User login
Ketogenic diets are what’s cooking for drug-refractory epilepsy
BANGKOK – For a form of epilepsy treatment that’s been around since the 1920s, ketogenic diet therapy has lately been the focus of a surprising wealth of clinical research and development, Suvasini Sharma, MD, observed at the International Epilepsy Congress.
This high-fat, low-carbohydrate diet is now well established as a valid and effective treatment option for children and adults with drug-refractory epilepsy who aren’t candidates for surgery. That’s about a third of all epilepsy patients. And as the recently overhauled pediatric ketogenic diet therapy (KDT) best practice consensus guidelines emphasize, KDT should be strongly considered after two antiepileptic drugs have failed, and even earlier for several epilepsy syndromes, noted Dr. Sharma, a pediatric neurologist at Lady Hardinge Medical College and Kalawati Saran Children’s Hospital in New Delhi, and a coauthor of the updated guidelines.
“The consensus guidelines recommend that you start thinking about the diet early, without waiting for every drug to fail,” she said at the congress, sponsored by the International League Against Epilepsy.
Among the KDT-related topics she highlighted were the recently revised best practice consensus guidelines; an expanding role for KDT in infants, critical care settings, and in epileptic encephalopathies; mounting evidence that KDT provides additional benefits beyond seizure control; and promising new alternative diet therapies. She also described the challenges of using KDT in a low-resource nation such as India, where most of the 1.3 billion people shop in markets where food isn’t packaged with the nutritional content labels essential to traditional KDTs, and low literacy is common.
KDT best practice guidelines
The latest guidelines, which include the details of standardized KDT protocols as well as a summary of recent translational research into mechanisms of action, replace the previous 10-year-old version. Flexibility is now the watchword. While the classic KDT was started as an inpatient intervention involving several days of fasting followed by multiday gradual reintroduction of calories, that approach is now deemed optional (Epilepsia Open. 2018 May 21;3[2]:175-92).
“By and large, the trend now is going to nonfasting initiation on an outpatient basis, but with more stringent monitoring,” according to Dr. Sharma.
The guidelines note that while the research literature shows that, on average, KDT results in about a 50% chance of at least a 50% reduction in seizure frequency in patients with drug-refractory epilepsy, there are a dozen specific conditions with 70% or greater responder rates: infantile spasms, tuberous sclerosis, epilepsy with myoclonic-atonic seizures, Dravet syndrome, glucose transporter 1 deficiency syndrome (Glut 1DS), pyruvate dehydrogenase deficiency (PDHD), febrile infection-related epilepsy syndrome (FIRES), super-refractory status epilepticus (SRSE), Ohtahara syndrome, complex I mitochondrial disorders, Angelman syndrome, and children with gastrostomy tubes. For Glut1DS and PDHD, KDTs should be considered the treatment of first choice.
Traditionally, KDTs weren’t recommended for children younger than age 2 years. There were concerns that maintaining ketosis and meeting growth requirements were contradictory goals. That’s no longer believed to be so. Indeed, current evidence shows that KDT is highly effective and well tolerated in infants with refractory epilepsy. European guidelines address patient selection, pre-KDT counseling, preferred methods of initiation and KDT discontinuation, and other key issues (Eur J Paediatr Neurol. 2016 Nov;20[6]:798-809).
The guidelines recognize four major, well-studied types of KDT: the classic long-chain triglyceride-centric diet; the medium-chain triglyceride diet; the more user-friendly modified Atkins diet; and low glycemic index therapy. Except in children younger than 2 years old, who should be started on the classic KDT, the consensus panel recommended that the specific KDT selected should be based on the family and child situation and the expertise at the local KDT center. Perceived differences in efficacy between the diets aren’t supported by persuasive evidence.
KDT benefits beyond seizure control
“Most of us who work in the diet scene are aware that patients often report increased alertness, and sometimes improved cognition,” said Dr. Sharma.
That subjective experience is now supported by evidence from a randomized, controlled trial. Dutch investigators who randomized 50 drug-refractory pediatric epilepsy patients to KDT or usual care documented a positive impact of the diet therapy on cognitive activation, mood, and anxious behavior (Epilepsy Behav. 2016 Jul;60:153-7).
More recently, a systematic review showed that while subjective assessments support claims of improved alertness, attention, and global cognition in patients on KDT for refractory epilepsy, structured neuropsychologic testing confirms the enhanced alertness but without significantly improved global cognition. The investigators reported that the improvements were unrelated to decreases in medication, the type of KDT or age at its introduction, or sleep improvement. Rather, the benefits appeared to be due to a combination of seizure reduction and direct effects of KDT on cognition (Epilepsy Behav. 2018 Oct;87:69-77).
There is also encouraging preliminary evidence of a possible protective effect of KDT against sudden unexpected death in epilepsy (SUDEP) in a mouse model (Epilepsia. 2016 Aug;57[8]:e178-82. doi: 10.1111/epi.13444).
The use of KDT in critical care settings
Investigators from the pediatric Status Epilepticus Research Group (pSERG) reported that 10 of 14 patients with convulsive refractory status epilepticus achieved EEG seizure resolution within 7 days after starting KDT. Moreover, 11 patients were able to be weaned off their continuous infusions within 14 days of starting KDT. Treatment-emergent gastroparesis and hypertriglyceridemia occurred in three patients (Epilepsy Res. 2018 Aug;144:1-6).
“It was reasonably well tolerated, but they started it quite late – a median of 13 days after onset of refractory status epilepticus. It should come much earlier on our list of therapies. We shouldn’t be waiting 2 weeks before going to the ketogenic diet, because we can diagnose refractory status epilepticus within 48 hours after arrival in the ICU most of the time,” Dr. Sharma said.
Austrian investigators have pioneered the use of intravenous KDT as a bridge when oral therapy is temporarily impossible because of status epilepticus, surgery, or other reasons. They reported that parental KDT with fat intake of 3.5-4 g/kg per day was safe and effective in their series of 17 young children with epilepsy (Epilepsia Open. 2017 Nov 16;3[1]:30-9).
The future: nonketogenic diet therapies
KDT in its various forms is just too demanding and restrictive for some patients. Nonketotic alternatives are being explored.
Triheptanoin is a synthetic medium-chain triglyceride in the form of an edible, odorless, tasteless oil. Its mechanism of action is by anaplerosis: that is, energy generation via replenishment of the tricarboxylic acid cycle. After demonstration of neuroprotective and anticonvulsant effects in several mouse models, Australian investigators conducted a pilot study of 30- to 100-mL/day of oral triheptanoin as add-on therapy in 12 children with drug-refractory epilepsy. Eight of the 12 took triheptanoin for longer than 12 weeks, and 5 of those 8 experienced a sustained greater than 50% reduction in seizure frequency, including 1 who remained seizure free for 30 weeks. Seven children had diarrhea or other GI side effects (Eur J Paediatr Neurol. 2018 Nov;22[6]:1074-80).
Parisian investigators have developed a nonketotic, palatable combination of amino acids, carbohydrates, and fatty acids with a low ratio of fat to protein-plus-carbohydrates that provided potent protection against seizures in a mouse model. This suggests that the traditional 4:1 ratio sought in KDT isn’t necessary for robust seizure reduction (Sci Rep. 2017 Jul 14;7[1]:5496).
“This is probably going to be the future of nutritional therapy in epilepsy,” Dr. Sharma predicted.
She reported having no financial conflicts regarding her presentation.
BANGKOK – For a form of epilepsy treatment that’s been around since the 1920s, ketogenic diet therapy has lately been the focus of a surprising wealth of clinical research and development, Suvasini Sharma, MD, observed at the International Epilepsy Congress.
This high-fat, low-carbohydrate diet is now well established as a valid and effective treatment option for children and adults with drug-refractory epilepsy who aren’t candidates for surgery. That’s about a third of all epilepsy patients. And as the recently overhauled pediatric ketogenic diet therapy (KDT) best practice consensus guidelines emphasize, KDT should be strongly considered after two antiepileptic drugs have failed, and even earlier for several epilepsy syndromes, noted Dr. Sharma, a pediatric neurologist at Lady Hardinge Medical College and Kalawati Saran Children’s Hospital in New Delhi, and a coauthor of the updated guidelines.
“The consensus guidelines recommend that you start thinking about the diet early, without waiting for every drug to fail,” she said at the congress, sponsored by the International League Against Epilepsy.
Among the KDT-related topics she highlighted were the recently revised best practice consensus guidelines; an expanding role for KDT in infants, critical care settings, and in epileptic encephalopathies; mounting evidence that KDT provides additional benefits beyond seizure control; and promising new alternative diet therapies. She also described the challenges of using KDT in a low-resource nation such as India, where most of the 1.3 billion people shop in markets where food isn’t packaged with the nutritional content labels essential to traditional KDTs, and low literacy is common.
KDT best practice guidelines
The latest guidelines, which include the details of standardized KDT protocols as well as a summary of recent translational research into mechanisms of action, replace the previous 10-year-old version. Flexibility is now the watchword. While the classic KDT was started as an inpatient intervention involving several days of fasting followed by multiday gradual reintroduction of calories, that approach is now deemed optional (Epilepsia Open. 2018 May 21;3[2]:175-92).
“By and large, the trend now is going to nonfasting initiation on an outpatient basis, but with more stringent monitoring,” according to Dr. Sharma.
The guidelines note that while the research literature shows that, on average, KDT results in about a 50% chance of at least a 50% reduction in seizure frequency in patients with drug-refractory epilepsy, there are a dozen specific conditions with 70% or greater responder rates: infantile spasms, tuberous sclerosis, epilepsy with myoclonic-atonic seizures, Dravet syndrome, glucose transporter 1 deficiency syndrome (Glut 1DS), pyruvate dehydrogenase deficiency (PDHD), febrile infection-related epilepsy syndrome (FIRES), super-refractory status epilepticus (SRSE), Ohtahara syndrome, complex I mitochondrial disorders, Angelman syndrome, and children with gastrostomy tubes. For Glut1DS and PDHD, KDTs should be considered the treatment of first choice.
Traditionally, KDTs weren’t recommended for children younger than age 2 years. There were concerns that maintaining ketosis and meeting growth requirements were contradictory goals. That’s no longer believed to be so. Indeed, current evidence shows that KDT is highly effective and well tolerated in infants with refractory epilepsy. European guidelines address patient selection, pre-KDT counseling, preferred methods of initiation and KDT discontinuation, and other key issues (Eur J Paediatr Neurol. 2016 Nov;20[6]:798-809).
The guidelines recognize four major, well-studied types of KDT: the classic long-chain triglyceride-centric diet; the medium-chain triglyceride diet; the more user-friendly modified Atkins diet; and low glycemic index therapy. Except in children younger than 2 years old, who should be started on the classic KDT, the consensus panel recommended that the specific KDT selected should be based on the family and child situation and the expertise at the local KDT center. Perceived differences in efficacy between the diets aren’t supported by persuasive evidence.
KDT benefits beyond seizure control
“Most of us who work in the diet scene are aware that patients often report increased alertness, and sometimes improved cognition,” said Dr. Sharma.
That subjective experience is now supported by evidence from a randomized, controlled trial. Dutch investigators who randomized 50 drug-refractory pediatric epilepsy patients to KDT or usual care documented a positive impact of the diet therapy on cognitive activation, mood, and anxious behavior (Epilepsy Behav. 2016 Jul;60:153-7).
More recently, a systematic review showed that while subjective assessments support claims of improved alertness, attention, and global cognition in patients on KDT for refractory epilepsy, structured neuropsychologic testing confirms the enhanced alertness but without significantly improved global cognition. The investigators reported that the improvements were unrelated to decreases in medication, the type of KDT or age at its introduction, or sleep improvement. Rather, the benefits appeared to be due to a combination of seizure reduction and direct effects of KDT on cognition (Epilepsy Behav. 2018 Oct;87:69-77).
There is also encouraging preliminary evidence of a possible protective effect of KDT against sudden unexpected death in epilepsy (SUDEP) in a mouse model (Epilepsia. 2016 Aug;57[8]:e178-82. doi: 10.1111/epi.13444).
The use of KDT in critical care settings
Investigators from the pediatric Status Epilepticus Research Group (pSERG) reported that 10 of 14 patients with convulsive refractory status epilepticus achieved EEG seizure resolution within 7 days after starting KDT. Moreover, 11 patients were able to be weaned off their continuous infusions within 14 days of starting KDT. Treatment-emergent gastroparesis and hypertriglyceridemia occurred in three patients (Epilepsy Res. 2018 Aug;144:1-6).
“It was reasonably well tolerated, but they started it quite late – a median of 13 days after onset of refractory status epilepticus. It should come much earlier on our list of therapies. We shouldn’t be waiting 2 weeks before going to the ketogenic diet, because we can diagnose refractory status epilepticus within 48 hours after arrival in the ICU most of the time,” Dr. Sharma said.
Austrian investigators have pioneered the use of intravenous KDT as a bridge when oral therapy is temporarily impossible because of status epilepticus, surgery, or other reasons. They reported that parental KDT with fat intake of 3.5-4 g/kg per day was safe and effective in their series of 17 young children with epilepsy (Epilepsia Open. 2017 Nov 16;3[1]:30-9).
The future: nonketogenic diet therapies
KDT in its various forms is just too demanding and restrictive for some patients. Nonketotic alternatives are being explored.
Triheptanoin is a synthetic medium-chain triglyceride in the form of an edible, odorless, tasteless oil. Its mechanism of action is by anaplerosis: that is, energy generation via replenishment of the tricarboxylic acid cycle. After demonstration of neuroprotective and anticonvulsant effects in several mouse models, Australian investigators conducted a pilot study of 30- to 100-mL/day of oral triheptanoin as add-on therapy in 12 children with drug-refractory epilepsy. Eight of the 12 took triheptanoin for longer than 12 weeks, and 5 of those 8 experienced a sustained greater than 50% reduction in seizure frequency, including 1 who remained seizure free for 30 weeks. Seven children had diarrhea or other GI side effects (Eur J Paediatr Neurol. 2018 Nov;22[6]:1074-80).
Parisian investigators have developed a nonketotic, palatable combination of amino acids, carbohydrates, and fatty acids with a low ratio of fat to protein-plus-carbohydrates that provided potent protection against seizures in a mouse model. This suggests that the traditional 4:1 ratio sought in KDT isn’t necessary for robust seizure reduction (Sci Rep. 2017 Jul 14;7[1]:5496).
“This is probably going to be the future of nutritional therapy in epilepsy,” Dr. Sharma predicted.
She reported having no financial conflicts regarding her presentation.
BANGKOK – For a form of epilepsy treatment that’s been around since the 1920s, ketogenic diet therapy has lately been the focus of a surprising wealth of clinical research and development, Suvasini Sharma, MD, observed at the International Epilepsy Congress.
This high-fat, low-carbohydrate diet is now well established as a valid and effective treatment option for children and adults with drug-refractory epilepsy who aren’t candidates for surgery. That’s about a third of all epilepsy patients. And as the recently overhauled pediatric ketogenic diet therapy (KDT) best practice consensus guidelines emphasize, KDT should be strongly considered after two antiepileptic drugs have failed, and even earlier for several epilepsy syndromes, noted Dr. Sharma, a pediatric neurologist at Lady Hardinge Medical College and Kalawati Saran Children’s Hospital in New Delhi, and a coauthor of the updated guidelines.
“The consensus guidelines recommend that you start thinking about the diet early, without waiting for every drug to fail,” she said at the congress, sponsored by the International League Against Epilepsy.
Among the KDT-related topics she highlighted were the recently revised best practice consensus guidelines; an expanding role for KDT in infants, critical care settings, and in epileptic encephalopathies; mounting evidence that KDT provides additional benefits beyond seizure control; and promising new alternative diet therapies. She also described the challenges of using KDT in a low-resource nation such as India, where most of the 1.3 billion people shop in markets where food isn’t packaged with the nutritional content labels essential to traditional KDTs, and low literacy is common.
KDT best practice guidelines
The latest guidelines, which include the details of standardized KDT protocols as well as a summary of recent translational research into mechanisms of action, replace the previous 10-year-old version. Flexibility is now the watchword. While the classic KDT was started as an inpatient intervention involving several days of fasting followed by multiday gradual reintroduction of calories, that approach is now deemed optional (Epilepsia Open. 2018 May 21;3[2]:175-92).
“By and large, the trend now is going to nonfasting initiation on an outpatient basis, but with more stringent monitoring,” according to Dr. Sharma.
The guidelines note that while the research literature shows that, on average, KDT results in about a 50% chance of at least a 50% reduction in seizure frequency in patients with drug-refractory epilepsy, there are a dozen specific conditions with 70% or greater responder rates: infantile spasms, tuberous sclerosis, epilepsy with myoclonic-atonic seizures, Dravet syndrome, glucose transporter 1 deficiency syndrome (Glut 1DS), pyruvate dehydrogenase deficiency (PDHD), febrile infection-related epilepsy syndrome (FIRES), super-refractory status epilepticus (SRSE), Ohtahara syndrome, complex I mitochondrial disorders, Angelman syndrome, and children with gastrostomy tubes. For Glut1DS and PDHD, KDTs should be considered the treatment of first choice.
Traditionally, KDTs weren’t recommended for children younger than age 2 years. There were concerns that maintaining ketosis and meeting growth requirements were contradictory goals. That’s no longer believed to be so. Indeed, current evidence shows that KDT is highly effective and well tolerated in infants with refractory epilepsy. European guidelines address patient selection, pre-KDT counseling, preferred methods of initiation and KDT discontinuation, and other key issues (Eur J Paediatr Neurol. 2016 Nov;20[6]:798-809).
The guidelines recognize four major, well-studied types of KDT: the classic long-chain triglyceride-centric diet; the medium-chain triglyceride diet; the more user-friendly modified Atkins diet; and low glycemic index therapy. Except in children younger than 2 years old, who should be started on the classic KDT, the consensus panel recommended that the specific KDT selected should be based on the family and child situation and the expertise at the local KDT center. Perceived differences in efficacy between the diets aren’t supported by persuasive evidence.
KDT benefits beyond seizure control
“Most of us who work in the diet scene are aware that patients often report increased alertness, and sometimes improved cognition,” said Dr. Sharma.
That subjective experience is now supported by evidence from a randomized, controlled trial. Dutch investigators who randomized 50 drug-refractory pediatric epilepsy patients to KDT or usual care documented a positive impact of the diet therapy on cognitive activation, mood, and anxious behavior (Epilepsy Behav. 2016 Jul;60:153-7).
More recently, a systematic review showed that while subjective assessments support claims of improved alertness, attention, and global cognition in patients on KDT for refractory epilepsy, structured neuropsychologic testing confirms the enhanced alertness but without significantly improved global cognition. The investigators reported that the improvements were unrelated to decreases in medication, the type of KDT or age at its introduction, or sleep improvement. Rather, the benefits appeared to be due to a combination of seizure reduction and direct effects of KDT on cognition (Epilepsy Behav. 2018 Oct;87:69-77).
There is also encouraging preliminary evidence of a possible protective effect of KDT against sudden unexpected death in epilepsy (SUDEP) in a mouse model (Epilepsia. 2016 Aug;57[8]:e178-82. doi: 10.1111/epi.13444).
The use of KDT in critical care settings
Investigators from the pediatric Status Epilepticus Research Group (pSERG) reported that 10 of 14 patients with convulsive refractory status epilepticus achieved EEG seizure resolution within 7 days after starting KDT. Moreover, 11 patients were able to be weaned off their continuous infusions within 14 days of starting KDT. Treatment-emergent gastroparesis and hypertriglyceridemia occurred in three patients (Epilepsy Res. 2018 Aug;144:1-6).
“It was reasonably well tolerated, but they started it quite late – a median of 13 days after onset of refractory status epilepticus. It should come much earlier on our list of therapies. We shouldn’t be waiting 2 weeks before going to the ketogenic diet, because we can diagnose refractory status epilepticus within 48 hours after arrival in the ICU most of the time,” Dr. Sharma said.
Austrian investigators have pioneered the use of intravenous KDT as a bridge when oral therapy is temporarily impossible because of status epilepticus, surgery, or other reasons. They reported that parental KDT with fat intake of 3.5-4 g/kg per day was safe and effective in their series of 17 young children with epilepsy (Epilepsia Open. 2017 Nov 16;3[1]:30-9).
The future: nonketogenic diet therapies
KDT in its various forms is just too demanding and restrictive for some patients. Nonketotic alternatives are being explored.
Triheptanoin is a synthetic medium-chain triglyceride in the form of an edible, odorless, tasteless oil. Its mechanism of action is by anaplerosis: that is, energy generation via replenishment of the tricarboxylic acid cycle. After demonstration of neuroprotective and anticonvulsant effects in several mouse models, Australian investigators conducted a pilot study of 30- to 100-mL/day of oral triheptanoin as add-on therapy in 12 children with drug-refractory epilepsy. Eight of the 12 took triheptanoin for longer than 12 weeks, and 5 of those 8 experienced a sustained greater than 50% reduction in seizure frequency, including 1 who remained seizure free for 30 weeks. Seven children had diarrhea or other GI side effects (Eur J Paediatr Neurol. 2018 Nov;22[6]:1074-80).
Parisian investigators have developed a nonketotic, palatable combination of amino acids, carbohydrates, and fatty acids with a low ratio of fat to protein-plus-carbohydrates that provided potent protection against seizures in a mouse model. This suggests that the traditional 4:1 ratio sought in KDT isn’t necessary for robust seizure reduction (Sci Rep. 2017 Jul 14;7[1]:5496).
“This is probably going to be the future of nutritional therapy in epilepsy,” Dr. Sharma predicted.
She reported having no financial conflicts regarding her presentation.
REPORTING FROM IEC 2019
Asthma hospitalization in kids linked with doubled migraine incidence
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
when compared with a similar pediatric population without asthma. The finding is based on an analysis of more than 11 million U.S. pediatric hospitalizations over the course of a decade.
Among children and adolescents aged 3-21 years who were hospitalized for asthma, migraine rates were significantly higher among girls, adolescents, and whites, compared with boys, children aged 12 years or younger, and nonwhites, respectively, in a trio of adjusted analyses, Riddhiben S. Patel, MD, and associates reported in a poster at the annual meeting of the American Headache Society.
“Our hope is that, by establishing an association between childhood asthma and migraine, [these children] may be more easily screened for, diagnosed, and treated early by providers,” wrote Dr. Patel, a pediatric neurologist and headache specialist at the University of Mississippi, Jackson, and associates.
Their analysis used administrative billing data collected by the Kids’ Inpatient Database, maintained by the U.S. Healthcare Cost and Utilization Project. The project includes a representative national sample of about 3 million pediatric hospital discharges every 3 years. The study used data from 11,483,103 hospitalizations of children and adolescents aged 3-21 years during 2003, 2006, 2009, and 2012, and found an overall hospitalization rate of 0.8% billed for migraine. For patients also hospitalized with a billing code for asthma, the rate jumped to 1.36%, a 120% statistically significant relative increase in migraine hospitalizations after adjustment for baseline demographic differences, the researchers said.
Among the children and adolescents hospitalized with an asthma billing code, the relative rate of also having a billing code for migraine after adjustment was a statistically significant 80% higher in girls, compared with boys, a statistically significant 7% higher in adolescents, compared with children 12 years or younger, and was significantly reduced by a relative 45% rate in nonwhites, compared with whites.
The mechanisms behind these associations are not known, but could involve mast-cell degranulation, autonomic dysfunction, or shared genetic or environmental etiologic factors, the authors said.
Dr. Patel reported no relevant disclosures.
SOURCE: Patel RS et al. Headache. 2019 June;59[S1]:1-208, Abstract P78.
REPORTING FROM AHS 2019
Criteria found largely interchangeable for classifying radiographic axSpA
, according to a comparative study first presented at the 2019 European League Against Rheumatism and now published.
“The major finding is that patients classified with one set of the criteria are essentially the same as those classified with the other,” according to Anne Boel, a researcher in the department of rheumatology at Leiden (the Netherlands) University Medical Center, and first author of the study.
The study addresses a controversy that has persisted since the introduction of ASAS criteria for defining axial spondyloarthritis (axSpA) with definite structural changes on conventional radiographs. It was unclear whether this ASAS diagnosis, called radiographic axSpA (r-axSpA), was the same as ankylosing spondylitis (AS) as defined by the older modified New York (mNY) criteria.
In this study, patients from eight cohorts were evaluated with the two classification sets. In addition to having radiographic sacroiliitis, all patients had to have back pain for at least 3 months, which is also mandatory for both classification sets.
Of the 3,434 fulfilling the ASAS criteria for r-axSpA, 96% fulfilled the mNY criteria for AS. Of the 3,882 meeting the mNY criteria for AS, 93% fulfilled the ASAS criteria for r-axSpA.
On the basis of this level of agreement, the authors called the terms r-axSpA and AS “interchangeable.” In the small proportion of cases when there was disagreement, the reason was considered to be minor and not to alter the conclusion that the disease entities are the same.
“Patients cannot be classified according to the ASAS criteria if they first develop back pain at age 45 years or older, so this is one difference between the two criteria sets that would affect classification,” Ms. Boel explained in an interview.
When tallied, 7% of the 4,041 patients with axSpA with radiographic sacroiliitis evaluated met only the mNY criteria, 3% met only the ASAS criteria, 89% met both sets of criteria, and 1% met neither, according to the published data.
Of those who met the mNY criteria but not the ASAS criteria, 99.7% would have potentially fulfilled the ASAS criteria for r-axSpA except for older age at onset. The remainder was attributed to an absence of inflammatory back pain or another spondyloarthritis feature.
Of the 3,434 patients fulfilling the ASAS criteria, 90% fulfilled the mNY criteria because of the presence of inflammatory back pain. Most of those without inflammatory back pain had a mobility restriction and so still met the mNY criteria. A small proportion without inflammatory back pain or mobility restriction fulfilled the ASAS criteria because of other SpA features.
The study resolves a persistent debate over whether AS patients identified by mNY criteria are the same as r-axSpA identified by ASAS criteria, according to the authors, reiterating that these data show that they can be considered the same disease.
This finding is particularly relevant when evaluating studies that have classified patients by either the mNY or the ASAS criteria.
This finding “has important implications for the axSpA research field,” the authors concluded. “Acknowledging that both criteria sets identify the same patients implies that older literature on AS and newer literature on r-axSpA can be directly compared.”
The study had no specific funding source. Ms. Boel reported having no potential conflicts of interest. Coauthors reported ties with pharmaceutical companies outside of this study.
SOURCE: Boel A et al. Ann Rheum Dis. 2019 Jul 30. doi: 10.1136/annrheumdis-2019-215707.
, according to a comparative study first presented at the 2019 European League Against Rheumatism and now published.
“The major finding is that patients classified with one set of the criteria are essentially the same as those classified with the other,” according to Anne Boel, a researcher in the department of rheumatology at Leiden (the Netherlands) University Medical Center, and first author of the study.
The study addresses a controversy that has persisted since the introduction of ASAS criteria for defining axial spondyloarthritis (axSpA) with definite structural changes on conventional radiographs. It was unclear whether this ASAS diagnosis, called radiographic axSpA (r-axSpA), was the same as ankylosing spondylitis (AS) as defined by the older modified New York (mNY) criteria.
In this study, patients from eight cohorts were evaluated with the two classification sets. In addition to having radiographic sacroiliitis, all patients had to have back pain for at least 3 months, which is also mandatory for both classification sets.
Of the 3,434 fulfilling the ASAS criteria for r-axSpA, 96% fulfilled the mNY criteria for AS. Of the 3,882 meeting the mNY criteria for AS, 93% fulfilled the ASAS criteria for r-axSpA.
On the basis of this level of agreement, the authors called the terms r-axSpA and AS “interchangeable.” In the small proportion of cases when there was disagreement, the reason was considered to be minor and not to alter the conclusion that the disease entities are the same.
“Patients cannot be classified according to the ASAS criteria if they first develop back pain at age 45 years or older, so this is one difference between the two criteria sets that would affect classification,” Ms. Boel explained in an interview.
When tallied, 7% of the 4,041 patients with axSpA with radiographic sacroiliitis evaluated met only the mNY criteria, 3% met only the ASAS criteria, 89% met both sets of criteria, and 1% met neither, according to the published data.
Of those who met the mNY criteria but not the ASAS criteria, 99.7% would have potentially fulfilled the ASAS criteria for r-axSpA except for older age at onset. The remainder was attributed to an absence of inflammatory back pain or another spondyloarthritis feature.
Of the 3,434 patients fulfilling the ASAS criteria, 90% fulfilled the mNY criteria because of the presence of inflammatory back pain. Most of those without inflammatory back pain had a mobility restriction and so still met the mNY criteria. A small proportion without inflammatory back pain or mobility restriction fulfilled the ASAS criteria because of other SpA features.
The study resolves a persistent debate over whether AS patients identified by mNY criteria are the same as r-axSpA identified by ASAS criteria, according to the authors, reiterating that these data show that they can be considered the same disease.
This finding is particularly relevant when evaluating studies that have classified patients by either the mNY or the ASAS criteria.
This finding “has important implications for the axSpA research field,” the authors concluded. “Acknowledging that both criteria sets identify the same patients implies that older literature on AS and newer literature on r-axSpA can be directly compared.”
The study had no specific funding source. Ms. Boel reported having no potential conflicts of interest. Coauthors reported ties with pharmaceutical companies outside of this study.
SOURCE: Boel A et al. Ann Rheum Dis. 2019 Jul 30. doi: 10.1136/annrheumdis-2019-215707.
, according to a comparative study first presented at the 2019 European League Against Rheumatism and now published.
“The major finding is that patients classified with one set of the criteria are essentially the same as those classified with the other,” according to Anne Boel, a researcher in the department of rheumatology at Leiden (the Netherlands) University Medical Center, and first author of the study.
The study addresses a controversy that has persisted since the introduction of ASAS criteria for defining axial spondyloarthritis (axSpA) with definite structural changes on conventional radiographs. It was unclear whether this ASAS diagnosis, called radiographic axSpA (r-axSpA), was the same as ankylosing spondylitis (AS) as defined by the older modified New York (mNY) criteria.
In this study, patients from eight cohorts were evaluated with the two classification sets. In addition to having radiographic sacroiliitis, all patients had to have back pain for at least 3 months, which is also mandatory for both classification sets.
Of the 3,434 fulfilling the ASAS criteria for r-axSpA, 96% fulfilled the mNY criteria for AS. Of the 3,882 meeting the mNY criteria for AS, 93% fulfilled the ASAS criteria for r-axSpA.
On the basis of this level of agreement, the authors called the terms r-axSpA and AS “interchangeable.” In the small proportion of cases when there was disagreement, the reason was considered to be minor and not to alter the conclusion that the disease entities are the same.
“Patients cannot be classified according to the ASAS criteria if they first develop back pain at age 45 years or older, so this is one difference between the two criteria sets that would affect classification,” Ms. Boel explained in an interview.
When tallied, 7% of the 4,041 patients with axSpA with radiographic sacroiliitis evaluated met only the mNY criteria, 3% met only the ASAS criteria, 89% met both sets of criteria, and 1% met neither, according to the published data.
Of those who met the mNY criteria but not the ASAS criteria, 99.7% would have potentially fulfilled the ASAS criteria for r-axSpA except for older age at onset. The remainder was attributed to an absence of inflammatory back pain or another spondyloarthritis feature.
Of the 3,434 patients fulfilling the ASAS criteria, 90% fulfilled the mNY criteria because of the presence of inflammatory back pain. Most of those without inflammatory back pain had a mobility restriction and so still met the mNY criteria. A small proportion without inflammatory back pain or mobility restriction fulfilled the ASAS criteria because of other SpA features.
The study resolves a persistent debate over whether AS patients identified by mNY criteria are the same as r-axSpA identified by ASAS criteria, according to the authors, reiterating that these data show that they can be considered the same disease.
This finding is particularly relevant when evaluating studies that have classified patients by either the mNY or the ASAS criteria.
This finding “has important implications for the axSpA research field,” the authors concluded. “Acknowledging that both criteria sets identify the same patients implies that older literature on AS and newer literature on r-axSpA can be directly compared.”
The study had no specific funding source. Ms. Boel reported having no potential conflicts of interest. Coauthors reported ties with pharmaceutical companies outside of this study.
SOURCE: Boel A et al. Ann Rheum Dis. 2019 Jul 30. doi: 10.1136/annrheumdis-2019-215707.
FROM ANNALS OF THE RHEUMATIC DISEASES
Fatal Drug-Resistant Invasive Pulmonary Aspergillus fumigatus in a 56-Year-Old Immunosuppressed Man (FULL)
Historically, aspergillosis in patients with hematopoietic stem cell transplantation (HSCT) has carried a high mortality rate. However, recent data demonstrate a dramatic improvement in outcomes for patients with HSCT: 90-day survival increased from 22% before 2000 to 45% over the past 15 years.1 Improved outcomes coincide with changes in transplant immunosuppression practices, use of cross-sectional imaging for early disease identification, galactomannan screening, and the development of novel treatment options.
Voriconazole is an azole drug that blocks the synthesis of ergosterol, a vital component of the cellular membrane of fungi. Voriconazole was approved in 2002 after a clinical trial demonstrated an improvement in 50% of patients with invasive aspergillosis in the voriconazole arm vs 30% in the amphotericin B arm at 12 weeks.2 Amphotericin B is a polyene antifungal drug that binds with ergosterol, creating leaks in the cell membrane that lead to cellular demise. Voriconazole quickly became the first-line therapy for invasive aspergillosis and is recommended by both the Infectious Disease Society of American (IDSA) and the European Conference on Infections in Leukemia.3
Case Presentation
A 55-year-old man with high-risk chronic myelogenous leukemia (CML) underwent a 10 of 10 human leukocyte antigen allele and antigen-matched peripheral blood allogeneic HSCT with a myeloablative-conditioning regimen of busulfan and cyclophosphamide, along with prophylactic voriconazole, sulfamethoxazole/trimethoprim, and acyclovir. After successful engraftment (without significant neutropenia), his posttransplant course was complicated by grade 2 graft vs host disease (GVHD) of the skin, eyes, and liver, which responded well to steroids and tacrolimus. Voriconazole was continued for 5 months until immunosuppression was minimized (tacrolimus 1 mg twice daily). Two months later, the patient’s GVHD worsened, necessitating treatment at an outside hospital with high-dose prednisone (2 mg/kg/d) and cyclosporine (300 mg twice daily). Voriconazole prophylaxis was not reinitiated at that time.
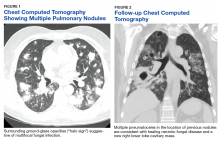
One year later, at a routine follow-up appointment, the patient endorsed several weeks of malaise, weight loss, and nonproductive cough. The patient’s immunosuppression recently had been reduced to 1 mg/kg/d of prednisone and 100 mg of cyclosporine twice daily. A chest X-ray demonstrated multiple pulmonary nodules; follow-up chest computed tomography (CT) confirmed multiple nodular infiltrates with surrounding ground-glass opacities suspicious with a fungal infection (Figure 1).
Treatment with oral voriconazole (300 mg twice daily) was initiated for probable pulmonary aspergillosis. Cyclosporine (150 mg twice daily) and prednisone (1 mg/kg/d) were continued throughout treatment out of concern for hepatic GVHD. The patient’s symptoms improved over the next 10 days, and follow-up chest imaging demonstrated improvement.
Two weeks after initiation of voriconazole treatment, the patient developed a new productive cough and dyspnea, associated with fevers and chills. Repeat imaging revealed right lower-lobe pneumonia. The serum voriconazole trough level was checked and was 3.1 mg/L, suggesting therapeutic dosing. The patient subsequently developed acute respiratory distress syndrome and required intubation and mechanical ventilation. Repeat BAL sampling demonstrated multidrug-resistant Escherichia coli, a BAL galactomannan level of 2.0 ODI, and negative fungal cultures. The patient’s hospital course was complicated by profound hypoxemia, requiring prone positioning and neuromuscular blockade. He was treated with meropenem and voriconazole. His immunosuppression was reduced, but he rapidly developed acute liver injury from hepatic GVHD that resolved after reinitiation of cyclosporine and prednisone at 0.75 mg/kg/d.
The patient improved over the next 3 weeks and was successfully extubated. Repeat chest CT imaging demonstrated numerous pneumatoceles in the location of previous nodules, consistent with healing necrotic fungal disease, and a new right lower-lobe cavitary mass (Figure 2). Two days after transferring out of the intensive care unit, the patient again developed hypoxemia and fevers to 39° C. Bronchoscopy with BAL of the right lower lobe revealed positive A fumigatus and Rhizopus sp polymerase chain reaction (PCR) assays, although fungal cultures were positive only for A fumigatus. Liposomal amphotericin B (5 mg/kg) was added to voriconazole therapy to treat mucormycosis and to provide a second active agent against A fumigatus.
Unfortunately, the patient’s clinical status continued to deteriorate with signs of progressive respiratory failure and infection despite empiric, broad-spectrum antibiotics and dual antifungal therapy. His serum voriconazole level continued to be therapeutic at 1.9 mg/L. The patient declined reintubation and invasive mechanical ventilation, and he ultimately transitioned to comfort measures and died with his family at the bedside.
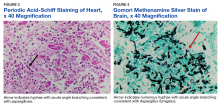
Autopsy demonstrated widely disseminated Aspergillus infection as the cause of death, with evidence of myocardial, neural, and vascular invasion of A fumigatus (Figures 3 and 4).
Discussion
This case of fatal, progressive, invasive, pulmonary aspergillosis demonstrates several important factors in the treatment of patients with this disease. Treatment failure usually relates to any of 4 possible factors: host immune status, severity or burden of disease, appropriate dosing of antifungal agents, and drug resistance. This patient’s immune system was heavily suppressed for a prolonged period. Attempts at reducing immunosuppression to the minimal required dosage to prevent a GVHD flare were unsuccessful and became an unmodifiable risk factor, a major contributor to his demise.
The risks of continuous high-dose immunosuppression in steroid-refractory GVHD is well understood and has been previously demonstrated to have up to 50% 4-year nonrelapse mortality, mainly due to overwhelming bacterial, viral, and fungal infections.4 All attempts should be made to cease or reduce immunosuppression in the setting of a severe infection, although this is sometimes impossible as in this case.
The patient’s disease burden was significant as evidenced by the bilateral, multifocal pulmonary nodules seen on chest imaging and the disseminated disease found at postmortem examination. His initial improvement in symptoms with voriconazole and the evolution of his images (with many of his initial pulmonary nodules becoming pneumatoceles) suggested a temporary positive immune response. The authors believe that the Rhizopus in his sputum represents noninvasive colonization of one of his pneumatoceles, because postmortem examination failed to reveal Rhizopus at any other location.
Voriconazole has excellent pulmonary and central nervous system penetration: In this patient serum levels were well within the therapeutic range. His peculiar drug resistance pattern (sensitivity to azoles and resistance to amphotericin) is unusual. Azole resistance in leukemia and patients with HSCT is more common than is amphotericin resistance, with current estimates of azole resistance close to 5%, ranging between 1% and 30%.5,6 Widespread use of antifungal prophylaxis with azoles likely selects for azole resistance.6
Despite this concern of azole resistance, current IDSA guidelines recommend against routine susceptibility testing of Aspergillus to azole therapy because of the current lack of consensus between the European Committee on Antibiotic Susceptibility Testing and Clinical and Laboratory Standards Institute on break points for resistance patterns.3,7 This is an area of emerging research, and proposed cut points for declaration of resistance do exist in the literature even if not globally agreed on.8
Combination antifungal therapy is an option for treatment in cases of possible drug resistance. Nonetheless, a recent randomized, double-blind, placebo-controlled, multicenter trial comparing voriconazole monotherapy with the combination of voriconazole and anidulafungin failed to demonstrate an overall mortality benefit in the primary analysis, although secondary analysis showed a mortality benefit with combination therapy in patients at highest risk for death.9
Despite the lack of unified standards with susceptibility testing, it may be reasonable to perform such tests in patients with demonstrating progressive disease. In this patient’s case, amphotericin B was added to treat the Rhizopus species found in his sputum, and while not the combination studied in the previously mentioned study, the drug should have provided an additional active agent for Aspergillus should this patient have had azole resistance.
Surprisingly, subsequent testing demonstrated the Aspergillus species to be resistant to amphotericin B. De novo amphotericin B-resistant A fumigates is extremely rare, with an expected incidence of 1% or less.10 The authors believe the patient may have demonstrated induction of amphotericin-B resistance through activation of fungal stress pathways by prior treatment with voriconazole. This has been demonstrated in vitro and should be considered should combination salvage therapy be required for the treatment of a refractory Aspergillus infection especially if patients have received prior treatment with voriconazole.11
Conclusion
This fatal case of invasive pulmonary aspergillosis illustrates the importance of considering the 4 main causes of treatment failure in an infection. Although the patient had a high burden of disease with a rare resistance pattern, he was treated with appropriate and well-dosed therapy. Ultimately, his unmodifiable immunosuppression was likely the driving factor leading to treatment failure and death. The indication for and number of bone marrow transplants continues to increase, thus exposure to and treatment of invasive fungal infections will increase accordingly. As such, providers should ensure that all causes of treatment failure are considered and addressed.
1. Upton A, Kirby KA, Carpenter P, Boeckh M, Marr KA. Invasive aspergillosis following hematopoietic cell transplantation: outcomes and prognostic factors associated with mortality. Clin Infect Dis. 2007;44(4):531-540.
2. Herbrecht R, Denning DW, Patterson TF, et al; Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347(6):408-415.
3. Patterson TF, Thompson GR III, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Disease Society of America. Clin Infect Dis. 2016;63(4):e1-e60.
4. García-Cadenas I, Rivera I, Martino R, et al. Patterns of infection and infection-related mortality in patients with steroid-refractory acute graft versus host disease. Bone Marrow Transplant. 2017;52(1):107-113.
5. Vermeulen E, Maertens J, De Bel A, et al. Nationwide surveillance of azole resistance in Aspergillus diseases. Antimicrob Agents Chemother. 2015;59(8):4569-4576.
6. Wiederhold NP, Patterson TF. Emergence of azole resistance in Aspergillus. Semin Respir Crit Care Med. 2015;36(5):673-680.
7. Cuenca-Estrella M, Moore CB, Barchiesi F, et al; AFST Subcommittee of the European Committee on Antimicrobial Susceptibility Testing. Multicenter evaluation of the reproducibility of the proposed antifungal susceptibility testing method for fermentative yeasts of the Antifungal Susceptibility Testing Subcommittee of the European Committee on Antimicrobial Susceptibility Testing (AFST-EUCAST). Clin Microbiol Infect. 2003;9(6):467-474.
8. Pfaller MA, Diekema DJ, Ghannoum MA, et al; Clinical and Laboratory Standards Institute Antifungal Testing Subcommittee. Wild-type MIC distribution and epidemiological cutoff values for Aspergillus fumigatus and three triazoles as determined by Clinical and Laboratory Standards Institute for broth microdilution methods. J Clin Microbiol. 2009;47(10):3142-3146.
9. Marr KA, Schlamm HT, Herbrecht R, et al. Combination antifungal therapy for invasive aspergillosis: a randomized trial. Ann Intern Med. 2015;162(2):81-89.
10. Tashiro M, Izumikawa K, Minematsu A, et al. Antifungal susceptibilities of Aspergillus fumigatus clinical isolates obtained in Nagasaki, Japan. Antimicrob Agents Chemother. 2012;56(1):584-587.
11. Rajendran R, Mowat E, Jones B, Williams C, Ramage G. Prior in vitro exposure to voriconazole confers resistance to amphotericin B in Aspergillus fumigatus biofilms. Int J Antimicrob Agents. 2015;46(3):342-345.
Historically, aspergillosis in patients with hematopoietic stem cell transplantation (HSCT) has carried a high mortality rate. However, recent data demonstrate a dramatic improvement in outcomes for patients with HSCT: 90-day survival increased from 22% before 2000 to 45% over the past 15 years.1 Improved outcomes coincide with changes in transplant immunosuppression practices, use of cross-sectional imaging for early disease identification, galactomannan screening, and the development of novel treatment options.
Voriconazole is an azole drug that blocks the synthesis of ergosterol, a vital component of the cellular membrane of fungi. Voriconazole was approved in 2002 after a clinical trial demonstrated an improvement in 50% of patients with invasive aspergillosis in the voriconazole arm vs 30% in the amphotericin B arm at 12 weeks.2 Amphotericin B is a polyene antifungal drug that binds with ergosterol, creating leaks in the cell membrane that lead to cellular demise. Voriconazole quickly became the first-line therapy for invasive aspergillosis and is recommended by both the Infectious Disease Society of American (IDSA) and the European Conference on Infections in Leukemia.3
Case Presentation
A 55-year-old man with high-risk chronic myelogenous leukemia (CML) underwent a 10 of 10 human leukocyte antigen allele and antigen-matched peripheral blood allogeneic HSCT with a myeloablative-conditioning regimen of busulfan and cyclophosphamide, along with prophylactic voriconazole, sulfamethoxazole/trimethoprim, and acyclovir. After successful engraftment (without significant neutropenia), his posttransplant course was complicated by grade 2 graft vs host disease (GVHD) of the skin, eyes, and liver, which responded well to steroids and tacrolimus. Voriconazole was continued for 5 months until immunosuppression was minimized (tacrolimus 1 mg twice daily). Two months later, the patient’s GVHD worsened, necessitating treatment at an outside hospital with high-dose prednisone (2 mg/kg/d) and cyclosporine (300 mg twice daily). Voriconazole prophylaxis was not reinitiated at that time.
One year later, at a routine follow-up appointment, the patient endorsed several weeks of malaise, weight loss, and nonproductive cough. The patient’s immunosuppression recently had been reduced to 1 mg/kg/d of prednisone and 100 mg of cyclosporine twice daily. A chest X-ray demonstrated multiple pulmonary nodules; follow-up chest computed tomography (CT) confirmed multiple nodular infiltrates with surrounding ground-glass opacities suspicious with a fungal infection (Figure 1).
Treatment with oral voriconazole (300 mg twice daily) was initiated for probable pulmonary aspergillosis. Cyclosporine (150 mg twice daily) and prednisone (1 mg/kg/d) were continued throughout treatment out of concern for hepatic GVHD. The patient’s symptoms improved over the next 10 days, and follow-up chest imaging demonstrated improvement.
Two weeks after initiation of voriconazole treatment, the patient developed a new productive cough and dyspnea, associated with fevers and chills. Repeat imaging revealed right lower-lobe pneumonia. The serum voriconazole trough level was checked and was 3.1 mg/L, suggesting therapeutic dosing. The patient subsequently developed acute respiratory distress syndrome and required intubation and mechanical ventilation. Repeat BAL sampling demonstrated multidrug-resistant Escherichia coli, a BAL galactomannan level of 2.0 ODI, and negative fungal cultures. The patient’s hospital course was complicated by profound hypoxemia, requiring prone positioning and neuromuscular blockade. He was treated with meropenem and voriconazole. His immunosuppression was reduced, but he rapidly developed acute liver injury from hepatic GVHD that resolved after reinitiation of cyclosporine and prednisone at 0.75 mg/kg/d.
The patient improved over the next 3 weeks and was successfully extubated. Repeat chest CT imaging demonstrated numerous pneumatoceles in the location of previous nodules, consistent with healing necrotic fungal disease, and a new right lower-lobe cavitary mass (Figure 2). Two days after transferring out of the intensive care unit, the patient again developed hypoxemia and fevers to 39° C. Bronchoscopy with BAL of the right lower lobe revealed positive A fumigatus and Rhizopus sp polymerase chain reaction (PCR) assays, although fungal cultures were positive only for A fumigatus. Liposomal amphotericin B (5 mg/kg) was added to voriconazole therapy to treat mucormycosis and to provide a second active agent against A fumigatus.
Unfortunately, the patient’s clinical status continued to deteriorate with signs of progressive respiratory failure and infection despite empiric, broad-spectrum antibiotics and dual antifungal therapy. His serum voriconazole level continued to be therapeutic at 1.9 mg/L. The patient declined reintubation and invasive mechanical ventilation, and he ultimately transitioned to comfort measures and died with his family at the bedside.
Autopsy demonstrated widely disseminated Aspergillus infection as the cause of death, with evidence of myocardial, neural, and vascular invasion of A fumigatus (Figures 3 and 4).
Discussion
This case of fatal, progressive, invasive, pulmonary aspergillosis demonstrates several important factors in the treatment of patients with this disease. Treatment failure usually relates to any of 4 possible factors: host immune status, severity or burden of disease, appropriate dosing of antifungal agents, and drug resistance. This patient’s immune system was heavily suppressed for a prolonged period. Attempts at reducing immunosuppression to the minimal required dosage to prevent a GVHD flare were unsuccessful and became an unmodifiable risk factor, a major contributor to his demise.
The risks of continuous high-dose immunosuppression in steroid-refractory GVHD is well understood and has been previously demonstrated to have up to 50% 4-year nonrelapse mortality, mainly due to overwhelming bacterial, viral, and fungal infections.4 All attempts should be made to cease or reduce immunosuppression in the setting of a severe infection, although this is sometimes impossible as in this case.
The patient’s disease burden was significant as evidenced by the bilateral, multifocal pulmonary nodules seen on chest imaging and the disseminated disease found at postmortem examination. His initial improvement in symptoms with voriconazole and the evolution of his images (with many of his initial pulmonary nodules becoming pneumatoceles) suggested a temporary positive immune response. The authors believe that the Rhizopus in his sputum represents noninvasive colonization of one of his pneumatoceles, because postmortem examination failed to reveal Rhizopus at any other location.
Voriconazole has excellent pulmonary and central nervous system penetration: In this patient serum levels were well within the therapeutic range. His peculiar drug resistance pattern (sensitivity to azoles and resistance to amphotericin) is unusual. Azole resistance in leukemia and patients with HSCT is more common than is amphotericin resistance, with current estimates of azole resistance close to 5%, ranging between 1% and 30%.5,6 Widespread use of antifungal prophylaxis with azoles likely selects for azole resistance.6
Despite this concern of azole resistance, current IDSA guidelines recommend against routine susceptibility testing of Aspergillus to azole therapy because of the current lack of consensus between the European Committee on Antibiotic Susceptibility Testing and Clinical and Laboratory Standards Institute on break points for resistance patterns.3,7 This is an area of emerging research, and proposed cut points for declaration of resistance do exist in the literature even if not globally agreed on.8
Combination antifungal therapy is an option for treatment in cases of possible drug resistance. Nonetheless, a recent randomized, double-blind, placebo-controlled, multicenter trial comparing voriconazole monotherapy with the combination of voriconazole and anidulafungin failed to demonstrate an overall mortality benefit in the primary analysis, although secondary analysis showed a mortality benefit with combination therapy in patients at highest risk for death.9
Despite the lack of unified standards with susceptibility testing, it may be reasonable to perform such tests in patients with demonstrating progressive disease. In this patient’s case, amphotericin B was added to treat the Rhizopus species found in his sputum, and while not the combination studied in the previously mentioned study, the drug should have provided an additional active agent for Aspergillus should this patient have had azole resistance.
Surprisingly, subsequent testing demonstrated the Aspergillus species to be resistant to amphotericin B. De novo amphotericin B-resistant A fumigates is extremely rare, with an expected incidence of 1% or less.10 The authors believe the patient may have demonstrated induction of amphotericin-B resistance through activation of fungal stress pathways by prior treatment with voriconazole. This has been demonstrated in vitro and should be considered should combination salvage therapy be required for the treatment of a refractory Aspergillus infection especially if patients have received prior treatment with voriconazole.11
Conclusion
This fatal case of invasive pulmonary aspergillosis illustrates the importance of considering the 4 main causes of treatment failure in an infection. Although the patient had a high burden of disease with a rare resistance pattern, he was treated with appropriate and well-dosed therapy. Ultimately, his unmodifiable immunosuppression was likely the driving factor leading to treatment failure and death. The indication for and number of bone marrow transplants continues to increase, thus exposure to and treatment of invasive fungal infections will increase accordingly. As such, providers should ensure that all causes of treatment failure are considered and addressed.
Historically, aspergillosis in patients with hematopoietic stem cell transplantation (HSCT) has carried a high mortality rate. However, recent data demonstrate a dramatic improvement in outcomes for patients with HSCT: 90-day survival increased from 22% before 2000 to 45% over the past 15 years.1 Improved outcomes coincide with changes in transplant immunosuppression practices, use of cross-sectional imaging for early disease identification, galactomannan screening, and the development of novel treatment options.
Voriconazole is an azole drug that blocks the synthesis of ergosterol, a vital component of the cellular membrane of fungi. Voriconazole was approved in 2002 after a clinical trial demonstrated an improvement in 50% of patients with invasive aspergillosis in the voriconazole arm vs 30% in the amphotericin B arm at 12 weeks.2 Amphotericin B is a polyene antifungal drug that binds with ergosterol, creating leaks in the cell membrane that lead to cellular demise. Voriconazole quickly became the first-line therapy for invasive aspergillosis and is recommended by both the Infectious Disease Society of American (IDSA) and the European Conference on Infections in Leukemia.3
Case Presentation
A 55-year-old man with high-risk chronic myelogenous leukemia (CML) underwent a 10 of 10 human leukocyte antigen allele and antigen-matched peripheral blood allogeneic HSCT with a myeloablative-conditioning regimen of busulfan and cyclophosphamide, along with prophylactic voriconazole, sulfamethoxazole/trimethoprim, and acyclovir. After successful engraftment (without significant neutropenia), his posttransplant course was complicated by grade 2 graft vs host disease (GVHD) of the skin, eyes, and liver, which responded well to steroids and tacrolimus. Voriconazole was continued for 5 months until immunosuppression was minimized (tacrolimus 1 mg twice daily). Two months later, the patient’s GVHD worsened, necessitating treatment at an outside hospital with high-dose prednisone (2 mg/kg/d) and cyclosporine (300 mg twice daily). Voriconazole prophylaxis was not reinitiated at that time.
One year later, at a routine follow-up appointment, the patient endorsed several weeks of malaise, weight loss, and nonproductive cough. The patient’s immunosuppression recently had been reduced to 1 mg/kg/d of prednisone and 100 mg of cyclosporine twice daily. A chest X-ray demonstrated multiple pulmonary nodules; follow-up chest computed tomography (CT) confirmed multiple nodular infiltrates with surrounding ground-glass opacities suspicious with a fungal infection (Figure 1).
Treatment with oral voriconazole (300 mg twice daily) was initiated for probable pulmonary aspergillosis. Cyclosporine (150 mg twice daily) and prednisone (1 mg/kg/d) were continued throughout treatment out of concern for hepatic GVHD. The patient’s symptoms improved over the next 10 days, and follow-up chest imaging demonstrated improvement.
Two weeks after initiation of voriconazole treatment, the patient developed a new productive cough and dyspnea, associated with fevers and chills. Repeat imaging revealed right lower-lobe pneumonia. The serum voriconazole trough level was checked and was 3.1 mg/L, suggesting therapeutic dosing. The patient subsequently developed acute respiratory distress syndrome and required intubation and mechanical ventilation. Repeat BAL sampling demonstrated multidrug-resistant Escherichia coli, a BAL galactomannan level of 2.0 ODI, and negative fungal cultures. The patient’s hospital course was complicated by profound hypoxemia, requiring prone positioning and neuromuscular blockade. He was treated with meropenem and voriconazole. His immunosuppression was reduced, but he rapidly developed acute liver injury from hepatic GVHD that resolved after reinitiation of cyclosporine and prednisone at 0.75 mg/kg/d.
The patient improved over the next 3 weeks and was successfully extubated. Repeat chest CT imaging demonstrated numerous pneumatoceles in the location of previous nodules, consistent with healing necrotic fungal disease, and a new right lower-lobe cavitary mass (Figure 2). Two days after transferring out of the intensive care unit, the patient again developed hypoxemia and fevers to 39° C. Bronchoscopy with BAL of the right lower lobe revealed positive A fumigatus and Rhizopus sp polymerase chain reaction (PCR) assays, although fungal cultures were positive only for A fumigatus. Liposomal amphotericin B (5 mg/kg) was added to voriconazole therapy to treat mucormycosis and to provide a second active agent against A fumigatus.
Unfortunately, the patient’s clinical status continued to deteriorate with signs of progressive respiratory failure and infection despite empiric, broad-spectrum antibiotics and dual antifungal therapy. His serum voriconazole level continued to be therapeutic at 1.9 mg/L. The patient declined reintubation and invasive mechanical ventilation, and he ultimately transitioned to comfort measures and died with his family at the bedside.
Autopsy demonstrated widely disseminated Aspergillus infection as the cause of death, with evidence of myocardial, neural, and vascular invasion of A fumigatus (Figures 3 and 4).
Discussion
This case of fatal, progressive, invasive, pulmonary aspergillosis demonstrates several important factors in the treatment of patients with this disease. Treatment failure usually relates to any of 4 possible factors: host immune status, severity or burden of disease, appropriate dosing of antifungal agents, and drug resistance. This patient’s immune system was heavily suppressed for a prolonged period. Attempts at reducing immunosuppression to the minimal required dosage to prevent a GVHD flare were unsuccessful and became an unmodifiable risk factor, a major contributor to his demise.
The risks of continuous high-dose immunosuppression in steroid-refractory GVHD is well understood and has been previously demonstrated to have up to 50% 4-year nonrelapse mortality, mainly due to overwhelming bacterial, viral, and fungal infections.4 All attempts should be made to cease or reduce immunosuppression in the setting of a severe infection, although this is sometimes impossible as in this case.
The patient’s disease burden was significant as evidenced by the bilateral, multifocal pulmonary nodules seen on chest imaging and the disseminated disease found at postmortem examination. His initial improvement in symptoms with voriconazole and the evolution of his images (with many of his initial pulmonary nodules becoming pneumatoceles) suggested a temporary positive immune response. The authors believe that the Rhizopus in his sputum represents noninvasive colonization of one of his pneumatoceles, because postmortem examination failed to reveal Rhizopus at any other location.
Voriconazole has excellent pulmonary and central nervous system penetration: In this patient serum levels were well within the therapeutic range. His peculiar drug resistance pattern (sensitivity to azoles and resistance to amphotericin) is unusual. Azole resistance in leukemia and patients with HSCT is more common than is amphotericin resistance, with current estimates of azole resistance close to 5%, ranging between 1% and 30%.5,6 Widespread use of antifungal prophylaxis with azoles likely selects for azole resistance.6
Despite this concern of azole resistance, current IDSA guidelines recommend against routine susceptibility testing of Aspergillus to azole therapy because of the current lack of consensus between the European Committee on Antibiotic Susceptibility Testing and Clinical and Laboratory Standards Institute on break points for resistance patterns.3,7 This is an area of emerging research, and proposed cut points for declaration of resistance do exist in the literature even if not globally agreed on.8
Combination antifungal therapy is an option for treatment in cases of possible drug resistance. Nonetheless, a recent randomized, double-blind, placebo-controlled, multicenter trial comparing voriconazole monotherapy with the combination of voriconazole and anidulafungin failed to demonstrate an overall mortality benefit in the primary analysis, although secondary analysis showed a mortality benefit with combination therapy in patients at highest risk for death.9
Despite the lack of unified standards with susceptibility testing, it may be reasonable to perform such tests in patients with demonstrating progressive disease. In this patient’s case, amphotericin B was added to treat the Rhizopus species found in his sputum, and while not the combination studied in the previously mentioned study, the drug should have provided an additional active agent for Aspergillus should this patient have had azole resistance.
Surprisingly, subsequent testing demonstrated the Aspergillus species to be resistant to amphotericin B. De novo amphotericin B-resistant A fumigates is extremely rare, with an expected incidence of 1% or less.10 The authors believe the patient may have demonstrated induction of amphotericin-B resistance through activation of fungal stress pathways by prior treatment with voriconazole. This has been demonstrated in vitro and should be considered should combination salvage therapy be required for the treatment of a refractory Aspergillus infection especially if patients have received prior treatment with voriconazole.11
Conclusion
This fatal case of invasive pulmonary aspergillosis illustrates the importance of considering the 4 main causes of treatment failure in an infection. Although the patient had a high burden of disease with a rare resistance pattern, he was treated with appropriate and well-dosed therapy. Ultimately, his unmodifiable immunosuppression was likely the driving factor leading to treatment failure and death. The indication for and number of bone marrow transplants continues to increase, thus exposure to and treatment of invasive fungal infections will increase accordingly. As such, providers should ensure that all causes of treatment failure are considered and addressed.
1. Upton A, Kirby KA, Carpenter P, Boeckh M, Marr KA. Invasive aspergillosis following hematopoietic cell transplantation: outcomes and prognostic factors associated with mortality. Clin Infect Dis. 2007;44(4):531-540.
2. Herbrecht R, Denning DW, Patterson TF, et al; Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347(6):408-415.
3. Patterson TF, Thompson GR III, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Disease Society of America. Clin Infect Dis. 2016;63(4):e1-e60.
4. García-Cadenas I, Rivera I, Martino R, et al. Patterns of infection and infection-related mortality in patients with steroid-refractory acute graft versus host disease. Bone Marrow Transplant. 2017;52(1):107-113.
5. Vermeulen E, Maertens J, De Bel A, et al. Nationwide surveillance of azole resistance in Aspergillus diseases. Antimicrob Agents Chemother. 2015;59(8):4569-4576.
6. Wiederhold NP, Patterson TF. Emergence of azole resistance in Aspergillus. Semin Respir Crit Care Med. 2015;36(5):673-680.
7. Cuenca-Estrella M, Moore CB, Barchiesi F, et al; AFST Subcommittee of the European Committee on Antimicrobial Susceptibility Testing. Multicenter evaluation of the reproducibility of the proposed antifungal susceptibility testing method for fermentative yeasts of the Antifungal Susceptibility Testing Subcommittee of the European Committee on Antimicrobial Susceptibility Testing (AFST-EUCAST). Clin Microbiol Infect. 2003;9(6):467-474.
8. Pfaller MA, Diekema DJ, Ghannoum MA, et al; Clinical and Laboratory Standards Institute Antifungal Testing Subcommittee. Wild-type MIC distribution and epidemiological cutoff values for Aspergillus fumigatus and three triazoles as determined by Clinical and Laboratory Standards Institute for broth microdilution methods. J Clin Microbiol. 2009;47(10):3142-3146.
9. Marr KA, Schlamm HT, Herbrecht R, et al. Combination antifungal therapy for invasive aspergillosis: a randomized trial. Ann Intern Med. 2015;162(2):81-89.
10. Tashiro M, Izumikawa K, Minematsu A, et al. Antifungal susceptibilities of Aspergillus fumigatus clinical isolates obtained in Nagasaki, Japan. Antimicrob Agents Chemother. 2012;56(1):584-587.
11. Rajendran R, Mowat E, Jones B, Williams C, Ramage G. Prior in vitro exposure to voriconazole confers resistance to amphotericin B in Aspergillus fumigatus biofilms. Int J Antimicrob Agents. 2015;46(3):342-345.
1. Upton A, Kirby KA, Carpenter P, Boeckh M, Marr KA. Invasive aspergillosis following hematopoietic cell transplantation: outcomes and prognostic factors associated with mortality. Clin Infect Dis. 2007;44(4):531-540.
2. Herbrecht R, Denning DW, Patterson TF, et al; Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347(6):408-415.
3. Patterson TF, Thompson GR III, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Disease Society of America. Clin Infect Dis. 2016;63(4):e1-e60.
4. García-Cadenas I, Rivera I, Martino R, et al. Patterns of infection and infection-related mortality in patients with steroid-refractory acute graft versus host disease. Bone Marrow Transplant. 2017;52(1):107-113.
5. Vermeulen E, Maertens J, De Bel A, et al. Nationwide surveillance of azole resistance in Aspergillus diseases. Antimicrob Agents Chemother. 2015;59(8):4569-4576.
6. Wiederhold NP, Patterson TF. Emergence of azole resistance in Aspergillus. Semin Respir Crit Care Med. 2015;36(5):673-680.
7. Cuenca-Estrella M, Moore CB, Barchiesi F, et al; AFST Subcommittee of the European Committee on Antimicrobial Susceptibility Testing. Multicenter evaluation of the reproducibility of the proposed antifungal susceptibility testing method for fermentative yeasts of the Antifungal Susceptibility Testing Subcommittee of the European Committee on Antimicrobial Susceptibility Testing (AFST-EUCAST). Clin Microbiol Infect. 2003;9(6):467-474.
8. Pfaller MA, Diekema DJ, Ghannoum MA, et al; Clinical and Laboratory Standards Institute Antifungal Testing Subcommittee. Wild-type MIC distribution and epidemiological cutoff values for Aspergillus fumigatus and three triazoles as determined by Clinical and Laboratory Standards Institute for broth microdilution methods. J Clin Microbiol. 2009;47(10):3142-3146.
9. Marr KA, Schlamm HT, Herbrecht R, et al. Combination antifungal therapy for invasive aspergillosis: a randomized trial. Ann Intern Med. 2015;162(2):81-89.
10. Tashiro M, Izumikawa K, Minematsu A, et al. Antifungal susceptibilities of Aspergillus fumigatus clinical isolates obtained in Nagasaki, Japan. Antimicrob Agents Chemother. 2012;56(1):584-587.
11. Rajendran R, Mowat E, Jones B, Williams C, Ramage G. Prior in vitro exposure to voriconazole confers resistance to amphotericin B in Aspergillus fumigatus biofilms. Int J Antimicrob Agents. 2015;46(3):342-345.
Nicotinamide-containing products gaining interest for aging, dermatologic disorders
NEW YORK – More patients are inquiring about the antiaging claims made for nicotinamide products, according to Christine DeWitt MD, of the department of dermatology, Georgetown University, Washington. She encouraged attendees at the American Academy of Dermatology summer meeting to gain familiarity with the underlying mechanisms and potential uses of nicotinamide for aging skin and prevention of skin cancer as well as for a variety of dermatologic disorders, including atopic dermatitis and bullous pemphigoid.
The ability of nicotinamide to increase oxidized nicotinamide adenine dinucleotide (NAD+) is credited for most of its dermatologic benefits, according to Dr. DeWitt. She explained that NAD+ has a central role in cell metabolism, including serving as a substrate for sirtuins, which help prevent deterioration of telomeres, now thought to be a critical event in aging.
Downstream effects include an improved barrier function to reduce transdermal water loss in patients with atopic dermatitis and anti-inflammatory effects that are relevant to acne and bullous pemphigoid.
The related but unique forms of vitamin B3, nicotinamide riboside and nicotinamide mononucleotide, appear to increase more directly and effectively NAD+ with the potential to provide more potent enzymatic antiaging effects, according to Dr. DeWitt. Not all of the more than 90 active and recruiting trials listed for these compounds on clinicaltrials.gov relate to aging, but many do list this or a related condition, such as frailty or sarcopenia, as the therapeutic target.
The trials are being conducted even as OTC nicotinamide riboside and nicotinamide mononucleotide products are being promoted with terms such as “antiaging DNA repair” and “sirtuins activator.” Dr. DeWitt said that favorable reviews of these products on Internet forums are leading many patients to ask her specifically about their clinical value.
“Patients are starting to look at aging and longevity as an entity to manage and to treat,” Dr. DeWitt explained. Increasingly, patients bring up terms like autophagy and ask about the science behind antiaging products.
The clinical role of nicotinamide-related products, whether to reduce events related to aging or provide other benefits, remains unproven.
Nevertheless, Dr. DeWitt often offers nicotinamide to her patients for such indications as acne and atopic dermatitis. In patients with bullous pemphigoid, nicotinamide is an adjunct to other therapies “in most of my patients.”
When recommending nicotinamide, Dr. DeWitt specifies a brand, not because there is evidence that one brand is better than another but because of a reputation of quality control with branded OTC products.
In general, nicotinamide, which is not generally associated with the flushing that accompanies niacin, is well tolerated. She recommends 500 mg twice daily for most indications.
Dr. DeWitt advised reviewing published studies on nicotinamide in order to respond appropriately to patient inquiries. She noted that many patients come to the clinician’s office already aware of the science behind the potential role of NAD+ to inhibit aging and will be seeking an objective point of view.
Dr. DeWitt reports no conflicts of interest.
NEW YORK – More patients are inquiring about the antiaging claims made for nicotinamide products, according to Christine DeWitt MD, of the department of dermatology, Georgetown University, Washington. She encouraged attendees at the American Academy of Dermatology summer meeting to gain familiarity with the underlying mechanisms and potential uses of nicotinamide for aging skin and prevention of skin cancer as well as for a variety of dermatologic disorders, including atopic dermatitis and bullous pemphigoid.
The ability of nicotinamide to increase oxidized nicotinamide adenine dinucleotide (NAD+) is credited for most of its dermatologic benefits, according to Dr. DeWitt. She explained that NAD+ has a central role in cell metabolism, including serving as a substrate for sirtuins, which help prevent deterioration of telomeres, now thought to be a critical event in aging.
Downstream effects include an improved barrier function to reduce transdermal water loss in patients with atopic dermatitis and anti-inflammatory effects that are relevant to acne and bullous pemphigoid.
The related but unique forms of vitamin B3, nicotinamide riboside and nicotinamide mononucleotide, appear to increase more directly and effectively NAD+ with the potential to provide more potent enzymatic antiaging effects, according to Dr. DeWitt. Not all of the more than 90 active and recruiting trials listed for these compounds on clinicaltrials.gov relate to aging, but many do list this or a related condition, such as frailty or sarcopenia, as the therapeutic target.
The trials are being conducted even as OTC nicotinamide riboside and nicotinamide mononucleotide products are being promoted with terms such as “antiaging DNA repair” and “sirtuins activator.” Dr. DeWitt said that favorable reviews of these products on Internet forums are leading many patients to ask her specifically about their clinical value.
“Patients are starting to look at aging and longevity as an entity to manage and to treat,” Dr. DeWitt explained. Increasingly, patients bring up terms like autophagy and ask about the science behind antiaging products.
The clinical role of nicotinamide-related products, whether to reduce events related to aging or provide other benefits, remains unproven.
Nevertheless, Dr. DeWitt often offers nicotinamide to her patients for such indications as acne and atopic dermatitis. In patients with bullous pemphigoid, nicotinamide is an adjunct to other therapies “in most of my patients.”
When recommending nicotinamide, Dr. DeWitt specifies a brand, not because there is evidence that one brand is better than another but because of a reputation of quality control with branded OTC products.
In general, nicotinamide, which is not generally associated with the flushing that accompanies niacin, is well tolerated. She recommends 500 mg twice daily for most indications.
Dr. DeWitt advised reviewing published studies on nicotinamide in order to respond appropriately to patient inquiries. She noted that many patients come to the clinician’s office already aware of the science behind the potential role of NAD+ to inhibit aging and will be seeking an objective point of view.
Dr. DeWitt reports no conflicts of interest.
NEW YORK – More patients are inquiring about the antiaging claims made for nicotinamide products, according to Christine DeWitt MD, of the department of dermatology, Georgetown University, Washington. She encouraged attendees at the American Academy of Dermatology summer meeting to gain familiarity with the underlying mechanisms and potential uses of nicotinamide for aging skin and prevention of skin cancer as well as for a variety of dermatologic disorders, including atopic dermatitis and bullous pemphigoid.
The ability of nicotinamide to increase oxidized nicotinamide adenine dinucleotide (NAD+) is credited for most of its dermatologic benefits, according to Dr. DeWitt. She explained that NAD+ has a central role in cell metabolism, including serving as a substrate for sirtuins, which help prevent deterioration of telomeres, now thought to be a critical event in aging.
Downstream effects include an improved barrier function to reduce transdermal water loss in patients with atopic dermatitis and anti-inflammatory effects that are relevant to acne and bullous pemphigoid.
The related but unique forms of vitamin B3, nicotinamide riboside and nicotinamide mononucleotide, appear to increase more directly and effectively NAD+ with the potential to provide more potent enzymatic antiaging effects, according to Dr. DeWitt. Not all of the more than 90 active and recruiting trials listed for these compounds on clinicaltrials.gov relate to aging, but many do list this or a related condition, such as frailty or sarcopenia, as the therapeutic target.
The trials are being conducted even as OTC nicotinamide riboside and nicotinamide mononucleotide products are being promoted with terms such as “antiaging DNA repair” and “sirtuins activator.” Dr. DeWitt said that favorable reviews of these products on Internet forums are leading many patients to ask her specifically about their clinical value.
“Patients are starting to look at aging and longevity as an entity to manage and to treat,” Dr. DeWitt explained. Increasingly, patients bring up terms like autophagy and ask about the science behind antiaging products.
The clinical role of nicotinamide-related products, whether to reduce events related to aging or provide other benefits, remains unproven.
Nevertheless, Dr. DeWitt often offers nicotinamide to her patients for such indications as acne and atopic dermatitis. In patients with bullous pemphigoid, nicotinamide is an adjunct to other therapies “in most of my patients.”
When recommending nicotinamide, Dr. DeWitt specifies a brand, not because there is evidence that one brand is better than another but because of a reputation of quality control with branded OTC products.
In general, nicotinamide, which is not generally associated with the flushing that accompanies niacin, is well tolerated. She recommends 500 mg twice daily for most indications.
Dr. DeWitt advised reviewing published studies on nicotinamide in order to respond appropriately to patient inquiries. She noted that many patients come to the clinician’s office already aware of the science behind the potential role of NAD+ to inhibit aging and will be seeking an objective point of view.
Dr. DeWitt reports no conflicts of interest.
EXPERT ANALYSIS FROM SUMMER AAD 2019
Botulinum toxin injections: Err on the side of undercorrecting in first-time users
NEW YORK – In patients receiving first-time botulinum toxin injections for cosmetic enhancements, it is prudent to use a relatively low dose, Gary Goldenberg, MD, advised at the American Academy of Dermatology summer meeting.
Optimal dosing varies by individual, and undertreatment is easier to correct than is excess treatment. “This is a pearl. I always undercorrect, especially if I am injecting a patient for the first time,” said Dr. Goldenberg, an assistant clinical professor of dermatology and pathology at the Icahn School of Medicine at Mount Sinai, New York.
All patients are invited to return 2 weeks after their initial treatments, when the maximum effect is reached. Dr. Goldenberg does not charge for touch-ups administered at that time. “I want the patient to have the best possible experience,” he said.
The demand for botulinum toxin injections is skyrocketing, even among patients in their 20s. Also, men now represent a substantial proportion of those seeking cosmetic botulinum toxin injections.
Botulinum toxin injections are a source of high levels of patient satisfaction, according to Dr. Goldenberg. They are also a good way to get started in performing cosmetic procedures as skills in the injection of botulinum toxin are readily acquired, While some primary care physicians and gynecologists also are offering botulinum toxin injections for cosmetic purposes, dermatologists “are going to do a better job because we know the anatomy the best,” he said.
Dr. Goldenberg said botulinum toxin injections should be offered as a service in promotional efforts for one’s practice, but any mention to patients should be tactful. Patients should be informed that there are solutions for damaged or wrinkled skin, but the topic should be dropped if there is no apparent interest.
“I only suggest. I do not push,” he said. “I never talk about money. If they want to know how much (injections) will cost, they must speak to my office staff.”
With the recent approval of prabotulinumtoxinA (Jeuveau), there are four botulinum toxin injection products available in the United States. These include the original product, onabotulinumtoxinA (Botox), incobotulinumtoxinA (Xeomin), and abobotulinumtoxinA (Dysport). Dr. Goldenberg, who has administered them all, is not so far convinced there are important differences between them in regard to either efficacy or safety.
“There is another product now in clinical trials, so perhaps we will have a fifth product in a year or so,” said Dr. Goldenberg, who noted that the competition has resulted in claims and counterclaims regarding such issues as speed of onset and durability.
For dermatologists new to providing botulinum toxin injections, Dr. Goldenberg suggested restricting initial procedures to the face, particularly glabellar lines for which all of the available products are indicated. The companies that make these products also should offer a broad array of resources for improving skills, he said.
Dr. Goldenberg reports no potential conflicts of interest with companies that make botulinum toxins.
NEW YORK – In patients receiving first-time botulinum toxin injections for cosmetic enhancements, it is prudent to use a relatively low dose, Gary Goldenberg, MD, advised at the American Academy of Dermatology summer meeting.
Optimal dosing varies by individual, and undertreatment is easier to correct than is excess treatment. “This is a pearl. I always undercorrect, especially if I am injecting a patient for the first time,” said Dr. Goldenberg, an assistant clinical professor of dermatology and pathology at the Icahn School of Medicine at Mount Sinai, New York.
All patients are invited to return 2 weeks after their initial treatments, when the maximum effect is reached. Dr. Goldenberg does not charge for touch-ups administered at that time. “I want the patient to have the best possible experience,” he said.
The demand for botulinum toxin injections is skyrocketing, even among patients in their 20s. Also, men now represent a substantial proportion of those seeking cosmetic botulinum toxin injections.
Botulinum toxin injections are a source of high levels of patient satisfaction, according to Dr. Goldenberg. They are also a good way to get started in performing cosmetic procedures as skills in the injection of botulinum toxin are readily acquired, While some primary care physicians and gynecologists also are offering botulinum toxin injections for cosmetic purposes, dermatologists “are going to do a better job because we know the anatomy the best,” he said.
Dr. Goldenberg said botulinum toxin injections should be offered as a service in promotional efforts for one’s practice, but any mention to patients should be tactful. Patients should be informed that there are solutions for damaged or wrinkled skin, but the topic should be dropped if there is no apparent interest.
“I only suggest. I do not push,” he said. “I never talk about money. If they want to know how much (injections) will cost, they must speak to my office staff.”
With the recent approval of prabotulinumtoxinA (Jeuveau), there are four botulinum toxin injection products available in the United States. These include the original product, onabotulinumtoxinA (Botox), incobotulinumtoxinA (Xeomin), and abobotulinumtoxinA (Dysport). Dr. Goldenberg, who has administered them all, is not so far convinced there are important differences between them in regard to either efficacy or safety.
“There is another product now in clinical trials, so perhaps we will have a fifth product in a year or so,” said Dr. Goldenberg, who noted that the competition has resulted in claims and counterclaims regarding such issues as speed of onset and durability.
For dermatologists new to providing botulinum toxin injections, Dr. Goldenberg suggested restricting initial procedures to the face, particularly glabellar lines for which all of the available products are indicated. The companies that make these products also should offer a broad array of resources for improving skills, he said.
Dr. Goldenberg reports no potential conflicts of interest with companies that make botulinum toxins.
NEW YORK – In patients receiving first-time botulinum toxin injections for cosmetic enhancements, it is prudent to use a relatively low dose, Gary Goldenberg, MD, advised at the American Academy of Dermatology summer meeting.
Optimal dosing varies by individual, and undertreatment is easier to correct than is excess treatment. “This is a pearl. I always undercorrect, especially if I am injecting a patient for the first time,” said Dr. Goldenberg, an assistant clinical professor of dermatology and pathology at the Icahn School of Medicine at Mount Sinai, New York.
All patients are invited to return 2 weeks after their initial treatments, when the maximum effect is reached. Dr. Goldenberg does not charge for touch-ups administered at that time. “I want the patient to have the best possible experience,” he said.
The demand for botulinum toxin injections is skyrocketing, even among patients in their 20s. Also, men now represent a substantial proportion of those seeking cosmetic botulinum toxin injections.
Botulinum toxin injections are a source of high levels of patient satisfaction, according to Dr. Goldenberg. They are also a good way to get started in performing cosmetic procedures as skills in the injection of botulinum toxin are readily acquired, While some primary care physicians and gynecologists also are offering botulinum toxin injections for cosmetic purposes, dermatologists “are going to do a better job because we know the anatomy the best,” he said.
Dr. Goldenberg said botulinum toxin injections should be offered as a service in promotional efforts for one’s practice, but any mention to patients should be tactful. Patients should be informed that there are solutions for damaged or wrinkled skin, but the topic should be dropped if there is no apparent interest.
“I only suggest. I do not push,” he said. “I never talk about money. If they want to know how much (injections) will cost, they must speak to my office staff.”
With the recent approval of prabotulinumtoxinA (Jeuveau), there are four botulinum toxin injection products available in the United States. These include the original product, onabotulinumtoxinA (Botox), incobotulinumtoxinA (Xeomin), and abobotulinumtoxinA (Dysport). Dr. Goldenberg, who has administered them all, is not so far convinced there are important differences between them in regard to either efficacy or safety.
“There is another product now in clinical trials, so perhaps we will have a fifth product in a year or so,” said Dr. Goldenberg, who noted that the competition has resulted in claims and counterclaims regarding such issues as speed of onset and durability.
For dermatologists new to providing botulinum toxin injections, Dr. Goldenberg suggested restricting initial procedures to the face, particularly glabellar lines for which all of the available products are indicated. The companies that make these products also should offer a broad array of resources for improving skills, he said.
Dr. Goldenberg reports no potential conflicts of interest with companies that make botulinum toxins.
EXPERT ANALYSIS FROM SUMMER AAD 2019
PCPs play role in identifying severe, difficult-to-treat asthma
ORLANDO – Clinicians at the primary care level should learn to distinguish the difference between severe and difficult-to-treat asthma to help facilitate referral to an asthma care specialist, according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
Care providers are seeing patients with severe asthma at their primary care practice, whether they realize it or not, and should therefore learn to recognize and diagnose these patients even if they are not directly treating them for asthma, said Michelle R. Dickens, MSN, RN, FNP-C, AE-C, a nurse practitioner at Ferrell-Duncan Clinic department of allergy, asthma, and immunology in Springfield, Mo., said in her presentation.
“There’s still a lot we can do to get the ball rolling,” Ms. Dickens said. “While you may not be prescribing some of these newer biologics and some of the high-level, $30,000-a-year medications for your asthmatic, you still have a role in this in identifying them and helping us to get to where they need to be.”
Ms. Dickens noted that patients may not even disclose their asthma history with their primary care provider if it is not the reason for the office visit. “Because asthma can be such an episodic disease, it’s not right on the top of their radar,” she said. “They have bigger issues they want to talk about with you, and they forget to mention the asthma part.”
Under Global Initiative for Asthma (GINA) criteria, severe asthma is defined as poorly controlled asthma even after patients demonstrate adherence and good technique. However, before diagnosing a patient with severe asthma, clinicians should first rule out whether the patient has asthma that is difficult to treat, said Ms. Dickens. Difficult-to-treat asthma is characterized by inadequate dosing of medication, noncompliance with medication dose (“spreading out” the medication), poor technique when self-administering the medication, and comorbid conditions. It is also possible that difficult-to-treat asthma is not well controlled because the asthma was misdiagnosed and is actually another condition, she added.
If a patient has difficult-to-treat asthma, ensure they are adhering to the therapy, using proper technique, and that the medicine is being administered at the proper dose. Using Expert Panel Report 3 (EPR-3) and Global Initiative for Asthma (GINA) guidelines, clinicians should maximize the treatment for a patient with severe asthma based on the stepwise approach outlined in the guidelines, and referring out to an asthma specialist for add-on therapy or stepping up therapy when indicated.
Researchers are beginning to explore the genotypes, phenotypes, and endotypes of asthma to learn more about severe asthma and potentially identify asthma subtypes, said Ms. Dickens. “We’re not there yet, but we are learning a little bit about why certain patients have certain types of asthma,” she said.
The Severe Asthma Research Program has found three clusters of likely severe asthma candidates: those with classic childhood asthma onset, those who have asthma with chronic obstructive pulmonary disease (COPD), and patients with both obesity and asthma characterized by “high impairment but mildly abnormal lung function.” Clinicians can use spirometry, complete blood count with differential, total immunoglobulin E, body mass index, allergy testing, and exhaled nitric oxide with these data and biomarkers to gain a better idea of a patient’s asthma situation.
Referrals to an asthma specialist should be considered if a patient experiences a life-threatening exacerbation, is not responding to therapy, has an unusual presentation of asthma symptoms, has comorbid conditions, or needs additional testing or additional education. Patients who are at step 2 or higher in EPR-3 guidelines and ready to move to step 3 and are under 4 years of age, and patients who are 5 years or older at step 4 of therapy or higher should be referred to an asthma specialist. “I think the younger the patient and the more severe the [symptoms], the more likely you should be referring to a specialist,” said Ms. Dickens.
Ms. Dickens reports no relevant financial disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
ORLANDO – Clinicians at the primary care level should learn to distinguish the difference between severe and difficult-to-treat asthma to help facilitate referral to an asthma care specialist, according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
Care providers are seeing patients with severe asthma at their primary care practice, whether they realize it or not, and should therefore learn to recognize and diagnose these patients even if they are not directly treating them for asthma, said Michelle R. Dickens, MSN, RN, FNP-C, AE-C, a nurse practitioner at Ferrell-Duncan Clinic department of allergy, asthma, and immunology in Springfield, Mo., said in her presentation.
“There’s still a lot we can do to get the ball rolling,” Ms. Dickens said. “While you may not be prescribing some of these newer biologics and some of the high-level, $30,000-a-year medications for your asthmatic, you still have a role in this in identifying them and helping us to get to where they need to be.”
Ms. Dickens noted that patients may not even disclose their asthma history with their primary care provider if it is not the reason for the office visit. “Because asthma can be such an episodic disease, it’s not right on the top of their radar,” she said. “They have bigger issues they want to talk about with you, and they forget to mention the asthma part.”
Under Global Initiative for Asthma (GINA) criteria, severe asthma is defined as poorly controlled asthma even after patients demonstrate adherence and good technique. However, before diagnosing a patient with severe asthma, clinicians should first rule out whether the patient has asthma that is difficult to treat, said Ms. Dickens. Difficult-to-treat asthma is characterized by inadequate dosing of medication, noncompliance with medication dose (“spreading out” the medication), poor technique when self-administering the medication, and comorbid conditions. It is also possible that difficult-to-treat asthma is not well controlled because the asthma was misdiagnosed and is actually another condition, she added.
If a patient has difficult-to-treat asthma, ensure they are adhering to the therapy, using proper technique, and that the medicine is being administered at the proper dose. Using Expert Panel Report 3 (EPR-3) and Global Initiative for Asthma (GINA) guidelines, clinicians should maximize the treatment for a patient with severe asthma based on the stepwise approach outlined in the guidelines, and referring out to an asthma specialist for add-on therapy or stepping up therapy when indicated.
Researchers are beginning to explore the genotypes, phenotypes, and endotypes of asthma to learn more about severe asthma and potentially identify asthma subtypes, said Ms. Dickens. “We’re not there yet, but we are learning a little bit about why certain patients have certain types of asthma,” she said.
The Severe Asthma Research Program has found three clusters of likely severe asthma candidates: those with classic childhood asthma onset, those who have asthma with chronic obstructive pulmonary disease (COPD), and patients with both obesity and asthma characterized by “high impairment but mildly abnormal lung function.” Clinicians can use spirometry, complete blood count with differential, total immunoglobulin E, body mass index, allergy testing, and exhaled nitric oxide with these data and biomarkers to gain a better idea of a patient’s asthma situation.
Referrals to an asthma specialist should be considered if a patient experiences a life-threatening exacerbation, is not responding to therapy, has an unusual presentation of asthma symptoms, has comorbid conditions, or needs additional testing or additional education. Patients who are at step 2 or higher in EPR-3 guidelines and ready to move to step 3 and are under 4 years of age, and patients who are 5 years or older at step 4 of therapy or higher should be referred to an asthma specialist. “I think the younger the patient and the more severe the [symptoms], the more likely you should be referring to a specialist,” said Ms. Dickens.
Ms. Dickens reports no relevant financial disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
ORLANDO – Clinicians at the primary care level should learn to distinguish the difference between severe and difficult-to-treat asthma to help facilitate referral to an asthma care specialist, according to a speaker at the Cardiovascular & Respiratory Summit by Global Academy for Medical Education.
Care providers are seeing patients with severe asthma at their primary care practice, whether they realize it or not, and should therefore learn to recognize and diagnose these patients even if they are not directly treating them for asthma, said Michelle R. Dickens, MSN, RN, FNP-C, AE-C, a nurse practitioner at Ferrell-Duncan Clinic department of allergy, asthma, and immunology in Springfield, Mo., said in her presentation.
“There’s still a lot we can do to get the ball rolling,” Ms. Dickens said. “While you may not be prescribing some of these newer biologics and some of the high-level, $30,000-a-year medications for your asthmatic, you still have a role in this in identifying them and helping us to get to where they need to be.”
Ms. Dickens noted that patients may not even disclose their asthma history with their primary care provider if it is not the reason for the office visit. “Because asthma can be such an episodic disease, it’s not right on the top of their radar,” she said. “They have bigger issues they want to talk about with you, and they forget to mention the asthma part.”
Under Global Initiative for Asthma (GINA) criteria, severe asthma is defined as poorly controlled asthma even after patients demonstrate adherence and good technique. However, before diagnosing a patient with severe asthma, clinicians should first rule out whether the patient has asthma that is difficult to treat, said Ms. Dickens. Difficult-to-treat asthma is characterized by inadequate dosing of medication, noncompliance with medication dose (“spreading out” the medication), poor technique when self-administering the medication, and comorbid conditions. It is also possible that difficult-to-treat asthma is not well controlled because the asthma was misdiagnosed and is actually another condition, she added.
If a patient has difficult-to-treat asthma, ensure they are adhering to the therapy, using proper technique, and that the medicine is being administered at the proper dose. Using Expert Panel Report 3 (EPR-3) and Global Initiative for Asthma (GINA) guidelines, clinicians should maximize the treatment for a patient with severe asthma based on the stepwise approach outlined in the guidelines, and referring out to an asthma specialist for add-on therapy or stepping up therapy when indicated.
Researchers are beginning to explore the genotypes, phenotypes, and endotypes of asthma to learn more about severe asthma and potentially identify asthma subtypes, said Ms. Dickens. “We’re not there yet, but we are learning a little bit about why certain patients have certain types of asthma,” she said.
The Severe Asthma Research Program has found three clusters of likely severe asthma candidates: those with classic childhood asthma onset, those who have asthma with chronic obstructive pulmonary disease (COPD), and patients with both obesity and asthma characterized by “high impairment but mildly abnormal lung function.” Clinicians can use spirometry, complete blood count with differential, total immunoglobulin E, body mass index, allergy testing, and exhaled nitric oxide with these data and biomarkers to gain a better idea of a patient’s asthma situation.
Referrals to an asthma specialist should be considered if a patient experiences a life-threatening exacerbation, is not responding to therapy, has an unusual presentation of asthma symptoms, has comorbid conditions, or needs additional testing or additional education. Patients who are at step 2 or higher in EPR-3 guidelines and ready to move to step 3 and are under 4 years of age, and patients who are 5 years or older at step 4 of therapy or higher should be referred to an asthma specialist. “I think the younger the patient and the more severe the [symptoms], the more likely you should be referring to a specialist,” said Ms. Dickens.
Ms. Dickens reports no relevant financial disclosures. Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM CARPS 2019
Keep your staff current – and happy
It goes without saying that as a physician, it’s essential to keep your knowledge and skills current. But too many private practitioners overlook the similar needs of their employees.
Like you, staff members provide better care to patients when they know the latest findings and techniques. They also provide better information: When patients ask questions of your staff, either in the office or over the phone (which happens more often than you probably think), you certainly want their answers to be accurate and up to date.
But there are lots of other good reasons to invest in ongoing staff training. It’s a win-win strategy for you, your staff, and for your practice.
The more your employees know, the more productive they will be. Not only will they complete everyday duties more efficiently, they will be stimulated to learn new tasks and accept more responsibility.
Staffers who have learned new skills are more willing to take on new challenges. And the better their skills and the greater their confidence, the less supervision they need from you, and the more they become involved in their work.
They will also be happier in their jobs. Investing in your employees’ competence makes them feel valued and appreciated. This leads to reduced turnover – which, alone, often pays for the training.
You probably already do some ongoing education: You do your yearly OSHA training because the law requires it, you run HIPAA updates as necessary, and you have everyone recertified periodically in basic or advanced CPR (I hope). But I’m talking about going beyond the basic stuff, which may satisfy legal requirements, but does not motivate your people to loftier goals.
An obvious example is sending your insurance people annually to coding and insurance processing courses – or at the very least, online refreshers – so they are always current on the latest third-party changes. The use of outdated or obsolete codes can cost you thousands of dollars every month. Other opportunities include keyboarding and computer courses for staff who work with your computers, and Excel and QuickBooks updates for your bookkeepers.
Continuing education does not have to be costly, and in some cases it can be free. For example, pharmaceutical representatives will be happy to run an in-service for your staff on a new medication or procedure or instrument, or refresh their memories on an established one. Be sure to make clear to the rep that the presentation must be as objective and impartial as possible, given the obvious potential conflict of interest involved.
Your office manager should join the Association of Dermatology Administrators and Managers. It holds annual meetings at the same time and in the same city as the American Academy of Dermatology winter meetings, with a good selection of refresher courses and lots of opportunities for networking with other managers, both personally or virtually.
Many other venues are available for employee education, in the cloud and in conventional classrooms. Courses are offered in many relevant subjects; a quick Google search turns up an eclectic mix, including medical terminology, record keeping and accounting, laboratory skills, diagnostic tests and procedures, pharmacology and medication administration, patient relations, medical law and ethics, and many others.
By far the most common question I receive on this issue is, “What if I pay for all that training, and then the employees leave?”
My reply: “What if you don’t, and they stay?”
Well-trained employees are vastly preferable to untrained ones. I suppose there is some risk of an occasional staffer accepting training and then moving on; but in 38 years, it has never happened in my office. In my experience, well-trained employees will stay. Education fosters loyalty. Employees who know you care enough about them to advance their skills will sense that they have a stake in the practice, and thus will be less likely to want to leave. Furthermore, continuing education will always be cheaper than training new employees from scratch.
In any case, everyone will benefit from a well-trained staff – you, your employees, your practice, and most importantly your patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
It goes without saying that as a physician, it’s essential to keep your knowledge and skills current. But too many private practitioners overlook the similar needs of their employees.
Like you, staff members provide better care to patients when they know the latest findings and techniques. They also provide better information: When patients ask questions of your staff, either in the office or over the phone (which happens more often than you probably think), you certainly want their answers to be accurate and up to date.
But there are lots of other good reasons to invest in ongoing staff training. It’s a win-win strategy for you, your staff, and for your practice.
The more your employees know, the more productive they will be. Not only will they complete everyday duties more efficiently, they will be stimulated to learn new tasks and accept more responsibility.
Staffers who have learned new skills are more willing to take on new challenges. And the better their skills and the greater their confidence, the less supervision they need from you, and the more they become involved in their work.
They will also be happier in their jobs. Investing in your employees’ competence makes them feel valued and appreciated. This leads to reduced turnover – which, alone, often pays for the training.
You probably already do some ongoing education: You do your yearly OSHA training because the law requires it, you run HIPAA updates as necessary, and you have everyone recertified periodically in basic or advanced CPR (I hope). But I’m talking about going beyond the basic stuff, which may satisfy legal requirements, but does not motivate your people to loftier goals.
An obvious example is sending your insurance people annually to coding and insurance processing courses – or at the very least, online refreshers – so they are always current on the latest third-party changes. The use of outdated or obsolete codes can cost you thousands of dollars every month. Other opportunities include keyboarding and computer courses for staff who work with your computers, and Excel and QuickBooks updates for your bookkeepers.
Continuing education does not have to be costly, and in some cases it can be free. For example, pharmaceutical representatives will be happy to run an in-service for your staff on a new medication or procedure or instrument, or refresh their memories on an established one. Be sure to make clear to the rep that the presentation must be as objective and impartial as possible, given the obvious potential conflict of interest involved.
Your office manager should join the Association of Dermatology Administrators and Managers. It holds annual meetings at the same time and in the same city as the American Academy of Dermatology winter meetings, with a good selection of refresher courses and lots of opportunities for networking with other managers, both personally or virtually.
Many other venues are available for employee education, in the cloud and in conventional classrooms. Courses are offered in many relevant subjects; a quick Google search turns up an eclectic mix, including medical terminology, record keeping and accounting, laboratory skills, diagnostic tests and procedures, pharmacology and medication administration, patient relations, medical law and ethics, and many others.
By far the most common question I receive on this issue is, “What if I pay for all that training, and then the employees leave?”
My reply: “What if you don’t, and they stay?”
Well-trained employees are vastly preferable to untrained ones. I suppose there is some risk of an occasional staffer accepting training and then moving on; but in 38 years, it has never happened in my office. In my experience, well-trained employees will stay. Education fosters loyalty. Employees who know you care enough about them to advance their skills will sense that they have a stake in the practice, and thus will be less likely to want to leave. Furthermore, continuing education will always be cheaper than training new employees from scratch.
In any case, everyone will benefit from a well-trained staff – you, your employees, your practice, and most importantly your patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
It goes without saying that as a physician, it’s essential to keep your knowledge and skills current. But too many private practitioners overlook the similar needs of their employees.
Like you, staff members provide better care to patients when they know the latest findings and techniques. They also provide better information: When patients ask questions of your staff, either in the office or over the phone (which happens more often than you probably think), you certainly want their answers to be accurate and up to date.
But there are lots of other good reasons to invest in ongoing staff training. It’s a win-win strategy for you, your staff, and for your practice.
The more your employees know, the more productive they will be. Not only will they complete everyday duties more efficiently, they will be stimulated to learn new tasks and accept more responsibility.
Staffers who have learned new skills are more willing to take on new challenges. And the better their skills and the greater their confidence, the less supervision they need from you, and the more they become involved in their work.
They will also be happier in their jobs. Investing in your employees’ competence makes them feel valued and appreciated. This leads to reduced turnover – which, alone, often pays for the training.
You probably already do some ongoing education: You do your yearly OSHA training because the law requires it, you run HIPAA updates as necessary, and you have everyone recertified periodically in basic or advanced CPR (I hope). But I’m talking about going beyond the basic stuff, which may satisfy legal requirements, but does not motivate your people to loftier goals.
An obvious example is sending your insurance people annually to coding and insurance processing courses – or at the very least, online refreshers – so they are always current on the latest third-party changes. The use of outdated or obsolete codes can cost you thousands of dollars every month. Other opportunities include keyboarding and computer courses for staff who work with your computers, and Excel and QuickBooks updates for your bookkeepers.
Continuing education does not have to be costly, and in some cases it can be free. For example, pharmaceutical representatives will be happy to run an in-service for your staff on a new medication or procedure or instrument, or refresh their memories on an established one. Be sure to make clear to the rep that the presentation must be as objective and impartial as possible, given the obvious potential conflict of interest involved.
Your office manager should join the Association of Dermatology Administrators and Managers. It holds annual meetings at the same time and in the same city as the American Academy of Dermatology winter meetings, with a good selection of refresher courses and lots of opportunities for networking with other managers, both personally or virtually.
Many other venues are available for employee education, in the cloud and in conventional classrooms. Courses are offered in many relevant subjects; a quick Google search turns up an eclectic mix, including medical terminology, record keeping and accounting, laboratory skills, diagnostic tests and procedures, pharmacology and medication administration, patient relations, medical law and ethics, and many others.
By far the most common question I receive on this issue is, “What if I pay for all that training, and then the employees leave?”
My reply: “What if you don’t, and they stay?”
Well-trained employees are vastly preferable to untrained ones. I suppose there is some risk of an occasional staffer accepting training and then moving on; but in 38 years, it has never happened in my office. In my experience, well-trained employees will stay. Education fosters loyalty. Employees who know you care enough about them to advance their skills will sense that they have a stake in the practice, and thus will be less likely to want to leave. Furthermore, continuing education will always be cheaper than training new employees from scratch.
In any case, everyone will benefit from a well-trained staff – you, your employees, your practice, and most importantly your patients.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Study: Cardiac biomarkers predicted CV events in CAP
in a recently conducted study.
These biomarkers were also used to predict late cardiovascular events at day 30 of community-acquired pneumonia (CAP) in patients who did not have a history of cardiovascular disease, according to Rosario Menéndez, MD, from the Hospital Universitario y Politécnico La Fe and Instituto de Investigación Sanitaria La Fe in Valencia, Spain, and colleagues.
“Some patients have still high levels of inflammatory and cardiac biomarkers at 30 days, when they are usually referred to primary care without receiving any specific additional recommendations,” Dr. Menéndez and colleagues wrote in CHEST. “Our results suggest that a change in usual practice is needed to reduce current and further cardiovascular CAP complications.”
Dr. Menéndez and colleagues prospectively followed 730 patients for 1 year who were hospitalized for CAP, measuring the cardiac biomarkers proadrenomedullin (proADM), pro b-type natriuretic peptide (proBNP), proendothelin-1, and troponin T, and the inflammatory biomarkers interleukin 6 (IL-6), C-reactive protein (CRP), and procalcitonin (PCT). The researchers also collected data on age, gender, smoking status, and vaccination history, as well as whether patients had any cardiac, renal, pulmonary, neurological or diabetes-related comorbidities.
Overall, 95 patients experienced early cardiovascular events, 67 patients had long-term cardiovascular events, and 20 patients experienced both early and late events. In hospital, the mortality rate was 4.7%; the 30-day mortality rate was 5.3%, and the 1-year mortality rate was 9.9%.
With regard to biomarkers, patients who experienced both early and late cardiovascular events had significantly higher initial levels of proADM, proendothelin-1, troponin, proBNP, and IL-6. Patients who experienced later events had consistent levels of these biomarkers until day 30, except for a decrease at day 4 or day 5.
After adjustment for age, sepsis, previous cardiac disease, and a partial pressure of oxygen in the alveoli to fractional inspired oxygen ratio (PaO2/FiO2) of less than 250mm Hg, cardiac biomarkers proendothelin-1 (odds ratio, 2.25; 95% confidence interval, 1.34-3.79), proADM (OR, 2.53; 95% CI, 1.53-4.20), proBNP (OR, 2.67; 95% CI, 1.59-4.49), and troponin T (OR, 2.70; 95% CI, 1.62-4.49) significantly predicted early cardiovascular events, while proendothelin-1 (OR, 3.13; 95% CI, 1.41-7.80), proADM (2.29; 95% CI, 1.01-5.19) and proBNP (OR, 2.34; 95% CI, 1.01-5.56) significantly predicted late cardiovascular events. For day 30 results, when researchers added IL-6 levels to proendothelin-1, the odds ratio for late events increased to 3.53, and when they added IL-6 levels to proADM, the odds ratio increased to 2.80.
Researchers noted the limitations of the study included that they did not analyze cardiac biomarkers to predict specific cardiovascular events, did not identify the cause for mortality at 1 year in most patients, and did not include a control group.
This study was supported in part by funding from Instituto de Salud Carlos III, Sociedad Española de Neumología y Cirugía Torácica, and the Center for Biomedical Research Network in Respiratory Diseases. The authors reported no relevant conflicts of interest.
SOURCE: Menéndez R et al. Chest. 2019 Aug 2. doi: 10.1016/j.chest.2019.06.040.
in a recently conducted study.
These biomarkers were also used to predict late cardiovascular events at day 30 of community-acquired pneumonia (CAP) in patients who did not have a history of cardiovascular disease, according to Rosario Menéndez, MD, from the Hospital Universitario y Politécnico La Fe and Instituto de Investigación Sanitaria La Fe in Valencia, Spain, and colleagues.
“Some patients have still high levels of inflammatory and cardiac biomarkers at 30 days, when they are usually referred to primary care without receiving any specific additional recommendations,” Dr. Menéndez and colleagues wrote in CHEST. “Our results suggest that a change in usual practice is needed to reduce current and further cardiovascular CAP complications.”
Dr. Menéndez and colleagues prospectively followed 730 patients for 1 year who were hospitalized for CAP, measuring the cardiac biomarkers proadrenomedullin (proADM), pro b-type natriuretic peptide (proBNP), proendothelin-1, and troponin T, and the inflammatory biomarkers interleukin 6 (IL-6), C-reactive protein (CRP), and procalcitonin (PCT). The researchers also collected data on age, gender, smoking status, and vaccination history, as well as whether patients had any cardiac, renal, pulmonary, neurological or diabetes-related comorbidities.
Overall, 95 patients experienced early cardiovascular events, 67 patients had long-term cardiovascular events, and 20 patients experienced both early and late events. In hospital, the mortality rate was 4.7%; the 30-day mortality rate was 5.3%, and the 1-year mortality rate was 9.9%.
With regard to biomarkers, patients who experienced both early and late cardiovascular events had significantly higher initial levels of proADM, proendothelin-1, troponin, proBNP, and IL-6. Patients who experienced later events had consistent levels of these biomarkers until day 30, except for a decrease at day 4 or day 5.
After adjustment for age, sepsis, previous cardiac disease, and a partial pressure of oxygen in the alveoli to fractional inspired oxygen ratio (PaO2/FiO2) of less than 250mm Hg, cardiac biomarkers proendothelin-1 (odds ratio, 2.25; 95% confidence interval, 1.34-3.79), proADM (OR, 2.53; 95% CI, 1.53-4.20), proBNP (OR, 2.67; 95% CI, 1.59-4.49), and troponin T (OR, 2.70; 95% CI, 1.62-4.49) significantly predicted early cardiovascular events, while proendothelin-1 (OR, 3.13; 95% CI, 1.41-7.80), proADM (2.29; 95% CI, 1.01-5.19) and proBNP (OR, 2.34; 95% CI, 1.01-5.56) significantly predicted late cardiovascular events. For day 30 results, when researchers added IL-6 levels to proendothelin-1, the odds ratio for late events increased to 3.53, and when they added IL-6 levels to proADM, the odds ratio increased to 2.80.
Researchers noted the limitations of the study included that they did not analyze cardiac biomarkers to predict specific cardiovascular events, did not identify the cause for mortality at 1 year in most patients, and did not include a control group.
This study was supported in part by funding from Instituto de Salud Carlos III, Sociedad Española de Neumología y Cirugía Torácica, and the Center for Biomedical Research Network in Respiratory Diseases. The authors reported no relevant conflicts of interest.
SOURCE: Menéndez R et al. Chest. 2019 Aug 2. doi: 10.1016/j.chest.2019.06.040.
in a recently conducted study.
These biomarkers were also used to predict late cardiovascular events at day 30 of community-acquired pneumonia (CAP) in patients who did not have a history of cardiovascular disease, according to Rosario Menéndez, MD, from the Hospital Universitario y Politécnico La Fe and Instituto de Investigación Sanitaria La Fe in Valencia, Spain, and colleagues.
“Some patients have still high levels of inflammatory and cardiac biomarkers at 30 days, when they are usually referred to primary care without receiving any specific additional recommendations,” Dr. Menéndez and colleagues wrote in CHEST. “Our results suggest that a change in usual practice is needed to reduce current and further cardiovascular CAP complications.”
Dr. Menéndez and colleagues prospectively followed 730 patients for 1 year who were hospitalized for CAP, measuring the cardiac biomarkers proadrenomedullin (proADM), pro b-type natriuretic peptide (proBNP), proendothelin-1, and troponin T, and the inflammatory biomarkers interleukin 6 (IL-6), C-reactive protein (CRP), and procalcitonin (PCT). The researchers also collected data on age, gender, smoking status, and vaccination history, as well as whether patients had any cardiac, renal, pulmonary, neurological or diabetes-related comorbidities.
Overall, 95 patients experienced early cardiovascular events, 67 patients had long-term cardiovascular events, and 20 patients experienced both early and late events. In hospital, the mortality rate was 4.7%; the 30-day mortality rate was 5.3%, and the 1-year mortality rate was 9.9%.
With regard to biomarkers, patients who experienced both early and late cardiovascular events had significantly higher initial levels of proADM, proendothelin-1, troponin, proBNP, and IL-6. Patients who experienced later events had consistent levels of these biomarkers until day 30, except for a decrease at day 4 or day 5.
After adjustment for age, sepsis, previous cardiac disease, and a partial pressure of oxygen in the alveoli to fractional inspired oxygen ratio (PaO2/FiO2) of less than 250mm Hg, cardiac biomarkers proendothelin-1 (odds ratio, 2.25; 95% confidence interval, 1.34-3.79), proADM (OR, 2.53; 95% CI, 1.53-4.20), proBNP (OR, 2.67; 95% CI, 1.59-4.49), and troponin T (OR, 2.70; 95% CI, 1.62-4.49) significantly predicted early cardiovascular events, while proendothelin-1 (OR, 3.13; 95% CI, 1.41-7.80), proADM (2.29; 95% CI, 1.01-5.19) and proBNP (OR, 2.34; 95% CI, 1.01-5.56) significantly predicted late cardiovascular events. For day 30 results, when researchers added IL-6 levels to proendothelin-1, the odds ratio for late events increased to 3.53, and when they added IL-6 levels to proADM, the odds ratio increased to 2.80.
Researchers noted the limitations of the study included that they did not analyze cardiac biomarkers to predict specific cardiovascular events, did not identify the cause for mortality at 1 year in most patients, and did not include a control group.
This study was supported in part by funding from Instituto de Salud Carlos III, Sociedad Española de Neumología y Cirugía Torácica, and the Center for Biomedical Research Network in Respiratory Diseases. The authors reported no relevant conflicts of interest.
SOURCE: Menéndez R et al. Chest. 2019 Aug 2. doi: 10.1016/j.chest.2019.06.040.
FROM CHEST
Lasmiditan is associated with driving impairment
Philadelphia – according to research presented at the annual meeting of the American Headache Society. This impairment coincides with the time of peak drug concentration and is resolved by 8 hours after dosing.
Lasmiditan, a 5-HT1F receptor agonist, is under regulatory review as an acute treatment of migraine in adults. In two phase 3 trials, a significant proportion of participants who received the treatment were pain-free at 2 hours and free of their most bothersome symptom at 2 hours, compared with controls. The most common treatment-emergent adverse events (dizziness, paresthesia, somnolence, fatigue, and hypoaesthesia) reflected the drug’s penetration of the CNS. Because CNS-related adverse events could affect a patient’s ability to drive, the effects of lasmiditan on simulated driving were studied, consistent with regulatory guidance.
Two studies in healthy participants
Eric Pearlman, MD, PhD, senior medical director for neuroscience, U.S. Medical Affairs, at Eli Lilly, and colleagues conducted two simulated driving studies with crossover designs. In the first study, the researchers randomized 90 healthy subjects (mean age, 34.9 years) to 50 mg, 100 mg, or 200 mg of lasmiditan; 1 mg of alprazolam (an active control); or placebo. After appropriate washout periods, participants received each treatment in random order. At 1.5 hours after each treatment, participants underwent a driving assessment using a driving simulator.
In the second study, Dr. Pearlman and colleagues randomized 68 healthy subjects (mean age, 32.8 years) to 100 mg or 200 mg of lasmiditan, 50 mg of diphenhydramine (an active control), or placebo. Participants underwent driving assessments at 8, 12, and 24 hours after baseline. Participants randomized to lasmiditan received treatment at baseline, but participants randomized to diphenhydramine received treatment 2 hours before each driving assessment. The diphenhydramine arm was intended to test the sensitivity of the driving assessment to impairment, as was the alprazolam arm in the first study.
During the driving assessments, participants were asked to maintain a speed of 100 km/h and to stay in the middle of the lane. The simulated road included gentle curves and hills, and oncoming traffic appeared occasionally. Participants also completed a secondary attention task, mimicking real-world conditions. Each assessment took about 1 hour. The primary endpoint was the standard deviation of lateral position (SDLP), which is known colloquially as weaving. The investigators defined noninferiority to placebo as an SDLP of 4.4 cm or less.
Participants reported that they could drive safely
In the first study, Dr. Pearlman and colleagues reported a dose-related increase in SDLP at 1.5 hours post treatment. All three doses of lasmiditan were inferior to placebo, in terms of their effect on SDLP. In the second study, both doses of lasmiditan were noninferior to placebo at 8 hours, 12 hours, and 24 hours. In both studies, the positive control confirmed the assay’s sensitivity to driving impairment. Secondary endpoints in the second study did not indicate an association between lasmiditan and clinically meaningful driving impairment at 8, 12, and 24 hours after dosing.
Single oral doses of lasmiditan were absorbed rapidly. The median time to peak concentration was approximately 2 hours, and the mean elimination half-life was about 4.25 hours. Exposure to lasmiditan was approximately dose proportional.
Before each driving assessment, investigators asked participants, “Do you feel safe to drive?” Depending on the dose, 55%-80% of participants responded affirmatively, but the majority of participants had clinically meaningful changes in SDLP. “This [result] is consistent with the FDA guidance in the literature that subject perception of safety to drive is faulty and supports the need for formal driving assessments,” said Dr. Pearlman.
Dizziness, somnolence, and headache were the most common adverse events in the study, and this result was similar to those of the phase 3 trials. Most of the adverse events were of mild to moderate severity.
Questions for further study
Among the questions that future research could address is whether the lasmiditan-related effects seen in these studies in healthy subjects are similar to those in patients with migraine when lasmiditan is taken to treat a migraine attack, said Dr. Pearlman. Another open question is whether migraine has ictal and interictal effects on driving performance.
Eli Lilly, which has developed lasmiditan, sponsored the studies. Dr. Pearlman and several of coinvestigators are employees of the company.
SOURCE: Pearlman E et al. AHS 2019, Abstract IOR06.
Philadelphia – according to research presented at the annual meeting of the American Headache Society. This impairment coincides with the time of peak drug concentration and is resolved by 8 hours after dosing.
Lasmiditan, a 5-HT1F receptor agonist, is under regulatory review as an acute treatment of migraine in adults. In two phase 3 trials, a significant proportion of participants who received the treatment were pain-free at 2 hours and free of their most bothersome symptom at 2 hours, compared with controls. The most common treatment-emergent adverse events (dizziness, paresthesia, somnolence, fatigue, and hypoaesthesia) reflected the drug’s penetration of the CNS. Because CNS-related adverse events could affect a patient’s ability to drive, the effects of lasmiditan on simulated driving were studied, consistent with regulatory guidance.
Two studies in healthy participants
Eric Pearlman, MD, PhD, senior medical director for neuroscience, U.S. Medical Affairs, at Eli Lilly, and colleagues conducted two simulated driving studies with crossover designs. In the first study, the researchers randomized 90 healthy subjects (mean age, 34.9 years) to 50 mg, 100 mg, or 200 mg of lasmiditan; 1 mg of alprazolam (an active control); or placebo. After appropriate washout periods, participants received each treatment in random order. At 1.5 hours after each treatment, participants underwent a driving assessment using a driving simulator.
In the second study, Dr. Pearlman and colleagues randomized 68 healthy subjects (mean age, 32.8 years) to 100 mg or 200 mg of lasmiditan, 50 mg of diphenhydramine (an active control), or placebo. Participants underwent driving assessments at 8, 12, and 24 hours after baseline. Participants randomized to lasmiditan received treatment at baseline, but participants randomized to diphenhydramine received treatment 2 hours before each driving assessment. The diphenhydramine arm was intended to test the sensitivity of the driving assessment to impairment, as was the alprazolam arm in the first study.
During the driving assessments, participants were asked to maintain a speed of 100 km/h and to stay in the middle of the lane. The simulated road included gentle curves and hills, and oncoming traffic appeared occasionally. Participants also completed a secondary attention task, mimicking real-world conditions. Each assessment took about 1 hour. The primary endpoint was the standard deviation of lateral position (SDLP), which is known colloquially as weaving. The investigators defined noninferiority to placebo as an SDLP of 4.4 cm or less.
Participants reported that they could drive safely
In the first study, Dr. Pearlman and colleagues reported a dose-related increase in SDLP at 1.5 hours post treatment. All three doses of lasmiditan were inferior to placebo, in terms of their effect on SDLP. In the second study, both doses of lasmiditan were noninferior to placebo at 8 hours, 12 hours, and 24 hours. In both studies, the positive control confirmed the assay’s sensitivity to driving impairment. Secondary endpoints in the second study did not indicate an association between lasmiditan and clinically meaningful driving impairment at 8, 12, and 24 hours after dosing.
Single oral doses of lasmiditan were absorbed rapidly. The median time to peak concentration was approximately 2 hours, and the mean elimination half-life was about 4.25 hours. Exposure to lasmiditan was approximately dose proportional.
Before each driving assessment, investigators asked participants, “Do you feel safe to drive?” Depending on the dose, 55%-80% of participants responded affirmatively, but the majority of participants had clinically meaningful changes in SDLP. “This [result] is consistent with the FDA guidance in the literature that subject perception of safety to drive is faulty and supports the need for formal driving assessments,” said Dr. Pearlman.
Dizziness, somnolence, and headache were the most common adverse events in the study, and this result was similar to those of the phase 3 trials. Most of the adverse events were of mild to moderate severity.
Questions for further study
Among the questions that future research could address is whether the lasmiditan-related effects seen in these studies in healthy subjects are similar to those in patients with migraine when lasmiditan is taken to treat a migraine attack, said Dr. Pearlman. Another open question is whether migraine has ictal and interictal effects on driving performance.
Eli Lilly, which has developed lasmiditan, sponsored the studies. Dr. Pearlman and several of coinvestigators are employees of the company.
SOURCE: Pearlman E et al. AHS 2019, Abstract IOR06.
Philadelphia – according to research presented at the annual meeting of the American Headache Society. This impairment coincides with the time of peak drug concentration and is resolved by 8 hours after dosing.
Lasmiditan, a 5-HT1F receptor agonist, is under regulatory review as an acute treatment of migraine in adults. In two phase 3 trials, a significant proportion of participants who received the treatment were pain-free at 2 hours and free of their most bothersome symptom at 2 hours, compared with controls. The most common treatment-emergent adverse events (dizziness, paresthesia, somnolence, fatigue, and hypoaesthesia) reflected the drug’s penetration of the CNS. Because CNS-related adverse events could affect a patient’s ability to drive, the effects of lasmiditan on simulated driving were studied, consistent with regulatory guidance.
Two studies in healthy participants
Eric Pearlman, MD, PhD, senior medical director for neuroscience, U.S. Medical Affairs, at Eli Lilly, and colleagues conducted two simulated driving studies with crossover designs. In the first study, the researchers randomized 90 healthy subjects (mean age, 34.9 years) to 50 mg, 100 mg, or 200 mg of lasmiditan; 1 mg of alprazolam (an active control); or placebo. After appropriate washout periods, participants received each treatment in random order. At 1.5 hours after each treatment, participants underwent a driving assessment using a driving simulator.
In the second study, Dr. Pearlman and colleagues randomized 68 healthy subjects (mean age, 32.8 years) to 100 mg or 200 mg of lasmiditan, 50 mg of diphenhydramine (an active control), or placebo. Participants underwent driving assessments at 8, 12, and 24 hours after baseline. Participants randomized to lasmiditan received treatment at baseline, but participants randomized to diphenhydramine received treatment 2 hours before each driving assessment. The diphenhydramine arm was intended to test the sensitivity of the driving assessment to impairment, as was the alprazolam arm in the first study.
During the driving assessments, participants were asked to maintain a speed of 100 km/h and to stay in the middle of the lane. The simulated road included gentle curves and hills, and oncoming traffic appeared occasionally. Participants also completed a secondary attention task, mimicking real-world conditions. Each assessment took about 1 hour. The primary endpoint was the standard deviation of lateral position (SDLP), which is known colloquially as weaving. The investigators defined noninferiority to placebo as an SDLP of 4.4 cm or less.
Participants reported that they could drive safely
In the first study, Dr. Pearlman and colleagues reported a dose-related increase in SDLP at 1.5 hours post treatment. All three doses of lasmiditan were inferior to placebo, in terms of their effect on SDLP. In the second study, both doses of lasmiditan were noninferior to placebo at 8 hours, 12 hours, and 24 hours. In both studies, the positive control confirmed the assay’s sensitivity to driving impairment. Secondary endpoints in the second study did not indicate an association between lasmiditan and clinically meaningful driving impairment at 8, 12, and 24 hours after dosing.
Single oral doses of lasmiditan were absorbed rapidly. The median time to peak concentration was approximately 2 hours, and the mean elimination half-life was about 4.25 hours. Exposure to lasmiditan was approximately dose proportional.
Before each driving assessment, investigators asked participants, “Do you feel safe to drive?” Depending on the dose, 55%-80% of participants responded affirmatively, but the majority of participants had clinically meaningful changes in SDLP. “This [result] is consistent with the FDA guidance in the literature that subject perception of safety to drive is faulty and supports the need for formal driving assessments,” said Dr. Pearlman.
Dizziness, somnolence, and headache were the most common adverse events in the study, and this result was similar to those of the phase 3 trials. Most of the adverse events were of mild to moderate severity.
Questions for further study
Among the questions that future research could address is whether the lasmiditan-related effects seen in these studies in healthy subjects are similar to those in patients with migraine when lasmiditan is taken to treat a migraine attack, said Dr. Pearlman. Another open question is whether migraine has ictal and interictal effects on driving performance.
Eli Lilly, which has developed lasmiditan, sponsored the studies. Dr. Pearlman and several of coinvestigators are employees of the company.
SOURCE: Pearlman E et al. AHS 2019, Abstract IOR06.
REPORTING FROM AHS 2019