User login
Elizabeth Wurtzel helped clear the air on stigma
When Elizabeth Wurtzel wrote “Prozac Nation,” an autobiographical account published in 1994 of her experience with depression and psychiatric medications, she helped shift the public dialogue about mental illness, and in doing so chipped away at the stigma that continues to haunt many of our patients.
Ms. Wurtzel, who died recently at age 52, wrote about depression passionately and matter-of-factly.
As she stated in “Prozac Nation”: “Depression was the loneliest &*%$ thing on earth. There were no halfway houses for depressives, no Depression Anonymous meetings that I knew of. Yes, of course, there were mental hospitals like McLean and Bellevue and Payne Whitney and the Menninger Clinic, but I couldn’t hope to end up in one of those places unless I made a suicide attempt serious enough to warrant oxygen or stitches or a stomach pump.
“I used to wish – to pray to God for the courage and strength – that I’d have the guts not to get better, but to slit my wrists and get a whole lot worse so I could land in some mental ward, where real help might have been possible.”
Think of where the public consciousness was in 1994. Peter D. Kramer, MD, had started the conversation on Prozac a year earlier with his book, “Listening to Prozac,” Kurt Cobain died by suicide in 1994, and 2 years later President Bill Clinton signed the Personal Responsibility and Work Opportunity Reconciliation Act, a law that “reformed” welfare and some say made it more difficult for low-income Americans to secure psychiatric and addiction services (Milbank Q. 2005 Mar;83[1]:65-99).
Prozac, as we know, was the first SSRI on the market in the late 1980s and was hailed as a major medication breakthrough in the treatment of depression. It lacked the side effects of the tricyclic antidepressants of previous years and did not have the potentially dangerous food restrictions associated with monoamine oxidase inhibitors.
Interestingly, the major reviews of Ms. Wurtzel’s book, mainly written by men, were negative. Those reviews focused more on the lifestyle of Ms. Wurtzel, her introspection, and how difficult life was for her, rather than the importance of the book. To me, her writing skills were exceptional, as was her willingness to put her lifestyle and suffering on the line.
The literary critics failed to recognize the book’s importance in unmasking the massive denial of mental illnesses and what Ms. Wurtzel was trying to get across. There have been many successful male writers over the years whose lives were difficult and replete with emotional pain and suffering, and their work was lauded. Regardless of the reviews’ negativity, readers found her book open and enlightening, making it a bestseller – thus paving the way for better and more-open discussion of mental disorders. It also became a touchstone in discussions of antidepressants in the psychiatric literature (Lancet. 1998 Sep 26. doi: 10.1016/S0140-6736(98)08418-9; Lancet. 2015 Oct 1. doi: 10.1016/S2215-0366[15]00430-7; and Biol Psychiatry. 2018 Dec 1;84[11]:e73-5).
However, unfortunately, the stigma still exists on many levels, often starting with the medical profession itself. In my experience over the years in teaching and supervising medical students, many of those not interested in becoming a psychiatrist all too often could not wait for their psych rotation to be over. Generally, they did not take the rotation seriously. I’ve even heard students making light of the delusions and paranoia seen in the suffering of acutely ill patients.
We can take this even further within the profession. I have had many referrals from far too many extremely competent physicians, across many medical specialties, who would refer to their patient as “sort of crazy.” Those physicians want the best for their patients, clearly, in making the referral, but they need to change their thinking and, therefore, their vocabulary about mental disorders. I’d like to see these physicians be more respectful of our patients – just as I would be if I were referring a patient complaining of fatigue and joint pain to a general internist or rheumatologist.
I once knew a brilliant orthopedic surgeon who, when he made a referral, would sit down with the patient and clearly explain why they were not crazy but had an anxiety or a mood problem that he didn’t treat but had a person to refer to who could help. Likewise, I know an ophthalmologist who tells his patients with some emotional symptoms that they are experiencing a difficult situation and would benefit from help that he is not able to provide but could be resolved with another type of specialist who works with their “difficulties.” We clearly need more docs like this who go out of their specialty to explain what patients might need – despite the administrative burden exacted by EMRs on doctors’ time and energy.
As we grow more tolerant in our culture and eliminate distasteful words about people and groups, maybe we should try and avoid the word crazy – even in our general vocabulary. Furthermore, in social situations, while out to dinner with friends, at the gym, or even while in the workplace, just as we may refer to our primary care doc as the best or report we have the best cardiologist or dermatologist, we rarely hear someone being open about the best psychiatrist, psychologist, or therapist in the same manner.
“If ‘Prozac Nation’ has any particular purpose,” she wrote in the afterword, “it would be to come out and say that clinical depression is a real problem, that it ruins lives, that it ends lives, that it very nearly ended my life, that it afflicts many, many people, many very bright and worthy and thoughtful and caring people, people who could probably save the world or at the very least do it some real good.” Those people are our patients, and medicine should take the lead in working further to destigmatize mental illness.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
When Elizabeth Wurtzel wrote “Prozac Nation,” an autobiographical account published in 1994 of her experience with depression and psychiatric medications, she helped shift the public dialogue about mental illness, and in doing so chipped away at the stigma that continues to haunt many of our patients.
Ms. Wurtzel, who died recently at age 52, wrote about depression passionately and matter-of-factly.
As she stated in “Prozac Nation”: “Depression was the loneliest &*%$ thing on earth. There were no halfway houses for depressives, no Depression Anonymous meetings that I knew of. Yes, of course, there were mental hospitals like McLean and Bellevue and Payne Whitney and the Menninger Clinic, but I couldn’t hope to end up in one of those places unless I made a suicide attempt serious enough to warrant oxygen or stitches or a stomach pump.
“I used to wish – to pray to God for the courage and strength – that I’d have the guts not to get better, but to slit my wrists and get a whole lot worse so I could land in some mental ward, where real help might have been possible.”
Think of where the public consciousness was in 1994. Peter D. Kramer, MD, had started the conversation on Prozac a year earlier with his book, “Listening to Prozac,” Kurt Cobain died by suicide in 1994, and 2 years later President Bill Clinton signed the Personal Responsibility and Work Opportunity Reconciliation Act, a law that “reformed” welfare and some say made it more difficult for low-income Americans to secure psychiatric and addiction services (Milbank Q. 2005 Mar;83[1]:65-99).
Prozac, as we know, was the first SSRI on the market in the late 1980s and was hailed as a major medication breakthrough in the treatment of depression. It lacked the side effects of the tricyclic antidepressants of previous years and did not have the potentially dangerous food restrictions associated with monoamine oxidase inhibitors.
Interestingly, the major reviews of Ms. Wurtzel’s book, mainly written by men, were negative. Those reviews focused more on the lifestyle of Ms. Wurtzel, her introspection, and how difficult life was for her, rather than the importance of the book. To me, her writing skills were exceptional, as was her willingness to put her lifestyle and suffering on the line.
The literary critics failed to recognize the book’s importance in unmasking the massive denial of mental illnesses and what Ms. Wurtzel was trying to get across. There have been many successful male writers over the years whose lives were difficult and replete with emotional pain and suffering, and their work was lauded. Regardless of the reviews’ negativity, readers found her book open and enlightening, making it a bestseller – thus paving the way for better and more-open discussion of mental disorders. It also became a touchstone in discussions of antidepressants in the psychiatric literature (Lancet. 1998 Sep 26. doi: 10.1016/S0140-6736(98)08418-9; Lancet. 2015 Oct 1. doi: 10.1016/S2215-0366[15]00430-7; and Biol Psychiatry. 2018 Dec 1;84[11]:e73-5).
However, unfortunately, the stigma still exists on many levels, often starting with the medical profession itself. In my experience over the years in teaching and supervising medical students, many of those not interested in becoming a psychiatrist all too often could not wait for their psych rotation to be over. Generally, they did not take the rotation seriously. I’ve even heard students making light of the delusions and paranoia seen in the suffering of acutely ill patients.
We can take this even further within the profession. I have had many referrals from far too many extremely competent physicians, across many medical specialties, who would refer to their patient as “sort of crazy.” Those physicians want the best for their patients, clearly, in making the referral, but they need to change their thinking and, therefore, their vocabulary about mental disorders. I’d like to see these physicians be more respectful of our patients – just as I would be if I were referring a patient complaining of fatigue and joint pain to a general internist or rheumatologist.
I once knew a brilliant orthopedic surgeon who, when he made a referral, would sit down with the patient and clearly explain why they were not crazy but had an anxiety or a mood problem that he didn’t treat but had a person to refer to who could help. Likewise, I know an ophthalmologist who tells his patients with some emotional symptoms that they are experiencing a difficult situation and would benefit from help that he is not able to provide but could be resolved with another type of specialist who works with their “difficulties.” We clearly need more docs like this who go out of their specialty to explain what patients might need – despite the administrative burden exacted by EMRs on doctors’ time and energy.
As we grow more tolerant in our culture and eliminate distasteful words about people and groups, maybe we should try and avoid the word crazy – even in our general vocabulary. Furthermore, in social situations, while out to dinner with friends, at the gym, or even while in the workplace, just as we may refer to our primary care doc as the best or report we have the best cardiologist or dermatologist, we rarely hear someone being open about the best psychiatrist, psychologist, or therapist in the same manner.
“If ‘Prozac Nation’ has any particular purpose,” she wrote in the afterword, “it would be to come out and say that clinical depression is a real problem, that it ruins lives, that it ends lives, that it very nearly ended my life, that it afflicts many, many people, many very bright and worthy and thoughtful and caring people, people who could probably save the world or at the very least do it some real good.” Those people are our patients, and medicine should take the lead in working further to destigmatize mental illness.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
When Elizabeth Wurtzel wrote “Prozac Nation,” an autobiographical account published in 1994 of her experience with depression and psychiatric medications, she helped shift the public dialogue about mental illness, and in doing so chipped away at the stigma that continues to haunt many of our patients.
Ms. Wurtzel, who died recently at age 52, wrote about depression passionately and matter-of-factly.
As she stated in “Prozac Nation”: “Depression was the loneliest &*%$ thing on earth. There were no halfway houses for depressives, no Depression Anonymous meetings that I knew of. Yes, of course, there were mental hospitals like McLean and Bellevue and Payne Whitney and the Menninger Clinic, but I couldn’t hope to end up in one of those places unless I made a suicide attempt serious enough to warrant oxygen or stitches or a stomach pump.
“I used to wish – to pray to God for the courage and strength – that I’d have the guts not to get better, but to slit my wrists and get a whole lot worse so I could land in some mental ward, where real help might have been possible.”
Think of where the public consciousness was in 1994. Peter D. Kramer, MD, had started the conversation on Prozac a year earlier with his book, “Listening to Prozac,” Kurt Cobain died by suicide in 1994, and 2 years later President Bill Clinton signed the Personal Responsibility and Work Opportunity Reconciliation Act, a law that “reformed” welfare and some say made it more difficult for low-income Americans to secure psychiatric and addiction services (Milbank Q. 2005 Mar;83[1]:65-99).
Prozac, as we know, was the first SSRI on the market in the late 1980s and was hailed as a major medication breakthrough in the treatment of depression. It lacked the side effects of the tricyclic antidepressants of previous years and did not have the potentially dangerous food restrictions associated with monoamine oxidase inhibitors.
Interestingly, the major reviews of Ms. Wurtzel’s book, mainly written by men, were negative. Those reviews focused more on the lifestyle of Ms. Wurtzel, her introspection, and how difficult life was for her, rather than the importance of the book. To me, her writing skills were exceptional, as was her willingness to put her lifestyle and suffering on the line.
The literary critics failed to recognize the book’s importance in unmasking the massive denial of mental illnesses and what Ms. Wurtzel was trying to get across. There have been many successful male writers over the years whose lives were difficult and replete with emotional pain and suffering, and their work was lauded. Regardless of the reviews’ negativity, readers found her book open and enlightening, making it a bestseller – thus paving the way for better and more-open discussion of mental disorders. It also became a touchstone in discussions of antidepressants in the psychiatric literature (Lancet. 1998 Sep 26. doi: 10.1016/S0140-6736(98)08418-9; Lancet. 2015 Oct 1. doi: 10.1016/S2215-0366[15]00430-7; and Biol Psychiatry. 2018 Dec 1;84[11]:e73-5).
However, unfortunately, the stigma still exists on many levels, often starting with the medical profession itself. In my experience over the years in teaching and supervising medical students, many of those not interested in becoming a psychiatrist all too often could not wait for their psych rotation to be over. Generally, they did not take the rotation seriously. I’ve even heard students making light of the delusions and paranoia seen in the suffering of acutely ill patients.
We can take this even further within the profession. I have had many referrals from far too many extremely competent physicians, across many medical specialties, who would refer to their patient as “sort of crazy.” Those physicians want the best for their patients, clearly, in making the referral, but they need to change their thinking and, therefore, their vocabulary about mental disorders. I’d like to see these physicians be more respectful of our patients – just as I would be if I were referring a patient complaining of fatigue and joint pain to a general internist or rheumatologist.
I once knew a brilliant orthopedic surgeon who, when he made a referral, would sit down with the patient and clearly explain why they were not crazy but had an anxiety or a mood problem that he didn’t treat but had a person to refer to who could help. Likewise, I know an ophthalmologist who tells his patients with some emotional symptoms that they are experiencing a difficult situation and would benefit from help that he is not able to provide but could be resolved with another type of specialist who works with their “difficulties.” We clearly need more docs like this who go out of their specialty to explain what patients might need – despite the administrative burden exacted by EMRs on doctors’ time and energy.
As we grow more tolerant in our culture and eliminate distasteful words about people and groups, maybe we should try and avoid the word crazy – even in our general vocabulary. Furthermore, in social situations, while out to dinner with friends, at the gym, or even while in the workplace, just as we may refer to our primary care doc as the best or report we have the best cardiologist or dermatologist, we rarely hear someone being open about the best psychiatrist, psychologist, or therapist in the same manner.
“If ‘Prozac Nation’ has any particular purpose,” she wrote in the afterword, “it would be to come out and say that clinical depression is a real problem, that it ruins lives, that it ends lives, that it very nearly ended my life, that it afflicts many, many people, many very bright and worthy and thoughtful and caring people, people who could probably save the world or at the very least do it some real good.” Those people are our patients, and medicine should take the lead in working further to destigmatize mental illness.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
What happens to clinically suspected arthralgia patients without RA?
About one-third of patients with clinically suspect arthralgia who do not develop RA have resolution of symptoms and subclinical joint inflammation on MRI by the end of 2 years, according to investigators from Leiden (the Netherlands) University.
“Thus far, most longitudinal studies performed in patients considered at risk for RA focused on the progression from arthralgia to RA, since (early) identification of individuals that will develop RA is a key point from a clinician’s perspective. However, there is also a group of patients that were considered at risk for RA but over time do not develop RA, meaning that, in hindsight, they possibly have not been truly ‘pre-RA’. This subgroup of patients is unexplored, and the course and outcome of joint symptoms and subclinical inflammation in these patients are yet unknown,” Robin M. ten Brinck and colleagues at Leiden wrote in Arthritis Research & Therapy.
The researchers followed 152 patients with clinically suspicious arthralgia (CSA) who did not develop RA during 2 years of follow-up. All patients had complete clinical data, and 98 had complete 2-year MRI data. Most of the 152 patients were women (74%), and they had a mean age of 47 years, a median of 5 tender joints (out of 68 evaluated), and 19% carried RA-related autoantibodies (rheumatoid factor and/or anti–citrullinated peptide antibody). None of the patients received disease-modifying antirheumatic drugs or glucocorticoids during the study; only NSAIDs were allowed.
Overall, 57 (38%) of the 152 reported resolution of symptoms by 2 years, including 32 (33%) of the 98 patients with serial MRI results available at 2 years. Of the remaining 95 patients who continued to have symptoms, 43 were diagnosed as having persistent CSA, 10 had osteoarthritis, and 13 had tendinomuscular complaints.
There was no statistically significant difference in mean baseline total MRI inflammation scores between those with and without symptom resolution, but among patients with a mean total MRI inflammation score greater than 0 at baseline, those who achieved resolution of symptoms over time had a mean score higher than that of symptom-free patients at baseline. Those patients with resolved symptoms also had a statistically significant decrease in MRI inflammation score at the 2-year follow-up. A smaller and not statistically significant decline in total MRI score was seen in patients without symptom resolution.
“Our study is the first to quantify the percentage of patients presenting with CSA that will have a resolution of symptoms over time. It consists of one-third of all nonprogressing patients and 27% of all patients that were identified as having CSA by rheumatologists,” the researchers wrote.
The study was sponsored by the European Research Council. The authors had no relevant disclosures.
SOURCE: ten Brinck RM et al. Arthritis Res Ther. 2020 Jan 16. doi: 10.1186/s13075-020-2102-9.
About one-third of patients with clinically suspect arthralgia who do not develop RA have resolution of symptoms and subclinical joint inflammation on MRI by the end of 2 years, according to investigators from Leiden (the Netherlands) University.
“Thus far, most longitudinal studies performed in patients considered at risk for RA focused on the progression from arthralgia to RA, since (early) identification of individuals that will develop RA is a key point from a clinician’s perspective. However, there is also a group of patients that were considered at risk for RA but over time do not develop RA, meaning that, in hindsight, they possibly have not been truly ‘pre-RA’. This subgroup of patients is unexplored, and the course and outcome of joint symptoms and subclinical inflammation in these patients are yet unknown,” Robin M. ten Brinck and colleagues at Leiden wrote in Arthritis Research & Therapy.
The researchers followed 152 patients with clinically suspicious arthralgia (CSA) who did not develop RA during 2 years of follow-up. All patients had complete clinical data, and 98 had complete 2-year MRI data. Most of the 152 patients were women (74%), and they had a mean age of 47 years, a median of 5 tender joints (out of 68 evaluated), and 19% carried RA-related autoantibodies (rheumatoid factor and/or anti–citrullinated peptide antibody). None of the patients received disease-modifying antirheumatic drugs or glucocorticoids during the study; only NSAIDs were allowed.
Overall, 57 (38%) of the 152 reported resolution of symptoms by 2 years, including 32 (33%) of the 98 patients with serial MRI results available at 2 years. Of the remaining 95 patients who continued to have symptoms, 43 were diagnosed as having persistent CSA, 10 had osteoarthritis, and 13 had tendinomuscular complaints.
There was no statistically significant difference in mean baseline total MRI inflammation scores between those with and without symptom resolution, but among patients with a mean total MRI inflammation score greater than 0 at baseline, those who achieved resolution of symptoms over time had a mean score higher than that of symptom-free patients at baseline. Those patients with resolved symptoms also had a statistically significant decrease in MRI inflammation score at the 2-year follow-up. A smaller and not statistically significant decline in total MRI score was seen in patients without symptom resolution.
“Our study is the first to quantify the percentage of patients presenting with CSA that will have a resolution of symptoms over time. It consists of one-third of all nonprogressing patients and 27% of all patients that were identified as having CSA by rheumatologists,” the researchers wrote.
The study was sponsored by the European Research Council. The authors had no relevant disclosures.
SOURCE: ten Brinck RM et al. Arthritis Res Ther. 2020 Jan 16. doi: 10.1186/s13075-020-2102-9.
About one-third of patients with clinically suspect arthralgia who do not develop RA have resolution of symptoms and subclinical joint inflammation on MRI by the end of 2 years, according to investigators from Leiden (the Netherlands) University.
“Thus far, most longitudinal studies performed in patients considered at risk for RA focused on the progression from arthralgia to RA, since (early) identification of individuals that will develop RA is a key point from a clinician’s perspective. However, there is also a group of patients that were considered at risk for RA but over time do not develop RA, meaning that, in hindsight, they possibly have not been truly ‘pre-RA’. This subgroup of patients is unexplored, and the course and outcome of joint symptoms and subclinical inflammation in these patients are yet unknown,” Robin M. ten Brinck and colleagues at Leiden wrote in Arthritis Research & Therapy.
The researchers followed 152 patients with clinically suspicious arthralgia (CSA) who did not develop RA during 2 years of follow-up. All patients had complete clinical data, and 98 had complete 2-year MRI data. Most of the 152 patients were women (74%), and they had a mean age of 47 years, a median of 5 tender joints (out of 68 evaluated), and 19% carried RA-related autoantibodies (rheumatoid factor and/or anti–citrullinated peptide antibody). None of the patients received disease-modifying antirheumatic drugs or glucocorticoids during the study; only NSAIDs were allowed.
Overall, 57 (38%) of the 152 reported resolution of symptoms by 2 years, including 32 (33%) of the 98 patients with serial MRI results available at 2 years. Of the remaining 95 patients who continued to have symptoms, 43 were diagnosed as having persistent CSA, 10 had osteoarthritis, and 13 had tendinomuscular complaints.
There was no statistically significant difference in mean baseline total MRI inflammation scores between those with and without symptom resolution, but among patients with a mean total MRI inflammation score greater than 0 at baseline, those who achieved resolution of symptoms over time had a mean score higher than that of symptom-free patients at baseline. Those patients with resolved symptoms also had a statistically significant decrease in MRI inflammation score at the 2-year follow-up. A smaller and not statistically significant decline in total MRI score was seen in patients without symptom resolution.
“Our study is the first to quantify the percentage of patients presenting with CSA that will have a resolution of symptoms over time. It consists of one-third of all nonprogressing patients and 27% of all patients that were identified as having CSA by rheumatologists,” the researchers wrote.
The study was sponsored by the European Research Council. The authors had no relevant disclosures.
SOURCE: ten Brinck RM et al. Arthritis Res Ther. 2020 Jan 16. doi: 10.1186/s13075-020-2102-9.
FROM ARTHRITIS RESEARCH & THERAPY
Sleep problems linked to worsening PTSD in veterans
Insomnia is a common problem for veterans with PTSD, and the frequency of sleep problems is associated with increasing severity of PTSD, according to a study published in of the Journal of Traumatic Stress.
Raymond C. Rosen, PhD, of the New England Research Institutes, Watertown, Mass., and coauthors wrote that exploration of the relationship between PTSD and insomnia is complicated by the fact that it can be difficult to separate out disturbed sleep from other elements of PTSD, and because of the presence of other comorbidities in veterans, such as depression and traumatic brain injury.
The cohort study involved 1,643 veterans – roughly equal numbers of women and men – of Iraq and Afghanistan. Around two-thirds of the cohort had a diagnosis of PTSD. The participants completed a self-administered survey online or by mail, and were also assessed in a telephone interview, then followed up within 2-4 years.
While the prevalence of sleep problems was high across the cohort, the study found that 74% of participants with PTSD at baseline said they had experienced sleep difficulties for at least half of the previous 30 days, and one-third had been prescribed for a sedative-hypnotic drug in the past year.
In comparison, veterans without PTSD had fewer sleep problems and were prescribed significantly fewer sedative-hypnotic drugs.
The prevalence of sleep problems was similar in men and women with PTSD, although women had significantly higher rates of sedative-hypnotic prescriptions than men (40.4% vs. 35%, P = .006). A similar gender difference in prescription rates was seen in individuals without PTSD.
The study found that, although there was only a weak association between the severity of PTSD symptoms at baseline and the frequency of sleep problems at follow-up, there was a stronger association in reverse. Veterans with a higher frequency of sleep problems at baseline showed a significant increase in PTSD symptoms at follow-up.
The authors commented that this was in line with previous studies finding a similar effect of sleep disturbance on PTSD severity, both in military personnel and civilians.
“From a neurobiological perspective, it has been proposed that chronic sleep loss can lead to emotional dysregulation or heightened autonomic arousal, which in turn may be a risk factor for PTSD in trauma-exposed individuals,” they wrote. “It has also been proposed that prior sleep disturbance may attenuate the effects of extinction learning, leading to more enduring or severe symptoms in trauma-exposed individuals with concomitant sleep disorders.”
Given this association, the authors called for more attention to be given to identifying, diagnosing, and treating sleep disorders in veterans with and without PTSD.
The authors noted that they did not have access to polysomnographic data for participants, and were also unable to assess the prevalence, frequency, or intensity of nightmares in the cohort.
The study was supported by the Department of Defense. Conflict of interest disclosures were unavailable.
SOURCE: Rosen RC et al. J Trauma Stress. 2020;32:936-45.
Insomnia is a common problem for veterans with PTSD, and the frequency of sleep problems is associated with increasing severity of PTSD, according to a study published in of the Journal of Traumatic Stress.
Raymond C. Rosen, PhD, of the New England Research Institutes, Watertown, Mass., and coauthors wrote that exploration of the relationship between PTSD and insomnia is complicated by the fact that it can be difficult to separate out disturbed sleep from other elements of PTSD, and because of the presence of other comorbidities in veterans, such as depression and traumatic brain injury.
The cohort study involved 1,643 veterans – roughly equal numbers of women and men – of Iraq and Afghanistan. Around two-thirds of the cohort had a diagnosis of PTSD. The participants completed a self-administered survey online or by mail, and were also assessed in a telephone interview, then followed up within 2-4 years.
While the prevalence of sleep problems was high across the cohort, the study found that 74% of participants with PTSD at baseline said they had experienced sleep difficulties for at least half of the previous 30 days, and one-third had been prescribed for a sedative-hypnotic drug in the past year.
In comparison, veterans without PTSD had fewer sleep problems and were prescribed significantly fewer sedative-hypnotic drugs.
The prevalence of sleep problems was similar in men and women with PTSD, although women had significantly higher rates of sedative-hypnotic prescriptions than men (40.4% vs. 35%, P = .006). A similar gender difference in prescription rates was seen in individuals without PTSD.
The study found that, although there was only a weak association between the severity of PTSD symptoms at baseline and the frequency of sleep problems at follow-up, there was a stronger association in reverse. Veterans with a higher frequency of sleep problems at baseline showed a significant increase in PTSD symptoms at follow-up.
The authors commented that this was in line with previous studies finding a similar effect of sleep disturbance on PTSD severity, both in military personnel and civilians.
“From a neurobiological perspective, it has been proposed that chronic sleep loss can lead to emotional dysregulation or heightened autonomic arousal, which in turn may be a risk factor for PTSD in trauma-exposed individuals,” they wrote. “It has also been proposed that prior sleep disturbance may attenuate the effects of extinction learning, leading to more enduring or severe symptoms in trauma-exposed individuals with concomitant sleep disorders.”
Given this association, the authors called for more attention to be given to identifying, diagnosing, and treating sleep disorders in veterans with and without PTSD.
The authors noted that they did not have access to polysomnographic data for participants, and were also unable to assess the prevalence, frequency, or intensity of nightmares in the cohort.
The study was supported by the Department of Defense. Conflict of interest disclosures were unavailable.
SOURCE: Rosen RC et al. J Trauma Stress. 2020;32:936-45.
Insomnia is a common problem for veterans with PTSD, and the frequency of sleep problems is associated with increasing severity of PTSD, according to a study published in of the Journal of Traumatic Stress.
Raymond C. Rosen, PhD, of the New England Research Institutes, Watertown, Mass., and coauthors wrote that exploration of the relationship between PTSD and insomnia is complicated by the fact that it can be difficult to separate out disturbed sleep from other elements of PTSD, and because of the presence of other comorbidities in veterans, such as depression and traumatic brain injury.
The cohort study involved 1,643 veterans – roughly equal numbers of women and men – of Iraq and Afghanistan. Around two-thirds of the cohort had a diagnosis of PTSD. The participants completed a self-administered survey online or by mail, and were also assessed in a telephone interview, then followed up within 2-4 years.
While the prevalence of sleep problems was high across the cohort, the study found that 74% of participants with PTSD at baseline said they had experienced sleep difficulties for at least half of the previous 30 days, and one-third had been prescribed for a sedative-hypnotic drug in the past year.
In comparison, veterans without PTSD had fewer sleep problems and were prescribed significantly fewer sedative-hypnotic drugs.
The prevalence of sleep problems was similar in men and women with PTSD, although women had significantly higher rates of sedative-hypnotic prescriptions than men (40.4% vs. 35%, P = .006). A similar gender difference in prescription rates was seen in individuals without PTSD.
The study found that, although there was only a weak association between the severity of PTSD symptoms at baseline and the frequency of sleep problems at follow-up, there was a stronger association in reverse. Veterans with a higher frequency of sleep problems at baseline showed a significant increase in PTSD symptoms at follow-up.
The authors commented that this was in line with previous studies finding a similar effect of sleep disturbance on PTSD severity, both in military personnel and civilians.
“From a neurobiological perspective, it has been proposed that chronic sleep loss can lead to emotional dysregulation or heightened autonomic arousal, which in turn may be a risk factor for PTSD in trauma-exposed individuals,” they wrote. “It has also been proposed that prior sleep disturbance may attenuate the effects of extinction learning, leading to more enduring or severe symptoms in trauma-exposed individuals with concomitant sleep disorders.”
Given this association, the authors called for more attention to be given to identifying, diagnosing, and treating sleep disorders in veterans with and without PTSD.
The authors noted that they did not have access to polysomnographic data for participants, and were also unable to assess the prevalence, frequency, or intensity of nightmares in the cohort.
The study was supported by the Department of Defense. Conflict of interest disclosures were unavailable.
SOURCE: Rosen RC et al. J Trauma Stress. 2020;32:936-45.
FROM THE JOURNAL OF TRAUMATIC STRESS
Nontuberculous mycobacterial lung disease cases on the rise across U.S.
To assess the NTM lung disease burden on a national level, Kevin L. Winthrop, MD, of Oregon Health & Science University, Portland, and associates analyzed patient data from a U.S. managed care claims database between 2008 and 2015. Their findings were published in the Annals of the American Thoracic Society.
A case of NTM lung disease was defined as a patient with at least two medical claims with the disease’s diagnostic codes – 031.0 and A31.0 – that were at least 30 days apart. Of the 74,984,596 beneficiaries in the database, 9,476 met the case definition for NTM lung disease; 69% (n = 6,530) were women.
From 2008 to 2015, the annual incidence of NTM lung disease increased from 3.13 (95% confidence interval, 2.88-3.40) to 4.73 (95% CI, 4.43-5.05) per 100,000 person-years, with the average rate of yearly change being +5.2% (95% CI, 4.0%-6.4%; P less than .01).The annual prevalence increased from 6.78 (95% CI, 6.45-7.14) to 11.70 (95% CI, 11.26-12.16) per 100,000 persons, with the average rate of yearly change being +7.5% (95% CI, 6.7-8.2%; P less than .01).
The majority of NTM lung disease in the United States is caused by Mycobacterium avium complex (17), although other species such as M. abscessus, M. kansasii, M. xenopi, and others contribute to this disease burden.
“It’s a classic chicken-or-egg scenario,” said Sachin Gupta, MD, a pulmonologist in San Francisco, in regard to the rising numbers. “Increased awareness of NTM lung disease is, in part, why we’re seeing prevalence and incidence go up. And yet the disease itself may also be growing in clusters and pockets, as the data show, in various places across the nation.
“The worrisome aspect here,” he added, “is that future studies will likely show that, as incidence is increasing, mortality is increasing as well. That speaks to the challenges with these bugs: Very hard to diagnose, very hard to treat.”
The authors acknowledged their study’s limitations, including the lack of microbiologic or radiographic confirmation of the NTM infection and the inherent shortcomings of claims data–based studies overall. They did note a previous report, however, that “claims-based case identification has a high positive predictive value of approximately 82% for NTM lung disease.”
The study was funded by Insmed; the Intramural Research Programs of the National Institute of Allergy and Infectious Diseases; and the National Heart, Lung, and Blood Institute. The authors reported no conflicts of interest.
SOURCE: Winthrop KL et al. Ann Am Thorac Soc. 2019 Dec 13. doi: 10.1513/AnnalsATS.201804-236OC.
To assess the NTM lung disease burden on a national level, Kevin L. Winthrop, MD, of Oregon Health & Science University, Portland, and associates analyzed patient data from a U.S. managed care claims database between 2008 and 2015. Their findings were published in the Annals of the American Thoracic Society.
A case of NTM lung disease was defined as a patient with at least two medical claims with the disease’s diagnostic codes – 031.0 and A31.0 – that were at least 30 days apart. Of the 74,984,596 beneficiaries in the database, 9,476 met the case definition for NTM lung disease; 69% (n = 6,530) were women.
From 2008 to 2015, the annual incidence of NTM lung disease increased from 3.13 (95% confidence interval, 2.88-3.40) to 4.73 (95% CI, 4.43-5.05) per 100,000 person-years, with the average rate of yearly change being +5.2% (95% CI, 4.0%-6.4%; P less than .01).The annual prevalence increased from 6.78 (95% CI, 6.45-7.14) to 11.70 (95% CI, 11.26-12.16) per 100,000 persons, with the average rate of yearly change being +7.5% (95% CI, 6.7-8.2%; P less than .01).
The majority of NTM lung disease in the United States is caused by Mycobacterium avium complex (17), although other species such as M. abscessus, M. kansasii, M. xenopi, and others contribute to this disease burden.
“It’s a classic chicken-or-egg scenario,” said Sachin Gupta, MD, a pulmonologist in San Francisco, in regard to the rising numbers. “Increased awareness of NTM lung disease is, in part, why we’re seeing prevalence and incidence go up. And yet the disease itself may also be growing in clusters and pockets, as the data show, in various places across the nation.
“The worrisome aspect here,” he added, “is that future studies will likely show that, as incidence is increasing, mortality is increasing as well. That speaks to the challenges with these bugs: Very hard to diagnose, very hard to treat.”
The authors acknowledged their study’s limitations, including the lack of microbiologic or radiographic confirmation of the NTM infection and the inherent shortcomings of claims data–based studies overall. They did note a previous report, however, that “claims-based case identification has a high positive predictive value of approximately 82% for NTM lung disease.”
The study was funded by Insmed; the Intramural Research Programs of the National Institute of Allergy and Infectious Diseases; and the National Heart, Lung, and Blood Institute. The authors reported no conflicts of interest.
SOURCE: Winthrop KL et al. Ann Am Thorac Soc. 2019 Dec 13. doi: 10.1513/AnnalsATS.201804-236OC.
To assess the NTM lung disease burden on a national level, Kevin L. Winthrop, MD, of Oregon Health & Science University, Portland, and associates analyzed patient data from a U.S. managed care claims database between 2008 and 2015. Their findings were published in the Annals of the American Thoracic Society.
A case of NTM lung disease was defined as a patient with at least two medical claims with the disease’s diagnostic codes – 031.0 and A31.0 – that were at least 30 days apart. Of the 74,984,596 beneficiaries in the database, 9,476 met the case definition for NTM lung disease; 69% (n = 6,530) were women.
From 2008 to 2015, the annual incidence of NTM lung disease increased from 3.13 (95% confidence interval, 2.88-3.40) to 4.73 (95% CI, 4.43-5.05) per 100,000 person-years, with the average rate of yearly change being +5.2% (95% CI, 4.0%-6.4%; P less than .01).The annual prevalence increased from 6.78 (95% CI, 6.45-7.14) to 11.70 (95% CI, 11.26-12.16) per 100,000 persons, with the average rate of yearly change being +7.5% (95% CI, 6.7-8.2%; P less than .01).
The majority of NTM lung disease in the United States is caused by Mycobacterium avium complex (17), although other species such as M. abscessus, M. kansasii, M. xenopi, and others contribute to this disease burden.
“It’s a classic chicken-or-egg scenario,” said Sachin Gupta, MD, a pulmonologist in San Francisco, in regard to the rising numbers. “Increased awareness of NTM lung disease is, in part, why we’re seeing prevalence and incidence go up. And yet the disease itself may also be growing in clusters and pockets, as the data show, in various places across the nation.
“The worrisome aspect here,” he added, “is that future studies will likely show that, as incidence is increasing, mortality is increasing as well. That speaks to the challenges with these bugs: Very hard to diagnose, very hard to treat.”
The authors acknowledged their study’s limitations, including the lack of microbiologic or radiographic confirmation of the NTM infection and the inherent shortcomings of claims data–based studies overall. They did note a previous report, however, that “claims-based case identification has a high positive predictive value of approximately 82% for NTM lung disease.”
The study was funded by Insmed; the Intramural Research Programs of the National Institute of Allergy and Infectious Diseases; and the National Heart, Lung, and Blood Institute. The authors reported no conflicts of interest.
SOURCE: Winthrop KL et al. Ann Am Thorac Soc. 2019 Dec 13. doi: 10.1513/AnnalsATS.201804-236OC.
FROM ANNALS OF THE AMERICAN THORACIC SOCIETY
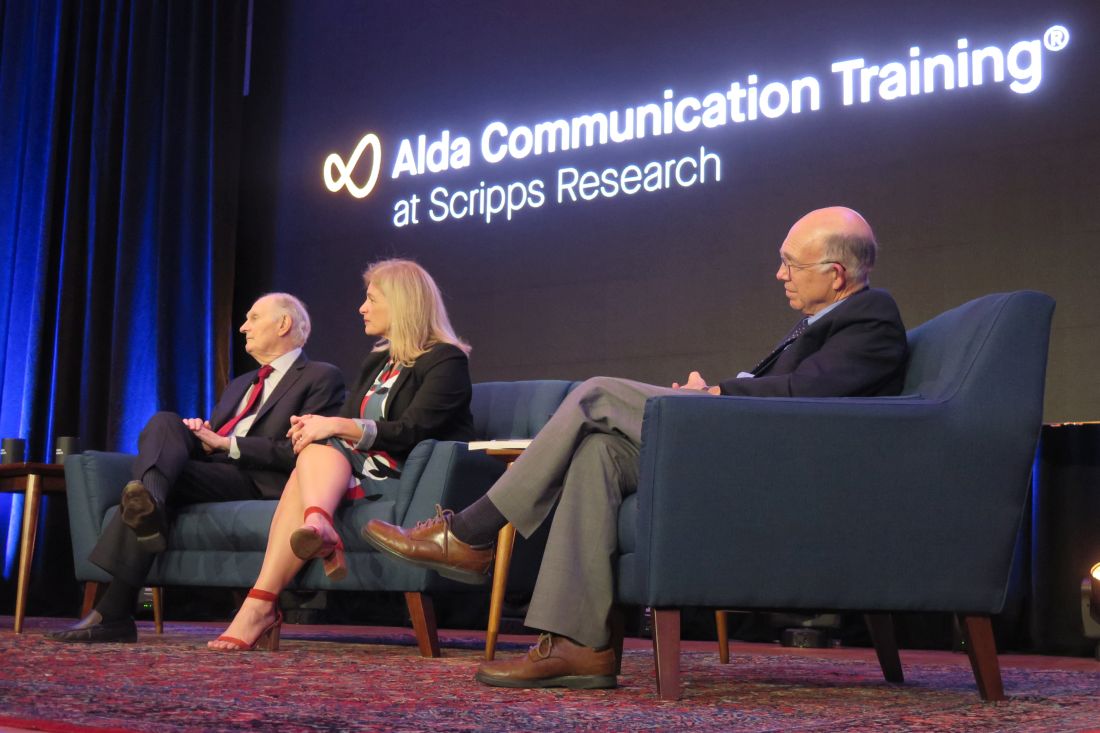
Alan Alda, Scripps Research join forces to improve science communication
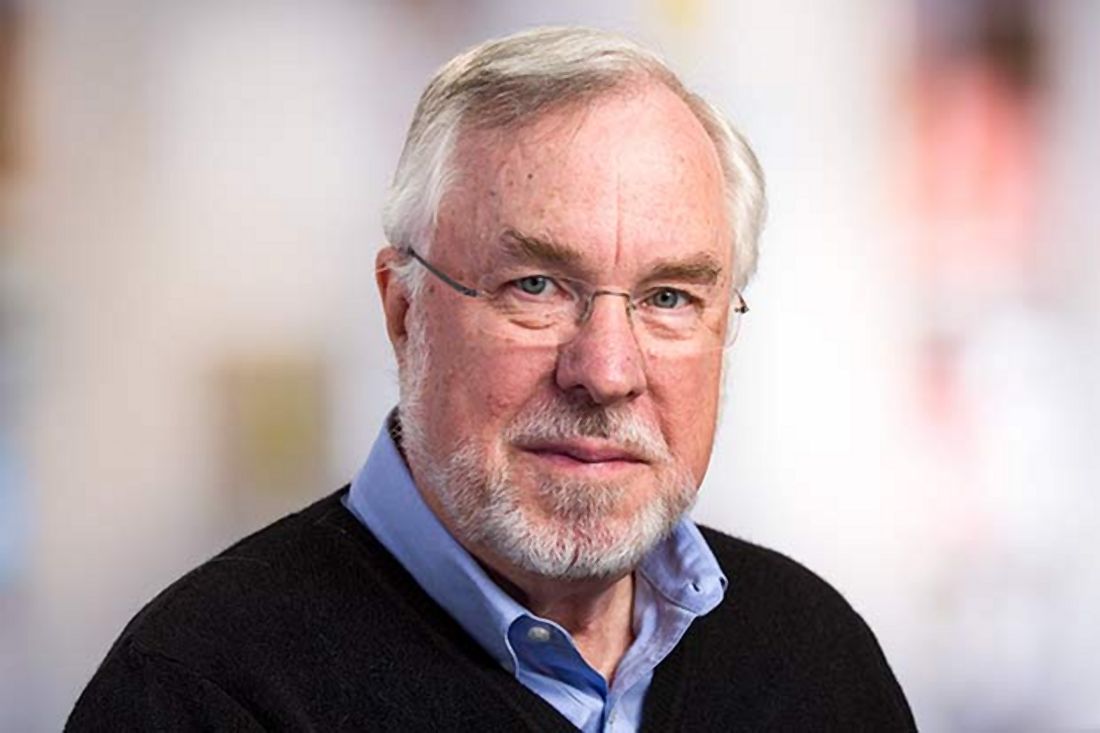
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
ctDNA and avapritinib in GI cancer management
In this edition of “How I Will Treat My Next Patient,” I highlight the potential role of circulating tumor DNA (ctDNA) monitoring in patients with a history of nonmetastatic colorectal cancer (CRC) and the approval of a new targeted agent for a subset of patients with gastrointestinal stromal tumors (GISTs). Taken together, this information may guide the management of selected patients with gastrointestinal malignancies, now and in the future.
ctDNA in colorectal cancer
Unfortunately, among patients with CRC with standard blood monitoring, multiple, incurable metastases are the predominant finding when relapse occurs. To improve upon the detection of potentially curable recurrent disease, researchers performed a cross-sectional, observational study of routine monitoring of ctDNA in patients with stage I-III CRC. The patients were also monitored with carcinoembryonic antigen (CEA) levels and imaging in accordance with guidelines from the National Comprehensive Cancer Network (Cancer. 2020 Jan 7. doi: 10.1002/cncr.32695). The investigators used the COLVERA assay of methylated CBAT1/IKZF1 for ctDNA monitoring and the LIAISON CEA plasma test.
Among the 50 patients with recurrence and 177 without recurrence of CRC who met all blood and imaging collection criteria, ctDNA testing offered a sensitivity of 68.1%, compared with 31.9% for CEA (P = .0002), with comparable specificity (97.9% vs. 96.4%; P = 1.000). Over about a 4-year time period, ctDNA detected an additional 18 patients (38%) with recurrence who did not have an elevated plasma CEA, whereas there was only 1 case (2.1%) with an elevated plasma CEA and negative ctDNA test.
Among recurrences considered amenable to surgery with curative intent, (n = 20), ctDNA was positive in 60% of patients, compared with only 20% for CEA (P = .010). Multivariate analysis indicated that ctDNA was an independent predictor of recurrence, whereas CEA was not.
The authors concluded that the methylated BCAT1/IKZF1 ctDNA test was superior to CEA monitoring after initial treatment for potentially curable CRC.
How these results influence practice
The current study adds to the body of work showing superior sensitivity of ctDNA monitoring in the detection of recurrence in patients with solid tumors. In May 2019, this column highlighted the work of Yuxuan Wang, MD, PhD, and colleagues in 58 patients with stages I-III CRC; over a similar duration of follow-up as in the current study (JAMA Oncol. 2019;5[8]:1118-23), Dr. Wang found that 10 of 13 recurrences (77%) were detected by monitoring ctDNA levels. CEA levels were detected 63% of recurrences.
The central, critical hypothesis of these efforts is that the earlier detection of metastatic disease will lead to improved survival for patients with CRC. As the authors state in their discussion, that hypothesis remains tantalizing but unproven.
Prospective, randomized trials like the recently opened COBRA trial (NRG-GI005), which tests ctDNA assay–directed therapy in patients with stage IIA CRC, deserve our enthusiastic support. Research with similar designs will establish the value of ctDNA monitoring as a biomarker for early intervention in patients with stage IV disease and for selecting patients after primary therapy who are unlikely to have been cured and who could potentially benefit from adjuvant therapy.
Monitoring ctDNA is a research tool that could be practice changing in the near future. It has shown enough promise to justify prospective, randomized trials to determine whether its superior sensitivity translates into improved survival.
Avapritinib for mutated GIST
The platelet-derived growth factor receptor–alpha (PDGFRA) gene encodes PDGFRA, a member of the type III tyrosine kinase receptor family, which includes the stem cell factor receptor, KIT (present in 95% of GISTs). PDGFRA and KIT have domains with specific roles in tyrosine kinase activation. Several PDGF isoforms bind and activate PDGFRA.
Among patients with GISTs, clinical responses to imatinib and other tyrosine kinase inhibitors (TKIs) correlate with tumor genotype. For example, many GISTs that progress within 6 months of TKI initiation lack mutations in KIT or PDGFRA or have a PDGFRA D842 mutation.
The Food and Drug Administration recently approved avapritinib (Ayvakit) for adults with unresectable or metastatic GISTs with a PDGFRA exon 18 mutation. The approval was based on the results of the NAVIGATOR trial, a single-arm, multicenter, open-label study of 43 patients with PDGFRA exon 18 mutations, including 38 patients with a PDGFRA D842V mutation.
The patients received 300 mg avapritinib once daily and 84% responded to avapritinib, though most were partial responses. Among patients with a D842V mutation, the response rate was also high – at 89% – but most responses were partial. At a median follow-up of 10.6 months, median response duration was not reached, but 61% of responses exceeded 6 months. Toxicity included asthenia, gastrointestinal and central nervous system side effects (including intracranial hemorrhage), hair color changes, lacrimation, and dizziness.
Avapritinib is the first drug approved specifically for patients with advanced or unresectable GISTs with a PDGFRA exon 18 mutation.
How these results influence practice
PDGFRA exon 18 mutations occur in 5%-7% of GISTs and are believed to stabilize the kinase activation loop, perhaps accounting for slow, steady growth of these tumors over a long time period and resistance to TKIs. The most frequent mutation results in an exon 18 D842V substitution (75% of all PDGFRA-mutated tumors). Although dramatic progress has been made in the treatment of patients with GIST since 2000, in patients with GISTs harboring PDGFRA exon 18 mutations, responses to treatment are rare and, when they occur, are more abbreviated.
With a high response rate and impressive response duration, avapritinib will be a valuable resource for oncologists treating this uncommon subset of patients with GISTs. The opportunity to convert unresectable tumors to potentially curable ones seems within reach.
The difficult dilemma will be to decide when treatment is needed and drug-related toxicity is justified in patients with slowly progressive tumors and few symptoms. As with so many decisions in oncology, until newer agents with fewer toxicities and higher complete response rates are developed, the proper time for any individual patient to embark on treatment with avapritinib will be found at the intersection of “precision medicine” and “clinical judgment.”
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I Will Treat My Next Patient,” I highlight the potential role of circulating tumor DNA (ctDNA) monitoring in patients with a history of nonmetastatic colorectal cancer (CRC) and the approval of a new targeted agent for a subset of patients with gastrointestinal stromal tumors (GISTs). Taken together, this information may guide the management of selected patients with gastrointestinal malignancies, now and in the future.
ctDNA in colorectal cancer
Unfortunately, among patients with CRC with standard blood monitoring, multiple, incurable metastases are the predominant finding when relapse occurs. To improve upon the detection of potentially curable recurrent disease, researchers performed a cross-sectional, observational study of routine monitoring of ctDNA in patients with stage I-III CRC. The patients were also monitored with carcinoembryonic antigen (CEA) levels and imaging in accordance with guidelines from the National Comprehensive Cancer Network (Cancer. 2020 Jan 7. doi: 10.1002/cncr.32695). The investigators used the COLVERA assay of methylated CBAT1/IKZF1 for ctDNA monitoring and the LIAISON CEA plasma test.
Among the 50 patients with recurrence and 177 without recurrence of CRC who met all blood and imaging collection criteria, ctDNA testing offered a sensitivity of 68.1%, compared with 31.9% for CEA (P = .0002), with comparable specificity (97.9% vs. 96.4%; P = 1.000). Over about a 4-year time period, ctDNA detected an additional 18 patients (38%) with recurrence who did not have an elevated plasma CEA, whereas there was only 1 case (2.1%) with an elevated plasma CEA and negative ctDNA test.
Among recurrences considered amenable to surgery with curative intent, (n = 20), ctDNA was positive in 60% of patients, compared with only 20% for CEA (P = .010). Multivariate analysis indicated that ctDNA was an independent predictor of recurrence, whereas CEA was not.
The authors concluded that the methylated BCAT1/IKZF1 ctDNA test was superior to CEA monitoring after initial treatment for potentially curable CRC.
How these results influence practice
The current study adds to the body of work showing superior sensitivity of ctDNA monitoring in the detection of recurrence in patients with solid tumors. In May 2019, this column highlighted the work of Yuxuan Wang, MD, PhD, and colleagues in 58 patients with stages I-III CRC; over a similar duration of follow-up as in the current study (JAMA Oncol. 2019;5[8]:1118-23), Dr. Wang found that 10 of 13 recurrences (77%) were detected by monitoring ctDNA levels. CEA levels were detected 63% of recurrences.
The central, critical hypothesis of these efforts is that the earlier detection of metastatic disease will lead to improved survival for patients with CRC. As the authors state in their discussion, that hypothesis remains tantalizing but unproven.
Prospective, randomized trials like the recently opened COBRA trial (NRG-GI005), which tests ctDNA assay–directed therapy in patients with stage IIA CRC, deserve our enthusiastic support. Research with similar designs will establish the value of ctDNA monitoring as a biomarker for early intervention in patients with stage IV disease and for selecting patients after primary therapy who are unlikely to have been cured and who could potentially benefit from adjuvant therapy.
Monitoring ctDNA is a research tool that could be practice changing in the near future. It has shown enough promise to justify prospective, randomized trials to determine whether its superior sensitivity translates into improved survival.
Avapritinib for mutated GIST
The platelet-derived growth factor receptor–alpha (PDGFRA) gene encodes PDGFRA, a member of the type III tyrosine kinase receptor family, which includes the stem cell factor receptor, KIT (present in 95% of GISTs). PDGFRA and KIT have domains with specific roles in tyrosine kinase activation. Several PDGF isoforms bind and activate PDGFRA.
Among patients with GISTs, clinical responses to imatinib and other tyrosine kinase inhibitors (TKIs) correlate with tumor genotype. For example, many GISTs that progress within 6 months of TKI initiation lack mutations in KIT or PDGFRA or have a PDGFRA D842 mutation.
The Food and Drug Administration recently approved avapritinib (Ayvakit) for adults with unresectable or metastatic GISTs with a PDGFRA exon 18 mutation. The approval was based on the results of the NAVIGATOR trial, a single-arm, multicenter, open-label study of 43 patients with PDGFRA exon 18 mutations, including 38 patients with a PDGFRA D842V mutation.
The patients received 300 mg avapritinib once daily and 84% responded to avapritinib, though most were partial responses. Among patients with a D842V mutation, the response rate was also high – at 89% – but most responses were partial. At a median follow-up of 10.6 months, median response duration was not reached, but 61% of responses exceeded 6 months. Toxicity included asthenia, gastrointestinal and central nervous system side effects (including intracranial hemorrhage), hair color changes, lacrimation, and dizziness.
Avapritinib is the first drug approved specifically for patients with advanced or unresectable GISTs with a PDGFRA exon 18 mutation.
How these results influence practice
PDGFRA exon 18 mutations occur in 5%-7% of GISTs and are believed to stabilize the kinase activation loop, perhaps accounting for slow, steady growth of these tumors over a long time period and resistance to TKIs. The most frequent mutation results in an exon 18 D842V substitution (75% of all PDGFRA-mutated tumors). Although dramatic progress has been made in the treatment of patients with GIST since 2000, in patients with GISTs harboring PDGFRA exon 18 mutations, responses to treatment are rare and, when they occur, are more abbreviated.
With a high response rate and impressive response duration, avapritinib will be a valuable resource for oncologists treating this uncommon subset of patients with GISTs. The opportunity to convert unresectable tumors to potentially curable ones seems within reach.
The difficult dilemma will be to decide when treatment is needed and drug-related toxicity is justified in patients with slowly progressive tumors and few symptoms. As with so many decisions in oncology, until newer agents with fewer toxicities and higher complete response rates are developed, the proper time for any individual patient to embark on treatment with avapritinib will be found at the intersection of “precision medicine” and “clinical judgment.”
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
In this edition of “How I Will Treat My Next Patient,” I highlight the potential role of circulating tumor DNA (ctDNA) monitoring in patients with a history of nonmetastatic colorectal cancer (CRC) and the approval of a new targeted agent for a subset of patients with gastrointestinal stromal tumors (GISTs). Taken together, this information may guide the management of selected patients with gastrointestinal malignancies, now and in the future.
ctDNA in colorectal cancer
Unfortunately, among patients with CRC with standard blood monitoring, multiple, incurable metastases are the predominant finding when relapse occurs. To improve upon the detection of potentially curable recurrent disease, researchers performed a cross-sectional, observational study of routine monitoring of ctDNA in patients with stage I-III CRC. The patients were also monitored with carcinoembryonic antigen (CEA) levels and imaging in accordance with guidelines from the National Comprehensive Cancer Network (Cancer. 2020 Jan 7. doi: 10.1002/cncr.32695). The investigators used the COLVERA assay of methylated CBAT1/IKZF1 for ctDNA monitoring and the LIAISON CEA plasma test.
Among the 50 patients with recurrence and 177 without recurrence of CRC who met all blood and imaging collection criteria, ctDNA testing offered a sensitivity of 68.1%, compared with 31.9% for CEA (P = .0002), with comparable specificity (97.9% vs. 96.4%; P = 1.000). Over about a 4-year time period, ctDNA detected an additional 18 patients (38%) with recurrence who did not have an elevated plasma CEA, whereas there was only 1 case (2.1%) with an elevated plasma CEA and negative ctDNA test.
Among recurrences considered amenable to surgery with curative intent, (n = 20), ctDNA was positive in 60% of patients, compared with only 20% for CEA (P = .010). Multivariate analysis indicated that ctDNA was an independent predictor of recurrence, whereas CEA was not.
The authors concluded that the methylated BCAT1/IKZF1 ctDNA test was superior to CEA monitoring after initial treatment for potentially curable CRC.
How these results influence practice
The current study adds to the body of work showing superior sensitivity of ctDNA monitoring in the detection of recurrence in patients with solid tumors. In May 2019, this column highlighted the work of Yuxuan Wang, MD, PhD, and colleagues in 58 patients with stages I-III CRC; over a similar duration of follow-up as in the current study (JAMA Oncol. 2019;5[8]:1118-23), Dr. Wang found that 10 of 13 recurrences (77%) were detected by monitoring ctDNA levels. CEA levels were detected 63% of recurrences.
The central, critical hypothesis of these efforts is that the earlier detection of metastatic disease will lead to improved survival for patients with CRC. As the authors state in their discussion, that hypothesis remains tantalizing but unproven.
Prospective, randomized trials like the recently opened COBRA trial (NRG-GI005), which tests ctDNA assay–directed therapy in patients with stage IIA CRC, deserve our enthusiastic support. Research with similar designs will establish the value of ctDNA monitoring as a biomarker for early intervention in patients with stage IV disease and for selecting patients after primary therapy who are unlikely to have been cured and who could potentially benefit from adjuvant therapy.
Monitoring ctDNA is a research tool that could be practice changing in the near future. It has shown enough promise to justify prospective, randomized trials to determine whether its superior sensitivity translates into improved survival.
Avapritinib for mutated GIST
The platelet-derived growth factor receptor–alpha (PDGFRA) gene encodes PDGFRA, a member of the type III tyrosine kinase receptor family, which includes the stem cell factor receptor, KIT (present in 95% of GISTs). PDGFRA and KIT have domains with specific roles in tyrosine kinase activation. Several PDGF isoforms bind and activate PDGFRA.
Among patients with GISTs, clinical responses to imatinib and other tyrosine kinase inhibitors (TKIs) correlate with tumor genotype. For example, many GISTs that progress within 6 months of TKI initiation lack mutations in KIT or PDGFRA or have a PDGFRA D842 mutation.
The Food and Drug Administration recently approved avapritinib (Ayvakit) for adults with unresectable or metastatic GISTs with a PDGFRA exon 18 mutation. The approval was based on the results of the NAVIGATOR trial, a single-arm, multicenter, open-label study of 43 patients with PDGFRA exon 18 mutations, including 38 patients with a PDGFRA D842V mutation.
The patients received 300 mg avapritinib once daily and 84% responded to avapritinib, though most were partial responses. Among patients with a D842V mutation, the response rate was also high – at 89% – but most responses were partial. At a median follow-up of 10.6 months, median response duration was not reached, but 61% of responses exceeded 6 months. Toxicity included asthenia, gastrointestinal and central nervous system side effects (including intracranial hemorrhage), hair color changes, lacrimation, and dizziness.
Avapritinib is the first drug approved specifically for patients with advanced or unresectable GISTs with a PDGFRA exon 18 mutation.
How these results influence practice
PDGFRA exon 18 mutations occur in 5%-7% of GISTs and are believed to stabilize the kinase activation loop, perhaps accounting for slow, steady growth of these tumors over a long time period and resistance to TKIs. The most frequent mutation results in an exon 18 D842V substitution (75% of all PDGFRA-mutated tumors). Although dramatic progress has been made in the treatment of patients with GIST since 2000, in patients with GISTs harboring PDGFRA exon 18 mutations, responses to treatment are rare and, when they occur, are more abbreviated.
With a high response rate and impressive response duration, avapritinib will be a valuable resource for oncologists treating this uncommon subset of patients with GISTs. The opportunity to convert unresectable tumors to potentially curable ones seems within reach.
The difficult dilemma will be to decide when treatment is needed and drug-related toxicity is justified in patients with slowly progressive tumors and few symptoms. As with so many decisions in oncology, until newer agents with fewer toxicities and higher complete response rates are developed, the proper time for any individual patient to embark on treatment with avapritinib will be found at the intersection of “precision medicine” and “clinical judgment.”
Dr. Lyss has been a community-based medical oncologist and clinical researcher for more than 35 years, practicing in St. Louis. His clinical and research interests are in the prevention, diagnosis, and treatment of breast and lung cancers and in expanding access to clinical trials to medically underserved populations.
Several factors may drive recent improvements in allo-HCT outcomes
A cancer center has seen improved outcomes of allogeneic transplant in recent years, despite increases in patient age and comorbidities.
Researchers compared patients who received allogeneic hematopoietic cell transplants (allo-HCTs) during two periods, 2003-2007 and 2013-2017.
Patients treated in the 2013-2017 period were older and had more HCT-specific comorbidities at baseline, but they had lower rates of mortality, relapse, and graft-versus-host disease (GVHD) post transplant. George B. McDonald, MD, an emeritus member at Fred Hutchinson Cancer Research Center in Seattle, and coauthors described these findings in Annals of Internal Medicine.
“The primary question being addressed by this study was whether the striking improvement in survival … from the 1990s to the early 2000s, that we and other transplant centers have reported, had reached a plateau or whether further improvements in survival were being seen,” Dr. McDonald said in an interview.
“We knew that older and sicker patients were now coming for transplant, compared to 10 years ago. Our transplant protocols have backed away from the highest doses of chemotherapy and irradiation used to prepare patients for transplant, toward less toxic therapies, including reduced-intensity conditioning,” he added. “Our investigators have sought to prevent and more effectively treat the myriad of complications of allogeneic transplant, based on research done at the Fred Hutchinson Cancer Research Center and at transplant centers throughout the world.”
Baseline characteristics and treatment
Dr. McDonald and his colleagues analyzed data on patients who received allo-HCTs at Seattle Cancer Care Alliance. There were 1,148 patients treated in the 2003-2007 period and 1,131 patients treated in the 2013-2017 period.
Indications for allo-HCT were similar between the time periods. Patients were diagnosed with aplastic anemia, acute and chronic leukemias, Hodgkin and non-Hodgkin lymphomas, myelodysplastic syndromes, and multiple myeloma.
Patients in the 2013-2017 group were older and had more HCT-specific comorbidities than did the patients in the 2003-2007 group. The median age was 50.0 years (range, 0.1-80.9 years) and 47.2 years (range, 0.4-78.9 years), respectively. The median score on the augmented HCT-specific comorbidity index was 4.0 and 3.0, respectively.
The 2013-2017 group was more likely to have intermediate-risk disease (73% vs. 54%) but less likely to have high-risk disease (14% vs. 31%). The 2013-2017 group was less likely to receive high-dose myeloablative conditioning (15% vs. 67%) but more likely to have an unrelated donor (70% vs. 59%) or receive a cord blood transplant (13% vs. 4%).
GVHD prophylaxis differed between the time periods, with patients in the 2013-2017 group being more likely to receive sirolimus, posttransplant cyclophosphamide, and abatacept.
Outcomes
Overall, outcomes were superior in the 2013-2017 group. The rate of nonrelapse mortality at day 200 was higher in the 2003-2007 group than in the 2013-2017 group – 16% and 11%, respectively (adjusted hazard ratio, 0.66; P = .008).
Relapse or progression was more common in the 2003-2007 group – 348 patients vs. 244 patients (aHR, 0.76; P = .011). More patients died from relapse in the 2003-2007 group – 307 patients vs. 186 patients (aHR, 0.69; P = .002). More patients died from any cause in the 2003-2007 group – 653 patients vs. 418 patients (aHR, 0.66; P less than .001). The rate of grade 2-4 acute GVHD was higher in the 2003-2007 group – 71% vs. 69% (aHR, 0.80) – and so was the rate of chronic GVHD – 44% vs. 29% (aHR, 0.40). The risk of developing gram-negative bacteremia was lower in the 2013-2017 group (aHR, 0.42), as was the risk of invasive mold infection (aHR, 0.55).
Patients in the 2013-2017 group had a higher risk of cytomegalovirus (CMV) infection (aHR = 1.15), but they were less likely to have high levels of CMV viremia (aHR, 0.78 for greater than 250 IU/mL; aHR, 0.46 for greater than 1,000 IU/mL). Having higher levels of CMV viremia was associated with an increased risk of non-relapse mortality.
Potential drivers of outcome
Dr. McDonald said this study’s design makes it difficult to determine the causes of improved outcomes in the 2013-2017 period. However, the researchers do have theories about which practice changes may have contributed to better allo-HCT outcomes.
Dr. McDonald said the decrease in GVHD over time was “likely owing to the introduction of newer preventive strategies and immune-suppressive drugs.”
The decrease in nonrelapse mortality may have been driven, in part, by a reduction in fatal infections. Dr. McDonald said these infections were less frequent in the 2013-2017 period because of “molecular methods of diagnosis (especially for herpesviruses) and newer treatments (especially for fungal infections).”
“Another reason for a lower frequency of serious infection was a change in practice for treating graft-versus-host disease,” Dr. McDonald added. “Based on a randomized trial comparing lower- versus higher-dose prednisone for less-severe GVHD … both initial doses of prednisone and total prednisone exposure were reduced.”
Another factor that may have improved allo-HCT outcomes is the center’s change in approach to conditioning therapy over time.
“The gradual shift from very-high-dose conditioning therapy to less-intense myeloablative therapy and to reduced-intensity conditioning was likely responsible for a reduction in damage to the liver, lungs, and kidneys over the last 10 years,” Dr. McDonald said. “We were able to identify patients who were at especially high risk for mortality during a screening process before transplant ... thus allowing patients at highest risk to receive less intense conditioning therapy.”
Dr. McDonald added that this study’s results are encouraging, particularly the reduction in nonrelapse mortality. However, there is still room for improvement when it comes to relapse and progression.
This research was funded by the National Institutes of Health, the American Cancer Society, and the Patient-Centered Outcomes Research Institute. Dr. McDonald reported relationships with Sangamo Therapeutics, Soligenix Therapeutics, and Lucent Medical Systems. His coauthors disclosed relationships with a range of companies.
SOURCE: McDonald GB et al. Ann Intern Med. 2020 Jan 20. doi: 10.7326/M19-2936.
A cancer center has seen improved outcomes of allogeneic transplant in recent years, despite increases in patient age and comorbidities.
Researchers compared patients who received allogeneic hematopoietic cell transplants (allo-HCTs) during two periods, 2003-2007 and 2013-2017.
Patients treated in the 2013-2017 period were older and had more HCT-specific comorbidities at baseline, but they had lower rates of mortality, relapse, and graft-versus-host disease (GVHD) post transplant. George B. McDonald, MD, an emeritus member at Fred Hutchinson Cancer Research Center in Seattle, and coauthors described these findings in Annals of Internal Medicine.
“The primary question being addressed by this study was whether the striking improvement in survival … from the 1990s to the early 2000s, that we and other transplant centers have reported, had reached a plateau or whether further improvements in survival were being seen,” Dr. McDonald said in an interview.
“We knew that older and sicker patients were now coming for transplant, compared to 10 years ago. Our transplant protocols have backed away from the highest doses of chemotherapy and irradiation used to prepare patients for transplant, toward less toxic therapies, including reduced-intensity conditioning,” he added. “Our investigators have sought to prevent and more effectively treat the myriad of complications of allogeneic transplant, based on research done at the Fred Hutchinson Cancer Research Center and at transplant centers throughout the world.”
Baseline characteristics and treatment
Dr. McDonald and his colleagues analyzed data on patients who received allo-HCTs at Seattle Cancer Care Alliance. There were 1,148 patients treated in the 2003-2007 period and 1,131 patients treated in the 2013-2017 period.
Indications for allo-HCT were similar between the time periods. Patients were diagnosed with aplastic anemia, acute and chronic leukemias, Hodgkin and non-Hodgkin lymphomas, myelodysplastic syndromes, and multiple myeloma.
Patients in the 2013-2017 group were older and had more HCT-specific comorbidities than did the patients in the 2003-2007 group. The median age was 50.0 years (range, 0.1-80.9 years) and 47.2 years (range, 0.4-78.9 years), respectively. The median score on the augmented HCT-specific comorbidity index was 4.0 and 3.0, respectively.
The 2013-2017 group was more likely to have intermediate-risk disease (73% vs. 54%) but less likely to have high-risk disease (14% vs. 31%). The 2013-2017 group was less likely to receive high-dose myeloablative conditioning (15% vs. 67%) but more likely to have an unrelated donor (70% vs. 59%) or receive a cord blood transplant (13% vs. 4%).
GVHD prophylaxis differed between the time periods, with patients in the 2013-2017 group being more likely to receive sirolimus, posttransplant cyclophosphamide, and abatacept.
Outcomes
Overall, outcomes were superior in the 2013-2017 group. The rate of nonrelapse mortality at day 200 was higher in the 2003-2007 group than in the 2013-2017 group – 16% and 11%, respectively (adjusted hazard ratio, 0.66; P = .008).
Relapse or progression was more common in the 2003-2007 group – 348 patients vs. 244 patients (aHR, 0.76; P = .011). More patients died from relapse in the 2003-2007 group – 307 patients vs. 186 patients (aHR, 0.69; P = .002). More patients died from any cause in the 2003-2007 group – 653 patients vs. 418 patients (aHR, 0.66; P less than .001). The rate of grade 2-4 acute GVHD was higher in the 2003-2007 group – 71% vs. 69% (aHR, 0.80) – and so was the rate of chronic GVHD – 44% vs. 29% (aHR, 0.40). The risk of developing gram-negative bacteremia was lower in the 2013-2017 group (aHR, 0.42), as was the risk of invasive mold infection (aHR, 0.55).
Patients in the 2013-2017 group had a higher risk of cytomegalovirus (CMV) infection (aHR = 1.15), but they were less likely to have high levels of CMV viremia (aHR, 0.78 for greater than 250 IU/mL; aHR, 0.46 for greater than 1,000 IU/mL). Having higher levels of CMV viremia was associated with an increased risk of non-relapse mortality.
Potential drivers of outcome
Dr. McDonald said this study’s design makes it difficult to determine the causes of improved outcomes in the 2013-2017 period. However, the researchers do have theories about which practice changes may have contributed to better allo-HCT outcomes.
Dr. McDonald said the decrease in GVHD over time was “likely owing to the introduction of newer preventive strategies and immune-suppressive drugs.”
The decrease in nonrelapse mortality may have been driven, in part, by a reduction in fatal infections. Dr. McDonald said these infections were less frequent in the 2013-2017 period because of “molecular methods of diagnosis (especially for herpesviruses) and newer treatments (especially for fungal infections).”
“Another reason for a lower frequency of serious infection was a change in practice for treating graft-versus-host disease,” Dr. McDonald added. “Based on a randomized trial comparing lower- versus higher-dose prednisone for less-severe GVHD … both initial doses of prednisone and total prednisone exposure were reduced.”
Another factor that may have improved allo-HCT outcomes is the center’s change in approach to conditioning therapy over time.
“The gradual shift from very-high-dose conditioning therapy to less-intense myeloablative therapy and to reduced-intensity conditioning was likely responsible for a reduction in damage to the liver, lungs, and kidneys over the last 10 years,” Dr. McDonald said. “We were able to identify patients who were at especially high risk for mortality during a screening process before transplant ... thus allowing patients at highest risk to receive less intense conditioning therapy.”
Dr. McDonald added that this study’s results are encouraging, particularly the reduction in nonrelapse mortality. However, there is still room for improvement when it comes to relapse and progression.
This research was funded by the National Institutes of Health, the American Cancer Society, and the Patient-Centered Outcomes Research Institute. Dr. McDonald reported relationships with Sangamo Therapeutics, Soligenix Therapeutics, and Lucent Medical Systems. His coauthors disclosed relationships with a range of companies.
SOURCE: McDonald GB et al. Ann Intern Med. 2020 Jan 20. doi: 10.7326/M19-2936.
A cancer center has seen improved outcomes of allogeneic transplant in recent years, despite increases in patient age and comorbidities.
Researchers compared patients who received allogeneic hematopoietic cell transplants (allo-HCTs) during two periods, 2003-2007 and 2013-2017.
Patients treated in the 2013-2017 period were older and had more HCT-specific comorbidities at baseline, but they had lower rates of mortality, relapse, and graft-versus-host disease (GVHD) post transplant. George B. McDonald, MD, an emeritus member at Fred Hutchinson Cancer Research Center in Seattle, and coauthors described these findings in Annals of Internal Medicine.
“The primary question being addressed by this study was whether the striking improvement in survival … from the 1990s to the early 2000s, that we and other transplant centers have reported, had reached a plateau or whether further improvements in survival were being seen,” Dr. McDonald said in an interview.
“We knew that older and sicker patients were now coming for transplant, compared to 10 years ago. Our transplant protocols have backed away from the highest doses of chemotherapy and irradiation used to prepare patients for transplant, toward less toxic therapies, including reduced-intensity conditioning,” he added. “Our investigators have sought to prevent and more effectively treat the myriad of complications of allogeneic transplant, based on research done at the Fred Hutchinson Cancer Research Center and at transplant centers throughout the world.”
Baseline characteristics and treatment
Dr. McDonald and his colleagues analyzed data on patients who received allo-HCTs at Seattle Cancer Care Alliance. There were 1,148 patients treated in the 2003-2007 period and 1,131 patients treated in the 2013-2017 period.
Indications for allo-HCT were similar between the time periods. Patients were diagnosed with aplastic anemia, acute and chronic leukemias, Hodgkin and non-Hodgkin lymphomas, myelodysplastic syndromes, and multiple myeloma.
Patients in the 2013-2017 group were older and had more HCT-specific comorbidities than did the patients in the 2003-2007 group. The median age was 50.0 years (range, 0.1-80.9 years) and 47.2 years (range, 0.4-78.9 years), respectively. The median score on the augmented HCT-specific comorbidity index was 4.0 and 3.0, respectively.
The 2013-2017 group was more likely to have intermediate-risk disease (73% vs. 54%) but less likely to have high-risk disease (14% vs. 31%). The 2013-2017 group was less likely to receive high-dose myeloablative conditioning (15% vs. 67%) but more likely to have an unrelated donor (70% vs. 59%) or receive a cord blood transplant (13% vs. 4%).
GVHD prophylaxis differed between the time periods, with patients in the 2013-2017 group being more likely to receive sirolimus, posttransplant cyclophosphamide, and abatacept.
Outcomes
Overall, outcomes were superior in the 2013-2017 group. The rate of nonrelapse mortality at day 200 was higher in the 2003-2007 group than in the 2013-2017 group – 16% and 11%, respectively (adjusted hazard ratio, 0.66; P = .008).
Relapse or progression was more common in the 2003-2007 group – 348 patients vs. 244 patients (aHR, 0.76; P = .011). More patients died from relapse in the 2003-2007 group – 307 patients vs. 186 patients (aHR, 0.69; P = .002). More patients died from any cause in the 2003-2007 group – 653 patients vs. 418 patients (aHR, 0.66; P less than .001). The rate of grade 2-4 acute GVHD was higher in the 2003-2007 group – 71% vs. 69% (aHR, 0.80) – and so was the rate of chronic GVHD – 44% vs. 29% (aHR, 0.40). The risk of developing gram-negative bacteremia was lower in the 2013-2017 group (aHR, 0.42), as was the risk of invasive mold infection (aHR, 0.55).
Patients in the 2013-2017 group had a higher risk of cytomegalovirus (CMV) infection (aHR = 1.15), but they were less likely to have high levels of CMV viremia (aHR, 0.78 for greater than 250 IU/mL; aHR, 0.46 for greater than 1,000 IU/mL). Having higher levels of CMV viremia was associated with an increased risk of non-relapse mortality.
Potential drivers of outcome
Dr. McDonald said this study’s design makes it difficult to determine the causes of improved outcomes in the 2013-2017 period. However, the researchers do have theories about which practice changes may have contributed to better allo-HCT outcomes.
Dr. McDonald said the decrease in GVHD over time was “likely owing to the introduction of newer preventive strategies and immune-suppressive drugs.”
The decrease in nonrelapse mortality may have been driven, in part, by a reduction in fatal infections. Dr. McDonald said these infections were less frequent in the 2013-2017 period because of “molecular methods of diagnosis (especially for herpesviruses) and newer treatments (especially for fungal infections).”
“Another reason for a lower frequency of serious infection was a change in practice for treating graft-versus-host disease,” Dr. McDonald added. “Based on a randomized trial comparing lower- versus higher-dose prednisone for less-severe GVHD … both initial doses of prednisone and total prednisone exposure were reduced.”
Another factor that may have improved allo-HCT outcomes is the center’s change in approach to conditioning therapy over time.
“The gradual shift from very-high-dose conditioning therapy to less-intense myeloablative therapy and to reduced-intensity conditioning was likely responsible for a reduction in damage to the liver, lungs, and kidneys over the last 10 years,” Dr. McDonald said. “We were able to identify patients who were at especially high risk for mortality during a screening process before transplant ... thus allowing patients at highest risk to receive less intense conditioning therapy.”
Dr. McDonald added that this study’s results are encouraging, particularly the reduction in nonrelapse mortality. However, there is still room for improvement when it comes to relapse and progression.
This research was funded by the National Institutes of Health, the American Cancer Society, and the Patient-Centered Outcomes Research Institute. Dr. McDonald reported relationships with Sangamo Therapeutics, Soligenix Therapeutics, and Lucent Medical Systems. His coauthors disclosed relationships with a range of companies.
SOURCE: McDonald GB et al. Ann Intern Med. 2020 Jan 20. doi: 10.7326/M19-2936.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: At a single center, outcomes of allogeneic hematopoietic cell transplant improved for patients treated in 2013-2017, compared with patients treated in 2003-2007.
Major finding: Rates of nonrelapse mortality at day 200 were higher in the 2003-2007 group than in the 2013-2017 group – 16% and 11%, respectively (adjusted hazard ratio, 0.66; P = .008).
Study details: A single-center study of 1,148 patients treated in the 2003-2007 period and 1,131 patients treated in the 2013-2017 period.
Disclosures: The research was funded by the National Institutes of Health, the American Cancer Society, and the Patient-Centered Outcomes Research Institute. Dr. McDonald reported relationships with Sangamo Therapeutics, Soligenix Therapeutics, and Lucent Medical Systems. His coauthors disclosed relationships with a range of companies.
Source: McDonald GB et al. Ann Intern Med. 2020 Jan 20. doi: 10.7326/M19-2936.
Cardiovascular risks associated with cannabis use
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Telehealth appears to help speed front end of liver transplant process
The incorporation of telehealth in the liver transplantation process is demonstrating the potential to expedite the evaluation of patients and get them listed on the transplant wait list.
New research shows “a ,” Binu V. John, MD, of McGuire VA Medical Center, Richmond, and colleagues wrote in a report published in Clinical Gastroenterology and Hepatology (2019 Dec 27. doi: 10.1016/j.cgh.2019.12.021).
Researchers looked at 465 patients who had evaluations for liver transplants at the Richmond Veterans Affairs Medical Center from 2005 through 2017. Nearly half (232 patients) were evaluated via telehealth, with the remaining 233 evaluated with traditional in-person evaluations.
“Patients in the telehealth group were evaluated significantly faster than patients in the usual care group (22 vs. 54 days, P less than .001),” Dr. John and colleagues wrote, adding that, after conducting a propensity-matched analysis, “telehealth was associated with an 85% reduction in time from referral to evaluation.”
Additionally, patients “who underwent the initial evaluation by telehealth were listed significantly earlier than the usual care group (95 vs. 149 days; P less than .001),” the authors stated, adding that “telehealth was associated with a 74% reduction in time to listing” after conducting a propensity-matched analysis.
However, while speeding up time to referral and listing, “the median time to transplant was not significantly different between the two groups on unadjusted (218 vs. 244 days; P = .084) or adjusted analysis (325 vs. 409 days; P = .08),” they added.
Additionally, “there was no difference in pretransplant mortality between [those] evaluated by telehealth or usual care in unadjusted analysis,” Dr. John and colleagues observed, noting that 169 of 465 patients (51 on the waiting list for a transplant and 118 who were not listed) who were referred died without receiving a liver transplant.
Researchers suggested that while evaluation times may have been shorter with the use of telehealth, they did not translate to shorter transplantation times “likely because the latter is a complex metric that is driven primarily by organ availability.”
Dr. John and colleagues cautioned that the centralized nature of the VA medical system could make the results of this study not generalizable across private care settings, particularly when care needs to cross state lines, which does not present an issue within the VA medical system.
That being said, the “ability to successfully evaluate and list patients via telehealth and obtain the same outcomes in terms of time to transplant and pretransplant mortality is significant because of the numerous advantages that telehealth offers to improve overall access to transplantation,” they stated, adding that more studies are needed, both in and out of the VA system, “to confirm that telehealth is a safe and effective way to expand access for patients undergoing evaluation for liver transplantation.”
Lead author Dr. Binu John serves on medical advisory boards for Gilead and Eisai and received research funding from a number of pharmaceutical manufacturers. No conflicts of interest were reported by the other authors.
SOURCE: John BV et al. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2019.12.021.
The incorporation of telehealth in the liver transplantation process is demonstrating the potential to expedite the evaluation of patients and get them listed on the transplant wait list.
New research shows “a ,” Binu V. John, MD, of McGuire VA Medical Center, Richmond, and colleagues wrote in a report published in Clinical Gastroenterology and Hepatology (2019 Dec 27. doi: 10.1016/j.cgh.2019.12.021).
Researchers looked at 465 patients who had evaluations for liver transplants at the Richmond Veterans Affairs Medical Center from 2005 through 2017. Nearly half (232 patients) were evaluated via telehealth, with the remaining 233 evaluated with traditional in-person evaluations.
“Patients in the telehealth group were evaluated significantly faster than patients in the usual care group (22 vs. 54 days, P less than .001),” Dr. John and colleagues wrote, adding that, after conducting a propensity-matched analysis, “telehealth was associated with an 85% reduction in time from referral to evaluation.”
Additionally, patients “who underwent the initial evaluation by telehealth were listed significantly earlier than the usual care group (95 vs. 149 days; P less than .001),” the authors stated, adding that “telehealth was associated with a 74% reduction in time to listing” after conducting a propensity-matched analysis.
However, while speeding up time to referral and listing, “the median time to transplant was not significantly different between the two groups on unadjusted (218 vs. 244 days; P = .084) or adjusted analysis (325 vs. 409 days; P = .08),” they added.
Additionally, “there was no difference in pretransplant mortality between [those] evaluated by telehealth or usual care in unadjusted analysis,” Dr. John and colleagues observed, noting that 169 of 465 patients (51 on the waiting list for a transplant and 118 who were not listed) who were referred died without receiving a liver transplant.
Researchers suggested that while evaluation times may have been shorter with the use of telehealth, they did not translate to shorter transplantation times “likely because the latter is a complex metric that is driven primarily by organ availability.”
Dr. John and colleagues cautioned that the centralized nature of the VA medical system could make the results of this study not generalizable across private care settings, particularly when care needs to cross state lines, which does not present an issue within the VA medical system.
That being said, the “ability to successfully evaluate and list patients via telehealth and obtain the same outcomes in terms of time to transplant and pretransplant mortality is significant because of the numerous advantages that telehealth offers to improve overall access to transplantation,” they stated, adding that more studies are needed, both in and out of the VA system, “to confirm that telehealth is a safe and effective way to expand access for patients undergoing evaluation for liver transplantation.”
Lead author Dr. Binu John serves on medical advisory boards for Gilead and Eisai and received research funding from a number of pharmaceutical manufacturers. No conflicts of interest were reported by the other authors.
SOURCE: John BV et al. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2019.12.021.
The incorporation of telehealth in the liver transplantation process is demonstrating the potential to expedite the evaluation of patients and get them listed on the transplant wait list.
New research shows “a ,” Binu V. John, MD, of McGuire VA Medical Center, Richmond, and colleagues wrote in a report published in Clinical Gastroenterology and Hepatology (2019 Dec 27. doi: 10.1016/j.cgh.2019.12.021).
Researchers looked at 465 patients who had evaluations for liver transplants at the Richmond Veterans Affairs Medical Center from 2005 through 2017. Nearly half (232 patients) were evaluated via telehealth, with the remaining 233 evaluated with traditional in-person evaluations.
“Patients in the telehealth group were evaluated significantly faster than patients in the usual care group (22 vs. 54 days, P less than .001),” Dr. John and colleagues wrote, adding that, after conducting a propensity-matched analysis, “telehealth was associated with an 85% reduction in time from referral to evaluation.”
Additionally, patients “who underwent the initial evaluation by telehealth were listed significantly earlier than the usual care group (95 vs. 149 days; P less than .001),” the authors stated, adding that “telehealth was associated with a 74% reduction in time to listing” after conducting a propensity-matched analysis.
However, while speeding up time to referral and listing, “the median time to transplant was not significantly different between the two groups on unadjusted (218 vs. 244 days; P = .084) or adjusted analysis (325 vs. 409 days; P = .08),” they added.
Additionally, “there was no difference in pretransplant mortality between [those] evaluated by telehealth or usual care in unadjusted analysis,” Dr. John and colleagues observed, noting that 169 of 465 patients (51 on the waiting list for a transplant and 118 who were not listed) who were referred died without receiving a liver transplant.
Researchers suggested that while evaluation times may have been shorter with the use of telehealth, they did not translate to shorter transplantation times “likely because the latter is a complex metric that is driven primarily by organ availability.”
Dr. John and colleagues cautioned that the centralized nature of the VA medical system could make the results of this study not generalizable across private care settings, particularly when care needs to cross state lines, which does not present an issue within the VA medical system.
That being said, the “ability to successfully evaluate and list patients via telehealth and obtain the same outcomes in terms of time to transplant and pretransplant mortality is significant because of the numerous advantages that telehealth offers to improve overall access to transplantation,” they stated, adding that more studies are needed, both in and out of the VA system, “to confirm that telehealth is a safe and effective way to expand access for patients undergoing evaluation for liver transplantation.”
Lead author Dr. Binu John serves on medical advisory boards for Gilead and Eisai and received research funding from a number of pharmaceutical manufacturers. No conflicts of interest were reported by the other authors.
SOURCE: John BV et al. Clin Gastroenterol Hepatol. doi: 10.1016/j.cgh.2019.12.021.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Travelers to three U.S. airports to be screened for novel coronavirus
according to an announcement from the Centers for Disease Control and Prevention.
Starting today, Jan. 17, 2020, people traveling from Wuhan to New York (JFK), San Francisco (SFO), and Los Angeles (LAX) airports will be screened for symptoms associated with 2019-nCoV, which include fever, cough, and difficulty breathing.
“Based on the information that CDC has today, we believe the current risk for this virus to the general public is low,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a CDC telebriefing.
To date, 45 cases of 2019-nCoV have been reported in Wuhan, according to the CDC. The Wuhan Municipal Health Commission said 15 patients have been cured and discharged, 5 severe cases are still being treated, and 2 patients have died. Both deaths occurred in older patients, one of whom was aged 69 years and one aged 61 years. One of the patients was known to have underlying health conditions.
Three cases of 2019-nCoV have been confirmed outside of Wuhan, one in Japan and two in Thailand. All three were travelers from Wuhan.
The virus is believed to have originated at Wuhan South China Seafood City, a market that sold seafood, chickens, bats, cats, marmots, and other wild animals. (The market has since been closed and disinfected.) The origin suggests animal-to-human transmission of 2019-nCoV, but it appears that human-to-human transmission can occur as well.
“While most of these infections seem to be happening from animals to people, there is some indication that limited person-to-person spread is happening,” Dr. Messonnier said.
Because of this potential risk, the CDC is working with the Department of Homeland Security’s Customs and Border Protection to screen travelers from Wuhan to the United States. The CDC is deploying about 100 additional staff to JFK, SFO, and LAX, where direct flights (JFK and SFO) or connecting flights (LAX) from Wuhan land.
The CDC could not confirm if exit screening is planned for people traveling abroad from Wuhan.
At the U.S. airports, travelers from Wuhan will be given a questionnaire asking about symptoms of 2019-nCoV (fever, cough, and difficulty breathing). People who exhibit symptoms will be assessed and questioned further. If they are believed to have 2019-nCoV, they will be sent to designated hospitals, where they will be examined, and samples will be collected.
Samples from patients with suspected 2019-nCoV will be sent to the CDC for analysis. Chinese health authorities made the full genome of 2019-nCoV publicly available, which will allow the CDC to confirm any cases that may arise in the United States. The CDC is currently working on a test to detect 2019-nCoV, which can be distributed to state health departments.
Earlier this month, the CDC issued a Level 1 Travel Health Notice for travelers to Wuhan and a Health Alert on 2019-nCoV. The latest information on 2019-nCoV can be found on the CDC’s Novel Coronavirus 2019 webpage.
according to an announcement from the Centers for Disease Control and Prevention.
Starting today, Jan. 17, 2020, people traveling from Wuhan to New York (JFK), San Francisco (SFO), and Los Angeles (LAX) airports will be screened for symptoms associated with 2019-nCoV, which include fever, cough, and difficulty breathing.
“Based on the information that CDC has today, we believe the current risk for this virus to the general public is low,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a CDC telebriefing.
To date, 45 cases of 2019-nCoV have been reported in Wuhan, according to the CDC. The Wuhan Municipal Health Commission said 15 patients have been cured and discharged, 5 severe cases are still being treated, and 2 patients have died. Both deaths occurred in older patients, one of whom was aged 69 years and one aged 61 years. One of the patients was known to have underlying health conditions.
Three cases of 2019-nCoV have been confirmed outside of Wuhan, one in Japan and two in Thailand. All three were travelers from Wuhan.
The virus is believed to have originated at Wuhan South China Seafood City, a market that sold seafood, chickens, bats, cats, marmots, and other wild animals. (The market has since been closed and disinfected.) The origin suggests animal-to-human transmission of 2019-nCoV, but it appears that human-to-human transmission can occur as well.
“While most of these infections seem to be happening from animals to people, there is some indication that limited person-to-person spread is happening,” Dr. Messonnier said.
Because of this potential risk, the CDC is working with the Department of Homeland Security’s Customs and Border Protection to screen travelers from Wuhan to the United States. The CDC is deploying about 100 additional staff to JFK, SFO, and LAX, where direct flights (JFK and SFO) or connecting flights (LAX) from Wuhan land.
The CDC could not confirm if exit screening is planned for people traveling abroad from Wuhan.
At the U.S. airports, travelers from Wuhan will be given a questionnaire asking about symptoms of 2019-nCoV (fever, cough, and difficulty breathing). People who exhibit symptoms will be assessed and questioned further. If they are believed to have 2019-nCoV, they will be sent to designated hospitals, where they will be examined, and samples will be collected.
Samples from patients with suspected 2019-nCoV will be sent to the CDC for analysis. Chinese health authorities made the full genome of 2019-nCoV publicly available, which will allow the CDC to confirm any cases that may arise in the United States. The CDC is currently working on a test to detect 2019-nCoV, which can be distributed to state health departments.
Earlier this month, the CDC issued a Level 1 Travel Health Notice for travelers to Wuhan and a Health Alert on 2019-nCoV. The latest information on 2019-nCoV can be found on the CDC’s Novel Coronavirus 2019 webpage.
according to an announcement from the Centers for Disease Control and Prevention.
Starting today, Jan. 17, 2020, people traveling from Wuhan to New York (JFK), San Francisco (SFO), and Los Angeles (LAX) airports will be screened for symptoms associated with 2019-nCoV, which include fever, cough, and difficulty breathing.
“Based on the information that CDC has today, we believe the current risk for this virus to the general public is low,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a CDC telebriefing.
To date, 45 cases of 2019-nCoV have been reported in Wuhan, according to the CDC. The Wuhan Municipal Health Commission said 15 patients have been cured and discharged, 5 severe cases are still being treated, and 2 patients have died. Both deaths occurred in older patients, one of whom was aged 69 years and one aged 61 years. One of the patients was known to have underlying health conditions.
Three cases of 2019-nCoV have been confirmed outside of Wuhan, one in Japan and two in Thailand. All three were travelers from Wuhan.
The virus is believed to have originated at Wuhan South China Seafood City, a market that sold seafood, chickens, bats, cats, marmots, and other wild animals. (The market has since been closed and disinfected.) The origin suggests animal-to-human transmission of 2019-nCoV, but it appears that human-to-human transmission can occur as well.
“While most of these infections seem to be happening from animals to people, there is some indication that limited person-to-person spread is happening,” Dr. Messonnier said.
Because of this potential risk, the CDC is working with the Department of Homeland Security’s Customs and Border Protection to screen travelers from Wuhan to the United States. The CDC is deploying about 100 additional staff to JFK, SFO, and LAX, where direct flights (JFK and SFO) or connecting flights (LAX) from Wuhan land.
The CDC could not confirm if exit screening is planned for people traveling abroad from Wuhan.
At the U.S. airports, travelers from Wuhan will be given a questionnaire asking about symptoms of 2019-nCoV (fever, cough, and difficulty breathing). People who exhibit symptoms will be assessed and questioned further. If they are believed to have 2019-nCoV, they will be sent to designated hospitals, where they will be examined, and samples will be collected.
Samples from patients with suspected 2019-nCoV will be sent to the CDC for analysis. Chinese health authorities made the full genome of 2019-nCoV publicly available, which will allow the CDC to confirm any cases that may arise in the United States. The CDC is currently working on a test to detect 2019-nCoV, which can be distributed to state health departments.
Earlier this month, the CDC issued a Level 1 Travel Health Notice for travelers to Wuhan and a Health Alert on 2019-nCoV. The latest information on 2019-nCoV can be found on the CDC’s Novel Coronavirus 2019 webpage.