User login
Study eyes liver transplantation after Region 5 UNOS downstaging
Liver transplantation led to “excellent outcomes” when performed after downstaging hepatocellular carcinoma using the UNOS (United Network for Organ Sharing) Region 5 protocol, investigators reported.
Downstaging succeeded for 58% of patients, and an estimated 87% of transplantation recipients were alive and recurrence free at 5 years, said Neil Mehta, MD, of the University of California, San Francisco, and his associates. The findings support expanding priority access to liver transplantation to include patients whose hepatocellular carcinoma (HCC) has been successfully downstaged, they said. “In the meantime, UNOS has recently approved the Region 5 downstaging protocol for receiving automatic HCC-MELD exception listing,” they wrote. The report was published in the June issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.11.037).
This is the first multicenter study of HCC downstaging according to a uniform protocol, the researchers noted. In multivariable analyses, downstaging was significantly more likely to fail in the setting of moderate to severe (Child Pugh B or C) hepatic impairment (hazard ratio, 3.3; 95% confidence interval, 3.0 to 3.6; P less than .001) or baseline alpha-fetoprotein level above 1,000 ng/mL (HR, 1.6; 95% CI, 1.4 to 1.9; P less than .001).
The incidence of HCC in the United States is expected to keep rising for at least another decade because of epidemic levels of fatty liver disease and chronic hepatitis C, the investigators noted. Downstaging HCC with local-regional therapy is a common bridge to transplantation, and successful treatment tends to reflect favorable tumor biology, which bodes well for transplantation. However, no multicenter study had evaluated these associations. Therefore, the investigators retrospectively studied 187 patients with HCC from three centers in California who underwent downstaging according to the UNOS Region 5 protocol between 2002 and 2012.
A total of 156 patients (83%) were successfully downstaged to within Milan criteria after a median of 2.7 months (interquartile range, 1.4 to 4.9 months), said the researchers. Among patients who were successfully downstaged but did not undergo transplantation, 37 patients had tumor progression or died from liver-related causes after a median of 6 months, while 10 patients remained on the transplant list. Among the 109 patients who underwent transplantation after a median of 13 months (interquartile range 6 to 19 months), median follow-up time was 4.3 years and estimated 5-year survival was 80%, and estimated recurrence-free survival was 87%.
Fully 68% of successfully downstaged patients required only one local-regional treatment, the researchers said. The Region 5 protocol considers patients eligible for downstaging if they have a single HCC lesion measuring up to 8 cm or multiple lesions whose combined diameters do not exceed 8 cm, and no evidence of extrahepatic disease or vascular invasion on multiphase computed tomography or magnetic resonance imaging.
The protocol considers downstaging successful if it results in one lesion measuring up to 5 cm or no more than three lesions of up to 3 cm each. Thus, patients who start out with four or five lesions must have complete necrosis of at least one to two tumors. Successfully downstaged patients must remain free of acute hepatic decompensation for at least 3 consecutive months before undergoing transplantation, according to the protocol.
“Slight refinements in the inclusion criteria for downstaging seem warranted [given] that all Child’s B/C patients with pretreatment alpha-fetoprotein greater than 1000 ng/mL suffered poor outcomes when downstaging was attempted,” the investigators noted. They reported that the 1-year risk of failed downstaging was 70% among patients with both Child’s B/C cirrhosis and alpha-fetoprotein level at or above 1000 ng/mL, 32% among patients with one risk factor, and 14% among patients with no risk factors (P less than .001).
The National Institutes of Health provided partial funding. The investigators reported having no conflicts of interest.
SOURCE: Mehta N, et al. Clin Gastroenterol Hepatol. 2017 Nov 23. doi: 10.1016/j.cgh.2017.11.037.
Liver transplantation of selected patients with hepatocellular carcinoma (HCC) is an accepted indication and associated with excellent outcomes. Until recently, criteria for liver transplantation were based on the Milan criteria that only took size and number of tumors under consideration. In this multicenter study, patients who were outside of Milan criteria were successfully downstaged to within Milan criteria with locoregional therapy and subsequently transplanted with excellent outcomes. Salient features included the following. 1) Six months waiting after the first treatment and 3 months after downstaging was required to ensure that the tumor stage remained within Milan criteria. 2) Any specific type of locoregional therapy was allowed. 3) Downstaging was possible in a majority of patients after a single treatment. 4) Patients with alpha-fetoprotein greater than 1000 ng/mL (approximately 10%) as well as presence of substantial decompensated liver disease (approximately 40%) did not have favorable outcomes. 4) On multivariable analysis, tumor biology was a stronger predictor of poor outcomes than was stage of liver disease.
Sumeet K. Asrani, MD, MSc, is associate professor in medicine and hepatologist at Baylor University Medical Center, and medical director of the Center for Advanced Liver Disease, Dallas. He has no conflicts of interest.
Liver transplantation of selected patients with hepatocellular carcinoma (HCC) is an accepted indication and associated with excellent outcomes. Until recently, criteria for liver transplantation were based on the Milan criteria that only took size and number of tumors under consideration. In this multicenter study, patients who were outside of Milan criteria were successfully downstaged to within Milan criteria with locoregional therapy and subsequently transplanted with excellent outcomes. Salient features included the following. 1) Six months waiting after the first treatment and 3 months after downstaging was required to ensure that the tumor stage remained within Milan criteria. 2) Any specific type of locoregional therapy was allowed. 3) Downstaging was possible in a majority of patients after a single treatment. 4) Patients with alpha-fetoprotein greater than 1000 ng/mL (approximately 10%) as well as presence of substantial decompensated liver disease (approximately 40%) did not have favorable outcomes. 4) On multivariable analysis, tumor biology was a stronger predictor of poor outcomes than was stage of liver disease.
Sumeet K. Asrani, MD, MSc, is associate professor in medicine and hepatologist at Baylor University Medical Center, and medical director of the Center for Advanced Liver Disease, Dallas. He has no conflicts of interest.
Liver transplantation of selected patients with hepatocellular carcinoma (HCC) is an accepted indication and associated with excellent outcomes. Until recently, criteria for liver transplantation were based on the Milan criteria that only took size and number of tumors under consideration. In this multicenter study, patients who were outside of Milan criteria were successfully downstaged to within Milan criteria with locoregional therapy and subsequently transplanted with excellent outcomes. Salient features included the following. 1) Six months waiting after the first treatment and 3 months after downstaging was required to ensure that the tumor stage remained within Milan criteria. 2) Any specific type of locoregional therapy was allowed. 3) Downstaging was possible in a majority of patients after a single treatment. 4) Patients with alpha-fetoprotein greater than 1000 ng/mL (approximately 10%) as well as presence of substantial decompensated liver disease (approximately 40%) did not have favorable outcomes. 4) On multivariable analysis, tumor biology was a stronger predictor of poor outcomes than was stage of liver disease.
Sumeet K. Asrani, MD, MSc, is associate professor in medicine and hepatologist at Baylor University Medical Center, and medical director of the Center for Advanced Liver Disease, Dallas. He has no conflicts of interest.
Liver transplantation led to “excellent outcomes” when performed after downstaging hepatocellular carcinoma using the UNOS (United Network for Organ Sharing) Region 5 protocol, investigators reported.
Downstaging succeeded for 58% of patients, and an estimated 87% of transplantation recipients were alive and recurrence free at 5 years, said Neil Mehta, MD, of the University of California, San Francisco, and his associates. The findings support expanding priority access to liver transplantation to include patients whose hepatocellular carcinoma (HCC) has been successfully downstaged, they said. “In the meantime, UNOS has recently approved the Region 5 downstaging protocol for receiving automatic HCC-MELD exception listing,” they wrote. The report was published in the June issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.11.037).
This is the first multicenter study of HCC downstaging according to a uniform protocol, the researchers noted. In multivariable analyses, downstaging was significantly more likely to fail in the setting of moderate to severe (Child Pugh B or C) hepatic impairment (hazard ratio, 3.3; 95% confidence interval, 3.0 to 3.6; P less than .001) or baseline alpha-fetoprotein level above 1,000 ng/mL (HR, 1.6; 95% CI, 1.4 to 1.9; P less than .001).
The incidence of HCC in the United States is expected to keep rising for at least another decade because of epidemic levels of fatty liver disease and chronic hepatitis C, the investigators noted. Downstaging HCC with local-regional therapy is a common bridge to transplantation, and successful treatment tends to reflect favorable tumor biology, which bodes well for transplantation. However, no multicenter study had evaluated these associations. Therefore, the investigators retrospectively studied 187 patients with HCC from three centers in California who underwent downstaging according to the UNOS Region 5 protocol between 2002 and 2012.
A total of 156 patients (83%) were successfully downstaged to within Milan criteria after a median of 2.7 months (interquartile range, 1.4 to 4.9 months), said the researchers. Among patients who were successfully downstaged but did not undergo transplantation, 37 patients had tumor progression or died from liver-related causes after a median of 6 months, while 10 patients remained on the transplant list. Among the 109 patients who underwent transplantation after a median of 13 months (interquartile range 6 to 19 months), median follow-up time was 4.3 years and estimated 5-year survival was 80%, and estimated recurrence-free survival was 87%.
Fully 68% of successfully downstaged patients required only one local-regional treatment, the researchers said. The Region 5 protocol considers patients eligible for downstaging if they have a single HCC lesion measuring up to 8 cm or multiple lesions whose combined diameters do not exceed 8 cm, and no evidence of extrahepatic disease or vascular invasion on multiphase computed tomography or magnetic resonance imaging.
The protocol considers downstaging successful if it results in one lesion measuring up to 5 cm or no more than three lesions of up to 3 cm each. Thus, patients who start out with four or five lesions must have complete necrosis of at least one to two tumors. Successfully downstaged patients must remain free of acute hepatic decompensation for at least 3 consecutive months before undergoing transplantation, according to the protocol.
“Slight refinements in the inclusion criteria for downstaging seem warranted [given] that all Child’s B/C patients with pretreatment alpha-fetoprotein greater than 1000 ng/mL suffered poor outcomes when downstaging was attempted,” the investigators noted. They reported that the 1-year risk of failed downstaging was 70% among patients with both Child’s B/C cirrhosis and alpha-fetoprotein level at or above 1000 ng/mL, 32% among patients with one risk factor, and 14% among patients with no risk factors (P less than .001).
The National Institutes of Health provided partial funding. The investigators reported having no conflicts of interest.
SOURCE: Mehta N, et al. Clin Gastroenterol Hepatol. 2017 Nov 23. doi: 10.1016/j.cgh.2017.11.037.
Liver transplantation led to “excellent outcomes” when performed after downstaging hepatocellular carcinoma using the UNOS (United Network for Organ Sharing) Region 5 protocol, investigators reported.
Downstaging succeeded for 58% of patients, and an estimated 87% of transplantation recipients were alive and recurrence free at 5 years, said Neil Mehta, MD, of the University of California, San Francisco, and his associates. The findings support expanding priority access to liver transplantation to include patients whose hepatocellular carcinoma (HCC) has been successfully downstaged, they said. “In the meantime, UNOS has recently approved the Region 5 downstaging protocol for receiving automatic HCC-MELD exception listing,” they wrote. The report was published in the June issue of Clinical Gastroenterology and Hepatology (doi: 10.1016/j.cgh.2017.11.037).
This is the first multicenter study of HCC downstaging according to a uniform protocol, the researchers noted. In multivariable analyses, downstaging was significantly more likely to fail in the setting of moderate to severe (Child Pugh B or C) hepatic impairment (hazard ratio, 3.3; 95% confidence interval, 3.0 to 3.6; P less than .001) or baseline alpha-fetoprotein level above 1,000 ng/mL (HR, 1.6; 95% CI, 1.4 to 1.9; P less than .001).
The incidence of HCC in the United States is expected to keep rising for at least another decade because of epidemic levels of fatty liver disease and chronic hepatitis C, the investigators noted. Downstaging HCC with local-regional therapy is a common bridge to transplantation, and successful treatment tends to reflect favorable tumor biology, which bodes well for transplantation. However, no multicenter study had evaluated these associations. Therefore, the investigators retrospectively studied 187 patients with HCC from three centers in California who underwent downstaging according to the UNOS Region 5 protocol between 2002 and 2012.
A total of 156 patients (83%) were successfully downstaged to within Milan criteria after a median of 2.7 months (interquartile range, 1.4 to 4.9 months), said the researchers. Among patients who were successfully downstaged but did not undergo transplantation, 37 patients had tumor progression or died from liver-related causes after a median of 6 months, while 10 patients remained on the transplant list. Among the 109 patients who underwent transplantation after a median of 13 months (interquartile range 6 to 19 months), median follow-up time was 4.3 years and estimated 5-year survival was 80%, and estimated recurrence-free survival was 87%.
Fully 68% of successfully downstaged patients required only one local-regional treatment, the researchers said. The Region 5 protocol considers patients eligible for downstaging if they have a single HCC lesion measuring up to 8 cm or multiple lesions whose combined diameters do not exceed 8 cm, and no evidence of extrahepatic disease or vascular invasion on multiphase computed tomography or magnetic resonance imaging.
The protocol considers downstaging successful if it results in one lesion measuring up to 5 cm or no more than three lesions of up to 3 cm each. Thus, patients who start out with four or five lesions must have complete necrosis of at least one to two tumors. Successfully downstaged patients must remain free of acute hepatic decompensation for at least 3 consecutive months before undergoing transplantation, according to the protocol.
“Slight refinements in the inclusion criteria for downstaging seem warranted [given] that all Child’s B/C patients with pretreatment alpha-fetoprotein greater than 1000 ng/mL suffered poor outcomes when downstaging was attempted,” the investigators noted. They reported that the 1-year risk of failed downstaging was 70% among patients with both Child’s B/C cirrhosis and alpha-fetoprotein level at or above 1000 ng/mL, 32% among patients with one risk factor, and 14% among patients with no risk factors (P less than .001).
The National Institutes of Health provided partial funding. The investigators reported having no conflicts of interest.
SOURCE: Mehta N, et al. Clin Gastroenterol Hepatol. 2017 Nov 23. doi: 10.1016/j.cgh.2017.11.037.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Liver transplantation led to excellent outcomes when performed after downstaging hepatocellular carcinoma according to the UNOS (United Network for Organ Sharing) Region 5 protocol.
Major finding: Downstaging succeeded in 58% of patients. Estimated 5-year posttransplantation recurrence-free survival was 87%.
Study details: Retrospective multicenter study of 187 patients with hepatocellular carcinoma.
Disclosures: The National Institutes of Health provided partial funding. The investigators reported having no conflicts of interest.
Source: Mehta N et al. Clin Gastroenterol Hepatol. 2017 Nov 23. doi: 10.1016/j.cgh.2017.11.037.
Severity of sepsis-associated coagulopathy predicts hospital mortality
Patients with appear to be at heightened risk of death, according to results of a large retrospective cohort study.
The risk of death in the study increased with the severity of the sepsis-associated coagulopathy, which was defined using international normalized ratio (INR) and platelet counts.
Those findings suggest that the severity of coagulation abnormalities might be used to quantify mortality risk, according to investigator Patrick G. Lyons, MD, of the division of pulmonary and critical care medicine, Washington University, St. Louis, and his coinvestigators.
“Future trials of sepsis therapies targeting the coagulation cascade should take into account the presence or absence of sepsis-associated coagulopathy, as well as the severity of sepsis-associated coagulopathy, when formulating potential trial designs,” the investigators wrote in the journal Critical Care Medicine.
Their retrospective cohort study included 6,148 consecutive patients with sepsis or septic shock hospitalized at a 1,300-bed urban academic medical center between 2010 and 2015. Of that group, 26% had sepsis-associated coagulopathy, defined as having both an INR of 1.2 or higher and a platelet count less than 150,000/mcL. Sepsis-associated coagulopathy was classified as mild for 4%, moderate for 16%, and severe for 6% of the cohort.
Hospital mortality was 25.4% for patients with no sepsis-associated coagulopathy, the research team found, increasing progressively from 27.0% for mild, 40.7% for moderate, and 56.1% for patients in the most severe category of sepsis-associated coagulopathy (P less than .001).
Hospital and ICU days also increased progressively according to the severity of coagulopathy, they reported.
Both presence and severity of sepsis-associated coagulopathy remained independently associated with hospital mortality even after adjustments were made for patient characteristics, hospitalization variables, and interactions between sepsis-associated coagulopathy and cancer, investigators said. Odds ratios ranged from 1.33 to 2.14 for presence of sepsis-associated coagulopathy, and from 1.18 to 1.51 for severity, they reported in the journal.
These data have potential implications for managing patients with sepsis, according to Dr. Lyons and coinvestigators. In particular, severity of sepsis-associated coagulopathy might be used as “another relatively simple way” to compare sepsis patient populations, similar to other markers of severity such as the Sequential Organ Failure Assessment score.
“This could have important implications for comparing the outcomes of patients with sepsis from different hospitals, especially with increasing requirements for public reporting of such data through systems such as the Severe Sepsis/Septic Shock Early Management Bundle-1 and New York State’s Rory’s Regulations,” the investigators wrote.
Reported disclosures for the study included institutional funding from Asahi Kasei Pharma America by one coauthor, and support from Barnes-Jewish Hospital Foundation by another. No other potential conflicts of interest were reported.
SOURCE: Lyons PG et al. Crit Care Med. 2018 May;46(5):736-42.
This study outlines a simplified classification scheme for coagulopathy with implications that are potentially “profound,” according to authors of an editorial accompanying the journal article.
“Despite the frequency with which hemostatic derangements occur in sepsis, there has not been a widely accepted system for stratification of coagulopathies,” said editorialists Garrett W. Britton, DO, Cody Babcock, PharmD, and Christopher J. Colombo, MD. “Of the most cited criteria, all have varying concordance, and one does not seem to have an advantage over another.”
In the present study, patients with sepsis-associated coagulopathy were stratified into mild, moderate, and severe categories based on international normalized ratio (INR) levels and platelet counts.
While the study has limitations including a sicker patient cohort and arbitrarily chosen severity thresholds, the investigators did find progressively increasing mortality rates that correlated with severity and were independent of confounding variables.
“Overall, this stratification system will prove useful in identifying target populations in future interventional studies,” the editorial authors wrote.
Since sepsis-related mortality remains high, the ultimate goal of research should be identifying varying phenotypes of the disease and targeting them with specific therapies, they added.
“Lyons et al. have aided the first steps in that process with their straightforward classification scheme for sepsis-associated coagulopathy,” they wrote. “Intelligently designed therapeutic trials ‘evaluating’ the response of these phenotypes to new (or old) pharmacotherapy should be the ultimate goal.”
Garrett W. Britton, DO, is with the department of medicine, critical care section, Walter Reed National Military Medical Center, Bethesda, Md. Cody Babcock, PharmD, and Christopher J. Colombo, MD, are with the department of medicine, critical care section, Dwight David Eisenhower Army Medical Center, Fort Gordon, Ga. These comments are derived from their editorial in Critical Care Medicine . The authors had no disclosures beyond reporting government work.
This study outlines a simplified classification scheme for coagulopathy with implications that are potentially “profound,” according to authors of an editorial accompanying the journal article.
“Despite the frequency with which hemostatic derangements occur in sepsis, there has not been a widely accepted system for stratification of coagulopathies,” said editorialists Garrett W. Britton, DO, Cody Babcock, PharmD, and Christopher J. Colombo, MD. “Of the most cited criteria, all have varying concordance, and one does not seem to have an advantage over another.”
In the present study, patients with sepsis-associated coagulopathy were stratified into mild, moderate, and severe categories based on international normalized ratio (INR) levels and platelet counts.
While the study has limitations including a sicker patient cohort and arbitrarily chosen severity thresholds, the investigators did find progressively increasing mortality rates that correlated with severity and were independent of confounding variables.
“Overall, this stratification system will prove useful in identifying target populations in future interventional studies,” the editorial authors wrote.
Since sepsis-related mortality remains high, the ultimate goal of research should be identifying varying phenotypes of the disease and targeting them with specific therapies, they added.
“Lyons et al. have aided the first steps in that process with their straightforward classification scheme for sepsis-associated coagulopathy,” they wrote. “Intelligently designed therapeutic trials ‘evaluating’ the response of these phenotypes to new (or old) pharmacotherapy should be the ultimate goal.”
Garrett W. Britton, DO, is with the department of medicine, critical care section, Walter Reed National Military Medical Center, Bethesda, Md. Cody Babcock, PharmD, and Christopher J. Colombo, MD, are with the department of medicine, critical care section, Dwight David Eisenhower Army Medical Center, Fort Gordon, Ga. These comments are derived from their editorial in Critical Care Medicine . The authors had no disclosures beyond reporting government work.
This study outlines a simplified classification scheme for coagulopathy with implications that are potentially “profound,” according to authors of an editorial accompanying the journal article.
“Despite the frequency with which hemostatic derangements occur in sepsis, there has not been a widely accepted system for stratification of coagulopathies,” said editorialists Garrett W. Britton, DO, Cody Babcock, PharmD, and Christopher J. Colombo, MD. “Of the most cited criteria, all have varying concordance, and one does not seem to have an advantage over another.”
In the present study, patients with sepsis-associated coagulopathy were stratified into mild, moderate, and severe categories based on international normalized ratio (INR) levels and platelet counts.
While the study has limitations including a sicker patient cohort and arbitrarily chosen severity thresholds, the investigators did find progressively increasing mortality rates that correlated with severity and were independent of confounding variables.
“Overall, this stratification system will prove useful in identifying target populations in future interventional studies,” the editorial authors wrote.
Since sepsis-related mortality remains high, the ultimate goal of research should be identifying varying phenotypes of the disease and targeting them with specific therapies, they added.
“Lyons et al. have aided the first steps in that process with their straightforward classification scheme for sepsis-associated coagulopathy,” they wrote. “Intelligently designed therapeutic trials ‘evaluating’ the response of these phenotypes to new (or old) pharmacotherapy should be the ultimate goal.”
Garrett W. Britton, DO, is with the department of medicine, critical care section, Walter Reed National Military Medical Center, Bethesda, Md. Cody Babcock, PharmD, and Christopher J. Colombo, MD, are with the department of medicine, critical care section, Dwight David Eisenhower Army Medical Center, Fort Gordon, Ga. These comments are derived from their editorial in Critical Care Medicine . The authors had no disclosures beyond reporting government work.
Patients with appear to be at heightened risk of death, according to results of a large retrospective cohort study.
The risk of death in the study increased with the severity of the sepsis-associated coagulopathy, which was defined using international normalized ratio (INR) and platelet counts.
Those findings suggest that the severity of coagulation abnormalities might be used to quantify mortality risk, according to investigator Patrick G. Lyons, MD, of the division of pulmonary and critical care medicine, Washington University, St. Louis, and his coinvestigators.
“Future trials of sepsis therapies targeting the coagulation cascade should take into account the presence or absence of sepsis-associated coagulopathy, as well as the severity of sepsis-associated coagulopathy, when formulating potential trial designs,” the investigators wrote in the journal Critical Care Medicine.
Their retrospective cohort study included 6,148 consecutive patients with sepsis or septic shock hospitalized at a 1,300-bed urban academic medical center between 2010 and 2015. Of that group, 26% had sepsis-associated coagulopathy, defined as having both an INR of 1.2 or higher and a platelet count less than 150,000/mcL. Sepsis-associated coagulopathy was classified as mild for 4%, moderate for 16%, and severe for 6% of the cohort.
Hospital mortality was 25.4% for patients with no sepsis-associated coagulopathy, the research team found, increasing progressively from 27.0% for mild, 40.7% for moderate, and 56.1% for patients in the most severe category of sepsis-associated coagulopathy (P less than .001).
Hospital and ICU days also increased progressively according to the severity of coagulopathy, they reported.
Both presence and severity of sepsis-associated coagulopathy remained independently associated with hospital mortality even after adjustments were made for patient characteristics, hospitalization variables, and interactions between sepsis-associated coagulopathy and cancer, investigators said. Odds ratios ranged from 1.33 to 2.14 for presence of sepsis-associated coagulopathy, and from 1.18 to 1.51 for severity, they reported in the journal.
These data have potential implications for managing patients with sepsis, according to Dr. Lyons and coinvestigators. In particular, severity of sepsis-associated coagulopathy might be used as “another relatively simple way” to compare sepsis patient populations, similar to other markers of severity such as the Sequential Organ Failure Assessment score.
“This could have important implications for comparing the outcomes of patients with sepsis from different hospitals, especially with increasing requirements for public reporting of such data through systems such as the Severe Sepsis/Septic Shock Early Management Bundle-1 and New York State’s Rory’s Regulations,” the investigators wrote.
Reported disclosures for the study included institutional funding from Asahi Kasei Pharma America by one coauthor, and support from Barnes-Jewish Hospital Foundation by another. No other potential conflicts of interest were reported.
SOURCE: Lyons PG et al. Crit Care Med. 2018 May;46(5):736-42.
Patients with appear to be at heightened risk of death, according to results of a large retrospective cohort study.
The risk of death in the study increased with the severity of the sepsis-associated coagulopathy, which was defined using international normalized ratio (INR) and platelet counts.
Those findings suggest that the severity of coagulation abnormalities might be used to quantify mortality risk, according to investigator Patrick G. Lyons, MD, of the division of pulmonary and critical care medicine, Washington University, St. Louis, and his coinvestigators.
“Future trials of sepsis therapies targeting the coagulation cascade should take into account the presence or absence of sepsis-associated coagulopathy, as well as the severity of sepsis-associated coagulopathy, when formulating potential trial designs,” the investigators wrote in the journal Critical Care Medicine.
Their retrospective cohort study included 6,148 consecutive patients with sepsis or septic shock hospitalized at a 1,300-bed urban academic medical center between 2010 and 2015. Of that group, 26% had sepsis-associated coagulopathy, defined as having both an INR of 1.2 or higher and a platelet count less than 150,000/mcL. Sepsis-associated coagulopathy was classified as mild for 4%, moderate for 16%, and severe for 6% of the cohort.
Hospital mortality was 25.4% for patients with no sepsis-associated coagulopathy, the research team found, increasing progressively from 27.0% for mild, 40.7% for moderate, and 56.1% for patients in the most severe category of sepsis-associated coagulopathy (P less than .001).
Hospital and ICU days also increased progressively according to the severity of coagulopathy, they reported.
Both presence and severity of sepsis-associated coagulopathy remained independently associated with hospital mortality even after adjustments were made for patient characteristics, hospitalization variables, and interactions between sepsis-associated coagulopathy and cancer, investigators said. Odds ratios ranged from 1.33 to 2.14 for presence of sepsis-associated coagulopathy, and from 1.18 to 1.51 for severity, they reported in the journal.
These data have potential implications for managing patients with sepsis, according to Dr. Lyons and coinvestigators. In particular, severity of sepsis-associated coagulopathy might be used as “another relatively simple way” to compare sepsis patient populations, similar to other markers of severity such as the Sequential Organ Failure Assessment score.
“This could have important implications for comparing the outcomes of patients with sepsis from different hospitals, especially with increasing requirements for public reporting of such data through systems such as the Severe Sepsis/Septic Shock Early Management Bundle-1 and New York State’s Rory’s Regulations,” the investigators wrote.
Reported disclosures for the study included institutional funding from Asahi Kasei Pharma America by one coauthor, and support from Barnes-Jewish Hospital Foundation by another. No other potential conflicts of interest were reported.
SOURCE: Lyons PG et al. Crit Care Med. 2018 May;46(5):736-42.
FROM CRITICAL CARE MEDICINE
Key clinical point: Risk of hospital mortality increased incrementally with the severity of sepsis-related coagulopathy.
Major finding: Hospital mortality was 25.4% for patients with no sepsis-associated coagulopathy, increasing progressively up to 56.1% for patients in the most severe category.
Study details: A retrospective cohort study including 6,148 consecutive patients hospitalized at a 1,300-bed urban academic medical center between 2010 and 2015.
Disclosures: One author reported institutional funding from Asahi Kasei Pharma America and another noted support from Barnes-Jewish Hospital Foundation. No other potential conflicts of interest were reported.
Source: Lyons PG et al. Crit Care Med. 2018 May;46(5):73642.
Pediatric Refractory Status Epilepticus Still Challenges Clinicians
Pediatric refractory status epilepticus (RSE) and super refractory status epilepticus (SRSE) remain life-threatening disorders whose etiology and effective management are elusive according to a review in Seizure.
- RSE is defined as a disorder that doesn’t respond to first and second line antiepileptic agents.
- SRSE refers to status epilepticus that continues for at least 24 hours after anesthetic agents have been given or which recurs once the drugs are stopped.
- The evidence to support current treatment options is not based on randomized clinical trials but instead relies on case series and expert opinions.
- The most common treatment for both disorders is continuous IV infusion of anesthetic drugs but the best dosing and the optimal administration rate remain controversial.
- Some clinicians have used non-drug approaches to RSE and SRSE but the evidence supporting these options is limited.
Vasquez A, Farias-Moeller R, Tatum W. Pediatric refractory and super refractory status epilepticus [Published online ahead of print May 19, 2018]. Seizure. DOI: https://doi.org/10.1016/j.seizure.2018.05.012.
Pediatric refractory status epilepticus (RSE) and super refractory status epilepticus (SRSE) remain life-threatening disorders whose etiology and effective management are elusive according to a review in Seizure.
- RSE is defined as a disorder that doesn’t respond to first and second line antiepileptic agents.
- SRSE refers to status epilepticus that continues for at least 24 hours after anesthetic agents have been given or which recurs once the drugs are stopped.
- The evidence to support current treatment options is not based on randomized clinical trials but instead relies on case series and expert opinions.
- The most common treatment for both disorders is continuous IV infusion of anesthetic drugs but the best dosing and the optimal administration rate remain controversial.
- Some clinicians have used non-drug approaches to RSE and SRSE but the evidence supporting these options is limited.
Vasquez A, Farias-Moeller R, Tatum W. Pediatric refractory and super refractory status epilepticus [Published online ahead of print May 19, 2018]. Seizure. DOI: https://doi.org/10.1016/j.seizure.2018.05.012.
Pediatric refractory status epilepticus (RSE) and super refractory status epilepticus (SRSE) remain life-threatening disorders whose etiology and effective management are elusive according to a review in Seizure.
- RSE is defined as a disorder that doesn’t respond to first and second line antiepileptic agents.
- SRSE refers to status epilepticus that continues for at least 24 hours after anesthetic agents have been given or which recurs once the drugs are stopped.
- The evidence to support current treatment options is not based on randomized clinical trials but instead relies on case series and expert opinions.
- The most common treatment for both disorders is continuous IV infusion of anesthetic drugs but the best dosing and the optimal administration rate remain controversial.
- Some clinicians have used non-drug approaches to RSE and SRSE but the evidence supporting these options is limited.
Vasquez A, Farias-Moeller R, Tatum W. Pediatric refractory and super refractory status epilepticus [Published online ahead of print May 19, 2018]. Seizure. DOI: https://doi.org/10.1016/j.seizure.2018.05.012.
Benzodiazepines Underutilized in Seizure Clusters
Patients with epilepsy clusters can benefit from rescue medications, but these drugs are underutilized according to a recent review of the medical literature.
- Saba Jafarpour from Boston Children’s Hospital, and associates found that the definition of epilepsy clusters differs among experts, including 3 or more seizures in 24 hours, 2 or more in 24 hours, and 2 or more in 6 hours.
- Most of the research analyzed by the investigators was conducted at tertiary centers on patients with refractory epilepsy.
- Although rectal diazepam gel is the only medication approved by the FDA as a rescue drug for seizure clusters, the researchers found that non-rectal oral benzodiazepines are effective and safe for outpatient treatment of these clusters.
- Acute treatment of seizure clusters can help prevent status epilepticus and reduce emergency department visits.
Jafarpour S, Hirsch LJ, Gaínza-Lein M, Kellinghaus C, Detyniecki K. Seizure cluster: definition, prevalence, consequences, and management [Published online ahead of print May 21,2018]. Seizure. DOI: https://doi.org/10.1016/j.seizure.2018.05.013.
Patients with epilepsy clusters can benefit from rescue medications, but these drugs are underutilized according to a recent review of the medical literature.
- Saba Jafarpour from Boston Children’s Hospital, and associates found that the definition of epilepsy clusters differs among experts, including 3 or more seizures in 24 hours, 2 or more in 24 hours, and 2 or more in 6 hours.
- Most of the research analyzed by the investigators was conducted at tertiary centers on patients with refractory epilepsy.
- Although rectal diazepam gel is the only medication approved by the FDA as a rescue drug for seizure clusters, the researchers found that non-rectal oral benzodiazepines are effective and safe for outpatient treatment of these clusters.
- Acute treatment of seizure clusters can help prevent status epilepticus and reduce emergency department visits.
Jafarpour S, Hirsch LJ, Gaínza-Lein M, Kellinghaus C, Detyniecki K. Seizure cluster: definition, prevalence, consequences, and management [Published online ahead of print May 21,2018]. Seizure. DOI: https://doi.org/10.1016/j.seizure.2018.05.013.
Patients with epilepsy clusters can benefit from rescue medications, but these drugs are underutilized according to a recent review of the medical literature.
- Saba Jafarpour from Boston Children’s Hospital, and associates found that the definition of epilepsy clusters differs among experts, including 3 or more seizures in 24 hours, 2 or more in 24 hours, and 2 or more in 6 hours.
- Most of the research analyzed by the investigators was conducted at tertiary centers on patients with refractory epilepsy.
- Although rectal diazepam gel is the only medication approved by the FDA as a rescue drug for seizure clusters, the researchers found that non-rectal oral benzodiazepines are effective and safe for outpatient treatment of these clusters.
- Acute treatment of seizure clusters can help prevent status epilepticus and reduce emergency department visits.
Jafarpour S, Hirsch LJ, Gaínza-Lein M, Kellinghaus C, Detyniecki K. Seizure cluster: definition, prevalence, consequences, and management [Published online ahead of print May 21,2018]. Seizure. DOI: https://doi.org/10.1016/j.seizure.2018.05.013.
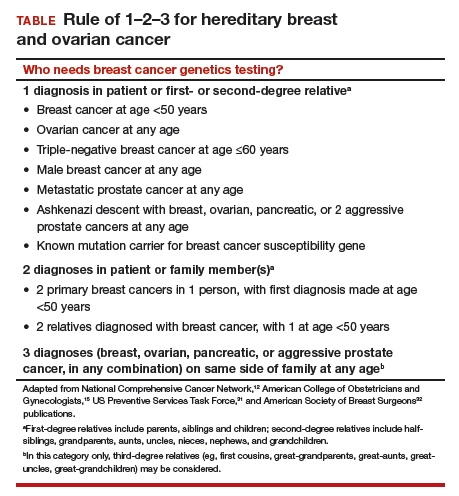
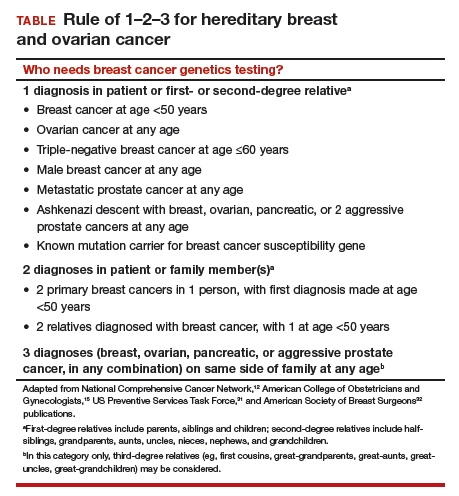
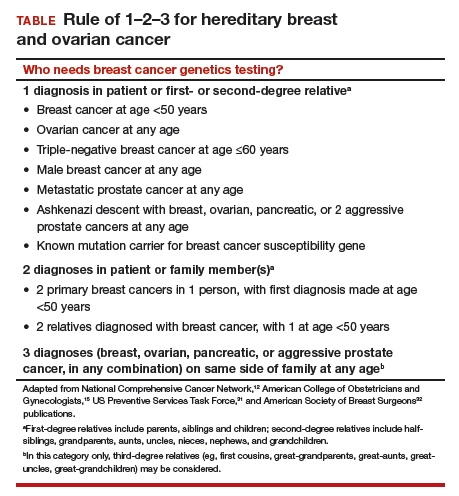
Who needs breast cancer genetics testing?
Advances in cancer genetics are rapidly changing how clinicians assess an individual’s risk for breast cancer. ObGyns counsel many women with a personal or family history of the disease, many of whom can benefit from genetics counseling and testing. As patients with a hereditary predisposition to breast cancer are at higher risk and are younger at diagnosis, it is imperative to identify them early so they can benefit from enhanced surveillance, chemoprevention, and discussions regarding risk-reducing surgeries. ObGyns are uniquely poised to identify young women at risk for hereditary cancer syndromes, and they play a crucial role in screening and prevention over the life span.
CASE Patient with breast cancer history asks about screening for her daughters
A 52-year-old woman presents for her annual examination. She underwent breast cancer treatment 10 years earlier and has done well since then. When asked about family history of breast cancer and ethnicity, she reports her mother had breast cancer later in life, and her mother’s father was of Ashkenazi Jewish ancestry.In addition, a maternal uncle had metastatic prostate cancer. You recall that breast cancer diagnosed before age 50 years and Ashkenazi ancestry are “red flags” for a hereditary cancer syndrome. The patient wonders how her daughters should be screened. What do you do next?
Having a risk assessment plan is crucial
Given increasing demands, limited time, and the abundance of information to be discussed with patients, primary care physicians may find it challenging to assess breast cancer risk, consider genetics testing for appropriate individuals, and counsel patients about risk management options. The process has become even more complex since the expansion in genetics knowledge and the advent of multigene panel testing. Not only is risk assessment crucial for this woman and her daughters, and for other patients, but a delay in diagnosing and treating breast cancer in patients with hereditary and familial cancer risks may represent a worrisome new trend in medical litigation.1,2 Clinicians must have a process in place for assessing risk in all patients and treating them appropriately.
The American Cancer Society (ACS) estimated that 252,710 cases of breast cancer would be diagnosed in 2017, leading to 40,610 deaths.3 Twelve percent to 14% of breast cancers are thought to be related to hereditary cancer predisposition syndromes.4–8 This means that, every year, almost 35,000 cases of breast cancer are attributable to hereditary risk. These cases can be detected early with enhanced surveillance, which carries the highest chance for cure, or prevented with risk-reducing surgery in identified genetic mutation carriers. Each child of a person with a genetic mutation predisposing to breast cancer has a 50% chance of inheriting the mutation and having a very high risk of cancer.
In this patient’s case, basic information is collected about her cancer-related personal and family history.
Asking a few key questions can help in stratifying risk:
- Have you or anyone in your family had cancer? What type, and at what age?
- If breast cancer, did it involve both breasts, or was it triple-negative?
- Is there a family history of ovarian cancer?
- Is there a family history of male breast cancer?
- Is there a family history of metastatic prostate cancer?
- Are you of Ashkenazi Jewish ethnicity?
- Have you or anyone in your family ever had genetics testing for cancer?
The hallmarks of hereditary cancer are multiple cancers in an individual or family; young age at diagnosis; and ovarian, pancreatic, or another rare cancer. Metastatic prostate cancer was added as a red flag for hereditary risk after a recent large series found that 11.8% of men with metastatic prostate cancer harbor germline mutations.9
CASE Continued
On further questioning, the patient reports she had triple-negative (estrogen receptor–, progesterone receptor–, and human epidermal growth factor receptor 2 [HER2]–negative) breast cancer, a feature of patients with germline BRCA1 (breast cancer susceptibility gene 1) mutations.10 In addition, her Ashkenazi ancestry is concerning, as there is a 1-in-40 chance of carrying 1 of the 3 Ashkenazi founder BRCA mutations.11 Is a genetics consultation needed?
Read about guidelines for referral and testing.
Guidelines for genetics referral and testing
According to the TABLE, which summarizes national guidelines for genetics referral, maternal and paternal family histories are equally important. Our patient was under age 50 at diagnosis, has a history of triple-negative breast cancer, is of Ashkenazi ancestry, and has a family history of metastatic prostate cancer. She meets the criteria for genetics testing, and screening for her daughters most certainly will depend on the findings of that testing. If she carries a BRCA1 mutation, as might be anticipated, each daughter would have a 50% chance of having inherited the mutation. If they carry the mutation as well, they would begin breast magnetic resonance imaging (MRI) screening at age 25.12 If they decide against genetics testing, they could still undergo MRI screening as untested first-degree relatives of a BRCA carrier, per ACS recommendations.13
Integrating evidence and experience
Over the past 10 to 20 years, other breast cancer susceptibility genes (eg, BRCA2, PALB2, CHEK2) have been identified. More recently, next-generation sequencing has become commercially available. Laboratories can use this newer method to sequence multiple genes rapidly and in parallel, and its cost is similar to that of single-syndrome testing.14 When more than 1 gene can explain an inherited cancer syndrome, multigene panel testing may be more efficient and cost-effective. Use of multigene panel testing is supported in guidelines issued by the National Comprehensive Cancer Network,12 the American College of Obstetricians and Gynecologists,15 and other medical societies.
For our patient, the most logical strategy would be to test for the 3 mutations most common in the Ashkenazi population and then, if no mutation is found, perform multigene panel testing.
Formal genetics counseling can be very helpful for a patient, particularly in the era of multigene panel testing.16,17 A detailed pedigree (family tree) is elicited, and a genetics specialist determines whether testing is indicated and which test is best for the patient. Possible test findings are explained. The patient may be found to have a pathogenic variant with associated increased cancer risk, a negative test result (informative or uninformative), or a variant of uncertain significance (VUS). VUS is a gene mutation identified with an unknown effect on protein function and an unclear association with cancer risk. A finding of VUS may make the patient anxious,18 create uncertainty in the treating physician,19 and lead to harmful overtreatment, excessive surveillance, or unnecessary use of a preventive measure.19–21 Genetics counseling allows the patient, even the patient with VUS, to make appropriate decisions.22 Counseling may also help a patient or family process emotional responses, such as fear and guilt. In addition, counselors are familiar with relevant laws and regulations, such as the Genetic Information Nondiscrimination Act of 2008 (GINA), which protects patients from insurance and employment discrimination. Many professional guidelines recommend providing genetics counseling in conjunction with genetics testing,12,23 and some insurance companies and some states require counseling for coverage of testing.
Cost of genetics counseling. If patients are concerned about the cost of genetics testing, they can be reassured with the following information24–26:
- The Patient Protection and Affordable Care Act (ACA) identifies BRCA testing as a preventive service
- Medicare provides coverage for affected patients with a qualifying personal history
- 97% of commercial insurers and most state Medicaid programs provide coverage for hereditary cancer testing
- Most commercial laboratories have affordability programs that may provide additional support.
If a BRCA mutation is found: Many patients question the value of knowing whether they have a BRCA mutation. What our patient, her daughters, and others may not realize is that, if a BRCA mutation is found, breast MRI screening can begin at age 25. Although contrast-enhanced MRI screening is highly sensitive in detecting breast cancer,27–29 it lacks specificity and commonly yields false positives.
Some patients also worry about overdiagnosis with this highly sensitive test. Many do not realize that preventively prescribed oral contraceptives can reduce the risk of ovarian cancer by 50%, and cosmetically acceptable risk-reducing breast surgeries can reduce the risk by 90%.
Many are unaware of the associated risks with ovarian, prostate, pancreatic, and other cancers; of risk management options; and of assisted reproduction options, such as preimplantation genetics diagnosis, which can prevent the passing of a genetic mutation to future generations. The guidelines on risk management options are increasingly clear and helpful,12,30–32 and women often turn to their ObGyns for advice about health and prevention.
ObGyns are often the first-line providers for women with a personal or family history of breast cancer. Identification of at-risk patients begins with taking a careful family history and becoming familiar with the rapidly evolving guidelines in this important field. Identification of appropriate candidates for breast cancer genetics testing is a key step toward prevention, value-based care, and avoidance of legal liability.
CASE Resolved
In this case, testing for the 3 common Ashkenazi BRCA founder mutations was negative, and multigene panel testing was also negative. Her husband is not of Ashkenazi Jewish descent and there is no significant family history of cancer on his side. The daughters are advised to begin high-risk screening at the age of 32, 10 years earlier than their mother was diagnosed, but no genetic testing is indicated for them.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Phillips RL Jr, Bartholomew LA, Dovey SM, Fryer GE Jr, Miyoshi TJ, Green LA. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13(2):121–126.
- Saber Tehrani AS, Lee H, Mathews SC, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- American Cancer Society. Breast Cancer Facts & Figures 2017-2018. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-factsand-figures/breast-cancer-facts-and-figures-2017-2018.pdf. Published 2017. Accessed December 28, 2017.
- Tung N, Battelli C, Allen B, et al. Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2 testing using next-generation sequencing with a 25-gene panel. Cancer. 2015;121(1):25–33.
- Tung N, Lin NU, Kidd J, et al. Frequency of germline mutations in 25 cancer susceptibility genes in a sequential series of patients with breast cancer. J Clin Oncol. 2016;34(13):1460–1468.
- Kurian AW, Hare EE, Mills MA, et al. Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment. J Clin Oncol. 2014;32(19):2001–2009.
- Easton DF, Pharoah PD, Antoniou AC, et al. Gene-panel sequencing and the prediction of breast-cancer risk. N Engl J Med. 2015;372(23):2243–2257.
- Yurgelun MB, Allen B, Kaldate RR, et al. Identification of a variety of mutations in cancer predisposition genes in patients with suspected Lynch syndrome. Gastroenterology. 2015;149(3):604–613.e20.
- Pritchard CC, Mateo J, Walsh MF, et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N Engl J Med. 2016;375(5):443–453.
- Mavaddat N, Barrowdale D, Andrulis IL, et al; Consortium of Investigators of Modifiers of BRCA1/2. Pathology of breast and ovarian cancers among BRCA1 and BRCA2 mutation carriers: results from the Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA). Cancer Epidemiol Biomarkers Prev. 2012;21(1):134–147.
- Struewing JP, Hartge P, Wacholder S, et al. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med. 1997;336(20):1401–1408.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Genetic/Familial High-Risk Assessment: Breast and Ovarian. Version 1.2018. https://www.nccn.org. Accessed December 28, 2017.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
- Heather JM, Chain B. The sequence of sequencers: the history of sequencing DNA. Genomics. 2016;107(1):1–8.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 182: Hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2017;130(3):e110–e126.
- Mester JL, Schreiber AH, Moran RT. Genetic counselors: your partners in clinical practice. Cleve Clin J Med. 2012;79(8):560–568.
- Smith M, Mester J, Eng C. How to spot heritable breast cancer: a primary care physician’s guide. Cleve Clin J Med. 2014;81(1):31–40.
- Welsh JL, Hoskin TL, Day CN, et al. Clinical decision-making in patients with variant of uncertain significance in BRCA1 or BRCA2 genes. Ann Surg Oncol. 2017;24(10):3067–3072.
- Kurian AW, Li Y, Hamilton AS, et al. Gaps in incorporating germline genetic testing into treatment decision-making for early-stage breast cancer. J Clin Oncol. 2017;35(20):2232–2239.
- Tung N, Domchek SM, Stadler Z, et al. Counselling framework for moderate-penetrance cancer-susceptibility mutations. Nat Rev Clin Oncol. 2016;13(9):581–588.
- Yu PP, Vose JM, Hayes DF. Genetic cancer susceptibility testing: increased technology, increased complexity. J Clin Oncol. 2015;33(31):3533–3534.
- Pederson HJ, Gopalakrishnan D, Noss R, Yanda C, Eng C, Grobmyer SR. Impact of multigene panel testing on surgical decision making in breast cancer patients. J Am Coll Surg. 2018;226(4):560–565.
- Robson ME, Bradbury AR, Arun B, et al. American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol. 2015;33(31):3660–3667.
- Preventive care benefits for women: What Marketplace health insurance plans cover. HealthCare.gov. https://www.healthcare.gov/coverage/what-marketplace-plans-cover/. Accessed May 15, 2018.
- Centers for Medicare & Medicaid Services. The Center for Consumer Information & Insurance Oversight: Affordable Care Act Implementation FAQs – Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.html. Accessed May 15, 2018.
- US Preventive Services Task Force. Final Recommendation Statement: BRCA-Related Cancer: Risk Assessment, Genetic Counseling, and Genetic Testing. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/brca-related-cancer-risk-assessment-genetic-counseling-and-genetic-testing. Published December 2013. Accessed May 15, 2018.
- Kuhl CK, Schrading S, Leutner CC, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol. 2005;23(33):8469–8476.
- Lehman CD, Blume JD, Weatherall P, et al; International Breast MRI Consortium Working Group. Screening women at high risk for breast cancer with mammography and magnetic resonance imaging. Cancer. 2005;103(9):1898–1905.
- Kriege M, Brekelmans CT, Boetes C, et al; Magnetic Resonance Imaging Screening Study Group. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351(5):427–437.
- Pederson HJ, Padia SA, May M, Grobmyer S. Managing patients at genetic risk of breast cancer. Cleve Clin J Med. 2016;83(3):199–206.
- Moyer VA; US Preventive Services Task Force. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(4):271–281.
- American Society of Breast Surgeons. Consensus Guideline on Hereditary Genetic Testing for Patients With and Without Breast Cancer. Columbia, MD: American Society of Breast Surgeons. https://www.breastsurgeons.org/new_layout/about/statements/PDF_Statements/BRCA_Testing.pdf. Published March 14, 2017. Accessed December 28, 2017.
Advances in cancer genetics are rapidly changing how clinicians assess an individual’s risk for breast cancer. ObGyns counsel many women with a personal or family history of the disease, many of whom can benefit from genetics counseling and testing. As patients with a hereditary predisposition to breast cancer are at higher risk and are younger at diagnosis, it is imperative to identify them early so they can benefit from enhanced surveillance, chemoprevention, and discussions regarding risk-reducing surgeries. ObGyns are uniquely poised to identify young women at risk for hereditary cancer syndromes, and they play a crucial role in screening and prevention over the life span.
CASE Patient with breast cancer history asks about screening for her daughters
A 52-year-old woman presents for her annual examination. She underwent breast cancer treatment 10 years earlier and has done well since then. When asked about family history of breast cancer and ethnicity, she reports her mother had breast cancer later in life, and her mother’s father was of Ashkenazi Jewish ancestry.In addition, a maternal uncle had metastatic prostate cancer. You recall that breast cancer diagnosed before age 50 years and Ashkenazi ancestry are “red flags” for a hereditary cancer syndrome. The patient wonders how her daughters should be screened. What do you do next?
Having a risk assessment plan is crucial
Given increasing demands, limited time, and the abundance of information to be discussed with patients, primary care physicians may find it challenging to assess breast cancer risk, consider genetics testing for appropriate individuals, and counsel patients about risk management options. The process has become even more complex since the expansion in genetics knowledge and the advent of multigene panel testing. Not only is risk assessment crucial for this woman and her daughters, and for other patients, but a delay in diagnosing and treating breast cancer in patients with hereditary and familial cancer risks may represent a worrisome new trend in medical litigation.1,2 Clinicians must have a process in place for assessing risk in all patients and treating them appropriately.
The American Cancer Society (ACS) estimated that 252,710 cases of breast cancer would be diagnosed in 2017, leading to 40,610 deaths.3 Twelve percent to 14% of breast cancers are thought to be related to hereditary cancer predisposition syndromes.4–8 This means that, every year, almost 35,000 cases of breast cancer are attributable to hereditary risk. These cases can be detected early with enhanced surveillance, which carries the highest chance for cure, or prevented with risk-reducing surgery in identified genetic mutation carriers. Each child of a person with a genetic mutation predisposing to breast cancer has a 50% chance of inheriting the mutation and having a very high risk of cancer.
In this patient’s case, basic information is collected about her cancer-related personal and family history.
Asking a few key questions can help in stratifying risk:
- Have you or anyone in your family had cancer? What type, and at what age?
- If breast cancer, did it involve both breasts, or was it triple-negative?
- Is there a family history of ovarian cancer?
- Is there a family history of male breast cancer?
- Is there a family history of metastatic prostate cancer?
- Are you of Ashkenazi Jewish ethnicity?
- Have you or anyone in your family ever had genetics testing for cancer?
The hallmarks of hereditary cancer are multiple cancers in an individual or family; young age at diagnosis; and ovarian, pancreatic, or another rare cancer. Metastatic prostate cancer was added as a red flag for hereditary risk after a recent large series found that 11.8% of men with metastatic prostate cancer harbor germline mutations.9
CASE Continued
On further questioning, the patient reports she had triple-negative (estrogen receptor–, progesterone receptor–, and human epidermal growth factor receptor 2 [HER2]–negative) breast cancer, a feature of patients with germline BRCA1 (breast cancer susceptibility gene 1) mutations.10 In addition, her Ashkenazi ancestry is concerning, as there is a 1-in-40 chance of carrying 1 of the 3 Ashkenazi founder BRCA mutations.11 Is a genetics consultation needed?
Read about guidelines for referral and testing.
Guidelines for genetics referral and testing
According to the TABLE, which summarizes national guidelines for genetics referral, maternal and paternal family histories are equally important. Our patient was under age 50 at diagnosis, has a history of triple-negative breast cancer, is of Ashkenazi ancestry, and has a family history of metastatic prostate cancer. She meets the criteria for genetics testing, and screening for her daughters most certainly will depend on the findings of that testing. If she carries a BRCA1 mutation, as might be anticipated, each daughter would have a 50% chance of having inherited the mutation. If they carry the mutation as well, they would begin breast magnetic resonance imaging (MRI) screening at age 25.12 If they decide against genetics testing, they could still undergo MRI screening as untested first-degree relatives of a BRCA carrier, per ACS recommendations.13
Integrating evidence and experience
Over the past 10 to 20 years, other breast cancer susceptibility genes (eg, BRCA2, PALB2, CHEK2) have been identified. More recently, next-generation sequencing has become commercially available. Laboratories can use this newer method to sequence multiple genes rapidly and in parallel, and its cost is similar to that of single-syndrome testing.14 When more than 1 gene can explain an inherited cancer syndrome, multigene panel testing may be more efficient and cost-effective. Use of multigene panel testing is supported in guidelines issued by the National Comprehensive Cancer Network,12 the American College of Obstetricians and Gynecologists,15 and other medical societies.
For our patient, the most logical strategy would be to test for the 3 mutations most common in the Ashkenazi population and then, if no mutation is found, perform multigene panel testing.
Formal genetics counseling can be very helpful for a patient, particularly in the era of multigene panel testing.16,17 A detailed pedigree (family tree) is elicited, and a genetics specialist determines whether testing is indicated and which test is best for the patient. Possible test findings are explained. The patient may be found to have a pathogenic variant with associated increased cancer risk, a negative test result (informative or uninformative), or a variant of uncertain significance (VUS). VUS is a gene mutation identified with an unknown effect on protein function and an unclear association with cancer risk. A finding of VUS may make the patient anxious,18 create uncertainty in the treating physician,19 and lead to harmful overtreatment, excessive surveillance, or unnecessary use of a preventive measure.19–21 Genetics counseling allows the patient, even the patient with VUS, to make appropriate decisions.22 Counseling may also help a patient or family process emotional responses, such as fear and guilt. In addition, counselors are familiar with relevant laws and regulations, such as the Genetic Information Nondiscrimination Act of 2008 (GINA), which protects patients from insurance and employment discrimination. Many professional guidelines recommend providing genetics counseling in conjunction with genetics testing,12,23 and some insurance companies and some states require counseling for coverage of testing.
Cost of genetics counseling. If patients are concerned about the cost of genetics testing, they can be reassured with the following information24–26:
- The Patient Protection and Affordable Care Act (ACA) identifies BRCA testing as a preventive service
- Medicare provides coverage for affected patients with a qualifying personal history
- 97% of commercial insurers and most state Medicaid programs provide coverage for hereditary cancer testing
- Most commercial laboratories have affordability programs that may provide additional support.
If a BRCA mutation is found: Many patients question the value of knowing whether they have a BRCA mutation. What our patient, her daughters, and others may not realize is that, if a BRCA mutation is found, breast MRI screening can begin at age 25. Although contrast-enhanced MRI screening is highly sensitive in detecting breast cancer,27–29 it lacks specificity and commonly yields false positives.
Some patients also worry about overdiagnosis with this highly sensitive test. Many do not realize that preventively prescribed oral contraceptives can reduce the risk of ovarian cancer by 50%, and cosmetically acceptable risk-reducing breast surgeries can reduce the risk by 90%.
Many are unaware of the associated risks with ovarian, prostate, pancreatic, and other cancers; of risk management options; and of assisted reproduction options, such as preimplantation genetics diagnosis, which can prevent the passing of a genetic mutation to future generations. The guidelines on risk management options are increasingly clear and helpful,12,30–32 and women often turn to their ObGyns for advice about health and prevention.
ObGyns are often the first-line providers for women with a personal or family history of breast cancer. Identification of at-risk patients begins with taking a careful family history and becoming familiar with the rapidly evolving guidelines in this important field. Identification of appropriate candidates for breast cancer genetics testing is a key step toward prevention, value-based care, and avoidance of legal liability.
CASE Resolved
In this case, testing for the 3 common Ashkenazi BRCA founder mutations was negative, and multigene panel testing was also negative. Her husband is not of Ashkenazi Jewish descent and there is no significant family history of cancer on his side. The daughters are advised to begin high-risk screening at the age of 32, 10 years earlier than their mother was diagnosed, but no genetic testing is indicated for them.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Advances in cancer genetics are rapidly changing how clinicians assess an individual’s risk for breast cancer. ObGyns counsel many women with a personal or family history of the disease, many of whom can benefit from genetics counseling and testing. As patients with a hereditary predisposition to breast cancer are at higher risk and are younger at diagnosis, it is imperative to identify them early so they can benefit from enhanced surveillance, chemoprevention, and discussions regarding risk-reducing surgeries. ObGyns are uniquely poised to identify young women at risk for hereditary cancer syndromes, and they play a crucial role in screening and prevention over the life span.
CASE Patient with breast cancer history asks about screening for her daughters
A 52-year-old woman presents for her annual examination. She underwent breast cancer treatment 10 years earlier and has done well since then. When asked about family history of breast cancer and ethnicity, she reports her mother had breast cancer later in life, and her mother’s father was of Ashkenazi Jewish ancestry.In addition, a maternal uncle had metastatic prostate cancer. You recall that breast cancer diagnosed before age 50 years and Ashkenazi ancestry are “red flags” for a hereditary cancer syndrome. The patient wonders how her daughters should be screened. What do you do next?
Having a risk assessment plan is crucial
Given increasing demands, limited time, and the abundance of information to be discussed with patients, primary care physicians may find it challenging to assess breast cancer risk, consider genetics testing for appropriate individuals, and counsel patients about risk management options. The process has become even more complex since the expansion in genetics knowledge and the advent of multigene panel testing. Not only is risk assessment crucial for this woman and her daughters, and for other patients, but a delay in diagnosing and treating breast cancer in patients with hereditary and familial cancer risks may represent a worrisome new trend in medical litigation.1,2 Clinicians must have a process in place for assessing risk in all patients and treating them appropriately.
The American Cancer Society (ACS) estimated that 252,710 cases of breast cancer would be diagnosed in 2017, leading to 40,610 deaths.3 Twelve percent to 14% of breast cancers are thought to be related to hereditary cancer predisposition syndromes.4–8 This means that, every year, almost 35,000 cases of breast cancer are attributable to hereditary risk. These cases can be detected early with enhanced surveillance, which carries the highest chance for cure, or prevented with risk-reducing surgery in identified genetic mutation carriers. Each child of a person with a genetic mutation predisposing to breast cancer has a 50% chance of inheriting the mutation and having a very high risk of cancer.
In this patient’s case, basic information is collected about her cancer-related personal and family history.
Asking a few key questions can help in stratifying risk:
- Have you or anyone in your family had cancer? What type, and at what age?
- If breast cancer, did it involve both breasts, or was it triple-negative?
- Is there a family history of ovarian cancer?
- Is there a family history of male breast cancer?
- Is there a family history of metastatic prostate cancer?
- Are you of Ashkenazi Jewish ethnicity?
- Have you or anyone in your family ever had genetics testing for cancer?
The hallmarks of hereditary cancer are multiple cancers in an individual or family; young age at diagnosis; and ovarian, pancreatic, or another rare cancer. Metastatic prostate cancer was added as a red flag for hereditary risk after a recent large series found that 11.8% of men with metastatic prostate cancer harbor germline mutations.9
CASE Continued
On further questioning, the patient reports she had triple-negative (estrogen receptor–, progesterone receptor–, and human epidermal growth factor receptor 2 [HER2]–negative) breast cancer, a feature of patients with germline BRCA1 (breast cancer susceptibility gene 1) mutations.10 In addition, her Ashkenazi ancestry is concerning, as there is a 1-in-40 chance of carrying 1 of the 3 Ashkenazi founder BRCA mutations.11 Is a genetics consultation needed?
Read about guidelines for referral and testing.
Guidelines for genetics referral and testing
According to the TABLE, which summarizes national guidelines for genetics referral, maternal and paternal family histories are equally important. Our patient was under age 50 at diagnosis, has a history of triple-negative breast cancer, is of Ashkenazi ancestry, and has a family history of metastatic prostate cancer. She meets the criteria for genetics testing, and screening for her daughters most certainly will depend on the findings of that testing. If she carries a BRCA1 mutation, as might be anticipated, each daughter would have a 50% chance of having inherited the mutation. If they carry the mutation as well, they would begin breast magnetic resonance imaging (MRI) screening at age 25.12 If they decide against genetics testing, they could still undergo MRI screening as untested first-degree relatives of a BRCA carrier, per ACS recommendations.13
Integrating evidence and experience
Over the past 10 to 20 years, other breast cancer susceptibility genes (eg, BRCA2, PALB2, CHEK2) have been identified. More recently, next-generation sequencing has become commercially available. Laboratories can use this newer method to sequence multiple genes rapidly and in parallel, and its cost is similar to that of single-syndrome testing.14 When more than 1 gene can explain an inherited cancer syndrome, multigene panel testing may be more efficient and cost-effective. Use of multigene panel testing is supported in guidelines issued by the National Comprehensive Cancer Network,12 the American College of Obstetricians and Gynecologists,15 and other medical societies.
For our patient, the most logical strategy would be to test for the 3 mutations most common in the Ashkenazi population and then, if no mutation is found, perform multigene panel testing.
Formal genetics counseling can be very helpful for a patient, particularly in the era of multigene panel testing.16,17 A detailed pedigree (family tree) is elicited, and a genetics specialist determines whether testing is indicated and which test is best for the patient. Possible test findings are explained. The patient may be found to have a pathogenic variant with associated increased cancer risk, a negative test result (informative or uninformative), or a variant of uncertain significance (VUS). VUS is a gene mutation identified with an unknown effect on protein function and an unclear association with cancer risk. A finding of VUS may make the patient anxious,18 create uncertainty in the treating physician,19 and lead to harmful overtreatment, excessive surveillance, or unnecessary use of a preventive measure.19–21 Genetics counseling allows the patient, even the patient with VUS, to make appropriate decisions.22 Counseling may also help a patient or family process emotional responses, such as fear and guilt. In addition, counselors are familiar with relevant laws and regulations, such as the Genetic Information Nondiscrimination Act of 2008 (GINA), which protects patients from insurance and employment discrimination. Many professional guidelines recommend providing genetics counseling in conjunction with genetics testing,12,23 and some insurance companies and some states require counseling for coverage of testing.
Cost of genetics counseling. If patients are concerned about the cost of genetics testing, they can be reassured with the following information24–26:
- The Patient Protection and Affordable Care Act (ACA) identifies BRCA testing as a preventive service
- Medicare provides coverage for affected patients with a qualifying personal history
- 97% of commercial insurers and most state Medicaid programs provide coverage for hereditary cancer testing
- Most commercial laboratories have affordability programs that may provide additional support.
If a BRCA mutation is found: Many patients question the value of knowing whether they have a BRCA mutation. What our patient, her daughters, and others may not realize is that, if a BRCA mutation is found, breast MRI screening can begin at age 25. Although contrast-enhanced MRI screening is highly sensitive in detecting breast cancer,27–29 it lacks specificity and commonly yields false positives.
Some patients also worry about overdiagnosis with this highly sensitive test. Many do not realize that preventively prescribed oral contraceptives can reduce the risk of ovarian cancer by 50%, and cosmetically acceptable risk-reducing breast surgeries can reduce the risk by 90%.
Many are unaware of the associated risks with ovarian, prostate, pancreatic, and other cancers; of risk management options; and of assisted reproduction options, such as preimplantation genetics diagnosis, which can prevent the passing of a genetic mutation to future generations. The guidelines on risk management options are increasingly clear and helpful,12,30–32 and women often turn to their ObGyns for advice about health and prevention.
ObGyns are often the first-line providers for women with a personal or family history of breast cancer. Identification of at-risk patients begins with taking a careful family history and becoming familiar with the rapidly evolving guidelines in this important field. Identification of appropriate candidates for breast cancer genetics testing is a key step toward prevention, value-based care, and avoidance of legal liability.
CASE Resolved
In this case, testing for the 3 common Ashkenazi BRCA founder mutations was negative, and multigene panel testing was also negative. Her husband is not of Ashkenazi Jewish descent and there is no significant family history of cancer on his side. The daughters are advised to begin high-risk screening at the age of 32, 10 years earlier than their mother was diagnosed, but no genetic testing is indicated for them.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Phillips RL Jr, Bartholomew LA, Dovey SM, Fryer GE Jr, Miyoshi TJ, Green LA. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13(2):121–126.
- Saber Tehrani AS, Lee H, Mathews SC, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- American Cancer Society. Breast Cancer Facts & Figures 2017-2018. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-factsand-figures/breast-cancer-facts-and-figures-2017-2018.pdf. Published 2017. Accessed December 28, 2017.
- Tung N, Battelli C, Allen B, et al. Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2 testing using next-generation sequencing with a 25-gene panel. Cancer. 2015;121(1):25–33.
- Tung N, Lin NU, Kidd J, et al. Frequency of germline mutations in 25 cancer susceptibility genes in a sequential series of patients with breast cancer. J Clin Oncol. 2016;34(13):1460–1468.
- Kurian AW, Hare EE, Mills MA, et al. Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment. J Clin Oncol. 2014;32(19):2001–2009.
- Easton DF, Pharoah PD, Antoniou AC, et al. Gene-panel sequencing and the prediction of breast-cancer risk. N Engl J Med. 2015;372(23):2243–2257.
- Yurgelun MB, Allen B, Kaldate RR, et al. Identification of a variety of mutations in cancer predisposition genes in patients with suspected Lynch syndrome. Gastroenterology. 2015;149(3):604–613.e20.
- Pritchard CC, Mateo J, Walsh MF, et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N Engl J Med. 2016;375(5):443–453.
- Mavaddat N, Barrowdale D, Andrulis IL, et al; Consortium of Investigators of Modifiers of BRCA1/2. Pathology of breast and ovarian cancers among BRCA1 and BRCA2 mutation carriers: results from the Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA). Cancer Epidemiol Biomarkers Prev. 2012;21(1):134–147.
- Struewing JP, Hartge P, Wacholder S, et al. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med. 1997;336(20):1401–1408.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Genetic/Familial High-Risk Assessment: Breast and Ovarian. Version 1.2018. https://www.nccn.org. Accessed December 28, 2017.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
- Heather JM, Chain B. The sequence of sequencers: the history of sequencing DNA. Genomics. 2016;107(1):1–8.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 182: Hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2017;130(3):e110–e126.
- Mester JL, Schreiber AH, Moran RT. Genetic counselors: your partners in clinical practice. Cleve Clin J Med. 2012;79(8):560–568.
- Smith M, Mester J, Eng C. How to spot heritable breast cancer: a primary care physician’s guide. Cleve Clin J Med. 2014;81(1):31–40.
- Welsh JL, Hoskin TL, Day CN, et al. Clinical decision-making in patients with variant of uncertain significance in BRCA1 or BRCA2 genes. Ann Surg Oncol. 2017;24(10):3067–3072.
- Kurian AW, Li Y, Hamilton AS, et al. Gaps in incorporating germline genetic testing into treatment decision-making for early-stage breast cancer. J Clin Oncol. 2017;35(20):2232–2239.
- Tung N, Domchek SM, Stadler Z, et al. Counselling framework for moderate-penetrance cancer-susceptibility mutations. Nat Rev Clin Oncol. 2016;13(9):581–588.
- Yu PP, Vose JM, Hayes DF. Genetic cancer susceptibility testing: increased technology, increased complexity. J Clin Oncol. 2015;33(31):3533–3534.
- Pederson HJ, Gopalakrishnan D, Noss R, Yanda C, Eng C, Grobmyer SR. Impact of multigene panel testing on surgical decision making in breast cancer patients. J Am Coll Surg. 2018;226(4):560–565.
- Robson ME, Bradbury AR, Arun B, et al. American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol. 2015;33(31):3660–3667.
- Preventive care benefits for women: What Marketplace health insurance plans cover. HealthCare.gov. https://www.healthcare.gov/coverage/what-marketplace-plans-cover/. Accessed May 15, 2018.
- Centers for Medicare & Medicaid Services. The Center for Consumer Information & Insurance Oversight: Affordable Care Act Implementation FAQs – Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.html. Accessed May 15, 2018.
- US Preventive Services Task Force. Final Recommendation Statement: BRCA-Related Cancer: Risk Assessment, Genetic Counseling, and Genetic Testing. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/brca-related-cancer-risk-assessment-genetic-counseling-and-genetic-testing. Published December 2013. Accessed May 15, 2018.
- Kuhl CK, Schrading S, Leutner CC, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol. 2005;23(33):8469–8476.
- Lehman CD, Blume JD, Weatherall P, et al; International Breast MRI Consortium Working Group. Screening women at high risk for breast cancer with mammography and magnetic resonance imaging. Cancer. 2005;103(9):1898–1905.
- Kriege M, Brekelmans CT, Boetes C, et al; Magnetic Resonance Imaging Screening Study Group. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351(5):427–437.
- Pederson HJ, Padia SA, May M, Grobmyer S. Managing patients at genetic risk of breast cancer. Cleve Clin J Med. 2016;83(3):199–206.
- Moyer VA; US Preventive Services Task Force. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(4):271–281.
- American Society of Breast Surgeons. Consensus Guideline on Hereditary Genetic Testing for Patients With and Without Breast Cancer. Columbia, MD: American Society of Breast Surgeons. https://www.breastsurgeons.org/new_layout/about/statements/PDF_Statements/BRCA_Testing.pdf. Published March 14, 2017. Accessed December 28, 2017.
- Phillips RL Jr, Bartholomew LA, Dovey SM, Fryer GE Jr, Miyoshi TJ, Green LA. Learning from malpractice claims about negligent, adverse events in primary care in the United States. Qual Saf Health Care. 2004;13(2):121–126.
- Saber Tehrani AS, Lee H, Mathews SC, et al. 25-year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672–680.
- American Cancer Society. Breast Cancer Facts & Figures 2017-2018. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-factsand-figures/breast-cancer-facts-and-figures-2017-2018.pdf. Published 2017. Accessed December 28, 2017.
- Tung N, Battelli C, Allen B, et al. Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2 testing using next-generation sequencing with a 25-gene panel. Cancer. 2015;121(1):25–33.
- Tung N, Lin NU, Kidd J, et al. Frequency of germline mutations in 25 cancer susceptibility genes in a sequential series of patients with breast cancer. J Clin Oncol. 2016;34(13):1460–1468.
- Kurian AW, Hare EE, Mills MA, et al. Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment. J Clin Oncol. 2014;32(19):2001–2009.
- Easton DF, Pharoah PD, Antoniou AC, et al. Gene-panel sequencing and the prediction of breast-cancer risk. N Engl J Med. 2015;372(23):2243–2257.
- Yurgelun MB, Allen B, Kaldate RR, et al. Identification of a variety of mutations in cancer predisposition genes in patients with suspected Lynch syndrome. Gastroenterology. 2015;149(3):604–613.e20.
- Pritchard CC, Mateo J, Walsh MF, et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N Engl J Med. 2016;375(5):443–453.
- Mavaddat N, Barrowdale D, Andrulis IL, et al; Consortium of Investigators of Modifiers of BRCA1/2. Pathology of breast and ovarian cancers among BRCA1 and BRCA2 mutation carriers: results from the Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA). Cancer Epidemiol Biomarkers Prev. 2012;21(1):134–147.
- Struewing JP, Hartge P, Wacholder S, et al. The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med. 1997;336(20):1401–1408.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Genetic/Familial High-Risk Assessment: Breast and Ovarian. Version 1.2018. https://www.nccn.org. Accessed December 28, 2017.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
- Heather JM, Chain B. The sequence of sequencers: the history of sequencing DNA. Genomics. 2016;107(1):1–8.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 182: Hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2017;130(3):e110–e126.
- Mester JL, Schreiber AH, Moran RT. Genetic counselors: your partners in clinical practice. Cleve Clin J Med. 2012;79(8):560–568.
- Smith M, Mester J, Eng C. How to spot heritable breast cancer: a primary care physician’s guide. Cleve Clin J Med. 2014;81(1):31–40.
- Welsh JL, Hoskin TL, Day CN, et al. Clinical decision-making in patients with variant of uncertain significance in BRCA1 or BRCA2 genes. Ann Surg Oncol. 2017;24(10):3067–3072.
- Kurian AW, Li Y, Hamilton AS, et al. Gaps in incorporating germline genetic testing into treatment decision-making for early-stage breast cancer. J Clin Oncol. 2017;35(20):2232–2239.
- Tung N, Domchek SM, Stadler Z, et al. Counselling framework for moderate-penetrance cancer-susceptibility mutations. Nat Rev Clin Oncol. 2016;13(9):581–588.
- Yu PP, Vose JM, Hayes DF. Genetic cancer susceptibility testing: increased technology, increased complexity. J Clin Oncol. 2015;33(31):3533–3534.
- Pederson HJ, Gopalakrishnan D, Noss R, Yanda C, Eng C, Grobmyer SR. Impact of multigene panel testing on surgical decision making in breast cancer patients. J Am Coll Surg. 2018;226(4):560–565.
- Robson ME, Bradbury AR, Arun B, et al. American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol. 2015;33(31):3660–3667.
- Preventive care benefits for women: What Marketplace health insurance plans cover. HealthCare.gov. https://www.healthcare.gov/coverage/what-marketplace-plans-cover/. Accessed May 15, 2018.
- Centers for Medicare & Medicaid Services. The Center for Consumer Information & Insurance Oversight: Affordable Care Act Implementation FAQs – Set 12. https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.html. Accessed May 15, 2018.
- US Preventive Services Task Force. Final Recommendation Statement: BRCA-Related Cancer: Risk Assessment, Genetic Counseling, and Genetic Testing. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/brca-related-cancer-risk-assessment-genetic-counseling-and-genetic-testing. Published December 2013. Accessed May 15, 2018.
- Kuhl CK, Schrading S, Leutner CC, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol. 2005;23(33):8469–8476.
- Lehman CD, Blume JD, Weatherall P, et al; International Breast MRI Consortium Working Group. Screening women at high risk for breast cancer with mammography and magnetic resonance imaging. Cancer. 2005;103(9):1898–1905.
- Kriege M, Brekelmans CT, Boetes C, et al; Magnetic Resonance Imaging Screening Study Group. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351(5):427–437.
- Pederson HJ, Padia SA, May M, Grobmyer S. Managing patients at genetic risk of breast cancer. Cleve Clin J Med. 2016;83(3):199–206.
- Moyer VA; US Preventive Services Task Force. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(4):271–281.
- American Society of Breast Surgeons. Consensus Guideline on Hereditary Genetic Testing for Patients With and Without Breast Cancer. Columbia, MD: American Society of Breast Surgeons. https://www.breastsurgeons.org/new_layout/about/statements/PDF_Statements/BRCA_Testing.pdf. Published March 14, 2017. Accessed December 28, 2017.
Take-home points
- The best genetics test is a good family history, updated annually
- Each year, 35,000 breast cancers are attributable to hereditary risk
- It is crucial to identify families at risk for hereditary breast cancer early, as cancers may begin in a woman's 30s; screening begins at age 25
- Multigene panel testing is efficient and cost-effective
- For patients who have highly penetrant pathogenic variants and are of childbearing age, preimplantation genetics diagnosis is an option
Glucose Hypometabolism Found in Pediatric Drug-Resistant Epilepsy
Children with drug-resistant epilepsy seem to have a lobar pattern of glucose hypometabolism according to PET scans performed on 41 patients with the disorder.
- Baseline positron emission tomography (PET) scans were performed on children with drug resistant epilepsy with a median age of 4.7 years.
- A follow-up PET scan was done 4.3 years (median) later.
- Children with space-occupying lesion-related epilepsy were not included in the study, nor were patients with progressive neurological disorders.
- Twenty-four children had unilateral glucose hypometabolism and 13 had bilateral hypometabolism at baseline.
- Follow-up PET scans revealed that 63% had interval expansion of the hypometabolic region of their brain; said expansion was associated with persistent seizures.
Govil-Dalela T, Kumar A Behen ME, Chugani HT, Juhász C. Evolution of lobar abnormalities of cerebral glucose metabolism in 41 children with drug-resistant epilepsy [Published online ahead of print May 22, 2018]. Epilepsia. doi: 10.1111/epi.14404.
Children with drug-resistant epilepsy seem to have a lobar pattern of glucose hypometabolism according to PET scans performed on 41 patients with the disorder.
- Baseline positron emission tomography (PET) scans were performed on children with drug resistant epilepsy with a median age of 4.7 years.
- A follow-up PET scan was done 4.3 years (median) later.
- Children with space-occupying lesion-related epilepsy were not included in the study, nor were patients with progressive neurological disorders.
- Twenty-four children had unilateral glucose hypometabolism and 13 had bilateral hypometabolism at baseline.
- Follow-up PET scans revealed that 63% had interval expansion of the hypometabolic region of their brain; said expansion was associated with persistent seizures.
Govil-Dalela T, Kumar A Behen ME, Chugani HT, Juhász C. Evolution of lobar abnormalities of cerebral glucose metabolism in 41 children with drug-resistant epilepsy [Published online ahead of print May 22, 2018]. Epilepsia. doi: 10.1111/epi.14404.
Children with drug-resistant epilepsy seem to have a lobar pattern of glucose hypometabolism according to PET scans performed on 41 patients with the disorder.
- Baseline positron emission tomography (PET) scans were performed on children with drug resistant epilepsy with a median age of 4.7 years.
- A follow-up PET scan was done 4.3 years (median) later.
- Children with space-occupying lesion-related epilepsy were not included in the study, nor were patients with progressive neurological disorders.
- Twenty-four children had unilateral glucose hypometabolism and 13 had bilateral hypometabolism at baseline.
- Follow-up PET scans revealed that 63% had interval expansion of the hypometabolic region of their brain; said expansion was associated with persistent seizures.
Govil-Dalela T, Kumar A Behen ME, Chugani HT, Juhász C. Evolution of lobar abnormalities of cerebral glucose metabolism in 41 children with drug-resistant epilepsy [Published online ahead of print May 22, 2018]. Epilepsia. doi: 10.1111/epi.14404.
Liver transplantation is on the rise for patients with severe alcoholic hepatitis
More transplant centers are offering liver transplantation as a viable therapeutic option for patients with severe alcoholic hepatitis who do not respond to steroid treatment.
“Alcoholic hepatitis is a disease caused by drinking alcohol. Excessive alcohol consumption causes fat to build up in your liver cells, as well as inflammation and scarring of the liver,” stated Saroja Bangaru, MD, chief resident at the University of Texas, Dallas. “Severe alcoholic hepatitis has an extremely high mortality and steroids are really the mainstay of therapy. Some alcoholic hepatitis patients do not respond to steroids and a significant percentage of them will die within 3 months. For these patients, liver transplantation is a therapeutic option.”
Dr. Bangaru and her colleagues conducted a survey that gathered data from 45 transplant centers in the United States and found that an increasing number have changed this practice and now offer liver transplantation to patients with severe alcoholic hepatitis.
The survey revealed that 51.1% of the 45 clinics offered liver transplantation to patients who had not yet been sober for 6 months, and 47.8% of transplant centers reported performing at least one liver transplant for severe alcoholic hepatitis. Just over a third (34.8%) of these centers had conducted three to five liver transplants, while only 8.9% of clinics performed at least six transplants. It is of note that most clinics have transplanted livers in fewer than five patients with severe alcoholic hepatitis, Dr. Bangaru said at the annual Digestive Disease Week®.
Patients experienced positive outcomes from these transplants, with almost 75% of surveyed clinics reporting 1-year survival rates of more than 90%, and 15% reporting 1-year survival rates of 80%-90%.
A factor that may have contributed to such positive outcomes was good patient selection based on liver transplant criteria for severe alcoholic hepatitis. More than 85% of center directors believed that liver transplant candidates should have a strong social support system, absence of severe psychiatric disorders, and a completed psychosocial evaluation, among other criteria.
Dr. Bangaru pointed out that the change in treating patients who have not abstained from alcohol is a break from traditional medical practice. “Historically, transplant centers would not consider a liver transplantation as an option unless a patient had abstained from drinking alcohol for 6 months. This rule was due to a concern that the patient would return to drinking after transplant as well as a perceived high risk that patients who continued drinking would miss medical appointments, fail to take their immunosuppressants and medications, and that this would lead to eventual graft failure.”
Another compounding issue was that patients were not counseled on their alcohol consumption habits, leading to further issues with transplantation. “Not infrequently, patients receive a diagnosis of severe alcoholic hepatitis during their initial visit and no one had previously told them to stop drinking. Since their presentation was preceded by active alcohol consumption, they would essentially be rendered ineligible for a transplant at that time,” she said.
Despite the history surrounding liver transplants in patients with severe alcoholic hepatitis, Dr. Bangaru hopes the shift in practice will improve the lives of more patients. “Because this practice of transplantation is being increasingly accepted and demonstrating positive outcomes, the hope is that more patients will be evaluated for transplantation and that transplant centers will improve their posttransplant support to ensure patients have great success after transplantation.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
More transplant centers are offering liver transplantation as a viable therapeutic option for patients with severe alcoholic hepatitis who do not respond to steroid treatment.
“Alcoholic hepatitis is a disease caused by drinking alcohol. Excessive alcohol consumption causes fat to build up in your liver cells, as well as inflammation and scarring of the liver,” stated Saroja Bangaru, MD, chief resident at the University of Texas, Dallas. “Severe alcoholic hepatitis has an extremely high mortality and steroids are really the mainstay of therapy. Some alcoholic hepatitis patients do not respond to steroids and a significant percentage of them will die within 3 months. For these patients, liver transplantation is a therapeutic option.”
Dr. Bangaru and her colleagues conducted a survey that gathered data from 45 transplant centers in the United States and found that an increasing number have changed this practice and now offer liver transplantation to patients with severe alcoholic hepatitis.
The survey revealed that 51.1% of the 45 clinics offered liver transplantation to patients who had not yet been sober for 6 months, and 47.8% of transplant centers reported performing at least one liver transplant for severe alcoholic hepatitis. Just over a third (34.8%) of these centers had conducted three to five liver transplants, while only 8.9% of clinics performed at least six transplants. It is of note that most clinics have transplanted livers in fewer than five patients with severe alcoholic hepatitis, Dr. Bangaru said at the annual Digestive Disease Week®.
Patients experienced positive outcomes from these transplants, with almost 75% of surveyed clinics reporting 1-year survival rates of more than 90%, and 15% reporting 1-year survival rates of 80%-90%.
A factor that may have contributed to such positive outcomes was good patient selection based on liver transplant criteria for severe alcoholic hepatitis. More than 85% of center directors believed that liver transplant candidates should have a strong social support system, absence of severe psychiatric disorders, and a completed psychosocial evaluation, among other criteria.
Dr. Bangaru pointed out that the change in treating patients who have not abstained from alcohol is a break from traditional medical practice. “Historically, transplant centers would not consider a liver transplantation as an option unless a patient had abstained from drinking alcohol for 6 months. This rule was due to a concern that the patient would return to drinking after transplant as well as a perceived high risk that patients who continued drinking would miss medical appointments, fail to take their immunosuppressants and medications, and that this would lead to eventual graft failure.”
Another compounding issue was that patients were not counseled on their alcohol consumption habits, leading to further issues with transplantation. “Not infrequently, patients receive a diagnosis of severe alcoholic hepatitis during their initial visit and no one had previously told them to stop drinking. Since their presentation was preceded by active alcohol consumption, they would essentially be rendered ineligible for a transplant at that time,” she said.
Despite the history surrounding liver transplants in patients with severe alcoholic hepatitis, Dr. Bangaru hopes the shift in practice will improve the lives of more patients. “Because this practice of transplantation is being increasingly accepted and demonstrating positive outcomes, the hope is that more patients will be evaluated for transplantation and that transplant centers will improve their posttransplant support to ensure patients have great success after transplantation.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
More transplant centers are offering liver transplantation as a viable therapeutic option for patients with severe alcoholic hepatitis who do not respond to steroid treatment.
“Alcoholic hepatitis is a disease caused by drinking alcohol. Excessive alcohol consumption causes fat to build up in your liver cells, as well as inflammation and scarring of the liver,” stated Saroja Bangaru, MD, chief resident at the University of Texas, Dallas. “Severe alcoholic hepatitis has an extremely high mortality and steroids are really the mainstay of therapy. Some alcoholic hepatitis patients do not respond to steroids and a significant percentage of them will die within 3 months. For these patients, liver transplantation is a therapeutic option.”
Dr. Bangaru and her colleagues conducted a survey that gathered data from 45 transplant centers in the United States and found that an increasing number have changed this practice and now offer liver transplantation to patients with severe alcoholic hepatitis.
The survey revealed that 51.1% of the 45 clinics offered liver transplantation to patients who had not yet been sober for 6 months, and 47.8% of transplant centers reported performing at least one liver transplant for severe alcoholic hepatitis. Just over a third (34.8%) of these centers had conducted three to five liver transplants, while only 8.9% of clinics performed at least six transplants. It is of note that most clinics have transplanted livers in fewer than five patients with severe alcoholic hepatitis, Dr. Bangaru said at the annual Digestive Disease Week®.
Patients experienced positive outcomes from these transplants, with almost 75% of surveyed clinics reporting 1-year survival rates of more than 90%, and 15% reporting 1-year survival rates of 80%-90%.
A factor that may have contributed to such positive outcomes was good patient selection based on liver transplant criteria for severe alcoholic hepatitis. More than 85% of center directors believed that liver transplant candidates should have a strong social support system, absence of severe psychiatric disorders, and a completed psychosocial evaluation, among other criteria.
Dr. Bangaru pointed out that the change in treating patients who have not abstained from alcohol is a break from traditional medical practice. “Historically, transplant centers would not consider a liver transplantation as an option unless a patient had abstained from drinking alcohol for 6 months. This rule was due to a concern that the patient would return to drinking after transplant as well as a perceived high risk that patients who continued drinking would miss medical appointments, fail to take their immunosuppressants and medications, and that this would lead to eventual graft failure.”
Another compounding issue was that patients were not counseled on their alcohol consumption habits, leading to further issues with transplantation. “Not infrequently, patients receive a diagnosis of severe alcoholic hepatitis during their initial visit and no one had previously told them to stop drinking. Since their presentation was preceded by active alcohol consumption, they would essentially be rendered ineligible for a transplant at that time,” she said.
Despite the history surrounding liver transplants in patients with severe alcoholic hepatitis, Dr. Bangaru hopes the shift in practice will improve the lives of more patients. “Because this practice of transplantation is being increasingly accepted and demonstrating positive outcomes, the hope is that more patients will be evaluated for transplantation and that transplant centers will improve their posttransplant support to ensure patients have great success after transplantation.”
Digestive Disease Week® is jointly sponsored by the American Association for the Study of Liver Diseases (AASLD), the American Gastroenterological Association (AGA) Institute, the American Society for Gastrointestinal Endoscopy (ASGE), and the Society for Surgery of the Alimentary Tract (SSAT).
REPORTING FROM DDW
Median time to progression from discoid to systemic lupus may be less than a year
ORLANDO – Progression from cutaneous to systemic lupus happens far more quickly than is commonly reported in the literature, according to an investigation from Brigham and Women’s Hospital, Boston.
Most studies have emphasized mean time to progression, which is generally said to be about 8 years. The problem is that the range is broad, anywhere from a few months to 30 or more years, so “the outliers influence the mean, and therefore, may not provide a fully accurate representation of the interval in which [most] patients progress” from discoid lupus erythematosus (DLE) to systemic lupus erythematosus (SLE), lead investigator Scott Elman, MD, said at the International Conference on Cutaneous Lupus Erythematosus.
He and his team thought it would be more useful to instead look at median time to progression, the point at which half of patients develop systemic disease. They found that , with the first quartile progressing by 303 days. The mean time to progression, meanwhile, was over 4 years, because of outliers who progressed at anywhere from 27 days to 30 years.
“The median progression of DLE to SLE occurs much sooner than previously reported” with mean progression times, said Dr. Elman, an internal medicine and dermatology resident at Brigham and Women’s. “We believe the use of median [time] is [more] clinically useful for both providers and patients in their understanding of what a diagnosis of DLE means for the risk of developing systemic disease.
“As clinicians seeing DLE patients, the primary question we are asking ourselves is how frequently we should be monitoring for signs and symptoms of systemic lupus,” he said. Relying on mean time instead of median time might give a false sense of security – and even delay checking for arthritis, nephritis, and other manifestations. There’s no current standard of practice about when monitoring should occur, but “I certainly think that closer monitoring of new patients with a diagnosis of DLE, especially in their first couple of years,” is a good idea, he noted, adding that for most patients, “it seems that if it’s going to happen, it’s going to happen sooner” rather than later. At Brigham and Women’s, newly diagnosed patients are generally brought back every 3-6 months for lab tests and a thorough review of symptoms, Dr. Elman said.
The next step is to identify risk factors for early progression. The study did not find any significant differences in lab values, medication exposures, or disease manifestations between early and late progressors, perhaps because of the small sample size. The work continues.
There was no external funding for the work. Dr. Elman had no disclosures.
ORLANDO – Progression from cutaneous to systemic lupus happens far more quickly than is commonly reported in the literature, according to an investigation from Brigham and Women’s Hospital, Boston.
Most studies have emphasized mean time to progression, which is generally said to be about 8 years. The problem is that the range is broad, anywhere from a few months to 30 or more years, so “the outliers influence the mean, and therefore, may not provide a fully accurate representation of the interval in which [most] patients progress” from discoid lupus erythematosus (DLE) to systemic lupus erythematosus (SLE), lead investigator Scott Elman, MD, said at the International Conference on Cutaneous Lupus Erythematosus.
He and his team thought it would be more useful to instead look at median time to progression, the point at which half of patients develop systemic disease. They found that , with the first quartile progressing by 303 days. The mean time to progression, meanwhile, was over 4 years, because of outliers who progressed at anywhere from 27 days to 30 years.
“The median progression of DLE to SLE occurs much sooner than previously reported” with mean progression times, said Dr. Elman, an internal medicine and dermatology resident at Brigham and Women’s. “We believe the use of median [time] is [more] clinically useful for both providers and patients in their understanding of what a diagnosis of DLE means for the risk of developing systemic disease.
“As clinicians seeing DLE patients, the primary question we are asking ourselves is how frequently we should be monitoring for signs and symptoms of systemic lupus,” he said. Relying on mean time instead of median time might give a false sense of security – and even delay checking for arthritis, nephritis, and other manifestations. There’s no current standard of practice about when monitoring should occur, but “I certainly think that closer monitoring of new patients with a diagnosis of DLE, especially in their first couple of years,” is a good idea, he noted, adding that for most patients, “it seems that if it’s going to happen, it’s going to happen sooner” rather than later. At Brigham and Women’s, newly diagnosed patients are generally brought back every 3-6 months for lab tests and a thorough review of symptoms, Dr. Elman said.
The next step is to identify risk factors for early progression. The study did not find any significant differences in lab values, medication exposures, or disease manifestations between early and late progressors, perhaps because of the small sample size. The work continues.
There was no external funding for the work. Dr. Elman had no disclosures.
ORLANDO – Progression from cutaneous to systemic lupus happens far more quickly than is commonly reported in the literature, according to an investigation from Brigham and Women’s Hospital, Boston.
Most studies have emphasized mean time to progression, which is generally said to be about 8 years. The problem is that the range is broad, anywhere from a few months to 30 or more years, so “the outliers influence the mean, and therefore, may not provide a fully accurate representation of the interval in which [most] patients progress” from discoid lupus erythematosus (DLE) to systemic lupus erythematosus (SLE), lead investigator Scott Elman, MD, said at the International Conference on Cutaneous Lupus Erythematosus.
He and his team thought it would be more useful to instead look at median time to progression, the point at which half of patients develop systemic disease. They found that , with the first quartile progressing by 303 days. The mean time to progression, meanwhile, was over 4 years, because of outliers who progressed at anywhere from 27 days to 30 years.
“The median progression of DLE to SLE occurs much sooner than previously reported” with mean progression times, said Dr. Elman, an internal medicine and dermatology resident at Brigham and Women’s. “We believe the use of median [time] is [more] clinically useful for both providers and patients in their understanding of what a diagnosis of DLE means for the risk of developing systemic disease.
“As clinicians seeing DLE patients, the primary question we are asking ourselves is how frequently we should be monitoring for signs and symptoms of systemic lupus,” he said. Relying on mean time instead of median time might give a false sense of security – and even delay checking for arthritis, nephritis, and other manifestations. There’s no current standard of practice about when monitoring should occur, but “I certainly think that closer monitoring of new patients with a diagnosis of DLE, especially in their first couple of years,” is a good idea, he noted, adding that for most patients, “it seems that if it’s going to happen, it’s going to happen sooner” rather than later. At Brigham and Women’s, newly diagnosed patients are generally brought back every 3-6 months for lab tests and a thorough review of symptoms, Dr. Elman said.
The next step is to identify risk factors for early progression. The study did not find any significant differences in lab values, medication exposures, or disease manifestations between early and late progressors, perhaps because of the small sample size. The work continues.
There was no external funding for the work. Dr. Elman had no disclosures.
REPORTING FROM ICCLE 2018
Key clinical point: Progression from cutaneous to systemic lupus happens far more quickly than is commonly reported in the literature.
Major finding: The median time to progression was 398 days, among a group of patients diagnosed with discoid lupus erythematosus.
Study details: A review of 32 patients who converted to systemic disease.
Disclosures: There was no external funding for the work, and the lead investigator had no disclosures.
Acute Generalized Exanthematous Pustulosis Caused by Pantoprazole
To the Editor:
A 34-year-old woman presented with a generalized pustular eruption with subjective fevers, chills, night sweats, and light-headedness. Ten days prior to admission she developed a generalized erythematous and pruritic rash; she had started pantoprazole for reflux 4 days prior to the rash. On admission, skin examination revealed facial edema and diffuse erythema covering 80% of the total body surface area with multiple 1- to 4-mm pustules coalescing into lakes of pus on the trunk as well as bilateral upper and lower arms and legs sparing the palms and soles. Desquamation and serous drainage with crust were observed on the skin of the head, upper trunk, and thighs (Figure 1). Vital signs were notable for hypotension. Laboratory tests on admission were remarkable for leukocytosis (white blood cell count: 22.5×103/μL [reference range, 4.5–11×103/μL]) with absolute eosinophilia but no neutrophilia. C-reactive protein (CRP) was elevated (237.9 mg/L [reference range, 5.0–9.9 mg/L]). Renal and hepatic functions were normal. Blood cultures grew methicillin-sensitive Staphylococcus aureus (MSSA). Further infectious disease workup for viral and fungal pathogens was negative.

Skin biopsy from the left thigh revealed subcorneal, pustular, acute spongiotic dermatitis with marked intraepidermal spongiosis and papillary edema; exocytosis of eosinophils; and single cell necrosis of keratinocytes (Figure 2). These findings were consistent with acute generalized exanthematous pustulosis (AGEP). Pantoprazole was discontinued, and cardiovascular support and antibiotic therapy for MSSA bacteremia were initiated. Respiratory, kidney, and liver functions remained normal throughout the 11-day hospitalization, and the pustular dermatitis, MSSA bacteremia, and cardiovascular symptoms resolved within 10 days.

Acute generalized exanthematous pustulosis is an uncommon, self-limited, generalized sterile pustular eruption notable for the usual absence of systemic symptoms and extracutaneous organ involvement. Hotz et al1 found that mean peripheral neutrophil counts (mean, 21.5×103/μL) and CRP levels (mean, 241.6 mg/L) were notably elevated in patients with systemic (ie, hepatic, pulmonary, renal, bone marrow) involvement. In our patient, only the CRP approached the elevated value reported by Hotz et al.1 However, the patient exhibited only cardiovascular instability in the context of secondary bacteremia and no other systemic symptoms. The combination of highly elevated neutrophilia and CRP may be a better marker for AGEP-precipitated extracutaneous organ involvement.
Although infectious pathogens such as Epstein-Barr virus and cytomegalovirus have been implicated, the majority of AGEP cases are adverse reactions (ARs) to medications, such as β-lactam antibiotics. In our patient, the widely prescribed proton pump inhibitor (PPI) pantoprazole was the most likely cause. Acute generalized exanthematous pustulosis was reported in a patient taking another PPI, omeprazole.2 However, PPIs are recognized to cause many cutaneous and other organ ARs, though prevalence of ARs is still low. In Thailand, Chularojanamontri et al3 reported 13.8 per 100,000 individuals developed a cutaneous AR to PPIs, and the ARs most frequently were attributed to omeprazole. They found that drug exanthems were the most common cutaneous ARs.3 However, more severe hypersensitivity reactions have been reported, including Stevens-Johnson syndrome, toxic epidermal necrolysis, and autoimmune eruptions such as cutaneous lupus erythematosus.3,4 Other systemic reactions to PPIs include increased risks for urticaria, pneumonia, Clostridium difficile infections, and acute interstitial nephritis.4,5
- Hotz C, Valeyrie-Allanore L, Haddad C, et al. Systemic involvement of acute generalized exanthematous pustulosis: a retrospective study on 58 patients. Br J Dermatol. 2013;169:1223-1232.
- Nantes Castillejo O, Zozaya Urmeneta JM, Valcayo Peñalba A, et al. Acute generalized exanthematous pustulosis induced by omeprazole [in Spanish]. Gastroenterol Hepatol. 2008;31:295-298.
- Chularojanamontri L, Jiamton S, Manapajon A, et al. Cutaneous reactions to proton pump inhibitors: a case-control study. J Drugs Dermatol. 2012;11:E43-E47.
- Chang YS. Hypersensitivity reactions to proton pump inhibitors. Curr Opin Allergy Clin Immunol. 2012;12:348-353.
- Wilhelm SM, Rjater RG, Kale-Pradhan PB. Perils and pitfalls of long-term effects of proton pump inhibitors. Expert Rev Clin Pharmacol. 2013;6:443-551.
To the Editor:
A 34-year-old woman presented with a generalized pustular eruption with subjective fevers, chills, night sweats, and light-headedness. Ten days prior to admission she developed a generalized erythematous and pruritic rash; she had started pantoprazole for reflux 4 days prior to the rash. On admission, skin examination revealed facial edema and diffuse erythema covering 80% of the total body surface area with multiple 1- to 4-mm pustules coalescing into lakes of pus on the trunk as well as bilateral upper and lower arms and legs sparing the palms and soles. Desquamation and serous drainage with crust were observed on the skin of the head, upper trunk, and thighs (Figure 1). Vital signs were notable for hypotension. Laboratory tests on admission were remarkable for leukocytosis (white blood cell count: 22.5×103/μL [reference range, 4.5–11×103/μL]) with absolute eosinophilia but no neutrophilia. C-reactive protein (CRP) was elevated (237.9 mg/L [reference range, 5.0–9.9 mg/L]). Renal and hepatic functions were normal. Blood cultures grew methicillin-sensitive Staphylococcus aureus (MSSA). Further infectious disease workup for viral and fungal pathogens was negative.

Skin biopsy from the left thigh revealed subcorneal, pustular, acute spongiotic dermatitis with marked intraepidermal spongiosis and papillary edema; exocytosis of eosinophils; and single cell necrosis of keratinocytes (Figure 2). These findings were consistent with acute generalized exanthematous pustulosis (AGEP). Pantoprazole was discontinued, and cardiovascular support and antibiotic therapy for MSSA bacteremia were initiated. Respiratory, kidney, and liver functions remained normal throughout the 11-day hospitalization, and the pustular dermatitis, MSSA bacteremia, and cardiovascular symptoms resolved within 10 days.

Acute generalized exanthematous pustulosis is an uncommon, self-limited, generalized sterile pustular eruption notable for the usual absence of systemic symptoms and extracutaneous organ involvement. Hotz et al1 found that mean peripheral neutrophil counts (mean, 21.5×103/μL) and CRP levels (mean, 241.6 mg/L) were notably elevated in patients with systemic (ie, hepatic, pulmonary, renal, bone marrow) involvement. In our patient, only the CRP approached the elevated value reported by Hotz et al.1 However, the patient exhibited only cardiovascular instability in the context of secondary bacteremia and no other systemic symptoms. The combination of highly elevated neutrophilia and CRP may be a better marker for AGEP-precipitated extracutaneous organ involvement.
Although infectious pathogens such as Epstein-Barr virus and cytomegalovirus have been implicated, the majority of AGEP cases are adverse reactions (ARs) to medications, such as β-lactam antibiotics. In our patient, the widely prescribed proton pump inhibitor (PPI) pantoprazole was the most likely cause. Acute generalized exanthematous pustulosis was reported in a patient taking another PPI, omeprazole.2 However, PPIs are recognized to cause many cutaneous and other organ ARs, though prevalence of ARs is still low. In Thailand, Chularojanamontri et al3 reported 13.8 per 100,000 individuals developed a cutaneous AR to PPIs, and the ARs most frequently were attributed to omeprazole. They found that drug exanthems were the most common cutaneous ARs.3 However, more severe hypersensitivity reactions have been reported, including Stevens-Johnson syndrome, toxic epidermal necrolysis, and autoimmune eruptions such as cutaneous lupus erythematosus.3,4 Other systemic reactions to PPIs include increased risks for urticaria, pneumonia, Clostridium difficile infections, and acute interstitial nephritis.4,5
To the Editor:
A 34-year-old woman presented with a generalized pustular eruption with subjective fevers, chills, night sweats, and light-headedness. Ten days prior to admission she developed a generalized erythematous and pruritic rash; she had started pantoprazole for reflux 4 days prior to the rash. On admission, skin examination revealed facial edema and diffuse erythema covering 80% of the total body surface area with multiple 1- to 4-mm pustules coalescing into lakes of pus on the trunk as well as bilateral upper and lower arms and legs sparing the palms and soles. Desquamation and serous drainage with crust were observed on the skin of the head, upper trunk, and thighs (Figure 1). Vital signs were notable for hypotension. Laboratory tests on admission were remarkable for leukocytosis (white blood cell count: 22.5×103/μL [reference range, 4.5–11×103/μL]) with absolute eosinophilia but no neutrophilia. C-reactive protein (CRP) was elevated (237.9 mg/L [reference range, 5.0–9.9 mg/L]). Renal and hepatic functions were normal. Blood cultures grew methicillin-sensitive Staphylococcus aureus (MSSA). Further infectious disease workup for viral and fungal pathogens was negative.

Skin biopsy from the left thigh revealed subcorneal, pustular, acute spongiotic dermatitis with marked intraepidermal spongiosis and papillary edema; exocytosis of eosinophils; and single cell necrosis of keratinocytes (Figure 2). These findings were consistent with acute generalized exanthematous pustulosis (AGEP). Pantoprazole was discontinued, and cardiovascular support and antibiotic therapy for MSSA bacteremia were initiated. Respiratory, kidney, and liver functions remained normal throughout the 11-day hospitalization, and the pustular dermatitis, MSSA bacteremia, and cardiovascular symptoms resolved within 10 days.

Acute generalized exanthematous pustulosis is an uncommon, self-limited, generalized sterile pustular eruption notable for the usual absence of systemic symptoms and extracutaneous organ involvement. Hotz et al1 found that mean peripheral neutrophil counts (mean, 21.5×103/μL) and CRP levels (mean, 241.6 mg/L) were notably elevated in patients with systemic (ie, hepatic, pulmonary, renal, bone marrow) involvement. In our patient, only the CRP approached the elevated value reported by Hotz et al.1 However, the patient exhibited only cardiovascular instability in the context of secondary bacteremia and no other systemic symptoms. The combination of highly elevated neutrophilia and CRP may be a better marker for AGEP-precipitated extracutaneous organ involvement.
Although infectious pathogens such as Epstein-Barr virus and cytomegalovirus have been implicated, the majority of AGEP cases are adverse reactions (ARs) to medications, such as β-lactam antibiotics. In our patient, the widely prescribed proton pump inhibitor (PPI) pantoprazole was the most likely cause. Acute generalized exanthematous pustulosis was reported in a patient taking another PPI, omeprazole.2 However, PPIs are recognized to cause many cutaneous and other organ ARs, though prevalence of ARs is still low. In Thailand, Chularojanamontri et al3 reported 13.8 per 100,000 individuals developed a cutaneous AR to PPIs, and the ARs most frequently were attributed to omeprazole. They found that drug exanthems were the most common cutaneous ARs.3 However, more severe hypersensitivity reactions have been reported, including Stevens-Johnson syndrome, toxic epidermal necrolysis, and autoimmune eruptions such as cutaneous lupus erythematosus.3,4 Other systemic reactions to PPIs include increased risks for urticaria, pneumonia, Clostridium difficile infections, and acute interstitial nephritis.4,5
- Hotz C, Valeyrie-Allanore L, Haddad C, et al. Systemic involvement of acute generalized exanthematous pustulosis: a retrospective study on 58 patients. Br J Dermatol. 2013;169:1223-1232.
- Nantes Castillejo O, Zozaya Urmeneta JM, Valcayo Peñalba A, et al. Acute generalized exanthematous pustulosis induced by omeprazole [in Spanish]. Gastroenterol Hepatol. 2008;31:295-298.
- Chularojanamontri L, Jiamton S, Manapajon A, et al. Cutaneous reactions to proton pump inhibitors: a case-control study. J Drugs Dermatol. 2012;11:E43-E47.
- Chang YS. Hypersensitivity reactions to proton pump inhibitors. Curr Opin Allergy Clin Immunol. 2012;12:348-353.
- Wilhelm SM, Rjater RG, Kale-Pradhan PB. Perils and pitfalls of long-term effects of proton pump inhibitors. Expert Rev Clin Pharmacol. 2013;6:443-551.
- Hotz C, Valeyrie-Allanore L, Haddad C, et al. Systemic involvement of acute generalized exanthematous pustulosis: a retrospective study on 58 patients. Br J Dermatol. 2013;169:1223-1232.
- Nantes Castillejo O, Zozaya Urmeneta JM, Valcayo Peñalba A, et al. Acute generalized exanthematous pustulosis induced by omeprazole [in Spanish]. Gastroenterol Hepatol. 2008;31:295-298.
- Chularojanamontri L, Jiamton S, Manapajon A, et al. Cutaneous reactions to proton pump inhibitors: a case-control study. J Drugs Dermatol. 2012;11:E43-E47.
- Chang YS. Hypersensitivity reactions to proton pump inhibitors. Curr Opin Allergy Clin Immunol. 2012;12:348-353.
- Wilhelm SM, Rjater RG, Kale-Pradhan PB. Perils and pitfalls of long-term effects of proton pump inhibitors. Expert Rev Clin Pharmacol. 2013;6:443-551.
Don’t trust interface dermatitis to diagnose dermatomyositis
ORLANDO – (DM), according to David Fiorentino, MD, PhD, professor of dermatology, rheumatology, and immunology at Stanford (Calif.) University.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Interface dermatitis on skin biopsy is “felt to be almost required by many people to make the diagnosis,” but he and his associates found that it was not present in about a quarter of a cohort of patients with DM. “We don’t want a clinician” to rule out the diagnosis based on its absence on a biopsy, “when its actually quite possible that the patient could have disease,” Dr. Fiorentino said at the International Conference on Cutaneous Lupus Erythematosus.
In general, skin biopsies in DM are tricky. “All of us take them, but we don’t really know how to interpret the information that comes back ... because we don’t really know how often many of [the associated] findings are seen” in DM patients, he noted.
One of the main concerns is to rule out lupus, but interface dermatitis is found in many of its cutaneous forms, as well as in graft-versus-host disease and other diseases.
So what’s a clinician to do? Fortunately, direct immunofluorescence can help. A positive lupus band test helps rule out DM, and the membrane attack complex helps rule it in, both with a good degree of certainty. In a video interview, Dr. Fiorentino explained these tests and how to use them.
Dr. Fiorentino had no relevant disclosures.
[email protected]
ORLANDO – (DM), according to David Fiorentino, MD, PhD, professor of dermatology, rheumatology, and immunology at Stanford (Calif.) University.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Interface dermatitis on skin biopsy is “felt to be almost required by many people to make the diagnosis,” but he and his associates found that it was not present in about a quarter of a cohort of patients with DM. “We don’t want a clinician” to rule out the diagnosis based on its absence on a biopsy, “when its actually quite possible that the patient could have disease,” Dr. Fiorentino said at the International Conference on Cutaneous Lupus Erythematosus.
In general, skin biopsies in DM are tricky. “All of us take them, but we don’t really know how to interpret the information that comes back ... because we don’t really know how often many of [the associated] findings are seen” in DM patients, he noted.
One of the main concerns is to rule out lupus, but interface dermatitis is found in many of its cutaneous forms, as well as in graft-versus-host disease and other diseases.
So what’s a clinician to do? Fortunately, direct immunofluorescence can help. A positive lupus band test helps rule out DM, and the membrane attack complex helps rule it in, both with a good degree of certainty. In a video interview, Dr. Fiorentino explained these tests and how to use them.
Dr. Fiorentino had no relevant disclosures.
[email protected]
ORLANDO – (DM), according to David Fiorentino, MD, PhD, professor of dermatology, rheumatology, and immunology at Stanford (Calif.) University.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Interface dermatitis on skin biopsy is “felt to be almost required by many people to make the diagnosis,” but he and his associates found that it was not present in about a quarter of a cohort of patients with DM. “We don’t want a clinician” to rule out the diagnosis based on its absence on a biopsy, “when its actually quite possible that the patient could have disease,” Dr. Fiorentino said at the International Conference on Cutaneous Lupus Erythematosus.
In general, skin biopsies in DM are tricky. “All of us take them, but we don’t really know how to interpret the information that comes back ... because we don’t really know how often many of [the associated] findings are seen” in DM patients, he noted.
One of the main concerns is to rule out lupus, but interface dermatitis is found in many of its cutaneous forms, as well as in graft-versus-host disease and other diseases.
So what’s a clinician to do? Fortunately, direct immunofluorescence can help. A positive lupus band test helps rule out DM, and the membrane attack complex helps rule it in, both with a good degree of certainty. In a video interview, Dr. Fiorentino explained these tests and how to use them.
Dr. Fiorentino had no relevant disclosures.
[email protected]
REPORTING FROM ICCLE 2018







