User login
Association Between Anemia and Fatigue in Hospitalized Patients: Does the Measure of Anemia Matter?
Fatigue is the most common clinical symptom of anemia and is a significant concern to patients.1,2 In ambulatory patients, lower hemoglobin (Hb) concentration is associated with increased fatigue.2,3 Accordingly, therapies that treat anemia by increasing Hb concentration, such as erythropoiesis stimulating agents,4-7 often use fatigue as an outcome measure.
In hospitalized patients, transfusion of red blood cell increases Hb concentration and is the primary treatment for anemia. However, the extent to which transfusion and changes in Hb concentration affect hospitalized patients’ fatigue levels is not well established. Guidelines support transfusing patients with symptoms of anemia, such as fatigue, on the assumption that the increased oxygen delivery will improve the symptoms of anemia. While transfusion studies in hospitalized patients have consistently reported that transfusion at lower or “restrictive” Hb concentrations is safe compared with transfusion at higher Hb concentrations,8-10 these studies have mainly used cardiac events and mortality as outcomes rather than patient symptoms, such as fatigue. Nevertheless, they have resulted in hospitals increasingly adopting restrictive transfusion policies that discourage transfusion at higher Hb levels.11,12 Consequently, the rate of transfusion in hospitalized patients has decreased,13 raising questions of whether some patients with lower Hb concentrations may experience increased fatigue as a result of restrictive transfusion policies. Fatigue among hospitalized patients is important not only because it is an adverse symptom but because it may result in decreased activity levels, deconditioning, and losses in functional status.14,15While the effect of alternative transfusion policies on fatigue in hospitalized patients could be answered by a randomized clinical trial using fatigue and functional status as outcomes, an important first step is to assess whether the Hb concentration of hospitalized patients is associated with their fatigue level during hospitalization. Because hospitalized patients often have acute illnesses that can cause fatigue in and of themselves, it is possible that anemia is not associated with fatigue in hospitalized patients despite anemia’s association with fatigue in ambulatory patients. Additionally, Hb concentration varies during hospitalization,16 raising the question of what measures of Hb during hospitalization might be most associated with anemia-related fatigue.
The objective of this study is to explore multiple Hb measures in hospitalized medical patients with anemia and test whether any of these Hb measures are associated with patients’ fatigue level.
METHODS
Study Design
We performed a prospective, observational study of hospitalized patients with anemia on the general medicine services at The University of Chicago Medical Center (UCMC). The institutional review board approved the study procedures, and all study subjects provided informed consent.
Study Eligibility
Between April 2014 and June 2015, all general medicine inpatients were approached for written consent for The University of Chicago Hospitalist Project,17 a research infrastructure at UCMC. Among patients consenting to participate in the Hospitalist Project, patients were eligible if they had Hb <9 g/dL at any point during their hospitalization and were age ≥50 years. Hb concentration of <9 g/dL was chosen to include the range of Hb values covered by most restrictive transfusion policies.8-10,18 Age ≥50 years was an inclusion criteria because anemia is more strongly associated with poor outcomes, including functional impairment, among older patients compared with younger patients.14,19-21 If patients were not eligible for inclusion at the time of consent for the Hospitalist Project, their Hb values were reviewed twice daily until hospital discharge to assess if their Hb was <9 g/dL. Proxies were sought to answer questions for patients who failed the Short Portable Mental Status Questionnaire.22
Patient Demographic Data Collection
Research assistants abstracted patient age and sex from the electronic health record (EHR), and asked patients to self-identify their race. The individual comorbidities included as part of the Charlson Comorbidity Index were identified using International Classification of Diseases, 9th Revision codes from hospital administrative data for each encounter and specifically included the following: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, liver disease, diabetes, hemiplegia and/or paraplegia, renal disease, cancer, and human immunodeficiency virus/acquired immunodeficiency syndrome.23 We also used Healthcare Cost and Utilization Project (www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp) diagnosis categories to identify whether patients had sickle cell (SC) anemia, gastrointestinal bleeding (GIB), or a depressive disorder (DD) because these conditions are associated with anemia (SC and GIB) and fatigue (DD).24
Measuring Anemia
Hb measures were available only when hospital providers ordered them as part of routine practice. The first Hb concentration <9 g/dL during a patient’s hospitalization, which made them eligible for study participation, was obtained through manual review of the EHR. All additional Hb values during the patient’s hospitalization were obtained from the hospital’s administrative data mart. All Hb values collected for each patient during the hospitalization were used to calculate summary measures of Hb during the hospitalization, including the mean Hb, median Hb, minimum Hb, maximum Hb, admission (first recorded) Hb, and discharge (last recorded) Hb. Hb measures were analyzed both as a continuous variable and as a categorical variable created by dividing the continuous Hb measures into integer ranges of 3 groups of approximately the same size.
Measuring Fatigue
Our primary outcome was patients’ level of fatigue reported during hospitalization, measured using the Functional Assessment of Chronic Illness Therapy (FACIT)-Anemia questionnaire. Fatigue was measured using a 13-question fatigue subscale,1,2,25 which measures fatigue within the past 7 days. Scores on the fatigue subscale range from 0 to 52, with lower scores reflecting greater levels of fatigue. As soon as patients met the eligibility criteria for study participation during their hospitalization (age ≥50 years and Hb <9 g/dL), they were approached to answer the FACIT questions. Values for missing data in the fatigue subscale for individual subjects were filled in using a prorated score from their answered questions as long as >50% of the items in the fatigue subscale were answered, in accordance with recommendations for addressing missing data in the FACIT.26 Fatigue was analyzed as a continuous variable and as a dichotomous variable created by dividing the sample into high (FACIT <27) and low (FACIT ≥27) levels of fatigue based on the median FACIT score of the population. Previous literature has shown a FACIT fatigue subscale score between 23 and 26 to be associated with an Eastern Cooperative Oncology Group (ECOG)27 C Performance Status rating of 2 to 33 compared to scores ≥27.
Statistical Analysis
Statistical analysis was performed using Stata statistical software (StataCorp, College Station, TX). Descriptive statistics were used to characterize patient demographics. Analysis of variance was used to test for differences in the mean fatigue levels across Hb measures. χ2 tests were performed to test for associations between high fatigue levels and the Hb measures. Multivariable analysis, including both linear and logistic regression models, were used to test the association of Hb concentration and fatigue. P values <0.05 using a 2-tailed test were deemed statistically significant.
RESULTS
Patient Characteristics
During the study period, 8559 patients were admitted to the general medicine service. Of those, 5073 (59%) consented for participation in the Hospitalist Project, and 3670 (72%) completed the Hospitalist Project inpatient interview. Of these patients, 1292 (35%) had Hb <9 g/dL, and 784 (61%) were 50 years or older and completed the FACIT questionnaire.
Table 1 reports the demographic characteristics and comorbidities for the sample, the mean (standard deviation [SD]) for the 6 Hb measures, and mean (SD) and median FACIT scores.
Bivariate Association of Fatigue and Hb
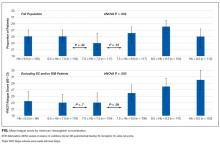
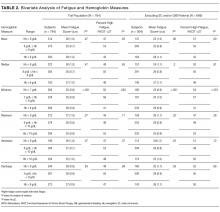
Categorizing patients into low, middle, or high Hb for each of the 6 Hb measures, minimum Hb was strongly associated with fatigue, with a weaker association for mean Hb and no statistically significant association for the other measures.
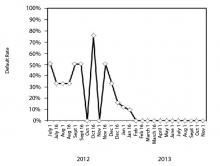
Minimum Hb. Patients with a minimum Hb <7 g/dL and patients with Hb 7-8 g/dL had higher fatigue levels (FACIT = 25 for each) than patients with a minimum Hb ≥8 g/dL (FACIT = 29; P < 0.001; Table 2). When excluding patients with SC and/or GIB because their average minimum Hb differed from the average minimum Hb of the full population (P < 0.001), patients with a minimum Hb <7 g/dL or 7-8 g/dL had even higher fatigue levels (FACIT = 23 and FACIT = 24, respectively), with no change in the fatigue level of patients with a minimum Hb ≥8 g/dL (FACIT = 29; P < 0.001; Table 2). Lower minimum Hb continued to be associated with higher fatigue levels when analyzed in 0.5 g/dL increments (Figure).
Mean Hb and Other Measures. Fatigue levels were high for 47% of patients with a mean Hb <8g /dL and 53% of patients with a mean Hb 8-9 g/dL compared with 43% of patients with a mean Hb ≥9 g/dL (P = 0.05). However, the association between high fatigue and mean Hb was not statistically significant when patients with SC and/or GIB were excluded (Table 2). None of the other 4 Hb measures was significantly associated with fatigue.
Linear Regression of Fatigue on Hb
In linear regression models, minimum Hb consistently predicted patient fatigue, mean Hb had a less robust association with fatigue, and the other Hb measures were not associated with patient fatigue. Increases in minimum Hb (analyzed as a continuous variable) were associated with reduced fatigue (higher FACIT score; β = 1.4; P = 0.005). In models in which minimum Hb was a categorical variable, patients with a minimum Hb of <7 g/dL or 7-8 g/dL had greater fatigue (lower FACIT score) than patients whose minimum Hb was ≥8 g/dL (Hb <7 g/dL: β = −4.2; P ≤ 0.001; Hb 7-8 g/dL: β = −4.1; P < 0.001). These results control for patients’ age, sex, individual comorbidities, and whether their minimum Hb occurred before or after the measurement of fatigue during hospitalization (Model 1), and the results are unchanged when also controlling for the number of Hb laboratory draws patients had during their hospitalization (Model 2; Table 3). In a stratified analysis excluding patients with either SC and/or GIB, changes in minimum Hb were associated with larger changes in patient fatigue levels (Supplemental Table 1). We also stratified our analysis to include only patients whose minimum Hb occurred before the measurement of their fatigue level during hospitalization to avoid a spurious association of fatigue with minimum Hb occurring after fatigue was measured. In both Models 1 and 2, minimum Hb remained a predictor of patients’ fatigue levels with similar effect sizes, although in Model 2, the results did not quite reach a statistically significant level, in part due to larger confidence intervals from the smaller sample size of this stratified analysis (Supplemental Table 2a). We further stratified this analysis to include only patients whose transfusion, if they received one, occurred after their minimum Hb and the measurement of their fatigue level to account for the possibility that a transfusion could affect the fatigue level patients report. In this analysis, most of the estimates of the effect of minimum Hb on fatigue were larger than those seen when only analyzing patients whose minimum Hb occurred before the measurement of their fatigue level, although again, the smaller sample size of this additional stratified analysis does produce larger confidence intervals for these estimates (Supplemental Table 2b).
No Hb measure other than minimum or mean had significant association with patient fatigue levels in linear regression models.
Logistic Regression of High Fatigue Level on Hb
Using logistic regression, minimum Hb analyzed as a categorical variable predicted increased odds of a high fatigue level. Patients with a minimum Hb <7 g/dL were 50% (odds ratio [OR] = 1.5; P = 0.03) more likely to have high fatigue and patients with a minimum Hb 7-8 g/dL were 90% (OR = 1.9; P < 0.001) more likely to have high fatigue compared with patients with a minimum Hb ≥8 g/dL in Model 1. These results were similar in Model 2, although the effect was only statistically significant in the 7-8 g/dL Hb group (Table 3). When excluding SC and/or GIB patients, the odds of having high fatigue as minimum Hb decreased were the same or higher for both models compared to the full population of patients. However, again, in Model 2, the effect was only statistically significant in the 7-8 g/dL Hb group (Supplemental Table 1).
Patients with a mean Hb <8 g/dL were 20% to 30% more likely to have high fatigue and patients with mean Hb 8-9 g/dL were 50% more likely to have high fatigue compared with patients with a mean Hb ≥9 g/dL, but the effects were only statistically significant for patients with a mean Hb 8-9 g/dL in both Models 1 and 2 (Table 3). These results were similar when excluding patients with SC and/or GIB, but they were only significant for patients with a mean Hb 8-9 g/dL in Model 1 and patients with a mean Hb <8 g/dL in the Model 2 (Supplemental Table 3).
DISCUSSION
These results demonstrate that minimum Hb during hospitalization is associated with fatigue in hospitalized patients age ≥50 years, and the association is stronger among patients without SC and/or GIB as comorbidities. The analysis of Hb as a continuous and categorical variable and the use of both linear and logistic regression models support the robustness of these associations and illuminate their clinical significance. For example, in linear regression with minimum Hb a continuous variable, the coefficient of 1.4 suggests that an increase of 2 g/dL in Hb, as might be expected from transfusion of 2 units of red blood cells, would be associated with about a 3-point improvement in fatigue. Additionally, as a categorical variable, a minimum Hb ≥8 g/dL compared with a minimum Hb <7 g/dL or 7-8 g/dL is associated with a 3- to 4-point improvement in fatigue. Previous literature suggests that a difference of 3 in the FACIT score is the minimum clinically important difference in fatigue,3 and changes in minimum Hb in either model predict changes in fatigue that are in the range of potential clinical significance.
The clinical significance of the findings is also reflected in the results of the logistic regressions, which may be mapped to potential effects on functional status. Specifically, the odds of having a high fatigue level (FACIT <27) increase 90% for persons with a minimum Hb 7–8 g/dL compared with persons with a minimum Hb ≥8 g/dL. For persons with a minimum Hb <7 g/dL, point estimates suggest a smaller (50%) increase in the odds of high fatigue, but the 95% confidence interval overlaps heavily with the estimate of patients whose minimum Hb is 7-8 g/dL. While it might be expected that patients with a minimum Hb <7 g/dL have greater levels of fatigue compared with patients with a minimum Hb 7-8 g/dL, we did not observe such a pattern. One reason may be that the confidence intervals of our estimated effects are wide enough that we cannot exclude such a pattern. Another possible explanation is that in both groups, the fatigue levels are sufficiently severe, such that the difference in their fatigue levels may not be clinically meaningful. For example, a FACIT score of 23 to 26 has been shown to be associated with an ECOG performance status of 2 to 3, requiring bed rest for at least part of the day.3 Therefore, patients with a minimum Hb 7-8 g/dL (mean FACIT score = 24; Table 2) or a minimum Hb of <7 g/dL (mean FACIT score = 23; Table 2) are already functionally limited to the point of being partially bed bound, such that further decreases in their Hb may not produce additional fatigue in part because they reduce their activity sufficiently to prevent an increase in fatigue. In such cases, the potential benefits of increased Hb may be better assessed by measuring fatigue in response to a specific and provoked activity level, a concept known as fatigability.20
That minimum Hb is more strongly associated with fatigue than any other measure of Hb during hospitalization may not be surprising. Mean, median, maximum, and discharge Hb may all be affected by transfusion during hospitalization that could affect fatigue. Admission Hb may not reflect true oxygen-carrying capacity because of hemoconcentration.
The association between Hb and fatigue in hospitalized patients is important because increased fatigue could contribute to slower clinical recovery in hospitalized patients. Additionally, increased fatigue during hospitalization and at hospital discharge could exacerbate the known deleterious consequences of fatigue on patients and their health outcomes14,15 after hospital discharge. Although one previous study, the Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair (FOCUS)8 trial, did not report differences in patients’ fatigue levels at 30 and 60 days postdischarge when transfused at restrictive (8 g/dL) compared with liberal (10 g/dL) Hb thresholds, confidence in the validity of this finding is reduced by the fact that more than half of the patients were lost to follow-up at the 30- and 60-day time points. Further, patients in the restrictive transfusion arm of FOCUS were transfused to maintain Hb levels at or above 8 g/dL. This transfusion threshold of 8 g/dL may have mitigated the high levels of fatigue that are seen in our study when patients’ Hb drops below 8 g/dL, and maintaining a Hb level of 7 g/dL is now the standard of care in stable hospitalized patients. Lastly, FOCUS was limited to postoperative hip fracture patients, and the generalizability of FOCUS to hospitalized medicine patients with anemia is limited.
Therefore, our results support guideline suggestions that practitioners incorporate the presence of patient symptoms such as fatigue into transfusion decisions, particularly if patients’ Hb is <8 g/dL.18 Though reasonable, the suggestion to incorporate symptoms such as fatigue into transfusion decisions has not been strongly supported by evidence so far, and it may often be neglected in practice. Definitive evidence to support such recommendations would benefit from study through an optimal trial18 that incorporates symptoms into decision making. Our findings add support for a study of transfusion strategies that incorporates patients’ fatigue level in addition to Hb concentration.
This study has several limitations. Although our sample size is large and includes patients with a range of comorbidities that we believe are representative of hospitalized general medicine patients, as a single-center, observational study, our results may not be generalizable to other centers. Additionally, although these data support a reliable association between hospitalized patients’ minimum Hb and fatigue level, the observational design of this study cannot prove that this relationship is causal. Also, patients’ Hb values were measured at the discretion of their clinician, and therefore, the measures of Hb were not uniformly measured for participating patients. In addition, fatigue was only measured at one time point during a patient’s hospitalization, and it is possible that patients’ fatigue levels change during hospitalization in relation to variables we did not consider. Finally, our study was not designed to assess the association of Hb with longer-term functional outcomes, which may be of greater concern than fatigue.
CONCLUSION
In hospitalized patients ≥50 years old, minimum Hb is reliably associated with patients’ fatigue level. Patients whose minimum Hb is <8 g/dL experience higher fatigue levels compared to patients whose minimum Hb is ≥8 g/dL. Additional studies are warranted to understand if patients may benefit from improved fatigue levels by correcting their anemia through transfusion.
1. Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13(2):63-74.
2. Cella D, Lai JS, Chang CH, Peterman A, Slavin M. Fatigue in cancer patients compared with fatigue in the general United States population. Cancer. 2002;94(2):528-538. doi:10.1002/cncr.10245.
3. Cella D, Eton DT, Lai J-S, Peterman AH, Merkel DE. Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manage. 2002;24(6):547-561.
4. Tonelli M, Hemmelgarn B, Reiman T, et al. Benefits and harms of erythropoiesis-stimulating agents for anemia related to cancer: a meta-analysis. CMAJ Can Med Assoc J J Assoc Medicale Can. 2009;180(11):E62-E71. doi:10.1503/cmaj.090470.
5. Foley RN, Curtis BM, Parfrey PS. Erythropoietin Therapy, Hemoglobin Targets, and Quality of Life in Healthy Hemodialysis Patients: A Randomized Trial. Clin J Am Soc Nephrol. 2009;4(4):726-733. doi:10.2215/CJN.04950908.
6. Keown PA, Churchill DN, Poulin-Costello M, et al. Dialysis patients treated with Epoetin alfa show improved anemia symptoms: A new analysis of the Canadian Erythropoietin Study Group trial. Hemodial Int Int Symp Home Hemodial. 2010;14(2):168-173. doi:10.1111/j.1542-4758.2009.00422.x.
7. Palmer SC, Saglimbene V, Mavridis D, et al. Erythropoiesis-stimulating agents for anaemia in adults with chronic kidney disease: a network meta-analysis. Cochrane Database Syst Rev. 2014:CD010590.
8. Carson JL, Terrin ML, Noveck H, et al. Liberal or Restrictive Transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453-2462. doi:10.1056/NEJMoa1012452.
9. Holst LB, Haase N, Wetterslev J, et al. Transfusion requirements in septic shock (TRISS) trial – comparing the effects and safety of liberal versus restrictive red blood cell transfusion in septic shock patients in the ICU: protocol for a randomised controlled trial. Trials. 2013;14:150. doi:10.1186/1745-6215-14-150.
10. Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340(6):409-417. doi:10.1056/NEJM199902113400601.
11. Corwin HL, Theus JW, Cargile CS, Lang NP. Red blood cell transfusion: Impact of an education program and a clinical guideline on transfusion practice. J Hosp Med. 2014;9(12):745-749. doi:10.1002/jhm.2237.
12. Saxena, S, editor. The Transfusion Committee: Putting Patient Safety First, 2nd Edition. Bethesda (MD): American Association of Blood Banks; 2013.
13. The 2011 National Blood Collection and Utilization Report. http://www.hhs.gov/ash/bloodsafety/2011-nbcus.pdf. Accessed August 16, 2017.
14. Vestergaard S, Nayfield SG, Patel KV, et al. Fatigue in a Representative Population of Older Persons and Its Association With Functional Impairment, Functional Limitation, and Disability. J Gerontol A Biol Sci Med Sci. 2009;64A(1):76-82. doi:10.1093/gerona/gln017.
15. Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135(5):313-321.
16. Koch CG, Li L, Sun Z, et al. Hospital-acquired anemia: Prevalence, outcomes, and healthcare implications. J Hosp Med. 2013;8(9):506-512. doi:10.1002/jhm.2061.
17. Meltzer D, Manning WG, Morrison J, et al. Effects of Physician Experience on Costs and Outcomes on an Academic General Medicine Service: Results of a Trial of Hospitalists. Ann Intern Med. 2002;137(11):866-874. doi:10.7326/0003-4819-137-11-200212030-00007.
18. Carson JL, Grossman BJ, Kleinman S, et al. Red Blood Cell Transfusion: A Clinical Practice Guideline From the AABB*. Ann Intern Med. 2012;157(1):49-58. doi:10.7326/0003-4819-157-1-201206190-00429.
19. Moreh E, Jacobs JM, Stessman J. Fatigue, function, and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2010;65(8):887-895. doi:10.1093/gerona/glq064.
20. Eldadah BA. Fatigue and Fatigability in Older Adults. PM&R. 2010;2(5):406-413. doi:10.1016/j.pmrj.2010.03.022.
21. Hardy SE, Studenski SA. Fatigue Predicts Mortality among Older Adults. J Am Geriatr Soc. 2008;56(10):1910-1914. doi:10.1111/j.1532-5415.2008.01957.x.
22. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433-441.
23. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139.
24. HCUP Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP). 2006-2009. Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed November 22, 2016.
25. Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol Off J Am Soc Clin Oncol. 1993;11(3):570-579.
26. Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79. doi:10.1186/1477-7525-1-79.
27. Oken MMMD a, Creech RHMD b, Tormey DCMD, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. J Clin Oncol. 1982;5(6):649-656.
Fatigue is the most common clinical symptom of anemia and is a significant concern to patients.1,2 In ambulatory patients, lower hemoglobin (Hb) concentration is associated with increased fatigue.2,3 Accordingly, therapies that treat anemia by increasing Hb concentration, such as erythropoiesis stimulating agents,4-7 often use fatigue as an outcome measure.
In hospitalized patients, transfusion of red blood cell increases Hb concentration and is the primary treatment for anemia. However, the extent to which transfusion and changes in Hb concentration affect hospitalized patients’ fatigue levels is not well established. Guidelines support transfusing patients with symptoms of anemia, such as fatigue, on the assumption that the increased oxygen delivery will improve the symptoms of anemia. While transfusion studies in hospitalized patients have consistently reported that transfusion at lower or “restrictive” Hb concentrations is safe compared with transfusion at higher Hb concentrations,8-10 these studies have mainly used cardiac events and mortality as outcomes rather than patient symptoms, such as fatigue. Nevertheless, they have resulted in hospitals increasingly adopting restrictive transfusion policies that discourage transfusion at higher Hb levels.11,12 Consequently, the rate of transfusion in hospitalized patients has decreased,13 raising questions of whether some patients with lower Hb concentrations may experience increased fatigue as a result of restrictive transfusion policies. Fatigue among hospitalized patients is important not only because it is an adverse symptom but because it may result in decreased activity levels, deconditioning, and losses in functional status.14,15While the effect of alternative transfusion policies on fatigue in hospitalized patients could be answered by a randomized clinical trial using fatigue and functional status as outcomes, an important first step is to assess whether the Hb concentration of hospitalized patients is associated with their fatigue level during hospitalization. Because hospitalized patients often have acute illnesses that can cause fatigue in and of themselves, it is possible that anemia is not associated with fatigue in hospitalized patients despite anemia’s association with fatigue in ambulatory patients. Additionally, Hb concentration varies during hospitalization,16 raising the question of what measures of Hb during hospitalization might be most associated with anemia-related fatigue.
The objective of this study is to explore multiple Hb measures in hospitalized medical patients with anemia and test whether any of these Hb measures are associated with patients’ fatigue level.
METHODS
Study Design
We performed a prospective, observational study of hospitalized patients with anemia on the general medicine services at The University of Chicago Medical Center (UCMC). The institutional review board approved the study procedures, and all study subjects provided informed consent.
Study Eligibility
Between April 2014 and June 2015, all general medicine inpatients were approached for written consent for The University of Chicago Hospitalist Project,17 a research infrastructure at UCMC. Among patients consenting to participate in the Hospitalist Project, patients were eligible if they had Hb <9 g/dL at any point during their hospitalization and were age ≥50 years. Hb concentration of <9 g/dL was chosen to include the range of Hb values covered by most restrictive transfusion policies.8-10,18 Age ≥50 years was an inclusion criteria because anemia is more strongly associated with poor outcomes, including functional impairment, among older patients compared with younger patients.14,19-21 If patients were not eligible for inclusion at the time of consent for the Hospitalist Project, their Hb values were reviewed twice daily until hospital discharge to assess if their Hb was <9 g/dL. Proxies were sought to answer questions for patients who failed the Short Portable Mental Status Questionnaire.22
Patient Demographic Data Collection
Research assistants abstracted patient age and sex from the electronic health record (EHR), and asked patients to self-identify their race. The individual comorbidities included as part of the Charlson Comorbidity Index were identified using International Classification of Diseases, 9th Revision codes from hospital administrative data for each encounter and specifically included the following: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, liver disease, diabetes, hemiplegia and/or paraplegia, renal disease, cancer, and human immunodeficiency virus/acquired immunodeficiency syndrome.23 We also used Healthcare Cost and Utilization Project (www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp) diagnosis categories to identify whether patients had sickle cell (SC) anemia, gastrointestinal bleeding (GIB), or a depressive disorder (DD) because these conditions are associated with anemia (SC and GIB) and fatigue (DD).24
Measuring Anemia
Hb measures were available only when hospital providers ordered them as part of routine practice. The first Hb concentration <9 g/dL during a patient’s hospitalization, which made them eligible for study participation, was obtained through manual review of the EHR. All additional Hb values during the patient’s hospitalization were obtained from the hospital’s administrative data mart. All Hb values collected for each patient during the hospitalization were used to calculate summary measures of Hb during the hospitalization, including the mean Hb, median Hb, minimum Hb, maximum Hb, admission (first recorded) Hb, and discharge (last recorded) Hb. Hb measures were analyzed both as a continuous variable and as a categorical variable created by dividing the continuous Hb measures into integer ranges of 3 groups of approximately the same size.
Measuring Fatigue
Our primary outcome was patients’ level of fatigue reported during hospitalization, measured using the Functional Assessment of Chronic Illness Therapy (FACIT)-Anemia questionnaire. Fatigue was measured using a 13-question fatigue subscale,1,2,25 which measures fatigue within the past 7 days. Scores on the fatigue subscale range from 0 to 52, with lower scores reflecting greater levels of fatigue. As soon as patients met the eligibility criteria for study participation during their hospitalization (age ≥50 years and Hb <9 g/dL), they were approached to answer the FACIT questions. Values for missing data in the fatigue subscale for individual subjects were filled in using a prorated score from their answered questions as long as >50% of the items in the fatigue subscale were answered, in accordance with recommendations for addressing missing data in the FACIT.26 Fatigue was analyzed as a continuous variable and as a dichotomous variable created by dividing the sample into high (FACIT <27) and low (FACIT ≥27) levels of fatigue based on the median FACIT score of the population. Previous literature has shown a FACIT fatigue subscale score between 23 and 26 to be associated with an Eastern Cooperative Oncology Group (ECOG)27 C Performance Status rating of 2 to 33 compared to scores ≥27.
Statistical Analysis
Statistical analysis was performed using Stata statistical software (StataCorp, College Station, TX). Descriptive statistics were used to characterize patient demographics. Analysis of variance was used to test for differences in the mean fatigue levels across Hb measures. χ2 tests were performed to test for associations between high fatigue levels and the Hb measures. Multivariable analysis, including both linear and logistic regression models, were used to test the association of Hb concentration and fatigue. P values <0.05 using a 2-tailed test were deemed statistically significant.
RESULTS
Patient Characteristics
During the study period, 8559 patients were admitted to the general medicine service. Of those, 5073 (59%) consented for participation in the Hospitalist Project, and 3670 (72%) completed the Hospitalist Project inpatient interview. Of these patients, 1292 (35%) had Hb <9 g/dL, and 784 (61%) were 50 years or older and completed the FACIT questionnaire.
Table 1 reports the demographic characteristics and comorbidities for the sample, the mean (standard deviation [SD]) for the 6 Hb measures, and mean (SD) and median FACIT scores.
Bivariate Association of Fatigue and Hb
Categorizing patients into low, middle, or high Hb for each of the 6 Hb measures, minimum Hb was strongly associated with fatigue, with a weaker association for mean Hb and no statistically significant association for the other measures.
Minimum Hb. Patients with a minimum Hb <7 g/dL and patients with Hb 7-8 g/dL had higher fatigue levels (FACIT = 25 for each) than patients with a minimum Hb ≥8 g/dL (FACIT = 29; P < 0.001; Table 2). When excluding patients with SC and/or GIB because their average minimum Hb differed from the average minimum Hb of the full population (P < 0.001), patients with a minimum Hb <7 g/dL or 7-8 g/dL had even higher fatigue levels (FACIT = 23 and FACIT = 24, respectively), with no change in the fatigue level of patients with a minimum Hb ≥8 g/dL (FACIT = 29; P < 0.001; Table 2). Lower minimum Hb continued to be associated with higher fatigue levels when analyzed in 0.5 g/dL increments (Figure).
Mean Hb and Other Measures. Fatigue levels were high for 47% of patients with a mean Hb <8g /dL and 53% of patients with a mean Hb 8-9 g/dL compared with 43% of patients with a mean Hb ≥9 g/dL (P = 0.05). However, the association between high fatigue and mean Hb was not statistically significant when patients with SC and/or GIB were excluded (Table 2). None of the other 4 Hb measures was significantly associated with fatigue.
Linear Regression of Fatigue on Hb
In linear regression models, minimum Hb consistently predicted patient fatigue, mean Hb had a less robust association with fatigue, and the other Hb measures were not associated with patient fatigue. Increases in minimum Hb (analyzed as a continuous variable) were associated with reduced fatigue (higher FACIT score; β = 1.4; P = 0.005). In models in which minimum Hb was a categorical variable, patients with a minimum Hb of <7 g/dL or 7-8 g/dL had greater fatigue (lower FACIT score) than patients whose minimum Hb was ≥8 g/dL (Hb <7 g/dL: β = −4.2; P ≤ 0.001; Hb 7-8 g/dL: β = −4.1; P < 0.001). These results control for patients’ age, sex, individual comorbidities, and whether their minimum Hb occurred before or after the measurement of fatigue during hospitalization (Model 1), and the results are unchanged when also controlling for the number of Hb laboratory draws patients had during their hospitalization (Model 2; Table 3). In a stratified analysis excluding patients with either SC and/or GIB, changes in minimum Hb were associated with larger changes in patient fatigue levels (Supplemental Table 1). We also stratified our analysis to include only patients whose minimum Hb occurred before the measurement of their fatigue level during hospitalization to avoid a spurious association of fatigue with minimum Hb occurring after fatigue was measured. In both Models 1 and 2, minimum Hb remained a predictor of patients’ fatigue levels with similar effect sizes, although in Model 2, the results did not quite reach a statistically significant level, in part due to larger confidence intervals from the smaller sample size of this stratified analysis (Supplemental Table 2a). We further stratified this analysis to include only patients whose transfusion, if they received one, occurred after their minimum Hb and the measurement of their fatigue level to account for the possibility that a transfusion could affect the fatigue level patients report. In this analysis, most of the estimates of the effect of minimum Hb on fatigue were larger than those seen when only analyzing patients whose minimum Hb occurred before the measurement of their fatigue level, although again, the smaller sample size of this additional stratified analysis does produce larger confidence intervals for these estimates (Supplemental Table 2b).
No Hb measure other than minimum or mean had significant association with patient fatigue levels in linear regression models.
Logistic Regression of High Fatigue Level on Hb
Using logistic regression, minimum Hb analyzed as a categorical variable predicted increased odds of a high fatigue level. Patients with a minimum Hb <7 g/dL were 50% (odds ratio [OR] = 1.5; P = 0.03) more likely to have high fatigue and patients with a minimum Hb 7-8 g/dL were 90% (OR = 1.9; P < 0.001) more likely to have high fatigue compared with patients with a minimum Hb ≥8 g/dL in Model 1. These results were similar in Model 2, although the effect was only statistically significant in the 7-8 g/dL Hb group (Table 3). When excluding SC and/or GIB patients, the odds of having high fatigue as minimum Hb decreased were the same or higher for both models compared to the full population of patients. However, again, in Model 2, the effect was only statistically significant in the 7-8 g/dL Hb group (Supplemental Table 1).
Patients with a mean Hb <8 g/dL were 20% to 30% more likely to have high fatigue and patients with mean Hb 8-9 g/dL were 50% more likely to have high fatigue compared with patients with a mean Hb ≥9 g/dL, but the effects were only statistically significant for patients with a mean Hb 8-9 g/dL in both Models 1 and 2 (Table 3). These results were similar when excluding patients with SC and/or GIB, but they were only significant for patients with a mean Hb 8-9 g/dL in Model 1 and patients with a mean Hb <8 g/dL in the Model 2 (Supplemental Table 3).
DISCUSSION
These results demonstrate that minimum Hb during hospitalization is associated with fatigue in hospitalized patients age ≥50 years, and the association is stronger among patients without SC and/or GIB as comorbidities. The analysis of Hb as a continuous and categorical variable and the use of both linear and logistic regression models support the robustness of these associations and illuminate their clinical significance. For example, in linear regression with minimum Hb a continuous variable, the coefficient of 1.4 suggests that an increase of 2 g/dL in Hb, as might be expected from transfusion of 2 units of red blood cells, would be associated with about a 3-point improvement in fatigue. Additionally, as a categorical variable, a minimum Hb ≥8 g/dL compared with a minimum Hb <7 g/dL or 7-8 g/dL is associated with a 3- to 4-point improvement in fatigue. Previous literature suggests that a difference of 3 in the FACIT score is the minimum clinically important difference in fatigue,3 and changes in minimum Hb in either model predict changes in fatigue that are in the range of potential clinical significance.
The clinical significance of the findings is also reflected in the results of the logistic regressions, which may be mapped to potential effects on functional status. Specifically, the odds of having a high fatigue level (FACIT <27) increase 90% for persons with a minimum Hb 7–8 g/dL compared with persons with a minimum Hb ≥8 g/dL. For persons with a minimum Hb <7 g/dL, point estimates suggest a smaller (50%) increase in the odds of high fatigue, but the 95% confidence interval overlaps heavily with the estimate of patients whose minimum Hb is 7-8 g/dL. While it might be expected that patients with a minimum Hb <7 g/dL have greater levels of fatigue compared with patients with a minimum Hb 7-8 g/dL, we did not observe such a pattern. One reason may be that the confidence intervals of our estimated effects are wide enough that we cannot exclude such a pattern. Another possible explanation is that in both groups, the fatigue levels are sufficiently severe, such that the difference in their fatigue levels may not be clinically meaningful. For example, a FACIT score of 23 to 26 has been shown to be associated with an ECOG performance status of 2 to 3, requiring bed rest for at least part of the day.3 Therefore, patients with a minimum Hb 7-8 g/dL (mean FACIT score = 24; Table 2) or a minimum Hb of <7 g/dL (mean FACIT score = 23; Table 2) are already functionally limited to the point of being partially bed bound, such that further decreases in their Hb may not produce additional fatigue in part because they reduce their activity sufficiently to prevent an increase in fatigue. In such cases, the potential benefits of increased Hb may be better assessed by measuring fatigue in response to a specific and provoked activity level, a concept known as fatigability.20
That minimum Hb is more strongly associated with fatigue than any other measure of Hb during hospitalization may not be surprising. Mean, median, maximum, and discharge Hb may all be affected by transfusion during hospitalization that could affect fatigue. Admission Hb may not reflect true oxygen-carrying capacity because of hemoconcentration.
The association between Hb and fatigue in hospitalized patients is important because increased fatigue could contribute to slower clinical recovery in hospitalized patients. Additionally, increased fatigue during hospitalization and at hospital discharge could exacerbate the known deleterious consequences of fatigue on patients and their health outcomes14,15 after hospital discharge. Although one previous study, the Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair (FOCUS)8 trial, did not report differences in patients’ fatigue levels at 30 and 60 days postdischarge when transfused at restrictive (8 g/dL) compared with liberal (10 g/dL) Hb thresholds, confidence in the validity of this finding is reduced by the fact that more than half of the patients were lost to follow-up at the 30- and 60-day time points. Further, patients in the restrictive transfusion arm of FOCUS were transfused to maintain Hb levels at or above 8 g/dL. This transfusion threshold of 8 g/dL may have mitigated the high levels of fatigue that are seen in our study when patients’ Hb drops below 8 g/dL, and maintaining a Hb level of 7 g/dL is now the standard of care in stable hospitalized patients. Lastly, FOCUS was limited to postoperative hip fracture patients, and the generalizability of FOCUS to hospitalized medicine patients with anemia is limited.
Therefore, our results support guideline suggestions that practitioners incorporate the presence of patient symptoms such as fatigue into transfusion decisions, particularly if patients’ Hb is <8 g/dL.18 Though reasonable, the suggestion to incorporate symptoms such as fatigue into transfusion decisions has not been strongly supported by evidence so far, and it may often be neglected in practice. Definitive evidence to support such recommendations would benefit from study through an optimal trial18 that incorporates symptoms into decision making. Our findings add support for a study of transfusion strategies that incorporates patients’ fatigue level in addition to Hb concentration.
This study has several limitations. Although our sample size is large and includes patients with a range of comorbidities that we believe are representative of hospitalized general medicine patients, as a single-center, observational study, our results may not be generalizable to other centers. Additionally, although these data support a reliable association between hospitalized patients’ minimum Hb and fatigue level, the observational design of this study cannot prove that this relationship is causal. Also, patients’ Hb values were measured at the discretion of their clinician, and therefore, the measures of Hb were not uniformly measured for participating patients. In addition, fatigue was only measured at one time point during a patient’s hospitalization, and it is possible that patients’ fatigue levels change during hospitalization in relation to variables we did not consider. Finally, our study was not designed to assess the association of Hb with longer-term functional outcomes, which may be of greater concern than fatigue.
CONCLUSION
In hospitalized patients ≥50 years old, minimum Hb is reliably associated with patients’ fatigue level. Patients whose minimum Hb is <8 g/dL experience higher fatigue levels compared to patients whose minimum Hb is ≥8 g/dL. Additional studies are warranted to understand if patients may benefit from improved fatigue levels by correcting their anemia through transfusion.
Fatigue is the most common clinical symptom of anemia and is a significant concern to patients.1,2 In ambulatory patients, lower hemoglobin (Hb) concentration is associated with increased fatigue.2,3 Accordingly, therapies that treat anemia by increasing Hb concentration, such as erythropoiesis stimulating agents,4-7 often use fatigue as an outcome measure.
In hospitalized patients, transfusion of red blood cell increases Hb concentration and is the primary treatment for anemia. However, the extent to which transfusion and changes in Hb concentration affect hospitalized patients’ fatigue levels is not well established. Guidelines support transfusing patients with symptoms of anemia, such as fatigue, on the assumption that the increased oxygen delivery will improve the symptoms of anemia. While transfusion studies in hospitalized patients have consistently reported that transfusion at lower or “restrictive” Hb concentrations is safe compared with transfusion at higher Hb concentrations,8-10 these studies have mainly used cardiac events and mortality as outcomes rather than patient symptoms, such as fatigue. Nevertheless, they have resulted in hospitals increasingly adopting restrictive transfusion policies that discourage transfusion at higher Hb levels.11,12 Consequently, the rate of transfusion in hospitalized patients has decreased,13 raising questions of whether some patients with lower Hb concentrations may experience increased fatigue as a result of restrictive transfusion policies. Fatigue among hospitalized patients is important not only because it is an adverse symptom but because it may result in decreased activity levels, deconditioning, and losses in functional status.14,15While the effect of alternative transfusion policies on fatigue in hospitalized patients could be answered by a randomized clinical trial using fatigue and functional status as outcomes, an important first step is to assess whether the Hb concentration of hospitalized patients is associated with their fatigue level during hospitalization. Because hospitalized patients often have acute illnesses that can cause fatigue in and of themselves, it is possible that anemia is not associated with fatigue in hospitalized patients despite anemia’s association with fatigue in ambulatory patients. Additionally, Hb concentration varies during hospitalization,16 raising the question of what measures of Hb during hospitalization might be most associated with anemia-related fatigue.
The objective of this study is to explore multiple Hb measures in hospitalized medical patients with anemia and test whether any of these Hb measures are associated with patients’ fatigue level.
METHODS
Study Design
We performed a prospective, observational study of hospitalized patients with anemia on the general medicine services at The University of Chicago Medical Center (UCMC). The institutional review board approved the study procedures, and all study subjects provided informed consent.
Study Eligibility
Between April 2014 and June 2015, all general medicine inpatients were approached for written consent for The University of Chicago Hospitalist Project,17 a research infrastructure at UCMC. Among patients consenting to participate in the Hospitalist Project, patients were eligible if they had Hb <9 g/dL at any point during their hospitalization and were age ≥50 years. Hb concentration of <9 g/dL was chosen to include the range of Hb values covered by most restrictive transfusion policies.8-10,18 Age ≥50 years was an inclusion criteria because anemia is more strongly associated with poor outcomes, including functional impairment, among older patients compared with younger patients.14,19-21 If patients were not eligible for inclusion at the time of consent for the Hospitalist Project, their Hb values were reviewed twice daily until hospital discharge to assess if their Hb was <9 g/dL. Proxies were sought to answer questions for patients who failed the Short Portable Mental Status Questionnaire.22
Patient Demographic Data Collection
Research assistants abstracted patient age and sex from the electronic health record (EHR), and asked patients to self-identify their race. The individual comorbidities included as part of the Charlson Comorbidity Index were identified using International Classification of Diseases, 9th Revision codes from hospital administrative data for each encounter and specifically included the following: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, liver disease, diabetes, hemiplegia and/or paraplegia, renal disease, cancer, and human immunodeficiency virus/acquired immunodeficiency syndrome.23 We also used Healthcare Cost and Utilization Project (www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp) diagnosis categories to identify whether patients had sickle cell (SC) anemia, gastrointestinal bleeding (GIB), or a depressive disorder (DD) because these conditions are associated with anemia (SC and GIB) and fatigue (DD).24
Measuring Anemia
Hb measures were available only when hospital providers ordered them as part of routine practice. The first Hb concentration <9 g/dL during a patient’s hospitalization, which made them eligible for study participation, was obtained through manual review of the EHR. All additional Hb values during the patient’s hospitalization were obtained from the hospital’s administrative data mart. All Hb values collected for each patient during the hospitalization were used to calculate summary measures of Hb during the hospitalization, including the mean Hb, median Hb, minimum Hb, maximum Hb, admission (first recorded) Hb, and discharge (last recorded) Hb. Hb measures were analyzed both as a continuous variable and as a categorical variable created by dividing the continuous Hb measures into integer ranges of 3 groups of approximately the same size.
Measuring Fatigue
Our primary outcome was patients’ level of fatigue reported during hospitalization, measured using the Functional Assessment of Chronic Illness Therapy (FACIT)-Anemia questionnaire. Fatigue was measured using a 13-question fatigue subscale,1,2,25 which measures fatigue within the past 7 days. Scores on the fatigue subscale range from 0 to 52, with lower scores reflecting greater levels of fatigue. As soon as patients met the eligibility criteria for study participation during their hospitalization (age ≥50 years and Hb <9 g/dL), they were approached to answer the FACIT questions. Values for missing data in the fatigue subscale for individual subjects were filled in using a prorated score from their answered questions as long as >50% of the items in the fatigue subscale were answered, in accordance with recommendations for addressing missing data in the FACIT.26 Fatigue was analyzed as a continuous variable and as a dichotomous variable created by dividing the sample into high (FACIT <27) and low (FACIT ≥27) levels of fatigue based on the median FACIT score of the population. Previous literature has shown a FACIT fatigue subscale score between 23 and 26 to be associated with an Eastern Cooperative Oncology Group (ECOG)27 C Performance Status rating of 2 to 33 compared to scores ≥27.
Statistical Analysis
Statistical analysis was performed using Stata statistical software (StataCorp, College Station, TX). Descriptive statistics were used to characterize patient demographics. Analysis of variance was used to test for differences in the mean fatigue levels across Hb measures. χ2 tests were performed to test for associations between high fatigue levels and the Hb measures. Multivariable analysis, including both linear and logistic regression models, were used to test the association of Hb concentration and fatigue. P values <0.05 using a 2-tailed test were deemed statistically significant.
RESULTS
Patient Characteristics
During the study period, 8559 patients were admitted to the general medicine service. Of those, 5073 (59%) consented for participation in the Hospitalist Project, and 3670 (72%) completed the Hospitalist Project inpatient interview. Of these patients, 1292 (35%) had Hb <9 g/dL, and 784 (61%) were 50 years or older and completed the FACIT questionnaire.
Table 1 reports the demographic characteristics and comorbidities for the sample, the mean (standard deviation [SD]) for the 6 Hb measures, and mean (SD) and median FACIT scores.
Bivariate Association of Fatigue and Hb
Categorizing patients into low, middle, or high Hb for each of the 6 Hb measures, minimum Hb was strongly associated with fatigue, with a weaker association for mean Hb and no statistically significant association for the other measures.
Minimum Hb. Patients with a minimum Hb <7 g/dL and patients with Hb 7-8 g/dL had higher fatigue levels (FACIT = 25 for each) than patients with a minimum Hb ≥8 g/dL (FACIT = 29; P < 0.001; Table 2). When excluding patients with SC and/or GIB because their average minimum Hb differed from the average minimum Hb of the full population (P < 0.001), patients with a minimum Hb <7 g/dL or 7-8 g/dL had even higher fatigue levels (FACIT = 23 and FACIT = 24, respectively), with no change in the fatigue level of patients with a minimum Hb ≥8 g/dL (FACIT = 29; P < 0.001; Table 2). Lower minimum Hb continued to be associated with higher fatigue levels when analyzed in 0.5 g/dL increments (Figure).
Mean Hb and Other Measures. Fatigue levels were high for 47% of patients with a mean Hb <8g /dL and 53% of patients with a mean Hb 8-9 g/dL compared with 43% of patients with a mean Hb ≥9 g/dL (P = 0.05). However, the association between high fatigue and mean Hb was not statistically significant when patients with SC and/or GIB were excluded (Table 2). None of the other 4 Hb measures was significantly associated with fatigue.
Linear Regression of Fatigue on Hb
In linear regression models, minimum Hb consistently predicted patient fatigue, mean Hb had a less robust association with fatigue, and the other Hb measures were not associated with patient fatigue. Increases in minimum Hb (analyzed as a continuous variable) were associated with reduced fatigue (higher FACIT score; β = 1.4; P = 0.005). In models in which minimum Hb was a categorical variable, patients with a minimum Hb of <7 g/dL or 7-8 g/dL had greater fatigue (lower FACIT score) than patients whose minimum Hb was ≥8 g/dL (Hb <7 g/dL: β = −4.2; P ≤ 0.001; Hb 7-8 g/dL: β = −4.1; P < 0.001). These results control for patients’ age, sex, individual comorbidities, and whether their minimum Hb occurred before or after the measurement of fatigue during hospitalization (Model 1), and the results are unchanged when also controlling for the number of Hb laboratory draws patients had during their hospitalization (Model 2; Table 3). In a stratified analysis excluding patients with either SC and/or GIB, changes in minimum Hb were associated with larger changes in patient fatigue levels (Supplemental Table 1). We also stratified our analysis to include only patients whose minimum Hb occurred before the measurement of their fatigue level during hospitalization to avoid a spurious association of fatigue with minimum Hb occurring after fatigue was measured. In both Models 1 and 2, minimum Hb remained a predictor of patients’ fatigue levels with similar effect sizes, although in Model 2, the results did not quite reach a statistically significant level, in part due to larger confidence intervals from the smaller sample size of this stratified analysis (Supplemental Table 2a). We further stratified this analysis to include only patients whose transfusion, if they received one, occurred after their minimum Hb and the measurement of their fatigue level to account for the possibility that a transfusion could affect the fatigue level patients report. In this analysis, most of the estimates of the effect of minimum Hb on fatigue were larger than those seen when only analyzing patients whose minimum Hb occurred before the measurement of their fatigue level, although again, the smaller sample size of this additional stratified analysis does produce larger confidence intervals for these estimates (Supplemental Table 2b).
No Hb measure other than minimum or mean had significant association with patient fatigue levels in linear regression models.
Logistic Regression of High Fatigue Level on Hb
Using logistic regression, minimum Hb analyzed as a categorical variable predicted increased odds of a high fatigue level. Patients with a minimum Hb <7 g/dL were 50% (odds ratio [OR] = 1.5; P = 0.03) more likely to have high fatigue and patients with a minimum Hb 7-8 g/dL were 90% (OR = 1.9; P < 0.001) more likely to have high fatigue compared with patients with a minimum Hb ≥8 g/dL in Model 1. These results were similar in Model 2, although the effect was only statistically significant in the 7-8 g/dL Hb group (Table 3). When excluding SC and/or GIB patients, the odds of having high fatigue as minimum Hb decreased were the same or higher for both models compared to the full population of patients. However, again, in Model 2, the effect was only statistically significant in the 7-8 g/dL Hb group (Supplemental Table 1).
Patients with a mean Hb <8 g/dL were 20% to 30% more likely to have high fatigue and patients with mean Hb 8-9 g/dL were 50% more likely to have high fatigue compared with patients with a mean Hb ≥9 g/dL, but the effects were only statistically significant for patients with a mean Hb 8-9 g/dL in both Models 1 and 2 (Table 3). These results were similar when excluding patients with SC and/or GIB, but they were only significant for patients with a mean Hb 8-9 g/dL in Model 1 and patients with a mean Hb <8 g/dL in the Model 2 (Supplemental Table 3).
DISCUSSION
These results demonstrate that minimum Hb during hospitalization is associated with fatigue in hospitalized patients age ≥50 years, and the association is stronger among patients without SC and/or GIB as comorbidities. The analysis of Hb as a continuous and categorical variable and the use of both linear and logistic regression models support the robustness of these associations and illuminate their clinical significance. For example, in linear regression with minimum Hb a continuous variable, the coefficient of 1.4 suggests that an increase of 2 g/dL in Hb, as might be expected from transfusion of 2 units of red blood cells, would be associated with about a 3-point improvement in fatigue. Additionally, as a categorical variable, a minimum Hb ≥8 g/dL compared with a minimum Hb <7 g/dL or 7-8 g/dL is associated with a 3- to 4-point improvement in fatigue. Previous literature suggests that a difference of 3 in the FACIT score is the minimum clinically important difference in fatigue,3 and changes in minimum Hb in either model predict changes in fatigue that are in the range of potential clinical significance.
The clinical significance of the findings is also reflected in the results of the logistic regressions, which may be mapped to potential effects on functional status. Specifically, the odds of having a high fatigue level (FACIT <27) increase 90% for persons with a minimum Hb 7–8 g/dL compared with persons with a minimum Hb ≥8 g/dL. For persons with a minimum Hb <7 g/dL, point estimates suggest a smaller (50%) increase in the odds of high fatigue, but the 95% confidence interval overlaps heavily with the estimate of patients whose minimum Hb is 7-8 g/dL. While it might be expected that patients with a minimum Hb <7 g/dL have greater levels of fatigue compared with patients with a minimum Hb 7-8 g/dL, we did not observe such a pattern. One reason may be that the confidence intervals of our estimated effects are wide enough that we cannot exclude such a pattern. Another possible explanation is that in both groups, the fatigue levels are sufficiently severe, such that the difference in their fatigue levels may not be clinically meaningful. For example, a FACIT score of 23 to 26 has been shown to be associated with an ECOG performance status of 2 to 3, requiring bed rest for at least part of the day.3 Therefore, patients with a minimum Hb 7-8 g/dL (mean FACIT score = 24; Table 2) or a minimum Hb of <7 g/dL (mean FACIT score = 23; Table 2) are already functionally limited to the point of being partially bed bound, such that further decreases in their Hb may not produce additional fatigue in part because they reduce their activity sufficiently to prevent an increase in fatigue. In such cases, the potential benefits of increased Hb may be better assessed by measuring fatigue in response to a specific and provoked activity level, a concept known as fatigability.20
That minimum Hb is more strongly associated with fatigue than any other measure of Hb during hospitalization may not be surprising. Mean, median, maximum, and discharge Hb may all be affected by transfusion during hospitalization that could affect fatigue. Admission Hb may not reflect true oxygen-carrying capacity because of hemoconcentration.
The association between Hb and fatigue in hospitalized patients is important because increased fatigue could contribute to slower clinical recovery in hospitalized patients. Additionally, increased fatigue during hospitalization and at hospital discharge could exacerbate the known deleterious consequences of fatigue on patients and their health outcomes14,15 after hospital discharge. Although one previous study, the Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair (FOCUS)8 trial, did not report differences in patients’ fatigue levels at 30 and 60 days postdischarge when transfused at restrictive (8 g/dL) compared with liberal (10 g/dL) Hb thresholds, confidence in the validity of this finding is reduced by the fact that more than half of the patients were lost to follow-up at the 30- and 60-day time points. Further, patients in the restrictive transfusion arm of FOCUS were transfused to maintain Hb levels at or above 8 g/dL. This transfusion threshold of 8 g/dL may have mitigated the high levels of fatigue that are seen in our study when patients’ Hb drops below 8 g/dL, and maintaining a Hb level of 7 g/dL is now the standard of care in stable hospitalized patients. Lastly, FOCUS was limited to postoperative hip fracture patients, and the generalizability of FOCUS to hospitalized medicine patients with anemia is limited.
Therefore, our results support guideline suggestions that practitioners incorporate the presence of patient symptoms such as fatigue into transfusion decisions, particularly if patients’ Hb is <8 g/dL.18 Though reasonable, the suggestion to incorporate symptoms such as fatigue into transfusion decisions has not been strongly supported by evidence so far, and it may often be neglected in practice. Definitive evidence to support such recommendations would benefit from study through an optimal trial18 that incorporates symptoms into decision making. Our findings add support for a study of transfusion strategies that incorporates patients’ fatigue level in addition to Hb concentration.
This study has several limitations. Although our sample size is large and includes patients with a range of comorbidities that we believe are representative of hospitalized general medicine patients, as a single-center, observational study, our results may not be generalizable to other centers. Additionally, although these data support a reliable association between hospitalized patients’ minimum Hb and fatigue level, the observational design of this study cannot prove that this relationship is causal. Also, patients’ Hb values were measured at the discretion of their clinician, and therefore, the measures of Hb were not uniformly measured for participating patients. In addition, fatigue was only measured at one time point during a patient’s hospitalization, and it is possible that patients’ fatigue levels change during hospitalization in relation to variables we did not consider. Finally, our study was not designed to assess the association of Hb with longer-term functional outcomes, which may be of greater concern than fatigue.
CONCLUSION
In hospitalized patients ≥50 years old, minimum Hb is reliably associated with patients’ fatigue level. Patients whose minimum Hb is <8 g/dL experience higher fatigue levels compared to patients whose minimum Hb is ≥8 g/dL. Additional studies are warranted to understand if patients may benefit from improved fatigue levels by correcting their anemia through transfusion.
1. Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13(2):63-74.
2. Cella D, Lai JS, Chang CH, Peterman A, Slavin M. Fatigue in cancer patients compared with fatigue in the general United States population. Cancer. 2002;94(2):528-538. doi:10.1002/cncr.10245.
3. Cella D, Eton DT, Lai J-S, Peterman AH, Merkel DE. Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manage. 2002;24(6):547-561.
4. Tonelli M, Hemmelgarn B, Reiman T, et al. Benefits and harms of erythropoiesis-stimulating agents for anemia related to cancer: a meta-analysis. CMAJ Can Med Assoc J J Assoc Medicale Can. 2009;180(11):E62-E71. doi:10.1503/cmaj.090470.
5. Foley RN, Curtis BM, Parfrey PS. Erythropoietin Therapy, Hemoglobin Targets, and Quality of Life in Healthy Hemodialysis Patients: A Randomized Trial. Clin J Am Soc Nephrol. 2009;4(4):726-733. doi:10.2215/CJN.04950908.
6. Keown PA, Churchill DN, Poulin-Costello M, et al. Dialysis patients treated with Epoetin alfa show improved anemia symptoms: A new analysis of the Canadian Erythropoietin Study Group trial. Hemodial Int Int Symp Home Hemodial. 2010;14(2):168-173. doi:10.1111/j.1542-4758.2009.00422.x.
7. Palmer SC, Saglimbene V, Mavridis D, et al. Erythropoiesis-stimulating agents for anaemia in adults with chronic kidney disease: a network meta-analysis. Cochrane Database Syst Rev. 2014:CD010590.
8. Carson JL, Terrin ML, Noveck H, et al. Liberal or Restrictive Transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453-2462. doi:10.1056/NEJMoa1012452.
9. Holst LB, Haase N, Wetterslev J, et al. Transfusion requirements in septic shock (TRISS) trial – comparing the effects and safety of liberal versus restrictive red blood cell transfusion in septic shock patients in the ICU: protocol for a randomised controlled trial. Trials. 2013;14:150. doi:10.1186/1745-6215-14-150.
10. Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340(6):409-417. doi:10.1056/NEJM199902113400601.
11. Corwin HL, Theus JW, Cargile CS, Lang NP. Red blood cell transfusion: Impact of an education program and a clinical guideline on transfusion practice. J Hosp Med. 2014;9(12):745-749. doi:10.1002/jhm.2237.
12. Saxena, S, editor. The Transfusion Committee: Putting Patient Safety First, 2nd Edition. Bethesda (MD): American Association of Blood Banks; 2013.
13. The 2011 National Blood Collection and Utilization Report. http://www.hhs.gov/ash/bloodsafety/2011-nbcus.pdf. Accessed August 16, 2017.
14. Vestergaard S, Nayfield SG, Patel KV, et al. Fatigue in a Representative Population of Older Persons and Its Association With Functional Impairment, Functional Limitation, and Disability. J Gerontol A Biol Sci Med Sci. 2009;64A(1):76-82. doi:10.1093/gerona/gln017.
15. Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135(5):313-321.
16. Koch CG, Li L, Sun Z, et al. Hospital-acquired anemia: Prevalence, outcomes, and healthcare implications. J Hosp Med. 2013;8(9):506-512. doi:10.1002/jhm.2061.
17. Meltzer D, Manning WG, Morrison J, et al. Effects of Physician Experience on Costs and Outcomes on an Academic General Medicine Service: Results of a Trial of Hospitalists. Ann Intern Med. 2002;137(11):866-874. doi:10.7326/0003-4819-137-11-200212030-00007.
18. Carson JL, Grossman BJ, Kleinman S, et al. Red Blood Cell Transfusion: A Clinical Practice Guideline From the AABB*. Ann Intern Med. 2012;157(1):49-58. doi:10.7326/0003-4819-157-1-201206190-00429.
19. Moreh E, Jacobs JM, Stessman J. Fatigue, function, and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2010;65(8):887-895. doi:10.1093/gerona/glq064.
20. Eldadah BA. Fatigue and Fatigability in Older Adults. PM&R. 2010;2(5):406-413. doi:10.1016/j.pmrj.2010.03.022.
21. Hardy SE, Studenski SA. Fatigue Predicts Mortality among Older Adults. J Am Geriatr Soc. 2008;56(10):1910-1914. doi:10.1111/j.1532-5415.2008.01957.x.
22. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433-441.
23. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139.
24. HCUP Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP). 2006-2009. Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed November 22, 2016.
25. Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol Off J Am Soc Clin Oncol. 1993;11(3):570-579.
26. Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79. doi:10.1186/1477-7525-1-79.
27. Oken MMMD a, Creech RHMD b, Tormey DCMD, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. J Clin Oncol. 1982;5(6):649-656.
1. Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13(2):63-74.
2. Cella D, Lai JS, Chang CH, Peterman A, Slavin M. Fatigue in cancer patients compared with fatigue in the general United States population. Cancer. 2002;94(2):528-538. doi:10.1002/cncr.10245.
3. Cella D, Eton DT, Lai J-S, Peterman AH, Merkel DE. Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manage. 2002;24(6):547-561.
4. Tonelli M, Hemmelgarn B, Reiman T, et al. Benefits and harms of erythropoiesis-stimulating agents for anemia related to cancer: a meta-analysis. CMAJ Can Med Assoc J J Assoc Medicale Can. 2009;180(11):E62-E71. doi:10.1503/cmaj.090470.
5. Foley RN, Curtis BM, Parfrey PS. Erythropoietin Therapy, Hemoglobin Targets, and Quality of Life in Healthy Hemodialysis Patients: A Randomized Trial. Clin J Am Soc Nephrol. 2009;4(4):726-733. doi:10.2215/CJN.04950908.
6. Keown PA, Churchill DN, Poulin-Costello M, et al. Dialysis patients treated with Epoetin alfa show improved anemia symptoms: A new analysis of the Canadian Erythropoietin Study Group trial. Hemodial Int Int Symp Home Hemodial. 2010;14(2):168-173. doi:10.1111/j.1542-4758.2009.00422.x.
7. Palmer SC, Saglimbene V, Mavridis D, et al. Erythropoiesis-stimulating agents for anaemia in adults with chronic kidney disease: a network meta-analysis. Cochrane Database Syst Rev. 2014:CD010590.
8. Carson JL, Terrin ML, Noveck H, et al. Liberal or Restrictive Transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453-2462. doi:10.1056/NEJMoa1012452.
9. Holst LB, Haase N, Wetterslev J, et al. Transfusion requirements in septic shock (TRISS) trial – comparing the effects and safety of liberal versus restrictive red blood cell transfusion in septic shock patients in the ICU: protocol for a randomised controlled trial. Trials. 2013;14:150. doi:10.1186/1745-6215-14-150.
10. Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med. 1999;340(6):409-417. doi:10.1056/NEJM199902113400601.
11. Corwin HL, Theus JW, Cargile CS, Lang NP. Red blood cell transfusion: Impact of an education program and a clinical guideline on transfusion practice. J Hosp Med. 2014;9(12):745-749. doi:10.1002/jhm.2237.
12. Saxena, S, editor. The Transfusion Committee: Putting Patient Safety First, 2nd Edition. Bethesda (MD): American Association of Blood Banks; 2013.
13. The 2011 National Blood Collection and Utilization Report. http://www.hhs.gov/ash/bloodsafety/2011-nbcus.pdf. Accessed August 16, 2017.
14. Vestergaard S, Nayfield SG, Patel KV, et al. Fatigue in a Representative Population of Older Persons and Its Association With Functional Impairment, Functional Limitation, and Disability. J Gerontol A Biol Sci Med Sci. 2009;64A(1):76-82. doi:10.1093/gerona/gln017.
15. Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135(5):313-321.
16. Koch CG, Li L, Sun Z, et al. Hospital-acquired anemia: Prevalence, outcomes, and healthcare implications. J Hosp Med. 2013;8(9):506-512. doi:10.1002/jhm.2061.
17. Meltzer D, Manning WG, Morrison J, et al. Effects of Physician Experience on Costs and Outcomes on an Academic General Medicine Service: Results of a Trial of Hospitalists. Ann Intern Med. 2002;137(11):866-874. doi:10.7326/0003-4819-137-11-200212030-00007.
18. Carson JL, Grossman BJ, Kleinman S, et al. Red Blood Cell Transfusion: A Clinical Practice Guideline From the AABB*. Ann Intern Med. 2012;157(1):49-58. doi:10.7326/0003-4819-157-1-201206190-00429.
19. Moreh E, Jacobs JM, Stessman J. Fatigue, function, and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2010;65(8):887-895. doi:10.1093/gerona/glq064.
20. Eldadah BA. Fatigue and Fatigability in Older Adults. PM&R. 2010;2(5):406-413. doi:10.1016/j.pmrj.2010.03.022.
21. Hardy SE, Studenski SA. Fatigue Predicts Mortality among Older Adults. J Am Geriatr Soc. 2008;56(10):1910-1914. doi:10.1111/j.1532-5415.2008.01957.x.
22. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433-441.
23. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139.
24. HCUP Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP). 2006-2009. Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed November 22, 2016.
25. Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol Off J Am Soc Clin Oncol. 1993;11(3):570-579.
26. Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79. doi:10.1186/1477-7525-1-79.
27. Oken MMMD a, Creech RHMD b, Tormey DCMD, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. J Clin Oncol. 1982;5(6):649-656.
© 2017 Society of Hospital Medicine
2017 Update on female sexual dysfunction
Sexual function is a complex, multifaceted process mediated by neurologic functions, hormonal regulation, and ps
As it turns out, quite a lot. Female sexual dysfunction is a common, vastly undertreated sexual health problem that can have wide-reaching effects on a woman’s life. These effects may include impaired body image, self-confidence, and self-worth. Sexual dysfunction also can contribute to relationship dissatisfaction and leave one feeling less connected with her partner.1,2 Studies have shown women with sexual dysfunction have higher health care expenditures3 and that depression and fatigue are common comorbidities, as is frequently seen in other chronic conditions such as diabetes and back pain.4
Understanding the pathogenesis of female sexual dysfunction helps to guide our approach to its management. Indeed, increased understanding of its pathology has helped to usher in new and emerging treatment options, as well as a personalized, biopsychosocial approach to its management.
Related article:
2016 Update on female sexual dysfunction
In this Update, I discuss the interplay of physiologic and psychological factors that affect female sexual function as well as the latest options for its management. I have also assembled a panel of experts to discuss 2 cases representative of sexual dysfunction that you may encounter in your clinical practice and how prescribing decisions are made for their management.
Read about factors that impact sexual function and agents to help manage dysfunction.
Multiple transmitters in the brain can increase or decrease sexual desire and function
Neurotransmitters involved in sexual excitation include brain dopamine, melanocortin, oxytocin, vasopressin, and norepinephrine, whereas brain opioids, serotonin, prolactin, and endocannabinoids function as sexual inhibitors. Inhibitory transmitters are activated normally during sexual refractoriness but also from primary aversion or secondary avoidance disorders.1 Drugs or conditions that reduce brain dopamine levels, increase the action of brain serotonin, or enhance brain opioid pathways have been shown to inhibit sexual desire, while those that increase hypothalamic and mesolimbic dopamine or decrease serotonin release have been shown to stimulate sexual desire.1
Estradiol and progesterone can impact sexual function and desire
In addition to the neurotransmitters, hormones are important modulators of female sexual function. Decreasing levels of circulating estrogen after menopause lead to physiologic, biologic, and clinical changes in the urogenital tissues, such as decreased elastin, thinning of the epithelium, reduced vaginal blood flow, diminished lubrication, and decreased flexibility and elasticity. These changes result in the symptoms of genitourinary syndrome of menopause (GSM), which affects as many as half of all menopausal women.5,6 In clinical trials, dyspareunia and vaginal dryness are the most bothersome GSM symptoms reported.7
The role of hormonal regulation in sexual dysfunction among premenopausal women is not yet fully understood, but we do know that estradiol has been shown to improve sexual desire, progesterone tends to dampen sexual desire, and that testosterone at physiological levels has been shown in most studies to have a neutral effect on sexual desire in a well-estrogenized patient.8
Related article:
Focus on treating genital atrophy symptoms
Experience and behavior modulate or reinforce sexual dysfunction
The most common psychological factors that trigger or amplify female sexual dysfunction are depression, anxiety, distraction, negative body image, sexual abuse, and emotional neglect.9 Contextual or sociocultural factors, such as relationship discord, life-stage stressors (the empty nest syndrome or anxiety and sleep deprivation from a new baby), as well as cultural or religious values that suppress sexuality, also should be considered.9 Experience-based neuroplasticity (changes in brain pathways that become solidified by negative or positive experiences) may elucidate how a multimodal approach, utilizing medical and psychological treatment, can be beneficial for patients, particularly those with hypoactive sexual desire disorder (HSDD).1
New and emerging approaches to managing female sexual dysfunction
Three agents, one of which has been available for prescription for some time, one that is newly available, and one in the pipeline, are or may soon be in the gynecologist's armamentarium.
Flibanserin
Medications that target excitatory pathways or blunt inhibitory pathways are in development, and one, flibanserin (Addyi), has been US Food and Drug Administration (FDA)-approved for the treatment of acquired, generalized HSDD in premenopausal women.1,10 Flibanserin is a nonhormonal, centrally acting, postsynaptic serotonin 1A receptor agonist and a serotonin 2A receptor antagonist that is taken daily at bedtime (100 mg); several weeks are usually needed before any effects are noted.1 It is not approved for postmenopausal women and has a boxed warning about the risks of hypotension and syncope; its use is contraindicated in women who drink alcohol, in those who have hepatic impairment, and with the use of moderate or strong CYP3A4 inhibitors.11
Also keep in mind that flibanserin is only available through a Risk Evaluation and Mitigation Strategy program, so clinicians who wish to prescribe it must enroll in and complete training to become certified providers.9
Related article:
What you need to know (and do) to prescribe the new drug flibanserin
Prasterone
Prasterone (Intrarosa), a once-daily intravaginal dehydroepiandrosterone (DHEA) product, is a prohormone that increases local estrogen and testosterone and has the advantage of improved sexual function, desire, arousal, lubrication, orgasm, satisfaction, as well as pain at sexual activity.12 It was approved by the FDA in November 2016 to treat moderate to severe dyspareunia and has been available for prescribing since July 2017. Its cost is comparable to topical estrogen products, with a $25 copay program.
Because prasterone is not an estrogen, it does not have the boxed warning that all estrogen products are mandated by the FDA to have. This may make it more acceptable to patients, who often decline to use an estrogen product after seeing the boxed warning on the package. The Centers for Medicare and Medicaid Services (CMS) does not have prasterone on its list of potentially hazardous drugs for the elderly. However, keep in mind that because its label is for dyspareunia and not specifically for GSM, CMS considers it a drug of choice--in other words, like sildenafil (Viagra), a lifestyle choice and not for treatment of a medical condition. As such, at the present time, Medicare does not cover it.
Bremelanotide
Late-stage trials of bremelanotide, a melanocortin receptor agonist, are underway. Its mechanism of action is somewhat like that of flibanserin in that both drugs increase dopamine and norepinephrine levels. The advantage of bremelanotide is that it is used as needed. It is dosed subcutaneously (1.75 mg) and it can be used as often as a woman would like to use it. The FDA is expected to consider it for approval in about a year. Unpublished data from poster sessions at recent meetings show that, in a phase 3 study of 1,247 premenopausal women with HSDD (who had already been screened for depression and were found to have a physiologic condition), improvements in desire, arousal, lubrication, and orgasm were shown with bremelanotide. About 18% of women stopped using the drug because of adverse effects (nausea, vomiting, flushing, or headache) versus 2% for placebo. Like flibanserin, it is expected to be approved for premenopausal women only.
Read how 3 experts would manage differing GSM symptoms.
What would you prescribe for these patients?
CASE Genitourinary syndrome of menopause (GSM) in a 55-year-old woman
A 55-year-old widow is beginning a new relationship. She has not had partnered sexual activity for several years, but she recently has begun a relationship. She describes pain with attempted penetration with her new partner. Her last menstrual period was 3 years ago and she has experienced very minor menopausal symptoms, which are not bothersome. On examination, the vulva and vagina are pale, with thin epithelium and absent rugae. The tissue lacks elasticity. A virginal speculum is needed to visualize the cervix.
How would you go about deciding which of the many options for management of GSM you will recommend for this patient? What do you weigh as you consider DHEA versus estrogen and topical versus oral therapy?
JoAnn V. Pinkerton, MD: Vulvovaginal atrophy (VVA), part of GSM, is associated with postmenopausal estrogen deficiency and includes the signs and symptoms seen on this patient's physical exam: vaginal narrowing, pallor, loss of elasticity, as well as pain with intercourse.6 Estrogen therapy is the most effective treatment for vaginal atrophy.13 Since she does not have significant menopausal symptoms, low-dose vaginal estrogen preparations are effective and generally safe treatments for VVA; these include creams, tablets containing estradiol or conjugated equine estrogen (CEE), and a low-dose vaginal estradiol ring--all available at doses that result in minimal systemic absorption.
Choice is usually made based on patient desire and likely adherence. If the patient prefers nonestrogen therapies that improve VVA and have been approved for relief of dyspareunia in postmenopausal women, I would discuss with the patient the oral selective estrogen receptor modulator ospemifene,14 and the new intravaginal DHEA suppositories, prasterone.15 Ospemifene is taken daily as an oral tablet, has a small risk of blood clots, and is my choice for women who do not need systemic hormone therapy and prefer to avoid vaginal therapy.
Andrew M. Kaunitz, MD: GSM is prevalent in menopausal women and, if not treated, causes progressive vaginal dryness and sexual discomfort. When the main indication for hormonal management in a menopausal woman is GSM (as opposed to treatment of vasomotor symptoms or prevention of osteoporosis), the treatment of choice is low-dose local vaginal estrogen, ospemifene, or prasterone (DHEA). Prasterone is a vaginally administered nonestrogen steroid that was approved by the FDA to treat dyspareunia associated with GSM. DHEA is an endogenous inactive steroid that is converted locally into androgens and estrogens; one vaginal insert is placed nightly.16,17
This 55-year-old widow has not been sexually active for some time. The facts that attempted penetration was painful and only an ultrathin (virginal) speculum could be used for examination indicate that contraction of the pelvic floor muscles is likely present. Simply starting medical management may not lead to comfortable/successful penetrative sex for this woman. In addition to medical management, she would likely benefit from referral for physical therapy. Using dilators and other strategies, along with the positive impact that medical management will have on the vaginal mucosa, a woman's physical therapist can work with this patient to help the pelvic floor muscles relax and facilitate comfortable penetrative sex.
James A. Simon, MD: With only minor vasomotor symptoms, I would assess the other potential benefits of a systemic therapy. These might include cardiovascular risk reduction (systemic estrogens or estrogens/progesterone in some), breast cancer risk reduction (some data suggesting ospemifene can accomplish this), osteoporosis prevention (systemic estrogens and estrogen/androgens), etc. If there is an option for a treatment to address more than one symptom, in this case GSM, assessing the risks/benefits of each of these therapies should be estimated for this specific patient.
If there are no systemic benefits to be had, then any of the local treatments should be helpful. As there are no head-to-head comparisons available, local estrogen cream, tablets, rings, local DHEA, or systemic ospemifene each should be considered possible treatments. I also feel this patient may benefit from supplementary self-dilation and/or physical therapy.
Related article:
2017 Update on menopause
CASE Dyspareunia and vasomotor symptoms in a 42-year-old breast cancer survivor
A 42-year-old woman with a BRCA1 mutation has undergone prophylactic mastectomies as well as hysterectomy with bilateral salpingo-oophorectomy. She reports mild to moderate hot flashes and bothersome vaginal dryness and dyspareunia. Examination confirms GSM.
Would you advise systemic hormone therapy for this patient? What would your recommendation be for management of her GSM symptoms?
Dr. Simon: While one's gut reaction would be to avoid systemic estrogen therapy in a patient with a BRCA1 mutation, the scientific information confirming this fear is lacking.18 Such patients may benefit significantly from systemic estrogen therapy (reduced risk of cardiovascular disease and cognitive decline, etc.), and with both breasts and both ovaries removed, estrogen's breast cancer risks, if any in this population, are largely avoided. The patient also may benefit from additional local therapy with either estrogens or DHEA.
Dr. Kaunitz: Due to her high lifetime risk of breast and ovarian cancer, this woman has proceeded with risk-reducing breast and gynecologic surgery. As more BRCA mutation carriers are being identified and undergo risk-reducing bilateral mastectomy (usually with reconstruction) and salpingo-oophorectomy, clinicians and mutation carriers more frequently face decisions regarding use of systemic hormone therapy.
Mutation carriers who have undergone bilateral risk-reducing mastectomy experience a very low baseline future risk for breast cancer; accordingly, concerns regarding this disease should not prevent use of systemic hormone therapy. Furthermore, without hormone replacement, induced menopause in women this age is associated with an elevated risk of osteoporosis, persistent vasomotor symptoms, cardiovascular disease, stroke, mood changes, dementia, Parkinson disease, and overall mortality. Recognizing the safety of estrogen therapy in this setting, this 42-year-old BRCA1 mutation carrier can initiate estrogen therapy. Standard dose estrogen therapy refers to oral estradiol 1.0 mg, conjugated equine estrogen 0.625 mg,or transdermal estradiol 0.05 mg. In younger women like this 42-year-old with surgically induced menopause, higher than standard replacement doses of estrogen are often appropriate.17
Due to concerns the hormone therapy might further increase future risk of breast cancer, some mutation carriers may delay or avoid risk-reducing bilateral salpingo-oophorectomy, a potentially lifesaving surgery which reduces not only future risk of ovarian cancer but also future risk for breast cancer.
Among mutation carriers with intact breasts, several studies address risk of breast cancer with use of systemic hormone therapy. Although limited in numbers of participants and years of follow-up, in aggregate, these studies provide reassurance that short-term use of systemic hormone therapy does not increase breast cancer risk in women with BRCA1 or BRCA2 mutations and intact breasts.19
Dr. Pinkerton: For this woman with early surgical menopause and hysterectomy, estrogen therapy could improve her vasomotor symptoms and decrease her risk of bone loss and GSM.17 In the Women's Health Initiative trial, there were 7 fewer breast cancers per 10,000 women-years in the estrogen-onlyarm.20 Observational studies suggest that hormone therapy, when given to the average age of menopause, decreases the risks of heart disease, Parkinson disease, and dementia.21 Limited observational evidence suggests that hormone therapy use does not further increase risk of breast cancer in women following oophorectomy for BRCA1 or BRCA2 gene mutation.22
The absolute risks observed with hormone therapy tended to be small, especially in younger, healthy women. Systemic hormone therapy could treat her hot flashes and her GSM symptoms and potentially decrease health risks associated with premature estrogen deficiency. Nonestrogen therapies for hot flashes include low-dose antidepressants, gabapentin, and mind-body options, such as cognitive behavioral therapy and hypnosis, but these would not decrease her health risks or treat her GSM.
If she only requests treatment of her GSM symptoms, she would be a candidate for low-dose vaginal estrogen therapy, given as a cream, tablet, or ring depending on her choice. I would not choose ospemifene as my first choice as she is having hot flashes, and there are no data yet on the drug's health benefits in early menopause. If she prefers nonestrogen vaginal therapy, the new intravaginal DHEA might be a good choice as both estrogen and testosterone are increased locally in the vagina while hormone levels remain in the postmenopausal range. There is no boxed warning on the patient insert, although safety in women with breast cancer or in those with elevated risk of breast cancer has not been tested.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Goldstein I, Kim NN, Clayton AH, et al. Hypoactive Sexual Desire Disorder: International Society for the Study of Women’s Sexual Health (ISSWSH) Expert Consensus Panel Review. Mayo Clin Proc. 2017;92(1):114–128.
- Kingsberg SA. Attitudinal survey of women living with low sexual desire. J Womens Health (Larchmt). 2014;23(10):817–823.
- Foley K, Foley D, Johnson BH. Healthcare resource utilization and expenditures of women diagnosed with hypoactive sexual desire disorder. J Med Econ. 2010;13(4):583–590.
- Biddle AK, West SL, D’Aloisio AA, Wheeler SB, Borisov NN, Thorp J. Hypoactive sexual desire disorder in postmenopausal women: quality of life and health burden. Value Health. 2009;12(5):763–772.
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–1068.
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902.
- Ettinger B, Hait H, Reape KZ, Shu H. Measuring symptom relief in studies of vaginal and vulvar atrophy: the most bothersome symptom approach. Menopause. 2008;15(5):885–889.
- Dennerstein L, Randolph J, Taffe J, Dudley E, Burger H. Hormones, mood, sexuality, and the menopausal transition. Fertil Steril. 2002;77(suppl 4):S42–S48.
- Brotto LA, Bitzer J, Laan E, Leiblum S, Luria M. Women’s sexual desire and arousal disorders [published correction appears in J Sex Med. 2010;7(2 pt 1):856]. J Sex Med. 2010;7(1 pt 2):586–614.
- US Food and Drug Administration website. FDA approves first treatment for sexual desire disorder. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm458734.htm. Accessed August 14, 2017.
- Addyi (flibanserin) [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals North America, LLC; 2016.
- Labrie F, Derogatis L, Archer DF, et al; Members of the VVA Prasterone Research Group. Effect of intravaginal prasterone on sexual dysfunction in postmenopausal women with vulvovaginal atrophy. J Sex Med. 2015;12(12):2401–2412.
- Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2016;8:CD001500.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20(6):623–630.
- Labrie F, Archer DF, Koltun, W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Kaunitz AM. Focus on treating genital atrophy symptoms. OBG Manag. 2017;29(1):14, 16–17.
- The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017;24(7):728–753.
- Crandall CJ, Hovey KM, Andrews CA, et al. Breast cancer, endometrial cancer, and cardiovascular events in participants who used vaginal estrogen in the Women’s Health Initiative Observational Study. Menopause. August 14, 2017. doi:10.1097/GME.0000000000000956.
- Domchek S, Kaunitz AM. Use of systemic hormone therapy in BRCA mutation carriers. Menopause. 2016;23(9):1026–1027.
- Anderson GL, Limacher M, Assaf AR, et al; Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–1712.
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483–491.
- Gabriel CA, Tigges-Cardwell J, Stopfer J, Erlichman J, Nathanson K, Domchek SM. Use of total abdominal hysterectomy and hormone replacement therapy in BRCA1 and BRCA2 mutation carriers undergoing risk-reducing salpingo-oophorectomy. Fam Cancer. 2009;8(1):23-28.
Sexual function is a complex, multifaceted process mediated by neurologic functions, hormonal regulation, and ps
As it turns out, quite a lot. Female sexual dysfunction is a common, vastly undertreated sexual health problem that can have wide-reaching effects on a woman’s life. These effects may include impaired body image, self-confidence, and self-worth. Sexual dysfunction also can contribute to relationship dissatisfaction and leave one feeling less connected with her partner.1,2 Studies have shown women with sexual dysfunction have higher health care expenditures3 and that depression and fatigue are common comorbidities, as is frequently seen in other chronic conditions such as diabetes and back pain.4
Understanding the pathogenesis of female sexual dysfunction helps to guide our approach to its management. Indeed, increased understanding of its pathology has helped to usher in new and emerging treatment options, as well as a personalized, biopsychosocial approach to its management.
Related article:
2016 Update on female sexual dysfunction
In this Update, I discuss the interplay of physiologic and psychological factors that affect female sexual function as well as the latest options for its management. I have also assembled a panel of experts to discuss 2 cases representative of sexual dysfunction that you may encounter in your clinical practice and how prescribing decisions are made for their management.
Read about factors that impact sexual function and agents to help manage dysfunction.
Multiple transmitters in the brain can increase or decrease sexual desire and function
Neurotransmitters involved in sexual excitation include brain dopamine, melanocortin, oxytocin, vasopressin, and norepinephrine, whereas brain opioids, serotonin, prolactin, and endocannabinoids function as sexual inhibitors. Inhibitory transmitters are activated normally during sexual refractoriness but also from primary aversion or secondary avoidance disorders.1 Drugs or conditions that reduce brain dopamine levels, increase the action of brain serotonin, or enhance brain opioid pathways have been shown to inhibit sexual desire, while those that increase hypothalamic and mesolimbic dopamine or decrease serotonin release have been shown to stimulate sexual desire.1
Estradiol and progesterone can impact sexual function and desire
In addition to the neurotransmitters, hormones are important modulators of female sexual function. Decreasing levels of circulating estrogen after menopause lead to physiologic, biologic, and clinical changes in the urogenital tissues, such as decreased elastin, thinning of the epithelium, reduced vaginal blood flow, diminished lubrication, and decreased flexibility and elasticity. These changes result in the symptoms of genitourinary syndrome of menopause (GSM), which affects as many as half of all menopausal women.5,6 In clinical trials, dyspareunia and vaginal dryness are the most bothersome GSM symptoms reported.7
The role of hormonal regulation in sexual dysfunction among premenopausal women is not yet fully understood, but we do know that estradiol has been shown to improve sexual desire, progesterone tends to dampen sexual desire, and that testosterone at physiological levels has been shown in most studies to have a neutral effect on sexual desire in a well-estrogenized patient.8
Related article:
Focus on treating genital atrophy symptoms
Experience and behavior modulate or reinforce sexual dysfunction
The most common psychological factors that trigger or amplify female sexual dysfunction are depression, anxiety, distraction, negative body image, sexual abuse, and emotional neglect.9 Contextual or sociocultural factors, such as relationship discord, life-stage stressors (the empty nest syndrome or anxiety and sleep deprivation from a new baby), as well as cultural or religious values that suppress sexuality, also should be considered.9 Experience-based neuroplasticity (changes in brain pathways that become solidified by negative or positive experiences) may elucidate how a multimodal approach, utilizing medical and psychological treatment, can be beneficial for patients, particularly those with hypoactive sexual desire disorder (HSDD).1
New and emerging approaches to managing female sexual dysfunction
Three agents, one of which has been available for prescription for some time, one that is newly available, and one in the pipeline, are or may soon be in the gynecologist's armamentarium.
Flibanserin
Medications that target excitatory pathways or blunt inhibitory pathways are in development, and one, flibanserin (Addyi), has been US Food and Drug Administration (FDA)-approved for the treatment of acquired, generalized HSDD in premenopausal women.1,10 Flibanserin is a nonhormonal, centrally acting, postsynaptic serotonin 1A receptor agonist and a serotonin 2A receptor antagonist that is taken daily at bedtime (100 mg); several weeks are usually needed before any effects are noted.1 It is not approved for postmenopausal women and has a boxed warning about the risks of hypotension and syncope; its use is contraindicated in women who drink alcohol, in those who have hepatic impairment, and with the use of moderate or strong CYP3A4 inhibitors.11
Also keep in mind that flibanserin is only available through a Risk Evaluation and Mitigation Strategy program, so clinicians who wish to prescribe it must enroll in and complete training to become certified providers.9
Related article:
What you need to know (and do) to prescribe the new drug flibanserin
Prasterone
Prasterone (Intrarosa), a once-daily intravaginal dehydroepiandrosterone (DHEA) product, is a prohormone that increases local estrogen and testosterone and has the advantage of improved sexual function, desire, arousal, lubrication, orgasm, satisfaction, as well as pain at sexual activity.12 It was approved by the FDA in November 2016 to treat moderate to severe dyspareunia and has been available for prescribing since July 2017. Its cost is comparable to topical estrogen products, with a $25 copay program.
Because prasterone is not an estrogen, it does not have the boxed warning that all estrogen products are mandated by the FDA to have. This may make it more acceptable to patients, who often decline to use an estrogen product after seeing the boxed warning on the package. The Centers for Medicare and Medicaid Services (CMS) does not have prasterone on its list of potentially hazardous drugs for the elderly. However, keep in mind that because its label is for dyspareunia and not specifically for GSM, CMS considers it a drug of choice--in other words, like sildenafil (Viagra), a lifestyle choice and not for treatment of a medical condition. As such, at the present time, Medicare does not cover it.
Bremelanotide
Late-stage trials of bremelanotide, a melanocortin receptor agonist, are underway. Its mechanism of action is somewhat like that of flibanserin in that both drugs increase dopamine and norepinephrine levels. The advantage of bremelanotide is that it is used as needed. It is dosed subcutaneously (1.75 mg) and it can be used as often as a woman would like to use it. The FDA is expected to consider it for approval in about a year. Unpublished data from poster sessions at recent meetings show that, in a phase 3 study of 1,247 premenopausal women with HSDD (who had already been screened for depression and were found to have a physiologic condition), improvements in desire, arousal, lubrication, and orgasm were shown with bremelanotide. About 18% of women stopped using the drug because of adverse effects (nausea, vomiting, flushing, or headache) versus 2% for placebo. Like flibanserin, it is expected to be approved for premenopausal women only.
Read how 3 experts would manage differing GSM symptoms.
What would you prescribe for these patients?
CASE Genitourinary syndrome of menopause (GSM) in a 55-year-old woman
A 55-year-old widow is beginning a new relationship. She has not had partnered sexual activity for several years, but she recently has begun a relationship. She describes pain with attempted penetration with her new partner. Her last menstrual period was 3 years ago and she has experienced very minor menopausal symptoms, which are not bothersome. On examination, the vulva and vagina are pale, with thin epithelium and absent rugae. The tissue lacks elasticity. A virginal speculum is needed to visualize the cervix.
How would you go about deciding which of the many options for management of GSM you will recommend for this patient? What do you weigh as you consider DHEA versus estrogen and topical versus oral therapy?
JoAnn V. Pinkerton, MD: Vulvovaginal atrophy (VVA), part of GSM, is associated with postmenopausal estrogen deficiency and includes the signs and symptoms seen on this patient's physical exam: vaginal narrowing, pallor, loss of elasticity, as well as pain with intercourse.6 Estrogen therapy is the most effective treatment for vaginal atrophy.13 Since she does not have significant menopausal symptoms, low-dose vaginal estrogen preparations are effective and generally safe treatments for VVA; these include creams, tablets containing estradiol or conjugated equine estrogen (CEE), and a low-dose vaginal estradiol ring--all available at doses that result in minimal systemic absorption.
Choice is usually made based on patient desire and likely adherence. If the patient prefers nonestrogen therapies that improve VVA and have been approved for relief of dyspareunia in postmenopausal women, I would discuss with the patient the oral selective estrogen receptor modulator ospemifene,14 and the new intravaginal DHEA suppositories, prasterone.15 Ospemifene is taken daily as an oral tablet, has a small risk of blood clots, and is my choice for women who do not need systemic hormone therapy and prefer to avoid vaginal therapy.
Andrew M. Kaunitz, MD: GSM is prevalent in menopausal women and, if not treated, causes progressive vaginal dryness and sexual discomfort. When the main indication for hormonal management in a menopausal woman is GSM (as opposed to treatment of vasomotor symptoms or prevention of osteoporosis), the treatment of choice is low-dose local vaginal estrogen, ospemifene, or prasterone (DHEA). Prasterone is a vaginally administered nonestrogen steroid that was approved by the FDA to treat dyspareunia associated with GSM. DHEA is an endogenous inactive steroid that is converted locally into androgens and estrogens; one vaginal insert is placed nightly.16,17
This 55-year-old widow has not been sexually active for some time. The facts that attempted penetration was painful and only an ultrathin (virginal) speculum could be used for examination indicate that contraction of the pelvic floor muscles is likely present. Simply starting medical management may not lead to comfortable/successful penetrative sex for this woman. In addition to medical management, she would likely benefit from referral for physical therapy. Using dilators and other strategies, along with the positive impact that medical management will have on the vaginal mucosa, a woman's physical therapist can work with this patient to help the pelvic floor muscles relax and facilitate comfortable penetrative sex.
James A. Simon, MD: With only minor vasomotor symptoms, I would assess the other potential benefits of a systemic therapy. These might include cardiovascular risk reduction (systemic estrogens or estrogens/progesterone in some), breast cancer risk reduction (some data suggesting ospemifene can accomplish this), osteoporosis prevention (systemic estrogens and estrogen/androgens), etc. If there is an option for a treatment to address more than one symptom, in this case GSM, assessing the risks/benefits of each of these therapies should be estimated for this specific patient.
If there are no systemic benefits to be had, then any of the local treatments should be helpful. As there are no head-to-head comparisons available, local estrogen cream, tablets, rings, local DHEA, or systemic ospemifene each should be considered possible treatments. I also feel this patient may benefit from supplementary self-dilation and/or physical therapy.
Related article:
2017 Update on menopause
CASE Dyspareunia and vasomotor symptoms in a 42-year-old breast cancer survivor
A 42-year-old woman with a BRCA1 mutation has undergone prophylactic mastectomies as well as hysterectomy with bilateral salpingo-oophorectomy. She reports mild to moderate hot flashes and bothersome vaginal dryness and dyspareunia. Examination confirms GSM.
Would you advise systemic hormone therapy for this patient? What would your recommendation be for management of her GSM symptoms?
Dr. Simon: While one's gut reaction would be to avoid systemic estrogen therapy in a patient with a BRCA1 mutation, the scientific information confirming this fear is lacking.18 Such patients may benefit significantly from systemic estrogen therapy (reduced risk of cardiovascular disease and cognitive decline, etc.), and with both breasts and both ovaries removed, estrogen's breast cancer risks, if any in this population, are largely avoided. The patient also may benefit from additional local therapy with either estrogens or DHEA.
Dr. Kaunitz: Due to her high lifetime risk of breast and ovarian cancer, this woman has proceeded with risk-reducing breast and gynecologic surgery. As more BRCA mutation carriers are being identified and undergo risk-reducing bilateral mastectomy (usually with reconstruction) and salpingo-oophorectomy, clinicians and mutation carriers more frequently face decisions regarding use of systemic hormone therapy.
Mutation carriers who have undergone bilateral risk-reducing mastectomy experience a very low baseline future risk for breast cancer; accordingly, concerns regarding this disease should not prevent use of systemic hormone therapy. Furthermore, without hormone replacement, induced menopause in women this age is associated with an elevated risk of osteoporosis, persistent vasomotor symptoms, cardiovascular disease, stroke, mood changes, dementia, Parkinson disease, and overall mortality. Recognizing the safety of estrogen therapy in this setting, this 42-year-old BRCA1 mutation carrier can initiate estrogen therapy. Standard dose estrogen therapy refers to oral estradiol 1.0 mg, conjugated equine estrogen 0.625 mg,or transdermal estradiol 0.05 mg. In younger women like this 42-year-old with surgically induced menopause, higher than standard replacement doses of estrogen are often appropriate.17
Due to concerns the hormone therapy might further increase future risk of breast cancer, some mutation carriers may delay or avoid risk-reducing bilateral salpingo-oophorectomy, a potentially lifesaving surgery which reduces not only future risk of ovarian cancer but also future risk for breast cancer.
Among mutation carriers with intact breasts, several studies address risk of breast cancer with use of systemic hormone therapy. Although limited in numbers of participants and years of follow-up, in aggregate, these studies provide reassurance that short-term use of systemic hormone therapy does not increase breast cancer risk in women with BRCA1 or BRCA2 mutations and intact breasts.19
Dr. Pinkerton: For this woman with early surgical menopause and hysterectomy, estrogen therapy could improve her vasomotor symptoms and decrease her risk of bone loss and GSM.17 In the Women's Health Initiative trial, there were 7 fewer breast cancers per 10,000 women-years in the estrogen-onlyarm.20 Observational studies suggest that hormone therapy, when given to the average age of menopause, decreases the risks of heart disease, Parkinson disease, and dementia.21 Limited observational evidence suggests that hormone therapy use does not further increase risk of breast cancer in women following oophorectomy for BRCA1 or BRCA2 gene mutation.22
The absolute risks observed with hormone therapy tended to be small, especially in younger, healthy women. Systemic hormone therapy could treat her hot flashes and her GSM symptoms and potentially decrease health risks associated with premature estrogen deficiency. Nonestrogen therapies for hot flashes include low-dose antidepressants, gabapentin, and mind-body options, such as cognitive behavioral therapy and hypnosis, but these would not decrease her health risks or treat her GSM.
If she only requests treatment of her GSM symptoms, she would be a candidate for low-dose vaginal estrogen therapy, given as a cream, tablet, or ring depending on her choice. I would not choose ospemifene as my first choice as she is having hot flashes, and there are no data yet on the drug's health benefits in early menopause. If she prefers nonestrogen vaginal therapy, the new intravaginal DHEA might be a good choice as both estrogen and testosterone are increased locally in the vagina while hormone levels remain in the postmenopausal range. There is no boxed warning on the patient insert, although safety in women with breast cancer or in those with elevated risk of breast cancer has not been tested.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Sexual function is a complex, multifaceted process mediated by neurologic functions, hormonal regulation, and ps
As it turns out, quite a lot. Female sexual dysfunction is a common, vastly undertreated sexual health problem that can have wide-reaching effects on a woman’s life. These effects may include impaired body image, self-confidence, and self-worth. Sexual dysfunction also can contribute to relationship dissatisfaction and leave one feeling less connected with her partner.1,2 Studies have shown women with sexual dysfunction have higher health care expenditures3 and that depression and fatigue are common comorbidities, as is frequently seen in other chronic conditions such as diabetes and back pain.4
Understanding the pathogenesis of female sexual dysfunction helps to guide our approach to its management. Indeed, increased understanding of its pathology has helped to usher in new and emerging treatment options, as well as a personalized, biopsychosocial approach to its management.
Related article:
2016 Update on female sexual dysfunction
In this Update, I discuss the interplay of physiologic and psychological factors that affect female sexual function as well as the latest options for its management. I have also assembled a panel of experts to discuss 2 cases representative of sexual dysfunction that you may encounter in your clinical practice and how prescribing decisions are made for their management.
Read about factors that impact sexual function and agents to help manage dysfunction.
Multiple transmitters in the brain can increase or decrease sexual desire and function
Neurotransmitters involved in sexual excitation include brain dopamine, melanocortin, oxytocin, vasopressin, and norepinephrine, whereas brain opioids, serotonin, prolactin, and endocannabinoids function as sexual inhibitors. Inhibitory transmitters are activated normally during sexual refractoriness but also from primary aversion or secondary avoidance disorders.1 Drugs or conditions that reduce brain dopamine levels, increase the action of brain serotonin, or enhance brain opioid pathways have been shown to inhibit sexual desire, while those that increase hypothalamic and mesolimbic dopamine or decrease serotonin release have been shown to stimulate sexual desire.1
Estradiol and progesterone can impact sexual function and desire
In addition to the neurotransmitters, hormones are important modulators of female sexual function. Decreasing levels of circulating estrogen after menopause lead to physiologic, biologic, and clinical changes in the urogenital tissues, such as decreased elastin, thinning of the epithelium, reduced vaginal blood flow, diminished lubrication, and decreased flexibility and elasticity. These changes result in the symptoms of genitourinary syndrome of menopause (GSM), which affects as many as half of all menopausal women.5,6 In clinical trials, dyspareunia and vaginal dryness are the most bothersome GSM symptoms reported.7
The role of hormonal regulation in sexual dysfunction among premenopausal women is not yet fully understood, but we do know that estradiol has been shown to improve sexual desire, progesterone tends to dampen sexual desire, and that testosterone at physiological levels has been shown in most studies to have a neutral effect on sexual desire in a well-estrogenized patient.8
Related article:
Focus on treating genital atrophy symptoms
Experience and behavior modulate or reinforce sexual dysfunction
The most common psychological factors that trigger or amplify female sexual dysfunction are depression, anxiety, distraction, negative body image, sexual abuse, and emotional neglect.9 Contextual or sociocultural factors, such as relationship discord, life-stage stressors (the empty nest syndrome or anxiety and sleep deprivation from a new baby), as well as cultural or religious values that suppress sexuality, also should be considered.9 Experience-based neuroplasticity (changes in brain pathways that become solidified by negative or positive experiences) may elucidate how a multimodal approach, utilizing medical and psychological treatment, can be beneficial for patients, particularly those with hypoactive sexual desire disorder (HSDD).1
New and emerging approaches to managing female sexual dysfunction
Three agents, one of which has been available for prescription for some time, one that is newly available, and one in the pipeline, are or may soon be in the gynecologist's armamentarium.
Flibanserin
Medications that target excitatory pathways or blunt inhibitory pathways are in development, and one, flibanserin (Addyi), has been US Food and Drug Administration (FDA)-approved for the treatment of acquired, generalized HSDD in premenopausal women.1,10 Flibanserin is a nonhormonal, centrally acting, postsynaptic serotonin 1A receptor agonist and a serotonin 2A receptor antagonist that is taken daily at bedtime (100 mg); several weeks are usually needed before any effects are noted.1 It is not approved for postmenopausal women and has a boxed warning about the risks of hypotension and syncope; its use is contraindicated in women who drink alcohol, in those who have hepatic impairment, and with the use of moderate or strong CYP3A4 inhibitors.11
Also keep in mind that flibanserin is only available through a Risk Evaluation and Mitigation Strategy program, so clinicians who wish to prescribe it must enroll in and complete training to become certified providers.9
Related article:
What you need to know (and do) to prescribe the new drug flibanserin
Prasterone
Prasterone (Intrarosa), a once-daily intravaginal dehydroepiandrosterone (DHEA) product, is a prohormone that increases local estrogen and testosterone and has the advantage of improved sexual function, desire, arousal, lubrication, orgasm, satisfaction, as well as pain at sexual activity.12 It was approved by the FDA in November 2016 to treat moderate to severe dyspareunia and has been available for prescribing since July 2017. Its cost is comparable to topical estrogen products, with a $25 copay program.
Because prasterone is not an estrogen, it does not have the boxed warning that all estrogen products are mandated by the FDA to have. This may make it more acceptable to patients, who often decline to use an estrogen product after seeing the boxed warning on the package. The Centers for Medicare and Medicaid Services (CMS) does not have prasterone on its list of potentially hazardous drugs for the elderly. However, keep in mind that because its label is for dyspareunia and not specifically for GSM, CMS considers it a drug of choice--in other words, like sildenafil (Viagra), a lifestyle choice and not for treatment of a medical condition. As such, at the present time, Medicare does not cover it.
Bremelanotide
Late-stage trials of bremelanotide, a melanocortin receptor agonist, are underway. Its mechanism of action is somewhat like that of flibanserin in that both drugs increase dopamine and norepinephrine levels. The advantage of bremelanotide is that it is used as needed. It is dosed subcutaneously (1.75 mg) and it can be used as often as a woman would like to use it. The FDA is expected to consider it for approval in about a year. Unpublished data from poster sessions at recent meetings show that, in a phase 3 study of 1,247 premenopausal women with HSDD (who had already been screened for depression and were found to have a physiologic condition), improvements in desire, arousal, lubrication, and orgasm were shown with bremelanotide. About 18% of women stopped using the drug because of adverse effects (nausea, vomiting, flushing, or headache) versus 2% for placebo. Like flibanserin, it is expected to be approved for premenopausal women only.
Read how 3 experts would manage differing GSM symptoms.
What would you prescribe for these patients?
CASE Genitourinary syndrome of menopause (GSM) in a 55-year-old woman
A 55-year-old widow is beginning a new relationship. She has not had partnered sexual activity for several years, but she recently has begun a relationship. She describes pain with attempted penetration with her new partner. Her last menstrual period was 3 years ago and she has experienced very minor menopausal symptoms, which are not bothersome. On examination, the vulva and vagina are pale, with thin epithelium and absent rugae. The tissue lacks elasticity. A virginal speculum is needed to visualize the cervix.
How would you go about deciding which of the many options for management of GSM you will recommend for this patient? What do you weigh as you consider DHEA versus estrogen and topical versus oral therapy?
JoAnn V. Pinkerton, MD: Vulvovaginal atrophy (VVA), part of GSM, is associated with postmenopausal estrogen deficiency and includes the signs and symptoms seen on this patient's physical exam: vaginal narrowing, pallor, loss of elasticity, as well as pain with intercourse.6 Estrogen therapy is the most effective treatment for vaginal atrophy.13 Since she does not have significant menopausal symptoms, low-dose vaginal estrogen preparations are effective and generally safe treatments for VVA; these include creams, tablets containing estradiol or conjugated equine estrogen (CEE), and a low-dose vaginal estradiol ring--all available at doses that result in minimal systemic absorption.
Choice is usually made based on patient desire and likely adherence. If the patient prefers nonestrogen therapies that improve VVA and have been approved for relief of dyspareunia in postmenopausal women, I would discuss with the patient the oral selective estrogen receptor modulator ospemifene,14 and the new intravaginal DHEA suppositories, prasterone.15 Ospemifene is taken daily as an oral tablet, has a small risk of blood clots, and is my choice for women who do not need systemic hormone therapy and prefer to avoid vaginal therapy.
Andrew M. Kaunitz, MD: GSM is prevalent in menopausal women and, if not treated, causes progressive vaginal dryness and sexual discomfort. When the main indication for hormonal management in a menopausal woman is GSM (as opposed to treatment of vasomotor symptoms or prevention of osteoporosis), the treatment of choice is low-dose local vaginal estrogen, ospemifene, or prasterone (DHEA). Prasterone is a vaginally administered nonestrogen steroid that was approved by the FDA to treat dyspareunia associated with GSM. DHEA is an endogenous inactive steroid that is converted locally into androgens and estrogens; one vaginal insert is placed nightly.16,17
This 55-year-old widow has not been sexually active for some time. The facts that attempted penetration was painful and only an ultrathin (virginal) speculum could be used for examination indicate that contraction of the pelvic floor muscles is likely present. Simply starting medical management may not lead to comfortable/successful penetrative sex for this woman. In addition to medical management, she would likely benefit from referral for physical therapy. Using dilators and other strategies, along with the positive impact that medical management will have on the vaginal mucosa, a woman's physical therapist can work with this patient to help the pelvic floor muscles relax and facilitate comfortable penetrative sex.
James A. Simon, MD: With only minor vasomotor symptoms, I would assess the other potential benefits of a systemic therapy. These might include cardiovascular risk reduction (systemic estrogens or estrogens/progesterone in some), breast cancer risk reduction (some data suggesting ospemifene can accomplish this), osteoporosis prevention (systemic estrogens and estrogen/androgens), etc. If there is an option for a treatment to address more than one symptom, in this case GSM, assessing the risks/benefits of each of these therapies should be estimated for this specific patient.
If there are no systemic benefits to be had, then any of the local treatments should be helpful. As there are no head-to-head comparisons available, local estrogen cream, tablets, rings, local DHEA, or systemic ospemifene each should be considered possible treatments. I also feel this patient may benefit from supplementary self-dilation and/or physical therapy.
Related article:
2017 Update on menopause
CASE Dyspareunia and vasomotor symptoms in a 42-year-old breast cancer survivor
A 42-year-old woman with a BRCA1 mutation has undergone prophylactic mastectomies as well as hysterectomy with bilateral salpingo-oophorectomy. She reports mild to moderate hot flashes and bothersome vaginal dryness and dyspareunia. Examination confirms GSM.
Would you advise systemic hormone therapy for this patient? What would your recommendation be for management of her GSM symptoms?
Dr. Simon: While one's gut reaction would be to avoid systemic estrogen therapy in a patient with a BRCA1 mutation, the scientific information confirming this fear is lacking.18 Such patients may benefit significantly from systemic estrogen therapy (reduced risk of cardiovascular disease and cognitive decline, etc.), and with both breasts and both ovaries removed, estrogen's breast cancer risks, if any in this population, are largely avoided. The patient also may benefit from additional local therapy with either estrogens or DHEA.
Dr. Kaunitz: Due to her high lifetime risk of breast and ovarian cancer, this woman has proceeded with risk-reducing breast and gynecologic surgery. As more BRCA mutation carriers are being identified and undergo risk-reducing bilateral mastectomy (usually with reconstruction) and salpingo-oophorectomy, clinicians and mutation carriers more frequently face decisions regarding use of systemic hormone therapy.
Mutation carriers who have undergone bilateral risk-reducing mastectomy experience a very low baseline future risk for breast cancer; accordingly, concerns regarding this disease should not prevent use of systemic hormone therapy. Furthermore, without hormone replacement, induced menopause in women this age is associated with an elevated risk of osteoporosis, persistent vasomotor symptoms, cardiovascular disease, stroke, mood changes, dementia, Parkinson disease, and overall mortality. Recognizing the safety of estrogen therapy in this setting, this 42-year-old BRCA1 mutation carrier can initiate estrogen therapy. Standard dose estrogen therapy refers to oral estradiol 1.0 mg, conjugated equine estrogen 0.625 mg,or transdermal estradiol 0.05 mg. In younger women like this 42-year-old with surgically induced menopause, higher than standard replacement doses of estrogen are often appropriate.17
Due to concerns the hormone therapy might further increase future risk of breast cancer, some mutation carriers may delay or avoid risk-reducing bilateral salpingo-oophorectomy, a potentially lifesaving surgery which reduces not only future risk of ovarian cancer but also future risk for breast cancer.
Among mutation carriers with intact breasts, several studies address risk of breast cancer with use of systemic hormone therapy. Although limited in numbers of participants and years of follow-up, in aggregate, these studies provide reassurance that short-term use of systemic hormone therapy does not increase breast cancer risk in women with BRCA1 or BRCA2 mutations and intact breasts.19
Dr. Pinkerton: For this woman with early surgical menopause and hysterectomy, estrogen therapy could improve her vasomotor symptoms and decrease her risk of bone loss and GSM.17 In the Women's Health Initiative trial, there were 7 fewer breast cancers per 10,000 women-years in the estrogen-onlyarm.20 Observational studies suggest that hormone therapy, when given to the average age of menopause, decreases the risks of heart disease, Parkinson disease, and dementia.21 Limited observational evidence suggests that hormone therapy use does not further increase risk of breast cancer in women following oophorectomy for BRCA1 or BRCA2 gene mutation.22
The absolute risks observed with hormone therapy tended to be small, especially in younger, healthy women. Systemic hormone therapy could treat her hot flashes and her GSM symptoms and potentially decrease health risks associated with premature estrogen deficiency. Nonestrogen therapies for hot flashes include low-dose antidepressants, gabapentin, and mind-body options, such as cognitive behavioral therapy and hypnosis, but these would not decrease her health risks or treat her GSM.
If she only requests treatment of her GSM symptoms, she would be a candidate for low-dose vaginal estrogen therapy, given as a cream, tablet, or ring depending on her choice. I would not choose ospemifene as my first choice as she is having hot flashes, and there are no data yet on the drug's health benefits in early menopause. If she prefers nonestrogen vaginal therapy, the new intravaginal DHEA might be a good choice as both estrogen and testosterone are increased locally in the vagina while hormone levels remain in the postmenopausal range. There is no boxed warning on the patient insert, although safety in women with breast cancer or in those with elevated risk of breast cancer has not been tested.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Goldstein I, Kim NN, Clayton AH, et al. Hypoactive Sexual Desire Disorder: International Society for the Study of Women’s Sexual Health (ISSWSH) Expert Consensus Panel Review. Mayo Clin Proc. 2017;92(1):114–128.
- Kingsberg SA. Attitudinal survey of women living with low sexual desire. J Womens Health (Larchmt). 2014;23(10):817–823.
- Foley K, Foley D, Johnson BH. Healthcare resource utilization and expenditures of women diagnosed with hypoactive sexual desire disorder. J Med Econ. 2010;13(4):583–590.
- Biddle AK, West SL, D’Aloisio AA, Wheeler SB, Borisov NN, Thorp J. Hypoactive sexual desire disorder in postmenopausal women: quality of life and health burden. Value Health. 2009;12(5):763–772.
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–1068.
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902.
- Ettinger B, Hait H, Reape KZ, Shu H. Measuring symptom relief in studies of vaginal and vulvar atrophy: the most bothersome symptom approach. Menopause. 2008;15(5):885–889.
- Dennerstein L, Randolph J, Taffe J, Dudley E, Burger H. Hormones, mood, sexuality, and the menopausal transition. Fertil Steril. 2002;77(suppl 4):S42–S48.
- Brotto LA, Bitzer J, Laan E, Leiblum S, Luria M. Women’s sexual desire and arousal disorders [published correction appears in J Sex Med. 2010;7(2 pt 1):856]. J Sex Med. 2010;7(1 pt 2):586–614.
- US Food and Drug Administration website. FDA approves first treatment for sexual desire disorder. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm458734.htm. Accessed August 14, 2017.
- Addyi (flibanserin) [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals North America, LLC; 2016.
- Labrie F, Derogatis L, Archer DF, et al; Members of the VVA Prasterone Research Group. Effect of intravaginal prasterone on sexual dysfunction in postmenopausal women with vulvovaginal atrophy. J Sex Med. 2015;12(12):2401–2412.
- Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2016;8:CD001500.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20(6):623–630.
- Labrie F, Archer DF, Koltun, W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Kaunitz AM. Focus on treating genital atrophy symptoms. OBG Manag. 2017;29(1):14, 16–17.
- The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017;24(7):728–753.
- Crandall CJ, Hovey KM, Andrews CA, et al. Breast cancer, endometrial cancer, and cardiovascular events in participants who used vaginal estrogen in the Women’s Health Initiative Observational Study. Menopause. August 14, 2017. doi:10.1097/GME.0000000000000956.
- Domchek S, Kaunitz AM. Use of systemic hormone therapy in BRCA mutation carriers. Menopause. 2016;23(9):1026–1027.
- Anderson GL, Limacher M, Assaf AR, et al; Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–1712.
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483–491.
- Gabriel CA, Tigges-Cardwell J, Stopfer J, Erlichman J, Nathanson K, Domchek SM. Use of total abdominal hysterectomy and hormone replacement therapy in BRCA1 and BRCA2 mutation carriers undergoing risk-reducing salpingo-oophorectomy. Fam Cancer. 2009;8(1):23-28.
- Goldstein I, Kim NN, Clayton AH, et al. Hypoactive Sexual Desire Disorder: International Society for the Study of Women’s Sexual Health (ISSWSH) Expert Consensus Panel Review. Mayo Clin Proc. 2017;92(1):114–128.
- Kingsberg SA. Attitudinal survey of women living with low sexual desire. J Womens Health (Larchmt). 2014;23(10):817–823.
- Foley K, Foley D, Johnson BH. Healthcare resource utilization and expenditures of women diagnosed with hypoactive sexual desire disorder. J Med Econ. 2010;13(4):583–590.
- Biddle AK, West SL, D’Aloisio AA, Wheeler SB, Borisov NN, Thorp J. Hypoactive sexual desire disorder in postmenopausal women: quality of life and health burden. Value Health. 2009;12(5):763–772.
- Portman DJ, Gass ML; Vulvovaginal Atrophy Terminology Consensus Conference Panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause. 2014;21(10):1063–1068.
- Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902.
- Ettinger B, Hait H, Reape KZ, Shu H. Measuring symptom relief in studies of vaginal and vulvar atrophy: the most bothersome symptom approach. Menopause. 2008;15(5):885–889.
- Dennerstein L, Randolph J, Taffe J, Dudley E, Burger H. Hormones, mood, sexuality, and the menopausal transition. Fertil Steril. 2002;77(suppl 4):S42–S48.
- Brotto LA, Bitzer J, Laan E, Leiblum S, Luria M. Women’s sexual desire and arousal disorders [published correction appears in J Sex Med. 2010;7(2 pt 1):856]. J Sex Med. 2010;7(1 pt 2):586–614.
- US Food and Drug Administration website. FDA approves first treatment for sexual desire disorder. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm458734.htm. Accessed August 14, 2017.
- Addyi (flibanserin) [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals North America, LLC; 2016.
- Labrie F, Derogatis L, Archer DF, et al; Members of the VVA Prasterone Research Group. Effect of intravaginal prasterone on sexual dysfunction in postmenopausal women with vulvovaginal atrophy. J Sex Med. 2015;12(12):2401–2412.
- Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2016;8:CD001500.
- Portman DJ, Bachmann GA, Simon JA; Ospemifene Study Group. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013;20(6):623–630.
- Labrie F, Archer DF, Koltun, W, et al; VVA Prasterone Research Group. Efficacy of intravaginal dehydroepiandrosterone (DHEA) on moderate to severe dyspareunia and vaginal dryness, symptoms of vulvovaginal atrophy, and of the genitourinary syndrome of menopause. Menopause. 2016;23(3):243–256.
- Kaunitz AM. Focus on treating genital atrophy symptoms. OBG Manag. 2017;29(1):14, 16–17.
- The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2017;24(7):728–753.
- Crandall CJ, Hovey KM, Andrews CA, et al. Breast cancer, endometrial cancer, and cardiovascular events in participants who used vaginal estrogen in the Women’s Health Initiative Observational Study. Menopause. August 14, 2017. doi:10.1097/GME.0000000000000956.
- Domchek S, Kaunitz AM. Use of systemic hormone therapy in BRCA mutation carriers. Menopause. 2016;23(9):1026–1027.
- Anderson GL, Limacher M, Assaf AR, et al; Women’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–1712.
- Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015;18(4):483–491.
- Gabriel CA, Tigges-Cardwell J, Stopfer J, Erlichman J, Nathanson K, Domchek SM. Use of total abdominal hysterectomy and hormone replacement therapy in BRCA1 and BRCA2 mutation carriers undergoing risk-reducing salpingo-oophorectomy. Fam Cancer. 2009;8(1):23-28.
Fast Tracks
- Although not fully understood how, estradiol can improve sexual desire, progesterone tends to dampen sexual desire, and testosterone has a neutral effect in premenopausal women
- Newly available since July 2017, prasterone is a once-daily intravaginal agent that treats moderate to severe dyspareunia and has costs similar to topical estrogens
- Estrogen therapy may be considered in a breast cancer mutation carrier who has undergone prophylactic mastectomies and bilateral salpingo-oophorectomy
Make the Diagnosis - September 2017
Nevus sebaceous (NS)
Nevus sebaceous (NS) is a congenital hamartoma of the sebaceous glands that was first described by Josef Jadassohn, MD, in 1895. The lesion is caused by a post-zygotic somatic mutation in the KRAS or HRAS genes, which can lead to variable clinical mosaicism. In addition, hamartomatous presentations within different cell lines may occur if the pluripotent stem cells are affected. The lesion is present in about 0.3% of newborns and is equally represented among gender, race, and geography.
NS has three stages of presentation. At birth or early childhood, NS most commonly presents as a solitary, well-circumscribed, smooth, yellow to tan-brown plaque with associated hair loss in the vertex of the scalp, although it may less commonly present on the face, neck, or trunk. The lesion may be raised at birth. During puberty, hormonal variations alter the form of the lesion and the NS can become more verrucous and nodular. The clinical differential diagnosis for NS includes seborrheic keratosis, congenital nevus, and epidermal nevus.
About 24% of patients may develop appendageal tumors arising from the primary lesion. The majority of these tumors are benign, with trichoblastoma and syringocystadenoma papilliferum as the most common secondary growths. The most common malignant tumor that arises is basal cell carcinoma. Deletion of the patched gene has been implicated in the development of basal cell carcinoma within NS lesions. Many other tumors arising from NS lesions have been reported in the literature, including keratoacanthoma, apocrine cystadenoma, leiomyoma, and sebaceous cell carcinoma. More rarely, development of an eccrine or apocrine carcinoma within the NS can lead to widespread metastasis and death.
Because there is a chance of secondary tumor development, the decision to surgically excise the lesion or closely follow for transformation is controversial. Advocates of surgical excision reason that adolescence is the optimal time for removal because it is before pubertal enlargement and the patient would be able to tolerate anesthesia. If the patient chooses to clinically monitor the lesion, he or she should be informed that a full-thickness excision with wide margins will have to be performed if malignant transformation occurs.
A biopsy was performed of the erythematous papule that revealed an atypical sebaceous neoplasm with features of a sebaceoma. The patient had subsequent excision of the entire lesion that was read by a different dermatopathologist and revealed nevus sebaceous with syringocystadenoma papilliferum, no residual atypical sebaceous neoplasm, and clear margins.
This case and photo were submitted by Victoria Billero, University of Miami, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
Nevus sebaceous (NS)
Nevus sebaceous (NS) is a congenital hamartoma of the sebaceous glands that was first described by Josef Jadassohn, MD, in 1895. The lesion is caused by a post-zygotic somatic mutation in the KRAS or HRAS genes, which can lead to variable clinical mosaicism. In addition, hamartomatous presentations within different cell lines may occur if the pluripotent stem cells are affected. The lesion is present in about 0.3% of newborns and is equally represented among gender, race, and geography.
NS has three stages of presentation. At birth or early childhood, NS most commonly presents as a solitary, well-circumscribed, smooth, yellow to tan-brown plaque with associated hair loss in the vertex of the scalp, although it may less commonly present on the face, neck, or trunk. The lesion may be raised at birth. During puberty, hormonal variations alter the form of the lesion and the NS can become more verrucous and nodular. The clinical differential diagnosis for NS includes seborrheic keratosis, congenital nevus, and epidermal nevus.
About 24% of patients may develop appendageal tumors arising from the primary lesion. The majority of these tumors are benign, with trichoblastoma and syringocystadenoma papilliferum as the most common secondary growths. The most common malignant tumor that arises is basal cell carcinoma. Deletion of the patched gene has been implicated in the development of basal cell carcinoma within NS lesions. Many other tumors arising from NS lesions have been reported in the literature, including keratoacanthoma, apocrine cystadenoma, leiomyoma, and sebaceous cell carcinoma. More rarely, development of an eccrine or apocrine carcinoma within the NS can lead to widespread metastasis and death.
Because there is a chance of secondary tumor development, the decision to surgically excise the lesion or closely follow for transformation is controversial. Advocates of surgical excision reason that adolescence is the optimal time for removal because it is before pubertal enlargement and the patient would be able to tolerate anesthesia. If the patient chooses to clinically monitor the lesion, he or she should be informed that a full-thickness excision with wide margins will have to be performed if malignant transformation occurs.
A biopsy was performed of the erythematous papule that revealed an atypical sebaceous neoplasm with features of a sebaceoma. The patient had subsequent excision of the entire lesion that was read by a different dermatopathologist and revealed nevus sebaceous with syringocystadenoma papilliferum, no residual atypical sebaceous neoplasm, and clear margins.
This case and photo were submitted by Victoria Billero, University of Miami, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
Nevus sebaceous (NS)
Nevus sebaceous (NS) is a congenital hamartoma of the sebaceous glands that was first described by Josef Jadassohn, MD, in 1895. The lesion is caused by a post-zygotic somatic mutation in the KRAS or HRAS genes, which can lead to variable clinical mosaicism. In addition, hamartomatous presentations within different cell lines may occur if the pluripotent stem cells are affected. The lesion is present in about 0.3% of newborns and is equally represented among gender, race, and geography.
NS has three stages of presentation. At birth or early childhood, NS most commonly presents as a solitary, well-circumscribed, smooth, yellow to tan-brown plaque with associated hair loss in the vertex of the scalp, although it may less commonly present on the face, neck, or trunk. The lesion may be raised at birth. During puberty, hormonal variations alter the form of the lesion and the NS can become more verrucous and nodular. The clinical differential diagnosis for NS includes seborrheic keratosis, congenital nevus, and epidermal nevus.
About 24% of patients may develop appendageal tumors arising from the primary lesion. The majority of these tumors are benign, with trichoblastoma and syringocystadenoma papilliferum as the most common secondary growths. The most common malignant tumor that arises is basal cell carcinoma. Deletion of the patched gene has been implicated in the development of basal cell carcinoma within NS lesions. Many other tumors arising from NS lesions have been reported in the literature, including keratoacanthoma, apocrine cystadenoma, leiomyoma, and sebaceous cell carcinoma. More rarely, development of an eccrine or apocrine carcinoma within the NS can lead to widespread metastasis and death.
Because there is a chance of secondary tumor development, the decision to surgically excise the lesion or closely follow for transformation is controversial. Advocates of surgical excision reason that adolescence is the optimal time for removal because it is before pubertal enlargement and the patient would be able to tolerate anesthesia. If the patient chooses to clinically monitor the lesion, he or she should be informed that a full-thickness excision with wide margins will have to be performed if malignant transformation occurs.
A biopsy was performed of the erythematous papule that revealed an atypical sebaceous neoplasm with features of a sebaceoma. The patient had subsequent excision of the entire lesion that was read by a different dermatopathologist and revealed nevus sebaceous with syringocystadenoma papilliferum, no residual atypical sebaceous neoplasm, and clear margins.
This case and photo were submitted by Victoria Billero, University of Miami, and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected].
A 30-year-old woman presented for a routine full body skin exam. Upon exam, was found to have a 4 cm x 1.7 cm smooth, yellow plaque on the left scalp with a prominent 5 mm erythematous papule. The plaque had been present since childhood. The papule developed over the past few months.
Successful Reduction of Catheter-Associated Urinary Tract Infection Rates in Nursing Homes Through a Multicomponent Prevention Intervention
Study Overview
Objective. To determine the effect of implementing an intervention to reduce catheter-associated urinary tract infections (CAUTIs) in nursing homes.
Design. Prospective implementation project.
Setting and participants. The study was conducted between March 2014 and August 2016 in 12-month cohorts of community-based nursing homes participating in the Agency for Healthcare Research and Quality Safety Program for Long-Term Care. A total of 568 nursing homes located across 48 states, Washington DC, and Puerto Rico were recruited to participate.
Intervention. The intervention was developed with the goal of modifying the elements of the Comprehensive Unit-Based Safety Program utilized in hospitals for adoption in nursing homes. The intervention included a technical bundle, that is, catheter removal, aseptic insertion, using regular assessments, training for catheter care, and incontinence care planning [1], as well as socioadaptive interventions focused on empowering teams, addressing implementation challenges, offering solutions, promoting resident safety culture, team building, leadership, and resident and family engagement. The interventions were implemented over a 12-month period. To be included in the data analysis, nursing homes need to remain active through the end of the 12-month period and report 2 months or more of outcome data and device-days. Nursing homes that reported large fluctuations in reported data were excluded from the analysis. A total of 433 nursing homes remained active throughout the intervention period.
Main outcome measures. The main study outcome measure was the CAUTI incidence rate, defined as the number of CAUTIs divided by the number of catheter-days and multiplied by 1000. National Healthcare Safety Network definitions were used. The criteria for UTI
included objective systemic and localizing clinical findings along with laboratory-based criteria. A secondary outcome was the urinary catheter utilization ratio, defined as the number of catheter-days divided by the number of resident-days multiplied by 100 and reported as a percentage. Participating nursing homes collected data on the daily number of CAUTIs, catheter days, resident days, and urine cultures for each month of the project period and these metrics were reported using the Health Research and Educational Trust, a research affiliate of the American Hospital Association, Comprehensive Data System.
Conclusion. A multicomponent intervention implemented in community-based nursing homes across the country was associated with a reduction in CAUTI rates. The study shows that the intervention to reduce CAUTI can be implemented on a large scale and can be associated with improvement in patient safety.
Commentary
Catheter-associated urinary tract infection is a common condition that affects nursing home residents, as nursing home residents often have an indwelling urinary catheter on admission to the nursing home. These infections can be costly, lead to hospital admissions, and can contribute to the development of multidrug-resistant organisms, which pose a significant public health threat [2]. CAUTIs, however, are potentially preventable through the use of practices that promote judicious use of urinary catheters and attention to aseptic insertion and catheter care [3,4]. Although prior randomized controlled trials demonstrated the potential impact of interventions that reduce incidence of urinary tract infections [5], the interventions have not been adopted widely.
Recognizing the importance of improving safety through reducing CAUTIs, the Agency for Healthcare Research and Quality has established toolkits and implementation guides for health care facilities to adopt better practices for reducing catheter-associated infections. This study adds to the current literature by demonstrating the feasibility and beneficial impact of widespread implementation of AHRQ tools.
The study evaluated the impact of the intervention in a large cohort of nursing homes, comparing outcome measures pre and post intervention. One limitation of the study is that other factors that were present concurrently may have contributed to the observed changes in CAUTI outcomes. The study also did not have a control group, and the changes in outcome rates were not compared with rates in homes that did not participate in the project. Also, it is not possible to examine the effect of the individual components of the intervention as this intervention had multiple components delivered simultaneously. Despite these drawbacks, the study makes a strong case that project implementation is associated with a reduction in CAUTI rates of more than 50%.
A next step to better understand how best to disseminate the intervention is to identify factors associated with greater improvements in outcomes among the cohort of nursing homes and also to understand the variations in how nursing homes are implementing the intervention and what impact these differences might have. This in turn may guide further efforts to broaden the impact through more nuanced application of the intervention.
Applications for Clinical Practice
This study demonstrates that CAUTI can be prevented through a multicomponent intervention that focuses on appropriate use and discontinuation of urinary catheters and proper catheter care. Given that these tools and guides are available for use through AHRQ, nursing homes should examine the potential for adoption in their facilities. This can enhance the safety for their residents by reducing the risk of a potentially preventable complication.
—William W. Hung, MD, MPH
1. Agency for Healthcare Research and Quality. Prevent catheter-associated urinary tract infection. CAUTI implementation guide. Accessed 11 Aug 2017 at www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/hais/cauti-tools/impl-guide/implementation-guide-appendix-k.pdf.
2. Chitnis AS, Edwards JR, Ricks PM, et al. Device-associated infection rates, device utilization, and antimicrobial resistance in long-term acute care hospitals reporting to the National Healthcare Safety Network, 2010. Infect Control Hosp Epidemiol 2012;33:993–1000.
3. Meddings J, Rogers MA, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf 2014;23:277–89.
4. Willson M, Wilde M, Webb ML, et al. Nursing interventions to reduce the risk of catheter-associated urinary tract infection: part 2: staff education, monitoring, and care techniques. J Wound Ostomy Continence Nurs 2009;36:137–54.
5. Meddings J, Saint S, Krein SL, et al. Systematic Review of interventions to reduce urinary tract infection in nursing home residents. J Hosp Med 2017;12:356–68.
Study Overview
Objective. To determine the effect of implementing an intervention to reduce catheter-associated urinary tract infections (CAUTIs) in nursing homes.
Design. Prospective implementation project.
Setting and participants. The study was conducted between March 2014 and August 2016 in 12-month cohorts of community-based nursing homes participating in the Agency for Healthcare Research and Quality Safety Program for Long-Term Care. A total of 568 nursing homes located across 48 states, Washington DC, and Puerto Rico were recruited to participate.
Intervention. The intervention was developed with the goal of modifying the elements of the Comprehensive Unit-Based Safety Program utilized in hospitals for adoption in nursing homes. The intervention included a technical bundle, that is, catheter removal, aseptic insertion, using regular assessments, training for catheter care, and incontinence care planning [1], as well as socioadaptive interventions focused on empowering teams, addressing implementation challenges, offering solutions, promoting resident safety culture, team building, leadership, and resident and family engagement. The interventions were implemented over a 12-month period. To be included in the data analysis, nursing homes need to remain active through the end of the 12-month period and report 2 months or more of outcome data and device-days. Nursing homes that reported large fluctuations in reported data were excluded from the analysis. A total of 433 nursing homes remained active throughout the intervention period.
Main outcome measures. The main study outcome measure was the CAUTI incidence rate, defined as the number of CAUTIs divided by the number of catheter-days and multiplied by 1000. National Healthcare Safety Network definitions were used. The criteria for UTI
included objective systemic and localizing clinical findings along with laboratory-based criteria. A secondary outcome was the urinary catheter utilization ratio, defined as the number of catheter-days divided by the number of resident-days multiplied by 100 and reported as a percentage. Participating nursing homes collected data on the daily number of CAUTIs, catheter days, resident days, and urine cultures for each month of the project period and these metrics were reported using the Health Research and Educational Trust, a research affiliate of the American Hospital Association, Comprehensive Data System.
Conclusion. A multicomponent intervention implemented in community-based nursing homes across the country was associated with a reduction in CAUTI rates. The study shows that the intervention to reduce CAUTI can be implemented on a large scale and can be associated with improvement in patient safety.
Commentary
Catheter-associated urinary tract infection is a common condition that affects nursing home residents, as nursing home residents often have an indwelling urinary catheter on admission to the nursing home. These infections can be costly, lead to hospital admissions, and can contribute to the development of multidrug-resistant organisms, which pose a significant public health threat [2]. CAUTIs, however, are potentially preventable through the use of practices that promote judicious use of urinary catheters and attention to aseptic insertion and catheter care [3,4]. Although prior randomized controlled trials demonstrated the potential impact of interventions that reduce incidence of urinary tract infections [5], the interventions have not been adopted widely.
Recognizing the importance of improving safety through reducing CAUTIs, the Agency for Healthcare Research and Quality has established toolkits and implementation guides for health care facilities to adopt better practices for reducing catheter-associated infections. This study adds to the current literature by demonstrating the feasibility and beneficial impact of widespread implementation of AHRQ tools.
The study evaluated the impact of the intervention in a large cohort of nursing homes, comparing outcome measures pre and post intervention. One limitation of the study is that other factors that were present concurrently may have contributed to the observed changes in CAUTI outcomes. The study also did not have a control group, and the changes in outcome rates were not compared with rates in homes that did not participate in the project. Also, it is not possible to examine the effect of the individual components of the intervention as this intervention had multiple components delivered simultaneously. Despite these drawbacks, the study makes a strong case that project implementation is associated with a reduction in CAUTI rates of more than 50%.
A next step to better understand how best to disseminate the intervention is to identify factors associated with greater improvements in outcomes among the cohort of nursing homes and also to understand the variations in how nursing homes are implementing the intervention and what impact these differences might have. This in turn may guide further efforts to broaden the impact through more nuanced application of the intervention.
Applications for Clinical Practice
This study demonstrates that CAUTI can be prevented through a multicomponent intervention that focuses on appropriate use and discontinuation of urinary catheters and proper catheter care. Given that these tools and guides are available for use through AHRQ, nursing homes should examine the potential for adoption in their facilities. This can enhance the safety for their residents by reducing the risk of a potentially preventable complication.
—William W. Hung, MD, MPH
Study Overview
Objective. To determine the effect of implementing an intervention to reduce catheter-associated urinary tract infections (CAUTIs) in nursing homes.
Design. Prospective implementation project.
Setting and participants. The study was conducted between March 2014 and August 2016 in 12-month cohorts of community-based nursing homes participating in the Agency for Healthcare Research and Quality Safety Program for Long-Term Care. A total of 568 nursing homes located across 48 states, Washington DC, and Puerto Rico were recruited to participate.
Intervention. The intervention was developed with the goal of modifying the elements of the Comprehensive Unit-Based Safety Program utilized in hospitals for adoption in nursing homes. The intervention included a technical bundle, that is, catheter removal, aseptic insertion, using regular assessments, training for catheter care, and incontinence care planning [1], as well as socioadaptive interventions focused on empowering teams, addressing implementation challenges, offering solutions, promoting resident safety culture, team building, leadership, and resident and family engagement. The interventions were implemented over a 12-month period. To be included in the data analysis, nursing homes need to remain active through the end of the 12-month period and report 2 months or more of outcome data and device-days. Nursing homes that reported large fluctuations in reported data were excluded from the analysis. A total of 433 nursing homes remained active throughout the intervention period.
Main outcome measures. The main study outcome measure was the CAUTI incidence rate, defined as the number of CAUTIs divided by the number of catheter-days and multiplied by 1000. National Healthcare Safety Network definitions were used. The criteria for UTI
included objective systemic and localizing clinical findings along with laboratory-based criteria. A secondary outcome was the urinary catheter utilization ratio, defined as the number of catheter-days divided by the number of resident-days multiplied by 100 and reported as a percentage. Participating nursing homes collected data on the daily number of CAUTIs, catheter days, resident days, and urine cultures for each month of the project period and these metrics were reported using the Health Research and Educational Trust, a research affiliate of the American Hospital Association, Comprehensive Data System.
Conclusion. A multicomponent intervention implemented in community-based nursing homes across the country was associated with a reduction in CAUTI rates. The study shows that the intervention to reduce CAUTI can be implemented on a large scale and can be associated with improvement in patient safety.
Commentary
Catheter-associated urinary tract infection is a common condition that affects nursing home residents, as nursing home residents often have an indwelling urinary catheter on admission to the nursing home. These infections can be costly, lead to hospital admissions, and can contribute to the development of multidrug-resistant organisms, which pose a significant public health threat [2]. CAUTIs, however, are potentially preventable through the use of practices that promote judicious use of urinary catheters and attention to aseptic insertion and catheter care [3,4]. Although prior randomized controlled trials demonstrated the potential impact of interventions that reduce incidence of urinary tract infections [5], the interventions have not been adopted widely.
Recognizing the importance of improving safety through reducing CAUTIs, the Agency for Healthcare Research and Quality has established toolkits and implementation guides for health care facilities to adopt better practices for reducing catheter-associated infections. This study adds to the current literature by demonstrating the feasibility and beneficial impact of widespread implementation of AHRQ tools.
The study evaluated the impact of the intervention in a large cohort of nursing homes, comparing outcome measures pre and post intervention. One limitation of the study is that other factors that were present concurrently may have contributed to the observed changes in CAUTI outcomes. The study also did not have a control group, and the changes in outcome rates were not compared with rates in homes that did not participate in the project. Also, it is not possible to examine the effect of the individual components of the intervention as this intervention had multiple components delivered simultaneously. Despite these drawbacks, the study makes a strong case that project implementation is associated with a reduction in CAUTI rates of more than 50%.
A next step to better understand how best to disseminate the intervention is to identify factors associated with greater improvements in outcomes among the cohort of nursing homes and also to understand the variations in how nursing homes are implementing the intervention and what impact these differences might have. This in turn may guide further efforts to broaden the impact through more nuanced application of the intervention.
Applications for Clinical Practice
This study demonstrates that CAUTI can be prevented through a multicomponent intervention that focuses on appropriate use and discontinuation of urinary catheters and proper catheter care. Given that these tools and guides are available for use through AHRQ, nursing homes should examine the potential for adoption in their facilities. This can enhance the safety for their residents by reducing the risk of a potentially preventable complication.
—William W. Hung, MD, MPH
1. Agency for Healthcare Research and Quality. Prevent catheter-associated urinary tract infection. CAUTI implementation guide. Accessed 11 Aug 2017 at www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/hais/cauti-tools/impl-guide/implementation-guide-appendix-k.pdf.
2. Chitnis AS, Edwards JR, Ricks PM, et al. Device-associated infection rates, device utilization, and antimicrobial resistance in long-term acute care hospitals reporting to the National Healthcare Safety Network, 2010. Infect Control Hosp Epidemiol 2012;33:993–1000.
3. Meddings J, Rogers MA, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf 2014;23:277–89.
4. Willson M, Wilde M, Webb ML, et al. Nursing interventions to reduce the risk of catheter-associated urinary tract infection: part 2: staff education, monitoring, and care techniques. J Wound Ostomy Continence Nurs 2009;36:137–54.
5. Meddings J, Saint S, Krein SL, et al. Systematic Review of interventions to reduce urinary tract infection in nursing home residents. J Hosp Med 2017;12:356–68.
1. Agency for Healthcare Research and Quality. Prevent catheter-associated urinary tract infection. CAUTI implementation guide. Accessed 11 Aug 2017 at www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/hais/cauti-tools/impl-guide/implementation-guide-appendix-k.pdf.
2. Chitnis AS, Edwards JR, Ricks PM, et al. Device-associated infection rates, device utilization, and antimicrobial resistance in long-term acute care hospitals reporting to the National Healthcare Safety Network, 2010. Infect Control Hosp Epidemiol 2012;33:993–1000.
3. Meddings J, Rogers MA, Krein SL, et al. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf 2014;23:277–89.
4. Willson M, Wilde M, Webb ML, et al. Nursing interventions to reduce the risk of catheter-associated urinary tract infection: part 2: staff education, monitoring, and care techniques. J Wound Ostomy Continence Nurs 2009;36:137–54.
5. Meddings J, Saint S, Krein SL, et al. Systematic Review of interventions to reduce urinary tract infection in nursing home residents. J Hosp Med 2017;12:356–68.
Does HPV testing lead to improved diagnosis of cervical dysplasia for patients with ASC-US cytology?
EXPERT COMMENTARY
The American Society for Colposcopy and Cervical Pathology (ASCCP) has recommended HPV triage for ASC-US cytology for more than 15 years. Since the ALTS trial demonstrated improved detection of CIN2+ in women with ASC-US cytology, HPV testing has become the preferred triage strategy for women with ASC-US cytology, except for women under age 25.1 However, we do not know the long-term outcomes for these women. The study by Cuzick and colleagues uniquely addresses this question.
Details of the study
The retrospective review of data from the New Mexico HPV Pap Registry examined the influence of HPV testing on outcomes in 20,677 women with ASC-US cytology between 2008 and 2012. Of those women, 80.5% had an HPV test, and the authors estimated that 80.6% of those HPV tests were for triage after ASC-US cytology as opposed to co-testing (that is, cytology and HPV testing together). Of note, the majority of these Pap tests were performed prior to the 2012 ASCCP guidelines that recommend HPV co-testing for all women aged 30 to 64 years regardless of cytology. Of the HPV tests performed, 43.1% were positive. The investigators then examined rates of CIN in the interval between ASC-US cytology and biopsy-confirmed CIN, and rates of loop electrosurgical excision procedures (LEEP) and results at 5 years.
The investigators found a non–statistically significant increase in overall detection of CIN3 (relative risk [RR], 1.16; 95% confidence interval [CI], 0.92–1.45) in women who had been triaged with HPV testing, and a significant increase in overall detection of CIN2 (RR, 1.27; 95% CI, 1.06–1.53) and CIN1 (RR, 1.76; 95% CI, 1.56–2.00). CIN1, CIN2, and CIN3 were detected significantly earlier in patients with HPV testing. As expected, the majority of CIN2 and CIN3 was diagnosed in women who were HPV positive.
Related article:
2017 Update on cervical disease
The proportion of women undergoing either endocervical curettage or cervical biopsy was higher in those with HPV testing (32.1% vs 20.6%, P<.001), as were LEEP rates (4.9% vs 4.0%, P = .03). LEEP rates were highest in the year after a positive HPV test and were mostly attributable to CIN1 results. However, the overall ratio of LEEP to CIN3+ diagnosis was similar in women who were tested for HPV compared with those who were not. A larger proportion of patients with HPV testing had follow-up compared with those without HPV testing (84.1% vs 78.9%, P<.001).
The authors concluded that HPV testing in women with ASC-US cytology leads to detecting high-grade disease earlier, but that HPV positivity results in more interventions, largely due to an overdiagnosis of CIN1. They also confirmed that the majority of high-grade lesions are found in women with positive HPV tests.
Related article:
2015 Update on cervical disease: New ammo for HPV prevention and screening
Study strengths and weaknesses
This is the first comprehensive long-term look at women with ASC-US cytology and the impact of HPV testing. The New Mexico HPV Pap Registry is the only US state-based registry with comprehensive follow-up data. This study’s results build on previous data that showed sensitivity is increased with the addition of HPV testing to cervical cytology,1 and they support current ASCCP guidelines that emphasize HPV triage or co-testing for women age 25 or older.
Potential bias. While this study has the benefit of a large cohort, it is limited by biases inherent in retrospective study design. One important potential bias is the differential utilization of HPV testing or procedures by providers. The authors acknowledge preliminary analyses that show that some clinics (rural, federally qualified health centers, public health clinics) serving underserved populations may underutilize or inappropriately utilize HPV testing.
Further, the 2008–2012 study period may make the results less generalizable to current practices since the ASCCP guidelines were adjusted to include more HPV testing in women aged 25 and older in 2012.
Finally, this study examines CIN but does not specifically look at the impact of HPV testing on the ultimate outcome of interest, cervical cancer rates.
The data from the study by Cuzick and colleagues support the importance of continued screening for cervical cancer and its precursors with HPV testing. However, the results also show that we need to improve our strategies for stratifying patients who actually need colposcopy. The authors assert an "enormous predictive value of HPV testing," but this comes at the expense of many unnecessary procedures. Clinicians should continue to use cytology with HPV triage in women aged 25 years and older, but the ASCCP should reconsider guidelines to improve screening specificity. The addition of other screening modalities, such as extended genotyping, methylation testing, and p16/Ki-67 staining, are considerations for ASC-US triage.
-- Sarah Dilley, MD, MPH, and Warner K. Huh, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- ASCUS-LSIL Triage Study (ALTS) Group. Results of a randomized trial on the management of cytology interpretations of atypical squamous cells of undetermined significance. Am J Obstet Gynecol. 2003;188(6):1383–1392.
EXPERT COMMENTARY
The American Society for Colposcopy and Cervical Pathology (ASCCP) has recommended HPV triage for ASC-US cytology for more than 15 years. Since the ALTS trial demonstrated improved detection of CIN2+ in women with ASC-US cytology, HPV testing has become the preferred triage strategy for women with ASC-US cytology, except for women under age 25.1 However, we do not know the long-term outcomes for these women. The study by Cuzick and colleagues uniquely addresses this question.
Details of the study
The retrospective review of data from the New Mexico HPV Pap Registry examined the influence of HPV testing on outcomes in 20,677 women with ASC-US cytology between 2008 and 2012. Of those women, 80.5% had an HPV test, and the authors estimated that 80.6% of those HPV tests were for triage after ASC-US cytology as opposed to co-testing (that is, cytology and HPV testing together). Of note, the majority of these Pap tests were performed prior to the 2012 ASCCP guidelines that recommend HPV co-testing for all women aged 30 to 64 years regardless of cytology. Of the HPV tests performed, 43.1% were positive. The investigators then examined rates of CIN in the interval between ASC-US cytology and biopsy-confirmed CIN, and rates of loop electrosurgical excision procedures (LEEP) and results at 5 years.
The investigators found a non–statistically significant increase in overall detection of CIN3 (relative risk [RR], 1.16; 95% confidence interval [CI], 0.92–1.45) in women who had been triaged with HPV testing, and a significant increase in overall detection of CIN2 (RR, 1.27; 95% CI, 1.06–1.53) and CIN1 (RR, 1.76; 95% CI, 1.56–2.00). CIN1, CIN2, and CIN3 were detected significantly earlier in patients with HPV testing. As expected, the majority of CIN2 and CIN3 was diagnosed in women who were HPV positive.
Related article:
2017 Update on cervical disease
The proportion of women undergoing either endocervical curettage or cervical biopsy was higher in those with HPV testing (32.1% vs 20.6%, P<.001), as were LEEP rates (4.9% vs 4.0%, P = .03). LEEP rates were highest in the year after a positive HPV test and were mostly attributable to CIN1 results. However, the overall ratio of LEEP to CIN3+ diagnosis was similar in women who were tested for HPV compared with those who were not. A larger proportion of patients with HPV testing had follow-up compared with those without HPV testing (84.1% vs 78.9%, P<.001).
The authors concluded that HPV testing in women with ASC-US cytology leads to detecting high-grade disease earlier, but that HPV positivity results in more interventions, largely due to an overdiagnosis of CIN1. They also confirmed that the majority of high-grade lesions are found in women with positive HPV tests.
Related article:
2015 Update on cervical disease: New ammo for HPV prevention and screening
Study strengths and weaknesses
This is the first comprehensive long-term look at women with ASC-US cytology and the impact of HPV testing. The New Mexico HPV Pap Registry is the only US state-based registry with comprehensive follow-up data. This study’s results build on previous data that showed sensitivity is increased with the addition of HPV testing to cervical cytology,1 and they support current ASCCP guidelines that emphasize HPV triage or co-testing for women age 25 or older.
Potential bias. While this study has the benefit of a large cohort, it is limited by biases inherent in retrospective study design. One important potential bias is the differential utilization of HPV testing or procedures by providers. The authors acknowledge preliminary analyses that show that some clinics (rural, federally qualified health centers, public health clinics) serving underserved populations may underutilize or inappropriately utilize HPV testing.
Further, the 2008–2012 study period may make the results less generalizable to current practices since the ASCCP guidelines were adjusted to include more HPV testing in women aged 25 and older in 2012.
Finally, this study examines CIN but does not specifically look at the impact of HPV testing on the ultimate outcome of interest, cervical cancer rates.
The data from the study by Cuzick and colleagues support the importance of continued screening for cervical cancer and its precursors with HPV testing. However, the results also show that we need to improve our strategies for stratifying patients who actually need colposcopy. The authors assert an "enormous predictive value of HPV testing," but this comes at the expense of many unnecessary procedures. Clinicians should continue to use cytology with HPV triage in women aged 25 years and older, but the ASCCP should reconsider guidelines to improve screening specificity. The addition of other screening modalities, such as extended genotyping, methylation testing, and p16/Ki-67 staining, are considerations for ASC-US triage.
-- Sarah Dilley, MD, MPH, and Warner K. Huh, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
EXPERT COMMENTARY
The American Society for Colposcopy and Cervical Pathology (ASCCP) has recommended HPV triage for ASC-US cytology for more than 15 years. Since the ALTS trial demonstrated improved detection of CIN2+ in women with ASC-US cytology, HPV testing has become the preferred triage strategy for women with ASC-US cytology, except for women under age 25.1 However, we do not know the long-term outcomes for these women. The study by Cuzick and colleagues uniquely addresses this question.
Details of the study
The retrospective review of data from the New Mexico HPV Pap Registry examined the influence of HPV testing on outcomes in 20,677 women with ASC-US cytology between 2008 and 2012. Of those women, 80.5% had an HPV test, and the authors estimated that 80.6% of those HPV tests were for triage after ASC-US cytology as opposed to co-testing (that is, cytology and HPV testing together). Of note, the majority of these Pap tests were performed prior to the 2012 ASCCP guidelines that recommend HPV co-testing for all women aged 30 to 64 years regardless of cytology. Of the HPV tests performed, 43.1% were positive. The investigators then examined rates of CIN in the interval between ASC-US cytology and biopsy-confirmed CIN, and rates of loop electrosurgical excision procedures (LEEP) and results at 5 years.
The investigators found a non–statistically significant increase in overall detection of CIN3 (relative risk [RR], 1.16; 95% confidence interval [CI], 0.92–1.45) in women who had been triaged with HPV testing, and a significant increase in overall detection of CIN2 (RR, 1.27; 95% CI, 1.06–1.53) and CIN1 (RR, 1.76; 95% CI, 1.56–2.00). CIN1, CIN2, and CIN3 were detected significantly earlier in patients with HPV testing. As expected, the majority of CIN2 and CIN3 was diagnosed in women who were HPV positive.
Related article:
2017 Update on cervical disease
The proportion of women undergoing either endocervical curettage or cervical biopsy was higher in those with HPV testing (32.1% vs 20.6%, P<.001), as were LEEP rates (4.9% vs 4.0%, P = .03). LEEP rates were highest in the year after a positive HPV test and were mostly attributable to CIN1 results. However, the overall ratio of LEEP to CIN3+ diagnosis was similar in women who were tested for HPV compared with those who were not. A larger proportion of patients with HPV testing had follow-up compared with those without HPV testing (84.1% vs 78.9%, P<.001).
The authors concluded that HPV testing in women with ASC-US cytology leads to detecting high-grade disease earlier, but that HPV positivity results in more interventions, largely due to an overdiagnosis of CIN1. They also confirmed that the majority of high-grade lesions are found in women with positive HPV tests.
Related article:
2015 Update on cervical disease: New ammo for HPV prevention and screening
Study strengths and weaknesses
This is the first comprehensive long-term look at women with ASC-US cytology and the impact of HPV testing. The New Mexico HPV Pap Registry is the only US state-based registry with comprehensive follow-up data. This study’s results build on previous data that showed sensitivity is increased with the addition of HPV testing to cervical cytology,1 and they support current ASCCP guidelines that emphasize HPV triage or co-testing for women age 25 or older.
Potential bias. While this study has the benefit of a large cohort, it is limited by biases inherent in retrospective study design. One important potential bias is the differential utilization of HPV testing or procedures by providers. The authors acknowledge preliminary analyses that show that some clinics (rural, federally qualified health centers, public health clinics) serving underserved populations may underutilize or inappropriately utilize HPV testing.
Further, the 2008–2012 study period may make the results less generalizable to current practices since the ASCCP guidelines were adjusted to include more HPV testing in women aged 25 and older in 2012.
Finally, this study examines CIN but does not specifically look at the impact of HPV testing on the ultimate outcome of interest, cervical cancer rates.
The data from the study by Cuzick and colleagues support the importance of continued screening for cervical cancer and its precursors with HPV testing. However, the results also show that we need to improve our strategies for stratifying patients who actually need colposcopy. The authors assert an "enormous predictive value of HPV testing," but this comes at the expense of many unnecessary procedures. Clinicians should continue to use cytology with HPV triage in women aged 25 years and older, but the ASCCP should reconsider guidelines to improve screening specificity. The addition of other screening modalities, such as extended genotyping, methylation testing, and p16/Ki-67 staining, are considerations for ASC-US triage.
-- Sarah Dilley, MD, MPH, and Warner K. Huh, MD
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- ASCUS-LSIL Triage Study (ALTS) Group. Results of a randomized trial on the management of cytology interpretations of atypical squamous cells of undetermined significance. Am J Obstet Gynecol. 2003;188(6):1383–1392.
- ASCUS-LSIL Triage Study (ALTS) Group. Results of a randomized trial on the management of cytology interpretations of atypical squamous cells of undetermined significance. Am J Obstet Gynecol. 2003;188(6):1383–1392.
Fast Tracks
- To assess long-term outcomes of women with ASC-US cytology and HPV triage, researchers examined the interval between ASC-US cytology and biopsy-confirmed CIN, LEEP rates, and results at 5 years
- HPV testing in women with ASC-US cytology leads to earlier detection of high-grade disease, but HPV positivity results in more interventions, largely due to overdiagnosis of CIN1
Impact of an Educational Training Program on Restorative Care Practice of Nursing Assistants Working with Hospitalized Older Patients
Abstract
- Background: Acute and prolonged exposure to hospital medical care can cause hospital-associated deconditioning with deleterious effects on patient care provision and quality of life. Physical rehabilitation provided by allied healthcare professionals can enable reacquisition of function via professional input into attainment of set goals. Separate to rehabilitative efforts, restorative care optimizes independence by motivating individuals to maintain and restore function. Nursing assistants (NAs) provide a significant amount of direct patient care and are well placed to deliver restorative care.
- Objective: To increase proportional restorative care interactions with hospitalized older adults by training NAs.
- Methods: A prospective cohort quality improvement (QI) project was undertaken at 3 acute hospital wards (patient minimum age 65 years) and 2 community subacute care wards in the UK. NAs working within the target settings received a 2-part restorative care training package. The primary evaluation tool was 51 hours in total of observation measuring the proportional change in restorative care events delivered by NAs.
- Results: NA-led restorative care events increased from 40 (pre-intervention) to 94 (post-intervention), representing a statistically significant proportional increase from 74% to 92% (χ2(1) 9.53, P = 0.002). NAs on occasions inadvertently emphasized restriction of function to manage risk and oblige with rest periods.
- Conclusion: Investing in NAs can influence the amount of restorative care delivered to hospitalized older adults at risk of hospital-associated deconditioning. Continued investment in NAs is indicated to influence top-down, mandated restorative care practice in this patient group.
Key words: older people; restorative care; hospital associated deconditioning; nursing assistants; rehabilitation; training.
Hospital-associated deconditioning is defined as a significant decline in functional abilities developed through acute and prolonged exposure to a medical care facility environment, and is independent of that attributed to primary pathologies resulting in acute admission [1]. Considerable research on iatrogenic complications in older hospitalized populations [1–5] has shown the impacts of hospital-associated deconditioning and associated dysfunctions on quality of life for patients and the resultant burden on health and social care provision [6].
Physical rehabilitation has been shown to restore function through high-dose repetition of task-specific activity [7], and the benefits attributed to extra physical therapy include improved mobility, activity, and participation [8]. Simply defined, physical rehabilitation is the reacquisition of function through multidisciplinary assessment and professional therapeutic input in attainment of set goals. A more recent nomenclature in health settings is “restorative care,” defined as a philosophy of care that encourages, enables, and motivates individuals to maintain and restore function, thereby optimizing independence [9]. It has been clearly defined as a philosophy separate from that of rehabilitation [9] and remote from task-related or “custodial care,” which is designed to assist in meeting patients’ daily activity needs without any therapeutic value.
In UK rehabilitation wards, nursing staff provide 4.5 times as much direct patient care time compared with allied health professionals, with paraprofessional nursing assistants (NAs, equivalent to certified nurse assistants [CNAs] in the United States) responsible for half of this direct nursing care [10]. Kessler’s group examined the evolving role of NAs in UK hospitals [11]. From a national survey of 700 NAs and 600 trained nurses, the authors upheld the view that NAs act as direct caregivers including through routine tasks traditionally delivered by nurses. They identified that NAs exhibit distinct qualities, which are valued by qualified nurses, including routine task fulfilment and abilities relating to patients, which enable NAs to enhance care quality. Indeed, the national findings of Kessler’s group were generalizable to our own clinical setting where a NA cohort was a well-placed, available, and motivated resource to deliver therapeutically focused care for our hospitalized older population.
The theoretical relationship between care approaches is complex and represents a challenge for service users and policy makers. For instance, comprehensive rehabilitation delivery during an acute care episode may lead to users not seeking custodial care at home. Conversely, day-to-day activities realized by custodial care at home may lead to users not seeking acute rehabilitative care [12]. With stable resources being assigned to more dependent users in higher numbers, reactive care regardless of environment has often been the model of choice.
However, an economic rationale has developed more recently where investment in maintenance and preventative models results in healthcare savings with models including the 4Rs; reablement, reactivation, rehabilitation, and restorative care [13]. In North America, restorative care approaches have resulted in favorable results in nursing home facilities [14] and at home [15], and restorative care education and motivation training for nursing assistants was effective in supporting a change in beliefs and practice behaviors [16]. While results show restorative care practices in the non-acute care sector are advantageous, it is unknown whether these approaches if adopted in hospital settings affect subsequent healthcare utilization in the non-acute facilities, or even if they are feasible to implement in acute facilities by a staff group able to do so. Therefore, the purpose of this QI project was to deploy a restorative care educational intervention for NA staff working with hospitalized older adults with the aim of increasing the proportion of restorative care delivered.
Methods
Context
This project was conducted at a UK National Health Service university teaching hospital trust at 3 acute hospital wards (patient minimum age 65 years) and 2 community subacute care wards for older patients. Participants consisted of all permanent or long-term temporary (> 3 months continuous employment) NAs working in the target settings (n = 36). The QI project design is summarized in Figure 1. The project applied the 4Es translational approach to regulate the QI intervention: Engage, Educate, Execute, and Evaluate [17]. The reporting of this study follows SQUIRE guidance [18].
Intervention
The QI activity was a holistic educational process for all NA participants.
Didactic Study Day
Each NA attended a study day led by a physical therapist (up to 10 NAs per group). A student-centered training approach was adopted, recognizing variations in adult learning styles [19], and included seminar style theory, video case scenarios, group work, practical skills, open discussion, and reflection. The training package outline was compiled following consensus among the multi-disciplinary team working in the target settings and the steering group. Topics covered were theory on the risk of hospitalization and benefits of early mobilization; case scenarios and examples of restorative care; identifying and overcoming barriers to restorative care; identifying appro-priate patients for a restorative care approach; practical skills, including assisting patients out of bed, ambulation, and eating/drinking; and challenging, problem-solving scenarios. All participants received a course handbook to facilitate learning.
Ward-Based Practice
Measures
Type of Care Event
The quantity and nature of all NA-patient functional task-related care events was established by independent systematic observation pre- and post-intervention. Observers rated the type of care for observed patients as either custodial or restorative events using a tool described below. In addition, the numbers of patients receiving no restorative care events at all during observation was calculated to capture changes in rates between patients observed. The observational tool used was adapted from that utilized in a North American study of a long-term care facility [20], which demonstrated favorable intra-rater reliability (person separation reliability of 0.77), inter-rater reliability (80% to 100% agreement on each of the care behaviors), and validity (evidence of unidimensionality and good fit of the items). Adaptations accommodated for data collection in a hospital environment and alteration to UK nomenclature.
Three blinded volunteer assessors undertook observations. The observers monitored for activity in any 1 of 8 functional domains: bed mobility, transfers, mobility, washing and dressing, exercise, hygiene (mouth care/shaving/hair/nail care), toileting, and eating. Patient activity observed within these domains was identified as either a restorative or custodial care event. For example: “asks or encourages patient to walk/independently propel wheelchair to bathroom/toilet/day room/activities and gives them time to perform activity” was identified as a restorative care event, while “utilizes wheelchair instead of encourages ambulation and does not encourage patient to self-propel” was considered a custodial care event. All observations were carried out by student physical therapists in training or physical therapy assistants, all of whom were familiar in working in the acute facility with hospitalized older people. In an attempt to optimize internal consistency, observer skill was quality-controlled by ensuring observers were trained and their competency assessed in the use of the evaluation measurement tool.
Bays of 3 to 6 beds comprised each observation space. Three 90-minute time epochs were selected for observation—awakening (early morning), lunchtime (middle of the day), and afternoon (before evening meal)—with the aim that each time frame be observed on a minimum of 1 occasion on each of the 5 wards to generate a minimum of 15 observation sessions. Resources dictated observational periods to be 90-minutes maximum, per epoch, on weekdays only. The mean (range) time between the didactic study day and the ward-based practice day was 4 (1–8) weeks, and between the ward-based practice day and the second observational period was 6 (1–14) weeks.
Patient Characteristics
Differences in the acuity of patients between pre- and post-QI activity in the observational environments could influence care demands. Therefore, patient characteristics before and after the QI activity were measured to assess for stability. Prior to each session, observers recorded patient demographic details and current STRATIFY score, a predictive tool used at the time to segment fall risk [21], from patients’ clinical records. Two measures were used to offer contemporaneous representation of the observed population in the observation environment: a modified Barthel index [22], which provides a measure of activities of daily living [23], and the Abbreviated Mental Test Score [24], a simple diagnostic screen for cognitive impairment. All patients were considered as recuperating and thus eligible for observation except those with a “Patient-At-Risk” score ≥ 4, indicating physiological factors associated with established or impending critical illness [25], or if an end of life care plan was clearly detailed in the clinical record.
Data Analysis
Patient demographics are reported descriptively. Ordinal data are summarized using median and inter-quartile ranges (IQR), interval/ratio data using mean and standard deviation (SD) unless otherwise stated. Categorical data are reported as percentages. Comparison of observed patient samples before and after the QI period were compared with the Mann-Whitney U-test for ordinal data, 2 sample t tests for interval/ratio data, and chi squared tests of proportions for other variables.
Analyses were carried out using STATA 11 ME (StataCorp, College Station, TX) and SPSS v17 (SPSS, Chicago). Statistical significance was set at P ≤ 0.05.
Ethical Issues
This study was approved by the local UK NHS Trust clinical audit committee (Quality Improvement project 2038).
Results
Care Events by NAs
Observations were undertaken across the 5 wards on 14 workdays (Monday–Friday) over 6 weeks in the pre-QI period, and on 16 workdays over 4 weeks in the post-QI period, yielding a total of 51 hours of observation.
Overall, across all care environments, there was a statistically significant proportional increase in restorative care from 74% to 92% [χ2(1) 9.53, P = 0.002] (Figure 2). This represents an increase in restorative care events from 40 to 94. Observed custodial care events decreased from 14 to 8, a 43% reduction in custodial care events overall, a difference which remained irrespective of the environment (acute or subacute care), pre- and post-QI activity (P = 0.538 and P = 0.695, respectively).
There was a marked decrease in the number of patients receiving no NA-led restorative care events from 59 (74%) to 32 (48%) before and after QI activity respectively, [χ2 (1) 10.63, P = 0.001].
Patients Observed
Patient population characteristics remained stable during the course of the QI activity; there were no significant differences in the observed patient characteristics pre- and post-QI activity (Table). In 51 hours of observation undertaken by 3 independent observers there were 80 and 71 occupied beds before and after QI activity, respectively, representing a stable bed occupancy rate of 94% and 83% (P = 0.074). Of the occupied beds, 98.7% and 98.6% of patients (pre- and post-QI activity, respectively) were considered recuperating and therefore appropriate for a restorative care approach.
Discussion
although significantly decreased from pre-QI proportions (74%). We therefore conclude that a meaningful decrease across patients receiving no restorative care and a meaningful increase in within-patient restorative care events post-QI intervention occurred.
Our study furthers research in methods of increasing restorative care events delivered by NAs. In a randomized controlled trial by Resnick et al [16], a structured 6-week restorative care program incorporating teaching NAs
restorative care philosophies (tier 1) and facilitating NAs to motivate residents to engage in functional activities (tier 2) was compared to placebo (a single 30-minute educational session in managing residents’ behavioral symptoms) [16]. Results showed the 6-week program led to more restorative care, with NAs demonstrating enhanced knowledge and expectations of restorative care outcomes and better job satisfaction. Our educational package (1 day) and ward-based-learning session (3–4 hours) was much shorter than Resnick et al’s 6-week intervention [16], and the optimal dose of educational packages for NAs is yet to be determined and needs to be addressed in future studies. Furthermore, while we found education increased restorative care across multiple environments, it is yet to be determined whether more restorative care has a positive impact on patient function downstream of an acute inpatient stay. In fact, determination of restorative care’s influence on augmenting rehabilitation outcomes is a neglected aspect of nursing-AHP practice that we aim to define and investigate in ongoing studies.
The patient population characteristics within the target wards were stable over the course of the QI project. Observed patients’ median Barthel (11) and Abbreviated Mental Test (6) scores remained stable and are indicative of high levels of day-to-day activity dependence [24,26–28]. Over the QI activity period it was therefore unsurprising that modest proportions of patients direc-ted their own care (28% and 33% pre and post-QI, respectively). Subsequently, demands on staff to lead patient care were substantial, leading to high risks of social or clinical iatrogenesis and hospital-associated deconditioning.
In a previous observational study, substantial patient inactivity was found in a highly dependent cohort of patients [29]. Fear of falling and insignificant emphasis on ambulation were cited as patient and organizational-centric reasons, respectively. Furthermore, in a selective observational study, patients receiving function-focused care (FFC; synonymous to restorative care) in an acute hospital environment developed less physical functional decline compared to those receiving custodial care [30]. However, patients who had fallen during their hospital stay received less FFC. The authors suggest limited FFC in fallers was deployed to minimize further risk but concluded there is need for nursing and therapy interventions that manage fall risks through endorsing functional activities instead of mobility restriction [30].
Limitations
While observational studies are more robust for measuring behavioral activities compared to self or proxy reporting [34], they are exposed to observer judgment and drift. An attempt was made to minimize this with the binary measurement of restorative versus custodial care and by random sampling of wards and time frames to capture an entire healthcare environment.
The observational study tool was based on one previously developed where acceptable reliability and validity was established and where observations were based on what individual care staff were practicing regardless of their operational environment [20]. In contrast, our observations were based in predetermined environmental spaces regardless of what care practice occurred within it. We consider our approach justifiable in minimizing observer influence on an individual’s practice by emphasizing to them that observers were interested in what happened in an environment [35,36]. However, we acknowledge the risk of under representation of care by observers not following the care delivery, and that local validity and reliability of our methods was not undertaken. Lastly, whilst training for observers was undertaken in this study to standardize the observations undertaken, validation of this method would be a feature required of any future experimental work.
Conclusions
Our findings support the current understanding of restorative care [14–16] and provides proof of concept that dedicating resources in a previously under-invested part of the workforce is feasible, well-accepted, and meaningful. The results are in keeping with the concept that the NA staff group is ready and able to fulfil their roles as direct caregivers, supporting and relieving other trained staff [11].
Corresponding author: Gareth D. Jones, MSc, Physiotherapy Dept, 3rd Fl Lambeth Wing, St Thomas’ Hospital, Westminster Bridge Rd, London SE1 7EH, UK, [email protected].
Funding/support: This work was supported by a small grants application to the Guy's and St Thomas' Charity, project code S100414.
Financial disclosures: No conflicts of interest to declare.
Acknowledgment: The authors acknowledge members of the steering group for their input: Rebekah Schiff, Carrie-Ann Wood, Judith Centofanti, Judith Hall, and Richard Page; Anne Bisset-Smith and Claudia Jacob for their initial pilot work; Amanda Buttery, Lottie Prowse, and Ryan Mackie for practical assistance; Siobhan Crichton for her statistical help; and Jacky Jones, Michael Thacker, Tisha Pryor, and Sarah Ritchie for helping review the manuscript.
1. Kortebein P. Rehabilitation for hospital-associated deconditioning. Am J Phys Med Rehabil 2009;88:66–77.
2. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med 1993;118:219–23.
3. Davydow DS, Hough CL, Levine DA, et al. Functional disability, cognitive impairment, and depression after hospitalization for pneumonia. Am J Med 2013;126:615–24.e5.
4. Sager MA, Franke T, Inouye SK, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 1996;156:645–52.
5. Warshaw GA, Moore JT, Friedman SW, et al. Functional disability in the hospitalized elderly. JAMA 1982;248:847–50.
6. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: "She was probably able to ambulate, but I'm not sure". JAMA 2011;306:1782–93.
7. Kwakkel G, Kollen B, Lindeman E. Understanding the pattern of functional recovery after stroke: facts and theories. Restor Neurol Neurosci 2004;22:281–99.
8. Peiris CL, Taylor NF, Shields N. Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med
Rehabil 2011;92:1490–500.
9. Resnick B, Boltz M, Galik E, Pretzer-Aboff I. Restorative care nursing for older adults: a guide for all care settings. 2nd ed. New York: Springer; 2012.
10. Rudd AG, Jenkinson D, Grant RL, Hoffman A. Staffing levels and patient dependence in English stroke units. Clin Med (Lond). 2009;9:110–5.
11. Kessler I, Heron P, Dopson S, et al. The nature and consequences of support workers in a hospital setting, Final Report. London: National Institute for Health Research, Service Delivery and Organization Programme; 2010.
12. Kashner TM, Krompholz B, McDonnell C, et al. Acute and custodial care among impaired aged. J Aging Health 1990;2:28–41.
13. Sims-Gould J, Tong CE, Wallis-Mayer L, Ashe MC. Reablement, reactivation, rehabilitation and restorative interventions with older adults in receipt of home care: a systematic review. J Am Med Dir Assoc 2017;18:653–63.
14. Shanti C, Johnson J, Meyers AM, et al. Evaluation of the restorative care education and training program for nursing homes. Can J Aging 2005;24:115–26.
15. Tinetti ME, Baker D, Gallo WT, et al. Evaluation of restorative care vs usual care for older adults receiving an acute episode of home care. JAMA 2002;287:2098–105.
16. Resnick B, Gruber-Baldini AL, Galik E, et al. Changing the philosophy of care in long-term care: testing of the restorative care intervention. Gerontologist 2009;49:175–84.
17. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008;337:a1714.
18. Davidoff F, Batalden P, Stevens D, et al; SQUIRE development group. Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ 2009;338:a3152.
19. Sweeney JF. Nurse education: learner-centred or teacher-centred? Nurse Educ Today 1986;6:257–62.
20. Resnick B, Rogers V, Galik E, Gruber-Baldini AL. Measuring restorative care provided by nursing assistants: reliability and validity of the Restorative Care Behavior Checklist. Nurs Res 2007;56:387–98.
21. Oliver D, Britton M, Seed P, et al. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ 1997;315:1049–53.
22. Colin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud 1988;10:61–3.
23. Richards SH, Peters TJ, Coast J, et al. Inter-rater reliability of the Barthel ADL index: how does a researcher compare to a nurse? Clin Rehabil 2000;14:72–8.
24. Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972;1:233–8.
25. Morgan CD, Baade LE. Neuropsychological testing and assessment scales for dementia of the Alzheimer's type. Psychiatr Clin North Am 1997;20:25–43.
26. Granger CV, Hamilton BB, Gresham GE, Kramer AA. The stroke rehabilitation outcome study: Part II. Relative merits of the total Barthel index score and a four-item subscore in predicting patient outcomes. Arch Phys Med Rehabil
1989;70:100–3.
27. MacKenzie DM, Copp P, Shaw RJ, Goodwin GM. Brief cognitive screening of the elderly: a comparison of the Mini-Mental State Examination (MMSE), Abbreviated Mental Test (AMT) and Mental Status Questionnaire (MSQ). Psychol Med
1996;26:427–30.
28. Uyttenboogaart M, Stewart RE, Vroomen PC, et al. Optimizing cutoff scores for the Barthel index and the modified Rankin scale for defining outcome in acute stroke trials. Stroke 2005;36:1984–7.
29. Callen BL, Mahoney JE, Grieves CB, et al. Frequency of hallway ambulation by hospitalized older adults on medical units of an academic hospital. Geriatr Nurs 2004;25:212–7.
30. Boltz M, Resnick B, Capezuti E, Shuluk J. Activity restriction vs. self-direction: hospitalised older adults' response to fear of falling. Int J Older People Nurs 2014;9:44–53.
31. Moyle W, Borbasi S, Wallis M, et al. Acute care management of older people with dementia: a qualitative perspective. J Clin Nurs 2011;20:420–8.
32. Olson DM, Borel CO, Laskowitz DT, et al. Quiet time: a nursing intervention to promote sleep in neurocritical care units. Am J Crit Care 2001;10:74–8.
33. Gardner C, Collins C, Osborne S, et al. Creating a therapeutic environment: a non-randomised controlled trial of a quiet time intervention for patients in acute care. Int J Nurs Stud 2009;46:778–86.
34. Kupek E. Bias and heteroscedastic memory error in self-reported health behavior: an investigation using covariance structure analysis. BMC Med Res Methodol 2002;2:14.
35. Fromme HB, Karani R, Downing SM. Direct observation in medical education: a review of the literature and evidence for validity. Mt Sinai J Med 2009;76:365–71.
36. Williams RG, Klamen DA, McGaghie WC. Cognitive, social and environmental sources of bias in clinical performance ratings. Teach Learn Med 2003;15:270–92.
Abstract
- Background: Acute and prolonged exposure to hospital medical care can cause hospital-associated deconditioning with deleterious effects on patient care provision and quality of life. Physical rehabilitation provided by allied healthcare professionals can enable reacquisition of function via professional input into attainment of set goals. Separate to rehabilitative efforts, restorative care optimizes independence by motivating individuals to maintain and restore function. Nursing assistants (NAs) provide a significant amount of direct patient care and are well placed to deliver restorative care.
- Objective: To increase proportional restorative care interactions with hospitalized older adults by training NAs.
- Methods: A prospective cohort quality improvement (QI) project was undertaken at 3 acute hospital wards (patient minimum age 65 years) and 2 community subacute care wards in the UK. NAs working within the target settings received a 2-part restorative care training package. The primary evaluation tool was 51 hours in total of observation measuring the proportional change in restorative care events delivered by NAs.
- Results: NA-led restorative care events increased from 40 (pre-intervention) to 94 (post-intervention), representing a statistically significant proportional increase from 74% to 92% (χ2(1) 9.53, P = 0.002). NAs on occasions inadvertently emphasized restriction of function to manage risk and oblige with rest periods.
- Conclusion: Investing in NAs can influence the amount of restorative care delivered to hospitalized older adults at risk of hospital-associated deconditioning. Continued investment in NAs is indicated to influence top-down, mandated restorative care practice in this patient group.
Key words: older people; restorative care; hospital associated deconditioning; nursing assistants; rehabilitation; training.
Hospital-associated deconditioning is defined as a significant decline in functional abilities developed through acute and prolonged exposure to a medical care facility environment, and is independent of that attributed to primary pathologies resulting in acute admission [1]. Considerable research on iatrogenic complications in older hospitalized populations [1–5] has shown the impacts of hospital-associated deconditioning and associated dysfunctions on quality of life for patients and the resultant burden on health and social care provision [6].
Physical rehabilitation has been shown to restore function through high-dose repetition of task-specific activity [7], and the benefits attributed to extra physical therapy include improved mobility, activity, and participation [8]. Simply defined, physical rehabilitation is the reacquisition of function through multidisciplinary assessment and professional therapeutic input in attainment of set goals. A more recent nomenclature in health settings is “restorative care,” defined as a philosophy of care that encourages, enables, and motivates individuals to maintain and restore function, thereby optimizing independence [9]. It has been clearly defined as a philosophy separate from that of rehabilitation [9] and remote from task-related or “custodial care,” which is designed to assist in meeting patients’ daily activity needs without any therapeutic value.
In UK rehabilitation wards, nursing staff provide 4.5 times as much direct patient care time compared with allied health professionals, with paraprofessional nursing assistants (NAs, equivalent to certified nurse assistants [CNAs] in the United States) responsible for half of this direct nursing care [10]. Kessler’s group examined the evolving role of NAs in UK hospitals [11]. From a national survey of 700 NAs and 600 trained nurses, the authors upheld the view that NAs act as direct caregivers including through routine tasks traditionally delivered by nurses. They identified that NAs exhibit distinct qualities, which are valued by qualified nurses, including routine task fulfilment and abilities relating to patients, which enable NAs to enhance care quality. Indeed, the national findings of Kessler’s group were generalizable to our own clinical setting where a NA cohort was a well-placed, available, and motivated resource to deliver therapeutically focused care for our hospitalized older population.
The theoretical relationship between care approaches is complex and represents a challenge for service users and policy makers. For instance, comprehensive rehabilitation delivery during an acute care episode may lead to users not seeking custodial care at home. Conversely, day-to-day activities realized by custodial care at home may lead to users not seeking acute rehabilitative care [12]. With stable resources being assigned to more dependent users in higher numbers, reactive care regardless of environment has often been the model of choice.
However, an economic rationale has developed more recently where investment in maintenance and preventative models results in healthcare savings with models including the 4Rs; reablement, reactivation, rehabilitation, and restorative care [13]. In North America, restorative care approaches have resulted in favorable results in nursing home facilities [14] and at home [15], and restorative care education and motivation training for nursing assistants was effective in supporting a change in beliefs and practice behaviors [16]. While results show restorative care practices in the non-acute care sector are advantageous, it is unknown whether these approaches if adopted in hospital settings affect subsequent healthcare utilization in the non-acute facilities, or even if they are feasible to implement in acute facilities by a staff group able to do so. Therefore, the purpose of this QI project was to deploy a restorative care educational intervention for NA staff working with hospitalized older adults with the aim of increasing the proportion of restorative care delivered.
Methods
Context
This project was conducted at a UK National Health Service university teaching hospital trust at 3 acute hospital wards (patient minimum age 65 years) and 2 community subacute care wards for older patients. Participants consisted of all permanent or long-term temporary (> 3 months continuous employment) NAs working in the target settings (n = 36). The QI project design is summarized in Figure 1. The project applied the 4Es translational approach to regulate the QI intervention: Engage, Educate, Execute, and Evaluate [17]. The reporting of this study follows SQUIRE guidance [18].
Intervention
The QI activity was a holistic educational process for all NA participants.
Didactic Study Day
Each NA attended a study day led by a physical therapist (up to 10 NAs per group). A student-centered training approach was adopted, recognizing variations in adult learning styles [19], and included seminar style theory, video case scenarios, group work, practical skills, open discussion, and reflection. The training package outline was compiled following consensus among the multi-disciplinary team working in the target settings and the steering group. Topics covered were theory on the risk of hospitalization and benefits of early mobilization; case scenarios and examples of restorative care; identifying and overcoming barriers to restorative care; identifying appro-priate patients for a restorative care approach; practical skills, including assisting patients out of bed, ambulation, and eating/drinking; and challenging, problem-solving scenarios. All participants received a course handbook to facilitate learning.
Ward-Based Practice
Measures
Type of Care Event
The quantity and nature of all NA-patient functional task-related care events was established by independent systematic observation pre- and post-intervention. Observers rated the type of care for observed patients as either custodial or restorative events using a tool described below. In addition, the numbers of patients receiving no restorative care events at all during observation was calculated to capture changes in rates between patients observed. The observational tool used was adapted from that utilized in a North American study of a long-term care facility [20], which demonstrated favorable intra-rater reliability (person separation reliability of 0.77), inter-rater reliability (80% to 100% agreement on each of the care behaviors), and validity (evidence of unidimensionality and good fit of the items). Adaptations accommodated for data collection in a hospital environment and alteration to UK nomenclature.
Three blinded volunteer assessors undertook observations. The observers monitored for activity in any 1 of 8 functional domains: bed mobility, transfers, mobility, washing and dressing, exercise, hygiene (mouth care/shaving/hair/nail care), toileting, and eating. Patient activity observed within these domains was identified as either a restorative or custodial care event. For example: “asks or encourages patient to walk/independently propel wheelchair to bathroom/toilet/day room/activities and gives them time to perform activity” was identified as a restorative care event, while “utilizes wheelchair instead of encourages ambulation and does not encourage patient to self-propel” was considered a custodial care event. All observations were carried out by student physical therapists in training or physical therapy assistants, all of whom were familiar in working in the acute facility with hospitalized older people. In an attempt to optimize internal consistency, observer skill was quality-controlled by ensuring observers were trained and their competency assessed in the use of the evaluation measurement tool.
Bays of 3 to 6 beds comprised each observation space. Three 90-minute time epochs were selected for observation—awakening (early morning), lunchtime (middle of the day), and afternoon (before evening meal)—with the aim that each time frame be observed on a minimum of 1 occasion on each of the 5 wards to generate a minimum of 15 observation sessions. Resources dictated observational periods to be 90-minutes maximum, per epoch, on weekdays only. The mean (range) time between the didactic study day and the ward-based practice day was 4 (1–8) weeks, and between the ward-based practice day and the second observational period was 6 (1–14) weeks.
Patient Characteristics
Differences in the acuity of patients between pre- and post-QI activity in the observational environments could influence care demands. Therefore, patient characteristics before and after the QI activity were measured to assess for stability. Prior to each session, observers recorded patient demographic details and current STRATIFY score, a predictive tool used at the time to segment fall risk [21], from patients’ clinical records. Two measures were used to offer contemporaneous representation of the observed population in the observation environment: a modified Barthel index [22], which provides a measure of activities of daily living [23], and the Abbreviated Mental Test Score [24], a simple diagnostic screen for cognitive impairment. All patients were considered as recuperating and thus eligible for observation except those with a “Patient-At-Risk” score ≥ 4, indicating physiological factors associated with established or impending critical illness [25], or if an end of life care plan was clearly detailed in the clinical record.
Data Analysis
Patient demographics are reported descriptively. Ordinal data are summarized using median and inter-quartile ranges (IQR), interval/ratio data using mean and standard deviation (SD) unless otherwise stated. Categorical data are reported as percentages. Comparison of observed patient samples before and after the QI period were compared with the Mann-Whitney U-test for ordinal data, 2 sample t tests for interval/ratio data, and chi squared tests of proportions for other variables.
Analyses were carried out using STATA 11 ME (StataCorp, College Station, TX) and SPSS v17 (SPSS, Chicago). Statistical significance was set at P ≤ 0.05.
Ethical Issues
This study was approved by the local UK NHS Trust clinical audit committee (Quality Improvement project 2038).
Results
Care Events by NAs
Observations were undertaken across the 5 wards on 14 workdays (Monday–Friday) over 6 weeks in the pre-QI period, and on 16 workdays over 4 weeks in the post-QI period, yielding a total of 51 hours of observation.
Overall, across all care environments, there was a statistically significant proportional increase in restorative care from 74% to 92% [χ2(1) 9.53, P = 0.002] (Figure 2). This represents an increase in restorative care events from 40 to 94. Observed custodial care events decreased from 14 to 8, a 43% reduction in custodial care events overall, a difference which remained irrespective of the environment (acute or subacute care), pre- and post-QI activity (P = 0.538 and P = 0.695, respectively).
There was a marked decrease in the number of patients receiving no NA-led restorative care events from 59 (74%) to 32 (48%) before and after QI activity respectively, [χ2 (1) 10.63, P = 0.001].
Patients Observed
Patient population characteristics remained stable during the course of the QI activity; there were no significant differences in the observed patient characteristics pre- and post-QI activity (Table). In 51 hours of observation undertaken by 3 independent observers there were 80 and 71 occupied beds before and after QI activity, respectively, representing a stable bed occupancy rate of 94% and 83% (P = 0.074). Of the occupied beds, 98.7% and 98.6% of patients (pre- and post-QI activity, respectively) were considered recuperating and therefore appropriate for a restorative care approach.
Discussion
although significantly decreased from pre-QI proportions (74%). We therefore conclude that a meaningful decrease across patients receiving no restorative care and a meaningful increase in within-patient restorative care events post-QI intervention occurred.
Our study furthers research in methods of increasing restorative care events delivered by NAs. In a randomized controlled trial by Resnick et al [16], a structured 6-week restorative care program incorporating teaching NAs
restorative care philosophies (tier 1) and facilitating NAs to motivate residents to engage in functional activities (tier 2) was compared to placebo (a single 30-minute educational session in managing residents’ behavioral symptoms) [16]. Results showed the 6-week program led to more restorative care, with NAs demonstrating enhanced knowledge and expectations of restorative care outcomes and better job satisfaction. Our educational package (1 day) and ward-based-learning session (3–4 hours) was much shorter than Resnick et al’s 6-week intervention [16], and the optimal dose of educational packages for NAs is yet to be determined and needs to be addressed in future studies. Furthermore, while we found education increased restorative care across multiple environments, it is yet to be determined whether more restorative care has a positive impact on patient function downstream of an acute inpatient stay. In fact, determination of restorative care’s influence on augmenting rehabilitation outcomes is a neglected aspect of nursing-AHP practice that we aim to define and investigate in ongoing studies.
The patient population characteristics within the target wards were stable over the course of the QI project. Observed patients’ median Barthel (11) and Abbreviated Mental Test (6) scores remained stable and are indicative of high levels of day-to-day activity dependence [24,26–28]. Over the QI activity period it was therefore unsurprising that modest proportions of patients direc-ted their own care (28% and 33% pre and post-QI, respectively). Subsequently, demands on staff to lead patient care were substantial, leading to high risks of social or clinical iatrogenesis and hospital-associated deconditioning.
In a previous observational study, substantial patient inactivity was found in a highly dependent cohort of patients [29]. Fear of falling and insignificant emphasis on ambulation were cited as patient and organizational-centric reasons, respectively. Furthermore, in a selective observational study, patients receiving function-focused care (FFC; synonymous to restorative care) in an acute hospital environment developed less physical functional decline compared to those receiving custodial care [30]. However, patients who had fallen during their hospital stay received less FFC. The authors suggest limited FFC in fallers was deployed to minimize further risk but concluded there is need for nursing and therapy interventions that manage fall risks through endorsing functional activities instead of mobility restriction [30].
Limitations
While observational studies are more robust for measuring behavioral activities compared to self or proxy reporting [34], they are exposed to observer judgment and drift. An attempt was made to minimize this with the binary measurement of restorative versus custodial care and by random sampling of wards and time frames to capture an entire healthcare environment.
The observational study tool was based on one previously developed where acceptable reliability and validity was established and where observations were based on what individual care staff were practicing regardless of their operational environment [20]. In contrast, our observations were based in predetermined environmental spaces regardless of what care practice occurred within it. We consider our approach justifiable in minimizing observer influence on an individual’s practice by emphasizing to them that observers were interested in what happened in an environment [35,36]. However, we acknowledge the risk of under representation of care by observers not following the care delivery, and that local validity and reliability of our methods was not undertaken. Lastly, whilst training for observers was undertaken in this study to standardize the observations undertaken, validation of this method would be a feature required of any future experimental work.
Conclusions
Our findings support the current understanding of restorative care [14–16] and provides proof of concept that dedicating resources in a previously under-invested part of the workforce is feasible, well-accepted, and meaningful. The results are in keeping with the concept that the NA staff group is ready and able to fulfil their roles as direct caregivers, supporting and relieving other trained staff [11].
Corresponding author: Gareth D. Jones, MSc, Physiotherapy Dept, 3rd Fl Lambeth Wing, St Thomas’ Hospital, Westminster Bridge Rd, London SE1 7EH, UK, [email protected].
Funding/support: This work was supported by a small grants application to the Guy's and St Thomas' Charity, project code S100414.
Financial disclosures: No conflicts of interest to declare.
Acknowledgment: The authors acknowledge members of the steering group for their input: Rebekah Schiff, Carrie-Ann Wood, Judith Centofanti, Judith Hall, and Richard Page; Anne Bisset-Smith and Claudia Jacob for their initial pilot work; Amanda Buttery, Lottie Prowse, and Ryan Mackie for practical assistance; Siobhan Crichton for her statistical help; and Jacky Jones, Michael Thacker, Tisha Pryor, and Sarah Ritchie for helping review the manuscript.
Abstract
- Background: Acute and prolonged exposure to hospital medical care can cause hospital-associated deconditioning with deleterious effects on patient care provision and quality of life. Physical rehabilitation provided by allied healthcare professionals can enable reacquisition of function via professional input into attainment of set goals. Separate to rehabilitative efforts, restorative care optimizes independence by motivating individuals to maintain and restore function. Nursing assistants (NAs) provide a significant amount of direct patient care and are well placed to deliver restorative care.
- Objective: To increase proportional restorative care interactions with hospitalized older adults by training NAs.
- Methods: A prospective cohort quality improvement (QI) project was undertaken at 3 acute hospital wards (patient minimum age 65 years) and 2 community subacute care wards in the UK. NAs working within the target settings received a 2-part restorative care training package. The primary evaluation tool was 51 hours in total of observation measuring the proportional change in restorative care events delivered by NAs.
- Results: NA-led restorative care events increased from 40 (pre-intervention) to 94 (post-intervention), representing a statistically significant proportional increase from 74% to 92% (χ2(1) 9.53, P = 0.002). NAs on occasions inadvertently emphasized restriction of function to manage risk and oblige with rest periods.
- Conclusion: Investing in NAs can influence the amount of restorative care delivered to hospitalized older adults at risk of hospital-associated deconditioning. Continued investment in NAs is indicated to influence top-down, mandated restorative care practice in this patient group.
Key words: older people; restorative care; hospital associated deconditioning; nursing assistants; rehabilitation; training.
Hospital-associated deconditioning is defined as a significant decline in functional abilities developed through acute and prolonged exposure to a medical care facility environment, and is independent of that attributed to primary pathologies resulting in acute admission [1]. Considerable research on iatrogenic complications in older hospitalized populations [1–5] has shown the impacts of hospital-associated deconditioning and associated dysfunctions on quality of life for patients and the resultant burden on health and social care provision [6].
Physical rehabilitation has been shown to restore function through high-dose repetition of task-specific activity [7], and the benefits attributed to extra physical therapy include improved mobility, activity, and participation [8]. Simply defined, physical rehabilitation is the reacquisition of function through multidisciplinary assessment and professional therapeutic input in attainment of set goals. A more recent nomenclature in health settings is “restorative care,” defined as a philosophy of care that encourages, enables, and motivates individuals to maintain and restore function, thereby optimizing independence [9]. It has been clearly defined as a philosophy separate from that of rehabilitation [9] and remote from task-related or “custodial care,” which is designed to assist in meeting patients’ daily activity needs without any therapeutic value.
In UK rehabilitation wards, nursing staff provide 4.5 times as much direct patient care time compared with allied health professionals, with paraprofessional nursing assistants (NAs, equivalent to certified nurse assistants [CNAs] in the United States) responsible for half of this direct nursing care [10]. Kessler’s group examined the evolving role of NAs in UK hospitals [11]. From a national survey of 700 NAs and 600 trained nurses, the authors upheld the view that NAs act as direct caregivers including through routine tasks traditionally delivered by nurses. They identified that NAs exhibit distinct qualities, which are valued by qualified nurses, including routine task fulfilment and abilities relating to patients, which enable NAs to enhance care quality. Indeed, the national findings of Kessler’s group were generalizable to our own clinical setting where a NA cohort was a well-placed, available, and motivated resource to deliver therapeutically focused care for our hospitalized older population.
The theoretical relationship between care approaches is complex and represents a challenge for service users and policy makers. For instance, comprehensive rehabilitation delivery during an acute care episode may lead to users not seeking custodial care at home. Conversely, day-to-day activities realized by custodial care at home may lead to users not seeking acute rehabilitative care [12]. With stable resources being assigned to more dependent users in higher numbers, reactive care regardless of environment has often been the model of choice.
However, an economic rationale has developed more recently where investment in maintenance and preventative models results in healthcare savings with models including the 4Rs; reablement, reactivation, rehabilitation, and restorative care [13]. In North America, restorative care approaches have resulted in favorable results in nursing home facilities [14] and at home [15], and restorative care education and motivation training for nursing assistants was effective in supporting a change in beliefs and practice behaviors [16]. While results show restorative care practices in the non-acute care sector are advantageous, it is unknown whether these approaches if adopted in hospital settings affect subsequent healthcare utilization in the non-acute facilities, or even if they are feasible to implement in acute facilities by a staff group able to do so. Therefore, the purpose of this QI project was to deploy a restorative care educational intervention for NA staff working with hospitalized older adults with the aim of increasing the proportion of restorative care delivered.
Methods
Context
This project was conducted at a UK National Health Service university teaching hospital trust at 3 acute hospital wards (patient minimum age 65 years) and 2 community subacute care wards for older patients. Participants consisted of all permanent or long-term temporary (> 3 months continuous employment) NAs working in the target settings (n = 36). The QI project design is summarized in Figure 1. The project applied the 4Es translational approach to regulate the QI intervention: Engage, Educate, Execute, and Evaluate [17]. The reporting of this study follows SQUIRE guidance [18].
Intervention
The QI activity was a holistic educational process for all NA participants.
Didactic Study Day
Each NA attended a study day led by a physical therapist (up to 10 NAs per group). A student-centered training approach was adopted, recognizing variations in adult learning styles [19], and included seminar style theory, video case scenarios, group work, practical skills, open discussion, and reflection. The training package outline was compiled following consensus among the multi-disciplinary team working in the target settings and the steering group. Topics covered were theory on the risk of hospitalization and benefits of early mobilization; case scenarios and examples of restorative care; identifying and overcoming barriers to restorative care; identifying appro-priate patients for a restorative care approach; practical skills, including assisting patients out of bed, ambulation, and eating/drinking; and challenging, problem-solving scenarios. All participants received a course handbook to facilitate learning.
Ward-Based Practice
Measures
Type of Care Event
The quantity and nature of all NA-patient functional task-related care events was established by independent systematic observation pre- and post-intervention. Observers rated the type of care for observed patients as either custodial or restorative events using a tool described below. In addition, the numbers of patients receiving no restorative care events at all during observation was calculated to capture changes in rates between patients observed. The observational tool used was adapted from that utilized in a North American study of a long-term care facility [20], which demonstrated favorable intra-rater reliability (person separation reliability of 0.77), inter-rater reliability (80% to 100% agreement on each of the care behaviors), and validity (evidence of unidimensionality and good fit of the items). Adaptations accommodated for data collection in a hospital environment and alteration to UK nomenclature.
Three blinded volunteer assessors undertook observations. The observers monitored for activity in any 1 of 8 functional domains: bed mobility, transfers, mobility, washing and dressing, exercise, hygiene (mouth care/shaving/hair/nail care), toileting, and eating. Patient activity observed within these domains was identified as either a restorative or custodial care event. For example: “asks or encourages patient to walk/independently propel wheelchair to bathroom/toilet/day room/activities and gives them time to perform activity” was identified as a restorative care event, while “utilizes wheelchair instead of encourages ambulation and does not encourage patient to self-propel” was considered a custodial care event. All observations were carried out by student physical therapists in training or physical therapy assistants, all of whom were familiar in working in the acute facility with hospitalized older people. In an attempt to optimize internal consistency, observer skill was quality-controlled by ensuring observers were trained and their competency assessed in the use of the evaluation measurement tool.
Bays of 3 to 6 beds comprised each observation space. Three 90-minute time epochs were selected for observation—awakening (early morning), lunchtime (middle of the day), and afternoon (before evening meal)—with the aim that each time frame be observed on a minimum of 1 occasion on each of the 5 wards to generate a minimum of 15 observation sessions. Resources dictated observational periods to be 90-minutes maximum, per epoch, on weekdays only. The mean (range) time between the didactic study day and the ward-based practice day was 4 (1–8) weeks, and between the ward-based practice day and the second observational period was 6 (1–14) weeks.
Patient Characteristics
Differences in the acuity of patients between pre- and post-QI activity in the observational environments could influence care demands. Therefore, patient characteristics before and after the QI activity were measured to assess for stability. Prior to each session, observers recorded patient demographic details and current STRATIFY score, a predictive tool used at the time to segment fall risk [21], from patients’ clinical records. Two measures were used to offer contemporaneous representation of the observed population in the observation environment: a modified Barthel index [22], which provides a measure of activities of daily living [23], and the Abbreviated Mental Test Score [24], a simple diagnostic screen for cognitive impairment. All patients were considered as recuperating and thus eligible for observation except those with a “Patient-At-Risk” score ≥ 4, indicating physiological factors associated with established or impending critical illness [25], or if an end of life care plan was clearly detailed in the clinical record.
Data Analysis
Patient demographics are reported descriptively. Ordinal data are summarized using median and inter-quartile ranges (IQR), interval/ratio data using mean and standard deviation (SD) unless otherwise stated. Categorical data are reported as percentages. Comparison of observed patient samples before and after the QI period were compared with the Mann-Whitney U-test for ordinal data, 2 sample t tests for interval/ratio data, and chi squared tests of proportions for other variables.
Analyses were carried out using STATA 11 ME (StataCorp, College Station, TX) and SPSS v17 (SPSS, Chicago). Statistical significance was set at P ≤ 0.05.
Ethical Issues
This study was approved by the local UK NHS Trust clinical audit committee (Quality Improvement project 2038).
Results
Care Events by NAs
Observations were undertaken across the 5 wards on 14 workdays (Monday–Friday) over 6 weeks in the pre-QI period, and on 16 workdays over 4 weeks in the post-QI period, yielding a total of 51 hours of observation.
Overall, across all care environments, there was a statistically significant proportional increase in restorative care from 74% to 92% [χ2(1) 9.53, P = 0.002] (Figure 2). This represents an increase in restorative care events from 40 to 94. Observed custodial care events decreased from 14 to 8, a 43% reduction in custodial care events overall, a difference which remained irrespective of the environment (acute or subacute care), pre- and post-QI activity (P = 0.538 and P = 0.695, respectively).
There was a marked decrease in the number of patients receiving no NA-led restorative care events from 59 (74%) to 32 (48%) before and after QI activity respectively, [χ2 (1) 10.63, P = 0.001].
Patients Observed
Patient population characteristics remained stable during the course of the QI activity; there were no significant differences in the observed patient characteristics pre- and post-QI activity (Table). In 51 hours of observation undertaken by 3 independent observers there were 80 and 71 occupied beds before and after QI activity, respectively, representing a stable bed occupancy rate of 94% and 83% (P = 0.074). Of the occupied beds, 98.7% and 98.6% of patients (pre- and post-QI activity, respectively) were considered recuperating and therefore appropriate for a restorative care approach.
Discussion
although significantly decreased from pre-QI proportions (74%). We therefore conclude that a meaningful decrease across patients receiving no restorative care and a meaningful increase in within-patient restorative care events post-QI intervention occurred.
Our study furthers research in methods of increasing restorative care events delivered by NAs. In a randomized controlled trial by Resnick et al [16], a structured 6-week restorative care program incorporating teaching NAs
restorative care philosophies (tier 1) and facilitating NAs to motivate residents to engage in functional activities (tier 2) was compared to placebo (a single 30-minute educational session in managing residents’ behavioral symptoms) [16]. Results showed the 6-week program led to more restorative care, with NAs demonstrating enhanced knowledge and expectations of restorative care outcomes and better job satisfaction. Our educational package (1 day) and ward-based-learning session (3–4 hours) was much shorter than Resnick et al’s 6-week intervention [16], and the optimal dose of educational packages for NAs is yet to be determined and needs to be addressed in future studies. Furthermore, while we found education increased restorative care across multiple environments, it is yet to be determined whether more restorative care has a positive impact on patient function downstream of an acute inpatient stay. In fact, determination of restorative care’s influence on augmenting rehabilitation outcomes is a neglected aspect of nursing-AHP practice that we aim to define and investigate in ongoing studies.
The patient population characteristics within the target wards were stable over the course of the QI project. Observed patients’ median Barthel (11) and Abbreviated Mental Test (6) scores remained stable and are indicative of high levels of day-to-day activity dependence [24,26–28]. Over the QI activity period it was therefore unsurprising that modest proportions of patients direc-ted their own care (28% and 33% pre and post-QI, respectively). Subsequently, demands on staff to lead patient care were substantial, leading to high risks of social or clinical iatrogenesis and hospital-associated deconditioning.
In a previous observational study, substantial patient inactivity was found in a highly dependent cohort of patients [29]. Fear of falling and insignificant emphasis on ambulation were cited as patient and organizational-centric reasons, respectively. Furthermore, in a selective observational study, patients receiving function-focused care (FFC; synonymous to restorative care) in an acute hospital environment developed less physical functional decline compared to those receiving custodial care [30]. However, patients who had fallen during their hospital stay received less FFC. The authors suggest limited FFC in fallers was deployed to minimize further risk but concluded there is need for nursing and therapy interventions that manage fall risks through endorsing functional activities instead of mobility restriction [30].
Limitations
While observational studies are more robust for measuring behavioral activities compared to self or proxy reporting [34], they are exposed to observer judgment and drift. An attempt was made to minimize this with the binary measurement of restorative versus custodial care and by random sampling of wards and time frames to capture an entire healthcare environment.
The observational study tool was based on one previously developed where acceptable reliability and validity was established and where observations were based on what individual care staff were practicing regardless of their operational environment [20]. In contrast, our observations were based in predetermined environmental spaces regardless of what care practice occurred within it. We consider our approach justifiable in minimizing observer influence on an individual’s practice by emphasizing to them that observers were interested in what happened in an environment [35,36]. However, we acknowledge the risk of under representation of care by observers not following the care delivery, and that local validity and reliability of our methods was not undertaken. Lastly, whilst training for observers was undertaken in this study to standardize the observations undertaken, validation of this method would be a feature required of any future experimental work.
Conclusions
Our findings support the current understanding of restorative care [14–16] and provides proof of concept that dedicating resources in a previously under-invested part of the workforce is feasible, well-accepted, and meaningful. The results are in keeping with the concept that the NA staff group is ready and able to fulfil their roles as direct caregivers, supporting and relieving other trained staff [11].
Corresponding author: Gareth D. Jones, MSc, Physiotherapy Dept, 3rd Fl Lambeth Wing, St Thomas’ Hospital, Westminster Bridge Rd, London SE1 7EH, UK, [email protected].
Funding/support: This work was supported by a small grants application to the Guy's and St Thomas' Charity, project code S100414.
Financial disclosures: No conflicts of interest to declare.
Acknowledgment: The authors acknowledge members of the steering group for their input: Rebekah Schiff, Carrie-Ann Wood, Judith Centofanti, Judith Hall, and Richard Page; Anne Bisset-Smith and Claudia Jacob for their initial pilot work; Amanda Buttery, Lottie Prowse, and Ryan Mackie for practical assistance; Siobhan Crichton for her statistical help; and Jacky Jones, Michael Thacker, Tisha Pryor, and Sarah Ritchie for helping review the manuscript.
1. Kortebein P. Rehabilitation for hospital-associated deconditioning. Am J Phys Med Rehabil 2009;88:66–77.
2. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med 1993;118:219–23.
3. Davydow DS, Hough CL, Levine DA, et al. Functional disability, cognitive impairment, and depression after hospitalization for pneumonia. Am J Med 2013;126:615–24.e5.
4. Sager MA, Franke T, Inouye SK, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 1996;156:645–52.
5. Warshaw GA, Moore JT, Friedman SW, et al. Functional disability in the hospitalized elderly. JAMA 1982;248:847–50.
6. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: "She was probably able to ambulate, but I'm not sure". JAMA 2011;306:1782–93.
7. Kwakkel G, Kollen B, Lindeman E. Understanding the pattern of functional recovery after stroke: facts and theories. Restor Neurol Neurosci 2004;22:281–99.
8. Peiris CL, Taylor NF, Shields N. Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med
Rehabil 2011;92:1490–500.
9. Resnick B, Boltz M, Galik E, Pretzer-Aboff I. Restorative care nursing for older adults: a guide for all care settings. 2nd ed. New York: Springer; 2012.
10. Rudd AG, Jenkinson D, Grant RL, Hoffman A. Staffing levels and patient dependence in English stroke units. Clin Med (Lond). 2009;9:110–5.
11. Kessler I, Heron P, Dopson S, et al. The nature and consequences of support workers in a hospital setting, Final Report. London: National Institute for Health Research, Service Delivery and Organization Programme; 2010.
12. Kashner TM, Krompholz B, McDonnell C, et al. Acute and custodial care among impaired aged. J Aging Health 1990;2:28–41.
13. Sims-Gould J, Tong CE, Wallis-Mayer L, Ashe MC. Reablement, reactivation, rehabilitation and restorative interventions with older adults in receipt of home care: a systematic review. J Am Med Dir Assoc 2017;18:653–63.
14. Shanti C, Johnson J, Meyers AM, et al. Evaluation of the restorative care education and training program for nursing homes. Can J Aging 2005;24:115–26.
15. Tinetti ME, Baker D, Gallo WT, et al. Evaluation of restorative care vs usual care for older adults receiving an acute episode of home care. JAMA 2002;287:2098–105.
16. Resnick B, Gruber-Baldini AL, Galik E, et al. Changing the philosophy of care in long-term care: testing of the restorative care intervention. Gerontologist 2009;49:175–84.
17. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008;337:a1714.
18. Davidoff F, Batalden P, Stevens D, et al; SQUIRE development group. Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ 2009;338:a3152.
19. Sweeney JF. Nurse education: learner-centred or teacher-centred? Nurse Educ Today 1986;6:257–62.
20. Resnick B, Rogers V, Galik E, Gruber-Baldini AL. Measuring restorative care provided by nursing assistants: reliability and validity of the Restorative Care Behavior Checklist. Nurs Res 2007;56:387–98.
21. Oliver D, Britton M, Seed P, et al. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ 1997;315:1049–53.
22. Colin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud 1988;10:61–3.
23. Richards SH, Peters TJ, Coast J, et al. Inter-rater reliability of the Barthel ADL index: how does a researcher compare to a nurse? Clin Rehabil 2000;14:72–8.
24. Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972;1:233–8.
25. Morgan CD, Baade LE. Neuropsychological testing and assessment scales for dementia of the Alzheimer's type. Psychiatr Clin North Am 1997;20:25–43.
26. Granger CV, Hamilton BB, Gresham GE, Kramer AA. The stroke rehabilitation outcome study: Part II. Relative merits of the total Barthel index score and a four-item subscore in predicting patient outcomes. Arch Phys Med Rehabil
1989;70:100–3.
27. MacKenzie DM, Copp P, Shaw RJ, Goodwin GM. Brief cognitive screening of the elderly: a comparison of the Mini-Mental State Examination (MMSE), Abbreviated Mental Test (AMT) and Mental Status Questionnaire (MSQ). Psychol Med
1996;26:427–30.
28. Uyttenboogaart M, Stewart RE, Vroomen PC, et al. Optimizing cutoff scores for the Barthel index and the modified Rankin scale for defining outcome in acute stroke trials. Stroke 2005;36:1984–7.
29. Callen BL, Mahoney JE, Grieves CB, et al. Frequency of hallway ambulation by hospitalized older adults on medical units of an academic hospital. Geriatr Nurs 2004;25:212–7.
30. Boltz M, Resnick B, Capezuti E, Shuluk J. Activity restriction vs. self-direction: hospitalised older adults' response to fear of falling. Int J Older People Nurs 2014;9:44–53.
31. Moyle W, Borbasi S, Wallis M, et al. Acute care management of older people with dementia: a qualitative perspective. J Clin Nurs 2011;20:420–8.
32. Olson DM, Borel CO, Laskowitz DT, et al. Quiet time: a nursing intervention to promote sleep in neurocritical care units. Am J Crit Care 2001;10:74–8.
33. Gardner C, Collins C, Osborne S, et al. Creating a therapeutic environment: a non-randomised controlled trial of a quiet time intervention for patients in acute care. Int J Nurs Stud 2009;46:778–86.
34. Kupek E. Bias and heteroscedastic memory error in self-reported health behavior: an investigation using covariance structure analysis. BMC Med Res Methodol 2002;2:14.
35. Fromme HB, Karani R, Downing SM. Direct observation in medical education: a review of the literature and evidence for validity. Mt Sinai J Med 2009;76:365–71.
36. Williams RG, Klamen DA, McGaghie WC. Cognitive, social and environmental sources of bias in clinical performance ratings. Teach Learn Med 2003;15:270–92.
1. Kortebein P. Rehabilitation for hospital-associated deconditioning. Am J Phys Med Rehabil 2009;88:66–77.
2. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med 1993;118:219–23.
3. Davydow DS, Hough CL, Levine DA, et al. Functional disability, cognitive impairment, and depression after hospitalization for pneumonia. Am J Med 2013;126:615–24.e5.
4. Sager MA, Franke T, Inouye SK, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 1996;156:645–52.
5. Warshaw GA, Moore JT, Friedman SW, et al. Functional disability in the hospitalized elderly. JAMA 1982;248:847–50.
6. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: "She was probably able to ambulate, but I'm not sure". JAMA 2011;306:1782–93.
7. Kwakkel G, Kollen B, Lindeman E. Understanding the pattern of functional recovery after stroke: facts and theories. Restor Neurol Neurosci 2004;22:281–99.
8. Peiris CL, Taylor NF, Shields N. Extra physical therapy reduces patient length of stay and improves functional outcomes and quality of life in people with acute or subacute conditions: a systematic review. Arch Phys Med
Rehabil 2011;92:1490–500.
9. Resnick B, Boltz M, Galik E, Pretzer-Aboff I. Restorative care nursing for older adults: a guide for all care settings. 2nd ed. New York: Springer; 2012.
10. Rudd AG, Jenkinson D, Grant RL, Hoffman A. Staffing levels and patient dependence in English stroke units. Clin Med (Lond). 2009;9:110–5.
11. Kessler I, Heron P, Dopson S, et al. The nature and consequences of support workers in a hospital setting, Final Report. London: National Institute for Health Research, Service Delivery and Organization Programme; 2010.
12. Kashner TM, Krompholz B, McDonnell C, et al. Acute and custodial care among impaired aged. J Aging Health 1990;2:28–41.
13. Sims-Gould J, Tong CE, Wallis-Mayer L, Ashe MC. Reablement, reactivation, rehabilitation and restorative interventions with older adults in receipt of home care: a systematic review. J Am Med Dir Assoc 2017;18:653–63.
14. Shanti C, Johnson J, Meyers AM, et al. Evaluation of the restorative care education and training program for nursing homes. Can J Aging 2005;24:115–26.
15. Tinetti ME, Baker D, Gallo WT, et al. Evaluation of restorative care vs usual care for older adults receiving an acute episode of home care. JAMA 2002;287:2098–105.
16. Resnick B, Gruber-Baldini AL, Galik E, et al. Changing the philosophy of care in long-term care: testing of the restorative care intervention. Gerontologist 2009;49:175–84.
17. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008;337:a1714.
18. Davidoff F, Batalden P, Stevens D, et al; SQUIRE development group. Publication guidelines for quality improvement studies in health care: evolution of the SQUIRE project. BMJ 2009;338:a3152.
19. Sweeney JF. Nurse education: learner-centred or teacher-centred? Nurse Educ Today 1986;6:257–62.
20. Resnick B, Rogers V, Galik E, Gruber-Baldini AL. Measuring restorative care provided by nursing assistants: reliability and validity of the Restorative Care Behavior Checklist. Nurs Res 2007;56:387–98.
21. Oliver D, Britton M, Seed P, et al. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ 1997;315:1049–53.
22. Colin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud 1988;10:61–3.
23. Richards SH, Peters TJ, Coast J, et al. Inter-rater reliability of the Barthel ADL index: how does a researcher compare to a nurse? Clin Rehabil 2000;14:72–8.
24. Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972;1:233–8.
25. Morgan CD, Baade LE. Neuropsychological testing and assessment scales for dementia of the Alzheimer's type. Psychiatr Clin North Am 1997;20:25–43.
26. Granger CV, Hamilton BB, Gresham GE, Kramer AA. The stroke rehabilitation outcome study: Part II. Relative merits of the total Barthel index score and a four-item subscore in predicting patient outcomes. Arch Phys Med Rehabil
1989;70:100–3.
27. MacKenzie DM, Copp P, Shaw RJ, Goodwin GM. Brief cognitive screening of the elderly: a comparison of the Mini-Mental State Examination (MMSE), Abbreviated Mental Test (AMT) and Mental Status Questionnaire (MSQ). Psychol Med
1996;26:427–30.
28. Uyttenboogaart M, Stewart RE, Vroomen PC, et al. Optimizing cutoff scores for the Barthel index and the modified Rankin scale for defining outcome in acute stroke trials. Stroke 2005;36:1984–7.
29. Callen BL, Mahoney JE, Grieves CB, et al. Frequency of hallway ambulation by hospitalized older adults on medical units of an academic hospital. Geriatr Nurs 2004;25:212–7.
30. Boltz M, Resnick B, Capezuti E, Shuluk J. Activity restriction vs. self-direction: hospitalised older adults' response to fear of falling. Int J Older People Nurs 2014;9:44–53.
31. Moyle W, Borbasi S, Wallis M, et al. Acute care management of older people with dementia: a qualitative perspective. J Clin Nurs 2011;20:420–8.
32. Olson DM, Borel CO, Laskowitz DT, et al. Quiet time: a nursing intervention to promote sleep in neurocritical care units. Am J Crit Care 2001;10:74–8.
33. Gardner C, Collins C, Osborne S, et al. Creating a therapeutic environment: a non-randomised controlled trial of a quiet time intervention for patients in acute care. Int J Nurs Stud 2009;46:778–86.
34. Kupek E. Bias and heteroscedastic memory error in self-reported health behavior: an investigation using covariance structure analysis. BMC Med Res Methodol 2002;2:14.
35. Fromme HB, Karani R, Downing SM. Direct observation in medical education: a review of the literature and evidence for validity. Mt Sinai J Med 2009;76:365–71.
36. Williams RG, Klamen DA, McGaghie WC. Cognitive, social and environmental sources of bias in clinical performance ratings. Teach Learn Med 2003;15:270–92.
Implementation of the ABCDEF Bundle in an Academic Medical Center
Abstract
- Objective: To describe the highlights of our medical center’s implementation of the Society of Critical Care Medicine’s ABCDEF bundle in 3 medical intensive care units (ICUs).
- Methods: After a review of our current clinical practices and written clinical guidelines, we evaluated deficiencies in clinical care and employed a variety of educational and clinical change interventions for each element of the bundle. We utilized an interdisciplinary team approach to facilitate the change process.
- Results: As a result of our efforts, improvement in the accuracy of assessments of pain, agitation, and delir-ium across all clinical disciplines and improved adherence to clinical practice guidelines, protocols, and instruments for all bundle elements was seen. These changes have been sustained following completion of the data collection phase of the project.
- Conclusion: ICU care is a team effort. As a result of participation in this initiative, there has been an increased awareness of the bundle elements, improved collaboration among team members, and increased patient and family communication.
Key words: intensive care; delirium; sedation; mobility.
Admission to the intensive care unit (ICU) is a stressful and challenging time for patients and their families. In addition, significant negative sequelae following an ICU stay have been reported in the literature, including such post-ICU complications as post-traumatic stress disorder [1–9], depression [10,11], ICU-acquired weakness [12–19], and post-intensive care syndrome [20–23]. Pain, anxiety, and delirium all contribute to patient distress and agitation, and the prevention or treatment of pain, anxiety, and delirium in the ICU is an important goal. The Society of Critical Care Medicine (SCCM) developed the ABCDEF bundle (Table) to facilitate implementation of their 2013 clinical practice guidelines for the management of pain, agitation, and delirium (PAD) [24]. The bundle emphasizes an integrated approach to assessing, treating and preventing significant pain, over or undersedation, and delirium in critically ill patients.
In 2015, SCCM began the ICU Liberation Collaborative, a clinical care collaborative designed to implement the ABCDEF bundle through team-based care at hospitals and health systems across the country. The Liberation Collaborative’s intent was to “liberate” patients from iatrogenic aspects of care [25]. Our medical center participated in the collaborative. In this article, we describe the highlights of our medical center’s implementation of the ABCDEF bundle in 3 medical ICUs.
Settings
The Ohio State University Wexner Medical Center is a 1000+–bed academic medical center located in Columbus, Ohio, containing more than 180 ICU beds. These ICU beds provide care to patients with medical, surgical, burn, trauma, oncology, and transplantation needs. The care of the critically ill patient is central to the organization’s mission “to improve people’s lives through innovation in research, education and patient care.”
At the start of our colloborative participation, all of the ABCDEF bundle elements were protocolized in these ICUs. However, there was a lack of knowledge of the content of the bundle elements and corresponding guidelines among all members of our interdisciplinary teams, and our written protocols and guidelines supporting many of the bundle elements had inconsistent application across the 3 clinical settings.
We convened an ABCDEF bundle/ICU liberation team consisting of an interdisciplinary group of clinicians. The team leader was a critical care clinical nurse specialist. The project required outcome and demographic data collection for all patients in the collaborative as well as concurrent (daily) data collection on each bundle element. The clinical pharmacists who work in the MICUs and are part of daily interdisciplinary rounds collected the daily bundle element data while the patient demographic and outcome data were collected by the clinical nurse specialist, nurse practitioner, and clinical quality manager. Oversight and accountability for the ABCDEF bundle/ICU liberation project was provided by an interdisciplinary critical care quality committee. Our ABCDEF bundle/ICU liberation team met weekly to discuss progress of the initiative and provided monthly updates to the larger quality committee.
Impacting the Bundle—Nursing Assessments
The PAD guidelines recommend the routine assessment of pain, agitation, and delirium in ICU patients. For pain, they recommend the use of patient self-report or the use of a behavioral pain scale as the most valid and reliable method for completing this assessment [24]. Our medical center had chosen to use the Critical Care Pain Observation Tool (CPOT), a valid and reliable pain scale, for assessment of pain in patients who are unable to communicate [26], which had been in use in the clinical setting for over a year when this project began. For agitation, the PAD guidelines recommended assessment of the adequacy and depth of sedation using the Richmond Agitation Sedation Scale (RASS) or Sedation Agitation Scale (SAS) [24] for all ICU patients. Our medical center has chosen to use the RASS as our delirium assessment. The RASS had been in use in the clinical setting for approximately 10 years when this project started. For delirium assessment, the Confusion Assessment Method for ICU (CAM-ICU) [27] or the Intensive Care Delirium Screening Checklist (ICDSC) [28] is recommended. Our medical center used the CAM-ICU, which had been in place for approximately 10 years prior to the start of this project. Even though the assessment tools were in place in our MICU unit and hospital-based policies and guidelines, the accuracy of the assessments for PAD was questioned by many clinicians.
To improve the accuracy of our nursing assessments for PAD, a group of clinical nurse specialists and nursing educators developed an education and competency program for all critical care nursing staff. This education program focused on the PAD guidelines and our medical center’s chosen assessment tools. Education included in-person continuing education lectures, online modules, demonstrations, and practice in the clinical setting. After several months of education and practice, all staff registered nurses (RNs) had to demonstrate PAD assessment competency on a live person. We used standardized patients who followed written scenarios for all of the testing. The RN was given 1 of 8 scenarios and was charged with completing a PAD assessment on the standardized patient. RNs who did not pass had to review the education materials and re-test at a later date. More than 600 RNs completed the PAD competency. After completion of the PAD competency, the clinical nurse specialists observed clinical practice and audited nursing documentation. The accuracy of assessments for PAD had increased. Anecdotally, many our critical care clinicians acknowledged that they had increased confidence in the accuracy of the PAD assessments. There was increased agreement between the results of the assessments performed by all members of the interdisciplinary team.
Impacting the Bundle—Standardized Nurse Early Report Facilitation
Communication among the members of the interdisciplinary team is essential in caring for critically ill patients. One of the ways that the members of the interdisciplinary team communicate is through daily patient rounds. Our ABCDEF bundle/ICU liberation team members attend and participate in daily patient rounds in our 3 MICUs on a regular basis. The ABCDEF bundle/ICU liberation team members wanted to improve communication during patient rounds for all elements of the bundle.
Nurse Early Report Facilitation was a standard that was implemented approximately 5 years prior to the start of the ICU Liberation Collaborative. Nurse early report facilitation requires that the bedside staff RN starts the daily patient rounds discussion on each of his/her patients. The report given by the bedside RN was designed to last 60 to 90 seconds and provide dynamic information on the patient’s condition. Requiring the bedside RN to start the patient rounding provides the following benefits: requires bedside RN presence, provides up-to-the-minute information, increases bedside RN engagement in the patient’s plan of care, and allows for questions and answers. Compliance from the bedside RNs with this process of beginning patient rounds was very high; however, the information that was shared when the bedside RN began rounds was variable. Some bedside RNs provided a lengthy report on the patient while others provided 1 or 2 words.
The ABCDEF bundle/ICU liberation team members thought that a way to hardwire the ABCDEF bundle elements would be to add structure to the nurse early report. By using the ABCDEF elements as a guide, the ABCDEF bundle/ICU liberation team members developed the Structured Nurse Early Report Facilitation in which the bedside RN provides the following information at the beginning of each patient discussion during rounds: name of patient, overnight events (travels, clinical changes, etc.), pain (pain score and PRN use), agitation (RASS and PRN use), delirium (results of CAM-ICU). When the bedside RN performs the nurse early report using the structured format, the team is primed to discuss the A, B, C, and D elements of the bundle.
To implement the Structured Nurse Early Report Facilitation in the MICUs, the critical care clinical nurse specialists provided in-person education at the monthly staff meetings. They also sent emails, developed education bulletin boards, made reminder cards that were placed on the in-room computers, and distributed “badge buddy” reminder cards that fit on the RNs’ hospital ID badges. We provided emails and in-person education to our physician and nurse practitioner teams so they were aware of the changes. Our physician and nurse practitioners were encouraged to ask for information about any elements missing from the Structured Nurse Early Report in the early days of the process change.
After a few months, the critical care clinical nurse specialists reported that the Structured Nurse Early Report Facilitation was occurring for more than 80% of MICU patients. Besides the increase in information related to pain, agitation, and delirium, the Structured Nurse Early Report Facilitation increased the interdisciplinary team’s use of the term “delirium.” Prior to the structured nurse early report, most of the interdisciplinary team members were not naming delirium as a diagnosis for our MICU patients and used terms such as ICU psychosis, confused, and disoriented to describe the mental status of patients with delirium. As a result of this lack of naming, there may have been a lack of recognition of delirium. Using the word “delirium” has increased our interdisciplinary team’s awareness of this diagnosis and has increased the treatment of delirium in patients who have the diagnosis.
In addition to improved assessment and diagnosis, the clinical pharmacist began leading the discussions around choice of sedation during daily rounds. Team members began to discuss the patient’s sedation level, sedation goals, and develop a plan for each patient. This discussion included input from all members of the interdisciplinary team and allowed for a comprehensive patient-specific plan to be formed during the daily patient rounds episode.
Impacting the Bundle—Focus on Mobility
There have been many articles published in the critical care literature on the topic of mobility in the ICU. The evidence shows that early mobilization and rehabilitation of patients in ICUs is safe and may improve physical function, and reduce the duration of delirium, mechanical ventilation, and ICU length of stay [29–31]. Our institution had developed a critical care mobility guideline in 2008 for staff RNs to follow in determining the level of mobility that the patient required during the shift. Over the years, the mobility guideline was used less and less. As other tasks and interventions became a priority, mobility became an intervention that was completed for very few patients.
Our ABCDEF bundle/ICU liberation team determined that increasing mobility of our MICU patients needed to be a plan of care priority. We organized an interdisciplinary team to discuss the issues and barriers to mobility for our MICU patients. The interdisciplinary mobility team had representatives from medicine, nursing, respiratory therapy, physical therapy, occupational therapy, and speech therapy. Initially, this team sent a survey to all disciplines who provided care for the patients in the MICU. Data from this survey was analyzed by the team to determine next steps.
Despite the fact that there were responses from 6 unique disciplines, several common barriers emerged. The largest barrier to overcome was staffing/time for mobility. It was clear from the survey respondents that all health care team members were busy providing patient care. Any change in the mobility guideline or practice needed to make efficient use of the practitioner’s time. Other barriers included space/equipment, communication, patient schedules, knowledge, patient and staff safety, and unit culture. The interdisciplinary mobility team divided into smaller workgroups to tackle the issues and barriers.
Mobility Rounds
Mobility rounds were implemented to attempt to decrease the barriers of time, communication, and know-ledge. Mobility rounds were designed as a start to the shift discussion on the topic of mobility. Mobility rounds included a clinical nurse specialist, a physical therapist (PT), an occupational therapist (OT), and a pulmonary physician/ nurse practitioner. This team met at 7:30 each weekday morning and walked room-to-room through our MICUs. The mobility rounds team laid eyes on each patient, developed a mobility plan for the day, and communicated this plan with the staff RN assigned to the patient. Mobility rounds were completed on all 48 MICU patients in 30 minutes.
Having the mobility rounds team at each patient’s bedside was important in several ways. First, it allowed the team members to see each patient, which gave the patient an opportunity to be part of his/her mobility plan. Also, the staff RNs and respiratory therapists (RTs) were often in the patient’s room. This improved communication as the staff RNs and RTs discussed the mobility plan with the PT and OT. For patients who required many resources for a mobility session, the morning bedside meeting allowed RNs, RTs, PTs, OTs, and physicians to set a schedule for the day’s mobility session. Having a scheduled time for mobility increased staff and patient communication. Also, it allowed all of the team members to adjust their workloads to be present for a complex mobility session.
Another benefit of mobility rounds was the opportunity for the PT and OT team members to provide education to their nursing and physician colleagues. Many nursing and physician providers do not understand the intricacies of physical and occupational therapy practice. This daily dialogue provided the PT/OT a forum to explain which patients would benefit from PT/OT services and which would not. It allowed the RNs and physicians to hear the type of therapy provided on past sessions. It allowed the PT/OT to discuss and evaluate the appropriateness of each patient consult. It allowed the RN and physician to communicate which patients they felt were highest priority for therapy for that day. Mobility rounds are ongoing. Data are being collected to determine the impact of mobility rounds on the intensity of mobility for our MICU patients.
Nurse-Driven Mobility Guideline
Another subgroup revised the outdated critical care mobility guideline and developed the new “Nurse-Driven Critical Care Mobility Guideline.” The guideline has been approved through all of the medical center quality committees and is in the final copyright and publication stages, with implementation training to begin in the fall. The updated guideline is in an easy-to-read flowchart format and provides the staff RN with a pathway to follow to determine if mobility is safe for the patient. After determining safety, the staff RN uses the guideline to determine and perform the patient’s correct mobility interventions for his/her shift. The guideline has built in consultation points with the provider team and the therapy experts.
Other Mobility Issues
A third subgroup from the interdisciplinary mobility team has been working on the equipment and space barriers. This subgroup is evaluating equipment such as bedside chairs, specialty beds, and assistive devices. Many of our MICU patient rooms have overhead lifts built into the ceilings. This equipment is available to all staff at all times. The equipment/space subgroup made sure that there were slings for use with the overhead lifts in all of the MICU equipment rooms. They provided staff education on proper use of the overhead lifts. They worked with the financial department and MICU nurse managers to purchase 2 bariatric chairs for patient use in the MICU.
A fourth subgroup has been working on the electronic documentation system. They are partnering with members of the information technology department to update the nursing and provider documentation regarding mobility. They have also worked on updating and elaborating on the electronic activity orders for our MICU patients. There have been many changes to various patient order sets to clarify mobility and activity restrictions. The admission order set for our MICU patients has an activity order that allows our staff RNs to fully utilize the new nurse-driven critical care mobility guideline.
Impacting the Bundle—Family Engagement and Empowerment
Family support is important for all hospitalized patients but is crucial for ICU patients. The medical center implemented an open visitation policy for all ICUs in 2015. Despite open visitation, the communication between patients, families, and interdisciplinary ICU teams was deficient. Families spoke to many different team members and had difficulty remembering all of the information that they received.
To increase family participation in the care of the MICU patient, we invited family members to participate in daily rounds. The families were invited to listen and encouraged to ask questions. During daily rounds, there is a time when all care providers stop talking and allow family members to inquire about the proposed plan of care for their family member. For family members who cannot attend daily rounds, our ICU teams arrange daily in-person or telephone meetings to discuss the patient’s plan of care. RNs provide a daily telefamily call to update the designated family member on the patient’s status, answer questions, and provide support.
In addition to the medical support for families, there is an art therapy program integrated into the ICU to assist families while they are in the medical center. This program is run by a certified art therapist who holds art therapy classes 2 afternoons a week. This provides family members with respite time during long hospital days. There are also nondenominational services offered multiple times during the week and a respite area is located in the lobby of the medical center.
In addition to these programs, the medical center added full-time social workers to be available 24 hours a day/ 7 days a week. The social worker can provide social support for our patients and families as well as help facilitate accommodations for those who travel a far distance. The social worker plays in integral part on the ICU team, often bridging the gap for families that can be overlooked by the medical team.
Conclusion
Care of the ICU patient is complex. Too often we work in our silos of responsibility with our list of tasks for the day. Participating in the ABCDEF bundle/ICU Liberation Collaborative required us to work together as a team. We were able to have candid conversations that improved our understanding of other team members’ perspectives, helping us to reflect on our behaviors and overcome barriers to improving patient care.
Even though the ICU Liberation Collaborative has ended, our work at the medical center continues. We are in the process of evaluating all of the interventions, processes, and guideline updates that our ABCEDF bundle/ICU liberation team worked on during our 18-month program. There have been many improvements such as increased accuracy of pain and delirium assessments, along with improved treatment of pain in the MICU patient. We have noticed increased communication with the patient and family and among all of the members of the interdisciplinary team. We have changed our language to accurately reflect the patient’s sedation level by using the correct RASS score and delirium status by using the term “delirium” when this condition exists. There is increased collaboration among team members in the area of mobility. More patients are out of bed on bedside chairs and more patients are walking in the halls. Over the next several months our ABCEDF bundle/ICU liberation team will continue to review and analyze the data that we collected in the collaborative. We will use that data and the clinical changes we see on a daily basis to continue to improve the care for our MICU patients.
Corresponding author: Michele L. Weber, DNP, RN, CCRN, CCNS, AOCNS, OCN, ANP-BC, The Ohio State University Wexner Medical Center, 410 West 10th Ave., Columbus, OH 43210, [email protected].
1. Svenningsen H, Egerod I, Christensen D, et al Symptoms of posttraumatic stress after intensive care delirium. Biomed Res Int 2015;2015:876–947.
2. Warlan H, Howland L. Posttraumatic stress syndrome associated with stays in the intensive care unit: importance of nurses; involvement. Crit Care Nurse 2015;35:44–52.
3. Bienvenu OJ, Gerstenblith TA. Posttraumatic stress disorder phenomena after critical illness. Crit Care Clin 2017;33:649–58.
4. Wintermann GB, Rosendahl J, Weidner K, et al. Risk factors of delayed onset posttraumatic stress disorder in chronically critically ill patients. J Nerv Ment Dis 2017 Jul 5.
5. Wolters AE, Peelen LM, Welling MC, et al. Long-term mental health problems after delirium in the ICU. Crit Care Med 2016;44:1808–13.
6. Wintermann GB, Weidner K, Stafuss B. Predictors of posttraumatic stress and quality of life in family members of chronically critically ill patients after intensive care Ann Intensive Care 2016;6:69.
7. Patel MD, Jackson JC, Morandi A et al. Incidence and risk factors for intensive care unit-related post-traumatic stress disorder in veterans and civilians Am J Respir Crit Care Med 2016;193:1373–81.
8. Girad TD, Shintani AK, Jackson JC et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care 2007;11:R28.
9. Jackson JC, Hart RP, Gordon SM, et al. Post-traumatic stress disorder and post-traumatic stress symptoms following critical illness in medical intensive care unit patients: assessing the magnitude of the problem. Crit Care 2007;11:R27.
10. Jackson JC, Pandharipande PP, Girad TD et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Resp Med 2014;2:369–79.
11. Davydow DS, Hough CL, Langa KM, Iwashyna TJ. Depressive symptoms in spouses of older patients with severe sepsis. Crit Care Med 2012;40:2335–41.
12. Farhan H, Moeno-Duarte I, Latronico N, et al. Acquired muscle weakness in the surgical intensive care unit: nosology, epidemiology, diagnosis and prevention. Anesthesiology 2016;124:207–34.
13. Stevens, RD, Zink EK. Inflammatory signatures in ICU-acquired weakness. Crit Care Med 2017;45:1098–100.
14. Lotronico, N, Herridge M, Hopkins O, et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med 2017 Mar 13.
15. Batt J, Herridge M, Dos Santos C. Mechanism of ICU-acquired weakness: skeletal muscle loss in critical illness. Intensive Care Med 2017 Mar 10.
16. Batt J, Mathur S, Katzberg HD. Mechanism of ICU-acquired weakness: muscle contractility in critical illness. Intensive Care Med 2017;43:584–86.
17. Schweickert WD, Hall J. ICU-acquired weakness. Chest 2007;131:1541–9.
18. Deem S. Intensive care unit-acquired muscle weakness. Repir Care 2006;51:1042–52.
19. Kahn J, Burnham EL, Moss M. Acquired weakness in the ICU: critical illness myopathy and polyneuropathy. Minerva Anesthesiol 2006;72:401–6.
20. Jeitziner MM, Hamers JP, Burgin R et al. Long-term consequences of pain, anxiety, and agitation for critically ill older patients after an intensive care unit stay. J Clin Nurs 2015;24:2419–28.
21. Svennigsen H, Langhorn L, Agard AS, Dereyer P. Post-ICU symptoms, consequences, and follow-up: an integrative review. Nurs Crit Care 2017;22:212–20.
22. Torres J, Carvalho D, Molinos E et al. The impact of the patient post-intensive care syndrome components upon caregiver burden. Med Intensiva 2017 Feb 7
23. Rawal G, Yadav S, Sumar R. Post-Intensive care syndrome: an overview. J Transl Int Med 2017;305:90–2.
24. Barr J, Fraser GL, Puntillo K , et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
25. Ely EW. The ABCDEF bundle: science and philosophy of how ICU liberation serves patients and families. Crit Care Med 2017;45:321–30.
26. Gelinas C, Fillion L, Puntillo K, et al. Validation of the critical-care pain observation tool in adult patients. Am J Crit Care 2006;15:420–7.
27. Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001;29:1370–9.
28. Bergeron N, Dubois MJ, Dumont M, et al. Intensive Care Delirium Screening Checklist: Evaluation of a new screening tool. Intensive Care Med 2001;27:859–64.
29. Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med 2007;35:139–45.
30. Morris PE. Moving our critically ill patients: Mobility barriers and benefits. Crit Care Clin 2007;23:1–20.
31. Nydahl P, Sricharoenchai T, Chandra S, et al. Safety of patient mobilization and rehabilitation in the intensive care unit. Systematic review with meta-analysis. Ann Am Thorac Soc 2017;14:766–77.
Abstract
- Objective: To describe the highlights of our medical center’s implementation of the Society of Critical Care Medicine’s ABCDEF bundle in 3 medical intensive care units (ICUs).
- Methods: After a review of our current clinical practices and written clinical guidelines, we evaluated deficiencies in clinical care and employed a variety of educational and clinical change interventions for each element of the bundle. We utilized an interdisciplinary team approach to facilitate the change process.
- Results: As a result of our efforts, improvement in the accuracy of assessments of pain, agitation, and delir-ium across all clinical disciplines and improved adherence to clinical practice guidelines, protocols, and instruments for all bundle elements was seen. These changes have been sustained following completion of the data collection phase of the project.
- Conclusion: ICU care is a team effort. As a result of participation in this initiative, there has been an increased awareness of the bundle elements, improved collaboration among team members, and increased patient and family communication.
Key words: intensive care; delirium; sedation; mobility.
Admission to the intensive care unit (ICU) is a stressful and challenging time for patients and their families. In addition, significant negative sequelae following an ICU stay have been reported in the literature, including such post-ICU complications as post-traumatic stress disorder [1–9], depression [10,11], ICU-acquired weakness [12–19], and post-intensive care syndrome [20–23]. Pain, anxiety, and delirium all contribute to patient distress and agitation, and the prevention or treatment of pain, anxiety, and delirium in the ICU is an important goal. The Society of Critical Care Medicine (SCCM) developed the ABCDEF bundle (Table) to facilitate implementation of their 2013 clinical practice guidelines for the management of pain, agitation, and delirium (PAD) [24]. The bundle emphasizes an integrated approach to assessing, treating and preventing significant pain, over or undersedation, and delirium in critically ill patients.
In 2015, SCCM began the ICU Liberation Collaborative, a clinical care collaborative designed to implement the ABCDEF bundle through team-based care at hospitals and health systems across the country. The Liberation Collaborative’s intent was to “liberate” patients from iatrogenic aspects of care [25]. Our medical center participated in the collaborative. In this article, we describe the highlights of our medical center’s implementation of the ABCDEF bundle in 3 medical ICUs.
Settings
The Ohio State University Wexner Medical Center is a 1000+–bed academic medical center located in Columbus, Ohio, containing more than 180 ICU beds. These ICU beds provide care to patients with medical, surgical, burn, trauma, oncology, and transplantation needs. The care of the critically ill patient is central to the organization’s mission “to improve people’s lives through innovation in research, education and patient care.”
At the start of our colloborative participation, all of the ABCDEF bundle elements were protocolized in these ICUs. However, there was a lack of knowledge of the content of the bundle elements and corresponding guidelines among all members of our interdisciplinary teams, and our written protocols and guidelines supporting many of the bundle elements had inconsistent application across the 3 clinical settings.
We convened an ABCDEF bundle/ICU liberation team consisting of an interdisciplinary group of clinicians. The team leader was a critical care clinical nurse specialist. The project required outcome and demographic data collection for all patients in the collaborative as well as concurrent (daily) data collection on each bundle element. The clinical pharmacists who work in the MICUs and are part of daily interdisciplinary rounds collected the daily bundle element data while the patient demographic and outcome data were collected by the clinical nurse specialist, nurse practitioner, and clinical quality manager. Oversight and accountability for the ABCDEF bundle/ICU liberation project was provided by an interdisciplinary critical care quality committee. Our ABCDEF bundle/ICU liberation team met weekly to discuss progress of the initiative and provided monthly updates to the larger quality committee.
Impacting the Bundle—Nursing Assessments
The PAD guidelines recommend the routine assessment of pain, agitation, and delirium in ICU patients. For pain, they recommend the use of patient self-report or the use of a behavioral pain scale as the most valid and reliable method for completing this assessment [24]. Our medical center had chosen to use the Critical Care Pain Observation Tool (CPOT), a valid and reliable pain scale, for assessment of pain in patients who are unable to communicate [26], which had been in use in the clinical setting for over a year when this project began. For agitation, the PAD guidelines recommended assessment of the adequacy and depth of sedation using the Richmond Agitation Sedation Scale (RASS) or Sedation Agitation Scale (SAS) [24] for all ICU patients. Our medical center has chosen to use the RASS as our delirium assessment. The RASS had been in use in the clinical setting for approximately 10 years when this project started. For delirium assessment, the Confusion Assessment Method for ICU (CAM-ICU) [27] or the Intensive Care Delirium Screening Checklist (ICDSC) [28] is recommended. Our medical center used the CAM-ICU, which had been in place for approximately 10 years prior to the start of this project. Even though the assessment tools were in place in our MICU unit and hospital-based policies and guidelines, the accuracy of the assessments for PAD was questioned by many clinicians.
To improve the accuracy of our nursing assessments for PAD, a group of clinical nurse specialists and nursing educators developed an education and competency program for all critical care nursing staff. This education program focused on the PAD guidelines and our medical center’s chosen assessment tools. Education included in-person continuing education lectures, online modules, demonstrations, and practice in the clinical setting. After several months of education and practice, all staff registered nurses (RNs) had to demonstrate PAD assessment competency on a live person. We used standardized patients who followed written scenarios for all of the testing. The RN was given 1 of 8 scenarios and was charged with completing a PAD assessment on the standardized patient. RNs who did not pass had to review the education materials and re-test at a later date. More than 600 RNs completed the PAD competency. After completion of the PAD competency, the clinical nurse specialists observed clinical practice and audited nursing documentation. The accuracy of assessments for PAD had increased. Anecdotally, many our critical care clinicians acknowledged that they had increased confidence in the accuracy of the PAD assessments. There was increased agreement between the results of the assessments performed by all members of the interdisciplinary team.
Impacting the Bundle—Standardized Nurse Early Report Facilitation
Communication among the members of the interdisciplinary team is essential in caring for critically ill patients. One of the ways that the members of the interdisciplinary team communicate is through daily patient rounds. Our ABCDEF bundle/ICU liberation team members attend and participate in daily patient rounds in our 3 MICUs on a regular basis. The ABCDEF bundle/ICU liberation team members wanted to improve communication during patient rounds for all elements of the bundle.
Nurse Early Report Facilitation was a standard that was implemented approximately 5 years prior to the start of the ICU Liberation Collaborative. Nurse early report facilitation requires that the bedside staff RN starts the daily patient rounds discussion on each of his/her patients. The report given by the bedside RN was designed to last 60 to 90 seconds and provide dynamic information on the patient’s condition. Requiring the bedside RN to start the patient rounding provides the following benefits: requires bedside RN presence, provides up-to-the-minute information, increases bedside RN engagement in the patient’s plan of care, and allows for questions and answers. Compliance from the bedside RNs with this process of beginning patient rounds was very high; however, the information that was shared when the bedside RN began rounds was variable. Some bedside RNs provided a lengthy report on the patient while others provided 1 or 2 words.
The ABCDEF bundle/ICU liberation team members thought that a way to hardwire the ABCDEF bundle elements would be to add structure to the nurse early report. By using the ABCDEF elements as a guide, the ABCDEF bundle/ICU liberation team members developed the Structured Nurse Early Report Facilitation in which the bedside RN provides the following information at the beginning of each patient discussion during rounds: name of patient, overnight events (travels, clinical changes, etc.), pain (pain score and PRN use), agitation (RASS and PRN use), delirium (results of CAM-ICU). When the bedside RN performs the nurse early report using the structured format, the team is primed to discuss the A, B, C, and D elements of the bundle.
To implement the Structured Nurse Early Report Facilitation in the MICUs, the critical care clinical nurse specialists provided in-person education at the monthly staff meetings. They also sent emails, developed education bulletin boards, made reminder cards that were placed on the in-room computers, and distributed “badge buddy” reminder cards that fit on the RNs’ hospital ID badges. We provided emails and in-person education to our physician and nurse practitioner teams so they were aware of the changes. Our physician and nurse practitioners were encouraged to ask for information about any elements missing from the Structured Nurse Early Report in the early days of the process change.
After a few months, the critical care clinical nurse specialists reported that the Structured Nurse Early Report Facilitation was occurring for more than 80% of MICU patients. Besides the increase in information related to pain, agitation, and delirium, the Structured Nurse Early Report Facilitation increased the interdisciplinary team’s use of the term “delirium.” Prior to the structured nurse early report, most of the interdisciplinary team members were not naming delirium as a diagnosis for our MICU patients and used terms such as ICU psychosis, confused, and disoriented to describe the mental status of patients with delirium. As a result of this lack of naming, there may have been a lack of recognition of delirium. Using the word “delirium” has increased our interdisciplinary team’s awareness of this diagnosis and has increased the treatment of delirium in patients who have the diagnosis.
In addition to improved assessment and diagnosis, the clinical pharmacist began leading the discussions around choice of sedation during daily rounds. Team members began to discuss the patient’s sedation level, sedation goals, and develop a plan for each patient. This discussion included input from all members of the interdisciplinary team and allowed for a comprehensive patient-specific plan to be formed during the daily patient rounds episode.
Impacting the Bundle—Focus on Mobility
There have been many articles published in the critical care literature on the topic of mobility in the ICU. The evidence shows that early mobilization and rehabilitation of patients in ICUs is safe and may improve physical function, and reduce the duration of delirium, mechanical ventilation, and ICU length of stay [29–31]. Our institution had developed a critical care mobility guideline in 2008 for staff RNs to follow in determining the level of mobility that the patient required during the shift. Over the years, the mobility guideline was used less and less. As other tasks and interventions became a priority, mobility became an intervention that was completed for very few patients.
Our ABCDEF bundle/ICU liberation team determined that increasing mobility of our MICU patients needed to be a plan of care priority. We organized an interdisciplinary team to discuss the issues and barriers to mobility for our MICU patients. The interdisciplinary mobility team had representatives from medicine, nursing, respiratory therapy, physical therapy, occupational therapy, and speech therapy. Initially, this team sent a survey to all disciplines who provided care for the patients in the MICU. Data from this survey was analyzed by the team to determine next steps.
Despite the fact that there were responses from 6 unique disciplines, several common barriers emerged. The largest barrier to overcome was staffing/time for mobility. It was clear from the survey respondents that all health care team members were busy providing patient care. Any change in the mobility guideline or practice needed to make efficient use of the practitioner’s time. Other barriers included space/equipment, communication, patient schedules, knowledge, patient and staff safety, and unit culture. The interdisciplinary mobility team divided into smaller workgroups to tackle the issues and barriers.
Mobility Rounds
Mobility rounds were implemented to attempt to decrease the barriers of time, communication, and know-ledge. Mobility rounds were designed as a start to the shift discussion on the topic of mobility. Mobility rounds included a clinical nurse specialist, a physical therapist (PT), an occupational therapist (OT), and a pulmonary physician/ nurse practitioner. This team met at 7:30 each weekday morning and walked room-to-room through our MICUs. The mobility rounds team laid eyes on each patient, developed a mobility plan for the day, and communicated this plan with the staff RN assigned to the patient. Mobility rounds were completed on all 48 MICU patients in 30 minutes.
Having the mobility rounds team at each patient’s bedside was important in several ways. First, it allowed the team members to see each patient, which gave the patient an opportunity to be part of his/her mobility plan. Also, the staff RNs and respiratory therapists (RTs) were often in the patient’s room. This improved communication as the staff RNs and RTs discussed the mobility plan with the PT and OT. For patients who required many resources for a mobility session, the morning bedside meeting allowed RNs, RTs, PTs, OTs, and physicians to set a schedule for the day’s mobility session. Having a scheduled time for mobility increased staff and patient communication. Also, it allowed all of the team members to adjust their workloads to be present for a complex mobility session.
Another benefit of mobility rounds was the opportunity for the PT and OT team members to provide education to their nursing and physician colleagues. Many nursing and physician providers do not understand the intricacies of physical and occupational therapy practice. This daily dialogue provided the PT/OT a forum to explain which patients would benefit from PT/OT services and which would not. It allowed the RNs and physicians to hear the type of therapy provided on past sessions. It allowed the PT/OT to discuss and evaluate the appropriateness of each patient consult. It allowed the RN and physician to communicate which patients they felt were highest priority for therapy for that day. Mobility rounds are ongoing. Data are being collected to determine the impact of mobility rounds on the intensity of mobility for our MICU patients.
Nurse-Driven Mobility Guideline
Another subgroup revised the outdated critical care mobility guideline and developed the new “Nurse-Driven Critical Care Mobility Guideline.” The guideline has been approved through all of the medical center quality committees and is in the final copyright and publication stages, with implementation training to begin in the fall. The updated guideline is in an easy-to-read flowchart format and provides the staff RN with a pathway to follow to determine if mobility is safe for the patient. After determining safety, the staff RN uses the guideline to determine and perform the patient’s correct mobility interventions for his/her shift. The guideline has built in consultation points with the provider team and the therapy experts.
Other Mobility Issues
A third subgroup from the interdisciplinary mobility team has been working on the equipment and space barriers. This subgroup is evaluating equipment such as bedside chairs, specialty beds, and assistive devices. Many of our MICU patient rooms have overhead lifts built into the ceilings. This equipment is available to all staff at all times. The equipment/space subgroup made sure that there were slings for use with the overhead lifts in all of the MICU equipment rooms. They provided staff education on proper use of the overhead lifts. They worked with the financial department and MICU nurse managers to purchase 2 bariatric chairs for patient use in the MICU.
A fourth subgroup has been working on the electronic documentation system. They are partnering with members of the information technology department to update the nursing and provider documentation regarding mobility. They have also worked on updating and elaborating on the electronic activity orders for our MICU patients. There have been many changes to various patient order sets to clarify mobility and activity restrictions. The admission order set for our MICU patients has an activity order that allows our staff RNs to fully utilize the new nurse-driven critical care mobility guideline.
Impacting the Bundle—Family Engagement and Empowerment
Family support is important for all hospitalized patients but is crucial for ICU patients. The medical center implemented an open visitation policy for all ICUs in 2015. Despite open visitation, the communication between patients, families, and interdisciplinary ICU teams was deficient. Families spoke to many different team members and had difficulty remembering all of the information that they received.
To increase family participation in the care of the MICU patient, we invited family members to participate in daily rounds. The families were invited to listen and encouraged to ask questions. During daily rounds, there is a time when all care providers stop talking and allow family members to inquire about the proposed plan of care for their family member. For family members who cannot attend daily rounds, our ICU teams arrange daily in-person or telephone meetings to discuss the patient’s plan of care. RNs provide a daily telefamily call to update the designated family member on the patient’s status, answer questions, and provide support.
In addition to the medical support for families, there is an art therapy program integrated into the ICU to assist families while they are in the medical center. This program is run by a certified art therapist who holds art therapy classes 2 afternoons a week. This provides family members with respite time during long hospital days. There are also nondenominational services offered multiple times during the week and a respite area is located in the lobby of the medical center.
In addition to these programs, the medical center added full-time social workers to be available 24 hours a day/ 7 days a week. The social worker can provide social support for our patients and families as well as help facilitate accommodations for those who travel a far distance. The social worker plays in integral part on the ICU team, often bridging the gap for families that can be overlooked by the medical team.
Conclusion
Care of the ICU patient is complex. Too often we work in our silos of responsibility with our list of tasks for the day. Participating in the ABCDEF bundle/ICU Liberation Collaborative required us to work together as a team. We were able to have candid conversations that improved our understanding of other team members’ perspectives, helping us to reflect on our behaviors and overcome barriers to improving patient care.
Even though the ICU Liberation Collaborative has ended, our work at the medical center continues. We are in the process of evaluating all of the interventions, processes, and guideline updates that our ABCEDF bundle/ICU liberation team worked on during our 18-month program. There have been many improvements such as increased accuracy of pain and delirium assessments, along with improved treatment of pain in the MICU patient. We have noticed increased communication with the patient and family and among all of the members of the interdisciplinary team. We have changed our language to accurately reflect the patient’s sedation level by using the correct RASS score and delirium status by using the term “delirium” when this condition exists. There is increased collaboration among team members in the area of mobility. More patients are out of bed on bedside chairs and more patients are walking in the halls. Over the next several months our ABCEDF bundle/ICU liberation team will continue to review and analyze the data that we collected in the collaborative. We will use that data and the clinical changes we see on a daily basis to continue to improve the care for our MICU patients.
Corresponding author: Michele L. Weber, DNP, RN, CCRN, CCNS, AOCNS, OCN, ANP-BC, The Ohio State University Wexner Medical Center, 410 West 10th Ave., Columbus, OH 43210, [email protected].
Abstract
- Objective: To describe the highlights of our medical center’s implementation of the Society of Critical Care Medicine’s ABCDEF bundle in 3 medical intensive care units (ICUs).
- Methods: After a review of our current clinical practices and written clinical guidelines, we evaluated deficiencies in clinical care and employed a variety of educational and clinical change interventions for each element of the bundle. We utilized an interdisciplinary team approach to facilitate the change process.
- Results: As a result of our efforts, improvement in the accuracy of assessments of pain, agitation, and delir-ium across all clinical disciplines and improved adherence to clinical practice guidelines, protocols, and instruments for all bundle elements was seen. These changes have been sustained following completion of the data collection phase of the project.
- Conclusion: ICU care is a team effort. As a result of participation in this initiative, there has been an increased awareness of the bundle elements, improved collaboration among team members, and increased patient and family communication.
Key words: intensive care; delirium; sedation; mobility.
Admission to the intensive care unit (ICU) is a stressful and challenging time for patients and their families. In addition, significant negative sequelae following an ICU stay have been reported in the literature, including such post-ICU complications as post-traumatic stress disorder [1–9], depression [10,11], ICU-acquired weakness [12–19], and post-intensive care syndrome [20–23]. Pain, anxiety, and delirium all contribute to patient distress and agitation, and the prevention or treatment of pain, anxiety, and delirium in the ICU is an important goal. The Society of Critical Care Medicine (SCCM) developed the ABCDEF bundle (Table) to facilitate implementation of their 2013 clinical practice guidelines for the management of pain, agitation, and delirium (PAD) [24]. The bundle emphasizes an integrated approach to assessing, treating and preventing significant pain, over or undersedation, and delirium in critically ill patients.
In 2015, SCCM began the ICU Liberation Collaborative, a clinical care collaborative designed to implement the ABCDEF bundle through team-based care at hospitals and health systems across the country. The Liberation Collaborative’s intent was to “liberate” patients from iatrogenic aspects of care [25]. Our medical center participated in the collaborative. In this article, we describe the highlights of our medical center’s implementation of the ABCDEF bundle in 3 medical ICUs.
Settings
The Ohio State University Wexner Medical Center is a 1000+–bed academic medical center located in Columbus, Ohio, containing more than 180 ICU beds. These ICU beds provide care to patients with medical, surgical, burn, trauma, oncology, and transplantation needs. The care of the critically ill patient is central to the organization’s mission “to improve people’s lives through innovation in research, education and patient care.”
At the start of our colloborative participation, all of the ABCDEF bundle elements were protocolized in these ICUs. However, there was a lack of knowledge of the content of the bundle elements and corresponding guidelines among all members of our interdisciplinary teams, and our written protocols and guidelines supporting many of the bundle elements had inconsistent application across the 3 clinical settings.
We convened an ABCDEF bundle/ICU liberation team consisting of an interdisciplinary group of clinicians. The team leader was a critical care clinical nurse specialist. The project required outcome and demographic data collection for all patients in the collaborative as well as concurrent (daily) data collection on each bundle element. The clinical pharmacists who work in the MICUs and are part of daily interdisciplinary rounds collected the daily bundle element data while the patient demographic and outcome data were collected by the clinical nurse specialist, nurse practitioner, and clinical quality manager. Oversight and accountability for the ABCDEF bundle/ICU liberation project was provided by an interdisciplinary critical care quality committee. Our ABCDEF bundle/ICU liberation team met weekly to discuss progress of the initiative and provided monthly updates to the larger quality committee.
Impacting the Bundle—Nursing Assessments
The PAD guidelines recommend the routine assessment of pain, agitation, and delirium in ICU patients. For pain, they recommend the use of patient self-report or the use of a behavioral pain scale as the most valid and reliable method for completing this assessment [24]. Our medical center had chosen to use the Critical Care Pain Observation Tool (CPOT), a valid and reliable pain scale, for assessment of pain in patients who are unable to communicate [26], which had been in use in the clinical setting for over a year when this project began. For agitation, the PAD guidelines recommended assessment of the adequacy and depth of sedation using the Richmond Agitation Sedation Scale (RASS) or Sedation Agitation Scale (SAS) [24] for all ICU patients. Our medical center has chosen to use the RASS as our delirium assessment. The RASS had been in use in the clinical setting for approximately 10 years when this project started. For delirium assessment, the Confusion Assessment Method for ICU (CAM-ICU) [27] or the Intensive Care Delirium Screening Checklist (ICDSC) [28] is recommended. Our medical center used the CAM-ICU, which had been in place for approximately 10 years prior to the start of this project. Even though the assessment tools were in place in our MICU unit and hospital-based policies and guidelines, the accuracy of the assessments for PAD was questioned by many clinicians.
To improve the accuracy of our nursing assessments for PAD, a group of clinical nurse specialists and nursing educators developed an education and competency program for all critical care nursing staff. This education program focused on the PAD guidelines and our medical center’s chosen assessment tools. Education included in-person continuing education lectures, online modules, demonstrations, and practice in the clinical setting. After several months of education and practice, all staff registered nurses (RNs) had to demonstrate PAD assessment competency on a live person. We used standardized patients who followed written scenarios for all of the testing. The RN was given 1 of 8 scenarios and was charged with completing a PAD assessment on the standardized patient. RNs who did not pass had to review the education materials and re-test at a later date. More than 600 RNs completed the PAD competency. After completion of the PAD competency, the clinical nurse specialists observed clinical practice and audited nursing documentation. The accuracy of assessments for PAD had increased. Anecdotally, many our critical care clinicians acknowledged that they had increased confidence in the accuracy of the PAD assessments. There was increased agreement between the results of the assessments performed by all members of the interdisciplinary team.
Impacting the Bundle—Standardized Nurse Early Report Facilitation
Communication among the members of the interdisciplinary team is essential in caring for critically ill patients. One of the ways that the members of the interdisciplinary team communicate is through daily patient rounds. Our ABCDEF bundle/ICU liberation team members attend and participate in daily patient rounds in our 3 MICUs on a regular basis. The ABCDEF bundle/ICU liberation team members wanted to improve communication during patient rounds for all elements of the bundle.
Nurse Early Report Facilitation was a standard that was implemented approximately 5 years prior to the start of the ICU Liberation Collaborative. Nurse early report facilitation requires that the bedside staff RN starts the daily patient rounds discussion on each of his/her patients. The report given by the bedside RN was designed to last 60 to 90 seconds and provide dynamic information on the patient’s condition. Requiring the bedside RN to start the patient rounding provides the following benefits: requires bedside RN presence, provides up-to-the-minute information, increases bedside RN engagement in the patient’s plan of care, and allows for questions and answers. Compliance from the bedside RNs with this process of beginning patient rounds was very high; however, the information that was shared when the bedside RN began rounds was variable. Some bedside RNs provided a lengthy report on the patient while others provided 1 or 2 words.
The ABCDEF bundle/ICU liberation team members thought that a way to hardwire the ABCDEF bundle elements would be to add structure to the nurse early report. By using the ABCDEF elements as a guide, the ABCDEF bundle/ICU liberation team members developed the Structured Nurse Early Report Facilitation in which the bedside RN provides the following information at the beginning of each patient discussion during rounds: name of patient, overnight events (travels, clinical changes, etc.), pain (pain score and PRN use), agitation (RASS and PRN use), delirium (results of CAM-ICU). When the bedside RN performs the nurse early report using the structured format, the team is primed to discuss the A, B, C, and D elements of the bundle.
To implement the Structured Nurse Early Report Facilitation in the MICUs, the critical care clinical nurse specialists provided in-person education at the monthly staff meetings. They also sent emails, developed education bulletin boards, made reminder cards that were placed on the in-room computers, and distributed “badge buddy” reminder cards that fit on the RNs’ hospital ID badges. We provided emails and in-person education to our physician and nurse practitioner teams so they were aware of the changes. Our physician and nurse practitioners were encouraged to ask for information about any elements missing from the Structured Nurse Early Report in the early days of the process change.
After a few months, the critical care clinical nurse specialists reported that the Structured Nurse Early Report Facilitation was occurring for more than 80% of MICU patients. Besides the increase in information related to pain, agitation, and delirium, the Structured Nurse Early Report Facilitation increased the interdisciplinary team’s use of the term “delirium.” Prior to the structured nurse early report, most of the interdisciplinary team members were not naming delirium as a diagnosis for our MICU patients and used terms such as ICU psychosis, confused, and disoriented to describe the mental status of patients with delirium. As a result of this lack of naming, there may have been a lack of recognition of delirium. Using the word “delirium” has increased our interdisciplinary team’s awareness of this diagnosis and has increased the treatment of delirium in patients who have the diagnosis.
In addition to improved assessment and diagnosis, the clinical pharmacist began leading the discussions around choice of sedation during daily rounds. Team members began to discuss the patient’s sedation level, sedation goals, and develop a plan for each patient. This discussion included input from all members of the interdisciplinary team and allowed for a comprehensive patient-specific plan to be formed during the daily patient rounds episode.
Impacting the Bundle—Focus on Mobility
There have been many articles published in the critical care literature on the topic of mobility in the ICU. The evidence shows that early mobilization and rehabilitation of patients in ICUs is safe and may improve physical function, and reduce the duration of delirium, mechanical ventilation, and ICU length of stay [29–31]. Our institution had developed a critical care mobility guideline in 2008 for staff RNs to follow in determining the level of mobility that the patient required during the shift. Over the years, the mobility guideline was used less and less. As other tasks and interventions became a priority, mobility became an intervention that was completed for very few patients.
Our ABCDEF bundle/ICU liberation team determined that increasing mobility of our MICU patients needed to be a plan of care priority. We organized an interdisciplinary team to discuss the issues and barriers to mobility for our MICU patients. The interdisciplinary mobility team had representatives from medicine, nursing, respiratory therapy, physical therapy, occupational therapy, and speech therapy. Initially, this team sent a survey to all disciplines who provided care for the patients in the MICU. Data from this survey was analyzed by the team to determine next steps.
Despite the fact that there were responses from 6 unique disciplines, several common barriers emerged. The largest barrier to overcome was staffing/time for mobility. It was clear from the survey respondents that all health care team members were busy providing patient care. Any change in the mobility guideline or practice needed to make efficient use of the practitioner’s time. Other barriers included space/equipment, communication, patient schedules, knowledge, patient and staff safety, and unit culture. The interdisciplinary mobility team divided into smaller workgroups to tackle the issues and barriers.
Mobility Rounds
Mobility rounds were implemented to attempt to decrease the barriers of time, communication, and know-ledge. Mobility rounds were designed as a start to the shift discussion on the topic of mobility. Mobility rounds included a clinical nurse specialist, a physical therapist (PT), an occupational therapist (OT), and a pulmonary physician/ nurse practitioner. This team met at 7:30 each weekday morning and walked room-to-room through our MICUs. The mobility rounds team laid eyes on each patient, developed a mobility plan for the day, and communicated this plan with the staff RN assigned to the patient. Mobility rounds were completed on all 48 MICU patients in 30 minutes.
Having the mobility rounds team at each patient’s bedside was important in several ways. First, it allowed the team members to see each patient, which gave the patient an opportunity to be part of his/her mobility plan. Also, the staff RNs and respiratory therapists (RTs) were often in the patient’s room. This improved communication as the staff RNs and RTs discussed the mobility plan with the PT and OT. For patients who required many resources for a mobility session, the morning bedside meeting allowed RNs, RTs, PTs, OTs, and physicians to set a schedule for the day’s mobility session. Having a scheduled time for mobility increased staff and patient communication. Also, it allowed all of the team members to adjust their workloads to be present for a complex mobility session.
Another benefit of mobility rounds was the opportunity for the PT and OT team members to provide education to their nursing and physician colleagues. Many nursing and physician providers do not understand the intricacies of physical and occupational therapy practice. This daily dialogue provided the PT/OT a forum to explain which patients would benefit from PT/OT services and which would not. It allowed the RNs and physicians to hear the type of therapy provided on past sessions. It allowed the PT/OT to discuss and evaluate the appropriateness of each patient consult. It allowed the RN and physician to communicate which patients they felt were highest priority for therapy for that day. Mobility rounds are ongoing. Data are being collected to determine the impact of mobility rounds on the intensity of mobility for our MICU patients.
Nurse-Driven Mobility Guideline
Another subgroup revised the outdated critical care mobility guideline and developed the new “Nurse-Driven Critical Care Mobility Guideline.” The guideline has been approved through all of the medical center quality committees and is in the final copyright and publication stages, with implementation training to begin in the fall. The updated guideline is in an easy-to-read flowchart format and provides the staff RN with a pathway to follow to determine if mobility is safe for the patient. After determining safety, the staff RN uses the guideline to determine and perform the patient’s correct mobility interventions for his/her shift. The guideline has built in consultation points with the provider team and the therapy experts.
Other Mobility Issues
A third subgroup from the interdisciplinary mobility team has been working on the equipment and space barriers. This subgroup is evaluating equipment such as bedside chairs, specialty beds, and assistive devices. Many of our MICU patient rooms have overhead lifts built into the ceilings. This equipment is available to all staff at all times. The equipment/space subgroup made sure that there were slings for use with the overhead lifts in all of the MICU equipment rooms. They provided staff education on proper use of the overhead lifts. They worked with the financial department and MICU nurse managers to purchase 2 bariatric chairs for patient use in the MICU.
A fourth subgroup has been working on the electronic documentation system. They are partnering with members of the information technology department to update the nursing and provider documentation regarding mobility. They have also worked on updating and elaborating on the electronic activity orders for our MICU patients. There have been many changes to various patient order sets to clarify mobility and activity restrictions. The admission order set for our MICU patients has an activity order that allows our staff RNs to fully utilize the new nurse-driven critical care mobility guideline.
Impacting the Bundle—Family Engagement and Empowerment
Family support is important for all hospitalized patients but is crucial for ICU patients. The medical center implemented an open visitation policy for all ICUs in 2015. Despite open visitation, the communication between patients, families, and interdisciplinary ICU teams was deficient. Families spoke to many different team members and had difficulty remembering all of the information that they received.
To increase family participation in the care of the MICU patient, we invited family members to participate in daily rounds. The families were invited to listen and encouraged to ask questions. During daily rounds, there is a time when all care providers stop talking and allow family members to inquire about the proposed plan of care for their family member. For family members who cannot attend daily rounds, our ICU teams arrange daily in-person or telephone meetings to discuss the patient’s plan of care. RNs provide a daily telefamily call to update the designated family member on the patient’s status, answer questions, and provide support.
In addition to the medical support for families, there is an art therapy program integrated into the ICU to assist families while they are in the medical center. This program is run by a certified art therapist who holds art therapy classes 2 afternoons a week. This provides family members with respite time during long hospital days. There are also nondenominational services offered multiple times during the week and a respite area is located in the lobby of the medical center.
In addition to these programs, the medical center added full-time social workers to be available 24 hours a day/ 7 days a week. The social worker can provide social support for our patients and families as well as help facilitate accommodations for those who travel a far distance. The social worker plays in integral part on the ICU team, often bridging the gap for families that can be overlooked by the medical team.
Conclusion
Care of the ICU patient is complex. Too often we work in our silos of responsibility with our list of tasks for the day. Participating in the ABCDEF bundle/ICU Liberation Collaborative required us to work together as a team. We were able to have candid conversations that improved our understanding of other team members’ perspectives, helping us to reflect on our behaviors and overcome barriers to improving patient care.
Even though the ICU Liberation Collaborative has ended, our work at the medical center continues. We are in the process of evaluating all of the interventions, processes, and guideline updates that our ABCEDF bundle/ICU liberation team worked on during our 18-month program. There have been many improvements such as increased accuracy of pain and delirium assessments, along with improved treatment of pain in the MICU patient. We have noticed increased communication with the patient and family and among all of the members of the interdisciplinary team. We have changed our language to accurately reflect the patient’s sedation level by using the correct RASS score and delirium status by using the term “delirium” when this condition exists. There is increased collaboration among team members in the area of mobility. More patients are out of bed on bedside chairs and more patients are walking in the halls. Over the next several months our ABCEDF bundle/ICU liberation team will continue to review and analyze the data that we collected in the collaborative. We will use that data and the clinical changes we see on a daily basis to continue to improve the care for our MICU patients.
Corresponding author: Michele L. Weber, DNP, RN, CCRN, CCNS, AOCNS, OCN, ANP-BC, The Ohio State University Wexner Medical Center, 410 West 10th Ave., Columbus, OH 43210, [email protected].
1. Svenningsen H, Egerod I, Christensen D, et al Symptoms of posttraumatic stress after intensive care delirium. Biomed Res Int 2015;2015:876–947.
2. Warlan H, Howland L. Posttraumatic stress syndrome associated with stays in the intensive care unit: importance of nurses; involvement. Crit Care Nurse 2015;35:44–52.
3. Bienvenu OJ, Gerstenblith TA. Posttraumatic stress disorder phenomena after critical illness. Crit Care Clin 2017;33:649–58.
4. Wintermann GB, Rosendahl J, Weidner K, et al. Risk factors of delayed onset posttraumatic stress disorder in chronically critically ill patients. J Nerv Ment Dis 2017 Jul 5.
5. Wolters AE, Peelen LM, Welling MC, et al. Long-term mental health problems after delirium in the ICU. Crit Care Med 2016;44:1808–13.
6. Wintermann GB, Weidner K, Stafuss B. Predictors of posttraumatic stress and quality of life in family members of chronically critically ill patients after intensive care Ann Intensive Care 2016;6:69.
7. Patel MD, Jackson JC, Morandi A et al. Incidence and risk factors for intensive care unit-related post-traumatic stress disorder in veterans and civilians Am J Respir Crit Care Med 2016;193:1373–81.
8. Girad TD, Shintani AK, Jackson JC et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care 2007;11:R28.
9. Jackson JC, Hart RP, Gordon SM, et al. Post-traumatic stress disorder and post-traumatic stress symptoms following critical illness in medical intensive care unit patients: assessing the magnitude of the problem. Crit Care 2007;11:R27.
10. Jackson JC, Pandharipande PP, Girad TD et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Resp Med 2014;2:369–79.
11. Davydow DS, Hough CL, Langa KM, Iwashyna TJ. Depressive symptoms in spouses of older patients with severe sepsis. Crit Care Med 2012;40:2335–41.
12. Farhan H, Moeno-Duarte I, Latronico N, et al. Acquired muscle weakness in the surgical intensive care unit: nosology, epidemiology, diagnosis and prevention. Anesthesiology 2016;124:207–34.
13. Stevens, RD, Zink EK. Inflammatory signatures in ICU-acquired weakness. Crit Care Med 2017;45:1098–100.
14. Lotronico, N, Herridge M, Hopkins O, et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med 2017 Mar 13.
15. Batt J, Herridge M, Dos Santos C. Mechanism of ICU-acquired weakness: skeletal muscle loss in critical illness. Intensive Care Med 2017 Mar 10.
16. Batt J, Mathur S, Katzberg HD. Mechanism of ICU-acquired weakness: muscle contractility in critical illness. Intensive Care Med 2017;43:584–86.
17. Schweickert WD, Hall J. ICU-acquired weakness. Chest 2007;131:1541–9.
18. Deem S. Intensive care unit-acquired muscle weakness. Repir Care 2006;51:1042–52.
19. Kahn J, Burnham EL, Moss M. Acquired weakness in the ICU: critical illness myopathy and polyneuropathy. Minerva Anesthesiol 2006;72:401–6.
20. Jeitziner MM, Hamers JP, Burgin R et al. Long-term consequences of pain, anxiety, and agitation for critically ill older patients after an intensive care unit stay. J Clin Nurs 2015;24:2419–28.
21. Svennigsen H, Langhorn L, Agard AS, Dereyer P. Post-ICU symptoms, consequences, and follow-up: an integrative review. Nurs Crit Care 2017;22:212–20.
22. Torres J, Carvalho D, Molinos E et al. The impact of the patient post-intensive care syndrome components upon caregiver burden. Med Intensiva 2017 Feb 7
23. Rawal G, Yadav S, Sumar R. Post-Intensive care syndrome: an overview. J Transl Int Med 2017;305:90–2.
24. Barr J, Fraser GL, Puntillo K , et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
25. Ely EW. The ABCDEF bundle: science and philosophy of how ICU liberation serves patients and families. Crit Care Med 2017;45:321–30.
26. Gelinas C, Fillion L, Puntillo K, et al. Validation of the critical-care pain observation tool in adult patients. Am J Crit Care 2006;15:420–7.
27. Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001;29:1370–9.
28. Bergeron N, Dubois MJ, Dumont M, et al. Intensive Care Delirium Screening Checklist: Evaluation of a new screening tool. Intensive Care Med 2001;27:859–64.
29. Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med 2007;35:139–45.
30. Morris PE. Moving our critically ill patients: Mobility barriers and benefits. Crit Care Clin 2007;23:1–20.
31. Nydahl P, Sricharoenchai T, Chandra S, et al. Safety of patient mobilization and rehabilitation in the intensive care unit. Systematic review with meta-analysis. Ann Am Thorac Soc 2017;14:766–77.
1. Svenningsen H, Egerod I, Christensen D, et al Symptoms of posttraumatic stress after intensive care delirium. Biomed Res Int 2015;2015:876–947.
2. Warlan H, Howland L. Posttraumatic stress syndrome associated with stays in the intensive care unit: importance of nurses; involvement. Crit Care Nurse 2015;35:44–52.
3. Bienvenu OJ, Gerstenblith TA. Posttraumatic stress disorder phenomena after critical illness. Crit Care Clin 2017;33:649–58.
4. Wintermann GB, Rosendahl J, Weidner K, et al. Risk factors of delayed onset posttraumatic stress disorder in chronically critically ill patients. J Nerv Ment Dis 2017 Jul 5.
5. Wolters AE, Peelen LM, Welling MC, et al. Long-term mental health problems after delirium in the ICU. Crit Care Med 2016;44:1808–13.
6. Wintermann GB, Weidner K, Stafuss B. Predictors of posttraumatic stress and quality of life in family members of chronically critically ill patients after intensive care Ann Intensive Care 2016;6:69.
7. Patel MD, Jackson JC, Morandi A et al. Incidence and risk factors for intensive care unit-related post-traumatic stress disorder in veterans and civilians Am J Respir Crit Care Med 2016;193:1373–81.
8. Girad TD, Shintani AK, Jackson JC et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care 2007;11:R28.
9. Jackson JC, Hart RP, Gordon SM, et al. Post-traumatic stress disorder and post-traumatic stress symptoms following critical illness in medical intensive care unit patients: assessing the magnitude of the problem. Crit Care 2007;11:R27.
10. Jackson JC, Pandharipande PP, Girad TD et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Resp Med 2014;2:369–79.
11. Davydow DS, Hough CL, Langa KM, Iwashyna TJ. Depressive symptoms in spouses of older patients with severe sepsis. Crit Care Med 2012;40:2335–41.
12. Farhan H, Moeno-Duarte I, Latronico N, et al. Acquired muscle weakness in the surgical intensive care unit: nosology, epidemiology, diagnosis and prevention. Anesthesiology 2016;124:207–34.
13. Stevens, RD, Zink EK. Inflammatory signatures in ICU-acquired weakness. Crit Care Med 2017;45:1098–100.
14. Lotronico, N, Herridge M, Hopkins O, et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med 2017 Mar 13.
15. Batt J, Herridge M, Dos Santos C. Mechanism of ICU-acquired weakness: skeletal muscle loss in critical illness. Intensive Care Med 2017 Mar 10.
16. Batt J, Mathur S, Katzberg HD. Mechanism of ICU-acquired weakness: muscle contractility in critical illness. Intensive Care Med 2017;43:584–86.
17. Schweickert WD, Hall J. ICU-acquired weakness. Chest 2007;131:1541–9.
18. Deem S. Intensive care unit-acquired muscle weakness. Repir Care 2006;51:1042–52.
19. Kahn J, Burnham EL, Moss M. Acquired weakness in the ICU: critical illness myopathy and polyneuropathy. Minerva Anesthesiol 2006;72:401–6.
20. Jeitziner MM, Hamers JP, Burgin R et al. Long-term consequences of pain, anxiety, and agitation for critically ill older patients after an intensive care unit stay. J Clin Nurs 2015;24:2419–28.
21. Svennigsen H, Langhorn L, Agard AS, Dereyer P. Post-ICU symptoms, consequences, and follow-up: an integrative review. Nurs Crit Care 2017;22:212–20.
22. Torres J, Carvalho D, Molinos E et al. The impact of the patient post-intensive care syndrome components upon caregiver burden. Med Intensiva 2017 Feb 7
23. Rawal G, Yadav S, Sumar R. Post-Intensive care syndrome: an overview. J Transl Int Med 2017;305:90–2.
24. Barr J, Fraser GL, Puntillo K , et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
25. Ely EW. The ABCDEF bundle: science and philosophy of how ICU liberation serves patients and families. Crit Care Med 2017;45:321–30.
26. Gelinas C, Fillion L, Puntillo K, et al. Validation of the critical-care pain observation tool in adult patients. Am J Crit Care 2006;15:420–7.
27. Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 2001;29:1370–9.
28. Bergeron N, Dubois MJ, Dumont M, et al. Intensive Care Delirium Screening Checklist: Evaluation of a new screening tool. Intensive Care Med 2001;27:859–64.
29. Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med 2007;35:139–45.
30. Morris PE. Moving our critically ill patients: Mobility barriers and benefits. Crit Care Clin 2007;23:1–20.
31. Nydahl P, Sricharoenchai T, Chandra S, et al. Safety of patient mobilization and rehabilitation in the intensive care unit. Systematic review with meta-analysis. Ann Am Thorac Soc 2017;14:766–77.
Reducing Lost-to-Follow-Up Rates in Patients Discharged from an Early Psychosis Intervention Program
From the Early Psychosis Intervention Program, Institute of Mental Health, Singapore.
Abstract
- Objective: To develop and apply interventions to reduce lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
- Methods: A team comprising clinical staff, case managers, and patients was formed to carry out a clinical practice improvement project. Tools such as brainstorming and root cause analysis were used to derive causes of patient loss to follow-up and interventions to address them were implemented. Plan, Do, Study, and Act cycles were used to evaluate the effectiveness of identified interventions.
- Results: After the 3 interventions were implemented, there was a decrease in the default rate, and the target default rate of 0% was achieved in less than 6 months.
- Conclusion: Easily implemented program changes led to rapid and sustained improvement in reducing lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
Key words: Transfusion; red blood cells; plasma; platelets; veterans.
Psychosis is a mental illness in which affected individuals lose contact with reality. The lifetime prevalence of all psychotic disorders is 3.06% [1]. The typical symptoms consist of hallucinations, delusions, disorganized speech and thinking and negative symptoms (apathy, avolition, alogia, affective flattening, and anhedonia). Treatment is primarily with antipsychotics and psychological and social therapies.
The key to better prognosis is shortening the duration of untreated psychoses (DUP), defined as the period of time between the onset of psychosis and initiation of adequate treatment [2]. Longer DUP is one of the poorer prognostic factors in the outcome of first episode psychosis patients [3]. Over the past 2 decades, there has been considerable interest in developing and implementing specialized treatment programs for first episode psychosis [4], and early intervention is now a well-established therapeutic approach [5]. Early intervention has 2 elements that are distinct from standard care: early detection and phase-specific treatment (phase-specific treatment is a psychological, social, or physical treatment developed, or modified, specifically for use with people at an early stage of the illness). It is not only the initial care that is important, but regular follow up in the stable phase is necessary to reduce chances of relapse.
The Early Psychosis Intervention Programme (EPIP) in Singapore is a national program whose mission is early detection of young people with early psychosis or at risk of developing a psychotic illness and engagement with these individuals and families with the aim of providing accessible, empowering, individualized, evidence-based care in a least restrictive environment. The program was initiated in April 2001 under the auspices of the Ministry of Health, Singapore. EPIP has a multidisciplinary team of doctors, case managers, occupational therapists, psychologists, family therapists, social workers, and nurses to provide a comprehensive and personalized client-centered service across inpatient, outpatient, and community settings. The program spans 3 years and has 3 phases, beginning with acute intervention, followed by the stabilization phase, and then the stable phase, which focuses on relapse prevention, healthy lifestyle, stress management and plan for transition to downstream care. The frequency of visits and interaction with the team is tailored to suit individual patient needs and phase of care and can range from every day to once every 3 months. Following the 3-year program, clients are discharged from EPIP to continuity care (community psychiatry teams).
The relapse signature card was used every 2 months in the last 6 months during the period that the improvement project was ongoing. As it was found effective, now we use it every 6 months until 30 months and then every 2 months until conclusion of the 3-year program.
In addition, an appreciation card (Figure 2) was designed that is given to patients who keep their first downstream appointment. The card highlights independence and responsibility for one’s own care.
3. Provide a designated contact person
To ensure a smooth transition to the new service, we provided a designated person to contact for continuity care. Arrangement was made to transfer care to a specific community team of specific doctors and case managers, and their hospital contact details were provided on a card that was given to patients. Of the 8 patients who were transferred, 1 defaulted, 1 went overseas, 1 followed up with a private psychiatrist and the remaining 5 came for their first visit appointments.
Results
shown).
Figure 3. Run chart showing percentage of patients who failed to attend their first appointment with continuity care following transfer out of the program. Pre-intervention, default rates ranged from 9% to 75%. In the first 2 months after all the interventions were instituted (Dec 1 2012–March 1 2013), 2 patients defaulted, after which the default rate decreased to 0%.
Discussion
Making 3 small changes in our early psychosis intervention program led to rewarding gains in improving our patients’ follow-up with continuity care and the changes have become part of our standard operating procedure. In reviewing our processes to identify the root causes for loss of patients to follow-up, we found that obtaining the patient’s perspective was invaluable. It was interesting to learn that the word “discharge” might be impacting the way patients thought about follow-up after completion of the early intervention program. The interventions have become part of our standard operating procedure and we continue to audit the results every month to ensure that 0% default is being maintained. We are also looking into improving out psychoeducational materials for patients and caregivers and using more visual and interactive materials.
Corresponding author: Basu Sutapa, MD, Institute of Mental Health, Buangkok Green Medical Park, 10 Buangkok View, Singapore, S539747, [email protected].
Financial disclosures: None.
1. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust NZJ Psychiatry 2005;39:964–71.
2. Chang WC, Chan GH, Jim OT, et al. Optimal duration of an early intervention programme for first-episode psychosis: randomised controlled trial. Br J Psychiatry. 2015;206:
492–500.
3. Koch A, Gillis LS. Non-attendance of psychiatric outpatients. S Afr Med J 1991;80:289–91.
4. Mueser KT, Penn DL, Addington J, et al. The NAVIGATE Program for first-episode psychosis: rationale, overview, and description of psychosocial components. Psychiatr Serv 2015;66:680–90.
5. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev 2011;(6):CD004718.
6. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat 2007;13:423–34.
7. Magnes RM. Outpatient appointments: a necessary evil? A literature review and survey of patient attendance records. Psychiatr Bull 2008;32:458–60.
8. Appleby L, Shaw J, Amos T, et al. Suicide within 12 months of contact with mental health services: national clinical survey. Br Med J 1999;318:1235–39.
9. Chen A. Noncompliance in community psychiatry: a review of clinical interventions. Hosp Community Psychiatry 1991;
42:282–7.
10. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric outpatient nonattendance: characteristics and outcome. Br J Psych 2000;176:160–5.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv 2000;51:885–9.
12. Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh D. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatr Epidemiol 2005;40:899–904.
13. Skarsholm H, Stoevring H, Nielsen B. Effect of a system-oriented intervention on compliance problems in schizophrenia: a pragmatic controlled trial. Schiz Res Treat 2014;
2014:789403.
14. The Clinical Practice Improvement Programme (CPIP), Institute of Healthcare Quality, National Healthcare Group 2002.
From the Early Psychosis Intervention Program, Institute of Mental Health, Singapore.
Abstract
- Objective: To develop and apply interventions to reduce lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
- Methods: A team comprising clinical staff, case managers, and patients was formed to carry out a clinical practice improvement project. Tools such as brainstorming and root cause analysis were used to derive causes of patient loss to follow-up and interventions to address them were implemented. Plan, Do, Study, and Act cycles were used to evaluate the effectiveness of identified interventions.
- Results: After the 3 interventions were implemented, there was a decrease in the default rate, and the target default rate of 0% was achieved in less than 6 months.
- Conclusion: Easily implemented program changes led to rapid and sustained improvement in reducing lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
Key words: Transfusion; red blood cells; plasma; platelets; veterans.
Psychosis is a mental illness in which affected individuals lose contact with reality. The lifetime prevalence of all psychotic disorders is 3.06% [1]. The typical symptoms consist of hallucinations, delusions, disorganized speech and thinking and negative symptoms (apathy, avolition, alogia, affective flattening, and anhedonia). Treatment is primarily with antipsychotics and psychological and social therapies.
The key to better prognosis is shortening the duration of untreated psychoses (DUP), defined as the period of time between the onset of psychosis and initiation of adequate treatment [2]. Longer DUP is one of the poorer prognostic factors in the outcome of first episode psychosis patients [3]. Over the past 2 decades, there has been considerable interest in developing and implementing specialized treatment programs for first episode psychosis [4], and early intervention is now a well-established therapeutic approach [5]. Early intervention has 2 elements that are distinct from standard care: early detection and phase-specific treatment (phase-specific treatment is a psychological, social, or physical treatment developed, or modified, specifically for use with people at an early stage of the illness). It is not only the initial care that is important, but regular follow up in the stable phase is necessary to reduce chances of relapse.
The Early Psychosis Intervention Programme (EPIP) in Singapore is a national program whose mission is early detection of young people with early psychosis or at risk of developing a psychotic illness and engagement with these individuals and families with the aim of providing accessible, empowering, individualized, evidence-based care in a least restrictive environment. The program was initiated in April 2001 under the auspices of the Ministry of Health, Singapore. EPIP has a multidisciplinary team of doctors, case managers, occupational therapists, psychologists, family therapists, social workers, and nurses to provide a comprehensive and personalized client-centered service across inpatient, outpatient, and community settings. The program spans 3 years and has 3 phases, beginning with acute intervention, followed by the stabilization phase, and then the stable phase, which focuses on relapse prevention, healthy lifestyle, stress management and plan for transition to downstream care. The frequency of visits and interaction with the team is tailored to suit individual patient needs and phase of care and can range from every day to once every 3 months. Following the 3-year program, clients are discharged from EPIP to continuity care (community psychiatry teams).
The relapse signature card was used every 2 months in the last 6 months during the period that the improvement project was ongoing. As it was found effective, now we use it every 6 months until 30 months and then every 2 months until conclusion of the 3-year program.
In addition, an appreciation card (Figure 2) was designed that is given to patients who keep their first downstream appointment. The card highlights independence and responsibility for one’s own care.
3. Provide a designated contact person
To ensure a smooth transition to the new service, we provided a designated person to contact for continuity care. Arrangement was made to transfer care to a specific community team of specific doctors and case managers, and their hospital contact details were provided on a card that was given to patients. Of the 8 patients who were transferred, 1 defaulted, 1 went overseas, 1 followed up with a private psychiatrist and the remaining 5 came for their first visit appointments.
Results
shown).
Figure 3. Run chart showing percentage of patients who failed to attend their first appointment with continuity care following transfer out of the program. Pre-intervention, default rates ranged from 9% to 75%. In the first 2 months after all the interventions were instituted (Dec 1 2012–March 1 2013), 2 patients defaulted, after which the default rate decreased to 0%.
Discussion
Making 3 small changes in our early psychosis intervention program led to rewarding gains in improving our patients’ follow-up with continuity care and the changes have become part of our standard operating procedure. In reviewing our processes to identify the root causes for loss of patients to follow-up, we found that obtaining the patient’s perspective was invaluable. It was interesting to learn that the word “discharge” might be impacting the way patients thought about follow-up after completion of the early intervention program. The interventions have become part of our standard operating procedure and we continue to audit the results every month to ensure that 0% default is being maintained. We are also looking into improving out psychoeducational materials for patients and caregivers and using more visual and interactive materials.
Corresponding author: Basu Sutapa, MD, Institute of Mental Health, Buangkok Green Medical Park, 10 Buangkok View, Singapore, S539747, [email protected].
Financial disclosures: None.
From the Early Psychosis Intervention Program, Institute of Mental Health, Singapore.
Abstract
- Objective: To develop and apply interventions to reduce lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
- Methods: A team comprising clinical staff, case managers, and patients was formed to carry out a clinical practice improvement project. Tools such as brainstorming and root cause analysis were used to derive causes of patient loss to follow-up and interventions to address them were implemented. Plan, Do, Study, and Act cycles were used to evaluate the effectiveness of identified interventions.
- Results: After the 3 interventions were implemented, there was a decrease in the default rate, and the target default rate of 0% was achieved in less than 6 months.
- Conclusion: Easily implemented program changes led to rapid and sustained improvement in reducing lost-to-follow-up rates in patients discharged from an early psychosis intervention program.
Key words: Transfusion; red blood cells; plasma; platelets; veterans.
Psychosis is a mental illness in which affected individuals lose contact with reality. The lifetime prevalence of all psychotic disorders is 3.06% [1]. The typical symptoms consist of hallucinations, delusions, disorganized speech and thinking and negative symptoms (apathy, avolition, alogia, affective flattening, and anhedonia). Treatment is primarily with antipsychotics and psychological and social therapies.
The key to better prognosis is shortening the duration of untreated psychoses (DUP), defined as the period of time between the onset of psychosis and initiation of adequate treatment [2]. Longer DUP is one of the poorer prognostic factors in the outcome of first episode psychosis patients [3]. Over the past 2 decades, there has been considerable interest in developing and implementing specialized treatment programs for first episode psychosis [4], and early intervention is now a well-established therapeutic approach [5]. Early intervention has 2 elements that are distinct from standard care: early detection and phase-specific treatment (phase-specific treatment is a psychological, social, or physical treatment developed, or modified, specifically for use with people at an early stage of the illness). It is not only the initial care that is important, but regular follow up in the stable phase is necessary to reduce chances of relapse.
The Early Psychosis Intervention Programme (EPIP) in Singapore is a national program whose mission is early detection of young people with early psychosis or at risk of developing a psychotic illness and engagement with these individuals and families with the aim of providing accessible, empowering, individualized, evidence-based care in a least restrictive environment. The program was initiated in April 2001 under the auspices of the Ministry of Health, Singapore. EPIP has a multidisciplinary team of doctors, case managers, occupational therapists, psychologists, family therapists, social workers, and nurses to provide a comprehensive and personalized client-centered service across inpatient, outpatient, and community settings. The program spans 3 years and has 3 phases, beginning with acute intervention, followed by the stabilization phase, and then the stable phase, which focuses on relapse prevention, healthy lifestyle, stress management and plan for transition to downstream care. The frequency of visits and interaction with the team is tailored to suit individual patient needs and phase of care and can range from every day to once every 3 months. Following the 3-year program, clients are discharged from EPIP to continuity care (community psychiatry teams).
The relapse signature card was used every 2 months in the last 6 months during the period that the improvement project was ongoing. As it was found effective, now we use it every 6 months until 30 months and then every 2 months until conclusion of the 3-year program.
In addition, an appreciation card (Figure 2) was designed that is given to patients who keep their first downstream appointment. The card highlights independence and responsibility for one’s own care.
3. Provide a designated contact person
To ensure a smooth transition to the new service, we provided a designated person to contact for continuity care. Arrangement was made to transfer care to a specific community team of specific doctors and case managers, and their hospital contact details were provided on a card that was given to patients. Of the 8 patients who were transferred, 1 defaulted, 1 went overseas, 1 followed up with a private psychiatrist and the remaining 5 came for their first visit appointments.
Results
shown).
Figure 3. Run chart showing percentage of patients who failed to attend their first appointment with continuity care following transfer out of the program. Pre-intervention, default rates ranged from 9% to 75%. In the first 2 months after all the interventions were instituted (Dec 1 2012–March 1 2013), 2 patients defaulted, after which the default rate decreased to 0%.
Discussion
Making 3 small changes in our early psychosis intervention program led to rewarding gains in improving our patients’ follow-up with continuity care and the changes have become part of our standard operating procedure. In reviewing our processes to identify the root causes for loss of patients to follow-up, we found that obtaining the patient’s perspective was invaluable. It was interesting to learn that the word “discharge” might be impacting the way patients thought about follow-up after completion of the early intervention program. The interventions have become part of our standard operating procedure and we continue to audit the results every month to ensure that 0% default is being maintained. We are also looking into improving out psychoeducational materials for patients and caregivers and using more visual and interactive materials.
Corresponding author: Basu Sutapa, MD, Institute of Mental Health, Buangkok Green Medical Park, 10 Buangkok View, Singapore, S539747, [email protected].
Financial disclosures: None.
1. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust NZJ Psychiatry 2005;39:964–71.
2. Chang WC, Chan GH, Jim OT, et al. Optimal duration of an early intervention programme for first-episode psychosis: randomised controlled trial. Br J Psychiatry. 2015;206:
492–500.
3. Koch A, Gillis LS. Non-attendance of psychiatric outpatients. S Afr Med J 1991;80:289–91.
4. Mueser KT, Penn DL, Addington J, et al. The NAVIGATE Program for first-episode psychosis: rationale, overview, and description of psychosocial components. Psychiatr Serv 2015;66:680–90.
5. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev 2011;(6):CD004718.
6. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat 2007;13:423–34.
7. Magnes RM. Outpatient appointments: a necessary evil? A literature review and survey of patient attendance records. Psychiatr Bull 2008;32:458–60.
8. Appleby L, Shaw J, Amos T, et al. Suicide within 12 months of contact with mental health services: national clinical survey. Br Med J 1999;318:1235–39.
9. Chen A. Noncompliance in community psychiatry: a review of clinical interventions. Hosp Community Psychiatry 1991;
42:282–7.
10. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric outpatient nonattendance: characteristics and outcome. Br J Psych 2000;176:160–5.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv 2000;51:885–9.
12. Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh D. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatr Epidemiol 2005;40:899–904.
13. Skarsholm H, Stoevring H, Nielsen B. Effect of a system-oriented intervention on compliance problems in schizophrenia: a pragmatic controlled trial. Schiz Res Treat 2014;
2014:789403.
14. The Clinical Practice Improvement Programme (CPIP), Institute of Healthcare Quality, National Healthcare Group 2002.
1. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust NZJ Psychiatry 2005;39:964–71.
2. Chang WC, Chan GH, Jim OT, et al. Optimal duration of an early intervention programme for first-episode psychosis: randomised controlled trial. Br J Psychiatry. 2015;206:
492–500.
3. Koch A, Gillis LS. Non-attendance of psychiatric outpatients. S Afr Med J 1991;80:289–91.
4. Mueser KT, Penn DL, Addington J, et al. The NAVIGATE Program for first-episode psychosis: rationale, overview, and description of psychosocial components. Psychiatr Serv 2015;66:680–90.
5. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev 2011;(6):CD004718.
6. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat 2007;13:423–34.
7. Magnes RM. Outpatient appointments: a necessary evil? A literature review and survey of patient attendance records. Psychiatr Bull 2008;32:458–60.
8. Appleby L, Shaw J, Amos T, et al. Suicide within 12 months of contact with mental health services: national clinical survey. Br Med J 1999;318:1235–39.
9. Chen A. Noncompliance in community psychiatry: a review of clinical interventions. Hosp Community Psychiatry 1991;
42:282–7.
10. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric outpatient nonattendance: characteristics and outcome. Br J Psych 2000;176:160–5.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv 2000;51:885–9.
12. Gutiérrez-Maldonado J, Caqueo-Urízar A, Kavanagh D. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatr Epidemiol 2005;40:899–904.
13. Skarsholm H, Stoevring H, Nielsen B. Effect of a system-oriented intervention on compliance problems in schizophrenia: a pragmatic controlled trial. Schiz Res Treat 2014;
2014:789403.
14. The Clinical Practice Improvement Programme (CPIP), Institute of Healthcare Quality, National Healthcare Group 2002.
Melanoma Prevention Via App That Photoages College Students’ Selfies
Study Overview
Objective. To develop and test a photoaging app designed for melanoma prevention through enhancing sun protective behaviors.
Design. Cross-sectional pilot study.
Setting and participants. 25 students (56% male) with a median age of 22 years (range 19–25) attending the University of Essen in Germany.
Intervention. The researchers tested a free mobile app called Sunface. The app has the user take a self-portrait (selfie) and then photoages the image based on self-reported Fitzpatrick skin type and individual UV protection behavior. The 6 categories of skin on the Fitzpatrick Scale are Type I – always burns, never tans; Type II – usually burns, tans minimally; Type III – sometimes mild burn, gradually tans; Type IV – rarely burns, tans with ease; Type V – very rarely burns, tans very easily; Type VI – never burns, tans very easily. Afterward, the app explains the results and provides recommendations on sun protection as well as the ABCDE rule for skin cancer detection (asymmetrical shape, border, color, diameter, evolution). An interviewer walked up to each student, asked for oral consent, handed them an iPod Touch with the app pre-installed, and let them use the app.
Main outcome measures. Student attitudes about the app as collected on an anonymous paper and pencil questionnaire. Items were statements (see Results below), and responses were on a Likert scale ranging from fully agree to fully disagree.
Results. The majority of students (82%) stated that they would download the app, that the intervention had the potential to motivate them to use sun protection (92%) and that they thought such an app could change their perceptions that tanning makes you attractive (76%). Only a minority of students disagreed or fully disagreed that they would download such an app (2/25, 8%) or that such an app could change their perceptions on tanning and attractiveness (4/25, 16%).
Conclusion. Based on previous studies and the initial study results presented here, it is reasonable to speculate that the app may induce behavioral change in the target population. Further work is required to implement and examine the effectiveness of app-based photoaging interventions within risk groups from various cultural backgrounds.
Commentary
The relationship between skin cancer and ultraviolet radiation is well established [1]. Despite the known risks, tanning behavior, including use of tanning beds, is common. Indoor tanning is prevalent, particularly among female adolescents, and aligns with other risk behaviors, appearance-related factors, and intentional sunbathing [2]. Behaviors such as seeking shade, avoiding sun exposure during peak hours of radiation, wearing protective clothing, or some combination of these behaviors can provide protection against ultraviolet radiation [1].Significantly lower frequencies of almost all recommended sun-protective measures are found in younger patient subgroups (age 14 to 25 years) [3]. Thus, it makes sense to target interventions at the adolescent age-group.
Counseling adolescents regarding the dangers of tanning can be difficult due to the pressure the media places on young women and men to enhance their appearance. As a result, appeals to the negative cosmetic impact of sun and indoor tanning may be more effective than health-based appeals [4].
In this pilot study, the authors tested a creative sun protection app that photoages the user’s image based on skin type and aging algorithms. The underlying aging algorithms are based on publications showing UV-induced skin damage by outdoor as well as indoor tanning. Afterward, the app explains the visual results and aims at increasing self-competence on skin cancer prevention by providing guideline recommendations on sun protection and the ABCDE rule for melanoma self-detection. The app was very well received by the partipating college students, and the researchers concluded that the app may aid in the prevention of melanoma by enhancing the adoption of sun protective behaviors. However, this study was very small.
Mobile phone apps are proliferating and they are recognized as a potential low cost way to deliver health interventions [5]. A previous trial by Buller [6] used a randomized controlled design to evaluate a smartphone app that delivered real-time advice about sun protection, such as alerts to apply or reapply sunscreen or wear a hat. Only 1 out of 7 sun-safety practices was used more frequently by intervention versus control participants. The authors of an evidence review of the effectiveness of mobile phone apps in achieving health-related behavior change note that adequately powered and relatively longer RCTs are needed to better determine the effectiveness of app-based interventions [5].
Applications for Clinical Practice
Warnings on the dangers of sunburn and indoor tanning at any age should be emphasized, and there is an important role for primary care physician and other clinician counseling as well as public health outreach. Phone apps have the benefit of being able to reach large numbers at low cost and can offer an interactive and personalized health education experience. Such nontraditional strategies offer promise. Further studies should shed light on what app features are most important to users and whether their deployment can have a measurable impact on cancer prevention.
1. Saraiya M, Glanz K, Briss PA, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med 2004;27:422–66.
2. Demko CA, Borawski EA, Debanne SM, et al. Use of indoor tanning facilities by white adolescents in the United States. Arch Pediatr Adolesc Med 2003;157:854–60.
3. Görig T, Diehl K, Greinert R, et al. Prevalence of sun-protective behaviour and intentional sun tanning in German adolescents and adults: results of a nationwide telephone survey.
J Eur Acad Dermatol Venereol 2017 Jun 2.
4. Blattner CM, Lal K, Murase JE. Non-traditional melanoma prevention strategies in the young adult and adolescent population. Dermatol Pract Concept 2014;4:73–4.
5. Zhao J, Freeman B, Li M. Can mobile phone apps influence people’s health behavior change? an evidence review. J Med Internet Res 2016;18:e287.
6. Buller DB, Berwick M, Lantz K, Buller MK, Shane J, Kane I, Liu X. Evaluation of immediate and 12-week effects of a smartphone sun-safety mobile application: a randomized clinical trial. JAMA Dermatol 2015;151:505–12.
Study Overview
Objective. To develop and test a photoaging app designed for melanoma prevention through enhancing sun protective behaviors.
Design. Cross-sectional pilot study.
Setting and participants. 25 students (56% male) with a median age of 22 years (range 19–25) attending the University of Essen in Germany.
Intervention. The researchers tested a free mobile app called Sunface. The app has the user take a self-portrait (selfie) and then photoages the image based on self-reported Fitzpatrick skin type and individual UV protection behavior. The 6 categories of skin on the Fitzpatrick Scale are Type I – always burns, never tans; Type II – usually burns, tans minimally; Type III – sometimes mild burn, gradually tans; Type IV – rarely burns, tans with ease; Type V – very rarely burns, tans very easily; Type VI – never burns, tans very easily. Afterward, the app explains the results and provides recommendations on sun protection as well as the ABCDE rule for skin cancer detection (asymmetrical shape, border, color, diameter, evolution). An interviewer walked up to each student, asked for oral consent, handed them an iPod Touch with the app pre-installed, and let them use the app.
Main outcome measures. Student attitudes about the app as collected on an anonymous paper and pencil questionnaire. Items were statements (see Results below), and responses were on a Likert scale ranging from fully agree to fully disagree.
Results. The majority of students (82%) stated that they would download the app, that the intervention had the potential to motivate them to use sun protection (92%) and that they thought such an app could change their perceptions that tanning makes you attractive (76%). Only a minority of students disagreed or fully disagreed that they would download such an app (2/25, 8%) or that such an app could change their perceptions on tanning and attractiveness (4/25, 16%).
Conclusion. Based on previous studies and the initial study results presented here, it is reasonable to speculate that the app may induce behavioral change in the target population. Further work is required to implement and examine the effectiveness of app-based photoaging interventions within risk groups from various cultural backgrounds.
Commentary
The relationship between skin cancer and ultraviolet radiation is well established [1]. Despite the known risks, tanning behavior, including use of tanning beds, is common. Indoor tanning is prevalent, particularly among female adolescents, and aligns with other risk behaviors, appearance-related factors, and intentional sunbathing [2]. Behaviors such as seeking shade, avoiding sun exposure during peak hours of radiation, wearing protective clothing, or some combination of these behaviors can provide protection against ultraviolet radiation [1].Significantly lower frequencies of almost all recommended sun-protective measures are found in younger patient subgroups (age 14 to 25 years) [3]. Thus, it makes sense to target interventions at the adolescent age-group.
Counseling adolescents regarding the dangers of tanning can be difficult due to the pressure the media places on young women and men to enhance their appearance. As a result, appeals to the negative cosmetic impact of sun and indoor tanning may be more effective than health-based appeals [4].
In this pilot study, the authors tested a creative sun protection app that photoages the user’s image based on skin type and aging algorithms. The underlying aging algorithms are based on publications showing UV-induced skin damage by outdoor as well as indoor tanning. Afterward, the app explains the visual results and aims at increasing self-competence on skin cancer prevention by providing guideline recommendations on sun protection and the ABCDE rule for melanoma self-detection. The app was very well received by the partipating college students, and the researchers concluded that the app may aid in the prevention of melanoma by enhancing the adoption of sun protective behaviors. However, this study was very small.
Mobile phone apps are proliferating and they are recognized as a potential low cost way to deliver health interventions [5]. A previous trial by Buller [6] used a randomized controlled design to evaluate a smartphone app that delivered real-time advice about sun protection, such as alerts to apply or reapply sunscreen or wear a hat. Only 1 out of 7 sun-safety practices was used more frequently by intervention versus control participants. The authors of an evidence review of the effectiveness of mobile phone apps in achieving health-related behavior change note that adequately powered and relatively longer RCTs are needed to better determine the effectiveness of app-based interventions [5].
Applications for Clinical Practice
Warnings on the dangers of sunburn and indoor tanning at any age should be emphasized, and there is an important role for primary care physician and other clinician counseling as well as public health outreach. Phone apps have the benefit of being able to reach large numbers at low cost and can offer an interactive and personalized health education experience. Such nontraditional strategies offer promise. Further studies should shed light on what app features are most important to users and whether their deployment can have a measurable impact on cancer prevention.
Study Overview
Objective. To develop and test a photoaging app designed for melanoma prevention through enhancing sun protective behaviors.
Design. Cross-sectional pilot study.
Setting and participants. 25 students (56% male) with a median age of 22 years (range 19–25) attending the University of Essen in Germany.
Intervention. The researchers tested a free mobile app called Sunface. The app has the user take a self-portrait (selfie) and then photoages the image based on self-reported Fitzpatrick skin type and individual UV protection behavior. The 6 categories of skin on the Fitzpatrick Scale are Type I – always burns, never tans; Type II – usually burns, tans minimally; Type III – sometimes mild burn, gradually tans; Type IV – rarely burns, tans with ease; Type V – very rarely burns, tans very easily; Type VI – never burns, tans very easily. Afterward, the app explains the results and provides recommendations on sun protection as well as the ABCDE rule for skin cancer detection (asymmetrical shape, border, color, diameter, evolution). An interviewer walked up to each student, asked for oral consent, handed them an iPod Touch with the app pre-installed, and let them use the app.
Main outcome measures. Student attitudes about the app as collected on an anonymous paper and pencil questionnaire. Items were statements (see Results below), and responses were on a Likert scale ranging from fully agree to fully disagree.
Results. The majority of students (82%) stated that they would download the app, that the intervention had the potential to motivate them to use sun protection (92%) and that they thought such an app could change their perceptions that tanning makes you attractive (76%). Only a minority of students disagreed or fully disagreed that they would download such an app (2/25, 8%) or that such an app could change their perceptions on tanning and attractiveness (4/25, 16%).
Conclusion. Based on previous studies and the initial study results presented here, it is reasonable to speculate that the app may induce behavioral change in the target population. Further work is required to implement and examine the effectiveness of app-based photoaging interventions within risk groups from various cultural backgrounds.
Commentary
The relationship between skin cancer and ultraviolet radiation is well established [1]. Despite the known risks, tanning behavior, including use of tanning beds, is common. Indoor tanning is prevalent, particularly among female adolescents, and aligns with other risk behaviors, appearance-related factors, and intentional sunbathing [2]. Behaviors such as seeking shade, avoiding sun exposure during peak hours of radiation, wearing protective clothing, or some combination of these behaviors can provide protection against ultraviolet radiation [1].Significantly lower frequencies of almost all recommended sun-protective measures are found in younger patient subgroups (age 14 to 25 years) [3]. Thus, it makes sense to target interventions at the adolescent age-group.
Counseling adolescents regarding the dangers of tanning can be difficult due to the pressure the media places on young women and men to enhance their appearance. As a result, appeals to the negative cosmetic impact of sun and indoor tanning may be more effective than health-based appeals [4].
In this pilot study, the authors tested a creative sun protection app that photoages the user’s image based on skin type and aging algorithms. The underlying aging algorithms are based on publications showing UV-induced skin damage by outdoor as well as indoor tanning. Afterward, the app explains the visual results and aims at increasing self-competence on skin cancer prevention by providing guideline recommendations on sun protection and the ABCDE rule for melanoma self-detection. The app was very well received by the partipating college students, and the researchers concluded that the app may aid in the prevention of melanoma by enhancing the adoption of sun protective behaviors. However, this study was very small.
Mobile phone apps are proliferating and they are recognized as a potential low cost way to deliver health interventions [5]. A previous trial by Buller [6] used a randomized controlled design to evaluate a smartphone app that delivered real-time advice about sun protection, such as alerts to apply or reapply sunscreen or wear a hat. Only 1 out of 7 sun-safety practices was used more frequently by intervention versus control participants. The authors of an evidence review of the effectiveness of mobile phone apps in achieving health-related behavior change note that adequately powered and relatively longer RCTs are needed to better determine the effectiveness of app-based interventions [5].
Applications for Clinical Practice
Warnings on the dangers of sunburn and indoor tanning at any age should be emphasized, and there is an important role for primary care physician and other clinician counseling as well as public health outreach. Phone apps have the benefit of being able to reach large numbers at low cost and can offer an interactive and personalized health education experience. Such nontraditional strategies offer promise. Further studies should shed light on what app features are most important to users and whether their deployment can have a measurable impact on cancer prevention.
1. Saraiya M, Glanz K, Briss PA, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med 2004;27:422–66.
2. Demko CA, Borawski EA, Debanne SM, et al. Use of indoor tanning facilities by white adolescents in the United States. Arch Pediatr Adolesc Med 2003;157:854–60.
3. Görig T, Diehl K, Greinert R, et al. Prevalence of sun-protective behaviour and intentional sun tanning in German adolescents and adults: results of a nationwide telephone survey.
J Eur Acad Dermatol Venereol 2017 Jun 2.
4. Blattner CM, Lal K, Murase JE. Non-traditional melanoma prevention strategies in the young adult and adolescent population. Dermatol Pract Concept 2014;4:73–4.
5. Zhao J, Freeman B, Li M. Can mobile phone apps influence people’s health behavior change? an evidence review. J Med Internet Res 2016;18:e287.
6. Buller DB, Berwick M, Lantz K, Buller MK, Shane J, Kane I, Liu X. Evaluation of immediate and 12-week effects of a smartphone sun-safety mobile application: a randomized clinical trial. JAMA Dermatol 2015;151:505–12.
1. Saraiya M, Glanz K, Briss PA, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: a systematic review. Am J Prev Med 2004;27:422–66.
2. Demko CA, Borawski EA, Debanne SM, et al. Use of indoor tanning facilities by white adolescents in the United States. Arch Pediatr Adolesc Med 2003;157:854–60.
3. Görig T, Diehl K, Greinert R, et al. Prevalence of sun-protective behaviour and intentional sun tanning in German adolescents and adults: results of a nationwide telephone survey.
J Eur Acad Dermatol Venereol 2017 Jun 2.
4. Blattner CM, Lal K, Murase JE. Non-traditional melanoma prevention strategies in the young adult and adolescent population. Dermatol Pract Concept 2014;4:73–4.
5. Zhao J, Freeman B, Li M. Can mobile phone apps influence people’s health behavior change? an evidence review. J Med Internet Res 2016;18:e287.
6. Buller DB, Berwick M, Lantz K, Buller MK, Shane J, Kane I, Liu X. Evaluation of immediate and 12-week effects of a smartphone sun-safety mobile application: a randomized clinical trial. JAMA Dermatol 2015;151:505–12.
On the Move: Group Exercise Program Targeting Timing and Coordination Improves Mobility in Community-Dwelling Adults
Study Overview
Objective. To compare the effectiveness of a group exercise program focusing on the timing and coordination of movement (ie, On the Move [OTM]) with a seated strength, endurance, and flexibility program (usual care) at improving function, disability, and walking ability in older adults.
Design. Cross-sectional pilot study.
Setting and participants. Participants were community-dwelling older adults who were residents or members of 32 independent living facilities, senior apartment buildings, and community centers in the greater Pittsburgh, Pennsylvania, area. Participants were recruted between April 2012 and January 2014. Inclusion criteria included age 65 years or older, ability to walk independently with a gait speed of at least 0.60 m/s, and ability to follow 2-step commands. Individuals were excluded if they were non-English speaking, medically unstable, planning to leave the area for an extended time period, or had abnormal blood pressure or heart rate following a 6-minute walk test. The 32 participating facilities were randomly assigned to the OTM intervention (16 sites, 152 participants) or usual care (16 sites, 146 participants). The OTM and usual care exercise programs had the same frequency and duration (50 minutes per session, twice weekly for 12 weeks), and all exercise sessions were held on site at the facilities. The usual care program was a strength, flexibility, and endurance program based on programs that were being conducted in the participating facilities. It included a warm-up (range-of-motion exercises and stretching), upper and lower extremity strength exercises, aerobic activities, and a cool-down and was conducted with the participants sitting.
Intervention. The OTM program consisted of warm-up, timing and coordination (stepping and walking patterns), strengthening, and cool down exercises, with most of the exercises conducted in a standing position (40 minutes) and the remainder (10 minutes) sitting. The stepping and walking patterns were designed to promote the timing and coordination of stepping, integrated with the phases of the gait pattern.
Main Results. The average participant age was 80.0 (SD, 8.1) years, most participants were female (84.2%) and white (83.65%), and the average number of chronic conditions was 2.8 (SD, 1.4). The 2 groups were similar except for small differences in facility type. 142 (93.4%) OTM participants and 139 (95.2%) usual care participants completed post-intervention testing. The OTM group had significantly greater mean (SD) improvements than the usual care group in gait speed (0.05 [0.13] m/s versus −0.01 [0.11] m/s; adjusted difference 0.05 [0.02] m/s; P = 0.002) and 6MWD (20.6 [57.1] m versus 4.1 [55.6] m; adjusted difference = 16.7 [7.4] m; P = 0.03). Class attendance was lower in the OTM group than in the usual care group (76 [50.0%] OTM participants versus 95 [65.1%] usual care participants attended at least 20 classes; P = 0.03). There were no other significant differences between the groups in primary or secondary outcomes.
Conclusion. The OTM intervention was more effective at improving mobility than a usual care exercise program.
Commentary
The ability to walk is fundamental to maintaining a high quality of life and living independently in the community. Walking difficulty is a common problem among older persons and is linked to higher rates of loss of independence, morbidity, disability, and mortality in this population [1,2]. Walking difficulty associated with aging is often reflected in reduced gait speed and walking distance. A decline in gait speed of as little as 1 m/s is associated with a 10% decrease in ability to perform activities of daily living [3,4].
According to the authors, previous studies that explored the impact of structured exercise programs on walking ability in older individuals have had mixed results. These studies typically used exercise interventions focused on improving lower extremity muscle strength, flexibility, and general conditioning. In this study, the authors examined a community-based group exercise program (OTM) that incorporated exercises targeting the timing and coordination of movement important for walking in addition to flexibility and strengthening exercises. The results showed that the OTM program was more effective at improving walking ability than usual care. This intervention produced changes in gait speed (0.5 m/s) and 6MWD (16.7 m) that met or nearly met the clinically meaningful change criteria established for research use (0.5 m/s and 20 m, respectively) [5].
The authors pointed out several strengths of this study. First, the OTM program was compared to a usual care exercise program taught by trained exercise professionals, making it more difficult to demonstrate a difference between the 2 interventions. Similar prior studies have used nonexercise controls as the comparator. In addition, the effectiveness of the OTM program was demonstrated in 3 different community settings, suggesting that it can be implemented in various settings. Finally, the study participants were frail, older-old adults, who typically are not included in exercise studies. An important limitation of this study is that because outcomes were measured only at the conclusion of the intervention, it is not known whether the walking improvements persist over time or what effects the intervention has on mobility, function, and disability over the long term.
Applications for Clinical Practice
This study adds to the current literature on group exercise programs for improving mobility among community-dwelling older adults and supports incorporation of timing and coordination exercises into such programs. As the authors note, however, follow-up studies exploring the impact of the OTM intervention on long-term disability outcomes are needed before routine implementation in clinical practice can be recommended.
—Ajay Dharod, MD, Wake Forest School of Medicine, Winston-Salem, NC
1. Khokhar SR, Stern Y, Bell K, et al. Persistent mobility deficit in the absence of deficits in activities of daily living: a risk factor for mortality. J Am Geriatr Soc 2001;49:1539–43.
2. Newman AB, Simonsick EM, Naydeck EM, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA 2006;295:2018–26.
3. Hortobagyi T, Lesinski M, Gabler M, et al. Effects of three types of exercise interventions on healthy old adults’ gait speed: a systematic review and meta-analysis. Sports Med 2015;
45:1627–43.
4. Judge JO, Schechtman K, Cress E. The relationship between physical performance measures and independence in instrumental activities of daily living. The FICSIT Group. Frailty and Injury: Cooperative Studies of Intervention Trials. J Am Geriatr Soc 1996;44:1332–41.
5. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743–9.
Study Overview
Objective. To compare the effectiveness of a group exercise program focusing on the timing and coordination of movement (ie, On the Move [OTM]) with a seated strength, endurance, and flexibility program (usual care) at improving function, disability, and walking ability in older adults.
Design. Cross-sectional pilot study.
Setting and participants. Participants were community-dwelling older adults who were residents or members of 32 independent living facilities, senior apartment buildings, and community centers in the greater Pittsburgh, Pennsylvania, area. Participants were recruted between April 2012 and January 2014. Inclusion criteria included age 65 years or older, ability to walk independently with a gait speed of at least 0.60 m/s, and ability to follow 2-step commands. Individuals were excluded if they were non-English speaking, medically unstable, planning to leave the area for an extended time period, or had abnormal blood pressure or heart rate following a 6-minute walk test. The 32 participating facilities were randomly assigned to the OTM intervention (16 sites, 152 participants) or usual care (16 sites, 146 participants). The OTM and usual care exercise programs had the same frequency and duration (50 minutes per session, twice weekly for 12 weeks), and all exercise sessions were held on site at the facilities. The usual care program was a strength, flexibility, and endurance program based on programs that were being conducted in the participating facilities. It included a warm-up (range-of-motion exercises and stretching), upper and lower extremity strength exercises, aerobic activities, and a cool-down and was conducted with the participants sitting.
Intervention. The OTM program consisted of warm-up, timing and coordination (stepping and walking patterns), strengthening, and cool down exercises, with most of the exercises conducted in a standing position (40 minutes) and the remainder (10 minutes) sitting. The stepping and walking patterns were designed to promote the timing and coordination of stepping, integrated with the phases of the gait pattern.
Main Results. The average participant age was 80.0 (SD, 8.1) years, most participants were female (84.2%) and white (83.65%), and the average number of chronic conditions was 2.8 (SD, 1.4). The 2 groups were similar except for small differences in facility type. 142 (93.4%) OTM participants and 139 (95.2%) usual care participants completed post-intervention testing. The OTM group had significantly greater mean (SD) improvements than the usual care group in gait speed (0.05 [0.13] m/s versus −0.01 [0.11] m/s; adjusted difference 0.05 [0.02] m/s; P = 0.002) and 6MWD (20.6 [57.1] m versus 4.1 [55.6] m; adjusted difference = 16.7 [7.4] m; P = 0.03). Class attendance was lower in the OTM group than in the usual care group (76 [50.0%] OTM participants versus 95 [65.1%] usual care participants attended at least 20 classes; P = 0.03). There were no other significant differences between the groups in primary or secondary outcomes.
Conclusion. The OTM intervention was more effective at improving mobility than a usual care exercise program.
Commentary
The ability to walk is fundamental to maintaining a high quality of life and living independently in the community. Walking difficulty is a common problem among older persons and is linked to higher rates of loss of independence, morbidity, disability, and mortality in this population [1,2]. Walking difficulty associated with aging is often reflected in reduced gait speed and walking distance. A decline in gait speed of as little as 1 m/s is associated with a 10% decrease in ability to perform activities of daily living [3,4].
According to the authors, previous studies that explored the impact of structured exercise programs on walking ability in older individuals have had mixed results. These studies typically used exercise interventions focused on improving lower extremity muscle strength, flexibility, and general conditioning. In this study, the authors examined a community-based group exercise program (OTM) that incorporated exercises targeting the timing and coordination of movement important for walking in addition to flexibility and strengthening exercises. The results showed that the OTM program was more effective at improving walking ability than usual care. This intervention produced changes in gait speed (0.5 m/s) and 6MWD (16.7 m) that met or nearly met the clinically meaningful change criteria established for research use (0.5 m/s and 20 m, respectively) [5].
The authors pointed out several strengths of this study. First, the OTM program was compared to a usual care exercise program taught by trained exercise professionals, making it more difficult to demonstrate a difference between the 2 interventions. Similar prior studies have used nonexercise controls as the comparator. In addition, the effectiveness of the OTM program was demonstrated in 3 different community settings, suggesting that it can be implemented in various settings. Finally, the study participants were frail, older-old adults, who typically are not included in exercise studies. An important limitation of this study is that because outcomes were measured only at the conclusion of the intervention, it is not known whether the walking improvements persist over time or what effects the intervention has on mobility, function, and disability over the long term.
Applications for Clinical Practice
This study adds to the current literature on group exercise programs for improving mobility among community-dwelling older adults and supports incorporation of timing and coordination exercises into such programs. As the authors note, however, follow-up studies exploring the impact of the OTM intervention on long-term disability outcomes are needed before routine implementation in clinical practice can be recommended.
—Ajay Dharod, MD, Wake Forest School of Medicine, Winston-Salem, NC
Study Overview
Objective. To compare the effectiveness of a group exercise program focusing on the timing and coordination of movement (ie, On the Move [OTM]) with a seated strength, endurance, and flexibility program (usual care) at improving function, disability, and walking ability in older adults.
Design. Cross-sectional pilot study.
Setting and participants. Participants were community-dwelling older adults who were residents or members of 32 independent living facilities, senior apartment buildings, and community centers in the greater Pittsburgh, Pennsylvania, area. Participants were recruted between April 2012 and January 2014. Inclusion criteria included age 65 years or older, ability to walk independently with a gait speed of at least 0.60 m/s, and ability to follow 2-step commands. Individuals were excluded if they were non-English speaking, medically unstable, planning to leave the area for an extended time period, or had abnormal blood pressure or heart rate following a 6-minute walk test. The 32 participating facilities were randomly assigned to the OTM intervention (16 sites, 152 participants) or usual care (16 sites, 146 participants). The OTM and usual care exercise programs had the same frequency and duration (50 minutes per session, twice weekly for 12 weeks), and all exercise sessions were held on site at the facilities. The usual care program was a strength, flexibility, and endurance program based on programs that were being conducted in the participating facilities. It included a warm-up (range-of-motion exercises and stretching), upper and lower extremity strength exercises, aerobic activities, and a cool-down and was conducted with the participants sitting.
Intervention. The OTM program consisted of warm-up, timing and coordination (stepping and walking patterns), strengthening, and cool down exercises, with most of the exercises conducted in a standing position (40 minutes) and the remainder (10 minutes) sitting. The stepping and walking patterns were designed to promote the timing and coordination of stepping, integrated with the phases of the gait pattern.
Main Results. The average participant age was 80.0 (SD, 8.1) years, most participants were female (84.2%) and white (83.65%), and the average number of chronic conditions was 2.8 (SD, 1.4). The 2 groups were similar except for small differences in facility type. 142 (93.4%) OTM participants and 139 (95.2%) usual care participants completed post-intervention testing. The OTM group had significantly greater mean (SD) improvements than the usual care group in gait speed (0.05 [0.13] m/s versus −0.01 [0.11] m/s; adjusted difference 0.05 [0.02] m/s; P = 0.002) and 6MWD (20.6 [57.1] m versus 4.1 [55.6] m; adjusted difference = 16.7 [7.4] m; P = 0.03). Class attendance was lower in the OTM group than in the usual care group (76 [50.0%] OTM participants versus 95 [65.1%] usual care participants attended at least 20 classes; P = 0.03). There were no other significant differences between the groups in primary or secondary outcomes.
Conclusion. The OTM intervention was more effective at improving mobility than a usual care exercise program.
Commentary
The ability to walk is fundamental to maintaining a high quality of life and living independently in the community. Walking difficulty is a common problem among older persons and is linked to higher rates of loss of independence, morbidity, disability, and mortality in this population [1,2]. Walking difficulty associated with aging is often reflected in reduced gait speed and walking distance. A decline in gait speed of as little as 1 m/s is associated with a 10% decrease in ability to perform activities of daily living [3,4].
According to the authors, previous studies that explored the impact of structured exercise programs on walking ability in older individuals have had mixed results. These studies typically used exercise interventions focused on improving lower extremity muscle strength, flexibility, and general conditioning. In this study, the authors examined a community-based group exercise program (OTM) that incorporated exercises targeting the timing and coordination of movement important for walking in addition to flexibility and strengthening exercises. The results showed that the OTM program was more effective at improving walking ability than usual care. This intervention produced changes in gait speed (0.5 m/s) and 6MWD (16.7 m) that met or nearly met the clinically meaningful change criteria established for research use (0.5 m/s and 20 m, respectively) [5].
The authors pointed out several strengths of this study. First, the OTM program was compared to a usual care exercise program taught by trained exercise professionals, making it more difficult to demonstrate a difference between the 2 interventions. Similar prior studies have used nonexercise controls as the comparator. In addition, the effectiveness of the OTM program was demonstrated in 3 different community settings, suggesting that it can be implemented in various settings. Finally, the study participants were frail, older-old adults, who typically are not included in exercise studies. An important limitation of this study is that because outcomes were measured only at the conclusion of the intervention, it is not known whether the walking improvements persist over time or what effects the intervention has on mobility, function, and disability over the long term.
Applications for Clinical Practice
This study adds to the current literature on group exercise programs for improving mobility among community-dwelling older adults and supports incorporation of timing and coordination exercises into such programs. As the authors note, however, follow-up studies exploring the impact of the OTM intervention on long-term disability outcomes are needed before routine implementation in clinical practice can be recommended.
—Ajay Dharod, MD, Wake Forest School of Medicine, Winston-Salem, NC
1. Khokhar SR, Stern Y, Bell K, et al. Persistent mobility deficit in the absence of deficits in activities of daily living: a risk factor for mortality. J Am Geriatr Soc 2001;49:1539–43.
2. Newman AB, Simonsick EM, Naydeck EM, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA 2006;295:2018–26.
3. Hortobagyi T, Lesinski M, Gabler M, et al. Effects of three types of exercise interventions on healthy old adults’ gait speed: a systematic review and meta-analysis. Sports Med 2015;
45:1627–43.
4. Judge JO, Schechtman K, Cress E. The relationship between physical performance measures and independence in instrumental activities of daily living. The FICSIT Group. Frailty and Injury: Cooperative Studies of Intervention Trials. J Am Geriatr Soc 1996;44:1332–41.
5. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743–9.
1. Khokhar SR, Stern Y, Bell K, et al. Persistent mobility deficit in the absence of deficits in activities of daily living: a risk factor for mortality. J Am Geriatr Soc 2001;49:1539–43.
2. Newman AB, Simonsick EM, Naydeck EM, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA 2006;295:2018–26.
3. Hortobagyi T, Lesinski M, Gabler M, et al. Effects of three types of exercise interventions on healthy old adults’ gait speed: a systematic review and meta-analysis. Sports Med 2015;
45:1627–43.
4. Judge JO, Schechtman K, Cress E. The relationship between physical performance measures and independence in instrumental activities of daily living. The FICSIT Group. Frailty and Injury: Cooperative Studies of Intervention Trials. J Am Geriatr Soc 1996;44:1332–41.
5. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743–9.