User login
Three-drug combo proves effective against multidrug-resistant UTIs
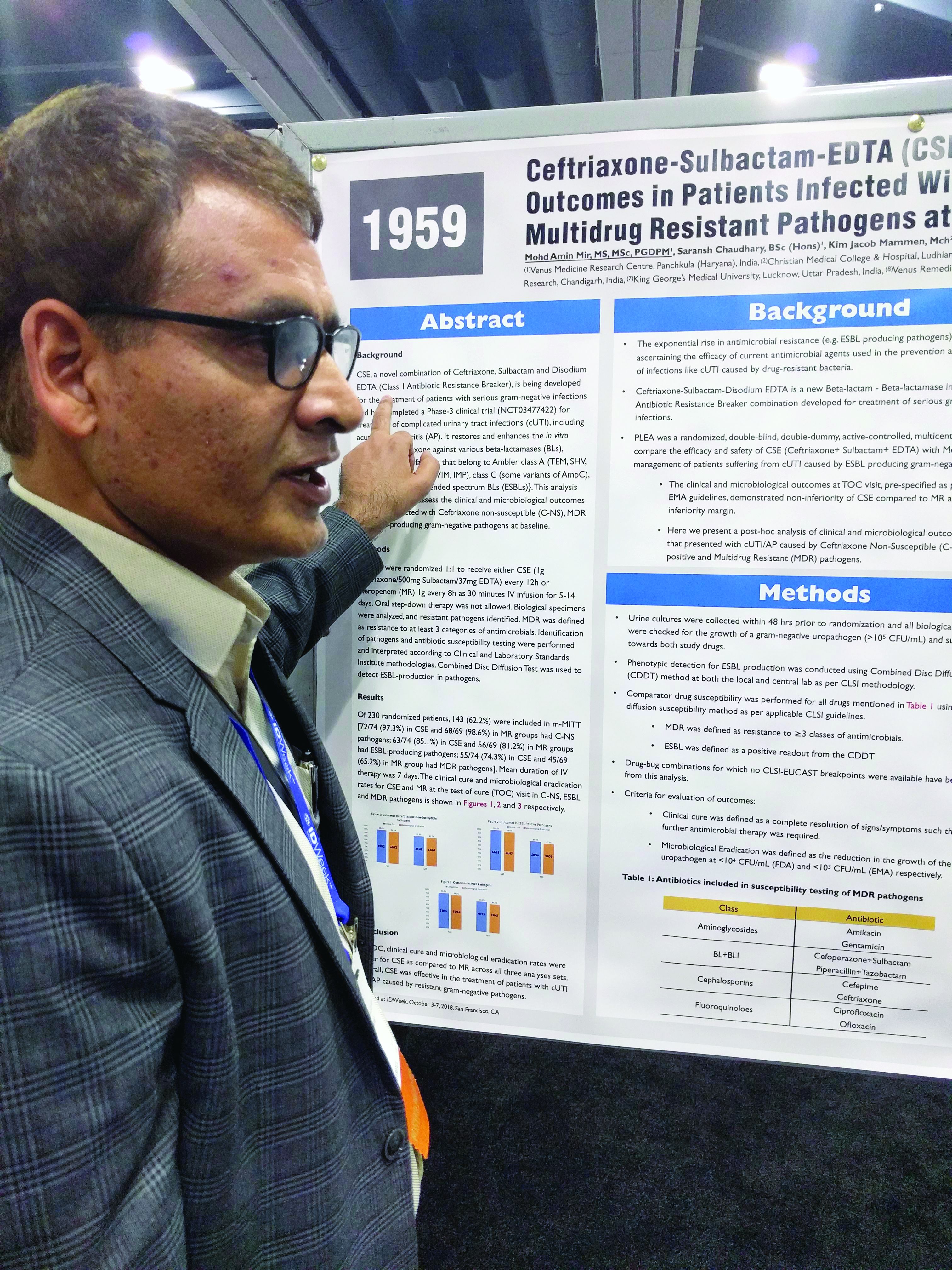
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
SAN FRANCISCO – A combination of ceftriaxone, a beta-lactamase inhibitor, and disodium ethylenediaminetetraacetic acid (EDTA) is superior to meropenem in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase (ESBL) gram-negative bacteria, according to a new study.
The post-hoc analysis also found that the three-drug combination – known as CSE – is noninferior to meropenem in multidrug-resistant (MDR) and ceftriaxone-nonsusceptible (C-NS) pathogens.
CSE is aimed at the growing problem of antibiotic resistance, particularly the mechanisms used by bacteria to counter beta-lactamase inhibitors. EDTA chelates zinc and calcium, and many of the resistance mechanisms rely on one or the other of these ions to function. In in vitro models, the combination of sulbactam and EDTA restores activity of ceftriaxone against various beta-lactamases.
Mohd Amin Mir, MD, head of clinical research at the Venus Medicine Research Center, Panchkula, India, and presenter of the study, said that, in the case of efflux pumps, “when there is EDTA present, it chelates the calcium, and that means there is no energy for the efflux pump to throw out the drug.”
The penems, which include meropenem, are a class of synthetic antibiotics with an unsaturated beta-lactam ring. Like other antibiotics, they are under assault from antibiotic resistance, especially beta-lactamase enzymes. “Penems are very precious drugs. The objective of developing [EDTA combinations] is to save the penems,” Dr. Mir said at an annual scientific meeting on infectious diseases.
The PLEA trial randomized 143 patients with complicated urinary tract infections or acute pyelonephritis to CSE (1 g ceftriaxone/500 mg sulbactam/37 mg EDTA) every 12 hours or 1 g meropenem (MR) as a 30-minute intravenous infusion over 30 minutes. Patients received treatment for 5-14 days.
The original study demonstrated that CSE is noninferior to meropenem at a 10% noninferiority margin. The researchers conducted a post-hoc analysis of patients who presented with complicated UTIs or acute pyelonephritis cases that were C-NS, ESBL-positive, or multidrug-resistant (MDR) pathogens. The researchers defined MDR as resistance to three or more categories of antimicrobial agents.
Of patients who received CSE, 97.3% had pathogens that were nonsusceptible to ceftriaxone, as did 98.6% of those who received MR; 85.1% of CSE and 81.2% of MR patients had an ESBL-producing pathogen; and 74.3% of infections in the CSE group were MDR, as were 65.2% of the MR group.
In all three resistant phenotypes, CSE at least trended to more favorable outcomes. In the MDR group, 96.4% of CSE patients achieved a clinical cure, compared with 88.9% in the MR group, and 94.5% achieved microbial eradication, compared with 86.75% in the MR group.
In the ESBL subgroup, 100% of patients in the CSE group achieved a clinical cure, compared with 89.3%, while 98.4% had complete eradication in the CSE group, compared with 87.5%. In the C-NS subgroup, 95.8% in the CSE group achieved a clinical cure, compared with 91.2%, and 94.4% achieved eradication, compared with 89.7% in the MR group.
In the ESBL subgroup, the lower bound of the 95% confidence interval of the between-group difference was greater than 0, indicating superiority of CSE over MR for both clinical cure and eradication. In the MDR and C-NS subgroups, CSE achieved noninferiority at a –10% margin.
CSE is currently commercially available in India, and the manufacturer is now seeking approval in Europe and the United States.
SOURCE: Mir MA et al. IDWeek 2018, Abstract 1959.
REPORTING FROM IDWEEK 2018
Key clinical point:
Major finding: The combination was noninferior in the context of different resistant subtypes.
Study details: Posthoc analysis of a randomized, controlled trial (n = 143).
Disclosures: The study was funded by Venus Medicine Research Center, which employs Dr. Mir.
Source: Mir MA et al. IDWeek 2018, Abstract 1959.
ACP beefs up firearms policy
The American College of Physicians supports appropriate regulations surrounding the purchase of firearms; best practices ownership, storage, and safe use to minimize the risk of accidental or intentional death or injury; and a ban on civilian use of semiautomatic weapons and large capacity magazines, according to an expanded and updated policy statement issued Oct. 29.
The updated policy statement was issued at the end of a week that saw a mass shooting at a Pittsburgh synagogue where 11 people were killed as well as an incident in which two others were shot to death in a Kentucky grocery store.
“Physicians regularly come face to face with the tragedy that gun violence brings, whether maliciously or unintentionally,” ACP President Ana María López, MD, said in a statement after the synagogue shooting. “The rate of injuries and deaths related to firearms and the growing incidence of mass shootings brings to light, once again, the glaring lack of firearm policy in the United States – a country with one of the highest rates of gun violence in the world. This most recent event makes it more important than ever that Congress and states implement common-sense policies that could prevent injuries and deaths from firearms.”
The policy statement reaffirms all policies included in the college’s 2014 policy.
New to the ACP policy is the college’s support for “appropriate regulation of the purchase of legal firearms to reduce firearms-related injuries and deaths.” ACP specifies that any policy “must be consistent with the Supreme Court ruling establishing that individual ownership of firearms is a constitutional right under the Second Amendment of the Bill of Rights.”
The expanded policy calls for universal criminal background checks for firearms purchase and completion of an educational program on firearm safety; strengthening and enforcing laws on prohibiting convicted domestic violence offenders from purchasing firearms; banning firearms that cannot be detected by metal detectors and standard security screening devices; and a reexamining of concealed carry laws. ACP also favors strong penalties and criminal prosecution for those who sell firearms illegally and for those who legally purchase firearms for the sole purpose of acting as the purchaser for someone who is not legally able to possess the firearm.
The policy also “favors enactment of legislation to ban the manufacture, sale, transfer, and subsequent ownership for civilian use of semiautomatic firearms that are designed to increase their rapid killing capacity (often called ‘assault weapons’) and large-capacity magazines, and retaining the current ban on automatic weapons for civilian use.”
As part of this, ACP is calling for a comprehensive definition of semiautomatic firearms that would be subject to the ban as well as a definition of sporting and hunting purposes that should be narrowly defined.
The policy also calls for raising of the minimum age to purchase a semiautomatic weapon to 21 years, prior to the full ban being put in place.
Finally, ACP is calling on firearm owners to “adhere to best practices to reduce the risk of accidental or intentional injuries or deaths from firearms,” including ensuring that firearms “cannot be accessed by children, adolescents, people with dementia, people with substance use disorder, and the subset of people with serious mental illness that are associated with greater risk of harming themselves and others.”
Finally, the expanded policy calls for enactment of extreme risk protection order laws, under which a family member or law enforcement officer can seek a court order to temporarily remove firearms from an individual who is at imminent risk of self-harm or to others, while preserving the individual’s due process protections.
[email protected]
SOURCE: Butkus R et al. Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-1530.
“Do you have guns in the home?”
This simple question should be asked as if it were any other question about health status and potentially unsafe behavior that doctors routinely ask.
It opens the door to further discuss firearms-related issues, especially if there is a concern regarding the patient’s mental state that could impact the health and safety of the patient or others around the individual.
James Kahn, MD, of Stanford (Calif.) University, makes this suggestion in an editorial accompanying the ACP policy statement (Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-2756).
“Do you have guns in the home?”
This simple question should be asked as if it were any other question about health status and potentially unsafe behavior that doctors routinely ask.
It opens the door to further discuss firearms-related issues, especially if there is a concern regarding the patient’s mental state that could impact the health and safety of the patient or others around the individual.
James Kahn, MD, of Stanford (Calif.) University, makes this suggestion in an editorial accompanying the ACP policy statement (Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-2756).
“Do you have guns in the home?”
This simple question should be asked as if it were any other question about health status and potentially unsafe behavior that doctors routinely ask.
It opens the door to further discuss firearms-related issues, especially if there is a concern regarding the patient’s mental state that could impact the health and safety of the patient or others around the individual.
James Kahn, MD, of Stanford (Calif.) University, makes this suggestion in an editorial accompanying the ACP policy statement (Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-2756).
The American College of Physicians supports appropriate regulations surrounding the purchase of firearms; best practices ownership, storage, and safe use to minimize the risk of accidental or intentional death or injury; and a ban on civilian use of semiautomatic weapons and large capacity magazines, according to an expanded and updated policy statement issued Oct. 29.
The updated policy statement was issued at the end of a week that saw a mass shooting at a Pittsburgh synagogue where 11 people were killed as well as an incident in which two others were shot to death in a Kentucky grocery store.
“Physicians regularly come face to face with the tragedy that gun violence brings, whether maliciously or unintentionally,” ACP President Ana María López, MD, said in a statement after the synagogue shooting. “The rate of injuries and deaths related to firearms and the growing incidence of mass shootings brings to light, once again, the glaring lack of firearm policy in the United States – a country with one of the highest rates of gun violence in the world. This most recent event makes it more important than ever that Congress and states implement common-sense policies that could prevent injuries and deaths from firearms.”
The policy statement reaffirms all policies included in the college’s 2014 policy.
New to the ACP policy is the college’s support for “appropriate regulation of the purchase of legal firearms to reduce firearms-related injuries and deaths.” ACP specifies that any policy “must be consistent with the Supreme Court ruling establishing that individual ownership of firearms is a constitutional right under the Second Amendment of the Bill of Rights.”
The expanded policy calls for universal criminal background checks for firearms purchase and completion of an educational program on firearm safety; strengthening and enforcing laws on prohibiting convicted domestic violence offenders from purchasing firearms; banning firearms that cannot be detected by metal detectors and standard security screening devices; and a reexamining of concealed carry laws. ACP also favors strong penalties and criminal prosecution for those who sell firearms illegally and for those who legally purchase firearms for the sole purpose of acting as the purchaser for someone who is not legally able to possess the firearm.
The policy also “favors enactment of legislation to ban the manufacture, sale, transfer, and subsequent ownership for civilian use of semiautomatic firearms that are designed to increase their rapid killing capacity (often called ‘assault weapons’) and large-capacity magazines, and retaining the current ban on automatic weapons for civilian use.”
As part of this, ACP is calling for a comprehensive definition of semiautomatic firearms that would be subject to the ban as well as a definition of sporting and hunting purposes that should be narrowly defined.
The policy also calls for raising of the minimum age to purchase a semiautomatic weapon to 21 years, prior to the full ban being put in place.
Finally, ACP is calling on firearm owners to “adhere to best practices to reduce the risk of accidental or intentional injuries or deaths from firearms,” including ensuring that firearms “cannot be accessed by children, adolescents, people with dementia, people with substance use disorder, and the subset of people with serious mental illness that are associated with greater risk of harming themselves and others.”
Finally, the expanded policy calls for enactment of extreme risk protection order laws, under which a family member or law enforcement officer can seek a court order to temporarily remove firearms from an individual who is at imminent risk of self-harm or to others, while preserving the individual’s due process protections.
[email protected]
SOURCE: Butkus R et al. Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-1530.
The American College of Physicians supports appropriate regulations surrounding the purchase of firearms; best practices ownership, storage, and safe use to minimize the risk of accidental or intentional death or injury; and a ban on civilian use of semiautomatic weapons and large capacity magazines, according to an expanded and updated policy statement issued Oct. 29.
The updated policy statement was issued at the end of a week that saw a mass shooting at a Pittsburgh synagogue where 11 people were killed as well as an incident in which two others were shot to death in a Kentucky grocery store.
“Physicians regularly come face to face with the tragedy that gun violence brings, whether maliciously or unintentionally,” ACP President Ana María López, MD, said in a statement after the synagogue shooting. “The rate of injuries and deaths related to firearms and the growing incidence of mass shootings brings to light, once again, the glaring lack of firearm policy in the United States – a country with one of the highest rates of gun violence in the world. This most recent event makes it more important than ever that Congress and states implement common-sense policies that could prevent injuries and deaths from firearms.”
The policy statement reaffirms all policies included in the college’s 2014 policy.
New to the ACP policy is the college’s support for “appropriate regulation of the purchase of legal firearms to reduce firearms-related injuries and deaths.” ACP specifies that any policy “must be consistent with the Supreme Court ruling establishing that individual ownership of firearms is a constitutional right under the Second Amendment of the Bill of Rights.”
The expanded policy calls for universal criminal background checks for firearms purchase and completion of an educational program on firearm safety; strengthening and enforcing laws on prohibiting convicted domestic violence offenders from purchasing firearms; banning firearms that cannot be detected by metal detectors and standard security screening devices; and a reexamining of concealed carry laws. ACP also favors strong penalties and criminal prosecution for those who sell firearms illegally and for those who legally purchase firearms for the sole purpose of acting as the purchaser for someone who is not legally able to possess the firearm.
The policy also “favors enactment of legislation to ban the manufacture, sale, transfer, and subsequent ownership for civilian use of semiautomatic firearms that are designed to increase their rapid killing capacity (often called ‘assault weapons’) and large-capacity magazines, and retaining the current ban on automatic weapons for civilian use.”
As part of this, ACP is calling for a comprehensive definition of semiautomatic firearms that would be subject to the ban as well as a definition of sporting and hunting purposes that should be narrowly defined.
The policy also calls for raising of the minimum age to purchase a semiautomatic weapon to 21 years, prior to the full ban being put in place.
Finally, ACP is calling on firearm owners to “adhere to best practices to reduce the risk of accidental or intentional injuries or deaths from firearms,” including ensuring that firearms “cannot be accessed by children, adolescents, people with dementia, people with substance use disorder, and the subset of people with serious mental illness that are associated with greater risk of harming themselves and others.”
Finally, the expanded policy calls for enactment of extreme risk protection order laws, under which a family member or law enforcement officer can seek a court order to temporarily remove firearms from an individual who is at imminent risk of self-harm or to others, while preserving the individual’s due process protections.
[email protected]
SOURCE: Butkus R et al. Ann Intern Med. 2018 Oct 29. doi: 10.7326/M18-1530.
FROM ANNALS OF INTERNAL MEDICINE
Few clinical outcomes convincingly linked to sickle cell trait
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Although sickle cell trait (SCT) has been linked to numerous adverse clinical outcomes in multiple studies, only a handful of those associations have strong supporting evidence, results of a systematic review suggest.
Venous and renal complications had the strongest evidence supporting an association with SCT, while exertion-related sudden death – perhaps the highest-profile potential complication of SCT – had moderate-strength evidence supporting a link, according to the review.
By contrast, most other associations between SCT and clinical outcomes had either low-strength evidence or insufficient data to support a link, according to Rakhi P. Naik, MD, of Johns Hopkins University, Baltimore, and coauthors of the review.
“Future rigorous studies are needed to address potential complications of SCT and to determine modifiers of risk,” they wrote. The report in the Annals of Internal Medicine.
The systematic review by Dr. Naik and colleagues focused on 41 studies, most of which were population-based cohort or case-control studies. They rated the evidence quality of each study and grouped 24 clinical outcomes of interest into six categories: exertion-related injury, renal, vascular, pediatric, surgery- and trauma-related outcomes, and mortality.
Exercise-related injury has received considerable attention, particularly in relation to the military and athletics.
The strength of evidence for a link between SCT and exertion-related death was low in their analysis, which included two studies evaluating the outcome. However, Dr. Naik and coauthors did note that SCT may be associated with a small absolute risk of exertion-related death in extreme conditions such a highly strenuous athletic training or the military.
“We do concur with the American Society of Hematology statement recommending against routine SCT screening in athletics and supporting the consistent use of universal precautions to mitigate exertion-related risk in all persons, regardless of SCT status,” they wrote.
Similarly, the absolute risk of exertional rhabdomyolysis in SCT is small and probably occurs only in high-intensity settings, with risk modified by other genetic and environmental factors, Dr. Naik and coauthors said, based on their analysis of two studies looking at this outcome.
Venous complications had a stronger body of evidence, including several studies showing high levels of procoagulants, which makes elevated venous thromboembolism risk plausible in individuals with SCT.
High-strength evidence linked pulmonary embolism, with or without deep-vein thrombosis, to SCT. In contrast, there was no increased risk of isolated deep-vein thrombosis in these individuals.
“The cause of this paradoxical observation is unknown but may be an increased risk for clot embolization in SCT,” Dr. Naik and colleagues wrote in a discussion of the results.
Renal outcomes were often attributed to SCT, and in this review, the authors said there was evidence to support SCT as a risk factor for both proteinuria and chronic kidney disease.
Out of six studies looking at proteinuria, the one high-quality study found a 1.86-fold increased risk for baseline albuminuria in African Americans with SCT versus those without, according to the review.
Out of four studies looking at chronic kidney disease, the two high-quality studies found 1.57- to 1.89-fold increased risk of those outcomes in African Americans with SCT.
Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
SOURCE: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point:
Major finding: Risks of 1.57-fold and higher were seen in high-quality studies linking SCT to venous and renal complications, while studies of moderate quality suggested small absolute risks of exertion-related mortality or rhabdomyolysis.
Study details: A systematic review including 41 mostly population-based cohort or case-control studies looking at 24 clinical outcomes of interest.
Disclosures: Support for the study came in part from the National Human Genome Research Institute and the National Heart, Lung, and Blood Institute. The authors reported disclosures related to Novartis, Addmedica, and Global Blood Therapeutics, among others.
Source: Naik RP et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1161.
Most Americans incorrectly identify homicide as more common than suicide
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
Most adults do not realize that suicide is a more frequent cause of death than homicide, according to the first nationally representative study of public perceptions of firearm and non-firearm-related violent death in the United States.
“These findings are consistent with the well-established relationship between risk perception and the ease with which a pertinent categorical example can be summoned from memory, which in most persons is probably affected by the salience of homicides in media coverage,” lead author Erin R. Morgan, MS, and her coauthors wrote in the Annals of Internal Medicine.
The coauthors reviewed 3,811 responses to a question in the National Firearms Survey on the intent and means of violent death; participants were given 4 options – homicide with a gun, homicide with a weapon other than a gun, suicide with a gun, and suicide by a method other than a gun – and asked to rank them by frequency. A study of those responses found that only 13.5% of U.S. adults could correctly identify their state’s most frequent cause of violent death. Of the 1,880 respondents who shared their occupations, only 20% of health care professionals answered the question correctly.
The survey was conducted in April 2015; between 2014 and 2015, suicide was more common than homicide in all 50 states. Suicide by firearm was also more common than homicide by firearm in every state but Illinois, Maryland, and New Jersey. When reviewing firearm options only, the percentage of respondents who identified suicide as most frequent increased to 25.9%, according to Ms. Morgan of the School of Public Health and of Harborview Injury Prevention & Research Center at the University of Washington in Seattle, and her colleagues.
The coauthors noted that accurate identification was not impacted by the respondents’ firearm ownership status, but also that future research should evaluate if promoting awareness of suicide frequency and risk might “motivate behavioral change regarding firearm storage.”
“Our findings suggest that correcting misperceptions about the relative frequency of firearm-related violent deaths may make persons more cognizant of the actuarial risks to themselves and their family, thus creating new opportunities for prevention,” they wrote.
The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
SOURCE: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Only 13.5% of U.S. adults – and 20% of health care professionals – could identify the most frequent cause of violent death in their state.
Major finding:
Study details: A study of 3,811 responses to the National Firearms Survey.
Disclosures: The study was funded by the Fund for a Safer Future and the Joyce Foundation. No conflicts of interest were reported.
Source: Morgan E et al. Ann Intern Med. 2018 Oct 30. doi:10.7326/M18-1533.
Investigational gene therapy for medically refractory Parkinson’s shows promise
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
ATLANTA – VY-AADC01, an investigational gene therapy for individuals with medically refractory Parkinson’s disease being developed by Voyager Therapeutics, was well tolerated and decreased the need for antiparkinsonian medications, results from an ongoing phase 1b study showed.
“Prior phase 1 trials also introduced the aromatic l-amino acid decarboxylase (AADC) gene using an adeno-associated virus serotype-2 (AAV2) vector into the putamen of people with Parkinson’s disease (PD),” lead study author Chad Christine, MD, said in an interview in advance of the annual meeting of the American Neurological Association. “Unlike the previous trials, here we increased both vector genome concentration and volume of the AAV2-AADC vector (VY-AADC01) across cohorts and used intraoperative MRI guidance to administer the gene product.”
According to Dr. Christine, a neurologist at the University of California, San Francisco, Parkinson’s Disease Clinic and Research Center, prior trials showed that AAV2-AADC was safe, but there was limited clinical efficacy. This may have been because of the limited volume of putamen treated with the gene therapy. “In our current trial, we admixed VY-AADC01 with gadoteridol (ProHance), an MR imaging agent, which allowed both near real-time MRI monitoring of the location and volume of product infused and postsurgical assessment of the area of the putamen covered by VY-AADC01,” he said. “In addition, we used 18F-Dopa PET, which allowed us to assess the activity of the AADC enzyme in the putamen.”
The researchers enrolled three cohorts of patients who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions. In cohort 1, five patients received up to 450 μL/putamen at a concentration of 8.3 × 1011 vg (viral genomes)/mL and were followed for 36 months. In cohort 2, five patients received up to 900 μL/putamen at 8.3 × 1011 vg/mL and were followed for 18 months. In cohort 3, five patients received up to 900 μL/putamen at 2.6 × 1012 vg/mL and were followed for 12 months.
At 12 months, Dr. Christine and his associates observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively; LED reductions were sustained to 18 months in cohorts 1 and 2. “We were impressed by how well the decrease in need for antiparkinsonian medications paralleled the AADC activity we measured in the putamen of our subjects, which is consistent with the proposed mechanism of action of VY-AADC01,” he said.
In addition, subjects in cohort 1 showed a mean 2.3-hour improvement in Parkinson’s diary-“on” time without troublesome dyskinesia at 24 months, which was maintained at 36 months, while subjects in cohort 2 showed a clinically meaningful 3.5-hour improvement at 18 months. Subjects in cohort 3 showed somewhat less improvement than the other cohorts (1.5 hours at 12 months), but they also had more severe baseline dyskinesia on the Unified Dyskinesia Rating Scale (a mean of 30.2 vs. 19.2 and 17.4 in cohorts 1 and 2, respectively). One patient in the trial experienced two surgery-related serious adverse events (pulmonary embolism and related heart arrhythmia) which resolved completely.
“I think we were somewhat surprised by some of the challenges of the surgical administration,” Dr. Christine said. “Our surgeons improved the administration technique throughout the trial and made a major transition from administering VY-AADC01 using a frontal approach to the putamen to using a posterior approach in our second phase 1 trial.”
He concluded that findings of the current trial suggest that AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated. “A number of outcomes suggest that it may offer clinical benefit to patients with advancing Parkinson’s disease, but this will have to be tested in a randomized trial which has recently started,” he said.
Dr. Christine acknowledged that the small sample size and the open-label design of the study limits the generalizability of the findings. The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
REPORTING FROM ANA 2018
Key clinical point: AAV2-AADC gene therapy, administered using intraoperative MRI guidance, appears to be safe and well tolerated.
Major finding: At 12 months, the researchers observed mean levodopa-equivalent dose (LED) reductions of –10.2%, –32.8%, and –39.3% in cohort 1, cohort 2, and cohort 3, respectively.
Study details: A study of 15 patients in three cohorts who received bilateral infusions of VY-AADC01, admixed with gadoteridol to facilitate intraoperative MRI monitoring of the infusions.
Disclosures: The trial received support from Voyager Therapeutics and the Michael J. Fox Foundation. Dr. Christine reported having no disclosures.
Source: Christine et al. ANA 2018, Abstract M300.
Many oromandibular dystonia patients report improvement after botulinum toxin injections
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
ATLANTA – A majority of oromandibular dystonia patients treated with botulinum toxin injections reported improvement in symptoms in the largest cohort of patients to date.
Improvements in the range of 50%-100% occurred in 78% of oromandibular dystonia (OMD) patients who received botulinum toxin injections in the retrospective, multicenter analysis, which was presented by Laura Scorr, MD, at the annual meeting of the American Neurological Association.
In an effort to better describe the clinical characteristics of patients with OMD, Dr. Scorr, a movement disorders specialist at Emory University, Atlanta, and her colleagues analyzed data collected from 164 OMD patients enrolled at 26 international sites in the Dystonia Coalition and 37 additional patients who were evaluated at the Emory University within the last year. Subjects enrolled at Dystonia Coalition centers underwent evaluation by a movement disorders specialist to determine distribution of dystonia, areas affected, and severity as measured by the Global Dystonia Rating Scale. A subgroup of patients also completed the SF 36-item Health Survey, the Beck Depression Scale, and the Liebowitz social anxiety scale. Meanwhile, the charts of patients seen at Emory underwent review for data on clinical characteristics, treatment type, botulinum toxin doses, and response.
Among all 201 patients, the average age of onset was 54 years and 65% were female. About 45% were determined to have focal dystonia, 36% had segmental dystonia, and 19% had generalized dystonia. Among a cohort of 47 patients evaluated in the Dystonia Coalition biorepository, the researchers observed significantly increased social anxiety and impaired quality of life on the Liebowitz social anxiety scale and the SF-36 Health Survey.
Of the 37 Emory patients, 31 (84%) received botulinum toxin injections. Of these, 39% reported symptom improvement that ranged from 75%-100% while 39% reported symptom improvement that ranged from 50%-74%. Only 13% had a minimal response, defined as improvement that ranged from 1%-24%.
“Oromandibular dystonia is particularly disabling,” Dr. Scorr said. “There have been a few reports in the literature that say it does not respond to botulinum toxin injections. But in our retrospective review, the majority of patients not only have a response, but a response that’s greater than 50% improvement, which is significant.” She acknowledged that the study’s retrospective design is a limitation. “I think we need more prospective studies, specifically on response to treatment with botulinum toxin,” she said.
The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr reported having no financial disclosures.
SOURCE: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
AT ANA 2018
Key clinical point: Oromandibular dystonia is associated with increased social anxiety and impaired quality of life.
Major finding: After receiving botulinum toxin injections, 78% of patients with oromandibular dystonia reported improvements in the range of 50%-100%.
Study details: A retrospective review of 201 patients with oromandibular dystonia.
Disclosures: The study was funded in part by the Dystonia Medical Research Foundation. Dr. Scorr researchers reported having no financial disclosures.
Source: Scorr L et al. Ann Neurol. 2018;84[S22]:S90, Abstract S216.
Kids and guns: Injury costs rose as incidence fell
Hospital costs for children with firearm-related injuries rose from 2006 to 2014, while the incidence of emergency department visits declined over the same period, according to the first national study of such visits in children.
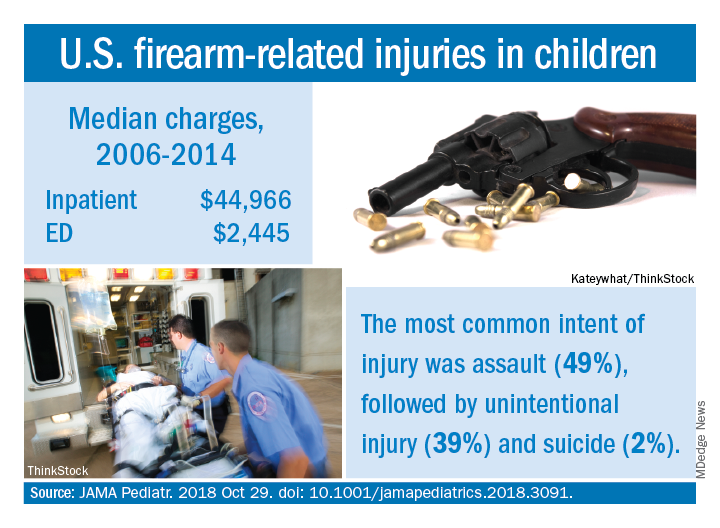
Median charges were $2,445 for an ED visit and $44,966 for inpatient management of individuals under 18 years of age for the entire study period, with both increasing over time and all data adjusted to 2018 dollars. The median charge for an ED visit rose from over $2,100 in 2006 to under $2,900 in 2014, while the inpatient median increased from approximately $43,000 to about $59,000. Total charges for firearm-related injuries in children were $2.5 billion during 2006-2014, with a mean of $270 million a year, Faiz Gani, MBBS, and Joseph K. Canner, MHS, said in JAMA Pediatrics.
The overall incidence of ED visits was 11.3/100,000 children under 18 years of age for the study period, with a steady decline seen from 2006, when incidence was about 15 visits/100,000, to 10/100,000 in 2014. The rate had dropped to about 7.5 visits/100,000 in 2013 before increasing in 2014, Dr. Gani and Mr. Canner of Johns Hopkins University, Baltimore, said based on data for 75,086 visits from the Nationwide Emergency Medicine Sample.
A trend observed throughout the course of the study was the higher incidence of ED visits among males, which was consistently more than five times higher than that of females. The highest incidence by age group was 85.9/100,000 for males aged 15-17 years. The most common intent of injury was assault at 49%, with unintentional injury next at 39% and suicide at 2%, the investigators reported.
This “first and largest nationally representative study” demonstrates the “substantial clinical and financial burden associated with firearm-related injuries among pediatric patients. Moving forward, additional resources and funds should be allocated to the study of firearm-related injuries. Only through further understanding of the social, political, and health-related risk factors for these injuries can we develop and implement effective policies to address this public health concern, wrote Dr. Gani and Mr. Canner, who reported no conflicts of interest.
SOURCE: JAMA Pediatr. 2018 Oct 29. doi: 10.1001/jamapediatrics.2018.3091.
Hospital costs for children with firearm-related injuries rose from 2006 to 2014, while the incidence of emergency department visits declined over the same period, according to the first national study of such visits in children.
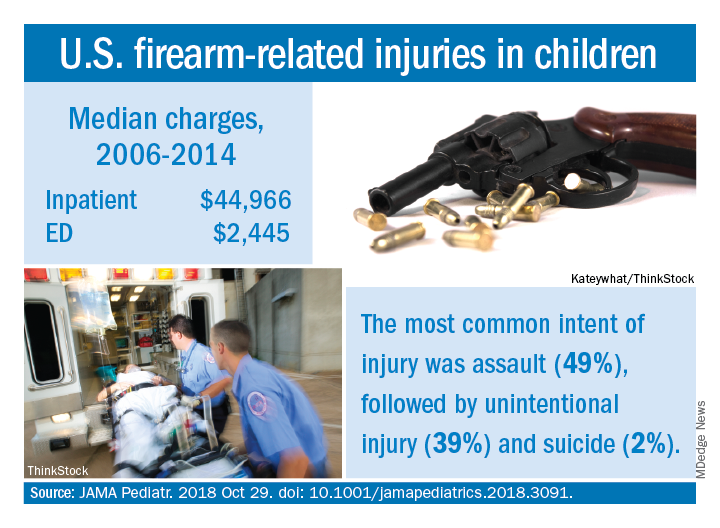
Median charges were $2,445 for an ED visit and $44,966 for inpatient management of individuals under 18 years of age for the entire study period, with both increasing over time and all data adjusted to 2018 dollars. The median charge for an ED visit rose from over $2,100 in 2006 to under $2,900 in 2014, while the inpatient median increased from approximately $43,000 to about $59,000. Total charges for firearm-related injuries in children were $2.5 billion during 2006-2014, with a mean of $270 million a year, Faiz Gani, MBBS, and Joseph K. Canner, MHS, said in JAMA Pediatrics.
The overall incidence of ED visits was 11.3/100,000 children under 18 years of age for the study period, with a steady decline seen from 2006, when incidence was about 15 visits/100,000, to 10/100,000 in 2014. The rate had dropped to about 7.5 visits/100,000 in 2013 before increasing in 2014, Dr. Gani and Mr. Canner of Johns Hopkins University, Baltimore, said based on data for 75,086 visits from the Nationwide Emergency Medicine Sample.
A trend observed throughout the course of the study was the higher incidence of ED visits among males, which was consistently more than five times higher than that of females. The highest incidence by age group was 85.9/100,000 for males aged 15-17 years. The most common intent of injury was assault at 49%, with unintentional injury next at 39% and suicide at 2%, the investigators reported.
This “first and largest nationally representative study” demonstrates the “substantial clinical and financial burden associated with firearm-related injuries among pediatric patients. Moving forward, additional resources and funds should be allocated to the study of firearm-related injuries. Only through further understanding of the social, political, and health-related risk factors for these injuries can we develop and implement effective policies to address this public health concern, wrote Dr. Gani and Mr. Canner, who reported no conflicts of interest.
SOURCE: JAMA Pediatr. 2018 Oct 29. doi: 10.1001/jamapediatrics.2018.3091.
Hospital costs for children with firearm-related injuries rose from 2006 to 2014, while the incidence of emergency department visits declined over the same period, according to the first national study of such visits in children.
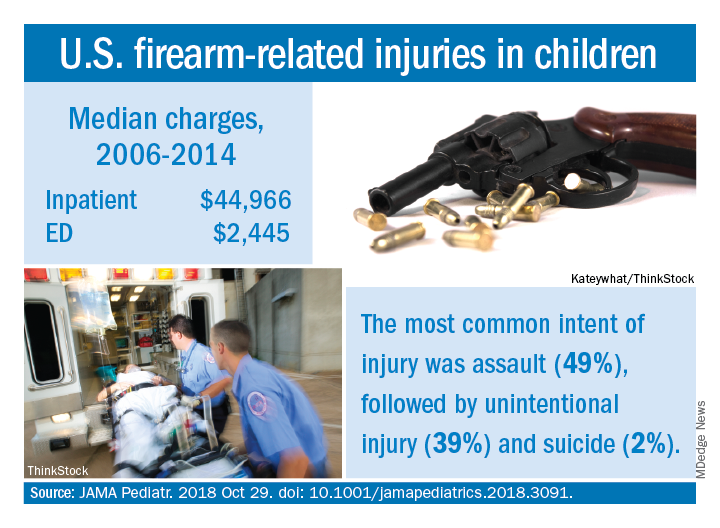
Median charges were $2,445 for an ED visit and $44,966 for inpatient management of individuals under 18 years of age for the entire study period, with both increasing over time and all data adjusted to 2018 dollars. The median charge for an ED visit rose from over $2,100 in 2006 to under $2,900 in 2014, while the inpatient median increased from approximately $43,000 to about $59,000. Total charges for firearm-related injuries in children were $2.5 billion during 2006-2014, with a mean of $270 million a year, Faiz Gani, MBBS, and Joseph K. Canner, MHS, said in JAMA Pediatrics.
The overall incidence of ED visits was 11.3/100,000 children under 18 years of age for the study period, with a steady decline seen from 2006, when incidence was about 15 visits/100,000, to 10/100,000 in 2014. The rate had dropped to about 7.5 visits/100,000 in 2013 before increasing in 2014, Dr. Gani and Mr. Canner of Johns Hopkins University, Baltimore, said based on data for 75,086 visits from the Nationwide Emergency Medicine Sample.
A trend observed throughout the course of the study was the higher incidence of ED visits among males, which was consistently more than five times higher than that of females. The highest incidence by age group was 85.9/100,000 for males aged 15-17 years. The most common intent of injury was assault at 49%, with unintentional injury next at 39% and suicide at 2%, the investigators reported.
This “first and largest nationally representative study” demonstrates the “substantial clinical and financial burden associated with firearm-related injuries among pediatric patients. Moving forward, additional resources and funds should be allocated to the study of firearm-related injuries. Only through further understanding of the social, political, and health-related risk factors for these injuries can we develop and implement effective policies to address this public health concern, wrote Dr. Gani and Mr. Canner, who reported no conflicts of interest.
SOURCE: JAMA Pediatr. 2018 Oct 29. doi: 10.1001/jamapediatrics.2018.3091.
FROM JAMA PEDIATRICS
ACIP resuscitates pertussis working group
The recent rise in pertussis rates may have peaked, but the experts are responding by reinstating a working group.
The new working group for pertussis was announced at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices. The ACIP’s new group, led by Fiona Havers, MD, of the CDC, heard data on the currently available pertussis vaccines and solicited ideas from ACIP members about what other data they would like before the February meeting.
One question on the agenda is whether the current recommendation that nonpregnant adults receive a single lifetime dose of Tdap and then tetanus-diphtheria (Td) boosters every 10 years be expanded to allow either Tdap or Td as the booster. Reasons for considering the change include possible changes in the circulating pertussis strain, improved diagnosis and reporting, and the waning of protection under the current guidelines, as well as the potential economic impact, Dr. Havers said.
This change could make booster administration easier for many physicians who do not routinely stock Td, some committee members noted. In addition, the Food and Drug Administration has approved a label change for one Tdap manufacturer to remove “single use” language.
In a study presented by David P. Greenberg, MD, associate vice president of Sanofi Pasteur, seroprotection rates to tetanus and diphtheria were similar in a comparison between groups of adults aged 18 years and older, receiving either Tdap (Adacel) or Td as a booster. “Seroprotection was greater than 99% in both groups,” he said.
Pain was the most common injection site reaction in both groups, rates of serious adverse events were similarly low (0.8% and 0.3%, respectively), and no deaths occurred in patients given either vaccine.
The postvaccination antipertussis geometric mean concentrations were noninferior in the Tdap group, compared with the Td group, Dr. Greenberg said.
A phase III open label study presented by Leonard Silverstein, MD, of GlaxoSmithKline also showed similar seroprotection rates for adults revaccinated with Tdap after an initial vaccination with either of two different Tdap vaccines.
Also at the February meeting, the committee will address whether any vaccine that contained Td should be allowed for use as tetanus prophylaxis in the setting of wound management, said Dr. Havers.
The committee members expressed interest in more information on several topics including pregnancy and pertussis, whether manufacturers could discuss vaccines in the pipeline, data on responses to multiple doses and if there is a point of diminishing returns, and whether some states are covering Tdap for adults.
The committee members had no financial conflicts to disclose.
The recent rise in pertussis rates may have peaked, but the experts are responding by reinstating a working group.
The new working group for pertussis was announced at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices. The ACIP’s new group, led by Fiona Havers, MD, of the CDC, heard data on the currently available pertussis vaccines and solicited ideas from ACIP members about what other data they would like before the February meeting.
One question on the agenda is whether the current recommendation that nonpregnant adults receive a single lifetime dose of Tdap and then tetanus-diphtheria (Td) boosters every 10 years be expanded to allow either Tdap or Td as the booster. Reasons for considering the change include possible changes in the circulating pertussis strain, improved diagnosis and reporting, and the waning of protection under the current guidelines, as well as the potential economic impact, Dr. Havers said.
This change could make booster administration easier for many physicians who do not routinely stock Td, some committee members noted. In addition, the Food and Drug Administration has approved a label change for one Tdap manufacturer to remove “single use” language.
In a study presented by David P. Greenberg, MD, associate vice president of Sanofi Pasteur, seroprotection rates to tetanus and diphtheria were similar in a comparison between groups of adults aged 18 years and older, receiving either Tdap (Adacel) or Td as a booster. “Seroprotection was greater than 99% in both groups,” he said.
Pain was the most common injection site reaction in both groups, rates of serious adverse events were similarly low (0.8% and 0.3%, respectively), and no deaths occurred in patients given either vaccine.
The postvaccination antipertussis geometric mean concentrations were noninferior in the Tdap group, compared with the Td group, Dr. Greenberg said.
A phase III open label study presented by Leonard Silverstein, MD, of GlaxoSmithKline also showed similar seroprotection rates for adults revaccinated with Tdap after an initial vaccination with either of two different Tdap vaccines.
Also at the February meeting, the committee will address whether any vaccine that contained Td should be allowed for use as tetanus prophylaxis in the setting of wound management, said Dr. Havers.
The committee members expressed interest in more information on several topics including pregnancy and pertussis, whether manufacturers could discuss vaccines in the pipeline, data on responses to multiple doses and if there is a point of diminishing returns, and whether some states are covering Tdap for adults.
The committee members had no financial conflicts to disclose.
The recent rise in pertussis rates may have peaked, but the experts are responding by reinstating a working group.
The new working group for pertussis was announced at a meeting of the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices. The ACIP’s new group, led by Fiona Havers, MD, of the CDC, heard data on the currently available pertussis vaccines and solicited ideas from ACIP members about what other data they would like before the February meeting.
One question on the agenda is whether the current recommendation that nonpregnant adults receive a single lifetime dose of Tdap and then tetanus-diphtheria (Td) boosters every 10 years be expanded to allow either Tdap or Td as the booster. Reasons for considering the change include possible changes in the circulating pertussis strain, improved diagnosis and reporting, and the waning of protection under the current guidelines, as well as the potential economic impact, Dr. Havers said.
This change could make booster administration easier for many physicians who do not routinely stock Td, some committee members noted. In addition, the Food and Drug Administration has approved a label change for one Tdap manufacturer to remove “single use” language.
In a study presented by David P. Greenberg, MD, associate vice president of Sanofi Pasteur, seroprotection rates to tetanus and diphtheria were similar in a comparison between groups of adults aged 18 years and older, receiving either Tdap (Adacel) or Td as a booster. “Seroprotection was greater than 99% in both groups,” he said.
Pain was the most common injection site reaction in both groups, rates of serious adverse events were similarly low (0.8% and 0.3%, respectively), and no deaths occurred in patients given either vaccine.
The postvaccination antipertussis geometric mean concentrations were noninferior in the Tdap group, compared with the Td group, Dr. Greenberg said.
A phase III open label study presented by Leonard Silverstein, MD, of GlaxoSmithKline also showed similar seroprotection rates for adults revaccinated with Tdap after an initial vaccination with either of two different Tdap vaccines.
Also at the February meeting, the committee will address whether any vaccine that contained Td should be allowed for use as tetanus prophylaxis in the setting of wound management, said Dr. Havers.
The committee members expressed interest in more information on several topics including pregnancy and pertussis, whether manufacturers could discuss vaccines in the pipeline, data on responses to multiple doses and if there is a point of diminishing returns, and whether some states are covering Tdap for adults.
The committee members had no financial conflicts to disclose.
AT AN ACIP MEETING
Geniculate Artery Injury During Primary Total Knee Arthroplasty
ABSTRACT
Major arterial injury associated with total knee arthroplasty (TKA) is a rare and potentially devastating complication. However, the rate of injury to smaller periarticular vessels and the clinical significance of such an injury have not been well investigated. The purpose of this study is to describe the rate and outcomes of geniculate artery (GA) injury, the time at which injury occurs, and any associations with tourniquet use.
From November 2015 to February 2016, 3 surgeons at a single institution performed 100 consecutive primary TKAs and documented the presence or absence and the timing of GA injury. The data were then retrospectively reviewed. All TKAs had no prior surgery on the operative extremity. Other variables collected included tourniquet use, tranexamic acid (TXA) administration, intraoperative blood loss, postoperative drain output, and blood transfusion.
The overall rate of GA injury was 38%, with lateral inferior and middle GA injury in 31% and 15% of TKAs, respectively. Most of the injuries were visualized during bone cuts or meniscectomy. The rate of overall or isolated GA injury was not significantly different (P > .05) with either use of intravenous (84 patients) or topical (14 patients) TXA administration. Comparing selective tourniquet use (only during cementation) vs routine use showed no differences in GA injury rate (P = .37), blood loss (P = .07), or drain output (P = .46).
There is a relatively high rate of GA injury, with injury to the lateral GA occurring more often than the middle GA. Routine or selective tourniquet use does not affect the rate of injury.
Continue to: Major arterial injury...
Major arterial injury associated with total knee arthroplasty (TKA) is a rare and potentially devastating complication. The majority of literature in this context consists of case reports, small case series, and large retrospective studies that have examined the type, location, and mechanism of injury present in these cases.1-13 Reported arterial injuries include occlusion, laceration, aneurysm, pseudoaneurysm, and arteriovenous fistula formation in the femoral (believed to be due to the tourniquet around the proximal thigh) and popliteal arteries causing combinations of ischemia and hemorrhage necessitating treatment ranging from endovascular arterial intervention to amputation.4,5,9-11,13-17 In addition, several studies have asserted that the risk of major arterial injury may be increased with tourniquet use, suggesting that tourniquet use should be minimized for routine primary TKAs.3,6
There are very few cases in the literature specifically addressing injury to the more commonly encountered geniculate arteries (GAs). The medial GAs are typically visualized and coagulated during the standard medial parapatellar approach. In addition, if performed, a lateral release can damage the lateral superior and inferior GAs and the middle GA can be cut with posterior cruciate ligament resection. However, the middle and lateral inferior GAs are anecdotally the most difficult to detect and treat intraoperatively, especially after implantation of TKA and deflation of the tourniquet. The potential lack of recognition of such GA injury can result in harmful sequelae, including ischemia of the patella, hemorrhage, and painful pseudoaneurysms.2,18-29 Currently, there are only 2 case reports of lateral inferior GA injury, 2 cases of medial inferior GA injury, and no reports of middle GA injury.2,23,24,29
The rate, the timing within surgery, the risk factors, including tourniquet use, and the clinical effects of GA injury are largely unknown. If these factors were better understood, prophylactic measures and/or awareness could be better applied to prevent adverse outcomes, especially in cases of the middle and lateral inferior GAs. The aims of this study are to elucidate the rate and timing of middle and lateral inferior GA injury during primary TKA; determine the factors related to injury, including intraoperative blood loss, postoperative drain output, and tranexamic (TXA) acid use; and investigate any differences in the rate of injury with and without the use of a tourniquet.
MATERIALS AND METHODS
PATIENT DEMOGRAPHICS AND SURGICAL TECHNIQUE
From November 2015 to February 2016, 3 surgeons (MJT, TMM, and RTT) at a single institution performed 100 consecutive unilateral primary TKAs and documented the presence or absence and the timing of GA injury. After obtaining approval from our Institutional Review Board, a retrospective study was performed to investigate the prospectively recorded rate of middle and lateral inferior GA injuries occurring during primary TKAs. Patients with a diagnosis of isolated osteoarthritis were included, and those with any previous surgery on the operative knee were excluded. The average age of patients at the time of surgery was 67 years (range, 25-91 years), the average body mass index was 33 kg/m2 (range, 18-54 kg/m2), and there were 63 (63%) female patients.
All TKAs were performed through a medial parapatellar approach with a posterior-stabilized, cemented design, and each patient received a postoperative surgical drain. One of the 3 lead surgeons (TMM) in this study used a tourniquet from the time of incision until the completion of cementation, and the other 2 (MJT and RTT) predominantly used the tourniquet only during cementation. To elucidate any differences in GA injury between these 2 methods of tourniquet use, the patients were categorized into 2 groups base d on tourniquet use. Group 1 included patients in whom a tourniquet was used to maintain a bloodless surgical field from the time of incision until the completion of cementation, and Group 2 included patients in whom tourniquet use was more selective (ie, applied only during cementation). Group 1 comprised 31% (31/100) of patients, while Group 2 comprised 67% (67/100) of patients; no tourniquet was used in 2% (2/100) of cases. In addition, TXA was used in 98% (98/100) of patients: 84 patients received intravenous (IV) and 14 received topical TXA administration.
Continue to: ANALYSIS OF GENICULATE ARTERY INJURY
ANALYSIS OF GENICULATE ARTERY INJURY
The senior authors critically evaluated the GA during the primary TKAs and documented the presence or absence of injury in the operative reports. GA injury was reported if there was intraoperative visualization of pulsatile bleeding or visualization of arterial lumen in the anatomic areas of the middle and lateral inferior GAs. At 3 separate occasions during the operation, the surgeon looked specifically for pulsatile bleeding or arterial lumen in the areas of the middle and lateral inferior GAs, including after all the femoral and tibial bone cuts were completed, immediately before preparing to cement (before the tourniquet was inflated if there was not one inflated from the start of the procedure), and immediately after the tourniquet was deflated (Figure 1). All bleeding GAs that were visualized were effectively coagulated by cautery. Details regarding the use of TXA (topical or IV), intraoperative blood loss, postsurgical drain output for 24 hours after surgery, and blood transfusion were collected from the patients’ medical records (Table 1).
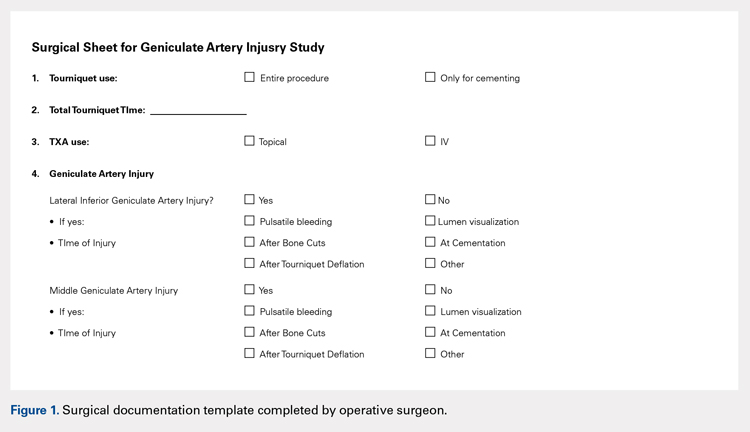
| Table 1. Operative Variables | |
Variable | Value |
Total number | 100 (100%) |
Intraoperative blood loss (mL) | 160 (25-500) |
Drain output 1st 24 hours (mL) | 488 (75-1980) |
Total output (mL) | 618 (75-2130) |
Use of TXA | 98 (98%) |
Topical TXA | 84 (84%) |
IV TXA | 14 (14%) |
Tourniquet entire procedure | 31 (31%) |
Operative variables other than geniculate artery injury. Data presented as mean (range) or n (%). TXA = tranexamic acid.
STATISTICAL METHODS
Statistical analysis was performed using the JMP software version 10.0.0 (SAS Institute, Inc). The overall rate of GA injury was determined, including the rates of GA injury based on location, time point, and method of diagnosis (pulsatile bleeding or arterial lumen visualization). If >1 GA injury occurred in the same knee, only 1 GA injury was calculated for the overall rate; however, each injury was specified separately when calculating the injury rate for the specific GA. Intraoperative blood loss, postoperative drain output, and the use of TXA were compared between cases in which a GA injury was detected and those in which it was not detected. Before conducting the retrospective review, a power analysis determined that we would require 100 patients to detect a difference in GA injury between Groups 1 and 2 (33 in Group 1 and 67 in Group 2), assuming a 30% rate in Group 1 and a 5% rate of GA injury in Group 2 using Fisher’s exact test. The Fisher’s exact test was used to compare categorical variables, and the Wilcoxon rank sum test was used to compare continuous variables. An alpha value of .05 was considered as statistically significant.
RESULTS
RATE OF GENICULATE ARTERY INJURY
The overall rate of any GA injury was 38% (38/100). Lateral inferior GA injury was more frequently detected than middle GA injury (31% vs 15% of TKAs, respectively; Table 2). Among the 31 lateral inferior GA injuries, 14 were identified as pulsatile bleeding, 7 as lumen visualizations, and 6 as both pulsatile bleeding and lumen visualization; 4 were detected by methods not recorded in the operative report. Of the lateral inferior GA injuries, 11 were identified after the bone cuts, 7 during meniscus removal, 3 during exposure, 1 after tourniquet deflation, and 9 at a time not recorded in the operative report. Of the 15 middle GA injuries, 9 were identified as pulsatile bleeding, 2 as lumen visualizations, and 4 as both pulsatile bleeding and lumen visualization. In addition, 7 of these GA injuries were identified after the bone cuts, 3 during cruciate removal, 1 after meniscus removal, 1 during exposure, and 3 at a time not recorded in the operative report (Table 3).
| Table 2. Rates of Geniculate Artery Injury Based on Location and Method | ||||
Location | Pulsatile Bleeding | Arterial Lumen | Both | Overall Rate |
Lateral inferior GA | 14 (14%) | 7 (7%) | 6 (6%) | 31 (31%) |
Middle GA | 9 (9%) | 2 (2%) | 4 (4%) | 15 (15%) |
Rates of geniculate artery injury based on location and method of diagnosis. Data presented as n (%). There were 4 additional lateral inferior and 9 middle GA injuries identified by a method not specified in the operative report. GA = geniculate artery.
Table 3. Rates of Geniculate Artery Injury Based on Time Point | ||
Time | Lateral Inferior GA | Middle GA |
After bone cuts | 11 (11%) | 7 (7%) |
During meniscus removal | 7 (7%) | 1 (1%) |
During exposure | 3 (3%) | 1 (1%) |
After tourniquet deflation | 1 (1%) | 0 (0%) |
During cruciate removal | 0 (0%) | 3 (3%) |
Not reported | 9 (9%) | 3 (3%) |
Rates of geniculate artery injury based on time point and method of diagnosis. GA = geniculate artery. Data presented as n (%).
FACTORS ASSOCIATED WITH GENICULATE ARTERY INJURY
Mean intraoperative estimated blood loss was 186 mL (standard deviation [SD], 111; range 50–500 mL) in those with a GA injury versus 147 mL (range, 82.25–400 mL) in those without injury (P = .14). Postoperative drain output in the 24 hours after surgery was 467 mL (SD 253, range 100–1105 mL) versus 502 mL (SD 378, range 75–1980 mL) in TKAs with and without GA injury, respectively (P = .82). Total estimated blood loss (combined intraoperative blood loss and 24-hour postoperative drain output) was 613 mL (SD 252, range 150–1105 mL) in TKAs with GA injury versus 620 mL (SD 393, range 75–2130 mL) without injury (P = .44) (Table 4). Overall, there was no statistical difference in blood loss, drain output, or combined output when analyzed according to lateral inferior or middle GA injury (P = .24–.82) (Table 5 and Table 6). No patients required blood transfusion postoperatively after TKA.
| Table 4. Factors Associated with GA Injury | |||
Outcome | GA Injury | No GA Injury | P Value |
Blood loss (mL) | 186 (50-500) | 147 (25-400) | .1366 |
24-Hour drain output (mL) | 467 (100-1105) | 502 (75-1980) | .8240 |
Total output (mL) | 613 (150-1105) | 620 (75-2130) | .4368 |
Differences in outcomes based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery.
| Table 5. Factors Associated with LIGA Injury | |||
Outcome | LIGA Injury | No LIGA Injury | P Value |
Blood loss (mL) | 178 (50-400) | 153 (25-500) | .2401 |
24-Hour drain output (mL) | 461 (100-890) | 501 (75-1980) | .8187 |
Total output (mL) | 610 (150-1080) | 621 (75-2130) | .4165 |
Differences in outcomes based on presence or absence of LIGA injury. Note that there were no significant differences. Values are reported as average (range). LIGA = lateral inferior geniculate artery.
| Table 6. Factors Associated with MGA Injury | |||
Outcome | MGA Injury | No MGA Injury | P Value |
Blood loss (mL) | 190 (75-500) | 156 (25-400) | .6225 |
24-Hour drain output (mL) | 455 (125-1105) | 494 (75-1980) | .6428 |
Total output (mL) | 582 (200-1105) | 624 (75-2130) | .6535 |
Differences in outcomes based on presence or absence of MGA injury. Note that there were no significant differences. Values are reported as average (range). MGA = middle geniculate artery.
IV administration of TXA was associated with a 37% (31/84) rate of GA injury, whereas topical TXA administration was associated with a 43% (6/14) rate of GA injury (P = .77). The rate of overall or isolated GA injury was not significantly different (P = .35–1.0) between IV and topical TXA administration (Table 7). In addition, total combined output was not significantly different (P = .1032) when comparing GA injury and noninjury in the subgroup analysis based on TXA use (IV or topical); however, topical administration was associated with lower intraoperative blood loss than IV administration (P = .0489), whereas IV administration was associated with lower 24-hour postoperative drain output than topical administration (P = .0169). There was no difference in blood loss, 24-hour drain output, or total output between those who did and did not sustain a GA injury in the group of patients who received IV TXA administration (Table 8, P = .2118–.7091). The same was true for those receiving topical TXA administration (Table 9, P = .0912–.9485).
Table 7. Factors Associated with TXA Injury | |||
Outcome | IV TXA (n = 84) | Topical TXA (n = 14) | P Value |
Any GA injury | 31 (37%) | 6 (43%) | .7683 |
LIGA injury | 24 (29%) | 6 (43%) | .3498 |
MGA injury | 13 (15%) | 2 (14%) | 1.0 |
Blood loss (mL) | 170 (25-500) | 113 (40-240) | .0489* |
24-Hour drain output (mL) | 454 (75-1980) | 662 (75-1800) | .0169* |
Total output (mL) | 592 (75-2130) | 751 (75-2130) | .1032 |
Differences in outcomes based on presence or absence of MGA injury. Note that there were no significant differences. Values are reported as n (%) or average (range). TXA = tranexamic acid, GA = geniculate artery, LIGA = lateral inferior geniculate artery, MGA = middle geniculate artery. *denotes statistical significance (P < .05).
| Table 8. Factors Associated with GA Injury Given IV TXA Use | ||||
Outcome | GA Injury | No GA Injury | Difference | P Value |
Blood loss (mL) | 195 (50-500) | 157 (25-400) | 38 | .2118 |
24-Hour drain output (mL) | 436 (100-1105) | 464 (75-1980) | 28 | .7091 |
Total output (mL) | 594 (150-1105) | 592 (75-2130) | 2 | .6982 |
Differences in outcomes of those patients who received IV TXA based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery, TXA = tranexamic acid.
| Table 9. Factors Associated with GA Injury Given Topical TXA Use | ||||
Outcome | GA Injury | No GA Injury | Difference | P Value |
Blood loss (mL) | 163 (100-250) | 84 (40-150) | 79 | .0912 |
24-Hour drain output (mL) | 610 (205-890) | 701 (415-1800) | 91 | .9485 |
Total output (mL) | 719 (405-960) | 775 (455-1900) | 56 | .6982 |
Differences in outcomes based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery.
Continue to: TOURNIQUET USE
TOURNIQUET USE
Comparison between Groups 1 (tourniquet use) and 2 (selective tourniquet use) revealed similar rates of overall and specific GA injury, intraoperative blood loss, and 24-hour postoperative drain output (Table 10). Group 1 demonstrated a 29% (9/31) rate of any GA injury versus 40% (27/67) in Group 2 (P = .37). For the specific lateral inferior GA injury, there was an equivalent rate of injury at 29% (9/31 in Group 1, 20/67 in Group 2; P = 1.0). Similarly, Group 1 patients had a 10% (3/31) rate of middle GA injury compared to 16% (11/67) in Group 2 patients (P = .53). Intraoperative estimated blood loss was lower in Group 1 (140 mL; range 25–400 mL) than in Group 2 (171 mL; range 40–500 mL) (P = .07), whereas the average 24-hour postoperative drain output was similar for Groups 1 (484 mL; range 75–1800 mL) and 2 (488 mL; range 100–1980 mL) (P = .46). Total estimated output was slightly less for Group 1 (593 mL; range 75–1900 mL) than for Group 2 (626 mL; range 125–2130 mL) (P = .38). A post hoc power analysis showed that with these rates of GA injury in Groups 1 and 2 and given a 2:1 ratio of the number of patients in Group 2 versus Group 1, a total of 185 patients in Group 1 and 370 patients in Group 2 would be needed to detect a statistically significant difference (P < .05) with a power of 80%.
| Table 10. Factors Associated with Tourniquet Use | ||||
Injury | Group 1 (n = 31) | Group 2 (n = 67) | Difference | P Value |
Overall GA injury | 9 (29%) | 27 (40%) | 11% | .3687 |
Lateral inferior GA | 9 (29%) | 20 (29%) | 0% | 1.0 |
Middle GA | 3 (10%) | 11 (16%) | 6% | .5382 |
Blood loss (mL) | 140 (25-400) | 171 (40-500) | 31 | .0661 |
24-Hour drain output (mL) | 484 (75-1800) | 488 (100-1980) | 4 | .4580 |
Total output (mL) | 593 (75-1900) | 626 (125-2130) | 33 | .3776 |
Differences in outcomes separated based on use of a tourniquet for the entire case (Group 1) vs use of a tourniquet only during cementation (Group 2). Note that there were no significant differences. Values are reported as n (%) or average (range). GA = geniculate artery.
DISCUSSION
Major arterial injury associated with TKA is a well-known, rare, and potentially devastating complication.1-13 However, the rate of injury to smaller periarticular vessels and the clinical significance of such injury have not been studied. The present study found a high rate of GA injury but no clinically significant difference in intraoperative blood loss or postoperative drain output between patients with GA injury (which was identified and managed with cautery) and those without GA injury. In addition, tourniquet use did not affect the rate of injury or the associated blood loss. To our knowledge, this is the first study that has critically evaluated the rate of GA injury occurring during TKA.
The overall rate of GA injury occurring during primary TKA was 38% with a higher predominance of lateral inferior than middle GA injury (31% vs 15%). Anatomically, it would follow that the lateral GA could be injured at a higher rate as it courses on top of the lateral meniscus, thus being susceptible to injury during cutting of the tibial plateau and meniscectomy. In addition, because the meniscectomy is performed longitudinally along the course of the artery, it may also be potentially lacerated in multiple locations and lengthwise. In theory, there should be a 100% rate of middle GA injury during posterior-stabilized TKA as this artery runs through the cruciate ligaments, which are resected during these cases. However, vessel injury was defined in this study as the visualization of pulsatile bleeding or vessel lumen. It is probable that in the cases in which injury to the middle GA was not visualized, it was cut but simultaneously cauterized. Thus, a lower rate (15%) of injury was detected. Nonetheless, these results still suggest that these periarticular arteries are injured at a higher rate; therefore, it is important for surgeons to specifically identify these injuries intraoperatively and adequately cauterize these vessels. As long as these arteries are cauterized, additional blood loss and potential vascular pseudoaneurysms should be prevented.
The effect of GA injury on intraoperative blood loss, 24-hour postoperative drain output, and total estimated blood loss showed no significant clinical findings in the present study cohort. In addition, examining the injury rate and blood loss based on TXA use also revealed no detrimental clinical associations. Although GA injury could inherently be associated with higher levels of blood loss and drain output, it is important to note that all GA injuries were also effectively coagulated, thus explaining the indifferent results. Accordingly, it should be recommended to surgeons performing primary TKAs to carefully evaluate for GA injury to prevent excessive blood loss or painful pseudoaneurysms. However, there is also a potential for beta error in this study in which a true difference did exist but no statistical difference was found due to the study being underpowered.
Full or selective tourniquet use during TKA did not appear to have any effect on the rate of GA injury, intraoperative blood loss, or 24-hour postoperative drain output. The similarity between GA injury rates perhaps further indicates an equivalent ability to detect these injuries between these two methods because of operative inspection for such injuries. With regard to intraoperative blood loss and drain output, the present findings are similar to previous studies demonstrating equivocal results despite variable tourniquet utilization in TKA.15,30 However, these results differ from those of Harvey and colleagues31, who demonstrated that blood loss inversely correlated with intraoperative tourniquet time. There are risks and benefits related to the use of both full and selective tourniquet methods, but either method does not appear to be advantageous in decreasing the rate of GA injury.
Continue to: Although this is the first study...
Although this is the first study to investigate the rates of GA injury and the potential clinical effects, there are limitations to this research. First, the study was retrospective in nature despite the fact that the data were collected prospectively. Only acute perioperative follow-up was performed, and thus, we were unable to evaluate longer term effects of GA injury on TKA outcomes. Furthermore, this study is potentially prone to beta error. As discussed above, 185 patients in Group 1 and 370 patients in Group 2 would be needed to detect a statistical difference in the rate of GA injury based on the rates found in this study. This study could also have been underpowered to identify differences in other aspects, such as differences in blood loss and drain. Furthermore, the data collected regarding intraoperative blood loss are estimated data and can be variable. Finally, visualization of vessel lumen and pulsatile bleeding is not a validated method to diagnose GA injuries, and potential injuries may have been missed. Despite such disadvantages, the strengths of this study include the concise results in consecutive patients, the generalizability of the data as multiple surgeons participated, and its first report of nonmajor periarticular artery injury.
CONCLUSIONS
There is a relatively high rate of GA injury, with injury to the lateral GA being visualized more often than injury to the middle GA. The majority of GA injuries occur around the time of bone cuts and meniscectomy, and tourniquet use does not affect the rate of injury. To reduce intraoperative blood loss and postoperative drain output, surgeons should identify and coagulate GA injuries routinely during primary TKA.
1. Calligaro KD, Dougherty MJ, Ryan S, Booth RE. Acute arterial complications associated with total hip and knee arthroplasty. J Vasc Surg. 2003;38(6):1170-1177. doi: 10.1016/S0741-5214(03)00918-2.
2. Dennis DA, Neumann RD, Toma P, Rosenberg G, Mallory TH. Arteriovenous fistula with false aneurysm of the inferior medial geniculate artery. A complication of total knee arthroplasty. Clin Orthop Relat Res. 1987(222):255-260.
3. Hagan PF, Kaufman EE. Vascular complication of knee arthroplasty under tourniquet. A case report. Clin Orthop Relat Res. 1990(257):159-161.
4. Holmberg A, Milbrink J, Bergqvist D. Arterial complications after knee arthroplasty: 4 cases and a review of the literature. Acta Orthop Scand. 1996;67(1):75-78. doi: 10.3109/17453679608995616.
5. Hozack WJ, Cole PA, Gardner R, Corces A. Popliteal aneurysm after total knee arthroplasty. Case reports and review of the literature. J Arthroplasty. 1990;5(4):301-305. doi: 10.1016/S0883-5403(08)80087-3.
6. Jeyaseelan S, Stevenson TM, Pfitzner J. Tourniquet failure and arterial calcification. Case report and theoretical dangers. Anaesthesia. 1981;36(1):48-50. doi: 10.1111/j.1365-2044.1981.tb08599.x
7. Mureebe L, Gahtan V, Kahn MB, Kerstein MD, Roberts AB. Popliteal artery injury after total knee arthroplasty. Am Surg. 1996;62(5):366-368.
8. O'Connor JV, Stocks G, Crabtree JD, Jr., Galasso P, Wallsh E. Popliteal pseudoaneurysm following total knee arthroplasty. J Arthroplasty. 1998;13(7):830-832. doi: 10.1016/S0883-5403(98)90039-0.
9. Ohira T, Fujimoto T, Taniwaki K. Acute popliteal artery occlusion after total knee arthroplasty. Arch Orthop Trauma Surg. 1997;116(6-7):429-430. doi: 10.1007/BF00434007.
10. Parfenchuck TA, Young TR. Intraoperative arterial occlusion in total joint arthroplasty. J Arthroplasty. 1994;9(2):217-220. doi: 10.1016/0883-5403(94)90071-X.
11. Rush JH, Vidovich JD, Johnson MA. Arterial complications of total knee replacement. The Australian experience. J Bone Joint Surg Br. 1987;69(3):400-402. doi: 10.1302/0301-620X.69B3.3584193.
12. Smith DE, McGraw RW, Taylor DC, Masri BA. Arterial complications and total knee arthroplasty. J Am Acad Orthop Surg. 2001;9(4):253-257.
13. Zahrani HA, Cuschieri RJ. Vascular complications after total knee replacement. J Cardiovasc Surg (Torino). 1989;30(6):951-952.
14. Isiklar ZU, Landon GC, Tullos HS. Amputation after failed total knee arthroplasty. Clin Orthop Relat Res. 1994(299):173-178.
15. Wakankar HM, Nicholl JE, Koka R, D'Arcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 1999;81(1):30-33. doi: 10.1302/0301-620X.81B1.0810030.
16. Kumar SN, Chapman JA, Rawlins I. Vascular injuries in total knee arthroplasty. A review of the problem with special reference to the possible effects of the tourniquet. J Arthroplasty. 1998;13(2):211-216. doi: 10.1016/S0883-5403(98)90102-4.
17. DeLaurentis DA, Levitsky KA, Booth RE, et al. Arterial and ischemic aspects of total knee arthroplasty. Am J Surg. 1992;164(3):237-240. doi: 10.1016/S0002-9610(05)81078-5.
18. Langkamer VG. Local vascular complications after knee replacement: a review with illustrative case reports. Knee. 2001;8(4):259-264. doi: 10.1016/S0968-0160(01)00103-X.
19. Moran M, Hodgkinson J, Tait W. False aneurysm of the superior lateral geniculate artery following Total Knee Replacement. Knee. 2002;9(4):349-351. doi: 10.1016/S0968-0160(02)00061-3.
20. Pritsch T, Parnes N, Menachem A. A bleeding pseudoaneurysm of the lateral genicular artery after total knee arthroplasty--a case report. Acta Orthop. 2005;76(1):138-140. doi: 10.1080/00016470510030463.
21. Gaheer RS, Chirputkar K, Sarungi M. Spontaneous resolution of superior medial geniculate artery pseudoaneurysm following total knee arthroplasty. Knee. 2014;21(2):586-588. doi: 10.1016/j.knee.2012.10.021.
22. Law KY, Cheung KW, Chiu KH, Antonio GE. Pseudoaneurysm of the geniculate artery following total knee arthroplasty: a report of two cases. J Orthop Surg (Hong Kong). 2007;15(3):386-389. /doi: 10.1177/230949900701500331.
23. Noorpuri BS, Maxwell-Armstrong CA, Lamerton AJ. Pseudo-aneurysm of a geniculate collateral artery complicating total knee replacement. Eur J Vasc Endovasc Surg. 1999;18(6):534-535.
24. Pai VS. Traumatic aneurysm of the inferior lateral geniculate artery after total knee replacement. J Arthroplasty. 1999;14(5):633-634. doi: 10.1016/S0883-5403(99)90089-X.
25. Julien TP, Gravereaux E, Martin S. Superior medial geniculate artery pseudoaneurysm after primary total knee arthroplasty. J Arthroplasty. 2012;27(2):323 e313-326. doi: 10.1016/j.arth.2011.02.009.
26. Kalsi PS, Carrington RJ, Skinner JS. Therapeutic embolization for the treatment of recurrent hemarthrosis after total knee arthroplasty due to an arteriovenous fistula. J Arthroplasty. 2007;22(8):1223-1225. /doi: 10.1016/j.arth.2006.11.012.
27. Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB. Patellofemoral complications following total knee arthroplasty. Effect of a lateral release and sacrifice of the superior lateral geniculate artery. J Arthroplasty. 1996;11(4):368-372. doi: 10.1016/S0883-5403(96)80024-6.
28. Aldrich D, Anschuetz R, LoPresti C, Fumich M, Pitluk H, O'Brien W. Pseudoaneurysm complicating knee arthroscopy. Arthroscopy. 1995;11(2):229-230. doi: 10.1016/0749-8063(95)90073-X.
29. Sharma H, Singh GK, Cavanagh SP, Kay D. Pseudoaneurysm of the inferior medial geniculate artery following primary total knee arthroplasty: delayed presentation with recurrent haemorrhagic episodes. Knee Surg Sports Traumatol Arthrosc. 2006;14(2):153-155. doi: 10.1007/s00167-005-0639-4.
30. Abdel-Salam A, Eyres KS. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J Bone Joint Surg Br. 1995;77(2):250-253. doi: 10.1302/0301-620X.77B2.7706340.
31. Harvey EJ, Leclerc J, Brooks CE, Burke DL. Effect of tourniquet use on blood loss and incidence of deep vein thrombosis in total knee arthroplasty. J Arthroplasty. 1997;12(3):291-296. doi: 10.1016/S0883-5403(97)90025-5.
ABSTRACT
Major arterial injury associated with total knee arthroplasty (TKA) is a rare and potentially devastating complication. However, the rate of injury to smaller periarticular vessels and the clinical significance of such an injury have not been well investigated. The purpose of this study is to describe the rate and outcomes of geniculate artery (GA) injury, the time at which injury occurs, and any associations with tourniquet use.
From November 2015 to February 2016, 3 surgeons at a single institution performed 100 consecutive primary TKAs and documented the presence or absence and the timing of GA injury. The data were then retrospectively reviewed. All TKAs had no prior surgery on the operative extremity. Other variables collected included tourniquet use, tranexamic acid (TXA) administration, intraoperative blood loss, postoperative drain output, and blood transfusion.
The overall rate of GA injury was 38%, with lateral inferior and middle GA injury in 31% and 15% of TKAs, respectively. Most of the injuries were visualized during bone cuts or meniscectomy. The rate of overall or isolated GA injury was not significantly different (P > .05) with either use of intravenous (84 patients) or topical (14 patients) TXA administration. Comparing selective tourniquet use (only during cementation) vs routine use showed no differences in GA injury rate (P = .37), blood loss (P = .07), or drain output (P = .46).
There is a relatively high rate of GA injury, with injury to the lateral GA occurring more often than the middle GA. Routine or selective tourniquet use does not affect the rate of injury.
Continue to: Major arterial injury...
Major arterial injury associated with total knee arthroplasty (TKA) is a rare and potentially devastating complication. The majority of literature in this context consists of case reports, small case series, and large retrospective studies that have examined the type, location, and mechanism of injury present in these cases.1-13 Reported arterial injuries include occlusion, laceration, aneurysm, pseudoaneurysm, and arteriovenous fistula formation in the femoral (believed to be due to the tourniquet around the proximal thigh) and popliteal arteries causing combinations of ischemia and hemorrhage necessitating treatment ranging from endovascular arterial intervention to amputation.4,5,9-11,13-17 In addition, several studies have asserted that the risk of major arterial injury may be increased with tourniquet use, suggesting that tourniquet use should be minimized for routine primary TKAs.3,6
There are very few cases in the literature specifically addressing injury to the more commonly encountered geniculate arteries (GAs). The medial GAs are typically visualized and coagulated during the standard medial parapatellar approach. In addition, if performed, a lateral release can damage the lateral superior and inferior GAs and the middle GA can be cut with posterior cruciate ligament resection. However, the middle and lateral inferior GAs are anecdotally the most difficult to detect and treat intraoperatively, especially after implantation of TKA and deflation of the tourniquet. The potential lack of recognition of such GA injury can result in harmful sequelae, including ischemia of the patella, hemorrhage, and painful pseudoaneurysms.2,18-29 Currently, there are only 2 case reports of lateral inferior GA injury, 2 cases of medial inferior GA injury, and no reports of middle GA injury.2,23,24,29
The rate, the timing within surgery, the risk factors, including tourniquet use, and the clinical effects of GA injury are largely unknown. If these factors were better understood, prophylactic measures and/or awareness could be better applied to prevent adverse outcomes, especially in cases of the middle and lateral inferior GAs. The aims of this study are to elucidate the rate and timing of middle and lateral inferior GA injury during primary TKA; determine the factors related to injury, including intraoperative blood loss, postoperative drain output, and tranexamic (TXA) acid use; and investigate any differences in the rate of injury with and without the use of a tourniquet.
MATERIALS AND METHODS
PATIENT DEMOGRAPHICS AND SURGICAL TECHNIQUE
From November 2015 to February 2016, 3 surgeons (MJT, TMM, and RTT) at a single institution performed 100 consecutive unilateral primary TKAs and documented the presence or absence and the timing of GA injury. After obtaining approval from our Institutional Review Board, a retrospective study was performed to investigate the prospectively recorded rate of middle and lateral inferior GA injuries occurring during primary TKAs. Patients with a diagnosis of isolated osteoarthritis were included, and those with any previous surgery on the operative knee were excluded. The average age of patients at the time of surgery was 67 years (range, 25-91 years), the average body mass index was 33 kg/m2 (range, 18-54 kg/m2), and there were 63 (63%) female patients.
All TKAs were performed through a medial parapatellar approach with a posterior-stabilized, cemented design, and each patient received a postoperative surgical drain. One of the 3 lead surgeons (TMM) in this study used a tourniquet from the time of incision until the completion of cementation, and the other 2 (MJT and RTT) predominantly used the tourniquet only during cementation. To elucidate any differences in GA injury between these 2 methods of tourniquet use, the patients were categorized into 2 groups base d on tourniquet use. Group 1 included patients in whom a tourniquet was used to maintain a bloodless surgical field from the time of incision until the completion of cementation, and Group 2 included patients in whom tourniquet use was more selective (ie, applied only during cementation). Group 1 comprised 31% (31/100) of patients, while Group 2 comprised 67% (67/100) of patients; no tourniquet was used in 2% (2/100) of cases. In addition, TXA was used in 98% (98/100) of patients: 84 patients received intravenous (IV) and 14 received topical TXA administration.
Continue to: ANALYSIS OF GENICULATE ARTERY INJURY
ANALYSIS OF GENICULATE ARTERY INJURY
The senior authors critically evaluated the GA during the primary TKAs and documented the presence or absence of injury in the operative reports. GA injury was reported if there was intraoperative visualization of pulsatile bleeding or visualization of arterial lumen in the anatomic areas of the middle and lateral inferior GAs. At 3 separate occasions during the operation, the surgeon looked specifically for pulsatile bleeding or arterial lumen in the areas of the middle and lateral inferior GAs, including after all the femoral and tibial bone cuts were completed, immediately before preparing to cement (before the tourniquet was inflated if there was not one inflated from the start of the procedure), and immediately after the tourniquet was deflated (Figure 1). All bleeding GAs that were visualized were effectively coagulated by cautery. Details regarding the use of TXA (topical or IV), intraoperative blood loss, postsurgical drain output for 24 hours after surgery, and blood transfusion were collected from the patients’ medical records (Table 1).
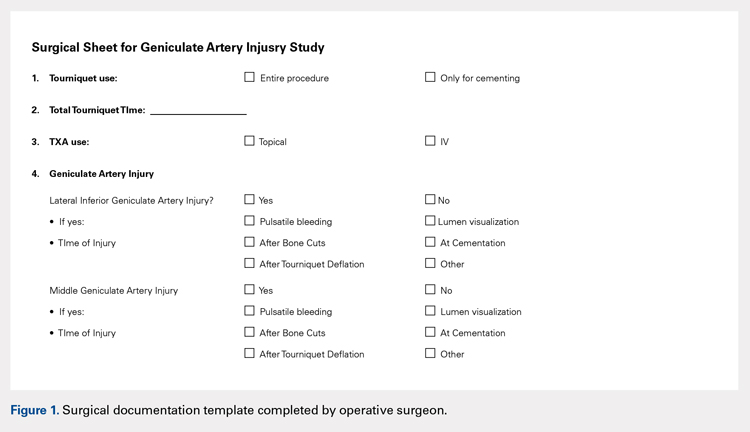
| Table 1. Operative Variables | |
Variable | Value |
Total number | 100 (100%) |
Intraoperative blood loss (mL) | 160 (25-500) |
Drain output 1st 24 hours (mL) | 488 (75-1980) |
Total output (mL) | 618 (75-2130) |
Use of TXA | 98 (98%) |
Topical TXA | 84 (84%) |
IV TXA | 14 (14%) |
Tourniquet entire procedure | 31 (31%) |
Operative variables other than geniculate artery injury. Data presented as mean (range) or n (%). TXA = tranexamic acid.
STATISTICAL METHODS
Statistical analysis was performed using the JMP software version 10.0.0 (SAS Institute, Inc). The overall rate of GA injury was determined, including the rates of GA injury based on location, time point, and method of diagnosis (pulsatile bleeding or arterial lumen visualization). If >1 GA injury occurred in the same knee, only 1 GA injury was calculated for the overall rate; however, each injury was specified separately when calculating the injury rate for the specific GA. Intraoperative blood loss, postoperative drain output, and the use of TXA were compared between cases in which a GA injury was detected and those in which it was not detected. Before conducting the retrospective review, a power analysis determined that we would require 100 patients to detect a difference in GA injury between Groups 1 and 2 (33 in Group 1 and 67 in Group 2), assuming a 30% rate in Group 1 and a 5% rate of GA injury in Group 2 using Fisher’s exact test. The Fisher’s exact test was used to compare categorical variables, and the Wilcoxon rank sum test was used to compare continuous variables. An alpha value of .05 was considered as statistically significant.
RESULTS
RATE OF GENICULATE ARTERY INJURY
The overall rate of any GA injury was 38% (38/100). Lateral inferior GA injury was more frequently detected than middle GA injury (31% vs 15% of TKAs, respectively; Table 2). Among the 31 lateral inferior GA injuries, 14 were identified as pulsatile bleeding, 7 as lumen visualizations, and 6 as both pulsatile bleeding and lumen visualization; 4 were detected by methods not recorded in the operative report. Of the lateral inferior GA injuries, 11 were identified after the bone cuts, 7 during meniscus removal, 3 during exposure, 1 after tourniquet deflation, and 9 at a time not recorded in the operative report. Of the 15 middle GA injuries, 9 were identified as pulsatile bleeding, 2 as lumen visualizations, and 4 as both pulsatile bleeding and lumen visualization. In addition, 7 of these GA injuries were identified after the bone cuts, 3 during cruciate removal, 1 after meniscus removal, 1 during exposure, and 3 at a time not recorded in the operative report (Table 3).
| Table 2. Rates of Geniculate Artery Injury Based on Location and Method | ||||
Location | Pulsatile Bleeding | Arterial Lumen | Both | Overall Rate |
Lateral inferior GA | 14 (14%) | 7 (7%) | 6 (6%) | 31 (31%) |
Middle GA | 9 (9%) | 2 (2%) | 4 (4%) | 15 (15%) |
Rates of geniculate artery injury based on location and method of diagnosis. Data presented as n (%). There were 4 additional lateral inferior and 9 middle GA injuries identified by a method not specified in the operative report. GA = geniculate artery.
Table 3. Rates of Geniculate Artery Injury Based on Time Point | ||
Time | Lateral Inferior GA | Middle GA |
After bone cuts | 11 (11%) | 7 (7%) |
During meniscus removal | 7 (7%) | 1 (1%) |
During exposure | 3 (3%) | 1 (1%) |
After tourniquet deflation | 1 (1%) | 0 (0%) |
During cruciate removal | 0 (0%) | 3 (3%) |
Not reported | 9 (9%) | 3 (3%) |
Rates of geniculate artery injury based on time point and method of diagnosis. GA = geniculate artery. Data presented as n (%).
FACTORS ASSOCIATED WITH GENICULATE ARTERY INJURY
Mean intraoperative estimated blood loss was 186 mL (standard deviation [SD], 111; range 50–500 mL) in those with a GA injury versus 147 mL (range, 82.25–400 mL) in those without injury (P = .14). Postoperative drain output in the 24 hours after surgery was 467 mL (SD 253, range 100–1105 mL) versus 502 mL (SD 378, range 75–1980 mL) in TKAs with and without GA injury, respectively (P = .82). Total estimated blood loss (combined intraoperative blood loss and 24-hour postoperative drain output) was 613 mL (SD 252, range 150–1105 mL) in TKAs with GA injury versus 620 mL (SD 393, range 75–2130 mL) without injury (P = .44) (Table 4). Overall, there was no statistical difference in blood loss, drain output, or combined output when analyzed according to lateral inferior or middle GA injury (P = .24–.82) (Table 5 and Table 6). No patients required blood transfusion postoperatively after TKA.
| Table 4. Factors Associated with GA Injury | |||
Outcome | GA Injury | No GA Injury | P Value |
Blood loss (mL) | 186 (50-500) | 147 (25-400) | .1366 |
24-Hour drain output (mL) | 467 (100-1105) | 502 (75-1980) | .8240 |
Total output (mL) | 613 (150-1105) | 620 (75-2130) | .4368 |
Differences in outcomes based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery.
| Table 5. Factors Associated with LIGA Injury | |||
Outcome | LIGA Injury | No LIGA Injury | P Value |
Blood loss (mL) | 178 (50-400) | 153 (25-500) | .2401 |
24-Hour drain output (mL) | 461 (100-890) | 501 (75-1980) | .8187 |
Total output (mL) | 610 (150-1080) | 621 (75-2130) | .4165 |
Differences in outcomes based on presence or absence of LIGA injury. Note that there were no significant differences. Values are reported as average (range). LIGA = lateral inferior geniculate artery.
| Table 6. Factors Associated with MGA Injury | |||
Outcome | MGA Injury | No MGA Injury | P Value |
Blood loss (mL) | 190 (75-500) | 156 (25-400) | .6225 |
24-Hour drain output (mL) | 455 (125-1105) | 494 (75-1980) | .6428 |
Total output (mL) | 582 (200-1105) | 624 (75-2130) | .6535 |
Differences in outcomes based on presence or absence of MGA injury. Note that there were no significant differences. Values are reported as average (range). MGA = middle geniculate artery.
IV administration of TXA was associated with a 37% (31/84) rate of GA injury, whereas topical TXA administration was associated with a 43% (6/14) rate of GA injury (P = .77). The rate of overall or isolated GA injury was not significantly different (P = .35–1.0) between IV and topical TXA administration (Table 7). In addition, total combined output was not significantly different (P = .1032) when comparing GA injury and noninjury in the subgroup analysis based on TXA use (IV or topical); however, topical administration was associated with lower intraoperative blood loss than IV administration (P = .0489), whereas IV administration was associated with lower 24-hour postoperative drain output than topical administration (P = .0169). There was no difference in blood loss, 24-hour drain output, or total output between those who did and did not sustain a GA injury in the group of patients who received IV TXA administration (Table 8, P = .2118–.7091). The same was true for those receiving topical TXA administration (Table 9, P = .0912–.9485).
Table 7. Factors Associated with TXA Injury | |||
Outcome | IV TXA (n = 84) | Topical TXA (n = 14) | P Value |
Any GA injury | 31 (37%) | 6 (43%) | .7683 |
LIGA injury | 24 (29%) | 6 (43%) | .3498 |
MGA injury | 13 (15%) | 2 (14%) | 1.0 |
Blood loss (mL) | 170 (25-500) | 113 (40-240) | .0489* |
24-Hour drain output (mL) | 454 (75-1980) | 662 (75-1800) | .0169* |
Total output (mL) | 592 (75-2130) | 751 (75-2130) | .1032 |
Differences in outcomes based on presence or absence of MGA injury. Note that there were no significant differences. Values are reported as n (%) or average (range). TXA = tranexamic acid, GA = geniculate artery, LIGA = lateral inferior geniculate artery, MGA = middle geniculate artery. *denotes statistical significance (P < .05).
| Table 8. Factors Associated with GA Injury Given IV TXA Use | ||||
Outcome | GA Injury | No GA Injury | Difference | P Value |
Blood loss (mL) | 195 (50-500) | 157 (25-400) | 38 | .2118 |
24-Hour drain output (mL) | 436 (100-1105) | 464 (75-1980) | 28 | .7091 |
Total output (mL) | 594 (150-1105) | 592 (75-2130) | 2 | .6982 |
Differences in outcomes of those patients who received IV TXA based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery, TXA = tranexamic acid.
| Table 9. Factors Associated with GA Injury Given Topical TXA Use | ||||
Outcome | GA Injury | No GA Injury | Difference | P Value |
Blood loss (mL) | 163 (100-250) | 84 (40-150) | 79 | .0912 |
24-Hour drain output (mL) | 610 (205-890) | 701 (415-1800) | 91 | .9485 |
Total output (mL) | 719 (405-960) | 775 (455-1900) | 56 | .6982 |
Differences in outcomes based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery.
Continue to: TOURNIQUET USE
TOURNIQUET USE
Comparison between Groups 1 (tourniquet use) and 2 (selective tourniquet use) revealed similar rates of overall and specific GA injury, intraoperative blood loss, and 24-hour postoperative drain output (Table 10). Group 1 demonstrated a 29% (9/31) rate of any GA injury versus 40% (27/67) in Group 2 (P = .37). For the specific lateral inferior GA injury, there was an equivalent rate of injury at 29% (9/31 in Group 1, 20/67 in Group 2; P = 1.0). Similarly, Group 1 patients had a 10% (3/31) rate of middle GA injury compared to 16% (11/67) in Group 2 patients (P = .53). Intraoperative estimated blood loss was lower in Group 1 (140 mL; range 25–400 mL) than in Group 2 (171 mL; range 40–500 mL) (P = .07), whereas the average 24-hour postoperative drain output was similar for Groups 1 (484 mL; range 75–1800 mL) and 2 (488 mL; range 100–1980 mL) (P = .46). Total estimated output was slightly less for Group 1 (593 mL; range 75–1900 mL) than for Group 2 (626 mL; range 125–2130 mL) (P = .38). A post hoc power analysis showed that with these rates of GA injury in Groups 1 and 2 and given a 2:1 ratio of the number of patients in Group 2 versus Group 1, a total of 185 patients in Group 1 and 370 patients in Group 2 would be needed to detect a statistically significant difference (P < .05) with a power of 80%.
| Table 10. Factors Associated with Tourniquet Use | ||||
Injury | Group 1 (n = 31) | Group 2 (n = 67) | Difference | P Value |
Overall GA injury | 9 (29%) | 27 (40%) | 11% | .3687 |
Lateral inferior GA | 9 (29%) | 20 (29%) | 0% | 1.0 |
Middle GA | 3 (10%) | 11 (16%) | 6% | .5382 |
Blood loss (mL) | 140 (25-400) | 171 (40-500) | 31 | .0661 |
24-Hour drain output (mL) | 484 (75-1800) | 488 (100-1980) | 4 | .4580 |
Total output (mL) | 593 (75-1900) | 626 (125-2130) | 33 | .3776 |
Differences in outcomes separated based on use of a tourniquet for the entire case (Group 1) vs use of a tourniquet only during cementation (Group 2). Note that there were no significant differences. Values are reported as n (%) or average (range). GA = geniculate artery.
DISCUSSION
Major arterial injury associated with TKA is a well-known, rare, and potentially devastating complication.1-13 However, the rate of injury to smaller periarticular vessels and the clinical significance of such injury have not been studied. The present study found a high rate of GA injury but no clinically significant difference in intraoperative blood loss or postoperative drain output between patients with GA injury (which was identified and managed with cautery) and those without GA injury. In addition, tourniquet use did not affect the rate of injury or the associated blood loss. To our knowledge, this is the first study that has critically evaluated the rate of GA injury occurring during TKA.
The overall rate of GA injury occurring during primary TKA was 38% with a higher predominance of lateral inferior than middle GA injury (31% vs 15%). Anatomically, it would follow that the lateral GA could be injured at a higher rate as it courses on top of the lateral meniscus, thus being susceptible to injury during cutting of the tibial plateau and meniscectomy. In addition, because the meniscectomy is performed longitudinally along the course of the artery, it may also be potentially lacerated in multiple locations and lengthwise. In theory, there should be a 100% rate of middle GA injury during posterior-stabilized TKA as this artery runs through the cruciate ligaments, which are resected during these cases. However, vessel injury was defined in this study as the visualization of pulsatile bleeding or vessel lumen. It is probable that in the cases in which injury to the middle GA was not visualized, it was cut but simultaneously cauterized. Thus, a lower rate (15%) of injury was detected. Nonetheless, these results still suggest that these periarticular arteries are injured at a higher rate; therefore, it is important for surgeons to specifically identify these injuries intraoperatively and adequately cauterize these vessels. As long as these arteries are cauterized, additional blood loss and potential vascular pseudoaneurysms should be prevented.
The effect of GA injury on intraoperative blood loss, 24-hour postoperative drain output, and total estimated blood loss showed no significant clinical findings in the present study cohort. In addition, examining the injury rate and blood loss based on TXA use also revealed no detrimental clinical associations. Although GA injury could inherently be associated with higher levels of blood loss and drain output, it is important to note that all GA injuries were also effectively coagulated, thus explaining the indifferent results. Accordingly, it should be recommended to surgeons performing primary TKAs to carefully evaluate for GA injury to prevent excessive blood loss or painful pseudoaneurysms. However, there is also a potential for beta error in this study in which a true difference did exist but no statistical difference was found due to the study being underpowered.
Full or selective tourniquet use during TKA did not appear to have any effect on the rate of GA injury, intraoperative blood loss, or 24-hour postoperative drain output. The similarity between GA injury rates perhaps further indicates an equivalent ability to detect these injuries between these two methods because of operative inspection for such injuries. With regard to intraoperative blood loss and drain output, the present findings are similar to previous studies demonstrating equivocal results despite variable tourniquet utilization in TKA.15,30 However, these results differ from those of Harvey and colleagues31, who demonstrated that blood loss inversely correlated with intraoperative tourniquet time. There are risks and benefits related to the use of both full and selective tourniquet methods, but either method does not appear to be advantageous in decreasing the rate of GA injury.
Continue to: Although this is the first study...
Although this is the first study to investigate the rates of GA injury and the potential clinical effects, there are limitations to this research. First, the study was retrospective in nature despite the fact that the data were collected prospectively. Only acute perioperative follow-up was performed, and thus, we were unable to evaluate longer term effects of GA injury on TKA outcomes. Furthermore, this study is potentially prone to beta error. As discussed above, 185 patients in Group 1 and 370 patients in Group 2 would be needed to detect a statistical difference in the rate of GA injury based on the rates found in this study. This study could also have been underpowered to identify differences in other aspects, such as differences in blood loss and drain. Furthermore, the data collected regarding intraoperative blood loss are estimated data and can be variable. Finally, visualization of vessel lumen and pulsatile bleeding is not a validated method to diagnose GA injuries, and potential injuries may have been missed. Despite such disadvantages, the strengths of this study include the concise results in consecutive patients, the generalizability of the data as multiple surgeons participated, and its first report of nonmajor periarticular artery injury.
CONCLUSIONS
There is a relatively high rate of GA injury, with injury to the lateral GA being visualized more often than injury to the middle GA. The majority of GA injuries occur around the time of bone cuts and meniscectomy, and tourniquet use does not affect the rate of injury. To reduce intraoperative blood loss and postoperative drain output, surgeons should identify and coagulate GA injuries routinely during primary TKA.
ABSTRACT
Major arterial injury associated with total knee arthroplasty (TKA) is a rare and potentially devastating complication. However, the rate of injury to smaller periarticular vessels and the clinical significance of such an injury have not been well investigated. The purpose of this study is to describe the rate and outcomes of geniculate artery (GA) injury, the time at which injury occurs, and any associations with tourniquet use.
From November 2015 to February 2016, 3 surgeons at a single institution performed 100 consecutive primary TKAs and documented the presence or absence and the timing of GA injury. The data were then retrospectively reviewed. All TKAs had no prior surgery on the operative extremity. Other variables collected included tourniquet use, tranexamic acid (TXA) administration, intraoperative blood loss, postoperative drain output, and blood transfusion.
The overall rate of GA injury was 38%, with lateral inferior and middle GA injury in 31% and 15% of TKAs, respectively. Most of the injuries were visualized during bone cuts or meniscectomy. The rate of overall or isolated GA injury was not significantly different (P > .05) with either use of intravenous (84 patients) or topical (14 patients) TXA administration. Comparing selective tourniquet use (only during cementation) vs routine use showed no differences in GA injury rate (P = .37), blood loss (P = .07), or drain output (P = .46).
There is a relatively high rate of GA injury, with injury to the lateral GA occurring more often than the middle GA. Routine or selective tourniquet use does not affect the rate of injury.
Continue to: Major arterial injury...
Major arterial injury associated with total knee arthroplasty (TKA) is a rare and potentially devastating complication. The majority of literature in this context consists of case reports, small case series, and large retrospective studies that have examined the type, location, and mechanism of injury present in these cases.1-13 Reported arterial injuries include occlusion, laceration, aneurysm, pseudoaneurysm, and arteriovenous fistula formation in the femoral (believed to be due to the tourniquet around the proximal thigh) and popliteal arteries causing combinations of ischemia and hemorrhage necessitating treatment ranging from endovascular arterial intervention to amputation.4,5,9-11,13-17 In addition, several studies have asserted that the risk of major arterial injury may be increased with tourniquet use, suggesting that tourniquet use should be minimized for routine primary TKAs.3,6
There are very few cases in the literature specifically addressing injury to the more commonly encountered geniculate arteries (GAs). The medial GAs are typically visualized and coagulated during the standard medial parapatellar approach. In addition, if performed, a lateral release can damage the lateral superior and inferior GAs and the middle GA can be cut with posterior cruciate ligament resection. However, the middle and lateral inferior GAs are anecdotally the most difficult to detect and treat intraoperatively, especially after implantation of TKA and deflation of the tourniquet. The potential lack of recognition of such GA injury can result in harmful sequelae, including ischemia of the patella, hemorrhage, and painful pseudoaneurysms.2,18-29 Currently, there are only 2 case reports of lateral inferior GA injury, 2 cases of medial inferior GA injury, and no reports of middle GA injury.2,23,24,29
The rate, the timing within surgery, the risk factors, including tourniquet use, and the clinical effects of GA injury are largely unknown. If these factors were better understood, prophylactic measures and/or awareness could be better applied to prevent adverse outcomes, especially in cases of the middle and lateral inferior GAs. The aims of this study are to elucidate the rate and timing of middle and lateral inferior GA injury during primary TKA; determine the factors related to injury, including intraoperative blood loss, postoperative drain output, and tranexamic (TXA) acid use; and investigate any differences in the rate of injury with and without the use of a tourniquet.
MATERIALS AND METHODS
PATIENT DEMOGRAPHICS AND SURGICAL TECHNIQUE
From November 2015 to February 2016, 3 surgeons (MJT, TMM, and RTT) at a single institution performed 100 consecutive unilateral primary TKAs and documented the presence or absence and the timing of GA injury. After obtaining approval from our Institutional Review Board, a retrospective study was performed to investigate the prospectively recorded rate of middle and lateral inferior GA injuries occurring during primary TKAs. Patients with a diagnosis of isolated osteoarthritis were included, and those with any previous surgery on the operative knee were excluded. The average age of patients at the time of surgery was 67 years (range, 25-91 years), the average body mass index was 33 kg/m2 (range, 18-54 kg/m2), and there were 63 (63%) female patients.
All TKAs were performed through a medial parapatellar approach with a posterior-stabilized, cemented design, and each patient received a postoperative surgical drain. One of the 3 lead surgeons (TMM) in this study used a tourniquet from the time of incision until the completion of cementation, and the other 2 (MJT and RTT) predominantly used the tourniquet only during cementation. To elucidate any differences in GA injury between these 2 methods of tourniquet use, the patients were categorized into 2 groups base d on tourniquet use. Group 1 included patients in whom a tourniquet was used to maintain a bloodless surgical field from the time of incision until the completion of cementation, and Group 2 included patients in whom tourniquet use was more selective (ie, applied only during cementation). Group 1 comprised 31% (31/100) of patients, while Group 2 comprised 67% (67/100) of patients; no tourniquet was used in 2% (2/100) of cases. In addition, TXA was used in 98% (98/100) of patients: 84 patients received intravenous (IV) and 14 received topical TXA administration.
Continue to: ANALYSIS OF GENICULATE ARTERY INJURY
ANALYSIS OF GENICULATE ARTERY INJURY
The senior authors critically evaluated the GA during the primary TKAs and documented the presence or absence of injury in the operative reports. GA injury was reported if there was intraoperative visualization of pulsatile bleeding or visualization of arterial lumen in the anatomic areas of the middle and lateral inferior GAs. At 3 separate occasions during the operation, the surgeon looked specifically for pulsatile bleeding or arterial lumen in the areas of the middle and lateral inferior GAs, including after all the femoral and tibial bone cuts were completed, immediately before preparing to cement (before the tourniquet was inflated if there was not one inflated from the start of the procedure), and immediately after the tourniquet was deflated (Figure 1). All bleeding GAs that were visualized were effectively coagulated by cautery. Details regarding the use of TXA (topical or IV), intraoperative blood loss, postsurgical drain output for 24 hours after surgery, and blood transfusion were collected from the patients’ medical records (Table 1).
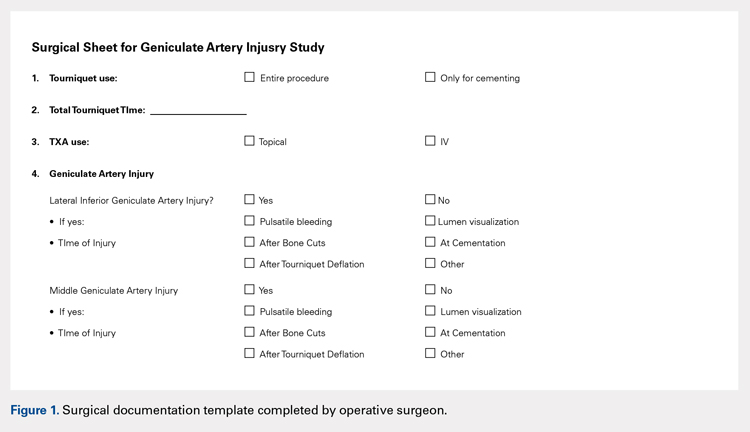
| Table 1. Operative Variables | |
Variable | Value |
Total number | 100 (100%) |
Intraoperative blood loss (mL) | 160 (25-500) |
Drain output 1st 24 hours (mL) | 488 (75-1980) |
Total output (mL) | 618 (75-2130) |
Use of TXA | 98 (98%) |
Topical TXA | 84 (84%) |
IV TXA | 14 (14%) |
Tourniquet entire procedure | 31 (31%) |
Operative variables other than geniculate artery injury. Data presented as mean (range) or n (%). TXA = tranexamic acid.
STATISTICAL METHODS
Statistical analysis was performed using the JMP software version 10.0.0 (SAS Institute, Inc). The overall rate of GA injury was determined, including the rates of GA injury based on location, time point, and method of diagnosis (pulsatile bleeding or arterial lumen visualization). If >1 GA injury occurred in the same knee, only 1 GA injury was calculated for the overall rate; however, each injury was specified separately when calculating the injury rate for the specific GA. Intraoperative blood loss, postoperative drain output, and the use of TXA were compared between cases in which a GA injury was detected and those in which it was not detected. Before conducting the retrospective review, a power analysis determined that we would require 100 patients to detect a difference in GA injury between Groups 1 and 2 (33 in Group 1 and 67 in Group 2), assuming a 30% rate in Group 1 and a 5% rate of GA injury in Group 2 using Fisher’s exact test. The Fisher’s exact test was used to compare categorical variables, and the Wilcoxon rank sum test was used to compare continuous variables. An alpha value of .05 was considered as statistically significant.
RESULTS
RATE OF GENICULATE ARTERY INJURY
The overall rate of any GA injury was 38% (38/100). Lateral inferior GA injury was more frequently detected than middle GA injury (31% vs 15% of TKAs, respectively; Table 2). Among the 31 lateral inferior GA injuries, 14 were identified as pulsatile bleeding, 7 as lumen visualizations, and 6 as both pulsatile bleeding and lumen visualization; 4 were detected by methods not recorded in the operative report. Of the lateral inferior GA injuries, 11 were identified after the bone cuts, 7 during meniscus removal, 3 during exposure, 1 after tourniquet deflation, and 9 at a time not recorded in the operative report. Of the 15 middle GA injuries, 9 were identified as pulsatile bleeding, 2 as lumen visualizations, and 4 as both pulsatile bleeding and lumen visualization. In addition, 7 of these GA injuries were identified after the bone cuts, 3 during cruciate removal, 1 after meniscus removal, 1 during exposure, and 3 at a time not recorded in the operative report (Table 3).
| Table 2. Rates of Geniculate Artery Injury Based on Location and Method | ||||
Location | Pulsatile Bleeding | Arterial Lumen | Both | Overall Rate |
Lateral inferior GA | 14 (14%) | 7 (7%) | 6 (6%) | 31 (31%) |
Middle GA | 9 (9%) | 2 (2%) | 4 (4%) | 15 (15%) |
Rates of geniculate artery injury based on location and method of diagnosis. Data presented as n (%). There were 4 additional lateral inferior and 9 middle GA injuries identified by a method not specified in the operative report. GA = geniculate artery.
Table 3. Rates of Geniculate Artery Injury Based on Time Point | ||
Time | Lateral Inferior GA | Middle GA |
After bone cuts | 11 (11%) | 7 (7%) |
During meniscus removal | 7 (7%) | 1 (1%) |
During exposure | 3 (3%) | 1 (1%) |
After tourniquet deflation | 1 (1%) | 0 (0%) |
During cruciate removal | 0 (0%) | 3 (3%) |
Not reported | 9 (9%) | 3 (3%) |
Rates of geniculate artery injury based on time point and method of diagnosis. GA = geniculate artery. Data presented as n (%).
FACTORS ASSOCIATED WITH GENICULATE ARTERY INJURY
Mean intraoperative estimated blood loss was 186 mL (standard deviation [SD], 111; range 50–500 mL) in those with a GA injury versus 147 mL (range, 82.25–400 mL) in those without injury (P = .14). Postoperative drain output in the 24 hours after surgery was 467 mL (SD 253, range 100–1105 mL) versus 502 mL (SD 378, range 75–1980 mL) in TKAs with and without GA injury, respectively (P = .82). Total estimated blood loss (combined intraoperative blood loss and 24-hour postoperative drain output) was 613 mL (SD 252, range 150–1105 mL) in TKAs with GA injury versus 620 mL (SD 393, range 75–2130 mL) without injury (P = .44) (Table 4). Overall, there was no statistical difference in blood loss, drain output, or combined output when analyzed according to lateral inferior or middle GA injury (P = .24–.82) (Table 5 and Table 6). No patients required blood transfusion postoperatively after TKA.
| Table 4. Factors Associated with GA Injury | |||
Outcome | GA Injury | No GA Injury | P Value |
Blood loss (mL) | 186 (50-500) | 147 (25-400) | .1366 |
24-Hour drain output (mL) | 467 (100-1105) | 502 (75-1980) | .8240 |
Total output (mL) | 613 (150-1105) | 620 (75-2130) | .4368 |
Differences in outcomes based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery.
| Table 5. Factors Associated with LIGA Injury | |||
Outcome | LIGA Injury | No LIGA Injury | P Value |
Blood loss (mL) | 178 (50-400) | 153 (25-500) | .2401 |
24-Hour drain output (mL) | 461 (100-890) | 501 (75-1980) | .8187 |
Total output (mL) | 610 (150-1080) | 621 (75-2130) | .4165 |
Differences in outcomes based on presence or absence of LIGA injury. Note that there were no significant differences. Values are reported as average (range). LIGA = lateral inferior geniculate artery.
| Table 6. Factors Associated with MGA Injury | |||
Outcome | MGA Injury | No MGA Injury | P Value |
Blood loss (mL) | 190 (75-500) | 156 (25-400) | .6225 |
24-Hour drain output (mL) | 455 (125-1105) | 494 (75-1980) | .6428 |
Total output (mL) | 582 (200-1105) | 624 (75-2130) | .6535 |
Differences in outcomes based on presence or absence of MGA injury. Note that there were no significant differences. Values are reported as average (range). MGA = middle geniculate artery.
IV administration of TXA was associated with a 37% (31/84) rate of GA injury, whereas topical TXA administration was associated with a 43% (6/14) rate of GA injury (P = .77). The rate of overall or isolated GA injury was not significantly different (P = .35–1.0) between IV and topical TXA administration (Table 7). In addition, total combined output was not significantly different (P = .1032) when comparing GA injury and noninjury in the subgroup analysis based on TXA use (IV or topical); however, topical administration was associated with lower intraoperative blood loss than IV administration (P = .0489), whereas IV administration was associated with lower 24-hour postoperative drain output than topical administration (P = .0169). There was no difference in blood loss, 24-hour drain output, or total output between those who did and did not sustain a GA injury in the group of patients who received IV TXA administration (Table 8, P = .2118–.7091). The same was true for those receiving topical TXA administration (Table 9, P = .0912–.9485).
Table 7. Factors Associated with TXA Injury | |||
Outcome | IV TXA (n = 84) | Topical TXA (n = 14) | P Value |
Any GA injury | 31 (37%) | 6 (43%) | .7683 |
LIGA injury | 24 (29%) | 6 (43%) | .3498 |
MGA injury | 13 (15%) | 2 (14%) | 1.0 |
Blood loss (mL) | 170 (25-500) | 113 (40-240) | .0489* |
24-Hour drain output (mL) | 454 (75-1980) | 662 (75-1800) | .0169* |
Total output (mL) | 592 (75-2130) | 751 (75-2130) | .1032 |
Differences in outcomes based on presence or absence of MGA injury. Note that there were no significant differences. Values are reported as n (%) or average (range). TXA = tranexamic acid, GA = geniculate artery, LIGA = lateral inferior geniculate artery, MGA = middle geniculate artery. *denotes statistical significance (P < .05).
| Table 8. Factors Associated with GA Injury Given IV TXA Use | ||||
Outcome | GA Injury | No GA Injury | Difference | P Value |
Blood loss (mL) | 195 (50-500) | 157 (25-400) | 38 | .2118 |
24-Hour drain output (mL) | 436 (100-1105) | 464 (75-1980) | 28 | .7091 |
Total output (mL) | 594 (150-1105) | 592 (75-2130) | 2 | .6982 |
Differences in outcomes of those patients who received IV TXA based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery, TXA = tranexamic acid.
| Table 9. Factors Associated with GA Injury Given Topical TXA Use | ||||
Outcome | GA Injury | No GA Injury | Difference | P Value |
Blood loss (mL) | 163 (100-250) | 84 (40-150) | 79 | .0912 |
24-Hour drain output (mL) | 610 (205-890) | 701 (415-1800) | 91 | .9485 |
Total output (mL) | 719 (405-960) | 775 (455-1900) | 56 | .6982 |
Differences in outcomes based on presence or absence of GA injury. Note that there were no significant differences. Values are reported as average (range). GA = geniculate artery.
Continue to: TOURNIQUET USE
TOURNIQUET USE
Comparison between Groups 1 (tourniquet use) and 2 (selective tourniquet use) revealed similar rates of overall and specific GA injury, intraoperative blood loss, and 24-hour postoperative drain output (Table 10). Group 1 demonstrated a 29% (9/31) rate of any GA injury versus 40% (27/67) in Group 2 (P = .37). For the specific lateral inferior GA injury, there was an equivalent rate of injury at 29% (9/31 in Group 1, 20/67 in Group 2; P = 1.0). Similarly, Group 1 patients had a 10% (3/31) rate of middle GA injury compared to 16% (11/67) in Group 2 patients (P = .53). Intraoperative estimated blood loss was lower in Group 1 (140 mL; range 25–400 mL) than in Group 2 (171 mL; range 40–500 mL) (P = .07), whereas the average 24-hour postoperative drain output was similar for Groups 1 (484 mL; range 75–1800 mL) and 2 (488 mL; range 100–1980 mL) (P = .46). Total estimated output was slightly less for Group 1 (593 mL; range 75–1900 mL) than for Group 2 (626 mL; range 125–2130 mL) (P = .38). A post hoc power analysis showed that with these rates of GA injury in Groups 1 and 2 and given a 2:1 ratio of the number of patients in Group 2 versus Group 1, a total of 185 patients in Group 1 and 370 patients in Group 2 would be needed to detect a statistically significant difference (P < .05) with a power of 80%.
| Table 10. Factors Associated with Tourniquet Use | ||||
Injury | Group 1 (n = 31) | Group 2 (n = 67) | Difference | P Value |
Overall GA injury | 9 (29%) | 27 (40%) | 11% | .3687 |
Lateral inferior GA | 9 (29%) | 20 (29%) | 0% | 1.0 |
Middle GA | 3 (10%) | 11 (16%) | 6% | .5382 |
Blood loss (mL) | 140 (25-400) | 171 (40-500) | 31 | .0661 |
24-Hour drain output (mL) | 484 (75-1800) | 488 (100-1980) | 4 | .4580 |
Total output (mL) | 593 (75-1900) | 626 (125-2130) | 33 | .3776 |
Differences in outcomes separated based on use of a tourniquet for the entire case (Group 1) vs use of a tourniquet only during cementation (Group 2). Note that there were no significant differences. Values are reported as n (%) or average (range). GA = geniculate artery.
DISCUSSION
Major arterial injury associated with TKA is a well-known, rare, and potentially devastating complication.1-13 However, the rate of injury to smaller periarticular vessels and the clinical significance of such injury have not been studied. The present study found a high rate of GA injury but no clinically significant difference in intraoperative blood loss or postoperative drain output between patients with GA injury (which was identified and managed with cautery) and those without GA injury. In addition, tourniquet use did not affect the rate of injury or the associated blood loss. To our knowledge, this is the first study that has critically evaluated the rate of GA injury occurring during TKA.
The overall rate of GA injury occurring during primary TKA was 38% with a higher predominance of lateral inferior than middle GA injury (31% vs 15%). Anatomically, it would follow that the lateral GA could be injured at a higher rate as it courses on top of the lateral meniscus, thus being susceptible to injury during cutting of the tibial plateau and meniscectomy. In addition, because the meniscectomy is performed longitudinally along the course of the artery, it may also be potentially lacerated in multiple locations and lengthwise. In theory, there should be a 100% rate of middle GA injury during posterior-stabilized TKA as this artery runs through the cruciate ligaments, which are resected during these cases. However, vessel injury was defined in this study as the visualization of pulsatile bleeding or vessel lumen. It is probable that in the cases in which injury to the middle GA was not visualized, it was cut but simultaneously cauterized. Thus, a lower rate (15%) of injury was detected. Nonetheless, these results still suggest that these periarticular arteries are injured at a higher rate; therefore, it is important for surgeons to specifically identify these injuries intraoperatively and adequately cauterize these vessels. As long as these arteries are cauterized, additional blood loss and potential vascular pseudoaneurysms should be prevented.
The effect of GA injury on intraoperative blood loss, 24-hour postoperative drain output, and total estimated blood loss showed no significant clinical findings in the present study cohort. In addition, examining the injury rate and blood loss based on TXA use also revealed no detrimental clinical associations. Although GA injury could inherently be associated with higher levels of blood loss and drain output, it is important to note that all GA injuries were also effectively coagulated, thus explaining the indifferent results. Accordingly, it should be recommended to surgeons performing primary TKAs to carefully evaluate for GA injury to prevent excessive blood loss or painful pseudoaneurysms. However, there is also a potential for beta error in this study in which a true difference did exist but no statistical difference was found due to the study being underpowered.
Full or selective tourniquet use during TKA did not appear to have any effect on the rate of GA injury, intraoperative blood loss, or 24-hour postoperative drain output. The similarity between GA injury rates perhaps further indicates an equivalent ability to detect these injuries between these two methods because of operative inspection for such injuries. With regard to intraoperative blood loss and drain output, the present findings are similar to previous studies demonstrating equivocal results despite variable tourniquet utilization in TKA.15,30 However, these results differ from those of Harvey and colleagues31, who demonstrated that blood loss inversely correlated with intraoperative tourniquet time. There are risks and benefits related to the use of both full and selective tourniquet methods, but either method does not appear to be advantageous in decreasing the rate of GA injury.
Continue to: Although this is the first study...
Although this is the first study to investigate the rates of GA injury and the potential clinical effects, there are limitations to this research. First, the study was retrospective in nature despite the fact that the data were collected prospectively. Only acute perioperative follow-up was performed, and thus, we were unable to evaluate longer term effects of GA injury on TKA outcomes. Furthermore, this study is potentially prone to beta error. As discussed above, 185 patients in Group 1 and 370 patients in Group 2 would be needed to detect a statistical difference in the rate of GA injury based on the rates found in this study. This study could also have been underpowered to identify differences in other aspects, such as differences in blood loss and drain. Furthermore, the data collected regarding intraoperative blood loss are estimated data and can be variable. Finally, visualization of vessel lumen and pulsatile bleeding is not a validated method to diagnose GA injuries, and potential injuries may have been missed. Despite such disadvantages, the strengths of this study include the concise results in consecutive patients, the generalizability of the data as multiple surgeons participated, and its first report of nonmajor periarticular artery injury.
CONCLUSIONS
There is a relatively high rate of GA injury, with injury to the lateral GA being visualized more often than injury to the middle GA. The majority of GA injuries occur around the time of bone cuts and meniscectomy, and tourniquet use does not affect the rate of injury. To reduce intraoperative blood loss and postoperative drain output, surgeons should identify and coagulate GA injuries routinely during primary TKA.
1. Calligaro KD, Dougherty MJ, Ryan S, Booth RE. Acute arterial complications associated with total hip and knee arthroplasty. J Vasc Surg. 2003;38(6):1170-1177. doi: 10.1016/S0741-5214(03)00918-2.
2. Dennis DA, Neumann RD, Toma P, Rosenberg G, Mallory TH. Arteriovenous fistula with false aneurysm of the inferior medial geniculate artery. A complication of total knee arthroplasty. Clin Orthop Relat Res. 1987(222):255-260.
3. Hagan PF, Kaufman EE. Vascular complication of knee arthroplasty under tourniquet. A case report. Clin Orthop Relat Res. 1990(257):159-161.
4. Holmberg A, Milbrink J, Bergqvist D. Arterial complications after knee arthroplasty: 4 cases and a review of the literature. Acta Orthop Scand. 1996;67(1):75-78. doi: 10.3109/17453679608995616.
5. Hozack WJ, Cole PA, Gardner R, Corces A. Popliteal aneurysm after total knee arthroplasty. Case reports and review of the literature. J Arthroplasty. 1990;5(4):301-305. doi: 10.1016/S0883-5403(08)80087-3.
6. Jeyaseelan S, Stevenson TM, Pfitzner J. Tourniquet failure and arterial calcification. Case report and theoretical dangers. Anaesthesia. 1981;36(1):48-50. doi: 10.1111/j.1365-2044.1981.tb08599.x
7. Mureebe L, Gahtan V, Kahn MB, Kerstein MD, Roberts AB. Popliteal artery injury after total knee arthroplasty. Am Surg. 1996;62(5):366-368.
8. O'Connor JV, Stocks G, Crabtree JD, Jr., Galasso P, Wallsh E. Popliteal pseudoaneurysm following total knee arthroplasty. J Arthroplasty. 1998;13(7):830-832. doi: 10.1016/S0883-5403(98)90039-0.
9. Ohira T, Fujimoto T, Taniwaki K. Acute popliteal artery occlusion after total knee arthroplasty. Arch Orthop Trauma Surg. 1997;116(6-7):429-430. doi: 10.1007/BF00434007.
10. Parfenchuck TA, Young TR. Intraoperative arterial occlusion in total joint arthroplasty. J Arthroplasty. 1994;9(2):217-220. doi: 10.1016/0883-5403(94)90071-X.
11. Rush JH, Vidovich JD, Johnson MA. Arterial complications of total knee replacement. The Australian experience. J Bone Joint Surg Br. 1987;69(3):400-402. doi: 10.1302/0301-620X.69B3.3584193.
12. Smith DE, McGraw RW, Taylor DC, Masri BA. Arterial complications and total knee arthroplasty. J Am Acad Orthop Surg. 2001;9(4):253-257.
13. Zahrani HA, Cuschieri RJ. Vascular complications after total knee replacement. J Cardiovasc Surg (Torino). 1989;30(6):951-952.
14. Isiklar ZU, Landon GC, Tullos HS. Amputation after failed total knee arthroplasty. Clin Orthop Relat Res. 1994(299):173-178.
15. Wakankar HM, Nicholl JE, Koka R, D'Arcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 1999;81(1):30-33. doi: 10.1302/0301-620X.81B1.0810030.
16. Kumar SN, Chapman JA, Rawlins I. Vascular injuries in total knee arthroplasty. A review of the problem with special reference to the possible effects of the tourniquet. J Arthroplasty. 1998;13(2):211-216. doi: 10.1016/S0883-5403(98)90102-4.
17. DeLaurentis DA, Levitsky KA, Booth RE, et al. Arterial and ischemic aspects of total knee arthroplasty. Am J Surg. 1992;164(3):237-240. doi: 10.1016/S0002-9610(05)81078-5.
18. Langkamer VG. Local vascular complications after knee replacement: a review with illustrative case reports. Knee. 2001;8(4):259-264. doi: 10.1016/S0968-0160(01)00103-X.
19. Moran M, Hodgkinson J, Tait W. False aneurysm of the superior lateral geniculate artery following Total Knee Replacement. Knee. 2002;9(4):349-351. doi: 10.1016/S0968-0160(02)00061-3.
20. Pritsch T, Parnes N, Menachem A. A bleeding pseudoaneurysm of the lateral genicular artery after total knee arthroplasty--a case report. Acta Orthop. 2005;76(1):138-140. doi: 10.1080/00016470510030463.
21. Gaheer RS, Chirputkar K, Sarungi M. Spontaneous resolution of superior medial geniculate artery pseudoaneurysm following total knee arthroplasty. Knee. 2014;21(2):586-588. doi: 10.1016/j.knee.2012.10.021.
22. Law KY, Cheung KW, Chiu KH, Antonio GE. Pseudoaneurysm of the geniculate artery following total knee arthroplasty: a report of two cases. J Orthop Surg (Hong Kong). 2007;15(3):386-389. /doi: 10.1177/230949900701500331.
23. Noorpuri BS, Maxwell-Armstrong CA, Lamerton AJ. Pseudo-aneurysm of a geniculate collateral artery complicating total knee replacement. Eur J Vasc Endovasc Surg. 1999;18(6):534-535.
24. Pai VS. Traumatic aneurysm of the inferior lateral geniculate artery after total knee replacement. J Arthroplasty. 1999;14(5):633-634. doi: 10.1016/S0883-5403(99)90089-X.
25. Julien TP, Gravereaux E, Martin S. Superior medial geniculate artery pseudoaneurysm after primary total knee arthroplasty. J Arthroplasty. 2012;27(2):323 e313-326. doi: 10.1016/j.arth.2011.02.009.
26. Kalsi PS, Carrington RJ, Skinner JS. Therapeutic embolization for the treatment of recurrent hemarthrosis after total knee arthroplasty due to an arteriovenous fistula. J Arthroplasty. 2007;22(8):1223-1225. /doi: 10.1016/j.arth.2006.11.012.
27. Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB. Patellofemoral complications following total knee arthroplasty. Effect of a lateral release and sacrifice of the superior lateral geniculate artery. J Arthroplasty. 1996;11(4):368-372. doi: 10.1016/S0883-5403(96)80024-6.
28. Aldrich D, Anschuetz R, LoPresti C, Fumich M, Pitluk H, O'Brien W. Pseudoaneurysm complicating knee arthroscopy. Arthroscopy. 1995;11(2):229-230. doi: 10.1016/0749-8063(95)90073-X.
29. Sharma H, Singh GK, Cavanagh SP, Kay D. Pseudoaneurysm of the inferior medial geniculate artery following primary total knee arthroplasty: delayed presentation with recurrent haemorrhagic episodes. Knee Surg Sports Traumatol Arthrosc. 2006;14(2):153-155. doi: 10.1007/s00167-005-0639-4.
30. Abdel-Salam A, Eyres KS. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J Bone Joint Surg Br. 1995;77(2):250-253. doi: 10.1302/0301-620X.77B2.7706340.
31. Harvey EJ, Leclerc J, Brooks CE, Burke DL. Effect of tourniquet use on blood loss and incidence of deep vein thrombosis in total knee arthroplasty. J Arthroplasty. 1997;12(3):291-296. doi: 10.1016/S0883-5403(97)90025-5.
1. Calligaro KD, Dougherty MJ, Ryan S, Booth RE. Acute arterial complications associated with total hip and knee arthroplasty. J Vasc Surg. 2003;38(6):1170-1177. doi: 10.1016/S0741-5214(03)00918-2.
2. Dennis DA, Neumann RD, Toma P, Rosenberg G, Mallory TH. Arteriovenous fistula with false aneurysm of the inferior medial geniculate artery. A complication of total knee arthroplasty. Clin Orthop Relat Res. 1987(222):255-260.
3. Hagan PF, Kaufman EE. Vascular complication of knee arthroplasty under tourniquet. A case report. Clin Orthop Relat Res. 1990(257):159-161.
4. Holmberg A, Milbrink J, Bergqvist D. Arterial complications after knee arthroplasty: 4 cases and a review of the literature. Acta Orthop Scand. 1996;67(1):75-78. doi: 10.3109/17453679608995616.
5. Hozack WJ, Cole PA, Gardner R, Corces A. Popliteal aneurysm after total knee arthroplasty. Case reports and review of the literature. J Arthroplasty. 1990;5(4):301-305. doi: 10.1016/S0883-5403(08)80087-3.
6. Jeyaseelan S, Stevenson TM, Pfitzner J. Tourniquet failure and arterial calcification. Case report and theoretical dangers. Anaesthesia. 1981;36(1):48-50. doi: 10.1111/j.1365-2044.1981.tb08599.x
7. Mureebe L, Gahtan V, Kahn MB, Kerstein MD, Roberts AB. Popliteal artery injury after total knee arthroplasty. Am Surg. 1996;62(5):366-368.
8. O'Connor JV, Stocks G, Crabtree JD, Jr., Galasso P, Wallsh E. Popliteal pseudoaneurysm following total knee arthroplasty. J Arthroplasty. 1998;13(7):830-832. doi: 10.1016/S0883-5403(98)90039-0.
9. Ohira T, Fujimoto T, Taniwaki K. Acute popliteal artery occlusion after total knee arthroplasty. Arch Orthop Trauma Surg. 1997;116(6-7):429-430. doi: 10.1007/BF00434007.
10. Parfenchuck TA, Young TR. Intraoperative arterial occlusion in total joint arthroplasty. J Arthroplasty. 1994;9(2):217-220. doi: 10.1016/0883-5403(94)90071-X.
11. Rush JH, Vidovich JD, Johnson MA. Arterial complications of total knee replacement. The Australian experience. J Bone Joint Surg Br. 1987;69(3):400-402. doi: 10.1302/0301-620X.69B3.3584193.
12. Smith DE, McGraw RW, Taylor DC, Masri BA. Arterial complications and total knee arthroplasty. J Am Acad Orthop Surg. 2001;9(4):253-257.
13. Zahrani HA, Cuschieri RJ. Vascular complications after total knee replacement. J Cardiovasc Surg (Torino). 1989;30(6):951-952.
14. Isiklar ZU, Landon GC, Tullos HS. Amputation after failed total knee arthroplasty. Clin Orthop Relat Res. 1994(299):173-178.
15. Wakankar HM, Nicholl JE, Koka R, D'Arcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 1999;81(1):30-33. doi: 10.1302/0301-620X.81B1.0810030.
16. Kumar SN, Chapman JA, Rawlins I. Vascular injuries in total knee arthroplasty. A review of the problem with special reference to the possible effects of the tourniquet. J Arthroplasty. 1998;13(2):211-216. doi: 10.1016/S0883-5403(98)90102-4.
17. DeLaurentis DA, Levitsky KA, Booth RE, et al. Arterial and ischemic aspects of total knee arthroplasty. Am J Surg. 1992;164(3):237-240. doi: 10.1016/S0002-9610(05)81078-5.
18. Langkamer VG. Local vascular complications after knee replacement: a review with illustrative case reports. Knee. 2001;8(4):259-264. doi: 10.1016/S0968-0160(01)00103-X.
19. Moran M, Hodgkinson J, Tait W. False aneurysm of the superior lateral geniculate artery following Total Knee Replacement. Knee. 2002;9(4):349-351. doi: 10.1016/S0968-0160(02)00061-3.
20. Pritsch T, Parnes N, Menachem A. A bleeding pseudoaneurysm of the lateral genicular artery after total knee arthroplasty--a case report. Acta Orthop. 2005;76(1):138-140. doi: 10.1080/00016470510030463.
21. Gaheer RS, Chirputkar K, Sarungi M. Spontaneous resolution of superior medial geniculate artery pseudoaneurysm following total knee arthroplasty. Knee. 2014;21(2):586-588. doi: 10.1016/j.knee.2012.10.021.
22. Law KY, Cheung KW, Chiu KH, Antonio GE. Pseudoaneurysm of the geniculate artery following total knee arthroplasty: a report of two cases. J Orthop Surg (Hong Kong). 2007;15(3):386-389. /doi: 10.1177/230949900701500331.
23. Noorpuri BS, Maxwell-Armstrong CA, Lamerton AJ. Pseudo-aneurysm of a geniculate collateral artery complicating total knee replacement. Eur J Vasc Endovasc Surg. 1999;18(6):534-535.
24. Pai VS. Traumatic aneurysm of the inferior lateral geniculate artery after total knee replacement. J Arthroplasty. 1999;14(5):633-634. doi: 10.1016/S0883-5403(99)90089-X.
25. Julien TP, Gravereaux E, Martin S. Superior medial geniculate artery pseudoaneurysm after primary total knee arthroplasty. J Arthroplasty. 2012;27(2):323 e313-326. doi: 10.1016/j.arth.2011.02.009.
26. Kalsi PS, Carrington RJ, Skinner JS. Therapeutic embolization for the treatment of recurrent hemarthrosis after total knee arthroplasty due to an arteriovenous fistula. J Arthroplasty. 2007;22(8):1223-1225. /doi: 10.1016/j.arth.2006.11.012.
27. Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB. Patellofemoral complications following total knee arthroplasty. Effect of a lateral release and sacrifice of the superior lateral geniculate artery. J Arthroplasty. 1996;11(4):368-372. doi: 10.1016/S0883-5403(96)80024-6.
28. Aldrich D, Anschuetz R, LoPresti C, Fumich M, Pitluk H, O'Brien W. Pseudoaneurysm complicating knee arthroscopy. Arthroscopy. 1995;11(2):229-230. doi: 10.1016/0749-8063(95)90073-X.
29. Sharma H, Singh GK, Cavanagh SP, Kay D. Pseudoaneurysm of the inferior medial geniculate artery following primary total knee arthroplasty: delayed presentation with recurrent haemorrhagic episodes. Knee Surg Sports Traumatol Arthrosc. 2006;14(2):153-155. doi: 10.1007/s00167-005-0639-4.
30. Abdel-Salam A, Eyres KS. Effects of tourniquet during total knee arthroplasty. A prospective randomised study. J Bone Joint Surg Br. 1995;77(2):250-253. doi: 10.1302/0301-620X.77B2.7706340.
31. Harvey EJ, Leclerc J, Brooks CE, Burke DL. Effect of tourniquet use on blood loss and incidence of deep vein thrombosis in total knee arthroplasty. J Arthroplasty. 1997;12(3):291-296. doi: 10.1016/S0883-5403(97)90025-5.
TAKE-HOME POINTS
- During total knee arthroscopy (TKA), 38% of patients will have an injury of a geniculate artery.
- The lateral inferior geniculate artery is most commonly injured, with a rate of injury of 31%.
- The middle geniculate artery is injured 15% of the time.
- The most common time of geniculate artery injury is during bone cutting or removal of the meniscus.
- There is no difference in rate of geniculate artery injury identification with or without the use of a tourniquet.
BAN2401 subanalyses attempt to ease concerns over study design and findings
BARCELONA – Alzheimer’s disease genetic risk status didn’t influence positive findings of the investigational monoclonal antibody, BAN2401, in a post hoc analysis of a phase 2 study’s secondary endpoint, Eisai said in a report released during the Clinical Trials on Alzheimer’s Disease conference.
In fact, according to the new analysis, the positive data presented last summer probably underestimated the molecule’s benefit to homozygous carriers of the apolipoprotein E epsilon-4 (APOE4), Chad Swanson, PhD, said at the meeting.
The new data cut was based on a small fraction of the 856 patients with early Alzheimer’s disease (AD) who were enrolled in Study 201: 10 APOE4 carriers and 69 noncarriers who completed 18 months on infusions of BAN2401 at 10 mg/kg biweekly, the only beneficial dose. The subanalysis determined that carriers benefited much more than did noncarriers on the three clinical measures, said Dr. Swanson, senior director of neurology clinical research at Eisai, and the study’s director:
- The Alzheimer’s Disease Composite Score (ADCOMS), a new measure of subtle cognitive changes in early disease: Carriers, 63% less decline than placebo vs. 7% less in noncarriers.
- Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog): Carriers, 84% less decline than placebo vs. 43% less in noncarriers.
- Clinical Dementia Rating-Sum of Boxes (CDR-SB): Carriers, 60% less decline than placebo vs. a 7% worsening in noncarriers.
To strengthen the power of the analysis, Dr. Swanson pooled data from the entire 18 months of both the 10 mg/kg biweekly and the next-highest dose (10 mg/kg monthly). This increased the numbers to 273 carriers and 141 noncarriers who had at least one exposure to the antibody.
He said this corrected the APOE4 imbalance and showed a 25% slowing of ADCOMS decline in carriers, a 6% slowing in noncarriers, and a 21% slowing overall, relative to placebo.
The somewhat counterintuitive findings took even copresenter Jeffrey L. Cummings, MD, by surprise.
“I would have hypothesized a greater effect in noncarriers than carriers, but that’s the great thing about data – they challenge our assumptions,” said Dr. Cummings, director of the Center for Neurodegeneration and Translational Neuroscience and director emeritus of the Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas and a consultant for both Eisai and Biogen, the company’s BAN2401 developmental partner. He postulated that APOE4-driven differences in plaque composition could have contributed to the observed benefit. “I think this also points to a very interesting biology that we don’t yet know. The plaque compactness is different, the distribution of diffuse plaques is different. This will bear a lot of additional analysis.”
Study 201 randomized patients with early Alzheimer’s to up to 18 months of treatment with placebo or infusions of BAN2401 at 2.5 mg/kg biweekly, 5 mg/kg monthly, 5 mg/kg biweekly, 10 mg/kg monthly, or 10 mg/kg biweekly. It had two unusual design features. First, patents were allocated to treatment arms by a Bayesian algorithm. The computer program examined results after every 50 enrollees and then allocated new subjects to what were, at that point, the most effective two doses. Additionally, the 18-month study was designed with a potential 12-month exit point, if computer modeling showed that it had at least an 80% probability of reaching at least a 25% cognitive benefit. In December, Eisai announced that the study hit just a 64% probability, missing the primary endpoint. But because Eisai felt the numbers were moving in the right direction, it continued with the additional 6 months of treatment, as allowed for in the study design, and then reanalyzed results with conventional statistics.
Thus, the successes reported at the Alzheimer’s Association International Conference in July and reanalyzed at CTAD, were secondary cognitive and functional outcomes.
Partway through the trial, a European regulatory body became alarmed at the rate of amyloid-related imaging abnormalities (ARIA) in the APOE4 carriers and excluded them from the highest-dose group. This meant that carriers comprised about 70%-80% of every unsuccessful treatment arm but just 29% of the successful one. The unbalanced randomization caused July’s skepticism. The CTAD subanalysis didn’t entirely alleviate it, and several acclaimed Alzheimer’s researchers gave it voice.
“You showed no difference in placebo rates of decline, but an increased benefit in the E4 carriers, which was really interesting,” said Reisa Sperling, MD, of Brigham and Women’s Hospital, Boston. “One difference in the E4 carriers was their rate of ARIA and how long they stayed in the study. How did you account for these issues in this analysis?”
“We didn’t specifically look at that kind of question,” Dr. Swanson said. “I think we feel that we actually see effects in both carriers and noncarriers, and we are still exploring the data and will keep looking through them to see what we can find.”
Gil Rabinovici, MD, also expressed some reservations.
“I agree that the post hoc analyses are encouraging, but I wouldn’t say they alleviate the concern when you have such a dramatic imbalance in a core feature of this disease, like APOE4 between the placebo and the high-dose group,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. “The people on this panel know far more than I do of the pitfalls of these kinds of analyses. We really need to see true randomization to put this issue to rest.”
Biomarkers support subanalysis finding
Dr. Swanson also presented new cerebrospinal fluid biomarker data showing changes in phosphorylated tau, neurogranin, and neurofilament light chain that support the overall 47% slowing of cognitive decline reported last summer. The 10 mg/kg biweekly and monthly groups were again combined to increase the sample size, but it remained quite small, with full data on 16 in the placebo group and 23 in the active group:
- Neurogranin, a synaptic protein that is a marker of neuronal damage, decreased by a median 58 pg/mL (11%), compared with a 13.5-pg/mL increase in the placebo group.
- Phosphorylated tau, a marker of tau pathology in the brain, decreased by a median 12 pg/mL (13%), compared with no change in the placebo group.
- Neurofilament light chain, a neuronal structural scaffold protein that is a marker of axonal degeneration, increased by a median 75 pg/mL in the active group, compared with a 156-pg/mL increase in the placebo group – a 48% difference.
The positive biomarker data bolstered the subanalysis to some extent, researchers felt. But in the end, Study 201 is just a first step for BAN2401, said Laurie Ryan, PhD, chief of the dementias of aging branch in the division of neuroscience at the National Institute on Aging.
“Today’s presentation gave us a new look at the trial data from the summer,” Dr. Ryan said in an interview. “The new analysis supports the findings previously released but is still preliminary. Nothing is definitive in a phase 2 study, so while it appears to suggest a potential positive, beneficial result, it needs further testing.”
Eisai has made its subanalysis presentation slides publicly available.
Dr. Swanson is an employee of Eisai. Dr. Cummings is a consultant for Eisai and Biogen. Dr. Sperling has consulted for numerous pharmaceutical companies. Dr. Rabinovici and Dr. Ryan have no disclosures.
SOURCE: Swanson C et al. CTAD, Symposium 3.
BARCELONA – Alzheimer’s disease genetic risk status didn’t influence positive findings of the investigational monoclonal antibody, BAN2401, in a post hoc analysis of a phase 2 study’s secondary endpoint, Eisai said in a report released during the Clinical Trials on Alzheimer’s Disease conference.
In fact, according to the new analysis, the positive data presented last summer probably underestimated the molecule’s benefit to homozygous carriers of the apolipoprotein E epsilon-4 (APOE4), Chad Swanson, PhD, said at the meeting.
The new data cut was based on a small fraction of the 856 patients with early Alzheimer’s disease (AD) who were enrolled in Study 201: 10 APOE4 carriers and 69 noncarriers who completed 18 months on infusions of BAN2401 at 10 mg/kg biweekly, the only beneficial dose. The subanalysis determined that carriers benefited much more than did noncarriers on the three clinical measures, said Dr. Swanson, senior director of neurology clinical research at Eisai, and the study’s director:
- The Alzheimer’s Disease Composite Score (ADCOMS), a new measure of subtle cognitive changes in early disease: Carriers, 63% less decline than placebo vs. 7% less in noncarriers.
- Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog): Carriers, 84% less decline than placebo vs. 43% less in noncarriers.
- Clinical Dementia Rating-Sum of Boxes (CDR-SB): Carriers, 60% less decline than placebo vs. a 7% worsening in noncarriers.
To strengthen the power of the analysis, Dr. Swanson pooled data from the entire 18 months of both the 10 mg/kg biweekly and the next-highest dose (10 mg/kg monthly). This increased the numbers to 273 carriers and 141 noncarriers who had at least one exposure to the antibody.
He said this corrected the APOE4 imbalance and showed a 25% slowing of ADCOMS decline in carriers, a 6% slowing in noncarriers, and a 21% slowing overall, relative to placebo.
The somewhat counterintuitive findings took even copresenter Jeffrey L. Cummings, MD, by surprise.
“I would have hypothesized a greater effect in noncarriers than carriers, but that’s the great thing about data – they challenge our assumptions,” said Dr. Cummings, director of the Center for Neurodegeneration and Translational Neuroscience and director emeritus of the Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas and a consultant for both Eisai and Biogen, the company’s BAN2401 developmental partner. He postulated that APOE4-driven differences in plaque composition could have contributed to the observed benefit. “I think this also points to a very interesting biology that we don’t yet know. The plaque compactness is different, the distribution of diffuse plaques is different. This will bear a lot of additional analysis.”
Study 201 randomized patients with early Alzheimer’s to up to 18 months of treatment with placebo or infusions of BAN2401 at 2.5 mg/kg biweekly, 5 mg/kg monthly, 5 mg/kg biweekly, 10 mg/kg monthly, or 10 mg/kg biweekly. It had two unusual design features. First, patents were allocated to treatment arms by a Bayesian algorithm. The computer program examined results after every 50 enrollees and then allocated new subjects to what were, at that point, the most effective two doses. Additionally, the 18-month study was designed with a potential 12-month exit point, if computer modeling showed that it had at least an 80% probability of reaching at least a 25% cognitive benefit. In December, Eisai announced that the study hit just a 64% probability, missing the primary endpoint. But because Eisai felt the numbers were moving in the right direction, it continued with the additional 6 months of treatment, as allowed for in the study design, and then reanalyzed results with conventional statistics.
Thus, the successes reported at the Alzheimer’s Association International Conference in July and reanalyzed at CTAD, were secondary cognitive and functional outcomes.
Partway through the trial, a European regulatory body became alarmed at the rate of amyloid-related imaging abnormalities (ARIA) in the APOE4 carriers and excluded them from the highest-dose group. This meant that carriers comprised about 70%-80% of every unsuccessful treatment arm but just 29% of the successful one. The unbalanced randomization caused July’s skepticism. The CTAD subanalysis didn’t entirely alleviate it, and several acclaimed Alzheimer’s researchers gave it voice.
“You showed no difference in placebo rates of decline, but an increased benefit in the E4 carriers, which was really interesting,” said Reisa Sperling, MD, of Brigham and Women’s Hospital, Boston. “One difference in the E4 carriers was their rate of ARIA and how long they stayed in the study. How did you account for these issues in this analysis?”
“We didn’t specifically look at that kind of question,” Dr. Swanson said. “I think we feel that we actually see effects in both carriers and noncarriers, and we are still exploring the data and will keep looking through them to see what we can find.”
Gil Rabinovici, MD, also expressed some reservations.
“I agree that the post hoc analyses are encouraging, but I wouldn’t say they alleviate the concern when you have such a dramatic imbalance in a core feature of this disease, like APOE4 between the placebo and the high-dose group,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. “The people on this panel know far more than I do of the pitfalls of these kinds of analyses. We really need to see true randomization to put this issue to rest.”
Biomarkers support subanalysis finding
Dr. Swanson also presented new cerebrospinal fluid biomarker data showing changes in phosphorylated tau, neurogranin, and neurofilament light chain that support the overall 47% slowing of cognitive decline reported last summer. The 10 mg/kg biweekly and monthly groups were again combined to increase the sample size, but it remained quite small, with full data on 16 in the placebo group and 23 in the active group:
- Neurogranin, a synaptic protein that is a marker of neuronal damage, decreased by a median 58 pg/mL (11%), compared with a 13.5-pg/mL increase in the placebo group.
- Phosphorylated tau, a marker of tau pathology in the brain, decreased by a median 12 pg/mL (13%), compared with no change in the placebo group.
- Neurofilament light chain, a neuronal structural scaffold protein that is a marker of axonal degeneration, increased by a median 75 pg/mL in the active group, compared with a 156-pg/mL increase in the placebo group – a 48% difference.
The positive biomarker data bolstered the subanalysis to some extent, researchers felt. But in the end, Study 201 is just a first step for BAN2401, said Laurie Ryan, PhD, chief of the dementias of aging branch in the division of neuroscience at the National Institute on Aging.
“Today’s presentation gave us a new look at the trial data from the summer,” Dr. Ryan said in an interview. “The new analysis supports the findings previously released but is still preliminary. Nothing is definitive in a phase 2 study, so while it appears to suggest a potential positive, beneficial result, it needs further testing.”
Eisai has made its subanalysis presentation slides publicly available.
Dr. Swanson is an employee of Eisai. Dr. Cummings is a consultant for Eisai and Biogen. Dr. Sperling has consulted for numerous pharmaceutical companies. Dr. Rabinovici and Dr. Ryan have no disclosures.
SOURCE: Swanson C et al. CTAD, Symposium 3.
BARCELONA – Alzheimer’s disease genetic risk status didn’t influence positive findings of the investigational monoclonal antibody, BAN2401, in a post hoc analysis of a phase 2 study’s secondary endpoint, Eisai said in a report released during the Clinical Trials on Alzheimer’s Disease conference.
In fact, according to the new analysis, the positive data presented last summer probably underestimated the molecule’s benefit to homozygous carriers of the apolipoprotein E epsilon-4 (APOE4), Chad Swanson, PhD, said at the meeting.
The new data cut was based on a small fraction of the 856 patients with early Alzheimer’s disease (AD) who were enrolled in Study 201: 10 APOE4 carriers and 69 noncarriers who completed 18 months on infusions of BAN2401 at 10 mg/kg biweekly, the only beneficial dose. The subanalysis determined that carriers benefited much more than did noncarriers on the three clinical measures, said Dr. Swanson, senior director of neurology clinical research at Eisai, and the study’s director:
- The Alzheimer’s Disease Composite Score (ADCOMS), a new measure of subtle cognitive changes in early disease: Carriers, 63% less decline than placebo vs. 7% less in noncarriers.
- Alzheimer’s Disease Assessment Scale-cognitive subscale (ADAS-Cog): Carriers, 84% less decline than placebo vs. 43% less in noncarriers.
- Clinical Dementia Rating-Sum of Boxes (CDR-SB): Carriers, 60% less decline than placebo vs. a 7% worsening in noncarriers.
To strengthen the power of the analysis, Dr. Swanson pooled data from the entire 18 months of both the 10 mg/kg biweekly and the next-highest dose (10 mg/kg monthly). This increased the numbers to 273 carriers and 141 noncarriers who had at least one exposure to the antibody.
He said this corrected the APOE4 imbalance and showed a 25% slowing of ADCOMS decline in carriers, a 6% slowing in noncarriers, and a 21% slowing overall, relative to placebo.
The somewhat counterintuitive findings took even copresenter Jeffrey L. Cummings, MD, by surprise.
“I would have hypothesized a greater effect in noncarriers than carriers, but that’s the great thing about data – they challenge our assumptions,” said Dr. Cummings, director of the Center for Neurodegeneration and Translational Neuroscience and director emeritus of the Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas and a consultant for both Eisai and Biogen, the company’s BAN2401 developmental partner. He postulated that APOE4-driven differences in plaque composition could have contributed to the observed benefit. “I think this also points to a very interesting biology that we don’t yet know. The plaque compactness is different, the distribution of diffuse plaques is different. This will bear a lot of additional analysis.”
Study 201 randomized patients with early Alzheimer’s to up to 18 months of treatment with placebo or infusions of BAN2401 at 2.5 mg/kg biweekly, 5 mg/kg monthly, 5 mg/kg biweekly, 10 mg/kg monthly, or 10 mg/kg biweekly. It had two unusual design features. First, patents were allocated to treatment arms by a Bayesian algorithm. The computer program examined results after every 50 enrollees and then allocated new subjects to what were, at that point, the most effective two doses. Additionally, the 18-month study was designed with a potential 12-month exit point, if computer modeling showed that it had at least an 80% probability of reaching at least a 25% cognitive benefit. In December, Eisai announced that the study hit just a 64% probability, missing the primary endpoint. But because Eisai felt the numbers were moving in the right direction, it continued with the additional 6 months of treatment, as allowed for in the study design, and then reanalyzed results with conventional statistics.
Thus, the successes reported at the Alzheimer’s Association International Conference in July and reanalyzed at CTAD, were secondary cognitive and functional outcomes.
Partway through the trial, a European regulatory body became alarmed at the rate of amyloid-related imaging abnormalities (ARIA) in the APOE4 carriers and excluded them from the highest-dose group. This meant that carriers comprised about 70%-80% of every unsuccessful treatment arm but just 29% of the successful one. The unbalanced randomization caused July’s skepticism. The CTAD subanalysis didn’t entirely alleviate it, and several acclaimed Alzheimer’s researchers gave it voice.
“You showed no difference in placebo rates of decline, but an increased benefit in the E4 carriers, which was really interesting,” said Reisa Sperling, MD, of Brigham and Women’s Hospital, Boston. “One difference in the E4 carriers was their rate of ARIA and how long they stayed in the study. How did you account for these issues in this analysis?”
“We didn’t specifically look at that kind of question,” Dr. Swanson said. “I think we feel that we actually see effects in both carriers and noncarriers, and we are still exploring the data and will keep looking through them to see what we can find.”
Gil Rabinovici, MD, also expressed some reservations.
“I agree that the post hoc analyses are encouraging, but I wouldn’t say they alleviate the concern when you have such a dramatic imbalance in a core feature of this disease, like APOE4 between the placebo and the high-dose group,” said Dr. Rabinovici, the Edward Fein and Pearl Landrith Endowed Professor in Memory & Aging at the University of California, San Francisco. “The people on this panel know far more than I do of the pitfalls of these kinds of analyses. We really need to see true randomization to put this issue to rest.”
Biomarkers support subanalysis finding
Dr. Swanson also presented new cerebrospinal fluid biomarker data showing changes in phosphorylated tau, neurogranin, and neurofilament light chain that support the overall 47% slowing of cognitive decline reported last summer. The 10 mg/kg biweekly and monthly groups were again combined to increase the sample size, but it remained quite small, with full data on 16 in the placebo group and 23 in the active group:
- Neurogranin, a synaptic protein that is a marker of neuronal damage, decreased by a median 58 pg/mL (11%), compared with a 13.5-pg/mL increase in the placebo group.
- Phosphorylated tau, a marker of tau pathology in the brain, decreased by a median 12 pg/mL (13%), compared with no change in the placebo group.
- Neurofilament light chain, a neuronal structural scaffold protein that is a marker of axonal degeneration, increased by a median 75 pg/mL in the active group, compared with a 156-pg/mL increase in the placebo group – a 48% difference.
The positive biomarker data bolstered the subanalysis to some extent, researchers felt. But in the end, Study 201 is just a first step for BAN2401, said Laurie Ryan, PhD, chief of the dementias of aging branch in the division of neuroscience at the National Institute on Aging.
“Today’s presentation gave us a new look at the trial data from the summer,” Dr. Ryan said in an interview. “The new analysis supports the findings previously released but is still preliminary. Nothing is definitive in a phase 2 study, so while it appears to suggest a potential positive, beneficial result, it needs further testing.”
Eisai has made its subanalysis presentation slides publicly available.
Dr. Swanson is an employee of Eisai. Dr. Cummings is a consultant for Eisai and Biogen. Dr. Sperling has consulted for numerous pharmaceutical companies. Dr. Rabinovici and Dr. Ryan have no disclosures.
SOURCE: Swanson C et al. CTAD, Symposium 3.
REPORTING FROM CTAD