User login
Upper and lower gastroenterology – the state of the art
In the upper GI section of the Postgraduate course program, Ikuo Hirano, MD, educated us on the refractory patient with eosinophilic esophagitis, reinforcing the need for chronic maintenance treatment and the complementary role of dilation. Gregory Ginsberg, MD, elucidated the specific strategies needed for gastric polyps with advice on which to leave and which to resect. Sachin Wani, MD, carefully outlined the changing landscape of Barrett’s esophagus with emphasis on our move to ablate rather than observe low-grade dysplasia. In the difficult area of treating gastroparesis, Linda Nguyen, MD, acquainted us with some of the newer medications for this disorder and discussed the emerging role of endoscopic pyloromyotomy. Michael Camilleri, MD, delivered a thorough analysis on the concept of leaky gut with data-driven recommendations on testing and the lack of adequate treatment. Finally, William Chey, MD, gave perspective to diagnosis and treatment of small-bowel bacterial overgrowth, particularly with its role in irritable bowel syndrome.
In the lower GI section of the course, Sunanda Kane, MD, gave a wonderful overview the present and emerging biologics for treatment of inflammatory bowel disease (IBD). David Rubin, MD, shared his expertise and vast experience for best management of ulcerative colitis while Edward Loftus Jr., MD, discussed the fact and fiction of diet-based therapy in IBD. This was followed by a timely lecture by Christina Ha, MD, on the need to think well outside the GI tract in IBD, discussing infections, cancers, and vaccinations in patients with IBD. The IBD section finished with an erudite and timely lecture by Marla Dubinsky, MD, evaluating the controversy over use of biosimilars in our clinical practice. The remainder of the lower GI section started with AGA President David Lieberman, MD, analyzing recent data on the need to move the colonic cancer screening age to 45 years, particularly in African Americans. Following this was a timely talk by Xavie Llor, MD, PhD, on when to suspect and how to test for the expanding definition of Lynch syndrome. Lin Chang, MD, delivered the penultimate clinical lecture on management of irritable bowel syndrome based on her many years of clinical expertise in this area. Finally, Gail Hecht, MD, AGAF, a former AGA president, summarized the exciting world of microbiome research from the recent annual Gut Microbiota for Health World Summit. All in all it was considered one of the best AGA Postgraduate courses by many and we look forward to even greater improvements for 2020.
This is a summary provided by the moderator of one of the AGA Postgraduate Course sessions held at DDW 2019. Dr. Katzka is professor of medicine and head of the Esophageal Interest Group at the Mayo Clinic in Rochester, Minn. He is on the advisory boards for Shire and Celgene.
In the upper GI section of the Postgraduate course program, Ikuo Hirano, MD, educated us on the refractory patient with eosinophilic esophagitis, reinforcing the need for chronic maintenance treatment and the complementary role of dilation. Gregory Ginsberg, MD, elucidated the specific strategies needed for gastric polyps with advice on which to leave and which to resect. Sachin Wani, MD, carefully outlined the changing landscape of Barrett’s esophagus with emphasis on our move to ablate rather than observe low-grade dysplasia. In the difficult area of treating gastroparesis, Linda Nguyen, MD, acquainted us with some of the newer medications for this disorder and discussed the emerging role of endoscopic pyloromyotomy. Michael Camilleri, MD, delivered a thorough analysis on the concept of leaky gut with data-driven recommendations on testing and the lack of adequate treatment. Finally, William Chey, MD, gave perspective to diagnosis and treatment of small-bowel bacterial overgrowth, particularly with its role in irritable bowel syndrome.
In the lower GI section of the course, Sunanda Kane, MD, gave a wonderful overview the present and emerging biologics for treatment of inflammatory bowel disease (IBD). David Rubin, MD, shared his expertise and vast experience for best management of ulcerative colitis while Edward Loftus Jr., MD, discussed the fact and fiction of diet-based therapy in IBD. This was followed by a timely lecture by Christina Ha, MD, on the need to think well outside the GI tract in IBD, discussing infections, cancers, and vaccinations in patients with IBD. The IBD section finished with an erudite and timely lecture by Marla Dubinsky, MD, evaluating the controversy over use of biosimilars in our clinical practice. The remainder of the lower GI section started with AGA President David Lieberman, MD, analyzing recent data on the need to move the colonic cancer screening age to 45 years, particularly in African Americans. Following this was a timely talk by Xavie Llor, MD, PhD, on when to suspect and how to test for the expanding definition of Lynch syndrome. Lin Chang, MD, delivered the penultimate clinical lecture on management of irritable bowel syndrome based on her many years of clinical expertise in this area. Finally, Gail Hecht, MD, AGAF, a former AGA president, summarized the exciting world of microbiome research from the recent annual Gut Microbiota for Health World Summit. All in all it was considered one of the best AGA Postgraduate courses by many and we look forward to even greater improvements for 2020.
This is a summary provided by the moderator of one of the AGA Postgraduate Course sessions held at DDW 2019. Dr. Katzka is professor of medicine and head of the Esophageal Interest Group at the Mayo Clinic in Rochester, Minn. He is on the advisory boards for Shire and Celgene.
In the upper GI section of the Postgraduate course program, Ikuo Hirano, MD, educated us on the refractory patient with eosinophilic esophagitis, reinforcing the need for chronic maintenance treatment and the complementary role of dilation. Gregory Ginsberg, MD, elucidated the specific strategies needed for gastric polyps with advice on which to leave and which to resect. Sachin Wani, MD, carefully outlined the changing landscape of Barrett’s esophagus with emphasis on our move to ablate rather than observe low-grade dysplasia. In the difficult area of treating gastroparesis, Linda Nguyen, MD, acquainted us with some of the newer medications for this disorder and discussed the emerging role of endoscopic pyloromyotomy. Michael Camilleri, MD, delivered a thorough analysis on the concept of leaky gut with data-driven recommendations on testing and the lack of adequate treatment. Finally, William Chey, MD, gave perspective to diagnosis and treatment of small-bowel bacterial overgrowth, particularly with its role in irritable bowel syndrome.
In the lower GI section of the course, Sunanda Kane, MD, gave a wonderful overview the present and emerging biologics for treatment of inflammatory bowel disease (IBD). David Rubin, MD, shared his expertise and vast experience for best management of ulcerative colitis while Edward Loftus Jr., MD, discussed the fact and fiction of diet-based therapy in IBD. This was followed by a timely lecture by Christina Ha, MD, on the need to think well outside the GI tract in IBD, discussing infections, cancers, and vaccinations in patients with IBD. The IBD section finished with an erudite and timely lecture by Marla Dubinsky, MD, evaluating the controversy over use of biosimilars in our clinical practice. The remainder of the lower GI section started with AGA President David Lieberman, MD, analyzing recent data on the need to move the colonic cancer screening age to 45 years, particularly in African Americans. Following this was a timely talk by Xavie Llor, MD, PhD, on when to suspect and how to test for the expanding definition of Lynch syndrome. Lin Chang, MD, delivered the penultimate clinical lecture on management of irritable bowel syndrome based on her many years of clinical expertise in this area. Finally, Gail Hecht, MD, AGAF, a former AGA president, summarized the exciting world of microbiome research from the recent annual Gut Microbiota for Health World Summit. All in all it was considered one of the best AGA Postgraduate courses by many and we look forward to even greater improvements for 2020.
This is a summary provided by the moderator of one of the AGA Postgraduate Course sessions held at DDW 2019. Dr. Katzka is professor of medicine and head of the Esophageal Interest Group at the Mayo Clinic in Rochester, Minn. He is on the advisory boards for Shire and Celgene.
Favorable Ebola results lead to drug trial termination, new focus
An investigational agent known as REGN-EB3 has met an early stopping criterion in the protocol of an Ebola therapeutics trial, according to a National Institutes of Health media advisory.
Preliminary results in 499 study participants showed that individuals receiving either of two treatments, REGN-EB3 or mAb114, had a greater chance of survival, compared with participants in the other two study arms.
The randomized, controlled Pamoja Tulinde Maisha (PALM) study, which began Nov. 20, 2018, was designed to evaluate four investigational agents (ZMapp, remdesivir, mAb114, and REGN-EB3) for the treatment of patients with Ebola virus disease in the Democratic Republic of the Congo (DRC) as part of the emergency response to an ongoing outbreak in the North Kivu and Ituri provinces.
As of Aug. 9, 2019, the trial had enrolled 681 patients at four Ebola treatment centers in live outbreak regions of the DRC, with the goal of enrolling 725 patients in total.
The trial investigators and study cosponsors accepted the recommendation for early termination, and staff at the trial sites in the DRC were promptly informed, according to the media advisory. Additional patient randomizations in the now-revised trial will be limited to treatment either with REGN-EB3 or mAb114. Patients randomized to the ZMapp or remdesivir arms in the last 10 days of the original trial will be given the option, at the discretion of their treating physician, to receive either of the two more effective treatments, according to the NIH.
“While the final analysis of the data can occur only after all the data are generated and collected (likely late September/early October 2019), the DSMB [Data and Safety Monitoring Board] and the study leadership felt the preliminary analysis of the existing data was compelling enough to recommend and implement these changes in the trial immediately. The complete results will be submitted for publication in the peer-reviewed medical literature as soon as possible,” the NIH stated.
The study is cosponsored and funded by the NIH, carried out by an international research consortium coordinated by the World Health Organization, and supported by four pharmaceutical companies (MappBio, Gilead, Regeneron, and Ridgeback Biotherapeutics).
An investigational agent known as REGN-EB3 has met an early stopping criterion in the protocol of an Ebola therapeutics trial, according to a National Institutes of Health media advisory.
Preliminary results in 499 study participants showed that individuals receiving either of two treatments, REGN-EB3 or mAb114, had a greater chance of survival, compared with participants in the other two study arms.
The randomized, controlled Pamoja Tulinde Maisha (PALM) study, which began Nov. 20, 2018, was designed to evaluate four investigational agents (ZMapp, remdesivir, mAb114, and REGN-EB3) for the treatment of patients with Ebola virus disease in the Democratic Republic of the Congo (DRC) as part of the emergency response to an ongoing outbreak in the North Kivu and Ituri provinces.
As of Aug. 9, 2019, the trial had enrolled 681 patients at four Ebola treatment centers in live outbreak regions of the DRC, with the goal of enrolling 725 patients in total.
The trial investigators and study cosponsors accepted the recommendation for early termination, and staff at the trial sites in the DRC were promptly informed, according to the media advisory. Additional patient randomizations in the now-revised trial will be limited to treatment either with REGN-EB3 or mAb114. Patients randomized to the ZMapp or remdesivir arms in the last 10 days of the original trial will be given the option, at the discretion of their treating physician, to receive either of the two more effective treatments, according to the NIH.
“While the final analysis of the data can occur only after all the data are generated and collected (likely late September/early October 2019), the DSMB [Data and Safety Monitoring Board] and the study leadership felt the preliminary analysis of the existing data was compelling enough to recommend and implement these changes in the trial immediately. The complete results will be submitted for publication in the peer-reviewed medical literature as soon as possible,” the NIH stated.
The study is cosponsored and funded by the NIH, carried out by an international research consortium coordinated by the World Health Organization, and supported by four pharmaceutical companies (MappBio, Gilead, Regeneron, and Ridgeback Biotherapeutics).
An investigational agent known as REGN-EB3 has met an early stopping criterion in the protocol of an Ebola therapeutics trial, according to a National Institutes of Health media advisory.
Preliminary results in 499 study participants showed that individuals receiving either of two treatments, REGN-EB3 or mAb114, had a greater chance of survival, compared with participants in the other two study arms.
The randomized, controlled Pamoja Tulinde Maisha (PALM) study, which began Nov. 20, 2018, was designed to evaluate four investigational agents (ZMapp, remdesivir, mAb114, and REGN-EB3) for the treatment of patients with Ebola virus disease in the Democratic Republic of the Congo (DRC) as part of the emergency response to an ongoing outbreak in the North Kivu and Ituri provinces.
As of Aug. 9, 2019, the trial had enrolled 681 patients at four Ebola treatment centers in live outbreak regions of the DRC, with the goal of enrolling 725 patients in total.
The trial investigators and study cosponsors accepted the recommendation for early termination, and staff at the trial sites in the DRC were promptly informed, according to the media advisory. Additional patient randomizations in the now-revised trial will be limited to treatment either with REGN-EB3 or mAb114. Patients randomized to the ZMapp or remdesivir arms in the last 10 days of the original trial will be given the option, at the discretion of their treating physician, to receive either of the two more effective treatments, according to the NIH.
“While the final analysis of the data can occur only after all the data are generated and collected (likely late September/early October 2019), the DSMB [Data and Safety Monitoring Board] and the study leadership felt the preliminary analysis of the existing data was compelling enough to recommend and implement these changes in the trial immediately. The complete results will be submitted for publication in the peer-reviewed medical literature as soon as possible,” the NIH stated.
The study is cosponsored and funded by the NIH, carried out by an international research consortium coordinated by the World Health Organization, and supported by four pharmaceutical companies (MappBio, Gilead, Regeneron, and Ridgeback Biotherapeutics).
Women underrepresented as oncology trial corresponding authors
Fewer than one in five oncologic phase 3 randomized controlled trials (RCTs) had female corresponding authors, but the proportion of women in this authorship role appears to be gradually increasing, investigators report.
“Through identification of the factors associated with gender disparities in RCT leadership, we hope that the academic oncology community will work to better understand and address the underlying reasons for such imbalances,” wrote Ethan B. Ludmir, MD, of the University of Texas MD Anderson Cancer Center, Houston, and associates. The report is in JAMA Oncology.
The authors searched ClinicalTrials.gov in late 2017 for all oncologic phase 3 RCTs. Of the 1,239 they initially turned up, the authors narrowed them down to the 598 that used multiple arms to test a therapeutic intervention, underwent peer review, and published results of primary endpoints. Among the trials, all published between 2003 and 2018, 17.9% had female corresponding authors.
Industry-funded trials, which comprised 77.8% of the sample, had half as many female corresponding authors (14.4%) as those not funded by industry (30.1%) (P less than .001), “possibly reflecting gender biases that are enhanced in the context of industry relationships with academic medicine,” the authors wrote. The opposite trend appeared in cooperative group trials, a quarter of which (25.9%) had female corresponding authors, compared with 14.3% of noncooperative trials (P = .001).
Trials for breast cancer and head and neck cancer were most likely to have female corresponding authors, while the trials with the lowest rates were those for gastrointestinal, genitourinary, and hematologic cancers (P less than .001). The researchers also found gender disparities in the type of intervention tested: Radiotherapy and supportive care studies were more likely to have female corresponding authors, yet none of the surgical trials had any (P less than .001).
In addition, female corresponding authorship was more likely when the institutions were based in the United States (n = 329) than when they were overseas (P = .001). Women were corresponding authors in 22.5% of U.S. studies and 20% of Canadian studies but only 12% of European trials and 2.3% of Asian trials (P = .001).
Within the United States, more than a third of studies from institutions in the Southeast had female corresponding authors (34.1%), followed by those in the Midwest (27.5%) and West (25.9%). Southwestern institutions were least likely to have female corresponding authors (8.7%). Approximately twice as many studies came from Northeastern institutions as from other regions (n = 112), but only 18.8% of these had female corresponding authors (P = .03).
The frequency of female corresponding authors has been increasing, however: The authors calculated a 1.2% increase each year, “echoing data showing an approximate 1.0% annual increase in the number of female academic hematologist-oncologists,” they noted. “However, the absolute female corresponding author rate for these trials is still lower than the percentage of female academic oncologists in this general study period, ranging from 27% in 2000 to 39% in 2015.”
SOURCE: Ludmir EB et al. JAMA Oncology. 8 Aug 2019. doi: 10.1001/jamaoncol.2019.2196.
Fewer than one in five oncologic phase 3 randomized controlled trials (RCTs) had female corresponding authors, but the proportion of women in this authorship role appears to be gradually increasing, investigators report.
“Through identification of the factors associated with gender disparities in RCT leadership, we hope that the academic oncology community will work to better understand and address the underlying reasons for such imbalances,” wrote Ethan B. Ludmir, MD, of the University of Texas MD Anderson Cancer Center, Houston, and associates. The report is in JAMA Oncology.
The authors searched ClinicalTrials.gov in late 2017 for all oncologic phase 3 RCTs. Of the 1,239 they initially turned up, the authors narrowed them down to the 598 that used multiple arms to test a therapeutic intervention, underwent peer review, and published results of primary endpoints. Among the trials, all published between 2003 and 2018, 17.9% had female corresponding authors.
Industry-funded trials, which comprised 77.8% of the sample, had half as many female corresponding authors (14.4%) as those not funded by industry (30.1%) (P less than .001), “possibly reflecting gender biases that are enhanced in the context of industry relationships with academic medicine,” the authors wrote. The opposite trend appeared in cooperative group trials, a quarter of which (25.9%) had female corresponding authors, compared with 14.3% of noncooperative trials (P = .001).
Trials for breast cancer and head and neck cancer were most likely to have female corresponding authors, while the trials with the lowest rates were those for gastrointestinal, genitourinary, and hematologic cancers (P less than .001). The researchers also found gender disparities in the type of intervention tested: Radiotherapy and supportive care studies were more likely to have female corresponding authors, yet none of the surgical trials had any (P less than .001).
In addition, female corresponding authorship was more likely when the institutions were based in the United States (n = 329) than when they were overseas (P = .001). Women were corresponding authors in 22.5% of U.S. studies and 20% of Canadian studies but only 12% of European trials and 2.3% of Asian trials (P = .001).
Within the United States, more than a third of studies from institutions in the Southeast had female corresponding authors (34.1%), followed by those in the Midwest (27.5%) and West (25.9%). Southwestern institutions were least likely to have female corresponding authors (8.7%). Approximately twice as many studies came from Northeastern institutions as from other regions (n = 112), but only 18.8% of these had female corresponding authors (P = .03).
The frequency of female corresponding authors has been increasing, however: The authors calculated a 1.2% increase each year, “echoing data showing an approximate 1.0% annual increase in the number of female academic hematologist-oncologists,” they noted. “However, the absolute female corresponding author rate for these trials is still lower than the percentage of female academic oncologists in this general study period, ranging from 27% in 2000 to 39% in 2015.”
SOURCE: Ludmir EB et al. JAMA Oncology. 8 Aug 2019. doi: 10.1001/jamaoncol.2019.2196.
Fewer than one in five oncologic phase 3 randomized controlled trials (RCTs) had female corresponding authors, but the proportion of women in this authorship role appears to be gradually increasing, investigators report.
“Through identification of the factors associated with gender disparities in RCT leadership, we hope that the academic oncology community will work to better understand and address the underlying reasons for such imbalances,” wrote Ethan B. Ludmir, MD, of the University of Texas MD Anderson Cancer Center, Houston, and associates. The report is in JAMA Oncology.
The authors searched ClinicalTrials.gov in late 2017 for all oncologic phase 3 RCTs. Of the 1,239 they initially turned up, the authors narrowed them down to the 598 that used multiple arms to test a therapeutic intervention, underwent peer review, and published results of primary endpoints. Among the trials, all published between 2003 and 2018, 17.9% had female corresponding authors.
Industry-funded trials, which comprised 77.8% of the sample, had half as many female corresponding authors (14.4%) as those not funded by industry (30.1%) (P less than .001), “possibly reflecting gender biases that are enhanced in the context of industry relationships with academic medicine,” the authors wrote. The opposite trend appeared in cooperative group trials, a quarter of which (25.9%) had female corresponding authors, compared with 14.3% of noncooperative trials (P = .001).
Trials for breast cancer and head and neck cancer were most likely to have female corresponding authors, while the trials with the lowest rates were those for gastrointestinal, genitourinary, and hematologic cancers (P less than .001). The researchers also found gender disparities in the type of intervention tested: Radiotherapy and supportive care studies were more likely to have female corresponding authors, yet none of the surgical trials had any (P less than .001).
In addition, female corresponding authorship was more likely when the institutions were based in the United States (n = 329) than when they were overseas (P = .001). Women were corresponding authors in 22.5% of U.S. studies and 20% of Canadian studies but only 12% of European trials and 2.3% of Asian trials (P = .001).
Within the United States, more than a third of studies from institutions in the Southeast had female corresponding authors (34.1%), followed by those in the Midwest (27.5%) and West (25.9%). Southwestern institutions were least likely to have female corresponding authors (8.7%). Approximately twice as many studies came from Northeastern institutions as from other regions (n = 112), but only 18.8% of these had female corresponding authors (P = .03).
The frequency of female corresponding authors has been increasing, however: The authors calculated a 1.2% increase each year, “echoing data showing an approximate 1.0% annual increase in the number of female academic hematologist-oncologists,” they noted. “However, the absolute female corresponding author rate for these trials is still lower than the percentage of female academic oncologists in this general study period, ranging from 27% in 2000 to 39% in 2015.”
SOURCE: Ludmir EB et al. JAMA Oncology. 8 Aug 2019. doi: 10.1001/jamaoncol.2019.2196.
FROM JAMA ONCOLOGY
Algorithm boosts MACE prediction in patients with chest pain
Adding electrocardiogram findings and clinical assessment to high-sensitivity cardiac troponin measurements in patients presenting with chest pain could improve predictions of their risk of 30-day major adverse cardiac events, particularly unstable angina, research suggests.
Investigators reported outcomes of a prospective study involving 3,123 patients with suspected acute myocardial infarction. The findings are in the Journal of the American College of Cardiology.
The aim of the researchers was to validate an extended algorithm that combined the European Society of Cardiology’s high-sensitivity cardiac troponin measurement at presentation and after 1 hour (ESC hs-cTn 0/1 h algorithm) with clinical assessment and ECG findings to aid prediction of major adverse cardiac events (MACE) within 30 days.
The clinical assessment involved the treating ED physician’s use of a visual analog scale to assess the patient’s pretest probability for an acute coronary syndrome (ACS), with a score above 70% qualifying as high likelihood.
The researchers found that the ESC hs-cTn 0/1 h algorithm alone triaged significantly more patients toward rule-out for MACE than did the extended algorithm (60% vs. 45%, P less than .001). This resulted in 487 patients being reclassified toward “observe” by the extended algorithm, and among this group the 30-day MACE rate was 1.1%.
However, the 30-day MACE rates were similar in the two groups – 0.6% among those ruled out by the ESC hs-cTn 0/1 h algorithm alone and 0.4% in those ruled out by the extended algorithm – resulting in a similar negative predictive value.
“These estimates will help clinicians to appropriately manage patients triaged toward rule-out according to the ESC hs-cTnT 0/1 h algorithm, in whom either the [visual analog scale] for ACS or the ECG still suggests the presence of an ACS,” wrote Thomas Nestelberger, MD, of the Cardiovascular Research Institute Basel (Switzerland) at the University of Basel, and coinvestigators.
The ESC hs-cTn 0/1 h algorithm also ruled in fewer patients than did the extended algorithm (16% vs. 26%, P less than .001), giving it a higher positive predictive value.
When the researchers added unstable angina to the major adverse cardiac event outcome, they found the ESC hs-cTn 0/1 h algorithm had a lower negative predictive value and a higher negative likelihood ratio compared with the extended algorithm for patients ruled out, but a higher positive predictive value and positive likelihood ratio for patients ruled in.
“Our findings corroborate and extend previous research regarding the development and validation of algorithms for the safe and effective rule-out and rule-in of MACE in patients with symptoms suggestive of AMI,” the authors wrote.
This study was supported by the Swiss National Science Foundation, the Swiss Heart Foundation, the European Union, the Cardiovascular Research Foundation Basel, the University Hospital Basel, Abbott, Beckman Coulter, Biomerieux, BRAHMS, Roche, Nanosphere, Siemens, Ortho Diagnostics, and Singulex. Several authors reported grants and support from the pharmaceutical sector.
SOURCE: Nestelberger T et al. J Am Coll Cardiol. 2019 Aug 20. doi: 10.1016/j.jacc.2019.06.025.
In patients presenting at the emergency department with chest pain, it’s important not only to diagnose acute myocardial infarction, but also to predict short-term risk of cardiac events to help guide management. This thoughtful and comprehensive analysis is the largest study assessing the added value of clinical and ECG assessment to the prognostication by high-sensitivity cardiac troponin algorithms in patients evaluated for chest pain. It reinforces the accuracy of hs-cTn at presentation and after 1 hour (ESC hs-cTn 0/1 h) algorithms to predict AMI and 30-day AMI-related events.
It is important to note that if unstable angina had been included as a major adverse cardiac event, the study would have found that the extended algorithm performs better than the hs-cTn 0/1 h algorithm in the prediction of this endpoint.
Germán Cediel, MD, is from Hospital Universitari Germans Trias i Pujol in Spain, Alfredo Bardají, MD, is from the Joan XXIII University Hospital in Spain, and José A. Barrabés, MD, is from Vall d’Hebron University Hospital and Research Institute, Universitat Autònoma de Barcelona. The comments are adapted from an editorial (J Am Coll Cardiol. 2019 Aug 20. doi: 10.1016/j.jacc.2019.05.065). The authors declared support from Instituto de Salud Carlos III, Spain, cofinanced by the European Regional Development Fund, and declared consultancies and educational activities with the pharmaceutical sector.
In patients presenting at the emergency department with chest pain, it’s important not only to diagnose acute myocardial infarction, but also to predict short-term risk of cardiac events to help guide management. This thoughtful and comprehensive analysis is the largest study assessing the added value of clinical and ECG assessment to the prognostication by high-sensitivity cardiac troponin algorithms in patients evaluated for chest pain. It reinforces the accuracy of hs-cTn at presentation and after 1 hour (ESC hs-cTn 0/1 h) algorithms to predict AMI and 30-day AMI-related events.
It is important to note that if unstable angina had been included as a major adverse cardiac event, the study would have found that the extended algorithm performs better than the hs-cTn 0/1 h algorithm in the prediction of this endpoint.
Germán Cediel, MD, is from Hospital Universitari Germans Trias i Pujol in Spain, Alfredo Bardají, MD, is from the Joan XXIII University Hospital in Spain, and José A. Barrabés, MD, is from Vall d’Hebron University Hospital and Research Institute, Universitat Autònoma de Barcelona. The comments are adapted from an editorial (J Am Coll Cardiol. 2019 Aug 20. doi: 10.1016/j.jacc.2019.05.065). The authors declared support from Instituto de Salud Carlos III, Spain, cofinanced by the European Regional Development Fund, and declared consultancies and educational activities with the pharmaceutical sector.
In patients presenting at the emergency department with chest pain, it’s important not only to diagnose acute myocardial infarction, but also to predict short-term risk of cardiac events to help guide management. This thoughtful and comprehensive analysis is the largest study assessing the added value of clinical and ECG assessment to the prognostication by high-sensitivity cardiac troponin algorithms in patients evaluated for chest pain. It reinforces the accuracy of hs-cTn at presentation and after 1 hour (ESC hs-cTn 0/1 h) algorithms to predict AMI and 30-day AMI-related events.
It is important to note that if unstable angina had been included as a major adverse cardiac event, the study would have found that the extended algorithm performs better than the hs-cTn 0/1 h algorithm in the prediction of this endpoint.
Germán Cediel, MD, is from Hospital Universitari Germans Trias i Pujol in Spain, Alfredo Bardají, MD, is from the Joan XXIII University Hospital in Spain, and José A. Barrabés, MD, is from Vall d’Hebron University Hospital and Research Institute, Universitat Autònoma de Barcelona. The comments are adapted from an editorial (J Am Coll Cardiol. 2019 Aug 20. doi: 10.1016/j.jacc.2019.05.065). The authors declared support from Instituto de Salud Carlos III, Spain, cofinanced by the European Regional Development Fund, and declared consultancies and educational activities with the pharmaceutical sector.
Adding electrocardiogram findings and clinical assessment to high-sensitivity cardiac troponin measurements in patients presenting with chest pain could improve predictions of their risk of 30-day major adverse cardiac events, particularly unstable angina, research suggests.
Investigators reported outcomes of a prospective study involving 3,123 patients with suspected acute myocardial infarction. The findings are in the Journal of the American College of Cardiology.
The aim of the researchers was to validate an extended algorithm that combined the European Society of Cardiology’s high-sensitivity cardiac troponin measurement at presentation and after 1 hour (ESC hs-cTn 0/1 h algorithm) with clinical assessment and ECG findings to aid prediction of major adverse cardiac events (MACE) within 30 days.
The clinical assessment involved the treating ED physician’s use of a visual analog scale to assess the patient’s pretest probability for an acute coronary syndrome (ACS), with a score above 70% qualifying as high likelihood.
The researchers found that the ESC hs-cTn 0/1 h algorithm alone triaged significantly more patients toward rule-out for MACE than did the extended algorithm (60% vs. 45%, P less than .001). This resulted in 487 patients being reclassified toward “observe” by the extended algorithm, and among this group the 30-day MACE rate was 1.1%.
However, the 30-day MACE rates were similar in the two groups – 0.6% among those ruled out by the ESC hs-cTn 0/1 h algorithm alone and 0.4% in those ruled out by the extended algorithm – resulting in a similar negative predictive value.
“These estimates will help clinicians to appropriately manage patients triaged toward rule-out according to the ESC hs-cTnT 0/1 h algorithm, in whom either the [visual analog scale] for ACS or the ECG still suggests the presence of an ACS,” wrote Thomas Nestelberger, MD, of the Cardiovascular Research Institute Basel (Switzerland) at the University of Basel, and coinvestigators.
The ESC hs-cTn 0/1 h algorithm also ruled in fewer patients than did the extended algorithm (16% vs. 26%, P less than .001), giving it a higher positive predictive value.
When the researchers added unstable angina to the major adverse cardiac event outcome, they found the ESC hs-cTn 0/1 h algorithm had a lower negative predictive value and a higher negative likelihood ratio compared with the extended algorithm for patients ruled out, but a higher positive predictive value and positive likelihood ratio for patients ruled in.
“Our findings corroborate and extend previous research regarding the development and validation of algorithms for the safe and effective rule-out and rule-in of MACE in patients with symptoms suggestive of AMI,” the authors wrote.
This study was supported by the Swiss National Science Foundation, the Swiss Heart Foundation, the European Union, the Cardiovascular Research Foundation Basel, the University Hospital Basel, Abbott, Beckman Coulter, Biomerieux, BRAHMS, Roche, Nanosphere, Siemens, Ortho Diagnostics, and Singulex. Several authors reported grants and support from the pharmaceutical sector.
SOURCE: Nestelberger T et al. J Am Coll Cardiol. 2019 Aug 20. doi: 10.1016/j.jacc.2019.06.025.
Adding electrocardiogram findings and clinical assessment to high-sensitivity cardiac troponin measurements in patients presenting with chest pain could improve predictions of their risk of 30-day major adverse cardiac events, particularly unstable angina, research suggests.
Investigators reported outcomes of a prospective study involving 3,123 patients with suspected acute myocardial infarction. The findings are in the Journal of the American College of Cardiology.
The aim of the researchers was to validate an extended algorithm that combined the European Society of Cardiology’s high-sensitivity cardiac troponin measurement at presentation and after 1 hour (ESC hs-cTn 0/1 h algorithm) with clinical assessment and ECG findings to aid prediction of major adverse cardiac events (MACE) within 30 days.
The clinical assessment involved the treating ED physician’s use of a visual analog scale to assess the patient’s pretest probability for an acute coronary syndrome (ACS), with a score above 70% qualifying as high likelihood.
The researchers found that the ESC hs-cTn 0/1 h algorithm alone triaged significantly more patients toward rule-out for MACE than did the extended algorithm (60% vs. 45%, P less than .001). This resulted in 487 patients being reclassified toward “observe” by the extended algorithm, and among this group the 30-day MACE rate was 1.1%.
However, the 30-day MACE rates were similar in the two groups – 0.6% among those ruled out by the ESC hs-cTn 0/1 h algorithm alone and 0.4% in those ruled out by the extended algorithm – resulting in a similar negative predictive value.
“These estimates will help clinicians to appropriately manage patients triaged toward rule-out according to the ESC hs-cTnT 0/1 h algorithm, in whom either the [visual analog scale] for ACS or the ECG still suggests the presence of an ACS,” wrote Thomas Nestelberger, MD, of the Cardiovascular Research Institute Basel (Switzerland) at the University of Basel, and coinvestigators.
The ESC hs-cTn 0/1 h algorithm also ruled in fewer patients than did the extended algorithm (16% vs. 26%, P less than .001), giving it a higher positive predictive value.
When the researchers added unstable angina to the major adverse cardiac event outcome, they found the ESC hs-cTn 0/1 h algorithm had a lower negative predictive value and a higher negative likelihood ratio compared with the extended algorithm for patients ruled out, but a higher positive predictive value and positive likelihood ratio for patients ruled in.
“Our findings corroborate and extend previous research regarding the development and validation of algorithms for the safe and effective rule-out and rule-in of MACE in patients with symptoms suggestive of AMI,” the authors wrote.
This study was supported by the Swiss National Science Foundation, the Swiss Heart Foundation, the European Union, the Cardiovascular Research Foundation Basel, the University Hospital Basel, Abbott, Beckman Coulter, Biomerieux, BRAHMS, Roche, Nanosphere, Siemens, Ortho Diagnostics, and Singulex. Several authors reported grants and support from the pharmaceutical sector.
SOURCE: Nestelberger T et al. J Am Coll Cardiol. 2019 Aug 20. doi: 10.1016/j.jacc.2019.06.025.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point:
Major finding: High-sensitivity cardiac troponin measurements combined with ECG and clinical assessment can help rule out MACE and unstable angina.
Study details: A prospective study of 3,123 patients with suspected acute myocardial infarction.
Disclosures: This study was supported by the Swiss National Science Foundation, the Swiss Heart Foundation, the European Union, the Cardiovascular Research Foundation Basel, the University Hospital Basel, Abbott, Beckman Coulter, Biomerieux, BRAHMS, Roche, NanoSphere, Siemens, Ortho Diagnostics, and Singulex. Several authors reported grants and support from the pharmaceutical sector.
Source: Nestelberger T et al. J Am Coll Cardiol. 2019 Aug 20. doi: 10.1016/j.jacc.2019.06.025.
Neonatal epileptic syndromes are surprisingly common
BANGKOK – Katherine B. Howell, MD, reported at the International Epilepsy Congress.
“This is an important finding. It’s a considerably larger number than might have been expected and likely has two contributing factors. Neonatal seizures were previously not considered epilepsy, so many previous studies excluded neonates and the conditions were underrecognized. And our large number of ictal EEGs allowed identification of ictal activation, which is a feature of EIMFS [epilepsy of infancy with migrating focal seizures]. Without those ictal recordings, the diagnosis of EIMFS may not have been made,” according to Dr. Howell, a neurologist at the Royal Children’s Hospital and University of Melbourne.
She presented a population-based study of all infants born with severe epilepsies of infancy (SEI) during a 2-year period in the Australian state of Victoria, which is considered an ideal environment for epidemiologic studies because government-funded health care is available to all. SEI was defined as seizures beginning before age 18 months, occurring at a rate of at least one per day for 1 week or weekly for 1 month, refractory to adequate trials of at least two antiepileptic drugs, and accompanied by an epileptiform EEG abnormality. Her focus was on the electroclinical phenotypes of the affected children because of the high clinical utility of this information.
“Assigning an epileptic syndrome is highly useful for clinician-to-clinician communication of an infant’s phenotype. It guides investigation of etiology and possibly selection of optimal therapy, such as steroids in West syndrome. And it can inform prognosis,” Dr. Howell said at the congress sponsored by the International League Against Epilepsy.
She and her coinvestigators analyzed the detailed records of all 114 infants with SEI born during the study period. The incidence was 1 in 2,000 live births.
“Among infants with epilepsy, this patient group with SEI is most critical to better understand. Effective treatment is often not available, the seizure and developmental outcomes are frequently devastating, and the health burden massive,” the neurologist observed.
The full spectrum of SEI
With the help of ictal EEGs, home seizure recordings, MRI scans, and genomic testing, the investigators were able to classify more than 85% of the infants. About 64% had a prototypic syndrome at onset, such as West syndrome, which accounted for 33% of all SEI, or Dravet syndrome, which was diagnosed in 3%.
The prevalence of the prototypic neonatal and early infantile epileptic syndromes was notably higher than previously reported by others: EIMFS accounted for 9% of total SEI, early infantile epileptic encephalopathy (EIEE) for 7%, and early myoclonic encephalopathy (EME) for 2%. This translated to an incidence of 1 in 28,000 live births for EIEE, 1 in 111,000 for EME, and 1 in 22,500 for EIMFS.
“While neither EIEE nor EIMFS are common, these incidences are actually not that much lower than the reported incidence of Dravet syndrome,” the neurologist pointed out.
About 36% of SEI didn’t fit into any of the prototypic syndromes. However, more than half of this subgroup, or 19% of total SEI, were prototypic syndrome like, a designation Dr. Howell and her coworkers used for cases that possessed most but not all of the well-recognized features of a particular prototypic syndrome; for example, West syndrome–like seizures but without hypsarrhythmia. Whether these prototypic syndrome-like SEI have etiologies and outcomes similar to or distinct from the prototypic syndromes remains a topic for further study.
SEI etiologies
A total of 14 patients had SEI because of an acquired syndrome attributed to brain injury, 31 were because of brain malformation, 21 involved single gene disorders, 9 were of chromosomal etiology, and 7 had a metabolic cause.
The key finding with regard to etiology was the glaring difference between children with West syndrome, its variants, or unifocal epilepsies as compared with the rest of the SEI patients. Those with West syndrome, a West syndrome–like designation, or unifocal epilepsies most commonly had a structural etiology for their SEI. Indeed, of the 52 children with West syndrome or a variant, 10 had an acquired brain injury as their etiology and 17 had a brain malformation. And of the 12 patients with unifocal SEI, 1 had a brain injury and 9 had brain malformations.
In contrast, children with neonatal or early infantile epileptic syndromes had predominantly genetic rather than structural etiologies. Of the 20 children with EIEE, EIMFS, or EME, none had brain injury as the etiology, only 1 had a brain malformation, but 9 had a single gene or chromosomal etiology.
Outcomes
“The outcome data highlight the extreme severity of SEI and the imperative for novel treatments: 16% mortality overall, so one in six was deceased by age 2 years. The infants who died after the neonatal period all had profound delays, and almost all had ongoing seizures until their death. Most survivors also had developmental delay, with severity ranging from mild to moderate in 49% to severe/profound in 41%. Just 10 of 114 children had normal development,” Dr. Howell reported.
However, there was a notable difference in outcomes between the various syndromes, and this information is highly relevant prognostically. Of the 20 children with neonatal and early infantile epileptic syndromes, 11 died and the other 9 had profound developmental delay. In contrast, the outlook was far better for children with West syndrome, West syndrome–like variants, or focal epilepsies: Among 64 affected patients, there were just 2 deaths, normal development in 9 patients, mild to moderate developmental delay in 34, and severe/profound delay in 19.
Dr. Howell reported having no financial conflicts regarding this study, which was supported by governmental research grants.
SOURCE: Howell KB et al. IEC 2019, Abstract P053.
BANGKOK – Katherine B. Howell, MD, reported at the International Epilepsy Congress.
“This is an important finding. It’s a considerably larger number than might have been expected and likely has two contributing factors. Neonatal seizures were previously not considered epilepsy, so many previous studies excluded neonates and the conditions were underrecognized. And our large number of ictal EEGs allowed identification of ictal activation, which is a feature of EIMFS [epilepsy of infancy with migrating focal seizures]. Without those ictal recordings, the diagnosis of EIMFS may not have been made,” according to Dr. Howell, a neurologist at the Royal Children’s Hospital and University of Melbourne.
She presented a population-based study of all infants born with severe epilepsies of infancy (SEI) during a 2-year period in the Australian state of Victoria, which is considered an ideal environment for epidemiologic studies because government-funded health care is available to all. SEI was defined as seizures beginning before age 18 months, occurring at a rate of at least one per day for 1 week or weekly for 1 month, refractory to adequate trials of at least two antiepileptic drugs, and accompanied by an epileptiform EEG abnormality. Her focus was on the electroclinical phenotypes of the affected children because of the high clinical utility of this information.
“Assigning an epileptic syndrome is highly useful for clinician-to-clinician communication of an infant’s phenotype. It guides investigation of etiology and possibly selection of optimal therapy, such as steroids in West syndrome. And it can inform prognosis,” Dr. Howell said at the congress sponsored by the International League Against Epilepsy.
She and her coinvestigators analyzed the detailed records of all 114 infants with SEI born during the study period. The incidence was 1 in 2,000 live births.
“Among infants with epilepsy, this patient group with SEI is most critical to better understand. Effective treatment is often not available, the seizure and developmental outcomes are frequently devastating, and the health burden massive,” the neurologist observed.
The full spectrum of SEI
With the help of ictal EEGs, home seizure recordings, MRI scans, and genomic testing, the investigators were able to classify more than 85% of the infants. About 64% had a prototypic syndrome at onset, such as West syndrome, which accounted for 33% of all SEI, or Dravet syndrome, which was diagnosed in 3%.
The prevalence of the prototypic neonatal and early infantile epileptic syndromes was notably higher than previously reported by others: EIMFS accounted for 9% of total SEI, early infantile epileptic encephalopathy (EIEE) for 7%, and early myoclonic encephalopathy (EME) for 2%. This translated to an incidence of 1 in 28,000 live births for EIEE, 1 in 111,000 for EME, and 1 in 22,500 for EIMFS.
“While neither EIEE nor EIMFS are common, these incidences are actually not that much lower than the reported incidence of Dravet syndrome,” the neurologist pointed out.
About 36% of SEI didn’t fit into any of the prototypic syndromes. However, more than half of this subgroup, or 19% of total SEI, were prototypic syndrome like, a designation Dr. Howell and her coworkers used for cases that possessed most but not all of the well-recognized features of a particular prototypic syndrome; for example, West syndrome–like seizures but without hypsarrhythmia. Whether these prototypic syndrome-like SEI have etiologies and outcomes similar to or distinct from the prototypic syndromes remains a topic for further study.
SEI etiologies
A total of 14 patients had SEI because of an acquired syndrome attributed to brain injury, 31 were because of brain malformation, 21 involved single gene disorders, 9 were of chromosomal etiology, and 7 had a metabolic cause.
The key finding with regard to etiology was the glaring difference between children with West syndrome, its variants, or unifocal epilepsies as compared with the rest of the SEI patients. Those with West syndrome, a West syndrome–like designation, or unifocal epilepsies most commonly had a structural etiology for their SEI. Indeed, of the 52 children with West syndrome or a variant, 10 had an acquired brain injury as their etiology and 17 had a brain malformation. And of the 12 patients with unifocal SEI, 1 had a brain injury and 9 had brain malformations.
In contrast, children with neonatal or early infantile epileptic syndromes had predominantly genetic rather than structural etiologies. Of the 20 children with EIEE, EIMFS, or EME, none had brain injury as the etiology, only 1 had a brain malformation, but 9 had a single gene or chromosomal etiology.
Outcomes
“The outcome data highlight the extreme severity of SEI and the imperative for novel treatments: 16% mortality overall, so one in six was deceased by age 2 years. The infants who died after the neonatal period all had profound delays, and almost all had ongoing seizures until their death. Most survivors also had developmental delay, with severity ranging from mild to moderate in 49% to severe/profound in 41%. Just 10 of 114 children had normal development,” Dr. Howell reported.
However, there was a notable difference in outcomes between the various syndromes, and this information is highly relevant prognostically. Of the 20 children with neonatal and early infantile epileptic syndromes, 11 died and the other 9 had profound developmental delay. In contrast, the outlook was far better for children with West syndrome, West syndrome–like variants, or focal epilepsies: Among 64 affected patients, there were just 2 deaths, normal development in 9 patients, mild to moderate developmental delay in 34, and severe/profound delay in 19.
Dr. Howell reported having no financial conflicts regarding this study, which was supported by governmental research grants.
SOURCE: Howell KB et al. IEC 2019, Abstract P053.
BANGKOK – Katherine B. Howell, MD, reported at the International Epilepsy Congress.
“This is an important finding. It’s a considerably larger number than might have been expected and likely has two contributing factors. Neonatal seizures were previously not considered epilepsy, so many previous studies excluded neonates and the conditions were underrecognized. And our large number of ictal EEGs allowed identification of ictal activation, which is a feature of EIMFS [epilepsy of infancy with migrating focal seizures]. Without those ictal recordings, the diagnosis of EIMFS may not have been made,” according to Dr. Howell, a neurologist at the Royal Children’s Hospital and University of Melbourne.
She presented a population-based study of all infants born with severe epilepsies of infancy (SEI) during a 2-year period in the Australian state of Victoria, which is considered an ideal environment for epidemiologic studies because government-funded health care is available to all. SEI was defined as seizures beginning before age 18 months, occurring at a rate of at least one per day for 1 week or weekly for 1 month, refractory to adequate trials of at least two antiepileptic drugs, and accompanied by an epileptiform EEG abnormality. Her focus was on the electroclinical phenotypes of the affected children because of the high clinical utility of this information.
“Assigning an epileptic syndrome is highly useful for clinician-to-clinician communication of an infant’s phenotype. It guides investigation of etiology and possibly selection of optimal therapy, such as steroids in West syndrome. And it can inform prognosis,” Dr. Howell said at the congress sponsored by the International League Against Epilepsy.
She and her coinvestigators analyzed the detailed records of all 114 infants with SEI born during the study period. The incidence was 1 in 2,000 live births.
“Among infants with epilepsy, this patient group with SEI is most critical to better understand. Effective treatment is often not available, the seizure and developmental outcomes are frequently devastating, and the health burden massive,” the neurologist observed.
The full spectrum of SEI
With the help of ictal EEGs, home seizure recordings, MRI scans, and genomic testing, the investigators were able to classify more than 85% of the infants. About 64% had a prototypic syndrome at onset, such as West syndrome, which accounted for 33% of all SEI, or Dravet syndrome, which was diagnosed in 3%.
The prevalence of the prototypic neonatal and early infantile epileptic syndromes was notably higher than previously reported by others: EIMFS accounted for 9% of total SEI, early infantile epileptic encephalopathy (EIEE) for 7%, and early myoclonic encephalopathy (EME) for 2%. This translated to an incidence of 1 in 28,000 live births for EIEE, 1 in 111,000 for EME, and 1 in 22,500 for EIMFS.
“While neither EIEE nor EIMFS are common, these incidences are actually not that much lower than the reported incidence of Dravet syndrome,” the neurologist pointed out.
About 36% of SEI didn’t fit into any of the prototypic syndromes. However, more than half of this subgroup, or 19% of total SEI, were prototypic syndrome like, a designation Dr. Howell and her coworkers used for cases that possessed most but not all of the well-recognized features of a particular prototypic syndrome; for example, West syndrome–like seizures but without hypsarrhythmia. Whether these prototypic syndrome-like SEI have etiologies and outcomes similar to or distinct from the prototypic syndromes remains a topic for further study.
SEI etiologies
A total of 14 patients had SEI because of an acquired syndrome attributed to brain injury, 31 were because of brain malformation, 21 involved single gene disorders, 9 were of chromosomal etiology, and 7 had a metabolic cause.
The key finding with regard to etiology was the glaring difference between children with West syndrome, its variants, or unifocal epilepsies as compared with the rest of the SEI patients. Those with West syndrome, a West syndrome–like designation, or unifocal epilepsies most commonly had a structural etiology for their SEI. Indeed, of the 52 children with West syndrome or a variant, 10 had an acquired brain injury as their etiology and 17 had a brain malformation. And of the 12 patients with unifocal SEI, 1 had a brain injury and 9 had brain malformations.
In contrast, children with neonatal or early infantile epileptic syndromes had predominantly genetic rather than structural etiologies. Of the 20 children with EIEE, EIMFS, or EME, none had brain injury as the etiology, only 1 had a brain malformation, but 9 had a single gene or chromosomal etiology.
Outcomes
“The outcome data highlight the extreme severity of SEI and the imperative for novel treatments: 16% mortality overall, so one in six was deceased by age 2 years. The infants who died after the neonatal period all had profound delays, and almost all had ongoing seizures until their death. Most survivors also had developmental delay, with severity ranging from mild to moderate in 49% to severe/profound in 41%. Just 10 of 114 children had normal development,” Dr. Howell reported.
However, there was a notable difference in outcomes between the various syndromes, and this information is highly relevant prognostically. Of the 20 children with neonatal and early infantile epileptic syndromes, 11 died and the other 9 had profound developmental delay. In contrast, the outlook was far better for children with West syndrome, West syndrome–like variants, or focal epilepsies: Among 64 affected patients, there were just 2 deaths, normal development in 9 patients, mild to moderate developmental delay in 34, and severe/profound delay in 19.
Dr. Howell reported having no financial conflicts regarding this study, which was supported by governmental research grants.
SOURCE: Howell KB et al. IEC 2019, Abstract P053.
REPORTING FROM IEC 2019
Ibrutinib/rituximab effective, safe as frontline treatment for older patients with MCL
LUGANO, SWITZERLAND – The chemotherapy-free combination of ibrutinib (Imbruvica) and rituximab is highly effective as frontline therapy for older, transplant-ineligible patients with nonblastoid mantle cell lymphoma, according to investigators.
In a phase 2 study of patients with a median age of 71 years, 38 of 41 patients (93%) had an objective response, and the regimen was both safe and easy to administer, reported Preetesh Jain, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“The adverse event profile was generally favorable, with specific monitoring recommended for patients with cardiovascular comorbidities and a history of atrial fibrillation,” he said at the International Conference on Malignant Lymphoma.
The investigators enrolled 48 patients aged 65 years and older with previously untreated mantle cell lymphoma (MCL), of whom 41 were evaluable for the primary endpoints of overall response rate (ORR) and safety. The patients had good performance status and normal organ function, with the largest tumor size less than 10 cm. Patients with atrial fibrillation could participate, if the fibrillation was controlled. Patients with Ki-67 protein levels of 50% or greater and blastoid/pleomorphic histology were excluded.
Patients were treated with ibrutinib 560 mg orally daily for each 28-day cycle, with therapy continued until disease progression, or until therapy was stopped for any other reason. Patients also received intravenous rituximab 375 mg/m2 on days 1, 8, 15 and 22, plus or minus one day for cycle 1, on day 1 of cycles 3-8, and on day 1 of every other cycle for up to 2 years.
Of the 41 patients evaluable for response, 26 (64%) had a complete response (CR) and 12 (29%) had a partial response. Three additional patients had stable disease, for an objective response rate of 93%.
Of 34 patients with PET scans, all had negative scans. Of 37 patients evaluable for minimal residual disease (MRD) by flow cytometry, 21 (58%) were MRD negative.
Patients with low or intermediate Mantle Cell Lymphoma International Prognostic Index (MIPI) scores had a higher ORR (100% vs. 89% for patients with high MIPI scores), and patients with low Ki-67 levels had a higher response rate than that of patients with KI-67 of 30% or greater (80% vs. 87%).
Neither median 3-year progression-free survival nor median 3-year overall survival have been reached, with respective 3-year rates of 87% and 95%.
Four patients experienced disease progression at 4, 10, 13 and 33 months of treatment. Three of these patients had disease that had transformed to blastoid/pleomorphic variant, two had Ki-67 of 30% or greater, one had mutations in TP53, and one had FAT1 and SF3B1 mutations.
Two patients died after ibrutinib therapy, one who had discontinued therapy because of bleeding, and the other who died on treatment at 13 months from transformed disease. Both of these patients had high Ki-67 levels.
Grade 3 or 4 hematological adverse events were neutropenia in four patients, and thrombocytopenia in two patients. There were no cases of grade 3 or 4 anemia.
Grade 3 or 4 nonhematological adverse events were fatigue, myalgia, and atrial fibrillation in seven patients each, diarrhea in six patients, and petechiae/bleeding in three patients.
Patients will continue to be followed for late adverse events, secondary cancers, and relapses, and further studies on clonal evolution, mutation profiling, and MRD are ongoing and will be reported at a later date, Dr. Jain said.
The National Cancer Institute supported the study. Dr. Jain reported having no financial disclosures.
SOURCE: Jain P et al. 15-ICML. Abstract 011.
LUGANO, SWITZERLAND – The chemotherapy-free combination of ibrutinib (Imbruvica) and rituximab is highly effective as frontline therapy for older, transplant-ineligible patients with nonblastoid mantle cell lymphoma, according to investigators.
In a phase 2 study of patients with a median age of 71 years, 38 of 41 patients (93%) had an objective response, and the regimen was both safe and easy to administer, reported Preetesh Jain, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“The adverse event profile was generally favorable, with specific monitoring recommended for patients with cardiovascular comorbidities and a history of atrial fibrillation,” he said at the International Conference on Malignant Lymphoma.
The investigators enrolled 48 patients aged 65 years and older with previously untreated mantle cell lymphoma (MCL), of whom 41 were evaluable for the primary endpoints of overall response rate (ORR) and safety. The patients had good performance status and normal organ function, with the largest tumor size less than 10 cm. Patients with atrial fibrillation could participate, if the fibrillation was controlled. Patients with Ki-67 protein levels of 50% or greater and blastoid/pleomorphic histology were excluded.
Patients were treated with ibrutinib 560 mg orally daily for each 28-day cycle, with therapy continued until disease progression, or until therapy was stopped for any other reason. Patients also received intravenous rituximab 375 mg/m2 on days 1, 8, 15 and 22, plus or minus one day for cycle 1, on day 1 of cycles 3-8, and on day 1 of every other cycle for up to 2 years.
Of the 41 patients evaluable for response, 26 (64%) had a complete response (CR) and 12 (29%) had a partial response. Three additional patients had stable disease, for an objective response rate of 93%.
Of 34 patients with PET scans, all had negative scans. Of 37 patients evaluable for minimal residual disease (MRD) by flow cytometry, 21 (58%) were MRD negative.
Patients with low or intermediate Mantle Cell Lymphoma International Prognostic Index (MIPI) scores had a higher ORR (100% vs. 89% for patients with high MIPI scores), and patients with low Ki-67 levels had a higher response rate than that of patients with KI-67 of 30% or greater (80% vs. 87%).
Neither median 3-year progression-free survival nor median 3-year overall survival have been reached, with respective 3-year rates of 87% and 95%.
Four patients experienced disease progression at 4, 10, 13 and 33 months of treatment. Three of these patients had disease that had transformed to blastoid/pleomorphic variant, two had Ki-67 of 30% or greater, one had mutations in TP53, and one had FAT1 and SF3B1 mutations.
Two patients died after ibrutinib therapy, one who had discontinued therapy because of bleeding, and the other who died on treatment at 13 months from transformed disease. Both of these patients had high Ki-67 levels.
Grade 3 or 4 hematological adverse events were neutropenia in four patients, and thrombocytopenia in two patients. There were no cases of grade 3 or 4 anemia.
Grade 3 or 4 nonhematological adverse events were fatigue, myalgia, and atrial fibrillation in seven patients each, diarrhea in six patients, and petechiae/bleeding in three patients.
Patients will continue to be followed for late adverse events, secondary cancers, and relapses, and further studies on clonal evolution, mutation profiling, and MRD are ongoing and will be reported at a later date, Dr. Jain said.
The National Cancer Institute supported the study. Dr. Jain reported having no financial disclosures.
SOURCE: Jain P et al. 15-ICML. Abstract 011.
LUGANO, SWITZERLAND – The chemotherapy-free combination of ibrutinib (Imbruvica) and rituximab is highly effective as frontline therapy for older, transplant-ineligible patients with nonblastoid mantle cell lymphoma, according to investigators.
In a phase 2 study of patients with a median age of 71 years, 38 of 41 patients (93%) had an objective response, and the regimen was both safe and easy to administer, reported Preetesh Jain, MD, PhD, of the University of Texas MD Anderson Cancer Center in Houston.
“The adverse event profile was generally favorable, with specific monitoring recommended for patients with cardiovascular comorbidities and a history of atrial fibrillation,” he said at the International Conference on Malignant Lymphoma.
The investigators enrolled 48 patients aged 65 years and older with previously untreated mantle cell lymphoma (MCL), of whom 41 were evaluable for the primary endpoints of overall response rate (ORR) and safety. The patients had good performance status and normal organ function, with the largest tumor size less than 10 cm. Patients with atrial fibrillation could participate, if the fibrillation was controlled. Patients with Ki-67 protein levels of 50% or greater and blastoid/pleomorphic histology were excluded.
Patients were treated with ibrutinib 560 mg orally daily for each 28-day cycle, with therapy continued until disease progression, or until therapy was stopped for any other reason. Patients also received intravenous rituximab 375 mg/m2 on days 1, 8, 15 and 22, plus or minus one day for cycle 1, on day 1 of cycles 3-8, and on day 1 of every other cycle for up to 2 years.
Of the 41 patients evaluable for response, 26 (64%) had a complete response (CR) and 12 (29%) had a partial response. Three additional patients had stable disease, for an objective response rate of 93%.
Of 34 patients with PET scans, all had negative scans. Of 37 patients evaluable for minimal residual disease (MRD) by flow cytometry, 21 (58%) were MRD negative.
Patients with low or intermediate Mantle Cell Lymphoma International Prognostic Index (MIPI) scores had a higher ORR (100% vs. 89% for patients with high MIPI scores), and patients with low Ki-67 levels had a higher response rate than that of patients with KI-67 of 30% or greater (80% vs. 87%).
Neither median 3-year progression-free survival nor median 3-year overall survival have been reached, with respective 3-year rates of 87% and 95%.
Four patients experienced disease progression at 4, 10, 13 and 33 months of treatment. Three of these patients had disease that had transformed to blastoid/pleomorphic variant, two had Ki-67 of 30% or greater, one had mutations in TP53, and one had FAT1 and SF3B1 mutations.
Two patients died after ibrutinib therapy, one who had discontinued therapy because of bleeding, and the other who died on treatment at 13 months from transformed disease. Both of these patients had high Ki-67 levels.
Grade 3 or 4 hematological adverse events were neutropenia in four patients, and thrombocytopenia in two patients. There were no cases of grade 3 or 4 anemia.
Grade 3 or 4 nonhematological adverse events were fatigue, myalgia, and atrial fibrillation in seven patients each, diarrhea in six patients, and petechiae/bleeding in three patients.
Patients will continue to be followed for late adverse events, secondary cancers, and relapses, and further studies on clonal evolution, mutation profiling, and MRD are ongoing and will be reported at a later date, Dr. Jain said.
The National Cancer Institute supported the study. Dr. Jain reported having no financial disclosures.
SOURCE: Jain P et al. 15-ICML. Abstract 011.
REPORTING FROM 15-ICML
Bevacizumab-erlotinib combo falls short in EGFR-mutant advanced NSCLC
according to a multicenter, phase 2, randomized, controlled trial.
“The development of erlotinib as a first-line therapy was an important advance, but there was interest in improving the efficacy of erlotinib,” noted the investigators, led by Thomas E. Stinchcombe, MD, of the Duke Cancer Institute in Durham, N.C. Preclinical data suggested that adding an antiangiogenic agent could overcome resistance, and subgroup analyses of a phase 3 trial hinted at greater efficacy of this combination in patients with EGFR-mutant disease (Lancet. 2011;377:1846-54).
The new trial was conducted among 88 patients with previously untreated stage 4 EGFR-mutant NSCLC eligible to receive bevacizumab. Two-thirds had an EGFR exon 19 deletion.
The patients were assigned evenly to receive erlotinib (Tarceva), an EGFR tyrosine kinase inhibitor, either alone or in combination with bevacizumab (Avastin), an antibody directed against vascular endothelial growth factor.
Results reported in JAMA Oncology showed that, during a median follow-up of 33 months, median progression-free survival (PFS) – the trial’s primary endpoint – was 17.9 months with the combination and 13.5 months with erlotinib alone, a nonsignificant difference (hazard ratio, 0.81; P = .39).
There was also no significant difference between groups in objective response rate (81% vs. 83%; P = .81) and overall survival (median, 32.4 vs. 50.6 months; HR, 1.41; P = .33).
Relative to the erlotinib monotherapy group, the combination therapy group had higher rates of grade 3 or worse acneiform rash (26% vs. 16%), hypertension (40% vs. 20%), and proteinuria (12% vs. 0%), but a lower rate of grade 3 or worse diarrhea (9% vs. 13%).
“Our study, unlike previous randomized clinical trials, did not reveal a significant improvement in PFS with the combination of erlotinib and bevacizumab. ... One consideration is that our trial used investigator assessment of response and disease progression, whereas previous randomized trials used blinded independent radiologic review,” Dr. Stinchcombe and coinvestigators summarized.
“Future studies will investigate novel osimertinib [Tagrisso] combinations and molecular markers to identify patients most likely to experience disease progression with single-agent EGFR TKIs,” they concluded.
Dr. Stinchcombe reported no relevant conflicts of interest. The trial was supported by Genentech/Roche.
SOURCE: Stinchcombe TE et al. JAMA Oncol. 2019 Aug 8. doi: 10.1001/jamaoncol.2019.1847.
according to a multicenter, phase 2, randomized, controlled trial.
“The development of erlotinib as a first-line therapy was an important advance, but there was interest in improving the efficacy of erlotinib,” noted the investigators, led by Thomas E. Stinchcombe, MD, of the Duke Cancer Institute in Durham, N.C. Preclinical data suggested that adding an antiangiogenic agent could overcome resistance, and subgroup analyses of a phase 3 trial hinted at greater efficacy of this combination in patients with EGFR-mutant disease (Lancet. 2011;377:1846-54).
The new trial was conducted among 88 patients with previously untreated stage 4 EGFR-mutant NSCLC eligible to receive bevacizumab. Two-thirds had an EGFR exon 19 deletion.
The patients were assigned evenly to receive erlotinib (Tarceva), an EGFR tyrosine kinase inhibitor, either alone or in combination with bevacizumab (Avastin), an antibody directed against vascular endothelial growth factor.
Results reported in JAMA Oncology showed that, during a median follow-up of 33 months, median progression-free survival (PFS) – the trial’s primary endpoint – was 17.9 months with the combination and 13.5 months with erlotinib alone, a nonsignificant difference (hazard ratio, 0.81; P = .39).
There was also no significant difference between groups in objective response rate (81% vs. 83%; P = .81) and overall survival (median, 32.4 vs. 50.6 months; HR, 1.41; P = .33).
Relative to the erlotinib monotherapy group, the combination therapy group had higher rates of grade 3 or worse acneiform rash (26% vs. 16%), hypertension (40% vs. 20%), and proteinuria (12% vs. 0%), but a lower rate of grade 3 or worse diarrhea (9% vs. 13%).
“Our study, unlike previous randomized clinical trials, did not reveal a significant improvement in PFS with the combination of erlotinib and bevacizumab. ... One consideration is that our trial used investigator assessment of response and disease progression, whereas previous randomized trials used blinded independent radiologic review,” Dr. Stinchcombe and coinvestigators summarized.
“Future studies will investigate novel osimertinib [Tagrisso] combinations and molecular markers to identify patients most likely to experience disease progression with single-agent EGFR TKIs,” they concluded.
Dr. Stinchcombe reported no relevant conflicts of interest. The trial was supported by Genentech/Roche.
SOURCE: Stinchcombe TE et al. JAMA Oncol. 2019 Aug 8. doi: 10.1001/jamaoncol.2019.1847.
according to a multicenter, phase 2, randomized, controlled trial.
“The development of erlotinib as a first-line therapy was an important advance, but there was interest in improving the efficacy of erlotinib,” noted the investigators, led by Thomas E. Stinchcombe, MD, of the Duke Cancer Institute in Durham, N.C. Preclinical data suggested that adding an antiangiogenic agent could overcome resistance, and subgroup analyses of a phase 3 trial hinted at greater efficacy of this combination in patients with EGFR-mutant disease (Lancet. 2011;377:1846-54).
The new trial was conducted among 88 patients with previously untreated stage 4 EGFR-mutant NSCLC eligible to receive bevacizumab. Two-thirds had an EGFR exon 19 deletion.
The patients were assigned evenly to receive erlotinib (Tarceva), an EGFR tyrosine kinase inhibitor, either alone or in combination with bevacizumab (Avastin), an antibody directed against vascular endothelial growth factor.
Results reported in JAMA Oncology showed that, during a median follow-up of 33 months, median progression-free survival (PFS) – the trial’s primary endpoint – was 17.9 months with the combination and 13.5 months with erlotinib alone, a nonsignificant difference (hazard ratio, 0.81; P = .39).
There was also no significant difference between groups in objective response rate (81% vs. 83%; P = .81) and overall survival (median, 32.4 vs. 50.6 months; HR, 1.41; P = .33).
Relative to the erlotinib monotherapy group, the combination therapy group had higher rates of grade 3 or worse acneiform rash (26% vs. 16%), hypertension (40% vs. 20%), and proteinuria (12% vs. 0%), but a lower rate of grade 3 or worse diarrhea (9% vs. 13%).
“Our study, unlike previous randomized clinical trials, did not reveal a significant improvement in PFS with the combination of erlotinib and bevacizumab. ... One consideration is that our trial used investigator assessment of response and disease progression, whereas previous randomized trials used blinded independent radiologic review,” Dr. Stinchcombe and coinvestigators summarized.
“Future studies will investigate novel osimertinib [Tagrisso] combinations and molecular markers to identify patients most likely to experience disease progression with single-agent EGFR TKIs,” they concluded.
Dr. Stinchcombe reported no relevant conflicts of interest. The trial was supported by Genentech/Roche.
SOURCE: Stinchcombe TE et al. JAMA Oncol. 2019 Aug 8. doi: 10.1001/jamaoncol.2019.1847.
FROM JAMA ONCOLOGY
PROMIS tools provide useful data for managing rheumatology patients
LAKE BUENA VISTA, FLA. –
The PROMIS tools – which like most patient-reported outcome (PRO) measurement tools are designed to evaluate and monitor physical, mental, and social health – can be used both for the general population and for individuals living with chronic conditions, Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham (UAB), said at the annual meeting of the Florida Society of Rheumatology.
The tools take a deeper dive into various symptoms and their effects; for instance, with respect to physical health, they measure fatigue, physical function, sleep disturbance, pain intensity, and pain interference – the extent to which pain “messes your patient’s life up,” explained Dr. Curtis, who also is codirector of the UAB Pharmacoepidemiology and Pharmacoeconomics Unit.
Additional physical health domains that PROs measure include dyspnea, gastrointestinal symptoms, pain behavior, pain quality, sexual function, and sleep-related impairment.
These are “things that, honestly, we don’t talk about much as a field, but absolutely affect patients with autoimmune diseases,” he said. “You know, sexual function – that doesn’t come up in my practice spontaneously very often, but there are ways you can quantify that, and for many patients that’s actually a big deal.”
The domains measured by PROMIS tools for mental health look at anxiety and depression, but also delve into alcohol use, anger, cognitive function, life satisfaction, self-efficacy for managing chronic conditions, substance use, and more. The domains for social health address ability to participate in social roles and activities, as well as companionship, satisfaction with social roles and activity, social isolation, and social support.
“You can’t go on a hike with friends [and] be far from a bathroom, because you have bad arthritis and you have Crohn’s disease. Well, that’s kind of an important thing that may or may not come up in your discussions about inflammatory arthritis associated with [inflammatory bowel disease],” he said.
Another example is a patient who is embarrassed attending social functions or wearing a swimsuit because of really bad psoriasis.
“These are the kinds of things that I’m suggesting you and I probably want to measure if we’re providing holistic care to rheumatology patients,” Dr. Curtis said.
The PROMIS tools provide a simple, user-friendly means for doing so in English, Spanish, and many other languages, he noted.
All the scales use the same 1-100 scoring range, which simplifies measurements. They are available for free by download and can be printed or used electronically for use in the office, at home, on the web, and via smartphone.
The NIH developed the PROMIS tools several years ago and validated them for multiple chronic disease populations, Dr. Curtis said, adding that the tools include multiple individual domains and overall “profiles” of varying lengths.
Most are fixed-length scales that are between 4 and 10 questions and can be completed within 30-60 seconds per scale, so several scales can be completed within 5-10 minutes.
However, some scales are longer and provide greater detail.
“The nice thing is that if you ask a few more questions you can get more precise information – there’s more of a floor and ceiling. You can detect people who do really well. You can distinguish between the marathon runners and the 5K-ers and the people who can walk 2 miles but aren’t going to run a race,” he explained.
Further, the PROMIS tools, like the 36-item Short Form Health Survey (SF-36), are benchmarked against the U.S. adult population, allowing for assessment of how a specific drug or treatment “impacts your arthritis patient on a scale that would also be relevant for somebody who doesn’t have arthritis, they have diabetes.”
The metrics and scales are the same, and that can be helpful when trying to get a payer to pay for a particular drug, he said.
“None of these are rheumatology specific; this puts PROs into a language that can help rheumatology contend for the value of the care that we provide on a scale that would be relevant for any other chronic illness, even for nonrheumatology patients,” he explained.
In addition, minimally important differences (group mean change of about 2-3 units) and minimally clinical important differences for individuals (5 units) have been established.
“So we know what the numbers mean, and this is true for all of the scales,” he said.
PROMIS tools also include computer-adaptive testing (CAT) versions, which helps to personalize the scales to provide more precise information for a given patient and eliminate irrelevant information.
Of note, PROMIS health measures are among the data that can be tracked on a smartphone using Arthritis Power, an arthritis research registry developed with the help of a recent infrastructure grant awarded to the Center for Education and Research and Therapeutics of Musculoskeletal Disorders at UAB, Dr. Curtis said.
The measures were also shown in the AWARE study to track closely with other measures, including the Clinical Disease Activity Index (CDAI), and with patient improvement on therapy.
“So these PROMIS scores are tracking with things that you and I are familiar with ... and it looks like these scores are faithfully tracking, over time, patients getting better on therapies that we would expect them to,” he said. “I think this is additional validation – not just from the National Institutes of Health and a decade of research by lots of different groups, but in our own field – that these actually correlate with disease activity ... and that when you start an effective therapy like a [tumor necrosis factor inhibitor] they’re going to improve as you would anticipate.”
Dr. Curtis reported funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Patient-Centered Outcomes Research Institute. He has also consulted for or received research grants from Amgen, AbbVie, Bristol-Myers Squibb, CORRONA, Lilly, Janssen, Myriad, Novartis, Roche, Pfizer, and Sanofi/Regeneron.
LAKE BUENA VISTA, FLA. –
The PROMIS tools – which like most patient-reported outcome (PRO) measurement tools are designed to evaluate and monitor physical, mental, and social health – can be used both for the general population and for individuals living with chronic conditions, Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham (UAB), said at the annual meeting of the Florida Society of Rheumatology.
The tools take a deeper dive into various symptoms and their effects; for instance, with respect to physical health, they measure fatigue, physical function, sleep disturbance, pain intensity, and pain interference – the extent to which pain “messes your patient’s life up,” explained Dr. Curtis, who also is codirector of the UAB Pharmacoepidemiology and Pharmacoeconomics Unit.
Additional physical health domains that PROs measure include dyspnea, gastrointestinal symptoms, pain behavior, pain quality, sexual function, and sleep-related impairment.
These are “things that, honestly, we don’t talk about much as a field, but absolutely affect patients with autoimmune diseases,” he said. “You know, sexual function – that doesn’t come up in my practice spontaneously very often, but there are ways you can quantify that, and for many patients that’s actually a big deal.”
The domains measured by PROMIS tools for mental health look at anxiety and depression, but also delve into alcohol use, anger, cognitive function, life satisfaction, self-efficacy for managing chronic conditions, substance use, and more. The domains for social health address ability to participate in social roles and activities, as well as companionship, satisfaction with social roles and activity, social isolation, and social support.
“You can’t go on a hike with friends [and] be far from a bathroom, because you have bad arthritis and you have Crohn’s disease. Well, that’s kind of an important thing that may or may not come up in your discussions about inflammatory arthritis associated with [inflammatory bowel disease],” he said.
Another example is a patient who is embarrassed attending social functions or wearing a swimsuit because of really bad psoriasis.
“These are the kinds of things that I’m suggesting you and I probably want to measure if we’re providing holistic care to rheumatology patients,” Dr. Curtis said.
The PROMIS tools provide a simple, user-friendly means for doing so in English, Spanish, and many other languages, he noted.
All the scales use the same 1-100 scoring range, which simplifies measurements. They are available for free by download and can be printed or used electronically for use in the office, at home, on the web, and via smartphone.
The NIH developed the PROMIS tools several years ago and validated them for multiple chronic disease populations, Dr. Curtis said, adding that the tools include multiple individual domains and overall “profiles” of varying lengths.
Most are fixed-length scales that are between 4 and 10 questions and can be completed within 30-60 seconds per scale, so several scales can be completed within 5-10 minutes.
However, some scales are longer and provide greater detail.
“The nice thing is that if you ask a few more questions you can get more precise information – there’s more of a floor and ceiling. You can detect people who do really well. You can distinguish between the marathon runners and the 5K-ers and the people who can walk 2 miles but aren’t going to run a race,” he explained.
Further, the PROMIS tools, like the 36-item Short Form Health Survey (SF-36), are benchmarked against the U.S. adult population, allowing for assessment of how a specific drug or treatment “impacts your arthritis patient on a scale that would also be relevant for somebody who doesn’t have arthritis, they have diabetes.”
The metrics and scales are the same, and that can be helpful when trying to get a payer to pay for a particular drug, he said.
“None of these are rheumatology specific; this puts PROs into a language that can help rheumatology contend for the value of the care that we provide on a scale that would be relevant for any other chronic illness, even for nonrheumatology patients,” he explained.
In addition, minimally important differences (group mean change of about 2-3 units) and minimally clinical important differences for individuals (5 units) have been established.
“So we know what the numbers mean, and this is true for all of the scales,” he said.
PROMIS tools also include computer-adaptive testing (CAT) versions, which helps to personalize the scales to provide more precise information for a given patient and eliminate irrelevant information.
Of note, PROMIS health measures are among the data that can be tracked on a smartphone using Arthritis Power, an arthritis research registry developed with the help of a recent infrastructure grant awarded to the Center for Education and Research and Therapeutics of Musculoskeletal Disorders at UAB, Dr. Curtis said.
The measures were also shown in the AWARE study to track closely with other measures, including the Clinical Disease Activity Index (CDAI), and with patient improvement on therapy.
“So these PROMIS scores are tracking with things that you and I are familiar with ... and it looks like these scores are faithfully tracking, over time, patients getting better on therapies that we would expect them to,” he said. “I think this is additional validation – not just from the National Institutes of Health and a decade of research by lots of different groups, but in our own field – that these actually correlate with disease activity ... and that when you start an effective therapy like a [tumor necrosis factor inhibitor] they’re going to improve as you would anticipate.”
Dr. Curtis reported funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Patient-Centered Outcomes Research Institute. He has also consulted for or received research grants from Amgen, AbbVie, Bristol-Myers Squibb, CORRONA, Lilly, Janssen, Myriad, Novartis, Roche, Pfizer, and Sanofi/Regeneron.
LAKE BUENA VISTA, FLA. –
The PROMIS tools – which like most patient-reported outcome (PRO) measurement tools are designed to evaluate and monitor physical, mental, and social health – can be used both for the general population and for individuals living with chronic conditions, Dr. Curtis, professor of medicine in the division of clinical immunology and rheumatology at the University of Alabama at Birmingham (UAB), said at the annual meeting of the Florida Society of Rheumatology.
The tools take a deeper dive into various symptoms and their effects; for instance, with respect to physical health, they measure fatigue, physical function, sleep disturbance, pain intensity, and pain interference – the extent to which pain “messes your patient’s life up,” explained Dr. Curtis, who also is codirector of the UAB Pharmacoepidemiology and Pharmacoeconomics Unit.
Additional physical health domains that PROs measure include dyspnea, gastrointestinal symptoms, pain behavior, pain quality, sexual function, and sleep-related impairment.
These are “things that, honestly, we don’t talk about much as a field, but absolutely affect patients with autoimmune diseases,” he said. “You know, sexual function – that doesn’t come up in my practice spontaneously very often, but there are ways you can quantify that, and for many patients that’s actually a big deal.”
The domains measured by PROMIS tools for mental health look at anxiety and depression, but also delve into alcohol use, anger, cognitive function, life satisfaction, self-efficacy for managing chronic conditions, substance use, and more. The domains for social health address ability to participate in social roles and activities, as well as companionship, satisfaction with social roles and activity, social isolation, and social support.
“You can’t go on a hike with friends [and] be far from a bathroom, because you have bad arthritis and you have Crohn’s disease. Well, that’s kind of an important thing that may or may not come up in your discussions about inflammatory arthritis associated with [inflammatory bowel disease],” he said.
Another example is a patient who is embarrassed attending social functions or wearing a swimsuit because of really bad psoriasis.
“These are the kinds of things that I’m suggesting you and I probably want to measure if we’re providing holistic care to rheumatology patients,” Dr. Curtis said.
The PROMIS tools provide a simple, user-friendly means for doing so in English, Spanish, and many other languages, he noted.
All the scales use the same 1-100 scoring range, which simplifies measurements. They are available for free by download and can be printed or used electronically for use in the office, at home, on the web, and via smartphone.
The NIH developed the PROMIS tools several years ago and validated them for multiple chronic disease populations, Dr. Curtis said, adding that the tools include multiple individual domains and overall “profiles” of varying lengths.
Most are fixed-length scales that are between 4 and 10 questions and can be completed within 30-60 seconds per scale, so several scales can be completed within 5-10 minutes.
However, some scales are longer and provide greater detail.
“The nice thing is that if you ask a few more questions you can get more precise information – there’s more of a floor and ceiling. You can detect people who do really well. You can distinguish between the marathon runners and the 5K-ers and the people who can walk 2 miles but aren’t going to run a race,” he explained.
Further, the PROMIS tools, like the 36-item Short Form Health Survey (SF-36), are benchmarked against the U.S. adult population, allowing for assessment of how a specific drug or treatment “impacts your arthritis patient on a scale that would also be relevant for somebody who doesn’t have arthritis, they have diabetes.”
The metrics and scales are the same, and that can be helpful when trying to get a payer to pay for a particular drug, he said.
“None of these are rheumatology specific; this puts PROs into a language that can help rheumatology contend for the value of the care that we provide on a scale that would be relevant for any other chronic illness, even for nonrheumatology patients,” he explained.
In addition, minimally important differences (group mean change of about 2-3 units) and minimally clinical important differences for individuals (5 units) have been established.
“So we know what the numbers mean, and this is true for all of the scales,” he said.
PROMIS tools also include computer-adaptive testing (CAT) versions, which helps to personalize the scales to provide more precise information for a given patient and eliminate irrelevant information.
Of note, PROMIS health measures are among the data that can be tracked on a smartphone using Arthritis Power, an arthritis research registry developed with the help of a recent infrastructure grant awarded to the Center for Education and Research and Therapeutics of Musculoskeletal Disorders at UAB, Dr. Curtis said.
The measures were also shown in the AWARE study to track closely with other measures, including the Clinical Disease Activity Index (CDAI), and with patient improvement on therapy.
“So these PROMIS scores are tracking with things that you and I are familiar with ... and it looks like these scores are faithfully tracking, over time, patients getting better on therapies that we would expect them to,” he said. “I think this is additional validation – not just from the National Institutes of Health and a decade of research by lots of different groups, but in our own field – that these actually correlate with disease activity ... and that when you start an effective therapy like a [tumor necrosis factor inhibitor] they’re going to improve as you would anticipate.”
Dr. Curtis reported funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the Patient-Centered Outcomes Research Institute. He has also consulted for or received research grants from Amgen, AbbVie, Bristol-Myers Squibb, CORRONA, Lilly, Janssen, Myriad, Novartis, Roche, Pfizer, and Sanofi/Regeneron.
EXPERT ANALYSIS FROM FSR 2019
PTSD in the inpatient setting
A problem hiding in plain sight
“I need to get out of here! I haven’t gotten any sleep, my medications never come on time, and I feel like a pincushion. I am leaving NOW!” The commotion interrupts your intern’s meticulous presentation as your team quickly files into the room. You find a disheveled, visibly frustrated man tearing at his intravenous line, surrounded by his half-eaten breakfast and multiple urinals filled to various levels. His IV pump is beeping, and telemetry wires hang haphazardly off his chest.
Mr. Smith had been admitted for a heart failure exacerbation. You’d been making steady progress with diuresis but are now faced with a likely discharge against medical advice if you can’t defuse the situation.
As hospitalists, this scenario might feel eerily familiar. Perhaps Mr. Smith had enough of being in the hospital and just wanted to go home to see his dog, or maybe the food was not up to his standards.
However, his next line stops your team dead in its tracks. “I feel like I am in Vietnam all over again. I am tied up with all these wires and feel like a prisoner! Please let me go.” It turns out that Mr. Smith had a comorbidity that was overlooked during his initial intake: posttraumatic stress disorder.
Impact of PTSD
PTSD is a diagnosis characterized by intrusive recurrent thoughts, dreams, or flashbacks that follow exposure to a traumatic event or series of events (see Table 1). While more common among veterans (for example, Vietnam veterans have an estimated lifetime prevalence of PTSD of 30.9% for men and 26.9% for women),1 a national survey of U.S. households estimated the lifetime prevalence of PTSD among adult Americans to be 6.8%.2 PTSD is often underdiagnosed and underreported by patients in the outpatient setting, leading to underrecognition and undertreatment of these patients in the inpatient setting.
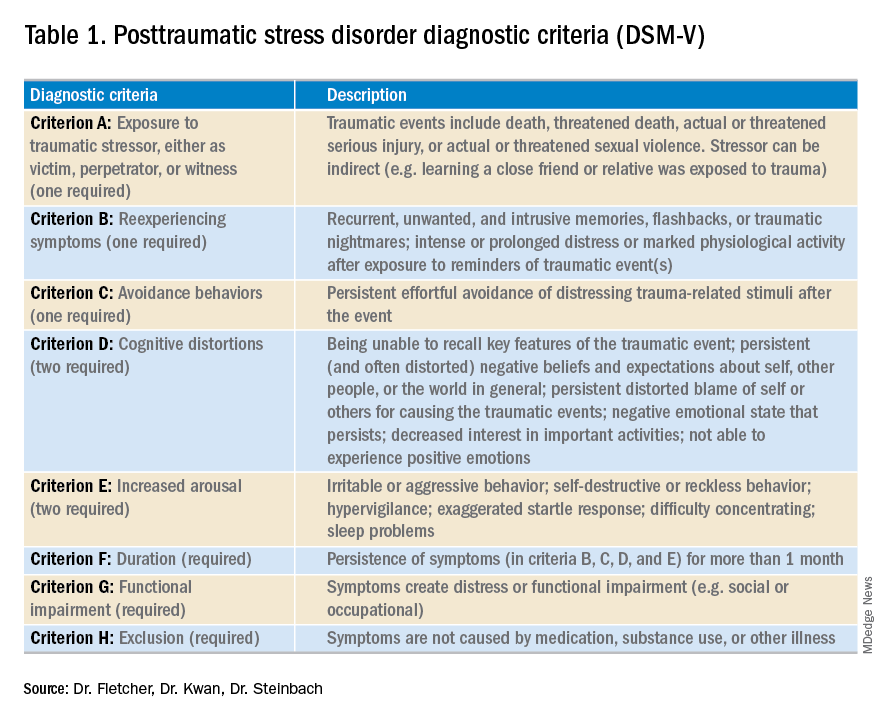
Although it may not be surprising that patients with PTSD use more mental health services, they are also more likely to use nonmental health services. In one study, total utilization of outpatient nonmental health services was 91% greater in veterans with PTSD, and these patients were three times more likely to be hospitalized than those without any mental health diagnoses.3 Additionally, they are likely to present later and stay longer when compared with patients without PTSD. One study estimated the cost of PTSD-related hospitalization in the United States from 2002 to 2011 as being $34.9 billion.4 Notably, close to 95% of hospitalizations in this study listed PTSD as a secondary rather than primary diagnosis, suggesting that the vast majority of these admitted patients are cared for by frontline providers who are not trained mental health professionals.
How PTSD manifests in the hospital
But, how exactly can the hospital environment contribute to decompensation of PTSD symptoms? Unfortunately, there is little empiric data to guide us. Based on what we do know of PTSD, we offer the following hypotheses.
Patients with PTSD may feel a loss of control or helplessness when admitted to the inpatient setting. For example, they cannot control when they receive their medications or when they get their meals. The act of showering or going outside requires approval. In addition, they might perceive they are being “ordered around” by staff and may be carted off to a study without knowing why the study is being done in the first place.
Triggers in the hospital environment may contribute to PTSD flares. Think about the loud, beeping IV pump that constantly goes off at random intervals, disrupting sleep. What about a blood draw in the early morning where the phlebotomist sticks a needle into the arm of a sleeping patient? Or the well-intentioned provider doing prerounds who wakes a sleeping patient with a shake of the shoulder or some other form of physical touch? The multidisciplinary team crowding around their hospital bed? For a patient suffering from PTSD, any of these could easily set off a cascade of escalating symptoms.
Knowing that these triggers exist, can anything be done to ameliorate their effects? We propose some practical suggestions for improving the hospital experience for patients with PTSD.
Strategies to combat PTSD in the inpatient setting
Perhaps the most practical place to start is with preserving sleep in hospitalized patients with PTSD. The majority of patients with PTSD have sleep disturbances, and interrupted sleep routines in these patients can exacerbate nightmares and underlying psychiatric issues.5 Therefore, we should strive to avoid unnecessary awakenings.
While this principle holds true for all hospitalized patients, it must be especially prioritized in patients with PTSD. Ask yourself these questions during your next admission: Must intravenous fluids run 24 hours a day, or could they be stopped at 6 p.m.? Are vital signs needed overnight? Could the last dose of furosemide occur at 4 p.m. to avoid nocturia?
Another strategy involves bedtime routines. Many of these patients may already follow a home sleep routine as part of their chronic PTSD management. To honor these habits in the hospital might mean that staff encourage turning the lights and the television off at a designated time. Additionally, the literature suggests music therapy can have a significant impact on enhanced sleep quality. When available, music therapy may reduce insomnia and decrease the amount of time prior to falling asleep.6
Other methods to counteract PTSD fall under the general principle of “trauma-informed care.” Trauma-informed care comprises practices promoting a culture of safety, empowerment, and healing.7 It is a mindful and sensitive approach that acknowledges the pervasive nature of trauma exposure, the reality of ongoing adverse effects in trauma survivors, and the fact that recovery is highly personal and complex.8
By definition, patients with PTSD have endured some traumatic event. Therefore, ideal care teams will ask patients about things that may trigger their anxiety and then work to mitigate them. For example, some patients with PTSD have a severe startle response when woken up by someone touching them. When patients feel that they can share their concerns with their care team and their team honors that observation by waking them in a different way, trust and control may be gained. This process of asking for patient guidance and adjusting accordingly is consistent with a trauma-informed care approach.9 A true trauma-informed care approach involves the entire practice environment but examining and adjusting our own behavior and assumptions are good places to start.
Summary of recommended treatments
Psychotherapy is preferable over pharmacotherapy, but both can be combined as needed. Individual trauma-focused psychotherapies utilizing a primary component of exposure and/or cognitive restructuring have strong evidence for effectiveness but are primarily outpatient based.
For pharmacologic treatment, selective serotonin reuptake inhibitors (for example, sertraline, paroxetine, or fluoxetine) and serotonin norepinephrine reuptake inhibitors (for example, venlafaxine) monotherapy have strong evidence for effectiveness and can be started while inpatient. However, these medications typically take weeks to produce benefits. Recent trials studying prazosin, an alpha1-adrenergic receptor antagonist used to alleviate nightmares associated with PTSD, have demonstrated inefficacy or even harm,leading experts to caution against its use.10,11 Finally, benzodiazepine and atypical antipsychotic usage should be restricted and used as a last resort.12
In summary, PTSD is common among veterans and nonveterans. While hospitalists may rarely admit patients because of their PTSD, they will often take care of patients who have PTSD as a comorbidity. Therefore, understanding the basics of PTSD and how hospitalization may exacerbate its symptoms can meaningfully improve care for these patients.
Dr. Fletcher is a hospitalist at the Milwaukee Veterans Affairs Medical Center and Froedtert Hospital in Wauwatosa, Wis. She is professor of internal medicine and program director for the internal medicine residency program at the Medical College of Wisconsin, Milwaukee. She is also faculty mentor for the VA’s Chief Resident for Quality and Safety. Dr. Kwan is a hospitalist at the VA San Diego Healthcare System and is associate professor at the University of California, San Diego, in the division of hospital medicine. He serves as an associate clerkship director of both the internal medicine clerkship and the medicine subinternship. He is the chair of SHM’s Physicians in Training committee. Dr. Steinbach is chief of hospital medicine at the Atlanta VA Medical Center and assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Kang HK et al. Posttraumatic stress disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157(2):141-8.
2. Kessler RC et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005; 62(6):593-602.
3. Cohen BE et al. Mental health diagnoses and utilization of VA nonmental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
4. Haviland MG et al. Posttraumatic stress disorder–related hospitalizations in the United States (2002-2011): Rates, co-occurring illnesses, suicidal ideation/self-harm, and hospital charges. J Nerv Ment Dis. 2016; 204(2):78-86.
5. Aurora RN et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
6. Blanaru M et al. The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment Illn. 2012;4(2):e13.
7. Tello M. (2018, Oct 16). Trauma-informed care: What it is, and why it’s important. Retrieved March 18, 2019, from https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562.
8. Harris M et al. Using trauma theory to design service systems. San Francisco: 2001.
9. Substance abuse and mental health services administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS publication no. SMA 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
10. Raskind MA et al. Trial of prazosin for posttraumatic stress disorder in military veterans. N Engl J Med. 2018 Feb 8;378(6):507-7.
11. McCall WV et al. A pilot, randomized clinical trial of bedtime doses of prazosin versus placebo in suicidal posttraumatic stress disorder patients with nightmares. J Clin Psychopharmacol. 2018 Dec;38(6):618-21.
12. U.S. Department of Veterans Affairs/U.S. Department of Defense. Clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction 2017. Accessed February 18, 2019.
A problem hiding in plain sight
A problem hiding in plain sight
“I need to get out of here! I haven’t gotten any sleep, my medications never come on time, and I feel like a pincushion. I am leaving NOW!” The commotion interrupts your intern’s meticulous presentation as your team quickly files into the room. You find a disheveled, visibly frustrated man tearing at his intravenous line, surrounded by his half-eaten breakfast and multiple urinals filled to various levels. His IV pump is beeping, and telemetry wires hang haphazardly off his chest.
Mr. Smith had been admitted for a heart failure exacerbation. You’d been making steady progress with diuresis but are now faced with a likely discharge against medical advice if you can’t defuse the situation.
As hospitalists, this scenario might feel eerily familiar. Perhaps Mr. Smith had enough of being in the hospital and just wanted to go home to see his dog, or maybe the food was not up to his standards.
However, his next line stops your team dead in its tracks. “I feel like I am in Vietnam all over again. I am tied up with all these wires and feel like a prisoner! Please let me go.” It turns out that Mr. Smith had a comorbidity that was overlooked during his initial intake: posttraumatic stress disorder.
Impact of PTSD
PTSD is a diagnosis characterized by intrusive recurrent thoughts, dreams, or flashbacks that follow exposure to a traumatic event or series of events (see Table 1). While more common among veterans (for example, Vietnam veterans have an estimated lifetime prevalence of PTSD of 30.9% for men and 26.9% for women),1 a national survey of U.S. households estimated the lifetime prevalence of PTSD among adult Americans to be 6.8%.2 PTSD is often underdiagnosed and underreported by patients in the outpatient setting, leading to underrecognition and undertreatment of these patients in the inpatient setting.
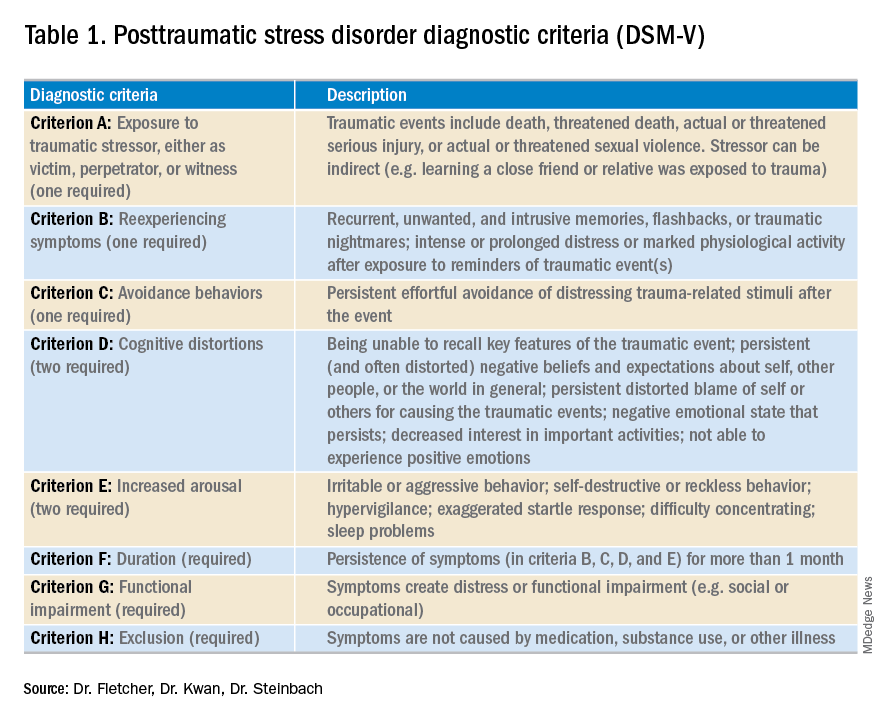
Although it may not be surprising that patients with PTSD use more mental health services, they are also more likely to use nonmental health services. In one study, total utilization of outpatient nonmental health services was 91% greater in veterans with PTSD, and these patients were three times more likely to be hospitalized than those without any mental health diagnoses.3 Additionally, they are likely to present later and stay longer when compared with patients without PTSD. One study estimated the cost of PTSD-related hospitalization in the United States from 2002 to 2011 as being $34.9 billion.4 Notably, close to 95% of hospitalizations in this study listed PTSD as a secondary rather than primary diagnosis, suggesting that the vast majority of these admitted patients are cared for by frontline providers who are not trained mental health professionals.
How PTSD manifests in the hospital
But, how exactly can the hospital environment contribute to decompensation of PTSD symptoms? Unfortunately, there is little empiric data to guide us. Based on what we do know of PTSD, we offer the following hypotheses.
Patients with PTSD may feel a loss of control or helplessness when admitted to the inpatient setting. For example, they cannot control when they receive their medications or when they get their meals. The act of showering or going outside requires approval. In addition, they might perceive they are being “ordered around” by staff and may be carted off to a study without knowing why the study is being done in the first place.
Triggers in the hospital environment may contribute to PTSD flares. Think about the loud, beeping IV pump that constantly goes off at random intervals, disrupting sleep. What about a blood draw in the early morning where the phlebotomist sticks a needle into the arm of a sleeping patient? Or the well-intentioned provider doing prerounds who wakes a sleeping patient with a shake of the shoulder or some other form of physical touch? The multidisciplinary team crowding around their hospital bed? For a patient suffering from PTSD, any of these could easily set off a cascade of escalating symptoms.
Knowing that these triggers exist, can anything be done to ameliorate their effects? We propose some practical suggestions for improving the hospital experience for patients with PTSD.
Strategies to combat PTSD in the inpatient setting
Perhaps the most practical place to start is with preserving sleep in hospitalized patients with PTSD. The majority of patients with PTSD have sleep disturbances, and interrupted sleep routines in these patients can exacerbate nightmares and underlying psychiatric issues.5 Therefore, we should strive to avoid unnecessary awakenings.
While this principle holds true for all hospitalized patients, it must be especially prioritized in patients with PTSD. Ask yourself these questions during your next admission: Must intravenous fluids run 24 hours a day, or could they be stopped at 6 p.m.? Are vital signs needed overnight? Could the last dose of furosemide occur at 4 p.m. to avoid nocturia?
Another strategy involves bedtime routines. Many of these patients may already follow a home sleep routine as part of their chronic PTSD management. To honor these habits in the hospital might mean that staff encourage turning the lights and the television off at a designated time. Additionally, the literature suggests music therapy can have a significant impact on enhanced sleep quality. When available, music therapy may reduce insomnia and decrease the amount of time prior to falling asleep.6
Other methods to counteract PTSD fall under the general principle of “trauma-informed care.” Trauma-informed care comprises practices promoting a culture of safety, empowerment, and healing.7 It is a mindful and sensitive approach that acknowledges the pervasive nature of trauma exposure, the reality of ongoing adverse effects in trauma survivors, and the fact that recovery is highly personal and complex.8
By definition, patients with PTSD have endured some traumatic event. Therefore, ideal care teams will ask patients about things that may trigger their anxiety and then work to mitigate them. For example, some patients with PTSD have a severe startle response when woken up by someone touching them. When patients feel that they can share their concerns with their care team and their team honors that observation by waking them in a different way, trust and control may be gained. This process of asking for patient guidance and adjusting accordingly is consistent with a trauma-informed care approach.9 A true trauma-informed care approach involves the entire practice environment but examining and adjusting our own behavior and assumptions are good places to start.
Summary of recommended treatments
Psychotherapy is preferable over pharmacotherapy, but both can be combined as needed. Individual trauma-focused psychotherapies utilizing a primary component of exposure and/or cognitive restructuring have strong evidence for effectiveness but are primarily outpatient based.
For pharmacologic treatment, selective serotonin reuptake inhibitors (for example, sertraline, paroxetine, or fluoxetine) and serotonin norepinephrine reuptake inhibitors (for example, venlafaxine) monotherapy have strong evidence for effectiveness and can be started while inpatient. However, these medications typically take weeks to produce benefits. Recent trials studying prazosin, an alpha1-adrenergic receptor antagonist used to alleviate nightmares associated with PTSD, have demonstrated inefficacy or even harm,leading experts to caution against its use.10,11 Finally, benzodiazepine and atypical antipsychotic usage should be restricted and used as a last resort.12
In summary, PTSD is common among veterans and nonveterans. While hospitalists may rarely admit patients because of their PTSD, they will often take care of patients who have PTSD as a comorbidity. Therefore, understanding the basics of PTSD and how hospitalization may exacerbate its symptoms can meaningfully improve care for these patients.
Dr. Fletcher is a hospitalist at the Milwaukee Veterans Affairs Medical Center and Froedtert Hospital in Wauwatosa, Wis. She is professor of internal medicine and program director for the internal medicine residency program at the Medical College of Wisconsin, Milwaukee. She is also faculty mentor for the VA’s Chief Resident for Quality and Safety. Dr. Kwan is a hospitalist at the VA San Diego Healthcare System and is associate professor at the University of California, San Diego, in the division of hospital medicine. He serves as an associate clerkship director of both the internal medicine clerkship and the medicine subinternship. He is the chair of SHM’s Physicians in Training committee. Dr. Steinbach is chief of hospital medicine at the Atlanta VA Medical Center and assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Kang HK et al. Posttraumatic stress disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157(2):141-8.
2. Kessler RC et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005; 62(6):593-602.
3. Cohen BE et al. Mental health diagnoses and utilization of VA nonmental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
4. Haviland MG et al. Posttraumatic stress disorder–related hospitalizations in the United States (2002-2011): Rates, co-occurring illnesses, suicidal ideation/self-harm, and hospital charges. J Nerv Ment Dis. 2016; 204(2):78-86.
5. Aurora RN et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
6. Blanaru M et al. The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment Illn. 2012;4(2):e13.
7. Tello M. (2018, Oct 16). Trauma-informed care: What it is, and why it’s important. Retrieved March 18, 2019, from https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562.
8. Harris M et al. Using trauma theory to design service systems. San Francisco: 2001.
9. Substance abuse and mental health services administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS publication no. SMA 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
10. Raskind MA et al. Trial of prazosin for posttraumatic stress disorder in military veterans. N Engl J Med. 2018 Feb 8;378(6):507-7.
11. McCall WV et al. A pilot, randomized clinical trial of bedtime doses of prazosin versus placebo in suicidal posttraumatic stress disorder patients with nightmares. J Clin Psychopharmacol. 2018 Dec;38(6):618-21.
12. U.S. Department of Veterans Affairs/U.S. Department of Defense. Clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction 2017. Accessed February 18, 2019.
“I need to get out of here! I haven’t gotten any sleep, my medications never come on time, and I feel like a pincushion. I am leaving NOW!” The commotion interrupts your intern’s meticulous presentation as your team quickly files into the room. You find a disheveled, visibly frustrated man tearing at his intravenous line, surrounded by his half-eaten breakfast and multiple urinals filled to various levels. His IV pump is beeping, and telemetry wires hang haphazardly off his chest.
Mr. Smith had been admitted for a heart failure exacerbation. You’d been making steady progress with diuresis but are now faced with a likely discharge against medical advice if you can’t defuse the situation.
As hospitalists, this scenario might feel eerily familiar. Perhaps Mr. Smith had enough of being in the hospital and just wanted to go home to see his dog, or maybe the food was not up to his standards.
However, his next line stops your team dead in its tracks. “I feel like I am in Vietnam all over again. I am tied up with all these wires and feel like a prisoner! Please let me go.” It turns out that Mr. Smith had a comorbidity that was overlooked during his initial intake: posttraumatic stress disorder.
Impact of PTSD
PTSD is a diagnosis characterized by intrusive recurrent thoughts, dreams, or flashbacks that follow exposure to a traumatic event or series of events (see Table 1). While more common among veterans (for example, Vietnam veterans have an estimated lifetime prevalence of PTSD of 30.9% for men and 26.9% for women),1 a national survey of U.S. households estimated the lifetime prevalence of PTSD among adult Americans to be 6.8%.2 PTSD is often underdiagnosed and underreported by patients in the outpatient setting, leading to underrecognition and undertreatment of these patients in the inpatient setting.
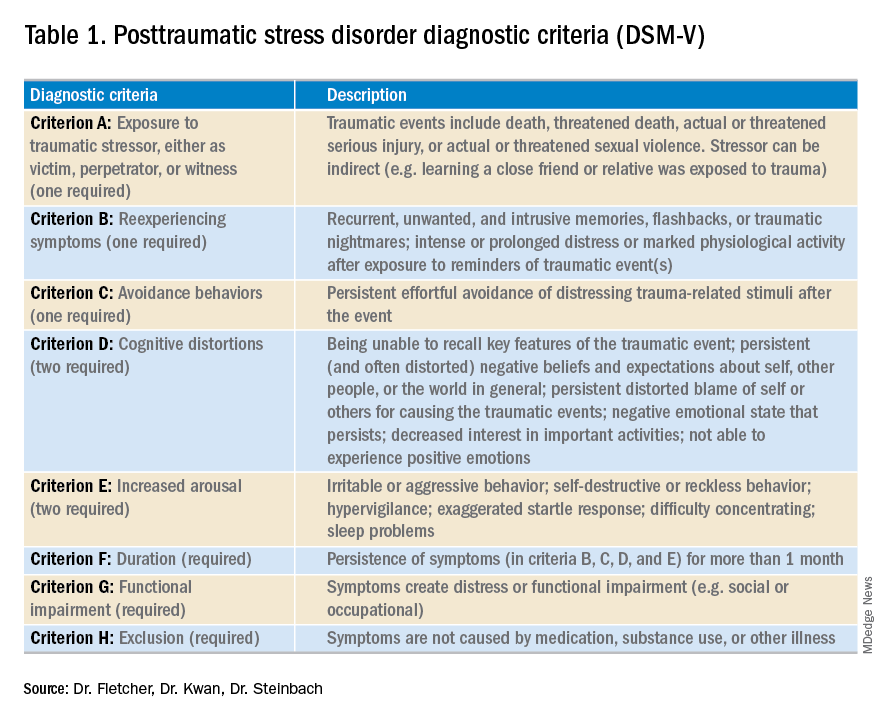
Although it may not be surprising that patients with PTSD use more mental health services, they are also more likely to use nonmental health services. In one study, total utilization of outpatient nonmental health services was 91% greater in veterans with PTSD, and these patients were three times more likely to be hospitalized than those without any mental health diagnoses.3 Additionally, they are likely to present later and stay longer when compared with patients without PTSD. One study estimated the cost of PTSD-related hospitalization in the United States from 2002 to 2011 as being $34.9 billion.4 Notably, close to 95% of hospitalizations in this study listed PTSD as a secondary rather than primary diagnosis, suggesting that the vast majority of these admitted patients are cared for by frontline providers who are not trained mental health professionals.
How PTSD manifests in the hospital
But, how exactly can the hospital environment contribute to decompensation of PTSD symptoms? Unfortunately, there is little empiric data to guide us. Based on what we do know of PTSD, we offer the following hypotheses.
Patients with PTSD may feel a loss of control or helplessness when admitted to the inpatient setting. For example, they cannot control when they receive their medications or when they get their meals. The act of showering or going outside requires approval. In addition, they might perceive they are being “ordered around” by staff and may be carted off to a study without knowing why the study is being done in the first place.
Triggers in the hospital environment may contribute to PTSD flares. Think about the loud, beeping IV pump that constantly goes off at random intervals, disrupting sleep. What about a blood draw in the early morning where the phlebotomist sticks a needle into the arm of a sleeping patient? Or the well-intentioned provider doing prerounds who wakes a sleeping patient with a shake of the shoulder or some other form of physical touch? The multidisciplinary team crowding around their hospital bed? For a patient suffering from PTSD, any of these could easily set off a cascade of escalating symptoms.
Knowing that these triggers exist, can anything be done to ameliorate their effects? We propose some practical suggestions for improving the hospital experience for patients with PTSD.
Strategies to combat PTSD in the inpatient setting
Perhaps the most practical place to start is with preserving sleep in hospitalized patients with PTSD. The majority of patients with PTSD have sleep disturbances, and interrupted sleep routines in these patients can exacerbate nightmares and underlying psychiatric issues.5 Therefore, we should strive to avoid unnecessary awakenings.
While this principle holds true for all hospitalized patients, it must be especially prioritized in patients with PTSD. Ask yourself these questions during your next admission: Must intravenous fluids run 24 hours a day, or could they be stopped at 6 p.m.? Are vital signs needed overnight? Could the last dose of furosemide occur at 4 p.m. to avoid nocturia?
Another strategy involves bedtime routines. Many of these patients may already follow a home sleep routine as part of their chronic PTSD management. To honor these habits in the hospital might mean that staff encourage turning the lights and the television off at a designated time. Additionally, the literature suggests music therapy can have a significant impact on enhanced sleep quality. When available, music therapy may reduce insomnia and decrease the amount of time prior to falling asleep.6
Other methods to counteract PTSD fall under the general principle of “trauma-informed care.” Trauma-informed care comprises practices promoting a culture of safety, empowerment, and healing.7 It is a mindful and sensitive approach that acknowledges the pervasive nature of trauma exposure, the reality of ongoing adverse effects in trauma survivors, and the fact that recovery is highly personal and complex.8
By definition, patients with PTSD have endured some traumatic event. Therefore, ideal care teams will ask patients about things that may trigger their anxiety and then work to mitigate them. For example, some patients with PTSD have a severe startle response when woken up by someone touching them. When patients feel that they can share their concerns with their care team and their team honors that observation by waking them in a different way, trust and control may be gained. This process of asking for patient guidance and adjusting accordingly is consistent with a trauma-informed care approach.9 A true trauma-informed care approach involves the entire practice environment but examining and adjusting our own behavior and assumptions are good places to start.
Summary of recommended treatments
Psychotherapy is preferable over pharmacotherapy, but both can be combined as needed. Individual trauma-focused psychotherapies utilizing a primary component of exposure and/or cognitive restructuring have strong evidence for effectiveness but are primarily outpatient based.
For pharmacologic treatment, selective serotonin reuptake inhibitors (for example, sertraline, paroxetine, or fluoxetine) and serotonin norepinephrine reuptake inhibitors (for example, venlafaxine) monotherapy have strong evidence for effectiveness and can be started while inpatient. However, these medications typically take weeks to produce benefits. Recent trials studying prazosin, an alpha1-adrenergic receptor antagonist used to alleviate nightmares associated with PTSD, have demonstrated inefficacy or even harm,leading experts to caution against its use.10,11 Finally, benzodiazepine and atypical antipsychotic usage should be restricted and used as a last resort.12
In summary, PTSD is common among veterans and nonveterans. While hospitalists may rarely admit patients because of their PTSD, they will often take care of patients who have PTSD as a comorbidity. Therefore, understanding the basics of PTSD and how hospitalization may exacerbate its symptoms can meaningfully improve care for these patients.
Dr. Fletcher is a hospitalist at the Milwaukee Veterans Affairs Medical Center and Froedtert Hospital in Wauwatosa, Wis. She is professor of internal medicine and program director for the internal medicine residency program at the Medical College of Wisconsin, Milwaukee. She is also faculty mentor for the VA’s Chief Resident for Quality and Safety. Dr. Kwan is a hospitalist at the VA San Diego Healthcare System and is associate professor at the University of California, San Diego, in the division of hospital medicine. He serves as an associate clerkship director of both the internal medicine clerkship and the medicine subinternship. He is the chair of SHM’s Physicians in Training committee. Dr. Steinbach is chief of hospital medicine at the Atlanta VA Medical Center and assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Kang HK et al. Posttraumatic stress disorder and chronic fatigue syndrome–like illness among Gulf War veterans: A population-based survey of 30,000 veterans. Am J Epidemiol. 2003;157(2):141-8.
2. Kessler RC et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005; 62(6):593-602.
3. Cohen BE et al. Mental health diagnoses and utilization of VA nonmental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18-24.
4. Haviland MG et al. Posttraumatic stress disorder–related hospitalizations in the United States (2002-2011): Rates, co-occurring illnesses, suicidal ideation/self-harm, and hospital charges. J Nerv Ment Dis. 2016; 204(2):78-86.
5. Aurora RN et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389-401.
6. Blanaru M et al. The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment Illn. 2012;4(2):e13.
7. Tello M. (2018, Oct 16). Trauma-informed care: What it is, and why it’s important. Retrieved March 18, 2019, from https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562.
8. Harris M et al. Using trauma theory to design service systems. San Francisco: 2001.
9. Substance abuse and mental health services administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS publication no. SMA 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014.
10. Raskind MA et al. Trial of prazosin for posttraumatic stress disorder in military veterans. N Engl J Med. 2018 Feb 8;378(6):507-7.
11. McCall WV et al. A pilot, randomized clinical trial of bedtime doses of prazosin versus placebo in suicidal posttraumatic stress disorder patients with nightmares. J Clin Psychopharmacol. 2018 Dec;38(6):618-21.
12. U.S. Department of Veterans Affairs/U.S. Department of Defense. Clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction 2017. Accessed February 18, 2019.
Apply for SVS Membership
The third membership deadline of 2019 is less than one month away on Sept. 1. SVS members enjoy many benefits such as SVSConnect, discounted pricing on publications and meeting registration, practice management resources and much more. Visit the membership page and start your application today. If you have any questions, please contact the SVS membership department at [email protected].
The third membership deadline of 2019 is less than one month away on Sept. 1. SVS members enjoy many benefits such as SVSConnect, discounted pricing on publications and meeting registration, practice management resources and much more. Visit the membership page and start your application today. If you have any questions, please contact the SVS membership department at [email protected].
The third membership deadline of 2019 is less than one month away on Sept. 1. SVS members enjoy many benefits such as SVSConnect, discounted pricing on publications and meeting registration, practice management resources and much more. Visit the membership page and start your application today. If you have any questions, please contact the SVS membership department at [email protected].












