User login
Collateral Damage: How COVID-19 Is Adversely Impacting Women Physicians
The coronavirus disease of 2019 (COVID-19) pandemic has affected every facet of our work and personal lives. While many hope we will return to “normal” with the pandemic’s passing, there is reason to believe medicine, and society, will experience irrevocable changes. Although the number of women pursuing and practicing medicine has increased, inequities remain in compensation, academic rank, and leadership positions.1,2 Within the workplace, women are more likely to be in frontline clinical positions, are more likely to be integral in promoting positive interpersonal relationships and collaborative work environments, and often are less represented in the high-level, decision-making roles in leadership or administration.3,4 These well-described issues may be exacerbated during this pandemic crisis. We describe how the current COVID-19 pandemic may intensify workplace inequities for women, and propose solutions for hospitalist groups, leaders, and administrators to ensure female hospitalists continue to prosper and thrive in these tenuous times.
HOW THE PANDEMIC MAY EXACERBATE EXISTING INEQUITIES
Increasing Demands at Home
Female physicians are more likely to have partners who are employed full-time and report spending more time on household activities including cleaning, cooking, and the care of children, compared with their male counterparts.5 With school and daycare closings, as well as stay-at-home orders in many US states, there has been an increase in household responsibilities and care needs for children remaining at home with a marked decrease in options for stable or emergency childcare.6 As compared with primary care and subspecialty colleagues who can provide a large percentage of their care through telemedicine, this is not the case for hospitalists who must be physically present to care for their patients. Therefore, hospitalists are unable to clinically “work from home” in the same way as many of their colleagues in other specialties. Increased childcare and schooling obligations, coupled with disproportionate household responsibilities and an inability to work from home, will likely result in female hospitalists struggling to meet family needs while pandemic-related work responsibilities are ramping up.7 In addition, women who are involved with administrative, leadership, or research activities may struggle to execute their responsibilities as a result of increased domestic duties.
Many hospitalists are also concerned about contracting COVID-19 and exposing their families to the illness given the high infection rate among healthcare workers and the shortage of personal protective equipment (PPE).8,9 Institutions and national organizations, including the Society of Hospital Medicine, have partnered with industry to provide discounted or complimentary hotel rooms for members to aid self-isolation while providing clinical care.10 One famous photo in popular and social media showed a pulmonary and critical care physician in a tent in his garage in order to self-isolate from his family.11 However, since women are often the primary caregivers for their children or other family members and may also be responsible for other important household activities, they may be unable or unwilling to remove themselves from their children and families. As a result, female hospitalists may encounter feelings of guilt or inadequacy if they’re unable to isolate in the same manner as male colleagues.8
Exaggerating Leadership Gap
One of the keys to a robust response to this pandemic is strong, thoughtful, and strategic leadership.12 Institutional, regional, and national leaders are at the forefront of designing the solutions to the many problems the COVID-19 pandemic has created. The paucity of women at high-level leadership positions in institutions across the United States, including university-based, community, public, and private institutions, means that there is a lack of female representation when institutional policy is being discussed and decided.4 This lack of representation may lead to policies and procedures that negatively affect female hospitalists or, at best, fail to consider the needs of or support female physicians. For example, leaders of a hospital medicine group may create mandatory “backup” coverage for night and weekend shifts for their group during surge periods of the pandemic without considering implications for childcare. Finding weekday, daytime coverage is challenging for many during this time when daycares and school are closed, and finding coverage during weekend or overnight hours will be even more challenging. With increased risks for older adults with high-risk medical conditions, grandparents or other friends or family members that previously would have assisted with childcare may no longer be an option. If a female hospitalist is not a member of the leadership group that helped design this coverage structure, there could be a lack of recognition of the undue strain this coverage model could create for women in the group. Even if not intentional, such policies may hinder women’s career stability and opportunities for further advancement, as well as their ability to adequately provide care for their families. Having women as a part of the leadership group that creates policies and schedules and makes pivotal decisions is imperative, especially regarding topics of providing access and compensation for “emergency childcare,” hazard pay, shift length, work conditions, job security, sick leave, workers compensation, advancement opportunities, and hiring practices.
Compensation
The gender pay gap in medicine has been consistently demonstrated among many specialties.13,14 The reasons for this inequity are multifactorial, and the COVID-19 pandemic has the potential to further widen this gap. With the unequal burden of unpaid care provided by women and their higher prevalence as frontline workers, they are at greater risk of needing to take unpaid leave to care for a sick family member or themselves.6,7 Similarly, without hazard pay, those with direct clinical responsibilities bear the risk of illness for themselves and their families without adequate compensation.
Impact on Physical and Mental Health
The overall well-being of the hospitalist workforce is critical to continue to provide the highest level of care for our patients. With higher workloads at home and at work, female hospitalists are at risk for increased burnout. Burnout has been linked to many negative outcomes including poor performance, depression, suicide, and leaving the profession.15 Burnout is documented to be higher in female physicians with several contributing factors that are aggravated by gender inequities, including having children at home, gender bias, and real or perceived lack of fairness in promotion and compensation.16 The COVID-19 pandemic has amplified the stress of having children in the home, as well as concerns around fair compensation as described above. The consequences of this have yet to be fully realized but may be dire.
PROPOSED RECOMMENDATIONS
We propose the following recommendations to help mitigate the effects of this epidemic and to continue to move our field forward on our path to equity.
1. Closely monitor the direct and indirect effects of COVID-19 on female hospitalists. While there has been a recent increase in scholarship on the pre–COVID-19 state of gender disparities, there is still much that is unknown. As we experience this upheaval in the way our institutions function, it is even more imperative to track gender deaggregated key indicators of wellness, burnout, and productivity. This includes the use of burnout inventories, salary equity reviews, procedures that track progress toward promotion, and even focus groups of female hospitalists.
2. Inquire about the needs of women in your organization and secure the support they need. This may take the form of including women on key task forces that address personal protective equipment allocation, design new processes, and prepare for surge capacity, as well as providing wellness initiatives, fostering collaborative social networks, or connecting them with emergency childcare resources.
3. Provide a mechanism to account for lack of academic productivity during this time. This period of decreased academic productivity may disproportionately derail progress toward promotion for women. Academic institutions should consider extending deadlines for promotion or tenure, as well as increasing flexibility in metrics used to determine appropriate progress in annual performance reviews.
4. Recognize and reward increased efforts in the areas of clinical or administrative contribution. In this time of crisis, women may be stepping up and leading efforts without titles or positions in ways that are significant and meaningful for their group or organization. Recognizing the ways women are contributing in a tangible and explicit way can provide an avenue for fair compensation, recognition, and career advancement. Female hospitalists should also “manage up” by speaking up and ensuring that leaders are aware of contributions. Amplification is another powerful technique whereby unrecognized contributions can be called out by other women or men.17
5. Support diversity, inclusion, and equity efforts. Keeping equity targets at the top of priority lists for goals moving forward will be imperative. Many institutions struggled to support strong diversity, inclusion, and equity efforts prior to COVID-19; however, the pandemic has highlighted the stark racial and socioeconomic disparities that exist in healthcare.18,19 As healthcare institutions and providers work to mitigate these disparities for patients, there would be no better time to look internally at how they pay, support, and promote their own employees. This would include actively identifying and mitigating any disparities that exist for employees by gender, race, religion, sexual orientation, ethnicity, age, or disability status.
6. Advocate for fair compensation for providers caring for COVID-19 patients. Frontline clinicians are bearing significant risks and increased workload during this crisis and should be compensated accordingly. Hazard pay, paid sick leave, medical and supplemental life insurance, and strong workers’ compensation protections for hospitalists who become ill at work are important for all clinicians, including women. Other long-term plans should include institutional interventions such as salary corrections and ongoing monitoring.20
SUMMARY
The COVID-19 pandemic will have long-term effects that are yet to be realized, including potentially widening gender disparities in medicine. With the current health and economic crises facing our institutions and nations, it can be tempting for diversity, equity, and inclusion initiatives to fall by the wayside. However, it is imperative that hospitalists, leaders, and institutions monitor the effects of the COVID-19 pandemic on women and proactively work to mitigate worsening disparities. Without this focus there is a risk that the recent gains in equity and advancement for women may be lost.
1. Association of American Medical Colleges. Table 13: US medical school faculty by sex, rank, and department, 2017-2018. December 31, 2019. Accessed January 16, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144(5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Rouse LP, Nagy-Agren S, Gebhard RE, Bernstein WK. Women physicians: gender and the medical workplace. J Womens Health (Larchmt). 2020;29(3):297‐309. https://doi.org/10.1089/jwh.2018.7290
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Starmer AJ, Frintner MP, Matos K, Somberg C, Freed G, Byrne BJ. Gender discrepancies related to pediatrician work-life balance and household responsibilities. Pediatrics. 2019;144(4):e20182926. https://doi.org/10.1542/peds.2018-2926
6. Alon TM, Doepke M, Olmstead-Rumsey J, Tertilt Ml. The impact of COVID-19 on gender equality. NBER Working Paper Series. 2020. https://doi.org/10.3386/w26947
7. Addati L, Cattaneo U, Esquivel V, Valarino I. Care work and care jobs for the future of decent work. Geneva: International Labour Office; 2018.
8. Maguire P. Should you steer clear of your own family? Hospitalists weigh living in isolation. Today’s Hospitalist. May 2020. Accessed May 4, 2020. https://www.todayshospitalist.com/treating-covid-patients/
9. Burrer SL, de Perio MA, Hughes MM, et al. Characteristics of health care personnel with COVID-19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477-481. DOI: http://dx.doi.org/10.15585/mmwr.mm6915e6
10. SHM Teams Up with Hilton and American Express to Provide Hotel Rooms for Members. SHM. April 13, 2020. Accessed May 7, 2020. https://www.hospitalmedicine.org/about/press-releases/SHM-One-Million-Beds-Hilton-AMEX/
11. Fichtel C, Kaufman S. Fearing COVID-19 spread to families, health care workers self-isolate at home. NBC News. March 31, 2020. Accessed May 7, 2020. https://www.nbcnews.com/health/health-news/fearing-covid-19-spread-families-health-care-workers-self-isolate-n1171726
12. Meier KA, Jerardi KE, Statile AM, Shah SS. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020;15(5):308‐310. https://doi.org/10.12788/jhm.3435
13. Frintner MP, Sisk B, Byrne BJ, Freed GL, Starmer AJ, Olson LM. Gender differences in earnings of early- and midcareer pediatricians. Pediatrics. 2019;144(4):e20183955. https://doi.org/10.1542/peds.2018-3955
14. Read S, Butkus R, Weissman A, Moyer DV. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169(9):658-661. https://doi.org/10.7326/m18-0693
15. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516‐529. https://doi.org/10.1111/joim.12752
16. Templeton K, Halpern L, Jumper C, Carroll RG. Leading and sustaining curricular change: workshop proceedings from the 2018 Sex and Gender Health Education Summit. J Womens Health (Larchmt). 2019;28(12):1743-1747. https://doi.org/10.1089/jwh.2018.7387
17. Eilperin J. White House women want to be in the room where it happens. The Washington Post. September 13, 2016. Accessed April 24, 2020. https://www.washingtonpost.com/news/powerpost/wp/2016/09/13/white-house-women-are-now-in-the-room-where-it-happens/
18. Choo EK. COVID-19 fault lines. Lancet. 2020;395(10233):1333. https://doi.org/10.1016/s0140-6736(20)30812-6
19. Núñez A, Madison M, Schiavo R, Elk R, Prigerson HG. Responding to healthcare disparities and challenges with access to care during COVID-19. Health Equity. 2020;4(1):117-128. https://doi.org/10.1089/heq.2020.29000.rtl
20. Paturel A. Closing the gender pay gap in medicine. AAMC News. April 16, 2019. Accessed April 21, 2020. https://www.aamc.org/news-insights/closing-gender-pay-gap-medicine
The coronavirus disease of 2019 (COVID-19) pandemic has affected every facet of our work and personal lives. While many hope we will return to “normal” with the pandemic’s passing, there is reason to believe medicine, and society, will experience irrevocable changes. Although the number of women pursuing and practicing medicine has increased, inequities remain in compensation, academic rank, and leadership positions.1,2 Within the workplace, women are more likely to be in frontline clinical positions, are more likely to be integral in promoting positive interpersonal relationships and collaborative work environments, and often are less represented in the high-level, decision-making roles in leadership or administration.3,4 These well-described issues may be exacerbated during this pandemic crisis. We describe how the current COVID-19 pandemic may intensify workplace inequities for women, and propose solutions for hospitalist groups, leaders, and administrators to ensure female hospitalists continue to prosper and thrive in these tenuous times.
HOW THE PANDEMIC MAY EXACERBATE EXISTING INEQUITIES
Increasing Demands at Home
Female physicians are more likely to have partners who are employed full-time and report spending more time on household activities including cleaning, cooking, and the care of children, compared with their male counterparts.5 With school and daycare closings, as well as stay-at-home orders in many US states, there has been an increase in household responsibilities and care needs for children remaining at home with a marked decrease in options for stable or emergency childcare.6 As compared with primary care and subspecialty colleagues who can provide a large percentage of their care through telemedicine, this is not the case for hospitalists who must be physically present to care for their patients. Therefore, hospitalists are unable to clinically “work from home” in the same way as many of their colleagues in other specialties. Increased childcare and schooling obligations, coupled with disproportionate household responsibilities and an inability to work from home, will likely result in female hospitalists struggling to meet family needs while pandemic-related work responsibilities are ramping up.7 In addition, women who are involved with administrative, leadership, or research activities may struggle to execute their responsibilities as a result of increased domestic duties.
Many hospitalists are also concerned about contracting COVID-19 and exposing their families to the illness given the high infection rate among healthcare workers and the shortage of personal protective equipment (PPE).8,9 Institutions and national organizations, including the Society of Hospital Medicine, have partnered with industry to provide discounted or complimentary hotel rooms for members to aid self-isolation while providing clinical care.10 One famous photo in popular and social media showed a pulmonary and critical care physician in a tent in his garage in order to self-isolate from his family.11 However, since women are often the primary caregivers for their children or other family members and may also be responsible for other important household activities, they may be unable or unwilling to remove themselves from their children and families. As a result, female hospitalists may encounter feelings of guilt or inadequacy if they’re unable to isolate in the same manner as male colleagues.8
Exaggerating Leadership Gap
One of the keys to a robust response to this pandemic is strong, thoughtful, and strategic leadership.12 Institutional, regional, and national leaders are at the forefront of designing the solutions to the many problems the COVID-19 pandemic has created. The paucity of women at high-level leadership positions in institutions across the United States, including university-based, community, public, and private institutions, means that there is a lack of female representation when institutional policy is being discussed and decided.4 This lack of representation may lead to policies and procedures that negatively affect female hospitalists or, at best, fail to consider the needs of or support female physicians. For example, leaders of a hospital medicine group may create mandatory “backup” coverage for night and weekend shifts for their group during surge periods of the pandemic without considering implications for childcare. Finding weekday, daytime coverage is challenging for many during this time when daycares and school are closed, and finding coverage during weekend or overnight hours will be even more challenging. With increased risks for older adults with high-risk medical conditions, grandparents or other friends or family members that previously would have assisted with childcare may no longer be an option. If a female hospitalist is not a member of the leadership group that helped design this coverage structure, there could be a lack of recognition of the undue strain this coverage model could create for women in the group. Even if not intentional, such policies may hinder women’s career stability and opportunities for further advancement, as well as their ability to adequately provide care for their families. Having women as a part of the leadership group that creates policies and schedules and makes pivotal decisions is imperative, especially regarding topics of providing access and compensation for “emergency childcare,” hazard pay, shift length, work conditions, job security, sick leave, workers compensation, advancement opportunities, and hiring practices.
Compensation
The gender pay gap in medicine has been consistently demonstrated among many specialties.13,14 The reasons for this inequity are multifactorial, and the COVID-19 pandemic has the potential to further widen this gap. With the unequal burden of unpaid care provided by women and their higher prevalence as frontline workers, they are at greater risk of needing to take unpaid leave to care for a sick family member or themselves.6,7 Similarly, without hazard pay, those with direct clinical responsibilities bear the risk of illness for themselves and their families without adequate compensation.
Impact on Physical and Mental Health
The overall well-being of the hospitalist workforce is critical to continue to provide the highest level of care for our patients. With higher workloads at home and at work, female hospitalists are at risk for increased burnout. Burnout has been linked to many negative outcomes including poor performance, depression, suicide, and leaving the profession.15 Burnout is documented to be higher in female physicians with several contributing factors that are aggravated by gender inequities, including having children at home, gender bias, and real or perceived lack of fairness in promotion and compensation.16 The COVID-19 pandemic has amplified the stress of having children in the home, as well as concerns around fair compensation as described above. The consequences of this have yet to be fully realized but may be dire.
PROPOSED RECOMMENDATIONS
We propose the following recommendations to help mitigate the effects of this epidemic and to continue to move our field forward on our path to equity.
1. Closely monitor the direct and indirect effects of COVID-19 on female hospitalists. While there has been a recent increase in scholarship on the pre–COVID-19 state of gender disparities, there is still much that is unknown. As we experience this upheaval in the way our institutions function, it is even more imperative to track gender deaggregated key indicators of wellness, burnout, and productivity. This includes the use of burnout inventories, salary equity reviews, procedures that track progress toward promotion, and even focus groups of female hospitalists.
2. Inquire about the needs of women in your organization and secure the support they need. This may take the form of including women on key task forces that address personal protective equipment allocation, design new processes, and prepare for surge capacity, as well as providing wellness initiatives, fostering collaborative social networks, or connecting them with emergency childcare resources.
3. Provide a mechanism to account for lack of academic productivity during this time. This period of decreased academic productivity may disproportionately derail progress toward promotion for women. Academic institutions should consider extending deadlines for promotion or tenure, as well as increasing flexibility in metrics used to determine appropriate progress in annual performance reviews.
4. Recognize and reward increased efforts in the areas of clinical or administrative contribution. In this time of crisis, women may be stepping up and leading efforts without titles or positions in ways that are significant and meaningful for their group or organization. Recognizing the ways women are contributing in a tangible and explicit way can provide an avenue for fair compensation, recognition, and career advancement. Female hospitalists should also “manage up” by speaking up and ensuring that leaders are aware of contributions. Amplification is another powerful technique whereby unrecognized contributions can be called out by other women or men.17
5. Support diversity, inclusion, and equity efforts. Keeping equity targets at the top of priority lists for goals moving forward will be imperative. Many institutions struggled to support strong diversity, inclusion, and equity efforts prior to COVID-19; however, the pandemic has highlighted the stark racial and socioeconomic disparities that exist in healthcare.18,19 As healthcare institutions and providers work to mitigate these disparities for patients, there would be no better time to look internally at how they pay, support, and promote their own employees. This would include actively identifying and mitigating any disparities that exist for employees by gender, race, religion, sexual orientation, ethnicity, age, or disability status.
6. Advocate for fair compensation for providers caring for COVID-19 patients. Frontline clinicians are bearing significant risks and increased workload during this crisis and should be compensated accordingly. Hazard pay, paid sick leave, medical and supplemental life insurance, and strong workers’ compensation protections for hospitalists who become ill at work are important for all clinicians, including women. Other long-term plans should include institutional interventions such as salary corrections and ongoing monitoring.20
SUMMARY
The COVID-19 pandemic will have long-term effects that are yet to be realized, including potentially widening gender disparities in medicine. With the current health and economic crises facing our institutions and nations, it can be tempting for diversity, equity, and inclusion initiatives to fall by the wayside. However, it is imperative that hospitalists, leaders, and institutions monitor the effects of the COVID-19 pandemic on women and proactively work to mitigate worsening disparities. Without this focus there is a risk that the recent gains in equity and advancement for women may be lost.
The coronavirus disease of 2019 (COVID-19) pandemic has affected every facet of our work and personal lives. While many hope we will return to “normal” with the pandemic’s passing, there is reason to believe medicine, and society, will experience irrevocable changes. Although the number of women pursuing and practicing medicine has increased, inequities remain in compensation, academic rank, and leadership positions.1,2 Within the workplace, women are more likely to be in frontline clinical positions, are more likely to be integral in promoting positive interpersonal relationships and collaborative work environments, and often are less represented in the high-level, decision-making roles in leadership or administration.3,4 These well-described issues may be exacerbated during this pandemic crisis. We describe how the current COVID-19 pandemic may intensify workplace inequities for women, and propose solutions for hospitalist groups, leaders, and administrators to ensure female hospitalists continue to prosper and thrive in these tenuous times.
HOW THE PANDEMIC MAY EXACERBATE EXISTING INEQUITIES
Increasing Demands at Home
Female physicians are more likely to have partners who are employed full-time and report spending more time on household activities including cleaning, cooking, and the care of children, compared with their male counterparts.5 With school and daycare closings, as well as stay-at-home orders in many US states, there has been an increase in household responsibilities and care needs for children remaining at home with a marked decrease in options for stable or emergency childcare.6 As compared with primary care and subspecialty colleagues who can provide a large percentage of their care through telemedicine, this is not the case for hospitalists who must be physically present to care for their patients. Therefore, hospitalists are unable to clinically “work from home” in the same way as many of their colleagues in other specialties. Increased childcare and schooling obligations, coupled with disproportionate household responsibilities and an inability to work from home, will likely result in female hospitalists struggling to meet family needs while pandemic-related work responsibilities are ramping up.7 In addition, women who are involved with administrative, leadership, or research activities may struggle to execute their responsibilities as a result of increased domestic duties.
Many hospitalists are also concerned about contracting COVID-19 and exposing their families to the illness given the high infection rate among healthcare workers and the shortage of personal protective equipment (PPE).8,9 Institutions and national organizations, including the Society of Hospital Medicine, have partnered with industry to provide discounted or complimentary hotel rooms for members to aid self-isolation while providing clinical care.10 One famous photo in popular and social media showed a pulmonary and critical care physician in a tent in his garage in order to self-isolate from his family.11 However, since women are often the primary caregivers for their children or other family members and may also be responsible for other important household activities, they may be unable or unwilling to remove themselves from their children and families. As a result, female hospitalists may encounter feelings of guilt or inadequacy if they’re unable to isolate in the same manner as male colleagues.8
Exaggerating Leadership Gap
One of the keys to a robust response to this pandemic is strong, thoughtful, and strategic leadership.12 Institutional, regional, and national leaders are at the forefront of designing the solutions to the many problems the COVID-19 pandemic has created. The paucity of women at high-level leadership positions in institutions across the United States, including university-based, community, public, and private institutions, means that there is a lack of female representation when institutional policy is being discussed and decided.4 This lack of representation may lead to policies and procedures that negatively affect female hospitalists or, at best, fail to consider the needs of or support female physicians. For example, leaders of a hospital medicine group may create mandatory “backup” coverage for night and weekend shifts for their group during surge periods of the pandemic without considering implications for childcare. Finding weekday, daytime coverage is challenging for many during this time when daycares and school are closed, and finding coverage during weekend or overnight hours will be even more challenging. With increased risks for older adults with high-risk medical conditions, grandparents or other friends or family members that previously would have assisted with childcare may no longer be an option. If a female hospitalist is not a member of the leadership group that helped design this coverage structure, there could be a lack of recognition of the undue strain this coverage model could create for women in the group. Even if not intentional, such policies may hinder women’s career stability and opportunities for further advancement, as well as their ability to adequately provide care for their families. Having women as a part of the leadership group that creates policies and schedules and makes pivotal decisions is imperative, especially regarding topics of providing access and compensation for “emergency childcare,” hazard pay, shift length, work conditions, job security, sick leave, workers compensation, advancement opportunities, and hiring practices.
Compensation
The gender pay gap in medicine has been consistently demonstrated among many specialties.13,14 The reasons for this inequity are multifactorial, and the COVID-19 pandemic has the potential to further widen this gap. With the unequal burden of unpaid care provided by women and their higher prevalence as frontline workers, they are at greater risk of needing to take unpaid leave to care for a sick family member or themselves.6,7 Similarly, without hazard pay, those with direct clinical responsibilities bear the risk of illness for themselves and their families without adequate compensation.
Impact on Physical and Mental Health
The overall well-being of the hospitalist workforce is critical to continue to provide the highest level of care for our patients. With higher workloads at home and at work, female hospitalists are at risk for increased burnout. Burnout has been linked to many negative outcomes including poor performance, depression, suicide, and leaving the profession.15 Burnout is documented to be higher in female physicians with several contributing factors that are aggravated by gender inequities, including having children at home, gender bias, and real or perceived lack of fairness in promotion and compensation.16 The COVID-19 pandemic has amplified the stress of having children in the home, as well as concerns around fair compensation as described above. The consequences of this have yet to be fully realized but may be dire.
PROPOSED RECOMMENDATIONS
We propose the following recommendations to help mitigate the effects of this epidemic and to continue to move our field forward on our path to equity.
1. Closely monitor the direct and indirect effects of COVID-19 on female hospitalists. While there has been a recent increase in scholarship on the pre–COVID-19 state of gender disparities, there is still much that is unknown. As we experience this upheaval in the way our institutions function, it is even more imperative to track gender deaggregated key indicators of wellness, burnout, and productivity. This includes the use of burnout inventories, salary equity reviews, procedures that track progress toward promotion, and even focus groups of female hospitalists.
2. Inquire about the needs of women in your organization and secure the support they need. This may take the form of including women on key task forces that address personal protective equipment allocation, design new processes, and prepare for surge capacity, as well as providing wellness initiatives, fostering collaborative social networks, or connecting them with emergency childcare resources.
3. Provide a mechanism to account for lack of academic productivity during this time. This period of decreased academic productivity may disproportionately derail progress toward promotion for women. Academic institutions should consider extending deadlines for promotion or tenure, as well as increasing flexibility in metrics used to determine appropriate progress in annual performance reviews.
4. Recognize and reward increased efforts in the areas of clinical or administrative contribution. In this time of crisis, women may be stepping up and leading efforts without titles or positions in ways that are significant and meaningful for their group or organization. Recognizing the ways women are contributing in a tangible and explicit way can provide an avenue for fair compensation, recognition, and career advancement. Female hospitalists should also “manage up” by speaking up and ensuring that leaders are aware of contributions. Amplification is another powerful technique whereby unrecognized contributions can be called out by other women or men.17
5. Support diversity, inclusion, and equity efforts. Keeping equity targets at the top of priority lists for goals moving forward will be imperative. Many institutions struggled to support strong diversity, inclusion, and equity efforts prior to COVID-19; however, the pandemic has highlighted the stark racial and socioeconomic disparities that exist in healthcare.18,19 As healthcare institutions and providers work to mitigate these disparities for patients, there would be no better time to look internally at how they pay, support, and promote their own employees. This would include actively identifying and mitigating any disparities that exist for employees by gender, race, religion, sexual orientation, ethnicity, age, or disability status.
6. Advocate for fair compensation for providers caring for COVID-19 patients. Frontline clinicians are bearing significant risks and increased workload during this crisis and should be compensated accordingly. Hazard pay, paid sick leave, medical and supplemental life insurance, and strong workers’ compensation protections for hospitalists who become ill at work are important for all clinicians, including women. Other long-term plans should include institutional interventions such as salary corrections and ongoing monitoring.20
SUMMARY
The COVID-19 pandemic will have long-term effects that are yet to be realized, including potentially widening gender disparities in medicine. With the current health and economic crises facing our institutions and nations, it can be tempting for diversity, equity, and inclusion initiatives to fall by the wayside. However, it is imperative that hospitalists, leaders, and institutions monitor the effects of the COVID-19 pandemic on women and proactively work to mitigate worsening disparities. Without this focus there is a risk that the recent gains in equity and advancement for women may be lost.
1. Association of American Medical Colleges. Table 13: US medical school faculty by sex, rank, and department, 2017-2018. December 31, 2019. Accessed January 16, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144(5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Rouse LP, Nagy-Agren S, Gebhard RE, Bernstein WK. Women physicians: gender and the medical workplace. J Womens Health (Larchmt). 2020;29(3):297‐309. https://doi.org/10.1089/jwh.2018.7290
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Starmer AJ, Frintner MP, Matos K, Somberg C, Freed G, Byrne BJ. Gender discrepancies related to pediatrician work-life balance and household responsibilities. Pediatrics. 2019;144(4):e20182926. https://doi.org/10.1542/peds.2018-2926
6. Alon TM, Doepke M, Olmstead-Rumsey J, Tertilt Ml. The impact of COVID-19 on gender equality. NBER Working Paper Series. 2020. https://doi.org/10.3386/w26947
7. Addati L, Cattaneo U, Esquivel V, Valarino I. Care work and care jobs for the future of decent work. Geneva: International Labour Office; 2018.
8. Maguire P. Should you steer clear of your own family? Hospitalists weigh living in isolation. Today’s Hospitalist. May 2020. Accessed May 4, 2020. https://www.todayshospitalist.com/treating-covid-patients/
9. Burrer SL, de Perio MA, Hughes MM, et al. Characteristics of health care personnel with COVID-19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477-481. DOI: http://dx.doi.org/10.15585/mmwr.mm6915e6
10. SHM Teams Up with Hilton and American Express to Provide Hotel Rooms for Members. SHM. April 13, 2020. Accessed May 7, 2020. https://www.hospitalmedicine.org/about/press-releases/SHM-One-Million-Beds-Hilton-AMEX/
11. Fichtel C, Kaufman S. Fearing COVID-19 spread to families, health care workers self-isolate at home. NBC News. March 31, 2020. Accessed May 7, 2020. https://www.nbcnews.com/health/health-news/fearing-covid-19-spread-families-health-care-workers-self-isolate-n1171726
12. Meier KA, Jerardi KE, Statile AM, Shah SS. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020;15(5):308‐310. https://doi.org/10.12788/jhm.3435
13. Frintner MP, Sisk B, Byrne BJ, Freed GL, Starmer AJ, Olson LM. Gender differences in earnings of early- and midcareer pediatricians. Pediatrics. 2019;144(4):e20183955. https://doi.org/10.1542/peds.2018-3955
14. Read S, Butkus R, Weissman A, Moyer DV. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169(9):658-661. https://doi.org/10.7326/m18-0693
15. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516‐529. https://doi.org/10.1111/joim.12752
16. Templeton K, Halpern L, Jumper C, Carroll RG. Leading and sustaining curricular change: workshop proceedings from the 2018 Sex and Gender Health Education Summit. J Womens Health (Larchmt). 2019;28(12):1743-1747. https://doi.org/10.1089/jwh.2018.7387
17. Eilperin J. White House women want to be in the room where it happens. The Washington Post. September 13, 2016. Accessed April 24, 2020. https://www.washingtonpost.com/news/powerpost/wp/2016/09/13/white-house-women-are-now-in-the-room-where-it-happens/
18. Choo EK. COVID-19 fault lines. Lancet. 2020;395(10233):1333. https://doi.org/10.1016/s0140-6736(20)30812-6
19. Núñez A, Madison M, Schiavo R, Elk R, Prigerson HG. Responding to healthcare disparities and challenges with access to care during COVID-19. Health Equity. 2020;4(1):117-128. https://doi.org/10.1089/heq.2020.29000.rtl
20. Paturel A. Closing the gender pay gap in medicine. AAMC News. April 16, 2019. Accessed April 21, 2020. https://www.aamc.org/news-insights/closing-gender-pay-gap-medicine
1. Association of American Medical Colleges. Table 13: US medical school faculty by sex, rank, and department, 2017-2018. December 31, 2019. Accessed January 16, 2020. https://www.aamc.org/download/486102/data/17table13.pdf
2. Spector ND, Asante PA, Marcelin JR, et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144(5):e20192149. https://doi.org/10.1542/peds.2019-2149
3. Rouse LP, Nagy-Agren S, Gebhard RE, Bernstein WK. Women physicians: gender and the medical workplace. J Womens Health (Larchmt). 2020;29(3):297‐309. https://doi.org/10.1089/jwh.2018.7290
4. Burden M, Frank MG, Keniston A, et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10(8):481-485. https://doi.org/10.1002/jhm.2340
5. Starmer AJ, Frintner MP, Matos K, Somberg C, Freed G, Byrne BJ. Gender discrepancies related to pediatrician work-life balance and household responsibilities. Pediatrics. 2019;144(4):e20182926. https://doi.org/10.1542/peds.2018-2926
6. Alon TM, Doepke M, Olmstead-Rumsey J, Tertilt Ml. The impact of COVID-19 on gender equality. NBER Working Paper Series. 2020. https://doi.org/10.3386/w26947
7. Addati L, Cattaneo U, Esquivel V, Valarino I. Care work and care jobs for the future of decent work. Geneva: International Labour Office; 2018.
8. Maguire P. Should you steer clear of your own family? Hospitalists weigh living in isolation. Today’s Hospitalist. May 2020. Accessed May 4, 2020. https://www.todayshospitalist.com/treating-covid-patients/
9. Burrer SL, de Perio MA, Hughes MM, et al. Characteristics of health care personnel with COVID-19 — United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477-481. DOI: http://dx.doi.org/10.15585/mmwr.mm6915e6
10. SHM Teams Up with Hilton and American Express to Provide Hotel Rooms for Members. SHM. April 13, 2020. Accessed May 7, 2020. https://www.hospitalmedicine.org/about/press-releases/SHM-One-Million-Beds-Hilton-AMEX/
11. Fichtel C, Kaufman S. Fearing COVID-19 spread to families, health care workers self-isolate at home. NBC News. March 31, 2020. Accessed May 7, 2020. https://www.nbcnews.com/health/health-news/fearing-covid-19-spread-families-health-care-workers-self-isolate-n1171726
12. Meier KA, Jerardi KE, Statile AM, Shah SS. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020;15(5):308‐310. https://doi.org/10.12788/jhm.3435
13. Frintner MP, Sisk B, Byrne BJ, Freed GL, Starmer AJ, Olson LM. Gender differences in earnings of early- and midcareer pediatricians. Pediatrics. 2019;144(4):e20183955. https://doi.org/10.1542/peds.2018-3955
14. Read S, Butkus R, Weissman A, Moyer DV. Compensation disparities by gender in internal medicine. Ann Intern Med. 2018;169(9):658-661. https://doi.org/10.7326/m18-0693
15. West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516‐529. https://doi.org/10.1111/joim.12752
16. Templeton K, Halpern L, Jumper C, Carroll RG. Leading and sustaining curricular change: workshop proceedings from the 2018 Sex and Gender Health Education Summit. J Womens Health (Larchmt). 2019;28(12):1743-1747. https://doi.org/10.1089/jwh.2018.7387
17. Eilperin J. White House women want to be in the room where it happens. The Washington Post. September 13, 2016. Accessed April 24, 2020. https://www.washingtonpost.com/news/powerpost/wp/2016/09/13/white-house-women-are-now-in-the-room-where-it-happens/
18. Choo EK. COVID-19 fault lines. Lancet. 2020;395(10233):1333. https://doi.org/10.1016/s0140-6736(20)30812-6
19. Núñez A, Madison M, Schiavo R, Elk R, Prigerson HG. Responding to healthcare disparities and challenges with access to care during COVID-19. Health Equity. 2020;4(1):117-128. https://doi.org/10.1089/heq.2020.29000.rtl
20. Paturel A. Closing the gender pay gap in medicine. AAMC News. April 16, 2019. Accessed April 21, 2020. https://www.aamc.org/news-insights/closing-gender-pay-gap-medicine
© 2020 Society of Hospital Medicine
CRC: Mailing fecal test kits appears cost effective, boosts screening
Mailing fecal immunochemical testing (FIT) kits with colorectal cancer (CRC) screening reminders appears cost effective and may boost screening rates across a variety of payers and providers, according to investigators.
Cost savings, when compared with mailing reminders alone, would be greatest from a Medicaid and state government perspective, reported lead author Stephanie B. Wheeler, PhD, MPH, of the University of North Carolina at Chapel Hill and colleagues.
“As payers and providers endeavor to increase the proportion of age-eligible adults who are up to date with CRC screening, according to the National Colorectal Cancer Roundtable target of 80% screened, understanding the comparative value of mailed FIT-based programs in low-income populations is urgently needed,” the investigators wrote in Cancer.
To address this need, Dr. Wheeler and colleagues coupled a randomized clinical trial with a cost-effectiveness analysis.
The trial involved 2,144 North Carolina Medicaid enrollees between 52 and 64 years of age who were overdue for CRC screening. Participants were randomly assigned to receive either a mailed reminder with an FIT kit or a mailed reminder alone. Those who received the reminder alone were provided with information about how to get an FIT kit or undergo screening colonoscopy.
The screening rate was significantly higher in the combination mailer group than it was the reminder-only group, at 21.1% versus 12.3% (P less than .01). Based on data from previous research, the investigators estimated that a number of participants also underwent colonoscopy screenings because of the reminders; this resulted in an estimated 23.3% screening rate among those who received an FIT kit, compared with 15.8% among those who received a reminder alone.
For cost analysis, these rates were entered into a model involving 35,000 Medicaid enrollees. Annual costs were compared from two perspectives: Medicaid/state and health clinic/facility, the latter of which included primary care providers, integrated health care systems, county health departments, and federally qualified health centers. The model incorporated a number of costs, such as those associated with equipment, mailing supplies, FIT kits, colonoscopy screenings, and personnel.
From a Medicaid/state perspective, the estimated total population screening cost of mailing both an FIT kit and reminder was $1.40 million, compared with $1.45 million for a reminder alone. This translated to a total cost per person screened of $172 for the combination mailer versus $262 for the reminder alone.
“Notably, compared with the reminder-only alternative, the reminder + FIT alternative was cost-saving or dominant from this perspective because it yielded more screenings at lower cost,” the investigators wrote.
The cost analysis from a health clinic/facility perspective was more nuanced.
While the estimated total population screening cost of a combination mailer was more than the reminder alone ($927,000 vs. $624,000), sending test kits led to screening of 2,598 additional individuals (8,131 vs. 5,533). The incremental cost-effectiveness ratio (ICER) for the combination mailer was $116 per person screened.
“This ICER fell within the range of what decision makers typically would be willing to pay for an additional person screened for CRC, previously shown to include ICERs as high as several hundred dollars or more,” the investigators noted.
According to Beverly B. Green, MD, MPH, of Kaiser Permanente Washington, Seattle, and Richard T. Meenan, PhD, MPH, of Kaiser Permanente Northwest, Portland, Oregon, who wrote a simultaneously published editorial, the study “suggests that direct FIT mailing can be highly cost effective if not cost saving within the Medicaid population, similar to tobacco-cessation programs or diabetes prevention programs in the same context of a Medicaid population.”
Still, practical details need to be resolved prior to real-world application, they added.
“[T]he analysis by Wheeler et al. raises an important question: Who should pay for mailed FIT screening programs?”
The answer, they suggested, may be health plans, since prevention of CRC could mitigate greater costs of care down the line. Further motivation could come from a program such as the Medicare 5-star program, which rewards higher screening rates with bonuses such as longer enrollment periods and higher payments, according to Dr. Green and Dr. Meenan.
“Unsurprisingly, Medicare CRC screening rates have been steadily increasing and now are approaching 80%,” they noted, “whereas Medicaid CRC screening rates remain low.”
The study was supported by the University of North Carolina, the Cancer Prevention and Control Research Network, the Centers for Disease Control and Prevention, and the National Cancer Institute. Dr. Wheeler reported grant funding from Pfizer.
SOURCE: Wheeler SB et al. Cancer. 2020 Jul 20. doi: 10.1002/cncr.32992.
Mailing fecal immunochemical testing (FIT) kits with colorectal cancer (CRC) screening reminders appears cost effective and may boost screening rates across a variety of payers and providers, according to investigators.
Cost savings, when compared with mailing reminders alone, would be greatest from a Medicaid and state government perspective, reported lead author Stephanie B. Wheeler, PhD, MPH, of the University of North Carolina at Chapel Hill and colleagues.
“As payers and providers endeavor to increase the proportion of age-eligible adults who are up to date with CRC screening, according to the National Colorectal Cancer Roundtable target of 80% screened, understanding the comparative value of mailed FIT-based programs in low-income populations is urgently needed,” the investigators wrote in Cancer.
To address this need, Dr. Wheeler and colleagues coupled a randomized clinical trial with a cost-effectiveness analysis.
The trial involved 2,144 North Carolina Medicaid enrollees between 52 and 64 years of age who were overdue for CRC screening. Participants were randomly assigned to receive either a mailed reminder with an FIT kit or a mailed reminder alone. Those who received the reminder alone were provided with information about how to get an FIT kit or undergo screening colonoscopy.
The screening rate was significantly higher in the combination mailer group than it was the reminder-only group, at 21.1% versus 12.3% (P less than .01). Based on data from previous research, the investigators estimated that a number of participants also underwent colonoscopy screenings because of the reminders; this resulted in an estimated 23.3% screening rate among those who received an FIT kit, compared with 15.8% among those who received a reminder alone.
For cost analysis, these rates were entered into a model involving 35,000 Medicaid enrollees. Annual costs were compared from two perspectives: Medicaid/state and health clinic/facility, the latter of which included primary care providers, integrated health care systems, county health departments, and federally qualified health centers. The model incorporated a number of costs, such as those associated with equipment, mailing supplies, FIT kits, colonoscopy screenings, and personnel.
From a Medicaid/state perspective, the estimated total population screening cost of mailing both an FIT kit and reminder was $1.40 million, compared with $1.45 million for a reminder alone. This translated to a total cost per person screened of $172 for the combination mailer versus $262 for the reminder alone.
“Notably, compared with the reminder-only alternative, the reminder + FIT alternative was cost-saving or dominant from this perspective because it yielded more screenings at lower cost,” the investigators wrote.
The cost analysis from a health clinic/facility perspective was more nuanced.
While the estimated total population screening cost of a combination mailer was more than the reminder alone ($927,000 vs. $624,000), sending test kits led to screening of 2,598 additional individuals (8,131 vs. 5,533). The incremental cost-effectiveness ratio (ICER) for the combination mailer was $116 per person screened.
“This ICER fell within the range of what decision makers typically would be willing to pay for an additional person screened for CRC, previously shown to include ICERs as high as several hundred dollars or more,” the investigators noted.
According to Beverly B. Green, MD, MPH, of Kaiser Permanente Washington, Seattle, and Richard T. Meenan, PhD, MPH, of Kaiser Permanente Northwest, Portland, Oregon, who wrote a simultaneously published editorial, the study “suggests that direct FIT mailing can be highly cost effective if not cost saving within the Medicaid population, similar to tobacco-cessation programs or diabetes prevention programs in the same context of a Medicaid population.”
Still, practical details need to be resolved prior to real-world application, they added.
“[T]he analysis by Wheeler et al. raises an important question: Who should pay for mailed FIT screening programs?”
The answer, they suggested, may be health plans, since prevention of CRC could mitigate greater costs of care down the line. Further motivation could come from a program such as the Medicare 5-star program, which rewards higher screening rates with bonuses such as longer enrollment periods and higher payments, according to Dr. Green and Dr. Meenan.
“Unsurprisingly, Medicare CRC screening rates have been steadily increasing and now are approaching 80%,” they noted, “whereas Medicaid CRC screening rates remain low.”
The study was supported by the University of North Carolina, the Cancer Prevention and Control Research Network, the Centers for Disease Control and Prevention, and the National Cancer Institute. Dr. Wheeler reported grant funding from Pfizer.
SOURCE: Wheeler SB et al. Cancer. 2020 Jul 20. doi: 10.1002/cncr.32992.
Mailing fecal immunochemical testing (FIT) kits with colorectal cancer (CRC) screening reminders appears cost effective and may boost screening rates across a variety of payers and providers, according to investigators.
Cost savings, when compared with mailing reminders alone, would be greatest from a Medicaid and state government perspective, reported lead author Stephanie B. Wheeler, PhD, MPH, of the University of North Carolina at Chapel Hill and colleagues.
“As payers and providers endeavor to increase the proportion of age-eligible adults who are up to date with CRC screening, according to the National Colorectal Cancer Roundtable target of 80% screened, understanding the comparative value of mailed FIT-based programs in low-income populations is urgently needed,” the investigators wrote in Cancer.
To address this need, Dr. Wheeler and colleagues coupled a randomized clinical trial with a cost-effectiveness analysis.
The trial involved 2,144 North Carolina Medicaid enrollees between 52 and 64 years of age who were overdue for CRC screening. Participants were randomly assigned to receive either a mailed reminder with an FIT kit or a mailed reminder alone. Those who received the reminder alone were provided with information about how to get an FIT kit or undergo screening colonoscopy.
The screening rate was significantly higher in the combination mailer group than it was the reminder-only group, at 21.1% versus 12.3% (P less than .01). Based on data from previous research, the investigators estimated that a number of participants also underwent colonoscopy screenings because of the reminders; this resulted in an estimated 23.3% screening rate among those who received an FIT kit, compared with 15.8% among those who received a reminder alone.
For cost analysis, these rates were entered into a model involving 35,000 Medicaid enrollees. Annual costs were compared from two perspectives: Medicaid/state and health clinic/facility, the latter of which included primary care providers, integrated health care systems, county health departments, and federally qualified health centers. The model incorporated a number of costs, such as those associated with equipment, mailing supplies, FIT kits, colonoscopy screenings, and personnel.
From a Medicaid/state perspective, the estimated total population screening cost of mailing both an FIT kit and reminder was $1.40 million, compared with $1.45 million for a reminder alone. This translated to a total cost per person screened of $172 for the combination mailer versus $262 for the reminder alone.
“Notably, compared with the reminder-only alternative, the reminder + FIT alternative was cost-saving or dominant from this perspective because it yielded more screenings at lower cost,” the investigators wrote.
The cost analysis from a health clinic/facility perspective was more nuanced.
While the estimated total population screening cost of a combination mailer was more than the reminder alone ($927,000 vs. $624,000), sending test kits led to screening of 2,598 additional individuals (8,131 vs. 5,533). The incremental cost-effectiveness ratio (ICER) for the combination mailer was $116 per person screened.
“This ICER fell within the range of what decision makers typically would be willing to pay for an additional person screened for CRC, previously shown to include ICERs as high as several hundred dollars or more,” the investigators noted.
According to Beverly B. Green, MD, MPH, of Kaiser Permanente Washington, Seattle, and Richard T. Meenan, PhD, MPH, of Kaiser Permanente Northwest, Portland, Oregon, who wrote a simultaneously published editorial, the study “suggests that direct FIT mailing can be highly cost effective if not cost saving within the Medicaid population, similar to tobacco-cessation programs or diabetes prevention programs in the same context of a Medicaid population.”
Still, practical details need to be resolved prior to real-world application, they added.
“[T]he analysis by Wheeler et al. raises an important question: Who should pay for mailed FIT screening programs?”
The answer, they suggested, may be health plans, since prevention of CRC could mitigate greater costs of care down the line. Further motivation could come from a program such as the Medicare 5-star program, which rewards higher screening rates with bonuses such as longer enrollment periods and higher payments, according to Dr. Green and Dr. Meenan.
“Unsurprisingly, Medicare CRC screening rates have been steadily increasing and now are approaching 80%,” they noted, “whereas Medicaid CRC screening rates remain low.”
The study was supported by the University of North Carolina, the Cancer Prevention and Control Research Network, the Centers for Disease Control and Prevention, and the National Cancer Institute. Dr. Wheeler reported grant funding from Pfizer.
SOURCE: Wheeler SB et al. Cancer. 2020 Jul 20. doi: 10.1002/cncr.32992.
FROM CANCER
Key clinical point: Mailing fecal immunochemical testing (FIT) kits along with colorectal cancer screening reminders appears cost effective and may lead to higher screening rates than mailing reminders alone.
Major finding: Individuals who received a reminder and a fecal immunochemical testing (FIT) kit had an estimated 23.3% colorectal cancer screening rate, compared with 15.8% among those who received a reminder alone.
Study details: A cost-effectiveness analysis of a randomized clinical trial involving Medicaid enrollees between 52 and 64 years of age.
Disclosures: The study was supported by the University of North Carolina, the Cancer Prevention and Control Research Network, the Centers for Disease Control and Prevention, and the National Cancer Institute. Dr. Wheeler reported grant funding from Pfizer.
Source: Wheeler SB et al. Cancer. 2020 Jul 20. doi: 10.1002/cncr.32992.
Schools can reopen safely with precautions, experts say
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
Clinicians address psoriatic disease risk in the era of COVID-19
COVID-19 has posed serious questions for patients with psoriatic disease and the clinicians who treat them. Both have serious concerns over whether psoriasis or the medications used to treat it pose additional risk for contracting COVID-19 or experiencing worse outcomes with illness.
At the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis, experts gathered to discuss these concerns and what is known about the special risk factors for psoriatic disease patients.
Studies from a few registries have been done already among patients with autoimmune disease, and the results so far suggest that patients may be able to breathe a little easier. “I don’t see any data that suggests that use of immunosuppressives or having autoimmune disease increases your risk of acquiring it. I think most of the risk is driven by risk of exposure,” said Kevin Winthrop, MD, MPH, a professor of public health, infectious diseases, ophthalmology at Oregon Health & Science University, Portland, during a presentation.
That assertion was reinforced by data presented by Rebecca Haberman, MD, a rheumatologist at New York University Langone Health. Her group created the Web-Based Assessment of Autoimmune, Immune-Mediated, and Rheumatic Patients during the COVID-19 Pandemic (WARCOV) cohort study to address the question of whether patients with immune-mediated inflammatory disease (IMID), including inflammatory arthritis, psoriasis, or inflammatory bowel disease, should discontinue or modify their immunotherapy regimens in the face of potential exposure to COVID-19.
To date, the study has data on 1,122 patients; 604 with inflammatory arthritis, 128 of whom have tested positive for COVID-19. The team established a cohort using the first 86 IMID patients confirmed to have contracted COVID-19. The hospitalization rate was 16% overall, and use of corticosteroids was associated with increased hospitalization risk. A follow-up analysis looking at the first 103 inflammatory arthritis patients who contracted COVID-19 showed a hospitalization rate of 26% and a mortality of 4%. That hospitalization rate is similar to the general hospitalization rate estimated by the New York Department of Health, Dr. Haberman said in her presentation.
Risk factors associated with hospitalization included being older and having asthma or COPD, which is similar to the general population. Use of oral glucocorticoids was linked to a big increase in risk for hospitalization, even with doses less than 10 mg prednisone daily (odds ratio, 14.31; 95% confidence interval, 3.55-57.70). There were no links between use of any cytokine therapy and risk, but use of TNF inhibitors was associated with a reduced risk (OR, 0.35; 95% CI, 0.13-0.97), while use of JAK inhibitors was associated with greater risk (OR, 6.30; 95% CI, 1.68-23.69). The latter result is tentative because of a small sample size, and it was driven largely by the experiences of patients with psoriatic arthritis.
Another study, run by the COVID-19 Global Rheumatology Alliance, looked at 600 patients with rheumatic disease from 40 countries, and “found no smoking gun,” said Leonard Calabrese, DO, who leads the Cleveland Clinic’s section of clinical immunology, during his presentation. “People can develop this when they’re on hydroxychloroquine. They seem to do not remarkably bad or remarkably good. There is no adverse signal for biologics, but being on prednisone [at a dose of] more than 10 mg is not great,” said Dr. Calabrese, who also noted that other publications have supported these conclusions.
So given these findings, how should clinicians address patient concerns? In the absence of probable exposure, “we say it’s better to have a well-controlled IMID on therapy than a poorly-controlled IMID on submaximal therapy. We say stick to therapy and try to wean the prednisone down as low as possible,” Dr. Calabrese said.
More controversially, what should patients do if they have had a significant exposure, such as a close proximity, prolonged exposure encounter with an individual with documented COVID-19, or at high-risk of disease? Dr. Calabrese noted that the American College of Rheumatology (ACR) guidelines recommend that low-level immunomodulation can be continued, “with an asterisk if it’s hydroxychloroquine, and it is in most of our minds now that we know that it is not effective, and the toxicity in the COVID setting is still being worked out,” he said.
With respect to other immunosuppressants, the ACR recommends stopping them temporarily, although IL-6 inhibitors may be continued in select circumstances. Resumption of the therapeutics can resume after a negative COVID test or completion of a 2-week observation period.
When patients contract COVID-19, antimalarial medications can be continued because they have been studied. “But medium-level immunomodulators, in particular methotrexate, I have grave concerns about because it can inhibit the adaptive immune response and antibody formation,” he said. COVID-19 is a serious infection, and all serious biologics have a package insert saying to stop them in a serious infection. Again, IL-6 inhibitors may be considered an exception in the right circumstances. When to resume these medications remains unknown. “I think that’s a work in progress. Test-based versus clinic-based strategies are a matter of controversy,” Dr. Calabrese said.
Ultimately, the question of what to do with immunosuppressive therapies in this population will continue to be a challenge. “The only good answer is to follow the rules of social distancing and to wear a mask,” said Kristina Callis Duffin, MD, a cochair of the department of dermatology and associate professor of dermatology at the University of Utah, Salt Lake City.
COVID-19 has posed serious questions for patients with psoriatic disease and the clinicians who treat them. Both have serious concerns over whether psoriasis or the medications used to treat it pose additional risk for contracting COVID-19 or experiencing worse outcomes with illness.
At the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis, experts gathered to discuss these concerns and what is known about the special risk factors for psoriatic disease patients.
Studies from a few registries have been done already among patients with autoimmune disease, and the results so far suggest that patients may be able to breathe a little easier. “I don’t see any data that suggests that use of immunosuppressives or having autoimmune disease increases your risk of acquiring it. I think most of the risk is driven by risk of exposure,” said Kevin Winthrop, MD, MPH, a professor of public health, infectious diseases, ophthalmology at Oregon Health & Science University, Portland, during a presentation.
That assertion was reinforced by data presented by Rebecca Haberman, MD, a rheumatologist at New York University Langone Health. Her group created the Web-Based Assessment of Autoimmune, Immune-Mediated, and Rheumatic Patients during the COVID-19 Pandemic (WARCOV) cohort study to address the question of whether patients with immune-mediated inflammatory disease (IMID), including inflammatory arthritis, psoriasis, or inflammatory bowel disease, should discontinue or modify their immunotherapy regimens in the face of potential exposure to COVID-19.
To date, the study has data on 1,122 patients; 604 with inflammatory arthritis, 128 of whom have tested positive for COVID-19. The team established a cohort using the first 86 IMID patients confirmed to have contracted COVID-19. The hospitalization rate was 16% overall, and use of corticosteroids was associated with increased hospitalization risk. A follow-up analysis looking at the first 103 inflammatory arthritis patients who contracted COVID-19 showed a hospitalization rate of 26% and a mortality of 4%. That hospitalization rate is similar to the general hospitalization rate estimated by the New York Department of Health, Dr. Haberman said in her presentation.
Risk factors associated with hospitalization included being older and having asthma or COPD, which is similar to the general population. Use of oral glucocorticoids was linked to a big increase in risk for hospitalization, even with doses less than 10 mg prednisone daily (odds ratio, 14.31; 95% confidence interval, 3.55-57.70). There were no links between use of any cytokine therapy and risk, but use of TNF inhibitors was associated with a reduced risk (OR, 0.35; 95% CI, 0.13-0.97), while use of JAK inhibitors was associated with greater risk (OR, 6.30; 95% CI, 1.68-23.69). The latter result is tentative because of a small sample size, and it was driven largely by the experiences of patients with psoriatic arthritis.
Another study, run by the COVID-19 Global Rheumatology Alliance, looked at 600 patients with rheumatic disease from 40 countries, and “found no smoking gun,” said Leonard Calabrese, DO, who leads the Cleveland Clinic’s section of clinical immunology, during his presentation. “People can develop this when they’re on hydroxychloroquine. They seem to do not remarkably bad or remarkably good. There is no adverse signal for biologics, but being on prednisone [at a dose of] more than 10 mg is not great,” said Dr. Calabrese, who also noted that other publications have supported these conclusions.
So given these findings, how should clinicians address patient concerns? In the absence of probable exposure, “we say it’s better to have a well-controlled IMID on therapy than a poorly-controlled IMID on submaximal therapy. We say stick to therapy and try to wean the prednisone down as low as possible,” Dr. Calabrese said.
More controversially, what should patients do if they have had a significant exposure, such as a close proximity, prolonged exposure encounter with an individual with documented COVID-19, or at high-risk of disease? Dr. Calabrese noted that the American College of Rheumatology (ACR) guidelines recommend that low-level immunomodulation can be continued, “with an asterisk if it’s hydroxychloroquine, and it is in most of our minds now that we know that it is not effective, and the toxicity in the COVID setting is still being worked out,” he said.
With respect to other immunosuppressants, the ACR recommends stopping them temporarily, although IL-6 inhibitors may be continued in select circumstances. Resumption of the therapeutics can resume after a negative COVID test or completion of a 2-week observation period.
When patients contract COVID-19, antimalarial medications can be continued because they have been studied. “But medium-level immunomodulators, in particular methotrexate, I have grave concerns about because it can inhibit the adaptive immune response and antibody formation,” he said. COVID-19 is a serious infection, and all serious biologics have a package insert saying to stop them in a serious infection. Again, IL-6 inhibitors may be considered an exception in the right circumstances. When to resume these medications remains unknown. “I think that’s a work in progress. Test-based versus clinic-based strategies are a matter of controversy,” Dr. Calabrese said.
Ultimately, the question of what to do with immunosuppressive therapies in this population will continue to be a challenge. “The only good answer is to follow the rules of social distancing and to wear a mask,” said Kristina Callis Duffin, MD, a cochair of the department of dermatology and associate professor of dermatology at the University of Utah, Salt Lake City.
COVID-19 has posed serious questions for patients with psoriatic disease and the clinicians who treat them. Both have serious concerns over whether psoriasis or the medications used to treat it pose additional risk for contracting COVID-19 or experiencing worse outcomes with illness.
At the virtual annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis, experts gathered to discuss these concerns and what is known about the special risk factors for psoriatic disease patients.
Studies from a few registries have been done already among patients with autoimmune disease, and the results so far suggest that patients may be able to breathe a little easier. “I don’t see any data that suggests that use of immunosuppressives or having autoimmune disease increases your risk of acquiring it. I think most of the risk is driven by risk of exposure,” said Kevin Winthrop, MD, MPH, a professor of public health, infectious diseases, ophthalmology at Oregon Health & Science University, Portland, during a presentation.
That assertion was reinforced by data presented by Rebecca Haberman, MD, a rheumatologist at New York University Langone Health. Her group created the Web-Based Assessment of Autoimmune, Immune-Mediated, and Rheumatic Patients during the COVID-19 Pandemic (WARCOV) cohort study to address the question of whether patients with immune-mediated inflammatory disease (IMID), including inflammatory arthritis, psoriasis, or inflammatory bowel disease, should discontinue or modify their immunotherapy regimens in the face of potential exposure to COVID-19.
To date, the study has data on 1,122 patients; 604 with inflammatory arthritis, 128 of whom have tested positive for COVID-19. The team established a cohort using the first 86 IMID patients confirmed to have contracted COVID-19. The hospitalization rate was 16% overall, and use of corticosteroids was associated with increased hospitalization risk. A follow-up analysis looking at the first 103 inflammatory arthritis patients who contracted COVID-19 showed a hospitalization rate of 26% and a mortality of 4%. That hospitalization rate is similar to the general hospitalization rate estimated by the New York Department of Health, Dr. Haberman said in her presentation.
Risk factors associated with hospitalization included being older and having asthma or COPD, which is similar to the general population. Use of oral glucocorticoids was linked to a big increase in risk for hospitalization, even with doses less than 10 mg prednisone daily (odds ratio, 14.31; 95% confidence interval, 3.55-57.70). There were no links between use of any cytokine therapy and risk, but use of TNF inhibitors was associated with a reduced risk (OR, 0.35; 95% CI, 0.13-0.97), while use of JAK inhibitors was associated with greater risk (OR, 6.30; 95% CI, 1.68-23.69). The latter result is tentative because of a small sample size, and it was driven largely by the experiences of patients with psoriatic arthritis.
Another study, run by the COVID-19 Global Rheumatology Alliance, looked at 600 patients with rheumatic disease from 40 countries, and “found no smoking gun,” said Leonard Calabrese, DO, who leads the Cleveland Clinic’s section of clinical immunology, during his presentation. “People can develop this when they’re on hydroxychloroquine. They seem to do not remarkably bad or remarkably good. There is no adverse signal for biologics, but being on prednisone [at a dose of] more than 10 mg is not great,” said Dr. Calabrese, who also noted that other publications have supported these conclusions.
So given these findings, how should clinicians address patient concerns? In the absence of probable exposure, “we say it’s better to have a well-controlled IMID on therapy than a poorly-controlled IMID on submaximal therapy. We say stick to therapy and try to wean the prednisone down as low as possible,” Dr. Calabrese said.
More controversially, what should patients do if they have had a significant exposure, such as a close proximity, prolonged exposure encounter with an individual with documented COVID-19, or at high-risk of disease? Dr. Calabrese noted that the American College of Rheumatology (ACR) guidelines recommend that low-level immunomodulation can be continued, “with an asterisk if it’s hydroxychloroquine, and it is in most of our minds now that we know that it is not effective, and the toxicity in the COVID setting is still being worked out,” he said.
With respect to other immunosuppressants, the ACR recommends stopping them temporarily, although IL-6 inhibitors may be continued in select circumstances. Resumption of the therapeutics can resume after a negative COVID test or completion of a 2-week observation period.
When patients contract COVID-19, antimalarial medications can be continued because they have been studied. “But medium-level immunomodulators, in particular methotrexate, I have grave concerns about because it can inhibit the adaptive immune response and antibody formation,” he said. COVID-19 is a serious infection, and all serious biologics have a package insert saying to stop them in a serious infection. Again, IL-6 inhibitors may be considered an exception in the right circumstances. When to resume these medications remains unknown. “I think that’s a work in progress. Test-based versus clinic-based strategies are a matter of controversy,” Dr. Calabrese said.
Ultimately, the question of what to do with immunosuppressive therapies in this population will continue to be a challenge. “The only good answer is to follow the rules of social distancing and to wear a mask,” said Kristina Callis Duffin, MD, a cochair of the department of dermatology and associate professor of dermatology at the University of Utah, Salt Lake City.
FROM THE GRAPPA 2020 VIRTUAL ANNUAL MEETING
Don’t overlook treating older patients with acute promyelocytic leukemia, expert says
The estimated one third of patients with acute promyelocytic leukemia (APL) who are older than 60 years now enjoy a notably better prognosis than in years past, thanks to the introduction of all-trans retinoic acid (ATRA) and arsenic trioxide (ATO). However, such patients still require special management considerations, and can only benefit from treatment advantages if properly identified.
In a recently published set of recommendations, the International Society of Geriatric Oncology Task Force outlined the latest information on the treatment of APL in older patients. Medscape spoke with the lead author of the article, Heidi Klepin, MD, MS, professor in the section on hematology and oncology at Wake Forest School of Medicine in Winston Salem, N.C., who highlighted the key points that clinicians need to know about this often highly treatable subtype of acute myeloid leukemia (AML). This interview has been edited for length and clarity.
Medscape: How do the potential benefits of therapy for APL compare with other AML subtypes in older persons?
Dr. Klepin: Potential benefits of therapy are dramatically better for APL, compared with other AML subtypes. The use of non–chemotherapy based regimens with ATRA and ATO has substantially changed options for APL management. ATRA+ATO are associated with high remission and cure rates. The chance of cure with less toxicity extends the clinical benefit to adults of advanced age and, to some extent, with comorbidities.
How has the management strategy for this subgroup of patients with APL changed in recent years?
Management options have changed dramatically with the advent of non–chemotherapy-based regimens. The majority of treated older adults could be expected to achieve remissions that are durable, with less risk of major side effects during treatment. Adults with comorbid conditions, at advanced age, and with some functional limitations could also still benefit from treatment.
Does that management strategy change based on whether patients are considered low-risk or high-risk?
Clinical trials are lacking to provide best evidence for the optimal treatment for adults over age 70 years. However, based on available data and experience, the expert consensus provided in this report recommends that older adults regardless of age with low-risk disease should be offered ATRA+ATO–based therapy if available.
The optimal approach for patients with high-risk disease is less clear based on available studies. For fit older adults without cardiac disease, the use of single-drug anthracycline chemotherapy with ATRA plus/minus ATO is appropriate. However, treatment with ATRA+ATO may also provide a good response with less side-effect risk. For older patients with high-risk disease and comorbidity or poor functional status, the use of non-chemotherapy regimen ATRA+ATO is preferred.
What role does frailty have in making treatment decisions in this population?
Although frail older adults have not been specifically studied in clinical trials, it is reasonable to offer treatment with a non–chemotherapy based regimen for many of these patients, particularly if frailty may in part be related to disease burden. Frailty is a dynamic state. Rapid initiation of therapy can improve function and symptoms, potentially reversing the phenotype of frailty if driven largely by disease burden.
What is the role of consolidation and maintenance therapy in older patients with APL?
Consolidation therapy is recommended with ATRA+ATO as a standard consideration for most patients when available, although protocol-based treatments may vary. For those older adults treated with chemotherapy+ATRA for high-risk disease, decreased anthracycline [chemotherapy] exposure during consolidation results in less mortality risk. Maintenance therapy is not needed when ATRA+ATO are used for induction and consolidation and after achieving a molecular remission.
What other patient factors should influence treatment decisions?
In practice, older age, concurrent comorbid conditions [particularly cardiac disease], and physical function may all influence treatment decisions. Regarding the disease itself, a high white blood cell count at diagnosis, which is classified as higher-risk disease, directs choice of therapy, particularly for fit older adults. Cardiac disease can limit certain treatment options because of risk of side effects. In particular, the use of anthracycline chemotherapy is contraindicated for people with heart failure, and the use of ATO can increase risk of arrhythmia and is not used with certain EKG findings.
Special considerations in older patients with APL
How would you characterize older individuals’ involvement in clinical trials?
Older adults are underrepresented on clinical trials, with very limited inclusion of those over age 75 years. Some APL trials have had upper age exclusions, which is something we have advocated to remove.
Are there unique challenges in diagnosing older adults with APL?
The presentation of APL with low blood counts can look similar to other types of AML or myelodysplastic syndrome when reviewing routine lab results. If additional testing is not done quickly, the diagnosis will be missed, as well as the opportunity for effective treatment. Rapid diagnosis is essential in this disease.
Are there age-related differences in the presentation of APL?
There are no available data to support more-aggressive APL biology in older adults.
How does age impact the outcomes of patients with APL?
Although the outcomes in APL have improved, the survival difference between age groups has not decreased in recent years and the magnitude of improvement in survival in older patients still lags behind younger patients. Older age is also associated with worse outcomes driven largely by increased early death, with greater rates of infection and multiorgan failure leading to a decreased overall survival.
How important is a geriatric assessment for older patients with APL? What role does it play in management?
There are no data on the use of a geriatric assessment specifically in APL, although a geriatric assessment is recommended for older adults starting new chemotherapy in general. A geriatric assessment may help determine who is fit enough to be treated like a younger patient, which has the greatest implications for those with high-risk disease where chemotherapy would be added.
A geriatric assessment can also play an important role in management by identifying vulnerabilities that could be addressed to minimize complications during treatment regardless of the type of treatment given. An example would be identifying and addressing polypharmacy (commonly defined as ≥5 medications). One challenge faced when treating older patients is the use of multiple concomitant medications. Polypharmacy is common among older patients with cancer. Among older adults, each new drug increases the risk of adverse drug events by 10%. Drugs commonly used for the treatment of APL, such as ATRA and ATO, have many potential drug interactions, which must be carefully assessed by a pharmacist prior to and during treatment. Active deprescribing of medications that are not critical during treatment for APL should be done to minimize risks.
What is differentiation syndrome? What role does age appear to play in the risk of developing it and in strategies for managing it?
Differentiation syndrome is a serious side effect that may occur in patients with APL who have been treated with certain anticancer drugs. Differentiation syndrome usually occurs within a week or 2 of starting treatment. It is caused by a large, rapid release of cytokines [immune substances] from leukemia cells. The most common symptoms include fever; cough; shortness of breath; weight gain; swelling of the arms, legs, and neck; build-up of excess fluid around the heart and lungs; low blood pressure; and kidney failure. Differentiation syndrome can be life-threatening if not recognized and treated early.
Some evidence suggests older adults may be at a higher risk for developing differentiation syndrome and may be less likely to tolerate it. A risk factor is kidney dysfunction, which is more common in older adults.
It is not clear that management should differ by age, but vigilance is critical. The use of prophylactic steroids is considered for high-risk patients [high white cell count or kidney disease]. The treatment for differentiation syndrome involves rapid use of steroids.
Does the management of infections differ in older people with APL?
There is no clear data to support a different management of infection prevention for older adults, although preventive antibiotics can be considered as older adults are at a higher risk for infectious complications. However, drug interactions need to be carefully considered in this context.
Guiding clinicians toward better treatment of APL
Why did you decide to formulate these recommendations now?
It is particularly important to draw attention to the management of older adults with APL given the availability of effective non–chemotherapy based therapies and the large distinction between expected outcomes with APL vs. other types of acute leukemia in this population. This diagnosis should not be missed. Further, we highlight the importance of ensuring that older adults are included in trials to provide best evidence for both treatment choice and supportive care management.
How do you see these recommendations affecting clinical practice?
We want to emphasize that advanced age should not preclude treatment, which can have meaningful benefit with expectation of remission and quality time gained.
We hope that these recommendations provide a useful blueprint for guiding the management of older adults, particularly consolidating information to help inform treatment for those patients older than 75 years that can provide best estimates of side effects and benefits when making a decision with patients. We also hope that these recommendations will be used to educate providers on the importance of looking for this diagnosis in our older patients.
From a practical standpoint, it will be important that this information gets to those providers who are making the referrals to oncologists, which can include primary care physicians and emergency room providers, to ensure prompt diagnostic workup. Treatment decisions can only be made once a diagnosis has been recognized, and time is critical with this disease.
Dr. Klepin disclosed a consultancy for Genentech and Pfizer and is a contributor to UpToDate.
A version of this article originally appeared on Medscape.com.
The estimated one third of patients with acute promyelocytic leukemia (APL) who are older than 60 years now enjoy a notably better prognosis than in years past, thanks to the introduction of all-trans retinoic acid (ATRA) and arsenic trioxide (ATO). However, such patients still require special management considerations, and can only benefit from treatment advantages if properly identified.
In a recently published set of recommendations, the International Society of Geriatric Oncology Task Force outlined the latest information on the treatment of APL in older patients. Medscape spoke with the lead author of the article, Heidi Klepin, MD, MS, professor in the section on hematology and oncology at Wake Forest School of Medicine in Winston Salem, N.C., who highlighted the key points that clinicians need to know about this often highly treatable subtype of acute myeloid leukemia (AML). This interview has been edited for length and clarity.
Medscape: How do the potential benefits of therapy for APL compare with other AML subtypes in older persons?
Dr. Klepin: Potential benefits of therapy are dramatically better for APL, compared with other AML subtypes. The use of non–chemotherapy based regimens with ATRA and ATO has substantially changed options for APL management. ATRA+ATO are associated with high remission and cure rates. The chance of cure with less toxicity extends the clinical benefit to adults of advanced age and, to some extent, with comorbidities.
How has the management strategy for this subgroup of patients with APL changed in recent years?
Management options have changed dramatically with the advent of non–chemotherapy-based regimens. The majority of treated older adults could be expected to achieve remissions that are durable, with less risk of major side effects during treatment. Adults with comorbid conditions, at advanced age, and with some functional limitations could also still benefit from treatment.
Does that management strategy change based on whether patients are considered low-risk or high-risk?
Clinical trials are lacking to provide best evidence for the optimal treatment for adults over age 70 years. However, based on available data and experience, the expert consensus provided in this report recommends that older adults regardless of age with low-risk disease should be offered ATRA+ATO–based therapy if available.
The optimal approach for patients with high-risk disease is less clear based on available studies. For fit older adults without cardiac disease, the use of single-drug anthracycline chemotherapy with ATRA plus/minus ATO is appropriate. However, treatment with ATRA+ATO may also provide a good response with less side-effect risk. For older patients with high-risk disease and comorbidity or poor functional status, the use of non-chemotherapy regimen ATRA+ATO is preferred.
What role does frailty have in making treatment decisions in this population?
Although frail older adults have not been specifically studied in clinical trials, it is reasonable to offer treatment with a non–chemotherapy based regimen for many of these patients, particularly if frailty may in part be related to disease burden. Frailty is a dynamic state. Rapid initiation of therapy can improve function and symptoms, potentially reversing the phenotype of frailty if driven largely by disease burden.
What is the role of consolidation and maintenance therapy in older patients with APL?
Consolidation therapy is recommended with ATRA+ATO as a standard consideration for most patients when available, although protocol-based treatments may vary. For those older adults treated with chemotherapy+ATRA for high-risk disease, decreased anthracycline [chemotherapy] exposure during consolidation results in less mortality risk. Maintenance therapy is not needed when ATRA+ATO are used for induction and consolidation and after achieving a molecular remission.
What other patient factors should influence treatment decisions?
In practice, older age, concurrent comorbid conditions [particularly cardiac disease], and physical function may all influence treatment decisions. Regarding the disease itself, a high white blood cell count at diagnosis, which is classified as higher-risk disease, directs choice of therapy, particularly for fit older adults. Cardiac disease can limit certain treatment options because of risk of side effects. In particular, the use of anthracycline chemotherapy is contraindicated for people with heart failure, and the use of ATO can increase risk of arrhythmia and is not used with certain EKG findings.
Special considerations in older patients with APL
How would you characterize older individuals’ involvement in clinical trials?
Older adults are underrepresented on clinical trials, with very limited inclusion of those over age 75 years. Some APL trials have had upper age exclusions, which is something we have advocated to remove.
Are there unique challenges in diagnosing older adults with APL?
The presentation of APL with low blood counts can look similar to other types of AML or myelodysplastic syndrome when reviewing routine lab results. If additional testing is not done quickly, the diagnosis will be missed, as well as the opportunity for effective treatment. Rapid diagnosis is essential in this disease.
Are there age-related differences in the presentation of APL?
There are no available data to support more-aggressive APL biology in older adults.
How does age impact the outcomes of patients with APL?
Although the outcomes in APL have improved, the survival difference between age groups has not decreased in recent years and the magnitude of improvement in survival in older patients still lags behind younger patients. Older age is also associated with worse outcomes driven largely by increased early death, with greater rates of infection and multiorgan failure leading to a decreased overall survival.
How important is a geriatric assessment for older patients with APL? What role does it play in management?
There are no data on the use of a geriatric assessment specifically in APL, although a geriatric assessment is recommended for older adults starting new chemotherapy in general. A geriatric assessment may help determine who is fit enough to be treated like a younger patient, which has the greatest implications for those with high-risk disease where chemotherapy would be added.
A geriatric assessment can also play an important role in management by identifying vulnerabilities that could be addressed to minimize complications during treatment regardless of the type of treatment given. An example would be identifying and addressing polypharmacy (commonly defined as ≥5 medications). One challenge faced when treating older patients is the use of multiple concomitant medications. Polypharmacy is common among older patients with cancer. Among older adults, each new drug increases the risk of adverse drug events by 10%. Drugs commonly used for the treatment of APL, such as ATRA and ATO, have many potential drug interactions, which must be carefully assessed by a pharmacist prior to and during treatment. Active deprescribing of medications that are not critical during treatment for APL should be done to minimize risks.
What is differentiation syndrome? What role does age appear to play in the risk of developing it and in strategies for managing it?
Differentiation syndrome is a serious side effect that may occur in patients with APL who have been treated with certain anticancer drugs. Differentiation syndrome usually occurs within a week or 2 of starting treatment. It is caused by a large, rapid release of cytokines [immune substances] from leukemia cells. The most common symptoms include fever; cough; shortness of breath; weight gain; swelling of the arms, legs, and neck; build-up of excess fluid around the heart and lungs; low blood pressure; and kidney failure. Differentiation syndrome can be life-threatening if not recognized and treated early.
Some evidence suggests older adults may be at a higher risk for developing differentiation syndrome and may be less likely to tolerate it. A risk factor is kidney dysfunction, which is more common in older adults.
It is not clear that management should differ by age, but vigilance is critical. The use of prophylactic steroids is considered for high-risk patients [high white cell count or kidney disease]. The treatment for differentiation syndrome involves rapid use of steroids.
Does the management of infections differ in older people with APL?
There is no clear data to support a different management of infection prevention for older adults, although preventive antibiotics can be considered as older adults are at a higher risk for infectious complications. However, drug interactions need to be carefully considered in this context.
Guiding clinicians toward better treatment of APL
Why did you decide to formulate these recommendations now?
It is particularly important to draw attention to the management of older adults with APL given the availability of effective non–chemotherapy based therapies and the large distinction between expected outcomes with APL vs. other types of acute leukemia in this population. This diagnosis should not be missed. Further, we highlight the importance of ensuring that older adults are included in trials to provide best evidence for both treatment choice and supportive care management.
How do you see these recommendations affecting clinical practice?
We want to emphasize that advanced age should not preclude treatment, which can have meaningful benefit with expectation of remission and quality time gained.
We hope that these recommendations provide a useful blueprint for guiding the management of older adults, particularly consolidating information to help inform treatment for those patients older than 75 years that can provide best estimates of side effects and benefits when making a decision with patients. We also hope that these recommendations will be used to educate providers on the importance of looking for this diagnosis in our older patients.
From a practical standpoint, it will be important that this information gets to those providers who are making the referrals to oncologists, which can include primary care physicians and emergency room providers, to ensure prompt diagnostic workup. Treatment decisions can only be made once a diagnosis has been recognized, and time is critical with this disease.
Dr. Klepin disclosed a consultancy for Genentech and Pfizer and is a contributor to UpToDate.
A version of this article originally appeared on Medscape.com.
The estimated one third of patients with acute promyelocytic leukemia (APL) who are older than 60 years now enjoy a notably better prognosis than in years past, thanks to the introduction of all-trans retinoic acid (ATRA) and arsenic trioxide (ATO). However, such patients still require special management considerations, and can only benefit from treatment advantages if properly identified.
In a recently published set of recommendations, the International Society of Geriatric Oncology Task Force outlined the latest information on the treatment of APL in older patients. Medscape spoke with the lead author of the article, Heidi Klepin, MD, MS, professor in the section on hematology and oncology at Wake Forest School of Medicine in Winston Salem, N.C., who highlighted the key points that clinicians need to know about this often highly treatable subtype of acute myeloid leukemia (AML). This interview has been edited for length and clarity.
Medscape: How do the potential benefits of therapy for APL compare with other AML subtypes in older persons?
Dr. Klepin: Potential benefits of therapy are dramatically better for APL, compared with other AML subtypes. The use of non–chemotherapy based regimens with ATRA and ATO has substantially changed options for APL management. ATRA+ATO are associated with high remission and cure rates. The chance of cure with less toxicity extends the clinical benefit to adults of advanced age and, to some extent, with comorbidities.
How has the management strategy for this subgroup of patients with APL changed in recent years?
Management options have changed dramatically with the advent of non–chemotherapy-based regimens. The majority of treated older adults could be expected to achieve remissions that are durable, with less risk of major side effects during treatment. Adults with comorbid conditions, at advanced age, and with some functional limitations could also still benefit from treatment.
Does that management strategy change based on whether patients are considered low-risk or high-risk?
Clinical trials are lacking to provide best evidence for the optimal treatment for adults over age 70 years. However, based on available data and experience, the expert consensus provided in this report recommends that older adults regardless of age with low-risk disease should be offered ATRA+ATO–based therapy if available.
The optimal approach for patients with high-risk disease is less clear based on available studies. For fit older adults without cardiac disease, the use of single-drug anthracycline chemotherapy with ATRA plus/minus ATO is appropriate. However, treatment with ATRA+ATO may also provide a good response with less side-effect risk. For older patients with high-risk disease and comorbidity or poor functional status, the use of non-chemotherapy regimen ATRA+ATO is preferred.
What role does frailty have in making treatment decisions in this population?
Although frail older adults have not been specifically studied in clinical trials, it is reasonable to offer treatment with a non–chemotherapy based regimen for many of these patients, particularly if frailty may in part be related to disease burden. Frailty is a dynamic state. Rapid initiation of therapy can improve function and symptoms, potentially reversing the phenotype of frailty if driven largely by disease burden.
What is the role of consolidation and maintenance therapy in older patients with APL?
Consolidation therapy is recommended with ATRA+ATO as a standard consideration for most patients when available, although protocol-based treatments may vary. For those older adults treated with chemotherapy+ATRA for high-risk disease, decreased anthracycline [chemotherapy] exposure during consolidation results in less mortality risk. Maintenance therapy is not needed when ATRA+ATO are used for induction and consolidation and after achieving a molecular remission.
What other patient factors should influence treatment decisions?
In practice, older age, concurrent comorbid conditions [particularly cardiac disease], and physical function may all influence treatment decisions. Regarding the disease itself, a high white blood cell count at diagnosis, which is classified as higher-risk disease, directs choice of therapy, particularly for fit older adults. Cardiac disease can limit certain treatment options because of risk of side effects. In particular, the use of anthracycline chemotherapy is contraindicated for people with heart failure, and the use of ATO can increase risk of arrhythmia and is not used with certain EKG findings.
Special considerations in older patients with APL
How would you characterize older individuals’ involvement in clinical trials?
Older adults are underrepresented on clinical trials, with very limited inclusion of those over age 75 years. Some APL trials have had upper age exclusions, which is something we have advocated to remove.
Are there unique challenges in diagnosing older adults with APL?
The presentation of APL with low blood counts can look similar to other types of AML or myelodysplastic syndrome when reviewing routine lab results. If additional testing is not done quickly, the diagnosis will be missed, as well as the opportunity for effective treatment. Rapid diagnosis is essential in this disease.
Are there age-related differences in the presentation of APL?
There are no available data to support more-aggressive APL biology in older adults.
How does age impact the outcomes of patients with APL?
Although the outcomes in APL have improved, the survival difference between age groups has not decreased in recent years and the magnitude of improvement in survival in older patients still lags behind younger patients. Older age is also associated with worse outcomes driven largely by increased early death, with greater rates of infection and multiorgan failure leading to a decreased overall survival.
How important is a geriatric assessment for older patients with APL? What role does it play in management?
There are no data on the use of a geriatric assessment specifically in APL, although a geriatric assessment is recommended for older adults starting new chemotherapy in general. A geriatric assessment may help determine who is fit enough to be treated like a younger patient, which has the greatest implications for those with high-risk disease where chemotherapy would be added.
A geriatric assessment can also play an important role in management by identifying vulnerabilities that could be addressed to minimize complications during treatment regardless of the type of treatment given. An example would be identifying and addressing polypharmacy (commonly defined as ≥5 medications). One challenge faced when treating older patients is the use of multiple concomitant medications. Polypharmacy is common among older patients with cancer. Among older adults, each new drug increases the risk of adverse drug events by 10%. Drugs commonly used for the treatment of APL, such as ATRA and ATO, have many potential drug interactions, which must be carefully assessed by a pharmacist prior to and during treatment. Active deprescribing of medications that are not critical during treatment for APL should be done to minimize risks.
What is differentiation syndrome? What role does age appear to play in the risk of developing it and in strategies for managing it?
Differentiation syndrome is a serious side effect that may occur in patients with APL who have been treated with certain anticancer drugs. Differentiation syndrome usually occurs within a week or 2 of starting treatment. It is caused by a large, rapid release of cytokines [immune substances] from leukemia cells. The most common symptoms include fever; cough; shortness of breath; weight gain; swelling of the arms, legs, and neck; build-up of excess fluid around the heart and lungs; low blood pressure; and kidney failure. Differentiation syndrome can be life-threatening if not recognized and treated early.
Some evidence suggests older adults may be at a higher risk for developing differentiation syndrome and may be less likely to tolerate it. A risk factor is kidney dysfunction, which is more common in older adults.
It is not clear that management should differ by age, but vigilance is critical. The use of prophylactic steroids is considered for high-risk patients [high white cell count or kidney disease]. The treatment for differentiation syndrome involves rapid use of steroids.
Does the management of infections differ in older people with APL?
There is no clear data to support a different management of infection prevention for older adults, although preventive antibiotics can be considered as older adults are at a higher risk for infectious complications. However, drug interactions need to be carefully considered in this context.
Guiding clinicians toward better treatment of APL
Why did you decide to formulate these recommendations now?
It is particularly important to draw attention to the management of older adults with APL given the availability of effective non–chemotherapy based therapies and the large distinction between expected outcomes with APL vs. other types of acute leukemia in this population. This diagnosis should not be missed. Further, we highlight the importance of ensuring that older adults are included in trials to provide best evidence for both treatment choice and supportive care management.
How do you see these recommendations affecting clinical practice?
We want to emphasize that advanced age should not preclude treatment, which can have meaningful benefit with expectation of remission and quality time gained.
We hope that these recommendations provide a useful blueprint for guiding the management of older adults, particularly consolidating information to help inform treatment for those patients older than 75 years that can provide best estimates of side effects and benefits when making a decision with patients. We also hope that these recommendations will be used to educate providers on the importance of looking for this diagnosis in our older patients.
From a practical standpoint, it will be important that this information gets to those providers who are making the referrals to oncologists, which can include primary care physicians and emergency room providers, to ensure prompt diagnostic workup. Treatment decisions can only be made once a diagnosis has been recognized, and time is critical with this disease.
Dr. Klepin disclosed a consultancy for Genentech and Pfizer and is a contributor to UpToDate.
A version of this article originally appeared on Medscape.com.
Rupioid Psoriasis and Psoriatic Arthritis in a Patient With Skin of Color
To the Editor:
A 49-year-old black woman presented with multiple hyperkeratotic papules that progressed over the last 2 months to circular plaques with central thick black crust resembling eschar. She first noticed these lesions as firm, small, black papules on the legs and continued to develop new lesions that eventually evolved into large, coin-shaped, hyperkeratotic plaques. Her medical history was notable for stage III non-Hodgkin follicular lymphoma in remission after treatment with rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate, and prednisone 7 months earlier, and chronic hepatitis B infection being treated with entecavir. Her family history was not remarkable for psoriasis or inflammatory arthritis.
She initially was seen by internal medicine and was started on topical triamcinolone with no improvement of the lesions. At presentation to dermatology, physical examination revealed firm, small, black, hyperkeratotic papules (Figure 1A) and circular plaques with a rim of erythema and central thick, smooth, black crust resembling eschar (Figure 1B). No other skin changes were noted at the time. The bilateral metacarpophalangeal, bilateral proximal interphalangeal, left wrist, and bilateral ankle joints were remarkable for tenderness, swelling, and reduced range of motion. She noted concomitant arthralgia and stiffness but denied fever. She had no other systemic symptoms including night sweats, weight loss, fatigue, malaise, sun sensitivity, oral ulcers, or hair loss. A radiograph of the hand was negative for erosive changes but showed mild periarticular osteopenia and fusiform soft tissue swelling of the third digit. Given the central appearance of eschar in the larger lesions, the initial differential diagnosis included Sweet syndrome, invasive fungal infection, vasculitis, and recurrent lymphoma.

A 4-mm punch biopsy specimen of a representative lesion on the right leg revealed psoriasiform epidermal hyperplasia, parakeratosis, neutrophils in the stratum corneum and spinosum, elongation of the rete ridges, and superficial vascular ectasia, which favored a diagnosis of psoriasis (Figure 2). A periodic acid-Schiff stain was negative for fungal hyphae. Fungal culture, bacterial tissue culture, and acid-fast bacilli smear were negative. Absence of deep dermal inflammation precluded a diagnosis of Sweet syndrome. Further notable laboratory studies included negative human immunodeficiency virus (HIV) antibody, rapid plasma reagin, hepatitis C antibody, and rheumatoid factor.
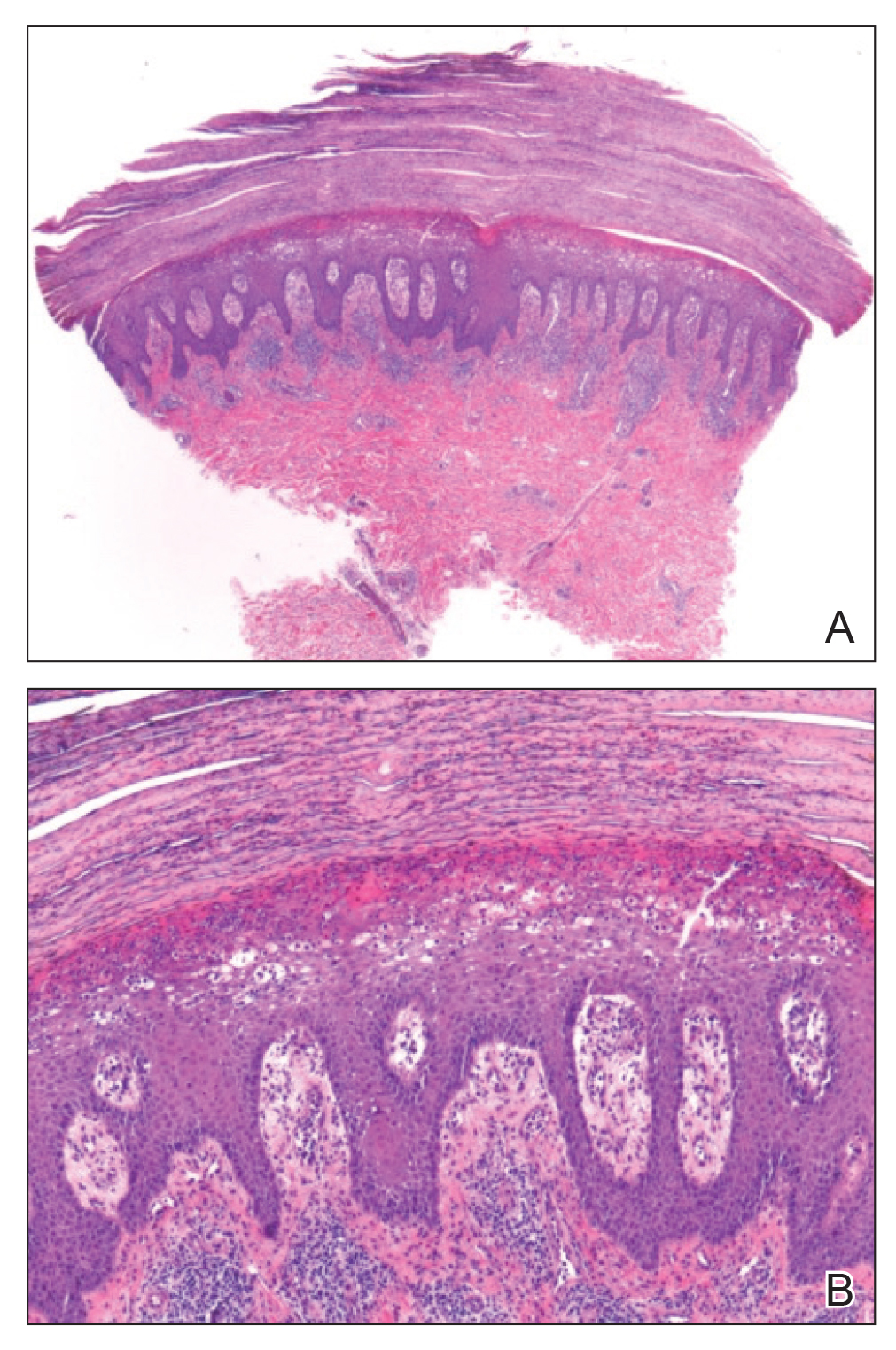
At follow-up 2 weeks later, the initial lesions were still present, and she had developed new widespread, well-demarcated, erythematous plaques with silver scale along the scalp, back, chest, and abdomen that were more typical of psoriasis. Oil spots were noted on several fingernails and toenails. Based on the clinicopathologic findings, nail changes, and asymmetric inflammatory arthritis, a diagnosis of rupioid psoriasis with psoriatic arthritis (PsA) was established. Treatment with clobetasol ointment 0.05% twice daily to active lesions was started. Initiation of systemic therapy with a steroid-sparing agent was deferred in anticipation of care coordination with rheumatology, hepatology, and hematology/oncology due to the patient's history of follicular lymphoma and chronic hepatitis B. Although attempts were made to avoid systemic corticosteroids due to the risk for a psoriasis flare upon discontinuation, because of the severity of arthralgia she was started on oral prednisone 20 mg daily by rheumatology with plans for a slow taper once an alternative systemic agent was started.1
At 10-week follow-up, the patient had marked improvement of psoriatic plaques with no active lesions while only on prednisone 20 mg daily. In consultation with her care team, she subsequently was started on methotrexate 10 mg weekly for 2 weeks followed by titration to 15 mg weekly. Plans were to start a prednisone taper after a month of methotrexate to allow her new treatment time for therapeutic effect. Notably, the patient chose to discontinue prednisone 2 weeks into methotrexate therapy after only two 10-mg doses of methotrexate weekly and well before therapeutic levels were achieved. Despite stopping prednisone early and without a taper, she did not experience a relapse in psoriatic skin lesions. Three months following initiation of methotrexate, she sustained resolution of the cutaneous lesions with only residual postinflammatory hyperpigmentation.
Psoriasis is a common chronic inflammatory skin disorder with multiple clinical presentations. There are several variants of psoriasis that are classified by their morphologic appearance including chronic plaque, guttate, erythrodermic, and pustular, with more than 90% of cases representing the plaque variant. Less common clinical presentations of psoriasis include rupioid, ostraceous, inverse, elephantine, and HIV associated.2 Rupioid psoriasis is a rare variant that presents with cone-shaped, limpetlike lesions.3,4 Similar to the limited epidemiological and clinical data pertaining to psoriasis in nonwhite racial groups, there also is a paucity of documented reports of rupioid psoriasis in skin of color.
Rupioid comes from the Greek word rhupos, meaning dirt or filth, and is used to describe well-demarcated lesions with thick, yellow, dirty-appearing, adherent crusts resembling oyster shells with a surrounding rim of erythema.5 Rupioid psoriasis initially was reported in 1948 and remains an uncommon and infrequently reported variant.6 The majority of reported cases have been associated with arthropathy, similar to our patient.3,4 Rupioid lesions also have been observed in an array of other diseases, such as secondary syphilis, crusted scabies, disseminated histoplasmosis, HIV, reactive arthritis, and aminoaciduria.7-11
Diagnosis of rupioid psoriasis can be confirmed with a skin biopsy, which demonstrates characteristic histopathologic findings of psoriasis.3 Laboratory analysis should be performed to rule out other causes of rupioid lesions, and PsA should be differentiated from rheumatoid arthritis if arthropathy is present. In our case, serum rapid plasma reagin, anti-HIV antibody, rheumatoid factor, and fungal cultures were negative. Usin0)g clinical findings, histopathology, laboratory analyses, and radiograph findings, the diagnosis of rupioid psoriasis with PsA was confirmed in our patient.
Psoriasis was not originally suspected in our patient due to the noncharacteristic lesions with smooth black crust--similar appearing to eschar--and the patient's complicated medical history. Variations in the presentation of psoriasis among white individuals and those with skin of color have been reported in the literature.12,13 Psoriatic lesions in darker skin tones may appear more violaceous or hyperpigmented with more conspicuous erythema and thicker plaques. Our patient lacked the classic rupioid appearance of concentric circular layers of dirty, yellow, oysterlike scale, and instead had thick, lamellate, black crust. A PubMed search of articles indexed for MEDLINE using the terms rupioid, coral reef psoriasis, rupioides, and rhupus revealed no other cases of rupioid psoriasis reported in black patients and no cases detailing the variations of rupioid lesions in skin of color. A case of rupioid psoriasis has been reported in a Hispanic patient, but the described psoriatic lesions were more characteristic of the dirty-appearing, conic plaques previously reported.14 Our case highlights a unique example of the variable presentations of cutaneous disorders in skin of color and black patients.
Our patient's case of rupioid psoriasis with PsA presented unique challenges for systemic treatment due to her multiple comorbidities. Rupioid psoriasis most often is treated with combination topical and systemic therapy, with agents such as methotrexate and cyclosporine having prior success.3,4 This variant of psoriasis is highly responsive to treatment, and marked improvement of lesions has been achieved with topical steroids alone with proper adherence.15 Our patient was started on clobetasol ointment 0.05% while a systemic agent was debated for her PsA. Although she did not have improvement with topical therapy alone, she experienced rapid resolution of the skin lesions after initiation of low-dose prednisone 20 mg daily. Interestingly, our patient did not experience a flare of the skin lesions upon discontinuation of systemic steroids despite the lack of an appropriate taper and methotrexate not having reached therapeutic levels.
The clinical nuances of rupioid psoriasis in skin of color have not yet been described and remain an important diagnostic consideration. Our patient achieved remission of skin lesions with sequential treatment of topical clobetasol, a low-dose systemic steroid, and methotrexate. Based on available reports, rupioid psoriasis may represent a variant of psoriasis that is highly responsive to treatment.
- Mrowietz U, Domm S. Systemic steroids in the treatment of psoriasis: what is fact, what is fiction? J Eur Acad Dermatol Venereol. 2013;27:1022-1025.
- Goldsmith LA, Katz SI, Gilchrest BA, eds. Fitzpatrick's Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Wang JL, Yang JH. Rupioid psoriasis associated with arthropathy. J Dermatol. 1997;24:46-49.
- Murakami T, Ohtsuki M, Nakagawa H. Rupioid psoriasis with arthropathy. Clin Exp Dermatol. 2000;25:409-412.
- Chung HJ, Marley-Kemp D, Keller M. Rupioid psoriasis and other skin diseases with rupioid manifestations. Cutis. 2014;94:119-121.
- Salamon M, Omulecki A, Sysa-Jedrzejowska A, et al. Psoriasisrupioides: a rare variant of a common disease. Cutis. 2011;88:135-137.
- Krase IZ, Cavanaugh K, Curiel-Lewandrowski C. A case of rupioid syphilis. JAAD Case Rep. 2016;2:141-143.
- Garofalo V, Saraceno R, Milana M, et al. Crusted scabies in a liver transplant patient mimicking rupioid psoriasis. Eur J Dermatol. 2016;26:495-496.
- Corti M, Villafane MF, Palmieri O, et al. Rupioid histoplasmosis: first case reported in an AIDS patient in Argentina. Rev Inst Med Trop Sao Paulo. 2010;52:279-280.
- Sehgal VN, Koranne RV, Shyam Prasad AL. Unusual manifestations of Reiter's disease in a child. Dermatologica. 1985;170:77-79.
- Haim S, Gilhar A, Cohen A. Cutaneous manifestations associated with aminoaciduria. report of two cases. Dermatologica. 1978;156:244-250.
- McMichael AJ, Vachiramon V, Guzman-Sanchez DA, et al. Psoriasis in African-Americans: a caregivers' survey. J Drugs Dermatol. 2012;11:478-482.
- Alexis AF, Blackcloud P. Psoriasis in skin of color: epidemiology, genetics, clinical presentation, and treatment nuances. J Clin Aesthet Dermatol. 2014;7:16-24.
- Posligua A, Maldonado C, Gonzalez MG. Rupioid psoriasis preceded by varicella presenting as Koebner phenomenon. J Am Acad Dermatol. 2016;74(5 suppl 1):AB268.
- Feldman SR, Feldman S, Brown K, et al. "Coral reef" psoriasis: a marker of resistance to topical treatment. J Dermatolog Treat. 2008;19:257-258.
To the Editor:
A 49-year-old black woman presented with multiple hyperkeratotic papules that progressed over the last 2 months to circular plaques with central thick black crust resembling eschar. She first noticed these lesions as firm, small, black papules on the legs and continued to develop new lesions that eventually evolved into large, coin-shaped, hyperkeratotic plaques. Her medical history was notable for stage III non-Hodgkin follicular lymphoma in remission after treatment with rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate, and prednisone 7 months earlier, and chronic hepatitis B infection being treated with entecavir. Her family history was not remarkable for psoriasis or inflammatory arthritis.
She initially was seen by internal medicine and was started on topical triamcinolone with no improvement of the lesions. At presentation to dermatology, physical examination revealed firm, small, black, hyperkeratotic papules (Figure 1A) and circular plaques with a rim of erythema and central thick, smooth, black crust resembling eschar (Figure 1B). No other skin changes were noted at the time. The bilateral metacarpophalangeal, bilateral proximal interphalangeal, left wrist, and bilateral ankle joints were remarkable for tenderness, swelling, and reduced range of motion. She noted concomitant arthralgia and stiffness but denied fever. She had no other systemic symptoms including night sweats, weight loss, fatigue, malaise, sun sensitivity, oral ulcers, or hair loss. A radiograph of the hand was negative for erosive changes but showed mild periarticular osteopenia and fusiform soft tissue swelling of the third digit. Given the central appearance of eschar in the larger lesions, the initial differential diagnosis included Sweet syndrome, invasive fungal infection, vasculitis, and recurrent lymphoma.

A 4-mm punch biopsy specimen of a representative lesion on the right leg revealed psoriasiform epidermal hyperplasia, parakeratosis, neutrophils in the stratum corneum and spinosum, elongation of the rete ridges, and superficial vascular ectasia, which favored a diagnosis of psoriasis (Figure 2). A periodic acid-Schiff stain was negative for fungal hyphae. Fungal culture, bacterial tissue culture, and acid-fast bacilli smear were negative. Absence of deep dermal inflammation precluded a diagnosis of Sweet syndrome. Further notable laboratory studies included negative human immunodeficiency virus (HIV) antibody, rapid plasma reagin, hepatitis C antibody, and rheumatoid factor.
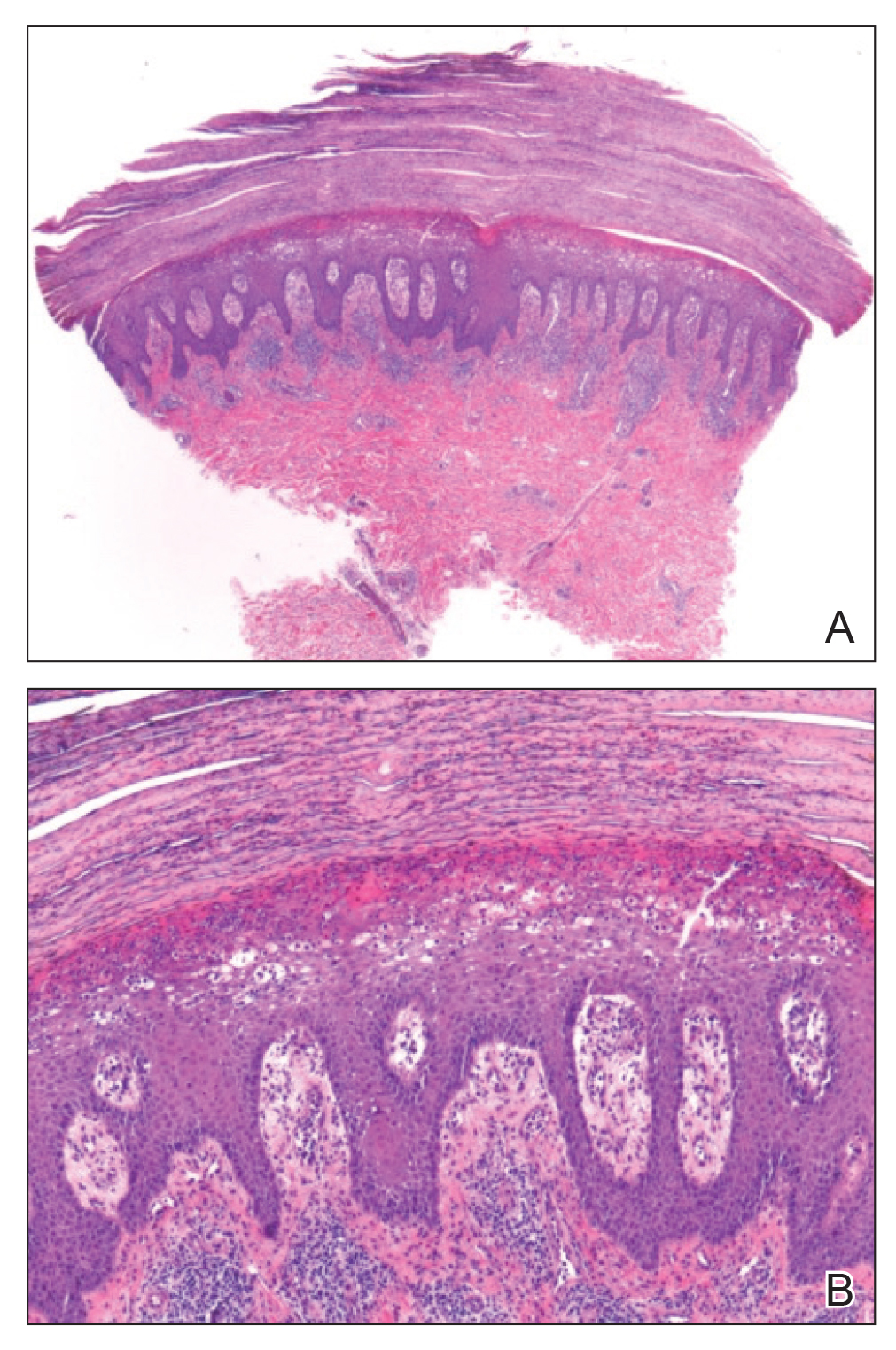
At follow-up 2 weeks later, the initial lesions were still present, and she had developed new widespread, well-demarcated, erythematous plaques with silver scale along the scalp, back, chest, and abdomen that were more typical of psoriasis. Oil spots were noted on several fingernails and toenails. Based on the clinicopathologic findings, nail changes, and asymmetric inflammatory arthritis, a diagnosis of rupioid psoriasis with psoriatic arthritis (PsA) was established. Treatment with clobetasol ointment 0.05% twice daily to active lesions was started. Initiation of systemic therapy with a steroid-sparing agent was deferred in anticipation of care coordination with rheumatology, hepatology, and hematology/oncology due to the patient's history of follicular lymphoma and chronic hepatitis B. Although attempts were made to avoid systemic corticosteroids due to the risk for a psoriasis flare upon discontinuation, because of the severity of arthralgia she was started on oral prednisone 20 mg daily by rheumatology with plans for a slow taper once an alternative systemic agent was started.1
At 10-week follow-up, the patient had marked improvement of psoriatic plaques with no active lesions while only on prednisone 20 mg daily. In consultation with her care team, she subsequently was started on methotrexate 10 mg weekly for 2 weeks followed by titration to 15 mg weekly. Plans were to start a prednisone taper after a month of methotrexate to allow her new treatment time for therapeutic effect. Notably, the patient chose to discontinue prednisone 2 weeks into methotrexate therapy after only two 10-mg doses of methotrexate weekly and well before therapeutic levels were achieved. Despite stopping prednisone early and without a taper, she did not experience a relapse in psoriatic skin lesions. Three months following initiation of methotrexate, she sustained resolution of the cutaneous lesions with only residual postinflammatory hyperpigmentation.
Psoriasis is a common chronic inflammatory skin disorder with multiple clinical presentations. There are several variants of psoriasis that are classified by their morphologic appearance including chronic plaque, guttate, erythrodermic, and pustular, with more than 90% of cases representing the plaque variant. Less common clinical presentations of psoriasis include rupioid, ostraceous, inverse, elephantine, and HIV associated.2 Rupioid psoriasis is a rare variant that presents with cone-shaped, limpetlike lesions.3,4 Similar to the limited epidemiological and clinical data pertaining to psoriasis in nonwhite racial groups, there also is a paucity of documented reports of rupioid psoriasis in skin of color.
Rupioid comes from the Greek word rhupos, meaning dirt or filth, and is used to describe well-demarcated lesions with thick, yellow, dirty-appearing, adherent crusts resembling oyster shells with a surrounding rim of erythema.5 Rupioid psoriasis initially was reported in 1948 and remains an uncommon and infrequently reported variant.6 The majority of reported cases have been associated with arthropathy, similar to our patient.3,4 Rupioid lesions also have been observed in an array of other diseases, such as secondary syphilis, crusted scabies, disseminated histoplasmosis, HIV, reactive arthritis, and aminoaciduria.7-11
Diagnosis of rupioid psoriasis can be confirmed with a skin biopsy, which demonstrates characteristic histopathologic findings of psoriasis.3 Laboratory analysis should be performed to rule out other causes of rupioid lesions, and PsA should be differentiated from rheumatoid arthritis if arthropathy is present. In our case, serum rapid plasma reagin, anti-HIV antibody, rheumatoid factor, and fungal cultures were negative. Usin0)g clinical findings, histopathology, laboratory analyses, and radiograph findings, the diagnosis of rupioid psoriasis with PsA was confirmed in our patient.
Psoriasis was not originally suspected in our patient due to the noncharacteristic lesions with smooth black crust--similar appearing to eschar--and the patient's complicated medical history. Variations in the presentation of psoriasis among white individuals and those with skin of color have been reported in the literature.12,13 Psoriatic lesions in darker skin tones may appear more violaceous or hyperpigmented with more conspicuous erythema and thicker plaques. Our patient lacked the classic rupioid appearance of concentric circular layers of dirty, yellow, oysterlike scale, and instead had thick, lamellate, black crust. A PubMed search of articles indexed for MEDLINE using the terms rupioid, coral reef psoriasis, rupioides, and rhupus revealed no other cases of rupioid psoriasis reported in black patients and no cases detailing the variations of rupioid lesions in skin of color. A case of rupioid psoriasis has been reported in a Hispanic patient, but the described psoriatic lesions were more characteristic of the dirty-appearing, conic plaques previously reported.14 Our case highlights a unique example of the variable presentations of cutaneous disorders in skin of color and black patients.
Our patient's case of rupioid psoriasis with PsA presented unique challenges for systemic treatment due to her multiple comorbidities. Rupioid psoriasis most often is treated with combination topical and systemic therapy, with agents such as methotrexate and cyclosporine having prior success.3,4 This variant of psoriasis is highly responsive to treatment, and marked improvement of lesions has been achieved with topical steroids alone with proper adherence.15 Our patient was started on clobetasol ointment 0.05% while a systemic agent was debated for her PsA. Although she did not have improvement with topical therapy alone, she experienced rapid resolution of the skin lesions after initiation of low-dose prednisone 20 mg daily. Interestingly, our patient did not experience a flare of the skin lesions upon discontinuation of systemic steroids despite the lack of an appropriate taper and methotrexate not having reached therapeutic levels.
The clinical nuances of rupioid psoriasis in skin of color have not yet been described and remain an important diagnostic consideration. Our patient achieved remission of skin lesions with sequential treatment of topical clobetasol, a low-dose systemic steroid, and methotrexate. Based on available reports, rupioid psoriasis may represent a variant of psoriasis that is highly responsive to treatment.
To the Editor:
A 49-year-old black woman presented with multiple hyperkeratotic papules that progressed over the last 2 months to circular plaques with central thick black crust resembling eschar. She first noticed these lesions as firm, small, black papules on the legs and continued to develop new lesions that eventually evolved into large, coin-shaped, hyperkeratotic plaques. Her medical history was notable for stage III non-Hodgkin follicular lymphoma in remission after treatment with rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate, and prednisone 7 months earlier, and chronic hepatitis B infection being treated with entecavir. Her family history was not remarkable for psoriasis or inflammatory arthritis.
She initially was seen by internal medicine and was started on topical triamcinolone with no improvement of the lesions. At presentation to dermatology, physical examination revealed firm, small, black, hyperkeratotic papules (Figure 1A) and circular plaques with a rim of erythema and central thick, smooth, black crust resembling eschar (Figure 1B). No other skin changes were noted at the time. The bilateral metacarpophalangeal, bilateral proximal interphalangeal, left wrist, and bilateral ankle joints were remarkable for tenderness, swelling, and reduced range of motion. She noted concomitant arthralgia and stiffness but denied fever. She had no other systemic symptoms including night sweats, weight loss, fatigue, malaise, sun sensitivity, oral ulcers, or hair loss. A radiograph of the hand was negative for erosive changes but showed mild periarticular osteopenia and fusiform soft tissue swelling of the third digit. Given the central appearance of eschar in the larger lesions, the initial differential diagnosis included Sweet syndrome, invasive fungal infection, vasculitis, and recurrent lymphoma.

A 4-mm punch biopsy specimen of a representative lesion on the right leg revealed psoriasiform epidermal hyperplasia, parakeratosis, neutrophils in the stratum corneum and spinosum, elongation of the rete ridges, and superficial vascular ectasia, which favored a diagnosis of psoriasis (Figure 2). A periodic acid-Schiff stain was negative for fungal hyphae. Fungal culture, bacterial tissue culture, and acid-fast bacilli smear were negative. Absence of deep dermal inflammation precluded a diagnosis of Sweet syndrome. Further notable laboratory studies included negative human immunodeficiency virus (HIV) antibody, rapid plasma reagin, hepatitis C antibody, and rheumatoid factor.
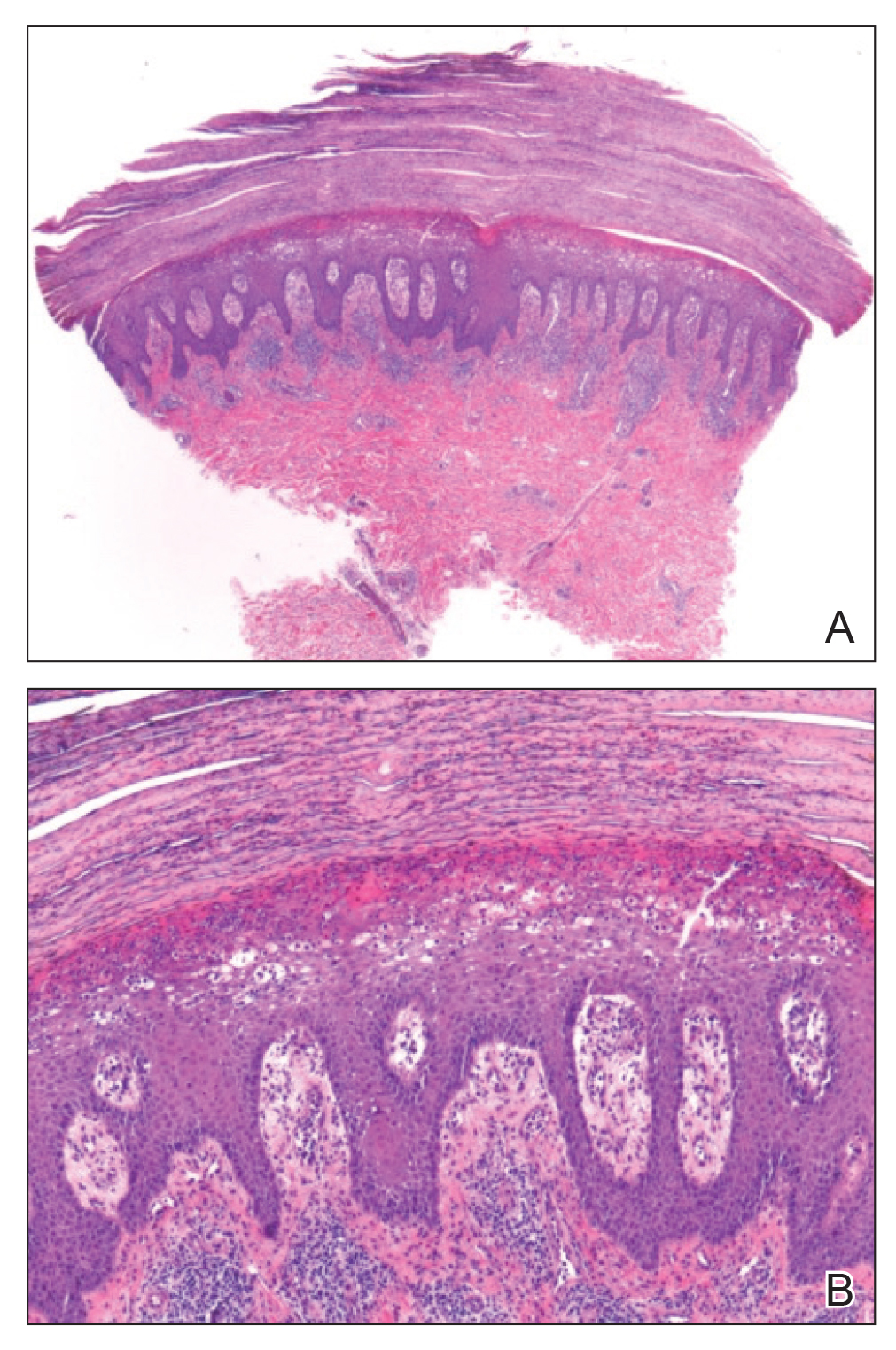
At follow-up 2 weeks later, the initial lesions were still present, and she had developed new widespread, well-demarcated, erythematous plaques with silver scale along the scalp, back, chest, and abdomen that were more typical of psoriasis. Oil spots were noted on several fingernails and toenails. Based on the clinicopathologic findings, nail changes, and asymmetric inflammatory arthritis, a diagnosis of rupioid psoriasis with psoriatic arthritis (PsA) was established. Treatment with clobetasol ointment 0.05% twice daily to active lesions was started. Initiation of systemic therapy with a steroid-sparing agent was deferred in anticipation of care coordination with rheumatology, hepatology, and hematology/oncology due to the patient's history of follicular lymphoma and chronic hepatitis B. Although attempts were made to avoid systemic corticosteroids due to the risk for a psoriasis flare upon discontinuation, because of the severity of arthralgia she was started on oral prednisone 20 mg daily by rheumatology with plans for a slow taper once an alternative systemic agent was started.1
At 10-week follow-up, the patient had marked improvement of psoriatic plaques with no active lesions while only on prednisone 20 mg daily. In consultation with her care team, she subsequently was started on methotrexate 10 mg weekly for 2 weeks followed by titration to 15 mg weekly. Plans were to start a prednisone taper after a month of methotrexate to allow her new treatment time for therapeutic effect. Notably, the patient chose to discontinue prednisone 2 weeks into methotrexate therapy after only two 10-mg doses of methotrexate weekly and well before therapeutic levels were achieved. Despite stopping prednisone early and without a taper, she did not experience a relapse in psoriatic skin lesions. Three months following initiation of methotrexate, she sustained resolution of the cutaneous lesions with only residual postinflammatory hyperpigmentation.
Psoriasis is a common chronic inflammatory skin disorder with multiple clinical presentations. There are several variants of psoriasis that are classified by their morphologic appearance including chronic plaque, guttate, erythrodermic, and pustular, with more than 90% of cases representing the plaque variant. Less common clinical presentations of psoriasis include rupioid, ostraceous, inverse, elephantine, and HIV associated.2 Rupioid psoriasis is a rare variant that presents with cone-shaped, limpetlike lesions.3,4 Similar to the limited epidemiological and clinical data pertaining to psoriasis in nonwhite racial groups, there also is a paucity of documented reports of rupioid psoriasis in skin of color.
Rupioid comes from the Greek word rhupos, meaning dirt or filth, and is used to describe well-demarcated lesions with thick, yellow, dirty-appearing, adherent crusts resembling oyster shells with a surrounding rim of erythema.5 Rupioid psoriasis initially was reported in 1948 and remains an uncommon and infrequently reported variant.6 The majority of reported cases have been associated with arthropathy, similar to our patient.3,4 Rupioid lesions also have been observed in an array of other diseases, such as secondary syphilis, crusted scabies, disseminated histoplasmosis, HIV, reactive arthritis, and aminoaciduria.7-11
Diagnosis of rupioid psoriasis can be confirmed with a skin biopsy, which demonstrates characteristic histopathologic findings of psoriasis.3 Laboratory analysis should be performed to rule out other causes of rupioid lesions, and PsA should be differentiated from rheumatoid arthritis if arthropathy is present. In our case, serum rapid plasma reagin, anti-HIV antibody, rheumatoid factor, and fungal cultures were negative. Usin0)g clinical findings, histopathology, laboratory analyses, and radiograph findings, the diagnosis of rupioid psoriasis with PsA was confirmed in our patient.
Psoriasis was not originally suspected in our patient due to the noncharacteristic lesions with smooth black crust--similar appearing to eschar--and the patient's complicated medical history. Variations in the presentation of psoriasis among white individuals and those with skin of color have been reported in the literature.12,13 Psoriatic lesions in darker skin tones may appear more violaceous or hyperpigmented with more conspicuous erythema and thicker plaques. Our patient lacked the classic rupioid appearance of concentric circular layers of dirty, yellow, oysterlike scale, and instead had thick, lamellate, black crust. A PubMed search of articles indexed for MEDLINE using the terms rupioid, coral reef psoriasis, rupioides, and rhupus revealed no other cases of rupioid psoriasis reported in black patients and no cases detailing the variations of rupioid lesions in skin of color. A case of rupioid psoriasis has been reported in a Hispanic patient, but the described psoriatic lesions were more characteristic of the dirty-appearing, conic plaques previously reported.14 Our case highlights a unique example of the variable presentations of cutaneous disorders in skin of color and black patients.
Our patient's case of rupioid psoriasis with PsA presented unique challenges for systemic treatment due to her multiple comorbidities. Rupioid psoriasis most often is treated with combination topical and systemic therapy, with agents such as methotrexate and cyclosporine having prior success.3,4 This variant of psoriasis is highly responsive to treatment, and marked improvement of lesions has been achieved with topical steroids alone with proper adherence.15 Our patient was started on clobetasol ointment 0.05% while a systemic agent was debated for her PsA. Although she did not have improvement with topical therapy alone, she experienced rapid resolution of the skin lesions after initiation of low-dose prednisone 20 mg daily. Interestingly, our patient did not experience a flare of the skin lesions upon discontinuation of systemic steroids despite the lack of an appropriate taper and methotrexate not having reached therapeutic levels.
The clinical nuances of rupioid psoriasis in skin of color have not yet been described and remain an important diagnostic consideration. Our patient achieved remission of skin lesions with sequential treatment of topical clobetasol, a low-dose systemic steroid, and methotrexate. Based on available reports, rupioid psoriasis may represent a variant of psoriasis that is highly responsive to treatment.
- Mrowietz U, Domm S. Systemic steroids in the treatment of psoriasis: what is fact, what is fiction? J Eur Acad Dermatol Venereol. 2013;27:1022-1025.
- Goldsmith LA, Katz SI, Gilchrest BA, eds. Fitzpatrick's Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Wang JL, Yang JH. Rupioid psoriasis associated with arthropathy. J Dermatol. 1997;24:46-49.
- Murakami T, Ohtsuki M, Nakagawa H. Rupioid psoriasis with arthropathy. Clin Exp Dermatol. 2000;25:409-412.
- Chung HJ, Marley-Kemp D, Keller M. Rupioid psoriasis and other skin diseases with rupioid manifestations. Cutis. 2014;94:119-121.
- Salamon M, Omulecki A, Sysa-Jedrzejowska A, et al. Psoriasisrupioides: a rare variant of a common disease. Cutis. 2011;88:135-137.
- Krase IZ, Cavanaugh K, Curiel-Lewandrowski C. A case of rupioid syphilis. JAAD Case Rep. 2016;2:141-143.
- Garofalo V, Saraceno R, Milana M, et al. Crusted scabies in a liver transplant patient mimicking rupioid psoriasis. Eur J Dermatol. 2016;26:495-496.
- Corti M, Villafane MF, Palmieri O, et al. Rupioid histoplasmosis: first case reported in an AIDS patient in Argentina. Rev Inst Med Trop Sao Paulo. 2010;52:279-280.
- Sehgal VN, Koranne RV, Shyam Prasad AL. Unusual manifestations of Reiter's disease in a child. Dermatologica. 1985;170:77-79.
- Haim S, Gilhar A, Cohen A. Cutaneous manifestations associated with aminoaciduria. report of two cases. Dermatologica. 1978;156:244-250.
- McMichael AJ, Vachiramon V, Guzman-Sanchez DA, et al. Psoriasis in African-Americans: a caregivers' survey. J Drugs Dermatol. 2012;11:478-482.
- Alexis AF, Blackcloud P. Psoriasis in skin of color: epidemiology, genetics, clinical presentation, and treatment nuances. J Clin Aesthet Dermatol. 2014;7:16-24.
- Posligua A, Maldonado C, Gonzalez MG. Rupioid psoriasis preceded by varicella presenting as Koebner phenomenon. J Am Acad Dermatol. 2016;74(5 suppl 1):AB268.
- Feldman SR, Feldman S, Brown K, et al. "Coral reef" psoriasis: a marker of resistance to topical treatment. J Dermatolog Treat. 2008;19:257-258.
- Mrowietz U, Domm S. Systemic steroids in the treatment of psoriasis: what is fact, what is fiction? J Eur Acad Dermatol Venereol. 2013;27:1022-1025.
- Goldsmith LA, Katz SI, Gilchrest BA, eds. Fitzpatrick's Dermatology in General Medicine. 8th ed. New York, NY: The McGraw-Hill Companies; 2012.
- Wang JL, Yang JH. Rupioid psoriasis associated with arthropathy. J Dermatol. 1997;24:46-49.
- Murakami T, Ohtsuki M, Nakagawa H. Rupioid psoriasis with arthropathy. Clin Exp Dermatol. 2000;25:409-412.
- Chung HJ, Marley-Kemp D, Keller M. Rupioid psoriasis and other skin diseases with rupioid manifestations. Cutis. 2014;94:119-121.
- Salamon M, Omulecki A, Sysa-Jedrzejowska A, et al. Psoriasisrupioides: a rare variant of a common disease. Cutis. 2011;88:135-137.
- Krase IZ, Cavanaugh K, Curiel-Lewandrowski C. A case of rupioid syphilis. JAAD Case Rep. 2016;2:141-143.
- Garofalo V, Saraceno R, Milana M, et al. Crusted scabies in a liver transplant patient mimicking rupioid psoriasis. Eur J Dermatol. 2016;26:495-496.
- Corti M, Villafane MF, Palmieri O, et al. Rupioid histoplasmosis: first case reported in an AIDS patient in Argentina. Rev Inst Med Trop Sao Paulo. 2010;52:279-280.
- Sehgal VN, Koranne RV, Shyam Prasad AL. Unusual manifestations of Reiter's disease in a child. Dermatologica. 1985;170:77-79.
- Haim S, Gilhar A, Cohen A. Cutaneous manifestations associated with aminoaciduria. report of two cases. Dermatologica. 1978;156:244-250.
- McMichael AJ, Vachiramon V, Guzman-Sanchez DA, et al. Psoriasis in African-Americans: a caregivers' survey. J Drugs Dermatol. 2012;11:478-482.
- Alexis AF, Blackcloud P. Psoriasis in skin of color: epidemiology, genetics, clinical presentation, and treatment nuances. J Clin Aesthet Dermatol. 2014;7:16-24.
- Posligua A, Maldonado C, Gonzalez MG. Rupioid psoriasis preceded by varicella presenting as Koebner phenomenon. J Am Acad Dermatol. 2016;74(5 suppl 1):AB268.
- Feldman SR, Feldman S, Brown K, et al. "Coral reef" psoriasis: a marker of resistance to topical treatment. J Dermatolog Treat. 2008;19:257-258.
Practice Points
- Rupioid psoriasis in skin of color may present a diagnostic challenge for health care providers.
- Rupioid psoriasis may represent a psoriasis variant that is highly responsive to treatment.
Terlipressin squeaks by FDA review for hepatorenal syndrome 1
The Food and Drug Administration’s Cardiovascular and Renal Drugs Advisory Committee narrowly recommended, by an 8-7 vote, that the agency grant marketing approval to terlipressin for the treatment of hepatorenal syndrome type 1, a severe, rare, and often rapidly lethal disease. No drugs are currently licensed in the United States for this indication.
The advisory committee’s discussion and vote on July 15 showcased the struggle the 15 members faced parsing data that hinted at efficacy but also featured clear flaws and limitations, with meager evidence showing clinically meaningful patient improvements.
Several advisory committee members voiced their dilemma balancing the desperation of patients and clinicians to have an effective agent to treat a frequently fatal condition against spotty evidence of efficacy.
Their uncertainty over benefit was exacerbated by the substantial rate of serious adverse events, compared with placebo. These events included respiratory failure, which occurred an absolute 9% more often among patients treated with terlipressin than among those who received placebo in the drug’s recent pivotal trial, and sepsis and septic shock, with an absolute 7% excess rate with terlipressin in comparison with placebo.
“This is an important, unmet need, and I want this drug, but the data are not clear that the benefits outweigh the risks,” commented Steven F. Solga, MD, a transplant hepatologist at the University of Pennsylvania, Philadelphia, who is a committee member.
“When you have sick patients with few treatment options, you grope for something to use, but I worry that this won’t help patients,” he said when explaining his vote against approval.
“I look forward to using this medication if I could figure out which patients could benefit from it,” he said.
‘Allow patients to decide if they want this treatment’
Experts estimate that the annual incidence of hepatorenal syndrome type 1 in the United States is about 35,000 patients.
“I would have liked to vote yes, because terlipressin was associated with a short-term increase in renal function, but there was also clear evidence for the risk of sepsis and respiratory failure, and no evidence that it improved survival,” said panel member Patrick H. Nachman, MD.
Dr. Nachman, professor of medicine and director of the division of nephrology and hypertension at the University of Minnesota, Minneapolis, voted against approval.
Several who voted in favor of terlipressin also shared these misgivings.
“The trend for benefit was quite small, I’m very worried about respiratory failure, and I’m uncomfortable with the postrandomization analyses” used by the developer of terlipressin (Mallinckrodt) to buttress the efficacy claims, explained panel member Paul M. Ridker, MD.
“So why did I vote yes? The problem is the enormous unmet need. Patients are in desperate shape, and the standard treatments are used off label, with no data. Here, we have data, and the primary endpoint was met,” said Dr. Ridker, who is professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital, both in Boston.
The effects of terlipressin appear to give clinicians a way to “stabilize renal function and buy time,” making it more feasible to try to rush the patient to liver transplantation or at least to “stop their downward spiral» as patients with decompensated liver failure develop inadequate renal blood flow that produces an acute fall in kidney function,” explained David N. Assis, MD, a hepatologist at Yale University, New Haven, Conn.
“The reality is, nothing else is available, aside from renal replacement therapy and pressors. There is a need for a treatment that buys time,” he said. He voted to recommend approval.
That sentiment was notably echoed in comments from the two nonclinical members of the advisory committee.
“This treatment addresses a major gap in care,” said Jacqueline D. Alikhaani, the panel’s consumer representative. “Allow patients to decide if they want this treatment,” said Daniel Bonner, the committee’s patient representative. Both voted in favor of FDA approval.
Terlipressin has been a long-standing linchpin for treating hepatorenal syndrome type 1 in Europe and other places outside the United States and Canada.
The most recent guidelines for managing patients with decompensated cirrhosis from the European Association for the Study of the Liver say that “[t]erlipressin plus albumin should be considered as the first-line therapeutic option for the treatment of hepatorenal syndrome and acute kidney injury” (J Hepatol. 2018 Aug 1;69).
According to company representatives who presented the case for terlipressin during the meeting, bringing the drug onto the U.S. market has been a 17-year journey, featuring three sequential trials.
- A 112-patient that the FDA accepted as the first of the two supportive trials needed for approval.
- A with 196 patients that tested terlipressin plus albumin against placebo plus albumin and showed a nominal benefit from terlipressin that failed to achieve statistical significance.
- The most recent trial, , which directly led to the advisory committee session. That trial enrolled 300 patients and met its primary endpoint. Data have not yet been published but have been at meetings.
One of the sources of controversy over the benefit from terlipressin centered on the primary endpoint used in CONFIRM, which required that the patient have two consecutive, low readings for serum creatinine, with levels no greater than 1.5 mg/dL while on treatment, and remain alive and free from need for renal replacement therapy for at least 10 days beyond this.
The FDA agreed to accept this as a primary endpoint but nonetheless considered it a surrogate.
According to FDA staffers who presented their take on the application, the agency accepted this primary endpoint “with the understanding that favorable trends in clinical outcomes, thought to be predicted by successful treatment of hepatic renal syndrome type 1, would be expected.”
The lack of many favorable trends in clinical outcomes helped foster the advisory committee’s divided response. The FDA’s staff uses its discretion when considering an advisory committee’s recommendations and making a final determination.
None of the advisory committee members disclosed any relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration’s Cardiovascular and Renal Drugs Advisory Committee narrowly recommended, by an 8-7 vote, that the agency grant marketing approval to terlipressin for the treatment of hepatorenal syndrome type 1, a severe, rare, and often rapidly lethal disease. No drugs are currently licensed in the United States for this indication.
The advisory committee’s discussion and vote on July 15 showcased the struggle the 15 members faced parsing data that hinted at efficacy but also featured clear flaws and limitations, with meager evidence showing clinically meaningful patient improvements.
Several advisory committee members voiced their dilemma balancing the desperation of patients and clinicians to have an effective agent to treat a frequently fatal condition against spotty evidence of efficacy.
Their uncertainty over benefit was exacerbated by the substantial rate of serious adverse events, compared with placebo. These events included respiratory failure, which occurred an absolute 9% more often among patients treated with terlipressin than among those who received placebo in the drug’s recent pivotal trial, and sepsis and septic shock, with an absolute 7% excess rate with terlipressin in comparison with placebo.
“This is an important, unmet need, and I want this drug, but the data are not clear that the benefits outweigh the risks,” commented Steven F. Solga, MD, a transplant hepatologist at the University of Pennsylvania, Philadelphia, who is a committee member.
“When you have sick patients with few treatment options, you grope for something to use, but I worry that this won’t help patients,” he said when explaining his vote against approval.
“I look forward to using this medication if I could figure out which patients could benefit from it,” he said.
‘Allow patients to decide if they want this treatment’
Experts estimate that the annual incidence of hepatorenal syndrome type 1 in the United States is about 35,000 patients.
“I would have liked to vote yes, because terlipressin was associated with a short-term increase in renal function, but there was also clear evidence for the risk of sepsis and respiratory failure, and no evidence that it improved survival,” said panel member Patrick H. Nachman, MD.
Dr. Nachman, professor of medicine and director of the division of nephrology and hypertension at the University of Minnesota, Minneapolis, voted against approval.
Several who voted in favor of terlipressin also shared these misgivings.
“The trend for benefit was quite small, I’m very worried about respiratory failure, and I’m uncomfortable with the postrandomization analyses” used by the developer of terlipressin (Mallinckrodt) to buttress the efficacy claims, explained panel member Paul M. Ridker, MD.
“So why did I vote yes? The problem is the enormous unmet need. Patients are in desperate shape, and the standard treatments are used off label, with no data. Here, we have data, and the primary endpoint was met,” said Dr. Ridker, who is professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital, both in Boston.
The effects of terlipressin appear to give clinicians a way to “stabilize renal function and buy time,” making it more feasible to try to rush the patient to liver transplantation or at least to “stop their downward spiral» as patients with decompensated liver failure develop inadequate renal blood flow that produces an acute fall in kidney function,” explained David N. Assis, MD, a hepatologist at Yale University, New Haven, Conn.
“The reality is, nothing else is available, aside from renal replacement therapy and pressors. There is a need for a treatment that buys time,” he said. He voted to recommend approval.
That sentiment was notably echoed in comments from the two nonclinical members of the advisory committee.
“This treatment addresses a major gap in care,” said Jacqueline D. Alikhaani, the panel’s consumer representative. “Allow patients to decide if they want this treatment,” said Daniel Bonner, the committee’s patient representative. Both voted in favor of FDA approval.
Terlipressin has been a long-standing linchpin for treating hepatorenal syndrome type 1 in Europe and other places outside the United States and Canada.
The most recent guidelines for managing patients with decompensated cirrhosis from the European Association for the Study of the Liver say that “[t]erlipressin plus albumin should be considered as the first-line therapeutic option for the treatment of hepatorenal syndrome and acute kidney injury” (J Hepatol. 2018 Aug 1;69).
According to company representatives who presented the case for terlipressin during the meeting, bringing the drug onto the U.S. market has been a 17-year journey, featuring three sequential trials.
- A 112-patient that the FDA accepted as the first of the two supportive trials needed for approval.
- A with 196 patients that tested terlipressin plus albumin against placebo plus albumin and showed a nominal benefit from terlipressin that failed to achieve statistical significance.
- The most recent trial, , which directly led to the advisory committee session. That trial enrolled 300 patients and met its primary endpoint. Data have not yet been published but have been at meetings.
One of the sources of controversy over the benefit from terlipressin centered on the primary endpoint used in CONFIRM, which required that the patient have two consecutive, low readings for serum creatinine, with levels no greater than 1.5 mg/dL while on treatment, and remain alive and free from need for renal replacement therapy for at least 10 days beyond this.
The FDA agreed to accept this as a primary endpoint but nonetheless considered it a surrogate.
According to FDA staffers who presented their take on the application, the agency accepted this primary endpoint “with the understanding that favorable trends in clinical outcomes, thought to be predicted by successful treatment of hepatic renal syndrome type 1, would be expected.”
The lack of many favorable trends in clinical outcomes helped foster the advisory committee’s divided response. The FDA’s staff uses its discretion when considering an advisory committee’s recommendations and making a final determination.
None of the advisory committee members disclosed any relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration’s Cardiovascular and Renal Drugs Advisory Committee narrowly recommended, by an 8-7 vote, that the agency grant marketing approval to terlipressin for the treatment of hepatorenal syndrome type 1, a severe, rare, and often rapidly lethal disease. No drugs are currently licensed in the United States for this indication.
The advisory committee’s discussion and vote on July 15 showcased the struggle the 15 members faced parsing data that hinted at efficacy but also featured clear flaws and limitations, with meager evidence showing clinically meaningful patient improvements.
Several advisory committee members voiced their dilemma balancing the desperation of patients and clinicians to have an effective agent to treat a frequently fatal condition against spotty evidence of efficacy.
Their uncertainty over benefit was exacerbated by the substantial rate of serious adverse events, compared with placebo. These events included respiratory failure, which occurred an absolute 9% more often among patients treated with terlipressin than among those who received placebo in the drug’s recent pivotal trial, and sepsis and septic shock, with an absolute 7% excess rate with terlipressin in comparison with placebo.
“This is an important, unmet need, and I want this drug, but the data are not clear that the benefits outweigh the risks,” commented Steven F. Solga, MD, a transplant hepatologist at the University of Pennsylvania, Philadelphia, who is a committee member.
“When you have sick patients with few treatment options, you grope for something to use, but I worry that this won’t help patients,” he said when explaining his vote against approval.
“I look forward to using this medication if I could figure out which patients could benefit from it,” he said.
‘Allow patients to decide if they want this treatment’
Experts estimate that the annual incidence of hepatorenal syndrome type 1 in the United States is about 35,000 patients.
“I would have liked to vote yes, because terlipressin was associated with a short-term increase in renal function, but there was also clear evidence for the risk of sepsis and respiratory failure, and no evidence that it improved survival,” said panel member Patrick H. Nachman, MD.
Dr. Nachman, professor of medicine and director of the division of nephrology and hypertension at the University of Minnesota, Minneapolis, voted against approval.
Several who voted in favor of terlipressin also shared these misgivings.
“The trend for benefit was quite small, I’m very worried about respiratory failure, and I’m uncomfortable with the postrandomization analyses” used by the developer of terlipressin (Mallinckrodt) to buttress the efficacy claims, explained panel member Paul M. Ridker, MD.
“So why did I vote yes? The problem is the enormous unmet need. Patients are in desperate shape, and the standard treatments are used off label, with no data. Here, we have data, and the primary endpoint was met,” said Dr. Ridker, who is professor of medicine at Harvard Medical School and director of the Center for Cardiovascular Disease Prevention at Brigham and Women’s Hospital, both in Boston.
The effects of terlipressin appear to give clinicians a way to “stabilize renal function and buy time,” making it more feasible to try to rush the patient to liver transplantation or at least to “stop their downward spiral» as patients with decompensated liver failure develop inadequate renal blood flow that produces an acute fall in kidney function,” explained David N. Assis, MD, a hepatologist at Yale University, New Haven, Conn.
“The reality is, nothing else is available, aside from renal replacement therapy and pressors. There is a need for a treatment that buys time,” he said. He voted to recommend approval.
That sentiment was notably echoed in comments from the two nonclinical members of the advisory committee.
“This treatment addresses a major gap in care,” said Jacqueline D. Alikhaani, the panel’s consumer representative. “Allow patients to decide if they want this treatment,” said Daniel Bonner, the committee’s patient representative. Both voted in favor of FDA approval.
Terlipressin has been a long-standing linchpin for treating hepatorenal syndrome type 1 in Europe and other places outside the United States and Canada.
The most recent guidelines for managing patients with decompensated cirrhosis from the European Association for the Study of the Liver say that “[t]erlipressin plus albumin should be considered as the first-line therapeutic option for the treatment of hepatorenal syndrome and acute kidney injury” (J Hepatol. 2018 Aug 1;69).
According to company representatives who presented the case for terlipressin during the meeting, bringing the drug onto the U.S. market has been a 17-year journey, featuring three sequential trials.
- A 112-patient that the FDA accepted as the first of the two supportive trials needed for approval.
- A with 196 patients that tested terlipressin plus albumin against placebo plus albumin and showed a nominal benefit from terlipressin that failed to achieve statistical significance.
- The most recent trial, , which directly led to the advisory committee session. That trial enrolled 300 patients and met its primary endpoint. Data have not yet been published but have been at meetings.
One of the sources of controversy over the benefit from terlipressin centered on the primary endpoint used in CONFIRM, which required that the patient have two consecutive, low readings for serum creatinine, with levels no greater than 1.5 mg/dL while on treatment, and remain alive and free from need for renal replacement therapy for at least 10 days beyond this.
The FDA agreed to accept this as a primary endpoint but nonetheless considered it a surrogate.
According to FDA staffers who presented their take on the application, the agency accepted this primary endpoint “with the understanding that favorable trends in clinical outcomes, thought to be predicted by successful treatment of hepatic renal syndrome type 1, would be expected.”
The lack of many favorable trends in clinical outcomes helped foster the advisory committee’s divided response. The FDA’s staff uses its discretion when considering an advisory committee’s recommendations and making a final determination.
None of the advisory committee members disclosed any relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Cancer patient organizations critically affected by pandemic
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The COVID-19 pandemic has disrupted every aspect of cancer care, from diagnosis, treatment, and follow-up to participation in clinical trials, according to a new report that collected responses from cancer patient organizations around the world.
The report includes responses from 157 organizations in 56 countries, representing some 350,000 patients with cancer.
“The COVID-19 global pandemic has quite literally wreaked havoc with all of our lives but especially for cancer patients,” said the report’s author, Frances Reid, MBA, program director, World Ovarian Cancer Coalition.
“To those who have the power or influence to ensure that cancer treatment and services are not set back several years, please listen to those organizations who can articulate clearly the impact on patients, work with them, and act on it as soon as you can,” she added.
The new report, entitled “The Impact of COVID-19 on Cancer Patient Organisations,” was released on June 12. The organizations were surveyed from May 11 to May 25.
Cancer diagnosis
Two-thirds of the organizations surveyed said cancer screening programs had been canceled in their country, and 59% indicated they had seen a drop in urgent referrals for suspected cancer.
Some 44% said that access to pathology services had been reduced. One group in Australia reported that “results of pathology tests are taking longer to be returned. Generally a result would be returned within 48 hours. Since COVID-19, results are taking up to 7 days to be returned.”
As for treatment, 68% of organizations reported delays or cancellations of surgery or other treatments; 58% reported there had been a need to modify treatment protocols; and 48% indicated there had been a drop in participation in clinical trials.
Respondents were also concerned about reported increases in stress, anxiety, and isolation among many cancer patients. “Often at increased risk of infection and serious illness themselves ... many have been required to ‘shield’ from others, totally withdrawing from life outside their homes, thus increasing the already high levels of isolation they feel because of their life-limiting conditions,” the report notes.
In addition, some 60% of the organizations said that the pandemic had increased financial hardship among cancer patients. One US group commented: “Unemployment levels in the States similar to depression era. This has been a real challenge as many have lost insurance as well as jobs.”
Only a minority of respondents reported that cancer care was being offered in hospitals with no special arrangements in place to treat concomitant COVID-19 patients.
On the other hand, only 15% of respondents indicated that patients were being treated in a hospital that was not also caring for COVID-19 patients.
“Cancer will not wait for COVID-19 to pass, if it ever will, and the patient organizations are the key to minimizing the devastating impact [COVID-19 is having] on people with cancer,” Reid emphasized.
“More than ever, the patient/support services should be strengthened,” commented a group from France.
Patient services affected
“Almost all organisations (89%) have had to alter their services for people with cancer,” the report notes.
Two thirds of organizations involved in professional educational activities have had to change their services in some way, either by moving them online or stopping programs altogether, at least temporarily. “Some found that doctors and nurses are too busy with the pandemic to participate, and that their appetite for such activity is also diminished,” the report notes.
The volume of phone calls and emails increased in almost 6 of 10 organizations that provide support services for patients. Compared to prepandemic levels, volume increased by an average of 44%.
The most common queries raised by people with cancer (accounting for 85% of all queries) were questions about the risks of contracting COVID-19 and cancer treatments during the pandemic.
Some of the organizations also commented about how they had been affected. One group from Uganda said: “We had a sudden lockdown and we could not access office to give face to face counselling. We stopped research due to national guidelines on research. We continued giving information via phone and social media especially WhatsApp. We created groups for patients and counsellors to continue interacting.”
A group in Costa Rica reported: “We developed a new program of transfers from their homes to the hospital for cancer patients in chemotherapy and radiotherapy. 200 monthly transfers. We created a virtual community instead of our face-to-face support group, we started in April and we have 108 members, virtual sessions are held every two weeks.”
An organization based in the United States reported that it was “totally revamping our educational programs to be delivered in new ways in an online format ― not just replicating the in-person formats, but reaching out to our community and asking them what they would find the most valuable.”
Impact on fundraising
Almost 9 in 10 organizations raise funds to support their activities, the report notes. “A shocking 79% of organisations say they predict a fall in income over the next 12 months, with a further 16% not sure, leaving only 5% confident of their financial stability.”
Every type of fund-raising has been affected by COVID-19, from grants and major donors to community fund-raising events. Sixty percent of organisations said they were trying to find new ways to raise funds.
However, as one organization in Japan noted: “At the moment we can survive and feel it is unethical to ask the public for money when many are facing dire financial personal circumstances.”
A group from Australia commented: “Fundraising has been extremely difficult due to COVID-19 with distancing laws and no group gatherings as well as the economic downturn. Crisis appeals have been unsuccessful and all outdoor events and major events have been cancelled. In Australia we have had to contend with also the fires earlier in the year where a lot of money was donated to leaving other foundations struggling to get donor support.”
A little more than half (55%) of the organizations surveyed have had to cut costs.
Staffing cuts have been made in 1 in 10 of the organizations surveyed. A similar proportion of organizations have furloughed staff. Many if not all staff from numerous organizations are working from home.
A little more than half of those surveyed either provide funding for research or conduct research themselves, but only one quarter of them indicated there had been no change in their research projects. The others have indicated that they had to either reduce the scope of their research, put it on pause, or stop it altogether.
Three quarters of survey respondents noted that they had engaged in advocacy activities prior to the pandemic, and almost two thirds of them said they had to delay these activities.
Several of the organizations expressed thanks to the survey authors.
“COVID-19 is a global pandemic and cancer patients all around the world have similar worries, concerns and questions ― we are a small/medium organisation working in one country but believe in the power of community and coalitions and so this survey is a very welcome part of looking at this from a greater perspective,” commented one British group.
Reid has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Cardiovascular risk factors tied to midlife cognitive decline
new research shows. The findings suggest that the relationship between CVRFs and cognition becomes evident much earlier than previously realized. Investigators found that individuals who smoked were 65% more likely to have accelerated cognitive decline, those with hypertension were 87% more likely, and individuals with diabetes had nearly a 200% increased risk.
“What is new here is that almost no one has looked at cardiovascular risk factors in such a young age [mean, 50 years] and cognitive change in middle age from 50 to 55 or so. Almost all other studies have looked at mid- or late-life cardiovascular risk factors and late-life cognition or dementia,” said study investigator Kristine Yaffe, MD.
The research was published online July 15 in Neurology.
New insight
Previous research has shown a strong association between CVRFs and a greater risk for cognitive decline and dementia in late life, but the investigators note that data about the influence of CVRFs on cognition in midlife are “sparse.” Longitudinal studies have also shown that several cognitive domains – particularly processing speed and executive function – may start to decline in midlife, but whether CVRFs, many of which also emerge in midlife, contribute to these changes is unclear.
To assess the effect of CVRFs on cognitive changes in midlife, the investigators analyzed data from the ongoing Coronary Artery Risk Development in Young Adults (CARDIA) study. CARDIA is a multicenter longitudinal study designed to measure risk factors for coronary artery disease in a large cohort of Black and White men and women.
The analysis was based on data from 2,675 participants who underwent CVRF assessment and cognitive testing at baseline and 5 years later. At baseline, participants’ mean age was 50.2 years. Approximately 57% of participants were women, 55% were White, and the mean number of years of education was 15. At study outset, 43% (n = 1,133) of participants were considered obese, 31% (n = 826) had hypertension, 15% (n = 701) were current smokers, 11% (n = 290) had diabetes, and 9% (n = 248) had high cholesterol.
Cognition was assessed using the Digit Symbol Substitution Test, which measures processing speed and executive function; the Stroop Test, which measures executive function; and the Rey Auditory Verbal Learning Test, which measures verbal memory.
Dose-dependent effect
Overall results showed that, for 5% of participants, cognitive decline was accelerated at 5 years. In unadjusted models, the odds of developing accelerated cognitive decline over 5 years was associated with hypertension (7.5% vs. 4.3%; odds ratio, 1.79, 95% confidence interval, 1.27-2.52), diabetes (10.3% vs. 4.7%; OR, 2.33; 95% CI, 1.53-3.56), and smoking (7.7% current smokers vs. 4.3% never smokers; OR, 1.87; 95% CI, 1.21-2.90). After adjusting for age, sex, and race, the associations remained significant.
The researchers found no significant effect of high cholesterol (6.9% vs. 5.2%; OR, 1.35; 95% CI, 0.80-2.28) or obesity (6.1% vs. 4.8%; OR, 1.29; 95% CI, 0.92-1.82) on accelerated cognitive decline.
Compared with participants with no CVRFs, the likelihood of accelerated cognitive decline was higher for individuals with one or two risk factors (OR, 1.94; 95% CI, 1.16-3.25) and was higher still for those with three or more risk factors (OR, 3.51; 95% CI, 2.05-6.00).
The fact that there was no association between midlife cognitive decline and obesity or high cholesterol did not come as a surprise, said Dr. Yaffe. “Most studies have not shown a consistent finding with high cholesterol and later-life cognition, so it is not surprising we did not see one in midlife, when there is not as much cognitive change.”
The study’s results, said Dr. Yaffe, provide physicians with another good reason to help patients address CVRFs and to work with them to lower blood pressure, stop smoking, reduce diabetes incidence, or control diabetes.
Dr. Yaffe said she and her colleagues plan further research into CVRFs and accelerated cognitive decline. “We want to know if this earlier cognitive decline [in midlife] is connected to greater decline later in life. We also want to know if improving these risk factors in midlife might prevent or slow dementia later.”
More to explore
Commenting on the findings, Michelle M. Mielke, PhD, professor of epidemiology and neurology at Mayo Clinic, Rochester, Minn., said one of the study’s main implications “is that the prevention and treatment of midlife hypertension and diabetes and smoking cessation directly impacts shorter-term changes in cognition.”
She added that the study also provides a foundation for answering further questions about the effects of CVRFs on cognition in midlife. For example, questions about sex differences remain unanswered. Men develop CVRFs earlier than women, but the investigators did not provide the prevalence of cardiovascular risk factors by sex.
“It was also not reported whether a specific midlife cardiovascular risk factor was more strongly associated with accelerated cognitive decline for women or for men,” she said. In addition, the mean age of the population at baseline is the approximate age of the onset of menopause, after which cardiovascular risk factors increase among women.
“Additional research is needed to understand the emergence of cardiovascular risk factors pre- versus post menopause on subsequent cognition and also consider the use of menopausal hormone therapy,” said Dr. Mielke.
“Another future research avenue is to further understand the impact of antihypertensive and diabetes medications,” she continued. “For example, in the current study, it was not clear how many [participants] with hypertension were treated versus untreated and whether this impacted subsequent cognition. Similarly, it is not known whether specific antihypertensives are more beneficial for cognition in midlife.”
CARDIA is supported by the National Heart, Lung, and Blood Institute; the University of Alabama at Birmingham; Northwestern University, Chicago; the University of Minnesota; and the Kaiser Foundation Research Institute. Dr. Yaffe serves on data safety monitoring boards for Eli Lilly and studies sponsored by the National Institute on Aging. She is a board member of Alector and is a member of the Beeson Scientific Advisory Board and the Global Council on Brain Health. Dr. Mielke has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research shows. The findings suggest that the relationship between CVRFs and cognition becomes evident much earlier than previously realized. Investigators found that individuals who smoked were 65% more likely to have accelerated cognitive decline, those with hypertension were 87% more likely, and individuals with diabetes had nearly a 200% increased risk.
“What is new here is that almost no one has looked at cardiovascular risk factors in such a young age [mean, 50 years] and cognitive change in middle age from 50 to 55 or so. Almost all other studies have looked at mid- or late-life cardiovascular risk factors and late-life cognition or dementia,” said study investigator Kristine Yaffe, MD.
The research was published online July 15 in Neurology.
New insight
Previous research has shown a strong association between CVRFs and a greater risk for cognitive decline and dementia in late life, but the investigators note that data about the influence of CVRFs on cognition in midlife are “sparse.” Longitudinal studies have also shown that several cognitive domains – particularly processing speed and executive function – may start to decline in midlife, but whether CVRFs, many of which also emerge in midlife, contribute to these changes is unclear.
To assess the effect of CVRFs on cognitive changes in midlife, the investigators analyzed data from the ongoing Coronary Artery Risk Development in Young Adults (CARDIA) study. CARDIA is a multicenter longitudinal study designed to measure risk factors for coronary artery disease in a large cohort of Black and White men and women.
The analysis was based on data from 2,675 participants who underwent CVRF assessment and cognitive testing at baseline and 5 years later. At baseline, participants’ mean age was 50.2 years. Approximately 57% of participants were women, 55% were White, and the mean number of years of education was 15. At study outset, 43% (n = 1,133) of participants were considered obese, 31% (n = 826) had hypertension, 15% (n = 701) were current smokers, 11% (n = 290) had diabetes, and 9% (n = 248) had high cholesterol.
Cognition was assessed using the Digit Symbol Substitution Test, which measures processing speed and executive function; the Stroop Test, which measures executive function; and the Rey Auditory Verbal Learning Test, which measures verbal memory.
Dose-dependent effect
Overall results showed that, for 5% of participants, cognitive decline was accelerated at 5 years. In unadjusted models, the odds of developing accelerated cognitive decline over 5 years was associated with hypertension (7.5% vs. 4.3%; odds ratio, 1.79, 95% confidence interval, 1.27-2.52), diabetes (10.3% vs. 4.7%; OR, 2.33; 95% CI, 1.53-3.56), and smoking (7.7% current smokers vs. 4.3% never smokers; OR, 1.87; 95% CI, 1.21-2.90). After adjusting for age, sex, and race, the associations remained significant.
The researchers found no significant effect of high cholesterol (6.9% vs. 5.2%; OR, 1.35; 95% CI, 0.80-2.28) or obesity (6.1% vs. 4.8%; OR, 1.29; 95% CI, 0.92-1.82) on accelerated cognitive decline.
Compared with participants with no CVRFs, the likelihood of accelerated cognitive decline was higher for individuals with one or two risk factors (OR, 1.94; 95% CI, 1.16-3.25) and was higher still for those with three or more risk factors (OR, 3.51; 95% CI, 2.05-6.00).
The fact that there was no association between midlife cognitive decline and obesity or high cholesterol did not come as a surprise, said Dr. Yaffe. “Most studies have not shown a consistent finding with high cholesterol and later-life cognition, so it is not surprising we did not see one in midlife, when there is not as much cognitive change.”
The study’s results, said Dr. Yaffe, provide physicians with another good reason to help patients address CVRFs and to work with them to lower blood pressure, stop smoking, reduce diabetes incidence, or control diabetes.
Dr. Yaffe said she and her colleagues plan further research into CVRFs and accelerated cognitive decline. “We want to know if this earlier cognitive decline [in midlife] is connected to greater decline later in life. We also want to know if improving these risk factors in midlife might prevent or slow dementia later.”
More to explore
Commenting on the findings, Michelle M. Mielke, PhD, professor of epidemiology and neurology at Mayo Clinic, Rochester, Minn., said one of the study’s main implications “is that the prevention and treatment of midlife hypertension and diabetes and smoking cessation directly impacts shorter-term changes in cognition.”
She added that the study also provides a foundation for answering further questions about the effects of CVRFs on cognition in midlife. For example, questions about sex differences remain unanswered. Men develop CVRFs earlier than women, but the investigators did not provide the prevalence of cardiovascular risk factors by sex.
“It was also not reported whether a specific midlife cardiovascular risk factor was more strongly associated with accelerated cognitive decline for women or for men,” she said. In addition, the mean age of the population at baseline is the approximate age of the onset of menopause, after which cardiovascular risk factors increase among women.
“Additional research is needed to understand the emergence of cardiovascular risk factors pre- versus post menopause on subsequent cognition and also consider the use of menopausal hormone therapy,” said Dr. Mielke.
“Another future research avenue is to further understand the impact of antihypertensive and diabetes medications,” she continued. “For example, in the current study, it was not clear how many [participants] with hypertension were treated versus untreated and whether this impacted subsequent cognition. Similarly, it is not known whether specific antihypertensives are more beneficial for cognition in midlife.”
CARDIA is supported by the National Heart, Lung, and Blood Institute; the University of Alabama at Birmingham; Northwestern University, Chicago; the University of Minnesota; and the Kaiser Foundation Research Institute. Dr. Yaffe serves on data safety monitoring boards for Eli Lilly and studies sponsored by the National Institute on Aging. She is a board member of Alector and is a member of the Beeson Scientific Advisory Board and the Global Council on Brain Health. Dr. Mielke has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
new research shows. The findings suggest that the relationship between CVRFs and cognition becomes evident much earlier than previously realized. Investigators found that individuals who smoked were 65% more likely to have accelerated cognitive decline, those with hypertension were 87% more likely, and individuals with diabetes had nearly a 200% increased risk.
“What is new here is that almost no one has looked at cardiovascular risk factors in such a young age [mean, 50 years] and cognitive change in middle age from 50 to 55 or so. Almost all other studies have looked at mid- or late-life cardiovascular risk factors and late-life cognition or dementia,” said study investigator Kristine Yaffe, MD.
The research was published online July 15 in Neurology.
New insight
Previous research has shown a strong association between CVRFs and a greater risk for cognitive decline and dementia in late life, but the investigators note that data about the influence of CVRFs on cognition in midlife are “sparse.” Longitudinal studies have also shown that several cognitive domains – particularly processing speed and executive function – may start to decline in midlife, but whether CVRFs, many of which also emerge in midlife, contribute to these changes is unclear.
To assess the effect of CVRFs on cognitive changes in midlife, the investigators analyzed data from the ongoing Coronary Artery Risk Development in Young Adults (CARDIA) study. CARDIA is a multicenter longitudinal study designed to measure risk factors for coronary artery disease in a large cohort of Black and White men and women.
The analysis was based on data from 2,675 participants who underwent CVRF assessment and cognitive testing at baseline and 5 years later. At baseline, participants’ mean age was 50.2 years. Approximately 57% of participants were women, 55% were White, and the mean number of years of education was 15. At study outset, 43% (n = 1,133) of participants were considered obese, 31% (n = 826) had hypertension, 15% (n = 701) were current smokers, 11% (n = 290) had diabetes, and 9% (n = 248) had high cholesterol.
Cognition was assessed using the Digit Symbol Substitution Test, which measures processing speed and executive function; the Stroop Test, which measures executive function; and the Rey Auditory Verbal Learning Test, which measures verbal memory.
Dose-dependent effect
Overall results showed that, for 5% of participants, cognitive decline was accelerated at 5 years. In unadjusted models, the odds of developing accelerated cognitive decline over 5 years was associated with hypertension (7.5% vs. 4.3%; odds ratio, 1.79, 95% confidence interval, 1.27-2.52), diabetes (10.3% vs. 4.7%; OR, 2.33; 95% CI, 1.53-3.56), and smoking (7.7% current smokers vs. 4.3% never smokers; OR, 1.87; 95% CI, 1.21-2.90). After adjusting for age, sex, and race, the associations remained significant.
The researchers found no significant effect of high cholesterol (6.9% vs. 5.2%; OR, 1.35; 95% CI, 0.80-2.28) or obesity (6.1% vs. 4.8%; OR, 1.29; 95% CI, 0.92-1.82) on accelerated cognitive decline.
Compared with participants with no CVRFs, the likelihood of accelerated cognitive decline was higher for individuals with one or two risk factors (OR, 1.94; 95% CI, 1.16-3.25) and was higher still for those with three or more risk factors (OR, 3.51; 95% CI, 2.05-6.00).
The fact that there was no association between midlife cognitive decline and obesity or high cholesterol did not come as a surprise, said Dr. Yaffe. “Most studies have not shown a consistent finding with high cholesterol and later-life cognition, so it is not surprising we did not see one in midlife, when there is not as much cognitive change.”
The study’s results, said Dr. Yaffe, provide physicians with another good reason to help patients address CVRFs and to work with them to lower blood pressure, stop smoking, reduce diabetes incidence, or control diabetes.
Dr. Yaffe said she and her colleagues plan further research into CVRFs and accelerated cognitive decline. “We want to know if this earlier cognitive decline [in midlife] is connected to greater decline later in life. We also want to know if improving these risk factors in midlife might prevent or slow dementia later.”
More to explore
Commenting on the findings, Michelle M. Mielke, PhD, professor of epidemiology and neurology at Mayo Clinic, Rochester, Minn., said one of the study’s main implications “is that the prevention and treatment of midlife hypertension and diabetes and smoking cessation directly impacts shorter-term changes in cognition.”
She added that the study also provides a foundation for answering further questions about the effects of CVRFs on cognition in midlife. For example, questions about sex differences remain unanswered. Men develop CVRFs earlier than women, but the investigators did not provide the prevalence of cardiovascular risk factors by sex.
“It was also not reported whether a specific midlife cardiovascular risk factor was more strongly associated with accelerated cognitive decline for women or for men,” she said. In addition, the mean age of the population at baseline is the approximate age of the onset of menopause, after which cardiovascular risk factors increase among women.
“Additional research is needed to understand the emergence of cardiovascular risk factors pre- versus post menopause on subsequent cognition and also consider the use of menopausal hormone therapy,” said Dr. Mielke.
“Another future research avenue is to further understand the impact of antihypertensive and diabetes medications,” she continued. “For example, in the current study, it was not clear how many [participants] with hypertension were treated versus untreated and whether this impacted subsequent cognition. Similarly, it is not known whether specific antihypertensives are more beneficial for cognition in midlife.”
CARDIA is supported by the National Heart, Lung, and Blood Institute; the University of Alabama at Birmingham; Northwestern University, Chicago; the University of Minnesota; and the Kaiser Foundation Research Institute. Dr. Yaffe serves on data safety monitoring boards for Eli Lilly and studies sponsored by the National Institute on Aging. She is a board member of Alector and is a member of the Beeson Scientific Advisory Board and the Global Council on Brain Health. Dr. Mielke has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Device improves physical exam completion rates in serious mental illness
Using a simple point-of-care (POC) finger prick device to measure blood glucose and lipid levels significantly increases rates of physical health checkups for patients with severe mental illness, new research shows.
In a UK pilot study, use of the Afinion 2 device (Abbott) was associated with a doubling of completed physical health checkups.
However, the effect only occurred in early-intervention services, in which clinicians may feel physical health checkups are most beneficial. This underlines the importance of staff training and payment incentives, the researchers note.
“Clearly, convenience is a great thing about these devices” for both the patient and the mental health clinician, Joseph Butler, MD, a psychiatry trainee at the University of Oxford, United Kingdom, told Medscape Medical News.
He noted that blood test results are rapid, which facilitates immediate discussion of a health management plan.
These tests are “independent from the lab, they’re independent from the general practitioner, and so in terms of convenience, we think it wins on both fronts,” Butler said.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society (SIRS) 2020, but the meeting was canceled because of the coronavirus pandemic.
Poor heart health
Previous research has shown that life expectancy of patients with severe mental illness is 15 to 20 years less than that of the general population, mostly because of complications from poor cardiovascular health.
In the United Kingdom, physical healthcare for patients with serious mental illness is provided by primary care clinicians and community mental health teams (CMHTs). The National Institute for Health and Care Excellence recommends an annual physical examination.
However, a recent audit in the south of England indicated that only 38% of patients with severe mental illness underwent complete physical examinations, primarily because blood glucose and lipid test panels had been omitted.
The researchers note that patients are typically advised to visit their general practitioner for blood tests, “which can be a challenge” for those with severe mental illness.
The Cardiovascular Monitoring in Mental Health (CARMEN) project involved distributing the Afinion 2 device for use in two CMHTs in Oxfordshire, United Kingdom, for 6 months. One CMHT was an early-intervention service, and the other was an adult mental health service.
Care coordinators received training on how to use the device as well as ongoing support to facilitate engagement with the device.
Rates of completion of blood testing and full physical examinations were compared between the intervention CMHTs and two matched control services – an early-intervention group, and an adult metal health services group in Buckinghamshire, a neighboring county.
Better completion rates
The investigators found that .
In contrast, the percentage of physical examinations that were completed remained low in the control CMHT early-intervention service, at just 7.8%.
Direct comparison between the two services showed that use of the POC device was associated with a significant increase in the number of complete physical examinations, at a relative rate of 5.18 (P < .001).
Results were similar when the investigators examined rates at which A1c and lipid panels were completed.
However, there was no difference in completion of physical examinations in the adult mental health service group, for which rates were comparable to those in the control service.
Butler speculated that the way health checkups are funded in the United Kingdom might have contributed to the poor results with the device in the adult mental health service.
In early-intervention services, there is increased awareness of the importance of physical examinations, and funding is contingent on whether clinicians persuade patients to have the examinations.
Overall, the findings show that use of a POC device for physical examinations is acceptable to patients who have severe mental illness as well as to mental health care clinicians, the investigators note.
“In teams where it is well adopted, POC testing can improve physical health check completion...although our qualitative findings highlight important considerations for maximizing clinician engagement,” they add.
The researchers plan to repeat the study across the whole of the south of England, with early-intervention services in the west equipped with POC devices and those in the east serving as controls.
Similar findings
Commenting on the findings for Medscape Medical News, Joe Parks, MD, vice president and practice improvement and medical director at the National Council for Behavioral Health, Washington, DC, noted that he and his colleagues conducted a similar study in the mid-2000s.
Starting in 2004, they distributed a POC finger prick test device for use by community mental health teams to measure blood glucose and lipid levels.
“We required as a condition of payment that the providers get these lab results for everybody they served and report them centrally. Then, we databased them and benchmarked them, and we were able to show significant reductions in HbA1c’s over time,” said Parks, who was not involved with the current research.
Moreover, that program achieved corresponding savings of $23 to $24 million, he noted.
Although his study and the current study show that POC devices work, he emphasized that it’s not enough to make the devices available to clinicians.
“You also have to ensure the providers put it in their clinic workflows and use it with everybody. To do that, it really helps if you have the providers report the results, then give them report cards so they can see who’s doing it and who isn’t,” Parks said.
It wasn’t surprising that in the current study, the introduction of the POC device made less of an impact in the adult community services, he noted.
Although weight reduction is much slower in that setting, “you can still get better control of their lipids and HbA1c›s, and you get at their weight over time. You just have to program for that, too,» said Parks.
He added that it’s hard to achieve weight reduction of more than 5% or 10%, but many of these patients need a 25% to 30% reduction. “The only thing that’s going to get that is bariatric surgery,” he noted.
POC devices are not widely used in the United States.
“The payer paying for the care basically has to insist that [it] be used and then provide the machine and train the staff to use it,” Parks said.
It requires payers “to get actually involved in how providers organize and manage care, which they tend to not like to do. It’s silly because the only way any payer has to make anybody better is through the provider,” he noted.
Parks added that to increase uptake beyond the “motivated few” requires that it be made part of the workflow and not left up to clinician discretion.
The study was funded by the National Institute for Health Research. Butler and Parks have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Using a simple point-of-care (POC) finger prick device to measure blood glucose and lipid levels significantly increases rates of physical health checkups for patients with severe mental illness, new research shows.
In a UK pilot study, use of the Afinion 2 device (Abbott) was associated with a doubling of completed physical health checkups.
However, the effect only occurred in early-intervention services, in which clinicians may feel physical health checkups are most beneficial. This underlines the importance of staff training and payment incentives, the researchers note.
“Clearly, convenience is a great thing about these devices” for both the patient and the mental health clinician, Joseph Butler, MD, a psychiatry trainee at the University of Oxford, United Kingdom, told Medscape Medical News.
He noted that blood test results are rapid, which facilitates immediate discussion of a health management plan.
These tests are “independent from the lab, they’re independent from the general practitioner, and so in terms of convenience, we think it wins on both fronts,” Butler said.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society (SIRS) 2020, but the meeting was canceled because of the coronavirus pandemic.
Poor heart health
Previous research has shown that life expectancy of patients with severe mental illness is 15 to 20 years less than that of the general population, mostly because of complications from poor cardiovascular health.
In the United Kingdom, physical healthcare for patients with serious mental illness is provided by primary care clinicians and community mental health teams (CMHTs). The National Institute for Health and Care Excellence recommends an annual physical examination.
However, a recent audit in the south of England indicated that only 38% of patients with severe mental illness underwent complete physical examinations, primarily because blood glucose and lipid test panels had been omitted.
The researchers note that patients are typically advised to visit their general practitioner for blood tests, “which can be a challenge” for those with severe mental illness.
The Cardiovascular Monitoring in Mental Health (CARMEN) project involved distributing the Afinion 2 device for use in two CMHTs in Oxfordshire, United Kingdom, for 6 months. One CMHT was an early-intervention service, and the other was an adult mental health service.
Care coordinators received training on how to use the device as well as ongoing support to facilitate engagement with the device.
Rates of completion of blood testing and full physical examinations were compared between the intervention CMHTs and two matched control services – an early-intervention group, and an adult metal health services group in Buckinghamshire, a neighboring county.
Better completion rates
The investigators found that .
In contrast, the percentage of physical examinations that were completed remained low in the control CMHT early-intervention service, at just 7.8%.
Direct comparison between the two services showed that use of the POC device was associated with a significant increase in the number of complete physical examinations, at a relative rate of 5.18 (P < .001).
Results were similar when the investigators examined rates at which A1c and lipid panels were completed.
However, there was no difference in completion of physical examinations in the adult mental health service group, for which rates were comparable to those in the control service.
Butler speculated that the way health checkups are funded in the United Kingdom might have contributed to the poor results with the device in the adult mental health service.
In early-intervention services, there is increased awareness of the importance of physical examinations, and funding is contingent on whether clinicians persuade patients to have the examinations.
Overall, the findings show that use of a POC device for physical examinations is acceptable to patients who have severe mental illness as well as to mental health care clinicians, the investigators note.
“In teams where it is well adopted, POC testing can improve physical health check completion...although our qualitative findings highlight important considerations for maximizing clinician engagement,” they add.
The researchers plan to repeat the study across the whole of the south of England, with early-intervention services in the west equipped with POC devices and those in the east serving as controls.
Similar findings
Commenting on the findings for Medscape Medical News, Joe Parks, MD, vice president and practice improvement and medical director at the National Council for Behavioral Health, Washington, DC, noted that he and his colleagues conducted a similar study in the mid-2000s.
Starting in 2004, they distributed a POC finger prick test device for use by community mental health teams to measure blood glucose and lipid levels.
“We required as a condition of payment that the providers get these lab results for everybody they served and report them centrally. Then, we databased them and benchmarked them, and we were able to show significant reductions in HbA1c’s over time,” said Parks, who was not involved with the current research.
Moreover, that program achieved corresponding savings of $23 to $24 million, he noted.
Although his study and the current study show that POC devices work, he emphasized that it’s not enough to make the devices available to clinicians.
“You also have to ensure the providers put it in their clinic workflows and use it with everybody. To do that, it really helps if you have the providers report the results, then give them report cards so they can see who’s doing it and who isn’t,” Parks said.
It wasn’t surprising that in the current study, the introduction of the POC device made less of an impact in the adult community services, he noted.
Although weight reduction is much slower in that setting, “you can still get better control of their lipids and HbA1c›s, and you get at their weight over time. You just have to program for that, too,» said Parks.
He added that it’s hard to achieve weight reduction of more than 5% or 10%, but many of these patients need a 25% to 30% reduction. “The only thing that’s going to get that is bariatric surgery,” he noted.
POC devices are not widely used in the United States.
“The payer paying for the care basically has to insist that [it] be used and then provide the machine and train the staff to use it,” Parks said.
It requires payers “to get actually involved in how providers organize and manage care, which they tend to not like to do. It’s silly because the only way any payer has to make anybody better is through the provider,” he noted.
Parks added that to increase uptake beyond the “motivated few” requires that it be made part of the workflow and not left up to clinician discretion.
The study was funded by the National Institute for Health Research. Butler and Parks have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Using a simple point-of-care (POC) finger prick device to measure blood glucose and lipid levels significantly increases rates of physical health checkups for patients with severe mental illness, new research shows.
In a UK pilot study, use of the Afinion 2 device (Abbott) was associated with a doubling of completed physical health checkups.
However, the effect only occurred in early-intervention services, in which clinicians may feel physical health checkups are most beneficial. This underlines the importance of staff training and payment incentives, the researchers note.
“Clearly, convenience is a great thing about these devices” for both the patient and the mental health clinician, Joseph Butler, MD, a psychiatry trainee at the University of Oxford, United Kingdom, told Medscape Medical News.
He noted that blood test results are rapid, which facilitates immediate discussion of a health management plan.
These tests are “independent from the lab, they’re independent from the general practitioner, and so in terms of convenience, we think it wins on both fronts,” Butler said.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society (SIRS) 2020, but the meeting was canceled because of the coronavirus pandemic.
Poor heart health
Previous research has shown that life expectancy of patients with severe mental illness is 15 to 20 years less than that of the general population, mostly because of complications from poor cardiovascular health.
In the United Kingdom, physical healthcare for patients with serious mental illness is provided by primary care clinicians and community mental health teams (CMHTs). The National Institute for Health and Care Excellence recommends an annual physical examination.
However, a recent audit in the south of England indicated that only 38% of patients with severe mental illness underwent complete physical examinations, primarily because blood glucose and lipid test panels had been omitted.
The researchers note that patients are typically advised to visit their general practitioner for blood tests, “which can be a challenge” for those with severe mental illness.
The Cardiovascular Monitoring in Mental Health (CARMEN) project involved distributing the Afinion 2 device for use in two CMHTs in Oxfordshire, United Kingdom, for 6 months. One CMHT was an early-intervention service, and the other was an adult mental health service.
Care coordinators received training on how to use the device as well as ongoing support to facilitate engagement with the device.
Rates of completion of blood testing and full physical examinations were compared between the intervention CMHTs and two matched control services – an early-intervention group, and an adult metal health services group in Buckinghamshire, a neighboring county.
Better completion rates
The investigators found that .
In contrast, the percentage of physical examinations that were completed remained low in the control CMHT early-intervention service, at just 7.8%.
Direct comparison between the two services showed that use of the POC device was associated with a significant increase in the number of complete physical examinations, at a relative rate of 5.18 (P < .001).
Results were similar when the investigators examined rates at which A1c and lipid panels were completed.
However, there was no difference in completion of physical examinations in the adult mental health service group, for which rates were comparable to those in the control service.
Butler speculated that the way health checkups are funded in the United Kingdom might have contributed to the poor results with the device in the adult mental health service.
In early-intervention services, there is increased awareness of the importance of physical examinations, and funding is contingent on whether clinicians persuade patients to have the examinations.
Overall, the findings show that use of a POC device for physical examinations is acceptable to patients who have severe mental illness as well as to mental health care clinicians, the investigators note.
“In teams where it is well adopted, POC testing can improve physical health check completion...although our qualitative findings highlight important considerations for maximizing clinician engagement,” they add.
The researchers plan to repeat the study across the whole of the south of England, with early-intervention services in the west equipped with POC devices and those in the east serving as controls.
Similar findings
Commenting on the findings for Medscape Medical News, Joe Parks, MD, vice president and practice improvement and medical director at the National Council for Behavioral Health, Washington, DC, noted that he and his colleagues conducted a similar study in the mid-2000s.
Starting in 2004, they distributed a POC finger prick test device for use by community mental health teams to measure blood glucose and lipid levels.
“We required as a condition of payment that the providers get these lab results for everybody they served and report them centrally. Then, we databased them and benchmarked them, and we were able to show significant reductions in HbA1c’s over time,” said Parks, who was not involved with the current research.
Moreover, that program achieved corresponding savings of $23 to $24 million, he noted.
Although his study and the current study show that POC devices work, he emphasized that it’s not enough to make the devices available to clinicians.
“You also have to ensure the providers put it in their clinic workflows and use it with everybody. To do that, it really helps if you have the providers report the results, then give them report cards so they can see who’s doing it and who isn’t,” Parks said.
It wasn’t surprising that in the current study, the introduction of the POC device made less of an impact in the adult community services, he noted.
Although weight reduction is much slower in that setting, “you can still get better control of their lipids and HbA1c›s, and you get at their weight over time. You just have to program for that, too,» said Parks.
He added that it’s hard to achieve weight reduction of more than 5% or 10%, but many of these patients need a 25% to 30% reduction. “The only thing that’s going to get that is bariatric surgery,” he noted.
POC devices are not widely used in the United States.
“The payer paying for the care basically has to insist that [it] be used and then provide the machine and train the staff to use it,” Parks said.
It requires payers “to get actually involved in how providers organize and manage care, which they tend to not like to do. It’s silly because the only way any payer has to make anybody better is through the provider,” he noted.
Parks added that to increase uptake beyond the “motivated few” requires that it be made part of the workflow and not left up to clinician discretion.
The study was funded by the National Institute for Health Research. Butler and Parks have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM SIRS 2020






