User login
Drug receives fast track designation for follicular lymphoma
The US Food and Drug Administration (FDA) has granted fast track designation to the EZH2 inhibitor tazemetostat as a treatment for relapsed or refractory follicular lymphoma, with or without EZH2-activating mutations.
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review.
In addition, the company developing the product may be allowed to submit sections of the new drug application or biologic license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
Tazemetostat also has fast track designation from the FDA as a treatment for patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) with EZH2-activating mutations.
Tazemetostat is under investigation as monotherapy and in combination with other agents as a treatment for multiple cancers.
Results from a phase 1 study suggested tazemetostat can produce durable responses in patients with advanced non-Hodgkin lymphomas, including follicular lymphoma and DLBCL. The study was presented at the 2015 ASH Annual Meeting.
Tazemetostat is currently under investigation in a phase 2 trial of adults with relapsed or refractory DLBCL or follicular lymphoma.
Interim efficacy and safety data from this study are scheduled to be presented at the International Conference on Malignant Lymphoma (ICML) in Lugano, Switzerland, on June 14, 2017, at 2:00 pm CET.
Tazemetostat is being developed by Epizyme, Inc. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to the EZH2 inhibitor tazemetostat as a treatment for relapsed or refractory follicular lymphoma, with or without EZH2-activating mutations.
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review.
In addition, the company developing the product may be allowed to submit sections of the new drug application or biologic license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
Tazemetostat also has fast track designation from the FDA as a treatment for patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) with EZH2-activating mutations.
Tazemetostat is under investigation as monotherapy and in combination with other agents as a treatment for multiple cancers.
Results from a phase 1 study suggested tazemetostat can produce durable responses in patients with advanced non-Hodgkin lymphomas, including follicular lymphoma and DLBCL. The study was presented at the 2015 ASH Annual Meeting.
Tazemetostat is currently under investigation in a phase 2 trial of adults with relapsed or refractory DLBCL or follicular lymphoma.
Interim efficacy and safety data from this study are scheduled to be presented at the International Conference on Malignant Lymphoma (ICML) in Lugano, Switzerland, on June 14, 2017, at 2:00 pm CET.
Tazemetostat is being developed by Epizyme, Inc. ![]()
The US Food and Drug Administration (FDA) has granted fast track designation to the EZH2 inhibitor tazemetostat as a treatment for relapsed or refractory follicular lymphoma, with or without EZH2-activating mutations.
The FDA’s fast track program is designed to facilitate the development and expedite the review of products intended to treat or prevent serious or life-threatening conditions and address unmet medical need.
Through the fast track program, a product may be eligible for priority review.
In addition, the company developing the product may be allowed to submit sections of the new drug application or biologic license application on a rolling basis as data become available.
Fast track designation also provides the company with opportunities for more frequent meetings and written communications with the FDA.
Tazemetostat also has fast track designation from the FDA as a treatment for patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) with EZH2-activating mutations.
Tazemetostat is under investigation as monotherapy and in combination with other agents as a treatment for multiple cancers.
Results from a phase 1 study suggested tazemetostat can produce durable responses in patients with advanced non-Hodgkin lymphomas, including follicular lymphoma and DLBCL. The study was presented at the 2015 ASH Annual Meeting.
Tazemetostat is currently under investigation in a phase 2 trial of adults with relapsed or refractory DLBCL or follicular lymphoma.
Interim efficacy and safety data from this study are scheduled to be presented at the International Conference on Malignant Lymphoma (ICML) in Lugano, Switzerland, on June 14, 2017, at 2:00 pm CET.
Tazemetostat is being developed by Epizyme, Inc. ![]()
Treatment granted PRIME designation for hemophilia B
The European Medicines Agency (EMA) has granted AMT-060 access to the agency’s PRIority MEdicines (PRIME) program.
AMT-060 is an investigational gene therapy intended for the treatment of patients with severe hemophilia B.
The goal of the EMA’s PRIME program is to accelerate the development of therapies that may offer a major advantage over existing treatments or benefit patients with no treatment options.
Through PRIME, the EMA offers early and enhanced support to developers in order to optimize development plans and speed regulatory evaluations to potentially bring therapies to patients more quickly.
To be accepted for PRIME, a therapy must demonstrate the potential to benefit patients with unmet medical need through early clinical or nonclinical data.
About AMT-060
AMT-060 consists of a codon-optimized wild-type factor IX (FIX) gene cassette, the LP1 liver promoter, and an AAV5 viral vector manufactured by uniQure using its proprietary insect cell-based technology platform. UniQure is the company developing AMT-060.
The EMA’s decision to grant AMT-060 access to the PRIME program is based on results from an ongoing phase 1/2 study. Updated data from this study were presented at the 2016 ASH Annual Meeting (abstract 2314).
The presentation included data on 10 patients. All patients had severe or moderately severe hemophilia at baseline, including documented FIX levels less than 1% to 2% of normal, and required chronic infusions of prophylactic or on-demand FIX therapy at the time of enrollment.
Each patient received a 1-time, 30-minute, intravenous dose of AMT-060, without the use of corticosteroids. Five patients received AMT-060 at 5 x 1012 gc/kg, and 5 received AMT-060 at 2 x 1013 gc/kg.
Patients in the low-dose cohort were followed for up to 52 weeks, and those in the higher-dose cohort were followed for up to 31 weeks.
Data from the higher-dose cohort showed a dose response with improvement in disease state in all 5 patients. Four patients who previously required prophylactic FIX therapy were able to stop this therapy.
As of the data cutoff date, 1 unconfirmed spontaneous bleed had been reported during an aggregate of 94 weeks of follow-up after the discontinuation of prophylaxis.
Researchers previously reported that 4 patients in the low-dose cohort were able to discontinue prophylactic therapy. The 1 patient who remained on prophylaxis sustained an improved disease phenotype and also required materially less FIX concentrate after treatment with AMT-060.
According to uniQure, all 5 patients in the low-dose cohort maintained “constant and clinically meaningful” levels of FIX activity for up to 52 weeks post-treatment. In fact, there were no spontaneous bleeds in these patients in the last 14 weeks of observation.
uniQure also said AMT-060 was well-tolerated, and there have been no severe adverse events.
Three patients (2 in the higher-dose cohort and 1 previously reported from the low-dose cohort) experienced mild, asymptomatic elevations of alanine aminotransferase and received a tapering course of corticosteroids per protocol.
These temporary alanine aminotransferase elevations were not associated with any loss of endogenous FIX activity or T-cell response to the AAV5 capsid.
None of the patients in either cohort have developed inhibitory antibodies against FIX, and none of the patients screened tested positive for anti-AAV5 antibodies. ![]()
The European Medicines Agency (EMA) has granted AMT-060 access to the agency’s PRIority MEdicines (PRIME) program.
AMT-060 is an investigational gene therapy intended for the treatment of patients with severe hemophilia B.
The goal of the EMA’s PRIME program is to accelerate the development of therapies that may offer a major advantage over existing treatments or benefit patients with no treatment options.
Through PRIME, the EMA offers early and enhanced support to developers in order to optimize development plans and speed regulatory evaluations to potentially bring therapies to patients more quickly.
To be accepted for PRIME, a therapy must demonstrate the potential to benefit patients with unmet medical need through early clinical or nonclinical data.
About AMT-060
AMT-060 consists of a codon-optimized wild-type factor IX (FIX) gene cassette, the LP1 liver promoter, and an AAV5 viral vector manufactured by uniQure using its proprietary insect cell-based technology platform. UniQure is the company developing AMT-060.
The EMA’s decision to grant AMT-060 access to the PRIME program is based on results from an ongoing phase 1/2 study. Updated data from this study were presented at the 2016 ASH Annual Meeting (abstract 2314).
The presentation included data on 10 patients. All patients had severe or moderately severe hemophilia at baseline, including documented FIX levels less than 1% to 2% of normal, and required chronic infusions of prophylactic or on-demand FIX therapy at the time of enrollment.
Each patient received a 1-time, 30-minute, intravenous dose of AMT-060, without the use of corticosteroids. Five patients received AMT-060 at 5 x 1012 gc/kg, and 5 received AMT-060 at 2 x 1013 gc/kg.
Patients in the low-dose cohort were followed for up to 52 weeks, and those in the higher-dose cohort were followed for up to 31 weeks.
Data from the higher-dose cohort showed a dose response with improvement in disease state in all 5 patients. Four patients who previously required prophylactic FIX therapy were able to stop this therapy.
As of the data cutoff date, 1 unconfirmed spontaneous bleed had been reported during an aggregate of 94 weeks of follow-up after the discontinuation of prophylaxis.
Researchers previously reported that 4 patients in the low-dose cohort were able to discontinue prophylactic therapy. The 1 patient who remained on prophylaxis sustained an improved disease phenotype and also required materially less FIX concentrate after treatment with AMT-060.
According to uniQure, all 5 patients in the low-dose cohort maintained “constant and clinically meaningful” levels of FIX activity for up to 52 weeks post-treatment. In fact, there were no spontaneous bleeds in these patients in the last 14 weeks of observation.
uniQure also said AMT-060 was well-tolerated, and there have been no severe adverse events.
Three patients (2 in the higher-dose cohort and 1 previously reported from the low-dose cohort) experienced mild, asymptomatic elevations of alanine aminotransferase and received a tapering course of corticosteroids per protocol.
These temporary alanine aminotransferase elevations were not associated with any loss of endogenous FIX activity or T-cell response to the AAV5 capsid.
None of the patients in either cohort have developed inhibitory antibodies against FIX, and none of the patients screened tested positive for anti-AAV5 antibodies. ![]()
The European Medicines Agency (EMA) has granted AMT-060 access to the agency’s PRIority MEdicines (PRIME) program.
AMT-060 is an investigational gene therapy intended for the treatment of patients with severe hemophilia B.
The goal of the EMA’s PRIME program is to accelerate the development of therapies that may offer a major advantage over existing treatments or benefit patients with no treatment options.
Through PRIME, the EMA offers early and enhanced support to developers in order to optimize development plans and speed regulatory evaluations to potentially bring therapies to patients more quickly.
To be accepted for PRIME, a therapy must demonstrate the potential to benefit patients with unmet medical need through early clinical or nonclinical data.
About AMT-060
AMT-060 consists of a codon-optimized wild-type factor IX (FIX) gene cassette, the LP1 liver promoter, and an AAV5 viral vector manufactured by uniQure using its proprietary insect cell-based technology platform. UniQure is the company developing AMT-060.
The EMA’s decision to grant AMT-060 access to the PRIME program is based on results from an ongoing phase 1/2 study. Updated data from this study were presented at the 2016 ASH Annual Meeting (abstract 2314).
The presentation included data on 10 patients. All patients had severe or moderately severe hemophilia at baseline, including documented FIX levels less than 1% to 2% of normal, and required chronic infusions of prophylactic or on-demand FIX therapy at the time of enrollment.
Each patient received a 1-time, 30-minute, intravenous dose of AMT-060, without the use of corticosteroids. Five patients received AMT-060 at 5 x 1012 gc/kg, and 5 received AMT-060 at 2 x 1013 gc/kg.
Patients in the low-dose cohort were followed for up to 52 weeks, and those in the higher-dose cohort were followed for up to 31 weeks.
Data from the higher-dose cohort showed a dose response with improvement in disease state in all 5 patients. Four patients who previously required prophylactic FIX therapy were able to stop this therapy.
As of the data cutoff date, 1 unconfirmed spontaneous bleed had been reported during an aggregate of 94 weeks of follow-up after the discontinuation of prophylaxis.
Researchers previously reported that 4 patients in the low-dose cohort were able to discontinue prophylactic therapy. The 1 patient who remained on prophylaxis sustained an improved disease phenotype and also required materially less FIX concentrate after treatment with AMT-060.
According to uniQure, all 5 patients in the low-dose cohort maintained “constant and clinically meaningful” levels of FIX activity for up to 52 weeks post-treatment. In fact, there were no spontaneous bleeds in these patients in the last 14 weeks of observation.
uniQure also said AMT-060 was well-tolerated, and there have been no severe adverse events.
Three patients (2 in the higher-dose cohort and 1 previously reported from the low-dose cohort) experienced mild, asymptomatic elevations of alanine aminotransferase and received a tapering course of corticosteroids per protocol.
These temporary alanine aminotransferase elevations were not associated with any loss of endogenous FIX activity or T-cell response to the AAV5 capsid.
None of the patients in either cohort have developed inhibitory antibodies against FIX, and none of the patients screened tested positive for anti-AAV5 antibodies. ![]()
FDA issues warnings about illegal ‘anticancer’ products
The US Food and Drug Administration (FDA) has posted warning letters addressed to 14 US-based companies illegally selling more than 65 products.
The companies are fraudulently claiming that these products prevent, diagnose, treat, or cure cancer.
The products are being marketed and sold without FDA approval, most commonly on websites and social media platforms.
“Consumers should not use these or similar unproven products because they may be unsafe and could prevent a person from seeking an appropriate and potentially life-saving cancer diagnosis or treatment,” said Douglas W. Stearn, director of the Office of Enforcement and Import Operations in the FDA’s Office of Regulatory Affairs.
“We encourage people to remain vigilant whether online or in a store, and avoid purchasing products marketed to treat cancer without any proof they will work. Patients should consult a healthcare professional about proper prevention, diagnosis, and treatment of cancer.”
It is a violation of the Federal Food, Drug and Cosmetic Act to market and sell products that claim to prevent, diagnose, treat, mitigate, or cure diseases without first demonstrating to the FDA that they are safe and effective for their labeled uses.
The illegally sold products cited in the FDA’s warning letters include a variety of product types, such as pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostics (such as thermography devices).
They include products marketed for use by humans or pets that make illegal, unproven claims regarding preventing, reversing, or curing cancer; killing/inhibiting cancer cells or tumors; or other similar anticancer claims.
The FDA has requested responses from the 14 companies stating how the violations will be corrected. Failure to correct the violations promptly may result in legal action, including product seizure, injunction, and/or criminal prosecution.
As part of the FDA’s effort to protect consumers from cancer health fraud, the FDA has issued more than 90 warning letters in the past 10 years to companies marketing hundreds of fraudulent cancer-related products on websites, social media, and in stores.
Although many of these companies have stopped selling the products or making fraudulent claims, numerous unsafe and unapproved products continue to be sold directly to consumers due, in part, to the ease with which companies can move their marketing operations to new websites.
The FDA continues to monitor and take action against companies promoting and selling unproven treatments in an effort to minimize the potential dangers to consumers and to educate consumers about the risks.
The FDA encourages healthcare professionals and consumers to report adverse reactions associated with these or similar products to the FDA’s MedWatch program. ![]()
The US Food and Drug Administration (FDA) has posted warning letters addressed to 14 US-based companies illegally selling more than 65 products.
The companies are fraudulently claiming that these products prevent, diagnose, treat, or cure cancer.
The products are being marketed and sold without FDA approval, most commonly on websites and social media platforms.
“Consumers should not use these or similar unproven products because they may be unsafe and could prevent a person from seeking an appropriate and potentially life-saving cancer diagnosis or treatment,” said Douglas W. Stearn, director of the Office of Enforcement and Import Operations in the FDA’s Office of Regulatory Affairs.
“We encourage people to remain vigilant whether online or in a store, and avoid purchasing products marketed to treat cancer without any proof they will work. Patients should consult a healthcare professional about proper prevention, diagnosis, and treatment of cancer.”
It is a violation of the Federal Food, Drug and Cosmetic Act to market and sell products that claim to prevent, diagnose, treat, mitigate, or cure diseases without first demonstrating to the FDA that they are safe and effective for their labeled uses.
The illegally sold products cited in the FDA’s warning letters include a variety of product types, such as pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostics (such as thermography devices).
They include products marketed for use by humans or pets that make illegal, unproven claims regarding preventing, reversing, or curing cancer; killing/inhibiting cancer cells or tumors; or other similar anticancer claims.
The FDA has requested responses from the 14 companies stating how the violations will be corrected. Failure to correct the violations promptly may result in legal action, including product seizure, injunction, and/or criminal prosecution.
As part of the FDA’s effort to protect consumers from cancer health fraud, the FDA has issued more than 90 warning letters in the past 10 years to companies marketing hundreds of fraudulent cancer-related products on websites, social media, and in stores.
Although many of these companies have stopped selling the products or making fraudulent claims, numerous unsafe and unapproved products continue to be sold directly to consumers due, in part, to the ease with which companies can move their marketing operations to new websites.
The FDA continues to monitor and take action against companies promoting and selling unproven treatments in an effort to minimize the potential dangers to consumers and to educate consumers about the risks.
The FDA encourages healthcare professionals and consumers to report adverse reactions associated with these or similar products to the FDA’s MedWatch program. ![]()
The US Food and Drug Administration (FDA) has posted warning letters addressed to 14 US-based companies illegally selling more than 65 products.
The companies are fraudulently claiming that these products prevent, diagnose, treat, or cure cancer.
The products are being marketed and sold without FDA approval, most commonly on websites and social media platforms.
“Consumers should not use these or similar unproven products because they may be unsafe and could prevent a person from seeking an appropriate and potentially life-saving cancer diagnosis or treatment,” said Douglas W. Stearn, director of the Office of Enforcement and Import Operations in the FDA’s Office of Regulatory Affairs.
“We encourage people to remain vigilant whether online or in a store, and avoid purchasing products marketed to treat cancer without any proof they will work. Patients should consult a healthcare professional about proper prevention, diagnosis, and treatment of cancer.”
It is a violation of the Federal Food, Drug and Cosmetic Act to market and sell products that claim to prevent, diagnose, treat, mitigate, or cure diseases without first demonstrating to the FDA that they are safe and effective for their labeled uses.
The illegally sold products cited in the FDA’s warning letters include a variety of product types, such as pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostics (such as thermography devices).
They include products marketed for use by humans or pets that make illegal, unproven claims regarding preventing, reversing, or curing cancer; killing/inhibiting cancer cells or tumors; or other similar anticancer claims.
The FDA has requested responses from the 14 companies stating how the violations will be corrected. Failure to correct the violations promptly may result in legal action, including product seizure, injunction, and/or criminal prosecution.
As part of the FDA’s effort to protect consumers from cancer health fraud, the FDA has issued more than 90 warning letters in the past 10 years to companies marketing hundreds of fraudulent cancer-related products on websites, social media, and in stores.
Although many of these companies have stopped selling the products or making fraudulent claims, numerous unsafe and unapproved products continue to be sold directly to consumers due, in part, to the ease with which companies can move their marketing operations to new websites.
The FDA continues to monitor and take action against companies promoting and selling unproven treatments in an effort to minimize the potential dangers to consumers and to educate consumers about the risks.
The FDA encourages healthcare professionals and consumers to report adverse reactions associated with these or similar products to the FDA’s MedWatch program. ![]()
Use of second-generation antidepressants in older adults is associated with increased hospitalization with hyponatremia
Clinical Question: Is there an increased risk of hyponatremia for older patients who are taking a second-generation antidepressant?
Background: Mood and anxiety disorders affect about one in eight older adults, and second-generation antidepressants are frequently recommended for treatment. A potential adverse effect of these agents is hyponatremia, which can lead to serious sequelae. The aim of this study was to investigate the 30-day risk for hospitalization with hyponatremia in older adults who were newly started on a second-generation antidepressant.
Setting: Ontario, Canada.
Synopsis: Multiple databases were utilized to obtain vital statistics and demographic information, diagnoses, prescriptions, and serum sodium measurements to establish a cohort population. One group of 172,552 was newly prescribed a second-generation antidepressant. A second control group of 297,501 was established in which patients were not prescribed antidepressants. Greedy matching was used to match each user to a nonuser based on similar characteristics of age, sex, evidence of mood disorder, chronic kidney disease, congestive heart failure, or diuretic use. After matching, 138,246 patients remained in each group and were nearly identical for all 10 0 measured characteristics. The primary outcome was that, compared with nonuse, second-generation antidepressant use was associated with higher 30-day risk of hospitalization with hyponatremia (relative risk, 5.46; 95% CI, 4.32-6.91). The secondary outcome showed that, compared with non-use, second-generation antidepressant use was associated with higher 30-day risk for hospitalization with concomitant hyponatremia and delirium (RR, 4.00; 95% CI, 1.74 - 9.16). Additionally, tests for specificity and temporality were employed.
Bottom Line: A robust association between second-generation antidepressant use and hospitalization with hyponatremia was determined in the large population-based cohort study.
Citation: Gandhi S, Shariff SZ, Al-Jaishi A, et al. “Second-generation antidepressants and hyponatremia risk: a population-based cohort study of older adults.” Am J Kidney Dis. 2017 Jan;69(1):87-96.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical Question: Is there an increased risk of hyponatremia for older patients who are taking a second-generation antidepressant?
Background: Mood and anxiety disorders affect about one in eight older adults, and second-generation antidepressants are frequently recommended for treatment. A potential adverse effect of these agents is hyponatremia, which can lead to serious sequelae. The aim of this study was to investigate the 30-day risk for hospitalization with hyponatremia in older adults who were newly started on a second-generation antidepressant.
Setting: Ontario, Canada.
Synopsis: Multiple databases were utilized to obtain vital statistics and demographic information, diagnoses, prescriptions, and serum sodium measurements to establish a cohort population. One group of 172,552 was newly prescribed a second-generation antidepressant. A second control group of 297,501 was established in which patients were not prescribed antidepressants. Greedy matching was used to match each user to a nonuser based on similar characteristics of age, sex, evidence of mood disorder, chronic kidney disease, congestive heart failure, or diuretic use. After matching, 138,246 patients remained in each group and were nearly identical for all 10 0 measured characteristics. The primary outcome was that, compared with nonuse, second-generation antidepressant use was associated with higher 30-day risk of hospitalization with hyponatremia (relative risk, 5.46; 95% CI, 4.32-6.91). The secondary outcome showed that, compared with non-use, second-generation antidepressant use was associated with higher 30-day risk for hospitalization with concomitant hyponatremia and delirium (RR, 4.00; 95% CI, 1.74 - 9.16). Additionally, tests for specificity and temporality were employed.
Bottom Line: A robust association between second-generation antidepressant use and hospitalization with hyponatremia was determined in the large population-based cohort study.
Citation: Gandhi S, Shariff SZ, Al-Jaishi A, et al. “Second-generation antidepressants and hyponatremia risk: a population-based cohort study of older adults.” Am J Kidney Dis. 2017 Jan;69(1):87-96.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
Clinical Question: Is there an increased risk of hyponatremia for older patients who are taking a second-generation antidepressant?
Background: Mood and anxiety disorders affect about one in eight older adults, and second-generation antidepressants are frequently recommended for treatment. A potential adverse effect of these agents is hyponatremia, which can lead to serious sequelae. The aim of this study was to investigate the 30-day risk for hospitalization with hyponatremia in older adults who were newly started on a second-generation antidepressant.
Setting: Ontario, Canada.
Synopsis: Multiple databases were utilized to obtain vital statistics and demographic information, diagnoses, prescriptions, and serum sodium measurements to establish a cohort population. One group of 172,552 was newly prescribed a second-generation antidepressant. A second control group of 297,501 was established in which patients were not prescribed antidepressants. Greedy matching was used to match each user to a nonuser based on similar characteristics of age, sex, evidence of mood disorder, chronic kidney disease, congestive heart failure, or diuretic use. After matching, 138,246 patients remained in each group and were nearly identical for all 10 0 measured characteristics. The primary outcome was that, compared with nonuse, second-generation antidepressant use was associated with higher 30-day risk of hospitalization with hyponatremia (relative risk, 5.46; 95% CI, 4.32-6.91). The secondary outcome showed that, compared with non-use, second-generation antidepressant use was associated with higher 30-day risk for hospitalization with concomitant hyponatremia and delirium (RR, 4.00; 95% CI, 1.74 - 9.16). Additionally, tests for specificity and temporality were employed.
Bottom Line: A robust association between second-generation antidepressant use and hospitalization with hyponatremia was determined in the large population-based cohort study.
Citation: Gandhi S, Shariff SZ, Al-Jaishi A, et al. “Second-generation antidepressants and hyponatremia risk: a population-based cohort study of older adults.” Am J Kidney Dis. 2017 Jan;69(1):87-96.
Dr. Kim is clinical assistant professor in the division of hospital medicine, Loyola University Chicago, Maywood, Ill.
FDA issues warning to companies selling illegal cancer treatments
The Food and Drug Administration has issued a warning to 14 U.S. companies that are illegally selling more than 65 products purported to prevent, diagnose, treat, or cure cancer, according to an FDA safety alert.
Product types include pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostic tools. The affected products are usually sold online or through social media.
Find the full safety alert on the FDA website.
The Food and Drug Administration has issued a warning to 14 U.S. companies that are illegally selling more than 65 products purported to prevent, diagnose, treat, or cure cancer, according to an FDA safety alert.
Product types include pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostic tools. The affected products are usually sold online or through social media.
Find the full safety alert on the FDA website.
The Food and Drug Administration has issued a warning to 14 U.S. companies that are illegally selling more than 65 products purported to prevent, diagnose, treat, or cure cancer, according to an FDA safety alert.
Product types include pills, topical creams, ointments, oils, drops, syrups, teas, and diagnostic tools. The affected products are usually sold online or through social media.
Find the full safety alert on the FDA website.
MDS genetic analysis identifies allogeneic HSCT candidates
NEW YORK – Genetic mutation analysis of patients with myelodysplastic syndrome (MDS) may have a useful role in routine practice based on recent reports that showed clear links between certain gene mutations and the outcomes of patients who underwent allogeneic hematopoietic stem cell transplantation (HSCT).
Two reports published in 2017 helped strengthen the case for routine mutation analysis in distinguishing patients with MDS or myeloproliferative neoplasms (MDN) who are very likely to have just a brief response to allogeneic HSCT from similar patients who seem likely to have several years of overall survival following transplantation.
Allogeneic HSCT is the only potentially curative procedure for patients with MDS or MDN. Although an increasing number of these patients undergo transplantation, clinicians need to choose the patients they select for the treatment carefully. “Molecular testing is playing an increasing role in selecting the best candidates,” Dr. Zeidan said.
The largest reported genetic study of allogeneic HSCT in MDS patients involved 1,514 patients entered into a U.S.-based dataset during 2005-2015. Testing identified at least one mutation in 1,196 (79%) of these patients.
Analysis of data from these patients found a disparate pattern of posttransplant survival that appeared to link with gene mutations and other risk factors. The highest risk patients were those with a mutation in their TP53 gene, found in 289 patients (19% of the 1,514 tested) who had a median overall survival (OS) of 0.7 years and a 3-year OS of 20% (New Engl J Med. 2017 Feb 9;376[6]:536-47).
Among patients without a TP53 mutation, OS depended on age, with the best survival seen among patients less than 40 years old. Patients in this subgroup who also had no other high-risk features – no therapy-related MDS, a platelet level of at least 30 x 109 at the time of transplantation, and bone marrow blasts less than 15% at diagnosis – had the best OS, 82% at 3-years of follow-up. The studied cohort included 116 patients (8%) who fell into this low-risk, best-outcome category, the optimal population for receiving an allogeneic HSCT, Dr. Zeidan said. Another 98 patients (6%) who had at least one of these high risk feature had a median OS of 2.6 years and a 3-year OS of 49%.
Additional gene mutations further subdivided the older patients in the study, those at least 40 years old, into various risk subgroups. Older patients with a mutation in a ras-pathway gene had a 0.9 year median OS and a 3-year OS of 30%. This subgroup included 129 patients (9%). Among older patients with no mutation in the ras-pathway gene, mutations in the JAK2 gene also linked with worse survival, a median OS of 0.5 years and a 3-year OS of 28% of a subgroup with 28 patients (2%). The largest subgroup in the study was older patients with no mutations in the TP53, JAK2, or ras-pathway genes, a subgroup with 854 patients (56%), who had a median OS of 2.3 years and a 3-year OS of 46%.
The second recent report was a Japanese study of 797 MDS patients who underwent genetic testing and received an allogeneic HSCT through the Japan Marrow Donor Program. The investigators found identifiable mutations in 617 patients (77%) and documented that patients with a TP53 or ras-pathway mutation had a “dismal prognosis” when associated with a complex karyotype and myelodysplastic or myeloproliferative neoplasms. However, among patients with a mutated TP53 gene or complex karyotype alone, long-term survival following transplantation appeared possible (Blood. 2017. doi: org/10.1182/blood-2016-12-754796.
Two smaller, earlier studies (J Clin Oncol. 2014 Sept 1;32[25]:2691-8; J Clin Oncol. 2016 Oct 20;34[30]:2627-37) also implicated mutations in the TET2, DNMT3A, ASXL1, and RUNX1 genes as identifying MDS patients with worse OS following allogeneic HSCT, Dr. Zeidan noted, but the combination of a TP53 gene mutation and a complex karyotype appears to confer the worst prognosis of all. Patients with mutations in more than one of these genes fared much worse than those with single mutations.
Dr. Zeidan had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
NEW YORK – Genetic mutation analysis of patients with myelodysplastic syndrome (MDS) may have a useful role in routine practice based on recent reports that showed clear links between certain gene mutations and the outcomes of patients who underwent allogeneic hematopoietic stem cell transplantation (HSCT).
Two reports published in 2017 helped strengthen the case for routine mutation analysis in distinguishing patients with MDS or myeloproliferative neoplasms (MDN) who are very likely to have just a brief response to allogeneic HSCT from similar patients who seem likely to have several years of overall survival following transplantation.
Allogeneic HSCT is the only potentially curative procedure for patients with MDS or MDN. Although an increasing number of these patients undergo transplantation, clinicians need to choose the patients they select for the treatment carefully. “Molecular testing is playing an increasing role in selecting the best candidates,” Dr. Zeidan said.
The largest reported genetic study of allogeneic HSCT in MDS patients involved 1,514 patients entered into a U.S.-based dataset during 2005-2015. Testing identified at least one mutation in 1,196 (79%) of these patients.
Analysis of data from these patients found a disparate pattern of posttransplant survival that appeared to link with gene mutations and other risk factors. The highest risk patients were those with a mutation in their TP53 gene, found in 289 patients (19% of the 1,514 tested) who had a median overall survival (OS) of 0.7 years and a 3-year OS of 20% (New Engl J Med. 2017 Feb 9;376[6]:536-47).
Among patients without a TP53 mutation, OS depended on age, with the best survival seen among patients less than 40 years old. Patients in this subgroup who also had no other high-risk features – no therapy-related MDS, a platelet level of at least 30 x 109 at the time of transplantation, and bone marrow blasts less than 15% at diagnosis – had the best OS, 82% at 3-years of follow-up. The studied cohort included 116 patients (8%) who fell into this low-risk, best-outcome category, the optimal population for receiving an allogeneic HSCT, Dr. Zeidan said. Another 98 patients (6%) who had at least one of these high risk feature had a median OS of 2.6 years and a 3-year OS of 49%.
Additional gene mutations further subdivided the older patients in the study, those at least 40 years old, into various risk subgroups. Older patients with a mutation in a ras-pathway gene had a 0.9 year median OS and a 3-year OS of 30%. This subgroup included 129 patients (9%). Among older patients with no mutation in the ras-pathway gene, mutations in the JAK2 gene also linked with worse survival, a median OS of 0.5 years and a 3-year OS of 28% of a subgroup with 28 patients (2%). The largest subgroup in the study was older patients with no mutations in the TP53, JAK2, or ras-pathway genes, a subgroup with 854 patients (56%), who had a median OS of 2.3 years and a 3-year OS of 46%.
The second recent report was a Japanese study of 797 MDS patients who underwent genetic testing and received an allogeneic HSCT through the Japan Marrow Donor Program. The investigators found identifiable mutations in 617 patients (77%) and documented that patients with a TP53 or ras-pathway mutation had a “dismal prognosis” when associated with a complex karyotype and myelodysplastic or myeloproliferative neoplasms. However, among patients with a mutated TP53 gene or complex karyotype alone, long-term survival following transplantation appeared possible (Blood. 2017. doi: org/10.1182/blood-2016-12-754796.
Two smaller, earlier studies (J Clin Oncol. 2014 Sept 1;32[25]:2691-8; J Clin Oncol. 2016 Oct 20;34[30]:2627-37) also implicated mutations in the TET2, DNMT3A, ASXL1, and RUNX1 genes as identifying MDS patients with worse OS following allogeneic HSCT, Dr. Zeidan noted, but the combination of a TP53 gene mutation and a complex karyotype appears to confer the worst prognosis of all. Patients with mutations in more than one of these genes fared much worse than those with single mutations.
Dr. Zeidan had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
NEW YORK – Genetic mutation analysis of patients with myelodysplastic syndrome (MDS) may have a useful role in routine practice based on recent reports that showed clear links between certain gene mutations and the outcomes of patients who underwent allogeneic hematopoietic stem cell transplantation (HSCT).
Two reports published in 2017 helped strengthen the case for routine mutation analysis in distinguishing patients with MDS or myeloproliferative neoplasms (MDN) who are very likely to have just a brief response to allogeneic HSCT from similar patients who seem likely to have several years of overall survival following transplantation.
Allogeneic HSCT is the only potentially curative procedure for patients with MDS or MDN. Although an increasing number of these patients undergo transplantation, clinicians need to choose the patients they select for the treatment carefully. “Molecular testing is playing an increasing role in selecting the best candidates,” Dr. Zeidan said.
The largest reported genetic study of allogeneic HSCT in MDS patients involved 1,514 patients entered into a U.S.-based dataset during 2005-2015. Testing identified at least one mutation in 1,196 (79%) of these patients.
Analysis of data from these patients found a disparate pattern of posttransplant survival that appeared to link with gene mutations and other risk factors. The highest risk patients were those with a mutation in their TP53 gene, found in 289 patients (19% of the 1,514 tested) who had a median overall survival (OS) of 0.7 years and a 3-year OS of 20% (New Engl J Med. 2017 Feb 9;376[6]:536-47).
Among patients without a TP53 mutation, OS depended on age, with the best survival seen among patients less than 40 years old. Patients in this subgroup who also had no other high-risk features – no therapy-related MDS, a platelet level of at least 30 x 109 at the time of transplantation, and bone marrow blasts less than 15% at diagnosis – had the best OS, 82% at 3-years of follow-up. The studied cohort included 116 patients (8%) who fell into this low-risk, best-outcome category, the optimal population for receiving an allogeneic HSCT, Dr. Zeidan said. Another 98 patients (6%) who had at least one of these high risk feature had a median OS of 2.6 years and a 3-year OS of 49%.
Additional gene mutations further subdivided the older patients in the study, those at least 40 years old, into various risk subgroups. Older patients with a mutation in a ras-pathway gene had a 0.9 year median OS and a 3-year OS of 30%. This subgroup included 129 patients (9%). Among older patients with no mutation in the ras-pathway gene, mutations in the JAK2 gene also linked with worse survival, a median OS of 0.5 years and a 3-year OS of 28% of a subgroup with 28 patients (2%). The largest subgroup in the study was older patients with no mutations in the TP53, JAK2, or ras-pathway genes, a subgroup with 854 patients (56%), who had a median OS of 2.3 years and a 3-year OS of 46%.
The second recent report was a Japanese study of 797 MDS patients who underwent genetic testing and received an allogeneic HSCT through the Japan Marrow Donor Program. The investigators found identifiable mutations in 617 patients (77%) and documented that patients with a TP53 or ras-pathway mutation had a “dismal prognosis” when associated with a complex karyotype and myelodysplastic or myeloproliferative neoplasms. However, among patients with a mutated TP53 gene or complex karyotype alone, long-term survival following transplantation appeared possible (Blood. 2017. doi: org/10.1182/blood-2016-12-754796.
Two smaller, earlier studies (J Clin Oncol. 2014 Sept 1;32[25]:2691-8; J Clin Oncol. 2016 Oct 20;34[30]:2627-37) also implicated mutations in the TET2, DNMT3A, ASXL1, and RUNX1 genes as identifying MDS patients with worse OS following allogeneic HSCT, Dr. Zeidan noted, but the combination of a TP53 gene mutation and a complex karyotype appears to confer the worst prognosis of all. Patients with mutations in more than one of these genes fared much worse than those with single mutations.
Dr. Zeidan had no relevant disclosures.
[email protected]
On Twitter @mitchelzoler
Pes planus: To treat or not to treat
Pes planus, or flat feet, is a common concern addressed during well-child visits. Many parents express concern more because of the appearance of the feet than actual symptomatology. But what is within the realm of normal and what is beyond?
Ninety percent of clinic visits for foot problems are for flat feet.1 Historically, the treatment of flat feet was wearing orthopedic shoes that were unappealing, so parents fear that is the fate of their child. Although the exact incidence rate of flat feet has not been determined, it clearly is quite common. Other contributing factors are joint hypermobility, obesity, and age. All children under the age of 2 years have flat feet because of the fat pad that is present. By the age of 10 years, this fat pad regresses and the normal arch is formed.
Given that the arch does not fully form until the end of the first decade of life, neither diagnosis nor treatment should be given until after that time. Evaluating for flat feet in the clinic is usually limited to inspection in weight bearing and non-weight bearing. There are more formal procedures using foot prints and x-rays, but practically speaking those are not necessary. It is key to examine the patient while he or she is standing, to see if the arch is present and to gauge the orientation of the talus bone. When the patient is supine, again note if the arch is present and check the degree of dorsiflexion and plantarflexion.
Determine whether the talus bone is straight or in a valgus position, and whether there is a shortened Achilles tendon. This is crucial in predicting whether symptoms will emerge if they haven’t already. Patients with rigid flat feet or flexible flat feet with shortened Achilles tendon usually begin to complain of discomfort with activity in the second or third decade of life. Those symptoms may be limited to pain in the foot near the head of the talus, or can be complaints of knee, hip, or back pain.1
For the asymptomatic patient, no intervention is needed. Although many clinicians recommend orthotics, studies have shown that after years of wearing orthotics, the feet remain flat. For symptomatic patients with flexible flat feet, there is increased intrinsic muscle activity, which can result in soreness and achiness of the feet. Orthotics can offer some relief, but for patients with shortened Achilles tendons, it potentially can cause more discomfort.2 Both OTC and hard custom orthotics have been shown to relieve pain without significant increase in the height of the arch. There is little information to support using one over the other.2
Heel cord stretching is another reasonable intervention to improve any discomfort. It is important to note that the knee must be extended and the subtalar joint must be in the neutral position for the stretch to be effective.
Surgery is reserved for flexible and rigid flat feet that are symptomatic despite conservative treatment. Bone reconstruction and tendon lengthening have shown reduction in symptoms.
In summary, the vast majority of patients with flat feet do not need any intervention. Proper categorization is important to determine if intervention will be needed. The use of orthotics should be reserved for symptomatic patients, but will not alter the height of the arch. Surgery is indicated for those patients with significant symptoms that have not improved with conservative measures. It has been found to be effective if all components of the deformity have been addressed.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Iran J Pediatr. 2013 Jun;23(3):247-60.
2. J Child Orthop. 2010;4(2):107-21.
Pes planus, or flat feet, is a common concern addressed during well-child visits. Many parents express concern more because of the appearance of the feet than actual symptomatology. But what is within the realm of normal and what is beyond?
Ninety percent of clinic visits for foot problems are for flat feet.1 Historically, the treatment of flat feet was wearing orthopedic shoes that were unappealing, so parents fear that is the fate of their child. Although the exact incidence rate of flat feet has not been determined, it clearly is quite common. Other contributing factors are joint hypermobility, obesity, and age. All children under the age of 2 years have flat feet because of the fat pad that is present. By the age of 10 years, this fat pad regresses and the normal arch is formed.
Given that the arch does not fully form until the end of the first decade of life, neither diagnosis nor treatment should be given until after that time. Evaluating for flat feet in the clinic is usually limited to inspection in weight bearing and non-weight bearing. There are more formal procedures using foot prints and x-rays, but practically speaking those are not necessary. It is key to examine the patient while he or she is standing, to see if the arch is present and to gauge the orientation of the talus bone. When the patient is supine, again note if the arch is present and check the degree of dorsiflexion and plantarflexion.
Determine whether the talus bone is straight or in a valgus position, and whether there is a shortened Achilles tendon. This is crucial in predicting whether symptoms will emerge if they haven’t already. Patients with rigid flat feet or flexible flat feet with shortened Achilles tendon usually begin to complain of discomfort with activity in the second or third decade of life. Those symptoms may be limited to pain in the foot near the head of the talus, or can be complaints of knee, hip, or back pain.1
For the asymptomatic patient, no intervention is needed. Although many clinicians recommend orthotics, studies have shown that after years of wearing orthotics, the feet remain flat. For symptomatic patients with flexible flat feet, there is increased intrinsic muscle activity, which can result in soreness and achiness of the feet. Orthotics can offer some relief, but for patients with shortened Achilles tendons, it potentially can cause more discomfort.2 Both OTC and hard custom orthotics have been shown to relieve pain without significant increase in the height of the arch. There is little information to support using one over the other.2
Heel cord stretching is another reasonable intervention to improve any discomfort. It is important to note that the knee must be extended and the subtalar joint must be in the neutral position for the stretch to be effective.
Surgery is reserved for flexible and rigid flat feet that are symptomatic despite conservative treatment. Bone reconstruction and tendon lengthening have shown reduction in symptoms.
In summary, the vast majority of patients with flat feet do not need any intervention. Proper categorization is important to determine if intervention will be needed. The use of orthotics should be reserved for symptomatic patients, but will not alter the height of the arch. Surgery is indicated for those patients with significant symptoms that have not improved with conservative measures. It has been found to be effective if all components of the deformity have been addressed.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Iran J Pediatr. 2013 Jun;23(3):247-60.
2. J Child Orthop. 2010;4(2):107-21.
Pes planus, or flat feet, is a common concern addressed during well-child visits. Many parents express concern more because of the appearance of the feet than actual symptomatology. But what is within the realm of normal and what is beyond?
Ninety percent of clinic visits for foot problems are for flat feet.1 Historically, the treatment of flat feet was wearing orthopedic shoes that were unappealing, so parents fear that is the fate of their child. Although the exact incidence rate of flat feet has not been determined, it clearly is quite common. Other contributing factors are joint hypermobility, obesity, and age. All children under the age of 2 years have flat feet because of the fat pad that is present. By the age of 10 years, this fat pad regresses and the normal arch is formed.
Given that the arch does not fully form until the end of the first decade of life, neither diagnosis nor treatment should be given until after that time. Evaluating for flat feet in the clinic is usually limited to inspection in weight bearing and non-weight bearing. There are more formal procedures using foot prints and x-rays, but practically speaking those are not necessary. It is key to examine the patient while he or she is standing, to see if the arch is present and to gauge the orientation of the talus bone. When the patient is supine, again note if the arch is present and check the degree of dorsiflexion and plantarflexion.
Determine whether the talus bone is straight or in a valgus position, and whether there is a shortened Achilles tendon. This is crucial in predicting whether symptoms will emerge if they haven’t already. Patients with rigid flat feet or flexible flat feet with shortened Achilles tendon usually begin to complain of discomfort with activity in the second or third decade of life. Those symptoms may be limited to pain in the foot near the head of the talus, or can be complaints of knee, hip, or back pain.1
For the asymptomatic patient, no intervention is needed. Although many clinicians recommend orthotics, studies have shown that after years of wearing orthotics, the feet remain flat. For symptomatic patients with flexible flat feet, there is increased intrinsic muscle activity, which can result in soreness and achiness of the feet. Orthotics can offer some relief, but for patients with shortened Achilles tendons, it potentially can cause more discomfort.2 Both OTC and hard custom orthotics have been shown to relieve pain without significant increase in the height of the arch. There is little information to support using one over the other.2
Heel cord stretching is another reasonable intervention to improve any discomfort. It is important to note that the knee must be extended and the subtalar joint must be in the neutral position for the stretch to be effective.
Surgery is reserved for flexible and rigid flat feet that are symptomatic despite conservative treatment. Bone reconstruction and tendon lengthening have shown reduction in symptoms.
In summary, the vast majority of patients with flat feet do not need any intervention. Proper categorization is important to determine if intervention will be needed. The use of orthotics should be reserved for symptomatic patients, but will not alter the height of the arch. Surgery is indicated for those patients with significant symptoms that have not improved with conservative measures. It has been found to be effective if all components of the deformity have been addressed.
Dr. Pearce is a pediatrician in Frankfort, Ill. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Iran J Pediatr. 2013 Jun;23(3):247-60.
2. J Child Orthop. 2010;4(2):107-21.
Primary Hyperparathyroidism: A Case-based Review
CE/CME No: CR-1705
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Differentiate primary hyperparathyroidism (PHPT) from other causes of hypercalcemia and types of hyerparathyroidism.
• Understand the calcium-parathyroid hormone feedback loop.
• Identify appropriate imaging studies and common laboratory findings in the patient with PHPT.
• Describe the common systemic manifestations of PHPT.
• Discuss medical versus surgical management of the patient with PHPT.
FACULTY
Barbara Austin is a Family Nurse Practitioner at Baptist Primary Care, Jacksonville, Florida, and is pursuing a Doctorate of Nursing Practice (DNP) at Jacksonville University.
The author has no financial relationships to disclose.

ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of May 2017.
Article begins on next page >>
Primary hyperparathyroidism (PHPT) is most often detected as hypercalcemia in an asymptomatic patient during routine blood work. Knowing the appropriate work-up of hypercalcemia is essential, since untreated PHPT can have significant complications affecting multiple organ systems—most notably, renal and musculoskeletal. Parathyroidectomy is curative in up to 95% of cases, but prevention of long-term complications relies on prompt recognition and appropriate follow-up.
Primary hyperparathyroidism (PHPT) is a common endocrine disorder, with a prevalence of approximately 1 to 3 cases per 1,000 persons.1 PHPT results from inappropriate overproduction of parathyroid hormone (PTH), the primary regulator of calcium homeostasis, and is characterized by hypercalcemia in the setting of an elevated or high-normal PTH level. In most cases of PHPT, unregulated PTH production is caused by a single parathyroid adenoma.
PHPT is the most common cause of hypercalcemia in outpatients and is typically diagnosed following incidental discovery during routine blood work in an asymptomatic patient.1,2 It is two to three times more common in women than in men, and incidence increases with age; as such, postmenopausal women are most commonly affected.1,3 PHPT often has an insidious course, and recognition of its clinical manifestations followed by appropriate diagnostic work-up and management are necessary to prevent sequelae.3
PATIENT PRESENTATION
A 68-year-old Caucasian woman presented to her family practice office for a third visit with continued complaints of nontraumatic right lower leg pain. She had previously been diagnosed with tendonitis, which was treated conservatively. The pain failed to improve, and an x-ray was ordered. The x-ray revealed no acute findings but did show osteopenia, prompting an order for a bone mineral density (BMD) test. The BMD test demonstrated osteoporosis, which warranted further investigation. She was prescribed alendronate but refused it, against medical advice, due to concern over potential adverse effects.
Her medical history included hyperlipidemia and hypertension under fair control with lisinopril. She took a low-dose aspirin and flaxseed supplement daily. She also had a history of radiation to the neck, having undergone tonsillar irradiation as a child (a common practice from the 1930s through the 1950s).3 Surgical history included a total hysterectomy with bilateral salpingo-oophorectomy, appendectomy, and tonsillectomy. There was no personal or family history of cancer or endocrine disorders, hypercalcemia, or nephrolithiasis. She was up to date on vaccines and preventive health care measures. Allergies included penicillin and sulfa, both resulting in hives. She was a nonsmoker and did not drink alcohol or engage in illicit drug use.
Review of systems revealed right lower anterior leg pain for four months, characterized as aching, deep, sharp, and throbbing with radiation to the ankle. The pain was worse with activity and prolonged standing; ibuprofen and application of ice provided partial relief. She had experienced some mood changes, including irritability. Physical exam was normal except for dominant right-sided thyromegaly, marked bony point tenderness to the right midshin area, and an antalgic gait.
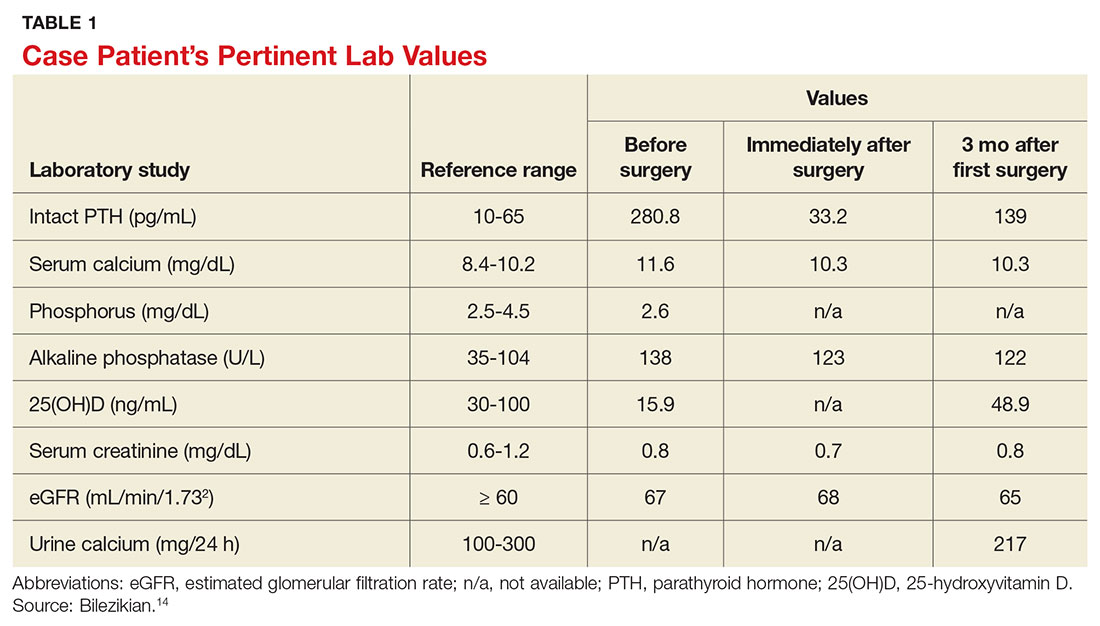
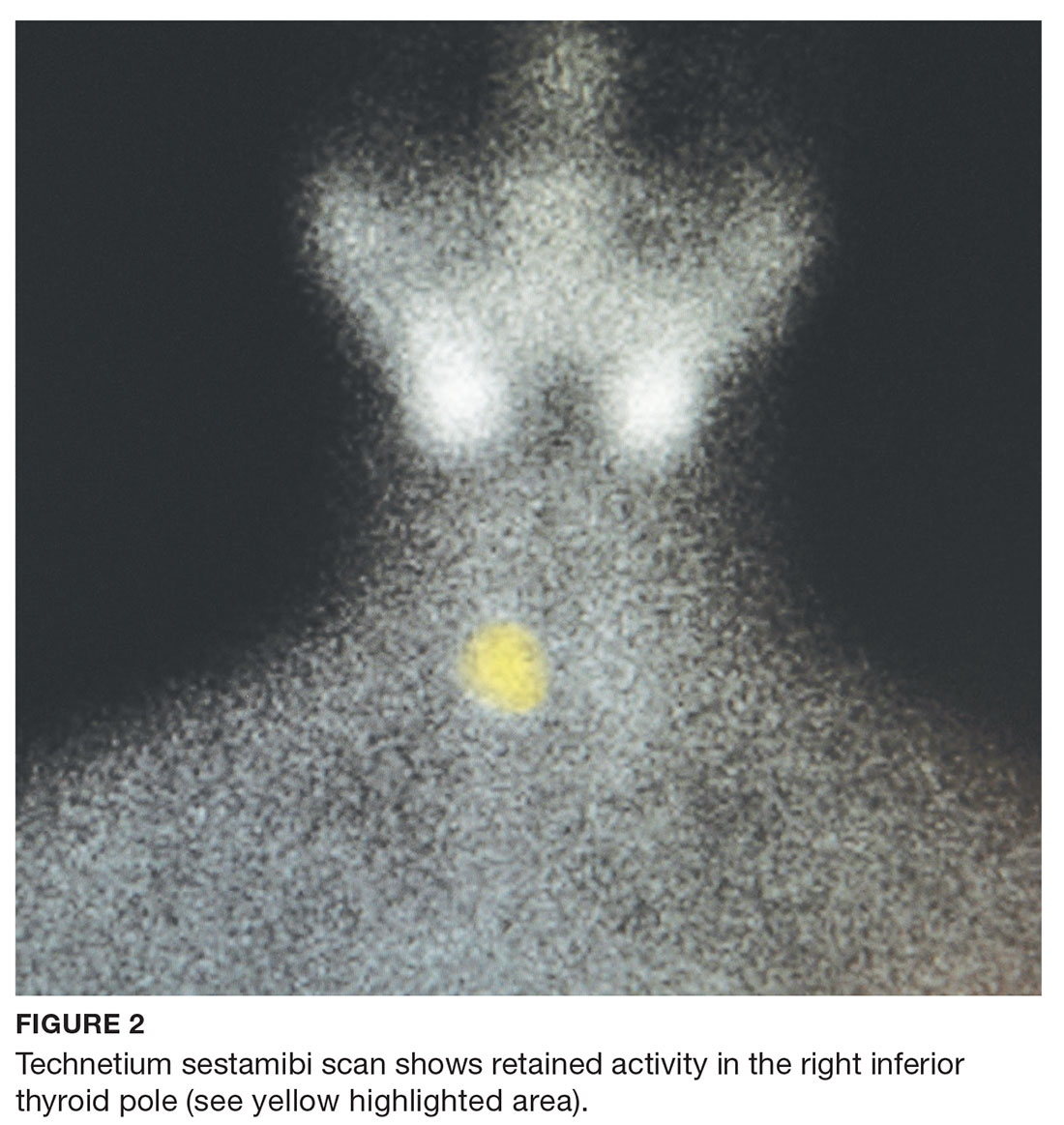
Laboratory work-up demonstrated elevated PTH, alkaline phosphatase, and calcium levels and a low 25-hydroxyvitamin D [25(OH)D] level (see Table 1). MRI of the right lower leg revealed a grade IV stress fracture (see Figure 1). The elevated serum calcium and PTH levels in addition to abnormal bone density findings led to the diagnosis of PHPT. She was referred to endocrinology and orthopedics for management of PHPT and the stress fracture, respectively, and was placed in an orthopedic walking boot for treatment of the midtibial stress fracture.
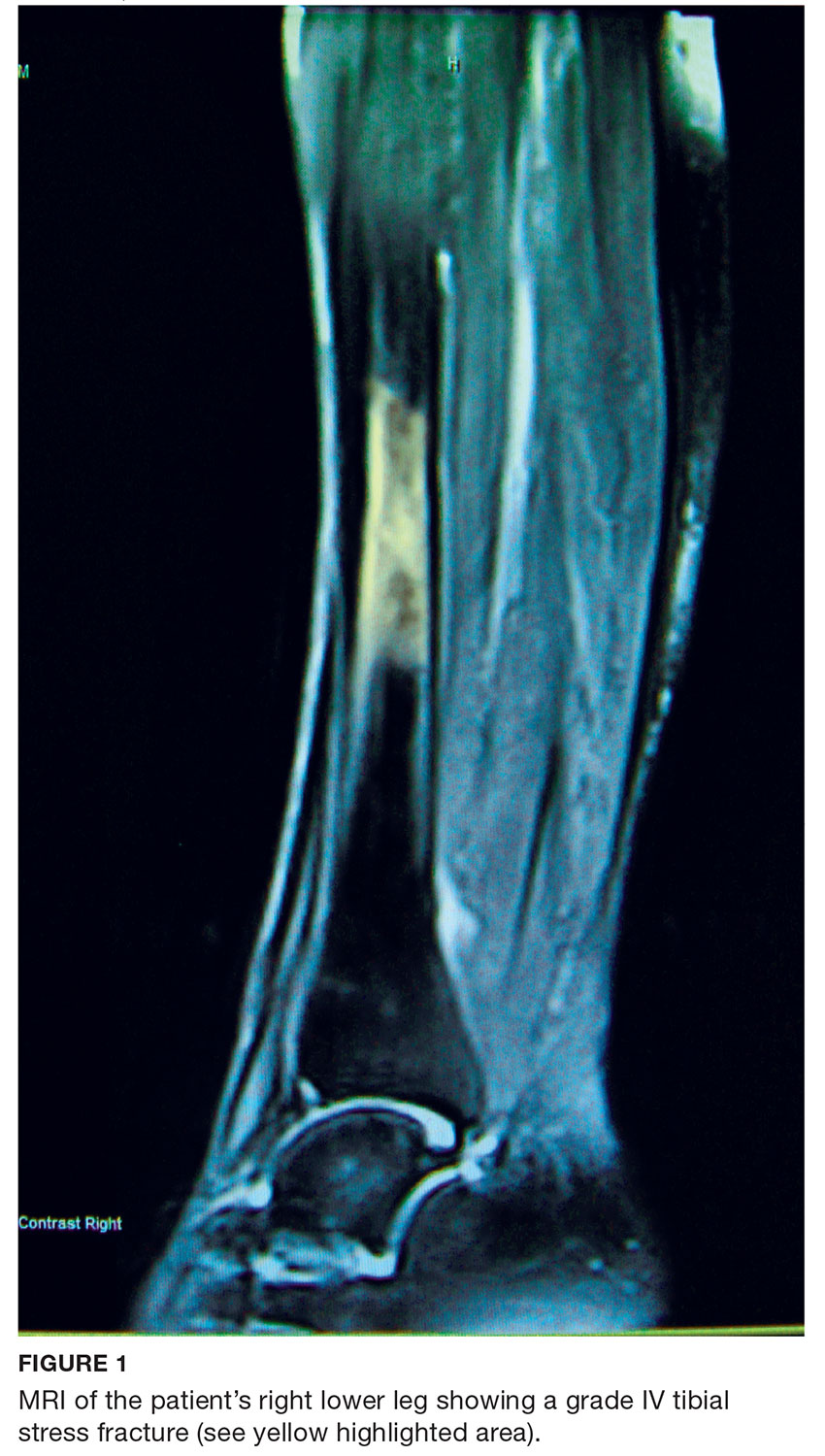
The endocrinologist referred her to an otolaryngologist trained in the surgical management of parathyroid adenomas, who ordered a thyroid ultrasound; this study was inconclusive. Additional imaging, including a Tc-99m sestamibi parathyroid scan and CT with contrast of the soft tissue of the neck, was obtained. The parathyroid scan of the neck and upper chest showed retained activity in the right inferior thyroid pole that was concerning for a parathyroid adenoma (see Figure 2). The CT identified a 1.5-cm parathyroid adenoma off the right inferior pole of the thyroid gland (concordant with the parathyroid scan). A single 300-mg parathyroid adenoma was removed from the right inferior pole of the thyroid. The surgery was deemed successful, with intraoperative normalization of the PTH level.
The patient was managed postoperatively by the endocrinologist and was started on calcium and vitamin D supplements. She was prescribed a bisphosphonate, as she had refused to take alendronate following her abnormal BMD test.
DIFFERENTIAL DIAGNOSIS
PHPT and malignancy are the most common causes of hypercalcemia, accounting for 90% of cases.2,4 A less common cause is familial hypocalciuric hypercalcemia (FHH), a rare benign disorder that imitates PHPT.1 FHH is ruled out by measurement of 24-hour urine calcium excretion and is characterized by hypocalciuria, defined as a urine calcium level of less than 100 mg/24 h (reference range, 100-300 mg/24 h).2 Low calcium excretion can also be identified by a calcium-creatinine excretion ratio.2 FHH is a benign autosomal dominant condition caused by a heterozygous mutation of the parathyroid glands’ calcium-sensing receptors.2,5,6 Young adults with FHH are asymptomatic, and mild hypercalcemia and a normal or slightly elevated PTH are the only laboratory findings.4
Measuring PTH levels is key in determining the underlying mechanism of hypercalcemia.2,7 If the hypercalcemia is not PTH-mediated, malignancy and granulomatous diseases such as sarcoidosis must be considered.2,7 PTH is suppressed in malignancy except for rare cases of PTH-producing tumors.4 Bone metastases cause calcium resorption, and sarcoidosis causes an excess of vitamin D, both resulting in hypercalcemia. Lymphomas and sarcoid granulomas express 1α-hydroxylase, an enzyme that increases the conversion of 25(OH)D to 1,25-dihydroxyvitamin D [1,25(OH)2D].2 When malignancy is suspected, it is appropriate to check a 1,25(OH)2D level. Thiazide diuretics, such as hydrochlorothiazide, decrease urinary calcium excretion and may result in mild hypercalcemia.2 Other possibilities in the differential include hypervitaminosis A or D, dehydration, and excess calcium ingestion, but these are less common.6,7
CALCIUM REGULATION
The parathyroid glands stem from four poles on the back of the thyroid gland; there are typically four, but the number can vary from two to 11. Secreted PTH, the primary regulator of calcium homeostasis, maintains calcium levels within a narrow physiologic range.2,8 PTH increases bone resorption, stimulating release of calcium into the blood, and signals the kidneys to increase reabsorption of calcium and excrete phosphorus. It also converts 25(OH)D to 1,25(OH)2 D, the active form of vitamin D that increases gastrointestinal calcium absorption. In a negative feedback loop, PTH secretion is regulated by serum calcium levels, stimulated when levels are low and suppressed when levels are high (see Figure 3).3 Calcium-sensing receptors, located in the chief cells of parathyroid tissue, are essential to calcium homeostasis. These receptors will either increase or decrease PTH release in response to small changes in blood ionized calcium levels. The receptors also play an independent role in the renal tubules by promoting secretion of calcium in the setting of hypercalcemia.5,9 The precise regulation of intracellular and extracellular calcium is necessary for normal functioning of physiologic processes, including bone metabolism, hormone release and regulation, neuromuscular function, and cell signaling.5

PATHOPHYSIOLOGY
Hyperparathyroidism is defined as excess secretion of PTH and is categorized as primary, secondary, or tertiary based on pathophysiologic mechanisms.
Primary hyperparathyroidism
PHPT is defined as PTH levels that are elevated or inappropriately normal in patients with hypercalcemia and no known history of kidney disease.2,6 This occurs when the normal feedback mechanism fails to inhibit excess hormone secretion by one or more of the parathyroid glands.6 With uninhibited PTH secretion, hypercalcemia will result from increased gastrointestinal absorption and bone resorption.
The most common causes of PHPT are an abnormal proliferation of parathyroid cells (parathyroid adenomas) and parathyroid tissue overgrowth (hyperplasia). PHPT may result from a single parathyroid adenoma (80%-90%), multigland hyperplasia (10%-15%), multiple adenomas (2%-3%), or malignancy (< 1%).6,10 Adenomas can occur sporadically or less commonly as part of an inherited syndrome.1 It is estimated that more than 10% of patients with PHPT have a mutation in one of 11 genes associated with PHPT.11 Approximately 5% of PHPT cases are familial, resulting from adenomas or carcinomas associated with mutations in the tumor suppressor genes MEN1 and CDC73 and the RET proto-oncogene.5 Multiple endocrine neoplasia (MEN) syndrome type 1 or 2a is associated with the development of parathyroid adenomas and other endocrine tumors.1,5 Mutations in the CDC73 gene can lead to parathyroid cancer, familial isolated hyperparathyroidism, and familial hyperparathyroidism-jaw tumor syndrome.5 Parathyroid cancer is rare and is linked to a history of radiation to the head and neck.3 Ectopic parathyroid adenomas represent 3% to 4% of all parathyroid adenomas and are often found in the mediastinum.12PHPT is the third most common endocrine disorder, with a prevalence of 1 case per 1,000 men and 2 to 3 cases per 1,000 women.5 Most women with PHPT are postmenopausal and older than 50.1 The condition can occur in younger adults but is rare in childhood and adolescence, with an incidence of 2 to 5 cases per 100,000.13
PHPT affects multiple organ systems, but the most commonly involved are the renal and musculoskeletal systems (see Table 2). The hypersecretory state causes excessive bone resorption and increased osteoclastic activity, resulting in osteoporosis and increased risk for pathologic fractures of the hip, wrist, and spine. The most common osteoporotic fractures are vertebral compression fractures.14 Fractures involving the thoracic spine contribute to the development of kyphosis.15
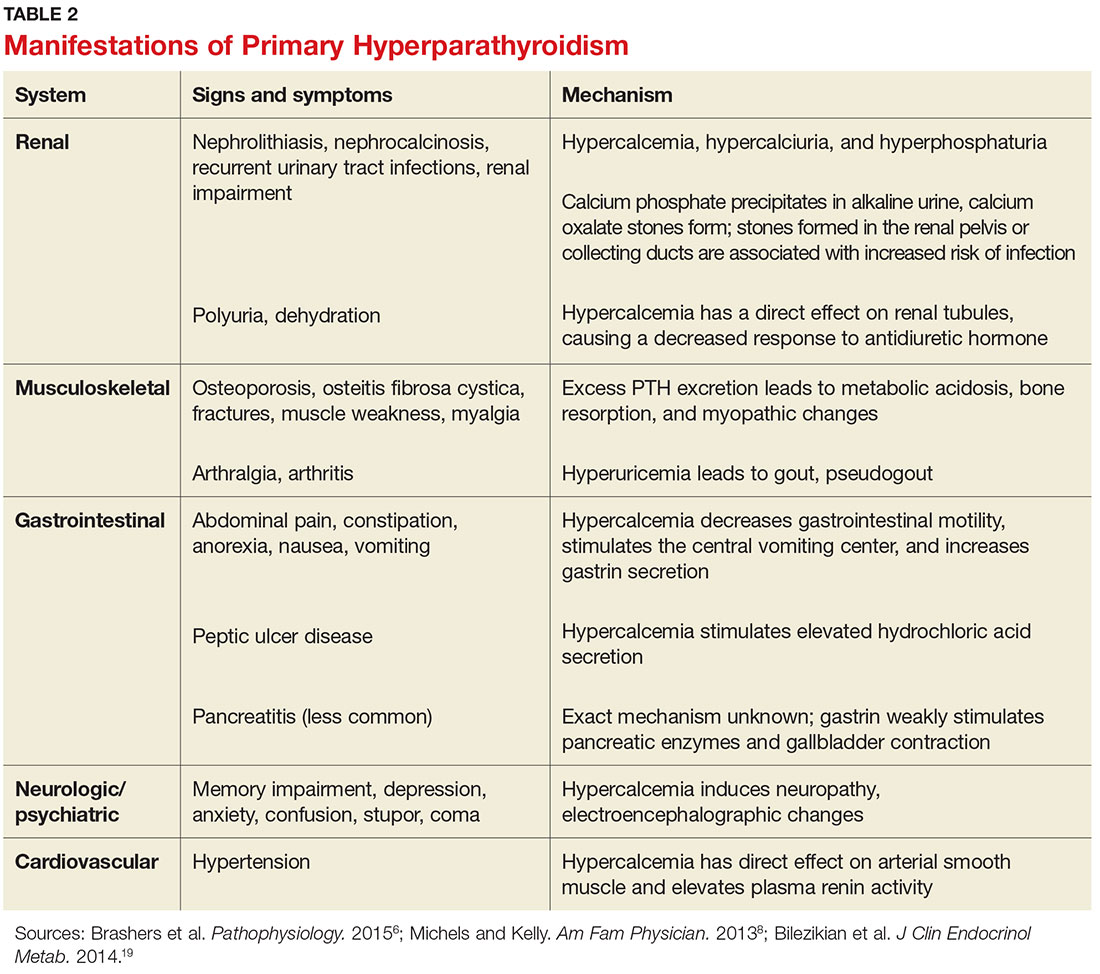
In the kidney, an increased filtered load of calcium leads to hypercalciuria, precipitation of calcium phosphate in the renal pelvis and collecting ducts, metabolic acidosis, alkaline urine, and hyperphosphaturia. The combination of alkaline urine, hyperphosphaturia, and hypercalciuria leads to the formation of kidney stones.6 Nephrolithiasis and alkaline urine predispose patients to recurrent urinary tract infections and subsequent renal impairment.6 In addition, hypercalcemia impairs the renal collecting system and decreases its response to antidiuretic hormone, resulting in polyuria.6
Secondary hyperparathyroidism
In secondary hyperparathyroidism, calcium levels are either normal or low. Normocalcemic hyperparathyroidism is characterized by normal ionized and total calcium levels and elevated PTH levels; it has no known cause.6 Secondary hyperparathyroidism occurs when excess PTH is excreted as a result of a chronic condition that leads to hypocalcemia. Examples of these disease states include vitamin D deficiency, chronic kidney disease (CKD), and intestinal malabsorption. The most common cause of secondary hyperparathyroidism is CKD; glomerular filtration insufficiency results in hyperphosphatemia, hypocalcemia, and low 1,25(OH)2D, stimulating the release of PTH. Other causes include deficient intake or decreased absorption of calcium or vitamin D; chronic use of medications such as lithium, phenobarbital, or phenytoin; bariatric surgery; celiac disease; and pancreatic disease.4,6,14 Lithium decreases urinary calcium excretion and reduces the sensitivity of the parathyroid gland to calcium.4
Tertiary hyperparathyroidism
Tertiary hyperparathyroidism, marked by hypercalcemia and excessive PTH secretion, can occur after prolonged secondary hyperparathyroidism. In this disorder, persistent parathyroid stimulation leads to gland hyperplasia, resulting in autonomous production of PTH despite correction of calcium levels.6 It most commonly occurs in patients with chronic secondary hyperparathyroidism with renal failure who receive a kidney transplant.2,6 In some cases, parathyroid hyperplasia may not regress after transplantation and parathyroidectomy may be necessary.
EVALUATION AND DIAGNOSTIC WORK-UP
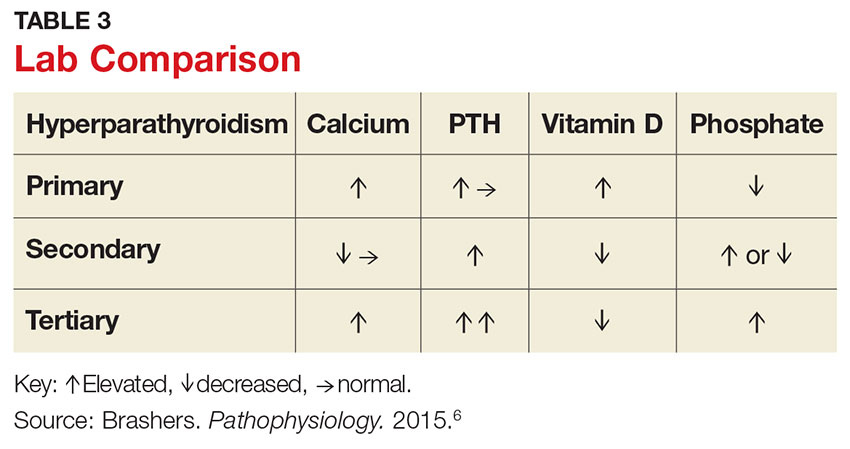
Laboratory tests
Hypercalcemia is the most common initial finding that leads to the diagnosis of PHPT. Elevated serum calcium and PTH is characteristic of the condition. When evaluating a patient with hypercalcemia, the diagnostic work-up includes tests to differentiate between PTH- and non–PTH-mediated causes of elevated calcium (see Table 3).7 Evaluation should begin with measurement of PTH by second- or third-generation immunoassay along with phosphorus, alkaline phosphatase, 25(OH)D, creatinine, estimated glomerular filtration rate (eGFR), and albumin. Additionally, a 24-hour urine collection for calcium, creatinine, and creatinine clearance should be considered in patients with overt nephrolithiasis or nephrocalcinosis. If the urine calcium is > 400 mg/24 h, a renal stone risk profile is indicated because nephrolithiasis is one of the most common complications of PHPT.14 There is a high prevalence of nephrolithiasis in patients with normocalcemic PHPT, even after parathyroidectomy.16 If the 24-hour urine calcium level is low, the diagnosis of FHH is considered. If the urine calcium is high and the intact PTH is elevated or inappropriately normal, the diagnosis of PHPT is considered; urine calcium will be normal in 60% of PHPT cases.4,11
Imaging studies
Imaging is useful for localization of adenomas and abnormal parathyroid tissue to guide surgical planning but is not necessary for diagnosis or medical management. Understanding the strengths and weaknesses of imaging modalities enables the clinician to order the most appropriate option. There are three primary imaging modalities used to locate parathyroid adenoma(s) or aberrant parathyroid tissue: ultrasound, nuclear medicine sestamibi parathyroid scans, and CT. Some clinicians start with an ultrasound, but its operator-dependent results can vary widely; in addition, ultrasound often provides poor anatomic definition and has limited value in locating ectopic parathyroid tissue.17
Nuclear medicine parathyroid scan with technetium-99m sestamibi is a sensitive method for localizing hyperfunctioning, enlarged parathyroid glands or tissue in normal anatomic positions or ectopic locations. Uptake is enhanced and prolonged in parathyroid adenomas as well as in aberrant tissue found in the mediastinum or subclavicular areas. Sestamibi parathyroid scan detects up to 89% of single adenomas, but studies of this imaging modality have demonstrated a wide range of sensitivities (44%-95%).5,17 A drawback of nuclear medicine studies is that they provide little anatomic detail.17 Nonetheless, the ability of the parathyroid scan to locate parathyroid glands has contributed to the success of the minimally invasive parathyroidectomy, and it is considered the most successful imaging modality available.5,10 Identifying the precise location of the parathyroid adenoma is essential for a successful surgical outcome; this is best achieved by combining the sestamibi parathyroid scan with CT.12
Emerging imaging modalities are the multidetector CT (MDCT) and 4D-CT techniques. In an evaluation of the diagnostic accuracy of contrast-enhanced MDCT in the detection of parathyroid adenomas and aberrant parathyroid tissue, MDCT demonstrated the ability to differentiate between adenomas and hyperplasia and display important anatomic structures such as nerves and blood vessels.17 The specificity of MDCT for ruling out abnormal parathyroid tissue was 75%, and the sensitivity for detecting a single adenoma was 80%. Overall, MDCT demonstrated an 88% positive predictive value (PPV) in localizing hyperfunctioning parathyroid glands but showed poor sensitivity in detecting multigland disease.17 The PPV is a key value in determining the ability of an imaging study to precisely locate aberrant parathyroid tissue. MDCT provides detailed definition of anatomy, locating ectopic parathyroid glands in the deeper paraesophageal areas and mediastinum while defining relationships between the tissue and its surrounding vasculature, lymph nodes, and thyroid tissue.17 The 4D-CT technique employs three-dimensional technology and accounts for the movement of the patient’s body over time (the “fourth dimension”). It is an accurate method for identifying parathyroid adenomas but exposes the patient to higher radiation doses.18 The sensitivity of 4D-CT in localizing abnormal parathyroid tissue is comparable to that of MDCT.16,18,19
Additional studies used during the management of the patient with PHPT are BMD testing and renal imaging. Secondary causes of bone loss are responsible for up to 30% of osteoporosis cases in postmenopausal women; one of these causes is PHPT.20 Elevated PTH causes increased bone turnover and results in decreased bone mass with subsequent increased fracture risk.9 Bone density should be measured by dual-energy x-ray absorptiometry (DEXA), and the skeletal survey should include the distal one-third of the radius, hip, and lumbar spine. The distal radius is rich in cortical bone and BMD is often lowest at this site in patients with PHPT, making it the most sensitive DEXA marker for early detection of bone loss.19,21 The hip contains an equal mix of cortical and trabecular bone and is the second most sensitive site for detecting bone loss in PHPT. The spine contains a high proportion of trabecular bone and is the least sensitive site.19,21 Renal imaging studies, including x-ray, ultrasound, and, less frequently, CT of the abdomen and pelvis, are used to assess for nephrolithiasis and nephrocalcinosis.19
TREATMENT/MANAGEMENT
Conservative medical management
PHPT is a complex disease process, and careful evaluation is required when determining whether medical versus surgical management is appropriate. Clinical presentation ranges from no symptoms to multisystem disease. Conservative medical management, which includes regular monitoring, is an acceptable strategy in an asymptomatic patient with a low fracture risk and no nephrolithiasis.1 Conservative care includes maintaining normal dietary calcium intake and adequate hydration, regular exercise, vitamin D supplementation, annual laboratory studies, BMD testing, and the avoidance of thiazide diuretics and lithium.1 Guidelines, from the Fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism, for monitoring asymptomatic PHPT patients recommend
- Annual measurement of serum calcium
- BMD measurement by DEXA every 1 to 2 years
- Annual assessment of eGFR and serum creatinine
- Renal imaging or a 24-h urine stone profile if nephrolithiasis is suspected.19
Long-term medical management of PHPT is difficult because no agents are available to suppress hypercalcemia or completely block PTH release.12
Maintaining serum 25(OH)D at a level > 20 ng/mL significantly reduces PTH secretion, in comparison to levels < 20 ng/mL, and does not aggravate hypercalcemia.22 The Endocrine Society recommends a minimum serum 25(OH)D level of 20 ng/mL and notes that targeting a higher threshold value of 30 ng/mL is reasonable.19 The daily requirement for vitamin D3, 800 IU to 1,000 IU, is a good starting point for supplementation.4 Measurement of 1,25(OH)2D levels lacks value and is not recommended for patients with PHPT. Calcium intake should follow established guidelines and is not limited in PHPT.19
Surgical management
Surgical management is indicated for symptomatic patients.23 Indications include nephrolithiasis, nephrocalcinosis, osteitis fibrosa cystica, or osteoporosis. Surgery is considered appropriate for individuals who do not meet these criteria if there are no medical contraindications.14 The Fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism revised the indications for surgery in 2014 to include asymptomatic patients, since surgery is the only definitive treatment for PHPT. Current guidelines for when to recommend surgery in the asymptomatic patient with PHPT are listed in Table 4.19
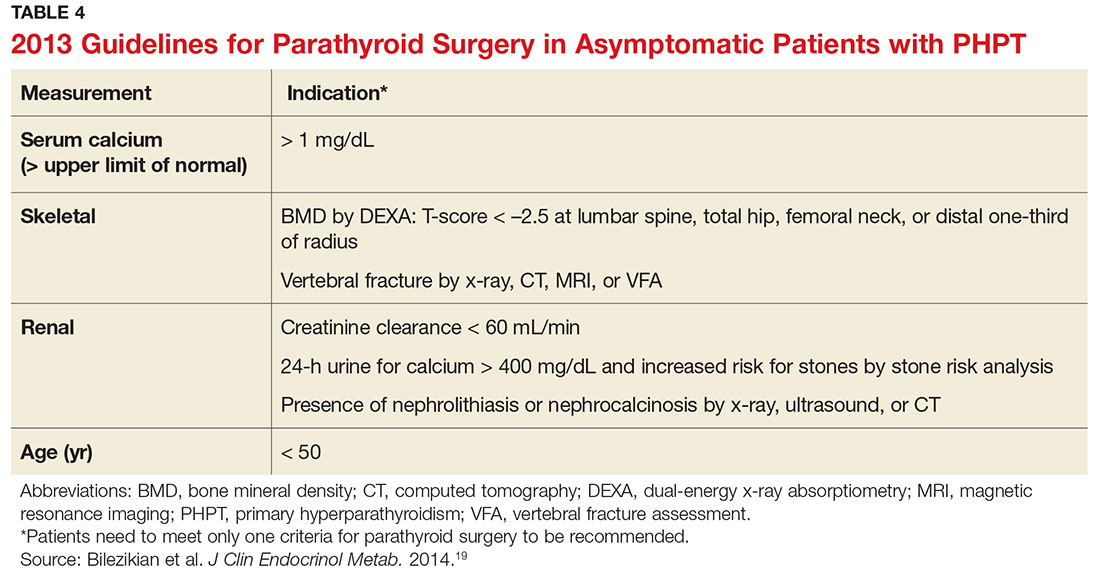
Preoperative localization and referral to an experienced surgeon is of utmost importance for a good outcome. An expert surgeon will usually perform a minimally invasive parathyroidectomy (MIP) and obtain intraoperative PTH levels; in some cases, a full neck exploration is necessary. PTH has a half-life of less than five minutes and is an accurate tool for determining whether the culprit gland has been successfully removed.5
Modern imaging studies, less invasive surgical techniques, and intraoperative measurements of PTH have decreased the need to conduct full neck exploration. MIP offers a smaller incision, less tissue dissection, and lower morbidity, and can be offered without the risks associated with general anesthesia.10 The goal of surgery is to restore normocalcemia and, in turn, prevent bone mineral loss and systemic effects of hypercalcemia over the long term.10 Surgical management for an ectopic parathyroid adenoma is controversial because these are often found in the mediastinum, requiring invasive surgery.12
Surgery is curative in up to 95% of cases and has a low rate of complications.2,24 A joint decision regarding treatment options is made among the patient, primary care clinician, and surgeon. Complications include vocal cord paralysis resulting from injury to the recurrent laryngeal nerve, bleeding or hematoma, laryngospasm, symptomatic hypocalcemia, and persistent hyperparathyroidism; seizures are very rare but can occur from transient hypocalcemia and hypomagnesemia.5 PTH levels drop by more than 50% intraoperatively if the procedure is successful; otherwise, exploration for another adenoma is indicated.10 Postoperative calcium and vitamin D supplementation are warranted once lab values are stable.
When surgery is contraindicated/refused
If surgery is indicated but the patient is a poor candidate or refuses surgery, management of hypercalcemia and bone loss with pharmacologic agents is warranted. The calcimimetic cinacalcet is a reasonable medical alternative that has been shown to adequately control hypercalcemia and hypophosphatemia and has proven effective in various patient subgroups.25 This agent is useful in the treatment of patients who are asymptomatic and refuse surgery, patients with refractory PHPT after parathyroidectomy, and patients with contraindications to surgery.24,25 The medication reduces calcium and modestly reduces PTH levels by binding parathyroid calcium-sensing receptors but does not improve bone density.2,12 Cinacalcet is approved by the FDA for use in patients with moderate to severe disease when surgery is contraindicated.24
Treatment options for osteoporosis, vertebral fractures, and progressive bone loss in the patient with PHPT include bisphosphonates. Raloxifene and estrogen replacements may be used in postmenopausal women. Oral bisphosphonates (alendronate or risedronate) are firstline therapies and have been shown to inhibit progression to osteoporosis in PHPT.9,26 They prevent osteoclastic activity, reducing bone resorption and turnover. Contraindications to oral bisphosphonates include esophageal disorders, gastrointestinal intolerance, or inability to follow the dosing requirements. Intravenous zoledronic acid provides an alternative route of administration.
Alendronate has the best evidence for improving bone density and preventing progression to osteoporosis in patients with PHPT, but the medication does not affect calcium or PTH levels.1,19 There is limited data on the effects of combining bisphosphonates with calcimimetics. Raloxifene is a selective estrogen receptor modulator that decreases bone resorption; it is approved for treating osteoporosis and may be used when a patient is not a good candidate for a bisphosphonate.20 Denosumab, currently under study for the treatment of PHPT, is a human monoclonal antibody that improves bone density but does not affect serum calcium.20 Nonpharmacologic therapies include alcohol moderation, decreased caffeine intake, weight-bearing exercise, smoking cessation, adequate hydration, and dietary modifications.20
OUTCOME FOR THE CASE PATIENT
Although PHPT is often discovered incidentally in routine blood work with hypercalcemia, the case patient had developed osteoporosis and a grade IV tibial stress fracture before the diagnosis was made. Following parathyroidectomy, her hypertension worsened, requiring an additional antihypertensive medication. She developed recurrent disease and was referred to a tertiary care center for revision parathyroidectomy due to persistent elevated calcium levels. A 24-hour urine calcium test ruled out concurrent FHH. A full neck exploration was conducted and a 340-mg hypercellular parathyroid gland was removed from the left superior pole. She will be monitored for recurrent disease and will remain on a vitamin D3 supplement and treatment for osteoporosis.
CONCLUSION
Primary care clinicians should have a low threshold for initiating the work-up of mild hypercalcemia in an effort to prevent sequelae. Patient education is essential throughout the process. Understanding the condition and treatment options is necessary for a patient’s active participation in clinical decision making. Conservative management of an asymptomatic patient includes avoiding thiazide diuretics and lithium, staying well hydrated with water, maintaining moderate dietary calcium (1,000-1,200 mg/d) and vitamin D (400-600 IU/d) intake, regular exercise, and appropriate lab and bone density monitoring. Surgical treatment is recommended for symptomatic patients exhibiting decreased bone density, fractures, renal impairment, or nephrolithiasis. Treating bone loss with bisphosphonates and hypercalcemia with calcimimetics is useful. Postmenopausal women may benefit from estrogen therapy or selective estrogen receptor modulators. These agents improve bone density and lower calcium, but are often contraindicated or have adverse effects. Surgery is the only cure.3
1. Turner J. Hypercalcaemia and primary hyperparathyroidism. Medicine. 2009;37(9):461-464.
2. Crowley R, Gittoes N. How to approach hypercalcaemia. Clin Med. 2013;13(3):287-290.
3. Kapustin JF, Schofield DL. Hyperparathyroidism: an incidental finding. Nurse Pract. 2012;37(11):9-14.
4. Cordellat IM. Hyperparathyroidism: primary or secondary disease? Rheumatol Clin. 2012;8(5):287-291.
5. MacKenzie-Feder J, Sirrs S, Anderson D, Sharif J, Khan A. Primary hyperparathyroidism: an overview. Int J Endocrinol. 2011;2011:251410.
6. Brashers VL, Jones RE, Huether SE. Alterations of hormonal regulation. In: McCance KL, Huether SE, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 7th ed. St. Louis, MO: Mosby; 2015:731-733.
7. Osborne JL, Klocko DJ. Woman, 66, with persistent abdominal and back pain. Clinician Reviews. 2014;24(11):34-37, 40.
8. Michels TC, Kelly KM. Parathyroid disorders. Am Fam Physician. 2013;88(4):249-257.
9. Rolighed L, Rejnmark L, Christiansen P. Bone involvement in primary hyperparathyroidism and changes after parathyroidectomy. US Endocrinol. 2013;9(2):181-184.
10. Karahan Ö, Okus A, Sevinç B, et al. Minimally invasive parathyroidectomy under local anesthesia. J Postgrad Med. 2013;59(1):21-24.
11. Fuleihan GE, Silverberg SJ. Primary hyperparathyroidism: diagnosis, differential diagnosis, and evaluation. Up-to-Date. www.uptodate.com/contents/primary-hyperparathyroidism-diagnosis-differential-diagnosis-and-evaluation. Accessed April 20, 2017.
12. Panchani R, Varma T, Goyal A, et al. A challenging case of an ectopic parathyroid adenoma. Indian J Endocrinol Metab. 2012;16:S408-S410.
13. Otasowie J, Hambleton BA. Aggression and homicidal thoughts in a patient with primary hyperparathyroidism: a case report. Br J Medical Pract. 2013;6(4):a630.
14. Bilezikian JP. Primary hyperparathyroidism: new insights, concepts and guidelines. Presented at: American Association of Clinical Endocrinologists 24th Annual Scientific and Clinical Congress; May 13-17, 2015; Nashville, TN. am2015.aace.com/presentations/Friday/F31/PrimaryHyperparathyroidismNew InsightsConceptsandGuidelines.pdf. Accessed April 20, 2017.
15. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 7th ed. St. Louis, MO: Mosby; 2015:1551-1555.
16. Amaral LM, Queiroz DC, Marques TF, et al. Clinical study: normocalcemic versus hypercalcemic primary hyperparathyroidism: more stone than bone? J Osteoporos. 2012;2012:128352.
17. Linda DD, Ng B, Rebello R, et al. The utility of multidetector computed tomography for detection of parathyroid disease in the setting of primary hyperparathyroidism. Can Assoc Radiol J. 2012;63(2):100-108.
18. Bann DV, Zacharia T, Goldenberg D, Goyal, N. Parathyroid localization using 4-D-computed tomography. Ear Nose Throat J. 2015;94(4-5):E55-E57.
19. Bilezikian JP, Brandi ML, Eastell R, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3561-3569.
20. Jeremiah MP, Unwin BK, Greenawald MH, Casiano VE. Diagnosis and management of osteoporosis. Am Fam Physician. 2015;92(4):261-268.
21. Wood K, Dhital S, Chen H, Sippel RS. What is the utility of distal forearm DXA in primary hyperparathyroidism? Oncologist. 2012;17(3):322-325.
22. Jayasena CN, Modi M, Palazzo F, et al. Associations of serum 25-hydroxyvitamin D with circulating PTH, phosphate and calcium in patients with primary hyperparathyroidism. Clin Endocrinol (Oxf). 2013;78(6):838-843.
23. Grey A. Nonsurgical management of mild primary hyperparathyroidism—a reasonable option. Clin Endocrinol. 2012;77(5):639-644.
24. Saponaro F, Faggiano A, Grimaldi F, et al. Cinacalcet in the management of primary hyperparathyroidism: post marketing experience of an Italian multicenter group. Clin Endocrinol (Oxf). 2013;79(1):20-26.
25. Rothe HM, Liangos O, Biggar P, et al. Cinacalcet treatment of primary hyperparathyroidism. Int J Endocrinol. 2011;2011:415719.
26. Farag N, Delbanco T, Strewler GJ. Update: a 64-year-old woman with primary hyperparathyroidism. JAMA. 2008;300(17):2044-2045.
CE/CME No: CR-1705
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Differentiate primary hyperparathyroidism (PHPT) from other causes of hypercalcemia and types of hyerparathyroidism.
• Understand the calcium-parathyroid hormone feedback loop.
• Identify appropriate imaging studies and common laboratory findings in the patient with PHPT.
• Describe the common systemic manifestations of PHPT.
• Discuss medical versus surgical management of the patient with PHPT.
FACULTY
Barbara Austin is a Family Nurse Practitioner at Baptist Primary Care, Jacksonville, Florida, and is pursuing a Doctorate of Nursing Practice (DNP) at Jacksonville University.
The author has no financial relationships to disclose.

ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of May 2017.
Article begins on next page >>
Primary hyperparathyroidism (PHPT) is most often detected as hypercalcemia in an asymptomatic patient during routine blood work. Knowing the appropriate work-up of hypercalcemia is essential, since untreated PHPT can have significant complications affecting multiple organ systems—most notably, renal and musculoskeletal. Parathyroidectomy is curative in up to 95% of cases, but prevention of long-term complications relies on prompt recognition and appropriate follow-up.
Primary hyperparathyroidism (PHPT) is a common endocrine disorder, with a prevalence of approximately 1 to 3 cases per 1,000 persons.1 PHPT results from inappropriate overproduction of parathyroid hormone (PTH), the primary regulator of calcium homeostasis, and is characterized by hypercalcemia in the setting of an elevated or high-normal PTH level. In most cases of PHPT, unregulated PTH production is caused by a single parathyroid adenoma.
PHPT is the most common cause of hypercalcemia in outpatients and is typically diagnosed following incidental discovery during routine blood work in an asymptomatic patient.1,2 It is two to three times more common in women than in men, and incidence increases with age; as such, postmenopausal women are most commonly affected.1,3 PHPT often has an insidious course, and recognition of its clinical manifestations followed by appropriate diagnostic work-up and management are necessary to prevent sequelae.3
PATIENT PRESENTATION
A 68-year-old Caucasian woman presented to her family practice office for a third visit with continued complaints of nontraumatic right lower leg pain. She had previously been diagnosed with tendonitis, which was treated conservatively. The pain failed to improve, and an x-ray was ordered. The x-ray revealed no acute findings but did show osteopenia, prompting an order for a bone mineral density (BMD) test. The BMD test demonstrated osteoporosis, which warranted further investigation. She was prescribed alendronate but refused it, against medical advice, due to concern over potential adverse effects.
Her medical history included hyperlipidemia and hypertension under fair control with lisinopril. She took a low-dose aspirin and flaxseed supplement daily. She also had a history of radiation to the neck, having undergone tonsillar irradiation as a child (a common practice from the 1930s through the 1950s).3 Surgical history included a total hysterectomy with bilateral salpingo-oophorectomy, appendectomy, and tonsillectomy. There was no personal or family history of cancer or endocrine disorders, hypercalcemia, or nephrolithiasis. She was up to date on vaccines and preventive health care measures. Allergies included penicillin and sulfa, both resulting in hives. She was a nonsmoker and did not drink alcohol or engage in illicit drug use.
Review of systems revealed right lower anterior leg pain for four months, characterized as aching, deep, sharp, and throbbing with radiation to the ankle. The pain was worse with activity and prolonged standing; ibuprofen and application of ice provided partial relief. She had experienced some mood changes, including irritability. Physical exam was normal except for dominant right-sided thyromegaly, marked bony point tenderness to the right midshin area, and an antalgic gait.
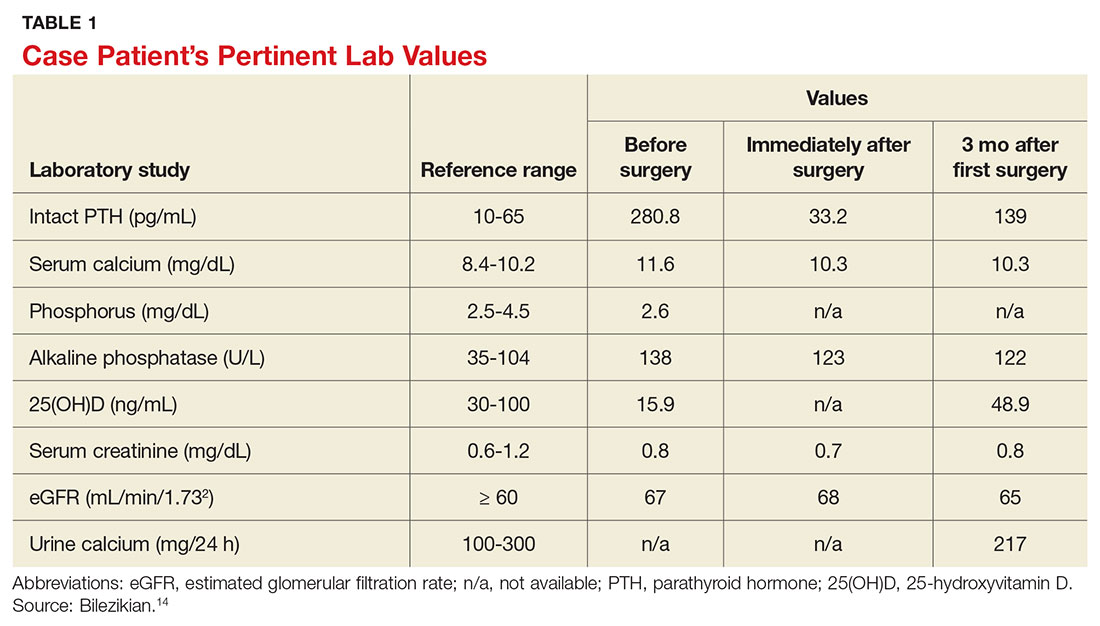
Laboratory work-up demonstrated elevated PTH, alkaline phosphatase, and calcium levels and a low 25-hydroxyvitamin D [25(OH)D] level (see Table 1). MRI of the right lower leg revealed a grade IV stress fracture (see Figure 1). The elevated serum calcium and PTH levels in addition to abnormal bone density findings led to the diagnosis of PHPT. She was referred to endocrinology and orthopedics for management of PHPT and the stress fracture, respectively, and was placed in an orthopedic walking boot for treatment of the midtibial stress fracture.
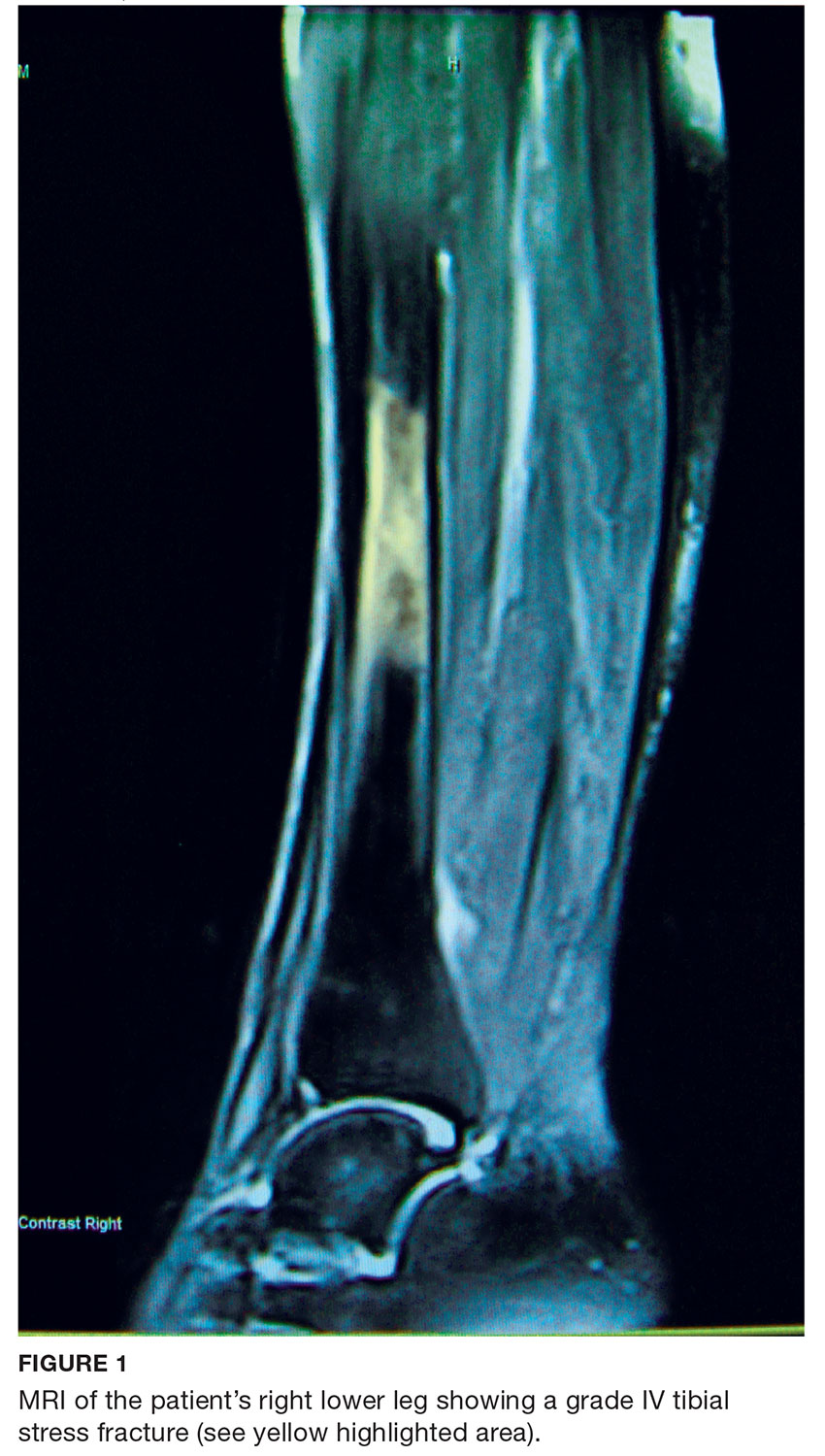
The endocrinologist referred her to an otolaryngologist trained in the surgical management of parathyroid adenomas, who ordered a thyroid ultrasound; this study was inconclusive. Additional imaging, including a Tc-99m sestamibi parathyroid scan and CT with contrast of the soft tissue of the neck, was obtained. The parathyroid scan of the neck and upper chest showed retained activity in the right inferior thyroid pole that was concerning for a parathyroid adenoma (see Figure 2). The CT identified a 1.5-cm parathyroid adenoma off the right inferior pole of the thyroid gland (concordant with the parathyroid scan). A single 300-mg parathyroid adenoma was removed from the right inferior pole of the thyroid. The surgery was deemed successful, with intraoperative normalization of the PTH level.
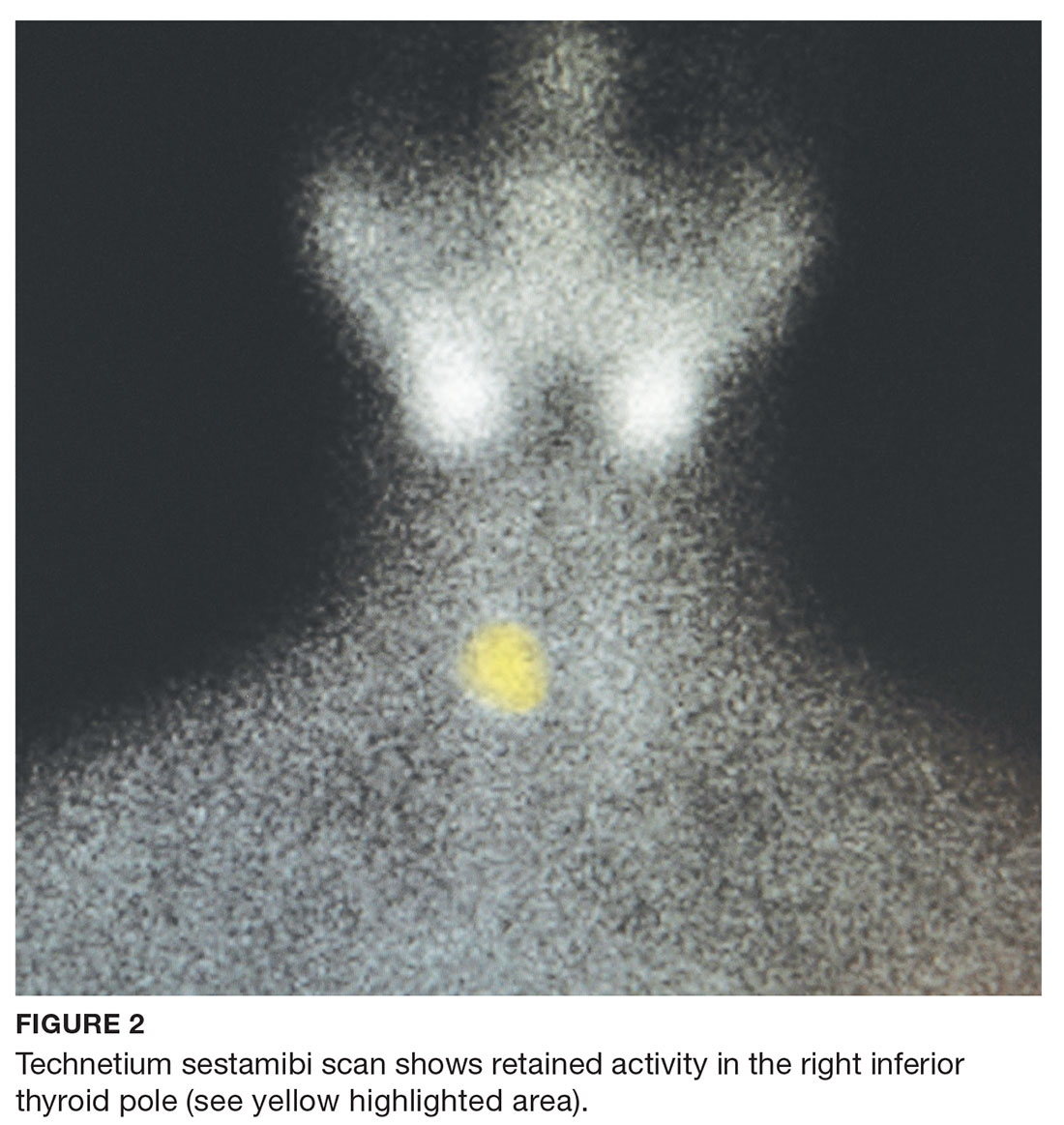
The patient was managed postoperatively by the endocrinologist and was started on calcium and vitamin D supplements. She was prescribed a bisphosphonate, as she had refused to take alendronate following her abnormal BMD test.
DIFFERENTIAL DIAGNOSIS
PHPT and malignancy are the most common causes of hypercalcemia, accounting for 90% of cases.2,4 A less common cause is familial hypocalciuric hypercalcemia (FHH), a rare benign disorder that imitates PHPT.1 FHH is ruled out by measurement of 24-hour urine calcium excretion and is characterized by hypocalciuria, defined as a urine calcium level of less than 100 mg/24 h (reference range, 100-300 mg/24 h).2 Low calcium excretion can also be identified by a calcium-creatinine excretion ratio.2 FHH is a benign autosomal dominant condition caused by a heterozygous mutation of the parathyroid glands’ calcium-sensing receptors.2,5,6 Young adults with FHH are asymptomatic, and mild hypercalcemia and a normal or slightly elevated PTH are the only laboratory findings.4
Measuring PTH levels is key in determining the underlying mechanism of hypercalcemia.2,7 If the hypercalcemia is not PTH-mediated, malignancy and granulomatous diseases such as sarcoidosis must be considered.2,7 PTH is suppressed in malignancy except for rare cases of PTH-producing tumors.4 Bone metastases cause calcium resorption, and sarcoidosis causes an excess of vitamin D, both resulting in hypercalcemia. Lymphomas and sarcoid granulomas express 1α-hydroxylase, an enzyme that increases the conversion of 25(OH)D to 1,25-dihydroxyvitamin D [1,25(OH)2D].2 When malignancy is suspected, it is appropriate to check a 1,25(OH)2D level. Thiazide diuretics, such as hydrochlorothiazide, decrease urinary calcium excretion and may result in mild hypercalcemia.2 Other possibilities in the differential include hypervitaminosis A or D, dehydration, and excess calcium ingestion, but these are less common.6,7
CALCIUM REGULATION
The parathyroid glands stem from four poles on the back of the thyroid gland; there are typically four, but the number can vary from two to 11. Secreted PTH, the primary regulator of calcium homeostasis, maintains calcium levels within a narrow physiologic range.2,8 PTH increases bone resorption, stimulating release of calcium into the blood, and signals the kidneys to increase reabsorption of calcium and excrete phosphorus. It also converts 25(OH)D to 1,25(OH)2 D, the active form of vitamin D that increases gastrointestinal calcium absorption. In a negative feedback loop, PTH secretion is regulated by serum calcium levels, stimulated when levels are low and suppressed when levels are high (see Figure 3).3 Calcium-sensing receptors, located in the chief cells of parathyroid tissue, are essential to calcium homeostasis. These receptors will either increase or decrease PTH release in response to small changes in blood ionized calcium levels. The receptors also play an independent role in the renal tubules by promoting secretion of calcium in the setting of hypercalcemia.5,9 The precise regulation of intracellular and extracellular calcium is necessary for normal functioning of physiologic processes, including bone metabolism, hormone release and regulation, neuromuscular function, and cell signaling.5

PATHOPHYSIOLOGY
Hyperparathyroidism is defined as excess secretion of PTH and is categorized as primary, secondary, or tertiary based on pathophysiologic mechanisms.
Primary hyperparathyroidism
PHPT is defined as PTH levels that are elevated or inappropriately normal in patients with hypercalcemia and no known history of kidney disease.2,6 This occurs when the normal feedback mechanism fails to inhibit excess hormone secretion by one or more of the parathyroid glands.6 With uninhibited PTH secretion, hypercalcemia will result from increased gastrointestinal absorption and bone resorption.
The most common causes of PHPT are an abnormal proliferation of parathyroid cells (parathyroid adenomas) and parathyroid tissue overgrowth (hyperplasia). PHPT may result from a single parathyroid adenoma (80%-90%), multigland hyperplasia (10%-15%), multiple adenomas (2%-3%), or malignancy (< 1%).6,10 Adenomas can occur sporadically or less commonly as part of an inherited syndrome.1 It is estimated that more than 10% of patients with PHPT have a mutation in one of 11 genes associated with PHPT.11 Approximately 5% of PHPT cases are familial, resulting from adenomas or carcinomas associated with mutations in the tumor suppressor genes MEN1 and CDC73 and the RET proto-oncogene.5 Multiple endocrine neoplasia (MEN) syndrome type 1 or 2a is associated with the development of parathyroid adenomas and other endocrine tumors.1,5 Mutations in the CDC73 gene can lead to parathyroid cancer, familial isolated hyperparathyroidism, and familial hyperparathyroidism-jaw tumor syndrome.5 Parathyroid cancer is rare and is linked to a history of radiation to the head and neck.3 Ectopic parathyroid adenomas represent 3% to 4% of all parathyroid adenomas and are often found in the mediastinum.12PHPT is the third most common endocrine disorder, with a prevalence of 1 case per 1,000 men and 2 to 3 cases per 1,000 women.5 Most women with PHPT are postmenopausal and older than 50.1 The condition can occur in younger adults but is rare in childhood and adolescence, with an incidence of 2 to 5 cases per 100,000.13
PHPT affects multiple organ systems, but the most commonly involved are the renal and musculoskeletal systems (see Table 2). The hypersecretory state causes excessive bone resorption and increased osteoclastic activity, resulting in osteoporosis and increased risk for pathologic fractures of the hip, wrist, and spine. The most common osteoporotic fractures are vertebral compression fractures.14 Fractures involving the thoracic spine contribute to the development of kyphosis.15
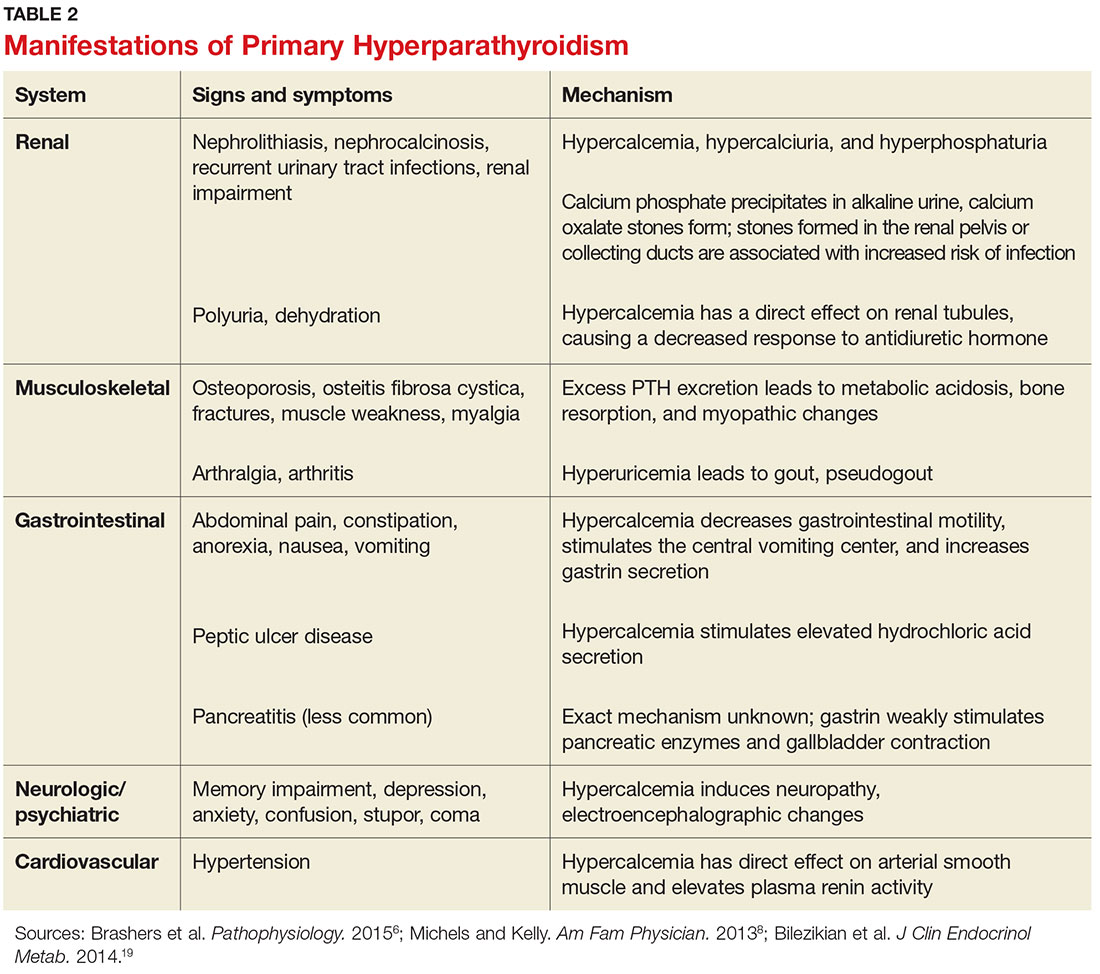
In the kidney, an increased filtered load of calcium leads to hypercalciuria, precipitation of calcium phosphate in the renal pelvis and collecting ducts, metabolic acidosis, alkaline urine, and hyperphosphaturia. The combination of alkaline urine, hyperphosphaturia, and hypercalciuria leads to the formation of kidney stones.6 Nephrolithiasis and alkaline urine predispose patients to recurrent urinary tract infections and subsequent renal impairment.6 In addition, hypercalcemia impairs the renal collecting system and decreases its response to antidiuretic hormone, resulting in polyuria.6
Secondary hyperparathyroidism
In secondary hyperparathyroidism, calcium levels are either normal or low. Normocalcemic hyperparathyroidism is characterized by normal ionized and total calcium levels and elevated PTH levels; it has no known cause.6 Secondary hyperparathyroidism occurs when excess PTH is excreted as a result of a chronic condition that leads to hypocalcemia. Examples of these disease states include vitamin D deficiency, chronic kidney disease (CKD), and intestinal malabsorption. The most common cause of secondary hyperparathyroidism is CKD; glomerular filtration insufficiency results in hyperphosphatemia, hypocalcemia, and low 1,25(OH)2D, stimulating the release of PTH. Other causes include deficient intake or decreased absorption of calcium or vitamin D; chronic use of medications such as lithium, phenobarbital, or phenytoin; bariatric surgery; celiac disease; and pancreatic disease.4,6,14 Lithium decreases urinary calcium excretion and reduces the sensitivity of the parathyroid gland to calcium.4
Tertiary hyperparathyroidism
Tertiary hyperparathyroidism, marked by hypercalcemia and excessive PTH secretion, can occur after prolonged secondary hyperparathyroidism. In this disorder, persistent parathyroid stimulation leads to gland hyperplasia, resulting in autonomous production of PTH despite correction of calcium levels.6 It most commonly occurs in patients with chronic secondary hyperparathyroidism with renal failure who receive a kidney transplant.2,6 In some cases, parathyroid hyperplasia may not regress after transplantation and parathyroidectomy may be necessary.
EVALUATION AND DIAGNOSTIC WORK-UP
Laboratory tests
Hypercalcemia is the most common initial finding that leads to the diagnosis of PHPT. Elevated serum calcium and PTH is characteristic of the condition. When evaluating a patient with hypercalcemia, the diagnostic work-up includes tests to differentiate between PTH- and non–PTH-mediated causes of elevated calcium (see Table 3).7 Evaluation should begin with measurement of PTH by second- or third-generation immunoassay along with phosphorus, alkaline phosphatase, 25(OH)D, creatinine, estimated glomerular filtration rate (eGFR), and albumin. Additionally, a 24-hour urine collection for calcium, creatinine, and creatinine clearance should be considered in patients with overt nephrolithiasis or nephrocalcinosis. If the urine calcium is > 400 mg/24 h, a renal stone risk profile is indicated because nephrolithiasis is one of the most common complications of PHPT.14 There is a high prevalence of nephrolithiasis in patients with normocalcemic PHPT, even after parathyroidectomy.16 If the 24-hour urine calcium level is low, the diagnosis of FHH is considered. If the urine calcium is high and the intact PTH is elevated or inappropriately normal, the diagnosis of PHPT is considered; urine calcium will be normal in 60% of PHPT cases.4,11
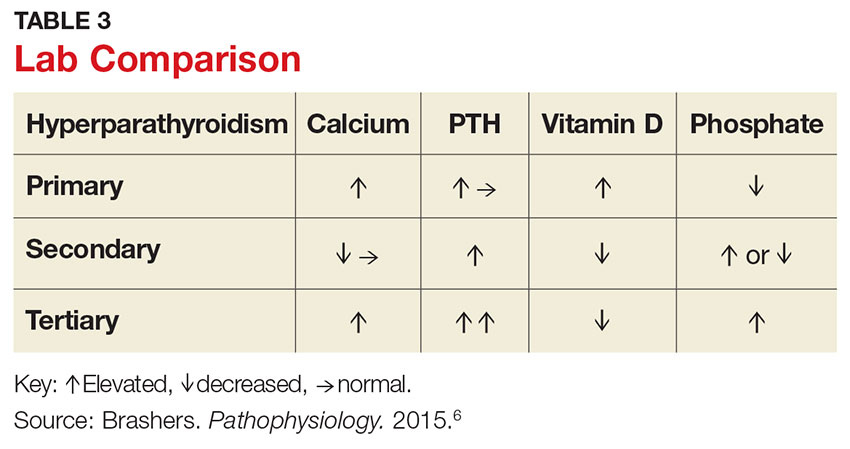
Imaging studies
Imaging is useful for localization of adenomas and abnormal parathyroid tissue to guide surgical planning but is not necessary for diagnosis or medical management. Understanding the strengths and weaknesses of imaging modalities enables the clinician to order the most appropriate option. There are three primary imaging modalities used to locate parathyroid adenoma(s) or aberrant parathyroid tissue: ultrasound, nuclear medicine sestamibi parathyroid scans, and CT. Some clinicians start with an ultrasound, but its operator-dependent results can vary widely; in addition, ultrasound often provides poor anatomic definition and has limited value in locating ectopic parathyroid tissue.17
Nuclear medicine parathyroid scan with technetium-99m sestamibi is a sensitive method for localizing hyperfunctioning, enlarged parathyroid glands or tissue in normal anatomic positions or ectopic locations. Uptake is enhanced and prolonged in parathyroid adenomas as well as in aberrant tissue found in the mediastinum or subclavicular areas. Sestamibi parathyroid scan detects up to 89% of single adenomas, but studies of this imaging modality have demonstrated a wide range of sensitivities (44%-95%).5,17 A drawback of nuclear medicine studies is that they provide little anatomic detail.17 Nonetheless, the ability of the parathyroid scan to locate parathyroid glands has contributed to the success of the minimally invasive parathyroidectomy, and it is considered the most successful imaging modality available.5,10 Identifying the precise location of the parathyroid adenoma is essential for a successful surgical outcome; this is best achieved by combining the sestamibi parathyroid scan with CT.12
Emerging imaging modalities are the multidetector CT (MDCT) and 4D-CT techniques. In an evaluation of the diagnostic accuracy of contrast-enhanced MDCT in the detection of parathyroid adenomas and aberrant parathyroid tissue, MDCT demonstrated the ability to differentiate between adenomas and hyperplasia and display important anatomic structures such as nerves and blood vessels.17 The specificity of MDCT for ruling out abnormal parathyroid tissue was 75%, and the sensitivity for detecting a single adenoma was 80%. Overall, MDCT demonstrated an 88% positive predictive value (PPV) in localizing hyperfunctioning parathyroid glands but showed poor sensitivity in detecting multigland disease.17 The PPV is a key value in determining the ability of an imaging study to precisely locate aberrant parathyroid tissue. MDCT provides detailed definition of anatomy, locating ectopic parathyroid glands in the deeper paraesophageal areas and mediastinum while defining relationships between the tissue and its surrounding vasculature, lymph nodes, and thyroid tissue.17 The 4D-CT technique employs three-dimensional technology and accounts for the movement of the patient’s body over time (the “fourth dimension”). It is an accurate method for identifying parathyroid adenomas but exposes the patient to higher radiation doses.18 The sensitivity of 4D-CT in localizing abnormal parathyroid tissue is comparable to that of MDCT.16,18,19
Additional studies used during the management of the patient with PHPT are BMD testing and renal imaging. Secondary causes of bone loss are responsible for up to 30% of osteoporosis cases in postmenopausal women; one of these causes is PHPT.20 Elevated PTH causes increased bone turnover and results in decreased bone mass with subsequent increased fracture risk.9 Bone density should be measured by dual-energy x-ray absorptiometry (DEXA), and the skeletal survey should include the distal one-third of the radius, hip, and lumbar spine. The distal radius is rich in cortical bone and BMD is often lowest at this site in patients with PHPT, making it the most sensitive DEXA marker for early detection of bone loss.19,21 The hip contains an equal mix of cortical and trabecular bone and is the second most sensitive site for detecting bone loss in PHPT. The spine contains a high proportion of trabecular bone and is the least sensitive site.19,21 Renal imaging studies, including x-ray, ultrasound, and, less frequently, CT of the abdomen and pelvis, are used to assess for nephrolithiasis and nephrocalcinosis.19
TREATMENT/MANAGEMENT
Conservative medical management
PHPT is a complex disease process, and careful evaluation is required when determining whether medical versus surgical management is appropriate. Clinical presentation ranges from no symptoms to multisystem disease. Conservative medical management, which includes regular monitoring, is an acceptable strategy in an asymptomatic patient with a low fracture risk and no nephrolithiasis.1 Conservative care includes maintaining normal dietary calcium intake and adequate hydration, regular exercise, vitamin D supplementation, annual laboratory studies, BMD testing, and the avoidance of thiazide diuretics and lithium.1 Guidelines, from the Fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism, for monitoring asymptomatic PHPT patients recommend
- Annual measurement of serum calcium
- BMD measurement by DEXA every 1 to 2 years
- Annual assessment of eGFR and serum creatinine
- Renal imaging or a 24-h urine stone profile if nephrolithiasis is suspected.19
Long-term medical management of PHPT is difficult because no agents are available to suppress hypercalcemia or completely block PTH release.12
Maintaining serum 25(OH)D at a level > 20 ng/mL significantly reduces PTH secretion, in comparison to levels < 20 ng/mL, and does not aggravate hypercalcemia.22 The Endocrine Society recommends a minimum serum 25(OH)D level of 20 ng/mL and notes that targeting a higher threshold value of 30 ng/mL is reasonable.19 The daily requirement for vitamin D3, 800 IU to 1,000 IU, is a good starting point for supplementation.4 Measurement of 1,25(OH)2D levels lacks value and is not recommended for patients with PHPT. Calcium intake should follow established guidelines and is not limited in PHPT.19
Surgical management
Surgical management is indicated for symptomatic patients.23 Indications include nephrolithiasis, nephrocalcinosis, osteitis fibrosa cystica, or osteoporosis. Surgery is considered appropriate for individuals who do not meet these criteria if there are no medical contraindications.14 The Fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism revised the indications for surgery in 2014 to include asymptomatic patients, since surgery is the only definitive treatment for PHPT. Current guidelines for when to recommend surgery in the asymptomatic patient with PHPT are listed in Table 4.19
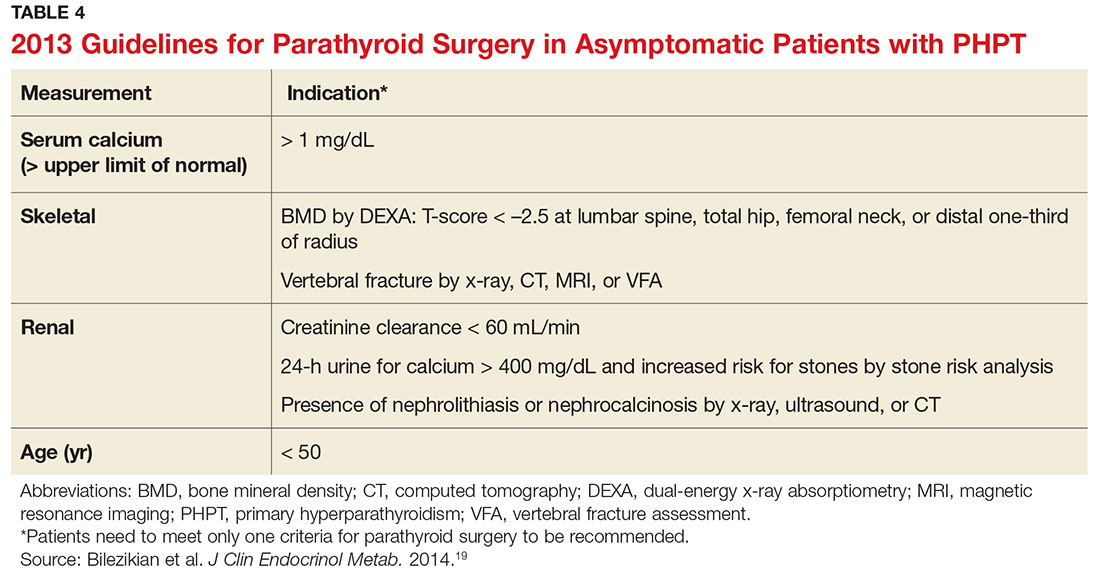
Preoperative localization and referral to an experienced surgeon is of utmost importance for a good outcome. An expert surgeon will usually perform a minimally invasive parathyroidectomy (MIP) and obtain intraoperative PTH levels; in some cases, a full neck exploration is necessary. PTH has a half-life of less than five minutes and is an accurate tool for determining whether the culprit gland has been successfully removed.5
Modern imaging studies, less invasive surgical techniques, and intraoperative measurements of PTH have decreased the need to conduct full neck exploration. MIP offers a smaller incision, less tissue dissection, and lower morbidity, and can be offered without the risks associated with general anesthesia.10 The goal of surgery is to restore normocalcemia and, in turn, prevent bone mineral loss and systemic effects of hypercalcemia over the long term.10 Surgical management for an ectopic parathyroid adenoma is controversial because these are often found in the mediastinum, requiring invasive surgery.12
Surgery is curative in up to 95% of cases and has a low rate of complications.2,24 A joint decision regarding treatment options is made among the patient, primary care clinician, and surgeon. Complications include vocal cord paralysis resulting from injury to the recurrent laryngeal nerve, bleeding or hematoma, laryngospasm, symptomatic hypocalcemia, and persistent hyperparathyroidism; seizures are very rare but can occur from transient hypocalcemia and hypomagnesemia.5 PTH levels drop by more than 50% intraoperatively if the procedure is successful; otherwise, exploration for another adenoma is indicated.10 Postoperative calcium and vitamin D supplementation are warranted once lab values are stable.
When surgery is contraindicated/refused
If surgery is indicated but the patient is a poor candidate or refuses surgery, management of hypercalcemia and bone loss with pharmacologic agents is warranted. The calcimimetic cinacalcet is a reasonable medical alternative that has been shown to adequately control hypercalcemia and hypophosphatemia and has proven effective in various patient subgroups.25 This agent is useful in the treatment of patients who are asymptomatic and refuse surgery, patients with refractory PHPT after parathyroidectomy, and patients with contraindications to surgery.24,25 The medication reduces calcium and modestly reduces PTH levels by binding parathyroid calcium-sensing receptors but does not improve bone density.2,12 Cinacalcet is approved by the FDA for use in patients with moderate to severe disease when surgery is contraindicated.24
Treatment options for osteoporosis, vertebral fractures, and progressive bone loss in the patient with PHPT include bisphosphonates. Raloxifene and estrogen replacements may be used in postmenopausal women. Oral bisphosphonates (alendronate or risedronate) are firstline therapies and have been shown to inhibit progression to osteoporosis in PHPT.9,26 They prevent osteoclastic activity, reducing bone resorption and turnover. Contraindications to oral bisphosphonates include esophageal disorders, gastrointestinal intolerance, or inability to follow the dosing requirements. Intravenous zoledronic acid provides an alternative route of administration.
Alendronate has the best evidence for improving bone density and preventing progression to osteoporosis in patients with PHPT, but the medication does not affect calcium or PTH levels.1,19 There is limited data on the effects of combining bisphosphonates with calcimimetics. Raloxifene is a selective estrogen receptor modulator that decreases bone resorption; it is approved for treating osteoporosis and may be used when a patient is not a good candidate for a bisphosphonate.20 Denosumab, currently under study for the treatment of PHPT, is a human monoclonal antibody that improves bone density but does not affect serum calcium.20 Nonpharmacologic therapies include alcohol moderation, decreased caffeine intake, weight-bearing exercise, smoking cessation, adequate hydration, and dietary modifications.20
OUTCOME FOR THE CASE PATIENT
Although PHPT is often discovered incidentally in routine blood work with hypercalcemia, the case patient had developed osteoporosis and a grade IV tibial stress fracture before the diagnosis was made. Following parathyroidectomy, her hypertension worsened, requiring an additional antihypertensive medication. She developed recurrent disease and was referred to a tertiary care center for revision parathyroidectomy due to persistent elevated calcium levels. A 24-hour urine calcium test ruled out concurrent FHH. A full neck exploration was conducted and a 340-mg hypercellular parathyroid gland was removed from the left superior pole. She will be monitored for recurrent disease and will remain on a vitamin D3 supplement and treatment for osteoporosis.
CONCLUSION
Primary care clinicians should have a low threshold for initiating the work-up of mild hypercalcemia in an effort to prevent sequelae. Patient education is essential throughout the process. Understanding the condition and treatment options is necessary for a patient’s active participation in clinical decision making. Conservative management of an asymptomatic patient includes avoiding thiazide diuretics and lithium, staying well hydrated with water, maintaining moderate dietary calcium (1,000-1,200 mg/d) and vitamin D (400-600 IU/d) intake, regular exercise, and appropriate lab and bone density monitoring. Surgical treatment is recommended for symptomatic patients exhibiting decreased bone density, fractures, renal impairment, or nephrolithiasis. Treating bone loss with bisphosphonates and hypercalcemia with calcimimetics is useful. Postmenopausal women may benefit from estrogen therapy or selective estrogen receptor modulators. These agents improve bone density and lower calcium, but are often contraindicated or have adverse effects. Surgery is the only cure.3
CE/CME No: CR-1705
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Differentiate primary hyperparathyroidism (PHPT) from other causes of hypercalcemia and types of hyerparathyroidism.
• Understand the calcium-parathyroid hormone feedback loop.
• Identify appropriate imaging studies and common laboratory findings in the patient with PHPT.
• Describe the common systemic manifestations of PHPT.
• Discuss medical versus surgical management of the patient with PHPT.
FACULTY
Barbara Austin is a Family Nurse Practitioner at Baptist Primary Care, Jacksonville, Florida, and is pursuing a Doctorate of Nursing Practice (DNP) at Jacksonville University.
The author has no financial relationships to disclose.

ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid for one year from the issue date of May 2017.
Article begins on next page >>
Primary hyperparathyroidism (PHPT) is most often detected as hypercalcemia in an asymptomatic patient during routine blood work. Knowing the appropriate work-up of hypercalcemia is essential, since untreated PHPT can have significant complications affecting multiple organ systems—most notably, renal and musculoskeletal. Parathyroidectomy is curative in up to 95% of cases, but prevention of long-term complications relies on prompt recognition and appropriate follow-up.
Primary hyperparathyroidism (PHPT) is a common endocrine disorder, with a prevalence of approximately 1 to 3 cases per 1,000 persons.1 PHPT results from inappropriate overproduction of parathyroid hormone (PTH), the primary regulator of calcium homeostasis, and is characterized by hypercalcemia in the setting of an elevated or high-normal PTH level. In most cases of PHPT, unregulated PTH production is caused by a single parathyroid adenoma.
PHPT is the most common cause of hypercalcemia in outpatients and is typically diagnosed following incidental discovery during routine blood work in an asymptomatic patient.1,2 It is two to three times more common in women than in men, and incidence increases with age; as such, postmenopausal women are most commonly affected.1,3 PHPT often has an insidious course, and recognition of its clinical manifestations followed by appropriate diagnostic work-up and management are necessary to prevent sequelae.3
PATIENT PRESENTATION
A 68-year-old Caucasian woman presented to her family practice office for a third visit with continued complaints of nontraumatic right lower leg pain. She had previously been diagnosed with tendonitis, which was treated conservatively. The pain failed to improve, and an x-ray was ordered. The x-ray revealed no acute findings but did show osteopenia, prompting an order for a bone mineral density (BMD) test. The BMD test demonstrated osteoporosis, which warranted further investigation. She was prescribed alendronate but refused it, against medical advice, due to concern over potential adverse effects.
Her medical history included hyperlipidemia and hypertension under fair control with lisinopril. She took a low-dose aspirin and flaxseed supplement daily. She also had a history of radiation to the neck, having undergone tonsillar irradiation as a child (a common practice from the 1930s through the 1950s).3 Surgical history included a total hysterectomy with bilateral salpingo-oophorectomy, appendectomy, and tonsillectomy. There was no personal or family history of cancer or endocrine disorders, hypercalcemia, or nephrolithiasis. She was up to date on vaccines and preventive health care measures. Allergies included penicillin and sulfa, both resulting in hives. She was a nonsmoker and did not drink alcohol or engage in illicit drug use.
Review of systems revealed right lower anterior leg pain for four months, characterized as aching, deep, sharp, and throbbing with radiation to the ankle. The pain was worse with activity and prolonged standing; ibuprofen and application of ice provided partial relief. She had experienced some mood changes, including irritability. Physical exam was normal except for dominant right-sided thyromegaly, marked bony point tenderness to the right midshin area, and an antalgic gait.
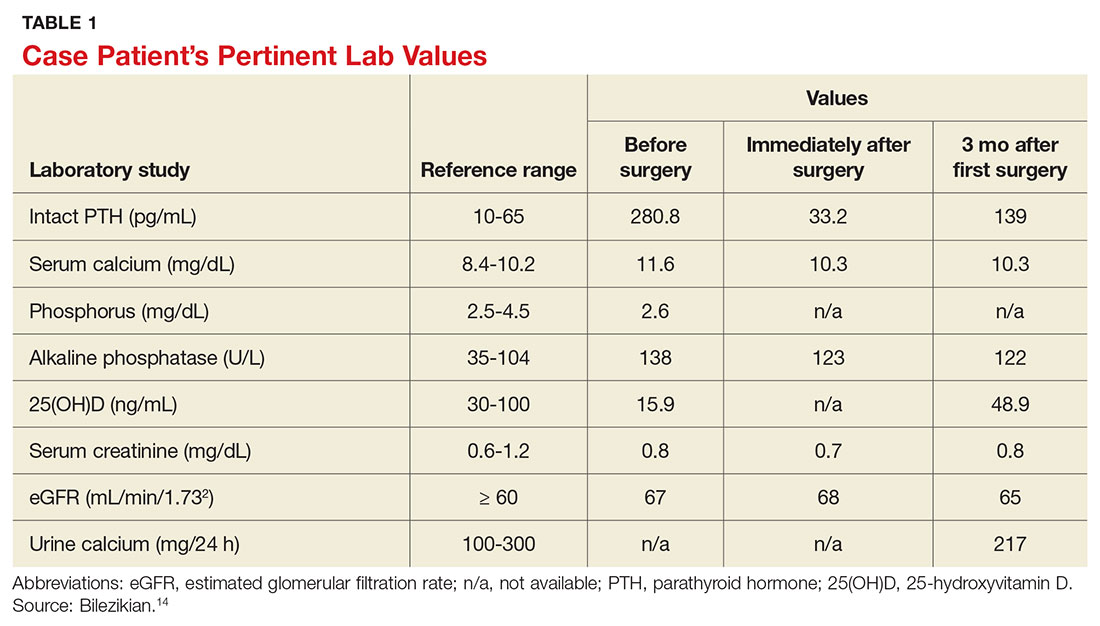
Laboratory work-up demonstrated elevated PTH, alkaline phosphatase, and calcium levels and a low 25-hydroxyvitamin D [25(OH)D] level (see Table 1). MRI of the right lower leg revealed a grade IV stress fracture (see Figure 1). The elevated serum calcium and PTH levels in addition to abnormal bone density findings led to the diagnosis of PHPT. She was referred to endocrinology and orthopedics for management of PHPT and the stress fracture, respectively, and was placed in an orthopedic walking boot for treatment of the midtibial stress fracture.
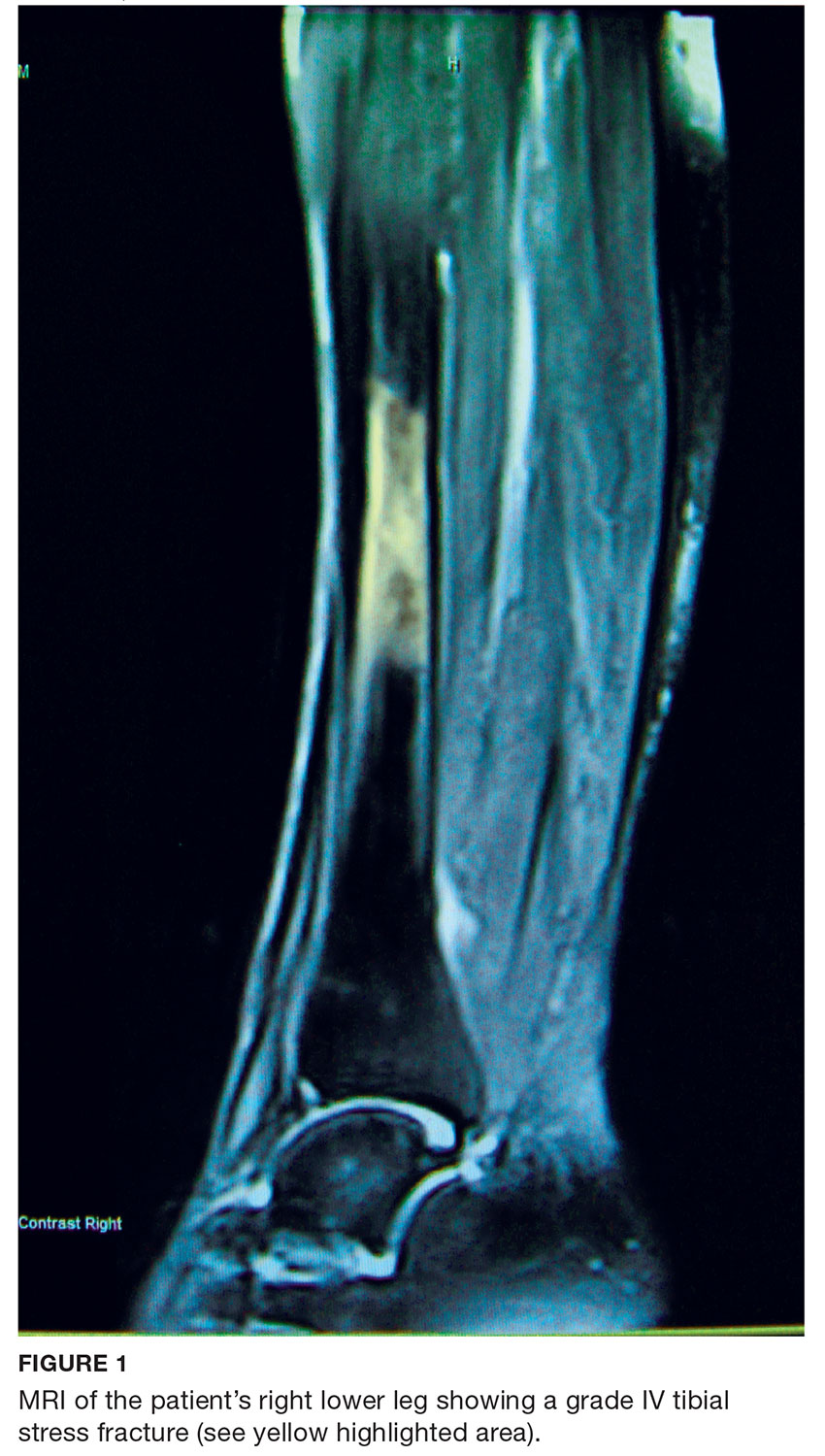
The endocrinologist referred her to an otolaryngologist trained in the surgical management of parathyroid adenomas, who ordered a thyroid ultrasound; this study was inconclusive. Additional imaging, including a Tc-99m sestamibi parathyroid scan and CT with contrast of the soft tissue of the neck, was obtained. The parathyroid scan of the neck and upper chest showed retained activity in the right inferior thyroid pole that was concerning for a parathyroid adenoma (see Figure 2). The CT identified a 1.5-cm parathyroid adenoma off the right inferior pole of the thyroid gland (concordant with the parathyroid scan). A single 300-mg parathyroid adenoma was removed from the right inferior pole of the thyroid. The surgery was deemed successful, with intraoperative normalization of the PTH level.
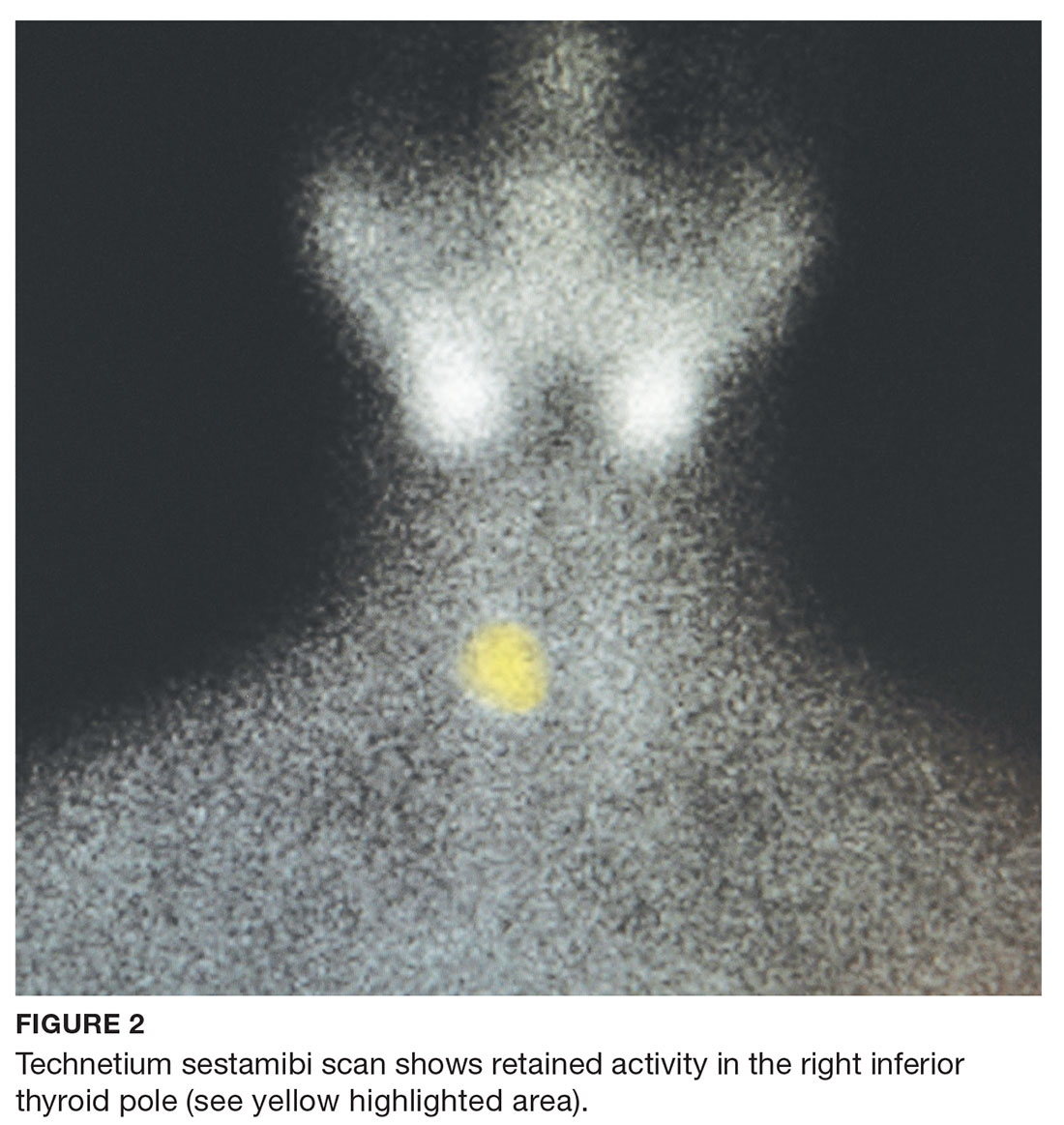
The patient was managed postoperatively by the endocrinologist and was started on calcium and vitamin D supplements. She was prescribed a bisphosphonate, as she had refused to take alendronate following her abnormal BMD test.
DIFFERENTIAL DIAGNOSIS
PHPT and malignancy are the most common causes of hypercalcemia, accounting for 90% of cases.2,4 A less common cause is familial hypocalciuric hypercalcemia (FHH), a rare benign disorder that imitates PHPT.1 FHH is ruled out by measurement of 24-hour urine calcium excretion and is characterized by hypocalciuria, defined as a urine calcium level of less than 100 mg/24 h (reference range, 100-300 mg/24 h).2 Low calcium excretion can also be identified by a calcium-creatinine excretion ratio.2 FHH is a benign autosomal dominant condition caused by a heterozygous mutation of the parathyroid glands’ calcium-sensing receptors.2,5,6 Young adults with FHH are asymptomatic, and mild hypercalcemia and a normal or slightly elevated PTH are the only laboratory findings.4
Measuring PTH levels is key in determining the underlying mechanism of hypercalcemia.2,7 If the hypercalcemia is not PTH-mediated, malignancy and granulomatous diseases such as sarcoidosis must be considered.2,7 PTH is suppressed in malignancy except for rare cases of PTH-producing tumors.4 Bone metastases cause calcium resorption, and sarcoidosis causes an excess of vitamin D, both resulting in hypercalcemia. Lymphomas and sarcoid granulomas express 1α-hydroxylase, an enzyme that increases the conversion of 25(OH)D to 1,25-dihydroxyvitamin D [1,25(OH)2D].2 When malignancy is suspected, it is appropriate to check a 1,25(OH)2D level. Thiazide diuretics, such as hydrochlorothiazide, decrease urinary calcium excretion and may result in mild hypercalcemia.2 Other possibilities in the differential include hypervitaminosis A or D, dehydration, and excess calcium ingestion, but these are less common.6,7
CALCIUM REGULATION
The parathyroid glands stem from four poles on the back of the thyroid gland; there are typically four, but the number can vary from two to 11. Secreted PTH, the primary regulator of calcium homeostasis, maintains calcium levels within a narrow physiologic range.2,8 PTH increases bone resorption, stimulating release of calcium into the blood, and signals the kidneys to increase reabsorption of calcium and excrete phosphorus. It also converts 25(OH)D to 1,25(OH)2 D, the active form of vitamin D that increases gastrointestinal calcium absorption. In a negative feedback loop, PTH secretion is regulated by serum calcium levels, stimulated when levels are low and suppressed when levels are high (see Figure 3).3 Calcium-sensing receptors, located in the chief cells of parathyroid tissue, are essential to calcium homeostasis. These receptors will either increase or decrease PTH release in response to small changes in blood ionized calcium levels. The receptors also play an independent role in the renal tubules by promoting secretion of calcium in the setting of hypercalcemia.5,9 The precise regulation of intracellular and extracellular calcium is necessary for normal functioning of physiologic processes, including bone metabolism, hormone release and regulation, neuromuscular function, and cell signaling.5

PATHOPHYSIOLOGY
Hyperparathyroidism is defined as excess secretion of PTH and is categorized as primary, secondary, or tertiary based on pathophysiologic mechanisms.
Primary hyperparathyroidism
PHPT is defined as PTH levels that are elevated or inappropriately normal in patients with hypercalcemia and no known history of kidney disease.2,6 This occurs when the normal feedback mechanism fails to inhibit excess hormone secretion by one or more of the parathyroid glands.6 With uninhibited PTH secretion, hypercalcemia will result from increased gastrointestinal absorption and bone resorption.
The most common causes of PHPT are an abnormal proliferation of parathyroid cells (parathyroid adenomas) and parathyroid tissue overgrowth (hyperplasia). PHPT may result from a single parathyroid adenoma (80%-90%), multigland hyperplasia (10%-15%), multiple adenomas (2%-3%), or malignancy (< 1%).6,10 Adenomas can occur sporadically or less commonly as part of an inherited syndrome.1 It is estimated that more than 10% of patients with PHPT have a mutation in one of 11 genes associated with PHPT.11 Approximately 5% of PHPT cases are familial, resulting from adenomas or carcinomas associated with mutations in the tumor suppressor genes MEN1 and CDC73 and the RET proto-oncogene.5 Multiple endocrine neoplasia (MEN) syndrome type 1 or 2a is associated with the development of parathyroid adenomas and other endocrine tumors.1,5 Mutations in the CDC73 gene can lead to parathyroid cancer, familial isolated hyperparathyroidism, and familial hyperparathyroidism-jaw tumor syndrome.5 Parathyroid cancer is rare and is linked to a history of radiation to the head and neck.3 Ectopic parathyroid adenomas represent 3% to 4% of all parathyroid adenomas and are often found in the mediastinum.12PHPT is the third most common endocrine disorder, with a prevalence of 1 case per 1,000 men and 2 to 3 cases per 1,000 women.5 Most women with PHPT are postmenopausal and older than 50.1 The condition can occur in younger adults but is rare in childhood and adolescence, with an incidence of 2 to 5 cases per 100,000.13
PHPT affects multiple organ systems, but the most commonly involved are the renal and musculoskeletal systems (see Table 2). The hypersecretory state causes excessive bone resorption and increased osteoclastic activity, resulting in osteoporosis and increased risk for pathologic fractures of the hip, wrist, and spine. The most common osteoporotic fractures are vertebral compression fractures.14 Fractures involving the thoracic spine contribute to the development of kyphosis.15
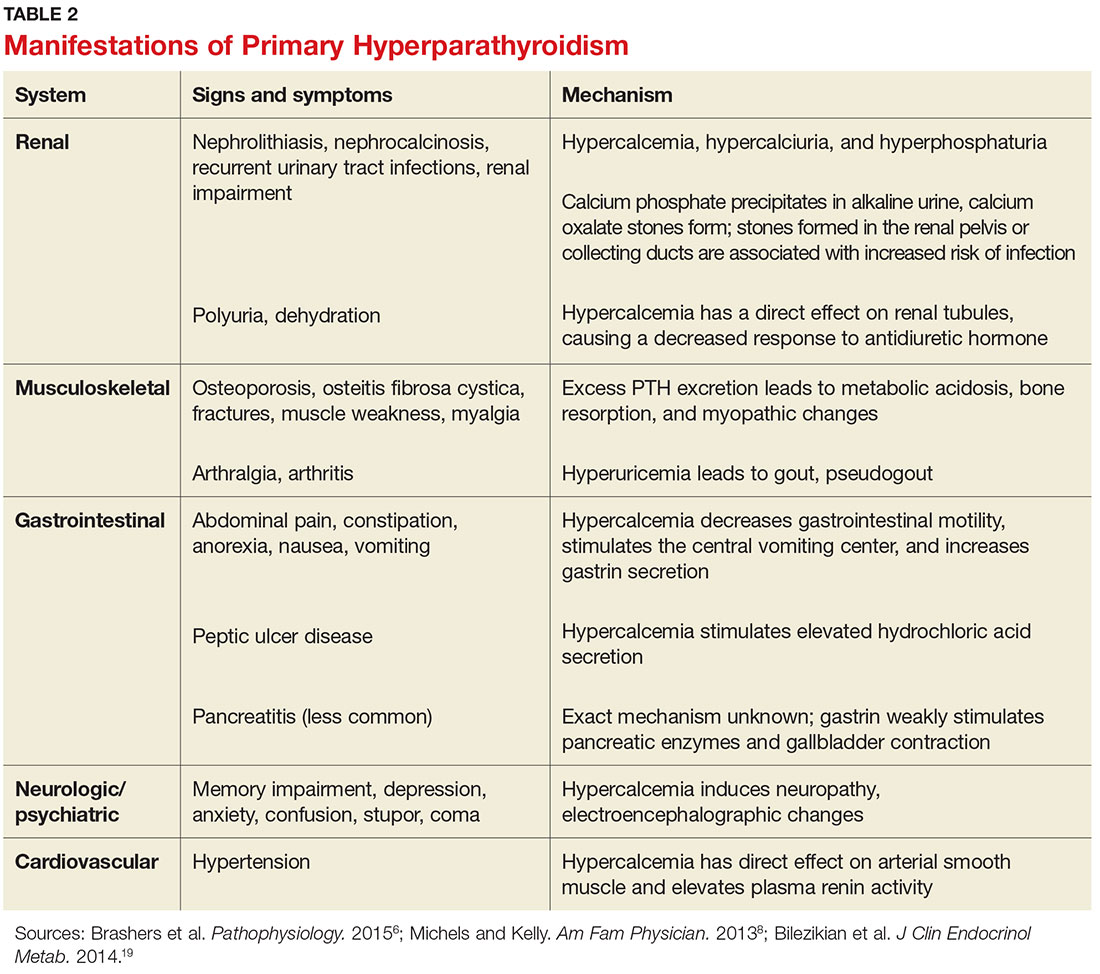
In the kidney, an increased filtered load of calcium leads to hypercalciuria, precipitation of calcium phosphate in the renal pelvis and collecting ducts, metabolic acidosis, alkaline urine, and hyperphosphaturia. The combination of alkaline urine, hyperphosphaturia, and hypercalciuria leads to the formation of kidney stones.6 Nephrolithiasis and alkaline urine predispose patients to recurrent urinary tract infections and subsequent renal impairment.6 In addition, hypercalcemia impairs the renal collecting system and decreases its response to antidiuretic hormone, resulting in polyuria.6
Secondary hyperparathyroidism
In secondary hyperparathyroidism, calcium levels are either normal or low. Normocalcemic hyperparathyroidism is characterized by normal ionized and total calcium levels and elevated PTH levels; it has no known cause.6 Secondary hyperparathyroidism occurs when excess PTH is excreted as a result of a chronic condition that leads to hypocalcemia. Examples of these disease states include vitamin D deficiency, chronic kidney disease (CKD), and intestinal malabsorption. The most common cause of secondary hyperparathyroidism is CKD; glomerular filtration insufficiency results in hyperphosphatemia, hypocalcemia, and low 1,25(OH)2D, stimulating the release of PTH. Other causes include deficient intake or decreased absorption of calcium or vitamin D; chronic use of medications such as lithium, phenobarbital, or phenytoin; bariatric surgery; celiac disease; and pancreatic disease.4,6,14 Lithium decreases urinary calcium excretion and reduces the sensitivity of the parathyroid gland to calcium.4
Tertiary hyperparathyroidism
Tertiary hyperparathyroidism, marked by hypercalcemia and excessive PTH secretion, can occur after prolonged secondary hyperparathyroidism. In this disorder, persistent parathyroid stimulation leads to gland hyperplasia, resulting in autonomous production of PTH despite correction of calcium levels.6 It most commonly occurs in patients with chronic secondary hyperparathyroidism with renal failure who receive a kidney transplant.2,6 In some cases, parathyroid hyperplasia may not regress after transplantation and parathyroidectomy may be necessary.
EVALUATION AND DIAGNOSTIC WORK-UP
Laboratory tests
Hypercalcemia is the most common initial finding that leads to the diagnosis of PHPT. Elevated serum calcium and PTH is characteristic of the condition. When evaluating a patient with hypercalcemia, the diagnostic work-up includes tests to differentiate between PTH- and non–PTH-mediated causes of elevated calcium (see Table 3).7 Evaluation should begin with measurement of PTH by second- or third-generation immunoassay along with phosphorus, alkaline phosphatase, 25(OH)D, creatinine, estimated glomerular filtration rate (eGFR), and albumin. Additionally, a 24-hour urine collection for calcium, creatinine, and creatinine clearance should be considered in patients with overt nephrolithiasis or nephrocalcinosis. If the urine calcium is > 400 mg/24 h, a renal stone risk profile is indicated because nephrolithiasis is one of the most common complications of PHPT.14 There is a high prevalence of nephrolithiasis in patients with normocalcemic PHPT, even after parathyroidectomy.16 If the 24-hour urine calcium level is low, the diagnosis of FHH is considered. If the urine calcium is high and the intact PTH is elevated or inappropriately normal, the diagnosis of PHPT is considered; urine calcium will be normal in 60% of PHPT cases.4,11
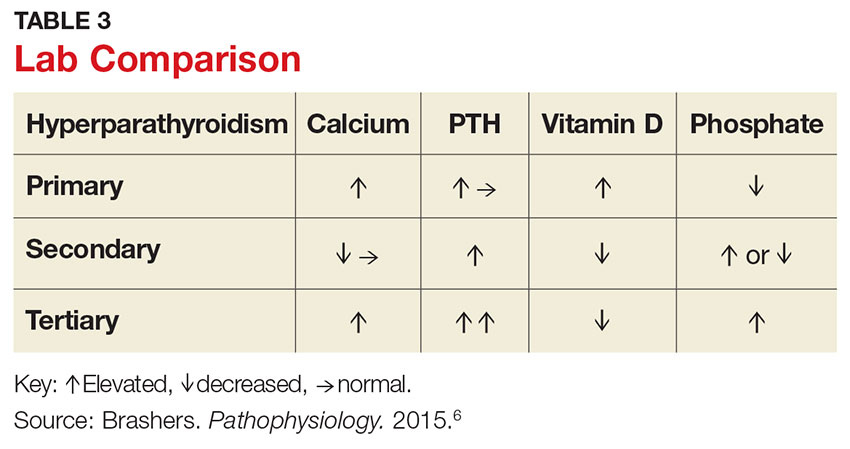
Imaging studies
Imaging is useful for localization of adenomas and abnormal parathyroid tissue to guide surgical planning but is not necessary for diagnosis or medical management. Understanding the strengths and weaknesses of imaging modalities enables the clinician to order the most appropriate option. There are three primary imaging modalities used to locate parathyroid adenoma(s) or aberrant parathyroid tissue: ultrasound, nuclear medicine sestamibi parathyroid scans, and CT. Some clinicians start with an ultrasound, but its operator-dependent results can vary widely; in addition, ultrasound often provides poor anatomic definition and has limited value in locating ectopic parathyroid tissue.17
Nuclear medicine parathyroid scan with technetium-99m sestamibi is a sensitive method for localizing hyperfunctioning, enlarged parathyroid glands or tissue in normal anatomic positions or ectopic locations. Uptake is enhanced and prolonged in parathyroid adenomas as well as in aberrant tissue found in the mediastinum or subclavicular areas. Sestamibi parathyroid scan detects up to 89% of single adenomas, but studies of this imaging modality have demonstrated a wide range of sensitivities (44%-95%).5,17 A drawback of nuclear medicine studies is that they provide little anatomic detail.17 Nonetheless, the ability of the parathyroid scan to locate parathyroid glands has contributed to the success of the minimally invasive parathyroidectomy, and it is considered the most successful imaging modality available.5,10 Identifying the precise location of the parathyroid adenoma is essential for a successful surgical outcome; this is best achieved by combining the sestamibi parathyroid scan with CT.12
Emerging imaging modalities are the multidetector CT (MDCT) and 4D-CT techniques. In an evaluation of the diagnostic accuracy of contrast-enhanced MDCT in the detection of parathyroid adenomas and aberrant parathyroid tissue, MDCT demonstrated the ability to differentiate between adenomas and hyperplasia and display important anatomic structures such as nerves and blood vessels.17 The specificity of MDCT for ruling out abnormal parathyroid tissue was 75%, and the sensitivity for detecting a single adenoma was 80%. Overall, MDCT demonstrated an 88% positive predictive value (PPV) in localizing hyperfunctioning parathyroid glands but showed poor sensitivity in detecting multigland disease.17 The PPV is a key value in determining the ability of an imaging study to precisely locate aberrant parathyroid tissue. MDCT provides detailed definition of anatomy, locating ectopic parathyroid glands in the deeper paraesophageal areas and mediastinum while defining relationships between the tissue and its surrounding vasculature, lymph nodes, and thyroid tissue.17 The 4D-CT technique employs three-dimensional technology and accounts for the movement of the patient’s body over time (the “fourth dimension”). It is an accurate method for identifying parathyroid adenomas but exposes the patient to higher radiation doses.18 The sensitivity of 4D-CT in localizing abnormal parathyroid tissue is comparable to that of MDCT.16,18,19
Additional studies used during the management of the patient with PHPT are BMD testing and renal imaging. Secondary causes of bone loss are responsible for up to 30% of osteoporosis cases in postmenopausal women; one of these causes is PHPT.20 Elevated PTH causes increased bone turnover and results in decreased bone mass with subsequent increased fracture risk.9 Bone density should be measured by dual-energy x-ray absorptiometry (DEXA), and the skeletal survey should include the distal one-third of the radius, hip, and lumbar spine. The distal radius is rich in cortical bone and BMD is often lowest at this site in patients with PHPT, making it the most sensitive DEXA marker for early detection of bone loss.19,21 The hip contains an equal mix of cortical and trabecular bone and is the second most sensitive site for detecting bone loss in PHPT. The spine contains a high proportion of trabecular bone and is the least sensitive site.19,21 Renal imaging studies, including x-ray, ultrasound, and, less frequently, CT of the abdomen and pelvis, are used to assess for nephrolithiasis and nephrocalcinosis.19
TREATMENT/MANAGEMENT
Conservative medical management
PHPT is a complex disease process, and careful evaluation is required when determining whether medical versus surgical management is appropriate. Clinical presentation ranges from no symptoms to multisystem disease. Conservative medical management, which includes regular monitoring, is an acceptable strategy in an asymptomatic patient with a low fracture risk and no nephrolithiasis.1 Conservative care includes maintaining normal dietary calcium intake and adequate hydration, regular exercise, vitamin D supplementation, annual laboratory studies, BMD testing, and the avoidance of thiazide diuretics and lithium.1 Guidelines, from the Fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism, for monitoring asymptomatic PHPT patients recommend
- Annual measurement of serum calcium
- BMD measurement by DEXA every 1 to 2 years
- Annual assessment of eGFR and serum creatinine
- Renal imaging or a 24-h urine stone profile if nephrolithiasis is suspected.19
Long-term medical management of PHPT is difficult because no agents are available to suppress hypercalcemia or completely block PTH release.12
Maintaining serum 25(OH)D at a level > 20 ng/mL significantly reduces PTH secretion, in comparison to levels < 20 ng/mL, and does not aggravate hypercalcemia.22 The Endocrine Society recommends a minimum serum 25(OH)D level of 20 ng/mL and notes that targeting a higher threshold value of 30 ng/mL is reasonable.19 The daily requirement for vitamin D3, 800 IU to 1,000 IU, is a good starting point for supplementation.4 Measurement of 1,25(OH)2D levels lacks value and is not recommended for patients with PHPT. Calcium intake should follow established guidelines and is not limited in PHPT.19
Surgical management
Surgical management is indicated for symptomatic patients.23 Indications include nephrolithiasis, nephrocalcinosis, osteitis fibrosa cystica, or osteoporosis. Surgery is considered appropriate for individuals who do not meet these criteria if there are no medical contraindications.14 The Fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism revised the indications for surgery in 2014 to include asymptomatic patients, since surgery is the only definitive treatment for PHPT. Current guidelines for when to recommend surgery in the asymptomatic patient with PHPT are listed in Table 4.19
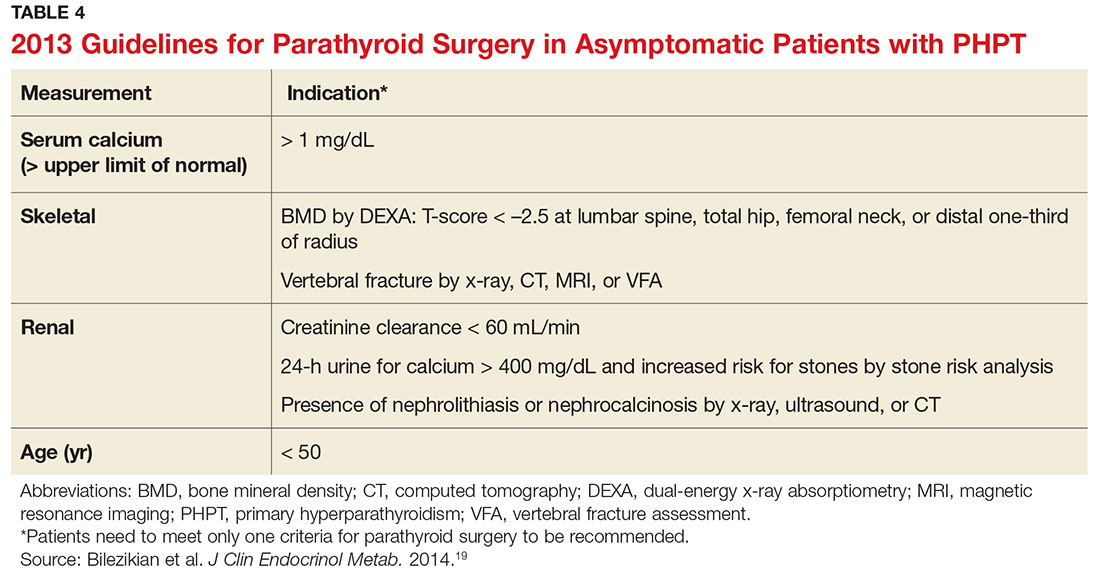
Preoperative localization and referral to an experienced surgeon is of utmost importance for a good outcome. An expert surgeon will usually perform a minimally invasive parathyroidectomy (MIP) and obtain intraoperative PTH levels; in some cases, a full neck exploration is necessary. PTH has a half-life of less than five minutes and is an accurate tool for determining whether the culprit gland has been successfully removed.5
Modern imaging studies, less invasive surgical techniques, and intraoperative measurements of PTH have decreased the need to conduct full neck exploration. MIP offers a smaller incision, less tissue dissection, and lower morbidity, and can be offered without the risks associated with general anesthesia.10 The goal of surgery is to restore normocalcemia and, in turn, prevent bone mineral loss and systemic effects of hypercalcemia over the long term.10 Surgical management for an ectopic parathyroid adenoma is controversial because these are often found in the mediastinum, requiring invasive surgery.12
Surgery is curative in up to 95% of cases and has a low rate of complications.2,24 A joint decision regarding treatment options is made among the patient, primary care clinician, and surgeon. Complications include vocal cord paralysis resulting from injury to the recurrent laryngeal nerve, bleeding or hematoma, laryngospasm, symptomatic hypocalcemia, and persistent hyperparathyroidism; seizures are very rare but can occur from transient hypocalcemia and hypomagnesemia.5 PTH levels drop by more than 50% intraoperatively if the procedure is successful; otherwise, exploration for another adenoma is indicated.10 Postoperative calcium and vitamin D supplementation are warranted once lab values are stable.
When surgery is contraindicated/refused
If surgery is indicated but the patient is a poor candidate or refuses surgery, management of hypercalcemia and bone loss with pharmacologic agents is warranted. The calcimimetic cinacalcet is a reasonable medical alternative that has been shown to adequately control hypercalcemia and hypophosphatemia and has proven effective in various patient subgroups.25 This agent is useful in the treatment of patients who are asymptomatic and refuse surgery, patients with refractory PHPT after parathyroidectomy, and patients with contraindications to surgery.24,25 The medication reduces calcium and modestly reduces PTH levels by binding parathyroid calcium-sensing receptors but does not improve bone density.2,12 Cinacalcet is approved by the FDA for use in patients with moderate to severe disease when surgery is contraindicated.24
Treatment options for osteoporosis, vertebral fractures, and progressive bone loss in the patient with PHPT include bisphosphonates. Raloxifene and estrogen replacements may be used in postmenopausal women. Oral bisphosphonates (alendronate or risedronate) are firstline therapies and have been shown to inhibit progression to osteoporosis in PHPT.9,26 They prevent osteoclastic activity, reducing bone resorption and turnover. Contraindications to oral bisphosphonates include esophageal disorders, gastrointestinal intolerance, or inability to follow the dosing requirements. Intravenous zoledronic acid provides an alternative route of administration.
Alendronate has the best evidence for improving bone density and preventing progression to osteoporosis in patients with PHPT, but the medication does not affect calcium or PTH levels.1,19 There is limited data on the effects of combining bisphosphonates with calcimimetics. Raloxifene is a selective estrogen receptor modulator that decreases bone resorption; it is approved for treating osteoporosis and may be used when a patient is not a good candidate for a bisphosphonate.20 Denosumab, currently under study for the treatment of PHPT, is a human monoclonal antibody that improves bone density but does not affect serum calcium.20 Nonpharmacologic therapies include alcohol moderation, decreased caffeine intake, weight-bearing exercise, smoking cessation, adequate hydration, and dietary modifications.20
OUTCOME FOR THE CASE PATIENT
Although PHPT is often discovered incidentally in routine blood work with hypercalcemia, the case patient had developed osteoporosis and a grade IV tibial stress fracture before the diagnosis was made. Following parathyroidectomy, her hypertension worsened, requiring an additional antihypertensive medication. She developed recurrent disease and was referred to a tertiary care center for revision parathyroidectomy due to persistent elevated calcium levels. A 24-hour urine calcium test ruled out concurrent FHH. A full neck exploration was conducted and a 340-mg hypercellular parathyroid gland was removed from the left superior pole. She will be monitored for recurrent disease and will remain on a vitamin D3 supplement and treatment for osteoporosis.
CONCLUSION
Primary care clinicians should have a low threshold for initiating the work-up of mild hypercalcemia in an effort to prevent sequelae. Patient education is essential throughout the process. Understanding the condition and treatment options is necessary for a patient’s active participation in clinical decision making. Conservative management of an asymptomatic patient includes avoiding thiazide diuretics and lithium, staying well hydrated with water, maintaining moderate dietary calcium (1,000-1,200 mg/d) and vitamin D (400-600 IU/d) intake, regular exercise, and appropriate lab and bone density monitoring. Surgical treatment is recommended for symptomatic patients exhibiting decreased bone density, fractures, renal impairment, or nephrolithiasis. Treating bone loss with bisphosphonates and hypercalcemia with calcimimetics is useful. Postmenopausal women may benefit from estrogen therapy or selective estrogen receptor modulators. These agents improve bone density and lower calcium, but are often contraindicated or have adverse effects. Surgery is the only cure.3
1. Turner J. Hypercalcaemia and primary hyperparathyroidism. Medicine. 2009;37(9):461-464.
2. Crowley R, Gittoes N. How to approach hypercalcaemia. Clin Med. 2013;13(3):287-290.
3. Kapustin JF, Schofield DL. Hyperparathyroidism: an incidental finding. Nurse Pract. 2012;37(11):9-14.
4. Cordellat IM. Hyperparathyroidism: primary or secondary disease? Rheumatol Clin. 2012;8(5):287-291.
5. MacKenzie-Feder J, Sirrs S, Anderson D, Sharif J, Khan A. Primary hyperparathyroidism: an overview. Int J Endocrinol. 2011;2011:251410.
6. Brashers VL, Jones RE, Huether SE. Alterations of hormonal regulation. In: McCance KL, Huether SE, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 7th ed. St. Louis, MO: Mosby; 2015:731-733.
7. Osborne JL, Klocko DJ. Woman, 66, with persistent abdominal and back pain. Clinician Reviews. 2014;24(11):34-37, 40.
8. Michels TC, Kelly KM. Parathyroid disorders. Am Fam Physician. 2013;88(4):249-257.
9. Rolighed L, Rejnmark L, Christiansen P. Bone involvement in primary hyperparathyroidism and changes after parathyroidectomy. US Endocrinol. 2013;9(2):181-184.
10. Karahan Ö, Okus A, Sevinç B, et al. Minimally invasive parathyroidectomy under local anesthesia. J Postgrad Med. 2013;59(1):21-24.
11. Fuleihan GE, Silverberg SJ. Primary hyperparathyroidism: diagnosis, differential diagnosis, and evaluation. Up-to-Date. www.uptodate.com/contents/primary-hyperparathyroidism-diagnosis-differential-diagnosis-and-evaluation. Accessed April 20, 2017.
12. Panchani R, Varma T, Goyal A, et al. A challenging case of an ectopic parathyroid adenoma. Indian J Endocrinol Metab. 2012;16:S408-S410.
13. Otasowie J, Hambleton BA. Aggression and homicidal thoughts in a patient with primary hyperparathyroidism: a case report. Br J Medical Pract. 2013;6(4):a630.
14. Bilezikian JP. Primary hyperparathyroidism: new insights, concepts and guidelines. Presented at: American Association of Clinical Endocrinologists 24th Annual Scientific and Clinical Congress; May 13-17, 2015; Nashville, TN. am2015.aace.com/presentations/Friday/F31/PrimaryHyperparathyroidismNew InsightsConceptsandGuidelines.pdf. Accessed April 20, 2017.
15. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 7th ed. St. Louis, MO: Mosby; 2015:1551-1555.
16. Amaral LM, Queiroz DC, Marques TF, et al. Clinical study: normocalcemic versus hypercalcemic primary hyperparathyroidism: more stone than bone? J Osteoporos. 2012;2012:128352.
17. Linda DD, Ng B, Rebello R, et al. The utility of multidetector computed tomography for detection of parathyroid disease in the setting of primary hyperparathyroidism. Can Assoc Radiol J. 2012;63(2):100-108.
18. Bann DV, Zacharia T, Goldenberg D, Goyal, N. Parathyroid localization using 4-D-computed tomography. Ear Nose Throat J. 2015;94(4-5):E55-E57.
19. Bilezikian JP, Brandi ML, Eastell R, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3561-3569.
20. Jeremiah MP, Unwin BK, Greenawald MH, Casiano VE. Diagnosis and management of osteoporosis. Am Fam Physician. 2015;92(4):261-268.
21. Wood K, Dhital S, Chen H, Sippel RS. What is the utility of distal forearm DXA in primary hyperparathyroidism? Oncologist. 2012;17(3):322-325.
22. Jayasena CN, Modi M, Palazzo F, et al. Associations of serum 25-hydroxyvitamin D with circulating PTH, phosphate and calcium in patients with primary hyperparathyroidism. Clin Endocrinol (Oxf). 2013;78(6):838-843.
23. Grey A. Nonsurgical management of mild primary hyperparathyroidism—a reasonable option. Clin Endocrinol. 2012;77(5):639-644.
24. Saponaro F, Faggiano A, Grimaldi F, et al. Cinacalcet in the management of primary hyperparathyroidism: post marketing experience of an Italian multicenter group. Clin Endocrinol (Oxf). 2013;79(1):20-26.
25. Rothe HM, Liangos O, Biggar P, et al. Cinacalcet treatment of primary hyperparathyroidism. Int J Endocrinol. 2011;2011:415719.
26. Farag N, Delbanco T, Strewler GJ. Update: a 64-year-old woman with primary hyperparathyroidism. JAMA. 2008;300(17):2044-2045.
1. Turner J. Hypercalcaemia and primary hyperparathyroidism. Medicine. 2009;37(9):461-464.
2. Crowley R, Gittoes N. How to approach hypercalcaemia. Clin Med. 2013;13(3):287-290.
3. Kapustin JF, Schofield DL. Hyperparathyroidism: an incidental finding. Nurse Pract. 2012;37(11):9-14.
4. Cordellat IM. Hyperparathyroidism: primary or secondary disease? Rheumatol Clin. 2012;8(5):287-291.
5. MacKenzie-Feder J, Sirrs S, Anderson D, Sharif J, Khan A. Primary hyperparathyroidism: an overview. Int J Endocrinol. 2011;2011:251410.
6. Brashers VL, Jones RE, Huether SE. Alterations of hormonal regulation. In: McCance KL, Huether SE, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 7th ed. St. Louis, MO: Mosby; 2015:731-733.
7. Osborne JL, Klocko DJ. Woman, 66, with persistent abdominal and back pain. Clinician Reviews. 2014;24(11):34-37, 40.
8. Michels TC, Kelly KM. Parathyroid disorders. Am Fam Physician. 2013;88(4):249-257.
9. Rolighed L, Rejnmark L, Christiansen P. Bone involvement in primary hyperparathyroidism and changes after parathyroidectomy. US Endocrinol. 2013;9(2):181-184.
10. Karahan Ö, Okus A, Sevinç B, et al. Minimally invasive parathyroidectomy under local anesthesia. J Postgrad Med. 2013;59(1):21-24.
11. Fuleihan GE, Silverberg SJ. Primary hyperparathyroidism: diagnosis, differential diagnosis, and evaluation. Up-to-Date. www.uptodate.com/contents/primary-hyperparathyroidism-diagnosis-differential-diagnosis-and-evaluation. Accessed April 20, 2017.
12. Panchani R, Varma T, Goyal A, et al. A challenging case of an ectopic parathyroid adenoma. Indian J Endocrinol Metab. 2012;16:S408-S410.
13. Otasowie J, Hambleton BA. Aggression and homicidal thoughts in a patient with primary hyperparathyroidism: a case report. Br J Medical Pract. 2013;6(4):a630.
14. Bilezikian JP. Primary hyperparathyroidism: new insights, concepts and guidelines. Presented at: American Association of Clinical Endocrinologists 24th Annual Scientific and Clinical Congress; May 13-17, 2015; Nashville, TN. am2015.aace.com/presentations/Friday/F31/PrimaryHyperparathyroidismNew InsightsConceptsandGuidelines.pdf. Accessed April 20, 2017.
15. Crowther-Radulewicz CL, McCance KL. Alterations of musculoskeletal function. In: McCance KL, Huether SE, eds. Pathophysiology: The Biologic Basis for Disease in Adults and Children. 7th ed. St. Louis, MO: Mosby; 2015:1551-1555.
16. Amaral LM, Queiroz DC, Marques TF, et al. Clinical study: normocalcemic versus hypercalcemic primary hyperparathyroidism: more stone than bone? J Osteoporos. 2012;2012:128352.
17. Linda DD, Ng B, Rebello R, et al. The utility of multidetector computed tomography for detection of parathyroid disease in the setting of primary hyperparathyroidism. Can Assoc Radiol J. 2012;63(2):100-108.
18. Bann DV, Zacharia T, Goldenberg D, Goyal, N. Parathyroid localization using 4-D-computed tomography. Ear Nose Throat J. 2015;94(4-5):E55-E57.
19. Bilezikian JP, Brandi ML, Eastell R, et al. Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99(10):3561-3569.
20. Jeremiah MP, Unwin BK, Greenawald MH, Casiano VE. Diagnosis and management of osteoporosis. Am Fam Physician. 2015;92(4):261-268.
21. Wood K, Dhital S, Chen H, Sippel RS. What is the utility of distal forearm DXA in primary hyperparathyroidism? Oncologist. 2012;17(3):322-325.
22. Jayasena CN, Modi M, Palazzo F, et al. Associations of serum 25-hydroxyvitamin D with circulating PTH, phosphate and calcium in patients with primary hyperparathyroidism. Clin Endocrinol (Oxf). 2013;78(6):838-843.
23. Grey A. Nonsurgical management of mild primary hyperparathyroidism—a reasonable option. Clin Endocrinol. 2012;77(5):639-644.
24. Saponaro F, Faggiano A, Grimaldi F, et al. Cinacalcet in the management of primary hyperparathyroidism: post marketing experience of an Italian multicenter group. Clin Endocrinol (Oxf). 2013;79(1):20-26.
25. Rothe HM, Liangos O, Biggar P, et al. Cinacalcet treatment of primary hyperparathyroidism. Int J Endocrinol. 2011;2011:415719.
26. Farag N, Delbanco T, Strewler GJ. Update: a 64-year-old woman with primary hyperparathyroidism. JAMA. 2008;300(17):2044-2045.
Can Botulinum Toxin Benefit People With Parkinson’s Disease?
Apraxia of Eyelid Opening
Apraxia of eyelid opening sometimes is associated with Parkinson’s disease and parkinsonian disorders such as progressive supranuclear palsy. Patients with this condition may be unable to open their eyes without contracting the frontalis muscle. The literature contains no randomized controlled trials of botulinum toxin for this indication, but open-label studies, such as one from Inoue and Rogers, suggest a benefit. Reports indicate that the pretarsal is the most appropriate injection target. An initial dose of 10–20 units of onabotulinum or incobotulinum toxin can be administered to the orbicularis oculi.
Sialorrhea
Sialorrhea is common among patients with Parkinson’s disease and may result from impaired swallowing or autonomic dysregulation. Anticholinergic drugs such as glycopyrrolate often have limited efficacy for sialorrhea and may cause side effects. Several randomized controlled trials have examined botulinum toxin as a potential treatment. A review by Seppi et al concluded that botulinum toxin types A and B are efficacious for this indication, although it is an off-label use.
Two injection sites have been considered for this treatment: the submandibular gland, which is responsible for continuous saliva secretion, and the parotid gland, which is responsible for stimulated secretion. Most studies have used the parotid gland or the parotid and submandibular glands as targets. One small study directly compared the two injection sites and found a trend toward a greater benefit from injection into the submandibular gland. “One approach could be to inject the parotid gland, and if it is still not effective, you can inject the submandibular gland,” said Dr. Chen. The dose for the parotid gland ranges between 5 and 50 units of onabotulinum or incobotulinum toxin, and a dose of 5 units generally is used for the submandibular gland.
The injection site may be localized using ultrasound or anatomical landmarks. A study in which the target was the parotid gland found slightly better results with ultrasound guidance, but ultrasound may be more necessary for injections into the submandibular gland, said Dr. Chen. Whether ultrasound guidance improves outcomes of botulinum toxin for sialorrhea thus has not been established, he added.
Jaw Tremor and Upper-Limb Tremor
Levodopa is the first-line treatment for tremor in Parkinson’s disease, but some patients do not respond well to this therapy. Schneider and colleagues studied abobotulinum toxin for jaw tremor in Parkinson’s disease. They administered the treatment to three people through bilateral masseter injection. Patients had an excellent response without side effects. Another protocol is an injection of 40 units of onabotulinum or incobotulinum toxin into the masseter and 10 units into the temporalis, said Dr. Chen.
No randomized controlled trials of botulinum toxin for arm tremor related to Parkinson’s disease have been published, but Rahimi et al published two case series. In one series published in 2015, the investigators administered injections to 28 patients at baseline, 16 weeks, and 32 weeks. The study was open-label, and muscles were selected using kinematic analysis. They found reduced tremor with treatment, and patients had mild muscle weakness.
Dystonia
Patients with Parkinson’s disease or multiple system atrophy may develop cervical dystonia that manifests as anterocollis. Patients with progressive supranuclear palsy may develop retrocollis. Although botulinum toxin is not indicated for it, case reports suggest that the treatment may be effective for cervical dystonia. The sternomastoid, scalene, and the longus colli are appropriate injection targets. Neurologists may need imaging guidance to inject botulinum toxin into the longus colli. For one patient with cervical dystonia secondary to corticobasal syndrome, Dr. Chen administered 30 units (onabotulinum or incobotulinum toxin) to the right trapezius, 60 units to the levator scapulae, and 20 units to the sternomastoid.
Dystonic clenched fists also may occur in Parkinson’s disease and Parkinson-plus syndromes. In 2001, Cordivari et al studied botulinum toxin as a treatment for dystonic clenched fists in seven patients with Parkinson’s disease and seven patients with other disorders. The researchers used electromyography to distinguish between muscle contraction and contracture. The injection sites were the flexor digitorum superficialis, flexor digitorum profundus, flexor pollicis longus, and lumbricals. The treatment reduced pain, relaxed muscles, and helped to resolve palmar infections.
Leg dystonia can be a presenting symptom in young-onset Parkinson’s disease and sometimes is observed in peak-dose dyskinesia. However, the typical presentation is off-period foot inversion and toe flexion. The big toe may be flexed or extended. The largest study of botulinum toxin for leg dystonia included 30 patients with Parkinson’s disease and painful off dystonia and was published in 1995. Open-label treatment improved pain and spasm for all patients, and seven patients with on dystonia had improved posture on walking. In 2016, Gupta et al administered 250–400 units of onabotulinum toxin to six patients with Parkinson’s disease and leg dystonia treated with deep brain stimulation. The treatment improved dystonia, pain, walking, gait velocity, and cadence.
Pain
Neurologists also have used botulinum toxin to treat pain in Parkinson’s disease. Bruno and colleagues performed a retrospective chart review of patients with Parkinson’s disease who received botulinum toxin for various indications over a 20-year period. The main indication for treatment was pain, and 81% of patients who received botulinum toxin for pain reported benefit after the first injection. The benefit was sustained with further injections.
Overactive Bladder
Overactive bladder affects between 38% and 71% of people with Parkinson’s disease. Symptoms include urinary urgency, urinary frequency, nocturia, and incontinence. Behavioral modification is the first-line treatment, and antimuscarinic agents may provide benefit. Overactive bladder is an approved indication for onabotulinum toxin. The usual dose is 200 units, but it can range between 100 and 300 units. Treatment is injected into the detrusor muscles, and the benefit lasts for six months to nine months. Urine retention is a potential side effect of this treatment.
—Erik Greb
Suggested Reading
Bruno VA, Fox SH, Mancini D, Miyasaki JM. Botulinum toxin use in refractory pain and other symptoms in parkinsonism. Can J Neurol Sci. 2016;43(5):697-702.
Cordivari C, Misra VP, Catania S, Lees AJ. Treatment of dystonic clenched fist with botulinum toxin. Mov Disord. 2001;16(5):907-913.
Giannantoni A, Conte A, Proietti S, et al. Botulinum toxin type A in patients with Parkinson’s disease and refractory overactive bladder. J Urol. 2011;186(3):960-964.
Glass GA, Ku S, Ostrem JL, et al. Fluoroscopic, EMG-guided injection of botulinum toxin into the longus colli for the treatment of anterocollis. Parkinsonism Relat Disord. 2009;15(8):610-613.
Gupta AD, Visvanathan R. Botulinum toxin for foot dystonia in patients with Parkinson’s disease having deep brain stimulation: A case series and a pilot study. J Rehabil Med. 2016;48(6):559-562.
Inoue K, Rogers JD. Botulinum toxin injection into Riolan’s muscle: somatosensory ‘trick’. Eur Neurol. 2007;58(3):138-141.
Pacchetti C, Albani G, Martignoni E, et al. “Off” painful dystonia in Parkinson’s disease treated with botulinum toxin. Mov Disord. 1995;10(3):333-336.
Rahimi F, Samotus O, Lee J, Jog M. Effective management of upper limb parkinsonian tremor by incobotulinumtoxinA injections using sensor-based biomechanical patterns. Tremor Other Hyperkinet Mov (NY). 2015;5:348.
Schneider SA, Edwards MJ, Cordivari C, et al. Botulinum toxin A may be efficacious as treatment for jaw tremor in Parkinson’s disease. Mov Disord. 2006;21(10):1722-1724.
Seppi K, Weintraub D, Coelho M, et al. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord. 2011;26 Suppl 3:S42-S80.
Apraxia of Eyelid Opening
Apraxia of eyelid opening sometimes is associated with Parkinson’s disease and parkinsonian disorders such as progressive supranuclear palsy. Patients with this condition may be unable to open their eyes without contracting the frontalis muscle. The literature contains no randomized controlled trials of botulinum toxin for this indication, but open-label studies, such as one from Inoue and Rogers, suggest a benefit. Reports indicate that the pretarsal is the most appropriate injection target. An initial dose of 10–20 units of onabotulinum or incobotulinum toxin can be administered to the orbicularis oculi.
Sialorrhea
Sialorrhea is common among patients with Parkinson’s disease and may result from impaired swallowing or autonomic dysregulation. Anticholinergic drugs such as glycopyrrolate often have limited efficacy for sialorrhea and may cause side effects. Several randomized controlled trials have examined botulinum toxin as a potential treatment. A review by Seppi et al concluded that botulinum toxin types A and B are efficacious for this indication, although it is an off-label use.
Two injection sites have been considered for this treatment: the submandibular gland, which is responsible for continuous saliva secretion, and the parotid gland, which is responsible for stimulated secretion. Most studies have used the parotid gland or the parotid and submandibular glands as targets. One small study directly compared the two injection sites and found a trend toward a greater benefit from injection into the submandibular gland. “One approach could be to inject the parotid gland, and if it is still not effective, you can inject the submandibular gland,” said Dr. Chen. The dose for the parotid gland ranges between 5 and 50 units of onabotulinum or incobotulinum toxin, and a dose of 5 units generally is used for the submandibular gland.
The injection site may be localized using ultrasound or anatomical landmarks. A study in which the target was the parotid gland found slightly better results with ultrasound guidance, but ultrasound may be more necessary for injections into the submandibular gland, said Dr. Chen. Whether ultrasound guidance improves outcomes of botulinum toxin for sialorrhea thus has not been established, he added.
Jaw Tremor and Upper-Limb Tremor
Levodopa is the first-line treatment for tremor in Parkinson’s disease, but some patients do not respond well to this therapy. Schneider and colleagues studied abobotulinum toxin for jaw tremor in Parkinson’s disease. They administered the treatment to three people through bilateral masseter injection. Patients had an excellent response without side effects. Another protocol is an injection of 40 units of onabotulinum or incobotulinum toxin into the masseter and 10 units into the temporalis, said Dr. Chen.
No randomized controlled trials of botulinum toxin for arm tremor related to Parkinson’s disease have been published, but Rahimi et al published two case series. In one series published in 2015, the investigators administered injections to 28 patients at baseline, 16 weeks, and 32 weeks. The study was open-label, and muscles were selected using kinematic analysis. They found reduced tremor with treatment, and patients had mild muscle weakness.
Dystonia
Patients with Parkinson’s disease or multiple system atrophy may develop cervical dystonia that manifests as anterocollis. Patients with progressive supranuclear palsy may develop retrocollis. Although botulinum toxin is not indicated for it, case reports suggest that the treatment may be effective for cervical dystonia. The sternomastoid, scalene, and the longus colli are appropriate injection targets. Neurologists may need imaging guidance to inject botulinum toxin into the longus colli. For one patient with cervical dystonia secondary to corticobasal syndrome, Dr. Chen administered 30 units (onabotulinum or incobotulinum toxin) to the right trapezius, 60 units to the levator scapulae, and 20 units to the sternomastoid.
Dystonic clenched fists also may occur in Parkinson’s disease and Parkinson-plus syndromes. In 2001, Cordivari et al studied botulinum toxin as a treatment for dystonic clenched fists in seven patients with Parkinson’s disease and seven patients with other disorders. The researchers used electromyography to distinguish between muscle contraction and contracture. The injection sites were the flexor digitorum superficialis, flexor digitorum profundus, flexor pollicis longus, and lumbricals. The treatment reduced pain, relaxed muscles, and helped to resolve palmar infections.
Leg dystonia can be a presenting symptom in young-onset Parkinson’s disease and sometimes is observed in peak-dose dyskinesia. However, the typical presentation is off-period foot inversion and toe flexion. The big toe may be flexed or extended. The largest study of botulinum toxin for leg dystonia included 30 patients with Parkinson’s disease and painful off dystonia and was published in 1995. Open-label treatment improved pain and spasm for all patients, and seven patients with on dystonia had improved posture on walking. In 2016, Gupta et al administered 250–400 units of onabotulinum toxin to six patients with Parkinson’s disease and leg dystonia treated with deep brain stimulation. The treatment improved dystonia, pain, walking, gait velocity, and cadence.
Pain
Neurologists also have used botulinum toxin to treat pain in Parkinson’s disease. Bruno and colleagues performed a retrospective chart review of patients with Parkinson’s disease who received botulinum toxin for various indications over a 20-year period. The main indication for treatment was pain, and 81% of patients who received botulinum toxin for pain reported benefit after the first injection. The benefit was sustained with further injections.
Overactive Bladder
Overactive bladder affects between 38% and 71% of people with Parkinson’s disease. Symptoms include urinary urgency, urinary frequency, nocturia, and incontinence. Behavioral modification is the first-line treatment, and antimuscarinic agents may provide benefit. Overactive bladder is an approved indication for onabotulinum toxin. The usual dose is 200 units, but it can range between 100 and 300 units. Treatment is injected into the detrusor muscles, and the benefit lasts for six months to nine months. Urine retention is a potential side effect of this treatment.
—Erik Greb
Suggested Reading
Bruno VA, Fox SH, Mancini D, Miyasaki JM. Botulinum toxin use in refractory pain and other symptoms in parkinsonism. Can J Neurol Sci. 2016;43(5):697-702.
Cordivari C, Misra VP, Catania S, Lees AJ. Treatment of dystonic clenched fist with botulinum toxin. Mov Disord. 2001;16(5):907-913.
Giannantoni A, Conte A, Proietti S, et al. Botulinum toxin type A in patients with Parkinson’s disease and refractory overactive bladder. J Urol. 2011;186(3):960-964.
Glass GA, Ku S, Ostrem JL, et al. Fluoroscopic, EMG-guided injection of botulinum toxin into the longus colli for the treatment of anterocollis. Parkinsonism Relat Disord. 2009;15(8):610-613.
Gupta AD, Visvanathan R. Botulinum toxin for foot dystonia in patients with Parkinson’s disease having deep brain stimulation: A case series and a pilot study. J Rehabil Med. 2016;48(6):559-562.
Inoue K, Rogers JD. Botulinum toxin injection into Riolan’s muscle: somatosensory ‘trick’. Eur Neurol. 2007;58(3):138-141.
Pacchetti C, Albani G, Martignoni E, et al. “Off” painful dystonia in Parkinson’s disease treated with botulinum toxin. Mov Disord. 1995;10(3):333-336.
Rahimi F, Samotus O, Lee J, Jog M. Effective management of upper limb parkinsonian tremor by incobotulinumtoxinA injections using sensor-based biomechanical patterns. Tremor Other Hyperkinet Mov (NY). 2015;5:348.
Schneider SA, Edwards MJ, Cordivari C, et al. Botulinum toxin A may be efficacious as treatment for jaw tremor in Parkinson’s disease. Mov Disord. 2006;21(10):1722-1724.
Seppi K, Weintraub D, Coelho M, et al. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord. 2011;26 Suppl 3:S42-S80.
Apraxia of Eyelid Opening
Apraxia of eyelid opening sometimes is associated with Parkinson’s disease and parkinsonian disorders such as progressive supranuclear palsy. Patients with this condition may be unable to open their eyes without contracting the frontalis muscle. The literature contains no randomized controlled trials of botulinum toxin for this indication, but open-label studies, such as one from Inoue and Rogers, suggest a benefit. Reports indicate that the pretarsal is the most appropriate injection target. An initial dose of 10–20 units of onabotulinum or incobotulinum toxin can be administered to the orbicularis oculi.
Sialorrhea
Sialorrhea is common among patients with Parkinson’s disease and may result from impaired swallowing or autonomic dysregulation. Anticholinergic drugs such as glycopyrrolate often have limited efficacy for sialorrhea and may cause side effects. Several randomized controlled trials have examined botulinum toxin as a potential treatment. A review by Seppi et al concluded that botulinum toxin types A and B are efficacious for this indication, although it is an off-label use.
Two injection sites have been considered for this treatment: the submandibular gland, which is responsible for continuous saliva secretion, and the parotid gland, which is responsible for stimulated secretion. Most studies have used the parotid gland or the parotid and submandibular glands as targets. One small study directly compared the two injection sites and found a trend toward a greater benefit from injection into the submandibular gland. “One approach could be to inject the parotid gland, and if it is still not effective, you can inject the submandibular gland,” said Dr. Chen. The dose for the parotid gland ranges between 5 and 50 units of onabotulinum or incobotulinum toxin, and a dose of 5 units generally is used for the submandibular gland.
The injection site may be localized using ultrasound or anatomical landmarks. A study in which the target was the parotid gland found slightly better results with ultrasound guidance, but ultrasound may be more necessary for injections into the submandibular gland, said Dr. Chen. Whether ultrasound guidance improves outcomes of botulinum toxin for sialorrhea thus has not been established, he added.
Jaw Tremor and Upper-Limb Tremor
Levodopa is the first-line treatment for tremor in Parkinson’s disease, but some patients do not respond well to this therapy. Schneider and colleagues studied abobotulinum toxin for jaw tremor in Parkinson’s disease. They administered the treatment to three people through bilateral masseter injection. Patients had an excellent response without side effects. Another protocol is an injection of 40 units of onabotulinum or incobotulinum toxin into the masseter and 10 units into the temporalis, said Dr. Chen.
No randomized controlled trials of botulinum toxin for arm tremor related to Parkinson’s disease have been published, but Rahimi et al published two case series. In one series published in 2015, the investigators administered injections to 28 patients at baseline, 16 weeks, and 32 weeks. The study was open-label, and muscles were selected using kinematic analysis. They found reduced tremor with treatment, and patients had mild muscle weakness.
Dystonia
Patients with Parkinson’s disease or multiple system atrophy may develop cervical dystonia that manifests as anterocollis. Patients with progressive supranuclear palsy may develop retrocollis. Although botulinum toxin is not indicated for it, case reports suggest that the treatment may be effective for cervical dystonia. The sternomastoid, scalene, and the longus colli are appropriate injection targets. Neurologists may need imaging guidance to inject botulinum toxin into the longus colli. For one patient with cervical dystonia secondary to corticobasal syndrome, Dr. Chen administered 30 units (onabotulinum or incobotulinum toxin) to the right trapezius, 60 units to the levator scapulae, and 20 units to the sternomastoid.
Dystonic clenched fists also may occur in Parkinson’s disease and Parkinson-plus syndromes. In 2001, Cordivari et al studied botulinum toxin as a treatment for dystonic clenched fists in seven patients with Parkinson’s disease and seven patients with other disorders. The researchers used electromyography to distinguish between muscle contraction and contracture. The injection sites were the flexor digitorum superficialis, flexor digitorum profundus, flexor pollicis longus, and lumbricals. The treatment reduced pain, relaxed muscles, and helped to resolve palmar infections.
Leg dystonia can be a presenting symptom in young-onset Parkinson’s disease and sometimes is observed in peak-dose dyskinesia. However, the typical presentation is off-period foot inversion and toe flexion. The big toe may be flexed or extended. The largest study of botulinum toxin for leg dystonia included 30 patients with Parkinson’s disease and painful off dystonia and was published in 1995. Open-label treatment improved pain and spasm for all patients, and seven patients with on dystonia had improved posture on walking. In 2016, Gupta et al administered 250–400 units of onabotulinum toxin to six patients with Parkinson’s disease and leg dystonia treated with deep brain stimulation. The treatment improved dystonia, pain, walking, gait velocity, and cadence.
Pain
Neurologists also have used botulinum toxin to treat pain in Parkinson’s disease. Bruno and colleagues performed a retrospective chart review of patients with Parkinson’s disease who received botulinum toxin for various indications over a 20-year period. The main indication for treatment was pain, and 81% of patients who received botulinum toxin for pain reported benefit after the first injection. The benefit was sustained with further injections.
Overactive Bladder
Overactive bladder affects between 38% and 71% of people with Parkinson’s disease. Symptoms include urinary urgency, urinary frequency, nocturia, and incontinence. Behavioral modification is the first-line treatment, and antimuscarinic agents may provide benefit. Overactive bladder is an approved indication for onabotulinum toxin. The usual dose is 200 units, but it can range between 100 and 300 units. Treatment is injected into the detrusor muscles, and the benefit lasts for six months to nine months. Urine retention is a potential side effect of this treatment.
—Erik Greb
Suggested Reading
Bruno VA, Fox SH, Mancini D, Miyasaki JM. Botulinum toxin use in refractory pain and other symptoms in parkinsonism. Can J Neurol Sci. 2016;43(5):697-702.
Cordivari C, Misra VP, Catania S, Lees AJ. Treatment of dystonic clenched fist with botulinum toxin. Mov Disord. 2001;16(5):907-913.
Giannantoni A, Conte A, Proietti S, et al. Botulinum toxin type A in patients with Parkinson’s disease and refractory overactive bladder. J Urol. 2011;186(3):960-964.
Glass GA, Ku S, Ostrem JL, et al. Fluoroscopic, EMG-guided injection of botulinum toxin into the longus colli for the treatment of anterocollis. Parkinsonism Relat Disord. 2009;15(8):610-613.
Gupta AD, Visvanathan R. Botulinum toxin for foot dystonia in patients with Parkinson’s disease having deep brain stimulation: A case series and a pilot study. J Rehabil Med. 2016;48(6):559-562.
Inoue K, Rogers JD. Botulinum toxin injection into Riolan’s muscle: somatosensory ‘trick’. Eur Neurol. 2007;58(3):138-141.
Pacchetti C, Albani G, Martignoni E, et al. “Off” painful dystonia in Parkinson’s disease treated with botulinum toxin. Mov Disord. 1995;10(3):333-336.
Rahimi F, Samotus O, Lee J, Jog M. Effective management of upper limb parkinsonian tremor by incobotulinumtoxinA injections using sensor-based biomechanical patterns. Tremor Other Hyperkinet Mov (NY). 2015;5:348.
Schneider SA, Edwards MJ, Cordivari C, et al. Botulinum toxin A may be efficacious as treatment for jaw tremor in Parkinson’s disease. Mov Disord. 2006;21(10):1722-1724.
Seppi K, Weintraub D, Coelho M, et al. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord. 2011;26 Suppl 3:S42-S80.
One in four practitioners doing FNAs are endocrinologists
AT ENDO 2017
ORLANDO – Endocrinologists made up about one in four of the practitioners performing fine needle aspiration (FNA) biopsies between 2012 and 2014, according to a review of data from the Centers for Medicare & Medicaid Services.
Similarly, endocrinologists performed 25% of image-guided thyroid biopsies.
Endocrine surgeons represent only a small percentage of all practitioners performing head and neck ultrasound exams and image-guided FNA, lead author Mamoona Khokhar, MD, said during a poster presentation at the annual meeting of the Endocrine Society. This is true even though the more portable nature of ultrasound has made it easier for motivated surgeons to incorporate its use into their practice, she said.
Examining 3 years of data from a provider utilization and payment database, Dr. Khokhar and her colleagues identified the types of practitioners who performed head and neck ultrasound, as well as image-guided FNA.
In their analysis, the researchers broadly divided practitioners into surgeons and nonsurgeons. Overall, of the 14,750 median annual practitioners performing head and neck ultrasound between 2012 and 2014, 97.2% were nonsurgeon practitioners, reported Dr. Khokhar, an endocrine surgery fellow at Columbia University Medical Center in New York.
Of all practitioners performing head and neck ultrasound, most (81%) were radiologists. Endocrinologists made up 8% of the overall pool performing ultrasounds.
Breaking the surgeon group down further showed that endocrine surgeons represented 14.7% of surgeons performing head and neck ultrasound, meaning that they made up just 0.4% of the practitioner pool for this procedure. Just over half (52%) of the surgeons performing ultrasounds were otolaryngologists.
The number of practitioners performing image-guided FNA was smaller, at a median 3,695 per year during the study period. Surgeons made up 10.7% of this number. Of the surgeons who performed image-guided FNA, 10.5% were endocrine surgeons. Endocrine surgeons made up 1.1% of all practitioners who billed for FNA.
Again, radiologists made up the majority (58%) of the practitioners performing FNA, and one in four (25%) of practitioners performing FNAs were endocrinologists. Just 5% of the practitioners performing FNAs were otolaryngologists.
More endocrine surgeons performed ultrasound than advanced practice providers (nurse practitioners or physician assistants, 0.2%), pathologists (0.1%), and surgical oncologists (0.04%; P for all, less than .0001). However, advanced practice providers and pathologists both performed significantly more FNAs than did endocrine surgeons (2.1% and 1.8%, P less than .0001).
Although the raw proportion of endocrine surgeons billing for these procedures increased during the study period, the increases were not statistically significant. Dr. Khokhar and her colleagues found that the proportion of American Association of Endocrine Surgeons members who performed head and neck ultrasound grew from 59% in 2012 to 72% in 2014 (P = 0.37), while the proportion performing FNA also increased, from 36% in 2012 to 46% in 2014 (P = .40).
Surgeons, however, may face a number of obstacles in setting up office-based ultrasound, which can lead to underutilization by surgeons, Dr. Khokhar noted, adding that “the results of this study suggest that endocrine surgeons may not be fully utilizing this critical tool in their clinical practice.”
The authors reported no outside sources of funding, and had no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
AT ENDO 2017
ORLANDO – Endocrinologists made up about one in four of the practitioners performing fine needle aspiration (FNA) biopsies between 2012 and 2014, according to a review of data from the Centers for Medicare & Medicaid Services.
Similarly, endocrinologists performed 25% of image-guided thyroid biopsies.
Endocrine surgeons represent only a small percentage of all practitioners performing head and neck ultrasound exams and image-guided FNA, lead author Mamoona Khokhar, MD, said during a poster presentation at the annual meeting of the Endocrine Society. This is true even though the more portable nature of ultrasound has made it easier for motivated surgeons to incorporate its use into their practice, she said.
Examining 3 years of data from a provider utilization and payment database, Dr. Khokhar and her colleagues identified the types of practitioners who performed head and neck ultrasound, as well as image-guided FNA.
In their analysis, the researchers broadly divided practitioners into surgeons and nonsurgeons. Overall, of the 14,750 median annual practitioners performing head and neck ultrasound between 2012 and 2014, 97.2% were nonsurgeon practitioners, reported Dr. Khokhar, an endocrine surgery fellow at Columbia University Medical Center in New York.
Of all practitioners performing head and neck ultrasound, most (81%) were radiologists. Endocrinologists made up 8% of the overall pool performing ultrasounds.
Breaking the surgeon group down further showed that endocrine surgeons represented 14.7% of surgeons performing head and neck ultrasound, meaning that they made up just 0.4% of the practitioner pool for this procedure. Just over half (52%) of the surgeons performing ultrasounds were otolaryngologists.
The number of practitioners performing image-guided FNA was smaller, at a median 3,695 per year during the study period. Surgeons made up 10.7% of this number. Of the surgeons who performed image-guided FNA, 10.5% were endocrine surgeons. Endocrine surgeons made up 1.1% of all practitioners who billed for FNA.
Again, radiologists made up the majority (58%) of the practitioners performing FNA, and one in four (25%) of practitioners performing FNAs were endocrinologists. Just 5% of the practitioners performing FNAs were otolaryngologists.
More endocrine surgeons performed ultrasound than advanced practice providers (nurse practitioners or physician assistants, 0.2%), pathologists (0.1%), and surgical oncologists (0.04%; P for all, less than .0001). However, advanced practice providers and pathologists both performed significantly more FNAs than did endocrine surgeons (2.1% and 1.8%, P less than .0001).
Although the raw proportion of endocrine surgeons billing for these procedures increased during the study period, the increases were not statistically significant. Dr. Khokhar and her colleagues found that the proportion of American Association of Endocrine Surgeons members who performed head and neck ultrasound grew from 59% in 2012 to 72% in 2014 (P = 0.37), while the proportion performing FNA also increased, from 36% in 2012 to 46% in 2014 (P = .40).
Surgeons, however, may face a number of obstacles in setting up office-based ultrasound, which can lead to underutilization by surgeons, Dr. Khokhar noted, adding that “the results of this study suggest that endocrine surgeons may not be fully utilizing this critical tool in their clinical practice.”
The authors reported no outside sources of funding, and had no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
AT ENDO 2017
ORLANDO – Endocrinologists made up about one in four of the practitioners performing fine needle aspiration (FNA) biopsies between 2012 and 2014, according to a review of data from the Centers for Medicare & Medicaid Services.
Similarly, endocrinologists performed 25% of image-guided thyroid biopsies.
Endocrine surgeons represent only a small percentage of all practitioners performing head and neck ultrasound exams and image-guided FNA, lead author Mamoona Khokhar, MD, said during a poster presentation at the annual meeting of the Endocrine Society. This is true even though the more portable nature of ultrasound has made it easier for motivated surgeons to incorporate its use into their practice, she said.
Examining 3 years of data from a provider utilization and payment database, Dr. Khokhar and her colleagues identified the types of practitioners who performed head and neck ultrasound, as well as image-guided FNA.
In their analysis, the researchers broadly divided practitioners into surgeons and nonsurgeons. Overall, of the 14,750 median annual practitioners performing head and neck ultrasound between 2012 and 2014, 97.2% were nonsurgeon practitioners, reported Dr. Khokhar, an endocrine surgery fellow at Columbia University Medical Center in New York.
Of all practitioners performing head and neck ultrasound, most (81%) were radiologists. Endocrinologists made up 8% of the overall pool performing ultrasounds.
Breaking the surgeon group down further showed that endocrine surgeons represented 14.7% of surgeons performing head and neck ultrasound, meaning that they made up just 0.4% of the practitioner pool for this procedure. Just over half (52%) of the surgeons performing ultrasounds were otolaryngologists.
The number of practitioners performing image-guided FNA was smaller, at a median 3,695 per year during the study period. Surgeons made up 10.7% of this number. Of the surgeons who performed image-guided FNA, 10.5% were endocrine surgeons. Endocrine surgeons made up 1.1% of all practitioners who billed for FNA.
Again, radiologists made up the majority (58%) of the practitioners performing FNA, and one in four (25%) of practitioners performing FNAs were endocrinologists. Just 5% of the practitioners performing FNAs were otolaryngologists.
More endocrine surgeons performed ultrasound than advanced practice providers (nurse practitioners or physician assistants, 0.2%), pathologists (0.1%), and surgical oncologists (0.04%; P for all, less than .0001). However, advanced practice providers and pathologists both performed significantly more FNAs than did endocrine surgeons (2.1% and 1.8%, P less than .0001).
Although the raw proportion of endocrine surgeons billing for these procedures increased during the study period, the increases were not statistically significant. Dr. Khokhar and her colleagues found that the proportion of American Association of Endocrine Surgeons members who performed head and neck ultrasound grew from 59% in 2012 to 72% in 2014 (P = 0.37), while the proportion performing FNA also increased, from 36% in 2012 to 46% in 2014 (P = .40).
Surgeons, however, may face a number of obstacles in setting up office-based ultrasound, which can lead to underutilization by surgeons, Dr. Khokhar noted, adding that “the results of this study suggest that endocrine surgeons may not be fully utilizing this critical tool in their clinical practice.”
The authors reported no outside sources of funding, and had no relevant conflicts of interest.
[email protected]
On Twitter @karioakes
Key clinical point:
Major finding: Endocrinologists made up 25% of the practitioners performing FNAs.
Data source: A retrospective analysis of 3 years’ worth of data on head and neck ultrasound and fine needle aspiration from the Centers for Medicare & Medicaid Services.
Disclosures: None of the study authors reported relevant disclosures, and no external source of funding was reported.