User login
CHMP endorses drug delivery system
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a label variation for Neulasta® (pegfilgrastim) to include the Neulasta® Onpro® Kit.
The Neulasta Onpro Kit is an on-body injector (OBI) delivery system for Neulasta, which is approved in the European Union to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).
The Neulasta Onpro Kit includes a specifically designed Neulasta pre-filled syringe along with a single-use OBI. The small, lightweight OBI is applied to a patient’s skin on the same day of chemotherapy.
The OBI is intended to facilitate timed delivery of the correct dose of Neulasta and eliminate the need for patients to return to a healthcare setting the day after they receive chemotherapy.
The CHMP’s opinion on the Neulasta Onpro Kit will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the centralized marketing authorization of Neulasta will be updated to include information on the Neulasta Onpro Kit in the drug’s label.
This change will be valid throughout the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions about Neulasta’s label on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a label variation for Neulasta® (pegfilgrastim) to include the Neulasta® Onpro® Kit.
The Neulasta Onpro Kit is an on-body injector (OBI) delivery system for Neulasta, which is approved in the European Union to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).
The Neulasta Onpro Kit includes a specifically designed Neulasta pre-filled syringe along with a single-use OBI. The small, lightweight OBI is applied to a patient’s skin on the same day of chemotherapy.
The OBI is intended to facilitate timed delivery of the correct dose of Neulasta and eliminate the need for patients to return to a healthcare setting the day after they receive chemotherapy.
The CHMP’s opinion on the Neulasta Onpro Kit will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the centralized marketing authorization of Neulasta will be updated to include information on the Neulasta Onpro Kit in the drug’s label.
This change will be valid throughout the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions about Neulasta’s label on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended a label variation for Neulasta® (pegfilgrastim) to include the Neulasta® Onpro® Kit.
The Neulasta Onpro Kit is an on-body injector (OBI) delivery system for Neulasta, which is approved in the European Union to reduce the duration of neutropenia and the incidence of febrile neutropenia in adults treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).
The Neulasta Onpro Kit includes a specifically designed Neulasta pre-filled syringe along with a single-use OBI. The small, lightweight OBI is applied to a patient’s skin on the same day of chemotherapy.
The OBI is intended to facilitate timed delivery of the correct dose of Neulasta and eliminate the need for patients to return to a healthcare setting the day after they receive chemotherapy.
The CHMP’s opinion on the Neulasta Onpro Kit will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the centralized marketing authorization of Neulasta will be updated to include information on the Neulasta Onpro Kit in the drug’s label.
This change will be valid throughout the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions about Neulasta’s label on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
Ketamine for mood disorders?
Audacious advances to discover new treatments for psychiatric brain disorders
In recent years, the pace of the development of novel new treatments for brain disorders in both psychiatry and neurology, including psychiatric disorders, has been the subject of much worry and hand-wringing.1
Some major pharmaceutical companies have stopped research programs in neuropsychiatry to focus on other, “easier” therapeutic areas where they think the biology is better understood and therefore drug development is more feasible.
However, I am now more optimistic than I have been in many years that we are on the verge of a promising era of pharmacotherapy that will usher in far better prevention, diagnosis, and management of neuropsychiatric disorders, and a better outcome for our patients. Why the optimism? There is a series of converging trends that justify it.
Funding for basic neuroscience research. Governments all over the world have woken up to the fact that brain disorders will account for the largest economic impact unless new treatments are developed. This has spurred multiple initiatives to better understand the underlying neurobiologic mechanisms of the brain in health and disease.2
Renewed enthusiasm for brain disorders from small pharmaceutical and mid-size biotechnology companies. While some of the larger pharmaceutical companies have withdrawn from pursuing new treatments for psychiatric disorders due to the need to satisfy “shareholders,” small and nimble biotechnology companies have stepped up, seeing an opportunity in a field that is not overcrowded and still has an extensive unmet need. These companies are developing truly novel treatments and approaches that can differentiate from current treatments. These include:
- rapid-acting antidepressants
- targeting specific symptom domains of psychiatric disorders, such as cognition, apathy, or anhedonia, that currently have no adequate or effective treatment
- novel therapeutic targets in a range of indications
- nonpharmacologic approaches.
Leading companies in this space include Allergan and Blackthorn Therapeutics. These companies and others have publicly discussed their commitment to developing new treatments for psychiatric disorders.
But large pharmaceutical companies should not be discounted. Examples of advances by larger companies include the recent FDA “breakthrough designation” for the development of balovaptan by Roche, a medication with the potential to improve “core social interaction and communication” in patients with autism, and the work Johnson & Johnson is conducting with S-ketamine for depression and acutely suicidal patients.
New scientific breakthroughs in areas such as synthetic biology, gene editing, nanotechnology, pluripotent cells, understanding the impact of the microbiome, and many other fields will dramatically accelerate the pace of scientific progress, allowing new treatment approaches not previously imagined.
New technologies. An array of new technologies—such as biosensors, artificial intelligence and machine learning, augmented and virtual reality, and other digital health tools—will impact every step of the “patient journey.” These will enable earlier detection and diagnosis, ongoing real-time assessment of symptoms, and more objective assessments, and they will facilitate the delivery of, and assessment of adherence to, treatments such as pharmacotherapy, neuromodulation, video games, apps, or a combination of these modalities.
Until recently, the idea of a video game or augmented reality glasses being viewed as serious and validated treatment modalities would have been considered science fiction. New ways of assessing patients—including voice, typing, activity on smartphones, diurnal rhythm, etc.—have the potential to dramatically improve the information clinicians will have about patient functioning in the real world. Another area where new technologies may eventually have a huge impact is in facilitating the prediction of suicide attempts.3
New digital therapeutics companies. It is no coincidence that the digital therapeutics companies that have been making the news and obtaining FDA approvals, such as Proteus Digital Health, Pear Therapeutics, Akili, and Click Therapeutics, are all addressing brain disorders.
Patient empowerment. With these new tools, the patient can become a true partner in the therapeutic alliance more than ever before. Patients can have an active role in diagnosis and be active participants in many new treatment modalities. There will be many new ways for patients to share their data to improve their care and to advance the science of these tools. Utilizing blockchain protocols, patients will have more control over how and with whom their data is shared, and even be compensated for it.
This may all seem like a medical “brave new world,” and perhaps a long way away. However, I believe these changes are happening at an exponential rate. It is hard to believe that common technological tools such as Google Maps, Gmail, and the smartphone first became available only a few years ago. The merging of biology and technology will have profound effects, and will be recognized as the momentous scientific achievement of the early 21st century.
Unlike clunky technologies such as electronic medical records, which have in fact made the clinician–patient experience worse, I believe that the technologies I describe above will enhance and augment the clinician–patient relationship. As health care practitioners, we need to be open to new technologies and ways of assessing and treating our patients while making sure our clinical insights and experience inform the development of these new technologies.
Let’s buckle up. Life in psychiatry is going to get more interesting than ever!
1. O’Hara M, Duncan P. The Guardian. Why ‘big pharma’ stopped searching for the next prozac. https://www.theguardian.com/society/2016/jan/27/prozac-next-psychiatric-wonder-drug-research-medicine-mental-illness. Published January 27, 2016. Accessed February 7, 2018.
2. Insel TR, Landis SC, Collins FS. The NIH BRAIN Initiative. Science. 2013;340(6133):687-688.
3. Vahabzadeh A, Sahin N, Kalali A. Digital suicide prevention: can technology become a game-changer? Innov Clin Neurosci. 2016;13(5-6):16-20.
In recent years, the pace of the development of novel new treatments for brain disorders in both psychiatry and neurology, including psychiatric disorders, has been the subject of much worry and hand-wringing.1
Some major pharmaceutical companies have stopped research programs in neuropsychiatry to focus on other, “easier” therapeutic areas where they think the biology is better understood and therefore drug development is more feasible.
However, I am now more optimistic than I have been in many years that we are on the verge of a promising era of pharmacotherapy that will usher in far better prevention, diagnosis, and management of neuropsychiatric disorders, and a better outcome for our patients. Why the optimism? There is a series of converging trends that justify it.
Funding for basic neuroscience research. Governments all over the world have woken up to the fact that brain disorders will account for the largest economic impact unless new treatments are developed. This has spurred multiple initiatives to better understand the underlying neurobiologic mechanisms of the brain in health and disease.2
Renewed enthusiasm for brain disorders from small pharmaceutical and mid-size biotechnology companies. While some of the larger pharmaceutical companies have withdrawn from pursuing new treatments for psychiatric disorders due to the need to satisfy “shareholders,” small and nimble biotechnology companies have stepped up, seeing an opportunity in a field that is not overcrowded and still has an extensive unmet need. These companies are developing truly novel treatments and approaches that can differentiate from current treatments. These include:
- rapid-acting antidepressants
- targeting specific symptom domains of psychiatric disorders, such as cognition, apathy, or anhedonia, that currently have no adequate or effective treatment
- novel therapeutic targets in a range of indications
- nonpharmacologic approaches.
Leading companies in this space include Allergan and Blackthorn Therapeutics. These companies and others have publicly discussed their commitment to developing new treatments for psychiatric disorders.
But large pharmaceutical companies should not be discounted. Examples of advances by larger companies include the recent FDA “breakthrough designation” for the development of balovaptan by Roche, a medication with the potential to improve “core social interaction and communication” in patients with autism, and the work Johnson & Johnson is conducting with S-ketamine for depression and acutely suicidal patients.
New scientific breakthroughs in areas such as synthetic biology, gene editing, nanotechnology, pluripotent cells, understanding the impact of the microbiome, and many other fields will dramatically accelerate the pace of scientific progress, allowing new treatment approaches not previously imagined.
New technologies. An array of new technologies—such as biosensors, artificial intelligence and machine learning, augmented and virtual reality, and other digital health tools—will impact every step of the “patient journey.” These will enable earlier detection and diagnosis, ongoing real-time assessment of symptoms, and more objective assessments, and they will facilitate the delivery of, and assessment of adherence to, treatments such as pharmacotherapy, neuromodulation, video games, apps, or a combination of these modalities.
Until recently, the idea of a video game or augmented reality glasses being viewed as serious and validated treatment modalities would have been considered science fiction. New ways of assessing patients—including voice, typing, activity on smartphones, diurnal rhythm, etc.—have the potential to dramatically improve the information clinicians will have about patient functioning in the real world. Another area where new technologies may eventually have a huge impact is in facilitating the prediction of suicide attempts.3
New digital therapeutics companies. It is no coincidence that the digital therapeutics companies that have been making the news and obtaining FDA approvals, such as Proteus Digital Health, Pear Therapeutics, Akili, and Click Therapeutics, are all addressing brain disorders.
Patient empowerment. With these new tools, the patient can become a true partner in the therapeutic alliance more than ever before. Patients can have an active role in diagnosis and be active participants in many new treatment modalities. There will be many new ways for patients to share their data to improve their care and to advance the science of these tools. Utilizing blockchain protocols, patients will have more control over how and with whom their data is shared, and even be compensated for it.
This may all seem like a medical “brave new world,” and perhaps a long way away. However, I believe these changes are happening at an exponential rate. It is hard to believe that common technological tools such as Google Maps, Gmail, and the smartphone first became available only a few years ago. The merging of biology and technology will have profound effects, and will be recognized as the momentous scientific achievement of the early 21st century.
Unlike clunky technologies such as electronic medical records, which have in fact made the clinician–patient experience worse, I believe that the technologies I describe above will enhance and augment the clinician–patient relationship. As health care practitioners, we need to be open to new technologies and ways of assessing and treating our patients while making sure our clinical insights and experience inform the development of these new technologies.
Let’s buckle up. Life in psychiatry is going to get more interesting than ever!
In recent years, the pace of the development of novel new treatments for brain disorders in both psychiatry and neurology, including psychiatric disorders, has been the subject of much worry and hand-wringing.1
Some major pharmaceutical companies have stopped research programs in neuropsychiatry to focus on other, “easier” therapeutic areas where they think the biology is better understood and therefore drug development is more feasible.
However, I am now more optimistic than I have been in many years that we are on the verge of a promising era of pharmacotherapy that will usher in far better prevention, diagnosis, and management of neuropsychiatric disorders, and a better outcome for our patients. Why the optimism? There is a series of converging trends that justify it.
Funding for basic neuroscience research. Governments all over the world have woken up to the fact that brain disorders will account for the largest economic impact unless new treatments are developed. This has spurred multiple initiatives to better understand the underlying neurobiologic mechanisms of the brain in health and disease.2
Renewed enthusiasm for brain disorders from small pharmaceutical and mid-size biotechnology companies. While some of the larger pharmaceutical companies have withdrawn from pursuing new treatments for psychiatric disorders due to the need to satisfy “shareholders,” small and nimble biotechnology companies have stepped up, seeing an opportunity in a field that is not overcrowded and still has an extensive unmet need. These companies are developing truly novel treatments and approaches that can differentiate from current treatments. These include:
- rapid-acting antidepressants
- targeting specific symptom domains of psychiatric disorders, such as cognition, apathy, or anhedonia, that currently have no adequate or effective treatment
- novel therapeutic targets in a range of indications
- nonpharmacologic approaches.
Leading companies in this space include Allergan and Blackthorn Therapeutics. These companies and others have publicly discussed their commitment to developing new treatments for psychiatric disorders.
But large pharmaceutical companies should not be discounted. Examples of advances by larger companies include the recent FDA “breakthrough designation” for the development of balovaptan by Roche, a medication with the potential to improve “core social interaction and communication” in patients with autism, and the work Johnson & Johnson is conducting with S-ketamine for depression and acutely suicidal patients.
New scientific breakthroughs in areas such as synthetic biology, gene editing, nanotechnology, pluripotent cells, understanding the impact of the microbiome, and many other fields will dramatically accelerate the pace of scientific progress, allowing new treatment approaches not previously imagined.
New technologies. An array of new technologies—such as biosensors, artificial intelligence and machine learning, augmented and virtual reality, and other digital health tools—will impact every step of the “patient journey.” These will enable earlier detection and diagnosis, ongoing real-time assessment of symptoms, and more objective assessments, and they will facilitate the delivery of, and assessment of adherence to, treatments such as pharmacotherapy, neuromodulation, video games, apps, or a combination of these modalities.
Until recently, the idea of a video game or augmented reality glasses being viewed as serious and validated treatment modalities would have been considered science fiction. New ways of assessing patients—including voice, typing, activity on smartphones, diurnal rhythm, etc.—have the potential to dramatically improve the information clinicians will have about patient functioning in the real world. Another area where new technologies may eventually have a huge impact is in facilitating the prediction of suicide attempts.3
New digital therapeutics companies. It is no coincidence that the digital therapeutics companies that have been making the news and obtaining FDA approvals, such as Proteus Digital Health, Pear Therapeutics, Akili, and Click Therapeutics, are all addressing brain disorders.
Patient empowerment. With these new tools, the patient can become a true partner in the therapeutic alliance more than ever before. Patients can have an active role in diagnosis and be active participants in many new treatment modalities. There will be many new ways for patients to share their data to improve their care and to advance the science of these tools. Utilizing blockchain protocols, patients will have more control over how and with whom their data is shared, and even be compensated for it.
This may all seem like a medical “brave new world,” and perhaps a long way away. However, I believe these changes are happening at an exponential rate. It is hard to believe that common technological tools such as Google Maps, Gmail, and the smartphone first became available only a few years ago. The merging of biology and technology will have profound effects, and will be recognized as the momentous scientific achievement of the early 21st century.
Unlike clunky technologies such as electronic medical records, which have in fact made the clinician–patient experience worse, I believe that the technologies I describe above will enhance and augment the clinician–patient relationship. As health care practitioners, we need to be open to new technologies and ways of assessing and treating our patients while making sure our clinical insights and experience inform the development of these new technologies.
Let’s buckle up. Life in psychiatry is going to get more interesting than ever!
1. O’Hara M, Duncan P. The Guardian. Why ‘big pharma’ stopped searching for the next prozac. https://www.theguardian.com/society/2016/jan/27/prozac-next-psychiatric-wonder-drug-research-medicine-mental-illness. Published January 27, 2016. Accessed February 7, 2018.
2. Insel TR, Landis SC, Collins FS. The NIH BRAIN Initiative. Science. 2013;340(6133):687-688.
3. Vahabzadeh A, Sahin N, Kalali A. Digital suicide prevention: can technology become a game-changer? Innov Clin Neurosci. 2016;13(5-6):16-20.
1. O’Hara M, Duncan P. The Guardian. Why ‘big pharma’ stopped searching for the next prozac. https://www.theguardian.com/society/2016/jan/27/prozac-next-psychiatric-wonder-drug-research-medicine-mental-illness. Published January 27, 2016. Accessed February 7, 2018.
2. Insel TR, Landis SC, Collins FS. The NIH BRAIN Initiative. Science. 2013;340(6133):687-688.
3. Vahabzadeh A, Sahin N, Kalali A. Digital suicide prevention: can technology become a game-changer? Innov Clin Neurosci. 2016;13(5-6):16-20.
Psychiatry 2.0: Experiencing psychiatry’s new challenges together
“It is beyond a doubt that all our knowledge begins with experience.”
- Immanuel Kant
Medicine, a highly experiential profession, is constantly evolving. The consistency of change and the psychiatrist’s inherent wonder offers a paradoxical sense of comfort and conundrum.
As students, we look to our predecessors, associations, and peers to master concepts both concrete and abstract. And once we achieve competence at understanding mechanisms, applying biopsychosocial formulations, and effectively teaching what we’ve learned—everything changes!
We journey through a new era of medicine together. With burgeoning technology, intense politics, and confounding social media, we are undergoing new applications, hurdles to health care, and personal exposure to extremes that have never been experienced before. The landscape of psychiatric practice is changing. Its transformation inherently challenges our existing practices and standards.
It wasn’t too long ago that classroom fodder included how to deal with seeing your patient at a cocktail party. Contemporary discussions are more likely to address the patient who follows you on Twitter (and whom you follow back). Long ago are the days of educating students through a didactic model. Learning now occurs in collaborative group settings with a focus on the practical and hands-on experience. Budding psychiatrists are interested these days in talking about setting up their own apps, establishing a start-up company for health care, working on policy reform, and innovating new approaches to achieve social justice.
A history of challenge and change
Developing variables and expectations in this Millennial Age makes it an exciting time for psychiatrists to explore, adapt, and lead into the future. Fortunately, the field has had ample practice with challenge and changes. Social constructs of how individuals with mental illness were treated altered with William Battie, an English physician whose 1758 Treatise on Madness called for treatments to be utilized on rich and poor mental patients alike in asylums.1 Remember the days of chaining patients to bedposts on psychiatric wards? Of course not! Such archaic practices thankfully disappeared, due in large part to French physician Philippe Pinel. Patient care has evolved to encompass empathy, rights, and dignity.2
German physician Johann Christian Reil, who coined the term “psychiatry” more than 200 years ago, asserted that mental illness should be treated by the most highly qualified physicians.3 Such thinking seems obvious in 2018, but before Reil, the mental and physical states were seen as unrelated.
Modern psychiatry has certainly come a long way.4 We recognize mental health as being essential to overall health. Medications have evolved beyond lithium, chlorpromazine, and fluoxetine. We now have quarterly injectable antipsychotics and pills that patients can swallow and actually be monitored by their clinicians!4
The American Psychiatric Association (APA) has published multiple iterations of the Diagnostic and Statistical Manual of Mental Disorders since its inception in 1968.5 And with those revisions have come changes that most contemporary colleagues could only describe as self-evident—such as the declassification of homosexuality as a mental disorder in 1973.
Despite these advances and the advent of the Mental Health Parity Act of 2008, experience has shown us that some things have seen little progress. Reil, who saw a nexus between mental and physical health, launched an anti-stigma campaign more than 200 years ago. This begs a question to colleagues: How far have we come? Or better yet, capitalizing on our knowledge, experience, and hopes: What else can we do?
The essential interaction between mental, chemical, and physical domains has given rise to psychiatry and its many subspecialties. Among them is forensic psychiatry, which deals with the overlap of mental health and legal matters.6
While often recognized for its relation to criminology, forensic psychiatry encompasses the entirety of legal mental health matters.7 These are things that the daily practitioner faces on a routine basis.
My mentor, Dr. Douglas Mossman, author of
A new department for a new era
The world is changing very rapidly, and we face new dilemmas in the midst of trying to uphold our duties to patients and the profession. There are emerging domains that psychiatrists will experience for the first time—leaving us with more questions than direction. And that is the impetus for this new department, Psychiatry 2.0.
The ever-evolving Internet opens doors for psychiatrists to access and educate a larger audience. It also provides a tool for psychiatrists to keep a web-based presence, something essential for competitive business practices to stay relevant. We are languishing in a political climate that challenges our sense of duty to the public, which often is in contrast with the ethical principles of our association. Technology also poses problems, whether it’s tracking our patients through the pills they ingest, following them on an app, or relying on data from wearable devices in lieu of a patient’s report. All of this suggests a potential for progress as well as problems.
The goal of Psychiatry 2.0 is to experience new challenges together. As Department Editor, I will cover an array of cutting-edge and controversial topics. Continuing with Dr. Mossman’s teachings—that forensic understanding enhances the clinical practice—this department will routinely combine evidence-based information with legal concepts.
Each article in Psychiatry 2.0 will be divided into 3 parts, focusing on a clinician’s dilemma, a duty, and a discussion. The dilemma will be relatable to the clinician in everyday practice. A practical and evidence-based approach will be taken to expound upon our duty as physicians. And finally, there will be discussion about where the field is going, and how it will likely change. In its quarterly publication, Psychiatry 2.0 will explore a diverse range of topics, including technology, social media, stigma, social justice, and politics.
In memoriam: Douglas Mossman, MD
In my role as Department Editor, I find myself already reflecting on the experience, wisdom, compassion, encouragement, and legacy of Dr. Mossman. A distinguished psychiatrist, gifted musician, and inspiring mentor and academician, Dr. Mossman embodied knowledge, creativity, and devotion.
Among Dr. Mossman’s many accolades, including more than 180 authored publications, he was recipient of the Guttmacher Award (2008, the APA) and Golden Apple (2017, the American Academy of Psychiatry and Law). Dr. Mossman was further known to many as a mentor and friend. He was generous with his experiences as a highly accomplished physician and thoughtful in his teachings and publications, leaving an enduring legacy.
Remembering Dr. Mossman’s sage voice and articulate writings will be essential to moving forward in this modern age of psychiatry, as we experience new dilemmas and opportunities.
1. Morris A. William Battie’s Treatise on Madness (1758) and John Monro’s remarks on Dr Battie’s Treatise (1758). Br J Psychiatry. 2008;192(4):257.
2. Scull A. Moral treatment reconsidered. Social order/mental disorder: Anglo-American psychiatry in historical perspective. Berkeley, CA: University of California Press; 1986;81-95.
3. Marneros A. Psychiatry’s 200th birthday. Br J Psychiatry. 2008;193(1):1-3.
4. Cade JF. Lithium salts in the treatment of psychotic excitement. Med J Aust. 1949;2(10):349-352.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
6. Gold LH. Rediscovering forensic psychiatry. The American Psychiatric Publishing Textbook of Forensic Psychiatry. Simon RI, Gold LH, eds. Washington, DC: American Psychiatric Publishing; 2004;3-36.
7. Gutheil TG. The history of forensic psychiatry. J Am Acad Psychiatry Law. 2005;33(2):259-262.
“It is beyond a doubt that all our knowledge begins with experience.”
- Immanuel Kant
Medicine, a highly experiential profession, is constantly evolving. The consistency of change and the psychiatrist’s inherent wonder offers a paradoxical sense of comfort and conundrum.
As students, we look to our predecessors, associations, and peers to master concepts both concrete and abstract. And once we achieve competence at understanding mechanisms, applying biopsychosocial formulations, and effectively teaching what we’ve learned—everything changes!
We journey through a new era of medicine together. With burgeoning technology, intense politics, and confounding social media, we are undergoing new applications, hurdles to health care, and personal exposure to extremes that have never been experienced before. The landscape of psychiatric practice is changing. Its transformation inherently challenges our existing practices and standards.
It wasn’t too long ago that classroom fodder included how to deal with seeing your patient at a cocktail party. Contemporary discussions are more likely to address the patient who follows you on Twitter (and whom you follow back). Long ago are the days of educating students through a didactic model. Learning now occurs in collaborative group settings with a focus on the practical and hands-on experience. Budding psychiatrists are interested these days in talking about setting up their own apps, establishing a start-up company for health care, working on policy reform, and innovating new approaches to achieve social justice.
A history of challenge and change
Developing variables and expectations in this Millennial Age makes it an exciting time for psychiatrists to explore, adapt, and lead into the future. Fortunately, the field has had ample practice with challenge and changes. Social constructs of how individuals with mental illness were treated altered with William Battie, an English physician whose 1758 Treatise on Madness called for treatments to be utilized on rich and poor mental patients alike in asylums.1 Remember the days of chaining patients to bedposts on psychiatric wards? Of course not! Such archaic practices thankfully disappeared, due in large part to French physician Philippe Pinel. Patient care has evolved to encompass empathy, rights, and dignity.2
German physician Johann Christian Reil, who coined the term “psychiatry” more than 200 years ago, asserted that mental illness should be treated by the most highly qualified physicians.3 Such thinking seems obvious in 2018, but before Reil, the mental and physical states were seen as unrelated.
Modern psychiatry has certainly come a long way.4 We recognize mental health as being essential to overall health. Medications have evolved beyond lithium, chlorpromazine, and fluoxetine. We now have quarterly injectable antipsychotics and pills that patients can swallow and actually be monitored by their clinicians!4
The American Psychiatric Association (APA) has published multiple iterations of the Diagnostic and Statistical Manual of Mental Disorders since its inception in 1968.5 And with those revisions have come changes that most contemporary colleagues could only describe as self-evident—such as the declassification of homosexuality as a mental disorder in 1973.
Despite these advances and the advent of the Mental Health Parity Act of 2008, experience has shown us that some things have seen little progress. Reil, who saw a nexus between mental and physical health, launched an anti-stigma campaign more than 200 years ago. This begs a question to colleagues: How far have we come? Or better yet, capitalizing on our knowledge, experience, and hopes: What else can we do?
The essential interaction between mental, chemical, and physical domains has given rise to psychiatry and its many subspecialties. Among them is forensic psychiatry, which deals with the overlap of mental health and legal matters.6
While often recognized for its relation to criminology, forensic psychiatry encompasses the entirety of legal mental health matters.7 These are things that the daily practitioner faces on a routine basis.
My mentor, Dr. Douglas Mossman, author of
A new department for a new era
The world is changing very rapidly, and we face new dilemmas in the midst of trying to uphold our duties to patients and the profession. There are emerging domains that psychiatrists will experience for the first time—leaving us with more questions than direction. And that is the impetus for this new department, Psychiatry 2.0.
The ever-evolving Internet opens doors for psychiatrists to access and educate a larger audience. It also provides a tool for psychiatrists to keep a web-based presence, something essential for competitive business practices to stay relevant. We are languishing in a political climate that challenges our sense of duty to the public, which often is in contrast with the ethical principles of our association. Technology also poses problems, whether it’s tracking our patients through the pills they ingest, following them on an app, or relying on data from wearable devices in lieu of a patient’s report. All of this suggests a potential for progress as well as problems.
The goal of Psychiatry 2.0 is to experience new challenges together. As Department Editor, I will cover an array of cutting-edge and controversial topics. Continuing with Dr. Mossman’s teachings—that forensic understanding enhances the clinical practice—this department will routinely combine evidence-based information with legal concepts.
Each article in Psychiatry 2.0 will be divided into 3 parts, focusing on a clinician’s dilemma, a duty, and a discussion. The dilemma will be relatable to the clinician in everyday practice. A practical and evidence-based approach will be taken to expound upon our duty as physicians. And finally, there will be discussion about where the field is going, and how it will likely change. In its quarterly publication, Psychiatry 2.0 will explore a diverse range of topics, including technology, social media, stigma, social justice, and politics.
In memoriam: Douglas Mossman, MD
In my role as Department Editor, I find myself already reflecting on the experience, wisdom, compassion, encouragement, and legacy of Dr. Mossman. A distinguished psychiatrist, gifted musician, and inspiring mentor and academician, Dr. Mossman embodied knowledge, creativity, and devotion.
Among Dr. Mossman’s many accolades, including more than 180 authored publications, he was recipient of the Guttmacher Award (2008, the APA) and Golden Apple (2017, the American Academy of Psychiatry and Law). Dr. Mossman was further known to many as a mentor and friend. He was generous with his experiences as a highly accomplished physician and thoughtful in his teachings and publications, leaving an enduring legacy.
Remembering Dr. Mossman’s sage voice and articulate writings will be essential to moving forward in this modern age of psychiatry, as we experience new dilemmas and opportunities.
“It is beyond a doubt that all our knowledge begins with experience.”
- Immanuel Kant
Medicine, a highly experiential profession, is constantly evolving. The consistency of change and the psychiatrist’s inherent wonder offers a paradoxical sense of comfort and conundrum.
As students, we look to our predecessors, associations, and peers to master concepts both concrete and abstract. And once we achieve competence at understanding mechanisms, applying biopsychosocial formulations, and effectively teaching what we’ve learned—everything changes!
We journey through a new era of medicine together. With burgeoning technology, intense politics, and confounding social media, we are undergoing new applications, hurdles to health care, and personal exposure to extremes that have never been experienced before. The landscape of psychiatric practice is changing. Its transformation inherently challenges our existing practices and standards.
It wasn’t too long ago that classroom fodder included how to deal with seeing your patient at a cocktail party. Contemporary discussions are more likely to address the patient who follows you on Twitter (and whom you follow back). Long ago are the days of educating students through a didactic model. Learning now occurs in collaborative group settings with a focus on the practical and hands-on experience. Budding psychiatrists are interested these days in talking about setting up their own apps, establishing a start-up company for health care, working on policy reform, and innovating new approaches to achieve social justice.
A history of challenge and change
Developing variables and expectations in this Millennial Age makes it an exciting time for psychiatrists to explore, adapt, and lead into the future. Fortunately, the field has had ample practice with challenge and changes. Social constructs of how individuals with mental illness were treated altered with William Battie, an English physician whose 1758 Treatise on Madness called for treatments to be utilized on rich and poor mental patients alike in asylums.1 Remember the days of chaining patients to bedposts on psychiatric wards? Of course not! Such archaic practices thankfully disappeared, due in large part to French physician Philippe Pinel. Patient care has evolved to encompass empathy, rights, and dignity.2
German physician Johann Christian Reil, who coined the term “psychiatry” more than 200 years ago, asserted that mental illness should be treated by the most highly qualified physicians.3 Such thinking seems obvious in 2018, but before Reil, the mental and physical states were seen as unrelated.
Modern psychiatry has certainly come a long way.4 We recognize mental health as being essential to overall health. Medications have evolved beyond lithium, chlorpromazine, and fluoxetine. We now have quarterly injectable antipsychotics and pills that patients can swallow and actually be monitored by their clinicians!4
The American Psychiatric Association (APA) has published multiple iterations of the Diagnostic and Statistical Manual of Mental Disorders since its inception in 1968.5 And with those revisions have come changes that most contemporary colleagues could only describe as self-evident—such as the declassification of homosexuality as a mental disorder in 1973.
Despite these advances and the advent of the Mental Health Parity Act of 2008, experience has shown us that some things have seen little progress. Reil, who saw a nexus between mental and physical health, launched an anti-stigma campaign more than 200 years ago. This begs a question to colleagues: How far have we come? Or better yet, capitalizing on our knowledge, experience, and hopes: What else can we do?
The essential interaction between mental, chemical, and physical domains has given rise to psychiatry and its many subspecialties. Among them is forensic psychiatry, which deals with the overlap of mental health and legal matters.6
While often recognized for its relation to criminology, forensic psychiatry encompasses the entirety of legal mental health matters.7 These are things that the daily practitioner faces on a routine basis.
My mentor, Dr. Douglas Mossman, author of
A new department for a new era
The world is changing very rapidly, and we face new dilemmas in the midst of trying to uphold our duties to patients and the profession. There are emerging domains that psychiatrists will experience for the first time—leaving us with more questions than direction. And that is the impetus for this new department, Psychiatry 2.0.
The ever-evolving Internet opens doors for psychiatrists to access and educate a larger audience. It also provides a tool for psychiatrists to keep a web-based presence, something essential for competitive business practices to stay relevant. We are languishing in a political climate that challenges our sense of duty to the public, which often is in contrast with the ethical principles of our association. Technology also poses problems, whether it’s tracking our patients through the pills they ingest, following them on an app, or relying on data from wearable devices in lieu of a patient’s report. All of this suggests a potential for progress as well as problems.
The goal of Psychiatry 2.0 is to experience new challenges together. As Department Editor, I will cover an array of cutting-edge and controversial topics. Continuing with Dr. Mossman’s teachings—that forensic understanding enhances the clinical practice—this department will routinely combine evidence-based information with legal concepts.
Each article in Psychiatry 2.0 will be divided into 3 parts, focusing on a clinician’s dilemma, a duty, and a discussion. The dilemma will be relatable to the clinician in everyday practice. A practical and evidence-based approach will be taken to expound upon our duty as physicians. And finally, there will be discussion about where the field is going, and how it will likely change. In its quarterly publication, Psychiatry 2.0 will explore a diverse range of topics, including technology, social media, stigma, social justice, and politics.
In memoriam: Douglas Mossman, MD
In my role as Department Editor, I find myself already reflecting on the experience, wisdom, compassion, encouragement, and legacy of Dr. Mossman. A distinguished psychiatrist, gifted musician, and inspiring mentor and academician, Dr. Mossman embodied knowledge, creativity, and devotion.
Among Dr. Mossman’s many accolades, including more than 180 authored publications, he was recipient of the Guttmacher Award (2008, the APA) and Golden Apple (2017, the American Academy of Psychiatry and Law). Dr. Mossman was further known to many as a mentor and friend. He was generous with his experiences as a highly accomplished physician and thoughtful in his teachings and publications, leaving an enduring legacy.
Remembering Dr. Mossman’s sage voice and articulate writings will be essential to moving forward in this modern age of psychiatry, as we experience new dilemmas and opportunities.
1. Morris A. William Battie’s Treatise on Madness (1758) and John Monro’s remarks on Dr Battie’s Treatise (1758). Br J Psychiatry. 2008;192(4):257.
2. Scull A. Moral treatment reconsidered. Social order/mental disorder: Anglo-American psychiatry in historical perspective. Berkeley, CA: University of California Press; 1986;81-95.
3. Marneros A. Psychiatry’s 200th birthday. Br J Psychiatry. 2008;193(1):1-3.
4. Cade JF. Lithium salts in the treatment of psychotic excitement. Med J Aust. 1949;2(10):349-352.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
6. Gold LH. Rediscovering forensic psychiatry. The American Psychiatric Publishing Textbook of Forensic Psychiatry. Simon RI, Gold LH, eds. Washington, DC: American Psychiatric Publishing; 2004;3-36.
7. Gutheil TG. The history of forensic psychiatry. J Am Acad Psychiatry Law. 2005;33(2):259-262.
1. Morris A. William Battie’s Treatise on Madness (1758) and John Monro’s remarks on Dr Battie’s Treatise (1758). Br J Psychiatry. 2008;192(4):257.
2. Scull A. Moral treatment reconsidered. Social order/mental disorder: Anglo-American psychiatry in historical perspective. Berkeley, CA: University of California Press; 1986;81-95.
3. Marneros A. Psychiatry’s 200th birthday. Br J Psychiatry. 2008;193(1):1-3.
4. Cade JF. Lithium salts in the treatment of psychotic excitement. Med J Aust. 1949;2(10):349-352.
5. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
6. Gold LH. Rediscovering forensic psychiatry. The American Psychiatric Publishing Textbook of Forensic Psychiatry. Simon RI, Gold LH, eds. Washington, DC: American Psychiatric Publishing; 2004;3-36.
7. Gutheil TG. The history of forensic psychiatry. J Am Acad Psychiatry Law. 2005;33(2):259-262.
Strategies for managing medication-induced hyperprolactinemia
Ms. E, age 23, presents to your office for a routine visit for management of bipolar I disorder and posttraumatic stress disorder with comorbid type 2 diabetes mellitus. She currently is taking
Ms. E has a history of self-discontinuing medication when adverse events occur. She has been hospitalized twice for psychosis and suicide attempts. Past psychotropic medications that have been discontinued due to adverse effects include ziprasidone (mild abnormal lip movement), olanzapine (ineffective and drowsy), valproic acid (tremor and abdominal discomfort), lithium (rash), and aripiprazole (increased fasting blood sugar and labile mood).
At her appointment today, Ms. E says she is concerned because she has been experiencing galactorrhea for the past 4 weeks. Her prolactin level is 14.4 ng/mL; a normal level for a woman who is not pregnant is <25 ng/mL. However, a repeat prolactin level is obtained, and is found to be elevated at 38 ng/mL.
Prolactin, a polypeptide hormone that is secreted from the pituitary gland, has many functions, including involvement in the synthesis and maintenance of breast milk production, in reproductive behavior, and in luteal function.1,2 Hyperprolactinemia—an elevated prolactin level—is a common endocrinologic disorder of the hypothalamic–pituitary–axis.3 Children, adolescents, premenopausal women, and women in the perinatal period are more vulnerable to medication-induced hyperprolactinemia.4 If not asymptomatic, patients with hyperprolactinemia may experience amenorrhea, galactorrhea, hypogonadism, sexual dysfunction, or infertility.1,4 Chronic hyperprolactinemia may increase the risk for long-term complications, such as decreased bone mineral density and osteoporosis, although available evidence has conflicting findings.1
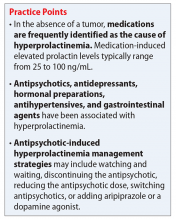
Hyperprolactinemia is diagnosed by a prolactin concentration above the upper reference range.3 Various hormones and neurotransmitters can impact inhibition or stimulation of prolactin release.5 For example, dopamine tonically inhibits prolactin release and synthesis, whereas estrogen stimulates prolactin secretion.1,5 Prolactin also can be elevated under several physiologic and pathologic conditions, such as during stressful situations, meals, or sexual activity.1,5 A prolactin level >250 ng/mL is usually indicative of a prolactinoma; however, some medications, such as strong D2 receptor antagonists (eg, risperidone, haloperidol), can cause significant elevation without evidence of prolactinoma.3 In the absence of a tumor, medications are often identified as the cause of hyperprolactinemia.3 According to the Endocrinology Society clinical practice guideline, medication-induced elevated prolactin levels are typically between 25 to 100 ng/mL.3
Medication-induced hyperprolactinemia
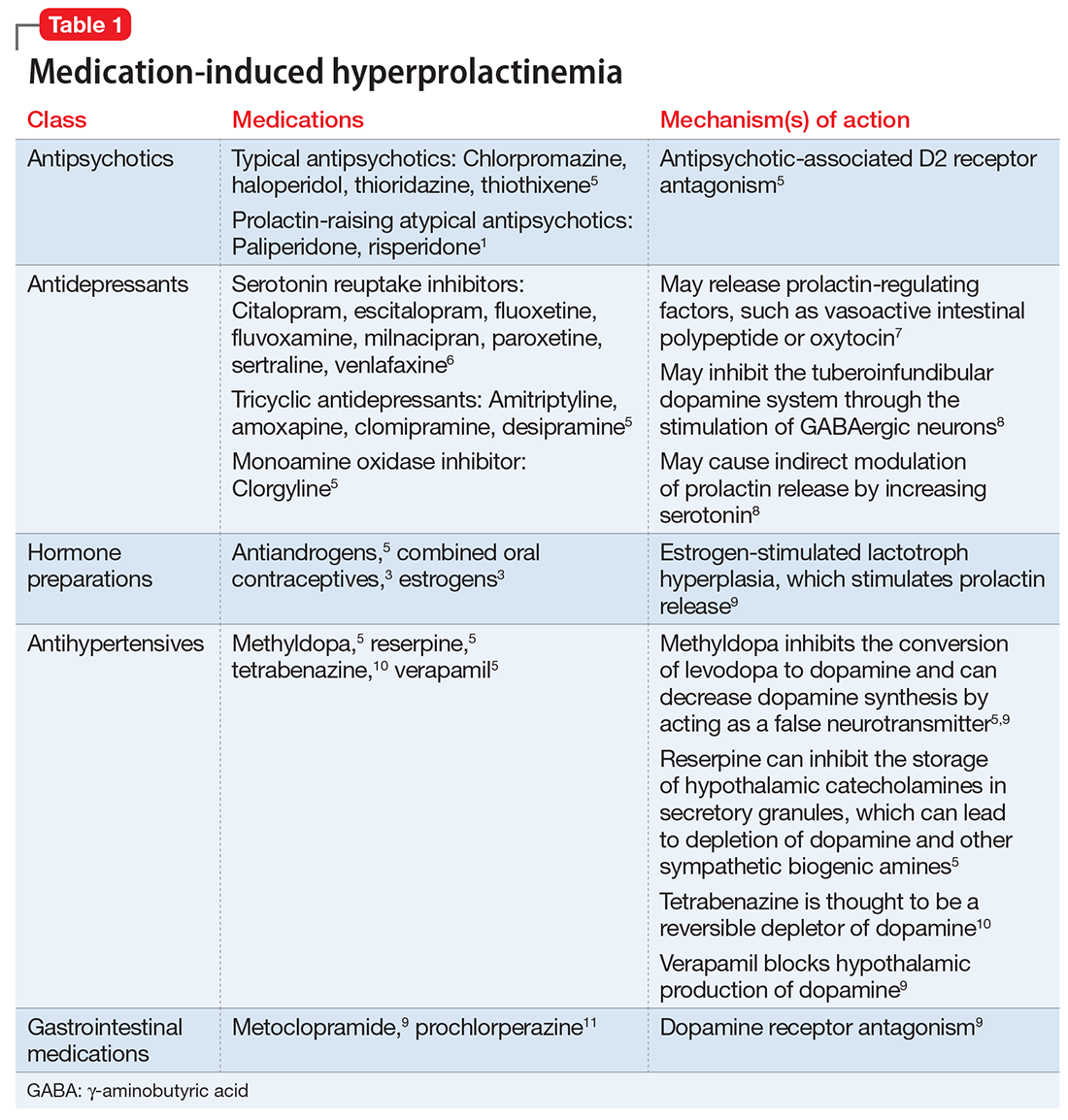
Antipsychotics, antidepressants, hormonal preparations, antihypertensives, and gastrointestinal agents have been associated with hyperprolactinemia (Table 11,3,5-11). These medication classes increase prolactin by decreasing dopamine, which facilitates disinhibition of prolactin synthesis and release, or increasing prolactin stimulating hormones, such as serotonin or estrogen.5
Antipsychotics are the most common medication-related cause of hyperprolactinemia.3 Typical antipsychotics are more likely to cause hyperprolactinemia than atypical antipsychotics; the incidence among patients taking typical antipsychotics is 40% to 90%.3 Atypical antipsychotics, except risperidone and paliperidone, are considered to cause less endocrinologic effects than typical antipsychotics through various mechanisms: serotonergic receptor antagonism, fast dissociation from D2 receptors, D2 receptor partial agonism, and preferential binding of D3 vs D2 receptors.1,5 By having transient D2 receptor association, clozapine and quetiapine are considered to have less risk of hyperprolactinemia compared with other atypical antipsychotics.1,5 Aripiprazole, brexpiprazole, and cariprazine are partial D2 receptor agonists, and cariprazine is the only agent that exhibits preferential binding to D3 receptors.12,13 Based on limited data, brexpiprazole and cariprazine may have prolactin-sparing properties given their partial D2 receptor agonism.12,13 However, one study found increased prolactin levels in some patients after treatment with brexpiprazole, 4 mg/d.14 Similarly, another study found that cariprazine could increase prolactin levels as much as 4.1 ng/mL, depending on the dose.15 Except for aripiprazole, brexpiprazole, cariprazine, and clozapine, all other atypical antipsychotics marketed in the United States have a standard warning in the package insert regarding prolactin elevations.1,16,17
Because antidepressants are less well-studied as a cause of medication-induced hyperprolactinemia, drawing definitive conclusions regarding incidence rates is limited, but the incidence seems to be fairly low.6,18 A French pharmacovigilance study found that of 182,836 spontaneous adverse drug events reported between 1985 and 2009, there were 159 reports of selective serotonin reuptake inhibitors (SSRIs) inducing hyperprolactinemia.6 F
Mirtazapine and bupropion have been found to be prolactin-neutral.5 Bupropion also has been reported to decrease prolactin levels, potentially via its ability to block dopamine reuptake.19
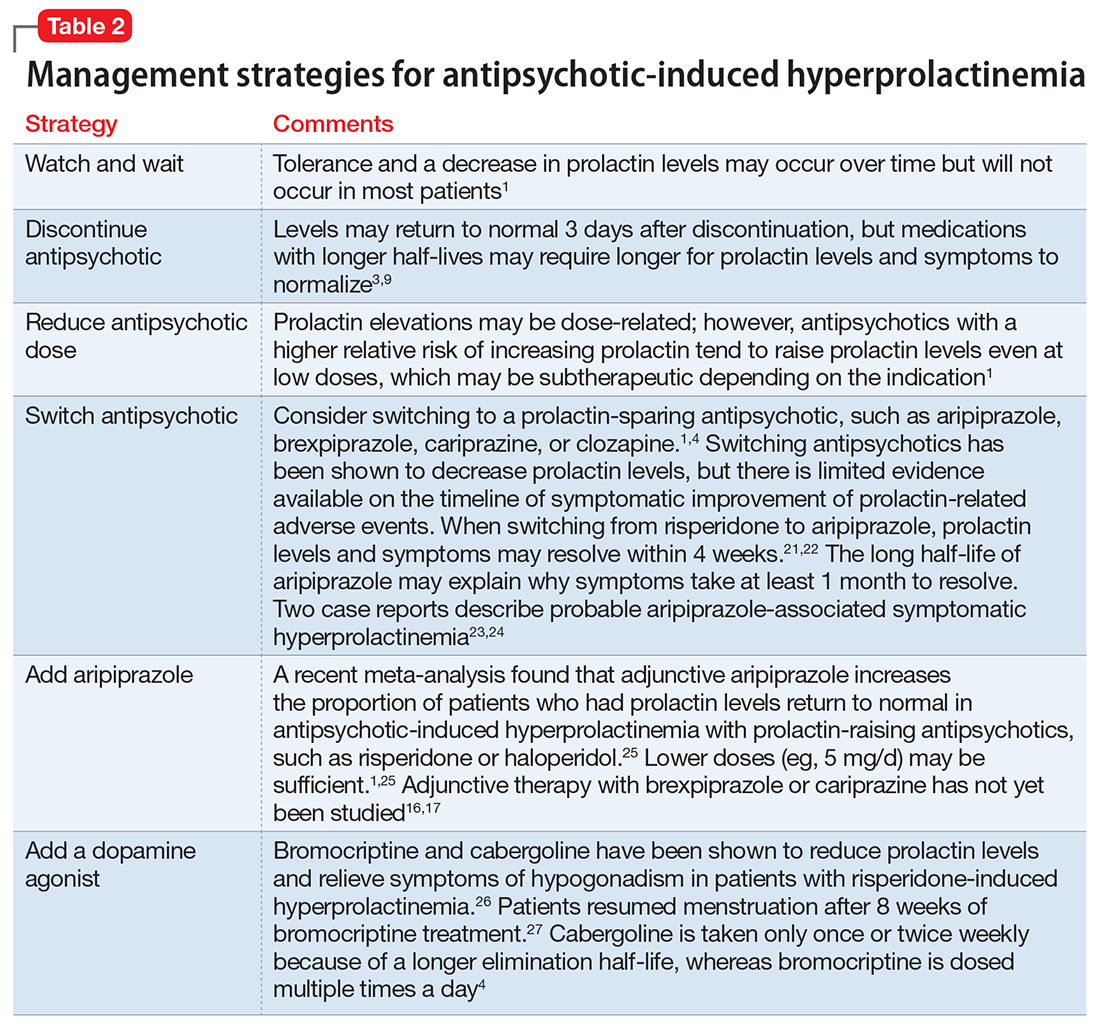
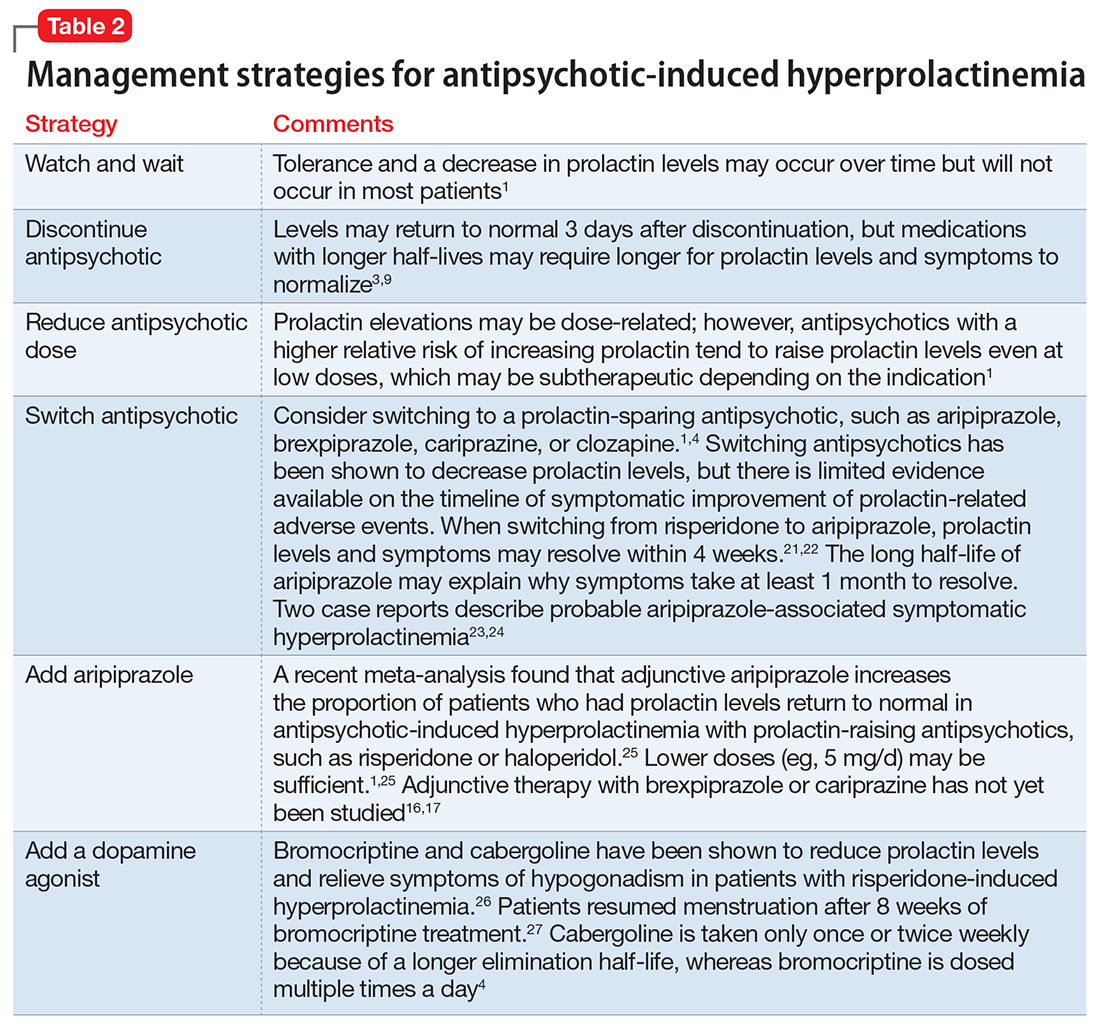
Managing medication-induced hyperprolactinemia
Screening for and identifying clinically significant hyperprolactinemia is critical, because adverse effects of medications can lead to nonadherence and clinical decompensation.20 Patients must be informed of potential symptoms of hyperprolactinemia, and clinicians should inquire about such symptoms at each visit. Routine monitoring of prolactin levels in asymptomatic patients is not necessary, because the Endocrine Society Clinical Practice Guideline does not recommend treating patients with asymptomatic medication-induced hyperprolactinemia.3
In patients who report hyperprolactinemia symptoms, clinicians should review the patient’s prescribed medications and past medical history (eg, chronic renal failure, hypothyroidism) for potential causes or exacerbations, and address these factors accordingly.3 Order a measurement of prolactin level. A patient with a prolactin level >100 ng/mL should be referred to Endocrinology to rule out prolactinoma.1
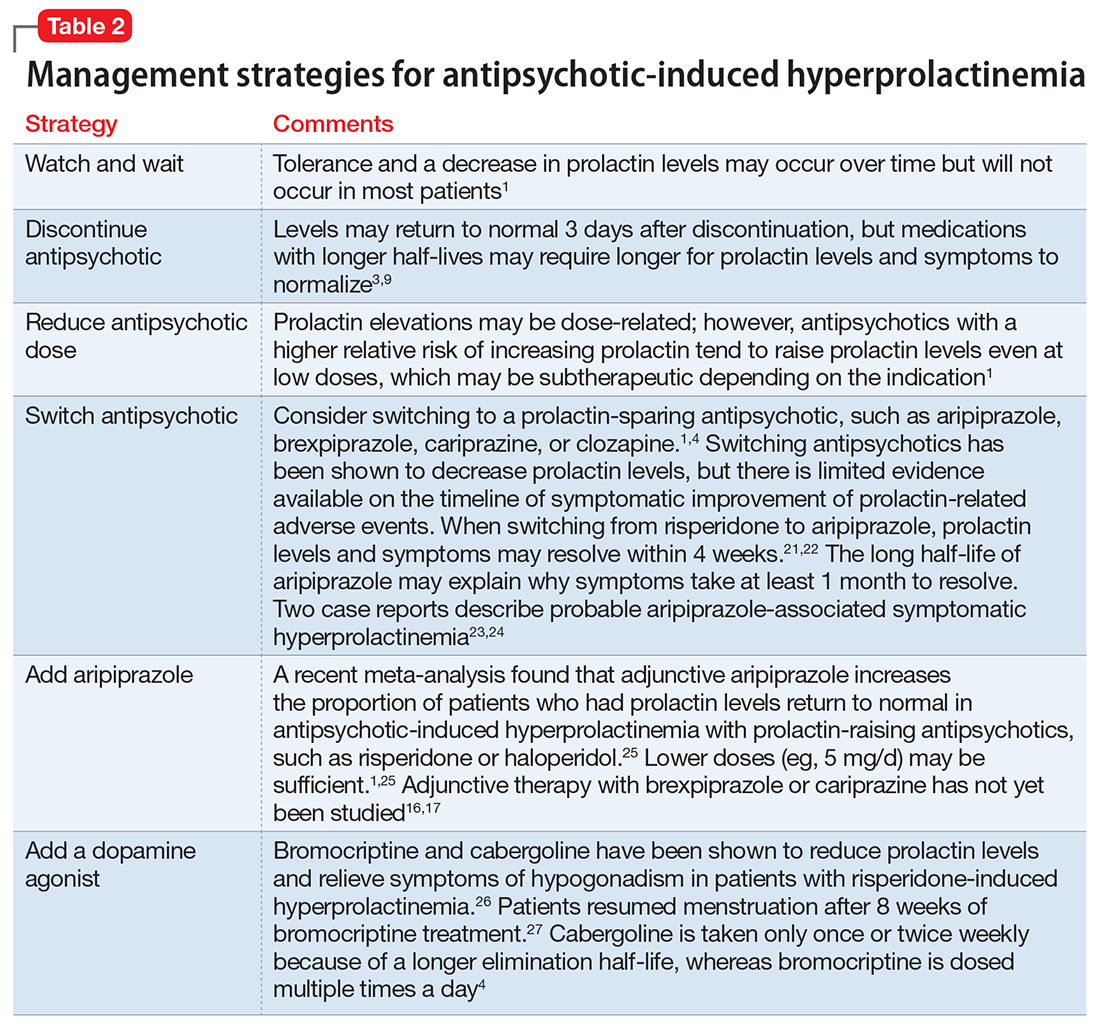
If a patient’s prolactin level is between 25 and 100 ng/mL, review the patient’s medications (Table 11,3,5-11), because prolactin levels within this range usually signal a medication-induced cause.3 For patients with antipsychotic-induced hyperprolactinemia, there are several management strategies (Table 21,3,4,9,16,17,21-27):
- Watch and wait may be warranted when the patient is experiencing mild hyperprolactinemia symptoms.
- Discontinue. If the patient can be maintained without an antipsychotic, discontinuing the antipsychotic would be a first-line option.3
- Reduce the dose. Reducing the antipsychotic dose may be the preferred strategy for patients with moderate to severe hyperprolactinemia symptoms who responded to the antipsychotic and do not wish to start adjunctive therapy.4
- Switching to a prolactin-sparing antipsychotic may help normalize prolactin levels and may be preferred when the risk of relapse is low.3 Dopamine agonists can treat medication-induced hyperprolactinemia, but may worsen psychiatric symptoms.28,29 Therefore, this may be the preferred strategy if the offending medication cannot be discontinued or switched, or if the patient has a comorbid prolactinoma.
Less data exist on managing hyperprolactinemia that is induced by a medication other than an antipsychotic; however, it seems reasonable that the same strategies could be implemented. Specifically, for SSRI–induced hyperprolactinemia, if clinically appropriate, switching to or adding an alternative antidepressant that may be prolactin-sparing, such as mirtazapine or bupropion, could be attempted.8 One study found that fluoxetine-induced galactorrhea ceased within 10 days of discontinuing the medication.30
CASE CONTINUED
Because Ms. E has been on the same medication regimen for 3 years and recently developed galactorrhea, it seems unlikely that her hyperprolactinemia is medication-induced. However, a tumor-related cause is less likely because the prolactin level is <100 ng/mL. Based on the literature, the only possible medication-induced cause of her galactorrhea is risperidone. Ms. E agrees to a trial of adjunctive oral aripiprazole, 5 mg/d, with close monitoring of her type 2 diabetes mellitus. Because of the long elimination half-life of aripiprazole, 1 month is required to monitor for improvement in galactorrhea. Ms. E is advised to use breast pads as a nonpharmacologic strategy in the interim. After 1 month of treatment, Ms. E denies galactorrhea symptoms and no longer requires the use of breast pads.
1. Peuskens J, Pani L, Detraux J, et al. The effects of novel and newly approved antipsychotics on serum prolactin levels: a comprehensive review. CNS Drugs.2014;28(5):421-453.
2. Freeman ME, Kanyicska B, Lerant A, et al. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80(4):1523-1631.
3. Melmed S, Casanueva FF, Hoffman AR, et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society Clinical practice guideline. J Clin Endocrinol Metab. 2011;96(2):273-288.
4. Bostwick JR, Guthrie SK, Ellingrod VL. Antipsychotic-induced hyperprolactinemia. Pharmacotherapy. 2009;29(1):64-73.
5. La Torre D, Falorni A. Pharmacological causes of hyperprolactinemia. Ther Clin Risk Manag. 2007;3(5):929-951.
6. Petit A, Piednoir D, Germain ML, et al. Drug-induced hyperprolactinemia: a case-non-case study from the national pharmacovigilance database [in French]. Therapie. 2003;58(2):159-163.
7. Emiliano AB, Fudge JL. From galactorrhea to osteopenia: rethinking serotonin-prolactin interactions. Neuropsychopharmacology. 2004;29(5):833-846.
8. Coker F, Taylor D. Antidepressant-induced hyperprolactinaemia: incidence, mechanisms and management. CNS Drugs. 2010;24(7):563-574.
9. Molitch ME. Medication induced hyperprolactinemia. Mayo Clin Proc. 2005;80(8):1050-1057.
10. Xenazine (tetrabenazine) [package insert]. Washington, DC: Prestwick Pharmaceuticals, Inc.; 2008.
11. Peña KS, Rosenfeld JA. Evaluation and treatment of galactorrhea. Am Fam Physician 2001;63(9):1763-1770.
12. Durgam S, Starace A, Li D, et al. The efficacy and tolerability of cariprazine in acute mania associated with bipolar I disorder: a phase II trial. Bipolar Disord. 2015;17(1):63-75.
13. Das S, Barnwal P, Winston AB, et al. Brexpiprazole: so far so good. Ther Adv Psychopharmacol. 2016;6(1):39-54.
14. Correll CU, Skuban A, Ouyang J, et al. Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2015;172(9):870-880.
15. Durgam S, Earley W, Guo H, et al. Efficacy and safety of adjunctive cariprazine in inadequate responders to antidepressants: a randomized, double-blind, placebo-controlled study in adult patients with major depressive disorder. J Clin Pscyhiatry. 2016;77(3):371-378.
16. Rexulti (brexpiprazole) [package insert]. Tokyo, Japan: Otsuka Pharmaceuticals Inc.; 2015.
17. Cariprazine (Vraylar) [package insert]. Parsippany, New Jersey: Actavis Pharmacueitcals Inc.; 2015.
18. Marken PA, Haykal RF, Fisher JN. Management of psychotropic-induced hyperprolactinemia. Clin Pharm. 1992;11(10):851-856.
19. Meltzer HY, Fang VS, Tricou BJ, et al. Effect of antidepressants on neuroendocrine axis in humans. Adv Biochem Psychopharmacol. 1982;32:303-316.
20. Tsuboi T, Bies RR, Suzuki T, et al. Hyperprolactinemia and estimated dopamine D2 receptor occupancy in patients with schizophrenia: analysis of the CATIE data. Prog Neuropsychopharmacol Biol Psychiatry. 2013;45:178-182.
21. Lee BH, Kim YK, Park SH. Using aripiprazole to resolve antipsychotic-induced symptomatic hyperprolactinemia: a pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(4):714-717.
22. Lu ML, Shen WW, Chen CH. Time course of the changes in antipsychotic-induced hyperprolactinemia following the switch to aripiprazole. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(8):1978-1981.
23. Mendhekar DN, Andrade C. Galactorrhea with aripiprazole. Can J Psychiatry. 2005;50(4):243.
24. Joseph SP. Aripiprazole induced hyperprolactinemia in a young female with delusional disorder. Indian J Psychol Med. 2016;38(3):260-262.
25. Meng M, Li W, Zhang S, et al. Using aripiprazole to reduce antipsychotic-induced hyperprolactinemia: meta-analysis of currently available randomized controlled trials. Shaghai Arch Psychiatry. 2015;27(1):4-17.
26. Tollin SR. Use of the dopamine agonists bromocriptine and cabergoline in the management of risperidone induced hyperprolactinemia in patients with psychotic disorders. J Endocrinol Invest. 2000;23(11):765-70.
27. Yuan HN, Wang CY, Sze CW, et al. A randomized, crossover comparison of herbal medicine and bromocriptine against risperidone-induced hyperprolactinemia in patients with schizophrenia. J Clin Psychopharmacol. 2008;28(3):264-370.
28. Chang SC, Chen CH, Lu ML. Cabergoline-induced psychotic exacerbation in schizophrenic patients. General Hospital Psychiatry. 2008;30(4):378-380.
29. Ishitobi M, Kosaka H, Shukunami K, et al. Adjunctive treatment with low-dosage pramipexole for risperidone-associated hyperprolactinemia and sexual dysfunction in a male patient with schizophrenia. J Clin Psychopharmacol 2011;31(2):243-245.
30. Peterson MC. Reversible galactorrhea and prolactin elevation related to fluoxetine use. Mayo Clin Proc. 2001;76(2):215-216.
Ms. E, age 23, presents to your office for a routine visit for management of bipolar I disorder and posttraumatic stress disorder with comorbid type 2 diabetes mellitus. She currently is taking
Ms. E has a history of self-discontinuing medication when adverse events occur. She has been hospitalized twice for psychosis and suicide attempts. Past psychotropic medications that have been discontinued due to adverse effects include ziprasidone (mild abnormal lip movement), olanzapine (ineffective and drowsy), valproic acid (tremor and abdominal discomfort), lithium (rash), and aripiprazole (increased fasting blood sugar and labile mood).
At her appointment today, Ms. E says she is concerned because she has been experiencing galactorrhea for the past 4 weeks. Her prolactin level is 14.4 ng/mL; a normal level for a woman who is not pregnant is <25 ng/mL. However, a repeat prolactin level is obtained, and is found to be elevated at 38 ng/mL.
Prolactin, a polypeptide hormone that is secreted from the pituitary gland, has many functions, including involvement in the synthesis and maintenance of breast milk production, in reproductive behavior, and in luteal function.1,2 Hyperprolactinemia—an elevated prolactin level—is a common endocrinologic disorder of the hypothalamic–pituitary–axis.3 Children, adolescents, premenopausal women, and women in the perinatal period are more vulnerable to medication-induced hyperprolactinemia.4 If not asymptomatic, patients with hyperprolactinemia may experience amenorrhea, galactorrhea, hypogonadism, sexual dysfunction, or infertility.1,4 Chronic hyperprolactinemia may increase the risk for long-term complications, such as decreased bone mineral density and osteoporosis, although available evidence has conflicting findings.1
Hyperprolactinemia is diagnosed by a prolactin concentration above the upper reference range.3 Various hormones and neurotransmitters can impact inhibition or stimulation of prolactin release.5 For example, dopamine tonically inhibits prolactin release and synthesis, whereas estrogen stimulates prolactin secretion.1,5 Prolactin also can be elevated under several physiologic and pathologic conditions, such as during stressful situations, meals, or sexual activity.1,5 A prolactin level >250 ng/mL is usually indicative of a prolactinoma; however, some medications, such as strong D2 receptor antagonists (eg, risperidone, haloperidol), can cause significant elevation without evidence of prolactinoma.3 In the absence of a tumor, medications are often identified as the cause of hyperprolactinemia.3 According to the Endocrinology Society clinical practice guideline, medication-induced elevated prolactin levels are typically between 25 to 100 ng/mL.3
Medication-induced hyperprolactinemia
Antipsychotics, antidepressants, hormonal preparations, antihypertensives, and gastrointestinal agents have been associated with hyperprolactinemia (Table 11,3,5-11). These medication classes increase prolactin by decreasing dopamine, which facilitates disinhibition of prolactin synthesis and release, or increasing prolactin stimulating hormones, such as serotonin or estrogen.5
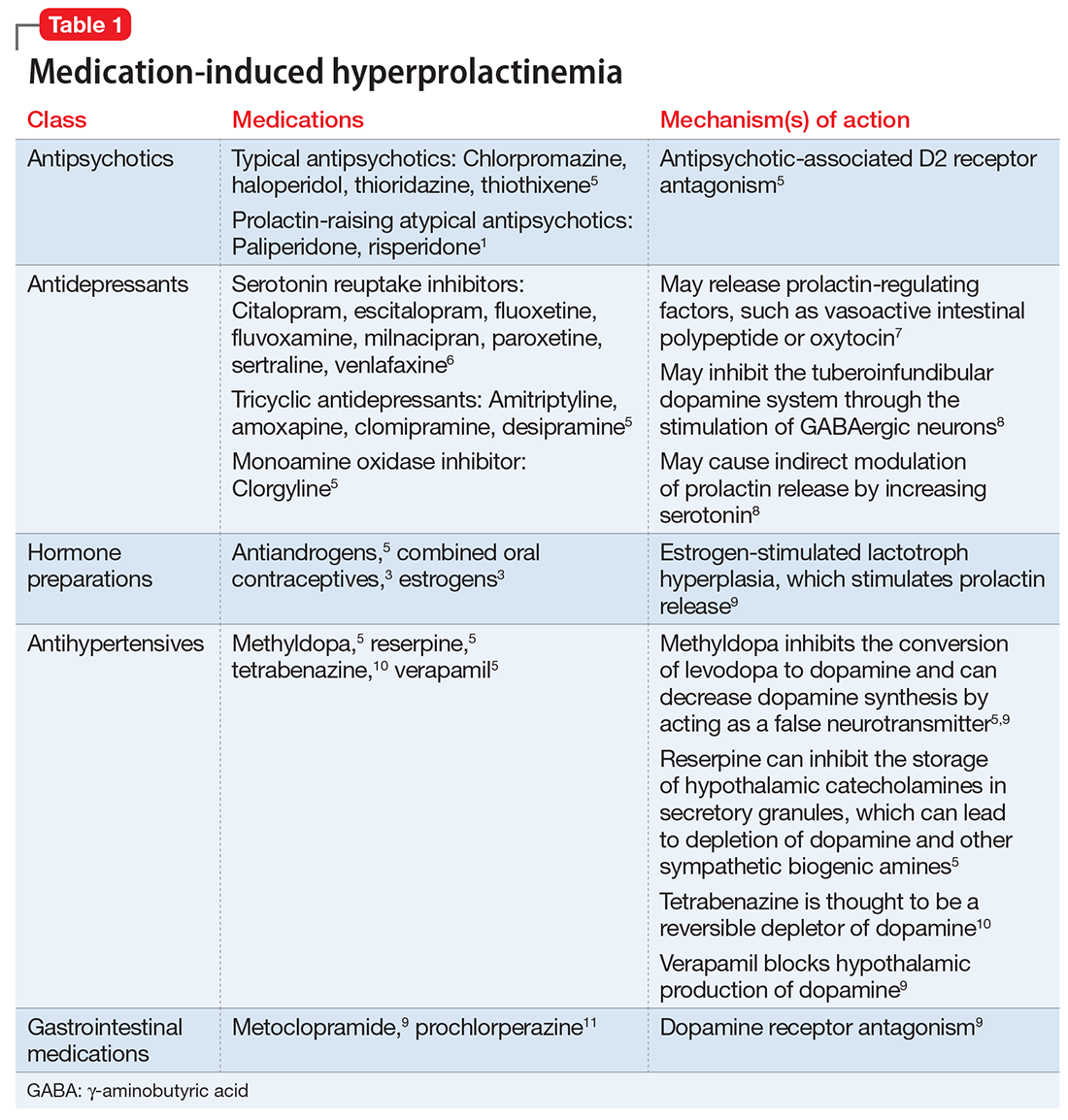
Antipsychotics are the most common medication-related cause of hyperprolactinemia.3 Typical antipsychotics are more likely to cause hyperprolactinemia than atypical antipsychotics; the incidence among patients taking typical antipsychotics is 40% to 90%.3 Atypical antipsychotics, except risperidone and paliperidone, are considered to cause less endocrinologic effects than typical antipsychotics through various mechanisms: serotonergic receptor antagonism, fast dissociation from D2 receptors, D2 receptor partial agonism, and preferential binding of D3 vs D2 receptors.1,5 By having transient D2 receptor association, clozapine and quetiapine are considered to have less risk of hyperprolactinemia compared with other atypical antipsychotics.1,5 Aripiprazole, brexpiprazole, and cariprazine are partial D2 receptor agonists, and cariprazine is the only agent that exhibits preferential binding to D3 receptors.12,13 Based on limited data, brexpiprazole and cariprazine may have prolactin-sparing properties given their partial D2 receptor agonism.12,13 However, one study found increased prolactin levels in some patients after treatment with brexpiprazole, 4 mg/d.14 Similarly, another study found that cariprazine could increase prolactin levels as much as 4.1 ng/mL, depending on the dose.15 Except for aripiprazole, brexpiprazole, cariprazine, and clozapine, all other atypical antipsychotics marketed in the United States have a standard warning in the package insert regarding prolactin elevations.1,16,17
Because antidepressants are less well-studied as a cause of medication-induced hyperprolactinemia, drawing definitive conclusions regarding incidence rates is limited, but the incidence seems to be fairly low.6,18 A French pharmacovigilance study found that of 182,836 spontaneous adverse drug events reported between 1985 and 2009, there were 159 reports of selective serotonin reuptake inhibitors (SSRIs) inducing hyperprolactinemia.6 F
Mirtazapine and bupropion have been found to be prolactin-neutral.5 Bupropion also has been reported to decrease prolactin levels, potentially via its ability to block dopamine reuptake.19
Managing medication-induced hyperprolactinemia
Screening for and identifying clinically significant hyperprolactinemia is critical, because adverse effects of medications can lead to nonadherence and clinical decompensation.20 Patients must be informed of potential symptoms of hyperprolactinemia, and clinicians should inquire about such symptoms at each visit. Routine monitoring of prolactin levels in asymptomatic patients is not necessary, because the Endocrine Society Clinical Practice Guideline does not recommend treating patients with asymptomatic medication-induced hyperprolactinemia.3
In patients who report hyperprolactinemia symptoms, clinicians should review the patient’s prescribed medications and past medical history (eg, chronic renal failure, hypothyroidism) for potential causes or exacerbations, and address these factors accordingly.3 Order a measurement of prolactin level. A patient with a prolactin level >100 ng/mL should be referred to Endocrinology to rule out prolactinoma.1
If a patient’s prolactin level is between 25 and 100 ng/mL, review the patient’s medications (Table 11,3,5-11), because prolactin levels within this range usually signal a medication-induced cause.3 For patients with antipsychotic-induced hyperprolactinemia, there are several management strategies (Table 21,3,4,9,16,17,21-27):
- Watch and wait may be warranted when the patient is experiencing mild hyperprolactinemia symptoms.
- Discontinue. If the patient can be maintained without an antipsychotic, discontinuing the antipsychotic would be a first-line option.3
- Reduce the dose. Reducing the antipsychotic dose may be the preferred strategy for patients with moderate to severe hyperprolactinemia symptoms who responded to the antipsychotic and do not wish to start adjunctive therapy.4
- Switching to a prolactin-sparing antipsychotic may help normalize prolactin levels and may be preferred when the risk of relapse is low.3 Dopamine agonists can treat medication-induced hyperprolactinemia, but may worsen psychiatric symptoms.28,29 Therefore, this may be the preferred strategy if the offending medication cannot be discontinued or switched, or if the patient has a comorbid prolactinoma.
Less data exist on managing hyperprolactinemia that is induced by a medication other than an antipsychotic; however, it seems reasonable that the same strategies could be implemented. Specifically, for SSRI–induced hyperprolactinemia, if clinically appropriate, switching to or adding an alternative antidepressant that may be prolactin-sparing, such as mirtazapine or bupropion, could be attempted.8 One study found that fluoxetine-induced galactorrhea ceased within 10 days of discontinuing the medication.30
CASE CONTINUED
Because Ms. E has been on the same medication regimen for 3 years and recently developed galactorrhea, it seems unlikely that her hyperprolactinemia is medication-induced. However, a tumor-related cause is less likely because the prolactin level is <100 ng/mL. Based on the literature, the only possible medication-induced cause of her galactorrhea is risperidone. Ms. E agrees to a trial of adjunctive oral aripiprazole, 5 mg/d, with close monitoring of her type 2 diabetes mellitus. Because of the long elimination half-life of aripiprazole, 1 month is required to monitor for improvement in galactorrhea. Ms. E is advised to use breast pads as a nonpharmacologic strategy in the interim. After 1 month of treatment, Ms. E denies galactorrhea symptoms and no longer requires the use of breast pads.
Ms. E, age 23, presents to your office for a routine visit for management of bipolar I disorder and posttraumatic stress disorder with comorbid type 2 diabetes mellitus. She currently is taking
Ms. E has a history of self-discontinuing medication when adverse events occur. She has been hospitalized twice for psychosis and suicide attempts. Past psychotropic medications that have been discontinued due to adverse effects include ziprasidone (mild abnormal lip movement), olanzapine (ineffective and drowsy), valproic acid (tremor and abdominal discomfort), lithium (rash), and aripiprazole (increased fasting blood sugar and labile mood).
At her appointment today, Ms. E says she is concerned because she has been experiencing galactorrhea for the past 4 weeks. Her prolactin level is 14.4 ng/mL; a normal level for a woman who is not pregnant is <25 ng/mL. However, a repeat prolactin level is obtained, and is found to be elevated at 38 ng/mL.
Prolactin, a polypeptide hormone that is secreted from the pituitary gland, has many functions, including involvement in the synthesis and maintenance of breast milk production, in reproductive behavior, and in luteal function.1,2 Hyperprolactinemia—an elevated prolactin level—is a common endocrinologic disorder of the hypothalamic–pituitary–axis.3 Children, adolescents, premenopausal women, and women in the perinatal period are more vulnerable to medication-induced hyperprolactinemia.4 If not asymptomatic, patients with hyperprolactinemia may experience amenorrhea, galactorrhea, hypogonadism, sexual dysfunction, or infertility.1,4 Chronic hyperprolactinemia may increase the risk for long-term complications, such as decreased bone mineral density and osteoporosis, although available evidence has conflicting findings.1
Hyperprolactinemia is diagnosed by a prolactin concentration above the upper reference range.3 Various hormones and neurotransmitters can impact inhibition or stimulation of prolactin release.5 For example, dopamine tonically inhibits prolactin release and synthesis, whereas estrogen stimulates prolactin secretion.1,5 Prolactin also can be elevated under several physiologic and pathologic conditions, such as during stressful situations, meals, or sexual activity.1,5 A prolactin level >250 ng/mL is usually indicative of a prolactinoma; however, some medications, such as strong D2 receptor antagonists (eg, risperidone, haloperidol), can cause significant elevation without evidence of prolactinoma.3 In the absence of a tumor, medications are often identified as the cause of hyperprolactinemia.3 According to the Endocrinology Society clinical practice guideline, medication-induced elevated prolactin levels are typically between 25 to 100 ng/mL.3
Medication-induced hyperprolactinemia
Antipsychotics, antidepressants, hormonal preparations, antihypertensives, and gastrointestinal agents have been associated with hyperprolactinemia (Table 11,3,5-11). These medication classes increase prolactin by decreasing dopamine, which facilitates disinhibition of prolactin synthesis and release, or increasing prolactin stimulating hormones, such as serotonin or estrogen.5
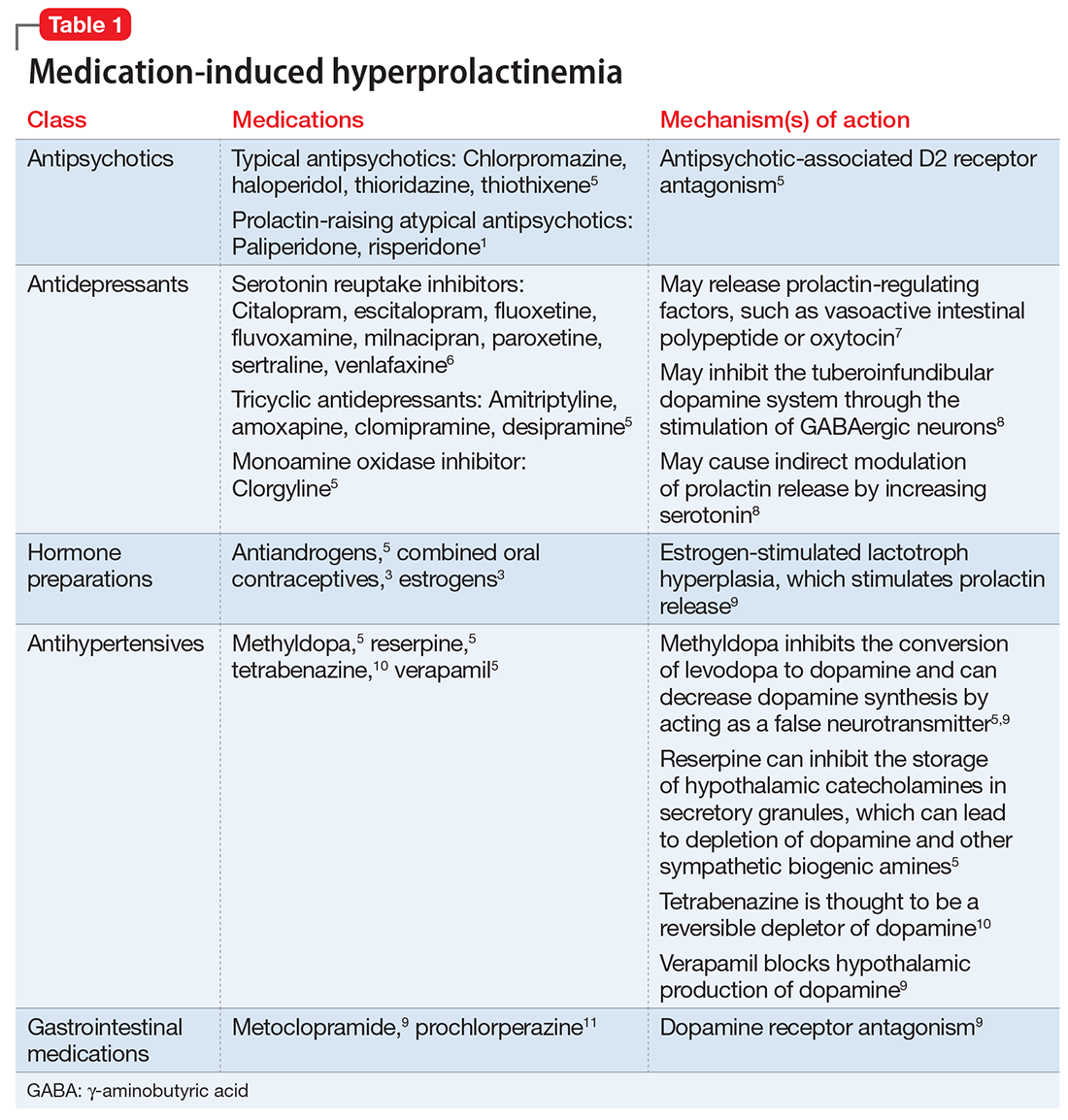
Antipsychotics are the most common medication-related cause of hyperprolactinemia.3 Typical antipsychotics are more likely to cause hyperprolactinemia than atypical antipsychotics; the incidence among patients taking typical antipsychotics is 40% to 90%.3 Atypical antipsychotics, except risperidone and paliperidone, are considered to cause less endocrinologic effects than typical antipsychotics through various mechanisms: serotonergic receptor antagonism, fast dissociation from D2 receptors, D2 receptor partial agonism, and preferential binding of D3 vs D2 receptors.1,5 By having transient D2 receptor association, clozapine and quetiapine are considered to have less risk of hyperprolactinemia compared with other atypical antipsychotics.1,5 Aripiprazole, brexpiprazole, and cariprazine are partial D2 receptor agonists, and cariprazine is the only agent that exhibits preferential binding to D3 receptors.12,13 Based on limited data, brexpiprazole and cariprazine may have prolactin-sparing properties given their partial D2 receptor agonism.12,13 However, one study found increased prolactin levels in some patients after treatment with brexpiprazole, 4 mg/d.14 Similarly, another study found that cariprazine could increase prolactin levels as much as 4.1 ng/mL, depending on the dose.15 Except for aripiprazole, brexpiprazole, cariprazine, and clozapine, all other atypical antipsychotics marketed in the United States have a standard warning in the package insert regarding prolactin elevations.1,16,17
Because antidepressants are less well-studied as a cause of medication-induced hyperprolactinemia, drawing definitive conclusions regarding incidence rates is limited, but the incidence seems to be fairly low.6,18 A French pharmacovigilance study found that of 182,836 spontaneous adverse drug events reported between 1985 and 2009, there were 159 reports of selective serotonin reuptake inhibitors (SSRIs) inducing hyperprolactinemia.6 F
Mirtazapine and bupropion have been found to be prolactin-neutral.5 Bupropion also has been reported to decrease prolactin levels, potentially via its ability to block dopamine reuptake.19
Managing medication-induced hyperprolactinemia
Screening for and identifying clinically significant hyperprolactinemia is critical, because adverse effects of medications can lead to nonadherence and clinical decompensation.20 Patients must be informed of potential symptoms of hyperprolactinemia, and clinicians should inquire about such symptoms at each visit. Routine monitoring of prolactin levels in asymptomatic patients is not necessary, because the Endocrine Society Clinical Practice Guideline does not recommend treating patients with asymptomatic medication-induced hyperprolactinemia.3
In patients who report hyperprolactinemia symptoms, clinicians should review the patient’s prescribed medications and past medical history (eg, chronic renal failure, hypothyroidism) for potential causes or exacerbations, and address these factors accordingly.3 Order a measurement of prolactin level. A patient with a prolactin level >100 ng/mL should be referred to Endocrinology to rule out prolactinoma.1
If a patient’s prolactin level is between 25 and 100 ng/mL, review the patient’s medications (Table 11,3,5-11), because prolactin levels within this range usually signal a medication-induced cause.3 For patients with antipsychotic-induced hyperprolactinemia, there are several management strategies (Table 21,3,4,9,16,17,21-27):
- Watch and wait may be warranted when the patient is experiencing mild hyperprolactinemia symptoms.
- Discontinue. If the patient can be maintained without an antipsychotic, discontinuing the antipsychotic would be a first-line option.3
- Reduce the dose. Reducing the antipsychotic dose may be the preferred strategy for patients with moderate to severe hyperprolactinemia symptoms who responded to the antipsychotic and do not wish to start adjunctive therapy.4
- Switching to a prolactin-sparing antipsychotic may help normalize prolactin levels and may be preferred when the risk of relapse is low.3 Dopamine agonists can treat medication-induced hyperprolactinemia, but may worsen psychiatric symptoms.28,29 Therefore, this may be the preferred strategy if the offending medication cannot be discontinued or switched, or if the patient has a comorbid prolactinoma.
Less data exist on managing hyperprolactinemia that is induced by a medication other than an antipsychotic; however, it seems reasonable that the same strategies could be implemented. Specifically, for SSRI–induced hyperprolactinemia, if clinically appropriate, switching to or adding an alternative antidepressant that may be prolactin-sparing, such as mirtazapine or bupropion, could be attempted.8 One study found that fluoxetine-induced galactorrhea ceased within 10 days of discontinuing the medication.30
CASE CONTINUED
Because Ms. E has been on the same medication regimen for 3 years and recently developed galactorrhea, it seems unlikely that her hyperprolactinemia is medication-induced. However, a tumor-related cause is less likely because the prolactin level is <100 ng/mL. Based on the literature, the only possible medication-induced cause of her galactorrhea is risperidone. Ms. E agrees to a trial of adjunctive oral aripiprazole, 5 mg/d, with close monitoring of her type 2 diabetes mellitus. Because of the long elimination half-life of aripiprazole, 1 month is required to monitor for improvement in galactorrhea. Ms. E is advised to use breast pads as a nonpharmacologic strategy in the interim. After 1 month of treatment, Ms. E denies galactorrhea symptoms and no longer requires the use of breast pads.
1. Peuskens J, Pani L, Detraux J, et al. The effects of novel and newly approved antipsychotics on serum prolactin levels: a comprehensive review. CNS Drugs.2014;28(5):421-453.
2. Freeman ME, Kanyicska B, Lerant A, et al. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80(4):1523-1631.
3. Melmed S, Casanueva FF, Hoffman AR, et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society Clinical practice guideline. J Clin Endocrinol Metab. 2011;96(2):273-288.
4. Bostwick JR, Guthrie SK, Ellingrod VL. Antipsychotic-induced hyperprolactinemia. Pharmacotherapy. 2009;29(1):64-73.
5. La Torre D, Falorni A. Pharmacological causes of hyperprolactinemia. Ther Clin Risk Manag. 2007;3(5):929-951.
6. Petit A, Piednoir D, Germain ML, et al. Drug-induced hyperprolactinemia: a case-non-case study from the national pharmacovigilance database [in French]. Therapie. 2003;58(2):159-163.
7. Emiliano AB, Fudge JL. From galactorrhea to osteopenia: rethinking serotonin-prolactin interactions. Neuropsychopharmacology. 2004;29(5):833-846.
8. Coker F, Taylor D. Antidepressant-induced hyperprolactinaemia: incidence, mechanisms and management. CNS Drugs. 2010;24(7):563-574.
9. Molitch ME. Medication induced hyperprolactinemia. Mayo Clin Proc. 2005;80(8):1050-1057.
10. Xenazine (tetrabenazine) [package insert]. Washington, DC: Prestwick Pharmaceuticals, Inc.; 2008.
11. Peña KS, Rosenfeld JA. Evaluation and treatment of galactorrhea. Am Fam Physician 2001;63(9):1763-1770.
12. Durgam S, Starace A, Li D, et al. The efficacy and tolerability of cariprazine in acute mania associated with bipolar I disorder: a phase II trial. Bipolar Disord. 2015;17(1):63-75.
13. Das S, Barnwal P, Winston AB, et al. Brexpiprazole: so far so good. Ther Adv Psychopharmacol. 2016;6(1):39-54.
14. Correll CU, Skuban A, Ouyang J, et al. Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2015;172(9):870-880.
15. Durgam S, Earley W, Guo H, et al. Efficacy and safety of adjunctive cariprazine in inadequate responders to antidepressants: a randomized, double-blind, placebo-controlled study in adult patients with major depressive disorder. J Clin Pscyhiatry. 2016;77(3):371-378.
16. Rexulti (brexpiprazole) [package insert]. Tokyo, Japan: Otsuka Pharmaceuticals Inc.; 2015.
17. Cariprazine (Vraylar) [package insert]. Parsippany, New Jersey: Actavis Pharmacueitcals Inc.; 2015.
18. Marken PA, Haykal RF, Fisher JN. Management of psychotropic-induced hyperprolactinemia. Clin Pharm. 1992;11(10):851-856.
19. Meltzer HY, Fang VS, Tricou BJ, et al. Effect of antidepressants on neuroendocrine axis in humans. Adv Biochem Psychopharmacol. 1982;32:303-316.
20. Tsuboi T, Bies RR, Suzuki T, et al. Hyperprolactinemia and estimated dopamine D2 receptor occupancy in patients with schizophrenia: analysis of the CATIE data. Prog Neuropsychopharmacol Biol Psychiatry. 2013;45:178-182.
21. Lee BH, Kim YK, Park SH. Using aripiprazole to resolve antipsychotic-induced symptomatic hyperprolactinemia: a pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(4):714-717.
22. Lu ML, Shen WW, Chen CH. Time course of the changes in antipsychotic-induced hyperprolactinemia following the switch to aripiprazole. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(8):1978-1981.
23. Mendhekar DN, Andrade C. Galactorrhea with aripiprazole. Can J Psychiatry. 2005;50(4):243.
24. Joseph SP. Aripiprazole induced hyperprolactinemia in a young female with delusional disorder. Indian J Psychol Med. 2016;38(3):260-262.
25. Meng M, Li W, Zhang S, et al. Using aripiprazole to reduce antipsychotic-induced hyperprolactinemia: meta-analysis of currently available randomized controlled trials. Shaghai Arch Psychiatry. 2015;27(1):4-17.
26. Tollin SR. Use of the dopamine agonists bromocriptine and cabergoline in the management of risperidone induced hyperprolactinemia in patients with psychotic disorders. J Endocrinol Invest. 2000;23(11):765-70.
27. Yuan HN, Wang CY, Sze CW, et al. A randomized, crossover comparison of herbal medicine and bromocriptine against risperidone-induced hyperprolactinemia in patients with schizophrenia. J Clin Psychopharmacol. 2008;28(3):264-370.
28. Chang SC, Chen CH, Lu ML. Cabergoline-induced psychotic exacerbation in schizophrenic patients. General Hospital Psychiatry. 2008;30(4):378-380.
29. Ishitobi M, Kosaka H, Shukunami K, et al. Adjunctive treatment with low-dosage pramipexole for risperidone-associated hyperprolactinemia and sexual dysfunction in a male patient with schizophrenia. J Clin Psychopharmacol 2011;31(2):243-245.
30. Peterson MC. Reversible galactorrhea and prolactin elevation related to fluoxetine use. Mayo Clin Proc. 2001;76(2):215-216.
1. Peuskens J, Pani L, Detraux J, et al. The effects of novel and newly approved antipsychotics on serum prolactin levels: a comprehensive review. CNS Drugs.2014;28(5):421-453.
2. Freeman ME, Kanyicska B, Lerant A, et al. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80(4):1523-1631.
3. Melmed S, Casanueva FF, Hoffman AR, et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society Clinical practice guideline. J Clin Endocrinol Metab. 2011;96(2):273-288.
4. Bostwick JR, Guthrie SK, Ellingrod VL. Antipsychotic-induced hyperprolactinemia. Pharmacotherapy. 2009;29(1):64-73.
5. La Torre D, Falorni A. Pharmacological causes of hyperprolactinemia. Ther Clin Risk Manag. 2007;3(5):929-951.
6. Petit A, Piednoir D, Germain ML, et al. Drug-induced hyperprolactinemia: a case-non-case study from the national pharmacovigilance database [in French]. Therapie. 2003;58(2):159-163.
7. Emiliano AB, Fudge JL. From galactorrhea to osteopenia: rethinking serotonin-prolactin interactions. Neuropsychopharmacology. 2004;29(5):833-846.
8. Coker F, Taylor D. Antidepressant-induced hyperprolactinaemia: incidence, mechanisms and management. CNS Drugs. 2010;24(7):563-574.
9. Molitch ME. Medication induced hyperprolactinemia. Mayo Clin Proc. 2005;80(8):1050-1057.
10. Xenazine (tetrabenazine) [package insert]. Washington, DC: Prestwick Pharmaceuticals, Inc.; 2008.
11. Peña KS, Rosenfeld JA. Evaluation and treatment of galactorrhea. Am Fam Physician 2001;63(9):1763-1770.
12. Durgam S, Starace A, Li D, et al. The efficacy and tolerability of cariprazine in acute mania associated with bipolar I disorder: a phase II trial. Bipolar Disord. 2015;17(1):63-75.
13. Das S, Barnwal P, Winston AB, et al. Brexpiprazole: so far so good. Ther Adv Psychopharmacol. 2016;6(1):39-54.
14. Correll CU, Skuban A, Ouyang J, et al. Efficacy and safety of brexpiprazole for the treatment of acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled trial. Am J Psychiatry. 2015;172(9):870-880.
15. Durgam S, Earley W, Guo H, et al. Efficacy and safety of adjunctive cariprazine in inadequate responders to antidepressants: a randomized, double-blind, placebo-controlled study in adult patients with major depressive disorder. J Clin Pscyhiatry. 2016;77(3):371-378.
16. Rexulti (brexpiprazole) [package insert]. Tokyo, Japan: Otsuka Pharmaceuticals Inc.; 2015.
17. Cariprazine (Vraylar) [package insert]. Parsippany, New Jersey: Actavis Pharmacueitcals Inc.; 2015.
18. Marken PA, Haykal RF, Fisher JN. Management of psychotropic-induced hyperprolactinemia. Clin Pharm. 1992;11(10):851-856.
19. Meltzer HY, Fang VS, Tricou BJ, et al. Effect of antidepressants on neuroendocrine axis in humans. Adv Biochem Psychopharmacol. 1982;32:303-316.
20. Tsuboi T, Bies RR, Suzuki T, et al. Hyperprolactinemia and estimated dopamine D2 receptor occupancy in patients with schizophrenia: analysis of the CATIE data. Prog Neuropsychopharmacol Biol Psychiatry. 2013;45:178-182.
21. Lee BH, Kim YK, Park SH. Using aripiprazole to resolve antipsychotic-induced symptomatic hyperprolactinemia: a pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(4):714-717.
22. Lu ML, Shen WW, Chen CH. Time course of the changes in antipsychotic-induced hyperprolactinemia following the switch to aripiprazole. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(8):1978-1981.
23. Mendhekar DN, Andrade C. Galactorrhea with aripiprazole. Can J Psychiatry. 2005;50(4):243.
24. Joseph SP. Aripiprazole induced hyperprolactinemia in a young female with delusional disorder. Indian J Psychol Med. 2016;38(3):260-262.
25. Meng M, Li W, Zhang S, et al. Using aripiprazole to reduce antipsychotic-induced hyperprolactinemia: meta-analysis of currently available randomized controlled trials. Shaghai Arch Psychiatry. 2015;27(1):4-17.
26. Tollin SR. Use of the dopamine agonists bromocriptine and cabergoline in the management of risperidone induced hyperprolactinemia in patients with psychotic disorders. J Endocrinol Invest. 2000;23(11):765-70.
27. Yuan HN, Wang CY, Sze CW, et al. A randomized, crossover comparison of herbal medicine and bromocriptine against risperidone-induced hyperprolactinemia in patients with schizophrenia. J Clin Psychopharmacol. 2008;28(3):264-370.
28. Chang SC, Chen CH, Lu ML. Cabergoline-induced psychotic exacerbation in schizophrenic patients. General Hospital Psychiatry. 2008;30(4):378-380.
29. Ishitobi M, Kosaka H, Shukunami K, et al. Adjunctive treatment with low-dosage pramipexole for risperidone-associated hyperprolactinemia and sexual dysfunction in a male patient with schizophrenia. J Clin Psychopharmacol 2011;31(2):243-245.
30. Peterson MC. Reversible galactorrhea and prolactin elevation related to fluoxetine use. Mayo Clin Proc. 2001;76(2):215-216.
Decompensation in a 51-year-old woman with schizophrenia
CASE Psychotic and reclusive
Ms. A, age 51, has schizophrenia and has been doing well living at a supervised residential facility. She was stable on haloperidol, 10 mg twice a day, for years but recently became agitated, threatening her roommate and yelling during the night. Ms. A begins to refuse to take her haloperidol. She also refuses to attend several outpatient appointments. As a result, Ms. A is admitted to the psychiatric unit on an involuntary basis.
In the hospital, Ms. A rarely comes out of her room. When she does come out, she usually sits in a chair, talking to herself and occasionally yelling or crying in apparent distress. Ms. A refuses to engage with her treatment team and lies mute in her bed when they attempt to interview her. Her records indicate that previous medication trials have included
Over the next week, Ms. A begins to interact more appropriately with nursing sta
[polldaddy:9945425]
The authors’ observations
As a class, antipsychotics lead to symptom reduction in approximately 70% of patients.1 However, the degree of response can vary markedly between individuals; although some patients may experience almost complete resolution of symptoms, others are still markedly impaired, as in Ms. A’s case.
A substantial amount of literature suggests that although the practice is common, use of >1 antipsychotic does not significantly increase efficacy but increases risk of adverse effects, such as type 2 diabetes mellitus, metabolic syndrome, cognitive impairment, and extrapyramidal symptoms.2-4 One exception is augmentation of clozapine with a second antipsychotic, which in certain cases appears to offer greater efficacy than clozapine alone.1 Practice guidelines and evidence generally do not support the use of multiple antipsychotics, but 20% of patients take >1 antipsychotic.5,6 Although antipsychotic polypharmacy may be appropriate for some patients, current literature suggests it is being done more often than recommended.
Clozapine is considered the most efficacious option for treatment-resistant schizophrenia.7 Because of Ms. A’s history of recurrent hospitalizations, her extensive list of trialed medications, and her ongoing symptoms despite a sufficient trial of haloperidol, the treatment team gives serious consideration to switching Ms. A to clozapine. However, Ms. A is not able to tolerate blood draws without significant support from nursing staff, and it is likely she would be unable to tolerate the frequent blood monitoring required of patients receiving clozapine.
Because many of Ms. A’s symptoms were negative or depressive, including hypersomnia, psychomotor retardation, sadness with frequent crying spells, and reduced interest in activities, adding an antidepressant to Ms. A’s medication regimen was considered. A recent systematic review and meta-analysis showed that adding an antidepressant to an antipsychotic in patients with schizophrenia had small but beneficial effects on depressive and negative symptoms and a low risk of adverse effects.8 However, Ms. A declined this option.
TREATMENT Adding long-acting haloperidol
Ms. A had previously achieved therapeutic blood levels9 with oral haloperidol. Data suggest that compared with the oral form, long-acting injectable antipsychotics can both improve compliance and decrease rehospitalization rates.10-12 Because Ms. A previously had done well with haloperidol decanoate, 200 mg every 2 weeks, achieving a blood level of 16.2 ng/mL, and because she had a partial response to oral haloperidol, we add haloperidol decanoate, 100 mg every 2 weeks, to her regimen, with the intention of transitioning her to all-depot dosing. In addition, the treatment team tries to engage Ms. A in a discussion of potential psychological contributions to her current presentation. They note that Ms. A has her basic needs met on the unit and reports feeling safe there; thus, a fear of discharge may be contributing to her lack of engagement with the team. However, because of her limited communication, it is challenging to investigate this hypothesis or explore other possible psychological issues.
Despite increasing the dosing of haloperidol, Ms. A shows minimal improvement. She continues to stonewall her treatment team, and is unwilling or unable to engage in meaningful conversation. A review of her chart suggests that this hospital course is different from previous ones in which her average stay was a few weeks, and she generally was able to converse with the treatment team, participate in discussions about her care, and make decisions about her desire for discharge.
The team considers if additional factors could be impacting Ms. A’s current presentation. They raise the possibility that she could be going through menopause, and hormonal fluctuations may be contributing to her symptoms. Despite being on the unit for nearly 2 months, Ms. A has not required the use of sanitary products. She also reports to nursing staff that at times she feels flushed and sweaty, but she is afebrile and does not have other signs or symptoms of infection.
[polldaddy:9945428]
The authors’ observations
Evidence suggests that estrogen levels can influence the development and severity of symptoms of schizophrenia (Table 113,14). Rates of schizophrenia are lower in women, and women typically have a later onset of illness with less severe symptoms.13 Women also have a second peak incidence of schizophrenia between ages 45 and 50, corresponding with the hormonal changes associated with menopause and the associated drop in estrogen.14 Symptoms also fluctuate with hormonal cycles—women experience worsening symptoms during the premenstrual phase of the menstrual cycle, when estrogen levels are low, and an improvement of symptoms during high-estrogen phases of the cycle.14 Overall, low levels of estrogen also have been observed in women with schizophrenia relative to controls, although this may be partially attributable to treatment with antipsychotics.14
Estrogen affects various regions of the brain implicated in schizophrenia and likely imparts its behavioral effects through several different mechanisms. Estrogen can act on cells to directly impact intracellular signaling and to alter gene expression.15 Although most often thought of as being related to reproductive functions, estrogen receptors can be found in many cortical and subcortical regions of the brain, such as the hippocampus, substantia nigra, and prefrontal cortex. Estrogen receptor expression levels in certain brain regions have been found to be altered in individuals with schizophrenia.15 Estrogen also enhances neurogenesis and neuroplasticity, playing a role in learning and memory.16 Particularly relevant, estrogen has been shown to directly impact both the dopaminergic and serotonergic systems.15,17 In animal models, estrogen has been shown to decrease the behavioral effects induced by dopamine agonists and decrease symptoms of schizophrenia.18 The underlying molecular mechanisms by which estrogen has these effects are uncertain.
Given estrogen’s potentially protective effects, clinical trials have explored the role of estrogen as an adjuvant to antipsychotics for treating schizophrenia. Studies have shown that estrogen can improve psychotic symptoms in patients with schizophrenia.19,20 However, because estrogen administration can increase the risk of breast and uterine cancer, researchers are instead investigating selective estrogen receptor modulators (SERMs).14 These medications have mixed agonist and antagonist effects, with different effects on different tissues. Raloxifene is a SERM that acts as an estrogen agonist in some tissues, but an antagonist in uterine and breast tissue, which may minimize potential deleterious adverse effects (Table 221-24). Repeated randomized controlled trials have found promising results for use of raloxifene as an adjunctive treatment in peri- and postmenopausal women with schizophrenia, including those refractory to antipsychotic treatment.13,25-27
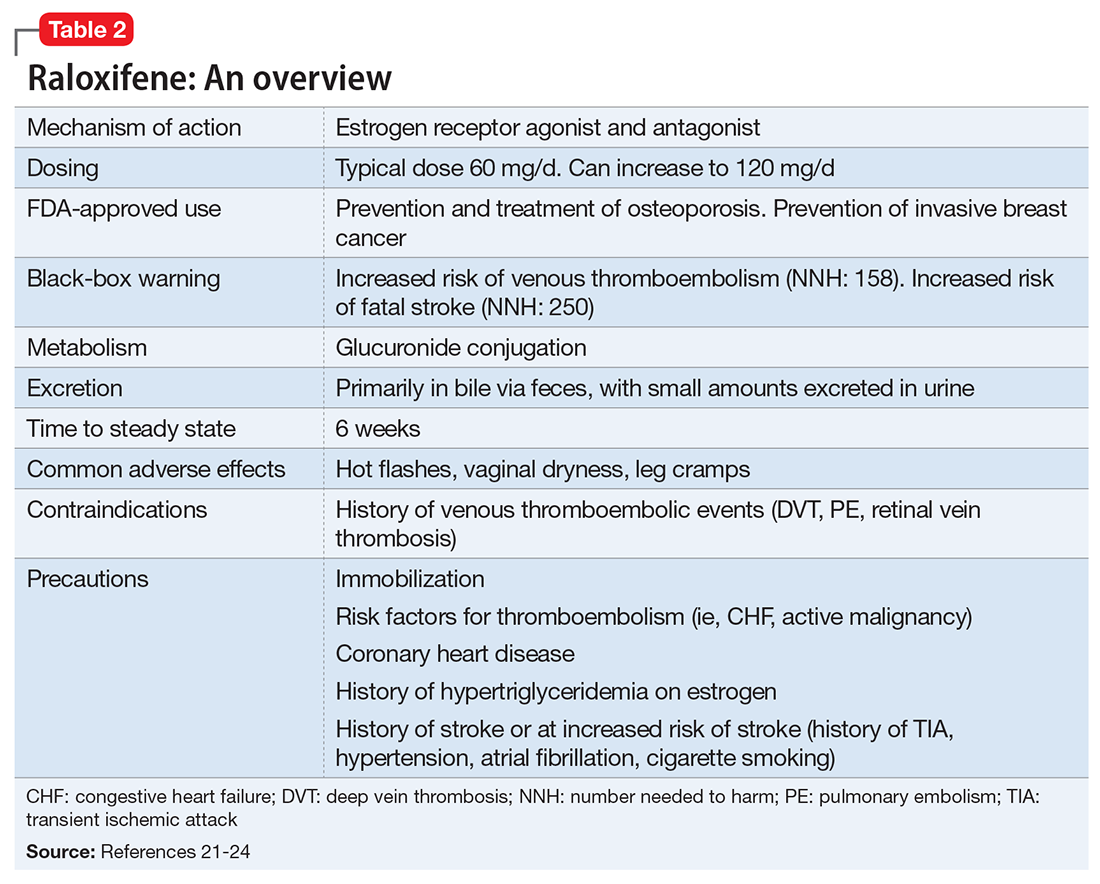
TREATMENT Address symptoms
The treatment team takes steps to address Ms. A’s perimenopausal symptoms. For mild to moderate hot flashes, primary interventions are nonpharmacologic.28 Because Ms. A primarily reports her hot flashes at night, she is given lightweight pajamas and moved to the coolest room on the unit. Both bring some relief, and her hot flashes appear to be less distressing. The treatment team decides to consult Endocrinology to further investigate the feasibility of starting raloxifene (Table 3) because of their experience using this medication to manage osteoporosis.
[polldaddy:9945429]
The authors’ observations
Raloxifene is FDA-approved for treating osteoporosis and preventing invasive breast cancer.29 Because it is an estrogen antagonist in both breast and uterine tissues, raloxifene does not increase the risk of uterine or breast cancer. Large studies have shown rates of cardiovascular events are similar for raloxifene and placebo, and some studies have found that raloxifene treatment is associated with improvement in cardiovascular risk factors, including lower blood pressure, lower low-density lipoprotein cholesterol, and increased high-density lipoprotein cholesterol.29 Raloxifene does, however, increase risk of venous thromboembolism, including deep vein thrombosis and pulmonary embolism, and fatal stroke.29,30 Overall, the risk remains relatively low, with an absolute risk increase of fatal stroke of 0.7 per 1,000 woman-years (number needed to harm [NNH]: 250) and an absolute risk increase of venous thromboembolic events of 1.88 per 1,000 women-years (NNH: 158).31 However, raloxifene may not be appropriate for patients with independent risk factors for these events. Despite this, a large meta-analysis found a 10% decrease in mortality for patients taking raloxifene compared with those receiving placebo.32 Raloxifene also can cause hot flashes, muscle cramps, and flu-like symptoms.29
Diagnosis of menopause and perimenopause is largely clinical, with hormone testing generally recommended for women age <45 in whom the diagnosis may be unclear.28 Thus, Ms. A’s vasomotor symptoms and absence of a menstrual cycle for at least 2 months were diagnostic of perimenopause; a 12-month cessation in menstrual cycles is required for a diagnosis of menopause.28
OUTCOME Improvement with raloxifene
Because Ms. A is at relatively low risk for a thromboembolism or stroke, the benefit of raloxifene is thought to outweigh the risk, and she is started on raloxifene, 60 mg/d. Over the next 2 weeks, Ms. A becomes increasingly interactive, and is seen sitting at a table talking with other patients on multiple occasions. She spends time looking at fashion magazines, and engages in conversation about fashion with staff and other patients. She participates in group therapy for the first time during this hospital stay and begins to talk about discharge. She occasionally smiles and waves at her treatment team and participates more in the daily interview, although these interactions remain limited and on her terms. She maintains this improvement and is transferred to a psychiatric facility in her home county for ongoing care and discharge planning.
2. Citrome L, Jaffe A, Levine J, et al. Relationship between antipsychotic medication treatment and new cases of diabetes among psychiatric inpatients. Psychiatr Serv. 2004;55(9):1006-1013.
3. Correll CU, Frederickson AM, Kane JM, et al. Does antipsychotic polypharmacy increase the risk for metabolic syndrome? Schizophr Res. 2007;89(1-3):91-100.
4. Gallego JA, Nielsen J, De Hert M, et al. Safety and tolerability of antipsychotic polypharmacy. Expert Opin Drug Saf. 2012;11(4):527-542.
5. Gallego JA, Bonetti J, Zhang J, et al. Prevalence and correlates of antipsychotic polypharmacy: a systematic review and meta-regression of global and regional trends from the 1970s to 2009. Schizophr Res. 2012;138(1):18-28.
6. Hasan A, Falkai P, Wobrock T, et al; WFSBP Task Force on Treatment Guidelines for Schizophrenia. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318-378.
7. McEvoy JP, Lieberman JA, Stroup TS, et al; CATIE Investigators. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610.
8. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9);876-886.
9. Ulrich S, Neuhof S, Braun V, et al. Therapeutic window of serum haloperidol concentration in acute schizophrenia and schizoaffective disorder. Pharmacopsychiatry. 1998;31(5):163-169.
10. Lafeuille MH, Dean J, Carter V, et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Curr Med Res Opin. 2014;30(8):1643-1655.
11. MacEwan JP, Kamat SA, Duffy RA, et al. Hospital readmission rates among patients with schizophrenia treated with long-acting injectables or oral antipsychotics. Psychiatr Serv. 2016;67(11):1183-1188.
12. Marcus SC, Zummo J, Pettit AR, et al. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768.
13. Usall J, Huerta-Ramos E, Iniesta R, et al; RALOPSYCAT Group. Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. J Clin Psychiatry. 2011;72(11):1552-1557.
14. Seeman MV. Treating schizophrenia at the time of menopause. Maturitas. 2012;72(2):117-120.
15. Gogos A, Sbisa AM, Sun J, et al. A role for estrogen in schizophrenia: clinical and preclinical findings. Int J Endocrinol. 2015;2015:615356. doi: 10.1155/2015/615356.
16. Khan MM. Neurocognitive, neuroprotective, and cardiometabolic effects of raloxifene: potential for improving therapeutic outcomes in schizophrenia. CNS Drugs. 2016;30(7):589-601.
17. Barth C, Villringer A, Sacher J. Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Front Neurosci. 2015;9:37.
18. Häfner H, Behrens S, De Vry J, et al. An animal model for the effects of estradiol on dopamine-mediated behavior: implications for sex differences in schizophrenia. Psychiatry Res. 1991;38(2):125-134.
19. Akhondzadeh S, Nejatisafa AA, Amini H, et al. Adjunctive estrogen treatment in women with chronic schizophrenia: a double-blind, randomized, and placebo-controlled trial. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(6):1007-1012.
20. Kulkarni J, de Castella A, Fitzgerald PB, et al. Estrogen in severe mental illness: a potential new treatment approach. Arch Gen Psychiatry. 2008;65(8):955-960.
21. Ellis AJ, Hendrick VM, Williams R, Komm BS. Selective estrogen receptor modulators in clinical practice: a safety overview. Expert Opin Drug Saf. 2015;14(6):921-934.
22. Morello KC, Wurz GT, DeGregorio MW. Pharmacokinetics of selective estrogen receptor modulators. Clin pharmacokinet. 2003;42(4):361-372.
23. Lewiecki EM, Miller PD, Harris ST, et al. Understanding and communicating the benefits and risks of denosumab, raloxifene, and teriparatide for the treatment of osteoporosis. J Clin Densitom. 2014;17(4):490-495.
24. Raloxifene Hydrochloride. Micromedex 2.0. Truven Health Analytics. www.micromedexsolutions.com. Accessed July 24, 2016.
25. Kulkarni J, Gavrilidis E, Gwini SM, et al. Effect of adjunctive raloxifene therapy on severity of refractory schizophrenia in women: a randomized clinical trial. JAMA Psychiatry. 2016;73(9):947-954.
26. Huerta-Ramos E, Iniesta R, Ochoa S, et al. Effects of raloxifene on cognition in postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. Eur Neuropsychopharmacol. 2014;24(2):223-231.
27. Kianimehr G, Fatehi F, Hashempoor S, et al. Raloxifene adjunctive therapy for postmenopausal women suffering from chronic schizophrenia: a randomized double-blind and placebo controlled trial. Daru. 2014;22:55.
28. Stuenkel CA, Davis SR, Gompel A, et al. Treatment of symptoms of the menopause: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(11):3975-4011.
29. Ellis AJ, Hendrick VM, Williams R, et al. Selective estrogen receptor modulators in clinical practice: a safety overview. Expert Opin Drug Saf. 2015;14(6):921-934.
30. Adomaityte J, Farooq M, Qayyum R. Effect of raloxifene therapy on venous thromboembolism in postmenopausal women. A meta-analysis. Thromb Haemost. 2008;99(2):338-342.
31. Lewiecki EM, Miller PD, Harris ST, et al. Understanding and communicating the benefits and risks of denosumab, raloxifene, and teriparatide for the treatment of osteoporosis. J Clin Densitom. 2014;17(4):490-495.
32. Grady D, Cauley JA, Stock JL, et al. Effect of raloxifene on all-cause mortality. Am J Med. 2010;123(5):469.e1-461.e7.
CASE Psychotic and reclusive
Ms. A, age 51, has schizophrenia and has been doing well living at a supervised residential facility. She was stable on haloperidol, 10 mg twice a day, for years but recently became agitated, threatening her roommate and yelling during the night. Ms. A begins to refuse to take her haloperidol. She also refuses to attend several outpatient appointments. As a result, Ms. A is admitted to the psychiatric unit on an involuntary basis.
In the hospital, Ms. A rarely comes out of her room. When she does come out, she usually sits in a chair, talking to herself and occasionally yelling or crying in apparent distress. Ms. A refuses to engage with her treatment team and lies mute in her bed when they attempt to interview her. Her records indicate that previous medication trials have included
Over the next week, Ms. A begins to interact more appropriately with nursing sta
[polldaddy:9945425]
The authors’ observations
As a class, antipsychotics lead to symptom reduction in approximately 70% of patients.1 However, the degree of response can vary markedly between individuals; although some patients may experience almost complete resolution of symptoms, others are still markedly impaired, as in Ms. A’s case.
A substantial amount of literature suggests that although the practice is common, use of >1 antipsychotic does not significantly increase efficacy but increases risk of adverse effects, such as type 2 diabetes mellitus, metabolic syndrome, cognitive impairment, and extrapyramidal symptoms.2-4 One exception is augmentation of clozapine with a second antipsychotic, which in certain cases appears to offer greater efficacy than clozapine alone.1 Practice guidelines and evidence generally do not support the use of multiple antipsychotics, but 20% of patients take >1 antipsychotic.5,6 Although antipsychotic polypharmacy may be appropriate for some patients, current literature suggests it is being done more often than recommended.
Clozapine is considered the most efficacious option for treatment-resistant schizophrenia.7 Because of Ms. A’s history of recurrent hospitalizations, her extensive list of trialed medications, and her ongoing symptoms despite a sufficient trial of haloperidol, the treatment team gives serious consideration to switching Ms. A to clozapine. However, Ms. A is not able to tolerate blood draws without significant support from nursing staff, and it is likely she would be unable to tolerate the frequent blood monitoring required of patients receiving clozapine.
Because many of Ms. A’s symptoms were negative or depressive, including hypersomnia, psychomotor retardation, sadness with frequent crying spells, and reduced interest in activities, adding an antidepressant to Ms. A’s medication regimen was considered. A recent systematic review and meta-analysis showed that adding an antidepressant to an antipsychotic in patients with schizophrenia had small but beneficial effects on depressive and negative symptoms and a low risk of adverse effects.8 However, Ms. A declined this option.
TREATMENT Adding long-acting haloperidol
Ms. A had previously achieved therapeutic blood levels9 with oral haloperidol. Data suggest that compared with the oral form, long-acting injectable antipsychotics can both improve compliance and decrease rehospitalization rates.10-12 Because Ms. A previously had done well with haloperidol decanoate, 200 mg every 2 weeks, achieving a blood level of 16.2 ng/mL, and because she had a partial response to oral haloperidol, we add haloperidol decanoate, 100 mg every 2 weeks, to her regimen, with the intention of transitioning her to all-depot dosing. In addition, the treatment team tries to engage Ms. A in a discussion of potential psychological contributions to her current presentation. They note that Ms. A has her basic needs met on the unit and reports feeling safe there; thus, a fear of discharge may be contributing to her lack of engagement with the team. However, because of her limited communication, it is challenging to investigate this hypothesis or explore other possible psychological issues.
Despite increasing the dosing of haloperidol, Ms. A shows minimal improvement. She continues to stonewall her treatment team, and is unwilling or unable to engage in meaningful conversation. A review of her chart suggests that this hospital course is different from previous ones in which her average stay was a few weeks, and she generally was able to converse with the treatment team, participate in discussions about her care, and make decisions about her desire for discharge.
The team considers if additional factors could be impacting Ms. A’s current presentation. They raise the possibility that she could be going through menopause, and hormonal fluctuations may be contributing to her symptoms. Despite being on the unit for nearly 2 months, Ms. A has not required the use of sanitary products. She also reports to nursing staff that at times she feels flushed and sweaty, but she is afebrile and does not have other signs or symptoms of infection.
[polldaddy:9945428]
The authors’ observations
Evidence suggests that estrogen levels can influence the development and severity of symptoms of schizophrenia (Table 113,14). Rates of schizophrenia are lower in women, and women typically have a later onset of illness with less severe symptoms.13 Women also have a second peak incidence of schizophrenia between ages 45 and 50, corresponding with the hormonal changes associated with menopause and the associated drop in estrogen.14 Symptoms also fluctuate with hormonal cycles—women experience worsening symptoms during the premenstrual phase of the menstrual cycle, when estrogen levels are low, and an improvement of symptoms during high-estrogen phases of the cycle.14 Overall, low levels of estrogen also have been observed in women with schizophrenia relative to controls, although this may be partially attributable to treatment with antipsychotics.14
Estrogen affects various regions of the brain implicated in schizophrenia and likely imparts its behavioral effects through several different mechanisms. Estrogen can act on cells to directly impact intracellular signaling and to alter gene expression.15 Although most often thought of as being related to reproductive functions, estrogen receptors can be found in many cortical and subcortical regions of the brain, such as the hippocampus, substantia nigra, and prefrontal cortex. Estrogen receptor expression levels in certain brain regions have been found to be altered in individuals with schizophrenia.15 Estrogen also enhances neurogenesis and neuroplasticity, playing a role in learning and memory.16 Particularly relevant, estrogen has been shown to directly impact both the dopaminergic and serotonergic systems.15,17 In animal models, estrogen has been shown to decrease the behavioral effects induced by dopamine agonists and decrease symptoms of schizophrenia.18 The underlying molecular mechanisms by which estrogen has these effects are uncertain.
Given estrogen’s potentially protective effects, clinical trials have explored the role of estrogen as an adjuvant to antipsychotics for treating schizophrenia. Studies have shown that estrogen can improve psychotic symptoms in patients with schizophrenia.19,20 However, because estrogen administration can increase the risk of breast and uterine cancer, researchers are instead investigating selective estrogen receptor modulators (SERMs).14 These medications have mixed agonist and antagonist effects, with different effects on different tissues. Raloxifene is a SERM that acts as an estrogen agonist in some tissues, but an antagonist in uterine and breast tissue, which may minimize potential deleterious adverse effects (Table 221-24). Repeated randomized controlled trials have found promising results for use of raloxifene as an adjunctive treatment in peri- and postmenopausal women with schizophrenia, including those refractory to antipsychotic treatment.13,25-27
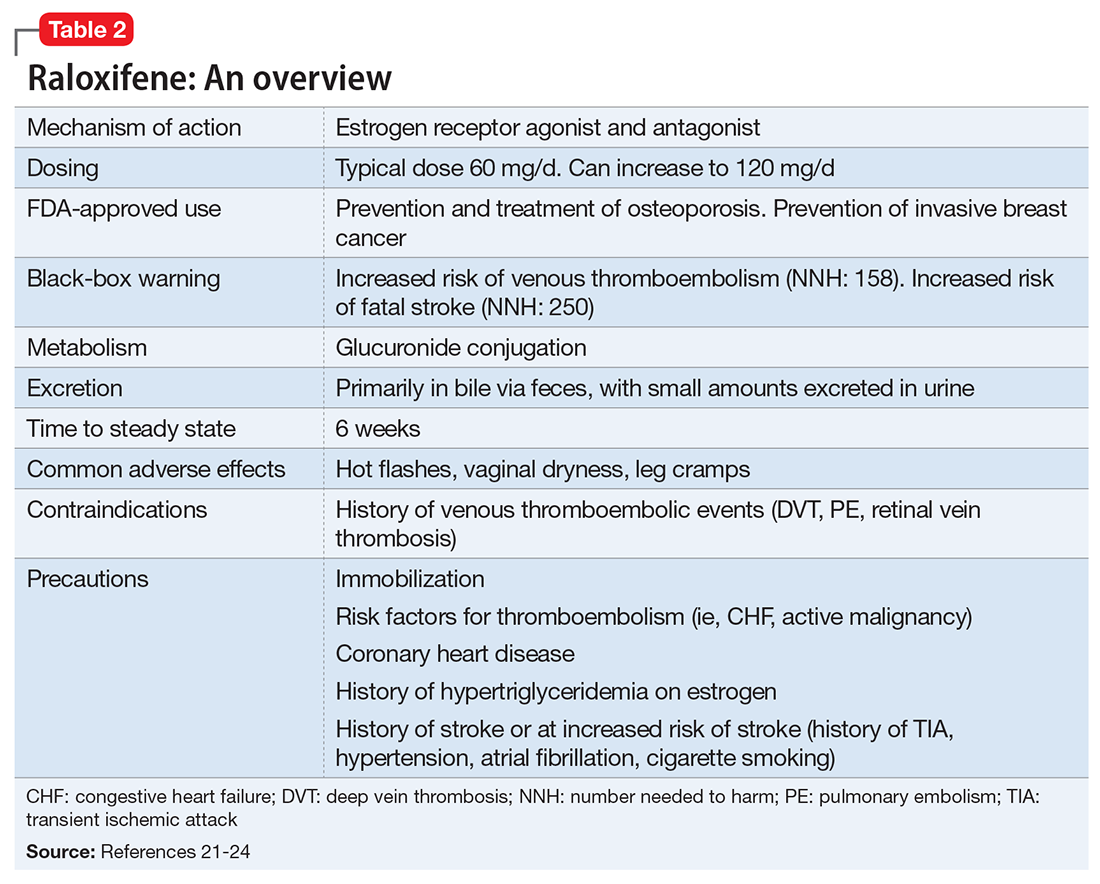
TREATMENT Address symptoms
The treatment team takes steps to address Ms. A’s perimenopausal symptoms. For mild to moderate hot flashes, primary interventions are nonpharmacologic.28 Because Ms. A primarily reports her hot flashes at night, she is given lightweight pajamas and moved to the coolest room on the unit. Both bring some relief, and her hot flashes appear to be less distressing. The treatment team decides to consult Endocrinology to further investigate the feasibility of starting raloxifene (Table 3) because of their experience using this medication to manage osteoporosis.
[polldaddy:9945429]
The authors’ observations
Raloxifene is FDA-approved for treating osteoporosis and preventing invasive breast cancer.29 Because it is an estrogen antagonist in both breast and uterine tissues, raloxifene does not increase the risk of uterine or breast cancer. Large studies have shown rates of cardiovascular events are similar for raloxifene and placebo, and some studies have found that raloxifene treatment is associated with improvement in cardiovascular risk factors, including lower blood pressure, lower low-density lipoprotein cholesterol, and increased high-density lipoprotein cholesterol.29 Raloxifene does, however, increase risk of venous thromboembolism, including deep vein thrombosis and pulmonary embolism, and fatal stroke.29,30 Overall, the risk remains relatively low, with an absolute risk increase of fatal stroke of 0.7 per 1,000 woman-years (number needed to harm [NNH]: 250) and an absolute risk increase of venous thromboembolic events of 1.88 per 1,000 women-years (NNH: 158).31 However, raloxifene may not be appropriate for patients with independent risk factors for these events. Despite this, a large meta-analysis found a 10% decrease in mortality for patients taking raloxifene compared with those receiving placebo.32 Raloxifene also can cause hot flashes, muscle cramps, and flu-like symptoms.29
Diagnosis of menopause and perimenopause is largely clinical, with hormone testing generally recommended for women age <45 in whom the diagnosis may be unclear.28 Thus, Ms. A’s vasomotor symptoms and absence of a menstrual cycle for at least 2 months were diagnostic of perimenopause; a 12-month cessation in menstrual cycles is required for a diagnosis of menopause.28
OUTCOME Improvement with raloxifene
Because Ms. A is at relatively low risk for a thromboembolism or stroke, the benefit of raloxifene is thought to outweigh the risk, and she is started on raloxifene, 60 mg/d. Over the next 2 weeks, Ms. A becomes increasingly interactive, and is seen sitting at a table talking with other patients on multiple occasions. She spends time looking at fashion magazines, and engages in conversation about fashion with staff and other patients. She participates in group therapy for the first time during this hospital stay and begins to talk about discharge. She occasionally smiles and waves at her treatment team and participates more in the daily interview, although these interactions remain limited and on her terms. She maintains this improvement and is transferred to a psychiatric facility in her home county for ongoing care and discharge planning.
CASE Psychotic and reclusive
Ms. A, age 51, has schizophrenia and has been doing well living at a supervised residential facility. She was stable on haloperidol, 10 mg twice a day, for years but recently became agitated, threatening her roommate and yelling during the night. Ms. A begins to refuse to take her haloperidol. She also refuses to attend several outpatient appointments. As a result, Ms. A is admitted to the psychiatric unit on an involuntary basis.
In the hospital, Ms. A rarely comes out of her room. When she does come out, she usually sits in a chair, talking to herself and occasionally yelling or crying in apparent distress. Ms. A refuses to engage with her treatment team and lies mute in her bed when they attempt to interview her. Her records indicate that previous medication trials have included
Over the next week, Ms. A begins to interact more appropriately with nursing sta
[polldaddy:9945425]
The authors’ observations
As a class, antipsychotics lead to symptom reduction in approximately 70% of patients.1 However, the degree of response can vary markedly between individuals; although some patients may experience almost complete resolution of symptoms, others are still markedly impaired, as in Ms. A’s case.
A substantial amount of literature suggests that although the practice is common, use of >1 antipsychotic does not significantly increase efficacy but increases risk of adverse effects, such as type 2 diabetes mellitus, metabolic syndrome, cognitive impairment, and extrapyramidal symptoms.2-4 One exception is augmentation of clozapine with a second antipsychotic, which in certain cases appears to offer greater efficacy than clozapine alone.1 Practice guidelines and evidence generally do not support the use of multiple antipsychotics, but 20% of patients take >1 antipsychotic.5,6 Although antipsychotic polypharmacy may be appropriate for some patients, current literature suggests it is being done more often than recommended.
Clozapine is considered the most efficacious option for treatment-resistant schizophrenia.7 Because of Ms. A’s history of recurrent hospitalizations, her extensive list of trialed medications, and her ongoing symptoms despite a sufficient trial of haloperidol, the treatment team gives serious consideration to switching Ms. A to clozapine. However, Ms. A is not able to tolerate blood draws without significant support from nursing staff, and it is likely she would be unable to tolerate the frequent blood monitoring required of patients receiving clozapine.
Because many of Ms. A’s symptoms were negative or depressive, including hypersomnia, psychomotor retardation, sadness with frequent crying spells, and reduced interest in activities, adding an antidepressant to Ms. A’s medication regimen was considered. A recent systematic review and meta-analysis showed that adding an antidepressant to an antipsychotic in patients with schizophrenia had small but beneficial effects on depressive and negative symptoms and a low risk of adverse effects.8 However, Ms. A declined this option.
TREATMENT Adding long-acting haloperidol
Ms. A had previously achieved therapeutic blood levels9 with oral haloperidol. Data suggest that compared with the oral form, long-acting injectable antipsychotics can both improve compliance and decrease rehospitalization rates.10-12 Because Ms. A previously had done well with haloperidol decanoate, 200 mg every 2 weeks, achieving a blood level of 16.2 ng/mL, and because she had a partial response to oral haloperidol, we add haloperidol decanoate, 100 mg every 2 weeks, to her regimen, with the intention of transitioning her to all-depot dosing. In addition, the treatment team tries to engage Ms. A in a discussion of potential psychological contributions to her current presentation. They note that Ms. A has her basic needs met on the unit and reports feeling safe there; thus, a fear of discharge may be contributing to her lack of engagement with the team. However, because of her limited communication, it is challenging to investigate this hypothesis or explore other possible psychological issues.
Despite increasing the dosing of haloperidol, Ms. A shows minimal improvement. She continues to stonewall her treatment team, and is unwilling or unable to engage in meaningful conversation. A review of her chart suggests that this hospital course is different from previous ones in which her average stay was a few weeks, and she generally was able to converse with the treatment team, participate in discussions about her care, and make decisions about her desire for discharge.
The team considers if additional factors could be impacting Ms. A’s current presentation. They raise the possibility that she could be going through menopause, and hormonal fluctuations may be contributing to her symptoms. Despite being on the unit for nearly 2 months, Ms. A has not required the use of sanitary products. She also reports to nursing staff that at times she feels flushed and sweaty, but she is afebrile and does not have other signs or symptoms of infection.
[polldaddy:9945428]
The authors’ observations
Evidence suggests that estrogen levels can influence the development and severity of symptoms of schizophrenia (Table 113,14). Rates of schizophrenia are lower in women, and women typically have a later onset of illness with less severe symptoms.13 Women also have a second peak incidence of schizophrenia between ages 45 and 50, corresponding with the hormonal changes associated with menopause and the associated drop in estrogen.14 Symptoms also fluctuate with hormonal cycles—women experience worsening symptoms during the premenstrual phase of the menstrual cycle, when estrogen levels are low, and an improvement of symptoms during high-estrogen phases of the cycle.14 Overall, low levels of estrogen also have been observed in women with schizophrenia relative to controls, although this may be partially attributable to treatment with antipsychotics.14
Estrogen affects various regions of the brain implicated in schizophrenia and likely imparts its behavioral effects through several different mechanisms. Estrogen can act on cells to directly impact intracellular signaling and to alter gene expression.15 Although most often thought of as being related to reproductive functions, estrogen receptors can be found in many cortical and subcortical regions of the brain, such as the hippocampus, substantia nigra, and prefrontal cortex. Estrogen receptor expression levels in certain brain regions have been found to be altered in individuals with schizophrenia.15 Estrogen also enhances neurogenesis and neuroplasticity, playing a role in learning and memory.16 Particularly relevant, estrogen has been shown to directly impact both the dopaminergic and serotonergic systems.15,17 In animal models, estrogen has been shown to decrease the behavioral effects induced by dopamine agonists and decrease symptoms of schizophrenia.18 The underlying molecular mechanisms by which estrogen has these effects are uncertain.
Given estrogen’s potentially protective effects, clinical trials have explored the role of estrogen as an adjuvant to antipsychotics for treating schizophrenia. Studies have shown that estrogen can improve psychotic symptoms in patients with schizophrenia.19,20 However, because estrogen administration can increase the risk of breast and uterine cancer, researchers are instead investigating selective estrogen receptor modulators (SERMs).14 These medications have mixed agonist and antagonist effects, with different effects on different tissues. Raloxifene is a SERM that acts as an estrogen agonist in some tissues, but an antagonist in uterine and breast tissue, which may minimize potential deleterious adverse effects (Table 221-24). Repeated randomized controlled trials have found promising results for use of raloxifene as an adjunctive treatment in peri- and postmenopausal women with schizophrenia, including those refractory to antipsychotic treatment.13,25-27
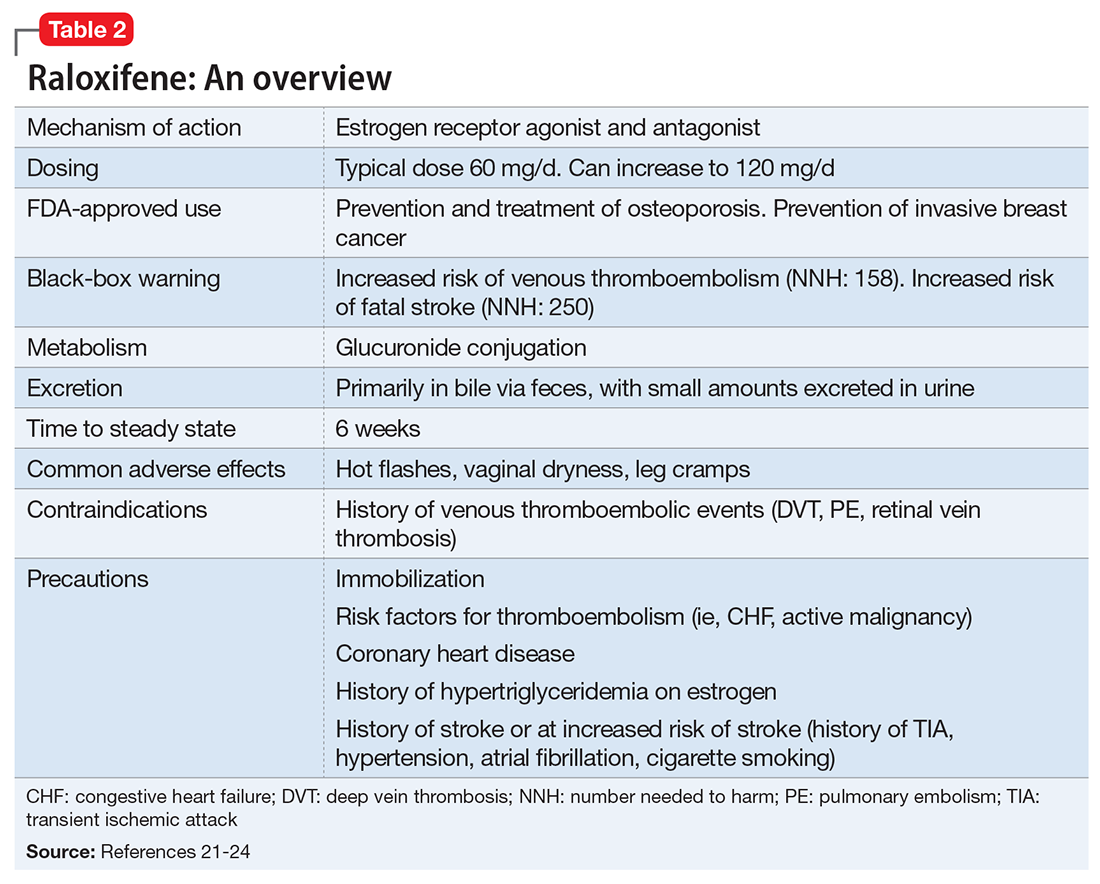
TREATMENT Address symptoms
The treatment team takes steps to address Ms. A’s perimenopausal symptoms. For mild to moderate hot flashes, primary interventions are nonpharmacologic.28 Because Ms. A primarily reports her hot flashes at night, she is given lightweight pajamas and moved to the coolest room on the unit. Both bring some relief, and her hot flashes appear to be less distressing. The treatment team decides to consult Endocrinology to further investigate the feasibility of starting raloxifene (Table 3) because of their experience using this medication to manage osteoporosis.
[polldaddy:9945429]
The authors’ observations
Raloxifene is FDA-approved for treating osteoporosis and preventing invasive breast cancer.29 Because it is an estrogen antagonist in both breast and uterine tissues, raloxifene does not increase the risk of uterine or breast cancer. Large studies have shown rates of cardiovascular events are similar for raloxifene and placebo, and some studies have found that raloxifene treatment is associated with improvement in cardiovascular risk factors, including lower blood pressure, lower low-density lipoprotein cholesterol, and increased high-density lipoprotein cholesterol.29 Raloxifene does, however, increase risk of venous thromboembolism, including deep vein thrombosis and pulmonary embolism, and fatal stroke.29,30 Overall, the risk remains relatively low, with an absolute risk increase of fatal stroke of 0.7 per 1,000 woman-years (number needed to harm [NNH]: 250) and an absolute risk increase of venous thromboembolic events of 1.88 per 1,000 women-years (NNH: 158).31 However, raloxifene may not be appropriate for patients with independent risk factors for these events. Despite this, a large meta-analysis found a 10% decrease in mortality for patients taking raloxifene compared with those receiving placebo.32 Raloxifene also can cause hot flashes, muscle cramps, and flu-like symptoms.29
Diagnosis of menopause and perimenopause is largely clinical, with hormone testing generally recommended for women age <45 in whom the diagnosis may be unclear.28 Thus, Ms. A’s vasomotor symptoms and absence of a menstrual cycle for at least 2 months were diagnostic of perimenopause; a 12-month cessation in menstrual cycles is required for a diagnosis of menopause.28
OUTCOME Improvement with raloxifene
Because Ms. A is at relatively low risk for a thromboembolism or stroke, the benefit of raloxifene is thought to outweigh the risk, and she is started on raloxifene, 60 mg/d. Over the next 2 weeks, Ms. A becomes increasingly interactive, and is seen sitting at a table talking with other patients on multiple occasions. She spends time looking at fashion magazines, and engages in conversation about fashion with staff and other patients. She participates in group therapy for the first time during this hospital stay and begins to talk about discharge. She occasionally smiles and waves at her treatment team and participates more in the daily interview, although these interactions remain limited and on her terms. She maintains this improvement and is transferred to a psychiatric facility in her home county for ongoing care and discharge planning.
2. Citrome L, Jaffe A, Levine J, et al. Relationship between antipsychotic medication treatment and new cases of diabetes among psychiatric inpatients. Psychiatr Serv. 2004;55(9):1006-1013.
3. Correll CU, Frederickson AM, Kane JM, et al. Does antipsychotic polypharmacy increase the risk for metabolic syndrome? Schizophr Res. 2007;89(1-3):91-100.
4. Gallego JA, Nielsen J, De Hert M, et al. Safety and tolerability of antipsychotic polypharmacy. Expert Opin Drug Saf. 2012;11(4):527-542.
5. Gallego JA, Bonetti J, Zhang J, et al. Prevalence and correlates of antipsychotic polypharmacy: a systematic review and meta-regression of global and regional trends from the 1970s to 2009. Schizophr Res. 2012;138(1):18-28.
6. Hasan A, Falkai P, Wobrock T, et al; WFSBP Task Force on Treatment Guidelines for Schizophrenia. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318-378.
7. McEvoy JP, Lieberman JA, Stroup TS, et al; CATIE Investigators. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610.
8. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9);876-886.
9. Ulrich S, Neuhof S, Braun V, et al. Therapeutic window of serum haloperidol concentration in acute schizophrenia and schizoaffective disorder. Pharmacopsychiatry. 1998;31(5):163-169.
10. Lafeuille MH, Dean J, Carter V, et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Curr Med Res Opin. 2014;30(8):1643-1655.
11. MacEwan JP, Kamat SA, Duffy RA, et al. Hospital readmission rates among patients with schizophrenia treated with long-acting injectables or oral antipsychotics. Psychiatr Serv. 2016;67(11):1183-1188.
12. Marcus SC, Zummo J, Pettit AR, et al. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768.
13. Usall J, Huerta-Ramos E, Iniesta R, et al; RALOPSYCAT Group. Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. J Clin Psychiatry. 2011;72(11):1552-1557.
14. Seeman MV. Treating schizophrenia at the time of menopause. Maturitas. 2012;72(2):117-120.
15. Gogos A, Sbisa AM, Sun J, et al. A role for estrogen in schizophrenia: clinical and preclinical findings. Int J Endocrinol. 2015;2015:615356. doi: 10.1155/2015/615356.
16. Khan MM. Neurocognitive, neuroprotective, and cardiometabolic effects of raloxifene: potential for improving therapeutic outcomes in schizophrenia. CNS Drugs. 2016;30(7):589-601.
17. Barth C, Villringer A, Sacher J. Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Front Neurosci. 2015;9:37.
18. Häfner H, Behrens S, De Vry J, et al. An animal model for the effects of estradiol on dopamine-mediated behavior: implications for sex differences in schizophrenia. Psychiatry Res. 1991;38(2):125-134.
19. Akhondzadeh S, Nejatisafa AA, Amini H, et al. Adjunctive estrogen treatment in women with chronic schizophrenia: a double-blind, randomized, and placebo-controlled trial. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(6):1007-1012.
20. Kulkarni J, de Castella A, Fitzgerald PB, et al. Estrogen in severe mental illness: a potential new treatment approach. Arch Gen Psychiatry. 2008;65(8):955-960.
21. Ellis AJ, Hendrick VM, Williams R, Komm BS. Selective estrogen receptor modulators in clinical practice: a safety overview. Expert Opin Drug Saf. 2015;14(6):921-934.
22. Morello KC, Wurz GT, DeGregorio MW. Pharmacokinetics of selective estrogen receptor modulators. Clin pharmacokinet. 2003;42(4):361-372.
23. Lewiecki EM, Miller PD, Harris ST, et al. Understanding and communicating the benefits and risks of denosumab, raloxifene, and teriparatide for the treatment of osteoporosis. J Clin Densitom. 2014;17(4):490-495.
24. Raloxifene Hydrochloride. Micromedex 2.0. Truven Health Analytics. www.micromedexsolutions.com. Accessed July 24, 2016.
25. Kulkarni J, Gavrilidis E, Gwini SM, et al. Effect of adjunctive raloxifene therapy on severity of refractory schizophrenia in women: a randomized clinical trial. JAMA Psychiatry. 2016;73(9):947-954.
26. Huerta-Ramos E, Iniesta R, Ochoa S, et al. Effects of raloxifene on cognition in postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. Eur Neuropsychopharmacol. 2014;24(2):223-231.
27. Kianimehr G, Fatehi F, Hashempoor S, et al. Raloxifene adjunctive therapy for postmenopausal women suffering from chronic schizophrenia: a randomized double-blind and placebo controlled trial. Daru. 2014;22:55.
28. Stuenkel CA, Davis SR, Gompel A, et al. Treatment of symptoms of the menopause: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(11):3975-4011.
29. Ellis AJ, Hendrick VM, Williams R, et al. Selective estrogen receptor modulators in clinical practice: a safety overview. Expert Opin Drug Saf. 2015;14(6):921-934.
30. Adomaityte J, Farooq M, Qayyum R. Effect of raloxifene therapy on venous thromboembolism in postmenopausal women. A meta-analysis. Thromb Haemost. 2008;99(2):338-342.
31. Lewiecki EM, Miller PD, Harris ST, et al. Understanding and communicating the benefits and risks of denosumab, raloxifene, and teriparatide for the treatment of osteoporosis. J Clin Densitom. 2014;17(4):490-495.
32. Grady D, Cauley JA, Stock JL, et al. Effect of raloxifene on all-cause mortality. Am J Med. 2010;123(5):469.e1-461.e7.
2. Citrome L, Jaffe A, Levine J, et al. Relationship between antipsychotic medication treatment and new cases of diabetes among psychiatric inpatients. Psychiatr Serv. 2004;55(9):1006-1013.
3. Correll CU, Frederickson AM, Kane JM, et al. Does antipsychotic polypharmacy increase the risk for metabolic syndrome? Schizophr Res. 2007;89(1-3):91-100.
4. Gallego JA, Nielsen J, De Hert M, et al. Safety and tolerability of antipsychotic polypharmacy. Expert Opin Drug Saf. 2012;11(4):527-542.
5. Gallego JA, Bonetti J, Zhang J, et al. Prevalence and correlates of antipsychotic polypharmacy: a systematic review and meta-regression of global and regional trends from the 1970s to 2009. Schizophr Res. 2012;138(1):18-28.
6. Hasan A, Falkai P, Wobrock T, et al; WFSBP Task Force on Treatment Guidelines for Schizophrenia. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318-378.
7. McEvoy JP, Lieberman JA, Stroup TS, et al; CATIE Investigators. Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia who did not respond to prior atypical antipsychotic treatment. Am J Psychiatry. 2006;163(4):600-610.
8. Helfer B, Samara MT, Huhn M, et al. Efficacy and safety of antidepressants added to antipsychotics for schizophrenia: a systematic review and meta-analysis. Am J Psychiatry. 2016;173(9);876-886.
9. Ulrich S, Neuhof S, Braun V, et al. Therapeutic window of serum haloperidol concentration in acute schizophrenia and schizoaffective disorder. Pharmacopsychiatry. 1998;31(5):163-169.
10. Lafeuille MH, Dean J, Carter V, et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Curr Med Res Opin. 2014;30(8):1643-1655.
11. MacEwan JP, Kamat SA, Duffy RA, et al. Hospital readmission rates among patients with schizophrenia treated with long-acting injectables or oral antipsychotics. Psychiatr Serv. 2016;67(11):1183-1188.
12. Marcus SC, Zummo J, Pettit AR, et al. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754-768.
13. Usall J, Huerta-Ramos E, Iniesta R, et al; RALOPSYCAT Group. Raloxifene as an adjunctive treatment for postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. J Clin Psychiatry. 2011;72(11):1552-1557.
14. Seeman MV. Treating schizophrenia at the time of menopause. Maturitas. 2012;72(2):117-120.
15. Gogos A, Sbisa AM, Sun J, et al. A role for estrogen in schizophrenia: clinical and preclinical findings. Int J Endocrinol. 2015;2015:615356. doi: 10.1155/2015/615356.
16. Khan MM. Neurocognitive, neuroprotective, and cardiometabolic effects of raloxifene: potential for improving therapeutic outcomes in schizophrenia. CNS Drugs. 2016;30(7):589-601.
17. Barth C, Villringer A, Sacher J. Sex hormones affect neurotransmitters and shape the adult female brain during hormonal transition periods. Front Neurosci. 2015;9:37.
18. Häfner H, Behrens S, De Vry J, et al. An animal model for the effects of estradiol on dopamine-mediated behavior: implications for sex differences in schizophrenia. Psychiatry Res. 1991;38(2):125-134.
19. Akhondzadeh S, Nejatisafa AA, Amini H, et al. Adjunctive estrogen treatment in women with chronic schizophrenia: a double-blind, randomized, and placebo-controlled trial. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(6):1007-1012.
20. Kulkarni J, de Castella A, Fitzgerald PB, et al. Estrogen in severe mental illness: a potential new treatment approach. Arch Gen Psychiatry. 2008;65(8):955-960.
21. Ellis AJ, Hendrick VM, Williams R, Komm BS. Selective estrogen receptor modulators in clinical practice: a safety overview. Expert Opin Drug Saf. 2015;14(6):921-934.
22. Morello KC, Wurz GT, DeGregorio MW. Pharmacokinetics of selective estrogen receptor modulators. Clin pharmacokinet. 2003;42(4):361-372.
23. Lewiecki EM, Miller PD, Harris ST, et al. Understanding and communicating the benefits and risks of denosumab, raloxifene, and teriparatide for the treatment of osteoporosis. J Clin Densitom. 2014;17(4):490-495.
24. Raloxifene Hydrochloride. Micromedex 2.0. Truven Health Analytics. www.micromedexsolutions.com. Accessed July 24, 2016.
25. Kulkarni J, Gavrilidis E, Gwini SM, et al. Effect of adjunctive raloxifene therapy on severity of refractory schizophrenia in women: a randomized clinical trial. JAMA Psychiatry. 2016;73(9):947-954.
26. Huerta-Ramos E, Iniesta R, Ochoa S, et al. Effects of raloxifene on cognition in postmenopausal women with schizophrenia: a double-blind, randomized, placebo-controlled trial. Eur Neuropsychopharmacol. 2014;24(2):223-231.
27. Kianimehr G, Fatehi F, Hashempoor S, et al. Raloxifene adjunctive therapy for postmenopausal women suffering from chronic schizophrenia: a randomized double-blind and placebo controlled trial. Daru. 2014;22:55.
28. Stuenkel CA, Davis SR, Gompel A, et al. Treatment of symptoms of the menopause: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(11):3975-4011.
29. Ellis AJ, Hendrick VM, Williams R, et al. Selective estrogen receptor modulators in clinical practice: a safety overview. Expert Opin Drug Saf. 2015;14(6):921-934.
30. Adomaityte J, Farooq M, Qayyum R. Effect of raloxifene therapy on venous thromboembolism in postmenopausal women. A meta-analysis. Thromb Haemost. 2008;99(2):338-342.
31. Lewiecki EM, Miller PD, Harris ST, et al. Understanding and communicating the benefits and risks of denosumab, raloxifene, and teriparatide for the treatment of osteoporosis. J Clin Densitom. 2014;17(4):490-495.
32. Grady D, Cauley JA, Stock JL, et al. Effect of raloxifene on all-cause mortality. Am J Med. 2010;123(5):469.e1-461.e7.
Admission to an inpatient psychiatry unit or a medical unit? Consider 3 Ms and 3 Ps
Hospital psychiatrists often are asked whether a patient with comorbid medical and psychiatric illnesses should be admitted to an inpatient psychiatry unit or to a medical unit. Psychiatric units vary widely in their capacity to manage patients’ medical conditions. Medical comorbidity also is associated with longer psychiatric hospitalizations.1 The decision of where to admit may be particularly challenging when presented with a patient with delirium, which often mimics primary psychiatric illnesses such as depression but will not resolve without treatment of the underlying illness. While diagnosis and treatment of delirium typically occur in the hospital setting, 1 study found that approximately 15% of 199 psychiatric inpatients were delirious and that these patients had hospital stays that were approximately 62% longer than those without delirium.2
When you need to determine whether a patient should be admitted to an inpatient psychiatry unit with a medical consult or vice versa, consider the following 3 Ms and 3 Ps.
Medications. Can medications, including those that are given intravenously or require serum monitoring, be administered on the psychiatric unit? Can the medical unit administer involuntary psychotropics?
Mobility. Does the patient require assistance with mobility? Does the patient pose a fall risk? A physical therapy consult may be helpful.
Monitoring. Suicide risk is the most common indication for patient sitters.3 Would a patient sitter be needed for the patient? On the other hand, can the psychiatry unit manage telemetry, frequent vital signs, or infectious disease precautions?
People. Would the patient benefit from the therapeutic milieu and specialized staff of an inpatient psychiatry unit?
Prognosis. What ongoing medical and psychiatric management is required? What are the medical and psychiatric prognoses?
Placement. To where will the patient be transferred after hospitalization? How does admission to inpatient psychiatry vs medical impact the ultimate disposition?
Help the treatment team make the decision
Determining the ideal patient placement often evokes strong feelings among treatment teams. Psychiatrists can help facilitate the conversation by asking the questions outlined above, and by keeping in mind, “What is best for this patient?”
1. Rodrigues-Silva N, Ribeiro L. Impact of medical comorbidity in psychiatric inpatient length of stay. J Ment Health. 2017:1-5 [epub ahead of print].
2. Ritchie J, Steiner W, Abrahamowicz M. Incidence of and risk factors for delirium among psychiatric inpatients. Psychiatr Serv. 1996;47(7):727-730.
3. Solimine S, Takeshita J, Goebert D, et al. Characteristics of patients with constant observers. Psychosomatics. 2018;59(1):67-74.
Hospital psychiatrists often are asked whether a patient with comorbid medical and psychiatric illnesses should be admitted to an inpatient psychiatry unit or to a medical unit. Psychiatric units vary widely in their capacity to manage patients’ medical conditions. Medical comorbidity also is associated with longer psychiatric hospitalizations.1 The decision of where to admit may be particularly challenging when presented with a patient with delirium, which often mimics primary psychiatric illnesses such as depression but will not resolve without treatment of the underlying illness. While diagnosis and treatment of delirium typically occur in the hospital setting, 1 study found that approximately 15% of 199 psychiatric inpatients were delirious and that these patients had hospital stays that were approximately 62% longer than those without delirium.2
When you need to determine whether a patient should be admitted to an inpatient psychiatry unit with a medical consult or vice versa, consider the following 3 Ms and 3 Ps.
Medications. Can medications, including those that are given intravenously or require serum monitoring, be administered on the psychiatric unit? Can the medical unit administer involuntary psychotropics?
Mobility. Does the patient require assistance with mobility? Does the patient pose a fall risk? A physical therapy consult may be helpful.
Monitoring. Suicide risk is the most common indication for patient sitters.3 Would a patient sitter be needed for the patient? On the other hand, can the psychiatry unit manage telemetry, frequent vital signs, or infectious disease precautions?
People. Would the patient benefit from the therapeutic milieu and specialized staff of an inpatient psychiatry unit?
Prognosis. What ongoing medical and psychiatric management is required? What are the medical and psychiatric prognoses?
Placement. To where will the patient be transferred after hospitalization? How does admission to inpatient psychiatry vs medical impact the ultimate disposition?
Help the treatment team make the decision
Determining the ideal patient placement often evokes strong feelings among treatment teams. Psychiatrists can help facilitate the conversation by asking the questions outlined above, and by keeping in mind, “What is best for this patient?”
Hospital psychiatrists often are asked whether a patient with comorbid medical and psychiatric illnesses should be admitted to an inpatient psychiatry unit or to a medical unit. Psychiatric units vary widely in their capacity to manage patients’ medical conditions. Medical comorbidity also is associated with longer psychiatric hospitalizations.1 The decision of where to admit may be particularly challenging when presented with a patient with delirium, which often mimics primary psychiatric illnesses such as depression but will not resolve without treatment of the underlying illness. While diagnosis and treatment of delirium typically occur in the hospital setting, 1 study found that approximately 15% of 199 psychiatric inpatients were delirious and that these patients had hospital stays that were approximately 62% longer than those without delirium.2
When you need to determine whether a patient should be admitted to an inpatient psychiatry unit with a medical consult or vice versa, consider the following 3 Ms and 3 Ps.
Medications. Can medications, including those that are given intravenously or require serum monitoring, be administered on the psychiatric unit? Can the medical unit administer involuntary psychotropics?
Mobility. Does the patient require assistance with mobility? Does the patient pose a fall risk? A physical therapy consult may be helpful.
Monitoring. Suicide risk is the most common indication for patient sitters.3 Would a patient sitter be needed for the patient? On the other hand, can the psychiatry unit manage telemetry, frequent vital signs, or infectious disease precautions?
People. Would the patient benefit from the therapeutic milieu and specialized staff of an inpatient psychiatry unit?
Prognosis. What ongoing medical and psychiatric management is required? What are the medical and psychiatric prognoses?
Placement. To where will the patient be transferred after hospitalization? How does admission to inpatient psychiatry vs medical impact the ultimate disposition?
Help the treatment team make the decision
Determining the ideal patient placement often evokes strong feelings among treatment teams. Psychiatrists can help facilitate the conversation by asking the questions outlined above, and by keeping in mind, “What is best for this patient?”
1. Rodrigues-Silva N, Ribeiro L. Impact of medical comorbidity in psychiatric inpatient length of stay. J Ment Health. 2017:1-5 [epub ahead of print].
2. Ritchie J, Steiner W, Abrahamowicz M. Incidence of and risk factors for delirium among psychiatric inpatients. Psychiatr Serv. 1996;47(7):727-730.
3. Solimine S, Takeshita J, Goebert D, et al. Characteristics of patients with constant observers. Psychosomatics. 2018;59(1):67-74.
1. Rodrigues-Silva N, Ribeiro L. Impact of medical comorbidity in psychiatric inpatient length of stay. J Ment Health. 2017:1-5 [epub ahead of print].
2. Ritchie J, Steiner W, Abrahamowicz M. Incidence of and risk factors for delirium among psychiatric inpatients. Psychiatr Serv. 1996;47(7):727-730.
3. Solimine S, Takeshita J, Goebert D, et al. Characteristics of patients with constant observers. Psychosomatics. 2018;59(1):67-74.
How to handle unsolicited e-mails
The ubiquitous use of e-mail has opened the proverbial “Pandora’s box” of access to psychiatrists. Our e-mail addresses are readily available online via search engines or on hospital Web sites. E-mail has become a convenient method of communicating with patients; however, it also has resulted in a proliferation of unsolicited e-mails sent to physicians from people they don’t know seeking professional advice.1 If you publish medical literature or make media appearances, you may be contacted by such individuals requesting your expertise.
Unsolicited e-mails present psychiatrists with ethical and legal quandaries that force them to consider how they can balance the human reflex to offer assistance against the potential ramifications of replying. These conundrums include:
- whether the sender is an actual person, and whether he or she is asking for advice
- the risks of replying vs not replying
- the possibility that there is a plausible crisis or danger to the sender or others
- the potential for establishing a doctor–patient relationship by replying
- the legal liability that might be incurred by replying.2
Take preemptive measures
There is guidance on how to e-mail your patients and respond to solicited e-mails, but there is a dearth of literature on how to respond to unsolicited e-mails. Anecdotal reports and limited literature suggest several possible measures you could take for managing unsolicited e-mails:
- Establish a policy of never opening unsolicited e-mails
- Create a strict junk-mail filter to prevent unsolicited e-mails from being delivered to your inbox
- Set up an automatic reply stating that unwanted or unsolicited e-mails will not be read and/or that no reply will be provided
- Read unsolicited e-mails, but immediately delete them without replying
- Acknowledge the sender in a reply, but state that you are unable to assist and decline further contact
- Send a generic reply clarifying that you are unable to provide medical assistance, and encourage the sender to seek help locally.2
Despite the urge to help, consider the consequences
In addition to taking up valuable time, unsolicited e-mails create legal and ethical predicaments that could subject you to legal liability if you choose to reply. Even though your intentions may be altruistic and you want to be helpfu
1. D’Alessandro DM, D’Alessandro MP, Colbert S. A proposed solution for addressing the challenge of patient cries for help through an analysis of unsolicited electronic email. Pediatrics. 2000;105(6):E74.
2. Friedman SH, Appel JM, Ash P, et al. Unsolicited e-mails to forensic psychiatrists. J Am Acad Psychiatry Law. 2016;44(4):470-478.
The ubiquitous use of e-mail has opened the proverbial “Pandora’s box” of access to psychiatrists. Our e-mail addresses are readily available online via search engines or on hospital Web sites. E-mail has become a convenient method of communicating with patients; however, it also has resulted in a proliferation of unsolicited e-mails sent to physicians from people they don’t know seeking professional advice.1 If you publish medical literature or make media appearances, you may be contacted by such individuals requesting your expertise.
Unsolicited e-mails present psychiatrists with ethical and legal quandaries that force them to consider how they can balance the human reflex to offer assistance against the potential ramifications of replying. These conundrums include:
- whether the sender is an actual person, and whether he or she is asking for advice
- the risks of replying vs not replying
- the possibility that there is a plausible crisis or danger to the sender or others
- the potential for establishing a doctor–patient relationship by replying
- the legal liability that might be incurred by replying.2
Take preemptive measures
There is guidance on how to e-mail your patients and respond to solicited e-mails, but there is a dearth of literature on how to respond to unsolicited e-mails. Anecdotal reports and limited literature suggest several possible measures you could take for managing unsolicited e-mails:
- Establish a policy of never opening unsolicited e-mails
- Create a strict junk-mail filter to prevent unsolicited e-mails from being delivered to your inbox
- Set up an automatic reply stating that unwanted or unsolicited e-mails will not be read and/or that no reply will be provided
- Read unsolicited e-mails, but immediately delete them without replying
- Acknowledge the sender in a reply, but state that you are unable to assist and decline further contact
- Send a generic reply clarifying that you are unable to provide medical assistance, and encourage the sender to seek help locally.2
Despite the urge to help, consider the consequences
In addition to taking up valuable time, unsolicited e-mails create legal and ethical predicaments that could subject you to legal liability if you choose to reply. Even though your intentions may be altruistic and you want to be helpfu
The ubiquitous use of e-mail has opened the proverbial “Pandora’s box” of access to psychiatrists. Our e-mail addresses are readily available online via search engines or on hospital Web sites. E-mail has become a convenient method of communicating with patients; however, it also has resulted in a proliferation of unsolicited e-mails sent to physicians from people they don’t know seeking professional advice.1 If you publish medical literature or make media appearances, you may be contacted by such individuals requesting your expertise.
Unsolicited e-mails present psychiatrists with ethical and legal quandaries that force them to consider how they can balance the human reflex to offer assistance against the potential ramifications of replying. These conundrums include:
- whether the sender is an actual person, and whether he or she is asking for advice
- the risks of replying vs not replying
- the possibility that there is a plausible crisis or danger to the sender or others
- the potential for establishing a doctor–patient relationship by replying
- the legal liability that might be incurred by replying.2
Take preemptive measures
There is guidance on how to e-mail your patients and respond to solicited e-mails, but there is a dearth of literature on how to respond to unsolicited e-mails. Anecdotal reports and limited literature suggest several possible measures you could take for managing unsolicited e-mails:
- Establish a policy of never opening unsolicited e-mails
- Create a strict junk-mail filter to prevent unsolicited e-mails from being delivered to your inbox
- Set up an automatic reply stating that unwanted or unsolicited e-mails will not be read and/or that no reply will be provided
- Read unsolicited e-mails, but immediately delete them without replying
- Acknowledge the sender in a reply, but state that you are unable to assist and decline further contact
- Send a generic reply clarifying that you are unable to provide medical assistance, and encourage the sender to seek help locally.2
Despite the urge to help, consider the consequences
In addition to taking up valuable time, unsolicited e-mails create legal and ethical predicaments that could subject you to legal liability if you choose to reply. Even though your intentions may be altruistic and you want to be helpfu
1. D’Alessandro DM, D’Alessandro MP, Colbert S. A proposed solution for addressing the challenge of patient cries for help through an analysis of unsolicited electronic email. Pediatrics. 2000;105(6):E74.
2. Friedman SH, Appel JM, Ash P, et al. Unsolicited e-mails to forensic psychiatrists. J Am Acad Psychiatry Law. 2016;44(4):470-478.
1. D’Alessandro DM, D’Alessandro MP, Colbert S. A proposed solution for addressing the challenge of patient cries for help through an analysis of unsolicited electronic email. Pediatrics. 2000;105(6):E74.
2. Friedman SH, Appel JM, Ash P, et al. Unsolicited e-mails to forensic psychiatrists. J Am Acad Psychiatry Law. 2016;44(4):470-478.
Can mood stabilizers reduce chronic pain in patients with bipolar disorder?
Misuse of prescription opioids has led to a staggering number of patients developing addiction, which the National Institutes of Health (NIH) and Department of Health and Human Services (HHS) have identified as a health care crisis. In the United States, approximately 29% of patients prescribed an opioid misuse it, and approximately 80% of heroin users started with prescription opioids.1,2 The NIH and HHS have outlined 5 priorities to help resolve this crisis:
- Improve access to prevention, treatment, and recovery support services
- Increase availability and distribution of overdose-reversing medications
- As the epidemic changes, strengthen what we know with improved public health surveillance
- Support research that advances the understanding of pain and addiction and that develops new treatments and interventions
- Improve pain management by utilizing evidence-based practices and reducing opioid misuse and opiate-related harm.3
Treating chronic pain in patients with bipolar disorder
At the Missouri University Psychiatric Center, an inpatient psychiatric ward, we recently conducted a retrospective cohort study to identify effective alternatives for treating pain, and to decrease opioid-related harm. Our study focused on 73 inpatients experiencing exacerbation of bipolar I disorder who also had chronic pain. These patients were treated with mood stabilizers, including lithium and carbamazepine. Patients also were taking medications, as needed, for agitation and their home medications for various medical problems. Selection of mood stabilizer therapy was non-random by standard of care based on best clinical practices. Dosing was based on blood-level monitoring adjusted to maintain therapeutic levels while receiving inpatient care. The average duration of inpatient treatment was approximately 1 to 5 weeks.
Pain was measured at baseline and compared with daily pain scores after mood stabilizer therapy using a 10-point scale, with 0 for no pain to 10 for worse pain, for the duration of the admission As expected based on the findings of previous research, carbamazepine resulted in a decrease in average daily pain score by 1.25 points after treatment (P = .048; F value = 4.3; F-crit = 4.23; calculated by one-way analysis of variance). However, patients who received lithium experienced a greater decrease in average daily pain score, by 2.17 points after treatment (P = .00035; F value = 14.56; F-crit = 4.02).
To further characterize the relationship between bipolar disorder and chronic pain, we looked at change in pain scores for mixed, manic, and depressive episodes of bipolar disorder by Clinical Global Impressions—Improvement (CGI-I) Scale categories (Figure). Participants who experienced the greatest clinical improvement also experienced the highest degree of analgesia. Those in the “Very much improved” CGI-I category experienced an almost 3-point decrease in average daily pain scores, with significance well below threshold (P = .0000967; F value = 19.83; F-crit = 4.11). Participants who showed no change in their bipolar I disorder symptoms or experienced exacerbation of their symptoms showed a significant increase in pain scores (P = .037; F value = 6.24; F-crit = 5.32).
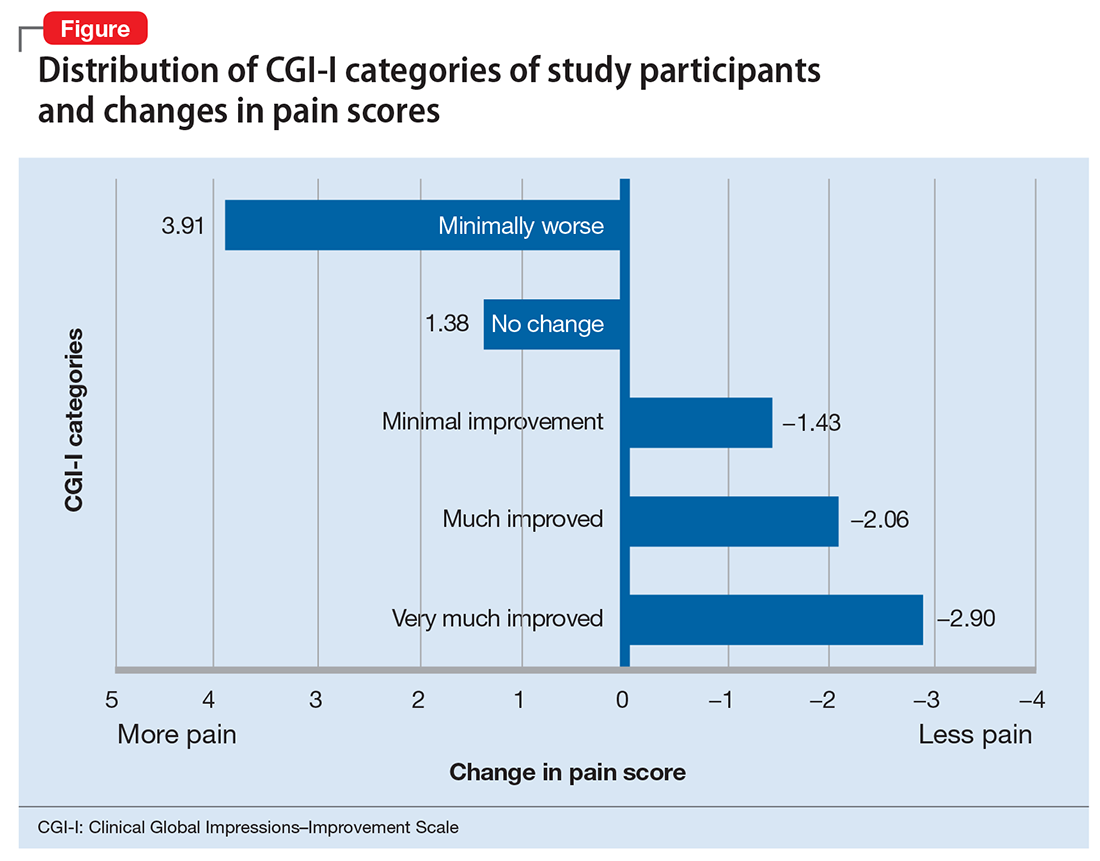
Our data show that lithium and carbamazepine provide clinically and statistically significant analgesia in patients with bipolar I disorder and chronic pain. Furthermore, exacerbation of bipolar I disorder symptoms was associated with an increase of approximately 4 points on a 10-point chronic pain scale.
Acknowledgments
We would like to acknowledge contributions of Yajie Yu, MD, Sailaja Bysani, MD, Emily Leary, PhD, and Oluwole Popoola, MD, for their work in this study.
1. Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4):569-576.
2. Muhuri PK, Gfroerer JC, Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Rev. 2013.
3. National Institutes of Health. Department of Health and Human Services. Opiate crisis. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-crisis. Updated January 2018. Accessed February 5, 2018.
Misuse of prescription opioids has led to a staggering number of patients developing addiction, which the National Institutes of Health (NIH) and Department of Health and Human Services (HHS) have identified as a health care crisis. In the United States, approximately 29% of patients prescribed an opioid misuse it, and approximately 80% of heroin users started with prescription opioids.1,2 The NIH and HHS have outlined 5 priorities to help resolve this crisis:
- Improve access to prevention, treatment, and recovery support services
- Increase availability and distribution of overdose-reversing medications
- As the epidemic changes, strengthen what we know with improved public health surveillance
- Support research that advances the understanding of pain and addiction and that develops new treatments and interventions
- Improve pain management by utilizing evidence-based practices and reducing opioid misuse and opiate-related harm.3
Treating chronic pain in patients with bipolar disorder
At the Missouri University Psychiatric Center, an inpatient psychiatric ward, we recently conducted a retrospective cohort study to identify effective alternatives for treating pain, and to decrease opioid-related harm. Our study focused on 73 inpatients experiencing exacerbation of bipolar I disorder who also had chronic pain. These patients were treated with mood stabilizers, including lithium and carbamazepine. Patients also were taking medications, as needed, for agitation and their home medications for various medical problems. Selection of mood stabilizer therapy was non-random by standard of care based on best clinical practices. Dosing was based on blood-level monitoring adjusted to maintain therapeutic levels while receiving inpatient care. The average duration of inpatient treatment was approximately 1 to 5 weeks.
Pain was measured at baseline and compared with daily pain scores after mood stabilizer therapy using a 10-point scale, with 0 for no pain to 10 for worse pain, for the duration of the admission As expected based on the findings of previous research, carbamazepine resulted in a decrease in average daily pain score by 1.25 points after treatment (P = .048; F value = 4.3; F-crit = 4.23; calculated by one-way analysis of variance). However, patients who received lithium experienced a greater decrease in average daily pain score, by 2.17 points after treatment (P = .00035; F value = 14.56; F-crit = 4.02).
To further characterize the relationship between bipolar disorder and chronic pain, we looked at change in pain scores for mixed, manic, and depressive episodes of bipolar disorder by Clinical Global Impressions—Improvement (CGI-I) Scale categories (Figure). Participants who experienced the greatest clinical improvement also experienced the highest degree of analgesia. Those in the “Very much improved” CGI-I category experienced an almost 3-point decrease in average daily pain scores, with significance well below threshold (P = .0000967; F value = 19.83; F-crit = 4.11). Participants who showed no change in their bipolar I disorder symptoms or experienced exacerbation of their symptoms showed a significant increase in pain scores (P = .037; F value = 6.24; F-crit = 5.32).
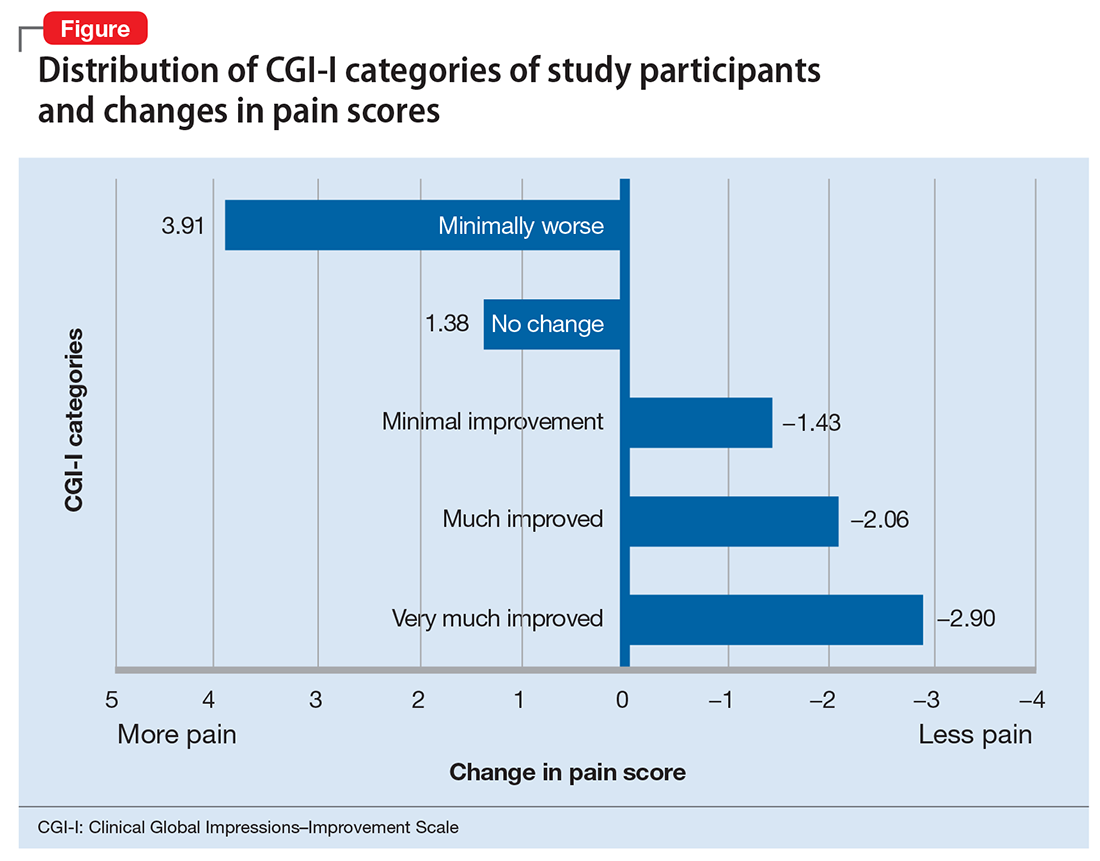
Our data show that lithium and carbamazepine provide clinically and statistically significant analgesia in patients with bipolar I disorder and chronic pain. Furthermore, exacerbation of bipolar I disorder symptoms was associated with an increase of approximately 4 points on a 10-point chronic pain scale.
Acknowledgments
We would like to acknowledge contributions of Yajie Yu, MD, Sailaja Bysani, MD, Emily Leary, PhD, and Oluwole Popoola, MD, for their work in this study.
Misuse of prescription opioids has led to a staggering number of patients developing addiction, which the National Institutes of Health (NIH) and Department of Health and Human Services (HHS) have identified as a health care crisis. In the United States, approximately 29% of patients prescribed an opioid misuse it, and approximately 80% of heroin users started with prescription opioids.1,2 The NIH and HHS have outlined 5 priorities to help resolve this crisis:
- Improve access to prevention, treatment, and recovery support services
- Increase availability and distribution of overdose-reversing medications
- As the epidemic changes, strengthen what we know with improved public health surveillance
- Support research that advances the understanding of pain and addiction and that develops new treatments and interventions
- Improve pain management by utilizing evidence-based practices and reducing opioid misuse and opiate-related harm.3
Treating chronic pain in patients with bipolar disorder
At the Missouri University Psychiatric Center, an inpatient psychiatric ward, we recently conducted a retrospective cohort study to identify effective alternatives for treating pain, and to decrease opioid-related harm. Our study focused on 73 inpatients experiencing exacerbation of bipolar I disorder who also had chronic pain. These patients were treated with mood stabilizers, including lithium and carbamazepine. Patients also were taking medications, as needed, for agitation and their home medications for various medical problems. Selection of mood stabilizer therapy was non-random by standard of care based on best clinical practices. Dosing was based on blood-level monitoring adjusted to maintain therapeutic levels while receiving inpatient care. The average duration of inpatient treatment was approximately 1 to 5 weeks.
Pain was measured at baseline and compared with daily pain scores after mood stabilizer therapy using a 10-point scale, with 0 for no pain to 10 for worse pain, for the duration of the admission As expected based on the findings of previous research, carbamazepine resulted in a decrease in average daily pain score by 1.25 points after treatment (P = .048; F value = 4.3; F-crit = 4.23; calculated by one-way analysis of variance). However, patients who received lithium experienced a greater decrease in average daily pain score, by 2.17 points after treatment (P = .00035; F value = 14.56; F-crit = 4.02).
To further characterize the relationship between bipolar disorder and chronic pain, we looked at change in pain scores for mixed, manic, and depressive episodes of bipolar disorder by Clinical Global Impressions—Improvement (CGI-I) Scale categories (Figure). Participants who experienced the greatest clinical improvement also experienced the highest degree of analgesia. Those in the “Very much improved” CGI-I category experienced an almost 3-point decrease in average daily pain scores, with significance well below threshold (P = .0000967; F value = 19.83; F-crit = 4.11). Participants who showed no change in their bipolar I disorder symptoms or experienced exacerbation of their symptoms showed a significant increase in pain scores (P = .037; F value = 6.24; F-crit = 5.32).
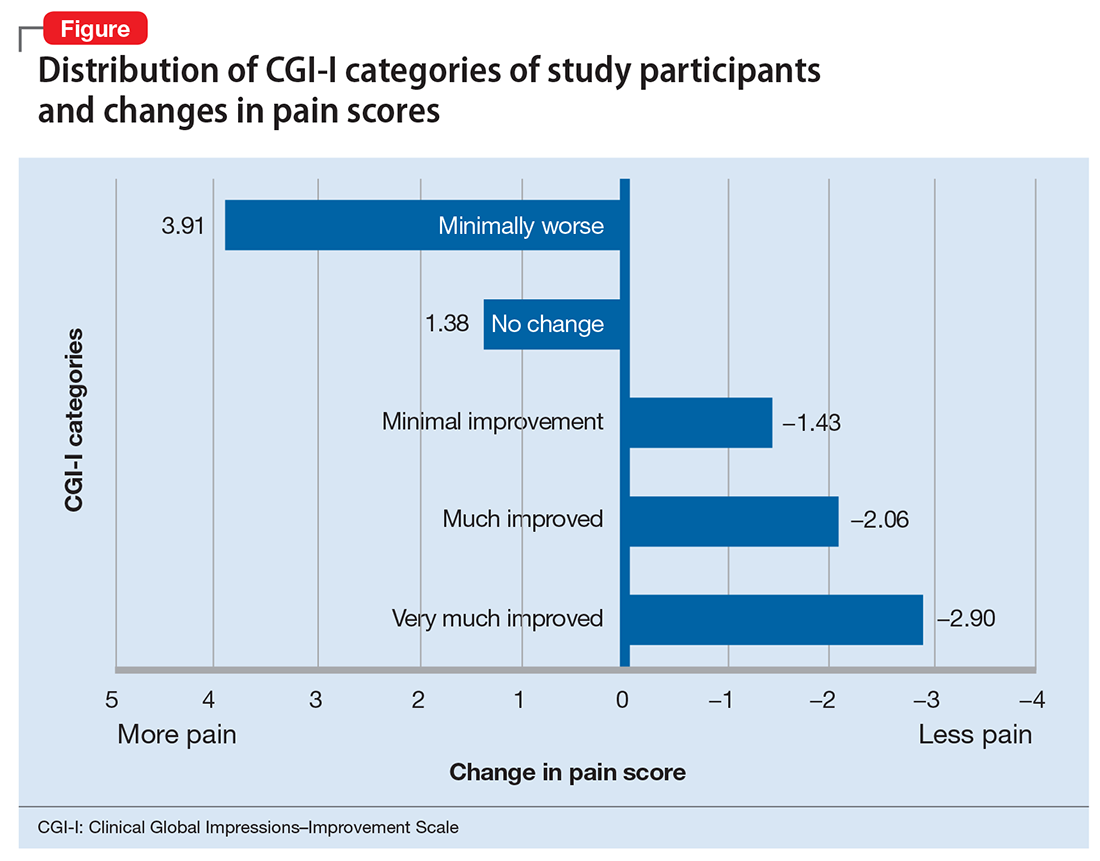
Our data show that lithium and carbamazepine provide clinically and statistically significant analgesia in patients with bipolar I disorder and chronic pain. Furthermore, exacerbation of bipolar I disorder symptoms was associated with an increase of approximately 4 points on a 10-point chronic pain scale.
Acknowledgments
We would like to acknowledge contributions of Yajie Yu, MD, Sailaja Bysani, MD, Emily Leary, PhD, and Oluwole Popoola, MD, for their work in this study.
1. Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4):569-576.
2. Muhuri PK, Gfroerer JC, Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Rev. 2013.
3. National Institutes of Health. Department of Health and Human Services. Opiate crisis. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-crisis. Updated January 2018. Accessed February 5, 2018.
1. Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015;156(4):569-576.
2. Muhuri PK, Gfroerer JC, Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Rev. 2013.
3. National Institutes of Health. Department of Health and Human Services. Opiate crisis. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-crisis. Updated January 2018. Accessed February 5, 2018.
Diffuse erythematous rash resistant to treatment
A 39-year-old woman presented to the emergency department for evaluation of diffuse redness, itching, and tenderness of her skin. The patient said the eruption began 4 months earlier as localized plaques on her scalp, elbows, and beneath both breasts. Over the course of a few days, the redness became more diffuse, affecting most of her body. She also noticed swelling and skin desquamation on her lower extremities.
The patient had visited multiple urgent care clinics and underwent several courses of prednisone with initial improvement of symptoms, but experienced recurrence shortly after finishing the tapers.
On physical examination, more than 95% of the patient’s skin was bright red and tender to the touch, with associated exfoliation (FIGURES 1A-1B). Her lower extremities had pitting edema with superficial erosions that were weeping serous fluid. She was afebrile and normotensive, but had shaking chills and was tachycardic, with a heart rate of 115 bpm. There was no nail pitting, pustules, or lymphadenopathy. Lab tests revealed a low albumin level of 2.2 g/dL (normal: 3.5-5.5 g/dL), an elevated white blood cell count of 14,700 cells/mcL (normal: 4500-11,000 cells/mcL), and normocytic anemia (low hemoglobin of 8.7 g/dL; normal: 12-15.5 g/dL). The patient was admitted.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Erythroderma
Based on the patient’s clinical presentation, we diagnosed severe erythroderma secondary to psoriasis. A punch biopsy was performed, and pathology demonstrated subacute spongiotic dermatitis with superficial neutrophilic infiltrates, consistent with psoriasis.
Erythroderma is widespread reddening of the skin associated with desquamation, typically involving more than 90% of the body’s surface area.1 In most instances, erythroderma is a clinical presentation of an existing dermatosis. The most common causative conditions include primary skin disorders (such as psoriasis or atopic dermatitis), idiopathic erythroderma, and drug eruptions. Less common causes include cutaneous T-cell lymphoma, pityriasis rubra pilaris, and contact dermatitis.1
It’s unclear why some skin diseases progress to erythroderma; the pathogenesis is complicated and involves keratinocytes and lymphocytes interacting with adhesion molecules and cytokines. Erythroderma can arise at any age and occurs in all races, but is more common in males and older adults, with a mean age of 42 to 61 years.2 The annual incidence of erythroderma is estimated to be one per 100,000 adults.3
A complete picture of the patient is essential to making the diagnosis
Diagnosis can be difficult and hinges on historical and physical exam findings, as well as lab evaluations and skin biopsies. The history should focus on current and former medications, while the physical exam should hone in on clinical manifestations of existing dermatoses. The most common extracutaneous finding is generalized lymphadenopathy, which if prominent, may warrant lymph node biopsy, with studies for evaluation of underlying lymphoma.
Tachycardia develops in 40% of patients, secondary to increased blood flow to the skin and fluid loss, with risk of high-output cardiac failure.2 Patients often have chills because their skin is not able to regulate their body temperature normally.4
The lab evaluation should include a complete blood count with differential and a comprehensive metabolic panel, as well as blood, skin, and urine cultures if infection is suspected as an inciting factor. Typical findings include mild anemia, leukocytosis, eosinophilia, and an elevated erythrocyte sedimentation rate.5 In addition, patients with chronic erythroderma commonly have low albumin.6 Unfortunately, lab studies don’t always reveal the underlying cause of the erythroderma.
Biopsies are commonly performed. However, the underlying etiology is often not clearly reflected in the result. Histology is typically nonspecific; findings frequently include hyperkeratosis, acanthosis, spongiosis, and perivascular inflammatory infiltrate. Additionally, the prominence of histologic features may vary depending on the stage of disease and the severity of inflammation. More specific findings may become evident later in the disease as the erythroderma clears, so repeated skin biopsies over time may be needed for diagnosis.7
Consider these conditions, which can lead to erythroderma
First and foremost, it is important to get a thorough history, particularly about prior skin conditions and symptoms that may indicate the presence of undiagnosed skin conditions.
Psoriasis is one of the most common causes of erythroderma. A history of pre-existing psoriasis is very helpful, but when this is not present, a biopsy can help confirm a clinical suspicion for psoriasis. It also helps to look for clues of psoriasis like nail changes or a history of plaques over the elbows and knees.
Atopic dermatitis is another common cause of erythroderma, and the history might include scaling and erythematous patches or plaques involving flexural surfaces before erythroderma occurs. Patients may have a history of atopic dermatitis from childhood and/or a history of other atopic conditions such as asthma and allergic rhinitis.
Drug eruptions occur following the administration of a new medication and can mimic a myriad of dermatoses.
Cutaneous T-cell lymphoma can lead to erythroderma and be differentiated with skin biopsy; pathology may show atypical lymphocytes, and Pautrier’s microabscesses may be seen.8
Pityriasis rubra pilaris is a relatively rare condition that presents with red-orange scaling patches and thickened yellowish palms and soles.9
Tx targets underlying etiology and associated complications
When treating a patient with erythroderma, it’s important to prevent hypothermia and secondary infections. If symptoms are severe, hospitalization should be considered. Nutrition should be assessed, and any fluid or electrolyte imbalances should be corrected.
Oral antihistamines are commonly administered to suppress associated pruritus. Topical treatment usually consists of corticosteroids under occlusion with bland emollients. Depending upon the underlying disease, the following systemic medications may be started: methotrexate 7.5 to 15 mg once/week; acitretin 10 to 25 mg/d; or cyclosporine 2.5 to 5 mg/kg/d; in addition to topical treatment.4
Our patient. Pathology for our patient was indicative of psoriasis. She was started on a regimen of cyclosporine 4 to 5 mg/kg/d, diphenhydramine 25 to 50 mg as needed for itching, triamcinolone 0.1% ointment under wet wraps to her trunk and extremities, and hydrocortisone 2.5% ointment to be applied to her face daily. She was released after 5 days in the hospital. At outpatient follow-up one week later, her erythroderma was resolving. One month later, her erythroderma was resolved (FIGURE 2), although she did have psoriatic plaques on her lower legs.

CORRESPONDENCE
Richard P. Usatine, MD, University of Texas Health San Antonio, 7703 Floyd Curl Dr., San Antonio, TX 78229; [email protected].
1. Keisham C, Sahoo B, Khurana N, et al. Clinicopathologic study of erythroderma. J Am Acad Dermatol. 2013;68:AB85.
2. Li J, Zheng H-Y. Erythroderma: a clinical and prognostic study. Dermatology. 2012;225:154-162.
3. Sigurdsson V, Steegmans PH, van Vioten WA. The incidence of erythroderma: a survey among all dermatologists in The Netherlands. J Am Acad Dermatol. 2001;45:675-678.
4. Bolognia J, Schaffer J, Duncan K, et al. Dermatology essentials. 1st ed. Oxford, England: Elsevier Saunders; 2014.
5. Karakayli G, Beckham G, Orengo I, et al. Exfoliative dermatitis. Am Fam Physician. 1999;59:625-630.
6. Rothe MJ, Bialy TL, Grant-Kels JM. Erythroderma. Dermatol Clin. 2000;18:405-415.
7. Walsh NM, Prokopetz R, Tron VA, et al. Histopathology in erythroderma: review of a series of cases by multiple observers. J Cutan Pathol. 1994;21:419-423.
8. Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. Diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70:205.e1-e16.
9. Abdel-Azim NE, Ismail SA, Fathy E. Differentiation of pityriasis rubra pilaris from plaque psoriasis by dermoscopy. Arch Dermatol Res. 2017;309:311-314.
A 39-year-old woman presented to the emergency department for evaluation of diffuse redness, itching, and tenderness of her skin. The patient said the eruption began 4 months earlier as localized plaques on her scalp, elbows, and beneath both breasts. Over the course of a few days, the redness became more diffuse, affecting most of her body. She also noticed swelling and skin desquamation on her lower extremities.
The patient had visited multiple urgent care clinics and underwent several courses of prednisone with initial improvement of symptoms, but experienced recurrence shortly after finishing the tapers.
On physical examination, more than 95% of the patient’s skin was bright red and tender to the touch, with associated exfoliation (FIGURES 1A-1B). Her lower extremities had pitting edema with superficial erosions that were weeping serous fluid. She was afebrile and normotensive, but had shaking chills and was tachycardic, with a heart rate of 115 bpm. There was no nail pitting, pustules, or lymphadenopathy. Lab tests revealed a low albumin level of 2.2 g/dL (normal: 3.5-5.5 g/dL), an elevated white blood cell count of 14,700 cells/mcL (normal: 4500-11,000 cells/mcL), and normocytic anemia (low hemoglobin of 8.7 g/dL; normal: 12-15.5 g/dL). The patient was admitted.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Erythroderma
Based on the patient’s clinical presentation, we diagnosed severe erythroderma secondary to psoriasis. A punch biopsy was performed, and pathology demonstrated subacute spongiotic dermatitis with superficial neutrophilic infiltrates, consistent with psoriasis.
Erythroderma is widespread reddening of the skin associated with desquamation, typically involving more than 90% of the body’s surface area.1 In most instances, erythroderma is a clinical presentation of an existing dermatosis. The most common causative conditions include primary skin disorders (such as psoriasis or atopic dermatitis), idiopathic erythroderma, and drug eruptions. Less common causes include cutaneous T-cell lymphoma, pityriasis rubra pilaris, and contact dermatitis.1
It’s unclear why some skin diseases progress to erythroderma; the pathogenesis is complicated and involves keratinocytes and lymphocytes interacting with adhesion molecules and cytokines. Erythroderma can arise at any age and occurs in all races, but is more common in males and older adults, with a mean age of 42 to 61 years.2 The annual incidence of erythroderma is estimated to be one per 100,000 adults.3
A complete picture of the patient is essential to making the diagnosis
Diagnosis can be difficult and hinges on historical and physical exam findings, as well as lab evaluations and skin biopsies. The history should focus on current and former medications, while the physical exam should hone in on clinical manifestations of existing dermatoses. The most common extracutaneous finding is generalized lymphadenopathy, which if prominent, may warrant lymph node biopsy, with studies for evaluation of underlying lymphoma.
Tachycardia develops in 40% of patients, secondary to increased blood flow to the skin and fluid loss, with risk of high-output cardiac failure.2 Patients often have chills because their skin is not able to regulate their body temperature normally.4
The lab evaluation should include a complete blood count with differential and a comprehensive metabolic panel, as well as blood, skin, and urine cultures if infection is suspected as an inciting factor. Typical findings include mild anemia, leukocytosis, eosinophilia, and an elevated erythrocyte sedimentation rate.5 In addition, patients with chronic erythroderma commonly have low albumin.6 Unfortunately, lab studies don’t always reveal the underlying cause of the erythroderma.
Biopsies are commonly performed. However, the underlying etiology is often not clearly reflected in the result. Histology is typically nonspecific; findings frequently include hyperkeratosis, acanthosis, spongiosis, and perivascular inflammatory infiltrate. Additionally, the prominence of histologic features may vary depending on the stage of disease and the severity of inflammation. More specific findings may become evident later in the disease as the erythroderma clears, so repeated skin biopsies over time may be needed for diagnosis.7
Consider these conditions, which can lead to erythroderma
First and foremost, it is important to get a thorough history, particularly about prior skin conditions and symptoms that may indicate the presence of undiagnosed skin conditions.
Psoriasis is one of the most common causes of erythroderma. A history of pre-existing psoriasis is very helpful, but when this is not present, a biopsy can help confirm a clinical suspicion for psoriasis. It also helps to look for clues of psoriasis like nail changes or a history of plaques over the elbows and knees.
Atopic dermatitis is another common cause of erythroderma, and the history might include scaling and erythematous patches or plaques involving flexural surfaces before erythroderma occurs. Patients may have a history of atopic dermatitis from childhood and/or a history of other atopic conditions such as asthma and allergic rhinitis.
Drug eruptions occur following the administration of a new medication and can mimic a myriad of dermatoses.
Cutaneous T-cell lymphoma can lead to erythroderma and be differentiated with skin biopsy; pathology may show atypical lymphocytes, and Pautrier’s microabscesses may be seen.8
Pityriasis rubra pilaris is a relatively rare condition that presents with red-orange scaling patches and thickened yellowish palms and soles.9
Tx targets underlying etiology and associated complications
When treating a patient with erythroderma, it’s important to prevent hypothermia and secondary infections. If symptoms are severe, hospitalization should be considered. Nutrition should be assessed, and any fluid or electrolyte imbalances should be corrected.
Oral antihistamines are commonly administered to suppress associated pruritus. Topical treatment usually consists of corticosteroids under occlusion with bland emollients. Depending upon the underlying disease, the following systemic medications may be started: methotrexate 7.5 to 15 mg once/week; acitretin 10 to 25 mg/d; or cyclosporine 2.5 to 5 mg/kg/d; in addition to topical treatment.4
Our patient. Pathology for our patient was indicative of psoriasis. She was started on a regimen of cyclosporine 4 to 5 mg/kg/d, diphenhydramine 25 to 50 mg as needed for itching, triamcinolone 0.1% ointment under wet wraps to her trunk and extremities, and hydrocortisone 2.5% ointment to be applied to her face daily. She was released after 5 days in the hospital. At outpatient follow-up one week later, her erythroderma was resolving. One month later, her erythroderma was resolved (FIGURE 2), although she did have psoriatic plaques on her lower legs.

CORRESPONDENCE
Richard P. Usatine, MD, University of Texas Health San Antonio, 7703 Floyd Curl Dr., San Antonio, TX 78229; [email protected].
A 39-year-old woman presented to the emergency department for evaluation of diffuse redness, itching, and tenderness of her skin. The patient said the eruption began 4 months earlier as localized plaques on her scalp, elbows, and beneath both breasts. Over the course of a few days, the redness became more diffuse, affecting most of her body. She also noticed swelling and skin desquamation on her lower extremities.
The patient had visited multiple urgent care clinics and underwent several courses of prednisone with initial improvement of symptoms, but experienced recurrence shortly after finishing the tapers.
On physical examination, more than 95% of the patient’s skin was bright red and tender to the touch, with associated exfoliation (FIGURES 1A-1B). Her lower extremities had pitting edema with superficial erosions that were weeping serous fluid. She was afebrile and normotensive, but had shaking chills and was tachycardic, with a heart rate of 115 bpm. There was no nail pitting, pustules, or lymphadenopathy. Lab tests revealed a low albumin level of 2.2 g/dL (normal: 3.5-5.5 g/dL), an elevated white blood cell count of 14,700 cells/mcL (normal: 4500-11,000 cells/mcL), and normocytic anemia (low hemoglobin of 8.7 g/dL; normal: 12-15.5 g/dL). The patient was admitted.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Erythroderma
Based on the patient’s clinical presentation, we diagnosed severe erythroderma secondary to psoriasis. A punch biopsy was performed, and pathology demonstrated subacute spongiotic dermatitis with superficial neutrophilic infiltrates, consistent with psoriasis.
Erythroderma is widespread reddening of the skin associated with desquamation, typically involving more than 90% of the body’s surface area.1 In most instances, erythroderma is a clinical presentation of an existing dermatosis. The most common causative conditions include primary skin disorders (such as psoriasis or atopic dermatitis), idiopathic erythroderma, and drug eruptions. Less common causes include cutaneous T-cell lymphoma, pityriasis rubra pilaris, and contact dermatitis.1
It’s unclear why some skin diseases progress to erythroderma; the pathogenesis is complicated and involves keratinocytes and lymphocytes interacting with adhesion molecules and cytokines. Erythroderma can arise at any age and occurs in all races, but is more common in males and older adults, with a mean age of 42 to 61 years.2 The annual incidence of erythroderma is estimated to be one per 100,000 adults.3
A complete picture of the patient is essential to making the diagnosis
Diagnosis can be difficult and hinges on historical and physical exam findings, as well as lab evaluations and skin biopsies. The history should focus on current and former medications, while the physical exam should hone in on clinical manifestations of existing dermatoses. The most common extracutaneous finding is generalized lymphadenopathy, which if prominent, may warrant lymph node biopsy, with studies for evaluation of underlying lymphoma.
Tachycardia develops in 40% of patients, secondary to increased blood flow to the skin and fluid loss, with risk of high-output cardiac failure.2 Patients often have chills because their skin is not able to regulate their body temperature normally.4
The lab evaluation should include a complete blood count with differential and a comprehensive metabolic panel, as well as blood, skin, and urine cultures if infection is suspected as an inciting factor. Typical findings include mild anemia, leukocytosis, eosinophilia, and an elevated erythrocyte sedimentation rate.5 In addition, patients with chronic erythroderma commonly have low albumin.6 Unfortunately, lab studies don’t always reveal the underlying cause of the erythroderma.
Biopsies are commonly performed. However, the underlying etiology is often not clearly reflected in the result. Histology is typically nonspecific; findings frequently include hyperkeratosis, acanthosis, spongiosis, and perivascular inflammatory infiltrate. Additionally, the prominence of histologic features may vary depending on the stage of disease and the severity of inflammation. More specific findings may become evident later in the disease as the erythroderma clears, so repeated skin biopsies over time may be needed for diagnosis.7
Consider these conditions, which can lead to erythroderma
First and foremost, it is important to get a thorough history, particularly about prior skin conditions and symptoms that may indicate the presence of undiagnosed skin conditions.
Psoriasis is one of the most common causes of erythroderma. A history of pre-existing psoriasis is very helpful, but when this is not present, a biopsy can help confirm a clinical suspicion for psoriasis. It also helps to look for clues of psoriasis like nail changes or a history of plaques over the elbows and knees.
Atopic dermatitis is another common cause of erythroderma, and the history might include scaling and erythematous patches or plaques involving flexural surfaces before erythroderma occurs. Patients may have a history of atopic dermatitis from childhood and/or a history of other atopic conditions such as asthma and allergic rhinitis.
Drug eruptions occur following the administration of a new medication and can mimic a myriad of dermatoses.
Cutaneous T-cell lymphoma can lead to erythroderma and be differentiated with skin biopsy; pathology may show atypical lymphocytes, and Pautrier’s microabscesses may be seen.8
Pityriasis rubra pilaris is a relatively rare condition that presents with red-orange scaling patches and thickened yellowish palms and soles.9
Tx targets underlying etiology and associated complications
When treating a patient with erythroderma, it’s important to prevent hypothermia and secondary infections. If symptoms are severe, hospitalization should be considered. Nutrition should be assessed, and any fluid or electrolyte imbalances should be corrected.
Oral antihistamines are commonly administered to suppress associated pruritus. Topical treatment usually consists of corticosteroids under occlusion with bland emollients. Depending upon the underlying disease, the following systemic medications may be started: methotrexate 7.5 to 15 mg once/week; acitretin 10 to 25 mg/d; or cyclosporine 2.5 to 5 mg/kg/d; in addition to topical treatment.4
Our patient. Pathology for our patient was indicative of psoriasis. She was started on a regimen of cyclosporine 4 to 5 mg/kg/d, diphenhydramine 25 to 50 mg as needed for itching, triamcinolone 0.1% ointment under wet wraps to her trunk and extremities, and hydrocortisone 2.5% ointment to be applied to her face daily. She was released after 5 days in the hospital. At outpatient follow-up one week later, her erythroderma was resolving. One month later, her erythroderma was resolved (FIGURE 2), although she did have psoriatic plaques on her lower legs.

CORRESPONDENCE
Richard P. Usatine, MD, University of Texas Health San Antonio, 7703 Floyd Curl Dr., San Antonio, TX 78229; [email protected].
1. Keisham C, Sahoo B, Khurana N, et al. Clinicopathologic study of erythroderma. J Am Acad Dermatol. 2013;68:AB85.
2. Li J, Zheng H-Y. Erythroderma: a clinical and prognostic study. Dermatology. 2012;225:154-162.
3. Sigurdsson V, Steegmans PH, van Vioten WA. The incidence of erythroderma: a survey among all dermatologists in The Netherlands. J Am Acad Dermatol. 2001;45:675-678.
4. Bolognia J, Schaffer J, Duncan K, et al. Dermatology essentials. 1st ed. Oxford, England: Elsevier Saunders; 2014.
5. Karakayli G, Beckham G, Orengo I, et al. Exfoliative dermatitis. Am Fam Physician. 1999;59:625-630.
6. Rothe MJ, Bialy TL, Grant-Kels JM. Erythroderma. Dermatol Clin. 2000;18:405-415.
7. Walsh NM, Prokopetz R, Tron VA, et al. Histopathology in erythroderma: review of a series of cases by multiple observers. J Cutan Pathol. 1994;21:419-423.
8. Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. Diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70:205.e1-e16.
9. Abdel-Azim NE, Ismail SA, Fathy E. Differentiation of pityriasis rubra pilaris from plaque psoriasis by dermoscopy. Arch Dermatol Res. 2017;309:311-314.
1. Keisham C, Sahoo B, Khurana N, et al. Clinicopathologic study of erythroderma. J Am Acad Dermatol. 2013;68:AB85.
2. Li J, Zheng H-Y. Erythroderma: a clinical and prognostic study. Dermatology. 2012;225:154-162.
3. Sigurdsson V, Steegmans PH, van Vioten WA. The incidence of erythroderma: a survey among all dermatologists in The Netherlands. J Am Acad Dermatol. 2001;45:675-678.
4. Bolognia J, Schaffer J, Duncan K, et al. Dermatology essentials. 1st ed. Oxford, England: Elsevier Saunders; 2014.
5. Karakayli G, Beckham G, Orengo I, et al. Exfoliative dermatitis. Am Fam Physician. 1999;59:625-630.
6. Rothe MJ, Bialy TL, Grant-Kels JM. Erythroderma. Dermatol Clin. 2000;18:405-415.
7. Walsh NM, Prokopetz R, Tron VA, et al. Histopathology in erythroderma: review of a series of cases by multiple observers. J Cutan Pathol. 1994;21:419-423.
8. Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part I. Diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70:205.e1-e16.
9. Abdel-Azim NE, Ismail SA, Fathy E. Differentiation of pityriasis rubra pilaris from plaque psoriasis by dermoscopy. Arch Dermatol Res. 2017;309:311-314.