User login
Polypharmacy in the Elderly: How to Reduce Adverse Drug Events
CE/CME No: CR-1802
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Identify patients who are at the greatest risk for the effects of polypharmacy.
• Recognize which medications are most likely to cause adverse drug events (ADEs) in the elderly population.
• Understand the effects of aging on the pharmacokinetics and pharmacodynamics of medications.
• Learn strategies to reduce the risk for polypharmacy and ADEs, including use of the Beers Criteria and the STOPP/START Criteria.
FACULTY
Kelsey Barclay practices in orthopedic surgery at Stanford Medical Center in Palo Alto, California. Amy Frassetto practices in Ob-Gyn at NewYork-Presbyterian in New York City. Julie Robb practices in emergency medicine at South Nassau Communities Hospital in Oceanside, New York. Ellen D. Mandel is a Clinical Professor in the Department of PA Studies at Pace University-Lenox Hill Hospital in New York City.

ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid through January 31, 2019.
Article begins on next page >>
Managing medications in the elderly can be complicated by the physiologic effects of aging and the prevalence of comorbidities. Consistent use of tools such as the Beers criteria and the STOPP/START criteria, as well as medication reconciliation, can reduce polypharmacy and its adverse drug effects, improving health outcomes in this population.
Older adults (those 65 and older) often have a number of comorbidities requiring pharmacologic intervention, making medication management a complicated but essential part of caring for the elderly. A recent analysis of trends in prescription drug use by community-dwelling adults found that 39% of older adults used five or more prescribed medications.1 Furthermore, about 72% of older adults also take a nonprescription medication (OTC or supplement); while OTC medication use has declined in this population in recent years, dietary supplement use has increased.2
These patients are also more susceptible to adverse drug events (ADEs)—including adverse drug reactions (ADRs)—resulting from the physiologic changes of aging. By one estimate, ADRs are about seven times more common in those older than 70 than in younger persons.3 One out of every 30 urgent hospital admissions in patients ages 65 and older is related to an ADR.4
Providers must therefore be cognizant of drug indications, dosing, and drug interactions when prescribing medications to elderly patients. Fortunately, tools and methods to avoid polypharmacy and the adverse effects of commonly prescribed medications—such as anticholinergics and psychotropic drugs—are available.
POLYPHARMACY AND PRESCRIPTION CASCADING
While there is no specific number of medications required to define polypharmacy, the term is generally used when a nonhospitalized individual is taking five or more medications.5 The more medications a patient is taking, the more at risk he or she will be for ADRs, drug interactions, and prescription cascading.
Prescription cascading begins when an ADR is thought to be a new symptom and a new drug is prescribed to control it. Ultimately, a cascade of prescriptions occurs to control avoidable ADRs, resulting in polypharmacy. As many as 57% of women older than 65 in the United States are currently prescribed five or more medications, with 12% prescribed nine or more drugs.6 Not only do these medications cause independent ADRs, but there is also increased risk for drug interactions—and potentially, additional avoidable ADRs.
The elderly population is at greater risk for ADEs because these patients are more likely to have multiple comorbidities and chronic diseases, requiring multiple therapies.7 Polypharmacy is also more dangerous in the elderly because the physiologic changes that occur during natural aging can affect both the pharmacokinetics and pharmacodynamics of medications. The absorption, distribution, metabolism, and excretion of drugs within the human body changes as a person ages, while certain drug classes can alter the way the body functions. For example, muscle mass naturally declines and the proportion of body fat to muscle increases; this change affects the distribution of drugs such as benzodiazepines or lithium.7 If the medication dosage is not corrected, the toxicity of the drug will be increased.7
Medication excretion is largely controlled by the kidneys. Renal perfusion and function decline with age, leading to a decrease in glomerular filtration rate—which requires closer monitoring of medication selection and dosing. The risk is heightened when the elderly patient becomes acutely ill. An acute decrease in kidney function results in decreased excretion of medications, leading to an increase in ADRs.7
Ultimately, the safety of many medications in the elderly patient is unknown.8 But there is a growing body of knowledge on the adverse effects of some classes of medication in this population.
COMMONLY PRESCRIBED MEDICATIONS—AND RISKS
ADEs result from medication errors, ADRs, allergic reactions, and overdoses. The incidence of ADEs—specifically ADRs and medication errors—is elevated in elderly patients who are prescribed certain classes of medications or multiple drugs simultaneously.8 Anticholinergic drugs and psychotropic drugs (specifically antipsychotics and benzodiazepines) are among the medications most commonly prescribed to elderly patients—and among the most likely to contribute to ADEs.9 Diabetes is a chronic condition whose treatment may also put elderly patients at risk for ADEs.10
Anticholinergic medications
Anticholinergic drugs—commonly prescribed for Parkinson disease, depression, urinary incontinence, pulmonary disorders, intestinal motility, and muscle spasms—competitively inhibit the binding of acetylcholine to muscarinic acetylcholine receptors.9 Because this mechanism tends to be nonselective, the adverse effects may be widespread. Central adverse effects include cognitive impairment, confusion, and delirium; peripheral adverse effects include constipation, urinary retention, dry mouth, blurred vision, peristaltic reduction, and tachycardia.9
Anticholinergic drugs are commonly prescribed to elderly patients for cardiovascular (CV) and neurologic disorders. (Medications for the former include ß-blockers, calcium channel blockers, diuretics, and ACE inhibitors; for the latter, amitriptyline, quetiapine, nortriptyline, prochlorperazine, haloperidol, and paroxetine.) An assessment of anticholinergic activity classified most neurologic medications as high activity and most CV medications as low—however, the latter are usually given in conjunction with other anticholinergic medications, increasing their ability to cause ADRs.11
In many cases, patients are prescribed anticholinergic medications to control symptoms of a disease, not to cure it—which means patients may be taking these medications for years. This cumulative exposure is called the anticholinergic burden. Many studies show that the anticholinergic burden is a predictor of cognitive and physical decline; a 2016 study of adults older than 65 who were exposed to 5 mg/d of oxybutynin for more than three years had a 23% increased risk for dementia, compared to low-risk or no exposure groups.9
In a retrospective, population-level study conducted in New Zealand, researchers assessed the anticholinergic effects of delirium, urinary retention, and constipation in 2,248 patients (65 and older) who were admitted to the hospital with at least one prescribed medication. Anticholinergic burden was found to be a significant independent predictor; patients taking five anticholinergic medications were more than three times as likely to develop an anticholinergic effect than those taking just one such medication (adjusted odds ratio, 3.21).11
Psychotropic drugs
Another often-prescribed medication group is psychotropic drugs, specifically antipsychotics and benzodiazepines, for agitation and behavioral disturbances in dementia. A year-long study of 851 patients in two long-term care nursing homes in Boston found that risk for ADRs—specifically, falls—was increased in those who had a change (initiation or dose increase) in psychotropic medication (ie, benzodiazepine, antipsychotic, or antidepressant).12
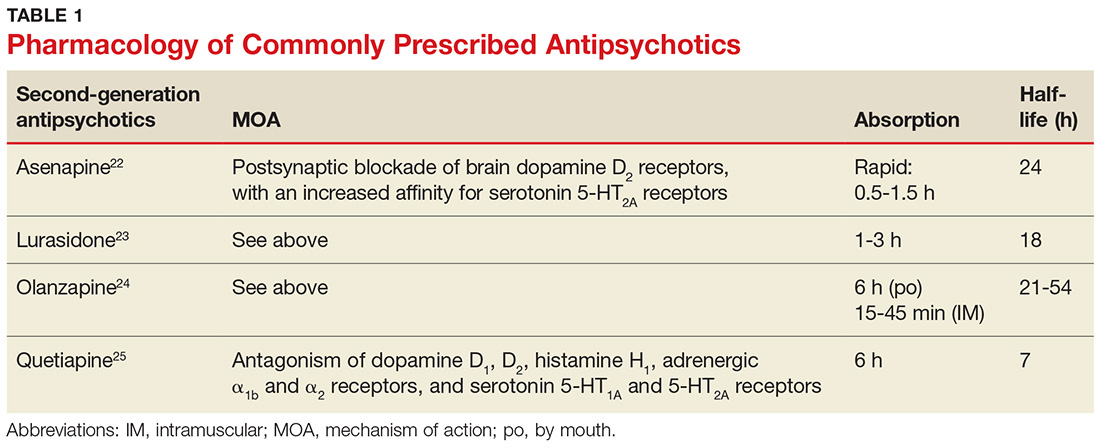
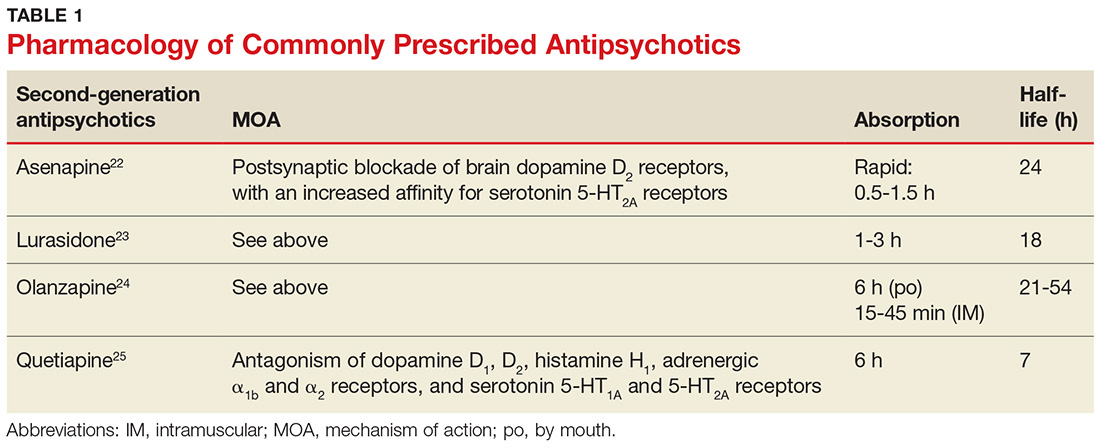
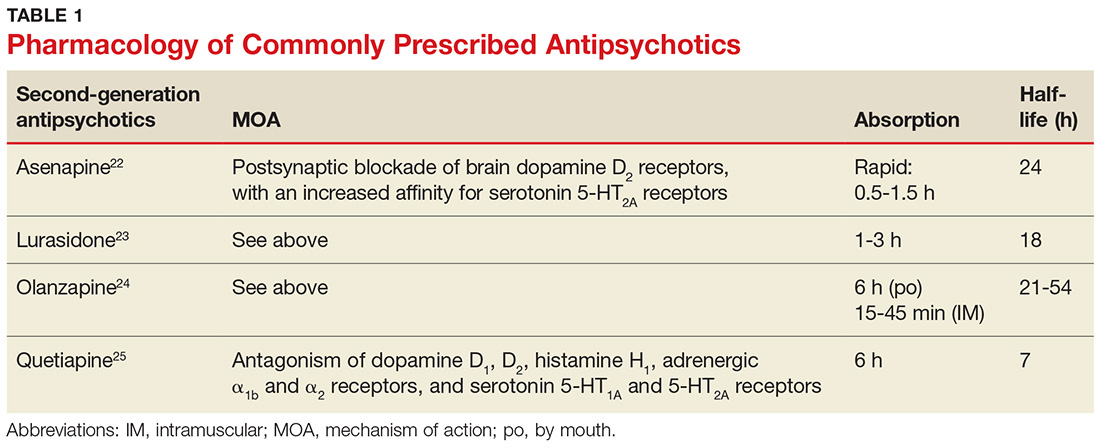
Second-generation antipsychotics, which are more commonly prescribed than first-generation agents, work on a postsynaptic blockade of brain dopamine D2 receptors and have an increased affinity for serotonin 5-HT2A receptors (see Table 1 for pharmacology of these medications).13,14 Adverse effects of these drugs include hypotension, sedation, and anticholinergic effects. Second-generation antipsychotics also carry a “black box warning” for increased risk for death in elderly patients with dementia-related psychosis.15
Benzodiazepines bind to receptors in the gamma-aminobutyric acid receptor complex, which enhances the binding of this inhibitory neurotransmitter (see Table 2 for pharmacology). Of this class of drugs, lorazepam has the highest potency, whereas midazolam and diazepam have lower potencies. Use of benzodiazepines increases risk for delirium and respiratory depression.16 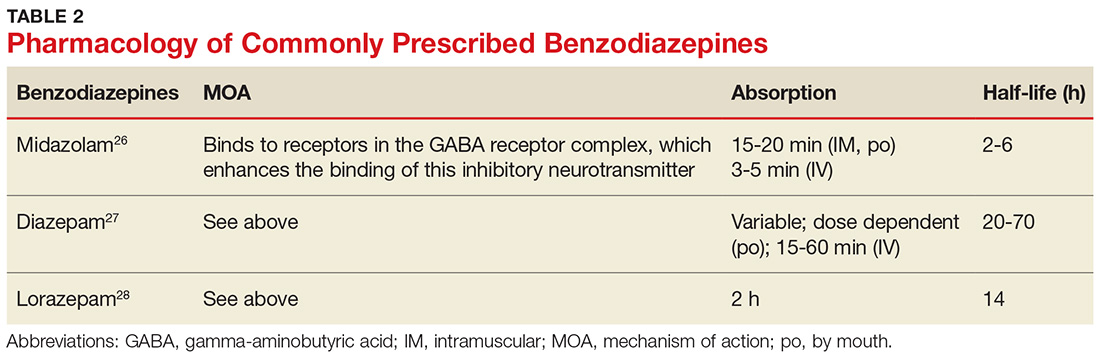
Diabetes treatment
People with diabetes have an increased risk for ADEs; this risk is elevated in older adults due to comorbidities such as peripheral neuropathy, retinopathy, coronary artery disease, and peripheral vascular disease.10 Hypoglycemic agents, such as insulin and insulin secretagogues, confer a higher risk for falls due to their hypoglycemic effect.10 Furthermore, metformin is known to increase risk for cognitive impairment in patients with diabetes.10
PREVENTING ADEs AND UNNECESSARY POLYPHARMACY
Predicting and preventing ADEs should be a health care provider’s priority when treating an elderly patient taking multiple medications—but it is often overlooked. Electronic medical records (EMRs) are helpful in preventing ADEs, specifically prescription errors, by flagging the patient’s chart when potentially problematic medications are ordered; however, this captures only a portion of ADEs occurring in this population.7
Other options to evaluate a patient for polypharmacy and possible ADRs include the Beers Criteria and the STOPP/START Criteria.17,18 Additionally, performing thorough and frequent medication reviews helps ensure that patients are prescribed essential medications to treat their comorbidities with the most opportunistic risk-benefit ratio. Patients’ medication lists across settings (eg, hospital, primary care, urgent care) can be accessed more easily, efficiently, and accurately with the integration of EMRs.
Beers Criteria
First published by Dr. Mark Beers in 1991 and endorsed by the American Geriatrics Society, the Beers Criteria identifies possible harmful effects of certain commonly prescribed medications to help guide and modify pharmacologic treatments, particularly in adults older than 65. The Beers Criteria classifies medications into three categories:
- Drugs that should be avoided or dose-adjusted
- Drugs that are potentially inappropriate in patients with certain conditions or syndromes
- Drugs that should be prescribed with caution in older adults.17
In the most recent update (2015), possible adverse effects of medications based on a patient’s hepatic or renal function, the effectiveness of the medication, and possible drug interactions were added. For example, nitrofurantoin and antiarrhythmics (eg, amiodarone and digoxin) should be avoided at a lower threshold of hepatic and renal impairment than previously recommended. The criteria suggest avoiding use of zolpidem, a nonbenzodiazepine receptor agonist, because of its elevated risk for adverse effects and minimal effectiveness in treating insomnia. More information about the 2015 criteria is available from the American Geriatrics Society (http://online library.wiley.com/doi/10.1111/jgs. 13702/full).19
The latest update also takes into account recently published evidence of increased ADEs resulting from drugs such as antipsychotics and proton pump inhibitors (PPIs).20 Antipsychotics are associated with an increased risk for morbidity and mortality, and PPIs are now recommended only for treatment duration of up to two months because of the possible increased risk for Clostridium difficile infection, as well as falls and fractures in patients older than 65.20 (PPIs indirectly reduce calcium absorption, which may lead to an increased fracture risk, particularly in postmenopausal women.20)
As with any guideline, the Beers Criteria was designed to supplement, not replace, clinical expertise and judgment. The risks and benefits of a medication should be weighed for the individual patient.
STOPP/START Criteria
Less widely used is the STOPP/START Criteria, an evidence-based set of guidelines consisting of 65 STOPP (Screening Tool of Older Person’s potentially inappropriate Prescriptions) and 22 START (Screening Tool to Alert doctors to the Right Treatment) criteria. Although they may be used individually, STOPP and START are best used together to determine the most appropriate medications for an elderly patient.
The STOPP guidelines help determine when the risks of a medication may outweigh the benefits in a given patient. STOPP includes recommendations for the appropriate length of time to use a medication; for example, PPIs should not be used for more than eight weeks (similar to the Beers recommendation) and benzodiazepines and neuroleptics for more than four weeks.18
START helps clinicians recognize potential prescribing omissions and to identify when a medication regimen should be implemented based on a patient’s history.18 Examples of START criteria include suggestions of when to initiate calcium and vitamin D supplementation for prevention of osteoporosis and when to begin statins in patients with diabetes, coronary artery disease, and cardiovascular disease.18
STOPP/START is organized by physiologic system, which allows for greater usability, and it addresses medications by class rather than specific medications. (The Beers Criteria was criticized for these reasons, as well as its limited transferability outside the United States.) When assessed in systematic reviews, the STOPP/START criteria were found to be fundamentally more sensitive than the Beers Criteria. Overall, it was concluded that the use of the STOPP/START criteria resulted in an absolute risk reduction of 21.2% to 35.7% and greatly improved the appropriateness of prescribing medication to the elderly. Its use also resulted in fewer follow-up appointments with a primary care physician (PCP).18
iPhone and Android applications such as iGeriatrics and Medstopper provide clinicians with easy access to Beers Criteria and STOPP/START Criteria, respectively.
Medication reconciliation
Medication reconciliation—in which health care providers review a patient’s medication list at hospital admission and discharge, and even at routine office visits—is an increasingly common practice, especially with the implementation of EMRs. The patient’s prescribed and OTC medications, as well as dose, route, frequency, and indication, are updated, with the goal of maintaining the most accurate list. Health care providers can utilize both the Beers Criteria and the STOPP/START criteria in their reconciliation process to help reduce polypharmacy in the elderly. It is an essential step in maintaining communication between providers and ultimately decreasing the incidence of ADEs.17
IMPROVE … continuity of care
Polypharmacy can decrease patient likelihood to adhere to the regimen, whether due to confusion or intolerance.8 Patients should be included, along with caregivers and all medical providers, in a holistic assessment of the patient’s best interests in terms of long-term care and pharmacologic treatment, since those who have a sense of control in their treatment goals and expectations often achieve a better understanding of their medical status.10
However, educating patients about their medications is time-consuming, and time is often at a premium during a typical office visit. A pilot study of 28 male veterans (ages 85 and older)—the Integrated Management and Polypharmacy Review of Vulnerable Elders (IMPROVE) project—devised a model to combat this problem.21 As an adjunct to a visit with the PCP, a clinical pharmacist trained in patient education and medication management performed face-to-face clinical consults with patients and their caregivers. The results indicated that medical management by both the PCP and the pharmacist resulted in better medication management. The pharmacist was able to spend time with the patient and caregiver, resulting in individualized instructions, education, and strategies for safe and effective medication use. The PCP remained involved by cosigning the note with the pharmacist and was available for consultation, if needed.
In IMPROVE, 79% of patients had at least one medication discontinued and 75% had one or more dosing or timing adjustments made. Potentially inappropriate medications were reduced by 14%.21 When the researchers compared the six-month period before the trial with the six-month period afterward, they found an average pharmacy cost savings of $64 per veteran per month. There was also a decreasing trend in phone calls and visits to the PCP. Cost savings were comparable to or greater than those reported for similar interventions.21 There has not been sufficient long-term follow-up to assess this method’s effects on ADEs, morbidity, and mortality, however.
CONCLUSION
Managing medications in the elderly population is difficult, and polypharmacy is common due to the prevalence of patients with comorbidities. It is important for providers to be aware of possible drug interactions, prescribing cascades, and ADEs. Medications such as anticholinergics and antipsychotics pose an increased risk for ADEs, but the regular implementation of criteria such as Beers or STOPP/START in clinical practice will minimize overprescribing and improve health outcomes. These criteria should be used to supplement the clinical judgment and expertise of providers as a mainstay of patient care in the elderly.
1. Kantor ED, Rehm CD, Haas JS, et al. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314:1818-1830.
2. Qato DM, Wilder J, Schumm LP. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med. 2016;176(4):473-482.
3. Beard K. Adverse reactions as a cause of hospital admission in the aged. Drugs Aging. 1992;2(4):356-367.
4. Pedros C, Formiga F, Corbella X, Arnau J. Adverse drug reactions leading to urgent hospital admission in an elderly population: prevalence and main features. Eur J Clin Pharmacol. 2016:72(2):219-226.
5. Maher RL Jr, Hanlon JT, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57-65.
6. Nguyen PV-Q, Spinelli C. Prescribing cascade in an elderly woman. Can Pharm J (Ott). 2016;149(3):122-124.
7. Lavan AH, Gallagher PF, O’Mahony D. Methods to reduce prescribing errors in elderly patients with multimorbidity. Clin Interv Aging. 2016;11:857-866.
8. Sivagnanam G. Deprescription: the prescription metabolism. J Pharmacol Pharmacother. 2016;7(3):133-137.
9. Koronkowski M, Eisenhower C, Marcum Z. An update on geriatric medication safety and challenges specific to the care of older adults. Ann Longterm Care. 2016; 24(3):37-40.
10. Peron EP, Ogbonna KC, Donohoe KL. Diabetic medications and polypharmacy. Clin Geriatr Med. 2015;31(1): 17-vii.
11. Salahudeen MS, Nishtala PS, Duffull SB. The influence of patient characteristics on anticholinergic events in older people. Dement Geriatr Cogn Dis Extra. 2015;5(3): 530-541.
12. Echt MA, Samelson EJ, Hannan MT, et al. Psychotropic drug initiation or increased dosage and the acute risk of falls: a prospective cohort study of nursing home residents. BMC Geriatrics. 2013;13:19.
13. Mauri MC, Paletta S, Maffini M, et al. Clinical pharmacology of antipsychotics: an update. EXCLI J. 2014;13: 1163-1191.
14. Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatry. 2002;47:29-40.
15. FDA. Public Health Advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances (2005). www. fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm053171. Accessed November 28, 2017.
16. Griffin CE III, Kaye AM, Bueno FR, Kaye AD. Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner J. 2013;13:214-223.
17. Flanagan N, Beizer J. Medication reconciliation and education for older adults: using the 2015 AGS Beers Criteria as a guide. Home Healthc Now. 2016;34(10): 542-549.
18. Hill-Taylor B, Sketris I, Hayden J, et al. Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther. 2013;38(5):360-372.
19. American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11): 2227-2246.
20. Salbu RL, Feuer J. A closer look at the 2015 Beers criteria. J Pharm Pract. 2017;30(4):419-424.
21. Mirk A, Echt KV, Vandenberg AE, et al. Polypharmacy review of vulnerable elders: can we IMPROVE outcomes? Fed Pract. 2016;33(3):39-41.
22. Saphris [package insert]. Irvine, CA: Allergan, USA, Inc; 2017.
23. Latuda [package insert]. Marlborough, MA: Sunovion Pharmaceuticals, Inc; 2017.
24. Zyprexa [package insert]. Indianapolis, IN: Lilly USA LLC; 2017.
25. Seroquel [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals; 2017.
26. Midazolam hydrochloride injection solution [package insert]. Lake Forest, IL: Hospira Inc; 2017.
27. Diazepam oral solution and Diazepam Intensol oral solution concentrate [package insert]. Eatontown, NJ: West-Ward Pharmaceuticals Corp; 2016.
28. Ativan tablet [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals; 2013.
CE/CME No: CR-1802
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Identify patients who are at the greatest risk for the effects of polypharmacy.
• Recognize which medications are most likely to cause adverse drug events (ADEs) in the elderly population.
• Understand the effects of aging on the pharmacokinetics and pharmacodynamics of medications.
• Learn strategies to reduce the risk for polypharmacy and ADEs, including use of the Beers Criteria and the STOPP/START Criteria.
FACULTY
Kelsey Barclay practices in orthopedic surgery at Stanford Medical Center in Palo Alto, California. Amy Frassetto practices in Ob-Gyn at NewYork-Presbyterian in New York City. Julie Robb practices in emergency medicine at South Nassau Communities Hospital in Oceanside, New York. Ellen D. Mandel is a Clinical Professor in the Department of PA Studies at Pace University-Lenox Hill Hospital in New York City.

ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid through January 31, 2019.
Article begins on next page >>
Managing medications in the elderly can be complicated by the physiologic effects of aging and the prevalence of comorbidities. Consistent use of tools such as the Beers criteria and the STOPP/START criteria, as well as medication reconciliation, can reduce polypharmacy and its adverse drug effects, improving health outcomes in this population.
Older adults (those 65 and older) often have a number of comorbidities requiring pharmacologic intervention, making medication management a complicated but essential part of caring for the elderly. A recent analysis of trends in prescription drug use by community-dwelling adults found that 39% of older adults used five or more prescribed medications.1 Furthermore, about 72% of older adults also take a nonprescription medication (OTC or supplement); while OTC medication use has declined in this population in recent years, dietary supplement use has increased.2
These patients are also more susceptible to adverse drug events (ADEs)—including adverse drug reactions (ADRs)—resulting from the physiologic changes of aging. By one estimate, ADRs are about seven times more common in those older than 70 than in younger persons.3 One out of every 30 urgent hospital admissions in patients ages 65 and older is related to an ADR.4
Providers must therefore be cognizant of drug indications, dosing, and drug interactions when prescribing medications to elderly patients. Fortunately, tools and methods to avoid polypharmacy and the adverse effects of commonly prescribed medications—such as anticholinergics and psychotropic drugs—are available.
POLYPHARMACY AND PRESCRIPTION CASCADING
While there is no specific number of medications required to define polypharmacy, the term is generally used when a nonhospitalized individual is taking five or more medications.5 The more medications a patient is taking, the more at risk he or she will be for ADRs, drug interactions, and prescription cascading.
Prescription cascading begins when an ADR is thought to be a new symptom and a new drug is prescribed to control it. Ultimately, a cascade of prescriptions occurs to control avoidable ADRs, resulting in polypharmacy. As many as 57% of women older than 65 in the United States are currently prescribed five or more medications, with 12% prescribed nine or more drugs.6 Not only do these medications cause independent ADRs, but there is also increased risk for drug interactions—and potentially, additional avoidable ADRs.
The elderly population is at greater risk for ADEs because these patients are more likely to have multiple comorbidities and chronic diseases, requiring multiple therapies.7 Polypharmacy is also more dangerous in the elderly because the physiologic changes that occur during natural aging can affect both the pharmacokinetics and pharmacodynamics of medications. The absorption, distribution, metabolism, and excretion of drugs within the human body changes as a person ages, while certain drug classes can alter the way the body functions. For example, muscle mass naturally declines and the proportion of body fat to muscle increases; this change affects the distribution of drugs such as benzodiazepines or lithium.7 If the medication dosage is not corrected, the toxicity of the drug will be increased.7
Medication excretion is largely controlled by the kidneys. Renal perfusion and function decline with age, leading to a decrease in glomerular filtration rate—which requires closer monitoring of medication selection and dosing. The risk is heightened when the elderly patient becomes acutely ill. An acute decrease in kidney function results in decreased excretion of medications, leading to an increase in ADRs.7
Ultimately, the safety of many medications in the elderly patient is unknown.8 But there is a growing body of knowledge on the adverse effects of some classes of medication in this population.
COMMONLY PRESCRIBED MEDICATIONS—AND RISKS
ADEs result from medication errors, ADRs, allergic reactions, and overdoses. The incidence of ADEs—specifically ADRs and medication errors—is elevated in elderly patients who are prescribed certain classes of medications or multiple drugs simultaneously.8 Anticholinergic drugs and psychotropic drugs (specifically antipsychotics and benzodiazepines) are among the medications most commonly prescribed to elderly patients—and among the most likely to contribute to ADEs.9 Diabetes is a chronic condition whose treatment may also put elderly patients at risk for ADEs.10
Anticholinergic medications
Anticholinergic drugs—commonly prescribed for Parkinson disease, depression, urinary incontinence, pulmonary disorders, intestinal motility, and muscle spasms—competitively inhibit the binding of acetylcholine to muscarinic acetylcholine receptors.9 Because this mechanism tends to be nonselective, the adverse effects may be widespread. Central adverse effects include cognitive impairment, confusion, and delirium; peripheral adverse effects include constipation, urinary retention, dry mouth, blurred vision, peristaltic reduction, and tachycardia.9
Anticholinergic drugs are commonly prescribed to elderly patients for cardiovascular (CV) and neurologic disorders. (Medications for the former include ß-blockers, calcium channel blockers, diuretics, and ACE inhibitors; for the latter, amitriptyline, quetiapine, nortriptyline, prochlorperazine, haloperidol, and paroxetine.) An assessment of anticholinergic activity classified most neurologic medications as high activity and most CV medications as low—however, the latter are usually given in conjunction with other anticholinergic medications, increasing their ability to cause ADRs.11
In many cases, patients are prescribed anticholinergic medications to control symptoms of a disease, not to cure it—which means patients may be taking these medications for years. This cumulative exposure is called the anticholinergic burden. Many studies show that the anticholinergic burden is a predictor of cognitive and physical decline; a 2016 study of adults older than 65 who were exposed to 5 mg/d of oxybutynin for more than three years had a 23% increased risk for dementia, compared to low-risk or no exposure groups.9
In a retrospective, population-level study conducted in New Zealand, researchers assessed the anticholinergic effects of delirium, urinary retention, and constipation in 2,248 patients (65 and older) who were admitted to the hospital with at least one prescribed medication. Anticholinergic burden was found to be a significant independent predictor; patients taking five anticholinergic medications were more than three times as likely to develop an anticholinergic effect than those taking just one such medication (adjusted odds ratio, 3.21).11
Psychotropic drugs
Another often-prescribed medication group is psychotropic drugs, specifically antipsychotics and benzodiazepines, for agitation and behavioral disturbances in dementia. A year-long study of 851 patients in two long-term care nursing homes in Boston found that risk for ADRs—specifically, falls—was increased in those who had a change (initiation or dose increase) in psychotropic medication (ie, benzodiazepine, antipsychotic, or antidepressant).12
Second-generation antipsychotics, which are more commonly prescribed than first-generation agents, work on a postsynaptic blockade of brain dopamine D2 receptors and have an increased affinity for serotonin 5-HT2A receptors (see Table 1 for pharmacology of these medications).13,14 Adverse effects of these drugs include hypotension, sedation, and anticholinergic effects. Second-generation antipsychotics also carry a “black box warning” for increased risk for death in elderly patients with dementia-related psychosis.15
Benzodiazepines bind to receptors in the gamma-aminobutyric acid receptor complex, which enhances the binding of this inhibitory neurotransmitter (see Table 2 for pharmacology). Of this class of drugs, lorazepam has the highest potency, whereas midazolam and diazepam have lower potencies. Use of benzodiazepines increases risk for delirium and respiratory depression.16 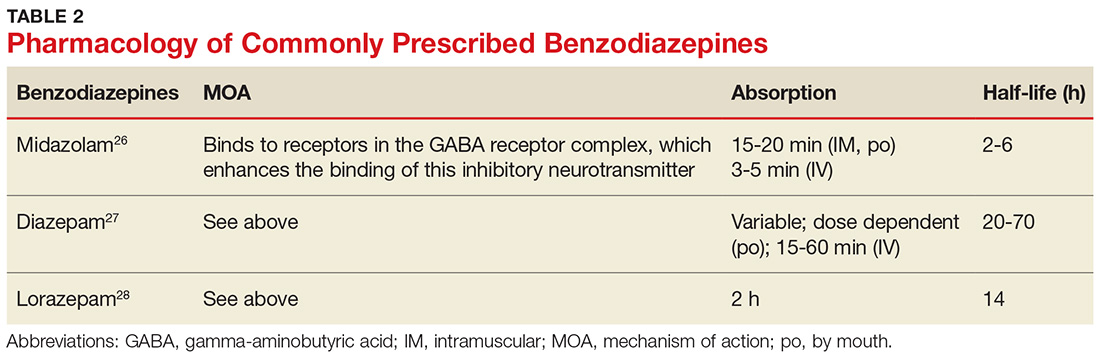
Diabetes treatment
People with diabetes have an increased risk for ADEs; this risk is elevated in older adults due to comorbidities such as peripheral neuropathy, retinopathy, coronary artery disease, and peripheral vascular disease.10 Hypoglycemic agents, such as insulin and insulin secretagogues, confer a higher risk for falls due to their hypoglycemic effect.10 Furthermore, metformin is known to increase risk for cognitive impairment in patients with diabetes.10
PREVENTING ADEs AND UNNECESSARY POLYPHARMACY
Predicting and preventing ADEs should be a health care provider’s priority when treating an elderly patient taking multiple medications—but it is often overlooked. Electronic medical records (EMRs) are helpful in preventing ADEs, specifically prescription errors, by flagging the patient’s chart when potentially problematic medications are ordered; however, this captures only a portion of ADEs occurring in this population.7
Other options to evaluate a patient for polypharmacy and possible ADRs include the Beers Criteria and the STOPP/START Criteria.17,18 Additionally, performing thorough and frequent medication reviews helps ensure that patients are prescribed essential medications to treat their comorbidities with the most opportunistic risk-benefit ratio. Patients’ medication lists across settings (eg, hospital, primary care, urgent care) can be accessed more easily, efficiently, and accurately with the integration of EMRs.
Beers Criteria
First published by Dr. Mark Beers in 1991 and endorsed by the American Geriatrics Society, the Beers Criteria identifies possible harmful effects of certain commonly prescribed medications to help guide and modify pharmacologic treatments, particularly in adults older than 65. The Beers Criteria classifies medications into three categories:
- Drugs that should be avoided or dose-adjusted
- Drugs that are potentially inappropriate in patients with certain conditions or syndromes
- Drugs that should be prescribed with caution in older adults.17
In the most recent update (2015), possible adverse effects of medications based on a patient’s hepatic or renal function, the effectiveness of the medication, and possible drug interactions were added. For example, nitrofurantoin and antiarrhythmics (eg, amiodarone and digoxin) should be avoided at a lower threshold of hepatic and renal impairment than previously recommended. The criteria suggest avoiding use of zolpidem, a nonbenzodiazepine receptor agonist, because of its elevated risk for adverse effects and minimal effectiveness in treating insomnia. More information about the 2015 criteria is available from the American Geriatrics Society (http://online library.wiley.com/doi/10.1111/jgs. 13702/full).19
The latest update also takes into account recently published evidence of increased ADEs resulting from drugs such as antipsychotics and proton pump inhibitors (PPIs).20 Antipsychotics are associated with an increased risk for morbidity and mortality, and PPIs are now recommended only for treatment duration of up to two months because of the possible increased risk for Clostridium difficile infection, as well as falls and fractures in patients older than 65.20 (PPIs indirectly reduce calcium absorption, which may lead to an increased fracture risk, particularly in postmenopausal women.20)
As with any guideline, the Beers Criteria was designed to supplement, not replace, clinical expertise and judgment. The risks and benefits of a medication should be weighed for the individual patient.
STOPP/START Criteria
Less widely used is the STOPP/START Criteria, an evidence-based set of guidelines consisting of 65 STOPP (Screening Tool of Older Person’s potentially inappropriate Prescriptions) and 22 START (Screening Tool to Alert doctors to the Right Treatment) criteria. Although they may be used individually, STOPP and START are best used together to determine the most appropriate medications for an elderly patient.
The STOPP guidelines help determine when the risks of a medication may outweigh the benefits in a given patient. STOPP includes recommendations for the appropriate length of time to use a medication; for example, PPIs should not be used for more than eight weeks (similar to the Beers recommendation) and benzodiazepines and neuroleptics for more than four weeks.18
START helps clinicians recognize potential prescribing omissions and to identify when a medication regimen should be implemented based on a patient’s history.18 Examples of START criteria include suggestions of when to initiate calcium and vitamin D supplementation for prevention of osteoporosis and when to begin statins in patients with diabetes, coronary artery disease, and cardiovascular disease.18
STOPP/START is organized by physiologic system, which allows for greater usability, and it addresses medications by class rather than specific medications. (The Beers Criteria was criticized for these reasons, as well as its limited transferability outside the United States.) When assessed in systematic reviews, the STOPP/START criteria were found to be fundamentally more sensitive than the Beers Criteria. Overall, it was concluded that the use of the STOPP/START criteria resulted in an absolute risk reduction of 21.2% to 35.7% and greatly improved the appropriateness of prescribing medication to the elderly. Its use also resulted in fewer follow-up appointments with a primary care physician (PCP).18
iPhone and Android applications such as iGeriatrics and Medstopper provide clinicians with easy access to Beers Criteria and STOPP/START Criteria, respectively.
Medication reconciliation
Medication reconciliation—in which health care providers review a patient’s medication list at hospital admission and discharge, and even at routine office visits—is an increasingly common practice, especially with the implementation of EMRs. The patient’s prescribed and OTC medications, as well as dose, route, frequency, and indication, are updated, with the goal of maintaining the most accurate list. Health care providers can utilize both the Beers Criteria and the STOPP/START criteria in their reconciliation process to help reduce polypharmacy in the elderly. It is an essential step in maintaining communication between providers and ultimately decreasing the incidence of ADEs.17
IMPROVE … continuity of care
Polypharmacy can decrease patient likelihood to adhere to the regimen, whether due to confusion or intolerance.8 Patients should be included, along with caregivers and all medical providers, in a holistic assessment of the patient’s best interests in terms of long-term care and pharmacologic treatment, since those who have a sense of control in their treatment goals and expectations often achieve a better understanding of their medical status.10
However, educating patients about their medications is time-consuming, and time is often at a premium during a typical office visit. A pilot study of 28 male veterans (ages 85 and older)—the Integrated Management and Polypharmacy Review of Vulnerable Elders (IMPROVE) project—devised a model to combat this problem.21 As an adjunct to a visit with the PCP, a clinical pharmacist trained in patient education and medication management performed face-to-face clinical consults with patients and their caregivers. The results indicated that medical management by both the PCP and the pharmacist resulted in better medication management. The pharmacist was able to spend time with the patient and caregiver, resulting in individualized instructions, education, and strategies for safe and effective medication use. The PCP remained involved by cosigning the note with the pharmacist and was available for consultation, if needed.
In IMPROVE, 79% of patients had at least one medication discontinued and 75% had one or more dosing or timing adjustments made. Potentially inappropriate medications were reduced by 14%.21 When the researchers compared the six-month period before the trial with the six-month period afterward, they found an average pharmacy cost savings of $64 per veteran per month. There was also a decreasing trend in phone calls and visits to the PCP. Cost savings were comparable to or greater than those reported for similar interventions.21 There has not been sufficient long-term follow-up to assess this method’s effects on ADEs, morbidity, and mortality, however.
CONCLUSION
Managing medications in the elderly population is difficult, and polypharmacy is common due to the prevalence of patients with comorbidities. It is important for providers to be aware of possible drug interactions, prescribing cascades, and ADEs. Medications such as anticholinergics and antipsychotics pose an increased risk for ADEs, but the regular implementation of criteria such as Beers or STOPP/START in clinical practice will minimize overprescribing and improve health outcomes. These criteria should be used to supplement the clinical judgment and expertise of providers as a mainstay of patient care in the elderly.
CE/CME No: CR-1802
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Identify patients who are at the greatest risk for the effects of polypharmacy.
• Recognize which medications are most likely to cause adverse drug events (ADEs) in the elderly population.
• Understand the effects of aging on the pharmacokinetics and pharmacodynamics of medications.
• Learn strategies to reduce the risk for polypharmacy and ADEs, including use of the Beers Criteria and the STOPP/START Criteria.
FACULTY
Kelsey Barclay practices in orthopedic surgery at Stanford Medical Center in Palo Alto, California. Amy Frassetto practices in Ob-Gyn at NewYork-Presbyterian in New York City. Julie Robb practices in emergency medicine at South Nassau Communities Hospital in Oceanside, New York. Ellen D. Mandel is a Clinical Professor in the Department of PA Studies at Pace University-Lenox Hill Hospital in New York City.

ACCREDITATION STATEMENT
This program has been reviewed and is approved for a maximum of 1.0 hour of American Academy of Physician Assistants (AAPA) Category 1 CME credit by the Physician Assistant Review Panel. [NPs: Both ANCC and the AANP Certification Program recognize AAPA as an approved provider of Category 1 credit.] Approval is valid through January 31, 2019.
Article begins on next page >>
Managing medications in the elderly can be complicated by the physiologic effects of aging and the prevalence of comorbidities. Consistent use of tools such as the Beers criteria and the STOPP/START criteria, as well as medication reconciliation, can reduce polypharmacy and its adverse drug effects, improving health outcomes in this population.
Older adults (those 65 and older) often have a number of comorbidities requiring pharmacologic intervention, making medication management a complicated but essential part of caring for the elderly. A recent analysis of trends in prescription drug use by community-dwelling adults found that 39% of older adults used five or more prescribed medications.1 Furthermore, about 72% of older adults also take a nonprescription medication (OTC or supplement); while OTC medication use has declined in this population in recent years, dietary supplement use has increased.2
These patients are also more susceptible to adverse drug events (ADEs)—including adverse drug reactions (ADRs)—resulting from the physiologic changes of aging. By one estimate, ADRs are about seven times more common in those older than 70 than in younger persons.3 One out of every 30 urgent hospital admissions in patients ages 65 and older is related to an ADR.4
Providers must therefore be cognizant of drug indications, dosing, and drug interactions when prescribing medications to elderly patients. Fortunately, tools and methods to avoid polypharmacy and the adverse effects of commonly prescribed medications—such as anticholinergics and psychotropic drugs—are available.
POLYPHARMACY AND PRESCRIPTION CASCADING
While there is no specific number of medications required to define polypharmacy, the term is generally used when a nonhospitalized individual is taking five or more medications.5 The more medications a patient is taking, the more at risk he or she will be for ADRs, drug interactions, and prescription cascading.
Prescription cascading begins when an ADR is thought to be a new symptom and a new drug is prescribed to control it. Ultimately, a cascade of prescriptions occurs to control avoidable ADRs, resulting in polypharmacy. As many as 57% of women older than 65 in the United States are currently prescribed five or more medications, with 12% prescribed nine or more drugs.6 Not only do these medications cause independent ADRs, but there is also increased risk for drug interactions—and potentially, additional avoidable ADRs.
The elderly population is at greater risk for ADEs because these patients are more likely to have multiple comorbidities and chronic diseases, requiring multiple therapies.7 Polypharmacy is also more dangerous in the elderly because the physiologic changes that occur during natural aging can affect both the pharmacokinetics and pharmacodynamics of medications. The absorption, distribution, metabolism, and excretion of drugs within the human body changes as a person ages, while certain drug classes can alter the way the body functions. For example, muscle mass naturally declines and the proportion of body fat to muscle increases; this change affects the distribution of drugs such as benzodiazepines or lithium.7 If the medication dosage is not corrected, the toxicity of the drug will be increased.7
Medication excretion is largely controlled by the kidneys. Renal perfusion and function decline with age, leading to a decrease in glomerular filtration rate—which requires closer monitoring of medication selection and dosing. The risk is heightened when the elderly patient becomes acutely ill. An acute decrease in kidney function results in decreased excretion of medications, leading to an increase in ADRs.7
Ultimately, the safety of many medications in the elderly patient is unknown.8 But there is a growing body of knowledge on the adverse effects of some classes of medication in this population.
COMMONLY PRESCRIBED MEDICATIONS—AND RISKS
ADEs result from medication errors, ADRs, allergic reactions, and overdoses. The incidence of ADEs—specifically ADRs and medication errors—is elevated in elderly patients who are prescribed certain classes of medications or multiple drugs simultaneously.8 Anticholinergic drugs and psychotropic drugs (specifically antipsychotics and benzodiazepines) are among the medications most commonly prescribed to elderly patients—and among the most likely to contribute to ADEs.9 Diabetes is a chronic condition whose treatment may also put elderly patients at risk for ADEs.10
Anticholinergic medications
Anticholinergic drugs—commonly prescribed for Parkinson disease, depression, urinary incontinence, pulmonary disorders, intestinal motility, and muscle spasms—competitively inhibit the binding of acetylcholine to muscarinic acetylcholine receptors.9 Because this mechanism tends to be nonselective, the adverse effects may be widespread. Central adverse effects include cognitive impairment, confusion, and delirium; peripheral adverse effects include constipation, urinary retention, dry mouth, blurred vision, peristaltic reduction, and tachycardia.9
Anticholinergic drugs are commonly prescribed to elderly patients for cardiovascular (CV) and neurologic disorders. (Medications for the former include ß-blockers, calcium channel blockers, diuretics, and ACE inhibitors; for the latter, amitriptyline, quetiapine, nortriptyline, prochlorperazine, haloperidol, and paroxetine.) An assessment of anticholinergic activity classified most neurologic medications as high activity and most CV medications as low—however, the latter are usually given in conjunction with other anticholinergic medications, increasing their ability to cause ADRs.11
In many cases, patients are prescribed anticholinergic medications to control symptoms of a disease, not to cure it—which means patients may be taking these medications for years. This cumulative exposure is called the anticholinergic burden. Many studies show that the anticholinergic burden is a predictor of cognitive and physical decline; a 2016 study of adults older than 65 who were exposed to 5 mg/d of oxybutynin for more than three years had a 23% increased risk for dementia, compared to low-risk or no exposure groups.9
In a retrospective, population-level study conducted in New Zealand, researchers assessed the anticholinergic effects of delirium, urinary retention, and constipation in 2,248 patients (65 and older) who were admitted to the hospital with at least one prescribed medication. Anticholinergic burden was found to be a significant independent predictor; patients taking five anticholinergic medications were more than three times as likely to develop an anticholinergic effect than those taking just one such medication (adjusted odds ratio, 3.21).11
Psychotropic drugs
Another often-prescribed medication group is psychotropic drugs, specifically antipsychotics and benzodiazepines, for agitation and behavioral disturbances in dementia. A year-long study of 851 patients in two long-term care nursing homes in Boston found that risk for ADRs—specifically, falls—was increased in those who had a change (initiation or dose increase) in psychotropic medication (ie, benzodiazepine, antipsychotic, or antidepressant).12
Second-generation antipsychotics, which are more commonly prescribed than first-generation agents, work on a postsynaptic blockade of brain dopamine D2 receptors and have an increased affinity for serotonin 5-HT2A receptors (see Table 1 for pharmacology of these medications).13,14 Adverse effects of these drugs include hypotension, sedation, and anticholinergic effects. Second-generation antipsychotics also carry a “black box warning” for increased risk for death in elderly patients with dementia-related psychosis.15
Benzodiazepines bind to receptors in the gamma-aminobutyric acid receptor complex, which enhances the binding of this inhibitory neurotransmitter (see Table 2 for pharmacology). Of this class of drugs, lorazepam has the highest potency, whereas midazolam and diazepam have lower potencies. Use of benzodiazepines increases risk for delirium and respiratory depression.16 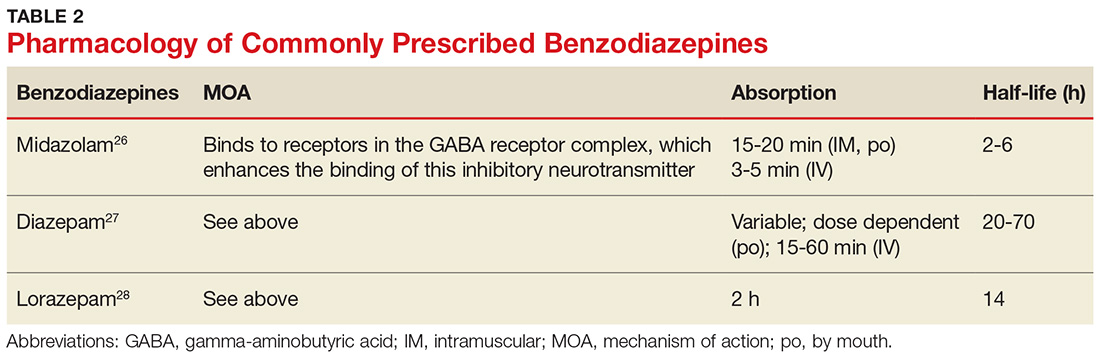
Diabetes treatment
People with diabetes have an increased risk for ADEs; this risk is elevated in older adults due to comorbidities such as peripheral neuropathy, retinopathy, coronary artery disease, and peripheral vascular disease.10 Hypoglycemic agents, such as insulin and insulin secretagogues, confer a higher risk for falls due to their hypoglycemic effect.10 Furthermore, metformin is known to increase risk for cognitive impairment in patients with diabetes.10
PREVENTING ADEs AND UNNECESSARY POLYPHARMACY
Predicting and preventing ADEs should be a health care provider’s priority when treating an elderly patient taking multiple medications—but it is often overlooked. Electronic medical records (EMRs) are helpful in preventing ADEs, specifically prescription errors, by flagging the patient’s chart when potentially problematic medications are ordered; however, this captures only a portion of ADEs occurring in this population.7
Other options to evaluate a patient for polypharmacy and possible ADRs include the Beers Criteria and the STOPP/START Criteria.17,18 Additionally, performing thorough and frequent medication reviews helps ensure that patients are prescribed essential medications to treat their comorbidities with the most opportunistic risk-benefit ratio. Patients’ medication lists across settings (eg, hospital, primary care, urgent care) can be accessed more easily, efficiently, and accurately with the integration of EMRs.
Beers Criteria
First published by Dr. Mark Beers in 1991 and endorsed by the American Geriatrics Society, the Beers Criteria identifies possible harmful effects of certain commonly prescribed medications to help guide and modify pharmacologic treatments, particularly in adults older than 65. The Beers Criteria classifies medications into three categories:
- Drugs that should be avoided or dose-adjusted
- Drugs that are potentially inappropriate in patients with certain conditions or syndromes
- Drugs that should be prescribed with caution in older adults.17
In the most recent update (2015), possible adverse effects of medications based on a patient’s hepatic or renal function, the effectiveness of the medication, and possible drug interactions were added. For example, nitrofurantoin and antiarrhythmics (eg, amiodarone and digoxin) should be avoided at a lower threshold of hepatic and renal impairment than previously recommended. The criteria suggest avoiding use of zolpidem, a nonbenzodiazepine receptor agonist, because of its elevated risk for adverse effects and minimal effectiveness in treating insomnia. More information about the 2015 criteria is available from the American Geriatrics Society (http://online library.wiley.com/doi/10.1111/jgs. 13702/full).19
The latest update also takes into account recently published evidence of increased ADEs resulting from drugs such as antipsychotics and proton pump inhibitors (PPIs).20 Antipsychotics are associated with an increased risk for morbidity and mortality, and PPIs are now recommended only for treatment duration of up to two months because of the possible increased risk for Clostridium difficile infection, as well as falls and fractures in patients older than 65.20 (PPIs indirectly reduce calcium absorption, which may lead to an increased fracture risk, particularly in postmenopausal women.20)
As with any guideline, the Beers Criteria was designed to supplement, not replace, clinical expertise and judgment. The risks and benefits of a medication should be weighed for the individual patient.
STOPP/START Criteria
Less widely used is the STOPP/START Criteria, an evidence-based set of guidelines consisting of 65 STOPP (Screening Tool of Older Person’s potentially inappropriate Prescriptions) and 22 START (Screening Tool to Alert doctors to the Right Treatment) criteria. Although they may be used individually, STOPP and START are best used together to determine the most appropriate medications for an elderly patient.
The STOPP guidelines help determine when the risks of a medication may outweigh the benefits in a given patient. STOPP includes recommendations for the appropriate length of time to use a medication; for example, PPIs should not be used for more than eight weeks (similar to the Beers recommendation) and benzodiazepines and neuroleptics for more than four weeks.18
START helps clinicians recognize potential prescribing omissions and to identify when a medication regimen should be implemented based on a patient’s history.18 Examples of START criteria include suggestions of when to initiate calcium and vitamin D supplementation for prevention of osteoporosis and when to begin statins in patients with diabetes, coronary artery disease, and cardiovascular disease.18
STOPP/START is organized by physiologic system, which allows for greater usability, and it addresses medications by class rather than specific medications. (The Beers Criteria was criticized for these reasons, as well as its limited transferability outside the United States.) When assessed in systematic reviews, the STOPP/START criteria were found to be fundamentally more sensitive than the Beers Criteria. Overall, it was concluded that the use of the STOPP/START criteria resulted in an absolute risk reduction of 21.2% to 35.7% and greatly improved the appropriateness of prescribing medication to the elderly. Its use also resulted in fewer follow-up appointments with a primary care physician (PCP).18
iPhone and Android applications such as iGeriatrics and Medstopper provide clinicians with easy access to Beers Criteria and STOPP/START Criteria, respectively.
Medication reconciliation
Medication reconciliation—in which health care providers review a patient’s medication list at hospital admission and discharge, and even at routine office visits—is an increasingly common practice, especially with the implementation of EMRs. The patient’s prescribed and OTC medications, as well as dose, route, frequency, and indication, are updated, with the goal of maintaining the most accurate list. Health care providers can utilize both the Beers Criteria and the STOPP/START criteria in their reconciliation process to help reduce polypharmacy in the elderly. It is an essential step in maintaining communication between providers and ultimately decreasing the incidence of ADEs.17
IMPROVE … continuity of care
Polypharmacy can decrease patient likelihood to adhere to the regimen, whether due to confusion or intolerance.8 Patients should be included, along with caregivers and all medical providers, in a holistic assessment of the patient’s best interests in terms of long-term care and pharmacologic treatment, since those who have a sense of control in their treatment goals and expectations often achieve a better understanding of their medical status.10
However, educating patients about their medications is time-consuming, and time is often at a premium during a typical office visit. A pilot study of 28 male veterans (ages 85 and older)—the Integrated Management and Polypharmacy Review of Vulnerable Elders (IMPROVE) project—devised a model to combat this problem.21 As an adjunct to a visit with the PCP, a clinical pharmacist trained in patient education and medication management performed face-to-face clinical consults with patients and their caregivers. The results indicated that medical management by both the PCP and the pharmacist resulted in better medication management. The pharmacist was able to spend time with the patient and caregiver, resulting in individualized instructions, education, and strategies for safe and effective medication use. The PCP remained involved by cosigning the note with the pharmacist and was available for consultation, if needed.
In IMPROVE, 79% of patients had at least one medication discontinued and 75% had one or more dosing or timing adjustments made. Potentially inappropriate medications were reduced by 14%.21 When the researchers compared the six-month period before the trial with the six-month period afterward, they found an average pharmacy cost savings of $64 per veteran per month. There was also a decreasing trend in phone calls and visits to the PCP. Cost savings were comparable to or greater than those reported for similar interventions.21 There has not been sufficient long-term follow-up to assess this method’s effects on ADEs, morbidity, and mortality, however.
CONCLUSION
Managing medications in the elderly population is difficult, and polypharmacy is common due to the prevalence of patients with comorbidities. It is important for providers to be aware of possible drug interactions, prescribing cascades, and ADEs. Medications such as anticholinergics and antipsychotics pose an increased risk for ADEs, but the regular implementation of criteria such as Beers or STOPP/START in clinical practice will minimize overprescribing and improve health outcomes. These criteria should be used to supplement the clinical judgment and expertise of providers as a mainstay of patient care in the elderly.
1. Kantor ED, Rehm CD, Haas JS, et al. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314:1818-1830.
2. Qato DM, Wilder J, Schumm LP. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med. 2016;176(4):473-482.
3. Beard K. Adverse reactions as a cause of hospital admission in the aged. Drugs Aging. 1992;2(4):356-367.
4. Pedros C, Formiga F, Corbella X, Arnau J. Adverse drug reactions leading to urgent hospital admission in an elderly population: prevalence and main features. Eur J Clin Pharmacol. 2016:72(2):219-226.
5. Maher RL Jr, Hanlon JT, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57-65.
6. Nguyen PV-Q, Spinelli C. Prescribing cascade in an elderly woman. Can Pharm J (Ott). 2016;149(3):122-124.
7. Lavan AH, Gallagher PF, O’Mahony D. Methods to reduce prescribing errors in elderly patients with multimorbidity. Clin Interv Aging. 2016;11:857-866.
8. Sivagnanam G. Deprescription: the prescription metabolism. J Pharmacol Pharmacother. 2016;7(3):133-137.
9. Koronkowski M, Eisenhower C, Marcum Z. An update on geriatric medication safety and challenges specific to the care of older adults. Ann Longterm Care. 2016; 24(3):37-40.
10. Peron EP, Ogbonna KC, Donohoe KL. Diabetic medications and polypharmacy. Clin Geriatr Med. 2015;31(1): 17-vii.
11. Salahudeen MS, Nishtala PS, Duffull SB. The influence of patient characteristics on anticholinergic events in older people. Dement Geriatr Cogn Dis Extra. 2015;5(3): 530-541.
12. Echt MA, Samelson EJ, Hannan MT, et al. Psychotropic drug initiation or increased dosage and the acute risk of falls: a prospective cohort study of nursing home residents. BMC Geriatrics. 2013;13:19.
13. Mauri MC, Paletta S, Maffini M, et al. Clinical pharmacology of antipsychotics: an update. EXCLI J. 2014;13: 1163-1191.
14. Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatry. 2002;47:29-40.
15. FDA. Public Health Advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances (2005). www. fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm053171. Accessed November 28, 2017.
16. Griffin CE III, Kaye AM, Bueno FR, Kaye AD. Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner J. 2013;13:214-223.
17. Flanagan N, Beizer J. Medication reconciliation and education for older adults: using the 2015 AGS Beers Criteria as a guide. Home Healthc Now. 2016;34(10): 542-549.
18. Hill-Taylor B, Sketris I, Hayden J, et al. Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther. 2013;38(5):360-372.
19. American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11): 2227-2246.
20. Salbu RL, Feuer J. A closer look at the 2015 Beers criteria. J Pharm Pract. 2017;30(4):419-424.
21. Mirk A, Echt KV, Vandenberg AE, et al. Polypharmacy review of vulnerable elders: can we IMPROVE outcomes? Fed Pract. 2016;33(3):39-41.
22. Saphris [package insert]. Irvine, CA: Allergan, USA, Inc; 2017.
23. Latuda [package insert]. Marlborough, MA: Sunovion Pharmaceuticals, Inc; 2017.
24. Zyprexa [package insert]. Indianapolis, IN: Lilly USA LLC; 2017.
25. Seroquel [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals; 2017.
26. Midazolam hydrochloride injection solution [package insert]. Lake Forest, IL: Hospira Inc; 2017.
27. Diazepam oral solution and Diazepam Intensol oral solution concentrate [package insert]. Eatontown, NJ: West-Ward Pharmaceuticals Corp; 2016.
28. Ativan tablet [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals; 2013.
1. Kantor ED, Rehm CD, Haas JS, et al. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314:1818-1830.
2. Qato DM, Wilder J, Schumm LP. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med. 2016;176(4):473-482.
3. Beard K. Adverse reactions as a cause of hospital admission in the aged. Drugs Aging. 1992;2(4):356-367.
4. Pedros C, Formiga F, Corbella X, Arnau J. Adverse drug reactions leading to urgent hospital admission in an elderly population: prevalence and main features. Eur J Clin Pharmacol. 2016:72(2):219-226.
5. Maher RL Jr, Hanlon JT, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57-65.
6. Nguyen PV-Q, Spinelli C. Prescribing cascade in an elderly woman. Can Pharm J (Ott). 2016;149(3):122-124.
7. Lavan AH, Gallagher PF, O’Mahony D. Methods to reduce prescribing errors in elderly patients with multimorbidity. Clin Interv Aging. 2016;11:857-866.
8. Sivagnanam G. Deprescription: the prescription metabolism. J Pharmacol Pharmacother. 2016;7(3):133-137.
9. Koronkowski M, Eisenhower C, Marcum Z. An update on geriatric medication safety and challenges specific to the care of older adults. Ann Longterm Care. 2016; 24(3):37-40.
10. Peron EP, Ogbonna KC, Donohoe KL. Diabetic medications and polypharmacy. Clin Geriatr Med. 2015;31(1): 17-vii.
11. Salahudeen MS, Nishtala PS, Duffull SB. The influence of patient characteristics on anticholinergic events in older people. Dement Geriatr Cogn Dis Extra. 2015;5(3): 530-541.
12. Echt MA, Samelson EJ, Hannan MT, et al. Psychotropic drug initiation or increased dosage and the acute risk of falls: a prospective cohort study of nursing home residents. BMC Geriatrics. 2013;13:19.
13. Mauri MC, Paletta S, Maffini M, et al. Clinical pharmacology of antipsychotics: an update. EXCLI J. 2014;13: 1163-1191.
14. Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatry. 2002;47:29-40.
15. FDA. Public Health Advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances (2005). www. fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm053171. Accessed November 28, 2017.
16. Griffin CE III, Kaye AM, Bueno FR, Kaye AD. Benzodiazepine pharmacology and central nervous system-mediated effects. Ochsner J. 2013;13:214-223.
17. Flanagan N, Beizer J. Medication reconciliation and education for older adults: using the 2015 AGS Beers Criteria as a guide. Home Healthc Now. 2016;34(10): 542-549.
18. Hill-Taylor B, Sketris I, Hayden J, et al. Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther. 2013;38(5):360-372.
19. American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11): 2227-2246.
20. Salbu RL, Feuer J. A closer look at the 2015 Beers criteria. J Pharm Pract. 2017;30(4):419-424.
21. Mirk A, Echt KV, Vandenberg AE, et al. Polypharmacy review of vulnerable elders: can we IMPROVE outcomes? Fed Pract. 2016;33(3):39-41.
22. Saphris [package insert]. Irvine, CA: Allergan, USA, Inc; 2017.
23. Latuda [package insert]. Marlborough, MA: Sunovion Pharmaceuticals, Inc; 2017.
24. Zyprexa [package insert]. Indianapolis, IN: Lilly USA LLC; 2017.
25. Seroquel [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals; 2017.
26. Midazolam hydrochloride injection solution [package insert]. Lake Forest, IL: Hospira Inc; 2017.
27. Diazepam oral solution and Diazepam Intensol oral solution concentrate [package insert]. Eatontown, NJ: West-Ward Pharmaceuticals Corp; 2016.
28. Ativan tablet [package insert]. Bridgewater, NJ: Valeant Pharmaceuticals; 2013.
Does fish oil during pregnancy help prevent asthma in kids?
ILLUSTRATIVE CASE
A 24-year-old G2P1 at 24 weeks’ gestation presents to your clinic for a routine prenatal visit. Her older daughter has asthma and she is inquiring as to whether there is anything she can do to lower the risk of her second child developing asthma in the future. What do you recommend?
Asthma is the most common chronic disease in children in resource-rich countries such as the United States.2 The Centers for Disease Control and Prevention (CDC) reported that 8.4% of children were diagnosed with asthma in 2015.3
Omega-3 fatty acids, found naturally in fish oil, are thought to confer anti-inflammatory properties that offer protection against asthma. Clinical trials have shown that fish oil supplementation in pregnancy results in higher levels of omega-3 fatty acids, along with anti-inflammatory changes, in offspring.4 Previous epidemiologic studies have also found that consumption of omega-3 fatty acids decreased the risk of atopy and asthma in offspring.5,6
A Cochrane review published in 2015, however, concluded that omega-3 supplementation during pregnancy had no benefit on wheeze or asthma in offspring.7 Five RCTs were included in the analysis. The largest trial by Palmer et al, which included 706 women, showed no benefit for omega-3 supplementation.8 The second largest by Olsen et al, which included 533 women, did show a benefit (hazard ratio [HR]=0.37; 95% confidence interval [CI], 0.15-0.92; number needed to treat [NNT]=19.6).9
These results, however, were limited by heterogeneity in the amount of fish oil supplemented and duration of follow-up. For example, the children in the Palmer study were followed only until 3 years of age, which is around the time that asthma can be formally diagnosed, potentially leading to under-reporting.8 In addition, the diagnosis of asthma was based on parent report of 3 episodes of wheezing, use of daily asthma medication, or use of a national registry—all of which can underestimate the incidence of asthma. The reported rate of childhood asthma with IgE-sensitization (they did not report the rate without sensitization) was 1.8% in both arms, which is much lower than the CDC’s rate of 8.4%, suggesting underdiagnosis.3,8 Due to these biases and other potential confounders, no firm conclusions can be drawn from the Cochrane review.
STUDY SUMMARY
Maternal fish oil supplementation reduces incidence of asthma in children
This single-center, double-blinded RCT of 736 pregnant women evaluated the effect of 2.4 g/d of n-3 long-chain polyunsaturated fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) or placebo (olive oil), starting at an estimated gestational age of 24 to 26 weeks, on wheeze or asthma incidence in their offspring.1
Eligible women were between 22 and 26 weeks’ pregnant at the time of recruitment. Exclusion criteria included supplementation of 600 IU/d or more of vitamin D, or having any endocrine, cardiac, or renal disorders. The investigators randomized the women in a 1:1 ratio to either fish oil or placebo. Maternal EPA and DHA blood levels were tested at the time of randomization and one week after birth.
The primary outcome was persistent wheeze or asthma (after 3 years of age, the diagnosis of persistent wheeze was termed asthma) based on daily diary recordings of 5 episodes of troublesome lung symptoms within the last 6 months (each lasting for at least 3 consecutive days), rescue use of inhaled beta2-agonists, and/or relapse after a 3-month course of inhaled glucocorticoids. Secondary outcomes included lower respiratory tract infections, asthma exacerbations, eczema, and allergic sensitization.
In total, 695 offspring were included in the study with 95.5% follow-up at 3 years and 93.1% follow-up at 5 years. The children had scheduled pediatric visits at 1 week; 1, 3, 6, 12, 18, 24, 30, and 36 months; and at 4 and 5 years, and acute visits for any pulmonary, allergic, or dermatologic symptoms that arose.
Results. The investigators found that the children of the mothers who received the fish oil had a lower risk of persistent wheeze or asthma at ages 3 to 5 years compared to those who received placebo (16.9% vs 23.7%; HR=0.69; 95% CI, 0.49-0.97; P=.035; NNT=14.7). But the effect of the fish oil supplementation was significant only in the children of the mothers with baseline EPA and DHA levels in the lowest third (17.5% vs 34.1%; HR=0.46; 95% CI, 0.25-0.83; P=.011; NNT=5.6). Similarly, in mothers who consumed the least EPA and DHA before the start of the study, fish oil supplementation had a greater benefit in terms of decreased wheeze and asthma (18.5% vs 32.4%; HR=0.55; 95% CI, 0.30-0.98; P=.043; NNT=7.2).
As for the secondary outcomes, only a reduction in lower respiratory tract infections was associated with the fish oil supplementation vs the control (38.8% vs 45.5%; HR=0.77; 95% CI, 0.61-0.99; P=.041; NNT=14.9). There was no reduction in asthma exacerbations, eczema, or risk of sensitization in the fish oil group.
WHAT'S NEW?
Study adds fuel to the fire
This study strengthens the case for fish oil supplementation during pregnancy to reduce the risk of asthma in offspring, despite the recent Cochrane review that showed no benefit.1,7 The Palmer study used a much lower amount of omega-3s (900 mg/d fish oil vs 2400 mg/d in the current trial).1,8 Olsen et al supplemented with a greater amount of omega-3s (2700 mg/d) and did find a benefit.9 The NNT from the Olsen study (19.6) is consistent with that of the current investigation, suggesting that a higher dosage may be necessary to prevent the onset of asthma.
Additionally, this study followed children for a longer period than did the Palmer study, which may have led to more accurate diagnoses of asthma.1,8 Lastly, the diagnosis of asthma in the Palmer study was based on parent survey data and use of daily asthma medicine rather than on daily diary cards, which are often more accurate.
Consider fish consumption. Both this study and the Olsen trial were performed in Denmark.1,9 While Denmark and the United States have had a relatively similar level of fish consumption since the 1990s, women in Denmark may eat a higher proportion of oily fish than women in the United States, given the more common inclusion of mackerel and herring in their diet.10 Thus, the effect of supplementation may be more pronounced in women in the United States.
CAVEATS
Questions remain: Ideal dose and which women to treat?
The US Food and Drug Administration currently recommends 8 to 12 ounces of fish per week for pregnant women, but there are no guidelines on the ideal amount of fish oil to be consumed.11 The Palmer study,8 using 900 mg/d fish oil, did not show a benefit, whereas there did appear to be benefit in this study (2400 mg/d)1 and the Olsen study (2700 mg/d).9 Further research is needed to determine the optimal dosage.
The decreased risk of persistent wheeze or asthma was seen only in the children of the women whose EPA and DHA blood levels were in the lowest third of the study population. Thus, only women whose blood levels are low to begin with will likely benefit from this intervention. Currently, EPA and DHA levels are not routinely checked, but there may be some benefit to doing so.
One proxy for blood levels is maternal intake of fish at baseline. The investigators found that there was an association between dietary intake of fish and blood levels of EPA and DHA (r=0.32; P<.001).1 Therefore, additional screening questions to determine fish consumption would be useful for identifying women most likely to benefit from supplementation.
CHALLENGES TO IMPLEMENTATION
Multiple pills and additional cost
Since omega-3 fatty acids are relatively safe and the NNT in the general population is low, it may be worth supplementing all pregnant women, even without a commercially-available blood test for EPA or DHA. Nevertheless, some women may find it challenging to take up to an additional 4 pills/d for 13 or more weeks. Also, there is an associated cost with these supplements, although it is low.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Bisgaard H, Stokholm J, Chawes BL, et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Engl J Med. 2016;375:2530-2539.
2. Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dessemination Committee Report. Allergy. 2004;59:469-478.
3. Centers for Disease Control and Prevention. Asthma. Available at: https://www.cdc.gov/asthma/most_recent_data.htm. Accessed October 9, 2017.
4. Miyata J, Arita M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol Int. 2015;64:27-34.
5. Salam MT, Li YF, Langholz B, et al. Maternal fish consumption during pregnancy and risk of early childhood asthma. J Asthma. 2005;42:513-518.
6. Calvani M, Alessandri C, Sopo SM, et al. Consumption of fish, butter and margarine during pregnancy and development of allergic sensitizations in the offspring: role of maternal atopy. Pediatr Allergy Immunol. 2006;17:94-102.
7. Gunaratne AW, Makrides M, Collins CT. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst Rev. 2015;22:CD010085.
8. Palmer D, Sullivan T, Gold M, et al. Randomized controlled trial of fish oil supplementation in pregnancy on childhood allergies. Allergy. 2013;68:1370-1376.
9. Olsen SF, Østerdal ML, Salvig JD, et al. Fish oil intake compared with olive oil intake in late pregnancy and asthma in the offspring: 16 y of registry-based follow-up from a randomized controlled trial. Am J Clin Nutr. 2008;88:167-175.
10. Helgi Library. Fish consumption per capita by country. Available at: http://www.helgilibrary.com/indicators/fish-consumption-per-capita/. Accessed September 27, 2017.
11. FDA Advice About Eating Fish, From the Environmental Protection Agency and Food and Drug Administration; Revised Fish Advice; Availability. Federal Register.2017;82:6571-6574.
ILLUSTRATIVE CASE
A 24-year-old G2P1 at 24 weeks’ gestation presents to your clinic for a routine prenatal visit. Her older daughter has asthma and she is inquiring as to whether there is anything she can do to lower the risk of her second child developing asthma in the future. What do you recommend?
Asthma is the most common chronic disease in children in resource-rich countries such as the United States.2 The Centers for Disease Control and Prevention (CDC) reported that 8.4% of children were diagnosed with asthma in 2015.3
Omega-3 fatty acids, found naturally in fish oil, are thought to confer anti-inflammatory properties that offer protection against asthma. Clinical trials have shown that fish oil supplementation in pregnancy results in higher levels of omega-3 fatty acids, along with anti-inflammatory changes, in offspring.4 Previous epidemiologic studies have also found that consumption of omega-3 fatty acids decreased the risk of atopy and asthma in offspring.5,6
A Cochrane review published in 2015, however, concluded that omega-3 supplementation during pregnancy had no benefit on wheeze or asthma in offspring.7 Five RCTs were included in the analysis. The largest trial by Palmer et al, which included 706 women, showed no benefit for omega-3 supplementation.8 The second largest by Olsen et al, which included 533 women, did show a benefit (hazard ratio [HR]=0.37; 95% confidence interval [CI], 0.15-0.92; number needed to treat [NNT]=19.6).9
These results, however, were limited by heterogeneity in the amount of fish oil supplemented and duration of follow-up. For example, the children in the Palmer study were followed only until 3 years of age, which is around the time that asthma can be formally diagnosed, potentially leading to under-reporting.8 In addition, the diagnosis of asthma was based on parent report of 3 episodes of wheezing, use of daily asthma medication, or use of a national registry—all of which can underestimate the incidence of asthma. The reported rate of childhood asthma with IgE-sensitization (they did not report the rate without sensitization) was 1.8% in both arms, which is much lower than the CDC’s rate of 8.4%, suggesting underdiagnosis.3,8 Due to these biases and other potential confounders, no firm conclusions can be drawn from the Cochrane review.
STUDY SUMMARY
Maternal fish oil supplementation reduces incidence of asthma in children
This single-center, double-blinded RCT of 736 pregnant women evaluated the effect of 2.4 g/d of n-3 long-chain polyunsaturated fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) or placebo (olive oil), starting at an estimated gestational age of 24 to 26 weeks, on wheeze or asthma incidence in their offspring.1
Eligible women were between 22 and 26 weeks’ pregnant at the time of recruitment. Exclusion criteria included supplementation of 600 IU/d or more of vitamin D, or having any endocrine, cardiac, or renal disorders. The investigators randomized the women in a 1:1 ratio to either fish oil or placebo. Maternal EPA and DHA blood levels were tested at the time of randomization and one week after birth.
The primary outcome was persistent wheeze or asthma (after 3 years of age, the diagnosis of persistent wheeze was termed asthma) based on daily diary recordings of 5 episodes of troublesome lung symptoms within the last 6 months (each lasting for at least 3 consecutive days), rescue use of inhaled beta2-agonists, and/or relapse after a 3-month course of inhaled glucocorticoids. Secondary outcomes included lower respiratory tract infections, asthma exacerbations, eczema, and allergic sensitization.
In total, 695 offspring were included in the study with 95.5% follow-up at 3 years and 93.1% follow-up at 5 years. The children had scheduled pediatric visits at 1 week; 1, 3, 6, 12, 18, 24, 30, and 36 months; and at 4 and 5 years, and acute visits for any pulmonary, allergic, or dermatologic symptoms that arose.
Results. The investigators found that the children of the mothers who received the fish oil had a lower risk of persistent wheeze or asthma at ages 3 to 5 years compared to those who received placebo (16.9% vs 23.7%; HR=0.69; 95% CI, 0.49-0.97; P=.035; NNT=14.7). But the effect of the fish oil supplementation was significant only in the children of the mothers with baseline EPA and DHA levels in the lowest third (17.5% vs 34.1%; HR=0.46; 95% CI, 0.25-0.83; P=.011; NNT=5.6). Similarly, in mothers who consumed the least EPA and DHA before the start of the study, fish oil supplementation had a greater benefit in terms of decreased wheeze and asthma (18.5% vs 32.4%; HR=0.55; 95% CI, 0.30-0.98; P=.043; NNT=7.2).
As for the secondary outcomes, only a reduction in lower respiratory tract infections was associated with the fish oil supplementation vs the control (38.8% vs 45.5%; HR=0.77; 95% CI, 0.61-0.99; P=.041; NNT=14.9). There was no reduction in asthma exacerbations, eczema, or risk of sensitization in the fish oil group.
WHAT'S NEW?
Study adds fuel to the fire
This study strengthens the case for fish oil supplementation during pregnancy to reduce the risk of asthma in offspring, despite the recent Cochrane review that showed no benefit.1,7 The Palmer study used a much lower amount of omega-3s (900 mg/d fish oil vs 2400 mg/d in the current trial).1,8 Olsen et al supplemented with a greater amount of omega-3s (2700 mg/d) and did find a benefit.9 The NNT from the Olsen study (19.6) is consistent with that of the current investigation, suggesting that a higher dosage may be necessary to prevent the onset of asthma.
Additionally, this study followed children for a longer period than did the Palmer study, which may have led to more accurate diagnoses of asthma.1,8 Lastly, the diagnosis of asthma in the Palmer study was based on parent survey data and use of daily asthma medicine rather than on daily diary cards, which are often more accurate.
Consider fish consumption. Both this study and the Olsen trial were performed in Denmark.1,9 While Denmark and the United States have had a relatively similar level of fish consumption since the 1990s, women in Denmark may eat a higher proportion of oily fish than women in the United States, given the more common inclusion of mackerel and herring in their diet.10 Thus, the effect of supplementation may be more pronounced in women in the United States.
CAVEATS
Questions remain: Ideal dose and which women to treat?
The US Food and Drug Administration currently recommends 8 to 12 ounces of fish per week for pregnant women, but there are no guidelines on the ideal amount of fish oil to be consumed.11 The Palmer study,8 using 900 mg/d fish oil, did not show a benefit, whereas there did appear to be benefit in this study (2400 mg/d)1 and the Olsen study (2700 mg/d).9 Further research is needed to determine the optimal dosage.
The decreased risk of persistent wheeze or asthma was seen only in the children of the women whose EPA and DHA blood levels were in the lowest third of the study population. Thus, only women whose blood levels are low to begin with will likely benefit from this intervention. Currently, EPA and DHA levels are not routinely checked, but there may be some benefit to doing so.
One proxy for blood levels is maternal intake of fish at baseline. The investigators found that there was an association between dietary intake of fish and blood levels of EPA and DHA (r=0.32; P<.001).1 Therefore, additional screening questions to determine fish consumption would be useful for identifying women most likely to benefit from supplementation.
CHALLENGES TO IMPLEMENTATION
Multiple pills and additional cost
Since omega-3 fatty acids are relatively safe and the NNT in the general population is low, it may be worth supplementing all pregnant women, even without a commercially-available blood test for EPA or DHA. Nevertheless, some women may find it challenging to take up to an additional 4 pills/d for 13 or more weeks. Also, there is an associated cost with these supplements, although it is low.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 24-year-old G2P1 at 24 weeks’ gestation presents to your clinic for a routine prenatal visit. Her older daughter has asthma and she is inquiring as to whether there is anything she can do to lower the risk of her second child developing asthma in the future. What do you recommend?
Asthma is the most common chronic disease in children in resource-rich countries such as the United States.2 The Centers for Disease Control and Prevention (CDC) reported that 8.4% of children were diagnosed with asthma in 2015.3
Omega-3 fatty acids, found naturally in fish oil, are thought to confer anti-inflammatory properties that offer protection against asthma. Clinical trials have shown that fish oil supplementation in pregnancy results in higher levels of omega-3 fatty acids, along with anti-inflammatory changes, in offspring.4 Previous epidemiologic studies have also found that consumption of omega-3 fatty acids decreased the risk of atopy and asthma in offspring.5,6
A Cochrane review published in 2015, however, concluded that omega-3 supplementation during pregnancy had no benefit on wheeze or asthma in offspring.7 Five RCTs were included in the analysis. The largest trial by Palmer et al, which included 706 women, showed no benefit for omega-3 supplementation.8 The second largest by Olsen et al, which included 533 women, did show a benefit (hazard ratio [HR]=0.37; 95% confidence interval [CI], 0.15-0.92; number needed to treat [NNT]=19.6).9
These results, however, were limited by heterogeneity in the amount of fish oil supplemented and duration of follow-up. For example, the children in the Palmer study were followed only until 3 years of age, which is around the time that asthma can be formally diagnosed, potentially leading to under-reporting.8 In addition, the diagnosis of asthma was based on parent report of 3 episodes of wheezing, use of daily asthma medication, or use of a national registry—all of which can underestimate the incidence of asthma. The reported rate of childhood asthma with IgE-sensitization (they did not report the rate without sensitization) was 1.8% in both arms, which is much lower than the CDC’s rate of 8.4%, suggesting underdiagnosis.3,8 Due to these biases and other potential confounders, no firm conclusions can be drawn from the Cochrane review.
STUDY SUMMARY
Maternal fish oil supplementation reduces incidence of asthma in children
This single-center, double-blinded RCT of 736 pregnant women evaluated the effect of 2.4 g/d of n-3 long-chain polyunsaturated fatty acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) or placebo (olive oil), starting at an estimated gestational age of 24 to 26 weeks, on wheeze or asthma incidence in their offspring.1
Eligible women were between 22 and 26 weeks’ pregnant at the time of recruitment. Exclusion criteria included supplementation of 600 IU/d or more of vitamin D, or having any endocrine, cardiac, or renal disorders. The investigators randomized the women in a 1:1 ratio to either fish oil or placebo. Maternal EPA and DHA blood levels were tested at the time of randomization and one week after birth.
The primary outcome was persistent wheeze or asthma (after 3 years of age, the diagnosis of persistent wheeze was termed asthma) based on daily diary recordings of 5 episodes of troublesome lung symptoms within the last 6 months (each lasting for at least 3 consecutive days), rescue use of inhaled beta2-agonists, and/or relapse after a 3-month course of inhaled glucocorticoids. Secondary outcomes included lower respiratory tract infections, asthma exacerbations, eczema, and allergic sensitization.
In total, 695 offspring were included in the study with 95.5% follow-up at 3 years and 93.1% follow-up at 5 years. The children had scheduled pediatric visits at 1 week; 1, 3, 6, 12, 18, 24, 30, and 36 months; and at 4 and 5 years, and acute visits for any pulmonary, allergic, or dermatologic symptoms that arose.
Results. The investigators found that the children of the mothers who received the fish oil had a lower risk of persistent wheeze or asthma at ages 3 to 5 years compared to those who received placebo (16.9% vs 23.7%; HR=0.69; 95% CI, 0.49-0.97; P=.035; NNT=14.7). But the effect of the fish oil supplementation was significant only in the children of the mothers with baseline EPA and DHA levels in the lowest third (17.5% vs 34.1%; HR=0.46; 95% CI, 0.25-0.83; P=.011; NNT=5.6). Similarly, in mothers who consumed the least EPA and DHA before the start of the study, fish oil supplementation had a greater benefit in terms of decreased wheeze and asthma (18.5% vs 32.4%; HR=0.55; 95% CI, 0.30-0.98; P=.043; NNT=7.2).
As for the secondary outcomes, only a reduction in lower respiratory tract infections was associated with the fish oil supplementation vs the control (38.8% vs 45.5%; HR=0.77; 95% CI, 0.61-0.99; P=.041; NNT=14.9). There was no reduction in asthma exacerbations, eczema, or risk of sensitization in the fish oil group.
WHAT'S NEW?
Study adds fuel to the fire
This study strengthens the case for fish oil supplementation during pregnancy to reduce the risk of asthma in offspring, despite the recent Cochrane review that showed no benefit.1,7 The Palmer study used a much lower amount of omega-3s (900 mg/d fish oil vs 2400 mg/d in the current trial).1,8 Olsen et al supplemented with a greater amount of omega-3s (2700 mg/d) and did find a benefit.9 The NNT from the Olsen study (19.6) is consistent with that of the current investigation, suggesting that a higher dosage may be necessary to prevent the onset of asthma.
Additionally, this study followed children for a longer period than did the Palmer study, which may have led to more accurate diagnoses of asthma.1,8 Lastly, the diagnosis of asthma in the Palmer study was based on parent survey data and use of daily asthma medicine rather than on daily diary cards, which are often more accurate.
Consider fish consumption. Both this study and the Olsen trial were performed in Denmark.1,9 While Denmark and the United States have had a relatively similar level of fish consumption since the 1990s, women in Denmark may eat a higher proportion of oily fish than women in the United States, given the more common inclusion of mackerel and herring in their diet.10 Thus, the effect of supplementation may be more pronounced in women in the United States.
CAVEATS
Questions remain: Ideal dose and which women to treat?
The US Food and Drug Administration currently recommends 8 to 12 ounces of fish per week for pregnant women, but there are no guidelines on the ideal amount of fish oil to be consumed.11 The Palmer study,8 using 900 mg/d fish oil, did not show a benefit, whereas there did appear to be benefit in this study (2400 mg/d)1 and the Olsen study (2700 mg/d).9 Further research is needed to determine the optimal dosage.
The decreased risk of persistent wheeze or asthma was seen only in the children of the women whose EPA and DHA blood levels were in the lowest third of the study population. Thus, only women whose blood levels are low to begin with will likely benefit from this intervention. Currently, EPA and DHA levels are not routinely checked, but there may be some benefit to doing so.
One proxy for blood levels is maternal intake of fish at baseline. The investigators found that there was an association between dietary intake of fish and blood levels of EPA and DHA (r=0.32; P<.001).1 Therefore, additional screening questions to determine fish consumption would be useful for identifying women most likely to benefit from supplementation.
CHALLENGES TO IMPLEMENTATION
Multiple pills and additional cost
Since omega-3 fatty acids are relatively safe and the NNT in the general population is low, it may be worth supplementing all pregnant women, even without a commercially-available blood test for EPA or DHA. Nevertheless, some women may find it challenging to take up to an additional 4 pills/d for 13 or more weeks. Also, there is an associated cost with these supplements, although it is low.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Bisgaard H, Stokholm J, Chawes BL, et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Engl J Med. 2016;375:2530-2539.
2. Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dessemination Committee Report. Allergy. 2004;59:469-478.
3. Centers for Disease Control and Prevention. Asthma. Available at: https://www.cdc.gov/asthma/most_recent_data.htm. Accessed October 9, 2017.
4. Miyata J, Arita M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol Int. 2015;64:27-34.
5. Salam MT, Li YF, Langholz B, et al. Maternal fish consumption during pregnancy and risk of early childhood asthma. J Asthma. 2005;42:513-518.
6. Calvani M, Alessandri C, Sopo SM, et al. Consumption of fish, butter and margarine during pregnancy and development of allergic sensitizations in the offspring: role of maternal atopy. Pediatr Allergy Immunol. 2006;17:94-102.
7. Gunaratne AW, Makrides M, Collins CT. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst Rev. 2015;22:CD010085.
8. Palmer D, Sullivan T, Gold M, et al. Randomized controlled trial of fish oil supplementation in pregnancy on childhood allergies. Allergy. 2013;68:1370-1376.
9. Olsen SF, Østerdal ML, Salvig JD, et al. Fish oil intake compared with olive oil intake in late pregnancy and asthma in the offspring: 16 y of registry-based follow-up from a randomized controlled trial. Am J Clin Nutr. 2008;88:167-175.
10. Helgi Library. Fish consumption per capita by country. Available at: http://www.helgilibrary.com/indicators/fish-consumption-per-capita/. Accessed September 27, 2017.
11. FDA Advice About Eating Fish, From the Environmental Protection Agency and Food and Drug Administration; Revised Fish Advice; Availability. Federal Register.2017;82:6571-6574.
1. Bisgaard H, Stokholm J, Chawes BL, et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Engl J Med. 2016;375:2530-2539.
2. Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dessemination Committee Report. Allergy. 2004;59:469-478.
3. Centers for Disease Control and Prevention. Asthma. Available at: https://www.cdc.gov/asthma/most_recent_data.htm. Accessed October 9, 2017.
4. Miyata J, Arita M. Role of omega-3 fatty acids and their metabolites in asthma and allergic diseases. Allergol Int. 2015;64:27-34.
5. Salam MT, Li YF, Langholz B, et al. Maternal fish consumption during pregnancy and risk of early childhood asthma. J Asthma. 2005;42:513-518.
6. Calvani M, Alessandri C, Sopo SM, et al. Consumption of fish, butter and margarine during pregnancy and development of allergic sensitizations in the offspring: role of maternal atopy. Pediatr Allergy Immunol. 2006;17:94-102.
7. Gunaratne AW, Makrides M, Collins CT. Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood. Cochrane Database Syst Rev. 2015;22:CD010085.
8. Palmer D, Sullivan T, Gold M, et al. Randomized controlled trial of fish oil supplementation in pregnancy on childhood allergies. Allergy. 2013;68:1370-1376.
9. Olsen SF, Østerdal ML, Salvig JD, et al. Fish oil intake compared with olive oil intake in late pregnancy and asthma in the offspring: 16 y of registry-based follow-up from a randomized controlled trial. Am J Clin Nutr. 2008;88:167-175.
10. Helgi Library. Fish consumption per capita by country. Available at: http://www.helgilibrary.com/indicators/fish-consumption-per-capita/. Accessed September 27, 2017.
11. FDA Advice About Eating Fish, From the Environmental Protection Agency and Food and Drug Administration; Revised Fish Advice; Availability. Federal Register.2017;82:6571-6574.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
PRACTICE CHANGER
Fish oil supplementation taken by women in the third trimester of pregnancy can reduce the risk of persistent wheeze, asthma, and infections of the lower respiratory tract in their children.1
STRENGTH OF RECOMMENDATION
B: Based on 2 double-blinded randomized controlled trials (RCTs).
Bisgaard H, Stokholm J, Chawes BL, et al. Fish oil-derived fatty acids in pregnancy and wheeze and asthma in offspring. N Engl J Med. 2016;375:2530-2539.1
Is megestrol acetate safe and effective for malnourished nursing home residents?
EVIDENCE SUMMARY
A 25-week double-blind, placebo-controlled RCT of 51 nursing home patients (mean age 76 years, range 50 to 95 years; 96% men) in 2000 found no difference in all-cause mortality between the MA treatment group and the placebo group (absolute risk reduction [ARR]=13.4%; 95% confidence interval [CI], -12.9% to 37.3%; number needed to harm [NNH]=7; 95% CI, -8 to 3).1
A 2007 case-control study of 17,328 nursing home residents (mean age 84 years [standard deviation, 9]; 71% women) found increased mortality for residents treated with at least 6 days of MA (median survival=23.9 months; 95% CI, 20.2-27.5) compared with untreated residents (median survival=31.2 months; 95% CI, 27.8-35.9).2 The decrease in median survival remained after adjusting for demographic variables, medical diagnoses, and cognitive and physical functioning (hazard ratio=1.37; 95% CI, 1.17-1.59). Follow-up ranged from 30 days to 44 months.
Risks related to megestrol acetate include deep vein thrombosis
The 2000 double-blind, placebo-controlled RCT of 51 nursing home patients found no difference in adverse events between the MA group and the placebo group (absolute risk increase=6.3%; 95% CI, -14.7% to 27.3%).1 No DVTs were reported as adverse events.
A 2003 retrospective chart review of 246 nursing home residents (mean age 87 years, 77% women) who were given MA 400 mg/d found an overall incidence of DVT of 4.1% (10 residents); 3.2% (8) residents were on MA at the time of DVT occurrence.3
A 2000 retrospective chart review of 19 nursing home residents who were prescribed MA (mean age 83 years, range 66 to 92 years; 84% women) found 32% (6) who developed Doppler-confirmed DVT after 50 days of therapy.4 DVT was not associated with known risk factors, age, body mass index, numbers of medications, or other medical diagnoses. The authors didn’t report MA dosage.
Patients on megestrol acetate don’t gain weight...
The 2000 double-blind, placebo-controlled RCT of 51 nursing home patients found no difference between the MA (800 mg/d for 12 weeks) and placebo groups in percentage of patients who gained ≥1.82 kg (ARR=-6.6%; 95% CI, -30.2% to 18.2%).1 At the 25-week follow-up (after the MA patients had been off the therapy for 13 weeks), a statistically, but not clinically, significant difference was observed in the number of MA patients who gained ≥1.82 kg (absolute benefit increase=40.2%; 95% CI, 13.4%-66.9%; number needed to treat [NNT]=2; 95% CI, 1-8). Of note, the authors based their statistics on a weight gain of ≥1.82 kg whereas 5 kg or 5% weight gain is the more commonly used definition for clinical significance.5
The 2007 case-control cohort study of 17,328 nursing home residents, who had lost 5% of total body weight in 3 months or 10% of total body weight in 6 months, also found no significant difference in weight gain between MA-treated patients (median dose=486 mg, range 20 to 2400 mg; median duration=90 days, range 7 to 934 days; median change=1 lb, interquartile range [IQR]=-8 to 10) and controls (median change=2 lb, IQR=-4 to 9) after 6 months of treatment.2
...And some lose weight
In a 2005 prospective case series of 17 nursing home residents (mean age 92 years [standard deviation, 6], 88% women), MA (400 mg/d for 63 days) was associated with weight loss (mean=-2.13±9.32 lb).6 Nine patients (53%) lost weight (mean=9.3±5.4 lb), and 8 patients (47%) gained weight (mean=5.9±4.9 lb).
A retrospective chart review in 2000 of 14 nursing home residents (mean age 84 years, range 74 to 97 years; 85% women) who received MA 40 to 800 mg/d for one to 15 weeks showed that 43% gained weight (mean=3.1 kg), 43% lost weight (mean=2.0 kg), and 14% had no weight change.7
A 2002 retrospective chart review of 50 nursing home residents (mean age 79 years, range 31 to 93 years; 74% women) who were treated with MA 200 to 2400 mg/d for at least 6 months found a mean weight loss of 1.1 to 2.2 kg.8 In the 6 months after MA discontinuation, weight gain for available subjects (5 to 16 patients) varied (mean monthly change=-0.17 kg to 3.07 kg). The study had a high attrition rate (26 patients were lost 6 months after MA initiation; 39 were lost 6 months after MA discontinuation).
RECOMMENDATIONS
The 2015 American Geriatrics Society Beers Criteria for potentially inappropriate medication use in older adults strongly advises against the use of MA because of limited increases in weight and increased risk of thrombotic events.9
1. Yeh SS, Wu SY, Lee TP, et al. Improvement in quality of life measures and stimulation of weight gain after treatment with megestrol acetate oral suspension in geriatric cachexia: results of a double-blind placebo controlled study. J Am Geriatr Soc. 2000;48:485-492.
2. Bodenner D, Spencer T, Riggs AT, et al., A retrospective study of the association between megestrol acetate administration and mortality among nursing home residents with clinically significant weight loss. Am J Geriatr Pharmacother. 2007;5:137-146.
3. Kropsky B, Shi Y, Cherniack EP. Incidence of deep-venous thrombosis in nursing home residents using megestrol acetate. J Am Med Dir Assoc. 2003;4:255-256.
4. Bolen JC, Andersen RE, Bennett RG. Deep vein thrombosis as a complication of megestrol acetate therapy among nursing home residents. J Am Med Dir Assoc. 2000;1:248-252.
5. Colman E. Food and Drug Administration’s Obesity Drug Guidance Document: a short history. Circulation. 2012;125:2156-2164.
6. Simmons SF, Walker KA, Osterwell D. The effect of megestrol acetate on oral food and fluid intake in nursing home residents: a pilot study. J Am Med Dir Assoc. 2005;6(3 Suppl):S5-S11.
7. Cicero LA, Rosenberg JM, Miyashiro A, et al. Megestrol acetate suspension for the treatment of involuntary weight loss in elderly nursing home residents: a retrospective chart review. Consult Pharm. 2000;15:811-814.
8. Dickerson LM, Jones KW. Retrospective review and intervention in the use of megestrol acetate in residents of skilled nursing facilities in South Carolina. Consult Pharm. 2002;17:1040-1042.
9. The American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2015;63:2227-2246.
EVIDENCE SUMMARY
A 25-week double-blind, placebo-controlled RCT of 51 nursing home patients (mean age 76 years, range 50 to 95 years; 96% men) in 2000 found no difference in all-cause mortality between the MA treatment group and the placebo group (absolute risk reduction [ARR]=13.4%; 95% confidence interval [CI], -12.9% to 37.3%; number needed to harm [NNH]=7; 95% CI, -8 to 3).1
A 2007 case-control study of 17,328 nursing home residents (mean age 84 years [standard deviation, 9]; 71% women) found increased mortality for residents treated with at least 6 days of MA (median survival=23.9 months; 95% CI, 20.2-27.5) compared with untreated residents (median survival=31.2 months; 95% CI, 27.8-35.9).2 The decrease in median survival remained after adjusting for demographic variables, medical diagnoses, and cognitive and physical functioning (hazard ratio=1.37; 95% CI, 1.17-1.59). Follow-up ranged from 30 days to 44 months.
Risks related to megestrol acetate include deep vein thrombosis
The 2000 double-blind, placebo-controlled RCT of 51 nursing home patients found no difference in adverse events between the MA group and the placebo group (absolute risk increase=6.3%; 95% CI, -14.7% to 27.3%).1 No DVTs were reported as adverse events.
A 2003 retrospective chart review of 246 nursing home residents (mean age 87 years, 77% women) who were given MA 400 mg/d found an overall incidence of DVT of 4.1% (10 residents); 3.2% (8) residents were on MA at the time of DVT occurrence.3
A 2000 retrospective chart review of 19 nursing home residents who were prescribed MA (mean age 83 years, range 66 to 92 years; 84% women) found 32% (6) who developed Doppler-confirmed DVT after 50 days of therapy.4 DVT was not associated with known risk factors, age, body mass index, numbers of medications, or other medical diagnoses. The authors didn’t report MA dosage.
Patients on megestrol acetate don’t gain weight...
The 2000 double-blind, placebo-controlled RCT of 51 nursing home patients found no difference between the MA (800 mg/d for 12 weeks) and placebo groups in percentage of patients who gained ≥1.82 kg (ARR=-6.6%; 95% CI, -30.2% to 18.2%).1 At the 25-week follow-up (after the MA patients had been off the therapy for 13 weeks), a statistically, but not clinically, significant difference was observed in the number of MA patients who gained ≥1.82 kg (absolute benefit increase=40.2%; 95% CI, 13.4%-66.9%; number needed to treat [NNT]=2; 95% CI, 1-8). Of note, the authors based their statistics on a weight gain of ≥1.82 kg whereas 5 kg or 5% weight gain is the more commonly used definition for clinical significance.5
The 2007 case-control cohort study of 17,328 nursing home residents, who had lost 5% of total body weight in 3 months or 10% of total body weight in 6 months, also found no significant difference in weight gain between MA-treated patients (median dose=486 mg, range 20 to 2400 mg; median duration=90 days, range 7 to 934 days; median change=1 lb, interquartile range [IQR]=-8 to 10) and controls (median change=2 lb, IQR=-4 to 9) after 6 months of treatment.2
...And some lose weight
In a 2005 prospective case series of 17 nursing home residents (mean age 92 years [standard deviation, 6], 88% women), MA (400 mg/d for 63 days) was associated with weight loss (mean=-2.13±9.32 lb).6 Nine patients (53%) lost weight (mean=9.3±5.4 lb), and 8 patients (47%) gained weight (mean=5.9±4.9 lb).
A retrospective chart review in 2000 of 14 nursing home residents (mean age 84 years, range 74 to 97 years; 85% women) who received MA 40 to 800 mg/d for one to 15 weeks showed that 43% gained weight (mean=3.1 kg), 43% lost weight (mean=2.0 kg), and 14% had no weight change.7
A 2002 retrospective chart review of 50 nursing home residents (mean age 79 years, range 31 to 93 years; 74% women) who were treated with MA 200 to 2400 mg/d for at least 6 months found a mean weight loss of 1.1 to 2.2 kg.8 In the 6 months after MA discontinuation, weight gain for available subjects (5 to 16 patients) varied (mean monthly change=-0.17 kg to 3.07 kg). The study had a high attrition rate (26 patients were lost 6 months after MA initiation; 39 were lost 6 months after MA discontinuation).
RECOMMENDATIONS
The 2015 American Geriatrics Society Beers Criteria for potentially inappropriate medication use in older adults strongly advises against the use of MA because of limited increases in weight and increased risk of thrombotic events.9
EVIDENCE SUMMARY
A 25-week double-blind, placebo-controlled RCT of 51 nursing home patients (mean age 76 years, range 50 to 95 years; 96% men) in 2000 found no difference in all-cause mortality between the MA treatment group and the placebo group (absolute risk reduction [ARR]=13.4%; 95% confidence interval [CI], -12.9% to 37.3%; number needed to harm [NNH]=7; 95% CI, -8 to 3).1
A 2007 case-control study of 17,328 nursing home residents (mean age 84 years [standard deviation, 9]; 71% women) found increased mortality for residents treated with at least 6 days of MA (median survival=23.9 months; 95% CI, 20.2-27.5) compared with untreated residents (median survival=31.2 months; 95% CI, 27.8-35.9).2 The decrease in median survival remained after adjusting for demographic variables, medical diagnoses, and cognitive and physical functioning (hazard ratio=1.37; 95% CI, 1.17-1.59). Follow-up ranged from 30 days to 44 months.
Risks related to megestrol acetate include deep vein thrombosis
The 2000 double-blind, placebo-controlled RCT of 51 nursing home patients found no difference in adverse events between the MA group and the placebo group (absolute risk increase=6.3%; 95% CI, -14.7% to 27.3%).1 No DVTs were reported as adverse events.
A 2003 retrospective chart review of 246 nursing home residents (mean age 87 years, 77% women) who were given MA 400 mg/d found an overall incidence of DVT of 4.1% (10 residents); 3.2% (8) residents were on MA at the time of DVT occurrence.3
A 2000 retrospective chart review of 19 nursing home residents who were prescribed MA (mean age 83 years, range 66 to 92 years; 84% women) found 32% (6) who developed Doppler-confirmed DVT after 50 days of therapy.4 DVT was not associated with known risk factors, age, body mass index, numbers of medications, or other medical diagnoses. The authors didn’t report MA dosage.
Patients on megestrol acetate don’t gain weight...
The 2000 double-blind, placebo-controlled RCT of 51 nursing home patients found no difference between the MA (800 mg/d for 12 weeks) and placebo groups in percentage of patients who gained ≥1.82 kg (ARR=-6.6%; 95% CI, -30.2% to 18.2%).1 At the 25-week follow-up (after the MA patients had been off the therapy for 13 weeks), a statistically, but not clinically, significant difference was observed in the number of MA patients who gained ≥1.82 kg (absolute benefit increase=40.2%; 95% CI, 13.4%-66.9%; number needed to treat [NNT]=2; 95% CI, 1-8). Of note, the authors based their statistics on a weight gain of ≥1.82 kg whereas 5 kg or 5% weight gain is the more commonly used definition for clinical significance.5
The 2007 case-control cohort study of 17,328 nursing home residents, who had lost 5% of total body weight in 3 months or 10% of total body weight in 6 months, also found no significant difference in weight gain between MA-treated patients (median dose=486 mg, range 20 to 2400 mg; median duration=90 days, range 7 to 934 days; median change=1 lb, interquartile range [IQR]=-8 to 10) and controls (median change=2 lb, IQR=-4 to 9) after 6 months of treatment.2
...And some lose weight
In a 2005 prospective case series of 17 nursing home residents (mean age 92 years [standard deviation, 6], 88% women), MA (400 mg/d for 63 days) was associated with weight loss (mean=-2.13±9.32 lb).6 Nine patients (53%) lost weight (mean=9.3±5.4 lb), and 8 patients (47%) gained weight (mean=5.9±4.9 lb).
A retrospective chart review in 2000 of 14 nursing home residents (mean age 84 years, range 74 to 97 years; 85% women) who received MA 40 to 800 mg/d for one to 15 weeks showed that 43% gained weight (mean=3.1 kg), 43% lost weight (mean=2.0 kg), and 14% had no weight change.7
A 2002 retrospective chart review of 50 nursing home residents (mean age 79 years, range 31 to 93 years; 74% women) who were treated with MA 200 to 2400 mg/d for at least 6 months found a mean weight loss of 1.1 to 2.2 kg.8 In the 6 months after MA discontinuation, weight gain for available subjects (5 to 16 patients) varied (mean monthly change=-0.17 kg to 3.07 kg). The study had a high attrition rate (26 patients were lost 6 months after MA initiation; 39 were lost 6 months after MA discontinuation).
RECOMMENDATIONS
The 2015 American Geriatrics Society Beers Criteria for potentially inappropriate medication use in older adults strongly advises against the use of MA because of limited increases in weight and increased risk of thrombotic events.9
1. Yeh SS, Wu SY, Lee TP, et al. Improvement in quality of life measures and stimulation of weight gain after treatment with megestrol acetate oral suspension in geriatric cachexia: results of a double-blind placebo controlled study. J Am Geriatr Soc. 2000;48:485-492.
2. Bodenner D, Spencer T, Riggs AT, et al., A retrospective study of the association between megestrol acetate administration and mortality among nursing home residents with clinically significant weight loss. Am J Geriatr Pharmacother. 2007;5:137-146.
3. Kropsky B, Shi Y, Cherniack EP. Incidence of deep-venous thrombosis in nursing home residents using megestrol acetate. J Am Med Dir Assoc. 2003;4:255-256.
4. Bolen JC, Andersen RE, Bennett RG. Deep vein thrombosis as a complication of megestrol acetate therapy among nursing home residents. J Am Med Dir Assoc. 2000;1:248-252.
5. Colman E. Food and Drug Administration’s Obesity Drug Guidance Document: a short history. Circulation. 2012;125:2156-2164.
6. Simmons SF, Walker KA, Osterwell D. The effect of megestrol acetate on oral food and fluid intake in nursing home residents: a pilot study. J Am Med Dir Assoc. 2005;6(3 Suppl):S5-S11.
7. Cicero LA, Rosenberg JM, Miyashiro A, et al. Megestrol acetate suspension for the treatment of involuntary weight loss in elderly nursing home residents: a retrospective chart review. Consult Pharm. 2000;15:811-814.
8. Dickerson LM, Jones KW. Retrospective review and intervention in the use of megestrol acetate in residents of skilled nursing facilities in South Carolina. Consult Pharm. 2002;17:1040-1042.
9. The American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2015;63:2227-2246.
1. Yeh SS, Wu SY, Lee TP, et al. Improvement in quality of life measures and stimulation of weight gain after treatment with megestrol acetate oral suspension in geriatric cachexia: results of a double-blind placebo controlled study. J Am Geriatr Soc. 2000;48:485-492.
2. Bodenner D, Spencer T, Riggs AT, et al., A retrospective study of the association between megestrol acetate administration and mortality among nursing home residents with clinically significant weight loss. Am J Geriatr Pharmacother. 2007;5:137-146.
3. Kropsky B, Shi Y, Cherniack EP. Incidence of deep-venous thrombosis in nursing home residents using megestrol acetate. J Am Med Dir Assoc. 2003;4:255-256.
4. Bolen JC, Andersen RE, Bennett RG. Deep vein thrombosis as a complication of megestrol acetate therapy among nursing home residents. J Am Med Dir Assoc. 2000;1:248-252.
5. Colman E. Food and Drug Administration’s Obesity Drug Guidance Document: a short history. Circulation. 2012;125:2156-2164.
6. Simmons SF, Walker KA, Osterwell D. The effect of megestrol acetate on oral food and fluid intake in nursing home residents: a pilot study. J Am Med Dir Assoc. 2005;6(3 Suppl):S5-S11.
7. Cicero LA, Rosenberg JM, Miyashiro A, et al. Megestrol acetate suspension for the treatment of involuntary weight loss in elderly nursing home residents: a retrospective chart review. Consult Pharm. 2000;15:811-814.
8. Dickerson LM, Jones KW. Retrospective review and intervention in the use of megestrol acetate in residents of skilled nursing facilities in South Carolina. Consult Pharm. 2002;17:1040-1042.
9. The American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2015;63:2227-2246.
Evidence-based answers from the Family Physicians Inquiries Network
EVIDENCE-BASED ANSWER:
No. Megestrol acetate (MA) is neither safe nor effective for stimulating appetite in malnourished nursing home residents. It increases the risk of deep vein thrombosis (DVT) (strength of recommendation [SOR]: C, 2 retrospective chart reviews), but isn’t associated with other new or worsening events or disorders (SOR: B, single randomized controlled trial [RCT]).
Over a 25-week period, MA wasn’t associated with increased mortality (SOR: B, single RCT). After 44 months, however, MA-treated patients showed decreased median survival (SOR: B, single case-control study).
Consistent, meaningful weight gain was not observed with MA treatment (SOR: B, single case-control study, single RCT, 2 retrospective chart reviews, single prospective case-series).
How do oral NSAIDs compare to other oral analgesics right after an acute musculoskeletal injury?
EVIDENCE SUMMARY
A Cochrane review of 16 RCTs (2144 patients) compared pain relief and return to function with oral NSAIDs and other oral analgesics (acetaminophen, opioids, or opioids plus acetaminophen) in patients who had suffered a soft tissue injury within the past 48 hours.1 No differences between NSAIDs and acetaminophen were seen in pain relief at fewer than 24 hours on a 100-point visual analog scale (VAS) (4 trials; 359 patients; mean difference [MD]=1.56; 95% confidence interval [CI], -3.9 to 7.0). Nor were differences observed in return to function at 7 days (3 trials, 386 patients; risk ratio [RR]=0.99; 95% CI, 0.90-1.09).
No differences in pain relief between NSAIDs and oral opioids were seen at fewer than 24 hours (2 trials, 757 patients; MD=-0.02; 95% CI, -3.71 to 3.68) nor at days 4 to 6 (one trial, 706 patients; MD=-2.9; 95% CI, -6.06 to 0.26). Compared with NSAIDs, opioids showed a small increase in return to function at 7 days (2 trials, 749 patients; RR=1.13; 95% CI, 1.03-1.25), but the combination of acetaminophen and opioids didn’t show a difference (one trial, 89 patients; RR= 1.28; 95% CI, 0.90-1.81).
Adverse gastrointestinal events (not defined) were no different between NSAIDs and acetaminophen (7 trials, 627 patients; RR=1.76; 95% CI, 0.99-3.14) and occurred less often with NSAIDs than with oral opioids (2 trials, 769 patients; RR=0.51; 95% CI, 0.37-0.69). Overall, the authors concluded that low-quality evidence consistently showed NSAIDs were at least equal to other oral analgesics in efficacy of pain relief and return to function.
Naproxen vs oxycodone: The opioid has more adverse effects
A double-blind, noninferiority, randomized trial (published after the Cochrane review search date) compared the effects of treatment with a single dose of oxycodone with a single dose of naproxen in 150 adult emergency department (ED) patients in a tertiary care academic center who had acute soft tissue injury and pain scores between 3 and 7 (on a 1-to-10 scale).2 Injuries included sprains, strains, contusions, low-back injury, and intervertebral disk problems. The authors didn’t clearly define “acute” with regard to time from injury.
Patients were randomized and given a single dose of oxycodone 10 mg or naproxen 250 mg with water. Pain scores and adverse effects were reassessed at 30 minutes and 60 minutes after administration, and a follow-up phone call was placed at 24 hours to evaluate further need for analgesics and adverse effects.
Baseline pain scores before medication administration were similar in the 2 groups (6.21 for the oxycodone group, 6 for the naproxen group). No difference in pain scores between oxycodone and naproxen was seen at 30 minutes (4.5 vs 4.4; P=.76) or 60 minutes (2.5 vs 2.6; P=.45). The number of patients who required more analgesics within 24 hours after administration didn’t differ significantly between the oxycodone group and the naproxen group (12 patients vs 5 patients; P=.07).
The study evaluated adverse effects, including nausea, vomiting, dizziness, drowsiness, pruritus, and epigastric pain. Overall, 22% of patients (33) from both groups combined experienced at least one adverse effect. The oxycodone group reported more adverse effects overall (36% vs 8%; RR=4.5; 95% CI, 2.0-10.2;). Ten patients experienced nausea, 6 vomiting, 4 dizziness, 3 drowsiness, and 2 pruritis. In the naproxen group, 4 patients experienced nausea; no other adverse effects were reported.
Acetaminophen, indomethacin, and diclofenac are equivalent
A double-blind RCT in a university hospital ED in Hong Kong compared patients older than 16 years with “isolated painful limb injury” after trauma who received combinations of analgesics or placebo.3 Patients were recruited during typical work-week hours (Monday to Friday, 9 am to 5 pm) and randomized into 4 groups: acetaminophen 1 g plus placebo (66 patients), placebo plus indomethacin 25 mg (71 patients), placebo plus diclofenac 25 mg (69 patients), or acetaminophen 1 g plus diclofenac 25 mg (94 patients).
Each patient was given the group’s designated combination of analgesics in the ED and asked to rate pain on a 0-to-100 visual analog pain scale (VAPS) at 0, 30, 60, 90, and 120 minutes after administration. Patients then left the ED with a 3-day course of their analgesic combination and were instructed to take the medication 4 times daily on the first day and 3 times daily thereafter. Patients recorded pain scores on the VAPS 3 times daily after discharge and at follow-up 5 to 8 days after initial presentation. Intention-to-treat analysis was done for patients lost to follow-up. A change in VAPS of 13 was considered clinically significant.
All groups started with similar pain scores (30 at rest and 70 with activity) and didn’t achieve clinically significant pain relief within the first hour (mean change in VAPS <13). At 90 minutes, all groups achieved a mean change in VAPS >13, with no statistically significant difference between the groups. Adverse effects were rare (7% total), and none were severe (no gastrointestinal hemorrhage or renal damage).
Outside the ED, the acetaminophen-diclofenac combination group showed the greatest pain score reduction at every time point at rest and with activity, but none of the reductions were statistically or clinically significant (results presented graphically). No difference was found between the groups in number of patients who completed the course of analgesics, took additional analgesia, tried Chinese medicine, or returned to the ED within 30 days.
Limitations to the study included that the medication dosages may be much lower than typical dosages given in the United States and therefore lack applicability. The study also didn’t include a true placebo arm.
1. Jones P, Dalziel SR, Lamdin R, et al. Oral non-steroidal anti-inflammatory drugs versus other oral analgesic agents for acute soft tissue injury. Cochrane Database Syst Rev. 2015;(7):CD007789.
2. Fathi M, Zare MA, Bahmani HR, et al. Comparison of oral oxycodone and naproxen in soft tissue injury pain control: a double-blind randomized clinical trial. Am J Emerg Med. 2015;33:1205-1208.
3. Woo WW, Man SY, Lam PK, et al. Randomized double-blind trial comparing oral paracetamol and oral nonsteroidal anti-inflammatory drugs for treating pain after musculoskeletal injury. Ann Emerg Med. 2005;46:352-361.
EVIDENCE SUMMARY
A Cochrane review of 16 RCTs (2144 patients) compared pain relief and return to function with oral NSAIDs and other oral analgesics (acetaminophen, opioids, or opioids plus acetaminophen) in patients who had suffered a soft tissue injury within the past 48 hours.1 No differences between NSAIDs and acetaminophen were seen in pain relief at fewer than 24 hours on a 100-point visual analog scale (VAS) (4 trials; 359 patients; mean difference [MD]=1.56; 95% confidence interval [CI], -3.9 to 7.0). Nor were differences observed in return to function at 7 days (3 trials, 386 patients; risk ratio [RR]=0.99; 95% CI, 0.90-1.09).
No differences in pain relief between NSAIDs and oral opioids were seen at fewer than 24 hours (2 trials, 757 patients; MD=-0.02; 95% CI, -3.71 to 3.68) nor at days 4 to 6 (one trial, 706 patients; MD=-2.9; 95% CI, -6.06 to 0.26). Compared with NSAIDs, opioids showed a small increase in return to function at 7 days (2 trials, 749 patients; RR=1.13; 95% CI, 1.03-1.25), but the combination of acetaminophen and opioids didn’t show a difference (one trial, 89 patients; RR= 1.28; 95% CI, 0.90-1.81).
Adverse gastrointestinal events (not defined) were no different between NSAIDs and acetaminophen (7 trials, 627 patients; RR=1.76; 95% CI, 0.99-3.14) and occurred less often with NSAIDs than with oral opioids (2 trials, 769 patients; RR=0.51; 95% CI, 0.37-0.69). Overall, the authors concluded that low-quality evidence consistently showed NSAIDs were at least equal to other oral analgesics in efficacy of pain relief and return to function.
Naproxen vs oxycodone: The opioid has more adverse effects
A double-blind, noninferiority, randomized trial (published after the Cochrane review search date) compared the effects of treatment with a single dose of oxycodone with a single dose of naproxen in 150 adult emergency department (ED) patients in a tertiary care academic center who had acute soft tissue injury and pain scores between 3 and 7 (on a 1-to-10 scale).2 Injuries included sprains, strains, contusions, low-back injury, and intervertebral disk problems. The authors didn’t clearly define “acute” with regard to time from injury.
Patients were randomized and given a single dose of oxycodone 10 mg or naproxen 250 mg with water. Pain scores and adverse effects were reassessed at 30 minutes and 60 minutes after administration, and a follow-up phone call was placed at 24 hours to evaluate further need for analgesics and adverse effects.
Baseline pain scores before medication administration were similar in the 2 groups (6.21 for the oxycodone group, 6 for the naproxen group). No difference in pain scores between oxycodone and naproxen was seen at 30 minutes (4.5 vs 4.4; P=.76) or 60 minutes (2.5 vs 2.6; P=.45). The number of patients who required more analgesics within 24 hours after administration didn’t differ significantly between the oxycodone group and the naproxen group (12 patients vs 5 patients; P=.07).
The study evaluated adverse effects, including nausea, vomiting, dizziness, drowsiness, pruritus, and epigastric pain. Overall, 22% of patients (33) from both groups combined experienced at least one adverse effect. The oxycodone group reported more adverse effects overall (36% vs 8%; RR=4.5; 95% CI, 2.0-10.2;). Ten patients experienced nausea, 6 vomiting, 4 dizziness, 3 drowsiness, and 2 pruritis. In the naproxen group, 4 patients experienced nausea; no other adverse effects were reported.
Acetaminophen, indomethacin, and diclofenac are equivalent
A double-blind RCT in a university hospital ED in Hong Kong compared patients older than 16 years with “isolated painful limb injury” after trauma who received combinations of analgesics or placebo.3 Patients were recruited during typical work-week hours (Monday to Friday, 9 am to 5 pm) and randomized into 4 groups: acetaminophen 1 g plus placebo (66 patients), placebo plus indomethacin 25 mg (71 patients), placebo plus diclofenac 25 mg (69 patients), or acetaminophen 1 g plus diclofenac 25 mg (94 patients).
Each patient was given the group’s designated combination of analgesics in the ED and asked to rate pain on a 0-to-100 visual analog pain scale (VAPS) at 0, 30, 60, 90, and 120 minutes after administration. Patients then left the ED with a 3-day course of their analgesic combination and were instructed to take the medication 4 times daily on the first day and 3 times daily thereafter. Patients recorded pain scores on the VAPS 3 times daily after discharge and at follow-up 5 to 8 days after initial presentation. Intention-to-treat analysis was done for patients lost to follow-up. A change in VAPS of 13 was considered clinically significant.
All groups started with similar pain scores (30 at rest and 70 with activity) and didn’t achieve clinically significant pain relief within the first hour (mean change in VAPS <13). At 90 minutes, all groups achieved a mean change in VAPS >13, with no statistically significant difference between the groups. Adverse effects were rare (7% total), and none were severe (no gastrointestinal hemorrhage or renal damage).
Outside the ED, the acetaminophen-diclofenac combination group showed the greatest pain score reduction at every time point at rest and with activity, but none of the reductions were statistically or clinically significant (results presented graphically). No difference was found between the groups in number of patients who completed the course of analgesics, took additional analgesia, tried Chinese medicine, or returned to the ED within 30 days.
Limitations to the study included that the medication dosages may be much lower than typical dosages given in the United States and therefore lack applicability. The study also didn’t include a true placebo arm.
EVIDENCE SUMMARY
A Cochrane review of 16 RCTs (2144 patients) compared pain relief and return to function with oral NSAIDs and other oral analgesics (acetaminophen, opioids, or opioids plus acetaminophen) in patients who had suffered a soft tissue injury within the past 48 hours.1 No differences between NSAIDs and acetaminophen were seen in pain relief at fewer than 24 hours on a 100-point visual analog scale (VAS) (4 trials; 359 patients; mean difference [MD]=1.56; 95% confidence interval [CI], -3.9 to 7.0). Nor were differences observed in return to function at 7 days (3 trials, 386 patients; risk ratio [RR]=0.99; 95% CI, 0.90-1.09).
No differences in pain relief between NSAIDs and oral opioids were seen at fewer than 24 hours (2 trials, 757 patients; MD=-0.02; 95% CI, -3.71 to 3.68) nor at days 4 to 6 (one trial, 706 patients; MD=-2.9; 95% CI, -6.06 to 0.26). Compared with NSAIDs, opioids showed a small increase in return to function at 7 days (2 trials, 749 patients; RR=1.13; 95% CI, 1.03-1.25), but the combination of acetaminophen and opioids didn’t show a difference (one trial, 89 patients; RR= 1.28; 95% CI, 0.90-1.81).
Adverse gastrointestinal events (not defined) were no different between NSAIDs and acetaminophen (7 trials, 627 patients; RR=1.76; 95% CI, 0.99-3.14) and occurred less often with NSAIDs than with oral opioids (2 trials, 769 patients; RR=0.51; 95% CI, 0.37-0.69). Overall, the authors concluded that low-quality evidence consistently showed NSAIDs were at least equal to other oral analgesics in efficacy of pain relief and return to function.
Naproxen vs oxycodone: The opioid has more adverse effects
A double-blind, noninferiority, randomized trial (published after the Cochrane review search date) compared the effects of treatment with a single dose of oxycodone with a single dose of naproxen in 150 adult emergency department (ED) patients in a tertiary care academic center who had acute soft tissue injury and pain scores between 3 and 7 (on a 1-to-10 scale).2 Injuries included sprains, strains, contusions, low-back injury, and intervertebral disk problems. The authors didn’t clearly define “acute” with regard to time from injury.
Patients were randomized and given a single dose of oxycodone 10 mg or naproxen 250 mg with water. Pain scores and adverse effects were reassessed at 30 minutes and 60 minutes after administration, and a follow-up phone call was placed at 24 hours to evaluate further need for analgesics and adverse effects.
Baseline pain scores before medication administration were similar in the 2 groups (6.21 for the oxycodone group, 6 for the naproxen group). No difference in pain scores between oxycodone and naproxen was seen at 30 minutes (4.5 vs 4.4; P=.76) or 60 minutes (2.5 vs 2.6; P=.45). The number of patients who required more analgesics within 24 hours after administration didn’t differ significantly between the oxycodone group and the naproxen group (12 patients vs 5 patients; P=.07).
The study evaluated adverse effects, including nausea, vomiting, dizziness, drowsiness, pruritus, and epigastric pain. Overall, 22% of patients (33) from both groups combined experienced at least one adverse effect. The oxycodone group reported more adverse effects overall (36% vs 8%; RR=4.5; 95% CI, 2.0-10.2;). Ten patients experienced nausea, 6 vomiting, 4 dizziness, 3 drowsiness, and 2 pruritis. In the naproxen group, 4 patients experienced nausea; no other adverse effects were reported.
Acetaminophen, indomethacin, and diclofenac are equivalent
A double-blind RCT in a university hospital ED in Hong Kong compared patients older than 16 years with “isolated painful limb injury” after trauma who received combinations of analgesics or placebo.3 Patients were recruited during typical work-week hours (Monday to Friday, 9 am to 5 pm) and randomized into 4 groups: acetaminophen 1 g plus placebo (66 patients), placebo plus indomethacin 25 mg (71 patients), placebo plus diclofenac 25 mg (69 patients), or acetaminophen 1 g plus diclofenac 25 mg (94 patients).
Each patient was given the group’s designated combination of analgesics in the ED and asked to rate pain on a 0-to-100 visual analog pain scale (VAPS) at 0, 30, 60, 90, and 120 minutes after administration. Patients then left the ED with a 3-day course of their analgesic combination and were instructed to take the medication 4 times daily on the first day and 3 times daily thereafter. Patients recorded pain scores on the VAPS 3 times daily after discharge and at follow-up 5 to 8 days after initial presentation. Intention-to-treat analysis was done for patients lost to follow-up. A change in VAPS of 13 was considered clinically significant.
All groups started with similar pain scores (30 at rest and 70 with activity) and didn’t achieve clinically significant pain relief within the first hour (mean change in VAPS <13). At 90 minutes, all groups achieved a mean change in VAPS >13, with no statistically significant difference between the groups. Adverse effects were rare (7% total), and none were severe (no gastrointestinal hemorrhage or renal damage).
Outside the ED, the acetaminophen-diclofenac combination group showed the greatest pain score reduction at every time point at rest and with activity, but none of the reductions were statistically or clinically significant (results presented graphically). No difference was found between the groups in number of patients who completed the course of analgesics, took additional analgesia, tried Chinese medicine, or returned to the ED within 30 days.
Limitations to the study included that the medication dosages may be much lower than typical dosages given in the United States and therefore lack applicability. The study also didn’t include a true placebo arm.
1. Jones P, Dalziel SR, Lamdin R, et al. Oral non-steroidal anti-inflammatory drugs versus other oral analgesic agents for acute soft tissue injury. Cochrane Database Syst Rev. 2015;(7):CD007789.
2. Fathi M, Zare MA, Bahmani HR, et al. Comparison of oral oxycodone and naproxen in soft tissue injury pain control: a double-blind randomized clinical trial. Am J Emerg Med. 2015;33:1205-1208.
3. Woo WW, Man SY, Lam PK, et al. Randomized double-blind trial comparing oral paracetamol and oral nonsteroidal anti-inflammatory drugs for treating pain after musculoskeletal injury. Ann Emerg Med. 2005;46:352-361.
1. Jones P, Dalziel SR, Lamdin R, et al. Oral non-steroidal anti-inflammatory drugs versus other oral analgesic agents for acute soft tissue injury. Cochrane Database Syst Rev. 2015;(7):CD007789.
2. Fathi M, Zare MA, Bahmani HR, et al. Comparison of oral oxycodone and naproxen in soft tissue injury pain control: a double-blind randomized clinical trial. Am J Emerg Med. 2015;33:1205-1208.
3. Woo WW, Man SY, Lam PK, et al. Randomized double-blind trial comparing oral paracetamol and oral nonsteroidal anti-inflammatory drugs for treating pain after musculoskeletal injury. Ann Emerg Med. 2005;46:352-361.
Evidence-based answers from the Family Physicians Inquiries Network
EVIDENCE-BASED ANSWER:
Nonsteroidal anti-inflammatory drugs (NSAIDs) are at least as effective as other oral analgesics (opioids, acetaminophen) in relieving pain in the first few days after an acute musculoskeletal injury. Evidence also indicates that using NSAIDs results in fewer adverse events than using narcotics (strength of recommendation [SOR]: A, systematic review of randomized controlled trials [RCTs], as well as individual RCTs).
Point-of-care ultrasound: Deploying in primary care
Two weeks ago, I saw a man with a swollen left leg in the office. It took me 2 days to get a Doppler study completed in my busy health care system. Point-of-care ultrasound (POCUS) would have been invaluable for this gentleman. As we know, though, POCUS has been “slow to grow” in primary care. However, as this month’s cover story suggests, things are changing.
Since the 1970s, ultrasound has been a standard diagnostic tool for many conditions. Initially considered the domain of radiologists and cardiologists with extensive training, technologic advances now allow accurate interpretation of ultrasound images by generalist physicians with a modest amount of training.
One of the first references to POCUS in general practice in the United States was published in 1988.1 Use of ultrasound in family medicine has developed slowly over the past 30 years, due to the high cost of equipment, a lack of training as a formal component of family medicine residency curricula, and a lack of evidence of its effectiveness in office practice. Only 6% of practicing family physicians (FPs) reported using non-obstetric POCUS in their practices in 2016, and only 2% of family medicine residency programs had established POCUS curricula in 2015.2,3
Ready for prime time. Although I had considered POCUS to be a relatively new and untested technology for primary care settings, my reading of the POCUS article has convinced me that POCUS is now ready for widespread deployment in family medicine office practice. Bornemann and colleagues review the evidence for the use of POCUS in 4 areas: the heart, the lung, screening for abdominal aortic aneurysm (AAA), and the diagnosis of deep vein thrombosis. They provide more than 30 references that support the accuracy and effectiveness of the use of POCUS by FPs for these areas. The equipment is affordable, there is ample evidence of accuracy and effectiveness, and, as they note, a curriculum for FP training has been published.
I certainly hope that POCUS continues to make its way into FPs’ offices. It would certainly help patients like the one I saw 2 weeks ago, and it would help us to screen for AAA in older male smokers, as recommended by the US Preventive Services Task Force.
I am delighted to see FP pioneers working to advance the use of POCUS in family medicine. Hopefully, it will become a standard part of family medicine training and practice sooner, rather than later.
1. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. J Fam Pract. 1988;5:129-135.
2. Clinical procedures performed by physicians at their practice. American Academy of Family Physicians Member Census, December 31, 2016. Available at: http://www.aafp.org/about/the-aafp/family-medicine-facts/table-12(rev).html. Accessed January 16, 2018.
3. Hall JW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: a CERA study. Fam Med. 2015;47:706-711.
Two weeks ago, I saw a man with a swollen left leg in the office. It took me 2 days to get a Doppler study completed in my busy health care system. Point-of-care ultrasound (POCUS) would have been invaluable for this gentleman. As we know, though, POCUS has been “slow to grow” in primary care. However, as this month’s cover story suggests, things are changing.
Since the 1970s, ultrasound has been a standard diagnostic tool for many conditions. Initially considered the domain of radiologists and cardiologists with extensive training, technologic advances now allow accurate interpretation of ultrasound images by generalist physicians with a modest amount of training.
One of the first references to POCUS in general practice in the United States was published in 1988.1 Use of ultrasound in family medicine has developed slowly over the past 30 years, due to the high cost of equipment, a lack of training as a formal component of family medicine residency curricula, and a lack of evidence of its effectiveness in office practice. Only 6% of practicing family physicians (FPs) reported using non-obstetric POCUS in their practices in 2016, and only 2% of family medicine residency programs had established POCUS curricula in 2015.2,3
Ready for prime time. Although I had considered POCUS to be a relatively new and untested technology for primary care settings, my reading of the POCUS article has convinced me that POCUS is now ready for widespread deployment in family medicine office practice. Bornemann and colleagues review the evidence for the use of POCUS in 4 areas: the heart, the lung, screening for abdominal aortic aneurysm (AAA), and the diagnosis of deep vein thrombosis. They provide more than 30 references that support the accuracy and effectiveness of the use of POCUS by FPs for these areas. The equipment is affordable, there is ample evidence of accuracy and effectiveness, and, as they note, a curriculum for FP training has been published.
I certainly hope that POCUS continues to make its way into FPs’ offices. It would certainly help patients like the one I saw 2 weeks ago, and it would help us to screen for AAA in older male smokers, as recommended by the US Preventive Services Task Force.
I am delighted to see FP pioneers working to advance the use of POCUS in family medicine. Hopefully, it will become a standard part of family medicine training and practice sooner, rather than later.
Two weeks ago, I saw a man with a swollen left leg in the office. It took me 2 days to get a Doppler study completed in my busy health care system. Point-of-care ultrasound (POCUS) would have been invaluable for this gentleman. As we know, though, POCUS has been “slow to grow” in primary care. However, as this month’s cover story suggests, things are changing.
Since the 1970s, ultrasound has been a standard diagnostic tool for many conditions. Initially considered the domain of radiologists and cardiologists with extensive training, technologic advances now allow accurate interpretation of ultrasound images by generalist physicians with a modest amount of training.
One of the first references to POCUS in general practice in the United States was published in 1988.1 Use of ultrasound in family medicine has developed slowly over the past 30 years, due to the high cost of equipment, a lack of training as a formal component of family medicine residency curricula, and a lack of evidence of its effectiveness in office practice. Only 6% of practicing family physicians (FPs) reported using non-obstetric POCUS in their practices in 2016, and only 2% of family medicine residency programs had established POCUS curricula in 2015.2,3
Ready for prime time. Although I had considered POCUS to be a relatively new and untested technology for primary care settings, my reading of the POCUS article has convinced me that POCUS is now ready for widespread deployment in family medicine office practice. Bornemann and colleagues review the evidence for the use of POCUS in 4 areas: the heart, the lung, screening for abdominal aortic aneurysm (AAA), and the diagnosis of deep vein thrombosis. They provide more than 30 references that support the accuracy and effectiveness of the use of POCUS by FPs for these areas. The equipment is affordable, there is ample evidence of accuracy and effectiveness, and, as they note, a curriculum for FP training has been published.
I certainly hope that POCUS continues to make its way into FPs’ offices. It would certainly help patients like the one I saw 2 weeks ago, and it would help us to screen for AAA in older male smokers, as recommended by the US Preventive Services Task Force.
I am delighted to see FP pioneers working to advance the use of POCUS in family medicine. Hopefully, it will become a standard part of family medicine training and practice sooner, rather than later.
1. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. J Fam Pract. 1988;5:129-135.
2. Clinical procedures performed by physicians at their practice. American Academy of Family Physicians Member Census, December 31, 2016. Available at: http://www.aafp.org/about/the-aafp/family-medicine-facts/table-12(rev).html. Accessed January 16, 2018.
3. Hall JW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: a CERA study. Fam Med. 2015;47:706-711.
1. Hahn RG, Davies TC, Rodney WM. Diagnostic ultrasound in general practice. J Fam Pract. 1988;5:129-135.
2. Clinical procedures performed by physicians at their practice. American Academy of Family Physicians Member Census, December 31, 2016. Available at: http://www.aafp.org/about/the-aafp/family-medicine-facts/table-12(rev).html. Accessed January 16, 2018.
3. Hall JW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: a CERA study. Fam Med. 2015;47:706-711.
Complex regional pain syndrome: Steps that FPs can take
USPSTF weighs in on postmenopausal hormone therapy to prevent chronic conditions
Resources
US Preventive Services Task Force. Final Recommendation Statement: Hormone Therapy in Postmenopausal Women: Primary Prevention of Chronic Conditions. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/menopausal-hormone-therapy-preventive-medication1. Accessed January 5, 2018.
Resources
US Preventive Services Task Force. Final Recommendation Statement: Hormone Therapy in Postmenopausal Women: Primary Prevention of Chronic Conditions. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/menopausal-hormone-therapy-preventive-medication1. Accessed January 5, 2018.
Resources
US Preventive Services Task Force. Final Recommendation Statement: Hormone Therapy in Postmenopausal Women: Primary Prevention of Chronic Conditions. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/menopausal-hormone-therapy-preventive-medication1. Accessed January 5, 2018.
Using oral and topical cosmeceuticals to prevent and treat skin aging, Part II
This month’s column resumes my review of prevention and treatment strategies for aging skin using oral and topical cosmeceutical agents.
Preventing and treating inflammation
Skin aging can result from inflammation through several mechanisms, including the formation of reactive oxygen species. Inflammation itself arises from myriad etiologic pathways, with multiple inflammatory mediators potentially involved, including histamines, cytokines, eicosanoids (for example, prostaglandins, thromboxanes, and leukotrienes), complement cascade components, kinins, fibrinopeptide enzymes, nuclear factor–kappa B, and free radicals.
Topically applied argan oil, caffeine, chamomile, feverfew, green tea, licorice extract, aloe, linoleic acid (found in high concentrations in argan oil and safflower oil), and niacinamide are among the anti-inflammatory ingredients that have been used successfully in topical skin care to reduce inflammation. The Food and Drug Administration does not allow cosmetics to make “anti-inflammatory” claims. For this reason, these products will state they have “soothing” effects or imply they improve of redness.
Oral polypodium leucotomos has been demonstrated to suppress the effect of UV radiation on COX-2 expression.2 Also, glycolic acid has exhibited the capacity to inhibit COX-2 signaling and other inflammatory mediators.3
Preventing and treating glycation
Glycation is produced by the Maillard reaction, a chemical reaction – particularly well known in cooking – between an amino acid and a sugar molecule that typically requires heat. This reaction was first described by Louis Camille Maillard in 1912 when he noted that amino acids can react with sugar to yield brown or golden-brown substances. It took until the 1980s for scientists to understand the importance of glycation in health.
When glycation occurs, sugar molecules attach to proteins, creating cross-linked proteins known as advanced glycation end products (or AGEs) and causing a series of chemical reactions. Glycation occurs in collagen fibers and results in the formation of cross-links that bind collagen fibers to each other, which leaves the skin stiffer. Glycosylated collagen is believed to be a factor in the appearance of aged skin.4 Glycation also can affect elastin: Recent research suggests that glycation can engender elastosis, which is elastin that is abnormally clumped together and presents more frequently in aged skin.
Several antiaging skin care products claim to treat glycation, but – unfortunately – glycation is not a reversible reaction. It must be prevented in the first place. Some studies suggest that antioxidants can prevent glycation, but it is more likely that they just divert the process down a different pathway that still leads to glycation. Reducing serum glucose levels is the optimum method of preventing glycation.5 Dietary intervention and oral metformin are recommended for lowering glycation.
REVERSING SKIN CELL AGING
Epidermal keratinocytes in aging
Young basal stem cells synthesize a plethora of new keratinocytes at a pace that leads to fast cell turnover and vigorous production of protective epidermal constituents. Old keratinocytes display less energy, show reduced responsiveness to cellular signals, and do not synthesize these protective components.6,7 Keratinocyte stem cell function declines over time while damage accumulates, as seen in a diminished response to growth factors, decreased keratinization, and impaired function.8
Dermal fibroblasts in cutaneous aging
Young fibroblasts produce key cellular constituents, including collagen, elastin, hyaluronic acid, and heparan sulfate. This production declines in older fibroblasts. Like aging keratinocytes, old fibroblasts lose energy and responsiveness to growth factors and other cellular signals.6,7
Rejuvenating aged skin with cosmeceuticals
Gene expression, growth factors, cytokines, chemokines, and receptor activation guide the function of keratinocytes and fibroblasts. To reverse or slow cellular skin aging, old keratinocytes and fibroblasts must be galvanized to respond to such signals or the signals must be enhanced.
Stimulating old keratinocytes and fibroblasts
Essential steps in stimulating aged keratinocytes and fibroblasts include: activating gene expression, adding growth factors, activating cytokines and chemokines, turning on receptors, and making cells more responsive to signals.
Influencing gene expression
Retinoids are known to affect collagen genes and increase activity of procollagen genes, thereby reducing the production of collagenase. Many studies have shown the efficacy of retinoids in treating aged skin and preventing cutaneous aging in both areas frequently exposed to the sun but also those that aren’t.9,10 Prescription retinoids (tretinoin, adapalene, tazarotene) and over-the-counter retinoids (retinol) are first-line options to treat and prevent aging by stimulating old keratinocytes and fibroblasts.10,11 However, exposing retinoic acid receptors to retinoids almost invariably leads to erythema and flaking in the first few weeks. Therefore, retinoids should be titrated slowly. Note that retinoid esters, such as retinyl palmitate and retinyl linoleate, do not penetrate well into the dermis;12 they also are not as effective as retinol, tretinoin, adapalene, and tazarotene. Compliance with retinoids is always an issue with patients. They should receive printed educational material about how to begin use and why it is important to use these products consistently.
Growth factors
The use of cosmetic formulations that contain growth factors can contribute to skin rejuvenation. There are various types of growth factors that have the capacity to stimulate old keratinocytes and fibroblasts to enhance function.17 Growth factors, which are inactive or vulnerable to degradation in their native, soluble form, can directly energize genes or act as a signaling mechanism. To exert their quintessential functions, growth factors must be transferred to the correct receptor site in order for the cell to respond to their signal.18
Heparan sulfate
Heparan sulfate (HS) plays a primary role in cell-to-cell communications. It increases cellular response to growth factors by facilitating the response of old, lazy fibroblasts to the cellular signals.18 HS binds, stores, and protects growth factors, which allows them to complete movement to their targets, and then presents them to the appropriate binding site.18,19 A topically applied analogue of HS has been demonstrated to rejuvenate aged skin.20
Stem cells
Stem cells included and pointedly marketed in cosmeceutical products are usually plant derived, are too large to penetrate the stratum corneum, display short shelf lives, and do not behave as human stem cells would. As a result, stem cells in cosmeceutical agents are essentially useless.
However, novel technologies have revealed ingredients that can incite native stem cells to repopulate the epidermis and dermis with young cells. Stem cells in skin include basal stem cells and 10 varieties of hair follicle stem cells. The LGR6+ hair follicle cells play a pivotal role in repopulating the epidermis after wounding has occurred.21,22 Aesthetic physicians have known for several years that inducing skin wounding with lasers, needles, and acidic peels leads to improvement in its appearance. Researchers have provided new data showing that wounding the skin prompts LGR6+ stem cells to repopulate the epidermis. Once wounding occurs, neutrophils release the peptide defensin, which stimulates the LGR6+ stem cells to repopulate the epidermis.23 Topical defensin that has been formulated to penetrate into hair follicles, where the LGR6+ stem cells reside, has been demonstrated to render a smoother, more youthful appearance to the skin.
Conclusion
It is important for practitioners to identify patients at risk for premature skin aging as early as possible and start them on an appropriate and consistent skin care regimen. This typically will include at least a daily sunscreen with an SPF 15 or higher, a nightly topical retinoid, and oral and topical antioxidants. The patient’s additional skin type proclivities (for example, dryness, inflammation, melanocyte activity) should guide the physician as to how to combine these baseline product types with cleansers, moisturizers, and formulations with hydroxy acids, growth factors, heparan sulfate, and defensin.
Several studies have revealed that patients exhibit poor compliance with recommended regimens.24 Informing patients about the need for skin protection and providing printed instructions can help to improve compliance.25 This can promote healthy lifestyle habits and compliance with scientifically proven antiaging therapies.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
1. Arch Dermatol Res. 2010 Jan;302(1):5-17.
2. Am J Pathol. 2009 Nov;175(5):1952-61.
3. J Dermatol Sci. 2017 Jun;86(3):238-48.
4. Eur J Dermatol. 2007 Jan-Feb;17(1):12-20.
5. “Advanced Glycation End Products (AGEs): Emerging Mediators of Skin Aging,” in Textbook of Aging Skin (Berlin: Springer, 2017, pp. 1675-86).
6. Mech Ageing Dev. 1986 Jul;35(2):185-98.
7. Exp Cell Res. 1996 Sep 15;227(2):252-5.
8. J Cutan Pathol. 2003 Jul;30(6):351-7.
9. PLoS One. 2015 Feb 6;10(2):e0117491.
10. Arch Dermatol. 2007 May;143(5):606-12.
11. JAMA. 1988 Jan 22-29;259(4):527-32.
12. J Invest Dermatol. 1997 Sep;109(3):301-5.
13. J Am Acad Dermatol. 1996 Feb;34(2 Pt 1):187-95.
14. J Am Acad Dermatol. 1996 Sep;35(3 Pt 1):388-91.
15. Dermatol Surg. 2001 May;27(5):429-33.
16. J Invest Dermatol. 1994 Aug;103(2):228-32.
17. Clin Cosmet Investig Dermatol. 2016 Nov 9;9:411-9.
18. Chem Biol Drug Des. 2008 Dec;72(6):455-82.
19. Front Immunol. 2013 Dec 18;4:470.
20. J Drugs Dermatol. 2015 Jul;14(7):669-74.
21. Science. 2010 Mar 12;327(5971):1385-9.
22. Plast Reconstr Surg. 2014 Mar;133(3):579-90.
23. Plast Reconstr Surg. 2013 Nov;132(5):1159-71.
24. J Am Acad Dermatol. 2008 Jul;59(1):27-33.
25. J Am Acad Dermatol. 2013 Mar;68(3):364.e1-10.
This month’s column resumes my review of prevention and treatment strategies for aging skin using oral and topical cosmeceutical agents.
Preventing and treating inflammation
Skin aging can result from inflammation through several mechanisms, including the formation of reactive oxygen species. Inflammation itself arises from myriad etiologic pathways, with multiple inflammatory mediators potentially involved, including histamines, cytokines, eicosanoids (for example, prostaglandins, thromboxanes, and leukotrienes), complement cascade components, kinins, fibrinopeptide enzymes, nuclear factor–kappa B, and free radicals.
Topically applied argan oil, caffeine, chamomile, feverfew, green tea, licorice extract, aloe, linoleic acid (found in high concentrations in argan oil and safflower oil), and niacinamide are among the anti-inflammatory ingredients that have been used successfully in topical skin care to reduce inflammation. The Food and Drug Administration does not allow cosmetics to make “anti-inflammatory” claims. For this reason, these products will state they have “soothing” effects or imply they improve of redness.
Oral polypodium leucotomos has been demonstrated to suppress the effect of UV radiation on COX-2 expression.2 Also, glycolic acid has exhibited the capacity to inhibit COX-2 signaling and other inflammatory mediators.3
Preventing and treating glycation
Glycation is produced by the Maillard reaction, a chemical reaction – particularly well known in cooking – between an amino acid and a sugar molecule that typically requires heat. This reaction was first described by Louis Camille Maillard in 1912 when he noted that amino acids can react with sugar to yield brown or golden-brown substances. It took until the 1980s for scientists to understand the importance of glycation in health.
When glycation occurs, sugar molecules attach to proteins, creating cross-linked proteins known as advanced glycation end products (or AGEs) and causing a series of chemical reactions. Glycation occurs in collagen fibers and results in the formation of cross-links that bind collagen fibers to each other, which leaves the skin stiffer. Glycosylated collagen is believed to be a factor in the appearance of aged skin.4 Glycation also can affect elastin: Recent research suggests that glycation can engender elastosis, which is elastin that is abnormally clumped together and presents more frequently in aged skin.
Several antiaging skin care products claim to treat glycation, but – unfortunately – glycation is not a reversible reaction. It must be prevented in the first place. Some studies suggest that antioxidants can prevent glycation, but it is more likely that they just divert the process down a different pathway that still leads to glycation. Reducing serum glucose levels is the optimum method of preventing glycation.5 Dietary intervention and oral metformin are recommended for lowering glycation.
REVERSING SKIN CELL AGING
Epidermal keratinocytes in aging
Young basal stem cells synthesize a plethora of new keratinocytes at a pace that leads to fast cell turnover and vigorous production of protective epidermal constituents. Old keratinocytes display less energy, show reduced responsiveness to cellular signals, and do not synthesize these protective components.6,7 Keratinocyte stem cell function declines over time while damage accumulates, as seen in a diminished response to growth factors, decreased keratinization, and impaired function.8
Dermal fibroblasts in cutaneous aging
Young fibroblasts produce key cellular constituents, including collagen, elastin, hyaluronic acid, and heparan sulfate. This production declines in older fibroblasts. Like aging keratinocytes, old fibroblasts lose energy and responsiveness to growth factors and other cellular signals.6,7
Rejuvenating aged skin with cosmeceuticals
Gene expression, growth factors, cytokines, chemokines, and receptor activation guide the function of keratinocytes and fibroblasts. To reverse or slow cellular skin aging, old keratinocytes and fibroblasts must be galvanized to respond to such signals or the signals must be enhanced.
Stimulating old keratinocytes and fibroblasts
Essential steps in stimulating aged keratinocytes and fibroblasts include: activating gene expression, adding growth factors, activating cytokines and chemokines, turning on receptors, and making cells more responsive to signals.
Influencing gene expression
Retinoids are known to affect collagen genes and increase activity of procollagen genes, thereby reducing the production of collagenase. Many studies have shown the efficacy of retinoids in treating aged skin and preventing cutaneous aging in both areas frequently exposed to the sun but also those that aren’t.9,10 Prescription retinoids (tretinoin, adapalene, tazarotene) and over-the-counter retinoids (retinol) are first-line options to treat and prevent aging by stimulating old keratinocytes and fibroblasts.10,11 However, exposing retinoic acid receptors to retinoids almost invariably leads to erythema and flaking in the first few weeks. Therefore, retinoids should be titrated slowly. Note that retinoid esters, such as retinyl palmitate and retinyl linoleate, do not penetrate well into the dermis;12 they also are not as effective as retinol, tretinoin, adapalene, and tazarotene. Compliance with retinoids is always an issue with patients. They should receive printed educational material about how to begin use and why it is important to use these products consistently.
Growth factors
The use of cosmetic formulations that contain growth factors can contribute to skin rejuvenation. There are various types of growth factors that have the capacity to stimulate old keratinocytes and fibroblasts to enhance function.17 Growth factors, which are inactive or vulnerable to degradation in their native, soluble form, can directly energize genes or act as a signaling mechanism. To exert their quintessential functions, growth factors must be transferred to the correct receptor site in order for the cell to respond to their signal.18
Heparan sulfate
Heparan sulfate (HS) plays a primary role in cell-to-cell communications. It increases cellular response to growth factors by facilitating the response of old, lazy fibroblasts to the cellular signals.18 HS binds, stores, and protects growth factors, which allows them to complete movement to their targets, and then presents them to the appropriate binding site.18,19 A topically applied analogue of HS has been demonstrated to rejuvenate aged skin.20
Stem cells
Stem cells included and pointedly marketed in cosmeceutical products are usually plant derived, are too large to penetrate the stratum corneum, display short shelf lives, and do not behave as human stem cells would. As a result, stem cells in cosmeceutical agents are essentially useless.
However, novel technologies have revealed ingredients that can incite native stem cells to repopulate the epidermis and dermis with young cells. Stem cells in skin include basal stem cells and 10 varieties of hair follicle stem cells. The LGR6+ hair follicle cells play a pivotal role in repopulating the epidermis after wounding has occurred.21,22 Aesthetic physicians have known for several years that inducing skin wounding with lasers, needles, and acidic peels leads to improvement in its appearance. Researchers have provided new data showing that wounding the skin prompts LGR6+ stem cells to repopulate the epidermis. Once wounding occurs, neutrophils release the peptide defensin, which stimulates the LGR6+ stem cells to repopulate the epidermis.23 Topical defensin that has been formulated to penetrate into hair follicles, where the LGR6+ stem cells reside, has been demonstrated to render a smoother, more youthful appearance to the skin.
Conclusion
It is important for practitioners to identify patients at risk for premature skin aging as early as possible and start them on an appropriate and consistent skin care regimen. This typically will include at least a daily sunscreen with an SPF 15 or higher, a nightly topical retinoid, and oral and topical antioxidants. The patient’s additional skin type proclivities (for example, dryness, inflammation, melanocyte activity) should guide the physician as to how to combine these baseline product types with cleansers, moisturizers, and formulations with hydroxy acids, growth factors, heparan sulfate, and defensin.
Several studies have revealed that patients exhibit poor compliance with recommended regimens.24 Informing patients about the need for skin protection and providing printed instructions can help to improve compliance.25 This can promote healthy lifestyle habits and compliance with scientifically proven antiaging therapies.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
1. Arch Dermatol Res. 2010 Jan;302(1):5-17.
2. Am J Pathol. 2009 Nov;175(5):1952-61.
3. J Dermatol Sci. 2017 Jun;86(3):238-48.
4. Eur J Dermatol. 2007 Jan-Feb;17(1):12-20.
5. “Advanced Glycation End Products (AGEs): Emerging Mediators of Skin Aging,” in Textbook of Aging Skin (Berlin: Springer, 2017, pp. 1675-86).
6. Mech Ageing Dev. 1986 Jul;35(2):185-98.
7. Exp Cell Res. 1996 Sep 15;227(2):252-5.
8. J Cutan Pathol. 2003 Jul;30(6):351-7.
9. PLoS One. 2015 Feb 6;10(2):e0117491.
10. Arch Dermatol. 2007 May;143(5):606-12.
11. JAMA. 1988 Jan 22-29;259(4):527-32.
12. J Invest Dermatol. 1997 Sep;109(3):301-5.
13. J Am Acad Dermatol. 1996 Feb;34(2 Pt 1):187-95.
14. J Am Acad Dermatol. 1996 Sep;35(3 Pt 1):388-91.
15. Dermatol Surg. 2001 May;27(5):429-33.
16. J Invest Dermatol. 1994 Aug;103(2):228-32.
17. Clin Cosmet Investig Dermatol. 2016 Nov 9;9:411-9.
18. Chem Biol Drug Des. 2008 Dec;72(6):455-82.
19. Front Immunol. 2013 Dec 18;4:470.
20. J Drugs Dermatol. 2015 Jul;14(7):669-74.
21. Science. 2010 Mar 12;327(5971):1385-9.
22. Plast Reconstr Surg. 2014 Mar;133(3):579-90.
23. Plast Reconstr Surg. 2013 Nov;132(5):1159-71.
24. J Am Acad Dermatol. 2008 Jul;59(1):27-33.
25. J Am Acad Dermatol. 2013 Mar;68(3):364.e1-10.
This month’s column resumes my review of prevention and treatment strategies for aging skin using oral and topical cosmeceutical agents.
Preventing and treating inflammation
Skin aging can result from inflammation through several mechanisms, including the formation of reactive oxygen species. Inflammation itself arises from myriad etiologic pathways, with multiple inflammatory mediators potentially involved, including histamines, cytokines, eicosanoids (for example, prostaglandins, thromboxanes, and leukotrienes), complement cascade components, kinins, fibrinopeptide enzymes, nuclear factor–kappa B, and free radicals.
Topically applied argan oil, caffeine, chamomile, feverfew, green tea, licorice extract, aloe, linoleic acid (found in high concentrations in argan oil and safflower oil), and niacinamide are among the anti-inflammatory ingredients that have been used successfully in topical skin care to reduce inflammation. The Food and Drug Administration does not allow cosmetics to make “anti-inflammatory” claims. For this reason, these products will state they have “soothing” effects or imply they improve of redness.
Oral polypodium leucotomos has been demonstrated to suppress the effect of UV radiation on COX-2 expression.2 Also, glycolic acid has exhibited the capacity to inhibit COX-2 signaling and other inflammatory mediators.3
Preventing and treating glycation
Glycation is produced by the Maillard reaction, a chemical reaction – particularly well known in cooking – between an amino acid and a sugar molecule that typically requires heat. This reaction was first described by Louis Camille Maillard in 1912 when he noted that amino acids can react with sugar to yield brown or golden-brown substances. It took until the 1980s for scientists to understand the importance of glycation in health.
When glycation occurs, sugar molecules attach to proteins, creating cross-linked proteins known as advanced glycation end products (or AGEs) and causing a series of chemical reactions. Glycation occurs in collagen fibers and results in the formation of cross-links that bind collagen fibers to each other, which leaves the skin stiffer. Glycosylated collagen is believed to be a factor in the appearance of aged skin.4 Glycation also can affect elastin: Recent research suggests that glycation can engender elastosis, which is elastin that is abnormally clumped together and presents more frequently in aged skin.
Several antiaging skin care products claim to treat glycation, but – unfortunately – glycation is not a reversible reaction. It must be prevented in the first place. Some studies suggest that antioxidants can prevent glycation, but it is more likely that they just divert the process down a different pathway that still leads to glycation. Reducing serum glucose levels is the optimum method of preventing glycation.5 Dietary intervention and oral metformin are recommended for lowering glycation.
REVERSING SKIN CELL AGING
Epidermal keratinocytes in aging
Young basal stem cells synthesize a plethora of new keratinocytes at a pace that leads to fast cell turnover and vigorous production of protective epidermal constituents. Old keratinocytes display less energy, show reduced responsiveness to cellular signals, and do not synthesize these protective components.6,7 Keratinocyte stem cell function declines over time while damage accumulates, as seen in a diminished response to growth factors, decreased keratinization, and impaired function.8
Dermal fibroblasts in cutaneous aging
Young fibroblasts produce key cellular constituents, including collagen, elastin, hyaluronic acid, and heparan sulfate. This production declines in older fibroblasts. Like aging keratinocytes, old fibroblasts lose energy and responsiveness to growth factors and other cellular signals.6,7
Rejuvenating aged skin with cosmeceuticals
Gene expression, growth factors, cytokines, chemokines, and receptor activation guide the function of keratinocytes and fibroblasts. To reverse or slow cellular skin aging, old keratinocytes and fibroblasts must be galvanized to respond to such signals or the signals must be enhanced.
Stimulating old keratinocytes and fibroblasts
Essential steps in stimulating aged keratinocytes and fibroblasts include: activating gene expression, adding growth factors, activating cytokines and chemokines, turning on receptors, and making cells more responsive to signals.
Influencing gene expression
Retinoids are known to affect collagen genes and increase activity of procollagen genes, thereby reducing the production of collagenase. Many studies have shown the efficacy of retinoids in treating aged skin and preventing cutaneous aging in both areas frequently exposed to the sun but also those that aren’t.9,10 Prescription retinoids (tretinoin, adapalene, tazarotene) and over-the-counter retinoids (retinol) are first-line options to treat and prevent aging by stimulating old keratinocytes and fibroblasts.10,11 However, exposing retinoic acid receptors to retinoids almost invariably leads to erythema and flaking in the first few weeks. Therefore, retinoids should be titrated slowly. Note that retinoid esters, such as retinyl palmitate and retinyl linoleate, do not penetrate well into the dermis;12 they also are not as effective as retinol, tretinoin, adapalene, and tazarotene. Compliance with retinoids is always an issue with patients. They should receive printed educational material about how to begin use and why it is important to use these products consistently.
Growth factors
The use of cosmetic formulations that contain growth factors can contribute to skin rejuvenation. There are various types of growth factors that have the capacity to stimulate old keratinocytes and fibroblasts to enhance function.17 Growth factors, which are inactive or vulnerable to degradation in their native, soluble form, can directly energize genes or act as a signaling mechanism. To exert their quintessential functions, growth factors must be transferred to the correct receptor site in order for the cell to respond to their signal.18
Heparan sulfate
Heparan sulfate (HS) plays a primary role in cell-to-cell communications. It increases cellular response to growth factors by facilitating the response of old, lazy fibroblasts to the cellular signals.18 HS binds, stores, and protects growth factors, which allows them to complete movement to their targets, and then presents them to the appropriate binding site.18,19 A topically applied analogue of HS has been demonstrated to rejuvenate aged skin.20
Stem cells
Stem cells included and pointedly marketed in cosmeceutical products are usually plant derived, are too large to penetrate the stratum corneum, display short shelf lives, and do not behave as human stem cells would. As a result, stem cells in cosmeceutical agents are essentially useless.
However, novel technologies have revealed ingredients that can incite native stem cells to repopulate the epidermis and dermis with young cells. Stem cells in skin include basal stem cells and 10 varieties of hair follicle stem cells. The LGR6+ hair follicle cells play a pivotal role in repopulating the epidermis after wounding has occurred.21,22 Aesthetic physicians have known for several years that inducing skin wounding with lasers, needles, and acidic peels leads to improvement in its appearance. Researchers have provided new data showing that wounding the skin prompts LGR6+ stem cells to repopulate the epidermis. Once wounding occurs, neutrophils release the peptide defensin, which stimulates the LGR6+ stem cells to repopulate the epidermis.23 Topical defensin that has been formulated to penetrate into hair follicles, where the LGR6+ stem cells reside, has been demonstrated to render a smoother, more youthful appearance to the skin.
Conclusion
It is important for practitioners to identify patients at risk for premature skin aging as early as possible and start them on an appropriate and consistent skin care regimen. This typically will include at least a daily sunscreen with an SPF 15 or higher, a nightly topical retinoid, and oral and topical antioxidants. The patient’s additional skin type proclivities (for example, dryness, inflammation, melanocyte activity) should guide the physician as to how to combine these baseline product types with cleansers, moisturizers, and formulations with hydroxy acids, growth factors, heparan sulfate, and defensin.
Several studies have revealed that patients exhibit poor compliance with recommended regimens.24 Informing patients about the need for skin protection and providing printed instructions can help to improve compliance.25 This can promote healthy lifestyle habits and compliance with scientifically proven antiaging therapies.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
1. Arch Dermatol Res. 2010 Jan;302(1):5-17.
2. Am J Pathol. 2009 Nov;175(5):1952-61.
3. J Dermatol Sci. 2017 Jun;86(3):238-48.
4. Eur J Dermatol. 2007 Jan-Feb;17(1):12-20.
5. “Advanced Glycation End Products (AGEs): Emerging Mediators of Skin Aging,” in Textbook of Aging Skin (Berlin: Springer, 2017, pp. 1675-86).
6. Mech Ageing Dev. 1986 Jul;35(2):185-98.
7. Exp Cell Res. 1996 Sep 15;227(2):252-5.
8. J Cutan Pathol. 2003 Jul;30(6):351-7.
9. PLoS One. 2015 Feb 6;10(2):e0117491.
10. Arch Dermatol. 2007 May;143(5):606-12.
11. JAMA. 1988 Jan 22-29;259(4):527-32.
12. J Invest Dermatol. 1997 Sep;109(3):301-5.
13. J Am Acad Dermatol. 1996 Feb;34(2 Pt 1):187-95.
14. J Am Acad Dermatol. 1996 Sep;35(3 Pt 1):388-91.
15. Dermatol Surg. 2001 May;27(5):429-33.
16. J Invest Dermatol. 1994 Aug;103(2):228-32.
17. Clin Cosmet Investig Dermatol. 2016 Nov 9;9:411-9.
18. Chem Biol Drug Des. 2008 Dec;72(6):455-82.
19. Front Immunol. 2013 Dec 18;4:470.
20. J Drugs Dermatol. 2015 Jul;14(7):669-74.
21. Science. 2010 Mar 12;327(5971):1385-9.
22. Plast Reconstr Surg. 2014 Mar;133(3):579-90.
23. Plast Reconstr Surg. 2013 Nov;132(5):1159-71.
24. J Am Acad Dermatol. 2008 Jul;59(1):27-33.
25. J Am Acad Dermatol. 2013 Mar;68(3):364.e1-10.
Antipsychotics for obsessive-compulsive disorder: Weighing risks vs benefits
Mr. E, age 37, has a 20-year history of obsessive-compulsive disorder (OCD), with comorbid generalized anxiety disorder and hypertension. His medication regimen consists of
Box
Antipsychotics for OCD: What the guidelines recommend
The 2013 American Psychiatric Association (APA) obsessive-compulsive disorder (OCD) treatment guidelines include recommendations regarding the use of antipsychotics in patients who do not respond to first-line treatment with selective serotonin reuptake inhibitors (SSRIs) and/or cognitive-behavioral therapy (CBT). The APA recommends evaluating contributing factors, including comorbidities, family support, and ability to tolerate psychotherapy or maximum recommended drug doses, before augmenting or switching therapies.1
In patients with a partial response to SSRIs and/or CBT, the APA suggests that augmentation may be preferable to switching treatments. Augmentation strategies for SSRIs include antipsychotics or CBT with Exposure Response Prevention (ERP); augmentation strategies for CBT include SSRIs. Combining SSRIs and CBT may decrease the chance of relapse when medication is discontinued. If the patient has a partial response to ERP, intensification of therapy also can be considered based on patient-specific factors. In non-responders, switching therapies may be necessary. Alternative treatments including a different SSRI; an antidepressant from a difference class, such as clomipramine or mirtazapine; an antipsychotic; or CBT.
The 2006 National Institute for Health and Clinical Excellence guidelines for OCD recommend additional high-intensity CBT, adding an antipsychotic to an SSRI or clomipramine, or combining clomipramine with citalopram in non-responders. There is no guidance regarding the order in which these treatments should be trialed. Antipsychotics are recommended as an entire class, and there are no recommendations regarding dosing or long-term risks. These guidelines are based on limited evidence, including only 1 trial of quetiapine and 1 trial of olanzapine.2,3
Efficacy
The 2013 National Institute for Health Care and Excellence Evidence Update included a 2010 Cochrane Review of 11 randomized controlled trials (RCTs) of antipsychotics as adjunctive treatment to SSRIs.5 All trials were <6 months, and most were limited regarding quality aspects. Two trials found no statistically significant difference with olanzapine in efficacy measures (Y-BOCS mean difference [MD] −2.96; 95% confidence interval [CI] −7.41 to 1.22; effect size d = −2.96 [−7.14, 1.22]). Among patients with no clinically significant change (defined as ≤35% reduction in Y-BOCS), there was no significant difference between groups (n = 44, 1 RCT, odds ratio [OR] 0.76; 95% CI 0.17 to 3.29; effect size d = 0.76 [0.17, 3.29]). Studies found increased weight gain with olanzapine compared with antidepressant monotherapy.
Statistically significant differences were demonstrated with the addition of quetiapine to antidepressant monotherapy as shown in Y-BOCS score at endpoint (Y-BOCS MD −2.28; 95% CI −4.05 to −0.52; effect size d −2.28 [−4.05, −0.52]). Quetiapine also demonstrated benefit for depressive and anxiety symptoms. Among patients with no clinically significant change (defined as ≤35% reduction in Y-BOCS), there was a significant difference between groups (n = 80, 2 RCTs, OR 0.27; 95% CI 0.09 to 0.87; effect size d = 0.27 [0.09, 0.87]).
Adjunctive treatment with risperidone was superior to antidepressant monotherapy for participants without a significant response in OCD symptom severity of at least 25% with validated measures (OR 0.17; 95% CI 0.04 to 0.66; effect size d = 0.17 [0.04, 0.66]), and in depressive and anxiety symptoms. Mean reduction in Y-BOCS scores was not statistically significant with risperidone (MD −3.35; 95% CI −8.25 to 1.55; effect size d = −3.35 [−8.25, 1.55]).5
A 2014 meta-analysis by Veale et al3 included double-blind, randomized trials that examined atypical antipsychotics compared with placebo for adults with OCD that used an intention-to-treat analysis. Unlike the Cochrane Review, these studies used the Y-BOCS as a primary outcome measure. Participants had a Y-BOCS score of ≥16; had at least 1 appropriate trial of an SSRI or clomipramine (defined as the maximum dose tolerated for at least 8 weeks); and had to continue taking the SSRI or
Fourteen articles were included in the meta-analysis, but all had small sample sizes and no long-term follow-up data.3 Antipsychotics in the meta-analysis included risperidone (4 studies), quetiapine (5 studies), olanzapine (2 studies),
The overall difference in Y-BOCS score change between drug and placebo groups was 2.34 points, which had an overall effect size of d = 0.40. Those taking antipsychotics had approximately a 10% reduction in Y-BOCS score over time. The overall difference was statistically significant with risperidone (overall mean reduction of 3.89 points on the Y-BOCS; 95% CI 1.43 to 5.48; effect size of d = 0.53) and aripiprazole (difference in Y-BOCS outcome 0.1 scores of 6.29 points; effect size of d = 1.11). One trial of risperidone used a low dose (0.5 mg) and had a larger effect size than the studies that used moderate doses. The overall difference was not statistically significant for quetiapine (difference of Y-BOCS outcome scores of 0.81 points) or olanzapine (difference in Y-BOCS outcome scores of −0.19; indicating <1 point difference on the Y-BOCS).3
Studies included in the meta-analysis ranged in durations from 6 to 16 weeks; duration of ≥4 weeks did not make a difference in response. One study demonstrated a worsening of symptoms in the quetiapine group between weeks 4 and 12. Only 4 studies included most patients that had a previous trial of CBT. One study with an additional treatment arm evaluating CBT found that adding CBT was superior to adjunctive risperidone or placebo. Another study found that adding clomipramine or placebo to
Two studies included in the meta-analysis classified OCD symptoms by subtype, such as by dimensions of checking; symmetry, ordering, counting, and repeating; contamination and cleaning; and hoarding. Currently, no clinically significant predictor of outcome of antipsychotic therapy has been identified. Two studies included in the meta-analysis assessed patients with comorbid tic disorders and found no difference by treatment. One study demonstrated benefit of haloperidol in patients with comorbid tic disorders compared with those without comorbid tic disorders. Of note, none of the studies included in the meta-analysis excluded patients with hoarding characteristics, which generally indicate a worse prognosis with treatment.3
In 2015, Dold et al6 provided an update to a 2013 meta-analysis7 assessing antipsychotic augmentation of SSRIs in treatment-resistant OCD. This update included 2 new RCTs. The 2013 analysis7 concluded that risperidone should be considered first-line and is preferred over olanzapine and quetiapine. However, the update found the highest effect size for aripiprazole (d = −1.35), followed by haloperidol (d = −0.82), risperidone (d = −0.59), quetiapine (d = −0.50), olanzapine (d = −0.49), and paliperidone (d = −0.21).6,7
The 2015 update6 concluded that the antipsychotic doses used in trials were moderate and that there was no association between dose and treatment response, indicating that high doses of antipsychotics may not be more effective. Dold et al6 postulated that the antipsychotic doses required for treating OCD are similar to those used in treating major depressive disorder and lower than doses used in treating schizophrenia. The 2013 meta-analysis demonstrated that moderate doses of antipsychotics resulted in statistically significant efficacy (relative risk [RR] = 3.99, 95% CI 1.92 to 8.27), while low doses did not demonstrate statistical significance (RR = 1.06, 95% CI 0.45 to 2.53).6,7
The 2015 subgroup analysis update evaluated the duration of SSRI treatment prior to the antipsychotic augmentation phase, but did not demonstrate statistically significant efficacy for studies with <8 weeks’ duration of SSRI treatment, further highlighting the need for extended duration of treatment with an SSRI prior to augmentation.6
The 2013 meta-analysis discussed populations with comorbid tic disorders, including a study that found that patients with OCD and comorbid tic disorders benefit more from adjunctive antipsychotic therapy than those without the comorbidity. The 2015 update excluded trials that included patients with comorbid tic disorders to reduce bias, which did not affect the overall effect sizes of the data.6,7
In summary, efficacy has been demonstrated for risperidone and aripiprazole. There has been no benefit demonstrated with olanzapine and limited benefit with quetiapine. One study suggested worsening of symptoms with quetiapine the longer that treatment persisted.3,5-7
Safety
Assessing potential harms related to the use of antipsychotics in treating OCD is complicated, because this information is not always assessed in trials. Instead, researchers often focus on exploring potential benefits because long-term effects of antipsychotics, including sedation, weight gain, metabolic syndrome, and extrapyramidal side effects, are well documented.3
Trials included in the meta-analysis by Veale et al3 had a maximum duration of 16 weeks, so it is likely that many of the potential harms of antipsychotic use would not yet have been measurable. The authors cautioned that, although aripiprazole and risperidone demonstrated benefit, their benefit must be weighed against the potential physical risks of long-term antipsychotic use.3One study that was not included in the meta-analysis by Veale et al3 evaluated individuals who did not respond to a SSRI, and randomly assigned them to quetiapine, olanzapine, or risperidone plus CBT. At 1-year follow-up, 50% of participants receiving an antipsychotic had an increase of >10% in body mass index (BMI) and had higher fasting blood sugars compared with only 15.2% of participants with increased BMI in the comparison group (SSRI responders).3
Foa et al8 investigated long-term outcomes (ie, 6 months) of SSRI augmentation with ERP or risperidone in patients with OCD. Forty patients were randomized to receive risperidone, and 9 were considered responders. Only 8 chose to enter the maintenance phase, and of those participants, 5 did not complete the study. Two withdrew due to worsening depression, 2 withdrew due to intolerable adverse effects, and 1 was lost to follow-up. Unfortunately, there was no further discussion of what the intolerable adverse effects were.8
Patients with comorbid schizophrenia and OCD face additional risks. Lifetime prevalence rates of OCD are greater in persons with schizophrenia compared with the general population (26% vs 8%, respectively). Most studies have demonstrated poor prognosis and medication adherence among patients with comorbid schizophrenia and OCD. Fonseka et al9 assessed the risk of antipsychotic induction and exacerbation of OCD symptoms in patients with schizophrenia. Induction and exacerbation of OCD symptoms
Evidence of olanzapine induction and exacerbation of OCD symptoms is also limited to case reports and retrospective studies. However, some studies have estimated induction of OCD symptoms with olanzapine in 11% to 20% of patients.9 There is insufficient evidence to form conclusions regarding other antipsychotics. Fonseka et al9 recommends switching to an antipsychotic with lower 5HT-2 binding affinity or adding an SSRI, such as fluvoxamine, if induction or exacerbation of OCD symptoms occurs.
Consider long-term risks
The evidence for benefits with antipsychotics in treatment-resistant OCD is limited by different populations recruited, small sample sizes, and lack of long-term follow-up. Most evidence supports using ERP over antipsychotics for treating OCD symptoms that have not responded to SSRIs. However, ERP poses its own challenges that may limit clinical utility, such as economic and time restraints. Therefore, benefits with antipsychotics, such as risperidone and aripiprazole, must be weighed against potential long-term risks of treatment, including sedation, weight gain, metabolic syndrome, and extrapyramidal side effects.
Regarding Mr. E’s case, because he had been maximized on SSRI therapy for an adequate duration (escitalopram, 40 mg/d, for 12 weeks) and completed CBT with ERP with a partial response, adding risperidone, 0.5 mg at bedtime, was an appropriate treatment option that is supported by the available guidelines and evidence. The risperidone dose is reflective of the initial dosing strategies used in clinical trials. It is recommended to assess efficacy of treatment at 8 weeks with a validated measure, such as the Y-BOCS. A dose increase may be needed to achieve clinically significant symptom improvement, because moderate doses of risperidone have demonstrated efficacy in trials; however, high doses of risperidone are unlikely to provide additional benefit and increase the risk of adverse effects. If risperidone does not provide a clinically favorable risk–benefit ratio for Mr. E, aripiprazole is a potential alternative.
1. American Psychiatric Association. Practice guideline for the treatment of patients with obsessive-compulsive disorder. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/ocd.pdf. Published July 2007. Accessed December 11, 2017.
2. National Institute for Health and Care Excellence (NICE). Obsessive compulsive disorder. http://arms.evidence.nhs.uk/resources/hub/1028833/attachment. Updated September 18, 2013. Accessed December 11, 2017.
3. Veale D, Miles S, Smallcombe N, et al. Atypical antipsychotic augmentation in SSRI treatment refractory obsessive-compulsive disorder: a systematic review and
4. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
5. Komossa K, Depping AM, Meyer M, et al. Second-generation antipsychotics for obsessive compulsive disorder. Cochrane Database Syst Rev. 2010;12:1-44.
6. Dold M, Aigner M, Lanzenberger R, et al. Antipsychotic augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: an update meta-analysis of double-blind, randomized, placebo-controlled trials. Int J Neuropsychopharmacol. 2015;18(9). doi: 10.1093/ijnp/pyv047.
7. Dold M, Aigner M, Lanzenberger R, et al. Antipsychotic augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: a meta-analysis of double-blind, randomized, placebo-controlled trials. Int J Neuropsychopharmacol. 2013;16(3):557-574.
8. Foa EB, Simpson HB, Rosenfield D, et al. Six-month outcomes from a randomized trial augmenting serotonin reuptake inhibitors with exposure and response prevention or risperidone in adults with obsessive-compulsive disorder. J Clin Psychiatry. 2015;76(4):440-446.
9. Fonseka TM, Richter MA, Muller DJ. Second generation antipsychotic-induced obsessive-compulsive symptoms in schizophrenia: a review of the experimental literature. Curr Psychiatry Rep. 2014;16(11):510.
Mr. E, age 37, has a 20-year history of obsessive-compulsive disorder (OCD), with comorbid generalized anxiety disorder and hypertension. His medication regimen consists of
Box
Antipsychotics for OCD: What the guidelines recommend
The 2013 American Psychiatric Association (APA) obsessive-compulsive disorder (OCD) treatment guidelines include recommendations regarding the use of antipsychotics in patients who do not respond to first-line treatment with selective serotonin reuptake inhibitors (SSRIs) and/or cognitive-behavioral therapy (CBT). The APA recommends evaluating contributing factors, including comorbidities, family support, and ability to tolerate psychotherapy or maximum recommended drug doses, before augmenting or switching therapies.1
In patients with a partial response to SSRIs and/or CBT, the APA suggests that augmentation may be preferable to switching treatments. Augmentation strategies for SSRIs include antipsychotics or CBT with Exposure Response Prevention (ERP); augmentation strategies for CBT include SSRIs. Combining SSRIs and CBT may decrease the chance of relapse when medication is discontinued. If the patient has a partial response to ERP, intensification of therapy also can be considered based on patient-specific factors. In non-responders, switching therapies may be necessary. Alternative treatments including a different SSRI; an antidepressant from a difference class, such as clomipramine or mirtazapine; an antipsychotic; or CBT.
The 2006 National Institute for Health and Clinical Excellence guidelines for OCD recommend additional high-intensity CBT, adding an antipsychotic to an SSRI or clomipramine, or combining clomipramine with citalopram in non-responders. There is no guidance regarding the order in which these treatments should be trialed. Antipsychotics are recommended as an entire class, and there are no recommendations regarding dosing or long-term risks. These guidelines are based on limited evidence, including only 1 trial of quetiapine and 1 trial of olanzapine.2,3
Efficacy
The 2013 National Institute for Health Care and Excellence Evidence Update included a 2010 Cochrane Review of 11 randomized controlled trials (RCTs) of antipsychotics as adjunctive treatment to SSRIs.5 All trials were <6 months, and most were limited regarding quality aspects. Two trials found no statistically significant difference with olanzapine in efficacy measures (Y-BOCS mean difference [MD] −2.96; 95% confidence interval [CI] −7.41 to 1.22; effect size d = −2.96 [−7.14, 1.22]). Among patients with no clinically significant change (defined as ≤35% reduction in Y-BOCS), there was no significant difference between groups (n = 44, 1 RCT, odds ratio [OR] 0.76; 95% CI 0.17 to 3.29; effect size d = 0.76 [0.17, 3.29]). Studies found increased weight gain with olanzapine compared with antidepressant monotherapy.
Statistically significant differences were demonstrated with the addition of quetiapine to antidepressant monotherapy as shown in Y-BOCS score at endpoint (Y-BOCS MD −2.28; 95% CI −4.05 to −0.52; effect size d −2.28 [−4.05, −0.52]). Quetiapine also demonstrated benefit for depressive and anxiety symptoms. Among patients with no clinically significant change (defined as ≤35% reduction in Y-BOCS), there was a significant difference between groups (n = 80, 2 RCTs, OR 0.27; 95% CI 0.09 to 0.87; effect size d = 0.27 [0.09, 0.87]).
Adjunctive treatment with risperidone was superior to antidepressant monotherapy for participants without a significant response in OCD symptom severity of at least 25% with validated measures (OR 0.17; 95% CI 0.04 to 0.66; effect size d = 0.17 [0.04, 0.66]), and in depressive and anxiety symptoms. Mean reduction in Y-BOCS scores was not statistically significant with risperidone (MD −3.35; 95% CI −8.25 to 1.55; effect size d = −3.35 [−8.25, 1.55]).5
A 2014 meta-analysis by Veale et al3 included double-blind, randomized trials that examined atypical antipsychotics compared with placebo for adults with OCD that used an intention-to-treat analysis. Unlike the Cochrane Review, these studies used the Y-BOCS as a primary outcome measure. Participants had a Y-BOCS score of ≥16; had at least 1 appropriate trial of an SSRI or clomipramine (defined as the maximum dose tolerated for at least 8 weeks); and had to continue taking the SSRI or
Fourteen articles were included in the meta-analysis, but all had small sample sizes and no long-term follow-up data.3 Antipsychotics in the meta-analysis included risperidone (4 studies), quetiapine (5 studies), olanzapine (2 studies),
The overall difference in Y-BOCS score change between drug and placebo groups was 2.34 points, which had an overall effect size of d = 0.40. Those taking antipsychotics had approximately a 10% reduction in Y-BOCS score over time. The overall difference was statistically significant with risperidone (overall mean reduction of 3.89 points on the Y-BOCS; 95% CI 1.43 to 5.48; effect size of d = 0.53) and aripiprazole (difference in Y-BOCS outcome 0.1 scores of 6.29 points; effect size of d = 1.11). One trial of risperidone used a low dose (0.5 mg) and had a larger effect size than the studies that used moderate doses. The overall difference was not statistically significant for quetiapine (difference of Y-BOCS outcome scores of 0.81 points) or olanzapine (difference in Y-BOCS outcome scores of −0.19; indicating <1 point difference on the Y-BOCS).3
Studies included in the meta-analysis ranged in durations from 6 to 16 weeks; duration of ≥4 weeks did not make a difference in response. One study demonstrated a worsening of symptoms in the quetiapine group between weeks 4 and 12. Only 4 studies included most patients that had a previous trial of CBT. One study with an additional treatment arm evaluating CBT found that adding CBT was superior to adjunctive risperidone or placebo. Another study found that adding clomipramine or placebo to
Two studies included in the meta-analysis classified OCD symptoms by subtype, such as by dimensions of checking; symmetry, ordering, counting, and repeating; contamination and cleaning; and hoarding. Currently, no clinically significant predictor of outcome of antipsychotic therapy has been identified. Two studies included in the meta-analysis assessed patients with comorbid tic disorders and found no difference by treatment. One study demonstrated benefit of haloperidol in patients with comorbid tic disorders compared with those without comorbid tic disorders. Of note, none of the studies included in the meta-analysis excluded patients with hoarding characteristics, which generally indicate a worse prognosis with treatment.3
In 2015, Dold et al6 provided an update to a 2013 meta-analysis7 assessing antipsychotic augmentation of SSRIs in treatment-resistant OCD. This update included 2 new RCTs. The 2013 analysis7 concluded that risperidone should be considered first-line and is preferred over olanzapine and quetiapine. However, the update found the highest effect size for aripiprazole (d = −1.35), followed by haloperidol (d = −0.82), risperidone (d = −0.59), quetiapine (d = −0.50), olanzapine (d = −0.49), and paliperidone (d = −0.21).6,7
The 2015 update6 concluded that the antipsychotic doses used in trials were moderate and that there was no association between dose and treatment response, indicating that high doses of antipsychotics may not be more effective. Dold et al6 postulated that the antipsychotic doses required for treating OCD are similar to those used in treating major depressive disorder and lower than doses used in treating schizophrenia. The 2013 meta-analysis demonstrated that moderate doses of antipsychotics resulted in statistically significant efficacy (relative risk [RR] = 3.99, 95% CI 1.92 to 8.27), while low doses did not demonstrate statistical significance (RR = 1.06, 95% CI 0.45 to 2.53).6,7
The 2015 subgroup analysis update evaluated the duration of SSRI treatment prior to the antipsychotic augmentation phase, but did not demonstrate statistically significant efficacy for studies with <8 weeks’ duration of SSRI treatment, further highlighting the need for extended duration of treatment with an SSRI prior to augmentation.6
The 2013 meta-analysis discussed populations with comorbid tic disorders, including a study that found that patients with OCD and comorbid tic disorders benefit more from adjunctive antipsychotic therapy than those without the comorbidity. The 2015 update excluded trials that included patients with comorbid tic disorders to reduce bias, which did not affect the overall effect sizes of the data.6,7
In summary, efficacy has been demonstrated for risperidone and aripiprazole. There has been no benefit demonstrated with olanzapine and limited benefit with quetiapine. One study suggested worsening of symptoms with quetiapine the longer that treatment persisted.3,5-7
Safety
Assessing potential harms related to the use of antipsychotics in treating OCD is complicated, because this information is not always assessed in trials. Instead, researchers often focus on exploring potential benefits because long-term effects of antipsychotics, including sedation, weight gain, metabolic syndrome, and extrapyramidal side effects, are well documented.3
Trials included in the meta-analysis by Veale et al3 had a maximum duration of 16 weeks, so it is likely that many of the potential harms of antipsychotic use would not yet have been measurable. The authors cautioned that, although aripiprazole and risperidone demonstrated benefit, their benefit must be weighed against the potential physical risks of long-term antipsychotic use.3One study that was not included in the meta-analysis by Veale et al3 evaluated individuals who did not respond to a SSRI, and randomly assigned them to quetiapine, olanzapine, or risperidone plus CBT. At 1-year follow-up, 50% of participants receiving an antipsychotic had an increase of >10% in body mass index (BMI) and had higher fasting blood sugars compared with only 15.2% of participants with increased BMI in the comparison group (SSRI responders).3
Foa et al8 investigated long-term outcomes (ie, 6 months) of SSRI augmentation with ERP or risperidone in patients with OCD. Forty patients were randomized to receive risperidone, and 9 were considered responders. Only 8 chose to enter the maintenance phase, and of those participants, 5 did not complete the study. Two withdrew due to worsening depression, 2 withdrew due to intolerable adverse effects, and 1 was lost to follow-up. Unfortunately, there was no further discussion of what the intolerable adverse effects were.8
Patients with comorbid schizophrenia and OCD face additional risks. Lifetime prevalence rates of OCD are greater in persons with schizophrenia compared with the general population (26% vs 8%, respectively). Most studies have demonstrated poor prognosis and medication adherence among patients with comorbid schizophrenia and OCD. Fonseka et al9 assessed the risk of antipsychotic induction and exacerbation of OCD symptoms in patients with schizophrenia. Induction and exacerbation of OCD symptoms
Evidence of olanzapine induction and exacerbation of OCD symptoms is also limited to case reports and retrospective studies. However, some studies have estimated induction of OCD symptoms with olanzapine in 11% to 20% of patients.9 There is insufficient evidence to form conclusions regarding other antipsychotics. Fonseka et al9 recommends switching to an antipsychotic with lower 5HT-2 binding affinity or adding an SSRI, such as fluvoxamine, if induction or exacerbation of OCD symptoms occurs.
Consider long-term risks
The evidence for benefits with antipsychotics in treatment-resistant OCD is limited by different populations recruited, small sample sizes, and lack of long-term follow-up. Most evidence supports using ERP over antipsychotics for treating OCD symptoms that have not responded to SSRIs. However, ERP poses its own challenges that may limit clinical utility, such as economic and time restraints. Therefore, benefits with antipsychotics, such as risperidone and aripiprazole, must be weighed against potential long-term risks of treatment, including sedation, weight gain, metabolic syndrome, and extrapyramidal side effects.
Regarding Mr. E’s case, because he had been maximized on SSRI therapy for an adequate duration (escitalopram, 40 mg/d, for 12 weeks) and completed CBT with ERP with a partial response, adding risperidone, 0.5 mg at bedtime, was an appropriate treatment option that is supported by the available guidelines and evidence. The risperidone dose is reflective of the initial dosing strategies used in clinical trials. It is recommended to assess efficacy of treatment at 8 weeks with a validated measure, such as the Y-BOCS. A dose increase may be needed to achieve clinically significant symptom improvement, because moderate doses of risperidone have demonstrated efficacy in trials; however, high doses of risperidone are unlikely to provide additional benefit and increase the risk of adverse effects. If risperidone does not provide a clinically favorable risk–benefit ratio for Mr. E, aripiprazole is a potential alternative.
Mr. E, age 37, has a 20-year history of obsessive-compulsive disorder (OCD), with comorbid generalized anxiety disorder and hypertension. His medication regimen consists of
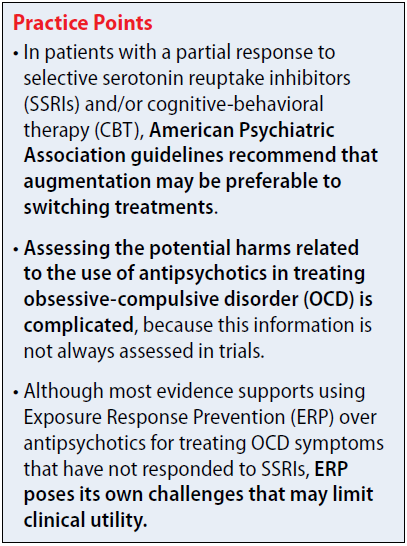
Box
Antipsychotics for OCD: What the guidelines recommend
The 2013 American Psychiatric Association (APA) obsessive-compulsive disorder (OCD) treatment guidelines include recommendations regarding the use of antipsychotics in patients who do not respond to first-line treatment with selective serotonin reuptake inhibitors (SSRIs) and/or cognitive-behavioral therapy (CBT). The APA recommends evaluating contributing factors, including comorbidities, family support, and ability to tolerate psychotherapy or maximum recommended drug doses, before augmenting or switching therapies.1
In patients with a partial response to SSRIs and/or CBT, the APA suggests that augmentation may be preferable to switching treatments. Augmentation strategies for SSRIs include antipsychotics or CBT with Exposure Response Prevention (ERP); augmentation strategies for CBT include SSRIs. Combining SSRIs and CBT may decrease the chance of relapse when medication is discontinued. If the patient has a partial response to ERP, intensification of therapy also can be considered based on patient-specific factors. In non-responders, switching therapies may be necessary. Alternative treatments including a different SSRI; an antidepressant from a difference class, such as clomipramine or mirtazapine; an antipsychotic; or CBT.
The 2006 National Institute for Health and Clinical Excellence guidelines for OCD recommend additional high-intensity CBT, adding an antipsychotic to an SSRI or clomipramine, or combining clomipramine with citalopram in non-responders. There is no guidance regarding the order in which these treatments should be trialed. Antipsychotics are recommended as an entire class, and there are no recommendations regarding dosing or long-term risks. These guidelines are based on limited evidence, including only 1 trial of quetiapine and 1 trial of olanzapine.2,3
Efficacy
The 2013 National Institute for Health Care and Excellence Evidence Update included a 2010 Cochrane Review of 11 randomized controlled trials (RCTs) of antipsychotics as adjunctive treatment to SSRIs.5 All trials were <6 months, and most were limited regarding quality aspects. Two trials found no statistically significant difference with olanzapine in efficacy measures (Y-BOCS mean difference [MD] −2.96; 95% confidence interval [CI] −7.41 to 1.22; effect size d = −2.96 [−7.14, 1.22]). Among patients with no clinically significant change (defined as ≤35% reduction in Y-BOCS), there was no significant difference between groups (n = 44, 1 RCT, odds ratio [OR] 0.76; 95% CI 0.17 to 3.29; effect size d = 0.76 [0.17, 3.29]). Studies found increased weight gain with olanzapine compared with antidepressant monotherapy.
Statistically significant differences were demonstrated with the addition of quetiapine to antidepressant monotherapy as shown in Y-BOCS score at endpoint (Y-BOCS MD −2.28; 95% CI −4.05 to −0.52; effect size d −2.28 [−4.05, −0.52]). Quetiapine also demonstrated benefit for depressive and anxiety symptoms. Among patients with no clinically significant change (defined as ≤35% reduction in Y-BOCS), there was a significant difference between groups (n = 80, 2 RCTs, OR 0.27; 95% CI 0.09 to 0.87; effect size d = 0.27 [0.09, 0.87]).
Adjunctive treatment with risperidone was superior to antidepressant monotherapy for participants without a significant response in OCD symptom severity of at least 25% with validated measures (OR 0.17; 95% CI 0.04 to 0.66; effect size d = 0.17 [0.04, 0.66]), and in depressive and anxiety symptoms. Mean reduction in Y-BOCS scores was not statistically significant with risperidone (MD −3.35; 95% CI −8.25 to 1.55; effect size d = −3.35 [−8.25, 1.55]).5
A 2014 meta-analysis by Veale et al3 included double-blind, randomized trials that examined atypical antipsychotics compared with placebo for adults with OCD that used an intention-to-treat analysis. Unlike the Cochrane Review, these studies used the Y-BOCS as a primary outcome measure. Participants had a Y-BOCS score of ≥16; had at least 1 appropriate trial of an SSRI or clomipramine (defined as the maximum dose tolerated for at least 8 weeks); and had to continue taking the SSRI or
Fourteen articles were included in the meta-analysis, but all had small sample sizes and no long-term follow-up data.3 Antipsychotics in the meta-analysis included risperidone (4 studies), quetiapine (5 studies), olanzapine (2 studies),
The overall difference in Y-BOCS score change between drug and placebo groups was 2.34 points, which had an overall effect size of d = 0.40. Those taking antipsychotics had approximately a 10% reduction in Y-BOCS score over time. The overall difference was statistically significant with risperidone (overall mean reduction of 3.89 points on the Y-BOCS; 95% CI 1.43 to 5.48; effect size of d = 0.53) and aripiprazole (difference in Y-BOCS outcome 0.1 scores of 6.29 points; effect size of d = 1.11). One trial of risperidone used a low dose (0.5 mg) and had a larger effect size than the studies that used moderate doses. The overall difference was not statistically significant for quetiapine (difference of Y-BOCS outcome scores of 0.81 points) or olanzapine (difference in Y-BOCS outcome scores of −0.19; indicating <1 point difference on the Y-BOCS).3
Studies included in the meta-analysis ranged in durations from 6 to 16 weeks; duration of ≥4 weeks did not make a difference in response. One study demonstrated a worsening of symptoms in the quetiapine group between weeks 4 and 12. Only 4 studies included most patients that had a previous trial of CBT. One study with an additional treatment arm evaluating CBT found that adding CBT was superior to adjunctive risperidone or placebo. Another study found that adding clomipramine or placebo to
Two studies included in the meta-analysis classified OCD symptoms by subtype, such as by dimensions of checking; symmetry, ordering, counting, and repeating; contamination and cleaning; and hoarding. Currently, no clinically significant predictor of outcome of antipsychotic therapy has been identified. Two studies included in the meta-analysis assessed patients with comorbid tic disorders and found no difference by treatment. One study demonstrated benefit of haloperidol in patients with comorbid tic disorders compared with those without comorbid tic disorders. Of note, none of the studies included in the meta-analysis excluded patients with hoarding characteristics, which generally indicate a worse prognosis with treatment.3
In 2015, Dold et al6 provided an update to a 2013 meta-analysis7 assessing antipsychotic augmentation of SSRIs in treatment-resistant OCD. This update included 2 new RCTs. The 2013 analysis7 concluded that risperidone should be considered first-line and is preferred over olanzapine and quetiapine. However, the update found the highest effect size for aripiprazole (d = −1.35), followed by haloperidol (d = −0.82), risperidone (d = −0.59), quetiapine (d = −0.50), olanzapine (d = −0.49), and paliperidone (d = −0.21).6,7
The 2015 update6 concluded that the antipsychotic doses used in trials were moderate and that there was no association between dose and treatment response, indicating that high doses of antipsychotics may not be more effective. Dold et al6 postulated that the antipsychotic doses required for treating OCD are similar to those used in treating major depressive disorder and lower than doses used in treating schizophrenia. The 2013 meta-analysis demonstrated that moderate doses of antipsychotics resulted in statistically significant efficacy (relative risk [RR] = 3.99, 95% CI 1.92 to 8.27), while low doses did not demonstrate statistical significance (RR = 1.06, 95% CI 0.45 to 2.53).6,7
The 2015 subgroup analysis update evaluated the duration of SSRI treatment prior to the antipsychotic augmentation phase, but did not demonstrate statistically significant efficacy for studies with <8 weeks’ duration of SSRI treatment, further highlighting the need for extended duration of treatment with an SSRI prior to augmentation.6
The 2013 meta-analysis discussed populations with comorbid tic disorders, including a study that found that patients with OCD and comorbid tic disorders benefit more from adjunctive antipsychotic therapy than those without the comorbidity. The 2015 update excluded trials that included patients with comorbid tic disorders to reduce bias, which did not affect the overall effect sizes of the data.6,7
In summary, efficacy has been demonstrated for risperidone and aripiprazole. There has been no benefit demonstrated with olanzapine and limited benefit with quetiapine. One study suggested worsening of symptoms with quetiapine the longer that treatment persisted.3,5-7
Safety
Assessing potential harms related to the use of antipsychotics in treating OCD is complicated, because this information is not always assessed in trials. Instead, researchers often focus on exploring potential benefits because long-term effects of antipsychotics, including sedation, weight gain, metabolic syndrome, and extrapyramidal side effects, are well documented.3
Trials included in the meta-analysis by Veale et al3 had a maximum duration of 16 weeks, so it is likely that many of the potential harms of antipsychotic use would not yet have been measurable. The authors cautioned that, although aripiprazole and risperidone demonstrated benefit, their benefit must be weighed against the potential physical risks of long-term antipsychotic use.3One study that was not included in the meta-analysis by Veale et al3 evaluated individuals who did not respond to a SSRI, and randomly assigned them to quetiapine, olanzapine, or risperidone plus CBT. At 1-year follow-up, 50% of participants receiving an antipsychotic had an increase of >10% in body mass index (BMI) and had higher fasting blood sugars compared with only 15.2% of participants with increased BMI in the comparison group (SSRI responders).3
Foa et al8 investigated long-term outcomes (ie, 6 months) of SSRI augmentation with ERP or risperidone in patients with OCD. Forty patients were randomized to receive risperidone, and 9 were considered responders. Only 8 chose to enter the maintenance phase, and of those participants, 5 did not complete the study. Two withdrew due to worsening depression, 2 withdrew due to intolerable adverse effects, and 1 was lost to follow-up. Unfortunately, there was no further discussion of what the intolerable adverse effects were.8
Patients with comorbid schizophrenia and OCD face additional risks. Lifetime prevalence rates of OCD are greater in persons with schizophrenia compared with the general population (26% vs 8%, respectively). Most studies have demonstrated poor prognosis and medication adherence among patients with comorbid schizophrenia and OCD. Fonseka et al9 assessed the risk of antipsychotic induction and exacerbation of OCD symptoms in patients with schizophrenia. Induction and exacerbation of OCD symptoms
Evidence of olanzapine induction and exacerbation of OCD symptoms is also limited to case reports and retrospective studies. However, some studies have estimated induction of OCD symptoms with olanzapine in 11% to 20% of patients.9 There is insufficient evidence to form conclusions regarding other antipsychotics. Fonseka et al9 recommends switching to an antipsychotic with lower 5HT-2 binding affinity or adding an SSRI, such as fluvoxamine, if induction or exacerbation of OCD symptoms occurs.
Consider long-term risks
The evidence for benefits with antipsychotics in treatment-resistant OCD is limited by different populations recruited, small sample sizes, and lack of long-term follow-up. Most evidence supports using ERP over antipsychotics for treating OCD symptoms that have not responded to SSRIs. However, ERP poses its own challenges that may limit clinical utility, such as economic and time restraints. Therefore, benefits with antipsychotics, such as risperidone and aripiprazole, must be weighed against potential long-term risks of treatment, including sedation, weight gain, metabolic syndrome, and extrapyramidal side effects.
Regarding Mr. E’s case, because he had been maximized on SSRI therapy for an adequate duration (escitalopram, 40 mg/d, for 12 weeks) and completed CBT with ERP with a partial response, adding risperidone, 0.5 mg at bedtime, was an appropriate treatment option that is supported by the available guidelines and evidence. The risperidone dose is reflective of the initial dosing strategies used in clinical trials. It is recommended to assess efficacy of treatment at 8 weeks with a validated measure, such as the Y-BOCS. A dose increase may be needed to achieve clinically significant symptom improvement, because moderate doses of risperidone have demonstrated efficacy in trials; however, high doses of risperidone are unlikely to provide additional benefit and increase the risk of adverse effects. If risperidone does not provide a clinically favorable risk–benefit ratio for Mr. E, aripiprazole is a potential alternative.
1. American Psychiatric Association. Practice guideline for the treatment of patients with obsessive-compulsive disorder. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/ocd.pdf. Published July 2007. Accessed December 11, 2017.
2. National Institute for Health and Care Excellence (NICE). Obsessive compulsive disorder. http://arms.evidence.nhs.uk/resources/hub/1028833/attachment. Updated September 18, 2013. Accessed December 11, 2017.
3. Veale D, Miles S, Smallcombe N, et al. Atypical antipsychotic augmentation in SSRI treatment refractory obsessive-compulsive disorder: a systematic review and
4. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
5. Komossa K, Depping AM, Meyer M, et al. Second-generation antipsychotics for obsessive compulsive disorder. Cochrane Database Syst Rev. 2010;12:1-44.
6. Dold M, Aigner M, Lanzenberger R, et al. Antipsychotic augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: an update meta-analysis of double-blind, randomized, placebo-controlled trials. Int J Neuropsychopharmacol. 2015;18(9). doi: 10.1093/ijnp/pyv047.
7. Dold M, Aigner M, Lanzenberger R, et al. Antipsychotic augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: a meta-analysis of double-blind, randomized, placebo-controlled trials. Int J Neuropsychopharmacol. 2013;16(3):557-574.
8. Foa EB, Simpson HB, Rosenfield D, et al. Six-month outcomes from a randomized trial augmenting serotonin reuptake inhibitors with exposure and response prevention or risperidone in adults with obsessive-compulsive disorder. J Clin Psychiatry. 2015;76(4):440-446.
9. Fonseka TM, Richter MA, Muller DJ. Second generation antipsychotic-induced obsessive-compulsive symptoms in schizophrenia: a review of the experimental literature. Curr Psychiatry Rep. 2014;16(11):510.
1. American Psychiatric Association. Practice guideline for the treatment of patients with obsessive-compulsive disorder. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/ocd.pdf. Published July 2007. Accessed December 11, 2017.
2. National Institute for Health and Care Excellence (NICE). Obsessive compulsive disorder. http://arms.evidence.nhs.uk/resources/hub/1028833/attachment. Updated September 18, 2013. Accessed December 11, 2017.
3. Veale D, Miles S, Smallcombe N, et al. Atypical antipsychotic augmentation in SSRI treatment refractory obsessive-compulsive disorder: a systematic review and
4. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
5. Komossa K, Depping AM, Meyer M, et al. Second-generation antipsychotics for obsessive compulsive disorder. Cochrane Database Syst Rev. 2010;12:1-44.
6. Dold M, Aigner M, Lanzenberger R, et al. Antipsychotic augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: an update meta-analysis of double-blind, randomized, placebo-controlled trials. Int J Neuropsychopharmacol. 2015;18(9). doi: 10.1093/ijnp/pyv047.
7. Dold M, Aigner M, Lanzenberger R, et al. Antipsychotic augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: a meta-analysis of double-blind, randomized, placebo-controlled trials. Int J Neuropsychopharmacol. 2013;16(3):557-574.
8. Foa EB, Simpson HB, Rosenfield D, et al. Six-month outcomes from a randomized trial augmenting serotonin reuptake inhibitors with exposure and response prevention or risperidone in adults with obsessive-compulsive disorder. J Clin Psychiatry. 2015;76(4):440-446.
9. Fonseka TM, Richter MA, Muller DJ. Second generation antipsychotic-induced obsessive-compulsive symptoms in schizophrenia: a review of the experimental literature. Curr Psychiatry Rep. 2014;16(11):510.
Welcome to The New Gastroenterologist online!
Dear Colleagues,
It is with great excitement that I introduce the first e-newsletter version of The New Gastroenterologist! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
In this issue of The New Gastroenterologist, our In Focus article provides a practical overview of the management of chronic constipation. This article, written by Nitin Ahuja and James Reynolds from the Neurogastroenterology and Motility Program at the University of Pennsylvania, Philadelphia, addresses a common topic in our field, and can also be found in the February print issue of GI & Hepatology News. To complement this article, there is a corresponding video abstract that can be viewed.
Also in this issue, Richard Peek (Vanderbilt University, Nashville, Tenn.) – one of the Coeditors in Chief of Gastroenterology – provides a summary of the newly created 1-year editorial fellowship for the AGA’s flagship journal. This is a fantastic new opportunity and you can learn firsthand about the experience of the inaugural editorial fellow, Eric Shah (University of Michigan, Ann Arbor), in an accompanying video. Additionally, as helping patients make a successful transition from a pediatric GI practice to an adult GI practice can be very challenging, in this issue Manreet Kaur and Allyson Wyatt (Baylor College of Medicine, Houston) provide a primer on how to successfully aid in this transition.
Are you considering a career in hospital administration? If so, you will enjoy reading about pursuing a career in hospital administration from Brijen Shah, who is the chief medical officer of Mount Sinai Queens (Icahn School of Medicine at Mount Sinai, New York). Have you been to one of the AGA’s Regional Practice Skills Workshops? These workshops are sponsored by the AGA Trainee and Early Career Committee and held in a growing number of cities across the country. In this issue, Munish Ashat (University of Iowa, Iowa City) provides a recap of the workshop he attended, complete with many useful career pearls.
I hope that you also enjoy the other features in the new e-newsletter format of The New Gastroenterologist. I especially want to point out one of our new sections entitled “In Case You Missed It.” As we all undoubtedly experience information overload with so many new articles released each month, this section collects relevant articles from the numerous AGA publications and consolidates them to ensure you don’t miss any of this great content.
If you are interested in contributing to future issues of The New Gastroenterologist or if there are topics that would interest you, please let us know. You can contact me ([email protected]) or the managing editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Dear Colleagues,
It is with great excitement that I introduce the first e-newsletter version of The New Gastroenterologist! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
In this issue of The New Gastroenterologist, our In Focus article provides a practical overview of the management of chronic constipation. This article, written by Nitin Ahuja and James Reynolds from the Neurogastroenterology and Motility Program at the University of Pennsylvania, Philadelphia, addresses a common topic in our field, and can also be found in the February print issue of GI & Hepatology News. To complement this article, there is a corresponding video abstract that can be viewed.
Also in this issue, Richard Peek (Vanderbilt University, Nashville, Tenn.) – one of the Coeditors in Chief of Gastroenterology – provides a summary of the newly created 1-year editorial fellowship for the AGA’s flagship journal. This is a fantastic new opportunity and you can learn firsthand about the experience of the inaugural editorial fellow, Eric Shah (University of Michigan, Ann Arbor), in an accompanying video. Additionally, as helping patients make a successful transition from a pediatric GI practice to an adult GI practice can be very challenging, in this issue Manreet Kaur and Allyson Wyatt (Baylor College of Medicine, Houston) provide a primer on how to successfully aid in this transition.
Are you considering a career in hospital administration? If so, you will enjoy reading about pursuing a career in hospital administration from Brijen Shah, who is the chief medical officer of Mount Sinai Queens (Icahn School of Medicine at Mount Sinai, New York). Have you been to one of the AGA’s Regional Practice Skills Workshops? These workshops are sponsored by the AGA Trainee and Early Career Committee and held in a growing number of cities across the country. In this issue, Munish Ashat (University of Iowa, Iowa City) provides a recap of the workshop he attended, complete with many useful career pearls.
I hope that you also enjoy the other features in the new e-newsletter format of The New Gastroenterologist. I especially want to point out one of our new sections entitled “In Case You Missed It.” As we all undoubtedly experience information overload with so many new articles released each month, this section collects relevant articles from the numerous AGA publications and consolidates them to ensure you don’t miss any of this great content.
If you are interested in contributing to future issues of The New Gastroenterologist or if there are topics that would interest you, please let us know. You can contact me ([email protected]) or the managing editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.
Dear Colleagues,
It is with great excitement that I introduce the first e-newsletter version of The New Gastroenterologist! As more content in medicine, and life in general, is moving toward digital platforms, we at the AGA believe this transition will improve both content dissemination and accessibility to all our readers. In this new format, we will continue to provide articles on topics of importance to the early-career community, expand our offerings by including the new “In Focus” articles (concise overviews of GI topics) both digitally and in GI & Hepatology News print issues, as well as increase the use of multimedia resources, such as videos, to further enhance our content.
In this issue of The New Gastroenterologist, our In Focus article provides a practical overview of the management of chronic constipation. This article, written by Nitin Ahuja and James Reynolds from the Neurogastroenterology and Motility Program at the University of Pennsylvania, Philadelphia, addresses a common topic in our field, and can also be found in the February print issue of GI & Hepatology News. To complement this article, there is a corresponding video abstract that can be viewed.
Also in this issue, Richard Peek (Vanderbilt University, Nashville, Tenn.) – one of the Coeditors in Chief of Gastroenterology – provides a summary of the newly created 1-year editorial fellowship for the AGA’s flagship journal. This is a fantastic new opportunity and you can learn firsthand about the experience of the inaugural editorial fellow, Eric Shah (University of Michigan, Ann Arbor), in an accompanying video. Additionally, as helping patients make a successful transition from a pediatric GI practice to an adult GI practice can be very challenging, in this issue Manreet Kaur and Allyson Wyatt (Baylor College of Medicine, Houston) provide a primer on how to successfully aid in this transition.
Are you considering a career in hospital administration? If so, you will enjoy reading about pursuing a career in hospital administration from Brijen Shah, who is the chief medical officer of Mount Sinai Queens (Icahn School of Medicine at Mount Sinai, New York). Have you been to one of the AGA’s Regional Practice Skills Workshops? These workshops are sponsored by the AGA Trainee and Early Career Committee and held in a growing number of cities across the country. In this issue, Munish Ashat (University of Iowa, Iowa City) provides a recap of the workshop he attended, complete with many useful career pearls.
I hope that you also enjoy the other features in the new e-newsletter format of The New Gastroenterologist. I especially want to point out one of our new sections entitled “In Case You Missed It.” As we all undoubtedly experience information overload with so many new articles released each month, this section collects relevant articles from the numerous AGA publications and consolidates them to ensure you don’t miss any of this great content.
If you are interested in contributing to future issues of The New Gastroenterologist or if there are topics that would interest you, please let us know. You can contact me ([email protected]) or the managing editor of The New Gastroenterologist, Ryan Farrell ([email protected]).
Sincerely,
Bryson W. Katona, MD, PhD
Editor in Chief
Dr. Katona is an instructor of medicine in the division of gastroenterology at the University of Pennsylvania, Philadelphia.









