User login
NIAID proposes 3-pronged plan for universal influenza vaccine
Three specific research areas were proposed by the National Institute of Allergy and Infectious Diseases (NIAID) in its development plan for a universal influenza vaccine, as detailed in a report published online in the Journal of Infectious Diseases.
Anthony S. Fauci, MD, director of the NIAID, spoke with Frontline Medical News in an interview regarding the plan and noted that he and his colleagues felt that it was important to accelerate the effort for a universal vaccine.
“The strategic plan also includes a description of research resources essential to advancing these three research areas that [the] NIAID will develop, support, and provide for the scientific community,” wrote Dr. Erbelding and her coauthors.
The development plan comes 8 months after scientists from academia, industry, and government convened for the NIAID Pathway to a Universal Influenza Vaccine workshop to address knowledge gaps and strategy, which was summarized last year in the journal Immunity (2017;47: 599-603). The scientists at the workshop developed criteria that would define a universal vaccine and decided that a universal vaccine for influenza should do three things: be at least 75% effective against symptomatic influenza infection; protect against group I and II influenza A viruses; and have durable protections that lasts at least 1 year and preferably through multiple seasons.
“Clearly, a vaccine that would cover most or all seasonal strains of influenza and also provide protection during a pandemic is highly desirable,” wrote Catharine I. Paules, MD, of the University of Maryland, Baltimore, and her coauthors in the workshop summary.
Dr. Fauci told Frontline Medical News how “experts from all over the country addressed their thoughts and concerns with us last year [at the workshop], and now we have a development plan,” he said. “But the next step will be doing the research and finding more resources. ... The work is yet to be done.”
The development plan was published amid an ongoing historic flu season.
Dr. Fauci noted that this season had particular circumstances that made it worse than normal. “I don’t think that, had we had this plan in place a year ago, it would have had an impact on this flu season,” he said.
The authors reported no relevant financial conflicts and that the National Institutes of Health produced this plan.
SOURCE: Erbelding E et al. J Infect Dis. 2018 Feb 28. doi: 10.1093/infdis/jiy103.
Three specific research areas were proposed by the National Institute of Allergy and Infectious Diseases (NIAID) in its development plan for a universal influenza vaccine, as detailed in a report published online in the Journal of Infectious Diseases.
Anthony S. Fauci, MD, director of the NIAID, spoke with Frontline Medical News in an interview regarding the plan and noted that he and his colleagues felt that it was important to accelerate the effort for a universal vaccine.
“The strategic plan also includes a description of research resources essential to advancing these three research areas that [the] NIAID will develop, support, and provide for the scientific community,” wrote Dr. Erbelding and her coauthors.
The development plan comes 8 months after scientists from academia, industry, and government convened for the NIAID Pathway to a Universal Influenza Vaccine workshop to address knowledge gaps and strategy, which was summarized last year in the journal Immunity (2017;47: 599-603). The scientists at the workshop developed criteria that would define a universal vaccine and decided that a universal vaccine for influenza should do three things: be at least 75% effective against symptomatic influenza infection; protect against group I and II influenza A viruses; and have durable protections that lasts at least 1 year and preferably through multiple seasons.
“Clearly, a vaccine that would cover most or all seasonal strains of influenza and also provide protection during a pandemic is highly desirable,” wrote Catharine I. Paules, MD, of the University of Maryland, Baltimore, and her coauthors in the workshop summary.
Dr. Fauci told Frontline Medical News how “experts from all over the country addressed their thoughts and concerns with us last year [at the workshop], and now we have a development plan,” he said. “But the next step will be doing the research and finding more resources. ... The work is yet to be done.”
The development plan was published amid an ongoing historic flu season.
Dr. Fauci noted that this season had particular circumstances that made it worse than normal. “I don’t think that, had we had this plan in place a year ago, it would have had an impact on this flu season,” he said.
The authors reported no relevant financial conflicts and that the National Institutes of Health produced this plan.
SOURCE: Erbelding E et al. J Infect Dis. 2018 Feb 28. doi: 10.1093/infdis/jiy103.
Three specific research areas were proposed by the National Institute of Allergy and Infectious Diseases (NIAID) in its development plan for a universal influenza vaccine, as detailed in a report published online in the Journal of Infectious Diseases.
Anthony S. Fauci, MD, director of the NIAID, spoke with Frontline Medical News in an interview regarding the plan and noted that he and his colleagues felt that it was important to accelerate the effort for a universal vaccine.
“The strategic plan also includes a description of research resources essential to advancing these three research areas that [the] NIAID will develop, support, and provide for the scientific community,” wrote Dr. Erbelding and her coauthors.
The development plan comes 8 months after scientists from academia, industry, and government convened for the NIAID Pathway to a Universal Influenza Vaccine workshop to address knowledge gaps and strategy, which was summarized last year in the journal Immunity (2017;47: 599-603). The scientists at the workshop developed criteria that would define a universal vaccine and decided that a universal vaccine for influenza should do three things: be at least 75% effective against symptomatic influenza infection; protect against group I and II influenza A viruses; and have durable protections that lasts at least 1 year and preferably through multiple seasons.
“Clearly, a vaccine that would cover most or all seasonal strains of influenza and also provide protection during a pandemic is highly desirable,” wrote Catharine I. Paules, MD, of the University of Maryland, Baltimore, and her coauthors in the workshop summary.
Dr. Fauci told Frontline Medical News how “experts from all over the country addressed their thoughts and concerns with us last year [at the workshop], and now we have a development plan,” he said. “But the next step will be doing the research and finding more resources. ... The work is yet to be done.”
The development plan was published amid an ongoing historic flu season.
Dr. Fauci noted that this season had particular circumstances that made it worse than normal. “I don’t think that, had we had this plan in place a year ago, it would have had an impact on this flu season,” he said.
The authors reported no relevant financial conflicts and that the National Institutes of Health produced this plan.
SOURCE: Erbelding E et al. J Infect Dis. 2018 Feb 28. doi: 10.1093/infdis/jiy103.
FROM THE JOURNAL OF INFECTIOUS DISEASES
Abruptio placenta brings increased cardiovascular risk – and soon
ANAHEIM, CALIF. – Women who experience placental abruption are at significantly increased risk for multiple forms of cardiovascular disease beginning within the first few years after their pregnancy complication, according to a study of more than 1.6 million California women.
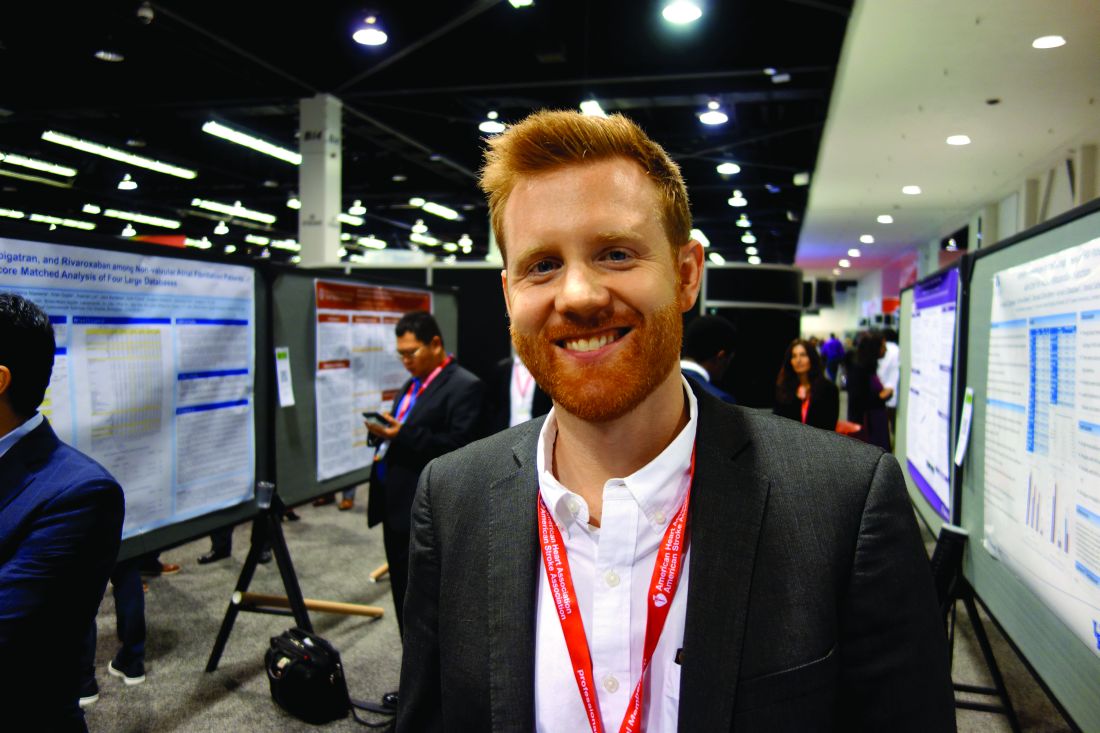
While gestational hypertension, preeclampsia, and fetal growth restriction have previously all been shown to be associated with increased risk of incident cardiovascular disease, this huge California study provides the first strong epidemiologic evidence that placental abruption is as well. Prior studies looking at the issue have been underpowered, Michael J. Healey, MD, said at the American Heart Association scientific sessions.
“Our hypothesis is that there might be some type of shared mechanism, probably involving microvascular dysfunction, that explains the relationships we see between these pregnancy complications and increased near-term risk of cardiovascular disease,” he explained in an interview.
Dr. Healy, a hospitalist attached to the heart failure service at the University of California, San Francisco, presented a retrospective study of a multiethnic cohort comprising 1,614,950 parous women aged 15-50 years who participated in the California Healthcare Cost and Utility Project during 2005-2009. Placental abruption occurred in 15,057 of them at a mean age of 29.2 years.
During a median 4.9 years of follow-up, women who experienced abruptio placenta were at 6% increased risk for heart failure, 11% greater risk for MI, 8% increased risk for hypertensive urgency, and 2% greater risk for myocardial infarction with no obstructive atherosclerosis (MINOCA) in an age- and race-adjusted analysis. All of these were statistically significant differences.
Of note, however, in a multivariate analysis fully adjusted for standard cardiovascular risk factors, as well as hypercoagulability, preterm birth, grand multiparity, and insurance status, placental abruption was independently associated with a 2.14-fold risk of MINOCA, but it was no longer linked to significantly increased risks of the other cardiovascular events.
The implication is that the increased risk of these other forms of cardiovascular disease is mediated through the women’s increased prevalence of the traditional cardiovascular risk factors, whereas a novel mechanism – most likely microvascular dysfunction – underlies the association between placental abruption and MINOCA, according to Dr. Healy.
He plans to extend this research by taking a look at the relationship between placental abruption and the various subtypes of MINOCA, including coronary dissection, vasospasm, thrombophilia disorders, and stress cardiomyopathy, in order to examine whether the increased risk posed by placental abruption is concentrated in certain forms of MINOCA. Data on MINOCA subtypes were recorded as part of the California project.
He reported having no financial conflicts of interest regarding his study.
ANAHEIM, CALIF. – Women who experience placental abruption are at significantly increased risk for multiple forms of cardiovascular disease beginning within the first few years after their pregnancy complication, according to a study of more than 1.6 million California women.
While gestational hypertension, preeclampsia, and fetal growth restriction have previously all been shown to be associated with increased risk of incident cardiovascular disease, this huge California study provides the first strong epidemiologic evidence that placental abruption is as well. Prior studies looking at the issue have been underpowered, Michael J. Healey, MD, said at the American Heart Association scientific sessions.
“Our hypothesis is that there might be some type of shared mechanism, probably involving microvascular dysfunction, that explains the relationships we see between these pregnancy complications and increased near-term risk of cardiovascular disease,” he explained in an interview.
Dr. Healy, a hospitalist attached to the heart failure service at the University of California, San Francisco, presented a retrospective study of a multiethnic cohort comprising 1,614,950 parous women aged 15-50 years who participated in the California Healthcare Cost and Utility Project during 2005-2009. Placental abruption occurred in 15,057 of them at a mean age of 29.2 years.
During a median 4.9 years of follow-up, women who experienced abruptio placenta were at 6% increased risk for heart failure, 11% greater risk for MI, 8% increased risk for hypertensive urgency, and 2% greater risk for myocardial infarction with no obstructive atherosclerosis (MINOCA) in an age- and race-adjusted analysis. All of these were statistically significant differences.
Of note, however, in a multivariate analysis fully adjusted for standard cardiovascular risk factors, as well as hypercoagulability, preterm birth, grand multiparity, and insurance status, placental abruption was independently associated with a 2.14-fold risk of MINOCA, but it was no longer linked to significantly increased risks of the other cardiovascular events.
The implication is that the increased risk of these other forms of cardiovascular disease is mediated through the women’s increased prevalence of the traditional cardiovascular risk factors, whereas a novel mechanism – most likely microvascular dysfunction – underlies the association between placental abruption and MINOCA, according to Dr. Healy.
He plans to extend this research by taking a look at the relationship between placental abruption and the various subtypes of MINOCA, including coronary dissection, vasospasm, thrombophilia disorders, and stress cardiomyopathy, in order to examine whether the increased risk posed by placental abruption is concentrated in certain forms of MINOCA. Data on MINOCA subtypes were recorded as part of the California project.
He reported having no financial conflicts of interest regarding his study.
ANAHEIM, CALIF. – Women who experience placental abruption are at significantly increased risk for multiple forms of cardiovascular disease beginning within the first few years after their pregnancy complication, according to a study of more than 1.6 million California women.
While gestational hypertension, preeclampsia, and fetal growth restriction have previously all been shown to be associated with increased risk of incident cardiovascular disease, this huge California study provides the first strong epidemiologic evidence that placental abruption is as well. Prior studies looking at the issue have been underpowered, Michael J. Healey, MD, said at the American Heart Association scientific sessions.
“Our hypothesis is that there might be some type of shared mechanism, probably involving microvascular dysfunction, that explains the relationships we see between these pregnancy complications and increased near-term risk of cardiovascular disease,” he explained in an interview.
Dr. Healy, a hospitalist attached to the heart failure service at the University of California, San Francisco, presented a retrospective study of a multiethnic cohort comprising 1,614,950 parous women aged 15-50 years who participated in the California Healthcare Cost and Utility Project during 2005-2009. Placental abruption occurred in 15,057 of them at a mean age of 29.2 years.
During a median 4.9 years of follow-up, women who experienced abruptio placenta were at 6% increased risk for heart failure, 11% greater risk for MI, 8% increased risk for hypertensive urgency, and 2% greater risk for myocardial infarction with no obstructive atherosclerosis (MINOCA) in an age- and race-adjusted analysis. All of these were statistically significant differences.
Of note, however, in a multivariate analysis fully adjusted for standard cardiovascular risk factors, as well as hypercoagulability, preterm birth, grand multiparity, and insurance status, placental abruption was independently associated with a 2.14-fold risk of MINOCA, but it was no longer linked to significantly increased risks of the other cardiovascular events.
The implication is that the increased risk of these other forms of cardiovascular disease is mediated through the women’s increased prevalence of the traditional cardiovascular risk factors, whereas a novel mechanism – most likely microvascular dysfunction – underlies the association between placental abruption and MINOCA, according to Dr. Healy.
He plans to extend this research by taking a look at the relationship between placental abruption and the various subtypes of MINOCA, including coronary dissection, vasospasm, thrombophilia disorders, and stress cardiomyopathy, in order to examine whether the increased risk posed by placental abruption is concentrated in certain forms of MINOCA. Data on MINOCA subtypes were recorded as part of the California project.
He reported having no financial conflicts of interest regarding his study.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
Key clinical point: Placental abruption is associated with increased risk of maternal cardiovascular events within a few years after delivery.
Major finding: Placental abruption was independently associated with a 2.14-fold increased risk of myocardial infarction with no obstructive atherosclerosis during a median 4.9 years of follow-up.
Study details: This was a retrospective study of more than 1.6 million parous women enrolled in the California Healthcare Cost and Utilization Project, including 15,057 with placental abruption.
Disclosures: The study presenter reported having no financial conflicts of interest.
Expert argues for improving MACRA, not scrapping it
Even given the notable problems and challenges associated with Medicare’s Merit-based Incentive Payment System (MIPS), the program should be improved via pilot programs and demonstration projects, according to Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush.
“Although I agree with MedPAC about the problems it has identified, I am also concerned about the commission’s proposal,” Dr. Wilensky wrote in an editorial published in the New England Journal of Medicine (doi: 10.1056/NEJMp1801673). She noted that a lack of support from major medical associations, combined with the impending midterm elections, means that it would be challenging to get a legislative fix through Congress.
Read her suggestions on how to improve MIPS in the New England Journal of Medicine.
Michael E. Nelson, MD, FCCP, comments: Dr. Wilensky made some cogent arguments as to why scrapping MIPS may not be such a good idea. In my mind, however, the final paragraph of the editorial was the most important. “Practicing physicians need make their views about the MIPS and its alternatives known to their representative medical groups and, if necessary, to their representatives in Congress as well. In the past, practicing clinicians have been woefully bad at making their voices heard. Now is a good time for that to change.” Your future is being decided without you. The squeaky wheel gets the grease.
Michael E. Nelson, MD, FCCP, comments: Dr. Wilensky made some cogent arguments as to why scrapping MIPS may not be such a good idea. In my mind, however, the final paragraph of the editorial was the most important. “Practicing physicians need make their views about the MIPS and its alternatives known to their representative medical groups and, if necessary, to their representatives in Congress as well. In the past, practicing clinicians have been woefully bad at making their voices heard. Now is a good time for that to change.” Your future is being decided without you. The squeaky wheel gets the grease.
Michael E. Nelson, MD, FCCP, comments: Dr. Wilensky made some cogent arguments as to why scrapping MIPS may not be such a good idea. In my mind, however, the final paragraph of the editorial was the most important. “Practicing physicians need make their views about the MIPS and its alternatives known to their representative medical groups and, if necessary, to their representatives in Congress as well. In the past, practicing clinicians have been woefully bad at making their voices heard. Now is a good time for that to change.” Your future is being decided without you. The squeaky wheel gets the grease.
Even given the notable problems and challenges associated with Medicare’s Merit-based Incentive Payment System (MIPS), the program should be improved via pilot programs and demonstration projects, according to Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush.
“Although I agree with MedPAC about the problems it has identified, I am also concerned about the commission’s proposal,” Dr. Wilensky wrote in an editorial published in the New England Journal of Medicine (doi: 10.1056/NEJMp1801673). She noted that a lack of support from major medical associations, combined with the impending midterm elections, means that it would be challenging to get a legislative fix through Congress.
Read her suggestions on how to improve MIPS in the New England Journal of Medicine.
Even given the notable problems and challenges associated with Medicare’s Merit-based Incentive Payment System (MIPS), the program should be improved via pilot programs and demonstration projects, according to Gail R. Wilensky, PhD, economist and senior fellow at Project Hope and a former top health aide to President George H.W. Bush.
“Although I agree with MedPAC about the problems it has identified, I am also concerned about the commission’s proposal,” Dr. Wilensky wrote in an editorial published in the New England Journal of Medicine (doi: 10.1056/NEJMp1801673). She noted that a lack of support from major medical associations, combined with the impending midterm elections, means that it would be challenging to get a legislative fix through Congress.
Read her suggestions on how to improve MIPS in the New England Journal of Medicine.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Mycosis fungoides increases risk for second cancers
LA JOLLA, CALIF. – Patients with mycosis fungoides are at increased risk for developing other cancers and should be screened for second primary and hematologic malignancies, results of a cancer registry survey suggest.
A study of data on 6,196 patients included in 18 population-based cancer registries comprising the SEER-18 (Surveillance, Epidemiology, and End Results 18) database who were diagnosed and followed from 2000 to 2014 showed that 514 (8.3%) developed second cancers, compared with the 70.8 secondary malignancies that would be expected in the general population. This difference translated into a standardized incidence ratio (SIR) of 7.3, reported Amrita Goyal, MD, and Aleksandr Lazaryan, MD, PhD, of the University of Minnesota, Minneapolis.
Patients with MF have a 500% greater risk for developing a second solid malignancy and a 2700% greater likelihood of developing a second hematologic malignancy, she said.
The investigators hypothesized that MF predisposes patients to second malignancies because of its immunocompromising effects.
Dr. Goyal said that, although the SEER data set does not include information on disease stage for all patients, when they looked at a separate cohort of 173 University of Minnesota patients with MF, they saw that patients with higher-stage MF were significantly more likely to develop secondary malignancies than patients with lower-stage disease.
The investigators looked at the actual and expected cancer incidence rates for the SEER-18 population sample, and used data on age, sex, race, and calendar year to generate incidence estimates for the general population.
They found that 514 patients in the SEER-18 population developed a total of 170 second primary hematologic malignancies, for a SIR of 27.4, compared with the general population. The most common hematologic cancers were Hodgkin lymphoma (SIR 69.8) and non-Hodgkin lymphoma (SIR 46.5), and other second hematologic malignancies included multiple myeloma (SIR 4.5), chronic lymphocytic leukemia (SIR 9.1). and acute leukemias (SIR 8.1).
The most frequently occurring second solid tumors included cancers of the nose, nasal cavity, and middle ear (SIR 30.4); thyroid (SIR 16.1); brain (SIR 15.1); and breast (SIR 8.0).
Other solid tumors with an approximately 400%-500% higher incidence included cancers of the prostate, bladder, colon, and kidneys.
Dr. Goyal and Dr. Lazaryan recommend development of targeted cancer screening strategies for patients with MF.
The study was funded in part by an American Society of Hematology HONORS grant. The researchers reported having no conflicts of interest. The T-Cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
SOURCE: Goyal A et al. TCLF 2018 Abstract EP18_2.
LA JOLLA, CALIF. – Patients with mycosis fungoides are at increased risk for developing other cancers and should be screened for second primary and hematologic malignancies, results of a cancer registry survey suggest.
A study of data on 6,196 patients included in 18 population-based cancer registries comprising the SEER-18 (Surveillance, Epidemiology, and End Results 18) database who were diagnosed and followed from 2000 to 2014 showed that 514 (8.3%) developed second cancers, compared with the 70.8 secondary malignancies that would be expected in the general population. This difference translated into a standardized incidence ratio (SIR) of 7.3, reported Amrita Goyal, MD, and Aleksandr Lazaryan, MD, PhD, of the University of Minnesota, Minneapolis.
Patients with MF have a 500% greater risk for developing a second solid malignancy and a 2700% greater likelihood of developing a second hematologic malignancy, she said.
The investigators hypothesized that MF predisposes patients to second malignancies because of its immunocompromising effects.
Dr. Goyal said that, although the SEER data set does not include information on disease stage for all patients, when they looked at a separate cohort of 173 University of Minnesota patients with MF, they saw that patients with higher-stage MF were significantly more likely to develop secondary malignancies than patients with lower-stage disease.
The investigators looked at the actual and expected cancer incidence rates for the SEER-18 population sample, and used data on age, sex, race, and calendar year to generate incidence estimates for the general population.
They found that 514 patients in the SEER-18 population developed a total of 170 second primary hematologic malignancies, for a SIR of 27.4, compared with the general population. The most common hematologic cancers were Hodgkin lymphoma (SIR 69.8) and non-Hodgkin lymphoma (SIR 46.5), and other second hematologic malignancies included multiple myeloma (SIR 4.5), chronic lymphocytic leukemia (SIR 9.1). and acute leukemias (SIR 8.1).
The most frequently occurring second solid tumors included cancers of the nose, nasal cavity, and middle ear (SIR 30.4); thyroid (SIR 16.1); brain (SIR 15.1); and breast (SIR 8.0).
Other solid tumors with an approximately 400%-500% higher incidence included cancers of the prostate, bladder, colon, and kidneys.
Dr. Goyal and Dr. Lazaryan recommend development of targeted cancer screening strategies for patients with MF.
The study was funded in part by an American Society of Hematology HONORS grant. The researchers reported having no conflicts of interest. The T-Cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
SOURCE: Goyal A et al. TCLF 2018 Abstract EP18_2.
LA JOLLA, CALIF. – Patients with mycosis fungoides are at increased risk for developing other cancers and should be screened for second primary and hematologic malignancies, results of a cancer registry survey suggest.
A study of data on 6,196 patients included in 18 population-based cancer registries comprising the SEER-18 (Surveillance, Epidemiology, and End Results 18) database who were diagnosed and followed from 2000 to 2014 showed that 514 (8.3%) developed second cancers, compared with the 70.8 secondary malignancies that would be expected in the general population. This difference translated into a standardized incidence ratio (SIR) of 7.3, reported Amrita Goyal, MD, and Aleksandr Lazaryan, MD, PhD, of the University of Minnesota, Minneapolis.
Patients with MF have a 500% greater risk for developing a second solid malignancy and a 2700% greater likelihood of developing a second hematologic malignancy, she said.
The investigators hypothesized that MF predisposes patients to second malignancies because of its immunocompromising effects.
Dr. Goyal said that, although the SEER data set does not include information on disease stage for all patients, when they looked at a separate cohort of 173 University of Minnesota patients with MF, they saw that patients with higher-stage MF were significantly more likely to develop secondary malignancies than patients with lower-stage disease.
The investigators looked at the actual and expected cancer incidence rates for the SEER-18 population sample, and used data on age, sex, race, and calendar year to generate incidence estimates for the general population.
They found that 514 patients in the SEER-18 population developed a total of 170 second primary hematologic malignancies, for a SIR of 27.4, compared with the general population. The most common hematologic cancers were Hodgkin lymphoma (SIR 69.8) and non-Hodgkin lymphoma (SIR 46.5), and other second hematologic malignancies included multiple myeloma (SIR 4.5), chronic lymphocytic leukemia (SIR 9.1). and acute leukemias (SIR 8.1).
The most frequently occurring second solid tumors included cancers of the nose, nasal cavity, and middle ear (SIR 30.4); thyroid (SIR 16.1); brain (SIR 15.1); and breast (SIR 8.0).
Other solid tumors with an approximately 400%-500% higher incidence included cancers of the prostate, bladder, colon, and kidneys.
Dr. Goyal and Dr. Lazaryan recommend development of targeted cancer screening strategies for patients with MF.
The study was funded in part by an American Society of Hematology HONORS grant. The researchers reported having no conflicts of interest. The T-Cell Lymphoma Forum is held by Jonathan Wood & Associates, which is owned by the same company as this news organization.
SOURCE: Goyal A et al. TCLF 2018 Abstract EP18_2.
REPORTING FROM TCLF 2018
Key clinical point:
Major finding: Patients with MF have a 730% greater likelihood of developing a second primary hematologic malignancy.
Study details: A retrospective review of data on 6,196 patients in the SEER-18 database.
Disclosures: The study was funded in part by an American Society of Hematology HONORS grant. The researchers reported having no conflicts of interest.
Source: Goyal A et al. TCLF 2018 Abstract EP18_2.
Characteristics, Frequency, and Disposition of Patients With a HeartMate II Left Ventricular Assist Device Presenting to the ED
Introduction
Approximately 6.5 million adults in the United States have heart failure, accounting for nearly 1 million ED visits annually.1 Advanced heart failure is particularly difficult to treat, and is associated with significant morbidity and mortality. While medical therapy is the initial treatment for patients with advanced heart failure, it has limited effectiveness; therefore, at the present time, heart transplant is the most effective treatment for heart failure refractory to medical management.
According to the 2013 Registry of the International Society for Heart and Lung Transplantation, 4,096 cardiac transplants were performed worldwide in 2011, approximately 2,000 of which were done in the United States.2
The average age of a heart transplant recipient in the United States is 55 years.2 In 2017, there were nearly 4,000 patients on the United Network for Organ Sharing, the organization that manages the national transplant waiting list in the United States and matches donors to recipients.3 Unfortunately, the number of patients requiring a heart transplant far exceeds the number of registered donors, and a large number of patients must wait years for transplantation. In addition to those awaiting a heart transplant, there are many patients with advanced heart failure who are not suitable candidates for transplant (usually due to age).
Left Ventricular Assist Devices
As of December 31, 2016, a total of 22,866 US Food and Drug Administration (FDA)-approved devices were listed in the Interagency Registry for Mechanically Assisted Circulatory Support, 17,016 of which were continuous-flow (CF) left ventricular assist devices (LVADs), including the HeartMate II (HMII) (Abbott Laboratories) and the HeartWare Ventricular Assist Device (HVAD) (Medtronic).4 Left ventricular assist devices, which have been in use for over 30 years, have evolved into smaller, quieter, and more durable devices. The current generation of LVADs has a CF design (as opposed to the older pulsatile-flow [PF] design). More importantly, CF LVADs are associated with higher survival rates and increased quality of life than the earlier PF models.5 For these reasons, CF LVADs are being used much more frequently today. As previously noted, LVADs serve as a temporizing measure for patients awaiting a heart transplant (ie, bridge-to-transplant therapy [BTT]) or as the primary treatment for patients who are not suitable candidates for transplant (ie, destination therapy [DT]).
The percentage of patients receiving an LVAD as a DT has increased from around 15% between 2006 to 2007 to nearly 46% in 2014.6Recently, several reports following LVAD patients demonstrated a reverse remodeling of the heart and recovery of native cardiac function that was sufficient enough in some patients as to permit LVAD removal (ie, bridge to recovery).7 In the United States, the number of patients undergoing LVAD removal due to recovery remains fewer than 3%.6With the increase in the number of patients receiving LVADs, there is an increased likelihood of LVAD patients presenting to an ED due to device-related complications. Recognized complications associated with LVADs include thrombosis, infection, bleeding, and issues with volume status.5,7 However, the frequency of LVAD-associated complications and the final disposition of these patients is less well known.
HeartMate II Patient ED Presentation Study
Purpose
The purpose of our study was to identify the reasons for LVAD patient presentation to the ED, the frequency of these presentations, and the final disposition of these patients. Our institution, Sentara Norfolk General Hospital (SNGH), is a level I trauma and a tertiary care referral center, and it is the only hospital in a large area of Virginia to perform LVAD implantation.
Our study involved only patients implanted with the HMII LVAD.
Methods
Patients and Study Design
This was a retrospective study of patients with an HMII LVAD who presented to the SNGH ED between April 1, 2009 and September 9, 2012. All patients implanted with an HMII LVAD during the study period were assigned a study number linking the patient to their medical record number and social security number. Study numbers were assigned at the time of LVAD implantation by one of the investigators. This document was kept in a secure and locked location in the department of emergency medicine and was not accessible to anyone other than study investigators.
The electronic medical records were retrospectively reviewed to identify any HMII LVAD patient presenting to the SNGH ED during the study period. Information abstracted from the ED medical records included patient age, sex, initial complaint, final diagnosis, and disposition. Only the patient’s assigned study number was used on the data collection form, and no personal identifying information was present.
This study was granted approval for human subject research by the Eastern Virginia Medical School Institutional Review Board. Eligible patients included all patients with an HMII LVAD implanted during the study period. Study patients who presented to the SNGH ED between April 1, 2009 and September 9, 2012 were identified by a retrospective chart review. These patients were instructed to specifically seek care at the SNGH ED in the event of an emergency. There were no exclusion criteria.
Data were collected and reported in real numbers and percentages. No formal statistical analysis was used in evaluating the results.
Results
Between April 1, 2009 and September 9, 2012, there were a total of 98 patients with an HMII LVAD that had been implanted during the study period at SNGH. The average patient age was 53.6 years, with a range from age 20 years to 78 years. Sixty-seven (68%) of the patients enrolled in the study required at least one ED visit. The HMII LVAD patients who presented to the ED ranged in age from 20 years to 78 years, with an average age of 53.1 years. The average number of ED visits by these 67 patients was 3.7, with a range of 1 to 12. Approximately 56% of the ED visits were directly LVAD-related. In all, 67 patients were responsible for a total of 248 ED visits.
The two most common reasons for presentation to the ED involved bleeding and volume overload. A total of 37 ED visits (14.9%), were related to bleeding, which included gastrointestinal (GI) bleeding (18/37 or 49%), epistaxis, hematuria, gingival bleeding, and postoperative bleeding following tooth extraction.
Volume overload accounted for 37 ED visits (14.9%), and the most common presenting symptom in these patients was shortness of breath. Other reasons patients presented to the ED were weakness/lightheadedness/dizziness/syncope (24/9.6%), device malfunction (20/8.1%), infection (7/2.8%), and transient ischemic attack/cerebrovascular accident (6/2.4%). For infection-related ED visits, two presentations (2.9%) involved a driveline infection. Common causes for ED visits related to device malfunction included battery failure and device-alarm activation. Overall, 142 of the 248 total ED visits (57.3%) resulted in hospital admission. One patient in the study presented in cardiac arrest and could not be resuscitated.
The remaining 108 LVAD patient ED visits (44%), did not appear to be related to the presence of the LVAD, but rather represented common reasons for presentation to an ED. These other non-LVAD-related reasons for presentation to the ED were due to motor vehicle incidents (3); assault (2); dental pain (3); mechanical fall (5); and upper respiratory tract infection (4), and represented small groupings of patient reasons for an ED visit.
Examples of singular reasons for presentation to the ED included one patient who presented with suicidal ideation, and another patient who presented for evaluation of symptoms suspicious for a sexually transmitted infection.
Discussion
As the number of patients with advanced heart failure continues to increase, the number of those with an LVAD also increases. Between 2006 and June 2013, nearly 9,000 adult patients in the United States received a durable LVAD.6 In the early years of LVAD implantation, patients were restricted to remain in proximity of geographical areas surrounding academic health care centers. An increased comfort level by both physicians and patients now allows LVAD patients to reside in more distant communities. This increase in LVAD implantation, coupled with the widening patient distribution, make it important for every emergency physician (EP) to have a working knowledge of the device and its associated complications. To date, the characteristics and frequency of LVAD patient presentations to the ED have not been well characterized.
Left ventricular assist devices are considered in patients who have significant symptoms associated with poor LV function or who cannot maintain normal hemodynamics and vital organ function. Continuous-flow LVADs account for almost all devices currently implanted. During our data-collection period, there were two FDA-approved implantable LVADs—the HMII, approved for BTT in 2008 and for DT in 2010; and the HVAD approved for BTT in 2012. In August 2017, HeartMate III (Abbott Laboratories) was approved by the FDA. All patients enrolled in our study were recipients of the HMII device, as this was the only type of LVAD implant performed at our hospital. Current survival with the HMII LVAD is 80% at 1 year and 69% at 2 years, and there has not been shown to be a significant difference when stratified by era of implant.6
Device Designs and Structures
The pump of the HMII is inserted into the abdominal cavity, whereas the HVAD is implanted in the chest cavity, with the inflow cannula in the apex of the LV and the outflow cannula connecting to the proximal aorta. Blood is continuously pumped through the system.8,9 The pump is connected to a driveline that exits the body and connects to a controller. Continuous-flow devices have either an axial or centrifugal blood pump. Axial devices have an impeller that is connected to ball-and-cup bearings that accelerate blood along its axis. Newer axial flow pumps incorporate magnetic levitation of the rotor and do not require the use of bearings. Centrifugal devices accelerate blood circumferentially with a rotor that is suspended within in the blood pool by electromagnetic or hydrodynamic forces.10 The controller is powered by two external batteries or connected to a power base unit where the pump can be interrogated. The controller is usually housed in a garment worn by the patient, one that also includes the batteries. The controller can also be powered by a base unit that can be plugged into an electrical outlet.11
There are, and continue to be, advances in both LVAD design and function. Since the time period of our study, changes have been made in the outflow bend relief (the tube at the junction of the outflow cannula and the pump housing designed to prevent kinking of the outflow cannula) and the LVAD controller. Older controllers have been replaced with newer models, but many of the LVAD pumps in this article remain in service.
Anticoagulation Therapy
Patients who have a CF LVAD require anticoagulation therapy with warfarin to a target international normalized ratio (INR) of 2 to 3, in addition to aspirin therapy of 325 mg daily.8,9Newer oral anticoagulant drugs are not routinely given to patients who have a CF LVAD.
Cardiopulmonary Evaluation
With CF LVADs, blood is pumped continuously, and a constant, machine-like murmur can be heard on auscultation rather than the typical heart sounds. Patients who have an LVAD may not have palpable arterial pulses. Doppler evaluation of the brachial artery and a manual blood pressure (BP) cuff are used to listen for the start of Korotkoff sounds as the cuff is released. The pressure at which the first sound is heard is used to estimate the patient’s mean arterial pressure (MAP) at the time when there is no pulse; and the systolic BP (SBP) is heard at the time when there is pulse. Patients with a CF LVAD with nonpulsatile flow should have a MAP between 70 mm Hg and 90 mm Hg (HMII), or 70 mm Hg and 80 mm Hg (HVAD). Patients who have a CF LVAD with a palpable pulse should have an SBP less than 120 mm Hg (HMII) or 105 mm Hg (HVAD). Readings outside of these ranges require an adjustment in the patient’s antihypertensive therapy, since high BP increases the risk of stroke and can impair the cardiac support provided by the LVAD.8Low BP may be the result of inadequate pump speed, dehydration, inflow cannula obstruction, or pump thrombus.
Bleeding
In our study, bleeding and volume overload were the two most common reasons LVAD patients presented to the ED. Interestingly, in a systematic review of clinical outcomes following CF LVAD implantation, bleeding was the most commonly recorded adverse event.12In fact, the majority of patients in all of the studies reviewed experienced at least one bleeding event. In one study of 139 HMII LVAD patients, the risk of bleeding was greatest within the first two weeks, and early bleeding was associated with increased mortality.13The most common source of bleeding complications in patients with a CF LVAD are GI, similar to our study.14
In a review and meta-analysis by Draper et al,15of GI bleeding in 1,697 patients with CF LVADs, the pooled prevalence was 23%.Subgroup analysis demonstrated an increased risk of bleeding in older patients and in those who had an elevated serum creatinine level.15 Upper GI bleeding occurred in 48% of patients, lower GI bleeding in 22%, small-bowel bleeding in 15%, and bleeding at an unknown site in 19%. The most common cause of the bleeding was from arteriovenous malformations (AVMs).15 In their review, Draper et al15 found a 9.3% prevalence of recurrent GI bleeding and a pooled event rate for an all-cause mortality rate of 23%.
They also noted that the increased risk of GI bleeding in CF LVAD patients is multifactorial. For example, there was decreased activity of type 2 von Willebrand factor multimers in patients with CF LVADs, leading to an acquired von Willebrand syndrome.15
Another finding seen in this review was that CF devices lead to a low pulse-pressure system, which is thought to cause some degree of intestinal hypoperfusion, potentially leading to vascular dilation and AVM formation.15 Based on findings, a neurovascular etiology involving increased sympathetic tone resulting in smooth muscle relaxation and AVM formation has been proposed. Lastly, the anticoagulation required with the CF LVADs to prevent pump thrombosis also increases the risk of GI bleeding, especially when combined with aspirin or other antiplatelet agents which are routinely prescribed.15
Volume Overload
Interestingly, in our study, volume overload as a cause for ED presentation was the same as for bleeding complications. In the systematic review of clinical outcomes in CF LVAD patients, volume overload or ongoing heart failure occurred in 18% of patients 1 year after device implantation.12
The clinical presentation of patients experiencing volume overload is typically dyspnea and fatigue; on physical examination they will frequently demonstrate evidence of fluid retention, such as dependent edema and pulmonary congestion.16Causes of volume overload in the LVAD patient includes medication noncompliance, inadequate pump speed, device malfunction, right ventricular failure, impaired renal function, and cardiac tamponade.16 These patients will frequently have MAPs greater than 90 mm Hg, and may require treatment with diuretics, calcium channel blockers, beta-blockers, or angiotensin-converting enzyme inhibitors.8
Weakness, Lightheadedness, Dizziness, Syncope
In our study, some combination of weakness, lightheadedness, dizziness, and syncope accounted for the third most common cause of ED presentation (9.6%). In the majority of cases, this was due to dehydration. Usually, these patients will have a MAP less than 60 mm Hg. Unfortunately, patients with pump thrombosis, sepsis, or cannula malposition can also present with a low MAP. It is important to differentiate the cause, as the management is quite different, depending on the etiology. Bedside ultrasound can play an important role in evaluating the volume status and cannula position.8 In addition, emergent consult with the patients ventricular assist device (VAD) treatment team is critical.8 Pump thrombus is a medical emergency and is usually associated with hematuria without red blood cells in the urine, acute kidney injury, and marked elevations in lactate dehydrogenase and serum free hemoglobin.8 If not treated promptly, renal failure and death may result. If dehydration is the cause, gentle rehydration with intravenous normal saline and electrolyte replacement may be all that is required.
Device Malfunction
Device malfunction was the next most common reason for ED presentation in our study, at 8.1%. This category included a number of different events, including battery failure, driveline fracture, and pump thrombosis. According to McIlvennan et al,12 causes of device malfunction include thrombus formation with hemolysis, mechanical failure of the impeller, and driveline lead fractures with electrical failure.Again, the VAD team should be consulted immediately, and the EP should plug the LVAD into a hospital power base, if available, to conserve battery life. If power is interrupted, the pump will stop working. The EP should examine all of the connections from the percutaneous lead to the controller and from the controller to the batteries to ensure they are intact. The exit site for the percutaneous lead should be examined for evidence of trauma or signs of infection. The patient should also be asked about recent trauma to the driveline.
Neurological Events
Interestingly, in other reviews, neurological events, including ischemic stroke, hemorrhagic stroke, and transient ischemic attack occur with higher frequency than was the case in the study, and are relatively common complications that can result in severe morbidity and mortality.12In the Interagency Registry for Mechanically Assisted Circulatory Support report, there was a 3% risk of stroke at 1 month, 5% at 3 months, 7% at 6 months, 11% at 12 months, 17% at 24 months, and 19% at 36 months post-implant.6,12Similarly, the HMII DT Trial demonstrated rates of ischemic and hemorrhagic stroke as high as 8% and 11% respectively, within the first 2 years following LVAD placement.5,6In our study, neurological events accounted for only six (2.4%) of ED visits. It is unclear why our numbers were less than those reported by others.
Cardiac Events and Management
During the study period, one LVAD patient presented to the ED in cardiac arrest. Patients who have an LVAD and are in cardiac arrest have unique considerations that deserve discussion. If the LVAD pump has stopped functioning, connections between the system controller and the pump and power source must be checked, as loose connections need to be refitted and the pump restarted. It is important to note that when an LVAD ceases operation, blood becomes stagnant in the pump and conduits. Delays of even several minutes pose a significant risk for pump thrombosis, stroke, and thromboembolism when the device is restarted. If the pump does not restart and the patient is connected to batteries, the batteries should be replaced with a new, fully charged pair, or the device should be connected to a base unit.17
Due to the location of the outflow graft on the aorta and the inflow conduit in the LV apex, external chest compressions pose a risk of dislodging the device and causing fatal hemorrhage. Clinical judgment should be used when deciding to perform external chest compressions. A recent American Heart Association scientific statement concluded that withholding chest compression in a patient with an LVAD who is truly in circulatory failure that is not attributable to a device failure would cause more harm to the patient than the potential to dislodge the device.18
Direct cardiac massage, performed by a skilled surgeon may be effective in patients that have had recent device implantation, especially if prior to mediastinal healing.16 If external defibrillation/cardioversion is required, the percutaneous lead should not be disconnected from the system controller and the pump should not be stopped prior to the delivery of a shock.17
Study Limitations
This was a retrospective study and has the limitations common to all such studies. It is possible that some of the patients in our study sought care at a hospital ED outside of our system, and therefore were not included in our study. This, however, is exceedingly unlikely as the cardiologists and care team continually emphasized and instructed all patients in our study only to present to the study hospital ED for any complaint. Similarly, the various emergency medical services agencies for our region were also instructed to bring all LVAD patients to the study hospital.
Another limitation of our study is the relatively small total number of patients (98) and that our findings may not apply to other patient populations. This limitation, however, would be true for any hospital system that limits the type of LVAD implant procedure to one manufacturer (HMII in this instance).
Conclusion
Emergency physicians must be prepared to evaluate the LVAD patient presenting to the ED. A little over 55% of the time, the visit will be directly related to the LVAD; in the remainder of cases, patient presentation will be due to a non-LVAD-related cause. At initial presentation, however, the EP should assume that the ED visit is related to the LVAD, until a thorough history and physical examination can exclude otherwise.
Because of the high incidence of GI bleeding in LVAD patients, a rectal examination for blood in the stool should be performed for any complaint that may be related, such as generalized weakness, syncope, or shortness of breath. In the majority of cases, a complete blood count; complete metabolic profile, including lactic acid dehydrogenase; and coagulation studies, including prothrombin time and INRs, are indicated. Most patients with an LVAD will require a member of the VAD team (typically the perfusionist or biomedical engineer) to interrogate the controller if there is any concern about its function, including alarm sounding or lights flashing.
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603. doi:10.1161/CIR.0000000000000485. Erratum in: Circulation. 2017;135(1):e646. doi:10.1161/CIR.0000000000000491.
2. Lund LH, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: thirtieth official adult heart transplant report—2013; focus theme: age. J Heart Lung Transplant. 2013;32(10):951-964. doi:10.1016/j.healun.2013.08.006.
3. UNOS (United Network for Organ Sharing) Web site. https://unos.org/data/transplant-trends/waiting-list-candidates-by-organ-type/. Accessed February 8, 2018.
4. Kirklin JK, Pagani FD, Kormos RL, et al. Eighth annual INTERMACS report: Special focus on framing the impact of adverse events. J Heart Lung Transplant. 2017;36(10):1080-1086. doi:10.1016/j.healun.2017.07.005.
5. Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous flow left ventricular assist device. N Engl J Med. 2009;361(23):2241-2251. doi:10.1056/NEJMoa0909938.
6. Kirklin JK, Naftel DC, Pagani FD, et al. Seventh INTERMACS annual report: 15,000 patients and counting. J Heart Lung Transplant. 2015;34(12):1495-1504. doi:10.1016/j.healun.2015.10.003.
7. Ambardekar AV, Buttrick PM. Reverse remodeling with left ventricular assist devices: a review of clinical, cellular and molecular effects. Circ Heart Fail. 2011;4(2):224-233. doi:10.1161/CIRCHEARTFAILURE.110.959684.
8. Slaughter MS, Pagani FD, Rogers JG, et al. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant. 2010;29 (suppl 4):1-39. doi:10.1016/j.healun.2010.01.011.
9. Lo BM, Devine AS. Patients with left ventricular assist devices. Critical Decisions in Emergency Medicine. 2014;28(7):2-9.
10. Feldman D, Pamboukian SV, Teuteberg JJ, et al. The 2013 International Society for Heart and Lung Transplantation guidelines for mechanical circulatory support: executive summary. J Heart Lung Transplant. 2013;32(2):157-187. doi:10.1016/j.healun.2012.09.013.
11. Miller LW, Pagani FD, Russell SD, et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357(9):885-896. doi:10.1056/NEJMoa067758.
12. McIlvennan CK, Magid KH, Ambardekar AV, et al. Clinical outcomes following continuous-flow left ventricular assist device: a systematic review. Circ Heart Fail. 2014;7(6):1003-1013. doi:10.1161/
13. Mulloy DP, Bhamidipati CM, Stone ML, et al. Cryoablation during left ventricular assist device implantation reduces postoperative ventricular tachyarrhythmias. J Thorac Cardiovasc Surg. 2013;145(5):1207-1213. doi:10.1016/j.jtcvs.2012.03.061.
14. Stern DR, Kazam J, Edwards P, et al. Increased incidence of gastrointestinal bleeding following implantation of the Heartmate II LVAD. J Card Surg. 2010;25(3):352-356. doi:10.1111/j.1540-8191.2010.01025.x.
15. Draper KV, Huang RJ, Gerson LB. GI bleeding in patients with continuous-flow left ventricular assist devices: a systematic review and meta-analysis. Gastrointest Endosc. 2014;80(3):435-446. doi:10.1016/j.gie.2014.03.040.
16. Aissaoui N, Morshuis M, Diebold B, et al. Heart failure while on ventricular assist device support: a true clinical entity? Arch Cardiovasc Dis. 2013:106(1):44-51. doi:10.1016/j.acvd.2012.09.006.
17. Thoratec HeartMate II Left Ventricular Assist System (LVAS) Information and Emergency Assistance Guide. Thoratec Corporation Web site. http://www.thoratec.com/_assets/download-tracker/HM_II_Info_Emergency_Assist_Guide_US_103873B_ENGLISH.pdf. Accessed July 5, 2017.
18. Peberdy MA, Gluck JA, Ornato JP, et al; American Heart Association Emergency Cardiovascular Care Committee; Council on Cardiopulmonary, Critical Care, Perioperative, and Resuscitation; Council on Cardiovascular Diseases in the Young; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. Cardiopulmonary resuscitation in adults and children with mechanical circulatory support a scientific statement from the American Heart Association. Circulation. 2017;135(24):e1115-e1134. doi:10.1161/CIR.0000000000000504.
Introduction
Approximately 6.5 million adults in the United States have heart failure, accounting for nearly 1 million ED visits annually.1 Advanced heart failure is particularly difficult to treat, and is associated with significant morbidity and mortality. While medical therapy is the initial treatment for patients with advanced heart failure, it has limited effectiveness; therefore, at the present time, heart transplant is the most effective treatment for heart failure refractory to medical management.
According to the 2013 Registry of the International Society for Heart and Lung Transplantation, 4,096 cardiac transplants were performed worldwide in 2011, approximately 2,000 of which were done in the United States.2
The average age of a heart transplant recipient in the United States is 55 years.2 In 2017, there were nearly 4,000 patients on the United Network for Organ Sharing, the organization that manages the national transplant waiting list in the United States and matches donors to recipients.3 Unfortunately, the number of patients requiring a heart transplant far exceeds the number of registered donors, and a large number of patients must wait years for transplantation. In addition to those awaiting a heart transplant, there are many patients with advanced heart failure who are not suitable candidates for transplant (usually due to age).
Left Ventricular Assist Devices
As of December 31, 2016, a total of 22,866 US Food and Drug Administration (FDA)-approved devices were listed in the Interagency Registry for Mechanically Assisted Circulatory Support, 17,016 of which were continuous-flow (CF) left ventricular assist devices (LVADs), including the HeartMate II (HMII) (Abbott Laboratories) and the HeartWare Ventricular Assist Device (HVAD) (Medtronic).4 Left ventricular assist devices, which have been in use for over 30 years, have evolved into smaller, quieter, and more durable devices. The current generation of LVADs has a CF design (as opposed to the older pulsatile-flow [PF] design). More importantly, CF LVADs are associated with higher survival rates and increased quality of life than the earlier PF models.5 For these reasons, CF LVADs are being used much more frequently today. As previously noted, LVADs serve as a temporizing measure for patients awaiting a heart transplant (ie, bridge-to-transplant therapy [BTT]) or as the primary treatment for patients who are not suitable candidates for transplant (ie, destination therapy [DT]).
The percentage of patients receiving an LVAD as a DT has increased from around 15% between 2006 to 2007 to nearly 46% in 2014.6Recently, several reports following LVAD patients demonstrated a reverse remodeling of the heart and recovery of native cardiac function that was sufficient enough in some patients as to permit LVAD removal (ie, bridge to recovery).7 In the United States, the number of patients undergoing LVAD removal due to recovery remains fewer than 3%.6With the increase in the number of patients receiving LVADs, there is an increased likelihood of LVAD patients presenting to an ED due to device-related complications. Recognized complications associated with LVADs include thrombosis, infection, bleeding, and issues with volume status.5,7 However, the frequency of LVAD-associated complications and the final disposition of these patients is less well known.
HeartMate II Patient ED Presentation Study
Purpose
The purpose of our study was to identify the reasons for LVAD patient presentation to the ED, the frequency of these presentations, and the final disposition of these patients. Our institution, Sentara Norfolk General Hospital (SNGH), is a level I trauma and a tertiary care referral center, and it is the only hospital in a large area of Virginia to perform LVAD implantation.
Our study involved only patients implanted with the HMII LVAD.
Methods
Patients and Study Design
This was a retrospective study of patients with an HMII LVAD who presented to the SNGH ED between April 1, 2009 and September 9, 2012. All patients implanted with an HMII LVAD during the study period were assigned a study number linking the patient to their medical record number and social security number. Study numbers were assigned at the time of LVAD implantation by one of the investigators. This document was kept in a secure and locked location in the department of emergency medicine and was not accessible to anyone other than study investigators.
The electronic medical records were retrospectively reviewed to identify any HMII LVAD patient presenting to the SNGH ED during the study period. Information abstracted from the ED medical records included patient age, sex, initial complaint, final diagnosis, and disposition. Only the patient’s assigned study number was used on the data collection form, and no personal identifying information was present.
This study was granted approval for human subject research by the Eastern Virginia Medical School Institutional Review Board. Eligible patients included all patients with an HMII LVAD implanted during the study period. Study patients who presented to the SNGH ED between April 1, 2009 and September 9, 2012 were identified by a retrospective chart review. These patients were instructed to specifically seek care at the SNGH ED in the event of an emergency. There were no exclusion criteria.
Data were collected and reported in real numbers and percentages. No formal statistical analysis was used in evaluating the results.
Results
Between April 1, 2009 and September 9, 2012, there were a total of 98 patients with an HMII LVAD that had been implanted during the study period at SNGH. The average patient age was 53.6 years, with a range from age 20 years to 78 years. Sixty-seven (68%) of the patients enrolled in the study required at least one ED visit. The HMII LVAD patients who presented to the ED ranged in age from 20 years to 78 years, with an average age of 53.1 years. The average number of ED visits by these 67 patients was 3.7, with a range of 1 to 12. Approximately 56% of the ED visits were directly LVAD-related. In all, 67 patients were responsible for a total of 248 ED visits.
The two most common reasons for presentation to the ED involved bleeding and volume overload. A total of 37 ED visits (14.9%), were related to bleeding, which included gastrointestinal (GI) bleeding (18/37 or 49%), epistaxis, hematuria, gingival bleeding, and postoperative bleeding following tooth extraction.
Volume overload accounted for 37 ED visits (14.9%), and the most common presenting symptom in these patients was shortness of breath. Other reasons patients presented to the ED were weakness/lightheadedness/dizziness/syncope (24/9.6%), device malfunction (20/8.1%), infection (7/2.8%), and transient ischemic attack/cerebrovascular accident (6/2.4%). For infection-related ED visits, two presentations (2.9%) involved a driveline infection. Common causes for ED visits related to device malfunction included battery failure and device-alarm activation. Overall, 142 of the 248 total ED visits (57.3%) resulted in hospital admission. One patient in the study presented in cardiac arrest and could not be resuscitated.
The remaining 108 LVAD patient ED visits (44%), did not appear to be related to the presence of the LVAD, but rather represented common reasons for presentation to an ED. These other non-LVAD-related reasons for presentation to the ED were due to motor vehicle incidents (3); assault (2); dental pain (3); mechanical fall (5); and upper respiratory tract infection (4), and represented small groupings of patient reasons for an ED visit.
Examples of singular reasons for presentation to the ED included one patient who presented with suicidal ideation, and another patient who presented for evaluation of symptoms suspicious for a sexually transmitted infection.
Discussion
As the number of patients with advanced heart failure continues to increase, the number of those with an LVAD also increases. Between 2006 and June 2013, nearly 9,000 adult patients in the United States received a durable LVAD.6 In the early years of LVAD implantation, patients were restricted to remain in proximity of geographical areas surrounding academic health care centers. An increased comfort level by both physicians and patients now allows LVAD patients to reside in more distant communities. This increase in LVAD implantation, coupled with the widening patient distribution, make it important for every emergency physician (EP) to have a working knowledge of the device and its associated complications. To date, the characteristics and frequency of LVAD patient presentations to the ED have not been well characterized.
Left ventricular assist devices are considered in patients who have significant symptoms associated with poor LV function or who cannot maintain normal hemodynamics and vital organ function. Continuous-flow LVADs account for almost all devices currently implanted. During our data-collection period, there were two FDA-approved implantable LVADs—the HMII, approved for BTT in 2008 and for DT in 2010; and the HVAD approved for BTT in 2012. In August 2017, HeartMate III (Abbott Laboratories) was approved by the FDA. All patients enrolled in our study were recipients of the HMII device, as this was the only type of LVAD implant performed at our hospital. Current survival with the HMII LVAD is 80% at 1 year and 69% at 2 years, and there has not been shown to be a significant difference when stratified by era of implant.6
Device Designs and Structures
The pump of the HMII is inserted into the abdominal cavity, whereas the HVAD is implanted in the chest cavity, with the inflow cannula in the apex of the LV and the outflow cannula connecting to the proximal aorta. Blood is continuously pumped through the system.8,9 The pump is connected to a driveline that exits the body and connects to a controller. Continuous-flow devices have either an axial or centrifugal blood pump. Axial devices have an impeller that is connected to ball-and-cup bearings that accelerate blood along its axis. Newer axial flow pumps incorporate magnetic levitation of the rotor and do not require the use of bearings. Centrifugal devices accelerate blood circumferentially with a rotor that is suspended within in the blood pool by electromagnetic or hydrodynamic forces.10 The controller is powered by two external batteries or connected to a power base unit where the pump can be interrogated. The controller is usually housed in a garment worn by the patient, one that also includes the batteries. The controller can also be powered by a base unit that can be plugged into an electrical outlet.11
There are, and continue to be, advances in both LVAD design and function. Since the time period of our study, changes have been made in the outflow bend relief (the tube at the junction of the outflow cannula and the pump housing designed to prevent kinking of the outflow cannula) and the LVAD controller. Older controllers have been replaced with newer models, but many of the LVAD pumps in this article remain in service.
Anticoagulation Therapy
Patients who have a CF LVAD require anticoagulation therapy with warfarin to a target international normalized ratio (INR) of 2 to 3, in addition to aspirin therapy of 325 mg daily.8,9Newer oral anticoagulant drugs are not routinely given to patients who have a CF LVAD.
Cardiopulmonary Evaluation
With CF LVADs, blood is pumped continuously, and a constant, machine-like murmur can be heard on auscultation rather than the typical heart sounds. Patients who have an LVAD may not have palpable arterial pulses. Doppler evaluation of the brachial artery and a manual blood pressure (BP) cuff are used to listen for the start of Korotkoff sounds as the cuff is released. The pressure at which the first sound is heard is used to estimate the patient’s mean arterial pressure (MAP) at the time when there is no pulse; and the systolic BP (SBP) is heard at the time when there is pulse. Patients with a CF LVAD with nonpulsatile flow should have a MAP between 70 mm Hg and 90 mm Hg (HMII), or 70 mm Hg and 80 mm Hg (HVAD). Patients who have a CF LVAD with a palpable pulse should have an SBP less than 120 mm Hg (HMII) or 105 mm Hg (HVAD). Readings outside of these ranges require an adjustment in the patient’s antihypertensive therapy, since high BP increases the risk of stroke and can impair the cardiac support provided by the LVAD.8Low BP may be the result of inadequate pump speed, dehydration, inflow cannula obstruction, or pump thrombus.
Bleeding
In our study, bleeding and volume overload were the two most common reasons LVAD patients presented to the ED. Interestingly, in a systematic review of clinical outcomes following CF LVAD implantation, bleeding was the most commonly recorded adverse event.12In fact, the majority of patients in all of the studies reviewed experienced at least one bleeding event. In one study of 139 HMII LVAD patients, the risk of bleeding was greatest within the first two weeks, and early bleeding was associated with increased mortality.13The most common source of bleeding complications in patients with a CF LVAD are GI, similar to our study.14
In a review and meta-analysis by Draper et al,15of GI bleeding in 1,697 patients with CF LVADs, the pooled prevalence was 23%.Subgroup analysis demonstrated an increased risk of bleeding in older patients and in those who had an elevated serum creatinine level.15 Upper GI bleeding occurred in 48% of patients, lower GI bleeding in 22%, small-bowel bleeding in 15%, and bleeding at an unknown site in 19%. The most common cause of the bleeding was from arteriovenous malformations (AVMs).15 In their review, Draper et al15 found a 9.3% prevalence of recurrent GI bleeding and a pooled event rate for an all-cause mortality rate of 23%.
They also noted that the increased risk of GI bleeding in CF LVAD patients is multifactorial. For example, there was decreased activity of type 2 von Willebrand factor multimers in patients with CF LVADs, leading to an acquired von Willebrand syndrome.15
Another finding seen in this review was that CF devices lead to a low pulse-pressure system, which is thought to cause some degree of intestinal hypoperfusion, potentially leading to vascular dilation and AVM formation.15 Based on findings, a neurovascular etiology involving increased sympathetic tone resulting in smooth muscle relaxation and AVM formation has been proposed. Lastly, the anticoagulation required with the CF LVADs to prevent pump thrombosis also increases the risk of GI bleeding, especially when combined with aspirin or other antiplatelet agents which are routinely prescribed.15
Volume Overload
Interestingly, in our study, volume overload as a cause for ED presentation was the same as for bleeding complications. In the systematic review of clinical outcomes in CF LVAD patients, volume overload or ongoing heart failure occurred in 18% of patients 1 year after device implantation.12
The clinical presentation of patients experiencing volume overload is typically dyspnea and fatigue; on physical examination they will frequently demonstrate evidence of fluid retention, such as dependent edema and pulmonary congestion.16Causes of volume overload in the LVAD patient includes medication noncompliance, inadequate pump speed, device malfunction, right ventricular failure, impaired renal function, and cardiac tamponade.16 These patients will frequently have MAPs greater than 90 mm Hg, and may require treatment with diuretics, calcium channel blockers, beta-blockers, or angiotensin-converting enzyme inhibitors.8
Weakness, Lightheadedness, Dizziness, Syncope
In our study, some combination of weakness, lightheadedness, dizziness, and syncope accounted for the third most common cause of ED presentation (9.6%). In the majority of cases, this was due to dehydration. Usually, these patients will have a MAP less than 60 mm Hg. Unfortunately, patients with pump thrombosis, sepsis, or cannula malposition can also present with a low MAP. It is important to differentiate the cause, as the management is quite different, depending on the etiology. Bedside ultrasound can play an important role in evaluating the volume status and cannula position.8 In addition, emergent consult with the patients ventricular assist device (VAD) treatment team is critical.8 Pump thrombus is a medical emergency and is usually associated with hematuria without red blood cells in the urine, acute kidney injury, and marked elevations in lactate dehydrogenase and serum free hemoglobin.8 If not treated promptly, renal failure and death may result. If dehydration is the cause, gentle rehydration with intravenous normal saline and electrolyte replacement may be all that is required.
Device Malfunction
Device malfunction was the next most common reason for ED presentation in our study, at 8.1%. This category included a number of different events, including battery failure, driveline fracture, and pump thrombosis. According to McIlvennan et al,12 causes of device malfunction include thrombus formation with hemolysis, mechanical failure of the impeller, and driveline lead fractures with electrical failure.Again, the VAD team should be consulted immediately, and the EP should plug the LVAD into a hospital power base, if available, to conserve battery life. If power is interrupted, the pump will stop working. The EP should examine all of the connections from the percutaneous lead to the controller and from the controller to the batteries to ensure they are intact. The exit site for the percutaneous lead should be examined for evidence of trauma or signs of infection. The patient should also be asked about recent trauma to the driveline.
Neurological Events
Interestingly, in other reviews, neurological events, including ischemic stroke, hemorrhagic stroke, and transient ischemic attack occur with higher frequency than was the case in the study, and are relatively common complications that can result in severe morbidity and mortality.12In the Interagency Registry for Mechanically Assisted Circulatory Support report, there was a 3% risk of stroke at 1 month, 5% at 3 months, 7% at 6 months, 11% at 12 months, 17% at 24 months, and 19% at 36 months post-implant.6,12Similarly, the HMII DT Trial demonstrated rates of ischemic and hemorrhagic stroke as high as 8% and 11% respectively, within the first 2 years following LVAD placement.5,6In our study, neurological events accounted for only six (2.4%) of ED visits. It is unclear why our numbers were less than those reported by others.
Cardiac Events and Management
During the study period, one LVAD patient presented to the ED in cardiac arrest. Patients who have an LVAD and are in cardiac arrest have unique considerations that deserve discussion. If the LVAD pump has stopped functioning, connections between the system controller and the pump and power source must be checked, as loose connections need to be refitted and the pump restarted. It is important to note that when an LVAD ceases operation, blood becomes stagnant in the pump and conduits. Delays of even several minutes pose a significant risk for pump thrombosis, stroke, and thromboembolism when the device is restarted. If the pump does not restart and the patient is connected to batteries, the batteries should be replaced with a new, fully charged pair, or the device should be connected to a base unit.17
Due to the location of the outflow graft on the aorta and the inflow conduit in the LV apex, external chest compressions pose a risk of dislodging the device and causing fatal hemorrhage. Clinical judgment should be used when deciding to perform external chest compressions. A recent American Heart Association scientific statement concluded that withholding chest compression in a patient with an LVAD who is truly in circulatory failure that is not attributable to a device failure would cause more harm to the patient than the potential to dislodge the device.18
Direct cardiac massage, performed by a skilled surgeon may be effective in patients that have had recent device implantation, especially if prior to mediastinal healing.16 If external defibrillation/cardioversion is required, the percutaneous lead should not be disconnected from the system controller and the pump should not be stopped prior to the delivery of a shock.17
Study Limitations
This was a retrospective study and has the limitations common to all such studies. It is possible that some of the patients in our study sought care at a hospital ED outside of our system, and therefore were not included in our study. This, however, is exceedingly unlikely as the cardiologists and care team continually emphasized and instructed all patients in our study only to present to the study hospital ED for any complaint. Similarly, the various emergency medical services agencies for our region were also instructed to bring all LVAD patients to the study hospital.
Another limitation of our study is the relatively small total number of patients (98) and that our findings may not apply to other patient populations. This limitation, however, would be true for any hospital system that limits the type of LVAD implant procedure to one manufacturer (HMII in this instance).
Conclusion
Emergency physicians must be prepared to evaluate the LVAD patient presenting to the ED. A little over 55% of the time, the visit will be directly related to the LVAD; in the remainder of cases, patient presentation will be due to a non-LVAD-related cause. At initial presentation, however, the EP should assume that the ED visit is related to the LVAD, until a thorough history and physical examination can exclude otherwise.
Because of the high incidence of GI bleeding in LVAD patients, a rectal examination for blood in the stool should be performed for any complaint that may be related, such as generalized weakness, syncope, or shortness of breath. In the majority of cases, a complete blood count; complete metabolic profile, including lactic acid dehydrogenase; and coagulation studies, including prothrombin time and INRs, are indicated. Most patients with an LVAD will require a member of the VAD team (typically the perfusionist or biomedical engineer) to interrogate the controller if there is any concern about its function, including alarm sounding or lights flashing.
Introduction
Approximately 6.5 million adults in the United States have heart failure, accounting for nearly 1 million ED visits annually.1 Advanced heart failure is particularly difficult to treat, and is associated with significant morbidity and mortality. While medical therapy is the initial treatment for patients with advanced heart failure, it has limited effectiveness; therefore, at the present time, heart transplant is the most effective treatment for heart failure refractory to medical management.
According to the 2013 Registry of the International Society for Heart and Lung Transplantation, 4,096 cardiac transplants were performed worldwide in 2011, approximately 2,000 of which were done in the United States.2
The average age of a heart transplant recipient in the United States is 55 years.2 In 2017, there were nearly 4,000 patients on the United Network for Organ Sharing, the organization that manages the national transplant waiting list in the United States and matches donors to recipients.3 Unfortunately, the number of patients requiring a heart transplant far exceeds the number of registered donors, and a large number of patients must wait years for transplantation. In addition to those awaiting a heart transplant, there are many patients with advanced heart failure who are not suitable candidates for transplant (usually due to age).
Left Ventricular Assist Devices
As of December 31, 2016, a total of 22,866 US Food and Drug Administration (FDA)-approved devices were listed in the Interagency Registry for Mechanically Assisted Circulatory Support, 17,016 of which were continuous-flow (CF) left ventricular assist devices (LVADs), including the HeartMate II (HMII) (Abbott Laboratories) and the HeartWare Ventricular Assist Device (HVAD) (Medtronic).4 Left ventricular assist devices, which have been in use for over 30 years, have evolved into smaller, quieter, and more durable devices. The current generation of LVADs has a CF design (as opposed to the older pulsatile-flow [PF] design). More importantly, CF LVADs are associated with higher survival rates and increased quality of life than the earlier PF models.5 For these reasons, CF LVADs are being used much more frequently today. As previously noted, LVADs serve as a temporizing measure for patients awaiting a heart transplant (ie, bridge-to-transplant therapy [BTT]) or as the primary treatment for patients who are not suitable candidates for transplant (ie, destination therapy [DT]).
The percentage of patients receiving an LVAD as a DT has increased from around 15% between 2006 to 2007 to nearly 46% in 2014.6Recently, several reports following LVAD patients demonstrated a reverse remodeling of the heart and recovery of native cardiac function that was sufficient enough in some patients as to permit LVAD removal (ie, bridge to recovery).7 In the United States, the number of patients undergoing LVAD removal due to recovery remains fewer than 3%.6With the increase in the number of patients receiving LVADs, there is an increased likelihood of LVAD patients presenting to an ED due to device-related complications. Recognized complications associated with LVADs include thrombosis, infection, bleeding, and issues with volume status.5,7 However, the frequency of LVAD-associated complications and the final disposition of these patients is less well known.
HeartMate II Patient ED Presentation Study
Purpose
The purpose of our study was to identify the reasons for LVAD patient presentation to the ED, the frequency of these presentations, and the final disposition of these patients. Our institution, Sentara Norfolk General Hospital (SNGH), is a level I trauma and a tertiary care referral center, and it is the only hospital in a large area of Virginia to perform LVAD implantation.
Our study involved only patients implanted with the HMII LVAD.
Methods
Patients and Study Design
This was a retrospective study of patients with an HMII LVAD who presented to the SNGH ED between April 1, 2009 and September 9, 2012. All patients implanted with an HMII LVAD during the study period were assigned a study number linking the patient to their medical record number and social security number. Study numbers were assigned at the time of LVAD implantation by one of the investigators. This document was kept in a secure and locked location in the department of emergency medicine and was not accessible to anyone other than study investigators.
The electronic medical records were retrospectively reviewed to identify any HMII LVAD patient presenting to the SNGH ED during the study period. Information abstracted from the ED medical records included patient age, sex, initial complaint, final diagnosis, and disposition. Only the patient’s assigned study number was used on the data collection form, and no personal identifying information was present.
This study was granted approval for human subject research by the Eastern Virginia Medical School Institutional Review Board. Eligible patients included all patients with an HMII LVAD implanted during the study period. Study patients who presented to the SNGH ED between April 1, 2009 and September 9, 2012 were identified by a retrospective chart review. These patients were instructed to specifically seek care at the SNGH ED in the event of an emergency. There were no exclusion criteria.
Data were collected and reported in real numbers and percentages. No formal statistical analysis was used in evaluating the results.
Results
Between April 1, 2009 and September 9, 2012, there were a total of 98 patients with an HMII LVAD that had been implanted during the study period at SNGH. The average patient age was 53.6 years, with a range from age 20 years to 78 years. Sixty-seven (68%) of the patients enrolled in the study required at least one ED visit. The HMII LVAD patients who presented to the ED ranged in age from 20 years to 78 years, with an average age of 53.1 years. The average number of ED visits by these 67 patients was 3.7, with a range of 1 to 12. Approximately 56% of the ED visits were directly LVAD-related. In all, 67 patients were responsible for a total of 248 ED visits.
The two most common reasons for presentation to the ED involved bleeding and volume overload. A total of 37 ED visits (14.9%), were related to bleeding, which included gastrointestinal (GI) bleeding (18/37 or 49%), epistaxis, hematuria, gingival bleeding, and postoperative bleeding following tooth extraction.
Volume overload accounted for 37 ED visits (14.9%), and the most common presenting symptom in these patients was shortness of breath. Other reasons patients presented to the ED were weakness/lightheadedness/dizziness/syncope (24/9.6%), device malfunction (20/8.1%), infection (7/2.8%), and transient ischemic attack/cerebrovascular accident (6/2.4%). For infection-related ED visits, two presentations (2.9%) involved a driveline infection. Common causes for ED visits related to device malfunction included battery failure and device-alarm activation. Overall, 142 of the 248 total ED visits (57.3%) resulted in hospital admission. One patient in the study presented in cardiac arrest and could not be resuscitated.
The remaining 108 LVAD patient ED visits (44%), did not appear to be related to the presence of the LVAD, but rather represented common reasons for presentation to an ED. These other non-LVAD-related reasons for presentation to the ED were due to motor vehicle incidents (3); assault (2); dental pain (3); mechanical fall (5); and upper respiratory tract infection (4), and represented small groupings of patient reasons for an ED visit.
Examples of singular reasons for presentation to the ED included one patient who presented with suicidal ideation, and another patient who presented for evaluation of symptoms suspicious for a sexually transmitted infection.
Discussion
As the number of patients with advanced heart failure continues to increase, the number of those with an LVAD also increases. Between 2006 and June 2013, nearly 9,000 adult patients in the United States received a durable LVAD.6 In the early years of LVAD implantation, patients were restricted to remain in proximity of geographical areas surrounding academic health care centers. An increased comfort level by both physicians and patients now allows LVAD patients to reside in more distant communities. This increase in LVAD implantation, coupled with the widening patient distribution, make it important for every emergency physician (EP) to have a working knowledge of the device and its associated complications. To date, the characteristics and frequency of LVAD patient presentations to the ED have not been well characterized.
Left ventricular assist devices are considered in patients who have significant symptoms associated with poor LV function or who cannot maintain normal hemodynamics and vital organ function. Continuous-flow LVADs account for almost all devices currently implanted. During our data-collection period, there were two FDA-approved implantable LVADs—the HMII, approved for BTT in 2008 and for DT in 2010; and the HVAD approved for BTT in 2012. In August 2017, HeartMate III (Abbott Laboratories) was approved by the FDA. All patients enrolled in our study were recipients of the HMII device, as this was the only type of LVAD implant performed at our hospital. Current survival with the HMII LVAD is 80% at 1 year and 69% at 2 years, and there has not been shown to be a significant difference when stratified by era of implant.6
Device Designs and Structures
The pump of the HMII is inserted into the abdominal cavity, whereas the HVAD is implanted in the chest cavity, with the inflow cannula in the apex of the LV and the outflow cannula connecting to the proximal aorta. Blood is continuously pumped through the system.8,9 The pump is connected to a driveline that exits the body and connects to a controller. Continuous-flow devices have either an axial or centrifugal blood pump. Axial devices have an impeller that is connected to ball-and-cup bearings that accelerate blood along its axis. Newer axial flow pumps incorporate magnetic levitation of the rotor and do not require the use of bearings. Centrifugal devices accelerate blood circumferentially with a rotor that is suspended within in the blood pool by electromagnetic or hydrodynamic forces.10 The controller is powered by two external batteries or connected to a power base unit where the pump can be interrogated. The controller is usually housed in a garment worn by the patient, one that also includes the batteries. The controller can also be powered by a base unit that can be plugged into an electrical outlet.11
There are, and continue to be, advances in both LVAD design and function. Since the time period of our study, changes have been made in the outflow bend relief (the tube at the junction of the outflow cannula and the pump housing designed to prevent kinking of the outflow cannula) and the LVAD controller. Older controllers have been replaced with newer models, but many of the LVAD pumps in this article remain in service.
Anticoagulation Therapy
Patients who have a CF LVAD require anticoagulation therapy with warfarin to a target international normalized ratio (INR) of 2 to 3, in addition to aspirin therapy of 325 mg daily.8,9Newer oral anticoagulant drugs are not routinely given to patients who have a CF LVAD.
Cardiopulmonary Evaluation
With CF LVADs, blood is pumped continuously, and a constant, machine-like murmur can be heard on auscultation rather than the typical heart sounds. Patients who have an LVAD may not have palpable arterial pulses. Doppler evaluation of the brachial artery and a manual blood pressure (BP) cuff are used to listen for the start of Korotkoff sounds as the cuff is released. The pressure at which the first sound is heard is used to estimate the patient’s mean arterial pressure (MAP) at the time when there is no pulse; and the systolic BP (SBP) is heard at the time when there is pulse. Patients with a CF LVAD with nonpulsatile flow should have a MAP between 70 mm Hg and 90 mm Hg (HMII), or 70 mm Hg and 80 mm Hg (HVAD). Patients who have a CF LVAD with a palpable pulse should have an SBP less than 120 mm Hg (HMII) or 105 mm Hg (HVAD). Readings outside of these ranges require an adjustment in the patient’s antihypertensive therapy, since high BP increases the risk of stroke and can impair the cardiac support provided by the LVAD.8Low BP may be the result of inadequate pump speed, dehydration, inflow cannula obstruction, or pump thrombus.
Bleeding
In our study, bleeding and volume overload were the two most common reasons LVAD patients presented to the ED. Interestingly, in a systematic review of clinical outcomes following CF LVAD implantation, bleeding was the most commonly recorded adverse event.12In fact, the majority of patients in all of the studies reviewed experienced at least one bleeding event. In one study of 139 HMII LVAD patients, the risk of bleeding was greatest within the first two weeks, and early bleeding was associated with increased mortality.13The most common source of bleeding complications in patients with a CF LVAD are GI, similar to our study.14
In a review and meta-analysis by Draper et al,15of GI bleeding in 1,697 patients with CF LVADs, the pooled prevalence was 23%.Subgroup analysis demonstrated an increased risk of bleeding in older patients and in those who had an elevated serum creatinine level.15 Upper GI bleeding occurred in 48% of patients, lower GI bleeding in 22%, small-bowel bleeding in 15%, and bleeding at an unknown site in 19%. The most common cause of the bleeding was from arteriovenous malformations (AVMs).15 In their review, Draper et al15 found a 9.3% prevalence of recurrent GI bleeding and a pooled event rate for an all-cause mortality rate of 23%.
They also noted that the increased risk of GI bleeding in CF LVAD patients is multifactorial. For example, there was decreased activity of type 2 von Willebrand factor multimers in patients with CF LVADs, leading to an acquired von Willebrand syndrome.15
Another finding seen in this review was that CF devices lead to a low pulse-pressure system, which is thought to cause some degree of intestinal hypoperfusion, potentially leading to vascular dilation and AVM formation.15 Based on findings, a neurovascular etiology involving increased sympathetic tone resulting in smooth muscle relaxation and AVM formation has been proposed. Lastly, the anticoagulation required with the CF LVADs to prevent pump thrombosis also increases the risk of GI bleeding, especially when combined with aspirin or other antiplatelet agents which are routinely prescribed.15
Volume Overload
Interestingly, in our study, volume overload as a cause for ED presentation was the same as for bleeding complications. In the systematic review of clinical outcomes in CF LVAD patients, volume overload or ongoing heart failure occurred in 18% of patients 1 year after device implantation.12
The clinical presentation of patients experiencing volume overload is typically dyspnea and fatigue; on physical examination they will frequently demonstrate evidence of fluid retention, such as dependent edema and pulmonary congestion.16Causes of volume overload in the LVAD patient includes medication noncompliance, inadequate pump speed, device malfunction, right ventricular failure, impaired renal function, and cardiac tamponade.16 These patients will frequently have MAPs greater than 90 mm Hg, and may require treatment with diuretics, calcium channel blockers, beta-blockers, or angiotensin-converting enzyme inhibitors.8
Weakness, Lightheadedness, Dizziness, Syncope
In our study, some combination of weakness, lightheadedness, dizziness, and syncope accounted for the third most common cause of ED presentation (9.6%). In the majority of cases, this was due to dehydration. Usually, these patients will have a MAP less than 60 mm Hg. Unfortunately, patients with pump thrombosis, sepsis, or cannula malposition can also present with a low MAP. It is important to differentiate the cause, as the management is quite different, depending on the etiology. Bedside ultrasound can play an important role in evaluating the volume status and cannula position.8 In addition, emergent consult with the patients ventricular assist device (VAD) treatment team is critical.8 Pump thrombus is a medical emergency and is usually associated with hematuria without red blood cells in the urine, acute kidney injury, and marked elevations in lactate dehydrogenase and serum free hemoglobin.8 If not treated promptly, renal failure and death may result. If dehydration is the cause, gentle rehydration with intravenous normal saline and electrolyte replacement may be all that is required.
Device Malfunction
Device malfunction was the next most common reason for ED presentation in our study, at 8.1%. This category included a number of different events, including battery failure, driveline fracture, and pump thrombosis. According to McIlvennan et al,12 causes of device malfunction include thrombus formation with hemolysis, mechanical failure of the impeller, and driveline lead fractures with electrical failure.Again, the VAD team should be consulted immediately, and the EP should plug the LVAD into a hospital power base, if available, to conserve battery life. If power is interrupted, the pump will stop working. The EP should examine all of the connections from the percutaneous lead to the controller and from the controller to the batteries to ensure they are intact. The exit site for the percutaneous lead should be examined for evidence of trauma or signs of infection. The patient should also be asked about recent trauma to the driveline.
Neurological Events
Interestingly, in other reviews, neurological events, including ischemic stroke, hemorrhagic stroke, and transient ischemic attack occur with higher frequency than was the case in the study, and are relatively common complications that can result in severe morbidity and mortality.12In the Interagency Registry for Mechanically Assisted Circulatory Support report, there was a 3% risk of stroke at 1 month, 5% at 3 months, 7% at 6 months, 11% at 12 months, 17% at 24 months, and 19% at 36 months post-implant.6,12Similarly, the HMII DT Trial demonstrated rates of ischemic and hemorrhagic stroke as high as 8% and 11% respectively, within the first 2 years following LVAD placement.5,6In our study, neurological events accounted for only six (2.4%) of ED visits. It is unclear why our numbers were less than those reported by others.
Cardiac Events and Management
During the study period, one LVAD patient presented to the ED in cardiac arrest. Patients who have an LVAD and are in cardiac arrest have unique considerations that deserve discussion. If the LVAD pump has stopped functioning, connections between the system controller and the pump and power source must be checked, as loose connections need to be refitted and the pump restarted. It is important to note that when an LVAD ceases operation, blood becomes stagnant in the pump and conduits. Delays of even several minutes pose a significant risk for pump thrombosis, stroke, and thromboembolism when the device is restarted. If the pump does not restart and the patient is connected to batteries, the batteries should be replaced with a new, fully charged pair, or the device should be connected to a base unit.17
Due to the location of the outflow graft on the aorta and the inflow conduit in the LV apex, external chest compressions pose a risk of dislodging the device and causing fatal hemorrhage. Clinical judgment should be used when deciding to perform external chest compressions. A recent American Heart Association scientific statement concluded that withholding chest compression in a patient with an LVAD who is truly in circulatory failure that is not attributable to a device failure would cause more harm to the patient than the potential to dislodge the device.18
Direct cardiac massage, performed by a skilled surgeon may be effective in patients that have had recent device implantation, especially if prior to mediastinal healing.16 If external defibrillation/cardioversion is required, the percutaneous lead should not be disconnected from the system controller and the pump should not be stopped prior to the delivery of a shock.17
Study Limitations
This was a retrospective study and has the limitations common to all such studies. It is possible that some of the patients in our study sought care at a hospital ED outside of our system, and therefore were not included in our study. This, however, is exceedingly unlikely as the cardiologists and care team continually emphasized and instructed all patients in our study only to present to the study hospital ED for any complaint. Similarly, the various emergency medical services agencies for our region were also instructed to bring all LVAD patients to the study hospital.
Another limitation of our study is the relatively small total number of patients (98) and that our findings may not apply to other patient populations. This limitation, however, would be true for any hospital system that limits the type of LVAD implant procedure to one manufacturer (HMII in this instance).
Conclusion
Emergency physicians must be prepared to evaluate the LVAD patient presenting to the ED. A little over 55% of the time, the visit will be directly related to the LVAD; in the remainder of cases, patient presentation will be due to a non-LVAD-related cause. At initial presentation, however, the EP should assume that the ED visit is related to the LVAD, until a thorough history and physical examination can exclude otherwise.
Because of the high incidence of GI bleeding in LVAD patients, a rectal examination for blood in the stool should be performed for any complaint that may be related, such as generalized weakness, syncope, or shortness of breath. In the majority of cases, a complete blood count; complete metabolic profile, including lactic acid dehydrogenase; and coagulation studies, including prothrombin time and INRs, are indicated. Most patients with an LVAD will require a member of the VAD team (typically the perfusionist or biomedical engineer) to interrogate the controller if there is any concern about its function, including alarm sounding or lights flashing.
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603. doi:10.1161/CIR.0000000000000485. Erratum in: Circulation. 2017;135(1):e646. doi:10.1161/CIR.0000000000000491.
2. Lund LH, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: thirtieth official adult heart transplant report—2013; focus theme: age. J Heart Lung Transplant. 2013;32(10):951-964. doi:10.1016/j.healun.2013.08.006.
3. UNOS (United Network for Organ Sharing) Web site. https://unos.org/data/transplant-trends/waiting-list-candidates-by-organ-type/. Accessed February 8, 2018.
4. Kirklin JK, Pagani FD, Kormos RL, et al. Eighth annual INTERMACS report: Special focus on framing the impact of adverse events. J Heart Lung Transplant. 2017;36(10):1080-1086. doi:10.1016/j.healun.2017.07.005.
5. Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous flow left ventricular assist device. N Engl J Med. 2009;361(23):2241-2251. doi:10.1056/NEJMoa0909938.
6. Kirklin JK, Naftel DC, Pagani FD, et al. Seventh INTERMACS annual report: 15,000 patients and counting. J Heart Lung Transplant. 2015;34(12):1495-1504. doi:10.1016/j.healun.2015.10.003.
7. Ambardekar AV, Buttrick PM. Reverse remodeling with left ventricular assist devices: a review of clinical, cellular and molecular effects. Circ Heart Fail. 2011;4(2):224-233. doi:10.1161/CIRCHEARTFAILURE.110.959684.
8. Slaughter MS, Pagani FD, Rogers JG, et al. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant. 2010;29 (suppl 4):1-39. doi:10.1016/j.healun.2010.01.011.
9. Lo BM, Devine AS. Patients with left ventricular assist devices. Critical Decisions in Emergency Medicine. 2014;28(7):2-9.
10. Feldman D, Pamboukian SV, Teuteberg JJ, et al. The 2013 International Society for Heart and Lung Transplantation guidelines for mechanical circulatory support: executive summary. J Heart Lung Transplant. 2013;32(2):157-187. doi:10.1016/j.healun.2012.09.013.
11. Miller LW, Pagani FD, Russell SD, et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357(9):885-896. doi:10.1056/NEJMoa067758.
12. McIlvennan CK, Magid KH, Ambardekar AV, et al. Clinical outcomes following continuous-flow left ventricular assist device: a systematic review. Circ Heart Fail. 2014;7(6):1003-1013. doi:10.1161/
13. Mulloy DP, Bhamidipati CM, Stone ML, et al. Cryoablation during left ventricular assist device implantation reduces postoperative ventricular tachyarrhythmias. J Thorac Cardiovasc Surg. 2013;145(5):1207-1213. doi:10.1016/j.jtcvs.2012.03.061.
14. Stern DR, Kazam J, Edwards P, et al. Increased incidence of gastrointestinal bleeding following implantation of the Heartmate II LVAD. J Card Surg. 2010;25(3):352-356. doi:10.1111/j.1540-8191.2010.01025.x.
15. Draper KV, Huang RJ, Gerson LB. GI bleeding in patients with continuous-flow left ventricular assist devices: a systematic review and meta-analysis. Gastrointest Endosc. 2014;80(3):435-446. doi:10.1016/j.gie.2014.03.040.
16. Aissaoui N, Morshuis M, Diebold B, et al. Heart failure while on ventricular assist device support: a true clinical entity? Arch Cardiovasc Dis. 2013:106(1):44-51. doi:10.1016/j.acvd.2012.09.006.
17. Thoratec HeartMate II Left Ventricular Assist System (LVAS) Information and Emergency Assistance Guide. Thoratec Corporation Web site. http://www.thoratec.com/_assets/download-tracker/HM_II_Info_Emergency_Assist_Guide_US_103873B_ENGLISH.pdf. Accessed July 5, 2017.
18. Peberdy MA, Gluck JA, Ornato JP, et al; American Heart Association Emergency Cardiovascular Care Committee; Council on Cardiopulmonary, Critical Care, Perioperative, and Resuscitation; Council on Cardiovascular Diseases in the Young; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. Cardiopulmonary resuscitation in adults and children with mechanical circulatory support a scientific statement from the American Heart Association. Circulation. 2017;135(24):e1115-e1134. doi:10.1161/CIR.0000000000000504.
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603. doi:10.1161/CIR.0000000000000485. Erratum in: Circulation. 2017;135(1):e646. doi:10.1161/CIR.0000000000000491.
2. Lund LH, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: thirtieth official adult heart transplant report—2013; focus theme: age. J Heart Lung Transplant. 2013;32(10):951-964. doi:10.1016/j.healun.2013.08.006.
3. UNOS (United Network for Organ Sharing) Web site. https://unos.org/data/transplant-trends/waiting-list-candidates-by-organ-type/. Accessed February 8, 2018.
4. Kirklin JK, Pagani FD, Kormos RL, et al. Eighth annual INTERMACS report: Special focus on framing the impact of adverse events. J Heart Lung Transplant. 2017;36(10):1080-1086. doi:10.1016/j.healun.2017.07.005.
5. Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous flow left ventricular assist device. N Engl J Med. 2009;361(23):2241-2251. doi:10.1056/NEJMoa0909938.
6. Kirklin JK, Naftel DC, Pagani FD, et al. Seventh INTERMACS annual report: 15,000 patients and counting. J Heart Lung Transplant. 2015;34(12):1495-1504. doi:10.1016/j.healun.2015.10.003.
7. Ambardekar AV, Buttrick PM. Reverse remodeling with left ventricular assist devices: a review of clinical, cellular and molecular effects. Circ Heart Fail. 2011;4(2):224-233. doi:10.1161/CIRCHEARTFAILURE.110.959684.
8. Slaughter MS, Pagani FD, Rogers JG, et al. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant. 2010;29 (suppl 4):1-39. doi:10.1016/j.healun.2010.01.011.
9. Lo BM, Devine AS. Patients with left ventricular assist devices. Critical Decisions in Emergency Medicine. 2014;28(7):2-9.
10. Feldman D, Pamboukian SV, Teuteberg JJ, et al. The 2013 International Society for Heart and Lung Transplantation guidelines for mechanical circulatory support: executive summary. J Heart Lung Transplant. 2013;32(2):157-187. doi:10.1016/j.healun.2012.09.013.
11. Miller LW, Pagani FD, Russell SD, et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357(9):885-896. doi:10.1056/NEJMoa067758.
12. McIlvennan CK, Magid KH, Ambardekar AV, et al. Clinical outcomes following continuous-flow left ventricular assist device: a systematic review. Circ Heart Fail. 2014;7(6):1003-1013. doi:10.1161/
13. Mulloy DP, Bhamidipati CM, Stone ML, et al. Cryoablation during left ventricular assist device implantation reduces postoperative ventricular tachyarrhythmias. J Thorac Cardiovasc Surg. 2013;145(5):1207-1213. doi:10.1016/j.jtcvs.2012.03.061.
14. Stern DR, Kazam J, Edwards P, et al. Increased incidence of gastrointestinal bleeding following implantation of the Heartmate II LVAD. J Card Surg. 2010;25(3):352-356. doi:10.1111/j.1540-8191.2010.01025.x.
15. Draper KV, Huang RJ, Gerson LB. GI bleeding in patients with continuous-flow left ventricular assist devices: a systematic review and meta-analysis. Gastrointest Endosc. 2014;80(3):435-446. doi:10.1016/j.gie.2014.03.040.
16. Aissaoui N, Morshuis M, Diebold B, et al. Heart failure while on ventricular assist device support: a true clinical entity? Arch Cardiovasc Dis. 2013:106(1):44-51. doi:10.1016/j.acvd.2012.09.006.
17. Thoratec HeartMate II Left Ventricular Assist System (LVAS) Information and Emergency Assistance Guide. Thoratec Corporation Web site. http://www.thoratec.com/_assets/download-tracker/HM_II_Info_Emergency_Assist_Guide_US_103873B_ENGLISH.pdf. Accessed July 5, 2017.
18. Peberdy MA, Gluck JA, Ornato JP, et al; American Heart Association Emergency Cardiovascular Care Committee; Council on Cardiopulmonary, Critical Care, Perioperative, and Resuscitation; Council on Cardiovascular Diseases in the Young; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular and Stroke Nursing; and Council on Clinical Cardiology. Cardiopulmonary resuscitation in adults and children with mechanical circulatory support a scientific statement from the American Heart Association. Circulation. 2017;135(24):e1115-e1134. doi:10.1161/CIR.0000000000000504.
Disruptive Physician Behavior: The Importance of Recognition and Intervention and Its Impact on Patient Safety
Dramatic stories of disruptive physician behavior (DPB) appear occasionally in the news, such as the physician who shot and killed a colleague within hospital confines or the gynecologist who secretly took photographs using a camera disguised as a pen during pelvic examinations. More common in hospitals, however, are incidents of inappropriate behavior that may generate complaints from patients or other providers and at times snowball into administrative or legal challenges.
“Professionalism” is one of the six competencies listed by the Accreditation Council for Graduate Medical Education (ACGME)1 and the American Board of Medical Specialties. Unfortunately, incidents of disruptive behavior can result in violation of the tenets of professionalism in the healthcare environment. These behaviors fall along a continuum ranging from outwardly aggressive and uncivil to overly passive and insidious. Although these behaviors can occur across all healthcare disciplines and settings and are not just limited to physicians, the behaviors of physicians often have a much greater impact on the healthcare system as a whole because of their positions of relative “power” within the system.2 Hence, this problem requires greater awareness and education. In this context, the aim of this article is to discuss disruptive behaviors in physicians
The AMA defines DPB as “personal conduct, verbal or physical that has the potential to negatively affect patient care or the ability to work with other members of the healthcare team.”3 The definition of DPB by the Joint Commission includes “all behaviors that undermine a culture of safety.”4 Both the Joint Commission and the AMA recognize the significance and patient safety implications of such behavior. Policy statements by both these organizations underscore the importance of confronting and remedying these potentially dangerous interpersonal behaviors.
Data regarding the prevalence of DPB have been inconsistent. One study estimated that 3%–5% of physicians demonstrate this behavior,5 whereas another study reported a DPB prevalence of 97% among physicians and nurses in the workplace.6 According to a 2004 survey of physician executives, more than 95% of them reported regular encounters of DPB.7
The etiology of such disruptive behaviors is multifactorial and complex. Explanations associated with ‘nature versus nurture’ have ranged from physician psychopathology to unhealthy modeling during training. Both extrinsic and intrinsic factors may also contribute to DPB. External stressors and negative experiences–professional and/or personal–can provoke disruptive behaviors. Overwork, fatigue, strife, and a dysfunctional environment that can arise in both work and home environments can contribute to the development of mental health problems. Stress, burnout, and depression have increasingly become prevalent among physicians and can play a significant role in causing impaired patterns of professional conduct.8, 9 These mental health problems can cause physicians to acquire maladaptive coping strategies such as substance abuse and drug or alcohol dependence. However, it is important to note that physician impairment and substance abuse are not the most frequent causes of DPB. In fact, fewer than 10% of physician behavior issues have been related to substance abuse.2, 5
Psychiatric disorders such as major depression and bipolar and anxiety disorders may also contribute to DPB.10 Most of these disorders (except for schizophrenia) are likely as common among physicians as among the general public.9 An essential clarification is that although DPB can be a manifestation of personality disorders or psychiatric disorders, it does not always stem from underlying psychopathology. Clarifying these distinctions is important for managing the problem and calls for expert professional evaluation in some cases.10
A person’s behavior is shaped by character, values, perceptions, and attitudes. Individuals who engage in DPB typically lack insight and justify their behaviors as a means to achieve a goal. Disrespectful behavior is rooted, in part, in characteristics such as insecurity, immaturity, and aggressiveness; however, it can also be learned, tolerated, and reinforced in the hierarchical hospital culture.11
Other intrinsic factors that may contribute to DPB include lack of emotional intelligence, poor social skills, cultural and ethnic issues, and generation and gender bias.12 Identifying the root causes of DPB can be challenging due to the complexity of the interaction between the healthcare environment and the key players within it; nevertheless, awareness of the contributing factors and early recognition are important. Those who take on the mantle of leadership within hospitals should be educated in this regard.
Repercussions of Disruptive Physician Behavior
An institution’s organizational culture often has an impact on how DPB is addressed. Tolerance of such behavior can have far-reaching consequences. The central tenets of a “culture of safety and respect”–teamwork across disciplines and a blame-free environment in which every member of the healthcare team feels equally empowered to report errors and openly discuss safety issues–would be negatively impacted.
DPB can diminish the quality of care provided, increase the risk of medical errors, and adversely affect patient safety and satisfaction.11-13 Such behavior can cause erosion of relationships and communication between individuals and contribute to a hostile work environment. For instance, nurses or trainees may be afraid to question a physician because of the fear of getting yelled at or being humiliated. Consequently, improperly written orders may be overlooked or a potentially “wrong-site” surgical procedure may not be questioned for fear of provoking a hostile response.
DPB can increase litigation risk and financial costs to institutions. Provider retention may be adversely affected; valued staff may leave hospitals and need to be replaced, and productivity may suffer. When physicians in training observe how their superiors model disruptive behaviors with impunity, a concerning problem that arises is that DPB becomes normalized in the workplace culture, especially if such behaviors are tolerated and result in a perceived gain.
Proposed Interventions
Confrontation of DPB can be challenging without appropriate infrastructure. Healthcare facilities should have a fair system in place for reliable reporting and monitoring of DPB, including a complaints’ verification process, appeals process, and an option for fair hearing.
It is best to initially address the issue in a direct, timely, yet informal manner through counseling or a verbal warning. In several situations, such informal counseling opportunities create a mindful awareness of the problem and the problematic behavior ceases without the need for further action.
When informal intervention is either not appropriate (eg, if the alleged event involved an assault or other illegal behavior) or has already been offered in the past, more formal intervention is required. Institutional progressive disciplinary polices should be in place and adhered to. For example, repeat offenders may be issued written warnings or even temporary suspension of privileges.
Institutional resources such as human resources departments, office of general counsel, office of medical affairs, and the hospital’s medical board may be consulted. Some medical centers have “employee assistance programs” staffed with clinicians skilled in dealing with DPB. Individuals diagnosed with substance abuse or a mental health disorder may require consultation with mental health professionals.14
Special “Professionalism Committees” can be instituted and tasked with investigating complaints and making recommendations for the involvement of resources outside the institution, such as a state medical society.15
Conclusion
Although the vast majority of physicians are well-behaved, it is important to acknowledge that disruptive behaviors can occur in the healthcare environment. Such behaviors have a major impact on workplace culture and patient safety and must be recognized early. Hospital executives and leaders must ensure that appropriate interventions are undertaken—before the quality of patient care is affected and before lives are endangered.
Acknowledgment
The authors would like to thank Ansu John for providing editorial assistance with the manuscript.
Disclosures
The authors have nothing to disclose (Conflict of Interest Form submitted as separate PDF document). Dr. Heitt consults with local hospitals, medical practices, and licensing boards regarding physicians and other healthcare practitioners who have been accused of engaging in disruptive behavior. In these situations he may be paid by the board, medical society, hospital, practice or the professional (patient).
1. Accreditation Council for Graduate Medical Education. Common program requirements: general competencies. https://www.acgme.org/Portals/0/PDFs/Common_Program_Requirements_07012011[2].pdf. Accessed July 25, 2017.
2. Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient safety and quality healthcare. Lionheart Publishing, Inc. 2006;3:16-24 https://www.psqh.com/julaug06/disruptive.html. Accessed October 1, 2017.
3. American Medical Association. Opinion E- 9.045–Physicians with disruptive behavior. Chicago, IL American Medical Association 2008.
4. Joint Commission: Behaviors that undermine a culture of safety. Sentinel event alert, July 9, 2008:40. http://www.jointcommission.org/sentinel_event_alert_issue_40_behaviors_that_undermine_a_culture_of_safety/. Accessed October 1, 2017.
5. Leape LL, Fromson JA. Problem doctors: is there a system-level solution? Ann Int Med. 2006;144:107-115. PubMed
6. Rosenstein AH, O’Daniel M. A survey of the impact of disruptive behaviors and communication defects on patient safety. Jt Comm J Qual Patient Saf. 2008;34(8):464-471. PubMed
7. Weber DO. Poll Results: Doctors’ disruptive behavior disturbs physician leaders. The Physician Executive. 2004;30(5):6. PubMed
8. Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289(23):3161-3166. PubMed
9. Brown S, Goske M, Johnson C. Beyond substance abuse: stress, burnout and depression as causes of physician impairment and disruptive behavior. J Am Coll Radiol. 2009 6;(7):479-485. PubMed
10. Reynolds NT. Disruptive physician behavior: use and misuse of the label. J Med Regulation. 2012;98(1):8-19.
11. Leape LL, Shore MF, Dienstag JL, et al. Perspective: a culture of respect, part 1: the nature and causes of disrespectful behavior by physicians. Acad Med. 2012;87(7):845-852. PubMed
12. Rosenstein AH, O’Daniel M. Impact and implications of disruptive behavior in the perioperative arena. J Am Coll Surg. 2006;203(1):96-105. PubMed
13. Patient Safety Primer: Disruptive and unprofessional behavior. Available at AHRQ Patient Safety Network: https://psnet.ahrq.gov/primers/primer/15/disruptive-and-unprofessional-behavior(Accessed October 1, 2017.
14. Williams BW, Williams MV. The disruptive physician: conceptual organization. JMed Licensure Discipline. 2008;94(3):12-19.
15. Speck R, Foster J, Mulhem V, et al. Development of a professionalism committee approach to address unprofessional medical staff behavior at an academic medical center. Jt Comm J Qual Patient Saf. 2004;40(4):161-167. PubMed
Dramatic stories of disruptive physician behavior (DPB) appear occasionally in the news, such as the physician who shot and killed a colleague within hospital confines or the gynecologist who secretly took photographs using a camera disguised as a pen during pelvic examinations. More common in hospitals, however, are incidents of inappropriate behavior that may generate complaints from patients or other providers and at times snowball into administrative or legal challenges.
“Professionalism” is one of the six competencies listed by the Accreditation Council for Graduate Medical Education (ACGME)1 and the American Board of Medical Specialties. Unfortunately, incidents of disruptive behavior can result in violation of the tenets of professionalism in the healthcare environment. These behaviors fall along a continuum ranging from outwardly aggressive and uncivil to overly passive and insidious. Although these behaviors can occur across all healthcare disciplines and settings and are not just limited to physicians, the behaviors of physicians often have a much greater impact on the healthcare system as a whole because of their positions of relative “power” within the system.2 Hence, this problem requires greater awareness and education. In this context, the aim of this article is to discuss disruptive behaviors in physicians
The AMA defines DPB as “personal conduct, verbal or physical that has the potential to negatively affect patient care or the ability to work with other members of the healthcare team.”3 The definition of DPB by the Joint Commission includes “all behaviors that undermine a culture of safety.”4 Both the Joint Commission and the AMA recognize the significance and patient safety implications of such behavior. Policy statements by both these organizations underscore the importance of confronting and remedying these potentially dangerous interpersonal behaviors.
Data regarding the prevalence of DPB have been inconsistent. One study estimated that 3%–5% of physicians demonstrate this behavior,5 whereas another study reported a DPB prevalence of 97% among physicians and nurses in the workplace.6 According to a 2004 survey of physician executives, more than 95% of them reported regular encounters of DPB.7
The etiology of such disruptive behaviors is multifactorial and complex. Explanations associated with ‘nature versus nurture’ have ranged from physician psychopathology to unhealthy modeling during training. Both extrinsic and intrinsic factors may also contribute to DPB. External stressors and negative experiences–professional and/or personal–can provoke disruptive behaviors. Overwork, fatigue, strife, and a dysfunctional environment that can arise in both work and home environments can contribute to the development of mental health problems. Stress, burnout, and depression have increasingly become prevalent among physicians and can play a significant role in causing impaired patterns of professional conduct.8, 9 These mental health problems can cause physicians to acquire maladaptive coping strategies such as substance abuse and drug or alcohol dependence. However, it is important to note that physician impairment and substance abuse are not the most frequent causes of DPB. In fact, fewer than 10% of physician behavior issues have been related to substance abuse.2, 5
Psychiatric disorders such as major depression and bipolar and anxiety disorders may also contribute to DPB.10 Most of these disorders (except for schizophrenia) are likely as common among physicians as among the general public.9 An essential clarification is that although DPB can be a manifestation of personality disorders or psychiatric disorders, it does not always stem from underlying psychopathology. Clarifying these distinctions is important for managing the problem and calls for expert professional evaluation in some cases.10
A person’s behavior is shaped by character, values, perceptions, and attitudes. Individuals who engage in DPB typically lack insight and justify their behaviors as a means to achieve a goal. Disrespectful behavior is rooted, in part, in characteristics such as insecurity, immaturity, and aggressiveness; however, it can also be learned, tolerated, and reinforced in the hierarchical hospital culture.11
Other intrinsic factors that may contribute to DPB include lack of emotional intelligence, poor social skills, cultural and ethnic issues, and generation and gender bias.12 Identifying the root causes of DPB can be challenging due to the complexity of the interaction between the healthcare environment and the key players within it; nevertheless, awareness of the contributing factors and early recognition are important. Those who take on the mantle of leadership within hospitals should be educated in this regard.
Repercussions of Disruptive Physician Behavior
An institution’s organizational culture often has an impact on how DPB is addressed. Tolerance of such behavior can have far-reaching consequences. The central tenets of a “culture of safety and respect”–teamwork across disciplines and a blame-free environment in which every member of the healthcare team feels equally empowered to report errors and openly discuss safety issues–would be negatively impacted.
DPB can diminish the quality of care provided, increase the risk of medical errors, and adversely affect patient safety and satisfaction.11-13 Such behavior can cause erosion of relationships and communication between individuals and contribute to a hostile work environment. For instance, nurses or trainees may be afraid to question a physician because of the fear of getting yelled at or being humiliated. Consequently, improperly written orders may be overlooked or a potentially “wrong-site” surgical procedure may not be questioned for fear of provoking a hostile response.
DPB can increase litigation risk and financial costs to institutions. Provider retention may be adversely affected; valued staff may leave hospitals and need to be replaced, and productivity may suffer. When physicians in training observe how their superiors model disruptive behaviors with impunity, a concerning problem that arises is that DPB becomes normalized in the workplace culture, especially if such behaviors are tolerated and result in a perceived gain.
Proposed Interventions
Confrontation of DPB can be challenging without appropriate infrastructure. Healthcare facilities should have a fair system in place for reliable reporting and monitoring of DPB, including a complaints’ verification process, appeals process, and an option for fair hearing.
It is best to initially address the issue in a direct, timely, yet informal manner through counseling or a verbal warning. In several situations, such informal counseling opportunities create a mindful awareness of the problem and the problematic behavior ceases without the need for further action.
When informal intervention is either not appropriate (eg, if the alleged event involved an assault or other illegal behavior) or has already been offered in the past, more formal intervention is required. Institutional progressive disciplinary polices should be in place and adhered to. For example, repeat offenders may be issued written warnings or even temporary suspension of privileges.
Institutional resources such as human resources departments, office of general counsel, office of medical affairs, and the hospital’s medical board may be consulted. Some medical centers have “employee assistance programs” staffed with clinicians skilled in dealing with DPB. Individuals diagnosed with substance abuse or a mental health disorder may require consultation with mental health professionals.14
Special “Professionalism Committees” can be instituted and tasked with investigating complaints and making recommendations for the involvement of resources outside the institution, such as a state medical society.15
Conclusion
Although the vast majority of physicians are well-behaved, it is important to acknowledge that disruptive behaviors can occur in the healthcare environment. Such behaviors have a major impact on workplace culture and patient safety and must be recognized early. Hospital executives and leaders must ensure that appropriate interventions are undertaken—before the quality of patient care is affected and before lives are endangered.
Acknowledgment
The authors would like to thank Ansu John for providing editorial assistance with the manuscript.
Disclosures
The authors have nothing to disclose (Conflict of Interest Form submitted as separate PDF document). Dr. Heitt consults with local hospitals, medical practices, and licensing boards regarding physicians and other healthcare practitioners who have been accused of engaging in disruptive behavior. In these situations he may be paid by the board, medical society, hospital, practice or the professional (patient).
Dramatic stories of disruptive physician behavior (DPB) appear occasionally in the news, such as the physician who shot and killed a colleague within hospital confines or the gynecologist who secretly took photographs using a camera disguised as a pen during pelvic examinations. More common in hospitals, however, are incidents of inappropriate behavior that may generate complaints from patients or other providers and at times snowball into administrative or legal challenges.
“Professionalism” is one of the six competencies listed by the Accreditation Council for Graduate Medical Education (ACGME)1 and the American Board of Medical Specialties. Unfortunately, incidents of disruptive behavior can result in violation of the tenets of professionalism in the healthcare environment. These behaviors fall along a continuum ranging from outwardly aggressive and uncivil to overly passive and insidious. Although these behaviors can occur across all healthcare disciplines and settings and are not just limited to physicians, the behaviors of physicians often have a much greater impact on the healthcare system as a whole because of their positions of relative “power” within the system.2 Hence, this problem requires greater awareness and education. In this context, the aim of this article is to discuss disruptive behaviors in physicians
The AMA defines DPB as “personal conduct, verbal or physical that has the potential to negatively affect patient care or the ability to work with other members of the healthcare team.”3 The definition of DPB by the Joint Commission includes “all behaviors that undermine a culture of safety.”4 Both the Joint Commission and the AMA recognize the significance and patient safety implications of such behavior. Policy statements by both these organizations underscore the importance of confronting and remedying these potentially dangerous interpersonal behaviors.
Data regarding the prevalence of DPB have been inconsistent. One study estimated that 3%–5% of physicians demonstrate this behavior,5 whereas another study reported a DPB prevalence of 97% among physicians and nurses in the workplace.6 According to a 2004 survey of physician executives, more than 95% of them reported regular encounters of DPB.7
The etiology of such disruptive behaviors is multifactorial and complex. Explanations associated with ‘nature versus nurture’ have ranged from physician psychopathology to unhealthy modeling during training. Both extrinsic and intrinsic factors may also contribute to DPB. External stressors and negative experiences–professional and/or personal–can provoke disruptive behaviors. Overwork, fatigue, strife, and a dysfunctional environment that can arise in both work and home environments can contribute to the development of mental health problems. Stress, burnout, and depression have increasingly become prevalent among physicians and can play a significant role in causing impaired patterns of professional conduct.8, 9 These mental health problems can cause physicians to acquire maladaptive coping strategies such as substance abuse and drug or alcohol dependence. However, it is important to note that physician impairment and substance abuse are not the most frequent causes of DPB. In fact, fewer than 10% of physician behavior issues have been related to substance abuse.2, 5
Psychiatric disorders such as major depression and bipolar and anxiety disorders may also contribute to DPB.10 Most of these disorders (except for schizophrenia) are likely as common among physicians as among the general public.9 An essential clarification is that although DPB can be a manifestation of personality disorders or psychiatric disorders, it does not always stem from underlying psychopathology. Clarifying these distinctions is important for managing the problem and calls for expert professional evaluation in some cases.10
A person’s behavior is shaped by character, values, perceptions, and attitudes. Individuals who engage in DPB typically lack insight and justify their behaviors as a means to achieve a goal. Disrespectful behavior is rooted, in part, in characteristics such as insecurity, immaturity, and aggressiveness; however, it can also be learned, tolerated, and reinforced in the hierarchical hospital culture.11
Other intrinsic factors that may contribute to DPB include lack of emotional intelligence, poor social skills, cultural and ethnic issues, and generation and gender bias.12 Identifying the root causes of DPB can be challenging due to the complexity of the interaction between the healthcare environment and the key players within it; nevertheless, awareness of the contributing factors and early recognition are important. Those who take on the mantle of leadership within hospitals should be educated in this regard.
Repercussions of Disruptive Physician Behavior
An institution’s organizational culture often has an impact on how DPB is addressed. Tolerance of such behavior can have far-reaching consequences. The central tenets of a “culture of safety and respect”–teamwork across disciplines and a blame-free environment in which every member of the healthcare team feels equally empowered to report errors and openly discuss safety issues–would be negatively impacted.
DPB can diminish the quality of care provided, increase the risk of medical errors, and adversely affect patient safety and satisfaction.11-13 Such behavior can cause erosion of relationships and communication between individuals and contribute to a hostile work environment. For instance, nurses or trainees may be afraid to question a physician because of the fear of getting yelled at or being humiliated. Consequently, improperly written orders may be overlooked or a potentially “wrong-site” surgical procedure may not be questioned for fear of provoking a hostile response.
DPB can increase litigation risk and financial costs to institutions. Provider retention may be adversely affected; valued staff may leave hospitals and need to be replaced, and productivity may suffer. When physicians in training observe how their superiors model disruptive behaviors with impunity, a concerning problem that arises is that DPB becomes normalized in the workplace culture, especially if such behaviors are tolerated and result in a perceived gain.
Proposed Interventions
Confrontation of DPB can be challenging without appropriate infrastructure. Healthcare facilities should have a fair system in place for reliable reporting and monitoring of DPB, including a complaints’ verification process, appeals process, and an option for fair hearing.
It is best to initially address the issue in a direct, timely, yet informal manner through counseling or a verbal warning. In several situations, such informal counseling opportunities create a mindful awareness of the problem and the problematic behavior ceases without the need for further action.
When informal intervention is either not appropriate (eg, if the alleged event involved an assault or other illegal behavior) or has already been offered in the past, more formal intervention is required. Institutional progressive disciplinary polices should be in place and adhered to. For example, repeat offenders may be issued written warnings or even temporary suspension of privileges.
Institutional resources such as human resources departments, office of general counsel, office of medical affairs, and the hospital’s medical board may be consulted. Some medical centers have “employee assistance programs” staffed with clinicians skilled in dealing with DPB. Individuals diagnosed with substance abuse or a mental health disorder may require consultation with mental health professionals.14
Special “Professionalism Committees” can be instituted and tasked with investigating complaints and making recommendations for the involvement of resources outside the institution, such as a state medical society.15
Conclusion
Although the vast majority of physicians are well-behaved, it is important to acknowledge that disruptive behaviors can occur in the healthcare environment. Such behaviors have a major impact on workplace culture and patient safety and must be recognized early. Hospital executives and leaders must ensure that appropriate interventions are undertaken—before the quality of patient care is affected and before lives are endangered.
Acknowledgment
The authors would like to thank Ansu John for providing editorial assistance with the manuscript.
Disclosures
The authors have nothing to disclose (Conflict of Interest Form submitted as separate PDF document). Dr. Heitt consults with local hospitals, medical practices, and licensing boards regarding physicians and other healthcare practitioners who have been accused of engaging in disruptive behavior. In these situations he may be paid by the board, medical society, hospital, practice or the professional (patient).
1. Accreditation Council for Graduate Medical Education. Common program requirements: general competencies. https://www.acgme.org/Portals/0/PDFs/Common_Program_Requirements_07012011[2].pdf. Accessed July 25, 2017.
2. Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient safety and quality healthcare. Lionheart Publishing, Inc. 2006;3:16-24 https://www.psqh.com/julaug06/disruptive.html. Accessed October 1, 2017.
3. American Medical Association. Opinion E- 9.045–Physicians with disruptive behavior. Chicago, IL American Medical Association 2008.
4. Joint Commission: Behaviors that undermine a culture of safety. Sentinel event alert, July 9, 2008:40. http://www.jointcommission.org/sentinel_event_alert_issue_40_behaviors_that_undermine_a_culture_of_safety/. Accessed October 1, 2017.
5. Leape LL, Fromson JA. Problem doctors: is there a system-level solution? Ann Int Med. 2006;144:107-115. PubMed
6. Rosenstein AH, O’Daniel M. A survey of the impact of disruptive behaviors and communication defects on patient safety. Jt Comm J Qual Patient Saf. 2008;34(8):464-471. PubMed
7. Weber DO. Poll Results: Doctors’ disruptive behavior disturbs physician leaders. The Physician Executive. 2004;30(5):6. PubMed
8. Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289(23):3161-3166. PubMed
9. Brown S, Goske M, Johnson C. Beyond substance abuse: stress, burnout and depression as causes of physician impairment and disruptive behavior. J Am Coll Radiol. 2009 6;(7):479-485. PubMed
10. Reynolds NT. Disruptive physician behavior: use and misuse of the label. J Med Regulation. 2012;98(1):8-19.
11. Leape LL, Shore MF, Dienstag JL, et al. Perspective: a culture of respect, part 1: the nature and causes of disrespectful behavior by physicians. Acad Med. 2012;87(7):845-852. PubMed
12. Rosenstein AH, O’Daniel M. Impact and implications of disruptive behavior in the perioperative arena. J Am Coll Surg. 2006;203(1):96-105. PubMed
13. Patient Safety Primer: Disruptive and unprofessional behavior. Available at AHRQ Patient Safety Network: https://psnet.ahrq.gov/primers/primer/15/disruptive-and-unprofessional-behavior(Accessed October 1, 2017.
14. Williams BW, Williams MV. The disruptive physician: conceptual organization. JMed Licensure Discipline. 2008;94(3):12-19.
15. Speck R, Foster J, Mulhem V, et al. Development of a professionalism committee approach to address unprofessional medical staff behavior at an academic medical center. Jt Comm J Qual Patient Saf. 2004;40(4):161-167. PubMed
1. Accreditation Council for Graduate Medical Education. Common program requirements: general competencies. https://www.acgme.org/Portals/0/PDFs/Common_Program_Requirements_07012011[2].pdf. Accessed July 25, 2017.
2. Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient safety and quality healthcare. Lionheart Publishing, Inc. 2006;3:16-24 https://www.psqh.com/julaug06/disruptive.html. Accessed October 1, 2017.
3. American Medical Association. Opinion E- 9.045–Physicians with disruptive behavior. Chicago, IL American Medical Association 2008.
4. Joint Commission: Behaviors that undermine a culture of safety. Sentinel event alert, July 9, 2008:40. http://www.jointcommission.org/sentinel_event_alert_issue_40_behaviors_that_undermine_a_culture_of_safety/. Accessed October 1, 2017.
5. Leape LL, Fromson JA. Problem doctors: is there a system-level solution? Ann Int Med. 2006;144:107-115. PubMed
6. Rosenstein AH, O’Daniel M. A survey of the impact of disruptive behaviors and communication defects on patient safety. Jt Comm J Qual Patient Saf. 2008;34(8):464-471. PubMed
7. Weber DO. Poll Results: Doctors’ disruptive behavior disturbs physician leaders. The Physician Executive. 2004;30(5):6. PubMed
8. Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289(23):3161-3166. PubMed
9. Brown S, Goske M, Johnson C. Beyond substance abuse: stress, burnout and depression as causes of physician impairment and disruptive behavior. J Am Coll Radiol. 2009 6;(7):479-485. PubMed
10. Reynolds NT. Disruptive physician behavior: use and misuse of the label. J Med Regulation. 2012;98(1):8-19.
11. Leape LL, Shore MF, Dienstag JL, et al. Perspective: a culture of respect, part 1: the nature and causes of disrespectful behavior by physicians. Acad Med. 2012;87(7):845-852. PubMed
12. Rosenstein AH, O’Daniel M. Impact and implications of disruptive behavior in the perioperative arena. J Am Coll Surg. 2006;203(1):96-105. PubMed
13. Patient Safety Primer: Disruptive and unprofessional behavior. Available at AHRQ Patient Safety Network: https://psnet.ahrq.gov/primers/primer/15/disruptive-and-unprofessional-behavior(Accessed October 1, 2017.
14. Williams BW, Williams MV. The disruptive physician: conceptual organization. JMed Licensure Discipline. 2008;94(3):12-19.
15. Speck R, Foster J, Mulhem V, et al. Development of a professionalism committee approach to address unprofessional medical staff behavior at an academic medical center. Jt Comm J Qual Patient Saf. 2004;40(4):161-167. PubMed
© 2018 Society of Hospital Medicine
Denah Joseph: “In the Hospital”
We recently spoke with Denah Joseph, a clinical chaplain who works with the Palliative Care team to provide spiritual services to patients with serious illness. In addition, Denah leads efforts to address burnout among healthcare providers.
Denah, tell us about yourself.
My first career was actually in clinical psychology, but I’ve been a Palliative Care chaplain for 15 years. I also teach skill-building for providers around burnout and resilience.
What brought you to Palliative Care?
I’ve lost three sisters and a partner to breast cancer, and my dad died when I was quite young, so I’ve had a lot of exposure to loss. The other big thread in my life has been my spiritual practice. My father was an Orthodox Jew, but exceptionally ecumenical for his time. His first wife was Irish Catholic, and my father used to go to church, sit, kneel, and say the rosary, and light candles for his Catholic friends. Three hundred nuns from the local diocese all came to my dad’s funeral. It was really remarkable.
I’ve been a practicing Buddhist since I was 19. When I went back to school to become a chaplain I wanted to bring more of my spiritual interest into counseling work, so chaplaincy seemed like a really interesting way to do that.
Tell us more about what a chaplain actually does.
As a field, healthcare chaplaincy is relatively new. The old model was if a person was religious, somebody would arrange for a rabbi or an imam or a priest to come into the hospital and take care of the pastoral needs of that patient. In the last 10 to 15 years, the consensus guidelines for quality patient care now include addressing the spiritual dimension of patients’ lives. Instead of relying on volunteers from the community with no quality assurance, it’s required that any hospital over 200 beds have spiritual care available. In order to be a board-certified chaplain, you need to be endorsed by a faith community, and have an advanced degree in either Pastoral Counseling or Theology.
Everybody has spiritual needs even if they don’t use that word “spiritual.” We define it in terms of meaning, relationships, impact on one’s life, hope, fears, reconciliation issues, legacy issues, etc. Approximately 80% of patients want their physicians to understand a little bit about their spiritual/existential/emotional world, and only 20% of doctors ask—so there’s a really big gap. This can be a 5-minute conversation about who are you, what’s important to you, what’s the biggest struggle with your illness that is not medically oriented.
Can you share a patient encounter where you learned something?
Recently I cared for a patient whose wish was to survive to see his only son graduate from college. His wife and son both were like, “You’ve got to hang in there, Dad. You’ve got to hang in there.” He had very advanced pancreatic cancer, and the chances of him making it to graduation were exceedingly small, but nobody was dealing with this.
During the hospitalization, I went to the patient and his wife and I said, “We’re all hoping that you’re going to make it until the graduation but in the event you don’t, would you like to write a letter to your son?” In the Jewish tradition, it is called an ethical will. It’s the idea of legacy work. Just like you would make a will for your material possessions, an ethical will expresses what you value, what you hope for and dream for your beloved. He wanted to do it. His wife said, “Absolutely not, that’s like believing you’re not going to make it.” He was a very gentle guy. He would generally completely defer to his wife, but this time he said, “No, I want to do this.”
So I met with the patient and asked questions like, “What are the things you would hope to be remembered for? What are you most proud of that you want your son to know? What would you want your son to know if he became a father?”
I had him just talk, while I took notes. Later on, I wrote it up on official stationery and gave it to the patient.
What was his reaction when you gave the letter to him?
He started to cry. He said it was perfect. I usually read it to them so they can make edits if they want to. It sort of brings the grief forward when you imagine talking to a beloved that you’re leaving behind.
A few days later the patient died in the hospital surrounded by family members.
His wife, who had advocated so strongly against the letter, hugged me. She said, “That letter is the most important thing that happened here in the hospital.” I was shocked she said that, I had no idea he even shared it with her.
If people have the opportunity to share what’s important to them, particularly generationally, it could address a very deep need to be remembered.
Reflecting on it, I actually see myself as a healer and all my work is in healing, whether it’s working with physicians or working with patients or working with students or working with people in my private practice. It’s a theme that runs through everything. It’s not a word we hear often enough in medicine.
Why not?
The culture of medicine has lost its roots, in that sense. I hear a lot of people say, “There’s nothing we can do medically, so we’re just supporting them through this.” Supporting people through the experience is often seen as less valuable, but I think, particularly for serious, terminal illness, supporting people is not optional.
Switching gears a bit, tell us about the skill-building and resilience work you’ve done.
I think if you don’t proactively care for the rest of your life then your work life takes over. Although it’s pronounced in medicine, it’s in all fields. The pace and stress of our contemporary culture can be contrary to well-being in general.
When I first came to UCSF, I saw a culture of silence around stress, anxiety, and burnout. I started reading about burnout and the numbers of people who qualified to be burnt out at any given time, which may be at least 50% and trending upward. It just seemed to me that in any other profession if half the workforce was impaired, somebody would be doing something. I’ve really become passionate about this in the last couple of years.
So I developed a burnout prevention and resilience skills training class for providers. We work on mindfulness, social connection and support, positive psychology emotions like gratitude, appreciation, self-compassion, and humor, and delve into the sources of meaning in our work.
Based on your work, what would you say are the key stressors in medicine, generally?
Well there’s research on the electronic medical record and the increasing focus on metrics and “value-driven medicine,” which can lead to reduced connection with patients. I hope that what I’m doing makes some difference, but fundamentally, I believe there needs to be a real commitment on the part of the health system, to understand and make the changes that need to happen.
What is the fundamental problem? How do you define that?
Well I don’t think anybody knows. I think that’s what we’re saying. How can it be that so many people aren’t happy in such privileged work? It’s not clinical. It’s the system. It’s yet another flow sheet that you have to fill out; the actual amount of time spent with patients is low. No wonder we get burned out. We’re just doing orders all the time and answering phone calls.
It’s the loss of interconnectedness.
Yes, it’s the loss of connection. That goes back to even why chaplains may not be recognized as adding value. You can’t put a metric on connection. You can’t say, “I made 5 connections.”
Anything else you would like to share?
I don’t know how you feel about it, but I feel so grateful to have the opportunity to be in people’s lives in the intimate way we get to be and I, especially, get to be in a way sometimes even more than doctors. You get to be there, and you may even want to talk about the things that we were mentioning, but they’re asking you about their creatinine and their platelets and their urinary incontinence, so that’s what you’re having to talk about. I don’t have to do that, so I feel like I get the best seat in the house that way.
I think the seriously ill have so much to share and often are wise, particularly the young ones, from having dealt with illness. I’m really interested in that idea of wisdom and how you develop wisdom. Traditionally wisdom is associated with being an elder and having lived a long time and having a lot of experience. I think our work gives us that opportunity. We don’t have to necessarily live through everything to develop that kind of wisdom, but just to be with people who are living through these things.
So here I am, almost 70. I’m working harder than I’ve ever worked in my life. My partner is retired. She’s like, “Come on, let’s play.” She rides bikes, takes the dog out, cooks, reads. But I just can’t stop. I think it’s because I feel like, what else would I want to be doing with my time? I think that’s an amazing thing to be given that gift that I learn from my patients all the time and learn about what’s important. Obviously people are different, but it all boils down to relationships in the end.
That’s the promise of medicine, and I think that’s the great sadness of what’s going on with the epidemic of burnout. People lose connection to that.
There is some element to being present in these hard and difficult times that can bring perspective to life; and to know the sadness, in some ways
…is to know the joy.
Thank you, Denah, for sharing your thoughts with us.
We recently spoke with Denah Joseph, a clinical chaplain who works with the Palliative Care team to provide spiritual services to patients with serious illness. In addition, Denah leads efforts to address burnout among healthcare providers.
Denah, tell us about yourself.
My first career was actually in clinical psychology, but I’ve been a Palliative Care chaplain for 15 years. I also teach skill-building for providers around burnout and resilience.
What brought you to Palliative Care?
I’ve lost three sisters and a partner to breast cancer, and my dad died when I was quite young, so I’ve had a lot of exposure to loss. The other big thread in my life has been my spiritual practice. My father was an Orthodox Jew, but exceptionally ecumenical for his time. His first wife was Irish Catholic, and my father used to go to church, sit, kneel, and say the rosary, and light candles for his Catholic friends. Three hundred nuns from the local diocese all came to my dad’s funeral. It was really remarkable.
I’ve been a practicing Buddhist since I was 19. When I went back to school to become a chaplain I wanted to bring more of my spiritual interest into counseling work, so chaplaincy seemed like a really interesting way to do that.
Tell us more about what a chaplain actually does.
As a field, healthcare chaplaincy is relatively new. The old model was if a person was religious, somebody would arrange for a rabbi or an imam or a priest to come into the hospital and take care of the pastoral needs of that patient. In the last 10 to 15 years, the consensus guidelines for quality patient care now include addressing the spiritual dimension of patients’ lives. Instead of relying on volunteers from the community with no quality assurance, it’s required that any hospital over 200 beds have spiritual care available. In order to be a board-certified chaplain, you need to be endorsed by a faith community, and have an advanced degree in either Pastoral Counseling or Theology.
Everybody has spiritual needs even if they don’t use that word “spiritual.” We define it in terms of meaning, relationships, impact on one’s life, hope, fears, reconciliation issues, legacy issues, etc. Approximately 80% of patients want their physicians to understand a little bit about their spiritual/existential/emotional world, and only 20% of doctors ask—so there’s a really big gap. This can be a 5-minute conversation about who are you, what’s important to you, what’s the biggest struggle with your illness that is not medically oriented.
Can you share a patient encounter where you learned something?
Recently I cared for a patient whose wish was to survive to see his only son graduate from college. His wife and son both were like, “You’ve got to hang in there, Dad. You’ve got to hang in there.” He had very advanced pancreatic cancer, and the chances of him making it to graduation were exceedingly small, but nobody was dealing with this.
During the hospitalization, I went to the patient and his wife and I said, “We’re all hoping that you’re going to make it until the graduation but in the event you don’t, would you like to write a letter to your son?” In the Jewish tradition, it is called an ethical will. It’s the idea of legacy work. Just like you would make a will for your material possessions, an ethical will expresses what you value, what you hope for and dream for your beloved. He wanted to do it. His wife said, “Absolutely not, that’s like believing you’re not going to make it.” He was a very gentle guy. He would generally completely defer to his wife, but this time he said, “No, I want to do this.”
So I met with the patient and asked questions like, “What are the things you would hope to be remembered for? What are you most proud of that you want your son to know? What would you want your son to know if he became a father?”
I had him just talk, while I took notes. Later on, I wrote it up on official stationery and gave it to the patient.
What was his reaction when you gave the letter to him?
He started to cry. He said it was perfect. I usually read it to them so they can make edits if they want to. It sort of brings the grief forward when you imagine talking to a beloved that you’re leaving behind.
A few days later the patient died in the hospital surrounded by family members.
His wife, who had advocated so strongly against the letter, hugged me. She said, “That letter is the most important thing that happened here in the hospital.” I was shocked she said that, I had no idea he even shared it with her.
If people have the opportunity to share what’s important to them, particularly generationally, it could address a very deep need to be remembered.
Reflecting on it, I actually see myself as a healer and all my work is in healing, whether it’s working with physicians or working with patients or working with students or working with people in my private practice. It’s a theme that runs through everything. It’s not a word we hear often enough in medicine.
Why not?
The culture of medicine has lost its roots, in that sense. I hear a lot of people say, “There’s nothing we can do medically, so we’re just supporting them through this.” Supporting people through the experience is often seen as less valuable, but I think, particularly for serious, terminal illness, supporting people is not optional.
Switching gears a bit, tell us about the skill-building and resilience work you’ve done.
I think if you don’t proactively care for the rest of your life then your work life takes over. Although it’s pronounced in medicine, it’s in all fields. The pace and stress of our contemporary culture can be contrary to well-being in general.
When I first came to UCSF, I saw a culture of silence around stress, anxiety, and burnout. I started reading about burnout and the numbers of people who qualified to be burnt out at any given time, which may be at least 50% and trending upward. It just seemed to me that in any other profession if half the workforce was impaired, somebody would be doing something. I’ve really become passionate about this in the last couple of years.
So I developed a burnout prevention and resilience skills training class for providers. We work on mindfulness, social connection and support, positive psychology emotions like gratitude, appreciation, self-compassion, and humor, and delve into the sources of meaning in our work.
Based on your work, what would you say are the key stressors in medicine, generally?
Well there’s research on the electronic medical record and the increasing focus on metrics and “value-driven medicine,” which can lead to reduced connection with patients. I hope that what I’m doing makes some difference, but fundamentally, I believe there needs to be a real commitment on the part of the health system, to understand and make the changes that need to happen.
What is the fundamental problem? How do you define that?
Well I don’t think anybody knows. I think that’s what we’re saying. How can it be that so many people aren’t happy in such privileged work? It’s not clinical. It’s the system. It’s yet another flow sheet that you have to fill out; the actual amount of time spent with patients is low. No wonder we get burned out. We’re just doing orders all the time and answering phone calls.
It’s the loss of interconnectedness.
Yes, it’s the loss of connection. That goes back to even why chaplains may not be recognized as adding value. You can’t put a metric on connection. You can’t say, “I made 5 connections.”
Anything else you would like to share?
I don’t know how you feel about it, but I feel so grateful to have the opportunity to be in people’s lives in the intimate way we get to be and I, especially, get to be in a way sometimes even more than doctors. You get to be there, and you may even want to talk about the things that we were mentioning, but they’re asking you about their creatinine and their platelets and their urinary incontinence, so that’s what you’re having to talk about. I don’t have to do that, so I feel like I get the best seat in the house that way.
I think the seriously ill have so much to share and often are wise, particularly the young ones, from having dealt with illness. I’m really interested in that idea of wisdom and how you develop wisdom. Traditionally wisdom is associated with being an elder and having lived a long time and having a lot of experience. I think our work gives us that opportunity. We don’t have to necessarily live through everything to develop that kind of wisdom, but just to be with people who are living through these things.
So here I am, almost 70. I’m working harder than I’ve ever worked in my life. My partner is retired. She’s like, “Come on, let’s play.” She rides bikes, takes the dog out, cooks, reads. But I just can’t stop. I think it’s because I feel like, what else would I want to be doing with my time? I think that’s an amazing thing to be given that gift that I learn from my patients all the time and learn about what’s important. Obviously people are different, but it all boils down to relationships in the end.
That’s the promise of medicine, and I think that’s the great sadness of what’s going on with the epidemic of burnout. People lose connection to that.
There is some element to being present in these hard and difficult times that can bring perspective to life; and to know the sadness, in some ways
…is to know the joy.
Thank you, Denah, for sharing your thoughts with us.
We recently spoke with Denah Joseph, a clinical chaplain who works with the Palliative Care team to provide spiritual services to patients with serious illness. In addition, Denah leads efforts to address burnout among healthcare providers.
Denah, tell us about yourself.
My first career was actually in clinical psychology, but I’ve been a Palliative Care chaplain for 15 years. I also teach skill-building for providers around burnout and resilience.
What brought you to Palliative Care?
I’ve lost three sisters and a partner to breast cancer, and my dad died when I was quite young, so I’ve had a lot of exposure to loss. The other big thread in my life has been my spiritual practice. My father was an Orthodox Jew, but exceptionally ecumenical for his time. His first wife was Irish Catholic, and my father used to go to church, sit, kneel, and say the rosary, and light candles for his Catholic friends. Three hundred nuns from the local diocese all came to my dad’s funeral. It was really remarkable.
I’ve been a practicing Buddhist since I was 19. When I went back to school to become a chaplain I wanted to bring more of my spiritual interest into counseling work, so chaplaincy seemed like a really interesting way to do that.
Tell us more about what a chaplain actually does.
As a field, healthcare chaplaincy is relatively new. The old model was if a person was religious, somebody would arrange for a rabbi or an imam or a priest to come into the hospital and take care of the pastoral needs of that patient. In the last 10 to 15 years, the consensus guidelines for quality patient care now include addressing the spiritual dimension of patients’ lives. Instead of relying on volunteers from the community with no quality assurance, it’s required that any hospital over 200 beds have spiritual care available. In order to be a board-certified chaplain, you need to be endorsed by a faith community, and have an advanced degree in either Pastoral Counseling or Theology.
Everybody has spiritual needs even if they don’t use that word “spiritual.” We define it in terms of meaning, relationships, impact on one’s life, hope, fears, reconciliation issues, legacy issues, etc. Approximately 80% of patients want their physicians to understand a little bit about their spiritual/existential/emotional world, and only 20% of doctors ask—so there’s a really big gap. This can be a 5-minute conversation about who are you, what’s important to you, what’s the biggest struggle with your illness that is not medically oriented.
Can you share a patient encounter where you learned something?
Recently I cared for a patient whose wish was to survive to see his only son graduate from college. His wife and son both were like, “You’ve got to hang in there, Dad. You’ve got to hang in there.” He had very advanced pancreatic cancer, and the chances of him making it to graduation were exceedingly small, but nobody was dealing with this.
During the hospitalization, I went to the patient and his wife and I said, “We’re all hoping that you’re going to make it until the graduation but in the event you don’t, would you like to write a letter to your son?” In the Jewish tradition, it is called an ethical will. It’s the idea of legacy work. Just like you would make a will for your material possessions, an ethical will expresses what you value, what you hope for and dream for your beloved. He wanted to do it. His wife said, “Absolutely not, that’s like believing you’re not going to make it.” He was a very gentle guy. He would generally completely defer to his wife, but this time he said, “No, I want to do this.”
So I met with the patient and asked questions like, “What are the things you would hope to be remembered for? What are you most proud of that you want your son to know? What would you want your son to know if he became a father?”
I had him just talk, while I took notes. Later on, I wrote it up on official stationery and gave it to the patient.
What was his reaction when you gave the letter to him?
He started to cry. He said it was perfect. I usually read it to them so they can make edits if they want to. It sort of brings the grief forward when you imagine talking to a beloved that you’re leaving behind.
A few days later the patient died in the hospital surrounded by family members.
His wife, who had advocated so strongly against the letter, hugged me. She said, “That letter is the most important thing that happened here in the hospital.” I was shocked she said that, I had no idea he even shared it with her.
If people have the opportunity to share what’s important to them, particularly generationally, it could address a very deep need to be remembered.
Reflecting on it, I actually see myself as a healer and all my work is in healing, whether it’s working with physicians or working with patients or working with students or working with people in my private practice. It’s a theme that runs through everything. It’s not a word we hear often enough in medicine.
Why not?
The culture of medicine has lost its roots, in that sense. I hear a lot of people say, “There’s nothing we can do medically, so we’re just supporting them through this.” Supporting people through the experience is often seen as less valuable, but I think, particularly for serious, terminal illness, supporting people is not optional.
Switching gears a bit, tell us about the skill-building and resilience work you’ve done.
I think if you don’t proactively care for the rest of your life then your work life takes over. Although it’s pronounced in medicine, it’s in all fields. The pace and stress of our contemporary culture can be contrary to well-being in general.
When I first came to UCSF, I saw a culture of silence around stress, anxiety, and burnout. I started reading about burnout and the numbers of people who qualified to be burnt out at any given time, which may be at least 50% and trending upward. It just seemed to me that in any other profession if half the workforce was impaired, somebody would be doing something. I’ve really become passionate about this in the last couple of years.
So I developed a burnout prevention and resilience skills training class for providers. We work on mindfulness, social connection and support, positive psychology emotions like gratitude, appreciation, self-compassion, and humor, and delve into the sources of meaning in our work.
Based on your work, what would you say are the key stressors in medicine, generally?
Well there’s research on the electronic medical record and the increasing focus on metrics and “value-driven medicine,” which can lead to reduced connection with patients. I hope that what I’m doing makes some difference, but fundamentally, I believe there needs to be a real commitment on the part of the health system, to understand and make the changes that need to happen.
What is the fundamental problem? How do you define that?
Well I don’t think anybody knows. I think that’s what we’re saying. How can it be that so many people aren’t happy in such privileged work? It’s not clinical. It’s the system. It’s yet another flow sheet that you have to fill out; the actual amount of time spent with patients is low. No wonder we get burned out. We’re just doing orders all the time and answering phone calls.
It’s the loss of interconnectedness.
Yes, it’s the loss of connection. That goes back to even why chaplains may not be recognized as adding value. You can’t put a metric on connection. You can’t say, “I made 5 connections.”
Anything else you would like to share?
I don’t know how you feel about it, but I feel so grateful to have the opportunity to be in people’s lives in the intimate way we get to be and I, especially, get to be in a way sometimes even more than doctors. You get to be there, and you may even want to talk about the things that we were mentioning, but they’re asking you about their creatinine and their platelets and their urinary incontinence, so that’s what you’re having to talk about. I don’t have to do that, so I feel like I get the best seat in the house that way.
I think the seriously ill have so much to share and often are wise, particularly the young ones, from having dealt with illness. I’m really interested in that idea of wisdom and how you develop wisdom. Traditionally wisdom is associated with being an elder and having lived a long time and having a lot of experience. I think our work gives us that opportunity. We don’t have to necessarily live through everything to develop that kind of wisdom, but just to be with people who are living through these things.
So here I am, almost 70. I’m working harder than I’ve ever worked in my life. My partner is retired. She’s like, “Come on, let’s play.” She rides bikes, takes the dog out, cooks, reads. But I just can’t stop. I think it’s because I feel like, what else would I want to be doing with my time? I think that’s an amazing thing to be given that gift that I learn from my patients all the time and learn about what’s important. Obviously people are different, but it all boils down to relationships in the end.
That’s the promise of medicine, and I think that’s the great sadness of what’s going on with the epidemic of burnout. People lose connection to that.
There is some element to being present in these hard and difficult times that can bring perspective to life; and to know the sadness, in some ways
…is to know the joy.
Thank you, Denah, for sharing your thoughts with us.
© 2018 Society of Hospital Medicine
In the Hospital: Series Introduction
The only real voyage of discovery consists not in seeking new landscapes but in having new eyes.
—Marcel Proust
Hospitals can be complex, challenging, and dehumanizing for both patients and practitioners. In a national survey, up to half of hospitalists were affected by burnout and scored highly on emotional exhaustion and depersonalization scales.1
Yet hospitals are also ripe with meaningful stories. In addition to patients’ narratives, the stories of multidisciplinary team members who make quality patient care possible reveal that we are bound together in more ways than we realize. Now, we have the opportunity to tell these stories.
This issue of Journal of Hospital Medicine introduces a new series: In the Hospital. Through selected interviews we explore the day-to-day lives of members of our hospital team. Highlighting the “team”
We invite readers to appreciate the common threads that bind these pieces together. These stories will introduce us to individuals who have discrete and often disparate job descriptions, but all of them care about patients and want the best for them. Some are frustrated with the health care system and the constraints it places on our efficiency. Many of them worry about how to balance the demands of work with the need to be available for their families and friends. Many are trying their best to maintain their humanism, build resilience, and sustain themselves in ways that meet their personal goals for excellence, empathy, and fulfillment.
This series begins with the story of a palliative-care clinical chaplain whose life experience and perspective brings to light issues of resilience, meaning, and purpose. Future stories in this series will include a variety of providers across a spectrum of practice environments. We look forward to engaging you in this journey and welcome feedback and contributions.
Disclosures
The authors have nothing to disclose.
1. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and out- patient general internists. J Hosp Med. 2014;9(3),176-181. PubMed
The only real voyage of discovery consists not in seeking new landscapes but in having new eyes.
—Marcel Proust
Hospitals can be complex, challenging, and dehumanizing for both patients and practitioners. In a national survey, up to half of hospitalists were affected by burnout and scored highly on emotional exhaustion and depersonalization scales.1
Yet hospitals are also ripe with meaningful stories. In addition to patients’ narratives, the stories of multidisciplinary team members who make quality patient care possible reveal that we are bound together in more ways than we realize. Now, we have the opportunity to tell these stories.
This issue of Journal of Hospital Medicine introduces a new series: In the Hospital. Through selected interviews we explore the day-to-day lives of members of our hospital team. Highlighting the “team”
We invite readers to appreciate the common threads that bind these pieces together. These stories will introduce us to individuals who have discrete and often disparate job descriptions, but all of them care about patients and want the best for them. Some are frustrated with the health care system and the constraints it places on our efficiency. Many of them worry about how to balance the demands of work with the need to be available for their families and friends. Many are trying their best to maintain their humanism, build resilience, and sustain themselves in ways that meet their personal goals for excellence, empathy, and fulfillment.
This series begins with the story of a palliative-care clinical chaplain whose life experience and perspective brings to light issues of resilience, meaning, and purpose. Future stories in this series will include a variety of providers across a spectrum of practice environments. We look forward to engaging you in this journey and welcome feedback and contributions.
Disclosures
The authors have nothing to disclose.
The only real voyage of discovery consists not in seeking new landscapes but in having new eyes.
—Marcel Proust
Hospitals can be complex, challenging, and dehumanizing for both patients and practitioners. In a national survey, up to half of hospitalists were affected by burnout and scored highly on emotional exhaustion and depersonalization scales.1
Yet hospitals are also ripe with meaningful stories. In addition to patients’ narratives, the stories of multidisciplinary team members who make quality patient care possible reveal that we are bound together in more ways than we realize. Now, we have the opportunity to tell these stories.
This issue of Journal of Hospital Medicine introduces a new series: In the Hospital. Through selected interviews we explore the day-to-day lives of members of our hospital team. Highlighting the “team”
We invite readers to appreciate the common threads that bind these pieces together. These stories will introduce us to individuals who have discrete and often disparate job descriptions, but all of them care about patients and want the best for them. Some are frustrated with the health care system and the constraints it places on our efficiency. Many of them worry about how to balance the demands of work with the need to be available for their families and friends. Many are trying their best to maintain their humanism, build resilience, and sustain themselves in ways that meet their personal goals for excellence, empathy, and fulfillment.
This series begins with the story of a palliative-care clinical chaplain whose life experience and perspective brings to light issues of resilience, meaning, and purpose. Future stories in this series will include a variety of providers across a spectrum of practice environments. We look forward to engaging you in this journey and welcome feedback and contributions.
Disclosures
The authors have nothing to disclose.
1. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and out- patient general internists. J Hosp Med. 2014;9(3),176-181. PubMed
1. Roberts DL, Shanafelt TD, Dyrbye LN, West CP. A national comparison of burnout and work-life balance among internal medicine hospitalists and out- patient general internists. J Hosp Med. 2014;9(3),176-181. PubMed
© 2018 Society of Hospital Medicine
Rivaroxaban Plus Aspirin Nearly Halves Ischemic Stroke Risk
LOS ANGELES—Combined treatment with a low dosage of the anticoagulant rivaroxaban plus aspirin cut the incidence of ischemic strokes nearly in half, compared with aspirin alone, in a multicenter, randomized trial of more than 27,000 patients with stable atherosclerotic vascular disease.
This dramatic reduction in ischemic strokes, as well as a 42% reduction in all-cause strokes, by adding low-dose rivaroxaban (Xarelto) occurred without a significant increase in hemorrhagic strokes, but with a small increase in total major bleeding events such as gastrointestinal bleeds, said Mike Sharma, MD, at the International Stroke Conference 2018.
“There was a consistent effect across all strata of stroke risk,” Dr. Sharma said. Among patients with a prior stroke, rivaroxaban plus aspirin provided the greatest benefit, with no increase in intracranial hemorrhages, Dr. Sharma said.
“We think these results will fundamentally change how we approach stroke prevention,” said Dr. Sharma, a stroke neurologist in the Population Health Research Institute of McMaster University in Hamilton, Ontario.
An Analysis of Data From COMPASS
Dr. Sharma reported results from a secondary analysis of data collected in the COMPASS (Rivaroxaban for the Prevention of Major Cardiovascular Events in Coronary or Peripheral Artery Disease) trial, which enrolled 27,395 patients with stable coronary or peripheral artery disease at 602 centers in 33 countries.
The primary outcome of the trial, reported in 2017, was the combined rate of cardiovascular death, myocardial infarction, or stroke during an average of 23 months of follow-up. Patients received rivaroxaban plus aspirin (ie, 2.5 mg of rivaroxaban twice daily plus 100 mg of aspirin once daily), aspirin alone (ie, 100 mg of aspirin daily), or rivaroxaban alone (ie, 5.0 mg of rivaroxaban twice daily). A primary outcome event occurred in 4.1% of patients treated with rivaroxaban plus aspirin, 4.9% of patients who received rivaroxaban alone, and 5.4% of patients who received aspirin alone—a statistically significant 24% relative risk reduction in the combined treatment group, compared with aspirin only. The rivaroxaban only–treated patients did not significantly differ from the control patients who received only aspirin. The rate of major bleeds in patients treated with rivaroxaban plus aspirin was 1.2% greater, compared with aspirin only, but the rate of nonfatal symptomatic intracranial hemorrhages was identical in the two treatment groups.
The present study focused on various measures of stroke. The rate of all strokes was 42% lower among the patients treated with rivaroxaban plus aspirin, compared with the aspirin-alone patients, and the rate of ischemic strokes was 49% lower with the dual therapy, compared with aspirin only. Both differences were statistically significant. In contrast, the rivaroxaban-alone regimen did not significantly reduce all-cause strokes. It did significantly reduce ischemic strokes, compared with aspirin only, but it also significantly increased hemorrhagic strokes, compared with aspirin only, an adverse effect not caused by the combination of low-dose rivaroxaban plus aspirin.
Benefit in High-Risk Patients
Rivaroxaban plus aspirin surpassed aspirin alone for preventing mild and severe strokes and for preventing strokes in patients with a history of a prior stroke and in those without a prior stroke. The stroke reduction produced by rivaroxaban plus aspirin was greatest in the highest risk patients—those with a prior stroke. On the combined regimen, these patients had an average stroke incidence of 0.7% per year, compared with an annual 3.4% rate among the patients on aspirin only. This 2.7% absolute reduction by using rivaroxaban plus aspirin translated into a number needed to treat of 37 patients with a history of stroke to prevent one new stroke per year.
The 2017 report of the main COMPASS results included a net clinical benefit analysis that factored together the primary end point events and major bleeding events. The net rate of all these events was 4.7% with rivaroxaban plus aspirin and 5.9% with aspirin only, a statistically significant 20% relative risk reduction for all adverse outcomes with dual therapy. Researchers are assessing the cost-effectiveness of adding rivaroxaban, Dr. Sharma said.
Rivaroxaban received FDA marketing approval in 2011 for preventing deep vein thrombosis and preventing stroke in patients with atrial fibrillation at dosages higher than those used in COMPASS. The approved rivaroxaban dosage is 10 mg/day for preventing deep vein thrombosis, and 20 mg/day for preventing stroke in patients with atrial fibrillation. The 2.5-mg formulation of rivaroxaban that was given twice daily had the best safety and efficacy in COMPASS, but it is not available now on the US market, although it is available in Europe. Johnson & Johnson, which markets rivaroxaban globally with Bayer, submitted an application to the FDA in December 2017 for marketing approval of the 2.5-mg formulation in twice-daily dosing for use as in the COMPASS trial.
COMPASS was sponsored by Bayer, and Dr. Sharma has been a consultant or adviser to Bayer.
—Mitchel L. Zoler
Suggested Reading
Eikelboom JW, Connolly SJ, Bosch J, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377(14):1319-1330.
LOS ANGELES—Combined treatment with a low dosage of the anticoagulant rivaroxaban plus aspirin cut the incidence of ischemic strokes nearly in half, compared with aspirin alone, in a multicenter, randomized trial of more than 27,000 patients with stable atherosclerotic vascular disease.
This dramatic reduction in ischemic strokes, as well as a 42% reduction in all-cause strokes, by adding low-dose rivaroxaban (Xarelto) occurred without a significant increase in hemorrhagic strokes, but with a small increase in total major bleeding events such as gastrointestinal bleeds, said Mike Sharma, MD, at the International Stroke Conference 2018.
“There was a consistent effect across all strata of stroke risk,” Dr. Sharma said. Among patients with a prior stroke, rivaroxaban plus aspirin provided the greatest benefit, with no increase in intracranial hemorrhages, Dr. Sharma said.
“We think these results will fundamentally change how we approach stroke prevention,” said Dr. Sharma, a stroke neurologist in the Population Health Research Institute of McMaster University in Hamilton, Ontario.
An Analysis of Data From COMPASS
Dr. Sharma reported results from a secondary analysis of data collected in the COMPASS (Rivaroxaban for the Prevention of Major Cardiovascular Events in Coronary or Peripheral Artery Disease) trial, which enrolled 27,395 patients with stable coronary or peripheral artery disease at 602 centers in 33 countries.
The primary outcome of the trial, reported in 2017, was the combined rate of cardiovascular death, myocardial infarction, or stroke during an average of 23 months of follow-up. Patients received rivaroxaban plus aspirin (ie, 2.5 mg of rivaroxaban twice daily plus 100 mg of aspirin once daily), aspirin alone (ie, 100 mg of aspirin daily), or rivaroxaban alone (ie, 5.0 mg of rivaroxaban twice daily). A primary outcome event occurred in 4.1% of patients treated with rivaroxaban plus aspirin, 4.9% of patients who received rivaroxaban alone, and 5.4% of patients who received aspirin alone—a statistically significant 24% relative risk reduction in the combined treatment group, compared with aspirin only. The rivaroxaban only–treated patients did not significantly differ from the control patients who received only aspirin. The rate of major bleeds in patients treated with rivaroxaban plus aspirin was 1.2% greater, compared with aspirin only, but the rate of nonfatal symptomatic intracranial hemorrhages was identical in the two treatment groups.
The present study focused on various measures of stroke. The rate of all strokes was 42% lower among the patients treated with rivaroxaban plus aspirin, compared with the aspirin-alone patients, and the rate of ischemic strokes was 49% lower with the dual therapy, compared with aspirin only. Both differences were statistically significant. In contrast, the rivaroxaban-alone regimen did not significantly reduce all-cause strokes. It did significantly reduce ischemic strokes, compared with aspirin only, but it also significantly increased hemorrhagic strokes, compared with aspirin only, an adverse effect not caused by the combination of low-dose rivaroxaban plus aspirin.
Benefit in High-Risk Patients
Rivaroxaban plus aspirin surpassed aspirin alone for preventing mild and severe strokes and for preventing strokes in patients with a history of a prior stroke and in those without a prior stroke. The stroke reduction produced by rivaroxaban plus aspirin was greatest in the highest risk patients—those with a prior stroke. On the combined regimen, these patients had an average stroke incidence of 0.7% per year, compared with an annual 3.4% rate among the patients on aspirin only. This 2.7% absolute reduction by using rivaroxaban plus aspirin translated into a number needed to treat of 37 patients with a history of stroke to prevent one new stroke per year.
The 2017 report of the main COMPASS results included a net clinical benefit analysis that factored together the primary end point events and major bleeding events. The net rate of all these events was 4.7% with rivaroxaban plus aspirin and 5.9% with aspirin only, a statistically significant 20% relative risk reduction for all adverse outcomes with dual therapy. Researchers are assessing the cost-effectiveness of adding rivaroxaban, Dr. Sharma said.
Rivaroxaban received FDA marketing approval in 2011 for preventing deep vein thrombosis and preventing stroke in patients with atrial fibrillation at dosages higher than those used in COMPASS. The approved rivaroxaban dosage is 10 mg/day for preventing deep vein thrombosis, and 20 mg/day for preventing stroke in patients with atrial fibrillation. The 2.5-mg formulation of rivaroxaban that was given twice daily had the best safety and efficacy in COMPASS, but it is not available now on the US market, although it is available in Europe. Johnson & Johnson, which markets rivaroxaban globally with Bayer, submitted an application to the FDA in December 2017 for marketing approval of the 2.5-mg formulation in twice-daily dosing for use as in the COMPASS trial.
COMPASS was sponsored by Bayer, and Dr. Sharma has been a consultant or adviser to Bayer.
—Mitchel L. Zoler
Suggested Reading
Eikelboom JW, Connolly SJ, Bosch J, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377(14):1319-1330.
LOS ANGELES—Combined treatment with a low dosage of the anticoagulant rivaroxaban plus aspirin cut the incidence of ischemic strokes nearly in half, compared with aspirin alone, in a multicenter, randomized trial of more than 27,000 patients with stable atherosclerotic vascular disease.
This dramatic reduction in ischemic strokes, as well as a 42% reduction in all-cause strokes, by adding low-dose rivaroxaban (Xarelto) occurred without a significant increase in hemorrhagic strokes, but with a small increase in total major bleeding events such as gastrointestinal bleeds, said Mike Sharma, MD, at the International Stroke Conference 2018.
“There was a consistent effect across all strata of stroke risk,” Dr. Sharma said. Among patients with a prior stroke, rivaroxaban plus aspirin provided the greatest benefit, with no increase in intracranial hemorrhages, Dr. Sharma said.
“We think these results will fundamentally change how we approach stroke prevention,” said Dr. Sharma, a stroke neurologist in the Population Health Research Institute of McMaster University in Hamilton, Ontario.
An Analysis of Data From COMPASS
Dr. Sharma reported results from a secondary analysis of data collected in the COMPASS (Rivaroxaban for the Prevention of Major Cardiovascular Events in Coronary or Peripheral Artery Disease) trial, which enrolled 27,395 patients with stable coronary or peripheral artery disease at 602 centers in 33 countries.
The primary outcome of the trial, reported in 2017, was the combined rate of cardiovascular death, myocardial infarction, or stroke during an average of 23 months of follow-up. Patients received rivaroxaban plus aspirin (ie, 2.5 mg of rivaroxaban twice daily plus 100 mg of aspirin once daily), aspirin alone (ie, 100 mg of aspirin daily), or rivaroxaban alone (ie, 5.0 mg of rivaroxaban twice daily). A primary outcome event occurred in 4.1% of patients treated with rivaroxaban plus aspirin, 4.9% of patients who received rivaroxaban alone, and 5.4% of patients who received aspirin alone—a statistically significant 24% relative risk reduction in the combined treatment group, compared with aspirin only. The rivaroxaban only–treated patients did not significantly differ from the control patients who received only aspirin. The rate of major bleeds in patients treated with rivaroxaban plus aspirin was 1.2% greater, compared with aspirin only, but the rate of nonfatal symptomatic intracranial hemorrhages was identical in the two treatment groups.
The present study focused on various measures of stroke. The rate of all strokes was 42% lower among the patients treated with rivaroxaban plus aspirin, compared with the aspirin-alone patients, and the rate of ischemic strokes was 49% lower with the dual therapy, compared with aspirin only. Both differences were statistically significant. In contrast, the rivaroxaban-alone regimen did not significantly reduce all-cause strokes. It did significantly reduce ischemic strokes, compared with aspirin only, but it also significantly increased hemorrhagic strokes, compared with aspirin only, an adverse effect not caused by the combination of low-dose rivaroxaban plus aspirin.
Benefit in High-Risk Patients
Rivaroxaban plus aspirin surpassed aspirin alone for preventing mild and severe strokes and for preventing strokes in patients with a history of a prior stroke and in those without a prior stroke. The stroke reduction produced by rivaroxaban plus aspirin was greatest in the highest risk patients—those with a prior stroke. On the combined regimen, these patients had an average stroke incidence of 0.7% per year, compared with an annual 3.4% rate among the patients on aspirin only. This 2.7% absolute reduction by using rivaroxaban plus aspirin translated into a number needed to treat of 37 patients with a history of stroke to prevent one new stroke per year.
The 2017 report of the main COMPASS results included a net clinical benefit analysis that factored together the primary end point events and major bleeding events. The net rate of all these events was 4.7% with rivaroxaban plus aspirin and 5.9% with aspirin only, a statistically significant 20% relative risk reduction for all adverse outcomes with dual therapy. Researchers are assessing the cost-effectiveness of adding rivaroxaban, Dr. Sharma said.
Rivaroxaban received FDA marketing approval in 2011 for preventing deep vein thrombosis and preventing stroke in patients with atrial fibrillation at dosages higher than those used in COMPASS. The approved rivaroxaban dosage is 10 mg/day for preventing deep vein thrombosis, and 20 mg/day for preventing stroke in patients with atrial fibrillation. The 2.5-mg formulation of rivaroxaban that was given twice daily had the best safety and efficacy in COMPASS, but it is not available now on the US market, although it is available in Europe. Johnson & Johnson, which markets rivaroxaban globally with Bayer, submitted an application to the FDA in December 2017 for marketing approval of the 2.5-mg formulation in twice-daily dosing for use as in the COMPASS trial.
COMPASS was sponsored by Bayer, and Dr. Sharma has been a consultant or adviser to Bayer.
—Mitchel L. Zoler
Suggested Reading
Eikelboom JW, Connolly SJ, Bosch J, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377(14):1319-1330.
Relationship between Hospital 30-Day Mortality Rates for Heart Failure and Patterns of Early Inpatient Comfort Care
In an effort to improve the quality of care delivered to heart failure (HF) patients, the Centers for Medicare & Medicaid Services (CMS) publish hospitals’ 30-day risk-standardized mortality rates (RSMRs) for HF.1 These mortality rates are also used by CMS to determine the financial penalties and bonuses that hospitals receive as part of the national Hospital Value-based Purchasing program.2 Whether or not these efforts effectively direct patients towards high-quality providers or motivate hospitals to provide better care, few would disagree with the overarching goal of decreasing the number of patients who die from HF.
However, for some patients with chronic disease at the end of life, goals of care may change. The quality of days lived may become more important than the quantity of days lived. As a consequence, high-quality care for some patients at the end of life is associated with withdrawing life-sustaining or life-extending therapies. Over time, this therapeutic perspective has become more common, with use of hospice care doubling from 23% to 47% between 2000 and 2012 among Medicare beneficiaries who died.3 For a national cohort of older patients admitted with HF—not just those patients who died in that same year—hospitals’ rates of referral to hospice are considerably lower, averaging 2.9% in 2010 in a national study.4 Nevertheless, it is possible that hospitals that more faithfully follow their dying patients’ wishes and withdraw life-prolonging interventions and provide comfort-focused care at the end of life might be unfairly penalized if such efforts resulted in higher mortality rates than other hospitals.
Therefore, we used Medicare data linked to a national HF registry with information about end-of-life care, to address 3 questions: (1) How much do hospitals vary in their rates of early comfort care and how has this changed over time; (2) What hospital and patient factors are associated with higher early comfort care rates; and (3) Is there a correlation between 30-day risk-adjusted mortality rates for HF with hospital rates of early comfort care?
METHODS
Data Sources
We used data from the American Heart Association’s Get With The Guidelines-Heart Failure (GWTG-HF) registry. GWTG-HF is a voluntary, inpatient, quality improvement registry5-7 that uses web-based tools and standard questionnaires to collect data on patients with HF admitted to participating hospitals nationwide. The data include information from admission (eg, sociodemographic characteristics, symptoms, medical history, and initial laboratory and test results), the inpatient stay (eg, therapies), and discharge (eg, discharge destination, whether and when comfort care was initiated). We linked the GWTG-HF registry data to Medicare claims data in order to obtain information about Medicare eligibility and patient comorbidities. Additionally, we used data from the American Hospital Association (2008) for hospital characteristics. Quintiles Real-World & Late Phase Research (Cambridge, MA) serves as the data coordinating center for GWTG-HF and the Duke Clinical Research Institute (Durham, NC) serves as the statistical analytic center. GWTG-HF participating sites have a waiver of informed consent because the data are de-identified and primarily used for quality improvement. All analyses performed on this data have been approved by the Duke Medical Center Institutional Review Board.
Study Population
Study Outcomes
Our outcome of interest was the correlation between a hospital’s rate of initiating early CMO for admitted HF patients and a hospital’s 30-day RSMR for HF. The GWTG-HF questionnaire8 asks “When is the earliest physician/advanced practice nurse/physician assistant documentation of comfort measures only?” and permits 4 responses: day 0 or 1, day 2 or after, timing unclear, or not documented/unable to determine. We defined early CMO as CMO on day 0 or 1, and late/no CMO as any other response. We chose to examine early comfort care because many hospitalized patients transition to comfort care before they die if the death is in any way predictable. Thus, if comfort care is measured at any time during the hospitalization, hospitals that have high mortality rates are likely to have high comfort care rates. Therefore, we chose to use the more precise measure of early comfort care. We created hospital-level, risk-standardized early comfort care rates using the same risk-adjustment model used for RSMRs but with the outcome of early comfort care instead of mortality.9,10
RSMRs were calculated using a validated GWTG-HF 30-day risk-standardized mortality model9 with additional variables identified from other GWTG-HF analyses.10 The 30 days are measured as the 30 days after the index admission date.
Statistical Analyses
We described trends in early comfort care rates over time, from February 17, 2008, to February 17, 2014, using the Cochran-Armitage test for trend. We then grouped hospitals into quintiles based on their unadjusted early comfort care rates. We described patient and hospital characteristics for each quintile, using χ2 tests to test for differences across quintiles for categorical variables and Wilcoxon rank sum tests to assess for differences across quintiles for continuous variables. We then examined the Spearman’s rank correlation between hospitals’ RSMR and risk-adjusted comfort care rates. Finally, we compared hospital-level RSMRs before and after adjusting for early comfort care.
We performed risk-adjustment for these last 2 analyses as follows. For each patient, covariates were obtained from the GWTG-HF registry. Clinical data captured for the index admission were utilized in the risk-adjustment model (for both RSMRs and risk-adjusted comfort care rates). Included covariates were as follows: age (per 10 years); race (black vs non-black); systolic blood pressure at admission ≤170 (per 10 mm Hg); respiratory rate (per 5 respirations/min); heart rate ≤105 (per 10 beats/min); weight ≤100 (per 5 kg); weight >100 (per 5 kg); blood urea nitrogen (per 10 mg/dl); brain natriuretic peptide ≤2000 (per 500 pg/ml); hemoglobin 10-14 (per 1 g/dl); troponin abnormal (vs normal); creatinine ≤1 (per 1 mg/dl); sodium 130-140 (per 5 mEq/l); and chronic obstructive pulmonary disease or asthma.
Hierarchical logistic regression modeling was used to calculate the hospital-specific RSMR. A predicted/expected ratio similar to an observed/expected (O/E) ratio was calculated using the following modifications: (1) instead of the observed (crude) number of deaths, the numerator is the number of deaths predicted by the hierarchical model among a hospital’s patients given the patients’ risk factors and the hospital-specific effect; (2) the denominator is the expected number of deaths among the hospital’s patients given the patients’ risk factors and the average of all hospital-specific effects overall; and (3) the ratio of the numerator and denominator are then multiplied by the observed overall mortality rate (same as O/E). This calculation is the method used by CMS to derive RSMRs.11 Multiple imputation was used to handle missing data in the models; 25 imputed datasets using the fully conditional specification method were created. Patients with missing prior comorbidities were assumed to not have those conditions. Hospital characteristics were not imputed; therefore, for analyses that required construction of risk-adjusted comfort care rates or RSMRs, we excluded 18,867 patients cared for at 82 hospitals missing hospital characteristics. We ran 2 sets of models for risk-adjusted comfort care rates and RSMRs: the first adjusted only for patient characteristics, and the second adjusted for both patient and hospital characteristics. Results from the 2 models were similar, so we present only results from the latter. Variance inflation factors were all <2, indicating the collinearity between covariates was not an issue.
All statistical analyses were performed by using SAS version 9.4 (SAS Institute, Cary, NC). We tested for statistical significance by using 2-tailed tests and considered P values <.05 to be statistically significant.
RESULTS
Of the 272 hospitals included in our final study cohort, the observed median overall rate of early comfort care in this study was 1.9% (25th to 75th percentile: 0.9% to 4.0%); hospitals varied widely in unadjusted early comfort care rates (0.00% to 0.46% in the lowest quintile, and 4.60% to 39.91% in the highest quintile; Table 1).
DISCUSSION
Among a national sample of US hospitals, we found wide variation in how frequently health care providers deliver comfort care within the first 2 days of admission for HF. A minority of hospitals reported no early comfort care on any patients throughout the 6-year study period, but hospitals in the highest quintile initiated early comfort care rates for at least 1 in 20 HF patients. Hospitals that were more likely to initiate early comfort care had a higher proportion of female and white patients and were less likely to have the capacity to deliver aggressive surgical interventions such as heart transplants. Hospital-level 30-day RSMRs were not correlated with rates of early comfort care.
While the appropriate rate of early comfort care for patients hospitalized with HF is unknown, given that the average hospital RSMR is approximately 12% for fee-for-service Medicare patients hospitalized with HF,12 it is surprising that some hospitals initiated early comfort care on none or very few of their HF patients. It is quite possible that many of these hospitals initiated comfort care for some of their patients after 48 hours of hospitalization. We were unable to estimate the average period of time patients received comfort care prior to dying, the degree to which this varies across hospitals or why it might vary, and whether the length of time between comfort care initiation and death is related to satisfaction with end-of-life care. Future research on these topics would help inform providers seeking to deliver better end-of-life care. In this study, we also were unable to estimate how often early comfort care was not initiated because patients had a good prognosis. However, prior studies have suggested low rates of comfort care or hospice referral even among patients at very high estimated mortality risk.4 It is also possible that providers and families had concerns about the ability to accurately prognosticate, although several models have been shown to perform acceptably for patients hospitalized with HF.13
We found that comfort care rates did not increase over time, even though use of hospice care doubled among Medicare beneficiaries between 2000 and 2012. By way of context, cancer—the second leading cause of death in the US—was responsible for 38% of hospice admissions in 2013, whereas heart disease (including but not limited to HF)—the leading cause of death— was responsible for 13% of hospice admissions.14 The 2013 American College of Cardiology Foundation and the American Heart Association guidelines for HF recommend consideration of hospice or palliative care for inpatient and transitional care.15 In future work, it would be important to better understand the drivers behind decisions around comfort care for patients hospitalized with HF.
With regards to the policy implications of our study, we found that on average, adjusting 30-day mortality rates for early comfort care was not associated with a change in hospital mortality rankings. For those hospitals with high comfort care rates, adjusting for comfort care did lower mortality rates, but the change was so small as to be clinically insignificant. CMS’ RSMR for HF excludes patients enrolled in hospice during the 12 months prior to index admission, including the first day of the index admission, acknowledging that death may not be an untoward outcome for such patients.16 Fee-for-service Medicare beneficiaries excluded for hospice enrollment comprised 1.29% of HF admissions from July 2012 to June 201516 and are likely a subset of early comfort care patients in our sample, both because of the inclusiveness of chart review (vs claims-based identification) and because we defined early comfort care as comfort care initiated on day 0 or 1 of hospitalization. Nevertheless, with our data we cannot assess to what degree our findings were due solely to hospice patients excluded from CMS’ current estimates.
Prior research has described the underuse of palliative care among patients with HF17 and the association of palliative care with better patient and family experiences at the end of life.18-20 We add to this literature by describing the epidemiology—prevalence, changes over time, and associated factors—of early comfort care for HF in a national sample of hospitals. This serves as a baseline for future work on end-of-life care among patients hospitalized for HF. Our findings also contribute to ongoing discussion about how best to risk-adjust mortality metrics used to assess hospital quality in pay-for-performance programs. Recent research on stroke and pneumonia based on California data suggests that not accounting for do-not-resuscitate (DNR) status biases hospital mortality rates.21,22 Earlier research examined the impact of adjusting hospital mortality rates for DNR for a broader range of conditions.23,24 We expand this line of inquiry by examining the hospital-level association of early comfort care with mortality rates for HF, utilizing a national, contemporary cohort of inpatient stays. In addition, while studies have found that DNR rates within the first 24 hours of admission are relatively high (median 15.8% for pneumonia; 13.3% for stroke),21,22 comfort care is distinct from DNR.
Our findings should be interpreted in the context of several potential limitations. First, we did not have any information about patient or family wishes regarding end-of-life care, or the exact timing of early comfort care (eg, day 0 or day 1). The initiation of comfort care usually follows conversations about end-of-life care involving a patient, his or her family, and the medical team. Thus, we do not know if low early comfort care rates represent the lack of such a conversation (and thus poor-quality care) or the desire by most patients not to initiate early comfort care (and thus high-quality care). This would be an important area for future research. Second, we included only patients admitted to hospitals that participate in GWTG-HF, a voluntary quality improvement initiative. This may limit the generalizability of our findings, but it is unclear how our sample might bias our findings. Hospitals engaged in quality improvement may be more likely to initiate early comfort care aligned with patients’ wishes; on the other hand, hospitals with advanced surgical capabilities are over-represented in our sample and these hospitals are less likely to initiate early comfort care. Third, we examined associations and cannot make conclusions about causality. Residual measured and unmeasured confounding may influence these findings.
In summary, we found that early comfort care rates for fee-for-service Medicare beneficiaries admitted for HF varies widely among hospitals, but median rates of early comfort care have not changed over time. On average, there was no correlation between hospital-level, 30-day, RSMRs and rates of early comfort care. This suggests that current efforts to lower mortality rates have not had unintended consequences for hospitals that institute early comfort care more commonly than their peers.
Acknowledgments
Dr. Chen and Ms. Cox take responsibility for the integrity of the data and the accuracy of the data analysis. Drs. Chen, Levine, and Hayward are responsible for the study concept and design. Drs. Chen and Fonarow acquired the data. Dr. Chen drafted the manuscript. Drs. Chen, Levin, Hayward, Cox, Fonarow, DeVore, Hernandez, Heidenreich, and Yancy revised the manuscript for important intellectual content. Drs. Chen, Hayward, Cox, and Schulte performed the statistical analysis. Drs. Chen and Fonarow obtained funding for the study. Drs. Hayward and Fonarow supervised the study. The authors thank Bailey Green, MPH, for the research assistance she provided. She was compensated for her work.
Disclosure
Dr. Fonarow reports research support from the National Institutes of Health, and consulting for Amgen, Janssen, Novartis, Medtronic, and St Jude Medical. Dr. DeVore reports research support from the American Heart Association, Amgen, and Novartis, and consulting for Amgen. The other authors have no relevant conflicts of interest. Dr. Chen was supported by a Career Development Grant Award (K08HS020671) from the Agency for Healthcare Research and Quality when the manuscript was being prepared. She currently receives support from the Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation for her work there. She also receives support from the Blue Cross Blue Shield of Michigan Foundation’s Investigator Initiated Research Program, the Agency for Healthcare Research and Quality (R01 HS024698), and the National Institute on Aging (P01 AG019783). These funding sources had no role in the preparation, review, or approval of the manuscript. The GWTG-HF program is provided by the American Heart Association. GWTG-HF has been funded in the past through support from Amgen, Medtronic, GlaxoSmithKline, Ortho-McNeil, and the American Heart Association Pharmaceutical Roundtable. These sponsors had no role in the study design, data analysis or manuscript preparation and revision.
1. Centers for Medicare & Medicaid Services. Hospital Compare. https://www.medicare.gov/hospitalcompare/. Accessed on November 27, 2016.
2. Centers for Medicare & Medicaid Services. Hospital Value-based Purchasing. https://www.medicare.gov/hospitalcompare/data/hospital-vbp.html. Accessed August 30, 2017.
3. Medicare Payment Advisory Comission. Report to the Congress: Medicare payment policy. 2014. http://www.medpac.gov/docs/default-source/reports/mar14_entirereport.pdf. Accessed August 31, 2017.
4. Whellan DJ, Cox M, Hernandez AF, et al. Utilization of hospice and predicted mortality risk among older patients hospitalized with heart failure: findings from GWTG-HF. J Card Fail. 2012;18(6):471-477. PubMed
5. Hong Y, LaBresh KA. Overview of the American Heart Association “Get with the Guidelines” programs: coronary heart disease, stroke, and heart failure. Crit Pathw Cardiol. 2006;5(4):179-186. PubMed
6. LaBresh KA, Gliklich R, Liljestrand J, Peto R, Ellrodt AG. Using “get with the guidelines” to improve cardiovascular secondary prevention. Jt Comm J Qual Saf. 2003;29(10):539-550. PubMed
7. Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA. 2007;298(13):1525-1532. PubMed
8. Get With The Guidelines-Heart Failure. HF Patient Management Tool, October 2016.
9. Eapen ZJ, Liang L, Fonarow GC, et al. Validated, electronic health record deployable prediction models for assessing patient risk of 30-day rehospitalization and mortality in older heart failure patients. JACC Heart Fail. 2013;1(3):245-251. PubMed
10. Peterson PN, Rumsfeld JS, Liang L, et al. A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association get with the guidelines program. Circ Cardiovasc Qual Outcomes. 2010;3(1):25-32. PubMed
11. Frequently Asked Questions (FAQs): Implementation and Maintenance of CMS Mortality Measures for AMI & HF. 2007. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/downloads/HospitalMortalityAboutAMI_HF.pdf. Accessed August 30, 2017.
12. Suter LG, Li SX, Grady JN, et al. National patterns of risk-standardized mortality and readmission after hospitalization for acute myocardial infarction, heart failure, and pneumonia: update on publicly reported outcomes measures based on the 2013 release. J Gen Intern Med. 2014;29(10):1333-1340. PubMed
13. Lagu T, Pekow PS, Shieh MS, et al. Validation and comparison of seven mortality prediction models for hospitalized patients with acute decompensated heart failure. Circ Heart Fail. Aug 2016;9(8):e002912. PubMed
14. National Hospice and Palliative Care Organization. NHPCO’s facts and figures: hospice care in america. 2015. https://www.nhpco.org/sites/default/files/public/Statistics_Research/2015_Facts_Figures.pdf. Accessed August 30, 2017.
15. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810-1852. PubMed
16. Centers for Medicare & Medicaid Services. 2016 Condition-Specific Measures Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Mortality Measures. https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228774398696. Accessed August 30, 2017.
17. Bakitas M, Macmartin M, Trzepkowski K, et al. Palliative care consultations for heart failure patients: how many, when, and why? J Card Fail. 2013;19(3):193-201. PubMed
18. Wachterman MW, Pilver C, Smith D, Ersek M, Lipsitz SR, Keating NL. Quality of End-of-Life Care Provided to Patients With Different Serious Illnesses. JAMA Intern Med. 2016;176(8):1095-1102. PubMed
19. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673. PubMed
20. Rogers JG, Patel CB, Mentz RJ, et al. Palliative care in heart failure: results of a randomized, controlled clinical trial. J Card Fail. 2016;22(11):940. PubMed
21. Kelly AG, Zahuranec DB, Holloway RG, Morgenstern LB, Burke JF. Variation in do-not-resuscitate orders for patients with ischemic stroke: implications for national hospital comparisons. Stroke. 2014;45(3):822-827. PubMed
22. Walkey AJ, Weinberg J, Wiener RS, Cooke CR, Lindenauer PK. Association of Do-Not-Resuscitate Orders and Hospital Mortality Rate Among Patients With Pneumonia. JAMA Intern Med. 2016;176(1):97-104. PubMed
23. Bardach N, Zhao S, Pantilat S, Johnston SC. Adjustment for do-not-resuscitate orders reverses the apparent in-hospital mortality advantage for minorities. Am J Med. 2005;118(4):400-408. PubMed
24. Tabak YP, Johannes RS, Silber JH, Kurtz SG. Should Do-Not-Resuscitate status be included as a mortality risk adjustor? The impact of DNR variations on performance reporting. Med Care. 2005;43(7):658-666. PubMed
In an effort to improve the quality of care delivered to heart failure (HF) patients, the Centers for Medicare & Medicaid Services (CMS) publish hospitals’ 30-day risk-standardized mortality rates (RSMRs) for HF.1 These mortality rates are also used by CMS to determine the financial penalties and bonuses that hospitals receive as part of the national Hospital Value-based Purchasing program.2 Whether or not these efforts effectively direct patients towards high-quality providers or motivate hospitals to provide better care, few would disagree with the overarching goal of decreasing the number of patients who die from HF.
However, for some patients with chronic disease at the end of life, goals of care may change. The quality of days lived may become more important than the quantity of days lived. As a consequence, high-quality care for some patients at the end of life is associated with withdrawing life-sustaining or life-extending therapies. Over time, this therapeutic perspective has become more common, with use of hospice care doubling from 23% to 47% between 2000 and 2012 among Medicare beneficiaries who died.3 For a national cohort of older patients admitted with HF—not just those patients who died in that same year—hospitals’ rates of referral to hospice are considerably lower, averaging 2.9% in 2010 in a national study.4 Nevertheless, it is possible that hospitals that more faithfully follow their dying patients’ wishes and withdraw life-prolonging interventions and provide comfort-focused care at the end of life might be unfairly penalized if such efforts resulted in higher mortality rates than other hospitals.
Therefore, we used Medicare data linked to a national HF registry with information about end-of-life care, to address 3 questions: (1) How much do hospitals vary in their rates of early comfort care and how has this changed over time; (2) What hospital and patient factors are associated with higher early comfort care rates; and (3) Is there a correlation between 30-day risk-adjusted mortality rates for HF with hospital rates of early comfort care?
METHODS
Data Sources
We used data from the American Heart Association’s Get With The Guidelines-Heart Failure (GWTG-HF) registry. GWTG-HF is a voluntary, inpatient, quality improvement registry5-7 that uses web-based tools and standard questionnaires to collect data on patients with HF admitted to participating hospitals nationwide. The data include information from admission (eg, sociodemographic characteristics, symptoms, medical history, and initial laboratory and test results), the inpatient stay (eg, therapies), and discharge (eg, discharge destination, whether and when comfort care was initiated). We linked the GWTG-HF registry data to Medicare claims data in order to obtain information about Medicare eligibility and patient comorbidities. Additionally, we used data from the American Hospital Association (2008) for hospital characteristics. Quintiles Real-World & Late Phase Research (Cambridge, MA) serves as the data coordinating center for GWTG-HF and the Duke Clinical Research Institute (Durham, NC) serves as the statistical analytic center. GWTG-HF participating sites have a waiver of informed consent because the data are de-identified and primarily used for quality improvement. All analyses performed on this data have been approved by the Duke Medical Center Institutional Review Board.
Study Population
Study Outcomes
Our outcome of interest was the correlation between a hospital’s rate of initiating early CMO for admitted HF patients and a hospital’s 30-day RSMR for HF. The GWTG-HF questionnaire8 asks “When is the earliest physician/advanced practice nurse/physician assistant documentation of comfort measures only?” and permits 4 responses: day 0 or 1, day 2 or after, timing unclear, or not documented/unable to determine. We defined early CMO as CMO on day 0 or 1, and late/no CMO as any other response. We chose to examine early comfort care because many hospitalized patients transition to comfort care before they die if the death is in any way predictable. Thus, if comfort care is measured at any time during the hospitalization, hospitals that have high mortality rates are likely to have high comfort care rates. Therefore, we chose to use the more precise measure of early comfort care. We created hospital-level, risk-standardized early comfort care rates using the same risk-adjustment model used for RSMRs but with the outcome of early comfort care instead of mortality.9,10
RSMRs were calculated using a validated GWTG-HF 30-day risk-standardized mortality model9 with additional variables identified from other GWTG-HF analyses.10 The 30 days are measured as the 30 days after the index admission date.
Statistical Analyses
We described trends in early comfort care rates over time, from February 17, 2008, to February 17, 2014, using the Cochran-Armitage test for trend. We then grouped hospitals into quintiles based on their unadjusted early comfort care rates. We described patient and hospital characteristics for each quintile, using χ2 tests to test for differences across quintiles for categorical variables and Wilcoxon rank sum tests to assess for differences across quintiles for continuous variables. We then examined the Spearman’s rank correlation between hospitals’ RSMR and risk-adjusted comfort care rates. Finally, we compared hospital-level RSMRs before and after adjusting for early comfort care.
We performed risk-adjustment for these last 2 analyses as follows. For each patient, covariates were obtained from the GWTG-HF registry. Clinical data captured for the index admission were utilized in the risk-adjustment model (for both RSMRs and risk-adjusted comfort care rates). Included covariates were as follows: age (per 10 years); race (black vs non-black); systolic blood pressure at admission ≤170 (per 10 mm Hg); respiratory rate (per 5 respirations/min); heart rate ≤105 (per 10 beats/min); weight ≤100 (per 5 kg); weight >100 (per 5 kg); blood urea nitrogen (per 10 mg/dl); brain natriuretic peptide ≤2000 (per 500 pg/ml); hemoglobin 10-14 (per 1 g/dl); troponin abnormal (vs normal); creatinine ≤1 (per 1 mg/dl); sodium 130-140 (per 5 mEq/l); and chronic obstructive pulmonary disease or asthma.
Hierarchical logistic regression modeling was used to calculate the hospital-specific RSMR. A predicted/expected ratio similar to an observed/expected (O/E) ratio was calculated using the following modifications: (1) instead of the observed (crude) number of deaths, the numerator is the number of deaths predicted by the hierarchical model among a hospital’s patients given the patients’ risk factors and the hospital-specific effect; (2) the denominator is the expected number of deaths among the hospital’s patients given the patients’ risk factors and the average of all hospital-specific effects overall; and (3) the ratio of the numerator and denominator are then multiplied by the observed overall mortality rate (same as O/E). This calculation is the method used by CMS to derive RSMRs.11 Multiple imputation was used to handle missing data in the models; 25 imputed datasets using the fully conditional specification method were created. Patients with missing prior comorbidities were assumed to not have those conditions. Hospital characteristics were not imputed; therefore, for analyses that required construction of risk-adjusted comfort care rates or RSMRs, we excluded 18,867 patients cared for at 82 hospitals missing hospital characteristics. We ran 2 sets of models for risk-adjusted comfort care rates and RSMRs: the first adjusted only for patient characteristics, and the second adjusted for both patient and hospital characteristics. Results from the 2 models were similar, so we present only results from the latter. Variance inflation factors were all <2, indicating the collinearity between covariates was not an issue.
All statistical analyses were performed by using SAS version 9.4 (SAS Institute, Cary, NC). We tested for statistical significance by using 2-tailed tests and considered P values <.05 to be statistically significant.
RESULTS
Of the 272 hospitals included in our final study cohort, the observed median overall rate of early comfort care in this study was 1.9% (25th to 75th percentile: 0.9% to 4.0%); hospitals varied widely in unadjusted early comfort care rates (0.00% to 0.46% in the lowest quintile, and 4.60% to 39.91% in the highest quintile; Table 1).
DISCUSSION
Among a national sample of US hospitals, we found wide variation in how frequently health care providers deliver comfort care within the first 2 days of admission for HF. A minority of hospitals reported no early comfort care on any patients throughout the 6-year study period, but hospitals in the highest quintile initiated early comfort care rates for at least 1 in 20 HF patients. Hospitals that were more likely to initiate early comfort care had a higher proportion of female and white patients and were less likely to have the capacity to deliver aggressive surgical interventions such as heart transplants. Hospital-level 30-day RSMRs were not correlated with rates of early comfort care.
While the appropriate rate of early comfort care for patients hospitalized with HF is unknown, given that the average hospital RSMR is approximately 12% for fee-for-service Medicare patients hospitalized with HF,12 it is surprising that some hospitals initiated early comfort care on none or very few of their HF patients. It is quite possible that many of these hospitals initiated comfort care for some of their patients after 48 hours of hospitalization. We were unable to estimate the average period of time patients received comfort care prior to dying, the degree to which this varies across hospitals or why it might vary, and whether the length of time between comfort care initiation and death is related to satisfaction with end-of-life care. Future research on these topics would help inform providers seeking to deliver better end-of-life care. In this study, we also were unable to estimate how often early comfort care was not initiated because patients had a good prognosis. However, prior studies have suggested low rates of comfort care or hospice referral even among patients at very high estimated mortality risk.4 It is also possible that providers and families had concerns about the ability to accurately prognosticate, although several models have been shown to perform acceptably for patients hospitalized with HF.13
We found that comfort care rates did not increase over time, even though use of hospice care doubled among Medicare beneficiaries between 2000 and 2012. By way of context, cancer—the second leading cause of death in the US—was responsible for 38% of hospice admissions in 2013, whereas heart disease (including but not limited to HF)—the leading cause of death— was responsible for 13% of hospice admissions.14 The 2013 American College of Cardiology Foundation and the American Heart Association guidelines for HF recommend consideration of hospice or palliative care for inpatient and transitional care.15 In future work, it would be important to better understand the drivers behind decisions around comfort care for patients hospitalized with HF.
With regards to the policy implications of our study, we found that on average, adjusting 30-day mortality rates for early comfort care was not associated with a change in hospital mortality rankings. For those hospitals with high comfort care rates, adjusting for comfort care did lower mortality rates, but the change was so small as to be clinically insignificant. CMS’ RSMR for HF excludes patients enrolled in hospice during the 12 months prior to index admission, including the first day of the index admission, acknowledging that death may not be an untoward outcome for such patients.16 Fee-for-service Medicare beneficiaries excluded for hospice enrollment comprised 1.29% of HF admissions from July 2012 to June 201516 and are likely a subset of early comfort care patients in our sample, both because of the inclusiveness of chart review (vs claims-based identification) and because we defined early comfort care as comfort care initiated on day 0 or 1 of hospitalization. Nevertheless, with our data we cannot assess to what degree our findings were due solely to hospice patients excluded from CMS’ current estimates.
Prior research has described the underuse of palliative care among patients with HF17 and the association of palliative care with better patient and family experiences at the end of life.18-20 We add to this literature by describing the epidemiology—prevalence, changes over time, and associated factors—of early comfort care for HF in a national sample of hospitals. This serves as a baseline for future work on end-of-life care among patients hospitalized for HF. Our findings also contribute to ongoing discussion about how best to risk-adjust mortality metrics used to assess hospital quality in pay-for-performance programs. Recent research on stroke and pneumonia based on California data suggests that not accounting for do-not-resuscitate (DNR) status biases hospital mortality rates.21,22 Earlier research examined the impact of adjusting hospital mortality rates for DNR for a broader range of conditions.23,24 We expand this line of inquiry by examining the hospital-level association of early comfort care with mortality rates for HF, utilizing a national, contemporary cohort of inpatient stays. In addition, while studies have found that DNR rates within the first 24 hours of admission are relatively high (median 15.8% for pneumonia; 13.3% for stroke),21,22 comfort care is distinct from DNR.
Our findings should be interpreted in the context of several potential limitations. First, we did not have any information about patient or family wishes regarding end-of-life care, or the exact timing of early comfort care (eg, day 0 or day 1). The initiation of comfort care usually follows conversations about end-of-life care involving a patient, his or her family, and the medical team. Thus, we do not know if low early comfort care rates represent the lack of such a conversation (and thus poor-quality care) or the desire by most patients not to initiate early comfort care (and thus high-quality care). This would be an important area for future research. Second, we included only patients admitted to hospitals that participate in GWTG-HF, a voluntary quality improvement initiative. This may limit the generalizability of our findings, but it is unclear how our sample might bias our findings. Hospitals engaged in quality improvement may be more likely to initiate early comfort care aligned with patients’ wishes; on the other hand, hospitals with advanced surgical capabilities are over-represented in our sample and these hospitals are less likely to initiate early comfort care. Third, we examined associations and cannot make conclusions about causality. Residual measured and unmeasured confounding may influence these findings.
In summary, we found that early comfort care rates for fee-for-service Medicare beneficiaries admitted for HF varies widely among hospitals, but median rates of early comfort care have not changed over time. On average, there was no correlation between hospital-level, 30-day, RSMRs and rates of early comfort care. This suggests that current efforts to lower mortality rates have not had unintended consequences for hospitals that institute early comfort care more commonly than their peers.
Acknowledgments
Dr. Chen and Ms. Cox take responsibility for the integrity of the data and the accuracy of the data analysis. Drs. Chen, Levine, and Hayward are responsible for the study concept and design. Drs. Chen and Fonarow acquired the data. Dr. Chen drafted the manuscript. Drs. Chen, Levin, Hayward, Cox, Fonarow, DeVore, Hernandez, Heidenreich, and Yancy revised the manuscript for important intellectual content. Drs. Chen, Hayward, Cox, and Schulte performed the statistical analysis. Drs. Chen and Fonarow obtained funding for the study. Drs. Hayward and Fonarow supervised the study. The authors thank Bailey Green, MPH, for the research assistance she provided. She was compensated for her work.
Disclosure
Dr. Fonarow reports research support from the National Institutes of Health, and consulting for Amgen, Janssen, Novartis, Medtronic, and St Jude Medical. Dr. DeVore reports research support from the American Heart Association, Amgen, and Novartis, and consulting for Amgen. The other authors have no relevant conflicts of interest. Dr. Chen was supported by a Career Development Grant Award (K08HS020671) from the Agency for Healthcare Research and Quality when the manuscript was being prepared. She currently receives support from the Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation for her work there. She also receives support from the Blue Cross Blue Shield of Michigan Foundation’s Investigator Initiated Research Program, the Agency for Healthcare Research and Quality (R01 HS024698), and the National Institute on Aging (P01 AG019783). These funding sources had no role in the preparation, review, or approval of the manuscript. The GWTG-HF program is provided by the American Heart Association. GWTG-HF has been funded in the past through support from Amgen, Medtronic, GlaxoSmithKline, Ortho-McNeil, and the American Heart Association Pharmaceutical Roundtable. These sponsors had no role in the study design, data analysis or manuscript preparation and revision.
In an effort to improve the quality of care delivered to heart failure (HF) patients, the Centers for Medicare & Medicaid Services (CMS) publish hospitals’ 30-day risk-standardized mortality rates (RSMRs) for HF.1 These mortality rates are also used by CMS to determine the financial penalties and bonuses that hospitals receive as part of the national Hospital Value-based Purchasing program.2 Whether or not these efforts effectively direct patients towards high-quality providers or motivate hospitals to provide better care, few would disagree with the overarching goal of decreasing the number of patients who die from HF.
However, for some patients with chronic disease at the end of life, goals of care may change. The quality of days lived may become more important than the quantity of days lived. As a consequence, high-quality care for some patients at the end of life is associated with withdrawing life-sustaining or life-extending therapies. Over time, this therapeutic perspective has become more common, with use of hospice care doubling from 23% to 47% between 2000 and 2012 among Medicare beneficiaries who died.3 For a national cohort of older patients admitted with HF—not just those patients who died in that same year—hospitals’ rates of referral to hospice are considerably lower, averaging 2.9% in 2010 in a national study.4 Nevertheless, it is possible that hospitals that more faithfully follow their dying patients’ wishes and withdraw life-prolonging interventions and provide comfort-focused care at the end of life might be unfairly penalized if such efforts resulted in higher mortality rates than other hospitals.
Therefore, we used Medicare data linked to a national HF registry with information about end-of-life care, to address 3 questions: (1) How much do hospitals vary in their rates of early comfort care and how has this changed over time; (2) What hospital and patient factors are associated with higher early comfort care rates; and (3) Is there a correlation between 30-day risk-adjusted mortality rates for HF with hospital rates of early comfort care?
METHODS
Data Sources
We used data from the American Heart Association’s Get With The Guidelines-Heart Failure (GWTG-HF) registry. GWTG-HF is a voluntary, inpatient, quality improvement registry5-7 that uses web-based tools and standard questionnaires to collect data on patients with HF admitted to participating hospitals nationwide. The data include information from admission (eg, sociodemographic characteristics, symptoms, medical history, and initial laboratory and test results), the inpatient stay (eg, therapies), and discharge (eg, discharge destination, whether and when comfort care was initiated). We linked the GWTG-HF registry data to Medicare claims data in order to obtain information about Medicare eligibility and patient comorbidities. Additionally, we used data from the American Hospital Association (2008) for hospital characteristics. Quintiles Real-World & Late Phase Research (Cambridge, MA) serves as the data coordinating center for GWTG-HF and the Duke Clinical Research Institute (Durham, NC) serves as the statistical analytic center. GWTG-HF participating sites have a waiver of informed consent because the data are de-identified and primarily used for quality improvement. All analyses performed on this data have been approved by the Duke Medical Center Institutional Review Board.
Study Population
Study Outcomes
Our outcome of interest was the correlation between a hospital’s rate of initiating early CMO for admitted HF patients and a hospital’s 30-day RSMR for HF. The GWTG-HF questionnaire8 asks “When is the earliest physician/advanced practice nurse/physician assistant documentation of comfort measures only?” and permits 4 responses: day 0 or 1, day 2 or after, timing unclear, or not documented/unable to determine. We defined early CMO as CMO on day 0 or 1, and late/no CMO as any other response. We chose to examine early comfort care because many hospitalized patients transition to comfort care before they die if the death is in any way predictable. Thus, if comfort care is measured at any time during the hospitalization, hospitals that have high mortality rates are likely to have high comfort care rates. Therefore, we chose to use the more precise measure of early comfort care. We created hospital-level, risk-standardized early comfort care rates using the same risk-adjustment model used for RSMRs but with the outcome of early comfort care instead of mortality.9,10
RSMRs were calculated using a validated GWTG-HF 30-day risk-standardized mortality model9 with additional variables identified from other GWTG-HF analyses.10 The 30 days are measured as the 30 days after the index admission date.
Statistical Analyses
We described trends in early comfort care rates over time, from February 17, 2008, to February 17, 2014, using the Cochran-Armitage test for trend. We then grouped hospitals into quintiles based on their unadjusted early comfort care rates. We described patient and hospital characteristics for each quintile, using χ2 tests to test for differences across quintiles for categorical variables and Wilcoxon rank sum tests to assess for differences across quintiles for continuous variables. We then examined the Spearman’s rank correlation between hospitals’ RSMR and risk-adjusted comfort care rates. Finally, we compared hospital-level RSMRs before and after adjusting for early comfort care.
We performed risk-adjustment for these last 2 analyses as follows. For each patient, covariates were obtained from the GWTG-HF registry. Clinical data captured for the index admission were utilized in the risk-adjustment model (for both RSMRs and risk-adjusted comfort care rates). Included covariates were as follows: age (per 10 years); race (black vs non-black); systolic blood pressure at admission ≤170 (per 10 mm Hg); respiratory rate (per 5 respirations/min); heart rate ≤105 (per 10 beats/min); weight ≤100 (per 5 kg); weight >100 (per 5 kg); blood urea nitrogen (per 10 mg/dl); brain natriuretic peptide ≤2000 (per 500 pg/ml); hemoglobin 10-14 (per 1 g/dl); troponin abnormal (vs normal); creatinine ≤1 (per 1 mg/dl); sodium 130-140 (per 5 mEq/l); and chronic obstructive pulmonary disease or asthma.
Hierarchical logistic regression modeling was used to calculate the hospital-specific RSMR. A predicted/expected ratio similar to an observed/expected (O/E) ratio was calculated using the following modifications: (1) instead of the observed (crude) number of deaths, the numerator is the number of deaths predicted by the hierarchical model among a hospital’s patients given the patients’ risk factors and the hospital-specific effect; (2) the denominator is the expected number of deaths among the hospital’s patients given the patients’ risk factors and the average of all hospital-specific effects overall; and (3) the ratio of the numerator and denominator are then multiplied by the observed overall mortality rate (same as O/E). This calculation is the method used by CMS to derive RSMRs.11 Multiple imputation was used to handle missing data in the models; 25 imputed datasets using the fully conditional specification method were created. Patients with missing prior comorbidities were assumed to not have those conditions. Hospital characteristics were not imputed; therefore, for analyses that required construction of risk-adjusted comfort care rates or RSMRs, we excluded 18,867 patients cared for at 82 hospitals missing hospital characteristics. We ran 2 sets of models for risk-adjusted comfort care rates and RSMRs: the first adjusted only for patient characteristics, and the second adjusted for both patient and hospital characteristics. Results from the 2 models were similar, so we present only results from the latter. Variance inflation factors were all <2, indicating the collinearity between covariates was not an issue.
All statistical analyses were performed by using SAS version 9.4 (SAS Institute, Cary, NC). We tested for statistical significance by using 2-tailed tests and considered P values <.05 to be statistically significant.
RESULTS
Of the 272 hospitals included in our final study cohort, the observed median overall rate of early comfort care in this study was 1.9% (25th to 75th percentile: 0.9% to 4.0%); hospitals varied widely in unadjusted early comfort care rates (0.00% to 0.46% in the lowest quintile, and 4.60% to 39.91% in the highest quintile; Table 1).
DISCUSSION
Among a national sample of US hospitals, we found wide variation in how frequently health care providers deliver comfort care within the first 2 days of admission for HF. A minority of hospitals reported no early comfort care on any patients throughout the 6-year study period, but hospitals in the highest quintile initiated early comfort care rates for at least 1 in 20 HF patients. Hospitals that were more likely to initiate early comfort care had a higher proportion of female and white patients and were less likely to have the capacity to deliver aggressive surgical interventions such as heart transplants. Hospital-level 30-day RSMRs were not correlated with rates of early comfort care.
While the appropriate rate of early comfort care for patients hospitalized with HF is unknown, given that the average hospital RSMR is approximately 12% for fee-for-service Medicare patients hospitalized with HF,12 it is surprising that some hospitals initiated early comfort care on none or very few of their HF patients. It is quite possible that many of these hospitals initiated comfort care for some of their patients after 48 hours of hospitalization. We were unable to estimate the average period of time patients received comfort care prior to dying, the degree to which this varies across hospitals or why it might vary, and whether the length of time between comfort care initiation and death is related to satisfaction with end-of-life care. Future research on these topics would help inform providers seeking to deliver better end-of-life care. In this study, we also were unable to estimate how often early comfort care was not initiated because patients had a good prognosis. However, prior studies have suggested low rates of comfort care or hospice referral even among patients at very high estimated mortality risk.4 It is also possible that providers and families had concerns about the ability to accurately prognosticate, although several models have been shown to perform acceptably for patients hospitalized with HF.13
We found that comfort care rates did not increase over time, even though use of hospice care doubled among Medicare beneficiaries between 2000 and 2012. By way of context, cancer—the second leading cause of death in the US—was responsible for 38% of hospice admissions in 2013, whereas heart disease (including but not limited to HF)—the leading cause of death— was responsible for 13% of hospice admissions.14 The 2013 American College of Cardiology Foundation and the American Heart Association guidelines for HF recommend consideration of hospice or palliative care for inpatient and transitional care.15 In future work, it would be important to better understand the drivers behind decisions around comfort care for patients hospitalized with HF.
With regards to the policy implications of our study, we found that on average, adjusting 30-day mortality rates for early comfort care was not associated with a change in hospital mortality rankings. For those hospitals with high comfort care rates, adjusting for comfort care did lower mortality rates, but the change was so small as to be clinically insignificant. CMS’ RSMR for HF excludes patients enrolled in hospice during the 12 months prior to index admission, including the first day of the index admission, acknowledging that death may not be an untoward outcome for such patients.16 Fee-for-service Medicare beneficiaries excluded for hospice enrollment comprised 1.29% of HF admissions from July 2012 to June 201516 and are likely a subset of early comfort care patients in our sample, both because of the inclusiveness of chart review (vs claims-based identification) and because we defined early comfort care as comfort care initiated on day 0 or 1 of hospitalization. Nevertheless, with our data we cannot assess to what degree our findings were due solely to hospice patients excluded from CMS’ current estimates.
Prior research has described the underuse of palliative care among patients with HF17 and the association of palliative care with better patient and family experiences at the end of life.18-20 We add to this literature by describing the epidemiology—prevalence, changes over time, and associated factors—of early comfort care for HF in a national sample of hospitals. This serves as a baseline for future work on end-of-life care among patients hospitalized for HF. Our findings also contribute to ongoing discussion about how best to risk-adjust mortality metrics used to assess hospital quality in pay-for-performance programs. Recent research on stroke and pneumonia based on California data suggests that not accounting for do-not-resuscitate (DNR) status biases hospital mortality rates.21,22 Earlier research examined the impact of adjusting hospital mortality rates for DNR for a broader range of conditions.23,24 We expand this line of inquiry by examining the hospital-level association of early comfort care with mortality rates for HF, utilizing a national, contemporary cohort of inpatient stays. In addition, while studies have found that DNR rates within the first 24 hours of admission are relatively high (median 15.8% for pneumonia; 13.3% for stroke),21,22 comfort care is distinct from DNR.
Our findings should be interpreted in the context of several potential limitations. First, we did not have any information about patient or family wishes regarding end-of-life care, or the exact timing of early comfort care (eg, day 0 or day 1). The initiation of comfort care usually follows conversations about end-of-life care involving a patient, his or her family, and the medical team. Thus, we do not know if low early comfort care rates represent the lack of such a conversation (and thus poor-quality care) or the desire by most patients not to initiate early comfort care (and thus high-quality care). This would be an important area for future research. Second, we included only patients admitted to hospitals that participate in GWTG-HF, a voluntary quality improvement initiative. This may limit the generalizability of our findings, but it is unclear how our sample might bias our findings. Hospitals engaged in quality improvement may be more likely to initiate early comfort care aligned with patients’ wishes; on the other hand, hospitals with advanced surgical capabilities are over-represented in our sample and these hospitals are less likely to initiate early comfort care. Third, we examined associations and cannot make conclusions about causality. Residual measured and unmeasured confounding may influence these findings.
In summary, we found that early comfort care rates for fee-for-service Medicare beneficiaries admitted for HF varies widely among hospitals, but median rates of early comfort care have not changed over time. On average, there was no correlation between hospital-level, 30-day, RSMRs and rates of early comfort care. This suggests that current efforts to lower mortality rates have not had unintended consequences for hospitals that institute early comfort care more commonly than their peers.
Acknowledgments
Dr. Chen and Ms. Cox take responsibility for the integrity of the data and the accuracy of the data analysis. Drs. Chen, Levine, and Hayward are responsible for the study concept and design. Drs. Chen and Fonarow acquired the data. Dr. Chen drafted the manuscript. Drs. Chen, Levin, Hayward, Cox, Fonarow, DeVore, Hernandez, Heidenreich, and Yancy revised the manuscript for important intellectual content. Drs. Chen, Hayward, Cox, and Schulte performed the statistical analysis. Drs. Chen and Fonarow obtained funding for the study. Drs. Hayward and Fonarow supervised the study. The authors thank Bailey Green, MPH, for the research assistance she provided. She was compensated for her work.
Disclosure
Dr. Fonarow reports research support from the National Institutes of Health, and consulting for Amgen, Janssen, Novartis, Medtronic, and St Jude Medical. Dr. DeVore reports research support from the American Heart Association, Amgen, and Novartis, and consulting for Amgen. The other authors have no relevant conflicts of interest. Dr. Chen was supported by a Career Development Grant Award (K08HS020671) from the Agency for Healthcare Research and Quality when the manuscript was being prepared. She currently receives support from the Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation for her work there. She also receives support from the Blue Cross Blue Shield of Michigan Foundation’s Investigator Initiated Research Program, the Agency for Healthcare Research and Quality (R01 HS024698), and the National Institute on Aging (P01 AG019783). These funding sources had no role in the preparation, review, or approval of the manuscript. The GWTG-HF program is provided by the American Heart Association. GWTG-HF has been funded in the past through support from Amgen, Medtronic, GlaxoSmithKline, Ortho-McNeil, and the American Heart Association Pharmaceutical Roundtable. These sponsors had no role in the study design, data analysis or manuscript preparation and revision.
1. Centers for Medicare & Medicaid Services. Hospital Compare. https://www.medicare.gov/hospitalcompare/. Accessed on November 27, 2016.
2. Centers for Medicare & Medicaid Services. Hospital Value-based Purchasing. https://www.medicare.gov/hospitalcompare/data/hospital-vbp.html. Accessed August 30, 2017.
3. Medicare Payment Advisory Comission. Report to the Congress: Medicare payment policy. 2014. http://www.medpac.gov/docs/default-source/reports/mar14_entirereport.pdf. Accessed August 31, 2017.
4. Whellan DJ, Cox M, Hernandez AF, et al. Utilization of hospice and predicted mortality risk among older patients hospitalized with heart failure: findings from GWTG-HF. J Card Fail. 2012;18(6):471-477. PubMed
5. Hong Y, LaBresh KA. Overview of the American Heart Association “Get with the Guidelines” programs: coronary heart disease, stroke, and heart failure. Crit Pathw Cardiol. 2006;5(4):179-186. PubMed
6. LaBresh KA, Gliklich R, Liljestrand J, Peto R, Ellrodt AG. Using “get with the guidelines” to improve cardiovascular secondary prevention. Jt Comm J Qual Saf. 2003;29(10):539-550. PubMed
7. Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA. 2007;298(13):1525-1532. PubMed
8. Get With The Guidelines-Heart Failure. HF Patient Management Tool, October 2016.
9. Eapen ZJ, Liang L, Fonarow GC, et al. Validated, electronic health record deployable prediction models for assessing patient risk of 30-day rehospitalization and mortality in older heart failure patients. JACC Heart Fail. 2013;1(3):245-251. PubMed
10. Peterson PN, Rumsfeld JS, Liang L, et al. A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association get with the guidelines program. Circ Cardiovasc Qual Outcomes. 2010;3(1):25-32. PubMed
11. Frequently Asked Questions (FAQs): Implementation and Maintenance of CMS Mortality Measures for AMI & HF. 2007. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/downloads/HospitalMortalityAboutAMI_HF.pdf. Accessed August 30, 2017.
12. Suter LG, Li SX, Grady JN, et al. National patterns of risk-standardized mortality and readmission after hospitalization for acute myocardial infarction, heart failure, and pneumonia: update on publicly reported outcomes measures based on the 2013 release. J Gen Intern Med. 2014;29(10):1333-1340. PubMed
13. Lagu T, Pekow PS, Shieh MS, et al. Validation and comparison of seven mortality prediction models for hospitalized patients with acute decompensated heart failure. Circ Heart Fail. Aug 2016;9(8):e002912. PubMed
14. National Hospice and Palliative Care Organization. NHPCO’s facts and figures: hospice care in america. 2015. https://www.nhpco.org/sites/default/files/public/Statistics_Research/2015_Facts_Figures.pdf. Accessed August 30, 2017.
15. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810-1852. PubMed
16. Centers for Medicare & Medicaid Services. 2016 Condition-Specific Measures Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Mortality Measures. https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228774398696. Accessed August 30, 2017.
17. Bakitas M, Macmartin M, Trzepkowski K, et al. Palliative care consultations for heart failure patients: how many, when, and why? J Card Fail. 2013;19(3):193-201. PubMed
18. Wachterman MW, Pilver C, Smith D, Ersek M, Lipsitz SR, Keating NL. Quality of End-of-Life Care Provided to Patients With Different Serious Illnesses. JAMA Intern Med. 2016;176(8):1095-1102. PubMed
19. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673. PubMed
20. Rogers JG, Patel CB, Mentz RJ, et al. Palliative care in heart failure: results of a randomized, controlled clinical trial. J Card Fail. 2016;22(11):940. PubMed
21. Kelly AG, Zahuranec DB, Holloway RG, Morgenstern LB, Burke JF. Variation in do-not-resuscitate orders for patients with ischemic stroke: implications for national hospital comparisons. Stroke. 2014;45(3):822-827. PubMed
22. Walkey AJ, Weinberg J, Wiener RS, Cooke CR, Lindenauer PK. Association of Do-Not-Resuscitate Orders and Hospital Mortality Rate Among Patients With Pneumonia. JAMA Intern Med. 2016;176(1):97-104. PubMed
23. Bardach N, Zhao S, Pantilat S, Johnston SC. Adjustment for do-not-resuscitate orders reverses the apparent in-hospital mortality advantage for minorities. Am J Med. 2005;118(4):400-408. PubMed
24. Tabak YP, Johannes RS, Silber JH, Kurtz SG. Should Do-Not-Resuscitate status be included as a mortality risk adjustor? The impact of DNR variations on performance reporting. Med Care. 2005;43(7):658-666. PubMed
1. Centers for Medicare & Medicaid Services. Hospital Compare. https://www.medicare.gov/hospitalcompare/. Accessed on November 27, 2016.
2. Centers for Medicare & Medicaid Services. Hospital Value-based Purchasing. https://www.medicare.gov/hospitalcompare/data/hospital-vbp.html. Accessed August 30, 2017.
3. Medicare Payment Advisory Comission. Report to the Congress: Medicare payment policy. 2014. http://www.medpac.gov/docs/default-source/reports/mar14_entirereport.pdf. Accessed August 31, 2017.
4. Whellan DJ, Cox M, Hernandez AF, et al. Utilization of hospice and predicted mortality risk among older patients hospitalized with heart failure: findings from GWTG-HF. J Card Fail. 2012;18(6):471-477. PubMed
5. Hong Y, LaBresh KA. Overview of the American Heart Association “Get with the Guidelines” programs: coronary heart disease, stroke, and heart failure. Crit Pathw Cardiol. 2006;5(4):179-186. PubMed
6. LaBresh KA, Gliklich R, Liljestrand J, Peto R, Ellrodt AG. Using “get with the guidelines” to improve cardiovascular secondary prevention. Jt Comm J Qual Saf. 2003;29(10):539-550. PubMed
7. Hernandez AF, Fonarow GC, Liang L, et al. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA. 2007;298(13):1525-1532. PubMed
8. Get With The Guidelines-Heart Failure. HF Patient Management Tool, October 2016.
9. Eapen ZJ, Liang L, Fonarow GC, et al. Validated, electronic health record deployable prediction models for assessing patient risk of 30-day rehospitalization and mortality in older heart failure patients. JACC Heart Fail. 2013;1(3):245-251. PubMed
10. Peterson PN, Rumsfeld JS, Liang L, et al. A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association get with the guidelines program. Circ Cardiovasc Qual Outcomes. 2010;3(1):25-32. PubMed
11. Frequently Asked Questions (FAQs): Implementation and Maintenance of CMS Mortality Measures for AMI & HF. 2007. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/downloads/HospitalMortalityAboutAMI_HF.pdf. Accessed August 30, 2017.
12. Suter LG, Li SX, Grady JN, et al. National patterns of risk-standardized mortality and readmission after hospitalization for acute myocardial infarction, heart failure, and pneumonia: update on publicly reported outcomes measures based on the 2013 release. J Gen Intern Med. 2014;29(10):1333-1340. PubMed
13. Lagu T, Pekow PS, Shieh MS, et al. Validation and comparison of seven mortality prediction models for hospitalized patients with acute decompensated heart failure. Circ Heart Fail. Aug 2016;9(8):e002912. PubMed
14. National Hospice and Palliative Care Organization. NHPCO’s facts and figures: hospice care in america. 2015. https://www.nhpco.org/sites/default/files/public/Statistics_Research/2015_Facts_Figures.pdf. Accessed August 30, 2017.
15. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):1810-1852. PubMed
16. Centers for Medicare & Medicaid Services. 2016 Condition-Specific Measures Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Mortality Measures. https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228774398696. Accessed August 30, 2017.
17. Bakitas M, Macmartin M, Trzepkowski K, et al. Palliative care consultations for heart failure patients: how many, when, and why? J Card Fail. 2013;19(3):193-201. PubMed
18. Wachterman MW, Pilver C, Smith D, Ersek M, Lipsitz SR, Keating NL. Quality of End-of-Life Care Provided to Patients With Different Serious Illnesses. JAMA Intern Med. 2016;176(8):1095-1102. PubMed
19. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673. PubMed
20. Rogers JG, Patel CB, Mentz RJ, et al. Palliative care in heart failure: results of a randomized, controlled clinical trial. J Card Fail. 2016;22(11):940. PubMed
21. Kelly AG, Zahuranec DB, Holloway RG, Morgenstern LB, Burke JF. Variation in do-not-resuscitate orders for patients with ischemic stroke: implications for national hospital comparisons. Stroke. 2014;45(3):822-827. PubMed
22. Walkey AJ, Weinberg J, Wiener RS, Cooke CR, Lindenauer PK. Association of Do-Not-Resuscitate Orders and Hospital Mortality Rate Among Patients With Pneumonia. JAMA Intern Med. 2016;176(1):97-104. PubMed
23. Bardach N, Zhao S, Pantilat S, Johnston SC. Adjustment for do-not-resuscitate orders reverses the apparent in-hospital mortality advantage for minorities. Am J Med. 2005;118(4):400-408. PubMed
24. Tabak YP, Johannes RS, Silber JH, Kurtz SG. Should Do-Not-Resuscitate status be included as a mortality risk adjustor? The impact of DNR variations on performance reporting. Med Care. 2005;43(7):658-666. PubMed
© 2018 Society of Hospital Medicine