hyperglycemia and subsequent increased levels of AGEs and OxPs in patients with long-standing T2D may have long-lasting adverse effects on the development of macrovascular complications,” the researchers concluded. They acknowledged certain limitations of the analysis, including the fact that it was conducted in an older, primarily male population. Therefore, “extrapolation of the study findings to other populations must be done with caution,” they wrote. “This study also does not allow us to make a definite claim of causation between AGEs and OxPs with the extent of atherosclerosis.”
The Veterans Affairs Cooperative Studies Program of the U.S. Department of Veterans Affairs Office of Research and Development funded the study. Additional support was received from National Institutes of Health, the American Diabetes Association, and the National Institute of Diabetes and Digestive and Kidney Diseases. Two study authors, Scott Howell, MS, and Paul J. Beisswenger, MD, disclosed that they are affiliated with PreventAGE Healthcare. The other researchers reported having no financial disclosures.
[email protected]
Key clinical point:
Major finding: Glyoxal hydroimidazolone was associated with the extent of carotid intima-media thickness as well as with the extent of coronary artery calcification.
Data source: An analysis of 411 patients the VA Diabetes Trial.
Disclosures: The Veterans Affairs Cooperative Studies Program of the U.S. Department of Veterans Affairs Office of Research and Development funded the study. Additional support was received from National Institutes of Health, the American Diabetes Association, and the National Institute of Diabetes and Digestive and Kidney Diseases. Two study authors, Scott Howell, MS, and Paul J. Beisswenger, MD, disclosed that they are affiliated with PreventAGE Healthcare. The other researchers reported having no financial disclosures.
Liver transplantation largely effective in critically ill children
The use of advanced critical care in children and infants with liver failure is justified because orthotopic liver transplantation can be performed on the sickest children and achieve acceptable outcomes, results from a large analysis demonstrated.
“Hand in hand with improved care for critically ill children with liver failure, posttransplant critical care has made tremendous strides,” Abbas Rana, MD, wrote in a study published online in the Journal of the American College of Surgeons. “Our recipients have gotten sicker while our postoperative outcomes have improved. The question then becomes, have our operative skills and postoperative critical care management kept up with the abilities to keep sick children with liver failure alive? Just because transplantation is now possible in our sickest children, is it justified?”
To find out, Dr. Rana of the division of abdominal transplantation and hepatobiliary surgery at Baylor College of Medicine, Houston, and colleagues retrospectively analyzed United Network for Organ Sharing data from all orthotopic liver transplantation (OLT) recipients between Sept. 1, 1987, and June 30, 2015. The analysis paired the liver registry data with data collected by the Organ Procurement and Transplantation Network, and was limited to transplant recipients younger than age 18. The researchers followed a total of 13,723 recipients from date of transplant until either death or the date of last known follow-up (J Am Coll Surg. 2016 Dec 25. doi: 10.1016/j.jamcollsurg.2016.12.025).
In another part of the study, the researchers retrospectively reviewed the charts of 354 patients under 18 years of age who underwent OLT between March 1, 2002, and June 30, 2015, at Texas Children’s Hospital, including 65 who were admitted to the ICU at the time of transplantation.
In the analysis of national data, the researchers found that the rates of 1-year survival following OLT in children in the ICU improved from 60% in 1987 to 92% in 2013 (P less than .001). The rates of 1-year survival also improved for children on dialysis at the time of transplant (from 50% in 1995 to 95% in 2013; P less than .001) and for those dependent on a mechanical ventilator at the time of transplant (from 49% in 1994 to 94% in 2013; P less than .001). The significant risk factors were two previous transplants (hazard ratio, 4.2), one previous transplant (HR, 2.5), serum sodium greater than 150 mEq/L (HR, 2.0), dialysis or glomerular filtration rate less than 30 mL/min per 1.73 m2 (HR, 2.0), mechanical ventilator dependence (HR, 1.8), body weight under 6 kg (HR, 1.8), encephalopathy (HR, 1.8), and annual center volume of fewer than five cases (HR, 1.7).
In the experience at Texas Children’s Hospital, the researchers observed “preserved and successful patient survival outcomes” in many markers of acuity. For example, the 10-year survival rates for patients dependent on mechanical ventilation and dialysis were 85% and 96%, respectively, and reached 100% for those requiring therapeutic plasma exchange, molescular adsorbent recirculating system (MARS) liver dialysis, and vasopressors.
“Our collective ability to keep sick children alive with liver failure has improved considerably over the years,” the researchers wrote. “Keeping pace, this analysis demonstrates that the posttransplant outcomes have also improved dramatically. The survival outcomes are comparable to the general population, justifying the use of scarce donors. Although we cannot declare in absolute that no child should be left behind, we can demonstrate acceptable outcomes to date and urge the continual revisiting of our concepts of futility.
“We have learned throughout our experience that almost every child with end-stage liver disease and acute liver failure should be offered liver replacement, as long as the vasoactive medication and mechanical support are not maximized prior to the initiation of the OLT procedure. Every effort should be made to transplant our sickest children.”
This study was supported by the Cade R. Alpard Foundation. The researchers reported having no relevant financial disclosures.
The use of advanced critical care in children and infants with liver failure is justified because orthotopic liver transplantation can be performed on the sickest children and achieve acceptable outcomes, results from a large analysis demonstrated.
“Hand in hand with improved care for critically ill children with liver failure, posttransplant critical care has made tremendous strides,” Abbas Rana, MD, wrote in a study published online in the Journal of the American College of Surgeons. “Our recipients have gotten sicker while our postoperative outcomes have improved. The question then becomes, have our operative skills and postoperative critical care management kept up with the abilities to keep sick children with liver failure alive? Just because transplantation is now possible in our sickest children, is it justified?”
To find out, Dr. Rana of the division of abdominal transplantation and hepatobiliary surgery at Baylor College of Medicine, Houston, and colleagues retrospectively analyzed United Network for Organ Sharing data from all orthotopic liver transplantation (OLT) recipients between Sept. 1, 1987, and June 30, 2015. The analysis paired the liver registry data with data collected by the Organ Procurement and Transplantation Network, and was limited to transplant recipients younger than age 18. The researchers followed a total of 13,723 recipients from date of transplant until either death or the date of last known follow-up (J Am Coll Surg. 2016 Dec 25. doi: 10.1016/j.jamcollsurg.2016.12.025).
In another part of the study, the researchers retrospectively reviewed the charts of 354 patients under 18 years of age who underwent OLT between March 1, 2002, and June 30, 2015, at Texas Children’s Hospital, including 65 who were admitted to the ICU at the time of transplantation.
In the analysis of national data, the researchers found that the rates of 1-year survival following OLT in children in the ICU improved from 60% in 1987 to 92% in 2013 (P less than .001). The rates of 1-year survival also improved for children on dialysis at the time of transplant (from 50% in 1995 to 95% in 2013; P less than .001) and for those dependent on a mechanical ventilator at the time of transplant (from 49% in 1994 to 94% in 2013; P less than .001). The significant risk factors were two previous transplants (hazard ratio, 4.2), one previous transplant (HR, 2.5), serum sodium greater than 150 mEq/L (HR, 2.0), dialysis or glomerular filtration rate less than 30 mL/min per 1.73 m2 (HR, 2.0), mechanical ventilator dependence (HR, 1.8), body weight under 6 kg (HR, 1.8), encephalopathy (HR, 1.8), and annual center volume of fewer than five cases (HR, 1.7).
In the experience at Texas Children’s Hospital, the researchers observed “preserved and successful patient survival outcomes” in many markers of acuity. For example, the 10-year survival rates for patients dependent on mechanical ventilation and dialysis were 85% and 96%, respectively, and reached 100% for those requiring therapeutic plasma exchange, molescular adsorbent recirculating system (MARS) liver dialysis, and vasopressors.
“Our collective ability to keep sick children alive with liver failure has improved considerably over the years,” the researchers wrote. “Keeping pace, this analysis demonstrates that the posttransplant outcomes have also improved dramatically. The survival outcomes are comparable to the general population, justifying the use of scarce donors. Although we cannot declare in absolute that no child should be left behind, we can demonstrate acceptable outcomes to date and urge the continual revisiting of our concepts of futility.
“We have learned throughout our experience that almost every child with end-stage liver disease and acute liver failure should be offered liver replacement, as long as the vasoactive medication and mechanical support are not maximized prior to the initiation of the OLT procedure. Every effort should be made to transplant our sickest children.”
This study was supported by the Cade R. Alpard Foundation. The researchers reported having no relevant financial disclosures.
The use of advanced critical care in children and infants with liver failure is justified because orthotopic liver transplantation can be performed on the sickest children and achieve acceptable outcomes, results from a large analysis demonstrated.
“Hand in hand with improved care for critically ill children with liver failure, posttransplant critical care has made tremendous strides,” Abbas Rana, MD, wrote in a study published online in the Journal of the American College of Surgeons. “Our recipients have gotten sicker while our postoperative outcomes have improved. The question then becomes, have our operative skills and postoperative critical care management kept up with the abilities to keep sick children with liver failure alive? Just because transplantation is now possible in our sickest children, is it justified?”
To find out, Dr. Rana of the division of abdominal transplantation and hepatobiliary surgery at Baylor College of Medicine, Houston, and colleagues retrospectively analyzed United Network for Organ Sharing data from all orthotopic liver transplantation (OLT) recipients between Sept. 1, 1987, and June 30, 2015. The analysis paired the liver registry data with data collected by the Organ Procurement and Transplantation Network, and was limited to transplant recipients younger than age 18. The researchers followed a total of 13,723 recipients from date of transplant until either death or the date of last known follow-up (J Am Coll Surg. 2016 Dec 25. doi: 10.1016/j.jamcollsurg.2016.12.025).
In another part of the study, the researchers retrospectively reviewed the charts of 354 patients under 18 years of age who underwent OLT between March 1, 2002, and June 30, 2015, at Texas Children’s Hospital, including 65 who were admitted to the ICU at the time of transplantation.
In the analysis of national data, the researchers found that the rates of 1-year survival following OLT in children in the ICU improved from 60% in 1987 to 92% in 2013 (P less than .001). The rates of 1-year survival also improved for children on dialysis at the time of transplant (from 50% in 1995 to 95% in 2013; P less than .001) and for those dependent on a mechanical ventilator at the time of transplant (from 49% in 1994 to 94% in 2013; P less than .001). The significant risk factors were two previous transplants (hazard ratio, 4.2), one previous transplant (HR, 2.5), serum sodium greater than 150 mEq/L (HR, 2.0), dialysis or glomerular filtration rate less than 30 mL/min per 1.73 m2 (HR, 2.0), mechanical ventilator dependence (HR, 1.8), body weight under 6 kg (HR, 1.8), encephalopathy (HR, 1.8), and annual center volume of fewer than five cases (HR, 1.7).
In the experience at Texas Children’s Hospital, the researchers observed “preserved and successful patient survival outcomes” in many markers of acuity. For example, the 10-year survival rates for patients dependent on mechanical ventilation and dialysis were 85% and 96%, respectively, and reached 100% for those requiring therapeutic plasma exchange, molescular adsorbent recirculating system (MARS) liver dialysis, and vasopressors.
“Our collective ability to keep sick children alive with liver failure has improved considerably over the years,” the researchers wrote. “Keeping pace, this analysis demonstrates that the posttransplant outcomes have also improved dramatically. The survival outcomes are comparable to the general population, justifying the use of scarce donors. Although we cannot declare in absolute that no child should be left behind, we can demonstrate acceptable outcomes to date and urge the continual revisiting of our concepts of futility.
“We have learned throughout our experience that almost every child with end-stage liver disease and acute liver failure should be offered liver replacement, as long as the vasoactive medication and mechanical support are not maximized prior to the initiation of the OLT procedure. Every effort should be made to transplant our sickest children.”
This study was supported by the Cade R. Alpard Foundation. The researchers reported having no relevant financial disclosures.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point:
Major finding: The rates of 1-year survival following orthotopic liver transplantation in ICU children improved from 60% in 1987 to 92% in 2013 (P less than .001).
Data source: An analysis of 13,723 patients under the age of 18 years who underwent OLT between Sept. 1, 1987, and June 30, 2015.
Disclosures: The study was supported by the Cade R. Alpard Foundation. The researchers reported having no relevant financial disclosures.
How Will the Trump Travel Ban Impact the VA?
Rural health care and the VA seem to be on the front line in the battle over President Trump’s executive order halting travel to the U.S. for citizens of 7 Muslim-majority countries. The executive order, which has been temporarily suspended by a federal judge, could affect as many as 15,000 doctors and possibly even more pharmacists, nurses, and other health care providers. The ban also is expected to impact nearly 9,000 physicians from Iran and another 3,500 from Syria and 1,500 from Iraq.
The VA has long depended on foreign-born health care providers, and given the VA’s challenges in filling its more than 45,000 vacancies, this reliance was only expected to grow.. The Conrad 30 program allows J-1 medical doctors to apply for a waiver to the 2-year residence requirement upon completion of the J-1 exchange visitor program. Over the years, many international medical graduates (IMGs) earned permanent residence by agreeing to work 3 or 5 years in an underserved area or VA facility.
“The United States is facing a serious shortage of physicians. IMGs play an important role in U.S. health care, representing roughly 25% of the workforce,” AAMC (Association of American Medical Colleges) President and CEO Darrell G. Kirch, MD said in a statement. “In the last decade, Conrad 30 alone has directed nearly 10,000 physicians into rural and urban underserved communities. Impeding these U.S. immigration pathways jeopardizes critical access to high-quality physician care for our nation’s most vulnerable populations.”
Related: Medical Organizations Respond to Trump’s Immigration Order
According to an analysis of 2010 census data from the Migration Policy Institute (MPI), foreign-born workers make up 15% of the 1.1 million health care providers in the U.S., which includes a significant proportion of physicians and surgeons (27%) and a smaller, but still significant number of registered nurses (15%), technologists and technicians (12%), and therapists (10%). Among support personnel foreign-born workers range from 19% of health care support workers to 22% of nursing, psychiatric, and home health aides.
In a more recent analysis from the George Mason Institute for Immigration Research, 22% of nursing, psychiatric, and home health aides are foreign born.
Most of the foreign-born health care providers have acquired U.S. citizenship, according to MPI, “with naturalization rates ranging from 55% for those working as nursing, psychiatric, or home health aides to 78% for other health care practitioners and technical occupations. According to American Association of Family Practitioners (AAFP), 42% of office visits in rural America are with foreign-born physicians.
“Many family physicians are IMGs, who have completed all or part of their education and training in the U.S.,” AAFP President John Meigs, Jr, MD, FAAFP, wrote in a letter to President Trump. “They are professionals who dedicate their careers to the service of their patients in communities large and small, urban and rural. In fact, 20% of our membership and over 25% of family medicine residents [comprise] IMGs. The AAFP applauds and supports wholly the contributions of these individual family physicians to their patients and communities and we celebrate their diversity.”
Rural health care and the VA seem to be on the front line in the battle over President Trump’s executive order halting travel to the U.S. for citizens of 7 Muslim-majority countries. The executive order, which has been temporarily suspended by a federal judge, could affect as many as 15,000 doctors and possibly even more pharmacists, nurses, and other health care providers. The ban also is expected to impact nearly 9,000 physicians from Iran and another 3,500 from Syria and 1,500 from Iraq.
The VA has long depended on foreign-born health care providers, and given the VA’s challenges in filling its more than 45,000 vacancies, this reliance was only expected to grow.. The Conrad 30 program allows J-1 medical doctors to apply for a waiver to the 2-year residence requirement upon completion of the J-1 exchange visitor program. Over the years, many international medical graduates (IMGs) earned permanent residence by agreeing to work 3 or 5 years in an underserved area or VA facility.
“The United States is facing a serious shortage of physicians. IMGs play an important role in U.S. health care, representing roughly 25% of the workforce,” AAMC (Association of American Medical Colleges) President and CEO Darrell G. Kirch, MD said in a statement. “In the last decade, Conrad 30 alone has directed nearly 10,000 physicians into rural and urban underserved communities. Impeding these U.S. immigration pathways jeopardizes critical access to high-quality physician care for our nation’s most vulnerable populations.”
Related: Medical Organizations Respond to Trump’s Immigration Order
According to an analysis of 2010 census data from the Migration Policy Institute (MPI), foreign-born workers make up 15% of the 1.1 million health care providers in the U.S., which includes a significant proportion of physicians and surgeons (27%) and a smaller, but still significant number of registered nurses (15%), technologists and technicians (12%), and therapists (10%). Among support personnel foreign-born workers range from 19% of health care support workers to 22% of nursing, psychiatric, and home health aides.
In a more recent analysis from the George Mason Institute for Immigration Research, 22% of nursing, psychiatric, and home health aides are foreign born.
Most of the foreign-born health care providers have acquired U.S. citizenship, according to MPI, “with naturalization rates ranging from 55% for those working as nursing, psychiatric, or home health aides to 78% for other health care practitioners and technical occupations. According to American Association of Family Practitioners (AAFP), 42% of office visits in rural America are with foreign-born physicians.
“Many family physicians are IMGs, who have completed all or part of their education and training in the U.S.,” AAFP President John Meigs, Jr, MD, FAAFP, wrote in a letter to President Trump. “They are professionals who dedicate their careers to the service of their patients in communities large and small, urban and rural. In fact, 20% of our membership and over 25% of family medicine residents [comprise] IMGs. The AAFP applauds and supports wholly the contributions of these individual family physicians to their patients and communities and we celebrate their diversity.”
Rural health care and the VA seem to be on the front line in the battle over President Trump’s executive order halting travel to the U.S. for citizens of 7 Muslim-majority countries. The executive order, which has been temporarily suspended by a federal judge, could affect as many as 15,000 doctors and possibly even more pharmacists, nurses, and other health care providers. The ban also is expected to impact nearly 9,000 physicians from Iran and another 3,500 from Syria and 1,500 from Iraq.
The VA has long depended on foreign-born health care providers, and given the VA’s challenges in filling its more than 45,000 vacancies, this reliance was only expected to grow.. The Conrad 30 program allows J-1 medical doctors to apply for a waiver to the 2-year residence requirement upon completion of the J-1 exchange visitor program. Over the years, many international medical graduates (IMGs) earned permanent residence by agreeing to work 3 or 5 years in an underserved area or VA facility.
“The United States is facing a serious shortage of physicians. IMGs play an important role in U.S. health care, representing roughly 25% of the workforce,” AAMC (Association of American Medical Colleges) President and CEO Darrell G. Kirch, MD said in a statement. “In the last decade, Conrad 30 alone has directed nearly 10,000 physicians into rural and urban underserved communities. Impeding these U.S. immigration pathways jeopardizes critical access to high-quality physician care for our nation’s most vulnerable populations.”
Related: Medical Organizations Respond to Trump’s Immigration Order
According to an analysis of 2010 census data from the Migration Policy Institute (MPI), foreign-born workers make up 15% of the 1.1 million health care providers in the U.S., which includes a significant proportion of physicians and surgeons (27%) and a smaller, but still significant number of registered nurses (15%), technologists and technicians (12%), and therapists (10%). Among support personnel foreign-born workers range from 19% of health care support workers to 22% of nursing, psychiatric, and home health aides.
In a more recent analysis from the George Mason Institute for Immigration Research, 22% of nursing, psychiatric, and home health aides are foreign born.
Most of the foreign-born health care providers have acquired U.S. citizenship, according to MPI, “with naturalization rates ranging from 55% for those working as nursing, psychiatric, or home health aides to 78% for other health care practitioners and technical occupations. According to American Association of Family Practitioners (AAFP), 42% of office visits in rural America are with foreign-born physicians.
“Many family physicians are IMGs, who have completed all or part of their education and training in the U.S.,” AAFP President John Meigs, Jr, MD, FAAFP, wrote in a letter to President Trump. “They are professionals who dedicate their careers to the service of their patients in communities large and small, urban and rural. In fact, 20% of our membership and over 25% of family medicine residents [comprise] IMGs. The AAFP applauds and supports wholly the contributions of these individual family physicians to their patients and communities and we celebrate their diversity.”
Widespread Poikilodermatous Dermatomyositis Associated With Chronic Lymphocytic Leukemia
To the Editor:
Dermatomyositis represents a rare idiopathic inflammatory process presenting with cutaneous lesions and muscular weakness. It often represents a paraneoplastic syndrome. We report the case of a 62-year-old man with a history of total-body poikiloderma and a recent diagnosis of chronic lymphocytic leukemia (CLL). Despite lacking typical features of the disease, a diagnosis of dermatomyositis was made. Our patient may represent a distinct poikilodermatous variant of dermatomyositis, sharing the generalized distribution of the erythrodermic subtype.
A 62-year-old man presented with pruritic poikiloderma involving the neck, arms, legs, abdomen, chest, and back of 2 years’ duration (Figure). He also experienced dysphagia and weakness of the legs. The rash was previously treated by other dermatologists with a combination of high-potency topical steroids and topical tacrolimus 0.1% without success. His history was notable for CLL, which had been diagnosed by a dermatologist 6 months prior to the current presentation. Prior to his visit to the dermatologist, the patient had received 6 chemotherapeutic sessions with a combination of rituximab and cyclophosphamide for the treatment of CLL. The rash did not improve with chemotherapy.

Repeat biopsies of affected regions only demonstrated features of mild interface dermatitis. Direct immunofluorescence studies showed scattered colloid body fluorescence for IgM. Because of bilateral weakness of the legs, a muscle biopsy was taken, which demonstrated severe atrophy and interstitial fibrosis, with neurogenic abnormalities detected in areas of lesser atrophy via abnormal muscle fiber–type grouping. Metabolic panel showed elevated muscle enzymes in the blood: creatine kinase, 243 U/L (reference range, 10–225 U/L); serum aldolase, 16 U/L (reference range, ≤8.1 U/L); lactate dehydrogenase, 314 U/L (reference range, 60–200 U/L). An autoimmune panel was negative for Jo-1, Scl-70, U1 ribonucleoprotein, DNA, desmoglein 1 and 3, and antiacetylcholine receptor antibodies. An elevated erythrocyte sedimentation rate was measured at 16 mm/h (reference range, 0–10 mm/h). Given these findings, the lesions were confirmed as a widespread poikilodermatous variant of dermatomyositis.
The patient was placed on a daily 50-mg dose of prednisone, which produced rapid improvement in scaling and erythema. Creatine kinase and serum aldolase levels normalized and motor strength increased. After 1 week the prednisone dosage was reduced to a daily 30-mg dose, and then 20 mg a week later. The skin lesions completely resolved within 4 to 5 months and the patient is currently on a prednisone dose of 5 mg, alternating with 2.5 mg of prednisone and rituximab infusion every 2 months.
Dermatomyositis is a rare entity with an incidence of approximately 0.5 to 1 per 100,000 individuals.1 It presents with a characteristic rash composed of Gottron papules; pathognomonic flat violaceous papules on the dorsal interphalangeal joints, elbows, or knees; and a heliotrope rash, a violaceous erythema involving the eyelids. Poikiloderma frequently is reported to present in a shawl-like distribution, encompassing the shoulders, arms, and upper back.1,2 Dermatomyositis of the poikilodermatous type can present in nonphotoexposed areas and photoexposed areas. The unusual feature is the total-body involvement, which is analogous to erythroderma.3
Our case may represent a distinct poikilodermatous manifestation sharing the distribution of the erythrodermic subtype. We believe that the skin lesions may have represented a paraneoplastic event presenting prior to diagnosis with CLL. Dermatomyositis has a strong association with cancer, with patients 3 times more likely to develop internal malignancy.4 Association is strongest for non-Hodgkin lymphoma, as well as ovarian, lung, colorectal, pancreatic, and gastric cancer. When associated with malignancy, symptoms of dermatomyositis or myositis typically precede the discovery of malignancy by an average of 1.9 years.5 Dermatomyositis has been previously reported to present as a paraneoplastic manifestation of CLL.6 One case has been reported of a patient with CLL who developed leukemia cutis presenting with poikiloderma in the characteristic dermatomyositis shawl-like distribution.7 The lack of dermal infiltration with leukemic cells in our patient, however, makes a paraneoplastic etiology much more likely.
Our patient’s rash did not initially improve with treatment of CLL, but dermatomyositis associated with hematological malignancy may precede, occur simultaneously, or follow the diagnosis of malignancy.8 Additionally, symptoms of dermatomyositis do not always parallel the course of hematological malignancy outcome. However, rituximab has been used as a treatment of dermatomyositis and may have contributed some synergistic effect in combination with prednisone in our patient.9
- Dourmishev LA, Dourmishev AL, Schwartz RA. Dermatomyositis: cutaneous manifestations of its variants. Int J Dermatol. 2002;41:625-630.
- Kovacs SO, Kovacs SC. Dermatomyositis. J Am Acad Dermatol. 1998;39:899-920; quiz 921-992.
- Liu ZH, Wang XD. Acute-onset adult dermatomyositis presenting with erythroderma and diplopia. Clin Exp Dermatol. 2007;32:751-752.
- Hill CL, Zhang Y, Sigurgeirsson B, et al. Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 2001;357:96-100.
- Bohan A, Peter JB, Bowman RL, et al. Computer-assisted analysis of 153 patients with polymyositis and dermatomyositis. Medicine (Baltimore). 1977;56:255-286.
- Ishida T, Aikawa K, Tamura T, et al. Chronic lymphocytic leukemia associated with nephrotic syndrome and dermatomyositis. Intern Med. 1995;34:15-17.
- Nousari HC, Kimyai-Asadi A, Huang CH, et al. T-cell chronic lymphocytic leukemia mimicking dermatomyositis. Int J Dermatol. 2000;39:144-146.
- Marie I, Guillevin L, Menard JF, et al. Hematological malignancy associated with polymyositis and dermatomyositis. Autoimmun Rev. 2012;11:615-620.
- Levine TD. Rituximab in the treatment of dermatomyositis: an open-label pilot study. Arthritis Rheum. 2005;52:601-607.
To the Editor:
Dermatomyositis represents a rare idiopathic inflammatory process presenting with cutaneous lesions and muscular weakness. It often represents a paraneoplastic syndrome. We report the case of a 62-year-old man with a history of total-body poikiloderma and a recent diagnosis of chronic lymphocytic leukemia (CLL). Despite lacking typical features of the disease, a diagnosis of dermatomyositis was made. Our patient may represent a distinct poikilodermatous variant of dermatomyositis, sharing the generalized distribution of the erythrodermic subtype.
A 62-year-old man presented with pruritic poikiloderma involving the neck, arms, legs, abdomen, chest, and back of 2 years’ duration (Figure). He also experienced dysphagia and weakness of the legs. The rash was previously treated by other dermatologists with a combination of high-potency topical steroids and topical tacrolimus 0.1% without success. His history was notable for CLL, which had been diagnosed by a dermatologist 6 months prior to the current presentation. Prior to his visit to the dermatologist, the patient had received 6 chemotherapeutic sessions with a combination of rituximab and cyclophosphamide for the treatment of CLL. The rash did not improve with chemotherapy.

Repeat biopsies of affected regions only demonstrated features of mild interface dermatitis. Direct immunofluorescence studies showed scattered colloid body fluorescence for IgM. Because of bilateral weakness of the legs, a muscle biopsy was taken, which demonstrated severe atrophy and interstitial fibrosis, with neurogenic abnormalities detected in areas of lesser atrophy via abnormal muscle fiber–type grouping. Metabolic panel showed elevated muscle enzymes in the blood: creatine kinase, 243 U/L (reference range, 10–225 U/L); serum aldolase, 16 U/L (reference range, ≤8.1 U/L); lactate dehydrogenase, 314 U/L (reference range, 60–200 U/L). An autoimmune panel was negative for Jo-1, Scl-70, U1 ribonucleoprotein, DNA, desmoglein 1 and 3, and antiacetylcholine receptor antibodies. An elevated erythrocyte sedimentation rate was measured at 16 mm/h (reference range, 0–10 mm/h). Given these findings, the lesions were confirmed as a widespread poikilodermatous variant of dermatomyositis.
The patient was placed on a daily 50-mg dose of prednisone, which produced rapid improvement in scaling and erythema. Creatine kinase and serum aldolase levels normalized and motor strength increased. After 1 week the prednisone dosage was reduced to a daily 30-mg dose, and then 20 mg a week later. The skin lesions completely resolved within 4 to 5 months and the patient is currently on a prednisone dose of 5 mg, alternating with 2.5 mg of prednisone and rituximab infusion every 2 months.
Dermatomyositis is a rare entity with an incidence of approximately 0.5 to 1 per 100,000 individuals.1 It presents with a characteristic rash composed of Gottron papules; pathognomonic flat violaceous papules on the dorsal interphalangeal joints, elbows, or knees; and a heliotrope rash, a violaceous erythema involving the eyelids. Poikiloderma frequently is reported to present in a shawl-like distribution, encompassing the shoulders, arms, and upper back.1,2 Dermatomyositis of the poikilodermatous type can present in nonphotoexposed areas and photoexposed areas. The unusual feature is the total-body involvement, which is analogous to erythroderma.3
Our case may represent a distinct poikilodermatous manifestation sharing the distribution of the erythrodermic subtype. We believe that the skin lesions may have represented a paraneoplastic event presenting prior to diagnosis with CLL. Dermatomyositis has a strong association with cancer, with patients 3 times more likely to develop internal malignancy.4 Association is strongest for non-Hodgkin lymphoma, as well as ovarian, lung, colorectal, pancreatic, and gastric cancer. When associated with malignancy, symptoms of dermatomyositis or myositis typically precede the discovery of malignancy by an average of 1.9 years.5 Dermatomyositis has been previously reported to present as a paraneoplastic manifestation of CLL.6 One case has been reported of a patient with CLL who developed leukemia cutis presenting with poikiloderma in the characteristic dermatomyositis shawl-like distribution.7 The lack of dermal infiltration with leukemic cells in our patient, however, makes a paraneoplastic etiology much more likely.
Our patient’s rash did not initially improve with treatment of CLL, but dermatomyositis associated with hematological malignancy may precede, occur simultaneously, or follow the diagnosis of malignancy.8 Additionally, symptoms of dermatomyositis do not always parallel the course of hematological malignancy outcome. However, rituximab has been used as a treatment of dermatomyositis and may have contributed some synergistic effect in combination with prednisone in our patient.9
To the Editor:
Dermatomyositis represents a rare idiopathic inflammatory process presenting with cutaneous lesions and muscular weakness. It often represents a paraneoplastic syndrome. We report the case of a 62-year-old man with a history of total-body poikiloderma and a recent diagnosis of chronic lymphocytic leukemia (CLL). Despite lacking typical features of the disease, a diagnosis of dermatomyositis was made. Our patient may represent a distinct poikilodermatous variant of dermatomyositis, sharing the generalized distribution of the erythrodermic subtype.
A 62-year-old man presented with pruritic poikiloderma involving the neck, arms, legs, abdomen, chest, and back of 2 years’ duration (Figure). He also experienced dysphagia and weakness of the legs. The rash was previously treated by other dermatologists with a combination of high-potency topical steroids and topical tacrolimus 0.1% without success. His history was notable for CLL, which had been diagnosed by a dermatologist 6 months prior to the current presentation. Prior to his visit to the dermatologist, the patient had received 6 chemotherapeutic sessions with a combination of rituximab and cyclophosphamide for the treatment of CLL. The rash did not improve with chemotherapy.

Repeat biopsies of affected regions only demonstrated features of mild interface dermatitis. Direct immunofluorescence studies showed scattered colloid body fluorescence for IgM. Because of bilateral weakness of the legs, a muscle biopsy was taken, which demonstrated severe atrophy and interstitial fibrosis, with neurogenic abnormalities detected in areas of lesser atrophy via abnormal muscle fiber–type grouping. Metabolic panel showed elevated muscle enzymes in the blood: creatine kinase, 243 U/L (reference range, 10–225 U/L); serum aldolase, 16 U/L (reference range, ≤8.1 U/L); lactate dehydrogenase, 314 U/L (reference range, 60–200 U/L). An autoimmune panel was negative for Jo-1, Scl-70, U1 ribonucleoprotein, DNA, desmoglein 1 and 3, and antiacetylcholine receptor antibodies. An elevated erythrocyte sedimentation rate was measured at 16 mm/h (reference range, 0–10 mm/h). Given these findings, the lesions were confirmed as a widespread poikilodermatous variant of dermatomyositis.
The patient was placed on a daily 50-mg dose of prednisone, which produced rapid improvement in scaling and erythema. Creatine kinase and serum aldolase levels normalized and motor strength increased. After 1 week the prednisone dosage was reduced to a daily 30-mg dose, and then 20 mg a week later. The skin lesions completely resolved within 4 to 5 months and the patient is currently on a prednisone dose of 5 mg, alternating with 2.5 mg of prednisone and rituximab infusion every 2 months.
Dermatomyositis is a rare entity with an incidence of approximately 0.5 to 1 per 100,000 individuals.1 It presents with a characteristic rash composed of Gottron papules; pathognomonic flat violaceous papules on the dorsal interphalangeal joints, elbows, or knees; and a heliotrope rash, a violaceous erythema involving the eyelids. Poikiloderma frequently is reported to present in a shawl-like distribution, encompassing the shoulders, arms, and upper back.1,2 Dermatomyositis of the poikilodermatous type can present in nonphotoexposed areas and photoexposed areas. The unusual feature is the total-body involvement, which is analogous to erythroderma.3
Our case may represent a distinct poikilodermatous manifestation sharing the distribution of the erythrodermic subtype. We believe that the skin lesions may have represented a paraneoplastic event presenting prior to diagnosis with CLL. Dermatomyositis has a strong association with cancer, with patients 3 times more likely to develop internal malignancy.4 Association is strongest for non-Hodgkin lymphoma, as well as ovarian, lung, colorectal, pancreatic, and gastric cancer. When associated with malignancy, symptoms of dermatomyositis or myositis typically precede the discovery of malignancy by an average of 1.9 years.5 Dermatomyositis has been previously reported to present as a paraneoplastic manifestation of CLL.6 One case has been reported of a patient with CLL who developed leukemia cutis presenting with poikiloderma in the characteristic dermatomyositis shawl-like distribution.7 The lack of dermal infiltration with leukemic cells in our patient, however, makes a paraneoplastic etiology much more likely.
Our patient’s rash did not initially improve with treatment of CLL, but dermatomyositis associated with hematological malignancy may precede, occur simultaneously, or follow the diagnosis of malignancy.8 Additionally, symptoms of dermatomyositis do not always parallel the course of hematological malignancy outcome. However, rituximab has been used as a treatment of dermatomyositis and may have contributed some synergistic effect in combination with prednisone in our patient.9
- Dourmishev LA, Dourmishev AL, Schwartz RA. Dermatomyositis: cutaneous manifestations of its variants. Int J Dermatol. 2002;41:625-630.
- Kovacs SO, Kovacs SC. Dermatomyositis. J Am Acad Dermatol. 1998;39:899-920; quiz 921-992.
- Liu ZH, Wang XD. Acute-onset adult dermatomyositis presenting with erythroderma and diplopia. Clin Exp Dermatol. 2007;32:751-752.
- Hill CL, Zhang Y, Sigurgeirsson B, et al. Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 2001;357:96-100.
- Bohan A, Peter JB, Bowman RL, et al. Computer-assisted analysis of 153 patients with polymyositis and dermatomyositis. Medicine (Baltimore). 1977;56:255-286.
- Ishida T, Aikawa K, Tamura T, et al. Chronic lymphocytic leukemia associated with nephrotic syndrome and dermatomyositis. Intern Med. 1995;34:15-17.
- Nousari HC, Kimyai-Asadi A, Huang CH, et al. T-cell chronic lymphocytic leukemia mimicking dermatomyositis. Int J Dermatol. 2000;39:144-146.
- Marie I, Guillevin L, Menard JF, et al. Hematological malignancy associated with polymyositis and dermatomyositis. Autoimmun Rev. 2012;11:615-620.
- Levine TD. Rituximab in the treatment of dermatomyositis: an open-label pilot study. Arthritis Rheum. 2005;52:601-607.
- Dourmishev LA, Dourmishev AL, Schwartz RA. Dermatomyositis: cutaneous manifestations of its variants. Int J Dermatol. 2002;41:625-630.
- Kovacs SO, Kovacs SC. Dermatomyositis. J Am Acad Dermatol. 1998;39:899-920; quiz 921-992.
- Liu ZH, Wang XD. Acute-onset adult dermatomyositis presenting with erythroderma and diplopia. Clin Exp Dermatol. 2007;32:751-752.
- Hill CL, Zhang Y, Sigurgeirsson B, et al. Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 2001;357:96-100.
- Bohan A, Peter JB, Bowman RL, et al. Computer-assisted analysis of 153 patients with polymyositis and dermatomyositis. Medicine (Baltimore). 1977;56:255-286.
- Ishida T, Aikawa K, Tamura T, et al. Chronic lymphocytic leukemia associated with nephrotic syndrome and dermatomyositis. Intern Med. 1995;34:15-17.
- Nousari HC, Kimyai-Asadi A, Huang CH, et al. T-cell chronic lymphocytic leukemia mimicking dermatomyositis. Int J Dermatol. 2000;39:144-146.
- Marie I, Guillevin L, Menard JF, et al. Hematological malignancy associated with polymyositis and dermatomyositis. Autoimmun Rev. 2012;11:615-620.
- Levine TD. Rituximab in the treatment of dermatomyositis: an open-label pilot study. Arthritis Rheum. 2005;52:601-607.
Practice Points
- Poikiloderma, even with an unusual clinical presentation, can be a useful clinical clue for the diagnosis of dermatomyositis or other collagen vascular disease.
- Dermatomyositis can be paraneoplastic and though often associated with epithelial malignancies and solid tumors can also be associated with leukemias.
Are Breast Cancer Patients Satisfied With Their Care?
Japan has a universal health care system with low copays and short wait times for appointments, including those with specialists. Yet patient satisfaction scores are low compared with those of other countries. Researchers from Juntendo Urayasu Hospital, a university hospital in a Tokyo suburb, conducted a study of 214 patients with breast cancer to find out which aspects of radiation oncology care might affect patient satisfaction. The survey included questions about overall treatment, time from diagnosis to treatment start, wait times in the hospital, and length of consultations.
In general, levels of satisfaction were high. However, wait time was significantly negatively associated with both overall satisfaction and satisfaction with the radiation oncologist. Wait time was just under an hour for an average 11-minute consultation. Although this was longer than the “notorious” Japanese situation of a “3 hours wait and 3 minutes consultation,” the researchers say, “We expect that an international audience will appreciate that even 11 minutes is an exceptionally short duration for a consultation visit with a specialist in radiation oncology.”
They note, though, a reasonable caveat. Anyone can walk into their hospital and, for an additional fee, see a specialist on the day they want, which can lead to extended wait times from sheer congestion. Their hospital’s chief breast cancer surgeon sees 60 to 70 patients a day; the radiation oncologist treats 500 to 600 patients a year without resident or trainee support. This situation is typical of Japanese university hospitals, the researchers add.
Related: Breast Cancer Treatment Among Rural and Urban Women at the Veterans Health Administration
Importantly, for Japanese patients, the researchers also included questions to measure patients’ opinions about sharing how they felt with their physicians. The level of sharing correlated with satisfaction, but the researchers point out that in Japan sharing feelings remains “challenging.” Their findings suggest, they say, that if this were improved, patients’ satisfaction might increase.
Japan has a universal health care system with low copays and short wait times for appointments, including those with specialists. Yet patient satisfaction scores are low compared with those of other countries. Researchers from Juntendo Urayasu Hospital, a university hospital in a Tokyo suburb, conducted a study of 214 patients with breast cancer to find out which aspects of radiation oncology care might affect patient satisfaction. The survey included questions about overall treatment, time from diagnosis to treatment start, wait times in the hospital, and length of consultations.
In general, levels of satisfaction were high. However, wait time was significantly negatively associated with both overall satisfaction and satisfaction with the radiation oncologist. Wait time was just under an hour for an average 11-minute consultation. Although this was longer than the “notorious” Japanese situation of a “3 hours wait and 3 minutes consultation,” the researchers say, “We expect that an international audience will appreciate that even 11 minutes is an exceptionally short duration for a consultation visit with a specialist in radiation oncology.”
They note, though, a reasonable caveat. Anyone can walk into their hospital and, for an additional fee, see a specialist on the day they want, which can lead to extended wait times from sheer congestion. Their hospital’s chief breast cancer surgeon sees 60 to 70 patients a day; the radiation oncologist treats 500 to 600 patients a year without resident or trainee support. This situation is typical of Japanese university hospitals, the researchers add.
Related: Breast Cancer Treatment Among Rural and Urban Women at the Veterans Health Administration
Importantly, for Japanese patients, the researchers also included questions to measure patients’ opinions about sharing how they felt with their physicians. The level of sharing correlated with satisfaction, but the researchers point out that in Japan sharing feelings remains “challenging.” Their findings suggest, they say, that if this were improved, patients’ satisfaction might increase.
Japan has a universal health care system with low copays and short wait times for appointments, including those with specialists. Yet patient satisfaction scores are low compared with those of other countries. Researchers from Juntendo Urayasu Hospital, a university hospital in a Tokyo suburb, conducted a study of 214 patients with breast cancer to find out which aspects of radiation oncology care might affect patient satisfaction. The survey included questions about overall treatment, time from diagnosis to treatment start, wait times in the hospital, and length of consultations.
In general, levels of satisfaction were high. However, wait time was significantly negatively associated with both overall satisfaction and satisfaction with the radiation oncologist. Wait time was just under an hour for an average 11-minute consultation. Although this was longer than the “notorious” Japanese situation of a “3 hours wait and 3 minutes consultation,” the researchers say, “We expect that an international audience will appreciate that even 11 minutes is an exceptionally short duration for a consultation visit with a specialist in radiation oncology.”
They note, though, a reasonable caveat. Anyone can walk into their hospital and, for an additional fee, see a specialist on the day they want, which can lead to extended wait times from sheer congestion. Their hospital’s chief breast cancer surgeon sees 60 to 70 patients a day; the radiation oncologist treats 500 to 600 patients a year without resident or trainee support. This situation is typical of Japanese university hospitals, the researchers add.
Related: Breast Cancer Treatment Among Rural and Urban Women at the Veterans Health Administration
Importantly, for Japanese patients, the researchers also included questions to measure patients’ opinions about sharing how they felt with their physicians. The level of sharing correlated with satisfaction, but the researchers point out that in Japan sharing feelings remains “challenging.” Their findings suggest, they say, that if this were improved, patients’ satisfaction might increase.
Intrathecal hydromorphone boosts post-op pain control
LAS VEGAS – Intrathecal hydromorphone, administered alone or with lidocaine, effectively controlled pain and decreased postoperative opioid use after colorectal surgery in a retrospective study.
The technique was so effective that 28% of patients required no postoperative opioids at all, Amit Merchea, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The intrathecal analgesic was part of an enhanced recovery pathway (ERP) for patients undergoing elective colorectal surgery at the Mayo Clinic, Jacksonville, Fla., where Dr. Merchea practices colorectal surgery.
Morphine has been the gold standard for this approach, he said. Dr. Merchea and his colleagues investigated the use of hydromorphone in 601 patients who underwent open or minimally invasive colorectal surgery at the Mayo Clinic from 2012 to 2013.
The patients were a median of 52 years old. The surgical approach was almost evenly split between open and laparoscopic. The median length of hospital stay was 3 days. All received intrathecal hydromorphone either alone (91%) or with a local anesthetic (9%).
Everyone was on the same presurgical and postsurgical pain control regimen, which consisted of celecoxib, gabapentin, and acetaminophen before surgery, followed by nonsteroidal anti-inflammatories and acetaminophen, with oxycodone as needed, after surgery.
Overall, the procedure was well tolerated, with seven cases of pruritus requiring Nubain (nalbuphine), one case of respiratory depression that required naloxone, and one postdural headache that required a patch. The rate of ileus was 16%.
At 4 hours, the median pain score was 3 on a 1- to 10-point scale. At 24 hours, it was a median of 4. By 48 hours, the median pain score was 6. This increase is to be expected as the hydrocodone exists in the intrathecal space for up to 36 hours, Dr. Merchea noted.
The median total oral morphine equivalent (OME) was 24; 170 patients (28%) needed no opioid medications after surgery.
He also presented outcomes by infusion composition. There was no difference in the rate of ileus among those who had hydromorphone alone and those who had it with lidocaine. The length of stay was 3 vs. 3.5 days, respectively. The only significant difference in pain scores was the 48-hour maximum, which was a median of 7 in the combination group and 6 in the hydromorphone-only group.
The combination group, however, required more postoperative opioids (33.8 vs. 22.5 OMEs). Significantly more patients in the hydromorphone-only group were able to go without any postoperative opioids (30% vs. 15%).
Dr. Merchea also broke down the results by hydromorphone dosage, but there were no significant differences in ileus rate, length of stay, or pain scores correlated with dosage. However, those who received higher doses were significantly more likely to need more postoperative opioids than those who had lower doses.
Session moderator Peter Muscarella, MD, of Montefiore Medical Center, New York, asked whether the intrathecal infusion was associated with hypotension. “Some of these procedures with epidural analgesics intraoperatively, we have seen shifts in blood pressure that result in excess fluid administration, sometimes leading to tissue complications.”
Dr. Merchea said hypotension was not an outcome of this trial, but that he has looked at it before. “We have previously reported that epidural analgesia was associated with a 15% occurrence of hypotension, but it had no clinical impact and didn’t warrant giving any additional fluids.”
Dr. Merchea had no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
LAS VEGAS – Intrathecal hydromorphone, administered alone or with lidocaine, effectively controlled pain and decreased postoperative opioid use after colorectal surgery in a retrospective study.
The technique was so effective that 28% of patients required no postoperative opioids at all, Amit Merchea, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The intrathecal analgesic was part of an enhanced recovery pathway (ERP) for patients undergoing elective colorectal surgery at the Mayo Clinic, Jacksonville, Fla., where Dr. Merchea practices colorectal surgery.
Morphine has been the gold standard for this approach, he said. Dr. Merchea and his colleagues investigated the use of hydromorphone in 601 patients who underwent open or minimally invasive colorectal surgery at the Mayo Clinic from 2012 to 2013.
The patients were a median of 52 years old. The surgical approach was almost evenly split between open and laparoscopic. The median length of hospital stay was 3 days. All received intrathecal hydromorphone either alone (91%) or with a local anesthetic (9%).
Everyone was on the same presurgical and postsurgical pain control regimen, which consisted of celecoxib, gabapentin, and acetaminophen before surgery, followed by nonsteroidal anti-inflammatories and acetaminophen, with oxycodone as needed, after surgery.
Overall, the procedure was well tolerated, with seven cases of pruritus requiring Nubain (nalbuphine), one case of respiratory depression that required naloxone, and one postdural headache that required a patch. The rate of ileus was 16%.
At 4 hours, the median pain score was 3 on a 1- to 10-point scale. At 24 hours, it was a median of 4. By 48 hours, the median pain score was 6. This increase is to be expected as the hydrocodone exists in the intrathecal space for up to 36 hours, Dr. Merchea noted.
The median total oral morphine equivalent (OME) was 24; 170 patients (28%) needed no opioid medications after surgery.
He also presented outcomes by infusion composition. There was no difference in the rate of ileus among those who had hydromorphone alone and those who had it with lidocaine. The length of stay was 3 vs. 3.5 days, respectively. The only significant difference in pain scores was the 48-hour maximum, which was a median of 7 in the combination group and 6 in the hydromorphone-only group.
The combination group, however, required more postoperative opioids (33.8 vs. 22.5 OMEs). Significantly more patients in the hydromorphone-only group were able to go without any postoperative opioids (30% vs. 15%).
Dr. Merchea also broke down the results by hydromorphone dosage, but there were no significant differences in ileus rate, length of stay, or pain scores correlated with dosage. However, those who received higher doses were significantly more likely to need more postoperative opioids than those who had lower doses.
Session moderator Peter Muscarella, MD, of Montefiore Medical Center, New York, asked whether the intrathecal infusion was associated with hypotension. “Some of these procedures with epidural analgesics intraoperatively, we have seen shifts in blood pressure that result in excess fluid administration, sometimes leading to tissue complications.”
Dr. Merchea said hypotension was not an outcome of this trial, but that he has looked at it before. “We have previously reported that epidural analgesia was associated with a 15% occurrence of hypotension, but it had no clinical impact and didn’t warrant giving any additional fluids.”
Dr. Merchea had no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
LAS VEGAS – Intrathecal hydromorphone, administered alone or with lidocaine, effectively controlled pain and decreased postoperative opioid use after colorectal surgery in a retrospective study.
The technique was so effective that 28% of patients required no postoperative opioids at all, Amit Merchea, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The intrathecal analgesic was part of an enhanced recovery pathway (ERP) for patients undergoing elective colorectal surgery at the Mayo Clinic, Jacksonville, Fla., where Dr. Merchea practices colorectal surgery.
Morphine has been the gold standard for this approach, he said. Dr. Merchea and his colleagues investigated the use of hydromorphone in 601 patients who underwent open or minimally invasive colorectal surgery at the Mayo Clinic from 2012 to 2013.
The patients were a median of 52 years old. The surgical approach was almost evenly split between open and laparoscopic. The median length of hospital stay was 3 days. All received intrathecal hydromorphone either alone (91%) or with a local anesthetic (9%).
Everyone was on the same presurgical and postsurgical pain control regimen, which consisted of celecoxib, gabapentin, and acetaminophen before surgery, followed by nonsteroidal anti-inflammatories and acetaminophen, with oxycodone as needed, after surgery.
Overall, the procedure was well tolerated, with seven cases of pruritus requiring Nubain (nalbuphine), one case of respiratory depression that required naloxone, and one postdural headache that required a patch. The rate of ileus was 16%.
At 4 hours, the median pain score was 3 on a 1- to 10-point scale. At 24 hours, it was a median of 4. By 48 hours, the median pain score was 6. This increase is to be expected as the hydrocodone exists in the intrathecal space for up to 36 hours, Dr. Merchea noted.
The median total oral morphine equivalent (OME) was 24; 170 patients (28%) needed no opioid medications after surgery.
He also presented outcomes by infusion composition. There was no difference in the rate of ileus among those who had hydromorphone alone and those who had it with lidocaine. The length of stay was 3 vs. 3.5 days, respectively. The only significant difference in pain scores was the 48-hour maximum, which was a median of 7 in the combination group and 6 in the hydromorphone-only group.
The combination group, however, required more postoperative opioids (33.8 vs. 22.5 OMEs). Significantly more patients in the hydromorphone-only group were able to go without any postoperative opioids (30% vs. 15%).
Dr. Merchea also broke down the results by hydromorphone dosage, but there were no significant differences in ileus rate, length of stay, or pain scores correlated with dosage. However, those who received higher doses were significantly more likely to need more postoperative opioids than those who had lower doses.
Session moderator Peter Muscarella, MD, of Montefiore Medical Center, New York, asked whether the intrathecal infusion was associated with hypotension. “Some of these procedures with epidural analgesics intraoperatively, we have seen shifts in blood pressure that result in excess fluid administration, sometimes leading to tissue complications.”
Dr. Merchea said hypotension was not an outcome of this trial, but that he has looked at it before. “We have previously reported that epidural analgesia was associated with a 15% occurrence of hypotension, but it had no clinical impact and didn’t warrant giving any additional fluids.”
Dr. Merchea had no relevant financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point:
Major finding: About a quarter of patients (28%) needed no postoperative opioids.
Data source: A retrospective study of 601 patients.
Disclosures: Dr. Merchea had no relevant financial disclosures.