User login
AGA Clinical Practice Update Expert Review: Management of malignant alimentary tract obstruction
The American Gastroenterological Association published a clinical practice update expert review for managing malignant alimentary tract obstructions (MATOs) that includes 14 best practice advice statements, ranging from general principles to specific clinical choices.
“There are many options available for the management of MATOs, with the addition of new modalities as interventional endoscopy continues to evolve,” Osman Ahmed, MD, of the University of Toronto and colleagues wrote in Clinical Gastroenterology and Hepatology. “The important concept to understand for any physician managing MATOs is that there is no longer a ‘one-size-fits-all’ approach that can be applied to all patients.”
First, the investigators called for an individualized, multidisciplinary approach that includes oncologists, surgeons, and endoscopists. They advised physicians to “take into account the characteristics of the obstruction, patient’s expectations, prognosis, expected subsequent therapies, and functional status.”
The remaining advice statements are organized by site of obstruction, with various management approaches based on candidacy for resection and other patient factors.
Esophageal obstruction
For patients with esophageal obstruction who are candidates for resection or chemoradiation, Dr. Ahmed and colleagues advised against routine use of self-expanding metal stents (SEMS) due to “high rates of stent migration, higher morbidity and mortality, and potentially lower R0 (microscopically negative margins) resection rates.”
If such patients are at risk of malnutrition, an enteral feeding tube may be considered, although patients should be counseled about associated procedural risks, such as abdominal wall tumor seeding.
Among patients with esophageal obstruction who are not candidates for resection, SEMS insertion or brachytherapy may be used separately or in combination, according to the investigators.
“Clinicians should not consider the use of laser therapy or photodynamic therapy because of the lack of evidence of better outcomes and superior alternatives,” the investigators noted.
If SEMS placement is elected, Dr. Ahmed and colleagues noted there remains ongoing debate. For this expert review, the authors advised using a fully covered stent, based on potentially higher risk for tumor ingrowth and reinterventions with uncovered SEMS.
Gastric outlet obstruction
According to the update, patients with gastric outlet obstruction who have good functional status and a life expectancy greater than 2 months should undergo surgical gastrojejunostomy, ideally via a laparoscopic approach instead of an open approach because of shorter hospital stays and less blood loss. If a sufficiently experienced endoscopist is available, an endoscopic ultrasound-guided gastrojejunostomy may be performed, although Dr. Ahmed and colleagues noted that no devices have been approved by the Food and Drug Administration for this technique.
For patients who are not candidates for gastrojejunostomy, enteral stent insertion should be considered; however, they should not be used in patients with severely impaired gastric motility or multiple luminal obstructions “because of limited benefit in these scenarios.” Instead, a venting gastrostomy may be elected.
Colonic obstruction
For patients with malignant colonic obstruction, SEMS may be considered as a “bridge to surgery,” wrote Dr. Ahmed and colleagues, and in the case of proximal or right-sided malignant obstruction, as a bridge to surgery or a palliative measure, keeping in mind “the technical challenges of SEMS insertion in those areas.”
Extracolonic obstruction
Finally, the expert panel suggested that SEMS may be appropriate for selective extracolonic malignancy if patients are not surgical candidates, noting that SEMS placement in this scenario “is more technically challenging, clinical success rates are more variable, and complications (including stent migration) are more frequent.”
The investigators concluded by advising clinicians to remain within the realm of their abilities when managing MATOs, and to refer when needed.
“[I]t is important for physicians to understand their limits and expertise and recognize when cases are best managed at experienced high-volume centers,” they wrote.
The clinical practice update expert review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Lee disclosed a relationship with Boston Scientific.
The American Gastroenterological Association published a clinical practice update expert review for managing malignant alimentary tract obstructions (MATOs) that includes 14 best practice advice statements, ranging from general principles to specific clinical choices.
“There are many options available for the management of MATOs, with the addition of new modalities as interventional endoscopy continues to evolve,” Osman Ahmed, MD, of the University of Toronto and colleagues wrote in Clinical Gastroenterology and Hepatology. “The important concept to understand for any physician managing MATOs is that there is no longer a ‘one-size-fits-all’ approach that can be applied to all patients.”
First, the investigators called for an individualized, multidisciplinary approach that includes oncologists, surgeons, and endoscopists. They advised physicians to “take into account the characteristics of the obstruction, patient’s expectations, prognosis, expected subsequent therapies, and functional status.”
The remaining advice statements are organized by site of obstruction, with various management approaches based on candidacy for resection and other patient factors.
Esophageal obstruction
For patients with esophageal obstruction who are candidates for resection or chemoradiation, Dr. Ahmed and colleagues advised against routine use of self-expanding metal stents (SEMS) due to “high rates of stent migration, higher morbidity and mortality, and potentially lower R0 (microscopically negative margins) resection rates.”
If such patients are at risk of malnutrition, an enteral feeding tube may be considered, although patients should be counseled about associated procedural risks, such as abdominal wall tumor seeding.
Among patients with esophageal obstruction who are not candidates for resection, SEMS insertion or brachytherapy may be used separately or in combination, according to the investigators.
“Clinicians should not consider the use of laser therapy or photodynamic therapy because of the lack of evidence of better outcomes and superior alternatives,” the investigators noted.
If SEMS placement is elected, Dr. Ahmed and colleagues noted there remains ongoing debate. For this expert review, the authors advised using a fully covered stent, based on potentially higher risk for tumor ingrowth and reinterventions with uncovered SEMS.
Gastric outlet obstruction
According to the update, patients with gastric outlet obstruction who have good functional status and a life expectancy greater than 2 months should undergo surgical gastrojejunostomy, ideally via a laparoscopic approach instead of an open approach because of shorter hospital stays and less blood loss. If a sufficiently experienced endoscopist is available, an endoscopic ultrasound-guided gastrojejunostomy may be performed, although Dr. Ahmed and colleagues noted that no devices have been approved by the Food and Drug Administration for this technique.
For patients who are not candidates for gastrojejunostomy, enteral stent insertion should be considered; however, they should not be used in patients with severely impaired gastric motility or multiple luminal obstructions “because of limited benefit in these scenarios.” Instead, a venting gastrostomy may be elected.
Colonic obstruction
For patients with malignant colonic obstruction, SEMS may be considered as a “bridge to surgery,” wrote Dr. Ahmed and colleagues, and in the case of proximal or right-sided malignant obstruction, as a bridge to surgery or a palliative measure, keeping in mind “the technical challenges of SEMS insertion in those areas.”
Extracolonic obstruction
Finally, the expert panel suggested that SEMS may be appropriate for selective extracolonic malignancy if patients are not surgical candidates, noting that SEMS placement in this scenario “is more technically challenging, clinical success rates are more variable, and complications (including stent migration) are more frequent.”
The investigators concluded by advising clinicians to remain within the realm of their abilities when managing MATOs, and to refer when needed.
“[I]t is important for physicians to understand their limits and expertise and recognize when cases are best managed at experienced high-volume centers,” they wrote.
The clinical practice update expert review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Lee disclosed a relationship with Boston Scientific.
The American Gastroenterological Association published a clinical practice update expert review for managing malignant alimentary tract obstructions (MATOs) that includes 14 best practice advice statements, ranging from general principles to specific clinical choices.
“There are many options available for the management of MATOs, with the addition of new modalities as interventional endoscopy continues to evolve,” Osman Ahmed, MD, of the University of Toronto and colleagues wrote in Clinical Gastroenterology and Hepatology. “The important concept to understand for any physician managing MATOs is that there is no longer a ‘one-size-fits-all’ approach that can be applied to all patients.”
First, the investigators called for an individualized, multidisciplinary approach that includes oncologists, surgeons, and endoscopists. They advised physicians to “take into account the characteristics of the obstruction, patient’s expectations, prognosis, expected subsequent therapies, and functional status.”
The remaining advice statements are organized by site of obstruction, with various management approaches based on candidacy for resection and other patient factors.
Esophageal obstruction
For patients with esophageal obstruction who are candidates for resection or chemoradiation, Dr. Ahmed and colleagues advised against routine use of self-expanding metal stents (SEMS) due to “high rates of stent migration, higher morbidity and mortality, and potentially lower R0 (microscopically negative margins) resection rates.”
If such patients are at risk of malnutrition, an enteral feeding tube may be considered, although patients should be counseled about associated procedural risks, such as abdominal wall tumor seeding.
Among patients with esophageal obstruction who are not candidates for resection, SEMS insertion or brachytherapy may be used separately or in combination, according to the investigators.
“Clinicians should not consider the use of laser therapy or photodynamic therapy because of the lack of evidence of better outcomes and superior alternatives,” the investigators noted.
If SEMS placement is elected, Dr. Ahmed and colleagues noted there remains ongoing debate. For this expert review, the authors advised using a fully covered stent, based on potentially higher risk for tumor ingrowth and reinterventions with uncovered SEMS.
Gastric outlet obstruction
According to the update, patients with gastric outlet obstruction who have good functional status and a life expectancy greater than 2 months should undergo surgical gastrojejunostomy, ideally via a laparoscopic approach instead of an open approach because of shorter hospital stays and less blood loss. If a sufficiently experienced endoscopist is available, an endoscopic ultrasound-guided gastrojejunostomy may be performed, although Dr. Ahmed and colleagues noted that no devices have been approved by the Food and Drug Administration for this technique.
For patients who are not candidates for gastrojejunostomy, enteral stent insertion should be considered; however, they should not be used in patients with severely impaired gastric motility or multiple luminal obstructions “because of limited benefit in these scenarios.” Instead, a venting gastrostomy may be elected.
Colonic obstruction
For patients with malignant colonic obstruction, SEMS may be considered as a “bridge to surgery,” wrote Dr. Ahmed and colleagues, and in the case of proximal or right-sided malignant obstruction, as a bridge to surgery or a palliative measure, keeping in mind “the technical challenges of SEMS insertion in those areas.”
Extracolonic obstruction
Finally, the expert panel suggested that SEMS may be appropriate for selective extracolonic malignancy if patients are not surgical candidates, noting that SEMS placement in this scenario “is more technically challenging, clinical success rates are more variable, and complications (including stent migration) are more frequent.”
The investigators concluded by advising clinicians to remain within the realm of their abilities when managing MATOs, and to refer when needed.
“[I]t is important for physicians to understand their limits and expertise and recognize when cases are best managed at experienced high-volume centers,” they wrote.
The clinical practice update expert review was commissioned and approved by the AGA Institute Clinical Practice Updates Committee and the AGA Governing Board. Dr. Lee disclosed a relationship with Boston Scientific.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Low-dose aspirin linked to lower dementia risk in some
, according to a retrospective analysis of two large cohorts. The association with all-cause dementia was weak, but much more pronounced in subjects with coronary heart disease.
The results underscore that individuals with cardiovascular disease risk factors should be prescribed LDASA, and they should be encouraged to be compliant. The study differed from previous observational and randomized, controlled trials, which yielded mixed results. Many looked at individuals older than age 65. The pathological changes associated with dementia may occur up to 2 decades before symptom onset, and it appears that LDASA cannot counter cognitive decline after a diagnosis is made. “The use of LDASA at this age may be already too late,” said Thi Ngoc Mai Nguyen, a PhD student at Network Aging Research, Heidelberg University, Germany. She presented the results at the 2021 Alzheimer’s Association International Conference.
Previous studies also included individuals using LDASA to prevent cardiovascular disease, and they didn’t always adjust for these risk factors. The current work used two large databases, UK Biobank and ESTHER, with a follow-up time of over 10 years for both. “We were able to balance out the distribution of measured baseline covariates (to be) similar between LDASA users and nonusers, and thus, we were able to adjust for confounders more comprehensively,” said Ms. Nguyen.
Not yet a definitive answer
Although the findings are promising, Ms. Nguyen noted that the study is not the final word. “Residual confounding is possible, and causation cannot be tested. The only way to answer this is to have clinical trials with at least 10 years of follow-up,” said Ms. Nguyen. She plans to conduct similar studies in non-White populations, and also to examine whether LDASA can help preserve cognitive function in middle-age adults.
The study is interesting, said Claire Sexton, DPhil, who was asked to comment, but she suggested that it is not practice changing. “There is not evidence from the dementia science perspective that should go against whatever the recommendations are for cardiovascular risk,” said Dr. Sexton, director of scientific programs and outreach at the Alzheimer’s Association. “I don’t think this study alone can provide a definitive answer on low-dose aspirin and its association with dementia and Alzheimer’s disease, but it’s an important addition to the literature,” she added.
Meta-analysis data
The researchers examined two prospective cohort studies, and combined them into a meta-analysis. It included the ESTHER cohort from Saarland, Germany, with 5,258 individuals and 14.3 years of follow-up, and the UK Biobank cohort, with 305,394 individuals and 11.6 years of follow-up. Subjects selected for analysis were 55 years old or older.
The meta-analysis showed no significant association between LDASA use and reduced risk of Alzheimer’s disease, but there was an association between LDASA use and all-cause dementia (hazard ratio [HR], 0.96; 95% confidence interval [CI], 0.93-0.99).
There were no sex differences with respect to Alzheimer’s dementia, but in males, LDASA was associated with lower risk of vascular dementia (HR, 0.85; 95% CI, 0.79-0.93) and all-cause dementia (HR, 0.87; 95% CI, 0.83-0.92). However, in females, LDASA was tied to greater risk of both vascular dementia (HR, 1.13; 95% CI, 1.02-1.24) and all-cause dementia (HR, 1.07; 95% CI, 1.02-1.13).
The strongest association between LDASA and reduced dementia risk was found in subjects with coronary heart disease (HR, 0.69; 95% CI, 0.59-0.80).
The researchers also used UK Biobank primary care data to analyze associations between longer use of LDASA and reduced dementia risk. Those who used LDASA for 0-5 years were at a higher than average risk of all-cause dementia (HR, 2.80; 95% CI, 2.48-3.16), Alzheimer’s disease (HR, 2.26; 95% CI, 1.84-2.77), and vascular dementia (HR, 3.79; 95% CI, 3.17-4.53). Long-term LDASA users, defined as 10 years or longer, had a lower risk of all-cause dementia (HR, 0.51; 95% CI, 0.47-0.56), Alzheimer’s disease (HR, 0.58; 95% CI, 0.51-0.68), and vascular dementia (HR, 0.48; 95% CI, 0.42-0.56).
Dr. Nguyen and Dr. Sexton have no relevant financial disclosures.
, according to a retrospective analysis of two large cohorts. The association with all-cause dementia was weak, but much more pronounced in subjects with coronary heart disease.
The results underscore that individuals with cardiovascular disease risk factors should be prescribed LDASA, and they should be encouraged to be compliant. The study differed from previous observational and randomized, controlled trials, which yielded mixed results. Many looked at individuals older than age 65. The pathological changes associated with dementia may occur up to 2 decades before symptom onset, and it appears that LDASA cannot counter cognitive decline after a diagnosis is made. “The use of LDASA at this age may be already too late,” said Thi Ngoc Mai Nguyen, a PhD student at Network Aging Research, Heidelberg University, Germany. She presented the results at the 2021 Alzheimer’s Association International Conference.
Previous studies also included individuals using LDASA to prevent cardiovascular disease, and they didn’t always adjust for these risk factors. The current work used two large databases, UK Biobank and ESTHER, with a follow-up time of over 10 years for both. “We were able to balance out the distribution of measured baseline covariates (to be) similar between LDASA users and nonusers, and thus, we were able to adjust for confounders more comprehensively,” said Ms. Nguyen.
Not yet a definitive answer
Although the findings are promising, Ms. Nguyen noted that the study is not the final word. “Residual confounding is possible, and causation cannot be tested. The only way to answer this is to have clinical trials with at least 10 years of follow-up,” said Ms. Nguyen. She plans to conduct similar studies in non-White populations, and also to examine whether LDASA can help preserve cognitive function in middle-age adults.
The study is interesting, said Claire Sexton, DPhil, who was asked to comment, but she suggested that it is not practice changing. “There is not evidence from the dementia science perspective that should go against whatever the recommendations are for cardiovascular risk,” said Dr. Sexton, director of scientific programs and outreach at the Alzheimer’s Association. “I don’t think this study alone can provide a definitive answer on low-dose aspirin and its association with dementia and Alzheimer’s disease, but it’s an important addition to the literature,” she added.
Meta-analysis data
The researchers examined two prospective cohort studies, and combined them into a meta-analysis. It included the ESTHER cohort from Saarland, Germany, with 5,258 individuals and 14.3 years of follow-up, and the UK Biobank cohort, with 305,394 individuals and 11.6 years of follow-up. Subjects selected for analysis were 55 years old or older.
The meta-analysis showed no significant association between LDASA use and reduced risk of Alzheimer’s disease, but there was an association between LDASA use and all-cause dementia (hazard ratio [HR], 0.96; 95% confidence interval [CI], 0.93-0.99).
There were no sex differences with respect to Alzheimer’s dementia, but in males, LDASA was associated with lower risk of vascular dementia (HR, 0.85; 95% CI, 0.79-0.93) and all-cause dementia (HR, 0.87; 95% CI, 0.83-0.92). However, in females, LDASA was tied to greater risk of both vascular dementia (HR, 1.13; 95% CI, 1.02-1.24) and all-cause dementia (HR, 1.07; 95% CI, 1.02-1.13).
The strongest association between LDASA and reduced dementia risk was found in subjects with coronary heart disease (HR, 0.69; 95% CI, 0.59-0.80).
The researchers also used UK Biobank primary care data to analyze associations between longer use of LDASA and reduced dementia risk. Those who used LDASA for 0-5 years were at a higher than average risk of all-cause dementia (HR, 2.80; 95% CI, 2.48-3.16), Alzheimer’s disease (HR, 2.26; 95% CI, 1.84-2.77), and vascular dementia (HR, 3.79; 95% CI, 3.17-4.53). Long-term LDASA users, defined as 10 years or longer, had a lower risk of all-cause dementia (HR, 0.51; 95% CI, 0.47-0.56), Alzheimer’s disease (HR, 0.58; 95% CI, 0.51-0.68), and vascular dementia (HR, 0.48; 95% CI, 0.42-0.56).
Dr. Nguyen and Dr. Sexton have no relevant financial disclosures.
, according to a retrospective analysis of two large cohorts. The association with all-cause dementia was weak, but much more pronounced in subjects with coronary heart disease.
The results underscore that individuals with cardiovascular disease risk factors should be prescribed LDASA, and they should be encouraged to be compliant. The study differed from previous observational and randomized, controlled trials, which yielded mixed results. Many looked at individuals older than age 65. The pathological changes associated with dementia may occur up to 2 decades before symptom onset, and it appears that LDASA cannot counter cognitive decline after a diagnosis is made. “The use of LDASA at this age may be already too late,” said Thi Ngoc Mai Nguyen, a PhD student at Network Aging Research, Heidelberg University, Germany. She presented the results at the 2021 Alzheimer’s Association International Conference.
Previous studies also included individuals using LDASA to prevent cardiovascular disease, and they didn’t always adjust for these risk factors. The current work used two large databases, UK Biobank and ESTHER, with a follow-up time of over 10 years for both. “We were able to balance out the distribution of measured baseline covariates (to be) similar between LDASA users and nonusers, and thus, we were able to adjust for confounders more comprehensively,” said Ms. Nguyen.
Not yet a definitive answer
Although the findings are promising, Ms. Nguyen noted that the study is not the final word. “Residual confounding is possible, and causation cannot be tested. The only way to answer this is to have clinical trials with at least 10 years of follow-up,” said Ms. Nguyen. She plans to conduct similar studies in non-White populations, and also to examine whether LDASA can help preserve cognitive function in middle-age adults.
The study is interesting, said Claire Sexton, DPhil, who was asked to comment, but she suggested that it is not practice changing. “There is not evidence from the dementia science perspective that should go against whatever the recommendations are for cardiovascular risk,” said Dr. Sexton, director of scientific programs and outreach at the Alzheimer’s Association. “I don’t think this study alone can provide a definitive answer on low-dose aspirin and its association with dementia and Alzheimer’s disease, but it’s an important addition to the literature,” she added.
Meta-analysis data
The researchers examined two prospective cohort studies, and combined them into a meta-analysis. It included the ESTHER cohort from Saarland, Germany, with 5,258 individuals and 14.3 years of follow-up, and the UK Biobank cohort, with 305,394 individuals and 11.6 years of follow-up. Subjects selected for analysis were 55 years old or older.
The meta-analysis showed no significant association between LDASA use and reduced risk of Alzheimer’s disease, but there was an association between LDASA use and all-cause dementia (hazard ratio [HR], 0.96; 95% confidence interval [CI], 0.93-0.99).
There were no sex differences with respect to Alzheimer’s dementia, but in males, LDASA was associated with lower risk of vascular dementia (HR, 0.85; 95% CI, 0.79-0.93) and all-cause dementia (HR, 0.87; 95% CI, 0.83-0.92). However, in females, LDASA was tied to greater risk of both vascular dementia (HR, 1.13; 95% CI, 1.02-1.24) and all-cause dementia (HR, 1.07; 95% CI, 1.02-1.13).
The strongest association between LDASA and reduced dementia risk was found in subjects with coronary heart disease (HR, 0.69; 95% CI, 0.59-0.80).
The researchers also used UK Biobank primary care data to analyze associations between longer use of LDASA and reduced dementia risk. Those who used LDASA for 0-5 years were at a higher than average risk of all-cause dementia (HR, 2.80; 95% CI, 2.48-3.16), Alzheimer’s disease (HR, 2.26; 95% CI, 1.84-2.77), and vascular dementia (HR, 3.79; 95% CI, 3.17-4.53). Long-term LDASA users, defined as 10 years or longer, had a lower risk of all-cause dementia (HR, 0.51; 95% CI, 0.47-0.56), Alzheimer’s disease (HR, 0.58; 95% CI, 0.51-0.68), and vascular dementia (HR, 0.48; 95% CI, 0.42-0.56).
Dr. Nguyen and Dr. Sexton have no relevant financial disclosures.
FROM AAIC 2021
Same-day discharge for elective PCI shown safe in real-world analysis
Based on a large registry, there appears to be no adverse consequences for same-day discharge following an elective percutaneous cardiovascular intervention (PCI), according to an analysis of a nationwide registry.
“Our data suggest there has been no negative impact on patient outcomes as a result of increasing use of same-day discharge,” lead investigator Steven M. Bradley, MD, said in an interview.
The analysis was based on data on 819,091 patients who underwent an elective PCI procedure during July 2009–December 2017 in the National CathPCI Registry. During this period, the proportion of elective PCIs performed with same-day discharge rose from 4.5% to 28.6%, a fivefold gain, according to Dr. Bradley, an associate cardiologist at the Minneapolis Heart Institute, and colleagues.
Within this study, outcomes in 212,369 patients were analyzed through a link to Centers for Medicare & Medicaid Services data. Despite the growth in same-day discharge PCIs over the study period, there was no change in 30-day mortality rates while the rate of 30-day rehospitalization fell after risk adjustment.
These data are considered to have a message for routine practice, particularly for those hospitals that have been slow to move to same-day discharge for elective PCI when lack of complications makes this appropriate.
However, “this does not mean same-day discharge is safe for all patients,” Dr. Bradley cautioned, but these data suggest “there is a clear opportunity at sites with low rates” to look for strategies that allow patients to recover at home, which is preferred by many patients and lowers costs.
In 2009, the first year in which the data were analyzed, there was relatively little variation in the rate of same day discharge for elective PCI among the 1,716 hospitals that contributed patients to the registry. At that point, almost all hospitals had rates below 10%, according to the report published in JACC: Cardiovascular Interventions on Aug 2, 2021 .
From 2011 onward, there were progressive gains at most hospitals, with an even steeper rise beginning in 2014. By 2017, even though some hospitals were still performing almost no same-day discharge PCIs, many were discharging up to 40%, and the outliers were discharging nearly all.
Expressed in interquartiles at the hospital level, the range climbed from 0.0% to 4.7% in 2009 and reached 4.5% to 41.0% by 2017. For 2017, relative to 2009, this produced an odds ratio for same-day discharge that was more than fourfold greater, after adjustment for year and access site.
Access site was an important variable. For those undergoing PCI with radial access, the median same-day discharge rates climbed from 21.8% in 2009 to 58.3% in 2017. Same-day discharge rates for elective PCI performed by femoral access, already lower in 2009, have consistently lagged. By 2017, the median rate of same-day discharge for those undergoing PCI by the femoral route was less than half of that associated with radial access.
Despite the faster rise in same-day discharge and radial access over the course of the study, these were not directly correlated. In 2017, 25% of sites performing PCI by radial access were still discharging fewer than 10% of patients on the same day as their elective PCI.
Several previous studies have also found that same-day discharge can be offered selectively after elective PCI without adversely affecting outcomes, according to multiple citations provided by the authors. The advantage of early discharge includes both convenience for the patient and lower costs, with some of the studies attempting to quantify savings. In one, it was estimated that per-case savings from performing radial-access elective PCI with same-day discharge was nearly $3,700 when compared with transfemoral access and an overnight stay.
Radial access key to same-day success
An accompanying editorial by Deepak Bhatt, MD, and Jonathan G. Sung, MBChB, who are both interventional cardiologists at Brigham and Women’s Hospital, Boston, generally agreed with the premise that these data support judicious use of same-day discharge for elective PCI.
They pointed out limitations in the study, including its retrospective design and the inability to look at important outcomes other than mortality and 30-day rehospitalization, such as bleeding, that are relevant to the safety of early discharge, but concluded that same-day discharge, as well as radial access procedures, are underused.
“For uncomplicated elective PCI, we should aim for same-day discharge,” Dr. Bhatt said in an interview. He linked this to radial access.
“Radial access certainly facilitates same-day discharge, though even beyond that aspect, it should be the default route of vascular access whenever possible,” Dr. Bhatt said. Yet he was careful to say that neither same-day discharge nor radial access can be recommended in all patients. While the operator needs “to be comfortable” with a radial access approach, there are multiple factors that might preclude early discharge.
“Of course, if a long procedure, high contrast use, bleeding, a long travel distance to get home, etc. [are considered], then an overnight stay may be warranted,” he said.
Dr. Bradley advised centers planning to increase their same-day discharge rates for elective PCI to use a systematic approach.
“Sites should identify areas for opportunity in the use of same-day discharge and then track the implications on patient outcomes to ensure that the approach being used maintains high-quality care,” he said.
Dr. Bradley reported no potential conflicts of interest. Dr. Bhatt has received research funding from a large number of pharmaceutical and device manufacturers, including those that make products relevant to PCI.
Based on a large registry, there appears to be no adverse consequences for same-day discharge following an elective percutaneous cardiovascular intervention (PCI), according to an analysis of a nationwide registry.
“Our data suggest there has been no negative impact on patient outcomes as a result of increasing use of same-day discharge,” lead investigator Steven M. Bradley, MD, said in an interview.
The analysis was based on data on 819,091 patients who underwent an elective PCI procedure during July 2009–December 2017 in the National CathPCI Registry. During this period, the proportion of elective PCIs performed with same-day discharge rose from 4.5% to 28.6%, a fivefold gain, according to Dr. Bradley, an associate cardiologist at the Minneapolis Heart Institute, and colleagues.
Within this study, outcomes in 212,369 patients were analyzed through a link to Centers for Medicare & Medicaid Services data. Despite the growth in same-day discharge PCIs over the study period, there was no change in 30-day mortality rates while the rate of 30-day rehospitalization fell after risk adjustment.
These data are considered to have a message for routine practice, particularly for those hospitals that have been slow to move to same-day discharge for elective PCI when lack of complications makes this appropriate.
However, “this does not mean same-day discharge is safe for all patients,” Dr. Bradley cautioned, but these data suggest “there is a clear opportunity at sites with low rates” to look for strategies that allow patients to recover at home, which is preferred by many patients and lowers costs.
In 2009, the first year in which the data were analyzed, there was relatively little variation in the rate of same day discharge for elective PCI among the 1,716 hospitals that contributed patients to the registry. At that point, almost all hospitals had rates below 10%, according to the report published in JACC: Cardiovascular Interventions on Aug 2, 2021 .
From 2011 onward, there were progressive gains at most hospitals, with an even steeper rise beginning in 2014. By 2017, even though some hospitals were still performing almost no same-day discharge PCIs, many were discharging up to 40%, and the outliers were discharging nearly all.
Expressed in interquartiles at the hospital level, the range climbed from 0.0% to 4.7% in 2009 and reached 4.5% to 41.0% by 2017. For 2017, relative to 2009, this produced an odds ratio for same-day discharge that was more than fourfold greater, after adjustment for year and access site.
Access site was an important variable. For those undergoing PCI with radial access, the median same-day discharge rates climbed from 21.8% in 2009 to 58.3% in 2017. Same-day discharge rates for elective PCI performed by femoral access, already lower in 2009, have consistently lagged. By 2017, the median rate of same-day discharge for those undergoing PCI by the femoral route was less than half of that associated with radial access.
Despite the faster rise in same-day discharge and radial access over the course of the study, these were not directly correlated. In 2017, 25% of sites performing PCI by radial access were still discharging fewer than 10% of patients on the same day as their elective PCI.
Several previous studies have also found that same-day discharge can be offered selectively after elective PCI without adversely affecting outcomes, according to multiple citations provided by the authors. The advantage of early discharge includes both convenience for the patient and lower costs, with some of the studies attempting to quantify savings. In one, it was estimated that per-case savings from performing radial-access elective PCI with same-day discharge was nearly $3,700 when compared with transfemoral access and an overnight stay.
Radial access key to same-day success
An accompanying editorial by Deepak Bhatt, MD, and Jonathan G. Sung, MBChB, who are both interventional cardiologists at Brigham and Women’s Hospital, Boston, generally agreed with the premise that these data support judicious use of same-day discharge for elective PCI.
They pointed out limitations in the study, including its retrospective design and the inability to look at important outcomes other than mortality and 30-day rehospitalization, such as bleeding, that are relevant to the safety of early discharge, but concluded that same-day discharge, as well as radial access procedures, are underused.
“For uncomplicated elective PCI, we should aim for same-day discharge,” Dr. Bhatt said in an interview. He linked this to radial access.
“Radial access certainly facilitates same-day discharge, though even beyond that aspect, it should be the default route of vascular access whenever possible,” Dr. Bhatt said. Yet he was careful to say that neither same-day discharge nor radial access can be recommended in all patients. While the operator needs “to be comfortable” with a radial access approach, there are multiple factors that might preclude early discharge.
“Of course, if a long procedure, high contrast use, bleeding, a long travel distance to get home, etc. [are considered], then an overnight stay may be warranted,” he said.
Dr. Bradley advised centers planning to increase their same-day discharge rates for elective PCI to use a systematic approach.
“Sites should identify areas for opportunity in the use of same-day discharge and then track the implications on patient outcomes to ensure that the approach being used maintains high-quality care,” he said.
Dr. Bradley reported no potential conflicts of interest. Dr. Bhatt has received research funding from a large number of pharmaceutical and device manufacturers, including those that make products relevant to PCI.
Based on a large registry, there appears to be no adverse consequences for same-day discharge following an elective percutaneous cardiovascular intervention (PCI), according to an analysis of a nationwide registry.
“Our data suggest there has been no negative impact on patient outcomes as a result of increasing use of same-day discharge,” lead investigator Steven M. Bradley, MD, said in an interview.
The analysis was based on data on 819,091 patients who underwent an elective PCI procedure during July 2009–December 2017 in the National CathPCI Registry. During this period, the proportion of elective PCIs performed with same-day discharge rose from 4.5% to 28.6%, a fivefold gain, according to Dr. Bradley, an associate cardiologist at the Minneapolis Heart Institute, and colleagues.
Within this study, outcomes in 212,369 patients were analyzed through a link to Centers for Medicare & Medicaid Services data. Despite the growth in same-day discharge PCIs over the study period, there was no change in 30-day mortality rates while the rate of 30-day rehospitalization fell after risk adjustment.
These data are considered to have a message for routine practice, particularly for those hospitals that have been slow to move to same-day discharge for elective PCI when lack of complications makes this appropriate.
However, “this does not mean same-day discharge is safe for all patients,” Dr. Bradley cautioned, but these data suggest “there is a clear opportunity at sites with low rates” to look for strategies that allow patients to recover at home, which is preferred by many patients and lowers costs.
In 2009, the first year in which the data were analyzed, there was relatively little variation in the rate of same day discharge for elective PCI among the 1,716 hospitals that contributed patients to the registry. At that point, almost all hospitals had rates below 10%, according to the report published in JACC: Cardiovascular Interventions on Aug 2, 2021 .
From 2011 onward, there were progressive gains at most hospitals, with an even steeper rise beginning in 2014. By 2017, even though some hospitals were still performing almost no same-day discharge PCIs, many were discharging up to 40%, and the outliers were discharging nearly all.
Expressed in interquartiles at the hospital level, the range climbed from 0.0% to 4.7% in 2009 and reached 4.5% to 41.0% by 2017. For 2017, relative to 2009, this produced an odds ratio for same-day discharge that was more than fourfold greater, after adjustment for year and access site.
Access site was an important variable. For those undergoing PCI with radial access, the median same-day discharge rates climbed from 21.8% in 2009 to 58.3% in 2017. Same-day discharge rates for elective PCI performed by femoral access, already lower in 2009, have consistently lagged. By 2017, the median rate of same-day discharge for those undergoing PCI by the femoral route was less than half of that associated with radial access.
Despite the faster rise in same-day discharge and radial access over the course of the study, these were not directly correlated. In 2017, 25% of sites performing PCI by radial access were still discharging fewer than 10% of patients on the same day as their elective PCI.
Several previous studies have also found that same-day discharge can be offered selectively after elective PCI without adversely affecting outcomes, according to multiple citations provided by the authors. The advantage of early discharge includes both convenience for the patient and lower costs, with some of the studies attempting to quantify savings. In one, it was estimated that per-case savings from performing radial-access elective PCI with same-day discharge was nearly $3,700 when compared with transfemoral access and an overnight stay.
Radial access key to same-day success
An accompanying editorial by Deepak Bhatt, MD, and Jonathan G. Sung, MBChB, who are both interventional cardiologists at Brigham and Women’s Hospital, Boston, generally agreed with the premise that these data support judicious use of same-day discharge for elective PCI.
They pointed out limitations in the study, including its retrospective design and the inability to look at important outcomes other than mortality and 30-day rehospitalization, such as bleeding, that are relevant to the safety of early discharge, but concluded that same-day discharge, as well as radial access procedures, are underused.
“For uncomplicated elective PCI, we should aim for same-day discharge,” Dr. Bhatt said in an interview. He linked this to radial access.
“Radial access certainly facilitates same-day discharge, though even beyond that aspect, it should be the default route of vascular access whenever possible,” Dr. Bhatt said. Yet he was careful to say that neither same-day discharge nor radial access can be recommended in all patients. While the operator needs “to be comfortable” with a radial access approach, there are multiple factors that might preclude early discharge.
“Of course, if a long procedure, high contrast use, bleeding, a long travel distance to get home, etc. [are considered], then an overnight stay may be warranted,” he said.
Dr. Bradley advised centers planning to increase their same-day discharge rates for elective PCI to use a systematic approach.
“Sites should identify areas for opportunity in the use of same-day discharge and then track the implications on patient outcomes to ensure that the approach being used maintains high-quality care,” he said.
Dr. Bradley reported no potential conflicts of interest. Dr. Bhatt has received research funding from a large number of pharmaceutical and device manufacturers, including those that make products relevant to PCI.
FROM JACC: CARDIOVASCULAR INTERVENTIONS
Never prouder to be a hospitalist
I have been a proud hospitalist for more than 20 years, and yet I have never been prouder to be a hospitalist than now. The pandemic has been brutal, killing more than 600,000 Americans as of this writing. It has stretched the health care system, its doctors, nurses, and other providers to the limit. Yet we will get through it, we are getting through it, and hospitalists deserve a huge portion of the credit.
According to the CDC, there have been over 2.3 million COVID-19 hospitalizations. In my home state of Maryland, between two-thirds and three-quarters of hospitalized COVID patients are cared for on general medical floors, the domain of hospitalists. When hospitals needed COVID units, hospitalists stepped up to design and staff them. When our ICU colleagues needed support, especially in those early dark days, hospitalists stepped in. When our outpatient colleagues were called into the hospital, hospitalists were there to help them on board. When the House of Medicine was in chaos due to COVID-19, hospitalists ran towards that fire. Our previous 20+ years of collective experience made us the ideal specialty to manage the inpatient challenges over the last 18 months.
Need a new clinical schedule by Sunday? Check.
Need help with new clinical protocols? Check.
Need to help other colleagues? Check.
Need to reprogram the EMR? Check.
Need a new way to teach residents and students on the wards? Check.
Need a whole new unit – no, wait – a new hospital wing? No, scratch that – a whole new COVID hospital in a few weeks? Check. (I personally did that last one at the Baltimore Convention Center!)
For me and many hospitalists like me, it is as if the last 20 years were prep work for the pandemic.
Here at SHM, we know the pandemic is hard work – exhausting, even. SHM has been actively focused on supporting hospitalists during this crisis so that hospitalists can focus on patients. Early in the pandemic, SHM quickly pivoted to supply hospitalists with COVID-19 resources in their fight against the coronavirus. Numerous COVID-19 webinars, a COVID addendum to the State of Hospital Medicine Report, and a dedicated COVID issue of the Journal of Hospital Medicine were early and successful information dissemination strategies.
As the world – and hospitalists – dug in for a multi-year pandemic, SHM continued to advance the care of patients by opening our library of educational content for free to anyone. Our Public Policy Committee was active around both COVID-19- and hospitalist-related topics: immigration, telehealth, wellbeing, and financial impacts, to name a few.
As the pandemic slogged on, our Wellbeing Task Force came up with innovative support measures, including a check-in guide for hospitalists and fellow health care workers and dedicated wellness sessions complete with a licensed therapist for members. All the while, despite the restrictions and hurdles the pandemic has thrown our way, SHM members keep meeting and collaborating through virtual chapter events, committee work, special interest groups, and our annual conference, SHM Converge. Thank you to the countless members who donated their time to SHM, so that SHM could support hospitalists and their patients.
Now, we are transitioning into a new phase of the pandemic. The medical miracles that are the COVID-19 vaccines have made that possible. Fully vaccinated, I no longer worry that every time someone sneezes, or when I care for patients with a fever, that I am playing a high stakes poker game with my life. Don’t get me wrong; as I write, the Delta variant has a hold on the nation, and I know it’s not over yet. But it does appear as if the medical war on COVID is shifting from national to regional (or even local) responses.
During this new phase, we must rebuild our personal and professional lives. If you haven’t read Retired Lieutenant General Mark Hertling’s perspective piece in the August issue of the Journal of Hospital Medicine, I strongly encourage you to do so. He shares profound lessons on transitioning from active combat that are directly applicable to hospitalists who have been “deployed” battling COVID-19.
SHM will continue to pivot to meet our members’ needs too. We are already gearing up for more in-person education and networking. Chapters are starting to meet in person, and SHM is happy to provide visiting faculty. I will visit members from Florida to Maine and places in between starting this fall! Our Board of Directors and other SHM leaders are also starting to meet with members in person. Our own Leadership Academy will take place at Amelia Island in Florida in October, where we can learn, network, and even decompress. We also can’t wait for SHM Converge 2022 in Nashville, where we hope to reunite with many of you after 2 years of virtual conferences.
Our response to the pandemic, a once in a century crisis where our own safety was at risk, where doing the right thing might mean death or harming loved ones, our response of running into the fire to save lives is truly inspiring. The power of care – for our patients, for our family and friends, and for our hospital medicine community and the community at large – is evident more now than ever.
There have always been good reasons to be proud of being a hospitalist: taking care of the acutely ill, helping hospitals improve, teaching young doctors, and watching my specialty grow by leaps and bounds, to name just a few. But I’ve never been prouder than I am now.
Dr. Howell is the CEO of the Society of Hospital Medicine.
I have been a proud hospitalist for more than 20 years, and yet I have never been prouder to be a hospitalist than now. The pandemic has been brutal, killing more than 600,000 Americans as of this writing. It has stretched the health care system, its doctors, nurses, and other providers to the limit. Yet we will get through it, we are getting through it, and hospitalists deserve a huge portion of the credit.
According to the CDC, there have been over 2.3 million COVID-19 hospitalizations. In my home state of Maryland, between two-thirds and three-quarters of hospitalized COVID patients are cared for on general medical floors, the domain of hospitalists. When hospitals needed COVID units, hospitalists stepped up to design and staff them. When our ICU colleagues needed support, especially in those early dark days, hospitalists stepped in. When our outpatient colleagues were called into the hospital, hospitalists were there to help them on board. When the House of Medicine was in chaos due to COVID-19, hospitalists ran towards that fire. Our previous 20+ years of collective experience made us the ideal specialty to manage the inpatient challenges over the last 18 months.
Need a new clinical schedule by Sunday? Check.
Need help with new clinical protocols? Check.
Need to help other colleagues? Check.
Need to reprogram the EMR? Check.
Need a new way to teach residents and students on the wards? Check.
Need a whole new unit – no, wait – a new hospital wing? No, scratch that – a whole new COVID hospital in a few weeks? Check. (I personally did that last one at the Baltimore Convention Center!)
For me and many hospitalists like me, it is as if the last 20 years were prep work for the pandemic.
Here at SHM, we know the pandemic is hard work – exhausting, even. SHM has been actively focused on supporting hospitalists during this crisis so that hospitalists can focus on patients. Early in the pandemic, SHM quickly pivoted to supply hospitalists with COVID-19 resources in their fight against the coronavirus. Numerous COVID-19 webinars, a COVID addendum to the State of Hospital Medicine Report, and a dedicated COVID issue of the Journal of Hospital Medicine were early and successful information dissemination strategies.
As the world – and hospitalists – dug in for a multi-year pandemic, SHM continued to advance the care of patients by opening our library of educational content for free to anyone. Our Public Policy Committee was active around both COVID-19- and hospitalist-related topics: immigration, telehealth, wellbeing, and financial impacts, to name a few.
As the pandemic slogged on, our Wellbeing Task Force came up with innovative support measures, including a check-in guide for hospitalists and fellow health care workers and dedicated wellness sessions complete with a licensed therapist for members. All the while, despite the restrictions and hurdles the pandemic has thrown our way, SHM members keep meeting and collaborating through virtual chapter events, committee work, special interest groups, and our annual conference, SHM Converge. Thank you to the countless members who donated their time to SHM, so that SHM could support hospitalists and their patients.
Now, we are transitioning into a new phase of the pandemic. The medical miracles that are the COVID-19 vaccines have made that possible. Fully vaccinated, I no longer worry that every time someone sneezes, or when I care for patients with a fever, that I am playing a high stakes poker game with my life. Don’t get me wrong; as I write, the Delta variant has a hold on the nation, and I know it’s not over yet. But it does appear as if the medical war on COVID is shifting from national to regional (or even local) responses.
During this new phase, we must rebuild our personal and professional lives. If you haven’t read Retired Lieutenant General Mark Hertling’s perspective piece in the August issue of the Journal of Hospital Medicine, I strongly encourage you to do so. He shares profound lessons on transitioning from active combat that are directly applicable to hospitalists who have been “deployed” battling COVID-19.
SHM will continue to pivot to meet our members’ needs too. We are already gearing up for more in-person education and networking. Chapters are starting to meet in person, and SHM is happy to provide visiting faculty. I will visit members from Florida to Maine and places in between starting this fall! Our Board of Directors and other SHM leaders are also starting to meet with members in person. Our own Leadership Academy will take place at Amelia Island in Florida in October, where we can learn, network, and even decompress. We also can’t wait for SHM Converge 2022 in Nashville, where we hope to reunite with many of you after 2 years of virtual conferences.
Our response to the pandemic, a once in a century crisis where our own safety was at risk, where doing the right thing might mean death or harming loved ones, our response of running into the fire to save lives is truly inspiring. The power of care – for our patients, for our family and friends, and for our hospital medicine community and the community at large – is evident more now than ever.
There have always been good reasons to be proud of being a hospitalist: taking care of the acutely ill, helping hospitals improve, teaching young doctors, and watching my specialty grow by leaps and bounds, to name just a few. But I’ve never been prouder than I am now.
Dr. Howell is the CEO of the Society of Hospital Medicine.
I have been a proud hospitalist for more than 20 years, and yet I have never been prouder to be a hospitalist than now. The pandemic has been brutal, killing more than 600,000 Americans as of this writing. It has stretched the health care system, its doctors, nurses, and other providers to the limit. Yet we will get through it, we are getting through it, and hospitalists deserve a huge portion of the credit.
According to the CDC, there have been over 2.3 million COVID-19 hospitalizations. In my home state of Maryland, between two-thirds and three-quarters of hospitalized COVID patients are cared for on general medical floors, the domain of hospitalists. When hospitals needed COVID units, hospitalists stepped up to design and staff them. When our ICU colleagues needed support, especially in those early dark days, hospitalists stepped in. When our outpatient colleagues were called into the hospital, hospitalists were there to help them on board. When the House of Medicine was in chaos due to COVID-19, hospitalists ran towards that fire. Our previous 20+ years of collective experience made us the ideal specialty to manage the inpatient challenges over the last 18 months.
Need a new clinical schedule by Sunday? Check.
Need help with new clinical protocols? Check.
Need to help other colleagues? Check.
Need to reprogram the EMR? Check.
Need a new way to teach residents and students on the wards? Check.
Need a whole new unit – no, wait – a new hospital wing? No, scratch that – a whole new COVID hospital in a few weeks? Check. (I personally did that last one at the Baltimore Convention Center!)
For me and many hospitalists like me, it is as if the last 20 years were prep work for the pandemic.
Here at SHM, we know the pandemic is hard work – exhausting, even. SHM has been actively focused on supporting hospitalists during this crisis so that hospitalists can focus on patients. Early in the pandemic, SHM quickly pivoted to supply hospitalists with COVID-19 resources in their fight against the coronavirus. Numerous COVID-19 webinars, a COVID addendum to the State of Hospital Medicine Report, and a dedicated COVID issue of the Journal of Hospital Medicine were early and successful information dissemination strategies.
As the world – and hospitalists – dug in for a multi-year pandemic, SHM continued to advance the care of patients by opening our library of educational content for free to anyone. Our Public Policy Committee was active around both COVID-19- and hospitalist-related topics: immigration, telehealth, wellbeing, and financial impacts, to name a few.
As the pandemic slogged on, our Wellbeing Task Force came up with innovative support measures, including a check-in guide for hospitalists and fellow health care workers and dedicated wellness sessions complete with a licensed therapist for members. All the while, despite the restrictions and hurdles the pandemic has thrown our way, SHM members keep meeting and collaborating through virtual chapter events, committee work, special interest groups, and our annual conference, SHM Converge. Thank you to the countless members who donated their time to SHM, so that SHM could support hospitalists and their patients.
Now, we are transitioning into a new phase of the pandemic. The medical miracles that are the COVID-19 vaccines have made that possible. Fully vaccinated, I no longer worry that every time someone sneezes, or when I care for patients with a fever, that I am playing a high stakes poker game with my life. Don’t get me wrong; as I write, the Delta variant has a hold on the nation, and I know it’s not over yet. But it does appear as if the medical war on COVID is shifting from national to regional (or even local) responses.
During this new phase, we must rebuild our personal and professional lives. If you haven’t read Retired Lieutenant General Mark Hertling’s perspective piece in the August issue of the Journal of Hospital Medicine, I strongly encourage you to do so. He shares profound lessons on transitioning from active combat that are directly applicable to hospitalists who have been “deployed” battling COVID-19.
SHM will continue to pivot to meet our members’ needs too. We are already gearing up for more in-person education and networking. Chapters are starting to meet in person, and SHM is happy to provide visiting faculty. I will visit members from Florida to Maine and places in between starting this fall! Our Board of Directors and other SHM leaders are also starting to meet with members in person. Our own Leadership Academy will take place at Amelia Island in Florida in October, where we can learn, network, and even decompress. We also can’t wait for SHM Converge 2022 in Nashville, where we hope to reunite with many of you after 2 years of virtual conferences.
Our response to the pandemic, a once in a century crisis where our own safety was at risk, where doing the right thing might mean death or harming loved ones, our response of running into the fire to save lives is truly inspiring. The power of care – for our patients, for our family and friends, and for our hospital medicine community and the community at large – is evident more now than ever.
There have always been good reasons to be proud of being a hospitalist: taking care of the acutely ill, helping hospitals improve, teaching young doctors, and watching my specialty grow by leaps and bounds, to name just a few. But I’ve never been prouder than I am now.
Dr. Howell is the CEO of the Society of Hospital Medicine.
ACOG, SMFM urge all pregnant women to get COVID-19 vaccine
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) strongly recommend that all pregnant women be vaccinated against COVID-19.
Only about 16% of pregnant people have received one or more doses of a COVID-19 vaccine, according to the Centers for Disease Control and Prevention, despite evidence that COVID-19 infection puts pregnant people at an increased risk of severe complications and death.
That CDC report in June also found that vaccination during pregnancy was lowest among Hispanic (11.9%) and non-Hispanic Black women (6%) and women aged 18-24 years (5.5%) and highest among non-Hispanic Asian women (24.7%) and women aged 35-49 years (22.7%).
Linda Eckert, MD, professor of obstetrics and gynecology at University of Washington, Seattle, and a member of ACOG’s immunization expert work group, said in an interview that previously, ACOG has said that pregnant women should have the opportunity to be vaccinated, should they choose it.
Now the urgency has increased, she said: “This is a strong recommendation.”
The recommendation comes after mounting evidence demonstrating that COVID-19 vaccines are safe during pregnancy “from tens of thousands of reporting individuals over the last several months, as well as the current low vaccination rates and concerning increase in cases,” ACOG and SMFM said in the statement.
Both organizations said the timing of the advisory comes amid growing concern about the Delta variant.
CDC Director Rochelle Walensky, MD, has called the variant “one of the most infectious respiratory viruses we know of.”
No evidence of maternal/fetal harm
There is no evidence that COVID-19 vaccines could cause maternal or fetal harm, ACOG stated.
“ACOG encourages its members to enthusiastically recommend vaccination to their patients. This means emphasizing the known safety of the vaccines and the increased risk of severe complications associated with COVID-19 infection, including death, during pregnancy,” said J. Martin Tucker, MD, FACOG, president of ACOG. “It is clear that pregnant people need to feel confident in the decision to choose vaccination, and a strong recommendation from their obstetrician-gynecologist could make a meaningful difference for many pregnant people.”
Pregnant women are considered high risk because of concerns about the effect of COVID-19 during and after pregnancy, and on their offspring.
As this news organization has reported, research published in The BMJ found that pregnant women with COVID-19 may be at higher risk of admission to a hospital intensive care unit.
Preterm birth rates also were found to be higher among pregnant women with COVID-19 than among pregnant women without the disease.
Dr. Eckert said several of her patients have declined the vaccine. Among the reasons are that they don’t want to take any medications while pregnant or that they have heard that effects of the vaccines were not studied in pregnant women.
“Sometimes as I review with them the ongoing data coming in from pregnant individuals and newborns, [these patients] may change their minds and get the vaccine,” Dr. Eckert said.
In some cases, a pregnant patient’s family has pressured the patient not to get the vaccine.
The ACOG/SMFM advice notes that pregnant women who have decided to wait until after delivery to be vaccinated “may be inadvertently exposing themselves to an increased risk of severe illness or death.”
The recommendation extends to those who have already given birth.
“Those who have recently delivered and were not vaccinated during pregnancy are also strongly encouraged to get vaccinated as soon as possible,” the statement reads.
ACOG has developed talking points about the safety and efficacy of COVID-19 vaccines for pregnant patients.
Dr. Eckert disclosed no relevant financial relationships.
Persistent Panniculitis in Dermatomyositis
To the Editor:
A 62-year-old woman with a history of dermatomyositis (DM) presented to dermatology clinic for evaluation of multiple subcutaneous nodules. Two years prior to the current presentation, the patient was diagnosed by her primary care physician with DM based on clinical presentation. She initially developed body aches, muscle pain, and weakness of the upper extremities, specifically around the shoulders, and later the lower extremities, specifically around the thighs. The initial physical examination revealed pain with movement, tenderness to palpation, and proximal extremity weakness. The patient also noted a 50-lb weight loss. Over the next year, she noted dysphagia and developed multiple subcutaneous nodules on the right arm, chest, and left axilla. Subsequently, she developed a violaceous, hyperpigmented, periorbital rash and erythema of the anterior chest. She did not experience hair loss, oral ulcers, photosensitivity, or joint pain.
Laboratory testing in the months following the initial presentation revealed a creatine phosphokinase level of 436 U/L (reference range, 20–200 U/L), an erythrocyte sedimentation rate of 60 mm/h (reference range, <31 mm/h), and an aldolase level of 10.4 U/L (reference range, 1.0–8.0 U/L). Lactate dehydrogenase and thyroid function tests were within normal limits. Antinuclear antibodies, anti–double-stranded DNA, anti-Smith antibodies, anti-ribonucleoprotein, anti–Jo-1 antibodies, and anti–smooth muscle antibodies all were negative. Total blood complement levels were elevated, but complement C3 and C4 were within normal limits. Imaging demonstrated normal chest radiographs, and a modified barium swallow confirmed swallowing dysfunction. A right quadricep muscle biopsy confirmed the diagnosis of DM. A malignancy work-up including mammography, colonoscopy, and computed tomography of the chest, abdomen, and pelvis was negative aside from nodular opacities in the chest. She was treated with prednisone (60 mg, 0.9 mg/kg) daily and methotrexate (15–20 mg) weekly for several months. While the treatment attenuated the rash and improved weakness, the nodules persisted, prompting a referral to dermatology.
Physical examination at the dermatology clinic demonstrated the persistent subcutaneous nodules were indurated and bilaterally located on the arms, axillae, chest, abdomen, buttocks, and thighs with no pain or erythema (Figure). Laboratory tests demonstrated a normal creatine phosphokinase level, elevated erythrocyte sedimentation rate (70 mm/h), and elevated aldolase level (9.3 U/L). Complement levels were elevated, though complement C3 and C4 remained within normal limits. Histopathology of nodules from the medial right upper arm and left thigh showed lobular panniculitis with fat necrosis, calcification, and interface changes. The patient was treated for several months with daily mycophenolate mofetil (1 g increased to 3 g) and daily hydroxychloroquine (200 mg) without any effect on the nodules.
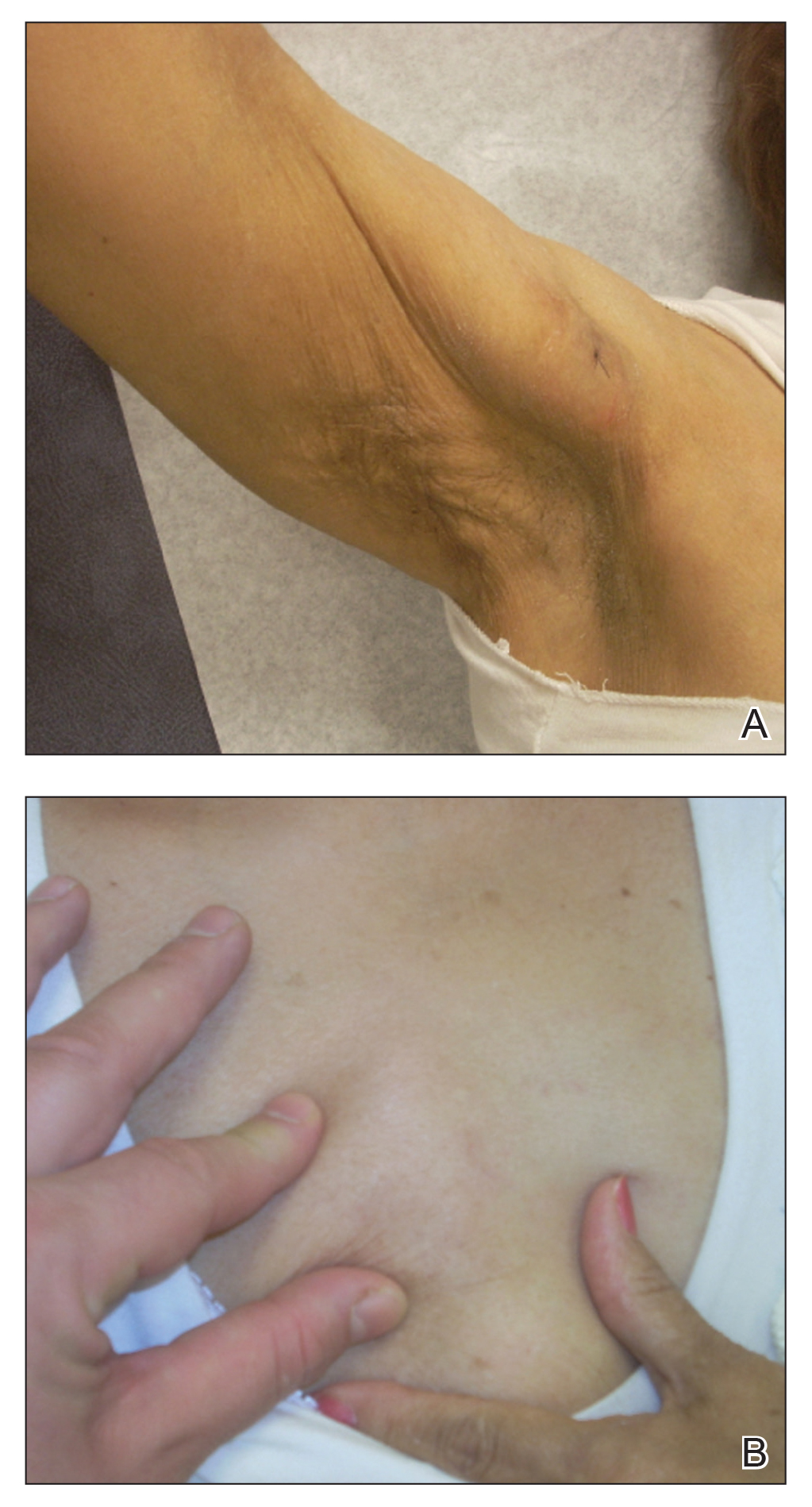
The histologic features of panniculitis in lupus and DM are similar and include multifocal hyalinization of the subcuticular fat and diffuse lobular infiltrates of mature lymphocytes without nuclear atypia.1 Though clinical panniculitis is a rare finding in DM, histologic panniculitis is a relatively common finding.2 Despite the similar histopathology of lupus and DM, the presence of typical DM clinical and laboratory features in our patient (body aches, muscle pain, proximal weakness, cutaneous manifestations, elevated creatine phosphokinase, normal complement C3 and C4) made a diagnosis of DM more likely.
Clinical panniculitis is a rare subcutaneous manifestation of DM with around 50 cases reported in the literature (Table). A PubMed search of articles indexed for MEDLINE was conducted using the terms dermatomyositis and panniculitis through July 2019. Additionally, a full-text review and search of references within these articles was used to identify all cases of patients presenting with panniculitis in the setting of DM. Exclusion criteria were cases in which another etiology was considered likely (infectious panniculitis and lupus panniculitis) as well as those without an English translation. We identified 43 cases; the average age of the patients was 39.6 years, and 36 (83.7%) of the cases were women. Patients typically presented with persistent, indurated, painful, erythematous, nodular lesions localized to the arms, abdomen, buttocks, and thighs.
While panniculitis has been reported preceding and concurrent with a diagnosis of DM, a number of cases described presentation as late as 5 years following onset of classic DM symptoms.12,13,31 In some cases (3/43 [7.0%]), panniculitis was the only cutaneous manifestation of DM.15,33,36 However, it occurred more commonly with other characteristic skin findings, such as heliotrope rash or Gottron sign.Some investigators have recommended that panniculitis be included as a diagnostic feature of DM and that DM be considered in the differential diagnosis in isolated cases of panniculitis.25,33
Though it seems panniculitis in DM may correlate with a better prognosis, we identified underlying malignancies in 3 cases. Malignancies associated with panniculitis in DM included ovarian adenocarcinoma, nasopharyngeal carcinoma, and parotid carcinoma, indicating that appropriate cancer screening still is critical in the diagnostic workup.2,11,22
A majority of the reported panniculitis cases in DM have responded to treatment with prednisone; however, treatment with prednisone has been more recalcitrant in other cases. Reports of successful additional therapies include methotrexate, cyclosporine, azathioprine, hydroxychloroquine, intravenous immunoglobulin, mepacrine, or a combination of these entities.19,22 In most cases, improvement of the panniculitis and other DM symptoms occurred simultaneously.25 It is noteworthy that the muscular symptoms often resolved more rapidly than cutaneous manifestations.33 Few reported cases (6 including the current case) found a persistent panniculitis despite improvement and remission of the myositis.3,5,10,11,30
Our patient was treated with both prednisone and methotrexate for several months, leading to remission of muscular symptoms (along with return to baseline of creatine phosphokinase), yet the panniculitis did not improve. The subcutaneous nodules also did not respond to treatment with mycophenolate mofetil and hydroxychloroquine.
Recent immunohistochemical studies have suggested that panniculitic lesions show better outcomes with immunosuppressive therapy when compared with other DM-related skin lesions.40 However, this was not the case for our patient, who after months of immunosuppressive therapy showed complete resolution of the periorbital and chest rashes with persistence of multiple indurated subcutaneous nodules.
Our case adds to a number of reports of DM presenting with panniculitis. Our patient fit the classic demographic of previously reported cases, as she was an adult woman without evidence of underlying malignancy; however, our case remains an example of the therapeutic challenge that exists when encountering a persistent, treatment-resistant panniculitis despite resolution of all other features of DM.
- Wick MR. Panniculitis: a summary. Semin Diagn Pathol. 2017;34:261-272.
- Girouard SD, Velez NF, Penson RT, et al. Panniculitis associated with dermatomyositis and recurrent ovarian cancer. Arch Dermatol. 2012;148:740-744.
- van Dongen HM, van Vugt RM, Stoof TJ. Extensive persistent panniculitis in the context of dermatomyositis. J Clin Rheumatol. 2020;26:E187-E188.
- Choi YJ, Yoo WH. Panniculitis, a rare presentation of onset and exacerbation of juvenile dermatomyositis: a case report and literature review. Arch Rheumatol. 2018;33:367-371.
- Azevedo PO, Castellen NR, Salai AF, et al. Panniculitis associated with amyopathic dermatomyositis. An Bras Dermatol. 2018;93:119-121.
- Agulló A, Hinds B, Larrea M, et al. Livedo racemosa, reticulated ulcerations, panniculitis and violaceous plaques in a 46-year-old woman. Indian Dermatol Online J. 2018;9:47-49.
- Hattori Y, Matsuyama K, Takahashi T, et al. Anti-MDA5 antibody-positive dermatomyositis presenting with cellulitis-like erythema on the mandible as an initial symptom. Case Rep Dermatol. 2018;10:110-114.
- Hasegawa A, Shimomura Y, Kibune N, et al. Panniculitis as the initial manifestation of dermatomyositis with anti-MDA5 antibody. Clin Exp Dermatol. 2017;42:551-553.
- Salman A, Kasapcopur O, Ergun T, et al. Panniculitis in juvenile dermatomyositis: report of a case and review of the published work. J Dermatol. 2016;43:951-953.
- Carroll M, Mellick N, Wagner G. Dermatomyositis panniculitis: a case report. Australas J Dermatol. 2015;56:224‐226.
- Chairatchaneeboon M, Kulthanan K, Manapajon A. Calcific panniculitis and nasopharyngeal cancer-associated adult-onset dermatomyositis: a case report and literature review. Springerplus. 2015;4:201.
- Otero Rivas MM, Vicente Villa A, González Lara L, et al. Panniculitis in juvenile dermatomyositis. Clin Exp Dermatol. 2015;40:574-575.
- Yanaba K, Tanito K, Hamaguchi Y, et al. Anti‐transcription intermediary factor‐1γ/α/β antibody‐positive dermatomyositis associated with multiple panniculitis lesions. Int J Rheum Dis. 2015;20:1831-1834.
- Pau-Charles I, Moreno PJ, Ortiz-Ibanez K, et al. Anti-MDA5 positive clinically amyopathic dermatomyositis presenting with severe cardiomyopathy. J Eur Acad Dermatol Venereol. 2014;28:1097-1102.
- Lamb R, Digby S, Stewart W, et al. Cutaneous ulceration: more than skin deep? Clin Exp Dermatol. 2013;38:443-445.
- Arias M, Hernández MI, Cunha LG, et al. Panniculitis in a patient with dermatomyositis. An Bras Dermatol. 2011;86:146-148.
- Hemmi S, Kushida R, Nishimura H, et al. Magnetic resonance imaging diagnosis of panniculitis in dermatomyositis. Muscle Nerve. 2010;41:151-153.
- Geddes MR, Sinnreich M, Chalk C. Minocycline-induced dermatomyositis. Muscle Nerve. 2010;41:547-549.
- Abdul‐Wahab A, Holden CA, Harland C, et al Calcific panniculitis in adult‐onset dermatomyositis. Clin Exp Dermatol. 2009;34:E854-E856.
- Carneiro S, Alvim G, Resende P, et al. Dermatomyositis with panniculitis. Skinmed. 2007;6:46-47.
- Carrera E, Lobrinus JA, Spertini O, et al. Dermatomyositis, lobarpanniculitis and inflammatory myopathy with abundant macrophages. Neuromuscul Disord. 2006;16:468-471.
- Lin JH, Chu CY, Lin RY. Panniculitis in adult onset dermatomyositis: report of two cases and review of the literature. Dermatol Sinica. 2006;24:194-200.
- Chen GY, Liu MF, Lee JY, et al. Combination of massive mucinosis, dermatomyositis, pyoderma gangrenosum-like ulcer, bullae and fatal intestinal vasculopathy in a young female. Eur J Dermatol. 2005;15:396-400.
- Nakamori A, Yamaguchi Y, Kurimoto I, et al. Vesiculobullous dermatomyositis with panniculitis without muscle disease. J Am Acad Dermatol. 2003;49:1136-1139.
- Solans R, Cortés J, Selva A, et al. Panniculitis: a cutaneous manifestation of dermatomyositis. J Am Acad Dermatol. 2002;46:S148-S150.
- Chao YY, Yang LJ. Dermatomyositis presenting as panniculitis. Int J Dermatol. 2000;39:141-144.
- Lee MW, Lim YS, Choi JH, et al. Panniculitis showing membranocystic changes in the dermatomyositis. J Dermatol. 1999;26:608‐610.
- Ghali FE, Reed AM, Groben PA, et al. Panniculitis in juvenile dermatomyositis. Pediatr Dermatol. 1999;16:270-272.
- Molnar K, Kemeny L, Korom I, et al. Panniculitis in dermatomyositis: report of two cases. Br J Dermatol. 1998;139:161‐163.
- Ishikawa O, Tamura A, Ryuzaki K, et al. Membranocystic changes in the panniculitis of dermatomyositis. Br J Dermatol. 1996;134:773-776.
- Sabroe RA, Wallington TB, Kennedy CT. Dermatomyositis treated with high-dose intravenous immunoglobulins and associated with panniculitis. Clin Exp Dermatol. 1995;20:164-167.
- Neidenbach PJ, Sahn EE, Helton J. Panniculitis in juvenile dermatomyositis. J Am Acad Dermatol. 1995;33:305-307.
- Fusade T, Belanyi P, Joly P, et al. Subcutaneous changes in dermatomyositis. Br J Dermatol. 1993;128:451-453.
- Winkelmann WJ, Billick RC, Srolovitz H. Dermatomyositis presenting as panniculitis. J Am Acad Dermatol. 1990;23:127-128.
- Commens C, O’Neill P, Walker G. Dermatomyositis associated with multifocal lipoatrophy. J Am Acad Dermatol. 1990;22:966-969.
- Raimer SS, Solomon AR, Daniels JC. Polymyositis presenting with panniculitis. J Am Acad Dermatol. 1985;13(2 pt 2):366‐369.
- Feldman D, Hochberg MC, Zizic TM, et al. Cutaneous vasculitis in adult polymyositis/dermatomyositis. J Rheumatol. 1983;10:85-89.
- Kimura S, Fukuyama Y. Tubular cytoplasmic inclusions in a case of childhood dermatomyositis with migratory subcutaneous nodules. Eur J Pediatr. 1977;125:275-283.
- Weber FP, Gray AMH. Chronic relapsing polydermatomyositis with predominant involvement of the subcutaneous fat. Br J Dermatol. 1924;36:544-560.
- Santos‐Briz A, Calle A, Linos K, et al. Dermatomyositis panniculitis: a clinicopathological and immunohistochemical study of 18 cases. J Eur Acad Dermatol Venereol. 2018;32:1352-1359.
To the Editor:
A 62-year-old woman with a history of dermatomyositis (DM) presented to dermatology clinic for evaluation of multiple subcutaneous nodules. Two years prior to the current presentation, the patient was diagnosed by her primary care physician with DM based on clinical presentation. She initially developed body aches, muscle pain, and weakness of the upper extremities, specifically around the shoulders, and later the lower extremities, specifically around the thighs. The initial physical examination revealed pain with movement, tenderness to palpation, and proximal extremity weakness. The patient also noted a 50-lb weight loss. Over the next year, she noted dysphagia and developed multiple subcutaneous nodules on the right arm, chest, and left axilla. Subsequently, she developed a violaceous, hyperpigmented, periorbital rash and erythema of the anterior chest. She did not experience hair loss, oral ulcers, photosensitivity, or joint pain.
Laboratory testing in the months following the initial presentation revealed a creatine phosphokinase level of 436 U/L (reference range, 20–200 U/L), an erythrocyte sedimentation rate of 60 mm/h (reference range, <31 mm/h), and an aldolase level of 10.4 U/L (reference range, 1.0–8.0 U/L). Lactate dehydrogenase and thyroid function tests were within normal limits. Antinuclear antibodies, anti–double-stranded DNA, anti-Smith antibodies, anti-ribonucleoprotein, anti–Jo-1 antibodies, and anti–smooth muscle antibodies all were negative. Total blood complement levels were elevated, but complement C3 and C4 were within normal limits. Imaging demonstrated normal chest radiographs, and a modified barium swallow confirmed swallowing dysfunction. A right quadricep muscle biopsy confirmed the diagnosis of DM. A malignancy work-up including mammography, colonoscopy, and computed tomography of the chest, abdomen, and pelvis was negative aside from nodular opacities in the chest. She was treated with prednisone (60 mg, 0.9 mg/kg) daily and methotrexate (15–20 mg) weekly for several months. While the treatment attenuated the rash and improved weakness, the nodules persisted, prompting a referral to dermatology.
Physical examination at the dermatology clinic demonstrated the persistent subcutaneous nodules were indurated and bilaterally located on the arms, axillae, chest, abdomen, buttocks, and thighs with no pain or erythema (Figure). Laboratory tests demonstrated a normal creatine phosphokinase level, elevated erythrocyte sedimentation rate (70 mm/h), and elevated aldolase level (9.3 U/L). Complement levels were elevated, though complement C3 and C4 remained within normal limits. Histopathology of nodules from the medial right upper arm and left thigh showed lobular panniculitis with fat necrosis, calcification, and interface changes. The patient was treated for several months with daily mycophenolate mofetil (1 g increased to 3 g) and daily hydroxychloroquine (200 mg) without any effect on the nodules.
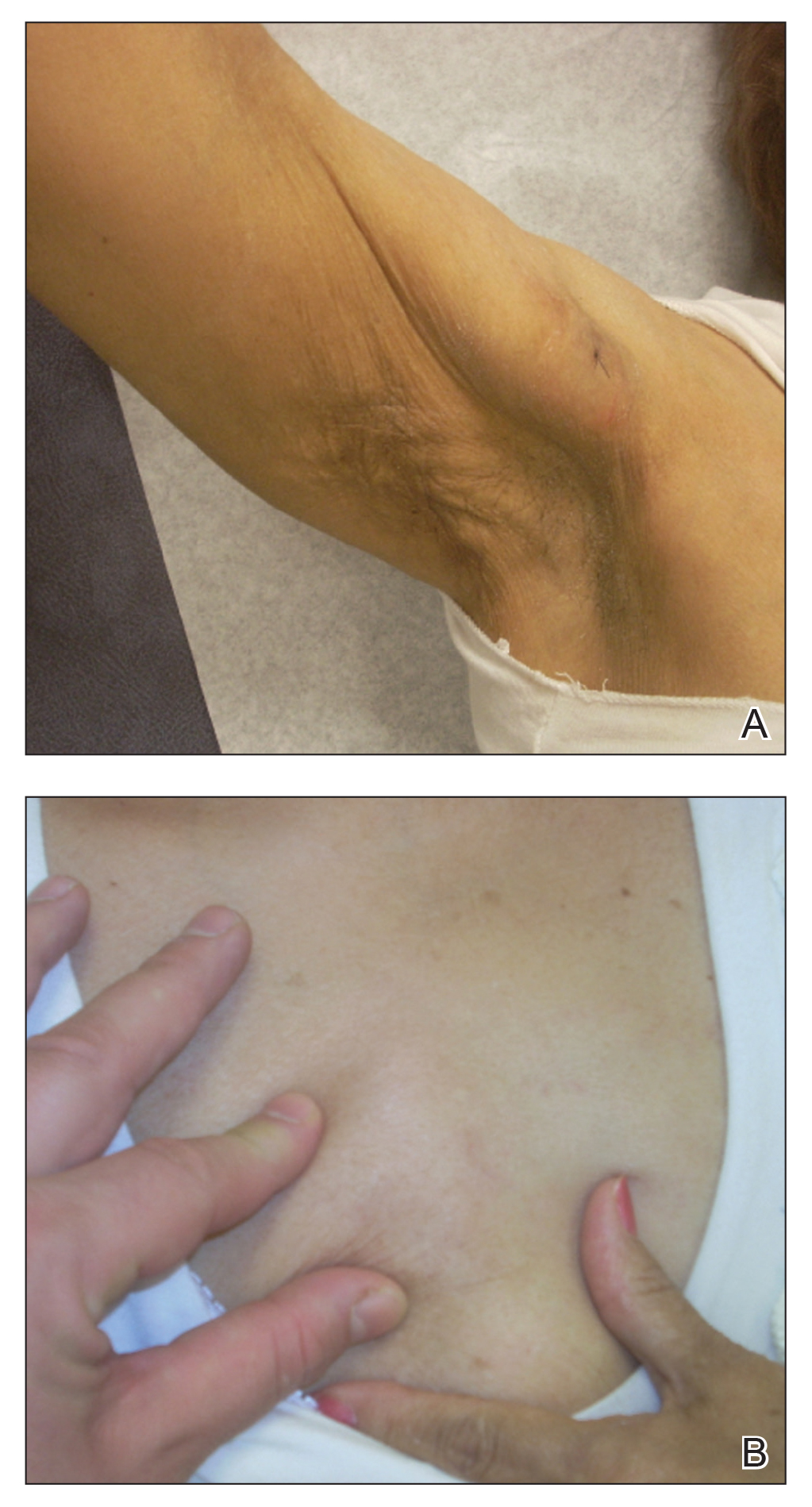
The histologic features of panniculitis in lupus and DM are similar and include multifocal hyalinization of the subcuticular fat and diffuse lobular infiltrates of mature lymphocytes without nuclear atypia.1 Though clinical panniculitis is a rare finding in DM, histologic panniculitis is a relatively common finding.2 Despite the similar histopathology of lupus and DM, the presence of typical DM clinical and laboratory features in our patient (body aches, muscle pain, proximal weakness, cutaneous manifestations, elevated creatine phosphokinase, normal complement C3 and C4) made a diagnosis of DM more likely.
Clinical panniculitis is a rare subcutaneous manifestation of DM with around 50 cases reported in the literature (Table). A PubMed search of articles indexed for MEDLINE was conducted using the terms dermatomyositis and panniculitis through July 2019. Additionally, a full-text review and search of references within these articles was used to identify all cases of patients presenting with panniculitis in the setting of DM. Exclusion criteria were cases in which another etiology was considered likely (infectious panniculitis and lupus panniculitis) as well as those without an English translation. We identified 43 cases; the average age of the patients was 39.6 years, and 36 (83.7%) of the cases were women. Patients typically presented with persistent, indurated, painful, erythematous, nodular lesions localized to the arms, abdomen, buttocks, and thighs.
While panniculitis has been reported preceding and concurrent with a diagnosis of DM, a number of cases described presentation as late as 5 years following onset of classic DM symptoms.12,13,31 In some cases (3/43 [7.0%]), panniculitis was the only cutaneous manifestation of DM.15,33,36 However, it occurred more commonly with other characteristic skin findings, such as heliotrope rash or Gottron sign.Some investigators have recommended that panniculitis be included as a diagnostic feature of DM and that DM be considered in the differential diagnosis in isolated cases of panniculitis.25,33
Though it seems panniculitis in DM may correlate with a better prognosis, we identified underlying malignancies in 3 cases. Malignancies associated with panniculitis in DM included ovarian adenocarcinoma, nasopharyngeal carcinoma, and parotid carcinoma, indicating that appropriate cancer screening still is critical in the diagnostic workup.2,11,22
A majority of the reported panniculitis cases in DM have responded to treatment with prednisone; however, treatment with prednisone has been more recalcitrant in other cases. Reports of successful additional therapies include methotrexate, cyclosporine, azathioprine, hydroxychloroquine, intravenous immunoglobulin, mepacrine, or a combination of these entities.19,22 In most cases, improvement of the panniculitis and other DM symptoms occurred simultaneously.25 It is noteworthy that the muscular symptoms often resolved more rapidly than cutaneous manifestations.33 Few reported cases (6 including the current case) found a persistent panniculitis despite improvement and remission of the myositis.3,5,10,11,30
Our patient was treated with both prednisone and methotrexate for several months, leading to remission of muscular symptoms (along with return to baseline of creatine phosphokinase), yet the panniculitis did not improve. The subcutaneous nodules also did not respond to treatment with mycophenolate mofetil and hydroxychloroquine.
Recent immunohistochemical studies have suggested that panniculitic lesions show better outcomes with immunosuppressive therapy when compared with other DM-related skin lesions.40 However, this was not the case for our patient, who after months of immunosuppressive therapy showed complete resolution of the periorbital and chest rashes with persistence of multiple indurated subcutaneous nodules.
Our case adds to a number of reports of DM presenting with panniculitis. Our patient fit the classic demographic of previously reported cases, as she was an adult woman without evidence of underlying malignancy; however, our case remains an example of the therapeutic challenge that exists when encountering a persistent, treatment-resistant panniculitis despite resolution of all other features of DM.
To the Editor:
A 62-year-old woman with a history of dermatomyositis (DM) presented to dermatology clinic for evaluation of multiple subcutaneous nodules. Two years prior to the current presentation, the patient was diagnosed by her primary care physician with DM based on clinical presentation. She initially developed body aches, muscle pain, and weakness of the upper extremities, specifically around the shoulders, and later the lower extremities, specifically around the thighs. The initial physical examination revealed pain with movement, tenderness to palpation, and proximal extremity weakness. The patient also noted a 50-lb weight loss. Over the next year, she noted dysphagia and developed multiple subcutaneous nodules on the right arm, chest, and left axilla. Subsequently, she developed a violaceous, hyperpigmented, periorbital rash and erythema of the anterior chest. She did not experience hair loss, oral ulcers, photosensitivity, or joint pain.
Laboratory testing in the months following the initial presentation revealed a creatine phosphokinase level of 436 U/L (reference range, 20–200 U/L), an erythrocyte sedimentation rate of 60 mm/h (reference range, <31 mm/h), and an aldolase level of 10.4 U/L (reference range, 1.0–8.0 U/L). Lactate dehydrogenase and thyroid function tests were within normal limits. Antinuclear antibodies, anti–double-stranded DNA, anti-Smith antibodies, anti-ribonucleoprotein, anti–Jo-1 antibodies, and anti–smooth muscle antibodies all were negative. Total blood complement levels were elevated, but complement C3 and C4 were within normal limits. Imaging demonstrated normal chest radiographs, and a modified barium swallow confirmed swallowing dysfunction. A right quadricep muscle biopsy confirmed the diagnosis of DM. A malignancy work-up including mammography, colonoscopy, and computed tomography of the chest, abdomen, and pelvis was negative aside from nodular opacities in the chest. She was treated with prednisone (60 mg, 0.9 mg/kg) daily and methotrexate (15–20 mg) weekly for several months. While the treatment attenuated the rash and improved weakness, the nodules persisted, prompting a referral to dermatology.
Physical examination at the dermatology clinic demonstrated the persistent subcutaneous nodules were indurated and bilaterally located on the arms, axillae, chest, abdomen, buttocks, and thighs with no pain or erythema (Figure). Laboratory tests demonstrated a normal creatine phosphokinase level, elevated erythrocyte sedimentation rate (70 mm/h), and elevated aldolase level (9.3 U/L). Complement levels were elevated, though complement C3 and C4 remained within normal limits. Histopathology of nodules from the medial right upper arm and left thigh showed lobular panniculitis with fat necrosis, calcification, and interface changes. The patient was treated for several months with daily mycophenolate mofetil (1 g increased to 3 g) and daily hydroxychloroquine (200 mg) without any effect on the nodules.
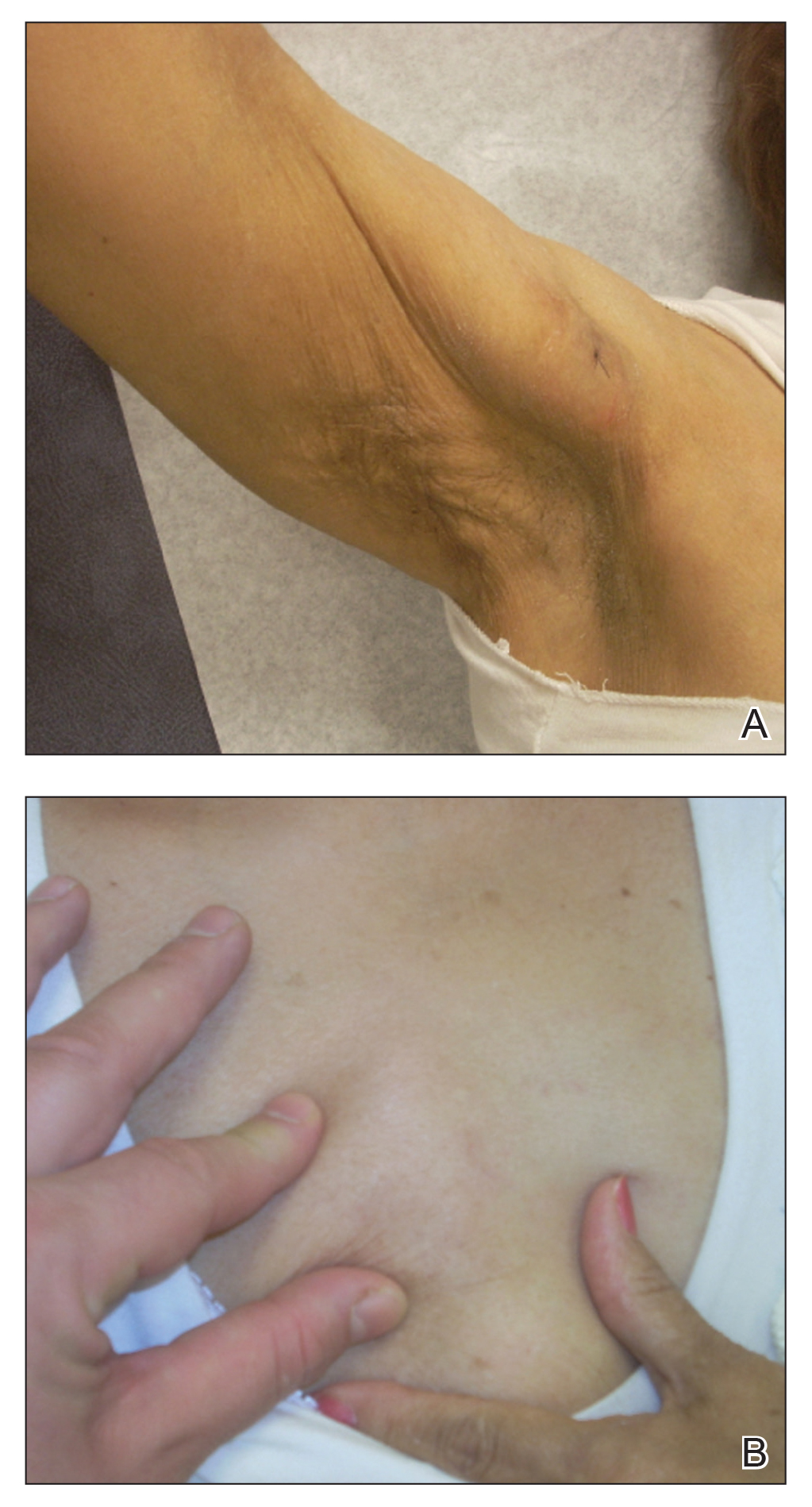
The histologic features of panniculitis in lupus and DM are similar and include multifocal hyalinization of the subcuticular fat and diffuse lobular infiltrates of mature lymphocytes without nuclear atypia.1 Though clinical panniculitis is a rare finding in DM, histologic panniculitis is a relatively common finding.2 Despite the similar histopathology of lupus and DM, the presence of typical DM clinical and laboratory features in our patient (body aches, muscle pain, proximal weakness, cutaneous manifestations, elevated creatine phosphokinase, normal complement C3 and C4) made a diagnosis of DM more likely.
Clinical panniculitis is a rare subcutaneous manifestation of DM with around 50 cases reported in the literature (Table). A PubMed search of articles indexed for MEDLINE was conducted using the terms dermatomyositis and panniculitis through July 2019. Additionally, a full-text review and search of references within these articles was used to identify all cases of patients presenting with panniculitis in the setting of DM. Exclusion criteria were cases in which another etiology was considered likely (infectious panniculitis and lupus panniculitis) as well as those without an English translation. We identified 43 cases; the average age of the patients was 39.6 years, and 36 (83.7%) of the cases were women. Patients typically presented with persistent, indurated, painful, erythematous, nodular lesions localized to the arms, abdomen, buttocks, and thighs.
While panniculitis has been reported preceding and concurrent with a diagnosis of DM, a number of cases described presentation as late as 5 years following onset of classic DM symptoms.12,13,31 In some cases (3/43 [7.0%]), panniculitis was the only cutaneous manifestation of DM.15,33,36 However, it occurred more commonly with other characteristic skin findings, such as heliotrope rash or Gottron sign.Some investigators have recommended that panniculitis be included as a diagnostic feature of DM and that DM be considered in the differential diagnosis in isolated cases of panniculitis.25,33
Though it seems panniculitis in DM may correlate with a better prognosis, we identified underlying malignancies in 3 cases. Malignancies associated with panniculitis in DM included ovarian adenocarcinoma, nasopharyngeal carcinoma, and parotid carcinoma, indicating that appropriate cancer screening still is critical in the diagnostic workup.2,11,22
A majority of the reported panniculitis cases in DM have responded to treatment with prednisone; however, treatment with prednisone has been more recalcitrant in other cases. Reports of successful additional therapies include methotrexate, cyclosporine, azathioprine, hydroxychloroquine, intravenous immunoglobulin, mepacrine, or a combination of these entities.19,22 In most cases, improvement of the panniculitis and other DM symptoms occurred simultaneously.25 It is noteworthy that the muscular symptoms often resolved more rapidly than cutaneous manifestations.33 Few reported cases (6 including the current case) found a persistent panniculitis despite improvement and remission of the myositis.3,5,10,11,30
Our patient was treated with both prednisone and methotrexate for several months, leading to remission of muscular symptoms (along with return to baseline of creatine phosphokinase), yet the panniculitis did not improve. The subcutaneous nodules also did not respond to treatment with mycophenolate mofetil and hydroxychloroquine.
Recent immunohistochemical studies have suggested that panniculitic lesions show better outcomes with immunosuppressive therapy when compared with other DM-related skin lesions.40 However, this was not the case for our patient, who after months of immunosuppressive therapy showed complete resolution of the periorbital and chest rashes with persistence of multiple indurated subcutaneous nodules.
Our case adds to a number of reports of DM presenting with panniculitis. Our patient fit the classic demographic of previously reported cases, as she was an adult woman without evidence of underlying malignancy; however, our case remains an example of the therapeutic challenge that exists when encountering a persistent, treatment-resistant panniculitis despite resolution of all other features of DM.
- Wick MR. Panniculitis: a summary. Semin Diagn Pathol. 2017;34:261-272.
- Girouard SD, Velez NF, Penson RT, et al. Panniculitis associated with dermatomyositis and recurrent ovarian cancer. Arch Dermatol. 2012;148:740-744.
- van Dongen HM, van Vugt RM, Stoof TJ. Extensive persistent panniculitis in the context of dermatomyositis. J Clin Rheumatol. 2020;26:E187-E188.
- Choi YJ, Yoo WH. Panniculitis, a rare presentation of onset and exacerbation of juvenile dermatomyositis: a case report and literature review. Arch Rheumatol. 2018;33:367-371.
- Azevedo PO, Castellen NR, Salai AF, et al. Panniculitis associated with amyopathic dermatomyositis. An Bras Dermatol. 2018;93:119-121.
- Agulló A, Hinds B, Larrea M, et al. Livedo racemosa, reticulated ulcerations, panniculitis and violaceous plaques in a 46-year-old woman. Indian Dermatol Online J. 2018;9:47-49.
- Hattori Y, Matsuyama K, Takahashi T, et al. Anti-MDA5 antibody-positive dermatomyositis presenting with cellulitis-like erythema on the mandible as an initial symptom. Case Rep Dermatol. 2018;10:110-114.
- Hasegawa A, Shimomura Y, Kibune N, et al. Panniculitis as the initial manifestation of dermatomyositis with anti-MDA5 antibody. Clin Exp Dermatol. 2017;42:551-553.
- Salman A, Kasapcopur O, Ergun T, et al. Panniculitis in juvenile dermatomyositis: report of a case and review of the published work. J Dermatol. 2016;43:951-953.
- Carroll M, Mellick N, Wagner G. Dermatomyositis panniculitis: a case report. Australas J Dermatol. 2015;56:224‐226.
- Chairatchaneeboon M, Kulthanan K, Manapajon A. Calcific panniculitis and nasopharyngeal cancer-associated adult-onset dermatomyositis: a case report and literature review. Springerplus. 2015;4:201.
- Otero Rivas MM, Vicente Villa A, González Lara L, et al. Panniculitis in juvenile dermatomyositis. Clin Exp Dermatol. 2015;40:574-575.
- Yanaba K, Tanito K, Hamaguchi Y, et al. Anti‐transcription intermediary factor‐1γ/α/β antibody‐positive dermatomyositis associated with multiple panniculitis lesions. Int J Rheum Dis. 2015;20:1831-1834.
- Pau-Charles I, Moreno PJ, Ortiz-Ibanez K, et al. Anti-MDA5 positive clinically amyopathic dermatomyositis presenting with severe cardiomyopathy. J Eur Acad Dermatol Venereol. 2014;28:1097-1102.
- Lamb R, Digby S, Stewart W, et al. Cutaneous ulceration: more than skin deep? Clin Exp Dermatol. 2013;38:443-445.
- Arias M, Hernández MI, Cunha LG, et al. Panniculitis in a patient with dermatomyositis. An Bras Dermatol. 2011;86:146-148.
- Hemmi S, Kushida R, Nishimura H, et al. Magnetic resonance imaging diagnosis of panniculitis in dermatomyositis. Muscle Nerve. 2010;41:151-153.
- Geddes MR, Sinnreich M, Chalk C. Minocycline-induced dermatomyositis. Muscle Nerve. 2010;41:547-549.
- Abdul‐Wahab A, Holden CA, Harland C, et al Calcific panniculitis in adult‐onset dermatomyositis. Clin Exp Dermatol. 2009;34:E854-E856.
- Carneiro S, Alvim G, Resende P, et al. Dermatomyositis with panniculitis. Skinmed. 2007;6:46-47.
- Carrera E, Lobrinus JA, Spertini O, et al. Dermatomyositis, lobarpanniculitis and inflammatory myopathy with abundant macrophages. Neuromuscul Disord. 2006;16:468-471.
- Lin JH, Chu CY, Lin RY. Panniculitis in adult onset dermatomyositis: report of two cases and review of the literature. Dermatol Sinica. 2006;24:194-200.
- Chen GY, Liu MF, Lee JY, et al. Combination of massive mucinosis, dermatomyositis, pyoderma gangrenosum-like ulcer, bullae and fatal intestinal vasculopathy in a young female. Eur J Dermatol. 2005;15:396-400.
- Nakamori A, Yamaguchi Y, Kurimoto I, et al. Vesiculobullous dermatomyositis with panniculitis without muscle disease. J Am Acad Dermatol. 2003;49:1136-1139.
- Solans R, Cortés J, Selva A, et al. Panniculitis: a cutaneous manifestation of dermatomyositis. J Am Acad Dermatol. 2002;46:S148-S150.
- Chao YY, Yang LJ. Dermatomyositis presenting as panniculitis. Int J Dermatol. 2000;39:141-144.
- Lee MW, Lim YS, Choi JH, et al. Panniculitis showing membranocystic changes in the dermatomyositis. J Dermatol. 1999;26:608‐610.
- Ghali FE, Reed AM, Groben PA, et al. Panniculitis in juvenile dermatomyositis. Pediatr Dermatol. 1999;16:270-272.
- Molnar K, Kemeny L, Korom I, et al. Panniculitis in dermatomyositis: report of two cases. Br J Dermatol. 1998;139:161‐163.
- Ishikawa O, Tamura A, Ryuzaki K, et al. Membranocystic changes in the panniculitis of dermatomyositis. Br J Dermatol. 1996;134:773-776.
- Sabroe RA, Wallington TB, Kennedy CT. Dermatomyositis treated with high-dose intravenous immunoglobulins and associated with panniculitis. Clin Exp Dermatol. 1995;20:164-167.
- Neidenbach PJ, Sahn EE, Helton J. Panniculitis in juvenile dermatomyositis. J Am Acad Dermatol. 1995;33:305-307.
- Fusade T, Belanyi P, Joly P, et al. Subcutaneous changes in dermatomyositis. Br J Dermatol. 1993;128:451-453.
- Winkelmann WJ, Billick RC, Srolovitz H. Dermatomyositis presenting as panniculitis. J Am Acad Dermatol. 1990;23:127-128.
- Commens C, O’Neill P, Walker G. Dermatomyositis associated with multifocal lipoatrophy. J Am Acad Dermatol. 1990;22:966-969.
- Raimer SS, Solomon AR, Daniels JC. Polymyositis presenting with panniculitis. J Am Acad Dermatol. 1985;13(2 pt 2):366‐369.
- Feldman D, Hochberg MC, Zizic TM, et al. Cutaneous vasculitis in adult polymyositis/dermatomyositis. J Rheumatol. 1983;10:85-89.
- Kimura S, Fukuyama Y. Tubular cytoplasmic inclusions in a case of childhood dermatomyositis with migratory subcutaneous nodules. Eur J Pediatr. 1977;125:275-283.
- Weber FP, Gray AMH. Chronic relapsing polydermatomyositis with predominant involvement of the subcutaneous fat. Br J Dermatol. 1924;36:544-560.
- Santos‐Briz A, Calle A, Linos K, et al. Dermatomyositis panniculitis: a clinicopathological and immunohistochemical study of 18 cases. J Eur Acad Dermatol Venereol. 2018;32:1352-1359.
- Wick MR. Panniculitis: a summary. Semin Diagn Pathol. 2017;34:261-272.
- Girouard SD, Velez NF, Penson RT, et al. Panniculitis associated with dermatomyositis and recurrent ovarian cancer. Arch Dermatol. 2012;148:740-744.
- van Dongen HM, van Vugt RM, Stoof TJ. Extensive persistent panniculitis in the context of dermatomyositis. J Clin Rheumatol. 2020;26:E187-E188.
- Choi YJ, Yoo WH. Panniculitis, a rare presentation of onset and exacerbation of juvenile dermatomyositis: a case report and literature review. Arch Rheumatol. 2018;33:367-371.
- Azevedo PO, Castellen NR, Salai AF, et al. Panniculitis associated with amyopathic dermatomyositis. An Bras Dermatol. 2018;93:119-121.
- Agulló A, Hinds B, Larrea M, et al. Livedo racemosa, reticulated ulcerations, panniculitis and violaceous plaques in a 46-year-old woman. Indian Dermatol Online J. 2018;9:47-49.
- Hattori Y, Matsuyama K, Takahashi T, et al. Anti-MDA5 antibody-positive dermatomyositis presenting with cellulitis-like erythema on the mandible as an initial symptom. Case Rep Dermatol. 2018;10:110-114.
- Hasegawa A, Shimomura Y, Kibune N, et al. Panniculitis as the initial manifestation of dermatomyositis with anti-MDA5 antibody. Clin Exp Dermatol. 2017;42:551-553.
- Salman A, Kasapcopur O, Ergun T, et al. Panniculitis in juvenile dermatomyositis: report of a case and review of the published work. J Dermatol. 2016;43:951-953.
- Carroll M, Mellick N, Wagner G. Dermatomyositis panniculitis: a case report. Australas J Dermatol. 2015;56:224‐226.
- Chairatchaneeboon M, Kulthanan K, Manapajon A. Calcific panniculitis and nasopharyngeal cancer-associated adult-onset dermatomyositis: a case report and literature review. Springerplus. 2015;4:201.
- Otero Rivas MM, Vicente Villa A, González Lara L, et al. Panniculitis in juvenile dermatomyositis. Clin Exp Dermatol. 2015;40:574-575.
- Yanaba K, Tanito K, Hamaguchi Y, et al. Anti‐transcription intermediary factor‐1γ/α/β antibody‐positive dermatomyositis associated with multiple panniculitis lesions. Int J Rheum Dis. 2015;20:1831-1834.
- Pau-Charles I, Moreno PJ, Ortiz-Ibanez K, et al. Anti-MDA5 positive clinically amyopathic dermatomyositis presenting with severe cardiomyopathy. J Eur Acad Dermatol Venereol. 2014;28:1097-1102.
- Lamb R, Digby S, Stewart W, et al. Cutaneous ulceration: more than skin deep? Clin Exp Dermatol. 2013;38:443-445.
- Arias M, Hernández MI, Cunha LG, et al. Panniculitis in a patient with dermatomyositis. An Bras Dermatol. 2011;86:146-148.
- Hemmi S, Kushida R, Nishimura H, et al. Magnetic resonance imaging diagnosis of panniculitis in dermatomyositis. Muscle Nerve. 2010;41:151-153.
- Geddes MR, Sinnreich M, Chalk C. Minocycline-induced dermatomyositis. Muscle Nerve. 2010;41:547-549.
- Abdul‐Wahab A, Holden CA, Harland C, et al Calcific panniculitis in adult‐onset dermatomyositis. Clin Exp Dermatol. 2009;34:E854-E856.
- Carneiro S, Alvim G, Resende P, et al. Dermatomyositis with panniculitis. Skinmed. 2007;6:46-47.
- Carrera E, Lobrinus JA, Spertini O, et al. Dermatomyositis, lobarpanniculitis and inflammatory myopathy with abundant macrophages. Neuromuscul Disord. 2006;16:468-471.
- Lin JH, Chu CY, Lin RY. Panniculitis in adult onset dermatomyositis: report of two cases and review of the literature. Dermatol Sinica. 2006;24:194-200.
- Chen GY, Liu MF, Lee JY, et al. Combination of massive mucinosis, dermatomyositis, pyoderma gangrenosum-like ulcer, bullae and fatal intestinal vasculopathy in a young female. Eur J Dermatol. 2005;15:396-400.
- Nakamori A, Yamaguchi Y, Kurimoto I, et al. Vesiculobullous dermatomyositis with panniculitis without muscle disease. J Am Acad Dermatol. 2003;49:1136-1139.
- Solans R, Cortés J, Selva A, et al. Panniculitis: a cutaneous manifestation of dermatomyositis. J Am Acad Dermatol. 2002;46:S148-S150.
- Chao YY, Yang LJ. Dermatomyositis presenting as panniculitis. Int J Dermatol. 2000;39:141-144.
- Lee MW, Lim YS, Choi JH, et al. Panniculitis showing membranocystic changes in the dermatomyositis. J Dermatol. 1999;26:608‐610.
- Ghali FE, Reed AM, Groben PA, et al. Panniculitis in juvenile dermatomyositis. Pediatr Dermatol. 1999;16:270-272.
- Molnar K, Kemeny L, Korom I, et al. Panniculitis in dermatomyositis: report of two cases. Br J Dermatol. 1998;139:161‐163.
- Ishikawa O, Tamura A, Ryuzaki K, et al. Membranocystic changes in the panniculitis of dermatomyositis. Br J Dermatol. 1996;134:773-776.
- Sabroe RA, Wallington TB, Kennedy CT. Dermatomyositis treated with high-dose intravenous immunoglobulins and associated with panniculitis. Clin Exp Dermatol. 1995;20:164-167.
- Neidenbach PJ, Sahn EE, Helton J. Panniculitis in juvenile dermatomyositis. J Am Acad Dermatol. 1995;33:305-307.
- Fusade T, Belanyi P, Joly P, et al. Subcutaneous changes in dermatomyositis. Br J Dermatol. 1993;128:451-453.
- Winkelmann WJ, Billick RC, Srolovitz H. Dermatomyositis presenting as panniculitis. J Am Acad Dermatol. 1990;23:127-128.
- Commens C, O’Neill P, Walker G. Dermatomyositis associated with multifocal lipoatrophy. J Am Acad Dermatol. 1990;22:966-969.
- Raimer SS, Solomon AR, Daniels JC. Polymyositis presenting with panniculitis. J Am Acad Dermatol. 1985;13(2 pt 2):366‐369.
- Feldman D, Hochberg MC, Zizic TM, et al. Cutaneous vasculitis in adult polymyositis/dermatomyositis. J Rheumatol. 1983;10:85-89.
- Kimura S, Fukuyama Y. Tubular cytoplasmic inclusions in a case of childhood dermatomyositis with migratory subcutaneous nodules. Eur J Pediatr. 1977;125:275-283.
- Weber FP, Gray AMH. Chronic relapsing polydermatomyositis with predominant involvement of the subcutaneous fat. Br J Dermatol. 1924;36:544-560.
- Santos‐Briz A, Calle A, Linos K, et al. Dermatomyositis panniculitis: a clinicopathological and immunohistochemical study of 18 cases. J Eur Acad Dermatol Venereol. 2018;32:1352-1359.
Practice Points
- Clinical panniculitis is a rare subcutaneous manifestation of dermatomyositis (DM) that dermatologists must consider when evaluating patients with this condition.
- Panniculitis can precede, occur simultaneously with, or develop up to 5 years after onset of DM.
- Many patients suffer from treatment-resistant panniculitis in DM, suggesting that therapeutic management of this condition may require long-term and more aggressive treatment modalities.
COVID-19: Delta variant is raising the stakes
Empathetic conversations with unvaccinated people desperately needed
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Empathetic conversations with unvaccinated people desperately needed
Empathetic conversations with unvaccinated people desperately needed
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Like many colleagues, I have been working to change the minds and behaviors of acquaintances and patients who are opting to forgo a COVID vaccine. The large numbers of these unvaccinated Americans, combined with the surging Delta coronavirus variant, are endangering the health of us all.
When I spoke with the 22-year-old daughter of a family friend about what was holding her back, she told me that she would “never” get vaccinated. I shared my vaccination experience and told her that, except for a sore arm both times for a day, I felt no side effects. Likewise, I said, all of my adult family members are vaccinated, and everyone is fine. She was neither moved nor convinced.
Finally, I asked her whether she attended school (knowing that she was a college graduate), and she said “yes.” So I told her that all 50 states require children attending public schools to be vaccinated for diseases such as diphtheria, tetanus, polio, and the chickenpox – with certain religious, philosophical, and medical exemptions. Her response was simple: “I didn’t know that. Anyway, my parents were in charge.” Suddenly, her thinking shifted. “You’re right,” she said. She got a COVID shot the next day. Success for me.
When I asked another acquaintance whether he’d been vaccinated, he said he’d heard people were getting very sick from the vaccine – and was going to wait. Another gentleman I spoke with said that, at age 45, he was healthy. Besides, he added, he “doesn’t get sick.” When I asked another acquaintance about her vaccination status, her retort was that this was none of my business. So far, I’m batting about .300.
But as a physician, I believe that we – and other health care providers – must continue to encourage the people in our lives to care for themselves and others by getting vaccinated. One concrete step advised by the Centers for Disease Control and Prevention is to help people make an appointment for a shot. Some sites no longer require appointments, and New York City, for example, offers in-home vaccinations to all NYC residents.
Also, NYC Mayor Bill de Blasio announced Aug. 3 the “Key to NYC Pass,” which he called a “first-in-the-nation approach” to vaccination. Under this new policy, vaccine-eligible people aged 12 and older in New York City will need to prove with a vaccination card, an app, or an Excelsior Pass that they have received at least one dose of vaccine before participating in indoor venues such as restaurants, bars, gyms, and movie theaters within the city. Mayor de Blasio said the new initiative, which is still being finalized, will be phased in starting the week of Aug. 16. I see this as a major public health measure that will keep people healthy – and get them vaccinated.
The medical community should support this move by the city of New York and encourage people to follow CDC guidance on wearing face coverings in public settings, especially schools. New research shows that physicians continue to be among the most trusted sources of vaccine-related information.
Another strategy we might use is to point to the longtime practices of surgeons. We could ask: Why do surgeons wear face masks in the operating room? For years, these coverings have been used to protect patients from the nasal and oral bacteria generated by operating room staff. Likewise, we can tell those who remain on the fence that, by wearing face masks, we are protecting others from all variants, but specifically from Delta – which the CDC now says can be transmitted by people who are fully vaccinated.
Why did the CDC lift face mask guidance for fully vaccinated people in indoor spaces in May? It was clear to me and other colleagues back then that this was not a good idea. Despite that guidance, I continued to wear a mask in public places and advised anyone who would listen to do the same.
The development of vaccines in the 20th and 21st centuries has saved millions of lives. The World Health Organization reports that 4 million to 5 million lives a year are saved by immunizations. In addition, research shows that, before the emergence of SARS-CoV-2, vaccinations led to the eradication of smallpox and polio, and a 74% drop in measles-related deaths between 2004 and 2014.
Protecting the most vulnerable
With COVID cases surging, particularly in parts of the South and Midwest, I am concerned about children under age 12 who do not yet qualify for a vaccine. Certainly, unvaccinated parents could spread the virus to their young children, and unvaccinated children could transmit the illness to immediate and extended family. Now that the CDC has said that there is a risk of SARS-CoV-2 breakthrough infection among fully vaccinated people in areas with high community transmission, should we worry about unvaccinated young children with vaccinated parents? I recently spoke with James C. Fagin, MD, a board-certified pediatrician and immunologist, to get his views on this issue.
Dr. Fagin, who is retired, said he is in complete agreement with the Food and Drug Administration when it comes to approving medications for children. However, given the seriousness of the pandemic and the need to get our children back to in-person learning, he would like to see the approval process safely expedited. Large numbers of unvaccinated people increase the pool for the Delta variant and could increase the likelihood of a new variant that is more resistant to the vaccines, said Dr. Fagin, former chief of academic pediatrics at North Shore University Hospital and a former faculty member in the allergy/immunology division of Cohen Children’s Medical Center, both in New York.
Meanwhile, I agree with the American Academy of Pediatrics’ recommendations that children, teachers, and school staff and other adults in school settings should wear masks regardless of vaccination status. Kids adjust well to masks – as my grandchildren and their friends have.
The bottom line is that we need to get as many people as possible vaccinated as soon as possible, and while doing so, we must continue to wear face coverings in public spaces. As clinicians, we have a special responsibility to do all that we can to change minds – and behaviors.
Dr. London is a practicing psychiatrist who has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Diabetes drug’s new weight-loss indication fuels cost-benefit debate
The long list of side effects that follow ads for newer expensive drugs to treat type 2 diabetes sometimes include an unusual warning: They might cause weight loss. That side effect is one that many people – especially those with type 2 diabetes, which is associated with obesity – may desperately want.
So it’s no surprise that some of the same drugs are being reformulated and renamed by manufacturers as a new obesity treatment. No longer limited to the crowded field of treatments for type 2 diabetes, which affects about 10% of Americans, they join the far smaller number of drugs for obesity, which affects 42% of Americans and is ready to be mined for profit.
One that recently hit the market – winning Food and Drug Administration approval in June – is Novo Nordisk’s Wegovy (semaglutide), a higher-dose version of the company’s injectable diabetes drug, Ozempic.
Ozempic’s peppy ads suggest that people who use it might lose weight, but also include a disclaimer: that it “is not a weight-loss drug.” Now – with a new name – it is. And clinical trials showed using it leads to significant weight loss for many patients.
“People who go on this medication lose more weight than with any drug we’ve seen, ever,” said Fatima Cody Stanford, MD, MPH, an obesity medicine specialist at Massachusetts General Hospital and Harvard Medical School, both in Boston, who was not involved with any of the clinical trials.
But that leaves employers and insurers in the uncomfortable position of deciding if it’s worth it.
Wegovy’s monthly wholesale price tag – set at $1,349 – is about 58% more than Ozempic’s, although, the company pointed out, the drug’s injector pens contain more than twice as much of the active ingredient. Studies so far show that patients may need to take it indefinitely to maintain weight loss, translating to a tab that could top $323,000 over 20 years at the current price. Weight-loss treatments are not universally covered by insurance policies.
The arrival of this new class of weight-loss drugs – one from Lilly may soon follow – has created a thicket of issues for those who will pay for them. The decision is complicated by many unknowables concerning their long-term use and whether competition might eventually lower the price.
“The metric we try to use is value,” said James Gelfand, senior vice president for health policy at the ERISA Industry Committee, which represents large, self-insured employers. “If we pay for this drug, how much is this going to cost and how much value will it provide to the beneficiaries?”
Weight-loss treatments have had a lackluster past in this regard, with only modest results. Many employers and insurers likely remember Fen-Phen, a combination of fenfluramine and dexfenfluramine that was pulled from the market in the late 1990s for causing heart valve problems.
New drugs like Wegovy, more effective but also pricier than previous weight-loss treatments, will add more fuel to that debate.
Past treatments were shown to prompt weight loss in the range of 5%-10% of body weight. But many had relatively serious or unpleasant side effects.
Wegovy, however, helped patients lose an average of 15% of their body weight over 68 weeks in the main clinical trial that led to its approval. A comparison group that got a placebo injection lost an average of 2.5% over the same period. On the high end, nearly a third of patients in the treatment group lost 20% or more. Both groups had counseling on diet and exercise.
Side effects, generally considered mild, included nausea, diarrhea, vomiting, and constipation. A few patients developed pancreatitis, a serious inflammation of the pancreas. Like the diabetes medication, the drug carries a warning about a potential risk of a type of thyroid cancer.
Weight loss in those taking Wegovy puts it close to the 20%-25% losses seen with bariatric surgery, said Stanford, and well above the 3%-4% seen with diet and other lifestyle changes alone.
Participants also saw reductions in their waistlines and improvements in their blood pressure and blood sugar levels, which may mean they won’t develop diabetes, said Sean Wharton, MD, an internal medicine specialist and adjunct professor at York University in Toronto who was among the coauthors of the report outlining the results of the first clinical trial on Wegovy.
Since weight loss is known to reduce the risk of heart attack, high blood pressure and diabetes, might the new drug type be worth it?
Covering such treatment would be a sea change for Medicare, which specifically bars coverage for obesity medications or drugs for “anorexia, weight loss, or weight gain,” although it does pay for bariatric surgery. Pharmaceutical companies, patient advocates, and some medical professionals are backing proposed federal legislation to allow coverage. But the legislation, the Treat and Reduce Obesity Act, has not made progress despite being reintroduced every year since 2012, and sponsors are now asking federal officials instead to rewrite existing rules.
Private insurers will have to consider a cost-benefit analysis of adding Wegovy to their list of covered treatments, either broadly or with limits. Obesity was first recognized as a disease by the American Medical Association, easing the path for insurance coverage, in 2013.
“Employers are going to have a bit of a challenge” deciding whether to add the benefit to insurance offerings, said Steve Pearson, founder and president of the Institute for Clinical and Economic Review, which provides cost-benefit analyses of medical treatments but has not yet looked at Wegovy.
The trade-offs are embodied in patients like Phylander Pannell, a 49-year-old Largo, Md., woman who said she lost 65 pounds in a clinical trial of Wegovy. That study gave the drug to all participants for the first 20 weeks, then randomly assigned patients to get either the drug or a placebo for the next 48 weeks to determine what happens when the medication is stopped. Only after the trial ended did she find out she was in the treatment group the entire time.
Her weight fell slowly at first, then ramped up, eventually bringing her 190-pound frame down to about 125. Pains in her joints eased; she felt better all around.
“I definitely feel the drug was it for me,” said Ms. Pannell, who also followed the trial’s guidance on diet and exercise.
The study found that both groups lost weight in the initial 20 weeks, but those who continued to get the drug lost an additional average of 7.9% of their body weight. Those who got a placebo gained back nearly 7%.
After the trial ended, and the COVID-19 pandemic hit, Ms. Pannell regained some weight and is now at 155. She is eager to get back on the medication and hopes her job-based insurance will cover it.
Many employers do cover obesity drugs. For example, about 40% of private employer plans include Novo Nordisk’s once-daily injection called Saxenda on their health plans, said Michael Bachner, Novo Nordisk’s director of media relations.
He said the $1,349-a-month wholesale acquisition price of Wegovy was determined by making it equivalent to that of Saxenda, which is less effective.
Still, that is more than the $851 monthly wholesale price of Ozempic. But, he pointed out, the recommended dosage of Wegovy is more than twice that of Ozempic. Four milligrams come in the Ozempic injector pens for the month, while Wegovy has 9.6.
“There’s more drug in the pen,” Mr. Bachner said. “That drives the price up.”
He added: “This is not a 20-year-old drug that we now have a new indication for and are pricing it higher. It’s a whole different clinical program,” which required new trials.
Now scientists, employers, physicians, and patients will have to decide whether the new drugs are worth it.
Earlier estimates – some commissioned by Novo Nordisk – of the potential cost of adding an obesity drug benefit to Medicare showed an overall reduction in spending when better health from the resulting weight loss was factored in.
Still, those earlier estimates considered much less expensive drugs, including a range of generic and branded drugs costing as little as $7 a month to more than $300, a small fraction of Wegovy’s cost.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The long list of side effects that follow ads for newer expensive drugs to treat type 2 diabetes sometimes include an unusual warning: They might cause weight loss. That side effect is one that many people – especially those with type 2 diabetes, which is associated with obesity – may desperately want.
So it’s no surprise that some of the same drugs are being reformulated and renamed by manufacturers as a new obesity treatment. No longer limited to the crowded field of treatments for type 2 diabetes, which affects about 10% of Americans, they join the far smaller number of drugs for obesity, which affects 42% of Americans and is ready to be mined for profit.
One that recently hit the market – winning Food and Drug Administration approval in June – is Novo Nordisk’s Wegovy (semaglutide), a higher-dose version of the company’s injectable diabetes drug, Ozempic.
Ozempic’s peppy ads suggest that people who use it might lose weight, but also include a disclaimer: that it “is not a weight-loss drug.” Now – with a new name – it is. And clinical trials showed using it leads to significant weight loss for many patients.
“People who go on this medication lose more weight than with any drug we’ve seen, ever,” said Fatima Cody Stanford, MD, MPH, an obesity medicine specialist at Massachusetts General Hospital and Harvard Medical School, both in Boston, who was not involved with any of the clinical trials.
But that leaves employers and insurers in the uncomfortable position of deciding if it’s worth it.
Wegovy’s monthly wholesale price tag – set at $1,349 – is about 58% more than Ozempic’s, although, the company pointed out, the drug’s injector pens contain more than twice as much of the active ingredient. Studies so far show that patients may need to take it indefinitely to maintain weight loss, translating to a tab that could top $323,000 over 20 years at the current price. Weight-loss treatments are not universally covered by insurance policies.
The arrival of this new class of weight-loss drugs – one from Lilly may soon follow – has created a thicket of issues for those who will pay for them. The decision is complicated by many unknowables concerning their long-term use and whether competition might eventually lower the price.
“The metric we try to use is value,” said James Gelfand, senior vice president for health policy at the ERISA Industry Committee, which represents large, self-insured employers. “If we pay for this drug, how much is this going to cost and how much value will it provide to the beneficiaries?”
Weight-loss treatments have had a lackluster past in this regard, with only modest results. Many employers and insurers likely remember Fen-Phen, a combination of fenfluramine and dexfenfluramine that was pulled from the market in the late 1990s for causing heart valve problems.
New drugs like Wegovy, more effective but also pricier than previous weight-loss treatments, will add more fuel to that debate.
Past treatments were shown to prompt weight loss in the range of 5%-10% of body weight. But many had relatively serious or unpleasant side effects.
Wegovy, however, helped patients lose an average of 15% of their body weight over 68 weeks in the main clinical trial that led to its approval. A comparison group that got a placebo injection lost an average of 2.5% over the same period. On the high end, nearly a third of patients in the treatment group lost 20% or more. Both groups had counseling on diet and exercise.
Side effects, generally considered mild, included nausea, diarrhea, vomiting, and constipation. A few patients developed pancreatitis, a serious inflammation of the pancreas. Like the diabetes medication, the drug carries a warning about a potential risk of a type of thyroid cancer.
Weight loss in those taking Wegovy puts it close to the 20%-25% losses seen with bariatric surgery, said Stanford, and well above the 3%-4% seen with diet and other lifestyle changes alone.
Participants also saw reductions in their waistlines and improvements in their blood pressure and blood sugar levels, which may mean they won’t develop diabetes, said Sean Wharton, MD, an internal medicine specialist and adjunct professor at York University in Toronto who was among the coauthors of the report outlining the results of the first clinical trial on Wegovy.
Since weight loss is known to reduce the risk of heart attack, high blood pressure and diabetes, might the new drug type be worth it?
Covering such treatment would be a sea change for Medicare, which specifically bars coverage for obesity medications or drugs for “anorexia, weight loss, or weight gain,” although it does pay for bariatric surgery. Pharmaceutical companies, patient advocates, and some medical professionals are backing proposed federal legislation to allow coverage. But the legislation, the Treat and Reduce Obesity Act, has not made progress despite being reintroduced every year since 2012, and sponsors are now asking federal officials instead to rewrite existing rules.
Private insurers will have to consider a cost-benefit analysis of adding Wegovy to their list of covered treatments, either broadly or with limits. Obesity was first recognized as a disease by the American Medical Association, easing the path for insurance coverage, in 2013.
“Employers are going to have a bit of a challenge” deciding whether to add the benefit to insurance offerings, said Steve Pearson, founder and president of the Institute for Clinical and Economic Review, which provides cost-benefit analyses of medical treatments but has not yet looked at Wegovy.
The trade-offs are embodied in patients like Phylander Pannell, a 49-year-old Largo, Md., woman who said she lost 65 pounds in a clinical trial of Wegovy. That study gave the drug to all participants for the first 20 weeks, then randomly assigned patients to get either the drug or a placebo for the next 48 weeks to determine what happens when the medication is stopped. Only after the trial ended did she find out she was in the treatment group the entire time.
Her weight fell slowly at first, then ramped up, eventually bringing her 190-pound frame down to about 125. Pains in her joints eased; she felt better all around.
“I definitely feel the drug was it for me,” said Ms. Pannell, who also followed the trial’s guidance on diet and exercise.
The study found that both groups lost weight in the initial 20 weeks, but those who continued to get the drug lost an additional average of 7.9% of their body weight. Those who got a placebo gained back nearly 7%.
After the trial ended, and the COVID-19 pandemic hit, Ms. Pannell regained some weight and is now at 155. She is eager to get back on the medication and hopes her job-based insurance will cover it.
Many employers do cover obesity drugs. For example, about 40% of private employer plans include Novo Nordisk’s once-daily injection called Saxenda on their health plans, said Michael Bachner, Novo Nordisk’s director of media relations.
He said the $1,349-a-month wholesale acquisition price of Wegovy was determined by making it equivalent to that of Saxenda, which is less effective.
Still, that is more than the $851 monthly wholesale price of Ozempic. But, he pointed out, the recommended dosage of Wegovy is more than twice that of Ozempic. Four milligrams come in the Ozempic injector pens for the month, while Wegovy has 9.6.
“There’s more drug in the pen,” Mr. Bachner said. “That drives the price up.”
He added: “This is not a 20-year-old drug that we now have a new indication for and are pricing it higher. It’s a whole different clinical program,” which required new trials.
Now scientists, employers, physicians, and patients will have to decide whether the new drugs are worth it.
Earlier estimates – some commissioned by Novo Nordisk – of the potential cost of adding an obesity drug benefit to Medicare showed an overall reduction in spending when better health from the resulting weight loss was factored in.
Still, those earlier estimates considered much less expensive drugs, including a range of generic and branded drugs costing as little as $7 a month to more than $300, a small fraction of Wegovy’s cost.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The long list of side effects that follow ads for newer expensive drugs to treat type 2 diabetes sometimes include an unusual warning: They might cause weight loss. That side effect is one that many people – especially those with type 2 diabetes, which is associated with obesity – may desperately want.
So it’s no surprise that some of the same drugs are being reformulated and renamed by manufacturers as a new obesity treatment. No longer limited to the crowded field of treatments for type 2 diabetes, which affects about 10% of Americans, they join the far smaller number of drugs for obesity, which affects 42% of Americans and is ready to be mined for profit.
One that recently hit the market – winning Food and Drug Administration approval in June – is Novo Nordisk’s Wegovy (semaglutide), a higher-dose version of the company’s injectable diabetes drug, Ozempic.
Ozempic’s peppy ads suggest that people who use it might lose weight, but also include a disclaimer: that it “is not a weight-loss drug.” Now – with a new name – it is. And clinical trials showed using it leads to significant weight loss for many patients.
“People who go on this medication lose more weight than with any drug we’ve seen, ever,” said Fatima Cody Stanford, MD, MPH, an obesity medicine specialist at Massachusetts General Hospital and Harvard Medical School, both in Boston, who was not involved with any of the clinical trials.
But that leaves employers and insurers in the uncomfortable position of deciding if it’s worth it.
Wegovy’s monthly wholesale price tag – set at $1,349 – is about 58% more than Ozempic’s, although, the company pointed out, the drug’s injector pens contain more than twice as much of the active ingredient. Studies so far show that patients may need to take it indefinitely to maintain weight loss, translating to a tab that could top $323,000 over 20 years at the current price. Weight-loss treatments are not universally covered by insurance policies.
The arrival of this new class of weight-loss drugs – one from Lilly may soon follow – has created a thicket of issues for those who will pay for them. The decision is complicated by many unknowables concerning their long-term use and whether competition might eventually lower the price.
“The metric we try to use is value,” said James Gelfand, senior vice president for health policy at the ERISA Industry Committee, which represents large, self-insured employers. “If we pay for this drug, how much is this going to cost and how much value will it provide to the beneficiaries?”
Weight-loss treatments have had a lackluster past in this regard, with only modest results. Many employers and insurers likely remember Fen-Phen, a combination of fenfluramine and dexfenfluramine that was pulled from the market in the late 1990s for causing heart valve problems.
New drugs like Wegovy, more effective but also pricier than previous weight-loss treatments, will add more fuel to that debate.
Past treatments were shown to prompt weight loss in the range of 5%-10% of body weight. But many had relatively serious or unpleasant side effects.
Wegovy, however, helped patients lose an average of 15% of their body weight over 68 weeks in the main clinical trial that led to its approval. A comparison group that got a placebo injection lost an average of 2.5% over the same period. On the high end, nearly a third of patients in the treatment group lost 20% or more. Both groups had counseling on diet and exercise.
Side effects, generally considered mild, included nausea, diarrhea, vomiting, and constipation. A few patients developed pancreatitis, a serious inflammation of the pancreas. Like the diabetes medication, the drug carries a warning about a potential risk of a type of thyroid cancer.
Weight loss in those taking Wegovy puts it close to the 20%-25% losses seen with bariatric surgery, said Stanford, and well above the 3%-4% seen with diet and other lifestyle changes alone.
Participants also saw reductions in their waistlines and improvements in their blood pressure and blood sugar levels, which may mean they won’t develop diabetes, said Sean Wharton, MD, an internal medicine specialist and adjunct professor at York University in Toronto who was among the coauthors of the report outlining the results of the first clinical trial on Wegovy.
Since weight loss is known to reduce the risk of heart attack, high blood pressure and diabetes, might the new drug type be worth it?
Covering such treatment would be a sea change for Medicare, which specifically bars coverage for obesity medications or drugs for “anorexia, weight loss, or weight gain,” although it does pay for bariatric surgery. Pharmaceutical companies, patient advocates, and some medical professionals are backing proposed federal legislation to allow coverage. But the legislation, the Treat and Reduce Obesity Act, has not made progress despite being reintroduced every year since 2012, and sponsors are now asking federal officials instead to rewrite existing rules.
Private insurers will have to consider a cost-benefit analysis of adding Wegovy to their list of covered treatments, either broadly or with limits. Obesity was first recognized as a disease by the American Medical Association, easing the path for insurance coverage, in 2013.
“Employers are going to have a bit of a challenge” deciding whether to add the benefit to insurance offerings, said Steve Pearson, founder and president of the Institute for Clinical and Economic Review, which provides cost-benefit analyses of medical treatments but has not yet looked at Wegovy.
The trade-offs are embodied in patients like Phylander Pannell, a 49-year-old Largo, Md., woman who said she lost 65 pounds in a clinical trial of Wegovy. That study gave the drug to all participants for the first 20 weeks, then randomly assigned patients to get either the drug or a placebo for the next 48 weeks to determine what happens when the medication is stopped. Only after the trial ended did she find out she was in the treatment group the entire time.
Her weight fell slowly at first, then ramped up, eventually bringing her 190-pound frame down to about 125. Pains in her joints eased; she felt better all around.
“I definitely feel the drug was it for me,” said Ms. Pannell, who also followed the trial’s guidance on diet and exercise.
The study found that both groups lost weight in the initial 20 weeks, but those who continued to get the drug lost an additional average of 7.9% of their body weight. Those who got a placebo gained back nearly 7%.
After the trial ended, and the COVID-19 pandemic hit, Ms. Pannell regained some weight and is now at 155. She is eager to get back on the medication and hopes her job-based insurance will cover it.
Many employers do cover obesity drugs. For example, about 40% of private employer plans include Novo Nordisk’s once-daily injection called Saxenda on their health plans, said Michael Bachner, Novo Nordisk’s director of media relations.
He said the $1,349-a-month wholesale acquisition price of Wegovy was determined by making it equivalent to that of Saxenda, which is less effective.
Still, that is more than the $851 monthly wholesale price of Ozempic. But, he pointed out, the recommended dosage of Wegovy is more than twice that of Ozempic. Four milligrams come in the Ozempic injector pens for the month, while Wegovy has 9.6.
“There’s more drug in the pen,” Mr. Bachner said. “That drives the price up.”
He added: “This is not a 20-year-old drug that we now have a new indication for and are pricing it higher. It’s a whole different clinical program,” which required new trials.
Now scientists, employers, physicians, and patients will have to decide whether the new drugs are worth it.
Earlier estimates – some commissioned by Novo Nordisk – of the potential cost of adding an obesity drug benefit to Medicare showed an overall reduction in spending when better health from the resulting weight loss was factored in.
Still, those earlier estimates considered much less expensive drugs, including a range of generic and branded drugs costing as little as $7 a month to more than $300, a small fraction of Wegovy’s cost.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Vaccination alone won’t counter rise of resistant variants: Study
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
Relaxation of nonpharmaceutical interventions once vaccination of the population has reached a tipping point short of herd immunity can increase the probability of the emergence of a resistant strain that natural selection then favors, according to new findings of a modeling study published online on July 30, 2021, in Scientific Reports.
Although vaccination is the best strategy for controlling viral spread, changes in our behavior and mindset will be increasingly required to stay ahead of vaccine-resistant strains, according to the authors of the report.
“We have become accustomed to thinking of the pandemic from the point of view of epidemiology, and advised to reduce transmission and the number of people getting sick and the death rate. As the pandemic spreads across years, there will be a new dimension to our thinking, both for policymakers and the public. And that’s the evolutionary perspective,” coauthor Fyodor Kondrashov, PhD, an evolutionary biologist at the Institute of Science and Technology, Klosterneuburg, Austria, said at a press briefing on July 299.
The coming “change of mentality” that Dr. Kondrashov foresees should reassure people that masking and social distancing even after being vaccinated aren’t futile. “It decreases the possibility that a vaccine-resistant strain is running around. We’re not just trying to prevent the spread, but the evolution of novel variants, which are so rare at this point that we haven’t yet identified them,” he said.
The study focused on evolution generically, rather than on specific variants. “We took the classical model used to study epidemiology of pandemics, the SIR [susceptible, infected, recovered] model, and we modified it to study the dynamics of rare mutations associated with emergence of a vaccine-resistant strain,” Simon A. Rella, the lead author of the study and a PhD student at the Institute of Science and Technology, explained at the briefing.
The researchers simulated the probability that a vaccine-resistant strain will emerge in a population of 10,000,000 individuals over 3 years, with vaccinations beginning after the first year. For eight scenarios, rates of infection, recovery, death, vaccination, and mutation and the percentage of individuals with resistant viral strains were factors in the model.
The model also simulated waves of low and high transmission, similar to the effects of large-scale interventions such as lockdowns.
Three factors
The study showed that a trio of factors increases the probability of a vaccine-resistant strain taking hold: slow rates of vaccination, high number of infected individuals, and faster mutation rate
These factors, Mr. Rella said, are obvious to some degree. “Every infected individual is like a mini-bioreactor, increasing the risk that mutations will appear that will endow the virus with the property of avoiding the immune system primed by a vaccine.”
Not as obvious, Mr. Rella added, is that, when most people are vaccinated, a vaccine-resistant strain has an advantage over the original strain and spreads faster.
But we can stop it, he said. “Our model shows that if at the time a vaccine campaign is close to finishing and nonpharmacological interventions are maintained, then there’s a chance to completely remove the vaccine-resistant mutations from the virus population.”
In scenarios in which a resistant strain became established, resistance initially emerged after about 60% of the population had been vaccinated. That makes nonpharmaceutical interventions such as masking and social distancing vitally important. Just under 50% of the U.S. population over the age of 12 has been fully vaccinated, according to the Centers for Disease Control and Prevention.
“Our results suggest that policymakers and individuals should consider maintaining nonpharmaceutical interventions and transmission-reducing behaviors throughout the entire vaccination period,” the investigators concluded.
A ‘powerful force’
“We hope for the best, that vaccine resistance has not developed, but caution that evolution is a very powerful force, and maintaining some precautions during vaccination may help to control that evolution,” said Dr. Kondrashov.
The investigators are relying on epidemiologists to determine which measures are most effective.
“It’s necessary to vaccinate as many people as fast as possible and as globally as possible and to maintain some level of nonpharmaceutical intervention to ensure rare variants have a chance to be suppressed instead of spread,” concluded Dr. Kondrashov.
He’s pessimistic because many countries are still having difficulty accessing vaccines, and vaccine efficacy wanes slightly over time. The authors warned that “the emergence of a partially or fully vaccine-resistant strain and its eventual establishment appears inevitable.”
The worst-case scenario is familiar to population biologists: rounds of “vaccine development playing catch up in the evolutionary arms race against novel strains,” the authors wrote.
Limitations of the study are that some parameters of the rate of evolution for vaccine-resistant strains aren’t known, and in creating the model, consideration was not given to effects of increased testing, rigorous contact tracing, rates of viral genome sequencing, and travel restrictions.
Rather, the model illustrates general principals by which vaccine resistance can evolve, Dr. Kondrashov said.
A version of this article first appeared on Medscape.com.
C. diff eradication not necessary for clinical cure of recurrent infections with fecal transplant
It’s not necessary to completely eradicate all Clostridioides difficile to successfully treat recurrent C. difficile infections with fecal microbiota transplant (FMT), according to a study presented online July 12 at the European Congress of Clinical Microbiology & Infectious Diseases.
C. difficile colonization persisted for 3 weeks after FMT in about one-quarter of patients, but it’s not clear whether this is a persistent infection, a newly acquired infection, or partial persistence of a mixed infection, said Elisabeth Terveer, MD, a medical microbiologist at Leiden (the Netherlands) University Medical Center. In addition, “82% of patients with detectable C. diff do not relapse, so it’s absolutely not necessary for a cure,” she said.
Several mechanisms explain why FMT is a highly effective therapy for recurrent C. difficile infections, including restoration of bacterial metabolism in the gut, immune modulation, and direct competition between bacteria, Dr. Terveer said, but it’s less clear whether eradication of C. difficile spores is among these mechanisms.
Between May 2016 and April 2020, the researchers analyzed fecal samples from 84 patients who took vancomycin for at least 4 days before undergoing FMT. The researchers took fecal samples from patients before FMT and 3 weeks after FMT to culture them and the donor samples for presence of C. difficile, and they assessed clinical outcomes at 3 weeks and 6 months after FMT.
After antibiotic treatment but prior to FMT, 19% of patients (n = 16) still had a toxigenic C. difficile culture while the other 81% had a negative culture. None of the donor samples had a positive C. difficile culture. After FMT treatment, five patients who had a positive pre-FMT culture remained positive, and the other 11 were negative. Among the 81% of patients (n = 68) who had a negative culture just before FMT, 22 had a positive culture and 46 had a negative culture after FMT. Overall, 26% of patients post FMT had a positive C. difficile culture, a finding that was 10-fold higher than another study that assessed C. difficile with PCR testing, Dr. Terveer said.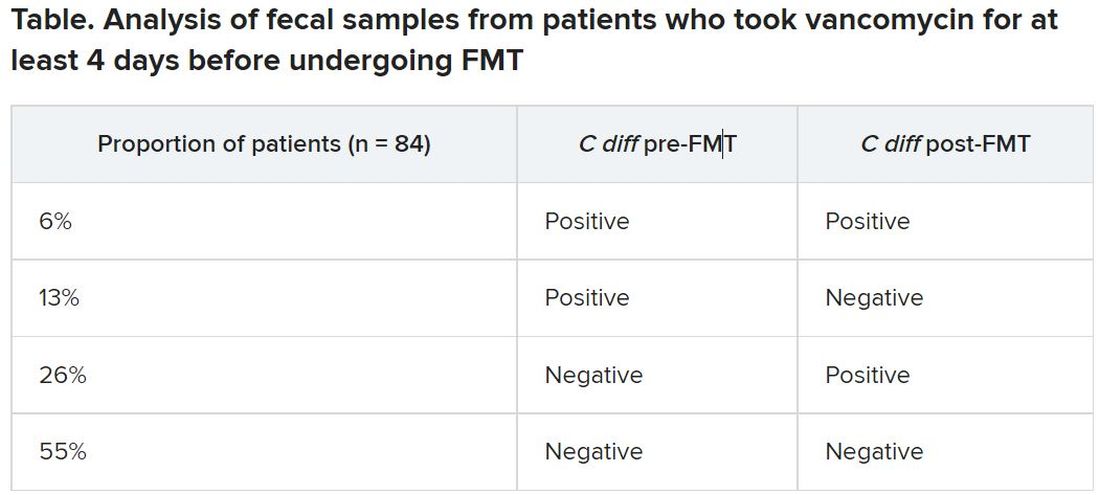
The clinical cure rate after FMT was 94%, and five patients had relapses within 2 months of their FMT. These relapses were more prevalent in patients with a positive C. difficile culture prior to FMT (odds ratio [OR], 7.6; P = .045) and a positive C. difficile culture after FMT (OR, 13.6; P = .016). Still, 82% of patients who had a positive C. difficile culture post FMT remained clinically cured 2 months later.
It’s unclear why 19% of patients had a positive culture after their antibiotic pretreatment prior to FMT, Dr. Terveer said, but it may be because the pretreatment was of such a short duration.
“I think the advice should be: Give a full anti–C. diff antibiotic course to treat the C. diff infection, and then give FMT afterward to restore the microbiota and prevent further relapses,” Dr. Terveer told attendees.
Dimitri Drekonja, MD, chief of the Minneapolis VA Infectious Disease Section, said the findings were not necessarily surprising, but it would have been interesting for the researchers to have conducted DNA sequencing of the patients’ fecal samples post FMT to see what the biological diversity looked like.
“One school of thought has been that you have to repopulate the normal diverse microbiota of the colon” with FMT, and the other “is that you need to get rid of the C. diff that›s there,” Dr. Drekonja, who was not involved in the study, said in an interview. “I think more people think it’s the diverse microbiota because if it’s just getting rid of C. diff, we can get do that with antibiotics – but that gets rid of the other organisms.”
As long as you have a diverse microbiota post FMT, Dr. Drekonja said, then “having a few residual organisms, even if they get magnified in the culture process, is probably not that big a deal.”
But there’s a third school of thought that Dr. Drekonja said he himself falls into: “I don’t really care how it works, just that in well-done trials, it does work.” As long as large, robust, well-blinded trials show that FMT works, “I’m open to all sorts of ideas of what the mechanism is,” he said. “The main thing is that it does or doesn’t work.”
These findings basically reinforce current guidance not to test patients’ stools if they are asymptomatic, Dr. Drekonja said. In the past, clinicians sometimes tested patients’ stool after therapy to ensure the C. difficile was eradicated, regardless of whether the patient had symptoms of infection, he said.
“We’ve since become much more attuned that there are lots of people who have detectable C. diff in their stool without any symptoms,” whether detectable by culture or PCR, Dr. Drekonja said. “Generally, if you’re doing well and you’re not having diarrhea, don’t test, and if someone does test and finds it, pretend you didn’t see the test,” he advised. “This is a big part of diagnostic stewardship, which is: You don’t go testing people who are doing well.”
The Netherlands Donor Feces Bank used in the research is funded by a grant from Vedanta Biosciences. Dr. Drekonja had no disclosures.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center: www.gastro.org/Cdiff.
A version of this article first appeared on Medscape.com.
It’s not necessary to completely eradicate all Clostridioides difficile to successfully treat recurrent C. difficile infections with fecal microbiota transplant (FMT), according to a study presented online July 12 at the European Congress of Clinical Microbiology & Infectious Diseases.
C. difficile colonization persisted for 3 weeks after FMT in about one-quarter of patients, but it’s not clear whether this is a persistent infection, a newly acquired infection, or partial persistence of a mixed infection, said Elisabeth Terveer, MD, a medical microbiologist at Leiden (the Netherlands) University Medical Center. In addition, “82% of patients with detectable C. diff do not relapse, so it’s absolutely not necessary for a cure,” she said.
Several mechanisms explain why FMT is a highly effective therapy for recurrent C. difficile infections, including restoration of bacterial metabolism in the gut, immune modulation, and direct competition between bacteria, Dr. Terveer said, but it’s less clear whether eradication of C. difficile spores is among these mechanisms.
Between May 2016 and April 2020, the researchers analyzed fecal samples from 84 patients who took vancomycin for at least 4 days before undergoing FMT. The researchers took fecal samples from patients before FMT and 3 weeks after FMT to culture them and the donor samples for presence of C. difficile, and they assessed clinical outcomes at 3 weeks and 6 months after FMT.
After antibiotic treatment but prior to FMT, 19% of patients (n = 16) still had a toxigenic C. difficile culture while the other 81% had a negative culture. None of the donor samples had a positive C. difficile culture. After FMT treatment, five patients who had a positive pre-FMT culture remained positive, and the other 11 were negative. Among the 81% of patients (n = 68) who had a negative culture just before FMT, 22 had a positive culture and 46 had a negative culture after FMT. Overall, 26% of patients post FMT had a positive C. difficile culture, a finding that was 10-fold higher than another study that assessed C. difficile with PCR testing, Dr. Terveer said.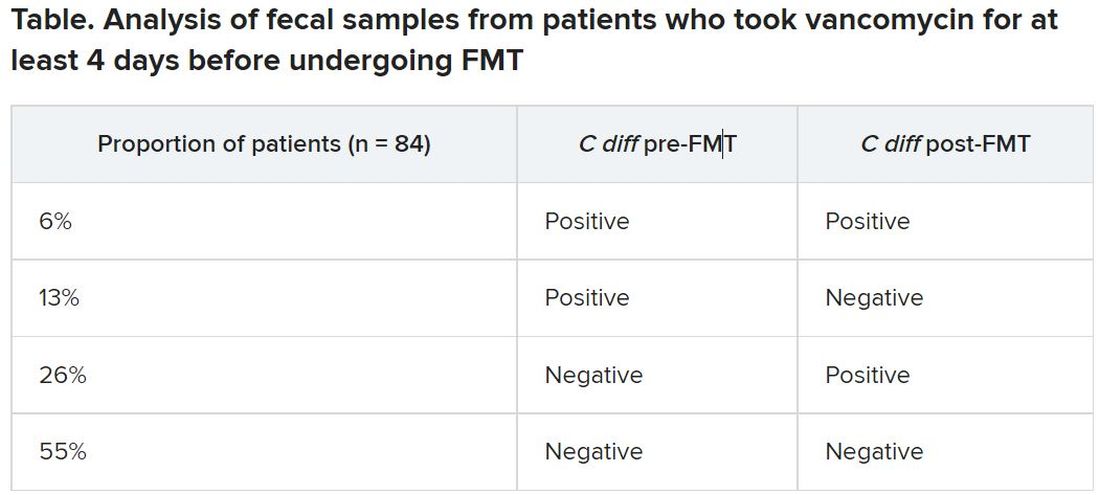
The clinical cure rate after FMT was 94%, and five patients had relapses within 2 months of their FMT. These relapses were more prevalent in patients with a positive C. difficile culture prior to FMT (odds ratio [OR], 7.6; P = .045) and a positive C. difficile culture after FMT (OR, 13.6; P = .016). Still, 82% of patients who had a positive C. difficile culture post FMT remained clinically cured 2 months later.
It’s unclear why 19% of patients had a positive culture after their antibiotic pretreatment prior to FMT, Dr. Terveer said, but it may be because the pretreatment was of such a short duration.
“I think the advice should be: Give a full anti–C. diff antibiotic course to treat the C. diff infection, and then give FMT afterward to restore the microbiota and prevent further relapses,” Dr. Terveer told attendees.
Dimitri Drekonja, MD, chief of the Minneapolis VA Infectious Disease Section, said the findings were not necessarily surprising, but it would have been interesting for the researchers to have conducted DNA sequencing of the patients’ fecal samples post FMT to see what the biological diversity looked like.
“One school of thought has been that you have to repopulate the normal diverse microbiota of the colon” with FMT, and the other “is that you need to get rid of the C. diff that›s there,” Dr. Drekonja, who was not involved in the study, said in an interview. “I think more people think it’s the diverse microbiota because if it’s just getting rid of C. diff, we can get do that with antibiotics – but that gets rid of the other organisms.”
As long as you have a diverse microbiota post FMT, Dr. Drekonja said, then “having a few residual organisms, even if they get magnified in the culture process, is probably not that big a deal.”
But there’s a third school of thought that Dr. Drekonja said he himself falls into: “I don’t really care how it works, just that in well-done trials, it does work.” As long as large, robust, well-blinded trials show that FMT works, “I’m open to all sorts of ideas of what the mechanism is,” he said. “The main thing is that it does or doesn’t work.”
These findings basically reinforce current guidance not to test patients’ stools if they are asymptomatic, Dr. Drekonja said. In the past, clinicians sometimes tested patients’ stool after therapy to ensure the C. difficile was eradicated, regardless of whether the patient had symptoms of infection, he said.
“We’ve since become much more attuned that there are lots of people who have detectable C. diff in their stool without any symptoms,” whether detectable by culture or PCR, Dr. Drekonja said. “Generally, if you’re doing well and you’re not having diarrhea, don’t test, and if someone does test and finds it, pretend you didn’t see the test,” he advised. “This is a big part of diagnostic stewardship, which is: You don’t go testing people who are doing well.”
The Netherlands Donor Feces Bank used in the research is funded by a grant from Vedanta Biosciences. Dr. Drekonja had no disclosures.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center: www.gastro.org/Cdiff.
A version of this article first appeared on Medscape.com.
It’s not necessary to completely eradicate all Clostridioides difficile to successfully treat recurrent C. difficile infections with fecal microbiota transplant (FMT), according to a study presented online July 12 at the European Congress of Clinical Microbiology & Infectious Diseases.
C. difficile colonization persisted for 3 weeks after FMT in about one-quarter of patients, but it’s not clear whether this is a persistent infection, a newly acquired infection, or partial persistence of a mixed infection, said Elisabeth Terveer, MD, a medical microbiologist at Leiden (the Netherlands) University Medical Center. In addition, “82% of patients with detectable C. diff do not relapse, so it’s absolutely not necessary for a cure,” she said.
Several mechanisms explain why FMT is a highly effective therapy for recurrent C. difficile infections, including restoration of bacterial metabolism in the gut, immune modulation, and direct competition between bacteria, Dr. Terveer said, but it’s less clear whether eradication of C. difficile spores is among these mechanisms.
Between May 2016 and April 2020, the researchers analyzed fecal samples from 84 patients who took vancomycin for at least 4 days before undergoing FMT. The researchers took fecal samples from patients before FMT and 3 weeks after FMT to culture them and the donor samples for presence of C. difficile, and they assessed clinical outcomes at 3 weeks and 6 months after FMT.
After antibiotic treatment but prior to FMT, 19% of patients (n = 16) still had a toxigenic C. difficile culture while the other 81% had a negative culture. None of the donor samples had a positive C. difficile culture. After FMT treatment, five patients who had a positive pre-FMT culture remained positive, and the other 11 were negative. Among the 81% of patients (n = 68) who had a negative culture just before FMT, 22 had a positive culture and 46 had a negative culture after FMT. Overall, 26% of patients post FMT had a positive C. difficile culture, a finding that was 10-fold higher than another study that assessed C. difficile with PCR testing, Dr. Terveer said.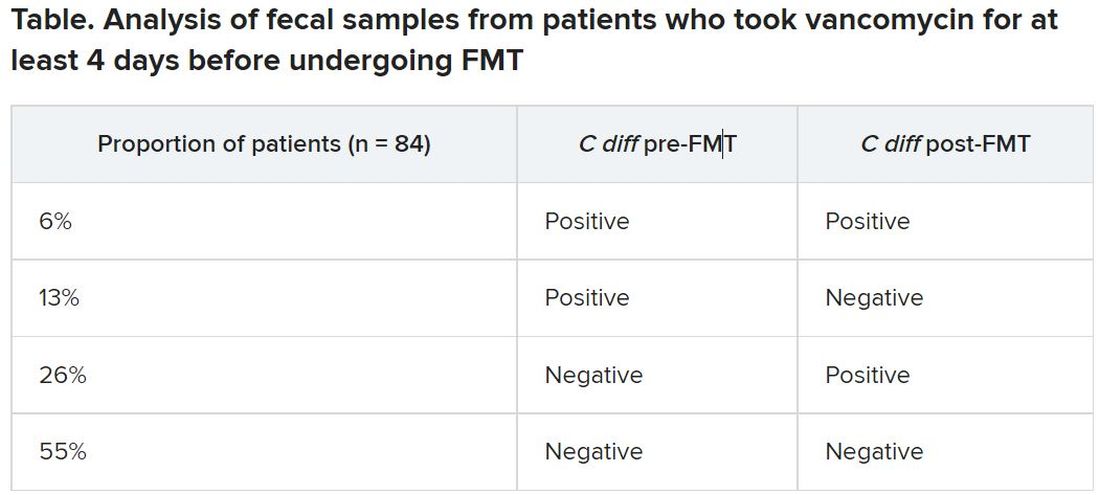
The clinical cure rate after FMT was 94%, and five patients had relapses within 2 months of their FMT. These relapses were more prevalent in patients with a positive C. difficile culture prior to FMT (odds ratio [OR], 7.6; P = .045) and a positive C. difficile culture after FMT (OR, 13.6; P = .016). Still, 82% of patients who had a positive C. difficile culture post FMT remained clinically cured 2 months later.
It’s unclear why 19% of patients had a positive culture after their antibiotic pretreatment prior to FMT, Dr. Terveer said, but it may be because the pretreatment was of such a short duration.
“I think the advice should be: Give a full anti–C. diff antibiotic course to treat the C. diff infection, and then give FMT afterward to restore the microbiota and prevent further relapses,” Dr. Terveer told attendees.
Dimitri Drekonja, MD, chief of the Minneapolis VA Infectious Disease Section, said the findings were not necessarily surprising, but it would have been interesting for the researchers to have conducted DNA sequencing of the patients’ fecal samples post FMT to see what the biological diversity looked like.
“One school of thought has been that you have to repopulate the normal diverse microbiota of the colon” with FMT, and the other “is that you need to get rid of the C. diff that›s there,” Dr. Drekonja, who was not involved in the study, said in an interview. “I think more people think it’s the diverse microbiota because if it’s just getting rid of C. diff, we can get do that with antibiotics – but that gets rid of the other organisms.”
As long as you have a diverse microbiota post FMT, Dr. Drekonja said, then “having a few residual organisms, even if they get magnified in the culture process, is probably not that big a deal.”
But there’s a third school of thought that Dr. Drekonja said he himself falls into: “I don’t really care how it works, just that in well-done trials, it does work.” As long as large, robust, well-blinded trials show that FMT works, “I’m open to all sorts of ideas of what the mechanism is,” he said. “The main thing is that it does or doesn’t work.”
These findings basically reinforce current guidance not to test patients’ stools if they are asymptomatic, Dr. Drekonja said. In the past, clinicians sometimes tested patients’ stool after therapy to ensure the C. difficile was eradicated, regardless of whether the patient had symptoms of infection, he said.
“We’ve since become much more attuned that there are lots of people who have detectable C. diff in their stool without any symptoms,” whether detectable by culture or PCR, Dr. Drekonja said. “Generally, if you’re doing well and you’re not having diarrhea, don’t test, and if someone does test and finds it, pretend you didn’t see the test,” he advised. “This is a big part of diagnostic stewardship, which is: You don’t go testing people who are doing well.”
The Netherlands Donor Feces Bank used in the research is funded by a grant from Vedanta Biosciences. Dr. Drekonja had no disclosures.
Help your patients understand their C. difficile diagnosis by sharing patient education from the AGA GI Patient Center: www.gastro.org/Cdiff.
A version of this article first appeared on Medscape.com.