User login
Herceptin linked to doubling of HF risk in women with breast cancer
Adding more evidence to an ongoing debate, a large new study suggests that patients with breast cancer who take trastuzumab (Herceptin) may face double the adjusted risk of developing heart failure, with older women at highest risk.
The study also found that most patients who took trastuzumab didn’t receive recommended cardiac screening.
The researchers said their findings are unique because they tracked both younger and older patients. “By examining the rates of both cardiac monitoring and cardiotoxicity, we could begin to address the controversial issue of whether cardiac monitoring is warranted in young breast cancer patients,” wrote Mariana Chavez-MacGregor, MD, MSC, of the University of Texas MD Anderson Cancer Center, and her associates. The report was published in JACC: Cardiovascular Imaging.
While Trastuzumab has boosted breast cancer survival rates for patients with HER2-positive tumors, it’s also raised concerns about cardiotoxicity that could be an indicator of subsequent congestive heart failure (Cochrane Database Syst Rev. 2014 Jun 12;(6):CD006242).
According to the new study, the risk of trastuzumab risk is linked to damage to cardiac myocytes that can cause reversible cardiotoxicity.
The prescribing information for trastuzumab advises patients to undergo cardiac monitoring before treatment with trastuzumab and every 3 months during treatment. Recommendations by medical organizations have varied.
Now, as a 2016 report put it, it’s “increasingly unclear” whether frequent routine monitoring is appropriate for all patients (J Clin Oncol. 2016 Apr 1;34[10]:1030-3).
For the current study, Dr. Chavez-MacGregor and her associates identified 16,456 adult women in the United States who were diagnosed with nonmetastatic invasive breast cancer from 2009 to 2014. Researchers tracked the group, with a median age of 56, through as late as 2015.
The women were treated with chemotherapy within 6 months of diagnosis, and 4,325 received trastuzumab.
Of all the subjects, 692 patients (4.2%) developed heart failure following chemotherapy. The rate among patients treated with trastuzumab was higher, at 8.3%, compared with 2.7% for those not treated with trastuzumab (P less than .001).
The researchers also looked at anthracycline users and found that they were slightly more likely to develop HF (4.6% vs. 4.0% among nonusers, P = .048).
Increased age boosted the risk of HF in the trastuzumab-treated patients, and the risk was highest in those treated with both anthracyclines and trastuzumab. Other factors linked to more risk were comorbidities, hypertension, and valve disease.
After adjusting for confounders, the researchers estimated that those treated with trastuzumab were 2.01 times more likely to develop HF (HR, 2.01; 95% confidence interval, 1.72-2.36), and those who took anthracycline were 1.53 times more likely (HR, 1.53; 95% CI, 1.30-1.80)
The researchers also examined medical records for evidence that subjects underwent cardiac screening at least once every 4 months, not 3 months, as the prescribing information recommends. The study team chose to focus on 4-month intervals “to compensate for differences in scheduling, resources, or levels of accessibility to medical care.”
Medical records suggest that 73.5% of patients who took trastuzumab underwent cardiac screening at the beginning of therapy, but only 46.2% continued to do so at least every 4 months.
An adjusted model linked more screening to the use of anthracyclines and taxanes, radiation treatment, and living in the Northeast vs. the West.
“HF was more frequently identified among patients undergoing recommended cardiac monitoring (10.4% compared with 6.5%, respectively; P less than.001), suggesting that, as more patients are screened, more patients are likely to be found having HF,” the researchers reported.
However, they added that “our sensitivity analysis using inpatient claims allowed us to determine that the HF identified using cardiac monitoring was not severe enough to require hospitalization and was likely asymptomatic. The clinical implications of the diagnosis of asymptomatic HF are hard to determine and are beyond the scope of this study.”
The researchers also noted that the findings suggest that screening has become more common in recent years.
“The number of cancer survivors is expected to increase over time, and we will continue to see patients develop treatment-related cardiotoxicity,” the researchers wrote. “Thus, more research, evidence-based guidelines, and tools for prediction of cancer treatment–related cardiotoxicity are needed.”
The National Cancer Institute and Cancer Prevention and Research Institute of Texas funded the study. Two study authors reported grant funding from the Susan G. Komen Breast Cancer Foundation, and one reports consulting for Pfizer and Roche. The other authors reported no disclosures.
SOURCE: Chavez-MacGregor M et al. JACC: Cardiovasc Imaging. 2018 Aug;11[8]1084-93.
While trastuzumab clearly benefits patients with HER2-positive breast cancer at various stages of progression, concerns about heart failure persist. Studies have suggested that the drug doesn’t boost the risk of late cardiac events, but it’s not clear if this is due to mandated screening in these trials. The new study provides more evidence that adherence to screening guidelines is limited, and recent trials offer evidence that the general cardiac risk may be overblown. Future studies could be designed to offer insight into the wisdom of adjusting screening regimens based on stratification of risk. A meta-analysis could also be helpful, and the upcoming results of the SAFE-HEART study will provide information about the safety of anti-HER2 antibody therapy in patients with low but asymptomatic left-ventricular ejection fraction.
These comments are excerpted from a commentary by Chau T. Dang, MD, of Memorial Sloan Kettering Cancer Center, New York, and her associates (JACC: Cardiovasc Imaging. 2018 Aug;11[8]:1094-7). Most of the commentary authors report various disclosures.
While trastuzumab clearly benefits patients with HER2-positive breast cancer at various stages of progression, concerns about heart failure persist. Studies have suggested that the drug doesn’t boost the risk of late cardiac events, but it’s not clear if this is due to mandated screening in these trials. The new study provides more evidence that adherence to screening guidelines is limited, and recent trials offer evidence that the general cardiac risk may be overblown. Future studies could be designed to offer insight into the wisdom of adjusting screening regimens based on stratification of risk. A meta-analysis could also be helpful, and the upcoming results of the SAFE-HEART study will provide information about the safety of anti-HER2 antibody therapy in patients with low but asymptomatic left-ventricular ejection fraction.
These comments are excerpted from a commentary by Chau T. Dang, MD, of Memorial Sloan Kettering Cancer Center, New York, and her associates (JACC: Cardiovasc Imaging. 2018 Aug;11[8]:1094-7). Most of the commentary authors report various disclosures.
While trastuzumab clearly benefits patients with HER2-positive breast cancer at various stages of progression, concerns about heart failure persist. Studies have suggested that the drug doesn’t boost the risk of late cardiac events, but it’s not clear if this is due to mandated screening in these trials. The new study provides more evidence that adherence to screening guidelines is limited, and recent trials offer evidence that the general cardiac risk may be overblown. Future studies could be designed to offer insight into the wisdom of adjusting screening regimens based on stratification of risk. A meta-analysis could also be helpful, and the upcoming results of the SAFE-HEART study will provide information about the safety of anti-HER2 antibody therapy in patients with low but asymptomatic left-ventricular ejection fraction.
These comments are excerpted from a commentary by Chau T. Dang, MD, of Memorial Sloan Kettering Cancer Center, New York, and her associates (JACC: Cardiovasc Imaging. 2018 Aug;11[8]:1094-7). Most of the commentary authors report various disclosures.
Adding more evidence to an ongoing debate, a large new study suggests that patients with breast cancer who take trastuzumab (Herceptin) may face double the adjusted risk of developing heart failure, with older women at highest risk.
The study also found that most patients who took trastuzumab didn’t receive recommended cardiac screening.
The researchers said their findings are unique because they tracked both younger and older patients. “By examining the rates of both cardiac monitoring and cardiotoxicity, we could begin to address the controversial issue of whether cardiac monitoring is warranted in young breast cancer patients,” wrote Mariana Chavez-MacGregor, MD, MSC, of the University of Texas MD Anderson Cancer Center, and her associates. The report was published in JACC: Cardiovascular Imaging.
While Trastuzumab has boosted breast cancer survival rates for patients with HER2-positive tumors, it’s also raised concerns about cardiotoxicity that could be an indicator of subsequent congestive heart failure (Cochrane Database Syst Rev. 2014 Jun 12;(6):CD006242).
According to the new study, the risk of trastuzumab risk is linked to damage to cardiac myocytes that can cause reversible cardiotoxicity.
The prescribing information for trastuzumab advises patients to undergo cardiac monitoring before treatment with trastuzumab and every 3 months during treatment. Recommendations by medical organizations have varied.
Now, as a 2016 report put it, it’s “increasingly unclear” whether frequent routine monitoring is appropriate for all patients (J Clin Oncol. 2016 Apr 1;34[10]:1030-3).
For the current study, Dr. Chavez-MacGregor and her associates identified 16,456 adult women in the United States who were diagnosed with nonmetastatic invasive breast cancer from 2009 to 2014. Researchers tracked the group, with a median age of 56, through as late as 2015.
The women were treated with chemotherapy within 6 months of diagnosis, and 4,325 received trastuzumab.
Of all the subjects, 692 patients (4.2%) developed heart failure following chemotherapy. The rate among patients treated with trastuzumab was higher, at 8.3%, compared with 2.7% for those not treated with trastuzumab (P less than .001).
The researchers also looked at anthracycline users and found that they were slightly more likely to develop HF (4.6% vs. 4.0% among nonusers, P = .048).
Increased age boosted the risk of HF in the trastuzumab-treated patients, and the risk was highest in those treated with both anthracyclines and trastuzumab. Other factors linked to more risk were comorbidities, hypertension, and valve disease.
After adjusting for confounders, the researchers estimated that those treated with trastuzumab were 2.01 times more likely to develop HF (HR, 2.01; 95% confidence interval, 1.72-2.36), and those who took anthracycline were 1.53 times more likely (HR, 1.53; 95% CI, 1.30-1.80)
The researchers also examined medical records for evidence that subjects underwent cardiac screening at least once every 4 months, not 3 months, as the prescribing information recommends. The study team chose to focus on 4-month intervals “to compensate for differences in scheduling, resources, or levels of accessibility to medical care.”
Medical records suggest that 73.5% of patients who took trastuzumab underwent cardiac screening at the beginning of therapy, but only 46.2% continued to do so at least every 4 months.
An adjusted model linked more screening to the use of anthracyclines and taxanes, radiation treatment, and living in the Northeast vs. the West.
“HF was more frequently identified among patients undergoing recommended cardiac monitoring (10.4% compared with 6.5%, respectively; P less than.001), suggesting that, as more patients are screened, more patients are likely to be found having HF,” the researchers reported.
However, they added that “our sensitivity analysis using inpatient claims allowed us to determine that the HF identified using cardiac monitoring was not severe enough to require hospitalization and was likely asymptomatic. The clinical implications of the diagnosis of asymptomatic HF are hard to determine and are beyond the scope of this study.”
The researchers also noted that the findings suggest that screening has become more common in recent years.
“The number of cancer survivors is expected to increase over time, and we will continue to see patients develop treatment-related cardiotoxicity,” the researchers wrote. “Thus, more research, evidence-based guidelines, and tools for prediction of cancer treatment–related cardiotoxicity are needed.”
The National Cancer Institute and Cancer Prevention and Research Institute of Texas funded the study. Two study authors reported grant funding from the Susan G. Komen Breast Cancer Foundation, and one reports consulting for Pfizer and Roche. The other authors reported no disclosures.
SOURCE: Chavez-MacGregor M et al. JACC: Cardiovasc Imaging. 2018 Aug;11[8]1084-93.
Adding more evidence to an ongoing debate, a large new study suggests that patients with breast cancer who take trastuzumab (Herceptin) may face double the adjusted risk of developing heart failure, with older women at highest risk.
The study also found that most patients who took trastuzumab didn’t receive recommended cardiac screening.
The researchers said their findings are unique because they tracked both younger and older patients. “By examining the rates of both cardiac monitoring and cardiotoxicity, we could begin to address the controversial issue of whether cardiac monitoring is warranted in young breast cancer patients,” wrote Mariana Chavez-MacGregor, MD, MSC, of the University of Texas MD Anderson Cancer Center, and her associates. The report was published in JACC: Cardiovascular Imaging.
While Trastuzumab has boosted breast cancer survival rates for patients with HER2-positive tumors, it’s also raised concerns about cardiotoxicity that could be an indicator of subsequent congestive heart failure (Cochrane Database Syst Rev. 2014 Jun 12;(6):CD006242).
According to the new study, the risk of trastuzumab risk is linked to damage to cardiac myocytes that can cause reversible cardiotoxicity.
The prescribing information for trastuzumab advises patients to undergo cardiac monitoring before treatment with trastuzumab and every 3 months during treatment. Recommendations by medical organizations have varied.
Now, as a 2016 report put it, it’s “increasingly unclear” whether frequent routine monitoring is appropriate for all patients (J Clin Oncol. 2016 Apr 1;34[10]:1030-3).
For the current study, Dr. Chavez-MacGregor and her associates identified 16,456 adult women in the United States who were diagnosed with nonmetastatic invasive breast cancer from 2009 to 2014. Researchers tracked the group, with a median age of 56, through as late as 2015.
The women were treated with chemotherapy within 6 months of diagnosis, and 4,325 received trastuzumab.
Of all the subjects, 692 patients (4.2%) developed heart failure following chemotherapy. The rate among patients treated with trastuzumab was higher, at 8.3%, compared with 2.7% for those not treated with trastuzumab (P less than .001).
The researchers also looked at anthracycline users and found that they were slightly more likely to develop HF (4.6% vs. 4.0% among nonusers, P = .048).
Increased age boosted the risk of HF in the trastuzumab-treated patients, and the risk was highest in those treated with both anthracyclines and trastuzumab. Other factors linked to more risk were comorbidities, hypertension, and valve disease.
After adjusting for confounders, the researchers estimated that those treated with trastuzumab were 2.01 times more likely to develop HF (HR, 2.01; 95% confidence interval, 1.72-2.36), and those who took anthracycline were 1.53 times more likely (HR, 1.53; 95% CI, 1.30-1.80)
The researchers also examined medical records for evidence that subjects underwent cardiac screening at least once every 4 months, not 3 months, as the prescribing information recommends. The study team chose to focus on 4-month intervals “to compensate for differences in scheduling, resources, or levels of accessibility to medical care.”
Medical records suggest that 73.5% of patients who took trastuzumab underwent cardiac screening at the beginning of therapy, but only 46.2% continued to do so at least every 4 months.
An adjusted model linked more screening to the use of anthracyclines and taxanes, radiation treatment, and living in the Northeast vs. the West.
“HF was more frequently identified among patients undergoing recommended cardiac monitoring (10.4% compared with 6.5%, respectively; P less than.001), suggesting that, as more patients are screened, more patients are likely to be found having HF,” the researchers reported.
However, they added that “our sensitivity analysis using inpatient claims allowed us to determine that the HF identified using cardiac monitoring was not severe enough to require hospitalization and was likely asymptomatic. The clinical implications of the diagnosis of asymptomatic HF are hard to determine and are beyond the scope of this study.”
The researchers also noted that the findings suggest that screening has become more common in recent years.
“The number of cancer survivors is expected to increase over time, and we will continue to see patients develop treatment-related cardiotoxicity,” the researchers wrote. “Thus, more research, evidence-based guidelines, and tools for prediction of cancer treatment–related cardiotoxicity are needed.”
The National Cancer Institute and Cancer Prevention and Research Institute of Texas funded the study. Two study authors reported grant funding from the Susan G. Komen Breast Cancer Foundation, and one reports consulting for Pfizer and Roche. The other authors reported no disclosures.
SOURCE: Chavez-MacGregor M et al. JACC: Cardiovasc Imaging. 2018 Aug;11[8]1084-93.
FROM JACC: CARDIOVASCULAR IMAGING
Key clinical point: Women with breast cancer who take trastuzumab (Herceptin) may face double the adjusted risk of heart failure, but most aren’t screened frequently.
Major finding: Patients who took trastuzumab were 2.01 times more likely to develop HF (HR, 95% CI, 1.72-2.36) than were those who didn’t. Of all patients who took the drug, fewer than half received recommended frequency of screening.
Study details: Analysis of 16,456 U.S. adult women with nonmetastatic breast cancer diagnosed from 2009 to 2014 and tracked through 2015. Of those, 4.2% developed HF.
Disclosures: The National Cancer Institute and Cancer Prevention and Research Institute of Texas funded the study. Two study authors report grant funding from the Susan G. Komen Breast Cancer Foundation, and one reports consulting for Pfizer and Roche. The other authors report no disclosures.
Source: Chavez-MacGregor M et al. JACC: Cardiovasc Imaging 2018 Aug;11[8]1084-93.
FDA warning shines light on vaginal rejuvenation
The Food and Drug Administration has issued a stern warning to several manufacturers and a statement of caution to the public concerning “vaginal rejuvenation,” an umbrella term for a host of procedures to alter vaginal tissue for therapeutic or cosmetic purposes.
Lasers and other energy-based devices have been approved to treat abnormal or precancerous cervical or vaginal tissue and general warts, but the FDA has not approved any to treat vaginal atrophy, urinary incontinence, or reduced sexual function.
Device manufacturers claim lasers can address these conditions despite limited scientific evidence for their safety or efficacy. Insurers do not reimburse the procedures, considering them to be cosmetic.
In a July 30 statement, FDA Commissioner Scott Gottlieb, MD, slammed “deceptive” marketing practices on the part of manufacturers.
The FDA has reviewed 12 complaints since December 2015 of adverse effects related to vaginal procedures using the devices. Two were from manufacturers reporting pain and bleeding in patients following treatment, FDA spokeswoman Deborah Kotz said in an interview. “The FDA has also received voluntary MedWatch reports from individual patients who experienced significant pain and discomfort from procedures performed with these devices.”
The agency has targeted seven firms: Alma Lasers, BTL Aesthetics, BTL Industries, Cynosure, InMode, Sciton, and ThermiGen, with letters demanding evidence of FDA approval, clearance, or intent to seek clearance for use of their products on female genitalia. They also asked for evidence backing specific claims.
In a July 26 letter to BTL Industries, for example, the FDA demanded to know why the firm was marketing its Exilis laser device, approved for the treatment of facial wrinkles, as “Ultra Femme 360,” which it called “a whole new approach to women’s intimate health.” The device, according to the manufacturer, “provides the shortest noninvasive radio-frequency treatment available for female intimate parts” and “is proven to increase elastin and collagen in the treatment area.”
The FDA asked Cynosure, the maker of the Mona Lisa Touch, a system marketed as an FDA-approved treatment for vaginal atrophy, for evidence to support its claims that Mona Lisa Touch “is the only technology for vaginal and vulvar health with over 18+ published clinical studies” and is clinically proven to treat “painful symptoms of menopause, including intimacy.” They also asked for information about a modification to the originally approved device that was not brought to the FDA’s attention.
In a letter to Alma Lasers, whose Pixel CO2 Laser System was approved for use in a broad use of surgical applications including gynecologic surgery, the FDA noted that the device was being marketed as “FEMILIFT,” a laser procedure designed to “improve vaginal irregularities” and to assist “in vaginal mucosa revitalization.” The FDA demanded evidence for those claims.
The manufacturers have 30 days to respond to the FDA, which has not ruled out seeking enforcement action against firms with unsatisfactory responses.
For more than a decade, researchers have shown that healthy vaginal morphology is exceptionally wide ranging, including a recent study in more than 650 women, the largest to date (BJOG. 2018 Jun 25. doi: 10.1111/1471-0528.15387). Nonetheless, interest in elective vaginal procedures has only increased, with an industry report from the International Society of Aesthetic and Plastic Surgery describing a 45% increase in the use of one surgery, vaginal labiaplasty, between 2014 and 2016. Most procedures were performed in Brazil and the United States.
While plastic surgery societies support vaginal rejuvenation procedures, the American College of Obstetricians and Gynecologists has long frowned on them, with its first critique issued in a 2007 committee opinion. “No adequate studies have been published assessing the long-term satisfaction, safety, and complication rates for these procedures,” the association said last year in its most recent update on the subject.
Gynecologist David M. Jaspan, DO, of the Einstein Healthcare Network in Philadelphia, echoed ACOG’s views and said he welcomed FDA interest in vaginal rejuvenation.
The practice has “never been endorsed by the College or a board. It’s been considered a cosmetic procedure and it’s been under scrutiny for at least a decade,” Dr. Jaspan said. “I have reservations about the clinical outcomes and the training surrounds these procedures and I anxiously await randomized controlled trials to further evaluate them.”
Gynecologists who offer the procedures caution that they may have a role, and that randomized trials are underway to determine which groups of women might be best helped.
Marie Paraiso, MD, professor of obstetrics and gynecology at the Cleveland Clinic, said she uses the Mona Lisa Touch, a CO2 fractionated laser, to treat patients with genitourinary syndrome of menopause (GSM). These patients, Dr. Paraiso said, “complain of vaginal dryness and are unable to have intercourse or experience significant pain during or after intercourse. Some of them also may have irritative voiding, urinary frequency and urgency, or mild stress incontinence.”
Dr. Paraiso’s group has performed some 300 treatments with the laser and “we have fortunately not had patients complaining of persistent vaginal pain or scarring.” About 80%-90% of patients respond, she said, with some 20%-25% seeking retreatment within a year. “I believe for women who have contraindications to hormonal therapy or do not tolerate or cannot afford prolonged hormonal therapy, the CO2 fractional vaginal laser has been effective.”
Dr. Paraiso is also leading a multisite clinical trial randomizing about 200 patients with GSM to the laser treatment or estrogen-based vaginal creams, and following them for 6 months; thus far, she said, 6 of 89 patients, half in the laser arm, have reported mild to moderate adverse events.
Dr. Paraiso said she does not have a financial relationship with the manufacturer of Mona Lisa Touch, and that the trial was funded by the Foundation for Female Health Awareness, which receives unrestricted research grants from some device makers. “Our institute owns the laser and I have never been paid to train anyone to perform these procedures,” Dr. Paraiso added. “Our onus was to study the laser in order to improve the lives of our patients.”
Other trials comparing vaginal lasers with sham treatment are currently underway or in planning.
The North American Menopause Society struck a cautious note in response to the FDA criticism. In a statement issued August 1, JoAnn Pinkerton, MD, the society’s executive director, said the field needed prospective, randomized, sham-controlled trials of the laser and energy therapies. The therapies “may turn out to be an appropriate choice for many women, particularly for those concerned about breast cancer risk” associated with hormonal treatments. But until more robust data are available, doctors should “discuss the benefits and risks of all available treatment options for vaginal symptoms, including over-the-counter lubricants, vaginal moisturizers, and FDA-approved vaginal therapies such as vaginal estrogen and intravaginal dehydroepiandrosterone and oral therapies such as hormone therapy and ospemifene to determine the best treatment for women with GSM.”
Any discussion of vaginal energy-based therapies, should include the disclosure that these have not been approved for the specific indication, Dr. Pinkerton cautioned.
The term “vaginal rejuvenation,” coined by cosmetic gynecologists, incorporates surgeries designed to modify the appearance of the vulva, reduce the redundancy of vaginal tissue, and improve vaginal tone.
Endorsed by some well-known academic gynecologists, these devices have been promoted as “safe and effective” without any prospective, randomized studies and without accountability for conflicts of interest including “educational stipends” from device manufacturers and clinicians’ need to recoup the high cost of the devices themselves.
Studies have generally been limited to fewer than 100 patients followed for 12 weeks or less. Companies are not informing doctors that the devices may not be FDA approved for the purposes advertised, nor are they providing adverse effects reports. Laser and radio-frequency procedures at best demonstrate temporary, marginal improvement in vaginal tone and dyspareunia, and at worst are associated with increased pelvic pain and dyspareunia, as well as vaginal, rectal, and bladder thermal burns. For those of us who specialize in cosmetic surgery, they have very limited benefit with a significant risk of injury to the patient even when properly used.
Julio Cesar Novoa, MD, is a private practice ob.gyn from El Paso, Tex. He reported no relevant conflicts of interest.
The term “vaginal rejuvenation,” coined by cosmetic gynecologists, incorporates surgeries designed to modify the appearance of the vulva, reduce the redundancy of vaginal tissue, and improve vaginal tone.
Endorsed by some well-known academic gynecologists, these devices have been promoted as “safe and effective” without any prospective, randomized studies and without accountability for conflicts of interest including “educational stipends” from device manufacturers and clinicians’ need to recoup the high cost of the devices themselves.
Studies have generally been limited to fewer than 100 patients followed for 12 weeks or less. Companies are not informing doctors that the devices may not be FDA approved for the purposes advertised, nor are they providing adverse effects reports. Laser and radio-frequency procedures at best demonstrate temporary, marginal improvement in vaginal tone and dyspareunia, and at worst are associated with increased pelvic pain and dyspareunia, as well as vaginal, rectal, and bladder thermal burns. For those of us who specialize in cosmetic surgery, they have very limited benefit with a significant risk of injury to the patient even when properly used.
Julio Cesar Novoa, MD, is a private practice ob.gyn from El Paso, Tex. He reported no relevant conflicts of interest.
The term “vaginal rejuvenation,” coined by cosmetic gynecologists, incorporates surgeries designed to modify the appearance of the vulva, reduce the redundancy of vaginal tissue, and improve vaginal tone.
Endorsed by some well-known academic gynecologists, these devices have been promoted as “safe and effective” without any prospective, randomized studies and without accountability for conflicts of interest including “educational stipends” from device manufacturers and clinicians’ need to recoup the high cost of the devices themselves.
Studies have generally been limited to fewer than 100 patients followed for 12 weeks or less. Companies are not informing doctors that the devices may not be FDA approved for the purposes advertised, nor are they providing adverse effects reports. Laser and radio-frequency procedures at best demonstrate temporary, marginal improvement in vaginal tone and dyspareunia, and at worst are associated with increased pelvic pain and dyspareunia, as well as vaginal, rectal, and bladder thermal burns. For those of us who specialize in cosmetic surgery, they have very limited benefit with a significant risk of injury to the patient even when properly used.
Julio Cesar Novoa, MD, is a private practice ob.gyn from El Paso, Tex. He reported no relevant conflicts of interest.
The Food and Drug Administration has issued a stern warning to several manufacturers and a statement of caution to the public concerning “vaginal rejuvenation,” an umbrella term for a host of procedures to alter vaginal tissue for therapeutic or cosmetic purposes.
Lasers and other energy-based devices have been approved to treat abnormal or precancerous cervical or vaginal tissue and general warts, but the FDA has not approved any to treat vaginal atrophy, urinary incontinence, or reduced sexual function.
Device manufacturers claim lasers can address these conditions despite limited scientific evidence for their safety or efficacy. Insurers do not reimburse the procedures, considering them to be cosmetic.
In a July 30 statement, FDA Commissioner Scott Gottlieb, MD, slammed “deceptive” marketing practices on the part of manufacturers.
The FDA has reviewed 12 complaints since December 2015 of adverse effects related to vaginal procedures using the devices. Two were from manufacturers reporting pain and bleeding in patients following treatment, FDA spokeswoman Deborah Kotz said in an interview. “The FDA has also received voluntary MedWatch reports from individual patients who experienced significant pain and discomfort from procedures performed with these devices.”
The agency has targeted seven firms: Alma Lasers, BTL Aesthetics, BTL Industries, Cynosure, InMode, Sciton, and ThermiGen, with letters demanding evidence of FDA approval, clearance, or intent to seek clearance for use of their products on female genitalia. They also asked for evidence backing specific claims.
In a July 26 letter to BTL Industries, for example, the FDA demanded to know why the firm was marketing its Exilis laser device, approved for the treatment of facial wrinkles, as “Ultra Femme 360,” which it called “a whole new approach to women’s intimate health.” The device, according to the manufacturer, “provides the shortest noninvasive radio-frequency treatment available for female intimate parts” and “is proven to increase elastin and collagen in the treatment area.”
The FDA asked Cynosure, the maker of the Mona Lisa Touch, a system marketed as an FDA-approved treatment for vaginal atrophy, for evidence to support its claims that Mona Lisa Touch “is the only technology for vaginal and vulvar health with over 18+ published clinical studies” and is clinically proven to treat “painful symptoms of menopause, including intimacy.” They also asked for information about a modification to the originally approved device that was not brought to the FDA’s attention.
In a letter to Alma Lasers, whose Pixel CO2 Laser System was approved for use in a broad use of surgical applications including gynecologic surgery, the FDA noted that the device was being marketed as “FEMILIFT,” a laser procedure designed to “improve vaginal irregularities” and to assist “in vaginal mucosa revitalization.” The FDA demanded evidence for those claims.
The manufacturers have 30 days to respond to the FDA, which has not ruled out seeking enforcement action against firms with unsatisfactory responses.
For more than a decade, researchers have shown that healthy vaginal morphology is exceptionally wide ranging, including a recent study in more than 650 women, the largest to date (BJOG. 2018 Jun 25. doi: 10.1111/1471-0528.15387). Nonetheless, interest in elective vaginal procedures has only increased, with an industry report from the International Society of Aesthetic and Plastic Surgery describing a 45% increase in the use of one surgery, vaginal labiaplasty, between 2014 and 2016. Most procedures were performed in Brazil and the United States.
While plastic surgery societies support vaginal rejuvenation procedures, the American College of Obstetricians and Gynecologists has long frowned on them, with its first critique issued in a 2007 committee opinion. “No adequate studies have been published assessing the long-term satisfaction, safety, and complication rates for these procedures,” the association said last year in its most recent update on the subject.
Gynecologist David M. Jaspan, DO, of the Einstein Healthcare Network in Philadelphia, echoed ACOG’s views and said he welcomed FDA interest in vaginal rejuvenation.
The practice has “never been endorsed by the College or a board. It’s been considered a cosmetic procedure and it’s been under scrutiny for at least a decade,” Dr. Jaspan said. “I have reservations about the clinical outcomes and the training surrounds these procedures and I anxiously await randomized controlled trials to further evaluate them.”
Gynecologists who offer the procedures caution that they may have a role, and that randomized trials are underway to determine which groups of women might be best helped.
Marie Paraiso, MD, professor of obstetrics and gynecology at the Cleveland Clinic, said she uses the Mona Lisa Touch, a CO2 fractionated laser, to treat patients with genitourinary syndrome of menopause (GSM). These patients, Dr. Paraiso said, “complain of vaginal dryness and are unable to have intercourse or experience significant pain during or after intercourse. Some of them also may have irritative voiding, urinary frequency and urgency, or mild stress incontinence.”
Dr. Paraiso’s group has performed some 300 treatments with the laser and “we have fortunately not had patients complaining of persistent vaginal pain or scarring.” About 80%-90% of patients respond, she said, with some 20%-25% seeking retreatment within a year. “I believe for women who have contraindications to hormonal therapy or do not tolerate or cannot afford prolonged hormonal therapy, the CO2 fractional vaginal laser has been effective.”
Dr. Paraiso is also leading a multisite clinical trial randomizing about 200 patients with GSM to the laser treatment or estrogen-based vaginal creams, and following them for 6 months; thus far, she said, 6 of 89 patients, half in the laser arm, have reported mild to moderate adverse events.
Dr. Paraiso said she does not have a financial relationship with the manufacturer of Mona Lisa Touch, and that the trial was funded by the Foundation for Female Health Awareness, which receives unrestricted research grants from some device makers. “Our institute owns the laser and I have never been paid to train anyone to perform these procedures,” Dr. Paraiso added. “Our onus was to study the laser in order to improve the lives of our patients.”
Other trials comparing vaginal lasers with sham treatment are currently underway or in planning.
The North American Menopause Society struck a cautious note in response to the FDA criticism. In a statement issued August 1, JoAnn Pinkerton, MD, the society’s executive director, said the field needed prospective, randomized, sham-controlled trials of the laser and energy therapies. The therapies “may turn out to be an appropriate choice for many women, particularly for those concerned about breast cancer risk” associated with hormonal treatments. But until more robust data are available, doctors should “discuss the benefits and risks of all available treatment options for vaginal symptoms, including over-the-counter lubricants, vaginal moisturizers, and FDA-approved vaginal therapies such as vaginal estrogen and intravaginal dehydroepiandrosterone and oral therapies such as hormone therapy and ospemifene to determine the best treatment for women with GSM.”
Any discussion of vaginal energy-based therapies, should include the disclosure that these have not been approved for the specific indication, Dr. Pinkerton cautioned.
The Food and Drug Administration has issued a stern warning to several manufacturers and a statement of caution to the public concerning “vaginal rejuvenation,” an umbrella term for a host of procedures to alter vaginal tissue for therapeutic or cosmetic purposes.
Lasers and other energy-based devices have been approved to treat abnormal or precancerous cervical or vaginal tissue and general warts, but the FDA has not approved any to treat vaginal atrophy, urinary incontinence, or reduced sexual function.
Device manufacturers claim lasers can address these conditions despite limited scientific evidence for their safety or efficacy. Insurers do not reimburse the procedures, considering them to be cosmetic.
In a July 30 statement, FDA Commissioner Scott Gottlieb, MD, slammed “deceptive” marketing practices on the part of manufacturers.
The FDA has reviewed 12 complaints since December 2015 of adverse effects related to vaginal procedures using the devices. Two were from manufacturers reporting pain and bleeding in patients following treatment, FDA spokeswoman Deborah Kotz said in an interview. “The FDA has also received voluntary MedWatch reports from individual patients who experienced significant pain and discomfort from procedures performed with these devices.”
The agency has targeted seven firms: Alma Lasers, BTL Aesthetics, BTL Industries, Cynosure, InMode, Sciton, and ThermiGen, with letters demanding evidence of FDA approval, clearance, or intent to seek clearance for use of their products on female genitalia. They also asked for evidence backing specific claims.
In a July 26 letter to BTL Industries, for example, the FDA demanded to know why the firm was marketing its Exilis laser device, approved for the treatment of facial wrinkles, as “Ultra Femme 360,” which it called “a whole new approach to women’s intimate health.” The device, according to the manufacturer, “provides the shortest noninvasive radio-frequency treatment available for female intimate parts” and “is proven to increase elastin and collagen in the treatment area.”
The FDA asked Cynosure, the maker of the Mona Lisa Touch, a system marketed as an FDA-approved treatment for vaginal atrophy, for evidence to support its claims that Mona Lisa Touch “is the only technology for vaginal and vulvar health with over 18+ published clinical studies” and is clinically proven to treat “painful symptoms of menopause, including intimacy.” They also asked for information about a modification to the originally approved device that was not brought to the FDA’s attention.
In a letter to Alma Lasers, whose Pixel CO2 Laser System was approved for use in a broad use of surgical applications including gynecologic surgery, the FDA noted that the device was being marketed as “FEMILIFT,” a laser procedure designed to “improve vaginal irregularities” and to assist “in vaginal mucosa revitalization.” The FDA demanded evidence for those claims.
The manufacturers have 30 days to respond to the FDA, which has not ruled out seeking enforcement action against firms with unsatisfactory responses.
For more than a decade, researchers have shown that healthy vaginal morphology is exceptionally wide ranging, including a recent study in more than 650 women, the largest to date (BJOG. 2018 Jun 25. doi: 10.1111/1471-0528.15387). Nonetheless, interest in elective vaginal procedures has only increased, with an industry report from the International Society of Aesthetic and Plastic Surgery describing a 45% increase in the use of one surgery, vaginal labiaplasty, between 2014 and 2016. Most procedures were performed in Brazil and the United States.
While plastic surgery societies support vaginal rejuvenation procedures, the American College of Obstetricians and Gynecologists has long frowned on them, with its first critique issued in a 2007 committee opinion. “No adequate studies have been published assessing the long-term satisfaction, safety, and complication rates for these procedures,” the association said last year in its most recent update on the subject.
Gynecologist David M. Jaspan, DO, of the Einstein Healthcare Network in Philadelphia, echoed ACOG’s views and said he welcomed FDA interest in vaginal rejuvenation.
The practice has “never been endorsed by the College or a board. It’s been considered a cosmetic procedure and it’s been under scrutiny for at least a decade,” Dr. Jaspan said. “I have reservations about the clinical outcomes and the training surrounds these procedures and I anxiously await randomized controlled trials to further evaluate them.”
Gynecologists who offer the procedures caution that they may have a role, and that randomized trials are underway to determine which groups of women might be best helped.
Marie Paraiso, MD, professor of obstetrics and gynecology at the Cleveland Clinic, said she uses the Mona Lisa Touch, a CO2 fractionated laser, to treat patients with genitourinary syndrome of menopause (GSM). These patients, Dr. Paraiso said, “complain of vaginal dryness and are unable to have intercourse or experience significant pain during or after intercourse. Some of them also may have irritative voiding, urinary frequency and urgency, or mild stress incontinence.”
Dr. Paraiso’s group has performed some 300 treatments with the laser and “we have fortunately not had patients complaining of persistent vaginal pain or scarring.” About 80%-90% of patients respond, she said, with some 20%-25% seeking retreatment within a year. “I believe for women who have contraindications to hormonal therapy or do not tolerate or cannot afford prolonged hormonal therapy, the CO2 fractional vaginal laser has been effective.”
Dr. Paraiso is also leading a multisite clinical trial randomizing about 200 patients with GSM to the laser treatment or estrogen-based vaginal creams, and following them for 6 months; thus far, she said, 6 of 89 patients, half in the laser arm, have reported mild to moderate adverse events.
Dr. Paraiso said she does not have a financial relationship with the manufacturer of Mona Lisa Touch, and that the trial was funded by the Foundation for Female Health Awareness, which receives unrestricted research grants from some device makers. “Our institute owns the laser and I have never been paid to train anyone to perform these procedures,” Dr. Paraiso added. “Our onus was to study the laser in order to improve the lives of our patients.”
Other trials comparing vaginal lasers with sham treatment are currently underway or in planning.
The North American Menopause Society struck a cautious note in response to the FDA criticism. In a statement issued August 1, JoAnn Pinkerton, MD, the society’s executive director, said the field needed prospective, randomized, sham-controlled trials of the laser and energy therapies. The therapies “may turn out to be an appropriate choice for many women, particularly for those concerned about breast cancer risk” associated with hormonal treatments. But until more robust data are available, doctors should “discuss the benefits and risks of all available treatment options for vaginal symptoms, including over-the-counter lubricants, vaginal moisturizers, and FDA-approved vaginal therapies such as vaginal estrogen and intravaginal dehydroepiandrosterone and oral therapies such as hormone therapy and ospemifene to determine the best treatment for women with GSM.”
Any discussion of vaginal energy-based therapies, should include the disclosure that these have not been approved for the specific indication, Dr. Pinkerton cautioned.
CMS proposal to level E/M payments raises concerns
Citing the need to reduce paperwork hassles, officials at the Centers for Medicare & Medicaid Services are proposing to flatten the payment for evaluation and management (E/M) visits coded at levels 2-5.
The CMS outlined how the proposal would affect payment using 2018 rates to model the change. The proposal would set the payment rate for level 1 E/M office visits for new patients at $44, down from the $45 using the current methodology. Levels 2-5 would receive $135. Currently, payments for level 2 visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For office visits with established patients, the proposed rate would be $24, up from the current payment of $22 for a level 1 visit. Levels 2-5 would receive $93. Under the current methodology, payments for level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
The change also comes with a reduced documentation burden, so the same documentation is needed regardless of which level between 2 and 5 the office visit is, a move that is expected to save some time each day.
The CMS outlined its vision for changes to the E/M payment in the proposed update to the 2019 Medicare physician fee schedule. Comments on the proposal are due Sept. 10, 2018.
The agency estimated that for most specialties, there would be minimal effect on this proposed change. However, for 10 specialties, payment reductions could result from this change.
Specialties identified as potentially losing less than 3% of their overall payment include allergy/immunology, audiologists, hematology/oncology, neurology, otolaryngology, pulmonary disease, and radiation oncology and radiation therapy centers.
Rheumatologists are expected to lose 3% of their pay from the proposal, while dermatologists and podiatrists are expected to lose 4%.
On the flip side, obstetricians/gynecologists are expected to see a 4% bump because of this proposal, while nurse practitioners could see a 3% increase. Specialties expected to see an increase of less than 3% include hand surgery, interventional pain management, optometry, physician assistants, psychiatry, and urology.
The proposal is raising concerns, particularly from those who stand to see their pay reduced by the proposal.
CMS "has proposed a disastrous plan that would force most neurologists not just to abandon Medicare participation, but also to refuse treatment to Medicare patients," Marc Raphaelson, MD, chair of the American Academy of Neurology's Coding Subcommittee and the Academy's representative to the Relative Value Scale Update Committee, wrote in a report. "The AAN is responding vigorously that one size does not fit all. One visit type does not fit our patients or our practices. Neurologists could not sustain our practices at the proposed payment rates."
Dr. Raphaelson noted that the AAN applauds the agency's "willingness to abandon medically irrelevant charting that contributes to our frustration and burnout. CMS has brought payment and documentation reform into a bright light. In return, it is up to the AAN, and our collegial medical societies, to propose a fair and transparent way to pay doctors for the work we really do."
The AAN recently joined the Americal College of Rheumatology (ACR) on Capitol Hill to raise awareness of the proposed cuts.
“Rheumatologists are pretty concerned about this,” Angus B. Worthing, MD, chair of the ACR’s Committee on Government Affairs, said in an interview. “Being a cognitive specialty ... we see patients who have complex or multiple issues and we focus more in the clinic on cognitive services, instead of procedural services.” He noted that rheumatologists bill across the E/M levels so it would be difficult to suggest a flat fee that would keep them from losing money.
Dr. Worthing, whose practice is in the Washington, D.C., metro area, said that about 70% of the Medicare payment covers overhead for the practice, leaving 30% to go toward the rheumatologist’s salary. To illustrate the impact of the proposed 3% cut, Dr. Worthing used the hypothetical of a current $100 payment turning into a $97 payment under the proposal. The overhead doesn’t change, so the physician’s portion that goes toward his salary drops 10% when it decreases from $30 to $27.
The Community Oncology Alliance made a similar observation.
“CMS is proposing to drastically cut payment for the critical evaluation and management of more complex cancer cases from $172 to $135 (a 22% payment cut) for a new patient and from $148 to $93 (a 37% payment cut) for an existing patient. Although CMS is proposing to streamline the reporting of these cases, the proposal severely undervalues the thorough and critical evaluation and management of seniors with cancer, especially life-threatening complex cases,” the organization said in a statement.
Dr. Worthing said the proposal has implications for recruiting medical trainees into rheumatology and for physicians in practice who may be considering whether to stop seeing Medicare patients. “Since we already have a shortage of rheumatologists in the U.S. that, per the ACR’s recent study, appears to be worsening, we are pretty concerned that if this proposal is finalized, we could be facing a situation with longer wait times to see a rheumatologist,” he said.
But Dr. Worthing praised the proposed reduction of documentation and said that it could save physicians some time. “If this proposal were finalized, I might be able to spend a minute or two less typing or documenting in a typical patient visit,” he said. “That might add up over time to seeing more patients.”
CMS officials estimate the proposal would save a lot more time. CMS Administrator Seema Verma said that the documentation change would result in an additional 51 hours for patient care per clinician per year.
However, Dr. Worthing said he was doubtful that any increase in volume would offset the losses from the proposed flat payment across levels 2-5 E/M visits, especially if the pay decrease results in access issues. “If doctors were seeing less and having a harder time covering their business expenses seeing Medicare patients, they might be incentivized to see more commercially insured patients and maintain their practice’s viability that way and not participate in Medicare anymore,” he said.
***This story was updated 8/8/2018.
SOURCE: CMS proposed rule, CMS-1693-P.
Citing the need to reduce paperwork hassles, officials at the Centers for Medicare & Medicaid Services are proposing to flatten the payment for evaluation and management (E/M) visits coded at levels 2-5.
The CMS outlined how the proposal would affect payment using 2018 rates to model the change. The proposal would set the payment rate for level 1 E/M office visits for new patients at $44, down from the $45 using the current methodology. Levels 2-5 would receive $135. Currently, payments for level 2 visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For office visits with established patients, the proposed rate would be $24, up from the current payment of $22 for a level 1 visit. Levels 2-5 would receive $93. Under the current methodology, payments for level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
The change also comes with a reduced documentation burden, so the same documentation is needed regardless of which level between 2 and 5 the office visit is, a move that is expected to save some time each day.
The CMS outlined its vision for changes to the E/M payment in the proposed update to the 2019 Medicare physician fee schedule. Comments on the proposal are due Sept. 10, 2018.
The agency estimated that for most specialties, there would be minimal effect on this proposed change. However, for 10 specialties, payment reductions could result from this change.
Specialties identified as potentially losing less than 3% of their overall payment include allergy/immunology, audiologists, hematology/oncology, neurology, otolaryngology, pulmonary disease, and radiation oncology and radiation therapy centers.
Rheumatologists are expected to lose 3% of their pay from the proposal, while dermatologists and podiatrists are expected to lose 4%.
On the flip side, obstetricians/gynecologists are expected to see a 4% bump because of this proposal, while nurse practitioners could see a 3% increase. Specialties expected to see an increase of less than 3% include hand surgery, interventional pain management, optometry, physician assistants, psychiatry, and urology.
The proposal is raising concerns, particularly from those who stand to see their pay reduced by the proposal.
CMS "has proposed a disastrous plan that would force most neurologists not just to abandon Medicare participation, but also to refuse treatment to Medicare patients," Marc Raphaelson, MD, chair of the American Academy of Neurology's Coding Subcommittee and the Academy's representative to the Relative Value Scale Update Committee, wrote in a report. "The AAN is responding vigorously that one size does not fit all. One visit type does not fit our patients or our practices. Neurologists could not sustain our practices at the proposed payment rates."
Dr. Raphaelson noted that the AAN applauds the agency's "willingness to abandon medically irrelevant charting that contributes to our frustration and burnout. CMS has brought payment and documentation reform into a bright light. In return, it is up to the AAN, and our collegial medical societies, to propose a fair and transparent way to pay doctors for the work we really do."
The AAN recently joined the Americal College of Rheumatology (ACR) on Capitol Hill to raise awareness of the proposed cuts.
“Rheumatologists are pretty concerned about this,” Angus B. Worthing, MD, chair of the ACR’s Committee on Government Affairs, said in an interview. “Being a cognitive specialty ... we see patients who have complex or multiple issues and we focus more in the clinic on cognitive services, instead of procedural services.” He noted that rheumatologists bill across the E/M levels so it would be difficult to suggest a flat fee that would keep them from losing money.
Dr. Worthing, whose practice is in the Washington, D.C., metro area, said that about 70% of the Medicare payment covers overhead for the practice, leaving 30% to go toward the rheumatologist’s salary. To illustrate the impact of the proposed 3% cut, Dr. Worthing used the hypothetical of a current $100 payment turning into a $97 payment under the proposal. The overhead doesn’t change, so the physician’s portion that goes toward his salary drops 10% when it decreases from $30 to $27.
The Community Oncology Alliance made a similar observation.
“CMS is proposing to drastically cut payment for the critical evaluation and management of more complex cancer cases from $172 to $135 (a 22% payment cut) for a new patient and from $148 to $93 (a 37% payment cut) for an existing patient. Although CMS is proposing to streamline the reporting of these cases, the proposal severely undervalues the thorough and critical evaluation and management of seniors with cancer, especially life-threatening complex cases,” the organization said in a statement.
Dr. Worthing said the proposal has implications for recruiting medical trainees into rheumatology and for physicians in practice who may be considering whether to stop seeing Medicare patients. “Since we already have a shortage of rheumatologists in the U.S. that, per the ACR’s recent study, appears to be worsening, we are pretty concerned that if this proposal is finalized, we could be facing a situation with longer wait times to see a rheumatologist,” he said.
But Dr. Worthing praised the proposed reduction of documentation and said that it could save physicians some time. “If this proposal were finalized, I might be able to spend a minute or two less typing or documenting in a typical patient visit,” he said. “That might add up over time to seeing more patients.”
CMS officials estimate the proposal would save a lot more time. CMS Administrator Seema Verma said that the documentation change would result in an additional 51 hours for patient care per clinician per year.
However, Dr. Worthing said he was doubtful that any increase in volume would offset the losses from the proposed flat payment across levels 2-5 E/M visits, especially if the pay decrease results in access issues. “If doctors were seeing less and having a harder time covering their business expenses seeing Medicare patients, they might be incentivized to see more commercially insured patients and maintain their practice’s viability that way and not participate in Medicare anymore,” he said.
***This story was updated 8/8/2018.
SOURCE: CMS proposed rule, CMS-1693-P.
Citing the need to reduce paperwork hassles, officials at the Centers for Medicare & Medicaid Services are proposing to flatten the payment for evaluation and management (E/M) visits coded at levels 2-5.
The CMS outlined how the proposal would affect payment using 2018 rates to model the change. The proposal would set the payment rate for level 1 E/M office visits for new patients at $44, down from the $45 using the current methodology. Levels 2-5 would receive $135. Currently, payments for level 2 visits are set at $76, level 3 at $110, level 4 at $167, and level 5 at $211.
For office visits with established patients, the proposed rate would be $24, up from the current payment of $22 for a level 1 visit. Levels 2-5 would receive $93. Under the current methodology, payments for level 2 visits are set at $45, level 3 at $74, level 4 at $109, and level 5 at $148.
The change also comes with a reduced documentation burden, so the same documentation is needed regardless of which level between 2 and 5 the office visit is, a move that is expected to save some time each day.
The CMS outlined its vision for changes to the E/M payment in the proposed update to the 2019 Medicare physician fee schedule. Comments on the proposal are due Sept. 10, 2018.
The agency estimated that for most specialties, there would be minimal effect on this proposed change. However, for 10 specialties, payment reductions could result from this change.
Specialties identified as potentially losing less than 3% of their overall payment include allergy/immunology, audiologists, hematology/oncology, neurology, otolaryngology, pulmonary disease, and radiation oncology and radiation therapy centers.
Rheumatologists are expected to lose 3% of their pay from the proposal, while dermatologists and podiatrists are expected to lose 4%.
On the flip side, obstetricians/gynecologists are expected to see a 4% bump because of this proposal, while nurse practitioners could see a 3% increase. Specialties expected to see an increase of less than 3% include hand surgery, interventional pain management, optometry, physician assistants, psychiatry, and urology.
The proposal is raising concerns, particularly from those who stand to see their pay reduced by the proposal.
CMS "has proposed a disastrous plan that would force most neurologists not just to abandon Medicare participation, but also to refuse treatment to Medicare patients," Marc Raphaelson, MD, chair of the American Academy of Neurology's Coding Subcommittee and the Academy's representative to the Relative Value Scale Update Committee, wrote in a report. "The AAN is responding vigorously that one size does not fit all. One visit type does not fit our patients or our practices. Neurologists could not sustain our practices at the proposed payment rates."
Dr. Raphaelson noted that the AAN applauds the agency's "willingness to abandon medically irrelevant charting that contributes to our frustration and burnout. CMS has brought payment and documentation reform into a bright light. In return, it is up to the AAN, and our collegial medical societies, to propose a fair and transparent way to pay doctors for the work we really do."
The AAN recently joined the Americal College of Rheumatology (ACR) on Capitol Hill to raise awareness of the proposed cuts.
“Rheumatologists are pretty concerned about this,” Angus B. Worthing, MD, chair of the ACR’s Committee on Government Affairs, said in an interview. “Being a cognitive specialty ... we see patients who have complex or multiple issues and we focus more in the clinic on cognitive services, instead of procedural services.” He noted that rheumatologists bill across the E/M levels so it would be difficult to suggest a flat fee that would keep them from losing money.
Dr. Worthing, whose practice is in the Washington, D.C., metro area, said that about 70% of the Medicare payment covers overhead for the practice, leaving 30% to go toward the rheumatologist’s salary. To illustrate the impact of the proposed 3% cut, Dr. Worthing used the hypothetical of a current $100 payment turning into a $97 payment under the proposal. The overhead doesn’t change, so the physician’s portion that goes toward his salary drops 10% when it decreases from $30 to $27.
The Community Oncology Alliance made a similar observation.
“CMS is proposing to drastically cut payment for the critical evaluation and management of more complex cancer cases from $172 to $135 (a 22% payment cut) for a new patient and from $148 to $93 (a 37% payment cut) for an existing patient. Although CMS is proposing to streamline the reporting of these cases, the proposal severely undervalues the thorough and critical evaluation and management of seniors with cancer, especially life-threatening complex cases,” the organization said in a statement.
Dr. Worthing said the proposal has implications for recruiting medical trainees into rheumatology and for physicians in practice who may be considering whether to stop seeing Medicare patients. “Since we already have a shortage of rheumatologists in the U.S. that, per the ACR’s recent study, appears to be worsening, we are pretty concerned that if this proposal is finalized, we could be facing a situation with longer wait times to see a rheumatologist,” he said.
But Dr. Worthing praised the proposed reduction of documentation and said that it could save physicians some time. “If this proposal were finalized, I might be able to spend a minute or two less typing or documenting in a typical patient visit,” he said. “That might add up over time to seeing more patients.”
CMS officials estimate the proposal would save a lot more time. CMS Administrator Seema Verma said that the documentation change would result in an additional 51 hours for patient care per clinician per year.
However, Dr. Worthing said he was doubtful that any increase in volume would offset the losses from the proposed flat payment across levels 2-5 E/M visits, especially if the pay decrease results in access issues. “If doctors were seeing less and having a harder time covering their business expenses seeing Medicare patients, they might be incentivized to see more commercially insured patients and maintain their practice’s viability that way and not participate in Medicare anymore,” he said.
***This story was updated 8/8/2018.
SOURCE: CMS proposed rule, CMS-1693-P.
Key clinical point: Some specialties would be paid less under proposed payment changes for 2019.
Major finding: New patient visits (levels 2-5) would be paid at $135 and established patient visits (levels 2-5) would be paid at $93.
Study details: The physician fee schedule proposal would pay level 2-5 E/M visits at the same rate, and reduce some documentation requirements.
Disclosures: No relevant financial disclosures were reported.
Source: CMS proposed rule, CMS-1693-P.
Medical associations want withdrawal of Title X changes
Leading medical societies are calling on the Trump administration to withdraw its proposed changes to the federal Title X family planning program, calling the modifications a threat to essential health care for women.
In late May, the Department of Health & Human Services proposed broad changes to Title X, including no longer allowing staff at Title X clinics to counsel, refer, or provide information to women about abortions and mandating that Title X clinics that offer abortions maintain a separate facility for abortion services. The proposed changes aim to “refocus” the Title X program and ensure that all Title X services align with its family planning mission, according to the proposed rule published June 1.
In a July 31 letter to HHS, the American Medical Association requested that HHS withdraw the proposal, citing concerns from the medical community.
“We are very concerned that the proposed changes, if implemented, would undermine patients’ access to high-quality medical care and information, dangerously interfere with the patient-physician relationship and conflict with physicians’ ethical obligations, exclude qualified providers, and jeopardize public health,” James L. Madara, MD, chief executive officer and vice president of the AMA, wrote in a letter. “We urge HHS to withdraw this [proposal].”
The American College of Obstetricians and Gynecologists, the American College of Physicians, the American Academy of Pediatrics, the American Psychiatric Association, and 13 other health care associations also have called on the HHS to rescind its proposed rule. According to a statement from these associations, the proposal endangers women’s lives by restricting access to medically accurate information and preventive health care.
Title X is a long-standing federal program that provides funding for women’s health care and comprehensive family planning services, primarily to low-income and uninsured patients. Federal law prohibits the use of Title X funds to pay for abortions.
Under the proposed regulations, the Trump administration would define “family planning” as the voluntary process of identifying goals and developing a plan for the number and spacing of children and the means by which those goals may be achieved. This includes planning methods and services “to limit or enhance the likelihood of conception, including contraceptive methods and natural family planning or other fertility awareness-based methods,” according to the proposal. HHS specifies that family planning does not include postconception care, obstetric or prenatal care, or abortion as a method of family planning. HHS has proposed that, if a woman comes to a Title X–funded clinic and is pregnant, she be referred externally for pregnancy services. However, the proposed rule would no longer allow Title X programs to provide abortion counseling and/or referral.
According to HHS, requiring separate facilities for abortion-related care would ensure that Title X funds are used for the purposes expressly mandated by Congress – to offer family planning methods and services – and that any infrastructure built with Title X funds would not be used for impermissible purposes.
More than 100,000 comments have been submitted on the proposed rule since June. Antiabortion organizations, such as the Susan B. Anthony List, have expressed strong support for the proposed rule.
“The American people have repeatedly expressed their predominant policy preferences by supporting Congressional enactments designed to distinguish and separate abortion from family planning,” SBA List President Marjorie Dannenfelser wrote in a comment. “Abortion is not health care, nor is abortion family planning. The Clinton administration and subsequent presidential administrations have erroneously allowed the blatant distribution of Title X funding to abortion centers and abortion-referral facilities for years and in direct violation of the original purpose of Title X funding.”
A group of 14 state governors, meanwhile, has threatened legal action if the Trump administration moves forward with finalizing its rule. In a May 31 letter, the 14 Democratic governors urged HHS to halt its changes to the Title X program and said they would explore all options, including legal avenues, to protect patients’ access to care. More recently, Democratic governors in Washington, Oregon, Hawaii, and New York have said they will refuse all Title X funding if the Trump administration does not rescind its proposed changes to the program.
“This is not an issue about life or choices. This is an issue about the rights of millions of individuals who deserve the best health care available,” Hawaii governor David Ige said in a July 30 statement. “Hawaii will not accept federal funds for these programs if the proposed rules are implemented.”
Public comment on the proposed rule closed on July 31.
Leading medical societies are calling on the Trump administration to withdraw its proposed changes to the federal Title X family planning program, calling the modifications a threat to essential health care for women.
In late May, the Department of Health & Human Services proposed broad changes to Title X, including no longer allowing staff at Title X clinics to counsel, refer, or provide information to women about abortions and mandating that Title X clinics that offer abortions maintain a separate facility for abortion services. The proposed changes aim to “refocus” the Title X program and ensure that all Title X services align with its family planning mission, according to the proposed rule published June 1.
In a July 31 letter to HHS, the American Medical Association requested that HHS withdraw the proposal, citing concerns from the medical community.
“We are very concerned that the proposed changes, if implemented, would undermine patients’ access to high-quality medical care and information, dangerously interfere with the patient-physician relationship and conflict with physicians’ ethical obligations, exclude qualified providers, and jeopardize public health,” James L. Madara, MD, chief executive officer and vice president of the AMA, wrote in a letter. “We urge HHS to withdraw this [proposal].”
The American College of Obstetricians and Gynecologists, the American College of Physicians, the American Academy of Pediatrics, the American Psychiatric Association, and 13 other health care associations also have called on the HHS to rescind its proposed rule. According to a statement from these associations, the proposal endangers women’s lives by restricting access to medically accurate information and preventive health care.
Title X is a long-standing federal program that provides funding for women’s health care and comprehensive family planning services, primarily to low-income and uninsured patients. Federal law prohibits the use of Title X funds to pay for abortions.
Under the proposed regulations, the Trump administration would define “family planning” as the voluntary process of identifying goals and developing a plan for the number and spacing of children and the means by which those goals may be achieved. This includes planning methods and services “to limit or enhance the likelihood of conception, including contraceptive methods and natural family planning or other fertility awareness-based methods,” according to the proposal. HHS specifies that family planning does not include postconception care, obstetric or prenatal care, or abortion as a method of family planning. HHS has proposed that, if a woman comes to a Title X–funded clinic and is pregnant, she be referred externally for pregnancy services. However, the proposed rule would no longer allow Title X programs to provide abortion counseling and/or referral.
According to HHS, requiring separate facilities for abortion-related care would ensure that Title X funds are used for the purposes expressly mandated by Congress – to offer family planning methods and services – and that any infrastructure built with Title X funds would not be used for impermissible purposes.
More than 100,000 comments have been submitted on the proposed rule since June. Antiabortion organizations, such as the Susan B. Anthony List, have expressed strong support for the proposed rule.
“The American people have repeatedly expressed their predominant policy preferences by supporting Congressional enactments designed to distinguish and separate abortion from family planning,” SBA List President Marjorie Dannenfelser wrote in a comment. “Abortion is not health care, nor is abortion family planning. The Clinton administration and subsequent presidential administrations have erroneously allowed the blatant distribution of Title X funding to abortion centers and abortion-referral facilities for years and in direct violation of the original purpose of Title X funding.”
A group of 14 state governors, meanwhile, has threatened legal action if the Trump administration moves forward with finalizing its rule. In a May 31 letter, the 14 Democratic governors urged HHS to halt its changes to the Title X program and said they would explore all options, including legal avenues, to protect patients’ access to care. More recently, Democratic governors in Washington, Oregon, Hawaii, and New York have said they will refuse all Title X funding if the Trump administration does not rescind its proposed changes to the program.
“This is not an issue about life or choices. This is an issue about the rights of millions of individuals who deserve the best health care available,” Hawaii governor David Ige said in a July 30 statement. “Hawaii will not accept federal funds for these programs if the proposed rules are implemented.”
Public comment on the proposed rule closed on July 31.
Leading medical societies are calling on the Trump administration to withdraw its proposed changes to the federal Title X family planning program, calling the modifications a threat to essential health care for women.
In late May, the Department of Health & Human Services proposed broad changes to Title X, including no longer allowing staff at Title X clinics to counsel, refer, or provide information to women about abortions and mandating that Title X clinics that offer abortions maintain a separate facility for abortion services. The proposed changes aim to “refocus” the Title X program and ensure that all Title X services align with its family planning mission, according to the proposed rule published June 1.
In a July 31 letter to HHS, the American Medical Association requested that HHS withdraw the proposal, citing concerns from the medical community.
“We are very concerned that the proposed changes, if implemented, would undermine patients’ access to high-quality medical care and information, dangerously interfere with the patient-physician relationship and conflict with physicians’ ethical obligations, exclude qualified providers, and jeopardize public health,” James L. Madara, MD, chief executive officer and vice president of the AMA, wrote in a letter. “We urge HHS to withdraw this [proposal].”
The American College of Obstetricians and Gynecologists, the American College of Physicians, the American Academy of Pediatrics, the American Psychiatric Association, and 13 other health care associations also have called on the HHS to rescind its proposed rule. According to a statement from these associations, the proposal endangers women’s lives by restricting access to medically accurate information and preventive health care.
Title X is a long-standing federal program that provides funding for women’s health care and comprehensive family planning services, primarily to low-income and uninsured patients. Federal law prohibits the use of Title X funds to pay for abortions.
Under the proposed regulations, the Trump administration would define “family planning” as the voluntary process of identifying goals and developing a plan for the number and spacing of children and the means by which those goals may be achieved. This includes planning methods and services “to limit or enhance the likelihood of conception, including contraceptive methods and natural family planning or other fertility awareness-based methods,” according to the proposal. HHS specifies that family planning does not include postconception care, obstetric or prenatal care, or abortion as a method of family planning. HHS has proposed that, if a woman comes to a Title X–funded clinic and is pregnant, she be referred externally for pregnancy services. However, the proposed rule would no longer allow Title X programs to provide abortion counseling and/or referral.
According to HHS, requiring separate facilities for abortion-related care would ensure that Title X funds are used for the purposes expressly mandated by Congress – to offer family planning methods and services – and that any infrastructure built with Title X funds would not be used for impermissible purposes.
More than 100,000 comments have been submitted on the proposed rule since June. Antiabortion organizations, such as the Susan B. Anthony List, have expressed strong support for the proposed rule.
“The American people have repeatedly expressed their predominant policy preferences by supporting Congressional enactments designed to distinguish and separate abortion from family planning,” SBA List President Marjorie Dannenfelser wrote in a comment. “Abortion is not health care, nor is abortion family planning. The Clinton administration and subsequent presidential administrations have erroneously allowed the blatant distribution of Title X funding to abortion centers and abortion-referral facilities for years and in direct violation of the original purpose of Title X funding.”
A group of 14 state governors, meanwhile, has threatened legal action if the Trump administration moves forward with finalizing its rule. In a May 31 letter, the 14 Democratic governors urged HHS to halt its changes to the Title X program and said they would explore all options, including legal avenues, to protect patients’ access to care. More recently, Democratic governors in Washington, Oregon, Hawaii, and New York have said they will refuse all Title X funding if the Trump administration does not rescind its proposed changes to the program.
“This is not an issue about life or choices. This is an issue about the rights of millions of individuals who deserve the best health care available,” Hawaii governor David Ige said in a July 30 statement. “Hawaii will not accept federal funds for these programs if the proposed rules are implemented.”
Public comment on the proposed rule closed on July 31.
What to expect from next-gen CGRP inhibitors for migraine, cluster headache
SAN FRANCISCO – Galcanezumab, the investigational calcitonin gene-related peptide inhibitor under development as preventive therapy for migraine, looks like a triple threat: Multiple phase 3 randomized trials have not only demonstrated safety and efficacy of the monoclonal antibody for prevention of both episodic and chronic migraine but for prevention of episodic cluster headache as well.
Galcanezumab’s demonstrated preventive benefit in patients with episodic cluster headache, if confirmed, would be a big deal. This type of headache is far less common than migraine, but often characterized as not merely debilitating but devastating. Phase 3 evidence of galcanezumab’s safety and efficacy for prevention of episodic cluster headache constitutes a unique advantage over fremanezumab and eptinezumab, the other two monoclonal antibodies directed against calcitonin gene-related peptide (CGRP) for which new phase 3 data were presented at the annual meeting of the American Headache Society. But the latter two novel agents showed advantages of their own.
While the efficacy of the CGRP inhibitors isn’t light-years ahead of the long-standard preventive therapies for migraine, such as topiramate, beta-blockers, antidepressants, and valproate, the new agents offer far greater tolerability and safety – side effect profiles are essentially the same as for placebo except for a modest increase in mild injection site reactions – along with documented substantial quality of life improvements using validated measures. And onset of benefit is far more rapid than with the long-time standard oral preventive medications.
Here are the highlights from the AHS annual meeting:
Galcanezumab
Sheena K. Aurora, MD, presented the results of the GCAL study, a phase 3 randomized, double-blind, 8-week study of subcutaneous galcanezumab at 300 mg once monthly or placebo administered for 2 months in 106 patients with ongoing episodic cluster headache attacks at baseline.
“This is really uncharted territory. The American Headache Society, in its 2016 cluster headache guidelines, reported that there was no high-quality evidence for prophylactic therapy,” noted Dr. Aurora of Eli Lilly in Indianapolis.
After the GCAL study, that’s no longer true. Study participants were a typical population of episodic cluster headache patients: that is, mostly middle-aged men. They averaged more than 17 cluster headache attacks per week during the baseline period, or 2-3 daily, with roughly a 16-year history of episodic cluster headaches, which typically occur in bursts lasting 6-8 weeks before temporarily fading. Of note, 14 of the 106 patients reported a history of prior suicidal ideation; while disturbing, that’s actually a lower rate than in some epidemiologic studies examining patients with this excruciating form of head pain.
The primary endpoint was the mean change in weekly cluster headache attack frequency during weeks 1-3. The difference was significant: a reduction of 8.7 attacks per week in the galcanezumab group, compared with 5.2 fewer in controls. The key secondary endpoint was the proportion of patients with at least a 50% reduction in weekly cluster attack frequency from baseline at week 3: This was achieved in 76% in the galcanezumab arm, versus 57% for placebo, again a significant difference.
At week 4, 73% of patients on galcanezumab rated themselves as very much or much better on the Patient Global Impression of Improvement, significantly greater than the 46% rate in controls. By week 8, this difference – while trending favorably – was no longer statistically significant, but it must be noted that by then 8 of the original 57 patients randomized to placebo had discontinued treatment because of the lack of efficacy, compared with just 1 of 49 in the galcanezumab group.
Adverse events in the two treatment arms were essentially the same as placebo except for an 8% rate of mild injection site reactions in the active treatment group.
Another double-blind, placebo-controlled phase 3 trial known as the CGAM study was conducted in 237 patients with chronic rather than episodic cluster headache. However, it proved negative for the same endpoints, Dr. Aurora said.
Separately, she presented a new post hoc analysis of the recently published EVOLVE-1 (JAMA Neurol. 2018 May 29. doi: 10.1001/jamaneurol.2018.1212) and EVOLVE-2 (Cephalalgia. 2018 Jul;38[8]:1442-54) trials. These two mirror-image pivotal phase 3, double-blind, placebo-controlled, 6-month studies of galcanezumab at 120 or 240 mg once monthly included a collective 1,773 episodic migraine patients with a baseline mean of 9.1 migraine headache days per month. Her analysis focused on the rapidity of onset of the humanized monoclonal antibody’s preventive effect.
“As most clinicians are aware, the current oral preventive treatments that we use require titration, and we don’t really see a good effect for maybe 2-3 months,” she observed.
In an ordinal logistic regression analysis, she and her coinvestigators first determined that the galcanezumab group separated from placebo in terms of reduced migraine headache days as early as 1 month in both studies. Next, they drilled down deeper into the participants’ daily headache diaries and determined that the onset of effect was seen at week 1, at which point the odds of a significant reduction in weekly migraine headache days were 2.71-fold greater with galcanezumab than placebo in EVOLVE-1 and 2.88-fold greater in EVOLVE-2.
“Patients would like to know how quickly they might see an effect, so the fact that we start seeing it for patients who’ve had migraine for 20 years with an average of 9.1 migraine headache days per month as early as week 1 is gratifying, even though the absolute numbers who benefit at that point are small,” Dr. Aurora said.
Fremanezumab
Fremanezumab is a fully humanized monoclonal antibody selectively targeting CGRP. Like galcanezumab and eptinezumab, it is now supported by phase 3 data from short-term, double-blind, placebo-controlled trials backed up by reassuring results from long-term, open-label studies.
During the 28 days prior to the start of the long-term, double-blind study, the chronic migraine patients averaged 16.4 migraine days, while the episodic migraine patients averaged 9.2. After 6 months on their assigned dosing regimen, the episodic migraine patients in the 225 mg monthly group had a mean 4.9 fewer monthly migraine days than at baseline, and the 675 mg quarterly group averaged 5.0 fewer days. The chronic migraine patients on 225 mg monthly had a mean 7.9-day reduction, while the 675 mg quarterly group averaged a 6.5-day reduction in monthly migraine days.
The key point in this interim analysis is that these clinically meaningful reductions in monthly number of migraine days at 6 months were of the same magnitude as at month 1, demonstrating solid maintenance of efficacy over time, noted Dr. Goadsby, professor of neurology at the University of California, San Francisco, and AHS president-elect.
Jessica Ailani, MD, presented evidence that fremanezumab is not only an effective migraine preventive therapy, it also shows potential as a medication for reversion from chronic migraine to episodic migraine.
She presented a post hoc analysis of the 1,130 chronic migraine patients who participated in the 12-week, placebo-controlled HALO CM trial. Thirty-two percent of them who were randomized to 675 mg of fremanezumab quarterly reverted from chronic to episodic migraine, meaning they had fewer than 15 headache days per month during all 3 months of the treatment period. So did 35% of patients who received 225 mg monthly. Both results were significantly better than the 23% placebo reversion rate, which is consistent with the effect of placebo in other studies.
The mean number of monthly headache days of at least moderate severity fell by 4.3 days from baseline in the fremanezumab quarterly group and by 4.6 with monthly therapy, significantly outperforming the 2.5-day reduction with placebo. And the patients who did well did very well indeed: those who reverted from chronic to episodic migraine went from a mean of 18-19 headache days per month at baseline to about 7 days during any month in the treatment period, she reported.
Two patients on 675 mg of fremanezumab quarterly developed antidrug antibodies.
Patients with MOH at baseline experienced a mean reduction of 4.7 headache days of at least moderate severity per month on fremanezumab at 675 mg quarterly and a 5.2-day reduction with monthly fremanezumab, both significantly better than the 2.5-day reduction with placebo. A total of 35% of the fremanezumab quarterly group achieved a 50% or greater reduction in the monthly average number of at least moderately severe headaches, as did 39% of patients on monthly fremanezumab and 14% on placebo.
Moreover, during the 12-week study period, 55% of patients with MOH at baseline who were on fremanezumab quarterly reported no medication overuse, as did 61% of those on 225 mg of fremanezumab once monthly and 46% of controls, according to Dr. Silberstein, professor of neurology and director of the headache center at Thomas Jefferson University in Philadelphia.
For the 1,034 participants who completed testing, the average baseline HIT-6 score was 64 points on a test that can range from 36-78, with higher scores indicating greater adverse impact. At repeat testing 4 weeks after the last dose, the quarterly dosing group showed a statistically significant and clinically meaningful 6.4-point reduction from baseline, and the monthly fremanezumab group had a 6.8-point reduction. Both of those outcomes were significantly better than the placebo group’s 4.5-point decrease, reported Dr. Winner, director of Palm Beach Neurology in West Palm Beach, Fla.
Those HIT-6 changes in fremanezumab-treated patients moved them from the severe disability category to moderate disability, he noted.
“We also evaluated other disability components in this study. The MSQ – the Migraine Specific Quality-of-Life Questionnaire – also showed significant improvement by patient assessment, and on a patient global assessment measure, over 50% of patients who got fremanezumab noted improvement in that 12-week study, getting back to work, functioning normally, etc.,” the neurologist added.
Eptinezumab
Unlike other anti-CGRP antibodies, eptinezumab is administered intravenously, once every 3 months, rather than by subcutaneous injection. This IgG1 anti-CGRP monoclonal antibody was engineered for reduced immune activation and a 30-day half-life. It’s onset of action is extremely rapid, with 100% of the agent being bioavailable within a few hours after administration.
The positive 12-week outcomes of the phase 3 randomized, double-blind, placebo-controlled PROMISE-2 trial of eptinezumab for prophylaxis against chronic migraine have previously been presented, as have the 1-year results in episodic migraine patients in PROMISE-1.
Of those on the higher dose of eptinezumab, 33% had at least a 75% reduction in monthly migraine days from baseline, a figure that climbed to 43% after the second infusion; and of those who received eptinezumab at the 300-mg dose, 61% experienced a 50% or greater reduction in monthly migraine days from baseline during weeks 1-12, as did 64% during weeks 13-24 following a second infusion.
A key secondary endpoint in PROMISE-2 was the proportion of patients having a migraine on any given day. During the 28-day baseline period, that figure was 58%. But the day after the first infusion that proportion dropped to 28% in both the eptinezumab 100- and 300-mg groups, and that rate held through the next 12 weeks. In contrast, roughly 45% of placebo-treated controls had a migraine on any given day during the 12 weeks.
“The key thing is on the day following infusion you have established pretty much the full preventive value of eptinezumab, and it is maintained stable all the way through 12 weeks,” according to Dr. Cady, vice president of neurology at Alder BioPharmaceuticals, which is developing the biologic.
When an audience member remarked on the placebo response rates in the CRGP inhibitor studies and indeed in clinical trials in migraine generally, Dr. Cady responded with one of the meeting’s more memorable comments: “If placebo brought you to the dance, you’re still at the party.”
Dr. Winner reported serving as a consultant to Alder BioPharmaceuticals, which sponsored the HALO trials and is developing eptinezumab, as well as to numerous other pharmaceutical companies. Similarly, Dr. Goadsby, Dr. Ailani, and Dr. Silberstein are consultants to many companies, including Teva Pharmaceuticals, which is developing fremanezumab.
SAN FRANCISCO – Galcanezumab, the investigational calcitonin gene-related peptide inhibitor under development as preventive therapy for migraine, looks like a triple threat: Multiple phase 3 randomized trials have not only demonstrated safety and efficacy of the monoclonal antibody for prevention of both episodic and chronic migraine but for prevention of episodic cluster headache as well.
Galcanezumab’s demonstrated preventive benefit in patients with episodic cluster headache, if confirmed, would be a big deal. This type of headache is far less common than migraine, but often characterized as not merely debilitating but devastating. Phase 3 evidence of galcanezumab’s safety and efficacy for prevention of episodic cluster headache constitutes a unique advantage over fremanezumab and eptinezumab, the other two monoclonal antibodies directed against calcitonin gene-related peptide (CGRP) for which new phase 3 data were presented at the annual meeting of the American Headache Society. But the latter two novel agents showed advantages of their own.
While the efficacy of the CGRP inhibitors isn’t light-years ahead of the long-standard preventive therapies for migraine, such as topiramate, beta-blockers, antidepressants, and valproate, the new agents offer far greater tolerability and safety – side effect profiles are essentially the same as for placebo except for a modest increase in mild injection site reactions – along with documented substantial quality of life improvements using validated measures. And onset of benefit is far more rapid than with the long-time standard oral preventive medications.
Here are the highlights from the AHS annual meeting:
Galcanezumab
Sheena K. Aurora, MD, presented the results of the GCAL study, a phase 3 randomized, double-blind, 8-week study of subcutaneous galcanezumab at 300 mg once monthly or placebo administered for 2 months in 106 patients with ongoing episodic cluster headache attacks at baseline.
“This is really uncharted territory. The American Headache Society, in its 2016 cluster headache guidelines, reported that there was no high-quality evidence for prophylactic therapy,” noted Dr. Aurora of Eli Lilly in Indianapolis.
After the GCAL study, that’s no longer true. Study participants were a typical population of episodic cluster headache patients: that is, mostly middle-aged men. They averaged more than 17 cluster headache attacks per week during the baseline period, or 2-3 daily, with roughly a 16-year history of episodic cluster headaches, which typically occur in bursts lasting 6-8 weeks before temporarily fading. Of note, 14 of the 106 patients reported a history of prior suicidal ideation; while disturbing, that’s actually a lower rate than in some epidemiologic studies examining patients with this excruciating form of head pain.
The primary endpoint was the mean change in weekly cluster headache attack frequency during weeks 1-3. The difference was significant: a reduction of 8.7 attacks per week in the galcanezumab group, compared with 5.2 fewer in controls. The key secondary endpoint was the proportion of patients with at least a 50% reduction in weekly cluster attack frequency from baseline at week 3: This was achieved in 76% in the galcanezumab arm, versus 57% for placebo, again a significant difference.
At week 4, 73% of patients on galcanezumab rated themselves as very much or much better on the Patient Global Impression of Improvement, significantly greater than the 46% rate in controls. By week 8, this difference – while trending favorably – was no longer statistically significant, but it must be noted that by then 8 of the original 57 patients randomized to placebo had discontinued treatment because of the lack of efficacy, compared with just 1 of 49 in the galcanezumab group.
Adverse events in the two treatment arms were essentially the same as placebo except for an 8% rate of mild injection site reactions in the active treatment group.
Another double-blind, placebo-controlled phase 3 trial known as the CGAM study was conducted in 237 patients with chronic rather than episodic cluster headache. However, it proved negative for the same endpoints, Dr. Aurora said.
Separately, she presented a new post hoc analysis of the recently published EVOLVE-1 (JAMA Neurol. 2018 May 29. doi: 10.1001/jamaneurol.2018.1212) and EVOLVE-2 (Cephalalgia. 2018 Jul;38[8]:1442-54) trials. These two mirror-image pivotal phase 3, double-blind, placebo-controlled, 6-month studies of galcanezumab at 120 or 240 mg once monthly included a collective 1,773 episodic migraine patients with a baseline mean of 9.1 migraine headache days per month. Her analysis focused on the rapidity of onset of the humanized monoclonal antibody’s preventive effect.
“As most clinicians are aware, the current oral preventive treatments that we use require titration, and we don’t really see a good effect for maybe 2-3 months,” she observed.
In an ordinal logistic regression analysis, she and her coinvestigators first determined that the galcanezumab group separated from placebo in terms of reduced migraine headache days as early as 1 month in both studies. Next, they drilled down deeper into the participants’ daily headache diaries and determined that the onset of effect was seen at week 1, at which point the odds of a significant reduction in weekly migraine headache days were 2.71-fold greater with galcanezumab than placebo in EVOLVE-1 and 2.88-fold greater in EVOLVE-2.
“Patients would like to know how quickly they might see an effect, so the fact that we start seeing it for patients who’ve had migraine for 20 years with an average of 9.1 migraine headache days per month as early as week 1 is gratifying, even though the absolute numbers who benefit at that point are small,” Dr. Aurora said.
Fremanezumab
Fremanezumab is a fully humanized monoclonal antibody selectively targeting CGRP. Like galcanezumab and eptinezumab, it is now supported by phase 3 data from short-term, double-blind, placebo-controlled trials backed up by reassuring results from long-term, open-label studies.
During the 28 days prior to the start of the long-term, double-blind study, the chronic migraine patients averaged 16.4 migraine days, while the episodic migraine patients averaged 9.2. After 6 months on their assigned dosing regimen, the episodic migraine patients in the 225 mg monthly group had a mean 4.9 fewer monthly migraine days than at baseline, and the 675 mg quarterly group averaged 5.0 fewer days. The chronic migraine patients on 225 mg monthly had a mean 7.9-day reduction, while the 675 mg quarterly group averaged a 6.5-day reduction in monthly migraine days.
The key point in this interim analysis is that these clinically meaningful reductions in monthly number of migraine days at 6 months were of the same magnitude as at month 1, demonstrating solid maintenance of efficacy over time, noted Dr. Goadsby, professor of neurology at the University of California, San Francisco, and AHS president-elect.
Jessica Ailani, MD, presented evidence that fremanezumab is not only an effective migraine preventive therapy, it also shows potential as a medication for reversion from chronic migraine to episodic migraine.
She presented a post hoc analysis of the 1,130 chronic migraine patients who participated in the 12-week, placebo-controlled HALO CM trial. Thirty-two percent of them who were randomized to 675 mg of fremanezumab quarterly reverted from chronic to episodic migraine, meaning they had fewer than 15 headache days per month during all 3 months of the treatment period. So did 35% of patients who received 225 mg monthly. Both results were significantly better than the 23% placebo reversion rate, which is consistent with the effect of placebo in other studies.
The mean number of monthly headache days of at least moderate severity fell by 4.3 days from baseline in the fremanezumab quarterly group and by 4.6 with monthly therapy, significantly outperforming the 2.5-day reduction with placebo. And the patients who did well did very well indeed: those who reverted from chronic to episodic migraine went from a mean of 18-19 headache days per month at baseline to about 7 days during any month in the treatment period, she reported.
Two patients on 675 mg of fremanezumab quarterly developed antidrug antibodies.
Patients with MOH at baseline experienced a mean reduction of 4.7 headache days of at least moderate severity per month on fremanezumab at 675 mg quarterly and a 5.2-day reduction with monthly fremanezumab, both significantly better than the 2.5-day reduction with placebo. A total of 35% of the fremanezumab quarterly group achieved a 50% or greater reduction in the monthly average number of at least moderately severe headaches, as did 39% of patients on monthly fremanezumab and 14% on placebo.
Moreover, during the 12-week study period, 55% of patients with MOH at baseline who were on fremanezumab quarterly reported no medication overuse, as did 61% of those on 225 mg of fremanezumab once monthly and 46% of controls, according to Dr. Silberstein, professor of neurology and director of the headache center at Thomas Jefferson University in Philadelphia.
For the 1,034 participants who completed testing, the average baseline HIT-6 score was 64 points on a test that can range from 36-78, with higher scores indicating greater adverse impact. At repeat testing 4 weeks after the last dose, the quarterly dosing group showed a statistically significant and clinically meaningful 6.4-point reduction from baseline, and the monthly fremanezumab group had a 6.8-point reduction. Both of those outcomes were significantly better than the placebo group’s 4.5-point decrease, reported Dr. Winner, director of Palm Beach Neurology in West Palm Beach, Fla.
Those HIT-6 changes in fremanezumab-treated patients moved them from the severe disability category to moderate disability, he noted.
“We also evaluated other disability components in this study. The MSQ – the Migraine Specific Quality-of-Life Questionnaire – also showed significant improvement by patient assessment, and on a patient global assessment measure, over 50% of patients who got fremanezumab noted improvement in that 12-week study, getting back to work, functioning normally, etc.,” the neurologist added.
Eptinezumab
Unlike other anti-CGRP antibodies, eptinezumab is administered intravenously, once every 3 months, rather than by subcutaneous injection. This IgG1 anti-CGRP monoclonal antibody was engineered for reduced immune activation and a 30-day half-life. It’s onset of action is extremely rapid, with 100% of the agent being bioavailable within a few hours after administration.
The positive 12-week outcomes of the phase 3 randomized, double-blind, placebo-controlled PROMISE-2 trial of eptinezumab for prophylaxis against chronic migraine have previously been presented, as have the 1-year results in episodic migraine patients in PROMISE-1.
Of those on the higher dose of eptinezumab, 33% had at least a 75% reduction in monthly migraine days from baseline, a figure that climbed to 43% after the second infusion; and of those who received eptinezumab at the 300-mg dose, 61% experienced a 50% or greater reduction in monthly migraine days from baseline during weeks 1-12, as did 64% during weeks 13-24 following a second infusion.
A key secondary endpoint in PROMISE-2 was the proportion of patients having a migraine on any given day. During the 28-day baseline period, that figure was 58%. But the day after the first infusion that proportion dropped to 28% in both the eptinezumab 100- and 300-mg groups, and that rate held through the next 12 weeks. In contrast, roughly 45% of placebo-treated controls had a migraine on any given day during the 12 weeks.
“The key thing is on the day following infusion you have established pretty much the full preventive value of eptinezumab, and it is maintained stable all the way through 12 weeks,” according to Dr. Cady, vice president of neurology at Alder BioPharmaceuticals, which is developing the biologic.
When an audience member remarked on the placebo response rates in the CRGP inhibitor studies and indeed in clinical trials in migraine generally, Dr. Cady responded with one of the meeting’s more memorable comments: “If placebo brought you to the dance, you’re still at the party.”
Dr. Winner reported serving as a consultant to Alder BioPharmaceuticals, which sponsored the HALO trials and is developing eptinezumab, as well as to numerous other pharmaceutical companies. Similarly, Dr. Goadsby, Dr. Ailani, and Dr. Silberstein are consultants to many companies, including Teva Pharmaceuticals, which is developing fremanezumab.
SAN FRANCISCO – Galcanezumab, the investigational calcitonin gene-related peptide inhibitor under development as preventive therapy for migraine, looks like a triple threat: Multiple phase 3 randomized trials have not only demonstrated safety and efficacy of the monoclonal antibody for prevention of both episodic and chronic migraine but for prevention of episodic cluster headache as well.
Galcanezumab’s demonstrated preventive benefit in patients with episodic cluster headache, if confirmed, would be a big deal. This type of headache is far less common than migraine, but often characterized as not merely debilitating but devastating. Phase 3 evidence of galcanezumab’s safety and efficacy for prevention of episodic cluster headache constitutes a unique advantage over fremanezumab and eptinezumab, the other two monoclonal antibodies directed against calcitonin gene-related peptide (CGRP) for which new phase 3 data were presented at the annual meeting of the American Headache Society. But the latter two novel agents showed advantages of their own.
While the efficacy of the CGRP inhibitors isn’t light-years ahead of the long-standard preventive therapies for migraine, such as topiramate, beta-blockers, antidepressants, and valproate, the new agents offer far greater tolerability and safety – side effect profiles are essentially the same as for placebo except for a modest increase in mild injection site reactions – along with documented substantial quality of life improvements using validated measures. And onset of benefit is far more rapid than with the long-time standard oral preventive medications.
Here are the highlights from the AHS annual meeting:
Galcanezumab
Sheena K. Aurora, MD, presented the results of the GCAL study, a phase 3 randomized, double-blind, 8-week study of subcutaneous galcanezumab at 300 mg once monthly or placebo administered for 2 months in 106 patients with ongoing episodic cluster headache attacks at baseline.
“This is really uncharted territory. The American Headache Society, in its 2016 cluster headache guidelines, reported that there was no high-quality evidence for prophylactic therapy,” noted Dr. Aurora of Eli Lilly in Indianapolis.
After the GCAL study, that’s no longer true. Study participants were a typical population of episodic cluster headache patients: that is, mostly middle-aged men. They averaged more than 17 cluster headache attacks per week during the baseline period, or 2-3 daily, with roughly a 16-year history of episodic cluster headaches, which typically occur in bursts lasting 6-8 weeks before temporarily fading. Of note, 14 of the 106 patients reported a history of prior suicidal ideation; while disturbing, that’s actually a lower rate than in some epidemiologic studies examining patients with this excruciating form of head pain.
The primary endpoint was the mean change in weekly cluster headache attack frequency during weeks 1-3. The difference was significant: a reduction of 8.7 attacks per week in the galcanezumab group, compared with 5.2 fewer in controls. The key secondary endpoint was the proportion of patients with at least a 50% reduction in weekly cluster attack frequency from baseline at week 3: This was achieved in 76% in the galcanezumab arm, versus 57% for placebo, again a significant difference.
At week 4, 73% of patients on galcanezumab rated themselves as very much or much better on the Patient Global Impression of Improvement, significantly greater than the 46% rate in controls. By week 8, this difference – while trending favorably – was no longer statistically significant, but it must be noted that by then 8 of the original 57 patients randomized to placebo had discontinued treatment because of the lack of efficacy, compared with just 1 of 49 in the galcanezumab group.
Adverse events in the two treatment arms were essentially the same as placebo except for an 8% rate of mild injection site reactions in the active treatment group.
Another double-blind, placebo-controlled phase 3 trial known as the CGAM study was conducted in 237 patients with chronic rather than episodic cluster headache. However, it proved negative for the same endpoints, Dr. Aurora said.
Separately, she presented a new post hoc analysis of the recently published EVOLVE-1 (JAMA Neurol. 2018 May 29. doi: 10.1001/jamaneurol.2018.1212) and EVOLVE-2 (Cephalalgia. 2018 Jul;38[8]:1442-54) trials. These two mirror-image pivotal phase 3, double-blind, placebo-controlled, 6-month studies of galcanezumab at 120 or 240 mg once monthly included a collective 1,773 episodic migraine patients with a baseline mean of 9.1 migraine headache days per month. Her analysis focused on the rapidity of onset of the humanized monoclonal antibody’s preventive effect.
“As most clinicians are aware, the current oral preventive treatments that we use require titration, and we don’t really see a good effect for maybe 2-3 months,” she observed.
In an ordinal logistic regression analysis, she and her coinvestigators first determined that the galcanezumab group separated from placebo in terms of reduced migraine headache days as early as 1 month in both studies. Next, they drilled down deeper into the participants’ daily headache diaries and determined that the onset of effect was seen at week 1, at which point the odds of a significant reduction in weekly migraine headache days were 2.71-fold greater with galcanezumab than placebo in EVOLVE-1 and 2.88-fold greater in EVOLVE-2.
“Patients would like to know how quickly they might see an effect, so the fact that we start seeing it for patients who’ve had migraine for 20 years with an average of 9.1 migraine headache days per month as early as week 1 is gratifying, even though the absolute numbers who benefit at that point are small,” Dr. Aurora said.
Fremanezumab
Fremanezumab is a fully humanized monoclonal antibody selectively targeting CGRP. Like galcanezumab and eptinezumab, it is now supported by phase 3 data from short-term, double-blind, placebo-controlled trials backed up by reassuring results from long-term, open-label studies.
During the 28 days prior to the start of the long-term, double-blind study, the chronic migraine patients averaged 16.4 migraine days, while the episodic migraine patients averaged 9.2. After 6 months on their assigned dosing regimen, the episodic migraine patients in the 225 mg monthly group had a mean 4.9 fewer monthly migraine days than at baseline, and the 675 mg quarterly group averaged 5.0 fewer days. The chronic migraine patients on 225 mg monthly had a mean 7.9-day reduction, while the 675 mg quarterly group averaged a 6.5-day reduction in monthly migraine days.
The key point in this interim analysis is that these clinically meaningful reductions in monthly number of migraine days at 6 months were of the same magnitude as at month 1, demonstrating solid maintenance of efficacy over time, noted Dr. Goadsby, professor of neurology at the University of California, San Francisco, and AHS president-elect.
Jessica Ailani, MD, presented evidence that fremanezumab is not only an effective migraine preventive therapy, it also shows potential as a medication for reversion from chronic migraine to episodic migraine.
She presented a post hoc analysis of the 1,130 chronic migraine patients who participated in the 12-week, placebo-controlled HALO CM trial. Thirty-two percent of them who were randomized to 675 mg of fremanezumab quarterly reverted from chronic to episodic migraine, meaning they had fewer than 15 headache days per month during all 3 months of the treatment period. So did 35% of patients who received 225 mg monthly. Both results were significantly better than the 23% placebo reversion rate, which is consistent with the effect of placebo in other studies.
The mean number of monthly headache days of at least moderate severity fell by 4.3 days from baseline in the fremanezumab quarterly group and by 4.6 with monthly therapy, significantly outperforming the 2.5-day reduction with placebo. And the patients who did well did very well indeed: those who reverted from chronic to episodic migraine went from a mean of 18-19 headache days per month at baseline to about 7 days during any month in the treatment period, she reported.
Two patients on 675 mg of fremanezumab quarterly developed antidrug antibodies.
Patients with MOH at baseline experienced a mean reduction of 4.7 headache days of at least moderate severity per month on fremanezumab at 675 mg quarterly and a 5.2-day reduction with monthly fremanezumab, both significantly better than the 2.5-day reduction with placebo. A total of 35% of the fremanezumab quarterly group achieved a 50% or greater reduction in the monthly average number of at least moderately severe headaches, as did 39% of patients on monthly fremanezumab and 14% on placebo.
Moreover, during the 12-week study period, 55% of patients with MOH at baseline who were on fremanezumab quarterly reported no medication overuse, as did 61% of those on 225 mg of fremanezumab once monthly and 46% of controls, according to Dr. Silberstein, professor of neurology and director of the headache center at Thomas Jefferson University in Philadelphia.
For the 1,034 participants who completed testing, the average baseline HIT-6 score was 64 points on a test that can range from 36-78, with higher scores indicating greater adverse impact. At repeat testing 4 weeks after the last dose, the quarterly dosing group showed a statistically significant and clinically meaningful 6.4-point reduction from baseline, and the monthly fremanezumab group had a 6.8-point reduction. Both of those outcomes were significantly better than the placebo group’s 4.5-point decrease, reported Dr. Winner, director of Palm Beach Neurology in West Palm Beach, Fla.
Those HIT-6 changes in fremanezumab-treated patients moved them from the severe disability category to moderate disability, he noted.
“We also evaluated other disability components in this study. The MSQ – the Migraine Specific Quality-of-Life Questionnaire – also showed significant improvement by patient assessment, and on a patient global assessment measure, over 50% of patients who got fremanezumab noted improvement in that 12-week study, getting back to work, functioning normally, etc.,” the neurologist added.
Eptinezumab
Unlike other anti-CGRP antibodies, eptinezumab is administered intravenously, once every 3 months, rather than by subcutaneous injection. This IgG1 anti-CGRP monoclonal antibody was engineered for reduced immune activation and a 30-day half-life. It’s onset of action is extremely rapid, with 100% of the agent being bioavailable within a few hours after administration.
The positive 12-week outcomes of the phase 3 randomized, double-blind, placebo-controlled PROMISE-2 trial of eptinezumab for prophylaxis against chronic migraine have previously been presented, as have the 1-year results in episodic migraine patients in PROMISE-1.
Of those on the higher dose of eptinezumab, 33% had at least a 75% reduction in monthly migraine days from baseline, a figure that climbed to 43% after the second infusion; and of those who received eptinezumab at the 300-mg dose, 61% experienced a 50% or greater reduction in monthly migraine days from baseline during weeks 1-12, as did 64% during weeks 13-24 following a second infusion.
A key secondary endpoint in PROMISE-2 was the proportion of patients having a migraine on any given day. During the 28-day baseline period, that figure was 58%. But the day after the first infusion that proportion dropped to 28% in both the eptinezumab 100- and 300-mg groups, and that rate held through the next 12 weeks. In contrast, roughly 45% of placebo-treated controls had a migraine on any given day during the 12 weeks.
“The key thing is on the day following infusion you have established pretty much the full preventive value of eptinezumab, and it is maintained stable all the way through 12 weeks,” according to Dr. Cady, vice president of neurology at Alder BioPharmaceuticals, which is developing the biologic.
When an audience member remarked on the placebo response rates in the CRGP inhibitor studies and indeed in clinical trials in migraine generally, Dr. Cady responded with one of the meeting’s more memorable comments: “If placebo brought you to the dance, you’re still at the party.”
Dr. Winner reported serving as a consultant to Alder BioPharmaceuticals, which sponsored the HALO trials and is developing eptinezumab, as well as to numerous other pharmaceutical companies. Similarly, Dr. Goadsby, Dr. Ailani, and Dr. Silberstein are consultants to many companies, including Teva Pharmaceuticals, which is developing fremanezumab.
REPORTING FROM THE AHS ANNUAL MEETING
Tranexamic Acid Reduces Perioperative Blood Loss and Hemarthrosis in Total Ankle Arthroplasty
ABSTRACT
Tranexamic acid (TXA) is an effective agent used for reducing perioperative blood loss and decreasing the potential for postoperative hemarthrosis. We hypothesized that patients who had received intraoperative TXA during total ankle arthroplasty (TAA) would have a reduction in postoperative drain output, thereby resulting in a reduced risk of postoperative hemarthrosis and lower wound complication rates.
A retrospective review was conducted on 50 consecutive patients, 25 receiving TXA (TXA-TAA) and 25 not receiving TXA (No TXA-TAA), who underwent an uncemented TAA between September 2011 and December 2015. Demographic characteristics, drain output, preoperative and postoperative hemoglobin levels, operative and postoperative course, and minor and major wound complications of the patients were reviewed.
Drain output was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (71.6 ± 60.3 vs 200.2 ± 117.0 mL, respectively, P < .0001). The overall wound complication rate in the No TXA-TAA group was higher (20%, 5/25) than that in the TXA-TAA group (8%, 2/25) (P = .114). The mean change in preoperative to postoperative hemoglobin level was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (1.5 ± 0.6 vs 2.0 ± 0.4 g/dL, respectively, P = .01).
TXA is an effective hemostatic agent when used during TAA. TXA reduces perioperative blood loss, hemarthrosis, and the risk of wound complications.
Continue to: End-stage ankle arthritis...
End-stage ankle arthritis is a disabling condition that may lead to poor quality of life and difficulties with activities of daily living.1 The associated mental and physical disability has been demonstrated to be as severe as in end-stage hip arthrosis.2 Operative treatment for symptomatic end-stage ankle arthritis includes arthrodesis or total ankle arthroplasty (TAA) in those refractory to nonoperative treatment.3 Newer generation implants have made TAA a more attractive option for both the surgeon and the patient.
Over the past decade, the utility of TAA has increased and attention has turned toward the management of perioperative factors that would maximize patient satisfaction and decrease the length of stay and complication rates, as well as hospital costs.4 Comprehensive literature on total knee arthroplasty (TKA) and total hip arthroplasty (THA) has demonstrated that the management of perioperative blood loss, specifically postoperative hemarthrosis, is a modifiable factor affecting patient recovery, complication rates, and hospital costs.5-8 Drain output has been used as a direct measure of intra-articular blood accumulation.9 Decreased drain output implies decreased hemarthrosis, which could potentially alleviate the pressure on the wound and decrease wound complications.
One of the major strategies that has been recognized for reducing blood loss and decreasing the potential for postoperative hemarthrosis is the use of intravenous (IV) or topical tranexamic acid (TXA).10,11 TXA is a synthetic antifibrinolytic medication that has been extensively used throughout the medical field since the 1960s to help control the bleeding cascade. This medication stabilizes clot formation without inducing a pro-coaguable state.12 Intraoperative administration of TXA has been shown to reduce drain output and decrease transfusion requirements after TKA and THA without an associated increase in patient morbidity and mortality.6,11,13-15
Currently, there is a lack of studies evaluating the utility of TXA during TAA. We hypothesize that compared with patients who had not received TXA, those who had received intraoperative TXA during TAA would have a reduction in postoperative drain output and therefore decreased hemarthrosis, lower wound complication rate, and a diminished change in preoperative to postoperative hemoglobin levels, reflecting a reduction in perioperative blood loss.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board at the University at Buffalo, State University of New York. A retrospective chart review was conducted on 50 consecutive patients who underwent an uncemented TAA with the Salto Talaris total ankle prosthesis (Tornier, Inc) between September 2011 and December 2015. All surgeries were performed at 1 institution by a single fellowship surgeon trained in foot and ankle surgery through the anterior approach where a midline incision was made over the ankle. The interval between the tibialis anterior tendon and the extensor hallucis longus tendon was used. We had incorporated intraoperative TXA into the TAA surgical protocol at our institution in January 2014. We evaluated the first 25 consecutive patients who underwent TAA after TXA use began (TXA-TAA) and another 25 consecutive patients who underwent TAA before the routine use of TXA (No TXA-TAA). Inclusion criteria were patients who presented with pain, decreased function, and radiographic parameters of end-stage tibiotalar arthritis due to degenerative arthritis, rheumatoid arthritis, or posttraumatic arthritis who subsequently underwent a TAA. Exclusion criteria were patients with a contraindication for IV TXA use, a preexisting coagulopathy, or where drain output was not recorded. Contraindications for IV TXA use included patients with impaired renal clearance, recent cardiac surgery, myocardial infarction, ischemic stroke, or venous thromboembolism (VTE). Seven patients were ultimately excluded from this study based on the inclusion and exclusion criteria, 3 patients from the TXA-TAA group and 4 patients from the No TXA-TAA group.
Continue to: Charts were reviewed for demographics...
Charts were reviewed for demographics, preoperative and postoperative hemoglobin levels, indications for surgery, surgical procedures, length of surgery, postoperative drain output, length of stay, postoperative pain visual analog scale (VAS) score, minor and major wound complications, and postoperative complications. Minor wound complications were defined as the anterior surgical incision that required local wound care in office or oral antibiotics without subsequent consequences. Major wound complications were defined as requiring surgical débridement and/or any additional treatment in the operating room.16 Postoperative complications other than wound complications were defined as those requiring a subsequent surgical intervention. Patient demographics and clinical and procedural characteristics of patients in both the TXA-TAA and the No TXA-TAA groups are outlined in Table 1. There were 14 males and 11 females in the TXA-TAA group and 16 males and 9 females in the No TXA-TAA group. The mean age was 65.8 ± 10.9 years in the TXA-TAA group and 66.9 ± 8.0 years in the No TXA-TAA group (P = .69). Mean body mass index (BMI) was 31.6 ± 6.3 in the TXA-TAA group and 29.4 ± 4.9 in the No TXA-TAA group (P = .18). The primary indication for TAA was degenerative osteoarthritis in 26 patients, posttraumatic arthritis in 21 patients, and rheumatoid arthritis in 3 patients. The most common associated procedure was Achilles tendon lengthening in both groups. The mean follow-up in the TXA-TAA group was 9.3 ± 5.8 months (range, 2.0-24.0 months). Postoperative complications due to TXA administration as described in previous literature were defined as VTE, myocardial infarction, or ischemic cerebral event. The TXA-TAA group received a standard 1 g dose of IV TXA 20 minutes prior to tourniquet inflation. A tourniquet was used intraoperatively on all patients included in this study. A postoperative 400-mL surgical drain (Hemovac, Zimmer Biomet) was placed in the ankle joint in all patients and subsequently discontinued on postoperative day 1. Recent literature has reported the minor wound complication rate associated with TAA to be as high as 25% and the major wound complication rate to be 8.5%.16 To assist in reducing the risk for wound complications, our protocol traditionally uses an intra-articular surgical drain to decrease any pressure on the wound from postoperative hemarthrosis.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
aP value was calculated from t-test continuous variables and Chi-square test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index.
Total drain output was recorded in milliliters (mL) in all patients. The change between the preoperative hemoglobin level and the hemoglobin level on postoperative day 1 was calculated for each patient. The calculated blood loss was determined using Meunier’s equation, which estimates the total blood volume using Nadler’s formula and then uses preoperative hemoglobin and postoperative day 1 hemoglobin values to calculate blood loss.17,18 VAS scores (scale, 1-10) were obtained every 4 hours on postoperative day 1 according to the nursing protocol. The number 1 on the scale represents the least amount of pain, whereas 10 indicates the worst pain. The VAS scores were then averaged for each patient.
A power analysis using preliminary data determined that 15 patients were needed in each group to detect a 50% reduction in drain output at a power of 80% and a P value of 0.05. Descriptive statistics were used to analyze demographic data. We compared the demographic and clinical characteristics of patients in the TXA-TAA group with those of patients in the No TXA-TAA group using unpaired student t-tests for continuous variables and Chi-square or Fischer’s exact tests for categorical variables. Simple and adjusted linear regression analyses were used to examine the difference in drain output and blood loss between the 2 groups (TXA-TAA vs No TXA-TAA). Multivariate models were adjusted for age, BMI, and length of surgery. A P value <.05 was considered to be statistically significant. We performed all analyses using a statistical software package (SAS version 9.2, SAS Institute).
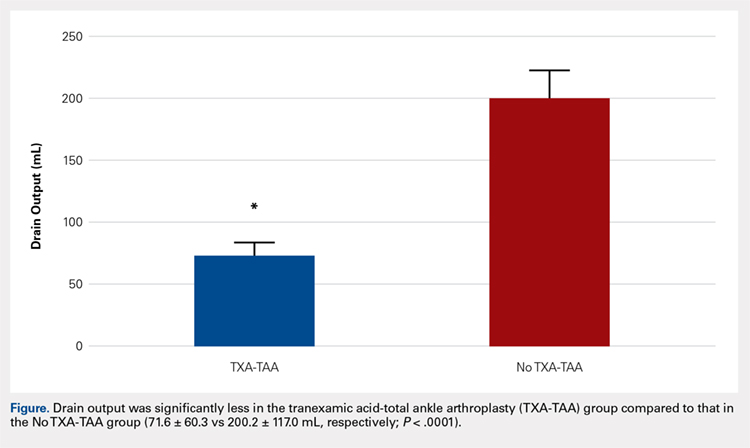
RESULTS
Drain output was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (71.6 ± 60.3 vs 200.2 ± 117.0 mL, respectively, P = .0001) (Figure). The clinical characteristics of the patients who underwent TAA with the use of TXA are outlined in Table 2. The mean change in preoperative to postoperative hemoglobin levels was significantly lower in the TXA-TAA group than in the No TXA-TAA group (1.5 ± 0.6 vs 2.0 ± 0.4 g/dL, respectively; P = .01). The calculated blood loss in patients in the TXA-TAA group was significantly lower than that in patients in the No TXA-TAA group (649.9 ± 332.7 vs 906.8 ± 287.4 mL, respectively; P = .01). No patient in either group received a blood transfusion. We did not observe a significant difference in the length of surgery between the TXA-TAA and the No TXA-TAA groups (112.8 ± 24.8 vs 108.6 ± 26.0 min, respectively; P = .57). The average American Society of Anesthesiologists’ (ASA) classification was similar between the groups (2.2 ± 0.6 and 2.2 ± 0.5, respectively; P = 1.00) as was the age-adjusted Charlson Comorbidity Index (2.8 ± 1.7 vs 2.9 ± 1.6, respectively; P = .93). Mean VAS scores on postoperative day 1 in the TXA-TAA and the No TXA-TAA group were 4.9 ± 1.7 and 5.3 ± 1.4, respectively (P = .71). The average length of stay in the TXA-TAA group was 1.6 ± 0.7 days vs 1.3 ± 0.6 days in the No TXA-TAA group (P = .23). Two patients in the TXA-TAA group had an extended hospital length of stay of 5 days due to discharge planning and social issues.
Table 2. Clinical Characteristics of Total Ankle Arthroplasty (TAA) Patients by Use of Tranexamic Acid (TXA), N = 50 | |||
|---|---|---|---|
| TXA use in TAA | P valuea | |
| Yes (n = 25 cases) | No (n = 25 controls) |
|
Clinical Characteristic |
|
|
|
Drain Output (ml), mean ± SD
| 71.6 ± 60.3 | 200.2 ± 117.0 | <0.0001 |
Preoperative to Postoperative Hgb Change (g/dL), mean ± SD
| 1.5 ± 0.6 | 2.0 ± 0.4 | 0.01 |
Blood Loss Calculated (ml), mean ± SD
| 649.9 ± 332.73 | 906.8 ± 287.4 | 0.01 |
Length of Surgery (min), mean ± SD
| 112.8 ± 24.8 | 108.6 ± 26.0 | 0.57 |
VAS scores on the POD (No.), mean ± SD
| 4.9 ± 1.7 | 5.3 ±1.4 | 0.71 |
LOS (day), mean ± SD
| 1.6 ± 0.7 | 1.3 ± 0.6 | 0.23 |
aP value was calculated from t-test for continuous variables, and Chi-square test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
Abbreviations: LOS, length of stay; VAS, visual analog scale; POD, postoperative day.
Table 3. Linear Regression Analyses of Drain Output and Blood Loss using Tranexamic Acid (TXA) in Total Ankle Arthroplasty (TAA), Unadjusted and Adjusted Models for Length of Surgery, N = 50 | ||||
| TXA Use in TAA (Yes vs No) | |||
Drain Output (mL)
| Regression coefficient (β) | SE | Test statistics (t) | P valuea |
Unadjusted Model | -128.6 | 26.3 | -4.89 | < 0.0001 |
Adjusted for Age | -129.6 | 26.5 | -4.89 | <0.0001 |
Adjusted for BMI | -121.8 | 26.6 | -4.57 | <0.0001 |
Adjusted for Length of Surgery | -129.6 | 26.6 | -4.86 | <0.0001 |
Multivariable Modelb | -123.4 | 27.1 | -4.55 | <0.0001 |
Blood Loss (mL)
|
|
|
|
|
Unadjusted Model | -257.0 | 87.9 | -2.92 | 0.005 |
Adjusted for Age | -263.7 | 87.4 | -3.02 | 0.004 |
Adjusted for BMI | -268.7 | 90.2 | -2.98 | 0.005 |
Adjusted for Length of Surgery | -261.3 | 88.6 | -2.94 | 0.005 |
Multivariable Modelb | -275.6 | 90.7 | -3.04 | 0.004 |
aLinear regression was used to calculate the P value. bAdjusted for age, BMI and length of surgery.
Abbreviation: BMI, body mass index.
Table 4. Patient Wound Complication Categories by Use of Tranexamic Acid (TXA) in Total Ankle Arthroplasty (TAA), N = 50 | |||
|---|---|---|---|
| TXA Use in TAA | P valuea | |
Wound Complication | Yes (n = 25 cases) | No (n = 25 controls) | 0.114 |
None, n = 46 (86%) | 23 (40%) | 20 (46%) |
|
Minor, n = 6 (12%) | 2 (4%) | 4 (8%) |
|
Major, n = 1 (2%) | 0 (0%) | 1 (4%) |
|
aP value was calculated from Fisher’s Exact test (67% cells had count <5) test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
The crude linear regression model revealed a significant difference in drain output between the TXA-TAA and the No TXA-TAA groups (β = −128.6 ± 26.3, P < .0001) (Table 3). Further adjustment for age and length of surgery slightly strengthened the association (β = −129.6 ± 26.6, P < .0001). The nature of regression coefficient β showed that the mean estimate of drain output was 129.6 mL lower in the TXA-TAA group than that in the No TXA-TAA group. There was a significant difference in blood loss between the TXA-TAA and the No TXA-TAA groups in the crude linear regression model (β = −257.0 ± 87.9, P = .005). Additional adjustment for age, BMI, and length of surgery slightly strengthened the association (β = −275.6 ± 90.7, P = .004). The nature of regression coefficient β showed that the mean estimate of blood loss was 275.6 mL lower in the TXA-TAA group than in the No TXA-TAA group (Table 3).
Continue to: There was no statistically significant difference...
There was no statistically significant difference in wound complications between the TXA-TAA and the No TXA-TAA groups in this study population (P = .114). However, our results showed a higher overall wound complication rate in the No TXA-TAA group than in the TXA-TAA group (20% (5/25) vs 8% (2/25), respectively) (Table 4). In the No TXA-TAA group, there were 4 minor and 1 major wound complications. All 5 patients experiencing a postoperative wound complication required oral antibiotics for a minimum of 4 weeks and local wound care. One patient underwent a surgical débridement meeting the criteria for major wound complications. In the TXA-TAA group, there were 2 minor wound complications and no major wound complications. One patient was administered prophylactic oral antibiotics for 7 days with local wound care for blister formation without evidence of infection. The second patient experiencing a minor wound complication required 3 weeks of oral antibiotics and local wound care. No patients in either group had a deep infection requiring implant removal, IV antibiotics, or subsequent hospital admission. The surgical incisions in all patients healed after the aforementioned treatments with no persistent drainage or development of chronic wounds.
In the TXA-TAA group, there was 1 patient who sustained an intraoperative medial malleolus fracture. One patient developed an extensor hallucis longus contracture 5 months postoperatively that subsequently underwent release and lengthening. There was 1 patient in this group who sustained a distal tibia fracture 5 cm proximal to the prosthesis 3 months postoperatively after a mechanical fall. In the No TXA-TAA group, there were 2 patients who sustained intraoperative medial malleolus fractures. One patient underwent a revision of the tibial component 24 months postoperatively due to aseptic loosening. In addition, another patient in this group who sustained an Achilles tendon rupture 5 months postoperatively after a fall subsequently underwent repair with tibialis anterior tendon allograft.
There were no patients in either group who experienced any hospital readmissions in the acute follow-up period as defined by a 90-day period after discharge. There were no complications associated with TXA administration in either group.
DISCUSSION
Recent advances in total ankle prosthetic design coupled with increased survival and improved short- to midterm follow-up results make TAA an effective treatment option for end-stage ankle arthritis. Management of perioperative blood loss and reducing the potential for significant hemarthrosis and subsequent wound complications are important factors to consider for patients undergoing TAA. TXA administration is used in several centers as part of an intraoperative strategy to reduce blood loss and decrease intra-articular blood accumulation. To our knowledge, this is the first study to evaluate the management of blood loss and hemarthrosis using TXA during TAA.
IV and topical administrations of TXA have been demonstrated to be highly effective hemostatic agents in the perioperative period for TKA and THA.11 Recent literature has demonstrated a significant reduction in drain output and mean change in preoperative to postoperative hemoglobin levels in patients who received TXA compared to that in patients who did not receive TXA. The patients who did not receive TXA had more than twice as much drain output.5,10,14,19-21
Continue to: The ankle has a thin...
The ankle has a thin soft tissue envelope that does not have elaborate elastic properties. The soft tissue release and bleeding surfaces of the bone during TAA are not as extensive when compared with TKA and THA, but the intra-articular volume is smaller and the surrounding soft tissues may be less yielding when blood accumulation occurs.22 The vascular supply can be rich surrounding the ankle in the absence of arterial disease and is not as apt to tolerate dislocation and subluxation as in the case of THA or TKA.23 Shear forces can easily tear the branches of the anterior tibial artery that lie within the fascia that is continuous with the periosteum on the distal tibia.24 Reduction of hemarthrosis within the ankle joint may lead to a decrease in postoperative swelling, decreased pain, and increased range of motion due to the diminished potential for fibrosis. We also believe that there could be a reduced risk for wound complications. The current literature reports the rate of wound complications to be anywhere from 2% to 25%, with diabetes, inflammatory conditions, coronary artery disease, peripheral vascular disease, and smoking history >12-pack-years as risk factors.16,25,26 In this study, we observed a significant reduction in drain output and an overall reduced percentage of postoperative wound complications in patients who received TXA. These results demonstrate that TXA use decreases postoperative hemarthrosis.
TXA use in TKA and THA has been shown to decrease direct hospital costs and hospital length of stay.7,14,27 A recent study by Moskal and colleagues7 showed that topical TXA use has the potential to significantly decrease hospital man-hours for those patients undergoing TKA and achieve larger cost savings. Although there was no significant difference in the length of stay between the 2 groups, the average length of stay after TAA was shorter in both groups compared to the reported national average (1.49 vs 2.2 days, respectively).4 The administration of TXA in the appropriate patient has the potential to decrease hospital costs by controlling postoperative pain and swelling, allowing for earlier discharge. Long-term cost benefits could also include decreased infection rates and wound complications, and improved clinical outcomes because of improved range of motion and function scores.
The limitations of this study include the retrospective nature of its design and the relatively small sample size. The results showed nonstatistically significant differences in wound complications between the TXA-TAA and the No TXA-TAA groups, consistent with an insufficient sample size and thus inadequate power to detect the significant difference. However, this study clearly showed that the wound complication rates were higher in the No TXA-TAA group than in the TXA-TAA group, suggesting the importance of further similar studies using a larger sample size.
CONCLUSION
Current TAA offers a viable alternative to arthrodesis for end-stage ankle arthritis. TXA is an inexpensive and effective hemostatic agent used during TAA. If no major contraindication is present, routine use of TXA is recommended to assist in blood loss management, decrease postoperative hemarthrosis, and help to reduce the risk of postoperative wound complications.
1. Saltzman CL, Salamon ML, Blanchard GM, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44-46.
2. Glazebrook M, Daniels T, Younger A, et al. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90(3):499-505. doi:10.2106/JBJS.F.01299.
3. Thomas RH, Daniels TR. Ankle arthritis. J Bone Joint Surg Am. 2003;85-A(5):923-936.
4. Zhou H, Yakavonis M, Shaw JJ, Patel A, Li X. In-patient trends and complications after total ankle arthroplasty in the United States. Orthopedics. 2016:1-6. doi:10.3928/01477447-20151228-05.
5. Benoni G, Fredin H. Fibrinolytic inhibition with tranexamic acid reduces blood loss and blood transfusion after knee arthroplasty: a prospective, randomised, double-blind study of 86 patients. J Bone Joint Surg Br. 1996;78(3):434-440.
6. Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM. A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J. 2014;96-B(8):1005-1015. doi:10.1302/0301-620X.96B8.33745.
7. Moskal JT, Harris RN, Capps SG. Transfusion cost savings with tranexamic acid in primary total knee arthroplasty from 2009 to 2012. J Arthroplasty. 2015;30(3):365-368. doi:10.1016/j.arth.2014.10.008.
8. Friedman R, Homering M, Holberg G, Berkowitz SD. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014;96(4):272-278. doi:10.2106/JBJS.L.01268.
9. Aggarwal AK, Singh N, Sudesh P. Topical vs intravenous tranexamic acid in reducing blood loss after bilateral total knee arthroplasty: a prospective study. J Arthroplasty. 2016;31(7):1442-1448. doi:10.1016/j.arth.2015.12.033.
10. Su EP, Su S. Strategies for reducing peri-operative blood loss in total knee arthroplasty. Bone Joint J. 2016;98-B(1 Suppl A):98-100. doi:10.1302/0301-620X.98B.36430.
11. Gomez-Barrena E, Ortega-Andreu M, Padilla-Eguiluz NG, Perez-Chrzanowska H, Figueredo-Zalve R. Topical intra-articular compared with intravenous tranexamic acid to reduce blood loss in primary total knee replacement: a double-blind, randomized, controlled, noninferiority clinical trial. J Bone Joint Surg Am. 2014;96(23):1937-1944. doi:10.2106/JBJS.N.00060.
12. Cap AP, Baer DG, Orman JA, Aden J, Ryan K, Blackbourne LH. Tranexamic acid for trauma patients: a critical review of the literature. J Trauma. 2011;71(1 Suppl):S9-14. doi:10.1097/TA.0b013e31822114af.
13. Duncan CM, Gillette BP, Jacob AK, Sierra RJ, Sanchez-Sotelo J, Smith HM. Venous thromboembolism and mortality associated with tranexamic acid use during total hip and knee arthroplasty. J Arthroplasty. 2015;30(2):272-276. doi:10.1016/j.arth.2014.08.022.
14. Alshryda S, Mason J, Vaghela M, et al. Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total knee replacement: a randomized controlled trial (TRANX-K). J Bone Joint Surg Am. 2013;95(21):1961-1968. doi:10.2106/JBJS.L.00907.
15. Ng W, Jerath A, Wasowicz M. Tranexamic acid: a clinical review. Anaesthesiol Intensive Ther. 2015;47(4):339-350. doi:10.5603/AIT.a2015.0011.
16. Raikin SM, Kane J, Ciminiello ME. Risk factors for incision-healing complications following total ankle arthroplasty. J Bone Joint Surg Am. 2010;92(12):2150-2155. doi:10.2106/JBJS.I.00870.
17. Meunier A, Petersson A, Good L, Berlin G. Validation of a haemoglobin dilution method for estimation of blood loss. Vox Sang. 2008;95(2):120-124. doi:10.1111/j.1423-0410.2008.01071.x.
18. Gibon E, Courpied JP, Hamadouche M. Total joint replacement and blood loss: what is the best equation? Int Orthop. 2013;37(4):735-739. doi:10.1007/s00264-013-1801-0
19. Chareancholvanich K, Siriwattanasakul P, Narkbunnam R, Pornrattanamaneewong C. Temporary clamping of drain combined with tranexamic acid reduce blood loss after total knee arthroplasty: a prospective randomized controlled trial. BMC Musculoskelet Disord. 2012;13:124.
20. Orpen NM, Little C, Walker G, Crawfurd EJ. Tranexamic acid reduces early post-operative blood loss after total knee arthroplasty: a prospective randomised controlled trial of 29 patients. Knee. 2006;13(2):106-110. doi:10.1016/j.knee.2005.11.001.
21. Veien M, Sorensen JV, Madsen F, Juelsgaard P. Tranexamic acid given intraoperatively reduces blood loss after total knee replacement: a randomized, controlled study. Acta Anaesthesiol Scand. 2002;46(10):1206-1211.
22. Draeger RW, Singh B, Parekh SG. Quantifying normal ankle joint volume: An anatomic study. Indian J Orthop. 2009;43(1):72-75. doi:10.4103/0019-5413.45326.
23. Gill LH. Challenges in total ankle arthroplasty. Foot Ankle Int. 2004;25(4):195-207. doi:10.1177/107110070402500402.
24. Taylor GI, Pan WR. Angiosomes of the leg: anatomic study and clinical implications. Plast Reconstr Surg. 1998;102(3):599-616; discussion 617-598. doi:10.1097/00006534-199809030-00001.
25. Gougoulias N, Khanna A, Maffulli N. How successful are current ankle replacements?: a systematic review of the literature. Clin Orthop Relat Res. 2010;468(1):199-208. doi:10.1007/s11999-009-0987-3.
26. Noelle S, Egidy CC, Cross MB, Gebauer M, Klauser W. Complication rates after total ankle arthroplasty in one hundred consecutive prostheses. Int Orthop. 2013;37(9):1789-1794. doi:10.1007/s00264-013-1971-9.
27. Chimento GF, Huff T, Ochsner JL Jr, Meyer M, Brandner L, Babin S. An evaluation of the use of topical tranexamic acid in total knee arthroplasty. J Arthroplasty. 2013;28(8 Suppl):74-77. doi:10.1016/j.arth.2013.06.037.
ABSTRACT
Tranexamic acid (TXA) is an effective agent used for reducing perioperative blood loss and decreasing the potential for postoperative hemarthrosis. We hypothesized that patients who had received intraoperative TXA during total ankle arthroplasty (TAA) would have a reduction in postoperative drain output, thereby resulting in a reduced risk of postoperative hemarthrosis and lower wound complication rates.
A retrospective review was conducted on 50 consecutive patients, 25 receiving TXA (TXA-TAA) and 25 not receiving TXA (No TXA-TAA), who underwent an uncemented TAA between September 2011 and December 2015. Demographic characteristics, drain output, preoperative and postoperative hemoglobin levels, operative and postoperative course, and minor and major wound complications of the patients were reviewed.
Drain output was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (71.6 ± 60.3 vs 200.2 ± 117.0 mL, respectively, P < .0001). The overall wound complication rate in the No TXA-TAA group was higher (20%, 5/25) than that in the TXA-TAA group (8%, 2/25) (P = .114). The mean change in preoperative to postoperative hemoglobin level was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (1.5 ± 0.6 vs 2.0 ± 0.4 g/dL, respectively, P = .01).
TXA is an effective hemostatic agent when used during TAA. TXA reduces perioperative blood loss, hemarthrosis, and the risk of wound complications.
Continue to: End-stage ankle arthritis...
End-stage ankle arthritis is a disabling condition that may lead to poor quality of life and difficulties with activities of daily living.1 The associated mental and physical disability has been demonstrated to be as severe as in end-stage hip arthrosis.2 Operative treatment for symptomatic end-stage ankle arthritis includes arthrodesis or total ankle arthroplasty (TAA) in those refractory to nonoperative treatment.3 Newer generation implants have made TAA a more attractive option for both the surgeon and the patient.
Over the past decade, the utility of TAA has increased and attention has turned toward the management of perioperative factors that would maximize patient satisfaction and decrease the length of stay and complication rates, as well as hospital costs.4 Comprehensive literature on total knee arthroplasty (TKA) and total hip arthroplasty (THA) has demonstrated that the management of perioperative blood loss, specifically postoperative hemarthrosis, is a modifiable factor affecting patient recovery, complication rates, and hospital costs.5-8 Drain output has been used as a direct measure of intra-articular blood accumulation.9 Decreased drain output implies decreased hemarthrosis, which could potentially alleviate the pressure on the wound and decrease wound complications.
One of the major strategies that has been recognized for reducing blood loss and decreasing the potential for postoperative hemarthrosis is the use of intravenous (IV) or topical tranexamic acid (TXA).10,11 TXA is a synthetic antifibrinolytic medication that has been extensively used throughout the medical field since the 1960s to help control the bleeding cascade. This medication stabilizes clot formation without inducing a pro-coaguable state.12 Intraoperative administration of TXA has been shown to reduce drain output and decrease transfusion requirements after TKA and THA without an associated increase in patient morbidity and mortality.6,11,13-15
Currently, there is a lack of studies evaluating the utility of TXA during TAA. We hypothesize that compared with patients who had not received TXA, those who had received intraoperative TXA during TAA would have a reduction in postoperative drain output and therefore decreased hemarthrosis, lower wound complication rate, and a diminished change in preoperative to postoperative hemoglobin levels, reflecting a reduction in perioperative blood loss.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board at the University at Buffalo, State University of New York. A retrospective chart review was conducted on 50 consecutive patients who underwent an uncemented TAA with the Salto Talaris total ankle prosthesis (Tornier, Inc) between September 2011 and December 2015. All surgeries were performed at 1 institution by a single fellowship surgeon trained in foot and ankle surgery through the anterior approach where a midline incision was made over the ankle. The interval between the tibialis anterior tendon and the extensor hallucis longus tendon was used. We had incorporated intraoperative TXA into the TAA surgical protocol at our institution in January 2014. We evaluated the first 25 consecutive patients who underwent TAA after TXA use began (TXA-TAA) and another 25 consecutive patients who underwent TAA before the routine use of TXA (No TXA-TAA). Inclusion criteria were patients who presented with pain, decreased function, and radiographic parameters of end-stage tibiotalar arthritis due to degenerative arthritis, rheumatoid arthritis, or posttraumatic arthritis who subsequently underwent a TAA. Exclusion criteria were patients with a contraindication for IV TXA use, a preexisting coagulopathy, or where drain output was not recorded. Contraindications for IV TXA use included patients with impaired renal clearance, recent cardiac surgery, myocardial infarction, ischemic stroke, or venous thromboembolism (VTE). Seven patients were ultimately excluded from this study based on the inclusion and exclusion criteria, 3 patients from the TXA-TAA group and 4 patients from the No TXA-TAA group.
Continue to: Charts were reviewed for demographics...
Charts were reviewed for demographics, preoperative and postoperative hemoglobin levels, indications for surgery, surgical procedures, length of surgery, postoperative drain output, length of stay, postoperative pain visual analog scale (VAS) score, minor and major wound complications, and postoperative complications. Minor wound complications were defined as the anterior surgical incision that required local wound care in office or oral antibiotics without subsequent consequences. Major wound complications were defined as requiring surgical débridement and/or any additional treatment in the operating room.16 Postoperative complications other than wound complications were defined as those requiring a subsequent surgical intervention. Patient demographics and clinical and procedural characteristics of patients in both the TXA-TAA and the No TXA-TAA groups are outlined in Table 1. There were 14 males and 11 females in the TXA-TAA group and 16 males and 9 females in the No TXA-TAA group. The mean age was 65.8 ± 10.9 years in the TXA-TAA group and 66.9 ± 8.0 years in the No TXA-TAA group (P = .69). Mean body mass index (BMI) was 31.6 ± 6.3 in the TXA-TAA group and 29.4 ± 4.9 in the No TXA-TAA group (P = .18). The primary indication for TAA was degenerative osteoarthritis in 26 patients, posttraumatic arthritis in 21 patients, and rheumatoid arthritis in 3 patients. The most common associated procedure was Achilles tendon lengthening in both groups. The mean follow-up in the TXA-TAA group was 9.3 ± 5.8 months (range, 2.0-24.0 months). Postoperative complications due to TXA administration as described in previous literature were defined as VTE, myocardial infarction, or ischemic cerebral event. The TXA-TAA group received a standard 1 g dose of IV TXA 20 minutes prior to tourniquet inflation. A tourniquet was used intraoperatively on all patients included in this study. A postoperative 400-mL surgical drain (Hemovac, Zimmer Biomet) was placed in the ankle joint in all patients and subsequently discontinued on postoperative day 1. Recent literature has reported the minor wound complication rate associated with TAA to be as high as 25% and the major wound complication rate to be 8.5%.16 To assist in reducing the risk for wound complications, our protocol traditionally uses an intra-articular surgical drain to decrease any pressure on the wound from postoperative hemarthrosis.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
aP value was calculated from t-test continuous variables and Chi-square test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index.
Total drain output was recorded in milliliters (mL) in all patients. The change between the preoperative hemoglobin level and the hemoglobin level on postoperative day 1 was calculated for each patient. The calculated blood loss was determined using Meunier’s equation, which estimates the total blood volume using Nadler’s formula and then uses preoperative hemoglobin and postoperative day 1 hemoglobin values to calculate blood loss.17,18 VAS scores (scale, 1-10) were obtained every 4 hours on postoperative day 1 according to the nursing protocol. The number 1 on the scale represents the least amount of pain, whereas 10 indicates the worst pain. The VAS scores were then averaged for each patient.
A power analysis using preliminary data determined that 15 patients were needed in each group to detect a 50% reduction in drain output at a power of 80% and a P value of 0.05. Descriptive statistics were used to analyze demographic data. We compared the demographic and clinical characteristics of patients in the TXA-TAA group with those of patients in the No TXA-TAA group using unpaired student t-tests for continuous variables and Chi-square or Fischer’s exact tests for categorical variables. Simple and adjusted linear regression analyses were used to examine the difference in drain output and blood loss between the 2 groups (TXA-TAA vs No TXA-TAA). Multivariate models were adjusted for age, BMI, and length of surgery. A P value <.05 was considered to be statistically significant. We performed all analyses using a statistical software package (SAS version 9.2, SAS Institute).
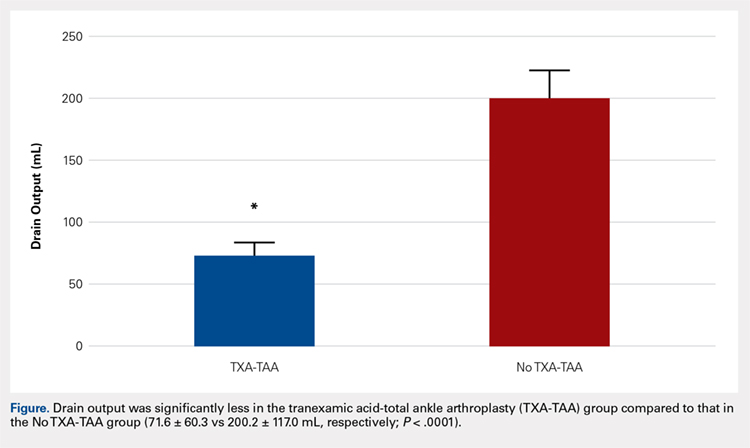
RESULTS
Drain output was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (71.6 ± 60.3 vs 200.2 ± 117.0 mL, respectively, P = .0001) (Figure). The clinical characteristics of the patients who underwent TAA with the use of TXA are outlined in Table 2. The mean change in preoperative to postoperative hemoglobin levels was significantly lower in the TXA-TAA group than in the No TXA-TAA group (1.5 ± 0.6 vs 2.0 ± 0.4 g/dL, respectively; P = .01). The calculated blood loss in patients in the TXA-TAA group was significantly lower than that in patients in the No TXA-TAA group (649.9 ± 332.7 vs 906.8 ± 287.4 mL, respectively; P = .01). No patient in either group received a blood transfusion. We did not observe a significant difference in the length of surgery between the TXA-TAA and the No TXA-TAA groups (112.8 ± 24.8 vs 108.6 ± 26.0 min, respectively; P = .57). The average American Society of Anesthesiologists’ (ASA) classification was similar between the groups (2.2 ± 0.6 and 2.2 ± 0.5, respectively; P = 1.00) as was the age-adjusted Charlson Comorbidity Index (2.8 ± 1.7 vs 2.9 ± 1.6, respectively; P = .93). Mean VAS scores on postoperative day 1 in the TXA-TAA and the No TXA-TAA group were 4.9 ± 1.7 and 5.3 ± 1.4, respectively (P = .71). The average length of stay in the TXA-TAA group was 1.6 ± 0.7 days vs 1.3 ± 0.6 days in the No TXA-TAA group (P = .23). Two patients in the TXA-TAA group had an extended hospital length of stay of 5 days due to discharge planning and social issues.
Table 2. Clinical Characteristics of Total Ankle Arthroplasty (TAA) Patients by Use of Tranexamic Acid (TXA), N = 50 | |||
|---|---|---|---|
| TXA use in TAA | P valuea | |
| Yes (n = 25 cases) | No (n = 25 controls) |
|
Clinical Characteristic |
|
|
|
Drain Output (ml), mean ± SD
| 71.6 ± 60.3 | 200.2 ± 117.0 | <0.0001 |
Preoperative to Postoperative Hgb Change (g/dL), mean ± SD
| 1.5 ± 0.6 | 2.0 ± 0.4 | 0.01 |
Blood Loss Calculated (ml), mean ± SD
| 649.9 ± 332.73 | 906.8 ± 287.4 | 0.01 |
Length of Surgery (min), mean ± SD
| 112.8 ± 24.8 | 108.6 ± 26.0 | 0.57 |
VAS scores on the POD (No.), mean ± SD
| 4.9 ± 1.7 | 5.3 ±1.4 | 0.71 |
LOS (day), mean ± SD
| 1.6 ± 0.7 | 1.3 ± 0.6 | 0.23 |
aP value was calculated from t-test for continuous variables, and Chi-square test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
Abbreviations: LOS, length of stay; VAS, visual analog scale; POD, postoperative day.
Table 3. Linear Regression Analyses of Drain Output and Blood Loss using Tranexamic Acid (TXA) in Total Ankle Arthroplasty (TAA), Unadjusted and Adjusted Models for Length of Surgery, N = 50 | ||||
| TXA Use in TAA (Yes vs No) | |||
Drain Output (mL)
| Regression coefficient (β) | SE | Test statistics (t) | P valuea |
Unadjusted Model | -128.6 | 26.3 | -4.89 | < 0.0001 |
Adjusted for Age | -129.6 | 26.5 | -4.89 | <0.0001 |
Adjusted for BMI | -121.8 | 26.6 | -4.57 | <0.0001 |
Adjusted for Length of Surgery | -129.6 | 26.6 | -4.86 | <0.0001 |
Multivariable Modelb | -123.4 | 27.1 | -4.55 | <0.0001 |
Blood Loss (mL)
|
|
|
|
|
Unadjusted Model | -257.0 | 87.9 | -2.92 | 0.005 |
Adjusted for Age | -263.7 | 87.4 | -3.02 | 0.004 |
Adjusted for BMI | -268.7 | 90.2 | -2.98 | 0.005 |
Adjusted for Length of Surgery | -261.3 | 88.6 | -2.94 | 0.005 |
Multivariable Modelb | -275.6 | 90.7 | -3.04 | 0.004 |
aLinear regression was used to calculate the P value. bAdjusted for age, BMI and length of surgery.
Abbreviation: BMI, body mass index.
Table 4. Patient Wound Complication Categories by Use of Tranexamic Acid (TXA) in Total Ankle Arthroplasty (TAA), N = 50 | |||
|---|---|---|---|
| TXA Use in TAA | P valuea | |
Wound Complication | Yes (n = 25 cases) | No (n = 25 controls) | 0.114 |
None, n = 46 (86%) | 23 (40%) | 20 (46%) |
|
Minor, n = 6 (12%) | 2 (4%) | 4 (8%) |
|
Major, n = 1 (2%) | 0 (0%) | 1 (4%) |
|
aP value was calculated from Fisher’s Exact test (67% cells had count <5) test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
The crude linear regression model revealed a significant difference in drain output between the TXA-TAA and the No TXA-TAA groups (β = −128.6 ± 26.3, P < .0001) (Table 3). Further adjustment for age and length of surgery slightly strengthened the association (β = −129.6 ± 26.6, P < .0001). The nature of regression coefficient β showed that the mean estimate of drain output was 129.6 mL lower in the TXA-TAA group than that in the No TXA-TAA group. There was a significant difference in blood loss between the TXA-TAA and the No TXA-TAA groups in the crude linear regression model (β = −257.0 ± 87.9, P = .005). Additional adjustment for age, BMI, and length of surgery slightly strengthened the association (β = −275.6 ± 90.7, P = .004). The nature of regression coefficient β showed that the mean estimate of blood loss was 275.6 mL lower in the TXA-TAA group than in the No TXA-TAA group (Table 3).
Continue to: There was no statistically significant difference...
There was no statistically significant difference in wound complications between the TXA-TAA and the No TXA-TAA groups in this study population (P = .114). However, our results showed a higher overall wound complication rate in the No TXA-TAA group than in the TXA-TAA group (20% (5/25) vs 8% (2/25), respectively) (Table 4). In the No TXA-TAA group, there were 4 minor and 1 major wound complications. All 5 patients experiencing a postoperative wound complication required oral antibiotics for a minimum of 4 weeks and local wound care. One patient underwent a surgical débridement meeting the criteria for major wound complications. In the TXA-TAA group, there were 2 minor wound complications and no major wound complications. One patient was administered prophylactic oral antibiotics for 7 days with local wound care for blister formation without evidence of infection. The second patient experiencing a minor wound complication required 3 weeks of oral antibiotics and local wound care. No patients in either group had a deep infection requiring implant removal, IV antibiotics, or subsequent hospital admission. The surgical incisions in all patients healed after the aforementioned treatments with no persistent drainage or development of chronic wounds.
In the TXA-TAA group, there was 1 patient who sustained an intraoperative medial malleolus fracture. One patient developed an extensor hallucis longus contracture 5 months postoperatively that subsequently underwent release and lengthening. There was 1 patient in this group who sustained a distal tibia fracture 5 cm proximal to the prosthesis 3 months postoperatively after a mechanical fall. In the No TXA-TAA group, there were 2 patients who sustained intraoperative medial malleolus fractures. One patient underwent a revision of the tibial component 24 months postoperatively due to aseptic loosening. In addition, another patient in this group who sustained an Achilles tendon rupture 5 months postoperatively after a fall subsequently underwent repair with tibialis anterior tendon allograft.
There were no patients in either group who experienced any hospital readmissions in the acute follow-up period as defined by a 90-day period after discharge. There were no complications associated with TXA administration in either group.
DISCUSSION
Recent advances in total ankle prosthetic design coupled with increased survival and improved short- to midterm follow-up results make TAA an effective treatment option for end-stage ankle arthritis. Management of perioperative blood loss and reducing the potential for significant hemarthrosis and subsequent wound complications are important factors to consider for patients undergoing TAA. TXA administration is used in several centers as part of an intraoperative strategy to reduce blood loss and decrease intra-articular blood accumulation. To our knowledge, this is the first study to evaluate the management of blood loss and hemarthrosis using TXA during TAA.
IV and topical administrations of TXA have been demonstrated to be highly effective hemostatic agents in the perioperative period for TKA and THA.11 Recent literature has demonstrated a significant reduction in drain output and mean change in preoperative to postoperative hemoglobin levels in patients who received TXA compared to that in patients who did not receive TXA. The patients who did not receive TXA had more than twice as much drain output.5,10,14,19-21
Continue to: The ankle has a thin...
The ankle has a thin soft tissue envelope that does not have elaborate elastic properties. The soft tissue release and bleeding surfaces of the bone during TAA are not as extensive when compared with TKA and THA, but the intra-articular volume is smaller and the surrounding soft tissues may be less yielding when blood accumulation occurs.22 The vascular supply can be rich surrounding the ankle in the absence of arterial disease and is not as apt to tolerate dislocation and subluxation as in the case of THA or TKA.23 Shear forces can easily tear the branches of the anterior tibial artery that lie within the fascia that is continuous with the periosteum on the distal tibia.24 Reduction of hemarthrosis within the ankle joint may lead to a decrease in postoperative swelling, decreased pain, and increased range of motion due to the diminished potential for fibrosis. We also believe that there could be a reduced risk for wound complications. The current literature reports the rate of wound complications to be anywhere from 2% to 25%, with diabetes, inflammatory conditions, coronary artery disease, peripheral vascular disease, and smoking history >12-pack-years as risk factors.16,25,26 In this study, we observed a significant reduction in drain output and an overall reduced percentage of postoperative wound complications in patients who received TXA. These results demonstrate that TXA use decreases postoperative hemarthrosis.
TXA use in TKA and THA has been shown to decrease direct hospital costs and hospital length of stay.7,14,27 A recent study by Moskal and colleagues7 showed that topical TXA use has the potential to significantly decrease hospital man-hours for those patients undergoing TKA and achieve larger cost savings. Although there was no significant difference in the length of stay between the 2 groups, the average length of stay after TAA was shorter in both groups compared to the reported national average (1.49 vs 2.2 days, respectively).4 The administration of TXA in the appropriate patient has the potential to decrease hospital costs by controlling postoperative pain and swelling, allowing for earlier discharge. Long-term cost benefits could also include decreased infection rates and wound complications, and improved clinical outcomes because of improved range of motion and function scores.
The limitations of this study include the retrospective nature of its design and the relatively small sample size. The results showed nonstatistically significant differences in wound complications between the TXA-TAA and the No TXA-TAA groups, consistent with an insufficient sample size and thus inadequate power to detect the significant difference. However, this study clearly showed that the wound complication rates were higher in the No TXA-TAA group than in the TXA-TAA group, suggesting the importance of further similar studies using a larger sample size.
CONCLUSION
Current TAA offers a viable alternative to arthrodesis for end-stage ankle arthritis. TXA is an inexpensive and effective hemostatic agent used during TAA. If no major contraindication is present, routine use of TXA is recommended to assist in blood loss management, decrease postoperative hemarthrosis, and help to reduce the risk of postoperative wound complications.
ABSTRACT
Tranexamic acid (TXA) is an effective agent used for reducing perioperative blood loss and decreasing the potential for postoperative hemarthrosis. We hypothesized that patients who had received intraoperative TXA during total ankle arthroplasty (TAA) would have a reduction in postoperative drain output, thereby resulting in a reduced risk of postoperative hemarthrosis and lower wound complication rates.
A retrospective review was conducted on 50 consecutive patients, 25 receiving TXA (TXA-TAA) and 25 not receiving TXA (No TXA-TAA), who underwent an uncemented TAA between September 2011 and December 2015. Demographic characteristics, drain output, preoperative and postoperative hemoglobin levels, operative and postoperative course, and minor and major wound complications of the patients were reviewed.
Drain output was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (71.6 ± 60.3 vs 200.2 ± 117.0 mL, respectively, P < .0001). The overall wound complication rate in the No TXA-TAA group was higher (20%, 5/25) than that in the TXA-TAA group (8%, 2/25) (P = .114). The mean change in preoperative to postoperative hemoglobin level was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (1.5 ± 0.6 vs 2.0 ± 0.4 g/dL, respectively, P = .01).
TXA is an effective hemostatic agent when used during TAA. TXA reduces perioperative blood loss, hemarthrosis, and the risk of wound complications.
Continue to: End-stage ankle arthritis...
End-stage ankle arthritis is a disabling condition that may lead to poor quality of life and difficulties with activities of daily living.1 The associated mental and physical disability has been demonstrated to be as severe as in end-stage hip arthrosis.2 Operative treatment for symptomatic end-stage ankle arthritis includes arthrodesis or total ankle arthroplasty (TAA) in those refractory to nonoperative treatment.3 Newer generation implants have made TAA a more attractive option for both the surgeon and the patient.
Over the past decade, the utility of TAA has increased and attention has turned toward the management of perioperative factors that would maximize patient satisfaction and decrease the length of stay and complication rates, as well as hospital costs.4 Comprehensive literature on total knee arthroplasty (TKA) and total hip arthroplasty (THA) has demonstrated that the management of perioperative blood loss, specifically postoperative hemarthrosis, is a modifiable factor affecting patient recovery, complication rates, and hospital costs.5-8 Drain output has been used as a direct measure of intra-articular blood accumulation.9 Decreased drain output implies decreased hemarthrosis, which could potentially alleviate the pressure on the wound and decrease wound complications.
One of the major strategies that has been recognized for reducing blood loss and decreasing the potential for postoperative hemarthrosis is the use of intravenous (IV) or topical tranexamic acid (TXA).10,11 TXA is a synthetic antifibrinolytic medication that has been extensively used throughout the medical field since the 1960s to help control the bleeding cascade. This medication stabilizes clot formation without inducing a pro-coaguable state.12 Intraoperative administration of TXA has been shown to reduce drain output and decrease transfusion requirements after TKA and THA without an associated increase in patient morbidity and mortality.6,11,13-15
Currently, there is a lack of studies evaluating the utility of TXA during TAA. We hypothesize that compared with patients who had not received TXA, those who had received intraoperative TXA during TAA would have a reduction in postoperative drain output and therefore decreased hemarthrosis, lower wound complication rate, and a diminished change in preoperative to postoperative hemoglobin levels, reflecting a reduction in perioperative blood loss.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board at the University at Buffalo, State University of New York. A retrospective chart review was conducted on 50 consecutive patients who underwent an uncemented TAA with the Salto Talaris total ankle prosthesis (Tornier, Inc) between September 2011 and December 2015. All surgeries were performed at 1 institution by a single fellowship surgeon trained in foot and ankle surgery through the anterior approach where a midline incision was made over the ankle. The interval between the tibialis anterior tendon and the extensor hallucis longus tendon was used. We had incorporated intraoperative TXA into the TAA surgical protocol at our institution in January 2014. We evaluated the first 25 consecutive patients who underwent TAA after TXA use began (TXA-TAA) and another 25 consecutive patients who underwent TAA before the routine use of TXA (No TXA-TAA). Inclusion criteria were patients who presented with pain, decreased function, and radiographic parameters of end-stage tibiotalar arthritis due to degenerative arthritis, rheumatoid arthritis, or posttraumatic arthritis who subsequently underwent a TAA. Exclusion criteria were patients with a contraindication for IV TXA use, a preexisting coagulopathy, or where drain output was not recorded. Contraindications for IV TXA use included patients with impaired renal clearance, recent cardiac surgery, myocardial infarction, ischemic stroke, or venous thromboembolism (VTE). Seven patients were ultimately excluded from this study based on the inclusion and exclusion criteria, 3 patients from the TXA-TAA group and 4 patients from the No TXA-TAA group.
Continue to: Charts were reviewed for demographics...
Charts were reviewed for demographics, preoperative and postoperative hemoglobin levels, indications for surgery, surgical procedures, length of surgery, postoperative drain output, length of stay, postoperative pain visual analog scale (VAS) score, minor and major wound complications, and postoperative complications. Minor wound complications were defined as the anterior surgical incision that required local wound care in office or oral antibiotics without subsequent consequences. Major wound complications were defined as requiring surgical débridement and/or any additional treatment in the operating room.16 Postoperative complications other than wound complications were defined as those requiring a subsequent surgical intervention. Patient demographics and clinical and procedural characteristics of patients in both the TXA-TAA and the No TXA-TAA groups are outlined in Table 1. There were 14 males and 11 females in the TXA-TAA group and 16 males and 9 females in the No TXA-TAA group. The mean age was 65.8 ± 10.9 years in the TXA-TAA group and 66.9 ± 8.0 years in the No TXA-TAA group (P = .69). Mean body mass index (BMI) was 31.6 ± 6.3 in the TXA-TAA group and 29.4 ± 4.9 in the No TXA-TAA group (P = .18). The primary indication for TAA was degenerative osteoarthritis in 26 patients, posttraumatic arthritis in 21 patients, and rheumatoid arthritis in 3 patients. The most common associated procedure was Achilles tendon lengthening in both groups. The mean follow-up in the TXA-TAA group was 9.3 ± 5.8 months (range, 2.0-24.0 months). Postoperative complications due to TXA administration as described in previous literature were defined as VTE, myocardial infarction, or ischemic cerebral event. The TXA-TAA group received a standard 1 g dose of IV TXA 20 minutes prior to tourniquet inflation. A tourniquet was used intraoperatively on all patients included in this study. A postoperative 400-mL surgical drain (Hemovac, Zimmer Biomet) was placed in the ankle joint in all patients and subsequently discontinued on postoperative day 1. Recent literature has reported the minor wound complication rate associated with TAA to be as high as 25% and the major wound complication rate to be 8.5%.16 To assist in reducing the risk for wound complications, our protocol traditionally uses an intra-articular surgical drain to decrease any pressure on the wound from postoperative hemarthrosis.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
aP value was calculated from t-test continuous variables and Chi-square test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index.
Total drain output was recorded in milliliters (mL) in all patients. The change between the preoperative hemoglobin level and the hemoglobin level on postoperative day 1 was calculated for each patient. The calculated blood loss was determined using Meunier’s equation, which estimates the total blood volume using Nadler’s formula and then uses preoperative hemoglobin and postoperative day 1 hemoglobin values to calculate blood loss.17,18 VAS scores (scale, 1-10) were obtained every 4 hours on postoperative day 1 according to the nursing protocol. The number 1 on the scale represents the least amount of pain, whereas 10 indicates the worst pain. The VAS scores were then averaged for each patient.
A power analysis using preliminary data determined that 15 patients were needed in each group to detect a 50% reduction in drain output at a power of 80% and a P value of 0.05. Descriptive statistics were used to analyze demographic data. We compared the demographic and clinical characteristics of patients in the TXA-TAA group with those of patients in the No TXA-TAA group using unpaired student t-tests for continuous variables and Chi-square or Fischer’s exact tests for categorical variables. Simple and adjusted linear regression analyses were used to examine the difference in drain output and blood loss between the 2 groups (TXA-TAA vs No TXA-TAA). Multivariate models were adjusted for age, BMI, and length of surgery. A P value <.05 was considered to be statistically significant. We performed all analyses using a statistical software package (SAS version 9.2, SAS Institute).
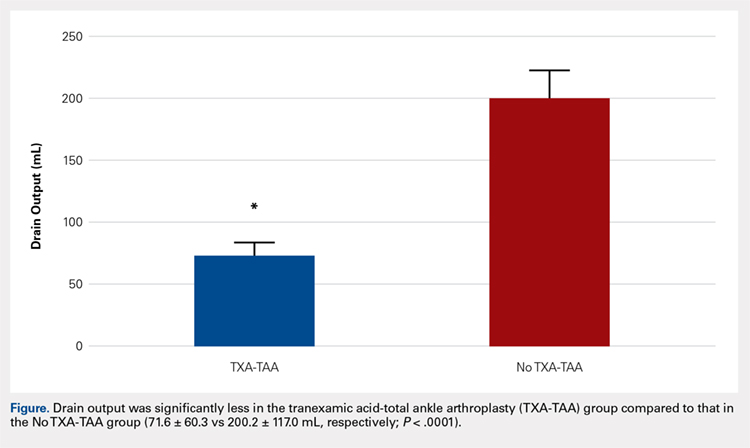
RESULTS
Drain output was significantly less in the TXA-TAA group compared to that in the No TXA-TAA group (71.6 ± 60.3 vs 200.2 ± 117.0 mL, respectively, P = .0001) (Figure). The clinical characteristics of the patients who underwent TAA with the use of TXA are outlined in Table 2. The mean change in preoperative to postoperative hemoglobin levels was significantly lower in the TXA-TAA group than in the No TXA-TAA group (1.5 ± 0.6 vs 2.0 ± 0.4 g/dL, respectively; P = .01). The calculated blood loss in patients in the TXA-TAA group was significantly lower than that in patients in the No TXA-TAA group (649.9 ± 332.7 vs 906.8 ± 287.4 mL, respectively; P = .01). No patient in either group received a blood transfusion. We did not observe a significant difference in the length of surgery between the TXA-TAA and the No TXA-TAA groups (112.8 ± 24.8 vs 108.6 ± 26.0 min, respectively; P = .57). The average American Society of Anesthesiologists’ (ASA) classification was similar between the groups (2.2 ± 0.6 and 2.2 ± 0.5, respectively; P = 1.00) as was the age-adjusted Charlson Comorbidity Index (2.8 ± 1.7 vs 2.9 ± 1.6, respectively; P = .93). Mean VAS scores on postoperative day 1 in the TXA-TAA and the No TXA-TAA group were 4.9 ± 1.7 and 5.3 ± 1.4, respectively (P = .71). The average length of stay in the TXA-TAA group was 1.6 ± 0.7 days vs 1.3 ± 0.6 days in the No TXA-TAA group (P = .23). Two patients in the TXA-TAA group had an extended hospital length of stay of 5 days due to discharge planning and social issues.
Table 2. Clinical Characteristics of Total Ankle Arthroplasty (TAA) Patients by Use of Tranexamic Acid (TXA), N = 50 | |||
|---|---|---|---|
| TXA use in TAA | P valuea | |
| Yes (n = 25 cases) | No (n = 25 controls) |
|
Clinical Characteristic |
|
|
|
Drain Output (ml), mean ± SD
| 71.6 ± 60.3 | 200.2 ± 117.0 | <0.0001 |
Preoperative to Postoperative Hgb Change (g/dL), mean ± SD
| 1.5 ± 0.6 | 2.0 ± 0.4 | 0.01 |
Blood Loss Calculated (ml), mean ± SD
| 649.9 ± 332.73 | 906.8 ± 287.4 | 0.01 |
Length of Surgery (min), mean ± SD
| 112.8 ± 24.8 | 108.6 ± 26.0 | 0.57 |
VAS scores on the POD (No.), mean ± SD
| 4.9 ± 1.7 | 5.3 ±1.4 | 0.71 |
LOS (day), mean ± SD
| 1.6 ± 0.7 | 1.3 ± 0.6 | 0.23 |
aP value was calculated from t-test for continuous variables, and Chi-square test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
Abbreviations: LOS, length of stay; VAS, visual analog scale; POD, postoperative day.
Table 3. Linear Regression Analyses of Drain Output and Blood Loss using Tranexamic Acid (TXA) in Total Ankle Arthroplasty (TAA), Unadjusted and Adjusted Models for Length of Surgery, N = 50 | ||||
| TXA Use in TAA (Yes vs No) | |||
Drain Output (mL)
| Regression coefficient (β) | SE | Test statistics (t) | P valuea |
Unadjusted Model | -128.6 | 26.3 | -4.89 | < 0.0001 |
Adjusted for Age | -129.6 | 26.5 | -4.89 | <0.0001 |
Adjusted for BMI | -121.8 | 26.6 | -4.57 | <0.0001 |
Adjusted for Length of Surgery | -129.6 | 26.6 | -4.86 | <0.0001 |
Multivariable Modelb | -123.4 | 27.1 | -4.55 | <0.0001 |
Blood Loss (mL)
|
|
|
|
|
Unadjusted Model | -257.0 | 87.9 | -2.92 | 0.005 |
Adjusted for Age | -263.7 | 87.4 | -3.02 | 0.004 |
Adjusted for BMI | -268.7 | 90.2 | -2.98 | 0.005 |
Adjusted for Length of Surgery | -261.3 | 88.6 | -2.94 | 0.005 |
Multivariable Modelb | -275.6 | 90.7 | -3.04 | 0.004 |
aLinear regression was used to calculate the P value. bAdjusted for age, BMI and length of surgery.
Abbreviation: BMI, body mass index.
Table 4. Patient Wound Complication Categories by Use of Tranexamic Acid (TXA) in Total Ankle Arthroplasty (TAA), N = 50 | |||
|---|---|---|---|
| TXA Use in TAA | P valuea | |
Wound Complication | Yes (n = 25 cases) | No (n = 25 controls) | 0.114 |
None, n = 46 (86%) | 23 (40%) | 20 (46%) |
|
Minor, n = 6 (12%) | 2 (4%) | 4 (8%) |
|
Major, n = 1 (2%) | 0 (0%) | 1 (4%) |
|
aP value was calculated from Fisher’s Exact test (67% cells had count <5) test for categorical variables (TXA-TAA vs No TXA-TAA comparison).
The crude linear regression model revealed a significant difference in drain output between the TXA-TAA and the No TXA-TAA groups (β = −128.6 ± 26.3, P < .0001) (Table 3). Further adjustment for age and length of surgery slightly strengthened the association (β = −129.6 ± 26.6, P < .0001). The nature of regression coefficient β showed that the mean estimate of drain output was 129.6 mL lower in the TXA-TAA group than that in the No TXA-TAA group. There was a significant difference in blood loss between the TXA-TAA and the No TXA-TAA groups in the crude linear regression model (β = −257.0 ± 87.9, P = .005). Additional adjustment for age, BMI, and length of surgery slightly strengthened the association (β = −275.6 ± 90.7, P = .004). The nature of regression coefficient β showed that the mean estimate of blood loss was 275.6 mL lower in the TXA-TAA group than in the No TXA-TAA group (Table 3).
Continue to: There was no statistically significant difference...
There was no statistically significant difference in wound complications between the TXA-TAA and the No TXA-TAA groups in this study population (P = .114). However, our results showed a higher overall wound complication rate in the No TXA-TAA group than in the TXA-TAA group (20% (5/25) vs 8% (2/25), respectively) (Table 4). In the No TXA-TAA group, there were 4 minor and 1 major wound complications. All 5 patients experiencing a postoperative wound complication required oral antibiotics for a minimum of 4 weeks and local wound care. One patient underwent a surgical débridement meeting the criteria for major wound complications. In the TXA-TAA group, there were 2 minor wound complications and no major wound complications. One patient was administered prophylactic oral antibiotics for 7 days with local wound care for blister formation without evidence of infection. The second patient experiencing a minor wound complication required 3 weeks of oral antibiotics and local wound care. No patients in either group had a deep infection requiring implant removal, IV antibiotics, or subsequent hospital admission. The surgical incisions in all patients healed after the aforementioned treatments with no persistent drainage or development of chronic wounds.
In the TXA-TAA group, there was 1 patient who sustained an intraoperative medial malleolus fracture. One patient developed an extensor hallucis longus contracture 5 months postoperatively that subsequently underwent release and lengthening. There was 1 patient in this group who sustained a distal tibia fracture 5 cm proximal to the prosthesis 3 months postoperatively after a mechanical fall. In the No TXA-TAA group, there were 2 patients who sustained intraoperative medial malleolus fractures. One patient underwent a revision of the tibial component 24 months postoperatively due to aseptic loosening. In addition, another patient in this group who sustained an Achilles tendon rupture 5 months postoperatively after a fall subsequently underwent repair with tibialis anterior tendon allograft.
There were no patients in either group who experienced any hospital readmissions in the acute follow-up period as defined by a 90-day period after discharge. There were no complications associated with TXA administration in either group.
DISCUSSION
Recent advances in total ankle prosthetic design coupled with increased survival and improved short- to midterm follow-up results make TAA an effective treatment option for end-stage ankle arthritis. Management of perioperative blood loss and reducing the potential for significant hemarthrosis and subsequent wound complications are important factors to consider for patients undergoing TAA. TXA administration is used in several centers as part of an intraoperative strategy to reduce blood loss and decrease intra-articular blood accumulation. To our knowledge, this is the first study to evaluate the management of blood loss and hemarthrosis using TXA during TAA.
IV and topical administrations of TXA have been demonstrated to be highly effective hemostatic agents in the perioperative period for TKA and THA.11 Recent literature has demonstrated a significant reduction in drain output and mean change in preoperative to postoperative hemoglobin levels in patients who received TXA compared to that in patients who did not receive TXA. The patients who did not receive TXA had more than twice as much drain output.5,10,14,19-21
Continue to: The ankle has a thin...
The ankle has a thin soft tissue envelope that does not have elaborate elastic properties. The soft tissue release and bleeding surfaces of the bone during TAA are not as extensive when compared with TKA and THA, but the intra-articular volume is smaller and the surrounding soft tissues may be less yielding when blood accumulation occurs.22 The vascular supply can be rich surrounding the ankle in the absence of arterial disease and is not as apt to tolerate dislocation and subluxation as in the case of THA or TKA.23 Shear forces can easily tear the branches of the anterior tibial artery that lie within the fascia that is continuous with the periosteum on the distal tibia.24 Reduction of hemarthrosis within the ankle joint may lead to a decrease in postoperative swelling, decreased pain, and increased range of motion due to the diminished potential for fibrosis. We also believe that there could be a reduced risk for wound complications. The current literature reports the rate of wound complications to be anywhere from 2% to 25%, with diabetes, inflammatory conditions, coronary artery disease, peripheral vascular disease, and smoking history >12-pack-years as risk factors.16,25,26 In this study, we observed a significant reduction in drain output and an overall reduced percentage of postoperative wound complications in patients who received TXA. These results demonstrate that TXA use decreases postoperative hemarthrosis.
TXA use in TKA and THA has been shown to decrease direct hospital costs and hospital length of stay.7,14,27 A recent study by Moskal and colleagues7 showed that topical TXA use has the potential to significantly decrease hospital man-hours for those patients undergoing TKA and achieve larger cost savings. Although there was no significant difference in the length of stay between the 2 groups, the average length of stay after TAA was shorter in both groups compared to the reported national average (1.49 vs 2.2 days, respectively).4 The administration of TXA in the appropriate patient has the potential to decrease hospital costs by controlling postoperative pain and swelling, allowing for earlier discharge. Long-term cost benefits could also include decreased infection rates and wound complications, and improved clinical outcomes because of improved range of motion and function scores.
The limitations of this study include the retrospective nature of its design and the relatively small sample size. The results showed nonstatistically significant differences in wound complications between the TXA-TAA and the No TXA-TAA groups, consistent with an insufficient sample size and thus inadequate power to detect the significant difference. However, this study clearly showed that the wound complication rates were higher in the No TXA-TAA group than in the TXA-TAA group, suggesting the importance of further similar studies using a larger sample size.
CONCLUSION
Current TAA offers a viable alternative to arthrodesis for end-stage ankle arthritis. TXA is an inexpensive and effective hemostatic agent used during TAA. If no major contraindication is present, routine use of TXA is recommended to assist in blood loss management, decrease postoperative hemarthrosis, and help to reduce the risk of postoperative wound complications.
1. Saltzman CL, Salamon ML, Blanchard GM, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44-46.
2. Glazebrook M, Daniels T, Younger A, et al. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90(3):499-505. doi:10.2106/JBJS.F.01299.
3. Thomas RH, Daniels TR. Ankle arthritis. J Bone Joint Surg Am. 2003;85-A(5):923-936.
4. Zhou H, Yakavonis M, Shaw JJ, Patel A, Li X. In-patient trends and complications after total ankle arthroplasty in the United States. Orthopedics. 2016:1-6. doi:10.3928/01477447-20151228-05.
5. Benoni G, Fredin H. Fibrinolytic inhibition with tranexamic acid reduces blood loss and blood transfusion after knee arthroplasty: a prospective, randomised, double-blind study of 86 patients. J Bone Joint Surg Br. 1996;78(3):434-440.
6. Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM. A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J. 2014;96-B(8):1005-1015. doi:10.1302/0301-620X.96B8.33745.
7. Moskal JT, Harris RN, Capps SG. Transfusion cost savings with tranexamic acid in primary total knee arthroplasty from 2009 to 2012. J Arthroplasty. 2015;30(3):365-368. doi:10.1016/j.arth.2014.10.008.
8. Friedman R, Homering M, Holberg G, Berkowitz SD. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014;96(4):272-278. doi:10.2106/JBJS.L.01268.
9. Aggarwal AK, Singh N, Sudesh P. Topical vs intravenous tranexamic acid in reducing blood loss after bilateral total knee arthroplasty: a prospective study. J Arthroplasty. 2016;31(7):1442-1448. doi:10.1016/j.arth.2015.12.033.
10. Su EP, Su S. Strategies for reducing peri-operative blood loss in total knee arthroplasty. Bone Joint J. 2016;98-B(1 Suppl A):98-100. doi:10.1302/0301-620X.98B.36430.
11. Gomez-Barrena E, Ortega-Andreu M, Padilla-Eguiluz NG, Perez-Chrzanowska H, Figueredo-Zalve R. Topical intra-articular compared with intravenous tranexamic acid to reduce blood loss in primary total knee replacement: a double-blind, randomized, controlled, noninferiority clinical trial. J Bone Joint Surg Am. 2014;96(23):1937-1944. doi:10.2106/JBJS.N.00060.
12. Cap AP, Baer DG, Orman JA, Aden J, Ryan K, Blackbourne LH. Tranexamic acid for trauma patients: a critical review of the literature. J Trauma. 2011;71(1 Suppl):S9-14. doi:10.1097/TA.0b013e31822114af.
13. Duncan CM, Gillette BP, Jacob AK, Sierra RJ, Sanchez-Sotelo J, Smith HM. Venous thromboembolism and mortality associated with tranexamic acid use during total hip and knee arthroplasty. J Arthroplasty. 2015;30(2):272-276. doi:10.1016/j.arth.2014.08.022.
14. Alshryda S, Mason J, Vaghela M, et al. Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total knee replacement: a randomized controlled trial (TRANX-K). J Bone Joint Surg Am. 2013;95(21):1961-1968. doi:10.2106/JBJS.L.00907.
15. Ng W, Jerath A, Wasowicz M. Tranexamic acid: a clinical review. Anaesthesiol Intensive Ther. 2015;47(4):339-350. doi:10.5603/AIT.a2015.0011.
16. Raikin SM, Kane J, Ciminiello ME. Risk factors for incision-healing complications following total ankle arthroplasty. J Bone Joint Surg Am. 2010;92(12):2150-2155. doi:10.2106/JBJS.I.00870.
17. Meunier A, Petersson A, Good L, Berlin G. Validation of a haemoglobin dilution method for estimation of blood loss. Vox Sang. 2008;95(2):120-124. doi:10.1111/j.1423-0410.2008.01071.x.
18. Gibon E, Courpied JP, Hamadouche M. Total joint replacement and blood loss: what is the best equation? Int Orthop. 2013;37(4):735-739. doi:10.1007/s00264-013-1801-0
19. Chareancholvanich K, Siriwattanasakul P, Narkbunnam R, Pornrattanamaneewong C. Temporary clamping of drain combined with tranexamic acid reduce blood loss after total knee arthroplasty: a prospective randomized controlled trial. BMC Musculoskelet Disord. 2012;13:124.
20. Orpen NM, Little C, Walker G, Crawfurd EJ. Tranexamic acid reduces early post-operative blood loss after total knee arthroplasty: a prospective randomised controlled trial of 29 patients. Knee. 2006;13(2):106-110. doi:10.1016/j.knee.2005.11.001.
21. Veien M, Sorensen JV, Madsen F, Juelsgaard P. Tranexamic acid given intraoperatively reduces blood loss after total knee replacement: a randomized, controlled study. Acta Anaesthesiol Scand. 2002;46(10):1206-1211.
22. Draeger RW, Singh B, Parekh SG. Quantifying normal ankle joint volume: An anatomic study. Indian J Orthop. 2009;43(1):72-75. doi:10.4103/0019-5413.45326.
23. Gill LH. Challenges in total ankle arthroplasty. Foot Ankle Int. 2004;25(4):195-207. doi:10.1177/107110070402500402.
24. Taylor GI, Pan WR. Angiosomes of the leg: anatomic study and clinical implications. Plast Reconstr Surg. 1998;102(3):599-616; discussion 617-598. doi:10.1097/00006534-199809030-00001.
25. Gougoulias N, Khanna A, Maffulli N. How successful are current ankle replacements?: a systematic review of the literature. Clin Orthop Relat Res. 2010;468(1):199-208. doi:10.1007/s11999-009-0987-3.
26. Noelle S, Egidy CC, Cross MB, Gebauer M, Klauser W. Complication rates after total ankle arthroplasty in one hundred consecutive prostheses. Int Orthop. 2013;37(9):1789-1794. doi:10.1007/s00264-013-1971-9.
27. Chimento GF, Huff T, Ochsner JL Jr, Meyer M, Brandner L, Babin S. An evaluation of the use of topical tranexamic acid in total knee arthroplasty. J Arthroplasty. 2013;28(8 Suppl):74-77. doi:10.1016/j.arth.2013.06.037.
1. Saltzman CL, Salamon ML, Blanchard GM, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44-46.
2. Glazebrook M, Daniels T, Younger A, et al. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90(3):499-505. doi:10.2106/JBJS.F.01299.
3. Thomas RH, Daniels TR. Ankle arthritis. J Bone Joint Surg Am. 2003;85-A(5):923-936.
4. Zhou H, Yakavonis M, Shaw JJ, Patel A, Li X. In-patient trends and complications after total ankle arthroplasty in the United States. Orthopedics. 2016:1-6. doi:10.3928/01477447-20151228-05.
5. Benoni G, Fredin H. Fibrinolytic inhibition with tranexamic acid reduces blood loss and blood transfusion after knee arthroplasty: a prospective, randomised, double-blind study of 86 patients. J Bone Joint Surg Br. 1996;78(3):434-440.
6. Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM. A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J. 2014;96-B(8):1005-1015. doi:10.1302/0301-620X.96B8.33745.
7. Moskal JT, Harris RN, Capps SG. Transfusion cost savings with tranexamic acid in primary total knee arthroplasty from 2009 to 2012. J Arthroplasty. 2015;30(3):365-368. doi:10.1016/j.arth.2014.10.008.
8. Friedman R, Homering M, Holberg G, Berkowitz SD. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J Bone Joint Surg Am. 2014;96(4):272-278. doi:10.2106/JBJS.L.01268.
9. Aggarwal AK, Singh N, Sudesh P. Topical vs intravenous tranexamic acid in reducing blood loss after bilateral total knee arthroplasty: a prospective study. J Arthroplasty. 2016;31(7):1442-1448. doi:10.1016/j.arth.2015.12.033.
10. Su EP, Su S. Strategies for reducing peri-operative blood loss in total knee arthroplasty. Bone Joint J. 2016;98-B(1 Suppl A):98-100. doi:10.1302/0301-620X.98B.36430.
11. Gomez-Barrena E, Ortega-Andreu M, Padilla-Eguiluz NG, Perez-Chrzanowska H, Figueredo-Zalve R. Topical intra-articular compared with intravenous tranexamic acid to reduce blood loss in primary total knee replacement: a double-blind, randomized, controlled, noninferiority clinical trial. J Bone Joint Surg Am. 2014;96(23):1937-1944. doi:10.2106/JBJS.N.00060.
12. Cap AP, Baer DG, Orman JA, Aden J, Ryan K, Blackbourne LH. Tranexamic acid for trauma patients: a critical review of the literature. J Trauma. 2011;71(1 Suppl):S9-14. doi:10.1097/TA.0b013e31822114af.
13. Duncan CM, Gillette BP, Jacob AK, Sierra RJ, Sanchez-Sotelo J, Smith HM. Venous thromboembolism and mortality associated with tranexamic acid use during total hip and knee arthroplasty. J Arthroplasty. 2015;30(2):272-276. doi:10.1016/j.arth.2014.08.022.
14. Alshryda S, Mason J, Vaghela M, et al. Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total knee replacement: a randomized controlled trial (TRANX-K). J Bone Joint Surg Am. 2013;95(21):1961-1968. doi:10.2106/JBJS.L.00907.
15. Ng W, Jerath A, Wasowicz M. Tranexamic acid: a clinical review. Anaesthesiol Intensive Ther. 2015;47(4):339-350. doi:10.5603/AIT.a2015.0011.
16. Raikin SM, Kane J, Ciminiello ME. Risk factors for incision-healing complications following total ankle arthroplasty. J Bone Joint Surg Am. 2010;92(12):2150-2155. doi:10.2106/JBJS.I.00870.
17. Meunier A, Petersson A, Good L, Berlin G. Validation of a haemoglobin dilution method for estimation of blood loss. Vox Sang. 2008;95(2):120-124. doi:10.1111/j.1423-0410.2008.01071.x.
18. Gibon E, Courpied JP, Hamadouche M. Total joint replacement and blood loss: what is the best equation? Int Orthop. 2013;37(4):735-739. doi:10.1007/s00264-013-1801-0
19. Chareancholvanich K, Siriwattanasakul P, Narkbunnam R, Pornrattanamaneewong C. Temporary clamping of drain combined with tranexamic acid reduce blood loss after total knee arthroplasty: a prospective randomized controlled trial. BMC Musculoskelet Disord. 2012;13:124.
20. Orpen NM, Little C, Walker G, Crawfurd EJ. Tranexamic acid reduces early post-operative blood loss after total knee arthroplasty: a prospective randomised controlled trial of 29 patients. Knee. 2006;13(2):106-110. doi:10.1016/j.knee.2005.11.001.
21. Veien M, Sorensen JV, Madsen F, Juelsgaard P. Tranexamic acid given intraoperatively reduces blood loss after total knee replacement: a randomized, controlled study. Acta Anaesthesiol Scand. 2002;46(10):1206-1211.
22. Draeger RW, Singh B, Parekh SG. Quantifying normal ankle joint volume: An anatomic study. Indian J Orthop. 2009;43(1):72-75. doi:10.4103/0019-5413.45326.
23. Gill LH. Challenges in total ankle arthroplasty. Foot Ankle Int. 2004;25(4):195-207. doi:10.1177/107110070402500402.
24. Taylor GI, Pan WR. Angiosomes of the leg: anatomic study and clinical implications. Plast Reconstr Surg. 1998;102(3):599-616; discussion 617-598. doi:10.1097/00006534-199809030-00001.
25. Gougoulias N, Khanna A, Maffulli N. How successful are current ankle replacements?: a systematic review of the literature. Clin Orthop Relat Res. 2010;468(1):199-208. doi:10.1007/s11999-009-0987-3.
26. Noelle S, Egidy CC, Cross MB, Gebauer M, Klauser W. Complication rates after total ankle arthroplasty in one hundred consecutive prostheses. Int Orthop. 2013;37(9):1789-1794. doi:10.1007/s00264-013-1971-9.
27. Chimento GF, Huff T, Ochsner JL Jr, Meyer M, Brandner L, Babin S. An evaluation of the use of topical tranexamic acid in total knee arthroplasty. J Arthroplasty. 2013;28(8 Suppl):74-77. doi:10.1016/j.arth.2013.06.037.
TAKE-HOME POINTS
- TXA is an inexpensive and effective hemostatic agent used during TAA.
- The ankle has a thin soft tissue envelope that does not have elaborate elastic properties. The soft tissue release and bleeding surfaces of bone during TAA are not as extensive when compared to TKA and THA, but the intra-articular volume is smaller and surrounding soft tissues may be less yielding when blood accumulation occurs.
- If no major contraindication is present, routine use of TXA is recommended to assist in blood loss management during TAA.
- TXA decreases postoperative hemarthrosis and helps to reduce the risk of postoperative wound complications.
- The administration of TXA in the appropriate patient has the potential to decrease hospital cost by controlling postoperative pain and swelling allowing for earlier discharge.
New MS criteria may create more false positives
The revised McDonald criteria for multiple sclerosis (MS) has led to more diagnoses in patients with clinically isolated syndrome (CIS), but a new study of the criteria has suggested that they may lead to a number of false positive MS diagnoses among patients with a less severe disease state.
“In our data, specificity of the 2017 criteria was significantly lower than for the 2010 criteria,” Roos M. van der Vuurst de Vries, MD, from the department of neurology at Erasmus Medical Center in Rotterdam, the Netherlands, and her colleagues wrote in JAMA Neurology. “Earlier data showed that the previous McDonald criteria lead to a higher number of MS diagnoses in patients who will not have a second attack.”
Dr. van der Vuurst de Vries and her colleagues analyzed data from 229 patients with a CIS who underwent an MRI of the spinal cord to assess for dissemination in space (DIS); of these, 180 patients were scored for both DIS and dissemination in time (DIT) and had a “baseline MRI scan that included T1 images after gadolinium administration or scans that did not show any T2 hyperintense lesions.” Some patients also underwent a baseline lumbar puncture if clinically required.
Patients were assessed using both the 2010 and 2017 McDonald criteria for MS, and results were measured using sensitivity, specificity, positive predictive and negative predictive values, and accuracy at 1-year, 3-year, and 5-year follow-up. “The most important addition is that the new criteria allow MS diagnosis when the MRI scan meets criteria for DIS and unique oligoclonal bands (OCB) are present in [cerebrospinal fluid], even in absence of DIT on the MRI scan,” the researchers wrote. “The other major difference is that not only asymptomatic but also symptomatic lesions can be used to demonstrate DIS and DIT on MRI. Furthermore, cortical lesions can be used to demonstrate dissemination in space.”
The researchers found that 124 patients met 2010 DIS criteria (54%) and that 74 patients (60%) went on to develop clinically definite MS, while 149 patients (65%) met 2017 DIS criteria, and 89 patients (60%) went on to clinically definite MS. There were 46 patients (26%) who met 2010 DIT criteria, and 33 of those patients (72%) were diagnosed with clinically definite MS; 126 patients (70%) met 2017 DIT criteria, and 76 of those patients (60%) had clinically definite MS. The sensitivity for the 2010 criteria was 36% (95% confidence interval, 27%-47%)versus 68% for the 2017 criteria (95% CI, 57%-77%; P less than .001). However, specificity for the 2017 criteria was lower (61%; 95% CI, 50%-71%) when compared with the 2010 criteria (85%; 95% CI, 76%-92%; P less than .001). Researchers found more baseline MS diagnoses with the 2017 criteria than with the 2010 criteria, but they noted that 14 of 22 patients (64%) under the 2010 criteria and 26 of 48 patients (54%) under the 2017 criteria with MS had a second attack within 5 years.
The study was supported by the Dutch Multiple Sclerosis Research Foundation. One or more authors received compensation from Teva, Merck, Roche, Sanofi Genzyme, Biogen, and Novartis in the form of honoraria, for advisory board membership, as travel grants, or for participation in trials.
SOURCE: van der Vuurst de Vries RM, et al. JAMA Neurol. 2018 Aug 6. doi: 10.1001/jamaneurol.2018.2160.
The revised McDonald criteria for multiple sclerosis (MS) has led to more diagnoses in patients with clinically isolated syndrome (CIS), but a new study of the criteria has suggested that they may lead to a number of false positive MS diagnoses among patients with a less severe disease state.
“In our data, specificity of the 2017 criteria was significantly lower than for the 2010 criteria,” Roos M. van der Vuurst de Vries, MD, from the department of neurology at Erasmus Medical Center in Rotterdam, the Netherlands, and her colleagues wrote in JAMA Neurology. “Earlier data showed that the previous McDonald criteria lead to a higher number of MS diagnoses in patients who will not have a second attack.”
Dr. van der Vuurst de Vries and her colleagues analyzed data from 229 patients with a CIS who underwent an MRI of the spinal cord to assess for dissemination in space (DIS); of these, 180 patients were scored for both DIS and dissemination in time (DIT) and had a “baseline MRI scan that included T1 images after gadolinium administration or scans that did not show any T2 hyperintense lesions.” Some patients also underwent a baseline lumbar puncture if clinically required.
Patients were assessed using both the 2010 and 2017 McDonald criteria for MS, and results were measured using sensitivity, specificity, positive predictive and negative predictive values, and accuracy at 1-year, 3-year, and 5-year follow-up. “The most important addition is that the new criteria allow MS diagnosis when the MRI scan meets criteria for DIS and unique oligoclonal bands (OCB) are present in [cerebrospinal fluid], even in absence of DIT on the MRI scan,” the researchers wrote. “The other major difference is that not only asymptomatic but also symptomatic lesions can be used to demonstrate DIS and DIT on MRI. Furthermore, cortical lesions can be used to demonstrate dissemination in space.”
The researchers found that 124 patients met 2010 DIS criteria (54%) and that 74 patients (60%) went on to develop clinically definite MS, while 149 patients (65%) met 2017 DIS criteria, and 89 patients (60%) went on to clinically definite MS. There were 46 patients (26%) who met 2010 DIT criteria, and 33 of those patients (72%) were diagnosed with clinically definite MS; 126 patients (70%) met 2017 DIT criteria, and 76 of those patients (60%) had clinically definite MS. The sensitivity for the 2010 criteria was 36% (95% confidence interval, 27%-47%)versus 68% for the 2017 criteria (95% CI, 57%-77%; P less than .001). However, specificity for the 2017 criteria was lower (61%; 95% CI, 50%-71%) when compared with the 2010 criteria (85%; 95% CI, 76%-92%; P less than .001). Researchers found more baseline MS diagnoses with the 2017 criteria than with the 2010 criteria, but they noted that 14 of 22 patients (64%) under the 2010 criteria and 26 of 48 patients (54%) under the 2017 criteria with MS had a second attack within 5 years.
The study was supported by the Dutch Multiple Sclerosis Research Foundation. One or more authors received compensation from Teva, Merck, Roche, Sanofi Genzyme, Biogen, and Novartis in the form of honoraria, for advisory board membership, as travel grants, or for participation in trials.
SOURCE: van der Vuurst de Vries RM, et al. JAMA Neurol. 2018 Aug 6. doi: 10.1001/jamaneurol.2018.2160.
The revised McDonald criteria for multiple sclerosis (MS) has led to more diagnoses in patients with clinically isolated syndrome (CIS), but a new study of the criteria has suggested that they may lead to a number of false positive MS diagnoses among patients with a less severe disease state.
“In our data, specificity of the 2017 criteria was significantly lower than for the 2010 criteria,” Roos M. van der Vuurst de Vries, MD, from the department of neurology at Erasmus Medical Center in Rotterdam, the Netherlands, and her colleagues wrote in JAMA Neurology. “Earlier data showed that the previous McDonald criteria lead to a higher number of MS diagnoses in patients who will not have a second attack.”
Dr. van der Vuurst de Vries and her colleagues analyzed data from 229 patients with a CIS who underwent an MRI of the spinal cord to assess for dissemination in space (DIS); of these, 180 patients were scored for both DIS and dissemination in time (DIT) and had a “baseline MRI scan that included T1 images after gadolinium administration or scans that did not show any T2 hyperintense lesions.” Some patients also underwent a baseline lumbar puncture if clinically required.
Patients were assessed using both the 2010 and 2017 McDonald criteria for MS, and results were measured using sensitivity, specificity, positive predictive and negative predictive values, and accuracy at 1-year, 3-year, and 5-year follow-up. “The most important addition is that the new criteria allow MS diagnosis when the MRI scan meets criteria for DIS and unique oligoclonal bands (OCB) are present in [cerebrospinal fluid], even in absence of DIT on the MRI scan,” the researchers wrote. “The other major difference is that not only asymptomatic but also symptomatic lesions can be used to demonstrate DIS and DIT on MRI. Furthermore, cortical lesions can be used to demonstrate dissemination in space.”
The researchers found that 124 patients met 2010 DIS criteria (54%) and that 74 patients (60%) went on to develop clinically definite MS, while 149 patients (65%) met 2017 DIS criteria, and 89 patients (60%) went on to clinically definite MS. There were 46 patients (26%) who met 2010 DIT criteria, and 33 of those patients (72%) were diagnosed with clinically definite MS; 126 patients (70%) met 2017 DIT criteria, and 76 of those patients (60%) had clinically definite MS. The sensitivity for the 2010 criteria was 36% (95% confidence interval, 27%-47%)versus 68% for the 2017 criteria (95% CI, 57%-77%; P less than .001). However, specificity for the 2017 criteria was lower (61%; 95% CI, 50%-71%) when compared with the 2010 criteria (85%; 95% CI, 76%-92%; P less than .001). Researchers found more baseline MS diagnoses with the 2017 criteria than with the 2010 criteria, but they noted that 14 of 22 patients (64%) under the 2010 criteria and 26 of 48 patients (54%) under the 2017 criteria with MS had a second attack within 5 years.
The study was supported by the Dutch Multiple Sclerosis Research Foundation. One or more authors received compensation from Teva, Merck, Roche, Sanofi Genzyme, Biogen, and Novartis in the form of honoraria, for advisory board membership, as travel grants, or for participation in trials.
SOURCE: van der Vuurst de Vries RM, et al. JAMA Neurol. 2018 Aug 6. doi: 10.1001/jamaneurol.2018.2160.
FROM JAMA NEUROLOGY
Key clinical point: The 2017 McDonald criteria for MS may diagnose more patients with a clinically isolated syndrome, but a lower specificity may also capture more patients who do not have a second CIS event.
Major finding: The sensitivity for the 2017 criteria was greater at 68%, compared with 36% in the 2010 criteria; however, specificity was significantly lower in the 2017 criteria at 61%, compared with 85% in the 2010 criteria.
Data source: An original study of 229 patients from the Netherlands with CIS who underwent an MRI scan within 3 months of symptoms.
Disclosures: The study was supported by the Dutch Multiple Sclerosis Research Foundation. One or more authors received compensation from Teva, Merck, Roche, Sanofi Genzyme, Biogen, and Novartis in the form of honoraria, for advisory board membership, as travel grants, or for participation in trials.
Source: van der Vuurst de Vries RM et al. JAMA Neurol. 2018 Aug 6. doi: 10.1001/jamaneurol.2018.2160.
Galcanezumab Reduces Attack Frequency in Patients With Cluster Headache
SAN FRANCISCO—Among patients with episodic cluster headache, galcanezumab significantly reduced weekly attack frequency, according to the results of a phase III trial presented at the 60th Annual Scientific Meeting of the American Headache Society. Results of an eight-week, double-blind, placebo-controlled clinical trial showed that galcanezumab (300 mg SC) significantly reduced the weekly cluster headache attack frequency across weeks one to three, which was the study’s primary end point, and resulted in a significantly greater percentage of patients achieving a 50% or greater reduction in their weekly cluster headache attack frequency at week three.
James M. Martinez, MD, a medical fellow at Eli Lilly, Indianapolis, Indiana, and study collaborators sought to determine if galcanezumab (aka LY2951742), a humanized monoclonal antibody that selectively binds to calcitonin gene-related peptide (CGRP), is efficacious as a preventive treatment of episodic cluster headache.
A phase III study was designed to assess the efficacy and safety of galcanezumab in individuals with episodic cluster headache, as defined by ICHD-3 beta criteria. This study comprised a screening period; a prospective baseline period; an eight-week, double-blind, placebo-controlled treatment period; and a four-month posttreatment washout period.
In the double-blind treatment period, participants were randomized 1:1 to galcanezumab 300 mg SC (n = 49) or placebo (n = 57) once monthly for two months. The primary end point was the overall mean change from baseline in weekly cluster headache attack frequency across weeks one to three. The key secondary end point was the proportion of participants achieving a response, defined as a reduction from baseline of 50% or greater in the weekly cluster headache attack frequency at week three. Other secondary end points included proportion of participants very much or much better based on Patient Global Impression of Improvement (PGI-I) at weeks four and eight.
Baseline demographics of the galcanezumab and placebo groups were similar. Mean age was 47 and 45, respectively; 84% and 82%, respectively, were male. The mean number of weekly cluster headache attacks in the baseline period was 17.8 for the galcanezumab group and 17.3 for the placebo group. Overall, four participants (8%) in the galcanezumab treatment group discontinued therapy during the double-blind period versus 12 (21%) in the placebo group. In the placebo group, eight participants (14%) discontinued treatment due to lack of efficacy versus one (2%) in the galcanezumab group. The mean change in weekly cluster headache attack frequency across weeks one to three was –8.7 for galcanezumab versus –5.2 for placebo (difference between treatment groups in mean change, –3.5). The proportion of participants achieving a 50% or greater reduction in weekly cluster headache attack frequency was 76% for galcanezumab versus 57% for placebo. The proportion of participants very much or much better based on PGI-I was significantly greater with galcanezumab versus placebo at week four (73% vs 46%) but not at week eight (72% vs 66%). There were no clinically meaningful differences between treatment groups on tolerability or safety parameters except for a statistically significantly greater incidence of injection site pain with galcanezumab versus placebo (8.2% vs 0%), which was similar to the safety profile seen previously in patients with episodic and chronic migraine.
—Glenn S. Williams
SAN FRANCISCO—Among patients with episodic cluster headache, galcanezumab significantly reduced weekly attack frequency, according to the results of a phase III trial presented at the 60th Annual Scientific Meeting of the American Headache Society. Results of an eight-week, double-blind, placebo-controlled clinical trial showed that galcanezumab (300 mg SC) significantly reduced the weekly cluster headache attack frequency across weeks one to three, which was the study’s primary end point, and resulted in a significantly greater percentage of patients achieving a 50% or greater reduction in their weekly cluster headache attack frequency at week three.
James M. Martinez, MD, a medical fellow at Eli Lilly, Indianapolis, Indiana, and study collaborators sought to determine if galcanezumab (aka LY2951742), a humanized monoclonal antibody that selectively binds to calcitonin gene-related peptide (CGRP), is efficacious as a preventive treatment of episodic cluster headache.
A phase III study was designed to assess the efficacy and safety of galcanezumab in individuals with episodic cluster headache, as defined by ICHD-3 beta criteria. This study comprised a screening period; a prospective baseline period; an eight-week, double-blind, placebo-controlled treatment period; and a four-month posttreatment washout period.
In the double-blind treatment period, participants were randomized 1:1 to galcanezumab 300 mg SC (n = 49) or placebo (n = 57) once monthly for two months. The primary end point was the overall mean change from baseline in weekly cluster headache attack frequency across weeks one to three. The key secondary end point was the proportion of participants achieving a response, defined as a reduction from baseline of 50% or greater in the weekly cluster headache attack frequency at week three. Other secondary end points included proportion of participants very much or much better based on Patient Global Impression of Improvement (PGI-I) at weeks four and eight.
Baseline demographics of the galcanezumab and placebo groups were similar. Mean age was 47 and 45, respectively; 84% and 82%, respectively, were male. The mean number of weekly cluster headache attacks in the baseline period was 17.8 for the galcanezumab group and 17.3 for the placebo group. Overall, four participants (8%) in the galcanezumab treatment group discontinued therapy during the double-blind period versus 12 (21%) in the placebo group. In the placebo group, eight participants (14%) discontinued treatment due to lack of efficacy versus one (2%) in the galcanezumab group. The mean change in weekly cluster headache attack frequency across weeks one to three was –8.7 for galcanezumab versus –5.2 for placebo (difference between treatment groups in mean change, –3.5). The proportion of participants achieving a 50% or greater reduction in weekly cluster headache attack frequency was 76% for galcanezumab versus 57% for placebo. The proportion of participants very much or much better based on PGI-I was significantly greater with galcanezumab versus placebo at week four (73% vs 46%) but not at week eight (72% vs 66%). There were no clinically meaningful differences between treatment groups on tolerability or safety parameters except for a statistically significantly greater incidence of injection site pain with galcanezumab versus placebo (8.2% vs 0%), which was similar to the safety profile seen previously in patients with episodic and chronic migraine.
—Glenn S. Williams
SAN FRANCISCO—Among patients with episodic cluster headache, galcanezumab significantly reduced weekly attack frequency, according to the results of a phase III trial presented at the 60th Annual Scientific Meeting of the American Headache Society. Results of an eight-week, double-blind, placebo-controlled clinical trial showed that galcanezumab (300 mg SC) significantly reduced the weekly cluster headache attack frequency across weeks one to three, which was the study’s primary end point, and resulted in a significantly greater percentage of patients achieving a 50% or greater reduction in their weekly cluster headache attack frequency at week three.
James M. Martinez, MD, a medical fellow at Eli Lilly, Indianapolis, Indiana, and study collaborators sought to determine if galcanezumab (aka LY2951742), a humanized monoclonal antibody that selectively binds to calcitonin gene-related peptide (CGRP), is efficacious as a preventive treatment of episodic cluster headache.
A phase III study was designed to assess the efficacy and safety of galcanezumab in individuals with episodic cluster headache, as defined by ICHD-3 beta criteria. This study comprised a screening period; a prospective baseline period; an eight-week, double-blind, placebo-controlled treatment period; and a four-month posttreatment washout period.
In the double-blind treatment period, participants were randomized 1:1 to galcanezumab 300 mg SC (n = 49) or placebo (n = 57) once monthly for two months. The primary end point was the overall mean change from baseline in weekly cluster headache attack frequency across weeks one to three. The key secondary end point was the proportion of participants achieving a response, defined as a reduction from baseline of 50% or greater in the weekly cluster headache attack frequency at week three. Other secondary end points included proportion of participants very much or much better based on Patient Global Impression of Improvement (PGI-I) at weeks four and eight.
Baseline demographics of the galcanezumab and placebo groups were similar. Mean age was 47 and 45, respectively; 84% and 82%, respectively, were male. The mean number of weekly cluster headache attacks in the baseline period was 17.8 for the galcanezumab group and 17.3 for the placebo group. Overall, four participants (8%) in the galcanezumab treatment group discontinued therapy during the double-blind period versus 12 (21%) in the placebo group. In the placebo group, eight participants (14%) discontinued treatment due to lack of efficacy versus one (2%) in the galcanezumab group. The mean change in weekly cluster headache attack frequency across weeks one to three was –8.7 for galcanezumab versus –5.2 for placebo (difference between treatment groups in mean change, –3.5). The proportion of participants achieving a 50% or greater reduction in weekly cluster headache attack frequency was 76% for galcanezumab versus 57% for placebo. The proportion of participants very much or much better based on PGI-I was significantly greater with galcanezumab versus placebo at week four (73% vs 46%) but not at week eight (72% vs 66%). There were no clinically meaningful differences between treatment groups on tolerability or safety parameters except for a statistically significantly greater incidence of injection site pain with galcanezumab versus placebo (8.2% vs 0%), which was similar to the safety profile seen previously in patients with episodic and chronic migraine.
—Glenn S. Williams
Aspirin May Be an Effective Pretreatment for Exercise in Patients With MS
Time to exhaustion was significantly greater after pretreatment with aspirin versus placebo.
LOS ANGELES—Aspirin may be an effective pretreatment for exercise in patients with multiple sclerosis (MS), according to a study described at the 70th Annual Meeting of the American Academy of Neurology.
“Exercise in MS we know to be beneficial on multiple levels,” said Victoria M. Leavitt, PhD, Assistant Professor of Neuropsychology at Columbia University Medical Center in New York. “In addition to physical benefits like gait, balance, and improved cardiovascular fitness, exercise is also associated with improved mood, reduced fatigue, and improved memory performance. The challenge, of course, is that exercise is only beneficial if people actually do it.”
Exercise-induced overheating, exhaustion, and symptom worsening (Uhtoff’s phenomenon) deter many patients with MS from exercise, and patients may have elevated resting body temperatures that are associated with worse fatigue.
To test whether aspirin pretreatment improves exercise performance in people with MS, Dr. Leavitt and colleagues conducted a randomized, placebo-controlled, crossover pilot study. The researchers studied aspirin because of its antipyretic effects and its efficacy in reducing fatigue in nonexercising patients with MS. The primary outcome was total time spent exercising. Change in exercise-induced body temperature was a secondary outcome.
In all, 12 patients participated in the study (nine females; mean age, 39.8; mean disease duration, 7.7 years; Expanded Disability Status Scale scores of 6.5 or less). Eight patients reported heat sensitivity during exercise.
Participants completed two maximal progressive ramped lower body cycle ergometer exercise tests one week apart after taking 650 mg of aspirin or placebo one hour before each test.
Patients exercised an average of 16.4 seconds longer after taking aspirin (9 minutes 28.6 seconds), versus placebo (9 minutes 12.2 seconds). In heat-sensitive patients, average body temperature increase after exercise with aspirin (0.41°F) was lower than the increase with placebo (0.88°F). This difference was not statistically significant.
Larger studies are needed, but the results are encouraging, Dr. Leavitt said. “The next thing we want to look at is how this translates to everyday exercise,” she said. “Does aspirin use in people with MS result in increased physical activity levels or increased adherence to exercise regimens?”
—Jake Remaly
Suggested Reading
Leavitt VM, Blanchard AR, Guo CY, et al. Aspirin is an effective pretreatment for exercise in multiple sclerosis: a double-blin
Wingerchuk DM, Benarroch EE, O’Brien PC, et al. A randomized controlled crossover trial of aspirin for fatigue in multiple sclerosis. Neurology. 2005;64(7):1267-1269.
Time to exhaustion was significantly greater after pretreatment with aspirin versus placebo.
Time to exhaustion was significantly greater after pretreatment with aspirin versus placebo.
LOS ANGELES—Aspirin may be an effective pretreatment for exercise in patients with multiple sclerosis (MS), according to a study described at the 70th Annual Meeting of the American Academy of Neurology.
“Exercise in MS we know to be beneficial on multiple levels,” said Victoria M. Leavitt, PhD, Assistant Professor of Neuropsychology at Columbia University Medical Center in New York. “In addition to physical benefits like gait, balance, and improved cardiovascular fitness, exercise is also associated with improved mood, reduced fatigue, and improved memory performance. The challenge, of course, is that exercise is only beneficial if people actually do it.”
Exercise-induced overheating, exhaustion, and symptom worsening (Uhtoff’s phenomenon) deter many patients with MS from exercise, and patients may have elevated resting body temperatures that are associated with worse fatigue.
To test whether aspirin pretreatment improves exercise performance in people with MS, Dr. Leavitt and colleagues conducted a randomized, placebo-controlled, crossover pilot study. The researchers studied aspirin because of its antipyretic effects and its efficacy in reducing fatigue in nonexercising patients with MS. The primary outcome was total time spent exercising. Change in exercise-induced body temperature was a secondary outcome.
In all, 12 patients participated in the study (nine females; mean age, 39.8; mean disease duration, 7.7 years; Expanded Disability Status Scale scores of 6.5 or less). Eight patients reported heat sensitivity during exercise.
Participants completed two maximal progressive ramped lower body cycle ergometer exercise tests one week apart after taking 650 mg of aspirin or placebo one hour before each test.
Patients exercised an average of 16.4 seconds longer after taking aspirin (9 minutes 28.6 seconds), versus placebo (9 minutes 12.2 seconds). In heat-sensitive patients, average body temperature increase after exercise with aspirin (0.41°F) was lower than the increase with placebo (0.88°F). This difference was not statistically significant.
Larger studies are needed, but the results are encouraging, Dr. Leavitt said. “The next thing we want to look at is how this translates to everyday exercise,” she said. “Does aspirin use in people with MS result in increased physical activity levels or increased adherence to exercise regimens?”
—Jake Remaly
Suggested Reading
Leavitt VM, Blanchard AR, Guo CY, et al. Aspirin is an effective pretreatment for exercise in multiple sclerosis: a double-blin
Wingerchuk DM, Benarroch EE, O’Brien PC, et al. A randomized controlled crossover trial of aspirin for fatigue in multiple sclerosis. Neurology. 2005;64(7):1267-1269.
LOS ANGELES—Aspirin may be an effective pretreatment for exercise in patients with multiple sclerosis (MS), according to a study described at the 70th Annual Meeting of the American Academy of Neurology.
“Exercise in MS we know to be beneficial on multiple levels,” said Victoria M. Leavitt, PhD, Assistant Professor of Neuropsychology at Columbia University Medical Center in New York. “In addition to physical benefits like gait, balance, and improved cardiovascular fitness, exercise is also associated with improved mood, reduced fatigue, and improved memory performance. The challenge, of course, is that exercise is only beneficial if people actually do it.”
Exercise-induced overheating, exhaustion, and symptom worsening (Uhtoff’s phenomenon) deter many patients with MS from exercise, and patients may have elevated resting body temperatures that are associated with worse fatigue.
To test whether aspirin pretreatment improves exercise performance in people with MS, Dr. Leavitt and colleagues conducted a randomized, placebo-controlled, crossover pilot study. The researchers studied aspirin because of its antipyretic effects and its efficacy in reducing fatigue in nonexercising patients with MS. The primary outcome was total time spent exercising. Change in exercise-induced body temperature was a secondary outcome.
In all, 12 patients participated in the study (nine females; mean age, 39.8; mean disease duration, 7.7 years; Expanded Disability Status Scale scores of 6.5 or less). Eight patients reported heat sensitivity during exercise.
Participants completed two maximal progressive ramped lower body cycle ergometer exercise tests one week apart after taking 650 mg of aspirin or placebo one hour before each test.
Patients exercised an average of 16.4 seconds longer after taking aspirin (9 minutes 28.6 seconds), versus placebo (9 minutes 12.2 seconds). In heat-sensitive patients, average body temperature increase after exercise with aspirin (0.41°F) was lower than the increase with placebo (0.88°F). This difference was not statistically significant.
Larger studies are needed, but the results are encouraging, Dr. Leavitt said. “The next thing we want to look at is how this translates to everyday exercise,” she said. “Does aspirin use in people with MS result in increased physical activity levels or increased adherence to exercise regimens?”
—Jake Remaly
Suggested Reading
Leavitt VM, Blanchard AR, Guo CY, et al. Aspirin is an effective pretreatment for exercise in multiple sclerosis: a double-blin
Wingerchuk DM, Benarroch EE, O’Brien PC, et al. A randomized controlled crossover trial of aspirin for fatigue in multiple sclerosis. Neurology. 2005;64(7):1267-1269.
Rare clear cell papillary RCC has indolent course
Clear cell papillary renal cell carcinoma (CCPRCC), a recently identified, rare type of renal tumor, appears to have an indolent course with low risk of either local invasion or distant metastasis, results of a small retrospective study suggest.
Among 25 patients with CCPRCC followed for as long as 119 months, there were no cases of local recurrence or distant metastasis, reported Wei-Jen Chen, MD, of Tapei (Taiwan) Veterans General Hospital, and colleagues.
“Based on our findings, CCPRCC has an indolent behavior even if the patients are immunosuppressed or if they receive less invasive therapy. Microscopically, CCPRCC is considered to be a tumor of low malignant potential, as all tumors in our series were of low nuclear grade,” they wrote in a study published online in the Journal of the Chinese Medical Association.
“Whenever the diagnosis is made in a high grade renal tumor, it should be carefully re-confirmed by either cytogenetic or molecular genetic methods,” the authors reported.
CCPRCC was newly recognized as a distinct renal malignancy in the 2016 World Health Organization Classification of Tumors of the Urinary System and Male Genital Organs. The classification describes CCPRCC as “a renal epithelial neoplasm composed of low-grade clear epithelial cells arranged in tubules and papillae with a predominantly linear nuclear alignment away from the basement membrane.”
Although rare, these tumors account for up to 5% of all resected renal tumors, and arise sporadically in patients with end-stage renal disease (ESRD) and von Hippel-Lindau syndrome, the classification states, adding that “according to current knowledge, these tumors have indolent behavior.”
To see if they could verify that last statement, Dr. Chen and associates collected data on all patients diagnosed at their institution with CCPRCC from January 2008 through September 2016.
They identified a total of 25 patients (11 men and 14 women) with a mean age at diagnosis of 62.8 years. Of this group, three patients with poor general condition underwent cryotherapy after a biopsy-confirmed diagnosis of CCPRCC.
All of the remaining 22 patients underwent surgical resection. Of this group, four had ESRD; three of these patients had received a kidney transplant prior to diagnosis of CCPRCC in the native kidneys, and one had three tumors over both kidneys.
“Three patients had other types of synchronous RCC; one with acquired cystic kidney disease-associated RCC, and the others with ccRCC. All CCPRCCs were localized and low grade (pT1a- pT1b, Fuhrman grade 2), and all of the patients are currently alive with no evidence of disease,” the investigators wrote.
Mean follow-up was 49.7 months (range 12 to 119 months).
One additional patient who was not included in the series was initially diagnosed with CCPRCC with lung metastasis. This patient, who died 3 years and 8 months after cytoreductive nephrectomy, had a clinical course distinct from that of all the other patients, leading the investigators to reexamine his kidney specimen with whole-exome sequencing. The sequencing led to a revision of the diagnosis to clear cell RCC.
The investigators noted that clear cell RCC, papillary RCC, and translocation RCC are three RCC subtypes that should be considered in the differential diagnosis of CCPRCC.
The investigators did not report a study funding source. They reported having no conflicts of interest relevant to the subject matter or materials discussed in the article.
SOURCE: Chen W-J et al. J Chinese Med Assoc. 2018 July 20. doi: 10.1016/j.jcma.2018.04.005.
Clear cell papillary renal cell carcinoma (CCPRCC), a recently identified, rare type of renal tumor, appears to have an indolent course with low risk of either local invasion or distant metastasis, results of a small retrospective study suggest.
Among 25 patients with CCPRCC followed for as long as 119 months, there were no cases of local recurrence or distant metastasis, reported Wei-Jen Chen, MD, of Tapei (Taiwan) Veterans General Hospital, and colleagues.
“Based on our findings, CCPRCC has an indolent behavior even if the patients are immunosuppressed or if they receive less invasive therapy. Microscopically, CCPRCC is considered to be a tumor of low malignant potential, as all tumors in our series were of low nuclear grade,” they wrote in a study published online in the Journal of the Chinese Medical Association.
“Whenever the diagnosis is made in a high grade renal tumor, it should be carefully re-confirmed by either cytogenetic or molecular genetic methods,” the authors reported.
CCPRCC was newly recognized as a distinct renal malignancy in the 2016 World Health Organization Classification of Tumors of the Urinary System and Male Genital Organs. The classification describes CCPRCC as “a renal epithelial neoplasm composed of low-grade clear epithelial cells arranged in tubules and papillae with a predominantly linear nuclear alignment away from the basement membrane.”
Although rare, these tumors account for up to 5% of all resected renal tumors, and arise sporadically in patients with end-stage renal disease (ESRD) and von Hippel-Lindau syndrome, the classification states, adding that “according to current knowledge, these tumors have indolent behavior.”
To see if they could verify that last statement, Dr. Chen and associates collected data on all patients diagnosed at their institution with CCPRCC from January 2008 through September 2016.
They identified a total of 25 patients (11 men and 14 women) with a mean age at diagnosis of 62.8 years. Of this group, three patients with poor general condition underwent cryotherapy after a biopsy-confirmed diagnosis of CCPRCC.
All of the remaining 22 patients underwent surgical resection. Of this group, four had ESRD; three of these patients had received a kidney transplant prior to diagnosis of CCPRCC in the native kidneys, and one had three tumors over both kidneys.
“Three patients had other types of synchronous RCC; one with acquired cystic kidney disease-associated RCC, and the others with ccRCC. All CCPRCCs were localized and low grade (pT1a- pT1b, Fuhrman grade 2), and all of the patients are currently alive with no evidence of disease,” the investigators wrote.
Mean follow-up was 49.7 months (range 12 to 119 months).
One additional patient who was not included in the series was initially diagnosed with CCPRCC with lung metastasis. This patient, who died 3 years and 8 months after cytoreductive nephrectomy, had a clinical course distinct from that of all the other patients, leading the investigators to reexamine his kidney specimen with whole-exome sequencing. The sequencing led to a revision of the diagnosis to clear cell RCC.
The investigators noted that clear cell RCC, papillary RCC, and translocation RCC are three RCC subtypes that should be considered in the differential diagnosis of CCPRCC.
The investigators did not report a study funding source. They reported having no conflicts of interest relevant to the subject matter or materials discussed in the article.
SOURCE: Chen W-J et al. J Chinese Med Assoc. 2018 July 20. doi: 10.1016/j.jcma.2018.04.005.
Clear cell papillary renal cell carcinoma (CCPRCC), a recently identified, rare type of renal tumor, appears to have an indolent course with low risk of either local invasion or distant metastasis, results of a small retrospective study suggest.
Among 25 patients with CCPRCC followed for as long as 119 months, there were no cases of local recurrence or distant metastasis, reported Wei-Jen Chen, MD, of Tapei (Taiwan) Veterans General Hospital, and colleagues.
“Based on our findings, CCPRCC has an indolent behavior even if the patients are immunosuppressed or if they receive less invasive therapy. Microscopically, CCPRCC is considered to be a tumor of low malignant potential, as all tumors in our series were of low nuclear grade,” they wrote in a study published online in the Journal of the Chinese Medical Association.
“Whenever the diagnosis is made in a high grade renal tumor, it should be carefully re-confirmed by either cytogenetic or molecular genetic methods,” the authors reported.
CCPRCC was newly recognized as a distinct renal malignancy in the 2016 World Health Organization Classification of Tumors of the Urinary System and Male Genital Organs. The classification describes CCPRCC as “a renal epithelial neoplasm composed of low-grade clear epithelial cells arranged in tubules and papillae with a predominantly linear nuclear alignment away from the basement membrane.”
Although rare, these tumors account for up to 5% of all resected renal tumors, and arise sporadically in patients with end-stage renal disease (ESRD) and von Hippel-Lindau syndrome, the classification states, adding that “according to current knowledge, these tumors have indolent behavior.”
To see if they could verify that last statement, Dr. Chen and associates collected data on all patients diagnosed at their institution with CCPRCC from January 2008 through September 2016.
They identified a total of 25 patients (11 men and 14 women) with a mean age at diagnosis of 62.8 years. Of this group, three patients with poor general condition underwent cryotherapy after a biopsy-confirmed diagnosis of CCPRCC.
All of the remaining 22 patients underwent surgical resection. Of this group, four had ESRD; three of these patients had received a kidney transplant prior to diagnosis of CCPRCC in the native kidneys, and one had three tumors over both kidneys.
“Three patients had other types of synchronous RCC; one with acquired cystic kidney disease-associated RCC, and the others with ccRCC. All CCPRCCs were localized and low grade (pT1a- pT1b, Fuhrman grade 2), and all of the patients are currently alive with no evidence of disease,” the investigators wrote.
Mean follow-up was 49.7 months (range 12 to 119 months).
One additional patient who was not included in the series was initially diagnosed with CCPRCC with lung metastasis. This patient, who died 3 years and 8 months after cytoreductive nephrectomy, had a clinical course distinct from that of all the other patients, leading the investigators to reexamine his kidney specimen with whole-exome sequencing. The sequencing led to a revision of the diagnosis to clear cell RCC.
The investigators noted that clear cell RCC, papillary RCC, and translocation RCC are three RCC subtypes that should be considered in the differential diagnosis of CCPRCC.
The investigators did not report a study funding source. They reported having no conflicts of interest relevant to the subject matter or materials discussed in the article.
SOURCE: Chen W-J et al. J Chinese Med Assoc. 2018 July 20. doi: 10.1016/j.jcma.2018.04.005.
FROM JOURNAL OF THE CHINESE MEDICAL SOCIETY
Key clinical point: Clear cell papillary renal cell carcinoma (CCPRCC) is a distinct renal tumor type with an apparently indolent clinical course.
Major finding: There were no cases of local recurrence or distant metastasis of CCPRCC after a mean of 49.7 months of follow-up (range 12-119 months).
Study details: Retrospective case study of 25 patients diagnosed and treated at a single center.
Disclosures: The investigators did not report a study funding source. They reported having no conflicts of interest relevant to the subject matter or materials discussed in the article.
Source: Chen W-J et al. J Chinese Med Assoc. 2018 July 20 doi: 10.1016/j.jcma.2018.04.005.