User login
Gotta catch ’em all: Is Pokémon Go an intervention for schizophrenia?
San Diego – A 22-year-old Minnesota patient with schizophrenia tried to “catch ’em all” during last year’s Pokémon Go craze, and he ended up landing something even more important: motivation to get outside and meet people.
That’s the word from clinicians who report that the game dramatically transformed the young man’s life, coaxing him to leave his house, chat with other players, and even stop worrying so much about his movement disorder.
Could Pokémon Go become a treatment for people with mental illness who need motivation to leave their homes? It’s not clear, and the decline of the Pokémon Go phenomenon may make it difficult for researchers to find out, at least until another version sweeps the nation.
The Minnesota clinicians want to study the idea; they also want to know why it seems – based on a tiny sample – that patients with schizophrenia may have trouble tolerating the “augmented reality” built into the game.
Dr. Elmaghraby and his coauthor Suzanne Geier Jasberg, MD, an attending psychiatrist with PrairieCare Medical Group in Minneapolis, described their findings in a poster at the International Congress on Schizophrenia Research.
The Pokémon Go game appeared in the summer of 2016, and during that time, many of the young patients attending a first-episode psychosis clinic began talking about playing it, Dr. Elmaghraby said in an interview.
“They have the negative symptoms – they’re socially isolated, withdrawing from friends and families, and don’t engage with society,” she said. But the game requires users to travel around the real world in search of Pokémon characters.
“People who hadn’t left the house in many days were getting multiple steps per day by going out in the environment and engaging with other people,” she said.
The poster focuses on the 22-year-old male, who had the disorganized type of schizophrenia with auditory and visual hallucinations. He also had residual dyskinetic movements related to a previous stint on risperidone.
His thought processes were improving, but he’d had trouble leaving the house for 6 months. Then, the game coaxed him into a new phase.
“He demonstrated remarkable improvement in his negative symptoms, most notably motivation,” the clinicians wrote. “The game seemed to have a unique ability to motivate this young person to engage more robustly in social interactions.”
They also noticed that several patients, including the young man, engaged in a peculiar behavior: They turned off the “augmented reality” in the game.
Normally, Pokémon Go players keep the augmented reality feature on, allowing them to see Pokémon characters as if they’re actually nearby. Smartphone screens create the illusion by blending their live camera view of the world with images of the characters. (Think about how Dick Van Dyke appears to dance with animated penguins in “Mary Poppins,” and you’ll get the idea.)
In this augmented reality, your smartphone screen may makes it appear as if a Pokémon character is on top of the coffee cup at your desk, said report coauthor Dr. Jasberg. This feature adds to the immediacy and fun of the game.
But players can turn off this feature, eliminating the view of the world through the smartphone camera. Instead of appearing as if they’re nearby in the real world, the characters simply show up on a green screen, Dr. Jasberg said. (Players still have to go places to find them.)
The patients couldn’t explain why they preferred to turn off the feature, which is easily done, Dr. Elmaghraby said. However, they indicated that it’s not in order to preserve battery life, she said.
Dr. Elmaghraby speculates that their choices may have something to do with their underlying sensory processing dysfunction.
The clinicians hope to study how the brains of patients with schizophrenia work when they play the game with the augmented reality turned off and on. And they’re intrigued by how such games as Pokémon Go might encourage people to move and become socially engaged.
There’s been fairly little published research into the effects of the Pokémon Go craze, possibly because it erupted so recently. Several studies have examined its effects on exercise, with one analysis of college students suggesting that it especially boosted activity levels in the formerly sedentary (Int J Health Geogr. 2017 Feb 22;16[1]:8). Another study of young adults found that the increase of activity in players was moderate and vanished after 6 weeks (BMJ. 2016 Dec 13;355:i6270).
For now, Dr. Jasberg encouraged clinicians to be aware of Pokémon Go and understand that it’s a low-risk intervention. The clinicians didn’t notice any negative impacts, although it’s possible that parents may have gotten zinged by a distinctly modern phenomenon – overtaxed smartphone data plans.
The authors reported no relevant disclosures.
San Diego – A 22-year-old Minnesota patient with schizophrenia tried to “catch ’em all” during last year’s Pokémon Go craze, and he ended up landing something even more important: motivation to get outside and meet people.
That’s the word from clinicians who report that the game dramatically transformed the young man’s life, coaxing him to leave his house, chat with other players, and even stop worrying so much about his movement disorder.
Could Pokémon Go become a treatment for people with mental illness who need motivation to leave their homes? It’s not clear, and the decline of the Pokémon Go phenomenon may make it difficult for researchers to find out, at least until another version sweeps the nation.
The Minnesota clinicians want to study the idea; they also want to know why it seems – based on a tiny sample – that patients with schizophrenia may have trouble tolerating the “augmented reality” built into the game.
Dr. Elmaghraby and his coauthor Suzanne Geier Jasberg, MD, an attending psychiatrist with PrairieCare Medical Group in Minneapolis, described their findings in a poster at the International Congress on Schizophrenia Research.
The Pokémon Go game appeared in the summer of 2016, and during that time, many of the young patients attending a first-episode psychosis clinic began talking about playing it, Dr. Elmaghraby said in an interview.
“They have the negative symptoms – they’re socially isolated, withdrawing from friends and families, and don’t engage with society,” she said. But the game requires users to travel around the real world in search of Pokémon characters.
“People who hadn’t left the house in many days were getting multiple steps per day by going out in the environment and engaging with other people,” she said.
The poster focuses on the 22-year-old male, who had the disorganized type of schizophrenia with auditory and visual hallucinations. He also had residual dyskinetic movements related to a previous stint on risperidone.
His thought processes were improving, but he’d had trouble leaving the house for 6 months. Then, the game coaxed him into a new phase.
“He demonstrated remarkable improvement in his negative symptoms, most notably motivation,” the clinicians wrote. “The game seemed to have a unique ability to motivate this young person to engage more robustly in social interactions.”
They also noticed that several patients, including the young man, engaged in a peculiar behavior: They turned off the “augmented reality” in the game.
Normally, Pokémon Go players keep the augmented reality feature on, allowing them to see Pokémon characters as if they’re actually nearby. Smartphone screens create the illusion by blending their live camera view of the world with images of the characters. (Think about how Dick Van Dyke appears to dance with animated penguins in “Mary Poppins,” and you’ll get the idea.)
In this augmented reality, your smartphone screen may makes it appear as if a Pokémon character is on top of the coffee cup at your desk, said report coauthor Dr. Jasberg. This feature adds to the immediacy and fun of the game.
But players can turn off this feature, eliminating the view of the world through the smartphone camera. Instead of appearing as if they’re nearby in the real world, the characters simply show up on a green screen, Dr. Jasberg said. (Players still have to go places to find them.)
The patients couldn’t explain why they preferred to turn off the feature, which is easily done, Dr. Elmaghraby said. However, they indicated that it’s not in order to preserve battery life, she said.
Dr. Elmaghraby speculates that their choices may have something to do with their underlying sensory processing dysfunction.
The clinicians hope to study how the brains of patients with schizophrenia work when they play the game with the augmented reality turned off and on. And they’re intrigued by how such games as Pokémon Go might encourage people to move and become socially engaged.
There’s been fairly little published research into the effects of the Pokémon Go craze, possibly because it erupted so recently. Several studies have examined its effects on exercise, with one analysis of college students suggesting that it especially boosted activity levels in the formerly sedentary (Int J Health Geogr. 2017 Feb 22;16[1]:8). Another study of young adults found that the increase of activity in players was moderate and vanished after 6 weeks (BMJ. 2016 Dec 13;355:i6270).
For now, Dr. Jasberg encouraged clinicians to be aware of Pokémon Go and understand that it’s a low-risk intervention. The clinicians didn’t notice any negative impacts, although it’s possible that parents may have gotten zinged by a distinctly modern phenomenon – overtaxed smartphone data plans.
The authors reported no relevant disclosures.
San Diego – A 22-year-old Minnesota patient with schizophrenia tried to “catch ’em all” during last year’s Pokémon Go craze, and he ended up landing something even more important: motivation to get outside and meet people.
That’s the word from clinicians who report that the game dramatically transformed the young man’s life, coaxing him to leave his house, chat with other players, and even stop worrying so much about his movement disorder.
Could Pokémon Go become a treatment for people with mental illness who need motivation to leave their homes? It’s not clear, and the decline of the Pokémon Go phenomenon may make it difficult for researchers to find out, at least until another version sweeps the nation.
The Minnesota clinicians want to study the idea; they also want to know why it seems – based on a tiny sample – that patients with schizophrenia may have trouble tolerating the “augmented reality” built into the game.
Dr. Elmaghraby and his coauthor Suzanne Geier Jasberg, MD, an attending psychiatrist with PrairieCare Medical Group in Minneapolis, described their findings in a poster at the International Congress on Schizophrenia Research.
The Pokémon Go game appeared in the summer of 2016, and during that time, many of the young patients attending a first-episode psychosis clinic began talking about playing it, Dr. Elmaghraby said in an interview.
“They have the negative symptoms – they’re socially isolated, withdrawing from friends and families, and don’t engage with society,” she said. But the game requires users to travel around the real world in search of Pokémon characters.
“People who hadn’t left the house in many days were getting multiple steps per day by going out in the environment and engaging with other people,” she said.
The poster focuses on the 22-year-old male, who had the disorganized type of schizophrenia with auditory and visual hallucinations. He also had residual dyskinetic movements related to a previous stint on risperidone.
His thought processes were improving, but he’d had trouble leaving the house for 6 months. Then, the game coaxed him into a new phase.
“He demonstrated remarkable improvement in his negative symptoms, most notably motivation,” the clinicians wrote. “The game seemed to have a unique ability to motivate this young person to engage more robustly in social interactions.”
They also noticed that several patients, including the young man, engaged in a peculiar behavior: They turned off the “augmented reality” in the game.
Normally, Pokémon Go players keep the augmented reality feature on, allowing them to see Pokémon characters as if they’re actually nearby. Smartphone screens create the illusion by blending their live camera view of the world with images of the characters. (Think about how Dick Van Dyke appears to dance with animated penguins in “Mary Poppins,” and you’ll get the idea.)
In this augmented reality, your smartphone screen may makes it appear as if a Pokémon character is on top of the coffee cup at your desk, said report coauthor Dr. Jasberg. This feature adds to the immediacy and fun of the game.
But players can turn off this feature, eliminating the view of the world through the smartphone camera. Instead of appearing as if they’re nearby in the real world, the characters simply show up on a green screen, Dr. Jasberg said. (Players still have to go places to find them.)
The patients couldn’t explain why they preferred to turn off the feature, which is easily done, Dr. Elmaghraby said. However, they indicated that it’s not in order to preserve battery life, she said.
Dr. Elmaghraby speculates that their choices may have something to do with their underlying sensory processing dysfunction.
The clinicians hope to study how the brains of patients with schizophrenia work when they play the game with the augmented reality turned off and on. And they’re intrigued by how such games as Pokémon Go might encourage people to move and become socially engaged.
There’s been fairly little published research into the effects of the Pokémon Go craze, possibly because it erupted so recently. Several studies have examined its effects on exercise, with one analysis of college students suggesting that it especially boosted activity levels in the formerly sedentary (Int J Health Geogr. 2017 Feb 22;16[1]:8). Another study of young adults found that the increase of activity in players was moderate and vanished after 6 weeks (BMJ. 2016 Dec 13;355:i6270).
For now, Dr. Jasberg encouraged clinicians to be aware of Pokémon Go and understand that it’s a low-risk intervention. The clinicians didn’t notice any negative impacts, although it’s possible that parents may have gotten zinged by a distinctly modern phenomenon – overtaxed smartphone data plans.
The authors reported no relevant disclosures.
AT THE ICSR BIENNIAL MEETING
Coronary flow reserve reveals hidden cardiovascular risk
SNOWMASS, COLO. – Mounting evidence attests to the value of noninvasive measurement of coronary flow reserve as a means of classifying cardiovascular risk in patients with stable coronary artery disease (CAD) more accurately than is possible via coronary angiography or measurement of fractional flow reserve, Marcelo F. Di Carli, MD, reported at the Annual Cardiovascular Conference at Snowmass.
“We use CFR [coronary flow reserve] as a way to exclude coronary disease. It’s a good practical measure of multivessel ischemic CAD. When the CFR is normal, you can with high confidence exclude the possibility of high-risk CAD,” according to Dr. Di Carli, executive director of the cardiovascular imaging program and chief of the division of nuclear medicine and molecular imaging at Brigham and Women’s Hospital, Boston.
Most recently, he and his coinvestigators utilized CFR to provide new insight into the paradox that women have a higher cardiovascular disease death rate than men, even though their prevalence of obstructive CAD is lower.
Their NIH-sponsored study included 329 consecutive patients with a left ventricular ejection fraction greater than 40% – 43% of them women – who underwent coronary angiography several days after noninvasive assessment of CFR via myocardial perfusion positron emission tomography. The women had a lower burden of angiographic CAD and a lower pretest clinical risk score than the men. Nevertheless, during a median of 3 years of follow-up, the women had an adjusted twofold greater risk of the composite endpoint of cardiovascular death, nonfatal MI, or heart failure.
This excess cardiovascular risk in women was independently associated with a very low CFR, defined as less than 1.6. Dr. Di Carli and his coinvestigators calculated that this impaired CFR mediated 40% of the excess risk in women. Thus, a low CFR represents a novel hidden biologic risk for ischemic heart disease (Circulation. 2017 Feb 7;135[6]:566-77).
CFR is defined as the ratio of absolute coronary flow or myocardial perfusion between drug-induced hyperemia and rest. It can be quantified noninvasively using positron emission tomography or MRI.
CFR integrates into a single measure the three components of CAD: the focal stenosis, the diffuse atherosclerotic plaque typically present to a varying degree throughout a target vessel, and microvascular dysfunction.
CFR is a measure of coronary physiology, as is invasive fractional flow reserve (FFR). However, FFR measures only the severity of stenosis and extent of diffuse disease; it doesn’t assess microvascular dysfunction. This is a limitation because it means FFR can give false-negative readings in patients without significant obstructive coronary disease who have severe microvascular dysfunction.
As for angiography, Dr. Di Carli continued, it’s now evident that this purely anatomic assessment is of limited value as a marker of clinical risk and is inadequate to guide management decisions in the setting of stable CAD. After all, angiographically guided revascularization has not reduced cardiovascular events in clinical trials comparing it with optimal medical therapy, as in the COURAGE and BARI-2D trials.
“It’s clear that there’s been a paradigm shift in how we manage patients with stable CAD. For many years the coronary angiogram was the cornerstone of what we did: how we understand the symptoms, the patient’s risk, and ultimately how we proceed with treatment. But there is no benefit in basing treatment solely on what the lesions look like anatomically. That’s why we’ve turned to functional testing of coronary physiology,” he said.
CFR has opened a window on the importance of microvascular dysfunction, which is present in about half of patients with stable CAD and has been shown to predict cardiovascular risk independent of whether or not severe obstructive disease is present.
In an earlier study, Dr. Di Carli and coworkers demonstrated that quantification of CFR enhances stratification for risk of cardiac death among diabetes patients (Circulation. 2012 Oct 9;126[15]:1858-68). The study included 2,783 patients, of whom 1,172 were diabetic, who underwent measurement of CFR and were subsequently followed for a median of 1.4 years, during which 137 cardiac deaths occurred.
Diabetes patients without known CAD who had a low CFR had a high cardiac death rate of 2.8%/year, similar to the 2.0%/year rate in nondiabetic patients with a history of acute MI or revascularization. On the other hand, diabetes patients with a normal CFR and without known CAD had a cardiac mortality rate of only 0.3%/year, comparable to the 0.5% rate in nondiabetics without known CAD who had preserved systolic function and a normal stress perfusion study.
In the future, CFR may aid in decision making as to whether an individual with stable CAD is best treated by percutaneous coronary intervention, surgical revascularization, or guideline-directed medical therapy. For example, if CFR indicates the presence of an isolated severe focal stenosis, and this is confirmed by angiography and FFR, PCI may be the best option, while diffuse disease as demonstrated by CFR may be better treated surgically or using optimal medical therapy. But this needs to be established in prospective clinical trials, added Dr. Di Carli.
He reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – Mounting evidence attests to the value of noninvasive measurement of coronary flow reserve as a means of classifying cardiovascular risk in patients with stable coronary artery disease (CAD) more accurately than is possible via coronary angiography or measurement of fractional flow reserve, Marcelo F. Di Carli, MD, reported at the Annual Cardiovascular Conference at Snowmass.
“We use CFR [coronary flow reserve] as a way to exclude coronary disease. It’s a good practical measure of multivessel ischemic CAD. When the CFR is normal, you can with high confidence exclude the possibility of high-risk CAD,” according to Dr. Di Carli, executive director of the cardiovascular imaging program and chief of the division of nuclear medicine and molecular imaging at Brigham and Women’s Hospital, Boston.
Most recently, he and his coinvestigators utilized CFR to provide new insight into the paradox that women have a higher cardiovascular disease death rate than men, even though their prevalence of obstructive CAD is lower.
Their NIH-sponsored study included 329 consecutive patients with a left ventricular ejection fraction greater than 40% – 43% of them women – who underwent coronary angiography several days after noninvasive assessment of CFR via myocardial perfusion positron emission tomography. The women had a lower burden of angiographic CAD and a lower pretest clinical risk score than the men. Nevertheless, during a median of 3 years of follow-up, the women had an adjusted twofold greater risk of the composite endpoint of cardiovascular death, nonfatal MI, or heart failure.
This excess cardiovascular risk in women was independently associated with a very low CFR, defined as less than 1.6. Dr. Di Carli and his coinvestigators calculated that this impaired CFR mediated 40% of the excess risk in women. Thus, a low CFR represents a novel hidden biologic risk for ischemic heart disease (Circulation. 2017 Feb 7;135[6]:566-77).
CFR is defined as the ratio of absolute coronary flow or myocardial perfusion between drug-induced hyperemia and rest. It can be quantified noninvasively using positron emission tomography or MRI.
CFR integrates into a single measure the three components of CAD: the focal stenosis, the diffuse atherosclerotic plaque typically present to a varying degree throughout a target vessel, and microvascular dysfunction.
CFR is a measure of coronary physiology, as is invasive fractional flow reserve (FFR). However, FFR measures only the severity of stenosis and extent of diffuse disease; it doesn’t assess microvascular dysfunction. This is a limitation because it means FFR can give false-negative readings in patients without significant obstructive coronary disease who have severe microvascular dysfunction.
As for angiography, Dr. Di Carli continued, it’s now evident that this purely anatomic assessment is of limited value as a marker of clinical risk and is inadequate to guide management decisions in the setting of stable CAD. After all, angiographically guided revascularization has not reduced cardiovascular events in clinical trials comparing it with optimal medical therapy, as in the COURAGE and BARI-2D trials.
“It’s clear that there’s been a paradigm shift in how we manage patients with stable CAD. For many years the coronary angiogram was the cornerstone of what we did: how we understand the symptoms, the patient’s risk, and ultimately how we proceed with treatment. But there is no benefit in basing treatment solely on what the lesions look like anatomically. That’s why we’ve turned to functional testing of coronary physiology,” he said.
CFR has opened a window on the importance of microvascular dysfunction, which is present in about half of patients with stable CAD and has been shown to predict cardiovascular risk independent of whether or not severe obstructive disease is present.
In an earlier study, Dr. Di Carli and coworkers demonstrated that quantification of CFR enhances stratification for risk of cardiac death among diabetes patients (Circulation. 2012 Oct 9;126[15]:1858-68). The study included 2,783 patients, of whom 1,172 were diabetic, who underwent measurement of CFR and were subsequently followed for a median of 1.4 years, during which 137 cardiac deaths occurred.
Diabetes patients without known CAD who had a low CFR had a high cardiac death rate of 2.8%/year, similar to the 2.0%/year rate in nondiabetic patients with a history of acute MI or revascularization. On the other hand, diabetes patients with a normal CFR and without known CAD had a cardiac mortality rate of only 0.3%/year, comparable to the 0.5% rate in nondiabetics without known CAD who had preserved systolic function and a normal stress perfusion study.
In the future, CFR may aid in decision making as to whether an individual with stable CAD is best treated by percutaneous coronary intervention, surgical revascularization, or guideline-directed medical therapy. For example, if CFR indicates the presence of an isolated severe focal stenosis, and this is confirmed by angiography and FFR, PCI may be the best option, while diffuse disease as demonstrated by CFR may be better treated surgically or using optimal medical therapy. But this needs to be established in prospective clinical trials, added Dr. Di Carli.
He reported having no financial conflicts regarding his presentation.
SNOWMASS, COLO. – Mounting evidence attests to the value of noninvasive measurement of coronary flow reserve as a means of classifying cardiovascular risk in patients with stable coronary artery disease (CAD) more accurately than is possible via coronary angiography or measurement of fractional flow reserve, Marcelo F. Di Carli, MD, reported at the Annual Cardiovascular Conference at Snowmass.
“We use CFR [coronary flow reserve] as a way to exclude coronary disease. It’s a good practical measure of multivessel ischemic CAD. When the CFR is normal, you can with high confidence exclude the possibility of high-risk CAD,” according to Dr. Di Carli, executive director of the cardiovascular imaging program and chief of the division of nuclear medicine and molecular imaging at Brigham and Women’s Hospital, Boston.
Most recently, he and his coinvestigators utilized CFR to provide new insight into the paradox that women have a higher cardiovascular disease death rate than men, even though their prevalence of obstructive CAD is lower.
Their NIH-sponsored study included 329 consecutive patients with a left ventricular ejection fraction greater than 40% – 43% of them women – who underwent coronary angiography several days after noninvasive assessment of CFR via myocardial perfusion positron emission tomography. The women had a lower burden of angiographic CAD and a lower pretest clinical risk score than the men. Nevertheless, during a median of 3 years of follow-up, the women had an adjusted twofold greater risk of the composite endpoint of cardiovascular death, nonfatal MI, or heart failure.
This excess cardiovascular risk in women was independently associated with a very low CFR, defined as less than 1.6. Dr. Di Carli and his coinvestigators calculated that this impaired CFR mediated 40% of the excess risk in women. Thus, a low CFR represents a novel hidden biologic risk for ischemic heart disease (Circulation. 2017 Feb 7;135[6]:566-77).
CFR is defined as the ratio of absolute coronary flow or myocardial perfusion between drug-induced hyperemia and rest. It can be quantified noninvasively using positron emission tomography or MRI.
CFR integrates into a single measure the three components of CAD: the focal stenosis, the diffuse atherosclerotic plaque typically present to a varying degree throughout a target vessel, and microvascular dysfunction.
CFR is a measure of coronary physiology, as is invasive fractional flow reserve (FFR). However, FFR measures only the severity of stenosis and extent of diffuse disease; it doesn’t assess microvascular dysfunction. This is a limitation because it means FFR can give false-negative readings in patients without significant obstructive coronary disease who have severe microvascular dysfunction.
As for angiography, Dr. Di Carli continued, it’s now evident that this purely anatomic assessment is of limited value as a marker of clinical risk and is inadequate to guide management decisions in the setting of stable CAD. After all, angiographically guided revascularization has not reduced cardiovascular events in clinical trials comparing it with optimal medical therapy, as in the COURAGE and BARI-2D trials.
“It’s clear that there’s been a paradigm shift in how we manage patients with stable CAD. For many years the coronary angiogram was the cornerstone of what we did: how we understand the symptoms, the patient’s risk, and ultimately how we proceed with treatment. But there is no benefit in basing treatment solely on what the lesions look like anatomically. That’s why we’ve turned to functional testing of coronary physiology,” he said.
CFR has opened a window on the importance of microvascular dysfunction, which is present in about half of patients with stable CAD and has been shown to predict cardiovascular risk independent of whether or not severe obstructive disease is present.
In an earlier study, Dr. Di Carli and coworkers demonstrated that quantification of CFR enhances stratification for risk of cardiac death among diabetes patients (Circulation. 2012 Oct 9;126[15]:1858-68). The study included 2,783 patients, of whom 1,172 were diabetic, who underwent measurement of CFR and were subsequently followed for a median of 1.4 years, during which 137 cardiac deaths occurred.
Diabetes patients without known CAD who had a low CFR had a high cardiac death rate of 2.8%/year, similar to the 2.0%/year rate in nondiabetic patients with a history of acute MI or revascularization. On the other hand, diabetes patients with a normal CFR and without known CAD had a cardiac mortality rate of only 0.3%/year, comparable to the 0.5% rate in nondiabetics without known CAD who had preserved systolic function and a normal stress perfusion study.
In the future, CFR may aid in decision making as to whether an individual with stable CAD is best treated by percutaneous coronary intervention, surgical revascularization, or guideline-directed medical therapy. For example, if CFR indicates the presence of an isolated severe focal stenosis, and this is confirmed by angiography and FFR, PCI may be the best option, while diffuse disease as demonstrated by CFR may be better treated surgically or using optimal medical therapy. But this needs to be established in prospective clinical trials, added Dr. Di Carli.
He reported having no financial conflicts regarding his presentation.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Bundled maternal HIV, well-baby visits boost ART adherence
SEATTLE – When new moms can get their well-baby visits and HIV care together in the same office, they have better antiretroviral adherence, better viral suppression, and breast-feed longer, according to a randomized trial of 472 new moms with HIV in Cape Town, South Africa.
“It’s a simple and highly effective strategy for promoting maternal postpartum engagement” in HIV care, said lead investigator Landon Myer, MD, professor and head of epidemiology and biostatistics at the University of Cape Town.
Antiretroviral treatment management is often a routine part of prenatal care, but care splits after birth, with moms generally sent to an adult HIV clinic and babies in follow-up care at the pediatrician’s office. It’s a logistics problem for many, and women tend to prioritize the care of their infants over their own HIV.
“There’s a big push [globally] to identify interventions that can enhance women’s antiretroviral therapy (ART) adherence post partum,” Dr. Myer said.
The investigators had a hunch that bundling care would help. They randomized 234 women to centers with combined HIV and pediatric care within a week of birth and 238 to the usual split care approach. In the latter group, the mothers were referred to adult HIV services soon after delivery.
At 12 months, 77% of the women in the integrated-care group had viral loads below 50 copies/mL, versus 56% of women in the split care group. Women in the integrated group breastfed for about 9 months, versus 3 months in the control group. The findings were statistically significant.
“We were surprised by how big the differences were,” Dr. Myer said at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Mother-to-child transmission was low, at about 0.55%, and did not differ by arm. Vaccination rates, vitamin use, and other infant outcomes were also similar in both groups. Just a few women in each arm dropped out before the 12-month, postpartum visit.
The mothers were a median of 28 years old, and all had started ART during pregnancy at a median of 21 weeks gestation, with a median pre-ART T-cell count of 354 cells/microL. Three-quarters had viral suppression below 50 copies/mL at randomization. About a quarter were giving birth for the first time. Mothers in the bundled-care group were referred back to adult HIV services at the end of breastfeeding.
Dr. Myer had no disclosures. The work was funded by the National Institutes of Health.
SEATTLE – When new moms can get their well-baby visits and HIV care together in the same office, they have better antiretroviral adherence, better viral suppression, and breast-feed longer, according to a randomized trial of 472 new moms with HIV in Cape Town, South Africa.
“It’s a simple and highly effective strategy for promoting maternal postpartum engagement” in HIV care, said lead investigator Landon Myer, MD, professor and head of epidemiology and biostatistics at the University of Cape Town.
Antiretroviral treatment management is often a routine part of prenatal care, but care splits after birth, with moms generally sent to an adult HIV clinic and babies in follow-up care at the pediatrician’s office. It’s a logistics problem for many, and women tend to prioritize the care of their infants over their own HIV.
“There’s a big push [globally] to identify interventions that can enhance women’s antiretroviral therapy (ART) adherence post partum,” Dr. Myer said.
The investigators had a hunch that bundling care would help. They randomized 234 women to centers with combined HIV and pediatric care within a week of birth and 238 to the usual split care approach. In the latter group, the mothers were referred to adult HIV services soon after delivery.
At 12 months, 77% of the women in the integrated-care group had viral loads below 50 copies/mL, versus 56% of women in the split care group. Women in the integrated group breastfed for about 9 months, versus 3 months in the control group. The findings were statistically significant.
“We were surprised by how big the differences were,” Dr. Myer said at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Mother-to-child transmission was low, at about 0.55%, and did not differ by arm. Vaccination rates, vitamin use, and other infant outcomes were also similar in both groups. Just a few women in each arm dropped out before the 12-month, postpartum visit.
The mothers were a median of 28 years old, and all had started ART during pregnancy at a median of 21 weeks gestation, with a median pre-ART T-cell count of 354 cells/microL. Three-quarters had viral suppression below 50 copies/mL at randomization. About a quarter were giving birth for the first time. Mothers in the bundled-care group were referred back to adult HIV services at the end of breastfeeding.
Dr. Myer had no disclosures. The work was funded by the National Institutes of Health.
SEATTLE – When new moms can get their well-baby visits and HIV care together in the same office, they have better antiretroviral adherence, better viral suppression, and breast-feed longer, according to a randomized trial of 472 new moms with HIV in Cape Town, South Africa.
“It’s a simple and highly effective strategy for promoting maternal postpartum engagement” in HIV care, said lead investigator Landon Myer, MD, professor and head of epidemiology and biostatistics at the University of Cape Town.
Antiretroviral treatment management is often a routine part of prenatal care, but care splits after birth, with moms generally sent to an adult HIV clinic and babies in follow-up care at the pediatrician’s office. It’s a logistics problem for many, and women tend to prioritize the care of their infants over their own HIV.
“There’s a big push [globally] to identify interventions that can enhance women’s antiretroviral therapy (ART) adherence post partum,” Dr. Myer said.
The investigators had a hunch that bundling care would help. They randomized 234 women to centers with combined HIV and pediatric care within a week of birth and 238 to the usual split care approach. In the latter group, the mothers were referred to adult HIV services soon after delivery.
At 12 months, 77% of the women in the integrated-care group had viral loads below 50 copies/mL, versus 56% of women in the split care group. Women in the integrated group breastfed for about 9 months, versus 3 months in the control group. The findings were statistically significant.
“We were surprised by how big the differences were,” Dr. Myer said at the Conference on Retroviruses & Opportunistic Infections in partnership with the International Antiviral Society.
Mother-to-child transmission was low, at about 0.55%, and did not differ by arm. Vaccination rates, vitamin use, and other infant outcomes were also similar in both groups. Just a few women in each arm dropped out before the 12-month, postpartum visit.
The mothers were a median of 28 years old, and all had started ART during pregnancy at a median of 21 weeks gestation, with a median pre-ART T-cell count of 354 cells/microL. Three-quarters had viral suppression below 50 copies/mL at randomization. About a quarter were giving birth for the first time. Mothers in the bundled-care group were referred back to adult HIV services at the end of breastfeeding.
Dr. Myer had no disclosures. The work was funded by the National Institutes of Health.
AT CROI
Key clinical point:
Major finding: At 12 months, 77% of the women in the integrated-care group had viral loads below 50 copies/mL, versus 56% of women in the control arm. Women in the integrated group breastfed for about 9 months, versus 3 months in the split-care group.
Data source: A randomized trial of 472 new moms with HIV and their babies in Cape Town, South Africa.
Disclosures: Dr. Myer had no disclosures. The work was funded by the National Institutes of Health.
Polycythemia vera test detects JAK2 V617F/G1849T mutation
The ipsogen JAK2 RGQ PCR Kit has been given marketing authorization by the Food and Drug Administration.
This is the first FDA-authorized test for use in evaluating patients for suspected polycythemia vera, according to an FDA press release. Manufactured by Qiagen, the kit detects the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The presence of JAK2 mutations is one of the major criteria for clinical confirmation of polycythemia vera. The V617F/G1849T mutation is detected in more than 94% of these patients. This test does not detect less common mutations including mutations in exon 12 and is not intended for stand-alone diagnosis, which is based on other clinicopathological factors of polycythemia vera.
Marketing authorization, granted March 27, 2017, was based on data from a clinical study of 216 patients with suspected polycythemia vera. The study compared results from the ipsogen JAK2 RGQ PCR Kit with results obtained with Sanger sequencing. In the study, the ipsogen JAK2 RGQ PCR Kit test detected polycythemia vera with 94.6% sensitivity and 98.1% specificity.
Further information about the JAK2 RGQ PCR Kit is available at https://www.accessdata.fda.gov/cdrh_docs/pdf16/DEN160028.pdf.
[email protected]
On Twitter @maryjodales
The ipsogen JAK2 RGQ PCR Kit has been given marketing authorization by the Food and Drug Administration.
This is the first FDA-authorized test for use in evaluating patients for suspected polycythemia vera, according to an FDA press release. Manufactured by Qiagen, the kit detects the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The presence of JAK2 mutations is one of the major criteria for clinical confirmation of polycythemia vera. The V617F/G1849T mutation is detected in more than 94% of these patients. This test does not detect less common mutations including mutations in exon 12 and is not intended for stand-alone diagnosis, which is based on other clinicopathological factors of polycythemia vera.
Marketing authorization, granted March 27, 2017, was based on data from a clinical study of 216 patients with suspected polycythemia vera. The study compared results from the ipsogen JAK2 RGQ PCR Kit with results obtained with Sanger sequencing. In the study, the ipsogen JAK2 RGQ PCR Kit test detected polycythemia vera with 94.6% sensitivity and 98.1% specificity.
Further information about the JAK2 RGQ PCR Kit is available at https://www.accessdata.fda.gov/cdrh_docs/pdf16/DEN160028.pdf.
[email protected]
On Twitter @maryjodales
The ipsogen JAK2 RGQ PCR Kit has been given marketing authorization by the Food and Drug Administration.
This is the first FDA-authorized test for use in evaluating patients for suspected polycythemia vera, according to an FDA press release. Manufactured by Qiagen, the kit detects the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The presence of JAK2 mutations is one of the major criteria for clinical confirmation of polycythemia vera. The V617F/G1849T mutation is detected in more than 94% of these patients. This test does not detect less common mutations including mutations in exon 12 and is not intended for stand-alone diagnosis, which is based on other clinicopathological factors of polycythemia vera.
Marketing authorization, granted March 27, 2017, was based on data from a clinical study of 216 patients with suspected polycythemia vera. The study compared results from the ipsogen JAK2 RGQ PCR Kit with results obtained with Sanger sequencing. In the study, the ipsogen JAK2 RGQ PCR Kit test detected polycythemia vera with 94.6% sensitivity and 98.1% specificity.
Further information about the JAK2 RGQ PCR Kit is available at https://www.accessdata.fda.gov/cdrh_docs/pdf16/DEN160028.pdf.
[email protected]
On Twitter @maryjodales
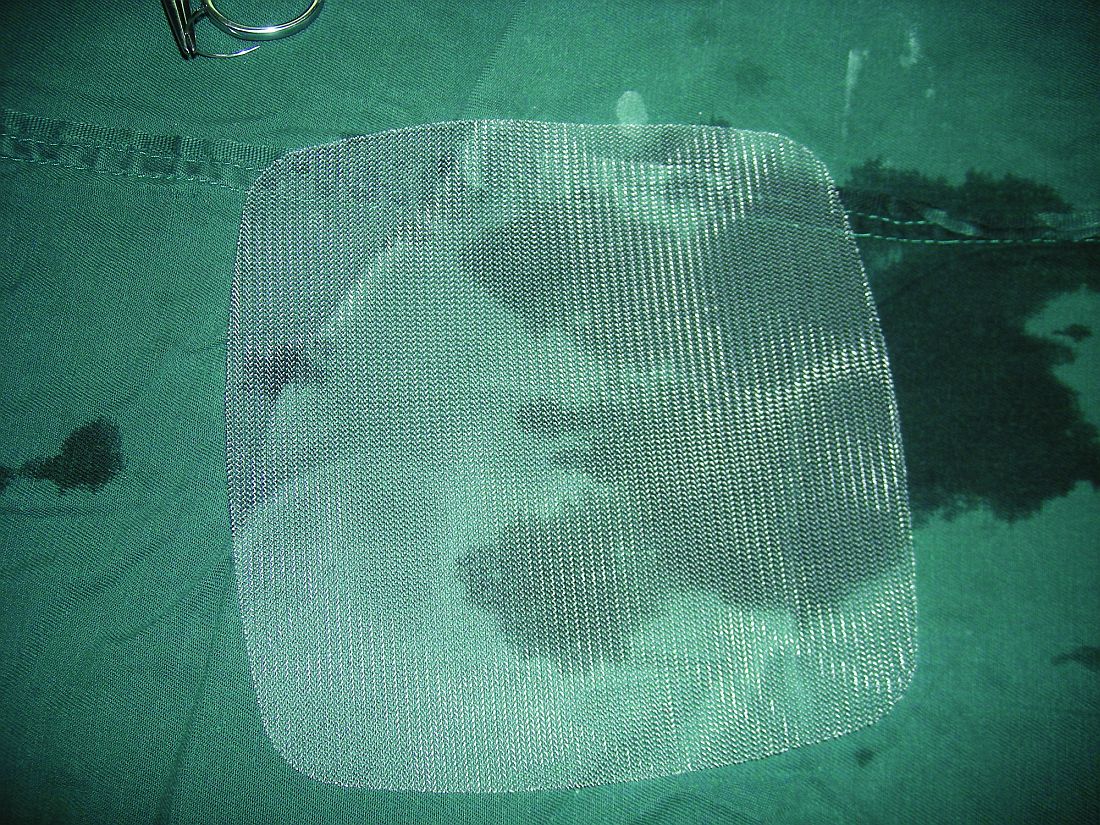
Lightweight mesh reduces erosion risk after sacrocolpopexy
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
SAN ANTONIO – Compared with heavier mesh types, ultralightweight polypropylene (Restorelle Y) did not increase the risk of mesh erosion after sacrocolpopexy in a retrospective, case-control study.
Delayed–absorbable monofilament polydioxanone suture (PDS) also decreased the risk, compared with nonabsorbable braided suture (Ethibond Excel) for vaginal mesh attachment.
The odds ratio for the ultralightweight polypropylene mesh exposure, versus heavier mesh, was not statistically significant (odds ratio, 2.18; 95% confidence interval, 0.33-14.57), which led to the main study conclusion.
“Mesh choice and suture selection [are] important independent predictors of” erosion, she said at the annual scientific meeting of the Society of Gynecologic Surgeons. “Based on this study, surgeons should consider use of [PDS over nonabsorbable braided suture] to reduce the risk of mesh exposure when using ultralightweight mesh.”
The team also found that prior surgery for incontinence, as well as immediate postoperative complications, which likely impede healing, increase erosion risk. The findings are useful in counseling patients and perhaps guiding follow-up, at least early on. Most of the 133 erosions in the study – out of 1,247 sacrocolpopexies performed at the university from 2003 to2013 – occurred in the first year, usually in the first 3 months.
The 133 women with erosions were randomly matched with 261 women who did not have erosions after sacrocolpopexy. The erosion rate hovered around 9.5% for most years. They shot up to 19% in 2006, the first year of robot-assisted sacrocolpopexies and fell to about 6% in 2011, 4% in 2012, and 2% in 2013, when surgeons started using the ultralightweight mesh.
“Our study also confirmed several known risk factors,” Dr. Durst said, including smoking, stage IV prolapse, nonabsorbable braided suture, and heavyweight polypropylene mesh.
On multivariate regression, prior surgery for incontinence (OR, 2.87; 95% CI, 1.19-6.96), porcine acellular collagen matrix with soft polypropylene mesh (Pelvicol with soft Prolene, OR, 4.95; 95% CI, 1.70-14.42), other polypropylene mesh (OR, 6.73; 95% CI, 1.12-40.63); braided suture for vaginal mesh attachment (OR, 4.52; 95% CI, 1.53-13.37), and immediate perioperative complications (OR, 1.04; 95% CI, 1.58-8.43) all remained independent risk factors for mesh exposure, as did duration of follow-up (OR, 1.04; 95% CI, 1.03-1.06).
There was no industry funding for the study, and the investigators reported having no financial disclosures.
* The meeting sponsor information was updated 6/9/2017.
AT SGS 2017
Key clinical point:
Major finding: The odds ratio for ultralightweight polypropylene (Restorelle Y) exposure, versus heavier polypropylene mesh, was not statistically significant (OR, 2.18; 95% CI, 0.33-14.57).
Data source: A single-center study matching 133 erosion cases to 261 controls.
Disclosures: There was no industry funding of the study, and the investigators reported no financial disclosures.
Decision tool helps patients compare SAVR, TAVR
WASHINGTON – A decision-assistance tool will soon be available that is designed to help intermediate-risk patients with severe aortic stenosis and their physicians better compare each patient’s expected outcome from surgical or transcatheter valve replacement based on each patient’s individual clinical and demographic features.
The decision tool will be available as both a web-based calculator and a downloadable app. It is derived from the outcomes of 4,732 patients who underwent surgical aortic valve replacement (SAVR) during 2011-2013 and who were included in the registry maintained by the Society of Thoracic Surgeons (STS), as well as an equal number of closely matched patients who underwent transcatheter aortic valve replacement (TAVR) during 2014-2015 and entered in the Transcatheter Valve (TVT) registry run by STS and the American College of Cardiology. Tool development also used longer-term outcomes data collected through Medicare.
After receiving patient-specific data, the decision tool estimates the patient’s short-term and 1-year predicted risks for death and stroke and likelihood of being discharged home, as well as the predicted number of days the patient would remain alive and out of the hospital during the first postprocedural year, J. Matthew Brennan, MD, said at the annual meeting of the American College of Cardiology.
Cardiologists and cardiac surgeons “are desperately looking for something like this” because, currently, the only option is to estimate a patient’s risk after SAVR or TAVR using tools developed only from patients who underwent one of these procedures. The new tool gives clinicians and patients a way to compare the two options for an individual patient in a way that “minimizes the biases,” said Dr. Brennan, an interventional cardiologist at Duke University in Durham, N.C., and principal investigator for development of the website and the tool.
Dr. Brennan and his associates developed the decision assistance tool with funding from the Patient-Center Outcomes Research Institute, and it will be available online at no cost at valveadvice.org. The website was already up and running when Dr. Brennan announced the tool during the meeting, and it currently has patient-centered information about aortic valve disease and the options available for treating it. He expects the decision tool to be posted on the site by April or May.
The data he and his associates used to create the decision tool came from a total of more than 197,000 SAVR patients entered into the STS SAVR database during 2011-2013 and more than 25,000 TAVR patients enrolled in the TVT registry during 2014-2015. They used propensity score matching to identify 4,732 matched patients from each group. The patients averaged 81-82 years old, nearly half were women, and their average STS risk score was 5.5-5.8, which meant that patients fell in an intermediate-risk range by this criterion. Just over three-quarters of the TAVR patients had their procedure done via a transfemoral route.
The analysis showed that, overall, 1-year mortality and stroke rates following each type of procedure were not significantly different, and several subgroup analyses failed to identify any type of patient who fell outside this overall pattern. The TAVR patients had a stroke rate that continued to rise during 12-month follow-up, compared with a much flatter pattern among the SAVR patients. While this did not result in an excess stroke rate, the pattern over time suggested that TAVR patients may not have received optimal anticoagulant treatment during the year following their procedure, Dr. Brennan said. The number of months that patients were alive and not hospitalized was also very similar in the SAVR and TAVR groups.
While the 1-year outcomes were very similar, the periprocedural outcomes showed several statistically significant differences. In-hospital mortality was significantly higher in the SAVR patients at 5%, compared with 3% in the TAVR patients. The SAVR patients also were significantly more likely to develop a need for dialysis and a need for red cells and to have a doubled duration in their ICU stay and in their postprocedural length of hospitalization, compared with TAVR patients. On the other hand, TAVR patients were significantly more likely to need a new pacemaker while hospitalized and had a 10 times higher rate of major vascular complications. The stroke rates were very similar in both arms, Dr. Brennan reported.
According to Dr. Brennan, the most striking difference in hospital outcomes was the discharge destination for patients: 70% of TAVR patients went home after their procedural hospitalization, compared with 41% of the SAVR patients. Discharges home following periprocedural hospitalization were “substantially higher” with TAVR, he said.
Another notable feature of these data was how they contrasted with the 1-year outcomes reported from the German Aortic Valve Registry at the American Heart Association Scientific Sessions in November 2016. In the German registry, 1-year mortality after propensity-score adjustment was about 11% among SAVR patients and about 14% among TAVR patients treated with a transfemoral approach, a statistically significant difference, reported Nicolas Werner, MD, of the Ludwigshafen (Germany) Clinic.
“I think the reason we see a difference in the German data is they weren’t able to remove from their analysis the really high-risk patients” who preferentially underwent TAVR, suggested Dr. Brennan. “We had the ability to match patients who had equipoise for undergoing SAVR or TAVR. That’s why our results are more consistent with the findings from the TAVR clinical trials.”
“One of the most important findings from [Dr. Brennan’s] study is [that] it makes the German Registry results look like the outliers rather than the results from the TAVR clinical trials,” commented Howard C. Hermann, MD, professor of cardiovascular disease and director of the cardiac catheterization laboratories at the University of Pennsylvania in Philadelphia.
The data analysis and development of the valveadvice.org website and decision tool received no commercial support. Dr. Brennan had no disclosures. Dr. Hermann has received honoraria and research support from Edwards Pharmaceuticals, research support from Medtronic, and honoraria and research support from several other companies.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – A decision-assistance tool will soon be available that is designed to help intermediate-risk patients with severe aortic stenosis and their physicians better compare each patient’s expected outcome from surgical or transcatheter valve replacement based on each patient’s individual clinical and demographic features.
The decision tool will be available as both a web-based calculator and a downloadable app. It is derived from the outcomes of 4,732 patients who underwent surgical aortic valve replacement (SAVR) during 2011-2013 and who were included in the registry maintained by the Society of Thoracic Surgeons (STS), as well as an equal number of closely matched patients who underwent transcatheter aortic valve replacement (TAVR) during 2014-2015 and entered in the Transcatheter Valve (TVT) registry run by STS and the American College of Cardiology. Tool development also used longer-term outcomes data collected through Medicare.
After receiving patient-specific data, the decision tool estimates the patient’s short-term and 1-year predicted risks for death and stroke and likelihood of being discharged home, as well as the predicted number of days the patient would remain alive and out of the hospital during the first postprocedural year, J. Matthew Brennan, MD, said at the annual meeting of the American College of Cardiology.
Cardiologists and cardiac surgeons “are desperately looking for something like this” because, currently, the only option is to estimate a patient’s risk after SAVR or TAVR using tools developed only from patients who underwent one of these procedures. The new tool gives clinicians and patients a way to compare the two options for an individual patient in a way that “minimizes the biases,” said Dr. Brennan, an interventional cardiologist at Duke University in Durham, N.C., and principal investigator for development of the website and the tool.
Dr. Brennan and his associates developed the decision assistance tool with funding from the Patient-Center Outcomes Research Institute, and it will be available online at no cost at valveadvice.org. The website was already up and running when Dr. Brennan announced the tool during the meeting, and it currently has patient-centered information about aortic valve disease and the options available for treating it. He expects the decision tool to be posted on the site by April or May.
The data he and his associates used to create the decision tool came from a total of more than 197,000 SAVR patients entered into the STS SAVR database during 2011-2013 and more than 25,000 TAVR patients enrolled in the TVT registry during 2014-2015. They used propensity score matching to identify 4,732 matched patients from each group. The patients averaged 81-82 years old, nearly half were women, and their average STS risk score was 5.5-5.8, which meant that patients fell in an intermediate-risk range by this criterion. Just over three-quarters of the TAVR patients had their procedure done via a transfemoral route.
The analysis showed that, overall, 1-year mortality and stroke rates following each type of procedure were not significantly different, and several subgroup analyses failed to identify any type of patient who fell outside this overall pattern. The TAVR patients had a stroke rate that continued to rise during 12-month follow-up, compared with a much flatter pattern among the SAVR patients. While this did not result in an excess stroke rate, the pattern over time suggested that TAVR patients may not have received optimal anticoagulant treatment during the year following their procedure, Dr. Brennan said. The number of months that patients were alive and not hospitalized was also very similar in the SAVR and TAVR groups.
While the 1-year outcomes were very similar, the periprocedural outcomes showed several statistically significant differences. In-hospital mortality was significantly higher in the SAVR patients at 5%, compared with 3% in the TAVR patients. The SAVR patients also were significantly more likely to develop a need for dialysis and a need for red cells and to have a doubled duration in their ICU stay and in their postprocedural length of hospitalization, compared with TAVR patients. On the other hand, TAVR patients were significantly more likely to need a new pacemaker while hospitalized and had a 10 times higher rate of major vascular complications. The stroke rates were very similar in both arms, Dr. Brennan reported.
According to Dr. Brennan, the most striking difference in hospital outcomes was the discharge destination for patients: 70% of TAVR patients went home after their procedural hospitalization, compared with 41% of the SAVR patients. Discharges home following periprocedural hospitalization were “substantially higher” with TAVR, he said.
Another notable feature of these data was how they contrasted with the 1-year outcomes reported from the German Aortic Valve Registry at the American Heart Association Scientific Sessions in November 2016. In the German registry, 1-year mortality after propensity-score adjustment was about 11% among SAVR patients and about 14% among TAVR patients treated with a transfemoral approach, a statistically significant difference, reported Nicolas Werner, MD, of the Ludwigshafen (Germany) Clinic.
“I think the reason we see a difference in the German data is they weren’t able to remove from their analysis the really high-risk patients” who preferentially underwent TAVR, suggested Dr. Brennan. “We had the ability to match patients who had equipoise for undergoing SAVR or TAVR. That’s why our results are more consistent with the findings from the TAVR clinical trials.”
“One of the most important findings from [Dr. Brennan’s] study is [that] it makes the German Registry results look like the outliers rather than the results from the TAVR clinical trials,” commented Howard C. Hermann, MD, professor of cardiovascular disease and director of the cardiac catheterization laboratories at the University of Pennsylvania in Philadelphia.
The data analysis and development of the valveadvice.org website and decision tool received no commercial support. Dr. Brennan had no disclosures. Dr. Hermann has received honoraria and research support from Edwards Pharmaceuticals, research support from Medtronic, and honoraria and research support from several other companies.
[email protected]
On Twitter @mitchelzoler
WASHINGTON – A decision-assistance tool will soon be available that is designed to help intermediate-risk patients with severe aortic stenosis and their physicians better compare each patient’s expected outcome from surgical or transcatheter valve replacement based on each patient’s individual clinical and demographic features.
The decision tool will be available as both a web-based calculator and a downloadable app. It is derived from the outcomes of 4,732 patients who underwent surgical aortic valve replacement (SAVR) during 2011-2013 and who were included in the registry maintained by the Society of Thoracic Surgeons (STS), as well as an equal number of closely matched patients who underwent transcatheter aortic valve replacement (TAVR) during 2014-2015 and entered in the Transcatheter Valve (TVT) registry run by STS and the American College of Cardiology. Tool development also used longer-term outcomes data collected through Medicare.
After receiving patient-specific data, the decision tool estimates the patient’s short-term and 1-year predicted risks for death and stroke and likelihood of being discharged home, as well as the predicted number of days the patient would remain alive and out of the hospital during the first postprocedural year, J. Matthew Brennan, MD, said at the annual meeting of the American College of Cardiology.
Cardiologists and cardiac surgeons “are desperately looking for something like this” because, currently, the only option is to estimate a patient’s risk after SAVR or TAVR using tools developed only from patients who underwent one of these procedures. The new tool gives clinicians and patients a way to compare the two options for an individual patient in a way that “minimizes the biases,” said Dr. Brennan, an interventional cardiologist at Duke University in Durham, N.C., and principal investigator for development of the website and the tool.
Dr. Brennan and his associates developed the decision assistance tool with funding from the Patient-Center Outcomes Research Institute, and it will be available online at no cost at valveadvice.org. The website was already up and running when Dr. Brennan announced the tool during the meeting, and it currently has patient-centered information about aortic valve disease and the options available for treating it. He expects the decision tool to be posted on the site by April or May.
The data he and his associates used to create the decision tool came from a total of more than 197,000 SAVR patients entered into the STS SAVR database during 2011-2013 and more than 25,000 TAVR patients enrolled in the TVT registry during 2014-2015. They used propensity score matching to identify 4,732 matched patients from each group. The patients averaged 81-82 years old, nearly half were women, and their average STS risk score was 5.5-5.8, which meant that patients fell in an intermediate-risk range by this criterion. Just over three-quarters of the TAVR patients had their procedure done via a transfemoral route.
The analysis showed that, overall, 1-year mortality and stroke rates following each type of procedure were not significantly different, and several subgroup analyses failed to identify any type of patient who fell outside this overall pattern. The TAVR patients had a stroke rate that continued to rise during 12-month follow-up, compared with a much flatter pattern among the SAVR patients. While this did not result in an excess stroke rate, the pattern over time suggested that TAVR patients may not have received optimal anticoagulant treatment during the year following their procedure, Dr. Brennan said. The number of months that patients were alive and not hospitalized was also very similar in the SAVR and TAVR groups.
While the 1-year outcomes were very similar, the periprocedural outcomes showed several statistically significant differences. In-hospital mortality was significantly higher in the SAVR patients at 5%, compared with 3% in the TAVR patients. The SAVR patients also were significantly more likely to develop a need for dialysis and a need for red cells and to have a doubled duration in their ICU stay and in their postprocedural length of hospitalization, compared with TAVR patients. On the other hand, TAVR patients were significantly more likely to need a new pacemaker while hospitalized and had a 10 times higher rate of major vascular complications. The stroke rates were very similar in both arms, Dr. Brennan reported.
According to Dr. Brennan, the most striking difference in hospital outcomes was the discharge destination for patients: 70% of TAVR patients went home after their procedural hospitalization, compared with 41% of the SAVR patients. Discharges home following periprocedural hospitalization were “substantially higher” with TAVR, he said.
Another notable feature of these data was how they contrasted with the 1-year outcomes reported from the German Aortic Valve Registry at the American Heart Association Scientific Sessions in November 2016. In the German registry, 1-year mortality after propensity-score adjustment was about 11% among SAVR patients and about 14% among TAVR patients treated with a transfemoral approach, a statistically significant difference, reported Nicolas Werner, MD, of the Ludwigshafen (Germany) Clinic.
“I think the reason we see a difference in the German data is they weren’t able to remove from their analysis the really high-risk patients” who preferentially underwent TAVR, suggested Dr. Brennan. “We had the ability to match patients who had equipoise for undergoing SAVR or TAVR. That’s why our results are more consistent with the findings from the TAVR clinical trials.”
“One of the most important findings from [Dr. Brennan’s] study is [that] it makes the German Registry results look like the outliers rather than the results from the TAVR clinical trials,” commented Howard C. Hermann, MD, professor of cardiovascular disease and director of the cardiac catheterization laboratories at the University of Pennsylvania in Philadelphia.
The data analysis and development of the valveadvice.org website and decision tool received no commercial support. Dr. Brennan had no disclosures. Dr. Hermann has received honoraria and research support from Edwards Pharmaceuticals, research support from Medtronic, and honoraria and research support from several other companies.
[email protected]
On Twitter @mitchelzoler
AT ACC 17
Key clinical point:
Major finding: In matched U.S. patients, TAVR led to 29% more patients being discharged home following their procedures, compared with SAVR.
Data source: Records for 9,464 U.S. patients who underwent TAVR or SAVR during 2011-2015.
Disclosures: Data analysis and development of the valveadvice.org website and decision tool received no commercial support. Dr. Brennan had no disclosures. Dr. Hermann has received honoraria and research support from Edwards Pharmaceuticals, research support from Medtronic, and honoraria and research support from several other companies.
BUN increase tracks with upper GI bleeding outcomes
In patients with acute nonvariceal upper GI bleeding (UGIB), increased blood urea nitrogen (BUN) levels at 24 hours were associated with worse outcomes. The marker, already proven useful in acute pancreatitis, could help physicians determine a patient’s prognosis.
Existing measures of UGIB risk are effective, but only about 30% of physicians ever calculate risk scores when evaluating UGIB patients, perhaps because they require measurements at multiple time points. “We personally think the reason for this is the busyness of clinical practices, especially the acute nature of upper GI bleeding. It’s often hard to step back to calculate a score that has multiple variables,” said study author Navin Kumar, MD, a fellow in gastroenterology at Brigham and Women’s Hospital, Boston.
The study was published in Gastrointestinal Endoscopy (2017. doi: 10.1016/j.gie.2017.03.1533).
Like acute pancreatitis, upper GI bleeding requires resuscitation management, which suggested that BUN levels might be a useful marker in this condition as well. To find out, the researchers analyzed data from 357 patients who were treated at the Brigham and Women’s Hospital emergency department and ultimately hospitalized for UGIB during 2004-2014.
The researchers analyzed BUN levels measured at admission and at the time closest to 24 hours after hospitalization, which ranged from 6 hours to 48 hours.
Thirty-seven patients (10%) experienced an increase in BUN level, while all the rest had levels that stayed steady or decreased. Those patients with BUN increases had a lower mean Glasgow-Blatchford score (7.8 vs. 9.6; P =.010), but there was no difference in AIMS65 scores.
Patients with BUN increases had greater odds of the composite outcome, which included inpatient death from any cause, inpatient rebleeding, a need for surgical or radiologic intervention, and/or a need for endoscopic reintervention during hospitalization (22% vs. 9%; P =.014). Inpatient mortality was higher in the increased BUN group (8% vs. 1%; P =.004).
Overall, BUN increase at 24 hours was associated with an odds ratio of 2.75 for the composite outcome (95% confidence interval, 1.13-6.70; P = .026).
A potential limitation to using the BUN is that it could just be catching patients with underlying renal disease. But when researchers adjusted for this, the odds ratio for increased BUN remained significant (OR, 3.00; P =.021).
“The nice part of the study is that it’s so easy to interpret and apply in a clinical setting. You just need two data points: BUN at presentation and at 24 hours. If the BUN level has risen, you need to have a higher degree of suspicion for the prognosis of those patients,” said Dr. Kumar.
The downside to BUN is that it doesn’t provide information for the first 24 hours. For that reason, BUN shouldn’t replace measures like the Glasgow-Blatchford score and the AIMS65 score. “But it’s very helpful to use this change in BUN score to get a sense of where the patient is trending. If it’s rising, there’s a higher risk of worse outcomes, and this could influence decisions about whether the patient should be in the ICU or the medical ward,” said Dr. Kumar.
In patients with acute nonvariceal upper GI bleeding (UGIB), increased blood urea nitrogen (BUN) levels at 24 hours were associated with worse outcomes. The marker, already proven useful in acute pancreatitis, could help physicians determine a patient’s prognosis.
Existing measures of UGIB risk are effective, but only about 30% of physicians ever calculate risk scores when evaluating UGIB patients, perhaps because they require measurements at multiple time points. “We personally think the reason for this is the busyness of clinical practices, especially the acute nature of upper GI bleeding. It’s often hard to step back to calculate a score that has multiple variables,” said study author Navin Kumar, MD, a fellow in gastroenterology at Brigham and Women’s Hospital, Boston.
The study was published in Gastrointestinal Endoscopy (2017. doi: 10.1016/j.gie.2017.03.1533).
Like acute pancreatitis, upper GI bleeding requires resuscitation management, which suggested that BUN levels might be a useful marker in this condition as well. To find out, the researchers analyzed data from 357 patients who were treated at the Brigham and Women’s Hospital emergency department and ultimately hospitalized for UGIB during 2004-2014.
The researchers analyzed BUN levels measured at admission and at the time closest to 24 hours after hospitalization, which ranged from 6 hours to 48 hours.
Thirty-seven patients (10%) experienced an increase in BUN level, while all the rest had levels that stayed steady or decreased. Those patients with BUN increases had a lower mean Glasgow-Blatchford score (7.8 vs. 9.6; P =.010), but there was no difference in AIMS65 scores.
Patients with BUN increases had greater odds of the composite outcome, which included inpatient death from any cause, inpatient rebleeding, a need for surgical or radiologic intervention, and/or a need for endoscopic reintervention during hospitalization (22% vs. 9%; P =.014). Inpatient mortality was higher in the increased BUN group (8% vs. 1%; P =.004).
Overall, BUN increase at 24 hours was associated with an odds ratio of 2.75 for the composite outcome (95% confidence interval, 1.13-6.70; P = .026).
A potential limitation to using the BUN is that it could just be catching patients with underlying renal disease. But when researchers adjusted for this, the odds ratio for increased BUN remained significant (OR, 3.00; P =.021).
“The nice part of the study is that it’s so easy to interpret and apply in a clinical setting. You just need two data points: BUN at presentation and at 24 hours. If the BUN level has risen, you need to have a higher degree of suspicion for the prognosis of those patients,” said Dr. Kumar.
The downside to BUN is that it doesn’t provide information for the first 24 hours. For that reason, BUN shouldn’t replace measures like the Glasgow-Blatchford score and the AIMS65 score. “But it’s very helpful to use this change in BUN score to get a sense of where the patient is trending. If it’s rising, there’s a higher risk of worse outcomes, and this could influence decisions about whether the patient should be in the ICU or the medical ward,” said Dr. Kumar.
In patients with acute nonvariceal upper GI bleeding (UGIB), increased blood urea nitrogen (BUN) levels at 24 hours were associated with worse outcomes. The marker, already proven useful in acute pancreatitis, could help physicians determine a patient’s prognosis.
Existing measures of UGIB risk are effective, but only about 30% of physicians ever calculate risk scores when evaluating UGIB patients, perhaps because they require measurements at multiple time points. “We personally think the reason for this is the busyness of clinical practices, especially the acute nature of upper GI bleeding. It’s often hard to step back to calculate a score that has multiple variables,” said study author Navin Kumar, MD, a fellow in gastroenterology at Brigham and Women’s Hospital, Boston.
The study was published in Gastrointestinal Endoscopy (2017. doi: 10.1016/j.gie.2017.03.1533).
Like acute pancreatitis, upper GI bleeding requires resuscitation management, which suggested that BUN levels might be a useful marker in this condition as well. To find out, the researchers analyzed data from 357 patients who were treated at the Brigham and Women’s Hospital emergency department and ultimately hospitalized for UGIB during 2004-2014.
The researchers analyzed BUN levels measured at admission and at the time closest to 24 hours after hospitalization, which ranged from 6 hours to 48 hours.
Thirty-seven patients (10%) experienced an increase in BUN level, while all the rest had levels that stayed steady or decreased. Those patients with BUN increases had a lower mean Glasgow-Blatchford score (7.8 vs. 9.6; P =.010), but there was no difference in AIMS65 scores.
Patients with BUN increases had greater odds of the composite outcome, which included inpatient death from any cause, inpatient rebleeding, a need for surgical or radiologic intervention, and/or a need for endoscopic reintervention during hospitalization (22% vs. 9%; P =.014). Inpatient mortality was higher in the increased BUN group (8% vs. 1%; P =.004).
Overall, BUN increase at 24 hours was associated with an odds ratio of 2.75 for the composite outcome (95% confidence interval, 1.13-6.70; P = .026).
A potential limitation to using the BUN is that it could just be catching patients with underlying renal disease. But when researchers adjusted for this, the odds ratio for increased BUN remained significant (OR, 3.00; P =.021).
“The nice part of the study is that it’s so easy to interpret and apply in a clinical setting. You just need two data points: BUN at presentation and at 24 hours. If the BUN level has risen, you need to have a higher degree of suspicion for the prognosis of those patients,” said Dr. Kumar.
The downside to BUN is that it doesn’t provide information for the first 24 hours. For that reason, BUN shouldn’t replace measures like the Glasgow-Blatchford score and the AIMS65 score. “But it’s very helpful to use this change in BUN score to get a sense of where the patient is trending. If it’s rising, there’s a higher risk of worse outcomes, and this could influence decisions about whether the patient should be in the ICU or the medical ward,” said Dr. Kumar.
FROM GASTROINTESTINAL ENDOSCOPY
Key clinical point: BUN could be a useful prognostic marker.
Major finding: BUN increase indicated a threefold increased risk of poor outcomes.
Data source: Retrospective analysis of 357 patients at a single center.
Disclosures: The study did not receive external funding. Dr. Kumar reported having no financial disclosures.
Transanal TME comparable to open, lap approaches to rectal cancer
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
HOUSTON – Transanal total mesorectal excision can consistently achieve good pathological results for obtaining specimens in rectal cancer, and overcome the shortcomings of the open and laparoscopic approaches to rectal cancer surgery, particularly in the distal part of the rectum where obtaining quality specimens can be technically challenging, researchers at the Hospital Clinic of Barcelona have found.
Reporting at the annual meeting of the Society of American Gastrointestinal and Endoscopic Surgeons, Jacqueline van Laarhoven, MD, PhD, said, “Pathologically, transanal total mesorectal excision [TME] provides good results on integrity of the mesorectum, negative circumferential and distal resection margins, and lymph nodes per specimen.” This study represents the first results of a relatively large, single-institution cohort, Dr. van Laarhoven said.
The study involved 187 patients with mid- or low-rectal cancer who had transanal TME from November 2011 to June 2016. Dr. van Laarhoven explained that obtaining high-quality specimens is an important prognostic factor for determining locoregional recurrence in rectal cancer. The study analyzed results of excised specimens in the mesorectum, circumferential and distal resected margins, and lymph nodes, and compared outcomes with those in two randomized clinical trials of both open and laparoscopic TME – the COLOR II (Lancet Oncol. 2013;14:210-8) and COREAN trials (Lancet Oncol. 2014;15:767-74) – where applicable.
In the Barcelona study population, 63.1% had tumors in the midrectum and 36.9% in the low rectum. Transanal TME yielded complete mesorectal quality in 95.7% of cases, almost-complete quality in 1.6% and incomplete in 1.1%, but comparison with COLOR II and COREAN trials was difficult because of differing inclusion criteria, Dr. van Laarhoven said.
Mean distal margin was 2.1 cm in midrectal cancer with a positive distal resection margin in 3.2%. In low-rectal cancer, the mean distal margin was 1.1 cm with a positive distal resection margin in 7.8%. Dr. van Laarhoven noted the overall circumferential resection margin (CRM) was 8.6% in this study, compared with 8.3% overall for the COREAN trial. As for COLOR II, the overall rate for positive CRM in mid- and low-rectal tumors was around 9%, Dr. van Laarhoven said, but in the open group the positive CRM was 3% in the midrectal excisions and 22% in low-rectal disease.
With regard to lymph nodes, the Barcelona study reported a median of 14 per specimen, with a range of 11 to 18, Dr. van Laarhoven said. However, in nonirradiated patients, the median was 15 per specimen. “This is consistent with the fact that neoadjuvant radiotherapy leads to a decrease in the lymph-node harvest,” she said. “These results are comparable to the COREAN and the COLOR II trials.”
Sixty-two percent of patients received neoadjuvant chemoradiotherapy, 3.2% received radiotherapy only, and 2.1% chemotherapy only.
On preoperative staging, 3.2% had T1 tumors, 20.3% T2, 67.9% T3, and 7.5% T4. The overall positive CRM (less than 1 mm) was 8.6% (including T4 tumors).
Postoperative pathological staging showed complete remission in 16% of patients, pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Dr. van Laarhoven commented, “As the quality of the surgical treatment is a surrogate marker for survival, transanal TME can be regarded as an oncologically safe method to treat patients with rectal cancer.”
Dr. van Laarhoven reported having no financial disclosures.
AT SAGES 2017
Key clinical point: Transanal total mesorectal excision (TME) is a viable alternative to open or laparoscopic TME in cancers of the low and midrectum.
Major finding: Postoperative pathological staging showed complete remission in 16%, with pT1 in 6.4%, pT2 in 28.9%, pT3 in 42.8%, pT4 in 2.7%, and pTis in 1.6%.
Data source: Analysis of 187 patients prospectively enrolled in a standardized database who had transanal TME from November 2011 to June 2016 at a single center.
Disclosures: Dr. van Laarhoven reported having no financial disclosures.
Young patients with first-episode psychosis face far higher mortality risk
Young people in the United States experiencing first-episode psychosis face a mortality risk that is 24 times greater than that of their peers in the general population, a new study shows.
“The hugely elevated mortality observed here underscores that young people experiencing psychosis warrant intensive clinical attention,” wrote Michael Schoenbaum, PhD, senior adviser for mental health services, epidemiology, and economics at the National Institute of Mental Health, and his associates. “In the general population, only individuals over 70 years of age have all-cause 12-month mortality approaching the rates we observed among young psychosis patients here.”
The researchers analyzed data on about 5,000 people aged 16-30 with commercial health insurance coverage who had a new ICD-9 diagnosis of schizophrenia, brief psychotic disorder, or psychotic disorder not otherwise specified, and followed them for 12 months. They limited the sample to people who had continuous insurance coverage over a period of 12 months or greater before their first observed diagnosis of psychosis – which they called the “index diagnosis.”
For the entire psychosis cohort, the 12-month mortality was 2.0% (1,968 per 100,000 people), compared with less than 0.1% in the general population (89 per 100,000). The researchers further found mortality “an order of magnitude higher in those with incident psychosis after age 25, compared with those with an incident diagnosis between ages 16 and 20” (Schizophr Bull. 2017 Apr 7. doi: 10.1093/schbul/sbx009).
Information on the cause of death was not available, but the researchers were able to look at the diagnoses that the decedents had received 12 months before their index psychosis diagnosis. Fifteen of the decedents had been diagnosed with cancer, nine with renal disease (end-stage), and one with cystic fibrosis. When those patients were removed from the mortality cohort, the 12-month mortality stood at 1.5%, a rate they said was 18 times higher than mortality in the general population.
“These findings show the importance of tracking mortality in individuals with mental illness,” Dr. Schoenbaum said in a statement. “Health systems do this in other areas of medicine, such as cancer and cardiology, but not for mental illness. Of course, we also need to learn how these young people are losing their lives.”
The study might not be generalizable because the cohort studied had access to continuous access to health insurance coverage “before and after the index psychosis diagnosis.” Also, the size of the cohort was relatively small. Nevertheless, they said, the findings are consistent with other studies showing that care for those with early psychosis falls short.
“Taken together, these findings provide a strong rationale for initiatives to improve early identification and integrated treatment for psychotic disorders in U.S. treatment settings,” Dr. Schoenbaum and his associates wrote.
The Commonwealth Fund provided support for the study. The researchers reported having no conflicts of interest, and said the views expressed in the study are their own and do not necessarily reflect those of the National Institute of Mental Health, or any other organizations or entities.
[email protected]
On Twitter @ginalhenderson
Young people in the United States experiencing first-episode psychosis face a mortality risk that is 24 times greater than that of their peers in the general population, a new study shows.
“The hugely elevated mortality observed here underscores that young people experiencing psychosis warrant intensive clinical attention,” wrote Michael Schoenbaum, PhD, senior adviser for mental health services, epidemiology, and economics at the National Institute of Mental Health, and his associates. “In the general population, only individuals over 70 years of age have all-cause 12-month mortality approaching the rates we observed among young psychosis patients here.”
The researchers analyzed data on about 5,000 people aged 16-30 with commercial health insurance coverage who had a new ICD-9 diagnosis of schizophrenia, brief psychotic disorder, or psychotic disorder not otherwise specified, and followed them for 12 months. They limited the sample to people who had continuous insurance coverage over a period of 12 months or greater before their first observed diagnosis of psychosis – which they called the “index diagnosis.”
For the entire psychosis cohort, the 12-month mortality was 2.0% (1,968 per 100,000 people), compared with less than 0.1% in the general population (89 per 100,000). The researchers further found mortality “an order of magnitude higher in those with incident psychosis after age 25, compared with those with an incident diagnosis between ages 16 and 20” (Schizophr Bull. 2017 Apr 7. doi: 10.1093/schbul/sbx009).
Information on the cause of death was not available, but the researchers were able to look at the diagnoses that the decedents had received 12 months before their index psychosis diagnosis. Fifteen of the decedents had been diagnosed with cancer, nine with renal disease (end-stage), and one with cystic fibrosis. When those patients were removed from the mortality cohort, the 12-month mortality stood at 1.5%, a rate they said was 18 times higher than mortality in the general population.
“These findings show the importance of tracking mortality in individuals with mental illness,” Dr. Schoenbaum said in a statement. “Health systems do this in other areas of medicine, such as cancer and cardiology, but not for mental illness. Of course, we also need to learn how these young people are losing their lives.”
The study might not be generalizable because the cohort studied had access to continuous access to health insurance coverage “before and after the index psychosis diagnosis.” Also, the size of the cohort was relatively small. Nevertheless, they said, the findings are consistent with other studies showing that care for those with early psychosis falls short.
“Taken together, these findings provide a strong rationale for initiatives to improve early identification and integrated treatment for psychotic disorders in U.S. treatment settings,” Dr. Schoenbaum and his associates wrote.
The Commonwealth Fund provided support for the study. The researchers reported having no conflicts of interest, and said the views expressed in the study are their own and do not necessarily reflect those of the National Institute of Mental Health, or any other organizations or entities.
[email protected]
On Twitter @ginalhenderson
Young people in the United States experiencing first-episode psychosis face a mortality risk that is 24 times greater than that of their peers in the general population, a new study shows.
“The hugely elevated mortality observed here underscores that young people experiencing psychosis warrant intensive clinical attention,” wrote Michael Schoenbaum, PhD, senior adviser for mental health services, epidemiology, and economics at the National Institute of Mental Health, and his associates. “In the general population, only individuals over 70 years of age have all-cause 12-month mortality approaching the rates we observed among young psychosis patients here.”
The researchers analyzed data on about 5,000 people aged 16-30 with commercial health insurance coverage who had a new ICD-9 diagnosis of schizophrenia, brief psychotic disorder, or psychotic disorder not otherwise specified, and followed them for 12 months. They limited the sample to people who had continuous insurance coverage over a period of 12 months or greater before their first observed diagnosis of psychosis – which they called the “index diagnosis.”
For the entire psychosis cohort, the 12-month mortality was 2.0% (1,968 per 100,000 people), compared with less than 0.1% in the general population (89 per 100,000). The researchers further found mortality “an order of magnitude higher in those with incident psychosis after age 25, compared with those with an incident diagnosis between ages 16 and 20” (Schizophr Bull. 2017 Apr 7. doi: 10.1093/schbul/sbx009).
Information on the cause of death was not available, but the researchers were able to look at the diagnoses that the decedents had received 12 months before their index psychosis diagnosis. Fifteen of the decedents had been diagnosed with cancer, nine with renal disease (end-stage), and one with cystic fibrosis. When those patients were removed from the mortality cohort, the 12-month mortality stood at 1.5%, a rate they said was 18 times higher than mortality in the general population.
“These findings show the importance of tracking mortality in individuals with mental illness,” Dr. Schoenbaum said in a statement. “Health systems do this in other areas of medicine, such as cancer and cardiology, but not for mental illness. Of course, we also need to learn how these young people are losing their lives.”
The study might not be generalizable because the cohort studied had access to continuous access to health insurance coverage “before and after the index psychosis diagnosis.” Also, the size of the cohort was relatively small. Nevertheless, they said, the findings are consistent with other studies showing that care for those with early psychosis falls short.
“Taken together, these findings provide a strong rationale for initiatives to improve early identification and integrated treatment for psychotic disorders in U.S. treatment settings,” Dr. Schoenbaum and his associates wrote.
The Commonwealth Fund provided support for the study. The researchers reported having no conflicts of interest, and said the views expressed in the study are their own and do not necessarily reflect those of the National Institute of Mental Health, or any other organizations or entities.
[email protected]
On Twitter @ginalhenderson
FROM SCHIZOPHRENIA BULLETIN
Myelofibrosis therapies moving beyond ruxolitinib
ORLANDO – Ruxolitinib is currently the only drug approved for the treatment of myelofibrosis, but a number of other therapies are in clinical trials and showing promise, according to Ruben A. Mesa, MD.
“Our field ... is rapidly in evolution,” he said at the annual conference of the National Comprehensive Cancer Network, adding that efforts are underway to determine where these drugs might fit in.
Among those being considered specifically for myelofibrosis are pacritinib, momelotinib, PRM-151, and imetelstat, he said.
Pacritinib
This JAK2/FT3 inhibitor reduces splenomegaly and its related symptoms, but may also help patients who have low platelet counts and a worse prognosis. Pacritinib has demonstrated safety in that population, said Dr. Mesa of Mayo Clinic Cancer Center, Phoenix, Ariz.
Concerns about increased mortality related to risk of intracranial hemorrhage and cardiovascular events led the Food and Drug Administration to place a full clinical hold on pacritinib in February 2016. That hold was lifted in January 2017 when data from the randomized, controlled, phase III PERSIST-2 study, as presented at the American Society of Hematology annual meeting in December 2016, showed the risks did not hold up among study patients.
PERSIST-2 compared pacritinib doses of 400 mg once daily and 200 mg twice daily with best alternative therapy, which was ruxolitinib in most patients, Dr. Mesa said. He noted that the study included patients who had marked thrombocytopenia and were allowed prior JAK2 inhibitor exposure.
The 200-mg twice-daily dosing was superior in achieving spleen volume reductions greater than 35%: 22% of patients in the 200-mg dosing group vs. 15% in the 400-mg once-daily dosing group, compared with 3% of those receiving best available therapy. The twice-daily dosing group also experienced greater symptom improvement: Thirty-two percent in the 200-mg twice-daily group vs. 17% in the 400-mg once-daily group achieved at least a 50% reduction in total symptom scale scores, compared with 14% of those receiving best available therapy.
Additional studies of pacritinib will begin enrolling soon, Dr. Mesa said, noting that these studies will look at lower doses in an effort to identify the minimally effective dose with the optimal balance of safety and efficacy.
Momelotinib
Momelotinib, a JAK1/JAK2 inhibitor, was evaluated in two large recently concluded phase III trials (SIMPLIFY-1 and SIMPLIFY-2). SIMPIFY-1 compared momelotinib to ruxolitinib in the front-line setting, and showed momelotinib to be noninferior for reducing splenomegaly.
“However, it was inferior for improvement in the symptom burden,” Dr. Mesa said, noting that while there seemed to be a favorable difference in terms of anemia, the study was structured in such a way that the agent needed to be noninferior for both spleen and symptoms for the anemia response to be evaluable.
SIMPLIFY-2 evaluated momelotinib in patients who had not responded to ruxolitinib. In this second-line setting, momelotinib was not superior to the best alternative therapy, but since the vast majority of the ruxolitinib failure patients remained on ruxolitinib, it is “a bit of a confounded study to assess,” he said.
The top-line data from these studies were issued in a press release from the manufacturer (Gilead) in November 2016, and the complete results are expected to be made public in the near future, at which time more will be known about the next steps for momelotinib, he said.
If approved, pacritinib and momelotinib could ultimately be positioned as a front-line and/or second-line treatment for myelofibrosis, Dr. Mesa predicted.
There has been a goal, in terms of trial design, to see if there is a niche for these drugs in the front-line setting based on blood counts.
“Those recommendations would clearly be very much dependent on the risk, the safety, and the efficacy,” he said.
PRM-151
This antifibrosing agent was shown to be active in early-phase trials – including in stage 1 of an adaptive phase II trial. PRM-151 is currently being evaluated in the fully-accrued ongoing phase II PROMOTE study to determine whether it improves splenomegaly, symptoms, and cytopenia. The primary endpoint of the study is the bone marrow response rate. Study subjects are patients with primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocythemia myelofibrosis, and grade 2-3 fibrosis, said Dr. Mesa, who is the principal investigator for the study.
Imetelstat
This telomerase inhibitor is being evaluated in the randomized, multicenter, phase II IMbark study, designed to assess spleen volume and total symptom score as primary end points. Earlier studies have shown deep responses in patients with myelofibrosis who were treated with imetelstat, Dr. Mesa said.
The IMbark study (NCT02426086) was originally designed to evaluate two dosing regimens administered as a single agent to participants with intermediate-2 or high-risk myelofibrosis who were refractory to or relapsed after JAK inhibitor treatment. Participants received either 9.4 mg/kg or 4.7 mg/kg intravenously every 3 weeks until disease progression, unacceptable toxicity, or study end.
According to information from Geron, which is developing the agent, enrollment of new participants is currently suspended following a planned internal data review, but enrollment “may be resumed after a second internal data review that is planned by the end of the second quarter of 2017.” If resumed, enrollment would be only to the higher-dose treatment arm; patients initially randomized to that arm may continue treatment, and those randomized to the lower-dose arm may see their dose increased at the investigator’s discretion.
If approved, PRM-151 and imetelstat would likely be positioned as second-line treatments for myelofibrosis, Dr. Mesa said, noting that determining which patients would be most likely to benefit from treatment with these agents would require a close look at the evidence from second-line studies.
Combination therapies
In addition to these investigational treatments, nearly 20 different combination treatments involving ruxolitinib plus another agent have been looked at to try to further improve activity. Some improvements in splenomegaly have been seen with combinations including ruxolitinib and either panobinostat (a histone deacytelase inhibitor), LDE225 (a hedgehog signaling pathway inhibitor), and BKM120 (a PI3-kinase inhibitor), he noted.
“For the area of greatest interest – which was to see incremental improvements in thrombocytopenia, anemia, or fibrosis – there have been favorable data, but they have been modest. It’s not quite clear that there is a combination that is ready for prime time, nor is there yet a combination that we have recommended through the treatment guidelines to be utilized for these patients,” he said.
Dr. Mesa has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals; Celgene Corporation, CTI BioPharma, the maker of pacritinib; Galena Biopharma; Gilead, the maker of momelotinib; Incyte, the maker of ruxolitinib; Novartis, the maker of panobinostat and BKM120; and Promedior, the maker of PRM-151.
ORLANDO – Ruxolitinib is currently the only drug approved for the treatment of myelofibrosis, but a number of other therapies are in clinical trials and showing promise, according to Ruben A. Mesa, MD.
“Our field ... is rapidly in evolution,” he said at the annual conference of the National Comprehensive Cancer Network, adding that efforts are underway to determine where these drugs might fit in.
Among those being considered specifically for myelofibrosis are pacritinib, momelotinib, PRM-151, and imetelstat, he said.
Pacritinib
This JAK2/FT3 inhibitor reduces splenomegaly and its related symptoms, but may also help patients who have low platelet counts and a worse prognosis. Pacritinib has demonstrated safety in that population, said Dr. Mesa of Mayo Clinic Cancer Center, Phoenix, Ariz.
Concerns about increased mortality related to risk of intracranial hemorrhage and cardiovascular events led the Food and Drug Administration to place a full clinical hold on pacritinib in February 2016. That hold was lifted in January 2017 when data from the randomized, controlled, phase III PERSIST-2 study, as presented at the American Society of Hematology annual meeting in December 2016, showed the risks did not hold up among study patients.
PERSIST-2 compared pacritinib doses of 400 mg once daily and 200 mg twice daily with best alternative therapy, which was ruxolitinib in most patients, Dr. Mesa said. He noted that the study included patients who had marked thrombocytopenia and were allowed prior JAK2 inhibitor exposure.
The 200-mg twice-daily dosing was superior in achieving spleen volume reductions greater than 35%: 22% of patients in the 200-mg dosing group vs. 15% in the 400-mg once-daily dosing group, compared with 3% of those receiving best available therapy. The twice-daily dosing group also experienced greater symptom improvement: Thirty-two percent in the 200-mg twice-daily group vs. 17% in the 400-mg once-daily group achieved at least a 50% reduction in total symptom scale scores, compared with 14% of those receiving best available therapy.
Additional studies of pacritinib will begin enrolling soon, Dr. Mesa said, noting that these studies will look at lower doses in an effort to identify the minimally effective dose with the optimal balance of safety and efficacy.
Momelotinib
Momelotinib, a JAK1/JAK2 inhibitor, was evaluated in two large recently concluded phase III trials (SIMPLIFY-1 and SIMPLIFY-2). SIMPIFY-1 compared momelotinib to ruxolitinib in the front-line setting, and showed momelotinib to be noninferior for reducing splenomegaly.
“However, it was inferior for improvement in the symptom burden,” Dr. Mesa said, noting that while there seemed to be a favorable difference in terms of anemia, the study was structured in such a way that the agent needed to be noninferior for both spleen and symptoms for the anemia response to be evaluable.
SIMPLIFY-2 evaluated momelotinib in patients who had not responded to ruxolitinib. In this second-line setting, momelotinib was not superior to the best alternative therapy, but since the vast majority of the ruxolitinib failure patients remained on ruxolitinib, it is “a bit of a confounded study to assess,” he said.
The top-line data from these studies were issued in a press release from the manufacturer (Gilead) in November 2016, and the complete results are expected to be made public in the near future, at which time more will be known about the next steps for momelotinib, he said.
If approved, pacritinib and momelotinib could ultimately be positioned as a front-line and/or second-line treatment for myelofibrosis, Dr. Mesa predicted.
There has been a goal, in terms of trial design, to see if there is a niche for these drugs in the front-line setting based on blood counts.
“Those recommendations would clearly be very much dependent on the risk, the safety, and the efficacy,” he said.
PRM-151
This antifibrosing agent was shown to be active in early-phase trials – including in stage 1 of an adaptive phase II trial. PRM-151 is currently being evaluated in the fully-accrued ongoing phase II PROMOTE study to determine whether it improves splenomegaly, symptoms, and cytopenia. The primary endpoint of the study is the bone marrow response rate. Study subjects are patients with primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocythemia myelofibrosis, and grade 2-3 fibrosis, said Dr. Mesa, who is the principal investigator for the study.
Imetelstat
This telomerase inhibitor is being evaluated in the randomized, multicenter, phase II IMbark study, designed to assess spleen volume and total symptom score as primary end points. Earlier studies have shown deep responses in patients with myelofibrosis who were treated with imetelstat, Dr. Mesa said.
The IMbark study (NCT02426086) was originally designed to evaluate two dosing regimens administered as a single agent to participants with intermediate-2 or high-risk myelofibrosis who were refractory to or relapsed after JAK inhibitor treatment. Participants received either 9.4 mg/kg or 4.7 mg/kg intravenously every 3 weeks until disease progression, unacceptable toxicity, or study end.
According to information from Geron, which is developing the agent, enrollment of new participants is currently suspended following a planned internal data review, but enrollment “may be resumed after a second internal data review that is planned by the end of the second quarter of 2017.” If resumed, enrollment would be only to the higher-dose treatment arm; patients initially randomized to that arm may continue treatment, and those randomized to the lower-dose arm may see their dose increased at the investigator’s discretion.
If approved, PRM-151 and imetelstat would likely be positioned as second-line treatments for myelofibrosis, Dr. Mesa said, noting that determining which patients would be most likely to benefit from treatment with these agents would require a close look at the evidence from second-line studies.
Combination therapies
In addition to these investigational treatments, nearly 20 different combination treatments involving ruxolitinib plus another agent have been looked at to try to further improve activity. Some improvements in splenomegaly have been seen with combinations including ruxolitinib and either panobinostat (a histone deacytelase inhibitor), LDE225 (a hedgehog signaling pathway inhibitor), and BKM120 (a PI3-kinase inhibitor), he noted.
“For the area of greatest interest – which was to see incremental improvements in thrombocytopenia, anemia, or fibrosis – there have been favorable data, but they have been modest. It’s not quite clear that there is a combination that is ready for prime time, nor is there yet a combination that we have recommended through the treatment guidelines to be utilized for these patients,” he said.
Dr. Mesa has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals; Celgene Corporation, CTI BioPharma, the maker of pacritinib; Galena Biopharma; Gilead, the maker of momelotinib; Incyte, the maker of ruxolitinib; Novartis, the maker of panobinostat and BKM120; and Promedior, the maker of PRM-151.
ORLANDO – Ruxolitinib is currently the only drug approved for the treatment of myelofibrosis, but a number of other therapies are in clinical trials and showing promise, according to Ruben A. Mesa, MD.
“Our field ... is rapidly in evolution,” he said at the annual conference of the National Comprehensive Cancer Network, adding that efforts are underway to determine where these drugs might fit in.
Among those being considered specifically for myelofibrosis are pacritinib, momelotinib, PRM-151, and imetelstat, he said.
Pacritinib
This JAK2/FT3 inhibitor reduces splenomegaly and its related symptoms, but may also help patients who have low platelet counts and a worse prognosis. Pacritinib has demonstrated safety in that population, said Dr. Mesa of Mayo Clinic Cancer Center, Phoenix, Ariz.
Concerns about increased mortality related to risk of intracranial hemorrhage and cardiovascular events led the Food and Drug Administration to place a full clinical hold on pacritinib in February 2016. That hold was lifted in January 2017 when data from the randomized, controlled, phase III PERSIST-2 study, as presented at the American Society of Hematology annual meeting in December 2016, showed the risks did not hold up among study patients.
PERSIST-2 compared pacritinib doses of 400 mg once daily and 200 mg twice daily with best alternative therapy, which was ruxolitinib in most patients, Dr. Mesa said. He noted that the study included patients who had marked thrombocytopenia and were allowed prior JAK2 inhibitor exposure.
The 200-mg twice-daily dosing was superior in achieving spleen volume reductions greater than 35%: 22% of patients in the 200-mg dosing group vs. 15% in the 400-mg once-daily dosing group, compared with 3% of those receiving best available therapy. The twice-daily dosing group also experienced greater symptom improvement: Thirty-two percent in the 200-mg twice-daily group vs. 17% in the 400-mg once-daily group achieved at least a 50% reduction in total symptom scale scores, compared with 14% of those receiving best available therapy.
Additional studies of pacritinib will begin enrolling soon, Dr. Mesa said, noting that these studies will look at lower doses in an effort to identify the minimally effective dose with the optimal balance of safety and efficacy.
Momelotinib
Momelotinib, a JAK1/JAK2 inhibitor, was evaluated in two large recently concluded phase III trials (SIMPLIFY-1 and SIMPLIFY-2). SIMPIFY-1 compared momelotinib to ruxolitinib in the front-line setting, and showed momelotinib to be noninferior for reducing splenomegaly.
“However, it was inferior for improvement in the symptom burden,” Dr. Mesa said, noting that while there seemed to be a favorable difference in terms of anemia, the study was structured in such a way that the agent needed to be noninferior for both spleen and symptoms for the anemia response to be evaluable.
SIMPLIFY-2 evaluated momelotinib in patients who had not responded to ruxolitinib. In this second-line setting, momelotinib was not superior to the best alternative therapy, but since the vast majority of the ruxolitinib failure patients remained on ruxolitinib, it is “a bit of a confounded study to assess,” he said.
The top-line data from these studies were issued in a press release from the manufacturer (Gilead) in November 2016, and the complete results are expected to be made public in the near future, at which time more will be known about the next steps for momelotinib, he said.
If approved, pacritinib and momelotinib could ultimately be positioned as a front-line and/or second-line treatment for myelofibrosis, Dr. Mesa predicted.
There has been a goal, in terms of trial design, to see if there is a niche for these drugs in the front-line setting based on blood counts.
“Those recommendations would clearly be very much dependent on the risk, the safety, and the efficacy,” he said.
PRM-151
This antifibrosing agent was shown to be active in early-phase trials – including in stage 1 of an adaptive phase II trial. PRM-151 is currently being evaluated in the fully-accrued ongoing phase II PROMOTE study to determine whether it improves splenomegaly, symptoms, and cytopenia. The primary endpoint of the study is the bone marrow response rate. Study subjects are patients with primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocythemia myelofibrosis, and grade 2-3 fibrosis, said Dr. Mesa, who is the principal investigator for the study.
Imetelstat
This telomerase inhibitor is being evaluated in the randomized, multicenter, phase II IMbark study, designed to assess spleen volume and total symptom score as primary end points. Earlier studies have shown deep responses in patients with myelofibrosis who were treated with imetelstat, Dr. Mesa said.
The IMbark study (NCT02426086) was originally designed to evaluate two dosing regimens administered as a single agent to participants with intermediate-2 or high-risk myelofibrosis who were refractory to or relapsed after JAK inhibitor treatment. Participants received either 9.4 mg/kg or 4.7 mg/kg intravenously every 3 weeks until disease progression, unacceptable toxicity, or study end.
According to information from Geron, which is developing the agent, enrollment of new participants is currently suspended following a planned internal data review, but enrollment “may be resumed after a second internal data review that is planned by the end of the second quarter of 2017.” If resumed, enrollment would be only to the higher-dose treatment arm; patients initially randomized to that arm may continue treatment, and those randomized to the lower-dose arm may see their dose increased at the investigator’s discretion.
If approved, PRM-151 and imetelstat would likely be positioned as second-line treatments for myelofibrosis, Dr. Mesa said, noting that determining which patients would be most likely to benefit from treatment with these agents would require a close look at the evidence from second-line studies.
Combination therapies
In addition to these investigational treatments, nearly 20 different combination treatments involving ruxolitinib plus another agent have been looked at to try to further improve activity. Some improvements in splenomegaly have been seen with combinations including ruxolitinib and either panobinostat (a histone deacytelase inhibitor), LDE225 (a hedgehog signaling pathway inhibitor), and BKM120 (a PI3-kinase inhibitor), he noted.
“For the area of greatest interest – which was to see incremental improvements in thrombocytopenia, anemia, or fibrosis – there have been favorable data, but they have been modest. It’s not quite clear that there is a combination that is ready for prime time, nor is there yet a combination that we have recommended through the treatment guidelines to be utilized for these patients,” he said.
Dr. Mesa has received consulting fees, honoraria, and/or grant/research support from ARIAD Pharmaceuticals; Celgene Corporation, CTI BioPharma, the maker of pacritinib; Galena Biopharma; Gilead, the maker of momelotinib; Incyte, the maker of ruxolitinib; Novartis, the maker of panobinostat and BKM120; and Promedior, the maker of PRM-151.
EXPERT ANALYSIS AT THE NCCN ANNUAL CONFERENCE