User login
Restriction of Foley catheters in older trauma patients improved outcomes
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
and led to earlier discharge, findings from a study revealed. The results of the study were reported in an abstract scheduled for release at the annual meeting of the American Academy of Orthopaedic Surgeons. The meeting was canceled because of COVID-19.
“We reduced the use of Foley catheters in our target population by more than 50%, which led to a decrease in the rate of hospital-acquired UTI and positively affected other perioperative outcomes,” reported Sanjit R. Konda, MD, an orthopedic surgeon with New York University Langone Health.
The quality initiative was introduced about 2 years ago specifically to reduce the risk of UTI in older patients admitted for femur or hip fractures. Previously at the level 1 trauma center where this quality initiative was introduced, placement of Foley catheters in these types of patients had been routine.
After the policy change, Foley catheters were only offered to these trauma patients 55 years of age or older when more than three episodes or urinary retention had been documented with a bladder scan. Urinary retention was defined as a volume of at least 600 mL.
When outcomes in 184 patients treated in the 15 months after the policy change were compared with 393 treated in the prior 38 months, Foley catheter use was substantially and significantly reduced (43.5% vs. 95.5%; P < .001), Dr. Konda said in an interview.
Although the lower rate of UTI following the policy change fell short of statistical significance (10.33% vs. 14.5%; P = .167), the policy change was associated with a decreased time to surgery (33.27 vs. 38.54 hours; P = .001), shorter length of stay (6.89 vs. 8.34 days; P < .001), and higher rate of home discharge (22.8% vs. 15.6%; P = .038).
When those who avoided a Foley catheter were compared with those who did not after the policy change, there was a significant reduction in UTI (4.81% vs. 17.4%; P = .014). In addition, patients who avoided a Foley catheter had a decreased time to surgery (P = .014), shorter length of stay (P < .001) and an almost 900% greater likelihood of home discharge (odds ratio, 9.9; P < .001).
“This quality initiative does increase the number of bladder scans required, meaning more work for nurses, but the program was developed in collaboration with our nursing staff, who were supportive of the goals,” Dr. Konda reported.
Reducing the incidence of UTI is an important initiative because the Centers for Medicare & Medicaid Services and other third-party payers employ this as a quality metric, according to Dr. Konda. This explains why hospital administrators generally embrace effective strategies to reduce UTI rates.
The improvement in outcomes, including the reduction in UTIs and length of stay, has cost implications, which will be evaluated in a future analysis, according to Dr. Konda.
Although this quality initiative was undertaken in a level 1 trauma center, Dr. Konda believes the same principles can be applied to other settings.
Jennifer A. Meddings, MD, an associate professor of medicine at the University of Michigan, Ann Arbor, agreed. Active in the evaluation of strategies to reduce hospital-acquired complications, Dr. Meddings published a study of procedural appropriateness ratings to guide strategies for improving the likelihood that catheters are employed only when needed (BMJ Qual Saf. 2019;28:56-66).
“In addition to avoiding UTI, reducing unnecessary placement of Foley catheters also eliminates the risk of trauma to the urinary tract,” Dr. Meddings said. This is a complication that is not well appreciated because the trauma is not always documented, according to Dr. Meddings, who believes increased risk of both UTI and urinary tract trauma should discourage use of Foley catheters when there is not a specific indication.
Although there are criteria other than excess bladder volume to determine when to consider a Foley catheter, Dr. Meddings encourages any systematic approach that increases the likelihood that catheters are not placed unnecessarily. She emphasized that a hip fracture by itself “is not a criterion for catheterization.”
Dr. Konda reported a financial relationship with Stryker.
FROM AAOS 2020
Risk index stratifies pediatric leukemia patients undergoing HSCT
A disease risk index is now available for pediatric patients with acute myeloid leukemia or acute lymphoblastic leukemia who undergo allogeneic hematopoietic stem cell transplantation.
The model, which was developed and validated using data from more than 2,000 patients, stratifies probabilities of leukemia-free survival (LFS) into four risk groups for acute myeloid leukemia (AML) and three risk groups for acute lymphoblastic leukemia (ALL), reported lead author Muna Qayed, MD, of Emory University, Atlanta, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
“The outcome of stem cell transplantation for hematologic malignancy is influenced by disease type, cytogenetics, and disease status at transplantation,” Dr. Qayed said. “In adults, these attributes were used to develop the disease risk index, or DRI, that can stratify patients for overall survival for purposes such as prognostication or clinical trial entry.”
But no such model exists for pediatric patients, Dr. Qayed said, noting that the adult DRI was found to be inaccurate when applied to children.
“[T]he [adult] DRI did not differentiate [pediatric] patients by overall survival,” Dr. Qayed said. “Therefore, knowing that pediatric AML and ALL differ biologically from adult leukemia, and further, treatment strategies differ between adults and children, we aimed to develop a pediatric-specific DRI.”
This involved analysis of data from 1,135 children with AML and 1,228 children with ALL who underwent transplantation between 2008 and 2017. All patients had myeloablative conditioning, and 75% received an unrelated donor graft. Haploidentical transplants were excluded because of small sample size.
Analyses were conducted in AML and ALL cohorts, with patients in each population randomized to training and validation subgroups in a 1:1 ratio. The primary outcome was LFS. Cox regression models were used to identify significant characteristics, which were then integrated into a prognostic scoring system for the training groups. These scoring systems were then tested in the validation subgroups. Maximum likelihood was used to identify age cutoffs, which were 3 years for AML and 2 years for ALL.
In both cohorts, disease status at transplantation was characterized by complete remission and minimal residual disease status.
In the AML cohort, approximately one-third of patients were in first complete remission with negative minimal residual disease. Risk was stratified into four groups, including good, intermediate, high, and very high risk, with respective 5-year LFS probabilities of 81%, 56%, 44%, and 21%. Independent predictors of poorer outcome included unfavorable cytogenetics, first or second complete remission with minimal residual disease positivity, relapse at transplantation, and age less than 3 years.
In the ALL cohort, risk was stratified into three risk tiers: good, intermediate, and high, with 5-year LFS probabilities of 68%, 50%, and 15%, respectively. Independent predictors of poorer outcome included age less than 2 years, relapse at transplantation, and second complete remission regardless of minimal residual disease status.
The models for each disease also predicted overall survival.
For AML, hazard ratios, ascending from good to very-high-risk tiers, were 1.00, 3.52, 4.67, and 8.62. For ALL risk tiers, ascending hazard ratios were 1.00, 2.16, and 3.86.
“In summary, the pediatric disease risk index validated for leukemia-free survival and overall survival successfully stratifies children with acute leukemia at the time of transplantation,” Dr. Qayed said.
She concluded her presentation by highlighting the practicality and relevance of the new scoring system.
“The components included in the scoring system used information that is readily available pretransplantation, lending support to the deliverability of the prognostic scoring system,” Dr. Qayed said. “It can further be used for improved interpretation of multicenter data and in clinical trials for risk stratification.”
In a virtual presentation, invited discussant Nirali N. Shah, MD, of the National Cancer Institute, Bethesda, Md., first emphasized the clinical importance of an accurate disease risk index for pediatric patients.
“When going into transplant, the No. 1 question that all parents will ask is: ‘Will my child be cured?’ ” she said.
According to Dr. Shah, the risk model developed by Dr. Qayed and colleagues is built on a strong foundation, including adequate sample size, comprehensive disease characterization, exclusion of patients that did not undergo myeloablative conditioning, and use of minimal residual disease status.
Still, more work is needed, Dr. Shah said.
“This DRI will need to be prospectively tested and compared to other established risk factors. For instance, minimal residual disease alone can be further stratified and has a significant role in establishing risk for posttransplant relapse. And the development of acute graft-versus-host disease also plays an important role in posttransplant relapse.”
Dr. Shah went on to outline potential areas of improvement.
“[F]uture directions for this study could include incorporation of early posttransplant events like graft-versus-host disease, potential stratification of the minimal residual disease results among those patients in complete remission, and potential application of this DRI to the adolescent and young adult population, which may have slight variation even from the adult DRI.”The study was funded by the National Institutes of Health. The investigators disclosed no conflicts of interest
SOURCE: Qayed M et al. ASCO 2020, Abstract 7503.
A disease risk index is now available for pediatric patients with acute myeloid leukemia or acute lymphoblastic leukemia who undergo allogeneic hematopoietic stem cell transplantation.
The model, which was developed and validated using data from more than 2,000 patients, stratifies probabilities of leukemia-free survival (LFS) into four risk groups for acute myeloid leukemia (AML) and three risk groups for acute lymphoblastic leukemia (ALL), reported lead author Muna Qayed, MD, of Emory University, Atlanta, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
“The outcome of stem cell transplantation for hematologic malignancy is influenced by disease type, cytogenetics, and disease status at transplantation,” Dr. Qayed said. “In adults, these attributes were used to develop the disease risk index, or DRI, that can stratify patients for overall survival for purposes such as prognostication or clinical trial entry.”
But no such model exists for pediatric patients, Dr. Qayed said, noting that the adult DRI was found to be inaccurate when applied to children.
“[T]he [adult] DRI did not differentiate [pediatric] patients by overall survival,” Dr. Qayed said. “Therefore, knowing that pediatric AML and ALL differ biologically from adult leukemia, and further, treatment strategies differ between adults and children, we aimed to develop a pediatric-specific DRI.”
This involved analysis of data from 1,135 children with AML and 1,228 children with ALL who underwent transplantation between 2008 and 2017. All patients had myeloablative conditioning, and 75% received an unrelated donor graft. Haploidentical transplants were excluded because of small sample size.
Analyses were conducted in AML and ALL cohorts, with patients in each population randomized to training and validation subgroups in a 1:1 ratio. The primary outcome was LFS. Cox regression models were used to identify significant characteristics, which were then integrated into a prognostic scoring system for the training groups. These scoring systems were then tested in the validation subgroups. Maximum likelihood was used to identify age cutoffs, which were 3 years for AML and 2 years for ALL.
In both cohorts, disease status at transplantation was characterized by complete remission and minimal residual disease status.
In the AML cohort, approximately one-third of patients were in first complete remission with negative minimal residual disease. Risk was stratified into four groups, including good, intermediate, high, and very high risk, with respective 5-year LFS probabilities of 81%, 56%, 44%, and 21%. Independent predictors of poorer outcome included unfavorable cytogenetics, first or second complete remission with minimal residual disease positivity, relapse at transplantation, and age less than 3 years.
In the ALL cohort, risk was stratified into three risk tiers: good, intermediate, and high, with 5-year LFS probabilities of 68%, 50%, and 15%, respectively. Independent predictors of poorer outcome included age less than 2 years, relapse at transplantation, and second complete remission regardless of minimal residual disease status.
The models for each disease also predicted overall survival.
For AML, hazard ratios, ascending from good to very-high-risk tiers, were 1.00, 3.52, 4.67, and 8.62. For ALL risk tiers, ascending hazard ratios were 1.00, 2.16, and 3.86.
“In summary, the pediatric disease risk index validated for leukemia-free survival and overall survival successfully stratifies children with acute leukemia at the time of transplantation,” Dr. Qayed said.
She concluded her presentation by highlighting the practicality and relevance of the new scoring system.
“The components included in the scoring system used information that is readily available pretransplantation, lending support to the deliverability of the prognostic scoring system,” Dr. Qayed said. “It can further be used for improved interpretation of multicenter data and in clinical trials for risk stratification.”
In a virtual presentation, invited discussant Nirali N. Shah, MD, of the National Cancer Institute, Bethesda, Md., first emphasized the clinical importance of an accurate disease risk index for pediatric patients.
“When going into transplant, the No. 1 question that all parents will ask is: ‘Will my child be cured?’ ” she said.
According to Dr. Shah, the risk model developed by Dr. Qayed and colleagues is built on a strong foundation, including adequate sample size, comprehensive disease characterization, exclusion of patients that did not undergo myeloablative conditioning, and use of minimal residual disease status.
Still, more work is needed, Dr. Shah said.
“This DRI will need to be prospectively tested and compared to other established risk factors. For instance, minimal residual disease alone can be further stratified and has a significant role in establishing risk for posttransplant relapse. And the development of acute graft-versus-host disease also plays an important role in posttransplant relapse.”
Dr. Shah went on to outline potential areas of improvement.
“[F]uture directions for this study could include incorporation of early posttransplant events like graft-versus-host disease, potential stratification of the minimal residual disease results among those patients in complete remission, and potential application of this DRI to the adolescent and young adult population, which may have slight variation even from the adult DRI.”The study was funded by the National Institutes of Health. The investigators disclosed no conflicts of interest
SOURCE: Qayed M et al. ASCO 2020, Abstract 7503.
A disease risk index is now available for pediatric patients with acute myeloid leukemia or acute lymphoblastic leukemia who undergo allogeneic hematopoietic stem cell transplantation.
The model, which was developed and validated using data from more than 2,000 patients, stratifies probabilities of leukemia-free survival (LFS) into four risk groups for acute myeloid leukemia (AML) and three risk groups for acute lymphoblastic leukemia (ALL), reported lead author Muna Qayed, MD, of Emory University, Atlanta, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
“The outcome of stem cell transplantation for hematologic malignancy is influenced by disease type, cytogenetics, and disease status at transplantation,” Dr. Qayed said. “In adults, these attributes were used to develop the disease risk index, or DRI, that can stratify patients for overall survival for purposes such as prognostication or clinical trial entry.”
But no such model exists for pediatric patients, Dr. Qayed said, noting that the adult DRI was found to be inaccurate when applied to children.
“[T]he [adult] DRI did not differentiate [pediatric] patients by overall survival,” Dr. Qayed said. “Therefore, knowing that pediatric AML and ALL differ biologically from adult leukemia, and further, treatment strategies differ between adults and children, we aimed to develop a pediatric-specific DRI.”
This involved analysis of data from 1,135 children with AML and 1,228 children with ALL who underwent transplantation between 2008 and 2017. All patients had myeloablative conditioning, and 75% received an unrelated donor graft. Haploidentical transplants were excluded because of small sample size.
Analyses were conducted in AML and ALL cohorts, with patients in each population randomized to training and validation subgroups in a 1:1 ratio. The primary outcome was LFS. Cox regression models were used to identify significant characteristics, which were then integrated into a prognostic scoring system for the training groups. These scoring systems were then tested in the validation subgroups. Maximum likelihood was used to identify age cutoffs, which were 3 years for AML and 2 years for ALL.
In both cohorts, disease status at transplantation was characterized by complete remission and minimal residual disease status.
In the AML cohort, approximately one-third of patients were in first complete remission with negative minimal residual disease. Risk was stratified into four groups, including good, intermediate, high, and very high risk, with respective 5-year LFS probabilities of 81%, 56%, 44%, and 21%. Independent predictors of poorer outcome included unfavorable cytogenetics, first or second complete remission with minimal residual disease positivity, relapse at transplantation, and age less than 3 years.
In the ALL cohort, risk was stratified into three risk tiers: good, intermediate, and high, with 5-year LFS probabilities of 68%, 50%, and 15%, respectively. Independent predictors of poorer outcome included age less than 2 years, relapse at transplantation, and second complete remission regardless of minimal residual disease status.
The models for each disease also predicted overall survival.
For AML, hazard ratios, ascending from good to very-high-risk tiers, were 1.00, 3.52, 4.67, and 8.62. For ALL risk tiers, ascending hazard ratios were 1.00, 2.16, and 3.86.
“In summary, the pediatric disease risk index validated for leukemia-free survival and overall survival successfully stratifies children with acute leukemia at the time of transplantation,” Dr. Qayed said.
She concluded her presentation by highlighting the practicality and relevance of the new scoring system.
“The components included in the scoring system used information that is readily available pretransplantation, lending support to the deliverability of the prognostic scoring system,” Dr. Qayed said. “It can further be used for improved interpretation of multicenter data and in clinical trials for risk stratification.”
In a virtual presentation, invited discussant Nirali N. Shah, MD, of the National Cancer Institute, Bethesda, Md., first emphasized the clinical importance of an accurate disease risk index for pediatric patients.
“When going into transplant, the No. 1 question that all parents will ask is: ‘Will my child be cured?’ ” she said.
According to Dr. Shah, the risk model developed by Dr. Qayed and colleagues is built on a strong foundation, including adequate sample size, comprehensive disease characterization, exclusion of patients that did not undergo myeloablative conditioning, and use of minimal residual disease status.
Still, more work is needed, Dr. Shah said.
“This DRI will need to be prospectively tested and compared to other established risk factors. For instance, minimal residual disease alone can be further stratified and has a significant role in establishing risk for posttransplant relapse. And the development of acute graft-versus-host disease also plays an important role in posttransplant relapse.”
Dr. Shah went on to outline potential areas of improvement.
“[F]uture directions for this study could include incorporation of early posttransplant events like graft-versus-host disease, potential stratification of the minimal residual disease results among those patients in complete remission, and potential application of this DRI to the adolescent and young adult population, which may have slight variation even from the adult DRI.”The study was funded by the National Institutes of Health. The investigators disclosed no conflicts of interest
SOURCE: Qayed M et al. ASCO 2020, Abstract 7503.
FROM ASCO 2020
TNF inhibitor plus methotrexate surpassed methotrexate monotherapy in PsA
Adding a tumor necrosis factor inhibitor to the treatment regimen of patients with psoriatic arthritis who failed to reach minimal disease activity on methotrexate monotherapy after 4 or more weeks had more than triple the rate of minimal disease activity after 16 weeks, compared with patients who had their methotrexate dosage escalated but received no second drug, in a multicenter, randomized study with 245 patients.
After 16 weeks, 42% of 123 patients with psoriatic arthritis (PsA) treated with methotrexate and the tumor necrosis factor (TNF) inhibitor adalimumab achieved minimal disease activity, compared with 13% of 122 patients randomized to receive escalated methotrexate monotherapy to their maximally tolerated dosage or to a maximum of 25 mg/week, Laura C. Coates, MBChB, PhD, reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
The findings are “supportive of the EULAR recommendations” for managing patients with PsA, said Dr. Coates, a rheumatologist at the University of Oxford (England). The EULAR recommendations call for starting a biologic disease-modifying antirheumatic drug (bDMARD) in patients with PsA and peripheral arthritis and “inadequate response to at least one [conventional synthetic] DMARD,” such as methotrexate (Ann Rheum Dis. 2019 Jun;79[6]:700-12). “A proportion of patients treated with methotrexate do well, but for those struggling on methotrexate, these results support use of a TNF inhibitor. It’s a balance of cost and benefit. If TNF inhibitors were as cheap as methotrexate, I suspect that would be first line more frequently,” Dr. Coates said in an interview. In contrast, the PsA management recommendations from the American College of Rheumatology make treatment with a TNF inhibitor first line, before starting with what these guidelines call an oral small molecule, the same as a conventional synthetic DMARD such as methotrexate (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
“It’s a well-known fact that adalimumab is more effective than methotrexate in [PsA] patients who do not respond sufficiently well to methotrexate. Patients failing on methotrexate have been escalated to a TNF inhibitor for years,” commented Robert B.M. Landewé, MD, a rheumatologist and professor of medicine at the University of Amsterdam, and a coauthor of the EULAR PsA treatment recommendations. “In the Netherlands and in my practice, every [PsA] patient starts on methotrexate until a dosage of at least 15 mg/week, but if they don’t have sufficient response we escalate to adding a TNF inhibitor,” he said in an interview. “A significant proportion of patients with PsA respond well to moderate to higher dosages of methotrexate,” and this monotherapy with escalation of methotrexate can be safely continued for more than 3 months in many patients without the risk of “losing too much time by waiting” to start a bDMARD.
Dr. Coates said that her practice was to look for some level of response to methotrexate by 12 weeks on treatment and for achievement of minimal disease activity within 24 weeks of treatment. If these targets are not reached, she then adds a TNF inhibitor.
The CONTROL study ran at 60 sites in the United States and in 12 other countries and enrolled patients with active PsA despite treatment with methotrexate for at least 4 weeks and no history of treatment with a bDMARD. Patients received either 40 mg adalimumab every other week plus 15 mg of methotrexate weekly, or maximum-tolerated methotrexate up to 25 mg/week. The results also showed that the primary endpoint of the rate of achieved minimal disease activity seen overall in each of the two study arms was consistent in both the roughly half of patients who had been on methotrexate monotherapy for 3 months or less before entering the study as well as those who had been on initial methotrexate monotherapy for a longer period. Other secondary endpoints examined also showed significantly better responses to adding adalimumab, including a tripling of the rate at which patients achieved complete resolution of their Psoriasis Area and Severity Index score, which occurred in 30% of patients on the TNF inhibitor plus methotrexate and in 9% of those on methotrexate monotherapy.
The results seen in the CONTROL study with adalimumab would likely be similar using a different TNF inhibitor or an agent that’s an adalimumab biosimilar, Dr. Coates said. The only patients with PsA and not achieving minimal disease activity on methotrexate monotherapy who should not then receive add-on treatment with a TNF inhibitor are those known to have a safety exclusion for this drug class or patients for whom the incremental cost poses a barrier, she added. In addition, patients with more substantial skin involvement may get greater benefit from a different class of bDMARD, such as a drug that inhibits interleukin-17 or IL-12 and -23 as recommended by the EULAR panel.
“We still get very good results with a TNF inhibitor for psoriasis, but in patients with severe psoriasis there is an argument to use a different drug,” Dr. Coates acknowledged. Skin responses with an IL-17 inhibitor or an IL-12/23 inhibitor “are far better” than with a TNF inhibitor, said Dr. Landewé. He also added the caution that longer-term use of adalimumab “may induce aggravation of PsA in a significant number of patients.”
CONTROL was sponsored by AbbVie, the company that markets adalimumab (Humira). Dr. Coates has been a consultant to AbbVie, as well as to Amgen, Biogen, Boehringer Ingelheim, Celgene, Jansen, Novartis, Pfizer, and UCB. Dr. Landewé has been a consultant to AbbVie, as well as to Eli Lilly, Novartis, Pfizer, and UCB.
SOURCE: Coates LC et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:33, Abstract OP0050.
Adding a tumor necrosis factor inhibitor to the treatment regimen of patients with psoriatic arthritis who failed to reach minimal disease activity on methotrexate monotherapy after 4 or more weeks had more than triple the rate of minimal disease activity after 16 weeks, compared with patients who had their methotrexate dosage escalated but received no second drug, in a multicenter, randomized study with 245 patients.
After 16 weeks, 42% of 123 patients with psoriatic arthritis (PsA) treated with methotrexate and the tumor necrosis factor (TNF) inhibitor adalimumab achieved minimal disease activity, compared with 13% of 122 patients randomized to receive escalated methotrexate monotherapy to their maximally tolerated dosage or to a maximum of 25 mg/week, Laura C. Coates, MBChB, PhD, reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
The findings are “supportive of the EULAR recommendations” for managing patients with PsA, said Dr. Coates, a rheumatologist at the University of Oxford (England). The EULAR recommendations call for starting a biologic disease-modifying antirheumatic drug (bDMARD) in patients with PsA and peripheral arthritis and “inadequate response to at least one [conventional synthetic] DMARD,” such as methotrexate (Ann Rheum Dis. 2019 Jun;79[6]:700-12). “A proportion of patients treated with methotrexate do well, but for those struggling on methotrexate, these results support use of a TNF inhibitor. It’s a balance of cost and benefit. If TNF inhibitors were as cheap as methotrexate, I suspect that would be first line more frequently,” Dr. Coates said in an interview. In contrast, the PsA management recommendations from the American College of Rheumatology make treatment with a TNF inhibitor first line, before starting with what these guidelines call an oral small molecule, the same as a conventional synthetic DMARD such as methotrexate (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
“It’s a well-known fact that adalimumab is more effective than methotrexate in [PsA] patients who do not respond sufficiently well to methotrexate. Patients failing on methotrexate have been escalated to a TNF inhibitor for years,” commented Robert B.M. Landewé, MD, a rheumatologist and professor of medicine at the University of Amsterdam, and a coauthor of the EULAR PsA treatment recommendations. “In the Netherlands and in my practice, every [PsA] patient starts on methotrexate until a dosage of at least 15 mg/week, but if they don’t have sufficient response we escalate to adding a TNF inhibitor,” he said in an interview. “A significant proportion of patients with PsA respond well to moderate to higher dosages of methotrexate,” and this monotherapy with escalation of methotrexate can be safely continued for more than 3 months in many patients without the risk of “losing too much time by waiting” to start a bDMARD.
Dr. Coates said that her practice was to look for some level of response to methotrexate by 12 weeks on treatment and for achievement of minimal disease activity within 24 weeks of treatment. If these targets are not reached, she then adds a TNF inhibitor.
The CONTROL study ran at 60 sites in the United States and in 12 other countries and enrolled patients with active PsA despite treatment with methotrexate for at least 4 weeks and no history of treatment with a bDMARD. Patients received either 40 mg adalimumab every other week plus 15 mg of methotrexate weekly, or maximum-tolerated methotrexate up to 25 mg/week. The results also showed that the primary endpoint of the rate of achieved minimal disease activity seen overall in each of the two study arms was consistent in both the roughly half of patients who had been on methotrexate monotherapy for 3 months or less before entering the study as well as those who had been on initial methotrexate monotherapy for a longer period. Other secondary endpoints examined also showed significantly better responses to adding adalimumab, including a tripling of the rate at which patients achieved complete resolution of their Psoriasis Area and Severity Index score, which occurred in 30% of patients on the TNF inhibitor plus methotrexate and in 9% of those on methotrexate monotherapy.
The results seen in the CONTROL study with adalimumab would likely be similar using a different TNF inhibitor or an agent that’s an adalimumab biosimilar, Dr. Coates said. The only patients with PsA and not achieving minimal disease activity on methotrexate monotherapy who should not then receive add-on treatment with a TNF inhibitor are those known to have a safety exclusion for this drug class or patients for whom the incremental cost poses a barrier, she added. In addition, patients with more substantial skin involvement may get greater benefit from a different class of bDMARD, such as a drug that inhibits interleukin-17 or IL-12 and -23 as recommended by the EULAR panel.
“We still get very good results with a TNF inhibitor for psoriasis, but in patients with severe psoriasis there is an argument to use a different drug,” Dr. Coates acknowledged. Skin responses with an IL-17 inhibitor or an IL-12/23 inhibitor “are far better” than with a TNF inhibitor, said Dr. Landewé. He also added the caution that longer-term use of adalimumab “may induce aggravation of PsA in a significant number of patients.”
CONTROL was sponsored by AbbVie, the company that markets adalimumab (Humira). Dr. Coates has been a consultant to AbbVie, as well as to Amgen, Biogen, Boehringer Ingelheim, Celgene, Jansen, Novartis, Pfizer, and UCB. Dr. Landewé has been a consultant to AbbVie, as well as to Eli Lilly, Novartis, Pfizer, and UCB.
SOURCE: Coates LC et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:33, Abstract OP0050.
Adding a tumor necrosis factor inhibitor to the treatment regimen of patients with psoriatic arthritis who failed to reach minimal disease activity on methotrexate monotherapy after 4 or more weeks had more than triple the rate of minimal disease activity after 16 weeks, compared with patients who had their methotrexate dosage escalated but received no second drug, in a multicenter, randomized study with 245 patients.
After 16 weeks, 42% of 123 patients with psoriatic arthritis (PsA) treated with methotrexate and the tumor necrosis factor (TNF) inhibitor adalimumab achieved minimal disease activity, compared with 13% of 122 patients randomized to receive escalated methotrexate monotherapy to their maximally tolerated dosage or to a maximum of 25 mg/week, Laura C. Coates, MBChB, PhD, reported at the annual European Congress of Rheumatology, held online this year due to COVID-19.
The findings are “supportive of the EULAR recommendations” for managing patients with PsA, said Dr. Coates, a rheumatologist at the University of Oxford (England). The EULAR recommendations call for starting a biologic disease-modifying antirheumatic drug (bDMARD) in patients with PsA and peripheral arthritis and “inadequate response to at least one [conventional synthetic] DMARD,” such as methotrexate (Ann Rheum Dis. 2019 Jun;79[6]:700-12). “A proportion of patients treated with methotrexate do well, but for those struggling on methotrexate, these results support use of a TNF inhibitor. It’s a balance of cost and benefit. If TNF inhibitors were as cheap as methotrexate, I suspect that would be first line more frequently,” Dr. Coates said in an interview. In contrast, the PsA management recommendations from the American College of Rheumatology make treatment with a TNF inhibitor first line, before starting with what these guidelines call an oral small molecule, the same as a conventional synthetic DMARD such as methotrexate (Arthritis Rheumatol. 2019 Jan;71[1]:5-32).
“It’s a well-known fact that adalimumab is more effective than methotrexate in [PsA] patients who do not respond sufficiently well to methotrexate. Patients failing on methotrexate have been escalated to a TNF inhibitor for years,” commented Robert B.M. Landewé, MD, a rheumatologist and professor of medicine at the University of Amsterdam, and a coauthor of the EULAR PsA treatment recommendations. “In the Netherlands and in my practice, every [PsA] patient starts on methotrexate until a dosage of at least 15 mg/week, but if they don’t have sufficient response we escalate to adding a TNF inhibitor,” he said in an interview. “A significant proportion of patients with PsA respond well to moderate to higher dosages of methotrexate,” and this monotherapy with escalation of methotrexate can be safely continued for more than 3 months in many patients without the risk of “losing too much time by waiting” to start a bDMARD.
Dr. Coates said that her practice was to look for some level of response to methotrexate by 12 weeks on treatment and for achievement of minimal disease activity within 24 weeks of treatment. If these targets are not reached, she then adds a TNF inhibitor.
The CONTROL study ran at 60 sites in the United States and in 12 other countries and enrolled patients with active PsA despite treatment with methotrexate for at least 4 weeks and no history of treatment with a bDMARD. Patients received either 40 mg adalimumab every other week plus 15 mg of methotrexate weekly, or maximum-tolerated methotrexate up to 25 mg/week. The results also showed that the primary endpoint of the rate of achieved minimal disease activity seen overall in each of the two study arms was consistent in both the roughly half of patients who had been on methotrexate monotherapy for 3 months or less before entering the study as well as those who had been on initial methotrexate monotherapy for a longer period. Other secondary endpoints examined also showed significantly better responses to adding adalimumab, including a tripling of the rate at which patients achieved complete resolution of their Psoriasis Area and Severity Index score, which occurred in 30% of patients on the TNF inhibitor plus methotrexate and in 9% of those on methotrexate monotherapy.
The results seen in the CONTROL study with adalimumab would likely be similar using a different TNF inhibitor or an agent that’s an adalimumab biosimilar, Dr. Coates said. The only patients with PsA and not achieving minimal disease activity on methotrexate monotherapy who should not then receive add-on treatment with a TNF inhibitor are those known to have a safety exclusion for this drug class or patients for whom the incremental cost poses a barrier, she added. In addition, patients with more substantial skin involvement may get greater benefit from a different class of bDMARD, such as a drug that inhibits interleukin-17 or IL-12 and -23 as recommended by the EULAR panel.
“We still get very good results with a TNF inhibitor for psoriasis, but in patients with severe psoriasis there is an argument to use a different drug,” Dr. Coates acknowledged. Skin responses with an IL-17 inhibitor or an IL-12/23 inhibitor “are far better” than with a TNF inhibitor, said Dr. Landewé. He also added the caution that longer-term use of adalimumab “may induce aggravation of PsA in a significant number of patients.”
CONTROL was sponsored by AbbVie, the company that markets adalimumab (Humira). Dr. Coates has been a consultant to AbbVie, as well as to Amgen, Biogen, Boehringer Ingelheim, Celgene, Jansen, Novartis, Pfizer, and UCB. Dr. Landewé has been a consultant to AbbVie, as well as to Eli Lilly, Novartis, Pfizer, and UCB.
SOURCE: Coates LC et al. Ann Rheum Dis. 2020 Jun;79[suppl 1]:33, Abstract OP0050.
FROM EULAR 2020 E-CONGRESS
Huntington’s disease biomarkers appear 24 years before clinical symptoms
, according to a study published in the June Lancet Neurology. The data come from the Huntington’s disease Young Adult Study (HD-YAS) conducted in the United Kingdom.
The genetic cause of Huntington’s disease provides a potential target for biomarker treatment, wrote joint first authors Rachael I. Scahill, PhD, and Paul Zeun, BMBS, of University College London and colleagues.
“A detailed characterization of the premanifest period in Huntington’s disease is crucial for disease staging, informing the optimum time to initiate treatments, and identifying biomarkers for future trials in people with premanifest Huntington’s disease (preHD),” they said.
Identifying biomarkers of pre-Huntington’s disease
For their study, the researchers recruited 64 young adults with presymptomatic Huntington’s disease (preHD) and 67 controls, with an average age of 29 years. Brain imaging was conducted between Aug. 2, 2017, and April 25, 2019. Individuals with preexisting measurable cognitive and psychiatric disorders were excluded.
The researchers found no significant evidence of cognitive or psychiatric impairment in the preHD group at 23.6 years from the predicted onset of symptoms. The preHD group showed smaller putamen volumes, compared with controls, but this difference had no apparent relation to the timing of symptom onset, the researchers said.
Brain imaging revealed elevations in the CSF mutant huntingtin, neurofilament light protein (NfL), YKL-40, and plasma NfL among individuals with preHD, compared with controls. Of these, CSF NfL showed the highest effect size of measures in the study and showed a significant increasing association with estimated years to the onset of clinical symptoms of HD carriers. Overall, 53% of individuals with preHD had CSF NfL values in the normal range, and 47% had elevated values, compared with controls.
“NfL is therefore a potential candidate to provide a measure of disease progression in early preHD and might eventually be used as a marker of response to treatment in future preventive trials,” the researchers said.
The study findings were limited by several factors including potential underpowering to detect associations with age and CAG gene segment repeats, the researchers noted.
However, “By identifying a cohort of individuals with preHD and no detectable functional impairment but who begin to exhibit subtle elevations in select biological measures of neurodegeneration, we have highlighted a crucial point early in the disease process,” they concluded.
“Intervening at this stage might offer the prospect of delaying or preventing further neurodegeneration while function is intact, giving gene carriers many more years of life without impairment,” they added.
What is the best window for treatment?
The study is “particularly important since the absence of any subclinical symptoms in preHD individuals far from onset shows that the abnormal developmental aspect of Huntington’s disease has no substantial effect on adults’ clinical pattern,” wrote Anne-Catherine Bachoud-Lévi, MD, of Université Paris Est, Créteil, France, in an accompanying comment.
“The most robust findings of [the study] are the sensitiveness of NfL, compared with mutant huntingtin in CSF of individuals with preHD, and that degenerative rather than developmental disorders are clinically relevant,” she said. However, potential limitations to the study include the exclusion absence of language and calculation as part of the cognitive assessments, she noted. “Ideally, more sensitive cognitive tasks including these domains should be designed for preHD participants.”
In addition, the risks versus benefits of any long-term treatment must be considered, Dr. Bachoud-Lévi noted.
“The best window for treatment should instead target the time when a detectable subclinical slope of cognitive performance allows for predicting disease onset within a few years,” she said. “Turning to machine learning methodology, such as that in oncology, might also permit combining the best window and the best disease-modifying therapy for individuals with preHD,” she added.
The study was supported by the Wellcome Trust, CHDI Foundation. The researchers had no financial conflicts to disclose. Dr. Bachoud-Lévi disclosed grants and personal fees from Roche, and grants from the French Ministry of Health and Direction de la Recherche Clinique.
SOURCES: Scahill RI et al. Lancet Neurol. 2020 June;19:502-12; Bachoud-Lévi A-C. Lancet Neurol. 2020 June;19:473-5.
, according to a study published in the June Lancet Neurology. The data come from the Huntington’s disease Young Adult Study (HD-YAS) conducted in the United Kingdom.
The genetic cause of Huntington’s disease provides a potential target for biomarker treatment, wrote joint first authors Rachael I. Scahill, PhD, and Paul Zeun, BMBS, of University College London and colleagues.
“A detailed characterization of the premanifest period in Huntington’s disease is crucial for disease staging, informing the optimum time to initiate treatments, and identifying biomarkers for future trials in people with premanifest Huntington’s disease (preHD),” they said.
Identifying biomarkers of pre-Huntington’s disease
For their study, the researchers recruited 64 young adults with presymptomatic Huntington’s disease (preHD) and 67 controls, with an average age of 29 years. Brain imaging was conducted between Aug. 2, 2017, and April 25, 2019. Individuals with preexisting measurable cognitive and psychiatric disorders were excluded.
The researchers found no significant evidence of cognitive or psychiatric impairment in the preHD group at 23.6 years from the predicted onset of symptoms. The preHD group showed smaller putamen volumes, compared with controls, but this difference had no apparent relation to the timing of symptom onset, the researchers said.
Brain imaging revealed elevations in the CSF mutant huntingtin, neurofilament light protein (NfL), YKL-40, and plasma NfL among individuals with preHD, compared with controls. Of these, CSF NfL showed the highest effect size of measures in the study and showed a significant increasing association with estimated years to the onset of clinical symptoms of HD carriers. Overall, 53% of individuals with preHD had CSF NfL values in the normal range, and 47% had elevated values, compared with controls.
“NfL is therefore a potential candidate to provide a measure of disease progression in early preHD and might eventually be used as a marker of response to treatment in future preventive trials,” the researchers said.
The study findings were limited by several factors including potential underpowering to detect associations with age and CAG gene segment repeats, the researchers noted.
However, “By identifying a cohort of individuals with preHD and no detectable functional impairment but who begin to exhibit subtle elevations in select biological measures of neurodegeneration, we have highlighted a crucial point early in the disease process,” they concluded.
“Intervening at this stage might offer the prospect of delaying or preventing further neurodegeneration while function is intact, giving gene carriers many more years of life without impairment,” they added.
What is the best window for treatment?
The study is “particularly important since the absence of any subclinical symptoms in preHD individuals far from onset shows that the abnormal developmental aspect of Huntington’s disease has no substantial effect on adults’ clinical pattern,” wrote Anne-Catherine Bachoud-Lévi, MD, of Université Paris Est, Créteil, France, in an accompanying comment.
“The most robust findings of [the study] are the sensitiveness of NfL, compared with mutant huntingtin in CSF of individuals with preHD, and that degenerative rather than developmental disorders are clinically relevant,” she said. However, potential limitations to the study include the exclusion absence of language and calculation as part of the cognitive assessments, she noted. “Ideally, more sensitive cognitive tasks including these domains should be designed for preHD participants.”
In addition, the risks versus benefits of any long-term treatment must be considered, Dr. Bachoud-Lévi noted.
“The best window for treatment should instead target the time when a detectable subclinical slope of cognitive performance allows for predicting disease onset within a few years,” she said. “Turning to machine learning methodology, such as that in oncology, might also permit combining the best window and the best disease-modifying therapy for individuals with preHD,” she added.
The study was supported by the Wellcome Trust, CHDI Foundation. The researchers had no financial conflicts to disclose. Dr. Bachoud-Lévi disclosed grants and personal fees from Roche, and grants from the French Ministry of Health and Direction de la Recherche Clinique.
SOURCES: Scahill RI et al. Lancet Neurol. 2020 June;19:502-12; Bachoud-Lévi A-C. Lancet Neurol. 2020 June;19:473-5.
, according to a study published in the June Lancet Neurology. The data come from the Huntington’s disease Young Adult Study (HD-YAS) conducted in the United Kingdom.
The genetic cause of Huntington’s disease provides a potential target for biomarker treatment, wrote joint first authors Rachael I. Scahill, PhD, and Paul Zeun, BMBS, of University College London and colleagues.
“A detailed characterization of the premanifest period in Huntington’s disease is crucial for disease staging, informing the optimum time to initiate treatments, and identifying biomarkers for future trials in people with premanifest Huntington’s disease (preHD),” they said.
Identifying biomarkers of pre-Huntington’s disease
For their study, the researchers recruited 64 young adults with presymptomatic Huntington’s disease (preHD) and 67 controls, with an average age of 29 years. Brain imaging was conducted between Aug. 2, 2017, and April 25, 2019. Individuals with preexisting measurable cognitive and psychiatric disorders were excluded.
The researchers found no significant evidence of cognitive or psychiatric impairment in the preHD group at 23.6 years from the predicted onset of symptoms. The preHD group showed smaller putamen volumes, compared with controls, but this difference had no apparent relation to the timing of symptom onset, the researchers said.
Brain imaging revealed elevations in the CSF mutant huntingtin, neurofilament light protein (NfL), YKL-40, and plasma NfL among individuals with preHD, compared with controls. Of these, CSF NfL showed the highest effect size of measures in the study and showed a significant increasing association with estimated years to the onset of clinical symptoms of HD carriers. Overall, 53% of individuals with preHD had CSF NfL values in the normal range, and 47% had elevated values, compared with controls.
“NfL is therefore a potential candidate to provide a measure of disease progression in early preHD and might eventually be used as a marker of response to treatment in future preventive trials,” the researchers said.
The study findings were limited by several factors including potential underpowering to detect associations with age and CAG gene segment repeats, the researchers noted.
However, “By identifying a cohort of individuals with preHD and no detectable functional impairment but who begin to exhibit subtle elevations in select biological measures of neurodegeneration, we have highlighted a crucial point early in the disease process,” they concluded.
“Intervening at this stage might offer the prospect of delaying or preventing further neurodegeneration while function is intact, giving gene carriers many more years of life without impairment,” they added.
What is the best window for treatment?
The study is “particularly important since the absence of any subclinical symptoms in preHD individuals far from onset shows that the abnormal developmental aspect of Huntington’s disease has no substantial effect on adults’ clinical pattern,” wrote Anne-Catherine Bachoud-Lévi, MD, of Université Paris Est, Créteil, France, in an accompanying comment.
“The most robust findings of [the study] are the sensitiveness of NfL, compared with mutant huntingtin in CSF of individuals with preHD, and that degenerative rather than developmental disorders are clinically relevant,” she said. However, potential limitations to the study include the exclusion absence of language and calculation as part of the cognitive assessments, she noted. “Ideally, more sensitive cognitive tasks including these domains should be designed for preHD participants.”
In addition, the risks versus benefits of any long-term treatment must be considered, Dr. Bachoud-Lévi noted.
“The best window for treatment should instead target the time when a detectable subclinical slope of cognitive performance allows for predicting disease onset within a few years,” she said. “Turning to machine learning methodology, such as that in oncology, might also permit combining the best window and the best disease-modifying therapy for individuals with preHD,” she added.
The study was supported by the Wellcome Trust, CHDI Foundation. The researchers had no financial conflicts to disclose. Dr. Bachoud-Lévi disclosed grants and personal fees from Roche, and grants from the French Ministry of Health and Direction de la Recherche Clinique.
SOURCES: Scahill RI et al. Lancet Neurol. 2020 June;19:502-12; Bachoud-Lévi A-C. Lancet Neurol. 2020 June;19:473-5.
FROM LANCET NEUROLOGY
JAK inhibitors have top risk for herpes zoster among newer RA DMARDs
Patients with rheumatoid arthritis (RA) who are treated with Janus kinase (JAK) inhibitors had the highest risk of developing herpes zoster among newer disease-modifying antirheumatic drugs (DMARDs), according to data released from the German biologics registry.
These are believed to be the first European data on the risk of herpes zoster with JAK inhibitors and showed that the crude incidence rate of herpes zoster per 1,000 patient-years was 24.9 with JAK inhibitors, compared with just 5.8 for controls taking conventional synthetic (cs) DMARDs.
The risk of herpes zoster was also increased with other biologic (b) and targeted synthetic (ts) DMARDs that were assessed, with crude rates per 1,000 patient-years of 10.4 for monoclonal tumor necrosis factor inhibitors (TNFi), 10.5 for B-cell targeted therapies, 9.4 for T-cell costimulation modulators, 9.0 for soluble TNF receptors, and 8.5 for interleukin (IL)-6 inhibitors.
Overall, JAK inhibitor treatment was associated with a fivefold higher risk of herpes zoster (hazard ratio, 5.0; P < .0001), compared with the control csDMARD population after adjustment using an inverse probability weights (IPW) method.
“The general risk of herpes zoster is [twofold] higher in patients with rheumatoid arthritis when you compare it with the general population,” said Anja Strangfeld, MD of the German Research Center, Berlin, and one of the three RABBIT [Rheumatoide Arthritis: Biobachtung der Biologika-Therapie] principal investigators.
“If you think of all the treatments that RA patients get, then the risk is further increased with bDMARD and [JAK inhibitor] treatments,” she added in an interview. While the risk was highest with JAK inhibitors, “we also saw that monoclonal TNF antibodies as well as all the other biologic DMARD treatments have a higher risk of herpes zoster in RA patients, compared to csDMARD therapy,” Dr. Strangfeld said.
Adjusted IPW HR for the other RA treatments showed an increased herpes zoster risk for all but the soluble TNF receptor agents, at 1.6 for IL-6 inhibitors (P = .0045) and monoclonal TNFi antibodies (P = .0003), and 1.7 for B-cell targeted therapies (P = .00026) and T-cell costimulation modulators (P = .0048).
Dr. Strangfeld presented these data during the annual European Congress of Rheumatology, held online this year due to COVID-19. The analysis included 12,470 patients with RA enrolled in RABBIT from 2007 onward and who had been treated with monoclonal TNF inhibitor antibodies, cell-targeted therapies, and tsDMARDs such as JAK inhibitors. In all, at the data cutoff at the end of April 2019, 452 cases of herpes zoster were recorded in 433 patients, of which 52 cases were serious.
“The reactivation of the varicella zoster virus causing the herpes zoster is triggered by a decline of cellular immunity. This can be due to aging or immune suppression of any kind,” Dr. Strangfeld said in her presentation.
“The Cox regression [analysis] revealed that higher age and intake of glucocorticoids were associated with an increased risk of herpes zoster,” she reported, with a dose dependent increase with glucocorticoids. IPW HR for age per 10 years was 1.3 (P < .0001) and 1.9 (P = .0022) for higher doses of glucocorticoids (>10 vs. 0 mg/day).
Commenting on the study, rheumatologist and epidemiologist Loreto Carmona, MD, PhD, said: “This is a very interesting study. The results are confident and precise. The frequency of herpes zoster infection [based on crude incidence rate estimates] is very high. However, we must focus on the [multivariable with IPW] analysis after taking into account baseline risk.”
Dr. Carmona, who is the chair of the congress’s Abstract Selection Committee and is the scientific director of the Instituto de Salud Musculoesquelética in Madrid, added: “Having a disease with high levels of activity or a disease refractory to treatments [both of which were very likely used in creating the IPW] levels off the risk a bit. Also, because RA by itself, glucocorticoids, and age all increase the risk. Still, jakinibs [JAK inhibitors] stand out as the treatment related to higher risk of herpes zoster infection.”
Dr. Strangfeld and fellow RABBIT investigators have previously looked at the risk of herpes zoster in patients treated with anti–TNF-alpha agents (JAMA. 2009;301[7]:737-44). They found that monoclonal anti–TNF-alpha agents may be associated with increased risk of herpes zoster, which is now confirmed by the current analysis. The reason for looking at herpes zoster risk again is that since that first analysis, many more therapies have become available for RA during the past 10 years, notably the tsDMARDs.
Herpes zoster may not always be a serious event, Dr. Strangfeld said in the interview, “but it diminishes your quality of life; it can also be associated with pain and may be followed by postherpetic neuralgia, which is very painful.” With new herpes zoster vaccinations available, it is now possible to vaccinate patients more easily. “This is advisable for all kinds of treatments,” she said.
“What we found was quite in agreement with the data that we know from the U.S., from the observational studies, for example from the Corrona database,” Dr. Strangfeld stated. The key finding is that the risk of herpes zoster is increased to some level, almost regardless of which drug is chosen, she said. “This gives a clear message that systematic herpes zoster vaccination should be done in patients with RA,” she suggested.
The German biologics registry RABBIT is supported by a joint unconditional grant from AbbVie, Amgen, Bristol-Myers Squibb, Celltrion, Hexal, Lilly, Merck Sharp & Dohme, Mylan, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Strangfeld has received speaker fees from AbbVie, Bristol-Myers Squibb, Merck Sharp & Dohme, Pfizer, Roche, Sanofi-Aventis, and UCB. Dr. Carmona had no relevant conflicts of interest to disclose.
SOURCE: Strangfeld A et al. Ann Rheum Dis. 2020;79[suppl 1]:150. Abstract OP0238.
Patients with rheumatoid arthritis (RA) who are treated with Janus kinase (JAK) inhibitors had the highest risk of developing herpes zoster among newer disease-modifying antirheumatic drugs (DMARDs), according to data released from the German biologics registry.
These are believed to be the first European data on the risk of herpes zoster with JAK inhibitors and showed that the crude incidence rate of herpes zoster per 1,000 patient-years was 24.9 with JAK inhibitors, compared with just 5.8 for controls taking conventional synthetic (cs) DMARDs.
The risk of herpes zoster was also increased with other biologic (b) and targeted synthetic (ts) DMARDs that were assessed, with crude rates per 1,000 patient-years of 10.4 for monoclonal tumor necrosis factor inhibitors (TNFi), 10.5 for B-cell targeted therapies, 9.4 for T-cell costimulation modulators, 9.0 for soluble TNF receptors, and 8.5 for interleukin (IL)-6 inhibitors.
Overall, JAK inhibitor treatment was associated with a fivefold higher risk of herpes zoster (hazard ratio, 5.0; P < .0001), compared with the control csDMARD population after adjustment using an inverse probability weights (IPW) method.
“The general risk of herpes zoster is [twofold] higher in patients with rheumatoid arthritis when you compare it with the general population,” said Anja Strangfeld, MD of the German Research Center, Berlin, and one of the three RABBIT [Rheumatoide Arthritis: Biobachtung der Biologika-Therapie] principal investigators.
“If you think of all the treatments that RA patients get, then the risk is further increased with bDMARD and [JAK inhibitor] treatments,” she added in an interview. While the risk was highest with JAK inhibitors, “we also saw that monoclonal TNF antibodies as well as all the other biologic DMARD treatments have a higher risk of herpes zoster in RA patients, compared to csDMARD therapy,” Dr. Strangfeld said.
Adjusted IPW HR for the other RA treatments showed an increased herpes zoster risk for all but the soluble TNF receptor agents, at 1.6 for IL-6 inhibitors (P = .0045) and monoclonal TNFi antibodies (P = .0003), and 1.7 for B-cell targeted therapies (P = .00026) and T-cell costimulation modulators (P = .0048).
Dr. Strangfeld presented these data during the annual European Congress of Rheumatology, held online this year due to COVID-19. The analysis included 12,470 patients with RA enrolled in RABBIT from 2007 onward and who had been treated with monoclonal TNF inhibitor antibodies, cell-targeted therapies, and tsDMARDs such as JAK inhibitors. In all, at the data cutoff at the end of April 2019, 452 cases of herpes zoster were recorded in 433 patients, of which 52 cases were serious.
“The reactivation of the varicella zoster virus causing the herpes zoster is triggered by a decline of cellular immunity. This can be due to aging or immune suppression of any kind,” Dr. Strangfeld said in her presentation.
“The Cox regression [analysis] revealed that higher age and intake of glucocorticoids were associated with an increased risk of herpes zoster,” she reported, with a dose dependent increase with glucocorticoids. IPW HR for age per 10 years was 1.3 (P < .0001) and 1.9 (P = .0022) for higher doses of glucocorticoids (>10 vs. 0 mg/day).
Commenting on the study, rheumatologist and epidemiologist Loreto Carmona, MD, PhD, said: “This is a very interesting study. The results are confident and precise. The frequency of herpes zoster infection [based on crude incidence rate estimates] is very high. However, we must focus on the [multivariable with IPW] analysis after taking into account baseline risk.”
Dr. Carmona, who is the chair of the congress’s Abstract Selection Committee and is the scientific director of the Instituto de Salud Musculoesquelética in Madrid, added: “Having a disease with high levels of activity or a disease refractory to treatments [both of which were very likely used in creating the IPW] levels off the risk a bit. Also, because RA by itself, glucocorticoids, and age all increase the risk. Still, jakinibs [JAK inhibitors] stand out as the treatment related to higher risk of herpes zoster infection.”
Dr. Strangfeld and fellow RABBIT investigators have previously looked at the risk of herpes zoster in patients treated with anti–TNF-alpha agents (JAMA. 2009;301[7]:737-44). They found that monoclonal anti–TNF-alpha agents may be associated with increased risk of herpes zoster, which is now confirmed by the current analysis. The reason for looking at herpes zoster risk again is that since that first analysis, many more therapies have become available for RA during the past 10 years, notably the tsDMARDs.
Herpes zoster may not always be a serious event, Dr. Strangfeld said in the interview, “but it diminishes your quality of life; it can also be associated with pain and may be followed by postherpetic neuralgia, which is very painful.” With new herpes zoster vaccinations available, it is now possible to vaccinate patients more easily. “This is advisable for all kinds of treatments,” she said.
“What we found was quite in agreement with the data that we know from the U.S., from the observational studies, for example from the Corrona database,” Dr. Strangfeld stated. The key finding is that the risk of herpes zoster is increased to some level, almost regardless of which drug is chosen, she said. “This gives a clear message that systematic herpes zoster vaccination should be done in patients with RA,” she suggested.
The German biologics registry RABBIT is supported by a joint unconditional grant from AbbVie, Amgen, Bristol-Myers Squibb, Celltrion, Hexal, Lilly, Merck Sharp & Dohme, Mylan, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Strangfeld has received speaker fees from AbbVie, Bristol-Myers Squibb, Merck Sharp & Dohme, Pfizer, Roche, Sanofi-Aventis, and UCB. Dr. Carmona had no relevant conflicts of interest to disclose.
SOURCE: Strangfeld A et al. Ann Rheum Dis. 2020;79[suppl 1]:150. Abstract OP0238.
Patients with rheumatoid arthritis (RA) who are treated with Janus kinase (JAK) inhibitors had the highest risk of developing herpes zoster among newer disease-modifying antirheumatic drugs (DMARDs), according to data released from the German biologics registry.
These are believed to be the first European data on the risk of herpes zoster with JAK inhibitors and showed that the crude incidence rate of herpes zoster per 1,000 patient-years was 24.9 with JAK inhibitors, compared with just 5.8 for controls taking conventional synthetic (cs) DMARDs.
The risk of herpes zoster was also increased with other biologic (b) and targeted synthetic (ts) DMARDs that were assessed, with crude rates per 1,000 patient-years of 10.4 for monoclonal tumor necrosis factor inhibitors (TNFi), 10.5 for B-cell targeted therapies, 9.4 for T-cell costimulation modulators, 9.0 for soluble TNF receptors, and 8.5 for interleukin (IL)-6 inhibitors.
Overall, JAK inhibitor treatment was associated with a fivefold higher risk of herpes zoster (hazard ratio, 5.0; P < .0001), compared with the control csDMARD population after adjustment using an inverse probability weights (IPW) method.
“The general risk of herpes zoster is [twofold] higher in patients with rheumatoid arthritis when you compare it with the general population,” said Anja Strangfeld, MD of the German Research Center, Berlin, and one of the three RABBIT [Rheumatoide Arthritis: Biobachtung der Biologika-Therapie] principal investigators.
“If you think of all the treatments that RA patients get, then the risk is further increased with bDMARD and [JAK inhibitor] treatments,” she added in an interview. While the risk was highest with JAK inhibitors, “we also saw that monoclonal TNF antibodies as well as all the other biologic DMARD treatments have a higher risk of herpes zoster in RA patients, compared to csDMARD therapy,” Dr. Strangfeld said.
Adjusted IPW HR for the other RA treatments showed an increased herpes zoster risk for all but the soluble TNF receptor agents, at 1.6 for IL-6 inhibitors (P = .0045) and monoclonal TNFi antibodies (P = .0003), and 1.7 for B-cell targeted therapies (P = .00026) and T-cell costimulation modulators (P = .0048).
Dr. Strangfeld presented these data during the annual European Congress of Rheumatology, held online this year due to COVID-19. The analysis included 12,470 patients with RA enrolled in RABBIT from 2007 onward and who had been treated with monoclonal TNF inhibitor antibodies, cell-targeted therapies, and tsDMARDs such as JAK inhibitors. In all, at the data cutoff at the end of April 2019, 452 cases of herpes zoster were recorded in 433 patients, of which 52 cases were serious.
“The reactivation of the varicella zoster virus causing the herpes zoster is triggered by a decline of cellular immunity. This can be due to aging or immune suppression of any kind,” Dr. Strangfeld said in her presentation.
“The Cox regression [analysis] revealed that higher age and intake of glucocorticoids were associated with an increased risk of herpes zoster,” she reported, with a dose dependent increase with glucocorticoids. IPW HR for age per 10 years was 1.3 (P < .0001) and 1.9 (P = .0022) for higher doses of glucocorticoids (>10 vs. 0 mg/day).
Commenting on the study, rheumatologist and epidemiologist Loreto Carmona, MD, PhD, said: “This is a very interesting study. The results are confident and precise. The frequency of herpes zoster infection [based on crude incidence rate estimates] is very high. However, we must focus on the [multivariable with IPW] analysis after taking into account baseline risk.”
Dr. Carmona, who is the chair of the congress’s Abstract Selection Committee and is the scientific director of the Instituto de Salud Musculoesquelética in Madrid, added: “Having a disease with high levels of activity or a disease refractory to treatments [both of which were very likely used in creating the IPW] levels off the risk a bit. Also, because RA by itself, glucocorticoids, and age all increase the risk. Still, jakinibs [JAK inhibitors] stand out as the treatment related to higher risk of herpes zoster infection.”
Dr. Strangfeld and fellow RABBIT investigators have previously looked at the risk of herpes zoster in patients treated with anti–TNF-alpha agents (JAMA. 2009;301[7]:737-44). They found that monoclonal anti–TNF-alpha agents may be associated with increased risk of herpes zoster, which is now confirmed by the current analysis. The reason for looking at herpes zoster risk again is that since that first analysis, many more therapies have become available for RA during the past 10 years, notably the tsDMARDs.
Herpes zoster may not always be a serious event, Dr. Strangfeld said in the interview, “but it diminishes your quality of life; it can also be associated with pain and may be followed by postherpetic neuralgia, which is very painful.” With new herpes zoster vaccinations available, it is now possible to vaccinate patients more easily. “This is advisable for all kinds of treatments,” she said.
“What we found was quite in agreement with the data that we know from the U.S., from the observational studies, for example from the Corrona database,” Dr. Strangfeld stated. The key finding is that the risk of herpes zoster is increased to some level, almost regardless of which drug is chosen, she said. “This gives a clear message that systematic herpes zoster vaccination should be done in patients with RA,” she suggested.
The German biologics registry RABBIT is supported by a joint unconditional grant from AbbVie, Amgen, Bristol-Myers Squibb, Celltrion, Hexal, Lilly, Merck Sharp & Dohme, Mylan, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Strangfeld has received speaker fees from AbbVie, Bristol-Myers Squibb, Merck Sharp & Dohme, Pfizer, Roche, Sanofi-Aventis, and UCB. Dr. Carmona had no relevant conflicts of interest to disclose.
SOURCE: Strangfeld A et al. Ann Rheum Dis. 2020;79[suppl 1]:150. Abstract OP0238.
FROM EULAR 2020 E-CONGRESS
Today’s Top News Highlights: Doctors protest racism, controversial studies retracted
Here are the stories our MDedge editors across specialties think you need to know about today:
#WhiteCoats4BlackLives stands up to racism
Participants in the growing #WhiteCoats4BlackLives protest against racism say it is a chance to use their status as trusted messengers, show themselves as allies of people of color, and demonstrate that they are familiar with how racism has contributed to health disparities.
The medical student-run group WhiteCoats4BlackLives has helped organize ongoing, large-scale events at hospitals, medical campuses, and city centers nationwide.“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in late last month in a city park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Read more.
A conversation on race
In this special episode of the Psychcast podast, host Lorenzo Norris, MD, and fourth-year psychiatry resident Brandon C. Newsome, MD, discuss race relations as physicians in the wake of the death of George Floyd. The pair discuss what their patients are experiencing and what they’re experiencing as black physicians.
“Racism – whether or not you witness it, whether or not you utilize it, whether or not you are the subject of it – affects and hurts us all,” Dr. Norris says. “We all have to start to own that. You can’t just stay siloed, because it is going to affect you.” Listen here.
Two journals retract studies on HCQ
The Lancet has retracted a highly cited study that suggested hydroxychloroquine (HCQ) may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
Three authors of the Lancet article wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO. The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote, leading them to request a retraction of the paper.
In a similar note, the authors requested that the New England Journal of Medicine retract the earlier article as well.
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
Read more.
FDA approves antibiotic to treat pneumonia
The Food and Drug Administration has approved Recarbrio (imipenem-cilastatin and relebactam) for the treatment of hospital-acquired and ventilator-associated bacterial pneumonia in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, of the agency’s Center for Drug Evaluation and Research.
Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
#WhiteCoats4BlackLives stands up to racism
Participants in the growing #WhiteCoats4BlackLives protest against racism say it is a chance to use their status as trusted messengers, show themselves as allies of people of color, and demonstrate that they are familiar with how racism has contributed to health disparities.
The medical student-run group WhiteCoats4BlackLives has helped organize ongoing, large-scale events at hospitals, medical campuses, and city centers nationwide.“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in late last month in a city park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Read more.
A conversation on race
In this special episode of the Psychcast podast, host Lorenzo Norris, MD, and fourth-year psychiatry resident Brandon C. Newsome, MD, discuss race relations as physicians in the wake of the death of George Floyd. The pair discuss what their patients are experiencing and what they’re experiencing as black physicians.
“Racism – whether or not you witness it, whether or not you utilize it, whether or not you are the subject of it – affects and hurts us all,” Dr. Norris says. “We all have to start to own that. You can’t just stay siloed, because it is going to affect you.” Listen here.
Two journals retract studies on HCQ
The Lancet has retracted a highly cited study that suggested hydroxychloroquine (HCQ) may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
Three authors of the Lancet article wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO. The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote, leading them to request a retraction of the paper.
In a similar note, the authors requested that the New England Journal of Medicine retract the earlier article as well.
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
Read more.
FDA approves antibiotic to treat pneumonia
The Food and Drug Administration has approved Recarbrio (imipenem-cilastatin and relebactam) for the treatment of hospital-acquired and ventilator-associated bacterial pneumonia in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, of the agency’s Center for Drug Evaluation and Research.
Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
#WhiteCoats4BlackLives stands up to racism
Participants in the growing #WhiteCoats4BlackLives protest against racism say it is a chance to use their status as trusted messengers, show themselves as allies of people of color, and demonstrate that they are familiar with how racism has contributed to health disparities.
The medical student-run group WhiteCoats4BlackLives has helped organize ongoing, large-scale events at hospitals, medical campuses, and city centers nationwide.“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in late last month in a city park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Read more.
A conversation on race
In this special episode of the Psychcast podast, host Lorenzo Norris, MD, and fourth-year psychiatry resident Brandon C. Newsome, MD, discuss race relations as physicians in the wake of the death of George Floyd. The pair discuss what their patients are experiencing and what they’re experiencing as black physicians.
“Racism – whether or not you witness it, whether or not you utilize it, whether or not you are the subject of it – affects and hurts us all,” Dr. Norris says. “We all have to start to own that. You can’t just stay siloed, because it is going to affect you.” Listen here.
Two journals retract studies on HCQ
The Lancet has retracted a highly cited study that suggested hydroxychloroquine (HCQ) may cause more harm than benefit in patients with COVID-19. Hours later, the New England Journal of Medicine announced that it had retracted a second article by some of the same authors, also on heart disease and COVID-19.
Three authors of the Lancet article wrote in a letter that the action came after concerns were raised about the integrity of the data, and about how the analysis was conducted by Chicago-based Surgisphere Corp and study coauthor Sapan Desai, MD, Surgisphere’s founder and CEO. The authors asked for an independent third-party review of Surgisphere to evaluate the integrity of the trial elements and to replicate the analyses in the article.
“Our independent peer reviewers informed us that Surgisphere would not transfer the full dataset, client contracts, and the full ISO audit report to their servers for analysis, as such transfer would violate client agreements and confidentiality requirements,” the authors wrote, leading them to request a retraction of the paper.
In a similar note, the authors requested that the New England Journal of Medicine retract the earlier article as well.
Both journals had already published “Expression of Concern” notices about the articles. The expression of concern followed an open letter, endorsed by more than 200 scientists, ethicists, and clinicians and posted on May 28, questioning the data and ethics of the study.
Read more.
FDA approves antibiotic to treat pneumonia
The Food and Drug Administration has approved Recarbrio (imipenem-cilastatin and relebactam) for the treatment of hospital-acquired and ventilator-associated bacterial pneumonia in people aged 18 years and older.
Approval for Recarbrio was based on results of a randomized, controlled clinical trial of 535 hospitalized adults with hospital-acquired and ventilator-associated bacterial pneumonia who received either Recarbrio or piperacillin-tazobactam. After 28 days, 16% of patients who received Recarbrio and 21% of patients who received piperacillin-tazobactam had died.
“As a public health agency, the FDA addresses the threat of antimicrobial-resistant infections by facilitating the development of safe and effective new treatments. These efforts provide more options to fight serious bacterial infections and get new, safe and effective therapies to patients as soon as possible,” said Sumathi Nambiar, MD, MPH, of the agency’s Center for Drug Evaluation and Research.
Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Adding avadomide shows promise for newly diagnosed DLBCL
For patients with newly diagnosed, high-risk diffuse large B-cell lymphoma (DLBCL), adding avadomide to standard therapy may reduce the likelihood of treatment failure, based on phase 1 results.
The regimen was well tolerated and had a complete response rate of 79%, reported lead author Neha Mehta-Shah, MD, of Washington University, St. Louis, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
Newly diagnosed DLBCL “remains a clinical challenge,” Dr. Mehta-Shah said, noting a treatment failure rate of 30%-50% for standard rituximab with cyclophosphamide, doxorubicin, vincristine, and prednisone every 21 days (R-CHOP-21), and worse outcomes among patients with high-risk disease.
In an effort to boost efficacy, the investigators turned to avadomide, a cereblon E3 ligase modulator, which previously demonstrated a complete response rate of 11% when used as monotherapy for patients with relapsed or refractory DLBCL.
The present phase 1 data included 35 adults with newly diagnosed DLBCL who had measurable lesions of at least 2.0 cm and International Prognostic Indices (IPI) between 3-5. Specifically, 51% of patients had an IPI of 3, while 49% had an IPI of 4-5.
All patients received standard R-CHOP with pegfilgrastim (to stimulate white blood cell growth), plus escalating doses of oral avadomide from 1-3 mg. Treatment was delivered, when tolerated, for up to six 21-day cycles. Depending on dose level, avadomide was given during either 2 or 3 out of 3 weeks. During treatment weeks, avadomide was given on 5 of 7 days.
The primary objectives were safety, tolerability, and complete response rate. Secondary objectives included biomarkers and additional efficacy measures, while exploratory analyses were also conducted to assess pharmacokinetics and pharmacodynamics.
Out of 34 patients evaluable for efficacy, the complete response rate was 79% and the objective response rate was 88%. After a median follow-up of 10 months, the 1-year progression-free survival rate was 80%.
“The combination showed promising efficacy,” Dr. Mehta-Shah said.
The regimen was also well tolerated and demonstrated an “acceptable safety profile consistent with either therapy alone,” Dr. Mehta-Shah added.
Most patients (91%) completed all six cycles of therapy. Median relative total dose intensities were 99% and 95% for avadomide and R-CHOP-21, respectively. Approximately two out of three patients (66%) required dose interruptions of avadomide, and 9% required dose reductions because of adverse events.
Dose-limiting toxicities occurred in six patients, including sepsis, febrile neutropenia caused by skin infections, febrile neutropenia with hypotension, febrile neutropenia, pneumonia, and neutropenia with bacterial hepatic infection. Based on these findings, the recommended phase 2 dose of avadomide was determined to be 3 mg given during 2 out of 3 weeks.
About 74% of patients had grade 3-4 treatment-emergent adverse events, the most common of which were neutropenia (54%), anemia (20%), leukopenia (20%), lymphopenia (14%), hypophosphatemia (14%), and febrile neutropenia (11%).
During the second cycle of therapy, one patient died because of concurrent pneumonia. After completion of therapy, two patients developed cardiac failure, and data gathered after each cycle showed that five patients had developed elevated levels of troponin or brain natriuretic peptide.
Flow cytometry showed that avadomide had proimmunomodulatory effects, including expansion of memory T-cell populations and enhanced proliferation of T cells and NK cells. The magnitude of this latter increase was greater than that observed in previous studies involving R-CHOP and durvalumab, Dr. Mehta-Shah noted.
“We look forward to following up on this data regarding the progression-free survival over a longer period of time,” Dr. Mehta-Shah said. “The results of this trial indicate that further evaluation of cereblon-modulating compounds combined with immunochemotherapy for patients with previously untreated diffuse large B-cell lymphoma is worthy of further exploration.”
Invited discussant Edward Yeh, MD, of the University of Missouri–Columbia, called cereblon modulators such as avadomide and thalidomide a “very exciting class of anticancer therapy.”
In a virtual presentation, Dr. Yeh noted that cereblon modulators have several advantages, including “good absorption, distribution, metabolism, [and] elimination,” plus relatively low susceptibility to mutation-directed drug resistance.
Despite some drawbacks, including difficulty to design and synthesize, Dr. Yeh suggested that this drug class may play a bigger role over time.
“We’re expecting more cancer therapy to come to fruition through the utilization of this posttranslational, protein-modification pathway,” he concluded.
The study was funded by Celgene. The investigators disclosed additional relationships with Kyowa Hakko Kirin, AstraZeneca, Roche, and others.
SOURCE: Mehta-Shah N et al. ASCO 2020, Abstract 3501.
For patients with newly diagnosed, high-risk diffuse large B-cell lymphoma (DLBCL), adding avadomide to standard therapy may reduce the likelihood of treatment failure, based on phase 1 results.
The regimen was well tolerated and had a complete response rate of 79%, reported lead author Neha Mehta-Shah, MD, of Washington University, St. Louis, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
Newly diagnosed DLBCL “remains a clinical challenge,” Dr. Mehta-Shah said, noting a treatment failure rate of 30%-50% for standard rituximab with cyclophosphamide, doxorubicin, vincristine, and prednisone every 21 days (R-CHOP-21), and worse outcomes among patients with high-risk disease.
In an effort to boost efficacy, the investigators turned to avadomide, a cereblon E3 ligase modulator, which previously demonstrated a complete response rate of 11% when used as monotherapy for patients with relapsed or refractory DLBCL.
The present phase 1 data included 35 adults with newly diagnosed DLBCL who had measurable lesions of at least 2.0 cm and International Prognostic Indices (IPI) between 3-5. Specifically, 51% of patients had an IPI of 3, while 49% had an IPI of 4-5.
All patients received standard R-CHOP with pegfilgrastim (to stimulate white blood cell growth), plus escalating doses of oral avadomide from 1-3 mg. Treatment was delivered, when tolerated, for up to six 21-day cycles. Depending on dose level, avadomide was given during either 2 or 3 out of 3 weeks. During treatment weeks, avadomide was given on 5 of 7 days.
The primary objectives were safety, tolerability, and complete response rate. Secondary objectives included biomarkers and additional efficacy measures, while exploratory analyses were also conducted to assess pharmacokinetics and pharmacodynamics.
Out of 34 patients evaluable for efficacy, the complete response rate was 79% and the objective response rate was 88%. After a median follow-up of 10 months, the 1-year progression-free survival rate was 80%.
“The combination showed promising efficacy,” Dr. Mehta-Shah said.
The regimen was also well tolerated and demonstrated an “acceptable safety profile consistent with either therapy alone,” Dr. Mehta-Shah added.
Most patients (91%) completed all six cycles of therapy. Median relative total dose intensities were 99% and 95% for avadomide and R-CHOP-21, respectively. Approximately two out of three patients (66%) required dose interruptions of avadomide, and 9% required dose reductions because of adverse events.
Dose-limiting toxicities occurred in six patients, including sepsis, febrile neutropenia caused by skin infections, febrile neutropenia with hypotension, febrile neutropenia, pneumonia, and neutropenia with bacterial hepatic infection. Based on these findings, the recommended phase 2 dose of avadomide was determined to be 3 mg given during 2 out of 3 weeks.
About 74% of patients had grade 3-4 treatment-emergent adverse events, the most common of which were neutropenia (54%), anemia (20%), leukopenia (20%), lymphopenia (14%), hypophosphatemia (14%), and febrile neutropenia (11%).
During the second cycle of therapy, one patient died because of concurrent pneumonia. After completion of therapy, two patients developed cardiac failure, and data gathered after each cycle showed that five patients had developed elevated levels of troponin or brain natriuretic peptide.
Flow cytometry showed that avadomide had proimmunomodulatory effects, including expansion of memory T-cell populations and enhanced proliferation of T cells and NK cells. The magnitude of this latter increase was greater than that observed in previous studies involving R-CHOP and durvalumab, Dr. Mehta-Shah noted.
“We look forward to following up on this data regarding the progression-free survival over a longer period of time,” Dr. Mehta-Shah said. “The results of this trial indicate that further evaluation of cereblon-modulating compounds combined with immunochemotherapy for patients with previously untreated diffuse large B-cell lymphoma is worthy of further exploration.”
Invited discussant Edward Yeh, MD, of the University of Missouri–Columbia, called cereblon modulators such as avadomide and thalidomide a “very exciting class of anticancer therapy.”
In a virtual presentation, Dr. Yeh noted that cereblon modulators have several advantages, including “good absorption, distribution, metabolism, [and] elimination,” plus relatively low susceptibility to mutation-directed drug resistance.
Despite some drawbacks, including difficulty to design and synthesize, Dr. Yeh suggested that this drug class may play a bigger role over time.
“We’re expecting more cancer therapy to come to fruition through the utilization of this posttranslational, protein-modification pathway,” he concluded.
The study was funded by Celgene. The investigators disclosed additional relationships with Kyowa Hakko Kirin, AstraZeneca, Roche, and others.
SOURCE: Mehta-Shah N et al. ASCO 2020, Abstract 3501.
For patients with newly diagnosed, high-risk diffuse large B-cell lymphoma (DLBCL), adding avadomide to standard therapy may reduce the likelihood of treatment failure, based on phase 1 results.
The regimen was well tolerated and had a complete response rate of 79%, reported lead author Neha Mehta-Shah, MD, of Washington University, St. Louis, who presented findings as part of the American Society of Clinical Oncology virtual scientific program.
Newly diagnosed DLBCL “remains a clinical challenge,” Dr. Mehta-Shah said, noting a treatment failure rate of 30%-50% for standard rituximab with cyclophosphamide, doxorubicin, vincristine, and prednisone every 21 days (R-CHOP-21), and worse outcomes among patients with high-risk disease.
In an effort to boost efficacy, the investigators turned to avadomide, a cereblon E3 ligase modulator, which previously demonstrated a complete response rate of 11% when used as monotherapy for patients with relapsed or refractory DLBCL.
The present phase 1 data included 35 adults with newly diagnosed DLBCL who had measurable lesions of at least 2.0 cm and International Prognostic Indices (IPI) between 3-5. Specifically, 51% of patients had an IPI of 3, while 49% had an IPI of 4-5.
All patients received standard R-CHOP with pegfilgrastim (to stimulate white blood cell growth), plus escalating doses of oral avadomide from 1-3 mg. Treatment was delivered, when tolerated, for up to six 21-day cycles. Depending on dose level, avadomide was given during either 2 or 3 out of 3 weeks. During treatment weeks, avadomide was given on 5 of 7 days.
The primary objectives were safety, tolerability, and complete response rate. Secondary objectives included biomarkers and additional efficacy measures, while exploratory analyses were also conducted to assess pharmacokinetics and pharmacodynamics.
Out of 34 patients evaluable for efficacy, the complete response rate was 79% and the objective response rate was 88%. After a median follow-up of 10 months, the 1-year progression-free survival rate was 80%.
“The combination showed promising efficacy,” Dr. Mehta-Shah said.
The regimen was also well tolerated and demonstrated an “acceptable safety profile consistent with either therapy alone,” Dr. Mehta-Shah added.
Most patients (91%) completed all six cycles of therapy. Median relative total dose intensities were 99% and 95% for avadomide and R-CHOP-21, respectively. Approximately two out of three patients (66%) required dose interruptions of avadomide, and 9% required dose reductions because of adverse events.
Dose-limiting toxicities occurred in six patients, including sepsis, febrile neutropenia caused by skin infections, febrile neutropenia with hypotension, febrile neutropenia, pneumonia, and neutropenia with bacterial hepatic infection. Based on these findings, the recommended phase 2 dose of avadomide was determined to be 3 mg given during 2 out of 3 weeks.
About 74% of patients had grade 3-4 treatment-emergent adverse events, the most common of which were neutropenia (54%), anemia (20%), leukopenia (20%), lymphopenia (14%), hypophosphatemia (14%), and febrile neutropenia (11%).
During the second cycle of therapy, one patient died because of concurrent pneumonia. After completion of therapy, two patients developed cardiac failure, and data gathered after each cycle showed that five patients had developed elevated levels of troponin or brain natriuretic peptide.
Flow cytometry showed that avadomide had proimmunomodulatory effects, including expansion of memory T-cell populations and enhanced proliferation of T cells and NK cells. The magnitude of this latter increase was greater than that observed in previous studies involving R-CHOP and durvalumab, Dr. Mehta-Shah noted.
“We look forward to following up on this data regarding the progression-free survival over a longer period of time,” Dr. Mehta-Shah said. “The results of this trial indicate that further evaluation of cereblon-modulating compounds combined with immunochemotherapy for patients with previously untreated diffuse large B-cell lymphoma is worthy of further exploration.”
Invited discussant Edward Yeh, MD, of the University of Missouri–Columbia, called cereblon modulators such as avadomide and thalidomide a “very exciting class of anticancer therapy.”
In a virtual presentation, Dr. Yeh noted that cereblon modulators have several advantages, including “good absorption, distribution, metabolism, [and] elimination,” plus relatively low susceptibility to mutation-directed drug resistance.
Despite some drawbacks, including difficulty to design and synthesize, Dr. Yeh suggested that this drug class may play a bigger role over time.
“We’re expecting more cancer therapy to come to fruition through the utilization of this posttranslational, protein-modification pathway,” he concluded.
The study was funded by Celgene. The investigators disclosed additional relationships with Kyowa Hakko Kirin, AstraZeneca, Roche, and others.
SOURCE: Mehta-Shah N et al. ASCO 2020, Abstract 3501.
FROM ASCO 2020
‘A good and peaceful death’: Cancer hospice during the pandemic
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.
Lillie Shockney, RN, MAS, a two-time breast cancer survivor and adjunct professor at Johns Hopkins School of Nursing in Baltimore, Maryland, mourns the many losses that her patients with advanced cancer now face in the midst of the COVID-19 pandemic. But in the void of the usual support networks and treatment plans, she sees the resurgence of something that has recently been crowded out: hospice.
The pandemic has forced patients and their physicians to reassess the risk/benefit balance of continuing or embarking on yet another cancer treatment.
“It’s one of the pearls that we will get out of this nightmare,” said Ms. Shockney, who recently retired as administrative director of the cancer survivorship programs at the Sidney Kimmel Comprehensive Cancer Center.
“Physicians have been taught to treat the disease – so as long as there’s a treatment they give another treatment,” she told Medscape Medical News during a Zoom call from her home. “But for some patients with advanced disease, those treatments were making them very sick, so they were trading longevity over quality of life.”
Of course, longevity has never been a guarantee with cancer treatment, and even less so now, with the risk of COVID-19.
“This is going to bring them to some hard discussions,” says Brenda Nevidjon, RN, MSN, chief executive officer at the Oncology Nursing Society.
“We’ve known for a long time that there are patients who are on third- and fourth-round treatment options that have very little evidence of prolonging life or quality of life,” she told Medscape Medical News. “Do we bring these people out of their home to a setting where there could be a fair number of COVID-positive patients? Do we expose them to that?”
Across the world, these dilemmas are pushing cancer specialists to initiate discussions of hospice sooner with patients who have advanced disease, and with more clarity than before.
One of the reasons such conversations have often been avoided is that the concept of hospice is generally misunderstood, said Ms. Shockney.
“Patients think ‘you’re giving up on me, you’ve abandoned me’, but hospice is all about preserving the remainder of their quality of life and letting them have time with family and time to fulfill those elements of experiencing a good and peaceful death,” she said.
Indeed, hospice is “a benefit meant for somebody with at least a 6-month horizon,” agrees Ms. Nevidjon. Yet the average length of hospice in the United States is just 5 days. “It’s at the very, very end, and yet for some of these patients the 6 months they could get in hospice might be a better quality of life than the 4 months on another whole plan of chemotherapy. I can’t imagine that on the backside of this pandemic we will not have learned and we won’t start to change practices around initiating more of these conversations.”
Silver lining of this pandemic?
It’s too early into the pandemic to have hard data on whether hospice uptake has increased, but “it’s encouraging to hear that hospice is being discussed and offered sooner as an alternative to that third- or fourth-round chemo,” said Lori Bishop, MHA, RN, vice president of palliative and advanced care at the National Hospice and Palliative Care Organization.
“I agree that improving informed-decision discussions and timely access to hospice is a silver lining of the pandemic,” she told Medscape Medical News.
But she points out that today’s hospice looks quite different than it did before the pandemic, with the immediate and very obvious difference being telehealth, which was not widely utilized previously.
In March, the Centers for Medicare & Medicaid Services expanded telehealth options for hospice providers, something that Ms. Bishop and other hospice providers hope will remain in place after the pandemic passes.
“Telehealth visits are offered to replace some in-home visits both to minimize risk of exposure to COVID-19 and reduce the drain on personal protective equipment,” Bishop explained.
“In-patient hospice programs are also finding unique ways to provide support and connect patients to their loved ones: visitors are allowed but limited to one or two. Music and pet therapy are being provided through the window or virtually and devices such as iPads are being used to help patients connect with loved ones,” she said.
Telehealth links patients out of loneliness, but the one thing it cannot do is provide the comfort of touch – an important part of any hospice program.
“Hand-holding ... I miss that a lot,” says Ms. Shockney, her eyes filling with tears. “When you take somebody’s hand, you don’t even have to speak; that connection, and eye contact, is all you need to help that person emotionally heal.”
This article first appeared on Medscape.com.
#WhiteCoats4BlackLives: A ‘platform for good’
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
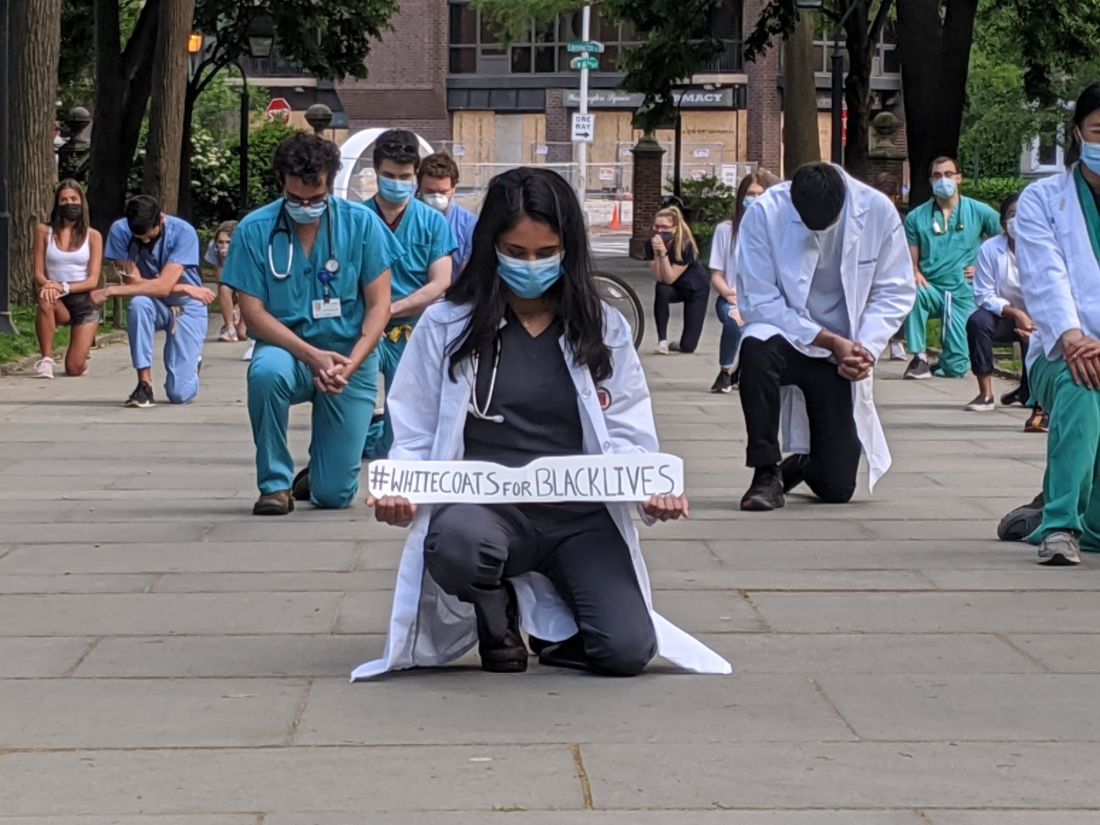
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
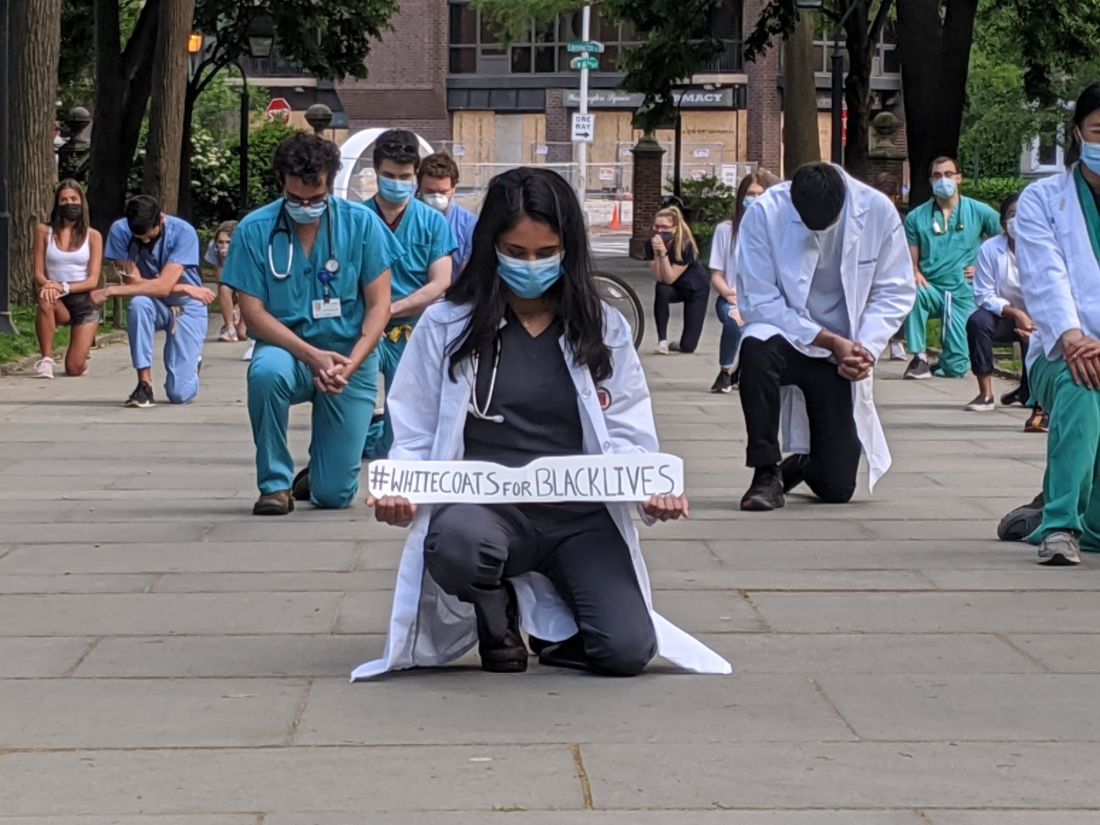
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
like those on vivid display during the COVID-19 pandemic.
Sporadic protests – with participants in scrubs or white coats kneeling for 8 minutes and 46 seconds in memory of George Floyd – have quickly grown into organized, ongoing, large-scale events at hospitals, medical campuses, and city centers in New York, Indianapolis, Atlanta, Austin, Houston, Boston, Miami, Portland, Sacramento, Los Angeles, Philadelphia, and Albuquerque, among others.
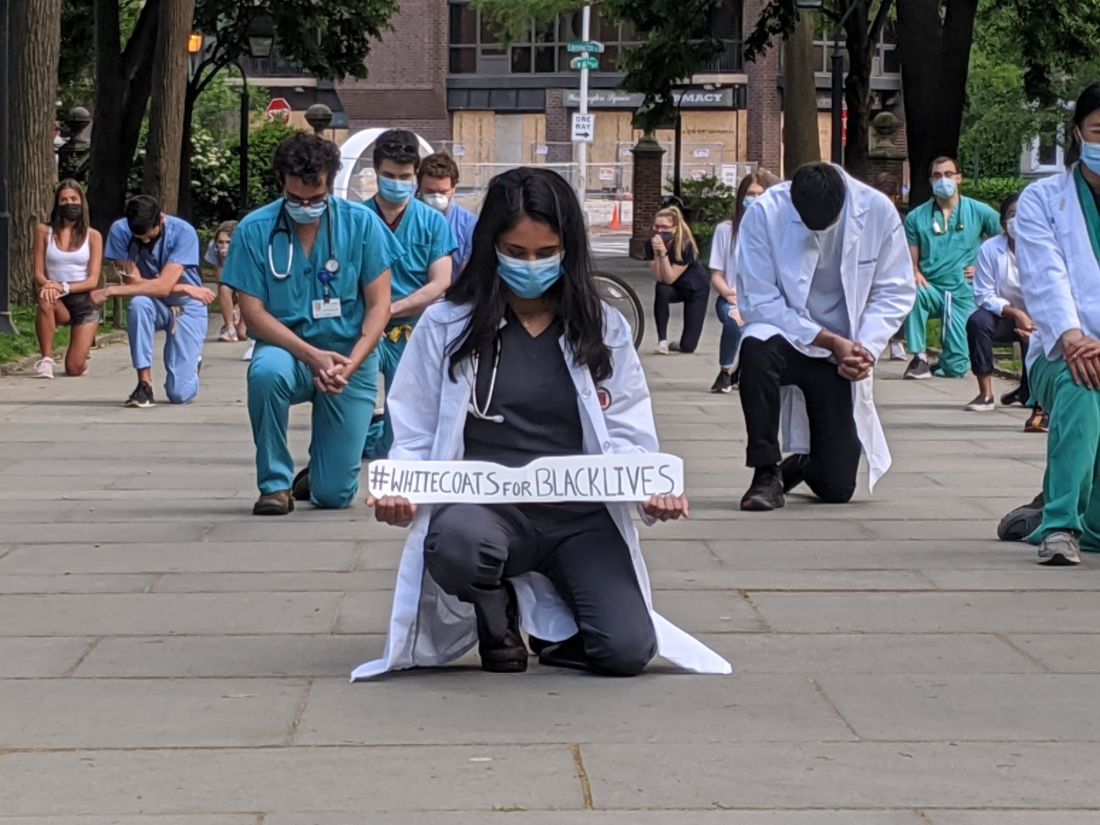
The group WhiteCoats4BlackLives began with a “die-in” protest in 2014, and the medical student–run organization continues to organize, with a large number of protests scheduled to occur simultaneously on June 5 at 1:00 p.m. Eastern Time.
“It’s important to use our platform for good,” said Danielle Verghese, MD, a first-year internal medicine resident at Thomas Jefferson University Hospital in Philadelphia, who helped recruit a small group of students, residents, and pharmacy school students to take part in a kneel-in on May 31 in the city’s Washington Square Park.
“As a doctor, most people in society regard me with a certain amount of respect and may listen if I say something,” Dr. Verghese said.
Crystal Nnenne Azu, MD, a third-year internal medicine resident at Indiana University, who has long worked on increasing diversity in medicine, said she helped organize a march and kneel-in at the school’s Eskenazi Hospital campus on June 3 to educate and show support.
Some 500-1,000 health care providers in scrubs and white coats turned out, tweeted one observer.
“Racism is a public health crisis,” Dr. Azu said. “This COVID epidemic has definitely raised that awareness even more for many of our colleagues.”
Disproportionate death rates in blacks and Latinos are “not just related to individual choices but also systemic racism,” she said.
The march also called out police brutality and the “angst” that many people feel about it, said Dr. Azu. “People want an avenue to express their discomfort, to raise awareness, and also show their solidarity and support for peaceful protests,” she said.
A June 4 protest and “die-in” – held to honor black and indigenous lives at the University of New Mexico Health Sciences campus in Albuquerque – was personal for Jaron Kee, MD, a first-year family medicine resident. He was raised on the Navajo reservation in Crystal, New Mexico, and has watched COVID-19 devastate the tribe, adding insult to years of health disparities, police brutality, and neglect of thousands of missing and murdered indigenous women, he said.
Participating is a means of reassuring the community that “we’re allies and that their suffering and their livelihood is something that we don’t underrecognize,” Dr. Kee said. These values spurred him to enter medicine, he said.
Eileen Barrett, MD, MPH, a hospitalist and assistant professor of internal medicine at the University of New Mexico School of Medicine, who also attended the “die-in,” said she hopes that peers, in particular people of color, see that they have allies at work “who are committed to being anti-racist.”
It’s also “a statement to the community at large that physicians and other healthcare workers strive to be anti-racist and do our best to support our African American and indigenous peers, students, patients, and community members,” she said.
Now is different
Some residents said they felt particularly moved to act now – as the country entered a second week of protests in response to George Floyd’s death and as the COVID-19 pandemic highlighted the devastating toll of health disparities.
“This protest feels different to me,” said Ian Fields, MD, a urogynecology fellow at Oregon Health Sciences University (OHSU) School of Medicine. “The events over the last couple of weeks were just a big catalyst for this to explode,” he said.
“I was very intent, as a white male physician, just coming to acknowledge the privilege that I have, and to do something,” Dr. Fields said, adding that as an obstetrician-gynecologist, he sees the results of health disparities daily. He took part in a kneel-in and demonstration with OHSU colleagues on June 2 at Portland’s Pioneer Courthouse Square.
It’s okay to be sad and mourn, Dr. Fields said, but, he added, “nobody needs our tears necessarily right now. They need us to show up and to speak up about what we see going on.”
“It feels like it’s a national conversation,” said Dr. Verghese. The White Coats movement is “not an issue that’s confined to the black community – this is not an issue that’s a ‘black thing’ – this is a humanitarian thing,” she said.
Dr. Verghese, an Indian American who said that no one would mistake her for being white, said she still wants to acknowledge that she has privilege, as well as biases. All the patients in the COVID-19 unit where she works are African American, but she said she hadn’t initially noticed.
“What’s shocking is that I didn’t think about it,” she said. “I do have to recognize my own biases.”
Protesting During a Pandemic
Despite the demands of treating COVID-19 patients, healthcare professionals have made the White Coat protests a priority, they said. Most – but not all – of the White Coats protests have been on medical campuses, allowing health care professionals to quickly assemble and get back to work. Plus, all of the protests have called on attendees to march and gather safely – with masks and distancing.
“Seeing that we are working in the hospital, it’s important for us to be wearing our masks, to be social distancing,” Dr. Azu said. Organizers asked attendees to ensure that they protested in a way that kept them “from worsening the COVID epidemic,” said Dr. Azu.
Unlike many others, the first protest in Portland was in conjunction with a larger group that assembles every evening in the square, said Dr. Fields. The physician protesters were wearing masks and maintaining distance from each other, especially when they kneeled, he said.
The protests have provided an escape from the futility of not being able to do anything for COVID-19 patients except to provide support, said Dr. Verghese. “In so many ways, we find ourselves powerless,” she said.
Protesting, Dr. Verghese added, was “one tiny moment where I got to regain my sense of agency, that I could actually do something about this.”
This article first appeared on Medscape.com.
QI initiative can decrease unnecessary IV treatment of asymptomatic hypertension
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Limited research suggests IV treatment of asymptomatic hypertension may be widespread and unhelpful. There is potential for unnecessary treatment to have adverse outcomes, such as hypotension.
Study design: Retrospective cohort study.
Setting: A single academic hospital.
Synopsis: Of 2,306 inpatients with asymptomatic hypertension, 11% were treated with IV medications to lower their blood pressure. Patients with indications for stricter blood pressure control (such as stroke, intracranial hemorrhage, aortic dissection) were excluded from the study. Following the baseline period, an education intervention was employed that included presentations, handouts, and posters. A second phase of quality improvement intervention included adjustment of the electronic medical record blood pressure alert parameters from more than 160/90 to more than 180/90. After these interventions, a lower percentage of patients received IV blood pressure medications for asymptomatic hypertension without a significant change in the number of rapid response calls, ICU transfers, or code blues. Limitations include that this is a single-center study and it is unclear if the performance improvement seen will be maintained over time.
Bottom line: IV antihypertensive use for asymptomatic hypertension is common despite lack of data to support its use, and reduced use is possible using quality improvement interventions.
Citation: Jacobs Z et al. Reducing unnecessary treatment of asymptomatic elevated blood pressure with intravenous medications on the general internal medicine wards: a quality improvement initiative. J Hosp Med. 2019 Mar;14(3):144-50.
Dr. Sharma is associate medical director for clinical education in hospital medicine at Duke Regional Hospital and an assistant professor of medicine at Duke University.