User login
Frailty tied to higher mortality after major vascular surgery
Frailty defined as functional dependence is a predictor of mortality risk in elderly patients having major vascular surgery, a meta-analysis of studies has found
“Functional dependency may be recommended for use in rapid screening for frailty in major vascular surgery because of the high quality of associated evidence. Additionally, information on central muscle mass also adds incremental predictive value to long-term survival of elderly patients after major vascular surgery,” the study investigaters stated. However, they pointed out that “other newly developed frailty tools require further validation in more studies” before they should be adopted.
The report, published in the European Journal of Vascular and Endovascular Surgery, evaluated the effect of frailty in major vascular surgery from a search of MEDLINE, Embase, Cochrane Database, and Scopus through May 2018. Data were extracted from the articles related to surgery for abdominal aortic aneurysms (AAA) and lower extremity artery disease (LEAD), and a modified Newcastle-Ottawa scale was used to assess the quality of the included studies, according to Jiarong Wang, MD, of the department of vascular surgery, Sichuan University, Sichuan Province, China, and colleagues. A total of 22 cohort studies and one randomized controlled trial was used in the final analysis. The reviewers expressed the impact of frailty on outcomes as odds ratios (OR) or hazard ratios (HR) using a random effects model.
The researchers found that frailty, in terms of functional dependence, was associated with a significantly increased 30-day mortality risk in patients with AAA without heterogeneity (OR 5.15) and also in LEAD patients (OR 3.29). Functionally dependent patients also had a significantly increased 30-day mortality risk, compared with independent patients (OR 4.49), and similar results were observed after stratifying those who underwent AAA repair (OR 5.14) or lower extremity revascularization (OR 4.18). Even for patients who underwent endovascular procedures rather than open surgery, functional dependency was also associated with a significantly increased 30-day mortality risk (OR 4.90). In addition, with regard to 30-day morbidity, frailty was associated with a significantly increased risk in both AAA (OR 2.79) and LEAD (OR 1.40) patients.
As far as long-term outcomes were concerned, frailty was associated with a significantly increased risk of long-term all-cause mortality in the overall studied population (HR 2.22), as well as in patients with AAA repair (HR 2.10) and LEAD revascularization (HR 2.46). Dr. Wang and colleagues found that central muscle mass was the only tool with moderate quality of evidence predicting long-term survival after major vascular surgery (HR .48), with other single-domain tools such as nutrition or cognition scoring being of low quality. The modified Frailty Index was the only multi-domain tool with moderate quality in predicting mortality for AAA, while others were scored as low or very low, the authors added.
“Future research is warranted to establish consensus on how to select the optimal frailty tool for certain clinical settings,” they concluded.
The authors reported that they had no conflicts of interest and no funding sources for the study.
SOURCE: Wang, J et al. Eur J Vasc Endovasc Surg. 2018;56:591-602.
Frailty defined as functional dependence is a predictor of mortality risk in elderly patients having major vascular surgery, a meta-analysis of studies has found
“Functional dependency may be recommended for use in rapid screening for frailty in major vascular surgery because of the high quality of associated evidence. Additionally, information on central muscle mass also adds incremental predictive value to long-term survival of elderly patients after major vascular surgery,” the study investigaters stated. However, they pointed out that “other newly developed frailty tools require further validation in more studies” before they should be adopted.
The report, published in the European Journal of Vascular and Endovascular Surgery, evaluated the effect of frailty in major vascular surgery from a search of MEDLINE, Embase, Cochrane Database, and Scopus through May 2018. Data were extracted from the articles related to surgery for abdominal aortic aneurysms (AAA) and lower extremity artery disease (LEAD), and a modified Newcastle-Ottawa scale was used to assess the quality of the included studies, according to Jiarong Wang, MD, of the department of vascular surgery, Sichuan University, Sichuan Province, China, and colleagues. A total of 22 cohort studies and one randomized controlled trial was used in the final analysis. The reviewers expressed the impact of frailty on outcomes as odds ratios (OR) or hazard ratios (HR) using a random effects model.
The researchers found that frailty, in terms of functional dependence, was associated with a significantly increased 30-day mortality risk in patients with AAA without heterogeneity (OR 5.15) and also in LEAD patients (OR 3.29). Functionally dependent patients also had a significantly increased 30-day mortality risk, compared with independent patients (OR 4.49), and similar results were observed after stratifying those who underwent AAA repair (OR 5.14) or lower extremity revascularization (OR 4.18). Even for patients who underwent endovascular procedures rather than open surgery, functional dependency was also associated with a significantly increased 30-day mortality risk (OR 4.90). In addition, with regard to 30-day morbidity, frailty was associated with a significantly increased risk in both AAA (OR 2.79) and LEAD (OR 1.40) patients.
As far as long-term outcomes were concerned, frailty was associated with a significantly increased risk of long-term all-cause mortality in the overall studied population (HR 2.22), as well as in patients with AAA repair (HR 2.10) and LEAD revascularization (HR 2.46). Dr. Wang and colleagues found that central muscle mass was the only tool with moderate quality of evidence predicting long-term survival after major vascular surgery (HR .48), with other single-domain tools such as nutrition or cognition scoring being of low quality. The modified Frailty Index was the only multi-domain tool with moderate quality in predicting mortality for AAA, while others were scored as low or very low, the authors added.
“Future research is warranted to establish consensus on how to select the optimal frailty tool for certain clinical settings,” they concluded.
The authors reported that they had no conflicts of interest and no funding sources for the study.
SOURCE: Wang, J et al. Eur J Vasc Endovasc Surg. 2018;56:591-602.
Frailty defined as functional dependence is a predictor of mortality risk in elderly patients having major vascular surgery, a meta-analysis of studies has found
“Functional dependency may be recommended for use in rapid screening for frailty in major vascular surgery because of the high quality of associated evidence. Additionally, information on central muscle mass also adds incremental predictive value to long-term survival of elderly patients after major vascular surgery,” the study investigaters stated. However, they pointed out that “other newly developed frailty tools require further validation in more studies” before they should be adopted.
The report, published in the European Journal of Vascular and Endovascular Surgery, evaluated the effect of frailty in major vascular surgery from a search of MEDLINE, Embase, Cochrane Database, and Scopus through May 2018. Data were extracted from the articles related to surgery for abdominal aortic aneurysms (AAA) and lower extremity artery disease (LEAD), and a modified Newcastle-Ottawa scale was used to assess the quality of the included studies, according to Jiarong Wang, MD, of the department of vascular surgery, Sichuan University, Sichuan Province, China, and colleagues. A total of 22 cohort studies and one randomized controlled trial was used in the final analysis. The reviewers expressed the impact of frailty on outcomes as odds ratios (OR) or hazard ratios (HR) using a random effects model.
The researchers found that frailty, in terms of functional dependence, was associated with a significantly increased 30-day mortality risk in patients with AAA without heterogeneity (OR 5.15) and also in LEAD patients (OR 3.29). Functionally dependent patients also had a significantly increased 30-day mortality risk, compared with independent patients (OR 4.49), and similar results were observed after stratifying those who underwent AAA repair (OR 5.14) or lower extremity revascularization (OR 4.18). Even for patients who underwent endovascular procedures rather than open surgery, functional dependency was also associated with a significantly increased 30-day mortality risk (OR 4.90). In addition, with regard to 30-day morbidity, frailty was associated with a significantly increased risk in both AAA (OR 2.79) and LEAD (OR 1.40) patients.
As far as long-term outcomes were concerned, frailty was associated with a significantly increased risk of long-term all-cause mortality in the overall studied population (HR 2.22), as well as in patients with AAA repair (HR 2.10) and LEAD revascularization (HR 2.46). Dr. Wang and colleagues found that central muscle mass was the only tool with moderate quality of evidence predicting long-term survival after major vascular surgery (HR .48), with other single-domain tools such as nutrition or cognition scoring being of low quality. The modified Frailty Index was the only multi-domain tool with moderate quality in predicting mortality for AAA, while others were scored as low or very low, the authors added.
“Future research is warranted to establish consensus on how to select the optimal frailty tool for certain clinical settings,” they concluded.
The authors reported that they had no conflicts of interest and no funding sources for the study.
SOURCE: Wang, J et al. Eur J Vasc Endovasc Surg. 2018;56:591-602.
FROM EUROPEAN JOURNAL OF VASCULAR AND ENDOVASCULAR SURGERY
Key clinical point: Frailty was associated with increased short- and long-term mortality in major vascular surgery.
Major finding: Frailty was associated with a fourfold increased risk of 30-day mortality and a doubled increased risk of long-term mortality after major vascular surgery.
Study details: A meta-analysis of 22 cohort studies and one randomized controlled trial.
Disclosures: The authors reported that they had no conflicts of interest and no funding sources for the study.
Source: Wang, J et al., 2018. Eur J Vasc Endovasc Surg. 56:591-602.
Post-mastectomy pain strategy allows for safe, same-day discharge
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
BOSTON – A multimodal pain regimen allowed for safe and effective same-day discharge of women undergoing mastectomy procedures, a recent study showed.
Women had little need for stronger oral narcotic use in the single center, retrospective study presented at the annual clinical congress of the American College of Surgeons.
The analysis included 72 consecutive mastectomies performed at a single center from November 2015 to July 2017. Most mastectomies were bilateral (61, or 84.7%) while 11 (15.3%) were unilateral.
Patients received a standardized pain regimen including 1 gram of IV acetaminophen interoperatively, combined with 30 mg of IV ketorolac and a 4-level intercostal nerve block with liposomal bupivacaine.
Liposomal bupivacaine has a longer half-life than other anesthetics, according to lead study author Radbeh Torabi, MD, a fifth-year plastic surgery resident at Louisiana State University (LSU) Health Science Center in New Orleans.
“That allows for prolonged pain control, especially during the time when the patient’s going to have the most amount of pain, which is the first day to two days postoperatively,” Dr. Torabi said in an interview.
All 72 patients were discharged home on the same day with just a 1-week prescription for acetaminophen with codeine.
Only 5 patients presented to the emergency room in the 30-day postoperative period, and of those, only 2 (2.8%) required readmission for reasons other than mastectomy-related pain, investigators said. The remaining 3 patients did present with pain, but did not require hospital admission.
Taken together, these findings suggest that this multimodal strategy offers excellent pain control and has the potential to minimize inpatient admissions while decreasing oral narcotic use, investigators said in an interview following their presentation.
“The main takeaway is reducing the amount of prescriptions we give,” Dr. Torabi said.
Study co-author Cameron T. Ward Coker, MD, a fourth-year general surgery resident at LSU, said the multimodal pain strategy used in this study could represent a step toward eliminating the risks associated with opioid prescribing.
“From the feedback we got from our lecture and the other surgeons in the room, it seems like that’s already becoming a widespread phenomenon,” Dr. Coker said.
Patients in the study had an average age of about 57 years and an average BMI of 30, according to the investigators.
Dr. Coker and Dr. Torabi had no disclosures related to the presentation.
SOURCE: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
REPORTING FROM THE ACS CLINICAL CONGRESS
Key clinical point:
Major finding: Of 72 women who had same-day discharge after mastectomy, only 3 presented for pain in the 30-day postoperative period.
Study details: A retrospective review of 72 consecutive mastectomies performed at a single surgical center.
Disclosures: The lead author had no disclosures related to the presentation.
Source: Torabi R, et al. Scientific forum abstract at American College of Surgeons Clinical Congress. 2018 Oct 23.
Ruxolitinib under priority review for acute GVHD
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for the JAK1/JAK2 inhibitor ruxolitinib (Jakafi®).
With this sNDA, Incyte Corporation is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host-disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” said Steven Stein, MD, chief medical officer at Incyte.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
In addition to priority review, ruxolitinib has received breakthrough therapy and orphan drug designations from the FDA as a treatment for acute GVHD.
The sNDA submission for ruxolitinib in acute GVHD is based on data from the phase 2 REACH1 trial (NCT02953678).
In this ongoing trial, researchers are evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced topline results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint—overall response rate at day 28—was met. Ruxolitinib produced an overall response rate of 55% (39/71) at that time.
However, 73% of patients (52/71) responded to ruxolitinib at some point during the trial.
Incyte said the most common treatment-emergent adverse events were anemia (61%), thrombocytopenia (61%), and neutropenia (56%).
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for the JAK1/JAK2 inhibitor ruxolitinib (Jakafi®).
With this sNDA, Incyte Corporation is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host-disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” said Steven Stein, MD, chief medical officer at Incyte.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
In addition to priority review, ruxolitinib has received breakthrough therapy and orphan drug designations from the FDA as a treatment for acute GVHD.
The sNDA submission for ruxolitinib in acute GVHD is based on data from the phase 2 REACH1 trial (NCT02953678).
In this ongoing trial, researchers are evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced topline results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint—overall response rate at day 28—was met. Ruxolitinib produced an overall response rate of 55% (39/71) at that time.
However, 73% of patients (52/71) responded to ruxolitinib at some point during the trial.
Incyte said the most common treatment-emergent adverse events were anemia (61%), thrombocytopenia (61%), and neutropenia (56%).
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for the JAK1/JAK2 inhibitor ruxolitinib (Jakafi®).
With this sNDA, Incyte Corporation is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host-disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” said Steven Stein, MD, chief medical officer at Incyte.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
In addition to priority review, ruxolitinib has received breakthrough therapy and orphan drug designations from the FDA as a treatment for acute GVHD.
The sNDA submission for ruxolitinib in acute GVHD is based on data from the phase 2 REACH1 trial (NCT02953678).
In this ongoing trial, researchers are evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced topline results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint—overall response rate at day 28—was met. Ruxolitinib produced an overall response rate of 55% (39/71) at that time.
However, 73% of patients (52/71) responded to ruxolitinib at some point during the trial.
Incyte said the most common treatment-emergent adverse events were anemia (61%), thrombocytopenia (61%), and neutropenia (56%).
Ruxolitinib receives priority review for acute GVHD
The Food and Drug Administration has accepted the JAK1/JAK2 inhibitor ruxolitinib (Jakafi) for priority review.
Incyte is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” Steven Stein, MD, chief medical officer at Incyte, said in a statement.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The designation generally means that the agency will act on the application within 6 months, rather than 10 months.
In addition to priority review, the FDA previously granted ruxolitinib breakthrough therapy and orphan drug designations.
The application is based on data from the ongoing, phase 2 REACH1 trial (NCT02953678), which is evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced top-line results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint – overall response rate at day 28 – was met. Ruxolitinib produced an overall response rate of 55% at that time. However, 73% of patients responded to ruxolitinib at some point during the trial. Incyte said the most common treatment-emergent adverse events were anemia, thrombocytopenia, and neutropenia.
The Food and Drug Administration has accepted the JAK1/JAK2 inhibitor ruxolitinib (Jakafi) for priority review.
Incyte is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” Steven Stein, MD, chief medical officer at Incyte, said in a statement.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The designation generally means that the agency will act on the application within 6 months, rather than 10 months.
In addition to priority review, the FDA previously granted ruxolitinib breakthrough therapy and orphan drug designations.
The application is based on data from the ongoing, phase 2 REACH1 trial (NCT02953678), which is evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced top-line results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint – overall response rate at day 28 – was met. Ruxolitinib produced an overall response rate of 55% at that time. However, 73% of patients responded to ruxolitinib at some point during the trial. Incyte said the most common treatment-emergent adverse events were anemia, thrombocytopenia, and neutropenia.
The Food and Drug Administration has accepted the JAK1/JAK2 inhibitor ruxolitinib (Jakafi) for priority review.
Incyte is seeking approval for ruxolitinib as a treatment for patients with acute graft-versus-host disease (GVHD) who have had an inadequate response to corticosteroids.
“If approved, ruxolitinib will be the first and only treatment available in the U.S. for patients with acute GVHD who have not responded adequately to corticosteroid therapy,” Steven Stein, MD, chief medical officer at Incyte, said in a statement.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The designation generally means that the agency will act on the application within 6 months, rather than 10 months.
In addition to priority review, the FDA previously granted ruxolitinib breakthrough therapy and orphan drug designations.
The application is based on data from the ongoing, phase 2 REACH1 trial (NCT02953678), which is evaluating ruxolitinib in combination with corticosteroids in patients who have steroid-refractory acute GVHD.
Incyte announced top-line results from REACH1 in June, reporting on outcomes in 71 patients.
The study’s primary endpoint – overall response rate at day 28 – was met. Ruxolitinib produced an overall response rate of 55% at that time. However, 73% of patients responded to ruxolitinib at some point during the trial. Incyte said the most common treatment-emergent adverse events were anemia, thrombocytopenia, and neutropenia.
OMS721 gains orphan designation for HSCT-associated thrombotic microangiopathy
The Food and Drug Administration has granted OMS721 orphan designation for the treatment of hematopoietic stem cell transplant–associated thrombotic microangiopathy (HSCT-TMA).
OMS721 is a monoclonal antibody targeting MASP-2, the effector enzyme of the lectin pathway of the complement system.
The FDA previously granted OMS721 breakthrough therapy designation for HSCT-TMA and orphan designation for the prevention of complement-mediated TMA, including HSCT-TMA.
Omeros, the company developing OMS721, has established a compassionate use program for OMS721, which is active in the United States and Europe.
Phase 3 clinical programs are in progress for OMS721 in atypical hemolytic uremic syndrome, immunoglobulin A nephropathy, and HSCT-TMA. Two phase 2 trials of OMS721 – one in TMA and one in immunoglobulin A nephropathy – are ongoing.
Omeros announced results from the phase 2 TMA trial (NCT02222545) in February. The study includes adults with HSCT-TMA persisting for at least 2 weeks following immunosuppressive regimen modification or more than 30 days post transplant. Patients receive weekly OMS721 treatments for 4-8 weeks at the discretion of the investigator.
At the time of Omeros’s announcement, 18 HSCT-TMA patients had been treated.
These patients had a significantly longer median overall survival at 347 days, compared with historical controls at 21 days (P less than .0001).
Omeros also reported that markers of TMA activity significantly improved following OMS721 treatment.
The mean platelet count increased from 18,100 x 106/mL at baseline to 52,300 x 106/mL (P = .017). The mean lactate dehydrogenase decreased from 591 U/L to 250 U/L (P less than .001). And the mean haptoglobin increased from 8 mg/dL to 141 mg/dL (P = .003).
The most commonly reported adverse events were diarrhea and neutropenia. Four deaths occurred during the study. One of these – attributable to acute renal and respiratory failure – was considered possibly related to OMS721.
The Food and Drug Administration has granted OMS721 orphan designation for the treatment of hematopoietic stem cell transplant–associated thrombotic microangiopathy (HSCT-TMA).
OMS721 is a monoclonal antibody targeting MASP-2, the effector enzyme of the lectin pathway of the complement system.
The FDA previously granted OMS721 breakthrough therapy designation for HSCT-TMA and orphan designation for the prevention of complement-mediated TMA, including HSCT-TMA.
Omeros, the company developing OMS721, has established a compassionate use program for OMS721, which is active in the United States and Europe.
Phase 3 clinical programs are in progress for OMS721 in atypical hemolytic uremic syndrome, immunoglobulin A nephropathy, and HSCT-TMA. Two phase 2 trials of OMS721 – one in TMA and one in immunoglobulin A nephropathy – are ongoing.
Omeros announced results from the phase 2 TMA trial (NCT02222545) in February. The study includes adults with HSCT-TMA persisting for at least 2 weeks following immunosuppressive regimen modification or more than 30 days post transplant. Patients receive weekly OMS721 treatments for 4-8 weeks at the discretion of the investigator.
At the time of Omeros’s announcement, 18 HSCT-TMA patients had been treated.
These patients had a significantly longer median overall survival at 347 days, compared with historical controls at 21 days (P less than .0001).
Omeros also reported that markers of TMA activity significantly improved following OMS721 treatment.
The mean platelet count increased from 18,100 x 106/mL at baseline to 52,300 x 106/mL (P = .017). The mean lactate dehydrogenase decreased from 591 U/L to 250 U/L (P less than .001). And the mean haptoglobin increased from 8 mg/dL to 141 mg/dL (P = .003).
The most commonly reported adverse events were diarrhea and neutropenia. Four deaths occurred during the study. One of these – attributable to acute renal and respiratory failure – was considered possibly related to OMS721.
The Food and Drug Administration has granted OMS721 orphan designation for the treatment of hematopoietic stem cell transplant–associated thrombotic microangiopathy (HSCT-TMA).
OMS721 is a monoclonal antibody targeting MASP-2, the effector enzyme of the lectin pathway of the complement system.
The FDA previously granted OMS721 breakthrough therapy designation for HSCT-TMA and orphan designation for the prevention of complement-mediated TMA, including HSCT-TMA.
Omeros, the company developing OMS721, has established a compassionate use program for OMS721, which is active in the United States and Europe.
Phase 3 clinical programs are in progress for OMS721 in atypical hemolytic uremic syndrome, immunoglobulin A nephropathy, and HSCT-TMA. Two phase 2 trials of OMS721 – one in TMA and one in immunoglobulin A nephropathy – are ongoing.
Omeros announced results from the phase 2 TMA trial (NCT02222545) in February. The study includes adults with HSCT-TMA persisting for at least 2 weeks following immunosuppressive regimen modification or more than 30 days post transplant. Patients receive weekly OMS721 treatments for 4-8 weeks at the discretion of the investigator.
At the time of Omeros’s announcement, 18 HSCT-TMA patients had been treated.
These patients had a significantly longer median overall survival at 347 days, compared with historical controls at 21 days (P less than .0001).
Omeros also reported that markers of TMA activity significantly improved following OMS721 treatment.
The mean platelet count increased from 18,100 x 106/mL at baseline to 52,300 x 106/mL (P = .017). The mean lactate dehydrogenase decreased from 591 U/L to 250 U/L (P less than .001). And the mean haptoglobin increased from 8 mg/dL to 141 mg/dL (P = .003).
The most commonly reported adverse events were diarrhea and neutropenia. Four deaths occurred during the study. One of these – attributable to acute renal and respiratory failure – was considered possibly related to OMS721.
Pigmented Pruritic Macules in the Genital Area
The Diagnosis: Pediculosis Pubis
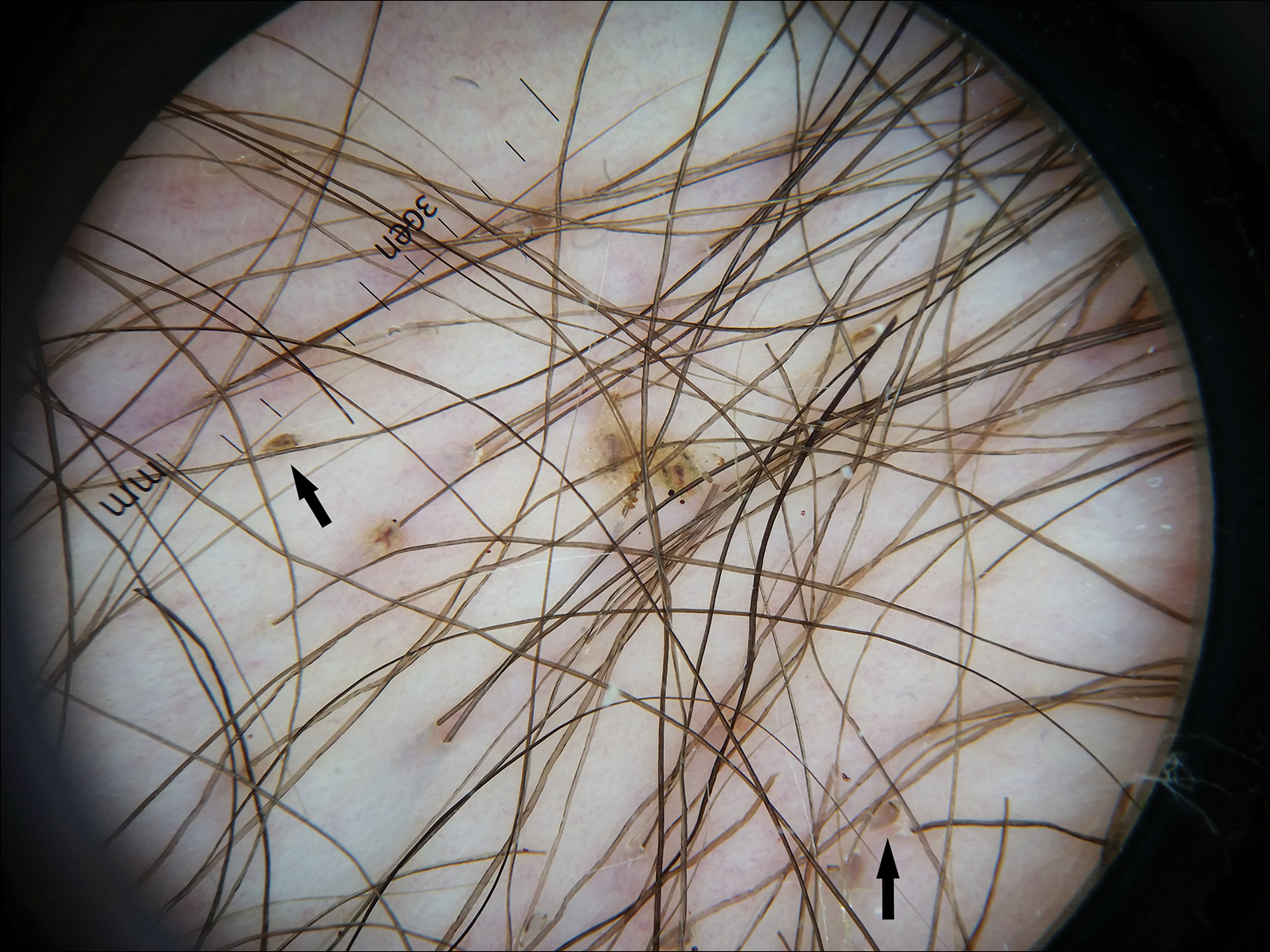
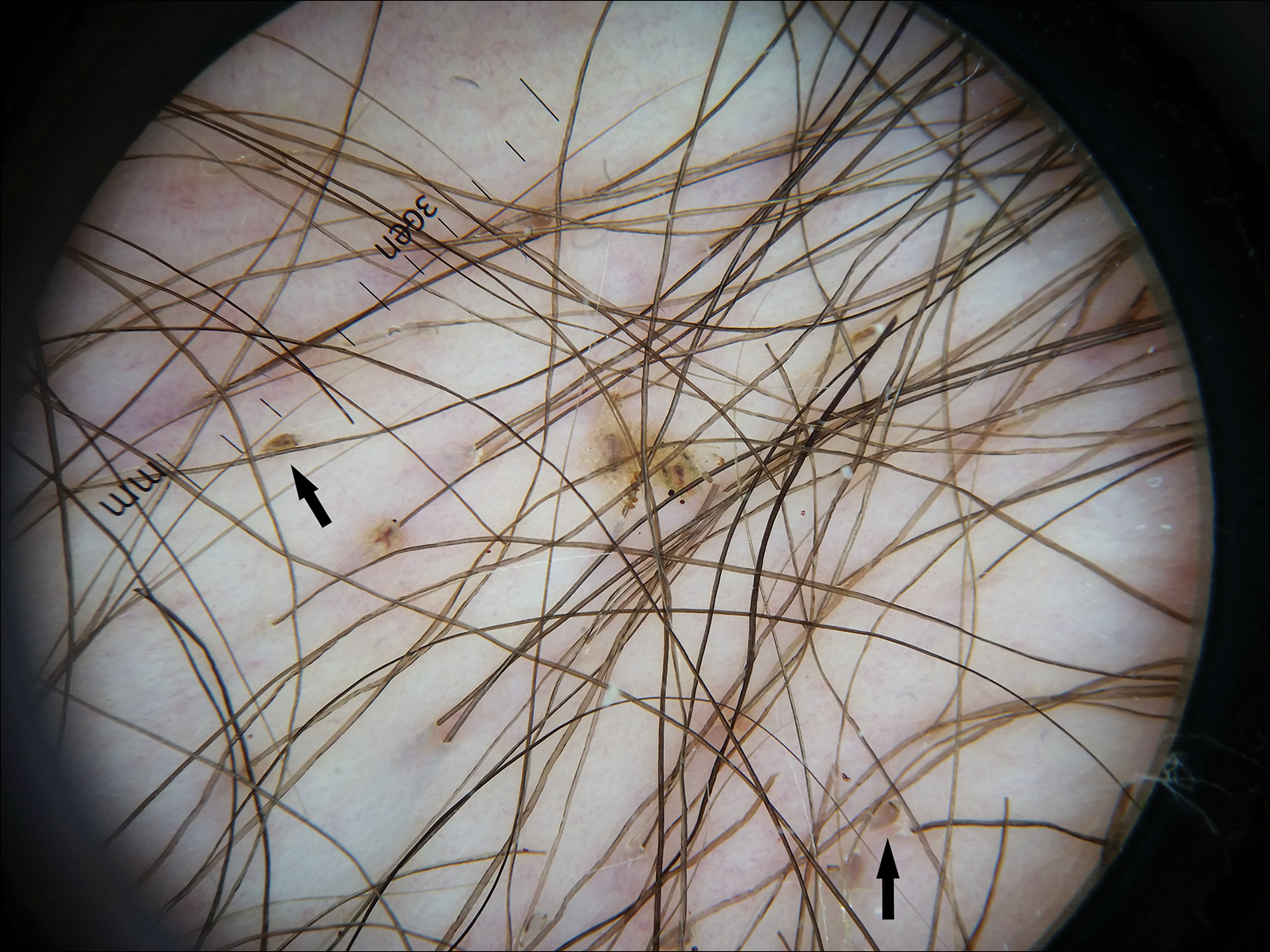
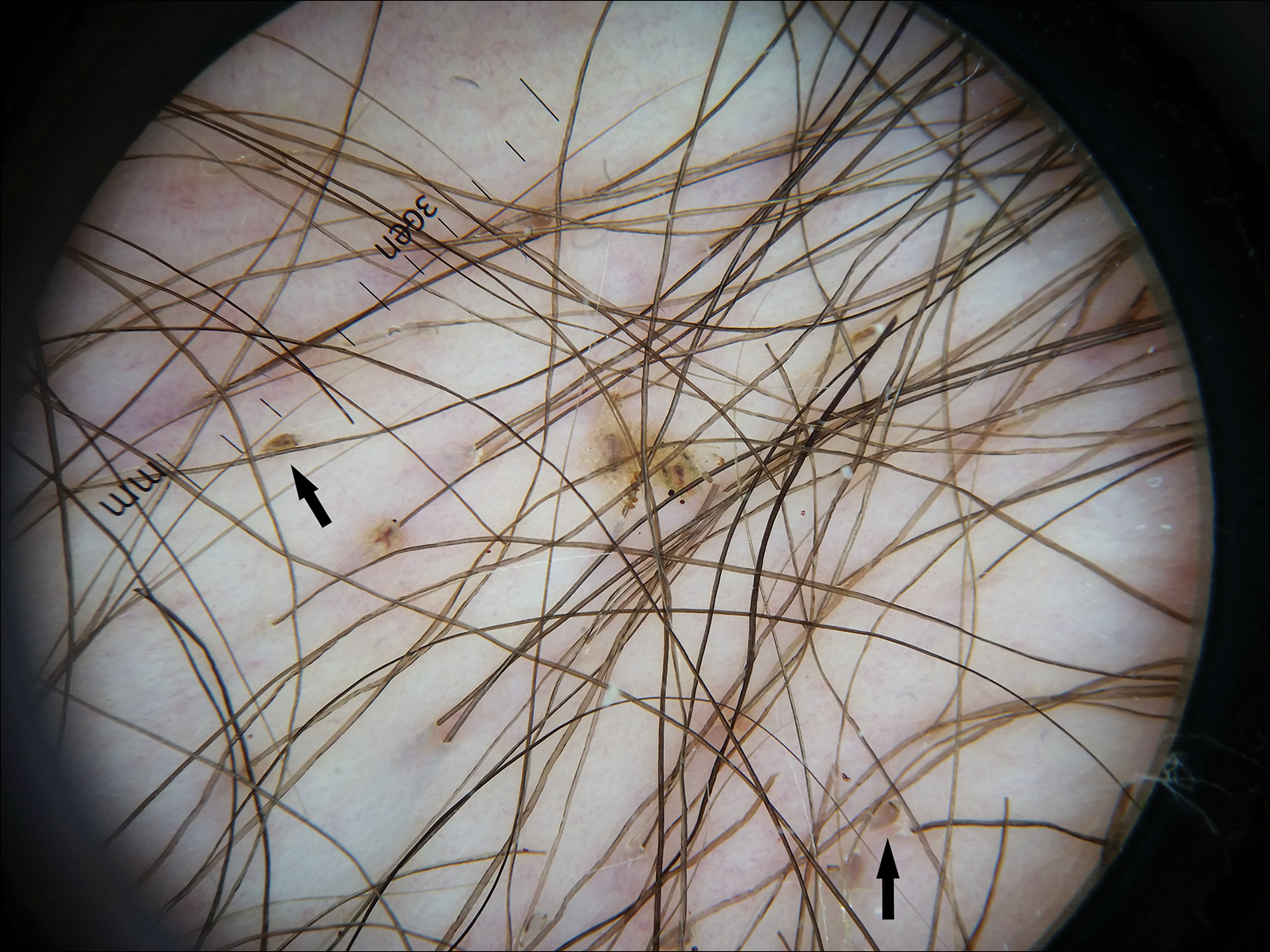
Dermoscopy of the pubic hair demonstrated a louse clutching multiple shafts of hairs (Figure) as well as scattered nits, confirming the presence of Phthirus pubis and diagnosis of pediculosis pubis. The key clinical diagnostic feature in this case was severe itching of the pubic area, with visible nits present on pubic hairs. Itching and infestation also can involve other hair-bearing areas such as the chest, legs, and axillae. The patient was treated with permethrin cream 5% applied to the pubic area and chest. Symptoms and infestation were resolved at 1-week follow-up.
Pediculosis pubis is an infestation of pubic hairs by the pubic (crab) louse P pubis, which feeds on host blood. Other body areas covered with dense hair also may be involved; 60% of patients are infested in at least 2 different sites.1 Pediculosis pubis is most commonly sexually transmitted through direct contact.2 Worldwide prevalence has been estimated at approximately 2% of the adult population, and a survey of 817 US college students in 2009 indicated a lifetime prevalence of 1.3%.3 The prevalence is slightly higher in men, highest in men who have sex with men, and rare in individuals with shaved pubic hair.1 The most common symptom is pruritus of the genital area. Infested patients also may develop asymptomatic bluish gray macules (maculae ceruleae) secondary to hemosiderin deposition from louse bites.4
The diagnosis of pediculosis pubis is made by identification of P pubis, either by examination with the naked eye or confirmation with dermoscopy or microscopy. Although the 0.8- to 1.2-mm lice are visible to the naked eye, they can be difficult to see if not filled with blood, and nits on the hairs can be mistaken for white piedra (fungal infection of the hair shafts) or trichomycosis pubis (bacterial infection of the hair shafts).4 Scabies and tinea cruris do not present with attachments to the hairs. Scabies may present with papules and burrows and tinea cruris with scaly erythematous plaques. Small numbers of lice and nits may be missed by the naked eye or a traditional magnifying glass.5 The use of dermoscopy allows for fast and accurate identification of the characteristic lice and nits, even in these more challenging cases.5 Accurate diagnosis is important, as approximately 31% of infested patients have other concurrent sexually transmitted infections that warrant screening.6
The Centers for Disease Control and Prevention recommends first-line treatment with permethrin cream (1% or 5%) or pyrethrin with piperonyl butoxide applied to all affected areas and washed off after 10 minutes.7 Patients should be reevaluated after 1 week if symptoms persist and re-treated if lice are found on examination.7,8 Malathion lotion 0.5% (applied and washed off after 8-12 hours) or oral ivermectin (250 µg/kg, repeated after 2 weeks) may be used for alternative therapies or cases of permethrin or pyrethrin resistance.7 Ivermectin also is effective for involvement of eyelashes where topical insecticides should not be used.9 Sexual partners should be treated to prevent repeat transmission.7,8 Bedding and clothing can be decontaminated by machine wash on hot cycle or isolating from body contact for 72 hours.7 Patients also should be screened for other sexually transmitted infections, including human immunodeficiency virus.6
- Burkhart CN, Burkhart CG, Morrell DS. Infestations. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. Vol 2. 3rd ed. China: Elsevier/Saunders; 2012:1429-1430.
- Chosidow O. Scabies and pediculosis. Lancet. 2000;355:819-826.
- Anderson AL, Chaney E. Pubic lice (Pthirus pubis): history, biology and treatment vs. knowledge and beliefs of US college students. Int J Environ Res Public Health. 2009;6:592-600.
- Ko CJ, Elston DM. Pediculosis. J Am Acad Dermatol. 2004;50:1-12; quiz 13-14.
- Chuh A, Lee A, Wong W, et al. Diagnosis of pediculosis pubis: a novel application of digital epiluminescence dermatoscopy. J Eur Acad Dermatol Venereol. 2007;21:837-838.
- Chapel TA, Katta T, Kuszmar T, et al. Pediculosis pubis in a clinic for treatment of sexually transmitted diseases. Sex Transm Dis. 1979;6:257-260.
- Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64:1-137.
- Leone PA. Scabies and pediculosis pubis: an update of treatment regimens and general review. Clin Infect Dis. 2007;44(suppl 3):S153-S159.
- Burkhart CN, Burkhart CG. Oral ivermectin therapy for phthiriasis palpebrum. Arch Ophthalmol. 2000;118:134-135.
The Diagnosis: Pediculosis Pubis
Dermoscopy of the pubic hair demonstrated a louse clutching multiple shafts of hairs (Figure) as well as scattered nits, confirming the presence of Phthirus pubis and diagnosis of pediculosis pubis. The key clinical diagnostic feature in this case was severe itching of the pubic area, with visible nits present on pubic hairs. Itching and infestation also can involve other hair-bearing areas such as the chest, legs, and axillae. The patient was treated with permethrin cream 5% applied to the pubic area and chest. Symptoms and infestation were resolved at 1-week follow-up.
Pediculosis pubis is an infestation of pubic hairs by the pubic (crab) louse P pubis, which feeds on host blood. Other body areas covered with dense hair also may be involved; 60% of patients are infested in at least 2 different sites.1 Pediculosis pubis is most commonly sexually transmitted through direct contact.2 Worldwide prevalence has been estimated at approximately 2% of the adult population, and a survey of 817 US college students in 2009 indicated a lifetime prevalence of 1.3%.3 The prevalence is slightly higher in men, highest in men who have sex with men, and rare in individuals with shaved pubic hair.1 The most common symptom is pruritus of the genital area. Infested patients also may develop asymptomatic bluish gray macules (maculae ceruleae) secondary to hemosiderin deposition from louse bites.4
The diagnosis of pediculosis pubis is made by identification of P pubis, either by examination with the naked eye or confirmation with dermoscopy or microscopy. Although the 0.8- to 1.2-mm lice are visible to the naked eye, they can be difficult to see if not filled with blood, and nits on the hairs can be mistaken for white piedra (fungal infection of the hair shafts) or trichomycosis pubis (bacterial infection of the hair shafts).4 Scabies and tinea cruris do not present with attachments to the hairs. Scabies may present with papules and burrows and tinea cruris with scaly erythematous plaques. Small numbers of lice and nits may be missed by the naked eye or a traditional magnifying glass.5 The use of dermoscopy allows for fast and accurate identification of the characteristic lice and nits, even in these more challenging cases.5 Accurate diagnosis is important, as approximately 31% of infested patients have other concurrent sexually transmitted infections that warrant screening.6
The Centers for Disease Control and Prevention recommends first-line treatment with permethrin cream (1% or 5%) or pyrethrin with piperonyl butoxide applied to all affected areas and washed off after 10 minutes.7 Patients should be reevaluated after 1 week if symptoms persist and re-treated if lice are found on examination.7,8 Malathion lotion 0.5% (applied and washed off after 8-12 hours) or oral ivermectin (250 µg/kg, repeated after 2 weeks) may be used for alternative therapies or cases of permethrin or pyrethrin resistance.7 Ivermectin also is effective for involvement of eyelashes where topical insecticides should not be used.9 Sexual partners should be treated to prevent repeat transmission.7,8 Bedding and clothing can be decontaminated by machine wash on hot cycle or isolating from body contact for 72 hours.7 Patients also should be screened for other sexually transmitted infections, including human immunodeficiency virus.6
The Diagnosis: Pediculosis Pubis
Dermoscopy of the pubic hair demonstrated a louse clutching multiple shafts of hairs (Figure) as well as scattered nits, confirming the presence of Phthirus pubis and diagnosis of pediculosis pubis. The key clinical diagnostic feature in this case was severe itching of the pubic area, with visible nits present on pubic hairs. Itching and infestation also can involve other hair-bearing areas such as the chest, legs, and axillae. The patient was treated with permethrin cream 5% applied to the pubic area and chest. Symptoms and infestation were resolved at 1-week follow-up.
Pediculosis pubis is an infestation of pubic hairs by the pubic (crab) louse P pubis, which feeds on host blood. Other body areas covered with dense hair also may be involved; 60% of patients are infested in at least 2 different sites.1 Pediculosis pubis is most commonly sexually transmitted through direct contact.2 Worldwide prevalence has been estimated at approximately 2% of the adult population, and a survey of 817 US college students in 2009 indicated a lifetime prevalence of 1.3%.3 The prevalence is slightly higher in men, highest in men who have sex with men, and rare in individuals with shaved pubic hair.1 The most common symptom is pruritus of the genital area. Infested patients also may develop asymptomatic bluish gray macules (maculae ceruleae) secondary to hemosiderin deposition from louse bites.4
The diagnosis of pediculosis pubis is made by identification of P pubis, either by examination with the naked eye or confirmation with dermoscopy or microscopy. Although the 0.8- to 1.2-mm lice are visible to the naked eye, they can be difficult to see if not filled with blood, and nits on the hairs can be mistaken for white piedra (fungal infection of the hair shafts) or trichomycosis pubis (bacterial infection of the hair shafts).4 Scabies and tinea cruris do not present with attachments to the hairs. Scabies may present with papules and burrows and tinea cruris with scaly erythematous plaques. Small numbers of lice and nits may be missed by the naked eye or a traditional magnifying glass.5 The use of dermoscopy allows for fast and accurate identification of the characteristic lice and nits, even in these more challenging cases.5 Accurate diagnosis is important, as approximately 31% of infested patients have other concurrent sexually transmitted infections that warrant screening.6
The Centers for Disease Control and Prevention recommends first-line treatment with permethrin cream (1% or 5%) or pyrethrin with piperonyl butoxide applied to all affected areas and washed off after 10 minutes.7 Patients should be reevaluated after 1 week if symptoms persist and re-treated if lice are found on examination.7,8 Malathion lotion 0.5% (applied and washed off after 8-12 hours) or oral ivermectin (250 µg/kg, repeated after 2 weeks) may be used for alternative therapies or cases of permethrin or pyrethrin resistance.7 Ivermectin also is effective for involvement of eyelashes where topical insecticides should not be used.9 Sexual partners should be treated to prevent repeat transmission.7,8 Bedding and clothing can be decontaminated by machine wash on hot cycle or isolating from body contact for 72 hours.7 Patients also should be screened for other sexually transmitted infections, including human immunodeficiency virus.6
- Burkhart CN, Burkhart CG, Morrell DS. Infestations. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. Vol 2. 3rd ed. China: Elsevier/Saunders; 2012:1429-1430.
- Chosidow O. Scabies and pediculosis. Lancet. 2000;355:819-826.
- Anderson AL, Chaney E. Pubic lice (Pthirus pubis): history, biology and treatment vs. knowledge and beliefs of US college students. Int J Environ Res Public Health. 2009;6:592-600.
- Ko CJ, Elston DM. Pediculosis. J Am Acad Dermatol. 2004;50:1-12; quiz 13-14.
- Chuh A, Lee A, Wong W, et al. Diagnosis of pediculosis pubis: a novel application of digital epiluminescence dermatoscopy. J Eur Acad Dermatol Venereol. 2007;21:837-838.
- Chapel TA, Katta T, Kuszmar T, et al. Pediculosis pubis in a clinic for treatment of sexually transmitted diseases. Sex Transm Dis. 1979;6:257-260.
- Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64:1-137.
- Leone PA. Scabies and pediculosis pubis: an update of treatment regimens and general review. Clin Infect Dis. 2007;44(suppl 3):S153-S159.
- Burkhart CN, Burkhart CG. Oral ivermectin therapy for phthiriasis palpebrum. Arch Ophthalmol. 2000;118:134-135.
- Burkhart CN, Burkhart CG, Morrell DS. Infestations. In: Bolognia J, Jorizzo JL, Schaffer JV, eds. Dermatology. Vol 2. 3rd ed. China: Elsevier/Saunders; 2012:1429-1430.
- Chosidow O. Scabies and pediculosis. Lancet. 2000;355:819-826.
- Anderson AL, Chaney E. Pubic lice (Pthirus pubis): history, biology and treatment vs. knowledge and beliefs of US college students. Int J Environ Res Public Health. 2009;6:592-600.
- Ko CJ, Elston DM. Pediculosis. J Am Acad Dermatol. 2004;50:1-12; quiz 13-14.
- Chuh A, Lee A, Wong W, et al. Diagnosis of pediculosis pubis: a novel application of digital epiluminescence dermatoscopy. J Eur Acad Dermatol Venereol. 2007;21:837-838.
- Chapel TA, Katta T, Kuszmar T, et al. Pediculosis pubis in a clinic for treatment of sexually transmitted diseases. Sex Transm Dis. 1979;6:257-260.
- Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep. 2015;64:1-137.
- Leone PA. Scabies and pediculosis pubis: an update of treatment regimens and general review. Clin Infect Dis. 2007;44(suppl 3):S153-S159.
- Burkhart CN, Burkhart CG. Oral ivermectin therapy for phthiriasis palpebrum. Arch Ophthalmol. 2000;118:134-135.

A 50-year-old man with a history of cerebrovascular accident presented with severe itching along the inguinal folds and over the chest of 2 months' duration. His last sexual encounter was 5 months prior. He had previously seen a primary care physician who told him he needed to clean the hair better. Examination of the genital area revealed pigmented macules and overlying particles among the pubic hair.
‘Woeful lack of awareness’ leads to delayed diagnoses for women with ovarian cancer
Lack of knowledge about ovarian cancer prevents many women from seeking medical attention, which delays diagnosis and treatment and may prove increasingly dangerous as incidence rises by an expected 55% over the next 2 decades, according to the World Ovarian Cancer Coalition.
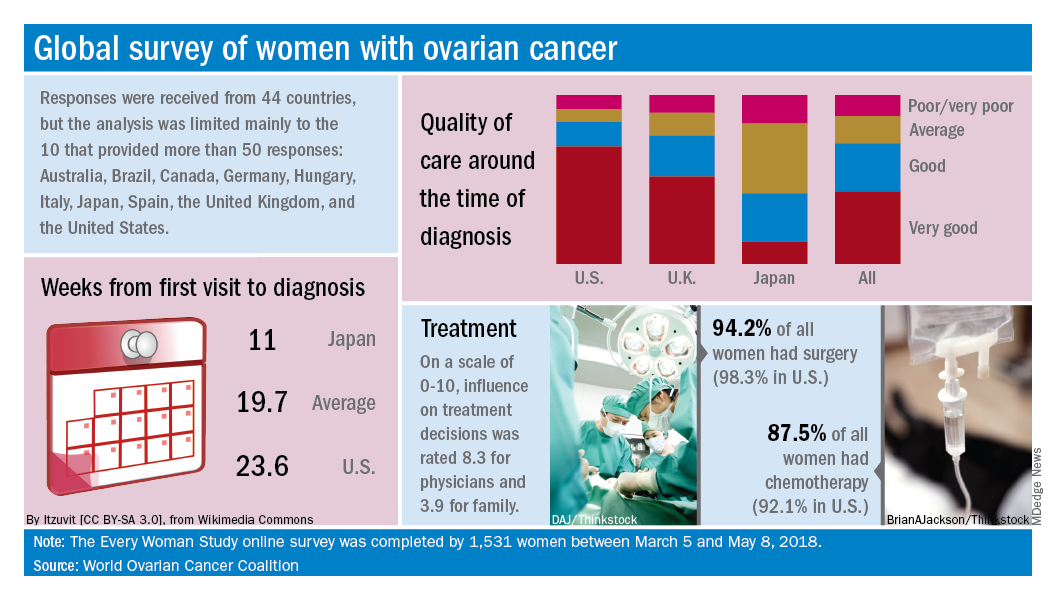
Data from the coalition’s 2018 survey of women with ovarian cancer show that 18% had never heard of the disease before their diagnosis and 51% had heard of it but did not know anything about it. The Every Women Study survey, completed by 1,531 women in 44 countries, also reveals that nine out of ten had experienced symptoms prior to diagnosis but fewer than half saw a physician within a month of noticing those symptoms, the coalition said.
“This study, for the first time, provides powerful evidence of the challenges faced by women diagnosed with ovarian cancer across the world and sets an agenda for global change. We were especially shocked by the widespread, woeful lack of awareness of ovarian cancer,” Annwen Jones, coalition vice-chair and cochair of the study, said in a separate written statement.
Results varied considerably by country, and only 10 countries provided enough responses to allow comparisons: Australia (120), Brazil (52), Canada (167), Germany (141), Hungary (58), Italy (92), Japan (250), Spain (70), the United Kingdom (176), and the United States (248).
Among those comparisons, women in Germany (5.5 weeks) and Spain (7.9 weeks) were the first to visit a physician after first experiencing symptoms, while those in Italy (15.2 weeks) and the United States (12.9 weeks) were last. The United States was also longest in time from first visit to diagnosis (23.6 weeks), and Japan was the shortest (11 weeks). Despite that world-longest time to diagnosis, however, over 69% of U.S. women said that their care around the time of diagnosis was very good, which was higher than any other country, the coalition reported.
Surgery statistics were closer among countries, with an average of 94% of all women undergoing surgery to treat their ovarian cancer. The United States, at 98.3%, was second to Spain’s 98.5%, and Hungary was the largest outlier on the low side at 59%. Over 87% of all women reported having chemotherapy to treat or control their cancer, and 9.8% of women said that they had received intraperitoneal chemotherapy. In the United States, 22.5% of women received intraperitoneal therapy, compared with 0.7% for the United Kingdom.
“No one country has all the answers, and whilst there is still an urgent need for a step-change in the level of investment in research for better treatments and tools for early diagnosis, there are significant opportunities to improve survival and quality of life for women in the immediate and short term to make a series of marginal gains if these variations are addressed by individual countries,” the coalition said in the report.
Lack of knowledge about ovarian cancer prevents many women from seeking medical attention, which delays diagnosis and treatment and may prove increasingly dangerous as incidence rises by an expected 55% over the next 2 decades, according to the World Ovarian Cancer Coalition.
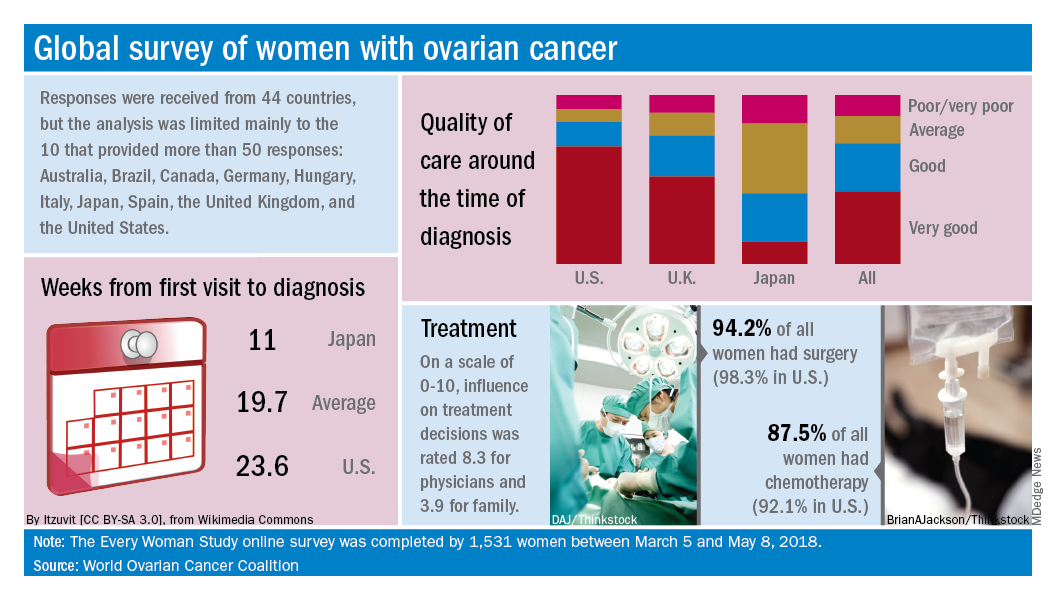
Data from the coalition’s 2018 survey of women with ovarian cancer show that 18% had never heard of the disease before their diagnosis and 51% had heard of it but did not know anything about it. The Every Women Study survey, completed by 1,531 women in 44 countries, also reveals that nine out of ten had experienced symptoms prior to diagnosis but fewer than half saw a physician within a month of noticing those symptoms, the coalition said.
“This study, for the first time, provides powerful evidence of the challenges faced by women diagnosed with ovarian cancer across the world and sets an agenda for global change. We were especially shocked by the widespread, woeful lack of awareness of ovarian cancer,” Annwen Jones, coalition vice-chair and cochair of the study, said in a separate written statement.
Results varied considerably by country, and only 10 countries provided enough responses to allow comparisons: Australia (120), Brazil (52), Canada (167), Germany (141), Hungary (58), Italy (92), Japan (250), Spain (70), the United Kingdom (176), and the United States (248).
Among those comparisons, women in Germany (5.5 weeks) and Spain (7.9 weeks) were the first to visit a physician after first experiencing symptoms, while those in Italy (15.2 weeks) and the United States (12.9 weeks) were last. The United States was also longest in time from first visit to diagnosis (23.6 weeks), and Japan was the shortest (11 weeks). Despite that world-longest time to diagnosis, however, over 69% of U.S. women said that their care around the time of diagnosis was very good, which was higher than any other country, the coalition reported.
Surgery statistics were closer among countries, with an average of 94% of all women undergoing surgery to treat their ovarian cancer. The United States, at 98.3%, was second to Spain’s 98.5%, and Hungary was the largest outlier on the low side at 59%. Over 87% of all women reported having chemotherapy to treat or control their cancer, and 9.8% of women said that they had received intraperitoneal chemotherapy. In the United States, 22.5% of women received intraperitoneal therapy, compared with 0.7% for the United Kingdom.
“No one country has all the answers, and whilst there is still an urgent need for a step-change in the level of investment in research for better treatments and tools for early diagnosis, there are significant opportunities to improve survival and quality of life for women in the immediate and short term to make a series of marginal gains if these variations are addressed by individual countries,” the coalition said in the report.
Lack of knowledge about ovarian cancer prevents many women from seeking medical attention, which delays diagnosis and treatment and may prove increasingly dangerous as incidence rises by an expected 55% over the next 2 decades, according to the World Ovarian Cancer Coalition.
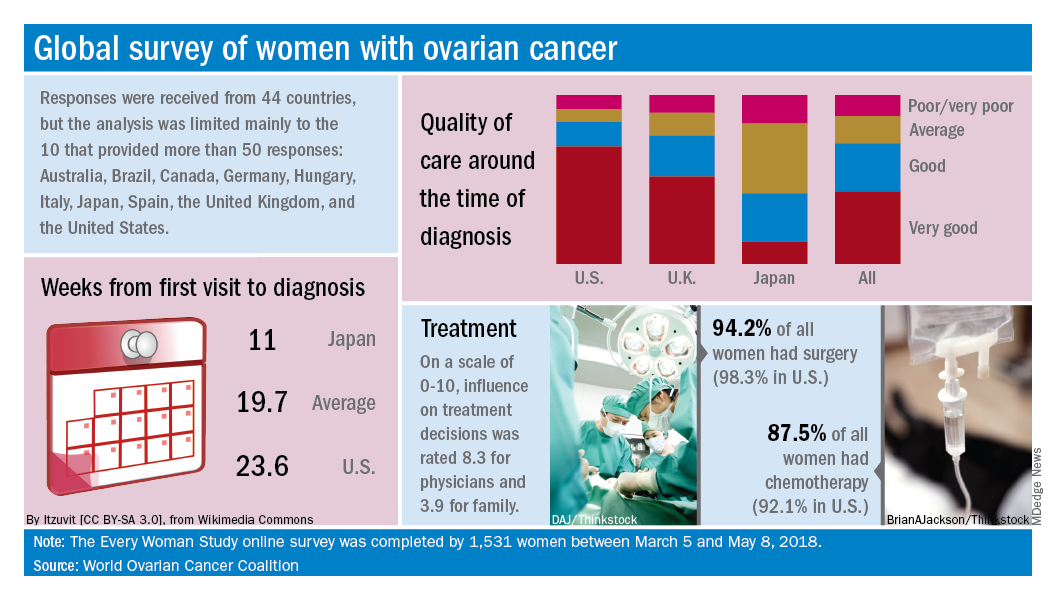
Data from the coalition’s 2018 survey of women with ovarian cancer show that 18% had never heard of the disease before their diagnosis and 51% had heard of it but did not know anything about it. The Every Women Study survey, completed by 1,531 women in 44 countries, also reveals that nine out of ten had experienced symptoms prior to diagnosis but fewer than half saw a physician within a month of noticing those symptoms, the coalition said.
“This study, for the first time, provides powerful evidence of the challenges faced by women diagnosed with ovarian cancer across the world and sets an agenda for global change. We were especially shocked by the widespread, woeful lack of awareness of ovarian cancer,” Annwen Jones, coalition vice-chair and cochair of the study, said in a separate written statement.
Results varied considerably by country, and only 10 countries provided enough responses to allow comparisons: Australia (120), Brazil (52), Canada (167), Germany (141), Hungary (58), Italy (92), Japan (250), Spain (70), the United Kingdom (176), and the United States (248).
Among those comparisons, women in Germany (5.5 weeks) and Spain (7.9 weeks) were the first to visit a physician after first experiencing symptoms, while those in Italy (15.2 weeks) and the United States (12.9 weeks) were last. The United States was also longest in time from first visit to diagnosis (23.6 weeks), and Japan was the shortest (11 weeks). Despite that world-longest time to diagnosis, however, over 69% of U.S. women said that their care around the time of diagnosis was very good, which was higher than any other country, the coalition reported.
Surgery statistics were closer among countries, with an average of 94% of all women undergoing surgery to treat their ovarian cancer. The United States, at 98.3%, was second to Spain’s 98.5%, and Hungary was the largest outlier on the low side at 59%. Over 87% of all women reported having chemotherapy to treat or control their cancer, and 9.8% of women said that they had received intraperitoneal chemotherapy. In the United States, 22.5% of women received intraperitoneal therapy, compared with 0.7% for the United Kingdom.
“No one country has all the answers, and whilst there is still an urgent need for a step-change in the level of investment in research for better treatments and tools for early diagnosis, there are significant opportunities to improve survival and quality of life for women in the immediate and short term to make a series of marginal gains if these variations are addressed by individual countries,” the coalition said in the report.
ACR readies first-ever guidelines on managing reproductive health in rheumatology
CHICAGO – Help is on the way for rheumatologists who may feel out of their depth regarding reproductive health issues in their patients.
for internal review in draft form. Lisa R. Sammaritano, MD, a leader of the expert panel that developed the evidence-based recommendations, shared highlights of the forthcoming guidelines at the annual meeting of the American College of Rheumatology.
“Our patients, fortunately, are pursuing pregnancy more often now than in years past. One of the key messages of the guidelines is that patients really do want to discuss these topics with their rheumatologist, even though that often does not happen now. What patients told us [in the guideline-development process] is their rheumatologist knows them better than their gynecologist or any of their other doctors because we have followed them for a long period of time and we understand their disease and their symptoms. They really want our input on questions about contraception, when to plan a pregnancy, and medication use,” said Dr. Sammaritano of the Hospital for Special Surgery and Cornell University in New York.
The guidelines were created over the course of a year and a half with extensive input from ob.gyns., as well as a patient panel. The project included a systematic review of more than 300 published studies in which guideline panelists attempt to find answers to an initial list of 370 questions. Dr. Sammaritano predicted that the guidelines will prove to be useful not only for rheumatologists, but for their colleagues in ob.gyn. as well. Just as rheumatologists likely haven’t kept up with the sea changes that have occurred in ob.gyn. since their medical school days, most ob.gyns. know little about rheumatic diseases.
“There’s room for education on both sides,” she observed in an interview. “I have had to write letters to gynecologists to get them to put my patients with antiphospholipid antibodies on a contraceptive that includes a progestin because the labeling says, ‘May increase risk of thrombosis.’ And yet if you look at the literature, most of the progestins do not increase the risk of thrombosis, even in patients who are already at increased risk because of a genetic prothrombotic abnormality. I practically had to sign my life away to get a gynecologist to put a progestin-containing IUD in my patient, whereas the risk of thrombosis to my patient with an unplanned pregnancy would have been 10-fold or 100-fold higher. Unplanned pregnancy is dangerous for patients with our diseases.”
And yet, she noted, half of all pregnancies in the United States are unplanned. Among women with rheumatic diseases, the proportion may well be even higher in light of their documented low rate of utilization of effective contraception.
A publication date for the guidelines won’t be set until the review is completed, but the plan is to issue three separate documents. One will address reproductive health outside of pregnancy, with key topics to include contraception, fertility preservation, menopause, and hormone replacement therapy. The second document will focus on pregnancy management, with special attention devoted to women with lupus or antiphospholipid antibodies because they are at particularly high risk of adverse pregnancy outcomes. The third document will be devoted to medications, covering issues including which medications can be continued during pregnancy and when to safely stop the ones that can’t. This section will address both maternal and paternal use of rheumatologic medications, the latter being a topic below the radar of ob.gyns.
The three medications whose paternal use in pregnancy generate the most questions in clinical practice are methotrexate, cyclophosphamide, and sulfasalazine.
“I cannot tell you how many times I’ve been asked whether male patients with rheumatic diseases need to stop their methotrexate before they plan to father a child – that’s been a big one. The answer is they don’t need to stop, but that’s a conditional recommendation because the product label still says to stop it 3 months before. But that’s based on theoretical concerns, and all the data support a lack of teratogenicity for men using methotrexate prior to and during pregnancy,” Dr. Sammaritano said.
Men on cyclophosphamide absolutely have to stop the drug 3 months before pregnancy because the drug causes DNA fragmentation in the sperm. Sulfasalazine is known to impair male fertility. The ACR guidelines will recommend that men continue the drug, but if pregnancy doesn’t occur within a reasonable time, then it’s appropriate to get a semen analysis rather than stopping sulfasalazine unnecessarily.
American College of Obstetricians and Gynecologists guidelines now recommend long-acting reversible contraception, including IUDs and progestin implants, as first-line contraception for all women. The ACR draft guidelines strongly recommend the same.
“That is new. The use of this form of contraception in women with rheumatic diseases is quite low. In general, our patients don’t use contraception as often as other women, and when they do, they don’t use effective contraception. There are many theories as to why that may be: perhaps it’s a focus on the more immediate issues of their rheumatic disease that doesn’t allow their rheumatologist to get to the point of discussing contraception,” according to Dr. Sammaritano.
Many rheumatologists will be pleasantly surprised to learn that the problem of increased risk of pelvic inflammatory disease associated with earlier-generation IUDs is no longer an issue with the current devices. And contrary to a misconception among some ob.gyns., autoimmune disease will not cause a woman to reject her IUD.
The ACR guidelines recommend continuing hydroxychloroquine in lupus patients during pregnancy – and considering starting the drug in those not already on it – because of strong evidence supporting both safety and benefit for mother and baby.
“We are recommending the use of low-dose aspirin for patients with lupus and antiphospholipid antibodies because those two conditions increase the risk for preeclampsia, and the ob.gyns. routinely use low-dose aspirin starting toward the end of the first trimester as preventive therapy. Large studies show that it reduces the risk,” she continued.
Dr. Sammaritano cautioned that the literature on the use of rheumatologic medications in pregnancy and breast feeding is generally weak – and in the case of the new oral small molecule JAK inhibitors, essentially nonexistent.
“A lot of our recommendations are conditional because we did not feel that the data support a strong recommendation. But you have to do something. As long as you communicate the idea that we’re doing the best we can with what information is available, I think patients will respond to that,” the rheumatologist said.
She reported having no financial conflicts regarding her presentation.
CHICAGO – Help is on the way for rheumatologists who may feel out of their depth regarding reproductive health issues in their patients.
for internal review in draft form. Lisa R. Sammaritano, MD, a leader of the expert panel that developed the evidence-based recommendations, shared highlights of the forthcoming guidelines at the annual meeting of the American College of Rheumatology.
“Our patients, fortunately, are pursuing pregnancy more often now than in years past. One of the key messages of the guidelines is that patients really do want to discuss these topics with their rheumatologist, even though that often does not happen now. What patients told us [in the guideline-development process] is their rheumatologist knows them better than their gynecologist or any of their other doctors because we have followed them for a long period of time and we understand their disease and their symptoms. They really want our input on questions about contraception, when to plan a pregnancy, and medication use,” said Dr. Sammaritano of the Hospital for Special Surgery and Cornell University in New York.
The guidelines were created over the course of a year and a half with extensive input from ob.gyns., as well as a patient panel. The project included a systematic review of more than 300 published studies in which guideline panelists attempt to find answers to an initial list of 370 questions. Dr. Sammaritano predicted that the guidelines will prove to be useful not only for rheumatologists, but for their colleagues in ob.gyn. as well. Just as rheumatologists likely haven’t kept up with the sea changes that have occurred in ob.gyn. since their medical school days, most ob.gyns. know little about rheumatic diseases.
“There’s room for education on both sides,” she observed in an interview. “I have had to write letters to gynecologists to get them to put my patients with antiphospholipid antibodies on a contraceptive that includes a progestin because the labeling says, ‘May increase risk of thrombosis.’ And yet if you look at the literature, most of the progestins do not increase the risk of thrombosis, even in patients who are already at increased risk because of a genetic prothrombotic abnormality. I practically had to sign my life away to get a gynecologist to put a progestin-containing IUD in my patient, whereas the risk of thrombosis to my patient with an unplanned pregnancy would have been 10-fold or 100-fold higher. Unplanned pregnancy is dangerous for patients with our diseases.”
And yet, she noted, half of all pregnancies in the United States are unplanned. Among women with rheumatic diseases, the proportion may well be even higher in light of their documented low rate of utilization of effective contraception.
A publication date for the guidelines won’t be set until the review is completed, but the plan is to issue three separate documents. One will address reproductive health outside of pregnancy, with key topics to include contraception, fertility preservation, menopause, and hormone replacement therapy. The second document will focus on pregnancy management, with special attention devoted to women with lupus or antiphospholipid antibodies because they are at particularly high risk of adverse pregnancy outcomes. The third document will be devoted to medications, covering issues including which medications can be continued during pregnancy and when to safely stop the ones that can’t. This section will address both maternal and paternal use of rheumatologic medications, the latter being a topic below the radar of ob.gyns.
The three medications whose paternal use in pregnancy generate the most questions in clinical practice are methotrexate, cyclophosphamide, and sulfasalazine.
“I cannot tell you how many times I’ve been asked whether male patients with rheumatic diseases need to stop their methotrexate before they plan to father a child – that’s been a big one. The answer is they don’t need to stop, but that’s a conditional recommendation because the product label still says to stop it 3 months before. But that’s based on theoretical concerns, and all the data support a lack of teratogenicity for men using methotrexate prior to and during pregnancy,” Dr. Sammaritano said.
Men on cyclophosphamide absolutely have to stop the drug 3 months before pregnancy because the drug causes DNA fragmentation in the sperm. Sulfasalazine is known to impair male fertility. The ACR guidelines will recommend that men continue the drug, but if pregnancy doesn’t occur within a reasonable time, then it’s appropriate to get a semen analysis rather than stopping sulfasalazine unnecessarily.
American College of Obstetricians and Gynecologists guidelines now recommend long-acting reversible contraception, including IUDs and progestin implants, as first-line contraception for all women. The ACR draft guidelines strongly recommend the same.
“That is new. The use of this form of contraception in women with rheumatic diseases is quite low. In general, our patients don’t use contraception as often as other women, and when they do, they don’t use effective contraception. There are many theories as to why that may be: perhaps it’s a focus on the more immediate issues of their rheumatic disease that doesn’t allow their rheumatologist to get to the point of discussing contraception,” according to Dr. Sammaritano.
Many rheumatologists will be pleasantly surprised to learn that the problem of increased risk of pelvic inflammatory disease associated with earlier-generation IUDs is no longer an issue with the current devices. And contrary to a misconception among some ob.gyns., autoimmune disease will not cause a woman to reject her IUD.
The ACR guidelines recommend continuing hydroxychloroquine in lupus patients during pregnancy – and considering starting the drug in those not already on it – because of strong evidence supporting both safety and benefit for mother and baby.
“We are recommending the use of low-dose aspirin for patients with lupus and antiphospholipid antibodies because those two conditions increase the risk for preeclampsia, and the ob.gyns. routinely use low-dose aspirin starting toward the end of the first trimester as preventive therapy. Large studies show that it reduces the risk,” she continued.
Dr. Sammaritano cautioned that the literature on the use of rheumatologic medications in pregnancy and breast feeding is generally weak – and in the case of the new oral small molecule JAK inhibitors, essentially nonexistent.
“A lot of our recommendations are conditional because we did not feel that the data support a strong recommendation. But you have to do something. As long as you communicate the idea that we’re doing the best we can with what information is available, I think patients will respond to that,” the rheumatologist said.
She reported having no financial conflicts regarding her presentation.
CHICAGO – Help is on the way for rheumatologists who may feel out of their depth regarding reproductive health issues in their patients.
for internal review in draft form. Lisa R. Sammaritano, MD, a leader of the expert panel that developed the evidence-based recommendations, shared highlights of the forthcoming guidelines at the annual meeting of the American College of Rheumatology.
“Our patients, fortunately, are pursuing pregnancy more often now than in years past. One of the key messages of the guidelines is that patients really do want to discuss these topics with their rheumatologist, even though that often does not happen now. What patients told us [in the guideline-development process] is their rheumatologist knows them better than their gynecologist or any of their other doctors because we have followed them for a long period of time and we understand their disease and their symptoms. They really want our input on questions about contraception, when to plan a pregnancy, and medication use,” said Dr. Sammaritano of the Hospital for Special Surgery and Cornell University in New York.
The guidelines were created over the course of a year and a half with extensive input from ob.gyns., as well as a patient panel. The project included a systematic review of more than 300 published studies in which guideline panelists attempt to find answers to an initial list of 370 questions. Dr. Sammaritano predicted that the guidelines will prove to be useful not only for rheumatologists, but for their colleagues in ob.gyn. as well. Just as rheumatologists likely haven’t kept up with the sea changes that have occurred in ob.gyn. since their medical school days, most ob.gyns. know little about rheumatic diseases.
“There’s room for education on both sides,” she observed in an interview. “I have had to write letters to gynecologists to get them to put my patients with antiphospholipid antibodies on a contraceptive that includes a progestin because the labeling says, ‘May increase risk of thrombosis.’ And yet if you look at the literature, most of the progestins do not increase the risk of thrombosis, even in patients who are already at increased risk because of a genetic prothrombotic abnormality. I practically had to sign my life away to get a gynecologist to put a progestin-containing IUD in my patient, whereas the risk of thrombosis to my patient with an unplanned pregnancy would have been 10-fold or 100-fold higher. Unplanned pregnancy is dangerous for patients with our diseases.”
And yet, she noted, half of all pregnancies in the United States are unplanned. Among women with rheumatic diseases, the proportion may well be even higher in light of their documented low rate of utilization of effective contraception.
A publication date for the guidelines won’t be set until the review is completed, but the plan is to issue three separate documents. One will address reproductive health outside of pregnancy, with key topics to include contraception, fertility preservation, menopause, and hormone replacement therapy. The second document will focus on pregnancy management, with special attention devoted to women with lupus or antiphospholipid antibodies because they are at particularly high risk of adverse pregnancy outcomes. The third document will be devoted to medications, covering issues including which medications can be continued during pregnancy and when to safely stop the ones that can’t. This section will address both maternal and paternal use of rheumatologic medications, the latter being a topic below the radar of ob.gyns.
The three medications whose paternal use in pregnancy generate the most questions in clinical practice are methotrexate, cyclophosphamide, and sulfasalazine.
“I cannot tell you how many times I’ve been asked whether male patients with rheumatic diseases need to stop their methotrexate before they plan to father a child – that’s been a big one. The answer is they don’t need to stop, but that’s a conditional recommendation because the product label still says to stop it 3 months before. But that’s based on theoretical concerns, and all the data support a lack of teratogenicity for men using methotrexate prior to and during pregnancy,” Dr. Sammaritano said.
Men on cyclophosphamide absolutely have to stop the drug 3 months before pregnancy because the drug causes DNA fragmentation in the sperm. Sulfasalazine is known to impair male fertility. The ACR guidelines will recommend that men continue the drug, but if pregnancy doesn’t occur within a reasonable time, then it’s appropriate to get a semen analysis rather than stopping sulfasalazine unnecessarily.
American College of Obstetricians and Gynecologists guidelines now recommend long-acting reversible contraception, including IUDs and progestin implants, as first-line contraception for all women. The ACR draft guidelines strongly recommend the same.
“That is new. The use of this form of contraception in women with rheumatic diseases is quite low. In general, our patients don’t use contraception as often as other women, and when they do, they don’t use effective contraception. There are many theories as to why that may be: perhaps it’s a focus on the more immediate issues of their rheumatic disease that doesn’t allow their rheumatologist to get to the point of discussing contraception,” according to Dr. Sammaritano.
Many rheumatologists will be pleasantly surprised to learn that the problem of increased risk of pelvic inflammatory disease associated with earlier-generation IUDs is no longer an issue with the current devices. And contrary to a misconception among some ob.gyns., autoimmune disease will not cause a woman to reject her IUD.
The ACR guidelines recommend continuing hydroxychloroquine in lupus patients during pregnancy – and considering starting the drug in those not already on it – because of strong evidence supporting both safety and benefit for mother and baby.
“We are recommending the use of low-dose aspirin for patients with lupus and antiphospholipid antibodies because those two conditions increase the risk for preeclampsia, and the ob.gyns. routinely use low-dose aspirin starting toward the end of the first trimester as preventive therapy. Large studies show that it reduces the risk,” she continued.
Dr. Sammaritano cautioned that the literature on the use of rheumatologic medications in pregnancy and breast feeding is generally weak – and in the case of the new oral small molecule JAK inhibitors, essentially nonexistent.
“A lot of our recommendations are conditional because we did not feel that the data support a strong recommendation. But you have to do something. As long as you communicate the idea that we’re doing the best we can with what information is available, I think patients will respond to that,” the rheumatologist said.
She reported having no financial conflicts regarding her presentation.
REPORTING FROM THE ACR ANNUAL MEETING
Trump scheme for Part B drugs raises red flags
A proposed Trump administration plan for paying for drugs under Medicare Part B has raised red flags for doctors.
The Centers for Medicare & Medicaid Services announced Oct. 25 that it will test paying for Part B drugs by more closely aligning those payments with international rates.
The so-called International Price Index (IPI) model “would test whether increasing competition for private-sector vendors to negotiate drug prices, and aligning Medicare payments for drugs with prices that are paid in foreign countries, improves beneficiary access and quality of care while reducing expenditures,” according to a government fact sheet.
Under the test, private vendors would “procure drugs, distribute them to physicians and hospitals, and take on the responsibility of billing Medicare. Vendors would aggregate purchasing, seek volume-based discounts, and compete for providers’ business, thereby creating competition where none exists today.”
Health care professionals and hospitals in certain geographic areas would receive their Part B drugs under this program, while the rest of the country would continue under the current buy-and-bill system. Eventually, over the 5-year phase-in period, half of the geographic regions would fall under this IPI model.
CMS officials note that the IPI model “would maintain beneficiaries’ choice of provider and treatments and would have meaningful beneficiary protections such as enhanced monitoring and Medicare Beneficiary Ombudsman supports.”
Initially, only single-source drugs and biologics with available international pricing data would be provided under the IPI model, which could be expanded over time to include drugs available via multiple sources.
Currently, Medicare typically pays average sales price (ASP) plus a 6% add-on for drugs under Part B. Under IPI, if the international price is determined to be lower than the ASP, the CMS would reimburse based on a target price derived from an international price index, with the hope that manufacturers would match the international price. The target price would be phased in over a 5-year period.
The plan also calls for an add-on price similar to the current buy-and-bill system; however, the CMS aims to bring the add-on back to 6% rather than the actual 4.3% under the budget sequestration.
Other add-ons are also under consideration, such as paying a fixed amount per encounter or per month as well as a unique payment based on drug class, physician specialty, or physician practice.
Early takes on the proposal were met with skepticism.
The Community Oncology Alliance (COA) said in a statement that it is “concerned that the IPI will either repeat past reform mistakes [such as the Competitive Acquisition Program] or introduce the same cancer treatment access challenges experienced by cancer patients today with pharmacy benefit managers and other middlemen under Medicare Part D.”
“What the administration is proposing is incredibly complex and extremely difficult to comprehend how it would be implemented in the real-world of medical practice,” said Ted Okon, executive director of the COA. “It is also disturbing that the administration is trying to end-run the Congress by forcing a mandatory CMS Innovation Center demonstration that will effectively change Medicare reimbursement, as the sequester cut to Part B drug reimbursement has already done.”
The American College of Rheumatology was more measured in its reaction, noting that any change in policy needs to be thoughtful in its process to ensure that patient care is not adversely affected.
“Efforts to address high costs can sometimes create significant access issues for patients while penalizing doctors for providing quality care,” ACR officials said in a statement. “These proposals include those restructuring reimbursement for Medicare Part B drugs through either flat fee payments or a competitive acquisition program, or allowing utilization management such as step therapy or ‘fail first’ protocols in the Medicare Part B program. It is imperative that policy makers stay focused on the players who control drug prices and not penalize Medicare patients who depend on timely access to needed therapies.”
The American Medical Association raised some concerns as well.
“The administration’s proposal for an International Pricing Index Model for Part B drugs raises a number of questions, and we need to have a greater understanding of the potential impact of the proposal on patients, physicians, and the health care system,” AMA President Barbara McAneny, MD, said in a statement. “We look forward to working constructively with the Administration as it seeks feedback.”
The advanced notice of proposed rulemaking was posted to the Federal Register website on Oct. 25 and is scheduled to be formally published in the publication on Oct. 30. Comments are due Dec. 24. The CMS plans to issue the proposed rule related to this model in the spring of 2019.
A proposed Trump administration plan for paying for drugs under Medicare Part B has raised red flags for doctors.
The Centers for Medicare & Medicaid Services announced Oct. 25 that it will test paying for Part B drugs by more closely aligning those payments with international rates.
The so-called International Price Index (IPI) model “would test whether increasing competition for private-sector vendors to negotiate drug prices, and aligning Medicare payments for drugs with prices that are paid in foreign countries, improves beneficiary access and quality of care while reducing expenditures,” according to a government fact sheet.
Under the test, private vendors would “procure drugs, distribute them to physicians and hospitals, and take on the responsibility of billing Medicare. Vendors would aggregate purchasing, seek volume-based discounts, and compete for providers’ business, thereby creating competition where none exists today.”
Health care professionals and hospitals in certain geographic areas would receive their Part B drugs under this program, while the rest of the country would continue under the current buy-and-bill system. Eventually, over the 5-year phase-in period, half of the geographic regions would fall under this IPI model.
CMS officials note that the IPI model “would maintain beneficiaries’ choice of provider and treatments and would have meaningful beneficiary protections such as enhanced monitoring and Medicare Beneficiary Ombudsman supports.”
Initially, only single-source drugs and biologics with available international pricing data would be provided under the IPI model, which could be expanded over time to include drugs available via multiple sources.
Currently, Medicare typically pays average sales price (ASP) plus a 6% add-on for drugs under Part B. Under IPI, if the international price is determined to be lower than the ASP, the CMS would reimburse based on a target price derived from an international price index, with the hope that manufacturers would match the international price. The target price would be phased in over a 5-year period.
The plan also calls for an add-on price similar to the current buy-and-bill system; however, the CMS aims to bring the add-on back to 6% rather than the actual 4.3% under the budget sequestration.
Other add-ons are also under consideration, such as paying a fixed amount per encounter or per month as well as a unique payment based on drug class, physician specialty, or physician practice.
Early takes on the proposal were met with skepticism.
The Community Oncology Alliance (COA) said in a statement that it is “concerned that the IPI will either repeat past reform mistakes [such as the Competitive Acquisition Program] or introduce the same cancer treatment access challenges experienced by cancer patients today with pharmacy benefit managers and other middlemen under Medicare Part D.”
“What the administration is proposing is incredibly complex and extremely difficult to comprehend how it would be implemented in the real-world of medical practice,” said Ted Okon, executive director of the COA. “It is also disturbing that the administration is trying to end-run the Congress by forcing a mandatory CMS Innovation Center demonstration that will effectively change Medicare reimbursement, as the sequester cut to Part B drug reimbursement has already done.”
The American College of Rheumatology was more measured in its reaction, noting that any change in policy needs to be thoughtful in its process to ensure that patient care is not adversely affected.
“Efforts to address high costs can sometimes create significant access issues for patients while penalizing doctors for providing quality care,” ACR officials said in a statement. “These proposals include those restructuring reimbursement for Medicare Part B drugs through either flat fee payments or a competitive acquisition program, or allowing utilization management such as step therapy or ‘fail first’ protocols in the Medicare Part B program. It is imperative that policy makers stay focused on the players who control drug prices and not penalize Medicare patients who depend on timely access to needed therapies.”
The American Medical Association raised some concerns as well.
“The administration’s proposal for an International Pricing Index Model for Part B drugs raises a number of questions, and we need to have a greater understanding of the potential impact of the proposal on patients, physicians, and the health care system,” AMA President Barbara McAneny, MD, said in a statement. “We look forward to working constructively with the Administration as it seeks feedback.”
The advanced notice of proposed rulemaking was posted to the Federal Register website on Oct. 25 and is scheduled to be formally published in the publication on Oct. 30. Comments are due Dec. 24. The CMS plans to issue the proposed rule related to this model in the spring of 2019.
A proposed Trump administration plan for paying for drugs under Medicare Part B has raised red flags for doctors.
The Centers for Medicare & Medicaid Services announced Oct. 25 that it will test paying for Part B drugs by more closely aligning those payments with international rates.
The so-called International Price Index (IPI) model “would test whether increasing competition for private-sector vendors to negotiate drug prices, and aligning Medicare payments for drugs with prices that are paid in foreign countries, improves beneficiary access and quality of care while reducing expenditures,” according to a government fact sheet.
Under the test, private vendors would “procure drugs, distribute them to physicians and hospitals, and take on the responsibility of billing Medicare. Vendors would aggregate purchasing, seek volume-based discounts, and compete for providers’ business, thereby creating competition where none exists today.”
Health care professionals and hospitals in certain geographic areas would receive their Part B drugs under this program, while the rest of the country would continue under the current buy-and-bill system. Eventually, over the 5-year phase-in period, half of the geographic regions would fall under this IPI model.
CMS officials note that the IPI model “would maintain beneficiaries’ choice of provider and treatments and would have meaningful beneficiary protections such as enhanced monitoring and Medicare Beneficiary Ombudsman supports.”
Initially, only single-source drugs and biologics with available international pricing data would be provided under the IPI model, which could be expanded over time to include drugs available via multiple sources.
Currently, Medicare typically pays average sales price (ASP) plus a 6% add-on for drugs under Part B. Under IPI, if the international price is determined to be lower than the ASP, the CMS would reimburse based on a target price derived from an international price index, with the hope that manufacturers would match the international price. The target price would be phased in over a 5-year period.
The plan also calls for an add-on price similar to the current buy-and-bill system; however, the CMS aims to bring the add-on back to 6% rather than the actual 4.3% under the budget sequestration.
Other add-ons are also under consideration, such as paying a fixed amount per encounter or per month as well as a unique payment based on drug class, physician specialty, or physician practice.
Early takes on the proposal were met with skepticism.
The Community Oncology Alliance (COA) said in a statement that it is “concerned that the IPI will either repeat past reform mistakes [such as the Competitive Acquisition Program] or introduce the same cancer treatment access challenges experienced by cancer patients today with pharmacy benefit managers and other middlemen under Medicare Part D.”
“What the administration is proposing is incredibly complex and extremely difficult to comprehend how it would be implemented in the real-world of medical practice,” said Ted Okon, executive director of the COA. “It is also disturbing that the administration is trying to end-run the Congress by forcing a mandatory CMS Innovation Center demonstration that will effectively change Medicare reimbursement, as the sequester cut to Part B drug reimbursement has already done.”
The American College of Rheumatology was more measured in its reaction, noting that any change in policy needs to be thoughtful in its process to ensure that patient care is not adversely affected.
“Efforts to address high costs can sometimes create significant access issues for patients while penalizing doctors for providing quality care,” ACR officials said in a statement. “These proposals include those restructuring reimbursement for Medicare Part B drugs through either flat fee payments or a competitive acquisition program, or allowing utilization management such as step therapy or ‘fail first’ protocols in the Medicare Part B program. It is imperative that policy makers stay focused on the players who control drug prices and not penalize Medicare patients who depend on timely access to needed therapies.”
The American Medical Association raised some concerns as well.
“The administration’s proposal for an International Pricing Index Model for Part B drugs raises a number of questions, and we need to have a greater understanding of the potential impact of the proposal on patients, physicians, and the health care system,” AMA President Barbara McAneny, MD, said in a statement. “We look forward to working constructively with the Administration as it seeks feedback.”
The advanced notice of proposed rulemaking was posted to the Federal Register website on Oct. 25 and is scheduled to be formally published in the publication on Oct. 30. Comments are due Dec. 24. The CMS plans to issue the proposed rule related to this model in the spring of 2019.
Acute kidney injury linked to later dementia
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
SAN DIEGO –
That’s according to a new study offering more evidence of a link between kidney disease and neurological problems.
“Clinicians should know that AKI is associated with poor long-term outcomes,” said lead author Jessica B. Kendrick MD, associate professor of medicine at the University of Colorado, Aurora. “We need to identify ways to prevent these long-term consequences.”
The findings were presented at Kidney Week 2018, sponsored by the American Society of Nephrology.
According to Dr. Kendrick, the acute neurological effects of AKI are well known. But no previous studies have examined the potential long-term cerebrovascular complications of AKI.
For the new study, Dr. Kendrick and her colleagues retrospectively analyzed 2,082 hospitalized patients in Utah from 1999 to 2009: 1,041 who completely recovered from AKI by discharge, and 1,041 who did not have AKI.
The average age was 61 years, and the average baseline creatinine was 0.9 ± 0.2 mg/dL. Over a median follow-up of 6 years, 97 patients developed dementia.
Those with AKI were more likely to develop dementia compared with the control group: 7% vs. 2% (hazard ratio, 3.4; 95% confidence interval, 2.14-5.40).
Other studies have linked kidney disease to cognitive impairment.
“There are a lot of theories as to why this is,” nephrologist Daniel Weiner, MD, of Tufts University, Boston, said in an interview. “It is most likely that the presence of kidney disease identifies individuals with a high burden of vascular disease, and that vascular disease, particularly of the small blood vessels, is an important contributor to cognitive impairment and dementia.”
That appears to be most notable in people who have protein in their urine, Dr. Weiner added. “The presence of protein in the urine identifies a severe enough process to affect the blood vessels in the kidney, and there is no reason to think that blood vessels elsewhere in the body, including in the brain, are not similarly affected.”
As for the current study, Dr. Weiner said it could support the vascular disease theory.
“People with vulnerable kidneys to acute injury also have vulnerable brains to acute injury,” he said. “People who get AKI usually have susceptibility to perfusion-related kidney injury. In other words, the small blood vessels that supply the kidney are unable to compensate to maintain sufficient blood flow during a time of low blood pressure or other systemic illness.”
That vulnerability “suggests to me that small blood vessels elsewhere in the body are less likely to be able to respond to challenges like low blood pressure,” Dr. Weiner explained. “If this occurs in the brain, it leads to microvascular disease and greater abnormal white-matter burden. This change in the brain anatomy is highly correlated with cognitive impairment.”
How can physicians put these finding to use? “These patients may require more monitoring,” Dr. Kendrick said. “For example, patients with AKI and complete recovery may not have any follow-up with a nephrologist, and perhaps they should.”
Moving forward, she said, “we are examining the association of AKI with cognitive dysfunction in different patient populations.” Researchers also are planning studies to better understand the mechanisms that are at work, she said.
The National Heart, Lung, and Blood Institute funded the study. The study authors had no disclosures.
SOURCE: Kendrick JB et al. Kidney Week 2018. Abstract TH-OR116.
REPORTING FROM KIDNEY WEEK 2018
Key clinical point: Patients with acute kidney injury seem to face a much higher risk of dementia.
Major finding: Hospitalized patients with AKI were 3.4 times more likely to develop dementia within a median of 6 years, compared with other hospitalized patients.
Study details: A retrospective study of 2,082 propensity-matched hospitalized patients, 1,041 who had AKI and fully recovered, and 1,041 who did not have AKI.
Disclosures: The National Heart, Lung, and Blood Institute funded the study. The authors had no disclosures.
Source: Kendrick JB et al. Kidney Week 2018. Abstract No. TH-OR116.