User login
Pneumonia with tender, dry, crusted lips
Mycoplasma pneumoniae infection commonly manifests as an upper or lower respiratory tract infection with associated fever, dyspnea, cough, and coryza. However, patients can present with extrapulmonary complications with dermatologic findings including mucocutaneous eruptions. M. pneumoniae–associated mucocutaneous disease has prominent mucositis and typically sparse cutaneous involvement. The mucositis usually involves the lips and oral mucosa, eye conjunctivae, and nasal mucosa and can involve urogenital lesions. It predominantly is observed in children and adolescents. This condition is essentially a subtype of Stevens-Johnson syndrome, with a specific infection-associated etiology, and has been called “Mycoplasma pneumoniae–induced rash and mucositis,” shortened to “MIRM.”
Severe reactive mucocutaneous eruptions include erythema multiforme (EM), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN). While there has been semantic confusion over the years, there are some distinctive characteristics.
EM is characterized by typical three-ringed target papules that are predominantly acral in location and often without mucosal involvement. The lesions are “multiforme” in that they can appear polymorphous and evolve during an episode, with erythematous macules progressing to edematous papules, sometimes with a halo of pallor and concentric “target-like” appearance. Lesions of EM are fixed, meaning individual lesions last 7-10 days, unlike urticarial lesions that last hours. EM classically is associated with herpes simplex virus infections which usually precede its development.
SJS and TEN display atypical macules and papules which develop into erythematous vesicles, bullae, and potentially extensive desquamation, usually presenting with fever and systemic symptoms, with multiple mucosal sites involved. SJS usually is defined by having bullae restricted to less than 10% of body surface area (BSA), TEN as greater than 30% BSA, and “overlap SJS-TEN” as 20%-30% skin detachment.1 SJS and TEN commonly are induced by medications and on a spectrum of drug hypersensitivity–induced epidermal necrolysis.
MIRM has been highlighted as a distinct, common condition, usually mucous-membrane predominant with involvement of two or more mucosal sites, less than 10% total BSA, the presence of few vesiculobullous lesions or scattered atypical targets with or without targetoid lesions (without rash is called MIRM sine rash), and clinical and laboratory evidence of atypical pneumonia.2 Other infections can cause similar eruptions (for example, Chlamydia pneumoniae), and a recent proposal by the Pediatric Dermatology Research Alliance has suggested the term “Reactive Infectious Mucocutaneous Eruption” (RIME) to include MIRM and other infection-induced reactions.
Laboratory diagnosis of M. pneumoniae is via serology or polymerase chain reaction. Antibody titers begin to rise approximately 7-9 days after infection and peak at 3-4 weeks. Enzyme immunoassay is more sensitive in detecting acute infection than culture and has sensitivity comparable to the polymerase chain reaction if there has been sufficient time to develop an antibody response.
The differential diagnosis between RIME/MIRM, SJS, and TEN may be difficult to distinguish in the first few days of presentation, and consideration of infections and possible medication causes is important. DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) also is in the differential diagnosis. DRESS usually has a long latency (2-8 weeks) between drug exposure and disease onset.
Treatment of RIME/MIRM is supportive care and treatment of any underlying infection. Steroids and intravenous immune globulin (IVIG) have been used to treat reactive mucositis, as well as cyclosporine and biologic agents (such as etanercept), in an attempt to minimize the extent and duration of mucous membrane vesiculation and denudation. While these drugs may help shorten the duration of the disease course, controlled trials are lacking and there is little comparative literature on efficacy or safety of these agents.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. Dr. Bhatti is a research fellow in pediatric dermatology at Rady Children’s Hospital and the University of California, San Diego. They said they have no financial disclosures. Email Dr. Eichenfield and Dr. Bhatti at [email protected].
References
1. Arch Dermatol. 1993 Jan;129(1):92-6.
2. J Am Acad Dermatol. 2015 Feb;72(2):239-45.
Mycoplasma pneumoniae infection commonly manifests as an upper or lower respiratory tract infection with associated fever, dyspnea, cough, and coryza. However, patients can present with extrapulmonary complications with dermatologic findings including mucocutaneous eruptions. M. pneumoniae–associated mucocutaneous disease has prominent mucositis and typically sparse cutaneous involvement. The mucositis usually involves the lips and oral mucosa, eye conjunctivae, and nasal mucosa and can involve urogenital lesions. It predominantly is observed in children and adolescents. This condition is essentially a subtype of Stevens-Johnson syndrome, with a specific infection-associated etiology, and has been called “Mycoplasma pneumoniae–induced rash and mucositis,” shortened to “MIRM.”
Severe reactive mucocutaneous eruptions include erythema multiforme (EM), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN). While there has been semantic confusion over the years, there are some distinctive characteristics.
EM is characterized by typical three-ringed target papules that are predominantly acral in location and often without mucosal involvement. The lesions are “multiforme” in that they can appear polymorphous and evolve during an episode, with erythematous macules progressing to edematous papules, sometimes with a halo of pallor and concentric “target-like” appearance. Lesions of EM are fixed, meaning individual lesions last 7-10 days, unlike urticarial lesions that last hours. EM classically is associated with herpes simplex virus infections which usually precede its development.
SJS and TEN display atypical macules and papules which develop into erythematous vesicles, bullae, and potentially extensive desquamation, usually presenting with fever and systemic symptoms, with multiple mucosal sites involved. SJS usually is defined by having bullae restricted to less than 10% of body surface area (BSA), TEN as greater than 30% BSA, and “overlap SJS-TEN” as 20%-30% skin detachment.1 SJS and TEN commonly are induced by medications and on a spectrum of drug hypersensitivity–induced epidermal necrolysis.
MIRM has been highlighted as a distinct, common condition, usually mucous-membrane predominant with involvement of two or more mucosal sites, less than 10% total BSA, the presence of few vesiculobullous lesions or scattered atypical targets with or without targetoid lesions (without rash is called MIRM sine rash), and clinical and laboratory evidence of atypical pneumonia.2 Other infections can cause similar eruptions (for example, Chlamydia pneumoniae), and a recent proposal by the Pediatric Dermatology Research Alliance has suggested the term “Reactive Infectious Mucocutaneous Eruption” (RIME) to include MIRM and other infection-induced reactions.
Laboratory diagnosis of M. pneumoniae is via serology or polymerase chain reaction. Antibody titers begin to rise approximately 7-9 days after infection and peak at 3-4 weeks. Enzyme immunoassay is more sensitive in detecting acute infection than culture and has sensitivity comparable to the polymerase chain reaction if there has been sufficient time to develop an antibody response.
The differential diagnosis between RIME/MIRM, SJS, and TEN may be difficult to distinguish in the first few days of presentation, and consideration of infections and possible medication causes is important. DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) also is in the differential diagnosis. DRESS usually has a long latency (2-8 weeks) between drug exposure and disease onset.
Treatment of RIME/MIRM is supportive care and treatment of any underlying infection. Steroids and intravenous immune globulin (IVIG) have been used to treat reactive mucositis, as well as cyclosporine and biologic agents (such as etanercept), in an attempt to minimize the extent and duration of mucous membrane vesiculation and denudation. While these drugs may help shorten the duration of the disease course, controlled trials are lacking and there is little comparative literature on efficacy or safety of these agents.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. Dr. Bhatti is a research fellow in pediatric dermatology at Rady Children’s Hospital and the University of California, San Diego. They said they have no financial disclosures. Email Dr. Eichenfield and Dr. Bhatti at [email protected].
References
1. Arch Dermatol. 1993 Jan;129(1):92-6.
2. J Am Acad Dermatol. 2015 Feb;72(2):239-45.
Mycoplasma pneumoniae infection commonly manifests as an upper or lower respiratory tract infection with associated fever, dyspnea, cough, and coryza. However, patients can present with extrapulmonary complications with dermatologic findings including mucocutaneous eruptions. M. pneumoniae–associated mucocutaneous disease has prominent mucositis and typically sparse cutaneous involvement. The mucositis usually involves the lips and oral mucosa, eye conjunctivae, and nasal mucosa and can involve urogenital lesions. It predominantly is observed in children and adolescents. This condition is essentially a subtype of Stevens-Johnson syndrome, with a specific infection-associated etiology, and has been called “Mycoplasma pneumoniae–induced rash and mucositis,” shortened to “MIRM.”
Severe reactive mucocutaneous eruptions include erythema multiforme (EM), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN). While there has been semantic confusion over the years, there are some distinctive characteristics.
EM is characterized by typical three-ringed target papules that are predominantly acral in location and often without mucosal involvement. The lesions are “multiforme” in that they can appear polymorphous and evolve during an episode, with erythematous macules progressing to edematous papules, sometimes with a halo of pallor and concentric “target-like” appearance. Lesions of EM are fixed, meaning individual lesions last 7-10 days, unlike urticarial lesions that last hours. EM classically is associated with herpes simplex virus infections which usually precede its development.
SJS and TEN display atypical macules and papules which develop into erythematous vesicles, bullae, and potentially extensive desquamation, usually presenting with fever and systemic symptoms, with multiple mucosal sites involved. SJS usually is defined by having bullae restricted to less than 10% of body surface area (BSA), TEN as greater than 30% BSA, and “overlap SJS-TEN” as 20%-30% skin detachment.1 SJS and TEN commonly are induced by medications and on a spectrum of drug hypersensitivity–induced epidermal necrolysis.
MIRM has been highlighted as a distinct, common condition, usually mucous-membrane predominant with involvement of two or more mucosal sites, less than 10% total BSA, the presence of few vesiculobullous lesions or scattered atypical targets with or without targetoid lesions (without rash is called MIRM sine rash), and clinical and laboratory evidence of atypical pneumonia.2 Other infections can cause similar eruptions (for example, Chlamydia pneumoniae), and a recent proposal by the Pediatric Dermatology Research Alliance has suggested the term “Reactive Infectious Mucocutaneous Eruption” (RIME) to include MIRM and other infection-induced reactions.
Laboratory diagnosis of M. pneumoniae is via serology or polymerase chain reaction. Antibody titers begin to rise approximately 7-9 days after infection and peak at 3-4 weeks. Enzyme immunoassay is more sensitive in detecting acute infection than culture and has sensitivity comparable to the polymerase chain reaction if there has been sufficient time to develop an antibody response.
The differential diagnosis between RIME/MIRM, SJS, and TEN may be difficult to distinguish in the first few days of presentation, and consideration of infections and possible medication causes is important. DRESS syndrome (drug reaction with eosinophilia and systemic symptoms) also is in the differential diagnosis. DRESS usually has a long latency (2-8 weeks) between drug exposure and disease onset.
Treatment of RIME/MIRM is supportive care and treatment of any underlying infection. Steroids and intravenous immune globulin (IVIG) have been used to treat reactive mucositis, as well as cyclosporine and biologic agents (such as etanercept), in an attempt to minimize the extent and duration of mucous membrane vesiculation and denudation. While these drugs may help shorten the duration of the disease course, controlled trials are lacking and there is little comparative literature on efficacy or safety of these agents.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children’s Hospital–San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. Dr. Bhatti is a research fellow in pediatric dermatology at Rady Children’s Hospital and the University of California, San Diego. They said they have no financial disclosures. Email Dr. Eichenfield and Dr. Bhatti at [email protected].
References
1. Arch Dermatol. 1993 Jan;129(1):92-6.
2. J Am Acad Dermatol. 2015 Feb;72(2):239-45.
Clinical trials in sarcoma bring hope and promise
In this issue of The Sarcoma Journal, we highlight research and developments presented at the 2019 ASCO annual meeting. Despite the rarity of sarcoma, it was not lost among the thousands of abstracts, posters, and talks presented during the four-and-a-half days of the meeting.
In the past 5 years, there has been a resurgence of phase 3 clinical trials in sarcoma, including several large first-line studies comparing combination therapies to doxorubicin—the gold standard since the mid-1970s. None have shown superiority. Despite this, there has been a gradual improvement in overall survival. This is attributed to advances in the multidisciplinary management of sarcomas and available supportive care services as well as a better understanding of and emergent therapies for individual sarcoma subtypes.
In the United States, we have seen the approval of several agents in sarcoma: pazopanib, with a 3-month improvement in progression-free survival (PFS) over placebo; trabectedin in liposarcoma and leiomyosarcoma, with a 2.7-month improvement in PFS over dacarbazine; and eribulin, based on a liposarcoma subgroup analysis that showed a 7-month improvement in overall survival over dacarbazine.None of these therapies are approved in the US in the front-line setting; rather, all after a patient generally receives a doxorubicin- based therapy.
We have learned a great deal from these studies. They highlight some of the challenges in designing clinical trials in a rare and heterogeneous group of malignancies. The sarcoma community is very much focused on overcoming these challenges by designing clinical trials appropriate to the disease and the therapy that is being studied. This includes the incorporation of novel endpoints, imaging modalities, patient-reported outcome measures, and statistical methodologies to best serve the patient and to determine whether and how the therapy is helping them.
There is tremendous hope and promise in sarcoma due to significant advancements in our understanding of mesenchymal biology and of the genetic diversity in these diseases. This has led to an influx of promising agents and trials, many of which have transformed treatment paradigms on specific sarcoma subtypes. This issue provides a glimpse into the progress being made.
From Dr. Tap’s plenary presentation at ASCO 2019
In this issue of The Sarcoma Journal, we highlight research and developments presented at the 2019 ASCO annual meeting. Despite the rarity of sarcoma, it was not lost among the thousands of abstracts, posters, and talks presented during the four-and-a-half days of the meeting.
In the past 5 years, there has been a resurgence of phase 3 clinical trials in sarcoma, including several large first-line studies comparing combination therapies to doxorubicin—the gold standard since the mid-1970s. None have shown superiority. Despite this, there has been a gradual improvement in overall survival. This is attributed to advances in the multidisciplinary management of sarcomas and available supportive care services as well as a better understanding of and emergent therapies for individual sarcoma subtypes.
In the United States, we have seen the approval of several agents in sarcoma: pazopanib, with a 3-month improvement in progression-free survival (PFS) over placebo; trabectedin in liposarcoma and leiomyosarcoma, with a 2.7-month improvement in PFS over dacarbazine; and eribulin, based on a liposarcoma subgroup analysis that showed a 7-month improvement in overall survival over dacarbazine.None of these therapies are approved in the US in the front-line setting; rather, all after a patient generally receives a doxorubicin- based therapy.
We have learned a great deal from these studies. They highlight some of the challenges in designing clinical trials in a rare and heterogeneous group of malignancies. The sarcoma community is very much focused on overcoming these challenges by designing clinical trials appropriate to the disease and the therapy that is being studied. This includes the incorporation of novel endpoints, imaging modalities, patient-reported outcome measures, and statistical methodologies to best serve the patient and to determine whether and how the therapy is helping them.
There is tremendous hope and promise in sarcoma due to significant advancements in our understanding of mesenchymal biology and of the genetic diversity in these diseases. This has led to an influx of promising agents and trials, many of which have transformed treatment paradigms on specific sarcoma subtypes. This issue provides a glimpse into the progress being made.
From Dr. Tap’s plenary presentation at ASCO 2019
In this issue of The Sarcoma Journal, we highlight research and developments presented at the 2019 ASCO annual meeting. Despite the rarity of sarcoma, it was not lost among the thousands of abstracts, posters, and talks presented during the four-and-a-half days of the meeting.
In the past 5 years, there has been a resurgence of phase 3 clinical trials in sarcoma, including several large first-line studies comparing combination therapies to doxorubicin—the gold standard since the mid-1970s. None have shown superiority. Despite this, there has been a gradual improvement in overall survival. This is attributed to advances in the multidisciplinary management of sarcomas and available supportive care services as well as a better understanding of and emergent therapies for individual sarcoma subtypes.
In the United States, we have seen the approval of several agents in sarcoma: pazopanib, with a 3-month improvement in progression-free survival (PFS) over placebo; trabectedin in liposarcoma and leiomyosarcoma, with a 2.7-month improvement in PFS over dacarbazine; and eribulin, based on a liposarcoma subgroup analysis that showed a 7-month improvement in overall survival over dacarbazine.None of these therapies are approved in the US in the front-line setting; rather, all after a patient generally receives a doxorubicin- based therapy.
We have learned a great deal from these studies. They highlight some of the challenges in designing clinical trials in a rare and heterogeneous group of malignancies. The sarcoma community is very much focused on overcoming these challenges by designing clinical trials appropriate to the disease and the therapy that is being studied. This includes the incorporation of novel endpoints, imaging modalities, patient-reported outcome measures, and statistical methodologies to best serve the patient and to determine whether and how the therapy is helping them.
There is tremendous hope and promise in sarcoma due to significant advancements in our understanding of mesenchymal biology and of the genetic diversity in these diseases. This has led to an influx of promising agents and trials, many of which have transformed treatment paradigms on specific sarcoma subtypes. This issue provides a glimpse into the progress being made.
From Dr. Tap’s plenary presentation at ASCO 2019
Meta-analysis finds platelet-rich plasma may improve hair growth
Treatment with intradermal injections of autologous compared with placebo, according to a meta-analysis of seven studies.
In the report of the results, published in the Journal of Cosmetic Dermatology, Gezim Dervishi, from University Hospital Cologne (Germany), and coauthors noted that autologous PRP contains cytokines and growth factors – including platelet‐derived growth factor, vascular endothelial growth factor, and insulinlike growth factor–1 – that are believed to play a role in new hair growth. While the evidence to support the clinical efficacy of this approach is currently limited and PRP is not approved for hair-loss treatment, it is being used in clinical trials and off label for hair restoration in Europe and the United States.
The authors reviewed 13 randomized, controlled trials involving 343 people with pattern hair loss randomized to PRP control treatment, or placebo in a simple-parallel or half-head design, and assessed at 3-6 months after starting treatment. The studies were conducted in countries that included the United States, Brazil, Spain, and Italy.
The meta-analysis included seven studies that used change in hair density as the primary outcome. Six of these studies compared PRP with placebo and one compared PRP plus minoxidil or finasteride versus placebo plus minoxidil or finasteride. Five evaluated outcomes 6 months after the intervention, and two studies evaluated outcomes 3 months afterwards.
Of these seven studies, five reported statistically significant increases in hair density in favor of PRP over placebo, while the remaining two did not find any significant treatment effect. In the seven studies, the pooled mean difference in increasing hair density between treatment and placebo was 30.35 (95% confidence interval, 1.77-58.93; P less than .00001).
The 13 studies involved applications of platelet-rich plasma one to eight times over treatment periods of 1-5 months. Three studies compared PRP in conjunction with either minoxidil, finasteride, or polydeoxyribonucleotide, compared with those same therapies without PRP, and 10 studies compared PRP with either normal saline or distilled water. Five studies were judged to be at high risk of bias for at least one item, but none of these studies were included in the meta-analysis.
None of the studies identified any significant short-term treatment-related adverse effects, but the authors suggested that future studies look at potential long-term adverse effects of treatment.
“We recommend further [randomized, controlled trials] that should ensure adequate random sequence generation, adequate allocation concealment, blinding of performance and detection, and that should prevent incomplete data and selective reporting,” they wrote.
Funding and conflicts of interest statements were not available.
SOURCE: Dervishi G et al. J Cosmet Dermatol. 2019 Aug 12. doi: 10.1111/jocd.13113.
Treatment with intradermal injections of autologous compared with placebo, according to a meta-analysis of seven studies.
In the report of the results, published in the Journal of Cosmetic Dermatology, Gezim Dervishi, from University Hospital Cologne (Germany), and coauthors noted that autologous PRP contains cytokines and growth factors – including platelet‐derived growth factor, vascular endothelial growth factor, and insulinlike growth factor–1 – that are believed to play a role in new hair growth. While the evidence to support the clinical efficacy of this approach is currently limited and PRP is not approved for hair-loss treatment, it is being used in clinical trials and off label for hair restoration in Europe and the United States.
The authors reviewed 13 randomized, controlled trials involving 343 people with pattern hair loss randomized to PRP control treatment, or placebo in a simple-parallel or half-head design, and assessed at 3-6 months after starting treatment. The studies were conducted in countries that included the United States, Brazil, Spain, and Italy.
The meta-analysis included seven studies that used change in hair density as the primary outcome. Six of these studies compared PRP with placebo and one compared PRP plus minoxidil or finasteride versus placebo plus minoxidil or finasteride. Five evaluated outcomes 6 months after the intervention, and two studies evaluated outcomes 3 months afterwards.
Of these seven studies, five reported statistically significant increases in hair density in favor of PRP over placebo, while the remaining two did not find any significant treatment effect. In the seven studies, the pooled mean difference in increasing hair density between treatment and placebo was 30.35 (95% confidence interval, 1.77-58.93; P less than .00001).
The 13 studies involved applications of platelet-rich plasma one to eight times over treatment periods of 1-5 months. Three studies compared PRP in conjunction with either minoxidil, finasteride, or polydeoxyribonucleotide, compared with those same therapies without PRP, and 10 studies compared PRP with either normal saline or distilled water. Five studies were judged to be at high risk of bias for at least one item, but none of these studies were included in the meta-analysis.
None of the studies identified any significant short-term treatment-related adverse effects, but the authors suggested that future studies look at potential long-term adverse effects of treatment.
“We recommend further [randomized, controlled trials] that should ensure adequate random sequence generation, adequate allocation concealment, blinding of performance and detection, and that should prevent incomplete data and selective reporting,” they wrote.
Funding and conflicts of interest statements were not available.
SOURCE: Dervishi G et al. J Cosmet Dermatol. 2019 Aug 12. doi: 10.1111/jocd.13113.
Treatment with intradermal injections of autologous compared with placebo, according to a meta-analysis of seven studies.
In the report of the results, published in the Journal of Cosmetic Dermatology, Gezim Dervishi, from University Hospital Cologne (Germany), and coauthors noted that autologous PRP contains cytokines and growth factors – including platelet‐derived growth factor, vascular endothelial growth factor, and insulinlike growth factor–1 – that are believed to play a role in new hair growth. While the evidence to support the clinical efficacy of this approach is currently limited and PRP is not approved for hair-loss treatment, it is being used in clinical trials and off label for hair restoration in Europe and the United States.
The authors reviewed 13 randomized, controlled trials involving 343 people with pattern hair loss randomized to PRP control treatment, or placebo in a simple-parallel or half-head design, and assessed at 3-6 months after starting treatment. The studies were conducted in countries that included the United States, Brazil, Spain, and Italy.
The meta-analysis included seven studies that used change in hair density as the primary outcome. Six of these studies compared PRP with placebo and one compared PRP plus minoxidil or finasteride versus placebo plus minoxidil or finasteride. Five evaluated outcomes 6 months after the intervention, and two studies evaluated outcomes 3 months afterwards.
Of these seven studies, five reported statistically significant increases in hair density in favor of PRP over placebo, while the remaining two did not find any significant treatment effect. In the seven studies, the pooled mean difference in increasing hair density between treatment and placebo was 30.35 (95% confidence interval, 1.77-58.93; P less than .00001).
The 13 studies involved applications of platelet-rich plasma one to eight times over treatment periods of 1-5 months. Three studies compared PRP in conjunction with either minoxidil, finasteride, or polydeoxyribonucleotide, compared with those same therapies without PRP, and 10 studies compared PRP with either normal saline or distilled water. Five studies were judged to be at high risk of bias for at least one item, but none of these studies were included in the meta-analysis.
None of the studies identified any significant short-term treatment-related adverse effects, but the authors suggested that future studies look at potential long-term adverse effects of treatment.
“We recommend further [randomized, controlled trials] that should ensure adequate random sequence generation, adequate allocation concealment, blinding of performance and detection, and that should prevent incomplete data and selective reporting,” they wrote.
Funding and conflicts of interest statements were not available.
SOURCE: Dervishi G et al. J Cosmet Dermatol. 2019 Aug 12. doi: 10.1111/jocd.13113.
FROM THE JOURNAL OF COSMETIC DERMATOLOGY
Benefits of peanut desensitization may not last
based on data from a phase 2 randomized trial of individuals with confirmed peanut allergies.
Previous studies have shown that desensitization to peanuts can be successful, but sustained response to oral immunotherapy after treatment reduction or discontinuation has not been well studied, wrote R. Sharon Chinthrajah, MD, of Stanford (Calif.)University, and colleagues.
“We found that OIT with peanut was able to desensitise people with peanut allergy to 4,000 mg of peanut protein, but that discontinuation of peanut, or even a reduction to 300 mg daily, increased the likelihood of regaining clinical reactivity to peanut,” they wrote. “With peanut allergy therapies in varying stages of clinical development, and some nearing [Food and Drug Administration] approval, vital questions remain regarding the durability of treatment effects and the appropriate maintenance doses.”
In the Peanut Oral Immunotherapy Study: Safety Efficacy and Discovery (POISED), published in The Lancet, the researchers randomized 120 participants to three groups:
• 60 patients built up to a maintenance dose of 4,000 mg of peanut protein for 104 weeks followed by total discontinuation (peanut-0).
• 35 patients built up to a maintenance dose of 4,000 mg of peanut protein for 104 weeks followed by a 300-mg maintenance dose of peanut protein in the form of peanut flour (peanut-300).
• 25 patients to an oat flour placebo.
All participants were trained on how and when to use epinephrine autoinjector devices to treat allergic symptoms such as respiratory problems (cough, shortness of breath, or change in voice), widespread hives or erythema, repetitive vomiting, persistent abdominal pain, angioedema of the face, or feeling faint.
The primary outcome was passing a double-blind, placebo-controlled, food challenge (DBPCFC) to 4,000 mg of peanut protein, which was measured at baseline and at weeks 104, 117, 130, 143, and 156.
Overall, 35% of the peanut-0 group passed the challenge at 104 and 117 weeks, compared with 4% of the placebo group. At week 156 after discontinuing OIT, 13% of the peanut-0 group met the DBPCFC challenge, compared with 4% of the placebo group. However, 37% of participants randomized to a reduced peanut protein dose of 300 mg passed the challenge at 156 weeks, suggesting that more data are needed on optimal maintenance dosing strategies.
Baseline demographics were similar across all groups. The median age at study enrollment was 11 years and the median allergy duration was 9 years. The most common adverse events were mild gastrointestinal and respiratory problems. Adverse events decreased over time in all three groups.
“Higher levels of peanut-specific IgE to total IgE ratio, peanut sIgE, Ara h 1, Ara h 2, and Ara h 1 IgE to peanut-specific IgE ratio at baseline in participants were associated with increased frequencies of adverse events during active peanut OIT,” the researchers noted.
The study findings were limited by several factors including the ability of participants to tolerate 4,000 mg of peanut protein after achieving a maintenance dose but conducting serial testing only for those who passed the challenge. In addition, the results may be limited to peanut and not generalizable to other food allergies, the researchers said.
However, the results suggest that OIT remains a promising treatment for peanut allergies, and the association of biomarkers with clinical outcomes “might help the practitioner in identifying good candidates for OIT and those individuals who warrant increased vigilance against allergic reactions during OIT,” they said.
The National Institutes of Health supported the study. The researchers had no financial conflicts to disclose.
SOURCE: Chinthrajah RS et al. Lancet. 2019 Sep 12. doi: 10.1016/S0140-6736(19)31793-3.
based on data from a phase 2 randomized trial of individuals with confirmed peanut allergies.
Previous studies have shown that desensitization to peanuts can be successful, but sustained response to oral immunotherapy after treatment reduction or discontinuation has not been well studied, wrote R. Sharon Chinthrajah, MD, of Stanford (Calif.)University, and colleagues.
“We found that OIT with peanut was able to desensitise people with peanut allergy to 4,000 mg of peanut protein, but that discontinuation of peanut, or even a reduction to 300 mg daily, increased the likelihood of regaining clinical reactivity to peanut,” they wrote. “With peanut allergy therapies in varying stages of clinical development, and some nearing [Food and Drug Administration] approval, vital questions remain regarding the durability of treatment effects and the appropriate maintenance doses.”
In the Peanut Oral Immunotherapy Study: Safety Efficacy and Discovery (POISED), published in The Lancet, the researchers randomized 120 participants to three groups:
• 60 patients built up to a maintenance dose of 4,000 mg of peanut protein for 104 weeks followed by total discontinuation (peanut-0).
• 35 patients built up to a maintenance dose of 4,000 mg of peanut protein for 104 weeks followed by a 300-mg maintenance dose of peanut protein in the form of peanut flour (peanut-300).
• 25 patients to an oat flour placebo.
All participants were trained on how and when to use epinephrine autoinjector devices to treat allergic symptoms such as respiratory problems (cough, shortness of breath, or change in voice), widespread hives or erythema, repetitive vomiting, persistent abdominal pain, angioedema of the face, or feeling faint.
The primary outcome was passing a double-blind, placebo-controlled, food challenge (DBPCFC) to 4,000 mg of peanut protein, which was measured at baseline and at weeks 104, 117, 130, 143, and 156.
Overall, 35% of the peanut-0 group passed the challenge at 104 and 117 weeks, compared with 4% of the placebo group. At week 156 after discontinuing OIT, 13% of the peanut-0 group met the DBPCFC challenge, compared with 4% of the placebo group. However, 37% of participants randomized to a reduced peanut protein dose of 300 mg passed the challenge at 156 weeks, suggesting that more data are needed on optimal maintenance dosing strategies.
Baseline demographics were similar across all groups. The median age at study enrollment was 11 years and the median allergy duration was 9 years. The most common adverse events were mild gastrointestinal and respiratory problems. Adverse events decreased over time in all three groups.
“Higher levels of peanut-specific IgE to total IgE ratio, peanut sIgE, Ara h 1, Ara h 2, and Ara h 1 IgE to peanut-specific IgE ratio at baseline in participants were associated with increased frequencies of adverse events during active peanut OIT,” the researchers noted.
The study findings were limited by several factors including the ability of participants to tolerate 4,000 mg of peanut protein after achieving a maintenance dose but conducting serial testing only for those who passed the challenge. In addition, the results may be limited to peanut and not generalizable to other food allergies, the researchers said.
However, the results suggest that OIT remains a promising treatment for peanut allergies, and the association of biomarkers with clinical outcomes “might help the practitioner in identifying good candidates for OIT and those individuals who warrant increased vigilance against allergic reactions during OIT,” they said.
The National Institutes of Health supported the study. The researchers had no financial conflicts to disclose.
SOURCE: Chinthrajah RS et al. Lancet. 2019 Sep 12. doi: 10.1016/S0140-6736(19)31793-3.
based on data from a phase 2 randomized trial of individuals with confirmed peanut allergies.
Previous studies have shown that desensitization to peanuts can be successful, but sustained response to oral immunotherapy after treatment reduction or discontinuation has not been well studied, wrote R. Sharon Chinthrajah, MD, of Stanford (Calif.)University, and colleagues.
“We found that OIT with peanut was able to desensitise people with peanut allergy to 4,000 mg of peanut protein, but that discontinuation of peanut, or even a reduction to 300 mg daily, increased the likelihood of regaining clinical reactivity to peanut,” they wrote. “With peanut allergy therapies in varying stages of clinical development, and some nearing [Food and Drug Administration] approval, vital questions remain regarding the durability of treatment effects and the appropriate maintenance doses.”
In the Peanut Oral Immunotherapy Study: Safety Efficacy and Discovery (POISED), published in The Lancet, the researchers randomized 120 participants to three groups:
• 60 patients built up to a maintenance dose of 4,000 mg of peanut protein for 104 weeks followed by total discontinuation (peanut-0).
• 35 patients built up to a maintenance dose of 4,000 mg of peanut protein for 104 weeks followed by a 300-mg maintenance dose of peanut protein in the form of peanut flour (peanut-300).
• 25 patients to an oat flour placebo.
All participants were trained on how and when to use epinephrine autoinjector devices to treat allergic symptoms such as respiratory problems (cough, shortness of breath, or change in voice), widespread hives or erythema, repetitive vomiting, persistent abdominal pain, angioedema of the face, or feeling faint.
The primary outcome was passing a double-blind, placebo-controlled, food challenge (DBPCFC) to 4,000 mg of peanut protein, which was measured at baseline and at weeks 104, 117, 130, 143, and 156.
Overall, 35% of the peanut-0 group passed the challenge at 104 and 117 weeks, compared with 4% of the placebo group. At week 156 after discontinuing OIT, 13% of the peanut-0 group met the DBPCFC challenge, compared with 4% of the placebo group. However, 37% of participants randomized to a reduced peanut protein dose of 300 mg passed the challenge at 156 weeks, suggesting that more data are needed on optimal maintenance dosing strategies.
Baseline demographics were similar across all groups. The median age at study enrollment was 11 years and the median allergy duration was 9 years. The most common adverse events were mild gastrointestinal and respiratory problems. Adverse events decreased over time in all three groups.
“Higher levels of peanut-specific IgE to total IgE ratio, peanut sIgE, Ara h 1, Ara h 2, and Ara h 1 IgE to peanut-specific IgE ratio at baseline in participants were associated with increased frequencies of adverse events during active peanut OIT,” the researchers noted.
The study findings were limited by several factors including the ability of participants to tolerate 4,000 mg of peanut protein after achieving a maintenance dose but conducting serial testing only for those who passed the challenge. In addition, the results may be limited to peanut and not generalizable to other food allergies, the researchers said.
However, the results suggest that OIT remains a promising treatment for peanut allergies, and the association of biomarkers with clinical outcomes “might help the practitioner in identifying good candidates for OIT and those individuals who warrant increased vigilance against allergic reactions during OIT,” they said.
The National Institutes of Health supported the study. The researchers had no financial conflicts to disclose.
SOURCE: Chinthrajah RS et al. Lancet. 2019 Sep 12. doi: 10.1016/S0140-6736(19)31793-3.
FROM THE LANCET
Prolonged Antibiotic Treatment in Newborns May Promote Multidrug Resistance
Antibiotics given to preterm infants can set them up for health problems later in life; research has shown, including allergies, psoriasis, diabetes, and inflammatory bowel disease. Researchers who conducted a National Institutes of Health (NIH)-funded study have added to that body of knowledge with their finding that treating preterm infants with long-term antibiotics could have lasting effects by promoting multidrug-resistant gut bacteria.
They used high-speed DNA sequencing and advanced computational analysis to study stool samples from 32 infants born very preterm who received antibiotic treatment for 21 months in the hospital and after discharge, then compared those with results from 9 very preterm infants treated with antibiotics for > 1 week and 17 healthy term and late-term infants who had not received antibiotics.
The infants on long-term antibiotics had less diverse bacterial populations in their gut, and those bacteria contained more antibiotic-resistant genes.
Strikingly, the genomes of the high-antibiotic-use samples contained genes for resistance to antibiotics typically not given to newborns, such as ciprofloxacin and chloramphenicol. The researchers say this may mean that the genes originate in multidrug-resistant bacteria. Using a particular antibiotic may trigger resistance to other antibiotics even if they were not used.
“The collateral damage of early-life antibiotic treatment and hospitalization in preterm infants is long lasting,” the researchers say. They urge development of strategies to protect these highly vulnerable patients.
Antibiotics given to preterm infants can set them up for health problems later in life; research has shown, including allergies, psoriasis, diabetes, and inflammatory bowel disease. Researchers who conducted a National Institutes of Health (NIH)-funded study have added to that body of knowledge with their finding that treating preterm infants with long-term antibiotics could have lasting effects by promoting multidrug-resistant gut bacteria.
They used high-speed DNA sequencing and advanced computational analysis to study stool samples from 32 infants born very preterm who received antibiotic treatment for 21 months in the hospital and after discharge, then compared those with results from 9 very preterm infants treated with antibiotics for > 1 week and 17 healthy term and late-term infants who had not received antibiotics.
The infants on long-term antibiotics had less diverse bacterial populations in their gut, and those bacteria contained more antibiotic-resistant genes.
Strikingly, the genomes of the high-antibiotic-use samples contained genes for resistance to antibiotics typically not given to newborns, such as ciprofloxacin and chloramphenicol. The researchers say this may mean that the genes originate in multidrug-resistant bacteria. Using a particular antibiotic may trigger resistance to other antibiotics even if they were not used.
“The collateral damage of early-life antibiotic treatment and hospitalization in preterm infants is long lasting,” the researchers say. They urge development of strategies to protect these highly vulnerable patients.
Antibiotics given to preterm infants can set them up for health problems later in life; research has shown, including allergies, psoriasis, diabetes, and inflammatory bowel disease. Researchers who conducted a National Institutes of Health (NIH)-funded study have added to that body of knowledge with their finding that treating preterm infants with long-term antibiotics could have lasting effects by promoting multidrug-resistant gut bacteria.
They used high-speed DNA sequencing and advanced computational analysis to study stool samples from 32 infants born very preterm who received antibiotic treatment for 21 months in the hospital and after discharge, then compared those with results from 9 very preterm infants treated with antibiotics for > 1 week and 17 healthy term and late-term infants who had not received antibiotics.
The infants on long-term antibiotics had less diverse bacterial populations in their gut, and those bacteria contained more antibiotic-resistant genes.
Strikingly, the genomes of the high-antibiotic-use samples contained genes for resistance to antibiotics typically not given to newborns, such as ciprofloxacin and chloramphenicol. The researchers say this may mean that the genes originate in multidrug-resistant bacteria. Using a particular antibiotic may trigger resistance to other antibiotics even if they were not used.
“The collateral damage of early-life antibiotic treatment and hospitalization in preterm infants is long lasting,” the researchers say. They urge development of strategies to protect these highly vulnerable patients.
Narrative Medicine: A Re-emerging Philosophy of Patient Care
Narrative medicine (NM) centers on understanding patients’ lives, caring for the caregivers (including the clinicians), and giving voice to the suffering.1 It is an antidote for medical “progress,” which often stresses technology and pharmacologic interventions, leaving the patient out of his/her own medical story—with negative consequences.
This missing patient narrative goes beyond the template information solicited and recorded in the history of present illness (HPI) and review of systems (ROS). It is well expressed by Francis W. Peabody, MD, (1881-1927) in a published lecture for Harvard Medical School students: “One of the essential qualities of the clinician is an interest in humanity, for the secret of the care of the patient is in caring for the patient.”2
This article serves as an introduction to NM, its evolution, and its power to improve medical diagnoses and reduce clinician burnout. While its roots are in palliative and chronic care, NM has a place in the day-to-day care of patients in acute settings as well.
VIGNETTE
It’s been a busy day in clinic; the clock ticks toward closing. Scanning the monitor, you permit a brief moment of relief as you spy the perfect end-of-shift, quickie patient case: “Sore throat x 2 days,” with a rapid strep test under way. You quickly check lab coat pockets for examination tools and hasten down the hall noting age 22, white female, self-pay. Vitals reveal a low-grade fever. Maybe this sore throat will be bacterial; all the easier as there will be no need to do the “antibiotics don’t work for viruses” sermon.
You knock briefly, enter the exam room, place the laptop on the counter, and immediately recognize the patient from multiple visits over the past 2 years, mostly for gynecologic issues. You recall treating her for gonorrhea and discussing her worry about HIV. She told you that she’s a graduate student, although she is overdressed for a week night, wearing a silk blouse, short skirt, and high heels. She offers a winning smile and tells you with her pleasant accent that she is running late for an appointment.
The patient describes her symptoms: unrelenting sore throat for 2 days and pain with swallowing. She complains of feeling feverish and fatigued, with no appetite and “swollen glands.” She denies cough and runny nose; she looks and sounds exhausted. She denies smoking and excessive alcohol intake. You vaguely hone in on the accent, thinking it might be South African. Her HPI and ROS completed, you record her physical findings of pharyngeal erythema, no exudates, and moderate anterior lymphadenopathy.
You have a nagging thought about her “story.” As an urgent care clinician, you know you are likely her only health care provider and you feel some connection. It is late, and the patient is in a rush, so you promise yourself to delve deeper the next time she presents.
Continue to: You confirm the negative strep test results...
You confirm the negative strep test results and deliver the well-rehearsed sermon. She appears surprised, asking if you are sure. You suggest that she schedule a full physical in the near future. She hops off the table, heels clicking on the tile floor, as you complete your note. You do not suspect she is off to meet her scheduled man of the evening as assigned by her escort service.
Before you clock out, you check the extended patient appointment schedule and do not see her name. You vow to call her the next day and discover that she has no listed phone number. An uncomfortable feeling settles in: Are you missing something?
IN URGENT CARE
NM is an interactive patient approach more often applied to seriously ill or chronic disease patients, for whom it meaningfully supports a patient’s existence as central to the diagnostic testing and treatment of health care concerns. One can professionally debate that NM has no place in urgent care; however, this is where many patients’ acute and chronic conditions are discovered. It is where elevated blood glucose becomes type 2 diabetes and abnormal complete blood counts become blood cancer. With deeper application of NM’s principles, our simple-appearing acute pharyngitis case might have received a different workup.
NM practitioners subscribe to careful listening. Rita Charon, MD, a leading proponent of NM, describes this approach to patient care as a “rigorous intellectual and clinical discipline to fortify health care with its capacity to skillfully receive the accounts persons give of themselves—to recognize, absorb, interpret, and be moved to action by the stories of others.”3 It is a patient care revival that helps clinicians recognize and shield themselves from the powerful stampede of technology, templated patient interviews, digital documentation, and diminution of clinician and patient bonding.
The clinician in this patient encounter has functionally intact radar, sensing something awry, but communication falls short. NM’s strength is to bond the clinician to the patient, enhancing subtle, and at times pivotal, information exchange. It generates patient trust even in brief encounters, fostering improved clinical decision-making. A stronger NM focus might have encouraged this clinician to investigate more deeply the patient’s fancy clothing and surprised response to the negative strep test results by posing a simple query, such as ”What do you think might be going on?”
Continue to: MEDICAL ERROR
MEDICAL ERROR
Pharyngitis is common, making it prime territory for medical error—even for experienced clinicians—because of 3 human tendencies that NM recognizes and seeks to avoid.4 These human tendencies, insightfully delineated decades ago by experimental psychologists Amos Tversky and Daniel Kahneman, authors of Anchoring, Availability and Attribution, appear most commonly under uncertain conditions and time pressures, such as in urgent care. How does this patient encounter reflect these tendencies?5
Anchoring refers to the tendency to grasp the first symptom, physical finding, or laboratory abnormality, and hold onto it tightly.5 Such initial diagnostic impressions/information may prove true; however, other unconsidered diagnoses may include the correct one. In this encounter, the clinician entered the exam room with an early fixed diagnosis and applied the rapid strep results to diagnose viral pharyngitis. Other, conflicting hints were fleetingly noted and not addressed.
Availability refers to the tendency to assume that a quickly recalled experience explains a novel situation.5 Clinicians regularly diagnose viral pharyngitis, leading to familiarity and availability. This is contrary to NM’s view of every patient having a unique and noteworthy story.
Attribution refers to the tendency to invoke stereotypical images and assign symptoms and findings to the stereotype, which is often negative (eg, hypochondriac, drinker).5
In this encounter, the clinician would have benefited from considering other categories of diagnoses that could occur in this patient, expanding the differential diagnosis list, by soliciting a deeper patient story, fostering trust, and following clinical intuition. Had this bond been cultivated over prior visits, even in an urgent care setting, the graduate student ruse would have been discovered and the patient’s true occupation—female sex worker—revealed. The clinician would have modified the laboratory testing, discovering human herpesvirus type 8 (HHV-8) as the pharyngitis etiology, which is disproportionately linked to HIV co-infection and increases the risk for Kaposi sarcoma (KS) 20,000-fold. The prevalence of HHV-8 is 17% in the United States and is much higher (50%) in South Africa, the origin of the patient’s accent.6 Deeper patient relationships enable uncomfortable history-taking questions, with improved reliability. This missed diagnosis has wide-ranging negative consequences for the patient and her escort encounters.6
Continue to: THE FLEXNER REPORT
THE FLEXNER REPORT: NARRATIVE MEDICINE'S EXCISION
It is clear that the scientific revolution prompted the removal of NM from clinical practice. The 1910 Flexner Report, funded by the Carnegie Foundation for the Advancement of Teaching Science and authored by research scholar and physician Abraham Flexner, analyzed the functioning of 155 US and Canadian medical schools.7 His report supported the socially desirable goal of reforming medical education by exposing mediocre quality, unsavory profit motives, inadequate facilities, and nonscientific approaches, and publishing a list of those falling below the gold standard (which was the German medical education system). Harvard and Johns Hopkins received a gold seal, many other medical schools closed, and several responded to the challenge and excelled.8
Medical school curricula transitioned to exclusively theoretical and scientific teaching, objectifying values and rewarding research and efficiency. The subjective patient story was surgically excised and replaced with objective science. Not all change is good, however, and years later, Flexner reflected that scientific medicine was “sadly deficient in cultural and philosophic background.”8 His report also dramatically suppressed the use of complementary and alternative medicine and psychiatry, another medical boomerang.9 Scientific rigor is desirable—but not to the exclusion of the central patient role and other potential health care modalities.
THE PROBLEM-ORIENTED MEDICAL RECORD AND EHR
Decades after Flexner’s report on medical education curricula, another reformer, Lawrence Weed, MD, trained his eye on medical documentation’s organization and structure. He published a seminal article, “Medical Records that Guide and Teach” in the New England Journal of Medicine.10 Truly a pioneer, he demonstrated how typical medical record case documentation circa 1967 could be more efficient and espoused the problem-oriented medical record. He conceptualized designs for reorganizing medical records, prophetically promoted use of “paramedical” personnel, and encouraged computer integration.10
Coinciding with the birth of the PA profession and the recent inception of the NP profession, Weed endorsed the use of trained interviewers who would apply a “branching” question algorithm with associated computer data entry designed to protect expensive physician time. The patient story would be a jigsaw puzzle, as physicians could fill in missing information.10
Weed’s goals had merit by stressing structure for the disorganized, then-handwritten medical record, benefitting the growth of team-based patient care. However, efficiency and precision continued to marginalize a key component of the patient’s illness narrative in favor of speed, objectivity, and achievable billing essentials.11 His recommendations have eradicated the free-text box, replacing it with a selection of pull-down choices or prewritten templates. With a series of clicks, the subjective patient’s own narrative is sterilized, removing valuable details from the team’s view.11 The “s” of the Subjective Objective Assessment and Plan note is washed away (Table 1).
Continue to: Weed's clinical documentation...
Weed’s clinical documentation efficiency system caught fire. However, similar to Flexner’s later second thoughts, Weed also cast doubt on the full effect of his recommendations. In a 2009 interview conducted by a former medical student of his, Weed revealed views that more closely resemble our current competency-based medical education and stress the value of interpersonal skills in patient care12:
- Computerization of the medical record—with its vast amount of information and physician-processing capacity—“inevitably” leads to dangerous cognitive shortcuts. Medical education seeks to instill “medical knowledge and clinical judgment,” giving students “misplaced faith in the completeness and accuracy of their own intellects and is the antithesis of a truly scientific education.”12
- Medical student recruitment and instruction have long emphasized memory and regurgitation of facts, while students should be selected for their hands-on and interpersonal skills. Medical school should be “teaching a core of behavior instead of a core of knowledge.”12 These are areas in which NM helps.
FLEXNER, WEED, AND NOW, CHARON
Medicine’s history is blemished by errors, some significant. Flexner neatly compartmentalized medical education, Weed digitized the clinician/patient interaction, and Charon revitalizes the reason clinicians chose a health care profession. Charon—as a practicing internist, as well as a professor in the Department of Medicine and Executive Director of the Program in Narrative Medicine at Columbia University’s Vagelos College of Physicians and Surgeons in New York City—is fully qualified to speak to the importance of NM in medical education and medical practice. Her 2006 book reminds us that sore throats are not always simple, boring, and routine; each one is as unique as the person housing that particular pharynx.13
How does NM drive clinicians to be better, countering cognitive errors while incorporating the patient’s cultural and philosophic background? According to Charon, the NM concept results from conversation among scholars and clinicians teaching and practicing at Columbia University in early 2000, fueled by decades of insight from literature, medical (health care) humanities, ethics, health care communication, and primary care medicine.3 NM supports patient-centric teaching and care, reminding us that it combines the historical doctor-at-bedside, who exhibited careful, empathetic questioning and listening, with the benefits of modern medical science.
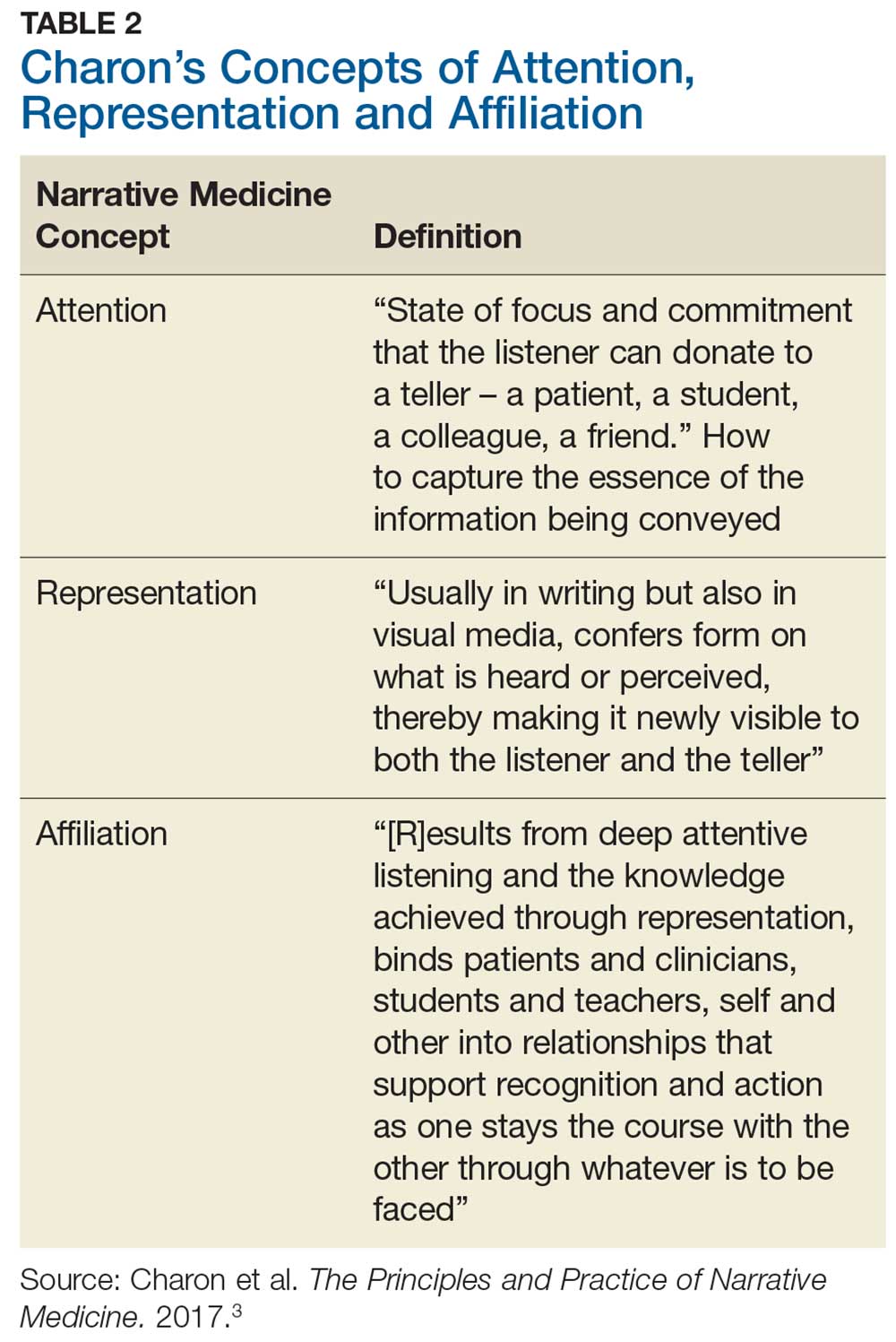
Charon describes 3 main clinician-to-patient interactions, allowing us to regain some of what we have lost: attention, representation, and affiliation (Table 2). In addition to medical error reduction, these 3 interactive behaviors counter the aforementioned 3As (anchoring, availability, and attribution) of cognitive error.5Attention initiates the clinician’s heightened and committed listening to the patient.3 In our patient encounter, essential information is undisclosed, leading to a missed diagnosis and an incomplete representation in the written note. The clinician, due to insufficient attention, missed important clues such as the patient’s dress, accent, and profession, which limited the representation. This almost seems nonsensical; who would care about a patient’s dress or accent and, of practical concern today, where would one record it? And could another urgent care clinician or specialist find these notes? How might a more serious future medical outcome be averted? Affiliation results in a connection of careful listening and full documentation as the clinician becomes invested in the whole patient, not just the sore throat.3
PREPROFESSIONAL AND PROFESSIONAL EDUCATION
Preprofessional humanities education may result in stronger NM conceptualization. The Association of American Medical Colleges (AAMC) recognizes the value of arts and humanities in medical education in developing qualities of professionalism, communication skills, and emotional intelligence in physicians. The AAMC Curriculum Inventory and Reports (2015-2016) shows that 119 medical schools require humanities education, including
- Visual arts to improve observational skills
- History education to frame modern-day Ebola outbreaks (eg, using the framework of the Black Death),
- Literature and poetry to enhance insight into different ways of living and thinking, fostering critical thinking.14
Continue to: NM has been offered in...
NM has been offered in medical schools with positive outcomes. Published results of a 2010 qualitative study of 130 Columbia University medical students who completed a required intensive half-semester of NM seminars testify to its salience.15 Students articulated NM’s importance to critical thinking and reflection, through improved attention and affiliation with their patients, improved ability to examine assumptions and develop new skills, and improved clarity of communication.15
A small number of PA programs, far fewer than medical schools, are incorporating NM coursework, through application of literature, visual media, creative writing, and other approaches based on the humanities.16 The nursing profession, which prefers the term narrative health care to narrative medicine, endorses its inclusion in nursing education. A 2018 article in Nursing Education Perspectives supports the study of humanities to complement technical competencies such as the ability to “absorb, analyze, and interpret complex artifacts” and to “participate effectively in deliberative conversations.”17
THE PRACTICING CLINICIAN: MENTAL HEALTH AND NARRATIVE MEDICINE
The value of NM extends beyond the patient to embrace caregivers as well; this is important, in light of increased attention to mental health status among clinicians. Although the term used most frequently is physician burnout, data indicate that patient management by MDs, NPs, and PAs is becoming indistinguishable—and thus risk for associated negative mental health consequences may be shared
The National Academy of Medicine is also addressing the issues of clinician well-being (see https://nam.edu/initiatives/clinician-resilience-and-well-being/). Former US Surgeon General Vivek Murthy, MD, has spoken about the epidemic of loneliness that affects clinicians. This can result from playing the physician role, lack of family support, and increased dependency on technology—yet, on a basic level, lack of interpersonal communication and connection are at the core.21 Communication between clinicians can lead to greater social cohesion and compassion, and effective uninterrupted listening and expression of their feelings helps. This begs the question: If physicians need to communicate better and practice active listening among themselves, how does this translate to the physician-to-patient bond?
THE CLINICIANS' PERSONAL BALM
Caruso Brown and Garden describe how the illness experiences of physicians, through their own reflective writing, create an empathy bridge between the professional healer and a sick patient, allowing them to be better and healthier clinicians.22 Recent best-selling physician narratives such as those by Atul Gawande,23 Siddhartha Mukherjee,24 and Paul Kalanithi25 support the similarities between the sick physician and the sick patient. Illness narratives written by physicians-turned-patients are not dissimilar to illness narratives written by patients. Reflective writing by clinicians fosters a deeper understanding not only of how patients feel, but also of the relationship they desire and deserve.22
Continue to: Writing a novel...
Writing a novel is beyond the time and ability of many clinicians. However, they can closely read literature (another NM tool), discuss books and other types of writing, participate in a book club, establish a hospital or office support group, and find a buddy or trustworthy confidant with whom to decompress and vent.3 Active journal clubs can alternate clinical guidelines with literature to expand their perspectives. An international voice, Maria Giulia Marini, Research and Health Director of the Fondazione ISTUD in Milan, Italy, and European proponent of NM, offers similar suggestions, indicating that making nonmedical works parts of a clinician’s life encourages empathy and promotes understanding between clinician and patient, as well as a holistic management approach, encourages personal and collegial reflection (eg, sharing tough experiences), sets a patient-centered agenda, and challenges the norm.26
NARRATIVE MEDICINE'S FUTURE ROLE
The field of medical humanities has experienced growth through publications, national and international conferences, and formal discussion between executives of the AAMC and the National Endowment for the Humanities to design and incorporate joint programs teaching humanities in medical schools.27 As of March 2019, there were 85 established baccalaureate health humanities programs in the US, with additional programs in development.28
Clinicians and professional organizations cannot help but see the suffering of patients, with its concomitant provider burden. The urgent care patient encounter in our example met the standard of care of the typical interaction that achieves billing protocols; the HPI, ROS, and physical exam would not raise an eyebrow. Yet, an NM approach provides more. Asking the atypical questions about accents, out-of-the-ordinary dress and behavior, and wondering about the mentioned late-night appointment attends to NM’s focused active listening, with resultant quality documentation and a whole patient encounter, even in an acute care case.
Don’t be afraid. Consider that as in novels and movies, strange things happen. The iconic book The House of God reminds clinicians that, upon hearing hoof beats, we should first think of horses—however, sometimes a zebra is correct.29 When an urgent care clinician interprets the hoof beats, a zebra may be in the differential diagnosis; in the case presented, the patient might fortunately be spared a future KS diagnosis. And the clinician may avoid personal anguish at what could have been a better outcome. NM can help clinicians remember that sore throats are as unique as people.
1. Krisberg K. Narrative medicine: Every patient has a story. AAMC News. March 28, 2018. https://news.aamc.org/medical-education/article/narrative-medicine-every-patient-has-story. Accessed October 10, 2018.
2. Peabody FW. The care of the patient. JAMA. 1927;80(12):877-882.
3. Charon R, DasGupta S, Hermann N, et al. The Principles and Practice of Narrative Medicine. New York, NY: Oxford University Press; 2017:1, 3.
4. Murphy JG , Stee LA, McAvoy MT, Oshiro J. Journal reporting of medical errors: the wisdom of Solomon, the bravery of Achilles, and the foolishness of Pan. Chest. 2007;131(3):890-896.
5. Groopman J, Hartzband P. Mindful medicine: Critical thinking leads to right diagnosis. ACP Internist. January 2008. https://acpinternist.org/archives/2008/01/groopman.htm. Accessed May 11, 2018.
6. Nzivo MM, Lwembe RM, Odari EO, Budambula NLM. Human herpes virus type 8 among female-sex workers. J Hum Virol Retrovirol 2017;5(6):00176.
7. Flexner A. Medical education in the United States and Canada—a report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. Boston, MA: DB Updike, Merrymount Press; 1910.
8. Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner Report. N Engl J Med. 2006;355(13):1339-1344.
9. Stahnisch FW, Verhoef M. The Flexner Report of 1910 and its impact on complementary and alternative medicine and psychiatry in North America in the 20th Century. Evid Based Complement Alternat Med. 2012;2012:647896.
10. Weed LL. Medical records that guide and teach. NEJM. 1968;278(12):652-657.
11. Ommaya AK, Cipriano PF, Hoyt DB, et al. Care-centered clinical documentation in the digital environment: solutions to alleviate burnout. NAM.edu/Perspectives. January 29, 2018. Accessed June 19, 2018.
12. Jacobs L. Interview with Lawrence Weed, MD - The father of the problem-oriented medical record looks ahead. The Permanente Journal. Summer 2009;13(3):84-89. https://doi.org/10.7812/TPP/09-068. Accessed August 2, 2019.
13. Charon R. Narrative Medicine: Honoring the Stories of Illness. New York, NY: Oxford University Press; 2006.
14. Mann S. Focusing on arts, humanities to develop well-rounded physicians. AAMC News. August 15, 2017. https://news.aamc.org/medical-education/article/focusing-arts-humanities-well-rounded-physicians/. Accessed Oct 10, 2018.
15. Miller E, Balmer D, Hermann N, et al. Sounding narrative medicine: studying students’ professional identity development at Columbia University College of Physicians and Surgeons. Acad Med. 2014;89(2):335-342.
16. Grant JP, Gregory T. The Sacred Seven elective: integrating the health humanities into physician assistant education. J Physician Assist Educ. 2017;28(4):220-222.
17. Lim F, Marsaglia MJ. Nursing humanities: teaching for a sense of salience. Nurs Educ Perspect. 2018;39(2):121-122.
18. Hooker RS. PAs, NPs, PAs, physicians and regression to the mean. JAAPA. 2018;31(7):13-14.
19. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;338:2272-2281.
20. Kearney MK, Weininger RB, Vachon ML, et al. Self-care of physicians caring for patients at the end of life: “Being connected … a key to my survival.” JAMA. 2009;301(11):1155–1164, E1.
21. Firth S. Former Surgeon General talks love, loneliness, and burnout: NAM panel addresses growing crisis in medicine. Medpage Today. May 4, 2018. www.medpagetoday.com/publichealthpolicy/generalprofessionalissues/72720. Accessed June 15, 2018.
22. Caruso Brown AE, Garden R. Images of healing and learning: from silence into language: Questioning the power of physician illness narratives. AMA J Ethics. 2017;19(5):501-507.
23. Gawande A. Being Mortal: Medicine and What Matters in the End. 1st ed. New York, NY: Metropolitan Books; 2014.
24. Mukherjee S. The Emperor of All Maladies: A Biography of Cancer. New York, NY: Simon & Schuster; 2010.
25. Kalanithi P. When Breath Becomes Air. New York, NY: Penguin Random House; 2016.
26. Marini MG. Narrative Medicine: Bridging the Gap Between Evidence-Based Care and Medical Humanities. Cham, Switzerland: Springer International Publishing; 2016.
27. Charon R. To see the suffering. Acad Med. 2017;92(12):1668-1670.
28. Lamb EG, Berry SL, Jones T. Health Humanities Baccalaureate Programs in the United States. Hiram, OH: Center for Literature and Medicine, Hiram College; March 2019.
29. Shem S. The House of God. New York, NY: Berkley Random House; 1978.
Narrative medicine (NM) centers on understanding patients’ lives, caring for the caregivers (including the clinicians), and giving voice to the suffering.1 It is an antidote for medical “progress,” which often stresses technology and pharmacologic interventions, leaving the patient out of his/her own medical story—with negative consequences.
This missing patient narrative goes beyond the template information solicited and recorded in the history of present illness (HPI) and review of systems (ROS). It is well expressed by Francis W. Peabody, MD, (1881-1927) in a published lecture for Harvard Medical School students: “One of the essential qualities of the clinician is an interest in humanity, for the secret of the care of the patient is in caring for the patient.”2
This article serves as an introduction to NM, its evolution, and its power to improve medical diagnoses and reduce clinician burnout. While its roots are in palliative and chronic care, NM has a place in the day-to-day care of patients in acute settings as well.
VIGNETTE
It’s been a busy day in clinic; the clock ticks toward closing. Scanning the monitor, you permit a brief moment of relief as you spy the perfect end-of-shift, quickie patient case: “Sore throat x 2 days,” with a rapid strep test under way. You quickly check lab coat pockets for examination tools and hasten down the hall noting age 22, white female, self-pay. Vitals reveal a low-grade fever. Maybe this sore throat will be bacterial; all the easier as there will be no need to do the “antibiotics don’t work for viruses” sermon.
You knock briefly, enter the exam room, place the laptop on the counter, and immediately recognize the patient from multiple visits over the past 2 years, mostly for gynecologic issues. You recall treating her for gonorrhea and discussing her worry about HIV. She told you that she’s a graduate student, although she is overdressed for a week night, wearing a silk blouse, short skirt, and high heels. She offers a winning smile and tells you with her pleasant accent that she is running late for an appointment.
The patient describes her symptoms: unrelenting sore throat for 2 days and pain with swallowing. She complains of feeling feverish and fatigued, with no appetite and “swollen glands.” She denies cough and runny nose; she looks and sounds exhausted. She denies smoking and excessive alcohol intake. You vaguely hone in on the accent, thinking it might be South African. Her HPI and ROS completed, you record her physical findings of pharyngeal erythema, no exudates, and moderate anterior lymphadenopathy.
You have a nagging thought about her “story.” As an urgent care clinician, you know you are likely her only health care provider and you feel some connection. It is late, and the patient is in a rush, so you promise yourself to delve deeper the next time she presents.
Continue to: You confirm the negative strep test results...
You confirm the negative strep test results and deliver the well-rehearsed sermon. She appears surprised, asking if you are sure. You suggest that she schedule a full physical in the near future. She hops off the table, heels clicking on the tile floor, as you complete your note. You do not suspect she is off to meet her scheduled man of the evening as assigned by her escort service.
Before you clock out, you check the extended patient appointment schedule and do not see her name. You vow to call her the next day and discover that she has no listed phone number. An uncomfortable feeling settles in: Are you missing something?
IN URGENT CARE
NM is an interactive patient approach more often applied to seriously ill or chronic disease patients, for whom it meaningfully supports a patient’s existence as central to the diagnostic testing and treatment of health care concerns. One can professionally debate that NM has no place in urgent care; however, this is where many patients’ acute and chronic conditions are discovered. It is where elevated blood glucose becomes type 2 diabetes and abnormal complete blood counts become blood cancer. With deeper application of NM’s principles, our simple-appearing acute pharyngitis case might have received a different workup.
NM practitioners subscribe to careful listening. Rita Charon, MD, a leading proponent of NM, describes this approach to patient care as a “rigorous intellectual and clinical discipline to fortify health care with its capacity to skillfully receive the accounts persons give of themselves—to recognize, absorb, interpret, and be moved to action by the stories of others.”3 It is a patient care revival that helps clinicians recognize and shield themselves from the powerful stampede of technology, templated patient interviews, digital documentation, and diminution of clinician and patient bonding.
The clinician in this patient encounter has functionally intact radar, sensing something awry, but communication falls short. NM’s strength is to bond the clinician to the patient, enhancing subtle, and at times pivotal, information exchange. It generates patient trust even in brief encounters, fostering improved clinical decision-making. A stronger NM focus might have encouraged this clinician to investigate more deeply the patient’s fancy clothing and surprised response to the negative strep test results by posing a simple query, such as ”What do you think might be going on?”
Continue to: MEDICAL ERROR
MEDICAL ERROR
Pharyngitis is common, making it prime territory for medical error—even for experienced clinicians—because of 3 human tendencies that NM recognizes and seeks to avoid.4 These human tendencies, insightfully delineated decades ago by experimental psychologists Amos Tversky and Daniel Kahneman, authors of Anchoring, Availability and Attribution, appear most commonly under uncertain conditions and time pressures, such as in urgent care. How does this patient encounter reflect these tendencies?5
Anchoring refers to the tendency to grasp the first symptom, physical finding, or laboratory abnormality, and hold onto it tightly.5 Such initial diagnostic impressions/information may prove true; however, other unconsidered diagnoses may include the correct one. In this encounter, the clinician entered the exam room with an early fixed diagnosis and applied the rapid strep results to diagnose viral pharyngitis. Other, conflicting hints were fleetingly noted and not addressed.
Availability refers to the tendency to assume that a quickly recalled experience explains a novel situation.5 Clinicians regularly diagnose viral pharyngitis, leading to familiarity and availability. This is contrary to NM’s view of every patient having a unique and noteworthy story.
Attribution refers to the tendency to invoke stereotypical images and assign symptoms and findings to the stereotype, which is often negative (eg, hypochondriac, drinker).5
In this encounter, the clinician would have benefited from considering other categories of diagnoses that could occur in this patient, expanding the differential diagnosis list, by soliciting a deeper patient story, fostering trust, and following clinical intuition. Had this bond been cultivated over prior visits, even in an urgent care setting, the graduate student ruse would have been discovered and the patient’s true occupation—female sex worker—revealed. The clinician would have modified the laboratory testing, discovering human herpesvirus type 8 (HHV-8) as the pharyngitis etiology, which is disproportionately linked to HIV co-infection and increases the risk for Kaposi sarcoma (KS) 20,000-fold. The prevalence of HHV-8 is 17% in the United States and is much higher (50%) in South Africa, the origin of the patient’s accent.6 Deeper patient relationships enable uncomfortable history-taking questions, with improved reliability. This missed diagnosis has wide-ranging negative consequences for the patient and her escort encounters.6
Continue to: THE FLEXNER REPORT
THE FLEXNER REPORT: NARRATIVE MEDICINE'S EXCISION
It is clear that the scientific revolution prompted the removal of NM from clinical practice. The 1910 Flexner Report, funded by the Carnegie Foundation for the Advancement of Teaching Science and authored by research scholar and physician Abraham Flexner, analyzed the functioning of 155 US and Canadian medical schools.7 His report supported the socially desirable goal of reforming medical education by exposing mediocre quality, unsavory profit motives, inadequate facilities, and nonscientific approaches, and publishing a list of those falling below the gold standard (which was the German medical education system). Harvard and Johns Hopkins received a gold seal, many other medical schools closed, and several responded to the challenge and excelled.8
Medical school curricula transitioned to exclusively theoretical and scientific teaching, objectifying values and rewarding research and efficiency. The subjective patient story was surgically excised and replaced with objective science. Not all change is good, however, and years later, Flexner reflected that scientific medicine was “sadly deficient in cultural and philosophic background.”8 His report also dramatically suppressed the use of complementary and alternative medicine and psychiatry, another medical boomerang.9 Scientific rigor is desirable—but not to the exclusion of the central patient role and other potential health care modalities.
THE PROBLEM-ORIENTED MEDICAL RECORD AND EHR
Decades after Flexner’s report on medical education curricula, another reformer, Lawrence Weed, MD, trained his eye on medical documentation’s organization and structure. He published a seminal article, “Medical Records that Guide and Teach” in the New England Journal of Medicine.10 Truly a pioneer, he demonstrated how typical medical record case documentation circa 1967 could be more efficient and espoused the problem-oriented medical record. He conceptualized designs for reorganizing medical records, prophetically promoted use of “paramedical” personnel, and encouraged computer integration.10
Coinciding with the birth of the PA profession and the recent inception of the NP profession, Weed endorsed the use of trained interviewers who would apply a “branching” question algorithm with associated computer data entry designed to protect expensive physician time. The patient story would be a jigsaw puzzle, as physicians could fill in missing information.10
Weed’s goals had merit by stressing structure for the disorganized, then-handwritten medical record, benefitting the growth of team-based patient care. However, efficiency and precision continued to marginalize a key component of the patient’s illness narrative in favor of speed, objectivity, and achievable billing essentials.11 His recommendations have eradicated the free-text box, replacing it with a selection of pull-down choices or prewritten templates. With a series of clicks, the subjective patient’s own narrative is sterilized, removing valuable details from the team’s view.11 The “s” of the Subjective Objective Assessment and Plan note is washed away (Table 1).
Continue to: Weed's clinical documentation...
Weed’s clinical documentation efficiency system caught fire. However, similar to Flexner’s later second thoughts, Weed also cast doubt on the full effect of his recommendations. In a 2009 interview conducted by a former medical student of his, Weed revealed views that more closely resemble our current competency-based medical education and stress the value of interpersonal skills in patient care12:
- Computerization of the medical record—with its vast amount of information and physician-processing capacity—“inevitably” leads to dangerous cognitive shortcuts. Medical education seeks to instill “medical knowledge and clinical judgment,” giving students “misplaced faith in the completeness and accuracy of their own intellects and is the antithesis of a truly scientific education.”12
- Medical student recruitment and instruction have long emphasized memory and regurgitation of facts, while students should be selected for their hands-on and interpersonal skills. Medical school should be “teaching a core of behavior instead of a core of knowledge.”12 These are areas in which NM helps.
FLEXNER, WEED, AND NOW, CHARON
Medicine’s history is blemished by errors, some significant. Flexner neatly compartmentalized medical education, Weed digitized the clinician/patient interaction, and Charon revitalizes the reason clinicians chose a health care profession. Charon—as a practicing internist, as well as a professor in the Department of Medicine and Executive Director of the Program in Narrative Medicine at Columbia University’s Vagelos College of Physicians and Surgeons in New York City—is fully qualified to speak to the importance of NM in medical education and medical practice. Her 2006 book reminds us that sore throats are not always simple, boring, and routine; each one is as unique as the person housing that particular pharynx.13
How does NM drive clinicians to be better, countering cognitive errors while incorporating the patient’s cultural and philosophic background? According to Charon, the NM concept results from conversation among scholars and clinicians teaching and practicing at Columbia University in early 2000, fueled by decades of insight from literature, medical (health care) humanities, ethics, health care communication, and primary care medicine.3 NM supports patient-centric teaching and care, reminding us that it combines the historical doctor-at-bedside, who exhibited careful, empathetic questioning and listening, with the benefits of modern medical science.
Charon describes 3 main clinician-to-patient interactions, allowing us to regain some of what we have lost: attention, representation, and affiliation (Table 2). In addition to medical error reduction, these 3 interactive behaviors counter the aforementioned 3As (anchoring, availability, and attribution) of cognitive error.5Attention initiates the clinician’s heightened and committed listening to the patient.3 In our patient encounter, essential information is undisclosed, leading to a missed diagnosis and an incomplete representation in the written note. The clinician, due to insufficient attention, missed important clues such as the patient’s dress, accent, and profession, which limited the representation. This almost seems nonsensical; who would care about a patient’s dress or accent and, of practical concern today, where would one record it? And could another urgent care clinician or specialist find these notes? How might a more serious future medical outcome be averted? Affiliation results in a connection of careful listening and full documentation as the clinician becomes invested in the whole patient, not just the sore throat.3
PREPROFESSIONAL AND PROFESSIONAL EDUCATION
Preprofessional humanities education may result in stronger NM conceptualization. The Association of American Medical Colleges (AAMC) recognizes the value of arts and humanities in medical education in developing qualities of professionalism, communication skills, and emotional intelligence in physicians. The AAMC Curriculum Inventory and Reports (2015-2016) shows that 119 medical schools require humanities education, including
- Visual arts to improve observational skills
- History education to frame modern-day Ebola outbreaks (eg, using the framework of the Black Death),
- Literature and poetry to enhance insight into different ways of living and thinking, fostering critical thinking.14
Continue to: NM has been offered in...
NM has been offered in medical schools with positive outcomes. Published results of a 2010 qualitative study of 130 Columbia University medical students who completed a required intensive half-semester of NM seminars testify to its salience.15 Students articulated NM’s importance to critical thinking and reflection, through improved attention and affiliation with their patients, improved ability to examine assumptions and develop new skills, and improved clarity of communication.15
A small number of PA programs, far fewer than medical schools, are incorporating NM coursework, through application of literature, visual media, creative writing, and other approaches based on the humanities.16 The nursing profession, which prefers the term narrative health care to narrative medicine, endorses its inclusion in nursing education. A 2018 article in Nursing Education Perspectives supports the study of humanities to complement technical competencies such as the ability to “absorb, analyze, and interpret complex artifacts” and to “participate effectively in deliberative conversations.”17
THE PRACTICING CLINICIAN: MENTAL HEALTH AND NARRATIVE MEDICINE
The value of NM extends beyond the patient to embrace caregivers as well; this is important, in light of increased attention to mental health status among clinicians. Although the term used most frequently is physician burnout, data indicate that patient management by MDs, NPs, and PAs is becoming indistinguishable—and thus risk for associated negative mental health consequences may be shared
The National Academy of Medicine is also addressing the issues of clinician well-being (see https://nam.edu/initiatives/clinician-resilience-and-well-being/). Former US Surgeon General Vivek Murthy, MD, has spoken about the epidemic of loneliness that affects clinicians. This can result from playing the physician role, lack of family support, and increased dependency on technology—yet, on a basic level, lack of interpersonal communication and connection are at the core.21 Communication between clinicians can lead to greater social cohesion and compassion, and effective uninterrupted listening and expression of their feelings helps. This begs the question: If physicians need to communicate better and practice active listening among themselves, how does this translate to the physician-to-patient bond?
THE CLINICIANS' PERSONAL BALM
Caruso Brown and Garden describe how the illness experiences of physicians, through their own reflective writing, create an empathy bridge between the professional healer and a sick patient, allowing them to be better and healthier clinicians.22 Recent best-selling physician narratives such as those by Atul Gawande,23 Siddhartha Mukherjee,24 and Paul Kalanithi25 support the similarities between the sick physician and the sick patient. Illness narratives written by physicians-turned-patients are not dissimilar to illness narratives written by patients. Reflective writing by clinicians fosters a deeper understanding not only of how patients feel, but also of the relationship they desire and deserve.22
Continue to: Writing a novel...
Writing a novel is beyond the time and ability of many clinicians. However, they can closely read literature (another NM tool), discuss books and other types of writing, participate in a book club, establish a hospital or office support group, and find a buddy or trustworthy confidant with whom to decompress and vent.3 Active journal clubs can alternate clinical guidelines with literature to expand their perspectives. An international voice, Maria Giulia Marini, Research and Health Director of the Fondazione ISTUD in Milan, Italy, and European proponent of NM, offers similar suggestions, indicating that making nonmedical works parts of a clinician’s life encourages empathy and promotes understanding between clinician and patient, as well as a holistic management approach, encourages personal and collegial reflection (eg, sharing tough experiences), sets a patient-centered agenda, and challenges the norm.26
NARRATIVE MEDICINE'S FUTURE ROLE
The field of medical humanities has experienced growth through publications, national and international conferences, and formal discussion between executives of the AAMC and the National Endowment for the Humanities to design and incorporate joint programs teaching humanities in medical schools.27 As of March 2019, there were 85 established baccalaureate health humanities programs in the US, with additional programs in development.28
Clinicians and professional organizations cannot help but see the suffering of patients, with its concomitant provider burden. The urgent care patient encounter in our example met the standard of care of the typical interaction that achieves billing protocols; the HPI, ROS, and physical exam would not raise an eyebrow. Yet, an NM approach provides more. Asking the atypical questions about accents, out-of-the-ordinary dress and behavior, and wondering about the mentioned late-night appointment attends to NM’s focused active listening, with resultant quality documentation and a whole patient encounter, even in an acute care case.
Don’t be afraid. Consider that as in novels and movies, strange things happen. The iconic book The House of God reminds clinicians that, upon hearing hoof beats, we should first think of horses—however, sometimes a zebra is correct.29 When an urgent care clinician interprets the hoof beats, a zebra may be in the differential diagnosis; in the case presented, the patient might fortunately be spared a future KS diagnosis. And the clinician may avoid personal anguish at what could have been a better outcome. NM can help clinicians remember that sore throats are as unique as people.
Narrative medicine (NM) centers on understanding patients’ lives, caring for the caregivers (including the clinicians), and giving voice to the suffering.1 It is an antidote for medical “progress,” which often stresses technology and pharmacologic interventions, leaving the patient out of his/her own medical story—with negative consequences.
This missing patient narrative goes beyond the template information solicited and recorded in the history of present illness (HPI) and review of systems (ROS). It is well expressed by Francis W. Peabody, MD, (1881-1927) in a published lecture for Harvard Medical School students: “One of the essential qualities of the clinician is an interest in humanity, for the secret of the care of the patient is in caring for the patient.”2
This article serves as an introduction to NM, its evolution, and its power to improve medical diagnoses and reduce clinician burnout. While its roots are in palliative and chronic care, NM has a place in the day-to-day care of patients in acute settings as well.
VIGNETTE
It’s been a busy day in clinic; the clock ticks toward closing. Scanning the monitor, you permit a brief moment of relief as you spy the perfect end-of-shift, quickie patient case: “Sore throat x 2 days,” with a rapid strep test under way. You quickly check lab coat pockets for examination tools and hasten down the hall noting age 22, white female, self-pay. Vitals reveal a low-grade fever. Maybe this sore throat will be bacterial; all the easier as there will be no need to do the “antibiotics don’t work for viruses” sermon.
You knock briefly, enter the exam room, place the laptop on the counter, and immediately recognize the patient from multiple visits over the past 2 years, mostly for gynecologic issues. You recall treating her for gonorrhea and discussing her worry about HIV. She told you that she’s a graduate student, although she is overdressed for a week night, wearing a silk blouse, short skirt, and high heels. She offers a winning smile and tells you with her pleasant accent that she is running late for an appointment.
The patient describes her symptoms: unrelenting sore throat for 2 days and pain with swallowing. She complains of feeling feverish and fatigued, with no appetite and “swollen glands.” She denies cough and runny nose; she looks and sounds exhausted. She denies smoking and excessive alcohol intake. You vaguely hone in on the accent, thinking it might be South African. Her HPI and ROS completed, you record her physical findings of pharyngeal erythema, no exudates, and moderate anterior lymphadenopathy.
You have a nagging thought about her “story.” As an urgent care clinician, you know you are likely her only health care provider and you feel some connection. It is late, and the patient is in a rush, so you promise yourself to delve deeper the next time she presents.
Continue to: You confirm the negative strep test results...
You confirm the negative strep test results and deliver the well-rehearsed sermon. She appears surprised, asking if you are sure. You suggest that she schedule a full physical in the near future. She hops off the table, heels clicking on the tile floor, as you complete your note. You do not suspect she is off to meet her scheduled man of the evening as assigned by her escort service.
Before you clock out, you check the extended patient appointment schedule and do not see her name. You vow to call her the next day and discover that she has no listed phone number. An uncomfortable feeling settles in: Are you missing something?
IN URGENT CARE
NM is an interactive patient approach more often applied to seriously ill or chronic disease patients, for whom it meaningfully supports a patient’s existence as central to the diagnostic testing and treatment of health care concerns. One can professionally debate that NM has no place in urgent care; however, this is where many patients’ acute and chronic conditions are discovered. It is where elevated blood glucose becomes type 2 diabetes and abnormal complete blood counts become blood cancer. With deeper application of NM’s principles, our simple-appearing acute pharyngitis case might have received a different workup.
NM practitioners subscribe to careful listening. Rita Charon, MD, a leading proponent of NM, describes this approach to patient care as a “rigorous intellectual and clinical discipline to fortify health care with its capacity to skillfully receive the accounts persons give of themselves—to recognize, absorb, interpret, and be moved to action by the stories of others.”3 It is a patient care revival that helps clinicians recognize and shield themselves from the powerful stampede of technology, templated patient interviews, digital documentation, and diminution of clinician and patient bonding.
The clinician in this patient encounter has functionally intact radar, sensing something awry, but communication falls short. NM’s strength is to bond the clinician to the patient, enhancing subtle, and at times pivotal, information exchange. It generates patient trust even in brief encounters, fostering improved clinical decision-making. A stronger NM focus might have encouraged this clinician to investigate more deeply the patient’s fancy clothing and surprised response to the negative strep test results by posing a simple query, such as ”What do you think might be going on?”
Continue to: MEDICAL ERROR
MEDICAL ERROR
Pharyngitis is common, making it prime territory for medical error—even for experienced clinicians—because of 3 human tendencies that NM recognizes and seeks to avoid.4 These human tendencies, insightfully delineated decades ago by experimental psychologists Amos Tversky and Daniel Kahneman, authors of Anchoring, Availability and Attribution, appear most commonly under uncertain conditions and time pressures, such as in urgent care. How does this patient encounter reflect these tendencies?5
Anchoring refers to the tendency to grasp the first symptom, physical finding, or laboratory abnormality, and hold onto it tightly.5 Such initial diagnostic impressions/information may prove true; however, other unconsidered diagnoses may include the correct one. In this encounter, the clinician entered the exam room with an early fixed diagnosis and applied the rapid strep results to diagnose viral pharyngitis. Other, conflicting hints were fleetingly noted and not addressed.
Availability refers to the tendency to assume that a quickly recalled experience explains a novel situation.5 Clinicians regularly diagnose viral pharyngitis, leading to familiarity and availability. This is contrary to NM’s view of every patient having a unique and noteworthy story.
Attribution refers to the tendency to invoke stereotypical images and assign symptoms and findings to the stereotype, which is often negative (eg, hypochondriac, drinker).5
In this encounter, the clinician would have benefited from considering other categories of diagnoses that could occur in this patient, expanding the differential diagnosis list, by soliciting a deeper patient story, fostering trust, and following clinical intuition. Had this bond been cultivated over prior visits, even in an urgent care setting, the graduate student ruse would have been discovered and the patient’s true occupation—female sex worker—revealed. The clinician would have modified the laboratory testing, discovering human herpesvirus type 8 (HHV-8) as the pharyngitis etiology, which is disproportionately linked to HIV co-infection and increases the risk for Kaposi sarcoma (KS) 20,000-fold. The prevalence of HHV-8 is 17% in the United States and is much higher (50%) in South Africa, the origin of the patient’s accent.6 Deeper patient relationships enable uncomfortable history-taking questions, with improved reliability. This missed diagnosis has wide-ranging negative consequences for the patient and her escort encounters.6
Continue to: THE FLEXNER REPORT
THE FLEXNER REPORT: NARRATIVE MEDICINE'S EXCISION
It is clear that the scientific revolution prompted the removal of NM from clinical practice. The 1910 Flexner Report, funded by the Carnegie Foundation for the Advancement of Teaching Science and authored by research scholar and physician Abraham Flexner, analyzed the functioning of 155 US and Canadian medical schools.7 His report supported the socially desirable goal of reforming medical education by exposing mediocre quality, unsavory profit motives, inadequate facilities, and nonscientific approaches, and publishing a list of those falling below the gold standard (which was the German medical education system). Harvard and Johns Hopkins received a gold seal, many other medical schools closed, and several responded to the challenge and excelled.8
Medical school curricula transitioned to exclusively theoretical and scientific teaching, objectifying values and rewarding research and efficiency. The subjective patient story was surgically excised and replaced with objective science. Not all change is good, however, and years later, Flexner reflected that scientific medicine was “sadly deficient in cultural and philosophic background.”8 His report also dramatically suppressed the use of complementary and alternative medicine and psychiatry, another medical boomerang.9 Scientific rigor is desirable—but not to the exclusion of the central patient role and other potential health care modalities.
THE PROBLEM-ORIENTED MEDICAL RECORD AND EHR
Decades after Flexner’s report on medical education curricula, another reformer, Lawrence Weed, MD, trained his eye on medical documentation’s organization and structure. He published a seminal article, “Medical Records that Guide and Teach” in the New England Journal of Medicine.10 Truly a pioneer, he demonstrated how typical medical record case documentation circa 1967 could be more efficient and espoused the problem-oriented medical record. He conceptualized designs for reorganizing medical records, prophetically promoted use of “paramedical” personnel, and encouraged computer integration.10
Coinciding with the birth of the PA profession and the recent inception of the NP profession, Weed endorsed the use of trained interviewers who would apply a “branching” question algorithm with associated computer data entry designed to protect expensive physician time. The patient story would be a jigsaw puzzle, as physicians could fill in missing information.10
Weed’s goals had merit by stressing structure for the disorganized, then-handwritten medical record, benefitting the growth of team-based patient care. However, efficiency and precision continued to marginalize a key component of the patient’s illness narrative in favor of speed, objectivity, and achievable billing essentials.11 His recommendations have eradicated the free-text box, replacing it with a selection of pull-down choices or prewritten templates. With a series of clicks, the subjective patient’s own narrative is sterilized, removing valuable details from the team’s view.11 The “s” of the Subjective Objective Assessment and Plan note is washed away (Table 1).
Continue to: Weed's clinical documentation...
Weed’s clinical documentation efficiency system caught fire. However, similar to Flexner’s later second thoughts, Weed also cast doubt on the full effect of his recommendations. In a 2009 interview conducted by a former medical student of his, Weed revealed views that more closely resemble our current competency-based medical education and stress the value of interpersonal skills in patient care12:
- Computerization of the medical record—with its vast amount of information and physician-processing capacity—“inevitably” leads to dangerous cognitive shortcuts. Medical education seeks to instill “medical knowledge and clinical judgment,” giving students “misplaced faith in the completeness and accuracy of their own intellects and is the antithesis of a truly scientific education.”12
- Medical student recruitment and instruction have long emphasized memory and regurgitation of facts, while students should be selected for their hands-on and interpersonal skills. Medical school should be “teaching a core of behavior instead of a core of knowledge.”12 These are areas in which NM helps.
FLEXNER, WEED, AND NOW, CHARON
Medicine’s history is blemished by errors, some significant. Flexner neatly compartmentalized medical education, Weed digitized the clinician/patient interaction, and Charon revitalizes the reason clinicians chose a health care profession. Charon—as a practicing internist, as well as a professor in the Department of Medicine and Executive Director of the Program in Narrative Medicine at Columbia University’s Vagelos College of Physicians and Surgeons in New York City—is fully qualified to speak to the importance of NM in medical education and medical practice. Her 2006 book reminds us that sore throats are not always simple, boring, and routine; each one is as unique as the person housing that particular pharynx.13
How does NM drive clinicians to be better, countering cognitive errors while incorporating the patient’s cultural and philosophic background? According to Charon, the NM concept results from conversation among scholars and clinicians teaching and practicing at Columbia University in early 2000, fueled by decades of insight from literature, medical (health care) humanities, ethics, health care communication, and primary care medicine.3 NM supports patient-centric teaching and care, reminding us that it combines the historical doctor-at-bedside, who exhibited careful, empathetic questioning and listening, with the benefits of modern medical science.
Charon describes 3 main clinician-to-patient interactions, allowing us to regain some of what we have lost: attention, representation, and affiliation (Table 2). In addition to medical error reduction, these 3 interactive behaviors counter the aforementioned 3As (anchoring, availability, and attribution) of cognitive error.5Attention initiates the clinician’s heightened and committed listening to the patient.3 In our patient encounter, essential information is undisclosed, leading to a missed diagnosis and an incomplete representation in the written note. The clinician, due to insufficient attention, missed important clues such as the patient’s dress, accent, and profession, which limited the representation. This almost seems nonsensical; who would care about a patient’s dress or accent and, of practical concern today, where would one record it? And could another urgent care clinician or specialist find these notes? How might a more serious future medical outcome be averted? Affiliation results in a connection of careful listening and full documentation as the clinician becomes invested in the whole patient, not just the sore throat.3
PREPROFESSIONAL AND PROFESSIONAL EDUCATION
Preprofessional humanities education may result in stronger NM conceptualization. The Association of American Medical Colleges (AAMC) recognizes the value of arts and humanities in medical education in developing qualities of professionalism, communication skills, and emotional intelligence in physicians. The AAMC Curriculum Inventory and Reports (2015-2016) shows that 119 medical schools require humanities education, including
- Visual arts to improve observational skills
- History education to frame modern-day Ebola outbreaks (eg, using the framework of the Black Death),
- Literature and poetry to enhance insight into different ways of living and thinking, fostering critical thinking.14
Continue to: NM has been offered in...
NM has been offered in medical schools with positive outcomes. Published results of a 2010 qualitative study of 130 Columbia University medical students who completed a required intensive half-semester of NM seminars testify to its salience.15 Students articulated NM’s importance to critical thinking and reflection, through improved attention and affiliation with their patients, improved ability to examine assumptions and develop new skills, and improved clarity of communication.15
A small number of PA programs, far fewer than medical schools, are incorporating NM coursework, through application of literature, visual media, creative writing, and other approaches based on the humanities.16 The nursing profession, which prefers the term narrative health care to narrative medicine, endorses its inclusion in nursing education. A 2018 article in Nursing Education Perspectives supports the study of humanities to complement technical competencies such as the ability to “absorb, analyze, and interpret complex artifacts” and to “participate effectively in deliberative conversations.”17
THE PRACTICING CLINICIAN: MENTAL HEALTH AND NARRATIVE MEDICINE
The value of NM extends beyond the patient to embrace caregivers as well; this is important, in light of increased attention to mental health status among clinicians. Although the term used most frequently is physician burnout, data indicate that patient management by MDs, NPs, and PAs is becoming indistinguishable—and thus risk for associated negative mental health consequences may be shared
The National Academy of Medicine is also addressing the issues of clinician well-being (see https://nam.edu/initiatives/clinician-resilience-and-well-being/). Former US Surgeon General Vivek Murthy, MD, has spoken about the epidemic of loneliness that affects clinicians. This can result from playing the physician role, lack of family support, and increased dependency on technology—yet, on a basic level, lack of interpersonal communication and connection are at the core.21 Communication between clinicians can lead to greater social cohesion and compassion, and effective uninterrupted listening and expression of their feelings helps. This begs the question: If physicians need to communicate better and practice active listening among themselves, how does this translate to the physician-to-patient bond?
THE CLINICIANS' PERSONAL BALM
Caruso Brown and Garden describe how the illness experiences of physicians, through their own reflective writing, create an empathy bridge between the professional healer and a sick patient, allowing them to be better and healthier clinicians.22 Recent best-selling physician narratives such as those by Atul Gawande,23 Siddhartha Mukherjee,24 and Paul Kalanithi25 support the similarities between the sick physician and the sick patient. Illness narratives written by physicians-turned-patients are not dissimilar to illness narratives written by patients. Reflective writing by clinicians fosters a deeper understanding not only of how patients feel, but also of the relationship they desire and deserve.22
Continue to: Writing a novel...
Writing a novel is beyond the time and ability of many clinicians. However, they can closely read literature (another NM tool), discuss books and other types of writing, participate in a book club, establish a hospital or office support group, and find a buddy or trustworthy confidant with whom to decompress and vent.3 Active journal clubs can alternate clinical guidelines with literature to expand their perspectives. An international voice, Maria Giulia Marini, Research and Health Director of the Fondazione ISTUD in Milan, Italy, and European proponent of NM, offers similar suggestions, indicating that making nonmedical works parts of a clinician’s life encourages empathy and promotes understanding between clinician and patient, as well as a holistic management approach, encourages personal and collegial reflection (eg, sharing tough experiences), sets a patient-centered agenda, and challenges the norm.26
NARRATIVE MEDICINE'S FUTURE ROLE
The field of medical humanities has experienced growth through publications, national and international conferences, and formal discussion between executives of the AAMC and the National Endowment for the Humanities to design and incorporate joint programs teaching humanities in medical schools.27 As of March 2019, there were 85 established baccalaureate health humanities programs in the US, with additional programs in development.28
Clinicians and professional organizations cannot help but see the suffering of patients, with its concomitant provider burden. The urgent care patient encounter in our example met the standard of care of the typical interaction that achieves billing protocols; the HPI, ROS, and physical exam would not raise an eyebrow. Yet, an NM approach provides more. Asking the atypical questions about accents, out-of-the-ordinary dress and behavior, and wondering about the mentioned late-night appointment attends to NM’s focused active listening, with resultant quality documentation and a whole patient encounter, even in an acute care case.
Don’t be afraid. Consider that as in novels and movies, strange things happen. The iconic book The House of God reminds clinicians that, upon hearing hoof beats, we should first think of horses—however, sometimes a zebra is correct.29 When an urgent care clinician interprets the hoof beats, a zebra may be in the differential diagnosis; in the case presented, the patient might fortunately be spared a future KS diagnosis. And the clinician may avoid personal anguish at what could have been a better outcome. NM can help clinicians remember that sore throats are as unique as people.
1. Krisberg K. Narrative medicine: Every patient has a story. AAMC News. March 28, 2018. https://news.aamc.org/medical-education/article/narrative-medicine-every-patient-has-story. Accessed October 10, 2018.
2. Peabody FW. The care of the patient. JAMA. 1927;80(12):877-882.
3. Charon R, DasGupta S, Hermann N, et al. The Principles and Practice of Narrative Medicine. New York, NY: Oxford University Press; 2017:1, 3.
4. Murphy JG , Stee LA, McAvoy MT, Oshiro J. Journal reporting of medical errors: the wisdom of Solomon, the bravery of Achilles, and the foolishness of Pan. Chest. 2007;131(3):890-896.
5. Groopman J, Hartzband P. Mindful medicine: Critical thinking leads to right diagnosis. ACP Internist. January 2008. https://acpinternist.org/archives/2008/01/groopman.htm. Accessed May 11, 2018.
6. Nzivo MM, Lwembe RM, Odari EO, Budambula NLM. Human herpes virus type 8 among female-sex workers. J Hum Virol Retrovirol 2017;5(6):00176.
7. Flexner A. Medical education in the United States and Canada—a report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. Boston, MA: DB Updike, Merrymount Press; 1910.
8. Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner Report. N Engl J Med. 2006;355(13):1339-1344.
9. Stahnisch FW, Verhoef M. The Flexner Report of 1910 and its impact on complementary and alternative medicine and psychiatry in North America in the 20th Century. Evid Based Complement Alternat Med. 2012;2012:647896.
10. Weed LL. Medical records that guide and teach. NEJM. 1968;278(12):652-657.
11. Ommaya AK, Cipriano PF, Hoyt DB, et al. Care-centered clinical documentation in the digital environment: solutions to alleviate burnout. NAM.edu/Perspectives. January 29, 2018. Accessed June 19, 2018.
12. Jacobs L. Interview with Lawrence Weed, MD - The father of the problem-oriented medical record looks ahead. The Permanente Journal. Summer 2009;13(3):84-89. https://doi.org/10.7812/TPP/09-068. Accessed August 2, 2019.
13. Charon R. Narrative Medicine: Honoring the Stories of Illness. New York, NY: Oxford University Press; 2006.
14. Mann S. Focusing on arts, humanities to develop well-rounded physicians. AAMC News. August 15, 2017. https://news.aamc.org/medical-education/article/focusing-arts-humanities-well-rounded-physicians/. Accessed Oct 10, 2018.
15. Miller E, Balmer D, Hermann N, et al. Sounding narrative medicine: studying students’ professional identity development at Columbia University College of Physicians and Surgeons. Acad Med. 2014;89(2):335-342.
16. Grant JP, Gregory T. The Sacred Seven elective: integrating the health humanities into physician assistant education. J Physician Assist Educ. 2017;28(4):220-222.
17. Lim F, Marsaglia MJ. Nursing humanities: teaching for a sense of salience. Nurs Educ Perspect. 2018;39(2):121-122.
18. Hooker RS. PAs, NPs, PAs, physicians and regression to the mean. JAAPA. 2018;31(7):13-14.
19. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;338:2272-2281.
20. Kearney MK, Weininger RB, Vachon ML, et al. Self-care of physicians caring for patients at the end of life: “Being connected … a key to my survival.” JAMA. 2009;301(11):1155–1164, E1.
21. Firth S. Former Surgeon General talks love, loneliness, and burnout: NAM panel addresses growing crisis in medicine. Medpage Today. May 4, 2018. www.medpagetoday.com/publichealthpolicy/generalprofessionalissues/72720. Accessed June 15, 2018.
22. Caruso Brown AE, Garden R. Images of healing and learning: from silence into language: Questioning the power of physician illness narratives. AMA J Ethics. 2017;19(5):501-507.
23. Gawande A. Being Mortal: Medicine and What Matters in the End. 1st ed. New York, NY: Metropolitan Books; 2014.
24. Mukherjee S. The Emperor of All Maladies: A Biography of Cancer. New York, NY: Simon & Schuster; 2010.
25. Kalanithi P. When Breath Becomes Air. New York, NY: Penguin Random House; 2016.
26. Marini MG. Narrative Medicine: Bridging the Gap Between Evidence-Based Care and Medical Humanities. Cham, Switzerland: Springer International Publishing; 2016.
27. Charon R. To see the suffering. Acad Med. 2017;92(12):1668-1670.
28. Lamb EG, Berry SL, Jones T. Health Humanities Baccalaureate Programs in the United States. Hiram, OH: Center for Literature and Medicine, Hiram College; March 2019.
29. Shem S. The House of God. New York, NY: Berkley Random House; 1978.
1. Krisberg K. Narrative medicine: Every patient has a story. AAMC News. March 28, 2018. https://news.aamc.org/medical-education/article/narrative-medicine-every-patient-has-story. Accessed October 10, 2018.
2. Peabody FW. The care of the patient. JAMA. 1927;80(12):877-882.
3. Charon R, DasGupta S, Hermann N, et al. The Principles and Practice of Narrative Medicine. New York, NY: Oxford University Press; 2017:1, 3.
4. Murphy JG , Stee LA, McAvoy MT, Oshiro J. Journal reporting of medical errors: the wisdom of Solomon, the bravery of Achilles, and the foolishness of Pan. Chest. 2007;131(3):890-896.
5. Groopman J, Hartzband P. Mindful medicine: Critical thinking leads to right diagnosis. ACP Internist. January 2008. https://acpinternist.org/archives/2008/01/groopman.htm. Accessed May 11, 2018.
6. Nzivo MM, Lwembe RM, Odari EO, Budambula NLM. Human herpes virus type 8 among female-sex workers. J Hum Virol Retrovirol 2017;5(6):00176.
7. Flexner A. Medical education in the United States and Canada—a report to the Carnegie Foundation for the Advancement of Teaching. Bulletin No. 4. Boston, MA: DB Updike, Merrymount Press; 1910.
8. Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner Report. N Engl J Med. 2006;355(13):1339-1344.
9. Stahnisch FW, Verhoef M. The Flexner Report of 1910 and its impact on complementary and alternative medicine and psychiatry in North America in the 20th Century. Evid Based Complement Alternat Med. 2012;2012:647896.
10. Weed LL. Medical records that guide and teach. NEJM. 1968;278(12):652-657.
11. Ommaya AK, Cipriano PF, Hoyt DB, et al. Care-centered clinical documentation in the digital environment: solutions to alleviate burnout. NAM.edu/Perspectives. January 29, 2018. Accessed June 19, 2018.
12. Jacobs L. Interview with Lawrence Weed, MD - The father of the problem-oriented medical record looks ahead. The Permanente Journal. Summer 2009;13(3):84-89. https://doi.org/10.7812/TPP/09-068. Accessed August 2, 2019.
13. Charon R. Narrative Medicine: Honoring the Stories of Illness. New York, NY: Oxford University Press; 2006.
14. Mann S. Focusing on arts, humanities to develop well-rounded physicians. AAMC News. August 15, 2017. https://news.aamc.org/medical-education/article/focusing-arts-humanities-well-rounded-physicians/. Accessed Oct 10, 2018.
15. Miller E, Balmer D, Hermann N, et al. Sounding narrative medicine: studying students’ professional identity development at Columbia University College of Physicians and Surgeons. Acad Med. 2014;89(2):335-342.
16. Grant JP, Gregory T. The Sacred Seven elective: integrating the health humanities into physician assistant education. J Physician Assist Educ. 2017;28(4):220-222.
17. Lim F, Marsaglia MJ. Nursing humanities: teaching for a sense of salience. Nurs Educ Perspect. 2018;39(2):121-122.
18. Hooker RS. PAs, NPs, PAs, physicians and regression to the mean. JAAPA. 2018;31(7):13-14.
19. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;338:2272-2281.
20. Kearney MK, Weininger RB, Vachon ML, et al. Self-care of physicians caring for patients at the end of life: “Being connected … a key to my survival.” JAMA. 2009;301(11):1155–1164, E1.
21. Firth S. Former Surgeon General talks love, loneliness, and burnout: NAM panel addresses growing crisis in medicine. Medpage Today. May 4, 2018. www.medpagetoday.com/publichealthpolicy/generalprofessionalissues/72720. Accessed June 15, 2018.
22. Caruso Brown AE, Garden R. Images of healing and learning: from silence into language: Questioning the power of physician illness narratives. AMA J Ethics. 2017;19(5):501-507.
23. Gawande A. Being Mortal: Medicine and What Matters in the End. 1st ed. New York, NY: Metropolitan Books; 2014.
24. Mukherjee S. The Emperor of All Maladies: A Biography of Cancer. New York, NY: Simon & Schuster; 2010.
25. Kalanithi P. When Breath Becomes Air. New York, NY: Penguin Random House; 2016.
26. Marini MG. Narrative Medicine: Bridging the Gap Between Evidence-Based Care and Medical Humanities. Cham, Switzerland: Springer International Publishing; 2016.
27. Charon R. To see the suffering. Acad Med. 2017;92(12):1668-1670.
28. Lamb EG, Berry SL, Jones T. Health Humanities Baccalaureate Programs in the United States. Hiram, OH: Center for Literature and Medicine, Hiram College; March 2019.
29. Shem S. The House of God. New York, NY: Berkley Random House; 1978.
Milrinone beats dobutamine in extending survival in HF
PHILADELPHIA – Milrinone was associated with a 50% reduction in mortality, compared with dobutamine, in patients with heart failure who were receiving home inotropes as a bridge to advanced therapies, according to results of a large U.S. registry study.
The survival profile for milrinone was more favorable than that for dobutamine across various indications for use, including bridge to transplant, bridge to mechanical support, and palliation.
The findings illustrate an “urgent need” for randomized trials that compare inotropic therapy strategies in patients with end-stage heart failure, said investigator Behram P. Mody, MD, of the division of cardiology at the University of California, San Diego, La Jolla.
“Although [there is] the possibility of selection bias and there are confounding variables, this consistent finding may reflect a true benefit of milrinone,” Dr. Mody said in a presentation at the annual scientific meeting of the Heart Failure Society of America
The evidence to support use of continuous outpatient intravenous inotropic therapy in stage D heart failure is limited and comes mainly from case series, and small, randomized trials demonstrating poor outcomes, Dr. Mody explained.
“Long-term survival associated with home inotropes in the modern era of guideline-directed medical and device therapy is poorly defined,” he said.
The retrospective study Dr. Mody presented at the meeting included 1,149 patients (mean age, 60 years; 29.9% women) who received continuous intravenous outpatient inotropic therapy (milrinone or dobutamine) from 2015 to 2017. This is possibly the largest body of data reported to date of patients receiving home inotropes, he said.
For the overall population, the estimated 1-year survival rate was 71% with milrinone, compared with 46% for dobutamine (P less than .0001), Dr. Mody reported. After adjusting for age, gender, weight, and indication, milrinone use was still significantly associated with lower mortality, compared with dobutamine (hazard ratio, 0.50; 95% confidence interval, 0.39-0.64; P less than .0001).
The survival benefit of milrinone over dobutamine was also significant in subsets of patients receiving home inotropes as bridge to transplant, bridge to mechanical support, or palliation. A similar trend, though not statistically significant, was seen for inotropes used as a bridge to decision, he added.
Mortality was generally higher in patients receiving inotropes as palliation, as opposed to bridge therapy, with 1-year survival of 55.0% and 65.6%, respectively, and median survival of 461 days and 584 days.
These findings suggest home inotropes can be “beneficial” in patients with end-stage heart failure in an era of guideline-directed medical therapy and greater defibrillator use, Dr. Mody said.
“I’m not saying that it should replace left ventricular assist devices as the bridge to transplant,” he added, “but it could be an alternative strategy for our patients.”
No funding source was given. Dr. Mody had no disclosures related to the study.
SOURCE: Mody BP et al. J Card Fail. 2019 Sep 14. doi: 10.1016/j.cardfail.2019.07.021.
PHILADELPHIA – Milrinone was associated with a 50% reduction in mortality, compared with dobutamine, in patients with heart failure who were receiving home inotropes as a bridge to advanced therapies, according to results of a large U.S. registry study.
The survival profile for milrinone was more favorable than that for dobutamine across various indications for use, including bridge to transplant, bridge to mechanical support, and palliation.
The findings illustrate an “urgent need” for randomized trials that compare inotropic therapy strategies in patients with end-stage heart failure, said investigator Behram P. Mody, MD, of the division of cardiology at the University of California, San Diego, La Jolla.
“Although [there is] the possibility of selection bias and there are confounding variables, this consistent finding may reflect a true benefit of milrinone,” Dr. Mody said in a presentation at the annual scientific meeting of the Heart Failure Society of America
The evidence to support use of continuous outpatient intravenous inotropic therapy in stage D heart failure is limited and comes mainly from case series, and small, randomized trials demonstrating poor outcomes, Dr. Mody explained.
“Long-term survival associated with home inotropes in the modern era of guideline-directed medical and device therapy is poorly defined,” he said.
The retrospective study Dr. Mody presented at the meeting included 1,149 patients (mean age, 60 years; 29.9% women) who received continuous intravenous outpatient inotropic therapy (milrinone or dobutamine) from 2015 to 2017. This is possibly the largest body of data reported to date of patients receiving home inotropes, he said.
For the overall population, the estimated 1-year survival rate was 71% with milrinone, compared with 46% for dobutamine (P less than .0001), Dr. Mody reported. After adjusting for age, gender, weight, and indication, milrinone use was still significantly associated with lower mortality, compared with dobutamine (hazard ratio, 0.50; 95% confidence interval, 0.39-0.64; P less than .0001).
The survival benefit of milrinone over dobutamine was also significant in subsets of patients receiving home inotropes as bridge to transplant, bridge to mechanical support, or palliation. A similar trend, though not statistically significant, was seen for inotropes used as a bridge to decision, he added.
Mortality was generally higher in patients receiving inotropes as palliation, as opposed to bridge therapy, with 1-year survival of 55.0% and 65.6%, respectively, and median survival of 461 days and 584 days.
These findings suggest home inotropes can be “beneficial” in patients with end-stage heart failure in an era of guideline-directed medical therapy and greater defibrillator use, Dr. Mody said.
“I’m not saying that it should replace left ventricular assist devices as the bridge to transplant,” he added, “but it could be an alternative strategy for our patients.”
No funding source was given. Dr. Mody had no disclosures related to the study.
SOURCE: Mody BP et al. J Card Fail. 2019 Sep 14. doi: 10.1016/j.cardfail.2019.07.021.
PHILADELPHIA – Milrinone was associated with a 50% reduction in mortality, compared with dobutamine, in patients with heart failure who were receiving home inotropes as a bridge to advanced therapies, according to results of a large U.S. registry study.
The survival profile for milrinone was more favorable than that for dobutamine across various indications for use, including bridge to transplant, bridge to mechanical support, and palliation.
The findings illustrate an “urgent need” for randomized trials that compare inotropic therapy strategies in patients with end-stage heart failure, said investigator Behram P. Mody, MD, of the division of cardiology at the University of California, San Diego, La Jolla.
“Although [there is] the possibility of selection bias and there are confounding variables, this consistent finding may reflect a true benefit of milrinone,” Dr. Mody said in a presentation at the annual scientific meeting of the Heart Failure Society of America
The evidence to support use of continuous outpatient intravenous inotropic therapy in stage D heart failure is limited and comes mainly from case series, and small, randomized trials demonstrating poor outcomes, Dr. Mody explained.
“Long-term survival associated with home inotropes in the modern era of guideline-directed medical and device therapy is poorly defined,” he said.
The retrospective study Dr. Mody presented at the meeting included 1,149 patients (mean age, 60 years; 29.9% women) who received continuous intravenous outpatient inotropic therapy (milrinone or dobutamine) from 2015 to 2017. This is possibly the largest body of data reported to date of patients receiving home inotropes, he said.
For the overall population, the estimated 1-year survival rate was 71% with milrinone, compared with 46% for dobutamine (P less than .0001), Dr. Mody reported. After adjusting for age, gender, weight, and indication, milrinone use was still significantly associated with lower mortality, compared with dobutamine (hazard ratio, 0.50; 95% confidence interval, 0.39-0.64; P less than .0001).
The survival benefit of milrinone over dobutamine was also significant in subsets of patients receiving home inotropes as bridge to transplant, bridge to mechanical support, or palliation. A similar trend, though not statistically significant, was seen for inotropes used as a bridge to decision, he added.
Mortality was generally higher in patients receiving inotropes as palliation, as opposed to bridge therapy, with 1-year survival of 55.0% and 65.6%, respectively, and median survival of 461 days and 584 days.
These findings suggest home inotropes can be “beneficial” in patients with end-stage heart failure in an era of guideline-directed medical therapy and greater defibrillator use, Dr. Mody said.
“I’m not saying that it should replace left ventricular assist devices as the bridge to transplant,” he added, “but it could be an alternative strategy for our patients.”
No funding source was given. Dr. Mody had no disclosures related to the study.
SOURCE: Mody BP et al. J Card Fail. 2019 Sep 14. doi: 10.1016/j.cardfail.2019.07.021.
REPORTING FROM HFSA 2019
Long-term survival in stage IV NSCLC
In this edition of “How I will treat my next patient,” I highlight two studies addressing long-term survival for patients with stage IV non–small cell lung cancer (NSCLC). One summarizes survival of patients who received nivolumab therapy in the second- or later-line setting. The other is a retrospective database query regarding whether local consolidation (LC) improves survival after systemic treatment of patients with oligometastatic NSCLC.
Nivolumab therapy
Scott J. Antonia, MD, PhD, and colleagues sought to determine the frequency of long-term survival among advanced NSCLC patients who received nivolumab in the second-line or later settings (Lancet Oncol. 2019 Aug 14. doi: 10.1016/S1470-2045[19]30407-3). They aggregated the results of four trials. Checkmate 017 and 057 were phase 3 comparisons of nivolumab with docetaxel for nonsquamous and squamous NSCLC, respectively – with crossover from docetaxel to nivolumab permitted. Checkmate 003 was a dose-escalation trial and Checkmate 063 was a phase 2 study of nivolumab in advanced, refractory squamous NSCLC. A minimum follow-up of 4 years was required.
In total, 664 patients participated in the four trials, more than 85% of whom received the fairly standard dose of 3 mg/kg every 2 weeks. In a very data-dense analysis, among all patients who received nivolumab, the 4-year overall survival was 14% (95% confidence interval, 11%-17%). Four-year overall survival was higher (19%; 95% CI, 15%-24%) in patients with at least 1% programmed death-ligand 1 (PD-L1) expression. There was no difference by histology (squamous vs. nonsquamous). Patients with Eastern Cooperative Oncology Group (ECOG) Performance Status of 0, PD-L1 greater than 10%, and absence of liver metastases were more likely to achieve 4-year overall survival.
Although progression-free survival was low (8%, overall; 19% for patients achieving complete remission or partial remission), depth of response correlated with the 4-year overall survival rate. Those patients in complete or partial remission at 6 months had an overall survival at 4 years of 56%. Stable disease at 6 months showed an overall survival at 4 years of 19%, which was superior to the results for patients with partial disease as best response (4%).
There were two treatment-related deaths with nivolumab, with no unexpected safety signals. Despite allowing continuous treatment in three of the four studies, most potentially immune-related toxic events occurred in the first 2-3 years of therapy. In the two randomized studies (017 and 057), 4-year overall survival was higher with nivolumab (14%) than with docetaxel (5%), with no overlap in the 95% confidence intervals.
What this means in practice
British prime minister, Benjamin Disraeli (and, later, Mark Twain) said, “There are three kinds of lies: lies, damned lies, and statistics.” There are no lies in Dr. Antonia’s paper, but there are plenty of statistics – which oncologists love. The reported data enable us to put some boundaries on the figures we quote when patients ask us, “How well could I do with this treatment?” Dr. Antonia’s paper significantly assists with these very practical discussions. For patients who want more detail, the boundaries can be further refined. Dr. Antonia and colleagues have given us clinical (depth of response, performance status, sites of metastasis) and molecular (proportion of cells with PD-L1) refinements to personalize our consultations with patients.
Unfortunately, the data do not allow us to predict who should not receive an immune checkpoint inhibitor and, instead, receive late-line chemotherapy or early hospice referral. The data summarize well-executed clinical trials, but it is well known that (as reported at the Quality Care Symposium 2019) NSCLC patients participating in clinical trials have significantly improved survival rates – perhaps as much as two times – compared with those not enrolled in trials. These realities, however, should not obscure the fact that immune checkpoint inhibitors are a major advance for metastatic NSCLC patients, including those who have progressed after prior treatment. They offer hope for cancer-free or cancer-controlled survival that would have properly been placed in the category of “a miracle” just a few years ago.
Local consolidation
Johannes Uhlig, MD, and colleagues analyzed 6 years of National Cancer Database records, identifying 34,887 stage IV NSCLC patients who had fewer than two distant metastatic lesions in the liver, lung, brain, or bone (JAMA Netw Open. 2019 Aug 21. doi: 10.1001/jamanetworkopen.2019.9702). Treatment groups were divided into patients who received systemic therapy alone (70.3% of the total patients), had surgical resection of the primary site plus systemic therapy (2.4%), or received external beam radiation therapy or thermal ablation (EBRT/TA) of the primary site plus systemic therapy (27.3%). Multivariable Cox proportional hazards models, incorporating a number of clinical variables, were used to compare overall survival between the three groups at a median follow-up of approximately 39 months.
They found that patients treated with surgical consolidation had a 41% lower mortality, in comparison with systemic therapy alone. EBRT/TA was also associated with lower mortality (by 5%), in comparison with systemic therapy alone, but the benefit was more nuanced. For instance, patients with squamous cell histology with low tumor bulk, low nodal burden, and fewer distant sites of disease benefited, but patients with adenocarcinoma and bulkier disease or more than two distant sites did not benefit.
The discussion emphasized all of the caveats that would be appropriate for a retrospective, telescopic record review – patient selection factors; lack of detail about systemic therapy; small numbers of patients in various subsets; exclusion of patients who had consolidative treatment of metastatic sites; and the potential for unbalanced allocation of patients with various actionable, prognostically relevant mutations. Further research, including ongoing trials such as NRG-LU002, was encouraged.
How these results influence clinical practice
Ralph R. Weichselbaum, MD, in his Karnofsky lecture at the 2018 annual meeting of the American Society of Clinical Oncology highlighted the hypothesis that metastatic tumors are enriched differentially for oligometastatic or polymetastatic miRNAs and that these miRNAs could influence future clinical behavior (J Clin Oncol. 2018;36[32]:3240-50). This work, coupled with clinical features (number of sites of disease, pace of progression) could elucidate which oligometastatic NSCLC patients might benefit from aggressive local treatment and achieve long-term, disease-free survival.
As previously reported, Daniel R. Gomez, MD, and colleagues found improved median progression-free survival (14.2 vs. 4.4 months; P = .022) and overall survival (41.2 vs. 17.0 months; P = .017) among patients with oligometastatic NSCLC who were randomized to local consolidation versus standard maintenance therapy/observation (J Clin Oncol. 8 May 2019. doi: 10. 1200/JCO.19.00201). Joshua M. Bauml and colleagues reported impressive results for systemically treated stage IV NSCLC patients who received local consolidation and checkpoint inhibitors for “oligo-remnant disease” (JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1449).
At the present time, clinical practice should remain governed by the general tendency to discourage aggressive local treatment except in highly selected cases with poorly resolved or impending life-altering symptoms. The publication by Dr. Uhlig and colleagues and the previously reported phase 2 trials, support phase 3 randomized trials of local treatment of isolated sites in oligometastatic NSCLC patients, particularly in an era of immune-based systemic treatment that offers finite potential for long-term survival.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I highlight two studies addressing long-term survival for patients with stage IV non–small cell lung cancer (NSCLC). One summarizes survival of patients who received nivolumab therapy in the second- or later-line setting. The other is a retrospective database query regarding whether local consolidation (LC) improves survival after systemic treatment of patients with oligometastatic NSCLC.
Nivolumab therapy
Scott J. Antonia, MD, PhD, and colleagues sought to determine the frequency of long-term survival among advanced NSCLC patients who received nivolumab in the second-line or later settings (Lancet Oncol. 2019 Aug 14. doi: 10.1016/S1470-2045[19]30407-3). They aggregated the results of four trials. Checkmate 017 and 057 were phase 3 comparisons of nivolumab with docetaxel for nonsquamous and squamous NSCLC, respectively – with crossover from docetaxel to nivolumab permitted. Checkmate 003 was a dose-escalation trial and Checkmate 063 was a phase 2 study of nivolumab in advanced, refractory squamous NSCLC. A minimum follow-up of 4 years was required.
In total, 664 patients participated in the four trials, more than 85% of whom received the fairly standard dose of 3 mg/kg every 2 weeks. In a very data-dense analysis, among all patients who received nivolumab, the 4-year overall survival was 14% (95% confidence interval, 11%-17%). Four-year overall survival was higher (19%; 95% CI, 15%-24%) in patients with at least 1% programmed death-ligand 1 (PD-L1) expression. There was no difference by histology (squamous vs. nonsquamous). Patients with Eastern Cooperative Oncology Group (ECOG) Performance Status of 0, PD-L1 greater than 10%, and absence of liver metastases were more likely to achieve 4-year overall survival.
Although progression-free survival was low (8%, overall; 19% for patients achieving complete remission or partial remission), depth of response correlated with the 4-year overall survival rate. Those patients in complete or partial remission at 6 months had an overall survival at 4 years of 56%. Stable disease at 6 months showed an overall survival at 4 years of 19%, which was superior to the results for patients with partial disease as best response (4%).
There were two treatment-related deaths with nivolumab, with no unexpected safety signals. Despite allowing continuous treatment in three of the four studies, most potentially immune-related toxic events occurred in the first 2-3 years of therapy. In the two randomized studies (017 and 057), 4-year overall survival was higher with nivolumab (14%) than with docetaxel (5%), with no overlap in the 95% confidence intervals.
What this means in practice
British prime minister, Benjamin Disraeli (and, later, Mark Twain) said, “There are three kinds of lies: lies, damned lies, and statistics.” There are no lies in Dr. Antonia’s paper, but there are plenty of statistics – which oncologists love. The reported data enable us to put some boundaries on the figures we quote when patients ask us, “How well could I do with this treatment?” Dr. Antonia’s paper significantly assists with these very practical discussions. For patients who want more detail, the boundaries can be further refined. Dr. Antonia and colleagues have given us clinical (depth of response, performance status, sites of metastasis) and molecular (proportion of cells with PD-L1) refinements to personalize our consultations with patients.
Unfortunately, the data do not allow us to predict who should not receive an immune checkpoint inhibitor and, instead, receive late-line chemotherapy or early hospice referral. The data summarize well-executed clinical trials, but it is well known that (as reported at the Quality Care Symposium 2019) NSCLC patients participating in clinical trials have significantly improved survival rates – perhaps as much as two times – compared with those not enrolled in trials. These realities, however, should not obscure the fact that immune checkpoint inhibitors are a major advance for metastatic NSCLC patients, including those who have progressed after prior treatment. They offer hope for cancer-free or cancer-controlled survival that would have properly been placed in the category of “a miracle” just a few years ago.
Local consolidation
Johannes Uhlig, MD, and colleagues analyzed 6 years of National Cancer Database records, identifying 34,887 stage IV NSCLC patients who had fewer than two distant metastatic lesions in the liver, lung, brain, or bone (JAMA Netw Open. 2019 Aug 21. doi: 10.1001/jamanetworkopen.2019.9702). Treatment groups were divided into patients who received systemic therapy alone (70.3% of the total patients), had surgical resection of the primary site plus systemic therapy (2.4%), or received external beam radiation therapy or thermal ablation (EBRT/TA) of the primary site plus systemic therapy (27.3%). Multivariable Cox proportional hazards models, incorporating a number of clinical variables, were used to compare overall survival between the three groups at a median follow-up of approximately 39 months.
They found that patients treated with surgical consolidation had a 41% lower mortality, in comparison with systemic therapy alone. EBRT/TA was also associated with lower mortality (by 5%), in comparison with systemic therapy alone, but the benefit was more nuanced. For instance, patients with squamous cell histology with low tumor bulk, low nodal burden, and fewer distant sites of disease benefited, but patients with adenocarcinoma and bulkier disease or more than two distant sites did not benefit.
The discussion emphasized all of the caveats that would be appropriate for a retrospective, telescopic record review – patient selection factors; lack of detail about systemic therapy; small numbers of patients in various subsets; exclusion of patients who had consolidative treatment of metastatic sites; and the potential for unbalanced allocation of patients with various actionable, prognostically relevant mutations. Further research, including ongoing trials such as NRG-LU002, was encouraged.
How these results influence clinical practice
Ralph R. Weichselbaum, MD, in his Karnofsky lecture at the 2018 annual meeting of the American Society of Clinical Oncology highlighted the hypothesis that metastatic tumors are enriched differentially for oligometastatic or polymetastatic miRNAs and that these miRNAs could influence future clinical behavior (J Clin Oncol. 2018;36[32]:3240-50). This work, coupled with clinical features (number of sites of disease, pace of progression) could elucidate which oligometastatic NSCLC patients might benefit from aggressive local treatment and achieve long-term, disease-free survival.
As previously reported, Daniel R. Gomez, MD, and colleagues found improved median progression-free survival (14.2 vs. 4.4 months; P = .022) and overall survival (41.2 vs. 17.0 months; P = .017) among patients with oligometastatic NSCLC who were randomized to local consolidation versus standard maintenance therapy/observation (J Clin Oncol. 8 May 2019. doi: 10. 1200/JCO.19.00201). Joshua M. Bauml and colleagues reported impressive results for systemically treated stage IV NSCLC patients who received local consolidation and checkpoint inhibitors for “oligo-remnant disease” (JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1449).
At the present time, clinical practice should remain governed by the general tendency to discourage aggressive local treatment except in highly selected cases with poorly resolved or impending life-altering symptoms. The publication by Dr. Uhlig and colleagues and the previously reported phase 2 trials, support phase 3 randomized trials of local treatment of isolated sites in oligometastatic NSCLC patients, particularly in an era of immune-based systemic treatment that offers finite potential for long-term survival.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I will treat my next patient,” I highlight two studies addressing long-term survival for patients with stage IV non–small cell lung cancer (NSCLC). One summarizes survival of patients who received nivolumab therapy in the second- or later-line setting. The other is a retrospective database query regarding whether local consolidation (LC) improves survival after systemic treatment of patients with oligometastatic NSCLC.
Nivolumab therapy
Scott J. Antonia, MD, PhD, and colleagues sought to determine the frequency of long-term survival among advanced NSCLC patients who received nivolumab in the second-line or later settings (Lancet Oncol. 2019 Aug 14. doi: 10.1016/S1470-2045[19]30407-3). They aggregated the results of four trials. Checkmate 017 and 057 were phase 3 comparisons of nivolumab with docetaxel for nonsquamous and squamous NSCLC, respectively – with crossover from docetaxel to nivolumab permitted. Checkmate 003 was a dose-escalation trial and Checkmate 063 was a phase 2 study of nivolumab in advanced, refractory squamous NSCLC. A minimum follow-up of 4 years was required.
In total, 664 patients participated in the four trials, more than 85% of whom received the fairly standard dose of 3 mg/kg every 2 weeks. In a very data-dense analysis, among all patients who received nivolumab, the 4-year overall survival was 14% (95% confidence interval, 11%-17%). Four-year overall survival was higher (19%; 95% CI, 15%-24%) in patients with at least 1% programmed death-ligand 1 (PD-L1) expression. There was no difference by histology (squamous vs. nonsquamous). Patients with Eastern Cooperative Oncology Group (ECOG) Performance Status of 0, PD-L1 greater than 10%, and absence of liver metastases were more likely to achieve 4-year overall survival.
Although progression-free survival was low (8%, overall; 19% for patients achieving complete remission or partial remission), depth of response correlated with the 4-year overall survival rate. Those patients in complete or partial remission at 6 months had an overall survival at 4 years of 56%. Stable disease at 6 months showed an overall survival at 4 years of 19%, which was superior to the results for patients with partial disease as best response (4%).
There were two treatment-related deaths with nivolumab, with no unexpected safety signals. Despite allowing continuous treatment in three of the four studies, most potentially immune-related toxic events occurred in the first 2-3 years of therapy. In the two randomized studies (017 and 057), 4-year overall survival was higher with nivolumab (14%) than with docetaxel (5%), with no overlap in the 95% confidence intervals.
What this means in practice
British prime minister, Benjamin Disraeli (and, later, Mark Twain) said, “There are three kinds of lies: lies, damned lies, and statistics.” There are no lies in Dr. Antonia’s paper, but there are plenty of statistics – which oncologists love. The reported data enable us to put some boundaries on the figures we quote when patients ask us, “How well could I do with this treatment?” Dr. Antonia’s paper significantly assists with these very practical discussions. For patients who want more detail, the boundaries can be further refined. Dr. Antonia and colleagues have given us clinical (depth of response, performance status, sites of metastasis) and molecular (proportion of cells with PD-L1) refinements to personalize our consultations with patients.
Unfortunately, the data do not allow us to predict who should not receive an immune checkpoint inhibitor and, instead, receive late-line chemotherapy or early hospice referral. The data summarize well-executed clinical trials, but it is well known that (as reported at the Quality Care Symposium 2019) NSCLC patients participating in clinical trials have significantly improved survival rates – perhaps as much as two times – compared with those not enrolled in trials. These realities, however, should not obscure the fact that immune checkpoint inhibitors are a major advance for metastatic NSCLC patients, including those who have progressed after prior treatment. They offer hope for cancer-free or cancer-controlled survival that would have properly been placed in the category of “a miracle” just a few years ago.
Local consolidation
Johannes Uhlig, MD, and colleagues analyzed 6 years of National Cancer Database records, identifying 34,887 stage IV NSCLC patients who had fewer than two distant metastatic lesions in the liver, lung, brain, or bone (JAMA Netw Open. 2019 Aug 21. doi: 10.1001/jamanetworkopen.2019.9702). Treatment groups were divided into patients who received systemic therapy alone (70.3% of the total patients), had surgical resection of the primary site plus systemic therapy (2.4%), or received external beam radiation therapy or thermal ablation (EBRT/TA) of the primary site plus systemic therapy (27.3%). Multivariable Cox proportional hazards models, incorporating a number of clinical variables, were used to compare overall survival between the three groups at a median follow-up of approximately 39 months.
They found that patients treated with surgical consolidation had a 41% lower mortality, in comparison with systemic therapy alone. EBRT/TA was also associated with lower mortality (by 5%), in comparison with systemic therapy alone, but the benefit was more nuanced. For instance, patients with squamous cell histology with low tumor bulk, low nodal burden, and fewer distant sites of disease benefited, but patients with adenocarcinoma and bulkier disease or more than two distant sites did not benefit.
The discussion emphasized all of the caveats that would be appropriate for a retrospective, telescopic record review – patient selection factors; lack of detail about systemic therapy; small numbers of patients in various subsets; exclusion of patients who had consolidative treatment of metastatic sites; and the potential for unbalanced allocation of patients with various actionable, prognostically relevant mutations. Further research, including ongoing trials such as NRG-LU002, was encouraged.
How these results influence clinical practice
Ralph R. Weichselbaum, MD, in his Karnofsky lecture at the 2018 annual meeting of the American Society of Clinical Oncology highlighted the hypothesis that metastatic tumors are enriched differentially for oligometastatic or polymetastatic miRNAs and that these miRNAs could influence future clinical behavior (J Clin Oncol. 2018;36[32]:3240-50). This work, coupled with clinical features (number of sites of disease, pace of progression) could elucidate which oligometastatic NSCLC patients might benefit from aggressive local treatment and achieve long-term, disease-free survival.
As previously reported, Daniel R. Gomez, MD, and colleagues found improved median progression-free survival (14.2 vs. 4.4 months; P = .022) and overall survival (41.2 vs. 17.0 months; P = .017) among patients with oligometastatic NSCLC who were randomized to local consolidation versus standard maintenance therapy/observation (J Clin Oncol. 8 May 2019. doi: 10. 1200/JCO.19.00201). Joshua M. Bauml and colleagues reported impressive results for systemically treated stage IV NSCLC patients who received local consolidation and checkpoint inhibitors for “oligo-remnant disease” (JAMA Oncol. 2019 Jul 11. doi: 10.1001/jamaoncol.2019.1449).
At the present time, clinical practice should remain governed by the general tendency to discourage aggressive local treatment except in highly selected cases with poorly resolved or impending life-altering symptoms. The publication by Dr. Uhlig and colleagues and the previously reported phase 2 trials, support phase 3 randomized trials of local treatment of isolated sites in oligometastatic NSCLC patients, particularly in an era of immune-based systemic treatment that offers finite potential for long-term survival.
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
CDC activates Emergency Operations Center to investigate vaping-associated lung injury
This move allows the CDC “to provide increased operational support” to CDC staff to meet the evolving challenges of the outbreak of vaping-related injuries and deaths, says a statement from the CDC.
“CDC has made it a priority to find out what is causing this outbreak,” noted CDC Director Robert Redfield, MD, in the statement.
The agency “continues to work closely with the U.S. Food and Drug Administration to collect information about recent e-cigarette product use, or vaping, among patients and to test the substances or chemicals within e-cigarette products used by case patients,” according to the statement.
The CDC provided email addresses and site addresses for gathering information and communicating about e-cigarettes.
Information about the collection of e-cigarettes for possible testing by FDA can be obtained through contacting [email protected].
To communicate with CDC about this public health response, clinicians and health officials can contact [email protected].
More information on the current outbreak related to e-cigarettes is available at https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
General information on electronic cigarette products, can be found at www.cdc.gov/e-cigarettes.
Individuals concerned about health risks of vaping should consider refraining from e-cigarette use while the cases of lung injury are being investigated, the CDC said.
This move allows the CDC “to provide increased operational support” to CDC staff to meet the evolving challenges of the outbreak of vaping-related injuries and deaths, says a statement from the CDC.
“CDC has made it a priority to find out what is causing this outbreak,” noted CDC Director Robert Redfield, MD, in the statement.
The agency “continues to work closely with the U.S. Food and Drug Administration to collect information about recent e-cigarette product use, or vaping, among patients and to test the substances or chemicals within e-cigarette products used by case patients,” according to the statement.
The CDC provided email addresses and site addresses for gathering information and communicating about e-cigarettes.
Information about the collection of e-cigarettes for possible testing by FDA can be obtained through contacting [email protected].
To communicate with CDC about this public health response, clinicians and health officials can contact [email protected].
More information on the current outbreak related to e-cigarettes is available at https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
General information on electronic cigarette products, can be found at www.cdc.gov/e-cigarettes.
Individuals concerned about health risks of vaping should consider refraining from e-cigarette use while the cases of lung injury are being investigated, the CDC said.
This move allows the CDC “to provide increased operational support” to CDC staff to meet the evolving challenges of the outbreak of vaping-related injuries and deaths, says a statement from the CDC.
“CDC has made it a priority to find out what is causing this outbreak,” noted CDC Director Robert Redfield, MD, in the statement.
The agency “continues to work closely with the U.S. Food and Drug Administration to collect information about recent e-cigarette product use, or vaping, among patients and to test the substances or chemicals within e-cigarette products used by case patients,” according to the statement.
The CDC provided email addresses and site addresses for gathering information and communicating about e-cigarettes.
Information about the collection of e-cigarettes for possible testing by FDA can be obtained through contacting [email protected].
To communicate with CDC about this public health response, clinicians and health officials can contact [email protected].
More information on the current outbreak related to e-cigarettes is available at https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html.
General information on electronic cigarette products, can be found at www.cdc.gov/e-cigarettes.
Individuals concerned about health risks of vaping should consider refraining from e-cigarette use while the cases of lung injury are being investigated, the CDC said.
NDMA found in samples of ranitidine, FDA says
According to the Food and Drug Administration,
“NDMA is a known environmental contaminant and found in water and foods, including meats, dairy products, and vegetables,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in a prepared statement issued on Sept. 13, 2019. “The FDA has been investigating NDMA and other nitrosamine impurities in blood pressure and heart failure medicines called Angiotensin II Receptor Blockers (ARBs) since last year. In the case of ARBs, the FDA has recommended numerous recalls as it discovered unacceptable levels of nitrosamines.”
Dr. Woodcock said that the agency is working with industry partners to determine whether the low levels of NDMA in ranitidine pose a risk to patients, and it plans to post that information when it becomes available. For now, “patients should be able to trust that their medicines are as safe as they can be and that the benefits of taking them outweigh any risk to their health,” she said. “Although NDMA may cause harm in large amounts, the levels the FDA is finding in ranitidine from preliminary tests barely exceed amounts you might expect to find in common foods.”
Dr. Woodcock emphasized that the FDA is not suggesting that individuals stop taking ranitidine at this time. “However, patients taking prescription ranitidine who wish to discontinue use should talk to their health care professional about other treatment options,” she said. “People taking OTC ranitidine could consider using other OTC medicines approved for their condition. There are multiple drugs on the market that are approved for the same or similar uses as ranitidine.”
She advised consumers and health care professionals to report any adverse reactions with ranitidine to the FDA’s MedWatch program to help the agency better understand the problem.
Visit the AGA GI Patient Center for education to share with your patients about GERD, including symptoms, testing, lifestyle modifications and drug treatments at https://www.gastro.org/practice-guidance/gi-patient-center/topic/gastroesophageal-reflux-disease-gerd.
According to the Food and Drug Administration,
“NDMA is a known environmental contaminant and found in water and foods, including meats, dairy products, and vegetables,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in a prepared statement issued on Sept. 13, 2019. “The FDA has been investigating NDMA and other nitrosamine impurities in blood pressure and heart failure medicines called Angiotensin II Receptor Blockers (ARBs) since last year. In the case of ARBs, the FDA has recommended numerous recalls as it discovered unacceptable levels of nitrosamines.”
Dr. Woodcock said that the agency is working with industry partners to determine whether the low levels of NDMA in ranitidine pose a risk to patients, and it plans to post that information when it becomes available. For now, “patients should be able to trust that their medicines are as safe as they can be and that the benefits of taking them outweigh any risk to their health,” she said. “Although NDMA may cause harm in large amounts, the levels the FDA is finding in ranitidine from preliminary tests barely exceed amounts you might expect to find in common foods.”
Dr. Woodcock emphasized that the FDA is not suggesting that individuals stop taking ranitidine at this time. “However, patients taking prescription ranitidine who wish to discontinue use should talk to their health care professional about other treatment options,” she said. “People taking OTC ranitidine could consider using other OTC medicines approved for their condition. There are multiple drugs on the market that are approved for the same or similar uses as ranitidine.”
She advised consumers and health care professionals to report any adverse reactions with ranitidine to the FDA’s MedWatch program to help the agency better understand the problem.
Visit the AGA GI Patient Center for education to share with your patients about GERD, including symptoms, testing, lifestyle modifications and drug treatments at https://www.gastro.org/practice-guidance/gi-patient-center/topic/gastroesophageal-reflux-disease-gerd.
According to the Food and Drug Administration,
“NDMA is a known environmental contaminant and found in water and foods, including meats, dairy products, and vegetables,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in a prepared statement issued on Sept. 13, 2019. “The FDA has been investigating NDMA and other nitrosamine impurities in blood pressure and heart failure medicines called Angiotensin II Receptor Blockers (ARBs) since last year. In the case of ARBs, the FDA has recommended numerous recalls as it discovered unacceptable levels of nitrosamines.”
Dr. Woodcock said that the agency is working with industry partners to determine whether the low levels of NDMA in ranitidine pose a risk to patients, and it plans to post that information when it becomes available. For now, “patients should be able to trust that their medicines are as safe as they can be and that the benefits of taking them outweigh any risk to their health,” she said. “Although NDMA may cause harm in large amounts, the levels the FDA is finding in ranitidine from preliminary tests barely exceed amounts you might expect to find in common foods.”
Dr. Woodcock emphasized that the FDA is not suggesting that individuals stop taking ranitidine at this time. “However, patients taking prescription ranitidine who wish to discontinue use should talk to their health care professional about other treatment options,” she said. “People taking OTC ranitidine could consider using other OTC medicines approved for their condition. There are multiple drugs on the market that are approved for the same or similar uses as ranitidine.”
She advised consumers and health care professionals to report any adverse reactions with ranitidine to the FDA’s MedWatch program to help the agency better understand the problem.
Visit the AGA GI Patient Center for education to share with your patients about GERD, including symptoms, testing, lifestyle modifications and drug treatments at https://www.gastro.org/practice-guidance/gi-patient-center/topic/gastroesophageal-reflux-disease-gerd.