User login
ASCO updates guidance on prophylaxis for adults with cancer-related immunosuppression
Fluoroquinolones are recommended for adults with cancer-related immunosuppression if they are at high risk of infection, according to an updated clinical practice guideline on antimicrobial prophylaxis.
By contrast, patients with solid tumors are not routinely recommended to receive antibiotic prophylaxis, according to the guideline, developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA).
The guideline includes antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions such as hand hygiene that may reduce infection risk.
Released in the Journal of Clinical Oncology, the updated guidelines were developed by an expert panel cochaired by Christopher R. Flowers, MD of Emory University, Atlanta, and Randy A. Taplitz, MD of the University of California, San Diego, Health.
For the most part, the panel endorsed the previous ASCO recommendations, published in 2013. However, the panel considered six new high-quality studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Fluoroquinolones, in the 2013 guideline, were recommended over trimethoprim-sulfamethoxazole because of fewer adverse events leading to treatment discontinuation. Panelists for the new guidelines said they continued to support that recommendation, based on an updated literature review.
That review showed significant reductions in both febrile neutropenia incidence and all-cause mortality, not only for patients at high risk of febrile neutropenia or profound, protracted neutropenia but also for lower-risk patients with solid tumors, they said.
However, the benefits did not sufficiently outweigh the harms to justify recommending fluoroquinolone prophylaxis for all patients with solid tumors or lymphoma, according to the report from the expert panel.
Those harms could include antibiotic-associated adverse effects, emergence of resistance, and Clostridium difficile infections, they said.
Accordingly, they recommended fluoroquinolone prophylaxis for the high-risk patients, including most patients with acute myeloid leukemia/myelodysplastic syndromes (AML/MDS) or those undergoing hematopoietic stem-cell transplantation (HSCT).
Similarly, the panel recommended that high-risk patients should receive antifungal prophylaxis with an oral triazole or parenteral echinocandin, while prophylaxis would not be routinely recommended for solid tumor patients.
By contrast, all patients undergoing chemotherapy for malignancy should receive yearly influenza vaccination with an inactivated quadrivalent vaccine, the panel said in its antiviral prophylaxis recommendations.
Family members, household contacts, and health care providers also should receive influenza vaccinations, said the panel, endorsing recommendations from the Centers for Disease Control and Prevention that were also cited in the 2013 ASCO guidelines.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce risk of pathogen transmission, the panel said, endorsing CDC recommendations cited in the previous guideline.
However, the panel said they recommend against interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks.
“Evidence of clinical benefit is lacking” for those interventions, they said.
Participants in the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.
SOURCE: Taplitz RA et al. J Clin Oncol. 2018 Sept 4. doi: 10.1200/JCO.18.00374.
Fluoroquinolones are recommended for adults with cancer-related immunosuppression if they are at high risk of infection, according to an updated clinical practice guideline on antimicrobial prophylaxis.
By contrast, patients with solid tumors are not routinely recommended to receive antibiotic prophylaxis, according to the guideline, developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA).
The guideline includes antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions such as hand hygiene that may reduce infection risk.
Released in the Journal of Clinical Oncology, the updated guidelines were developed by an expert panel cochaired by Christopher R. Flowers, MD of Emory University, Atlanta, and Randy A. Taplitz, MD of the University of California, San Diego, Health.
For the most part, the panel endorsed the previous ASCO recommendations, published in 2013. However, the panel considered six new high-quality studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Fluoroquinolones, in the 2013 guideline, were recommended over trimethoprim-sulfamethoxazole because of fewer adverse events leading to treatment discontinuation. Panelists for the new guidelines said they continued to support that recommendation, based on an updated literature review.
That review showed significant reductions in both febrile neutropenia incidence and all-cause mortality, not only for patients at high risk of febrile neutropenia or profound, protracted neutropenia but also for lower-risk patients with solid tumors, they said.
However, the benefits did not sufficiently outweigh the harms to justify recommending fluoroquinolone prophylaxis for all patients with solid tumors or lymphoma, according to the report from the expert panel.
Those harms could include antibiotic-associated adverse effects, emergence of resistance, and Clostridium difficile infections, they said.
Accordingly, they recommended fluoroquinolone prophylaxis for the high-risk patients, including most patients with acute myeloid leukemia/myelodysplastic syndromes (AML/MDS) or those undergoing hematopoietic stem-cell transplantation (HSCT).
Similarly, the panel recommended that high-risk patients should receive antifungal prophylaxis with an oral triazole or parenteral echinocandin, while prophylaxis would not be routinely recommended for solid tumor patients.
By contrast, all patients undergoing chemotherapy for malignancy should receive yearly influenza vaccination with an inactivated quadrivalent vaccine, the panel said in its antiviral prophylaxis recommendations.
Family members, household contacts, and health care providers also should receive influenza vaccinations, said the panel, endorsing recommendations from the Centers for Disease Control and Prevention that were also cited in the 2013 ASCO guidelines.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce risk of pathogen transmission, the panel said, endorsing CDC recommendations cited in the previous guideline.
However, the panel said they recommend against interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks.
“Evidence of clinical benefit is lacking” for those interventions, they said.
Participants in the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.
SOURCE: Taplitz RA et al. J Clin Oncol. 2018 Sept 4. doi: 10.1200/JCO.18.00374.
Fluoroquinolones are recommended for adults with cancer-related immunosuppression if they are at high risk of infection, according to an updated clinical practice guideline on antimicrobial prophylaxis.
By contrast, patients with solid tumors are not routinely recommended to receive antibiotic prophylaxis, according to the guideline, developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA).
The guideline includes antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions such as hand hygiene that may reduce infection risk.
Released in the Journal of Clinical Oncology, the updated guidelines were developed by an expert panel cochaired by Christopher R. Flowers, MD of Emory University, Atlanta, and Randy A. Taplitz, MD of the University of California, San Diego, Health.
For the most part, the panel endorsed the previous ASCO recommendations, published in 2013. However, the panel considered six new high-quality studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Fluoroquinolones, in the 2013 guideline, were recommended over trimethoprim-sulfamethoxazole because of fewer adverse events leading to treatment discontinuation. Panelists for the new guidelines said they continued to support that recommendation, based on an updated literature review.
That review showed significant reductions in both febrile neutropenia incidence and all-cause mortality, not only for patients at high risk of febrile neutropenia or profound, protracted neutropenia but also for lower-risk patients with solid tumors, they said.
However, the benefits did not sufficiently outweigh the harms to justify recommending fluoroquinolone prophylaxis for all patients with solid tumors or lymphoma, according to the report from the expert panel.
Those harms could include antibiotic-associated adverse effects, emergence of resistance, and Clostridium difficile infections, they said.
Accordingly, they recommended fluoroquinolone prophylaxis for the high-risk patients, including most patients with acute myeloid leukemia/myelodysplastic syndromes (AML/MDS) or those undergoing hematopoietic stem-cell transplantation (HSCT).
Similarly, the panel recommended that high-risk patients should receive antifungal prophylaxis with an oral triazole or parenteral echinocandin, while prophylaxis would not be routinely recommended for solid tumor patients.
By contrast, all patients undergoing chemotherapy for malignancy should receive yearly influenza vaccination with an inactivated quadrivalent vaccine, the panel said in its antiviral prophylaxis recommendations.
Family members, household contacts, and health care providers also should receive influenza vaccinations, said the panel, endorsing recommendations from the Centers for Disease Control and Prevention that were also cited in the 2013 ASCO guidelines.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce risk of pathogen transmission, the panel said, endorsing CDC recommendations cited in the previous guideline.
However, the panel said they recommend against interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks.
“Evidence of clinical benefit is lacking” for those interventions, they said.
Participants in the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.
SOURCE: Taplitz RA et al. J Clin Oncol. 2018 Sept 4. doi: 10.1200/JCO.18.00374.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
A Three-View Radiographic Approach to Femoroacetabular Impingement
ABSTRACT
Femoroacetabular impingement (FAI) is an abnormality of the hip joint that is increasingly being recognized as a cause of athletic disability and early degenerative hip disease. Despite significant advances in the knowledge of FAI, it remains a frequently unrecognized cause of hip pain in adolescents and young adults among orthopedic providers. The purpose of this article is to present a simple 3-view radiographic approach to young adults with hip pain. The radiographs include a standing anteroposterior view of the pelvis, a cross-table lateral view, and a false profile view. Good quality radiographs showing the common sites of potential impingement combined with a basic understanding of certain radiographic parameters may allow faster diagnosis, eliminate unnecessary studies, and allow earlier referral and management.
Continue to: The prevalence of femoroacetabular impingement...
The prevalence of femoroacetabular impingement (FAI) in the general population is estimated at 23.1%.1 While FAI is often bilateral,2 patients usually present with unilateral symptoms.3 Young, highly active individuals are most commonly affected.3 Despite significant improvement in our understanding of FAI in recent years, it remains a poorly recognized cause of hip pain among orthopedic providers. Clohisy and colleagues3 found that the average time to diagnosis was 3.1 years (range, 3-15 years) and the average number of providers seen before correct diagnosis was 4.2 (range, 1-16) with nearly half those providers being orthopedic specialists. This is likely attributed to limited training and lack of appropriate imaging. Multiple comprehensive radiographic approaches have been described, including plain films, computed tomography, and magnetic resonance imaging.2,4 The objective of this article is to present a simple 3-view plain film approach for young adults with hip pain. While history and physical examination remain key to FAI diagnosis, a basic knowledge of the common sites of impingement with appropriate radiographic views to visualize these sites may help eliminate unnecessary imaging and delayed diagnosis.
STANDING ANTEROPOSTERIOR VIEW OF THE PELVIS
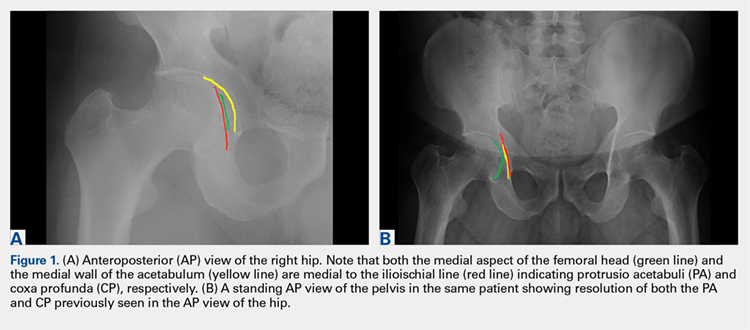
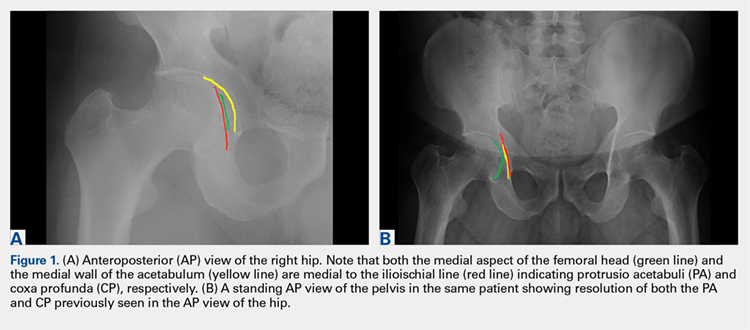
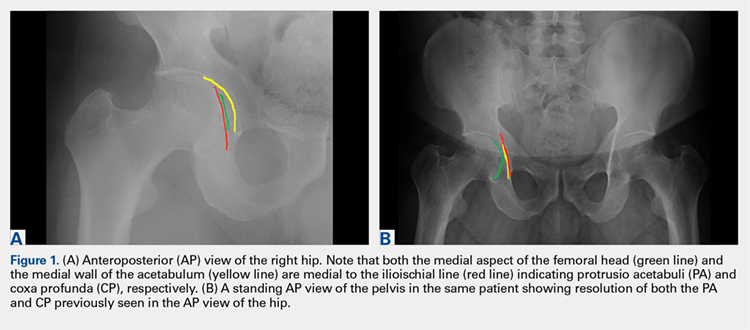
An anteroposterior (AP) view of the pelvis, as opposed to an AP view of the hip, is an important first radiograph in the evaluation of young patients presenting with hip pain. Not only does it permit visualization of the contralateral hip for comparison, but it also allows more accurate measurements of several radiographic parameters (Table). An AP view of the hip often gives the false impression of global over coverage, such as coxa profunda2 and protrusio acetabuli (Figures 1A, 1B), and may overestimate the amount of acetabular anteversion.2
Table. Summary of Common Radiographic Parameters When Assessing Young Adults with Hip Pain2,4
Sign | Best Radiographic View | Measurement | Quoted Normal Valuesa | Clinical Relevance of Abnormal Values |
Acetabular depth | AP pelvis | Medial wall of the acetabulum (MWA) relative to the ilioischial line (IIL) | MWA is lateral to IIL | Global overcoverage (ie, coxa profunda) |
Femoral depth | AP pelvis | Medial surface of the femoral head (MFH) relative to the IIL | MFH is lateral and within 10 mm of the IIL | >10 mm may indicate undercoverage (ie, dysplasia)
MFH medial to IIL may indicate overcoverage (ie, protrusio acetabuli) |
Tonnis angle | AP pelvis | Angle between the weight-bearing surface of the acetabulum and a line parallel to the horizontal axis of the pelvis (eg, inter-teardrop line) | 0°-10° | >10° may indicate undercoverage (ie, dysplasia)
<0° may indicate overcoverage (ie, pincer-type FAI) |
Lateral center edge angle | AP pelvis | Angle between a line perpendicular to the horizontal axis of the pelvis through the center of the femoral head and a line connecting the center of the femoral head to the lateral most edge of the acetabular weight-bearing surface | 25°-40° | >40° may indicate overcoverage (ie, pincer-type FAI)
<25° may indicate undercoverage (ie, dysplasia) |
Crossover sign | AP pelvis | Intersection between the anterior and posterior rims of the acetabulum | Crossover occurs at the lateral most aspect of the acetabular weight-bearing surface | Crossover occurring distal to the lateral most aspect of the acetabular weight-bearing surface may indicate acetabular retroversion |
Femoral neck-shaft angle | AP pelvis | Angle between the femoral shaft and the longitudinal axis of the neck | 135° ± 5° | >140° may indicate coxa valga
<130° may indicate coxa vara |
Alpha angle | Cross-table lateral | Angle between a line connecting the center of the femoral neck to the center of the femoral head and a line connecting the center of the head to a point on the anterolateral aspect of the head-neck junction where the head sphericity ends | >55° | Decreased head-neck offset (ie, cam-type impingement) |
Anterior head-neck offset | Cross-table lateral | Distance between 2 lines parallel to the longitudinal axis of the femoral neck: 1 line tangent to the anterior most aspect of the neck and 1 line tangent to the anterior surface of the femoral head | >10 mm | Decreased head-neck offset (ie, cam-type impingement) |
Anterior head-neck offset ratio | Cross-table lateral | Anterior head-neck offset divided by the diameter of the femoral head | >0.14 | Decreased head-neck offset (ie, cam-type impingement) |
Femoral version | Cross-table lateral | Angle between the longitudinal axis of the femoral neck and the longitudinal axis of the femoral shaft | 15° ± 5° | Developmental disorders (eg, dysplasia, slipped capital femoral epiphysis) |
Anterior center edge angle | False profile view | Angle between a vertical line through the center of the femoral head and a line connecting the center of the femoral head to the anterior most edge of the acetabular weight-bearing surface | >20° | Undercoverage (ie, dysplasia) |
aNormal values are provided for reference only and should not be solely relied on for diagnosis.
Abbreviations: AP, anteroposterior; FAI, femoroacetabular impingement.
A good quality radiograph is important for accurate assessment. The X-ray beam should be perpendicular to the coronal plane of the pelvis. Neutral rotation of the pelvis is a prerequisite and can be confirmed by the presence of symmetric obturator foramina, iliac wings, and coccyx vertically in line with the pubic symphysis. Deviations from this configuration can significantly affect the ability to accurately assess the acetabular version. This is because the rotational profile of the acetabulum is sensitive to pelvic rotation.5,6
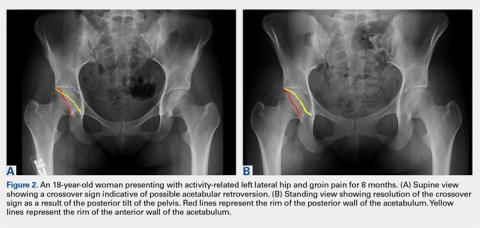
While the AP view of the pelvis can be obtained in either supine or standing positions, the standing position is recommended. A supine view tends to increase the likelihood of finding a crossover sign that often disappears in the standing position (Figures 2A, 2B). This is attributed to the posterior tilt of the pelvis in the sagittal plane with standing, which functionally increases acetabular anteversion, eliminating the crossover sign.5,6 In contrast, a crossover sign that persists in the standing position combined with other abnormal radiographic parameters, such as a negative Tonnis angle and/or increased lateral center edge angle, are concerning for pincer-type FAI (Figures 3A, 3B). An isolated crossover sign may be a normal variant in young asymptomatic patients7 and is not a reliable indicator of acetabular retroversion.5
In addition to assessing the acetabular coverage and version (Figures 1A, 1B, 3A, 3B, and 4A, 4B), the AP view of the pelvis can provide valuable information regarding the proximal femur. One should pay attention to the sphericity of the head (pistol grip cam lesions are most obvious on this view), congruency between the femoral head and the acetabulum, femoral offset, and neck-shaft angle. While we tend to traditionally classify FAI into cam and pincer osseous bumps, alterations in hip dynamics (i.e., coxa vara and coxa breva) can result in functional impingement even in the absence of the osseous bumps.
Continue to: CROSS-TABLE LATERAL...
CROSS-TABLE LATERAL
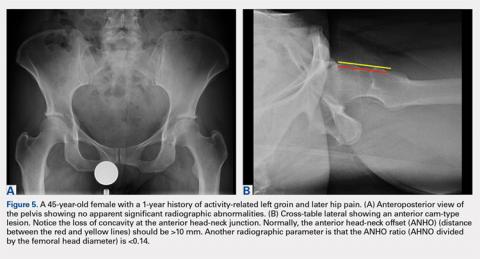
A cross-table lateral of the affected hip is another important radiographic adjunct in the evaluation of hip pain in young patients. This view provides AP axial visualization of the hip joint identifying potential pathologies such as anterior cam lesions that may not be apparent on frog-leg lateral radiographs (Figures 5A, 5B and 6A, 6B). The cross-table lateral view can also show posterior impingement and/or joint space narrowing from countercoup lesions associated with pincer-type FAI (Figures 3A, 3B). In addition, the rotational profile of the proximal femur is best assessed in this view (Figure 4B). The challenge with a cross-table lateral, however, is that it is operator-dependent. In circumstances where a good quality cross-table lateral cannot be obtained, we default to a frog-leg lateral to avoid excess radiation exposure.
FALSE PROFILE VIEW
A false profile view provides a good visualization of the anterosuperior aspect of the acetabulum. It can show anterior acetabular over or under coverage. It may also show sub-spine impingement (Figures 7A, 7B). Sub-spine impingement is characterized by a prominent anterior inferior iliac spine (AIIS) that extends to the level of the anterosuperior acetabular rim. The prominent AIIS can impinge on the femoral head-neck junction during hip flexion. A prominent AIIS has also been shown to give the false impression of a crossover sign.8
CONCLUSION
Even to the trained eye, radiographic findings of FAI can be quite subtle and easily missed. A systematic approach when interpreting plain radiographs is important. Radiographic assessment starts with good quality X-rays with the pelvis in neutral rotation. Because of the young age of most patients, radiation exposure should be minimized. An understanding of the potential sites of impingement and the specific radiographs to visualize these sites minimizes radiation exposure and other unnecessary imaging. In our experience, the 3-view radiographic approach presented combined with supportive history and physical examination findings are highly sensitive to identify cases of FAI. Advanced imaging is reserved for patients who have failed conservative management or considering surgical intervention.
1. Fernquest S, Arnold C, Palmer A, et al. Osseous impingement occurs early in flexion in cam-type femoroacetabular impingement: a 4D CT model. Bone Joint J. 2017;99-B(4 Supple B):41-48. doi:10.1302/0301-620X.99B4.BJJ-2016-1274.R1.
2. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188(6):1540-1552. doi:10.2214/AJR.06.0921.
3. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638-644. doi:10.1007/s11999-008-0680-y.
4. Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90 Suppl 4:47-66. doi:10.2106/JBJS.H.00756.
5. Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91(8):1031-1036. doi:10.1302/0301-620X.91B8.22389.
6. Dandachli W, Kannan V, Richards R, Shah Z, Hall-Craggs M, Witt J. Analysis of cover of the femoral head in normal and dysplastic hips: new CT-based technique. J Bone Joint Surg Br. 2008;90(11):1428-1434. doi:10.1302/0301-620X.90B11.20073.
7. Larson CM, Moreau-Gaudry A, Kelly BT, et al. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473(4):1247-1254. doi:10.1007/s11999-014-4055-2.
8. Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471(8):2463-2470. doi:10.1007/s11999-012-2689-5.
ABSTRACT
Femoroacetabular impingement (FAI) is an abnormality of the hip joint that is increasingly being recognized as a cause of athletic disability and early degenerative hip disease. Despite significant advances in the knowledge of FAI, it remains a frequently unrecognized cause of hip pain in adolescents and young adults among orthopedic providers. The purpose of this article is to present a simple 3-view radiographic approach to young adults with hip pain. The radiographs include a standing anteroposterior view of the pelvis, a cross-table lateral view, and a false profile view. Good quality radiographs showing the common sites of potential impingement combined with a basic understanding of certain radiographic parameters may allow faster diagnosis, eliminate unnecessary studies, and allow earlier referral and management.
Continue to: The prevalence of femoroacetabular impingement...
The prevalence of femoroacetabular impingement (FAI) in the general population is estimated at 23.1%.1 While FAI is often bilateral,2 patients usually present with unilateral symptoms.3 Young, highly active individuals are most commonly affected.3 Despite significant improvement in our understanding of FAI in recent years, it remains a poorly recognized cause of hip pain among orthopedic providers. Clohisy and colleagues3 found that the average time to diagnosis was 3.1 years (range, 3-15 years) and the average number of providers seen before correct diagnosis was 4.2 (range, 1-16) with nearly half those providers being orthopedic specialists. This is likely attributed to limited training and lack of appropriate imaging. Multiple comprehensive radiographic approaches have been described, including plain films, computed tomography, and magnetic resonance imaging.2,4 The objective of this article is to present a simple 3-view plain film approach for young adults with hip pain. While history and physical examination remain key to FAI diagnosis, a basic knowledge of the common sites of impingement with appropriate radiographic views to visualize these sites may help eliminate unnecessary imaging and delayed diagnosis.
STANDING ANTEROPOSTERIOR VIEW OF THE PELVIS
An anteroposterior (AP) view of the pelvis, as opposed to an AP view of the hip, is an important first radiograph in the evaluation of young patients presenting with hip pain. Not only does it permit visualization of the contralateral hip for comparison, but it also allows more accurate measurements of several radiographic parameters (Table). An AP view of the hip often gives the false impression of global over coverage, such as coxa profunda2 and protrusio acetabuli (Figures 1A, 1B), and may overestimate the amount of acetabular anteversion.2
Table. Summary of Common Radiographic Parameters When Assessing Young Adults with Hip Pain2,4
Sign | Best Radiographic View | Measurement | Quoted Normal Valuesa | Clinical Relevance of Abnormal Values |
Acetabular depth | AP pelvis | Medial wall of the acetabulum (MWA) relative to the ilioischial line (IIL) | MWA is lateral to IIL | Global overcoverage (ie, coxa profunda) |
Femoral depth | AP pelvis | Medial surface of the femoral head (MFH) relative to the IIL | MFH is lateral and within 10 mm of the IIL | >10 mm may indicate undercoverage (ie, dysplasia)
MFH medial to IIL may indicate overcoverage (ie, protrusio acetabuli) |
Tonnis angle | AP pelvis | Angle between the weight-bearing surface of the acetabulum and a line parallel to the horizontal axis of the pelvis (eg, inter-teardrop line) | 0°-10° | >10° may indicate undercoverage (ie, dysplasia)
<0° may indicate overcoverage (ie, pincer-type FAI) |
Lateral center edge angle | AP pelvis | Angle between a line perpendicular to the horizontal axis of the pelvis through the center of the femoral head and a line connecting the center of the femoral head to the lateral most edge of the acetabular weight-bearing surface | 25°-40° | >40° may indicate overcoverage (ie, pincer-type FAI)
<25° may indicate undercoverage (ie, dysplasia) |
Crossover sign | AP pelvis | Intersection between the anterior and posterior rims of the acetabulum | Crossover occurs at the lateral most aspect of the acetabular weight-bearing surface | Crossover occurring distal to the lateral most aspect of the acetabular weight-bearing surface may indicate acetabular retroversion |
Femoral neck-shaft angle | AP pelvis | Angle between the femoral shaft and the longitudinal axis of the neck | 135° ± 5° | >140° may indicate coxa valga
<130° may indicate coxa vara |
Alpha angle | Cross-table lateral | Angle between a line connecting the center of the femoral neck to the center of the femoral head and a line connecting the center of the head to a point on the anterolateral aspect of the head-neck junction where the head sphericity ends | >55° | Decreased head-neck offset (ie, cam-type impingement) |
Anterior head-neck offset | Cross-table lateral | Distance between 2 lines parallel to the longitudinal axis of the femoral neck: 1 line tangent to the anterior most aspect of the neck and 1 line tangent to the anterior surface of the femoral head | >10 mm | Decreased head-neck offset (ie, cam-type impingement) |
Anterior head-neck offset ratio | Cross-table lateral | Anterior head-neck offset divided by the diameter of the femoral head | >0.14 | Decreased head-neck offset (ie, cam-type impingement) |
Femoral version | Cross-table lateral | Angle between the longitudinal axis of the femoral neck and the longitudinal axis of the femoral shaft | 15° ± 5° | Developmental disorders (eg, dysplasia, slipped capital femoral epiphysis) |
Anterior center edge angle | False profile view | Angle between a vertical line through the center of the femoral head and a line connecting the center of the femoral head to the anterior most edge of the acetabular weight-bearing surface | >20° | Undercoverage (ie, dysplasia) |
aNormal values are provided for reference only and should not be solely relied on for diagnosis.
Abbreviations: AP, anteroposterior; FAI, femoroacetabular impingement.
A good quality radiograph is important for accurate assessment. The X-ray beam should be perpendicular to the coronal plane of the pelvis. Neutral rotation of the pelvis is a prerequisite and can be confirmed by the presence of symmetric obturator foramina, iliac wings, and coccyx vertically in line with the pubic symphysis. Deviations from this configuration can significantly affect the ability to accurately assess the acetabular version. This is because the rotational profile of the acetabulum is sensitive to pelvic rotation.5,6
While the AP view of the pelvis can be obtained in either supine or standing positions, the standing position is recommended. A supine view tends to increase the likelihood of finding a crossover sign that often disappears in the standing position (Figures 2A, 2B). This is attributed to the posterior tilt of the pelvis in the sagittal plane with standing, which functionally increases acetabular anteversion, eliminating the crossover sign.5,6 In contrast, a crossover sign that persists in the standing position combined with other abnormal radiographic parameters, such as a negative Tonnis angle and/or increased lateral center edge angle, are concerning for pincer-type FAI (Figures 3A, 3B). An isolated crossover sign may be a normal variant in young asymptomatic patients7 and is not a reliable indicator of acetabular retroversion.5
In addition to assessing the acetabular coverage and version (Figures 1A, 1B, 3A, 3B, and 4A, 4B), the AP view of the pelvis can provide valuable information regarding the proximal femur. One should pay attention to the sphericity of the head (pistol grip cam lesions are most obvious on this view), congruency between the femoral head and the acetabulum, femoral offset, and neck-shaft angle. While we tend to traditionally classify FAI into cam and pincer osseous bumps, alterations in hip dynamics (i.e., coxa vara and coxa breva) can result in functional impingement even in the absence of the osseous bumps.
Continue to: CROSS-TABLE LATERAL...
CROSS-TABLE LATERAL
A cross-table lateral of the affected hip is another important radiographic adjunct in the evaluation of hip pain in young patients. This view provides AP axial visualization of the hip joint identifying potential pathologies such as anterior cam lesions that may not be apparent on frog-leg lateral radiographs (Figures 5A, 5B and 6A, 6B). The cross-table lateral view can also show posterior impingement and/or joint space narrowing from countercoup lesions associated with pincer-type FAI (Figures 3A, 3B). In addition, the rotational profile of the proximal femur is best assessed in this view (Figure 4B). The challenge with a cross-table lateral, however, is that it is operator-dependent. In circumstances where a good quality cross-table lateral cannot be obtained, we default to a frog-leg lateral to avoid excess radiation exposure.
FALSE PROFILE VIEW
A false profile view provides a good visualization of the anterosuperior aspect of the acetabulum. It can show anterior acetabular over or under coverage. It may also show sub-spine impingement (Figures 7A, 7B). Sub-spine impingement is characterized by a prominent anterior inferior iliac spine (AIIS) that extends to the level of the anterosuperior acetabular rim. The prominent AIIS can impinge on the femoral head-neck junction during hip flexion. A prominent AIIS has also been shown to give the false impression of a crossover sign.8
CONCLUSION
Even to the trained eye, radiographic findings of FAI can be quite subtle and easily missed. A systematic approach when interpreting plain radiographs is important. Radiographic assessment starts with good quality X-rays with the pelvis in neutral rotation. Because of the young age of most patients, radiation exposure should be minimized. An understanding of the potential sites of impingement and the specific radiographs to visualize these sites minimizes radiation exposure and other unnecessary imaging. In our experience, the 3-view radiographic approach presented combined with supportive history and physical examination findings are highly sensitive to identify cases of FAI. Advanced imaging is reserved for patients who have failed conservative management or considering surgical intervention.
ABSTRACT
Femoroacetabular impingement (FAI) is an abnormality of the hip joint that is increasingly being recognized as a cause of athletic disability and early degenerative hip disease. Despite significant advances in the knowledge of FAI, it remains a frequently unrecognized cause of hip pain in adolescents and young adults among orthopedic providers. The purpose of this article is to present a simple 3-view radiographic approach to young adults with hip pain. The radiographs include a standing anteroposterior view of the pelvis, a cross-table lateral view, and a false profile view. Good quality radiographs showing the common sites of potential impingement combined with a basic understanding of certain radiographic parameters may allow faster diagnosis, eliminate unnecessary studies, and allow earlier referral and management.
Continue to: The prevalence of femoroacetabular impingement...
The prevalence of femoroacetabular impingement (FAI) in the general population is estimated at 23.1%.1 While FAI is often bilateral,2 patients usually present with unilateral symptoms.3 Young, highly active individuals are most commonly affected.3 Despite significant improvement in our understanding of FAI in recent years, it remains a poorly recognized cause of hip pain among orthopedic providers. Clohisy and colleagues3 found that the average time to diagnosis was 3.1 years (range, 3-15 years) and the average number of providers seen before correct diagnosis was 4.2 (range, 1-16) with nearly half those providers being orthopedic specialists. This is likely attributed to limited training and lack of appropriate imaging. Multiple comprehensive radiographic approaches have been described, including plain films, computed tomography, and magnetic resonance imaging.2,4 The objective of this article is to present a simple 3-view plain film approach for young adults with hip pain. While history and physical examination remain key to FAI diagnosis, a basic knowledge of the common sites of impingement with appropriate radiographic views to visualize these sites may help eliminate unnecessary imaging and delayed diagnosis.
STANDING ANTEROPOSTERIOR VIEW OF THE PELVIS
An anteroposterior (AP) view of the pelvis, as opposed to an AP view of the hip, is an important first radiograph in the evaluation of young patients presenting with hip pain. Not only does it permit visualization of the contralateral hip for comparison, but it also allows more accurate measurements of several radiographic parameters (Table). An AP view of the hip often gives the false impression of global over coverage, such as coxa profunda2 and protrusio acetabuli (Figures 1A, 1B), and may overestimate the amount of acetabular anteversion.2
Table. Summary of Common Radiographic Parameters When Assessing Young Adults with Hip Pain2,4
Sign | Best Radiographic View | Measurement | Quoted Normal Valuesa | Clinical Relevance of Abnormal Values |
Acetabular depth | AP pelvis | Medial wall of the acetabulum (MWA) relative to the ilioischial line (IIL) | MWA is lateral to IIL | Global overcoverage (ie, coxa profunda) |
Femoral depth | AP pelvis | Medial surface of the femoral head (MFH) relative to the IIL | MFH is lateral and within 10 mm of the IIL | >10 mm may indicate undercoverage (ie, dysplasia)
MFH medial to IIL may indicate overcoverage (ie, protrusio acetabuli) |
Tonnis angle | AP pelvis | Angle between the weight-bearing surface of the acetabulum and a line parallel to the horizontal axis of the pelvis (eg, inter-teardrop line) | 0°-10° | >10° may indicate undercoverage (ie, dysplasia)
<0° may indicate overcoverage (ie, pincer-type FAI) |
Lateral center edge angle | AP pelvis | Angle between a line perpendicular to the horizontal axis of the pelvis through the center of the femoral head and a line connecting the center of the femoral head to the lateral most edge of the acetabular weight-bearing surface | 25°-40° | >40° may indicate overcoverage (ie, pincer-type FAI)
<25° may indicate undercoverage (ie, dysplasia) |
Crossover sign | AP pelvis | Intersection between the anterior and posterior rims of the acetabulum | Crossover occurs at the lateral most aspect of the acetabular weight-bearing surface | Crossover occurring distal to the lateral most aspect of the acetabular weight-bearing surface may indicate acetabular retroversion |
Femoral neck-shaft angle | AP pelvis | Angle between the femoral shaft and the longitudinal axis of the neck | 135° ± 5° | >140° may indicate coxa valga
<130° may indicate coxa vara |
Alpha angle | Cross-table lateral | Angle between a line connecting the center of the femoral neck to the center of the femoral head and a line connecting the center of the head to a point on the anterolateral aspect of the head-neck junction where the head sphericity ends | >55° | Decreased head-neck offset (ie, cam-type impingement) |
Anterior head-neck offset | Cross-table lateral | Distance between 2 lines parallel to the longitudinal axis of the femoral neck: 1 line tangent to the anterior most aspect of the neck and 1 line tangent to the anterior surface of the femoral head | >10 mm | Decreased head-neck offset (ie, cam-type impingement) |
Anterior head-neck offset ratio | Cross-table lateral | Anterior head-neck offset divided by the diameter of the femoral head | >0.14 | Decreased head-neck offset (ie, cam-type impingement) |
Femoral version | Cross-table lateral | Angle between the longitudinal axis of the femoral neck and the longitudinal axis of the femoral shaft | 15° ± 5° | Developmental disorders (eg, dysplasia, slipped capital femoral epiphysis) |
Anterior center edge angle | False profile view | Angle between a vertical line through the center of the femoral head and a line connecting the center of the femoral head to the anterior most edge of the acetabular weight-bearing surface | >20° | Undercoverage (ie, dysplasia) |
aNormal values are provided for reference only and should not be solely relied on for diagnosis.
Abbreviations: AP, anteroposterior; FAI, femoroacetabular impingement.
A good quality radiograph is important for accurate assessment. The X-ray beam should be perpendicular to the coronal plane of the pelvis. Neutral rotation of the pelvis is a prerequisite and can be confirmed by the presence of symmetric obturator foramina, iliac wings, and coccyx vertically in line with the pubic symphysis. Deviations from this configuration can significantly affect the ability to accurately assess the acetabular version. This is because the rotational profile of the acetabulum is sensitive to pelvic rotation.5,6
While the AP view of the pelvis can be obtained in either supine or standing positions, the standing position is recommended. A supine view tends to increase the likelihood of finding a crossover sign that often disappears in the standing position (Figures 2A, 2B). This is attributed to the posterior tilt of the pelvis in the sagittal plane with standing, which functionally increases acetabular anteversion, eliminating the crossover sign.5,6 In contrast, a crossover sign that persists in the standing position combined with other abnormal radiographic parameters, such as a negative Tonnis angle and/or increased lateral center edge angle, are concerning for pincer-type FAI (Figures 3A, 3B). An isolated crossover sign may be a normal variant in young asymptomatic patients7 and is not a reliable indicator of acetabular retroversion.5
In addition to assessing the acetabular coverage and version (Figures 1A, 1B, 3A, 3B, and 4A, 4B), the AP view of the pelvis can provide valuable information regarding the proximal femur. One should pay attention to the sphericity of the head (pistol grip cam lesions are most obvious on this view), congruency between the femoral head and the acetabulum, femoral offset, and neck-shaft angle. While we tend to traditionally classify FAI into cam and pincer osseous bumps, alterations in hip dynamics (i.e., coxa vara and coxa breva) can result in functional impingement even in the absence of the osseous bumps.
Continue to: CROSS-TABLE LATERAL...
CROSS-TABLE LATERAL
A cross-table lateral of the affected hip is another important radiographic adjunct in the evaluation of hip pain in young patients. This view provides AP axial visualization of the hip joint identifying potential pathologies such as anterior cam lesions that may not be apparent on frog-leg lateral radiographs (Figures 5A, 5B and 6A, 6B). The cross-table lateral view can also show posterior impingement and/or joint space narrowing from countercoup lesions associated with pincer-type FAI (Figures 3A, 3B). In addition, the rotational profile of the proximal femur is best assessed in this view (Figure 4B). The challenge with a cross-table lateral, however, is that it is operator-dependent. In circumstances where a good quality cross-table lateral cannot be obtained, we default to a frog-leg lateral to avoid excess radiation exposure.
FALSE PROFILE VIEW
A false profile view provides a good visualization of the anterosuperior aspect of the acetabulum. It can show anterior acetabular over or under coverage. It may also show sub-spine impingement (Figures 7A, 7B). Sub-spine impingement is characterized by a prominent anterior inferior iliac spine (AIIS) that extends to the level of the anterosuperior acetabular rim. The prominent AIIS can impinge on the femoral head-neck junction during hip flexion. A prominent AIIS has also been shown to give the false impression of a crossover sign.8
CONCLUSION
Even to the trained eye, radiographic findings of FAI can be quite subtle and easily missed. A systematic approach when interpreting plain radiographs is important. Radiographic assessment starts with good quality X-rays with the pelvis in neutral rotation. Because of the young age of most patients, radiation exposure should be minimized. An understanding of the potential sites of impingement and the specific radiographs to visualize these sites minimizes radiation exposure and other unnecessary imaging. In our experience, the 3-view radiographic approach presented combined with supportive history and physical examination findings are highly sensitive to identify cases of FAI. Advanced imaging is reserved for patients who have failed conservative management or considering surgical intervention.
1. Fernquest S, Arnold C, Palmer A, et al. Osseous impingement occurs early in flexion in cam-type femoroacetabular impingement: a 4D CT model. Bone Joint J. 2017;99-B(4 Supple B):41-48. doi:10.1302/0301-620X.99B4.BJJ-2016-1274.R1.
2. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188(6):1540-1552. doi:10.2214/AJR.06.0921.
3. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638-644. doi:10.1007/s11999-008-0680-y.
4. Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90 Suppl 4:47-66. doi:10.2106/JBJS.H.00756.
5. Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91(8):1031-1036. doi:10.1302/0301-620X.91B8.22389.
6. Dandachli W, Kannan V, Richards R, Shah Z, Hall-Craggs M, Witt J. Analysis of cover of the femoral head in normal and dysplastic hips: new CT-based technique. J Bone Joint Surg Br. 2008;90(11):1428-1434. doi:10.1302/0301-620X.90B11.20073.
7. Larson CM, Moreau-Gaudry A, Kelly BT, et al. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473(4):1247-1254. doi:10.1007/s11999-014-4055-2.
8. Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471(8):2463-2470. doi:10.1007/s11999-012-2689-5.
1. Fernquest S, Arnold C, Palmer A, et al. Osseous impingement occurs early in flexion in cam-type femoroacetabular impingement: a 4D CT model. Bone Joint J. 2017;99-B(4 Supple B):41-48. doi:10.1302/0301-620X.99B4.BJJ-2016-1274.R1.
2. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188(6):1540-1552. doi:10.2214/AJR.06.0921.
3. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638-644. doi:10.1007/s11999-008-0680-y.
4. Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90 Suppl 4:47-66. doi:10.2106/JBJS.H.00756.
5. Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91(8):1031-1036. doi:10.1302/0301-620X.91B8.22389.
6. Dandachli W, Kannan V, Richards R, Shah Z, Hall-Craggs M, Witt J. Analysis of cover of the femoral head in normal and dysplastic hips: new CT-based technique. J Bone Joint Surg Br. 2008;90(11):1428-1434. doi:10.1302/0301-620X.90B11.20073.
7. Larson CM, Moreau-Gaudry A, Kelly BT, et al. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473(4):1247-1254. doi:10.1007/s11999-014-4055-2.
8. Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471(8):2463-2470. doi:10.1007/s11999-012-2689-5.
TAKE-HOME POINTS
- FAI is a frequently unrecognized cause of hip pain in adolescents and young adults.
- Understanding the potential sites of impingement and the specific radiographs to visualize these sites can help avoid unnecessary imaging and delayed diagnosis.
- A simple radiographic approach consisting of a standing AP view of the pelvis, a cross-table lateral view, and a false profile view is often a sufficient screening tool.
- While we tend to classify FAI into cam and pincer osseous bumps, alterations in hip dynamics can result in functional impingement even in the absence of the osseous bumps.
- Advanced imaging is reserved for patients who have failed conservative management or are considering surgical intervention.
Novartis nabs first CAR T approval in Canada
the first chimeric antigen receptor (CAR) T-cell therapy to receive regulatory approval in Canada.
Tisagenlecleucel is approved to treat patients aged 3-25 years who have B-cell acute lymphoblastic leukemia (ALL) and relapsed after allogenic stem cell transplant (SCT) or are otherwise ineligible for SCT, have experienced second or later relapse, or have refractory disease.
Tisagenlecleucel is also approved in Canada to treat adults who have received two or more lines of systemic therapy and have relapsed or refractory diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high-grade B-cell lymphoma, or DLBCL arising from follicular lymphoma.
Novartis, the company marketing tisagenlecleucel, said it is working with qualified treatment centers in Canada to prepare for the delivery of tisagenlecleucel. Certification and training are underway at these centers and Novartis is enhancing manufacturing capacity to meet patient needs.
Tisagenlecleucel has been studied in a pair of phase 2 trials – JULIET and ELIANA.
JULIET enrolled 165 adults with relapsed/refractory DLBCL, 111 of whom received a single infusion of tisagenlecleucel.
The overall response rate was 52% and the complete response (CR) rate was 40%. The median duration of response was not reached with a median follow-up of 13.9 months. At last follow-up, none of the responders had gone on to SCT.
The 12-month overall survival (OS) rate was 49%; the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome.
These results were presented at the 2018 annual congress of the European Hematology Association in June.
The ELIANA trial included 75 children and young adults with relapsed/refractory ALL. All patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The overall remission rate was 81%, with 60% of patients achieving a CR and 21% achieving CR with incomplete hematologic recovery. All patients whose best response was CR with incomplete hematologic recovery were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to SCT while in remission. At last follow-up, four were still in remission, and four had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
About 95% of patients had adverse events thought to be related to tisagenlecleucel. The incidence of treatment-related grade 3/4 adverse eventss was 73% (N Engl J Med 2018; 378:439-48).
the first chimeric antigen receptor (CAR) T-cell therapy to receive regulatory approval in Canada.
Tisagenlecleucel is approved to treat patients aged 3-25 years who have B-cell acute lymphoblastic leukemia (ALL) and relapsed after allogenic stem cell transplant (SCT) or are otherwise ineligible for SCT, have experienced second or later relapse, or have refractory disease.
Tisagenlecleucel is also approved in Canada to treat adults who have received two or more lines of systemic therapy and have relapsed or refractory diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high-grade B-cell lymphoma, or DLBCL arising from follicular lymphoma.
Novartis, the company marketing tisagenlecleucel, said it is working with qualified treatment centers in Canada to prepare for the delivery of tisagenlecleucel. Certification and training are underway at these centers and Novartis is enhancing manufacturing capacity to meet patient needs.
Tisagenlecleucel has been studied in a pair of phase 2 trials – JULIET and ELIANA.
JULIET enrolled 165 adults with relapsed/refractory DLBCL, 111 of whom received a single infusion of tisagenlecleucel.
The overall response rate was 52% and the complete response (CR) rate was 40%. The median duration of response was not reached with a median follow-up of 13.9 months. At last follow-up, none of the responders had gone on to SCT.
The 12-month overall survival (OS) rate was 49%; the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome.
These results were presented at the 2018 annual congress of the European Hematology Association in June.
The ELIANA trial included 75 children and young adults with relapsed/refractory ALL. All patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The overall remission rate was 81%, with 60% of patients achieving a CR and 21% achieving CR with incomplete hematologic recovery. All patients whose best response was CR with incomplete hematologic recovery were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to SCT while in remission. At last follow-up, four were still in remission, and four had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
About 95% of patients had adverse events thought to be related to tisagenlecleucel. The incidence of treatment-related grade 3/4 adverse eventss was 73% (N Engl J Med 2018; 378:439-48).
the first chimeric antigen receptor (CAR) T-cell therapy to receive regulatory approval in Canada.
Tisagenlecleucel is approved to treat patients aged 3-25 years who have B-cell acute lymphoblastic leukemia (ALL) and relapsed after allogenic stem cell transplant (SCT) or are otherwise ineligible for SCT, have experienced second or later relapse, or have refractory disease.
Tisagenlecleucel is also approved in Canada to treat adults who have received two or more lines of systemic therapy and have relapsed or refractory diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high-grade B-cell lymphoma, or DLBCL arising from follicular lymphoma.
Novartis, the company marketing tisagenlecleucel, said it is working with qualified treatment centers in Canada to prepare for the delivery of tisagenlecleucel. Certification and training are underway at these centers and Novartis is enhancing manufacturing capacity to meet patient needs.
Tisagenlecleucel has been studied in a pair of phase 2 trials – JULIET and ELIANA.
JULIET enrolled 165 adults with relapsed/refractory DLBCL, 111 of whom received a single infusion of tisagenlecleucel.
The overall response rate was 52% and the complete response (CR) rate was 40%. The median duration of response was not reached with a median follow-up of 13.9 months. At last follow-up, none of the responders had gone on to SCT.
The 12-month overall survival (OS) rate was 49%; the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome.
These results were presented at the 2018 annual congress of the European Hematology Association in June.
The ELIANA trial included 75 children and young adults with relapsed/refractory ALL. All patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The overall remission rate was 81%, with 60% of patients achieving a CR and 21% achieving CR with incomplete hematologic recovery. All patients whose best response was CR with incomplete hematologic recovery were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to SCT while in remission. At last follow-up, four were still in remission, and four had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
About 95% of patients had adverse events thought to be related to tisagenlecleucel. The incidence of treatment-related grade 3/4 adverse eventss was 73% (N Engl J Med 2018; 378:439-48).
CDC releases guidelines for pediatric mTBI
and should base management and prognostication on clinical decision-making tools and symptom rating scales, according to new practice guidelines issued by a working group of the Centers for Disease Control and Prevention (JAMA Pediatrics. 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2853.
The guidelines were released simultaneously with a systematic review, conducted by the same authors, of the existing literature regarding pediatric mTBI (JAMA Pediatrics 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2847). As the evaluators sorted through the literature to find high-quality studies for this population, the funnel rapidly narrowed: From an initial pool of over 15,000 studies conducted between 1990 and 2015, findings from just 75 studies were eventually included in the systematic review.
The review’s findings formed the basis for the guidelines and allowed Angela Lumba-Brown, MD, a pediatric emergency medicine physician at Stanford (Calif.) University, and her coauthors to ascribe a level of confidence in the inference from study data for a given recommendation. Recommendations also are categorized by strength and accordingly indicate that clinicians “should” or “may” follow them. Exceptions are carved out for practices, such as the use of hypertonic 3% saline solution for acute headache in the ED, that should not be used outside research settings.
In the end, the guidelines cover 19 main topics, sorted into guidance regarding the diagnosis, prognosis, and management and treatment of mTBI in children.
Diagnosis
The recommendations regarding mTBI diagnosis center around determining which children are at risk for significant intracranial injury (ICI). The guidelines recommend, with moderate confidence, that clinicians usually should not obtain a head CT for children with mTBI. Validated clinical decision rules should be used for risk stratification to determine which children can safely avoid imaging and which children should be considered for head CT, wrote Dr. Lumba-Brown and her coauthors. Magnetic resonance imaging is not recommended for initial evaluation of mTBI, nor should skull radiographs be ordered in the absence of clinical suspicion for skull fracture.
From the systematic review, Dr. Lumba-Brown and her colleagues found that several risk factors taken together may mean that significant ICI is more likely. These include patient age younger than 2 years; any vomiting, loss of consciousness, or amnesia; a severe mechanism of injury, severe or worsening headache, or nonfrontal scalp hematoma; a Glasgow Coma Scale (GCS) score of less than 15; and clinical suspicion for skull fracture. Clinicians should give consideration to the risks of ionizing radiation to the head, and balance this against their assessment of risk for severe – and perhaps actionable – injury.
A validated symptom rating scale, used in an age-appropriate way, should be used as part of the evaluation of children with mTBI. For children aged 6 and older, the Graded Symptom Checklist is an appropriate tool within 2 days after injury, while the Post Concussion Symptom Scale as part of computerized neurocognitive testing can differentiate which high school athletes have mTBI when used within 4 days of injury, according to the guidelines, which also identify other validated symptom rating scales.
The guidelines authors recommend, with high confidence, that serum biomarkers should not be used outside of research settings in the diagnosis of mTBI in children at present.
Prognosis
Families should be counseled that symptoms mostly resolve within 1-3 months for up to 80% of children with mTBI, but families also should know that “each child’s recovery from mTBI is unique and will follow its own trajectory,” wrote Dr. Lumba-Brown and her coauthors, in a moderate-strength recommendation.
Some factors have been associated with slower recovery from mTBI, and either upon evaluation for mTBI or in routine sports examinations, families should be told about this potential if risk factors are present, said the guidelines, although the evidence supporting the associations is of “varying strength,” wrote Dr. Lumba-Brown and her coauthors. Children with previous mTBIs and those with a history of premorbid neurologic and psychiatric problems, learning problems, or family and social stress all may have delayed recovery. For children with ICI, lower cognitive ability also is associated with delayed recovery.
Demographic factors such as lower socioeconomic status and being of Hispanic ethnicity also may increase the risk for delayed mTBI recovery. Older children and adolescents may recover more slowly. Those with more severe initial presentation and more symptoms in the immediate post-mTBI phase also may have a slower recovery course, said Dr. Lumba-Brown and her coauthors.
A validated prediction rule can be used in the ED to gather information about these discrete risk factors to guide family counseling, according to the guidelines, which note that research has found that “an empirically derived set of risk factors predicted the risk of persistent post-concussion symptoms at 28 days” for children seen in the ED with mTBI.
During the recovery phase, a combination of tools should be used to track recovery from mTBI; these can include validated symptom scales, validated cognitive testing, reaction time measures, and, in adolescent athletes, balance testing. Using a combination of tools is a valuable strategy, the researchers wrote. “No single assessment tool is strongly predictive of outcome in children with mTBI,” they noted.
When prognosis is poor, or recovery is not proceeding as expected, clinicians should have a low threshold for initiating other interventions and referrals.
Management and treatment
Although the guideline authors acknowledged significant knowledge gaps in all areas of pediatric mTBI diagnosis and management, evidence is especially scant for best practices for treatment, rest, and return to play and school after a child sustains mTBI, said Dr. Lumba-Brown and her coauthors.
However, families should be given information about warning signs for serious head injury and how to monitor symptoms, as well as information about mTBI and the expected recovery course. Other forward-looking instructions should cover the importance of preventing new head injuries, managing the gradual return to normal cognitive and physical activities, and clear instructions regarding return to school and recreational activities. The guideline authors made a strong recommendation to provide this information, with high confidence in the data.
However, little strong evidence points the way to a clear set of criteria for when children are ready for school, play, and athletic participation. These decisions must be customized to the individual child, and decision making, particularly about return to school and academic activities, should be a collaborative affair, with schools, clinicians, and families all communicating to make sure the pace of return to normal life is keeping pace with the child’s recovery. “Because postconcussive symptoms resolve at different rates in different children after mTBI, individualization of return-to-school programming is necessary,” wrote Dr. Lumba-Brown and her coauthors.
The guideline authors cite evidence that “suggests that early rest (within the first 3 days) may be beneficial but that inactivity beyond this period for most children may worsen their self-reported symptoms.”
Psychosocial support may be beneficial for certain children, wrote the researchers, drawing on evidence showing that such support is beneficial in frank TBI, and is probably beneficial in mTBI.
Active rehabilitation as tolerated is recommended after an initial period of rest, with exertion kept to a level that does not exacerbate symptoms. Children should not participate in contact activities until symptoms are fully resolved.
A posttraumatic headache that is severe or worsens in the ED should prompt consideration of emergent neuroimaging, according to the guidelines. In the postacute phase, however, children can have nonopioid analgesia, although parents should know about such risks as rebound headache. When chronic headache follows a mTBI, the guidelines recommend that clinicians refer patients for a multidisciplinary evaluation that can assess the many factors – including analgesic overuse – that can be contributors.
Drawing on the larger body of adult TBI research, the authors recommend that insufficient or disordered sleep be addressed, because “the maintenance of appropriate sleep and the management of disrupted sleep may be a critical target of treatment for the child with mTBI.”
Children who suffer a mTBI may experience cognitive dysfunction as a direct result of injury to the brain or secondary to the effects of other symptoms such as sleep disruptions, headache pain, fatigue, or low tolerance of frustration. Clinicians may want to perform or refer their patients for a neuropsychological evaluation to determine what is causing the cognitive dysfunction, the authors said.
Dr. Lumba-Brown and her coauthors, who formed the CDC’s Pediatric Mild Traumatic Brain Injury Guideline Workgroup, also recommended that clinicians use the term “mild traumatic brain injury” to describe head injuries that cause confusion or disorientation, without loss of consciousness, or loss of consciousness of up to 30 minutes or less, or posttraumatic amnesia of less than 24 hours duration, and that are associated with a GCS of 13-15 by 30 minutes after injury or at the time of initial medical assessment. This practice, they said, may reduce the risk of misinterpretation by medical professionals and the public that can occur when the terms “mTBI,” “concussion,” and “minor head injury” all may refer to the same injury.
The CDC has developed a suite of materials to assist both health care providers and the public in guideline implementation. The agency also is using its HEADS UP campaign to publicize the guidelines and related materials, and plans ongoing evaluation of the guidelines and implementation materials.
Many study authors, including Dr. Lumba-Brown, had relationships with medical device or pharmaceutical companies. The systematic review and guideline development were funded by the CDC.
A growing realization that mTBI can have persistent and significant deleterious effects has informed medical and public attitudes toward concussion in children, which now results in almost 1 million annual ED visits.
Progress at the laboratory bench has elucidated much of the neurometabolic cascade that occurs with the insult of mTBI, and has allowed researchers to document the path of brain healing after injury. Neuroimaging now can go beyond static images to trace neural networks and detect previously unseen and subtle functional deficits engendered by mTBI.
In particular, 21st century magnetic resonance imaging (MRI) has shown increased sensitivity over CT alone. In the TRACK-TBI study, over one in four patients whose CTs were read as normal had MRI findings consistent with trauma-induced pathology. Both multimodal MRI and serum biomarkers show promise, although more research regarding their utility is needed, particularly in the case of proteomic biomarkers.
Still, high-quality studies of pediatric mTBI are scant, and translation of burgeoning research into clinical practice is severely impeded by the numerous knowledge gaps that exist in the field.
Dr. Lumba-Brown and her colleagues have synthesized research that supports a neurobiopsychosocial model of mTBI in children that comes into play most prominently in the postacute phase, when non–injury-related factors such as demographics, socioeconomic status, and premorbid psychological conditions are strong mediators of the recovery trajectory.
With children as with adults, scant research guides the path forward for treatment and recovery from mTBI. For children, clinicians are still grappling with issues surrounding return to full participation in the academic and recreational activities of the school environment.
Data from two currently active studies should help light the way forward, however. The TRACK-TBI study, funded by the National Institutes of Health, will include almost 200 children among its 2,700 enrollees who have sustained all levels of TBI.
The Concussion Assessment, Research, and Education (CARE) Consortium is funded jointly by the National College Athletic Association and the Department of Defense. Between student athletes and military cadets, over 40,000 individuals are now part of the study.
The two studies’ testing modalities and methodologies align, offering the opportunity for a powerful pooled analysis that includes civilians, athletes, and those in the military.
Until then, these guidelines provide a way forward to an individualized approach to the best care for a child with mTBI.
Michael McCrea, PhD, is professor of neurology and neurosurgery, and director of brain injury research at the Medical College of Wisconsin, Milwaukee. Geoff Manley, MD, PhD, is professor of neurologic surgery at the University of California, San Francisco. Neither author reported conflicts of interest. These remarks were drawn from an editorial accompanying the guidelines and systematic review (JAMA Pediatrics. 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2846).
A growing realization that mTBI can have persistent and significant deleterious effects has informed medical and public attitudes toward concussion in children, which now results in almost 1 million annual ED visits.
Progress at the laboratory bench has elucidated much of the neurometabolic cascade that occurs with the insult of mTBI, and has allowed researchers to document the path of brain healing after injury. Neuroimaging now can go beyond static images to trace neural networks and detect previously unseen and subtle functional deficits engendered by mTBI.
In particular, 21st century magnetic resonance imaging (MRI) has shown increased sensitivity over CT alone. In the TRACK-TBI study, over one in four patients whose CTs were read as normal had MRI findings consistent with trauma-induced pathology. Both multimodal MRI and serum biomarkers show promise, although more research regarding their utility is needed, particularly in the case of proteomic biomarkers.
Still, high-quality studies of pediatric mTBI are scant, and translation of burgeoning research into clinical practice is severely impeded by the numerous knowledge gaps that exist in the field.
Dr. Lumba-Brown and her colleagues have synthesized research that supports a neurobiopsychosocial model of mTBI in children that comes into play most prominently in the postacute phase, when non–injury-related factors such as demographics, socioeconomic status, and premorbid psychological conditions are strong mediators of the recovery trajectory.
With children as with adults, scant research guides the path forward for treatment and recovery from mTBI. For children, clinicians are still grappling with issues surrounding return to full participation in the academic and recreational activities of the school environment.
Data from two currently active studies should help light the way forward, however. The TRACK-TBI study, funded by the National Institutes of Health, will include almost 200 children among its 2,700 enrollees who have sustained all levels of TBI.
The Concussion Assessment, Research, and Education (CARE) Consortium is funded jointly by the National College Athletic Association and the Department of Defense. Between student athletes and military cadets, over 40,000 individuals are now part of the study.
The two studies’ testing modalities and methodologies align, offering the opportunity for a powerful pooled analysis that includes civilians, athletes, and those in the military.
Until then, these guidelines provide a way forward to an individualized approach to the best care for a child with mTBI.
Michael McCrea, PhD, is professor of neurology and neurosurgery, and director of brain injury research at the Medical College of Wisconsin, Milwaukee. Geoff Manley, MD, PhD, is professor of neurologic surgery at the University of California, San Francisco. Neither author reported conflicts of interest. These remarks were drawn from an editorial accompanying the guidelines and systematic review (JAMA Pediatrics. 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2846).
A growing realization that mTBI can have persistent and significant deleterious effects has informed medical and public attitudes toward concussion in children, which now results in almost 1 million annual ED visits.
Progress at the laboratory bench has elucidated much of the neurometabolic cascade that occurs with the insult of mTBI, and has allowed researchers to document the path of brain healing after injury. Neuroimaging now can go beyond static images to trace neural networks and detect previously unseen and subtle functional deficits engendered by mTBI.
In particular, 21st century magnetic resonance imaging (MRI) has shown increased sensitivity over CT alone. In the TRACK-TBI study, over one in four patients whose CTs were read as normal had MRI findings consistent with trauma-induced pathology. Both multimodal MRI and serum biomarkers show promise, although more research regarding their utility is needed, particularly in the case of proteomic biomarkers.
Still, high-quality studies of pediatric mTBI are scant, and translation of burgeoning research into clinical practice is severely impeded by the numerous knowledge gaps that exist in the field.
Dr. Lumba-Brown and her colleagues have synthesized research that supports a neurobiopsychosocial model of mTBI in children that comes into play most prominently in the postacute phase, when non–injury-related factors such as demographics, socioeconomic status, and premorbid psychological conditions are strong mediators of the recovery trajectory.
With children as with adults, scant research guides the path forward for treatment and recovery from mTBI. For children, clinicians are still grappling with issues surrounding return to full participation in the academic and recreational activities of the school environment.
Data from two currently active studies should help light the way forward, however. The TRACK-TBI study, funded by the National Institutes of Health, will include almost 200 children among its 2,700 enrollees who have sustained all levels of TBI.
The Concussion Assessment, Research, and Education (CARE) Consortium is funded jointly by the National College Athletic Association and the Department of Defense. Between student athletes and military cadets, over 40,000 individuals are now part of the study.
The two studies’ testing modalities and methodologies align, offering the opportunity for a powerful pooled analysis that includes civilians, athletes, and those in the military.
Until then, these guidelines provide a way forward to an individualized approach to the best care for a child with mTBI.
Michael McCrea, PhD, is professor of neurology and neurosurgery, and director of brain injury research at the Medical College of Wisconsin, Milwaukee. Geoff Manley, MD, PhD, is professor of neurologic surgery at the University of California, San Francisco. Neither author reported conflicts of interest. These remarks were drawn from an editorial accompanying the guidelines and systematic review (JAMA Pediatrics. 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2846).
and should base management and prognostication on clinical decision-making tools and symptom rating scales, according to new practice guidelines issued by a working group of the Centers for Disease Control and Prevention (JAMA Pediatrics. 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2853.
The guidelines were released simultaneously with a systematic review, conducted by the same authors, of the existing literature regarding pediatric mTBI (JAMA Pediatrics 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2847). As the evaluators sorted through the literature to find high-quality studies for this population, the funnel rapidly narrowed: From an initial pool of over 15,000 studies conducted between 1990 and 2015, findings from just 75 studies were eventually included in the systematic review.
The review’s findings formed the basis for the guidelines and allowed Angela Lumba-Brown, MD, a pediatric emergency medicine physician at Stanford (Calif.) University, and her coauthors to ascribe a level of confidence in the inference from study data for a given recommendation. Recommendations also are categorized by strength and accordingly indicate that clinicians “should” or “may” follow them. Exceptions are carved out for practices, such as the use of hypertonic 3% saline solution for acute headache in the ED, that should not be used outside research settings.
In the end, the guidelines cover 19 main topics, sorted into guidance regarding the diagnosis, prognosis, and management and treatment of mTBI in children.
Diagnosis
The recommendations regarding mTBI diagnosis center around determining which children are at risk for significant intracranial injury (ICI). The guidelines recommend, with moderate confidence, that clinicians usually should not obtain a head CT for children with mTBI. Validated clinical decision rules should be used for risk stratification to determine which children can safely avoid imaging and which children should be considered for head CT, wrote Dr. Lumba-Brown and her coauthors. Magnetic resonance imaging is not recommended for initial evaluation of mTBI, nor should skull radiographs be ordered in the absence of clinical suspicion for skull fracture.
From the systematic review, Dr. Lumba-Brown and her colleagues found that several risk factors taken together may mean that significant ICI is more likely. These include patient age younger than 2 years; any vomiting, loss of consciousness, or amnesia; a severe mechanism of injury, severe or worsening headache, or nonfrontal scalp hematoma; a Glasgow Coma Scale (GCS) score of less than 15; and clinical suspicion for skull fracture. Clinicians should give consideration to the risks of ionizing radiation to the head, and balance this against their assessment of risk for severe – and perhaps actionable – injury.
A validated symptom rating scale, used in an age-appropriate way, should be used as part of the evaluation of children with mTBI. For children aged 6 and older, the Graded Symptom Checklist is an appropriate tool within 2 days after injury, while the Post Concussion Symptom Scale as part of computerized neurocognitive testing can differentiate which high school athletes have mTBI when used within 4 days of injury, according to the guidelines, which also identify other validated symptom rating scales.
The guidelines authors recommend, with high confidence, that serum biomarkers should not be used outside of research settings in the diagnosis of mTBI in children at present.
Prognosis
Families should be counseled that symptoms mostly resolve within 1-3 months for up to 80% of children with mTBI, but families also should know that “each child’s recovery from mTBI is unique and will follow its own trajectory,” wrote Dr. Lumba-Brown and her coauthors, in a moderate-strength recommendation.
Some factors have been associated with slower recovery from mTBI, and either upon evaluation for mTBI or in routine sports examinations, families should be told about this potential if risk factors are present, said the guidelines, although the evidence supporting the associations is of “varying strength,” wrote Dr. Lumba-Brown and her coauthors. Children with previous mTBIs and those with a history of premorbid neurologic and psychiatric problems, learning problems, or family and social stress all may have delayed recovery. For children with ICI, lower cognitive ability also is associated with delayed recovery.
Demographic factors such as lower socioeconomic status and being of Hispanic ethnicity also may increase the risk for delayed mTBI recovery. Older children and adolescents may recover more slowly. Those with more severe initial presentation and more symptoms in the immediate post-mTBI phase also may have a slower recovery course, said Dr. Lumba-Brown and her coauthors.
A validated prediction rule can be used in the ED to gather information about these discrete risk factors to guide family counseling, according to the guidelines, which note that research has found that “an empirically derived set of risk factors predicted the risk of persistent post-concussion symptoms at 28 days” for children seen in the ED with mTBI.
During the recovery phase, a combination of tools should be used to track recovery from mTBI; these can include validated symptom scales, validated cognitive testing, reaction time measures, and, in adolescent athletes, balance testing. Using a combination of tools is a valuable strategy, the researchers wrote. “No single assessment tool is strongly predictive of outcome in children with mTBI,” they noted.
When prognosis is poor, or recovery is not proceeding as expected, clinicians should have a low threshold for initiating other interventions and referrals.
Management and treatment
Although the guideline authors acknowledged significant knowledge gaps in all areas of pediatric mTBI diagnosis and management, evidence is especially scant for best practices for treatment, rest, and return to play and school after a child sustains mTBI, said Dr. Lumba-Brown and her coauthors.
However, families should be given information about warning signs for serious head injury and how to monitor symptoms, as well as information about mTBI and the expected recovery course. Other forward-looking instructions should cover the importance of preventing new head injuries, managing the gradual return to normal cognitive and physical activities, and clear instructions regarding return to school and recreational activities. The guideline authors made a strong recommendation to provide this information, with high confidence in the data.
However, little strong evidence points the way to a clear set of criteria for when children are ready for school, play, and athletic participation. These decisions must be customized to the individual child, and decision making, particularly about return to school and academic activities, should be a collaborative affair, with schools, clinicians, and families all communicating to make sure the pace of return to normal life is keeping pace with the child’s recovery. “Because postconcussive symptoms resolve at different rates in different children after mTBI, individualization of return-to-school programming is necessary,” wrote Dr. Lumba-Brown and her coauthors.
The guideline authors cite evidence that “suggests that early rest (within the first 3 days) may be beneficial but that inactivity beyond this period for most children may worsen their self-reported symptoms.”
Psychosocial support may be beneficial for certain children, wrote the researchers, drawing on evidence showing that such support is beneficial in frank TBI, and is probably beneficial in mTBI.
Active rehabilitation as tolerated is recommended after an initial period of rest, with exertion kept to a level that does not exacerbate symptoms. Children should not participate in contact activities until symptoms are fully resolved.
A posttraumatic headache that is severe or worsens in the ED should prompt consideration of emergent neuroimaging, according to the guidelines. In the postacute phase, however, children can have nonopioid analgesia, although parents should know about such risks as rebound headache. When chronic headache follows a mTBI, the guidelines recommend that clinicians refer patients for a multidisciplinary evaluation that can assess the many factors – including analgesic overuse – that can be contributors.
Drawing on the larger body of adult TBI research, the authors recommend that insufficient or disordered sleep be addressed, because “the maintenance of appropriate sleep and the management of disrupted sleep may be a critical target of treatment for the child with mTBI.”
Children who suffer a mTBI may experience cognitive dysfunction as a direct result of injury to the brain or secondary to the effects of other symptoms such as sleep disruptions, headache pain, fatigue, or low tolerance of frustration. Clinicians may want to perform or refer their patients for a neuropsychological evaluation to determine what is causing the cognitive dysfunction, the authors said.
Dr. Lumba-Brown and her coauthors, who formed the CDC’s Pediatric Mild Traumatic Brain Injury Guideline Workgroup, also recommended that clinicians use the term “mild traumatic brain injury” to describe head injuries that cause confusion or disorientation, without loss of consciousness, or loss of consciousness of up to 30 minutes or less, or posttraumatic amnesia of less than 24 hours duration, and that are associated with a GCS of 13-15 by 30 minutes after injury or at the time of initial medical assessment. This practice, they said, may reduce the risk of misinterpretation by medical professionals and the public that can occur when the terms “mTBI,” “concussion,” and “minor head injury” all may refer to the same injury.
The CDC has developed a suite of materials to assist both health care providers and the public in guideline implementation. The agency also is using its HEADS UP campaign to publicize the guidelines and related materials, and plans ongoing evaluation of the guidelines and implementation materials.
Many study authors, including Dr. Lumba-Brown, had relationships with medical device or pharmaceutical companies. The systematic review and guideline development were funded by the CDC.
and should base management and prognostication on clinical decision-making tools and symptom rating scales, according to new practice guidelines issued by a working group of the Centers for Disease Control and Prevention (JAMA Pediatrics. 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2853.
The guidelines were released simultaneously with a systematic review, conducted by the same authors, of the existing literature regarding pediatric mTBI (JAMA Pediatrics 2018 Sep 4. doi: 10.1001/jamapediatrics.2018.2847). As the evaluators sorted through the literature to find high-quality studies for this population, the funnel rapidly narrowed: From an initial pool of over 15,000 studies conducted between 1990 and 2015, findings from just 75 studies were eventually included in the systematic review.
The review’s findings formed the basis for the guidelines and allowed Angela Lumba-Brown, MD, a pediatric emergency medicine physician at Stanford (Calif.) University, and her coauthors to ascribe a level of confidence in the inference from study data for a given recommendation. Recommendations also are categorized by strength and accordingly indicate that clinicians “should” or “may” follow them. Exceptions are carved out for practices, such as the use of hypertonic 3% saline solution for acute headache in the ED, that should not be used outside research settings.
In the end, the guidelines cover 19 main topics, sorted into guidance regarding the diagnosis, prognosis, and management and treatment of mTBI in children.
Diagnosis
The recommendations regarding mTBI diagnosis center around determining which children are at risk for significant intracranial injury (ICI). The guidelines recommend, with moderate confidence, that clinicians usually should not obtain a head CT for children with mTBI. Validated clinical decision rules should be used for risk stratification to determine which children can safely avoid imaging and which children should be considered for head CT, wrote Dr. Lumba-Brown and her coauthors. Magnetic resonance imaging is not recommended for initial evaluation of mTBI, nor should skull radiographs be ordered in the absence of clinical suspicion for skull fracture.
From the systematic review, Dr. Lumba-Brown and her colleagues found that several risk factors taken together may mean that significant ICI is more likely. These include patient age younger than 2 years; any vomiting, loss of consciousness, or amnesia; a severe mechanism of injury, severe or worsening headache, or nonfrontal scalp hematoma; a Glasgow Coma Scale (GCS) score of less than 15; and clinical suspicion for skull fracture. Clinicians should give consideration to the risks of ionizing radiation to the head, and balance this against their assessment of risk for severe – and perhaps actionable – injury.
A validated symptom rating scale, used in an age-appropriate way, should be used as part of the evaluation of children with mTBI. For children aged 6 and older, the Graded Symptom Checklist is an appropriate tool within 2 days after injury, while the Post Concussion Symptom Scale as part of computerized neurocognitive testing can differentiate which high school athletes have mTBI when used within 4 days of injury, according to the guidelines, which also identify other validated symptom rating scales.
The guidelines authors recommend, with high confidence, that serum biomarkers should not be used outside of research settings in the diagnosis of mTBI in children at present.
Prognosis
Families should be counseled that symptoms mostly resolve within 1-3 months for up to 80% of children with mTBI, but families also should know that “each child’s recovery from mTBI is unique and will follow its own trajectory,” wrote Dr. Lumba-Brown and her coauthors, in a moderate-strength recommendation.
Some factors have been associated with slower recovery from mTBI, and either upon evaluation for mTBI or in routine sports examinations, families should be told about this potential if risk factors are present, said the guidelines, although the evidence supporting the associations is of “varying strength,” wrote Dr. Lumba-Brown and her coauthors. Children with previous mTBIs and those with a history of premorbid neurologic and psychiatric problems, learning problems, or family and social stress all may have delayed recovery. For children with ICI, lower cognitive ability also is associated with delayed recovery.
Demographic factors such as lower socioeconomic status and being of Hispanic ethnicity also may increase the risk for delayed mTBI recovery. Older children and adolescents may recover more slowly. Those with more severe initial presentation and more symptoms in the immediate post-mTBI phase also may have a slower recovery course, said Dr. Lumba-Brown and her coauthors.
A validated prediction rule can be used in the ED to gather information about these discrete risk factors to guide family counseling, according to the guidelines, which note that research has found that “an empirically derived set of risk factors predicted the risk of persistent post-concussion symptoms at 28 days” for children seen in the ED with mTBI.
During the recovery phase, a combination of tools should be used to track recovery from mTBI; these can include validated symptom scales, validated cognitive testing, reaction time measures, and, in adolescent athletes, balance testing. Using a combination of tools is a valuable strategy, the researchers wrote. “No single assessment tool is strongly predictive of outcome in children with mTBI,” they noted.
When prognosis is poor, or recovery is not proceeding as expected, clinicians should have a low threshold for initiating other interventions and referrals.
Management and treatment
Although the guideline authors acknowledged significant knowledge gaps in all areas of pediatric mTBI diagnosis and management, evidence is especially scant for best practices for treatment, rest, and return to play and school after a child sustains mTBI, said Dr. Lumba-Brown and her coauthors.
However, families should be given information about warning signs for serious head injury and how to monitor symptoms, as well as information about mTBI and the expected recovery course. Other forward-looking instructions should cover the importance of preventing new head injuries, managing the gradual return to normal cognitive and physical activities, and clear instructions regarding return to school and recreational activities. The guideline authors made a strong recommendation to provide this information, with high confidence in the data.
However, little strong evidence points the way to a clear set of criteria for when children are ready for school, play, and athletic participation. These decisions must be customized to the individual child, and decision making, particularly about return to school and academic activities, should be a collaborative affair, with schools, clinicians, and families all communicating to make sure the pace of return to normal life is keeping pace with the child’s recovery. “Because postconcussive symptoms resolve at different rates in different children after mTBI, individualization of return-to-school programming is necessary,” wrote Dr. Lumba-Brown and her coauthors.
The guideline authors cite evidence that “suggests that early rest (within the first 3 days) may be beneficial but that inactivity beyond this period for most children may worsen their self-reported symptoms.”
Psychosocial support may be beneficial for certain children, wrote the researchers, drawing on evidence showing that such support is beneficial in frank TBI, and is probably beneficial in mTBI.
Active rehabilitation as tolerated is recommended after an initial period of rest, with exertion kept to a level that does not exacerbate symptoms. Children should not participate in contact activities until symptoms are fully resolved.
A posttraumatic headache that is severe or worsens in the ED should prompt consideration of emergent neuroimaging, according to the guidelines. In the postacute phase, however, children can have nonopioid analgesia, although parents should know about such risks as rebound headache. When chronic headache follows a mTBI, the guidelines recommend that clinicians refer patients for a multidisciplinary evaluation that can assess the many factors – including analgesic overuse – that can be contributors.
Drawing on the larger body of adult TBI research, the authors recommend that insufficient or disordered sleep be addressed, because “the maintenance of appropriate sleep and the management of disrupted sleep may be a critical target of treatment for the child with mTBI.”
Children who suffer a mTBI may experience cognitive dysfunction as a direct result of injury to the brain or secondary to the effects of other symptoms such as sleep disruptions, headache pain, fatigue, or low tolerance of frustration. Clinicians may want to perform or refer their patients for a neuropsychological evaluation to determine what is causing the cognitive dysfunction, the authors said.
Dr. Lumba-Brown and her coauthors, who formed the CDC’s Pediatric Mild Traumatic Brain Injury Guideline Workgroup, also recommended that clinicians use the term “mild traumatic brain injury” to describe head injuries that cause confusion or disorientation, without loss of consciousness, or loss of consciousness of up to 30 minutes or less, or posttraumatic amnesia of less than 24 hours duration, and that are associated with a GCS of 13-15 by 30 minutes after injury or at the time of initial medical assessment. This practice, they said, may reduce the risk of misinterpretation by medical professionals and the public that can occur when the terms “mTBI,” “concussion,” and “minor head injury” all may refer to the same injury.
The CDC has developed a suite of materials to assist both health care providers and the public in guideline implementation. The agency also is using its HEADS UP campaign to publicize the guidelines and related materials, and plans ongoing evaluation of the guidelines and implementation materials.
Many study authors, including Dr. Lumba-Brown, had relationships with medical device or pharmaceutical companies. The systematic review and guideline development were funded by the CDC.
FROM JAMA PEDIATRICS
ARRIVE: What are the perinatal and maternal consequences of labor induction at 39 weeks compared with expectant management?
WHAT DOES THIS MEAN FOR PRACTICE?
- Induction of labor at 39 weeks in low-risk nulliparas, irrespective of Bishop score, seems to be a reasonable option to be included in route of delivery discussions with patients as part of the principle of shared decision-making.
- The data in this trial would suggest that such an approach not only reduces adverse perinatal outcomes but also may reduce the need for subsequent cesarean delivery.
Updates to EULAR hand OA management recommendations reflect current evidence
Updated EULAR recommendations on the management of hand osteoarthritis include five overarching principles as well as two new recommendations that reflect new research in the field.
The task force, led by Margreet Kloppenburg, MD, PhD, of the department of rheumatology at Leiden (the Netherlands) University Medical Center, noted that a decade had passed since the first recommendations were published in 2007.
“It was timely to update the recommendations, as many new studies had emerged during this period. In light of this new evidence, many of the 2007 recommendations were modified and new recommendations were added,” wrote Dr. Kloppenburg and her colleagues. The recommendations were published online in Annals of the Rheumatic Diseases.
They noted that the recommendations were targeted to all health professionals across primary and secondary care but also aimed to inform patients about their disease to “support shared decision making.”
In line with other EULAR sets of management recommendations, the update included five overarching principles that cover treatment goals, information and education for patients, individualization of treatment, shared decision making between clinicians and patients, and the need to take into consideration a multidisciplinary and multimodal (pharmacologic and nonpharmacologic) treatment approach.
The authors noted that for a long time hand OA was a “forgotten disease” and this was reflected by the paucity of clinical trials in the area. As a direct consequence, previous recommendations were based on expert opinion rather than evidence.
However, new data allowed the task force to recommend not to treat patients with hand OA with conventional synthetic or biologic disease-modifying antirheumatic drugs (DMARDs). The recommendation achieved the strongest level of evidence and a high level of agreement from the 19-member expert panel, which included 2 patient research partners. The authors said the recommendation was based on newer studies that demonstrated a lack of efficacy of csDMARDs and bDMARDs.
The authors also advised adapting the long-term follow-up of patients with hand OA to individual needs, although they noted this was based on expert opinion alone and that in the absence of a disease-modifying treatment, the goal of follow-up differs from that of many other rheumatic diseases. Individual needs will dictate the degree of follow-up required, based on the severity of symptoms, presence of erosive disease, reevaluation of the use of pharmacologic therapy, and a patient’s wishes and expectations. They also noted that “for most patients, standard radiographic follow-up is not useful at this moment” and that “follow-up does not necessarily have to be performed by a rheumatologist.
“Follow-up will likely increase adherence to nonpharmacological therapies like exercise or orthoses, and provides an opportunity for reevaluation of treatment,” they wrote.
The recommendations advise offering education and training in ergonomic principles and exercises to patients to improve function and muscle strength, as well as considering the use of orthoses in some patients.
Treatment recommendations suggested preferring topical treatments over systemic treatments and that oral analgesics, particularly NSAIDs, should be considered for a limited duration. The authors advised that chondroitin sulfate may be used in patients for pain relief and improvement in functioning and that intra-articular glucocorticoids should not generally be used but may be considered in patients with painful interphalangeal joints. Surgery should be considered for patients with structural abnormalities when other treatment modalities have not been sufficiently effective in relieving pain.
The recommendations were funded by EULAR. Several of the authors reported receiving consultancy fees and/or honoraria as well as research funding from industry.
SOURCE: Kloppenburg M et al. Ann Rheum Dis. 2018 Aug 28. doi: 10.1136/annrheumdis-2018-213826.
EULAR has updated its 2007 guidelines for the management of hand osteoarthritis. I find the recommendations helpful, and I have no disagreements.
The authors performed a systematic literature review that was more complete than the original guidelines. In addition, the methodology in developing the guidelines was updated utilizing the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) system to guide the expert opinion. The manuscript presents recommendations that are carefully supported in the text. To understand guidelines, one really needs to read the text.
The update lists a set of research questions, similar to the 2007 recommendations.
The authors group their therapeutic recommendations according to nonpharmacologic, pharmacologic, and surgical approaches, as well as about the need for follow-up. The three nonpharmacologic recommendations include education and training, exercise and muscle strengthening, and the use of orthoses. The pharmacologic approach includes topical therapy as a first-line, oral NSAIDs and analgesics, chondroitin sulfate, and intra-articular injections. There is a negative recommendation for the use of biologics. The surgical recommendation is directed at the relief of pain. The last recommendation emphasizes the need for follow-up and individual care.
The differences between the recommendations include the removal of acetaminophen as a first-line therapy. Indeed, it seems to be barely recommended at all. In addition, there is an emphasis on topical therapy, particularly NSAIDs. The authors are equivocal on the recommendations for intra-articular therapy. Paraffin and local heat are no longer included. The recommendation against biologic therapy is new. They included agents used for rheumatoid arthritis, such as methotrexate, in this negative recommendation.
These new recommendations are an update of guidelines that are over 10 years old. They are practical and helpful. Unfortunately, more research is needed as the present day therapy is often inadequate.
Roy D. Altman, MD, is professor emeritus of medicine in the division of rheumatology and immunology at the University of California, Los Angeles. He is a consultant to Ferring, Flexion, GlaxoSmithKline, Novartis, Olatec, Pfizer, and Sorrento Therapeutics.
EULAR has updated its 2007 guidelines for the management of hand osteoarthritis. I find the recommendations helpful, and I have no disagreements.
The authors performed a systematic literature review that was more complete than the original guidelines. In addition, the methodology in developing the guidelines was updated utilizing the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) system to guide the expert opinion. The manuscript presents recommendations that are carefully supported in the text. To understand guidelines, one really needs to read the text.
The update lists a set of research questions, similar to the 2007 recommendations.
The authors group their therapeutic recommendations according to nonpharmacologic, pharmacologic, and surgical approaches, as well as about the need for follow-up. The three nonpharmacologic recommendations include education and training, exercise and muscle strengthening, and the use of orthoses. The pharmacologic approach includes topical therapy as a first-line, oral NSAIDs and analgesics, chondroitin sulfate, and intra-articular injections. There is a negative recommendation for the use of biologics. The surgical recommendation is directed at the relief of pain. The last recommendation emphasizes the need for follow-up and individual care.
The differences between the recommendations include the removal of acetaminophen as a first-line therapy. Indeed, it seems to be barely recommended at all. In addition, there is an emphasis on topical therapy, particularly NSAIDs. The authors are equivocal on the recommendations for intra-articular therapy. Paraffin and local heat are no longer included. The recommendation against biologic therapy is new. They included agents used for rheumatoid arthritis, such as methotrexate, in this negative recommendation.
These new recommendations are an update of guidelines that are over 10 years old. They are practical and helpful. Unfortunately, more research is needed as the present day therapy is often inadequate.
Roy D. Altman, MD, is professor emeritus of medicine in the division of rheumatology and immunology at the University of California, Los Angeles. He is a consultant to Ferring, Flexion, GlaxoSmithKline, Novartis, Olatec, Pfizer, and Sorrento Therapeutics.
EULAR has updated its 2007 guidelines for the management of hand osteoarthritis. I find the recommendations helpful, and I have no disagreements.
The authors performed a systematic literature review that was more complete than the original guidelines. In addition, the methodology in developing the guidelines was updated utilizing the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) system to guide the expert opinion. The manuscript presents recommendations that are carefully supported in the text. To understand guidelines, one really needs to read the text.
The update lists a set of research questions, similar to the 2007 recommendations.
The authors group their therapeutic recommendations according to nonpharmacologic, pharmacologic, and surgical approaches, as well as about the need for follow-up. The three nonpharmacologic recommendations include education and training, exercise and muscle strengthening, and the use of orthoses. The pharmacologic approach includes topical therapy as a first-line, oral NSAIDs and analgesics, chondroitin sulfate, and intra-articular injections. There is a negative recommendation for the use of biologics. The surgical recommendation is directed at the relief of pain. The last recommendation emphasizes the need for follow-up and individual care.
The differences between the recommendations include the removal of acetaminophen as a first-line therapy. Indeed, it seems to be barely recommended at all. In addition, there is an emphasis on topical therapy, particularly NSAIDs. The authors are equivocal on the recommendations for intra-articular therapy. Paraffin and local heat are no longer included. The recommendation against biologic therapy is new. They included agents used for rheumatoid arthritis, such as methotrexate, in this negative recommendation.
These new recommendations are an update of guidelines that are over 10 years old. They are practical and helpful. Unfortunately, more research is needed as the present day therapy is often inadequate.
Roy D. Altman, MD, is professor emeritus of medicine in the division of rheumatology and immunology at the University of California, Los Angeles. He is a consultant to Ferring, Flexion, GlaxoSmithKline, Novartis, Olatec, Pfizer, and Sorrento Therapeutics.
Updated EULAR recommendations on the management of hand osteoarthritis include five overarching principles as well as two new recommendations that reflect new research in the field.
The task force, led by Margreet Kloppenburg, MD, PhD, of the department of rheumatology at Leiden (the Netherlands) University Medical Center, noted that a decade had passed since the first recommendations were published in 2007.
“It was timely to update the recommendations, as many new studies had emerged during this period. In light of this new evidence, many of the 2007 recommendations were modified and new recommendations were added,” wrote Dr. Kloppenburg and her colleagues. The recommendations were published online in Annals of the Rheumatic Diseases.
They noted that the recommendations were targeted to all health professionals across primary and secondary care but also aimed to inform patients about their disease to “support shared decision making.”
In line with other EULAR sets of management recommendations, the update included five overarching principles that cover treatment goals, information and education for patients, individualization of treatment, shared decision making between clinicians and patients, and the need to take into consideration a multidisciplinary and multimodal (pharmacologic and nonpharmacologic) treatment approach.
The authors noted that for a long time hand OA was a “forgotten disease” and this was reflected by the paucity of clinical trials in the area. As a direct consequence, previous recommendations were based on expert opinion rather than evidence.
However, new data allowed the task force to recommend not to treat patients with hand OA with conventional synthetic or biologic disease-modifying antirheumatic drugs (DMARDs). The recommendation achieved the strongest level of evidence and a high level of agreement from the 19-member expert panel, which included 2 patient research partners. The authors said the recommendation was based on newer studies that demonstrated a lack of efficacy of csDMARDs and bDMARDs.
The authors also advised adapting the long-term follow-up of patients with hand OA to individual needs, although they noted this was based on expert opinion alone and that in the absence of a disease-modifying treatment, the goal of follow-up differs from that of many other rheumatic diseases. Individual needs will dictate the degree of follow-up required, based on the severity of symptoms, presence of erosive disease, reevaluation of the use of pharmacologic therapy, and a patient’s wishes and expectations. They also noted that “for most patients, standard radiographic follow-up is not useful at this moment” and that “follow-up does not necessarily have to be performed by a rheumatologist.
“Follow-up will likely increase adherence to nonpharmacological therapies like exercise or orthoses, and provides an opportunity for reevaluation of treatment,” they wrote.
The recommendations advise offering education and training in ergonomic principles and exercises to patients to improve function and muscle strength, as well as considering the use of orthoses in some patients.
Treatment recommendations suggested preferring topical treatments over systemic treatments and that oral analgesics, particularly NSAIDs, should be considered for a limited duration. The authors advised that chondroitin sulfate may be used in patients for pain relief and improvement in functioning and that intra-articular glucocorticoids should not generally be used but may be considered in patients with painful interphalangeal joints. Surgery should be considered for patients with structural abnormalities when other treatment modalities have not been sufficiently effective in relieving pain.
The recommendations were funded by EULAR. Several of the authors reported receiving consultancy fees and/or honoraria as well as research funding from industry.
SOURCE: Kloppenburg M et al. Ann Rheum Dis. 2018 Aug 28. doi: 10.1136/annrheumdis-2018-213826.
Updated EULAR recommendations on the management of hand osteoarthritis include five overarching principles as well as two new recommendations that reflect new research in the field.
The task force, led by Margreet Kloppenburg, MD, PhD, of the department of rheumatology at Leiden (the Netherlands) University Medical Center, noted that a decade had passed since the first recommendations were published in 2007.
“It was timely to update the recommendations, as many new studies had emerged during this period. In light of this new evidence, many of the 2007 recommendations were modified and new recommendations were added,” wrote Dr. Kloppenburg and her colleagues. The recommendations were published online in Annals of the Rheumatic Diseases.
They noted that the recommendations were targeted to all health professionals across primary and secondary care but also aimed to inform patients about their disease to “support shared decision making.”
In line with other EULAR sets of management recommendations, the update included five overarching principles that cover treatment goals, information and education for patients, individualization of treatment, shared decision making between clinicians and patients, and the need to take into consideration a multidisciplinary and multimodal (pharmacologic and nonpharmacologic) treatment approach.
The authors noted that for a long time hand OA was a “forgotten disease” and this was reflected by the paucity of clinical trials in the area. As a direct consequence, previous recommendations were based on expert opinion rather than evidence.
However, new data allowed the task force to recommend not to treat patients with hand OA with conventional synthetic or biologic disease-modifying antirheumatic drugs (DMARDs). The recommendation achieved the strongest level of evidence and a high level of agreement from the 19-member expert panel, which included 2 patient research partners. The authors said the recommendation was based on newer studies that demonstrated a lack of efficacy of csDMARDs and bDMARDs.
The authors also advised adapting the long-term follow-up of patients with hand OA to individual needs, although they noted this was based on expert opinion alone and that in the absence of a disease-modifying treatment, the goal of follow-up differs from that of many other rheumatic diseases. Individual needs will dictate the degree of follow-up required, based on the severity of symptoms, presence of erosive disease, reevaluation of the use of pharmacologic therapy, and a patient’s wishes and expectations. They also noted that “for most patients, standard radiographic follow-up is not useful at this moment” and that “follow-up does not necessarily have to be performed by a rheumatologist.
“Follow-up will likely increase adherence to nonpharmacological therapies like exercise or orthoses, and provides an opportunity for reevaluation of treatment,” they wrote.
The recommendations advise offering education and training in ergonomic principles and exercises to patients to improve function and muscle strength, as well as considering the use of orthoses in some patients.
Treatment recommendations suggested preferring topical treatments over systemic treatments and that oral analgesics, particularly NSAIDs, should be considered for a limited duration. The authors advised that chondroitin sulfate may be used in patients for pain relief and improvement in functioning and that intra-articular glucocorticoids should not generally be used but may be considered in patients with painful interphalangeal joints. Surgery should be considered for patients with structural abnormalities when other treatment modalities have not been sufficiently effective in relieving pain.
The recommendations were funded by EULAR. Several of the authors reported receiving consultancy fees and/or honoraria as well as research funding from industry.
SOURCE: Kloppenburg M et al. Ann Rheum Dis. 2018 Aug 28. doi: 10.1136/annrheumdis-2018-213826.
FROM ANNALS OF THE RHEUMATIC DISEASES
Benign MS is real in small minority of patients
Nearly 3% of patients with multiple sclerosis (MS) are estimated to have a truly benign course of disease over at least 15 years without the use of disease-modifying therapy, based on findings from a U.K. population-based study that also showed how poorly benign disease tracks with disability measures and lacks agreement between patients and physicians.
“The study of the individuals with extremely favorable outcomes may uncover insights about disease pathogenesis or repair. However, the insensitivity of EDSS [Expanded Disability Status Scale]–based definitions of benign MS and the discrepancy between patient and clinician perception of benign MS undermine use of the term ‘benign’ in the clinical setting,” Emma Clare Tallantyre, MD, of Cardiff (Wales) University, and her colleagues wrote in the Journal of Neurology, Neurosurgery & Psychiatry.
Dr. Tallantyre and her colleagues found that, of 1,049 patients with disease duration longer than 15 years, 200 had a recent EDSS score of less than 4.0. Of those 200, 60 were clinically assessed and 9 (15%) were found to have truly benign MS, defined as having an EDSS less than 3.0 and having no significant fatigue, mood disturbance, cognitive impairment, or disruption to employment in the absence of disease-modifying therapy at least 15 years after symptom onset.
The investigators extrapolated these data to estimate that 30 patients in the study population of 1,049 had truly benign MS, for a prevalence of 2.9%. However, of the 60 patients who were clinically assessed, 39 thought they had benign MS based on the lay definition provided: “When referring to illness, ‘benign’ usually means a condition which has little or no harmful effects on a person. There are no complications and there is a good outcome or prognosis.”
Patients who self-reported benign MS had significantly lower EDSS scores, fewer depressive symptoms, lower fatigue severity, and lower reported MS impact than did patients who did not report benign MS. “Self-reported benign MS status showed poor agreement with our composite definition of benign MS status and only fair agreement with EDSS-based definitions of benign MS status,” the investigators wrote.
SOURCE: Tallantyre EC et al. J Neurol Neurosurg Psychiatry. 2018 Sep 3. doi: 10.1136/jnnp-2018-318802.
Nearly 3% of patients with multiple sclerosis (MS) are estimated to have a truly benign course of disease over at least 15 years without the use of disease-modifying therapy, based on findings from a U.K. population-based study that also showed how poorly benign disease tracks with disability measures and lacks agreement between patients and physicians.
“The study of the individuals with extremely favorable outcomes may uncover insights about disease pathogenesis or repair. However, the insensitivity of EDSS [Expanded Disability Status Scale]–based definitions of benign MS and the discrepancy between patient and clinician perception of benign MS undermine use of the term ‘benign’ in the clinical setting,” Emma Clare Tallantyre, MD, of Cardiff (Wales) University, and her colleagues wrote in the Journal of Neurology, Neurosurgery & Psychiatry.
Dr. Tallantyre and her colleagues found that, of 1,049 patients with disease duration longer than 15 years, 200 had a recent EDSS score of less than 4.0. Of those 200, 60 were clinically assessed and 9 (15%) were found to have truly benign MS, defined as having an EDSS less than 3.0 and having no significant fatigue, mood disturbance, cognitive impairment, or disruption to employment in the absence of disease-modifying therapy at least 15 years after symptom onset.
The investigators extrapolated these data to estimate that 30 patients in the study population of 1,049 had truly benign MS, for a prevalence of 2.9%. However, of the 60 patients who were clinically assessed, 39 thought they had benign MS based on the lay definition provided: “When referring to illness, ‘benign’ usually means a condition which has little or no harmful effects on a person. There are no complications and there is a good outcome or prognosis.”
Patients who self-reported benign MS had significantly lower EDSS scores, fewer depressive symptoms, lower fatigue severity, and lower reported MS impact than did patients who did not report benign MS. “Self-reported benign MS status showed poor agreement with our composite definition of benign MS status and only fair agreement with EDSS-based definitions of benign MS status,” the investigators wrote.
SOURCE: Tallantyre EC et al. J Neurol Neurosurg Psychiatry. 2018 Sep 3. doi: 10.1136/jnnp-2018-318802.
Nearly 3% of patients with multiple sclerosis (MS) are estimated to have a truly benign course of disease over at least 15 years without the use of disease-modifying therapy, based on findings from a U.K. population-based study that also showed how poorly benign disease tracks with disability measures and lacks agreement between patients and physicians.
“The study of the individuals with extremely favorable outcomes may uncover insights about disease pathogenesis or repair. However, the insensitivity of EDSS [Expanded Disability Status Scale]–based definitions of benign MS and the discrepancy between patient and clinician perception of benign MS undermine use of the term ‘benign’ in the clinical setting,” Emma Clare Tallantyre, MD, of Cardiff (Wales) University, and her colleagues wrote in the Journal of Neurology, Neurosurgery & Psychiatry.
Dr. Tallantyre and her colleagues found that, of 1,049 patients with disease duration longer than 15 years, 200 had a recent EDSS score of less than 4.0. Of those 200, 60 were clinically assessed and 9 (15%) were found to have truly benign MS, defined as having an EDSS less than 3.0 and having no significant fatigue, mood disturbance, cognitive impairment, or disruption to employment in the absence of disease-modifying therapy at least 15 years after symptom onset.
The investigators extrapolated these data to estimate that 30 patients in the study population of 1,049 had truly benign MS, for a prevalence of 2.9%. However, of the 60 patients who were clinically assessed, 39 thought they had benign MS based on the lay definition provided: “When referring to illness, ‘benign’ usually means a condition which has little or no harmful effects on a person. There are no complications and there is a good outcome or prognosis.”
Patients who self-reported benign MS had significantly lower EDSS scores, fewer depressive symptoms, lower fatigue severity, and lower reported MS impact than did patients who did not report benign MS. “Self-reported benign MS status showed poor agreement with our composite definition of benign MS status and only fair agreement with EDSS-based definitions of benign MS status,” the investigators wrote.
SOURCE: Tallantyre EC et al. J Neurol Neurosurg Psychiatry. 2018 Sep 3. doi: 10.1136/jnnp-2018-318802.
FROM THE JOURNAL OF NEUROLOGY, NEUROSURGERY & PSYCHIATRY
Time-to-Surgery for Definitive Fixation of Hip Fractures: A Look at Outcomes Based Upon Delay
ABSTRACT
The morbidity and mortality after hip fracture in the elderly are influenced by non-modifiable comorbidities. Time-to-surgery is a modifiable factor that may play a role in postoperative morbidity. This study investigates the outcomes and complications in the elderly hip fracture surgery as a function of time-to-surgery.
Using the American College of Surgeons-National Surgical Quality Improvement Program data from 2011 to 2012, a study population was generated using the Current Procedural Terminology codes for percutaneous or open treatment of femoral neck fractures (27235, 27236) and fixation with a screw and side plate or intramedullary fixation (27244, 27245) for peritrochanteric fractures. Three time-to-surgery groups (<24 hours to surgical intervention, 24-48 hours, and >48 hours) were created and matched for surgery type, sex, age, and American Society of Anesthesiologists class. Time-to-surgery was then studied for its effect on the post-surgical outcomes using the adjusted regression modeling.
A study population of 6036 hip fractures was created, and 2012 patients were assigned to each matched time-to-surgery group. The unadjusted models showed that the earlier surgical intervention groups (<24 hours and 24-48 hours) exhibited a lower overall complication rate (P = .034) compared with the group waiting for surgery >48 hours. The unadjusted mortality rates increased with delay to surgical intervention (P = .039). Time-to-surgery caused no effect on the return to the operating room rate (P = .554) nor readmission rate (P = .285). Compared with other time-to-surgeries, the time-to-surgery of >48 hours was associated with prolonged total hospital length of stay (10.9 days) (P < .001) and a longer surgery-to-discharge time (hazard ratio, 95% confidence interval: 0.74, 0.69-0.79) (P < .001). Adjusted analyses showed no time-to-surgery related difference in complications (P = .143) but presented an increase in the total length of stay (P < .001) and surgery-to-discharge time (P < .001).
Timeliness of surgical intervention in a comorbidity-adjusted population of elderly hip fracture patients causes no effect on the overall complications, readmissions, nor 30-day mortality. However, time-to-surgery of >48 hours is associated with costly increase in the total length of stay, including an increased post-surgery-to-discharge time.
Continue to: Despite the best efforts to optimize surgical care...
Despite the best efforts to optimize surgical care and postoperative rehabilitation following hip fracture, elderly patients feature alarmingly high in-hospital and 1-year mortality rates of 4.35% to 9.2%1-4 and 36%,5 respectively. Those who survive are unlikely to return to independent living, with only 17% of the patients following hip fracture being able to walk independently 6 months postoperatively, and 12% being able to climb stairs6. Possibly, these poor outcomes reflect a preoperative medical comorbidity burden rather than a measure of medical or surgical quality. Given the absence of consensus regarding optimal time-to-surgery, treating physicians often opt to delay surgical intervention for the purposes of medically optimizing highly comorbid patients without significant data to suggest clinical benefit of such practice.
Numerous investigators have attempted to identify the modifiable risk factors for complication after surgical care of elderly hip fracture patients. However, consensus guidelines of care are missing. This condition is largely due to the difficulties in effectively modifying preoperative demographic and medical comorbidities on a semi-urgent basis. However, timeliness to surgery is one area for study that the care team can affect. Although time-to-surgery is dependent on multiple factors, including time of presentation, day of week of admission, difficulties with scheduling, and administrative delays, the care team plays a role in hastening or retarding time-to-surgery. Several studies have considered various time cut-offs (24, 48, 72, and 120 hours) to define early intervention, but none have defined a specific role for early or delayed surgery. Several investigators have discovered a positive association between delayed time-to-surgery and mortality;4,8-14 however, the most rigorously conducted studies that stringently control for preoperative comorbidities and demographics conclude that variance in time-to-surgery causes no effect on the in-hospital or 1-year mortality risk.1-3,15-18
Other investigators have shown that with early surgical intervention for hip fracture, patients experience shorter hospital stays,1,3,16,17,19-22 less days in pain,19 decreased risk of decubitus ulcers,15,17,19,22 and an increased likelihood of independence following fracture,22-25 regardless of preoperative medical status. Despite this evidence of improved outcomes with early surgery, 40% to 54% of hip fracture patients in the United States experience surgical delays of more than 24 to 48 hours. Additionally, with the recent (2013) national estimates of cost per day spent in the hospital falling between $1791 to $2289,26 minimizing the days spent in the hospital would likely lead to significant cost-savings, presuming no adverse effect on health-related outcomes. To this end, we hypothesize that the value (outcomes per associated cost)7 of hip fracture surgical care can be positively influenced by minimizing surgical wait-times. We assessed the effect of early surgical intervention, within 24 or 48 hours of presentation, on 30-day mortality, postoperative morbidity, hospital length of stay, and readmission rates in a comorbidity-adjusted population from a nationally representative cohort.
Continue to: METHODS AND MATERIALS...
METHODS AND MATERIALS
This study used the data from the American College of Surgeon-National Surgical Quality Improvement Program (ACS-NSQIP) database. With over 258 participating hospitals, this database has been widely used to identify national trends in various surgical specialties.27-34 The database includes information from participants in 43 states with hospitals ranging from rural community hospitals to large academic centers. Each site employs surgical clinical reviewers who are rigorously trained to collect data through chart review and discussion with the treating surgeon and/or patient,35 allowing for the use of robust and quality data with proven inter-rater reliability.36,37
Using the 2011 to 2012 NSQIP database, we used primary Current Procedural Terminology codes to identify all patients who underwent percutaneous (27235) or open (27236) fixation of femoral neck fractures; and fixation with a screw and side plate (27244) or intramedullary fixation (27245) for peritrochanteric fractures. The sample was divided into 3 time-to-surgery groups (<24 hours from presentation to surgery, 24-48 hours, and >48 hours) which were matched for fracture type (femoral neck or peritrochanteric), sex, age (under 75 years or ≥75 years), and American Society of Anesthesiologists (ASA) class used as a surrogate for severity of medical infirmary. The subjects were randomly matched 1:1:1 to create 3 statistically equivalent time-to-surgery groups using Proc SurveySelect (SAS version 9.2, SAS Institute).
Generalized linear models using logit link function for binary variables and identity link function for normally distributed characteristics were used to compare the 3 time-to-surgery groups. Descriptive statistics are presented as counts and percentages or least-square means with standard deviations. Preoperative lab values that were not normally distributed were log transformed and presented in their original scales with median values and 25th to 75th percentiles. Outcomes were similarly modeled.
Total hospital stay was modeled with a negative binomial distribution. Proportional hazards models were used to model the time from operating room (OR) to discharge, censoring patients who died before discharge, with results presented as hazard ratios (HR) and 95% confidence intervals (CI) (Figure). The assumption of the proportional hazards was tested using a Wald test. Using this model, a HR of <1 denotes a longer postoperative hospital stay, as a longer hospital stay decreases the “risk” for discharge.
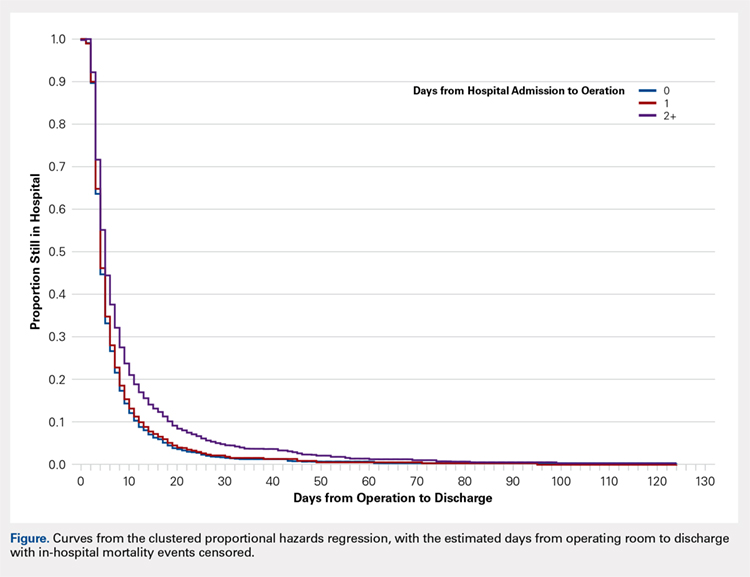
All models were adjusted for confounders, including race, body mass index (BMI), hypertension, chronic obstructive pulmonary disease, cancer, bleeding disorders, transfusion within 72 hours before surgery, preoperative levels of creatinine, platelet count, white blood cells (WBCs), hematocrit anesthesia type, and wound infection. These covariates were selected based upon their observed relationship to the studied outcomes and time-to-surgery groups, and were evaluated across the models for all outcomes for consistency and clarity. All statistical analyses were run at a type I error rate of 5% and performed in SAS version 9.2 software.
Continue to: RESULTS...
RESULTS
A study population of 6036 hip fractures was identified and divided into 3 groups of 2012 subjects each based upon time-to-surgery. The groups were successfully matched for surgery type, age (≥75 years old), gender, and ASA class. In each group, 594 of the 2012 (29.5%) patients were male, 1525 (75.8%) were ≥75 years of age, 9 (.5%) were ASA Class I, 269 (13.4%) were ASA Class II, 1424 (70.8%) were ASA class III, and 309 (15.4%) were ASA class IV.
Significant differences in preoperative comorbidity burden and preoperative lab values were identified between the 3 cohorts. Increased time-to-surgery was associated with differences in race (P < .001), elevated BMI (P = .010), higher rates of congestive heart failure (P < .001), hypertension medication (P = .020), bleeding disorders (P < .001), blood transfusion within 72 hours of surgery (P < .001), and systemic sepsis (P = .001). Delay to surgery was also associated with lower preoperative sodium (P = .005), blood urea nitrogen (P = .013), serum WBC (P < .001), hematocrit (P < .001), and platelets (P < .001) (Table 1).
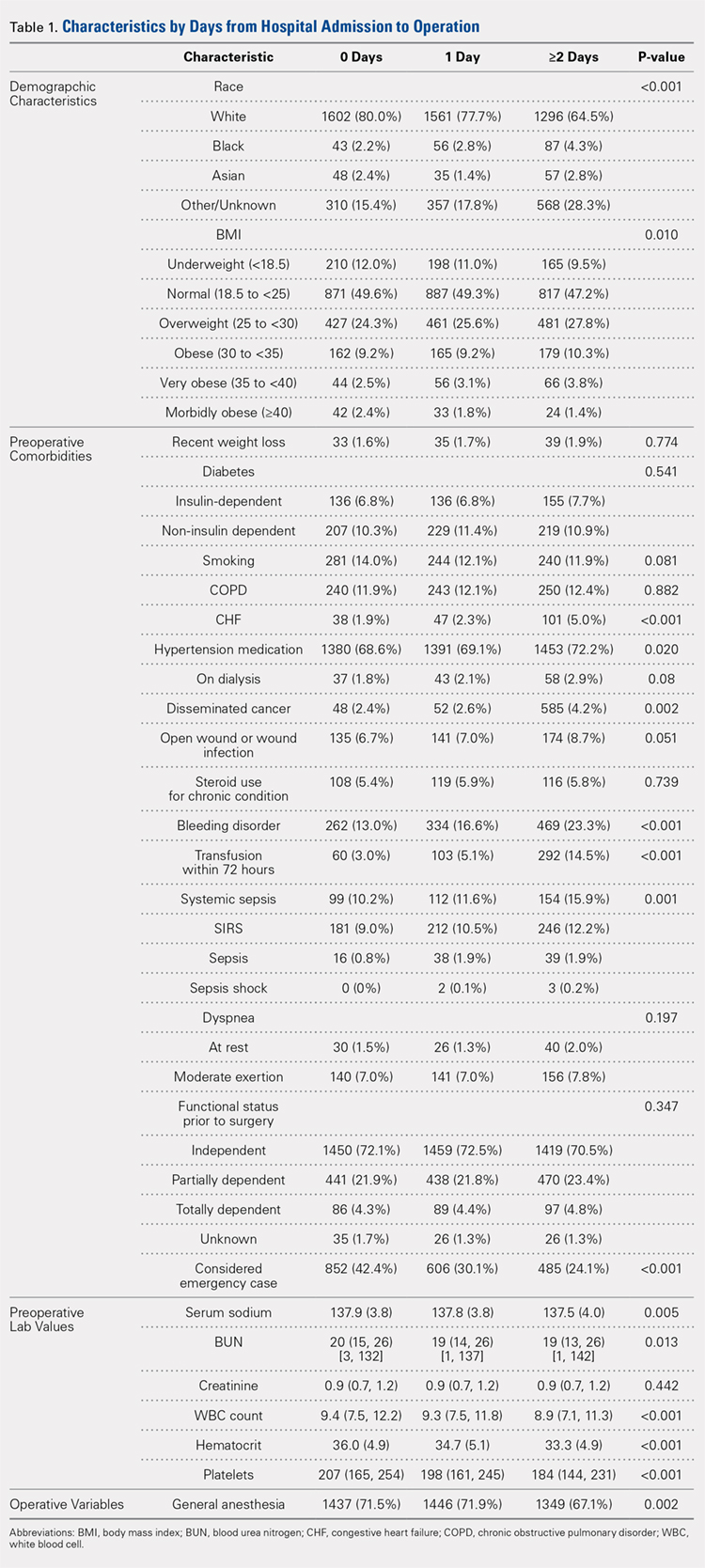
The unadjusted analyses revealed no association between time-to-surgery and return to OR (P = .554) nor readmission (P = .285). However, increasing time-to-surgery was associated with an increase in overall complications (P = .034), total length of hospital stay (P < .001), and 30-day mortality (P = .039) (Table 2).
Table 2. Estimated Event Rates from Matched Cohorts (Unadjusted)
| Time From Presentation to Definitive Fixation | |||
Outcomes | <24 hours | 24-48 hours | >48 hours | P-value |
Overall complication rate | 15.30% | 15.30% | 17.90% | 0.034 |
Total length of stay | 5.4 | 6.7 | 10.9 | <0.001 |
(mean days, 95% confidence interval) | (5.2, 5.7) | (6.5, 7.0) | (10.3, 11.5) | |
Time from OR to discharge | -ref- | 0.96 | 0.74 | <0.001 |
(Hazard ratio) | (0.90,1.02) | (0.69, 0.79) | ||
Return to OR | 2.40% | 2.40% | 2.00% | 0.554 |
Readmission | 9.60% | 8.40% | 8.30% | 0.285 |
30-day mortality rate | 5.80% | 5.30% | 7.20% | 0.039 |
Abbreviation: OR, operating room.
The adjusted analysis controlling for preoperative demographic and comorbidity variables revealed trends toward the increased overall complications and 30-day mortality with increased time-to-surgery; these trends showed no statistical significance (P = .143 and P = .08). No statistical relationship was observed between return to OR nor readmission and time-to-surgery. Increasing time-to-surgery remained significantly associated with the increased total length of hospital stay (P < .001). The adjusted analysis also revealed that the delay of >48 hours in time-to-surgery resulted in a longer surgery-to-discharge time (P < .001) (Table 3). No evidence of violation of the proportional hazards assumption was observed in the unadjusted nor adjusted clustered proportional hazards models (Wald test, P = .27 and P = .25, respectively).
Table 3. Estimated Event Rates from Matched Cohorts (Adjusteda)
| Time from Presentation to Definitive Fixation | |||
Outcomes | <24 hours | 24-48 hours | >48 hours | P-value |
Overall complication rate | 11.70% | 10.70% | 12.60% | 0.143 |
Total length of stay | 4.2 | 5.1 | 7.6 | <0.001 |
(mean days, 95% confidence interval) | (4.0, 4.5) | (4.8, 5.5) | (7.1, 8.3) | |
Time from OR to discharge | -ref- | 1.03 | 0.87 | <0.001 |
(Hazard ratio) | (0.97, 1.09) | (0.81, 0.92) | ||
Return to OR | 2.10% | 2.10% | 1.60% | 0.541 |
Readmission | 7.20% | 6.40% | 6.00% | 0.304 |
30-day mortality rate | 4.20% | 3.70% | 5.20% | 0.08 |
aModel adjusted for race, hypertension medication, cancer, bleeding disorders, transfusion within 72 hours before surgery, emergency status, wound infection, anesthesia type (general), body mass index (18.5-25), history of chronic obstructive pulmonary disease, and preoperative levels of creatinine, platelet count, white blood cell count, and hematocrit.
Continue to: DISCUSSION...
DISCUSSION
Previous research has demonstrated an association between age,3,4,25 comorbidity burden,1,3,25 gender,3,4 and ASA class4,18,21 with outcomes following hip fractures and serves as the basis of our matched analysis statistical methodology in assessing the effect of time-to-surgery on the outcome following hip fracture surgery. Prior investigators have also established the positive correlation between increased preoperative comorbidity burden and delay in time-to-surgery.10,15 This finding was confirmed in our unadjusted comparison of 3 time-to-surgery groups. However, prior investigations have not established a clear association between time-to-surgical intervention and postoperative morbidity and mortality.1,15,16,18,20,38 This study utilized a nationally representative dataset known for its data integrity and from which 6036 patients with surgically treated hip fractures, matched for surgery type, age, gender, and ASA class (a surrogate for severity of medical infirmary), were studied using adjusted regression modeling to afford an isolated statistical assessment of the effect of time-to-surgery on outcomes following hip fracture surgery.
Despite a large sample size and rigorous statistical methodology, for many outcome measures, our results show no support for the early or late operative intervention following hip fracture. We found no difference in 30-day mortality, readmission rate, nor total complication rate between the 3 time-to-surgery cohorts. This result indicates that the care of elderly patients following hip fracture is inherently complicated and that perioperative complication risk is probably only modestly modifiable by best medical practices, including optimizing time from clinical presentation to surgery.
As expected, patients who experienced longer delays from presentation to surgery were on average, more comorbid and more likely to yield abnormal preoperative lab values. However, in the adjusted analysis, delay in time-to-surgery, presumably for medical management, was not found to be associated with improved outcomes. In the same adjusted analysis, we uniquely identified that in the patients whose surgeries were delayed for more than 48 hours, the time from surgery-to-discharge was significantly increased. As a result, these patients spent extra days in the hospital both preoperatively and postoperatively, but without any corollary improvement in the outcomes.
Continue to: Recent estimates of the cost of hospital admission...
Recent estimates of the cost of hospital admission is approximated nationally at $2000/day.26 Although our data fail to support the formal cost-analysis of the effect of time-to-surgery in hip fracture care, a simple value-based analysis indicates that quality is preserved (no difference in outcome), whereas costly hospital days are eliminated with earlier surgery. The value in elderly hip fracture care. defined as the outcomes relative to the costs,7 is ultimately optimized by earlier time-to-surgery.
Although using a large, multi-institutional database is advantageous for finding population-based trends that are representative of a large cohort, using the ACS-NSQIP database features its limitations. Our analysis was limited to the defined scope of NSQIP and nature of the injury, whereas root cause for delay was not available for study. We were unable to identify which patients were delayed for administrative reasons or surgical convenience and which were delayed for medical optimization. Participation in the ACS-NSQIP database is voluntary, and no randomized hospital sampling was conducted. Participating hospitals were de-identified in the database. As expected, we were unable to identify the specific institution-based hip fracture protocols that may affect the outcomes following treatment for these fractures. Further, socioeconomic information and payer-status are unavailable for the study. Additionally, observations are limited to 30 days postoperative, and we cannot comment on longer-term outcomes. Finally, discharge disposition and functional outcome data are not represented, and we were unable to correlate time-to-surgery and functional recovery. However, previous studies have established that delay in time-to-surgery following hip fractures is negatively correlated with functional outcomes.22-25
Nevertheless, the ACS-NSQIP database remains one of the largest American surgical databases available, and includes care centers from nearly every state with variable demographics including rural, urban, and academic centers. The ACS performs broad-based inter-rater reliability audits on every participating site and has found an overall disagreement rate of only 1.8%. As such, although discrepancies exist between the complete patient chart and the data entered, the data found in the ACS-NSQIP database are reliable and considered a valid source of study.34,35 The large sample size, quality of data collection, wide geographic representation, and varied hospital types within the dataset possibly make our findings relevant in the majority of American healthcare settings.
CONCLUSION
This study demonstrates an associated increased length of hospital stay, including the increased time from surgery-to-discharge, in patients with hip fractures whose surgical intervention is delayed for >48 hours after presentation. Given the prior evidence that early surgical intervention improves the functional outcomes and the current evidence that surgical delay for any cause increases costly hospital length of stay without corollary improvement in the outcomes, a value-based assessment of hip fracture care argues for early surgical intervention whenever possible. Our findings should inform physician, institution, and policy maker value-based decision making regarding the best practices in geriatric hip fracture care.
1. Vidán MT, Sánchez E, Gracia Y, Marañón E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med. 2011;155(4):226-233. doi:10.7326/0003-4819-155-4-201108160-00006.
2. Verbeek DO, Ponsen KJ, Goslings JC, Heetveld MJ. Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop. 2008;32(1):13-18. doi:10.1007/s00264-006-0290-9.
3. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009;91(7):922-927. doi:10.1302/0301-620X.91B7.22446.
4. Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726-729. doi:10.1016/j.injury.2012.08.025.
5. Zuckerman JD. Hip fracture. N Engl J Med. 1996;334(23):1519-1525. doi:10.1056/NEJM199606063342307.
6. Marottoli RA, Berkman LF, Cooney LM Jr. Decline in physical function following hip fracture. J Am Geriatr Soc. 1992;40(9):861-866. doi:10.1111/j.1532-5415.1992.tb01980.x.
7. Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477-2481. doi:10.1056/NEJMp1011024.
8. Radcliff TA, Henderson WG, Stoner TJ, Khuri SF, Dohm M, Hutt E. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008;90(1):34-42. doi:10.2106/JBJS.G.00065.
9. Novack V, Jotkowitz A, Etzion O, Porath A. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int J Qual Health Care. 2007;19(3):170-176. doi:10.1093/intqhc/mzm003.
10. Weller I, Wai EK, Jaglal S, Kreder HJ. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005;87(3):361-366. doi:10.1302/0301-620X.87B3.15300.
11. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483-489. doi:10.2106/JBJS.D.01796.
12. Holt G, Smith R, Duncan K, McKeown DW. Does delay to theatre for medical reasons affect the peri-operative mortality in patients with a fracture of the hip? J Bone Joint Surg Br. 2010;92(6):835-841. doi:10.1302/0301-620X.92B6.24463.
13. Pioli G, Lauretani F, Davoli ML, et al. Older people with hip fracture and IADL disability require earlier surgery. J Gerontol A Biol Sci Med Sci. 2012;67(11):1272-1277. doi:10.1093/gerona/gls097.
14. Mackenzie DG, Wild S, Muir R. Mortality associated with delay in operation after hip fracture: Scottish data provide additional information. BMJ. 2006;332(7549):1093. doi:10.1136/bmj.332.7549.1093.
15. Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112(9):702-709. doi:10.1016/S0002-9343(02)01119-1.
16. Majumdar SR, Beaupre LA, Johnston DW, Dick DA, Cinats JG, Jiang HX. Lack of association between mortality and timing of surgical fixation in elderly patients with hip fracture: results of a retrospective population-based cohort study. Med Care. 2006;44(6):552-559. doi:10.1097/01.mlr.0000215812.13720.2e.
17. Hommel A, Ulander K, Bjorkelund KB, Norrman PO, Wingstrand H, Thorngren KG. Influence of optimised treatment of people with hip fracture on time to operation, length of hospital stay, reoperations and mortality within 1 year. Injury. 2008;39(10):1164-1174. doi:10.1016/j.injury.2008.01.048.
18. Rae HC, Harris IA, McEvoy L, Todorova T. Delay to surgery and mortality after hip fracture. ANZ J Surg. 2007;77(10):889-891. doi:10.1111/j.1445-2197.2007.04267.x.
19. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738-1743. doi:10.1001/jama.291.14.1738.
20. Bergeron E, Lavoie A, Moore L, et al. Is the delay to surgery for isolated hip fracture predictive of outcome in efficient systems? J Trauma. 2006;60(4):753-757. doi:10.1097/01.ta.0000214649.53190.2a.
21. Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8):1123-1126. doi:10.1302/0301-620X.87B8.16357.
22. Al-Ani AN, Samuelsson B, Tidermark J, et al. Early operation on patients with a hip fracture improved the ability to return to independent living. A prospective study of 850 patients. J Bone Joint Surg Am. 2008;90(7):1436-1442. doi:10.2106/JBJS.G.00890.
23. Hoenig H, Rubenstein LV, Sloane R, Horner R, Kahn K. What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med. 1997;157(5):513-520.
24. Doruk H, Mas MR, Yildiz C, Sonmez A, Kýrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39(2):179-185. doi:10.1016/j.archger.2004.03.004.
25. Yonezawa T, Yamazaki K, Atsumi T, Obara S. Influence of the timing of surgery on mortality and activity of hip fracture in elderly patients. J Orthop Sci Off J Jpn Orthop Assoc. 2009;14(5):566-573. doi:10.1007/s00776-009-1380-5.
26. Henry J Kaiser Family Foundation. Hospital adjusted expenses per inpatient day by ownership. https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day-by-ownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed March 14, 2013.
27. Belmont PJ Jr, Davey S, Orr JD, Ochoa LM, Bader JO, Schoenfeld AJ. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg. 2011;213(3):370-378. doi:10.1016/j.jamcollsurg.2011.05.019.
28. Davis SS Jr, Husain FA, Lin E, Nandipati KC, Perez S, Sweeney JF. Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg. 2013;216(1):96-104. doi:10.1016/j.jamcollsurg.2012.08.014.
29. Gart MS, Smetona JT, Hanwright PJ, et al. Autologous options for postmastectomy breast reconstruction: a comparison of outcomes based on the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216(2):229-238. doi:10.1016/j.jamcollsurg.2012.11.003.
30. Greenblatt DY, Rajamanickam V, Pugely AJ, Heise CP, Foley EF, Kennedy GD. Short-term outcomes after laparoscopic-assisted proctectomy for rectal cancer: results from the ACS NSQIP. J Am Coll Surg. 2011;212(5):844-854. doi:10.1016/j.jamcollsurg.2011.01.005.
31. Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013;95(3):193-199. doi:10.2106/JBJS.K.01682.
32. Rao RD. Risk factors for complications and mortality after spine surgery assessed with the NSQIP database: where do we go from here? Commentary on an article by Andrew J Schoenfeld, MD, et al.: "Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program". J Bone Joint Surg Am. 2011;93(17):e101:(101-102). doi:10.2106/JBJS.K.00786.
33. Schilling PL, Hallstrom BR, Birkmeyer JD, Carpenter JE. Prioritizing perioperative quality improvement in orthopaedic surgery. J Bone Joint Surg Am. 2010;92(9):1884-1889. doi:10.2106/JBJS.I.00735.
34. Tsilimparis N, Perez S, Dayama A, Ricotta JJ 2nd. Age-stratified results from 20,095 aortoiliac aneurysm repairs: should we approach octogenarians and nonagenarians differently? J Am Coll Surg. 2012;215(5):690-701. doi:10.1016/j.jamcollsurg.2012.06.411.
35. ACS National Surgical Quality Improvement Program. American College of Surgeons Web site. https://www.facs.org/quality-programs/acs-nsqip?. Accessed March 14, 2013.
36. Henderson WG, Daley J. Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg. 2009;198(5 Suppl):S19-S27. doi:10.1016/j.amjsurg.2009.07.025.
37. Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210(1):6-16. doi:10.1016/j.jamcollsurg.2009.09.031.
38. Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40(7):692-697. doi:10.1016/j.injury.2009.01.010.
ABSTRACT
The morbidity and mortality after hip fracture in the elderly are influenced by non-modifiable comorbidities. Time-to-surgery is a modifiable factor that may play a role in postoperative morbidity. This study investigates the outcomes and complications in the elderly hip fracture surgery as a function of time-to-surgery.
Using the American College of Surgeons-National Surgical Quality Improvement Program data from 2011 to 2012, a study population was generated using the Current Procedural Terminology codes for percutaneous or open treatment of femoral neck fractures (27235, 27236) and fixation with a screw and side plate or intramedullary fixation (27244, 27245) for peritrochanteric fractures. Three time-to-surgery groups (<24 hours to surgical intervention, 24-48 hours, and >48 hours) were created and matched for surgery type, sex, age, and American Society of Anesthesiologists class. Time-to-surgery was then studied for its effect on the post-surgical outcomes using the adjusted regression modeling.
A study population of 6036 hip fractures was created, and 2012 patients were assigned to each matched time-to-surgery group. The unadjusted models showed that the earlier surgical intervention groups (<24 hours and 24-48 hours) exhibited a lower overall complication rate (P = .034) compared with the group waiting for surgery >48 hours. The unadjusted mortality rates increased with delay to surgical intervention (P = .039). Time-to-surgery caused no effect on the return to the operating room rate (P = .554) nor readmission rate (P = .285). Compared with other time-to-surgeries, the time-to-surgery of >48 hours was associated with prolonged total hospital length of stay (10.9 days) (P < .001) and a longer surgery-to-discharge time (hazard ratio, 95% confidence interval: 0.74, 0.69-0.79) (P < .001). Adjusted analyses showed no time-to-surgery related difference in complications (P = .143) but presented an increase in the total length of stay (P < .001) and surgery-to-discharge time (P < .001).
Timeliness of surgical intervention in a comorbidity-adjusted population of elderly hip fracture patients causes no effect on the overall complications, readmissions, nor 30-day mortality. However, time-to-surgery of >48 hours is associated with costly increase in the total length of stay, including an increased post-surgery-to-discharge time.
Continue to: Despite the best efforts to optimize surgical care...
Despite the best efforts to optimize surgical care and postoperative rehabilitation following hip fracture, elderly patients feature alarmingly high in-hospital and 1-year mortality rates of 4.35% to 9.2%1-4 and 36%,5 respectively. Those who survive are unlikely to return to independent living, with only 17% of the patients following hip fracture being able to walk independently 6 months postoperatively, and 12% being able to climb stairs6. Possibly, these poor outcomes reflect a preoperative medical comorbidity burden rather than a measure of medical or surgical quality. Given the absence of consensus regarding optimal time-to-surgery, treating physicians often opt to delay surgical intervention for the purposes of medically optimizing highly comorbid patients without significant data to suggest clinical benefit of such practice.
Numerous investigators have attempted to identify the modifiable risk factors for complication after surgical care of elderly hip fracture patients. However, consensus guidelines of care are missing. This condition is largely due to the difficulties in effectively modifying preoperative demographic and medical comorbidities on a semi-urgent basis. However, timeliness to surgery is one area for study that the care team can affect. Although time-to-surgery is dependent on multiple factors, including time of presentation, day of week of admission, difficulties with scheduling, and administrative delays, the care team plays a role in hastening or retarding time-to-surgery. Several studies have considered various time cut-offs (24, 48, 72, and 120 hours) to define early intervention, but none have defined a specific role for early or delayed surgery. Several investigators have discovered a positive association between delayed time-to-surgery and mortality;4,8-14 however, the most rigorously conducted studies that stringently control for preoperative comorbidities and demographics conclude that variance in time-to-surgery causes no effect on the in-hospital or 1-year mortality risk.1-3,15-18
Other investigators have shown that with early surgical intervention for hip fracture, patients experience shorter hospital stays,1,3,16,17,19-22 less days in pain,19 decreased risk of decubitus ulcers,15,17,19,22 and an increased likelihood of independence following fracture,22-25 regardless of preoperative medical status. Despite this evidence of improved outcomes with early surgery, 40% to 54% of hip fracture patients in the United States experience surgical delays of more than 24 to 48 hours. Additionally, with the recent (2013) national estimates of cost per day spent in the hospital falling between $1791 to $2289,26 minimizing the days spent in the hospital would likely lead to significant cost-savings, presuming no adverse effect on health-related outcomes. To this end, we hypothesize that the value (outcomes per associated cost)7 of hip fracture surgical care can be positively influenced by minimizing surgical wait-times. We assessed the effect of early surgical intervention, within 24 or 48 hours of presentation, on 30-day mortality, postoperative morbidity, hospital length of stay, and readmission rates in a comorbidity-adjusted population from a nationally representative cohort.
Continue to: METHODS AND MATERIALS...
METHODS AND MATERIALS
This study used the data from the American College of Surgeon-National Surgical Quality Improvement Program (ACS-NSQIP) database. With over 258 participating hospitals, this database has been widely used to identify national trends in various surgical specialties.27-34 The database includes information from participants in 43 states with hospitals ranging from rural community hospitals to large academic centers. Each site employs surgical clinical reviewers who are rigorously trained to collect data through chart review and discussion with the treating surgeon and/or patient,35 allowing for the use of robust and quality data with proven inter-rater reliability.36,37
Using the 2011 to 2012 NSQIP database, we used primary Current Procedural Terminology codes to identify all patients who underwent percutaneous (27235) or open (27236) fixation of femoral neck fractures; and fixation with a screw and side plate (27244) or intramedullary fixation (27245) for peritrochanteric fractures. The sample was divided into 3 time-to-surgery groups (<24 hours from presentation to surgery, 24-48 hours, and >48 hours) which were matched for fracture type (femoral neck or peritrochanteric), sex, age (under 75 years or ≥75 years), and American Society of Anesthesiologists (ASA) class used as a surrogate for severity of medical infirmary. The subjects were randomly matched 1:1:1 to create 3 statistically equivalent time-to-surgery groups using Proc SurveySelect (SAS version 9.2, SAS Institute).
Generalized linear models using logit link function for binary variables and identity link function for normally distributed characteristics were used to compare the 3 time-to-surgery groups. Descriptive statistics are presented as counts and percentages or least-square means with standard deviations. Preoperative lab values that were not normally distributed were log transformed and presented in their original scales with median values and 25th to 75th percentiles. Outcomes were similarly modeled.
Total hospital stay was modeled with a negative binomial distribution. Proportional hazards models were used to model the time from operating room (OR) to discharge, censoring patients who died before discharge, with results presented as hazard ratios (HR) and 95% confidence intervals (CI) (Figure). The assumption of the proportional hazards was tested using a Wald test. Using this model, a HR of <1 denotes a longer postoperative hospital stay, as a longer hospital stay decreases the “risk” for discharge.
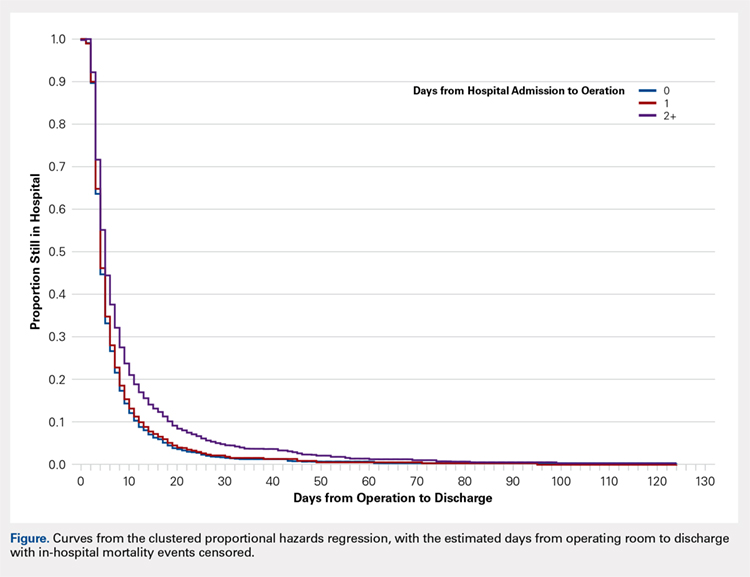
All models were adjusted for confounders, including race, body mass index (BMI), hypertension, chronic obstructive pulmonary disease, cancer, bleeding disorders, transfusion within 72 hours before surgery, preoperative levels of creatinine, platelet count, white blood cells (WBCs), hematocrit anesthesia type, and wound infection. These covariates were selected based upon their observed relationship to the studied outcomes and time-to-surgery groups, and were evaluated across the models for all outcomes for consistency and clarity. All statistical analyses were run at a type I error rate of 5% and performed in SAS version 9.2 software.
Continue to: RESULTS...
RESULTS
A study population of 6036 hip fractures was identified and divided into 3 groups of 2012 subjects each based upon time-to-surgery. The groups were successfully matched for surgery type, age (≥75 years old), gender, and ASA class. In each group, 594 of the 2012 (29.5%) patients were male, 1525 (75.8%) were ≥75 years of age, 9 (.5%) were ASA Class I, 269 (13.4%) were ASA Class II, 1424 (70.8%) were ASA class III, and 309 (15.4%) were ASA class IV.
Significant differences in preoperative comorbidity burden and preoperative lab values were identified between the 3 cohorts. Increased time-to-surgery was associated with differences in race (P < .001), elevated BMI (P = .010), higher rates of congestive heart failure (P < .001), hypertension medication (P = .020), bleeding disorders (P < .001), blood transfusion within 72 hours of surgery (P < .001), and systemic sepsis (P = .001). Delay to surgery was also associated with lower preoperative sodium (P = .005), blood urea nitrogen (P = .013), serum WBC (P < .001), hematocrit (P < .001), and platelets (P < .001) (Table 1).
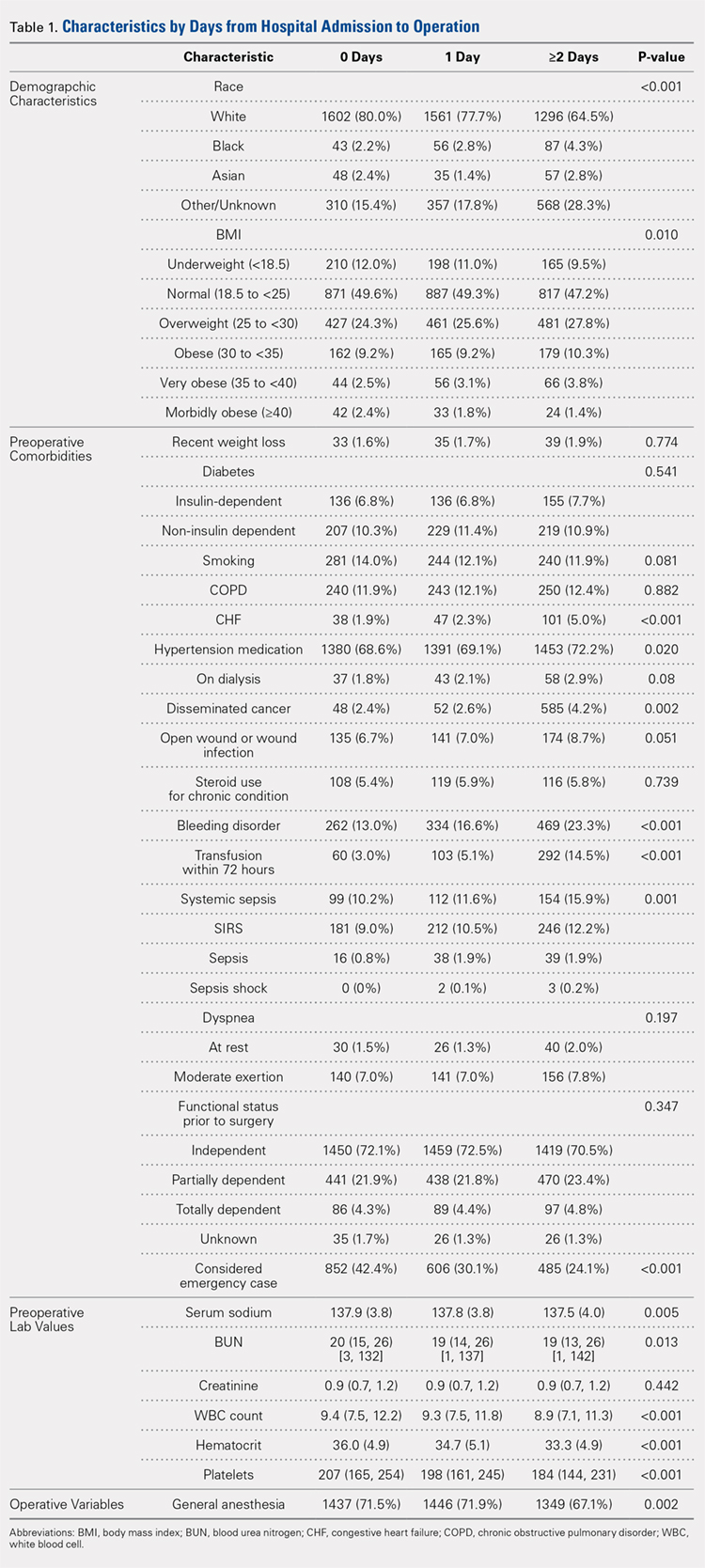
The unadjusted analyses revealed no association between time-to-surgery and return to OR (P = .554) nor readmission (P = .285). However, increasing time-to-surgery was associated with an increase in overall complications (P = .034), total length of hospital stay (P < .001), and 30-day mortality (P = .039) (Table 2).
Table 2. Estimated Event Rates from Matched Cohorts (Unadjusted)
| Time From Presentation to Definitive Fixation | |||
Outcomes | <24 hours | 24-48 hours | >48 hours | P-value |
Overall complication rate | 15.30% | 15.30% | 17.90% | 0.034 |
Total length of stay | 5.4 | 6.7 | 10.9 | <0.001 |
(mean days, 95% confidence interval) | (5.2, 5.7) | (6.5, 7.0) | (10.3, 11.5) | |
Time from OR to discharge | -ref- | 0.96 | 0.74 | <0.001 |
(Hazard ratio) | (0.90,1.02) | (0.69, 0.79) | ||
Return to OR | 2.40% | 2.40% | 2.00% | 0.554 |
Readmission | 9.60% | 8.40% | 8.30% | 0.285 |
30-day mortality rate | 5.80% | 5.30% | 7.20% | 0.039 |
Abbreviation: OR, operating room.
The adjusted analysis controlling for preoperative demographic and comorbidity variables revealed trends toward the increased overall complications and 30-day mortality with increased time-to-surgery; these trends showed no statistical significance (P = .143 and P = .08). No statistical relationship was observed between return to OR nor readmission and time-to-surgery. Increasing time-to-surgery remained significantly associated with the increased total length of hospital stay (P < .001). The adjusted analysis also revealed that the delay of >48 hours in time-to-surgery resulted in a longer surgery-to-discharge time (P < .001) (Table 3). No evidence of violation of the proportional hazards assumption was observed in the unadjusted nor adjusted clustered proportional hazards models (Wald test, P = .27 and P = .25, respectively).
Table 3. Estimated Event Rates from Matched Cohorts (Adjusteda)
| Time from Presentation to Definitive Fixation | |||
Outcomes | <24 hours | 24-48 hours | >48 hours | P-value |
Overall complication rate | 11.70% | 10.70% | 12.60% | 0.143 |
Total length of stay | 4.2 | 5.1 | 7.6 | <0.001 |
(mean days, 95% confidence interval) | (4.0, 4.5) | (4.8, 5.5) | (7.1, 8.3) | |
Time from OR to discharge | -ref- | 1.03 | 0.87 | <0.001 |
(Hazard ratio) | (0.97, 1.09) | (0.81, 0.92) | ||
Return to OR | 2.10% | 2.10% | 1.60% | 0.541 |
Readmission | 7.20% | 6.40% | 6.00% | 0.304 |
30-day mortality rate | 4.20% | 3.70% | 5.20% | 0.08 |
aModel adjusted for race, hypertension medication, cancer, bleeding disorders, transfusion within 72 hours before surgery, emergency status, wound infection, anesthesia type (general), body mass index (18.5-25), history of chronic obstructive pulmonary disease, and preoperative levels of creatinine, platelet count, white blood cell count, and hematocrit.
Continue to: DISCUSSION...
DISCUSSION
Previous research has demonstrated an association between age,3,4,25 comorbidity burden,1,3,25 gender,3,4 and ASA class4,18,21 with outcomes following hip fractures and serves as the basis of our matched analysis statistical methodology in assessing the effect of time-to-surgery on the outcome following hip fracture surgery. Prior investigators have also established the positive correlation between increased preoperative comorbidity burden and delay in time-to-surgery.10,15 This finding was confirmed in our unadjusted comparison of 3 time-to-surgery groups. However, prior investigations have not established a clear association between time-to-surgical intervention and postoperative morbidity and mortality.1,15,16,18,20,38 This study utilized a nationally representative dataset known for its data integrity and from which 6036 patients with surgically treated hip fractures, matched for surgery type, age, gender, and ASA class (a surrogate for severity of medical infirmary), were studied using adjusted regression modeling to afford an isolated statistical assessment of the effect of time-to-surgery on outcomes following hip fracture surgery.
Despite a large sample size and rigorous statistical methodology, for many outcome measures, our results show no support for the early or late operative intervention following hip fracture. We found no difference in 30-day mortality, readmission rate, nor total complication rate between the 3 time-to-surgery cohorts. This result indicates that the care of elderly patients following hip fracture is inherently complicated and that perioperative complication risk is probably only modestly modifiable by best medical practices, including optimizing time from clinical presentation to surgery.
As expected, patients who experienced longer delays from presentation to surgery were on average, more comorbid and more likely to yield abnormal preoperative lab values. However, in the adjusted analysis, delay in time-to-surgery, presumably for medical management, was not found to be associated with improved outcomes. In the same adjusted analysis, we uniquely identified that in the patients whose surgeries were delayed for more than 48 hours, the time from surgery-to-discharge was significantly increased. As a result, these patients spent extra days in the hospital both preoperatively and postoperatively, but without any corollary improvement in the outcomes.
Continue to: Recent estimates of the cost of hospital admission...
Recent estimates of the cost of hospital admission is approximated nationally at $2000/day.26 Although our data fail to support the formal cost-analysis of the effect of time-to-surgery in hip fracture care, a simple value-based analysis indicates that quality is preserved (no difference in outcome), whereas costly hospital days are eliminated with earlier surgery. The value in elderly hip fracture care. defined as the outcomes relative to the costs,7 is ultimately optimized by earlier time-to-surgery.
Although using a large, multi-institutional database is advantageous for finding population-based trends that are representative of a large cohort, using the ACS-NSQIP database features its limitations. Our analysis was limited to the defined scope of NSQIP and nature of the injury, whereas root cause for delay was not available for study. We were unable to identify which patients were delayed for administrative reasons or surgical convenience and which were delayed for medical optimization. Participation in the ACS-NSQIP database is voluntary, and no randomized hospital sampling was conducted. Participating hospitals were de-identified in the database. As expected, we were unable to identify the specific institution-based hip fracture protocols that may affect the outcomes following treatment for these fractures. Further, socioeconomic information and payer-status are unavailable for the study. Additionally, observations are limited to 30 days postoperative, and we cannot comment on longer-term outcomes. Finally, discharge disposition and functional outcome data are not represented, and we were unable to correlate time-to-surgery and functional recovery. However, previous studies have established that delay in time-to-surgery following hip fractures is negatively correlated with functional outcomes.22-25
Nevertheless, the ACS-NSQIP database remains one of the largest American surgical databases available, and includes care centers from nearly every state with variable demographics including rural, urban, and academic centers. The ACS performs broad-based inter-rater reliability audits on every participating site and has found an overall disagreement rate of only 1.8%. As such, although discrepancies exist between the complete patient chart and the data entered, the data found in the ACS-NSQIP database are reliable and considered a valid source of study.34,35 The large sample size, quality of data collection, wide geographic representation, and varied hospital types within the dataset possibly make our findings relevant in the majority of American healthcare settings.
CONCLUSION
This study demonstrates an associated increased length of hospital stay, including the increased time from surgery-to-discharge, in patients with hip fractures whose surgical intervention is delayed for >48 hours after presentation. Given the prior evidence that early surgical intervention improves the functional outcomes and the current evidence that surgical delay for any cause increases costly hospital length of stay without corollary improvement in the outcomes, a value-based assessment of hip fracture care argues for early surgical intervention whenever possible. Our findings should inform physician, institution, and policy maker value-based decision making regarding the best practices in geriatric hip fracture care.
ABSTRACT
The morbidity and mortality after hip fracture in the elderly are influenced by non-modifiable comorbidities. Time-to-surgery is a modifiable factor that may play a role in postoperative morbidity. This study investigates the outcomes and complications in the elderly hip fracture surgery as a function of time-to-surgery.
Using the American College of Surgeons-National Surgical Quality Improvement Program data from 2011 to 2012, a study population was generated using the Current Procedural Terminology codes for percutaneous or open treatment of femoral neck fractures (27235, 27236) and fixation with a screw and side plate or intramedullary fixation (27244, 27245) for peritrochanteric fractures. Three time-to-surgery groups (<24 hours to surgical intervention, 24-48 hours, and >48 hours) were created and matched for surgery type, sex, age, and American Society of Anesthesiologists class. Time-to-surgery was then studied for its effect on the post-surgical outcomes using the adjusted regression modeling.
A study population of 6036 hip fractures was created, and 2012 patients were assigned to each matched time-to-surgery group. The unadjusted models showed that the earlier surgical intervention groups (<24 hours and 24-48 hours) exhibited a lower overall complication rate (P = .034) compared with the group waiting for surgery >48 hours. The unadjusted mortality rates increased with delay to surgical intervention (P = .039). Time-to-surgery caused no effect on the return to the operating room rate (P = .554) nor readmission rate (P = .285). Compared with other time-to-surgeries, the time-to-surgery of >48 hours was associated with prolonged total hospital length of stay (10.9 days) (P < .001) and a longer surgery-to-discharge time (hazard ratio, 95% confidence interval: 0.74, 0.69-0.79) (P < .001). Adjusted analyses showed no time-to-surgery related difference in complications (P = .143) but presented an increase in the total length of stay (P < .001) and surgery-to-discharge time (P < .001).
Timeliness of surgical intervention in a comorbidity-adjusted population of elderly hip fracture patients causes no effect on the overall complications, readmissions, nor 30-day mortality. However, time-to-surgery of >48 hours is associated with costly increase in the total length of stay, including an increased post-surgery-to-discharge time.
Continue to: Despite the best efforts to optimize surgical care...
Despite the best efforts to optimize surgical care and postoperative rehabilitation following hip fracture, elderly patients feature alarmingly high in-hospital and 1-year mortality rates of 4.35% to 9.2%1-4 and 36%,5 respectively. Those who survive are unlikely to return to independent living, with only 17% of the patients following hip fracture being able to walk independently 6 months postoperatively, and 12% being able to climb stairs6. Possibly, these poor outcomes reflect a preoperative medical comorbidity burden rather than a measure of medical or surgical quality. Given the absence of consensus regarding optimal time-to-surgery, treating physicians often opt to delay surgical intervention for the purposes of medically optimizing highly comorbid patients without significant data to suggest clinical benefit of such practice.
Numerous investigators have attempted to identify the modifiable risk factors for complication after surgical care of elderly hip fracture patients. However, consensus guidelines of care are missing. This condition is largely due to the difficulties in effectively modifying preoperative demographic and medical comorbidities on a semi-urgent basis. However, timeliness to surgery is one area for study that the care team can affect. Although time-to-surgery is dependent on multiple factors, including time of presentation, day of week of admission, difficulties with scheduling, and administrative delays, the care team plays a role in hastening or retarding time-to-surgery. Several studies have considered various time cut-offs (24, 48, 72, and 120 hours) to define early intervention, but none have defined a specific role for early or delayed surgery. Several investigators have discovered a positive association between delayed time-to-surgery and mortality;4,8-14 however, the most rigorously conducted studies that stringently control for preoperative comorbidities and demographics conclude that variance in time-to-surgery causes no effect on the in-hospital or 1-year mortality risk.1-3,15-18
Other investigators have shown that with early surgical intervention for hip fracture, patients experience shorter hospital stays,1,3,16,17,19-22 less days in pain,19 decreased risk of decubitus ulcers,15,17,19,22 and an increased likelihood of independence following fracture,22-25 regardless of preoperative medical status. Despite this evidence of improved outcomes with early surgery, 40% to 54% of hip fracture patients in the United States experience surgical delays of more than 24 to 48 hours. Additionally, with the recent (2013) national estimates of cost per day spent in the hospital falling between $1791 to $2289,26 minimizing the days spent in the hospital would likely lead to significant cost-savings, presuming no adverse effect on health-related outcomes. To this end, we hypothesize that the value (outcomes per associated cost)7 of hip fracture surgical care can be positively influenced by minimizing surgical wait-times. We assessed the effect of early surgical intervention, within 24 or 48 hours of presentation, on 30-day mortality, postoperative morbidity, hospital length of stay, and readmission rates in a comorbidity-adjusted population from a nationally representative cohort.
Continue to: METHODS AND MATERIALS...
METHODS AND MATERIALS
This study used the data from the American College of Surgeon-National Surgical Quality Improvement Program (ACS-NSQIP) database. With over 258 participating hospitals, this database has been widely used to identify national trends in various surgical specialties.27-34 The database includes information from participants in 43 states with hospitals ranging from rural community hospitals to large academic centers. Each site employs surgical clinical reviewers who are rigorously trained to collect data through chart review and discussion with the treating surgeon and/or patient,35 allowing for the use of robust and quality data with proven inter-rater reliability.36,37
Using the 2011 to 2012 NSQIP database, we used primary Current Procedural Terminology codes to identify all patients who underwent percutaneous (27235) or open (27236) fixation of femoral neck fractures; and fixation with a screw and side plate (27244) or intramedullary fixation (27245) for peritrochanteric fractures. The sample was divided into 3 time-to-surgery groups (<24 hours from presentation to surgery, 24-48 hours, and >48 hours) which were matched for fracture type (femoral neck or peritrochanteric), sex, age (under 75 years or ≥75 years), and American Society of Anesthesiologists (ASA) class used as a surrogate for severity of medical infirmary. The subjects were randomly matched 1:1:1 to create 3 statistically equivalent time-to-surgery groups using Proc SurveySelect (SAS version 9.2, SAS Institute).
Generalized linear models using logit link function for binary variables and identity link function for normally distributed characteristics were used to compare the 3 time-to-surgery groups. Descriptive statistics are presented as counts and percentages or least-square means with standard deviations. Preoperative lab values that were not normally distributed were log transformed and presented in their original scales with median values and 25th to 75th percentiles. Outcomes were similarly modeled.
Total hospital stay was modeled with a negative binomial distribution. Proportional hazards models were used to model the time from operating room (OR) to discharge, censoring patients who died before discharge, with results presented as hazard ratios (HR) and 95% confidence intervals (CI) (Figure). The assumption of the proportional hazards was tested using a Wald test. Using this model, a HR of <1 denotes a longer postoperative hospital stay, as a longer hospital stay decreases the “risk” for discharge.
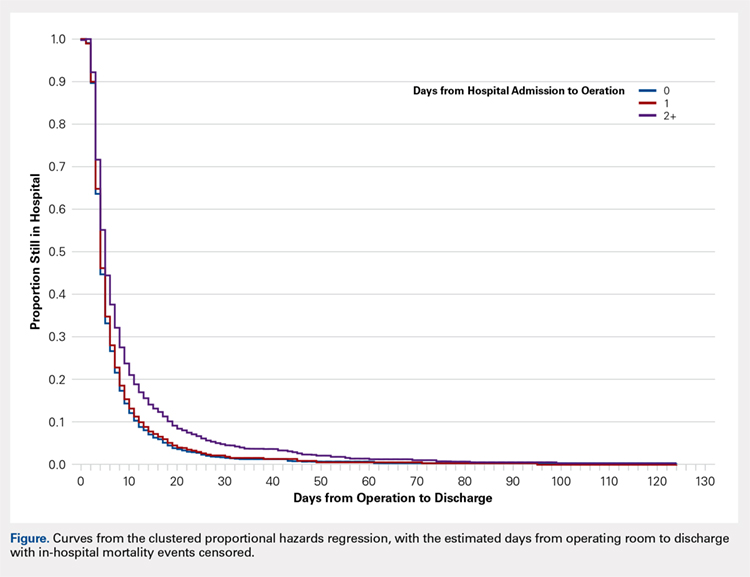
All models were adjusted for confounders, including race, body mass index (BMI), hypertension, chronic obstructive pulmonary disease, cancer, bleeding disorders, transfusion within 72 hours before surgery, preoperative levels of creatinine, platelet count, white blood cells (WBCs), hematocrit anesthesia type, and wound infection. These covariates were selected based upon their observed relationship to the studied outcomes and time-to-surgery groups, and were evaluated across the models for all outcomes for consistency and clarity. All statistical analyses were run at a type I error rate of 5% and performed in SAS version 9.2 software.
Continue to: RESULTS...
RESULTS
A study population of 6036 hip fractures was identified and divided into 3 groups of 2012 subjects each based upon time-to-surgery. The groups were successfully matched for surgery type, age (≥75 years old), gender, and ASA class. In each group, 594 of the 2012 (29.5%) patients were male, 1525 (75.8%) were ≥75 years of age, 9 (.5%) were ASA Class I, 269 (13.4%) were ASA Class II, 1424 (70.8%) were ASA class III, and 309 (15.4%) were ASA class IV.
Significant differences in preoperative comorbidity burden and preoperative lab values were identified between the 3 cohorts. Increased time-to-surgery was associated with differences in race (P < .001), elevated BMI (P = .010), higher rates of congestive heart failure (P < .001), hypertension medication (P = .020), bleeding disorders (P < .001), blood transfusion within 72 hours of surgery (P < .001), and systemic sepsis (P = .001). Delay to surgery was also associated with lower preoperative sodium (P = .005), blood urea nitrogen (P = .013), serum WBC (P < .001), hematocrit (P < .001), and platelets (P < .001) (Table 1).
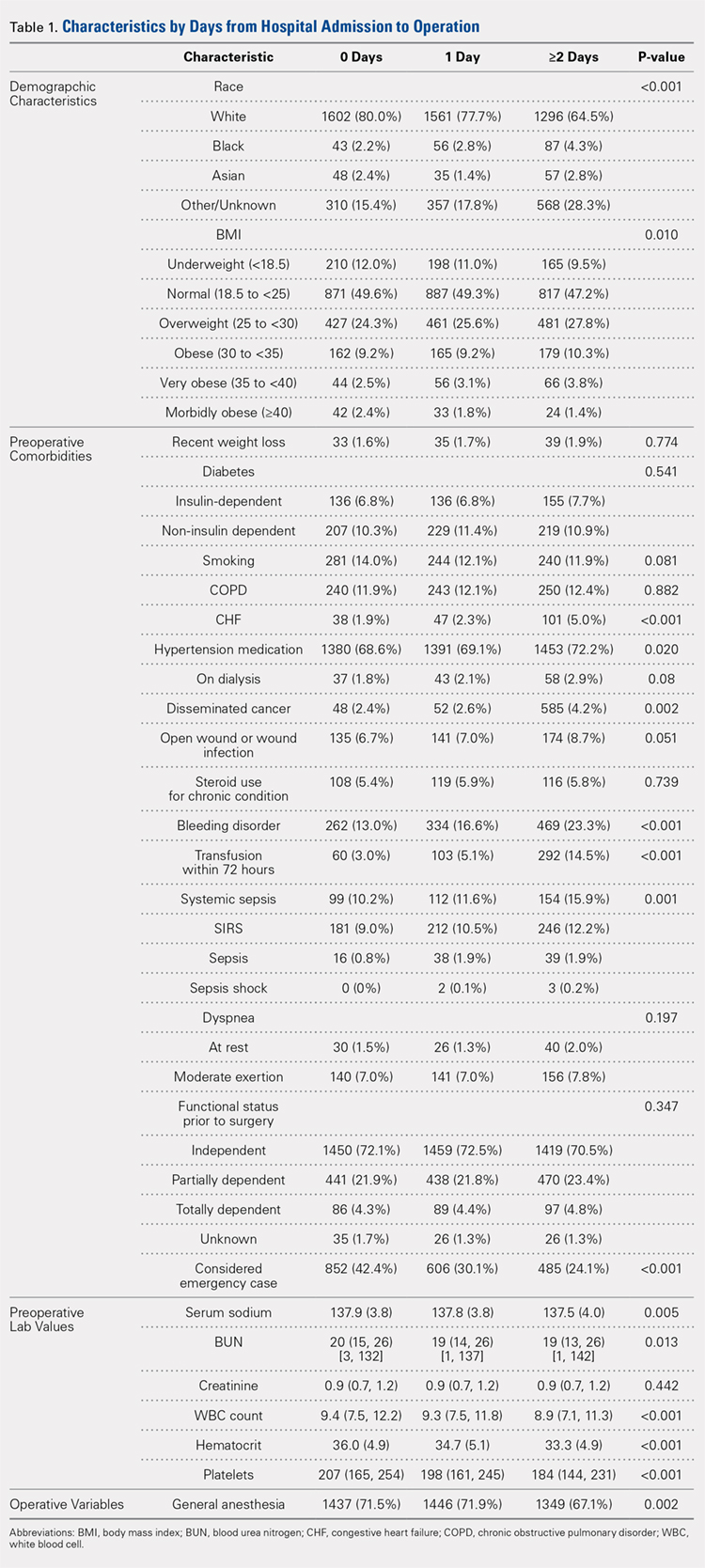
The unadjusted analyses revealed no association between time-to-surgery and return to OR (P = .554) nor readmission (P = .285). However, increasing time-to-surgery was associated with an increase in overall complications (P = .034), total length of hospital stay (P < .001), and 30-day mortality (P = .039) (Table 2).
Table 2. Estimated Event Rates from Matched Cohorts (Unadjusted)
| Time From Presentation to Definitive Fixation | |||
Outcomes | <24 hours | 24-48 hours | >48 hours | P-value |
Overall complication rate | 15.30% | 15.30% | 17.90% | 0.034 |
Total length of stay | 5.4 | 6.7 | 10.9 | <0.001 |
(mean days, 95% confidence interval) | (5.2, 5.7) | (6.5, 7.0) | (10.3, 11.5) | |
Time from OR to discharge | -ref- | 0.96 | 0.74 | <0.001 |
(Hazard ratio) | (0.90,1.02) | (0.69, 0.79) | ||
Return to OR | 2.40% | 2.40% | 2.00% | 0.554 |
Readmission | 9.60% | 8.40% | 8.30% | 0.285 |
30-day mortality rate | 5.80% | 5.30% | 7.20% | 0.039 |
Abbreviation: OR, operating room.
The adjusted analysis controlling for preoperative demographic and comorbidity variables revealed trends toward the increased overall complications and 30-day mortality with increased time-to-surgery; these trends showed no statistical significance (P = .143 and P = .08). No statistical relationship was observed between return to OR nor readmission and time-to-surgery. Increasing time-to-surgery remained significantly associated with the increased total length of hospital stay (P < .001). The adjusted analysis also revealed that the delay of >48 hours in time-to-surgery resulted in a longer surgery-to-discharge time (P < .001) (Table 3). No evidence of violation of the proportional hazards assumption was observed in the unadjusted nor adjusted clustered proportional hazards models (Wald test, P = .27 and P = .25, respectively).
Table 3. Estimated Event Rates from Matched Cohorts (Adjusteda)
| Time from Presentation to Definitive Fixation | |||
Outcomes | <24 hours | 24-48 hours | >48 hours | P-value |
Overall complication rate | 11.70% | 10.70% | 12.60% | 0.143 |
Total length of stay | 4.2 | 5.1 | 7.6 | <0.001 |
(mean days, 95% confidence interval) | (4.0, 4.5) | (4.8, 5.5) | (7.1, 8.3) | |
Time from OR to discharge | -ref- | 1.03 | 0.87 | <0.001 |
(Hazard ratio) | (0.97, 1.09) | (0.81, 0.92) | ||
Return to OR | 2.10% | 2.10% | 1.60% | 0.541 |
Readmission | 7.20% | 6.40% | 6.00% | 0.304 |
30-day mortality rate | 4.20% | 3.70% | 5.20% | 0.08 |
aModel adjusted for race, hypertension medication, cancer, bleeding disorders, transfusion within 72 hours before surgery, emergency status, wound infection, anesthesia type (general), body mass index (18.5-25), history of chronic obstructive pulmonary disease, and preoperative levels of creatinine, platelet count, white blood cell count, and hematocrit.
Continue to: DISCUSSION...
DISCUSSION
Previous research has demonstrated an association between age,3,4,25 comorbidity burden,1,3,25 gender,3,4 and ASA class4,18,21 with outcomes following hip fractures and serves as the basis of our matched analysis statistical methodology in assessing the effect of time-to-surgery on the outcome following hip fracture surgery. Prior investigators have also established the positive correlation between increased preoperative comorbidity burden and delay in time-to-surgery.10,15 This finding was confirmed in our unadjusted comparison of 3 time-to-surgery groups. However, prior investigations have not established a clear association between time-to-surgical intervention and postoperative morbidity and mortality.1,15,16,18,20,38 This study utilized a nationally representative dataset known for its data integrity and from which 6036 patients with surgically treated hip fractures, matched for surgery type, age, gender, and ASA class (a surrogate for severity of medical infirmary), were studied using adjusted regression modeling to afford an isolated statistical assessment of the effect of time-to-surgery on outcomes following hip fracture surgery.
Despite a large sample size and rigorous statistical methodology, for many outcome measures, our results show no support for the early or late operative intervention following hip fracture. We found no difference in 30-day mortality, readmission rate, nor total complication rate between the 3 time-to-surgery cohorts. This result indicates that the care of elderly patients following hip fracture is inherently complicated and that perioperative complication risk is probably only modestly modifiable by best medical practices, including optimizing time from clinical presentation to surgery.
As expected, patients who experienced longer delays from presentation to surgery were on average, more comorbid and more likely to yield abnormal preoperative lab values. However, in the adjusted analysis, delay in time-to-surgery, presumably for medical management, was not found to be associated with improved outcomes. In the same adjusted analysis, we uniquely identified that in the patients whose surgeries were delayed for more than 48 hours, the time from surgery-to-discharge was significantly increased. As a result, these patients spent extra days in the hospital both preoperatively and postoperatively, but without any corollary improvement in the outcomes.
Continue to: Recent estimates of the cost of hospital admission...
Recent estimates of the cost of hospital admission is approximated nationally at $2000/day.26 Although our data fail to support the formal cost-analysis of the effect of time-to-surgery in hip fracture care, a simple value-based analysis indicates that quality is preserved (no difference in outcome), whereas costly hospital days are eliminated with earlier surgery. The value in elderly hip fracture care. defined as the outcomes relative to the costs,7 is ultimately optimized by earlier time-to-surgery.
Although using a large, multi-institutional database is advantageous for finding population-based trends that are representative of a large cohort, using the ACS-NSQIP database features its limitations. Our analysis was limited to the defined scope of NSQIP and nature of the injury, whereas root cause for delay was not available for study. We were unable to identify which patients were delayed for administrative reasons or surgical convenience and which were delayed for medical optimization. Participation in the ACS-NSQIP database is voluntary, and no randomized hospital sampling was conducted. Participating hospitals were de-identified in the database. As expected, we were unable to identify the specific institution-based hip fracture protocols that may affect the outcomes following treatment for these fractures. Further, socioeconomic information and payer-status are unavailable for the study. Additionally, observations are limited to 30 days postoperative, and we cannot comment on longer-term outcomes. Finally, discharge disposition and functional outcome data are not represented, and we were unable to correlate time-to-surgery and functional recovery. However, previous studies have established that delay in time-to-surgery following hip fractures is negatively correlated with functional outcomes.22-25
Nevertheless, the ACS-NSQIP database remains one of the largest American surgical databases available, and includes care centers from nearly every state with variable demographics including rural, urban, and academic centers. The ACS performs broad-based inter-rater reliability audits on every participating site and has found an overall disagreement rate of only 1.8%. As such, although discrepancies exist between the complete patient chart and the data entered, the data found in the ACS-NSQIP database are reliable and considered a valid source of study.34,35 The large sample size, quality of data collection, wide geographic representation, and varied hospital types within the dataset possibly make our findings relevant in the majority of American healthcare settings.
CONCLUSION
This study demonstrates an associated increased length of hospital stay, including the increased time from surgery-to-discharge, in patients with hip fractures whose surgical intervention is delayed for >48 hours after presentation. Given the prior evidence that early surgical intervention improves the functional outcomes and the current evidence that surgical delay for any cause increases costly hospital length of stay without corollary improvement in the outcomes, a value-based assessment of hip fracture care argues for early surgical intervention whenever possible. Our findings should inform physician, institution, and policy maker value-based decision making regarding the best practices in geriatric hip fracture care.
1. Vidán MT, Sánchez E, Gracia Y, Marañón E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med. 2011;155(4):226-233. doi:10.7326/0003-4819-155-4-201108160-00006.
2. Verbeek DO, Ponsen KJ, Goslings JC, Heetveld MJ. Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop. 2008;32(1):13-18. doi:10.1007/s00264-006-0290-9.
3. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009;91(7):922-927. doi:10.1302/0301-620X.91B7.22446.
4. Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726-729. doi:10.1016/j.injury.2012.08.025.
5. Zuckerman JD. Hip fracture. N Engl J Med. 1996;334(23):1519-1525. doi:10.1056/NEJM199606063342307.
6. Marottoli RA, Berkman LF, Cooney LM Jr. Decline in physical function following hip fracture. J Am Geriatr Soc. 1992;40(9):861-866. doi:10.1111/j.1532-5415.1992.tb01980.x.
7. Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477-2481. doi:10.1056/NEJMp1011024.
8. Radcliff TA, Henderson WG, Stoner TJ, Khuri SF, Dohm M, Hutt E. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008;90(1):34-42. doi:10.2106/JBJS.G.00065.
9. Novack V, Jotkowitz A, Etzion O, Porath A. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int J Qual Health Care. 2007;19(3):170-176. doi:10.1093/intqhc/mzm003.
10. Weller I, Wai EK, Jaglal S, Kreder HJ. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005;87(3):361-366. doi:10.1302/0301-620X.87B3.15300.
11. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483-489. doi:10.2106/JBJS.D.01796.
12. Holt G, Smith R, Duncan K, McKeown DW. Does delay to theatre for medical reasons affect the peri-operative mortality in patients with a fracture of the hip? J Bone Joint Surg Br. 2010;92(6):835-841. doi:10.1302/0301-620X.92B6.24463.
13. Pioli G, Lauretani F, Davoli ML, et al. Older people with hip fracture and IADL disability require earlier surgery. J Gerontol A Biol Sci Med Sci. 2012;67(11):1272-1277. doi:10.1093/gerona/gls097.
14. Mackenzie DG, Wild S, Muir R. Mortality associated with delay in operation after hip fracture: Scottish data provide additional information. BMJ. 2006;332(7549):1093. doi:10.1136/bmj.332.7549.1093.
15. Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112(9):702-709. doi:10.1016/S0002-9343(02)01119-1.
16. Majumdar SR, Beaupre LA, Johnston DW, Dick DA, Cinats JG, Jiang HX. Lack of association between mortality and timing of surgical fixation in elderly patients with hip fracture: results of a retrospective population-based cohort study. Med Care. 2006;44(6):552-559. doi:10.1097/01.mlr.0000215812.13720.2e.
17. Hommel A, Ulander K, Bjorkelund KB, Norrman PO, Wingstrand H, Thorngren KG. Influence of optimised treatment of people with hip fracture on time to operation, length of hospital stay, reoperations and mortality within 1 year. Injury. 2008;39(10):1164-1174. doi:10.1016/j.injury.2008.01.048.
18. Rae HC, Harris IA, McEvoy L, Todorova T. Delay to surgery and mortality after hip fracture. ANZ J Surg. 2007;77(10):889-891. doi:10.1111/j.1445-2197.2007.04267.x.
19. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738-1743. doi:10.1001/jama.291.14.1738.
20. Bergeron E, Lavoie A, Moore L, et al. Is the delay to surgery for isolated hip fracture predictive of outcome in efficient systems? J Trauma. 2006;60(4):753-757. doi:10.1097/01.ta.0000214649.53190.2a.
21. Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8):1123-1126. doi:10.1302/0301-620X.87B8.16357.
22. Al-Ani AN, Samuelsson B, Tidermark J, et al. Early operation on patients with a hip fracture improved the ability to return to independent living. A prospective study of 850 patients. J Bone Joint Surg Am. 2008;90(7):1436-1442. doi:10.2106/JBJS.G.00890.
23. Hoenig H, Rubenstein LV, Sloane R, Horner R, Kahn K. What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med. 1997;157(5):513-520.
24. Doruk H, Mas MR, Yildiz C, Sonmez A, Kýrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39(2):179-185. doi:10.1016/j.archger.2004.03.004.
25. Yonezawa T, Yamazaki K, Atsumi T, Obara S. Influence of the timing of surgery on mortality and activity of hip fracture in elderly patients. J Orthop Sci Off J Jpn Orthop Assoc. 2009;14(5):566-573. doi:10.1007/s00776-009-1380-5.
26. Henry J Kaiser Family Foundation. Hospital adjusted expenses per inpatient day by ownership. https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day-by-ownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed March 14, 2013.
27. Belmont PJ Jr, Davey S, Orr JD, Ochoa LM, Bader JO, Schoenfeld AJ. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg. 2011;213(3):370-378. doi:10.1016/j.jamcollsurg.2011.05.019.
28. Davis SS Jr, Husain FA, Lin E, Nandipati KC, Perez S, Sweeney JF. Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg. 2013;216(1):96-104. doi:10.1016/j.jamcollsurg.2012.08.014.
29. Gart MS, Smetona JT, Hanwright PJ, et al. Autologous options for postmastectomy breast reconstruction: a comparison of outcomes based on the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216(2):229-238. doi:10.1016/j.jamcollsurg.2012.11.003.
30. Greenblatt DY, Rajamanickam V, Pugely AJ, Heise CP, Foley EF, Kennedy GD. Short-term outcomes after laparoscopic-assisted proctectomy for rectal cancer: results from the ACS NSQIP. J Am Coll Surg. 2011;212(5):844-854. doi:10.1016/j.jamcollsurg.2011.01.005.
31. Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013;95(3):193-199. doi:10.2106/JBJS.K.01682.
32. Rao RD. Risk factors for complications and mortality after spine surgery assessed with the NSQIP database: where do we go from here? Commentary on an article by Andrew J Schoenfeld, MD, et al.: "Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program". J Bone Joint Surg Am. 2011;93(17):e101:(101-102). doi:10.2106/JBJS.K.00786.
33. Schilling PL, Hallstrom BR, Birkmeyer JD, Carpenter JE. Prioritizing perioperative quality improvement in orthopaedic surgery. J Bone Joint Surg Am. 2010;92(9):1884-1889. doi:10.2106/JBJS.I.00735.
34. Tsilimparis N, Perez S, Dayama A, Ricotta JJ 2nd. Age-stratified results from 20,095 aortoiliac aneurysm repairs: should we approach octogenarians and nonagenarians differently? J Am Coll Surg. 2012;215(5):690-701. doi:10.1016/j.jamcollsurg.2012.06.411.
35. ACS National Surgical Quality Improvement Program. American College of Surgeons Web site. https://www.facs.org/quality-programs/acs-nsqip?. Accessed March 14, 2013.
36. Henderson WG, Daley J. Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg. 2009;198(5 Suppl):S19-S27. doi:10.1016/j.amjsurg.2009.07.025.
37. Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210(1):6-16. doi:10.1016/j.jamcollsurg.2009.09.031.
38. Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40(7):692-697. doi:10.1016/j.injury.2009.01.010.
1. Vidán MT, Sánchez E, Gracia Y, Marañón E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med. 2011;155(4):226-233. doi:10.7326/0003-4819-155-4-201108160-00006.
2. Verbeek DO, Ponsen KJ, Goslings JC, Heetveld MJ. Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop. 2008;32(1):13-18. doi:10.1007/s00264-006-0290-9.
3. Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM. Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br. 2009;91(7):922-927. doi:10.1302/0301-620X.91B7.22446.
4. Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726-729. doi:10.1016/j.injury.2012.08.025.
5. Zuckerman JD. Hip fracture. N Engl J Med. 1996;334(23):1519-1525. doi:10.1056/NEJM199606063342307.
6. Marottoli RA, Berkman LF, Cooney LM Jr. Decline in physical function following hip fracture. J Am Geriatr Soc. 1992;40(9):861-866. doi:10.1111/j.1532-5415.1992.tb01980.x.
7. Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477-2481. doi:10.1056/NEJMp1011024.
8. Radcliff TA, Henderson WG, Stoner TJ, Khuri SF, Dohm M, Hutt E. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008;90(1):34-42. doi:10.2106/JBJS.G.00065.
9. Novack V, Jotkowitz A, Etzion O, Porath A. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int J Qual Health Care. 2007;19(3):170-176. doi:10.1093/intqhc/mzm003.
10. Weller I, Wai EK, Jaglal S, Kreder HJ. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br. 2005;87(3):361-366. doi:10.1302/0301-620X.87B3.15300.
11. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483-489. doi:10.2106/JBJS.D.01796.
12. Holt G, Smith R, Duncan K, McKeown DW. Does delay to theatre for medical reasons affect the peri-operative mortality in patients with a fracture of the hip? J Bone Joint Surg Br. 2010;92(6):835-841. doi:10.1302/0301-620X.92B6.24463.
13. Pioli G, Lauretani F, Davoli ML, et al. Older people with hip fracture and IADL disability require earlier surgery. J Gerontol A Biol Sci Med Sci. 2012;67(11):1272-1277. doi:10.1093/gerona/gls097.
14. Mackenzie DG, Wild S, Muir R. Mortality associated with delay in operation after hip fracture: Scottish data provide additional information. BMJ. 2006;332(7549):1093. doi:10.1136/bmj.332.7549.1093.
15. Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112(9):702-709. doi:10.1016/S0002-9343(02)01119-1.
16. Majumdar SR, Beaupre LA, Johnston DW, Dick DA, Cinats JG, Jiang HX. Lack of association between mortality and timing of surgical fixation in elderly patients with hip fracture: results of a retrospective population-based cohort study. Med Care. 2006;44(6):552-559. doi:10.1097/01.mlr.0000215812.13720.2e.
17. Hommel A, Ulander K, Bjorkelund KB, Norrman PO, Wingstrand H, Thorngren KG. Influence of optimised treatment of people with hip fracture on time to operation, length of hospital stay, reoperations and mortality within 1 year. Injury. 2008;39(10):1164-1174. doi:10.1016/j.injury.2008.01.048.
18. Rae HC, Harris IA, McEvoy L, Todorova T. Delay to surgery and mortality after hip fracture. ANZ J Surg. 2007;77(10):889-891. doi:10.1111/j.1445-2197.2007.04267.x.
19. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738-1743. doi:10.1001/jama.291.14.1738.
20. Bergeron E, Lavoie A, Moore L, et al. Is the delay to surgery for isolated hip fracture predictive of outcome in efficient systems? J Trauma. 2006;60(4):753-757. doi:10.1097/01.ta.0000214649.53190.2a.
21. Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8):1123-1126. doi:10.1302/0301-620X.87B8.16357.
22. Al-Ani AN, Samuelsson B, Tidermark J, et al. Early operation on patients with a hip fracture improved the ability to return to independent living. A prospective study of 850 patients. J Bone Joint Surg Am. 2008;90(7):1436-1442. doi:10.2106/JBJS.G.00890.
23. Hoenig H, Rubenstein LV, Sloane R, Horner R, Kahn K. What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture? Arch Intern Med. 1997;157(5):513-520.
24. Doruk H, Mas MR, Yildiz C, Sonmez A, Kýrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39(2):179-185. doi:10.1016/j.archger.2004.03.004.
25. Yonezawa T, Yamazaki K, Atsumi T, Obara S. Influence of the timing of surgery on mortality and activity of hip fracture in elderly patients. J Orthop Sci Off J Jpn Orthop Assoc. 2009;14(5):566-573. doi:10.1007/s00776-009-1380-5.
26. Henry J Kaiser Family Foundation. Hospital adjusted expenses per inpatient day by ownership. https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day-by-ownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed March 14, 2013.
27. Belmont PJ Jr, Davey S, Orr JD, Ochoa LM, Bader JO, Schoenfeld AJ. Risk factors for 30-day postoperative complications and mortality after below-knee amputation: a study of 2,911 patients from the national surgical quality improvement program. J Am Coll Surg. 2011;213(3):370-378. doi:10.1016/j.jamcollsurg.2011.05.019.
28. Davis SS Jr, Husain FA, Lin E, Nandipati KC, Perez S, Sweeney JF. Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg. 2013;216(1):96-104. doi:10.1016/j.jamcollsurg.2012.08.014.
29. Gart MS, Smetona JT, Hanwright PJ, et al. Autologous options for postmastectomy breast reconstruction: a comparison of outcomes based on the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216(2):229-238. doi:10.1016/j.jamcollsurg.2012.11.003.
30. Greenblatt DY, Rajamanickam V, Pugely AJ, Heise CP, Foley EF, Kennedy GD. Short-term outcomes after laparoscopic-assisted proctectomy for rectal cancer: results from the ACS NSQIP. J Am Coll Surg. 2011;212(5):844-854. doi:10.1016/j.jamcollsurg.2011.01.005.
31. Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013;95(3):193-199. doi:10.2106/JBJS.K.01682.
32. Rao RD. Risk factors for complications and mortality after spine surgery assessed with the NSQIP database: where do we go from here? Commentary on an article by Andrew J Schoenfeld, MD, et al.: "Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program". J Bone Joint Surg Am. 2011;93(17):e101:(101-102). doi:10.2106/JBJS.K.00786.
33. Schilling PL, Hallstrom BR, Birkmeyer JD, Carpenter JE. Prioritizing perioperative quality improvement in orthopaedic surgery. J Bone Joint Surg Am. 2010;92(9):1884-1889. doi:10.2106/JBJS.I.00735.
34. Tsilimparis N, Perez S, Dayama A, Ricotta JJ 2nd. Age-stratified results from 20,095 aortoiliac aneurysm repairs: should we approach octogenarians and nonagenarians differently? J Am Coll Surg. 2012;215(5):690-701. doi:10.1016/j.jamcollsurg.2012.06.411.
35. ACS National Surgical Quality Improvement Program. American College of Surgeons Web site. https://www.facs.org/quality-programs/acs-nsqip?. Accessed March 14, 2013.
36. Henderson WG, Daley J. Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg. 2009;198(5 Suppl):S19-S27. doi:10.1016/j.amjsurg.2009.07.025.
37. Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210(1):6-16. doi:10.1016/j.jamcollsurg.2009.09.031.
38. Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40(7):692-697. doi:10.1016/j.injury.2009.01.010.
TAKE-HOME POINTS
- Time-to-surgery for definitive fixation of hip fractures is a modifiable risk factor.
- This study fails to demonstrate a benefit in delaying surgery for medical optimization as there were no time-to-surgery related differences in complications (P = 1.43).
- Delay in definitive surgery results in an increase in the total length of stay (P < .001) and surgery-to-discharge time (P < .001) without an improvement in overall complications, readmission or 30-day mortality rates.
- Despite numerous investigations, there are no consensus guidelines to decrease complications and mortality rates following hip fracture surgery.
- ACS-NSQIP database is a reliable and validated database.
Recommendations to Improve Asthma Outcomes: Work Group Call to Action
Click here to read the supplement.
What can be done to address the burden of asthma beyond pharmacotherapy? A panel of experts discuss steps for addressing sensitization to allergens that trigger increased asthma burden.
Topics Include:
- Identifying Patients with Allergic Components of Asthma
- Identifying and Addressing Allergen Exposure in Daily Practice
- The Opportunity for Payers and Health Systems for Supporting Trigger Avoidance Education
Click here to read the supplement.
Click here to read the supplement.
What can be done to address the burden of asthma beyond pharmacotherapy? A panel of experts discuss steps for addressing sensitization to allergens that trigger increased asthma burden.
Topics Include:
- Identifying Patients with Allergic Components of Asthma
- Identifying and Addressing Allergen Exposure in Daily Practice
- The Opportunity for Payers and Health Systems for Supporting Trigger Avoidance Education
Click here to read the supplement.
Click here to read the supplement.
What can be done to address the burden of asthma beyond pharmacotherapy? A panel of experts discuss steps for addressing sensitization to allergens that trigger increased asthma burden.
Topics Include:
- Identifying Patients with Allergic Components of Asthma
- Identifying and Addressing Allergen Exposure in Daily Practice
- The Opportunity for Payers and Health Systems for Supporting Trigger Avoidance Education
Click here to read the supplement.
Glenn Close fights stigma; empty nesters share pleasures, pains
Glenn Close is infamous for her portrayal of a woman whose reactions to a one-night stand in “Fatal Attraction” become increasingly bizarre and hostile. Whether the character was in the throes of a mental disorder was never broached in the movie. But Ms. Close has real-life family experience; her sister has bipolar disorder and a nephew has schizophrenia.
“When I became an advocate, I realized that is a family affair for one in four of us. One in four is touched in some way by mental illness. So, it became obvious to me that we have to talk about it,” Ms. Close said in an interview on CBS Sunday Morning. In 2010, Ms. Close and her sister Jessie began Bring Change to Mind, a foundation that strives to move discussions about mental health into the mainstream.
Harm reduction and opioids
The “just say no” mantra to drug abstinence espoused by Nancy Reagan decades ago remains an option for some people today. However, according to an article in The Walrus, this approach does not cut it for many drug users. What may resonate is the harm they are inflicting on themselves and how they can lessen it by curbing drug use. In Ottawa, Canada, a program that features an individualized and flexible approach to opioid addiction, which continues to offer drugs while focusing on health instead of abstinence, is having a positive effect.
“I’m an opioid addict. That goes without saying if you’re in this program,” one participant says. “Struggling with addiction while being homeless creates a unique set of challenges ... the [program] provides not only freedom from drug addiction on the street but freedom from homelessness.”
Empty nesters’ new lives
The ritual of being a parent, for many, is the bittersweet day when the last or only child heads off to college or university. A recent segment on National Public Radio gauged the reactions of some parents. For some, the initial feeling is one of relief, with days that are quieter and perhaps encouraging of more personal exploration. “After 20 years of every moment being about the girls, it was once again just the two of us. Some things are really great – walking around the house naked, going to bed before it’s dark and not having children mock us, and having a tidy house,” says Michael Pusateri of South Pasadena, Calif.
“But, we do miss the girls,” he adds. “I miss the sound of them bumping around the house. And as corny as it sounds, I miss seeing them sleep.”
For others, the polar opposite prevails. “My job as a full-time, stay-at-home mom to four kids has finally come to an end after 31 years when our baby left for college last week. I’ve been dreading drop-off day for about a decade. The hardest part was walking back into the now empty house, feeling swallowed up by the silence. The tears flowed when I walked by her room for the first time knowing she won’t be saying goodnight, Mom, from behind that door every night. Saying goodbye to the last is especially difficult as I sit here in my empty nest, missing my daughter and wondering, now what?” relates Beth Smizlof of Saratoga Springs, N.Y.
“A hundred people will tell you how to raise your son, but very few will talk about how to let him go,” says Julie Stewart of Birmingham, Ala.
What is a hyperpolyglot?
An article in The New Yorker considers people whose linguistic mastery encompasses dozens of languages. To be a hyperpolyglot – defined as someone who can speak 11 or more languages – requires a lot of effort. And there may be a genetic predisposition, since there is evidence (which still requires confirmation) that “an extreme language learner has a more-than-random chance of being a gay, left-handed male on the autism spectrum, with an autoimmune disorder, such as asthma or allergies,” writes Judith Thurman.
A brain that is more apt to process the information needed to learn a new language may also be part of the picture.
Coffee and cancer warning
On Aug. 29, the Food and Drug Administration released a statement from Commissioner Scott Gottlieb, MD, that supports a proposal to exempt coffee from California’s cancer warning law. The action was prompted by a recent ruling by a California court that the state’s Proposition 65 could require labeling of coffee with a cancer warning, because of the presence of a chemical called acrylamide, which can form in many foods during frying, roasting, and baking.
“In coffee, acrylamide forms during the roasting of coffee beans. Although acrylamide at high doses has been linked to cancer in animals, and coffee contains acrylamide, current science indicates that consuming coffee poses no significant risk of cancer,” the statement reads in part.
Glenn Close is infamous for her portrayal of a woman whose reactions to a one-night stand in “Fatal Attraction” become increasingly bizarre and hostile. Whether the character was in the throes of a mental disorder was never broached in the movie. But Ms. Close has real-life family experience; her sister has bipolar disorder and a nephew has schizophrenia.
“When I became an advocate, I realized that is a family affair for one in four of us. One in four is touched in some way by mental illness. So, it became obvious to me that we have to talk about it,” Ms. Close said in an interview on CBS Sunday Morning. In 2010, Ms. Close and her sister Jessie began Bring Change to Mind, a foundation that strives to move discussions about mental health into the mainstream.
Harm reduction and opioids
The “just say no” mantra to drug abstinence espoused by Nancy Reagan decades ago remains an option for some people today. However, according to an article in The Walrus, this approach does not cut it for many drug users. What may resonate is the harm they are inflicting on themselves and how they can lessen it by curbing drug use. In Ottawa, Canada, a program that features an individualized and flexible approach to opioid addiction, which continues to offer drugs while focusing on health instead of abstinence, is having a positive effect.
“I’m an opioid addict. That goes without saying if you’re in this program,” one participant says. “Struggling with addiction while being homeless creates a unique set of challenges ... the [program] provides not only freedom from drug addiction on the street but freedom from homelessness.”
Empty nesters’ new lives
The ritual of being a parent, for many, is the bittersweet day when the last or only child heads off to college or university. A recent segment on National Public Radio gauged the reactions of some parents. For some, the initial feeling is one of relief, with days that are quieter and perhaps encouraging of more personal exploration. “After 20 years of every moment being about the girls, it was once again just the two of us. Some things are really great – walking around the house naked, going to bed before it’s dark and not having children mock us, and having a tidy house,” says Michael Pusateri of South Pasadena, Calif.
“But, we do miss the girls,” he adds. “I miss the sound of them bumping around the house. And as corny as it sounds, I miss seeing them sleep.”
For others, the polar opposite prevails. “My job as a full-time, stay-at-home mom to four kids has finally come to an end after 31 years when our baby left for college last week. I’ve been dreading drop-off day for about a decade. The hardest part was walking back into the now empty house, feeling swallowed up by the silence. The tears flowed when I walked by her room for the first time knowing she won’t be saying goodnight, Mom, from behind that door every night. Saying goodbye to the last is especially difficult as I sit here in my empty nest, missing my daughter and wondering, now what?” relates Beth Smizlof of Saratoga Springs, N.Y.
“A hundred people will tell you how to raise your son, but very few will talk about how to let him go,” says Julie Stewart of Birmingham, Ala.
What is a hyperpolyglot?
An article in The New Yorker considers people whose linguistic mastery encompasses dozens of languages. To be a hyperpolyglot – defined as someone who can speak 11 or more languages – requires a lot of effort. And there may be a genetic predisposition, since there is evidence (which still requires confirmation) that “an extreme language learner has a more-than-random chance of being a gay, left-handed male on the autism spectrum, with an autoimmune disorder, such as asthma or allergies,” writes Judith Thurman.
A brain that is more apt to process the information needed to learn a new language may also be part of the picture.
Coffee and cancer warning
On Aug. 29, the Food and Drug Administration released a statement from Commissioner Scott Gottlieb, MD, that supports a proposal to exempt coffee from California’s cancer warning law. The action was prompted by a recent ruling by a California court that the state’s Proposition 65 could require labeling of coffee with a cancer warning, because of the presence of a chemical called acrylamide, which can form in many foods during frying, roasting, and baking.
“In coffee, acrylamide forms during the roasting of coffee beans. Although acrylamide at high doses has been linked to cancer in animals, and coffee contains acrylamide, current science indicates that consuming coffee poses no significant risk of cancer,” the statement reads in part.
Glenn Close is infamous for her portrayal of a woman whose reactions to a one-night stand in “Fatal Attraction” become increasingly bizarre and hostile. Whether the character was in the throes of a mental disorder was never broached in the movie. But Ms. Close has real-life family experience; her sister has bipolar disorder and a nephew has schizophrenia.
“When I became an advocate, I realized that is a family affair for one in four of us. One in four is touched in some way by mental illness. So, it became obvious to me that we have to talk about it,” Ms. Close said in an interview on CBS Sunday Morning. In 2010, Ms. Close and her sister Jessie began Bring Change to Mind, a foundation that strives to move discussions about mental health into the mainstream.
Harm reduction and opioids
The “just say no” mantra to drug abstinence espoused by Nancy Reagan decades ago remains an option for some people today. However, according to an article in The Walrus, this approach does not cut it for many drug users. What may resonate is the harm they are inflicting on themselves and how they can lessen it by curbing drug use. In Ottawa, Canada, a program that features an individualized and flexible approach to opioid addiction, which continues to offer drugs while focusing on health instead of abstinence, is having a positive effect.
“I’m an opioid addict. That goes without saying if you’re in this program,” one participant says. “Struggling with addiction while being homeless creates a unique set of challenges ... the [program] provides not only freedom from drug addiction on the street but freedom from homelessness.”
Empty nesters’ new lives
The ritual of being a parent, for many, is the bittersweet day when the last or only child heads off to college or university. A recent segment on National Public Radio gauged the reactions of some parents. For some, the initial feeling is one of relief, with days that are quieter and perhaps encouraging of more personal exploration. “After 20 years of every moment being about the girls, it was once again just the two of us. Some things are really great – walking around the house naked, going to bed before it’s dark and not having children mock us, and having a tidy house,” says Michael Pusateri of South Pasadena, Calif.
“But, we do miss the girls,” he adds. “I miss the sound of them bumping around the house. And as corny as it sounds, I miss seeing them sleep.”
For others, the polar opposite prevails. “My job as a full-time, stay-at-home mom to four kids has finally come to an end after 31 years when our baby left for college last week. I’ve been dreading drop-off day for about a decade. The hardest part was walking back into the now empty house, feeling swallowed up by the silence. The tears flowed when I walked by her room for the first time knowing she won’t be saying goodnight, Mom, from behind that door every night. Saying goodbye to the last is especially difficult as I sit here in my empty nest, missing my daughter and wondering, now what?” relates Beth Smizlof of Saratoga Springs, N.Y.
“A hundred people will tell you how to raise your son, but very few will talk about how to let him go,” says Julie Stewart of Birmingham, Ala.
What is a hyperpolyglot?
An article in The New Yorker considers people whose linguistic mastery encompasses dozens of languages. To be a hyperpolyglot – defined as someone who can speak 11 or more languages – requires a lot of effort. And there may be a genetic predisposition, since there is evidence (which still requires confirmation) that “an extreme language learner has a more-than-random chance of being a gay, left-handed male on the autism spectrum, with an autoimmune disorder, such as asthma or allergies,” writes Judith Thurman.
A brain that is more apt to process the information needed to learn a new language may also be part of the picture.
Coffee and cancer warning
On Aug. 29, the Food and Drug Administration released a statement from Commissioner Scott Gottlieb, MD, that supports a proposal to exempt coffee from California’s cancer warning law. The action was prompted by a recent ruling by a California court that the state’s Proposition 65 could require labeling of coffee with a cancer warning, because of the presence of a chemical called acrylamide, which can form in many foods during frying, roasting, and baking.
“In coffee, acrylamide forms during the roasting of coffee beans. Although acrylamide at high doses has been linked to cancer in animals, and coffee contains acrylamide, current science indicates that consuming coffee poses no significant risk of cancer,” the statement reads in part.