User login
What’s Eating You? Chiggers
Identifying Characteristics and Disease Transmission
Chiggers belong to the Trombiculidae family of mites and also are referred to as harvest mites, harvest bugs, harvest lice, mower’s mites, and redbugs.1 The term chigger specifically describes the larval stage of this mite’s life cycle, as it is the only stage responsible for chigger bites. The nymph and adult phases feed on vegetable matter. Trombiculid mites are most often found in forests, grassy areas, gardens, and moist areas of soil near bodies of water. Trombicula alfreddugesi is the most common species in the United States, and these mites mainly live in the southeastern and south central regions of the country. Conversely, Trombicula autumnalis is most predominant in Western Europe and East Asia.1
The life cycle of the mite includes the egg, larval, nymphal, and adult stages.2 Due to their need for air humidity greater than 80%, mites lay their eggs on low leaves, blades of grass, or on the ground. They spend most of their lives on vegetation no more than 30 cm above ground level.3 Eggs remain dormant for approximately 6 days until the hatching of the prelarvae, which have 6 legs and are nonfeeding. It takes another 6 days for the prelarvae to mature into larvae. Measuring 0.15 to 0.3 mm in length, mite larvae are a mere fraction of the size of adult mites, which generally are 1 to 2 mm in length, and are bright red or brown-red in color (Figure 1).

The biting larvae have many acceptable hosts including turtles, toads, birds, small mammals, and humans, which act as accidental hosts. Larvae remain on vegetation waiting for a suitable host to pass by so they may attach to its skin and remain there for several days. In the exploration for an ideal area to begin feeding (eg, thin epidermis,4 localized increased air humidity5), larvae can travel extensively on the skin; however, they often are stopped by tight-fitting sections of clothing (eg, waistbands), so bites are mostly found in clusters. To feed, mite larvae latch onto the skin using chelicerae, jawlike appendages found in the front of the mouth in arachnids.6 They then inject digestive enzymes that liquefy epidermal cells on direct contact, which results in the formation of a stylostome from which the mites may suck up lymph fluid and broken down tissue.7 Although the actual initial bite is painless, this feeding process leads to the localized inflammation and irritation noticed by infested patients.8
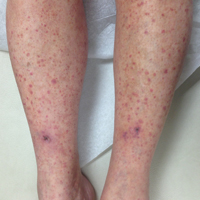
The classic clinical presentation includes severe pruritus and cutaneous swelling as well as erythema caused by the combination of several factors, such as enzyme-induced cellular mechanical damage, human immune response, and sometimes a superimposed bacterial infection. Papules and papulovesicles appear in groups, most commonly affecting the legs and waistline (Figure 2).9 Itching generally occurs within hours of larval latching and subsides within 72 hours. Cutaneous lesions typically take 1 to 2 weeks to heal. In some rare cases, patients may react with urticarial, bullous, or morbilliform eruptions, and the inflammation and pruritus can last for weeks.6 Summer penile syndrome has been noted in boys who display a local hypersensitivity to chigger bites.10 This syndrome represents a triad of penile swelling, dysuria, and pruritus, which lasts for a few days to a few weeks.

Disease Management
Because the lesions are self-healing, treatment is focused on symptomatic relief of itching by means of topical antipruritics (eg, camphor and menthol, pramoxine lotion) or oral antihistamines (eg, diphenhydramine, hydroxyzine). Potent topical corticosteroids may be used to alleviate inflammation and pruritus, especially when occluded under plastic wrap to increase absorption. In severe cases, an intralesional triamcinolone acetonide (2.5–5 mg/mL) injection may be required.9 The best practice, however, is to take preventative measures to avoid becoming a host for the mites. Patients should take special care when traveling in infested areas by completely covering their skin, tucking pant cuffs into their socks, and applying products containing DEET (N,N-diethyl-meta-toluamide or N,N-diethyl-3-methylbenzamide) to the skin and clothing. The odds of prevention are increased even further when clothing also is treated with permethrin.11
In parts of Asia and Australia, these mites may transmit Orientia tsutsugamushi, the organism responsible for scrub typhus, through their saliva during a bite.12 Scrub typhus is associated with an eschar, as well as fever, intense headache, and diffuse myalgia. It responds well to treatment with doxycycline 100 mg twice daily.13 Studies investigating genetic material found in trombiculid mites across the globe have detected Ehrlichia-specific DNA in Spain,14Borrelia-specific DNA in the Czech Republic,15,16 and Hantavirus-specific RNA in Texas.17 There is evidence that the mites play a role in maintenance of zoonotic reservoirs, while humans are infected via ingestion or inhalation of infectious rodent extreta.18
- McClain D, Dana AN, Goldenberg G. Mite infestations. Dermatol Ther. 2009;22:327-346.
- Lane RP, Crosskey RW. Medical Insects and Arachnids. London, England: Chapman & Hall; 1993.
- Gasser R, Wyniger R. Distribution and control of Trombiculidae with special reference to Trombicula autumnalis [article in German]. Acta Trop. 1955;12:308-326.
- Jones BM. The penetration of the host tissue by the harvest mite, Trombicula autumnalis Shaw. Parasitology. 1950;40:247-260.
- Farkas J. Concerning the predilected localisation of the manifestations of trombidiosis. predilected localisation and its relation to the ways of invasion [article in German]. Dermatol Monatsschr. 1979;165:858-861.
- Jones JG. Chiggers. Am Fam Physician. 1987;36:149-152.
- Shatrov AB. Stylostome formation in trombiculid mites (Acariformes: Trombiculidae). Exp Appl Acarol. 2009;49:261-280.
- Potts J. Eradication of ectoparasites in children. how to treat infestations of lice, scabies, and chiggers. Postgrad Med. 2001;110:57-59, 63-64.
- Elston DM. Arthropods and infestations. Infectious Diseases of the Skin. Boca Raton, FL; CRC Press; 2009:112-116.
- Smith GA, Sharma V, Knapp JF, et al. The summer penile syndrome: seasonal acute hypersensitivity reaction caused by chigger bites on the penis. Pediatr Emerg Care. 1998;14:116-118.
- Young GD, Evans S. Safety of DEET and permethrin in the prevention of arthropod attack. Military Med. 1998;163:324-330.
- Watt G, Parola P. Scrub typhus and tropical rickettsioses. Curr Opin Infect Dis. 2003;16:429-436.
- Panpanich R, Garner P. Antibiotics for treating scrub typhus. Cochrane Database Syst Rev. 2000;2:CD002150.
- Fernández-Soto P, Pérez-Sánchez R, Encinas-Grandes A. Molecular detection of Ehrlichia phagocytophila genogroup organisms in larvae of Neotrombicula autumnalis (Acari: Trombiculidae) captured in Spain. J Parasitol. 2001;87:1482-1483.
- Literak I, Stekolnikov AA, Sychra O, et al. Larvae of chigger mites Neotrombicula spp. (Acari: Trombiculidae) exhibited Borrelia but no Anaplasma infections: a field study including birds from the Czech Carpathians as hosts of chiggers. Exp Appl Acarol. 2008;44:307-314.
- Kampen H, Schöler A, Metzen M, et al. Neotrombicula autumnalis (Acari, Trombiculidae) as a vector for Borrelia burgdorferi sensu lato? Exp Appl Acarol. 2004;33:93-102.
- Houck MA, Qin H, Roberts HR. Hantavirus transmission: potential role of ectoparasites. Vector Borne Zoonotic Dis. 2001;1:75-79.
- Yu XJ, Tesh RB. The role of mites in the transmission and maintenance of Hantaan virus (Hantavirus: Bunyaviridae). J Infect Dis. 2014;210:1693-1699.
Identifying Characteristics and Disease Transmission
Chiggers belong to the Trombiculidae family of mites and also are referred to as harvest mites, harvest bugs, harvest lice, mower’s mites, and redbugs.1 The term chigger specifically describes the larval stage of this mite’s life cycle, as it is the only stage responsible for chigger bites. The nymph and adult phases feed on vegetable matter. Trombiculid mites are most often found in forests, grassy areas, gardens, and moist areas of soil near bodies of water. Trombicula alfreddugesi is the most common species in the United States, and these mites mainly live in the southeastern and south central regions of the country. Conversely, Trombicula autumnalis is most predominant in Western Europe and East Asia.1
The life cycle of the mite includes the egg, larval, nymphal, and adult stages.2 Due to their need for air humidity greater than 80%, mites lay their eggs on low leaves, blades of grass, or on the ground. They spend most of their lives on vegetation no more than 30 cm above ground level.3 Eggs remain dormant for approximately 6 days until the hatching of the prelarvae, which have 6 legs and are nonfeeding. It takes another 6 days for the prelarvae to mature into larvae. Measuring 0.15 to 0.3 mm in length, mite larvae are a mere fraction of the size of adult mites, which generally are 1 to 2 mm in length, and are bright red or brown-red in color (Figure 1).

The biting larvae have many acceptable hosts including turtles, toads, birds, small mammals, and humans, which act as accidental hosts. Larvae remain on vegetation waiting for a suitable host to pass by so they may attach to its skin and remain there for several days. In the exploration for an ideal area to begin feeding (eg, thin epidermis,4 localized increased air humidity5), larvae can travel extensively on the skin; however, they often are stopped by tight-fitting sections of clothing (eg, waistbands), so bites are mostly found in clusters. To feed, mite larvae latch onto the skin using chelicerae, jawlike appendages found in the front of the mouth in arachnids.6 They then inject digestive enzymes that liquefy epidermal cells on direct contact, which results in the formation of a stylostome from which the mites may suck up lymph fluid and broken down tissue.7 Although the actual initial bite is painless, this feeding process leads to the localized inflammation and irritation noticed by infested patients.8
The classic clinical presentation includes severe pruritus and cutaneous swelling as well as erythema caused by the combination of several factors, such as enzyme-induced cellular mechanical damage, human immune response, and sometimes a superimposed bacterial infection. Papules and papulovesicles appear in groups, most commonly affecting the legs and waistline (Figure 2).9 Itching generally occurs within hours of larval latching and subsides within 72 hours. Cutaneous lesions typically take 1 to 2 weeks to heal. In some rare cases, patients may react with urticarial, bullous, or morbilliform eruptions, and the inflammation and pruritus can last for weeks.6 Summer penile syndrome has been noted in boys who display a local hypersensitivity to chigger bites.10 This syndrome represents a triad of penile swelling, dysuria, and pruritus, which lasts for a few days to a few weeks.

Disease Management
Because the lesions are self-healing, treatment is focused on symptomatic relief of itching by means of topical antipruritics (eg, camphor and menthol, pramoxine lotion) or oral antihistamines (eg, diphenhydramine, hydroxyzine). Potent topical corticosteroids may be used to alleviate inflammation and pruritus, especially when occluded under plastic wrap to increase absorption. In severe cases, an intralesional triamcinolone acetonide (2.5–5 mg/mL) injection may be required.9 The best practice, however, is to take preventative measures to avoid becoming a host for the mites. Patients should take special care when traveling in infested areas by completely covering their skin, tucking pant cuffs into their socks, and applying products containing DEET (N,N-diethyl-meta-toluamide or N,N-diethyl-3-methylbenzamide) to the skin and clothing. The odds of prevention are increased even further when clothing also is treated with permethrin.11
In parts of Asia and Australia, these mites may transmit Orientia tsutsugamushi, the organism responsible for scrub typhus, through their saliva during a bite.12 Scrub typhus is associated with an eschar, as well as fever, intense headache, and diffuse myalgia. It responds well to treatment with doxycycline 100 mg twice daily.13 Studies investigating genetic material found in trombiculid mites across the globe have detected Ehrlichia-specific DNA in Spain,14Borrelia-specific DNA in the Czech Republic,15,16 and Hantavirus-specific RNA in Texas.17 There is evidence that the mites play a role in maintenance of zoonotic reservoirs, while humans are infected via ingestion or inhalation of infectious rodent extreta.18
Identifying Characteristics and Disease Transmission
Chiggers belong to the Trombiculidae family of mites and also are referred to as harvest mites, harvest bugs, harvest lice, mower’s mites, and redbugs.1 The term chigger specifically describes the larval stage of this mite’s life cycle, as it is the only stage responsible for chigger bites. The nymph and adult phases feed on vegetable matter. Trombiculid mites are most often found in forests, grassy areas, gardens, and moist areas of soil near bodies of water. Trombicula alfreddugesi is the most common species in the United States, and these mites mainly live in the southeastern and south central regions of the country. Conversely, Trombicula autumnalis is most predominant in Western Europe and East Asia.1
The life cycle of the mite includes the egg, larval, nymphal, and adult stages.2 Due to their need for air humidity greater than 80%, mites lay their eggs on low leaves, blades of grass, or on the ground. They spend most of their lives on vegetation no more than 30 cm above ground level.3 Eggs remain dormant for approximately 6 days until the hatching of the prelarvae, which have 6 legs and are nonfeeding. It takes another 6 days for the prelarvae to mature into larvae. Measuring 0.15 to 0.3 mm in length, mite larvae are a mere fraction of the size of adult mites, which generally are 1 to 2 mm in length, and are bright red or brown-red in color (Figure 1).

The biting larvae have many acceptable hosts including turtles, toads, birds, small mammals, and humans, which act as accidental hosts. Larvae remain on vegetation waiting for a suitable host to pass by so they may attach to its skin and remain there for several days. In the exploration for an ideal area to begin feeding (eg, thin epidermis,4 localized increased air humidity5), larvae can travel extensively on the skin; however, they often are stopped by tight-fitting sections of clothing (eg, waistbands), so bites are mostly found in clusters. To feed, mite larvae latch onto the skin using chelicerae, jawlike appendages found in the front of the mouth in arachnids.6 They then inject digestive enzymes that liquefy epidermal cells on direct contact, which results in the formation of a stylostome from which the mites may suck up lymph fluid and broken down tissue.7 Although the actual initial bite is painless, this feeding process leads to the localized inflammation and irritation noticed by infested patients.8
The classic clinical presentation includes severe pruritus and cutaneous swelling as well as erythema caused by the combination of several factors, such as enzyme-induced cellular mechanical damage, human immune response, and sometimes a superimposed bacterial infection. Papules and papulovesicles appear in groups, most commonly affecting the legs and waistline (Figure 2).9 Itching generally occurs within hours of larval latching and subsides within 72 hours. Cutaneous lesions typically take 1 to 2 weeks to heal. In some rare cases, patients may react with urticarial, bullous, or morbilliform eruptions, and the inflammation and pruritus can last for weeks.6 Summer penile syndrome has been noted in boys who display a local hypersensitivity to chigger bites.10 This syndrome represents a triad of penile swelling, dysuria, and pruritus, which lasts for a few days to a few weeks.

Disease Management
Because the lesions are self-healing, treatment is focused on symptomatic relief of itching by means of topical antipruritics (eg, camphor and menthol, pramoxine lotion) or oral antihistamines (eg, diphenhydramine, hydroxyzine). Potent topical corticosteroids may be used to alleviate inflammation and pruritus, especially when occluded under plastic wrap to increase absorption. In severe cases, an intralesional triamcinolone acetonide (2.5–5 mg/mL) injection may be required.9 The best practice, however, is to take preventative measures to avoid becoming a host for the mites. Patients should take special care when traveling in infested areas by completely covering their skin, tucking pant cuffs into their socks, and applying products containing DEET (N,N-diethyl-meta-toluamide or N,N-diethyl-3-methylbenzamide) to the skin and clothing. The odds of prevention are increased even further when clothing also is treated with permethrin.11
In parts of Asia and Australia, these mites may transmit Orientia tsutsugamushi, the organism responsible for scrub typhus, through their saliva during a bite.12 Scrub typhus is associated with an eschar, as well as fever, intense headache, and diffuse myalgia. It responds well to treatment with doxycycline 100 mg twice daily.13 Studies investigating genetic material found in trombiculid mites across the globe have detected Ehrlichia-specific DNA in Spain,14Borrelia-specific DNA in the Czech Republic,15,16 and Hantavirus-specific RNA in Texas.17 There is evidence that the mites play a role in maintenance of zoonotic reservoirs, while humans are infected via ingestion or inhalation of infectious rodent extreta.18
- McClain D, Dana AN, Goldenberg G. Mite infestations. Dermatol Ther. 2009;22:327-346.
- Lane RP, Crosskey RW. Medical Insects and Arachnids. London, England: Chapman & Hall; 1993.
- Gasser R, Wyniger R. Distribution and control of Trombiculidae with special reference to Trombicula autumnalis [article in German]. Acta Trop. 1955;12:308-326.
- Jones BM. The penetration of the host tissue by the harvest mite, Trombicula autumnalis Shaw. Parasitology. 1950;40:247-260.
- Farkas J. Concerning the predilected localisation of the manifestations of trombidiosis. predilected localisation and its relation to the ways of invasion [article in German]. Dermatol Monatsschr. 1979;165:858-861.
- Jones JG. Chiggers. Am Fam Physician. 1987;36:149-152.
- Shatrov AB. Stylostome formation in trombiculid mites (Acariformes: Trombiculidae). Exp Appl Acarol. 2009;49:261-280.
- Potts J. Eradication of ectoparasites in children. how to treat infestations of lice, scabies, and chiggers. Postgrad Med. 2001;110:57-59, 63-64.
- Elston DM. Arthropods and infestations. Infectious Diseases of the Skin. Boca Raton, FL; CRC Press; 2009:112-116.
- Smith GA, Sharma V, Knapp JF, et al. The summer penile syndrome: seasonal acute hypersensitivity reaction caused by chigger bites on the penis. Pediatr Emerg Care. 1998;14:116-118.
- Young GD, Evans S. Safety of DEET and permethrin in the prevention of arthropod attack. Military Med. 1998;163:324-330.
- Watt G, Parola P. Scrub typhus and tropical rickettsioses. Curr Opin Infect Dis. 2003;16:429-436.
- Panpanich R, Garner P. Antibiotics for treating scrub typhus. Cochrane Database Syst Rev. 2000;2:CD002150.
- Fernández-Soto P, Pérez-Sánchez R, Encinas-Grandes A. Molecular detection of Ehrlichia phagocytophila genogroup organisms in larvae of Neotrombicula autumnalis (Acari: Trombiculidae) captured in Spain. J Parasitol. 2001;87:1482-1483.
- Literak I, Stekolnikov AA, Sychra O, et al. Larvae of chigger mites Neotrombicula spp. (Acari: Trombiculidae) exhibited Borrelia but no Anaplasma infections: a field study including birds from the Czech Carpathians as hosts of chiggers. Exp Appl Acarol. 2008;44:307-314.
- Kampen H, Schöler A, Metzen M, et al. Neotrombicula autumnalis (Acari, Trombiculidae) as a vector for Borrelia burgdorferi sensu lato? Exp Appl Acarol. 2004;33:93-102.
- Houck MA, Qin H, Roberts HR. Hantavirus transmission: potential role of ectoparasites. Vector Borne Zoonotic Dis. 2001;1:75-79.
- Yu XJ, Tesh RB. The role of mites in the transmission and maintenance of Hantaan virus (Hantavirus: Bunyaviridae). J Infect Dis. 2014;210:1693-1699.
- McClain D, Dana AN, Goldenberg G. Mite infestations. Dermatol Ther. 2009;22:327-346.
- Lane RP, Crosskey RW. Medical Insects and Arachnids. London, England: Chapman & Hall; 1993.
- Gasser R, Wyniger R. Distribution and control of Trombiculidae with special reference to Trombicula autumnalis [article in German]. Acta Trop. 1955;12:308-326.
- Jones BM. The penetration of the host tissue by the harvest mite, Trombicula autumnalis Shaw. Parasitology. 1950;40:247-260.
- Farkas J. Concerning the predilected localisation of the manifestations of trombidiosis. predilected localisation and its relation to the ways of invasion [article in German]. Dermatol Monatsschr. 1979;165:858-861.
- Jones JG. Chiggers. Am Fam Physician. 1987;36:149-152.
- Shatrov AB. Stylostome formation in trombiculid mites (Acariformes: Trombiculidae). Exp Appl Acarol. 2009;49:261-280.
- Potts J. Eradication of ectoparasites in children. how to treat infestations of lice, scabies, and chiggers. Postgrad Med. 2001;110:57-59, 63-64.
- Elston DM. Arthropods and infestations. Infectious Diseases of the Skin. Boca Raton, FL; CRC Press; 2009:112-116.
- Smith GA, Sharma V, Knapp JF, et al. The summer penile syndrome: seasonal acute hypersensitivity reaction caused by chigger bites on the penis. Pediatr Emerg Care. 1998;14:116-118.
- Young GD, Evans S. Safety of DEET and permethrin in the prevention of arthropod attack. Military Med. 1998;163:324-330.
- Watt G, Parola P. Scrub typhus and tropical rickettsioses. Curr Opin Infect Dis. 2003;16:429-436.
- Panpanich R, Garner P. Antibiotics for treating scrub typhus. Cochrane Database Syst Rev. 2000;2:CD002150.
- Fernández-Soto P, Pérez-Sánchez R, Encinas-Grandes A. Molecular detection of Ehrlichia phagocytophila genogroup organisms in larvae of Neotrombicula autumnalis (Acari: Trombiculidae) captured in Spain. J Parasitol. 2001;87:1482-1483.
- Literak I, Stekolnikov AA, Sychra O, et al. Larvae of chigger mites Neotrombicula spp. (Acari: Trombiculidae) exhibited Borrelia but no Anaplasma infections: a field study including birds from the Czech Carpathians as hosts of chiggers. Exp Appl Acarol. 2008;44:307-314.
- Kampen H, Schöler A, Metzen M, et al. Neotrombicula autumnalis (Acari, Trombiculidae) as a vector for Borrelia burgdorferi sensu lato? Exp Appl Acarol. 2004;33:93-102.
- Houck MA, Qin H, Roberts HR. Hantavirus transmission: potential role of ectoparasites. Vector Borne Zoonotic Dis. 2001;1:75-79.
- Yu XJ, Tesh RB. The role of mites in the transmission and maintenance of Hantaan virus (Hantavirus: Bunyaviridae). J Infect Dis. 2014;210:1693-1699.
Practice Points
- The classic clinical presentation of chigger bites includes severe pruritus, cutaneous swelling, and erythematous papules and papulovesicles appearing in groups, most commonly affecting the legs and waistline.
- Because itching generally subsides within 72 hours of the chigger bite and cutaneous lesions typically heal within 1 to 2 weeks, treatment is focused on symptomatic relief.
- Symptomatic relief may be achieved by means of topical antipruritics or oral antihistamines as well as potent topical corticosteroids or an intralesional triamcinolone acetonide injection in severe cases.
NOTCH1 mutation predicts reduced ofatumumab efficacy in CLL
NEW YORK – NOTCH1 gene mutation appears to predict reduced efficacy of ofatumumab in patients with relapsed/refractory chronic lymphocytic leukemia, according to an analysis of patient DNA samples and data from the phase III COMPLEMENT 2 trial.
Recurrent mutations in NOTCH1, TP53, and SF3B1 are common in CLL and have been associated with adverse outcomes in previous studies; NOTCH1 mutation, in particular, was associated with poor outcome when rituximab was added to standard chemotherapy, indicating that the mutation is a predictive factor in the context of chemoimmunotherapy, Eugen Tausch, MD, of the University of Ulm, Germany, said at the annual International Workshop on Chronic Lymphocytic Leukemia.
The incidence and clinical impact of all three mutations were evaluated in relapsed/refractory CLL patients who were part of the COMPLEMENT 2 trial, which compared fludarabine and cyclophosphamide (FC) with FC+ofatumumab (FCO).
The mutation analysis of 325 available patient samples (out of 365) identified 221 mutations in 142 patients: 56 NOTCH1, 96 TP53, and 69 SF3B1 mutations, Dr. Tausch said.
The current study cohort was representative of the full COMPLEMENT 2 analysis set, he noted.
Additional TP53 mutations were found in 20 of 61 TP53 mutation patients, whereas only 4 of 64 SF3B1 mutation patients and 3 of 53 NOTCH1 mutation patients had additional mutations in SF3B1 and NOTCH1, respectively. TP53 mutation was associated with del(17p), and NOTCH1 mutation with +12q and elevated b2MG.
“We did not find associations with IGHV, gender, age, Binet stage, ECOG performance state, B symptoms, or WBC,” Dr. Tausch said.
In terms of outcomes as associated with the mutations, patients with TP53 mutation or SF3B1 mutation had a significantly worse overall response to treatment (overall response rate 67.8% vs. 84.4% for TP53 mutated vs. wild type, and 71.9% vs. 83.75% SF3B1 mutated vs. wild type, respectively). The findings were similar when looking at the treatment arms separately, he noted.
However, as in the full analysis set, progression-free survival among the subset of patients included in the current analysis was better in those who received FCO than in those who received FC (28.1 months vs. 18.1 months; hazard ratio, 0.67). TP53 mutation was an adverse prognostic factor overall in the current analysis (HR, 1.93), as well as in each treatment arm (HR for the FC arm, 2.14, and for the FCO arm, 1.81). TP53 mutation also was associated with decreased overall survival (HR, 2.11). Neither SF3B1 mutation nor NOTCH1 mutation were associated with differences in progression-free or overall survival, Dr. Tausch said.
CD20 expression on cell surface as measured using flow cytometry did not differ in wild-type vs. mutated patients, he said.
Multivariate analysis showed that independent prognostic factors for progression-free survival included FCO therapy (HR, 0.66), del(17p) (HR, 4.47), unmutated IGHV (HR, 2.17), and TP53 mutation (HR, 1.80), and independent prognostic factors for overall survival included del(17p) (HR, 5.02), unmutated IGHV (HR, 1.85), and TP53 mutation (HR, 1.68).
Adding ofatumumab to chemotherapy was beneficial, irrespective of TP53 mutation (HR, 0.52 for TP53 mutation, and HR, 0.68 for TP53 wild type), which confirms the prognostic value of TP53 mutation, he said.
With respect to NOTCH1, ofatumumab was beneficial in patients with NOTCH1 wild type but not in patients with NOTCH1 mutation (HR, 0.64 and 0.86, respectively).
This effect was not explained by CD20 expression levels, Dr. Tausch said.
The findings of this analysis suggest that NOTCH1 mutation is an independent predictive factor for reduced efficacy of ofatumumab, he said.
“Therefore, patients with a NOTCH1 mutation may be considered for chemotherapy without type1 CD20 antibodies or a treatment with novel compounds,” he concluded.
Dr. Tausch reported receiving research support from Novartis.
NEW YORK – NOTCH1 gene mutation appears to predict reduced efficacy of ofatumumab in patients with relapsed/refractory chronic lymphocytic leukemia, according to an analysis of patient DNA samples and data from the phase III COMPLEMENT 2 trial.
Recurrent mutations in NOTCH1, TP53, and SF3B1 are common in CLL and have been associated with adverse outcomes in previous studies; NOTCH1 mutation, in particular, was associated with poor outcome when rituximab was added to standard chemotherapy, indicating that the mutation is a predictive factor in the context of chemoimmunotherapy, Eugen Tausch, MD, of the University of Ulm, Germany, said at the annual International Workshop on Chronic Lymphocytic Leukemia.
The incidence and clinical impact of all three mutations were evaluated in relapsed/refractory CLL patients who were part of the COMPLEMENT 2 trial, which compared fludarabine and cyclophosphamide (FC) with FC+ofatumumab (FCO).
The mutation analysis of 325 available patient samples (out of 365) identified 221 mutations in 142 patients: 56 NOTCH1, 96 TP53, and 69 SF3B1 mutations, Dr. Tausch said.
The current study cohort was representative of the full COMPLEMENT 2 analysis set, he noted.
Additional TP53 mutations were found in 20 of 61 TP53 mutation patients, whereas only 4 of 64 SF3B1 mutation patients and 3 of 53 NOTCH1 mutation patients had additional mutations in SF3B1 and NOTCH1, respectively. TP53 mutation was associated with del(17p), and NOTCH1 mutation with +12q and elevated b2MG.
“We did not find associations with IGHV, gender, age, Binet stage, ECOG performance state, B symptoms, or WBC,” Dr. Tausch said.
In terms of outcomes as associated with the mutations, patients with TP53 mutation or SF3B1 mutation had a significantly worse overall response to treatment (overall response rate 67.8% vs. 84.4% for TP53 mutated vs. wild type, and 71.9% vs. 83.75% SF3B1 mutated vs. wild type, respectively). The findings were similar when looking at the treatment arms separately, he noted.
However, as in the full analysis set, progression-free survival among the subset of patients included in the current analysis was better in those who received FCO than in those who received FC (28.1 months vs. 18.1 months; hazard ratio, 0.67). TP53 mutation was an adverse prognostic factor overall in the current analysis (HR, 1.93), as well as in each treatment arm (HR for the FC arm, 2.14, and for the FCO arm, 1.81). TP53 mutation also was associated with decreased overall survival (HR, 2.11). Neither SF3B1 mutation nor NOTCH1 mutation were associated with differences in progression-free or overall survival, Dr. Tausch said.
CD20 expression on cell surface as measured using flow cytometry did not differ in wild-type vs. mutated patients, he said.
Multivariate analysis showed that independent prognostic factors for progression-free survival included FCO therapy (HR, 0.66), del(17p) (HR, 4.47), unmutated IGHV (HR, 2.17), and TP53 mutation (HR, 1.80), and independent prognostic factors for overall survival included del(17p) (HR, 5.02), unmutated IGHV (HR, 1.85), and TP53 mutation (HR, 1.68).
Adding ofatumumab to chemotherapy was beneficial, irrespective of TP53 mutation (HR, 0.52 for TP53 mutation, and HR, 0.68 for TP53 wild type), which confirms the prognostic value of TP53 mutation, he said.
With respect to NOTCH1, ofatumumab was beneficial in patients with NOTCH1 wild type but not in patients with NOTCH1 mutation (HR, 0.64 and 0.86, respectively).
This effect was not explained by CD20 expression levels, Dr. Tausch said.
The findings of this analysis suggest that NOTCH1 mutation is an independent predictive factor for reduced efficacy of ofatumumab, he said.
“Therefore, patients with a NOTCH1 mutation may be considered for chemotherapy without type1 CD20 antibodies or a treatment with novel compounds,” he concluded.
Dr. Tausch reported receiving research support from Novartis.
NEW YORK – NOTCH1 gene mutation appears to predict reduced efficacy of ofatumumab in patients with relapsed/refractory chronic lymphocytic leukemia, according to an analysis of patient DNA samples and data from the phase III COMPLEMENT 2 trial.
Recurrent mutations in NOTCH1, TP53, and SF3B1 are common in CLL and have been associated with adverse outcomes in previous studies; NOTCH1 mutation, in particular, was associated with poor outcome when rituximab was added to standard chemotherapy, indicating that the mutation is a predictive factor in the context of chemoimmunotherapy, Eugen Tausch, MD, of the University of Ulm, Germany, said at the annual International Workshop on Chronic Lymphocytic Leukemia.
The incidence and clinical impact of all three mutations were evaluated in relapsed/refractory CLL patients who were part of the COMPLEMENT 2 trial, which compared fludarabine and cyclophosphamide (FC) with FC+ofatumumab (FCO).
The mutation analysis of 325 available patient samples (out of 365) identified 221 mutations in 142 patients: 56 NOTCH1, 96 TP53, and 69 SF3B1 mutations, Dr. Tausch said.
The current study cohort was representative of the full COMPLEMENT 2 analysis set, he noted.
Additional TP53 mutations were found in 20 of 61 TP53 mutation patients, whereas only 4 of 64 SF3B1 mutation patients and 3 of 53 NOTCH1 mutation patients had additional mutations in SF3B1 and NOTCH1, respectively. TP53 mutation was associated with del(17p), and NOTCH1 mutation with +12q and elevated b2MG.
“We did not find associations with IGHV, gender, age, Binet stage, ECOG performance state, B symptoms, or WBC,” Dr. Tausch said.
In terms of outcomes as associated with the mutations, patients with TP53 mutation or SF3B1 mutation had a significantly worse overall response to treatment (overall response rate 67.8% vs. 84.4% for TP53 mutated vs. wild type, and 71.9% vs. 83.75% SF3B1 mutated vs. wild type, respectively). The findings were similar when looking at the treatment arms separately, he noted.
However, as in the full analysis set, progression-free survival among the subset of patients included in the current analysis was better in those who received FCO than in those who received FC (28.1 months vs. 18.1 months; hazard ratio, 0.67). TP53 mutation was an adverse prognostic factor overall in the current analysis (HR, 1.93), as well as in each treatment arm (HR for the FC arm, 2.14, and for the FCO arm, 1.81). TP53 mutation also was associated with decreased overall survival (HR, 2.11). Neither SF3B1 mutation nor NOTCH1 mutation were associated with differences in progression-free or overall survival, Dr. Tausch said.
CD20 expression on cell surface as measured using flow cytometry did not differ in wild-type vs. mutated patients, he said.
Multivariate analysis showed that independent prognostic factors for progression-free survival included FCO therapy (HR, 0.66), del(17p) (HR, 4.47), unmutated IGHV (HR, 2.17), and TP53 mutation (HR, 1.80), and independent prognostic factors for overall survival included del(17p) (HR, 5.02), unmutated IGHV (HR, 1.85), and TP53 mutation (HR, 1.68).
Adding ofatumumab to chemotherapy was beneficial, irrespective of TP53 mutation (HR, 0.52 for TP53 mutation, and HR, 0.68 for TP53 wild type), which confirms the prognostic value of TP53 mutation, he said.
With respect to NOTCH1, ofatumumab was beneficial in patients with NOTCH1 wild type but not in patients with NOTCH1 mutation (HR, 0.64 and 0.86, respectively).
This effect was not explained by CD20 expression levels, Dr. Tausch said.
The findings of this analysis suggest that NOTCH1 mutation is an independent predictive factor for reduced efficacy of ofatumumab, he said.
“Therefore, patients with a NOTCH1 mutation may be considered for chemotherapy without type1 CD20 antibodies or a treatment with novel compounds,” he concluded.
Dr. Tausch reported receiving research support from Novartis.
AT iwCLL MEETING
Key clinical point:
Major finding: Ofatumumab was beneficial in patients with NOTCH1 wild-type, but not in patients with NOTCH1 mutation (hazard ratios, 0.64 and 0.86, respectively).
Data source: A mutation analysis of 325 DNA samples from patients in the phase III COMPLEMENT 2 trial.
Disclosures: Dr. Tausch reported receiving research support from Novartis.
For Americans, less salt is still too much
Americans are buying less packaged food and beverages these days, and they’re getting less salt in the food that they do buy, but very few are getting the optimal sodium density in their purchases, according to a study involving more than 170,000 households.
First, salt content: In 2014, the households taking part in the Nielsen Homescan Consumer Panel were getting 361 mg of salt per 100 g of packaged food purchased, which is 12% less than the 411 mg per 100 g of food purchased in 2000. Overall sodium content, which includes beverages, dropped from 192 mg/100 g to 186 mg/100 g, said Jennifer M. Poti, PhD, of the University of North Carolina at Chapel Hill, and her associates.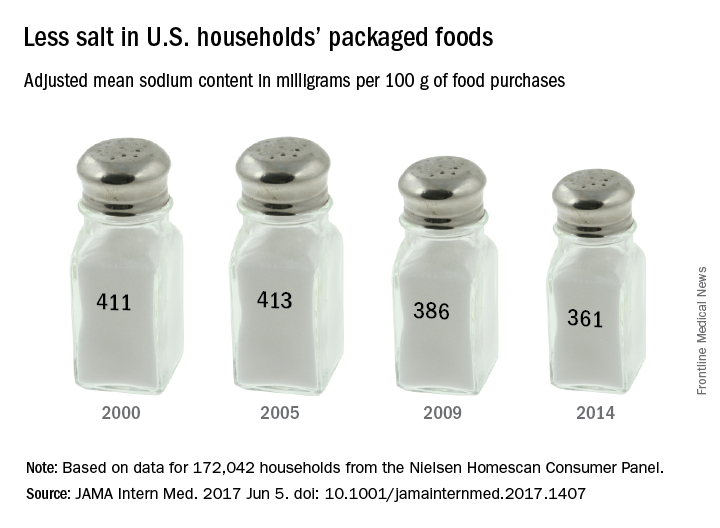
Total food and beverage purchases also were down from 1,328 g/day in 2000 to 1,134 in 2014, and the total sodium content of those purchases followed suit, dropping from 2,363 mg/day in 2000 to 1,967 mg/day in 2014. The decline in total purchases, however, was driven largely by beverages, which fell 21% from 2000 to 2014, while packaged food purchases fell by only 2%, the investigators reported (JAMA Intern Med. 2017 June 5. doi: 10.1001/jamainternmed.2017.1407).
Median sodium density was down significantly from 1,712 to 1,628 mg of sodium per 1,000 kcal, but by 2014, only 1.2% of the 172,042 households included in the study were purchasing the optimal level of 1,100 mg per 1,000 kcal, based on the DASH-Sodium trial and the Health Eating Index-2010, Dr. Poti and her associates said.
“Additional studies are needed to examine whether decreases in sodium from packaged foods were offset by increases in sodium from away-from-home sources,” they said, and since “there were no major shifts in the amount purchased for key food groups … sodium declines may relate mainly to reformulation.”
The study was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Carolina Population Center at the University of North Carolina. One of the investigators is supported by a National Health and Medical Research Council of Australia Early Career Fellowship. The investigators did not report any conflicts of interest.
Americans are buying less packaged food and beverages these days, and they’re getting less salt in the food that they do buy, but very few are getting the optimal sodium density in their purchases, according to a study involving more than 170,000 households.
First, salt content: In 2014, the households taking part in the Nielsen Homescan Consumer Panel were getting 361 mg of salt per 100 g of packaged food purchased, which is 12% less than the 411 mg per 100 g of food purchased in 2000. Overall sodium content, which includes beverages, dropped from 192 mg/100 g to 186 mg/100 g, said Jennifer M. Poti, PhD, of the University of North Carolina at Chapel Hill, and her associates.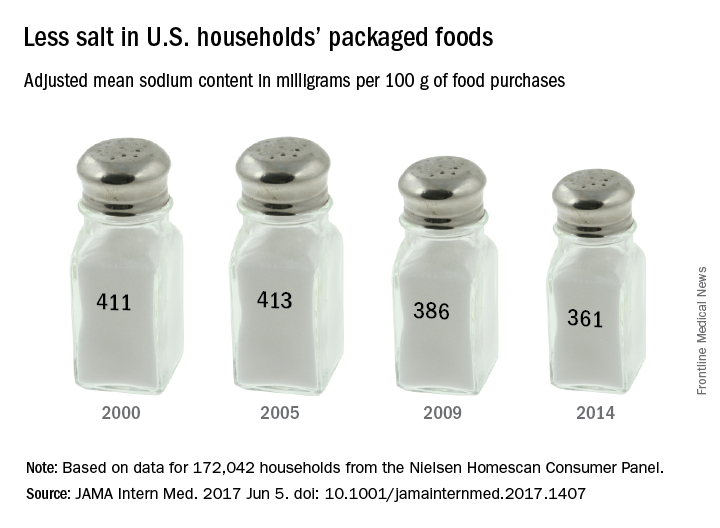
Total food and beverage purchases also were down from 1,328 g/day in 2000 to 1,134 in 2014, and the total sodium content of those purchases followed suit, dropping from 2,363 mg/day in 2000 to 1,967 mg/day in 2014. The decline in total purchases, however, was driven largely by beverages, which fell 21% from 2000 to 2014, while packaged food purchases fell by only 2%, the investigators reported (JAMA Intern Med. 2017 June 5. doi: 10.1001/jamainternmed.2017.1407).
Median sodium density was down significantly from 1,712 to 1,628 mg of sodium per 1,000 kcal, but by 2014, only 1.2% of the 172,042 households included in the study were purchasing the optimal level of 1,100 mg per 1,000 kcal, based on the DASH-Sodium trial and the Health Eating Index-2010, Dr. Poti and her associates said.
“Additional studies are needed to examine whether decreases in sodium from packaged foods were offset by increases in sodium from away-from-home sources,” they said, and since “there were no major shifts in the amount purchased for key food groups … sodium declines may relate mainly to reformulation.”
The study was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Carolina Population Center at the University of North Carolina. One of the investigators is supported by a National Health and Medical Research Council of Australia Early Career Fellowship. The investigators did not report any conflicts of interest.
Americans are buying less packaged food and beverages these days, and they’re getting less salt in the food that they do buy, but very few are getting the optimal sodium density in their purchases, according to a study involving more than 170,000 households.
First, salt content: In 2014, the households taking part in the Nielsen Homescan Consumer Panel were getting 361 mg of salt per 100 g of packaged food purchased, which is 12% less than the 411 mg per 100 g of food purchased in 2000. Overall sodium content, which includes beverages, dropped from 192 mg/100 g to 186 mg/100 g, said Jennifer M. Poti, PhD, of the University of North Carolina at Chapel Hill, and her associates.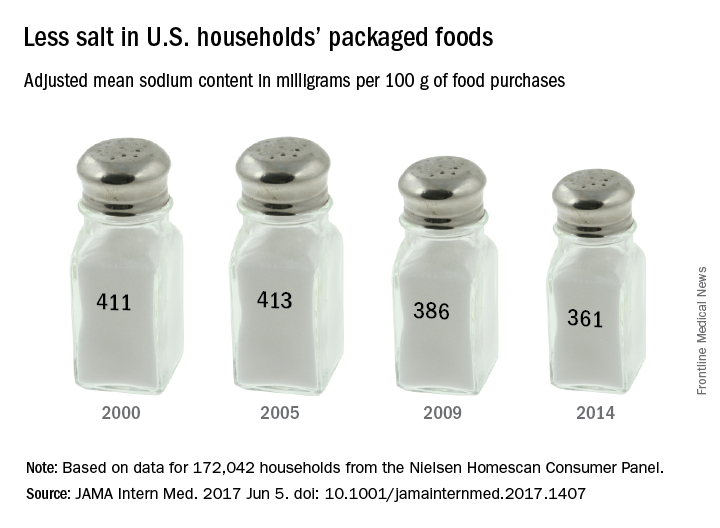
Total food and beverage purchases also were down from 1,328 g/day in 2000 to 1,134 in 2014, and the total sodium content of those purchases followed suit, dropping from 2,363 mg/day in 2000 to 1,967 mg/day in 2014. The decline in total purchases, however, was driven largely by beverages, which fell 21% from 2000 to 2014, while packaged food purchases fell by only 2%, the investigators reported (JAMA Intern Med. 2017 June 5. doi: 10.1001/jamainternmed.2017.1407).
Median sodium density was down significantly from 1,712 to 1,628 mg of sodium per 1,000 kcal, but by 2014, only 1.2% of the 172,042 households included in the study were purchasing the optimal level of 1,100 mg per 1,000 kcal, based on the DASH-Sodium trial and the Health Eating Index-2010, Dr. Poti and her associates said.
“Additional studies are needed to examine whether decreases in sodium from packaged foods were offset by increases in sodium from away-from-home sources,” they said, and since “there were no major shifts in the amount purchased for key food groups … sodium declines may relate mainly to reformulation.”
The study was funded by the Robert Wood Johnson Foundation, the National Institutes of Health, and the Carolina Population Center at the University of North Carolina. One of the investigators is supported by a National Health and Medical Research Council of Australia Early Career Fellowship. The investigators did not report any conflicts of interest.
FROM JAMA INTERNAL MEDICINE
Narrowband UVB Treatment Increases Serum 25-Hydroxyvitamin D Levels in Patients With Chronic Plaque Psoriasis
Psoriasis is a chronic, inflammatory, T-cell–mediated skin disease. Phototherapy, which consists of light used at various wavelengths, is a well-established treatment method for psoriasis vulgaris. Although successful results have been obtained with phototherapy in psoriasis, its mechanism of action is not fully understood. UV light has been shown to have an effect on T-lymphocyte function as well as various components of the natural and acquired immune response. It also has a suppressive effect on the immune system caused by many independent effects.1 Phototherapy currently is available using broadband UVB (290–320 nm), narrowband UVB (NB-UVB)(311–313 nm), 308-nm excimer laser, UVA1 (340–400 nm), psoralen plus UVA, and photopheresis.2 Narrowband UVB treatment with light sources that peak at 311 to 313 nm have been used with high efficacy and a low side-effect profile, becoming the standard phototherapy method for chronic plaque-type psoriasis.3
More than 90% of vitamin D synthesis is formed in the skin following UV exposure, and the wavelengths and the solar spectrum that stimulate vitamin D synthesis have been a focus of research.4 7-Dehydrocholesterol (provitamin D3) is first converted to previtamin D3. Although the necessary UV wavelength for previtamin D3 synthesis is 295 to 300 nm, it is known that production stops below 260 nm and above 315 nm.4-6 Previtamin D3 is unstable and is quickly converted to vitamin D3 in the skinand then to the biologically active form of 1,25-dihydroxyvitamin D3 (calcitriol) following hydroxylation in the liver and kidneys. Calcitriol shows its effect by binding to the special nuclear receptor for vitamin D.7 Many tissues including the keratinocytes, dendritic cells, melanocytes, and sebocytes in the skin have been shown to possess the enzymatic mechanism necessary for 1,25-dihydroxyvitamin D3 production. Vitamin D also is known to have paracrine, autocrine, and intracrine effects on immunomodulation, cell proliferation, differentiation, and apoptosis, in addition to its role in calcium metabolism.5-9 Topical vitamin D and its analogues are used effectively and safely in psoriasis treatment with these effects.10 A correlation between low serum vitamin D levels and chronic inflammation severity has been shown in psoriasis patients in some studies.11,12
In this study, we sought to evaluate the effect of NB-UVB on vitamin D status and related metabolic markers in patients with psoriasis.
Methods
This prospective, single-center study included patients living in or around Eskisehir, Turkey, who were 18 years of age or older and had been diagnosed with chronic plaque psoriasis with a psoriasis area and severity index (PASI) score of 5 or higher. Permission was granted by the local ethics committee. Patients provided written informed consent prior to enrollment. Patients were excluded if they were younger than 18 years; were pregnant or breastfeeding; stayed in open environments for more than 2 hours per day during the summer months (May through September); used drugs affecting calcium metabolism in the last 8 weeks (eg, barbiturates, anticonvulsants, corticosteroids, vitamin D supplements, bisphosphonates); used systemic treatment for psoriasis in the last 8 weeks; used phototherapy or sunbathing in the last 8 weeks; used topical vitamin D analogues in the last 4 weeks; or had a history of psoriatic arthritis and other inflammatory disorders, renal disease, known calcium metabolism disorders, granulomatous disorders, thyroid disease, diabetes mellitus, skin cancer, or abnormal photosensitivity and known lack of response or hypersensitivity to phototherapy.
Clinical Evaluation and Laboratory Studies
The participants’ age, gender, Fitzpatrick skin type, disease duration, dairy intake and vitamin supplement levels, hours of sun exposure per week, detailed medical history, and medications were obtained and documented in the medical records.
Serum 25(OH)D levels were measured using high-performance liquid chromatography/mass spectrometry, serum calcium and phosphorus levels using colorimetric analysis, serum alkaline phosphatase (ALP) levels using the enzymatic colorimetric method, and serum parathyroid hormone (PTH) levels using electrochemiluminescence at baseline and after PASI 75 was achieved with treatment. Vitamin D levels were classified in 3 groups: (1) deficient (<20 ng/mL); (2) inadequate (20–30 ng/mL); and (3) adequate (>30 ng/mL). The PASI scores at baseline and posttreatment were calculated by the same dermatologist (S.S.).
Treatment Protocol and Patient Follow-up
Narrowband UVB treatment was started at 70% of the minimal erythema dose (MED). Phototherapy was administered 3 times weekly for 6 months or until PASI 75 response was achieved. An increase of 20% to 30% from the prior dose was made according to the participants’ clinical status at each treatment session, and the dose was stabilized once the maximum dose was achieved according to skin type—up to 2000 mJ/cm2 for Fitzpatrick skin types I and II, 3000 mJ/cm2 for skin types III and IV, and 5000 mJ/cm2 for skin types V and VI. Participants were allowed to use low- and moderate-potency topical corticosteroids and moisturizers containing urea during the course of treatment. The study physician (S.S.) clinically evaluated participants every 4 weeks for 6 months or until PASI 75 was achieved, and the clinical improvement was calculated as the percentage decrease in PASI score.
Statistical Analysis
The Shapiro-Wilk normalcy test was used for the continuous variables in the study. Variables with a normal distribution were analyzed with the paired t test and 1-way analysis of variance test and presented as mean (SD). Variables without a normal distribution were analyzed with the Wilcoxon t test and the Kruskal-Wallis test and presented as the median and 25th and 75th quartiles. The serum 25(OH)D levels were evaluated according to the seasons with the Kruskal-Wallis test. Categorical variables were expressed as frequency and percentages. The Pearson and Spearman correlation analysis and regression analysis were used to show the relationship between the variables (ie, age, Fitzpatrick skin type, PASI score, maximum NB-UVB dose, and number of sessions). The statistical significance level was set at P≤.05. Statistical analyses were performed using SPSS software version 21.
Results
A total of 49 participants (30 [61.22%] males; 19 [38.78%] females) were included in the study. The mean age (SD) was 40.27 (14.62) years (range, 19–74 years). Three (6.12%) participants were Fitzpatrick skin type I, 15 (30.61%) were skin type II, and 31 (63.27%) were skin type III.
The baseline median PASI score for the 49 participants was 10.20 (7.85–13.65). Baseline serum 25(OH)D levels were noted to be deficient in 40 participants (81.63%) and inadequate in 9 participants (18.37%). The distribution of the serum 25(OH)D levels of the participants according to the season was evaluated with the Kruskal-Wallis test and no association was found between serum 25(OH)D levels and seasonal changes (P=.685). Comparison of 25(OH)D basal values with Fitzpatrick skin type revealed a statistically significant relationship between skin type and vitamin D level (P=.024). The basal serum 25(OH)D levels were significantly lower in Fitzpatrick skin type II versus skin type I (P=.039).
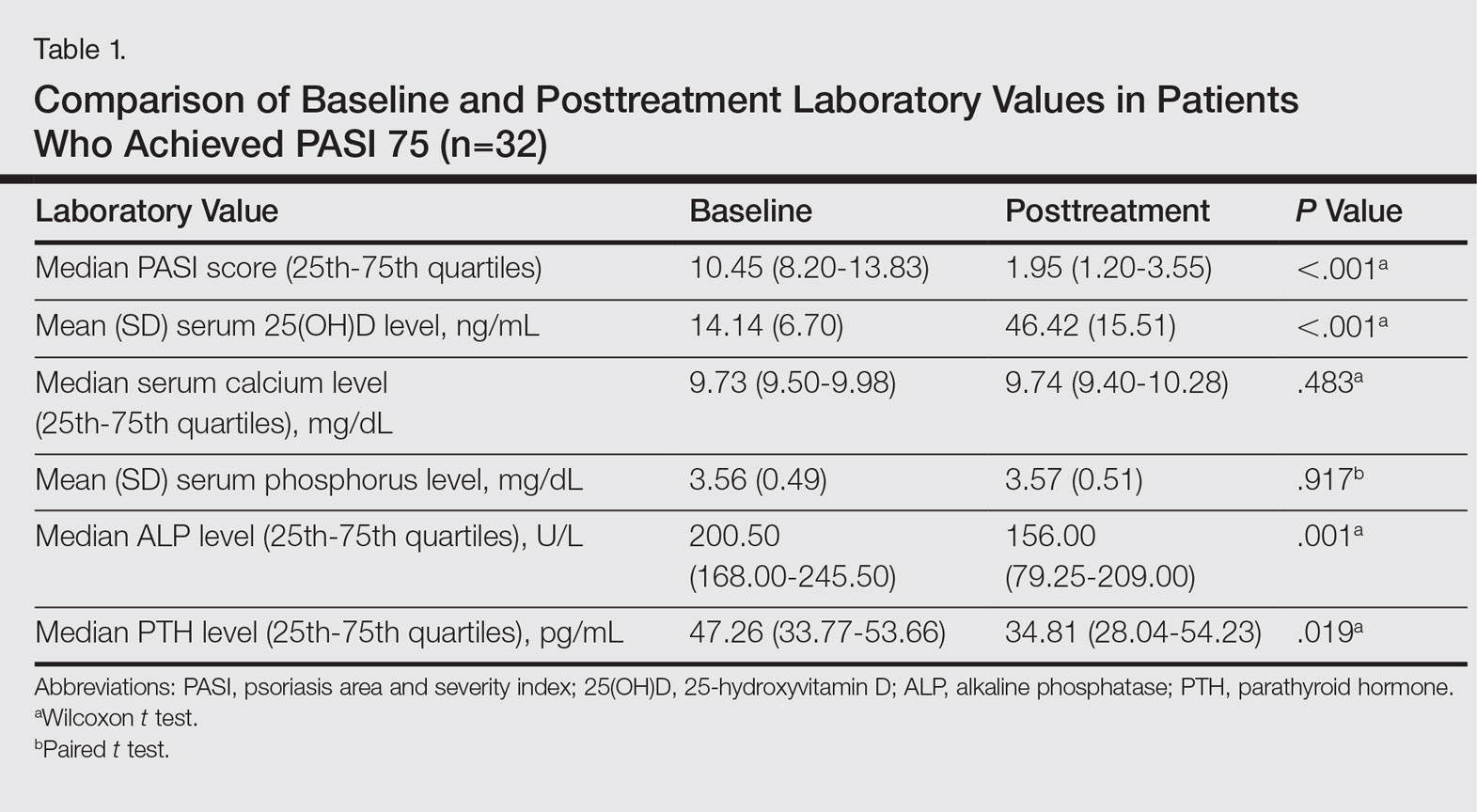
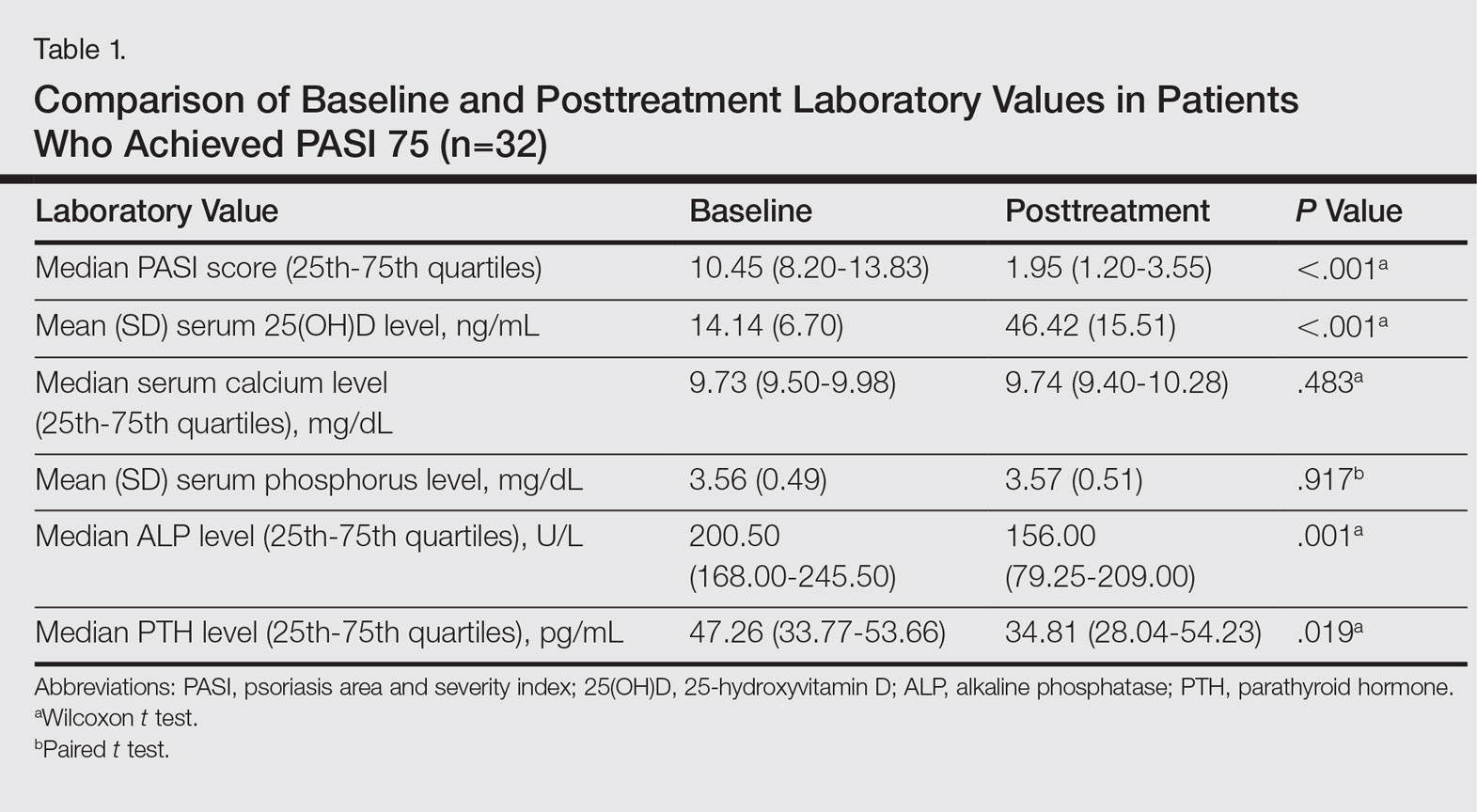
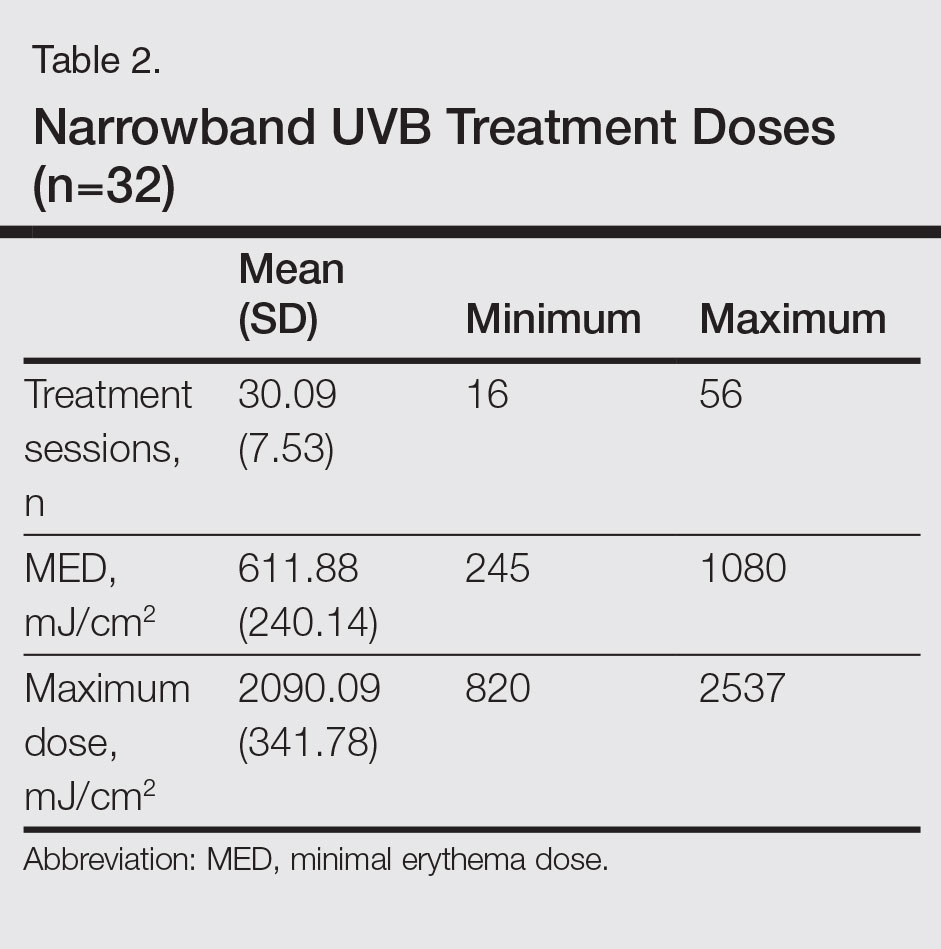
Thirty-two (65.31%) participants achieved PASI 75 by the end of treatment. The baseline median PASI score (25th-75th quartiles) for the 32 patients was 10.45 (8.20-13.83) and the posttreatment PASI score was 1.95 (1.20-3.55), a statistically significant decrease following treatment (P<.001)(Table 1). Mean (SD) baseline serum 25(OH)D levels were 14.14 (6.70) ng/mL and posttreatment levels were 46.42 (15.51) ng/mL in these participants, which demonstrated a statistically significant increase during NB-UVB treatment (P<.001). None of the participants reached the toxicity levels (>80 ng/mL) for serum 25(OH)D. There were no significant changes in serum calcium or phosphorus levels posttreatment (Table 1), but statistically significant decreases in serum ALP and PTH levels were noted (P=.001 and P=.019, respectively)(Table 1).
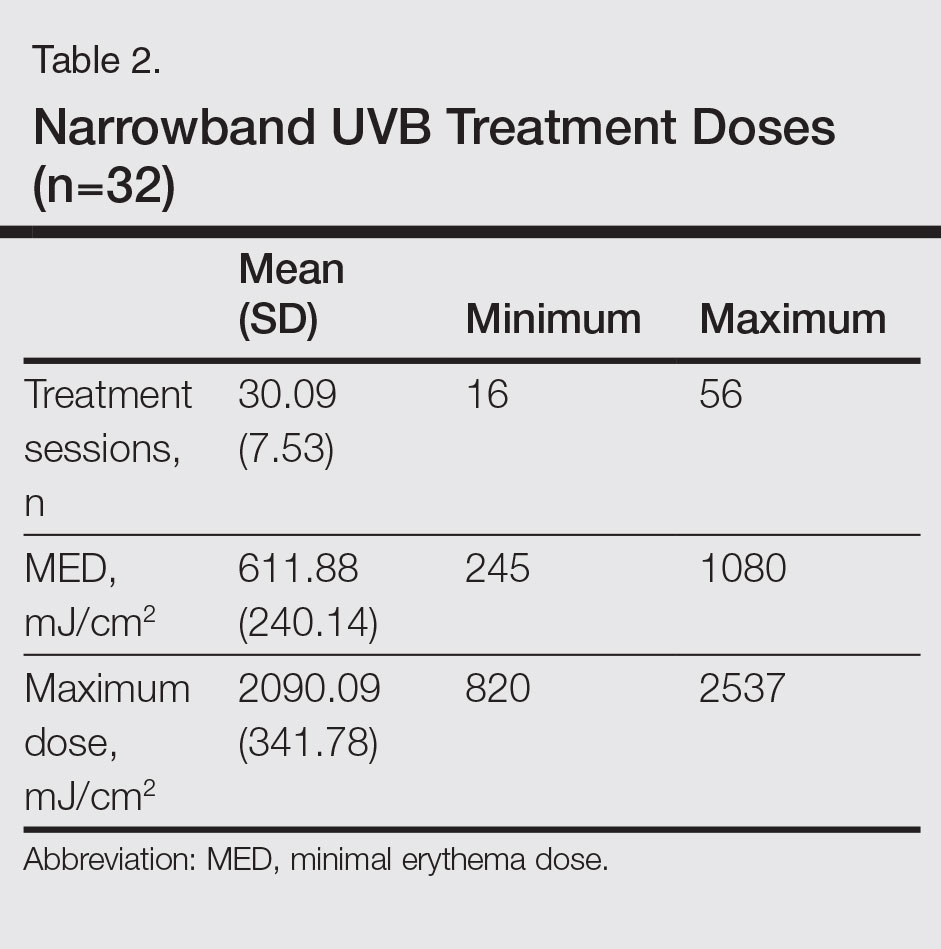
Participants who completed the study (n=32) received an average (SD) of 30.09 (7.53) sessions of NB-UVB treatment and the mean (SD) MED was 611.88 (240.14) mJ/cm2. The mean (SD) maximum dose was 2090.09 (341.78) mJ/cm2 (Table 2).
Posttreatment serum 25(OH)D levels were compared with the number of NB-UVB phototherapy sessions and the maximum dose values. We found that the posttreatment serum 25(OH)D levels correlated with the number of sessions (P=.031) but not with the maximum dose (P=.498).
Using regression analysis, we also evaluated the effect of the increase in vitamin D levels—posttreatment serum 25(OH)D level minus baseline serum 25(OH)D levels—on the decrease in PASI scores—baseline PASI score minus posttreatment PASI score—and found no effect of serum 25(OH)D level increase on PASI decrease (P=.530). There was no correlation between increased serum 25(OH)D levels and age, Fitzpatrick skin type, or baseline PASI score.
Comment
The most effective UV wavelength for vitamin D synthesis is 295 to 300 nm, and therefore broadband UVB is frequently studied when determining the relationship between phototherapy and serum vitamin D levels.4 The current study demonstrated a statistically significant increase in serum 25(OH)D levels following NB-UVB treatment in patients with moderate to severe chronic plaque psoriasis (P<.001). This result supports other studies reporting that NB-UVB treatment in psoriasis patients increases serum 25(OH)D levels.13-18
The main factor in the effective UVB level for vitamin D synthesis is the angle at which solar radiation reaches the earth, which is affected by the longitude, latitude, and time of day.19 For this reason, we planned to perform our study at a single center. Patients who stayed in open areas for more than 2 hours per day during the summer months (May through September) were excluded from the study to decrease the effect of seasonal changes on vitamin D levels. We evaluated the seasonal variation of vitamin D levels and found no relationship between seasonal changes and serum 25(OH)D levels. Therefore, the potential effect of seasonal changes on the vitamin D levels of study participants was excluded from the study.
The response to UV radiation changes according to age and Fitzpatrick skin type because 7-dehydrocholesterol levels decrease with age and melanin prevents the access of UVB photons to 7-dehydrocholesterol.20 The basal serum 25(OH)D levels were deficient in 81.63% of participants and inadequate in 18.37%. In this study, we also observed that the basal serum 25(OH)D levels were significantly lower in patients with Fitzpatrick skin type II than in Fitzpatrick skin type I (P=.039). The mean (SD) serum 25(OH)D level at baseline was 14.14 (6.70) ng/mL and posttreatment was 46.42 (15.51) ng/mL in the 32 patients who completed the study. Serum 25(OH)D levels showed a statistically significant increase after NB-UVB treatment (P<.001). The increased serum 25(OH)D levels after NB-UVB phototherapy were not associated with Fitzpatrick skin type, which was consistent with the results of Osmancevic et al.17 The adjusted NB-UVB doses according to the different skin types might be responsible for this result in our study.
Participant age did not have a significant effect on serum 25(OH)D levels, similar to other studies in the literature.13,17 We believe that artificial UVB radiation at high doses can compensate for the 7-dehydrocholesterol that decreases in the skin with aging.
We observed no significant change in the serum calcium and phosphorus levels with NB-UVB treatment in our study. None of the participants had a metabolic disorder related to increased 25(OH)D levels. The serum ALP and PTH levels decreased significantly following treatment (P=.001 and P=.019, respectively), which may have been secondary to increased serum 25(OH)D levels.
Posttreatment serum 25(OH)D levels were compared with the number of NB-UVB phototherapy sessions and maximum dose values. The posttreatment serum 25(OH)D levels were found to be related to the number of sessions received, but this value was not correlated with the maximum dose received. The MED and maximum dose were determined according to the Fitzpatrick skin type of the participants. Therefore, increased serum 25(OH)D levels with an increased number of sessions was an expected result. Our observation is in accordance with the finding described by Ryan et al.14 On the other hand, an in vitro study conducted by Olds et al21 reported that the relationship between UV light and cholecalciferol synthesis was not linear.
We found that increased serum 25(OH)D levels after treatment were not correlated with the decrease in PASI score, similar to studies by Romaní et al18 and Ryan et al.14 These results suggest that the clinical improvement following NB-UVB treatment is independent of the increased serum 25(OH)D levels in psoriasis patients.
Conclusion
In conclusion, we found that the serum 25(OH)D levels that increase as a result of NB-UVB therapy for the treatment of chronic plaque psoriasis has no statistically significant relationship with the age, Fitzpatrick skin type, baseline PASI score, changes in PASI, or maximum dose, while a positive relationship is present between the serum 25(OH)D levels and the number of sessions of NB-UVB.
- Şavk E. Immunology of Photo(chemo)therapy. Turkderm. 2010;44(suppl 2):62-66.
- Ferahbaş A. Phototherapy modalities and protocols. Turkderm. 2010;44(suppl 2):67-72.
- Ibbotson SH, Bilsland D, Cox NH, et al. An update and guidance on narrowband ultraviolet B phototherapy: a British Photodermatology Group Workshop report. Br J Dermatol. 2004;151:283-297.
- Norval M, Björn LO, de Gruijl FR. Is the action spectrum for the UV-induced production of previtamin D3 in human skin correct? Photochem Photobiol Sci. 2010;9:11-17.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-281.
- McKenzie RL, Liley JB, Björn LO. UV radiation: balancing risks and benefits. Photochem Photobiol. 2009;85:88-98.
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353-373.
- May E, Asadullah K, Zügel U. Immunoregulation through 1,25-dihydroxyvitamin D3 and its analogs. Curr Drug Targets Inflamm Allergy. 2004;3:377-393.
- Reichrath J. Vitamin D and the skin: an ancient friend, revisited. Exp Dermatol. 2007;16:618-625.
- Fu LW, Vender R. Systemic role for vitamin D in the treatment of psoriasis and metabolic syndrome. Dermatol Res Pract. 2011;2011:276079.
- Gisondi P, Rossini M, Di Cesare A, et al. Vitamin D status in patients with chronic plaque psoriasis. Br J Dermatol. 2012;166:505-510.
- Orgaz-Molina J, Buendía-Eisman A, Arrabal-Polo MA, et al. Deficiency of serum concentration of 25-hydroxyvitamin D in psoriatic patients: a case-control study. J Am Acad Dermatol. 2012;67:931-938.
- Osmancevic A, Landin-Wilhelmsen K, Larkö O, et al. UVB therapy increases 25 (OH) vitamin D syntheses in postmenopausal women with psoriasis. Photodermatol Photoimmunol Photomed. 2007;23:172-178.
- Ryan C, Moran B, McKenna MJ, et al. The effect of narrowband UV-B treatment for psoriasis on vitamin D status during wintertime in Ireland. Arch Dermatol. 2010;146:836-842.
- Vahavihu K, Ala-Houhala M, Peric M, et al. Narrowband ultraviolet B treatment improves vitamin D balance and alters antimicrobial peptide expression in skin lesions of psoriasis and atopic dermatitis. Br J Dermatol. 2010;163:321-328.
- Lesiak A, Narbutt J, Pawlaczyk M, et al. Vitamin D serum level changes in psoriatic patients treated with narrowband ultraviolet B phototherapy are related to the season of the irradiation. Photodermatol Photoimmunol Photomed. 2011;27:304-310.
- Osmancevic A, Landin-Wilhelmsen K, Larko O, et al.Vitamin D production in psoriasis patients increases less with narrowband than with broadband ultraviolet B phototherapy. Photodermatol Photoimmunol Photomed. 2009;25:119-123.
- Romaní J, Caixàs A, Carrascosa JM, et al. Effect of narrowband ultraviolet B therapy on inflammatory markers and body fat composition in moderate to severe psoriasis. Br J Dermatol. 2012;166:1237-1244.
- Diehl JW, Chiu MW. Effects of ambient sunlight and photoprotection on vitamin D status. Dermatol Ther. 2010;23:48-60.
- Armas LA, Dowell S, Akhter M, et al. Ultraviolet-B radiation increases serum 25-hydroxyvitamin D levels: the effect of UVB dose and skin color. J Am Acad Dermatol. 2007;57:588-593.
- Olds WJ, McKinley AR, Moore MR, et al. In vitro model of vitamin D3 (cholecalciferol) synthesis by UV radiation: dose-response relationships. J Photochem Photobiol B. 2008;93:88-93.
Psoriasis is a chronic, inflammatory, T-cell–mediated skin disease. Phototherapy, which consists of light used at various wavelengths, is a well-established treatment method for psoriasis vulgaris. Although successful results have been obtained with phototherapy in psoriasis, its mechanism of action is not fully understood. UV light has been shown to have an effect on T-lymphocyte function as well as various components of the natural and acquired immune response. It also has a suppressive effect on the immune system caused by many independent effects.1 Phototherapy currently is available using broadband UVB (290–320 nm), narrowband UVB (NB-UVB)(311–313 nm), 308-nm excimer laser, UVA1 (340–400 nm), psoralen plus UVA, and photopheresis.2 Narrowband UVB treatment with light sources that peak at 311 to 313 nm have been used with high efficacy and a low side-effect profile, becoming the standard phototherapy method for chronic plaque-type psoriasis.3
More than 90% of vitamin D synthesis is formed in the skin following UV exposure, and the wavelengths and the solar spectrum that stimulate vitamin D synthesis have been a focus of research.4 7-Dehydrocholesterol (provitamin D3) is first converted to previtamin D3. Although the necessary UV wavelength for previtamin D3 synthesis is 295 to 300 nm, it is known that production stops below 260 nm and above 315 nm.4-6 Previtamin D3 is unstable and is quickly converted to vitamin D3 in the skinand then to the biologically active form of 1,25-dihydroxyvitamin D3 (calcitriol) following hydroxylation in the liver and kidneys. Calcitriol shows its effect by binding to the special nuclear receptor for vitamin D.7 Many tissues including the keratinocytes, dendritic cells, melanocytes, and sebocytes in the skin have been shown to possess the enzymatic mechanism necessary for 1,25-dihydroxyvitamin D3 production. Vitamin D also is known to have paracrine, autocrine, and intracrine effects on immunomodulation, cell proliferation, differentiation, and apoptosis, in addition to its role in calcium metabolism.5-9 Topical vitamin D and its analogues are used effectively and safely in psoriasis treatment with these effects.10 A correlation between low serum vitamin D levels and chronic inflammation severity has been shown in psoriasis patients in some studies.11,12
In this study, we sought to evaluate the effect of NB-UVB on vitamin D status and related metabolic markers in patients with psoriasis.
Methods
This prospective, single-center study included patients living in or around Eskisehir, Turkey, who were 18 years of age or older and had been diagnosed with chronic plaque psoriasis with a psoriasis area and severity index (PASI) score of 5 or higher. Permission was granted by the local ethics committee. Patients provided written informed consent prior to enrollment. Patients were excluded if they were younger than 18 years; were pregnant or breastfeeding; stayed in open environments for more than 2 hours per day during the summer months (May through September); used drugs affecting calcium metabolism in the last 8 weeks (eg, barbiturates, anticonvulsants, corticosteroids, vitamin D supplements, bisphosphonates); used systemic treatment for psoriasis in the last 8 weeks; used phototherapy or sunbathing in the last 8 weeks; used topical vitamin D analogues in the last 4 weeks; or had a history of psoriatic arthritis and other inflammatory disorders, renal disease, known calcium metabolism disorders, granulomatous disorders, thyroid disease, diabetes mellitus, skin cancer, or abnormal photosensitivity and known lack of response or hypersensitivity to phototherapy.
Clinical Evaluation and Laboratory Studies
The participants’ age, gender, Fitzpatrick skin type, disease duration, dairy intake and vitamin supplement levels, hours of sun exposure per week, detailed medical history, and medications were obtained and documented in the medical records.
Serum 25(OH)D levels were measured using high-performance liquid chromatography/mass spectrometry, serum calcium and phosphorus levels using colorimetric analysis, serum alkaline phosphatase (ALP) levels using the enzymatic colorimetric method, and serum parathyroid hormone (PTH) levels using electrochemiluminescence at baseline and after PASI 75 was achieved with treatment. Vitamin D levels were classified in 3 groups: (1) deficient (<20 ng/mL); (2) inadequate (20–30 ng/mL); and (3) adequate (>30 ng/mL). The PASI scores at baseline and posttreatment were calculated by the same dermatologist (S.S.).
Treatment Protocol and Patient Follow-up
Narrowband UVB treatment was started at 70% of the minimal erythema dose (MED). Phototherapy was administered 3 times weekly for 6 months or until PASI 75 response was achieved. An increase of 20% to 30% from the prior dose was made according to the participants’ clinical status at each treatment session, and the dose was stabilized once the maximum dose was achieved according to skin type—up to 2000 mJ/cm2 for Fitzpatrick skin types I and II, 3000 mJ/cm2 for skin types III and IV, and 5000 mJ/cm2 for skin types V and VI. Participants were allowed to use low- and moderate-potency topical corticosteroids and moisturizers containing urea during the course of treatment. The study physician (S.S.) clinically evaluated participants every 4 weeks for 6 months or until PASI 75 was achieved, and the clinical improvement was calculated as the percentage decrease in PASI score.
Statistical Analysis
The Shapiro-Wilk normalcy test was used for the continuous variables in the study. Variables with a normal distribution were analyzed with the paired t test and 1-way analysis of variance test and presented as mean (SD). Variables without a normal distribution were analyzed with the Wilcoxon t test and the Kruskal-Wallis test and presented as the median and 25th and 75th quartiles. The serum 25(OH)D levels were evaluated according to the seasons with the Kruskal-Wallis test. Categorical variables were expressed as frequency and percentages. The Pearson and Spearman correlation analysis and regression analysis were used to show the relationship between the variables (ie, age, Fitzpatrick skin type, PASI score, maximum NB-UVB dose, and number of sessions). The statistical significance level was set at P≤.05. Statistical analyses were performed using SPSS software version 21.
Results
A total of 49 participants (30 [61.22%] males; 19 [38.78%] females) were included in the study. The mean age (SD) was 40.27 (14.62) years (range, 19–74 years). Three (6.12%) participants were Fitzpatrick skin type I, 15 (30.61%) were skin type II, and 31 (63.27%) were skin type III.
The baseline median PASI score for the 49 participants was 10.20 (7.85–13.65). Baseline serum 25(OH)D levels were noted to be deficient in 40 participants (81.63%) and inadequate in 9 participants (18.37%). The distribution of the serum 25(OH)D levels of the participants according to the season was evaluated with the Kruskal-Wallis test and no association was found between serum 25(OH)D levels and seasonal changes (P=.685). Comparison of 25(OH)D basal values with Fitzpatrick skin type revealed a statistically significant relationship between skin type and vitamin D level (P=.024). The basal serum 25(OH)D levels were significantly lower in Fitzpatrick skin type II versus skin type I (P=.039).
Thirty-two (65.31%) participants achieved PASI 75 by the end of treatment. The baseline median PASI score (25th-75th quartiles) for the 32 patients was 10.45 (8.20-13.83) and the posttreatment PASI score was 1.95 (1.20-3.55), a statistically significant decrease following treatment (P<.001)(Table 1). Mean (SD) baseline serum 25(OH)D levels were 14.14 (6.70) ng/mL and posttreatment levels were 46.42 (15.51) ng/mL in these participants, which demonstrated a statistically significant increase during NB-UVB treatment (P<.001). None of the participants reached the toxicity levels (>80 ng/mL) for serum 25(OH)D. There were no significant changes in serum calcium or phosphorus levels posttreatment (Table 1), but statistically significant decreases in serum ALP and PTH levels were noted (P=.001 and P=.019, respectively)(Table 1).
Participants who completed the study (n=32) received an average (SD) of 30.09 (7.53) sessions of NB-UVB treatment and the mean (SD) MED was 611.88 (240.14) mJ/cm2. The mean (SD) maximum dose was 2090.09 (341.78) mJ/cm2 (Table 2).
Posttreatment serum 25(OH)D levels were compared with the number of NB-UVB phototherapy sessions and the maximum dose values. We found that the posttreatment serum 25(OH)D levels correlated with the number of sessions (P=.031) but not with the maximum dose (P=.498).
Using regression analysis, we also evaluated the effect of the increase in vitamin D levels—posttreatment serum 25(OH)D level minus baseline serum 25(OH)D levels—on the decrease in PASI scores—baseline PASI score minus posttreatment PASI score—and found no effect of serum 25(OH)D level increase on PASI decrease (P=.530). There was no correlation between increased serum 25(OH)D levels and age, Fitzpatrick skin type, or baseline PASI score.
Comment
The most effective UV wavelength for vitamin D synthesis is 295 to 300 nm, and therefore broadband UVB is frequently studied when determining the relationship between phototherapy and serum vitamin D levels.4 The current study demonstrated a statistically significant increase in serum 25(OH)D levels following NB-UVB treatment in patients with moderate to severe chronic plaque psoriasis (P<.001). This result supports other studies reporting that NB-UVB treatment in psoriasis patients increases serum 25(OH)D levels.13-18
The main factor in the effective UVB level for vitamin D synthesis is the angle at which solar radiation reaches the earth, which is affected by the longitude, latitude, and time of day.19 For this reason, we planned to perform our study at a single center. Patients who stayed in open areas for more than 2 hours per day during the summer months (May through September) were excluded from the study to decrease the effect of seasonal changes on vitamin D levels. We evaluated the seasonal variation of vitamin D levels and found no relationship between seasonal changes and serum 25(OH)D levels. Therefore, the potential effect of seasonal changes on the vitamin D levels of study participants was excluded from the study.
The response to UV radiation changes according to age and Fitzpatrick skin type because 7-dehydrocholesterol levels decrease with age and melanin prevents the access of UVB photons to 7-dehydrocholesterol.20 The basal serum 25(OH)D levels were deficient in 81.63% of participants and inadequate in 18.37%. In this study, we also observed that the basal serum 25(OH)D levels were significantly lower in patients with Fitzpatrick skin type II than in Fitzpatrick skin type I (P=.039). The mean (SD) serum 25(OH)D level at baseline was 14.14 (6.70) ng/mL and posttreatment was 46.42 (15.51) ng/mL in the 32 patients who completed the study. Serum 25(OH)D levels showed a statistically significant increase after NB-UVB treatment (P<.001). The increased serum 25(OH)D levels after NB-UVB phototherapy were not associated with Fitzpatrick skin type, which was consistent with the results of Osmancevic et al.17 The adjusted NB-UVB doses according to the different skin types might be responsible for this result in our study.
Participant age did not have a significant effect on serum 25(OH)D levels, similar to other studies in the literature.13,17 We believe that artificial UVB radiation at high doses can compensate for the 7-dehydrocholesterol that decreases in the skin with aging.
We observed no significant change in the serum calcium and phosphorus levels with NB-UVB treatment in our study. None of the participants had a metabolic disorder related to increased 25(OH)D levels. The serum ALP and PTH levels decreased significantly following treatment (P=.001 and P=.019, respectively), which may have been secondary to increased serum 25(OH)D levels.
Posttreatment serum 25(OH)D levels were compared with the number of NB-UVB phototherapy sessions and maximum dose values. The posttreatment serum 25(OH)D levels were found to be related to the number of sessions received, but this value was not correlated with the maximum dose received. The MED and maximum dose were determined according to the Fitzpatrick skin type of the participants. Therefore, increased serum 25(OH)D levels with an increased number of sessions was an expected result. Our observation is in accordance with the finding described by Ryan et al.14 On the other hand, an in vitro study conducted by Olds et al21 reported that the relationship between UV light and cholecalciferol synthesis was not linear.
We found that increased serum 25(OH)D levels after treatment were not correlated with the decrease in PASI score, similar to studies by Romaní et al18 and Ryan et al.14 These results suggest that the clinical improvement following NB-UVB treatment is independent of the increased serum 25(OH)D levels in psoriasis patients.
Conclusion
In conclusion, we found that the serum 25(OH)D levels that increase as a result of NB-UVB therapy for the treatment of chronic plaque psoriasis has no statistically significant relationship with the age, Fitzpatrick skin type, baseline PASI score, changes in PASI, or maximum dose, while a positive relationship is present between the serum 25(OH)D levels and the number of sessions of NB-UVB.
Psoriasis is a chronic, inflammatory, T-cell–mediated skin disease. Phototherapy, which consists of light used at various wavelengths, is a well-established treatment method for psoriasis vulgaris. Although successful results have been obtained with phototherapy in psoriasis, its mechanism of action is not fully understood. UV light has been shown to have an effect on T-lymphocyte function as well as various components of the natural and acquired immune response. It also has a suppressive effect on the immune system caused by many independent effects.1 Phototherapy currently is available using broadband UVB (290–320 nm), narrowband UVB (NB-UVB)(311–313 nm), 308-nm excimer laser, UVA1 (340–400 nm), psoralen plus UVA, and photopheresis.2 Narrowband UVB treatment with light sources that peak at 311 to 313 nm have been used with high efficacy and a low side-effect profile, becoming the standard phototherapy method for chronic plaque-type psoriasis.3
More than 90% of vitamin D synthesis is formed in the skin following UV exposure, and the wavelengths and the solar spectrum that stimulate vitamin D synthesis have been a focus of research.4 7-Dehydrocholesterol (provitamin D3) is first converted to previtamin D3. Although the necessary UV wavelength for previtamin D3 synthesis is 295 to 300 nm, it is known that production stops below 260 nm and above 315 nm.4-6 Previtamin D3 is unstable and is quickly converted to vitamin D3 in the skinand then to the biologically active form of 1,25-dihydroxyvitamin D3 (calcitriol) following hydroxylation in the liver and kidneys. Calcitriol shows its effect by binding to the special nuclear receptor for vitamin D.7 Many tissues including the keratinocytes, dendritic cells, melanocytes, and sebocytes in the skin have been shown to possess the enzymatic mechanism necessary for 1,25-dihydroxyvitamin D3 production. Vitamin D also is known to have paracrine, autocrine, and intracrine effects on immunomodulation, cell proliferation, differentiation, and apoptosis, in addition to its role in calcium metabolism.5-9 Topical vitamin D and its analogues are used effectively and safely in psoriasis treatment with these effects.10 A correlation between low serum vitamin D levels and chronic inflammation severity has been shown in psoriasis patients in some studies.11,12
In this study, we sought to evaluate the effect of NB-UVB on vitamin D status and related metabolic markers in patients with psoriasis.
Methods
This prospective, single-center study included patients living in or around Eskisehir, Turkey, who were 18 years of age or older and had been diagnosed with chronic plaque psoriasis with a psoriasis area and severity index (PASI) score of 5 or higher. Permission was granted by the local ethics committee. Patients provided written informed consent prior to enrollment. Patients were excluded if they were younger than 18 years; were pregnant or breastfeeding; stayed in open environments for more than 2 hours per day during the summer months (May through September); used drugs affecting calcium metabolism in the last 8 weeks (eg, barbiturates, anticonvulsants, corticosteroids, vitamin D supplements, bisphosphonates); used systemic treatment for psoriasis in the last 8 weeks; used phototherapy or sunbathing in the last 8 weeks; used topical vitamin D analogues in the last 4 weeks; or had a history of psoriatic arthritis and other inflammatory disorders, renal disease, known calcium metabolism disorders, granulomatous disorders, thyroid disease, diabetes mellitus, skin cancer, or abnormal photosensitivity and known lack of response or hypersensitivity to phototherapy.
Clinical Evaluation and Laboratory Studies
The participants’ age, gender, Fitzpatrick skin type, disease duration, dairy intake and vitamin supplement levels, hours of sun exposure per week, detailed medical history, and medications were obtained and documented in the medical records.
Serum 25(OH)D levels were measured using high-performance liquid chromatography/mass spectrometry, serum calcium and phosphorus levels using colorimetric analysis, serum alkaline phosphatase (ALP) levels using the enzymatic colorimetric method, and serum parathyroid hormone (PTH) levels using electrochemiluminescence at baseline and after PASI 75 was achieved with treatment. Vitamin D levels were classified in 3 groups: (1) deficient (<20 ng/mL); (2) inadequate (20–30 ng/mL); and (3) adequate (>30 ng/mL). The PASI scores at baseline and posttreatment were calculated by the same dermatologist (S.S.).
Treatment Protocol and Patient Follow-up
Narrowband UVB treatment was started at 70% of the minimal erythema dose (MED). Phototherapy was administered 3 times weekly for 6 months or until PASI 75 response was achieved. An increase of 20% to 30% from the prior dose was made according to the participants’ clinical status at each treatment session, and the dose was stabilized once the maximum dose was achieved according to skin type—up to 2000 mJ/cm2 for Fitzpatrick skin types I and II, 3000 mJ/cm2 for skin types III and IV, and 5000 mJ/cm2 for skin types V and VI. Participants were allowed to use low- and moderate-potency topical corticosteroids and moisturizers containing urea during the course of treatment. The study physician (S.S.) clinically evaluated participants every 4 weeks for 6 months or until PASI 75 was achieved, and the clinical improvement was calculated as the percentage decrease in PASI score.
Statistical Analysis
The Shapiro-Wilk normalcy test was used for the continuous variables in the study. Variables with a normal distribution were analyzed with the paired t test and 1-way analysis of variance test and presented as mean (SD). Variables without a normal distribution were analyzed with the Wilcoxon t test and the Kruskal-Wallis test and presented as the median and 25th and 75th quartiles. The serum 25(OH)D levels were evaluated according to the seasons with the Kruskal-Wallis test. Categorical variables were expressed as frequency and percentages. The Pearson and Spearman correlation analysis and regression analysis were used to show the relationship between the variables (ie, age, Fitzpatrick skin type, PASI score, maximum NB-UVB dose, and number of sessions). The statistical significance level was set at P≤.05. Statistical analyses were performed using SPSS software version 21.
Results
A total of 49 participants (30 [61.22%] males; 19 [38.78%] females) were included in the study. The mean age (SD) was 40.27 (14.62) years (range, 19–74 years). Three (6.12%) participants were Fitzpatrick skin type I, 15 (30.61%) were skin type II, and 31 (63.27%) were skin type III.
The baseline median PASI score for the 49 participants was 10.20 (7.85–13.65). Baseline serum 25(OH)D levels were noted to be deficient in 40 participants (81.63%) and inadequate in 9 participants (18.37%). The distribution of the serum 25(OH)D levels of the participants according to the season was evaluated with the Kruskal-Wallis test and no association was found between serum 25(OH)D levels and seasonal changes (P=.685). Comparison of 25(OH)D basal values with Fitzpatrick skin type revealed a statistically significant relationship between skin type and vitamin D level (P=.024). The basal serum 25(OH)D levels were significantly lower in Fitzpatrick skin type II versus skin type I (P=.039).
Thirty-two (65.31%) participants achieved PASI 75 by the end of treatment. The baseline median PASI score (25th-75th quartiles) for the 32 patients was 10.45 (8.20-13.83) and the posttreatment PASI score was 1.95 (1.20-3.55), a statistically significant decrease following treatment (P<.001)(Table 1). Mean (SD) baseline serum 25(OH)D levels were 14.14 (6.70) ng/mL and posttreatment levels were 46.42 (15.51) ng/mL in these participants, which demonstrated a statistically significant increase during NB-UVB treatment (P<.001). None of the participants reached the toxicity levels (>80 ng/mL) for serum 25(OH)D. There were no significant changes in serum calcium or phosphorus levels posttreatment (Table 1), but statistically significant decreases in serum ALP and PTH levels were noted (P=.001 and P=.019, respectively)(Table 1).
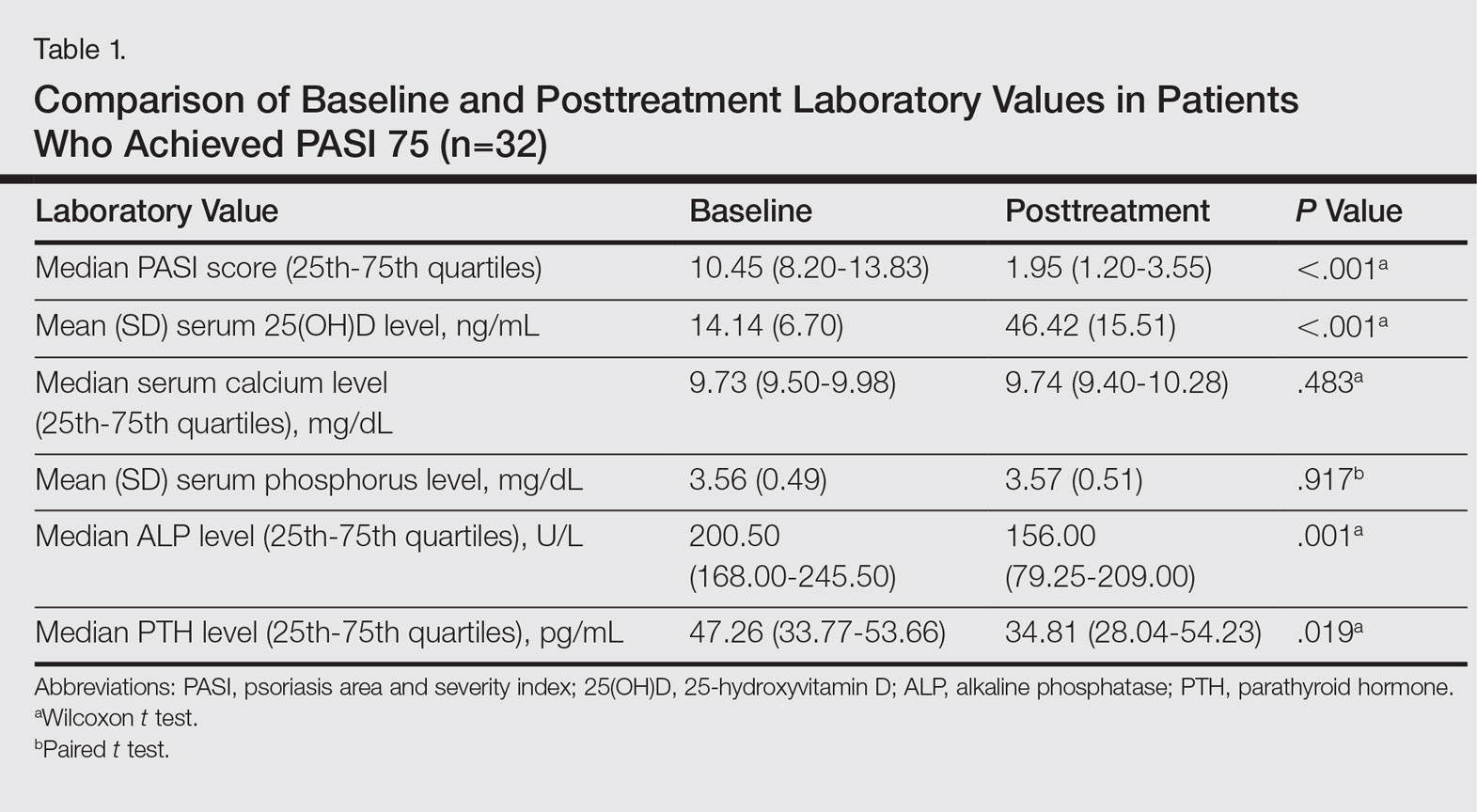
Participants who completed the study (n=32) received an average (SD) of 30.09 (7.53) sessions of NB-UVB treatment and the mean (SD) MED was 611.88 (240.14) mJ/cm2. The mean (SD) maximum dose was 2090.09 (341.78) mJ/cm2 (Table 2).
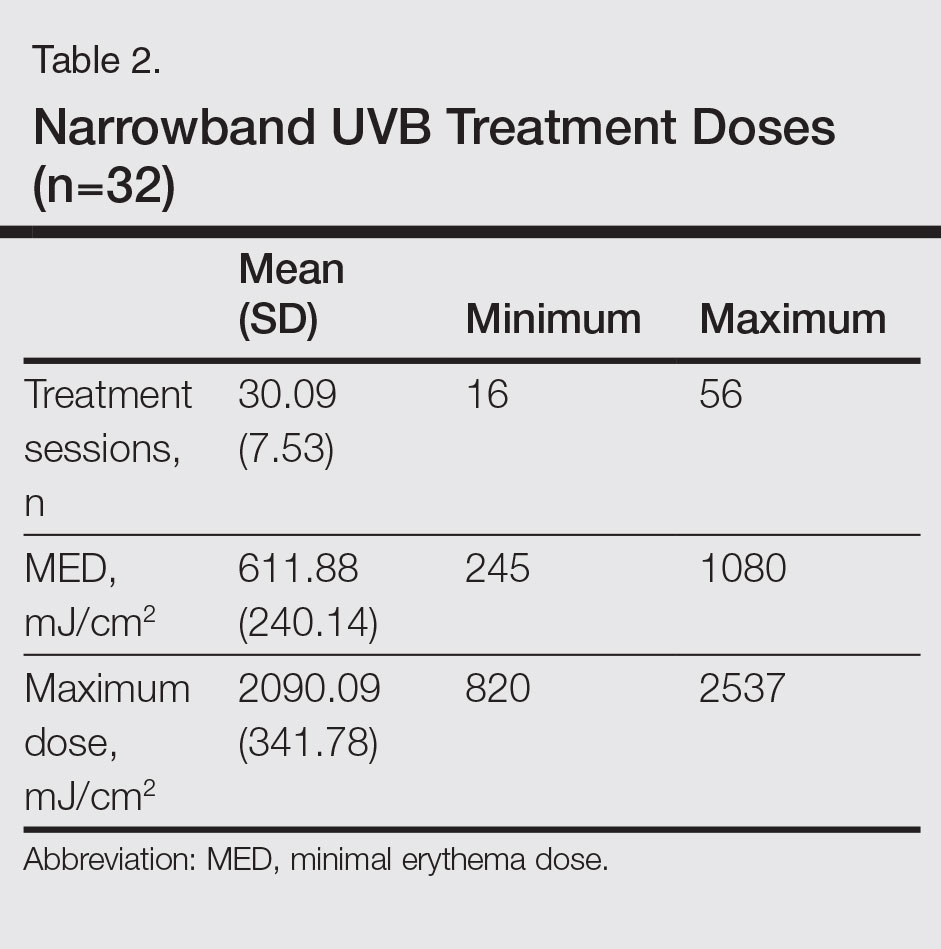
Posttreatment serum 25(OH)D levels were compared with the number of NB-UVB phototherapy sessions and the maximum dose values. We found that the posttreatment serum 25(OH)D levels correlated with the number of sessions (P=.031) but not with the maximum dose (P=.498).
Using regression analysis, we also evaluated the effect of the increase in vitamin D levels—posttreatment serum 25(OH)D level minus baseline serum 25(OH)D levels—on the decrease in PASI scores—baseline PASI score minus posttreatment PASI score—and found no effect of serum 25(OH)D level increase on PASI decrease (P=.530). There was no correlation between increased serum 25(OH)D levels and age, Fitzpatrick skin type, or baseline PASI score.
Comment
The most effective UV wavelength for vitamin D synthesis is 295 to 300 nm, and therefore broadband UVB is frequently studied when determining the relationship between phototherapy and serum vitamin D levels.4 The current study demonstrated a statistically significant increase in serum 25(OH)D levels following NB-UVB treatment in patients with moderate to severe chronic plaque psoriasis (P<.001). This result supports other studies reporting that NB-UVB treatment in psoriasis patients increases serum 25(OH)D levels.13-18
The main factor in the effective UVB level for vitamin D synthesis is the angle at which solar radiation reaches the earth, which is affected by the longitude, latitude, and time of day.19 For this reason, we planned to perform our study at a single center. Patients who stayed in open areas for more than 2 hours per day during the summer months (May through September) were excluded from the study to decrease the effect of seasonal changes on vitamin D levels. We evaluated the seasonal variation of vitamin D levels and found no relationship between seasonal changes and serum 25(OH)D levels. Therefore, the potential effect of seasonal changes on the vitamin D levels of study participants was excluded from the study.
The response to UV radiation changes according to age and Fitzpatrick skin type because 7-dehydrocholesterol levels decrease with age and melanin prevents the access of UVB photons to 7-dehydrocholesterol.20 The basal serum 25(OH)D levels were deficient in 81.63% of participants and inadequate in 18.37%. In this study, we also observed that the basal serum 25(OH)D levels were significantly lower in patients with Fitzpatrick skin type II than in Fitzpatrick skin type I (P=.039). The mean (SD) serum 25(OH)D level at baseline was 14.14 (6.70) ng/mL and posttreatment was 46.42 (15.51) ng/mL in the 32 patients who completed the study. Serum 25(OH)D levels showed a statistically significant increase after NB-UVB treatment (P<.001). The increased serum 25(OH)D levels after NB-UVB phototherapy were not associated with Fitzpatrick skin type, which was consistent with the results of Osmancevic et al.17 The adjusted NB-UVB doses according to the different skin types might be responsible for this result in our study.
Participant age did not have a significant effect on serum 25(OH)D levels, similar to other studies in the literature.13,17 We believe that artificial UVB radiation at high doses can compensate for the 7-dehydrocholesterol that decreases in the skin with aging.
We observed no significant change in the serum calcium and phosphorus levels with NB-UVB treatment in our study. None of the participants had a metabolic disorder related to increased 25(OH)D levels. The serum ALP and PTH levels decreased significantly following treatment (P=.001 and P=.019, respectively), which may have been secondary to increased serum 25(OH)D levels.
Posttreatment serum 25(OH)D levels were compared with the number of NB-UVB phototherapy sessions and maximum dose values. The posttreatment serum 25(OH)D levels were found to be related to the number of sessions received, but this value was not correlated with the maximum dose received. The MED and maximum dose were determined according to the Fitzpatrick skin type of the participants. Therefore, increased serum 25(OH)D levels with an increased number of sessions was an expected result. Our observation is in accordance with the finding described by Ryan et al.14 On the other hand, an in vitro study conducted by Olds et al21 reported that the relationship between UV light and cholecalciferol synthesis was not linear.
We found that increased serum 25(OH)D levels after treatment were not correlated with the decrease in PASI score, similar to studies by Romaní et al18 and Ryan et al.14 These results suggest that the clinical improvement following NB-UVB treatment is independent of the increased serum 25(OH)D levels in psoriasis patients.
Conclusion
In conclusion, we found that the serum 25(OH)D levels that increase as a result of NB-UVB therapy for the treatment of chronic plaque psoriasis has no statistically significant relationship with the age, Fitzpatrick skin type, baseline PASI score, changes in PASI, or maximum dose, while a positive relationship is present between the serum 25(OH)D levels and the number of sessions of NB-UVB.
- Şavk E. Immunology of Photo(chemo)therapy. Turkderm. 2010;44(suppl 2):62-66.
- Ferahbaş A. Phototherapy modalities and protocols. Turkderm. 2010;44(suppl 2):67-72.
- Ibbotson SH, Bilsland D, Cox NH, et al. An update and guidance on narrowband ultraviolet B phototherapy: a British Photodermatology Group Workshop report. Br J Dermatol. 2004;151:283-297.
- Norval M, Björn LO, de Gruijl FR. Is the action spectrum for the UV-induced production of previtamin D3 in human skin correct? Photochem Photobiol Sci. 2010;9:11-17.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-281.
- McKenzie RL, Liley JB, Björn LO. UV radiation: balancing risks and benefits. Photochem Photobiol. 2009;85:88-98.
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353-373.
- May E, Asadullah K, Zügel U. Immunoregulation through 1,25-dihydroxyvitamin D3 and its analogs. Curr Drug Targets Inflamm Allergy. 2004;3:377-393.
- Reichrath J. Vitamin D and the skin: an ancient friend, revisited. Exp Dermatol. 2007;16:618-625.
- Fu LW, Vender R. Systemic role for vitamin D in the treatment of psoriasis and metabolic syndrome. Dermatol Res Pract. 2011;2011:276079.
- Gisondi P, Rossini M, Di Cesare A, et al. Vitamin D status in patients with chronic plaque psoriasis. Br J Dermatol. 2012;166:505-510.
- Orgaz-Molina J, Buendía-Eisman A, Arrabal-Polo MA, et al. Deficiency of serum concentration of 25-hydroxyvitamin D in psoriatic patients: a case-control study. J Am Acad Dermatol. 2012;67:931-938.
- Osmancevic A, Landin-Wilhelmsen K, Larkö O, et al. UVB therapy increases 25 (OH) vitamin D syntheses in postmenopausal women with psoriasis. Photodermatol Photoimmunol Photomed. 2007;23:172-178.
- Ryan C, Moran B, McKenna MJ, et al. The effect of narrowband UV-B treatment for psoriasis on vitamin D status during wintertime in Ireland. Arch Dermatol. 2010;146:836-842.
- Vahavihu K, Ala-Houhala M, Peric M, et al. Narrowband ultraviolet B treatment improves vitamin D balance and alters antimicrobial peptide expression in skin lesions of psoriasis and atopic dermatitis. Br J Dermatol. 2010;163:321-328.
- Lesiak A, Narbutt J, Pawlaczyk M, et al. Vitamin D serum level changes in psoriatic patients treated with narrowband ultraviolet B phototherapy are related to the season of the irradiation. Photodermatol Photoimmunol Photomed. 2011;27:304-310.
- Osmancevic A, Landin-Wilhelmsen K, Larko O, et al.Vitamin D production in psoriasis patients increases less with narrowband than with broadband ultraviolet B phototherapy. Photodermatol Photoimmunol Photomed. 2009;25:119-123.
- Romaní J, Caixàs A, Carrascosa JM, et al. Effect of narrowband ultraviolet B therapy on inflammatory markers and body fat composition in moderate to severe psoriasis. Br J Dermatol. 2012;166:1237-1244.
- Diehl JW, Chiu MW. Effects of ambient sunlight and photoprotection on vitamin D status. Dermatol Ther. 2010;23:48-60.
- Armas LA, Dowell S, Akhter M, et al. Ultraviolet-B radiation increases serum 25-hydroxyvitamin D levels: the effect of UVB dose and skin color. J Am Acad Dermatol. 2007;57:588-593.
- Olds WJ, McKinley AR, Moore MR, et al. In vitro model of vitamin D3 (cholecalciferol) synthesis by UV radiation: dose-response relationships. J Photochem Photobiol B. 2008;93:88-93.
- Şavk E. Immunology of Photo(chemo)therapy. Turkderm. 2010;44(suppl 2):62-66.
- Ferahbaş A. Phototherapy modalities and protocols. Turkderm. 2010;44(suppl 2):67-72.
- Ibbotson SH, Bilsland D, Cox NH, et al. An update and guidance on narrowband ultraviolet B phototherapy: a British Photodermatology Group Workshop report. Br J Dermatol. 2004;151:283-297.
- Norval M, Björn LO, de Gruijl FR. Is the action spectrum for the UV-induced production of previtamin D3 in human skin correct? Photochem Photobiol Sci. 2010;9:11-17.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-281.
- McKenzie RL, Liley JB, Björn LO. UV radiation: balancing risks and benefits. Photochem Photobiol. 2009;85:88-98.
- Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353-373.
- May E, Asadullah K, Zügel U. Immunoregulation through 1,25-dihydroxyvitamin D3 and its analogs. Curr Drug Targets Inflamm Allergy. 2004;3:377-393.
- Reichrath J. Vitamin D and the skin: an ancient friend, revisited. Exp Dermatol. 2007;16:618-625.
- Fu LW, Vender R. Systemic role for vitamin D in the treatment of psoriasis and metabolic syndrome. Dermatol Res Pract. 2011;2011:276079.
- Gisondi P, Rossini M, Di Cesare A, et al. Vitamin D status in patients with chronic plaque psoriasis. Br J Dermatol. 2012;166:505-510.
- Orgaz-Molina J, Buendía-Eisman A, Arrabal-Polo MA, et al. Deficiency of serum concentration of 25-hydroxyvitamin D in psoriatic patients: a case-control study. J Am Acad Dermatol. 2012;67:931-938.
- Osmancevic A, Landin-Wilhelmsen K, Larkö O, et al. UVB therapy increases 25 (OH) vitamin D syntheses in postmenopausal women with psoriasis. Photodermatol Photoimmunol Photomed. 2007;23:172-178.
- Ryan C, Moran B, McKenna MJ, et al. The effect of narrowband UV-B treatment for psoriasis on vitamin D status during wintertime in Ireland. Arch Dermatol. 2010;146:836-842.
- Vahavihu K, Ala-Houhala M, Peric M, et al. Narrowband ultraviolet B treatment improves vitamin D balance and alters antimicrobial peptide expression in skin lesions of psoriasis and atopic dermatitis. Br J Dermatol. 2010;163:321-328.
- Lesiak A, Narbutt J, Pawlaczyk M, et al. Vitamin D serum level changes in psoriatic patients treated with narrowband ultraviolet B phototherapy are related to the season of the irradiation. Photodermatol Photoimmunol Photomed. 2011;27:304-310.
- Osmancevic A, Landin-Wilhelmsen K, Larko O, et al.Vitamin D production in psoriasis patients increases less with narrowband than with broadband ultraviolet B phototherapy. Photodermatol Photoimmunol Photomed. 2009;25:119-123.
- Romaní J, Caixàs A, Carrascosa JM, et al. Effect of narrowband ultraviolet B therapy on inflammatory markers and body fat composition in moderate to severe psoriasis. Br J Dermatol. 2012;166:1237-1244.
- Diehl JW, Chiu MW. Effects of ambient sunlight and photoprotection on vitamin D status. Dermatol Ther. 2010;23:48-60.
- Armas LA, Dowell S, Akhter M, et al. Ultraviolet-B radiation increases serum 25-hydroxyvitamin D levels: the effect of UVB dose and skin color. J Am Acad Dermatol. 2007;57:588-593.
- Olds WJ, McKinley AR, Moore MR, et al. In vitro model of vitamin D3 (cholecalciferol) synthesis by UV radiation: dose-response relationships. J Photochem Photobiol B. 2008;93:88-93.
Practice Points
- The 25-hydroxyvitamin D (25[OH]D) levels are increased by narrowband UVB (NB-UVB) treatment in psoriasis patients.
- The number of sessions of NB-UVB is associated with increased 25(OH)D levels.
Leukocytoclastic Vasculitis Resolution With Topical Dapsone
Leukocytoclastic vasculitis (LCV) is a disease characterized by inflammation of small vessels with characteristic clinical findings of petechiae and palpable purpura.1 Numerous etiologies have been described, but the disease commonly remains idiopathic.2,3 Leukocytoclastic vasculitis often spontaneously resolves within weeks and requires only symptomatic treatment. Chronic or severe disease can require systemic medical treatment with agents such as colchicine, dapsone, and corticosteroids. These agents are effective but carry risks of serious side effects.4,5 These side effects and/or medical contraindications prevent some patients from taking systemic medications for LCV. We present a case of LCV that resolved after treatment with topical dapsone, highlighting a potential new treatment ofLCV with a markedly better side-effect profile.
Case Report
A 60-year-old woman with recent upper respiratory tract and sinus infections presented to our dermatology clinic with painful palpable purpura on the bilateral shins, thighs, and dorsal aspects of the feet of several months’ duration (Figure, A). Her primary care provider initiated treatment with amoxicillin and doxycycline for the infections. When the rash developed approximately 1.5 weeks following initiation of her symptoms, the patient was referred to the dermatology and rheumatology departments at our institution. The treating dermatologist (M.B.T.) obtained a 4-mm punch biopsy from the right lower leg and LCV was shown on histology. The patient completed a 14-day course of doxycycline and amoxicillin without resolution of the eruption. After an extensive investigation, the treating rheumatologist concluded that the LCV was idiopathic or secondary to an infection or drug exposure. The rheumatologist started the patient on oral prednisone for the chronic symptomatic LCV, but she was intolerant of this medication and discontinued it after 1 week. Our dermatology clinic started her on triamcinolone cream 0.1% twice daily, but she continued to experience new and worsening lesions. At her follow-up appointment 1 month later, triamcinolone cream was discontinued and dapsone gel 5% twice daily was started. She experienced resolution of her previously recalcitrant LCV within 3 weeks (Figure, B).
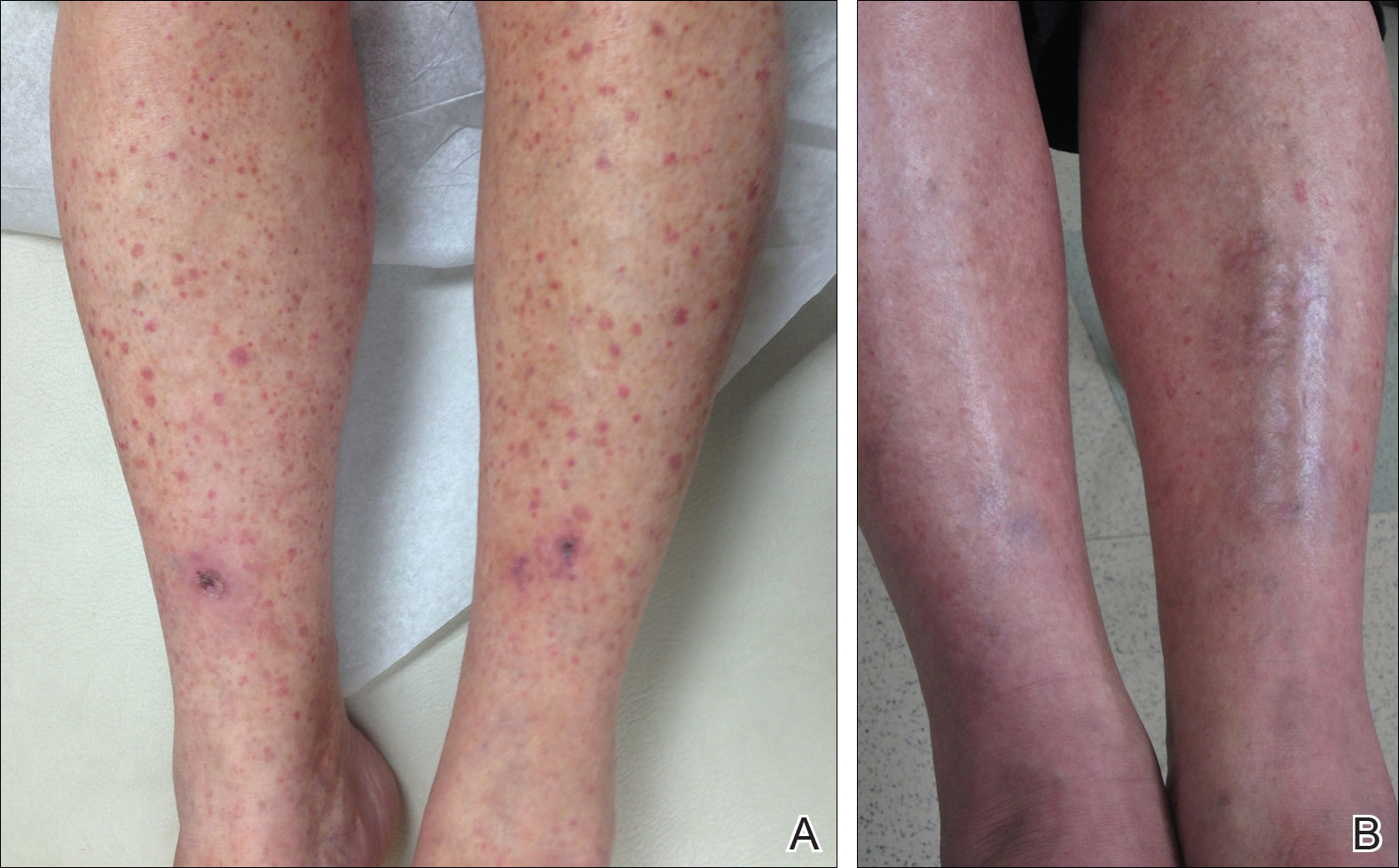
Comment
Established therapies for LCV carry serious side-effect profiles, which can preclude their use.5 Therefore, a topical therapeutic alternative for LCV would be ideal. Systemic prednisone is the first-line therapy for chronic and/or symptomatic LCV, but its side effects include suppression of the hypothalamic-pituitary-adrenal axis, immunosuppression, osteonecrosis, and glucose intolerance.5 Colchicine therapy carries risks for blood dyscrasia, immunosuppression, and gastrointestinal tract upset. Systemic dapsone also is an effective therapy for chronic and/or symptomatic LCV.5,6 However, systemic dapsone requires glucose-6-phosphate dehydrogenase deficiency screening and routine monitoring of blood counts, and it also carries the risk for serious adverse effects including neuropathy, blood dyscrasia, and hypersensitivity syndrome.5,6 Topical dapsone may provide similar efficacy with far fewer adverse effects and has proven to be a safe treatment of acne, even when used in patients with glucose-6-phosphate dehydrogenase deficiency. It displays low systemic absorption and does not accumulate over time once a steady state is reached.7 It also has been shown to be beneficial in other vasculopathies such as erythema elevatum diutinum and in other neutrophilic inflammatory disorders such as pyoderma gangrenosum.8,9 A case of methemoglobinemia due to topical dapsone has been reported.10 Although this effect is rare, clinicians should be aware of such adverse effects when using medications for off-label purposes.
Leukocytoclastic vasculitis can spontaneously resolve; however, our patient’s disease was chronic for several months, and she continued to develop new lesions without signs of resolution. After initiating topical dapsone, she experienced resolution within 3 weeks.
Conclusion
Topical dapsone is a novel approach for treating LCV. Given this drug’s favorable side-effect profile compared to the currently available therapeutic alternatives, we believe it is a reasonable option in select patients. Further investigation is needed to prove its efficacy, but it could be an ideal alternative for patients with contraindications to traditional therapies and/or for those unable to tolerate systemic therapy.
- Koutkia P, Mylonakis E, Rounds S, et al. Leucocytoclastic vasculitis: an update for the clinician. Scand J Rheumatol. 2001;30:315-322.
- Af Ekenstam E, Callen JP. Cutaneous leukocytoclastic vasculitis. clinical and laboratory features of 82 patients seen in private practice. Arch Dermatol. 1984;120:484-489.
- Gyselbrecht L, de Keyser F, Ongenae K, et al. Etiological factors and underlying conditions in patientswith leucocytoclastic vasculitis. Clin Exp Rheumatol. 1996;14:665-668.
- Sais G, Vidaller A, Jucglà A, et al. Colchicine in the treatment of cutaneous leukocytoclastic vasculitis. results of a prospective, randomized controlled trial. Arch Dermatol. 1995;131:1399-1402.
- Sunderkotter C, Bonsmann G, Sindrilaru A, et al. Management of leukocytoclastic vasculitis: clinical review. J Dermatol Treat. 2005;16:193-206.
- Zhu YI, Stiller MJ. Dapsone and sulfones in dermatology: overview and update. J Am Acad Dermatol. 2001;45:420-434.
- Stotland M, Shalita AR, Kissling RF. Dapsone 5% gel: a review of its efficacy and safety in the treatment of acne vulgaris. Am J Clin Dermatol. 2009;10:221-227.
- Frieling GW, Williams NL, Lim SJ, et al. Novel use of topical dapsone 5% gel for erythema elevatum diutinum: safer and effective. J Drugs Dermatol. 2013;12:481-484.
- Handler MZ, Hamilton H, Aires D. Treatment of peristomal pyoderma gangrenosum with topical crushed dapsone. J Drugs Dermatol. 2011;10:1059-1061.
- Swartzentruber GS, Yanta JH, Pizon AF. Methemoglobi-nemia as a complication of topical dapsone. N Engl J Med. 2015;372:491-492.
Leukocytoclastic vasculitis (LCV) is a disease characterized by inflammation of small vessels with characteristic clinical findings of petechiae and palpable purpura.1 Numerous etiologies have been described, but the disease commonly remains idiopathic.2,3 Leukocytoclastic vasculitis often spontaneously resolves within weeks and requires only symptomatic treatment. Chronic or severe disease can require systemic medical treatment with agents such as colchicine, dapsone, and corticosteroids. These agents are effective but carry risks of serious side effects.4,5 These side effects and/or medical contraindications prevent some patients from taking systemic medications for LCV. We present a case of LCV that resolved after treatment with topical dapsone, highlighting a potential new treatment ofLCV with a markedly better side-effect profile.
Case Report
A 60-year-old woman with recent upper respiratory tract and sinus infections presented to our dermatology clinic with painful palpable purpura on the bilateral shins, thighs, and dorsal aspects of the feet of several months’ duration (Figure, A). Her primary care provider initiated treatment with amoxicillin and doxycycline for the infections. When the rash developed approximately 1.5 weeks following initiation of her symptoms, the patient was referred to the dermatology and rheumatology departments at our institution. The treating dermatologist (M.B.T.) obtained a 4-mm punch biopsy from the right lower leg and LCV was shown on histology. The patient completed a 14-day course of doxycycline and amoxicillin without resolution of the eruption. After an extensive investigation, the treating rheumatologist concluded that the LCV was idiopathic or secondary to an infection or drug exposure. The rheumatologist started the patient on oral prednisone for the chronic symptomatic LCV, but she was intolerant of this medication and discontinued it after 1 week. Our dermatology clinic started her on triamcinolone cream 0.1% twice daily, but she continued to experience new and worsening lesions. At her follow-up appointment 1 month later, triamcinolone cream was discontinued and dapsone gel 5% twice daily was started. She experienced resolution of her previously recalcitrant LCV within 3 weeks (Figure, B).
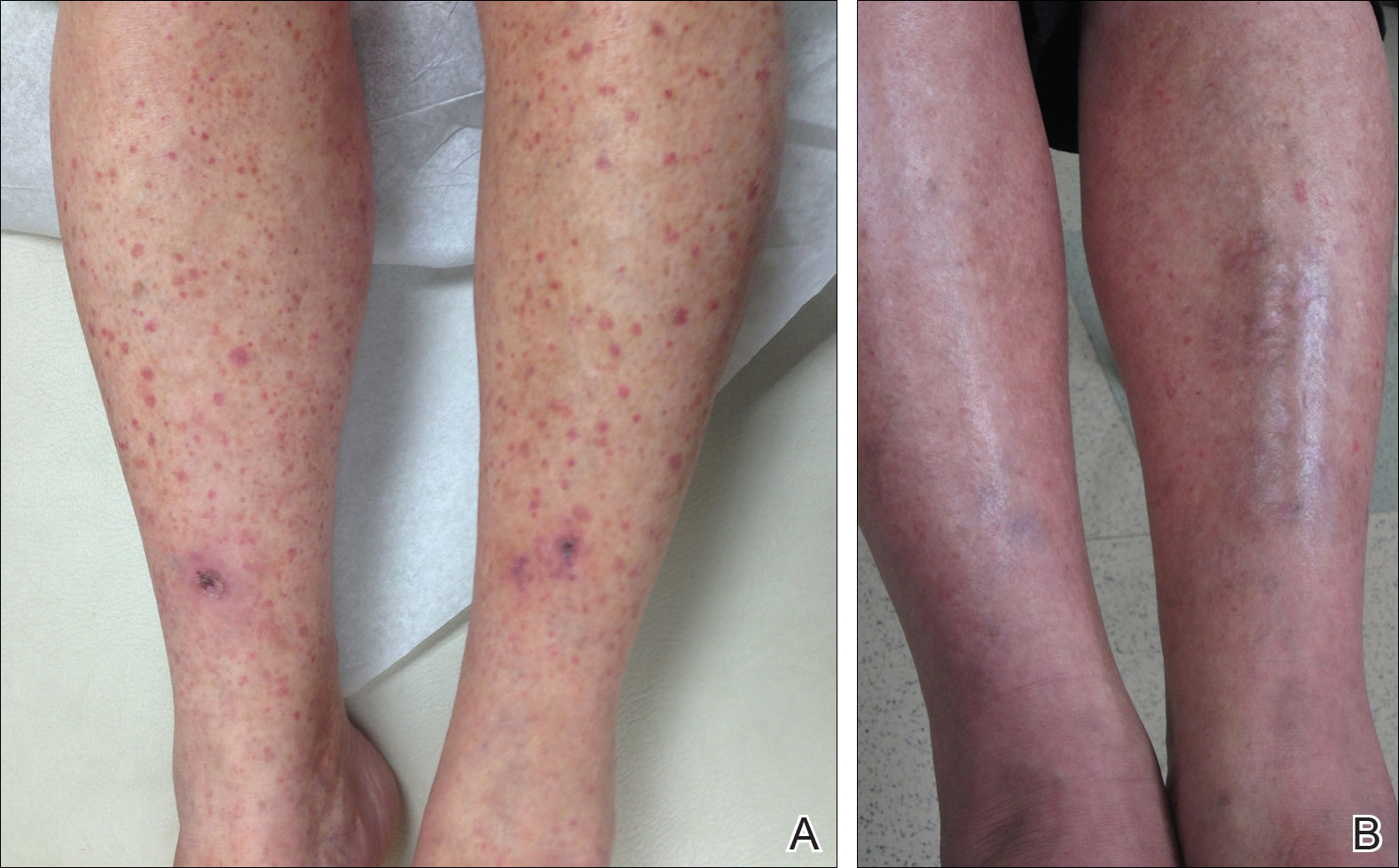
Comment
Established therapies for LCV carry serious side-effect profiles, which can preclude their use.5 Therefore, a topical therapeutic alternative for LCV would be ideal. Systemic prednisone is the first-line therapy for chronic and/or symptomatic LCV, but its side effects include suppression of the hypothalamic-pituitary-adrenal axis, immunosuppression, osteonecrosis, and glucose intolerance.5 Colchicine therapy carries risks for blood dyscrasia, immunosuppression, and gastrointestinal tract upset. Systemic dapsone also is an effective therapy for chronic and/or symptomatic LCV.5,6 However, systemic dapsone requires glucose-6-phosphate dehydrogenase deficiency screening and routine monitoring of blood counts, and it also carries the risk for serious adverse effects including neuropathy, blood dyscrasia, and hypersensitivity syndrome.5,6 Topical dapsone may provide similar efficacy with far fewer adverse effects and has proven to be a safe treatment of acne, even when used in patients with glucose-6-phosphate dehydrogenase deficiency. It displays low systemic absorption and does not accumulate over time once a steady state is reached.7 It also has been shown to be beneficial in other vasculopathies such as erythema elevatum diutinum and in other neutrophilic inflammatory disorders such as pyoderma gangrenosum.8,9 A case of methemoglobinemia due to topical dapsone has been reported.10 Although this effect is rare, clinicians should be aware of such adverse effects when using medications for off-label purposes.
Leukocytoclastic vasculitis can spontaneously resolve; however, our patient’s disease was chronic for several months, and she continued to develop new lesions without signs of resolution. After initiating topical dapsone, she experienced resolution within 3 weeks.
Conclusion
Topical dapsone is a novel approach for treating LCV. Given this drug’s favorable side-effect profile compared to the currently available therapeutic alternatives, we believe it is a reasonable option in select patients. Further investigation is needed to prove its efficacy, but it could be an ideal alternative for patients with contraindications to traditional therapies and/or for those unable to tolerate systemic therapy.
Leukocytoclastic vasculitis (LCV) is a disease characterized by inflammation of small vessels with characteristic clinical findings of petechiae and palpable purpura.1 Numerous etiologies have been described, but the disease commonly remains idiopathic.2,3 Leukocytoclastic vasculitis often spontaneously resolves within weeks and requires only symptomatic treatment. Chronic or severe disease can require systemic medical treatment with agents such as colchicine, dapsone, and corticosteroids. These agents are effective but carry risks of serious side effects.4,5 These side effects and/or medical contraindications prevent some patients from taking systemic medications for LCV. We present a case of LCV that resolved after treatment with topical dapsone, highlighting a potential new treatment ofLCV with a markedly better side-effect profile.
Case Report
A 60-year-old woman with recent upper respiratory tract and sinus infections presented to our dermatology clinic with painful palpable purpura on the bilateral shins, thighs, and dorsal aspects of the feet of several months’ duration (Figure, A). Her primary care provider initiated treatment with amoxicillin and doxycycline for the infections. When the rash developed approximately 1.5 weeks following initiation of her symptoms, the patient was referred to the dermatology and rheumatology departments at our institution. The treating dermatologist (M.B.T.) obtained a 4-mm punch biopsy from the right lower leg and LCV was shown on histology. The patient completed a 14-day course of doxycycline and amoxicillin without resolution of the eruption. After an extensive investigation, the treating rheumatologist concluded that the LCV was idiopathic or secondary to an infection or drug exposure. The rheumatologist started the patient on oral prednisone for the chronic symptomatic LCV, but she was intolerant of this medication and discontinued it after 1 week. Our dermatology clinic started her on triamcinolone cream 0.1% twice daily, but she continued to experience new and worsening lesions. At her follow-up appointment 1 month later, triamcinolone cream was discontinued and dapsone gel 5% twice daily was started. She experienced resolution of her previously recalcitrant LCV within 3 weeks (Figure, B).
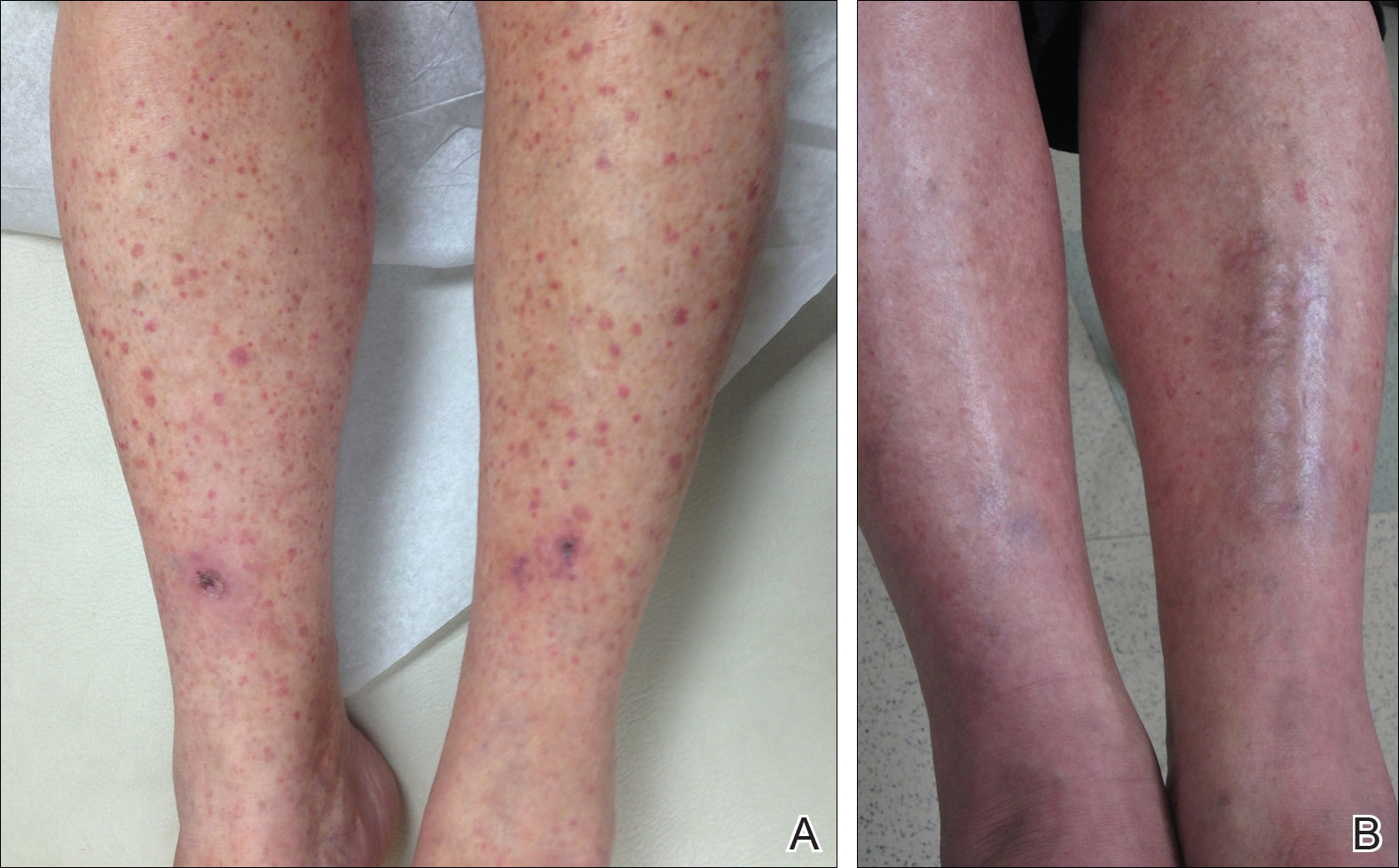
Comment
Established therapies for LCV carry serious side-effect profiles, which can preclude their use.5 Therefore, a topical therapeutic alternative for LCV would be ideal. Systemic prednisone is the first-line therapy for chronic and/or symptomatic LCV, but its side effects include suppression of the hypothalamic-pituitary-adrenal axis, immunosuppression, osteonecrosis, and glucose intolerance.5 Colchicine therapy carries risks for blood dyscrasia, immunosuppression, and gastrointestinal tract upset. Systemic dapsone also is an effective therapy for chronic and/or symptomatic LCV.5,6 However, systemic dapsone requires glucose-6-phosphate dehydrogenase deficiency screening and routine monitoring of blood counts, and it also carries the risk for serious adverse effects including neuropathy, blood dyscrasia, and hypersensitivity syndrome.5,6 Topical dapsone may provide similar efficacy with far fewer adverse effects and has proven to be a safe treatment of acne, even when used in patients with glucose-6-phosphate dehydrogenase deficiency. It displays low systemic absorption and does not accumulate over time once a steady state is reached.7 It also has been shown to be beneficial in other vasculopathies such as erythema elevatum diutinum and in other neutrophilic inflammatory disorders such as pyoderma gangrenosum.8,9 A case of methemoglobinemia due to topical dapsone has been reported.10 Although this effect is rare, clinicians should be aware of such adverse effects when using medications for off-label purposes.
Leukocytoclastic vasculitis can spontaneously resolve; however, our patient’s disease was chronic for several months, and she continued to develop new lesions without signs of resolution. After initiating topical dapsone, she experienced resolution within 3 weeks.
Conclusion
Topical dapsone is a novel approach for treating LCV. Given this drug’s favorable side-effect profile compared to the currently available therapeutic alternatives, we believe it is a reasonable option in select patients. Further investigation is needed to prove its efficacy, but it could be an ideal alternative for patients with contraindications to traditional therapies and/or for those unable to tolerate systemic therapy.
- Koutkia P, Mylonakis E, Rounds S, et al. Leucocytoclastic vasculitis: an update for the clinician. Scand J Rheumatol. 2001;30:315-322.
- Af Ekenstam E, Callen JP. Cutaneous leukocytoclastic vasculitis. clinical and laboratory features of 82 patients seen in private practice. Arch Dermatol. 1984;120:484-489.
- Gyselbrecht L, de Keyser F, Ongenae K, et al. Etiological factors and underlying conditions in patientswith leucocytoclastic vasculitis. Clin Exp Rheumatol. 1996;14:665-668.
- Sais G, Vidaller A, Jucglà A, et al. Colchicine in the treatment of cutaneous leukocytoclastic vasculitis. results of a prospective, randomized controlled trial. Arch Dermatol. 1995;131:1399-1402.
- Sunderkotter C, Bonsmann G, Sindrilaru A, et al. Management of leukocytoclastic vasculitis: clinical review. J Dermatol Treat. 2005;16:193-206.
- Zhu YI, Stiller MJ. Dapsone and sulfones in dermatology: overview and update. J Am Acad Dermatol. 2001;45:420-434.
- Stotland M, Shalita AR, Kissling RF. Dapsone 5% gel: a review of its efficacy and safety in the treatment of acne vulgaris. Am J Clin Dermatol. 2009;10:221-227.
- Frieling GW, Williams NL, Lim SJ, et al. Novel use of topical dapsone 5% gel for erythema elevatum diutinum: safer and effective. J Drugs Dermatol. 2013;12:481-484.
- Handler MZ, Hamilton H, Aires D. Treatment of peristomal pyoderma gangrenosum with topical crushed dapsone. J Drugs Dermatol. 2011;10:1059-1061.
- Swartzentruber GS, Yanta JH, Pizon AF. Methemoglobi-nemia as a complication of topical dapsone. N Engl J Med. 2015;372:491-492.
- Koutkia P, Mylonakis E, Rounds S, et al. Leucocytoclastic vasculitis: an update for the clinician. Scand J Rheumatol. 2001;30:315-322.
- Af Ekenstam E, Callen JP. Cutaneous leukocytoclastic vasculitis. clinical and laboratory features of 82 patients seen in private practice. Arch Dermatol. 1984;120:484-489.
- Gyselbrecht L, de Keyser F, Ongenae K, et al. Etiological factors and underlying conditions in patientswith leucocytoclastic vasculitis. Clin Exp Rheumatol. 1996;14:665-668.
- Sais G, Vidaller A, Jucglà A, et al. Colchicine in the treatment of cutaneous leukocytoclastic vasculitis. results of a prospective, randomized controlled trial. Arch Dermatol. 1995;131:1399-1402.
- Sunderkotter C, Bonsmann G, Sindrilaru A, et al. Management of leukocytoclastic vasculitis: clinical review. J Dermatol Treat. 2005;16:193-206.
- Zhu YI, Stiller MJ. Dapsone and sulfones in dermatology: overview and update. J Am Acad Dermatol. 2001;45:420-434.
- Stotland M, Shalita AR, Kissling RF. Dapsone 5% gel: a review of its efficacy and safety in the treatment of acne vulgaris. Am J Clin Dermatol. 2009;10:221-227.
- Frieling GW, Williams NL, Lim SJ, et al. Novel use of topical dapsone 5% gel for erythema elevatum diutinum: safer and effective. J Drugs Dermatol. 2013;12:481-484.
- Handler MZ, Hamilton H, Aires D. Treatment of peristomal pyoderma gangrenosum with topical crushed dapsone. J Drugs Dermatol. 2011;10:1059-1061.
- Swartzentruber GS, Yanta JH, Pizon AF. Methemoglobi-nemia as a complication of topical dapsone. N Engl J Med. 2015;372:491-492.
Practice Points
- Leukocytoclastic vasculitis is characterized by inflammation of small vessels with characteristic clinical findings of petechiae and palpable purpura.
- Leukocytoclastic vasculitis often spontaneously resolves within weeks and requires only symptomatic treatment, but chronic or severe disease can require systemic medical treatment with agents such as colchicine, dapsone, and corticosteroids.
Long-acting injectables may be best at preventing relapse in psychosis
SAN DIEGO – A new meta-analysis suggests that second-generation long-acting injectable antipsychotics (LAIs) are slightly better than oral antipsychotics at preventing relapse after a first psychotic incident.
The meta-analysis, released at the annual meeting of the American Psychiatric Association, is limited because it looks at only three studies. Still, study lead author Christine Tran-Boynes, DO, said the findings are useful for psychiatrists.
“For a long time, LAIs were associated with severely ill psychotic patients who were frequently hospitalized and not compliant with their oral meds,” Dr. Tran-Boynes, a resident at the University of Maryland, Baltimore, said in an interview. “The purpose of this paper is to change the perception of LAIs. They are not just a medication of last resort in those with severe, chronic psychosis but, instead, can be used in the early stages of psychosis as prophylaxis against relapse.”
Injectable antipsychotics are more commonly used in Europe, where “there also seemed to be a greater willingness among patients to receive this treatment,” said Peter F. Buckley, MD, dean of the medical school at Virginia Commonwealth University, Richmond.
The APA’s schizophrenia treatment guidelines recommend LAIs for patients with “recurrent relapses related to nonadherence” and patients who prefer the shots. Dr. Tran-Boynes notes that “the most common cause of relapse in patients with schizophrenia is partial adherence or nonadherence to oral antipsychotics. If LAIs can improve adherence in patients and monitoring of adherence for clinicians, they could have a role in preventing relapse during this critical period in psychosis.”
The meta-analysis examines three randomized controlled studies – two from 2015 and one from 2013 – that compare second-generation LAIs to first- and second-generation oral antipsychotics after first episodes of psychosis. Dr. Tran-Boynes said researchers could not find any studies comparing first-generation long-acting antipsychotics to oral antipsychotics.
The largest study had 769 participants; the others had 85 and 86. The subjects, all adults, had diagnoses of schizophrenia, schizoaffective disorder, or schizophreniform disorder. Their diagnoses must have been made within the previous 5 years.
According to the meta-analysis, relapses after first-episode psychosis were more likely (relative risk, 1.078; 95% confidence interval, 1.007-1.154; P = 0.012) in patients taking first- or second-generation oral antipsychotics, compared with those on second-generation LAIs.
“There was an 8% greater efficacy for LAIs preventing relapse after early psychosis, compared to oral antipsychotics,” Dr. Tran-Boynes said. She calculated the number needed to treat as 14.
The percentages of patients who did not relapse while taking second-generation LAIs ranged from 73% (31 of 42 patients randomized to an injectable risperidone arm over 24 months) to 95% (38 of 40 patients over a 12-month study, also of injectable risperidone), Dr. Tran-Boynes said.
When asked about the meta-analysis, Robert Rosenheck, MD, expressed concern.
“While well done, it is based on too few studies to give useful guidance to practice,” said Dr. Rosenheck, professor of psychiatry, epidemiology and public health at Yale University, New Haven, Conn.
Dr. Buckley also noted that the meta-analysis includes a small number of studies. “The effect is sizable for a first-episode population, but other studies to date are more mixed,” he added. “For instance, in a study among a more chronic schizophrenic population, we found no difference between a group receiving long-acting injectable risperidone and oral second-generation antipsychotics” (Schizophr Bull. 2015 Mar;41[2]:449-59).
What should psychiatrists know when they consider prescribing LAIs to prevent psychotic relapse? “If a patient expresses willingness to take an oral antipsychotic on a daily basis and/or has someone to monitor his medication intake, then prescribing an oral antipsychotic would be the ideal route,” Dr. Tran-Boynes said. “However, I would recommend LAIs to patients who have demonstrated poor compliance with previous medications in general, poor awareness of psychosis, poor awareness of need for treatment, poor availability of social support to ensure that the patient will take his/her medication daily, and/or if a patient expresses preference for LAIs.”
She cautioned that LAIs have disadvantages. Compared with oral antipsychotics, it’s harder to adjust patients’ dosages in response to side effects or when they improve, she said. LAIs are also more expensive in the short term, she said.
However, LAIs also may have produced fewer side effects, and there aren’t any questions about compliance, she said. In addition, “there’s less pain at the injection site with second-generation LAIs, compared to first-generation LAIs, due to the water-based solution of the former. The oil-based solutions that are characteristic of first-generation LAIs have been shown in studies to be very painful.”
Dr. Tran-Boynes and Dr. Rosenheck reported no relevant disclosures. Dr. Buckley disclosed that he is a research consultant for the National Institute of Mental Health.
SAN DIEGO – A new meta-analysis suggests that second-generation long-acting injectable antipsychotics (LAIs) are slightly better than oral antipsychotics at preventing relapse after a first psychotic incident.
The meta-analysis, released at the annual meeting of the American Psychiatric Association, is limited because it looks at only three studies. Still, study lead author Christine Tran-Boynes, DO, said the findings are useful for psychiatrists.
“For a long time, LAIs were associated with severely ill psychotic patients who were frequently hospitalized and not compliant with their oral meds,” Dr. Tran-Boynes, a resident at the University of Maryland, Baltimore, said in an interview. “The purpose of this paper is to change the perception of LAIs. They are not just a medication of last resort in those with severe, chronic psychosis but, instead, can be used in the early stages of psychosis as prophylaxis against relapse.”
Injectable antipsychotics are more commonly used in Europe, where “there also seemed to be a greater willingness among patients to receive this treatment,” said Peter F. Buckley, MD, dean of the medical school at Virginia Commonwealth University, Richmond.
The APA’s schizophrenia treatment guidelines recommend LAIs for patients with “recurrent relapses related to nonadherence” and patients who prefer the shots. Dr. Tran-Boynes notes that “the most common cause of relapse in patients with schizophrenia is partial adherence or nonadherence to oral antipsychotics. If LAIs can improve adherence in patients and monitoring of adherence for clinicians, they could have a role in preventing relapse during this critical period in psychosis.”
The meta-analysis examines three randomized controlled studies – two from 2015 and one from 2013 – that compare second-generation LAIs to first- and second-generation oral antipsychotics after first episodes of psychosis. Dr. Tran-Boynes said researchers could not find any studies comparing first-generation long-acting antipsychotics to oral antipsychotics.
The largest study had 769 participants; the others had 85 and 86. The subjects, all adults, had diagnoses of schizophrenia, schizoaffective disorder, or schizophreniform disorder. Their diagnoses must have been made within the previous 5 years.
According to the meta-analysis, relapses after first-episode psychosis were more likely (relative risk, 1.078; 95% confidence interval, 1.007-1.154; P = 0.012) in patients taking first- or second-generation oral antipsychotics, compared with those on second-generation LAIs.
“There was an 8% greater efficacy for LAIs preventing relapse after early psychosis, compared to oral antipsychotics,” Dr. Tran-Boynes said. She calculated the number needed to treat as 14.
The percentages of patients who did not relapse while taking second-generation LAIs ranged from 73% (31 of 42 patients randomized to an injectable risperidone arm over 24 months) to 95% (38 of 40 patients over a 12-month study, also of injectable risperidone), Dr. Tran-Boynes said.
When asked about the meta-analysis, Robert Rosenheck, MD, expressed concern.
“While well done, it is based on too few studies to give useful guidance to practice,” said Dr. Rosenheck, professor of psychiatry, epidemiology and public health at Yale University, New Haven, Conn.
Dr. Buckley also noted that the meta-analysis includes a small number of studies. “The effect is sizable for a first-episode population, but other studies to date are more mixed,” he added. “For instance, in a study among a more chronic schizophrenic population, we found no difference between a group receiving long-acting injectable risperidone and oral second-generation antipsychotics” (Schizophr Bull. 2015 Mar;41[2]:449-59).
What should psychiatrists know when they consider prescribing LAIs to prevent psychotic relapse? “If a patient expresses willingness to take an oral antipsychotic on a daily basis and/or has someone to monitor his medication intake, then prescribing an oral antipsychotic would be the ideal route,” Dr. Tran-Boynes said. “However, I would recommend LAIs to patients who have demonstrated poor compliance with previous medications in general, poor awareness of psychosis, poor awareness of need for treatment, poor availability of social support to ensure that the patient will take his/her medication daily, and/or if a patient expresses preference for LAIs.”
She cautioned that LAIs have disadvantages. Compared with oral antipsychotics, it’s harder to adjust patients’ dosages in response to side effects or when they improve, she said. LAIs are also more expensive in the short term, she said.
However, LAIs also may have produced fewer side effects, and there aren’t any questions about compliance, she said. In addition, “there’s less pain at the injection site with second-generation LAIs, compared to first-generation LAIs, due to the water-based solution of the former. The oil-based solutions that are characteristic of first-generation LAIs have been shown in studies to be very painful.”
Dr. Tran-Boynes and Dr. Rosenheck reported no relevant disclosures. Dr. Buckley disclosed that he is a research consultant for the National Institute of Mental Health.
SAN DIEGO – A new meta-analysis suggests that second-generation long-acting injectable antipsychotics (LAIs) are slightly better than oral antipsychotics at preventing relapse after a first psychotic incident.
The meta-analysis, released at the annual meeting of the American Psychiatric Association, is limited because it looks at only three studies. Still, study lead author Christine Tran-Boynes, DO, said the findings are useful for psychiatrists.
“For a long time, LAIs were associated with severely ill psychotic patients who were frequently hospitalized and not compliant with their oral meds,” Dr. Tran-Boynes, a resident at the University of Maryland, Baltimore, said in an interview. “The purpose of this paper is to change the perception of LAIs. They are not just a medication of last resort in those with severe, chronic psychosis but, instead, can be used in the early stages of psychosis as prophylaxis against relapse.”
Injectable antipsychotics are more commonly used in Europe, where “there also seemed to be a greater willingness among patients to receive this treatment,” said Peter F. Buckley, MD, dean of the medical school at Virginia Commonwealth University, Richmond.
The APA’s schizophrenia treatment guidelines recommend LAIs for patients with “recurrent relapses related to nonadherence” and patients who prefer the shots. Dr. Tran-Boynes notes that “the most common cause of relapse in patients with schizophrenia is partial adherence or nonadherence to oral antipsychotics. If LAIs can improve adherence in patients and monitoring of adherence for clinicians, they could have a role in preventing relapse during this critical period in psychosis.”
The meta-analysis examines three randomized controlled studies – two from 2015 and one from 2013 – that compare second-generation LAIs to first- and second-generation oral antipsychotics after first episodes of psychosis. Dr. Tran-Boynes said researchers could not find any studies comparing first-generation long-acting antipsychotics to oral antipsychotics.
The largest study had 769 participants; the others had 85 and 86. The subjects, all adults, had diagnoses of schizophrenia, schizoaffective disorder, or schizophreniform disorder. Their diagnoses must have been made within the previous 5 years.
According to the meta-analysis, relapses after first-episode psychosis were more likely (relative risk, 1.078; 95% confidence interval, 1.007-1.154; P = 0.012) in patients taking first- or second-generation oral antipsychotics, compared with those on second-generation LAIs.
“There was an 8% greater efficacy for LAIs preventing relapse after early psychosis, compared to oral antipsychotics,” Dr. Tran-Boynes said. She calculated the number needed to treat as 14.
The percentages of patients who did not relapse while taking second-generation LAIs ranged from 73% (31 of 42 patients randomized to an injectable risperidone arm over 24 months) to 95% (38 of 40 patients over a 12-month study, also of injectable risperidone), Dr. Tran-Boynes said.
When asked about the meta-analysis, Robert Rosenheck, MD, expressed concern.
“While well done, it is based on too few studies to give useful guidance to practice,” said Dr. Rosenheck, professor of psychiatry, epidemiology and public health at Yale University, New Haven, Conn.
Dr. Buckley also noted that the meta-analysis includes a small number of studies. “The effect is sizable for a first-episode population, but other studies to date are more mixed,” he added. “For instance, in a study among a more chronic schizophrenic population, we found no difference between a group receiving long-acting injectable risperidone and oral second-generation antipsychotics” (Schizophr Bull. 2015 Mar;41[2]:449-59).
What should psychiatrists know when they consider prescribing LAIs to prevent psychotic relapse? “If a patient expresses willingness to take an oral antipsychotic on a daily basis and/or has someone to monitor his medication intake, then prescribing an oral antipsychotic would be the ideal route,” Dr. Tran-Boynes said. “However, I would recommend LAIs to patients who have demonstrated poor compliance with previous medications in general, poor awareness of psychosis, poor awareness of need for treatment, poor availability of social support to ensure that the patient will take his/her medication daily, and/or if a patient expresses preference for LAIs.”
She cautioned that LAIs have disadvantages. Compared with oral antipsychotics, it’s harder to adjust patients’ dosages in response to side effects or when they improve, she said. LAIs are also more expensive in the short term, she said.
However, LAIs also may have produced fewer side effects, and there aren’t any questions about compliance, she said. In addition, “there’s less pain at the injection site with second-generation LAIs, compared to first-generation LAIs, due to the water-based solution of the former. The oil-based solutions that are characteristic of first-generation LAIs have been shown in studies to be very painful.”
Dr. Tran-Boynes and Dr. Rosenheck reported no relevant disclosures. Dr. Buckley disclosed that he is a research consultant for the National Institute of Mental Health.
AT APA
Key clinical point: Second-generation long-acting injectable antipsychotics (LAIs) may be better than oral antipsychotics at preventing relapse after first episode of psychosis.
Major finding: Relapses after first-episode psychosis were more likely (RR, 1.078; 95% CI, 1.007-1.154; P = 0.012) in patients on first- and second-generation oral antipsychotics, compared with second-generation LAIs.
Data source: Meta-analysis of three randomized controlled trials with 940 total patients.
Disclosures: Dr. Tran-Boynes reported having no relevant disclosures.
Make the Diagnosis - June 2017
Diagnosis: Porokeratotic eccrine ostial and dermal duct nevus (PEODDN)
Porokeratotic eccrine ostial and dermal duct nevus (PEODDN) is a rare, benign adnexal hamartoma first reported by Marsden et al. in 1979 as “comedo nevus of the palm” (Br J Dermatol. 1979 Dec;101[6]:717-22).
To date, 77 cases of PEODDN have been reported in the literature, with 53% having congenital onset. The average age of onset for the acquired lesions was 6 years. PEODDN affects males and females equally. Acral location is the most common (94%), but lesions have been reported less commonly on the trunk and face. A review of the literature found that most cases of PEODDN were independent, not associated with other conditions. Rarely, Bowen’s disease and squamous cell carcinoma have been reported to arise within PEODDN. Interestingly, two cases have been associated with keratitis-ichthyosis-deafness syndrome (KID).
Common differential diagnoses for PEODDN include porokeratosis of Mibelli, linear psoriasis, and linear epidermal nevus. Linear porokeratosis and porokeratosis of Mibelli are characterized by sharply demarcated hyperkeratotic annular lesions with distinct keratotic edges but do not have eccrine gland involvement on histopathology. Linear psoriasis, a rare form of psoriasis, is characterized by late onset linear psoriatic lesions along Blaschko lines. Linear epidermal nevus is a disease characterized by pruritic, erythematous scaly lesions following Blaschko lines that occurs in the first months of life and is slowly progressive. Histopathological features of PEODDN are diagnostic and distinguish it from these other clinical entities. A prominent parakeratotic column within an epidermal invagination that displays loss of the granular layer is found overlaying an eccrine duct with a dilated acrosyringium. Vacuolated and dyskeratotic keratinocytes are also typically present within the epidermal invagination.
The treatment for PEODDN remains elusive. Topical keratolytics, topical retinoids, topical steroids, topical calcipotriol, cryosurgery, phototherapy, and anthralin have been used to treat PEODDN unsuccessfully. Thus far, the most efficacious treatments include CO2 laser and surgical excision for small lesions. Given the young age of this patient, emollient therapy was chosen as treatment until the patient reaches an age at which the lesion is cosmetically more disturbing and other therapies may be safely attempted.
In conclusion, this patient represents a classic case of the rare entity, PEODDN, and draws attention to recent discoveries that a genetic mutation in GJB2 is causative. Because PEODDN shares its pathogenic mutation with KID syndrome, clinicians should be aware that, if the same mutation also affects germline cells, offspring have the potential to express manifestations of KID syndrome.
This case and photo are courtesy of Molly B. Hirt, a medical student at Indiana University, Indianapolis; Carrie L. Davis, MD, of the Dermatology Center of Southern Indiana and Indiana University, Bloomington; and Anita N. Haggstrom, MD, of the departments of dermatology and pediatrics, Indiana University, Indianapolis.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
Diagnosis: Porokeratotic eccrine ostial and dermal duct nevus (PEODDN)
Porokeratotic eccrine ostial and dermal duct nevus (PEODDN) is a rare, benign adnexal hamartoma first reported by Marsden et al. in 1979 as “comedo nevus of the palm” (Br J Dermatol. 1979 Dec;101[6]:717-22).
To date, 77 cases of PEODDN have been reported in the literature, with 53% having congenital onset. The average age of onset for the acquired lesions was 6 years. PEODDN affects males and females equally. Acral location is the most common (94%), but lesions have been reported less commonly on the trunk and face. A review of the literature found that most cases of PEODDN were independent, not associated with other conditions. Rarely, Bowen’s disease and squamous cell carcinoma have been reported to arise within PEODDN. Interestingly, two cases have been associated with keratitis-ichthyosis-deafness syndrome (KID).
Common differential diagnoses for PEODDN include porokeratosis of Mibelli, linear psoriasis, and linear epidermal nevus. Linear porokeratosis and porokeratosis of Mibelli are characterized by sharply demarcated hyperkeratotic annular lesions with distinct keratotic edges but do not have eccrine gland involvement on histopathology. Linear psoriasis, a rare form of psoriasis, is characterized by late onset linear psoriatic lesions along Blaschko lines. Linear epidermal nevus is a disease characterized by pruritic, erythematous scaly lesions following Blaschko lines that occurs in the first months of life and is slowly progressive. Histopathological features of PEODDN are diagnostic and distinguish it from these other clinical entities. A prominent parakeratotic column within an epidermal invagination that displays loss of the granular layer is found overlaying an eccrine duct with a dilated acrosyringium. Vacuolated and dyskeratotic keratinocytes are also typically present within the epidermal invagination.
The treatment for PEODDN remains elusive. Topical keratolytics, topical retinoids, topical steroids, topical calcipotriol, cryosurgery, phototherapy, and anthralin have been used to treat PEODDN unsuccessfully. Thus far, the most efficacious treatments include CO2 laser and surgical excision for small lesions. Given the young age of this patient, emollient therapy was chosen as treatment until the patient reaches an age at which the lesion is cosmetically more disturbing and other therapies may be safely attempted.
In conclusion, this patient represents a classic case of the rare entity, PEODDN, and draws attention to recent discoveries that a genetic mutation in GJB2 is causative. Because PEODDN shares its pathogenic mutation with KID syndrome, clinicians should be aware that, if the same mutation also affects germline cells, offspring have the potential to express manifestations of KID syndrome.
This case and photo are courtesy of Molly B. Hirt, a medical student at Indiana University, Indianapolis; Carrie L. Davis, MD, of the Dermatology Center of Southern Indiana and Indiana University, Bloomington; and Anita N. Haggstrom, MD, of the departments of dermatology and pediatrics, Indiana University, Indianapolis.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
Diagnosis: Porokeratotic eccrine ostial and dermal duct nevus (PEODDN)
Porokeratotic eccrine ostial and dermal duct nevus (PEODDN) is a rare, benign adnexal hamartoma first reported by Marsden et al. in 1979 as “comedo nevus of the palm” (Br J Dermatol. 1979 Dec;101[6]:717-22).
To date, 77 cases of PEODDN have been reported in the literature, with 53% having congenital onset. The average age of onset for the acquired lesions was 6 years. PEODDN affects males and females equally. Acral location is the most common (94%), but lesions have been reported less commonly on the trunk and face. A review of the literature found that most cases of PEODDN were independent, not associated with other conditions. Rarely, Bowen’s disease and squamous cell carcinoma have been reported to arise within PEODDN. Interestingly, two cases have been associated with keratitis-ichthyosis-deafness syndrome (KID).
Common differential diagnoses for PEODDN include porokeratosis of Mibelli, linear psoriasis, and linear epidermal nevus. Linear porokeratosis and porokeratosis of Mibelli are characterized by sharply demarcated hyperkeratotic annular lesions with distinct keratotic edges but do not have eccrine gland involvement on histopathology. Linear psoriasis, a rare form of psoriasis, is characterized by late onset linear psoriatic lesions along Blaschko lines. Linear epidermal nevus is a disease characterized by pruritic, erythematous scaly lesions following Blaschko lines that occurs in the first months of life and is slowly progressive. Histopathological features of PEODDN are diagnostic and distinguish it from these other clinical entities. A prominent parakeratotic column within an epidermal invagination that displays loss of the granular layer is found overlaying an eccrine duct with a dilated acrosyringium. Vacuolated and dyskeratotic keratinocytes are also typically present within the epidermal invagination.
The treatment for PEODDN remains elusive. Topical keratolytics, topical retinoids, topical steroids, topical calcipotriol, cryosurgery, phototherapy, and anthralin have been used to treat PEODDN unsuccessfully. Thus far, the most efficacious treatments include CO2 laser and surgical excision for small lesions. Given the young age of this patient, emollient therapy was chosen as treatment until the patient reaches an age at which the lesion is cosmetically more disturbing and other therapies may be safely attempted.
In conclusion, this patient represents a classic case of the rare entity, PEODDN, and draws attention to recent discoveries that a genetic mutation in GJB2 is causative. Because PEODDN shares its pathogenic mutation with KID syndrome, clinicians should be aware that, if the same mutation also affects germline cells, offspring have the potential to express manifestations of KID syndrome.
This case and photo are courtesy of Molly B. Hirt, a medical student at Indiana University, Indianapolis; Carrie L. Davis, MD, of the Dermatology Center of Southern Indiana and Indiana University, Bloomington; and Anita N. Haggstrom, MD, of the departments of dermatology and pediatrics, Indiana University, Indianapolis.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].

Segmental Vitiligo–like Hypopigmentation Associated With Metastatic Melanoma
To the Editor:
Melanoma-associated hypopigmentation frequently has been reported during the disease course and can include different characteristics such as regression of the primary melanoma and/or its metastases as well as common vitiligolike hypopigmentation at sites distant from the melanoma.1,2 Among patients who present with hypopigmentation, the most common clinical presentation is hypopigmented patches in a bilateral symmetric distribution that is similar to vitiligo.1 We report a case of segmental vitiligo–like hypopigmentation associated with melanoma.
RELATED ARTICLE: Novel Melanoma Therapies and Their Side Effects
A 37-year-old man presented with achromic patches on the right side of the neck and lower face of 2 months’ duration. He had a history of melanoma (Breslow thickness, 1.37 mm; mitotic rate, 4/mm2) on the right retroauricular region that was treated by wide local excision 12 years prior; after 10 years, he began to have headaches. At that time, imaging studies including computed tomography, magnetic resonance imaging, and positron emission tomography–computed tomography revealed multiple nodules on the brain, lungs, pancreas, left scapula, and left suprarenal gland. A lung biopsy confirmed metastatic melanoma. Intr
On physical examination using a Wood lamp at the current presentation 2 months later, the achromic patches were linearly distributed on the inferior portion of the right cheek (Figure). A 2×3-cm atrophic scar was present on the right retroauricular region. No regional or distant lymph nodes were enlarged or hard on examination. Although vitiligo is diagnosed using clinical findings,3 a biopsy was performed and showed absence of melanocytes at the dermoepidermal junction (hematoxylin and eosin stain) and complete absence of melanin pigment (Fontana-Masson stain). The patient was treated with topical tacrolimus with poor improvement after 2 months.
The relationship between melanoma and vitiligolike hypopigmentation is a fascinating and controversial topic. Its association is considered to be a consequence of the immune-mediated response against antigens shared by normal melanocytes and melanoma cells.4 Vitiligolike hypopigmentation occurs in 2.8%2 of melanoma patients and is reported in metastatic disease1 as well as those undergoing immunotherapy with or without chemotherapy.5 Its development in patients with stage III or IV melanoma seems to represent an independent positive prognostic factor2 and correlates with a better therapeutic outcome in patients undergoing treatment with biotherapy.5

In most cases, the onset of achromic lesions follows the diagnosis of melanoma. Hypopigmentation appears on average 4.8 years after the initial diagnosis and approximately 1 to 2 years after lymph node or distant metastasis.1 In our case, it occurred 12 years after the initial diagnosis and 2 years after metastatic disease was diagnosed.
Despite having widespread metastatic melanoma, our patient only developed achromic patches on the area near the prior melanoma. However, most affected patients present with hypopigmented patches in a bilateral symmetric distribution pattern similar to common vitiligo. No correlation has been found between the hypopigmentation distribution and the location of the primary tumor.1
Because fotemustine is not likely to induce hypopigmentation, we believe that the vitiligolike hypopigmentation in our patient was related to an immune-mediated response associated with melanoma. To help explain our findings, one hypothesis considered was that cutaneous mosaicism may be involved in segmental vitiligo.6 The tumor may have triggered an immune response that affected a close susceptible area of mosaic vitiligo, leading to these clinical findings.
- Hartmann A, Bedenk C, Keikavoussi P, et al. Vitiligo and melanoma-associated hypopigmentation (MAH): shared and discriminative features. J Dtsch Dermatol Ges. 2008;6:1053-1059.
- Quaglino P, Marenco F, Osella-Abate S, et al. Vitiligo is an independent favourable prognostic factor in stage III and IV metastatic melanoma patients: results from a single-institution hospital-based observational cohort study. Ann Oncol. 2010;21:409-414.
- Taïeb A, Picardo M, VETF Members. The definition and assessment of vitiligo: a consensus report of the Vitiligo European Task Force. Pigment Cell Res. 2007;20:27-35.
- Becker JC, Guldberg P, Zeuthen J, et al. Accumulation of identical T cells in melanoma and vitiligo-like leukoderma. J Invest Dermatol. 1999;113:1033-1038.
- Boasberg PD, Hoon DS, Piro LD, et al. Enhanced survival associated with vitiligo expression during maintenance biotherapy for metastatic melanoma. J Invest Dermatol. 2006;126:2658-2663.
- Van Geel N, Speeckaert R, Melsens E, et al. The distribution pattern of segmental vitiligo: clues for somatic mosaicism. Br J Dermatol. 2013;168:56-64.
To the Editor:
Melanoma-associated hypopigmentation frequently has been reported during the disease course and can include different characteristics such as regression of the primary melanoma and/or its metastases as well as common vitiligolike hypopigmentation at sites distant from the melanoma.1,2 Among patients who present with hypopigmentation, the most common clinical presentation is hypopigmented patches in a bilateral symmetric distribution that is similar to vitiligo.1 We report a case of segmental vitiligo–like hypopigmentation associated with melanoma.
RELATED ARTICLE: Novel Melanoma Therapies and Their Side Effects
A 37-year-old man presented with achromic patches on the right side of the neck and lower face of 2 months’ duration. He had a history of melanoma (Breslow thickness, 1.37 mm; mitotic rate, 4/mm2) on the right retroauricular region that was treated by wide local excision 12 years prior; after 10 years, he began to have headaches. At that time, imaging studies including computed tomography, magnetic resonance imaging, and positron emission tomography–computed tomography revealed multiple nodules on the brain, lungs, pancreas, left scapula, and left suprarenal gland. A lung biopsy confirmed metastatic melanoma. Intr
On physical examination using a Wood lamp at the current presentation 2 months later, the achromic patches were linearly distributed on the inferior portion of the right cheek (Figure). A 2×3-cm atrophic scar was present on the right retroauricular region. No regional or distant lymph nodes were enlarged or hard on examination. Although vitiligo is diagnosed using clinical findings,3 a biopsy was performed and showed absence of melanocytes at the dermoepidermal junction (hematoxylin and eosin stain) and complete absence of melanin pigment (Fontana-Masson stain). The patient was treated with topical tacrolimus with poor improvement after 2 months.
The relationship between melanoma and vitiligolike hypopigmentation is a fascinating and controversial topic. Its association is considered to be a consequence of the immune-mediated response against antigens shared by normal melanocytes and melanoma cells.4 Vitiligolike hypopigmentation occurs in 2.8%2 of melanoma patients and is reported in metastatic disease1 as well as those undergoing immunotherapy with or without chemotherapy.5 Its development in patients with stage III or IV melanoma seems to represent an independent positive prognostic factor2 and correlates with a better therapeutic outcome in patients undergoing treatment with biotherapy.5

In most cases, the onset of achromic lesions follows the diagnosis of melanoma. Hypopigmentation appears on average 4.8 years after the initial diagnosis and approximately 1 to 2 years after lymph node or distant metastasis.1 In our case, it occurred 12 years after the initial diagnosis and 2 years after metastatic disease was diagnosed.
Despite having widespread metastatic melanoma, our patient only developed achromic patches on the area near the prior melanoma. However, most affected patients present with hypopigmented patches in a bilateral symmetric distribution pattern similar to common vitiligo. No correlation has been found between the hypopigmentation distribution and the location of the primary tumor.1
Because fotemustine is not likely to induce hypopigmentation, we believe that the vitiligolike hypopigmentation in our patient was related to an immune-mediated response associated with melanoma. To help explain our findings, one hypothesis considered was that cutaneous mosaicism may be involved in segmental vitiligo.6 The tumor may have triggered an immune response that affected a close susceptible area of mosaic vitiligo, leading to these clinical findings.
To the Editor:
Melanoma-associated hypopigmentation frequently has been reported during the disease course and can include different characteristics such as regression of the primary melanoma and/or its metastases as well as common vitiligolike hypopigmentation at sites distant from the melanoma.1,2 Among patients who present with hypopigmentation, the most common clinical presentation is hypopigmented patches in a bilateral symmetric distribution that is similar to vitiligo.1 We report a case of segmental vitiligo–like hypopigmentation associated with melanoma.
RELATED ARTICLE: Novel Melanoma Therapies and Their Side Effects
A 37-year-old man presented with achromic patches on the right side of the neck and lower face of 2 months’ duration. He had a history of melanoma (Breslow thickness, 1.37 mm; mitotic rate, 4/mm2) on the right retroauricular region that was treated by wide local excision 12 years prior; after 10 years, he began to have headaches. At that time, imaging studies including computed tomography, magnetic resonance imaging, and positron emission tomography–computed tomography revealed multiple nodules on the brain, lungs, pancreas, left scapula, and left suprarenal gland. A lung biopsy confirmed metastatic melanoma. Intr
On physical examination using a Wood lamp at the current presentation 2 months later, the achromic patches were linearly distributed on the inferior portion of the right cheek (Figure). A 2×3-cm atrophic scar was present on the right retroauricular region. No regional or distant lymph nodes were enlarged or hard on examination. Although vitiligo is diagnosed using clinical findings,3 a biopsy was performed and showed absence of melanocytes at the dermoepidermal junction (hematoxylin and eosin stain) and complete absence of melanin pigment (Fontana-Masson stain). The patient was treated with topical tacrolimus with poor improvement after 2 months.
The relationship between melanoma and vitiligolike hypopigmentation is a fascinating and controversial topic. Its association is considered to be a consequence of the immune-mediated response against antigens shared by normal melanocytes and melanoma cells.4 Vitiligolike hypopigmentation occurs in 2.8%2 of melanoma patients and is reported in metastatic disease1 as well as those undergoing immunotherapy with or without chemotherapy.5 Its development in patients with stage III or IV melanoma seems to represent an independent positive prognostic factor2 and correlates with a better therapeutic outcome in patients undergoing treatment with biotherapy.5

In most cases, the onset of achromic lesions follows the diagnosis of melanoma. Hypopigmentation appears on average 4.8 years after the initial diagnosis and approximately 1 to 2 years after lymph node or distant metastasis.1 In our case, it occurred 12 years after the initial diagnosis and 2 years after metastatic disease was diagnosed.
Despite having widespread metastatic melanoma, our patient only developed achromic patches on the area near the prior melanoma. However, most affected patients present with hypopigmented patches in a bilateral symmetric distribution pattern similar to common vitiligo. No correlation has been found between the hypopigmentation distribution and the location of the primary tumor.1
Because fotemustine is not likely to induce hypopigmentation, we believe that the vitiligolike hypopigmentation in our patient was related to an immune-mediated response associated with melanoma. To help explain our findings, one hypothesis considered was that cutaneous mosaicism may be involved in segmental vitiligo.6 The tumor may have triggered an immune response that affected a close susceptible area of mosaic vitiligo, leading to these clinical findings.
- Hartmann A, Bedenk C, Keikavoussi P, et al. Vitiligo and melanoma-associated hypopigmentation (MAH): shared and discriminative features. J Dtsch Dermatol Ges. 2008;6:1053-1059.
- Quaglino P, Marenco F, Osella-Abate S, et al. Vitiligo is an independent favourable prognostic factor in stage III and IV metastatic melanoma patients: results from a single-institution hospital-based observational cohort study. Ann Oncol. 2010;21:409-414.
- Taïeb A, Picardo M, VETF Members. The definition and assessment of vitiligo: a consensus report of the Vitiligo European Task Force. Pigment Cell Res. 2007;20:27-35.
- Becker JC, Guldberg P, Zeuthen J, et al. Accumulation of identical T cells in melanoma and vitiligo-like leukoderma. J Invest Dermatol. 1999;113:1033-1038.
- Boasberg PD, Hoon DS, Piro LD, et al. Enhanced survival associated with vitiligo expression during maintenance biotherapy for metastatic melanoma. J Invest Dermatol. 2006;126:2658-2663.
- Van Geel N, Speeckaert R, Melsens E, et al. The distribution pattern of segmental vitiligo: clues for somatic mosaicism. Br J Dermatol. 2013;168:56-64.
- Hartmann A, Bedenk C, Keikavoussi P, et al. Vitiligo and melanoma-associated hypopigmentation (MAH): shared and discriminative features. J Dtsch Dermatol Ges. 2008;6:1053-1059.
- Quaglino P, Marenco F, Osella-Abate S, et al. Vitiligo is an independent favourable prognostic factor in stage III and IV metastatic melanoma patients: results from a single-institution hospital-based observational cohort study. Ann Oncol. 2010;21:409-414.
- Taïeb A, Picardo M, VETF Members. The definition and assessment of vitiligo: a consensus report of the Vitiligo European Task Force. Pigment Cell Res. 2007;20:27-35.
- Becker JC, Guldberg P, Zeuthen J, et al. Accumulation of identical T cells in melanoma and vitiligo-like leukoderma. J Invest Dermatol. 1999;113:1033-1038.
- Boasberg PD, Hoon DS, Piro LD, et al. Enhanced survival associated with vitiligo expression during maintenance biotherapy for metastatic melanoma. J Invest Dermatol. 2006;126:2658-2663.
- Van Geel N, Speeckaert R, Melsens E, et al. The distribution pattern of segmental vitiligo: clues for somatic mosaicism. Br J Dermatol. 2013;168:56-64.
Prac
- Melanoma-associated hypopigmentation usually manifests as common vitiligo; however, little is known about the pathophysiology of segmental vitiligo–like hypopigmentation associated with melanoma.
- This case of segmental vitiligo–like hypopigmentation associated with melanoma sheds light on possible autoimmune and mosaic disease etiology.
Rapid lab test predicts pediatric pneumococcal pneumonia severity
MADRID – Thomsen-Friedenreich antigen activation is useful as a novel early predictor of empyema in pediatric community-acquired pneumonia, Chi-Jung Chang, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
In her retrospective study of 142 Taiwanese children and adolescents hospitalized for community-acquired pneumonia (CAP), Thomsen-Friedenreich antigen (TA) activation had 100% specificity, 100% positive predictive value, and 31% sensitivity for Streptococcus pneumoniae as the causative microorganism.
Moreover, the higher the TA activation titer, the more severe the pneumonia complications that followed, according to Dr. Chang of MacKay Children’s Hospital in Taipei, Taiwan.
The value of this lab test lies in its speed and accuracy for detection of S. pneumoniae CAP. Conventional culture methods are relatively slow and have poor sensitivity, because a child often already has been on empiric antimicrobial therapy and the culture specimen is unwittingly obtained from a sterile site, she explained.
Twenty-two of the 142 children and adolescents hospitalized for lobar CAP were TA activation positive at admission. They were considerably sicker than were the 120 patients who were TA activation negative. Their initial C-reactive protein level was 31.9 mg/dL, twice that of the negative group. Their peak CRP during the hospital stay was significantly higher as well, as was their peak WBC.
Hospital lengths of stay were longer in the TA activation–positive group. Eighteen of 22 TA activation–positive patients (82%) were admitted to the ICU for an average of 8 days, compared with 9% of the negative group.
All TA activation–positive patients had complicated pneumonia with parapneumonic effusions, empyema, necrotizing pneumonia, and/or lung abscesses, as did 36% of the negative group.
S. pneumoniae was the most common pathogen in this study of CAP. It was the responsible microbe in all 22 of the TA activation–positive patients and in 29% of the TA activation–negative ones. The most common serotype in the TA activation group was 19A, which accounted for 12 of the 22 cases. This also was the predominant serotype found in CAP across all Taiwan during the first half of this decade, when the study took place.
In a multivariate logistic regression analysis, TA activation was far and away the strongest independent predictor of empyema, with an associated 15.8-fold increased risk. The other two independent predictors – longer fever duration prior to hospitalization and a higher initial CRP level – were far less robust, according to Dr. Chang.
How TA activation works as a predictor
TA is present on the surface of erythrocytes, platelets, and glomeruli, but ordinarily it is covered by a layer of N-acetylneuraminic acid. Streptococcus pneumoniae produces circulating neuraminidases, which cleave the N-acetylneuraminic acid and expose the underlying TA. The TA then quickly becomes activated through interaction with the anti-TA antibodies, which are normally present in plasma. Once activated, the TA stays so for weeks to months.
Other neuraminidase-producing microorganisms include Clostridium perfringens, Escherichia coli, and Bacteroides.
Dr. Chang and her colleagues used the peanut lectin agglutination method in their TA activation testing.
She reported having no financial conflicts regarding her study.
MADRID – Thomsen-Friedenreich antigen activation is useful as a novel early predictor of empyema in pediatric community-acquired pneumonia, Chi-Jung Chang, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
In her retrospective study of 142 Taiwanese children and adolescents hospitalized for community-acquired pneumonia (CAP), Thomsen-Friedenreich antigen (TA) activation had 100% specificity, 100% positive predictive value, and 31% sensitivity for Streptococcus pneumoniae as the causative microorganism.
Moreover, the higher the TA activation titer, the more severe the pneumonia complications that followed, according to Dr. Chang of MacKay Children’s Hospital in Taipei, Taiwan.
The value of this lab test lies in its speed and accuracy for detection of S. pneumoniae CAP. Conventional culture methods are relatively slow and have poor sensitivity, because a child often already has been on empiric antimicrobial therapy and the culture specimen is unwittingly obtained from a sterile site, she explained.
Twenty-two of the 142 children and adolescents hospitalized for lobar CAP were TA activation positive at admission. They were considerably sicker than were the 120 patients who were TA activation negative. Their initial C-reactive protein level was 31.9 mg/dL, twice that of the negative group. Their peak CRP during the hospital stay was significantly higher as well, as was their peak WBC.
Hospital lengths of stay were longer in the TA activation–positive group. Eighteen of 22 TA activation–positive patients (82%) were admitted to the ICU for an average of 8 days, compared with 9% of the negative group.
All TA activation–positive patients had complicated pneumonia with parapneumonic effusions, empyema, necrotizing pneumonia, and/or lung abscesses, as did 36% of the negative group.
S. pneumoniae was the most common pathogen in this study of CAP. It was the responsible microbe in all 22 of the TA activation–positive patients and in 29% of the TA activation–negative ones. The most common serotype in the TA activation group was 19A, which accounted for 12 of the 22 cases. This also was the predominant serotype found in CAP across all Taiwan during the first half of this decade, when the study took place.
In a multivariate logistic regression analysis, TA activation was far and away the strongest independent predictor of empyema, with an associated 15.8-fold increased risk. The other two independent predictors – longer fever duration prior to hospitalization and a higher initial CRP level – were far less robust, according to Dr. Chang.
How TA activation works as a predictor
TA is present on the surface of erythrocytes, platelets, and glomeruli, but ordinarily it is covered by a layer of N-acetylneuraminic acid. Streptococcus pneumoniae produces circulating neuraminidases, which cleave the N-acetylneuraminic acid and expose the underlying TA. The TA then quickly becomes activated through interaction with the anti-TA antibodies, which are normally present in plasma. Once activated, the TA stays so for weeks to months.
Other neuraminidase-producing microorganisms include Clostridium perfringens, Escherichia coli, and Bacteroides.
Dr. Chang and her colleagues used the peanut lectin agglutination method in their TA activation testing.
She reported having no financial conflicts regarding her study.
MADRID – Thomsen-Friedenreich antigen activation is useful as a novel early predictor of empyema in pediatric community-acquired pneumonia, Chi-Jung Chang, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
In her retrospective study of 142 Taiwanese children and adolescents hospitalized for community-acquired pneumonia (CAP), Thomsen-Friedenreich antigen (TA) activation had 100% specificity, 100% positive predictive value, and 31% sensitivity for Streptococcus pneumoniae as the causative microorganism.
Moreover, the higher the TA activation titer, the more severe the pneumonia complications that followed, according to Dr. Chang of MacKay Children’s Hospital in Taipei, Taiwan.
The value of this lab test lies in its speed and accuracy for detection of S. pneumoniae CAP. Conventional culture methods are relatively slow and have poor sensitivity, because a child often already has been on empiric antimicrobial therapy and the culture specimen is unwittingly obtained from a sterile site, she explained.
Twenty-two of the 142 children and adolescents hospitalized for lobar CAP were TA activation positive at admission. They were considerably sicker than were the 120 patients who were TA activation negative. Their initial C-reactive protein level was 31.9 mg/dL, twice that of the negative group. Their peak CRP during the hospital stay was significantly higher as well, as was their peak WBC.
Hospital lengths of stay were longer in the TA activation–positive group. Eighteen of 22 TA activation–positive patients (82%) were admitted to the ICU for an average of 8 days, compared with 9% of the negative group.
All TA activation–positive patients had complicated pneumonia with parapneumonic effusions, empyema, necrotizing pneumonia, and/or lung abscesses, as did 36% of the negative group.
S. pneumoniae was the most common pathogen in this study of CAP. It was the responsible microbe in all 22 of the TA activation–positive patients and in 29% of the TA activation–negative ones. The most common serotype in the TA activation group was 19A, which accounted for 12 of the 22 cases. This also was the predominant serotype found in CAP across all Taiwan during the first half of this decade, when the study took place.
In a multivariate logistic regression analysis, TA activation was far and away the strongest independent predictor of empyema, with an associated 15.8-fold increased risk. The other two independent predictors – longer fever duration prior to hospitalization and a higher initial CRP level – were far less robust, according to Dr. Chang.
How TA activation works as a predictor
TA is present on the surface of erythrocytes, platelets, and glomeruli, but ordinarily it is covered by a layer of N-acetylneuraminic acid. Streptococcus pneumoniae produces circulating neuraminidases, which cleave the N-acetylneuraminic acid and expose the underlying TA. The TA then quickly becomes activated through interaction with the anti-TA antibodies, which are normally present in plasma. Once activated, the TA stays so for weeks to months.
Other neuraminidase-producing microorganisms include Clostridium perfringens, Escherichia coli, and Bacteroides.
Dr. Chang and her colleagues used the peanut lectin agglutination method in their TA activation testing.
She reported having no financial conflicts regarding her study.
AT ESPID 2017
Key clinical point:
Major finding: A positive Thomsen-Friedenreich antigen activation test in pediatric community-acquired pneumonia had 100% specificity, 100% positive predictive value, and 31% sensitivity for S. pneumoniae as the causative microorganism.
Data source: A retrospective study of 142 Taiwanese children and teens hospitalized for lobular community-acquired pneumonia.
Disclosures: The study presenter reported having no financial conflicts of interest.
Isotretinoin for Acne: Tips for Prescribing and Managing Patient Concerns
What does your patient need to know at the first visit?
Most important is what you need to know before the first visit. As the prescribing physician, you must be familiar with the iPLEDGE program. Because of the complexity of the program, consider identifying a physician in your area to refer patients if you are not going to be a regular prescriber of the medication.
If you are enrolled in iPLEDGE, let your patients (and/or their parents/guardians) know that there is a great deal of misinformation on the Internet. Reiterate that you and your staff are available to discuss their concerns. Also, give them reliable sources of information, such as the American Academy of Dermatology's patient information sheet as well as the Mayo Clinic's acne information. Drugs.com is another resource.
All patients—males, females who cannot become pregnant, and females of childbearing potential (FCBPs)—must be aware that this medication can cause birth defects if taken during pregnancy. They must be informed that the medication is not to be shared with anyone and that they should not give blood while taking this medication.
What treatment course do you recommend?
My evidence-based approach is a course of isotretinoin totaling a minimum of 150 mg per kilogram body weight. Do not give a more abbreviated course unless the patient has cleared early; even then I tend to complete 150 mg when possible. There is published evidence that pushing the course to a total of 220 mg per kilogram body weight results in a longer remission.
Generally, I do few laboratory tests other than pretreatment lipid panels as well as 1 or 2 follow-up lipid panels at monthly intervals. To comply with the iPLEDGE program, FCBP patients must have a monthly pregnancy test, which is reported on the iPLEDGE website before the patient can be prescribed the drug and receive the drug from a pharmacist who is participating in the iPLEDGE program.
One of the defects of the iPLEDGE system is that although only a 30-day supply of pills can be prescribed, it is difficult to always bring a patient back in exactly 30 days; for example, we work on a 4-week cycle and 30 days brings us into the next week or uncommonly the weekend when we do not see patients. Our male patients or females not of childbearing potential are not affected, but for our FCBP patients, it means usually scheduling visits at 35-day intervals because the pregnancy tests must be performed at minimum 28-day intervals and the prescription cannot be written and the pregnancy test recorded until after at least 30 days.
What are the side effects?
The common side effects are what you would expect from a medicine that is supposed to dry up the oil on your skin: dryness of the lips, mouth, and skin, as well as rashes due to the dryness. There also can be minor swelling of the eyelids or lips, nosebleeds, upset stomach, and thinning of the hair; dryness of the scalp may occur. I recommend using a little petroleum jelly inside the nostrils at night to counteract the dryness that leads to nosebleeds, and saline drops or gel for the eyes, especially for contact lens wearers.
Joint aches and pains have been reported, though I rarely see those effects in patients who are physically active such as those participating in competitive sports. Mood changes have been reported, including suicidal ideation.
What do you do if patients refuse treatment?
There is so much false information on the Internet about the dangers of isotretinoin, leaving some patients (and parents/guardians) too afraid to use it. I sympathize with this anxiety, but I do endeavor to point out that the birth defects occur only in women taking the drug while pregnant and have not been reported to occur after the drug is out of the patient's system.
Similarly, I point out that almost all of the evidence-based studies failed to confirm any association between the use of isotretinoin and depression, teenage suicide, and subsequent inflammatory bowel disease. Nonetheless, I mention these issues and recommend that the parents/guardians observe the teenager; in the case of adult patients, they themselves must be sensitive to symptoms.
Suggested Readings
American Academy of Dermatology Association. Position statement on isotretinoin. https://www.aad.org/Forms/Policies/Uploads/PS/PS-Isotretinoin.pdf. Published December 9, 2000. Updated November 13, 2010. Accessed May 18, 2017.
Blasiak RC, Stamey CR, Burkhart CN, et al. High-dose isotretinoin treatment and the rate of retrial, relapse, and adverse effects in patients with acne vulgaris. JAMA Dermatol. 2013;149:1392-1398.
What does your patient need to know at the first visit?
Most important is what you need to know before the first visit. As the prescribing physician, you must be familiar with the iPLEDGE program. Because of the complexity of the program, consider identifying a physician in your area to refer patients if you are not going to be a regular prescriber of the medication.
If you are enrolled in iPLEDGE, let your patients (and/or their parents/guardians) know that there is a great deal of misinformation on the Internet. Reiterate that you and your staff are available to discuss their concerns. Also, give them reliable sources of information, such as the American Academy of Dermatology's patient information sheet as well as the Mayo Clinic's acne information. Drugs.com is another resource.
All patients—males, females who cannot become pregnant, and females of childbearing potential (FCBPs)—must be aware that this medication can cause birth defects if taken during pregnancy. They must be informed that the medication is not to be shared with anyone and that they should not give blood while taking this medication.
What treatment course do you recommend?
My evidence-based approach is a course of isotretinoin totaling a minimum of 150 mg per kilogram body weight. Do not give a more abbreviated course unless the patient has cleared early; even then I tend to complete 150 mg when possible. There is published evidence that pushing the course to a total of 220 mg per kilogram body weight results in a longer remission.
Generally, I do few laboratory tests other than pretreatment lipid panels as well as 1 or 2 follow-up lipid panels at monthly intervals. To comply with the iPLEDGE program, FCBP patients must have a monthly pregnancy test, which is reported on the iPLEDGE website before the patient can be prescribed the drug and receive the drug from a pharmacist who is participating in the iPLEDGE program.
One of the defects of the iPLEDGE system is that although only a 30-day supply of pills can be prescribed, it is difficult to always bring a patient back in exactly 30 days; for example, we work on a 4-week cycle and 30 days brings us into the next week or uncommonly the weekend when we do not see patients. Our male patients or females not of childbearing potential are not affected, but for our FCBP patients, it means usually scheduling visits at 35-day intervals because the pregnancy tests must be performed at minimum 28-day intervals and the prescription cannot be written and the pregnancy test recorded until after at least 30 days.
What are the side effects?
The common side effects are what you would expect from a medicine that is supposed to dry up the oil on your skin: dryness of the lips, mouth, and skin, as well as rashes due to the dryness. There also can be minor swelling of the eyelids or lips, nosebleeds, upset stomach, and thinning of the hair; dryness of the scalp may occur. I recommend using a little petroleum jelly inside the nostrils at night to counteract the dryness that leads to nosebleeds, and saline drops or gel for the eyes, especially for contact lens wearers.
Joint aches and pains have been reported, though I rarely see those effects in patients who are physically active such as those participating in competitive sports. Mood changes have been reported, including suicidal ideation.
What do you do if patients refuse treatment?
There is so much false information on the Internet about the dangers of isotretinoin, leaving some patients (and parents/guardians) too afraid to use it. I sympathize with this anxiety, but I do endeavor to point out that the birth defects occur only in women taking the drug while pregnant and have not been reported to occur after the drug is out of the patient's system.
Similarly, I point out that almost all of the evidence-based studies failed to confirm any association between the use of isotretinoin and depression, teenage suicide, and subsequent inflammatory bowel disease. Nonetheless, I mention these issues and recommend that the parents/guardians observe the teenager; in the case of adult patients, they themselves must be sensitive to symptoms.
Suggested Readings
American Academy of Dermatology Association. Position statement on isotretinoin. https://www.aad.org/Forms/Policies/Uploads/PS/PS-Isotretinoin.pdf. Published December 9, 2000. Updated November 13, 2010. Accessed May 18, 2017.
Blasiak RC, Stamey CR, Burkhart CN, et al. High-dose isotretinoin treatment and the rate of retrial, relapse, and adverse effects in patients with acne vulgaris. JAMA Dermatol. 2013;149:1392-1398.
What does your patient need to know at the first visit?
Most important is what you need to know before the first visit. As the prescribing physician, you must be familiar with the iPLEDGE program. Because of the complexity of the program, consider identifying a physician in your area to refer patients if you are not going to be a regular prescriber of the medication.
If you are enrolled in iPLEDGE, let your patients (and/or their parents/guardians) know that there is a great deal of misinformation on the Internet. Reiterate that you and your staff are available to discuss their concerns. Also, give them reliable sources of information, such as the American Academy of Dermatology's patient information sheet as well as the Mayo Clinic's acne information. Drugs.com is another resource.
All patients—males, females who cannot become pregnant, and females of childbearing potential (FCBPs)—must be aware that this medication can cause birth defects if taken during pregnancy. They must be informed that the medication is not to be shared with anyone and that they should not give blood while taking this medication.
What treatment course do you recommend?
My evidence-based approach is a course of isotretinoin totaling a minimum of 150 mg per kilogram body weight. Do not give a more abbreviated course unless the patient has cleared early; even then I tend to complete 150 mg when possible. There is published evidence that pushing the course to a total of 220 mg per kilogram body weight results in a longer remission.
Generally, I do few laboratory tests other than pretreatment lipid panels as well as 1 or 2 follow-up lipid panels at monthly intervals. To comply with the iPLEDGE program, FCBP patients must have a monthly pregnancy test, which is reported on the iPLEDGE website before the patient can be prescribed the drug and receive the drug from a pharmacist who is participating in the iPLEDGE program.
One of the defects of the iPLEDGE system is that although only a 30-day supply of pills can be prescribed, it is difficult to always bring a patient back in exactly 30 days; for example, we work on a 4-week cycle and 30 days brings us into the next week or uncommonly the weekend when we do not see patients. Our male patients or females not of childbearing potential are not affected, but for our FCBP patients, it means usually scheduling visits at 35-day intervals because the pregnancy tests must be performed at minimum 28-day intervals and the prescription cannot be written and the pregnancy test recorded until after at least 30 days.
What are the side effects?
The common side effects are what you would expect from a medicine that is supposed to dry up the oil on your skin: dryness of the lips, mouth, and skin, as well as rashes due to the dryness. There also can be minor swelling of the eyelids or lips, nosebleeds, upset stomach, and thinning of the hair; dryness of the scalp may occur. I recommend using a little petroleum jelly inside the nostrils at night to counteract the dryness that leads to nosebleeds, and saline drops or gel for the eyes, especially for contact lens wearers.
Joint aches and pains have been reported, though I rarely see those effects in patients who are physically active such as those participating in competitive sports. Mood changes have been reported, including suicidal ideation.
What do you do if patients refuse treatment?
There is so much false information on the Internet about the dangers of isotretinoin, leaving some patients (and parents/guardians) too afraid to use it. I sympathize with this anxiety, but I do endeavor to point out that the birth defects occur only in women taking the drug while pregnant and have not been reported to occur after the drug is out of the patient's system.
Similarly, I point out that almost all of the evidence-based studies failed to confirm any association between the use of isotretinoin and depression, teenage suicide, and subsequent inflammatory bowel disease. Nonetheless, I mention these issues and recommend that the parents/guardians observe the teenager; in the case of adult patients, they themselves must be sensitive to symptoms.
Suggested Readings
American Academy of Dermatology Association. Position statement on isotretinoin. https://www.aad.org/Forms/Policies/Uploads/PS/PS-Isotretinoin.pdf. Published December 9, 2000. Updated November 13, 2010. Accessed May 18, 2017.
Blasiak RC, Stamey CR, Burkhart CN, et al. High-dose isotretinoin treatment and the rate of retrial, relapse, and adverse effects in patients with acne vulgaris. JAMA Dermatol. 2013;149:1392-1398.