User login
No good reason to not use ultrasound during embryo transfer, expert says
CORONADO, CALIF. – according to William Schoolcraft, MD, HCLD.
At a meeting on IVF and embryo transfer sponsored by the University of California, San Diego, Dr. Schoolcraft said that ultrasound-guided embryo transfer helps clinicians avoid difficult transfers, minimizes contamination with blood, facilitates proper placement of the catheter tip, and minimizes the stimulation of uterine contractions. “We know that contaminating the catheter either with blood or mucous or endometrial tissue lowers clinical pregnancy rates, compared to a clean catheter,” said Dr. Schoolcraft, founder and medical director of the Colorado Center for Reproductive Medicine, Denver.
“Ultrasound guidance can help you follow the contour of the cervix and avoid touching the fundus. Your catheter should be free of blood, mucous, or endometrial cells when the embryologist examines it,” he said. In his clinical opinion, it’s hard to argue against using ultrasound guidance for embryo transfer. “It’s also very popular with IVF patients, because they get to visualize the transfer and have some reassurance that the embryo is delivered to their uterus,” he said.
The potential benefit of using three-dimensional ultrasound for embryo transfer is less clear. “It does require more expensive equipment and it’s a little more skill dependent, but in a randomized trial it didn’t lead to any difference in outcomes,” Dr. Schoolcraft said. “I think if you’re good with two-dimensional ultrasound, three-dimensional ultrasound doesn’t seem to have much benefit in terms of pregnancy outcomes.”
In a study published in 2017, researchers from Barcelona analyzed 7,714 embryo transfers to determine the impact of maneuvers during embryo transfers on the pregnancy rate (Fertil Steril. 2017 Mar;107[3]:657-63.e1). Using the direct embryo transfer as a reference, each instrumentation needed to successfully deposit the embryos in the fundus served as an index of the difficulty of transfer. A difficult transfer occurred in 7.7% of cycles, and the researchers found that the clinical pregnancy rate decreased progressively with the use of additional maneuvers during embryo transfer. Specifically, the clinical pregnancy rate was 39.4% when no additional maneuvers were required, 36.9% when an outer catheter sheath was used (odds ratio, 0.89), 31.7% when a Wallace stylet was used (OR, 0.71), and 26.1% when a tenaculum was used (OR, 0.54). “I think without question, avoiding a difficult transfer is important and certainly a key to our success,” said Dr. Schoolcraft, who was not involved with the study.
The ideal depth of embryo transfer is “a bit complicated,” he said, but according to the best available evidence, a depth of 15-20 mm from the fundus by ultrasound guidance appears to optimize implantation by avoiding the lower cavity where implantation is compromised. This range of depth also avoids problems with upper cavity transfers, including trauma, contractions, and tubal pregnancy. “I think that transfers which are close to the fundus, and possibly in some cases touching the fundus, may lead to uterine contractions, plugging the catheter with endometrium and generating bleeding,” Dr. Schoolcraft said. He pointed out that during natural pregnancies, embryos implant in the upper fundus nearly 90% of the time, compared with 66% of the time during IVF pregnancies. “To mimic Mother Nature we don’t want to be too low, either,” he said. “We all know that placenta previa is increased with IVF. This may be due to placing the embryos too low.”
According to Dr. Schoolcraft, many published studies have found that significantly higher pregnancy rates occur with routine bladder distension prior to embryo transfer, probably because of the smooth and easy insertion of the embryo transfer. A Scandinavian meta-analysis found that the odds ratio favoring ultrasound guidance and a full bladder for ongoing pregnancy was 1.44 and clinical pregnancy was 1.55, which is similar to that seen during an earlier review from The Cochrane Collaborative, with an OR of 1.47 for ongoing pregnancy and OR 1.53 for live birth (Cochrane Database Syst Rev. 2016 Mar 17. doi: 10.1002/14651858.CD006107.pub4).
Dr. Schoolcraft reported having no financial disclosures.
CORONADO, CALIF. – according to William Schoolcraft, MD, HCLD.
At a meeting on IVF and embryo transfer sponsored by the University of California, San Diego, Dr. Schoolcraft said that ultrasound-guided embryo transfer helps clinicians avoid difficult transfers, minimizes contamination with blood, facilitates proper placement of the catheter tip, and minimizes the stimulation of uterine contractions. “We know that contaminating the catheter either with blood or mucous or endometrial tissue lowers clinical pregnancy rates, compared to a clean catheter,” said Dr. Schoolcraft, founder and medical director of the Colorado Center for Reproductive Medicine, Denver.
“Ultrasound guidance can help you follow the contour of the cervix and avoid touching the fundus. Your catheter should be free of blood, mucous, or endometrial cells when the embryologist examines it,” he said. In his clinical opinion, it’s hard to argue against using ultrasound guidance for embryo transfer. “It’s also very popular with IVF patients, because they get to visualize the transfer and have some reassurance that the embryo is delivered to their uterus,” he said.
The potential benefit of using three-dimensional ultrasound for embryo transfer is less clear. “It does require more expensive equipment and it’s a little more skill dependent, but in a randomized trial it didn’t lead to any difference in outcomes,” Dr. Schoolcraft said. “I think if you’re good with two-dimensional ultrasound, three-dimensional ultrasound doesn’t seem to have much benefit in terms of pregnancy outcomes.”
In a study published in 2017, researchers from Barcelona analyzed 7,714 embryo transfers to determine the impact of maneuvers during embryo transfers on the pregnancy rate (Fertil Steril. 2017 Mar;107[3]:657-63.e1). Using the direct embryo transfer as a reference, each instrumentation needed to successfully deposit the embryos in the fundus served as an index of the difficulty of transfer. A difficult transfer occurred in 7.7% of cycles, and the researchers found that the clinical pregnancy rate decreased progressively with the use of additional maneuvers during embryo transfer. Specifically, the clinical pregnancy rate was 39.4% when no additional maneuvers were required, 36.9% when an outer catheter sheath was used (odds ratio, 0.89), 31.7% when a Wallace stylet was used (OR, 0.71), and 26.1% when a tenaculum was used (OR, 0.54). “I think without question, avoiding a difficult transfer is important and certainly a key to our success,” said Dr. Schoolcraft, who was not involved with the study.
The ideal depth of embryo transfer is “a bit complicated,” he said, but according to the best available evidence, a depth of 15-20 mm from the fundus by ultrasound guidance appears to optimize implantation by avoiding the lower cavity where implantation is compromised. This range of depth also avoids problems with upper cavity transfers, including trauma, contractions, and tubal pregnancy. “I think that transfers which are close to the fundus, and possibly in some cases touching the fundus, may lead to uterine contractions, plugging the catheter with endometrium and generating bleeding,” Dr. Schoolcraft said. He pointed out that during natural pregnancies, embryos implant in the upper fundus nearly 90% of the time, compared with 66% of the time during IVF pregnancies. “To mimic Mother Nature we don’t want to be too low, either,” he said. “We all know that placenta previa is increased with IVF. This may be due to placing the embryos too low.”
According to Dr. Schoolcraft, many published studies have found that significantly higher pregnancy rates occur with routine bladder distension prior to embryo transfer, probably because of the smooth and easy insertion of the embryo transfer. A Scandinavian meta-analysis found that the odds ratio favoring ultrasound guidance and a full bladder for ongoing pregnancy was 1.44 and clinical pregnancy was 1.55, which is similar to that seen during an earlier review from The Cochrane Collaborative, with an OR of 1.47 for ongoing pregnancy and OR 1.53 for live birth (Cochrane Database Syst Rev. 2016 Mar 17. doi: 10.1002/14651858.CD006107.pub4).
Dr. Schoolcraft reported having no financial disclosures.
CORONADO, CALIF. – according to William Schoolcraft, MD, HCLD.
At a meeting on IVF and embryo transfer sponsored by the University of California, San Diego, Dr. Schoolcraft said that ultrasound-guided embryo transfer helps clinicians avoid difficult transfers, minimizes contamination with blood, facilitates proper placement of the catheter tip, and minimizes the stimulation of uterine contractions. “We know that contaminating the catheter either with blood or mucous or endometrial tissue lowers clinical pregnancy rates, compared to a clean catheter,” said Dr. Schoolcraft, founder and medical director of the Colorado Center for Reproductive Medicine, Denver.
“Ultrasound guidance can help you follow the contour of the cervix and avoid touching the fundus. Your catheter should be free of blood, mucous, or endometrial cells when the embryologist examines it,” he said. In his clinical opinion, it’s hard to argue against using ultrasound guidance for embryo transfer. “It’s also very popular with IVF patients, because they get to visualize the transfer and have some reassurance that the embryo is delivered to their uterus,” he said.
The potential benefit of using three-dimensional ultrasound for embryo transfer is less clear. “It does require more expensive equipment and it’s a little more skill dependent, but in a randomized trial it didn’t lead to any difference in outcomes,” Dr. Schoolcraft said. “I think if you’re good with two-dimensional ultrasound, three-dimensional ultrasound doesn’t seem to have much benefit in terms of pregnancy outcomes.”
In a study published in 2017, researchers from Barcelona analyzed 7,714 embryo transfers to determine the impact of maneuvers during embryo transfers on the pregnancy rate (Fertil Steril. 2017 Mar;107[3]:657-63.e1). Using the direct embryo transfer as a reference, each instrumentation needed to successfully deposit the embryos in the fundus served as an index of the difficulty of transfer. A difficult transfer occurred in 7.7% of cycles, and the researchers found that the clinical pregnancy rate decreased progressively with the use of additional maneuvers during embryo transfer. Specifically, the clinical pregnancy rate was 39.4% when no additional maneuvers were required, 36.9% when an outer catheter sheath was used (odds ratio, 0.89), 31.7% when a Wallace stylet was used (OR, 0.71), and 26.1% when a tenaculum was used (OR, 0.54). “I think without question, avoiding a difficult transfer is important and certainly a key to our success,” said Dr. Schoolcraft, who was not involved with the study.
The ideal depth of embryo transfer is “a bit complicated,” he said, but according to the best available evidence, a depth of 15-20 mm from the fundus by ultrasound guidance appears to optimize implantation by avoiding the lower cavity where implantation is compromised. This range of depth also avoids problems with upper cavity transfers, including trauma, contractions, and tubal pregnancy. “I think that transfers which are close to the fundus, and possibly in some cases touching the fundus, may lead to uterine contractions, plugging the catheter with endometrium and generating bleeding,” Dr. Schoolcraft said. He pointed out that during natural pregnancies, embryos implant in the upper fundus nearly 90% of the time, compared with 66% of the time during IVF pregnancies. “To mimic Mother Nature we don’t want to be too low, either,” he said. “We all know that placenta previa is increased with IVF. This may be due to placing the embryos too low.”
According to Dr. Schoolcraft, many published studies have found that significantly higher pregnancy rates occur with routine bladder distension prior to embryo transfer, probably because of the smooth and easy insertion of the embryo transfer. A Scandinavian meta-analysis found that the odds ratio favoring ultrasound guidance and a full bladder for ongoing pregnancy was 1.44 and clinical pregnancy was 1.55, which is similar to that seen during an earlier review from The Cochrane Collaborative, with an OR of 1.47 for ongoing pregnancy and OR 1.53 for live birth (Cochrane Database Syst Rev. 2016 Mar 17. doi: 10.1002/14651858.CD006107.pub4).
Dr. Schoolcraft reported having no financial disclosures.
EXPERT ANALYSIS FROM A CME MEETING SPONSORED BY UCSD
Live attenuated flu vaccine gets ACIP nod for 2018-2019 season
The latest seasonal influenza vaccine recommendations from the Advisory Committee on Immunization Practices provide several key updates that will impact clinical practice in the 2018-2019 influenza season.
Of note, , following two seasons in which the committee recommended it not be used.
ACIP also updated its recommendations for individuals with a history of egg allergy, described the vaccine strains chosen for 2018-2019 season, and detailed the changes in age indications for Afluria Quadrivalent and Fluarix Quadrivalent that have been made since publication of its previous guidelines.
Published in MMWR Recommendations and Reports, the updated ACIP recommendations reflect discussions and decisions from the three public meetings of ACIP that have taken place since the last annual update.
All individuals 6 months of age and older who have no contraindications to influenza vaccine should receive routine annual influenza vaccine, ACIP also said in its report, reinforcing a key recommendation that has been in place since 2010.
“To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations,” wrote authors of the report, including lead author Lisa A. Grohskopf, MD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Dr. Grohskopf and coauthors made no specific recommendations on which vaccine to use. They said providers should choose licensed, age-appropriate recommended vaccines expected to be available for the 2018-2019 season, including inactivated influenza vaccines (IIV), a recombinant influenza vaccine (RIV4), and the LAIV option.
FluMist Quadrivalent, the one LAIV product expected to be available for the 2018-2019 season, is licensed for individuals aged 2-49 years.
In its deliberations over the updated LAIV recommendation, ACIP reviewed observational data from previous seasons suggesting that the vaccine was poorly effective, and significantly less effective than IIV, against influenza A(H1N1) pdm09 viruses.
The current formulation of FluMist includes a new H1N1pdm09-like vaccine virus. While no effectiveness estimates were available at the time of review, ACIP said it did consider manufacturer data on shedding and immunogenicity for the current vaccine in children between the ages of 24 months through less than 4 years.
“These data suggest that this new H1N1pdm09-like virus has improved replicative fitness over previous H1N1pdm09-like viruses included in LAIV,” Dr. Grohskopf and colleagues wrote.
Individuals with an egg allergy history also can receive any licensed, recommended, age-appropriate IIV, RIV, or LAIV vaccine, said ACIP. This updated recommendation was based in part on the committee’s review and discussion of three studies that showed no cases of anaphylaxis in egg-allergic children receiving LAIV.
The ACIP recommendation update also outlines the strains selected earlier this year for the 2018-2019 season. Trivalent influenza vaccines in the United States will include an A/Michigan/45/2015 (H1N1) pdm09–like virus, an A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus, and a B/Colorado/06/2017–like virus (Victoria lineage). Quadrivalent vaccines will include those strains plus a B/Phuket/3073/2013–like virus (Yamagata lineage).
The report also acknowledges the recent expansion of age indication for two vaccines that have occurred since the last ACIP recommendations.
Afluria Quadrivalent was previously licensed for individuals 18 years of age and older. In August 2017, the Food and Drug Administration approved expansion of the indication to individuals 5 years of age or older. In January 2018, FDA approved expansion of the Fluarix Quadrivalent indication, previously licensed for age 3 and older, to individuals 6 months and older.
Report coauthor Emmanuel B. Walter disclosed grants from Novavax and Merck. The remaining report authors reported no relevant financial disclosures.
SOURCE: Grohskopf LA et al. MMWR Recomm Rep. 2018 Aug 24;67(3):1-20.
The latest seasonal influenza vaccine recommendations from the Advisory Committee on Immunization Practices provide several key updates that will impact clinical practice in the 2018-2019 influenza season.
Of note, , following two seasons in which the committee recommended it not be used.
ACIP also updated its recommendations for individuals with a history of egg allergy, described the vaccine strains chosen for 2018-2019 season, and detailed the changes in age indications for Afluria Quadrivalent and Fluarix Quadrivalent that have been made since publication of its previous guidelines.
Published in MMWR Recommendations and Reports, the updated ACIP recommendations reflect discussions and decisions from the three public meetings of ACIP that have taken place since the last annual update.
All individuals 6 months of age and older who have no contraindications to influenza vaccine should receive routine annual influenza vaccine, ACIP also said in its report, reinforcing a key recommendation that has been in place since 2010.
“To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations,” wrote authors of the report, including lead author Lisa A. Grohskopf, MD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Dr. Grohskopf and coauthors made no specific recommendations on which vaccine to use. They said providers should choose licensed, age-appropriate recommended vaccines expected to be available for the 2018-2019 season, including inactivated influenza vaccines (IIV), a recombinant influenza vaccine (RIV4), and the LAIV option.
FluMist Quadrivalent, the one LAIV product expected to be available for the 2018-2019 season, is licensed for individuals aged 2-49 years.
In its deliberations over the updated LAIV recommendation, ACIP reviewed observational data from previous seasons suggesting that the vaccine was poorly effective, and significantly less effective than IIV, against influenza A(H1N1) pdm09 viruses.
The current formulation of FluMist includes a new H1N1pdm09-like vaccine virus. While no effectiveness estimates were available at the time of review, ACIP said it did consider manufacturer data on shedding and immunogenicity for the current vaccine in children between the ages of 24 months through less than 4 years.
“These data suggest that this new H1N1pdm09-like virus has improved replicative fitness over previous H1N1pdm09-like viruses included in LAIV,” Dr. Grohskopf and colleagues wrote.
Individuals with an egg allergy history also can receive any licensed, recommended, age-appropriate IIV, RIV, or LAIV vaccine, said ACIP. This updated recommendation was based in part on the committee’s review and discussion of three studies that showed no cases of anaphylaxis in egg-allergic children receiving LAIV.
The ACIP recommendation update also outlines the strains selected earlier this year for the 2018-2019 season. Trivalent influenza vaccines in the United States will include an A/Michigan/45/2015 (H1N1) pdm09–like virus, an A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus, and a B/Colorado/06/2017–like virus (Victoria lineage). Quadrivalent vaccines will include those strains plus a B/Phuket/3073/2013–like virus (Yamagata lineage).
The report also acknowledges the recent expansion of age indication for two vaccines that have occurred since the last ACIP recommendations.
Afluria Quadrivalent was previously licensed for individuals 18 years of age and older. In August 2017, the Food and Drug Administration approved expansion of the indication to individuals 5 years of age or older. In January 2018, FDA approved expansion of the Fluarix Quadrivalent indication, previously licensed for age 3 and older, to individuals 6 months and older.
Report coauthor Emmanuel B. Walter disclosed grants from Novavax and Merck. The remaining report authors reported no relevant financial disclosures.
SOURCE: Grohskopf LA et al. MMWR Recomm Rep. 2018 Aug 24;67(3):1-20.
The latest seasonal influenza vaccine recommendations from the Advisory Committee on Immunization Practices provide several key updates that will impact clinical practice in the 2018-2019 influenza season.
Of note, , following two seasons in which the committee recommended it not be used.
ACIP also updated its recommendations for individuals with a history of egg allergy, described the vaccine strains chosen for 2018-2019 season, and detailed the changes in age indications for Afluria Quadrivalent and Fluarix Quadrivalent that have been made since publication of its previous guidelines.
Published in MMWR Recommendations and Reports, the updated ACIP recommendations reflect discussions and decisions from the three public meetings of ACIP that have taken place since the last annual update.
All individuals 6 months of age and older who have no contraindications to influenza vaccine should receive routine annual influenza vaccine, ACIP also said in its report, reinforcing a key recommendation that has been in place since 2010.
“To avoid missed opportunities for vaccination, providers should offer vaccination during routine health care visits and hospitalizations,” wrote authors of the report, including lead author Lisa A. Grohskopf, MD, of the National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta.
Dr. Grohskopf and coauthors made no specific recommendations on which vaccine to use. They said providers should choose licensed, age-appropriate recommended vaccines expected to be available for the 2018-2019 season, including inactivated influenza vaccines (IIV), a recombinant influenza vaccine (RIV4), and the LAIV option.
FluMist Quadrivalent, the one LAIV product expected to be available for the 2018-2019 season, is licensed for individuals aged 2-49 years.
In its deliberations over the updated LAIV recommendation, ACIP reviewed observational data from previous seasons suggesting that the vaccine was poorly effective, and significantly less effective than IIV, against influenza A(H1N1) pdm09 viruses.
The current formulation of FluMist includes a new H1N1pdm09-like vaccine virus. While no effectiveness estimates were available at the time of review, ACIP said it did consider manufacturer data on shedding and immunogenicity for the current vaccine in children between the ages of 24 months through less than 4 years.
“These data suggest that this new H1N1pdm09-like virus has improved replicative fitness over previous H1N1pdm09-like viruses included in LAIV,” Dr. Grohskopf and colleagues wrote.
Individuals with an egg allergy history also can receive any licensed, recommended, age-appropriate IIV, RIV, or LAIV vaccine, said ACIP. This updated recommendation was based in part on the committee’s review and discussion of three studies that showed no cases of anaphylaxis in egg-allergic children receiving LAIV.
The ACIP recommendation update also outlines the strains selected earlier this year for the 2018-2019 season. Trivalent influenza vaccines in the United States will include an A/Michigan/45/2015 (H1N1) pdm09–like virus, an A/Singapore/INFIMH-16-0019/2016 (H3N2)-like virus, and a B/Colorado/06/2017–like virus (Victoria lineage). Quadrivalent vaccines will include those strains plus a B/Phuket/3073/2013–like virus (Yamagata lineage).
The report also acknowledges the recent expansion of age indication for two vaccines that have occurred since the last ACIP recommendations.
Afluria Quadrivalent was previously licensed for individuals 18 years of age and older. In August 2017, the Food and Drug Administration approved expansion of the indication to individuals 5 years of age or older. In January 2018, FDA approved expansion of the Fluarix Quadrivalent indication, previously licensed for age 3 and older, to individuals 6 months and older.
Report coauthor Emmanuel B. Walter disclosed grants from Novavax and Merck. The remaining report authors reported no relevant financial disclosures.
SOURCE: Grohskopf LA et al. MMWR Recomm Rep. 2018 Aug 24;67(3):1-20.
FROM MMWR
More frequent CT surveillance in NSCLC doesn’t improve survival
More even after researchers controlled for tumor histology and recurrence.
Compared with those followed every 3 months, the hazard ratio for 6-month follow-up with CT scanning was 1.16, and 1.06 for annual follow-up – a nonsignificant difference. Nor did more frequent imaging improve survival among the subgroup of patients who were cancer free 9 months after their surgery or among those who had recurrences, Timothy L. McMurry, PhD, and his colleagues reported in the Annals of Surgery. The paper was presented at the annual meeting of the American Surgical Association.
The results probably reflect the very poor survival rates of any patients who develop recurrent non–small cell lung cancer (NSCLC), wrote Dr. McMurry, a biostatistician at the University of Virginia, Charlottesville, and his coauthors.
“Surveillance recommendations need to be considered in the context of potential harms and benefits to patients and their caregivers,” they said. “Follow-up imaging and office visits increase cost and can lead to patient anxiety. Although it seems intuitive that earlier detection of asymptomatic recurrence could improve outcomes, patients with recurrent NSCLC do very poorly … poor survival after recurrence helps explain why more intense surveillance after surgical resection was not associated with improvement in overall survival.”
However, they noted, treatment advances for recurrent and metastatic disease may already be changing the outlook for these patients, “systemic therapy and targeted agents are demonstrating clinically significant survival benefits for small patient subgroups, which, in the future, may augment the benefits of early recurrence detection.”
The team undertook this retrospective study – the largest of its kind in NSCLC patients – in light of current follow-up recommendations that are based almost solely on expert consensus, with low-level data.
“Because there is a paucity of high-quality data on NSCLC surveillance, practice guidelines are based on small retrospective analyses and expert opinion. This results in wide variation in practice including both underuse and overuse of surveillance services.”
The study plumbed the National Cancer Database, extracting information on patients who underwent surgery for NSCLC stages I-III during 2006-2007. All had complete resection and negative margins. Patients were followed through 2012, or until they had a recurrence, a new primary cancer, or they died.
The cohort comprised 4,463 who were followed with CT imaging: 1,614 every 3 months, 1,999 every 6 months, and 850 annually. These intervals correspond to the three different major recommendations. The most common procedure was a lobectomy (about 80%). Patients with higher-stage cancers were significantly more likely to receive more frequent imaging. The regression model controlled for age, sex, comorbidities, tumor stage, and surgical procedure.
After 14 months, 3,552 patients (79.5%) were alive and cancer free. However, during the rest of the follow-up period, 11% developed a new primary cancer and 24% a recurrence of their lung cancer, with no between-group differences. The regression analysis showed no significant difference in recurrence related to surveillance interval, whether 6 months was compared with 3 months (hazard ratio, 1.16) or 1 year with 3 months (HR, 1.06).
Results were much the same for the subgroup of 3,165 who were alive and cancer free 9 months after surgery. In this group, 11% developed a new primary cancer and 29% a recurrence of their lung cancer, with similar numbers in each of the surveillance groups (HR, 1.12 for 6 months vs. 3 months).
Finally, a model including only those who had recurrence, new cancers, or were lost to follow-up within 14 months of surgery also showed no benefit for more frequent surveillance.
“More recent prerecurrence imaging was not associated with postrecurrence survival (HR, 1.02 per month since imaging), and patients who had gone more than 14 months without imaging were at no greater risk of death (HR, 1.01),” the investigators wrote.
The significant predictors of worse survival were nothing surprising, the authors noted. These included symptomatic recurrence (HR, 1.49), distant recurrence, age, male sex, congestive heart failure, coronary artery disease, and peripheral vascular disease.
The findings are not to say, however, that CT surveillance confers no benefit, the authors noted.
“Historically, 5-year survival for the earliest stage of lung cancer, stage IA, was only 70%. Increased use of CT scanning has, however, resulted in a decrease in the median tumor size of resected NSCLC and a shift toward earlier-stage disease. … The National Lung Screening Trial prospectively evaluated annual low-dose screening CT scans and demonstrated a 20% reduction in mortality from lung cancer. This enormous improvement in survival for NSCLC patients provides great promise for the future and is likely to increase the volume of lung cancer resections performed and the number of lung cancer survivors needing routine surveillance.”
However, the data do show that “at least annual CT surveillance is appropriate but that there is no benefit to more than biannual surveillance.”
The authors reported no financial conflicts.
SOURCE: McMurry TL et al. Ann Surg 2018 Jul 12. doi: 10.1097/SLA.0000000000002955.
More even after researchers controlled for tumor histology and recurrence.
Compared with those followed every 3 months, the hazard ratio for 6-month follow-up with CT scanning was 1.16, and 1.06 for annual follow-up – a nonsignificant difference. Nor did more frequent imaging improve survival among the subgroup of patients who were cancer free 9 months after their surgery or among those who had recurrences, Timothy L. McMurry, PhD, and his colleagues reported in the Annals of Surgery. The paper was presented at the annual meeting of the American Surgical Association.
The results probably reflect the very poor survival rates of any patients who develop recurrent non–small cell lung cancer (NSCLC), wrote Dr. McMurry, a biostatistician at the University of Virginia, Charlottesville, and his coauthors.
“Surveillance recommendations need to be considered in the context of potential harms and benefits to patients and their caregivers,” they said. “Follow-up imaging and office visits increase cost and can lead to patient anxiety. Although it seems intuitive that earlier detection of asymptomatic recurrence could improve outcomes, patients with recurrent NSCLC do very poorly … poor survival after recurrence helps explain why more intense surveillance after surgical resection was not associated with improvement in overall survival.”
However, they noted, treatment advances for recurrent and metastatic disease may already be changing the outlook for these patients, “systemic therapy and targeted agents are demonstrating clinically significant survival benefits for small patient subgroups, which, in the future, may augment the benefits of early recurrence detection.”
The team undertook this retrospective study – the largest of its kind in NSCLC patients – in light of current follow-up recommendations that are based almost solely on expert consensus, with low-level data.
“Because there is a paucity of high-quality data on NSCLC surveillance, practice guidelines are based on small retrospective analyses and expert opinion. This results in wide variation in practice including both underuse and overuse of surveillance services.”
The study plumbed the National Cancer Database, extracting information on patients who underwent surgery for NSCLC stages I-III during 2006-2007. All had complete resection and negative margins. Patients were followed through 2012, or until they had a recurrence, a new primary cancer, or they died.
The cohort comprised 4,463 who were followed with CT imaging: 1,614 every 3 months, 1,999 every 6 months, and 850 annually. These intervals correspond to the three different major recommendations. The most common procedure was a lobectomy (about 80%). Patients with higher-stage cancers were significantly more likely to receive more frequent imaging. The regression model controlled for age, sex, comorbidities, tumor stage, and surgical procedure.
After 14 months, 3,552 patients (79.5%) were alive and cancer free. However, during the rest of the follow-up period, 11% developed a new primary cancer and 24% a recurrence of their lung cancer, with no between-group differences. The regression analysis showed no significant difference in recurrence related to surveillance interval, whether 6 months was compared with 3 months (hazard ratio, 1.16) or 1 year with 3 months (HR, 1.06).
Results were much the same for the subgroup of 3,165 who were alive and cancer free 9 months after surgery. In this group, 11% developed a new primary cancer and 29% a recurrence of their lung cancer, with similar numbers in each of the surveillance groups (HR, 1.12 for 6 months vs. 3 months).
Finally, a model including only those who had recurrence, new cancers, or were lost to follow-up within 14 months of surgery also showed no benefit for more frequent surveillance.
“More recent prerecurrence imaging was not associated with postrecurrence survival (HR, 1.02 per month since imaging), and patients who had gone more than 14 months without imaging were at no greater risk of death (HR, 1.01),” the investigators wrote.
The significant predictors of worse survival were nothing surprising, the authors noted. These included symptomatic recurrence (HR, 1.49), distant recurrence, age, male sex, congestive heart failure, coronary artery disease, and peripheral vascular disease.
The findings are not to say, however, that CT surveillance confers no benefit, the authors noted.
“Historically, 5-year survival for the earliest stage of lung cancer, stage IA, was only 70%. Increased use of CT scanning has, however, resulted in a decrease in the median tumor size of resected NSCLC and a shift toward earlier-stage disease. … The National Lung Screening Trial prospectively evaluated annual low-dose screening CT scans and demonstrated a 20% reduction in mortality from lung cancer. This enormous improvement in survival for NSCLC patients provides great promise for the future and is likely to increase the volume of lung cancer resections performed and the number of lung cancer survivors needing routine surveillance.”
However, the data do show that “at least annual CT surveillance is appropriate but that there is no benefit to more than biannual surveillance.”
The authors reported no financial conflicts.
SOURCE: McMurry TL et al. Ann Surg 2018 Jul 12. doi: 10.1097/SLA.0000000000002955.
More even after researchers controlled for tumor histology and recurrence.
Compared with those followed every 3 months, the hazard ratio for 6-month follow-up with CT scanning was 1.16, and 1.06 for annual follow-up – a nonsignificant difference. Nor did more frequent imaging improve survival among the subgroup of patients who were cancer free 9 months after their surgery or among those who had recurrences, Timothy L. McMurry, PhD, and his colleagues reported in the Annals of Surgery. The paper was presented at the annual meeting of the American Surgical Association.
The results probably reflect the very poor survival rates of any patients who develop recurrent non–small cell lung cancer (NSCLC), wrote Dr. McMurry, a biostatistician at the University of Virginia, Charlottesville, and his coauthors.
“Surveillance recommendations need to be considered in the context of potential harms and benefits to patients and their caregivers,” they said. “Follow-up imaging and office visits increase cost and can lead to patient anxiety. Although it seems intuitive that earlier detection of asymptomatic recurrence could improve outcomes, patients with recurrent NSCLC do very poorly … poor survival after recurrence helps explain why more intense surveillance after surgical resection was not associated with improvement in overall survival.”
However, they noted, treatment advances for recurrent and metastatic disease may already be changing the outlook for these patients, “systemic therapy and targeted agents are demonstrating clinically significant survival benefits for small patient subgroups, which, in the future, may augment the benefits of early recurrence detection.”
The team undertook this retrospective study – the largest of its kind in NSCLC patients – in light of current follow-up recommendations that are based almost solely on expert consensus, with low-level data.
“Because there is a paucity of high-quality data on NSCLC surveillance, practice guidelines are based on small retrospective analyses and expert opinion. This results in wide variation in practice including both underuse and overuse of surveillance services.”
The study plumbed the National Cancer Database, extracting information on patients who underwent surgery for NSCLC stages I-III during 2006-2007. All had complete resection and negative margins. Patients were followed through 2012, or until they had a recurrence, a new primary cancer, or they died.
The cohort comprised 4,463 who were followed with CT imaging: 1,614 every 3 months, 1,999 every 6 months, and 850 annually. These intervals correspond to the three different major recommendations. The most common procedure was a lobectomy (about 80%). Patients with higher-stage cancers were significantly more likely to receive more frequent imaging. The regression model controlled for age, sex, comorbidities, tumor stage, and surgical procedure.
After 14 months, 3,552 patients (79.5%) were alive and cancer free. However, during the rest of the follow-up period, 11% developed a new primary cancer and 24% a recurrence of their lung cancer, with no between-group differences. The regression analysis showed no significant difference in recurrence related to surveillance interval, whether 6 months was compared with 3 months (hazard ratio, 1.16) or 1 year with 3 months (HR, 1.06).
Results were much the same for the subgroup of 3,165 who were alive and cancer free 9 months after surgery. In this group, 11% developed a new primary cancer and 29% a recurrence of their lung cancer, with similar numbers in each of the surveillance groups (HR, 1.12 for 6 months vs. 3 months).
Finally, a model including only those who had recurrence, new cancers, or were lost to follow-up within 14 months of surgery also showed no benefit for more frequent surveillance.
“More recent prerecurrence imaging was not associated with postrecurrence survival (HR, 1.02 per month since imaging), and patients who had gone more than 14 months without imaging were at no greater risk of death (HR, 1.01),” the investigators wrote.
The significant predictors of worse survival were nothing surprising, the authors noted. These included symptomatic recurrence (HR, 1.49), distant recurrence, age, male sex, congestive heart failure, coronary artery disease, and peripheral vascular disease.
The findings are not to say, however, that CT surveillance confers no benefit, the authors noted.
“Historically, 5-year survival for the earliest stage of lung cancer, stage IA, was only 70%. Increased use of CT scanning has, however, resulted in a decrease in the median tumor size of resected NSCLC and a shift toward earlier-stage disease. … The National Lung Screening Trial prospectively evaluated annual low-dose screening CT scans and demonstrated a 20% reduction in mortality from lung cancer. This enormous improvement in survival for NSCLC patients provides great promise for the future and is likely to increase the volume of lung cancer resections performed and the number of lung cancer survivors needing routine surveillance.”
However, the data do show that “at least annual CT surveillance is appropriate but that there is no benefit to more than biannual surveillance.”
The authors reported no financial conflicts.
SOURCE: McMurry TL et al. Ann Surg 2018 Jul 12. doi: 10.1097/SLA.0000000000002955.
FROM THE ANNALS OF SURGERY
Key clinical point: More frequent CT surveillance did not improve survival in patients with resected non–small cell lung cancer.
Major finding: Survival among those who got scans every 6 months was not significantly different than every 3 months (HR, 1.16)
Study details: The retrospective study comprised 4,463 patients.
Disclosures: The authors had no financial conflicts.
Source: McMurry TL et al. Ann Surg. 2018 Jul 12. doi: 10.1097/SLA.0000000000002955.
Mailing out fecal tests may improve CRC screening rates
Mailing fecal immunochemical tests (FITs) to overdue patients improved the rate of colorectal cancer screening in community health centers, results of a recent randomized trial show.
Outreach by mail led to a 3.4–percentage point increase in completion of FIT, compared with clinics who did not participate in the intervention, according to results of the randomized Strategies and Opportunities to STOP Colon Cancer in Priority Populations (STOP CRC) trial.
Although that difference was statistically significant, investigators said the improvement was less than expected based on previous experience, including a pilot study showing that the strategy of mailing fecal tests boosted completion rates by 38%.
Based on that discrepancy, additional strategies may be needed to support implementation of FIT mailing programs in low-resource health centers, reported Gloria D. Coronado, PhD, Kaiser Permanente Center for Health Research, Portland, Ore., and coinvestigators.
“This work demonstrates that mailed FIT outreach programs can have clinical impact when integrated into clinical work flows, but emphasizes the need to identify additional strategies to support program implementation in low-resource health centers,” Dr. Coronado and coauthors said in JAMA Internal Medicine.
The STOP CRC study included 26 federally qualified health center clinics serving low-income populations in Oregon and California. Investigators identified a total of 41,193 adults overdue for colorectal cancer screening between Feb. 4, 2014 and Feb. 3, 2015.
The core of the intervention was a set of electronic health record–embedded tools that identified adults due for screening and allowed staff to generate letters and mailing labels for a series of three mailings. The first mailing was an introductory letter, the second was a FIT kit packet that included wordless instructions, and the third was a reminder letter.
For clinics that participated in the intervention, the rate of FIT completion was 13.9%, versus 10.4%, a difference that was statistically significant (95% confidence interval, 0.1%-6.8%; P = .047), according to investigators. Likewise, the proportion of participants completing any CRC screening was significantly higher in the intervention clinics (18.3% versus 14.5%; 3.8 percentage points difference; 95% CI, 0.6%-7.0%; P = .024).
Somewhat larger effects were seen in an analysis that accounted for delays in implementation of the program. In that analysis, FIT completion rates were 17.6% for the intervention clinics and 12.8% for the usual care clinics (95% CI, 0.9-8.6%; P = .020), with similar increases seen in the proportion of patients receiving any CRC screening.
These increases in screening occurred despite “relatively low” implementation of the program, Dr. Coronado and colleagues said.
In the pilot study, a concerted effort was made to ensure all eligible adults got the intervention; in this study, 6,925 out of 21,134 intervention participants (33%) got an introductory letter, and of those, 91% received the FIT and 59% got the reminder letter.
Implementation varied widely by health center, ranging from 6.5% to 68.2%, investigators said in their report.
One reason for low implementation may be that the program competed with other priorities in the clinics. In interviews, health center leaders said challenges in the clinic included time burden, limited organizational capacity, and challenges with the EHR and associated reporting tools.
“For most participating health centers, STOP CRC represented the first time EHR tools were used to deliver cancer screening services outside the clinic,” Dr. Coronado said. “Implementation might have increased with experience.”
The research reported by Dr. Coronado and coinvestigators was supported by the National Institutes of Health. Dr. Coronado reported serving as a coinvestigator on a study of an experimental blood test for colorectal cancer funded by EpiGenomics and as principal investigator on a study of an experimental FIT funded by Quidel Corporation. No other disclosures were reported.
AGA patient education materials on colorectal cancer will help your patients better understand all of their screening options. Learn more at patient.gastro.org.
SOURCE: Coronado GD et al. JAMA Intern Med. 2018 Aug 6. doi: 10.1001/jamainternmed.2018.3629.
Mailing fecal immunochemical tests (FITs) to overdue patients improved the rate of colorectal cancer screening in community health centers, results of a recent randomized trial show.
Outreach by mail led to a 3.4–percentage point increase in completion of FIT, compared with clinics who did not participate in the intervention, according to results of the randomized Strategies and Opportunities to STOP Colon Cancer in Priority Populations (STOP CRC) trial.
Although that difference was statistically significant, investigators said the improvement was less than expected based on previous experience, including a pilot study showing that the strategy of mailing fecal tests boosted completion rates by 38%.
Based on that discrepancy, additional strategies may be needed to support implementation of FIT mailing programs in low-resource health centers, reported Gloria D. Coronado, PhD, Kaiser Permanente Center for Health Research, Portland, Ore., and coinvestigators.
“This work demonstrates that mailed FIT outreach programs can have clinical impact when integrated into clinical work flows, but emphasizes the need to identify additional strategies to support program implementation in low-resource health centers,” Dr. Coronado and coauthors said in JAMA Internal Medicine.
The STOP CRC study included 26 federally qualified health center clinics serving low-income populations in Oregon and California. Investigators identified a total of 41,193 adults overdue for colorectal cancer screening between Feb. 4, 2014 and Feb. 3, 2015.
The core of the intervention was a set of electronic health record–embedded tools that identified adults due for screening and allowed staff to generate letters and mailing labels for a series of three mailings. The first mailing was an introductory letter, the second was a FIT kit packet that included wordless instructions, and the third was a reminder letter.
For clinics that participated in the intervention, the rate of FIT completion was 13.9%, versus 10.4%, a difference that was statistically significant (95% confidence interval, 0.1%-6.8%; P = .047), according to investigators. Likewise, the proportion of participants completing any CRC screening was significantly higher in the intervention clinics (18.3% versus 14.5%; 3.8 percentage points difference; 95% CI, 0.6%-7.0%; P = .024).
Somewhat larger effects were seen in an analysis that accounted for delays in implementation of the program. In that analysis, FIT completion rates were 17.6% for the intervention clinics and 12.8% for the usual care clinics (95% CI, 0.9-8.6%; P = .020), with similar increases seen in the proportion of patients receiving any CRC screening.
These increases in screening occurred despite “relatively low” implementation of the program, Dr. Coronado and colleagues said.
In the pilot study, a concerted effort was made to ensure all eligible adults got the intervention; in this study, 6,925 out of 21,134 intervention participants (33%) got an introductory letter, and of those, 91% received the FIT and 59% got the reminder letter.
Implementation varied widely by health center, ranging from 6.5% to 68.2%, investigators said in their report.
One reason for low implementation may be that the program competed with other priorities in the clinics. In interviews, health center leaders said challenges in the clinic included time burden, limited organizational capacity, and challenges with the EHR and associated reporting tools.
“For most participating health centers, STOP CRC represented the first time EHR tools were used to deliver cancer screening services outside the clinic,” Dr. Coronado said. “Implementation might have increased with experience.”
The research reported by Dr. Coronado and coinvestigators was supported by the National Institutes of Health. Dr. Coronado reported serving as a coinvestigator on a study of an experimental blood test for colorectal cancer funded by EpiGenomics and as principal investigator on a study of an experimental FIT funded by Quidel Corporation. No other disclosures were reported.
AGA patient education materials on colorectal cancer will help your patients better understand all of their screening options. Learn more at patient.gastro.org.
SOURCE: Coronado GD et al. JAMA Intern Med. 2018 Aug 6. doi: 10.1001/jamainternmed.2018.3629.
Mailing fecal immunochemical tests (FITs) to overdue patients improved the rate of colorectal cancer screening in community health centers, results of a recent randomized trial show.
Outreach by mail led to a 3.4–percentage point increase in completion of FIT, compared with clinics who did not participate in the intervention, according to results of the randomized Strategies and Opportunities to STOP Colon Cancer in Priority Populations (STOP CRC) trial.
Although that difference was statistically significant, investigators said the improvement was less than expected based on previous experience, including a pilot study showing that the strategy of mailing fecal tests boosted completion rates by 38%.
Based on that discrepancy, additional strategies may be needed to support implementation of FIT mailing programs in low-resource health centers, reported Gloria D. Coronado, PhD, Kaiser Permanente Center for Health Research, Portland, Ore., and coinvestigators.
“This work demonstrates that mailed FIT outreach programs can have clinical impact when integrated into clinical work flows, but emphasizes the need to identify additional strategies to support program implementation in low-resource health centers,” Dr. Coronado and coauthors said in JAMA Internal Medicine.
The STOP CRC study included 26 federally qualified health center clinics serving low-income populations in Oregon and California. Investigators identified a total of 41,193 adults overdue for colorectal cancer screening between Feb. 4, 2014 and Feb. 3, 2015.
The core of the intervention was a set of electronic health record–embedded tools that identified adults due for screening and allowed staff to generate letters and mailing labels for a series of three mailings. The first mailing was an introductory letter, the second was a FIT kit packet that included wordless instructions, and the third was a reminder letter.
For clinics that participated in the intervention, the rate of FIT completion was 13.9%, versus 10.4%, a difference that was statistically significant (95% confidence interval, 0.1%-6.8%; P = .047), according to investigators. Likewise, the proportion of participants completing any CRC screening was significantly higher in the intervention clinics (18.3% versus 14.5%; 3.8 percentage points difference; 95% CI, 0.6%-7.0%; P = .024).
Somewhat larger effects were seen in an analysis that accounted for delays in implementation of the program. In that analysis, FIT completion rates were 17.6% for the intervention clinics and 12.8% for the usual care clinics (95% CI, 0.9-8.6%; P = .020), with similar increases seen in the proportion of patients receiving any CRC screening.
These increases in screening occurred despite “relatively low” implementation of the program, Dr. Coronado and colleagues said.
In the pilot study, a concerted effort was made to ensure all eligible adults got the intervention; in this study, 6,925 out of 21,134 intervention participants (33%) got an introductory letter, and of those, 91% received the FIT and 59% got the reminder letter.
Implementation varied widely by health center, ranging from 6.5% to 68.2%, investigators said in their report.
One reason for low implementation may be that the program competed with other priorities in the clinics. In interviews, health center leaders said challenges in the clinic included time burden, limited organizational capacity, and challenges with the EHR and associated reporting tools.
“For most participating health centers, STOP CRC represented the first time EHR tools were used to deliver cancer screening services outside the clinic,” Dr. Coronado said. “Implementation might have increased with experience.”
The research reported by Dr. Coronado and coinvestigators was supported by the National Institutes of Health. Dr. Coronado reported serving as a coinvestigator on a study of an experimental blood test for colorectal cancer funded by EpiGenomics and as principal investigator on a study of an experimental FIT funded by Quidel Corporation. No other disclosures were reported.
AGA patient education materials on colorectal cancer will help your patients better understand all of their screening options. Learn more at patient.gastro.org.
SOURCE: Coronado GD et al. JAMA Intern Med. 2018 Aug 6. doi: 10.1001/jamainternmed.2018.3629.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Mailing fecal immunochemical tests (FITs) to overdue patients improved the rate of colorectal cancer screening, though not to the extent that had been seen in a pilot study.
Major finding: Outreach by mail led to a 3.4–percentage point increase in FIT completion for participating clinics versus clinics that implemented usual care.
Study details: STOP CRC, a cluster-randomized pragmatic clinical trial including 26 federally qualified health center clinics and a total of 41,193 adults overdue for colorectal cancer screening.
Disclosures: The research was supported by the National Institutes of Health. One investigator reported disclosures related to EpiGenomics and Quidel Corporation.
Source: Coronado GD et al. JAMA Intern Med. 2018 Aug 6. doi: 10.1001/jamainternmed.2018.3629.
Early HbA1c levels may predict gestational diabetes
according to a case-control study drawn from the prospective NICHD Fetal Growth Studies-Singleton cohort.
Women who went on to develop GDM had higher HbA1c levels, and measuring this factor improved prediction when added to traditional GDM risk factors, Stefanie N. Hinkle, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and her associates reported in Scientific Reports.
A previous report showed that GDM-associated fetal overgrowth begins before GDM diagnosis, which suggests a need to identify GDM earlier in pregnancy (Int J Epidemiol. 2018 Feb;47[1]:25–25l).
HbA1c is already used to screen for type 2 diabetes mellitus outside of pregnancy. Previous studies that examined its potential utility for GDM have focused on high-risk patients, examined an HbA1c threshold of 5.7%, used GDM during the first trimester only as the outcome, or had other limitations. There is little research on HbA1c levels and GDM in population-based samples.
Dr. Hinkle and her associates conducted a secondary analysis of a case-control study that involved 2,334 low-risk pregnancies among nonobese women and 468 low-risk pregnancies among obese women (n = 2,802) at 12 U.S. centers. The women were recruited during gestational weeks 8-13 and then followed until the end of the pregnancy. The researchers did a nested GDM case-control study of 107 GDM cases and 214 matched non-GDM controls.
GDM cases had higher HbA1c levels throughout their pregnancies (P less than .03). The researchers found a linear association between HbA1c at enrollment and GDM risk (P = .001). Women with a first trimester HbA1c level of 5.7% had an odds ratio of 2.73 for GDM, compared with women at the median level of 5.2%.
In the adjusted model, for each increment of 0.1% at enrollment, women had an OR of 1.22 for GDM (P less than .001). For every 0.1% difference between HbA1c levels at enrollment and the second visit (24-29 weeks), the OR was 1.21 (P = .04). When the researchers excluded women who were obese, had smoked, had prior GDM, or had a hematologic disorder, the OR per 0.1% increase was similar (OR, 1.23; 95% confidence interval, 1.10-1.38).
A potential optimal cutoff point is 5.1%, which had a sensitivity of 47% (95% CI, 34%-60%) and a specificity of 79% (95% CI, 62%-88%). At 5.7%, which is used as the cutoff for prediabetes in nonpregnant women, the sensitivity was 21% (95% CI, 8%-36%) and the specificity was 95% (95% CI, 91%-99%).
When the model was added to conventional risk factors such as age, race/ethnicity, being overweight or obese before pregnancy, family history of diabetes, previous GDM, and nulliparity, the area under the curve of HbA1c levels at enrollment increased from 0.59 to 0.65.
Robert Atlas, MD, chair of obstetrics and gynecology at Mercy Medical Center, Baltimore, said in an interview, “This is just the first study that needs to be replicated in different patient populations. No one has looked at a continuum of HbA1c and what value above puts you at an increased risk. I think this is a very powerful study that sets the stage for further investigation into how to utilize HbA1c in a better way than we’ve ever looked at it before.”
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development intramural funding and by American Recovery and Reinvestment Act funding. Dr. Hinkle and her associates had no relevant financial disclosures. Dr. Atlas had no relevant financial disclosures.
SOURCE: Hinkle SN et al. Sci Rep. 2018 Aug 16;8(1):12249.
“I don’t think clinically this particular finding can make a change right off the bat. What it shows us is we need to understand, at a deeper level, what mechanistic processes might be going on. What underlying process is going on in the woman that looks apparently normal but has a slightly elevated HbA1c. What are the factors that are making this woman become at (greater) risk?”
Suchi Chandrasekaran, MD, MSCE, is an assistant professor of obstetrics and gynecology in the division of maternal fetal medicine at the University of Washington, Yakima. She had no relevant financial disclosures. She was not associated with the study.
“I don’t think clinically this particular finding can make a change right off the bat. What it shows us is we need to understand, at a deeper level, what mechanistic processes might be going on. What underlying process is going on in the woman that looks apparently normal but has a slightly elevated HbA1c. What are the factors that are making this woman become at (greater) risk?”
Suchi Chandrasekaran, MD, MSCE, is an assistant professor of obstetrics and gynecology in the division of maternal fetal medicine at the University of Washington, Yakima. She had no relevant financial disclosures. She was not associated with the study.
“I don’t think clinically this particular finding can make a change right off the bat. What it shows us is we need to understand, at a deeper level, what mechanistic processes might be going on. What underlying process is going on in the woman that looks apparently normal but has a slightly elevated HbA1c. What are the factors that are making this woman become at (greater) risk?”
Suchi Chandrasekaran, MD, MSCE, is an assistant professor of obstetrics and gynecology in the division of maternal fetal medicine at the University of Washington, Yakima. She had no relevant financial disclosures. She was not associated with the study.
according to a case-control study drawn from the prospective NICHD Fetal Growth Studies-Singleton cohort.
Women who went on to develop GDM had higher HbA1c levels, and measuring this factor improved prediction when added to traditional GDM risk factors, Stefanie N. Hinkle, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and her associates reported in Scientific Reports.
A previous report showed that GDM-associated fetal overgrowth begins before GDM diagnosis, which suggests a need to identify GDM earlier in pregnancy (Int J Epidemiol. 2018 Feb;47[1]:25–25l).
HbA1c is already used to screen for type 2 diabetes mellitus outside of pregnancy. Previous studies that examined its potential utility for GDM have focused on high-risk patients, examined an HbA1c threshold of 5.7%, used GDM during the first trimester only as the outcome, or had other limitations. There is little research on HbA1c levels and GDM in population-based samples.
Dr. Hinkle and her associates conducted a secondary analysis of a case-control study that involved 2,334 low-risk pregnancies among nonobese women and 468 low-risk pregnancies among obese women (n = 2,802) at 12 U.S. centers. The women were recruited during gestational weeks 8-13 and then followed until the end of the pregnancy. The researchers did a nested GDM case-control study of 107 GDM cases and 214 matched non-GDM controls.
GDM cases had higher HbA1c levels throughout their pregnancies (P less than .03). The researchers found a linear association between HbA1c at enrollment and GDM risk (P = .001). Women with a first trimester HbA1c level of 5.7% had an odds ratio of 2.73 for GDM, compared with women at the median level of 5.2%.
In the adjusted model, for each increment of 0.1% at enrollment, women had an OR of 1.22 for GDM (P less than .001). For every 0.1% difference between HbA1c levels at enrollment and the second visit (24-29 weeks), the OR was 1.21 (P = .04). When the researchers excluded women who were obese, had smoked, had prior GDM, or had a hematologic disorder, the OR per 0.1% increase was similar (OR, 1.23; 95% confidence interval, 1.10-1.38).
A potential optimal cutoff point is 5.1%, which had a sensitivity of 47% (95% CI, 34%-60%) and a specificity of 79% (95% CI, 62%-88%). At 5.7%, which is used as the cutoff for prediabetes in nonpregnant women, the sensitivity was 21% (95% CI, 8%-36%) and the specificity was 95% (95% CI, 91%-99%).
When the model was added to conventional risk factors such as age, race/ethnicity, being overweight or obese before pregnancy, family history of diabetes, previous GDM, and nulliparity, the area under the curve of HbA1c levels at enrollment increased from 0.59 to 0.65.
Robert Atlas, MD, chair of obstetrics and gynecology at Mercy Medical Center, Baltimore, said in an interview, “This is just the first study that needs to be replicated in different patient populations. No one has looked at a continuum of HbA1c and what value above puts you at an increased risk. I think this is a very powerful study that sets the stage for further investigation into how to utilize HbA1c in a better way than we’ve ever looked at it before.”
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development intramural funding and by American Recovery and Reinvestment Act funding. Dr. Hinkle and her associates had no relevant financial disclosures. Dr. Atlas had no relevant financial disclosures.
SOURCE: Hinkle SN et al. Sci Rep. 2018 Aug 16;8(1):12249.
according to a case-control study drawn from the prospective NICHD Fetal Growth Studies-Singleton cohort.
Women who went on to develop GDM had higher HbA1c levels, and measuring this factor improved prediction when added to traditional GDM risk factors, Stefanie N. Hinkle, PhD, of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and her associates reported in Scientific Reports.
A previous report showed that GDM-associated fetal overgrowth begins before GDM diagnosis, which suggests a need to identify GDM earlier in pregnancy (Int J Epidemiol. 2018 Feb;47[1]:25–25l).
HbA1c is already used to screen for type 2 diabetes mellitus outside of pregnancy. Previous studies that examined its potential utility for GDM have focused on high-risk patients, examined an HbA1c threshold of 5.7%, used GDM during the first trimester only as the outcome, or had other limitations. There is little research on HbA1c levels and GDM in population-based samples.
Dr. Hinkle and her associates conducted a secondary analysis of a case-control study that involved 2,334 low-risk pregnancies among nonobese women and 468 low-risk pregnancies among obese women (n = 2,802) at 12 U.S. centers. The women were recruited during gestational weeks 8-13 and then followed until the end of the pregnancy. The researchers did a nested GDM case-control study of 107 GDM cases and 214 matched non-GDM controls.
GDM cases had higher HbA1c levels throughout their pregnancies (P less than .03). The researchers found a linear association between HbA1c at enrollment and GDM risk (P = .001). Women with a first trimester HbA1c level of 5.7% had an odds ratio of 2.73 for GDM, compared with women at the median level of 5.2%.
In the adjusted model, for each increment of 0.1% at enrollment, women had an OR of 1.22 for GDM (P less than .001). For every 0.1% difference between HbA1c levels at enrollment and the second visit (24-29 weeks), the OR was 1.21 (P = .04). When the researchers excluded women who were obese, had smoked, had prior GDM, or had a hematologic disorder, the OR per 0.1% increase was similar (OR, 1.23; 95% confidence interval, 1.10-1.38).
A potential optimal cutoff point is 5.1%, which had a sensitivity of 47% (95% CI, 34%-60%) and a specificity of 79% (95% CI, 62%-88%). At 5.7%, which is used as the cutoff for prediabetes in nonpregnant women, the sensitivity was 21% (95% CI, 8%-36%) and the specificity was 95% (95% CI, 91%-99%).
When the model was added to conventional risk factors such as age, race/ethnicity, being overweight or obese before pregnancy, family history of diabetes, previous GDM, and nulliparity, the area under the curve of HbA1c levels at enrollment increased from 0.59 to 0.65.
Robert Atlas, MD, chair of obstetrics and gynecology at Mercy Medical Center, Baltimore, said in an interview, “This is just the first study that needs to be replicated in different patient populations. No one has looked at a continuum of HbA1c and what value above puts you at an increased risk. I think this is a very powerful study that sets the stage for further investigation into how to utilize HbA1c in a better way than we’ve ever looked at it before.”
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development intramural funding and by American Recovery and Reinvestment Act funding. Dr. Hinkle and her associates had no relevant financial disclosures. Dr. Atlas had no relevant financial disclosures.
SOURCE: Hinkle SN et al. Sci Rep. 2018 Aug 16;8(1):12249.
FROM SCIENTIFIC REPORTS
Key clinical point: First trimester HbA1c levels could improve early diagnosis.
Major finding: HbA1c levels of 5.1% predicted later gestational diabetes with a sensitivity of 47% and a specificity of 79%
Study details: Nested case-control study of 107 gestational diabetes cases and 214 controls.
Disclosures: The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development intramural funding and by the American Recovery and Reinvestment Act funding. .
Source: Hinkle SN et al. Sci Rep. 2018 Aug 16;8(1):12249.
Baseline steroids may reduce efficacy of checkpoint inhibitors
Immune checkpoint inhibitor therapy may be less effective if the patient is receiving corticosteroids at the time that treatment is initiated, results of a retrospective, two-center analysis suggest.
Corticosteroid use at the time of starting a PD-1 or PD-L1 inhibitor was associated with significantly reduced overall survival and progression-free survival in patients with non–small-cell lung cancer, the authors of the analysis reported.
“Prudent use of corticosteroids at the time of initiating PD-1/PD-L1 blockade is warranted,” said Matthew D. Hellmann, MD, of Memorial Sloan Kettering Cancer Center, New York, and his coauthors. The report is in the Journal of Clinical Oncology.
The retrospective analysis from Dr. Hellmann and his colleagues comprised 640 patients treated with single-agent atezolizumab, durvalumab, nivolumab, or pembrolizumab at Memorial Sloan Kettering Cancer Center or Gustave Roussy Cancer Center, Villejuif, France, between April 2011 and September 2017.
Ninety of those patients (14%) were receiving at least 10 mg of prednisone equivalent at the time the immune checkpoint inhibitor was started, a review of patient records revealed. About one-third were receiving corticosteroids for dyspnea or other respiratory symptoms. Another 21% had fatigue and 19% had brain metastases prompting corticosteroid treatment.
Corticosteroid use at the time of PD-1/PD-L1 blockade was associated with decreased progression-free survival (hazard ratio, 1.31; P = .03) and overall survival (HR, 1.66; P less than .001), as well as decreased overall response rate in a multivariable analysis adjusted for performance status, history of smoking, and history of brain metastases, the investigators reported.
Reduced efficacy also was seen in analyses that looked at each center separately. For the Memorial Sloan Kettering cohort (455 patients), baseline corticosteroid use was associated with significantly decreased overall response rate, shorter progression-free survival, and shorter overall survival.
For the smaller French cohort, (185 patients), there was a statistically nonsignificant decrease in overall response rate, along with significant reductions in progression-free survival and overall survival.
Based on these data, it may be prudent to try other pharmacologic or nonpharmacologic strategies to manage cancer symptoms if treatment with a PD-1/PD-L1 blocker is planned, Dr. Hellmann and his coauthors said.
“These strategies could enable patients to be tapered off corticosteroids before the start of PD-1/PD-L1 blockade to potentially achieve maximum benefit from these agents,” they wrote.
However, medically necessary corticosteroids should not be avoided, such as those given for management of brain metastases, they added.
Interestingly, other recent studies have suggested that patients already on PD-1/PD-L1 inhibitors do not seem to have decreased efficacy when corticosteroids are prescribed to manage emergent immune-related adverse events.
That’s “fortunate,” given that corticosteroids are a mainstay for the management of these characteristic adverse events in patients receiving immune checkpoint inhibitors, they said.
Dr. Hellmann reported research funding from Bristol-Myers Squibb, and a consulting or advisory role with AstraZeneca, Bristol-Myers Squibb, Genentech, Janssen Pharmaceuticals, MedImmune, Merck, Mirati Therapeutics, Shattuck Labs, and Syndax. Coauthors reported disclosures related to Amgen, Boehringer Ingelheim, Pfizer, and Roche, among others.
SOURCE: Arbour KC et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.79.0006.
Immune checkpoint inhibitor therapy may be less effective if the patient is receiving corticosteroids at the time that treatment is initiated, results of a retrospective, two-center analysis suggest.
Corticosteroid use at the time of starting a PD-1 or PD-L1 inhibitor was associated with significantly reduced overall survival and progression-free survival in patients with non–small-cell lung cancer, the authors of the analysis reported.
“Prudent use of corticosteroids at the time of initiating PD-1/PD-L1 blockade is warranted,” said Matthew D. Hellmann, MD, of Memorial Sloan Kettering Cancer Center, New York, and his coauthors. The report is in the Journal of Clinical Oncology.
The retrospective analysis from Dr. Hellmann and his colleagues comprised 640 patients treated with single-agent atezolizumab, durvalumab, nivolumab, or pembrolizumab at Memorial Sloan Kettering Cancer Center or Gustave Roussy Cancer Center, Villejuif, France, between April 2011 and September 2017.
Ninety of those patients (14%) were receiving at least 10 mg of prednisone equivalent at the time the immune checkpoint inhibitor was started, a review of patient records revealed. About one-third were receiving corticosteroids for dyspnea or other respiratory symptoms. Another 21% had fatigue and 19% had brain metastases prompting corticosteroid treatment.
Corticosteroid use at the time of PD-1/PD-L1 blockade was associated with decreased progression-free survival (hazard ratio, 1.31; P = .03) and overall survival (HR, 1.66; P less than .001), as well as decreased overall response rate in a multivariable analysis adjusted for performance status, history of smoking, and history of brain metastases, the investigators reported.
Reduced efficacy also was seen in analyses that looked at each center separately. For the Memorial Sloan Kettering cohort (455 patients), baseline corticosteroid use was associated with significantly decreased overall response rate, shorter progression-free survival, and shorter overall survival.
For the smaller French cohort, (185 patients), there was a statistically nonsignificant decrease in overall response rate, along with significant reductions in progression-free survival and overall survival.
Based on these data, it may be prudent to try other pharmacologic or nonpharmacologic strategies to manage cancer symptoms if treatment with a PD-1/PD-L1 blocker is planned, Dr. Hellmann and his coauthors said.
“These strategies could enable patients to be tapered off corticosteroids before the start of PD-1/PD-L1 blockade to potentially achieve maximum benefit from these agents,” they wrote.
However, medically necessary corticosteroids should not be avoided, such as those given for management of brain metastases, they added.
Interestingly, other recent studies have suggested that patients already on PD-1/PD-L1 inhibitors do not seem to have decreased efficacy when corticosteroids are prescribed to manage emergent immune-related adverse events.
That’s “fortunate,” given that corticosteroids are a mainstay for the management of these characteristic adverse events in patients receiving immune checkpoint inhibitors, they said.
Dr. Hellmann reported research funding from Bristol-Myers Squibb, and a consulting or advisory role with AstraZeneca, Bristol-Myers Squibb, Genentech, Janssen Pharmaceuticals, MedImmune, Merck, Mirati Therapeutics, Shattuck Labs, and Syndax. Coauthors reported disclosures related to Amgen, Boehringer Ingelheim, Pfizer, and Roche, among others.
SOURCE: Arbour KC et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.79.0006.
Immune checkpoint inhibitor therapy may be less effective if the patient is receiving corticosteroids at the time that treatment is initiated, results of a retrospective, two-center analysis suggest.
Corticosteroid use at the time of starting a PD-1 or PD-L1 inhibitor was associated with significantly reduced overall survival and progression-free survival in patients with non–small-cell lung cancer, the authors of the analysis reported.
“Prudent use of corticosteroids at the time of initiating PD-1/PD-L1 blockade is warranted,” said Matthew D. Hellmann, MD, of Memorial Sloan Kettering Cancer Center, New York, and his coauthors. The report is in the Journal of Clinical Oncology.
The retrospective analysis from Dr. Hellmann and his colleagues comprised 640 patients treated with single-agent atezolizumab, durvalumab, nivolumab, or pembrolizumab at Memorial Sloan Kettering Cancer Center or Gustave Roussy Cancer Center, Villejuif, France, between April 2011 and September 2017.
Ninety of those patients (14%) were receiving at least 10 mg of prednisone equivalent at the time the immune checkpoint inhibitor was started, a review of patient records revealed. About one-third were receiving corticosteroids for dyspnea or other respiratory symptoms. Another 21% had fatigue and 19% had brain metastases prompting corticosteroid treatment.
Corticosteroid use at the time of PD-1/PD-L1 blockade was associated with decreased progression-free survival (hazard ratio, 1.31; P = .03) and overall survival (HR, 1.66; P less than .001), as well as decreased overall response rate in a multivariable analysis adjusted for performance status, history of smoking, and history of brain metastases, the investigators reported.
Reduced efficacy also was seen in analyses that looked at each center separately. For the Memorial Sloan Kettering cohort (455 patients), baseline corticosteroid use was associated with significantly decreased overall response rate, shorter progression-free survival, and shorter overall survival.
For the smaller French cohort, (185 patients), there was a statistically nonsignificant decrease in overall response rate, along with significant reductions in progression-free survival and overall survival.
Based on these data, it may be prudent to try other pharmacologic or nonpharmacologic strategies to manage cancer symptoms if treatment with a PD-1/PD-L1 blocker is planned, Dr. Hellmann and his coauthors said.
“These strategies could enable patients to be tapered off corticosteroids before the start of PD-1/PD-L1 blockade to potentially achieve maximum benefit from these agents,” they wrote.
However, medically necessary corticosteroids should not be avoided, such as those given for management of brain metastases, they added.
Interestingly, other recent studies have suggested that patients already on PD-1/PD-L1 inhibitors do not seem to have decreased efficacy when corticosteroids are prescribed to manage emergent immune-related adverse events.
That’s “fortunate,” given that corticosteroids are a mainstay for the management of these characteristic adverse events in patients receiving immune checkpoint inhibitors, they said.
Dr. Hellmann reported research funding from Bristol-Myers Squibb, and a consulting or advisory role with AstraZeneca, Bristol-Myers Squibb, Genentech, Janssen Pharmaceuticals, MedImmune, Merck, Mirati Therapeutics, Shattuck Labs, and Syndax. Coauthors reported disclosures related to Amgen, Boehringer Ingelheim, Pfizer, and Roche, among others.
SOURCE: Arbour KC et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.79.0006.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Immune checkpoint inhibitors may be less effective if the patient is receiving corticosteroids at the time treatment is started.
Major finding: Corticosteroid use at the time of PD-1/PD-L1 blockade was associated with decreased progression-free survival (hazard ratio, 1.31; P = .03) and overall survival (HR, 1.66; P less than .001) in multivariate analysis.
Study details: Retrospective analysis of 640 patients treated with atezolizumab, durvalumab, nivolumab, or pembrolizumab at Memorial Sloan Kettering Cancer Center or Gustave Roussy Cancer Center.
Disclosures: The authors reported disclosures related to Amgen, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Genentech, Janssen Pharmaceuticals, MedImmune, Merck, Mirati Therapeutics, Pfizer, Roche, Shattuck Labs, and Syndax, among others.
Source: Arbour KC et al. J Clin Oncol. 2018 Aug 20. doi: 10.1200/JCO.2018.79.0006.
Applications for the 2019 Resident Corner Column Now Being Accepted
The Cutis Editorial Board is now accepting applications for the 2019 Resident Corner column. The Editorial Board will select 2 residents to serve as the Resident Corner columnists for 1 year (3 articles each). Articles are posted online only but will be referenced in Index Medicus. All applicants must be current residents and will still be in residency throughout 2019.
For consideration, send your curriculum vitae along with a brief (not to exceed 500 words) statement of why you enjoy Cutis and what you can offer your fellow residents in contributing a monthly column.
All materials should be submitted via email as 1 Word document to Melissa Sears by November 1. The residents who are selected to write the column for the upcoming year will be notified by November 15.
We look forward to continuing to educate dermatology residents on topics that are most important to them!
The Cutis Editorial Board is now accepting applications for the 2019 Resident Corner column. The Editorial Board will select 2 residents to serve as the Resident Corner columnists for 1 year (3 articles each). Articles are posted online only but will be referenced in Index Medicus. All applicants must be current residents and will still be in residency throughout 2019.
For consideration, send your curriculum vitae along with a brief (not to exceed 500 words) statement of why you enjoy Cutis and what you can offer your fellow residents in contributing a monthly column.
All materials should be submitted via email as 1 Word document to Melissa Sears by November 1. The residents who are selected to write the column for the upcoming year will be notified by November 15.
We look forward to continuing to educate dermatology residents on topics that are most important to them!
The Cutis Editorial Board is now accepting applications for the 2019 Resident Corner column. The Editorial Board will select 2 residents to serve as the Resident Corner columnists for 1 year (3 articles each). Articles are posted online only but will be referenced in Index Medicus. All applicants must be current residents and will still be in residency throughout 2019.
For consideration, send your curriculum vitae along with a brief (not to exceed 500 words) statement of why you enjoy Cutis and what you can offer your fellow residents in contributing a monthly column.
All materials should be submitted via email as 1 Word document to Melissa Sears by November 1. The residents who are selected to write the column for the upcoming year will be notified by November 15.
We look forward to continuing to educate dermatology residents on topics that are most important to them!
Mindfulness training for migraine just beginning to gather steam
SAN FRANCISCO – A brief course of mindfulness training for chronic migraine patients after their withdrawal from overuse of acute migraine medications proved as effective as prophylactic medication over the course of 12 months of follow-up, Frank Andrasik, PhD, reported at the annual meeting of the American Headache Society.
“The effects of mindfulness by and large rivaled those for medication alone. And although not specifically assessed, patients commented that mindfulness didn’t have side effects and promoted greater involvement and adherence,” said Dr. Andrasik, professor and chair, department of psychology, and director of the Center for Behavioral Medicine at the University of Memphis.
He noted that his recently published study (J Headache Pain. 2017 Dec;18[1]:15. doi: 10.1186/s10194-017-0728-z) is best considered exploratory because of its small size and nonrandomized design. Participants, after 5 days of structured acute medication withdrawal in a day hospital setting, got to choose whether to opt for pharmacologic prophylaxis for migraine – most often using botulinum toxin – or a brief course in mindfulness training entailing six once-weekly 45-minute sessions plus home practice for 7-10 minutes per day. And while this study design doesn’t rise to the status of level 1 randomized trial evidence, it does reflect real-world clinical practice, where patients often have a big say in choosing their treatment plan, the psychologist observed.
At baseline, all 44 patients met diagnostic criteria for chronic migraine with associated acute medication overuse. They averaged 20.5 headache days per month, with 18.4 days of acute migraine medication use.
At 3, 6, and 12 months of follow-up, the 22 patients in the mindfulness group averaged 8.3, 10.4, and 12.4 headache days per month, while the 22 on preventive migraine drugs averaged 8.8, 11, and 8.6 headache days per month. Both groups averaged similar 7- to 10-day reductions in days of acute migraine medication use per month.
Using the widely accepted endpoint of at least a 50% reduction in headache days per month, 50% of the mindfulness-only group and 52.6% of the prophylactic medication-only group met that standard at 12 months of follow-up. Moreover, at 12 months, 65% of the mindfulness therapy group and a similar 73.7% of the preventive medication group no longer met diagnostic criteria for chronic migraine.
The mindfulness protocol used in the study was based upon the popular mindfulness-based stress reduction program developed by Jon Kabat-Zinn, PhD.
Scores on the Migraine Disability Assessment (MIDAS) measure improved significantly and to a similar extent over baseline in both groups. So did scores on the Beck Depression Inventory. In contrast, scores on the State-Trait Anxiety Inventory didn’t change significantly in either study arm.
Both Dr. Andrasik and session chair Elizabeth K. Seng, PhD, cautioned that despite solid evidence of efficacy for mindfulness training in the treatment of depression and a number of chronic pain disorders, . Large randomized, controlled clinical trials are ongoing or in the planning stages, with no results yet available.
Dr. Seng, a clinical psychologist at Albert Einstein College of Medicine in New York, described mindfulness and acceptance as “third wave” behavioral treatments for migraine. The first wave therapies focused on fostering behavioral changes to reduce perceived stress in order to avoid triggering migraine attacks. The second wave involved therapeutic interactions aimed at helping patients reframe maladaptive automatic thoughts to reduce stress stemming from the daily hassles of life.
“The focus in the first- and second-wave therapies is, ‘Change something and your life will be better. Change your behaviors, clean up your act, change your thoughts because your thoughts are not helping you, and thereby reduce stress and reduce migraine.’ These mindfulness therapies are incredibly different from that,” she explained.
Indeed, the third-wave therapies aren’t trying to change daily hassles or automatic thoughts; instead, they seek to change the patient’s relationship to them such that they no longer create barriers to engaging in life activities that the patient finds nourishing and meaningful. It’s a matter of creating a willingness to experience pain in order to achieve worthwhile objectives, Dr. Seng continued.
It’s unclear that a reduction in migraine days – the traditional yardstick for therapeutic efficacy in migraine research – is the right primary outcome measure for third-wave therapies, according to the psychologist.
“So far, our evidence would suggest that mindfulness-based therapies do not reduce migraine days as much as other behavioral treatments, but what they’re doing is increasing migraine-related quality of life and reducing migraine-related disability to the same or possibly larger extent than our other behavioral treatments,“ she said. “Maybe what these third-wave therapies are actually doing is impacting our cognitive and emotional functioning, and that even if patients still experience similar levels of headache frequency, their reaction to those headache days no longer leads to a bunch of suffering. And that could be a clinically relevant outcome.”
Dr. Seng is particularly eager to formally study mindfulness therapies in a subgroup of migraine patients with high levels of depression. They might respond especially well, since mindfulness was originally developed as a treatment for severe depression. “Patients who are depressed have a hard time overcoming barriers to engaging in nourishing life activities, and when they have a headache day it’s even worse. That’s one of the things that’s leading them to have migraine-related disability,” she said.
Dr. Andrasik, whose study was supported by the European Commission and an Italian research foundation, reported having no financial conflicts of interest regarding his presentation. Dr. Seng reported serving as a consultant to GlaxoSmithKline.
SAN FRANCISCO – A brief course of mindfulness training for chronic migraine patients after their withdrawal from overuse of acute migraine medications proved as effective as prophylactic medication over the course of 12 months of follow-up, Frank Andrasik, PhD, reported at the annual meeting of the American Headache Society.
“The effects of mindfulness by and large rivaled those for medication alone. And although not specifically assessed, patients commented that mindfulness didn’t have side effects and promoted greater involvement and adherence,” said Dr. Andrasik, professor and chair, department of psychology, and director of the Center for Behavioral Medicine at the University of Memphis.
He noted that his recently published study (J Headache Pain. 2017 Dec;18[1]:15. doi: 10.1186/s10194-017-0728-z) is best considered exploratory because of its small size and nonrandomized design. Participants, after 5 days of structured acute medication withdrawal in a day hospital setting, got to choose whether to opt for pharmacologic prophylaxis for migraine – most often using botulinum toxin – or a brief course in mindfulness training entailing six once-weekly 45-minute sessions plus home practice for 7-10 minutes per day. And while this study design doesn’t rise to the status of level 1 randomized trial evidence, it does reflect real-world clinical practice, where patients often have a big say in choosing their treatment plan, the psychologist observed.
At baseline, all 44 patients met diagnostic criteria for chronic migraine with associated acute medication overuse. They averaged 20.5 headache days per month, with 18.4 days of acute migraine medication use.
At 3, 6, and 12 months of follow-up, the 22 patients in the mindfulness group averaged 8.3, 10.4, and 12.4 headache days per month, while the 22 on preventive migraine drugs averaged 8.8, 11, and 8.6 headache days per month. Both groups averaged similar 7- to 10-day reductions in days of acute migraine medication use per month.
Using the widely accepted endpoint of at least a 50% reduction in headache days per month, 50% of the mindfulness-only group and 52.6% of the prophylactic medication-only group met that standard at 12 months of follow-up. Moreover, at 12 months, 65% of the mindfulness therapy group and a similar 73.7% of the preventive medication group no longer met diagnostic criteria for chronic migraine.
The mindfulness protocol used in the study was based upon the popular mindfulness-based stress reduction program developed by Jon Kabat-Zinn, PhD.
Scores on the Migraine Disability Assessment (MIDAS) measure improved significantly and to a similar extent over baseline in both groups. So did scores on the Beck Depression Inventory. In contrast, scores on the State-Trait Anxiety Inventory didn’t change significantly in either study arm.
Both Dr. Andrasik and session chair Elizabeth K. Seng, PhD, cautioned that despite solid evidence of efficacy for mindfulness training in the treatment of depression and a number of chronic pain disorders, . Large randomized, controlled clinical trials are ongoing or in the planning stages, with no results yet available.
Dr. Seng, a clinical psychologist at Albert Einstein College of Medicine in New York, described mindfulness and acceptance as “third wave” behavioral treatments for migraine. The first wave therapies focused on fostering behavioral changes to reduce perceived stress in order to avoid triggering migraine attacks. The second wave involved therapeutic interactions aimed at helping patients reframe maladaptive automatic thoughts to reduce stress stemming from the daily hassles of life.
“The focus in the first- and second-wave therapies is, ‘Change something and your life will be better. Change your behaviors, clean up your act, change your thoughts because your thoughts are not helping you, and thereby reduce stress and reduce migraine.’ These mindfulness therapies are incredibly different from that,” she explained.
Indeed, the third-wave therapies aren’t trying to change daily hassles or automatic thoughts; instead, they seek to change the patient’s relationship to them such that they no longer create barriers to engaging in life activities that the patient finds nourishing and meaningful. It’s a matter of creating a willingness to experience pain in order to achieve worthwhile objectives, Dr. Seng continued.
It’s unclear that a reduction in migraine days – the traditional yardstick for therapeutic efficacy in migraine research – is the right primary outcome measure for third-wave therapies, according to the psychologist.
“So far, our evidence would suggest that mindfulness-based therapies do not reduce migraine days as much as other behavioral treatments, but what they’re doing is increasing migraine-related quality of life and reducing migraine-related disability to the same or possibly larger extent than our other behavioral treatments,“ she said. “Maybe what these third-wave therapies are actually doing is impacting our cognitive and emotional functioning, and that even if patients still experience similar levels of headache frequency, their reaction to those headache days no longer leads to a bunch of suffering. And that could be a clinically relevant outcome.”
Dr. Seng is particularly eager to formally study mindfulness therapies in a subgroup of migraine patients with high levels of depression. They might respond especially well, since mindfulness was originally developed as a treatment for severe depression. “Patients who are depressed have a hard time overcoming barriers to engaging in nourishing life activities, and when they have a headache day it’s even worse. That’s one of the things that’s leading them to have migraine-related disability,” she said.
Dr. Andrasik, whose study was supported by the European Commission and an Italian research foundation, reported having no financial conflicts of interest regarding his presentation. Dr. Seng reported serving as a consultant to GlaxoSmithKline.
SAN FRANCISCO – A brief course of mindfulness training for chronic migraine patients after their withdrawal from overuse of acute migraine medications proved as effective as prophylactic medication over the course of 12 months of follow-up, Frank Andrasik, PhD, reported at the annual meeting of the American Headache Society.
“The effects of mindfulness by and large rivaled those for medication alone. And although not specifically assessed, patients commented that mindfulness didn’t have side effects and promoted greater involvement and adherence,” said Dr. Andrasik, professor and chair, department of psychology, and director of the Center for Behavioral Medicine at the University of Memphis.
He noted that his recently published study (J Headache Pain. 2017 Dec;18[1]:15. doi: 10.1186/s10194-017-0728-z) is best considered exploratory because of its small size and nonrandomized design. Participants, after 5 days of structured acute medication withdrawal in a day hospital setting, got to choose whether to opt for pharmacologic prophylaxis for migraine – most often using botulinum toxin – or a brief course in mindfulness training entailing six once-weekly 45-minute sessions plus home practice for 7-10 minutes per day. And while this study design doesn’t rise to the status of level 1 randomized trial evidence, it does reflect real-world clinical practice, where patients often have a big say in choosing their treatment plan, the psychologist observed.
At baseline, all 44 patients met diagnostic criteria for chronic migraine with associated acute medication overuse. They averaged 20.5 headache days per month, with 18.4 days of acute migraine medication use.
At 3, 6, and 12 months of follow-up, the 22 patients in the mindfulness group averaged 8.3, 10.4, and 12.4 headache days per month, while the 22 on preventive migraine drugs averaged 8.8, 11, and 8.6 headache days per month. Both groups averaged similar 7- to 10-day reductions in days of acute migraine medication use per month.
Using the widely accepted endpoint of at least a 50% reduction in headache days per month, 50% of the mindfulness-only group and 52.6% of the prophylactic medication-only group met that standard at 12 months of follow-up. Moreover, at 12 months, 65% of the mindfulness therapy group and a similar 73.7% of the preventive medication group no longer met diagnostic criteria for chronic migraine.
The mindfulness protocol used in the study was based upon the popular mindfulness-based stress reduction program developed by Jon Kabat-Zinn, PhD.
Scores on the Migraine Disability Assessment (MIDAS) measure improved significantly and to a similar extent over baseline in both groups. So did scores on the Beck Depression Inventory. In contrast, scores on the State-Trait Anxiety Inventory didn’t change significantly in either study arm.
Both Dr. Andrasik and session chair Elizabeth K. Seng, PhD, cautioned that despite solid evidence of efficacy for mindfulness training in the treatment of depression and a number of chronic pain disorders, . Large randomized, controlled clinical trials are ongoing or in the planning stages, with no results yet available.
Dr. Seng, a clinical psychologist at Albert Einstein College of Medicine in New York, described mindfulness and acceptance as “third wave” behavioral treatments for migraine. The first wave therapies focused on fostering behavioral changes to reduce perceived stress in order to avoid triggering migraine attacks. The second wave involved therapeutic interactions aimed at helping patients reframe maladaptive automatic thoughts to reduce stress stemming from the daily hassles of life.
“The focus in the first- and second-wave therapies is, ‘Change something and your life will be better. Change your behaviors, clean up your act, change your thoughts because your thoughts are not helping you, and thereby reduce stress and reduce migraine.’ These mindfulness therapies are incredibly different from that,” she explained.
Indeed, the third-wave therapies aren’t trying to change daily hassles or automatic thoughts; instead, they seek to change the patient’s relationship to them such that they no longer create barriers to engaging in life activities that the patient finds nourishing and meaningful. It’s a matter of creating a willingness to experience pain in order to achieve worthwhile objectives, Dr. Seng continued.
It’s unclear that a reduction in migraine days – the traditional yardstick for therapeutic efficacy in migraine research – is the right primary outcome measure for third-wave therapies, according to the psychologist.
“So far, our evidence would suggest that mindfulness-based therapies do not reduce migraine days as much as other behavioral treatments, but what they’re doing is increasing migraine-related quality of life and reducing migraine-related disability to the same or possibly larger extent than our other behavioral treatments,“ she said. “Maybe what these third-wave therapies are actually doing is impacting our cognitive and emotional functioning, and that even if patients still experience similar levels of headache frequency, their reaction to those headache days no longer leads to a bunch of suffering. And that could be a clinically relevant outcome.”
Dr. Seng is particularly eager to formally study mindfulness therapies in a subgroup of migraine patients with high levels of depression. They might respond especially well, since mindfulness was originally developed as a treatment for severe depression. “Patients who are depressed have a hard time overcoming barriers to engaging in nourishing life activities, and when they have a headache day it’s even worse. That’s one of the things that’s leading them to have migraine-related disability,” she said.
Dr. Andrasik, whose study was supported by the European Commission and an Italian research foundation, reported having no financial conflicts of interest regarding his presentation. Dr. Seng reported serving as a consultant to GlaxoSmithKline.
REPORTING FROM THE AHS ANNUAL MEETING
Study sheds new light on prognostic factors in PRCC
Although the two major subtypes of papillary renal cell carcinoma (PRCC) differ on a variety of measures of aggressiveness, subtype is not independently prognostic, according to a retrospective cohort study conducted by the German Network of Kidney Cancer.
Investigators led by Iris Polifka, an intern at the Institute of Pathology at the University Hospital Erlangen (Germany), characterized 376 renal tumors initially diagnosed as PRCC. They reviewed histologic features and performed immunohistochemical staining for a range of markers.
Main study results, which were reported in Human Pathology, showed that 65.4% of the tumors were PRCC subtype 1 and 34.6% were PRCC subtype 2. The former more commonly had foamy macrophages and expressed cytokeratin 7, whereas the latter more commonly had abundant cytoplasm, expressed E-cadherin and p53, and had high MIB1 expression (staining of more than 15% of cells), which indicated a high proliferation rate (P less than .05 for each). The latter also had higher stage and higher grade.
Univariate analysis in the entire study cohort showed that racemase expression and cytokeratin 7 expression were favorable prognostic factors for overall survival, whereas presence of abundant cytoplasm and psammoma bodies, high MIB1 expression, and PRCC subtype 2 were unfavorable prognostic factors.
However, in multivariate analysis, only four factors were independent predictors of death: high tumor MIB1 expression (hazard ratio, 2.465; P = .033), higher T stage (P = .036), metastases (HR, 4.334; P = .011), and age older than the median of 63 years at surgery (HR, 2.384; P = .005). Notably, tumor subtype did not independently predict this outcome.
“[T]he better [overall survival] in PRCC1 is mainly a reflection of its encapsulated nature associated with lower TNM stage … while enhanced proliferation might add to the aggressive nature of high grade and high stage tumors independently from PRCC subtype,” the investigators propose.
“PRCC subtype on its own is not suitable for estimating survival. More data focusing on PRCC tumor biology is needed to define prognostic subgroups, especially in PRCC2,” they conclude.
The investigators disclosed that they had no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Polifka I et al. Hum Pathol. 2018 Aug 16. doi: 10.1016/j.humpath.2018.08.006.
Although the two major subtypes of papillary renal cell carcinoma (PRCC) differ on a variety of measures of aggressiveness, subtype is not independently prognostic, according to a retrospective cohort study conducted by the German Network of Kidney Cancer.
Investigators led by Iris Polifka, an intern at the Institute of Pathology at the University Hospital Erlangen (Germany), characterized 376 renal tumors initially diagnosed as PRCC. They reviewed histologic features and performed immunohistochemical staining for a range of markers.
Main study results, which were reported in Human Pathology, showed that 65.4% of the tumors were PRCC subtype 1 and 34.6% were PRCC subtype 2. The former more commonly had foamy macrophages and expressed cytokeratin 7, whereas the latter more commonly had abundant cytoplasm, expressed E-cadherin and p53, and had high MIB1 expression (staining of more than 15% of cells), which indicated a high proliferation rate (P less than .05 for each). The latter also had higher stage and higher grade.
Univariate analysis in the entire study cohort showed that racemase expression and cytokeratin 7 expression were favorable prognostic factors for overall survival, whereas presence of abundant cytoplasm and psammoma bodies, high MIB1 expression, and PRCC subtype 2 were unfavorable prognostic factors.
However, in multivariate analysis, only four factors were independent predictors of death: high tumor MIB1 expression (hazard ratio, 2.465; P = .033), higher T stage (P = .036), metastases (HR, 4.334; P = .011), and age older than the median of 63 years at surgery (HR, 2.384; P = .005). Notably, tumor subtype did not independently predict this outcome.
“[T]he better [overall survival] in PRCC1 is mainly a reflection of its encapsulated nature associated with lower TNM stage … while enhanced proliferation might add to the aggressive nature of high grade and high stage tumors independently from PRCC subtype,” the investigators propose.
“PRCC subtype on its own is not suitable for estimating survival. More data focusing on PRCC tumor biology is needed to define prognostic subgroups, especially in PRCC2,” they conclude.
The investigators disclosed that they had no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Polifka I et al. Hum Pathol. 2018 Aug 16. doi: 10.1016/j.humpath.2018.08.006.
Although the two major subtypes of papillary renal cell carcinoma (PRCC) differ on a variety of measures of aggressiveness, subtype is not independently prognostic, according to a retrospective cohort study conducted by the German Network of Kidney Cancer.
Investigators led by Iris Polifka, an intern at the Institute of Pathology at the University Hospital Erlangen (Germany), characterized 376 renal tumors initially diagnosed as PRCC. They reviewed histologic features and performed immunohistochemical staining for a range of markers.
Main study results, which were reported in Human Pathology, showed that 65.4% of the tumors were PRCC subtype 1 and 34.6% were PRCC subtype 2. The former more commonly had foamy macrophages and expressed cytokeratin 7, whereas the latter more commonly had abundant cytoplasm, expressed E-cadherin and p53, and had high MIB1 expression (staining of more than 15% of cells), which indicated a high proliferation rate (P less than .05 for each). The latter also had higher stage and higher grade.
Univariate analysis in the entire study cohort showed that racemase expression and cytokeratin 7 expression were favorable prognostic factors for overall survival, whereas presence of abundant cytoplasm and psammoma bodies, high MIB1 expression, and PRCC subtype 2 were unfavorable prognostic factors.
However, in multivariate analysis, only four factors were independent predictors of death: high tumor MIB1 expression (hazard ratio, 2.465; P = .033), higher T stage (P = .036), metastases (HR, 4.334; P = .011), and age older than the median of 63 years at surgery (HR, 2.384; P = .005). Notably, tumor subtype did not independently predict this outcome.
“[T]he better [overall survival] in PRCC1 is mainly a reflection of its encapsulated nature associated with lower TNM stage … while enhanced proliferation might add to the aggressive nature of high grade and high stage tumors independently from PRCC subtype,” the investigators propose.
“PRCC subtype on its own is not suitable for estimating survival. More data focusing on PRCC tumor biology is needed to define prognostic subgroups, especially in PRCC2,” they conclude.
The investigators disclosed that they had no relevant conflicts of interest. The study did not receive any specific funding.
SOURCE: Polifka I et al. Hum Pathol. 2018 Aug 16. doi: 10.1016/j.humpath.2018.08.006.
FROM HUMAN PATHOLOGY
Key clinical point: Tumor proliferation, TNM stage, and patient age are independently prognostic in PRCC, whereas tumor subtype is not.
Major finding: Patients had poorer overall survival if they had high tumor MIB1 expression (hazard ratio, 2.465), higher tumor T stage (P = .036), or metastases (hazard ratio, 4.334), or were older (hazard ratio, 2.384).
Study details: A multicenter retrospective cohort study of 376 renal tumors initially diagnosed as PRCC.
Disclosures: The investigators disclosed that they had no relevant conflicts of interest. The study did not receive any specific funding.
Source: Polifka I et al. Hum Pathol. 2018 Aug 16. doi: 10.1016/j.humpath.2018.08.006.
Metastatic Vulvovaginal Crohn Disease in the Setting of Well-Controlled Intestinal Disease
The cutaneous manifestations of Crohn disease (CD) are varied, including pyoderma gangrenosum, erythema nodosum, and metastatic CD (MCD). First described by Parks et al,1 MCD is defined as the occurrence of granulomatous lesions at a skin site distant from the gastrointestinal tract.1-20 Metastatic CD presents a diagnostic challenge because it is a rare component in the spectrum of inflammatory bowel disease complications, and many physicians are unaware of its existence. It may precede, coincide with, or develop after the diagnosis of intestinal disease.2-5 Vulvoperineal involvement is particularly problematic because a multitude of other, more likely disease processes are considered first. Typically it is initially diagnosed as a presumed infection prompting reflexive treatment with antivirals, antifungals, and antibiotics. Patients may experience symptoms for years prior to correct diagnosis and institution of proper therapy. A variety of clinical presentations have been described, including nonspecific pain and swelling, erythematous papules and plaques, and nonhealing ulcers. Skin biopsy characteristically confirms the diagnosis and reveals dermal noncaseating granulomas. Multiple oral and parenteral therapies are available, with surgical intervention reserved for resistant cases. We present a case of vulvovaginal MCD in the setting of well-controlled intestinal disease. We also provide a review of the literature regarding genital CD and emphasize the need to keep MCD in the differential of vulvoperineal pathology.
Case Report
A 29-year-old woman was referred to the dermatology clinic with vulvar pain, swelling, and pruritus of 14 months’ duration. Her medical history was remarkable for CD following a colectomy with colostomy. Prior therapies included methotrexate with infliximab for 5 years followed by a 2-year regimen with adalimumab, which induced remission of the intestinal disease.
The patient previously had taken a variety of topical and oral antimicrobials based on treatment from a primary care physician because fungal, bacterial, and viral infections initially were suspected; however, the vulvar disease persisted, and drug-induced immunosuppression was considered to be an underlying factor. Thus, adalimumab was discontinued. Despite elimination of the biologic, the vulvar disease progressed, which prompted referral to the dermatology clinic.
Physical examination revealed diffuse vulvar edema with overlying erythema and scale (Figure 1A). Upon closer inspection, scattered violaceous papules atop a backdrop of lichenification were evident, imparting a cobblestone appearance (Figure 1B). Additionally, a fissure was present on the gluteal cleft. Biopsy from the left labia majora demonstrated well-formed granulomas within a fibrotic reticular dermis (Figures 2A and 2B). The granulomas consisted of both mononucleated and multinucleated histiocytes, rimmed peripherally by lymphocytes and plasma cells (Figure 2C). Periodic acid–Schiff–diastase and acid-fast bacilli stains as well as polarizing microscopy were negative.

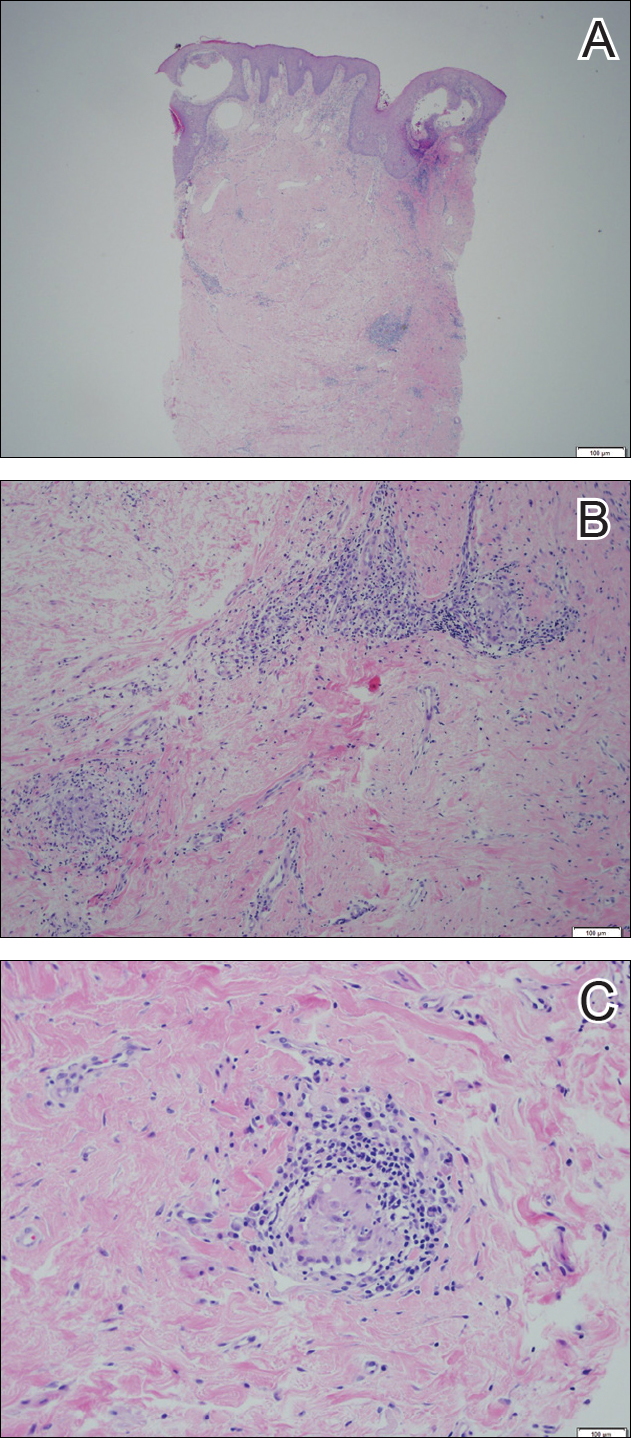
Given the patient’s history, a diagnosis of vulvoperineal MCD was rendered. The patient was started on oral metronidazole 250 mg 3 times daily with topical fluocinonide and tacrolimus. She responded well to this treatment regimen and was referred back to the gastroenterologist for management of the intestinal disease.
Comment
Crohn disease is an idiopathic chronic inflammatory condition that primarily affects the gastrointestinal tract, anywhere from the mouth to the anus. It is characterized by transmural inflammation and fissures that can extend beyond the muscularis propria.4,6 Extraintestinal manifestations are common.3
Cutaneous CD often presents as perianal, perifistular, or peristomal inflammation or ulceration.7 Other skin manifestations include pyoderma gangrenosum, erythema nodosum, erythema multiforme, epidermolysis bullosa acquisita, and palmar erythema.7 Metastatic CD involves skin noncontiguous with the gastrointestinal tract1-20 and may involve any portion of the cutis. Although rare, MCD is the typical etiology underlying vulvar CD.8
Approximately 20% of MCD patients have cutaneous lesions without a history of gastrointestinal disease. More than half of cases in adults and approximately two-thirds in children involve the genitalia. Although more common in adults, vulvar involvement has been reported in children as young as 6 years of age.2 Diagnosis is especially challenging when bowel symptoms are absent; those patients should be evaluated and followed for subsequent intestinal involvement.6
Clinically, symptoms may include general discomfort, pain, pruritus, and dyspareunia. Psychosocial and sexual dysfunction are prevalent and also should be addressed.9 Depending on the stage of the disease, physical examination may reveal erythema, edema, papules, pustules, nodules, condylomatous lesions, abscesses, fissures, fistulas, ulceration, acrochordons, and scarring.2-6,10,11
A host of infections (ie, mycobacterial, actinomycosis, deep fungal, sexually transmitted, schistosomiasis), inflammatory conditions (ie, sarcoid, hidradenitis suppurativa), foreign body reactions, Melkersson-Rosenthal syndrome, and sexual abuse should be included in the differential diagnosis.2,6,10-12 Once infection, sarcoid, and foreign body reaction have been ruled out, noncaseating granulomas in skin are highly suggestive of CD.7
Histopathologic findings of MCD reveal myriad morphological reaction patterns,5,13 including high-grade dysplasia and carcinoma of the vulva; therefore, it may be imprudent to withhold diagnosis based on the absence of the historically pathognomonic noncaseating granulomas.5
The etiopathogenesis of MCD remains an enigma. Dermatopathologic examinations consistently reveal a vascular injury syndrome,13 implicating a possible circulatory system contribution via deposition of immune complexes or antigens in skin.7 Bacterial infection has been implicated in the intestinal manifestations of CD; however, failure to detect microbial ribosomal RNA in MCD biopsies refutes theories of hematogenous spread of microbes.13 Another plausible explanation is that antibodies are formed to conserved microbial epitopes following loss of tolerance to gut flora, which results in an excessive immunologic response at distinct sites in susceptible individuals.13 A T-lymphocyte–mediated type IV hypersensitivity reaction also has been proposed via cross-reactivity of lymphocytes, with skin antigens precipitating extraintestinal granuloma formation and vascular injury.3 Clearly, further investigation is needed.
Magnetic resonanance imaging can identify the extent and anatomy of intestinal and pelvic disease and can assist in the diagnosis of vulvar CD.10,11,14 For these reasons, some experts propose that imaging should be instituted prior to therapy,12,15,16 especially when direct extension is suspected.17
Treatment is challenging and often involves collaboration among several specialties.12 Many treatment options exist because therapeutic responses vary and genital MCD is frequently recalcitrant to therapy.4 Medical therapy includes antibiotics such as metronidazole, corticosteroids (ie, topical, intralesional, systemic), and immune modulators (eg, azathioprine, 6-mercaptopurine, cyclosporine, methotrexate, mycophenolate mofetil, tumor necrosis factor α inhibitors).2,3,6,10,16,18 Thalidomide has been used for refractory cases.19 These treatments can be used alone or in combination. Patients should be monitored for side effects and informed that many treatment regimens may be required before a sustained response is achieved.4,16,18 Surgery is reserved for the most resistant cases. Extensive radical excision of the involved area is the best approach, as limited local excision often is followed by recurrence.20
Conclusion
Our case highlights that vulvar CD can develop in the setting of well-controlled intestinal disease. Vulvoperineal CD should be considered in the differential diagnosis of chronic vulvar pain, swelling, and pruritus, especially in cases resistant to standard therapies and regardless of whether or not gastrointestinal tract symptoms are present. Physicians must be cognizant that vulvar signs and symptoms may precede, coincide with, or follow the diagnosis of intestinal CD. Increased awareness of this entity may facilitate its early recognition and prompt more timely treatment among women with vulvar disease caused by MCD.
- Parks AG, Morson BC, Pegum JS. Crohn’s disease with cutaneous involvement. Proc R Soc Med. 1965;58:241-242.
- Ploysangam T, Heubi JE, Eisen D, et al. Cutaneous Crohn’s disease in children. J Am Acad Dermatol. 1997;36:697-704.
- Palamaras I, El-Jabbour J, Pietropaolo N, et al. Metastatic Crohn’s disease: a review. J Eur Acad Dermatol Venereol. 2008;22:1033-1043.
- Leu S, Sun PK, Collyer J, et al. Clinical spectrum of vulvar metastatic Crohn’s disease. Dig Dis Sci. 2009;54:1565-1571.
- Foo WC, Papalas JA, Robboy SJ, et al. Vulvar manifestations of Crohn’s disease. Am J Dermatopathol. 2001;33:588-593.
- Urbanek M, Neill SM, McKee PH. Vulval Crohn’s disease: difficulties in diagnosis. Clin Exp Dermatol. 1996;21:211-214.
- Burgdorf W. Cutaneous manifestations of Crohn’s disease. J Am Acad Dermatol. 1981;5:689-695.
- Andreani SM, Ratnasingham K, Dang HH, et al. Crohn’s disease of the vulva. Int J Surg. 2010;8:2-5.
- Feller E, Ribaudo S, Jackson N. Gynecologic aspects of Crohn’s disease. Am Fam Physician. 2001;64:1725-1728.
- Corbett SL, Walsh CM, Spitzer RF, et al. Vulvar inflammation as the only clinical manifestation of Crohn disease in an 8-year-old girl [published online May 10, 2010]. Pediatrics. 2010;125:E1518-E1522.
- Tonolini M, Villa C, Campari A, et al. Common and unusual urogenital Crohn’s disease complications: spectrum of cross-sectional imaging findings. Abdom Imaging. 2013;38:32-41.
- Bhaduri S, Jenkinson S, Lewis F. Vulval Crohn’s disease—a multi-specialty approach. Int J STD AIDS. 2005;16:512-514.
- Crowson AN, Nuovo GJ, Mihm MC Jr, et al. Cutaneous manifestations of Crohn’s disease, its spectrum, and its pathogenesis: intracellular consensus bacterial 16S rRNA is associated with the gastrointestinal but not the cutaneous manifestations of Crohn’s disease. Hum Pathol. 2003;34:1185-1192.
- Pai D, Dillman JR, Mahani MG, et al. MRI of vulvar Crohn disease. Pediatr Radiol. 2011;41:537-541.
- Madnani NA, Desai D, Gandhi N, et al. Isolated Crohn’s disease of the vulva. Indian J Dermatol Venereol Leprol. 2011;77:342-344.
- Makhija S, Trotter M, Wagner E, et al. Refractory Crohn’s disease of the vulva treated with infliximab: a case report. Can J Gastroenterol. 2007;21:835-837.
- Fahmy N, Kalidindi M, Khan R. Direct colo-labial Crohn’s abscess mimicking bartholinitis. Am J Obstret Gynecol. 2010;30:741-742.
- Preston PW, Hudson N, Lewis FM. Treatment of vulval Crohn’s disease with infliximab. Clin Exp Derm. 2006;31:378-380.
- Kolivras A, De Maubeuge J, André J, et al. Thalidomide in refractory vulvar ulcerations associated with Crohn’s disease. Dermatology. 2003;206:381-383.
- Kao MS, Paulson JD, Askin FB. Crohn’s disease of the vulva. Obstet Gynecol. 1975;46:329-333.
The cutaneous manifestations of Crohn disease (CD) are varied, including pyoderma gangrenosum, erythema nodosum, and metastatic CD (MCD). First described by Parks et al,1 MCD is defined as the occurrence of granulomatous lesions at a skin site distant from the gastrointestinal tract.1-20 Metastatic CD presents a diagnostic challenge because it is a rare component in the spectrum of inflammatory bowel disease complications, and many physicians are unaware of its existence. It may precede, coincide with, or develop after the diagnosis of intestinal disease.2-5 Vulvoperineal involvement is particularly problematic because a multitude of other, more likely disease processes are considered first. Typically it is initially diagnosed as a presumed infection prompting reflexive treatment with antivirals, antifungals, and antibiotics. Patients may experience symptoms for years prior to correct diagnosis and institution of proper therapy. A variety of clinical presentations have been described, including nonspecific pain and swelling, erythematous papules and plaques, and nonhealing ulcers. Skin biopsy characteristically confirms the diagnosis and reveals dermal noncaseating granulomas. Multiple oral and parenteral therapies are available, with surgical intervention reserved for resistant cases. We present a case of vulvovaginal MCD in the setting of well-controlled intestinal disease. We also provide a review of the literature regarding genital CD and emphasize the need to keep MCD in the differential of vulvoperineal pathology.
Case Report
A 29-year-old woman was referred to the dermatology clinic with vulvar pain, swelling, and pruritus of 14 months’ duration. Her medical history was remarkable for CD following a colectomy with colostomy. Prior therapies included methotrexate with infliximab for 5 years followed by a 2-year regimen with adalimumab, which induced remission of the intestinal disease.
The patient previously had taken a variety of topical and oral antimicrobials based on treatment from a primary care physician because fungal, bacterial, and viral infections initially were suspected; however, the vulvar disease persisted, and drug-induced immunosuppression was considered to be an underlying factor. Thus, adalimumab was discontinued. Despite elimination of the biologic, the vulvar disease progressed, which prompted referral to the dermatology clinic.
Physical examination revealed diffuse vulvar edema with overlying erythema and scale (Figure 1A). Upon closer inspection, scattered violaceous papules atop a backdrop of lichenification were evident, imparting a cobblestone appearance (Figure 1B). Additionally, a fissure was present on the gluteal cleft. Biopsy from the left labia majora demonstrated well-formed granulomas within a fibrotic reticular dermis (Figures 2A and 2B). The granulomas consisted of both mononucleated and multinucleated histiocytes, rimmed peripherally by lymphocytes and plasma cells (Figure 2C). Periodic acid–Schiff–diastase and acid-fast bacilli stains as well as polarizing microscopy were negative.

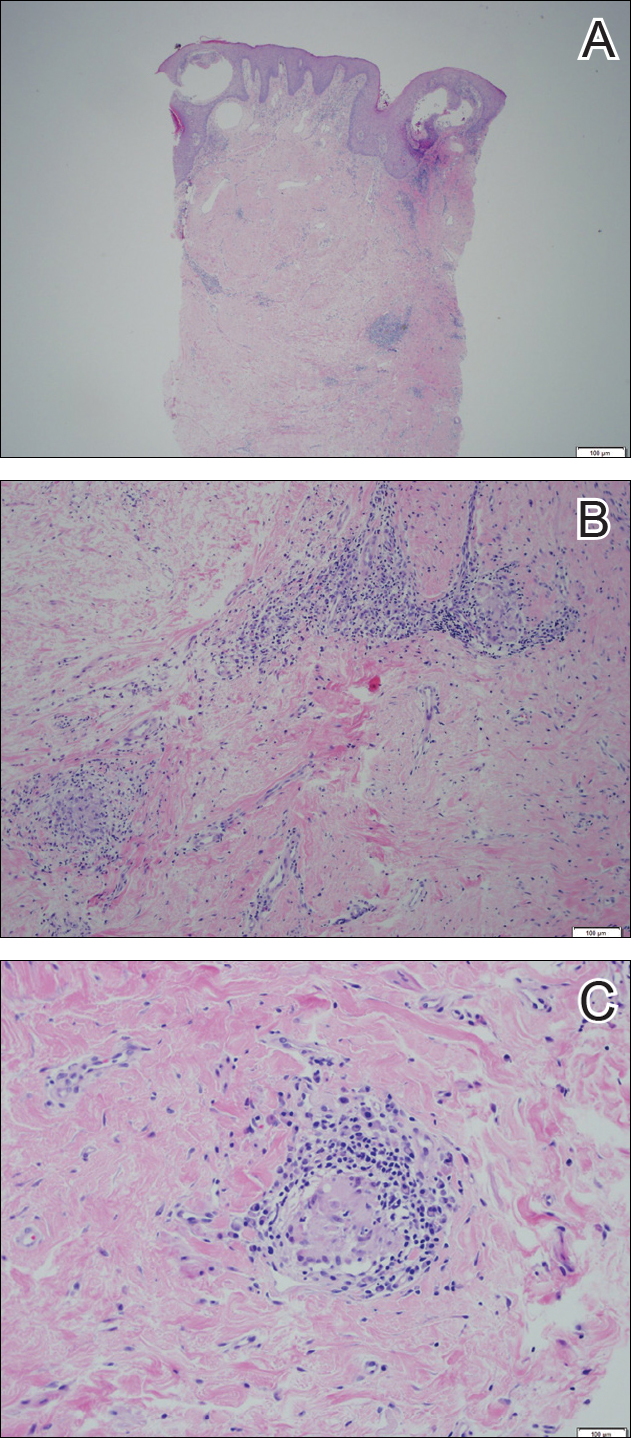
Given the patient’s history, a diagnosis of vulvoperineal MCD was rendered. The patient was started on oral metronidazole 250 mg 3 times daily with topical fluocinonide and tacrolimus. She responded well to this treatment regimen and was referred back to the gastroenterologist for management of the intestinal disease.
Comment
Crohn disease is an idiopathic chronic inflammatory condition that primarily affects the gastrointestinal tract, anywhere from the mouth to the anus. It is characterized by transmural inflammation and fissures that can extend beyond the muscularis propria.4,6 Extraintestinal manifestations are common.3
Cutaneous CD often presents as perianal, perifistular, or peristomal inflammation or ulceration.7 Other skin manifestations include pyoderma gangrenosum, erythema nodosum, erythema multiforme, epidermolysis bullosa acquisita, and palmar erythema.7 Metastatic CD involves skin noncontiguous with the gastrointestinal tract1-20 and may involve any portion of the cutis. Although rare, MCD is the typical etiology underlying vulvar CD.8
Approximately 20% of MCD patients have cutaneous lesions without a history of gastrointestinal disease. More than half of cases in adults and approximately two-thirds in children involve the genitalia. Although more common in adults, vulvar involvement has been reported in children as young as 6 years of age.2 Diagnosis is especially challenging when bowel symptoms are absent; those patients should be evaluated and followed for subsequent intestinal involvement.6
Clinically, symptoms may include general discomfort, pain, pruritus, and dyspareunia. Psychosocial and sexual dysfunction are prevalent and also should be addressed.9 Depending on the stage of the disease, physical examination may reveal erythema, edema, papules, pustules, nodules, condylomatous lesions, abscesses, fissures, fistulas, ulceration, acrochordons, and scarring.2-6,10,11
A host of infections (ie, mycobacterial, actinomycosis, deep fungal, sexually transmitted, schistosomiasis), inflammatory conditions (ie, sarcoid, hidradenitis suppurativa), foreign body reactions, Melkersson-Rosenthal syndrome, and sexual abuse should be included in the differential diagnosis.2,6,10-12 Once infection, sarcoid, and foreign body reaction have been ruled out, noncaseating granulomas in skin are highly suggestive of CD.7
Histopathologic findings of MCD reveal myriad morphological reaction patterns,5,13 including high-grade dysplasia and carcinoma of the vulva; therefore, it may be imprudent to withhold diagnosis based on the absence of the historically pathognomonic noncaseating granulomas.5
The etiopathogenesis of MCD remains an enigma. Dermatopathologic examinations consistently reveal a vascular injury syndrome,13 implicating a possible circulatory system contribution via deposition of immune complexes or antigens in skin.7 Bacterial infection has been implicated in the intestinal manifestations of CD; however, failure to detect microbial ribosomal RNA in MCD biopsies refutes theories of hematogenous spread of microbes.13 Another plausible explanation is that antibodies are formed to conserved microbial epitopes following loss of tolerance to gut flora, which results in an excessive immunologic response at distinct sites in susceptible individuals.13 A T-lymphocyte–mediated type IV hypersensitivity reaction also has been proposed via cross-reactivity of lymphocytes, with skin antigens precipitating extraintestinal granuloma formation and vascular injury.3 Clearly, further investigation is needed.
Magnetic resonanance imaging can identify the extent and anatomy of intestinal and pelvic disease and can assist in the diagnosis of vulvar CD.10,11,14 For these reasons, some experts propose that imaging should be instituted prior to therapy,12,15,16 especially when direct extension is suspected.17
Treatment is challenging and often involves collaboration among several specialties.12 Many treatment options exist because therapeutic responses vary and genital MCD is frequently recalcitrant to therapy.4 Medical therapy includes antibiotics such as metronidazole, corticosteroids (ie, topical, intralesional, systemic), and immune modulators (eg, azathioprine, 6-mercaptopurine, cyclosporine, methotrexate, mycophenolate mofetil, tumor necrosis factor α inhibitors).2,3,6,10,16,18 Thalidomide has been used for refractory cases.19 These treatments can be used alone or in combination. Patients should be monitored for side effects and informed that many treatment regimens may be required before a sustained response is achieved.4,16,18 Surgery is reserved for the most resistant cases. Extensive radical excision of the involved area is the best approach, as limited local excision often is followed by recurrence.20
Conclusion
Our case highlights that vulvar CD can develop in the setting of well-controlled intestinal disease. Vulvoperineal CD should be considered in the differential diagnosis of chronic vulvar pain, swelling, and pruritus, especially in cases resistant to standard therapies and regardless of whether or not gastrointestinal tract symptoms are present. Physicians must be cognizant that vulvar signs and symptoms may precede, coincide with, or follow the diagnosis of intestinal CD. Increased awareness of this entity may facilitate its early recognition and prompt more timely treatment among women with vulvar disease caused by MCD.
The cutaneous manifestations of Crohn disease (CD) are varied, including pyoderma gangrenosum, erythema nodosum, and metastatic CD (MCD). First described by Parks et al,1 MCD is defined as the occurrence of granulomatous lesions at a skin site distant from the gastrointestinal tract.1-20 Metastatic CD presents a diagnostic challenge because it is a rare component in the spectrum of inflammatory bowel disease complications, and many physicians are unaware of its existence. It may precede, coincide with, or develop after the diagnosis of intestinal disease.2-5 Vulvoperineal involvement is particularly problematic because a multitude of other, more likely disease processes are considered first. Typically it is initially diagnosed as a presumed infection prompting reflexive treatment with antivirals, antifungals, and antibiotics. Patients may experience symptoms for years prior to correct diagnosis and institution of proper therapy. A variety of clinical presentations have been described, including nonspecific pain and swelling, erythematous papules and plaques, and nonhealing ulcers. Skin biopsy characteristically confirms the diagnosis and reveals dermal noncaseating granulomas. Multiple oral and parenteral therapies are available, with surgical intervention reserved for resistant cases. We present a case of vulvovaginal MCD in the setting of well-controlled intestinal disease. We also provide a review of the literature regarding genital CD and emphasize the need to keep MCD in the differential of vulvoperineal pathology.
Case Report
A 29-year-old woman was referred to the dermatology clinic with vulvar pain, swelling, and pruritus of 14 months’ duration. Her medical history was remarkable for CD following a colectomy with colostomy. Prior therapies included methotrexate with infliximab for 5 years followed by a 2-year regimen with adalimumab, which induced remission of the intestinal disease.
The patient previously had taken a variety of topical and oral antimicrobials based on treatment from a primary care physician because fungal, bacterial, and viral infections initially were suspected; however, the vulvar disease persisted, and drug-induced immunosuppression was considered to be an underlying factor. Thus, adalimumab was discontinued. Despite elimination of the biologic, the vulvar disease progressed, which prompted referral to the dermatology clinic.
Physical examination revealed diffuse vulvar edema with overlying erythema and scale (Figure 1A). Upon closer inspection, scattered violaceous papules atop a backdrop of lichenification were evident, imparting a cobblestone appearance (Figure 1B). Additionally, a fissure was present on the gluteal cleft. Biopsy from the left labia majora demonstrated well-formed granulomas within a fibrotic reticular dermis (Figures 2A and 2B). The granulomas consisted of both mononucleated and multinucleated histiocytes, rimmed peripherally by lymphocytes and plasma cells (Figure 2C). Periodic acid–Schiff–diastase and acid-fast bacilli stains as well as polarizing microscopy were negative.

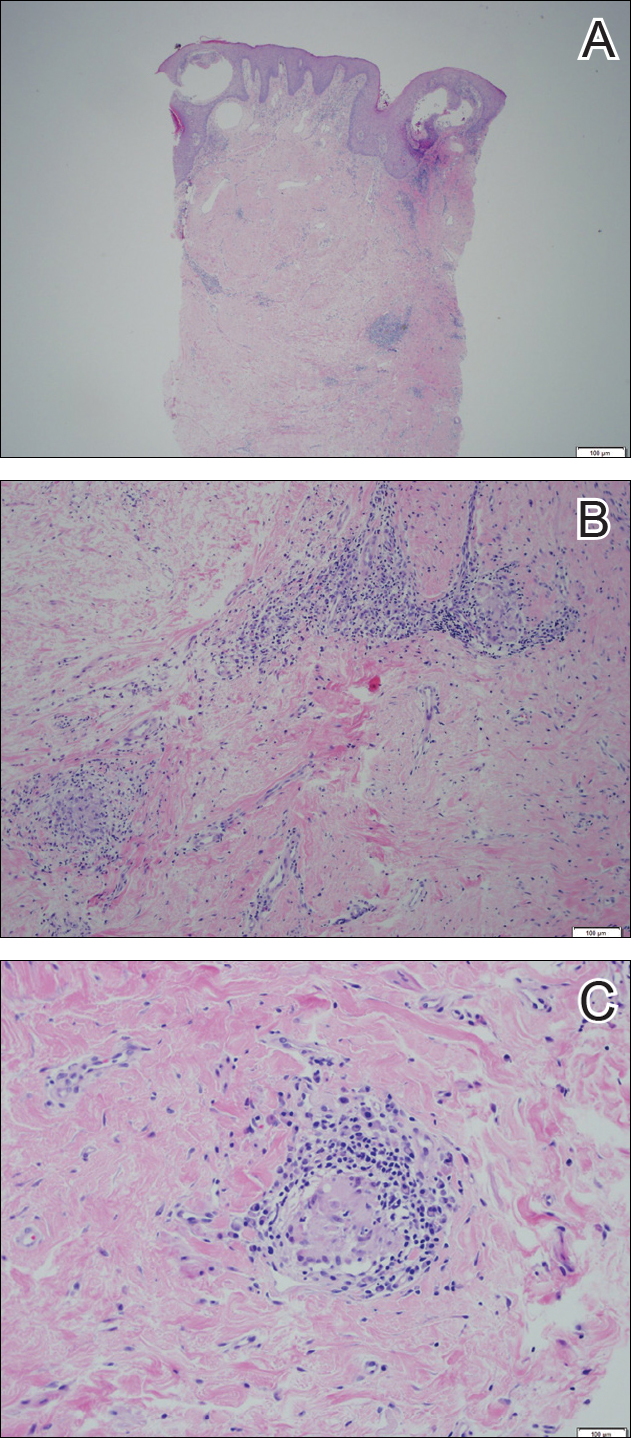
Given the patient’s history, a diagnosis of vulvoperineal MCD was rendered. The patient was started on oral metronidazole 250 mg 3 times daily with topical fluocinonide and tacrolimus. She responded well to this treatment regimen and was referred back to the gastroenterologist for management of the intestinal disease.
Comment
Crohn disease is an idiopathic chronic inflammatory condition that primarily affects the gastrointestinal tract, anywhere from the mouth to the anus. It is characterized by transmural inflammation and fissures that can extend beyond the muscularis propria.4,6 Extraintestinal manifestations are common.3
Cutaneous CD often presents as perianal, perifistular, or peristomal inflammation or ulceration.7 Other skin manifestations include pyoderma gangrenosum, erythema nodosum, erythema multiforme, epidermolysis bullosa acquisita, and palmar erythema.7 Metastatic CD involves skin noncontiguous with the gastrointestinal tract1-20 and may involve any portion of the cutis. Although rare, MCD is the typical etiology underlying vulvar CD.8
Approximately 20% of MCD patients have cutaneous lesions without a history of gastrointestinal disease. More than half of cases in adults and approximately two-thirds in children involve the genitalia. Although more common in adults, vulvar involvement has been reported in children as young as 6 years of age.2 Diagnosis is especially challenging when bowel symptoms are absent; those patients should be evaluated and followed for subsequent intestinal involvement.6
Clinically, symptoms may include general discomfort, pain, pruritus, and dyspareunia. Psychosocial and sexual dysfunction are prevalent and also should be addressed.9 Depending on the stage of the disease, physical examination may reveal erythema, edema, papules, pustules, nodules, condylomatous lesions, abscesses, fissures, fistulas, ulceration, acrochordons, and scarring.2-6,10,11
A host of infections (ie, mycobacterial, actinomycosis, deep fungal, sexually transmitted, schistosomiasis), inflammatory conditions (ie, sarcoid, hidradenitis suppurativa), foreign body reactions, Melkersson-Rosenthal syndrome, and sexual abuse should be included in the differential diagnosis.2,6,10-12 Once infection, sarcoid, and foreign body reaction have been ruled out, noncaseating granulomas in skin are highly suggestive of CD.7
Histopathologic findings of MCD reveal myriad morphological reaction patterns,5,13 including high-grade dysplasia and carcinoma of the vulva; therefore, it may be imprudent to withhold diagnosis based on the absence of the historically pathognomonic noncaseating granulomas.5
The etiopathogenesis of MCD remains an enigma. Dermatopathologic examinations consistently reveal a vascular injury syndrome,13 implicating a possible circulatory system contribution via deposition of immune complexes or antigens in skin.7 Bacterial infection has been implicated in the intestinal manifestations of CD; however, failure to detect microbial ribosomal RNA in MCD biopsies refutes theories of hematogenous spread of microbes.13 Another plausible explanation is that antibodies are formed to conserved microbial epitopes following loss of tolerance to gut flora, which results in an excessive immunologic response at distinct sites in susceptible individuals.13 A T-lymphocyte–mediated type IV hypersensitivity reaction also has been proposed via cross-reactivity of lymphocytes, with skin antigens precipitating extraintestinal granuloma formation and vascular injury.3 Clearly, further investigation is needed.
Magnetic resonanance imaging can identify the extent and anatomy of intestinal and pelvic disease and can assist in the diagnosis of vulvar CD.10,11,14 For these reasons, some experts propose that imaging should be instituted prior to therapy,12,15,16 especially when direct extension is suspected.17
Treatment is challenging and often involves collaboration among several specialties.12 Many treatment options exist because therapeutic responses vary and genital MCD is frequently recalcitrant to therapy.4 Medical therapy includes antibiotics such as metronidazole, corticosteroids (ie, topical, intralesional, systemic), and immune modulators (eg, azathioprine, 6-mercaptopurine, cyclosporine, methotrexate, mycophenolate mofetil, tumor necrosis factor α inhibitors).2,3,6,10,16,18 Thalidomide has been used for refractory cases.19 These treatments can be used alone or in combination. Patients should be monitored for side effects and informed that many treatment regimens may be required before a sustained response is achieved.4,16,18 Surgery is reserved for the most resistant cases. Extensive radical excision of the involved area is the best approach, as limited local excision often is followed by recurrence.20
Conclusion
Our case highlights that vulvar CD can develop in the setting of well-controlled intestinal disease. Vulvoperineal CD should be considered in the differential diagnosis of chronic vulvar pain, swelling, and pruritus, especially in cases resistant to standard therapies and regardless of whether or not gastrointestinal tract symptoms are present. Physicians must be cognizant that vulvar signs and symptoms may precede, coincide with, or follow the diagnosis of intestinal CD. Increased awareness of this entity may facilitate its early recognition and prompt more timely treatment among women with vulvar disease caused by MCD.
- Parks AG, Morson BC, Pegum JS. Crohn’s disease with cutaneous involvement. Proc R Soc Med. 1965;58:241-242.
- Ploysangam T, Heubi JE, Eisen D, et al. Cutaneous Crohn’s disease in children. J Am Acad Dermatol. 1997;36:697-704.
- Palamaras I, El-Jabbour J, Pietropaolo N, et al. Metastatic Crohn’s disease: a review. J Eur Acad Dermatol Venereol. 2008;22:1033-1043.
- Leu S, Sun PK, Collyer J, et al. Clinical spectrum of vulvar metastatic Crohn’s disease. Dig Dis Sci. 2009;54:1565-1571.
- Foo WC, Papalas JA, Robboy SJ, et al. Vulvar manifestations of Crohn’s disease. Am J Dermatopathol. 2001;33:588-593.
- Urbanek M, Neill SM, McKee PH. Vulval Crohn’s disease: difficulties in diagnosis. Clin Exp Dermatol. 1996;21:211-214.
- Burgdorf W. Cutaneous manifestations of Crohn’s disease. J Am Acad Dermatol. 1981;5:689-695.
- Andreani SM, Ratnasingham K, Dang HH, et al. Crohn’s disease of the vulva. Int J Surg. 2010;8:2-5.
- Feller E, Ribaudo S, Jackson N. Gynecologic aspects of Crohn’s disease. Am Fam Physician. 2001;64:1725-1728.
- Corbett SL, Walsh CM, Spitzer RF, et al. Vulvar inflammation as the only clinical manifestation of Crohn disease in an 8-year-old girl [published online May 10, 2010]. Pediatrics. 2010;125:E1518-E1522.
- Tonolini M, Villa C, Campari A, et al. Common and unusual urogenital Crohn’s disease complications: spectrum of cross-sectional imaging findings. Abdom Imaging. 2013;38:32-41.
- Bhaduri S, Jenkinson S, Lewis F. Vulval Crohn’s disease—a multi-specialty approach. Int J STD AIDS. 2005;16:512-514.
- Crowson AN, Nuovo GJ, Mihm MC Jr, et al. Cutaneous manifestations of Crohn’s disease, its spectrum, and its pathogenesis: intracellular consensus bacterial 16S rRNA is associated with the gastrointestinal but not the cutaneous manifestations of Crohn’s disease. Hum Pathol. 2003;34:1185-1192.
- Pai D, Dillman JR, Mahani MG, et al. MRI of vulvar Crohn disease. Pediatr Radiol. 2011;41:537-541.
- Madnani NA, Desai D, Gandhi N, et al. Isolated Crohn’s disease of the vulva. Indian J Dermatol Venereol Leprol. 2011;77:342-344.
- Makhija S, Trotter M, Wagner E, et al. Refractory Crohn’s disease of the vulva treated with infliximab: a case report. Can J Gastroenterol. 2007;21:835-837.
- Fahmy N, Kalidindi M, Khan R. Direct colo-labial Crohn’s abscess mimicking bartholinitis. Am J Obstret Gynecol. 2010;30:741-742.
- Preston PW, Hudson N, Lewis FM. Treatment of vulval Crohn’s disease with infliximab. Clin Exp Derm. 2006;31:378-380.
- Kolivras A, De Maubeuge J, André J, et al. Thalidomide in refractory vulvar ulcerations associated with Crohn’s disease. Dermatology. 2003;206:381-383.
- Kao MS, Paulson JD, Askin FB. Crohn’s disease of the vulva. Obstet Gynecol. 1975;46:329-333.
- Parks AG, Morson BC, Pegum JS. Crohn’s disease with cutaneous involvement. Proc R Soc Med. 1965;58:241-242.
- Ploysangam T, Heubi JE, Eisen D, et al. Cutaneous Crohn’s disease in children. J Am Acad Dermatol. 1997;36:697-704.
- Palamaras I, El-Jabbour J, Pietropaolo N, et al. Metastatic Crohn’s disease: a review. J Eur Acad Dermatol Venereol. 2008;22:1033-1043.
- Leu S, Sun PK, Collyer J, et al. Clinical spectrum of vulvar metastatic Crohn’s disease. Dig Dis Sci. 2009;54:1565-1571.
- Foo WC, Papalas JA, Robboy SJ, et al. Vulvar manifestations of Crohn’s disease. Am J Dermatopathol. 2001;33:588-593.
- Urbanek M, Neill SM, McKee PH. Vulval Crohn’s disease: difficulties in diagnosis. Clin Exp Dermatol. 1996;21:211-214.
- Burgdorf W. Cutaneous manifestations of Crohn’s disease. J Am Acad Dermatol. 1981;5:689-695.
- Andreani SM, Ratnasingham K, Dang HH, et al. Crohn’s disease of the vulva. Int J Surg. 2010;8:2-5.
- Feller E, Ribaudo S, Jackson N. Gynecologic aspects of Crohn’s disease. Am Fam Physician. 2001;64:1725-1728.
- Corbett SL, Walsh CM, Spitzer RF, et al. Vulvar inflammation as the only clinical manifestation of Crohn disease in an 8-year-old girl [published online May 10, 2010]. Pediatrics. 2010;125:E1518-E1522.
- Tonolini M, Villa C, Campari A, et al. Common and unusual urogenital Crohn’s disease complications: spectrum of cross-sectional imaging findings. Abdom Imaging. 2013;38:32-41.
- Bhaduri S, Jenkinson S, Lewis F. Vulval Crohn’s disease—a multi-specialty approach. Int J STD AIDS. 2005;16:512-514.
- Crowson AN, Nuovo GJ, Mihm MC Jr, et al. Cutaneous manifestations of Crohn’s disease, its spectrum, and its pathogenesis: intracellular consensus bacterial 16S rRNA is associated with the gastrointestinal but not the cutaneous manifestations of Crohn’s disease. Hum Pathol. 2003;34:1185-1192.
- Pai D, Dillman JR, Mahani MG, et al. MRI of vulvar Crohn disease. Pediatr Radiol. 2011;41:537-541.
- Madnani NA, Desai D, Gandhi N, et al. Isolated Crohn’s disease of the vulva. Indian J Dermatol Venereol Leprol. 2011;77:342-344.
- Makhija S, Trotter M, Wagner E, et al. Refractory Crohn’s disease of the vulva treated with infliximab: a case report. Can J Gastroenterol. 2007;21:835-837.
- Fahmy N, Kalidindi M, Khan R. Direct colo-labial Crohn’s abscess mimicking bartholinitis. Am J Obstret Gynecol. 2010;30:741-742.
- Preston PW, Hudson N, Lewis FM. Treatment of vulval Crohn’s disease with infliximab. Clin Exp Derm. 2006;31:378-380.
- Kolivras A, De Maubeuge J, André J, et al. Thalidomide in refractory vulvar ulcerations associated with Crohn’s disease. Dermatology. 2003;206:381-383.
- Kao MS, Paulson JD, Askin FB. Crohn’s disease of the vulva. Obstet Gynecol. 1975;46:329-333.