User login
Poor gut health tied to increased systemic disease risk
LAKE TAHOE, CALIF. – according to Mark A. Underwood, MD.
“Antibiotic exposure changes the composition of the intestinal microbiota,” he said at the annual meeting of the Society for Pediatric Dermatology. “That clearly causes both antibiotic-associated diarrhea and Clostridium difficile colitis. The bigger question is, is it possible that intestinal dysbiosis is related to a whole bunch of other systemic diseases? In other words, does an insult during a critical window of development cause changes in the intestinal microbiota that can lead to systemic diseases in the brain, the lung, the liver, or the immune system?”
According Dr. Underwood, a pediatrician who is chief of the division of neonatology at the University of California, Davis, the prevalence of dysbiosis is increasing worldwide, particularly in developed countries, where Bifidobacteria are decreasing and Enterobacteriaceae are increasing. “Those changes are associated with gut permeability and alterations in both local and systemic inflammation, and the risk for a number of diseases, including atopic dermatitis,” he said. Key reasons for the increasing prevalence of dysbiosis, he continued, include the use of antibiotics, cesarean section delivery, formula feeding, changes in hygiene that alter the intestinal biota, the high-fat, high-sugar Western diet, and a loss of vertical and horizontal transmission over generations.
In an effort to evaluate the association between early childhood antibiotic use with allergic diseases in later childhood, Japanese researchers followed 1,200 infants to the age of 5 years (Ann Allergy Asthma Immunol. 2017;119:54-8). They found that antibiotic exposure within the first 2 years of life was associated with an increased risk of asthma (adjusted odds ratio 1.72), allergic rhinitis (adjusted OR 1.65), and atopic dermatitis (adjusted OR 1.40). In a more recent, smaller prospective study, 436 Dutch infants were followed to 1 year of age (Pediatr Allergy Immunol. 2018;29[2]:151-8). The researchers found that antibiotic exposure within the first week of life was associated with allergic sensitization (adjusted OR 3.26), colic (adjusted OR 1.66), and wheezing (adjusted OR 1.56).
In a study of 44 term infants with a family history of allergy, changes in the fecal microbiota, especially colonization with Ruminococcus gnavus, preceded the onset of allergic symptoms (Gastroenterol. 2018;154[1]:154-67). The same researchers observed similar findings in an animal model.
One potential mechanism by which intestinal dysbiosis causes systemic disease is stimulation of toll-like receptor 4 (TLR4), “which is a receptor on a variety of mucosal cells that senses the presence of a microbial pathogen-associated patterns, particularly those of Gram-negative Enterobacteriaceae,” Dr. Underwood explained. Other potential mechanisms include increased intestinal permeability, an increase in the pH and decreases in short-chain fatty acids within the gut lumen, and a loss of intraluminal hypoxia. “Think of the colon as an anaerobic chamber,” he said. “The colon lumen should be very low in oxygen. It should be dominated by obligate anaerobes.”
Efforts to prevent or treat dysbiosis-related diseases include the use of probiotics and fecal transplantation. A recent Cochrane review of 8,672 patients found “moderate certainty evidence” that probiotics are effective for preventing C. difficile-associated diarrhea. The analysis included 31 randomized, controlled trials of adults who were treated either with a probiotic or with a placebo. When pooled, the risk ratio was 0.40, which represented a significant protection. In addition, a summary of 7 randomized controlled trials and 30 case series suggests that fecal microbial transplantation is superior to vancomycin for adults with recurrent C. difficile colitis (relative risk 0.23) (Aliment Pharmacol Ther. 2017;46[5]:470-93).
To date, the effect of giving probiotics to pregnant women who have a family history of allergy is less clear. One pooled analysis of such studies put the overall risk ratio at 0.74 (Mil Med. 2014;179[6]:580-92). “While I think the jury’s still out on how to best prevent atopic dermatitis in these families, it looks like there is some potential benefit in treating these moms during pregnancy with probiotics and treating the infant during the first few months of life,” Dr. Underwood said. The most effective were mixtures including one or more Lactobacillus species or L. rhamnosus, mixtures including one or more Bifidobacterium species, or B. lactis by itself. The use of probiotics also has been found to prevent necrotizing enterocolitis, sepsis, and death in premature infants (Semin Pediatr Surg. 2018;27[1]:39-46).
Dr. Underwood disclosed that he has received honoraria from Abbott and that he was a member of the scientific review board for Avexegen. He also chaired the data safety and monitoring board for Infant Bacterial Therapeutics and has received support from Evolve BioSystems to perform a clinical trial.
[email protected]
LAKE TAHOE, CALIF. – according to Mark A. Underwood, MD.
“Antibiotic exposure changes the composition of the intestinal microbiota,” he said at the annual meeting of the Society for Pediatric Dermatology. “That clearly causes both antibiotic-associated diarrhea and Clostridium difficile colitis. The bigger question is, is it possible that intestinal dysbiosis is related to a whole bunch of other systemic diseases? In other words, does an insult during a critical window of development cause changes in the intestinal microbiota that can lead to systemic diseases in the brain, the lung, the liver, or the immune system?”
According Dr. Underwood, a pediatrician who is chief of the division of neonatology at the University of California, Davis, the prevalence of dysbiosis is increasing worldwide, particularly in developed countries, where Bifidobacteria are decreasing and Enterobacteriaceae are increasing. “Those changes are associated with gut permeability and alterations in both local and systemic inflammation, and the risk for a number of diseases, including atopic dermatitis,” he said. Key reasons for the increasing prevalence of dysbiosis, he continued, include the use of antibiotics, cesarean section delivery, formula feeding, changes in hygiene that alter the intestinal biota, the high-fat, high-sugar Western diet, and a loss of vertical and horizontal transmission over generations.
In an effort to evaluate the association between early childhood antibiotic use with allergic diseases in later childhood, Japanese researchers followed 1,200 infants to the age of 5 years (Ann Allergy Asthma Immunol. 2017;119:54-8). They found that antibiotic exposure within the first 2 years of life was associated with an increased risk of asthma (adjusted odds ratio 1.72), allergic rhinitis (adjusted OR 1.65), and atopic dermatitis (adjusted OR 1.40). In a more recent, smaller prospective study, 436 Dutch infants were followed to 1 year of age (Pediatr Allergy Immunol. 2018;29[2]:151-8). The researchers found that antibiotic exposure within the first week of life was associated with allergic sensitization (adjusted OR 3.26), colic (adjusted OR 1.66), and wheezing (adjusted OR 1.56).
In a study of 44 term infants with a family history of allergy, changes in the fecal microbiota, especially colonization with Ruminococcus gnavus, preceded the onset of allergic symptoms (Gastroenterol. 2018;154[1]:154-67). The same researchers observed similar findings in an animal model.
One potential mechanism by which intestinal dysbiosis causes systemic disease is stimulation of toll-like receptor 4 (TLR4), “which is a receptor on a variety of mucosal cells that senses the presence of a microbial pathogen-associated patterns, particularly those of Gram-negative Enterobacteriaceae,” Dr. Underwood explained. Other potential mechanisms include increased intestinal permeability, an increase in the pH and decreases in short-chain fatty acids within the gut lumen, and a loss of intraluminal hypoxia. “Think of the colon as an anaerobic chamber,” he said. “The colon lumen should be very low in oxygen. It should be dominated by obligate anaerobes.”
Efforts to prevent or treat dysbiosis-related diseases include the use of probiotics and fecal transplantation. A recent Cochrane review of 8,672 patients found “moderate certainty evidence” that probiotics are effective for preventing C. difficile-associated diarrhea. The analysis included 31 randomized, controlled trials of adults who were treated either with a probiotic or with a placebo. When pooled, the risk ratio was 0.40, which represented a significant protection. In addition, a summary of 7 randomized controlled trials and 30 case series suggests that fecal microbial transplantation is superior to vancomycin for adults with recurrent C. difficile colitis (relative risk 0.23) (Aliment Pharmacol Ther. 2017;46[5]:470-93).
To date, the effect of giving probiotics to pregnant women who have a family history of allergy is less clear. One pooled analysis of such studies put the overall risk ratio at 0.74 (Mil Med. 2014;179[6]:580-92). “While I think the jury’s still out on how to best prevent atopic dermatitis in these families, it looks like there is some potential benefit in treating these moms during pregnancy with probiotics and treating the infant during the first few months of life,” Dr. Underwood said. The most effective were mixtures including one or more Lactobacillus species or L. rhamnosus, mixtures including one or more Bifidobacterium species, or B. lactis by itself. The use of probiotics also has been found to prevent necrotizing enterocolitis, sepsis, and death in premature infants (Semin Pediatr Surg. 2018;27[1]:39-46).
Dr. Underwood disclosed that he has received honoraria from Abbott and that he was a member of the scientific review board for Avexegen. He also chaired the data safety and monitoring board for Infant Bacterial Therapeutics and has received support from Evolve BioSystems to perform a clinical trial.
[email protected]
LAKE TAHOE, CALIF. – according to Mark A. Underwood, MD.
“Antibiotic exposure changes the composition of the intestinal microbiota,” he said at the annual meeting of the Society for Pediatric Dermatology. “That clearly causes both antibiotic-associated diarrhea and Clostridium difficile colitis. The bigger question is, is it possible that intestinal dysbiosis is related to a whole bunch of other systemic diseases? In other words, does an insult during a critical window of development cause changes in the intestinal microbiota that can lead to systemic diseases in the brain, the lung, the liver, or the immune system?”
According Dr. Underwood, a pediatrician who is chief of the division of neonatology at the University of California, Davis, the prevalence of dysbiosis is increasing worldwide, particularly in developed countries, where Bifidobacteria are decreasing and Enterobacteriaceae are increasing. “Those changes are associated with gut permeability and alterations in both local and systemic inflammation, and the risk for a number of diseases, including atopic dermatitis,” he said. Key reasons for the increasing prevalence of dysbiosis, he continued, include the use of antibiotics, cesarean section delivery, formula feeding, changes in hygiene that alter the intestinal biota, the high-fat, high-sugar Western diet, and a loss of vertical and horizontal transmission over generations.
In an effort to evaluate the association between early childhood antibiotic use with allergic diseases in later childhood, Japanese researchers followed 1,200 infants to the age of 5 years (Ann Allergy Asthma Immunol. 2017;119:54-8). They found that antibiotic exposure within the first 2 years of life was associated with an increased risk of asthma (adjusted odds ratio 1.72), allergic rhinitis (adjusted OR 1.65), and atopic dermatitis (adjusted OR 1.40). In a more recent, smaller prospective study, 436 Dutch infants were followed to 1 year of age (Pediatr Allergy Immunol. 2018;29[2]:151-8). The researchers found that antibiotic exposure within the first week of life was associated with allergic sensitization (adjusted OR 3.26), colic (adjusted OR 1.66), and wheezing (adjusted OR 1.56).
In a study of 44 term infants with a family history of allergy, changes in the fecal microbiota, especially colonization with Ruminococcus gnavus, preceded the onset of allergic symptoms (Gastroenterol. 2018;154[1]:154-67). The same researchers observed similar findings in an animal model.
One potential mechanism by which intestinal dysbiosis causes systemic disease is stimulation of toll-like receptor 4 (TLR4), “which is a receptor on a variety of mucosal cells that senses the presence of a microbial pathogen-associated patterns, particularly those of Gram-negative Enterobacteriaceae,” Dr. Underwood explained. Other potential mechanisms include increased intestinal permeability, an increase in the pH and decreases in short-chain fatty acids within the gut lumen, and a loss of intraluminal hypoxia. “Think of the colon as an anaerobic chamber,” he said. “The colon lumen should be very low in oxygen. It should be dominated by obligate anaerobes.”
Efforts to prevent or treat dysbiosis-related diseases include the use of probiotics and fecal transplantation. A recent Cochrane review of 8,672 patients found “moderate certainty evidence” that probiotics are effective for preventing C. difficile-associated diarrhea. The analysis included 31 randomized, controlled trials of adults who were treated either with a probiotic or with a placebo. When pooled, the risk ratio was 0.40, which represented a significant protection. In addition, a summary of 7 randomized controlled trials and 30 case series suggests that fecal microbial transplantation is superior to vancomycin for adults with recurrent C. difficile colitis (relative risk 0.23) (Aliment Pharmacol Ther. 2017;46[5]:470-93).
To date, the effect of giving probiotics to pregnant women who have a family history of allergy is less clear. One pooled analysis of such studies put the overall risk ratio at 0.74 (Mil Med. 2014;179[6]:580-92). “While I think the jury’s still out on how to best prevent atopic dermatitis in these families, it looks like there is some potential benefit in treating these moms during pregnancy with probiotics and treating the infant during the first few months of life,” Dr. Underwood said. The most effective were mixtures including one or more Lactobacillus species or L. rhamnosus, mixtures including one or more Bifidobacterium species, or B. lactis by itself. The use of probiotics also has been found to prevent necrotizing enterocolitis, sepsis, and death in premature infants (Semin Pediatr Surg. 2018;27[1]:39-46).
Dr. Underwood disclosed that he has received honoraria from Abbott and that he was a member of the scientific review board for Avexegen. He also chaired the data safety and monitoring board for Infant Bacterial Therapeutics and has received support from Evolve BioSystems to perform a clinical trial.
[email protected]
EXPERT ANALYSIS FROM THE SPD ANNUAL MEETING
So it’s pediatric onychomycosis. Now what?
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
[email protected]
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
[email protected]
CHICAGO – Though research shows that nail fungus occurs in just 0.3% of pediatric patients in the United States, that’s not what Sheila Friedlander, MD, is seeing in her southern California practice, where it’s not uncommon to see children whose nails, toe nails in particular, have fungal involvement.
said Dr. Friedlander during a nail-focused session at the annual summer meeting of the American Academy of Dermatology. Dr. Friedlander, professor of dermatology and pediatrics at the University of California San Diego and Rady Children’s Hospital, said that she suspects that more participation in organized sports at a young age may be contributing to the increase, with occlusive sports footwear replacing bare feet or sandals for more hours of the day, presenting more opportunities for toenail trauma in sports such as soccer.
When making the clinical call about a nail problem, bear in mind that the younger the child, the less likely a nail problem is fungal, Dr. Friedlander noted. “Little children are much less likely than older children to have nail fungus. Pediatric nails are thinner, and they are faster growing, with better blood supply to the matrix.”
And if frank onychomadesis is observed, think about the time of year, and ask about recent fevers and rashes, because coxsackievirus may be the culprit. “Be not afraid, and look everywhere if the nail is confusing to you,” she said. In all ages, the diagnosis is primarily clinical, “but I culture them, I ‘PAS’ [periodic acid-Schiff stain] them, too. If you do both, you’ll increase your yield,” Dr. Friedlander said, adding, “the beauty of PAS is you can use it to give your families an answer very soon.”
Once you’ve established that fungus is to blame for a nail problem, there’s a conundrum: There are no Food and Drug Administration-approved therapies, either topical or systemic, for pediatric onychomycosis, Dr. Friedlander said. She, along with coauthors and first author Aditya Gupta, MD, of Mediprobe Research, London, Ontario, Canada, recently published an article reviewing the safety and efficacy of antifungal agents in this age group (Pediatr Dermatol. 2018 Jun 26. doi: 10.1111/pde.13561).
Reviewing information available in the United States and Canada, Dr. Friedlander and her coauthors came up with three topical and four oral options for children, along with recommendations for dosage and duration.
In response to an audience question about the use of topical antifungal treatment for nail involvement, Dr. Friedlander responded, “I think topicals would be great for kids, but it’s for kids where there is no nail matrix involvement. Also, cost is a problem. Nobody will cover it. But some families are willing to do this to avoid systemic therapy,” and if the family budget can accommodate a topical choice, it’s a logical option, she said, noting that partial reimbursement via a coupon system is available from some pharmaceutical companies.
Where appropriate, ciclopirox 8%, efinaconazole 10%, and tavaborole 5% can each be considered. Dr. Friedlander cited one study she coauthored, which reported that 70% of pediatric participants with nonmatrix onychomycosis saw effective treatment, with a 71% mycological cure rate (P = .03), after 32 weeks of treatment with ciclopirox lacquer versus vehicle (Pediatr Dermatol. 2013 May-Jun;30[3]:316-22).
Systemic therapies – which, when studied, have been given at tinea capitis doses – could include griseofulvin, terbinafine, itraconazole, and fluconazole.
In terms of oral options, Dr. Friedlander said, griseofulvin has some practical limitations. While prolonged treatment is required in any case, terbinafine may produce results in about 3 months, whereas griseofulvin may require up to 9 months of therapy. “I always try to use terbinafine … griseofulvin takes a year and a day,” she said.
She also shared some tips to improve pediatric adherence with oral antifungals: “You can tell parents to crush terbinafine tablets and mix in peanut butter or applesauce to improve adherence. Griseofulvin can be flavored by the pharmacy, but volumes are big with griseofulvin, so it’s a challenge to get kids to take it all,” she said.
Dr. Friedlander reported that she had no relevant financial disclosures.
[email protected]
EXPERT ANALYSIS FROM SUMMER AAD 2018
New guidelines on antimicrobial prophylaxis
Experts have published updated guidelines on antimicrobial prophylaxis for adults with cancer-related immunosuppression.
The guidelines include antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions, such as hand hygiene, that may reduce infection risk.
The guidelines were developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA) and published in the Journal of Clinical Oncology.
For the most part, the expert panel that created these guidelines endorsed the previous ASCO recommendations, published in 2013.
However, the panel considered six new studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Recommendations
The ASCO/IDSA guidelines say health care providers should systematically assess the risk of febrile neutropenia, taking into account patient-, cancer-, and treatment-related factors.
Fluoroquinolone prophylaxis is recommended for patients at high risk of febrile neutropenia or profound, protracted neutropenia. This includes most patients with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) and patients undergoing hematopoietic stem cell transplant (HSCT) who are treated with myeloablative conditioning regimens.
Antifungal prophylaxis with an oral triazole or parenteral echinocandin is recommended for patients at risk of profound, protracted neutropenia, which includes HSCT recipients and most patients with AML/MDS.
However, neither antifungal nor antibiotic prophylaxis are routinely recommended for patients with solid tumors.
Prophylaxis with a nucleoside analog, such as acyclovir, is recommended in patients who are herpes simplex virus–seropositive and are undergoing allogeneic HSCT or leukemia induction.
Pneumocystis jirovecii prophylaxis, such as trimethoprim-sulfamethoxazole, is recommended for patients receiving chemotherapy regimens associated with a greater than 3.5% risk for pneumonia from P jirovecii.
Treatment with a nucleoside reverse transcription inhibitor, such as entecavir or tenofovir, is recommended for patients at high risk of hepatitis B virus reactivation.
Yearly influenza vaccination with an inactivated quadrivalent vaccine is recommended for all patients undergoing chemotherapy for malignancy as well as their family members, household contacts, and health care providers.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce the risk of pathogen transmission, according to the guidelines.
The guidelines also note that outpatients who develop neutropenia following cancer therapy should avoid prolonged contact with environments that have high concentrations of airborne fungal spores.
The guidelines do not recommend interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks. “Evidence of clinical benefit is lacking” for those interventions, the expert panel said.
Members of the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.
Experts have published updated guidelines on antimicrobial prophylaxis for adults with cancer-related immunosuppression.
The guidelines include antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions, such as hand hygiene, that may reduce infection risk.
The guidelines were developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA) and published in the Journal of Clinical Oncology.
For the most part, the expert panel that created these guidelines endorsed the previous ASCO recommendations, published in 2013.
However, the panel considered six new studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Recommendations
The ASCO/IDSA guidelines say health care providers should systematically assess the risk of febrile neutropenia, taking into account patient-, cancer-, and treatment-related factors.
Fluoroquinolone prophylaxis is recommended for patients at high risk of febrile neutropenia or profound, protracted neutropenia. This includes most patients with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) and patients undergoing hematopoietic stem cell transplant (HSCT) who are treated with myeloablative conditioning regimens.
Antifungal prophylaxis with an oral triazole or parenteral echinocandin is recommended for patients at risk of profound, protracted neutropenia, which includes HSCT recipients and most patients with AML/MDS.
However, neither antifungal nor antibiotic prophylaxis are routinely recommended for patients with solid tumors.
Prophylaxis with a nucleoside analog, such as acyclovir, is recommended in patients who are herpes simplex virus–seropositive and are undergoing allogeneic HSCT or leukemia induction.
Pneumocystis jirovecii prophylaxis, such as trimethoprim-sulfamethoxazole, is recommended for patients receiving chemotherapy regimens associated with a greater than 3.5% risk for pneumonia from P jirovecii.
Treatment with a nucleoside reverse transcription inhibitor, such as entecavir or tenofovir, is recommended for patients at high risk of hepatitis B virus reactivation.
Yearly influenza vaccination with an inactivated quadrivalent vaccine is recommended for all patients undergoing chemotherapy for malignancy as well as their family members, household contacts, and health care providers.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce the risk of pathogen transmission, according to the guidelines.
The guidelines also note that outpatients who develop neutropenia following cancer therapy should avoid prolonged contact with environments that have high concentrations of airborne fungal spores.
The guidelines do not recommend interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks. “Evidence of clinical benefit is lacking” for those interventions, the expert panel said.
Members of the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.
Experts have published updated guidelines on antimicrobial prophylaxis for adults with cancer-related immunosuppression.
The guidelines include antibacterial, antifungal, and antiviral prophylaxis recommendations, along with additional precautions, such as hand hygiene, that may reduce infection risk.
The guidelines were developed by the American Society of Clinical Oncology (ASCO) with the Infectious Diseases Society of America (IDSA) and published in the Journal of Clinical Oncology.
For the most part, the expert panel that created these guidelines endorsed the previous ASCO recommendations, published in 2013.
However, the panel considered six new studies and six new or updated meta-analyses to make modifications and add some new recommendations.
Recommendations
The ASCO/IDSA guidelines say health care providers should systematically assess the risk of febrile neutropenia, taking into account patient-, cancer-, and treatment-related factors.
Fluoroquinolone prophylaxis is recommended for patients at high risk of febrile neutropenia or profound, protracted neutropenia. This includes most patients with acute myeloid leukemia (AML) or myelodysplastic syndromes (MDS) and patients undergoing hematopoietic stem cell transplant (HSCT) who are treated with myeloablative conditioning regimens.
Antifungal prophylaxis with an oral triazole or parenteral echinocandin is recommended for patients at risk of profound, protracted neutropenia, which includes HSCT recipients and most patients with AML/MDS.
However, neither antifungal nor antibiotic prophylaxis are routinely recommended for patients with solid tumors.
Prophylaxis with a nucleoside analog, such as acyclovir, is recommended in patients who are herpes simplex virus–seropositive and are undergoing allogeneic HSCT or leukemia induction.
Pneumocystis jirovecii prophylaxis, such as trimethoprim-sulfamethoxazole, is recommended for patients receiving chemotherapy regimens associated with a greater than 3.5% risk for pneumonia from P jirovecii.
Treatment with a nucleoside reverse transcription inhibitor, such as entecavir or tenofovir, is recommended for patients at high risk of hepatitis B virus reactivation.
Yearly influenza vaccination with an inactivated quadrivalent vaccine is recommended for all patients undergoing chemotherapy for malignancy as well as their family members, household contacts, and health care providers.
Health care workers should follow hand hygiene and respiratory hygiene/cough etiquette to reduce the risk of pathogen transmission, according to the guidelines.
The guidelines also note that outpatients who develop neutropenia following cancer therapy should avoid prolonged contact with environments that have high concentrations of airborne fungal spores.
The guidelines do not recommend interventions such as neutropenic diet, footwear exchange, nutritional supplements, and surgical masks. “Evidence of clinical benefit is lacking” for those interventions, the expert panel said.
Members of the expert panel disclosed potential conflicts of interest related to Merck, Chimerix, GlyPharma Therapeutic, Pfizer, Cidara Therapeutics, Celgene, Astellas Pharma, Gilead Sciences, and Allergan, among other entities.
Receptor occupancy and drug response: Understanding the relationship
Most clinicians do not think about receptor occupancy when they prescribe a medication. Most simply assume that if they use a low dose of a medication, they will get a small effect, and if they use a higher dose, they will get a larger effect. However, this is frequently not accurate. Clinicians need to understand the relationship between receptor occupancy and drug response.
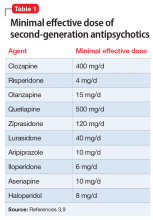
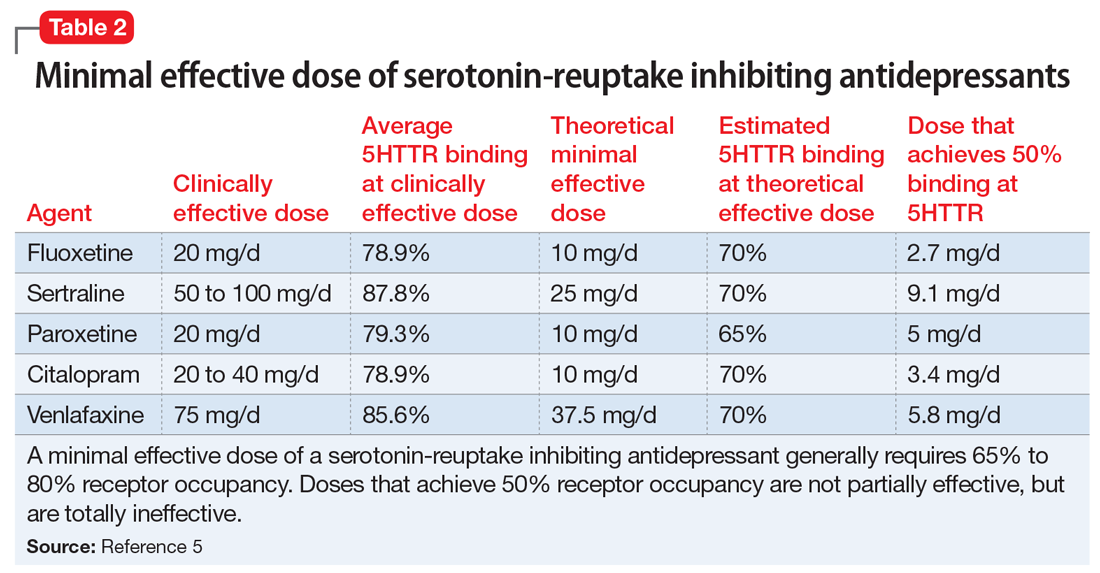
In general, when an antagonist of a neurotransmitter receptor is used, it must occupy a minimum of 65% to 70% of the target receptor to be effective. This is clearly the case when the target is a postsynaptic receptor, such as the dopamine D2 receptor.1-3 Similarly, despite significant variability in antidepressant response,4 blockade of 65% to 80% of presynaptic transport proteins—such as the serotonin reuptake pumps when considering serotoninergic antidepressants,5,6 or the norepinephrine reuptake pumps when considering noradrenergic agents such as nortriptyline7—is necessary for these medications to be effective.
It is reasonable to think of the drug response of such agents as following a “threshold” model (Figure 1). This model makes 2 predictions. The first prediction is that a low dose of the drug might result in <50% receptor occupancy, but is not associated with a smaller response; it is simply ineffective. The second prediction is that a very high dose of the drug (eg, one that may exceed 90% receptor occupancy) does not result in any additional benefit, but may cause additional adverse consequences.8

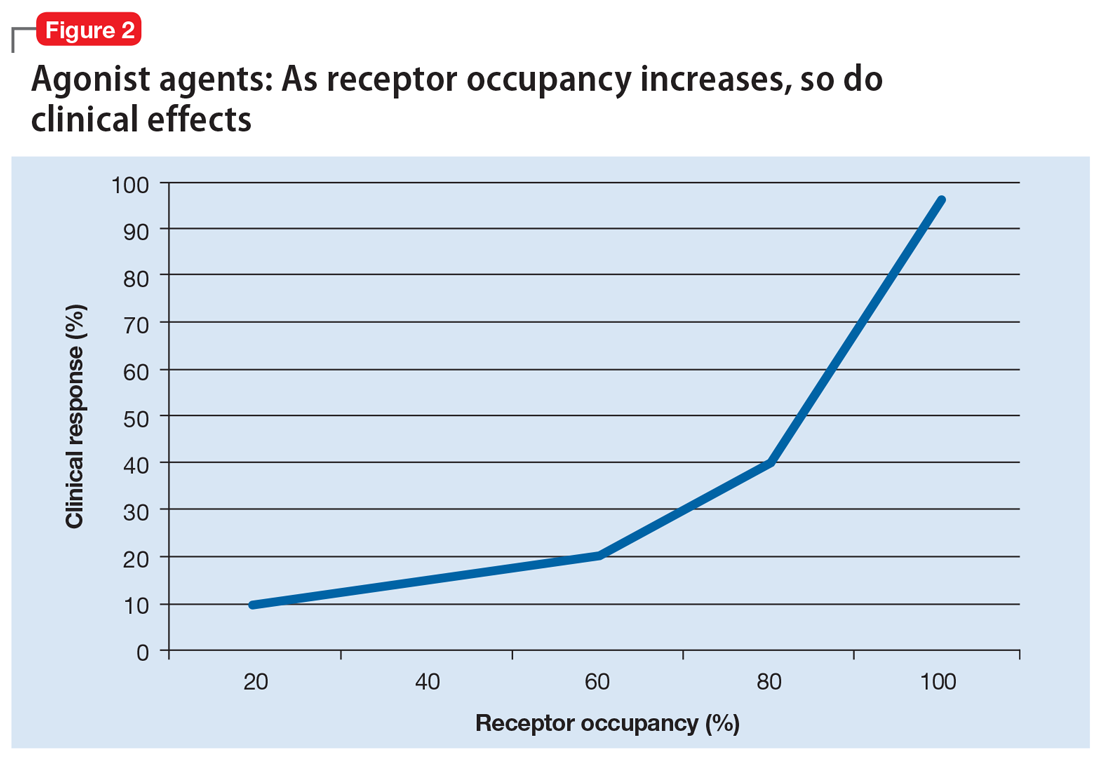
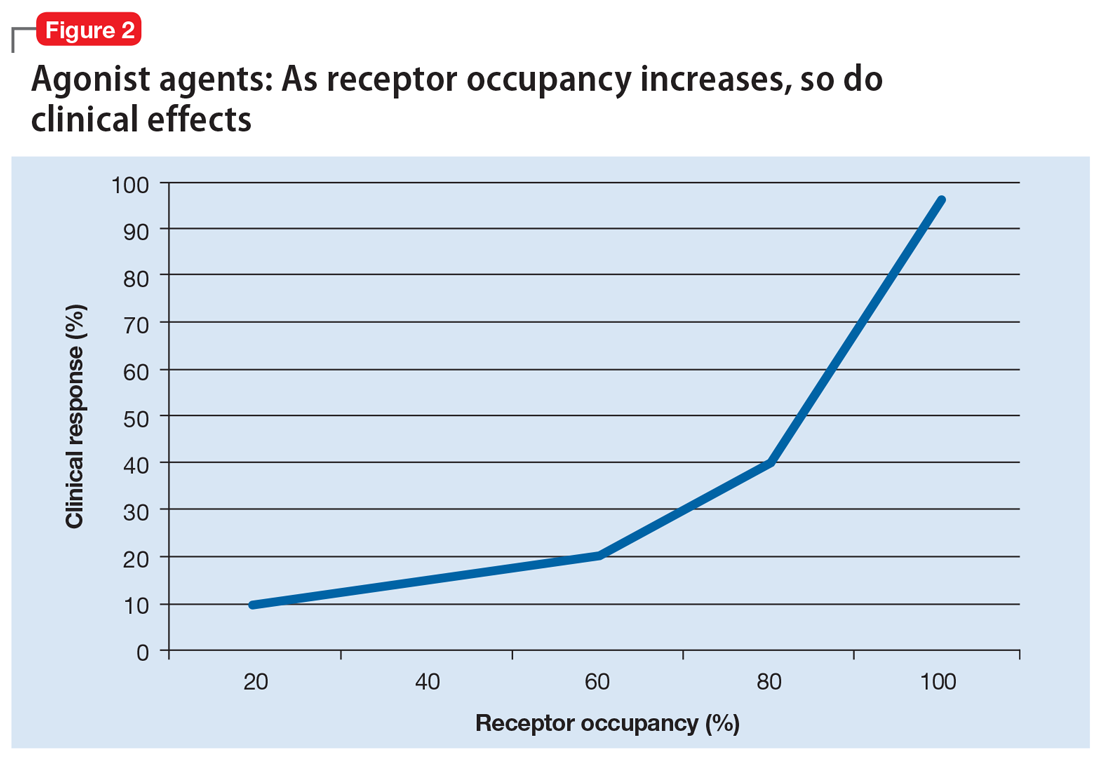
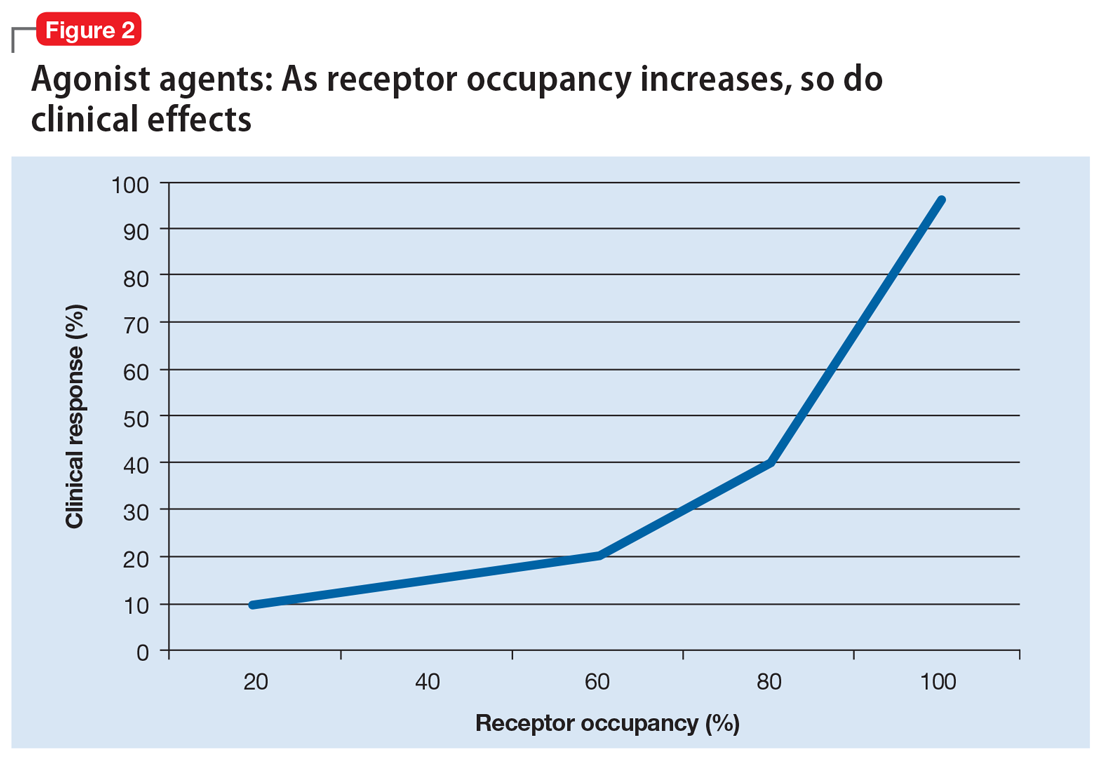
Alternatively, agonist medications, such as benzodiazepines or opiates, have their efficacy in a continuous dose-dependent fashion (Figure 2). Titrating these medications for clinical response is necessary, and minimal effective doses are highly individual. Agonist medications will not be addressed further in this article.
In this article, the term “response” is used to denote the average (population) symptom change in a study population. This term is not used as clinicians often use it to mean that their specific patient’s illness has improved, or that the patient has gone into remission. Furthermore, the information described in this article does not optimize clinical outcome, but instead is intended to help clinicians optimize the use of their pharmacologic tools.
Minimal effective dose
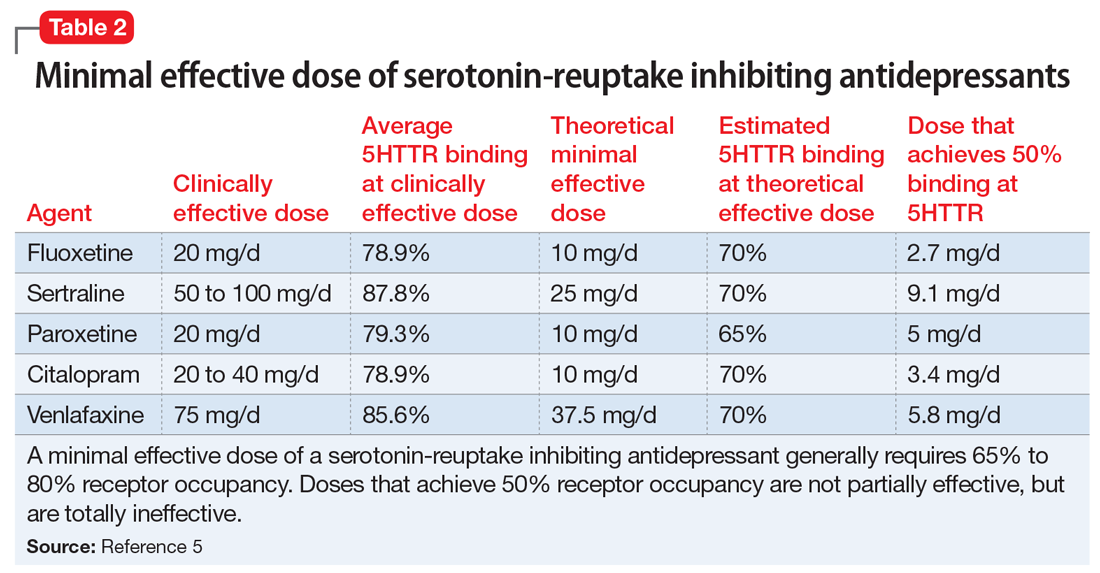
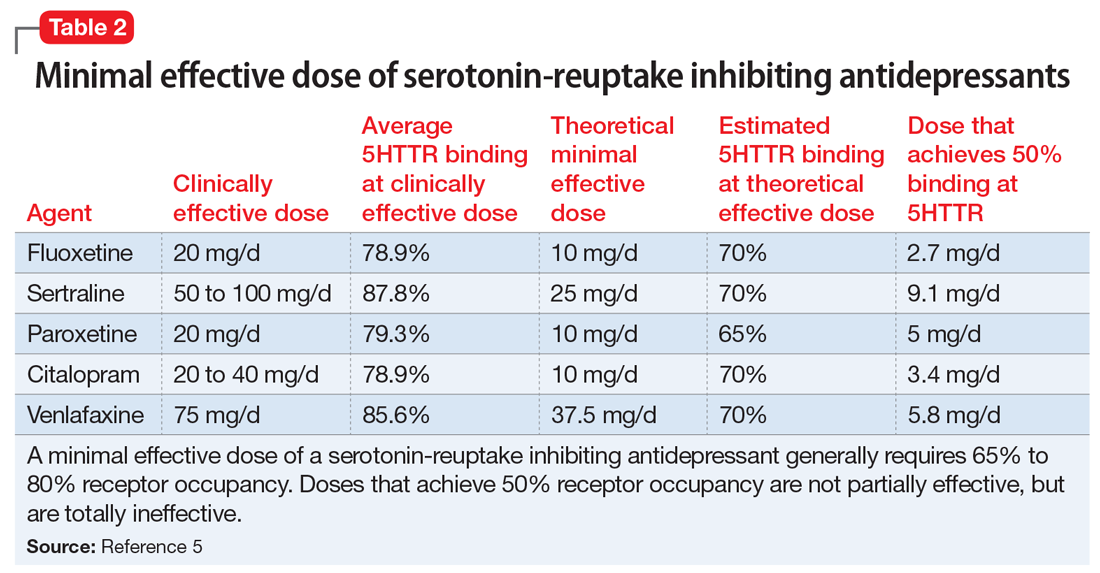
Medications that have a threshold for activity will display that clinically in a minimal effective dose (Table 13,9 and Table 25). The minimal effective dose of medications that act by blocking a neurotransmitter receptor is usually the dose that achieves 65% to 80% receptor occupancy in typical individuals (Table 25). The minimal effective doses for antipsychotics are listed in Table 1.3,9 These doses are known to occupy approximately 65% to 70% of postsynaptic D2 receptors in living humans as confirmed by positron emission tomography (PET) scans.10 Similar minimal effective doses can be determined for serotonin-reuptake inhibiting (SRI) antidepressants (Table 25). In placebo-controlled trials, doses that were smaller than the minimal effective dose did not provide any benefit.
There are important caveats to this. First is the use of partial agonists. Depending on the level of intrinsic activity of a partial agonist and clinical goal, the clinician may aim for a different level of receptor occupancy. For example, aripiprazole will act as a dopamine agonist at lower concentrations, but blocks the receptor at higher concentrations.11 Unlike antagonist antipsychotics, which require only 65% to 70% D2 receptor occupancy to be effective, aripiprazole receptor binding at effective antipsychotic doses is 90% to 95%.12-14 Since aripiprazole has an intrinsic activity of approximately 30% (ie, when it binds, it stimulates the D2 receptor to about 30% of the effect of dopamine binding to the receptor15), binding to 90% of the receptors, and displacing endogenous dopamine, allows aripiprazole to replace the background or tonic tone of dopamine, which has been measured at 19% in people with schizophrenia and 9% in controls.16 Clinically, this still appears as the minimal effective dose achieving maximal response17-19 without significant parkinsonism despite >90% receptor occupancy.12
Continue to: The second caveat is...
The second caveat is the action of low D2 receptor affinity antipsychotics, such as clozapine and quetiapine. These agents generally achieve adequate D2 receptor occupancy for only a brief period of time.20 It has been suggested that continuous receptor occupancy at ≥65% may not be necessary to obtain antipsychotic control.21,22 There may also be specific limbic and cortical (vs striatal) D2 receptor selectivity by clozapine23 compared with other second-generation antipsychotics such as risperidone and olanzapine,24,25 although this point remains debatable.26 Furthermore, the antipsychotic efficacy of low D2 receptor affinity drugs is unreliable, even in controlled, blinded studies (eg, a failed large quetiapine study27). Thus far, the actual antipsychotic mechanism of these agents is yet to be fully understood.
Minimal effective dose achieves maximal response
An interesting aspect of the threshold phenomenon of drug response is that once the minimal effective dose is reached, maximal response is achieved. In other words, there is no additional efficacy with additional dose increases. This is readily demonstrated in some studies in which patients were randomly assigned to different fixed doses or dose ranges. In these studies, there was generally no difference in response rates of different doses, so that once 65% to 80% receptor occupancy is achieved, minimal and maximal clinical response is simultaneously reached.18,28,29
For example, in the original risperidone studies, 6 mg/d was essentially equivalent to 16 mg/d.28 Similarly, lurasidone, 40 mg/d, achieves approximately 65% D2 occupancy.30 When the daily dose is increased to 120 mg, there is no additional benefit in controlling psychosis in schizophrenia.29 This pattern is also seen in partial agonists, where there are no differences between lower and higher doses in terms of response.18
Upon reading this, many clinicians may think “I don’t care what the studies say, I have seen additional benefits with additional doses.” There are several explanations for this. One is that individual patients have genetic variants that may prevent them from responding in a typical fashion. Hints of this are seen in an apparent disconnect between dosage and drug levels, so that it is not surprising that drug levels are a much better predictor of receptor occupancy than dosage.31 Nonetheless, as previously pointed out, for a population, dosage does predict receptor occupancy and outcome. However, for individuals, genetic variations make dosages less reliable. For example, ultrarapid metabolizers of cytochrome P450 (CYP) 2D6 may discontinue risperidone due to nonresponse, or require a higher dose or longer time period to respond.32,33 Similarly, patients who smoke may require an increase in doses of CYP1A2 substrates such as clozapine and olanzapine.34
Alternatively, the clinician may note improvement in mood, sleep, appetite, or other symptoms at lower doses, and then note additional improvements in psychosis or mania at higher doses.3 This occurs due to the varying affinity of different receptors. For example, in bipolar depression trials that used quetiapine in a fixed-dose design, patients who received 300 or 600 mg/d responded in the same fashion, with no additional benefit in improving depression with the higher dose.35 Similarly, in a flexible dose range study that evaluated lurasidone in bipolar depression, an average dose of 34 mg/d (range 20 to 60 mg/d) and an average dose of 83 mg/d (range 80 to 120 mg/d) both resulted in the same response (a 15.4-point reduction in depression ratings and an effect size of 0.51).36 For both quetiapine and lurasidone, higher doses are generally required to control psychosis.29,37 Note that for lurasidone, agitation, but not psychosis, improves with higher doses, which suggests that recruitment of additional receptors results in improvement in a different set of symptoms.9
Continue to: Clinical implications
Clinical implications
The implications for clinicians are relatively clear. Knowing the minimal effective doses for depression, psychosis, or mania informs the target dose. If improvement is seen at lower doses, the clinician needs to assess the profile of symptoms that improved, potential drug–drug interactions, or potential irregularities in the patient’s metabolic pathways. Clinicians need to increase doses above the minimally effective dose carefully, and expend additional effort in analyzing changes in their patient’s symptoms and adverse effects; this analysis should be performed with skepticism and willingness to reduce a dosage if no additional benefit is seen. Attention to these receptor-symptom interactions will improve response and reduce adverse consequences in the majority of patients.
Related Resource
- Lako IM, van den Heuvel ER, Knegtering H, et al. Estimating dopamine D2 receptor occupancy for doses of 8 antipsychotics: a meta-analysis. J Clin Psychopharmacol. 2013;33(5):675-681.
Drug Brand Names
Aripiprazole • Abilify
Asenapine • Saphris
Citalopram • Celexa
Clozapine • Clozaril
Fluoxetine • Prozac
Haloperidol • Haldol
Iloperidone • Fanapt
Lurasidone • Latuda
Nortriptyline • Pamelor
Olanzapine • Zyprexa
Paroxetine • Paxil
Quetiapine • Seroquel
Risperidone • Risperdal
Sertraline • Zoloft
Venlafaxine • Effexor
Ziprasidone • Geodon
1. Farde L, Nordström AL, Wiesel FA, et al. Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry. 1992;49(7):538-544.
2. Kapur S, Zipursky R, Jones C, et al. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry. 2000;157(4):514-520.
3. Roberts RJ, Lohano KK, El-Mallakh RS. Antipsychotics as antidepressants. Asia Pacific Psychiatry. 2016;8(3):179-188.
4. Quitkin FM, Rabkin JG, Gerald J, et al. Validity of clinical trials of antidepressants. Am J Psychiatry. 2000;157(3):327-337.
5. Meyer JH, Wilson AA, Sagrati S, et al. Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry. 2004;161(5):826-835.
6. Lundberg J, Tiger M, Landén M, et al. Serotonin transporter occupancy with TCAs and SSRIs: a PET study in patients with major depressive disorder. Int J Neuropsychopharmacol. 2012;15(8):1167-1172.
7. Takano H, Arakawa R, Nogami T, et al. Norepinephrine transporter occupancy by nortriptyline in patients with depression: a positron emission tomography study with (S,S)-[¹8F]FMeNER-D2. Int J Neuropsychopharmacol. 2014;17(4):553-560.
8. Johnson M, Kozielska M, Pilla Reddy V, et al. Dopamine D2 receptor occupancy as a predictor of catalepsy in rats: a pharmacokinetic-pharmacodynamic modeling approach. Pharm Res. 2014;31(10):2605-2617.
9. Allen MH, Citrome L, Pikalov A, et al. Efficacy of lurasidone in the treatment of agitation: a post hoc analysis of five short-term studies in acutely ill patients with schizophrenia. Gen Hosp Psychiatry. 2017;47:75-82.
10. Sekine M, Maeda J, Shimada H, et al. Central nervous system drug evaluation using positron emission tomography. Clin Psychopharmacol Neurosci. 2011;9(1):9-16.
11. Ma GF, Raivio N, Sabrià J, et al. Agonist and antagonist effects of aripiprazole on D2-like receptors controlling rat brain dopamine synthesis depend on the dopaminergic tone. Int J Neuropsychopharmacol. 2014;18(4):pii: pyu046. doi: 10.1093/ijnp/pyu046.
12. Yokoi F, Gründer G, Biziere K, et al. Dopamine D2 and D3 receptor occupancy in normal humans treated with the antipsychotic drug aripiprazole (OPC 14597): a study using positron emission tomography and [11C]raclopride. Neuropsychopharmacology. 2002;27(2):248-259.
13. Gründer G, Carlsson A, Wong DF. Mechanism of new antipsychotic medications: occupancy is not just antagonism. Arch Gen Psychiatry. 2003;60(10):974-977.
14. Mamo D, Graff A, Mizrahi R, et al. Differential effects of aripiprazole on D(2), 5-HT(2), and 5-HT(1A)receptor occupancy in patients with schizophrenia: a triple tracer PET study. Am J Psychiatry. 2007;164(9):1411-1417.
15. Weiden PJ, Preskorn SH, Fahnestock PA, et al. Translating the psychopharmacology of antipsychotics to individualized treatment for severe mental illness: a roadmap. J Clin Psychiatry. 2007;68(suppl 7):1-48.
16. Abi-Dargham A, Rodenhiser J, Printz D, et al. Increased baseline occupancy of D2 receptors by dopamine in schizophrenia. Proc Natl Acad Sci U S A. 2000;97(14):8104-8109.
17. Kane JM, Carson WH, Saha AR, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2002;63(9):763-771.
18. Potkin SG, Saha AR, Kujawa MJ, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry. 2003;60(7):681-690.
19. Cutler AJ, Marcus RN, Hardy SA, et al. The efficacy and safety of lower doses of aripiprazole for the treatment of patients with acute exacerbation of schizophrenia. CNS Spectr. 2006;11(9):691-702; quiz 719.
20. Gründer G, Landvogt C, Vernaleken I, et al. The striatal and extrastriatal D2/D3 receptor-binding profile of clozapine in patients with schizophrenia. Neuropsychopharmacology. 2006;31(5):1027-1035.
21. Mizuno Y, Bies RR, Remington G, et al. Dopamine D2 receptor occupancy with risperidone or olanzapine during maintenance treatment of schizophrenia: a cross-sectional study. Prog Neuropsychopharmacol Biol Psychiatry. 2012;37(1):182-187.
22. Moriguchi S, Bies RR, Remington G, et al. Estimated dopamine D2 receptor occupancy and remission in schizophrenia: analysis of the CATIE data. J Clin Psychopharmacol. 2013;33(5):682-685.
23. Pilowsky LS, Mulligan RS, Acton PD, et al. Limbic selectivity of clozapine. Lancet. 1997;350(9076):490-491.
24. Ito H, Arakawa R, Takahashi H, et al. No regional difference in dopamine D2 receptor occupancy by the second-generation antipsychotic drug risperidone in humans: a positron emission tomography study. Int J Neuropsychopharmacol. 2009;12(5):667-675.
25. Arakawa R, Ito H, Okumura M, et al. Extrastriatal dopamine D(2) receptor occupancy in olanzapine-treated patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2010;260(4):345-350.
26. Xiberas X, Martinot JL, Mallet L, et al. Extrastriatal and striatal D(2) dopamine receptor blockade with haloperidol or new antipsychotic drugs in patients with schizophrenia. Br J Psychiatry. 2001;179:503-508.
27. Cutler AJ, Tran-Johnson T, Kalali A, et al. A failed 6-week, randomized, double-blind, placebo-controlled study of once-daily extended release quetiapine fumarate in patients with acute schizophrenia: lessons learned. Psychopharmacol Bull. 2010;43(4):37-69.
28. Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry. 1994;151(6):825-835.
29. Meltzer HY, Cucchiaro J, Silva R, et al. Lurasidone in the treatment of schizophrenia: a randomized, double-blind, placebo- and olanzapine-controlled study. Am J Psychiatry. 2011;168(9):957-967.
30. Wong DF, Kuwabara H, Brašic JR, et al. Determination of dopamine D2 receptor occupancy by lurasidone using positron emission tomography in healthy male subjects. Psychopharmacology (Berl). 2013;229(2):245-252.
31. Potkin SG, Keator DB, Kesler-West ML, et al. D2 receptor occupancy following lurasidone treatment in patients with schizophrenia or schizoaffective disorder. CNS Spectr. 2014;19(2):176-181.
32. de Leon J, Susce MT, Pan RM, et al. The CYP2D6 poor metabolizer phenotype may be associated with risperidone adverse drug reactions and discontinuation. J Clin Psychiatry. 2005;66(1):15-27.
33. de Leon J, Susce MT, Pan RM, et al. A study of genetic (CYP2D6 and ABCB1) and environmental (drug inhibitors and inducers) variables that may influence plasma risperidone levels. Pharmacopsychiatry. 2007;40(3):93-102.
34. Narahari A, El-Mallakh RS, Kolikonda MK, et al. How coffee and cigarettes can affect the response to psychopharmacotherapy. Current Psychiatry. 2015;14(10):79-80.
35. Calabrese JR, Keck PE Jr, Macfadden W, et al. A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry. 2005;162(7):1351-1360.
36. Loebel A, Cucchiaro J, Silva R, et al. Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. 2014;171(2):160-168.
37. Lindenmayer JP, Brown D, Liu S, et al. The efficacy and tolerability of once-daily extended release quetiapine fumarate in hospitalized patients with acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled study. Psychopharmacol Bull. 2008;41(3):11-35.
Most clinicians do not think about receptor occupancy when they prescribe a medication. Most simply assume that if they use a low dose of a medication, they will get a small effect, and if they use a higher dose, they will get a larger effect. However, this is frequently not accurate. Clinicians need to understand the relationship between receptor occupancy and drug response.
In general, when an antagonist of a neurotransmitter receptor is used, it must occupy a minimum of 65% to 70% of the target receptor to be effective. This is clearly the case when the target is a postsynaptic receptor, such as the dopamine D2 receptor.1-3 Similarly, despite significant variability in antidepressant response,4 blockade of 65% to 80% of presynaptic transport proteins—such as the serotonin reuptake pumps when considering serotoninergic antidepressants,5,6 or the norepinephrine reuptake pumps when considering noradrenergic agents such as nortriptyline7—is necessary for these medications to be effective.
It is reasonable to think of the drug response of such agents as following a “threshold” model (Figure 1). This model makes 2 predictions. The first prediction is that a low dose of the drug might result in <50% receptor occupancy, but is not associated with a smaller response; it is simply ineffective. The second prediction is that a very high dose of the drug (eg, one that may exceed 90% receptor occupancy) does not result in any additional benefit, but may cause additional adverse consequences.8

Alternatively, agonist medications, such as benzodiazepines or opiates, have their efficacy in a continuous dose-dependent fashion (Figure 2). Titrating these medications for clinical response is necessary, and minimal effective doses are highly individual. Agonist medications will not be addressed further in this article.
In this article, the term “response” is used to denote the average (population) symptom change in a study population. This term is not used as clinicians often use it to mean that their specific patient’s illness has improved, or that the patient has gone into remission. Furthermore, the information described in this article does not optimize clinical outcome, but instead is intended to help clinicians optimize the use of their pharmacologic tools.
Minimal effective dose
Medications that have a threshold for activity will display that clinically in a minimal effective dose (Table 13,9 and Table 25). The minimal effective dose of medications that act by blocking a neurotransmitter receptor is usually the dose that achieves 65% to 80% receptor occupancy in typical individuals (Table 25). The minimal effective doses for antipsychotics are listed in Table 1.3,9 These doses are known to occupy approximately 65% to 70% of postsynaptic D2 receptors in living humans as confirmed by positron emission tomography (PET) scans.10 Similar minimal effective doses can be determined for serotonin-reuptake inhibiting (SRI) antidepressants (Table 25). In placebo-controlled trials, doses that were smaller than the minimal effective dose did not provide any benefit.
There are important caveats to this. First is the use of partial agonists. Depending on the level of intrinsic activity of a partial agonist and clinical goal, the clinician may aim for a different level of receptor occupancy. For example, aripiprazole will act as a dopamine agonist at lower concentrations, but blocks the receptor at higher concentrations.11 Unlike antagonist antipsychotics, which require only 65% to 70% D2 receptor occupancy to be effective, aripiprazole receptor binding at effective antipsychotic doses is 90% to 95%.12-14 Since aripiprazole has an intrinsic activity of approximately 30% (ie, when it binds, it stimulates the D2 receptor to about 30% of the effect of dopamine binding to the receptor15), binding to 90% of the receptors, and displacing endogenous dopamine, allows aripiprazole to replace the background or tonic tone of dopamine, which has been measured at 19% in people with schizophrenia and 9% in controls.16 Clinically, this still appears as the minimal effective dose achieving maximal response17-19 without significant parkinsonism despite >90% receptor occupancy.12
Continue to: The second caveat is...
The second caveat is the action of low D2 receptor affinity antipsychotics, such as clozapine and quetiapine. These agents generally achieve adequate D2 receptor occupancy for only a brief period of time.20 It has been suggested that continuous receptor occupancy at ≥65% may not be necessary to obtain antipsychotic control.21,22 There may also be specific limbic and cortical (vs striatal) D2 receptor selectivity by clozapine23 compared with other second-generation antipsychotics such as risperidone and olanzapine,24,25 although this point remains debatable.26 Furthermore, the antipsychotic efficacy of low D2 receptor affinity drugs is unreliable, even in controlled, blinded studies (eg, a failed large quetiapine study27). Thus far, the actual antipsychotic mechanism of these agents is yet to be fully understood.
Minimal effective dose achieves maximal response
An interesting aspect of the threshold phenomenon of drug response is that once the minimal effective dose is reached, maximal response is achieved. In other words, there is no additional efficacy with additional dose increases. This is readily demonstrated in some studies in which patients were randomly assigned to different fixed doses or dose ranges. In these studies, there was generally no difference in response rates of different doses, so that once 65% to 80% receptor occupancy is achieved, minimal and maximal clinical response is simultaneously reached.18,28,29
For example, in the original risperidone studies, 6 mg/d was essentially equivalent to 16 mg/d.28 Similarly, lurasidone, 40 mg/d, achieves approximately 65% D2 occupancy.30 When the daily dose is increased to 120 mg, there is no additional benefit in controlling psychosis in schizophrenia.29 This pattern is also seen in partial agonists, where there are no differences between lower and higher doses in terms of response.18
Upon reading this, many clinicians may think “I don’t care what the studies say, I have seen additional benefits with additional doses.” There are several explanations for this. One is that individual patients have genetic variants that may prevent them from responding in a typical fashion. Hints of this are seen in an apparent disconnect between dosage and drug levels, so that it is not surprising that drug levels are a much better predictor of receptor occupancy than dosage.31 Nonetheless, as previously pointed out, for a population, dosage does predict receptor occupancy and outcome. However, for individuals, genetic variations make dosages less reliable. For example, ultrarapid metabolizers of cytochrome P450 (CYP) 2D6 may discontinue risperidone due to nonresponse, or require a higher dose or longer time period to respond.32,33 Similarly, patients who smoke may require an increase in doses of CYP1A2 substrates such as clozapine and olanzapine.34
Alternatively, the clinician may note improvement in mood, sleep, appetite, or other symptoms at lower doses, and then note additional improvements in psychosis or mania at higher doses.3 This occurs due to the varying affinity of different receptors. For example, in bipolar depression trials that used quetiapine in a fixed-dose design, patients who received 300 or 600 mg/d responded in the same fashion, with no additional benefit in improving depression with the higher dose.35 Similarly, in a flexible dose range study that evaluated lurasidone in bipolar depression, an average dose of 34 mg/d (range 20 to 60 mg/d) and an average dose of 83 mg/d (range 80 to 120 mg/d) both resulted in the same response (a 15.4-point reduction in depression ratings and an effect size of 0.51).36 For both quetiapine and lurasidone, higher doses are generally required to control psychosis.29,37 Note that for lurasidone, agitation, but not psychosis, improves with higher doses, which suggests that recruitment of additional receptors results in improvement in a different set of symptoms.9
Continue to: Clinical implications
Clinical implications
The implications for clinicians are relatively clear. Knowing the minimal effective doses for depression, psychosis, or mania informs the target dose. If improvement is seen at lower doses, the clinician needs to assess the profile of symptoms that improved, potential drug–drug interactions, or potential irregularities in the patient’s metabolic pathways. Clinicians need to increase doses above the minimally effective dose carefully, and expend additional effort in analyzing changes in their patient’s symptoms and adverse effects; this analysis should be performed with skepticism and willingness to reduce a dosage if no additional benefit is seen. Attention to these receptor-symptom interactions will improve response and reduce adverse consequences in the majority of patients.
Related Resource
- Lako IM, van den Heuvel ER, Knegtering H, et al. Estimating dopamine D2 receptor occupancy for doses of 8 antipsychotics: a meta-analysis. J Clin Psychopharmacol. 2013;33(5):675-681.
Drug Brand Names
Aripiprazole • Abilify
Asenapine • Saphris
Citalopram • Celexa
Clozapine • Clozaril
Fluoxetine • Prozac
Haloperidol • Haldol
Iloperidone • Fanapt
Lurasidone • Latuda
Nortriptyline • Pamelor
Olanzapine • Zyprexa
Paroxetine • Paxil
Quetiapine • Seroquel
Risperidone • Risperdal
Sertraline • Zoloft
Venlafaxine • Effexor
Ziprasidone • Geodon
Most clinicians do not think about receptor occupancy when they prescribe a medication. Most simply assume that if they use a low dose of a medication, they will get a small effect, and if they use a higher dose, they will get a larger effect. However, this is frequently not accurate. Clinicians need to understand the relationship between receptor occupancy and drug response.
In general, when an antagonist of a neurotransmitter receptor is used, it must occupy a minimum of 65% to 70% of the target receptor to be effective. This is clearly the case when the target is a postsynaptic receptor, such as the dopamine D2 receptor.1-3 Similarly, despite significant variability in antidepressant response,4 blockade of 65% to 80% of presynaptic transport proteins—such as the serotonin reuptake pumps when considering serotoninergic antidepressants,5,6 or the norepinephrine reuptake pumps when considering noradrenergic agents such as nortriptyline7—is necessary for these medications to be effective.
It is reasonable to think of the drug response of such agents as following a “threshold” model (Figure 1). This model makes 2 predictions. The first prediction is that a low dose of the drug might result in <50% receptor occupancy, but is not associated with a smaller response; it is simply ineffective. The second prediction is that a very high dose of the drug (eg, one that may exceed 90% receptor occupancy) does not result in any additional benefit, but may cause additional adverse consequences.8

Alternatively, agonist medications, such as benzodiazepines or opiates, have their efficacy in a continuous dose-dependent fashion (Figure 2). Titrating these medications for clinical response is necessary, and minimal effective doses are highly individual. Agonist medications will not be addressed further in this article.
In this article, the term “response” is used to denote the average (population) symptom change in a study population. This term is not used as clinicians often use it to mean that their specific patient’s illness has improved, or that the patient has gone into remission. Furthermore, the information described in this article does not optimize clinical outcome, but instead is intended to help clinicians optimize the use of their pharmacologic tools.
Minimal effective dose
Medications that have a threshold for activity will display that clinically in a minimal effective dose (Table 13,9 and Table 25). The minimal effective dose of medications that act by blocking a neurotransmitter receptor is usually the dose that achieves 65% to 80% receptor occupancy in typical individuals (Table 25). The minimal effective doses for antipsychotics are listed in Table 1.3,9 These doses are known to occupy approximately 65% to 70% of postsynaptic D2 receptors in living humans as confirmed by positron emission tomography (PET) scans.10 Similar minimal effective doses can be determined for serotonin-reuptake inhibiting (SRI) antidepressants (Table 25). In placebo-controlled trials, doses that were smaller than the minimal effective dose did not provide any benefit.
There are important caveats to this. First is the use of partial agonists. Depending on the level of intrinsic activity of a partial agonist and clinical goal, the clinician may aim for a different level of receptor occupancy. For example, aripiprazole will act as a dopamine agonist at lower concentrations, but blocks the receptor at higher concentrations.11 Unlike antagonist antipsychotics, which require only 65% to 70% D2 receptor occupancy to be effective, aripiprazole receptor binding at effective antipsychotic doses is 90% to 95%.12-14 Since aripiprazole has an intrinsic activity of approximately 30% (ie, when it binds, it stimulates the D2 receptor to about 30% of the effect of dopamine binding to the receptor15), binding to 90% of the receptors, and displacing endogenous dopamine, allows aripiprazole to replace the background or tonic tone of dopamine, which has been measured at 19% in people with schizophrenia and 9% in controls.16 Clinically, this still appears as the minimal effective dose achieving maximal response17-19 without significant parkinsonism despite >90% receptor occupancy.12
Continue to: The second caveat is...
The second caveat is the action of low D2 receptor affinity antipsychotics, such as clozapine and quetiapine. These agents generally achieve adequate D2 receptor occupancy for only a brief period of time.20 It has been suggested that continuous receptor occupancy at ≥65% may not be necessary to obtain antipsychotic control.21,22 There may also be specific limbic and cortical (vs striatal) D2 receptor selectivity by clozapine23 compared with other second-generation antipsychotics such as risperidone and olanzapine,24,25 although this point remains debatable.26 Furthermore, the antipsychotic efficacy of low D2 receptor affinity drugs is unreliable, even in controlled, blinded studies (eg, a failed large quetiapine study27). Thus far, the actual antipsychotic mechanism of these agents is yet to be fully understood.
Minimal effective dose achieves maximal response
An interesting aspect of the threshold phenomenon of drug response is that once the minimal effective dose is reached, maximal response is achieved. In other words, there is no additional efficacy with additional dose increases. This is readily demonstrated in some studies in which patients were randomly assigned to different fixed doses or dose ranges. In these studies, there was generally no difference in response rates of different doses, so that once 65% to 80% receptor occupancy is achieved, minimal and maximal clinical response is simultaneously reached.18,28,29
For example, in the original risperidone studies, 6 mg/d was essentially equivalent to 16 mg/d.28 Similarly, lurasidone, 40 mg/d, achieves approximately 65% D2 occupancy.30 When the daily dose is increased to 120 mg, there is no additional benefit in controlling psychosis in schizophrenia.29 This pattern is also seen in partial agonists, where there are no differences between lower and higher doses in terms of response.18
Upon reading this, many clinicians may think “I don’t care what the studies say, I have seen additional benefits with additional doses.” There are several explanations for this. One is that individual patients have genetic variants that may prevent them from responding in a typical fashion. Hints of this are seen in an apparent disconnect between dosage and drug levels, so that it is not surprising that drug levels are a much better predictor of receptor occupancy than dosage.31 Nonetheless, as previously pointed out, for a population, dosage does predict receptor occupancy and outcome. However, for individuals, genetic variations make dosages less reliable. For example, ultrarapid metabolizers of cytochrome P450 (CYP) 2D6 may discontinue risperidone due to nonresponse, or require a higher dose or longer time period to respond.32,33 Similarly, patients who smoke may require an increase in doses of CYP1A2 substrates such as clozapine and olanzapine.34
Alternatively, the clinician may note improvement in mood, sleep, appetite, or other symptoms at lower doses, and then note additional improvements in psychosis or mania at higher doses.3 This occurs due to the varying affinity of different receptors. For example, in bipolar depression trials that used quetiapine in a fixed-dose design, patients who received 300 or 600 mg/d responded in the same fashion, with no additional benefit in improving depression with the higher dose.35 Similarly, in a flexible dose range study that evaluated lurasidone in bipolar depression, an average dose of 34 mg/d (range 20 to 60 mg/d) and an average dose of 83 mg/d (range 80 to 120 mg/d) both resulted in the same response (a 15.4-point reduction in depression ratings and an effect size of 0.51).36 For both quetiapine and lurasidone, higher doses are generally required to control psychosis.29,37 Note that for lurasidone, agitation, but not psychosis, improves with higher doses, which suggests that recruitment of additional receptors results in improvement in a different set of symptoms.9
Continue to: Clinical implications
Clinical implications
The implications for clinicians are relatively clear. Knowing the minimal effective doses for depression, psychosis, or mania informs the target dose. If improvement is seen at lower doses, the clinician needs to assess the profile of symptoms that improved, potential drug–drug interactions, or potential irregularities in the patient’s metabolic pathways. Clinicians need to increase doses above the minimally effective dose carefully, and expend additional effort in analyzing changes in their patient’s symptoms and adverse effects; this analysis should be performed with skepticism and willingness to reduce a dosage if no additional benefit is seen. Attention to these receptor-symptom interactions will improve response and reduce adverse consequences in the majority of patients.
Related Resource
- Lako IM, van den Heuvel ER, Knegtering H, et al. Estimating dopamine D2 receptor occupancy for doses of 8 antipsychotics: a meta-analysis. J Clin Psychopharmacol. 2013;33(5):675-681.
Drug Brand Names
Aripiprazole • Abilify
Asenapine • Saphris
Citalopram • Celexa
Clozapine • Clozaril
Fluoxetine • Prozac
Haloperidol • Haldol
Iloperidone • Fanapt
Lurasidone • Latuda
Nortriptyline • Pamelor
Olanzapine • Zyprexa
Paroxetine • Paxil
Quetiapine • Seroquel
Risperidone • Risperdal
Sertraline • Zoloft
Venlafaxine • Effexor
Ziprasidone • Geodon
1. Farde L, Nordström AL, Wiesel FA, et al. Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry. 1992;49(7):538-544.
2. Kapur S, Zipursky R, Jones C, et al. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry. 2000;157(4):514-520.
3. Roberts RJ, Lohano KK, El-Mallakh RS. Antipsychotics as antidepressants. Asia Pacific Psychiatry. 2016;8(3):179-188.
4. Quitkin FM, Rabkin JG, Gerald J, et al. Validity of clinical trials of antidepressants. Am J Psychiatry. 2000;157(3):327-337.
5. Meyer JH, Wilson AA, Sagrati S, et al. Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry. 2004;161(5):826-835.
6. Lundberg J, Tiger M, Landén M, et al. Serotonin transporter occupancy with TCAs and SSRIs: a PET study in patients with major depressive disorder. Int J Neuropsychopharmacol. 2012;15(8):1167-1172.
7. Takano H, Arakawa R, Nogami T, et al. Norepinephrine transporter occupancy by nortriptyline in patients with depression: a positron emission tomography study with (S,S)-[¹8F]FMeNER-D2. Int J Neuropsychopharmacol. 2014;17(4):553-560.
8. Johnson M, Kozielska M, Pilla Reddy V, et al. Dopamine D2 receptor occupancy as a predictor of catalepsy in rats: a pharmacokinetic-pharmacodynamic modeling approach. Pharm Res. 2014;31(10):2605-2617.
9. Allen MH, Citrome L, Pikalov A, et al. Efficacy of lurasidone in the treatment of agitation: a post hoc analysis of five short-term studies in acutely ill patients with schizophrenia. Gen Hosp Psychiatry. 2017;47:75-82.
10. Sekine M, Maeda J, Shimada H, et al. Central nervous system drug evaluation using positron emission tomography. Clin Psychopharmacol Neurosci. 2011;9(1):9-16.
11. Ma GF, Raivio N, Sabrià J, et al. Agonist and antagonist effects of aripiprazole on D2-like receptors controlling rat brain dopamine synthesis depend on the dopaminergic tone. Int J Neuropsychopharmacol. 2014;18(4):pii: pyu046. doi: 10.1093/ijnp/pyu046.
12. Yokoi F, Gründer G, Biziere K, et al. Dopamine D2 and D3 receptor occupancy in normal humans treated with the antipsychotic drug aripiprazole (OPC 14597): a study using positron emission tomography and [11C]raclopride. Neuropsychopharmacology. 2002;27(2):248-259.
13. Gründer G, Carlsson A, Wong DF. Mechanism of new antipsychotic medications: occupancy is not just antagonism. Arch Gen Psychiatry. 2003;60(10):974-977.
14. Mamo D, Graff A, Mizrahi R, et al. Differential effects of aripiprazole on D(2), 5-HT(2), and 5-HT(1A)receptor occupancy in patients with schizophrenia: a triple tracer PET study. Am J Psychiatry. 2007;164(9):1411-1417.
15. Weiden PJ, Preskorn SH, Fahnestock PA, et al. Translating the psychopharmacology of antipsychotics to individualized treatment for severe mental illness: a roadmap. J Clin Psychiatry. 2007;68(suppl 7):1-48.
16. Abi-Dargham A, Rodenhiser J, Printz D, et al. Increased baseline occupancy of D2 receptors by dopamine in schizophrenia. Proc Natl Acad Sci U S A. 2000;97(14):8104-8109.
17. Kane JM, Carson WH, Saha AR, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2002;63(9):763-771.
18. Potkin SG, Saha AR, Kujawa MJ, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry. 2003;60(7):681-690.
19. Cutler AJ, Marcus RN, Hardy SA, et al. The efficacy and safety of lower doses of aripiprazole for the treatment of patients with acute exacerbation of schizophrenia. CNS Spectr. 2006;11(9):691-702; quiz 719.
20. Gründer G, Landvogt C, Vernaleken I, et al. The striatal and extrastriatal D2/D3 receptor-binding profile of clozapine in patients with schizophrenia. Neuropsychopharmacology. 2006;31(5):1027-1035.
21. Mizuno Y, Bies RR, Remington G, et al. Dopamine D2 receptor occupancy with risperidone or olanzapine during maintenance treatment of schizophrenia: a cross-sectional study. Prog Neuropsychopharmacol Biol Psychiatry. 2012;37(1):182-187.
22. Moriguchi S, Bies RR, Remington G, et al. Estimated dopamine D2 receptor occupancy and remission in schizophrenia: analysis of the CATIE data. J Clin Psychopharmacol. 2013;33(5):682-685.
23. Pilowsky LS, Mulligan RS, Acton PD, et al. Limbic selectivity of clozapine. Lancet. 1997;350(9076):490-491.
24. Ito H, Arakawa R, Takahashi H, et al. No regional difference in dopamine D2 receptor occupancy by the second-generation antipsychotic drug risperidone in humans: a positron emission tomography study. Int J Neuropsychopharmacol. 2009;12(5):667-675.
25. Arakawa R, Ito H, Okumura M, et al. Extrastriatal dopamine D(2) receptor occupancy in olanzapine-treated patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2010;260(4):345-350.
26. Xiberas X, Martinot JL, Mallet L, et al. Extrastriatal and striatal D(2) dopamine receptor blockade with haloperidol or new antipsychotic drugs in patients with schizophrenia. Br J Psychiatry. 2001;179:503-508.
27. Cutler AJ, Tran-Johnson T, Kalali A, et al. A failed 6-week, randomized, double-blind, placebo-controlled study of once-daily extended release quetiapine fumarate in patients with acute schizophrenia: lessons learned. Psychopharmacol Bull. 2010;43(4):37-69.
28. Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry. 1994;151(6):825-835.
29. Meltzer HY, Cucchiaro J, Silva R, et al. Lurasidone in the treatment of schizophrenia: a randomized, double-blind, placebo- and olanzapine-controlled study. Am J Psychiatry. 2011;168(9):957-967.
30. Wong DF, Kuwabara H, Brašic JR, et al. Determination of dopamine D2 receptor occupancy by lurasidone using positron emission tomography in healthy male subjects. Psychopharmacology (Berl). 2013;229(2):245-252.
31. Potkin SG, Keator DB, Kesler-West ML, et al. D2 receptor occupancy following lurasidone treatment in patients with schizophrenia or schizoaffective disorder. CNS Spectr. 2014;19(2):176-181.
32. de Leon J, Susce MT, Pan RM, et al. The CYP2D6 poor metabolizer phenotype may be associated with risperidone adverse drug reactions and discontinuation. J Clin Psychiatry. 2005;66(1):15-27.
33. de Leon J, Susce MT, Pan RM, et al. A study of genetic (CYP2D6 and ABCB1) and environmental (drug inhibitors and inducers) variables that may influence plasma risperidone levels. Pharmacopsychiatry. 2007;40(3):93-102.
34. Narahari A, El-Mallakh RS, Kolikonda MK, et al. How coffee and cigarettes can affect the response to psychopharmacotherapy. Current Psychiatry. 2015;14(10):79-80.
35. Calabrese JR, Keck PE Jr, Macfadden W, et al. A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry. 2005;162(7):1351-1360.
36. Loebel A, Cucchiaro J, Silva R, et al. Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. 2014;171(2):160-168.
37. Lindenmayer JP, Brown D, Liu S, et al. The efficacy and tolerability of once-daily extended release quetiapine fumarate in hospitalized patients with acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled study. Psychopharmacol Bull. 2008;41(3):11-35.
1. Farde L, Nordström AL, Wiesel FA, et al. Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry. 1992;49(7):538-544.
2. Kapur S, Zipursky R, Jones C, et al. Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry. 2000;157(4):514-520.
3. Roberts RJ, Lohano KK, El-Mallakh RS. Antipsychotics as antidepressants. Asia Pacific Psychiatry. 2016;8(3):179-188.
4. Quitkin FM, Rabkin JG, Gerald J, et al. Validity of clinical trials of antidepressants. Am J Psychiatry. 2000;157(3):327-337.
5. Meyer JH, Wilson AA, Sagrati S, et al. Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry. 2004;161(5):826-835.
6. Lundberg J, Tiger M, Landén M, et al. Serotonin transporter occupancy with TCAs and SSRIs: a PET study in patients with major depressive disorder. Int J Neuropsychopharmacol. 2012;15(8):1167-1172.
7. Takano H, Arakawa R, Nogami T, et al. Norepinephrine transporter occupancy by nortriptyline in patients with depression: a positron emission tomography study with (S,S)-[¹8F]FMeNER-D2. Int J Neuropsychopharmacol. 2014;17(4):553-560.
8. Johnson M, Kozielska M, Pilla Reddy V, et al. Dopamine D2 receptor occupancy as a predictor of catalepsy in rats: a pharmacokinetic-pharmacodynamic modeling approach. Pharm Res. 2014;31(10):2605-2617.
9. Allen MH, Citrome L, Pikalov A, et al. Efficacy of lurasidone in the treatment of agitation: a post hoc analysis of five short-term studies in acutely ill patients with schizophrenia. Gen Hosp Psychiatry. 2017;47:75-82.
10. Sekine M, Maeda J, Shimada H, et al. Central nervous system drug evaluation using positron emission tomography. Clin Psychopharmacol Neurosci. 2011;9(1):9-16.
11. Ma GF, Raivio N, Sabrià J, et al. Agonist and antagonist effects of aripiprazole on D2-like receptors controlling rat brain dopamine synthesis depend on the dopaminergic tone. Int J Neuropsychopharmacol. 2014;18(4):pii: pyu046. doi: 10.1093/ijnp/pyu046.
12. Yokoi F, Gründer G, Biziere K, et al. Dopamine D2 and D3 receptor occupancy in normal humans treated with the antipsychotic drug aripiprazole (OPC 14597): a study using positron emission tomography and [11C]raclopride. Neuropsychopharmacology. 2002;27(2):248-259.
13. Gründer G, Carlsson A, Wong DF. Mechanism of new antipsychotic medications: occupancy is not just antagonism. Arch Gen Psychiatry. 2003;60(10):974-977.
14. Mamo D, Graff A, Mizrahi R, et al. Differential effects of aripiprazole on D(2), 5-HT(2), and 5-HT(1A)receptor occupancy in patients with schizophrenia: a triple tracer PET study. Am J Psychiatry. 2007;164(9):1411-1417.
15. Weiden PJ, Preskorn SH, Fahnestock PA, et al. Translating the psychopharmacology of antipsychotics to individualized treatment for severe mental illness: a roadmap. J Clin Psychiatry. 2007;68(suppl 7):1-48.
16. Abi-Dargham A, Rodenhiser J, Printz D, et al. Increased baseline occupancy of D2 receptors by dopamine in schizophrenia. Proc Natl Acad Sci U S A. 2000;97(14):8104-8109.
17. Kane JM, Carson WH, Saha AR, et al. Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry. 2002;63(9):763-771.
18. Potkin SG, Saha AR, Kujawa MJ, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry. 2003;60(7):681-690.
19. Cutler AJ, Marcus RN, Hardy SA, et al. The efficacy and safety of lower doses of aripiprazole for the treatment of patients with acute exacerbation of schizophrenia. CNS Spectr. 2006;11(9):691-702; quiz 719.
20. Gründer G, Landvogt C, Vernaleken I, et al. The striatal and extrastriatal D2/D3 receptor-binding profile of clozapine in patients with schizophrenia. Neuropsychopharmacology. 2006;31(5):1027-1035.
21. Mizuno Y, Bies RR, Remington G, et al. Dopamine D2 receptor occupancy with risperidone or olanzapine during maintenance treatment of schizophrenia: a cross-sectional study. Prog Neuropsychopharmacol Biol Psychiatry. 2012;37(1):182-187.
22. Moriguchi S, Bies RR, Remington G, et al. Estimated dopamine D2 receptor occupancy and remission in schizophrenia: analysis of the CATIE data. J Clin Psychopharmacol. 2013;33(5):682-685.
23. Pilowsky LS, Mulligan RS, Acton PD, et al. Limbic selectivity of clozapine. Lancet. 1997;350(9076):490-491.
24. Ito H, Arakawa R, Takahashi H, et al. No regional difference in dopamine D2 receptor occupancy by the second-generation antipsychotic drug risperidone in humans: a positron emission tomography study. Int J Neuropsychopharmacol. 2009;12(5):667-675.
25. Arakawa R, Ito H, Okumura M, et al. Extrastriatal dopamine D(2) receptor occupancy in olanzapine-treated patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2010;260(4):345-350.
26. Xiberas X, Martinot JL, Mallet L, et al. Extrastriatal and striatal D(2) dopamine receptor blockade with haloperidol or new antipsychotic drugs in patients with schizophrenia. Br J Psychiatry. 2001;179:503-508.
27. Cutler AJ, Tran-Johnson T, Kalali A, et al. A failed 6-week, randomized, double-blind, placebo-controlled study of once-daily extended release quetiapine fumarate in patients with acute schizophrenia: lessons learned. Psychopharmacol Bull. 2010;43(4):37-69.
28. Marder SR, Meibach RC. Risperidone in the treatment of schizophrenia. Am J Psychiatry. 1994;151(6):825-835.
29. Meltzer HY, Cucchiaro J, Silva R, et al. Lurasidone in the treatment of schizophrenia: a randomized, double-blind, placebo- and olanzapine-controlled study. Am J Psychiatry. 2011;168(9):957-967.
30. Wong DF, Kuwabara H, Brašic JR, et al. Determination of dopamine D2 receptor occupancy by lurasidone using positron emission tomography in healthy male subjects. Psychopharmacology (Berl). 2013;229(2):245-252.
31. Potkin SG, Keator DB, Kesler-West ML, et al. D2 receptor occupancy following lurasidone treatment in patients with schizophrenia or schizoaffective disorder. CNS Spectr. 2014;19(2):176-181.
32. de Leon J, Susce MT, Pan RM, et al. The CYP2D6 poor metabolizer phenotype may be associated with risperidone adverse drug reactions and discontinuation. J Clin Psychiatry. 2005;66(1):15-27.
33. de Leon J, Susce MT, Pan RM, et al. A study of genetic (CYP2D6 and ABCB1) and environmental (drug inhibitors and inducers) variables that may influence plasma risperidone levels. Pharmacopsychiatry. 2007;40(3):93-102.
34. Narahari A, El-Mallakh RS, Kolikonda MK, et al. How coffee and cigarettes can affect the response to psychopharmacotherapy. Current Psychiatry. 2015;14(10):79-80.
35. Calabrese JR, Keck PE Jr, Macfadden W, et al. A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry. 2005;162(7):1351-1360.
36. Loebel A, Cucchiaro J, Silva R, et al. Lurasidone monotherapy in the treatment of bipolar I depression: a randomized, double-blind, placebo-controlled study. Am J Psychiatry. 2014;171(2):160-168.
37. Lindenmayer JP, Brown D, Liu S, et al. The efficacy and tolerability of once-daily extended release quetiapine fumarate in hospitalized patients with acute schizophrenia: a 6-week randomized, double-blind, placebo-controlled study. Psychopharmacol Bull. 2008;41(3):11-35.
Extended propranolol use boosts success in high-risk infantile hemangioma
Extending oral propranolol treatment up to 12 months of age increased the success rate for high-risk infantile hemangioma, according to results published in Pediatrics.
Previous studies of oral propranol for infantile hemangiomas (IH) have revealed its efficacy, although there is no consensus on the optimal treatment duration. Nonetheless, treatment up to 12 months of age has been proposed if patients don’t respond after 6 months. Infants with high-risk hemangiomas, however, have been excluded from previous studies, authors of the current study explained.
In an open-label study of patients aged 35-150 days the success rate of oral propranolol was 47% after 6 months of treatment. The rate increased to 76% after the initial treatment period, reported Eulalia Baselga, MD, of the department of dermatology at Hospital de la Santa Creu i Sant Pau in Barcelona, and coauthors.
Investigators studied 45 patients from 10 hospitals in Spain and Poland between June 2015 and February 2017. The patients had high-risk IH in the proliferative phase. High-risk hemangiomas were defined as those that were life threatening, at risk for functional impact, disfiguring, or ulcerated nonresponsive to standard wound care measures.
Oral propranolol was administered twice daily at a dosage of 3 mg/kg per day. During the initial treatment period (ITP), patients received propranolol for a minimum of 6 months, and if treatment was not successful, it continued until success or up to 12 months of age.
Patients who achieved success in the initial phase were managed for 3 months with no treatment, and if there was rebound growth, treatment was restarted for up to 6 months at the provider’s discretion.
Treatment was considered a success if the target hemangioma resolved and there was no functional impact. The IH was considered resolved if it disappeared, even if there were minimal telangiectasias, erythema, skin thickening, soft tissue swelling, or the presence of sequelae.
Treatment success was achieved by 21 (47%) patients after 6 months and by 34 (76%) patients by the end of the ITP. Functional impact was determined using the Hemangioma Severity and Hemangioma Dynamic Complication scales. Adverse events, reported by 80% of patients, were resolved by the end of the study and included respiratory syncytial virus bronchiolitis, ulcerated hemangioma, pneumonia and respiratory failure, inguinal hernia, upper respiratory tract infection, dehydration, bronchitis, choking, and thermal burn. Although no patients experienced adverse events that resulted in discontinuation of treatment, 35 events led to temporary discontinuation, primarily due to respiratory events, the authors reported.
The results indicate that “oral propranolol is effective in treating high-risk IH with a favorable safety profile,” the authors concluded.
The study was funded by the Institut de Recherche Pierre Fabre Several authors were employed by or had other relationships with Pierre Fabre. The other authors had no conflicts of interest.
SOURCE: Baselga E et al. Pediatrics. 2018. doi: 10.1542/peds.2017-3866.
Extending oral propranolol treatment up to 12 months of age increased the success rate for high-risk infantile hemangioma, according to results published in Pediatrics.
Previous studies of oral propranol for infantile hemangiomas (IH) have revealed its efficacy, although there is no consensus on the optimal treatment duration. Nonetheless, treatment up to 12 months of age has been proposed if patients don’t respond after 6 months. Infants with high-risk hemangiomas, however, have been excluded from previous studies, authors of the current study explained.
In an open-label study of patients aged 35-150 days the success rate of oral propranolol was 47% after 6 months of treatment. The rate increased to 76% after the initial treatment period, reported Eulalia Baselga, MD, of the department of dermatology at Hospital de la Santa Creu i Sant Pau in Barcelona, and coauthors.
Investigators studied 45 patients from 10 hospitals in Spain and Poland between June 2015 and February 2017. The patients had high-risk IH in the proliferative phase. High-risk hemangiomas were defined as those that were life threatening, at risk for functional impact, disfiguring, or ulcerated nonresponsive to standard wound care measures.
Oral propranolol was administered twice daily at a dosage of 3 mg/kg per day. During the initial treatment period (ITP), patients received propranolol for a minimum of 6 months, and if treatment was not successful, it continued until success or up to 12 months of age.
Patients who achieved success in the initial phase were managed for 3 months with no treatment, and if there was rebound growth, treatment was restarted for up to 6 months at the provider’s discretion.
Treatment was considered a success if the target hemangioma resolved and there was no functional impact. The IH was considered resolved if it disappeared, even if there were minimal telangiectasias, erythema, skin thickening, soft tissue swelling, or the presence of sequelae.
Treatment success was achieved by 21 (47%) patients after 6 months and by 34 (76%) patients by the end of the ITP. Functional impact was determined using the Hemangioma Severity and Hemangioma Dynamic Complication scales. Adverse events, reported by 80% of patients, were resolved by the end of the study and included respiratory syncytial virus bronchiolitis, ulcerated hemangioma, pneumonia and respiratory failure, inguinal hernia, upper respiratory tract infection, dehydration, bronchitis, choking, and thermal burn. Although no patients experienced adverse events that resulted in discontinuation of treatment, 35 events led to temporary discontinuation, primarily due to respiratory events, the authors reported.
The results indicate that “oral propranolol is effective in treating high-risk IH with a favorable safety profile,” the authors concluded.
The study was funded by the Institut de Recherche Pierre Fabre Several authors were employed by or had other relationships with Pierre Fabre. The other authors had no conflicts of interest.
SOURCE: Baselga E et al. Pediatrics. 2018. doi: 10.1542/peds.2017-3866.
Extending oral propranolol treatment up to 12 months of age increased the success rate for high-risk infantile hemangioma, according to results published in Pediatrics.
Previous studies of oral propranol for infantile hemangiomas (IH) have revealed its efficacy, although there is no consensus on the optimal treatment duration. Nonetheless, treatment up to 12 months of age has been proposed if patients don’t respond after 6 months. Infants with high-risk hemangiomas, however, have been excluded from previous studies, authors of the current study explained.
In an open-label study of patients aged 35-150 days the success rate of oral propranolol was 47% after 6 months of treatment. The rate increased to 76% after the initial treatment period, reported Eulalia Baselga, MD, of the department of dermatology at Hospital de la Santa Creu i Sant Pau in Barcelona, and coauthors.
Investigators studied 45 patients from 10 hospitals in Spain and Poland between June 2015 and February 2017. The patients had high-risk IH in the proliferative phase. High-risk hemangiomas were defined as those that were life threatening, at risk for functional impact, disfiguring, or ulcerated nonresponsive to standard wound care measures.
Oral propranolol was administered twice daily at a dosage of 3 mg/kg per day. During the initial treatment period (ITP), patients received propranolol for a minimum of 6 months, and if treatment was not successful, it continued until success or up to 12 months of age.
Patients who achieved success in the initial phase were managed for 3 months with no treatment, and if there was rebound growth, treatment was restarted for up to 6 months at the provider’s discretion.
Treatment was considered a success if the target hemangioma resolved and there was no functional impact. The IH was considered resolved if it disappeared, even if there were minimal telangiectasias, erythema, skin thickening, soft tissue swelling, or the presence of sequelae.
Treatment success was achieved by 21 (47%) patients after 6 months and by 34 (76%) patients by the end of the ITP. Functional impact was determined using the Hemangioma Severity and Hemangioma Dynamic Complication scales. Adverse events, reported by 80% of patients, were resolved by the end of the study and included respiratory syncytial virus bronchiolitis, ulcerated hemangioma, pneumonia and respiratory failure, inguinal hernia, upper respiratory tract infection, dehydration, bronchitis, choking, and thermal burn. Although no patients experienced adverse events that resulted in discontinuation of treatment, 35 events led to temporary discontinuation, primarily due to respiratory events, the authors reported.
The results indicate that “oral propranolol is effective in treating high-risk IH with a favorable safety profile,” the authors concluded.
The study was funded by the Institut de Recherche Pierre Fabre Several authors were employed by or had other relationships with Pierre Fabre. The other authors had no conflicts of interest.
SOURCE: Baselga E et al. Pediatrics. 2018. doi: 10.1542/peds.2017-3866.
FROM PEDIATRICS
Key clinical point:
Major finding: After 6 months of treatment, the success rate was 47%, and it rose to 76% at the end of the treatment period.
Study details: A phase 3 study of 45 patients aged 35-150 days with high-risk IH.
Disclosures: The study was funded by the Institut de Recherche Pierre Fabre Several authors were employed by or had other relationships with Pierre Fabre. The other authors had no conflicts of interest.
Source: Baselga E et al. Pediatrics. 2018. doi: 10.1542/peds.2017-3866
Mechanism of cGVHD response to ECP still unclear
A prospective study did not reveal the mechanism driving response to extracorporeal photopheresis (ECP) in patients with chronic graft-versus-host disease (cGVHD).
However, researchers did find that responses occurred independent of risk factors, and results suggested that regulatory T cells (Tregs) are not the dominant mechanism of response to ECP.
Madan Jagasia, MBBS, of Vanderbilt University School of Medicine in Nashville, Tennessee, and his colleagues conducted this research and detailed the findings in Biology of Blood and Marrow Transplantation.
The study was funded by Therakos, Inc., a Mallinckrodt Pharmaceuticals Company.
The study included 77 patients with cGVHD. The median age at transplant was 49, 88% of patients were white, and 62% were male.
Patients had moderate (48%) or severe (52%) cGVHD. Sites of involvement included skin (86%), mouth (52%), gastrointestinal tract (29%), eye (62%), joint and fascia (51%), genital tract (11%), and lung (28%).
Patients had received a median of 2 (range, 0 to 7) prior lines of cGVHD therapy.
For this study, patients received 1689 ECP treatments, an average of 21.9 treatments per patient. The most common regimen was ECP twice a week for 4 weeks, then twice a week every 2 weeks for 8 weeks, then further tapering at the treating physician’s discretion.
Forty-eight patients (62.3%) completed all 6 months of ECP treatment. Reasons for early discontinuation included cGVHD progression (n=6), infection (n=4), cGVHD improvement (n=2), death from cGVHD-related cause (n=2), logistical issues (n=2), loss to follow-up (n=2), unknown reasons (n=4), and other various reasons (n=7) such as a finance issue and non-adherence.
Response
Provider-assessed response rates differed from response rates according to 2005 National Institutes of Health (NIH) consensus criteria.
According to providers, the response rate was 62.3% (48/77), with 14% of patients (n=11) achieving a complete response and 48% (n=37) attaining a partial response. Nineteen percent of patients (n=15) had stable disease, 14% (n=11) progressed, and 4% (n=3) did not have follow-up for cGVHD-related reasons.
Eight patients did not have enough data to assess NIH response. For the 69 evaluable patients, the NIH response rate was 43.5% (n=30), with 6% of patients (n=4) achieving a complete response and 38% (n=26) attaining a partial response. Fifteen percent of patients (n=10) had stable disease, 38% (n=26) progressed, and 4% (n=3) did not have follow-up for cGVHD-related reasons.
Risk factors
The researchers said there was no significant difference between responders and nonresponders when it came to age at treatment, platelet count, cGVHD severity, donor gender, and donor type.
For provider-assessed response, the median Karnofsky performance score at study entry was significantly higher in responders than nonresponders (90 vs 80; P=0.001). Responders also had a significantly shorter time from transplant to study entry compared to nonresponders (1.43 vs 2.06 years; P=0.051).
Similarly, according to NIH response, time from transplant to study entry was significantly shorter for responders than nonresponders (1.23 vs 1.92 years; P=0.04).
However, in a logistic regression model, time from transplant to study entry was not associated with provider-assessed or NIH response.
Tregs
The researchers found no significant difference in Treg percentages between responders and nonresponders.
For provider-assessed response, the baseline Treg frequency was 4.4% in responders and 4.8% in nonresponders (P=0.4). Treg percentages at the end of study were 4.2% and 5.5%, respectively (P=0.2). And the change in Treg frequency was 0.3% and 1.3%, respectively (P=0.3).
For NIH response, the baseline Treg frequency was 4.7% in responders and 4.4% in nonresponders (P=0.3). Treg percentages at the end of study were 4.4% and 4.7%, respectively (P=0.6). And the change in Treg percentages was 0.3% and 0.7%, respectively (P=0.4).
These findings run contrary to the researchers’ hypothesis that response to ECP would be associated with an increase in the percentage of Tregs.
The researchers did note that the number of Tregs varied between patients, and the team raised the possibility that the mechanism of Tregs in ECP is not visible by measuring cell abundance.
However, the researchers also said future studies should explore additional mechanisms of action for ECP and look particularly at other T-cell populations, dendritic cells, inhibitory cytokines, and proinflammatory cytokines.
A prospective study did not reveal the mechanism driving response to extracorporeal photopheresis (ECP) in patients with chronic graft-versus-host disease (cGVHD).
However, researchers did find that responses occurred independent of risk factors, and results suggested that regulatory T cells (Tregs) are not the dominant mechanism of response to ECP.
Madan Jagasia, MBBS, of Vanderbilt University School of Medicine in Nashville, Tennessee, and his colleagues conducted this research and detailed the findings in Biology of Blood and Marrow Transplantation.
The study was funded by Therakos, Inc., a Mallinckrodt Pharmaceuticals Company.
The study included 77 patients with cGVHD. The median age at transplant was 49, 88% of patients were white, and 62% were male.
Patients had moderate (48%) or severe (52%) cGVHD. Sites of involvement included skin (86%), mouth (52%), gastrointestinal tract (29%), eye (62%), joint and fascia (51%), genital tract (11%), and lung (28%).
Patients had received a median of 2 (range, 0 to 7) prior lines of cGVHD therapy.
For this study, patients received 1689 ECP treatments, an average of 21.9 treatments per patient. The most common regimen was ECP twice a week for 4 weeks, then twice a week every 2 weeks for 8 weeks, then further tapering at the treating physician’s discretion.
Forty-eight patients (62.3%) completed all 6 months of ECP treatment. Reasons for early discontinuation included cGVHD progression (n=6), infection (n=4), cGVHD improvement (n=2), death from cGVHD-related cause (n=2), logistical issues (n=2), loss to follow-up (n=2), unknown reasons (n=4), and other various reasons (n=7) such as a finance issue and non-adherence.
Response
Provider-assessed response rates differed from response rates according to 2005 National Institutes of Health (NIH) consensus criteria.
According to providers, the response rate was 62.3% (48/77), with 14% of patients (n=11) achieving a complete response and 48% (n=37) attaining a partial response. Nineteen percent of patients (n=15) had stable disease, 14% (n=11) progressed, and 4% (n=3) did not have follow-up for cGVHD-related reasons.
Eight patients did not have enough data to assess NIH response. For the 69 evaluable patients, the NIH response rate was 43.5% (n=30), with 6% of patients (n=4) achieving a complete response and 38% (n=26) attaining a partial response. Fifteen percent of patients (n=10) had stable disease, 38% (n=26) progressed, and 4% (n=3) did not have follow-up for cGVHD-related reasons.
Risk factors
The researchers said there was no significant difference between responders and nonresponders when it came to age at treatment, platelet count, cGVHD severity, donor gender, and donor type.
For provider-assessed response, the median Karnofsky performance score at study entry was significantly higher in responders than nonresponders (90 vs 80; P=0.001). Responders also had a significantly shorter time from transplant to study entry compared to nonresponders (1.43 vs 2.06 years; P=0.051).
Similarly, according to NIH response, time from transplant to study entry was significantly shorter for responders than nonresponders (1.23 vs 1.92 years; P=0.04).
However, in a logistic regression model, time from transplant to study entry was not associated with provider-assessed or NIH response.
Tregs
The researchers found no significant difference in Treg percentages between responders and nonresponders.
For provider-assessed response, the baseline Treg frequency was 4.4% in responders and 4.8% in nonresponders (P=0.4). Treg percentages at the end of study were 4.2% and 5.5%, respectively (P=0.2). And the change in Treg frequency was 0.3% and 1.3%, respectively (P=0.3).
For NIH response, the baseline Treg frequency was 4.7% in responders and 4.4% in nonresponders (P=0.3). Treg percentages at the end of study were 4.4% and 4.7%, respectively (P=0.6). And the change in Treg percentages was 0.3% and 0.7%, respectively (P=0.4).
These findings run contrary to the researchers’ hypothesis that response to ECP would be associated with an increase in the percentage of Tregs.
The researchers did note that the number of Tregs varied between patients, and the team raised the possibility that the mechanism of Tregs in ECP is not visible by measuring cell abundance.
However, the researchers also said future studies should explore additional mechanisms of action for ECP and look particularly at other T-cell populations, dendritic cells, inhibitory cytokines, and proinflammatory cytokines.
A prospective study did not reveal the mechanism driving response to extracorporeal photopheresis (ECP) in patients with chronic graft-versus-host disease (cGVHD).
However, researchers did find that responses occurred independent of risk factors, and results suggested that regulatory T cells (Tregs) are not the dominant mechanism of response to ECP.
Madan Jagasia, MBBS, of Vanderbilt University School of Medicine in Nashville, Tennessee, and his colleagues conducted this research and detailed the findings in Biology of Blood and Marrow Transplantation.
The study was funded by Therakos, Inc., a Mallinckrodt Pharmaceuticals Company.
The study included 77 patients with cGVHD. The median age at transplant was 49, 88% of patients were white, and 62% were male.
Patients had moderate (48%) or severe (52%) cGVHD. Sites of involvement included skin (86%), mouth (52%), gastrointestinal tract (29%), eye (62%), joint and fascia (51%), genital tract (11%), and lung (28%).
Patients had received a median of 2 (range, 0 to 7) prior lines of cGVHD therapy.
For this study, patients received 1689 ECP treatments, an average of 21.9 treatments per patient. The most common regimen was ECP twice a week for 4 weeks, then twice a week every 2 weeks for 8 weeks, then further tapering at the treating physician’s discretion.
Forty-eight patients (62.3%) completed all 6 months of ECP treatment. Reasons for early discontinuation included cGVHD progression (n=6), infection (n=4), cGVHD improvement (n=2), death from cGVHD-related cause (n=2), logistical issues (n=2), loss to follow-up (n=2), unknown reasons (n=4), and other various reasons (n=7) such as a finance issue and non-adherence.
Response
Provider-assessed response rates differed from response rates according to 2005 National Institutes of Health (NIH) consensus criteria.
According to providers, the response rate was 62.3% (48/77), with 14% of patients (n=11) achieving a complete response and 48% (n=37) attaining a partial response. Nineteen percent of patients (n=15) had stable disease, 14% (n=11) progressed, and 4% (n=3) did not have follow-up for cGVHD-related reasons.
Eight patients did not have enough data to assess NIH response. For the 69 evaluable patients, the NIH response rate was 43.5% (n=30), with 6% of patients (n=4) achieving a complete response and 38% (n=26) attaining a partial response. Fifteen percent of patients (n=10) had stable disease, 38% (n=26) progressed, and 4% (n=3) did not have follow-up for cGVHD-related reasons.
Risk factors
The researchers said there was no significant difference between responders and nonresponders when it came to age at treatment, platelet count, cGVHD severity, donor gender, and donor type.
For provider-assessed response, the median Karnofsky performance score at study entry was significantly higher in responders than nonresponders (90 vs 80; P=0.001). Responders also had a significantly shorter time from transplant to study entry compared to nonresponders (1.43 vs 2.06 years; P=0.051).
Similarly, according to NIH response, time from transplant to study entry was significantly shorter for responders than nonresponders (1.23 vs 1.92 years; P=0.04).
However, in a logistic regression model, time from transplant to study entry was not associated with provider-assessed or NIH response.
Tregs
The researchers found no significant difference in Treg percentages between responders and nonresponders.
For provider-assessed response, the baseline Treg frequency was 4.4% in responders and 4.8% in nonresponders (P=0.4). Treg percentages at the end of study were 4.2% and 5.5%, respectively (P=0.2). And the change in Treg frequency was 0.3% and 1.3%, respectively (P=0.3).
For NIH response, the baseline Treg frequency was 4.7% in responders and 4.4% in nonresponders (P=0.3). Treg percentages at the end of study were 4.4% and 4.7%, respectively (P=0.6). And the change in Treg percentages was 0.3% and 0.7%, respectively (P=0.4).
These findings run contrary to the researchers’ hypothesis that response to ECP would be associated with an increase in the percentage of Tregs.
The researchers did note that the number of Tregs varied between patients, and the team raised the possibility that the mechanism of Tregs in ECP is not visible by measuring cell abundance.
However, the researchers also said future studies should explore additional mechanisms of action for ECP and look particularly at other T-cell populations, dendritic cells, inhibitory cytokines, and proinflammatory cytokines.
FDA approves Cassipa for opioid dependence
Cassipa sublingual film, made by Teva Pharmaceuticals, is a 16 mg/4 mg dosage of buprenorphine and naloxone for the maintenance treatment of opioid dependence. Buprenorphine and naloxone sublingual film also is approved in both brand name and generic versions and in various strengths, the FDA said in a press release.
Cassipa should be used as part of a complete treatment plan that includes counseling and psychosocial support and should be used only after patient induction and stabilization up to a dose of 16 mg of buprenorphine using another marketed product. These products may only be prescribed by Drug Addiction Treatment Act (DATA)–certified prescribers.
“There’s an urgent need to ensure access to, and wider use and understanding of, medication-assisted treatment for opioid use disorder ... the FDA recently described a streamlined approach to drug development for certain medication-assisted treatments that are based on buprenorphine. This streamlined approach can reduce drug development costs, so products may be offered at a lower price to patients and we can broaden access to treatment,” FDA Commissioner Scott Gottlieb, MD, said in the statement.
He added that “individuals who successfully transition onto medication-assisted treatment are not swapping one addiction for another. Opioid replacement therapy can be an important part of effective treatment. Opioid use disorder should be viewed similarly to any other chronic condition that is treated with medication.”
Medication-assisted treatment (MAT) is a comprehensive approach that combines FDA-approved medications (currently methadone, buprenorphine, or naltrexone) with counseling and other behavioral therapies to treat patients with opioid use disorder. Regular adherence to MAT with buprenorphine reduces opioid withdrawal symptoms and the desire to use opioids. According to the Substance Abuse and Mental Health Services Administration, patients receiving MAT for treatment of their opioid use disorder cut their risk of death from all causes in half.
Improving access to prevention, treatment, and recovery services, including the full range of MAT, is part of the Department of Health and Human Services’ Five-Point Strategy to Combat the Opioid Crisis. Last month, the FDA issued draft guidance outlining new ways for drug developers to consider measuring and demonstrating the effectiveness and benefits of new or existing MAT products, building on another draft guidance issued in April outlining the agency’s current thinking about drug development and trial design issues relevant to the study of depot buprenorphine products (i.e., modified-release products for injection or implantation). In June, the agency also approved the first generic versions of Suboxone (buprenorphine and naloxone) sublingual film in multiple strengths, the statement said.
Cassipa was approved through the abbreviated 505(b)(2) approval pathway and its application relied, in part, on the FDA’s finding of safety and effectiveness for Suboxone sublingual film to support approval. The applicant demonstrated that reliance on the FDA’s finding of safety and effectiveness for Suboxone was scientifically justified and provided Cassipa-specific pharmacokinetic data to establish the drug’s safety and efficacy for its approved uses, according to the FDA.
Adverse events commonly observed with the buprenorphine and naloxone sublingual film are oral hypoesthesia, glossodynia, oral mucosal erythema, headache, nausea, vomiting, hyperhidrosis, constipation, signs and symptoms of withdrawal, insomnia, pain, and peripheral edema.
Cassipa sublingual film, made by Teva Pharmaceuticals, is a 16 mg/4 mg dosage of buprenorphine and naloxone for the maintenance treatment of opioid dependence. Buprenorphine and naloxone sublingual film also is approved in both brand name and generic versions and in various strengths, the FDA said in a press release.
Cassipa should be used as part of a complete treatment plan that includes counseling and psychosocial support and should be used only after patient induction and stabilization up to a dose of 16 mg of buprenorphine using another marketed product. These products may only be prescribed by Drug Addiction Treatment Act (DATA)–certified prescribers.
“There’s an urgent need to ensure access to, and wider use and understanding of, medication-assisted treatment for opioid use disorder ... the FDA recently described a streamlined approach to drug development for certain medication-assisted treatments that are based on buprenorphine. This streamlined approach can reduce drug development costs, so products may be offered at a lower price to patients and we can broaden access to treatment,” FDA Commissioner Scott Gottlieb, MD, said in the statement.
He added that “individuals who successfully transition onto medication-assisted treatment are not swapping one addiction for another. Opioid replacement therapy can be an important part of effective treatment. Opioid use disorder should be viewed similarly to any other chronic condition that is treated with medication.”
Medication-assisted treatment (MAT) is a comprehensive approach that combines FDA-approved medications (currently methadone, buprenorphine, or naltrexone) with counseling and other behavioral therapies to treat patients with opioid use disorder. Regular adherence to MAT with buprenorphine reduces opioid withdrawal symptoms and the desire to use opioids. According to the Substance Abuse and Mental Health Services Administration, patients receiving MAT for treatment of their opioid use disorder cut their risk of death from all causes in half.
Improving access to prevention, treatment, and recovery services, including the full range of MAT, is part of the Department of Health and Human Services’ Five-Point Strategy to Combat the Opioid Crisis. Last month, the FDA issued draft guidance outlining new ways for drug developers to consider measuring and demonstrating the effectiveness and benefits of new or existing MAT products, building on another draft guidance issued in April outlining the agency’s current thinking about drug development and trial design issues relevant to the study of depot buprenorphine products (i.e., modified-release products for injection or implantation). In June, the agency also approved the first generic versions of Suboxone (buprenorphine and naloxone) sublingual film in multiple strengths, the statement said.
Cassipa was approved through the abbreviated 505(b)(2) approval pathway and its application relied, in part, on the FDA’s finding of safety and effectiveness for Suboxone sublingual film to support approval. The applicant demonstrated that reliance on the FDA’s finding of safety and effectiveness for Suboxone was scientifically justified and provided Cassipa-specific pharmacokinetic data to establish the drug’s safety and efficacy for its approved uses, according to the FDA.
Adverse events commonly observed with the buprenorphine and naloxone sublingual film are oral hypoesthesia, glossodynia, oral mucosal erythema, headache, nausea, vomiting, hyperhidrosis, constipation, signs and symptoms of withdrawal, insomnia, pain, and peripheral edema.
Cassipa sublingual film, made by Teva Pharmaceuticals, is a 16 mg/4 mg dosage of buprenorphine and naloxone for the maintenance treatment of opioid dependence. Buprenorphine and naloxone sublingual film also is approved in both brand name and generic versions and in various strengths, the FDA said in a press release.
Cassipa should be used as part of a complete treatment plan that includes counseling and psychosocial support and should be used only after patient induction and stabilization up to a dose of 16 mg of buprenorphine using another marketed product. These products may only be prescribed by Drug Addiction Treatment Act (DATA)–certified prescribers.
“There’s an urgent need to ensure access to, and wider use and understanding of, medication-assisted treatment for opioid use disorder ... the FDA recently described a streamlined approach to drug development for certain medication-assisted treatments that are based on buprenorphine. This streamlined approach can reduce drug development costs, so products may be offered at a lower price to patients and we can broaden access to treatment,” FDA Commissioner Scott Gottlieb, MD, said in the statement.
He added that “individuals who successfully transition onto medication-assisted treatment are not swapping one addiction for another. Opioid replacement therapy can be an important part of effective treatment. Opioid use disorder should be viewed similarly to any other chronic condition that is treated with medication.”
Medication-assisted treatment (MAT) is a comprehensive approach that combines FDA-approved medications (currently methadone, buprenorphine, or naltrexone) with counseling and other behavioral therapies to treat patients with opioid use disorder. Regular adherence to MAT with buprenorphine reduces opioid withdrawal symptoms and the desire to use opioids. According to the Substance Abuse and Mental Health Services Administration, patients receiving MAT for treatment of their opioid use disorder cut their risk of death from all causes in half.
Improving access to prevention, treatment, and recovery services, including the full range of MAT, is part of the Department of Health and Human Services’ Five-Point Strategy to Combat the Opioid Crisis. Last month, the FDA issued draft guidance outlining new ways for drug developers to consider measuring and demonstrating the effectiveness and benefits of new or existing MAT products, building on another draft guidance issued in April outlining the agency’s current thinking about drug development and trial design issues relevant to the study of depot buprenorphine products (i.e., modified-release products for injection or implantation). In June, the agency also approved the first generic versions of Suboxone (buprenorphine and naloxone) sublingual film in multiple strengths, the statement said.
Cassipa was approved through the abbreviated 505(b)(2) approval pathway and its application relied, in part, on the FDA’s finding of safety and effectiveness for Suboxone sublingual film to support approval. The applicant demonstrated that reliance on the FDA’s finding of safety and effectiveness for Suboxone was scientifically justified and provided Cassipa-specific pharmacokinetic data to establish the drug’s safety and efficacy for its approved uses, according to the FDA.
Adverse events commonly observed with the buprenorphine and naloxone sublingual film are oral hypoesthesia, glossodynia, oral mucosal erythema, headache, nausea, vomiting, hyperhidrosis, constipation, signs and symptoms of withdrawal, insomnia, pain, and peripheral edema.
Risk Factors for Epilepsy after Traumatic Brain Injury
Among patients who have experienced a traumatic brain injury (TBI), the likelihood of developing post-traumatic epilepsy (PTE) increases with age, the early onset of seizures, and the severity of the brain injury, according to an analysis of insurance claims from 2004 to 2014.
- There were approximately 2.8 million emergency room visits, hospitalizations and deaths from traumatic brain injuries in the US in 2013.
- Early seizures occurred in 0.5% of patients with TBI.
- Over a 9 year period, the incidence of post-traumatic epilepsy (PTE) increased from 1 to 4% in this population.
- Early onset of seizures, older age, and TBI severity increased the likelihood of PTE.
- Prophylactic acetazolamide seemed to reduce the risk of PTE, when compared to patients who had received no anti-epilepsy drugs.
DeGrauw X, Thurman D, Xu L, et al. Epidemiology of traumatic brain injury-associated epilepsy and early use of anti-epilepsy drugs: An analysis of insurance claims data, 2004-2014. [Published online ahead of print July 23, 2018] Epilepsy Res. doi: 10.1016/j.eplepsyres.2018.07.012
Among patients who have experienced a traumatic brain injury (TBI), the likelihood of developing post-traumatic epilepsy (PTE) increases with age, the early onset of seizures, and the severity of the brain injury, according to an analysis of insurance claims from 2004 to 2014.
- There were approximately 2.8 million emergency room visits, hospitalizations and deaths from traumatic brain injuries in the US in 2013.
- Early seizures occurred in 0.5% of patients with TBI.
- Over a 9 year period, the incidence of post-traumatic epilepsy (PTE) increased from 1 to 4% in this population.
- Early onset of seizures, older age, and TBI severity increased the likelihood of PTE.
- Prophylactic acetazolamide seemed to reduce the risk of PTE, when compared to patients who had received no anti-epilepsy drugs.
DeGrauw X, Thurman D, Xu L, et al. Epidemiology of traumatic brain injury-associated epilepsy and early use of anti-epilepsy drugs: An analysis of insurance claims data, 2004-2014. [Published online ahead of print July 23, 2018] Epilepsy Res. doi: 10.1016/j.eplepsyres.2018.07.012
Among patients who have experienced a traumatic brain injury (TBI), the likelihood of developing post-traumatic epilepsy (PTE) increases with age, the early onset of seizures, and the severity of the brain injury, according to an analysis of insurance claims from 2004 to 2014.
- There were approximately 2.8 million emergency room visits, hospitalizations and deaths from traumatic brain injuries in the US in 2013.
- Early seizures occurred in 0.5% of patients with TBI.
- Over a 9 year period, the incidence of post-traumatic epilepsy (PTE) increased from 1 to 4% in this population.
- Early onset of seizures, older age, and TBI severity increased the likelihood of PTE.
- Prophylactic acetazolamide seemed to reduce the risk of PTE, when compared to patients who had received no anti-epilepsy drugs.
DeGrauw X, Thurman D, Xu L, et al. Epidemiology of traumatic brain injury-associated epilepsy and early use of anti-epilepsy drugs: An analysis of insurance claims data, 2004-2014. [Published online ahead of print July 23, 2018] Epilepsy Res. doi: 10.1016/j.eplepsyres.2018.07.012
Is It Possible to Predict Seizures?
Conventional medical wisdom insists that it is not possible to predict the onset of seizures with any certainty, but recent research suggests otherwise, according to a review published in Nature Reviews Neurology.
- An influential 2007 review of the medical literature concluded that there was insufficient evidence to foresee the onset of seizures.
- However, an international team of experts summarized several recent advances that suggest seizure prediction may be possible.
- The new review discusses a small experiment in which intracranial EEGs were used prospectively to predict seizures.
- Additional advances include EEG databases, seizure prediction competitions, and a better understanding of the mechanism of action behind seizures.
Kuhlmann L, Lehnertz K, Richardson MP, et al. Seizure prediction - ready for a new era. [Published online ahead of print August 21, 2018] Nat Rev Neurol. doi: 10.1038/s41582-018-0055-2
Conventional medical wisdom insists that it is not possible to predict the onset of seizures with any certainty, but recent research suggests otherwise, according to a review published in Nature Reviews Neurology.
- An influential 2007 review of the medical literature concluded that there was insufficient evidence to foresee the onset of seizures.
- However, an international team of experts summarized several recent advances that suggest seizure prediction may be possible.
- The new review discusses a small experiment in which intracranial EEGs were used prospectively to predict seizures.
- Additional advances include EEG databases, seizure prediction competitions, and a better understanding of the mechanism of action behind seizures.
Kuhlmann L, Lehnertz K, Richardson MP, et al. Seizure prediction - ready for a new era. [Published online ahead of print August 21, 2018] Nat Rev Neurol. doi: 10.1038/s41582-018-0055-2
Conventional medical wisdom insists that it is not possible to predict the onset of seizures with any certainty, but recent research suggests otherwise, according to a review published in Nature Reviews Neurology.
- An influential 2007 review of the medical literature concluded that there was insufficient evidence to foresee the onset of seizures.
- However, an international team of experts summarized several recent advances that suggest seizure prediction may be possible.
- The new review discusses a small experiment in which intracranial EEGs were used prospectively to predict seizures.
- Additional advances include EEG databases, seizure prediction competitions, and a better understanding of the mechanism of action behind seizures.
Kuhlmann L, Lehnertz K, Richardson MP, et al. Seizure prediction - ready for a new era. [Published online ahead of print August 21, 2018] Nat Rev Neurol. doi: 10.1038/s41582-018-0055-2
Managing Sleep Disorders in Epilepsy
Understanding the relationship between epilepsy and sleep disorders can help clinicians improve the management of both disorders according to a recent review in Epilepsy Research.
- Sleep apnea, insomnia, restless legs syndrome and parasomnias often occur in patients with epilepsy.
- Researchers from Brigham and Women’s Hospital in Boston and Mayo Clinic reviewed the symptoms and diagnosis of these sleep disorders to help clinicians screen patients with epilepsy at risk for these problems.
- The review also explores treatment options and several case reports that illustrate the consequences of said sleep disorders in those with epilepsy.
- Latreille et al believe that employing the latest diagnostic and treatment approaches to co-morbid sleep disorders may improve patients’ functional status, alertness, quality of life and seizure burden.
Latreille V, St. Louis EK, Pavlova M. Co-morbid sleep disorders and epilepsy: A narrative review and case examples. Epilepsy Res. 2018; 145:185-197. https://doi.org/10.1016/j.eplepsyres.2018.07.005
Understanding the relationship between epilepsy and sleep disorders can help clinicians improve the management of both disorders according to a recent review in Epilepsy Research.
- Sleep apnea, insomnia, restless legs syndrome and parasomnias often occur in patients with epilepsy.
- Researchers from Brigham and Women’s Hospital in Boston and Mayo Clinic reviewed the symptoms and diagnosis of these sleep disorders to help clinicians screen patients with epilepsy at risk for these problems.
- The review also explores treatment options and several case reports that illustrate the consequences of said sleep disorders in those with epilepsy.
- Latreille et al believe that employing the latest diagnostic and treatment approaches to co-morbid sleep disorders may improve patients’ functional status, alertness, quality of life and seizure burden.
Latreille V, St. Louis EK, Pavlova M. Co-morbid sleep disorders and epilepsy: A narrative review and case examples. Epilepsy Res. 2018; 145:185-197. https://doi.org/10.1016/j.eplepsyres.2018.07.005
Understanding the relationship between epilepsy and sleep disorders can help clinicians improve the management of both disorders according to a recent review in Epilepsy Research.
- Sleep apnea, insomnia, restless legs syndrome and parasomnias often occur in patients with epilepsy.
- Researchers from Brigham and Women’s Hospital in Boston and Mayo Clinic reviewed the symptoms and diagnosis of these sleep disorders to help clinicians screen patients with epilepsy at risk for these problems.
- The review also explores treatment options and several case reports that illustrate the consequences of said sleep disorders in those with epilepsy.
- Latreille et al believe that employing the latest diagnostic and treatment approaches to co-morbid sleep disorders may improve patients’ functional status, alertness, quality of life and seizure burden.
Latreille V, St. Louis EK, Pavlova M. Co-morbid sleep disorders and epilepsy: A narrative review and case examples. Epilepsy Res. 2018; 145:185-197. https://doi.org/10.1016/j.eplepsyres.2018.07.005