User login
European marketing of Picato suspended while skin cancer risk reviewed
As a precaution, the European Medicines Agency (EMA) has recommended that patients stop using ingenol mebutate (Picato) while the agency continues to review the safety of the topical treatment, which is indicated for the treatment of actinic keratosis in Europe and the United States.
No such action has been taken in the United States.
The EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) is reviewing data on skin cancer in patients treated with ingenol mebutate. In a trial comparing Picato and imiquimod, skin cancer was more common in the areas treated with Picato than in areas treated with imiquimod, the statement said.
“While uncertainties remain, the EMA said in a Jan. 17 news release. “The PRAC has therefore recommended suspending the medicine’s marketing authorization as a precaution and noted that alternative treatments are available.”
FDA is looking at the situation
LEO Pharma, the company that markets Picato, announced on Jan. 9 that it was initiating voluntary withdrawal of marketing authorization and possible voluntary withdrawal of Picato in the European Union (EU) and European Economic Area (EEA). The statement says, however, that “LEO Pharma has carefully reviewed the information received from PRAC, and the company disagrees with the ongoing assessment of PRAC.” There are “no additional safety data and it is LEO Pharma’s position that there is no evidence of a causal relationship or plausible mechanism hypothesis between the use of Picato and the development of skin malignancies.” An update added to the press release on Jan. 17 restates that the company disagrees with the assessment of PRAC.
“This matter does not affect Picato in the U.S., and there are no new developments in the [United States]. Picato continues to be available to patients in the U.S. We remain in dialogue with the U.S. Food and Drug Administration about Picato in the EU/EEA,” Rhonda Sciarra, associate director of global external communications for LEO Pharma, said in an email. “We remain committed to ensuring patient safety, rigorous pharmacovigilance monitoring, and transparency,” she added.
The FDA “is gathering data and information to investigate the safety concern related to Picato,” a spokesperson for the FDA told Dermatology News. “We are committed to sharing relevant findings when we have sufficient understanding of the situation and of what actions should be taken,” he added.
Examining the data
The EMA announcement described data about the risk of skin cancer in studies of Picato. A 3-year study in 484 patients found a higher incidence of skin malignancy with ingenol mebutate than with the comparator, imiquimod. In all, 3.3% of patients developed cancer in the ingenol mebutate group, compared with 0.4% in the comparator group.
In an 8-week vehicle-controlled trial in 1,262 patients, there were more skin tumors in patients who received ingenol mebutate than in those in the vehicle arm (1.0% vs. 0.1%).
In addition, according to the EMA statement, in four trials of a related ester that included 1,234 patients, a higher incidence of skin tumors occurred with the related drug, ingenol disoxate, than with a vehicle control (7.7% vs. 2.9%). PRAC considered these data because ingenol disoxate and ingenol mebutate are closely related, the EMA said.
“Health care professionals should stop prescribing Picato and consider different treatment options while authorities review the data,” according to the European agency. “Health care professionals should advise patients to be vigilant for any skin lesions developing and to seek medical advice promptly should any occur,” the statement adds.
Picato has been authorized in the EU since 2012, and the FDA approved Picato the same year. Patients have received about 2.8 million treatment courses in that time, according to the LEO Pharma press release.
As a precaution, the European Medicines Agency (EMA) has recommended that patients stop using ingenol mebutate (Picato) while the agency continues to review the safety of the topical treatment, which is indicated for the treatment of actinic keratosis in Europe and the United States.
No such action has been taken in the United States.
The EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) is reviewing data on skin cancer in patients treated with ingenol mebutate. In a trial comparing Picato and imiquimod, skin cancer was more common in the areas treated with Picato than in areas treated with imiquimod, the statement said.
“While uncertainties remain, the EMA said in a Jan. 17 news release. “The PRAC has therefore recommended suspending the medicine’s marketing authorization as a precaution and noted that alternative treatments are available.”
FDA is looking at the situation
LEO Pharma, the company that markets Picato, announced on Jan. 9 that it was initiating voluntary withdrawal of marketing authorization and possible voluntary withdrawal of Picato in the European Union (EU) and European Economic Area (EEA). The statement says, however, that “LEO Pharma has carefully reviewed the information received from PRAC, and the company disagrees with the ongoing assessment of PRAC.” There are “no additional safety data and it is LEO Pharma’s position that there is no evidence of a causal relationship or plausible mechanism hypothesis between the use of Picato and the development of skin malignancies.” An update added to the press release on Jan. 17 restates that the company disagrees with the assessment of PRAC.
“This matter does not affect Picato in the U.S., and there are no new developments in the [United States]. Picato continues to be available to patients in the U.S. We remain in dialogue with the U.S. Food and Drug Administration about Picato in the EU/EEA,” Rhonda Sciarra, associate director of global external communications for LEO Pharma, said in an email. “We remain committed to ensuring patient safety, rigorous pharmacovigilance monitoring, and transparency,” she added.
The FDA “is gathering data and information to investigate the safety concern related to Picato,” a spokesperson for the FDA told Dermatology News. “We are committed to sharing relevant findings when we have sufficient understanding of the situation and of what actions should be taken,” he added.
Examining the data
The EMA announcement described data about the risk of skin cancer in studies of Picato. A 3-year study in 484 patients found a higher incidence of skin malignancy with ingenol mebutate than with the comparator, imiquimod. In all, 3.3% of patients developed cancer in the ingenol mebutate group, compared with 0.4% in the comparator group.
In an 8-week vehicle-controlled trial in 1,262 patients, there were more skin tumors in patients who received ingenol mebutate than in those in the vehicle arm (1.0% vs. 0.1%).
In addition, according to the EMA statement, in four trials of a related ester that included 1,234 patients, a higher incidence of skin tumors occurred with the related drug, ingenol disoxate, than with a vehicle control (7.7% vs. 2.9%). PRAC considered these data because ingenol disoxate and ingenol mebutate are closely related, the EMA said.
“Health care professionals should stop prescribing Picato and consider different treatment options while authorities review the data,” according to the European agency. “Health care professionals should advise patients to be vigilant for any skin lesions developing and to seek medical advice promptly should any occur,” the statement adds.
Picato has been authorized in the EU since 2012, and the FDA approved Picato the same year. Patients have received about 2.8 million treatment courses in that time, according to the LEO Pharma press release.
As a precaution, the European Medicines Agency (EMA) has recommended that patients stop using ingenol mebutate (Picato) while the agency continues to review the safety of the topical treatment, which is indicated for the treatment of actinic keratosis in Europe and the United States.
No such action has been taken in the United States.
The EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) is reviewing data on skin cancer in patients treated with ingenol mebutate. In a trial comparing Picato and imiquimod, skin cancer was more common in the areas treated with Picato than in areas treated with imiquimod, the statement said.
“While uncertainties remain, the EMA said in a Jan. 17 news release. “The PRAC has therefore recommended suspending the medicine’s marketing authorization as a precaution and noted that alternative treatments are available.”
FDA is looking at the situation
LEO Pharma, the company that markets Picato, announced on Jan. 9 that it was initiating voluntary withdrawal of marketing authorization and possible voluntary withdrawal of Picato in the European Union (EU) and European Economic Area (EEA). The statement says, however, that “LEO Pharma has carefully reviewed the information received from PRAC, and the company disagrees with the ongoing assessment of PRAC.” There are “no additional safety data and it is LEO Pharma’s position that there is no evidence of a causal relationship or plausible mechanism hypothesis between the use of Picato and the development of skin malignancies.” An update added to the press release on Jan. 17 restates that the company disagrees with the assessment of PRAC.
“This matter does not affect Picato in the U.S., and there are no new developments in the [United States]. Picato continues to be available to patients in the U.S. We remain in dialogue with the U.S. Food and Drug Administration about Picato in the EU/EEA,” Rhonda Sciarra, associate director of global external communications for LEO Pharma, said in an email. “We remain committed to ensuring patient safety, rigorous pharmacovigilance monitoring, and transparency,” she added.
The FDA “is gathering data and information to investigate the safety concern related to Picato,” a spokesperson for the FDA told Dermatology News. “We are committed to sharing relevant findings when we have sufficient understanding of the situation and of what actions should be taken,” he added.
Examining the data
The EMA announcement described data about the risk of skin cancer in studies of Picato. A 3-year study in 484 patients found a higher incidence of skin malignancy with ingenol mebutate than with the comparator, imiquimod. In all, 3.3% of patients developed cancer in the ingenol mebutate group, compared with 0.4% in the comparator group.
In an 8-week vehicle-controlled trial in 1,262 patients, there were more skin tumors in patients who received ingenol mebutate than in those in the vehicle arm (1.0% vs. 0.1%).
In addition, according to the EMA statement, in four trials of a related ester that included 1,234 patients, a higher incidence of skin tumors occurred with the related drug, ingenol disoxate, than with a vehicle control (7.7% vs. 2.9%). PRAC considered these data because ingenol disoxate and ingenol mebutate are closely related, the EMA said.
“Health care professionals should stop prescribing Picato and consider different treatment options while authorities review the data,” according to the European agency. “Health care professionals should advise patients to be vigilant for any skin lesions developing and to seek medical advice promptly should any occur,” the statement adds.
Picato has been authorized in the EU since 2012, and the FDA approved Picato the same year. Patients have received about 2.8 million treatment courses in that time, according to the LEO Pharma press release.
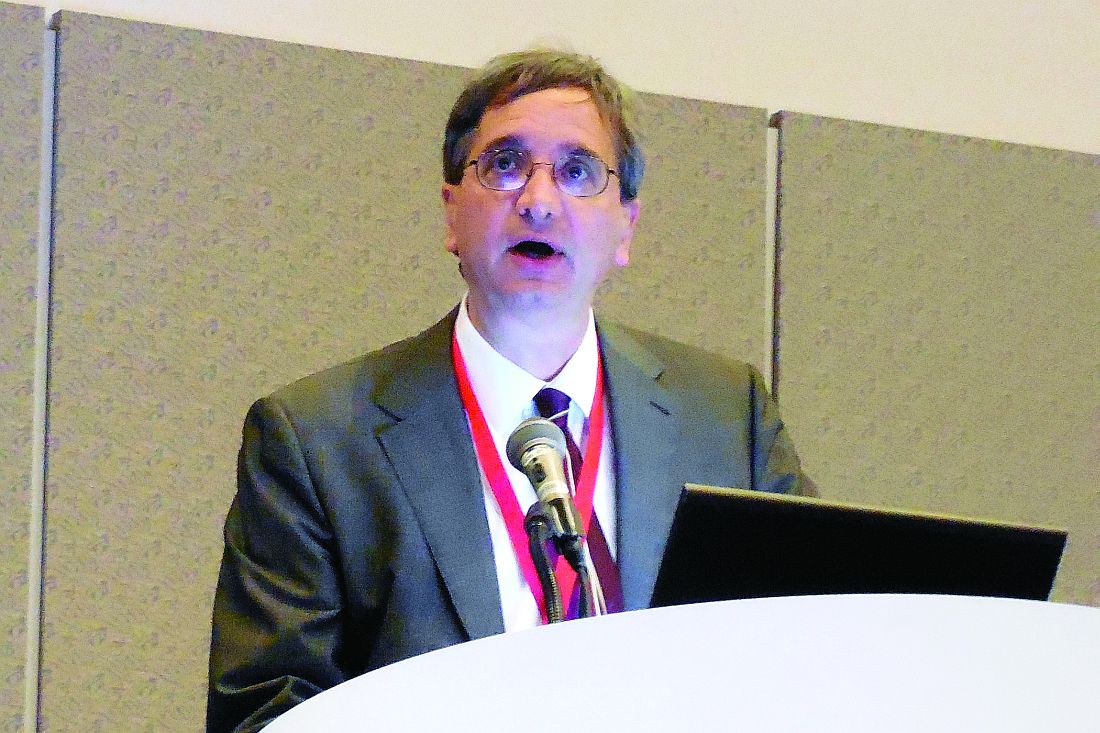
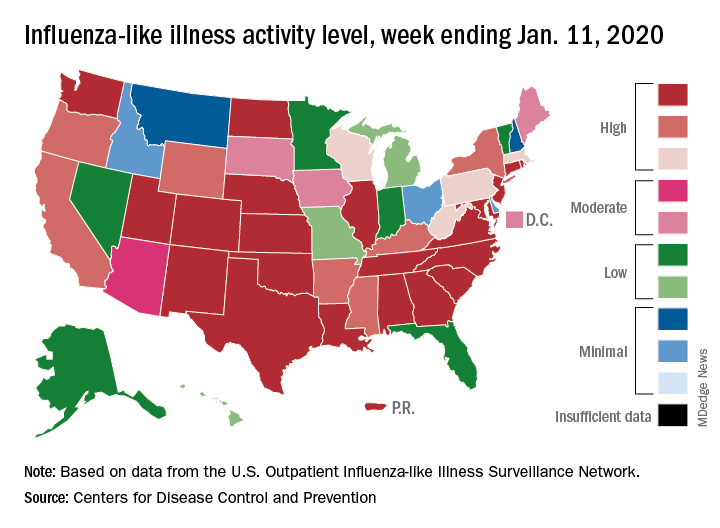
Flu activity declines for second straight week
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
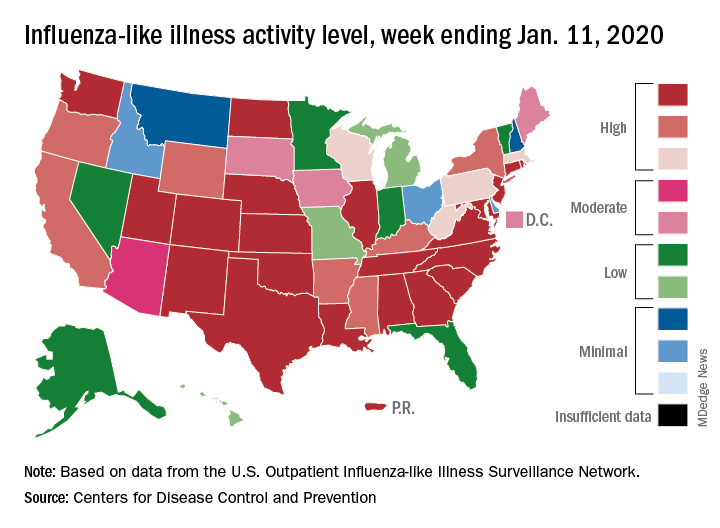
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.
Flu activity dropped nationally for a second consecutive week, but the changing predominance in type from influenza B to A suggests that “it is too early to know whether the season has peaked,” the Centers for Disease Control and Prevention said Jan. 17.
Patients with influenza-like illness (ILI) dropped from 5.7% to 4.7% of all visits to outpatient providers for the week ending Jan. 11, and the proportion of respiratory specimens positive for influenza decreased from 23.6% the week before to 22.9%, the CDC’s influenza division reported.
Despite that overall drop in positive specimens, however, “the percent positive for influenza A viruses increased and some regions are seeing increases in the proportion of influenza A(H1N1)pdm09 viruses compared to other influenza viruses,” the influenza division noted.
Outpatient activity on the state level also was down for the week. There were 23 jurisdictions – 21 states, New York City, and Puerto Rico – at level 10 on the CDC’s 1-10 scale of ILI activity for the week ending Jan. 11, compared with 33 the previous week, data from the CDC’s Outpatient Influenza-like Illness Surveillance Network show.
Indicators of ILI severity have not risen to high levels. “The percentage of deaths attributed to pneumonia and influenza increased from 6.0% to 6.9% but remains below the epidemic threshold” of 7.0% for the week, and the hospitalization rate remains at a fairly typical level for this time of year, the influenza division said.
For the week ending Jan. 11, 7 new ILI-related pediatric deaths were reported, which brings the total to 39 for the 2019-2020 season. Children aged 0-4 years are the second-most likely age group to be hospitalized with the flu (34.4/100,000 population) after adults aged 65 years and older, who have a cumulative rate of 47.6/100,000 for the season, the CDC reported.
Value analysis of JAK inhibitors for RA hampered by limited data
Adequate evidence shows that adding a Janus kinase (JAK) inhibitor to conventional disease-modifying antirheumatic drug therapy provides a net health benefit for patients with rheumatoid arthritis, compared with conventional drugs alone, according to a report by an independent research institute. But the long-term economic value of JAK inhibitors for rheumatoid arthritis is less clear, the report by the Institute for Clinical and Economic Review (ICER) indicates.
ICER on Jan. 9 released a finalized report and policy recommendations on JAK inhibitors and biosimilars for rheumatoid arthritis. The report reviews current evidence for JAK inhibitors for adults with moderately active to severely active rheumatoid arthritis.
Since the nonprofit’s 2017 review of targeted immune modulators for rheumatoid arthritis, two JAK inhibitors, baricitinib (Olumiant) and upadacitinib (Rinvoq), were approved by the Food and Drug Administration. At a December 2019 public meeting of the California Technology Assessment Forum (CTAF), one of ICER’s independent evidence appraisal committees, panelists reviewed recent evidence.
A pricey comparator
In ICER’s analysis, the JAK inhibitor upadacitinib reached common thresholds for cost-effectiveness when compared with adalimumab (Humira). Nevertheless, the 14 members of the independent evidence appraisal committee voted that upadacitinib’s long-term economic value was “low” (8 votes) or “intermediate” (6 votes). Concerns about the generalizability of phase 3 clinical trial data to patients in the real world were among the reservations noted by panelists. Furthermore, “legitimate questions remain about whether or not adalimumab, launched 17 years ago, is fairly priced to begin with,” Pamela Bradt, MD, MPH, ICER’s chief scientific officer, said in a news release.
The panel did not vote on the economic value of tofacitinib (Xeljanz) or baricitinib, the two other JAK inhibitors that are approved for rheumatoid arthritis, because head-to-head evidence against adalimumab was insufficient, ICER said.
“Rheumatoid arthritis is a progressively disabling condition, and patients are fortunate to have multiple therapy options – including biosimilars – that effectively slow disease progression,” Dr. Bradt said. “Many economists might expect medicines to become more affordable in an increasingly crowded therapeutic class; however, because the current rebate structure has erected barriers between patients and several emerging RA therapies, traditional market dynamics have been unable to drive down prices.”
Weighing efficacy and cost
Panelists found that the net health benefit provided by upadacitinib is superior to that provided by adalimumab. At the same time, they said that there is insufficient head-to-head evidence to distinguish between the net health benefit of upadacitinib and tofacitinib or to demonstrate that tofacitinib is superior to adalimumab. Evidence comparing baricitinib to adalimumab does not exist.
CTAF members unanimously agreed that adequate evidence demonstrates that the biosimilar infliximab-dyyb (Inflectra) is clinically equivalent to its reference biologic, infliximab (Remicade).
Economic modeling demonstrated that upadacitinib plus a conventional drug achieves marginally higher quality of life than adalimumab plus a conventional drug does, at similar costs. “Based on this comparison with adalimumab, ICER’s value-based price benchmark range for upadacitinib is between $44,000 and $45,000,” according to the ICER news release. “This benchmark represents a 25% discount off of upadacitinib’s annual list price of $59,860, a suggested discount that is consistent with the rebates we assume the manufacturer is currently offering.”
After the voting session, various experts, including clinicians, patient advocates, and representatives from manufacturers and insurance companies, made the following policy recommendations:
- Regulatory intervention may be needed to ensure that drug prices do not continue to increase further from reasonable alignment with added benefits for patients.
- Insurers, pharmacy benefit managers, and employers should increase transparency around the role of discounts and rebates in formulary design.
- Policymakers should aim to create a system that rewards lower-priced biosimilar treatment options.
The findings of the clinical review by the Institute for Clinical and Economic Review (ICER) are generally in line with our clinical perceptions. We have an increasing number of treatment options for our RA patients, and the results of this review support the efficacy of tofacitinib and upadacitinib, compared with currently available biologic treatments. While ICER’s voting panel did find the data supported the superiority of upadacitinib over adalimumab, the cost analysis notes a WAC (wholesale acquisition cost) for upadacitinib of $59,860. While at expected discounted rates it is felt to be cost effective when compared with adalimumab, it is difficult to know what this means since ICER found adalimumab itself not to be cost effective, compared with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), in its 2017 review.
ICER’s focus is drug pricing and cost effectiveness, so obviously our biologic drugs are in the institute’s crosshairs. This review provided context for a policy roundtable discussion that included patient, payer, and manufacturer input, as well as American College of Rheumatology (ACR) input. We are thankful that ACR had a seat at the table, and thankful ICER is attempting to bring light to the important issues and barriers that perpetuate high drug prices in our marketplace. The discussion was wide ranging but focused on step-edit policies, the role of pharmacy benefit managers (PBMs) in perpetuating high drug prices and the relatively slow uptake of biosimilars in our marketplace.
These issues are critical to every practicing rheumatologist because we each deal daily with the hassles of step-edit/fail-first policies, which hijack our otherwise thoughtful and evidence-based decision making regarding the best treatments for our patients. We know how much (unreimbursed) time it takes our staff to sort through these step edits and prior authorizations, and we have seen recent data regarding how these policies delay care and harm patients. We were thankful to see ICER validate these concerns and note that their suggested guidelines for rational step therapy somewhat mirror those in the Safe Step Act, which ACR supports on a federal legislative level. ACR continues to vigorously support the grandfathering of any patient on an effective treatment, regardless of changes in insurance or formulary; this was an issue of robust debate at their meeting, and this patient-centric position is not uniformly held among policymakers, unfortunately.
ACR agrees with ICER’s conclusion that transparency in the PBM system regarding rebates should be promoted and that opaque rebate negotiations between PBMs and manufacturers both incentivize higher prices and block access to the marketplace for cheaper biosimilar options.
Additionally, ICER and ACR agree about the critical role that biosimilar uptake will play in controlling drug costs. While we do not yet have any biosimilars that have been deemed interchangeable by the Food and Drug Administration, we agree with ICER that data regarding comparable efficacy and safety of biosimilars to their originator products is very reassuring. While the decision to switch to a biosimilar should be an individual decision between a provider and patient, and while we recognize with frustration that many FDA-approved biosimilars are not commercially available because of patent law, it is clear that the current costs of our biologic drugs are not sustainable and the uptake of biosimilars will be critical if we hope our health care economy can continue to support coverage of these life-changing drugs in years to come. We agree with ICER that it is incumbent upon prescribers to reassure our patients regarding the safety and efficacy of these drugs.
Christopher Phillips, MD , is a community rheumatologist in Paducah, Ky., who serves as chair of the insurance subcommittee of the ACR, under the guidance of the Committee on Rheumatologic Care. He attended the initial ICER rheumatoid arthritis review meeting in 2017 on behalf of ACR. In 2019, Dr. Phillips served as a reviewer and clinical expert to the ICER panel and participated in the policy roundtable discussion.
The findings of the clinical review by the Institute for Clinical and Economic Review (ICER) are generally in line with our clinical perceptions. We have an increasing number of treatment options for our RA patients, and the results of this review support the efficacy of tofacitinib and upadacitinib, compared with currently available biologic treatments. While ICER’s voting panel did find the data supported the superiority of upadacitinib over adalimumab, the cost analysis notes a WAC (wholesale acquisition cost) for upadacitinib of $59,860. While at expected discounted rates it is felt to be cost effective when compared with adalimumab, it is difficult to know what this means since ICER found adalimumab itself not to be cost effective, compared with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), in its 2017 review.
ICER’s focus is drug pricing and cost effectiveness, so obviously our biologic drugs are in the institute’s crosshairs. This review provided context for a policy roundtable discussion that included patient, payer, and manufacturer input, as well as American College of Rheumatology (ACR) input. We are thankful that ACR had a seat at the table, and thankful ICER is attempting to bring light to the important issues and barriers that perpetuate high drug prices in our marketplace. The discussion was wide ranging but focused on step-edit policies, the role of pharmacy benefit managers (PBMs) in perpetuating high drug prices and the relatively slow uptake of biosimilars in our marketplace.
These issues are critical to every practicing rheumatologist because we each deal daily with the hassles of step-edit/fail-first policies, which hijack our otherwise thoughtful and evidence-based decision making regarding the best treatments for our patients. We know how much (unreimbursed) time it takes our staff to sort through these step edits and prior authorizations, and we have seen recent data regarding how these policies delay care and harm patients. We were thankful to see ICER validate these concerns and note that their suggested guidelines for rational step therapy somewhat mirror those in the Safe Step Act, which ACR supports on a federal legislative level. ACR continues to vigorously support the grandfathering of any patient on an effective treatment, regardless of changes in insurance or formulary; this was an issue of robust debate at their meeting, and this patient-centric position is not uniformly held among policymakers, unfortunately.
ACR agrees with ICER’s conclusion that transparency in the PBM system regarding rebates should be promoted and that opaque rebate negotiations between PBMs and manufacturers both incentivize higher prices and block access to the marketplace for cheaper biosimilar options.
Additionally, ICER and ACR agree about the critical role that biosimilar uptake will play in controlling drug costs. While we do not yet have any biosimilars that have been deemed interchangeable by the Food and Drug Administration, we agree with ICER that data regarding comparable efficacy and safety of biosimilars to their originator products is very reassuring. While the decision to switch to a biosimilar should be an individual decision between a provider and patient, and while we recognize with frustration that many FDA-approved biosimilars are not commercially available because of patent law, it is clear that the current costs of our biologic drugs are not sustainable and the uptake of biosimilars will be critical if we hope our health care economy can continue to support coverage of these life-changing drugs in years to come. We agree with ICER that it is incumbent upon prescribers to reassure our patients regarding the safety and efficacy of these drugs.
Christopher Phillips, MD , is a community rheumatologist in Paducah, Ky., who serves as chair of the insurance subcommittee of the ACR, under the guidance of the Committee on Rheumatologic Care. He attended the initial ICER rheumatoid arthritis review meeting in 2017 on behalf of ACR. In 2019, Dr. Phillips served as a reviewer and clinical expert to the ICER panel and participated in the policy roundtable discussion.
The findings of the clinical review by the Institute for Clinical and Economic Review (ICER) are generally in line with our clinical perceptions. We have an increasing number of treatment options for our RA patients, and the results of this review support the efficacy of tofacitinib and upadacitinib, compared with currently available biologic treatments. While ICER’s voting panel did find the data supported the superiority of upadacitinib over adalimumab, the cost analysis notes a WAC (wholesale acquisition cost) for upadacitinib of $59,860. While at expected discounted rates it is felt to be cost effective when compared with adalimumab, it is difficult to know what this means since ICER found adalimumab itself not to be cost effective, compared with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs), in its 2017 review.
ICER’s focus is drug pricing and cost effectiveness, so obviously our biologic drugs are in the institute’s crosshairs. This review provided context for a policy roundtable discussion that included patient, payer, and manufacturer input, as well as American College of Rheumatology (ACR) input. We are thankful that ACR had a seat at the table, and thankful ICER is attempting to bring light to the important issues and barriers that perpetuate high drug prices in our marketplace. The discussion was wide ranging but focused on step-edit policies, the role of pharmacy benefit managers (PBMs) in perpetuating high drug prices and the relatively slow uptake of biosimilars in our marketplace.
These issues are critical to every practicing rheumatologist because we each deal daily with the hassles of step-edit/fail-first policies, which hijack our otherwise thoughtful and evidence-based decision making regarding the best treatments for our patients. We know how much (unreimbursed) time it takes our staff to sort through these step edits and prior authorizations, and we have seen recent data regarding how these policies delay care and harm patients. We were thankful to see ICER validate these concerns and note that their suggested guidelines for rational step therapy somewhat mirror those in the Safe Step Act, which ACR supports on a federal legislative level. ACR continues to vigorously support the grandfathering of any patient on an effective treatment, regardless of changes in insurance or formulary; this was an issue of robust debate at their meeting, and this patient-centric position is not uniformly held among policymakers, unfortunately.
ACR agrees with ICER’s conclusion that transparency in the PBM system regarding rebates should be promoted and that opaque rebate negotiations between PBMs and manufacturers both incentivize higher prices and block access to the marketplace for cheaper biosimilar options.
Additionally, ICER and ACR agree about the critical role that biosimilar uptake will play in controlling drug costs. While we do not yet have any biosimilars that have been deemed interchangeable by the Food and Drug Administration, we agree with ICER that data regarding comparable efficacy and safety of biosimilars to their originator products is very reassuring. While the decision to switch to a biosimilar should be an individual decision between a provider and patient, and while we recognize with frustration that many FDA-approved biosimilars are not commercially available because of patent law, it is clear that the current costs of our biologic drugs are not sustainable and the uptake of biosimilars will be critical if we hope our health care economy can continue to support coverage of these life-changing drugs in years to come. We agree with ICER that it is incumbent upon prescribers to reassure our patients regarding the safety and efficacy of these drugs.
Christopher Phillips, MD , is a community rheumatologist in Paducah, Ky., who serves as chair of the insurance subcommittee of the ACR, under the guidance of the Committee on Rheumatologic Care. He attended the initial ICER rheumatoid arthritis review meeting in 2017 on behalf of ACR. In 2019, Dr. Phillips served as a reviewer and clinical expert to the ICER panel and participated in the policy roundtable discussion.
Adequate evidence shows that adding a Janus kinase (JAK) inhibitor to conventional disease-modifying antirheumatic drug therapy provides a net health benefit for patients with rheumatoid arthritis, compared with conventional drugs alone, according to a report by an independent research institute. But the long-term economic value of JAK inhibitors for rheumatoid arthritis is less clear, the report by the Institute for Clinical and Economic Review (ICER) indicates.
ICER on Jan. 9 released a finalized report and policy recommendations on JAK inhibitors and biosimilars for rheumatoid arthritis. The report reviews current evidence for JAK inhibitors for adults with moderately active to severely active rheumatoid arthritis.
Since the nonprofit’s 2017 review of targeted immune modulators for rheumatoid arthritis, two JAK inhibitors, baricitinib (Olumiant) and upadacitinib (Rinvoq), were approved by the Food and Drug Administration. At a December 2019 public meeting of the California Technology Assessment Forum (CTAF), one of ICER’s independent evidence appraisal committees, panelists reviewed recent evidence.
A pricey comparator
In ICER’s analysis, the JAK inhibitor upadacitinib reached common thresholds for cost-effectiveness when compared with adalimumab (Humira). Nevertheless, the 14 members of the independent evidence appraisal committee voted that upadacitinib’s long-term economic value was “low” (8 votes) or “intermediate” (6 votes). Concerns about the generalizability of phase 3 clinical trial data to patients in the real world were among the reservations noted by panelists. Furthermore, “legitimate questions remain about whether or not adalimumab, launched 17 years ago, is fairly priced to begin with,” Pamela Bradt, MD, MPH, ICER’s chief scientific officer, said in a news release.
The panel did not vote on the economic value of tofacitinib (Xeljanz) or baricitinib, the two other JAK inhibitors that are approved for rheumatoid arthritis, because head-to-head evidence against adalimumab was insufficient, ICER said.
“Rheumatoid arthritis is a progressively disabling condition, and patients are fortunate to have multiple therapy options – including biosimilars – that effectively slow disease progression,” Dr. Bradt said. “Many economists might expect medicines to become more affordable in an increasingly crowded therapeutic class; however, because the current rebate structure has erected barriers between patients and several emerging RA therapies, traditional market dynamics have been unable to drive down prices.”
Weighing efficacy and cost
Panelists found that the net health benefit provided by upadacitinib is superior to that provided by adalimumab. At the same time, they said that there is insufficient head-to-head evidence to distinguish between the net health benefit of upadacitinib and tofacitinib or to demonstrate that tofacitinib is superior to adalimumab. Evidence comparing baricitinib to adalimumab does not exist.
CTAF members unanimously agreed that adequate evidence demonstrates that the biosimilar infliximab-dyyb (Inflectra) is clinically equivalent to its reference biologic, infliximab (Remicade).
Economic modeling demonstrated that upadacitinib plus a conventional drug achieves marginally higher quality of life than adalimumab plus a conventional drug does, at similar costs. “Based on this comparison with adalimumab, ICER’s value-based price benchmark range for upadacitinib is between $44,000 and $45,000,” according to the ICER news release. “This benchmark represents a 25% discount off of upadacitinib’s annual list price of $59,860, a suggested discount that is consistent with the rebates we assume the manufacturer is currently offering.”
After the voting session, various experts, including clinicians, patient advocates, and representatives from manufacturers and insurance companies, made the following policy recommendations:
- Regulatory intervention may be needed to ensure that drug prices do not continue to increase further from reasonable alignment with added benefits for patients.
- Insurers, pharmacy benefit managers, and employers should increase transparency around the role of discounts and rebates in formulary design.
- Policymakers should aim to create a system that rewards lower-priced biosimilar treatment options.
Adequate evidence shows that adding a Janus kinase (JAK) inhibitor to conventional disease-modifying antirheumatic drug therapy provides a net health benefit for patients with rheumatoid arthritis, compared with conventional drugs alone, according to a report by an independent research institute. But the long-term economic value of JAK inhibitors for rheumatoid arthritis is less clear, the report by the Institute for Clinical and Economic Review (ICER) indicates.
ICER on Jan. 9 released a finalized report and policy recommendations on JAK inhibitors and biosimilars for rheumatoid arthritis. The report reviews current evidence for JAK inhibitors for adults with moderately active to severely active rheumatoid arthritis.
Since the nonprofit’s 2017 review of targeted immune modulators for rheumatoid arthritis, two JAK inhibitors, baricitinib (Olumiant) and upadacitinib (Rinvoq), were approved by the Food and Drug Administration. At a December 2019 public meeting of the California Technology Assessment Forum (CTAF), one of ICER’s independent evidence appraisal committees, panelists reviewed recent evidence.
A pricey comparator
In ICER’s analysis, the JAK inhibitor upadacitinib reached common thresholds for cost-effectiveness when compared with adalimumab (Humira). Nevertheless, the 14 members of the independent evidence appraisal committee voted that upadacitinib’s long-term economic value was “low” (8 votes) or “intermediate” (6 votes). Concerns about the generalizability of phase 3 clinical trial data to patients in the real world were among the reservations noted by panelists. Furthermore, “legitimate questions remain about whether or not adalimumab, launched 17 years ago, is fairly priced to begin with,” Pamela Bradt, MD, MPH, ICER’s chief scientific officer, said in a news release.
The panel did not vote on the economic value of tofacitinib (Xeljanz) or baricitinib, the two other JAK inhibitors that are approved for rheumatoid arthritis, because head-to-head evidence against adalimumab was insufficient, ICER said.
“Rheumatoid arthritis is a progressively disabling condition, and patients are fortunate to have multiple therapy options – including biosimilars – that effectively slow disease progression,” Dr. Bradt said. “Many economists might expect medicines to become more affordable in an increasingly crowded therapeutic class; however, because the current rebate structure has erected barriers between patients and several emerging RA therapies, traditional market dynamics have been unable to drive down prices.”
Weighing efficacy and cost
Panelists found that the net health benefit provided by upadacitinib is superior to that provided by adalimumab. At the same time, they said that there is insufficient head-to-head evidence to distinguish between the net health benefit of upadacitinib and tofacitinib or to demonstrate that tofacitinib is superior to adalimumab. Evidence comparing baricitinib to adalimumab does not exist.
CTAF members unanimously agreed that adequate evidence demonstrates that the biosimilar infliximab-dyyb (Inflectra) is clinically equivalent to its reference biologic, infliximab (Remicade).
Economic modeling demonstrated that upadacitinib plus a conventional drug achieves marginally higher quality of life than adalimumab plus a conventional drug does, at similar costs. “Based on this comparison with adalimumab, ICER’s value-based price benchmark range for upadacitinib is between $44,000 and $45,000,” according to the ICER news release. “This benchmark represents a 25% discount off of upadacitinib’s annual list price of $59,860, a suggested discount that is consistent with the rebates we assume the manufacturer is currently offering.”
After the voting session, various experts, including clinicians, patient advocates, and representatives from manufacturers and insurance companies, made the following policy recommendations:
- Regulatory intervention may be needed to ensure that drug prices do not continue to increase further from reasonable alignment with added benefits for patients.
- Insurers, pharmacy benefit managers, and employers should increase transparency around the role of discounts and rebates in formulary design.
- Policymakers should aim to create a system that rewards lower-priced biosimilar treatment options.
Cognitive screening of older physicians: What’s fair?
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
FROM JAMA
Reducing alarm fatigue in the hospital
Noise increases patient anxiety
Researchers are exploring ways to make alarms and monitors less irritating and more informative.
“Hospitals today can be sonic hellscapes, which studies have shown regularly exceed levels set by the World Health Organization: droning IV pumps, ding-donging nurse call buttons, voices crackling on loudspeakers, ringing telephones, beeping elevators, buzzing ID scanners, clattering carts, coughing, screaming, vomiting,” according to a recent article in the New York Times.
And that’s not to mention all the alarms that blare regularly, day and night. “A single patient might trigger hundreds each day, challenging caregivers to figure out which machine is beeping, and what is wrong with the patient, if anything,” according to the article.
All this noise contributes to patient anxiety and delirium and to staff burnout too. Alarm fatigue is a serious problem, related to the high rate of false alarms, the lack of alarm standardization, and the number of medical devices that emit an alarm. Its effect is to make caregivers less responsive.
A group of researchers is developing new sounds that could replace current alarms. These new signals might mimic electronic dance music or the sounds of a heartbeat; they may combine audible alarms with visual cues such as interactive screens; they will certainly be quieter. Testing remains to be done around how quickly clinicians will be able to learn the sounds and how loud they need to be. The researchers say a new standard is likely to go into effect in 2020.
Reference
1. Rueb ES. To Reduce Hospital Noise, Researchers Create Alarms That Whistle and Sing. New York Times. July 9, 2019.
Noise increases patient anxiety
Noise increases patient anxiety
Researchers are exploring ways to make alarms and monitors less irritating and more informative.
“Hospitals today can be sonic hellscapes, which studies have shown regularly exceed levels set by the World Health Organization: droning IV pumps, ding-donging nurse call buttons, voices crackling on loudspeakers, ringing telephones, beeping elevators, buzzing ID scanners, clattering carts, coughing, screaming, vomiting,” according to a recent article in the New York Times.
And that’s not to mention all the alarms that blare regularly, day and night. “A single patient might trigger hundreds each day, challenging caregivers to figure out which machine is beeping, and what is wrong with the patient, if anything,” according to the article.
All this noise contributes to patient anxiety and delirium and to staff burnout too. Alarm fatigue is a serious problem, related to the high rate of false alarms, the lack of alarm standardization, and the number of medical devices that emit an alarm. Its effect is to make caregivers less responsive.
A group of researchers is developing new sounds that could replace current alarms. These new signals might mimic electronic dance music or the sounds of a heartbeat; they may combine audible alarms with visual cues such as interactive screens; they will certainly be quieter. Testing remains to be done around how quickly clinicians will be able to learn the sounds and how loud they need to be. The researchers say a new standard is likely to go into effect in 2020.
Reference
1. Rueb ES. To Reduce Hospital Noise, Researchers Create Alarms That Whistle and Sing. New York Times. July 9, 2019.
Researchers are exploring ways to make alarms and monitors less irritating and more informative.
“Hospitals today can be sonic hellscapes, which studies have shown regularly exceed levels set by the World Health Organization: droning IV pumps, ding-donging nurse call buttons, voices crackling on loudspeakers, ringing telephones, beeping elevators, buzzing ID scanners, clattering carts, coughing, screaming, vomiting,” according to a recent article in the New York Times.
And that’s not to mention all the alarms that blare regularly, day and night. “A single patient might trigger hundreds each day, challenging caregivers to figure out which machine is beeping, and what is wrong with the patient, if anything,” according to the article.
All this noise contributes to patient anxiety and delirium and to staff burnout too. Alarm fatigue is a serious problem, related to the high rate of false alarms, the lack of alarm standardization, and the number of medical devices that emit an alarm. Its effect is to make caregivers less responsive.
A group of researchers is developing new sounds that could replace current alarms. These new signals might mimic electronic dance music or the sounds of a heartbeat; they may combine audible alarms with visual cues such as interactive screens; they will certainly be quieter. Testing remains to be done around how quickly clinicians will be able to learn the sounds and how loud they need to be. The researchers say a new standard is likely to go into effect in 2020.
Reference
1. Rueb ES. To Reduce Hospital Noise, Researchers Create Alarms That Whistle and Sing. New York Times. July 9, 2019.
Cannabis users struggle to quit cigarettes
a large national survey has found.
“Over the past decade, there has been an increase in the use of cannabis among cigarette smokers and prevalence of cigarettes and cannabis co-use, suggesting that the negative consequences of cigarette–cannabis co-use may also become more prevalent over time,” wrote Andrea H. Weinberger, PhD, of Yeshiva University, New York, and colleagues. They noted that the prevalence of cigarette smoking is nearly three times higher among persons who use cannabis and have cannabis use disorders relative to those who do not.
The 2019 National Survey of Drug Use and Health estimated that 15.9% of Americans aged 12 years or older used cannabis in the past year. This number has been rising throughout the 2000s.
In that same report, cannabis use disorder (or marijuana use disorder) was defined as when an individual experiences clinically significant impairment caused by the recurrent use of marijuana, including health problems, persistent or increasing use, and failure to meet major responsibilities at work, school, or home. The report stated that approximately 1.6% of Americans aged 12 or older in 2018 had marijuana use disorder.
In the study published in Tobacco Control, the researchers used the National Survey on Drug Use and Health data to analyze cigarette smoking quit ratios among U.S. adults with and without cannabis use and cannabis use disorders. “Quit ratio was calculated as the proportion of former smokers among lifetime smokers and is considered a measure of total cessation in a population,” the researchers said.
In 2016, the quit ratios for adults with a history of cannabis use or cannabis use disorders were 23% and 15%, respectively, compared with 51% and 48%, respectively, in those with no cannabis use or cannabis use disorders.
Overall, quit ratios did not change significantly from 2002 to 2016 for individuals with cannabis use disorders after controlling for multiple demographic factors and other substance use disorders. However, during the same time period, quit ratios showed a nonlinear increase in cannabis users, nonusers, and individuals without cannabis use disorders.
The study findings were limited by several factors including the inability to generalize results to youth or individuals living outside the United States, the use of DSM-IV criteria to identify cannabis use disorder, the use of self-reports, and the inability to examine the timing of cannabis use as related to attempts to quit smoking, the researchers noted. However, the results highlight the need to consider offering smoking cessation treatment to individuals being treated for cannabis use disorders, and to include cannabis users in smoking cessation programs, the researchers noted.
“Based on our results, both public health and clinical efforts to improve cigarette quit outcomes may benefit from including those with any cannabis use,” they said. More research is needed to determine whether trends in the quit ratio change over time for cannabis users or those with cannabis use disorder, they added.
The study was funded by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose.
SOURCE: Weinberger AH et al. Tob Control. 2020;29(1):74-80. doi: 10.1136/tobaccocontrol-2018-054590.
a large national survey has found.
“Over the past decade, there has been an increase in the use of cannabis among cigarette smokers and prevalence of cigarettes and cannabis co-use, suggesting that the negative consequences of cigarette–cannabis co-use may also become more prevalent over time,” wrote Andrea H. Weinberger, PhD, of Yeshiva University, New York, and colleagues. They noted that the prevalence of cigarette smoking is nearly three times higher among persons who use cannabis and have cannabis use disorders relative to those who do not.
The 2019 National Survey of Drug Use and Health estimated that 15.9% of Americans aged 12 years or older used cannabis in the past year. This number has been rising throughout the 2000s.
In that same report, cannabis use disorder (or marijuana use disorder) was defined as when an individual experiences clinically significant impairment caused by the recurrent use of marijuana, including health problems, persistent or increasing use, and failure to meet major responsibilities at work, school, or home. The report stated that approximately 1.6% of Americans aged 12 or older in 2018 had marijuana use disorder.
In the study published in Tobacco Control, the researchers used the National Survey on Drug Use and Health data to analyze cigarette smoking quit ratios among U.S. adults with and without cannabis use and cannabis use disorders. “Quit ratio was calculated as the proportion of former smokers among lifetime smokers and is considered a measure of total cessation in a population,” the researchers said.
In 2016, the quit ratios for adults with a history of cannabis use or cannabis use disorders were 23% and 15%, respectively, compared with 51% and 48%, respectively, in those with no cannabis use or cannabis use disorders.
Overall, quit ratios did not change significantly from 2002 to 2016 for individuals with cannabis use disorders after controlling for multiple demographic factors and other substance use disorders. However, during the same time period, quit ratios showed a nonlinear increase in cannabis users, nonusers, and individuals without cannabis use disorders.
The study findings were limited by several factors including the inability to generalize results to youth or individuals living outside the United States, the use of DSM-IV criteria to identify cannabis use disorder, the use of self-reports, and the inability to examine the timing of cannabis use as related to attempts to quit smoking, the researchers noted. However, the results highlight the need to consider offering smoking cessation treatment to individuals being treated for cannabis use disorders, and to include cannabis users in smoking cessation programs, the researchers noted.
“Based on our results, both public health and clinical efforts to improve cigarette quit outcomes may benefit from including those with any cannabis use,” they said. More research is needed to determine whether trends in the quit ratio change over time for cannabis users or those with cannabis use disorder, they added.
The study was funded by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose.
SOURCE: Weinberger AH et al. Tob Control. 2020;29(1):74-80. doi: 10.1136/tobaccocontrol-2018-054590.
a large national survey has found.
“Over the past decade, there has been an increase in the use of cannabis among cigarette smokers and prevalence of cigarettes and cannabis co-use, suggesting that the negative consequences of cigarette–cannabis co-use may also become more prevalent over time,” wrote Andrea H. Weinberger, PhD, of Yeshiva University, New York, and colleagues. They noted that the prevalence of cigarette smoking is nearly three times higher among persons who use cannabis and have cannabis use disorders relative to those who do not.
The 2019 National Survey of Drug Use and Health estimated that 15.9% of Americans aged 12 years or older used cannabis in the past year. This number has been rising throughout the 2000s.
In that same report, cannabis use disorder (or marijuana use disorder) was defined as when an individual experiences clinically significant impairment caused by the recurrent use of marijuana, including health problems, persistent or increasing use, and failure to meet major responsibilities at work, school, or home. The report stated that approximately 1.6% of Americans aged 12 or older in 2018 had marijuana use disorder.
In the study published in Tobacco Control, the researchers used the National Survey on Drug Use and Health data to analyze cigarette smoking quit ratios among U.S. adults with and without cannabis use and cannabis use disorders. “Quit ratio was calculated as the proportion of former smokers among lifetime smokers and is considered a measure of total cessation in a population,” the researchers said.
In 2016, the quit ratios for adults with a history of cannabis use or cannabis use disorders were 23% and 15%, respectively, compared with 51% and 48%, respectively, in those with no cannabis use or cannabis use disorders.
Overall, quit ratios did not change significantly from 2002 to 2016 for individuals with cannabis use disorders after controlling for multiple demographic factors and other substance use disorders. However, during the same time period, quit ratios showed a nonlinear increase in cannabis users, nonusers, and individuals without cannabis use disorders.
The study findings were limited by several factors including the inability to generalize results to youth or individuals living outside the United States, the use of DSM-IV criteria to identify cannabis use disorder, the use of self-reports, and the inability to examine the timing of cannabis use as related to attempts to quit smoking, the researchers noted. However, the results highlight the need to consider offering smoking cessation treatment to individuals being treated for cannabis use disorders, and to include cannabis users in smoking cessation programs, the researchers noted.
“Based on our results, both public health and clinical efforts to improve cigarette quit outcomes may benefit from including those with any cannabis use,” they said. More research is needed to determine whether trends in the quit ratio change over time for cannabis users or those with cannabis use disorder, they added.
The study was funded by the National Institute on Drug Abuse. The researchers had no financial conflicts to disclose.
SOURCE: Weinberger AH et al. Tob Control. 2020;29(1):74-80. doi: 10.1136/tobaccocontrol-2018-054590.
FROM TOBACCO CONTROL
Big data breaks down Sjögren’s syndrome
The severity of Sjögren’s syndrome and its organ involvement has direct links to clinical characteristics that include age, gender, ethnicity, and geographical location, according to new research findings from a large, worldwide database of primary Sjögren’s syndrome patients.
Risk factors for more severe disease included male sex, earlier age at diagnosis, black/African-American (BAA) ethnicity, and living in more southerly countries, including below the equator. The authors hailed these factors as potentially helping to predict the presence of systemic disease in newly-diagnosed patients, as well as helping to determine the optimum follow-up strategy.
But not everyone agrees. In interviews, other experts suggested that the data were interesting and valuable, but were not ready to make reliable clinical predictions. “The predictive value of these data are limited when it comes to an individual patient sitting in front of you in the office,” said Tomas Mustelin, MD, professor of medicine at the University of Washington, Seattle.
“It would be an important clinical thing if you can figure out who’s at risk for systemic complications and who isn’t. This is a nice step in that direction,” said Hal Scofield, MD, professor of medicine and pathology at the University of Oklahoma, Oklahoma City, agreeing that the data were too preliminary to be broadly useful because there is too much overlap between different patient groups.
If there is one clinical message, it is that physicians should be looking beyond dry eyes and dry mouth in newly diagnosed Sjögren’s syndrome, according to Sarah Chung, MD, who is an acting instructor of rheumatology at the University of Washington. “It’s a reminder to investigate these extra-glandular manifestations, and a reminder that it is a heterogeneous presentation, so we have to keep an open mind and investigate thoroughly,” she said.
In the research published online in Rheumatology, first author Pilar Brito-Zerón, MD, PhD, of the University of Barcelona Hospital Clínic, and colleagues in the Sjögren Big Data Consortium used European League Against Rheumatism Sjögren’s syndrome disease activity index (ESSDAI) scores to examine phenotype and patient characteristics among 10,007 subjects drawn from the international consortium.
Overall, 93.5% of subjects were women, and the mean age at diagnosis was 53 (standard deviation [SD], 14.1 years). The mean total ESSDAI score was 6.1 (SD, 7.5).
Men had higher mean ESSDAI (8.1 vs. 6.0; P less than .001) and clinical ESSDAI (8.4 vs. 6.1; P less than .001) scores and were more likely to have a high disease activity state (22.5% vs. 11.7%; P less than .001). Domains that scored higher in men included lymphadenopathy (P less than .001), glandular (P less than .001), pulmonary (P = .001), peripheral nervous system (PNS) (P less than .001), and CNS (P less than .001).
The highest global ESSDAI scores were reported in patients younger than 35, but organ dominance differed by age group: The constitutional, lymphadenopathy, glandular, cutaneous, renal, hematologic, and biologic domains were highest in this age group, but pulmonary and peripheral nervous system were highest in patients over 65.
By ethnicity, the highest ESSDAI scores occurred in black/African-American patients (6.7), followed by white (6.5), Asian (5.4), and Hispanic (4.8; P less than .001). The organ-specific domains also tracked by ethnicity, with BAA patients experiencing the highest frequencies of activity in the lymphadenopathy, articular, neurologic, and biologic domains. White patients were more often affected in the glandular, cutaneous, and muscular domains, whereas Asians most often experienced the pulmonary, renal, and hematologic domains, and Hispanics the constitutional domain.
The survey included Europe, America, and Asia, and global ESSDAI scores were higher in the southern countries of Asia and Europe, and higher in countries below the equator in the Americas. The organ-by-organ activity scores had a differentiated pattern between northern and southern locales. Worldwide, the gradient of patients with moderate systemic activity (global ESSDAI score of 5 or higher) at diagnosis followed a north-south gradient.
The study had no specific funding, and the authors have no relevant financial disclosures. Dr. Mustelin, Dr. Scofield, and Dr. Chung have no relevant financial disclosures.
SOURCE: Brito-Zerón P et al. Rheumatology. 2019 Dec 24. doi: 10.1093/rheumatology/kez578.
The severity of Sjögren’s syndrome and its organ involvement has direct links to clinical characteristics that include age, gender, ethnicity, and geographical location, according to new research findings from a large, worldwide database of primary Sjögren’s syndrome patients.
Risk factors for more severe disease included male sex, earlier age at diagnosis, black/African-American (BAA) ethnicity, and living in more southerly countries, including below the equator. The authors hailed these factors as potentially helping to predict the presence of systemic disease in newly-diagnosed patients, as well as helping to determine the optimum follow-up strategy.
But not everyone agrees. In interviews, other experts suggested that the data were interesting and valuable, but were not ready to make reliable clinical predictions. “The predictive value of these data are limited when it comes to an individual patient sitting in front of you in the office,” said Tomas Mustelin, MD, professor of medicine at the University of Washington, Seattle.
“It would be an important clinical thing if you can figure out who’s at risk for systemic complications and who isn’t. This is a nice step in that direction,” said Hal Scofield, MD, professor of medicine and pathology at the University of Oklahoma, Oklahoma City, agreeing that the data were too preliminary to be broadly useful because there is too much overlap between different patient groups.
If there is one clinical message, it is that physicians should be looking beyond dry eyes and dry mouth in newly diagnosed Sjögren’s syndrome, according to Sarah Chung, MD, who is an acting instructor of rheumatology at the University of Washington. “It’s a reminder to investigate these extra-glandular manifestations, and a reminder that it is a heterogeneous presentation, so we have to keep an open mind and investigate thoroughly,” she said.
In the research published online in Rheumatology, first author Pilar Brito-Zerón, MD, PhD, of the University of Barcelona Hospital Clínic, and colleagues in the Sjögren Big Data Consortium used European League Against Rheumatism Sjögren’s syndrome disease activity index (ESSDAI) scores to examine phenotype and patient characteristics among 10,007 subjects drawn from the international consortium.
Overall, 93.5% of subjects were women, and the mean age at diagnosis was 53 (standard deviation [SD], 14.1 years). The mean total ESSDAI score was 6.1 (SD, 7.5).
Men had higher mean ESSDAI (8.1 vs. 6.0; P less than .001) and clinical ESSDAI (8.4 vs. 6.1; P less than .001) scores and were more likely to have a high disease activity state (22.5% vs. 11.7%; P less than .001). Domains that scored higher in men included lymphadenopathy (P less than .001), glandular (P less than .001), pulmonary (P = .001), peripheral nervous system (PNS) (P less than .001), and CNS (P less than .001).
The highest global ESSDAI scores were reported in patients younger than 35, but organ dominance differed by age group: The constitutional, lymphadenopathy, glandular, cutaneous, renal, hematologic, and biologic domains were highest in this age group, but pulmonary and peripheral nervous system were highest in patients over 65.
By ethnicity, the highest ESSDAI scores occurred in black/African-American patients (6.7), followed by white (6.5), Asian (5.4), and Hispanic (4.8; P less than .001). The organ-specific domains also tracked by ethnicity, with BAA patients experiencing the highest frequencies of activity in the lymphadenopathy, articular, neurologic, and biologic domains. White patients were more often affected in the glandular, cutaneous, and muscular domains, whereas Asians most often experienced the pulmonary, renal, and hematologic domains, and Hispanics the constitutional domain.
The survey included Europe, America, and Asia, and global ESSDAI scores were higher in the southern countries of Asia and Europe, and higher in countries below the equator in the Americas. The organ-by-organ activity scores had a differentiated pattern between northern and southern locales. Worldwide, the gradient of patients with moderate systemic activity (global ESSDAI score of 5 or higher) at diagnosis followed a north-south gradient.
The study had no specific funding, and the authors have no relevant financial disclosures. Dr. Mustelin, Dr. Scofield, and Dr. Chung have no relevant financial disclosures.
SOURCE: Brito-Zerón P et al. Rheumatology. 2019 Dec 24. doi: 10.1093/rheumatology/kez578.
The severity of Sjögren’s syndrome and its organ involvement has direct links to clinical characteristics that include age, gender, ethnicity, and geographical location, according to new research findings from a large, worldwide database of primary Sjögren’s syndrome patients.
Risk factors for more severe disease included male sex, earlier age at diagnosis, black/African-American (BAA) ethnicity, and living in more southerly countries, including below the equator. The authors hailed these factors as potentially helping to predict the presence of systemic disease in newly-diagnosed patients, as well as helping to determine the optimum follow-up strategy.
But not everyone agrees. In interviews, other experts suggested that the data were interesting and valuable, but were not ready to make reliable clinical predictions. “The predictive value of these data are limited when it comes to an individual patient sitting in front of you in the office,” said Tomas Mustelin, MD, professor of medicine at the University of Washington, Seattle.
“It would be an important clinical thing if you can figure out who’s at risk for systemic complications and who isn’t. This is a nice step in that direction,” said Hal Scofield, MD, professor of medicine and pathology at the University of Oklahoma, Oklahoma City, agreeing that the data were too preliminary to be broadly useful because there is too much overlap between different patient groups.
If there is one clinical message, it is that physicians should be looking beyond dry eyes and dry mouth in newly diagnosed Sjögren’s syndrome, according to Sarah Chung, MD, who is an acting instructor of rheumatology at the University of Washington. “It’s a reminder to investigate these extra-glandular manifestations, and a reminder that it is a heterogeneous presentation, so we have to keep an open mind and investigate thoroughly,” she said.
In the research published online in Rheumatology, first author Pilar Brito-Zerón, MD, PhD, of the University of Barcelona Hospital Clínic, and colleagues in the Sjögren Big Data Consortium used European League Against Rheumatism Sjögren’s syndrome disease activity index (ESSDAI) scores to examine phenotype and patient characteristics among 10,007 subjects drawn from the international consortium.
Overall, 93.5% of subjects were women, and the mean age at diagnosis was 53 (standard deviation [SD], 14.1 years). The mean total ESSDAI score was 6.1 (SD, 7.5).
Men had higher mean ESSDAI (8.1 vs. 6.0; P less than .001) and clinical ESSDAI (8.4 vs. 6.1; P less than .001) scores and were more likely to have a high disease activity state (22.5% vs. 11.7%; P less than .001). Domains that scored higher in men included lymphadenopathy (P less than .001), glandular (P less than .001), pulmonary (P = .001), peripheral nervous system (PNS) (P less than .001), and CNS (P less than .001).
The highest global ESSDAI scores were reported in patients younger than 35, but organ dominance differed by age group: The constitutional, lymphadenopathy, glandular, cutaneous, renal, hematologic, and biologic domains were highest in this age group, but pulmonary and peripheral nervous system were highest in patients over 65.
By ethnicity, the highest ESSDAI scores occurred in black/African-American patients (6.7), followed by white (6.5), Asian (5.4), and Hispanic (4.8; P less than .001). The organ-specific domains also tracked by ethnicity, with BAA patients experiencing the highest frequencies of activity in the lymphadenopathy, articular, neurologic, and biologic domains. White patients were more often affected in the glandular, cutaneous, and muscular domains, whereas Asians most often experienced the pulmonary, renal, and hematologic domains, and Hispanics the constitutional domain.
The survey included Europe, America, and Asia, and global ESSDAI scores were higher in the southern countries of Asia and Europe, and higher in countries below the equator in the Americas. The organ-by-organ activity scores had a differentiated pattern between northern and southern locales. Worldwide, the gradient of patients with moderate systemic activity (global ESSDAI score of 5 or higher) at diagnosis followed a north-south gradient.
The study had no specific funding, and the authors have no relevant financial disclosures. Dr. Mustelin, Dr. Scofield, and Dr. Chung have no relevant financial disclosures.
SOURCE: Brito-Zerón P et al. Rheumatology. 2019 Dec 24. doi: 10.1093/rheumatology/kez578.
FROM RHEUMATOLOGY
Children with resistant UTIs unexpectedly may respond to discordant antibiotics
Children with urinary tract infections (UTIs) may improve clinically, and pyuria may resolve, during empiric treatment with an antibiotic that turns out to be discordant, according a retrospective study in Pediatrics.
“The low rate of care escalation and high rate of clinical improvement while on discordant antibiotics suggests that, for most patients, it would be reasonable to continue current empiric antibiotic practices until urine culture sensitivities return,” said first author Marie E. Wang, MD, a pediatric hospitalist at Stanford (Calif.) University, and colleagues.
The researchers examined the initial clinical response and escalation of care for 316 children with UTIs who received therapy to which the infecting isolate was not susceptible. The study included patients who had infections that were resistant to third-generation cephalosporins – that is, urinalysis found that the infections were not susceptible to ceftriaxone or cefotaxime in vitro. Before the resistant organisms were identified, however, the patients were started on discordant antibiotics.
Escalation of care was uncommon
The patients had a median age of 2.4 years, and 78% were girls. Approximately 90% were started on a cephalosporin, and about 65% received a first-generation cephalosporin. Patients presented during 2012-2017 to one of five children’s hospitals or to a large managed care organization with 10 hospitals in the United States. The investigators defined care escalation as a visit to the emergency department, hospitalization, or transfer to the ICU.
In all, seven patients (2%) had escalation of care on discordant antibiotics. Four children visited an emergency department without hospitalization, and three children were hospitalized because of persistent symptoms.
Among 230 cases for which the researchers had data about clinical response at a median follow-up of 3 days, 84% “had overall clinical improvement while on discordant antibiotics,” the authors said.
For 22 children who had repeat urine testing while on discordant antibiotics, 53% had resolution of pyuria, and 32% had improvement of pyuria, whereas 16% did not have improvement. Of the three patients without improvement, one had no change, and two had worsening.
Of 17 patients who had a repeat urine culture on discordant therapy, 65% had a negative repeat culture, and 18% grew the same pathogen with a decreased colony count. Two patients had a colony count that remained unchanged, and one patient had an increased colony count.
Small studies outside the United States have reported similar results, the researchers noted. Spontaneous resolution of UTIs or antibiotics reaching a sufficient concentration in the urine and renal parenchyma to achieve a clinical response are possible explanations for the findings, they wrote.
“Few children required escalation of care and most experienced initial clinical improvement,” noted Dr. Wang and colleagues. “Furthermore, in the small group of children that underwent repeat urine testing while on discordant therapy, most had resolution or improvement in pyuria and sterilization of their urine cultures. Our findings suggest that Additionally, given that these patients initially received what would generally be considered inadequate treatment, our findings may provide some insight into the natural history of UTIs and/or trigger further investigation into the relationship between in vitro urine culture susceptibilities and in vivo clinical response to treatment.”
‘Caution is needed’
The study “highlights an intriguing observation about children with UTIs unexpectedly responding to discordant antibiotic therapy,” Tej K. Mattoo, MD, and Basim I. Asmar, MD, wrote in an accompanying commentary.(doi: 10.1542/peds.2019-3512). Dr. Mattoo and Dr. Asmar, a pediatric nephrologist and a specialist in pediatric infectious diseases, respectively, at Wayne State University and affiliated with Children’s Hospital of Michigan, both in Detroit.
In an inpatient setting, it may be easy for physicians to reassess patients “once urine culture results reveal resistance to the treating antibiotic,” they noted. In an ambulatory setting, however, “it is likely that some patients will receive a full course of an antibiotic that does not have in vitro activity against the urinary pathogen.”
Physicians have a responsibility to use antibiotics judiciously, they said. Widely accepted principles include avoiding repeated courses of antibiotics, diagnosing UTIs appropriately, and not treating asymptomatic bacteriuria.
The study had no external funding. The authors had no relevant financial disclosures.
SOURCE: Wang ME et al. Pediatrics. 2020 Jan 17. doi: 10.1542/peds.2019-1608.
This article was updated 2/4/2020.
Children with urinary tract infections (UTIs) may improve clinically, and pyuria may resolve, during empiric treatment with an antibiotic that turns out to be discordant, according a retrospective study in Pediatrics.
“The low rate of care escalation and high rate of clinical improvement while on discordant antibiotics suggests that, for most patients, it would be reasonable to continue current empiric antibiotic practices until urine culture sensitivities return,” said first author Marie E. Wang, MD, a pediatric hospitalist at Stanford (Calif.) University, and colleagues.
The researchers examined the initial clinical response and escalation of care for 316 children with UTIs who received therapy to which the infecting isolate was not susceptible. The study included patients who had infections that were resistant to third-generation cephalosporins – that is, urinalysis found that the infections were not susceptible to ceftriaxone or cefotaxime in vitro. Before the resistant organisms were identified, however, the patients were started on discordant antibiotics.
Escalation of care was uncommon
The patients had a median age of 2.4 years, and 78% were girls. Approximately 90% were started on a cephalosporin, and about 65% received a first-generation cephalosporin. Patients presented during 2012-2017 to one of five children’s hospitals or to a large managed care organization with 10 hospitals in the United States. The investigators defined care escalation as a visit to the emergency department, hospitalization, or transfer to the ICU.
In all, seven patients (2%) had escalation of care on discordant antibiotics. Four children visited an emergency department without hospitalization, and three children were hospitalized because of persistent symptoms.
Among 230 cases for which the researchers had data about clinical response at a median follow-up of 3 days, 84% “had overall clinical improvement while on discordant antibiotics,” the authors said.
For 22 children who had repeat urine testing while on discordant antibiotics, 53% had resolution of pyuria, and 32% had improvement of pyuria, whereas 16% did not have improvement. Of the three patients without improvement, one had no change, and two had worsening.
Of 17 patients who had a repeat urine culture on discordant therapy, 65% had a negative repeat culture, and 18% grew the same pathogen with a decreased colony count. Two patients had a colony count that remained unchanged, and one patient had an increased colony count.
Small studies outside the United States have reported similar results, the researchers noted. Spontaneous resolution of UTIs or antibiotics reaching a sufficient concentration in the urine and renal parenchyma to achieve a clinical response are possible explanations for the findings, they wrote.
“Few children required escalation of care and most experienced initial clinical improvement,” noted Dr. Wang and colleagues. “Furthermore, in the small group of children that underwent repeat urine testing while on discordant therapy, most had resolution or improvement in pyuria and sterilization of their urine cultures. Our findings suggest that Additionally, given that these patients initially received what would generally be considered inadequate treatment, our findings may provide some insight into the natural history of UTIs and/or trigger further investigation into the relationship between in vitro urine culture susceptibilities and in vivo clinical response to treatment.”
‘Caution is needed’
The study “highlights an intriguing observation about children with UTIs unexpectedly responding to discordant antibiotic therapy,” Tej K. Mattoo, MD, and Basim I. Asmar, MD, wrote in an accompanying commentary.(doi: 10.1542/peds.2019-3512). Dr. Mattoo and Dr. Asmar, a pediatric nephrologist and a specialist in pediatric infectious diseases, respectively, at Wayne State University and affiliated with Children’s Hospital of Michigan, both in Detroit.
In an inpatient setting, it may be easy for physicians to reassess patients “once urine culture results reveal resistance to the treating antibiotic,” they noted. In an ambulatory setting, however, “it is likely that some patients will receive a full course of an antibiotic that does not have in vitro activity against the urinary pathogen.”
Physicians have a responsibility to use antibiotics judiciously, they said. Widely accepted principles include avoiding repeated courses of antibiotics, diagnosing UTIs appropriately, and not treating asymptomatic bacteriuria.
The study had no external funding. The authors had no relevant financial disclosures.
SOURCE: Wang ME et al. Pediatrics. 2020 Jan 17. doi: 10.1542/peds.2019-1608.
This article was updated 2/4/2020.
Children with urinary tract infections (UTIs) may improve clinically, and pyuria may resolve, during empiric treatment with an antibiotic that turns out to be discordant, according a retrospective study in Pediatrics.
“The low rate of care escalation and high rate of clinical improvement while on discordant antibiotics suggests that, for most patients, it would be reasonable to continue current empiric antibiotic practices until urine culture sensitivities return,” said first author Marie E. Wang, MD, a pediatric hospitalist at Stanford (Calif.) University, and colleagues.
The researchers examined the initial clinical response and escalation of care for 316 children with UTIs who received therapy to which the infecting isolate was not susceptible. The study included patients who had infections that were resistant to third-generation cephalosporins – that is, urinalysis found that the infections were not susceptible to ceftriaxone or cefotaxime in vitro. Before the resistant organisms were identified, however, the patients were started on discordant antibiotics.
Escalation of care was uncommon
The patients had a median age of 2.4 years, and 78% were girls. Approximately 90% were started on a cephalosporin, and about 65% received a first-generation cephalosporin. Patients presented during 2012-2017 to one of five children’s hospitals or to a large managed care organization with 10 hospitals in the United States. The investigators defined care escalation as a visit to the emergency department, hospitalization, or transfer to the ICU.
In all, seven patients (2%) had escalation of care on discordant antibiotics. Four children visited an emergency department without hospitalization, and three children were hospitalized because of persistent symptoms.
Among 230 cases for which the researchers had data about clinical response at a median follow-up of 3 days, 84% “had overall clinical improvement while on discordant antibiotics,” the authors said.
For 22 children who had repeat urine testing while on discordant antibiotics, 53% had resolution of pyuria, and 32% had improvement of pyuria, whereas 16% did not have improvement. Of the three patients without improvement, one had no change, and two had worsening.
Of 17 patients who had a repeat urine culture on discordant therapy, 65% had a negative repeat culture, and 18% grew the same pathogen with a decreased colony count. Two patients had a colony count that remained unchanged, and one patient had an increased colony count.
Small studies outside the United States have reported similar results, the researchers noted. Spontaneous resolution of UTIs or antibiotics reaching a sufficient concentration in the urine and renal parenchyma to achieve a clinical response are possible explanations for the findings, they wrote.
“Few children required escalation of care and most experienced initial clinical improvement,” noted Dr. Wang and colleagues. “Furthermore, in the small group of children that underwent repeat urine testing while on discordant therapy, most had resolution or improvement in pyuria and sterilization of their urine cultures. Our findings suggest that Additionally, given that these patients initially received what would generally be considered inadequate treatment, our findings may provide some insight into the natural history of UTIs and/or trigger further investigation into the relationship between in vitro urine culture susceptibilities and in vivo clinical response to treatment.”
‘Caution is needed’
The study “highlights an intriguing observation about children with UTIs unexpectedly responding to discordant antibiotic therapy,” Tej K. Mattoo, MD, and Basim I. Asmar, MD, wrote in an accompanying commentary.(doi: 10.1542/peds.2019-3512). Dr. Mattoo and Dr. Asmar, a pediatric nephrologist and a specialist in pediatric infectious diseases, respectively, at Wayne State University and affiliated with Children’s Hospital of Michigan, both in Detroit.
In an inpatient setting, it may be easy for physicians to reassess patients “once urine culture results reveal resistance to the treating antibiotic,” they noted. In an ambulatory setting, however, “it is likely that some patients will receive a full course of an antibiotic that does not have in vitro activity against the urinary pathogen.”
Physicians have a responsibility to use antibiotics judiciously, they said. Widely accepted principles include avoiding repeated courses of antibiotics, diagnosing UTIs appropriately, and not treating asymptomatic bacteriuria.
The study had no external funding. The authors had no relevant financial disclosures.
SOURCE: Wang ME et al. Pediatrics. 2020 Jan 17. doi: 10.1542/peds.2019-1608.
This article was updated 2/4/2020.
FROM PEDIATRICS
FDA approves CV disease benefit for once-weekly semaglutide
(Ozempic, Novo Nordisk) in the treatment of type 2 diabetes and has added new trial data information to the label of the oral version (Rybelsus, Novo Nordisk) pertaining to CV safety.
The agency expanded the once-weekly injectable semaglutide’s label to include an indication for reducing the risk for major adverse cardiovascular events (MACE), including CV death, nonfatal myocardial infarction (MI), or nonfatal stroke, in adults with type 2 diabetes who have established CV disease.
Initially approved for the treatment of type 2 diabetes in adults in December 2017, once-weekly subcutaneously injectable semaglutide comes in 0.5-mg and 1.0-mg doses in a dedicated prefilled pen device.
The approval for the new indication was based on data from the 2-year randomized Trial to Evaluate Cardiovascular and Other Long-term Outcomes With Semaglutide in Subjects With Type 2 Diabetes (SUSTAIN 6), in which injectable semaglutide or placebo was added to standard of care in 3,297 adults with type 2 diabetes and established CV disease.
As reported by Medscape Medical News in September 2016, patients who underwent treatment with one of the two doses of semaglutide had a significant 26% lower risk for the primary composite outcome of first occurrence of CV death, nonfatal MI, or nonfatal stroke, compared with those who received placebo.
The reduced CV risk was driven primarily by significant reductions in nonfatal stroke and nonfatal MI (39% and 26%, respectively). There was no difference in CV death between drug and placebo groups. Gastrointestinal adverse events were more frequent with semaglutide than placebo, with the majority occurring during the first 30 weeks.
The oral semaglutide formulation, taken daily in 7-mg or 14-mg doses, was approved for the treatment of type 2 diabetes in September 2019, the first orally available GLP-1 agonist.
Now, the FDA has updated the prescribing information in the clinical studies section (section 14) to include results from the randomized, placebo-controlled, 3,183-subject Trial Investigating the Cardiovascular Safety of Oral Semaglutide in Subjects With Type 2 Diabetes (PIONEER 6), reported in June 2019, which found a nonsignificant 21% reduction in three-component MACE with oral semaglutide. The addition to the label for Rybelsus is with regard to CV safety, not benefit.
SOUL: Large ongoing CV outcomes trial for oral semaglutide
In June 2019, Novo Nordisk initiated a larger CV outcomes trial of oral semaglutide, A Heart Disease Study of Semaglutide in Patients With Type 2 Diabetes (SOUL). The trial, which includes 9,642 adults with type 2 diabetes and established CV disease, is further investigating the drug’s effects on the incidence of MACE. The estimated completion date is July 2024.
Semaglutide joins a growing list of drugs approved for treating type 2 diabetes that have been granted additional label indications for benefits beyond the lowering of glucose.
These include Novo Nordisk’s other injectable GLP-1 agonist, liraglutide (Victoza), additionally approved for reducing CV events in high-risk patients with type 2 diabetes, and the sodium-glucose transport 2 inhibitors empagliflozin (Jardiance, Boehringer Ingelheim/Lilly), for reducing CV death; canagliflozin (Invokana, Janssen), for reducing major adverse CV events,; kidney disease, CV death, and heart failure hospitalization; and dapagliflozin (Farxiga, AstraZeneca), for reducing heart failure hospitalization.
Recently, in an exclusive Medscape Medical News article, some experts questioned the design of these CV outcomes trials, suggesting that imbalances in glycemic control, blood pressure, and diuretic use between treatment and placebo arms could have biased the CV and renal outcomes of the trials in favor of the study drugs
A version of this story originally appeared on Medscape.com.
(Ozempic, Novo Nordisk) in the treatment of type 2 diabetes and has added new trial data information to the label of the oral version (Rybelsus, Novo Nordisk) pertaining to CV safety.
The agency expanded the once-weekly injectable semaglutide’s label to include an indication for reducing the risk for major adverse cardiovascular events (MACE), including CV death, nonfatal myocardial infarction (MI), or nonfatal stroke, in adults with type 2 diabetes who have established CV disease.
Initially approved for the treatment of type 2 diabetes in adults in December 2017, once-weekly subcutaneously injectable semaglutide comes in 0.5-mg and 1.0-mg doses in a dedicated prefilled pen device.
The approval for the new indication was based on data from the 2-year randomized Trial to Evaluate Cardiovascular and Other Long-term Outcomes With Semaglutide in Subjects With Type 2 Diabetes (SUSTAIN 6), in which injectable semaglutide or placebo was added to standard of care in 3,297 adults with type 2 diabetes and established CV disease.
As reported by Medscape Medical News in September 2016, patients who underwent treatment with one of the two doses of semaglutide had a significant 26% lower risk for the primary composite outcome of first occurrence of CV death, nonfatal MI, or nonfatal stroke, compared with those who received placebo.
The reduced CV risk was driven primarily by significant reductions in nonfatal stroke and nonfatal MI (39% and 26%, respectively). There was no difference in CV death between drug and placebo groups. Gastrointestinal adverse events were more frequent with semaglutide than placebo, with the majority occurring during the first 30 weeks.
The oral semaglutide formulation, taken daily in 7-mg or 14-mg doses, was approved for the treatment of type 2 diabetes in September 2019, the first orally available GLP-1 agonist.
Now, the FDA has updated the prescribing information in the clinical studies section (section 14) to include results from the randomized, placebo-controlled, 3,183-subject Trial Investigating the Cardiovascular Safety of Oral Semaglutide in Subjects With Type 2 Diabetes (PIONEER 6), reported in June 2019, which found a nonsignificant 21% reduction in three-component MACE with oral semaglutide. The addition to the label for Rybelsus is with regard to CV safety, not benefit.
SOUL: Large ongoing CV outcomes trial for oral semaglutide
In June 2019, Novo Nordisk initiated a larger CV outcomes trial of oral semaglutide, A Heart Disease Study of Semaglutide in Patients With Type 2 Diabetes (SOUL). The trial, which includes 9,642 adults with type 2 diabetes and established CV disease, is further investigating the drug’s effects on the incidence of MACE. The estimated completion date is July 2024.
Semaglutide joins a growing list of drugs approved for treating type 2 diabetes that have been granted additional label indications for benefits beyond the lowering of glucose.
These include Novo Nordisk’s other injectable GLP-1 agonist, liraglutide (Victoza), additionally approved for reducing CV events in high-risk patients with type 2 diabetes, and the sodium-glucose transport 2 inhibitors empagliflozin (Jardiance, Boehringer Ingelheim/Lilly), for reducing CV death; canagliflozin (Invokana, Janssen), for reducing major adverse CV events,; kidney disease, CV death, and heart failure hospitalization; and dapagliflozin (Farxiga, AstraZeneca), for reducing heart failure hospitalization.
Recently, in an exclusive Medscape Medical News article, some experts questioned the design of these CV outcomes trials, suggesting that imbalances in glycemic control, blood pressure, and diuretic use between treatment and placebo arms could have biased the CV and renal outcomes of the trials in favor of the study drugs
A version of this story originally appeared on Medscape.com.
(Ozempic, Novo Nordisk) in the treatment of type 2 diabetes and has added new trial data information to the label of the oral version (Rybelsus, Novo Nordisk) pertaining to CV safety.
The agency expanded the once-weekly injectable semaglutide’s label to include an indication for reducing the risk for major adverse cardiovascular events (MACE), including CV death, nonfatal myocardial infarction (MI), or nonfatal stroke, in adults with type 2 diabetes who have established CV disease.
Initially approved for the treatment of type 2 diabetes in adults in December 2017, once-weekly subcutaneously injectable semaglutide comes in 0.5-mg and 1.0-mg doses in a dedicated prefilled pen device.
The approval for the new indication was based on data from the 2-year randomized Trial to Evaluate Cardiovascular and Other Long-term Outcomes With Semaglutide in Subjects With Type 2 Diabetes (SUSTAIN 6), in which injectable semaglutide or placebo was added to standard of care in 3,297 adults with type 2 diabetes and established CV disease.
As reported by Medscape Medical News in September 2016, patients who underwent treatment with one of the two doses of semaglutide had a significant 26% lower risk for the primary composite outcome of first occurrence of CV death, nonfatal MI, or nonfatal stroke, compared with those who received placebo.
The reduced CV risk was driven primarily by significant reductions in nonfatal stroke and nonfatal MI (39% and 26%, respectively). There was no difference in CV death between drug and placebo groups. Gastrointestinal adverse events were more frequent with semaglutide than placebo, with the majority occurring during the first 30 weeks.
The oral semaglutide formulation, taken daily in 7-mg or 14-mg doses, was approved for the treatment of type 2 diabetes in September 2019, the first orally available GLP-1 agonist.
Now, the FDA has updated the prescribing information in the clinical studies section (section 14) to include results from the randomized, placebo-controlled, 3,183-subject Trial Investigating the Cardiovascular Safety of Oral Semaglutide in Subjects With Type 2 Diabetes (PIONEER 6), reported in June 2019, which found a nonsignificant 21% reduction in three-component MACE with oral semaglutide. The addition to the label for Rybelsus is with regard to CV safety, not benefit.
SOUL: Large ongoing CV outcomes trial for oral semaglutide
In June 2019, Novo Nordisk initiated a larger CV outcomes trial of oral semaglutide, A Heart Disease Study of Semaglutide in Patients With Type 2 Diabetes (SOUL). The trial, which includes 9,642 adults with type 2 diabetes and established CV disease, is further investigating the drug’s effects on the incidence of MACE. The estimated completion date is July 2024.
Semaglutide joins a growing list of drugs approved for treating type 2 diabetes that have been granted additional label indications for benefits beyond the lowering of glucose.
These include Novo Nordisk’s other injectable GLP-1 agonist, liraglutide (Victoza), additionally approved for reducing CV events in high-risk patients with type 2 diabetes, and the sodium-glucose transport 2 inhibitors empagliflozin (Jardiance, Boehringer Ingelheim/Lilly), for reducing CV death; canagliflozin (Invokana, Janssen), for reducing major adverse CV events,; kidney disease, CV death, and heart failure hospitalization; and dapagliflozin (Farxiga, AstraZeneca), for reducing heart failure hospitalization.
Recently, in an exclusive Medscape Medical News article, some experts questioned the design of these CV outcomes trials, suggesting that imbalances in glycemic control, blood pressure, and diuretic use between treatment and placebo arms could have biased the CV and renal outcomes of the trials in favor of the study drugs
A version of this story originally appeared on Medscape.com.
Pyrrolidone carboxylic acid may be a key cutaneous biomarker
Pyrrolidone carboxylic acid (PCA), the primary constituent of the natural moisturizing factor (NMF),1 including its derivatives – such as simple2 and novel3 esters as well as sugar complexes4 – is the subject of great interest and research regarding its capacity to moisturize the stratum corneum via topical application.
Creams and lotions containing the sodium salt of PCA are widely reported to aid in hydrating the skin and ameliorating dry flaky skin conditions.5,6 In addition, the zinc salt of L-pyrrolidone carboxylate is a longtime cosmetic ingredient due to antimicrobial and astringent qualities. This column briefly addresses the role of PCA in skin health.7
Dry skin
In a comprehensive literature review from 1981, Clar and Fourtanier reported conclusive evidence that PCA acts as a hydrating agent and that all the cosmetic formulations with a minimum of 2% PCA and PCA salt that they tested in their own 8-year study enhanced dry skin in short- and long-term conditions given suitable vehicles (no aqueous solutions).6
In a 2014 clinical study of 64 healthy white women with either normal or cosmetic dry skin, Feng et al. noted that tape stripped samples of stratum corneum revealed significantly lower ratios of free amino acids to protein and PCA to protein. This was associated with decreased hydration levels compared with normal skin. The investigators concluded that lower NMF levels across the depth of the stratum corneum and reduced cohesivity characterize cosmetic dry skin and that these clinical endpoints merit attention in evaluating the usefulness of treatments for dry skin.8
In 2016, Wei et al. reported on their assessment of the barrier function, hydration, and dryness of the lower leg skin of 25 female patients during the winter and then in the subsequent summer. They found that PCA levels were significantly greater during the summer, as were keratins. Hydration was also higher during the summer, while transepidermal water loss and visual dryness grades were substantially lower.9
Atopic dermatitis
A 2014 clinical study by Brandt et al. in patients with skin prone to developing atopic dermatitis (AD) revealed that a body wash composed of the filaggrin metabolites arginine and PCA was well tolerated and diminished pruritus. Patients reported liking the product and suggested that it improved their quality of life.10
Later that year, Jung et al. characterized the relationship of PCA levels, and other factors, with the clinical severity of AD. Specifically, in a study of 73 subjects (21 with mild AD, 21 with moderate to severe AD, 13 with X-linked ichthyosis as a negative control for filaggrin gene mutation, and 18 healthy controls), the investigators assessed transepidermal water loss, stratum corneum hydration, and skin surface pH. They found that PCA levels and caspase-14 were lower in inflammatory lesions compared with nonlesional skin in subjects with AD. These levels also were associated with clinical AD severity as measured by eczema area and severity index scores as well as skin barrier function.11
PCA as a biomarker
In 2009, Kezic et al. determined that the use of tape stripping to cull PCA in the stratum corneum was effective in revealing that PCA concentration in the outermost skin layer is a viable biomarker of filaggrin genotype.12
Raj et al. conducted an interesting study in 2016 in which they set out to describe the various markers for total NMF levels and link them to the activities of plasmin and corneocyte maturation in the photoexposed cheek and photoprotected postauricular regions of healthy white, black African, and albino African women in South Africa. PCA levels were highest among the albino African group, followed by black African and then white participants. The investigators also found that bleomycin hydrolase was linked to PCA synthesis, as suggested by higher bleomycin levels in albino African participants. In this group, corneocyte maturation was also observed to be impeded.13
The next year, the same team studied stratum corneum physiology and biochemistry of the cheeks in 48 white women with sensitive skin. The goal was to ascertain the connections between bleomycin hydrolase and calpain-1, PCA levels, corneocyte maturation, and transglutaminase and plasmin activities. Capsaicin sensitivity was observed in 52% of subjects, with PCA levels and bleomycin hydrolase activity found to be lower in the capsaicin-sensitive panel and correlated in subjects not sensitive to capsaicin. The researchers concluded that reduced levels of PCA, bleomycin hydrolase, and transglutaminase combined with a larger volume of immature corneocytes suggest comparatively poor stratum corneum maturation in individuals with sensitive skin.14
Other uses
In 2012, Takino et al. used cultured normal human dermal fibroblasts to show that zinc l-pyrrolidone carboxylate blocked UVA induction of activator protein-1, diminished matrix metalloproteinase-1 synthesis, and spurred type I collagen production. The researchers suggested that such results suggest the potential of zinc PCA for further investigation as an agent to combat photoaging.7
Conclusion
. Recent research suggests that it may serve as an important biomarker of filaggrin, NMF levels, and skin hydration. In addition, new data point to its usefulness as a gauge for ADs. More investigations are necessary to ascertain the feasibility of adjusting PCA levels through topical administration and what effects topically applied PCA may have on various skin parameters.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), as well as a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
References
1. Björklund S et al. Soft Matter. 2014 Jul 7;10(25):4535-46.
2. Hall KJ, Hill JC. J Soc Cosmet Chem. 1986;37(6):397-407.
3. Tezuka T et al. Dermatology. 1994;188(1):21-4.
4. Kwoya Hakko Kogyo Co. Pyrrolidone carboxylic acid esters containing composition used to prevent loss of moisture from the skin. Patent JA 48 82 046 (1982).
5. Org Santerre. l-pyrrolidone carboxylic acid-sugar compounds as rehydrating ingredients in cosmetics. Patent Fr 2 277 823 (1977).
6. Clar EJ, Fourtanier A. Int J Cosmet Sci. 1981 Jun;3(3):101-13.
7. Takino Y et al. Int J Cosmet Sci. 2012 Feb;34(1):23-8.
8. Feng L et al. Int J Cosmet Sci. 2014 Jun;36(3):231-8.
9. Wei KS et al. J Cosmet Sci. 2016 May-Jun;67(3):185-203.
10. Brandt S et al. J Drugs Dermatol. 2014 Sep;13(9):1108-11.
11. Jung M et al. J Dermatol Sci. 2014 Dec;76(3):231-9.
12. Kezic S et al. Br J Dermatol. 2009 Nov;161(5):1098-104.
13. Raj N et al. Int J Cosmet Sci. 2016 Dec;38(6):567-75.
14. Raj N et al. Int J Cosmet Sci. 2017 Feb;39(1):2-10.
Pyrrolidone carboxylic acid (PCA), the primary constituent of the natural moisturizing factor (NMF),1 including its derivatives – such as simple2 and novel3 esters as well as sugar complexes4 – is the subject of great interest and research regarding its capacity to moisturize the stratum corneum via topical application.
Creams and lotions containing the sodium salt of PCA are widely reported to aid in hydrating the skin and ameliorating dry flaky skin conditions.5,6 In addition, the zinc salt of L-pyrrolidone carboxylate is a longtime cosmetic ingredient due to antimicrobial and astringent qualities. This column briefly addresses the role of PCA in skin health.7
Dry skin
In a comprehensive literature review from 1981, Clar and Fourtanier reported conclusive evidence that PCA acts as a hydrating agent and that all the cosmetic formulations with a minimum of 2% PCA and PCA salt that they tested in their own 8-year study enhanced dry skin in short- and long-term conditions given suitable vehicles (no aqueous solutions).6
In a 2014 clinical study of 64 healthy white women with either normal or cosmetic dry skin, Feng et al. noted that tape stripped samples of stratum corneum revealed significantly lower ratios of free amino acids to protein and PCA to protein. This was associated with decreased hydration levels compared with normal skin. The investigators concluded that lower NMF levels across the depth of the stratum corneum and reduced cohesivity characterize cosmetic dry skin and that these clinical endpoints merit attention in evaluating the usefulness of treatments for dry skin.8
In 2016, Wei et al. reported on their assessment of the barrier function, hydration, and dryness of the lower leg skin of 25 female patients during the winter and then in the subsequent summer. They found that PCA levels were significantly greater during the summer, as were keratins. Hydration was also higher during the summer, while transepidermal water loss and visual dryness grades were substantially lower.9
Atopic dermatitis
A 2014 clinical study by Brandt et al. in patients with skin prone to developing atopic dermatitis (AD) revealed that a body wash composed of the filaggrin metabolites arginine and PCA was well tolerated and diminished pruritus. Patients reported liking the product and suggested that it improved their quality of life.10
Later that year, Jung et al. characterized the relationship of PCA levels, and other factors, with the clinical severity of AD. Specifically, in a study of 73 subjects (21 with mild AD, 21 with moderate to severe AD, 13 with X-linked ichthyosis as a negative control for filaggrin gene mutation, and 18 healthy controls), the investigators assessed transepidermal water loss, stratum corneum hydration, and skin surface pH. They found that PCA levels and caspase-14 were lower in inflammatory lesions compared with nonlesional skin in subjects with AD. These levels also were associated with clinical AD severity as measured by eczema area and severity index scores as well as skin barrier function.11
PCA as a biomarker
In 2009, Kezic et al. determined that the use of tape stripping to cull PCA in the stratum corneum was effective in revealing that PCA concentration in the outermost skin layer is a viable biomarker of filaggrin genotype.12
Raj et al. conducted an interesting study in 2016 in which they set out to describe the various markers for total NMF levels and link them to the activities of plasmin and corneocyte maturation in the photoexposed cheek and photoprotected postauricular regions of healthy white, black African, and albino African women in South Africa. PCA levels were highest among the albino African group, followed by black African and then white participants. The investigators also found that bleomycin hydrolase was linked to PCA synthesis, as suggested by higher bleomycin levels in albino African participants. In this group, corneocyte maturation was also observed to be impeded.13
The next year, the same team studied stratum corneum physiology and biochemistry of the cheeks in 48 white women with sensitive skin. The goal was to ascertain the connections between bleomycin hydrolase and calpain-1, PCA levels, corneocyte maturation, and transglutaminase and plasmin activities. Capsaicin sensitivity was observed in 52% of subjects, with PCA levels and bleomycin hydrolase activity found to be lower in the capsaicin-sensitive panel and correlated in subjects not sensitive to capsaicin. The researchers concluded that reduced levels of PCA, bleomycin hydrolase, and transglutaminase combined with a larger volume of immature corneocytes suggest comparatively poor stratum corneum maturation in individuals with sensitive skin.14
Other uses
In 2012, Takino et al. used cultured normal human dermal fibroblasts to show that zinc l-pyrrolidone carboxylate blocked UVA induction of activator protein-1, diminished matrix metalloproteinase-1 synthesis, and spurred type I collagen production. The researchers suggested that such results suggest the potential of zinc PCA for further investigation as an agent to combat photoaging.7
Conclusion
. Recent research suggests that it may serve as an important biomarker of filaggrin, NMF levels, and skin hydration. In addition, new data point to its usefulness as a gauge for ADs. More investigations are necessary to ascertain the feasibility of adjusting PCA levels through topical administration and what effects topically applied PCA may have on various skin parameters.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), as well as a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
References
1. Björklund S et al. Soft Matter. 2014 Jul 7;10(25):4535-46.
2. Hall KJ, Hill JC. J Soc Cosmet Chem. 1986;37(6):397-407.
3. Tezuka T et al. Dermatology. 1994;188(1):21-4.
4. Kwoya Hakko Kogyo Co. Pyrrolidone carboxylic acid esters containing composition used to prevent loss of moisture from the skin. Patent JA 48 82 046 (1982).
5. Org Santerre. l-pyrrolidone carboxylic acid-sugar compounds as rehydrating ingredients in cosmetics. Patent Fr 2 277 823 (1977).
6. Clar EJ, Fourtanier A. Int J Cosmet Sci. 1981 Jun;3(3):101-13.
7. Takino Y et al. Int J Cosmet Sci. 2012 Feb;34(1):23-8.
8. Feng L et al. Int J Cosmet Sci. 2014 Jun;36(3):231-8.
9. Wei KS et al. J Cosmet Sci. 2016 May-Jun;67(3):185-203.
10. Brandt S et al. J Drugs Dermatol. 2014 Sep;13(9):1108-11.
11. Jung M et al. J Dermatol Sci. 2014 Dec;76(3):231-9.
12. Kezic S et al. Br J Dermatol. 2009 Nov;161(5):1098-104.
13. Raj N et al. Int J Cosmet Sci. 2016 Dec;38(6):567-75.
14. Raj N et al. Int J Cosmet Sci. 2017 Feb;39(1):2-10.
Pyrrolidone carboxylic acid (PCA), the primary constituent of the natural moisturizing factor (NMF),1 including its derivatives – such as simple2 and novel3 esters as well as sugar complexes4 – is the subject of great interest and research regarding its capacity to moisturize the stratum corneum via topical application.
Creams and lotions containing the sodium salt of PCA are widely reported to aid in hydrating the skin and ameliorating dry flaky skin conditions.5,6 In addition, the zinc salt of L-pyrrolidone carboxylate is a longtime cosmetic ingredient due to antimicrobial and astringent qualities. This column briefly addresses the role of PCA in skin health.7
Dry skin
In a comprehensive literature review from 1981, Clar and Fourtanier reported conclusive evidence that PCA acts as a hydrating agent and that all the cosmetic formulations with a minimum of 2% PCA and PCA salt that they tested in their own 8-year study enhanced dry skin in short- and long-term conditions given suitable vehicles (no aqueous solutions).6
In a 2014 clinical study of 64 healthy white women with either normal or cosmetic dry skin, Feng et al. noted that tape stripped samples of stratum corneum revealed significantly lower ratios of free amino acids to protein and PCA to protein. This was associated with decreased hydration levels compared with normal skin. The investigators concluded that lower NMF levels across the depth of the stratum corneum and reduced cohesivity characterize cosmetic dry skin and that these clinical endpoints merit attention in evaluating the usefulness of treatments for dry skin.8
In 2016, Wei et al. reported on their assessment of the barrier function, hydration, and dryness of the lower leg skin of 25 female patients during the winter and then in the subsequent summer. They found that PCA levels were significantly greater during the summer, as were keratins. Hydration was also higher during the summer, while transepidermal water loss and visual dryness grades were substantially lower.9
Atopic dermatitis
A 2014 clinical study by Brandt et al. in patients with skin prone to developing atopic dermatitis (AD) revealed that a body wash composed of the filaggrin metabolites arginine and PCA was well tolerated and diminished pruritus. Patients reported liking the product and suggested that it improved their quality of life.10
Later that year, Jung et al. characterized the relationship of PCA levels, and other factors, with the clinical severity of AD. Specifically, in a study of 73 subjects (21 with mild AD, 21 with moderate to severe AD, 13 with X-linked ichthyosis as a negative control for filaggrin gene mutation, and 18 healthy controls), the investigators assessed transepidermal water loss, stratum corneum hydration, and skin surface pH. They found that PCA levels and caspase-14 were lower in inflammatory lesions compared with nonlesional skin in subjects with AD. These levels also were associated with clinical AD severity as measured by eczema area and severity index scores as well as skin barrier function.11
PCA as a biomarker
In 2009, Kezic et al. determined that the use of tape stripping to cull PCA in the stratum corneum was effective in revealing that PCA concentration in the outermost skin layer is a viable biomarker of filaggrin genotype.12
Raj et al. conducted an interesting study in 2016 in which they set out to describe the various markers for total NMF levels and link them to the activities of plasmin and corneocyte maturation in the photoexposed cheek and photoprotected postauricular regions of healthy white, black African, and albino African women in South Africa. PCA levels were highest among the albino African group, followed by black African and then white participants. The investigators also found that bleomycin hydrolase was linked to PCA synthesis, as suggested by higher bleomycin levels in albino African participants. In this group, corneocyte maturation was also observed to be impeded.13
The next year, the same team studied stratum corneum physiology and biochemistry of the cheeks in 48 white women with sensitive skin. The goal was to ascertain the connections between bleomycin hydrolase and calpain-1, PCA levels, corneocyte maturation, and transglutaminase and plasmin activities. Capsaicin sensitivity was observed in 52% of subjects, with PCA levels and bleomycin hydrolase activity found to be lower in the capsaicin-sensitive panel and correlated in subjects not sensitive to capsaicin. The researchers concluded that reduced levels of PCA, bleomycin hydrolase, and transglutaminase combined with a larger volume of immature corneocytes suggest comparatively poor stratum corneum maturation in individuals with sensitive skin.14
Other uses
In 2012, Takino et al. used cultured normal human dermal fibroblasts to show that zinc l-pyrrolidone carboxylate blocked UVA induction of activator protein-1, diminished matrix metalloproteinase-1 synthesis, and spurred type I collagen production. The researchers suggested that such results suggest the potential of zinc PCA for further investigation as an agent to combat photoaging.7
Conclusion
. Recent research suggests that it may serve as an important biomarker of filaggrin, NMF levels, and skin hydration. In addition, new data point to its usefulness as a gauge for ADs. More investigations are necessary to ascertain the feasibility of adjusting PCA levels through topical administration and what effects topically applied PCA may have on various skin parameters.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks, “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), as well as a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
References
1. Björklund S et al. Soft Matter. 2014 Jul 7;10(25):4535-46.
2. Hall KJ, Hill JC. J Soc Cosmet Chem. 1986;37(6):397-407.
3. Tezuka T et al. Dermatology. 1994;188(1):21-4.
4. Kwoya Hakko Kogyo Co. Pyrrolidone carboxylic acid esters containing composition used to prevent loss of moisture from the skin. Patent JA 48 82 046 (1982).
5. Org Santerre. l-pyrrolidone carboxylic acid-sugar compounds as rehydrating ingredients in cosmetics. Patent Fr 2 277 823 (1977).
6. Clar EJ, Fourtanier A. Int J Cosmet Sci. 1981 Jun;3(3):101-13.
7. Takino Y et al. Int J Cosmet Sci. 2012 Feb;34(1):23-8.
8. Feng L et al. Int J Cosmet Sci. 2014 Jun;36(3):231-8.
9. Wei KS et al. J Cosmet Sci. 2016 May-Jun;67(3):185-203.
10. Brandt S et al. J Drugs Dermatol. 2014 Sep;13(9):1108-11.
11. Jung M et al. J Dermatol Sci. 2014 Dec;76(3):231-9.
12. Kezic S et al. Br J Dermatol. 2009 Nov;161(5):1098-104.
13. Raj N et al. Int J Cosmet Sci. 2016 Dec;38(6):567-75.
14. Raj N et al. Int J Cosmet Sci. 2017 Feb;39(1):2-10.