User login
Medicare’s CAR T-cell coverage decision draws praise, but cost issues linger
Physicians are praising the decision by officials at the Centers for Medicare & Medicaid Services to provide coverage of chimeric antigen receptor T-cell therapy, though they say the planned payment structure will still leave hospitals in the red when treatment is administered.
On Aug. 7, 2019, the agency issued a national coverage determination that outlines Medicare coverage of chimeric antigen receptor (CAR) T-cell therapies when they are provided in health care facilities enrolled in the Food and Drug Administration’s Risk Evaluation and Mitigation Strategies program. Medicare will cover treatments for both FDA-approved indications and off-label uses that are recommended in CMS-approved compendia.
“What you’ve seen in both the [Medicare Inpatient Prospective Payment System] rule, as well as this coverage determination, is recognition by CMS that, with CAR T cells, we are dealing with something different and something extraordinary,” Joseph Alvarnas, MD, vice president of government affairs at City of Hope, Duarte, Calif., said in an interview. “For a lot of patients who suffer with non-Hodgkin’s lymphoma, the consequences of being refractory to standard therapies mean that many patients have few great prospects for moving forward with curative treatments. CAR T cells represent a really innovative set of treatments for patients.”
A proposed national coverage determination, issued in February 2019, would have put in place a coverage with evidence development (CED) requirement for CAR T-cell therapy, covering treatment nationwide if it was offered through CMS-approved registries or clinical studies in which patients were monitored for 2 or more years following treatment.
Physicians applauded the decision not to restrict access by imposing the CED requirement.
“I think what CMS has put out is a good thing,” said Navneet Majhail, MD, director of the Cleveland Clinic’s blood and marrow transplant program, and president of the American Society for Transplantation and Cellular Therapy.
“Both at the Cleveland Clinic level and the society level, we have been asking CMS for something similar and we are really glad and excited that CMS did do this. The concern was that CMS might do this in the context of some other regulatory requirements like CED that they sometimes do. I am glad that CMS decided not to put that mechanism into place for the CAR T-cell therapies,” Dr. Majhail said.
Dr. Alvarnas, who also serves as chair of the American Society of Hematology Committee on Practice, agreed. “I see good. I don’t see bad. I have read through this and it strikes me as being written with fairly great clarity.”
Dr. Alvarnas added that he had been worried about potential restrictions, such as CED. “Once you put something under that whole rubric of coverage with evidence development, then what you do is you create a bottleneck around access to therapy because you have to have an accruing clinical trial for patients to, in fact, be able to participate in that form of therapy.”
By not imposing a CED requirement, it opens the door to better understanding the role CAR T cells play in treatment, Dr. Alvarnas noted.
“Over time, the number of patients for whom these therapeutics work, based upon real medical evidence, will escalate and grow at a pace that can far exceed the restrictions placed under a CED model,” he said, adding that the national coverage determination “gives us the license to deliver therapeutics to the right patients based upon medical evidence as it evolves, provided that these things get listed as part of the compendia. I think that is a fantastic recognition that new roles for drugs, agents, therapeutics ... are going to evolve at a pace far faster than what CMS can write rules about.”
While Medicare’s coverage determination garnered positive reviews, the agency’s Inpatient Prospective Payment System final rule – which outlines reimbursement for CAR T-cell therapy and other new technologies – got a more tepid response.
In the final rule, CMS raised the payment it makes to hospitals for administering CAR T-cell therapies through its new technology add-on payment. Payments will rise from 50% of the technology to 65%, an increase from $186,500 to $242,450 for CAR T-cell therapies, beginning on Oct. 1, 2019.
But even the bump up to 65% may not be enough.
“I see the move to 65% as a new technology add-on payment as an incremental step in the correct direction, but what we’ve done to some extent is that we’ve delayed getting to some sort of more wholly conceived system,” Dr. Alvarnas said, noting that a new system will be needed as the new technology add-on payment goes away in 2021.
Abhinav Deol, MD, of the Karmanos Cancer Institute in Detroit said it’s a challenge to cover costs for the treatment. “If you just look at the simple math, it is still going to be an economic challenge. The cells that are approved for lymphoma patients that will probably fall into the Medicare category, the list price of those cells is $373,000. Even with the 65% coverage, it’s about $235,000-$240,000 in reimbursement,” he said. “For a facility to be able to provide the care for patients, you have that delta that is still not covered. It is still going to be an economic challenge for many of the facilities to provide this care.”
Thomas LeBlanc, MD, an associate professor of medicine at Duke University, Durham, N.C., said that, while the coverage determination is a positive step, it’s not clear that it will provide meaningful access to CAR T-cell therapy because of the cost.
“These products are incredibly expensive, and the total cost of providing them is woefully underestimated in only focusing on the sticker price of the product,” he said. “Doing so ignores the significant hospital care, sometimes even critical care, as well as specialized knowledge and high touch supportive care, all of which is required to safely get patients through this revolutionary yet often risky treatment. So when CMS offers to pay just 65% of the sticker price, I suspect that many institutions will still lose six figures for each patient treated.”
Dr. LeBlanc predicted that many centers will decline to provide CAR T-cell therapy despite the increase in the new technology add-on payment, though he added that “I’d love to be wrong about this.”
Dr. Majhail agreed, noting that, even with the bump in the add-on payment, hospitals “won’t be whole in terms of providing care for these patients.”
“The reimbursement piece continues to be a challenge,” he said. “It is better than what it was, but there is still more work to be done. That is something we will have to keep working with the agency on.”
Physicians are praising the decision by officials at the Centers for Medicare & Medicaid Services to provide coverage of chimeric antigen receptor T-cell therapy, though they say the planned payment structure will still leave hospitals in the red when treatment is administered.
On Aug. 7, 2019, the agency issued a national coverage determination that outlines Medicare coverage of chimeric antigen receptor (CAR) T-cell therapies when they are provided in health care facilities enrolled in the Food and Drug Administration’s Risk Evaluation and Mitigation Strategies program. Medicare will cover treatments for both FDA-approved indications and off-label uses that are recommended in CMS-approved compendia.
“What you’ve seen in both the [Medicare Inpatient Prospective Payment System] rule, as well as this coverage determination, is recognition by CMS that, with CAR T cells, we are dealing with something different and something extraordinary,” Joseph Alvarnas, MD, vice president of government affairs at City of Hope, Duarte, Calif., said in an interview. “For a lot of patients who suffer with non-Hodgkin’s lymphoma, the consequences of being refractory to standard therapies mean that many patients have few great prospects for moving forward with curative treatments. CAR T cells represent a really innovative set of treatments for patients.”
A proposed national coverage determination, issued in February 2019, would have put in place a coverage with evidence development (CED) requirement for CAR T-cell therapy, covering treatment nationwide if it was offered through CMS-approved registries or clinical studies in which patients were monitored for 2 or more years following treatment.
Physicians applauded the decision not to restrict access by imposing the CED requirement.
“I think what CMS has put out is a good thing,” said Navneet Majhail, MD, director of the Cleveland Clinic’s blood and marrow transplant program, and president of the American Society for Transplantation and Cellular Therapy.
“Both at the Cleveland Clinic level and the society level, we have been asking CMS for something similar and we are really glad and excited that CMS did do this. The concern was that CMS might do this in the context of some other regulatory requirements like CED that they sometimes do. I am glad that CMS decided not to put that mechanism into place for the CAR T-cell therapies,” Dr. Majhail said.
Dr. Alvarnas, who also serves as chair of the American Society of Hematology Committee on Practice, agreed. “I see good. I don’t see bad. I have read through this and it strikes me as being written with fairly great clarity.”
Dr. Alvarnas added that he had been worried about potential restrictions, such as CED. “Once you put something under that whole rubric of coverage with evidence development, then what you do is you create a bottleneck around access to therapy because you have to have an accruing clinical trial for patients to, in fact, be able to participate in that form of therapy.”
By not imposing a CED requirement, it opens the door to better understanding the role CAR T cells play in treatment, Dr. Alvarnas noted.
“Over time, the number of patients for whom these therapeutics work, based upon real medical evidence, will escalate and grow at a pace that can far exceed the restrictions placed under a CED model,” he said, adding that the national coverage determination “gives us the license to deliver therapeutics to the right patients based upon medical evidence as it evolves, provided that these things get listed as part of the compendia. I think that is a fantastic recognition that new roles for drugs, agents, therapeutics ... are going to evolve at a pace far faster than what CMS can write rules about.”
While Medicare’s coverage determination garnered positive reviews, the agency’s Inpatient Prospective Payment System final rule – which outlines reimbursement for CAR T-cell therapy and other new technologies – got a more tepid response.
In the final rule, CMS raised the payment it makes to hospitals for administering CAR T-cell therapies through its new technology add-on payment. Payments will rise from 50% of the technology to 65%, an increase from $186,500 to $242,450 for CAR T-cell therapies, beginning on Oct. 1, 2019.
But even the bump up to 65% may not be enough.
“I see the move to 65% as a new technology add-on payment as an incremental step in the correct direction, but what we’ve done to some extent is that we’ve delayed getting to some sort of more wholly conceived system,” Dr. Alvarnas said, noting that a new system will be needed as the new technology add-on payment goes away in 2021.
Abhinav Deol, MD, of the Karmanos Cancer Institute in Detroit said it’s a challenge to cover costs for the treatment. “If you just look at the simple math, it is still going to be an economic challenge. The cells that are approved for lymphoma patients that will probably fall into the Medicare category, the list price of those cells is $373,000. Even with the 65% coverage, it’s about $235,000-$240,000 in reimbursement,” he said. “For a facility to be able to provide the care for patients, you have that delta that is still not covered. It is still going to be an economic challenge for many of the facilities to provide this care.”
Thomas LeBlanc, MD, an associate professor of medicine at Duke University, Durham, N.C., said that, while the coverage determination is a positive step, it’s not clear that it will provide meaningful access to CAR T-cell therapy because of the cost.
“These products are incredibly expensive, and the total cost of providing them is woefully underestimated in only focusing on the sticker price of the product,” he said. “Doing so ignores the significant hospital care, sometimes even critical care, as well as specialized knowledge and high touch supportive care, all of which is required to safely get patients through this revolutionary yet often risky treatment. So when CMS offers to pay just 65% of the sticker price, I suspect that many institutions will still lose six figures for each patient treated.”
Dr. LeBlanc predicted that many centers will decline to provide CAR T-cell therapy despite the increase in the new technology add-on payment, though he added that “I’d love to be wrong about this.”
Dr. Majhail agreed, noting that, even with the bump in the add-on payment, hospitals “won’t be whole in terms of providing care for these patients.”
“The reimbursement piece continues to be a challenge,” he said. “It is better than what it was, but there is still more work to be done. That is something we will have to keep working with the agency on.”
Physicians are praising the decision by officials at the Centers for Medicare & Medicaid Services to provide coverage of chimeric antigen receptor T-cell therapy, though they say the planned payment structure will still leave hospitals in the red when treatment is administered.
On Aug. 7, 2019, the agency issued a national coverage determination that outlines Medicare coverage of chimeric antigen receptor (CAR) T-cell therapies when they are provided in health care facilities enrolled in the Food and Drug Administration’s Risk Evaluation and Mitigation Strategies program. Medicare will cover treatments for both FDA-approved indications and off-label uses that are recommended in CMS-approved compendia.
“What you’ve seen in both the [Medicare Inpatient Prospective Payment System] rule, as well as this coverage determination, is recognition by CMS that, with CAR T cells, we are dealing with something different and something extraordinary,” Joseph Alvarnas, MD, vice president of government affairs at City of Hope, Duarte, Calif., said in an interview. “For a lot of patients who suffer with non-Hodgkin’s lymphoma, the consequences of being refractory to standard therapies mean that many patients have few great prospects for moving forward with curative treatments. CAR T cells represent a really innovative set of treatments for patients.”
A proposed national coverage determination, issued in February 2019, would have put in place a coverage with evidence development (CED) requirement for CAR T-cell therapy, covering treatment nationwide if it was offered through CMS-approved registries or clinical studies in which patients were monitored for 2 or more years following treatment.
Physicians applauded the decision not to restrict access by imposing the CED requirement.
“I think what CMS has put out is a good thing,” said Navneet Majhail, MD, director of the Cleveland Clinic’s blood and marrow transplant program, and president of the American Society for Transplantation and Cellular Therapy.
“Both at the Cleveland Clinic level and the society level, we have been asking CMS for something similar and we are really glad and excited that CMS did do this. The concern was that CMS might do this in the context of some other regulatory requirements like CED that they sometimes do. I am glad that CMS decided not to put that mechanism into place for the CAR T-cell therapies,” Dr. Majhail said.
Dr. Alvarnas, who also serves as chair of the American Society of Hematology Committee on Practice, agreed. “I see good. I don’t see bad. I have read through this and it strikes me as being written with fairly great clarity.”
Dr. Alvarnas added that he had been worried about potential restrictions, such as CED. “Once you put something under that whole rubric of coverage with evidence development, then what you do is you create a bottleneck around access to therapy because you have to have an accruing clinical trial for patients to, in fact, be able to participate in that form of therapy.”
By not imposing a CED requirement, it opens the door to better understanding the role CAR T cells play in treatment, Dr. Alvarnas noted.
“Over time, the number of patients for whom these therapeutics work, based upon real medical evidence, will escalate and grow at a pace that can far exceed the restrictions placed under a CED model,” he said, adding that the national coverage determination “gives us the license to deliver therapeutics to the right patients based upon medical evidence as it evolves, provided that these things get listed as part of the compendia. I think that is a fantastic recognition that new roles for drugs, agents, therapeutics ... are going to evolve at a pace far faster than what CMS can write rules about.”
While Medicare’s coverage determination garnered positive reviews, the agency’s Inpatient Prospective Payment System final rule – which outlines reimbursement for CAR T-cell therapy and other new technologies – got a more tepid response.
In the final rule, CMS raised the payment it makes to hospitals for administering CAR T-cell therapies through its new technology add-on payment. Payments will rise from 50% of the technology to 65%, an increase from $186,500 to $242,450 for CAR T-cell therapies, beginning on Oct. 1, 2019.
But even the bump up to 65% may not be enough.
“I see the move to 65% as a new technology add-on payment as an incremental step in the correct direction, but what we’ve done to some extent is that we’ve delayed getting to some sort of more wholly conceived system,” Dr. Alvarnas said, noting that a new system will be needed as the new technology add-on payment goes away in 2021.
Abhinav Deol, MD, of the Karmanos Cancer Institute in Detroit said it’s a challenge to cover costs for the treatment. “If you just look at the simple math, it is still going to be an economic challenge. The cells that are approved for lymphoma patients that will probably fall into the Medicare category, the list price of those cells is $373,000. Even with the 65% coverage, it’s about $235,000-$240,000 in reimbursement,” he said. “For a facility to be able to provide the care for patients, you have that delta that is still not covered. It is still going to be an economic challenge for many of the facilities to provide this care.”
Thomas LeBlanc, MD, an associate professor of medicine at Duke University, Durham, N.C., said that, while the coverage determination is a positive step, it’s not clear that it will provide meaningful access to CAR T-cell therapy because of the cost.
“These products are incredibly expensive, and the total cost of providing them is woefully underestimated in only focusing on the sticker price of the product,” he said. “Doing so ignores the significant hospital care, sometimes even critical care, as well as specialized knowledge and high touch supportive care, all of which is required to safely get patients through this revolutionary yet often risky treatment. So when CMS offers to pay just 65% of the sticker price, I suspect that many institutions will still lose six figures for each patient treated.”
Dr. LeBlanc predicted that many centers will decline to provide CAR T-cell therapy despite the increase in the new technology add-on payment, though he added that “I’d love to be wrong about this.”
Dr. Majhail agreed, noting that, even with the bump in the add-on payment, hospitals “won’t be whole in terms of providing care for these patients.”
“The reimbursement piece continues to be a challenge,” he said. “It is better than what it was, but there is still more work to be done. That is something we will have to keep working with the agency on.”
Treatment of episodic cluster headache deviates from recommendations
PHILADELPHIA – , according to an analysis presented at the annual meeting of the American Headache Society.
Although consensus treatment guidelines do not exist for episodic cluster headache, treatment of this disorder did not follow many established recommendations that call for the use of preventive medications (e.g., MacGregor et al., 2010; Sarchielli et al., 2012; and May et al., 2006). Additional preventive medication options may be needed.
Patients with episodic cluster headache have several unilateral headache attacks per day. Little information is available to guide the selection of treatments for this population, and little is known about how available treatments are used in routine practice.
Analyzing cross-sectional survey data
To address this paucity of evidence, Jeffrey Scott Andrews, PharmD, a senior research scientist at Eli Lilly in Indianapolis, and colleagues examined data from the Adelphi 2017 Cluster Headache Disease Specific Programme, a large, international, cross-sectional survey. Physicians and patients in Germany, the United Kingdom, and the United States responded to the survey. Eligible physicians consulted with at least four patients with cluster headache per month, and eligible patients had a diagnosis of episodic cluster headache that was consistent with ICHD-3 beta criteria. Additional data were collected from all participants through questionnaires.
The analysis included 309 patients in Germany, 328 in the United Kingdom, and 375 in the United States. The average age of the patients was 40 years, and most of the patients were male. Less than 70% of patients reported working full time, which may indicate “the impact of this condition on work status,” said Dr. Andrews. Patients’ average number of attacks per day within an active period was 2.4. The two most commonly reported comorbidities were anxiety and depression. About 40% of cases of depression were reported to have occurred after the receipt of a diagnosis of cluster headache.
Use of inhaled oxygen was low
Most patients received acute treatments. The proportion of patients who received acute therapy only was 53% in Germany, 48% in the United Kingdom, and 43% in the United States. Approximately 34% of patients in Germany received a combination of acute and preventive therapy, compared with 37% in the United Kingdom and 42% in the United States. The proportion of patients who received preventive therapy only was 10% in Germany, 8% in the United Kingdom, and 12% in the United States.
The most commonly prescribed acute treatment, regardless of formulation, was sumatriptan. About 60% of patients received this medication. Less than one-third of patients used inhaled oxygen. Oxygen was prescribed more often in Germany (45%) and the United Kingdom (33%), compared with the United States (19%). U.S. patients face well-known obstacles in getting access to, and reimbursement for, oxygen, said Dr. Andrews. “That’s an area that deserves increased attention.” Zolmitriptan was the third most commonly prescribed acute medication.
Among prescriptions for sumatriptan, oral and injectable formulations were approximately equally common. Recommendations, however, indicate formulations with potentially fast onset of action. “The average duration of one of these attacks is between 15 and 180 minutes, so that certainly suggests that a formulation that gives you a faster onset of action might improve outcomes,” said Dr. Andrews. The use of injectable sumatriptan was lowest in the United States and highest in the United Kingdom.
“The most common decision regarding preventive treatment was [to give] no preventive treatment,” said Dr. Andrews. Verapamil was the most commonly prescribed preventive therapy (34% in Germany, 29% in the United States, and 25% in the United Kingdom), followed by topiramate, lithium, and valproate.
Nonadherence and noncompliance was common
Fewer U.K. patients (32%) reported taking their preventive therapy as advised, compared with German patients (60%) and U.S. patients (80%). Common reasons for noncompliance, regardless of location, were forgetfulness, the belief that a dose was not needed, and side effects. Most patients in the United Kingdom (60%) and the United States (54%) reported the need to take an extra dose of their acute medication to relieve pain symptoms, compared with 30% in Germany. Furthermore, 13% of U.S. patients indicated that they took extra doses all the time or nearly all the time, compared with 2% in Germany and 7% in the United Kingdom. Among patients who had discontinued a preventive treatment in the past, the most common reasons for discontinuation were lack of efficacy and problems with tolerability.
One limitation of the study was that the survey was not designed to represent the general cluster headache or treating physician populations fully. The data may reflect selection bias in favor of physicians who treat high volumes of patients and in favor of patients who frequently seek health care. In addition, the data were based on self-reports.
“Increased awareness and educational efforts that aim at promoting the need and benefit of the preventive treatment for these patients is warranted,” Dr. Andrews concluded.
Dr. Andrews is an employee of Eli Lilly, which funded the study.
SOURCE: Nichols R et al. AHS 2019. Abstract OR04.
PHILADELPHIA – , according to an analysis presented at the annual meeting of the American Headache Society.
Although consensus treatment guidelines do not exist for episodic cluster headache, treatment of this disorder did not follow many established recommendations that call for the use of preventive medications (e.g., MacGregor et al., 2010; Sarchielli et al., 2012; and May et al., 2006). Additional preventive medication options may be needed.
Patients with episodic cluster headache have several unilateral headache attacks per day. Little information is available to guide the selection of treatments for this population, and little is known about how available treatments are used in routine practice.
Analyzing cross-sectional survey data
To address this paucity of evidence, Jeffrey Scott Andrews, PharmD, a senior research scientist at Eli Lilly in Indianapolis, and colleagues examined data from the Adelphi 2017 Cluster Headache Disease Specific Programme, a large, international, cross-sectional survey. Physicians and patients in Germany, the United Kingdom, and the United States responded to the survey. Eligible physicians consulted with at least four patients with cluster headache per month, and eligible patients had a diagnosis of episodic cluster headache that was consistent with ICHD-3 beta criteria. Additional data were collected from all participants through questionnaires.
The analysis included 309 patients in Germany, 328 in the United Kingdom, and 375 in the United States. The average age of the patients was 40 years, and most of the patients were male. Less than 70% of patients reported working full time, which may indicate “the impact of this condition on work status,” said Dr. Andrews. Patients’ average number of attacks per day within an active period was 2.4. The two most commonly reported comorbidities were anxiety and depression. About 40% of cases of depression were reported to have occurred after the receipt of a diagnosis of cluster headache.
Use of inhaled oxygen was low
Most patients received acute treatments. The proportion of patients who received acute therapy only was 53% in Germany, 48% in the United Kingdom, and 43% in the United States. Approximately 34% of patients in Germany received a combination of acute and preventive therapy, compared with 37% in the United Kingdom and 42% in the United States. The proportion of patients who received preventive therapy only was 10% in Germany, 8% in the United Kingdom, and 12% in the United States.
The most commonly prescribed acute treatment, regardless of formulation, was sumatriptan. About 60% of patients received this medication. Less than one-third of patients used inhaled oxygen. Oxygen was prescribed more often in Germany (45%) and the United Kingdom (33%), compared with the United States (19%). U.S. patients face well-known obstacles in getting access to, and reimbursement for, oxygen, said Dr. Andrews. “That’s an area that deserves increased attention.” Zolmitriptan was the third most commonly prescribed acute medication.
Among prescriptions for sumatriptan, oral and injectable formulations were approximately equally common. Recommendations, however, indicate formulations with potentially fast onset of action. “The average duration of one of these attacks is between 15 and 180 minutes, so that certainly suggests that a formulation that gives you a faster onset of action might improve outcomes,” said Dr. Andrews. The use of injectable sumatriptan was lowest in the United States and highest in the United Kingdom.
“The most common decision regarding preventive treatment was [to give] no preventive treatment,” said Dr. Andrews. Verapamil was the most commonly prescribed preventive therapy (34% in Germany, 29% in the United States, and 25% in the United Kingdom), followed by topiramate, lithium, and valproate.
Nonadherence and noncompliance was common
Fewer U.K. patients (32%) reported taking their preventive therapy as advised, compared with German patients (60%) and U.S. patients (80%). Common reasons for noncompliance, regardless of location, were forgetfulness, the belief that a dose was not needed, and side effects. Most patients in the United Kingdom (60%) and the United States (54%) reported the need to take an extra dose of their acute medication to relieve pain symptoms, compared with 30% in Germany. Furthermore, 13% of U.S. patients indicated that they took extra doses all the time or nearly all the time, compared with 2% in Germany and 7% in the United Kingdom. Among patients who had discontinued a preventive treatment in the past, the most common reasons for discontinuation were lack of efficacy and problems with tolerability.
One limitation of the study was that the survey was not designed to represent the general cluster headache or treating physician populations fully. The data may reflect selection bias in favor of physicians who treat high volumes of patients and in favor of patients who frequently seek health care. In addition, the data were based on self-reports.
“Increased awareness and educational efforts that aim at promoting the need and benefit of the preventive treatment for these patients is warranted,” Dr. Andrews concluded.
Dr. Andrews is an employee of Eli Lilly, which funded the study.
SOURCE: Nichols R et al. AHS 2019. Abstract OR04.
PHILADELPHIA – , according to an analysis presented at the annual meeting of the American Headache Society.
Although consensus treatment guidelines do not exist for episodic cluster headache, treatment of this disorder did not follow many established recommendations that call for the use of preventive medications (e.g., MacGregor et al., 2010; Sarchielli et al., 2012; and May et al., 2006). Additional preventive medication options may be needed.
Patients with episodic cluster headache have several unilateral headache attacks per day. Little information is available to guide the selection of treatments for this population, and little is known about how available treatments are used in routine practice.
Analyzing cross-sectional survey data
To address this paucity of evidence, Jeffrey Scott Andrews, PharmD, a senior research scientist at Eli Lilly in Indianapolis, and colleagues examined data from the Adelphi 2017 Cluster Headache Disease Specific Programme, a large, international, cross-sectional survey. Physicians and patients in Germany, the United Kingdom, and the United States responded to the survey. Eligible physicians consulted with at least four patients with cluster headache per month, and eligible patients had a diagnosis of episodic cluster headache that was consistent with ICHD-3 beta criteria. Additional data were collected from all participants through questionnaires.
The analysis included 309 patients in Germany, 328 in the United Kingdom, and 375 in the United States. The average age of the patients was 40 years, and most of the patients were male. Less than 70% of patients reported working full time, which may indicate “the impact of this condition on work status,” said Dr. Andrews. Patients’ average number of attacks per day within an active period was 2.4. The two most commonly reported comorbidities were anxiety and depression. About 40% of cases of depression were reported to have occurred after the receipt of a diagnosis of cluster headache.
Use of inhaled oxygen was low
Most patients received acute treatments. The proportion of patients who received acute therapy only was 53% in Germany, 48% in the United Kingdom, and 43% in the United States. Approximately 34% of patients in Germany received a combination of acute and preventive therapy, compared with 37% in the United Kingdom and 42% in the United States. The proportion of patients who received preventive therapy only was 10% in Germany, 8% in the United Kingdom, and 12% in the United States.
The most commonly prescribed acute treatment, regardless of formulation, was sumatriptan. About 60% of patients received this medication. Less than one-third of patients used inhaled oxygen. Oxygen was prescribed more often in Germany (45%) and the United Kingdom (33%), compared with the United States (19%). U.S. patients face well-known obstacles in getting access to, and reimbursement for, oxygen, said Dr. Andrews. “That’s an area that deserves increased attention.” Zolmitriptan was the third most commonly prescribed acute medication.
Among prescriptions for sumatriptan, oral and injectable formulations were approximately equally common. Recommendations, however, indicate formulations with potentially fast onset of action. “The average duration of one of these attacks is between 15 and 180 minutes, so that certainly suggests that a formulation that gives you a faster onset of action might improve outcomes,” said Dr. Andrews. The use of injectable sumatriptan was lowest in the United States and highest in the United Kingdom.
“The most common decision regarding preventive treatment was [to give] no preventive treatment,” said Dr. Andrews. Verapamil was the most commonly prescribed preventive therapy (34% in Germany, 29% in the United States, and 25% in the United Kingdom), followed by topiramate, lithium, and valproate.
Nonadherence and noncompliance was common
Fewer U.K. patients (32%) reported taking their preventive therapy as advised, compared with German patients (60%) and U.S. patients (80%). Common reasons for noncompliance, regardless of location, were forgetfulness, the belief that a dose was not needed, and side effects. Most patients in the United Kingdom (60%) and the United States (54%) reported the need to take an extra dose of their acute medication to relieve pain symptoms, compared with 30% in Germany. Furthermore, 13% of U.S. patients indicated that they took extra doses all the time or nearly all the time, compared with 2% in Germany and 7% in the United Kingdom. Among patients who had discontinued a preventive treatment in the past, the most common reasons for discontinuation were lack of efficacy and problems with tolerability.
One limitation of the study was that the survey was not designed to represent the general cluster headache or treating physician populations fully. The data may reflect selection bias in favor of physicians who treat high volumes of patients and in favor of patients who frequently seek health care. In addition, the data were based on self-reports.
“Increased awareness and educational efforts that aim at promoting the need and benefit of the preventive treatment for these patients is warranted,” Dr. Andrews concluded.
Dr. Andrews is an employee of Eli Lilly, which funded the study.
SOURCE: Nichols R et al. AHS 2019. Abstract OR04.
REPORTING FROM AHS 2019
What is the future of celiac disease management?
CHICAGO – according to a lecture delivered at the 2019 James W. Freston Conference: Food at the Intersection of Gut Health and Disease.
Home testing services and portable gluten-detection devices enable patients to diagnose and manage themselves without medical supervision, but these strategies raise concerns about accuracy and efficacy, said Benjamin Lebwohl, MD, director of clinical research at the Celiac Disease Center at Columbia University in New York.
Potential treatments on the horizon
The gluten-free diet is the only treatment proven effective for celiac disease, but it can be expensive or unpalatable for some patients. The diet also entails risks of bowel irregularity and weight gain. “The gluten-free diet remains an inadequate treatment for many people with celiac disease,” said Dr. Lebwohl.
Tennyson et al. found that 66% of patients with biopsy-proven celiac disease are interested in nondietary therapy (Therap Adv Gastroenterol. 2013;6[5]:358-64.). Such patients are more likely to be male and older than 50 years.
Latiglutenase, a gluten enzyme derived from bacteria and cereal, is among the pharmacotherapies being investigated as a treatment for nonresponsive celiac disease. It reduces or eliminates the toxicity of gluten. In a recent phase 2b trial, however, the treatment did not achieve the primary outcome measure of histologic improvement (Gastroenterology. 2017;152[4]:787-98.). Compared with placebo, the drug was not associated with significant improvements in histologic and symptom scores.
Another drug in development is the tight-junction modulator larazotide acetate. Studies of zonula occludens toxin and its mammalian analogue zonulin led to the development of larazotide acetate. Leffler et al. found that a 0.5-mg dose of the drug reduced symptoms of nonresponsive celiac disease in patients who were following a gluten-free diet, compared with patients treated with the diet alone (Gastroenterology. 2015;148[7]:1311-9.). Innovate Pharmaceuticals plans to study the drug in phase 3 trials, said Dr. Lebwohl.
ImmunosanT has studied Nexvax2, which promotes gluten peptide desensitization. A phase 2 study examined the drug’s efficacy in reducing symptoms during a masked food challenge. The company discontinued this study when an interim analysis showed that the drug provided no more protection from gluten exposure than placebo. Nexvax2 was safe and well tolerated, and the study revealed no new safety signals.
In addition to newly developed therapies, researchers are studying whether drugs marketed for other indications could be effective treatments for celiac disease. For example, budesonide, a treatment for asthma and chronic obstructive pulmonary disease, is being investigated for nonresponsive celiac disease and refractory celiac disease. Other research is examining whether budesonide could provide effective protection after inadvertent gluten exposure. Systemic steroids, immunosuppressants such as azathioprine, chemotherapeutics such as cladribine, and mesalamine, which is a treatment for inflammatory bowel disease, also are under investigation.
But several questions related to drug development for celiac disease remain unanswered. For example, whether researchers should choose clinical or histologic endpoints for their trials is a subject of debate. “Probably, we’re going to be looking for two endpoints,” said Dr. Lebwohl. No consensus has been established about whether trials should include patients for whom diagnosis is based on a test other than a biopsy. Also, the effect of nondietary therapy on adherence to the gluten-free diet remains to be clarified.
Self-management of celiac disease
“We’re in a new era” of self-monitoring and direct-to-consumer advertising aimed at patients with celiac disease, said Dr. Lebwohl. Products and services that enable patients to diagnose and manage themselves independently are broadly available. For example, 23andMe provides at-home testing for HLA-DQ2.5 and HLA-DQ8, which could support a diagnosis of celiac disease. The service does not, however, test for HLA-DQ2.2, which is present in about 5% of patients with celiac disease. This testing consequently has high negative-predictive value, but poor positive-predictive value, said Dr. Lebwohl.
Similarly, ImAware provides blood tests that patients can take at home and send to the company for results. The tests look for antibodies such as tissue transglutaminase immunoglobulin A/immunoglobulin G and deamidated gliadin peptide IgA/IgG. The company advises patients to share their results with a health care professional.
Furthermore, portable devices such as Nima are marketed as gluten detectors. One study of the device included 804 users from all 50 states. The device found gluten in 32% of all restaurant food tested advertised as gluten-free. The interpretation of these results should take into account the fact that the device may detect gluten levels lower than 20 ppm, which generally are safe for patients with celiac disease. Furthermore, the data were uploaded voluntarily by users, and thus are not a random sample (Am J Gastroenterol. 2019;114[5]:792-7.). The device cannot detect certain forms of gluten such as barley malt. Because of limitations like these, the Nima device has “vocal critics,” said Dr. Lebwohl.
A profusion of books that offer dietary advice for patients with celiac disease also has become available. Data from Google Trends indicate that the popularity of the gluten-free diet spread from small pockets of the country in 2006 to most of the states in 2015.
Yet this “do-it-yourself” approach to celiac disease raises several concerns, said Dr. Lebwohl. Patients are at risk of interpreting their test results incorrectly, for example. Failing to consult a dietitian or physician, each of whom could have expertise in the field, entails risks as well. “Knowledgeable and empathetic care-giving is more important than ever,” Dr. Lebwohl concluded.
Dr. Lebwohl is on the medical advisory board of Innovate Biopharmaceuticals, a consultant for Takeda, and an unpaid advisor for the Nima Sensor.
CHICAGO – according to a lecture delivered at the 2019 James W. Freston Conference: Food at the Intersection of Gut Health and Disease.
Home testing services and portable gluten-detection devices enable patients to diagnose and manage themselves without medical supervision, but these strategies raise concerns about accuracy and efficacy, said Benjamin Lebwohl, MD, director of clinical research at the Celiac Disease Center at Columbia University in New York.
Potential treatments on the horizon
The gluten-free diet is the only treatment proven effective for celiac disease, but it can be expensive or unpalatable for some patients. The diet also entails risks of bowel irregularity and weight gain. “The gluten-free diet remains an inadequate treatment for many people with celiac disease,” said Dr. Lebwohl.
Tennyson et al. found that 66% of patients with biopsy-proven celiac disease are interested in nondietary therapy (Therap Adv Gastroenterol. 2013;6[5]:358-64.). Such patients are more likely to be male and older than 50 years.
Latiglutenase, a gluten enzyme derived from bacteria and cereal, is among the pharmacotherapies being investigated as a treatment for nonresponsive celiac disease. It reduces or eliminates the toxicity of gluten. In a recent phase 2b trial, however, the treatment did not achieve the primary outcome measure of histologic improvement (Gastroenterology. 2017;152[4]:787-98.). Compared with placebo, the drug was not associated with significant improvements in histologic and symptom scores.
Another drug in development is the tight-junction modulator larazotide acetate. Studies of zonula occludens toxin and its mammalian analogue zonulin led to the development of larazotide acetate. Leffler et al. found that a 0.5-mg dose of the drug reduced symptoms of nonresponsive celiac disease in patients who were following a gluten-free diet, compared with patients treated with the diet alone (Gastroenterology. 2015;148[7]:1311-9.). Innovate Pharmaceuticals plans to study the drug in phase 3 trials, said Dr. Lebwohl.
ImmunosanT has studied Nexvax2, which promotes gluten peptide desensitization. A phase 2 study examined the drug’s efficacy in reducing symptoms during a masked food challenge. The company discontinued this study when an interim analysis showed that the drug provided no more protection from gluten exposure than placebo. Nexvax2 was safe and well tolerated, and the study revealed no new safety signals.
In addition to newly developed therapies, researchers are studying whether drugs marketed for other indications could be effective treatments for celiac disease. For example, budesonide, a treatment for asthma and chronic obstructive pulmonary disease, is being investigated for nonresponsive celiac disease and refractory celiac disease. Other research is examining whether budesonide could provide effective protection after inadvertent gluten exposure. Systemic steroids, immunosuppressants such as azathioprine, chemotherapeutics such as cladribine, and mesalamine, which is a treatment for inflammatory bowel disease, also are under investigation.
But several questions related to drug development for celiac disease remain unanswered. For example, whether researchers should choose clinical or histologic endpoints for their trials is a subject of debate. “Probably, we’re going to be looking for two endpoints,” said Dr. Lebwohl. No consensus has been established about whether trials should include patients for whom diagnosis is based on a test other than a biopsy. Also, the effect of nondietary therapy on adherence to the gluten-free diet remains to be clarified.
Self-management of celiac disease
“We’re in a new era” of self-monitoring and direct-to-consumer advertising aimed at patients with celiac disease, said Dr. Lebwohl. Products and services that enable patients to diagnose and manage themselves independently are broadly available. For example, 23andMe provides at-home testing for HLA-DQ2.5 and HLA-DQ8, which could support a diagnosis of celiac disease. The service does not, however, test for HLA-DQ2.2, which is present in about 5% of patients with celiac disease. This testing consequently has high negative-predictive value, but poor positive-predictive value, said Dr. Lebwohl.
Similarly, ImAware provides blood tests that patients can take at home and send to the company for results. The tests look for antibodies such as tissue transglutaminase immunoglobulin A/immunoglobulin G and deamidated gliadin peptide IgA/IgG. The company advises patients to share their results with a health care professional.
Furthermore, portable devices such as Nima are marketed as gluten detectors. One study of the device included 804 users from all 50 states. The device found gluten in 32% of all restaurant food tested advertised as gluten-free. The interpretation of these results should take into account the fact that the device may detect gluten levels lower than 20 ppm, which generally are safe for patients with celiac disease. Furthermore, the data were uploaded voluntarily by users, and thus are not a random sample (Am J Gastroenterol. 2019;114[5]:792-7.). The device cannot detect certain forms of gluten such as barley malt. Because of limitations like these, the Nima device has “vocal critics,” said Dr. Lebwohl.
A profusion of books that offer dietary advice for patients with celiac disease also has become available. Data from Google Trends indicate that the popularity of the gluten-free diet spread from small pockets of the country in 2006 to most of the states in 2015.
Yet this “do-it-yourself” approach to celiac disease raises several concerns, said Dr. Lebwohl. Patients are at risk of interpreting their test results incorrectly, for example. Failing to consult a dietitian or physician, each of whom could have expertise in the field, entails risks as well. “Knowledgeable and empathetic care-giving is more important than ever,” Dr. Lebwohl concluded.
Dr. Lebwohl is on the medical advisory board of Innovate Biopharmaceuticals, a consultant for Takeda, and an unpaid advisor for the Nima Sensor.
CHICAGO – according to a lecture delivered at the 2019 James W. Freston Conference: Food at the Intersection of Gut Health and Disease.
Home testing services and portable gluten-detection devices enable patients to diagnose and manage themselves without medical supervision, but these strategies raise concerns about accuracy and efficacy, said Benjamin Lebwohl, MD, director of clinical research at the Celiac Disease Center at Columbia University in New York.
Potential treatments on the horizon
The gluten-free diet is the only treatment proven effective for celiac disease, but it can be expensive or unpalatable for some patients. The diet also entails risks of bowel irregularity and weight gain. “The gluten-free diet remains an inadequate treatment for many people with celiac disease,” said Dr. Lebwohl.
Tennyson et al. found that 66% of patients with biopsy-proven celiac disease are interested in nondietary therapy (Therap Adv Gastroenterol. 2013;6[5]:358-64.). Such patients are more likely to be male and older than 50 years.
Latiglutenase, a gluten enzyme derived from bacteria and cereal, is among the pharmacotherapies being investigated as a treatment for nonresponsive celiac disease. It reduces or eliminates the toxicity of gluten. In a recent phase 2b trial, however, the treatment did not achieve the primary outcome measure of histologic improvement (Gastroenterology. 2017;152[4]:787-98.). Compared with placebo, the drug was not associated with significant improvements in histologic and symptom scores.
Another drug in development is the tight-junction modulator larazotide acetate. Studies of zonula occludens toxin and its mammalian analogue zonulin led to the development of larazotide acetate. Leffler et al. found that a 0.5-mg dose of the drug reduced symptoms of nonresponsive celiac disease in patients who were following a gluten-free diet, compared with patients treated with the diet alone (Gastroenterology. 2015;148[7]:1311-9.). Innovate Pharmaceuticals plans to study the drug in phase 3 trials, said Dr. Lebwohl.
ImmunosanT has studied Nexvax2, which promotes gluten peptide desensitization. A phase 2 study examined the drug’s efficacy in reducing symptoms during a masked food challenge. The company discontinued this study when an interim analysis showed that the drug provided no more protection from gluten exposure than placebo. Nexvax2 was safe and well tolerated, and the study revealed no new safety signals.
In addition to newly developed therapies, researchers are studying whether drugs marketed for other indications could be effective treatments for celiac disease. For example, budesonide, a treatment for asthma and chronic obstructive pulmonary disease, is being investigated for nonresponsive celiac disease and refractory celiac disease. Other research is examining whether budesonide could provide effective protection after inadvertent gluten exposure. Systemic steroids, immunosuppressants such as azathioprine, chemotherapeutics such as cladribine, and mesalamine, which is a treatment for inflammatory bowel disease, also are under investigation.
But several questions related to drug development for celiac disease remain unanswered. For example, whether researchers should choose clinical or histologic endpoints for their trials is a subject of debate. “Probably, we’re going to be looking for two endpoints,” said Dr. Lebwohl. No consensus has been established about whether trials should include patients for whom diagnosis is based on a test other than a biopsy. Also, the effect of nondietary therapy on adherence to the gluten-free diet remains to be clarified.
Self-management of celiac disease
“We’re in a new era” of self-monitoring and direct-to-consumer advertising aimed at patients with celiac disease, said Dr. Lebwohl. Products and services that enable patients to diagnose and manage themselves independently are broadly available. For example, 23andMe provides at-home testing for HLA-DQ2.5 and HLA-DQ8, which could support a diagnosis of celiac disease. The service does not, however, test for HLA-DQ2.2, which is present in about 5% of patients with celiac disease. This testing consequently has high negative-predictive value, but poor positive-predictive value, said Dr. Lebwohl.
Similarly, ImAware provides blood tests that patients can take at home and send to the company for results. The tests look for antibodies such as tissue transglutaminase immunoglobulin A/immunoglobulin G and deamidated gliadin peptide IgA/IgG. The company advises patients to share their results with a health care professional.
Furthermore, portable devices such as Nima are marketed as gluten detectors. One study of the device included 804 users from all 50 states. The device found gluten in 32% of all restaurant food tested advertised as gluten-free. The interpretation of these results should take into account the fact that the device may detect gluten levels lower than 20 ppm, which generally are safe for patients with celiac disease. Furthermore, the data were uploaded voluntarily by users, and thus are not a random sample (Am J Gastroenterol. 2019;114[5]:792-7.). The device cannot detect certain forms of gluten such as barley malt. Because of limitations like these, the Nima device has “vocal critics,” said Dr. Lebwohl.
A profusion of books that offer dietary advice for patients with celiac disease also has become available. Data from Google Trends indicate that the popularity of the gluten-free diet spread from small pockets of the country in 2006 to most of the states in 2015.
Yet this “do-it-yourself” approach to celiac disease raises several concerns, said Dr. Lebwohl. Patients are at risk of interpreting their test results incorrectly, for example. Failing to consult a dietitian or physician, each of whom could have expertise in the field, entails risks as well. “Knowledgeable and empathetic care-giving is more important than ever,” Dr. Lebwohl concluded.
Dr. Lebwohl is on the medical advisory board of Innovate Biopharmaceuticals, a consultant for Takeda, and an unpaid advisor for the Nima Sensor.
EXPERT ANALYSIS FROM THE 2019 FRESTON CONFERENCE
Are rigid HPV vaccination schedules really necessary?
LJUBLJANA, SLOVENIA – Vladimir Gilca, MD, PhD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
This novel observation from a post hoc analysis of two clinical trials conducted by the same research team has important potential implications for both clinical practice and public health, according to Dr. Gilca of the Quebec National Institute of Public Health and Laval University, Quebec City.
“A less rigid immunization schedule might facilitate the coadministration of HPV vaccine with other vaccines, such as meningococcal or Tdap, and reduce the number of vaccination visits. Also, our data support the decision to offer only one dose in cases of vaccine shortage, like we have presently in many countries around the world, with the possibility of giving the second dose several years later when the shortage is resolved,” he said.
He presented a comparison of anti-HPV geometric mean IgG antibody titers and their distribution in two clinical trials with serologic assays performed in the same lab using the same enzyme-linked immunosorbent assay procedures. In the first study, 173 boys and girls aged 9-10 years received two doses of a 9-valent HPV vaccine 6 months apart. In the second trial, 31 girls were vaccinated with one dose of a quadrivalent HPV vaccine at age 9-14 years and then received a dose of the 9-valent vaccine at a mean of 5.4 years and maximum of 8 years later. Blood samples were obtained before and 1 month after the second dose in both trials.
Despite the enormous differences in the time between the first and second doses in the two studies, 100% of subjects in both trials were seropositive to HPV 6, 11, 16, and 18, with similar geometric mean titers and titer distributions before dose number two. Moreover, 1 month after the second dose, the geometric mean titers jumped 40-91 times in study participants with a 6-month dosing interval, and similarly by 60-82 times in those with the far lengthier interval. Titer distributions after the second dose were equivalent in the two studies.
Dr. Gilca and coinvestigators looked at subgroups who received their second dose 3-4 years, 6, or 7-8 years after the first. The time difference didn’t affect the distribution of antibodies.
“We conclude that delayed administration of the second dose has no negative impact on the magnitude of the immune response,” he declared.
There are abundant precedents for this phenomenon of high immunogenicity of delayed doses of vaccine. Rabies, anthrax, hepatitis A and B, and tick-borne encephalitis vaccines have all been shown to elicit at least a similar magnitude of immune response after delayed administration of a second or third dose, compared with dosing at the guideline-recommended intervals, he noted.
Asked about the possible approach of giving just one dose of HPV vaccine, as was supported based upon retrospective data in a high-profile presentation earlier at ESPID 2019, Dr. Gilca replied, “The data we’ve seen so far show clinical noninferiority between one, two, and three doses. An approach that might be used by at least some countries is to give, for example, one dose of HPV vaccine in grade 4 and to then wait for confirmatory data about the efficacy of one dose, which we expect in the next 4-5 years. At least five or six clinical trials are ongoing on one dose versus two or three doses.”
He reported having no financial conflicts of interest regarding his presentation.
SOURCE: Gilca V et al. ESPID 2019, Abstract.
LJUBLJANA, SLOVENIA – Vladimir Gilca, MD, PhD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
This novel observation from a post hoc analysis of two clinical trials conducted by the same research team has important potential implications for both clinical practice and public health, according to Dr. Gilca of the Quebec National Institute of Public Health and Laval University, Quebec City.
“A less rigid immunization schedule might facilitate the coadministration of HPV vaccine with other vaccines, such as meningococcal or Tdap, and reduce the number of vaccination visits. Also, our data support the decision to offer only one dose in cases of vaccine shortage, like we have presently in many countries around the world, with the possibility of giving the second dose several years later when the shortage is resolved,” he said.
He presented a comparison of anti-HPV geometric mean IgG antibody titers and their distribution in two clinical trials with serologic assays performed in the same lab using the same enzyme-linked immunosorbent assay procedures. In the first study, 173 boys and girls aged 9-10 years received two doses of a 9-valent HPV vaccine 6 months apart. In the second trial, 31 girls were vaccinated with one dose of a quadrivalent HPV vaccine at age 9-14 years and then received a dose of the 9-valent vaccine at a mean of 5.4 years and maximum of 8 years later. Blood samples were obtained before and 1 month after the second dose in both trials.
Despite the enormous differences in the time between the first and second doses in the two studies, 100% of subjects in both trials were seropositive to HPV 6, 11, 16, and 18, with similar geometric mean titers and titer distributions before dose number two. Moreover, 1 month after the second dose, the geometric mean titers jumped 40-91 times in study participants with a 6-month dosing interval, and similarly by 60-82 times in those with the far lengthier interval. Titer distributions after the second dose were equivalent in the two studies.
Dr. Gilca and coinvestigators looked at subgroups who received their second dose 3-4 years, 6, or 7-8 years after the first. The time difference didn’t affect the distribution of antibodies.
“We conclude that delayed administration of the second dose has no negative impact on the magnitude of the immune response,” he declared.
There are abundant precedents for this phenomenon of high immunogenicity of delayed doses of vaccine. Rabies, anthrax, hepatitis A and B, and tick-borne encephalitis vaccines have all been shown to elicit at least a similar magnitude of immune response after delayed administration of a second or third dose, compared with dosing at the guideline-recommended intervals, he noted.
Asked about the possible approach of giving just one dose of HPV vaccine, as was supported based upon retrospective data in a high-profile presentation earlier at ESPID 2019, Dr. Gilca replied, “The data we’ve seen so far show clinical noninferiority between one, two, and three doses. An approach that might be used by at least some countries is to give, for example, one dose of HPV vaccine in grade 4 and to then wait for confirmatory data about the efficacy of one dose, which we expect in the next 4-5 years. At least five or six clinical trials are ongoing on one dose versus two or three doses.”
He reported having no financial conflicts of interest regarding his presentation.
SOURCE: Gilca V et al. ESPID 2019, Abstract.
LJUBLJANA, SLOVENIA – Vladimir Gilca, MD, PhD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
This novel observation from a post hoc analysis of two clinical trials conducted by the same research team has important potential implications for both clinical practice and public health, according to Dr. Gilca of the Quebec National Institute of Public Health and Laval University, Quebec City.
“A less rigid immunization schedule might facilitate the coadministration of HPV vaccine with other vaccines, such as meningococcal or Tdap, and reduce the number of vaccination visits. Also, our data support the decision to offer only one dose in cases of vaccine shortage, like we have presently in many countries around the world, with the possibility of giving the second dose several years later when the shortage is resolved,” he said.
He presented a comparison of anti-HPV geometric mean IgG antibody titers and their distribution in two clinical trials with serologic assays performed in the same lab using the same enzyme-linked immunosorbent assay procedures. In the first study, 173 boys and girls aged 9-10 years received two doses of a 9-valent HPV vaccine 6 months apart. In the second trial, 31 girls were vaccinated with one dose of a quadrivalent HPV vaccine at age 9-14 years and then received a dose of the 9-valent vaccine at a mean of 5.4 years and maximum of 8 years later. Blood samples were obtained before and 1 month after the second dose in both trials.
Despite the enormous differences in the time between the first and second doses in the two studies, 100% of subjects in both trials were seropositive to HPV 6, 11, 16, and 18, with similar geometric mean titers and titer distributions before dose number two. Moreover, 1 month after the second dose, the geometric mean titers jumped 40-91 times in study participants with a 6-month dosing interval, and similarly by 60-82 times in those with the far lengthier interval. Titer distributions after the second dose were equivalent in the two studies.
Dr. Gilca and coinvestigators looked at subgroups who received their second dose 3-4 years, 6, or 7-8 years after the first. The time difference didn’t affect the distribution of antibodies.
“We conclude that delayed administration of the second dose has no negative impact on the magnitude of the immune response,” he declared.
There are abundant precedents for this phenomenon of high immunogenicity of delayed doses of vaccine. Rabies, anthrax, hepatitis A and B, and tick-borne encephalitis vaccines have all been shown to elicit at least a similar magnitude of immune response after delayed administration of a second or third dose, compared with dosing at the guideline-recommended intervals, he noted.
Asked about the possible approach of giving just one dose of HPV vaccine, as was supported based upon retrospective data in a high-profile presentation earlier at ESPID 2019, Dr. Gilca replied, “The data we’ve seen so far show clinical noninferiority between one, two, and three doses. An approach that might be used by at least some countries is to give, for example, one dose of HPV vaccine in grade 4 and to then wait for confirmatory data about the efficacy of one dose, which we expect in the next 4-5 years. At least five or six clinical trials are ongoing on one dose versus two or three doses.”
He reported having no financial conflicts of interest regarding his presentation.
SOURCE: Gilca V et al. ESPID 2019, Abstract.
REPORTING FROM ESPID 2019
Exposure to outdoor air pollutants linked to increased emphysema
Long-term exposure to ambient air pollutants was significantly associated with increases in emphysema and decreases in lung function, according to a diverse cohort study of six U.S. metropolitan areas.
“These associations in a community-based population demonstrate novel evidence that air pollution contributes to worsening lung health,” wrote Meng Wang, PhD, of the University of Washington, Seattle, and coauthors. The study was published in JAMA.
To determine whether exposure to outdoor air pollutants was associated with emphysema progression and change in lung function, the Multiethnic Study of Atherosclerosis (MESA) assessed 6,860 participants from six areas: Winston-Salem, N.C.; New York City; Baltimore; St. Paul, Minn.; Chicago; and Los Angeles. Percent emphysema was calculated based on all available CT scans; lung function was assessed via spirometry.
Spatiotemporal exposure models were developed for ozone, fine particulate matter less than 2.5 mcm in aerodynamic diameter, and oxides of nitrogen in each area based on Environmental Protection Agency measurements and the study’s cohort-specific monitoring. Annual mean concentrations of fine particulate matter and nitrogen decreased during follow-up, while ozone concentrations did not.
All participants underwent a cardiac CT scan at baseline, and 5,780 had at least one follow-up CT scan over a median period of 10 years. Ambient concentrations of ozone, fine particulate matter, nitrogen, and black carbon at baseline were significantly associated with greater increases in percent emphysema per 10 years, as were concentrations of zone and nitrogen during follow-up, reported Dr. Wang, formerly with the State University of New York at Buffalo.
Of the 3,636 participants who had at least one spirometric assessment, there was a mean decline in forced expiratory volume in 1 second (FEV1) of 309 mL (95% CI, 299-319 mL) and in forced vital capacity of 331 mL (95% CI, 317-345 mL) over 10 years. Ambient concentrations of ozone were significantly associated with a decline in FEV1, both at baseline and during follow-up.
The coauthors acknowledged their study’s limitations, including that general outdoor air pollution concentrations might not reflect individual exposure or concentrations indoors, where people spend most of their time. In addition, percent emphysema was only measured in the lower two-thirds of the lung, though they noted that “percent emphysema measured in the lower two-thirds of the lung correlates well with full-lung percent emphysema in this cohort and a cohort of smokers.”
This article was developed by the EPA and the University of Washington Center for Clean Air Research. MESA was funded by the National Institutes of Health and the National Heart, Lung, and Blood Institute, and supported by the National Institute of Environmental Health Sciences. The authors reported numerous conflicts of interest, including receiving grants and fees from the University of Washington, the EPA, the NIH, and various other pharmaceutical companies, foundations, and governmental entities.
SOURCE: Wang M et al. JAMA. 2019 Aug 13. doi: 10.1001/jama.2019.10255
Long-term exposure to ambient air pollutants was significantly associated with increases in emphysema and decreases in lung function, according to a diverse cohort study of six U.S. metropolitan areas.
“These associations in a community-based population demonstrate novel evidence that air pollution contributes to worsening lung health,” wrote Meng Wang, PhD, of the University of Washington, Seattle, and coauthors. The study was published in JAMA.
To determine whether exposure to outdoor air pollutants was associated with emphysema progression and change in lung function, the Multiethnic Study of Atherosclerosis (MESA) assessed 6,860 participants from six areas: Winston-Salem, N.C.; New York City; Baltimore; St. Paul, Minn.; Chicago; and Los Angeles. Percent emphysema was calculated based on all available CT scans; lung function was assessed via spirometry.
Spatiotemporal exposure models were developed for ozone, fine particulate matter less than 2.5 mcm in aerodynamic diameter, and oxides of nitrogen in each area based on Environmental Protection Agency measurements and the study’s cohort-specific monitoring. Annual mean concentrations of fine particulate matter and nitrogen decreased during follow-up, while ozone concentrations did not.
All participants underwent a cardiac CT scan at baseline, and 5,780 had at least one follow-up CT scan over a median period of 10 years. Ambient concentrations of ozone, fine particulate matter, nitrogen, and black carbon at baseline were significantly associated with greater increases in percent emphysema per 10 years, as were concentrations of zone and nitrogen during follow-up, reported Dr. Wang, formerly with the State University of New York at Buffalo.
Of the 3,636 participants who had at least one spirometric assessment, there was a mean decline in forced expiratory volume in 1 second (FEV1) of 309 mL (95% CI, 299-319 mL) and in forced vital capacity of 331 mL (95% CI, 317-345 mL) over 10 years. Ambient concentrations of ozone were significantly associated with a decline in FEV1, both at baseline and during follow-up.
The coauthors acknowledged their study’s limitations, including that general outdoor air pollution concentrations might not reflect individual exposure or concentrations indoors, where people spend most of their time. In addition, percent emphysema was only measured in the lower two-thirds of the lung, though they noted that “percent emphysema measured in the lower two-thirds of the lung correlates well with full-lung percent emphysema in this cohort and a cohort of smokers.”
This article was developed by the EPA and the University of Washington Center for Clean Air Research. MESA was funded by the National Institutes of Health and the National Heart, Lung, and Blood Institute, and supported by the National Institute of Environmental Health Sciences. The authors reported numerous conflicts of interest, including receiving grants and fees from the University of Washington, the EPA, the NIH, and various other pharmaceutical companies, foundations, and governmental entities.
SOURCE: Wang M et al. JAMA. 2019 Aug 13. doi: 10.1001/jama.2019.10255
Long-term exposure to ambient air pollutants was significantly associated with increases in emphysema and decreases in lung function, according to a diverse cohort study of six U.S. metropolitan areas.
“These associations in a community-based population demonstrate novel evidence that air pollution contributes to worsening lung health,” wrote Meng Wang, PhD, of the University of Washington, Seattle, and coauthors. The study was published in JAMA.
To determine whether exposure to outdoor air pollutants was associated with emphysema progression and change in lung function, the Multiethnic Study of Atherosclerosis (MESA) assessed 6,860 participants from six areas: Winston-Salem, N.C.; New York City; Baltimore; St. Paul, Minn.; Chicago; and Los Angeles. Percent emphysema was calculated based on all available CT scans; lung function was assessed via spirometry.
Spatiotemporal exposure models were developed for ozone, fine particulate matter less than 2.5 mcm in aerodynamic diameter, and oxides of nitrogen in each area based on Environmental Protection Agency measurements and the study’s cohort-specific monitoring. Annual mean concentrations of fine particulate matter and nitrogen decreased during follow-up, while ozone concentrations did not.
All participants underwent a cardiac CT scan at baseline, and 5,780 had at least one follow-up CT scan over a median period of 10 years. Ambient concentrations of ozone, fine particulate matter, nitrogen, and black carbon at baseline were significantly associated with greater increases in percent emphysema per 10 years, as were concentrations of zone and nitrogen during follow-up, reported Dr. Wang, formerly with the State University of New York at Buffalo.
Of the 3,636 participants who had at least one spirometric assessment, there was a mean decline in forced expiratory volume in 1 second (FEV1) of 309 mL (95% CI, 299-319 mL) and in forced vital capacity of 331 mL (95% CI, 317-345 mL) over 10 years. Ambient concentrations of ozone were significantly associated with a decline in FEV1, both at baseline and during follow-up.
The coauthors acknowledged their study’s limitations, including that general outdoor air pollution concentrations might not reflect individual exposure or concentrations indoors, where people spend most of their time. In addition, percent emphysema was only measured in the lower two-thirds of the lung, though they noted that “percent emphysema measured in the lower two-thirds of the lung correlates well with full-lung percent emphysema in this cohort and a cohort of smokers.”
This article was developed by the EPA and the University of Washington Center for Clean Air Research. MESA was funded by the National Institutes of Health and the National Heart, Lung, and Blood Institute, and supported by the National Institute of Environmental Health Sciences. The authors reported numerous conflicts of interest, including receiving grants and fees from the University of Washington, the EPA, the NIH, and various other pharmaceutical companies, foundations, and governmental entities.
SOURCE: Wang M et al. JAMA. 2019 Aug 13. doi: 10.1001/jama.2019.10255
FROM JAMA
The Impact of Diet on Psoriasis
Psoriasis is a chronic cutaneous disease associated with immune-mediated inflammation. The disease has a complex etiology, with factors such as genetics, smoking, alcohol use, diet, and stress all believed to be implicated in its appearance and severity. Specific factors, including increased body mass index and weight gain, have been associated with a higher prevalence of psoriasis and are risk factors for the disease. Because psoriasis varies in severity and incidence, patients often can experience a substantial negative impact on their quality of life, with increased incidences of anxiety and depression.1 Because diet is an accessible and controllable variable, many patients choose to alter their diets to help relieve symptoms of the disease. This article aims to review and summarize the existing literature for possible relationships and correlations between diet and psoriasis.
Because diet is a factor contributing to psoriasis, it is a lifestyle change that patients often make. In a 2017 survey of 1206 patients with psoriasis, 86% reported modifying their diets.2 Furthermore, when patients were compared with control individuals of the same sex and of similar age, it was shown that those with psoriasis consumed statistically significant lower amounts of sugar, whole-grain fiber, dairy products, and calcium (P<.001). The survey also found that patient diets included significantly more fruits, vegetables, and legumes (P<.01). Although no single diet was adhered to by patients, 40% did report attempting a specialized diet to improve their psoriasis. The most common diets were gluten free (35.6%), low carbohydrate/high protein (16.6%), and Paleolithic (11.6%). In addition to these diets, the Mediterranean diet and a vegetarian diet were both among those reported to improve psoriatic symptoms. Finally, certain foods stood out as more frequently reported to affect symptoms, particularly fish oil, fruits, vegetables, and water, which were all reported by at least 10% of respondents to positively affect their psoriasis. Reductions in consumption of alcohol, gluten, nightshades, and junk foods were associated with skin improvements in at least 50% of patients.2 These baseline differences in diet informed our search of the literature and showed that dietary changes can serve as an important adjunct to treatment for many patients.
Mediterranean Diet
The Mediterranean diet consists of a high amount of fruits, vegetables, nuts and legumes, cereals, and olive oil, while restricting consumption of red meats, dairy products, and alcohol (besides red wine) at meals.3 Adherence to the diet has been associated with a reduced risk for cardiovascular diseases,4 rheumatoid arthritis, and Crohn disease,3 among others, possibly because the diet contains a high proportion and variety of foods that contain antioxidants and anti-inflammatory compounds, including the monounsaturated fatty acids (MUFAs) in olive oil and the polyphenols in fruits and vegetables. Consumption of both MUFAs and highly anti-inflammatory nutrients has been associated with reduced prevalence of risk factors for chronic inflammatory diseases, and consumption levels of MUFAs in particular have been reported to be a predictive factor in psoriasis severity.3
Recent studies have tried to quantify an association between consumption of the Mediterranean diet and psoriasis. One cross-sectional study in 2015 evaluated 62 patients with psoriasis for their adherence to the Mediterranean diet and psoriasis severity.4 Utilizing a 14-question evaluation, the study found that patients with a higher severity of psoriasis, as evaluated by a psoriasis area and severity index (PASI) score and C-reactive protein levels, had a lower adherence to the diet. Notably, consumption of extra-virgin olive oil was found to be an independent predictor of PASI score, and consumption of fish was an independent predictor of C-reactive protein levels.4
A second cross-sectional questionnaire study found similar results in a larger population of 3557 patients. The same association between patients with severe psoriasis and low levels of adherence to the Mediterranean diet was reported.3 Although neither study showed a causal relationship between the diet and psoriasis severity, both did report the potential impacts of proinflammatory and anti-inflammatory foods. General foods and nutrients listed by the studies as having anti-inflammatory properties include MUFAs; fish; vitamins A, C, D, and E; and omega-3 fatty acids.3 Because of the large number of confounding factors in dietary studies that rely on questionnaires, it is hard to definitively label the Mediterranean diet as beneficial topsoriasis. However, individual components of the diet may be used as predictors of psoriasis severity, and the diet itself may be used in tandem with other treatments for psoriasis.
Gluten-Free Diet
Celiac disease is an inflammatory enteropathy caused by an immune reaction to the protein gliadin, which is found in foods containing gluten, such as wheat.5 Immune system assault on the intestinal enterocytes leads to the stripping away of villi, negatively affecting nutrient absorption. Multiple studies have reported an association between having psoriasis and having celiac disease as well as the reverse, including a 3-fold increased risk of celiac disease for patients with psoriasis in a 2017 meta-analysis.6 Even if patients with psoriasis did not have celiac disease, studies have found that a notable percentage of patients with psoriasis have elevated antigliadin IgA antibody levels.7 Many hypotheses have been proposed to explain this association. One article suggested that the malabsorption associated with celiac disease predisposes patients to vitamin D deficiency, which is a contributing risk factor for psoriasis.8 Other explanations involve common immune cells involved in the response to both diseases and a shared genetic background between the 2 diseases.8 As a gluten-free diet is standard for patients with celiac disease, it stands to reason that IgA could be used as a serum biomarker for patients who also could see improvements by adopting the diet.
This result could help explain the proportion of respondents to the 2017 survey who experienced improvements to their psoriasis if the gluten-free diet was in fact not triggering the inflammatory effects that a regular diet would, which also may help to explain the mixed results that the gluten-free diet has had as a treatment for psoriasis. One 3-month study of patients who were positive for antigliadin antibodies found that the majority (82%) experienced a decrease in antibody levels and affected skin area after following a gluten-free diet. Only half the patients had been diagnosed with celiac disease prior to the study, lending credibility to the idea that antigliadin antibody could be used as a marker for patients with psoriasis who would benefit from a gluten-free diet.9 Other case studies have reported no improvement of psoriasis following implementation of a gluten-free diet,10 despite the patients having elevated gliadin antibodies or celiac disease. More studies are required to discern the exact nature of the benefits of a gluten-free diet on psoriasis; however, it does serve as a promising option for patients with both psoriasis and celiac disease.
Ketogenic Diet
As obesity and weight gain are factors associated with psoriasis, some patients turn to diets that restrict calories with the goal of losing weight to improve their symptoms. One 2015 case report studied a patient who restored her response to systemic treatment of psoriasis following an intensive 4-week, calorie-restricted ketogenic diet.11 The ketogenic diet is a high-fat, adequate-protein, low-carbohydrate diet. Animal studies have shown the diet to have anti-inflammatory effects, including lowering levels of proinflammatory cytokines and reduced fever.12 In the 2015 case report, the rapid and consistent weight loss experienced by the patient because of the ketogenic diet was thought to be the cause of the restoration of treatment effectiveness,11 which is interesting, since the role of the ketogenic diet was not to supplement any deficiencies but to move the patient to a physiologic state that was once again receptive to treatment. This finding suggests that a variety of diets could improve psoriasis symptoms, so long as they do not cause inflammation or reduce overall body mass. One study of patients on a calorie-restricted diet over 8 weeks did see a trend of patients on the diet showing improvement in both their PASI scores and Dermatology Life Quality Index, though the improvement was not statistically significant.13 To determine if the ketogenic diet has a significant association with psoriasis improvement, controlled, large-population studies should be performed in the future with age, sex, and weight-matched controls, which may be difficult to do. Further studies looking at the association between weight loss and psoriasis also could be another direction.
Vegetarian Diet
Both vegetarian and vegan diets have been evaluated for their efficacy in relieving symptoms of chronic inflammatory disorders. Although the 2 diets are similar in avoiding consumption of meat, fish, and poultry, vegan diets often have additional food restrictions, including avoiding eggs, honey, and dairy products. One study noted the impact of these diets on patients with a variety of skin conditions following a period of fasting. It was observed that some patients with psoriasis saw an improvement in their symptoms during the period when they were eating a vegetarian or vegan diet, which was attributed to a return to normal levels of activity of neutrophils, extrapolated from serum levels of lactoferrin.14 Vegetarian diets have been shown to be associated with higher ratios of anti-inflammatory to proinflammatory adipokines compared to omnivorous diets,15 as well as lower expression levels of proinflammatory genes in the gut microbiota and lower expression levels of IgE.16 Perhaps the anti-inflammatory impacts of the diet affected the symptoms of psoriasis. The benefits of a vegetarian diet also have been attributed to the high amount of potassium consumed,17 which is used in the body to synthesize cortisol, a common treatment for psoriasis. Potassium supplementation has been shown to raise serum cortisol levels in patients.6 Although additional studies are needed to discern the significance of potassium in the vegetarian diet, both hypotheses are reasonable explanations for the observations seen in these studies.
Vitamin D and Other Nutritional Supplements
Because it is not always feasible for patients to alter their diets, many have turned to dietary supplements as an alternative method of treatment and lifestyle change. Two of the more prominently represented nutritional additives in the literature are fish oils and vitamin D.18 Supplemental vitamin D is a prohormone that can be endogenously converted to its active 1,25-dihydroxyvitamin D.19 Vitamin D plays important roles in the regulation of calcium and magnesium in the bones as well as the maturation and differentiation of keratinocytes in the skin.16 Topical vitamin D analogues are standard treatments for psoriasis, as they are used to modulate the immune system to great effect.20 Some patients with psoriasis present with vitamin D insufficiency,21 and it stands to reason that oral supplementation may be a treatment option. There have been multiple studies assessing the efficacy of oral vitamin D for the treatment of psoriasis; however, in the only randomized and placebo-controlled trial, there was only a slight nonsignificant improvement in the group supplemented with vitamin D.20 Another small, open-label study reported remarkably improved PASI scores in 9 vitamin D–supplemented, dietary calcium–restricted patients.22 The lack of recent, large-sample studies makes it hard to draw notable conclusions from these studies.
The polyunsaturated fatty acids found in fish oils also have been considered as a treatment option for psoriasis.23 Millsop et al20 conducted an analysis of the literature reviewing the efficacy of fish oil in the treatment of psoriasis. Twelve of 15 compiled trials showed an improvement in psoriasis, ranging from slight improvements from baseline levels of the disease to statistically significant decreases in PASI scores (P<.05). It is notable that the amount of fish oil given in these studies varied widely, but the amount given did not necessarily correlate with strength of impact.20 For example, Mayser et al,24 Bittiner et al,25 and Grimminger et al26 each performed prospective, double-blind studies with
Studies also have shown little to no improvement in the use of fish oil to treat psoriasis. One such study was conducted by Soyland et al27 in 1993 in Norway. Utilizing a prospective, double-blind, placebo-controlled design over 4 months on 145 patients with moderate to severe psoriasis, researchers evaluated the treatment effectiveness via PASI scores; subjective reports from the patients; clinical manifestations; and factors such as cellular infiltration, desquamation, and redness. The results were mixed, with the placebo (corn oil) group having less redness and cellular desquamation and the fish oil group showing less cellular infiltration. In the other categories, there was no significant difference between the 2 groups, and researchers concluded there was no significant benefit to treating psoriasis using fish oil vs corn oil.27 As with many of the other diets, there have been no recent, large-scale studies performed on the effect of fish oil supplementation on psoriasis; however, of the studies we reviewed, none showed fish oil supplementation to have a significant negative impact on psoriasis.
Conclusion
Dietary modifications have a complex multifactorial effect on psoriasis, often dependent on the variations of psoriasis and the lifestyle of the patient, including level of exercise, activities such as smoking and drinking, and genetic susceptibilities to conditions such as obesity. Thus, it is difficult for one diet to have a significant impact on psoriasis symptoms that applies to the majority of individuals. However, it appears that certain foods or nutritional supplements can be modified from all diets for general improvement. Foods with systemic anti-inflammatory effects, such as olive oil and fish oil, seem to be beneficial in treating psoriasis. As an extension, a gluten-free diet may help psoriasis patients with celiac disease by reducing the inflammatory environment of the body. On the opposite side of the spectrum, proinflammatory foods such as dietary fat and alcohol should be avoided.28
In general, larger and more recent population-based studies are needed to add to the literature on this subject. Nationwide voluntary web-based surveys such as the NutriNet-Santé study in France may be one way to quickly amass large quantities of data (ClinicalTrials.gov Identifier NCT03335644). Participants are recruited through multimedia campaigns and return online questionnaires annually for 1 decade. A subset of participants also contributes biologic samples and participates in clinical examinations. This type of data gathering would capture many variables, provide a large sample size, and perhaps shed light on regional differences in diet and lifestyle that could then be targeted with treatments.
- Madrid Álvarez MB, Carretero Hernández G, González Quesada A, et al. Measurement of the psychological impact of psoriasis on patients receiving systemic treatment. Actas Dermosifiliogr (English edition). 2018;109:733-740.
- Afifi L, Danesh MJ, Lee KM, et al. Dietary behaviors in psoriasis: patient-reported outcomes from a U.S. national survey. Dermatol Ther (Heidelb). 2017;7:227-242.
- Phan C, Touvier M, Kesse-Guyot E, et al. Association between Mediterranean anti-inflammatory dietary profile and severity of psoriasis: results from the NutriNet-Santé cohort. JAMA Dermatol. 2018;154:1017-1024.
- Barrea L, Balato N, Di Somma C, et al. Nutrition and psoriasis: is there any association between the severity of the disease and adherence to the Mediterranean diet? J Transl Med. 2015;13:18.
- Bhatia BK, Millsop JW, Debbaneh M, et al. Diet and psoriasis, part II: celiac disease and role of a gluten-free diet. J Am Acad Dermatol. 2014;71:350-358.
- Ungprasert P, Wijarnpreecha K, Kittanamongkolchai W. Psoriasis and risk of celiac disease: a systematic review and meta-analysis. Indian J Dermatol. 2017;62:41-46.
- Kolchak NA, Tetarnikova MK, Theodoropoulou MS, et al. Prevalence of antigliadin IgA antibodies in psoriasis vulgaris and response of seropositive patients to a gluten-free diet. J Multidiscip Healthc. 2017;11:13-19.
- Ludvigsson JF, Lindelöf B, Zingone F, et al. Psoriasis in a nationwide cohort study of patients with celiac disease. J Invest Dermatol. 2011;131:2010-2016.
- De Bastiani R, Gabrielli M, Lora L, et al. Association between coeliac disease and psoriasis: Italian primary care multicentre study. Dermatology. 2015;230:156-160.
- Pietrzak D, Pietrzak A, Krasowska D, et al. Digestive system in psoriasis: an update. Arch Dermatol Res. 2017;309:679-693.
- Castaldo G, Galdo G, Rotondi Aufiero F, et al. Very low-calorie ketogenic diet may allow restoring response to systemic therapy in relapsing plaque psoriasis [published online November 11, 2015]. Obes Res Clin Pract. 2016;10:348-352.
- Dupuis N, Curatolo N, Benoist J-F, et al. Ketogenic diet exhibits anti-inflammatory properties. Epilepsia. 2015;56:e95-e98.
- Jensen P, Zachariae C, Christensen R, et al. Effect of weight loss on the severity of psoriasis: a randomized clinical study. JAMA Dermatol. 2013;149:795-801.
- Lithell H, Bruce A, Gustafsson IB, et al. A fasting and vegetarian diet treatment trial on chronic inflammatory disorders. Acta Derm Venereol. 1983;63:397-403.
- Ambroszkiewicz J, Chełchowska M, Rowicka G, et al. Anti-inflammatory and pro-inflammatory adipokine profiles in children on vegetarian and omnivorous diets. Nutrients. 2018;10;pii E1241.
- Rastmanesh R. Psoriasis and vegetarian diets: a role for cortisol and potassium? Med Hypotheses. 2009;72:368.
- Zhang C, Björkman A, Cai K, et al. Impact of a 3-months vegetarian diet on the gut microbiota and immune repertoire. Front Immunol. 2018;9:908.
- Wolters M. Diet and psoriasis: experimental data and clinical evidence. Br J Dermatol. 2005;153:706-714.
- Zuccotti E, Oliveri M, Girometta C, et al. Nutritional strategies for psoriasis: current scientific evidence in clinical trials. Eur Rev Med Pharmacol Sci. 2018;22:8537-8551.
- Millsop JW, Bhatia BK, Debbaneh M, et al. Diet and psoriasis: part 3. role of nutritional supplements. J Am Acad Dermatol. 2014;71:561-569.
- El-Moaty Zaher HA, El-Komy MHM, Hegazy RA, et al. Assessment of interleukin-17 and vitamin D serum levels in psoriatic patients. J Am Acad Dermatol. 2013;69:840-842.
- Finamor DC, Sinigaglia-Coimbra R, Neves LCM, et al. A pilot study assessing the effect of prolonged administration of high daily doses of vitamin D on the clinical course of vitiligo and psoriasis. Dermatoendocrinol. 2013;5:222-234.
- Pona A, Haidari W, Kolli SS, et al. Diet and psoriasis. Dermatol Online J. 2019;25. https://escholarship.org/uc/item/1p37435s. Accessed April 14, 2019.
- Mayser P, Mrowietz U, Arenberger P, et al. ω-3 fatty acid–based lipid infusion in patients with chronic plaque psoriasis: results of a double-blind, randomized, placebo-controlled, multicenter trial. J Am Acad Dermatol. 1998;38:539-547.
- Bittiner SB, Tucker WF, Cartwright I, et al. A double-blind, randomised, placebo-controlled trial of fish oil in psoriasis. Lancet. 1988;1:378-380.
- Grimminger F, Mayser P, Papavassilis C, et al. A double-blind, randomized, placebo-controlled trial of n-3 fatty acid based lipid infusion in acute, extended guttate psoriasis: rapid improvement of clinical manifestations and changes in neutrophil leukotriene profile. Clin Investig. 1993;71:634-643.
- Soyland E, Funk J, Rajka G, et al. Effect of dietary supplementation with very-long-chain n-3 fatty acids in patients with psoriasis. N Engl J Med. 1993;328:1812-1816.
- Cunningham E. Is there research to support a specific diet for psoriasis? J Acad Nutr Diet. 2014;114:508.
Psoriasis is a chronic cutaneous disease associated with immune-mediated inflammation. The disease has a complex etiology, with factors such as genetics, smoking, alcohol use, diet, and stress all believed to be implicated in its appearance and severity. Specific factors, including increased body mass index and weight gain, have been associated with a higher prevalence of psoriasis and are risk factors for the disease. Because psoriasis varies in severity and incidence, patients often can experience a substantial negative impact on their quality of life, with increased incidences of anxiety and depression.1 Because diet is an accessible and controllable variable, many patients choose to alter their diets to help relieve symptoms of the disease. This article aims to review and summarize the existing literature for possible relationships and correlations between diet and psoriasis.
Because diet is a factor contributing to psoriasis, it is a lifestyle change that patients often make. In a 2017 survey of 1206 patients with psoriasis, 86% reported modifying their diets.2 Furthermore, when patients were compared with control individuals of the same sex and of similar age, it was shown that those with psoriasis consumed statistically significant lower amounts of sugar, whole-grain fiber, dairy products, and calcium (P<.001). The survey also found that patient diets included significantly more fruits, vegetables, and legumes (P<.01). Although no single diet was adhered to by patients, 40% did report attempting a specialized diet to improve their psoriasis. The most common diets were gluten free (35.6%), low carbohydrate/high protein (16.6%), and Paleolithic (11.6%). In addition to these diets, the Mediterranean diet and a vegetarian diet were both among those reported to improve psoriatic symptoms. Finally, certain foods stood out as more frequently reported to affect symptoms, particularly fish oil, fruits, vegetables, and water, which were all reported by at least 10% of respondents to positively affect their psoriasis. Reductions in consumption of alcohol, gluten, nightshades, and junk foods were associated with skin improvements in at least 50% of patients.2 These baseline differences in diet informed our search of the literature and showed that dietary changes can serve as an important adjunct to treatment for many patients.
Mediterranean Diet
The Mediterranean diet consists of a high amount of fruits, vegetables, nuts and legumes, cereals, and olive oil, while restricting consumption of red meats, dairy products, and alcohol (besides red wine) at meals.3 Adherence to the diet has been associated with a reduced risk for cardiovascular diseases,4 rheumatoid arthritis, and Crohn disease,3 among others, possibly because the diet contains a high proportion and variety of foods that contain antioxidants and anti-inflammatory compounds, including the monounsaturated fatty acids (MUFAs) in olive oil and the polyphenols in fruits and vegetables. Consumption of both MUFAs and highly anti-inflammatory nutrients has been associated with reduced prevalence of risk factors for chronic inflammatory diseases, and consumption levels of MUFAs in particular have been reported to be a predictive factor in psoriasis severity.3
Recent studies have tried to quantify an association between consumption of the Mediterranean diet and psoriasis. One cross-sectional study in 2015 evaluated 62 patients with psoriasis for their adherence to the Mediterranean diet and psoriasis severity.4 Utilizing a 14-question evaluation, the study found that patients with a higher severity of psoriasis, as evaluated by a psoriasis area and severity index (PASI) score and C-reactive protein levels, had a lower adherence to the diet. Notably, consumption of extra-virgin olive oil was found to be an independent predictor of PASI score, and consumption of fish was an independent predictor of C-reactive protein levels.4
A second cross-sectional questionnaire study found similar results in a larger population of 3557 patients. The same association between patients with severe psoriasis and low levels of adherence to the Mediterranean diet was reported.3 Although neither study showed a causal relationship between the diet and psoriasis severity, both did report the potential impacts of proinflammatory and anti-inflammatory foods. General foods and nutrients listed by the studies as having anti-inflammatory properties include MUFAs; fish; vitamins A, C, D, and E; and omega-3 fatty acids.3 Because of the large number of confounding factors in dietary studies that rely on questionnaires, it is hard to definitively label the Mediterranean diet as beneficial topsoriasis. However, individual components of the diet may be used as predictors of psoriasis severity, and the diet itself may be used in tandem with other treatments for psoriasis.
Gluten-Free Diet
Celiac disease is an inflammatory enteropathy caused by an immune reaction to the protein gliadin, which is found in foods containing gluten, such as wheat.5 Immune system assault on the intestinal enterocytes leads to the stripping away of villi, negatively affecting nutrient absorption. Multiple studies have reported an association between having psoriasis and having celiac disease as well as the reverse, including a 3-fold increased risk of celiac disease for patients with psoriasis in a 2017 meta-analysis.6 Even if patients with psoriasis did not have celiac disease, studies have found that a notable percentage of patients with psoriasis have elevated antigliadin IgA antibody levels.7 Many hypotheses have been proposed to explain this association. One article suggested that the malabsorption associated with celiac disease predisposes patients to vitamin D deficiency, which is a contributing risk factor for psoriasis.8 Other explanations involve common immune cells involved in the response to both diseases and a shared genetic background between the 2 diseases.8 As a gluten-free diet is standard for patients with celiac disease, it stands to reason that IgA could be used as a serum biomarker for patients who also could see improvements by adopting the diet.
This result could help explain the proportion of respondents to the 2017 survey who experienced improvements to their psoriasis if the gluten-free diet was in fact not triggering the inflammatory effects that a regular diet would, which also may help to explain the mixed results that the gluten-free diet has had as a treatment for psoriasis. One 3-month study of patients who were positive for antigliadin antibodies found that the majority (82%) experienced a decrease in antibody levels and affected skin area after following a gluten-free diet. Only half the patients had been diagnosed with celiac disease prior to the study, lending credibility to the idea that antigliadin antibody could be used as a marker for patients with psoriasis who would benefit from a gluten-free diet.9 Other case studies have reported no improvement of psoriasis following implementation of a gluten-free diet,10 despite the patients having elevated gliadin antibodies or celiac disease. More studies are required to discern the exact nature of the benefits of a gluten-free diet on psoriasis; however, it does serve as a promising option for patients with both psoriasis and celiac disease.
Ketogenic Diet
As obesity and weight gain are factors associated with psoriasis, some patients turn to diets that restrict calories with the goal of losing weight to improve their symptoms. One 2015 case report studied a patient who restored her response to systemic treatment of psoriasis following an intensive 4-week, calorie-restricted ketogenic diet.11 The ketogenic diet is a high-fat, adequate-protein, low-carbohydrate diet. Animal studies have shown the diet to have anti-inflammatory effects, including lowering levels of proinflammatory cytokines and reduced fever.12 In the 2015 case report, the rapid and consistent weight loss experienced by the patient because of the ketogenic diet was thought to be the cause of the restoration of treatment effectiveness,11 which is interesting, since the role of the ketogenic diet was not to supplement any deficiencies but to move the patient to a physiologic state that was once again receptive to treatment. This finding suggests that a variety of diets could improve psoriasis symptoms, so long as they do not cause inflammation or reduce overall body mass. One study of patients on a calorie-restricted diet over 8 weeks did see a trend of patients on the diet showing improvement in both their PASI scores and Dermatology Life Quality Index, though the improvement was not statistically significant.13 To determine if the ketogenic diet has a significant association with psoriasis improvement, controlled, large-population studies should be performed in the future with age, sex, and weight-matched controls, which may be difficult to do. Further studies looking at the association between weight loss and psoriasis also could be another direction.
Vegetarian Diet
Both vegetarian and vegan diets have been evaluated for their efficacy in relieving symptoms of chronic inflammatory disorders. Although the 2 diets are similar in avoiding consumption of meat, fish, and poultry, vegan diets often have additional food restrictions, including avoiding eggs, honey, and dairy products. One study noted the impact of these diets on patients with a variety of skin conditions following a period of fasting. It was observed that some patients with psoriasis saw an improvement in their symptoms during the period when they were eating a vegetarian or vegan diet, which was attributed to a return to normal levels of activity of neutrophils, extrapolated from serum levels of lactoferrin.14 Vegetarian diets have been shown to be associated with higher ratios of anti-inflammatory to proinflammatory adipokines compared to omnivorous diets,15 as well as lower expression levels of proinflammatory genes in the gut microbiota and lower expression levels of IgE.16 Perhaps the anti-inflammatory impacts of the diet affected the symptoms of psoriasis. The benefits of a vegetarian diet also have been attributed to the high amount of potassium consumed,17 which is used in the body to synthesize cortisol, a common treatment for psoriasis. Potassium supplementation has been shown to raise serum cortisol levels in patients.6 Although additional studies are needed to discern the significance of potassium in the vegetarian diet, both hypotheses are reasonable explanations for the observations seen in these studies.
Vitamin D and Other Nutritional Supplements
Because it is not always feasible for patients to alter their diets, many have turned to dietary supplements as an alternative method of treatment and lifestyle change. Two of the more prominently represented nutritional additives in the literature are fish oils and vitamin D.18 Supplemental vitamin D is a prohormone that can be endogenously converted to its active 1,25-dihydroxyvitamin D.19 Vitamin D plays important roles in the regulation of calcium and magnesium in the bones as well as the maturation and differentiation of keratinocytes in the skin.16 Topical vitamin D analogues are standard treatments for psoriasis, as they are used to modulate the immune system to great effect.20 Some patients with psoriasis present with vitamin D insufficiency,21 and it stands to reason that oral supplementation may be a treatment option. There have been multiple studies assessing the efficacy of oral vitamin D for the treatment of psoriasis; however, in the only randomized and placebo-controlled trial, there was only a slight nonsignificant improvement in the group supplemented with vitamin D.20 Another small, open-label study reported remarkably improved PASI scores in 9 vitamin D–supplemented, dietary calcium–restricted patients.22 The lack of recent, large-sample studies makes it hard to draw notable conclusions from these studies.
The polyunsaturated fatty acids found in fish oils also have been considered as a treatment option for psoriasis.23 Millsop et al20 conducted an analysis of the literature reviewing the efficacy of fish oil in the treatment of psoriasis. Twelve of 15 compiled trials showed an improvement in psoriasis, ranging from slight improvements from baseline levels of the disease to statistically significant decreases in PASI scores (P<.05). It is notable that the amount of fish oil given in these studies varied widely, but the amount given did not necessarily correlate with strength of impact.20 For example, Mayser et al,24 Bittiner et al,25 and Grimminger et al26 each performed prospective, double-blind studies with
Studies also have shown little to no improvement in the use of fish oil to treat psoriasis. One such study was conducted by Soyland et al27 in 1993 in Norway. Utilizing a prospective, double-blind, placebo-controlled design over 4 months on 145 patients with moderate to severe psoriasis, researchers evaluated the treatment effectiveness via PASI scores; subjective reports from the patients; clinical manifestations; and factors such as cellular infiltration, desquamation, and redness. The results were mixed, with the placebo (corn oil) group having less redness and cellular desquamation and the fish oil group showing less cellular infiltration. In the other categories, there was no significant difference between the 2 groups, and researchers concluded there was no significant benefit to treating psoriasis using fish oil vs corn oil.27 As with many of the other diets, there have been no recent, large-scale studies performed on the effect of fish oil supplementation on psoriasis; however, of the studies we reviewed, none showed fish oil supplementation to have a significant negative impact on psoriasis.
Conclusion
Dietary modifications have a complex multifactorial effect on psoriasis, often dependent on the variations of psoriasis and the lifestyle of the patient, including level of exercise, activities such as smoking and drinking, and genetic susceptibilities to conditions such as obesity. Thus, it is difficult for one diet to have a significant impact on psoriasis symptoms that applies to the majority of individuals. However, it appears that certain foods or nutritional supplements can be modified from all diets for general improvement. Foods with systemic anti-inflammatory effects, such as olive oil and fish oil, seem to be beneficial in treating psoriasis. As an extension, a gluten-free diet may help psoriasis patients with celiac disease by reducing the inflammatory environment of the body. On the opposite side of the spectrum, proinflammatory foods such as dietary fat and alcohol should be avoided.28
In general, larger and more recent population-based studies are needed to add to the literature on this subject. Nationwide voluntary web-based surveys such as the NutriNet-Santé study in France may be one way to quickly amass large quantities of data (ClinicalTrials.gov Identifier NCT03335644). Participants are recruited through multimedia campaigns and return online questionnaires annually for 1 decade. A subset of participants also contributes biologic samples and participates in clinical examinations. This type of data gathering would capture many variables, provide a large sample size, and perhaps shed light on regional differences in diet and lifestyle that could then be targeted with treatments.
Psoriasis is a chronic cutaneous disease associated with immune-mediated inflammation. The disease has a complex etiology, with factors such as genetics, smoking, alcohol use, diet, and stress all believed to be implicated in its appearance and severity. Specific factors, including increased body mass index and weight gain, have been associated with a higher prevalence of psoriasis and are risk factors for the disease. Because psoriasis varies in severity and incidence, patients often can experience a substantial negative impact on their quality of life, with increased incidences of anxiety and depression.1 Because diet is an accessible and controllable variable, many patients choose to alter their diets to help relieve symptoms of the disease. This article aims to review and summarize the existing literature for possible relationships and correlations between diet and psoriasis.
Because diet is a factor contributing to psoriasis, it is a lifestyle change that patients often make. In a 2017 survey of 1206 patients with psoriasis, 86% reported modifying their diets.2 Furthermore, when patients were compared with control individuals of the same sex and of similar age, it was shown that those with psoriasis consumed statistically significant lower amounts of sugar, whole-grain fiber, dairy products, and calcium (P<.001). The survey also found that patient diets included significantly more fruits, vegetables, and legumes (P<.01). Although no single diet was adhered to by patients, 40% did report attempting a specialized diet to improve their psoriasis. The most common diets were gluten free (35.6%), low carbohydrate/high protein (16.6%), and Paleolithic (11.6%). In addition to these diets, the Mediterranean diet and a vegetarian diet were both among those reported to improve psoriatic symptoms. Finally, certain foods stood out as more frequently reported to affect symptoms, particularly fish oil, fruits, vegetables, and water, which were all reported by at least 10% of respondents to positively affect their psoriasis. Reductions in consumption of alcohol, gluten, nightshades, and junk foods were associated with skin improvements in at least 50% of patients.2 These baseline differences in diet informed our search of the literature and showed that dietary changes can serve as an important adjunct to treatment for many patients.
Mediterranean Diet
The Mediterranean diet consists of a high amount of fruits, vegetables, nuts and legumes, cereals, and olive oil, while restricting consumption of red meats, dairy products, and alcohol (besides red wine) at meals.3 Adherence to the diet has been associated with a reduced risk for cardiovascular diseases,4 rheumatoid arthritis, and Crohn disease,3 among others, possibly because the diet contains a high proportion and variety of foods that contain antioxidants and anti-inflammatory compounds, including the monounsaturated fatty acids (MUFAs) in olive oil and the polyphenols in fruits and vegetables. Consumption of both MUFAs and highly anti-inflammatory nutrients has been associated with reduced prevalence of risk factors for chronic inflammatory diseases, and consumption levels of MUFAs in particular have been reported to be a predictive factor in psoriasis severity.3
Recent studies have tried to quantify an association between consumption of the Mediterranean diet and psoriasis. One cross-sectional study in 2015 evaluated 62 patients with psoriasis for their adherence to the Mediterranean diet and psoriasis severity.4 Utilizing a 14-question evaluation, the study found that patients with a higher severity of psoriasis, as evaluated by a psoriasis area and severity index (PASI) score and C-reactive protein levels, had a lower adherence to the diet. Notably, consumption of extra-virgin olive oil was found to be an independent predictor of PASI score, and consumption of fish was an independent predictor of C-reactive protein levels.4
A second cross-sectional questionnaire study found similar results in a larger population of 3557 patients. The same association between patients with severe psoriasis and low levels of adherence to the Mediterranean diet was reported.3 Although neither study showed a causal relationship between the diet and psoriasis severity, both did report the potential impacts of proinflammatory and anti-inflammatory foods. General foods and nutrients listed by the studies as having anti-inflammatory properties include MUFAs; fish; vitamins A, C, D, and E; and omega-3 fatty acids.3 Because of the large number of confounding factors in dietary studies that rely on questionnaires, it is hard to definitively label the Mediterranean diet as beneficial topsoriasis. However, individual components of the diet may be used as predictors of psoriasis severity, and the diet itself may be used in tandem with other treatments for psoriasis.
Gluten-Free Diet
Celiac disease is an inflammatory enteropathy caused by an immune reaction to the protein gliadin, which is found in foods containing gluten, such as wheat.5 Immune system assault on the intestinal enterocytes leads to the stripping away of villi, negatively affecting nutrient absorption. Multiple studies have reported an association between having psoriasis and having celiac disease as well as the reverse, including a 3-fold increased risk of celiac disease for patients with psoriasis in a 2017 meta-analysis.6 Even if patients with psoriasis did not have celiac disease, studies have found that a notable percentage of patients with psoriasis have elevated antigliadin IgA antibody levels.7 Many hypotheses have been proposed to explain this association. One article suggested that the malabsorption associated with celiac disease predisposes patients to vitamin D deficiency, which is a contributing risk factor for psoriasis.8 Other explanations involve common immune cells involved in the response to both diseases and a shared genetic background between the 2 diseases.8 As a gluten-free diet is standard for patients with celiac disease, it stands to reason that IgA could be used as a serum biomarker for patients who also could see improvements by adopting the diet.
This result could help explain the proportion of respondents to the 2017 survey who experienced improvements to their psoriasis if the gluten-free diet was in fact not triggering the inflammatory effects that a regular diet would, which also may help to explain the mixed results that the gluten-free diet has had as a treatment for psoriasis. One 3-month study of patients who were positive for antigliadin antibodies found that the majority (82%) experienced a decrease in antibody levels and affected skin area after following a gluten-free diet. Only half the patients had been diagnosed with celiac disease prior to the study, lending credibility to the idea that antigliadin antibody could be used as a marker for patients with psoriasis who would benefit from a gluten-free diet.9 Other case studies have reported no improvement of psoriasis following implementation of a gluten-free diet,10 despite the patients having elevated gliadin antibodies or celiac disease. More studies are required to discern the exact nature of the benefits of a gluten-free diet on psoriasis; however, it does serve as a promising option for patients with both psoriasis and celiac disease.
Ketogenic Diet
As obesity and weight gain are factors associated with psoriasis, some patients turn to diets that restrict calories with the goal of losing weight to improve their symptoms. One 2015 case report studied a patient who restored her response to systemic treatment of psoriasis following an intensive 4-week, calorie-restricted ketogenic diet.11 The ketogenic diet is a high-fat, adequate-protein, low-carbohydrate diet. Animal studies have shown the diet to have anti-inflammatory effects, including lowering levels of proinflammatory cytokines and reduced fever.12 In the 2015 case report, the rapid and consistent weight loss experienced by the patient because of the ketogenic diet was thought to be the cause of the restoration of treatment effectiveness,11 which is interesting, since the role of the ketogenic diet was not to supplement any deficiencies but to move the patient to a physiologic state that was once again receptive to treatment. This finding suggests that a variety of diets could improve psoriasis symptoms, so long as they do not cause inflammation or reduce overall body mass. One study of patients on a calorie-restricted diet over 8 weeks did see a trend of patients on the diet showing improvement in both their PASI scores and Dermatology Life Quality Index, though the improvement was not statistically significant.13 To determine if the ketogenic diet has a significant association with psoriasis improvement, controlled, large-population studies should be performed in the future with age, sex, and weight-matched controls, which may be difficult to do. Further studies looking at the association between weight loss and psoriasis also could be another direction.
Vegetarian Diet
Both vegetarian and vegan diets have been evaluated for their efficacy in relieving symptoms of chronic inflammatory disorders. Although the 2 diets are similar in avoiding consumption of meat, fish, and poultry, vegan diets often have additional food restrictions, including avoiding eggs, honey, and dairy products. One study noted the impact of these diets on patients with a variety of skin conditions following a period of fasting. It was observed that some patients with psoriasis saw an improvement in their symptoms during the period when they were eating a vegetarian or vegan diet, which was attributed to a return to normal levels of activity of neutrophils, extrapolated from serum levels of lactoferrin.14 Vegetarian diets have been shown to be associated with higher ratios of anti-inflammatory to proinflammatory adipokines compared to omnivorous diets,15 as well as lower expression levels of proinflammatory genes in the gut microbiota and lower expression levels of IgE.16 Perhaps the anti-inflammatory impacts of the diet affected the symptoms of psoriasis. The benefits of a vegetarian diet also have been attributed to the high amount of potassium consumed,17 which is used in the body to synthesize cortisol, a common treatment for psoriasis. Potassium supplementation has been shown to raise serum cortisol levels in patients.6 Although additional studies are needed to discern the significance of potassium in the vegetarian diet, both hypotheses are reasonable explanations for the observations seen in these studies.
Vitamin D and Other Nutritional Supplements
Because it is not always feasible for patients to alter their diets, many have turned to dietary supplements as an alternative method of treatment and lifestyle change. Two of the more prominently represented nutritional additives in the literature are fish oils and vitamin D.18 Supplemental vitamin D is a prohormone that can be endogenously converted to its active 1,25-dihydroxyvitamin D.19 Vitamin D plays important roles in the regulation of calcium and magnesium in the bones as well as the maturation and differentiation of keratinocytes in the skin.16 Topical vitamin D analogues are standard treatments for psoriasis, as they are used to modulate the immune system to great effect.20 Some patients with psoriasis present with vitamin D insufficiency,21 and it stands to reason that oral supplementation may be a treatment option. There have been multiple studies assessing the efficacy of oral vitamin D for the treatment of psoriasis; however, in the only randomized and placebo-controlled trial, there was only a slight nonsignificant improvement in the group supplemented with vitamin D.20 Another small, open-label study reported remarkably improved PASI scores in 9 vitamin D–supplemented, dietary calcium–restricted patients.22 The lack of recent, large-sample studies makes it hard to draw notable conclusions from these studies.
The polyunsaturated fatty acids found in fish oils also have been considered as a treatment option for psoriasis.23 Millsop et al20 conducted an analysis of the literature reviewing the efficacy of fish oil in the treatment of psoriasis. Twelve of 15 compiled trials showed an improvement in psoriasis, ranging from slight improvements from baseline levels of the disease to statistically significant decreases in PASI scores (P<.05). It is notable that the amount of fish oil given in these studies varied widely, but the amount given did not necessarily correlate with strength of impact.20 For example, Mayser et al,24 Bittiner et al,25 and Grimminger et al26 each performed prospective, double-blind studies with
Studies also have shown little to no improvement in the use of fish oil to treat psoriasis. One such study was conducted by Soyland et al27 in 1993 in Norway. Utilizing a prospective, double-blind, placebo-controlled design over 4 months on 145 patients with moderate to severe psoriasis, researchers evaluated the treatment effectiveness via PASI scores; subjective reports from the patients; clinical manifestations; and factors such as cellular infiltration, desquamation, and redness. The results were mixed, with the placebo (corn oil) group having less redness and cellular desquamation and the fish oil group showing less cellular infiltration. In the other categories, there was no significant difference between the 2 groups, and researchers concluded there was no significant benefit to treating psoriasis using fish oil vs corn oil.27 As with many of the other diets, there have been no recent, large-scale studies performed on the effect of fish oil supplementation on psoriasis; however, of the studies we reviewed, none showed fish oil supplementation to have a significant negative impact on psoriasis.
Conclusion
Dietary modifications have a complex multifactorial effect on psoriasis, often dependent on the variations of psoriasis and the lifestyle of the patient, including level of exercise, activities such as smoking and drinking, and genetic susceptibilities to conditions such as obesity. Thus, it is difficult for one diet to have a significant impact on psoriasis symptoms that applies to the majority of individuals. However, it appears that certain foods or nutritional supplements can be modified from all diets for general improvement. Foods with systemic anti-inflammatory effects, such as olive oil and fish oil, seem to be beneficial in treating psoriasis. As an extension, a gluten-free diet may help psoriasis patients with celiac disease by reducing the inflammatory environment of the body. On the opposite side of the spectrum, proinflammatory foods such as dietary fat and alcohol should be avoided.28
In general, larger and more recent population-based studies are needed to add to the literature on this subject. Nationwide voluntary web-based surveys such as the NutriNet-Santé study in France may be one way to quickly amass large quantities of data (ClinicalTrials.gov Identifier NCT03335644). Participants are recruited through multimedia campaigns and return online questionnaires annually for 1 decade. A subset of participants also contributes biologic samples and participates in clinical examinations. This type of data gathering would capture many variables, provide a large sample size, and perhaps shed light on regional differences in diet and lifestyle that could then be targeted with treatments.
- Madrid Álvarez MB, Carretero Hernández G, González Quesada A, et al. Measurement of the psychological impact of psoriasis on patients receiving systemic treatment. Actas Dermosifiliogr (English edition). 2018;109:733-740.
- Afifi L, Danesh MJ, Lee KM, et al. Dietary behaviors in psoriasis: patient-reported outcomes from a U.S. national survey. Dermatol Ther (Heidelb). 2017;7:227-242.
- Phan C, Touvier M, Kesse-Guyot E, et al. Association between Mediterranean anti-inflammatory dietary profile and severity of psoriasis: results from the NutriNet-Santé cohort. JAMA Dermatol. 2018;154:1017-1024.
- Barrea L, Balato N, Di Somma C, et al. Nutrition and psoriasis: is there any association between the severity of the disease and adherence to the Mediterranean diet? J Transl Med. 2015;13:18.
- Bhatia BK, Millsop JW, Debbaneh M, et al. Diet and psoriasis, part II: celiac disease and role of a gluten-free diet. J Am Acad Dermatol. 2014;71:350-358.
- Ungprasert P, Wijarnpreecha K, Kittanamongkolchai W. Psoriasis and risk of celiac disease: a systematic review and meta-analysis. Indian J Dermatol. 2017;62:41-46.
- Kolchak NA, Tetarnikova MK, Theodoropoulou MS, et al. Prevalence of antigliadin IgA antibodies in psoriasis vulgaris and response of seropositive patients to a gluten-free diet. J Multidiscip Healthc. 2017;11:13-19.
- Ludvigsson JF, Lindelöf B, Zingone F, et al. Psoriasis in a nationwide cohort study of patients with celiac disease. J Invest Dermatol. 2011;131:2010-2016.
- De Bastiani R, Gabrielli M, Lora L, et al. Association between coeliac disease and psoriasis: Italian primary care multicentre study. Dermatology. 2015;230:156-160.
- Pietrzak D, Pietrzak A, Krasowska D, et al. Digestive system in psoriasis: an update. Arch Dermatol Res. 2017;309:679-693.
- Castaldo G, Galdo G, Rotondi Aufiero F, et al. Very low-calorie ketogenic diet may allow restoring response to systemic therapy in relapsing plaque psoriasis [published online November 11, 2015]. Obes Res Clin Pract. 2016;10:348-352.
- Dupuis N, Curatolo N, Benoist J-F, et al. Ketogenic diet exhibits anti-inflammatory properties. Epilepsia. 2015;56:e95-e98.
- Jensen P, Zachariae C, Christensen R, et al. Effect of weight loss on the severity of psoriasis: a randomized clinical study. JAMA Dermatol. 2013;149:795-801.
- Lithell H, Bruce A, Gustafsson IB, et al. A fasting and vegetarian diet treatment trial on chronic inflammatory disorders. Acta Derm Venereol. 1983;63:397-403.
- Ambroszkiewicz J, Chełchowska M, Rowicka G, et al. Anti-inflammatory and pro-inflammatory adipokine profiles in children on vegetarian and omnivorous diets. Nutrients. 2018;10;pii E1241.
- Rastmanesh R. Psoriasis and vegetarian diets: a role for cortisol and potassium? Med Hypotheses. 2009;72:368.
- Zhang C, Björkman A, Cai K, et al. Impact of a 3-months vegetarian diet on the gut microbiota and immune repertoire. Front Immunol. 2018;9:908.
- Wolters M. Diet and psoriasis: experimental data and clinical evidence. Br J Dermatol. 2005;153:706-714.
- Zuccotti E, Oliveri M, Girometta C, et al. Nutritional strategies for psoriasis: current scientific evidence in clinical trials. Eur Rev Med Pharmacol Sci. 2018;22:8537-8551.
- Millsop JW, Bhatia BK, Debbaneh M, et al. Diet and psoriasis: part 3. role of nutritional supplements. J Am Acad Dermatol. 2014;71:561-569.
- El-Moaty Zaher HA, El-Komy MHM, Hegazy RA, et al. Assessment of interleukin-17 and vitamin D serum levels in psoriatic patients. J Am Acad Dermatol. 2013;69:840-842.
- Finamor DC, Sinigaglia-Coimbra R, Neves LCM, et al. A pilot study assessing the effect of prolonged administration of high daily doses of vitamin D on the clinical course of vitiligo and psoriasis. Dermatoendocrinol. 2013;5:222-234.
- Pona A, Haidari W, Kolli SS, et al. Diet and psoriasis. Dermatol Online J. 2019;25. https://escholarship.org/uc/item/1p37435s. Accessed April 14, 2019.
- Mayser P, Mrowietz U, Arenberger P, et al. ω-3 fatty acid–based lipid infusion in patients with chronic plaque psoriasis: results of a double-blind, randomized, placebo-controlled, multicenter trial. J Am Acad Dermatol. 1998;38:539-547.
- Bittiner SB, Tucker WF, Cartwright I, et al. A double-blind, randomised, placebo-controlled trial of fish oil in psoriasis. Lancet. 1988;1:378-380.
- Grimminger F, Mayser P, Papavassilis C, et al. A double-blind, randomized, placebo-controlled trial of n-3 fatty acid based lipid infusion in acute, extended guttate psoriasis: rapid improvement of clinical manifestations and changes in neutrophil leukotriene profile. Clin Investig. 1993;71:634-643.
- Soyland E, Funk J, Rajka G, et al. Effect of dietary supplementation with very-long-chain n-3 fatty acids in patients with psoriasis. N Engl J Med. 1993;328:1812-1816.
- Cunningham E. Is there research to support a specific diet for psoriasis? J Acad Nutr Diet. 2014;114:508.
- Madrid Álvarez MB, Carretero Hernández G, González Quesada A, et al. Measurement of the psychological impact of psoriasis on patients receiving systemic treatment. Actas Dermosifiliogr (English edition). 2018;109:733-740.
- Afifi L, Danesh MJ, Lee KM, et al. Dietary behaviors in psoriasis: patient-reported outcomes from a U.S. national survey. Dermatol Ther (Heidelb). 2017;7:227-242.
- Phan C, Touvier M, Kesse-Guyot E, et al. Association between Mediterranean anti-inflammatory dietary profile and severity of psoriasis: results from the NutriNet-Santé cohort. JAMA Dermatol. 2018;154:1017-1024.
- Barrea L, Balato N, Di Somma C, et al. Nutrition and psoriasis: is there any association between the severity of the disease and adherence to the Mediterranean diet? J Transl Med. 2015;13:18.
- Bhatia BK, Millsop JW, Debbaneh M, et al. Diet and psoriasis, part II: celiac disease and role of a gluten-free diet. J Am Acad Dermatol. 2014;71:350-358.
- Ungprasert P, Wijarnpreecha K, Kittanamongkolchai W. Psoriasis and risk of celiac disease: a systematic review and meta-analysis. Indian J Dermatol. 2017;62:41-46.
- Kolchak NA, Tetarnikova MK, Theodoropoulou MS, et al. Prevalence of antigliadin IgA antibodies in psoriasis vulgaris and response of seropositive patients to a gluten-free diet. J Multidiscip Healthc. 2017;11:13-19.
- Ludvigsson JF, Lindelöf B, Zingone F, et al. Psoriasis in a nationwide cohort study of patients with celiac disease. J Invest Dermatol. 2011;131:2010-2016.
- De Bastiani R, Gabrielli M, Lora L, et al. Association between coeliac disease and psoriasis: Italian primary care multicentre study. Dermatology. 2015;230:156-160.
- Pietrzak D, Pietrzak A, Krasowska D, et al. Digestive system in psoriasis: an update. Arch Dermatol Res. 2017;309:679-693.
- Castaldo G, Galdo G, Rotondi Aufiero F, et al. Very low-calorie ketogenic diet may allow restoring response to systemic therapy in relapsing plaque psoriasis [published online November 11, 2015]. Obes Res Clin Pract. 2016;10:348-352.
- Dupuis N, Curatolo N, Benoist J-F, et al. Ketogenic diet exhibits anti-inflammatory properties. Epilepsia. 2015;56:e95-e98.
- Jensen P, Zachariae C, Christensen R, et al. Effect of weight loss on the severity of psoriasis: a randomized clinical study. JAMA Dermatol. 2013;149:795-801.
- Lithell H, Bruce A, Gustafsson IB, et al. A fasting and vegetarian diet treatment trial on chronic inflammatory disorders. Acta Derm Venereol. 1983;63:397-403.
- Ambroszkiewicz J, Chełchowska M, Rowicka G, et al. Anti-inflammatory and pro-inflammatory adipokine profiles in children on vegetarian and omnivorous diets. Nutrients. 2018;10;pii E1241.
- Rastmanesh R. Psoriasis and vegetarian diets: a role for cortisol and potassium? Med Hypotheses. 2009;72:368.
- Zhang C, Björkman A, Cai K, et al. Impact of a 3-months vegetarian diet on the gut microbiota and immune repertoire. Front Immunol. 2018;9:908.
- Wolters M. Diet and psoriasis: experimental data and clinical evidence. Br J Dermatol. 2005;153:706-714.
- Zuccotti E, Oliveri M, Girometta C, et al. Nutritional strategies for psoriasis: current scientific evidence in clinical trials. Eur Rev Med Pharmacol Sci. 2018;22:8537-8551.
- Millsop JW, Bhatia BK, Debbaneh M, et al. Diet and psoriasis: part 3. role of nutritional supplements. J Am Acad Dermatol. 2014;71:561-569.
- El-Moaty Zaher HA, El-Komy MHM, Hegazy RA, et al. Assessment of interleukin-17 and vitamin D serum levels in psoriatic patients. J Am Acad Dermatol. 2013;69:840-842.
- Finamor DC, Sinigaglia-Coimbra R, Neves LCM, et al. A pilot study assessing the effect of prolonged administration of high daily doses of vitamin D on the clinical course of vitiligo and psoriasis. Dermatoendocrinol. 2013;5:222-234.
- Pona A, Haidari W, Kolli SS, et al. Diet and psoriasis. Dermatol Online J. 2019;25. https://escholarship.org/uc/item/1p37435s. Accessed April 14, 2019.
- Mayser P, Mrowietz U, Arenberger P, et al. ω-3 fatty acid–based lipid infusion in patients with chronic plaque psoriasis: results of a double-blind, randomized, placebo-controlled, multicenter trial. J Am Acad Dermatol. 1998;38:539-547.
- Bittiner SB, Tucker WF, Cartwright I, et al. A double-blind, randomised, placebo-controlled trial of fish oil in psoriasis. Lancet. 1988;1:378-380.
- Grimminger F, Mayser P, Papavassilis C, et al. A double-blind, randomized, placebo-controlled trial of n-3 fatty acid based lipid infusion in acute, extended guttate psoriasis: rapid improvement of clinical manifestations and changes in neutrophil leukotriene profile. Clin Investig. 1993;71:634-643.
- Soyland E, Funk J, Rajka G, et al. Effect of dietary supplementation with very-long-chain n-3 fatty acids in patients with psoriasis. N Engl J Med. 1993;328:1812-1816.
- Cunningham E. Is there research to support a specific diet for psoriasis? J Acad Nutr Diet. 2014;114:508.
Practice Points
- No single food, supplement, or diet has been shown to have a notable positive impact on all variations of psoriasis. However, foods with systemic anti-inflammatory effects may be worth testing and adding to the patient’s diet.
- A considerable proportion of patients with psoriasis also have elevated levels of antigliadin antibody. If patients have celiac disease or high levels of antigliadin antibody, switching them to a gluten-free diet could have a positive impact on their psoriasis.
- Elevated body mass index, weight gain, smoking, and obesity are all associated with a higher risk for psoriasis appearance and severity.
Translating the 2019 AAD-NPF Guidelines of Care for the Management of Psoriasis With Biologics to Clinical Practice
Psoriasis is a systemic immune-mediated disorder characterized by erythematous, scaly, well-demarcated plaques on the skin that affects approximately 3% of the world’s population.1 The disease is moderate to severe for approximately 1 in 6 individuals with psoriasis.2 These patients, particularly those with symptoms that are refractory to topical therapy and/or phototherapy, can benefit from the use of biologic agents, which are monoclonal antibodies and fusion proteins engineered to inhibit the action of cytokines that drive psoriatic inflammation.
In February 2019, the American Academy of Dermatology (AAD) and National Psoriasis Foundation (NPF) released an updated set of guidelines for the use of biologics in treating adult patients with psoriasis.3 The prior guidelines were released in 2008 when just 3 biologics—etanercept, infliximab, and adalimumab—were approved by the US Food and Drug Administration (FDA) for the management of psoriasis. These older recommendations were mostly based on studies of the efficacy and safety of biologics for patients with psoriatic arthritis.4 Over the last 11 years, 8 novel biologics have gained FDA approval, and numerous large phase 2 and phase 3 trials evaluating the risks and benefits of biologics have been conducted. The new guidelines contain considerably more detail and are based on evidence more specific to psoriasis rather than to psoriatic arthritis. Given the large repertoire of biologics available today and the increased amount of published research regarding each one, these guidelines may aid dermatologists in choosing the optimal biologic and managing therapy.
The AAD-NPF recommendations discuss the mechanism of action, efficacy, safety, and adverse events of the 10 biologics that have been FDA approved for the treatment of psoriasis as of March 2019, plus risankizumab, which was pending FDA approval at the time of publication and was later approved in April 2019. They also address dosing regimens, potential to combine biologics with other therapies, and different forms of psoriasis for which each may be effective.3 The purpose of this discussion is to present these guidelines in a condensed form to prescribers of biologic therapies and review the most clinically significant considerations during each step of treatment. Of note, we highlight only treatment of adult patients and do not discuss information relevant to risankizumab, as it was not FDA approved when the AAD-NPF guidelines were released.
Choosing a Biologic
Biologic therapy may be considered for patients with psoriasis that affects more than 3% of the body’s surface and is recalcitrant to localized therapies. There is no particular first-line biologic recommended for all patients with psoriasis; rather, choice of therapy should be individualized to the patient, considering factors such as body parts affected, comorbidities, lifestyle, and drug cost.
All 10 FDA-approved biologics (Table) have been ranked by the AAD and NPF as having grade A evidence for efficacy as monotherapy in the treatment of moderate to severe plaque-type psoriasis. Involvement of difficult-to-treat areas may be considered when choosing a specific therapy. The tumor necrosis factor α (TNF-α) inhibitors etanercept and adalimumab, the IL-17 inhibitor secukinumab, and the IL-23 inhibitor guselkumab have the greatest evidence for efficacy in treatment of nail disease. For scalp involvement, etanercept and guselkumab have the highest-quality evidence, and for palmoplantar disease, adalimumab, secukinumab, and guselkumab are considered the most effective. The TNF-α inhibitors are considered the optimal treatment option for concurrent psoriatic arthritis, though the IL-12/IL-23 inhibitor ustekinumab and the IL-17 inhibitors secukinumab and ixekizumab also have shown grade A evidence of efficacy. Of note, because TNF-α inhibitors received the earliest FDA approval, there is most evidence available for this class. Therapies with lower evidence quality for certain forms of psoriasis may show real-world effectiveness in individual patients, though more trials will be necessary to generate a body of evidence to change these clinical recommendations.
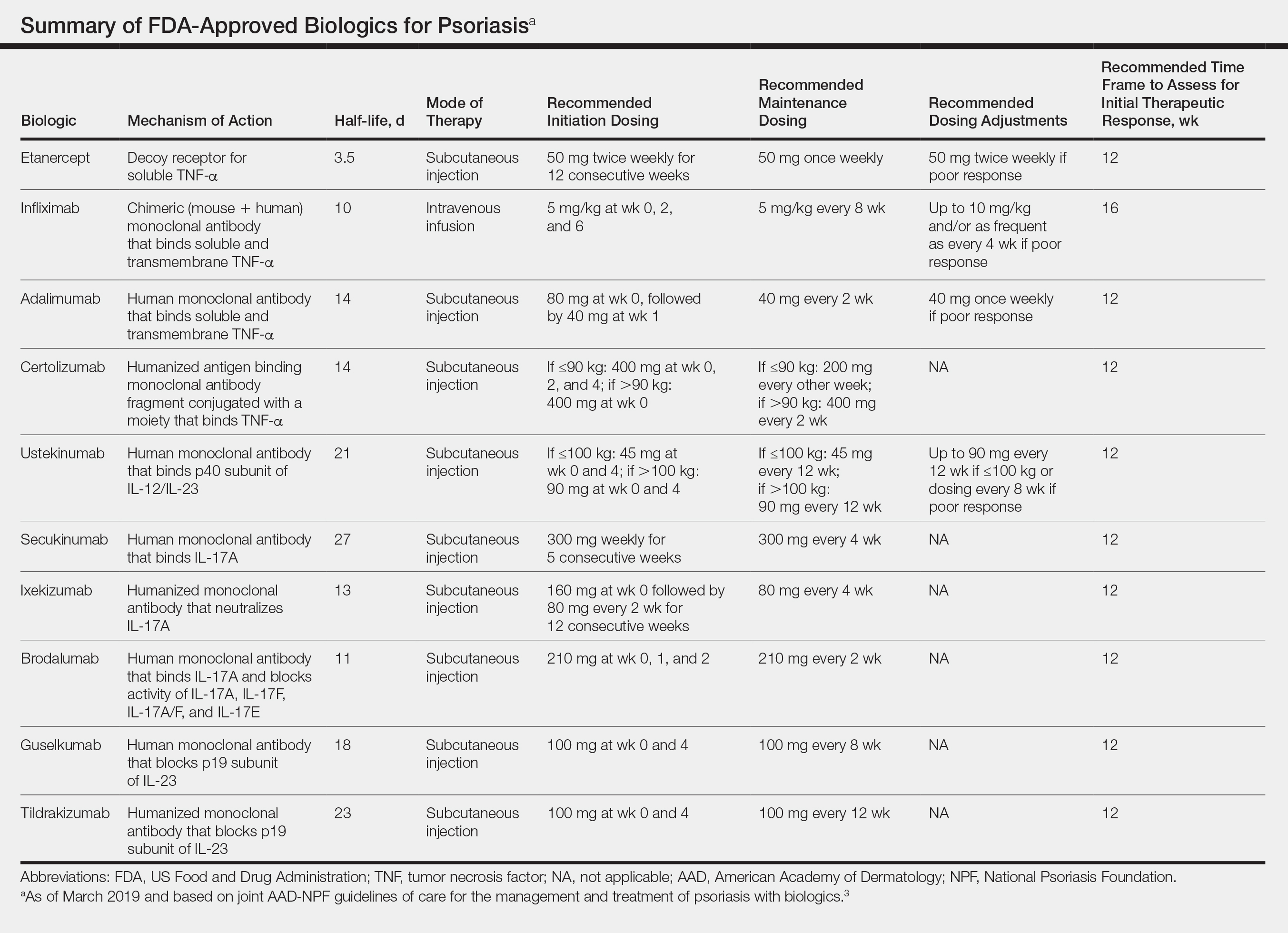
In pregnant women or those are anticipating pregnancy, certolizumab may be considered, as it is the only biologic shown to have minimal to no placental transfer. Other TNF-α inhibitors may undergo active placental transfer, particularly during the latter half of pregnancy,5 and the greatest theoretical risk of transfer occurs in the third trimester. Although these drugs may not directly harm the fetus, they do cause fetal immunosuppression for up to the first 3 months of life. All TNF-α inhibitors are considered safe during lactation. There are inadequate data regarding the safety of other classes of biologics during pregnancy and lactation.
Overweight and obese patients also require unique considerations when choosing a biologic. Infliximab is the only approved psoriasis biologic that utilizes proportional-to-weight dosing and hence may be particularly efficacious in patients with higher body mass. Ustekinumab dosing also takes patient weight into consideration; patients heavier than 100 kg should receive 90-mg doses at initiation and during maintenance compared to 45 mg for patients who weigh 100 kg or less. Other approved biologics also may be utilized in these patients but may require closer monitoring of treatment efficacy.
There are few serious contraindications for specific biologic therapies. Any history of allergic reaction to a particular therapy is an absolute contraindication to its use. In patients for whom IL-17 inhibitor treatment is being considered, inflammatory bowel disease (IBD) should be ruled out given the likelihood that IL-17 could reactivate or worsen IBD. Of note, TNF-α inhibitors and ustekinumab are approved therapies for patients with IBD and may be recommended in patients with comorbid psoriasis. Phase 2 and phase 3 trials have found no reactivation or worsening of IBD in patients with psoriasis who were treated with the IL-23 inhibitor tildrakizumab,6 and phase 2 trials of treatment of IBD with guselkumab are currently underway (ClinicalTrials.gov Identifier NCT03466411). In patients with New York Heart Association class III and class IV congestive heart failure or multiple sclerosis, initiation of TNF-α inhibitors should be avoided. Among 3 phase 3 trials encompassing nearly 3000 patients treated with the IL-17 inhibitor brodalumab, a total of 3 patients died by suicide7,8; hence, the FDA has issued a black box warning cautioning against use of this drug in patients with history of suicidal ideation or recent suicidal behavior. Although a causal relationship between brodalumab and suicide has not been well established,9 a thorough psychiatric history should be obtained in those initiating treatment with brodalumab.
Initiation of Therapy
Prior to initiating biologic therapy, it is important to obtain a complete blood cell count, complete metabolic panel, tuberculosis testing, and hepatitis B virus (HBV) and hepatitis C virus serologies. Testing for human immunodeficiency virus may be pursued at the clinician’s discretion. It is important to address any positive or concerning results prior to starting biologics. In patients with active infections, therapy may be initiated alongside guidance from an infectious disease specialist. Those with a positive purified protein derivative test, T-SPOT test, or QuantiFERON-TB Gold test must be referred for chest radiographs to rule out active tuberculosis. Patients with active HBV infection should receive appropriate referral to initiate antiviral therapy as well as core antibody testing, and those with active hepatitis C virus infection may only receive biologics under the combined discretion of a dermatologist and an appropriate specialist. Patients with human immunodeficiency virus must concurrently receive highly active antiretroviral therapy, show normal CD4+ T-cell count and undetectable viral load, and have no recent history of opportunistic infection.
Therapy should be commenced using specific dosing regimens, which are unique for each biologic (Table). Patients also must be educated on routine follow-up to assess treatment response and tolerability.
Assessment and Optimization of Treatment Response
Patients taking biologics may experience primary treatment failure, defined as lack of response to therapy from initiation. One predisposing factor may be increased body mass; patients who are overweight and obese are less likely to respond to standard regimens of TNF-α inhibitors and 45-mg dosing of ustekinumab. In most cases, however, the cause of primary nonresponse is unpredictable. For patients in whom therapy has failed within the recommended initial time frame (Table), dose escalation or shortening of dosing intervals may be pursued. Recommended dosing adjustments are outlined in the Table. Alternatively, patients may be switched to a different biologic.
If desired effectiveness is not reached with biologic monotherapy, topical corticosteroids, topical vitamin D analogues, or narrowband UVB light therapy may be concurrently used for difficult-to-treat areas. Evidence for safety and effectiveness of systemic adjuncts to biologics is moderate to low, warranting caution with their use. Methotrexate, cyclosporine, and apremilast have synergistic effects with biologics, though they may increase the risk for immunosuppression-related complications. Acitretin, an oral retinoid, likely is the most reasonable systemic adjunct to biologics because of its lack of immunosuppressive properties.
In patients with a suboptimal response to biologics, particularly those taking therapies that require frequent dosing, poor compliance should be considered.10 These patients may be switched to a biologic with less-frequent maintenance dosing (Table). Ustekinumab and tildrakizumab may be the best options for optimizing compliance, as they require dosing only once every 12 weeks after administration of loading doses.
Secondary treatment failure is diminished efficacy of treatment following successful initial response despite no changes in regimen. The best-known factor contributing to secondary nonresponse to biologics is the development of antidrug antibodies (ADAs), a phenomenon known as immunogenicity. The development of efficacy-limiting ADAs has been observed in response to most biologics, though ADAs against etanercept and guselkumab do not limit therapeutic response. Patients taking adalimumab and infliximab have particularly well-documented efficacy-limiting immunogenicity, and those who develop ADAs to infliximab are considered more prone to developing infusion reactions. Methotrexate, which limits antibody formation, may concomitantly be prescribed in patients who experience secondary treatment failure. It should be considered in all patients taking infliximab to increase efficacy and tolerability of therapy.
Considerations During Active Therapy
In addition to monitoring adherence and response to regimens, dermatologists must be heavily involved in counseling patients regarding the risks and adverse effects associated with these therapies. During maintenance therapy with biologics, patients must follow up with the prescriber at minimum every 3 to 6 months to evaluate for continued efficacy of treatment, extent of side effects, and effects of treatment on overall health and quality of life. Given the immunosuppressive effects of biologics, annual testing for tuberculosis should be considered in high-risk individuals. In those who are considered at low risk, tuberculosis testing may be done at the discretion of the dermatologist. In those with a history of HBV infection, HBV serologies should be pursued routinely given the risk for reactivation.
Annual screening for nonmelanoma skin cancer should be performed in all patients taking biologics. Tumor necrosis factor α inhibitor therapy in particular confers an elevated risk for cutaneous squamous cell carcinoma, especially in patients who are immunosuppressed at baseline and those with history of UV phototherapy. Use of acitretin alongside TNF-α inhibitors or ustekinumab may prevent squamous cell carcinoma formation in high-risk patients.
Because infliximab treatment poses an elevated risk of liver injury,11 liver function tests should be repeated 3 months following initiation of treatment and then every 6 to 12 months subsequently if results are normal. Periodic assessment of suicidal ideation is recommended in patients on brodalumab therapy, which may necessitate more frequent follow-up visits and potentially psychiatry referrals in certain patients. Patients taking IL-17 inhibitors, particularly those who are concurrently taking methotrexate, are at increased risk for developing mucocutaneous Candida infections; these patients should be monitored for such infections and treated appropriately.12
It is additionally important for prescribing dermatologists to ensure that patients on biologics are following up with their general providers to receive timely age-appropriate preventative screenings and vaccines. Inactivated vaccinations may be administered during therapy with any biologic; however, live vaccinations may induce systemic infection in those who are immunocompromised, which theoretically includes individuals taking biologic agents, though incidence data in this patient population are scarce.13 Some experts believe that administration of live vaccines warrants temporary discontinuation of biologic therapy for 2 to 3 half-lives before and after vaccination (Table). Others recommend stopping treatment at least 4 weeks before and until 2 weeks after vaccination. For patients taking biologics with half-lives greater than 20 days, which would theoretically require stopping the drug 2 months prior to vaccination, the benefit of vaccination should be weighed against the risk of prolonged discontinuation of therapy. Until recently, this recommendation was particularly important, as a live herpes zoster vaccination was recommended by the Centers for Disease Control and Prevention for adults older than 60 years. In 2017, a new inactivated herpes zoster vaccine was introduced and is now the preferred vaccine for all patients older than 50 years.14 It is especially important that patients on biologics receive this vaccine to avoid temporary drug discontinuation.
Evidence that any particular class of biologics increases risk for solid tumors or lymphoreticular malignancy is limited. One case-control analysis reported that more than 12 months of treatment with TNF-α inhibitors may increase risk for malignancy; however, the confidence interval reported hardly allows for statistical significance.15 Another retrospective cohort study found no elevated incidence of cancer in patients on TNF-α inhibitors compared to nonbiologic comparators.16 Ustekinumab was shown to confer no increased risk for malignancy in 1 large study,15 but no large studies have been conducted for other classes of drugs. Given the limited and inconclusive evidence available, the guidelines recommend that age-appropriate cancer screenings recommended for the general population should be pursued in patients taking biologics.
Surgery while taking biologics may lead to stress-induced augmentation of immunosuppression, resulting in elevated risk of infection.17 Low-risk surgeries that do not warrant discontinuation of treatment include endoscopic, ophthalmologic, dermatologic, orthopedic, and breast procedures. In patients preparing for elective surgery in which respiratory, gastrointestinal, or genitourinary tracts will be entered, biologics may be discontinued at least 3 half-lives (Table) prior to surgery if the dermatologist and surgeon collaboratively deem that risk of infection outweighs benefit of continued therapy.18 Therapy may be resumed within 1 to 2 weeks postoperatively if there are no surgical complications.
Switching Biologics
Changing therapy to another biologic should be considered if there is no response to treatment or the patient experiences adverse effects while taking a particular biologic. Because evidence is limited regarding the ideal time frame between discontinuation of a prior medication and initiation of a new biologic, this interval should be determined at the discretion of the provider based on the patient’s disease severity and response to prior treatment. For individuals who experience primary or secondary treatment failure while maintaining appropriate dosing and treatment compliance, switching to a different biologic is recommended to maximize treatment response.19 Changing therapy to a biologic within the same class is generally effective,20 and switching to a biologic with another mechanism of action should be considered if a class-specific adverse effect is the major reason for altering the regimen. Nonetheless, some patients may be unresponsive to biologic changes. Further research is necessary to determine which biologics may be most effective when previously used biologics have failed and particular factors that may predispose patients to biologic unresponsiveness.
Resuming Biologic Treatment Following Cessation
In cases where therapy is discontinued for any reason, it may be necessary to repeat initiation dosing when resuming treatment. In patients with severe or flaring disease or if more than 3 to 4 half-lives have passed since the most recent dose, it may be necessary to restart therapy with the loading dose (Table). Unfortunately, restarting therapy may preclude some patients from experiencing the maximal response that they attained prior to cessation. In such cases, switching biologic therapy to a different class may prove beneficial.
Final Thoughts
These recommendations contain valuable information that will assist dermatologists when initiating biologics and managing outcomes of their psoriasis patients. It is, however, crucial to bear in mind that these guidelines serve as merely a tool. Given the paucity of comprehensive research, particularly regarding some of the more recently approved therapies, there are many questions that are unanswered within the guidelines. Their utility for each individual patient situation is therefore limited, and clinical judgement may outweigh the information presented. The recommendations nevertheless provide a pivotal and unprecedented framework that promotes discourse among patients, dermatologists, and other providers to optimize the efficacy of biologic therapy for psoriasis.
- Michalek IM, Loring B, John SM. A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol. 2017;31:205-212.
- Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
- Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics [published online February 13, 2019]. J Am Acad Dermatol. 2019;80:1029-1072.
- Menter A, Gottlieb A, Feldman SR, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 1. overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008;58:826-850.
- Förger F, Villiger PM. Treatment of rheumatoid arthritis during pregnancy: present and future. Expert Rev Clin Immunol. 2016;12:937-944.
- Gooderham M, Elewski B, Pariser D, et al. Incidence of serious gastrointestinal events and inflammatory bowel disease among tildrakizumab-treated patients with moderate-to-severe plaque psoriasis: data from 3 large randomized clinical trials [abstract]. J Am Acad Dermatol. 2018;79(suppl 1):AB166.
- Lebwohl M, Strober B, Menter A, et al. Phase 3 studies comparing brodalumab with ustekinumab in psoriasis. N Engl J Med. 2015;373:1318-328.
- Papp KA, Reich K, Paul C, et al. A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. Br J Dermatol. 2016;175:273-286
- Beck KM, Koo J. Brodalumab for the treatment of plaque psoriasis: up-to-date. Expert Opin Biol Ther. 2019;19:287-292.
- Fouéré S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19(suppl 3):2-6.
- Björnsson ES, Bergmann OM, Björnsson HK, et al. Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419-1425, 1425.e1-3; quiz e19-20.
- Saunte DM, Mrowietz U, Puig L, et al. Candida infections in patients with psoriasis and psoriatic arthritis treated with interleukin-17 inhibitors and their practical management. Br J Dermatol. 2017;177:47-62.
- Huber F, Ehrensperger B, Hatz C, et al. Safety of live vaccines on immunosuppressive or immunomodulatory therapy—a retrospective study in three Swiss Travel Clinics [published online January 1, 2018]. J Travel Med. doi:10.1093/jtm/tax082.
- Dooling KL, Guo A, Patel M, et al. Recommendations of the Advisory Committee on Immunization Practices for Use of Herpes Zoster Vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103-108.
- Fiorentino D, Ho V, Lebwohl MG, et al. Risk of malignancy with systemic psoriasis treatment in the Psoriasis Longitudinal Assessment Registry. J Am Acad Dermatol. 2017;77:845-854.e5.
- Haynes K, Beukelman T, Curtis JR, et al. Tumor necrosis factor α inhibitor therapy and cancer risk in chronic immune-mediated diseases. Arthritis Rheum. 2013;65:48-58.
- Fabiano A, De Simone C, Gisondi P, et al. Management of patients with psoriasis treated with biologic drugs needing a surgical treatment. Drug Dev Res. 2014;75(suppl 1):S24-S26.
- Choi YM, Debbaneh M, Weinberg JM, et al. From the Medical Board of the National Psoriasis Foundation: perioperative management of systemic immunomodulatory agents in patients with psoriasis and psoriatic arthritis. J Am Acad Dermatol. 2016;75:798-805.e7.
- Honda H, Umezawa Y, Kikuchi S, et al. Switching of biologics in psoriasis: reasons and results. J Dermatol. 2017;44:1015-1019.
- Bracke S, Lambert J. Viewpoint on handling anti-TNF failure in psoriasis. Arch Dermatol Res. 2013;305:945-950.
Psoriasis is a systemic immune-mediated disorder characterized by erythematous, scaly, well-demarcated plaques on the skin that affects approximately 3% of the world’s population.1 The disease is moderate to severe for approximately 1 in 6 individuals with psoriasis.2 These patients, particularly those with symptoms that are refractory to topical therapy and/or phototherapy, can benefit from the use of biologic agents, which are monoclonal antibodies and fusion proteins engineered to inhibit the action of cytokines that drive psoriatic inflammation.
In February 2019, the American Academy of Dermatology (AAD) and National Psoriasis Foundation (NPF) released an updated set of guidelines for the use of biologics in treating adult patients with psoriasis.3 The prior guidelines were released in 2008 when just 3 biologics—etanercept, infliximab, and adalimumab—were approved by the US Food and Drug Administration (FDA) for the management of psoriasis. These older recommendations were mostly based on studies of the efficacy and safety of biologics for patients with psoriatic arthritis.4 Over the last 11 years, 8 novel biologics have gained FDA approval, and numerous large phase 2 and phase 3 trials evaluating the risks and benefits of biologics have been conducted. The new guidelines contain considerably more detail and are based on evidence more specific to psoriasis rather than to psoriatic arthritis. Given the large repertoire of biologics available today and the increased amount of published research regarding each one, these guidelines may aid dermatologists in choosing the optimal biologic and managing therapy.
The AAD-NPF recommendations discuss the mechanism of action, efficacy, safety, and adverse events of the 10 biologics that have been FDA approved for the treatment of psoriasis as of March 2019, plus risankizumab, which was pending FDA approval at the time of publication and was later approved in April 2019. They also address dosing regimens, potential to combine biologics with other therapies, and different forms of psoriasis for which each may be effective.3 The purpose of this discussion is to present these guidelines in a condensed form to prescribers of biologic therapies and review the most clinically significant considerations during each step of treatment. Of note, we highlight only treatment of adult patients and do not discuss information relevant to risankizumab, as it was not FDA approved when the AAD-NPF guidelines were released.
Choosing a Biologic
Biologic therapy may be considered for patients with psoriasis that affects more than 3% of the body’s surface and is recalcitrant to localized therapies. There is no particular first-line biologic recommended for all patients with psoriasis; rather, choice of therapy should be individualized to the patient, considering factors such as body parts affected, comorbidities, lifestyle, and drug cost.
All 10 FDA-approved biologics (Table) have been ranked by the AAD and NPF as having grade A evidence for efficacy as monotherapy in the treatment of moderate to severe plaque-type psoriasis. Involvement of difficult-to-treat areas may be considered when choosing a specific therapy. The tumor necrosis factor α (TNF-α) inhibitors etanercept and adalimumab, the IL-17 inhibitor secukinumab, and the IL-23 inhibitor guselkumab have the greatest evidence for efficacy in treatment of nail disease. For scalp involvement, etanercept and guselkumab have the highest-quality evidence, and for palmoplantar disease, adalimumab, secukinumab, and guselkumab are considered the most effective. The TNF-α inhibitors are considered the optimal treatment option for concurrent psoriatic arthritis, though the IL-12/IL-23 inhibitor ustekinumab and the IL-17 inhibitors secukinumab and ixekizumab also have shown grade A evidence of efficacy. Of note, because TNF-α inhibitors received the earliest FDA approval, there is most evidence available for this class. Therapies with lower evidence quality for certain forms of psoriasis may show real-world effectiveness in individual patients, though more trials will be necessary to generate a body of evidence to change these clinical recommendations.
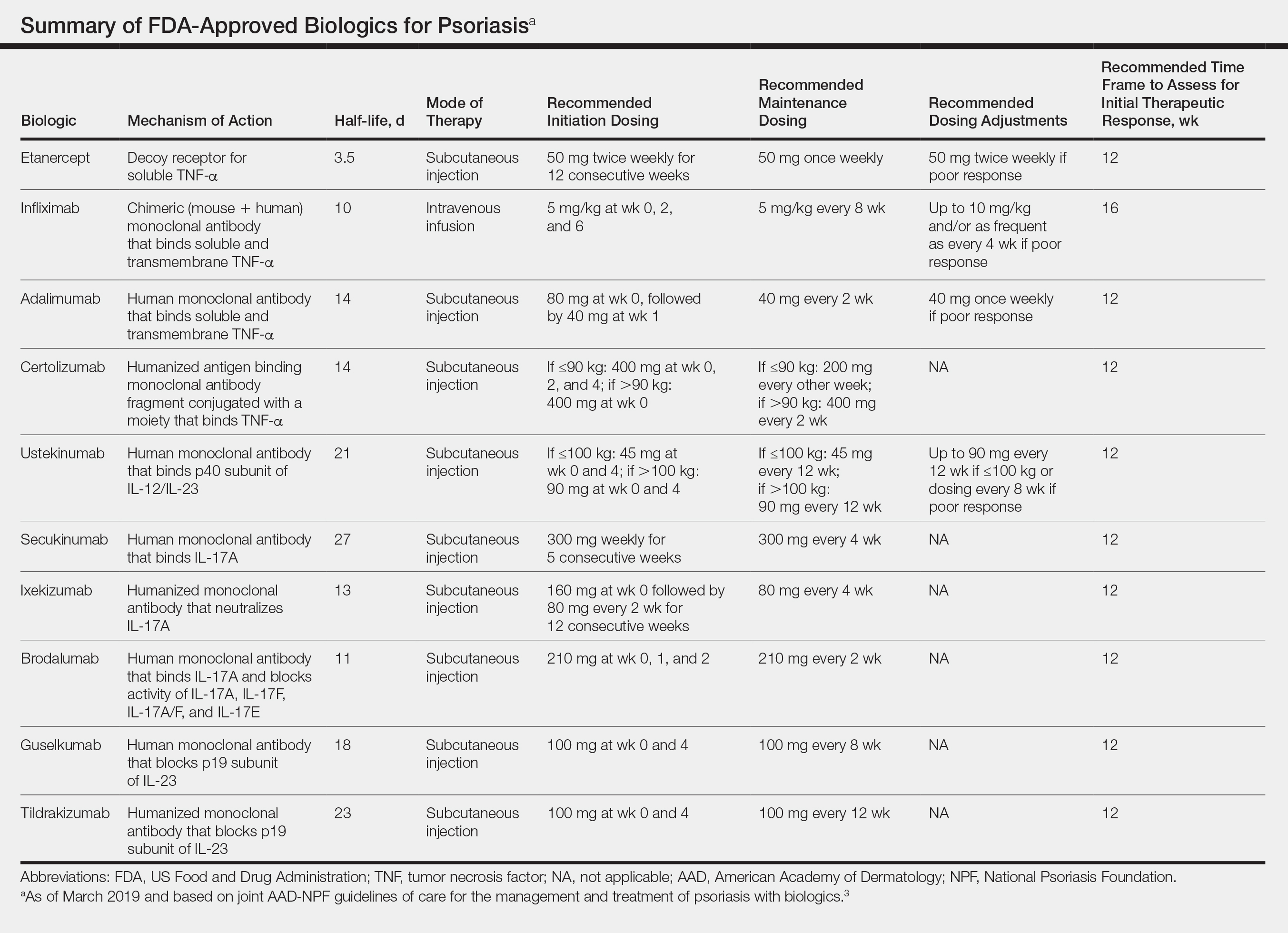
In pregnant women or those are anticipating pregnancy, certolizumab may be considered, as it is the only biologic shown to have minimal to no placental transfer. Other TNF-α inhibitors may undergo active placental transfer, particularly during the latter half of pregnancy,5 and the greatest theoretical risk of transfer occurs in the third trimester. Although these drugs may not directly harm the fetus, they do cause fetal immunosuppression for up to the first 3 months of life. All TNF-α inhibitors are considered safe during lactation. There are inadequate data regarding the safety of other classes of biologics during pregnancy and lactation.
Overweight and obese patients also require unique considerations when choosing a biologic. Infliximab is the only approved psoriasis biologic that utilizes proportional-to-weight dosing and hence may be particularly efficacious in patients with higher body mass. Ustekinumab dosing also takes patient weight into consideration; patients heavier than 100 kg should receive 90-mg doses at initiation and during maintenance compared to 45 mg for patients who weigh 100 kg or less. Other approved biologics also may be utilized in these patients but may require closer monitoring of treatment efficacy.
There are few serious contraindications for specific biologic therapies. Any history of allergic reaction to a particular therapy is an absolute contraindication to its use. In patients for whom IL-17 inhibitor treatment is being considered, inflammatory bowel disease (IBD) should be ruled out given the likelihood that IL-17 could reactivate or worsen IBD. Of note, TNF-α inhibitors and ustekinumab are approved therapies for patients with IBD and may be recommended in patients with comorbid psoriasis. Phase 2 and phase 3 trials have found no reactivation or worsening of IBD in patients with psoriasis who were treated with the IL-23 inhibitor tildrakizumab,6 and phase 2 trials of treatment of IBD with guselkumab are currently underway (ClinicalTrials.gov Identifier NCT03466411). In patients with New York Heart Association class III and class IV congestive heart failure or multiple sclerosis, initiation of TNF-α inhibitors should be avoided. Among 3 phase 3 trials encompassing nearly 3000 patients treated with the IL-17 inhibitor brodalumab, a total of 3 patients died by suicide7,8; hence, the FDA has issued a black box warning cautioning against use of this drug in patients with history of suicidal ideation or recent suicidal behavior. Although a causal relationship between brodalumab and suicide has not been well established,9 a thorough psychiatric history should be obtained in those initiating treatment with brodalumab.
Initiation of Therapy
Prior to initiating biologic therapy, it is important to obtain a complete blood cell count, complete metabolic panel, tuberculosis testing, and hepatitis B virus (HBV) and hepatitis C virus serologies. Testing for human immunodeficiency virus may be pursued at the clinician’s discretion. It is important to address any positive or concerning results prior to starting biologics. In patients with active infections, therapy may be initiated alongside guidance from an infectious disease specialist. Those with a positive purified protein derivative test, T-SPOT test, or QuantiFERON-TB Gold test must be referred for chest radiographs to rule out active tuberculosis. Patients with active HBV infection should receive appropriate referral to initiate antiviral therapy as well as core antibody testing, and those with active hepatitis C virus infection may only receive biologics under the combined discretion of a dermatologist and an appropriate specialist. Patients with human immunodeficiency virus must concurrently receive highly active antiretroviral therapy, show normal CD4+ T-cell count and undetectable viral load, and have no recent history of opportunistic infection.
Therapy should be commenced using specific dosing regimens, which are unique for each biologic (Table). Patients also must be educated on routine follow-up to assess treatment response and tolerability.
Assessment and Optimization of Treatment Response
Patients taking biologics may experience primary treatment failure, defined as lack of response to therapy from initiation. One predisposing factor may be increased body mass; patients who are overweight and obese are less likely to respond to standard regimens of TNF-α inhibitors and 45-mg dosing of ustekinumab. In most cases, however, the cause of primary nonresponse is unpredictable. For patients in whom therapy has failed within the recommended initial time frame (Table), dose escalation or shortening of dosing intervals may be pursued. Recommended dosing adjustments are outlined in the Table. Alternatively, patients may be switched to a different biologic.
If desired effectiveness is not reached with biologic monotherapy, topical corticosteroids, topical vitamin D analogues, or narrowband UVB light therapy may be concurrently used for difficult-to-treat areas. Evidence for safety and effectiveness of systemic adjuncts to biologics is moderate to low, warranting caution with their use. Methotrexate, cyclosporine, and apremilast have synergistic effects with biologics, though they may increase the risk for immunosuppression-related complications. Acitretin, an oral retinoid, likely is the most reasonable systemic adjunct to biologics because of its lack of immunosuppressive properties.
In patients with a suboptimal response to biologics, particularly those taking therapies that require frequent dosing, poor compliance should be considered.10 These patients may be switched to a biologic with less-frequent maintenance dosing (Table). Ustekinumab and tildrakizumab may be the best options for optimizing compliance, as they require dosing only once every 12 weeks after administration of loading doses.
Secondary treatment failure is diminished efficacy of treatment following successful initial response despite no changes in regimen. The best-known factor contributing to secondary nonresponse to biologics is the development of antidrug antibodies (ADAs), a phenomenon known as immunogenicity. The development of efficacy-limiting ADAs has been observed in response to most biologics, though ADAs against etanercept and guselkumab do not limit therapeutic response. Patients taking adalimumab and infliximab have particularly well-documented efficacy-limiting immunogenicity, and those who develop ADAs to infliximab are considered more prone to developing infusion reactions. Methotrexate, which limits antibody formation, may concomitantly be prescribed in patients who experience secondary treatment failure. It should be considered in all patients taking infliximab to increase efficacy and tolerability of therapy.
Considerations During Active Therapy
In addition to monitoring adherence and response to regimens, dermatologists must be heavily involved in counseling patients regarding the risks and adverse effects associated with these therapies. During maintenance therapy with biologics, patients must follow up with the prescriber at minimum every 3 to 6 months to evaluate for continued efficacy of treatment, extent of side effects, and effects of treatment on overall health and quality of life. Given the immunosuppressive effects of biologics, annual testing for tuberculosis should be considered in high-risk individuals. In those who are considered at low risk, tuberculosis testing may be done at the discretion of the dermatologist. In those with a history of HBV infection, HBV serologies should be pursued routinely given the risk for reactivation.
Annual screening for nonmelanoma skin cancer should be performed in all patients taking biologics. Tumor necrosis factor α inhibitor therapy in particular confers an elevated risk for cutaneous squamous cell carcinoma, especially in patients who are immunosuppressed at baseline and those with history of UV phototherapy. Use of acitretin alongside TNF-α inhibitors or ustekinumab may prevent squamous cell carcinoma formation in high-risk patients.
Because infliximab treatment poses an elevated risk of liver injury,11 liver function tests should be repeated 3 months following initiation of treatment and then every 6 to 12 months subsequently if results are normal. Periodic assessment of suicidal ideation is recommended in patients on brodalumab therapy, which may necessitate more frequent follow-up visits and potentially psychiatry referrals in certain patients. Patients taking IL-17 inhibitors, particularly those who are concurrently taking methotrexate, are at increased risk for developing mucocutaneous Candida infections; these patients should be monitored for such infections and treated appropriately.12
It is additionally important for prescribing dermatologists to ensure that patients on biologics are following up with their general providers to receive timely age-appropriate preventative screenings and vaccines. Inactivated vaccinations may be administered during therapy with any biologic; however, live vaccinations may induce systemic infection in those who are immunocompromised, which theoretically includes individuals taking biologic agents, though incidence data in this patient population are scarce.13 Some experts believe that administration of live vaccines warrants temporary discontinuation of biologic therapy for 2 to 3 half-lives before and after vaccination (Table). Others recommend stopping treatment at least 4 weeks before and until 2 weeks after vaccination. For patients taking biologics with half-lives greater than 20 days, which would theoretically require stopping the drug 2 months prior to vaccination, the benefit of vaccination should be weighed against the risk of prolonged discontinuation of therapy. Until recently, this recommendation was particularly important, as a live herpes zoster vaccination was recommended by the Centers for Disease Control and Prevention for adults older than 60 years. In 2017, a new inactivated herpes zoster vaccine was introduced and is now the preferred vaccine for all patients older than 50 years.14 It is especially important that patients on biologics receive this vaccine to avoid temporary drug discontinuation.
Evidence that any particular class of biologics increases risk for solid tumors or lymphoreticular malignancy is limited. One case-control analysis reported that more than 12 months of treatment with TNF-α inhibitors may increase risk for malignancy; however, the confidence interval reported hardly allows for statistical significance.15 Another retrospective cohort study found no elevated incidence of cancer in patients on TNF-α inhibitors compared to nonbiologic comparators.16 Ustekinumab was shown to confer no increased risk for malignancy in 1 large study,15 but no large studies have been conducted for other classes of drugs. Given the limited and inconclusive evidence available, the guidelines recommend that age-appropriate cancer screenings recommended for the general population should be pursued in patients taking biologics.
Surgery while taking biologics may lead to stress-induced augmentation of immunosuppression, resulting in elevated risk of infection.17 Low-risk surgeries that do not warrant discontinuation of treatment include endoscopic, ophthalmologic, dermatologic, orthopedic, and breast procedures. In patients preparing for elective surgery in which respiratory, gastrointestinal, or genitourinary tracts will be entered, biologics may be discontinued at least 3 half-lives (Table) prior to surgery if the dermatologist and surgeon collaboratively deem that risk of infection outweighs benefit of continued therapy.18 Therapy may be resumed within 1 to 2 weeks postoperatively if there are no surgical complications.
Switching Biologics
Changing therapy to another biologic should be considered if there is no response to treatment or the patient experiences adverse effects while taking a particular biologic. Because evidence is limited regarding the ideal time frame between discontinuation of a prior medication and initiation of a new biologic, this interval should be determined at the discretion of the provider based on the patient’s disease severity and response to prior treatment. For individuals who experience primary or secondary treatment failure while maintaining appropriate dosing and treatment compliance, switching to a different biologic is recommended to maximize treatment response.19 Changing therapy to a biologic within the same class is generally effective,20 and switching to a biologic with another mechanism of action should be considered if a class-specific adverse effect is the major reason for altering the regimen. Nonetheless, some patients may be unresponsive to biologic changes. Further research is necessary to determine which biologics may be most effective when previously used biologics have failed and particular factors that may predispose patients to biologic unresponsiveness.
Resuming Biologic Treatment Following Cessation
In cases where therapy is discontinued for any reason, it may be necessary to repeat initiation dosing when resuming treatment. In patients with severe or flaring disease or if more than 3 to 4 half-lives have passed since the most recent dose, it may be necessary to restart therapy with the loading dose (Table). Unfortunately, restarting therapy may preclude some patients from experiencing the maximal response that they attained prior to cessation. In such cases, switching biologic therapy to a different class may prove beneficial.
Final Thoughts
These recommendations contain valuable information that will assist dermatologists when initiating biologics and managing outcomes of their psoriasis patients. It is, however, crucial to bear in mind that these guidelines serve as merely a tool. Given the paucity of comprehensive research, particularly regarding some of the more recently approved therapies, there are many questions that are unanswered within the guidelines. Their utility for each individual patient situation is therefore limited, and clinical judgement may outweigh the information presented. The recommendations nevertheless provide a pivotal and unprecedented framework that promotes discourse among patients, dermatologists, and other providers to optimize the efficacy of biologic therapy for psoriasis.
Psoriasis is a systemic immune-mediated disorder characterized by erythematous, scaly, well-demarcated plaques on the skin that affects approximately 3% of the world’s population.1 The disease is moderate to severe for approximately 1 in 6 individuals with psoriasis.2 These patients, particularly those with symptoms that are refractory to topical therapy and/or phototherapy, can benefit from the use of biologic agents, which are monoclonal antibodies and fusion proteins engineered to inhibit the action of cytokines that drive psoriatic inflammation.
In February 2019, the American Academy of Dermatology (AAD) and National Psoriasis Foundation (NPF) released an updated set of guidelines for the use of biologics in treating adult patients with psoriasis.3 The prior guidelines were released in 2008 when just 3 biologics—etanercept, infliximab, and adalimumab—were approved by the US Food and Drug Administration (FDA) for the management of psoriasis. These older recommendations were mostly based on studies of the efficacy and safety of biologics for patients with psoriatic arthritis.4 Over the last 11 years, 8 novel biologics have gained FDA approval, and numerous large phase 2 and phase 3 trials evaluating the risks and benefits of biologics have been conducted. The new guidelines contain considerably more detail and are based on evidence more specific to psoriasis rather than to psoriatic arthritis. Given the large repertoire of biologics available today and the increased amount of published research regarding each one, these guidelines may aid dermatologists in choosing the optimal biologic and managing therapy.
The AAD-NPF recommendations discuss the mechanism of action, efficacy, safety, and adverse events of the 10 biologics that have been FDA approved for the treatment of psoriasis as of March 2019, plus risankizumab, which was pending FDA approval at the time of publication and was later approved in April 2019. They also address dosing regimens, potential to combine biologics with other therapies, and different forms of psoriasis for which each may be effective.3 The purpose of this discussion is to present these guidelines in a condensed form to prescribers of biologic therapies and review the most clinically significant considerations during each step of treatment. Of note, we highlight only treatment of adult patients and do not discuss information relevant to risankizumab, as it was not FDA approved when the AAD-NPF guidelines were released.
Choosing a Biologic
Biologic therapy may be considered for patients with psoriasis that affects more than 3% of the body’s surface and is recalcitrant to localized therapies. There is no particular first-line biologic recommended for all patients with psoriasis; rather, choice of therapy should be individualized to the patient, considering factors such as body parts affected, comorbidities, lifestyle, and drug cost.
All 10 FDA-approved biologics (Table) have been ranked by the AAD and NPF as having grade A evidence for efficacy as monotherapy in the treatment of moderate to severe plaque-type psoriasis. Involvement of difficult-to-treat areas may be considered when choosing a specific therapy. The tumor necrosis factor α (TNF-α) inhibitors etanercept and adalimumab, the IL-17 inhibitor secukinumab, and the IL-23 inhibitor guselkumab have the greatest evidence for efficacy in treatment of nail disease. For scalp involvement, etanercept and guselkumab have the highest-quality evidence, and for palmoplantar disease, adalimumab, secukinumab, and guselkumab are considered the most effective. The TNF-α inhibitors are considered the optimal treatment option for concurrent psoriatic arthritis, though the IL-12/IL-23 inhibitor ustekinumab and the IL-17 inhibitors secukinumab and ixekizumab also have shown grade A evidence of efficacy. Of note, because TNF-α inhibitors received the earliest FDA approval, there is most evidence available for this class. Therapies with lower evidence quality for certain forms of psoriasis may show real-world effectiveness in individual patients, though more trials will be necessary to generate a body of evidence to change these clinical recommendations.
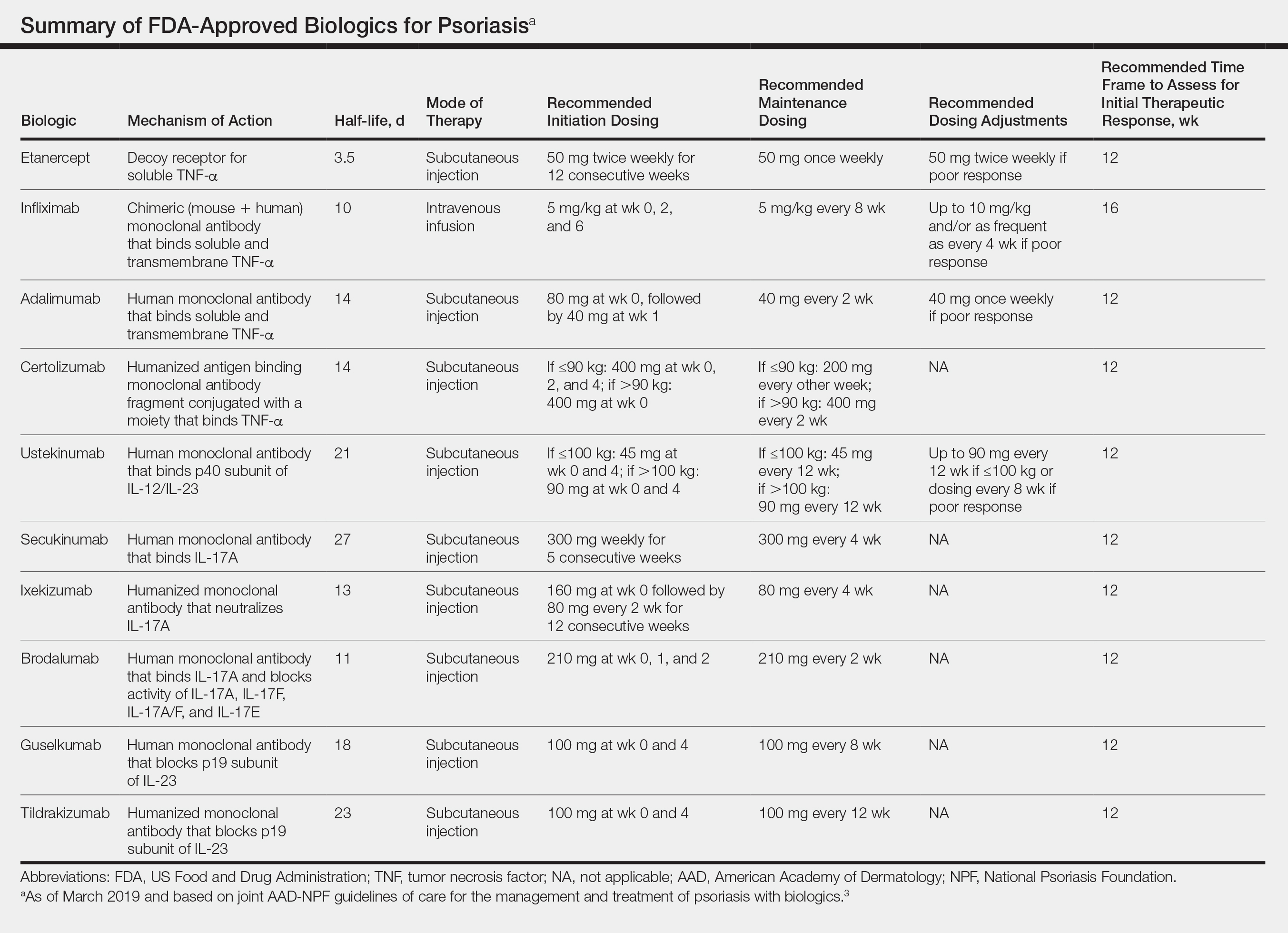
In pregnant women or those are anticipating pregnancy, certolizumab may be considered, as it is the only biologic shown to have minimal to no placental transfer. Other TNF-α inhibitors may undergo active placental transfer, particularly during the latter half of pregnancy,5 and the greatest theoretical risk of transfer occurs in the third trimester. Although these drugs may not directly harm the fetus, they do cause fetal immunosuppression for up to the first 3 months of life. All TNF-α inhibitors are considered safe during lactation. There are inadequate data regarding the safety of other classes of biologics during pregnancy and lactation.
Overweight and obese patients also require unique considerations when choosing a biologic. Infliximab is the only approved psoriasis biologic that utilizes proportional-to-weight dosing and hence may be particularly efficacious in patients with higher body mass. Ustekinumab dosing also takes patient weight into consideration; patients heavier than 100 kg should receive 90-mg doses at initiation and during maintenance compared to 45 mg for patients who weigh 100 kg or less. Other approved biologics also may be utilized in these patients but may require closer monitoring of treatment efficacy.
There are few serious contraindications for specific biologic therapies. Any history of allergic reaction to a particular therapy is an absolute contraindication to its use. In patients for whom IL-17 inhibitor treatment is being considered, inflammatory bowel disease (IBD) should be ruled out given the likelihood that IL-17 could reactivate or worsen IBD. Of note, TNF-α inhibitors and ustekinumab are approved therapies for patients with IBD and may be recommended in patients with comorbid psoriasis. Phase 2 and phase 3 trials have found no reactivation or worsening of IBD in patients with psoriasis who were treated with the IL-23 inhibitor tildrakizumab,6 and phase 2 trials of treatment of IBD with guselkumab are currently underway (ClinicalTrials.gov Identifier NCT03466411). In patients with New York Heart Association class III and class IV congestive heart failure or multiple sclerosis, initiation of TNF-α inhibitors should be avoided. Among 3 phase 3 trials encompassing nearly 3000 patients treated with the IL-17 inhibitor brodalumab, a total of 3 patients died by suicide7,8; hence, the FDA has issued a black box warning cautioning against use of this drug in patients with history of suicidal ideation or recent suicidal behavior. Although a causal relationship between brodalumab and suicide has not been well established,9 a thorough psychiatric history should be obtained in those initiating treatment with brodalumab.
Initiation of Therapy
Prior to initiating biologic therapy, it is important to obtain a complete blood cell count, complete metabolic panel, tuberculosis testing, and hepatitis B virus (HBV) and hepatitis C virus serologies. Testing for human immunodeficiency virus may be pursued at the clinician’s discretion. It is important to address any positive or concerning results prior to starting biologics. In patients with active infections, therapy may be initiated alongside guidance from an infectious disease specialist. Those with a positive purified protein derivative test, T-SPOT test, or QuantiFERON-TB Gold test must be referred for chest radiographs to rule out active tuberculosis. Patients with active HBV infection should receive appropriate referral to initiate antiviral therapy as well as core antibody testing, and those with active hepatitis C virus infection may only receive biologics under the combined discretion of a dermatologist and an appropriate specialist. Patients with human immunodeficiency virus must concurrently receive highly active antiretroviral therapy, show normal CD4+ T-cell count and undetectable viral load, and have no recent history of opportunistic infection.
Therapy should be commenced using specific dosing regimens, which are unique for each biologic (Table). Patients also must be educated on routine follow-up to assess treatment response and tolerability.
Assessment and Optimization of Treatment Response
Patients taking biologics may experience primary treatment failure, defined as lack of response to therapy from initiation. One predisposing factor may be increased body mass; patients who are overweight and obese are less likely to respond to standard regimens of TNF-α inhibitors and 45-mg dosing of ustekinumab. In most cases, however, the cause of primary nonresponse is unpredictable. For patients in whom therapy has failed within the recommended initial time frame (Table), dose escalation or shortening of dosing intervals may be pursued. Recommended dosing adjustments are outlined in the Table. Alternatively, patients may be switched to a different biologic.
If desired effectiveness is not reached with biologic monotherapy, topical corticosteroids, topical vitamin D analogues, or narrowband UVB light therapy may be concurrently used for difficult-to-treat areas. Evidence for safety and effectiveness of systemic adjuncts to biologics is moderate to low, warranting caution with their use. Methotrexate, cyclosporine, and apremilast have synergistic effects with biologics, though they may increase the risk for immunosuppression-related complications. Acitretin, an oral retinoid, likely is the most reasonable systemic adjunct to biologics because of its lack of immunosuppressive properties.
In patients with a suboptimal response to biologics, particularly those taking therapies that require frequent dosing, poor compliance should be considered.10 These patients may be switched to a biologic with less-frequent maintenance dosing (Table). Ustekinumab and tildrakizumab may be the best options for optimizing compliance, as they require dosing only once every 12 weeks after administration of loading doses.
Secondary treatment failure is diminished efficacy of treatment following successful initial response despite no changes in regimen. The best-known factor contributing to secondary nonresponse to biologics is the development of antidrug antibodies (ADAs), a phenomenon known as immunogenicity. The development of efficacy-limiting ADAs has been observed in response to most biologics, though ADAs against etanercept and guselkumab do not limit therapeutic response. Patients taking adalimumab and infliximab have particularly well-documented efficacy-limiting immunogenicity, and those who develop ADAs to infliximab are considered more prone to developing infusion reactions. Methotrexate, which limits antibody formation, may concomitantly be prescribed in patients who experience secondary treatment failure. It should be considered in all patients taking infliximab to increase efficacy and tolerability of therapy.
Considerations During Active Therapy
In addition to monitoring adherence and response to regimens, dermatologists must be heavily involved in counseling patients regarding the risks and adverse effects associated with these therapies. During maintenance therapy with biologics, patients must follow up with the prescriber at minimum every 3 to 6 months to evaluate for continued efficacy of treatment, extent of side effects, and effects of treatment on overall health and quality of life. Given the immunosuppressive effects of biologics, annual testing for tuberculosis should be considered in high-risk individuals. In those who are considered at low risk, tuberculosis testing may be done at the discretion of the dermatologist. In those with a history of HBV infection, HBV serologies should be pursued routinely given the risk for reactivation.
Annual screening for nonmelanoma skin cancer should be performed in all patients taking biologics. Tumor necrosis factor α inhibitor therapy in particular confers an elevated risk for cutaneous squamous cell carcinoma, especially in patients who are immunosuppressed at baseline and those with history of UV phototherapy. Use of acitretin alongside TNF-α inhibitors or ustekinumab may prevent squamous cell carcinoma formation in high-risk patients.
Because infliximab treatment poses an elevated risk of liver injury,11 liver function tests should be repeated 3 months following initiation of treatment and then every 6 to 12 months subsequently if results are normal. Periodic assessment of suicidal ideation is recommended in patients on brodalumab therapy, which may necessitate more frequent follow-up visits and potentially psychiatry referrals in certain patients. Patients taking IL-17 inhibitors, particularly those who are concurrently taking methotrexate, are at increased risk for developing mucocutaneous Candida infections; these patients should be monitored for such infections and treated appropriately.12
It is additionally important for prescribing dermatologists to ensure that patients on biologics are following up with their general providers to receive timely age-appropriate preventative screenings and vaccines. Inactivated vaccinations may be administered during therapy with any biologic; however, live vaccinations may induce systemic infection in those who are immunocompromised, which theoretically includes individuals taking biologic agents, though incidence data in this patient population are scarce.13 Some experts believe that administration of live vaccines warrants temporary discontinuation of biologic therapy for 2 to 3 half-lives before and after vaccination (Table). Others recommend stopping treatment at least 4 weeks before and until 2 weeks after vaccination. For patients taking biologics with half-lives greater than 20 days, which would theoretically require stopping the drug 2 months prior to vaccination, the benefit of vaccination should be weighed against the risk of prolonged discontinuation of therapy. Until recently, this recommendation was particularly important, as a live herpes zoster vaccination was recommended by the Centers for Disease Control and Prevention for adults older than 60 years. In 2017, a new inactivated herpes zoster vaccine was introduced and is now the preferred vaccine for all patients older than 50 years.14 It is especially important that patients on biologics receive this vaccine to avoid temporary drug discontinuation.
Evidence that any particular class of biologics increases risk for solid tumors or lymphoreticular malignancy is limited. One case-control analysis reported that more than 12 months of treatment with TNF-α inhibitors may increase risk for malignancy; however, the confidence interval reported hardly allows for statistical significance.15 Another retrospective cohort study found no elevated incidence of cancer in patients on TNF-α inhibitors compared to nonbiologic comparators.16 Ustekinumab was shown to confer no increased risk for malignancy in 1 large study,15 but no large studies have been conducted for other classes of drugs. Given the limited and inconclusive evidence available, the guidelines recommend that age-appropriate cancer screenings recommended for the general population should be pursued in patients taking biologics.
Surgery while taking biologics may lead to stress-induced augmentation of immunosuppression, resulting in elevated risk of infection.17 Low-risk surgeries that do not warrant discontinuation of treatment include endoscopic, ophthalmologic, dermatologic, orthopedic, and breast procedures. In patients preparing for elective surgery in which respiratory, gastrointestinal, or genitourinary tracts will be entered, biologics may be discontinued at least 3 half-lives (Table) prior to surgery if the dermatologist and surgeon collaboratively deem that risk of infection outweighs benefit of continued therapy.18 Therapy may be resumed within 1 to 2 weeks postoperatively if there are no surgical complications.
Switching Biologics
Changing therapy to another biologic should be considered if there is no response to treatment or the patient experiences adverse effects while taking a particular biologic. Because evidence is limited regarding the ideal time frame between discontinuation of a prior medication and initiation of a new biologic, this interval should be determined at the discretion of the provider based on the patient’s disease severity and response to prior treatment. For individuals who experience primary or secondary treatment failure while maintaining appropriate dosing and treatment compliance, switching to a different biologic is recommended to maximize treatment response.19 Changing therapy to a biologic within the same class is generally effective,20 and switching to a biologic with another mechanism of action should be considered if a class-specific adverse effect is the major reason for altering the regimen. Nonetheless, some patients may be unresponsive to biologic changes. Further research is necessary to determine which biologics may be most effective when previously used biologics have failed and particular factors that may predispose patients to biologic unresponsiveness.
Resuming Biologic Treatment Following Cessation
In cases where therapy is discontinued for any reason, it may be necessary to repeat initiation dosing when resuming treatment. In patients with severe or flaring disease or if more than 3 to 4 half-lives have passed since the most recent dose, it may be necessary to restart therapy with the loading dose (Table). Unfortunately, restarting therapy may preclude some patients from experiencing the maximal response that they attained prior to cessation. In such cases, switching biologic therapy to a different class may prove beneficial.
Final Thoughts
These recommendations contain valuable information that will assist dermatologists when initiating biologics and managing outcomes of their psoriasis patients. It is, however, crucial to bear in mind that these guidelines serve as merely a tool. Given the paucity of comprehensive research, particularly regarding some of the more recently approved therapies, there are many questions that are unanswered within the guidelines. Their utility for each individual patient situation is therefore limited, and clinical judgement may outweigh the information presented. The recommendations nevertheless provide a pivotal and unprecedented framework that promotes discourse among patients, dermatologists, and other providers to optimize the efficacy of biologic therapy for psoriasis.
- Michalek IM, Loring B, John SM. A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol. 2017;31:205-212.
- Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
- Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics [published online February 13, 2019]. J Am Acad Dermatol. 2019;80:1029-1072.
- Menter A, Gottlieb A, Feldman SR, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 1. overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008;58:826-850.
- Förger F, Villiger PM. Treatment of rheumatoid arthritis during pregnancy: present and future. Expert Rev Clin Immunol. 2016;12:937-944.
- Gooderham M, Elewski B, Pariser D, et al. Incidence of serious gastrointestinal events and inflammatory bowel disease among tildrakizumab-treated patients with moderate-to-severe plaque psoriasis: data from 3 large randomized clinical trials [abstract]. J Am Acad Dermatol. 2018;79(suppl 1):AB166.
- Lebwohl M, Strober B, Menter A, et al. Phase 3 studies comparing brodalumab with ustekinumab in psoriasis. N Engl J Med. 2015;373:1318-328.
- Papp KA, Reich K, Paul C, et al. A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. Br J Dermatol. 2016;175:273-286
- Beck KM, Koo J. Brodalumab for the treatment of plaque psoriasis: up-to-date. Expert Opin Biol Ther. 2019;19:287-292.
- Fouéré S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19(suppl 3):2-6.
- Björnsson ES, Bergmann OM, Björnsson HK, et al. Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419-1425, 1425.e1-3; quiz e19-20.
- Saunte DM, Mrowietz U, Puig L, et al. Candida infections in patients with psoriasis and psoriatic arthritis treated with interleukin-17 inhibitors and their practical management. Br J Dermatol. 2017;177:47-62.
- Huber F, Ehrensperger B, Hatz C, et al. Safety of live vaccines on immunosuppressive or immunomodulatory therapy—a retrospective study in three Swiss Travel Clinics [published online January 1, 2018]. J Travel Med. doi:10.1093/jtm/tax082.
- Dooling KL, Guo A, Patel M, et al. Recommendations of the Advisory Committee on Immunization Practices for Use of Herpes Zoster Vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103-108.
- Fiorentino D, Ho V, Lebwohl MG, et al. Risk of malignancy with systemic psoriasis treatment in the Psoriasis Longitudinal Assessment Registry. J Am Acad Dermatol. 2017;77:845-854.e5.
- Haynes K, Beukelman T, Curtis JR, et al. Tumor necrosis factor α inhibitor therapy and cancer risk in chronic immune-mediated diseases. Arthritis Rheum. 2013;65:48-58.
- Fabiano A, De Simone C, Gisondi P, et al. Management of patients with psoriasis treated with biologic drugs needing a surgical treatment. Drug Dev Res. 2014;75(suppl 1):S24-S26.
- Choi YM, Debbaneh M, Weinberg JM, et al. From the Medical Board of the National Psoriasis Foundation: perioperative management of systemic immunomodulatory agents in patients with psoriasis and psoriatic arthritis. J Am Acad Dermatol. 2016;75:798-805.e7.
- Honda H, Umezawa Y, Kikuchi S, et al. Switching of biologics in psoriasis: reasons and results. J Dermatol. 2017;44:1015-1019.
- Bracke S, Lambert J. Viewpoint on handling anti-TNF failure in psoriasis. Arch Dermatol Res. 2013;305:945-950.
- Michalek IM, Loring B, John SM. A systematic review of worldwide epidemiology of psoriasis. J Eur Acad Dermatol Venereol. 2017;31:205-212.
- Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60:218-224.
- Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics [published online February 13, 2019]. J Am Acad Dermatol. 2019;80:1029-1072.
- Menter A, Gottlieb A, Feldman SR, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 1. overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008;58:826-850.
- Förger F, Villiger PM. Treatment of rheumatoid arthritis during pregnancy: present and future. Expert Rev Clin Immunol. 2016;12:937-944.
- Gooderham M, Elewski B, Pariser D, et al. Incidence of serious gastrointestinal events and inflammatory bowel disease among tildrakizumab-treated patients with moderate-to-severe plaque psoriasis: data from 3 large randomized clinical trials [abstract]. J Am Acad Dermatol. 2018;79(suppl 1):AB166.
- Lebwohl M, Strober B, Menter A, et al. Phase 3 studies comparing brodalumab with ustekinumab in psoriasis. N Engl J Med. 2015;373:1318-328.
- Papp KA, Reich K, Paul C, et al. A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. Br J Dermatol. 2016;175:273-286
- Beck KM, Koo J. Brodalumab for the treatment of plaque psoriasis: up-to-date. Expert Opin Biol Ther. 2019;19:287-292.
- Fouéré S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19(suppl 3):2-6.
- Björnsson ES, Bergmann OM, Björnsson HK, et al. Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419-1425, 1425.e1-3; quiz e19-20.
- Saunte DM, Mrowietz U, Puig L, et al. Candida infections in patients with psoriasis and psoriatic arthritis treated with interleukin-17 inhibitors and their practical management. Br J Dermatol. 2017;177:47-62.
- Huber F, Ehrensperger B, Hatz C, et al. Safety of live vaccines on immunosuppressive or immunomodulatory therapy—a retrospective study in three Swiss Travel Clinics [published online January 1, 2018]. J Travel Med. doi:10.1093/jtm/tax082.
- Dooling KL, Guo A, Patel M, et al. Recommendations of the Advisory Committee on Immunization Practices for Use of Herpes Zoster Vaccines. MMWR Morb Mortal Wkly Rep. 2018;67:103-108.
- Fiorentino D, Ho V, Lebwohl MG, et al. Risk of malignancy with systemic psoriasis treatment in the Psoriasis Longitudinal Assessment Registry. J Am Acad Dermatol. 2017;77:845-854.e5.
- Haynes K, Beukelman T, Curtis JR, et al. Tumor necrosis factor α inhibitor therapy and cancer risk in chronic immune-mediated diseases. Arthritis Rheum. 2013;65:48-58.
- Fabiano A, De Simone C, Gisondi P, et al. Management of patients with psoriasis treated with biologic drugs needing a surgical treatment. Drug Dev Res. 2014;75(suppl 1):S24-S26.
- Choi YM, Debbaneh M, Weinberg JM, et al. From the Medical Board of the National Psoriasis Foundation: perioperative management of systemic immunomodulatory agents in patients with psoriasis and psoriatic arthritis. J Am Acad Dermatol. 2016;75:798-805.e7.
- Honda H, Umezawa Y, Kikuchi S, et al. Switching of biologics in psoriasis: reasons and results. J Dermatol. 2017;44:1015-1019.
- Bracke S, Lambert J. Viewpoint on handling anti-TNF failure in psoriasis. Arch Dermatol Res. 2013;305:945-950.
Practice Points
- There are currently 11 biologics approved for psoriasis, but there is no first-line or optimalbiologic. The choice must be made using clinical judgment based on a variety of medical and social factors.
- Frequent assessment for efficacy of and adverse events due to biologic therapy is warranted, as lack of response, loss of response, or severe side effects may warrant addition of concurrent therapies or switching to a different biologic.
- There are important considerations to make when immunizing and planning for surgery in patients on biologics.
Systemic Therapies in Psoriasis: An Update on Newly Approved and Pipeline Biologics and Oral Treatments
Recent advances in our understanding of psoriatic immune pathways have led to new generations of targeted therapies developed over the last 5 years. Although the pathogenesis of psoriasis remains to be fully elucidated, the success of these targeted therapies has confirmed a critical role of the IL-23/helper T cell (TH17) axis in maintaining the psoriatic immune cascade, a positive feedback loop in which IL-17, IL-12, and IL-23 released from myeloid dendritic cells lead to activation of helperT cells. Activated helper T cells—namely TH1, TH17, and TH22—release IL-17, IL-22, and other proinflammatory cytokines, amplifying the immune response and leading to keratinocyte proliferation and immune cell migration to psoriatic lesions. Inhibition of IL-17 and IL-23 by several biologics disrupts this aberrant inflammatory cascade and has led to dramatic improvements in outcomes, particularly among patients with moderate to severe disease.
Numerous biologics targeting these pathways and several oral treatments have been approved by the US Food and Drug Administration (FDA) for the treatment of psoriasis; in addition, a number of promising therapies are on the horizon, and knowledge of these medications might help guide our treatment approach to the patient with psoriasis. This article provides an update on the most recent (as of 2019) approved therapies and medications in the pipeline for moderate to severe plaque psoriasis, with a focus on systemic agents in phase 3 clinical trials. (Medications targeting psoriatic arthritis, biosimilars, and existing medications approved by the FDA prior to 2019 will not be discussed.)
Risankizumab
Risankizumab-rzaa (formerly BI 655066) is a humanized IgG1 monoclonal antibody that targets the p19 subunit of IL-23, selectively inhibiting the role of this critical cytokine in psoriatic inflammation.
Phase 1 Trial
In a phase 1 proof-of-concept study, 39 patients with moderate to severe plaque psoriasis received varying dosages of intravenous or subcutaneous risankizumab or placebo.1 At week 12, the percentage of risankizumab-treated patients achieving reduction in the psoriasis area and severity index (PASI) score by 75% (PASI 75), 90% (PASI 90), and 100% (PASI 100) was 87% (27/31; P<.001 vs placebo), 58% (18/31; P=.007 vs placebo), and 16% (5/31; P=.590 vs placebo), respectively. Improvements in PASI scores were observed as early as week 2. Adverse events (AEs) were reported by 65% of the risankizumab group and 88% of the placebo group. Serious AEs were reported in 4 patients receiving risankizumab, none of which were considered related to the study medication.1
Phase 2 Trial
A phase 2 comparator trial demonstrated noninferiority at higher dosages of risankizumab in comparison to the IL-12/IL-23 inhibitor ustekinumab.2 Among 166 participants with moderate to severe plaque psoriasis, PASI 90 at week 12 was met by 77% of participants receiving 90 or 180 mg of risankizumab compared to 40% receiving ustekinumab (P<.001). Onset of activity with risankizumab was faster and the duration of effect longer vs ustekinumab; by week 8, at least PASI 75 was achieved by approximately 80% of participants in the 90-mg and 180-mg risankizumab groups compared to 60% in the ustekinumab group; PASI score reductions generally were maintained for as long as 20 weeks after the final dose of risankizumab was administered.2
Phase 3 Trials
The 52-week UltIMMa-1 and UltIMMa-2 phase 3 trials compared subcutaneous risankizumab (150 mg) to ustekinumab (45 or 90 mg [weight-based dosing]) or placebo administered at weeks 0, 4, 16, 28, and 40 in approximately 1000 patients with moderate to severe plaque psoriasis.3 Patients initially assigned to placebo switched to risankizumab 150 mg at week 16. At week 16, PASI 90 was achieved by 75.3% of risankizumab-treated patients, 42.0% of ustekinumab-treated patients, and 4.9% of placebo-treated patients in UltIMMa-1, and by 74.8% of risankizumab-treated patients, 47.5% of ustekinumab-treated patients, and 2.0% of placebo-treated patients in UltIMMa-2 (P<.0001 vs placebo and ustekinumab for both studies). Achievement of a static physician’s global assessment (sPGA) score of 0 or 1 at week 16 similarly favored risankizumab, with 87.8%, 63.0%, and 7.8% of patients in UltIMMa-1 meeting an sPGA score of 0 or 1 in the risankizumab, ustekinumab, and placebo groups, respectively, and 83.7%, 61.6%, and 5.1% in UltIMMa-2 meeting an sPGA score of 0 or 1 in the risankizumab, ustekinumab, and placebo groups, respectively (P<.0001 vs placebo and ustekinumab for both studies). Among patients initially assigned to risankizumab, improvements in PASI and sPGA continued to increase until week 52, with 81.9% achieving PASI 90 at week 52 compared to 44.0% on ustekinumab in UltIMMa-1, and 80.6% achieving PASI 90 at week 52 compared to 50.5% on ustekinumab in UltIMMa-2 (P<.0001 vs ustekinumab for both studies). Treatment-emergent AE profiles were similar for risankizumab and ustekinumab in both studies, and there were no unexpected safety findings.3
Risankizumab received FDA approval for the treatment of moderate to severe plaque psoriasis in April 2019.
Bimekizumab
Bimekizumab (UCB4940), a humanized IgG1 monoclonal antibody, selectively neutralizes the biologic functions of IL-17A and IL-17F, the latter of which has only recently been implicated in contributing to the psoriatic immune cascade.4
First-in-Human Study
Thirty-nine participants with mild psoriasis demonstrated efficacy after single-dose intravenous bimekizumab, with maximal improvements in all measures of disease activity observed between weeks 8 and 12 in participants receiving 160 to 640 mg.5
Proof-of-Concept Phase 1b Study
A subsequent trial of 53 participants with psoriatic arthritis demonstrated sustained efficacy to week 20 with varying dosages of intravenous bimekizumab.6 At week 8, PASI 100 was met by 86.7% of participants receiving the top 3 dosages of bimekizumab compared to none of the placebo-treated participants. Treatment-emergent AEs, including neutropenia and elevation of liver transaminases, were mostly mild to moderate and resolved spontaneously. There were 3 severe AEs and 3 serious AEs, none of which were related to treatment.6
Importantly, bimekizumab was shown in this small study to have the potential to be highly effective at treating psoriatic arthritis. American College of Rheumatology ACR20, ACR50, and ACR70 response criteria were very high, with an ACR20 of 80% and an ACR50 of 40%.6 Further trials are necessary to gather more data and confirm these findings; however, these levels of response are higher than those of any other biologic on the market.
Phase 2b Dose-Ranging Study
In this trial, 250 participants with moderate to severe plaque psoriasis received either 64 mg, 160 mg with a 320-mg loading dose, 320 mg, or 480 mg of subcutaneous bimekizumab or placebo at weeks 0, 4, and 8.7 At week 12, PASI 90 was achieved by significantly more patients in all bimekizumab-treated groups compared to the placebo group (46.2%–79.1% vs 0%; P<.0001 for all dosages); PASI 100 also was achieved by significantly more bimekizumab-treated patients (27.9%–60.0% vs 0%; P<.0002). Improvement began as early as week 4, with clinically meaningful responses observed in all bimekizumab groups across all measures of disease activity. Treatment-emergent AEs occurred more frequently in bimekizumab-treated participants (61%) than in placebo-treated participants (36%); the most common AEs were nasopharyngitis and upper respiratory tract infection. Of note, fungal infections were reported by 4.3% of participants receiving bimekizumab; all cases were localized superficial infection, and none led to discontinuation. Three serious AEs were reported, none of which were considered related to the study treatment.7
Mirikizumab
Mirikizumab (LY3074828) is a humanized IgG4 monoclonal antibody that selectively binds and inhibits the p19 subunit of IL-23, with no action on IL-12.
Phase 1 Trial
Mirikizumab was shown to improve PASI scores in patients with plaque psoriasis.8
Phase 2 Trial
Subsequently, a trial of 205 participants with moderate to severe plaque psoriasis compared 3 dosing regimens of subcutaneous mirikizumab—30, 100, or 300 mg—at weeks 0 and 8 compared to placebo.9 Primary end point results at week 16 demonstrated PASI 90 response rates of 0%, 29% (P=.009), 59% (P<.001), and 67% (P<.001) in the placebo, 30-mg, 100-mg, and 300-mg mirikizumab groups, respectively. Complete clearance of psoriasis, measured by PASI 100 and sPGA 0, was achieved by 0%, 16%, 31%, and 31%, respectively (P=.039 for 30 mg vs placebo; P=.007 for the higher dosage groups vs placebo). Response rates for all efficacy outcomes were statistically significantly higher for all mirikizumab treatment groups compared to placebo and were highest in the 100-mg and 300-mg treatment groups. Frequencies of participants reporting AEs were similar across treatment and placebo groups.9
Oral Medications
Only a few small-molecule, orally bioavailable therapies are on the market for the treatment of psoriasis, some of which are associated with unfavorable side-effect profiles that preclude long-term therapy.
BMS-986165
The intracellular signaling enzyme tyrosine kinase 2 is involved in functional responses of IL-12 and IL-23. BMS-986165, a potent oral inhibitor of tyrosine kinase 2 with greater selectivity than other tyrosine kinase inhibitors, demonstrated efficacy in a phase 2 trial of 267 participants with moderate to severe plaque psoriasis receiving any of 5 dosing regimens—3 mg every other day, 3 mg daily, 3 mg twice daily, 6 mg twice daily, and 12 mg daily—compared to placebo.10 At week 12, the percentage of patients with a 75% or greater reduction in PASI was 7% with placebo, 9% with 3 mg every other day (P=.49 vs placebo), 39% with 3 mg daily (P<.001 vs placebo), 69% with 3 mg twice daily (P<.001 vs placebo), 67% with 6 mg twice daily (P<.001 vs placebo), and 75% with 12 mg once daily (P<.001 vs placebo). Adverse events occurred in 51% of patients in the placebo group and in 55% to 80% of BMS-986165–treated patients; the most common AEs were nasopharyngitis, headache, diarrhea, nausea, and upper respiratory tract infection.10
A phase 3 trial comparing BMS-986165 with placebo and apremilast is underway (ClinicalTrials.gov Identifier NCT03611751).
Piclidenoson (CF101)
A novel small molecule that binds the Gi protein–associated A3 adenosine receptor piclidenoson induces an anti-inflammatory response via deregulation of the Wnt and nuclear factor κB signal transduction pathways, leading to downregulation of proinflammatory cytokines, including IL-17 and IL-23.11
In a phase 2 dose-ranging study, 75 patients with moderate to severe plaque psoriasis received varying dosages—1, 2, or 4 mg—of oral piclidenoson or placebo twice daily for 12 weeks.12 Progressive improvement in the mean change from baseline PASI score was observed in the 2-mg group, with statistically significant differences at weeks 8 and 12 compared to placebo (P=.047 and P=.031, respectively). At week 12, 35.3% of the 2-mg group achieved at least PASI 50. Improvements in PASI were less pronounced in the 4-mg group, and no therapeutic benefit was observed in the 1-mg group. Of the 20 AEs reported, 15 possibly were related to the study drug; 1 AE was severe.12
In a subsequent phase 2/3 trial, patients with moderate to severe plaque psoriasis received piclidenoson—1 or 2 mg—or placebo twice daily.13 At week 12, PASI 75 was achieved by 8.5% of patients in the 2-mg group and by 6.9% of patients receiving placebo (P=.621), thereby not meeting the primary study end point. Results at week 32 were more encouraging. In the 2-mg group, PASI mean percentage improvement was 57% (P<.002) compared to baseline, with linear improvements observed in PASI 50 (63.5%), PASI 75 (35.5%), PASI 90 (24.7%), and PASI 100 (10.6%).13
A phase 3 trial comparing piclidenoson 2 and 3 mg to apremilast and placebo is in progress (ClinicalTrials.gov Identifier NCT03168256).
Future Directions
Despite abundant options for treating moderate to severe plaque psoriasis and psoriatic arthritis, the pipeline remains rich. Novel treatments might have improved efficacy, favorable safety profiles, and different modes of administration compared to current medications. In addition to the novel therapeutics covered here, several treatments are in development further down the pipeline, with only phase 1 or 2 data available. Remtolumab (ABT-122), a tumor necrosis factor α– and IL-17A–targeted immunoglobulin, is unique among biologics, given its dual inhibition of tumor necrosis factor α and IL-17A.14 M1095 (ALX-0761), a novel trivalent bispecific nanobody, is another intriguing candidate. This dual inhibitor of IL-17A/F might exhibit a number of advantages over conventional antibodies, including better tissue penetration, reduced immunogenicity, and a longer half-life (ClinicalTrials.gov Identifier NCT03384745).15,16
As always with drug development, numerous medications that were under development failed to meet primary end points in phase 2 trials and have therefore been discontinued, including namilumab and prurisol. It is reassuring that the pace of drug discovery and development in psoriasis does not seem to be slowing; to our patients’ benefit, we will have an array of treatments available to tailor therapy to the individual.
- Krueger JG, Ferris LK, Menter A, et al. Anti-IL-23A mAb BI 655066 for treatment of moderate-to-severe psoriasis: safety, efficacy, pharmacokinetics, and biomarker results of a single-rising-dose, randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol. 2015;136:116-124.e7.
- Papp KA, Blauvelt A, Bukhalo M, et al. Risankizumab versus ustekinumab for moderate-to-severe plaque psoriasis. N Engl J Med. 2017;376:1551-1560.
- Gordon KB, Strober B, Lebwohl M, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392:650-661.
- Maroof A, Baeten D, Archer S, et al. 02.13 Il-17f contributes to human chronic inflammation in synovial tissue: preclinical evidence with dual IL-17a and IL-17f inhibition with bimekizumab in psoriatic arthritis. Ann Rheum Dis. 2017;76(Suppl 1):A13.
- Glatt S, Helmer E, Haier B, et al. First-in-human randomized study of bimekizumab, a humanized monoclonal antibody and selective dual inhibitor of IL-17A and IL-17F, in mild psoriasis. Br J Clin Pharmacol. 2017;83:991-1001.
- Glatt S, Baeten D, Baker T, et al. Dual IL-17A and IL-17F neutralisation by bimekizumab in psoriatic arthritis: evidence from preclinical experiments and a randomised placebo-controlled clinical trial that IL-17F contributes to human chronic tissue inflammation. Ann Rheum Dis. 2018;77:523-532.
- Papp KA, Merola JF, Gottlieb AB, et al. Dual neutralization of bothinterleukin 17A and interleukin 17F with bimekizumab in patients with psoriasis: results from BE ABLE 1, a 12-week randomized, double-blinded, placebo-controlled phase 2b trial. J Am Acad Dermatol. 2018;79:277-286.e10.
- Maari C. Safety, efficacy, and pharmacokinetics of a p19-directed IL-23 antibody in patients with plaque psoriasis and healthy subjects. Presented at: 25th European Academy of Dermatology and Venereology Congress; Vienna, Austria; September 28-October 2, 2016.
- Reich K, Rich P, Maari C, et al. Efficacy and safety of mirikizumab (LY3074828) in the treatment of moderate-to-severe plaque psoriasis: results from a randomized phase II study. Br J Dermatol. 2019;181:88-95.
- Papp K, Gordon K, Thaçi D, et al. Phase 2 trial of selective tyrosine kinase 2 inhibition in psoriasis. N Engl J Med. 2018;379:1313-1321.
- Cohen S, Barer F, Itzhak I, et al. Inhibition of IL-17 and IL-23 in human keratinocytes by the A3 adenosine receptor agonist piclidenoson. J Immunol Res. 2018;2018:2310970.
- David M, Akerman L, Ziv M, et al. Treatment of plaque-type psoriasis with oral CF101: data from an exploratory randomized phase 2 clinical trial. J Eur Acad Dermatol Venereol. 2012;26:361-367.
- 13. David M, Gospodinov DK, Gheorghe N, et al. Treatment of plaque-type psoriasis with oral CF101: data from a phase II/III multicenter, randomized, controlled trial. J Drugs Dermatol. 2016;15:931-938.
- Mease PJ, Genovese MC, Weinblatt ME, et al. Phase II study of ABT-122, a tumor necrosis factor- and interleukin-17A-targeted dual variable domain immunoglobulin, in patients with psoriatic arthritis with an inadequate response to methotrexate. Arthritis Rheumatol. 2018;70:1778-1789.
- Nanobodies’ competitive features. Ablynx website. http://www.ablynx.com/technology-innovation/nanobodies-competitive-features. Accessed July 4, 2019.
- Svecova D, Lubell MW, Casset-Semanaz F, et al. A randomized, double-blind, placebo-controlled phase 1 study of multiple ascending doses of subcutaneous M1095, an anti-interleukin-17A/F nanobody, in moderate-to-severe psoriasis. J Am Acad Dermatol. 2019;81:196-203.
Recent advances in our understanding of psoriatic immune pathways have led to new generations of targeted therapies developed over the last 5 years. Although the pathogenesis of psoriasis remains to be fully elucidated, the success of these targeted therapies has confirmed a critical role of the IL-23/helper T cell (TH17) axis in maintaining the psoriatic immune cascade, a positive feedback loop in which IL-17, IL-12, and IL-23 released from myeloid dendritic cells lead to activation of helperT cells. Activated helper T cells—namely TH1, TH17, and TH22—release IL-17, IL-22, and other proinflammatory cytokines, amplifying the immune response and leading to keratinocyte proliferation and immune cell migration to psoriatic lesions. Inhibition of IL-17 and IL-23 by several biologics disrupts this aberrant inflammatory cascade and has led to dramatic improvements in outcomes, particularly among patients with moderate to severe disease.
Numerous biologics targeting these pathways and several oral treatments have been approved by the US Food and Drug Administration (FDA) for the treatment of psoriasis; in addition, a number of promising therapies are on the horizon, and knowledge of these medications might help guide our treatment approach to the patient with psoriasis. This article provides an update on the most recent (as of 2019) approved therapies and medications in the pipeline for moderate to severe plaque psoriasis, with a focus on systemic agents in phase 3 clinical trials. (Medications targeting psoriatic arthritis, biosimilars, and existing medications approved by the FDA prior to 2019 will not be discussed.)
Risankizumab
Risankizumab-rzaa (formerly BI 655066) is a humanized IgG1 monoclonal antibody that targets the p19 subunit of IL-23, selectively inhibiting the role of this critical cytokine in psoriatic inflammation.
Phase 1 Trial
In a phase 1 proof-of-concept study, 39 patients with moderate to severe plaque psoriasis received varying dosages of intravenous or subcutaneous risankizumab or placebo.1 At week 12, the percentage of risankizumab-treated patients achieving reduction in the psoriasis area and severity index (PASI) score by 75% (PASI 75), 90% (PASI 90), and 100% (PASI 100) was 87% (27/31; P<.001 vs placebo), 58% (18/31; P=.007 vs placebo), and 16% (5/31; P=.590 vs placebo), respectively. Improvements in PASI scores were observed as early as week 2. Adverse events (AEs) were reported by 65% of the risankizumab group and 88% of the placebo group. Serious AEs were reported in 4 patients receiving risankizumab, none of which were considered related to the study medication.1
Phase 2 Trial
A phase 2 comparator trial demonstrated noninferiority at higher dosages of risankizumab in comparison to the IL-12/IL-23 inhibitor ustekinumab.2 Among 166 participants with moderate to severe plaque psoriasis, PASI 90 at week 12 was met by 77% of participants receiving 90 or 180 mg of risankizumab compared to 40% receiving ustekinumab (P<.001). Onset of activity with risankizumab was faster and the duration of effect longer vs ustekinumab; by week 8, at least PASI 75 was achieved by approximately 80% of participants in the 90-mg and 180-mg risankizumab groups compared to 60% in the ustekinumab group; PASI score reductions generally were maintained for as long as 20 weeks after the final dose of risankizumab was administered.2
Phase 3 Trials
The 52-week UltIMMa-1 and UltIMMa-2 phase 3 trials compared subcutaneous risankizumab (150 mg) to ustekinumab (45 or 90 mg [weight-based dosing]) or placebo administered at weeks 0, 4, 16, 28, and 40 in approximately 1000 patients with moderate to severe plaque psoriasis.3 Patients initially assigned to placebo switched to risankizumab 150 mg at week 16. At week 16, PASI 90 was achieved by 75.3% of risankizumab-treated patients, 42.0% of ustekinumab-treated patients, and 4.9% of placebo-treated patients in UltIMMa-1, and by 74.8% of risankizumab-treated patients, 47.5% of ustekinumab-treated patients, and 2.0% of placebo-treated patients in UltIMMa-2 (P<.0001 vs placebo and ustekinumab for both studies). Achievement of a static physician’s global assessment (sPGA) score of 0 or 1 at week 16 similarly favored risankizumab, with 87.8%, 63.0%, and 7.8% of patients in UltIMMa-1 meeting an sPGA score of 0 or 1 in the risankizumab, ustekinumab, and placebo groups, respectively, and 83.7%, 61.6%, and 5.1% in UltIMMa-2 meeting an sPGA score of 0 or 1 in the risankizumab, ustekinumab, and placebo groups, respectively (P<.0001 vs placebo and ustekinumab for both studies). Among patients initially assigned to risankizumab, improvements in PASI and sPGA continued to increase until week 52, with 81.9% achieving PASI 90 at week 52 compared to 44.0% on ustekinumab in UltIMMa-1, and 80.6% achieving PASI 90 at week 52 compared to 50.5% on ustekinumab in UltIMMa-2 (P<.0001 vs ustekinumab for both studies). Treatment-emergent AE profiles were similar for risankizumab and ustekinumab in both studies, and there were no unexpected safety findings.3
Risankizumab received FDA approval for the treatment of moderate to severe plaque psoriasis in April 2019.
Bimekizumab
Bimekizumab (UCB4940), a humanized IgG1 monoclonal antibody, selectively neutralizes the biologic functions of IL-17A and IL-17F, the latter of which has only recently been implicated in contributing to the psoriatic immune cascade.4
First-in-Human Study
Thirty-nine participants with mild psoriasis demonstrated efficacy after single-dose intravenous bimekizumab, with maximal improvements in all measures of disease activity observed between weeks 8 and 12 in participants receiving 160 to 640 mg.5
Proof-of-Concept Phase 1b Study
A subsequent trial of 53 participants with psoriatic arthritis demonstrated sustained efficacy to week 20 with varying dosages of intravenous bimekizumab.6 At week 8, PASI 100 was met by 86.7% of participants receiving the top 3 dosages of bimekizumab compared to none of the placebo-treated participants. Treatment-emergent AEs, including neutropenia and elevation of liver transaminases, were mostly mild to moderate and resolved spontaneously. There were 3 severe AEs and 3 serious AEs, none of which were related to treatment.6
Importantly, bimekizumab was shown in this small study to have the potential to be highly effective at treating psoriatic arthritis. American College of Rheumatology ACR20, ACR50, and ACR70 response criteria were very high, with an ACR20 of 80% and an ACR50 of 40%.6 Further trials are necessary to gather more data and confirm these findings; however, these levels of response are higher than those of any other biologic on the market.
Phase 2b Dose-Ranging Study
In this trial, 250 participants with moderate to severe plaque psoriasis received either 64 mg, 160 mg with a 320-mg loading dose, 320 mg, or 480 mg of subcutaneous bimekizumab or placebo at weeks 0, 4, and 8.7 At week 12, PASI 90 was achieved by significantly more patients in all bimekizumab-treated groups compared to the placebo group (46.2%–79.1% vs 0%; P<.0001 for all dosages); PASI 100 also was achieved by significantly more bimekizumab-treated patients (27.9%–60.0% vs 0%; P<.0002). Improvement began as early as week 4, with clinically meaningful responses observed in all bimekizumab groups across all measures of disease activity. Treatment-emergent AEs occurred more frequently in bimekizumab-treated participants (61%) than in placebo-treated participants (36%); the most common AEs were nasopharyngitis and upper respiratory tract infection. Of note, fungal infections were reported by 4.3% of participants receiving bimekizumab; all cases were localized superficial infection, and none led to discontinuation. Three serious AEs were reported, none of which were considered related to the study treatment.7
Mirikizumab
Mirikizumab (LY3074828) is a humanized IgG4 monoclonal antibody that selectively binds and inhibits the p19 subunit of IL-23, with no action on IL-12.
Phase 1 Trial
Mirikizumab was shown to improve PASI scores in patients with plaque psoriasis.8
Phase 2 Trial
Subsequently, a trial of 205 participants with moderate to severe plaque psoriasis compared 3 dosing regimens of subcutaneous mirikizumab—30, 100, or 300 mg—at weeks 0 and 8 compared to placebo.9 Primary end point results at week 16 demonstrated PASI 90 response rates of 0%, 29% (P=.009), 59% (P<.001), and 67% (P<.001) in the placebo, 30-mg, 100-mg, and 300-mg mirikizumab groups, respectively. Complete clearance of psoriasis, measured by PASI 100 and sPGA 0, was achieved by 0%, 16%, 31%, and 31%, respectively (P=.039 for 30 mg vs placebo; P=.007 for the higher dosage groups vs placebo). Response rates for all efficacy outcomes were statistically significantly higher for all mirikizumab treatment groups compared to placebo and were highest in the 100-mg and 300-mg treatment groups. Frequencies of participants reporting AEs were similar across treatment and placebo groups.9
Oral Medications
Only a few small-molecule, orally bioavailable therapies are on the market for the treatment of psoriasis, some of which are associated with unfavorable side-effect profiles that preclude long-term therapy.
BMS-986165
The intracellular signaling enzyme tyrosine kinase 2 is involved in functional responses of IL-12 and IL-23. BMS-986165, a potent oral inhibitor of tyrosine kinase 2 with greater selectivity than other tyrosine kinase inhibitors, demonstrated efficacy in a phase 2 trial of 267 participants with moderate to severe plaque psoriasis receiving any of 5 dosing regimens—3 mg every other day, 3 mg daily, 3 mg twice daily, 6 mg twice daily, and 12 mg daily—compared to placebo.10 At week 12, the percentage of patients with a 75% or greater reduction in PASI was 7% with placebo, 9% with 3 mg every other day (P=.49 vs placebo), 39% with 3 mg daily (P<.001 vs placebo), 69% with 3 mg twice daily (P<.001 vs placebo), 67% with 6 mg twice daily (P<.001 vs placebo), and 75% with 12 mg once daily (P<.001 vs placebo). Adverse events occurred in 51% of patients in the placebo group and in 55% to 80% of BMS-986165–treated patients; the most common AEs were nasopharyngitis, headache, diarrhea, nausea, and upper respiratory tract infection.10
A phase 3 trial comparing BMS-986165 with placebo and apremilast is underway (ClinicalTrials.gov Identifier NCT03611751).
Piclidenoson (CF101)
A novel small molecule that binds the Gi protein–associated A3 adenosine receptor piclidenoson induces an anti-inflammatory response via deregulation of the Wnt and nuclear factor κB signal transduction pathways, leading to downregulation of proinflammatory cytokines, including IL-17 and IL-23.11
In a phase 2 dose-ranging study, 75 patients with moderate to severe plaque psoriasis received varying dosages—1, 2, or 4 mg—of oral piclidenoson or placebo twice daily for 12 weeks.12 Progressive improvement in the mean change from baseline PASI score was observed in the 2-mg group, with statistically significant differences at weeks 8 and 12 compared to placebo (P=.047 and P=.031, respectively). At week 12, 35.3% of the 2-mg group achieved at least PASI 50. Improvements in PASI were less pronounced in the 4-mg group, and no therapeutic benefit was observed in the 1-mg group. Of the 20 AEs reported, 15 possibly were related to the study drug; 1 AE was severe.12
In a subsequent phase 2/3 trial, patients with moderate to severe plaque psoriasis received piclidenoson—1 or 2 mg—or placebo twice daily.13 At week 12, PASI 75 was achieved by 8.5% of patients in the 2-mg group and by 6.9% of patients receiving placebo (P=.621), thereby not meeting the primary study end point. Results at week 32 were more encouraging. In the 2-mg group, PASI mean percentage improvement was 57% (P<.002) compared to baseline, with linear improvements observed in PASI 50 (63.5%), PASI 75 (35.5%), PASI 90 (24.7%), and PASI 100 (10.6%).13
A phase 3 trial comparing piclidenoson 2 and 3 mg to apremilast and placebo is in progress (ClinicalTrials.gov Identifier NCT03168256).
Future Directions
Despite abundant options for treating moderate to severe plaque psoriasis and psoriatic arthritis, the pipeline remains rich. Novel treatments might have improved efficacy, favorable safety profiles, and different modes of administration compared to current medications. In addition to the novel therapeutics covered here, several treatments are in development further down the pipeline, with only phase 1 or 2 data available. Remtolumab (ABT-122), a tumor necrosis factor α– and IL-17A–targeted immunoglobulin, is unique among biologics, given its dual inhibition of tumor necrosis factor α and IL-17A.14 M1095 (ALX-0761), a novel trivalent bispecific nanobody, is another intriguing candidate. This dual inhibitor of IL-17A/F might exhibit a number of advantages over conventional antibodies, including better tissue penetration, reduced immunogenicity, and a longer half-life (ClinicalTrials.gov Identifier NCT03384745).15,16
As always with drug development, numerous medications that were under development failed to meet primary end points in phase 2 trials and have therefore been discontinued, including namilumab and prurisol. It is reassuring that the pace of drug discovery and development in psoriasis does not seem to be slowing; to our patients’ benefit, we will have an array of treatments available to tailor therapy to the individual.
Recent advances in our understanding of psoriatic immune pathways have led to new generations of targeted therapies developed over the last 5 years. Although the pathogenesis of psoriasis remains to be fully elucidated, the success of these targeted therapies has confirmed a critical role of the IL-23/helper T cell (TH17) axis in maintaining the psoriatic immune cascade, a positive feedback loop in which IL-17, IL-12, and IL-23 released from myeloid dendritic cells lead to activation of helperT cells. Activated helper T cells—namely TH1, TH17, and TH22—release IL-17, IL-22, and other proinflammatory cytokines, amplifying the immune response and leading to keratinocyte proliferation and immune cell migration to psoriatic lesions. Inhibition of IL-17 and IL-23 by several biologics disrupts this aberrant inflammatory cascade and has led to dramatic improvements in outcomes, particularly among patients with moderate to severe disease.
Numerous biologics targeting these pathways and several oral treatments have been approved by the US Food and Drug Administration (FDA) for the treatment of psoriasis; in addition, a number of promising therapies are on the horizon, and knowledge of these medications might help guide our treatment approach to the patient with psoriasis. This article provides an update on the most recent (as of 2019) approved therapies and medications in the pipeline for moderate to severe plaque psoriasis, with a focus on systemic agents in phase 3 clinical trials. (Medications targeting psoriatic arthritis, biosimilars, and existing medications approved by the FDA prior to 2019 will not be discussed.)
Risankizumab
Risankizumab-rzaa (formerly BI 655066) is a humanized IgG1 monoclonal antibody that targets the p19 subunit of IL-23, selectively inhibiting the role of this critical cytokine in psoriatic inflammation.
Phase 1 Trial
In a phase 1 proof-of-concept study, 39 patients with moderate to severe plaque psoriasis received varying dosages of intravenous or subcutaneous risankizumab or placebo.1 At week 12, the percentage of risankizumab-treated patients achieving reduction in the psoriasis area and severity index (PASI) score by 75% (PASI 75), 90% (PASI 90), and 100% (PASI 100) was 87% (27/31; P<.001 vs placebo), 58% (18/31; P=.007 vs placebo), and 16% (5/31; P=.590 vs placebo), respectively. Improvements in PASI scores were observed as early as week 2. Adverse events (AEs) were reported by 65% of the risankizumab group and 88% of the placebo group. Serious AEs were reported in 4 patients receiving risankizumab, none of which were considered related to the study medication.1
Phase 2 Trial
A phase 2 comparator trial demonstrated noninferiority at higher dosages of risankizumab in comparison to the IL-12/IL-23 inhibitor ustekinumab.2 Among 166 participants with moderate to severe plaque psoriasis, PASI 90 at week 12 was met by 77% of participants receiving 90 or 180 mg of risankizumab compared to 40% receiving ustekinumab (P<.001). Onset of activity with risankizumab was faster and the duration of effect longer vs ustekinumab; by week 8, at least PASI 75 was achieved by approximately 80% of participants in the 90-mg and 180-mg risankizumab groups compared to 60% in the ustekinumab group; PASI score reductions generally were maintained for as long as 20 weeks after the final dose of risankizumab was administered.2
Phase 3 Trials
The 52-week UltIMMa-1 and UltIMMa-2 phase 3 trials compared subcutaneous risankizumab (150 mg) to ustekinumab (45 or 90 mg [weight-based dosing]) or placebo administered at weeks 0, 4, 16, 28, and 40 in approximately 1000 patients with moderate to severe plaque psoriasis.3 Patients initially assigned to placebo switched to risankizumab 150 mg at week 16. At week 16, PASI 90 was achieved by 75.3% of risankizumab-treated patients, 42.0% of ustekinumab-treated patients, and 4.9% of placebo-treated patients in UltIMMa-1, and by 74.8% of risankizumab-treated patients, 47.5% of ustekinumab-treated patients, and 2.0% of placebo-treated patients in UltIMMa-2 (P<.0001 vs placebo and ustekinumab for both studies). Achievement of a static physician’s global assessment (sPGA) score of 0 or 1 at week 16 similarly favored risankizumab, with 87.8%, 63.0%, and 7.8% of patients in UltIMMa-1 meeting an sPGA score of 0 or 1 in the risankizumab, ustekinumab, and placebo groups, respectively, and 83.7%, 61.6%, and 5.1% in UltIMMa-2 meeting an sPGA score of 0 or 1 in the risankizumab, ustekinumab, and placebo groups, respectively (P<.0001 vs placebo and ustekinumab for both studies). Among patients initially assigned to risankizumab, improvements in PASI and sPGA continued to increase until week 52, with 81.9% achieving PASI 90 at week 52 compared to 44.0% on ustekinumab in UltIMMa-1, and 80.6% achieving PASI 90 at week 52 compared to 50.5% on ustekinumab in UltIMMa-2 (P<.0001 vs ustekinumab for both studies). Treatment-emergent AE profiles were similar for risankizumab and ustekinumab in both studies, and there were no unexpected safety findings.3
Risankizumab received FDA approval for the treatment of moderate to severe plaque psoriasis in April 2019.
Bimekizumab
Bimekizumab (UCB4940), a humanized IgG1 monoclonal antibody, selectively neutralizes the biologic functions of IL-17A and IL-17F, the latter of which has only recently been implicated in contributing to the psoriatic immune cascade.4
First-in-Human Study
Thirty-nine participants with mild psoriasis demonstrated efficacy after single-dose intravenous bimekizumab, with maximal improvements in all measures of disease activity observed between weeks 8 and 12 in participants receiving 160 to 640 mg.5
Proof-of-Concept Phase 1b Study
A subsequent trial of 53 participants with psoriatic arthritis demonstrated sustained efficacy to week 20 with varying dosages of intravenous bimekizumab.6 At week 8, PASI 100 was met by 86.7% of participants receiving the top 3 dosages of bimekizumab compared to none of the placebo-treated participants. Treatment-emergent AEs, including neutropenia and elevation of liver transaminases, were mostly mild to moderate and resolved spontaneously. There were 3 severe AEs and 3 serious AEs, none of which were related to treatment.6
Importantly, bimekizumab was shown in this small study to have the potential to be highly effective at treating psoriatic arthritis. American College of Rheumatology ACR20, ACR50, and ACR70 response criteria were very high, with an ACR20 of 80% and an ACR50 of 40%.6 Further trials are necessary to gather more data and confirm these findings; however, these levels of response are higher than those of any other biologic on the market.
Phase 2b Dose-Ranging Study
In this trial, 250 participants with moderate to severe plaque psoriasis received either 64 mg, 160 mg with a 320-mg loading dose, 320 mg, or 480 mg of subcutaneous bimekizumab or placebo at weeks 0, 4, and 8.7 At week 12, PASI 90 was achieved by significantly more patients in all bimekizumab-treated groups compared to the placebo group (46.2%–79.1% vs 0%; P<.0001 for all dosages); PASI 100 also was achieved by significantly more bimekizumab-treated patients (27.9%–60.0% vs 0%; P<.0002). Improvement began as early as week 4, with clinically meaningful responses observed in all bimekizumab groups across all measures of disease activity. Treatment-emergent AEs occurred more frequently in bimekizumab-treated participants (61%) than in placebo-treated participants (36%); the most common AEs were nasopharyngitis and upper respiratory tract infection. Of note, fungal infections were reported by 4.3% of participants receiving bimekizumab; all cases were localized superficial infection, and none led to discontinuation. Three serious AEs were reported, none of which were considered related to the study treatment.7
Mirikizumab
Mirikizumab (LY3074828) is a humanized IgG4 monoclonal antibody that selectively binds and inhibits the p19 subunit of IL-23, with no action on IL-12.
Phase 1 Trial
Mirikizumab was shown to improve PASI scores in patients with plaque psoriasis.8
Phase 2 Trial
Subsequently, a trial of 205 participants with moderate to severe plaque psoriasis compared 3 dosing regimens of subcutaneous mirikizumab—30, 100, or 300 mg—at weeks 0 and 8 compared to placebo.9 Primary end point results at week 16 demonstrated PASI 90 response rates of 0%, 29% (P=.009), 59% (P<.001), and 67% (P<.001) in the placebo, 30-mg, 100-mg, and 300-mg mirikizumab groups, respectively. Complete clearance of psoriasis, measured by PASI 100 and sPGA 0, was achieved by 0%, 16%, 31%, and 31%, respectively (P=.039 for 30 mg vs placebo; P=.007 for the higher dosage groups vs placebo). Response rates for all efficacy outcomes were statistically significantly higher for all mirikizumab treatment groups compared to placebo and were highest in the 100-mg and 300-mg treatment groups. Frequencies of participants reporting AEs were similar across treatment and placebo groups.9
Oral Medications
Only a few small-molecule, orally bioavailable therapies are on the market for the treatment of psoriasis, some of which are associated with unfavorable side-effect profiles that preclude long-term therapy.
BMS-986165
The intracellular signaling enzyme tyrosine kinase 2 is involved in functional responses of IL-12 and IL-23. BMS-986165, a potent oral inhibitor of tyrosine kinase 2 with greater selectivity than other tyrosine kinase inhibitors, demonstrated efficacy in a phase 2 trial of 267 participants with moderate to severe plaque psoriasis receiving any of 5 dosing regimens—3 mg every other day, 3 mg daily, 3 mg twice daily, 6 mg twice daily, and 12 mg daily—compared to placebo.10 At week 12, the percentage of patients with a 75% or greater reduction in PASI was 7% with placebo, 9% with 3 mg every other day (P=.49 vs placebo), 39% with 3 mg daily (P<.001 vs placebo), 69% with 3 mg twice daily (P<.001 vs placebo), 67% with 6 mg twice daily (P<.001 vs placebo), and 75% with 12 mg once daily (P<.001 vs placebo). Adverse events occurred in 51% of patients in the placebo group and in 55% to 80% of BMS-986165–treated patients; the most common AEs were nasopharyngitis, headache, diarrhea, nausea, and upper respiratory tract infection.10
A phase 3 trial comparing BMS-986165 with placebo and apremilast is underway (ClinicalTrials.gov Identifier NCT03611751).
Piclidenoson (CF101)
A novel small molecule that binds the Gi protein–associated A3 adenosine receptor piclidenoson induces an anti-inflammatory response via deregulation of the Wnt and nuclear factor κB signal transduction pathways, leading to downregulation of proinflammatory cytokines, including IL-17 and IL-23.11
In a phase 2 dose-ranging study, 75 patients with moderate to severe plaque psoriasis received varying dosages—1, 2, or 4 mg—of oral piclidenoson or placebo twice daily for 12 weeks.12 Progressive improvement in the mean change from baseline PASI score was observed in the 2-mg group, with statistically significant differences at weeks 8 and 12 compared to placebo (P=.047 and P=.031, respectively). At week 12, 35.3% of the 2-mg group achieved at least PASI 50. Improvements in PASI were less pronounced in the 4-mg group, and no therapeutic benefit was observed in the 1-mg group. Of the 20 AEs reported, 15 possibly were related to the study drug; 1 AE was severe.12
In a subsequent phase 2/3 trial, patients with moderate to severe plaque psoriasis received piclidenoson—1 or 2 mg—or placebo twice daily.13 At week 12, PASI 75 was achieved by 8.5% of patients in the 2-mg group and by 6.9% of patients receiving placebo (P=.621), thereby not meeting the primary study end point. Results at week 32 were more encouraging. In the 2-mg group, PASI mean percentage improvement was 57% (P<.002) compared to baseline, with linear improvements observed in PASI 50 (63.5%), PASI 75 (35.5%), PASI 90 (24.7%), and PASI 100 (10.6%).13
A phase 3 trial comparing piclidenoson 2 and 3 mg to apremilast and placebo is in progress (ClinicalTrials.gov Identifier NCT03168256).
Future Directions
Despite abundant options for treating moderate to severe plaque psoriasis and psoriatic arthritis, the pipeline remains rich. Novel treatments might have improved efficacy, favorable safety profiles, and different modes of administration compared to current medications. In addition to the novel therapeutics covered here, several treatments are in development further down the pipeline, with only phase 1 or 2 data available. Remtolumab (ABT-122), a tumor necrosis factor α– and IL-17A–targeted immunoglobulin, is unique among biologics, given its dual inhibition of tumor necrosis factor α and IL-17A.14 M1095 (ALX-0761), a novel trivalent bispecific nanobody, is another intriguing candidate. This dual inhibitor of IL-17A/F might exhibit a number of advantages over conventional antibodies, including better tissue penetration, reduced immunogenicity, and a longer half-life (ClinicalTrials.gov Identifier NCT03384745).15,16
As always with drug development, numerous medications that were under development failed to meet primary end points in phase 2 trials and have therefore been discontinued, including namilumab and prurisol. It is reassuring that the pace of drug discovery and development in psoriasis does not seem to be slowing; to our patients’ benefit, we will have an array of treatments available to tailor therapy to the individual.
- Krueger JG, Ferris LK, Menter A, et al. Anti-IL-23A mAb BI 655066 for treatment of moderate-to-severe psoriasis: safety, efficacy, pharmacokinetics, and biomarker results of a single-rising-dose, randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol. 2015;136:116-124.e7.
- Papp KA, Blauvelt A, Bukhalo M, et al. Risankizumab versus ustekinumab for moderate-to-severe plaque psoriasis. N Engl J Med. 2017;376:1551-1560.
- Gordon KB, Strober B, Lebwohl M, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392:650-661.
- Maroof A, Baeten D, Archer S, et al. 02.13 Il-17f contributes to human chronic inflammation in synovial tissue: preclinical evidence with dual IL-17a and IL-17f inhibition with bimekizumab in psoriatic arthritis. Ann Rheum Dis. 2017;76(Suppl 1):A13.
- Glatt S, Helmer E, Haier B, et al. First-in-human randomized study of bimekizumab, a humanized monoclonal antibody and selective dual inhibitor of IL-17A and IL-17F, in mild psoriasis. Br J Clin Pharmacol. 2017;83:991-1001.
- Glatt S, Baeten D, Baker T, et al. Dual IL-17A and IL-17F neutralisation by bimekizumab in psoriatic arthritis: evidence from preclinical experiments and a randomised placebo-controlled clinical trial that IL-17F contributes to human chronic tissue inflammation. Ann Rheum Dis. 2018;77:523-532.
- Papp KA, Merola JF, Gottlieb AB, et al. Dual neutralization of bothinterleukin 17A and interleukin 17F with bimekizumab in patients with psoriasis: results from BE ABLE 1, a 12-week randomized, double-blinded, placebo-controlled phase 2b trial. J Am Acad Dermatol. 2018;79:277-286.e10.
- Maari C. Safety, efficacy, and pharmacokinetics of a p19-directed IL-23 antibody in patients with plaque psoriasis and healthy subjects. Presented at: 25th European Academy of Dermatology and Venereology Congress; Vienna, Austria; September 28-October 2, 2016.
- Reich K, Rich P, Maari C, et al. Efficacy and safety of mirikizumab (LY3074828) in the treatment of moderate-to-severe plaque psoriasis: results from a randomized phase II study. Br J Dermatol. 2019;181:88-95.
- Papp K, Gordon K, Thaçi D, et al. Phase 2 trial of selective tyrosine kinase 2 inhibition in psoriasis. N Engl J Med. 2018;379:1313-1321.
- Cohen S, Barer F, Itzhak I, et al. Inhibition of IL-17 and IL-23 in human keratinocytes by the A3 adenosine receptor agonist piclidenoson. J Immunol Res. 2018;2018:2310970.
- David M, Akerman L, Ziv M, et al. Treatment of plaque-type psoriasis with oral CF101: data from an exploratory randomized phase 2 clinical trial. J Eur Acad Dermatol Venereol. 2012;26:361-367.
- 13. David M, Gospodinov DK, Gheorghe N, et al. Treatment of plaque-type psoriasis with oral CF101: data from a phase II/III multicenter, randomized, controlled trial. J Drugs Dermatol. 2016;15:931-938.
- Mease PJ, Genovese MC, Weinblatt ME, et al. Phase II study of ABT-122, a tumor necrosis factor- and interleukin-17A-targeted dual variable domain immunoglobulin, in patients with psoriatic arthritis with an inadequate response to methotrexate. Arthritis Rheumatol. 2018;70:1778-1789.
- Nanobodies’ competitive features. Ablynx website. http://www.ablynx.com/technology-innovation/nanobodies-competitive-features. Accessed July 4, 2019.
- Svecova D, Lubell MW, Casset-Semanaz F, et al. A randomized, double-blind, placebo-controlled phase 1 study of multiple ascending doses of subcutaneous M1095, an anti-interleukin-17A/F nanobody, in moderate-to-severe psoriasis. J Am Acad Dermatol. 2019;81:196-203.
- Krueger JG, Ferris LK, Menter A, et al. Anti-IL-23A mAb BI 655066 for treatment of moderate-to-severe psoriasis: safety, efficacy, pharmacokinetics, and biomarker results of a single-rising-dose, randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol. 2015;136:116-124.e7.
- Papp KA, Blauvelt A, Bukhalo M, et al. Risankizumab versus ustekinumab for moderate-to-severe plaque psoriasis. N Engl J Med. 2017;376:1551-1560.
- Gordon KB, Strober B, Lebwohl M, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet. 2018;392:650-661.
- Maroof A, Baeten D, Archer S, et al. 02.13 Il-17f contributes to human chronic inflammation in synovial tissue: preclinical evidence with dual IL-17a and IL-17f inhibition with bimekizumab in psoriatic arthritis. Ann Rheum Dis. 2017;76(Suppl 1):A13.
- Glatt S, Helmer E, Haier B, et al. First-in-human randomized study of bimekizumab, a humanized monoclonal antibody and selective dual inhibitor of IL-17A and IL-17F, in mild psoriasis. Br J Clin Pharmacol. 2017;83:991-1001.
- Glatt S, Baeten D, Baker T, et al. Dual IL-17A and IL-17F neutralisation by bimekizumab in psoriatic arthritis: evidence from preclinical experiments and a randomised placebo-controlled clinical trial that IL-17F contributes to human chronic tissue inflammation. Ann Rheum Dis. 2018;77:523-532.
- Papp KA, Merola JF, Gottlieb AB, et al. Dual neutralization of bothinterleukin 17A and interleukin 17F with bimekizumab in patients with psoriasis: results from BE ABLE 1, a 12-week randomized, double-blinded, placebo-controlled phase 2b trial. J Am Acad Dermatol. 2018;79:277-286.e10.
- Maari C. Safety, efficacy, and pharmacokinetics of a p19-directed IL-23 antibody in patients with plaque psoriasis and healthy subjects. Presented at: 25th European Academy of Dermatology and Venereology Congress; Vienna, Austria; September 28-October 2, 2016.
- Reich K, Rich P, Maari C, et al. Efficacy and safety of mirikizumab (LY3074828) in the treatment of moderate-to-severe plaque psoriasis: results from a randomized phase II study. Br J Dermatol. 2019;181:88-95.
- Papp K, Gordon K, Thaçi D, et al. Phase 2 trial of selective tyrosine kinase 2 inhibition in psoriasis. N Engl J Med. 2018;379:1313-1321.
- Cohen S, Barer F, Itzhak I, et al. Inhibition of IL-17 and IL-23 in human keratinocytes by the A3 adenosine receptor agonist piclidenoson. J Immunol Res. 2018;2018:2310970.
- David M, Akerman L, Ziv M, et al. Treatment of plaque-type psoriasis with oral CF101: data from an exploratory randomized phase 2 clinical trial. J Eur Acad Dermatol Venereol. 2012;26:361-367.
- 13. David M, Gospodinov DK, Gheorghe N, et al. Treatment of plaque-type psoriasis with oral CF101: data from a phase II/III multicenter, randomized, controlled trial. J Drugs Dermatol. 2016;15:931-938.
- Mease PJ, Genovese MC, Weinblatt ME, et al. Phase II study of ABT-122, a tumor necrosis factor- and interleukin-17A-targeted dual variable domain immunoglobulin, in patients with psoriatic arthritis with an inadequate response to methotrexate. Arthritis Rheumatol. 2018;70:1778-1789.
- Nanobodies’ competitive features. Ablynx website. http://www.ablynx.com/technology-innovation/nanobodies-competitive-features. Accessed July 4, 2019.
- Svecova D, Lubell MW, Casset-Semanaz F, et al. A randomized, double-blind, placebo-controlled phase 1 study of multiple ascending doses of subcutaneous M1095, an anti-interleukin-17A/F nanobody, in moderate-to-severe psoriasis. J Am Acad Dermatol. 2019;81:196-203.
Practice Points
- New systemic options for the treatment of psoriasis continue to emerge.
- With more choices, we can now tailor therapeutic approaches to the patient rather than base treatment choices purely on efficacy.
- New and upcoming biologics may offer improved skin clearance in line with the National Psoriasis Foundation’s treat-to-target approach, while others may offer increased efficacy in treating psoriatic arthritis.
- Novel small-molecule oral medications are in development and may have improved efficacy over current options.
ECT breaks super-refractory status epilepticus
BANGKOK –
“These were highly refractory patients and ECT did contribute to their status termination,” she reported at the congress, sponsored by the International League Against Epilepsy.
Dr. Nguyen, a neurologist at Oregon Health and Science University, Portland, presented a single-center retrospective case series composed of four ECT-treated patients with NORSE (new onset refractory status epilepticus), three of whom experienced marked improvement in their seizure activity, including cessation of their status epilepticus, after completing a course of eight or nine ECT sessions.
A four-patient series may not seem to be compelling evidence, but it’s a significant contribution to the sparse literature regarding this off-label usage of ECT. Indeed, the biggest case series to date consists of eight patients treated at Indiana University, five of whom displayed neurotelemetry or clinical evidence of improvement within 24 hours after completing a full course of ECT (J ECT. 2018 Mar;34[1]:e5-e9. doi: 10.1097/YCT.0000000000000450).
And realistically, these small case series are as good as the supporting evidence is likely to get.
“It would be incredibly difficult to perform a randomized trial, and even a case-control study in such refractory patients would be quite difficult,” she observed.
Super-refractory status epilepticus is the term for seizures persisting despite 24 hours of adequate treatment with benzodiazepines, loading doses of antiepileptic drugs, and anesthetic agents for medically-induced coma, or for seizures that resume after withdrawal of general anesthesia. NORSE is defined as refractory status epilepticus without a history of seizures or a readily identifiable etiology. It is often associated with an autoimmune or paraneoplastic encephalitis. Outcomes are generally poor.
The four ECT-treated patients in the Oregon series were aged 27-48 years. Two had a prodromal viral illness, and a third had a vague prodrome but a negative infectious disease workup. Three patients were on four antiepileptic drugs at the time they began ECT, one was on seven. Two patients had generalized seizures, while the other two had both generalized and focal seizures. Two had normal brain MRI scans and the other two had abnormal MRIs. The patients had CSF white blood cell counts of 2, 5, 10, and 58 per mm3. All patients were on immunotherapy with intravenous corticosteroids, and three of the four were on additional immunomodulatory drugs.
ECT was started on a compassionate-use basis 16-49 days after hospital admission. These were patients who had run out of options, according to Dr. Nguyen.
Three of the four patients returned to consciousness after completing their course of ECT and withdrawal of their general anesthesia, with attenuation of their seizure activity and cessation of their super-refractory status epilepticus. Two of the three were discharged to a rehabilitation facility, including one who eventually could ambulate with slight assistance. Another patient died after discharge, while the fourth patient died during the initial hospital stay due to septic shock unrelated to the ECT.
At discharge, one patient had a modified Rankin Scale score (mRS) of 4, and two had a score of 5. At follow-up, two patients had a score of 3 and one was a 6.
Dr. Nguyen’s presentation met with undisguised audience skepticism.
“What is the theoretical basis to treat very severe epileptic seizures with another epileptic seizure? I mean, what made you do this?” one neurologist asked.
Dr. Nguyen replied that the mechanism of benefit isn’t clear. One possibility is enhanced inhibition of gamma-aminobutyric acid.
“When I describe ECT to the family, the way I think of it is as a hard reset. We tried burst suppression. This is an alternative approach,” she explained.
Another audience member said the treatment strategy smacks of homeopathy.
“These patients have a terrible disorder,” said session co-chair Gregory Krauss, MD. “Three of your four patients ultimately did not do very well.
“The question is, what are you really accomplishing in terms of the underlying encephalopathy and irritability that’s causing this? And are the seizures really a primary factor in their outcome? Is this treatment warranted to try to improve their overall outcome?” asked Dr. Krauss, professor of neurology at Johns Hopkins University, Baltimore.
Dr. Nguyen answered that she can’t say if the seizures are the cause or result of the encephalopathy.
“ECT was done well into the patients’ admission. Our difficulty is that while we were able to stop the seizures, unfortunately we weren’t able to go back in time and save the brain that was lost due to the convulsive and nonconvulsive activity,” she said. Dr. Nguyen added that she and her coinvestigators are interested in exploring the possibility that utilizing ECT earlier might abort the super-refractory status epilepticus sooner and thereby result in better outcomes.
Still, she noted, three of the four patients were able to leave the hospital, and the two survivors show improved cognitive abilities at 51 and 100 months of follow-up.
Dr. Nguyen reported having no financial conflicts.
SOURCE: Nguyen MTV et al. IEC 2019, Abstract P031.
BANGKOK –
“These were highly refractory patients and ECT did contribute to their status termination,” she reported at the congress, sponsored by the International League Against Epilepsy.
Dr. Nguyen, a neurologist at Oregon Health and Science University, Portland, presented a single-center retrospective case series composed of four ECT-treated patients with NORSE (new onset refractory status epilepticus), three of whom experienced marked improvement in their seizure activity, including cessation of their status epilepticus, after completing a course of eight or nine ECT sessions.
A four-patient series may not seem to be compelling evidence, but it’s a significant contribution to the sparse literature regarding this off-label usage of ECT. Indeed, the biggest case series to date consists of eight patients treated at Indiana University, five of whom displayed neurotelemetry or clinical evidence of improvement within 24 hours after completing a full course of ECT (J ECT. 2018 Mar;34[1]:e5-e9. doi: 10.1097/YCT.0000000000000450).
And realistically, these small case series are as good as the supporting evidence is likely to get.
“It would be incredibly difficult to perform a randomized trial, and even a case-control study in such refractory patients would be quite difficult,” she observed.
Super-refractory status epilepticus is the term for seizures persisting despite 24 hours of adequate treatment with benzodiazepines, loading doses of antiepileptic drugs, and anesthetic agents for medically-induced coma, or for seizures that resume after withdrawal of general anesthesia. NORSE is defined as refractory status epilepticus without a history of seizures or a readily identifiable etiology. It is often associated with an autoimmune or paraneoplastic encephalitis. Outcomes are generally poor.
The four ECT-treated patients in the Oregon series were aged 27-48 years. Two had a prodromal viral illness, and a third had a vague prodrome but a negative infectious disease workup. Three patients were on four antiepileptic drugs at the time they began ECT, one was on seven. Two patients had generalized seizures, while the other two had both generalized and focal seizures. Two had normal brain MRI scans and the other two had abnormal MRIs. The patients had CSF white blood cell counts of 2, 5, 10, and 58 per mm3. All patients were on immunotherapy with intravenous corticosteroids, and three of the four were on additional immunomodulatory drugs.
ECT was started on a compassionate-use basis 16-49 days after hospital admission. These were patients who had run out of options, according to Dr. Nguyen.
Three of the four patients returned to consciousness after completing their course of ECT and withdrawal of their general anesthesia, with attenuation of their seizure activity and cessation of their super-refractory status epilepticus. Two of the three were discharged to a rehabilitation facility, including one who eventually could ambulate with slight assistance. Another patient died after discharge, while the fourth patient died during the initial hospital stay due to septic shock unrelated to the ECT.
At discharge, one patient had a modified Rankin Scale score (mRS) of 4, and two had a score of 5. At follow-up, two patients had a score of 3 and one was a 6.
Dr. Nguyen’s presentation met with undisguised audience skepticism.
“What is the theoretical basis to treat very severe epileptic seizures with another epileptic seizure? I mean, what made you do this?” one neurologist asked.
Dr. Nguyen replied that the mechanism of benefit isn’t clear. One possibility is enhanced inhibition of gamma-aminobutyric acid.
“When I describe ECT to the family, the way I think of it is as a hard reset. We tried burst suppression. This is an alternative approach,” she explained.
Another audience member said the treatment strategy smacks of homeopathy.
“These patients have a terrible disorder,” said session co-chair Gregory Krauss, MD. “Three of your four patients ultimately did not do very well.
“The question is, what are you really accomplishing in terms of the underlying encephalopathy and irritability that’s causing this? And are the seizures really a primary factor in their outcome? Is this treatment warranted to try to improve their overall outcome?” asked Dr. Krauss, professor of neurology at Johns Hopkins University, Baltimore.
Dr. Nguyen answered that she can’t say if the seizures are the cause or result of the encephalopathy.
“ECT was done well into the patients’ admission. Our difficulty is that while we were able to stop the seizures, unfortunately we weren’t able to go back in time and save the brain that was lost due to the convulsive and nonconvulsive activity,” she said. Dr. Nguyen added that she and her coinvestigators are interested in exploring the possibility that utilizing ECT earlier might abort the super-refractory status epilepticus sooner and thereby result in better outcomes.
Still, she noted, three of the four patients were able to leave the hospital, and the two survivors show improved cognitive abilities at 51 and 100 months of follow-up.
Dr. Nguyen reported having no financial conflicts.
SOURCE: Nguyen MTV et al. IEC 2019, Abstract P031.
BANGKOK –
“These were highly refractory patients and ECT did contribute to their status termination,” she reported at the congress, sponsored by the International League Against Epilepsy.
Dr. Nguyen, a neurologist at Oregon Health and Science University, Portland, presented a single-center retrospective case series composed of four ECT-treated patients with NORSE (new onset refractory status epilepticus), three of whom experienced marked improvement in their seizure activity, including cessation of their status epilepticus, after completing a course of eight or nine ECT sessions.
A four-patient series may not seem to be compelling evidence, but it’s a significant contribution to the sparse literature regarding this off-label usage of ECT. Indeed, the biggest case series to date consists of eight patients treated at Indiana University, five of whom displayed neurotelemetry or clinical evidence of improvement within 24 hours after completing a full course of ECT (J ECT. 2018 Mar;34[1]:e5-e9. doi: 10.1097/YCT.0000000000000450).
And realistically, these small case series are as good as the supporting evidence is likely to get.
“It would be incredibly difficult to perform a randomized trial, and even a case-control study in such refractory patients would be quite difficult,” she observed.
Super-refractory status epilepticus is the term for seizures persisting despite 24 hours of adequate treatment with benzodiazepines, loading doses of antiepileptic drugs, and anesthetic agents for medically-induced coma, or for seizures that resume after withdrawal of general anesthesia. NORSE is defined as refractory status epilepticus without a history of seizures or a readily identifiable etiology. It is often associated with an autoimmune or paraneoplastic encephalitis. Outcomes are generally poor.
The four ECT-treated patients in the Oregon series were aged 27-48 years. Two had a prodromal viral illness, and a third had a vague prodrome but a negative infectious disease workup. Three patients were on four antiepileptic drugs at the time they began ECT, one was on seven. Two patients had generalized seizures, while the other two had both generalized and focal seizures. Two had normal brain MRI scans and the other two had abnormal MRIs. The patients had CSF white blood cell counts of 2, 5, 10, and 58 per mm3. All patients were on immunotherapy with intravenous corticosteroids, and three of the four were on additional immunomodulatory drugs.
ECT was started on a compassionate-use basis 16-49 days after hospital admission. These were patients who had run out of options, according to Dr. Nguyen.
Three of the four patients returned to consciousness after completing their course of ECT and withdrawal of their general anesthesia, with attenuation of their seizure activity and cessation of their super-refractory status epilepticus. Two of the three were discharged to a rehabilitation facility, including one who eventually could ambulate with slight assistance. Another patient died after discharge, while the fourth patient died during the initial hospital stay due to septic shock unrelated to the ECT.
At discharge, one patient had a modified Rankin Scale score (mRS) of 4, and two had a score of 5. At follow-up, two patients had a score of 3 and one was a 6.
Dr. Nguyen’s presentation met with undisguised audience skepticism.
“What is the theoretical basis to treat very severe epileptic seizures with another epileptic seizure? I mean, what made you do this?” one neurologist asked.
Dr. Nguyen replied that the mechanism of benefit isn’t clear. One possibility is enhanced inhibition of gamma-aminobutyric acid.
“When I describe ECT to the family, the way I think of it is as a hard reset. We tried burst suppression. This is an alternative approach,” she explained.
Another audience member said the treatment strategy smacks of homeopathy.
“These patients have a terrible disorder,” said session co-chair Gregory Krauss, MD. “Three of your four patients ultimately did not do very well.
“The question is, what are you really accomplishing in terms of the underlying encephalopathy and irritability that’s causing this? And are the seizures really a primary factor in their outcome? Is this treatment warranted to try to improve their overall outcome?” asked Dr. Krauss, professor of neurology at Johns Hopkins University, Baltimore.
Dr. Nguyen answered that she can’t say if the seizures are the cause or result of the encephalopathy.
“ECT was done well into the patients’ admission. Our difficulty is that while we were able to stop the seizures, unfortunately we weren’t able to go back in time and save the brain that was lost due to the convulsive and nonconvulsive activity,” she said. Dr. Nguyen added that she and her coinvestigators are interested in exploring the possibility that utilizing ECT earlier might abort the super-refractory status epilepticus sooner and thereby result in better outcomes.
Still, she noted, three of the four patients were able to leave the hospital, and the two survivors show improved cognitive abilities at 51 and 100 months of follow-up.
Dr. Nguyen reported having no financial conflicts.
SOURCE: Nguyen MTV et al. IEC 2019, Abstract P031.
REPORTING FROM IEC 2019
Novel score spots high-risk febrile children in ED
LJUBLJANA, SLOVENIA – A new age-adjusted quick Sequential Organ Failure Assessment (qSOFA) score designed for use in children presenting to the ED with fever showed good predictive value for admission to critical care within the next 48 hours, Aakash Khanijau, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“In the needle-in-a-haystack scenario that’s seen in pediatric emergency departments, our novel, age-adjusted qSOFA score could potentially improve the rapid identification and treatment of children with suspected sepsis presenting to the ED,” said Dr. Khanijau of the University of Liverpool (England).
He presented an exceptionally large retrospective validation study of the score’s performance in 12,393 children (median age, 2.5 years) who presented to EDs with fever, of whom 1,521 were admitted for suspected sepsis. Of the hospitalized children, 145 were admitted to critical care within the first 48 hours.
The pediatric qSOFA score had 72% sensitivity and 85% specificity for critical care admission within 48 hours, with a positive predictive value of 5.4% and, more importantly, a whopping negative predictive value of 99.6%.
“That very high negative predictive value underlines the powerful discriminatory nature of our tool in the emergency department setting,” Dr. Khanijau observed, adding that the score’s area under the receiver operating characteristic curve was 0.81, which is considered a good predictive value.
The impetus for developing an age-adjusted pediatric qSOFA score stems from the fact that the original qSOFA score was designed for rapid assessment of adults with suspected sepsis and isn’t applicable in children. Other existing scores, including SIRS (the Systemic Inflammatory Response Syndrome criteria), the full SOFA, and PELOD-2 (the Pediatric Logistic Organ Dysfunction score), take longer to determine than the adapted qSOFA in a setting where speed is of the essence, he explained.
The original qSOFA components are altered mentation, systolic blood pressure, and respiratory rate. The novel score developed by Dr. Khanijau and coworkers swaps out systolic BP in favor of capillary refill time and age-adjusted heart rate using the thresholds previously established in a landmark study from the Children’s Hospital of Philadelphia (Pediatrics. 2013 Apr;131[4]:e1150-7.)
“Our reasoning here is that arterial hypertension is known to be a much later sign of circulatory compromise in children and may provide less discriminatory value than signs such as delayed capillary refill time and tachycardia early in presentation in the emergency department,” according to Dr. Khanijau.
The novel scoring system features four criteria. One point each is given for a capillary refill time of 3 seconds or longer; anything less than “Alert” on the Alert, Responds to Voice, Respond to Pain, and Unresponsive scale; a heart rate above the 99th percentile on the age-adjusted curves; and a respiratory rate above the age-adjusted 99th percentile. Thus, scores can range from 0 to 4. In the validation study, a score of 2 or more spelled a 890% increased likelihood of being admitted to a critical care setting within 48 hours. It was also associated with a 100-fold increased likelihood of death during the hospitalization, which occurred in 10 children.
Asked how the new predictive score could change clinical management, Dr. Khanijau replied, “I think the key thing it does here is it identifies the children at risk of requiring critical care and should therefore motivate us in the children achieving that threshold to promptly investigate thoroughly for suspected sepsis using the more comprehensive tools, like the full SOFA.”
He reported having no financial conflicts of interest regarding his study.
SOURCE: Khanijau A et al. ESPID 2019, Abstract.
LJUBLJANA, SLOVENIA – A new age-adjusted quick Sequential Organ Failure Assessment (qSOFA) score designed for use in children presenting to the ED with fever showed good predictive value for admission to critical care within the next 48 hours, Aakash Khanijau, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“In the needle-in-a-haystack scenario that’s seen in pediatric emergency departments, our novel, age-adjusted qSOFA score could potentially improve the rapid identification and treatment of children with suspected sepsis presenting to the ED,” said Dr. Khanijau of the University of Liverpool (England).
He presented an exceptionally large retrospective validation study of the score’s performance in 12,393 children (median age, 2.5 years) who presented to EDs with fever, of whom 1,521 were admitted for suspected sepsis. Of the hospitalized children, 145 were admitted to critical care within the first 48 hours.
The pediatric qSOFA score had 72% sensitivity and 85% specificity for critical care admission within 48 hours, with a positive predictive value of 5.4% and, more importantly, a whopping negative predictive value of 99.6%.
“That very high negative predictive value underlines the powerful discriminatory nature of our tool in the emergency department setting,” Dr. Khanijau observed, adding that the score’s area under the receiver operating characteristic curve was 0.81, which is considered a good predictive value.
The impetus for developing an age-adjusted pediatric qSOFA score stems from the fact that the original qSOFA score was designed for rapid assessment of adults with suspected sepsis and isn’t applicable in children. Other existing scores, including SIRS (the Systemic Inflammatory Response Syndrome criteria), the full SOFA, and PELOD-2 (the Pediatric Logistic Organ Dysfunction score), take longer to determine than the adapted qSOFA in a setting where speed is of the essence, he explained.
The original qSOFA components are altered mentation, systolic blood pressure, and respiratory rate. The novel score developed by Dr. Khanijau and coworkers swaps out systolic BP in favor of capillary refill time and age-adjusted heart rate using the thresholds previously established in a landmark study from the Children’s Hospital of Philadelphia (Pediatrics. 2013 Apr;131[4]:e1150-7.)
“Our reasoning here is that arterial hypertension is known to be a much later sign of circulatory compromise in children and may provide less discriminatory value than signs such as delayed capillary refill time and tachycardia early in presentation in the emergency department,” according to Dr. Khanijau.
The novel scoring system features four criteria. One point each is given for a capillary refill time of 3 seconds or longer; anything less than “Alert” on the Alert, Responds to Voice, Respond to Pain, and Unresponsive scale; a heart rate above the 99th percentile on the age-adjusted curves; and a respiratory rate above the age-adjusted 99th percentile. Thus, scores can range from 0 to 4. In the validation study, a score of 2 or more spelled a 890% increased likelihood of being admitted to a critical care setting within 48 hours. It was also associated with a 100-fold increased likelihood of death during the hospitalization, which occurred in 10 children.
Asked how the new predictive score could change clinical management, Dr. Khanijau replied, “I think the key thing it does here is it identifies the children at risk of requiring critical care and should therefore motivate us in the children achieving that threshold to promptly investigate thoroughly for suspected sepsis using the more comprehensive tools, like the full SOFA.”
He reported having no financial conflicts of interest regarding his study.
SOURCE: Khanijau A et al. ESPID 2019, Abstract.
LJUBLJANA, SLOVENIA – A new age-adjusted quick Sequential Organ Failure Assessment (qSOFA) score designed for use in children presenting to the ED with fever showed good predictive value for admission to critical care within the next 48 hours, Aakash Khanijau, MD, reported at the annual meeting of the European Society for Paediatric Infectious Diseases.
“In the needle-in-a-haystack scenario that’s seen in pediatric emergency departments, our novel, age-adjusted qSOFA score could potentially improve the rapid identification and treatment of children with suspected sepsis presenting to the ED,” said Dr. Khanijau of the University of Liverpool (England).
He presented an exceptionally large retrospective validation study of the score’s performance in 12,393 children (median age, 2.5 years) who presented to EDs with fever, of whom 1,521 were admitted for suspected sepsis. Of the hospitalized children, 145 were admitted to critical care within the first 48 hours.
The pediatric qSOFA score had 72% sensitivity and 85% specificity for critical care admission within 48 hours, with a positive predictive value of 5.4% and, more importantly, a whopping negative predictive value of 99.6%.
“That very high negative predictive value underlines the powerful discriminatory nature of our tool in the emergency department setting,” Dr. Khanijau observed, adding that the score’s area under the receiver operating characteristic curve was 0.81, which is considered a good predictive value.
The impetus for developing an age-adjusted pediatric qSOFA score stems from the fact that the original qSOFA score was designed for rapid assessment of adults with suspected sepsis and isn’t applicable in children. Other existing scores, including SIRS (the Systemic Inflammatory Response Syndrome criteria), the full SOFA, and PELOD-2 (the Pediatric Logistic Organ Dysfunction score), take longer to determine than the adapted qSOFA in a setting where speed is of the essence, he explained.
The original qSOFA components are altered mentation, systolic blood pressure, and respiratory rate. The novel score developed by Dr. Khanijau and coworkers swaps out systolic BP in favor of capillary refill time and age-adjusted heart rate using the thresholds previously established in a landmark study from the Children’s Hospital of Philadelphia (Pediatrics. 2013 Apr;131[4]:e1150-7.)
“Our reasoning here is that arterial hypertension is known to be a much later sign of circulatory compromise in children and may provide less discriminatory value than signs such as delayed capillary refill time and tachycardia early in presentation in the emergency department,” according to Dr. Khanijau.
The novel scoring system features four criteria. One point each is given for a capillary refill time of 3 seconds or longer; anything less than “Alert” on the Alert, Responds to Voice, Respond to Pain, and Unresponsive scale; a heart rate above the 99th percentile on the age-adjusted curves; and a respiratory rate above the age-adjusted 99th percentile. Thus, scores can range from 0 to 4. In the validation study, a score of 2 or more spelled a 890% increased likelihood of being admitted to a critical care setting within 48 hours. It was also associated with a 100-fold increased likelihood of death during the hospitalization, which occurred in 10 children.
Asked how the new predictive score could change clinical management, Dr. Khanijau replied, “I think the key thing it does here is it identifies the children at risk of requiring critical care and should therefore motivate us in the children achieving that threshold to promptly investigate thoroughly for suspected sepsis using the more comprehensive tools, like the full SOFA.”
He reported having no financial conflicts of interest regarding his study.
SOURCE: Khanijau A et al. ESPID 2019, Abstract.
REPORTING FROM ESPID 2019















