User login
Debris left after TAVR varies by device
WASHINGTON – All transcatheter aortic valve replacement devices generate debris into the bloodstream, including debris larger than 1 mm, but the amount of the debris differs between devices, according to a study based on collections from a cerebral embolic protection system.
“The quantity of the debris measured by different methods and techniques revealed more debris in patients receiving the Evolut R or Lotus TAVR [transcatheter aortic valve replacement] devices than in patients receiving a Sapien 3 or Sapien XT prosthesis,” reported Tobias Schmidt, MD, a cardiologist at Asklepios Klinik St. Georg, Hamburg, Germany.
Of the 246 patients, 145 (59%) received a Sapien 3 device, 40 (16%) received an Evolut R, 36 (14%) received a Lotus, and 25 (10%) received a Sapien XT. Particle features based on histopathological and histomorphological analyses were compared. A multivariate analysis was conducted to test for interaction with the amount of debris according to patient demographics and procedural characteristics, which differed for the devices evaluated.
Debris was captured in essentially all patients (99%) and with every TAVR device. On automated histomorphometry, the Lotus device had significantly higher median particle counts relative to the Evolut R (P = .004), the Sapien S3 (P less than .001), and the Sapien XT (P = .02) devices. When stratified by particle size, the Evolut R generated significantly more particles greater than 500 mcm than either the Sapien S3 or the Sapien XT (both P less than .05).
For particle sizes greater than 1 mm, there were significantly higher counts for both the Lotus and Evolut R (both P less than .05) relative to the Sapien S3, but Dr. Schmidt emphasized all devices generated at least some debris this size and that particles greater than 1 mm were retrieved from 53% of all patients. Similarly, when median total particle area was calculated by histomorphometry, the Lotus (P = .0007) and Evolut R (P = .0009) devices were more likely to have particles greater than 1 mm than the Sapien devices, but again, debris with a large total particle area was retrieved from at least some patients in all device groups.
There were significant differences in patient demographics and procedural characteristics by device. For example, patients receiving an Evolut R were significantly more likely than those receiving the Lotus or Sapien S3 valves to have undergone dilation prior to TAVR. Patients receiving the Sapien XT were significantly older than patients receiving any of the other valve types.
In an effort to control for these differences, “multivariate analysis was performed to text for interaction with the amount of debris captured,” Dr. Schmidt explained. “This analysis showed that transcatheter valve type was the only significant predictor for the morphometric findings.”
In this study, most of the debris was found to come from the vascular bed, but foreign body debris and debris from myocardium was also identified. One hypothesis for the greater debris from the Lotus and Evolut R devices is that these are positionable, raising the possibility that manipulation of the devices was the source of the debris, according to Dr. Schmidt. However, this hypothesis needs verification.
One message from this study is that “capture of debris is universal across different transcatheter valve types,” Dr. Schmidt said, adding that this “supports the benefit of using a CPS device in all TAVR procedures.”
Several commentators, including Jeffrey Popma, MD, director of the Interventional Cardiology Clinical Service at Beth Israel Deaconess Hospital, Boston, observed that it would be inappropriate to conclude that the greater debris observed in this study would necessarily translate into a difference in risk of embolic events for the devices evaluated with or without a CPS device. He and others emphasized no relationship to clinical risk was demonstrated in this study.
Dr. Schmidt reports no potential conflicts of interest.
SOURCE: Schmidt T et al. CROI 2018.
WASHINGTON – All transcatheter aortic valve replacement devices generate debris into the bloodstream, including debris larger than 1 mm, but the amount of the debris differs between devices, according to a study based on collections from a cerebral embolic protection system.
“The quantity of the debris measured by different methods and techniques revealed more debris in patients receiving the Evolut R or Lotus TAVR [transcatheter aortic valve replacement] devices than in patients receiving a Sapien 3 or Sapien XT prosthesis,” reported Tobias Schmidt, MD, a cardiologist at Asklepios Klinik St. Georg, Hamburg, Germany.
Of the 246 patients, 145 (59%) received a Sapien 3 device, 40 (16%) received an Evolut R, 36 (14%) received a Lotus, and 25 (10%) received a Sapien XT. Particle features based on histopathological and histomorphological analyses were compared. A multivariate analysis was conducted to test for interaction with the amount of debris according to patient demographics and procedural characteristics, which differed for the devices evaluated.
Debris was captured in essentially all patients (99%) and with every TAVR device. On automated histomorphometry, the Lotus device had significantly higher median particle counts relative to the Evolut R (P = .004), the Sapien S3 (P less than .001), and the Sapien XT (P = .02) devices. When stratified by particle size, the Evolut R generated significantly more particles greater than 500 mcm than either the Sapien S3 or the Sapien XT (both P less than .05).
For particle sizes greater than 1 mm, there were significantly higher counts for both the Lotus and Evolut R (both P less than .05) relative to the Sapien S3, but Dr. Schmidt emphasized all devices generated at least some debris this size and that particles greater than 1 mm were retrieved from 53% of all patients. Similarly, when median total particle area was calculated by histomorphometry, the Lotus (P = .0007) and Evolut R (P = .0009) devices were more likely to have particles greater than 1 mm than the Sapien devices, but again, debris with a large total particle area was retrieved from at least some patients in all device groups.
There were significant differences in patient demographics and procedural characteristics by device. For example, patients receiving an Evolut R were significantly more likely than those receiving the Lotus or Sapien S3 valves to have undergone dilation prior to TAVR. Patients receiving the Sapien XT were significantly older than patients receiving any of the other valve types.
In an effort to control for these differences, “multivariate analysis was performed to text for interaction with the amount of debris captured,” Dr. Schmidt explained. “This analysis showed that transcatheter valve type was the only significant predictor for the morphometric findings.”
In this study, most of the debris was found to come from the vascular bed, but foreign body debris and debris from myocardium was also identified. One hypothesis for the greater debris from the Lotus and Evolut R devices is that these are positionable, raising the possibility that manipulation of the devices was the source of the debris, according to Dr. Schmidt. However, this hypothesis needs verification.
One message from this study is that “capture of debris is universal across different transcatheter valve types,” Dr. Schmidt said, adding that this “supports the benefit of using a CPS device in all TAVR procedures.”
Several commentators, including Jeffrey Popma, MD, director of the Interventional Cardiology Clinical Service at Beth Israel Deaconess Hospital, Boston, observed that it would be inappropriate to conclude that the greater debris observed in this study would necessarily translate into a difference in risk of embolic events for the devices evaluated with or without a CPS device. He and others emphasized no relationship to clinical risk was demonstrated in this study.
Dr. Schmidt reports no potential conflicts of interest.
SOURCE: Schmidt T et al. CROI 2018.
WASHINGTON – All transcatheter aortic valve replacement devices generate debris into the bloodstream, including debris larger than 1 mm, but the amount of the debris differs between devices, according to a study based on collections from a cerebral embolic protection system.
“The quantity of the debris measured by different methods and techniques revealed more debris in patients receiving the Evolut R or Lotus TAVR [transcatheter aortic valve replacement] devices than in patients receiving a Sapien 3 or Sapien XT prosthesis,” reported Tobias Schmidt, MD, a cardiologist at Asklepios Klinik St. Georg, Hamburg, Germany.
Of the 246 patients, 145 (59%) received a Sapien 3 device, 40 (16%) received an Evolut R, 36 (14%) received a Lotus, and 25 (10%) received a Sapien XT. Particle features based on histopathological and histomorphological analyses were compared. A multivariate analysis was conducted to test for interaction with the amount of debris according to patient demographics and procedural characteristics, which differed for the devices evaluated.
Debris was captured in essentially all patients (99%) and with every TAVR device. On automated histomorphometry, the Lotus device had significantly higher median particle counts relative to the Evolut R (P = .004), the Sapien S3 (P less than .001), and the Sapien XT (P = .02) devices. When stratified by particle size, the Evolut R generated significantly more particles greater than 500 mcm than either the Sapien S3 or the Sapien XT (both P less than .05).
For particle sizes greater than 1 mm, there were significantly higher counts for both the Lotus and Evolut R (both P less than .05) relative to the Sapien S3, but Dr. Schmidt emphasized all devices generated at least some debris this size and that particles greater than 1 mm were retrieved from 53% of all patients. Similarly, when median total particle area was calculated by histomorphometry, the Lotus (P = .0007) and Evolut R (P = .0009) devices were more likely to have particles greater than 1 mm than the Sapien devices, but again, debris with a large total particle area was retrieved from at least some patients in all device groups.
There were significant differences in patient demographics and procedural characteristics by device. For example, patients receiving an Evolut R were significantly more likely than those receiving the Lotus or Sapien S3 valves to have undergone dilation prior to TAVR. Patients receiving the Sapien XT were significantly older than patients receiving any of the other valve types.
In an effort to control for these differences, “multivariate analysis was performed to text for interaction with the amount of debris captured,” Dr. Schmidt explained. “This analysis showed that transcatheter valve type was the only significant predictor for the morphometric findings.”
In this study, most of the debris was found to come from the vascular bed, but foreign body debris and debris from myocardium was also identified. One hypothesis for the greater debris from the Lotus and Evolut R devices is that these are positionable, raising the possibility that manipulation of the devices was the source of the debris, according to Dr. Schmidt. However, this hypothesis needs verification.
One message from this study is that “capture of debris is universal across different transcatheter valve types,” Dr. Schmidt said, adding that this “supports the benefit of using a CPS device in all TAVR procedures.”
Several commentators, including Jeffrey Popma, MD, director of the Interventional Cardiology Clinical Service at Beth Israel Deaconess Hospital, Boston, observed that it would be inappropriate to conclude that the greater debris observed in this study would necessarily translate into a difference in risk of embolic events for the devices evaluated with or without a CPS device. He and others emphasized no relationship to clinical risk was demonstrated in this study.
Dr. Schmidt reports no potential conflicts of interest.
SOURCE: Schmidt T et al. CROI 2018.
AT CRT 2018
Key clinical point: Based on a study with a cerebral embolic collection system, transcatheter aortic valve replacement devices generate unequal debris.
Major finding: .
Data source: Data analysis from two randomized trials.
Disclosures: Dr. Schmidt reports no potential conflicts of interest.
Source: Schmidt T et al. CROI 2018.
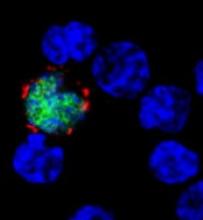
Mortality in patients with PTLD
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
Top hospital heart failure performance translates to longer survival
ORLANDO – Hospitals in the first quartile of short-term performance in treating heart failure patients had higher long-term survival rates for those patients, based on data from 317 hospitals that participated in a voluntary quality improvement program.
The burden of heart failure remains substantial in the United States, and health policies are increasingly focused on improving care for heart failure patients, said Ambarish Pandey, MD, of the University of Texas, Dallas, in a presentation at the annual meeting of the American College of Cardiology.
The researchers assessed hospital performance based on 30-day risk-standardized mortality rates (RSMR) in hospitals participating in the Get With the Guidelines–Heart Failure (GWTG-HF) registry, using a hierarchical, logistic regression model to calculate hospital-specific 30-day RSMRs.
Get With the Guidelines is a voluntary, observational quality improvement program that has been linked with CMS to capture long-term follow-up data, Dr. Pandey explained.
The study included 106,304 heart failure patients older than 65 years at 317 GWTG hospitals across the United States during 2005-2013. The hospitals were divided into performance quartiles based on 30-day RSMR. The 30-day RSMRs were 8.6%, 9.4%, 9.9%, and 10.7% in the first, second, third, and fourth quartiles, respectively.
There was a strong association between the top-performing hospitals and long-term survival rates for the patients that persisted beyond 30 days, said Dr. Pandey. The mortality rates after 5 years were 75.6%, 76.2%, 76.9%, and 79.6%, in the first, second, third, and fourth quartiles, respectively.
The hospitals in the first quartile were more likely than those in the fourth quartile to have primary percutaneous coronary intervention capabilities (80% vs. 73%), in-house cardiac surgery (66% vs. 57%), and a heart transplant center (13% vs. 2%).
In addition, the hospitals in the highest quartile had higher rates of adherence than those in the lowest quartile to guideline-directed heart failure therapies, including evidence-based beta-blocker use, ACE inhibitor and angiotensin receptor blocker use, postdischarge heart failure follow-up, implantable cardioverter defibrillator placement prior to discharge, and cardiac resynchronization therapy prior to discharge.The study was limited by a possible lack of generalizability to hospitals not participating in the GWTG program, Dr. Pandey said. In addition, “we cannot establish causation between hospital performance based on 30-day RSMR and long-term survival.”
However, the long-term survival advantage for heart failure patients treated at hospitals with the highest measures of short-term performance suggests that the 30-day RSMR could be used as an incentive for quality care and the improvement of long-term outcomes, he said.
Dr. Pandey had no financial conflicts to disclose. The Get With the Guidelines–Heart Failure program is supported by the American Heart Association, and has been previously funded by Medtronic, GlaxoSmithKline, Ortho-McNeil, and the AHA Pharmaceutical Roundtable. The findings were published simultaneously in JAMA Cardiology (2018 Mar 12. doi:10.1001/jamacardio.2018.0579).
SOURCE: Pandy A. ACC 2018.
ORLANDO – Hospitals in the first quartile of short-term performance in treating heart failure patients had higher long-term survival rates for those patients, based on data from 317 hospitals that participated in a voluntary quality improvement program.
The burden of heart failure remains substantial in the United States, and health policies are increasingly focused on improving care for heart failure patients, said Ambarish Pandey, MD, of the University of Texas, Dallas, in a presentation at the annual meeting of the American College of Cardiology.
The researchers assessed hospital performance based on 30-day risk-standardized mortality rates (RSMR) in hospitals participating in the Get With the Guidelines–Heart Failure (GWTG-HF) registry, using a hierarchical, logistic regression model to calculate hospital-specific 30-day RSMRs.
Get With the Guidelines is a voluntary, observational quality improvement program that has been linked with CMS to capture long-term follow-up data, Dr. Pandey explained.
The study included 106,304 heart failure patients older than 65 years at 317 GWTG hospitals across the United States during 2005-2013. The hospitals were divided into performance quartiles based on 30-day RSMR. The 30-day RSMRs were 8.6%, 9.4%, 9.9%, and 10.7% in the first, second, third, and fourth quartiles, respectively.
There was a strong association between the top-performing hospitals and long-term survival rates for the patients that persisted beyond 30 days, said Dr. Pandey. The mortality rates after 5 years were 75.6%, 76.2%, 76.9%, and 79.6%, in the first, second, third, and fourth quartiles, respectively.
The hospitals in the first quartile were more likely than those in the fourth quartile to have primary percutaneous coronary intervention capabilities (80% vs. 73%), in-house cardiac surgery (66% vs. 57%), and a heart transplant center (13% vs. 2%).
In addition, the hospitals in the highest quartile had higher rates of adherence than those in the lowest quartile to guideline-directed heart failure therapies, including evidence-based beta-blocker use, ACE inhibitor and angiotensin receptor blocker use, postdischarge heart failure follow-up, implantable cardioverter defibrillator placement prior to discharge, and cardiac resynchronization therapy prior to discharge.The study was limited by a possible lack of generalizability to hospitals not participating in the GWTG program, Dr. Pandey said. In addition, “we cannot establish causation between hospital performance based on 30-day RSMR and long-term survival.”
However, the long-term survival advantage for heart failure patients treated at hospitals with the highest measures of short-term performance suggests that the 30-day RSMR could be used as an incentive for quality care and the improvement of long-term outcomes, he said.
Dr. Pandey had no financial conflicts to disclose. The Get With the Guidelines–Heart Failure program is supported by the American Heart Association, and has been previously funded by Medtronic, GlaxoSmithKline, Ortho-McNeil, and the AHA Pharmaceutical Roundtable. The findings were published simultaneously in JAMA Cardiology (2018 Mar 12. doi:10.1001/jamacardio.2018.0579).
SOURCE: Pandy A. ACC 2018.
ORLANDO – Hospitals in the first quartile of short-term performance in treating heart failure patients had higher long-term survival rates for those patients, based on data from 317 hospitals that participated in a voluntary quality improvement program.
The burden of heart failure remains substantial in the United States, and health policies are increasingly focused on improving care for heart failure patients, said Ambarish Pandey, MD, of the University of Texas, Dallas, in a presentation at the annual meeting of the American College of Cardiology.
The researchers assessed hospital performance based on 30-day risk-standardized mortality rates (RSMR) in hospitals participating in the Get With the Guidelines–Heart Failure (GWTG-HF) registry, using a hierarchical, logistic regression model to calculate hospital-specific 30-day RSMRs.
Get With the Guidelines is a voluntary, observational quality improvement program that has been linked with CMS to capture long-term follow-up data, Dr. Pandey explained.
The study included 106,304 heart failure patients older than 65 years at 317 GWTG hospitals across the United States during 2005-2013. The hospitals were divided into performance quartiles based on 30-day RSMR. The 30-day RSMRs were 8.6%, 9.4%, 9.9%, and 10.7% in the first, second, third, and fourth quartiles, respectively.
There was a strong association between the top-performing hospitals and long-term survival rates for the patients that persisted beyond 30 days, said Dr. Pandey. The mortality rates after 5 years were 75.6%, 76.2%, 76.9%, and 79.6%, in the first, second, third, and fourth quartiles, respectively.
The hospitals in the first quartile were more likely than those in the fourth quartile to have primary percutaneous coronary intervention capabilities (80% vs. 73%), in-house cardiac surgery (66% vs. 57%), and a heart transplant center (13% vs. 2%).
In addition, the hospitals in the highest quartile had higher rates of adherence than those in the lowest quartile to guideline-directed heart failure therapies, including evidence-based beta-blocker use, ACE inhibitor and angiotensin receptor blocker use, postdischarge heart failure follow-up, implantable cardioverter defibrillator placement prior to discharge, and cardiac resynchronization therapy prior to discharge.The study was limited by a possible lack of generalizability to hospitals not participating in the GWTG program, Dr. Pandey said. In addition, “we cannot establish causation between hospital performance based on 30-day RSMR and long-term survival.”
However, the long-term survival advantage for heart failure patients treated at hospitals with the highest measures of short-term performance suggests that the 30-day RSMR could be used as an incentive for quality care and the improvement of long-term outcomes, he said.
Dr. Pandey had no financial conflicts to disclose. The Get With the Guidelines–Heart Failure program is supported by the American Heart Association, and has been previously funded by Medtronic, GlaxoSmithKline, Ortho-McNeil, and the AHA Pharmaceutical Roundtable. The findings were published simultaneously in JAMA Cardiology (2018 Mar 12. doi:10.1001/jamacardio.2018.0579).
SOURCE: Pandy A. ACC 2018.
REPORTING FROM ACC 2018
Key clinical point:
Major finding: Hospitals in the lowest quartile had a 22% higher 5-year mortality rate for heart failure patients compared with the highest quartile hospitals.
Study details: The data come from 106,304 heart failure patients admitted to 317 hospitals participating in a voluntary quality improvement program.
Disclosures: Dr. Pandey had no financial conflicts to disclose. The Get With the Guidelines–Heart Failure program is supported by the American Heart Association, and has been previously funded by Medtronic, GlaxoSmithKline, Ortho-McNeil, and the AHA Pharmaceutical Roundtable.
Source: Pandey A. ACC 2018.
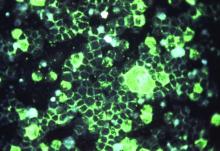
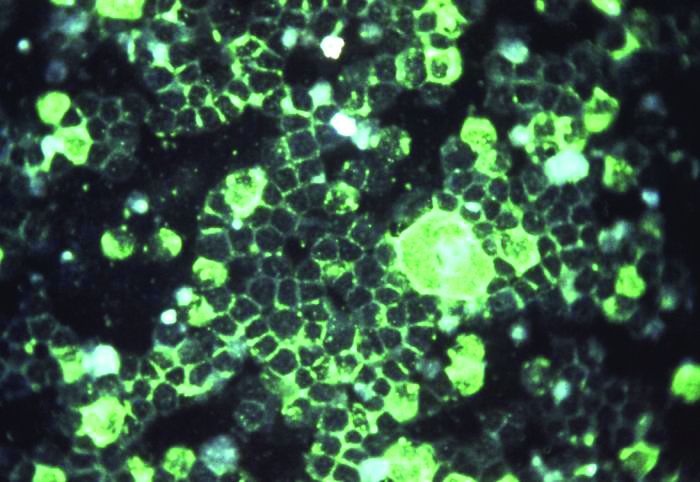
Clinical pattern may help distinguish pediatric NMN from subungal melanoma
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
When longitudinal melanonychia appears as a sharply demarcated pigment band of even width against normal nail in a child, Hutchinson’s sign with longitudinal brushy pigmentation may be a useful clinical pattern suggesting a diagnosis of nail matrix nevus rather than subungual melanoma, said Jae Ho Lee, MD, of Sungkyunkwan University, Seoul, South Korea, and associates.
with 14 children having melanonychia greater than 20% the width of the nail, compared with 2 adults. Total melanonychia occurred just twice, in two children. A total of 12 children had nail dystrophy, while none of the adults did; nail dystrophy was more frequent in wider lesions.
Hutchinson’s sign was seen in seven pediatric patients, but no adult patients. In most cases, Hutchinson’s sign had hyponychial pigmentation, and on dermoscopy showed a pigment pattern presenting longitudinally and resembling a brush mark (longitudinal brushy pigmentation or LBP). LBP of nail matrix nevi is different from the Hutchinson’s sign that occurs in subungual melanoma (SUM), where it is typically a “haphazard pigmentation pattern involving periungual skin.
“We propose that Hutchinson’s sign occurs more commonly in pediatric NMN than in adult NMN, and that the presence of the LBP pattern can help distinguish pediatric NMN from SUM,” the investigators said.
Histologically, the biopsies of the NMN in this study showed some important differences from known SUM histology. All the study biopsies “showed a melanocytic proliferation exhibiting a predominantly nested growth pattern, with the nests mostly located at the dermoepithelial junction and with retraction artifact surrounding the nests. There were variable nuclear hyperchromatism, nuclear sizes, and cytologic atypia within the NMN biopsy specimens,” the researchers said. “In contrast, the histology of SUM demonstrates a predominance of atypical single melanocytes over nests, retraction artifacts around individual melanocytes, and uniform atypia of melanocytes throughout the biopsy specimen.”
SOURCE: Lee JH et al. J Am Acad Dermatol. 2018 Mar;78(3):479-89.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Psoriasis patients often have history of childhood trauma
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
reported Maria Luigia Crosta, of Catholic University of the Sacred Heart, Rome, and her associates.
Other studies have shown that among dermatologic disorders, psoriasis has the highest link to psychiatric illness such as mood, anxiety, and personality disorders, and that patients with psoriasis have an increased risk of suicidal ideation, the investigators said.
“Improving resilience with a multidisciplinary approach and an early psychological intervention could facilitate the management of psoriasis, by promoting the establishment of a stronger therapeutic alliance and a better acceptance of disease. Programs for psoriasis patients should focus on self-motivation and strengthening of self-efficacy,” Dr. Crosta and her associates concluded.
SOURCE: Crosta ML et al. J Psychosom Res. 2018;106:25-8.
FROM THE JOURNAL OF PSYCHOSOMATIC RESEARCH
Efavirenz-based ART may hamper vaginal ring contraception
BOSTON – Efavirenz-based antiretroviral therapy may significantly impair the effectiveness of vaginal ring contraceptives, investigators reported.
Over a 21-day period, levels of estrogen among women who used a vaginal ring (NuvaRing) while on efavirenz-based antiretroviral therapy (ART) were up to 79% lower, and levels of progestin were up to 57% lower, than in women with HIV infection who used the vaginal ring before starting ART, reported Kimberly K. Scarsi, PharmD, of the University of Nebraska, Omaha.
In contrast, women on an atazanavir-based ART regimen had lower estrogen levels than untreated controls who used a vaginal ring, but higher levels of progestin – the primary antiovulatory component of the ring – suggesting that it would retain contraceptive effectiveness, she said at the annual Conference on Retroviruses and Opportunistic Infections.
“In a broader context, these data can be applied to other drugs that behave similarly. So for example, erythromycins are also known to interfere with hormones in this way, as well as some anticonvulsant agents that may also impair the effectiveness of vaginal ring contraceptives,” she said at a brief, following her presentation of the data in an oral abstract session.
She noted that the findings have important implications for developers of vaginal rings designed to prevent HIV transmission as well as provide hormone-based contraception.
Dr. Scarsi and colleagues conducted a phase 2, international, nonrandomized, parallel pharmacokinetic study comparing levels of estrogen in the form of ethinyl estradiol (EE) and progestin in the form of etonogestrel among women with HIV infection who had not yet begun ART, as well as women on efavirenz- or atazanavir-based regimens.
Participants 16 years and older from centers in Africa, Asia, and North and South America were enrolled. The patients had to be willing to use a second, nonhormonal form of effective contraceptive, and if they were not on ART had to have CD4 cell counts of 350 cells/m3 or higher at screening. Participants on ART had to be on stable therapy for at least 30 days, and have HIV-1 RNA of 400 copies/mL or less.
A total of 25 control subjects, 25 women on efavirenz, and 24 on atazanavir were available for the primary pharmacokinetic analysis.
Over 21 days, EE levels among the efavirenz groups were 53%-57% lower than those of controls. Levels among the atazanavir groups were 29%-59% lower.
On days 7, 14, and 21, the EE geometric means ratios in efavirenz-treated patients versus controls were 0.47, 0.45, and 0.43, respectively (P less than .05 for each comparison).
In the atazanavir group, the EE geometric mean ratios versus controls at the same time points were 0.68 (P nonsignificant), 0.71 (P less than .05), and 0.65 (P less than .05).
For those in the efavirenz group, etonogestrel levels over 21 days were 76%-79% lower than in controls. In contrast, levels in the atazanavir group were 71%-79% higher than in controls.
The geometric mean ratios for the efavirenz group at 7, 14, and 21 days versus controls were 0.21, 0.22, and 0.24 (P less than .05 for all comparisons). In the atazanavir group, the respective geometric mean ratios were 1.71, 1.79, and 1.74 (P less than .05 for all comparisons).
Safety and tolerability of the ring, a secondary endpoint, was similar among the groups, with slightly more than one-fourth of participants in each arm having a mild adverse event, most commonly associated with abnormal vaginal discharge or menstrual irregularities such as spotting.
The investigators also looked at endogenous progesterone levels as a surrogate for ovulation. Although the ring’s package insert recommends to start using it within the first 5 days after the start of menses, the median enrollment time was 9 days after menses in all groups. Nonetheless, all participants in the control and atazanavir groups had undetectable progesterone values (less than 5 ng/mL) by day 14.
In contrast, among women in the efavirenz group, all women had undetectable progesterone values only at day 21.
The findings suggest that, when considering contraception and ART in HIV-infected women, developers of intravaginally administered drugs should consider systemic drug-drug interactions, because hormones released from a vaginal ring are extensively absorbed and act systemically. It is also important to consider local drug-drug interactions with the microbiome, because although it is known that dapivirine released from a vaginal ring can concentrate in the vaginal tract, possible interactions with the local microbiome, local drug transporters, and local drug-metabolizing enzymes are not known, Dr. Scarsi cautioned.
The study was supported by the National Institutes of Health. Merck provided the vaginal ring used in the study. Dr. Scarsi reported having no conflicts of interest to disclose.
SOURCE: Scarsi KK et al. CROI 2018, Abstract 141.
BOSTON – Efavirenz-based antiretroviral therapy may significantly impair the effectiveness of vaginal ring contraceptives, investigators reported.
Over a 21-day period, levels of estrogen among women who used a vaginal ring (NuvaRing) while on efavirenz-based antiretroviral therapy (ART) were up to 79% lower, and levels of progestin were up to 57% lower, than in women with HIV infection who used the vaginal ring before starting ART, reported Kimberly K. Scarsi, PharmD, of the University of Nebraska, Omaha.
In contrast, women on an atazanavir-based ART regimen had lower estrogen levels than untreated controls who used a vaginal ring, but higher levels of progestin – the primary antiovulatory component of the ring – suggesting that it would retain contraceptive effectiveness, she said at the annual Conference on Retroviruses and Opportunistic Infections.
“In a broader context, these data can be applied to other drugs that behave similarly. So for example, erythromycins are also known to interfere with hormones in this way, as well as some anticonvulsant agents that may also impair the effectiveness of vaginal ring contraceptives,” she said at a brief, following her presentation of the data in an oral abstract session.
She noted that the findings have important implications for developers of vaginal rings designed to prevent HIV transmission as well as provide hormone-based contraception.
Dr. Scarsi and colleagues conducted a phase 2, international, nonrandomized, parallel pharmacokinetic study comparing levels of estrogen in the form of ethinyl estradiol (EE) and progestin in the form of etonogestrel among women with HIV infection who had not yet begun ART, as well as women on efavirenz- or atazanavir-based regimens.
Participants 16 years and older from centers in Africa, Asia, and North and South America were enrolled. The patients had to be willing to use a second, nonhormonal form of effective contraceptive, and if they were not on ART had to have CD4 cell counts of 350 cells/m3 or higher at screening. Participants on ART had to be on stable therapy for at least 30 days, and have HIV-1 RNA of 400 copies/mL or less.
A total of 25 control subjects, 25 women on efavirenz, and 24 on atazanavir were available for the primary pharmacokinetic analysis.
Over 21 days, EE levels among the efavirenz groups were 53%-57% lower than those of controls. Levels among the atazanavir groups were 29%-59% lower.
On days 7, 14, and 21, the EE geometric means ratios in efavirenz-treated patients versus controls were 0.47, 0.45, and 0.43, respectively (P less than .05 for each comparison).
In the atazanavir group, the EE geometric mean ratios versus controls at the same time points were 0.68 (P nonsignificant), 0.71 (P less than .05), and 0.65 (P less than .05).
For those in the efavirenz group, etonogestrel levels over 21 days were 76%-79% lower than in controls. In contrast, levels in the atazanavir group were 71%-79% higher than in controls.
The geometric mean ratios for the efavirenz group at 7, 14, and 21 days versus controls were 0.21, 0.22, and 0.24 (P less than .05 for all comparisons). In the atazanavir group, the respective geometric mean ratios were 1.71, 1.79, and 1.74 (P less than .05 for all comparisons).
Safety and tolerability of the ring, a secondary endpoint, was similar among the groups, with slightly more than one-fourth of participants in each arm having a mild adverse event, most commonly associated with abnormal vaginal discharge or menstrual irregularities such as spotting.
The investigators also looked at endogenous progesterone levels as a surrogate for ovulation. Although the ring’s package insert recommends to start using it within the first 5 days after the start of menses, the median enrollment time was 9 days after menses in all groups. Nonetheless, all participants in the control and atazanavir groups had undetectable progesterone values (less than 5 ng/mL) by day 14.
In contrast, among women in the efavirenz group, all women had undetectable progesterone values only at day 21.
The findings suggest that, when considering contraception and ART in HIV-infected women, developers of intravaginally administered drugs should consider systemic drug-drug interactions, because hormones released from a vaginal ring are extensively absorbed and act systemically. It is also important to consider local drug-drug interactions with the microbiome, because although it is known that dapivirine released from a vaginal ring can concentrate in the vaginal tract, possible interactions with the local microbiome, local drug transporters, and local drug-metabolizing enzymes are not known, Dr. Scarsi cautioned.
The study was supported by the National Institutes of Health. Merck provided the vaginal ring used in the study. Dr. Scarsi reported having no conflicts of interest to disclose.
SOURCE: Scarsi KK et al. CROI 2018, Abstract 141.
BOSTON – Efavirenz-based antiretroviral therapy may significantly impair the effectiveness of vaginal ring contraceptives, investigators reported.
Over a 21-day period, levels of estrogen among women who used a vaginal ring (NuvaRing) while on efavirenz-based antiretroviral therapy (ART) were up to 79% lower, and levels of progestin were up to 57% lower, than in women with HIV infection who used the vaginal ring before starting ART, reported Kimberly K. Scarsi, PharmD, of the University of Nebraska, Omaha.
In contrast, women on an atazanavir-based ART regimen had lower estrogen levels than untreated controls who used a vaginal ring, but higher levels of progestin – the primary antiovulatory component of the ring – suggesting that it would retain contraceptive effectiveness, she said at the annual Conference on Retroviruses and Opportunistic Infections.
“In a broader context, these data can be applied to other drugs that behave similarly. So for example, erythromycins are also known to interfere with hormones in this way, as well as some anticonvulsant agents that may also impair the effectiveness of vaginal ring contraceptives,” she said at a brief, following her presentation of the data in an oral abstract session.
She noted that the findings have important implications for developers of vaginal rings designed to prevent HIV transmission as well as provide hormone-based contraception.
Dr. Scarsi and colleagues conducted a phase 2, international, nonrandomized, parallel pharmacokinetic study comparing levels of estrogen in the form of ethinyl estradiol (EE) and progestin in the form of etonogestrel among women with HIV infection who had not yet begun ART, as well as women on efavirenz- or atazanavir-based regimens.
Participants 16 years and older from centers in Africa, Asia, and North and South America were enrolled. The patients had to be willing to use a second, nonhormonal form of effective contraceptive, and if they were not on ART had to have CD4 cell counts of 350 cells/m3 or higher at screening. Participants on ART had to be on stable therapy for at least 30 days, and have HIV-1 RNA of 400 copies/mL or less.
A total of 25 control subjects, 25 women on efavirenz, and 24 on atazanavir were available for the primary pharmacokinetic analysis.
Over 21 days, EE levels among the efavirenz groups were 53%-57% lower than those of controls. Levels among the atazanavir groups were 29%-59% lower.
On days 7, 14, and 21, the EE geometric means ratios in efavirenz-treated patients versus controls were 0.47, 0.45, and 0.43, respectively (P less than .05 for each comparison).
In the atazanavir group, the EE geometric mean ratios versus controls at the same time points were 0.68 (P nonsignificant), 0.71 (P less than .05), and 0.65 (P less than .05).
For those in the efavirenz group, etonogestrel levels over 21 days were 76%-79% lower than in controls. In contrast, levels in the atazanavir group were 71%-79% higher than in controls.
The geometric mean ratios for the efavirenz group at 7, 14, and 21 days versus controls were 0.21, 0.22, and 0.24 (P less than .05 for all comparisons). In the atazanavir group, the respective geometric mean ratios were 1.71, 1.79, and 1.74 (P less than .05 for all comparisons).
Safety and tolerability of the ring, a secondary endpoint, was similar among the groups, with slightly more than one-fourth of participants in each arm having a mild adverse event, most commonly associated with abnormal vaginal discharge or menstrual irregularities such as spotting.
The investigators also looked at endogenous progesterone levels as a surrogate for ovulation. Although the ring’s package insert recommends to start using it within the first 5 days after the start of menses, the median enrollment time was 9 days after menses in all groups. Nonetheless, all participants in the control and atazanavir groups had undetectable progesterone values (less than 5 ng/mL) by day 14.
In contrast, among women in the efavirenz group, all women had undetectable progesterone values only at day 21.
The findings suggest that, when considering contraception and ART in HIV-infected women, developers of intravaginally administered drugs should consider systemic drug-drug interactions, because hormones released from a vaginal ring are extensively absorbed and act systemically. It is also important to consider local drug-drug interactions with the microbiome, because although it is known that dapivirine released from a vaginal ring can concentrate in the vaginal tract, possible interactions with the local microbiome, local drug transporters, and local drug-metabolizing enzymes are not known, Dr. Scarsi cautioned.
The study was supported by the National Institutes of Health. Merck provided the vaginal ring used in the study. Dr. Scarsi reported having no conflicts of interest to disclose.
SOURCE: Scarsi KK et al. CROI 2018, Abstract 141.
REPORTING FROM CROI 2018
Key clinical point:
Major finding: Estrogen exposure in women on efavirenz was 53%-57% lower than among controls.
Study details: A pharmacokinetic study in 74 HIV-infected women.
Disclosures: The study was supported by the National Institutes of Health. Merck provided the vaginal ring used in the study. Dr. Scarsi reported having no conflicts of interest to disclose.
Source: Scarsi KK et al. CROI 2018, Abstract 141.
RSV immunoprophylaxis in premature infants doesn’t prevent later asthma
reported Nienke M. Scheltema, MD, of Wilhelmina Children’s Hospital, Utrecht, the Netherlands, and associates.
In a study of 395 otherwise healthy premature infants who were randomized to receive palivizumab for respiratory syncytial virus (RSV) immunoprophylaxis or placebo and followed for 6 years, 14% of the 199 infants in the RSV prevention group had parent-reported asthma, compared with 24% of the 196 in the placebo group (absolute risk reduction, 9.9%). This was explained mostly by differences in infrequent wheeze, the researchers said. However, physician-diagnosed asthma in the past 12 months was not significantly different between the two groups at 6 years: 10.3% in the RSV prevention group and 9.9% in the placebo group.
SOURCE: Scheltema NM et al. Lancet. 2018 Feb 27. doi: 10.1016/S2213-2600(18)30055-9.
reported Nienke M. Scheltema, MD, of Wilhelmina Children’s Hospital, Utrecht, the Netherlands, and associates.
In a study of 395 otherwise healthy premature infants who were randomized to receive palivizumab for respiratory syncytial virus (RSV) immunoprophylaxis or placebo and followed for 6 years, 14% of the 199 infants in the RSV prevention group had parent-reported asthma, compared with 24% of the 196 in the placebo group (absolute risk reduction, 9.9%). This was explained mostly by differences in infrequent wheeze, the researchers said. However, physician-diagnosed asthma in the past 12 months was not significantly different between the two groups at 6 years: 10.3% in the RSV prevention group and 9.9% in the placebo group.
SOURCE: Scheltema NM et al. Lancet. 2018 Feb 27. doi: 10.1016/S2213-2600(18)30055-9.
reported Nienke M. Scheltema, MD, of Wilhelmina Children’s Hospital, Utrecht, the Netherlands, and associates.
In a study of 395 otherwise healthy premature infants who were randomized to receive palivizumab for respiratory syncytial virus (RSV) immunoprophylaxis or placebo and followed for 6 years, 14% of the 199 infants in the RSV prevention group had parent-reported asthma, compared with 24% of the 196 in the placebo group (absolute risk reduction, 9.9%). This was explained mostly by differences in infrequent wheeze, the researchers said. However, physician-diagnosed asthma in the past 12 months was not significantly different between the two groups at 6 years: 10.3% in the RSV prevention group and 9.9% in the placebo group.
SOURCE: Scheltema NM et al. Lancet. 2018 Feb 27. doi: 10.1016/S2213-2600(18)30055-9.
FROM THE LANCET
Telehealth for Rural Veterans With Neurologic Disorders (FULL)
Dr. Geppert. I have the pleasure of interviewing Dr. Larry Davis, Distinguished Professor of Neurology at the University of New Mexico School of Medicine in Albuquerque and chief of the NMVAHCS Neurology Service. Welcome, Dr. Davis. Can you describe a teleneurology visit?
Dr. Davis. The NMVAHCS is the only VA located in a large rural state. Location is a real challenge because we treat a lot of veterans who live rurally, and they often have to travel 5 to 6 hours to Albuquerque. When the VA set up its telehealth systems, it was obvious to the NMVAHCS Neurology Service that this was a gold mine. We have many patients who are unable to drive because of their neurologic condition, and they need a caregiver—sometimes a spouse—to drive them to NMVAHCS to see a neurologist, usually in an outpatient setting, often for 30 to 45 minutes, and then drive back 5 hours.
When I get a consult from a rural CBOC, I invite the patient to come to NMVAHCS for the first visit. First, I examine the patient face-to-face so the patient can get to know me. Second, I order special tests or imaging, which are not available in rural areas. Sometimes, for complicated cases, the patient stays overnight.
We discuss the diagnosis with the patient, and make the decision whether the patient is a good candidate for telehealth. If the patient consents and wants to be seen at a local community VA center, we set it up. On a given day, the patient travels—often 15, 20 minutes at most—to the VA facility and goes into a modified examination room. The patient sits in front of a TV screen with a camera focused on him or her. The patient can see me on the screen. In my office I have 2 screens, one has the patient record; the other allows me to see the patient.
Over the years, I have discovered that once I know the patient, it’s just like talking across the table. I can get a history of what has changed either with medications or chronic illness since the last follow-up.
Dr. Geppert. What are the issues and challenges in treating patients with epilepsy, multiple sclerosis, and other neurologic conditions?
Dr. Davis. We have the most difficultly with sensory examinations. I can perform a good motor examination via telehealth, but it is more difficult if I need to look carefully at the patient’s reflexes. We follow individuals with headaches, seizures, multiple sclerosis, Parkinson disease, and a variety of other illnesses. There are not too many we cannot follow that way. If patients have questions, I can look at their medical record and laboratory data while they are on the screen.
The caregiver or spouse can sit next to the patient, so they can be part of the conversation. If the patient is having trouble describing what is going on, the caregiver can offer comments.
Dr. Geppert. If I’m the patient and I’ve had a previous stroke and it looks as though I might have had another, wouldn’t you like to do a neurologic exam but can’t via telehealth?
Dr. Davis. That’s a very good point. When I talk to a patient and I don’t like what I see, I have the ability to ask the patient to come to NMVAHCS. I had one patient who suddenly started getting chest pains during the exam, so we called the CBOC primary care doctor to immediately move the patient to the local hospital. I had another patient who started talking about suicide. I kept the patient on the phone, but we got the primary care doctor in the room. We do have backup.
Dr. Geppert. You mentioned that you often involve family and that you work with local CBOC registered nurses (RNs). Can you tell us how you extend the reach of teleneurology through self-care and family education?
Dr. Davis. We have 2 qualified RN patient educators. One is an expert in Parkinson disease; the other follows up with the patient who has had a stroke, to reduce risk factors for a second stroke.
When I see a patient for a limited time, I deal with the drugs and things like that. I am less focused on what type of chair the patient should sit on, whether the patient might fall, how to safely get up, etc. So I set up a separate appointment with the nurse educator, who goes through all the day-to-day activities that the patient has to be able to do. Patients with Parkinson disease do not like to sit on low sofas, for example. What are the tricks for constipation? If a patient falls, how do you safely get up? The nurse will have the patient get down right in front of the camera and walk them through how to get up.
Dr. Geppert. I know that in many rural areas, especially in our state, there are real shortages of neurologists and psychiatrists. Can you talk about how this helps multiply your ability to care for patients?
Dr. Davis. With the exception of 3 different communities, there are no neurologists within 50 to 100 miles.
Dr. Geppert. Or neuropsychiatrists.
Dr. Davis. Or neuropsychiatrists or even a psychiatry office. So patients are very limited. We have an extremely loyal population of VA patients because it isn’t easy to say, “I’m just going to go down the street and get another doc.”
Dr. Geppert. What type of feedback do you get from patients and family about doing this virtually?
Dr. Davis. We sent a carefully worded satisfaction survey and received 700 responses. We found the following responses: 90% agreed that they received good care during their visit. Ninety-one percent reported that they were able to communicate and 87% would continue their care via teleneurology. Was the teleneurology more convenient than driving here? Yes, 90% said that it was. And did they have overall satisfaction with the visit? Literally 90% reported that they did. It’s a very high satisfaction rate.
We know that patients will say, “Oh, you can see me every 3 months, but I want to come down to see you face-to-face from time-to-time.” When I ask why, the most common answers are either “I live so rurally, there are no stores.” Or “I have family, and I want to come down.” So we then try to set up that face-to-face visit on a Friday.
If they’re traveling, they get their travel pay, but then they get to spend the weekend with a friend or family. There are often secondary reasons. Occasionally, they have to come back for another specialist; we make great efforts to put both those visits on the same day so they don’t have to go back and forth.
Dr. Geppert. So Dr. Davis, you’re a world-famous neurologist, but do you have to have special training or expertise to do teleneurology?
Dr. Davis. It helps to be a good clinician; I’ve been doing this for many years. Because we see patients on a sequence by television, I have to keep track of the time, whereas in the face-to-face clinic if something is really going wrong, I have the ability to shift things around right away and spend more time with that patient. I try to set up longer times for telehealth. I work with a clinical nurse practitioner colleague who takes care of headache patients, and she has a shorter time between visits. I never quite know what’s going to happen, and I want to leave a lot of time for the patient or the spouse to ask questions.
Dr. Geppert. We are both, certainly, senior clinicians and technology is a little different and new. Did you have problems learning to use the teleneurology?
Dr. Davis. Believe it or not, no. The television system is very similar to Skype. It is called Jabber and is encrypted, so it’s safe to transmit. You have to feel comfortable talking to somebody on a TV screen. And the first time I did it, I felt a little awkward. Within a day or two, I was fine.
Dr. Geppert. Federal Practitioner readers may want to start teleneurology or get more involved in it. Are you in touch with other VA and DoD providers?
Dr. Davis. Practitioners can contact me if they want to talk about how we do patient education. We’ve also spent a fair amount of effort developing a handbook that we send out on the ABCs of how to do it.
Dr. Geppert. Do you involve residents in this?
Dr. Davis. No, not at this point. My goal is to do it, but ironically enough, I’m trying to get students who rotate out here to get a feel for what telehealth could be. They don’t do the exam and everything else, but they get a chance to see what telehealth can be. If they want to live in a rural state, they may be involved in it.
Dr. Geppert. If the primary care provider was seeing a patient with multiple sclerosis, which we both know can have symptom flare ups, would they be able to contact you and say, “Hey, Dr. Davis, I’m seeing so and so, and she looks like she’s having some visual problems today.”
Dr. Davis. That’s harder to do because we’re not the only ones using the telehealth system. Telemental health, dietitians, and others are using it all the time, so I have to have a scheduled time to be able to see patients. I’m surprised that more rural states aren’t using it because it really is very enjoyable.
Dr. Geppert. What has the VA learned about telehealth from this program?
Dr. Davis. We know that it actually saves NMVAHCS a lot of money because we don’t pay as much travel pay. The patients like it. The CBOC physicians like it because if I have to, I can type the note right away, and they can read it if the patient is staying there.
Author disclosures
Dr. Hixson has received a collaborative grant from UCB Inc. for research on online epilepsy resources.
Disclaimer
The opinions expressed herein do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Dr. Geppert. I have the pleasure of interviewing Dr. Larry Davis, Distinguished Professor of Neurology at the University of New Mexico School of Medicine in Albuquerque and chief of the NMVAHCS Neurology Service. Welcome, Dr. Davis. Can you describe a teleneurology visit?
Dr. Davis. The NMVAHCS is the only VA located in a large rural state. Location is a real challenge because we treat a lot of veterans who live rurally, and they often have to travel 5 to 6 hours to Albuquerque. When the VA set up its telehealth systems, it was obvious to the NMVAHCS Neurology Service that this was a gold mine. We have many patients who are unable to drive because of their neurologic condition, and they need a caregiver—sometimes a spouse—to drive them to NMVAHCS to see a neurologist, usually in an outpatient setting, often for 30 to 45 minutes, and then drive back 5 hours.
When I get a consult from a rural CBOC, I invite the patient to come to NMVAHCS for the first visit. First, I examine the patient face-to-face so the patient can get to know me. Second, I order special tests or imaging, which are not available in rural areas. Sometimes, for complicated cases, the patient stays overnight.
We discuss the diagnosis with the patient, and make the decision whether the patient is a good candidate for telehealth. If the patient consents and wants to be seen at a local community VA center, we set it up. On a given day, the patient travels—often 15, 20 minutes at most—to the VA facility and goes into a modified examination room. The patient sits in front of a TV screen with a camera focused on him or her. The patient can see me on the screen. In my office I have 2 screens, one has the patient record; the other allows me to see the patient.
Over the years, I have discovered that once I know the patient, it’s just like talking across the table. I can get a history of what has changed either with medications or chronic illness since the last follow-up.
Dr. Geppert. What are the issues and challenges in treating patients with epilepsy, multiple sclerosis, and other neurologic conditions?
Dr. Davis. We have the most difficultly with sensory examinations. I can perform a good motor examination via telehealth, but it is more difficult if I need to look carefully at the patient’s reflexes. We follow individuals with headaches, seizures, multiple sclerosis, Parkinson disease, and a variety of other illnesses. There are not too many we cannot follow that way. If patients have questions, I can look at their medical record and laboratory data while they are on the screen.
The caregiver or spouse can sit next to the patient, so they can be part of the conversation. If the patient is having trouble describing what is going on, the caregiver can offer comments.
Dr. Geppert. If I’m the patient and I’ve had a previous stroke and it looks as though I might have had another, wouldn’t you like to do a neurologic exam but can’t via telehealth?
Dr. Davis. That’s a very good point. When I talk to a patient and I don’t like what I see, I have the ability to ask the patient to come to NMVAHCS. I had one patient who suddenly started getting chest pains during the exam, so we called the CBOC primary care doctor to immediately move the patient to the local hospital. I had another patient who started talking about suicide. I kept the patient on the phone, but we got the primary care doctor in the room. We do have backup.
Dr. Geppert. You mentioned that you often involve family and that you work with local CBOC registered nurses (RNs). Can you tell us how you extend the reach of teleneurology through self-care and family education?
Dr. Davis. We have 2 qualified RN patient educators. One is an expert in Parkinson disease; the other follows up with the patient who has had a stroke, to reduce risk factors for a second stroke.
When I see a patient for a limited time, I deal with the drugs and things like that. I am less focused on what type of chair the patient should sit on, whether the patient might fall, how to safely get up, etc. So I set up a separate appointment with the nurse educator, who goes through all the day-to-day activities that the patient has to be able to do. Patients with Parkinson disease do not like to sit on low sofas, for example. What are the tricks for constipation? If a patient falls, how do you safely get up? The nurse will have the patient get down right in front of the camera and walk them through how to get up.
Dr. Geppert. I know that in many rural areas, especially in our state, there are real shortages of neurologists and psychiatrists. Can you talk about how this helps multiply your ability to care for patients?
Dr. Davis. With the exception of 3 different communities, there are no neurologists within 50 to 100 miles.
Dr. Geppert. Or neuropsychiatrists.
Dr. Davis. Or neuropsychiatrists or even a psychiatry office. So patients are very limited. We have an extremely loyal population of VA patients because it isn’t easy to say, “I’m just going to go down the street and get another doc.”
Dr. Geppert. What type of feedback do you get from patients and family about doing this virtually?
Dr. Davis. We sent a carefully worded satisfaction survey and received 700 responses. We found the following responses: 90% agreed that they received good care during their visit. Ninety-one percent reported that they were able to communicate and 87% would continue their care via teleneurology. Was the teleneurology more convenient than driving here? Yes, 90% said that it was. And did they have overall satisfaction with the visit? Literally 90% reported that they did. It’s a very high satisfaction rate.
We know that patients will say, “Oh, you can see me every 3 months, but I want to come down to see you face-to-face from time-to-time.” When I ask why, the most common answers are either “I live so rurally, there are no stores.” Or “I have family, and I want to come down.” So we then try to set up that face-to-face visit on a Friday.
If they’re traveling, they get their travel pay, but then they get to spend the weekend with a friend or family. There are often secondary reasons. Occasionally, they have to come back for another specialist; we make great efforts to put both those visits on the same day so they don’t have to go back and forth.
Dr. Geppert. So Dr. Davis, you’re a world-famous neurologist, but do you have to have special training or expertise to do teleneurology?
Dr. Davis. It helps to be a good clinician; I’ve been doing this for many years. Because we see patients on a sequence by television, I have to keep track of the time, whereas in the face-to-face clinic if something is really going wrong, I have the ability to shift things around right away and spend more time with that patient. I try to set up longer times for telehealth. I work with a clinical nurse practitioner colleague who takes care of headache patients, and she has a shorter time between visits. I never quite know what’s going to happen, and I want to leave a lot of time for the patient or the spouse to ask questions.
Dr. Geppert. We are both, certainly, senior clinicians and technology is a little different and new. Did you have problems learning to use the teleneurology?
Dr. Davis. Believe it or not, no. The television system is very similar to Skype. It is called Jabber and is encrypted, so it’s safe to transmit. You have to feel comfortable talking to somebody on a TV screen. And the first time I did it, I felt a little awkward. Within a day or two, I was fine.
Dr. Geppert. Federal Practitioner readers may want to start teleneurology or get more involved in it. Are you in touch with other VA and DoD providers?
Dr. Davis. Practitioners can contact me if they want to talk about how we do patient education. We’ve also spent a fair amount of effort developing a handbook that we send out on the ABCs of how to do it.
Dr. Geppert. Do you involve residents in this?
Dr. Davis. No, not at this point. My goal is to do it, but ironically enough, I’m trying to get students who rotate out here to get a feel for what telehealth could be. They don’t do the exam and everything else, but they get a chance to see what telehealth can be. If they want to live in a rural state, they may be involved in it.
Dr. Geppert. If the primary care provider was seeing a patient with multiple sclerosis, which we both know can have symptom flare ups, would they be able to contact you and say, “Hey, Dr. Davis, I’m seeing so and so, and she looks like she’s having some visual problems today.”
Dr. Davis. That’s harder to do because we’re not the only ones using the telehealth system. Telemental health, dietitians, and others are using it all the time, so I have to have a scheduled time to be able to see patients. I’m surprised that more rural states aren’t using it because it really is very enjoyable.
Dr. Geppert. What has the VA learned about telehealth from this program?
Dr. Davis. We know that it actually saves NMVAHCS a lot of money because we don’t pay as much travel pay. The patients like it. The CBOC physicians like it because if I have to, I can type the note right away, and they can read it if the patient is staying there.
Author disclosures
Dr. Hixson has received a collaborative grant from UCB Inc. for research on online epilepsy resources.
Disclaimer
The opinions expressed herein do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Dr. Geppert. I have the pleasure of interviewing Dr. Larry Davis, Distinguished Professor of Neurology at the University of New Mexico School of Medicine in Albuquerque and chief of the NMVAHCS Neurology Service. Welcome, Dr. Davis. Can you describe a teleneurology visit?
Dr. Davis. The NMVAHCS is the only VA located in a large rural state. Location is a real challenge because we treat a lot of veterans who live rurally, and they often have to travel 5 to 6 hours to Albuquerque. When the VA set up its telehealth systems, it was obvious to the NMVAHCS Neurology Service that this was a gold mine. We have many patients who are unable to drive because of their neurologic condition, and they need a caregiver—sometimes a spouse—to drive them to NMVAHCS to see a neurologist, usually in an outpatient setting, often for 30 to 45 minutes, and then drive back 5 hours.
When I get a consult from a rural CBOC, I invite the patient to come to NMVAHCS for the first visit. First, I examine the patient face-to-face so the patient can get to know me. Second, I order special tests or imaging, which are not available in rural areas. Sometimes, for complicated cases, the patient stays overnight.
We discuss the diagnosis with the patient, and make the decision whether the patient is a good candidate for telehealth. If the patient consents and wants to be seen at a local community VA center, we set it up. On a given day, the patient travels—often 15, 20 minutes at most—to the VA facility and goes into a modified examination room. The patient sits in front of a TV screen with a camera focused on him or her. The patient can see me on the screen. In my office I have 2 screens, one has the patient record; the other allows me to see the patient.
Over the years, I have discovered that once I know the patient, it’s just like talking across the table. I can get a history of what has changed either with medications or chronic illness since the last follow-up.
Dr. Geppert. What are the issues and challenges in treating patients with epilepsy, multiple sclerosis, and other neurologic conditions?
Dr. Davis. We have the most difficultly with sensory examinations. I can perform a good motor examination via telehealth, but it is more difficult if I need to look carefully at the patient’s reflexes. We follow individuals with headaches, seizures, multiple sclerosis, Parkinson disease, and a variety of other illnesses. There are not too many we cannot follow that way. If patients have questions, I can look at their medical record and laboratory data while they are on the screen.
The caregiver or spouse can sit next to the patient, so they can be part of the conversation. If the patient is having trouble describing what is going on, the caregiver can offer comments.
Dr. Geppert. If I’m the patient and I’ve had a previous stroke and it looks as though I might have had another, wouldn’t you like to do a neurologic exam but can’t via telehealth?
Dr. Davis. That’s a very good point. When I talk to a patient and I don’t like what I see, I have the ability to ask the patient to come to NMVAHCS. I had one patient who suddenly started getting chest pains during the exam, so we called the CBOC primary care doctor to immediately move the patient to the local hospital. I had another patient who started talking about suicide. I kept the patient on the phone, but we got the primary care doctor in the room. We do have backup.
Dr. Geppert. You mentioned that you often involve family and that you work with local CBOC registered nurses (RNs). Can you tell us how you extend the reach of teleneurology through self-care and family education?
Dr. Davis. We have 2 qualified RN patient educators. One is an expert in Parkinson disease; the other follows up with the patient who has had a stroke, to reduce risk factors for a second stroke.
When I see a patient for a limited time, I deal with the drugs and things like that. I am less focused on what type of chair the patient should sit on, whether the patient might fall, how to safely get up, etc. So I set up a separate appointment with the nurse educator, who goes through all the day-to-day activities that the patient has to be able to do. Patients with Parkinson disease do not like to sit on low sofas, for example. What are the tricks for constipation? If a patient falls, how do you safely get up? The nurse will have the patient get down right in front of the camera and walk them through how to get up.
Dr. Geppert. I know that in many rural areas, especially in our state, there are real shortages of neurologists and psychiatrists. Can you talk about how this helps multiply your ability to care for patients?
Dr. Davis. With the exception of 3 different communities, there are no neurologists within 50 to 100 miles.
Dr. Geppert. Or neuropsychiatrists.
Dr. Davis. Or neuropsychiatrists or even a psychiatry office. So patients are very limited. We have an extremely loyal population of VA patients because it isn’t easy to say, “I’m just going to go down the street and get another doc.”
Dr. Geppert. What type of feedback do you get from patients and family about doing this virtually?
Dr. Davis. We sent a carefully worded satisfaction survey and received 700 responses. We found the following responses: 90% agreed that they received good care during their visit. Ninety-one percent reported that they were able to communicate and 87% would continue their care via teleneurology. Was the teleneurology more convenient than driving here? Yes, 90% said that it was. And did they have overall satisfaction with the visit? Literally 90% reported that they did. It’s a very high satisfaction rate.
We know that patients will say, “Oh, you can see me every 3 months, but I want to come down to see you face-to-face from time-to-time.” When I ask why, the most common answers are either “I live so rurally, there are no stores.” Or “I have family, and I want to come down.” So we then try to set up that face-to-face visit on a Friday.
If they’re traveling, they get their travel pay, but then they get to spend the weekend with a friend or family. There are often secondary reasons. Occasionally, they have to come back for another specialist; we make great efforts to put both those visits on the same day so they don’t have to go back and forth.
Dr. Geppert. So Dr. Davis, you’re a world-famous neurologist, but do you have to have special training or expertise to do teleneurology?
Dr. Davis. It helps to be a good clinician; I’ve been doing this for many years. Because we see patients on a sequence by television, I have to keep track of the time, whereas in the face-to-face clinic if something is really going wrong, I have the ability to shift things around right away and spend more time with that patient. I try to set up longer times for telehealth. I work with a clinical nurse practitioner colleague who takes care of headache patients, and she has a shorter time between visits. I never quite know what’s going to happen, and I want to leave a lot of time for the patient or the spouse to ask questions.
Dr. Geppert. We are both, certainly, senior clinicians and technology is a little different and new. Did you have problems learning to use the teleneurology?
Dr. Davis. Believe it or not, no. The television system is very similar to Skype. It is called Jabber and is encrypted, so it’s safe to transmit. You have to feel comfortable talking to somebody on a TV screen. And the first time I did it, I felt a little awkward. Within a day or two, I was fine.
Dr. Geppert. Federal Practitioner readers may want to start teleneurology or get more involved in it. Are you in touch with other VA and DoD providers?
Dr. Davis. Practitioners can contact me if they want to talk about how we do patient education. We’ve also spent a fair amount of effort developing a handbook that we send out on the ABCs of how to do it.
Dr. Geppert. Do you involve residents in this?
Dr. Davis. No, not at this point. My goal is to do it, but ironically enough, I’m trying to get students who rotate out here to get a feel for what telehealth could be. They don’t do the exam and everything else, but they get a chance to see what telehealth can be. If they want to live in a rural state, they may be involved in it.
Dr. Geppert. If the primary care provider was seeing a patient with multiple sclerosis, which we both know can have symptom flare ups, would they be able to contact you and say, “Hey, Dr. Davis, I’m seeing so and so, and she looks like she’s having some visual problems today.”
Dr. Davis. That’s harder to do because we’re not the only ones using the telehealth system. Telemental health, dietitians, and others are using it all the time, so I have to have a scheduled time to be able to see patients. I’m surprised that more rural states aren’t using it because it really is very enjoyable.
Dr. Geppert. What has the VA learned about telehealth from this program?
Dr. Davis. We know that it actually saves NMVAHCS a lot of money because we don’t pay as much travel pay. The patients like it. The CBOC physicians like it because if I have to, I can type the note right away, and they can read it if the patient is staying there.
Author disclosures
Dr. Hixson has received a collaborative grant from UCB Inc. for research on online epilepsy resources.
Disclaimer
The opinions expressed herein do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Amgen withdraws application for darbepoetin alfa
Amgen has withdrawn its application to expand the existing marketing authorization for darbepoetin alfa (Aranesp), according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The goal with this application was to extend the authorization for darbepoetin alfa to include the treatment of anemia in adults with low-risk or intermediate-1-risk myelodysplastic syndromes (MDS) who have low transfusion demand.
Darbepoetin alfa is currently approved in the European Union (EU) to treat anemia in adults and children with chronic renal failure and adults who are receiving chemotherapy for non-myeloid malignancies.
Amgen withdrew the application for darbepoetin alfa in MDS patients after the CHMP had evaluated initial documentation provided by the company and formulated a list of questions. Amgen had not yet responded to the questions when it notified the CHMP of the withdrawal.
At the time of the withdrawal, the CHMP was of the provisional opinion that darbepoetin alfa could not have been approved for the treatment of anemia in adults with MDS.
This opinion was based on concerns about the data supporting the application—results from the phase 3 ARCADE trial (NCT01362140) and a phase 2 trial (NCT00095264).
The CHMP said changes to the design of the phase 3 trial and the exclusion of a high number of patients from the analysis of the results raise questions about the validity of the data.
In addition, the phase 2 trial, which was conducted in the US, was not in line with EU recommendations for the treatment of MDS patients.
Therefore, at the time of the withdrawal, the CHMP had decided the marketing authorization could not be expanded based on the data provided.
In a letter to the CHMP, Amgen said its decision to withdraw the application is based on the CHMP’s negative opinion.
Amgen has withdrawn its application to expand the existing marketing authorization for darbepoetin alfa (Aranesp), according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The goal with this application was to extend the authorization for darbepoetin alfa to include the treatment of anemia in adults with low-risk or intermediate-1-risk myelodysplastic syndromes (MDS) who have low transfusion demand.
Darbepoetin alfa is currently approved in the European Union (EU) to treat anemia in adults and children with chronic renal failure and adults who are receiving chemotherapy for non-myeloid malignancies.
Amgen withdrew the application for darbepoetin alfa in MDS patients after the CHMP had evaluated initial documentation provided by the company and formulated a list of questions. Amgen had not yet responded to the questions when it notified the CHMP of the withdrawal.
At the time of the withdrawal, the CHMP was of the provisional opinion that darbepoetin alfa could not have been approved for the treatment of anemia in adults with MDS.
This opinion was based on concerns about the data supporting the application—results from the phase 3 ARCADE trial (NCT01362140) and a phase 2 trial (NCT00095264).
The CHMP said changes to the design of the phase 3 trial and the exclusion of a high number of patients from the analysis of the results raise questions about the validity of the data.
In addition, the phase 2 trial, which was conducted in the US, was not in line with EU recommendations for the treatment of MDS patients.
Therefore, at the time of the withdrawal, the CHMP had decided the marketing authorization could not be expanded based on the data provided.
In a letter to the CHMP, Amgen said its decision to withdraw the application is based on the CHMP’s negative opinion.
Amgen has withdrawn its application to expand the existing marketing authorization for darbepoetin alfa (Aranesp), according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The goal with this application was to extend the authorization for darbepoetin alfa to include the treatment of anemia in adults with low-risk or intermediate-1-risk myelodysplastic syndromes (MDS) who have low transfusion demand.
Darbepoetin alfa is currently approved in the European Union (EU) to treat anemia in adults and children with chronic renal failure and adults who are receiving chemotherapy for non-myeloid malignancies.
Amgen withdrew the application for darbepoetin alfa in MDS patients after the CHMP had evaluated initial documentation provided by the company and formulated a list of questions. Amgen had not yet responded to the questions when it notified the CHMP of the withdrawal.
At the time of the withdrawal, the CHMP was of the provisional opinion that darbepoetin alfa could not have been approved for the treatment of anemia in adults with MDS.
This opinion was based on concerns about the data supporting the application—results from the phase 3 ARCADE trial (NCT01362140) and a phase 2 trial (NCT00095264).
The CHMP said changes to the design of the phase 3 trial and the exclusion of a high number of patients from the analysis of the results raise questions about the validity of the data.
In addition, the phase 2 trial, which was conducted in the US, was not in line with EU recommendations for the treatment of MDS patients.
Therefore, at the time of the withdrawal, the CHMP had decided the marketing authorization could not be expanded based on the data provided.
In a letter to the CHMP, Amgen said its decision to withdraw the application is based on the CHMP’s negative opinion.
Infection risk from reprocessed duodenoscopes is low, but the goal is zero
BOSTON – Once attributed to human error, the outbreaks of infection from persistent contamination of reprocessed duodenoscopes have eluded an easy fix, according to three experts addressing the problem at the 2018 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. This session is part of the AGA Center for GI Innovation and Technology’s ongoing efforts to convene stakeholders, including endoscope manufacturers and the Food and Drug Administration, and to collaborate on a solution to ensure zero device-transmitted infections.
Since the problem first was recognized, changes in device design and cleaning protocols have produced a fivefold reduction in the risk of infection.
“The risk is now very low and well beneath the benefits provided by endoscopy, but we will not settle for anything less than complete resolution of the problem,” said David R. Lichtenstein, MD, the director of the endoscopy program at Boston University. Leading off a program that outlined the problem and possible solutions, Dr. Lichtenstein said, “We need to make this a historical issue.”
After scrutiny by the many stakeholders, including the manufacturers, gastroenterologists, and regulatory agencies, the elevator mechanism has remained one focus of concern. The difficulty of cleaning this mechanism was recognized in the earliest devices, but redesigns to permit these channels to be flushed did not resolve the problem completely. In the AGA Tech Summit session, there was general consensus that even dedicated reprocessing technicians fully adherent to current protocols cannot reliably completely clean the currently available duodenoscopes in every case.
“In most instances, it is not the technician at fault and it is extremely difficult to get a flexible scope clean after a messy procedure,” explained Cori Ofstead, MSPH, an epidemiologist and president of Ofstead & Associates. In one study she conducted in endoscopes reprocessed using best practice recommendations, microbial presence could still be detected.
Although risk of contamination increases with repeated use of scopes, with damaged scopes, and after scopes have been used in procedures generating relatively high amounts of debris, Ms. Ofstead said, “If you look, you will find contamination.” While she emphasized the importance of developing incentives that reward quality over efficiency when attempting to reduce human error in duodenoscope reprocessing, she, like Dr. Lichtenstein, believes new strategies are needed to achieve zero tolerance for infection risk.
“Disinfection simply may not be enough,” Ms. Ofstead said. “The solution is likely to be something else, such as single-use scopes or sterilization.” Explaining how processes of sterilization and disinfection differ, David Weber, MD, MPH, professor of epidemiology, University of North Carolina School of Medicine, Chapel Hill, outlined the relative advantages and disadvantages of current options. Dr. Weber, who has been involved in numerous studies regarding duodenoscope decontamination, emphasized that that rigorous cleaning of biological debris is a central tenet of any solution, but he outlined evidence that the current standard of high level disinfection (HLD) has not been sufficient to bring the infection risk to zero.
“There is no simple answer, because every solution so far has introduced some challenges,” Dr. Lichtenstein observed. Listing some examples, he noted that autoclaving results in damage to endoscopes since they are heat labile; that some proposed sterilization techniques may be limited by sterilants that can’t penetrate biofilm formation into deeper layers that harbor viable bacteria and are associated with a risk of toxicity to technicians or patients; and that disposable endoscopes or elevator mechanisms may involve unacceptable costs or operating characteristics. However, he is convinced there is a solution.
“The problem is being addressed from different angles, and I think we will find the solution within several years. This may involve a series of additional incremental improvements, but I think no one with a stake in this issue will sit comfortably until it is no longer a problem,” Dr. Lichtenstein said.
In the discussion that followed the formal presentations, it was generally acknowledged that the ultimate solution remains unclear even though incremental progress is being made. In fact, there have been no major outbreaks in the United States in the last year following the attention given to this issue, which is likely to have promoted more diligence in disinfection, according to Dr. Lichtenstein.
“Disposable endoscopes or disposable parts on endoscopes that facilitate cleaning may be coming, but I think the best current step is a standardized method of testing scopes after cleaning to verify that disinfection has been achieved,” Dr. Lichtenstein said.
Other solutions, including new sterilization techniques may also emerge, but there was general consensus that the human factor will always be important even if the best solution proves to be a disposable endoscope. Dr. Weber said, “You can still place a disposable scope on a contaminated surface. The human factor is always important.”
Michael L. Kochman, MD, the Wilmott Professor of Medicine and director of the Center for Endoscopic Innovation, Research and Training at the University of Pennsylvania, Philadelphia, and past chair of the AGA Center for GI Innovation and Technology, added, “AGA will build on the relationships that we have with the manufacturers of the endoscopes along with companies developing other novel approaches to reprocessing, as well as the FDA and CDC, to further the discussion. Ultimately, we hope to see the availability of devices that are effective and reliably clean so that we do not have to be concerned about patient-to-patient transmission of infection.”
BOSTON – Once attributed to human error, the outbreaks of infection from persistent contamination of reprocessed duodenoscopes have eluded an easy fix, according to three experts addressing the problem at the 2018 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. This session is part of the AGA Center for GI Innovation and Technology’s ongoing efforts to convene stakeholders, including endoscope manufacturers and the Food and Drug Administration, and to collaborate on a solution to ensure zero device-transmitted infections.
Since the problem first was recognized, changes in device design and cleaning protocols have produced a fivefold reduction in the risk of infection.
“The risk is now very low and well beneath the benefits provided by endoscopy, but we will not settle for anything less than complete resolution of the problem,” said David R. Lichtenstein, MD, the director of the endoscopy program at Boston University. Leading off a program that outlined the problem and possible solutions, Dr. Lichtenstein said, “We need to make this a historical issue.”
After scrutiny by the many stakeholders, including the manufacturers, gastroenterologists, and regulatory agencies, the elevator mechanism has remained one focus of concern. The difficulty of cleaning this mechanism was recognized in the earliest devices, but redesigns to permit these channels to be flushed did not resolve the problem completely. In the AGA Tech Summit session, there was general consensus that even dedicated reprocessing technicians fully adherent to current protocols cannot reliably completely clean the currently available duodenoscopes in every case.
“In most instances, it is not the technician at fault and it is extremely difficult to get a flexible scope clean after a messy procedure,” explained Cori Ofstead, MSPH, an epidemiologist and president of Ofstead & Associates. In one study she conducted in endoscopes reprocessed using best practice recommendations, microbial presence could still be detected.
Although risk of contamination increases with repeated use of scopes, with damaged scopes, and after scopes have been used in procedures generating relatively high amounts of debris, Ms. Ofstead said, “If you look, you will find contamination.” While she emphasized the importance of developing incentives that reward quality over efficiency when attempting to reduce human error in duodenoscope reprocessing, she, like Dr. Lichtenstein, believes new strategies are needed to achieve zero tolerance for infection risk.
“Disinfection simply may not be enough,” Ms. Ofstead said. “The solution is likely to be something else, such as single-use scopes or sterilization.” Explaining how processes of sterilization and disinfection differ, David Weber, MD, MPH, professor of epidemiology, University of North Carolina School of Medicine, Chapel Hill, outlined the relative advantages and disadvantages of current options. Dr. Weber, who has been involved in numerous studies regarding duodenoscope decontamination, emphasized that that rigorous cleaning of biological debris is a central tenet of any solution, but he outlined evidence that the current standard of high level disinfection (HLD) has not been sufficient to bring the infection risk to zero.
“There is no simple answer, because every solution so far has introduced some challenges,” Dr. Lichtenstein observed. Listing some examples, he noted that autoclaving results in damage to endoscopes since they are heat labile; that some proposed sterilization techniques may be limited by sterilants that can’t penetrate biofilm formation into deeper layers that harbor viable bacteria and are associated with a risk of toxicity to technicians or patients; and that disposable endoscopes or elevator mechanisms may involve unacceptable costs or operating characteristics. However, he is convinced there is a solution.
“The problem is being addressed from different angles, and I think we will find the solution within several years. This may involve a series of additional incremental improvements, but I think no one with a stake in this issue will sit comfortably until it is no longer a problem,” Dr. Lichtenstein said.
In the discussion that followed the formal presentations, it was generally acknowledged that the ultimate solution remains unclear even though incremental progress is being made. In fact, there have been no major outbreaks in the United States in the last year following the attention given to this issue, which is likely to have promoted more diligence in disinfection, according to Dr. Lichtenstein.
“Disposable endoscopes or disposable parts on endoscopes that facilitate cleaning may be coming, but I think the best current step is a standardized method of testing scopes after cleaning to verify that disinfection has been achieved,” Dr. Lichtenstein said.
Other solutions, including new sterilization techniques may also emerge, but there was general consensus that the human factor will always be important even if the best solution proves to be a disposable endoscope. Dr. Weber said, “You can still place a disposable scope on a contaminated surface. The human factor is always important.”
Michael L. Kochman, MD, the Wilmott Professor of Medicine and director of the Center for Endoscopic Innovation, Research and Training at the University of Pennsylvania, Philadelphia, and past chair of the AGA Center for GI Innovation and Technology, added, “AGA will build on the relationships that we have with the manufacturers of the endoscopes along with companies developing other novel approaches to reprocessing, as well as the FDA and CDC, to further the discussion. Ultimately, we hope to see the availability of devices that are effective and reliably clean so that we do not have to be concerned about patient-to-patient transmission of infection.”
BOSTON – Once attributed to human error, the outbreaks of infection from persistent contamination of reprocessed duodenoscopes have eluded an easy fix, according to three experts addressing the problem at the 2018 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology. This session is part of the AGA Center for GI Innovation and Technology’s ongoing efforts to convene stakeholders, including endoscope manufacturers and the Food and Drug Administration, and to collaborate on a solution to ensure zero device-transmitted infections.
Since the problem first was recognized, changes in device design and cleaning protocols have produced a fivefold reduction in the risk of infection.
“The risk is now very low and well beneath the benefits provided by endoscopy, but we will not settle for anything less than complete resolution of the problem,” said David R. Lichtenstein, MD, the director of the endoscopy program at Boston University. Leading off a program that outlined the problem and possible solutions, Dr. Lichtenstein said, “We need to make this a historical issue.”
After scrutiny by the many stakeholders, including the manufacturers, gastroenterologists, and regulatory agencies, the elevator mechanism has remained one focus of concern. The difficulty of cleaning this mechanism was recognized in the earliest devices, but redesigns to permit these channels to be flushed did not resolve the problem completely. In the AGA Tech Summit session, there was general consensus that even dedicated reprocessing technicians fully adherent to current protocols cannot reliably completely clean the currently available duodenoscopes in every case.
“In most instances, it is not the technician at fault and it is extremely difficult to get a flexible scope clean after a messy procedure,” explained Cori Ofstead, MSPH, an epidemiologist and president of Ofstead & Associates. In one study she conducted in endoscopes reprocessed using best practice recommendations, microbial presence could still be detected.
Although risk of contamination increases with repeated use of scopes, with damaged scopes, and after scopes have been used in procedures generating relatively high amounts of debris, Ms. Ofstead said, “If you look, you will find contamination.” While she emphasized the importance of developing incentives that reward quality over efficiency when attempting to reduce human error in duodenoscope reprocessing, she, like Dr. Lichtenstein, believes new strategies are needed to achieve zero tolerance for infection risk.
“Disinfection simply may not be enough,” Ms. Ofstead said. “The solution is likely to be something else, such as single-use scopes or sterilization.” Explaining how processes of sterilization and disinfection differ, David Weber, MD, MPH, professor of epidemiology, University of North Carolina School of Medicine, Chapel Hill, outlined the relative advantages and disadvantages of current options. Dr. Weber, who has been involved in numerous studies regarding duodenoscope decontamination, emphasized that that rigorous cleaning of biological debris is a central tenet of any solution, but he outlined evidence that the current standard of high level disinfection (HLD) has not been sufficient to bring the infection risk to zero.
“There is no simple answer, because every solution so far has introduced some challenges,” Dr. Lichtenstein observed. Listing some examples, he noted that autoclaving results in damage to endoscopes since they are heat labile; that some proposed sterilization techniques may be limited by sterilants that can’t penetrate biofilm formation into deeper layers that harbor viable bacteria and are associated with a risk of toxicity to technicians or patients; and that disposable endoscopes or elevator mechanisms may involve unacceptable costs or operating characteristics. However, he is convinced there is a solution.
“The problem is being addressed from different angles, and I think we will find the solution within several years. This may involve a series of additional incremental improvements, but I think no one with a stake in this issue will sit comfortably until it is no longer a problem,” Dr. Lichtenstein said.
In the discussion that followed the formal presentations, it was generally acknowledged that the ultimate solution remains unclear even though incremental progress is being made. In fact, there have been no major outbreaks in the United States in the last year following the attention given to this issue, which is likely to have promoted more diligence in disinfection, according to Dr. Lichtenstein.
“Disposable endoscopes or disposable parts on endoscopes that facilitate cleaning may be coming, but I think the best current step is a standardized method of testing scopes after cleaning to verify that disinfection has been achieved,” Dr. Lichtenstein said.
Other solutions, including new sterilization techniques may also emerge, but there was general consensus that the human factor will always be important even if the best solution proves to be a disposable endoscope. Dr. Weber said, “You can still place a disposable scope on a contaminated surface. The human factor is always important.”
Michael L. Kochman, MD, the Wilmott Professor of Medicine and director of the Center for Endoscopic Innovation, Research and Training at the University of Pennsylvania, Philadelphia, and past chair of the AGA Center for GI Innovation and Technology, added, “AGA will build on the relationships that we have with the manufacturers of the endoscopes along with companies developing other novel approaches to reprocessing, as well as the FDA and CDC, to further the discussion. Ultimately, we hope to see the availability of devices that are effective and reliably clean so that we do not have to be concerned about patient-to-patient transmission of infection.”
EXPERT ANALYSIS FROM 2018 AGA TECH SUMMIT