User login
Early Diagnosis and Management of Tardive Dyskinesia
Tardive dyskinesia (TD) is a delayed movement disorder resulting from treatment with dopamine receptor–blocking medications, Dr Karen Anderson of Georgetown University School of Medicine explains. TD is most commonly associated with long-term use of antipsychotic drugs.
TD is characterized by involuntary, jerking movements of the tongue, lips, face, trunk, extremities, or the whole body. Although its characteristic movements are sometimes viewed as cosmetic, TD can interfere with patients’ quality of life and add to the stigma of mental illness.
The sooner TD is diagnosed, the more likely it is for patients to achieve remission spontaneously and without treatment. To that end, patients who are prescribed antipsychotic medication should be evaluated at baseline and regularly thereafter using the Abnormal Involuntary Movement Scale (AIMS), which rates abnormal movements.
The optimal first step in TD management is to stop the dopamine receptor–blocking medication, but this option may not be possible in patients with chronic conditions, such as manic depression and schizophrenia. In these patients, dose reduction or switching to a newer antipsychotic may provide relief.
Two vesicular monoamine transporter 2 (VMAT2) inhibitors are approved to treat TD and have been found to not worsen patients’ underlying psychiatric condition. Dr Anderson cautions that patients treated with a VMAT2 inhibitor will require monitoring because side effects of these agents include suicidal ideation.
--
Karen Anderson, MD, Professor, Department of Psychiatry and Neurology, Georgetown University School of Medicine; Washington, DC
Karen Anderson, MD, has disclosed the following relevant financial relationships:
Received income in an amount equal to or greater than $250 from: Neurocrine; Teva
Tardive dyskinesia (TD) is a delayed movement disorder resulting from treatment with dopamine receptor–blocking medications, Dr Karen Anderson of Georgetown University School of Medicine explains. TD is most commonly associated with long-term use of antipsychotic drugs.
TD is characterized by involuntary, jerking movements of the tongue, lips, face, trunk, extremities, or the whole body. Although its characteristic movements are sometimes viewed as cosmetic, TD can interfere with patients’ quality of life and add to the stigma of mental illness.
The sooner TD is diagnosed, the more likely it is for patients to achieve remission spontaneously and without treatment. To that end, patients who are prescribed antipsychotic medication should be evaluated at baseline and regularly thereafter using the Abnormal Involuntary Movement Scale (AIMS), which rates abnormal movements.
The optimal first step in TD management is to stop the dopamine receptor–blocking medication, but this option may not be possible in patients with chronic conditions, such as manic depression and schizophrenia. In these patients, dose reduction or switching to a newer antipsychotic may provide relief.
Two vesicular monoamine transporter 2 (VMAT2) inhibitors are approved to treat TD and have been found to not worsen patients’ underlying psychiatric condition. Dr Anderson cautions that patients treated with a VMAT2 inhibitor will require monitoring because side effects of these agents include suicidal ideation.
--
Karen Anderson, MD, Professor, Department of Psychiatry and Neurology, Georgetown University School of Medicine; Washington, DC
Karen Anderson, MD, has disclosed the following relevant financial relationships:
Received income in an amount equal to or greater than $250 from: Neurocrine; Teva
Tardive dyskinesia (TD) is a delayed movement disorder resulting from treatment with dopamine receptor–blocking medications, Dr Karen Anderson of Georgetown University School of Medicine explains. TD is most commonly associated with long-term use of antipsychotic drugs.
TD is characterized by involuntary, jerking movements of the tongue, lips, face, trunk, extremities, or the whole body. Although its characteristic movements are sometimes viewed as cosmetic, TD can interfere with patients’ quality of life and add to the stigma of mental illness.
The sooner TD is diagnosed, the more likely it is for patients to achieve remission spontaneously and without treatment. To that end, patients who are prescribed antipsychotic medication should be evaluated at baseline and regularly thereafter using the Abnormal Involuntary Movement Scale (AIMS), which rates abnormal movements.
The optimal first step in TD management is to stop the dopamine receptor–blocking medication, but this option may not be possible in patients with chronic conditions, such as manic depression and schizophrenia. In these patients, dose reduction or switching to a newer antipsychotic may provide relief.
Two vesicular monoamine transporter 2 (VMAT2) inhibitors are approved to treat TD and have been found to not worsen patients’ underlying psychiatric condition. Dr Anderson cautions that patients treated with a VMAT2 inhibitor will require monitoring because side effects of these agents include suicidal ideation.
--
Karen Anderson, MD, Professor, Department of Psychiatry and Neurology, Georgetown University School of Medicine; Washington, DC
Karen Anderson, MD, has disclosed the following relevant financial relationships:
Received income in an amount equal to or greater than $250 from: Neurocrine; Teva

PAH care turns corner with new therapies, intensified monitoring
Aggressive up-front combination therapy, more lofty treatment goals, and earlier and more frequent reassessments to guide treatment are improving care of patients with pulmonary arterial hypertension (PAH) while at the same time making it more complex.
A larger number of oral and generic treatment options have in some respects ushered in more management ease. But overall, “I don’t know if management of these patients has ever been more complicated, given the treatment options and strategies,” said Murali M. Chakinala, MD, professor of medicine at Washington University, St. Louis. “We’re always thinking through approaches.”
Diagnosis continues to be challenging given the rarity of PAH and its nonspecific presentation – and in some cases it’s now harder. Experts such as Dr. Chakinala are seeing increasing number of aging patients with left heart disease, chronic kidney disease, and other comorbidities who have significant precapillary pulmonary hypertension and who exhibit hemodynamics consistent with PAH, or group 1 PH.
The question experts face is, do such patients have “true PAH,” as do a reported 25-50 people per million, or do they have another type of PH in the classification schema – or a mixture?
Deciding which patients “really fit into group 1 and should be managed like group 1,” Dr. Chakinala said, requires clinical acumen and has important implications, as patients with PAH are the main beneficiaries of vasodilator therapy. Most other patients with PH will not respond to or tolerate such treatment.
“These older patients may be getting PAH through different mechanisms than our younger patients, but because we define PAH through hemodynamic criteria and by ruling out other obvious explanations, they all get lumped together,” said Dr. Chakinala. “We need to parse these patients out better in the future, much like our oncology colleagues are doing.”
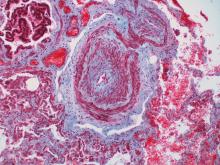
Personalized medicine hopefully is the next horizon for this condition, characterized by severe remodeling of the distal pulmonary arteries. Researchers are pushing to achieve deep phenotyping, identify biomarkers and improve risk assessment tools.
And with 80 or so centers now accredited by the Pulmonary Hypertension Association as Pulmonary Hypertension Care Centers, referred patients are accessing clinical trials of new nonvasodilatory drugs. Currently available therapies improve hemodynamics and symptoms, and can slow disease progression, but are not truly disease modifying, sources say.
“The endothelin, nitric oxide, and prostacyclin pathways have been exhaustively studied and we now have great drugs for those pathways,” said Dr. Chakinala, who leads the PHA’s scientific leadership council. But “we’re not going to put a greater dent into this disease until we have new drugs that work on different biologic pathways.”
Diagnostic challenges
The diagnosis of PAH – a remarkably heterogeneous condition that encompasses heritable forms and idiopathic forms, and that comprises a broad mix of predisposing conditions and exposures, from scleroderma to methamphetamine use – is still too often missed or delayed. Delayed diagnoses and misdiagnoses of PAH and other types of PH have been reported in up to 85% of at-risk patients, according to a 2016 literature review.
Being able to pivot from thinking about common pulmonary ailments or heart failure to considering PAH is a key part of earlier diagnosis and better treatment outcomes. “If someone has unexplained dyspnea or if they’re treated for other lung diseases and are not improving, think about a screening echocardiogram,” said Timothy L. Williamson, MD, vice president of quality and safety and a pulmonary and critical care physician at the University of Kansas Health Center, Kansas City.
One of the most common reasons Dr. Chakinala sees for missed diagnoses are right heart catheterizations that are incomplete or misinterpreted. (Right heart catheterizations are required to confirm the diagnosis.) “One can’t simply measure pressures and stop,” he said. “We need the full hemodynamic profile to know that it’s truly precapillary PAH ... and we need proper interpretation of [elements like] the waveforms.”
The 2019 World Symposium on Pulmonary Hypertension shifted the definition of PH from an arbitrarily defined mean pulmonary arterial pressure of at least 25 mm Hg at rest (as measured by right heart catheterization) to a more scientifically determined mPAP of at least 20 mm Hg.
The classification document also requires pulmonary vascular resistance (PVR) of at least 3 Wood units in the definition of all forms of precapillary PH. PAH specifically is defined as the presence of mPAP of at least 20 mm Hg, PVR of at least 3 Wood units, and pulmonary arterial wedge pressure 15 mm Hg or less.
Trends in treatment
The value of initial combination therapy with an endothelin receptor antagonist (ERA) and a phosphodiesterase-5 (PDE5) inhibitor in treatment-naive PAH was cemented in 2015 by the AMBITION trial. The primary endpoint (death, PAH hospitalization, or unsatisfactory clinical response) occurred in 18%, 34%, and 28% of patients who were randomized, respectively, to combination therapy, monotherapy with the ERA ambrisentan, or monotherapy with the PDE-5 inhibitor tadalafil – and in 31% of the two monotherapy groups combined.
The trial reported a 50% reduction in the primary endpoint in the combination-therapy group versus the pooled monotherapy group, as well as greater reductions in N-terminal of the prohormone brain natriuretic peptide levels, more satisfactory clinical response and greater improvement in 6-minute walking distance.
In practice, a minority of patients – typically older patients with multiple comorbidities – still receive initial monotherapy with sequential add-on therapies based on tolerance, but “for the most part PAH patients will start on combination therapy, most commonly with a ERA and PDE5 inhibitor,” Dr. Chakinala said.
For patients who are not improving on the ERA-PDE5 inhibitor approach – typically those who remain in the intermediate-risk category for intermediate-term mortality – substitution of the PDE5 inhibitor with the soluble guanylate cyclase stimulator riociguat may be considered, he and Dr. Williamson said. Clinical improvement with this substitution was demonstrated in the REPLACE trial.
Experts at PH care centers are also utilizing triple therapy for patients who do not improve to low-risk status after 2-4 months of dual combination therapy. The availability of oral prostacyclin analogues (selexipag and treprostinil) makes it easier to consider adding these agents early on, Dr. Chakinala and Dr. Richardson said.
Patients who fall into the high-risk category, at any point, are still best managed with parenteral prostacyclin analogues, Dr. Chakinala said.
In general, said Dr. Williamson, who also directs the University of Kansas Pulmonary Hypertension Comprehensive Care Center, “the PH community tends to be fairly aggressive up front, and with a low threshold for using prostacyclin analogues.”
The agents are “always part of the picture for someone who is really ill, in functional class IV, or has really impaired right ventricular function,” he said. “And we’re finding increased roles in patients who are not as ill but still have decompensated right ventricular dysfunction. It’s something we now consider.”
Recently published research on up-front oral triple therapy suggests possible benefit for some patients – but it’s far from conclusive, said Dr. Chakinala. The TRITON study randomized treatment-naive patients to the traditional ERA-PDE5 combination and either oral selexipag (a selective prostacyclin receptor agonist) or placebo as a third agent. It found no significant difference in reduction in PVR, the primary outcome, at week 26. However, the authors reported a “possible signal” for improved long-term outcomes with triple therapy.
“Based on this best evidence from a randomized clinical trial, I think it’s unfair to say that all patients should be on triple combination therapy right out of the gate,” he said. “Having said that, more recent [European] data showed that two drugs fell short of the mark in some patients, with high rates of clinical progression. And even in AMBITION, there were a number of patients in the combination arm who didn’t have a robust response.”
A 2021 retrospective analysis from the French Pulmonary Hypertension Registry – one of the European studies – assessed survival with monotherapy, dual therapy, or triple-combination therapy (two orals with a parenteral prostacyclin), and found no difference between monotherapy and dual therapy in high-risk patients.
Experts have been upping the ante, therefore, on early assessment and frequent reassessment of treatment response. Not long ago, patients were typically reassessed 6-12 months after the initiation of treatment. Now, experts at the PH care centers want to assess patients at 3-4 months and adjust or intensify treatment regimens for those who don’t yet qualify as low risk using a multidimensional risk score calculator.
The REVEAL (Registry to Evaluate Early and Long-Term PAH Management) risk score calculator, for instance, predicts the probability of 1-year survival and assigns patients to a strata of risk level based on either 12 or 6 variables (for the full or “lite” versions).]
Even better monitoring and risk assessment is needed, however, to “help sift out which patients are not improving enough on initial therapy or who are starting to fall off after being on a regimen for a period of time,” Dr. Chakinala said.
Today, with a network of accredited centers of expertise and a desire and need for many patients to remain close to home, Dr. Chakinala encourages finding a balance. Well-resourced clinicians can strive for early diagnosis and management – potentially initiating ERA–PDE-5 inhibitor combination therapy – but still should collaborate with PH experts.
“It’s a good idea to comanage these patients and let the experts see them periodically to help you determine when your patient may be declining,” he said. “The timetable for reassessment, the complexity of the reassessment, and the need to escalate to more advanced therapies has never been more important.”
Research highlights
Therapies that target inflammation and altered metabolism – including metformin – are among those being investigated for PAH. So are therapies targeting dysfunctional bone morphogenetic protein pathway signaling, which has been shown to be associated with hereditary, idiopathic, and likely other forms of PAH; one such drug, called sotatercept, is currently at the phase 3 trial stage.
Most promising for PAH may be the research efforts involving deep phenotyping, said Andrew J. Sweatt, MD, of Stanford (Calif.) University and the Vera Moulton Wall Center for Pulmonary Vascular Disease.
“It’s where a lot of research is headed – deep phenotyping to deconstruct the molecular and clinical heterogeneity that exists within PAH ... to detect distinct subphenotypes of patients who would respond to particular therapies,” said Dr. Sweatt, who led a review of PH clinical research presented at the 2020 American Thoracic Society International Conference
“Right now, we largely treat all patients the same ... [while] we know that patients have a wide response to therapies and there’s a lot of clinical heterogeneity in how their disease evolves over time,” he said.
Data from a large National Institutes of Health–funded multicenter phenotyping study of PH is being analyzed and should yield findings and publications starting this year, said Anna R. Hemnes, MD, associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., and an investigator with the initiative, coined “Redefining Pulmonary Hypertension through Pulmonary Disease Phenomics (PVDOMICS).”
Patients have undergone advanced imaging (for example, echocardiography, cardiac MRI, chest CT, ventilation/perfusion scans), advanced testing through right heart catheterization, body composition testing, quality of life questionnaires, and blood draws that have been analyzed for DNA and RNA expression, proteomics, and metabolomics, said Dr. Hemnes, assistant director of Vanderbilt’s Pulmonary Vascular Center.
The initiative aims to refine the classification of all kinds of PH and “to bring precision medicine to the field so we’re no longer characterizing somebody [based on imaging] and right heart catheterization, but we also incorporating molecular pieces and biomarkers into the diagnostic evaluation,” she said.
In the short term, the results of deep phenotyping should “allow us to be more effective with our therapy recommendations,” Dr. Hemnes said. “Then hopefully in the longer term, [identified biomarkers] will help us to develop new, more effective therapies.”
Dr. Sweatt and Dr. Williamson reported that they have no relevant financial disclosures. Dr. Hemnes reported that she holds stock in Tenax (which is studying a tyrosine kinase inhibitor for PAH) and serves as a consultant for Acceleron, Bayer, GossamerBio, United Therapeutics, and Janssen. She also receives research funding from Imara. Dr. Chakinala reported that he is an investigator on clinical trials for a number of pharmaceutical companies. He also serves on advisory boards for Phase Bio, Liquidia/Rare Gen, Bayer, Janssen, Trio Health Analytics, and Aerovate.
Aggressive up-front combination therapy, more lofty treatment goals, and earlier and more frequent reassessments to guide treatment are improving care of patients with pulmonary arterial hypertension (PAH) while at the same time making it more complex.
A larger number of oral and generic treatment options have in some respects ushered in more management ease. But overall, “I don’t know if management of these patients has ever been more complicated, given the treatment options and strategies,” said Murali M. Chakinala, MD, professor of medicine at Washington University, St. Louis. “We’re always thinking through approaches.”
Diagnosis continues to be challenging given the rarity of PAH and its nonspecific presentation – and in some cases it’s now harder. Experts such as Dr. Chakinala are seeing increasing number of aging patients with left heart disease, chronic kidney disease, and other comorbidities who have significant precapillary pulmonary hypertension and who exhibit hemodynamics consistent with PAH, or group 1 PH.
The question experts face is, do such patients have “true PAH,” as do a reported 25-50 people per million, or do they have another type of PH in the classification schema – or a mixture?
Deciding which patients “really fit into group 1 and should be managed like group 1,” Dr. Chakinala said, requires clinical acumen and has important implications, as patients with PAH are the main beneficiaries of vasodilator therapy. Most other patients with PH will not respond to or tolerate such treatment.
“These older patients may be getting PAH through different mechanisms than our younger patients, but because we define PAH through hemodynamic criteria and by ruling out other obvious explanations, they all get lumped together,” said Dr. Chakinala. “We need to parse these patients out better in the future, much like our oncology colleagues are doing.”
Personalized medicine hopefully is the next horizon for this condition, characterized by severe remodeling of the distal pulmonary arteries. Researchers are pushing to achieve deep phenotyping, identify biomarkers and improve risk assessment tools.
And with 80 or so centers now accredited by the Pulmonary Hypertension Association as Pulmonary Hypertension Care Centers, referred patients are accessing clinical trials of new nonvasodilatory drugs. Currently available therapies improve hemodynamics and symptoms, and can slow disease progression, but are not truly disease modifying, sources say.
“The endothelin, nitric oxide, and prostacyclin pathways have been exhaustively studied and we now have great drugs for those pathways,” said Dr. Chakinala, who leads the PHA’s scientific leadership council. But “we’re not going to put a greater dent into this disease until we have new drugs that work on different biologic pathways.”
Diagnostic challenges
The diagnosis of PAH – a remarkably heterogeneous condition that encompasses heritable forms and idiopathic forms, and that comprises a broad mix of predisposing conditions and exposures, from scleroderma to methamphetamine use – is still too often missed or delayed. Delayed diagnoses and misdiagnoses of PAH and other types of PH have been reported in up to 85% of at-risk patients, according to a 2016 literature review.
Being able to pivot from thinking about common pulmonary ailments or heart failure to considering PAH is a key part of earlier diagnosis and better treatment outcomes. “If someone has unexplained dyspnea or if they’re treated for other lung diseases and are not improving, think about a screening echocardiogram,” said Timothy L. Williamson, MD, vice president of quality and safety and a pulmonary and critical care physician at the University of Kansas Health Center, Kansas City.
One of the most common reasons Dr. Chakinala sees for missed diagnoses are right heart catheterizations that are incomplete or misinterpreted. (Right heart catheterizations are required to confirm the diagnosis.) “One can’t simply measure pressures and stop,” he said. “We need the full hemodynamic profile to know that it’s truly precapillary PAH ... and we need proper interpretation of [elements like] the waveforms.”
The 2019 World Symposium on Pulmonary Hypertension shifted the definition of PH from an arbitrarily defined mean pulmonary arterial pressure of at least 25 mm Hg at rest (as measured by right heart catheterization) to a more scientifically determined mPAP of at least 20 mm Hg.
The classification document also requires pulmonary vascular resistance (PVR) of at least 3 Wood units in the definition of all forms of precapillary PH. PAH specifically is defined as the presence of mPAP of at least 20 mm Hg, PVR of at least 3 Wood units, and pulmonary arterial wedge pressure 15 mm Hg or less.
Trends in treatment
The value of initial combination therapy with an endothelin receptor antagonist (ERA) and a phosphodiesterase-5 (PDE5) inhibitor in treatment-naive PAH was cemented in 2015 by the AMBITION trial. The primary endpoint (death, PAH hospitalization, or unsatisfactory clinical response) occurred in 18%, 34%, and 28% of patients who were randomized, respectively, to combination therapy, monotherapy with the ERA ambrisentan, or monotherapy with the PDE-5 inhibitor tadalafil – and in 31% of the two monotherapy groups combined.
The trial reported a 50% reduction in the primary endpoint in the combination-therapy group versus the pooled monotherapy group, as well as greater reductions in N-terminal of the prohormone brain natriuretic peptide levels, more satisfactory clinical response and greater improvement in 6-minute walking distance.
In practice, a minority of patients – typically older patients with multiple comorbidities – still receive initial monotherapy with sequential add-on therapies based on tolerance, but “for the most part PAH patients will start on combination therapy, most commonly with a ERA and PDE5 inhibitor,” Dr. Chakinala said.
For patients who are not improving on the ERA-PDE5 inhibitor approach – typically those who remain in the intermediate-risk category for intermediate-term mortality – substitution of the PDE5 inhibitor with the soluble guanylate cyclase stimulator riociguat may be considered, he and Dr. Williamson said. Clinical improvement with this substitution was demonstrated in the REPLACE trial.
Experts at PH care centers are also utilizing triple therapy for patients who do not improve to low-risk status after 2-4 months of dual combination therapy. The availability of oral prostacyclin analogues (selexipag and treprostinil) makes it easier to consider adding these agents early on, Dr. Chakinala and Dr. Richardson said.
Patients who fall into the high-risk category, at any point, are still best managed with parenteral prostacyclin analogues, Dr. Chakinala said.
In general, said Dr. Williamson, who also directs the University of Kansas Pulmonary Hypertension Comprehensive Care Center, “the PH community tends to be fairly aggressive up front, and with a low threshold for using prostacyclin analogues.”
The agents are “always part of the picture for someone who is really ill, in functional class IV, or has really impaired right ventricular function,” he said. “And we’re finding increased roles in patients who are not as ill but still have decompensated right ventricular dysfunction. It’s something we now consider.”
Recently published research on up-front oral triple therapy suggests possible benefit for some patients – but it’s far from conclusive, said Dr. Chakinala. The TRITON study randomized treatment-naive patients to the traditional ERA-PDE5 combination and either oral selexipag (a selective prostacyclin receptor agonist) or placebo as a third agent. It found no significant difference in reduction in PVR, the primary outcome, at week 26. However, the authors reported a “possible signal” for improved long-term outcomes with triple therapy.
“Based on this best evidence from a randomized clinical trial, I think it’s unfair to say that all patients should be on triple combination therapy right out of the gate,” he said. “Having said that, more recent [European] data showed that two drugs fell short of the mark in some patients, with high rates of clinical progression. And even in AMBITION, there were a number of patients in the combination arm who didn’t have a robust response.”
A 2021 retrospective analysis from the French Pulmonary Hypertension Registry – one of the European studies – assessed survival with monotherapy, dual therapy, or triple-combination therapy (two orals with a parenteral prostacyclin), and found no difference between monotherapy and dual therapy in high-risk patients.
Experts have been upping the ante, therefore, on early assessment and frequent reassessment of treatment response. Not long ago, patients were typically reassessed 6-12 months after the initiation of treatment. Now, experts at the PH care centers want to assess patients at 3-4 months and adjust or intensify treatment regimens for those who don’t yet qualify as low risk using a multidimensional risk score calculator.
The REVEAL (Registry to Evaluate Early and Long-Term PAH Management) risk score calculator, for instance, predicts the probability of 1-year survival and assigns patients to a strata of risk level based on either 12 or 6 variables (for the full or “lite” versions).]
Even better monitoring and risk assessment is needed, however, to “help sift out which patients are not improving enough on initial therapy or who are starting to fall off after being on a regimen for a period of time,” Dr. Chakinala said.
Today, with a network of accredited centers of expertise and a desire and need for many patients to remain close to home, Dr. Chakinala encourages finding a balance. Well-resourced clinicians can strive for early diagnosis and management – potentially initiating ERA–PDE-5 inhibitor combination therapy – but still should collaborate with PH experts.
“It’s a good idea to comanage these patients and let the experts see them periodically to help you determine when your patient may be declining,” he said. “The timetable for reassessment, the complexity of the reassessment, and the need to escalate to more advanced therapies has never been more important.”
Research highlights
Therapies that target inflammation and altered metabolism – including metformin – are among those being investigated for PAH. So are therapies targeting dysfunctional bone morphogenetic protein pathway signaling, which has been shown to be associated with hereditary, idiopathic, and likely other forms of PAH; one such drug, called sotatercept, is currently at the phase 3 trial stage.
Most promising for PAH may be the research efforts involving deep phenotyping, said Andrew J. Sweatt, MD, of Stanford (Calif.) University and the Vera Moulton Wall Center for Pulmonary Vascular Disease.
“It’s where a lot of research is headed – deep phenotyping to deconstruct the molecular and clinical heterogeneity that exists within PAH ... to detect distinct subphenotypes of patients who would respond to particular therapies,” said Dr. Sweatt, who led a review of PH clinical research presented at the 2020 American Thoracic Society International Conference
“Right now, we largely treat all patients the same ... [while] we know that patients have a wide response to therapies and there’s a lot of clinical heterogeneity in how their disease evolves over time,” he said.
Data from a large National Institutes of Health–funded multicenter phenotyping study of PH is being analyzed and should yield findings and publications starting this year, said Anna R. Hemnes, MD, associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., and an investigator with the initiative, coined “Redefining Pulmonary Hypertension through Pulmonary Disease Phenomics (PVDOMICS).”
Patients have undergone advanced imaging (for example, echocardiography, cardiac MRI, chest CT, ventilation/perfusion scans), advanced testing through right heart catheterization, body composition testing, quality of life questionnaires, and blood draws that have been analyzed for DNA and RNA expression, proteomics, and metabolomics, said Dr. Hemnes, assistant director of Vanderbilt’s Pulmonary Vascular Center.
The initiative aims to refine the classification of all kinds of PH and “to bring precision medicine to the field so we’re no longer characterizing somebody [based on imaging] and right heart catheterization, but we also incorporating molecular pieces and biomarkers into the diagnostic evaluation,” she said.
In the short term, the results of deep phenotyping should “allow us to be more effective with our therapy recommendations,” Dr. Hemnes said. “Then hopefully in the longer term, [identified biomarkers] will help us to develop new, more effective therapies.”
Dr. Sweatt and Dr. Williamson reported that they have no relevant financial disclosures. Dr. Hemnes reported that she holds stock in Tenax (which is studying a tyrosine kinase inhibitor for PAH) and serves as a consultant for Acceleron, Bayer, GossamerBio, United Therapeutics, and Janssen. She also receives research funding from Imara. Dr. Chakinala reported that he is an investigator on clinical trials for a number of pharmaceutical companies. He also serves on advisory boards for Phase Bio, Liquidia/Rare Gen, Bayer, Janssen, Trio Health Analytics, and Aerovate.
Aggressive up-front combination therapy, more lofty treatment goals, and earlier and more frequent reassessments to guide treatment are improving care of patients with pulmonary arterial hypertension (PAH) while at the same time making it more complex.
A larger number of oral and generic treatment options have in some respects ushered in more management ease. But overall, “I don’t know if management of these patients has ever been more complicated, given the treatment options and strategies,” said Murali M. Chakinala, MD, professor of medicine at Washington University, St. Louis. “We’re always thinking through approaches.”
Diagnosis continues to be challenging given the rarity of PAH and its nonspecific presentation – and in some cases it’s now harder. Experts such as Dr. Chakinala are seeing increasing number of aging patients with left heart disease, chronic kidney disease, and other comorbidities who have significant precapillary pulmonary hypertension and who exhibit hemodynamics consistent with PAH, or group 1 PH.
The question experts face is, do such patients have “true PAH,” as do a reported 25-50 people per million, or do they have another type of PH in the classification schema – or a mixture?
Deciding which patients “really fit into group 1 and should be managed like group 1,” Dr. Chakinala said, requires clinical acumen and has important implications, as patients with PAH are the main beneficiaries of vasodilator therapy. Most other patients with PH will not respond to or tolerate such treatment.
“These older patients may be getting PAH through different mechanisms than our younger patients, but because we define PAH through hemodynamic criteria and by ruling out other obvious explanations, they all get lumped together,” said Dr. Chakinala. “We need to parse these patients out better in the future, much like our oncology colleagues are doing.”
Personalized medicine hopefully is the next horizon for this condition, characterized by severe remodeling of the distal pulmonary arteries. Researchers are pushing to achieve deep phenotyping, identify biomarkers and improve risk assessment tools.
And with 80 or so centers now accredited by the Pulmonary Hypertension Association as Pulmonary Hypertension Care Centers, referred patients are accessing clinical trials of new nonvasodilatory drugs. Currently available therapies improve hemodynamics and symptoms, and can slow disease progression, but are not truly disease modifying, sources say.
“The endothelin, nitric oxide, and prostacyclin pathways have been exhaustively studied and we now have great drugs for those pathways,” said Dr. Chakinala, who leads the PHA’s scientific leadership council. But “we’re not going to put a greater dent into this disease until we have new drugs that work on different biologic pathways.”
Diagnostic challenges
The diagnosis of PAH – a remarkably heterogeneous condition that encompasses heritable forms and idiopathic forms, and that comprises a broad mix of predisposing conditions and exposures, from scleroderma to methamphetamine use – is still too often missed or delayed. Delayed diagnoses and misdiagnoses of PAH and other types of PH have been reported in up to 85% of at-risk patients, according to a 2016 literature review.
Being able to pivot from thinking about common pulmonary ailments or heart failure to considering PAH is a key part of earlier diagnosis and better treatment outcomes. “If someone has unexplained dyspnea or if they’re treated for other lung diseases and are not improving, think about a screening echocardiogram,” said Timothy L. Williamson, MD, vice president of quality and safety and a pulmonary and critical care physician at the University of Kansas Health Center, Kansas City.
One of the most common reasons Dr. Chakinala sees for missed diagnoses are right heart catheterizations that are incomplete or misinterpreted. (Right heart catheterizations are required to confirm the diagnosis.) “One can’t simply measure pressures and stop,” he said. “We need the full hemodynamic profile to know that it’s truly precapillary PAH ... and we need proper interpretation of [elements like] the waveforms.”
The 2019 World Symposium on Pulmonary Hypertension shifted the definition of PH from an arbitrarily defined mean pulmonary arterial pressure of at least 25 mm Hg at rest (as measured by right heart catheterization) to a more scientifically determined mPAP of at least 20 mm Hg.
The classification document also requires pulmonary vascular resistance (PVR) of at least 3 Wood units in the definition of all forms of precapillary PH. PAH specifically is defined as the presence of mPAP of at least 20 mm Hg, PVR of at least 3 Wood units, and pulmonary arterial wedge pressure 15 mm Hg or less.
Trends in treatment
The value of initial combination therapy with an endothelin receptor antagonist (ERA) and a phosphodiesterase-5 (PDE5) inhibitor in treatment-naive PAH was cemented in 2015 by the AMBITION trial. The primary endpoint (death, PAH hospitalization, or unsatisfactory clinical response) occurred in 18%, 34%, and 28% of patients who were randomized, respectively, to combination therapy, monotherapy with the ERA ambrisentan, or monotherapy with the PDE-5 inhibitor tadalafil – and in 31% of the two monotherapy groups combined.
The trial reported a 50% reduction in the primary endpoint in the combination-therapy group versus the pooled monotherapy group, as well as greater reductions in N-terminal of the prohormone brain natriuretic peptide levels, more satisfactory clinical response and greater improvement in 6-minute walking distance.
In practice, a minority of patients – typically older patients with multiple comorbidities – still receive initial monotherapy with sequential add-on therapies based on tolerance, but “for the most part PAH patients will start on combination therapy, most commonly with a ERA and PDE5 inhibitor,” Dr. Chakinala said.
For patients who are not improving on the ERA-PDE5 inhibitor approach – typically those who remain in the intermediate-risk category for intermediate-term mortality – substitution of the PDE5 inhibitor with the soluble guanylate cyclase stimulator riociguat may be considered, he and Dr. Williamson said. Clinical improvement with this substitution was demonstrated in the REPLACE trial.
Experts at PH care centers are also utilizing triple therapy for patients who do not improve to low-risk status after 2-4 months of dual combination therapy. The availability of oral prostacyclin analogues (selexipag and treprostinil) makes it easier to consider adding these agents early on, Dr. Chakinala and Dr. Richardson said.
Patients who fall into the high-risk category, at any point, are still best managed with parenteral prostacyclin analogues, Dr. Chakinala said.
In general, said Dr. Williamson, who also directs the University of Kansas Pulmonary Hypertension Comprehensive Care Center, “the PH community tends to be fairly aggressive up front, and with a low threshold for using prostacyclin analogues.”
The agents are “always part of the picture for someone who is really ill, in functional class IV, or has really impaired right ventricular function,” he said. “And we’re finding increased roles in patients who are not as ill but still have decompensated right ventricular dysfunction. It’s something we now consider.”
Recently published research on up-front oral triple therapy suggests possible benefit for some patients – but it’s far from conclusive, said Dr. Chakinala. The TRITON study randomized treatment-naive patients to the traditional ERA-PDE5 combination and either oral selexipag (a selective prostacyclin receptor agonist) or placebo as a third agent. It found no significant difference in reduction in PVR, the primary outcome, at week 26. However, the authors reported a “possible signal” for improved long-term outcomes with triple therapy.
“Based on this best evidence from a randomized clinical trial, I think it’s unfair to say that all patients should be on triple combination therapy right out of the gate,” he said. “Having said that, more recent [European] data showed that two drugs fell short of the mark in some patients, with high rates of clinical progression. And even in AMBITION, there were a number of patients in the combination arm who didn’t have a robust response.”
A 2021 retrospective analysis from the French Pulmonary Hypertension Registry – one of the European studies – assessed survival with monotherapy, dual therapy, or triple-combination therapy (two orals with a parenteral prostacyclin), and found no difference between monotherapy and dual therapy in high-risk patients.
Experts have been upping the ante, therefore, on early assessment and frequent reassessment of treatment response. Not long ago, patients were typically reassessed 6-12 months after the initiation of treatment. Now, experts at the PH care centers want to assess patients at 3-4 months and adjust or intensify treatment regimens for those who don’t yet qualify as low risk using a multidimensional risk score calculator.
The REVEAL (Registry to Evaluate Early and Long-Term PAH Management) risk score calculator, for instance, predicts the probability of 1-year survival and assigns patients to a strata of risk level based on either 12 or 6 variables (for the full or “lite” versions).]
Even better monitoring and risk assessment is needed, however, to “help sift out which patients are not improving enough on initial therapy or who are starting to fall off after being on a regimen for a period of time,” Dr. Chakinala said.
Today, with a network of accredited centers of expertise and a desire and need for many patients to remain close to home, Dr. Chakinala encourages finding a balance. Well-resourced clinicians can strive for early diagnosis and management – potentially initiating ERA–PDE-5 inhibitor combination therapy – but still should collaborate with PH experts.
“It’s a good idea to comanage these patients and let the experts see them periodically to help you determine when your patient may be declining,” he said. “The timetable for reassessment, the complexity of the reassessment, and the need to escalate to more advanced therapies has never been more important.”
Research highlights
Therapies that target inflammation and altered metabolism – including metformin – are among those being investigated for PAH. So are therapies targeting dysfunctional bone morphogenetic protein pathway signaling, which has been shown to be associated with hereditary, idiopathic, and likely other forms of PAH; one such drug, called sotatercept, is currently at the phase 3 trial stage.
Most promising for PAH may be the research efforts involving deep phenotyping, said Andrew J. Sweatt, MD, of Stanford (Calif.) University and the Vera Moulton Wall Center for Pulmonary Vascular Disease.
“It’s where a lot of research is headed – deep phenotyping to deconstruct the molecular and clinical heterogeneity that exists within PAH ... to detect distinct subphenotypes of patients who would respond to particular therapies,” said Dr. Sweatt, who led a review of PH clinical research presented at the 2020 American Thoracic Society International Conference
“Right now, we largely treat all patients the same ... [while] we know that patients have a wide response to therapies and there’s a lot of clinical heterogeneity in how their disease evolves over time,” he said.
Data from a large National Institutes of Health–funded multicenter phenotyping study of PH is being analyzed and should yield findings and publications starting this year, said Anna R. Hemnes, MD, associate professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., and an investigator with the initiative, coined “Redefining Pulmonary Hypertension through Pulmonary Disease Phenomics (PVDOMICS).”
Patients have undergone advanced imaging (for example, echocardiography, cardiac MRI, chest CT, ventilation/perfusion scans), advanced testing through right heart catheterization, body composition testing, quality of life questionnaires, and blood draws that have been analyzed for DNA and RNA expression, proteomics, and metabolomics, said Dr. Hemnes, assistant director of Vanderbilt’s Pulmonary Vascular Center.
The initiative aims to refine the classification of all kinds of PH and “to bring precision medicine to the field so we’re no longer characterizing somebody [based on imaging] and right heart catheterization, but we also incorporating molecular pieces and biomarkers into the diagnostic evaluation,” she said.
In the short term, the results of deep phenotyping should “allow us to be more effective with our therapy recommendations,” Dr. Hemnes said. “Then hopefully in the longer term, [identified biomarkers] will help us to develop new, more effective therapies.”
Dr. Sweatt and Dr. Williamson reported that they have no relevant financial disclosures. Dr. Hemnes reported that she holds stock in Tenax (which is studying a tyrosine kinase inhibitor for PAH) and serves as a consultant for Acceleron, Bayer, GossamerBio, United Therapeutics, and Janssen. She also receives research funding from Imara. Dr. Chakinala reported that he is an investigator on clinical trials for a number of pharmaceutical companies. He also serves on advisory boards for Phase Bio, Liquidia/Rare Gen, Bayer, Janssen, Trio Health Analytics, and Aerovate.
Multifactorial Effects of Endometriosis as a Chronic Systemic Disease
Can you talk about your research thus far and what your overall lab work has shown regarding endometriosis as a chronic systemic disease?
Dr. Flores: Endometriosis has traditionally been characterized by its pelvic manifestation however, it is important to understand that it is profoundly more than a pelvic disease—it is a chronic, systemic disease with multifactorial effects throughout the body.
We and other groups have found increased expression of several inflammatory cytokines in women with endometriosis. Our lab has found that compared to women without endometriosis, women with endometriosis not only have certain inflammatory cytokines elevated but also have altered expression of microRNAs. MicroRNAs are small noncoding RNAs that bind to and modulate translation of mRNA. To help determine whether these miRNAs were involved in mediating increased expression of inflammatory cytokines in women with endometriosis, we then transfected these miRNAs into a macrophage cell line, and again found altered inflammatory cytokine expression. We and others have also found a role for stem cells (from bone marrow and other sources) in the pathogenesis of endometriosis. In addition, we have found that in endometriosis, women have a low body-mass index and altered metabolism, which is related to induction of induction of hepatic (anorexigenic) gene expression and microRNA-mediated changes in adipocyte (metabolic) gene expression. Furthermore, we have found altered gene expression in regions of the brain associated with anxiety and depression and altered pain sensitization. Taken together, this work helps provide support for the systemic nature of endometriosis.
How can your findings in this space help us in diagnosing clinically and ultimately avoid diagnostic delay?
Dr. Flores: It’s about understanding that endometriosis is not just a pelvic disease and understanding that endometriosis is leading to inflammation and altered expression of miRNAs which allows endometriosis to have long-range effects. For example, women with endometriosis commonly have anxiety and depression and low BMI. As mentioned earlier, we have found that in a murine model of endometriosis, there is altered gene expression in regions of the brain associated with anxiety and depression and altered metabolism in a murine model of endometriosis. Other groups have also found changes in brain volume in these same areas in women with endometriosis, and we have seen low BMI in women with endometriosis. In fact, a common misconception was that being thin was a risk factor for endometriosis, however we have found that the endometriosis itself, is causing women alteration in genes associated with metabolism.
With respect to the endometrium, in addition to being a pelvic pain disorder, we also see that women with endometriosis have a higher likelihood of having infertility. And we think that's in part because one, just like the lesions can be resistant to progesterone, the endometrium of these women can also be resistant to progesterone. Progesterone is necessary for decidualization/implantation. We have also seen that stem cells can be recruited and ultimately incorrectly incorporated into the endometrium, which may also contribute to infertility in women with endometriosis.
If we can understand this multifactorial nature of endometriosis, I think this will help us not only shift toward diagnosing endometriosis clinically, but also avoid diagnostic delay. If we can understand that endometriosis is not just a pelvic disorder, but that It can also involve altered mood, bowel/bladder symptoms, inflammation, altered metabolism and/or cause infertility, I think that will ultimately help us to diagnosing earlier.
In addition, we can also utilize pelvic pain symptomatology to help with diagnosis as well. We can ask about cyclic pelvic pain that's been getting progressively worse over the years, not responding to non-steroidal anti-inflammatory medications. Also, in understanding that endometriosis can affect other organs, asking about cyclic pain/symptoms in other areas, such as cyclical bowel or bladder symptoms.
Thinking about the fact that if you do have a patient like that, you're seeing that they have altered mood symptoms, or alterations in inflammatory markers. Maybe that will help us shift from a disease that was typically only considered to be diagnosed by surgery, by switching to a clinical diagnosis for endometriosis. Doing that will hopefully help avoid diagnostic delay.
If we understand that while we typically describe endometriosis as causing cyclic pain symptoms, sometimes because of the existing diagnostic delay, ultimately women can present with chronic pelvic pain. Thus, it's also important to ask patients presenting with chronic pelvic pain what the symptoms were like beforehand (i.e., was the pain cyclic and progressively worsening over the years/before it became chronic) doing so will also help in terms of diagnosing sooner.
Lastly, circulating miRNAs have been considered promising biomarker candidates because they are stable in circulation and have highly specific expression profiles. We have found that the combination of several miRNAs reliably distinguished endometriosis patients from controls, and a prospective, blinded study showed that the combination of several miRNAs could be used to accurately identify patients with endometriosis, with an area under the receiver operating characteristic curve of 0.93.
Roughly 11%, or more than 6.5 million, women in the United States between the ages of 15–44 years, may have endometriosis. Is this disease more common in any particular age range or ethnicity?
Dr. Flores: We’re actually actively investigating that right now. And I think what makes it challenging, especially with respect to the age range, is now we're -- I think in part because of so much more awareness and more research is being done looking at this disease as a chronic systemic disease-- we're now starting to see/diagnose adolescents with endometriosis.
I think as we start gathering more information about these individuals, we'll be able to better say if there is a particular age range. Right now, we usually say it's in the reproductive years, however for some women it may be later if they were not diagnosed earlier. Conversely, some who are hopefully reading this, and also who conduct research on endometriosis, may be able to diagnose someone earlier that may have been missed until they were in their 30s or 40s, for example.
With respect to ethnicity, I'm the task force leader for diversity, equity, and inclusion in research and recruitment. This is something that I'm actively starting to work on, as are other groups. I don't have the answer for that yet, but as we continue to collect more data, we will have more information on this.
What are some of the existing hormonal therapies you rely upon as well as the biomarkers in predicting response to treatment, and are there any new research or treatments on the horizon?
Dr. Flores: I'll first start by telling you a bit about our existing treatment regimens, and then how I decide who would benefit from a given one. First line has always been progestin-based therapy, either in the form of a combined oral contraceptive pill or as progesterone only pills. However, up to 1/3 of women fail progestin-based therapy—this is termed progesterone resistance.
When progestin-based therapies fail, we then rely on other agents that are focused more on estrogen deprivation because, while we don't know the complete etiology of endometriosis, we do know that it is estrogen-dependent. There are two classes— gonadotropin releasing hormone (GnRH) agonists and GnRH antagonists. The agonist binds to the GnRH receptors, and initially can cause a flare effect due to its agonist properties, initially stimulate release of estradiol, and ultimately the GnRH receptor becomes downregulated and estradiol is decreased to the menopausal range. As a result we routinely provided add-back therapy with norethindrone to help prevent hot flashes and ensure bone protection.
Within the past three years, there has been a new oral GnRH receptor antagonist approved for treating endometriosis. The medication is available as a once a day or twice a day dosing regimen. As this is a GnRH antagonist, upon binding to the GnRH receptor, it blocks receptor activity, thus avoiding the flare affect; essentially, within 24 hours, there is a decrease in estradiol production.
As two doses are available, you can tailor how much you dial down estrogen for a given patient. The low dose lowers estradiol to a range of 40 picograms while the high (twice a day) dosing lowers your estrogen to about 6 picograms. Also, although it was not studied originally in terms of giving add-back therapy for the higher dose, given the safety (and effectiveness) of add-back therapy with GnRH agonists we are using the same norethindrone add-back therapy for women who are taking the GnRH receptor antagonist.
The next question is, how do we decide which medication a given patient receives? To answer that, I will tell you a bit about my precision-based medicine research. As mentioned before, while progestin-based therapy is first-line, failure rates are high, and unfortunately, we previously have not been able to identify who will or will not respond to first-line therapy. As such, I decided to assess progesterone receptor expression in endometriotic lesions from women who had undergone surgery for endometriosis, and determine whether progesterone receptor expression levels in lesions could be used to predict response to progestin-based therapy. I found that in women that had high levels of the progesterone receptor, they responded completely to progestin-based therapy-- there was a 100% response rate to progestin-based therapy. This is in sharp contrast to women who had low PR expression, where there was only a 6% response rate to progestin-based therapy.
While this is great with respect to being able to predict who will or will not respond to first line therapy, the one limitation is that would mean that women have to undergo surgery in order to determine progesterone receptor status/response to progestin-based therapy. However, given that within two to five years following surgery, up to 50% of women will have recurrence of pain symptoms, where I see my test coming into play is postoperatively. This is because many times , women who had pain, or who were failing a given agent, are placed back on that same medical therapy they were failing after surgery. Usually that was a progestin. Therefore, instead of putting them on that same therapy that they were failing, we can use my test to place them on an alternative therapy (such as a GnRH analogue) that more specifically targets estradiol production.
In terms of future directions with respect to treatment, there is a microRNA that has been found to be low in women with endometriosis—miRNALet-7b. In a murine model of endometriosis, we have found that if we supplement with Let-7, there is decreased inflammation and decreased lesion size of endometriosis. We have also found that supplementing miRNA Let-7b in human endometriotic lesions results in decreased inflammation in cell culture.
That would be future directions in terms of focusing on microRNAs and seeing how we can manipulate those to essentially block inflammation and lesion growth. Furthermore, such treatment would be non-hormonal, which would be a novel therapeutic approach.
As-Sanie S, Harris RE, Napadow V, et al. Changes in regional gray matter volume in women with chronic pelvic pain: a voxel-based morphometry study. Pain. 2012;153(5):1006-1014.
Ballard K, Lowton K, Wright J. What's the delay? A qualitative study of women's experiences of reaching a diagnosis of endometriosis. Fertil Steril. 2006;86(5):1296-1301
Cosar E, Mamillapalli R, Ersoy GS, Cho S, Seifer B, Taylor HS. Serum microRNAs as diagnostic markers of endometriosis: a comprehensive array-based analysis. Fertil Steril. 2016;106(2):402-409.
Flores VA, Vanhie A, Dang T, Taylor HS. Progesterone Receptor Status Predicts Response to Progestin Therapy in Endometriosis. J Clin Endocrinol Metab. 2018 Dec 1;103(12):4561-4568
Goetz TG, Mamillapalli R, Taylor HS. Low Body Mass Index in Endometriosis Is Promoted by Hepatic Metabolic Gene Dysregulation in Mice. Biol Reprod. 2016;95(6):115.
Li T, et al. Endometriosis alters brain electrophysiology, gene expression and increases pain sensitization, anxiety, and depression in female mice. Biol Reprod. 2018;99(2):349-359.
Moustafa S, Burn M, Mamillapalli R, Nematian S, Flores V, Taylor HS. Accurate diagnosis of endometriosis using serum microRNAs. Am J Obstet Gynecol. 2020;223(4):557.e1-557.e11.
Nematian SE, et al. Systemic Inflammation Induced by microRNAs: Endometriosis-Derived Alterations in Circulating microRNA 125b-5p and Let-7b-5p Regulate Macrophage Cytokine Production. J Clin Endocrinol Metab. 2018;103(1):64-74.
Nnoaham KE, Hummelshoj L, Webster P, et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2011;96(2):366-373.e8.
Rogers PA, D'Hooghe TM, Fazleabas A, et al. Defining future directions for endometriosis research: workshop report from the 2011 World Congress of Endometriosis In Montpellier, France. Reprod Sci. 2013;20(5):483-499.
Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations. Lancet. 2021 Feb 27
Zolbin MM, et al. Adipocyte alterations in endometriosis: reduced numbers of stem cells and microRNA induced alterations in adipocyte metabolic gene expression. Reprod Biol Endocrinol. 2019;17(1):36.
Can you talk about your research thus far and what your overall lab work has shown regarding endometriosis as a chronic systemic disease?
Dr. Flores: Endometriosis has traditionally been characterized by its pelvic manifestation however, it is important to understand that it is profoundly more than a pelvic disease—it is a chronic, systemic disease with multifactorial effects throughout the body.
We and other groups have found increased expression of several inflammatory cytokines in women with endometriosis. Our lab has found that compared to women without endometriosis, women with endometriosis not only have certain inflammatory cytokines elevated but also have altered expression of microRNAs. MicroRNAs are small noncoding RNAs that bind to and modulate translation of mRNA. To help determine whether these miRNAs were involved in mediating increased expression of inflammatory cytokines in women with endometriosis, we then transfected these miRNAs into a macrophage cell line, and again found altered inflammatory cytokine expression. We and others have also found a role for stem cells (from bone marrow and other sources) in the pathogenesis of endometriosis. In addition, we have found that in endometriosis, women have a low body-mass index and altered metabolism, which is related to induction of induction of hepatic (anorexigenic) gene expression and microRNA-mediated changes in adipocyte (metabolic) gene expression. Furthermore, we have found altered gene expression in regions of the brain associated with anxiety and depression and altered pain sensitization. Taken together, this work helps provide support for the systemic nature of endometriosis.
How can your findings in this space help us in diagnosing clinically and ultimately avoid diagnostic delay?
Dr. Flores: It’s about understanding that endometriosis is not just a pelvic disease and understanding that endometriosis is leading to inflammation and altered expression of miRNAs which allows endometriosis to have long-range effects. For example, women with endometriosis commonly have anxiety and depression and low BMI. As mentioned earlier, we have found that in a murine model of endometriosis, there is altered gene expression in regions of the brain associated with anxiety and depression and altered metabolism in a murine model of endometriosis. Other groups have also found changes in brain volume in these same areas in women with endometriosis, and we have seen low BMI in women with endometriosis. In fact, a common misconception was that being thin was a risk factor for endometriosis, however we have found that the endometriosis itself, is causing women alteration in genes associated with metabolism.
With respect to the endometrium, in addition to being a pelvic pain disorder, we also see that women with endometriosis have a higher likelihood of having infertility. And we think that's in part because one, just like the lesions can be resistant to progesterone, the endometrium of these women can also be resistant to progesterone. Progesterone is necessary for decidualization/implantation. We have also seen that stem cells can be recruited and ultimately incorrectly incorporated into the endometrium, which may also contribute to infertility in women with endometriosis.
If we can understand this multifactorial nature of endometriosis, I think this will help us not only shift toward diagnosing endometriosis clinically, but also avoid diagnostic delay. If we can understand that endometriosis is not just a pelvic disorder, but that It can also involve altered mood, bowel/bladder symptoms, inflammation, altered metabolism and/or cause infertility, I think that will ultimately help us to diagnosing earlier.
In addition, we can also utilize pelvic pain symptomatology to help with diagnosis as well. We can ask about cyclic pelvic pain that's been getting progressively worse over the years, not responding to non-steroidal anti-inflammatory medications. Also, in understanding that endometriosis can affect other organs, asking about cyclic pain/symptoms in other areas, such as cyclical bowel or bladder symptoms.
Thinking about the fact that if you do have a patient like that, you're seeing that they have altered mood symptoms, or alterations in inflammatory markers. Maybe that will help us shift from a disease that was typically only considered to be diagnosed by surgery, by switching to a clinical diagnosis for endometriosis. Doing that will hopefully help avoid diagnostic delay.
If we understand that while we typically describe endometriosis as causing cyclic pain symptoms, sometimes because of the existing diagnostic delay, ultimately women can present with chronic pelvic pain. Thus, it's also important to ask patients presenting with chronic pelvic pain what the symptoms were like beforehand (i.e., was the pain cyclic and progressively worsening over the years/before it became chronic) doing so will also help in terms of diagnosing sooner.
Lastly, circulating miRNAs have been considered promising biomarker candidates because they are stable in circulation and have highly specific expression profiles. We have found that the combination of several miRNAs reliably distinguished endometriosis patients from controls, and a prospective, blinded study showed that the combination of several miRNAs could be used to accurately identify patients with endometriosis, with an area under the receiver operating characteristic curve of 0.93.
Roughly 11%, or more than 6.5 million, women in the United States between the ages of 15–44 years, may have endometriosis. Is this disease more common in any particular age range or ethnicity?
Dr. Flores: We’re actually actively investigating that right now. And I think what makes it challenging, especially with respect to the age range, is now we're -- I think in part because of so much more awareness and more research is being done looking at this disease as a chronic systemic disease-- we're now starting to see/diagnose adolescents with endometriosis.
I think as we start gathering more information about these individuals, we'll be able to better say if there is a particular age range. Right now, we usually say it's in the reproductive years, however for some women it may be later if they were not diagnosed earlier. Conversely, some who are hopefully reading this, and also who conduct research on endometriosis, may be able to diagnose someone earlier that may have been missed until they were in their 30s or 40s, for example.
With respect to ethnicity, I'm the task force leader for diversity, equity, and inclusion in research and recruitment. This is something that I'm actively starting to work on, as are other groups. I don't have the answer for that yet, but as we continue to collect more data, we will have more information on this.
What are some of the existing hormonal therapies you rely upon as well as the biomarkers in predicting response to treatment, and are there any new research or treatments on the horizon?
Dr. Flores: I'll first start by telling you a bit about our existing treatment regimens, and then how I decide who would benefit from a given one. First line has always been progestin-based therapy, either in the form of a combined oral contraceptive pill or as progesterone only pills. However, up to 1/3 of women fail progestin-based therapy—this is termed progesterone resistance.
When progestin-based therapies fail, we then rely on other agents that are focused more on estrogen deprivation because, while we don't know the complete etiology of endometriosis, we do know that it is estrogen-dependent. There are two classes— gonadotropin releasing hormone (GnRH) agonists and GnRH antagonists. The agonist binds to the GnRH receptors, and initially can cause a flare effect due to its agonist properties, initially stimulate release of estradiol, and ultimately the GnRH receptor becomes downregulated and estradiol is decreased to the menopausal range. As a result we routinely provided add-back therapy with norethindrone to help prevent hot flashes and ensure bone protection.
Within the past three years, there has been a new oral GnRH receptor antagonist approved for treating endometriosis. The medication is available as a once a day or twice a day dosing regimen. As this is a GnRH antagonist, upon binding to the GnRH receptor, it blocks receptor activity, thus avoiding the flare affect; essentially, within 24 hours, there is a decrease in estradiol production.
As two doses are available, you can tailor how much you dial down estrogen for a given patient. The low dose lowers estradiol to a range of 40 picograms while the high (twice a day) dosing lowers your estrogen to about 6 picograms. Also, although it was not studied originally in terms of giving add-back therapy for the higher dose, given the safety (and effectiveness) of add-back therapy with GnRH agonists we are using the same norethindrone add-back therapy for women who are taking the GnRH receptor antagonist.
The next question is, how do we decide which medication a given patient receives? To answer that, I will tell you a bit about my precision-based medicine research. As mentioned before, while progestin-based therapy is first-line, failure rates are high, and unfortunately, we previously have not been able to identify who will or will not respond to first-line therapy. As such, I decided to assess progesterone receptor expression in endometriotic lesions from women who had undergone surgery for endometriosis, and determine whether progesterone receptor expression levels in lesions could be used to predict response to progestin-based therapy. I found that in women that had high levels of the progesterone receptor, they responded completely to progestin-based therapy-- there was a 100% response rate to progestin-based therapy. This is in sharp contrast to women who had low PR expression, where there was only a 6% response rate to progestin-based therapy.
While this is great with respect to being able to predict who will or will not respond to first line therapy, the one limitation is that would mean that women have to undergo surgery in order to determine progesterone receptor status/response to progestin-based therapy. However, given that within two to five years following surgery, up to 50% of women will have recurrence of pain symptoms, where I see my test coming into play is postoperatively. This is because many times , women who had pain, or who were failing a given agent, are placed back on that same medical therapy they were failing after surgery. Usually that was a progestin. Therefore, instead of putting them on that same therapy that they were failing, we can use my test to place them on an alternative therapy (such as a GnRH analogue) that more specifically targets estradiol production.
In terms of future directions with respect to treatment, there is a microRNA that has been found to be low in women with endometriosis—miRNALet-7b. In a murine model of endometriosis, we have found that if we supplement with Let-7, there is decreased inflammation and decreased lesion size of endometriosis. We have also found that supplementing miRNA Let-7b in human endometriotic lesions results in decreased inflammation in cell culture.
That would be future directions in terms of focusing on microRNAs and seeing how we can manipulate those to essentially block inflammation and lesion growth. Furthermore, such treatment would be non-hormonal, which would be a novel therapeutic approach.
Can you talk about your research thus far and what your overall lab work has shown regarding endometriosis as a chronic systemic disease?
Dr. Flores: Endometriosis has traditionally been characterized by its pelvic manifestation however, it is important to understand that it is profoundly more than a pelvic disease—it is a chronic, systemic disease with multifactorial effects throughout the body.
We and other groups have found increased expression of several inflammatory cytokines in women with endometriosis. Our lab has found that compared to women without endometriosis, women with endometriosis not only have certain inflammatory cytokines elevated but also have altered expression of microRNAs. MicroRNAs are small noncoding RNAs that bind to and modulate translation of mRNA. To help determine whether these miRNAs were involved in mediating increased expression of inflammatory cytokines in women with endometriosis, we then transfected these miRNAs into a macrophage cell line, and again found altered inflammatory cytokine expression. We and others have also found a role for stem cells (from bone marrow and other sources) in the pathogenesis of endometriosis. In addition, we have found that in endometriosis, women have a low body-mass index and altered metabolism, which is related to induction of induction of hepatic (anorexigenic) gene expression and microRNA-mediated changes in adipocyte (metabolic) gene expression. Furthermore, we have found altered gene expression in regions of the brain associated with anxiety and depression and altered pain sensitization. Taken together, this work helps provide support for the systemic nature of endometriosis.
How can your findings in this space help us in diagnosing clinically and ultimately avoid diagnostic delay?
Dr. Flores: It’s about understanding that endometriosis is not just a pelvic disease and understanding that endometriosis is leading to inflammation and altered expression of miRNAs which allows endometriosis to have long-range effects. For example, women with endometriosis commonly have anxiety and depression and low BMI. As mentioned earlier, we have found that in a murine model of endometriosis, there is altered gene expression in regions of the brain associated with anxiety and depression and altered metabolism in a murine model of endometriosis. Other groups have also found changes in brain volume in these same areas in women with endometriosis, and we have seen low BMI in women with endometriosis. In fact, a common misconception was that being thin was a risk factor for endometriosis, however we have found that the endometriosis itself, is causing women alteration in genes associated with metabolism.
With respect to the endometrium, in addition to being a pelvic pain disorder, we also see that women with endometriosis have a higher likelihood of having infertility. And we think that's in part because one, just like the lesions can be resistant to progesterone, the endometrium of these women can also be resistant to progesterone. Progesterone is necessary for decidualization/implantation. We have also seen that stem cells can be recruited and ultimately incorrectly incorporated into the endometrium, which may also contribute to infertility in women with endometriosis.
If we can understand this multifactorial nature of endometriosis, I think this will help us not only shift toward diagnosing endometriosis clinically, but also avoid diagnostic delay. If we can understand that endometriosis is not just a pelvic disorder, but that It can also involve altered mood, bowel/bladder symptoms, inflammation, altered metabolism and/or cause infertility, I think that will ultimately help us to diagnosing earlier.
In addition, we can also utilize pelvic pain symptomatology to help with diagnosis as well. We can ask about cyclic pelvic pain that's been getting progressively worse over the years, not responding to non-steroidal anti-inflammatory medications. Also, in understanding that endometriosis can affect other organs, asking about cyclic pain/symptoms in other areas, such as cyclical bowel or bladder symptoms.
Thinking about the fact that if you do have a patient like that, you're seeing that they have altered mood symptoms, or alterations in inflammatory markers. Maybe that will help us shift from a disease that was typically only considered to be diagnosed by surgery, by switching to a clinical diagnosis for endometriosis. Doing that will hopefully help avoid diagnostic delay.
If we understand that while we typically describe endometriosis as causing cyclic pain symptoms, sometimes because of the existing diagnostic delay, ultimately women can present with chronic pelvic pain. Thus, it's also important to ask patients presenting with chronic pelvic pain what the symptoms were like beforehand (i.e., was the pain cyclic and progressively worsening over the years/before it became chronic) doing so will also help in terms of diagnosing sooner.
Lastly, circulating miRNAs have been considered promising biomarker candidates because they are stable in circulation and have highly specific expression profiles. We have found that the combination of several miRNAs reliably distinguished endometriosis patients from controls, and a prospective, blinded study showed that the combination of several miRNAs could be used to accurately identify patients with endometriosis, with an area under the receiver operating characteristic curve of 0.93.
Roughly 11%, or more than 6.5 million, women in the United States between the ages of 15–44 years, may have endometriosis. Is this disease more common in any particular age range or ethnicity?
Dr. Flores: We’re actually actively investigating that right now. And I think what makes it challenging, especially with respect to the age range, is now we're -- I think in part because of so much more awareness and more research is being done looking at this disease as a chronic systemic disease-- we're now starting to see/diagnose adolescents with endometriosis.
I think as we start gathering more information about these individuals, we'll be able to better say if there is a particular age range. Right now, we usually say it's in the reproductive years, however for some women it may be later if they were not diagnosed earlier. Conversely, some who are hopefully reading this, and also who conduct research on endometriosis, may be able to diagnose someone earlier that may have been missed until they were in their 30s or 40s, for example.
With respect to ethnicity, I'm the task force leader for diversity, equity, and inclusion in research and recruitment. This is something that I'm actively starting to work on, as are other groups. I don't have the answer for that yet, but as we continue to collect more data, we will have more information on this.
What are some of the existing hormonal therapies you rely upon as well as the biomarkers in predicting response to treatment, and are there any new research or treatments on the horizon?
Dr. Flores: I'll first start by telling you a bit about our existing treatment regimens, and then how I decide who would benefit from a given one. First line has always been progestin-based therapy, either in the form of a combined oral contraceptive pill or as progesterone only pills. However, up to 1/3 of women fail progestin-based therapy—this is termed progesterone resistance.
When progestin-based therapies fail, we then rely on other agents that are focused more on estrogen deprivation because, while we don't know the complete etiology of endometriosis, we do know that it is estrogen-dependent. There are two classes— gonadotropin releasing hormone (GnRH) agonists and GnRH antagonists. The agonist binds to the GnRH receptors, and initially can cause a flare effect due to its agonist properties, initially stimulate release of estradiol, and ultimately the GnRH receptor becomes downregulated and estradiol is decreased to the menopausal range. As a result we routinely provided add-back therapy with norethindrone to help prevent hot flashes and ensure bone protection.
Within the past three years, there has been a new oral GnRH receptor antagonist approved for treating endometriosis. The medication is available as a once a day or twice a day dosing regimen. As this is a GnRH antagonist, upon binding to the GnRH receptor, it blocks receptor activity, thus avoiding the flare affect; essentially, within 24 hours, there is a decrease in estradiol production.
As two doses are available, you can tailor how much you dial down estrogen for a given patient. The low dose lowers estradiol to a range of 40 picograms while the high (twice a day) dosing lowers your estrogen to about 6 picograms. Also, although it was not studied originally in terms of giving add-back therapy for the higher dose, given the safety (and effectiveness) of add-back therapy with GnRH agonists we are using the same norethindrone add-back therapy for women who are taking the GnRH receptor antagonist.
The next question is, how do we decide which medication a given patient receives? To answer that, I will tell you a bit about my precision-based medicine research. As mentioned before, while progestin-based therapy is first-line, failure rates are high, and unfortunately, we previously have not been able to identify who will or will not respond to first-line therapy. As such, I decided to assess progesterone receptor expression in endometriotic lesions from women who had undergone surgery for endometriosis, and determine whether progesterone receptor expression levels in lesions could be used to predict response to progestin-based therapy. I found that in women that had high levels of the progesterone receptor, they responded completely to progestin-based therapy-- there was a 100% response rate to progestin-based therapy. This is in sharp contrast to women who had low PR expression, where there was only a 6% response rate to progestin-based therapy.
While this is great with respect to being able to predict who will or will not respond to first line therapy, the one limitation is that would mean that women have to undergo surgery in order to determine progesterone receptor status/response to progestin-based therapy. However, given that within two to five years following surgery, up to 50% of women will have recurrence of pain symptoms, where I see my test coming into play is postoperatively. This is because many times , women who had pain, or who were failing a given agent, are placed back on that same medical therapy they were failing after surgery. Usually that was a progestin. Therefore, instead of putting them on that same therapy that they were failing, we can use my test to place them on an alternative therapy (such as a GnRH analogue) that more specifically targets estradiol production.
In terms of future directions with respect to treatment, there is a microRNA that has been found to be low in women with endometriosis—miRNALet-7b. In a murine model of endometriosis, we have found that if we supplement with Let-7, there is decreased inflammation and decreased lesion size of endometriosis. We have also found that supplementing miRNA Let-7b in human endometriotic lesions results in decreased inflammation in cell culture.
That would be future directions in terms of focusing on microRNAs and seeing how we can manipulate those to essentially block inflammation and lesion growth. Furthermore, such treatment would be non-hormonal, which would be a novel therapeutic approach.
As-Sanie S, Harris RE, Napadow V, et al. Changes in regional gray matter volume in women with chronic pelvic pain: a voxel-based morphometry study. Pain. 2012;153(5):1006-1014.
Ballard K, Lowton K, Wright J. What's the delay? A qualitative study of women's experiences of reaching a diagnosis of endometriosis. Fertil Steril. 2006;86(5):1296-1301
Cosar E, Mamillapalli R, Ersoy GS, Cho S, Seifer B, Taylor HS. Serum microRNAs as diagnostic markers of endometriosis: a comprehensive array-based analysis. Fertil Steril. 2016;106(2):402-409.
Flores VA, Vanhie A, Dang T, Taylor HS. Progesterone Receptor Status Predicts Response to Progestin Therapy in Endometriosis. J Clin Endocrinol Metab. 2018 Dec 1;103(12):4561-4568
Goetz TG, Mamillapalli R, Taylor HS. Low Body Mass Index in Endometriosis Is Promoted by Hepatic Metabolic Gene Dysregulation in Mice. Biol Reprod. 2016;95(6):115.
Li T, et al. Endometriosis alters brain electrophysiology, gene expression and increases pain sensitization, anxiety, and depression in female mice. Biol Reprod. 2018;99(2):349-359.
Moustafa S, Burn M, Mamillapalli R, Nematian S, Flores V, Taylor HS. Accurate diagnosis of endometriosis using serum microRNAs. Am J Obstet Gynecol. 2020;223(4):557.e1-557.e11.
Nematian SE, et al. Systemic Inflammation Induced by microRNAs: Endometriosis-Derived Alterations in Circulating microRNA 125b-5p and Let-7b-5p Regulate Macrophage Cytokine Production. J Clin Endocrinol Metab. 2018;103(1):64-74.
Nnoaham KE, Hummelshoj L, Webster P, et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2011;96(2):366-373.e8.
Rogers PA, D'Hooghe TM, Fazleabas A, et al. Defining future directions for endometriosis research: workshop report from the 2011 World Congress of Endometriosis In Montpellier, France. Reprod Sci. 2013;20(5):483-499.
Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations. Lancet. 2021 Feb 27
Zolbin MM, et al. Adipocyte alterations in endometriosis: reduced numbers of stem cells and microRNA induced alterations in adipocyte metabolic gene expression. Reprod Biol Endocrinol. 2019;17(1):36.
As-Sanie S, Harris RE, Napadow V, et al. Changes in regional gray matter volume in women with chronic pelvic pain: a voxel-based morphometry study. Pain. 2012;153(5):1006-1014.
Ballard K, Lowton K, Wright J. What's the delay? A qualitative study of women's experiences of reaching a diagnosis of endometriosis. Fertil Steril. 2006;86(5):1296-1301
Cosar E, Mamillapalli R, Ersoy GS, Cho S, Seifer B, Taylor HS. Serum microRNAs as diagnostic markers of endometriosis: a comprehensive array-based analysis. Fertil Steril. 2016;106(2):402-409.
Flores VA, Vanhie A, Dang T, Taylor HS. Progesterone Receptor Status Predicts Response to Progestin Therapy in Endometriosis. J Clin Endocrinol Metab. 2018 Dec 1;103(12):4561-4568
Goetz TG, Mamillapalli R, Taylor HS. Low Body Mass Index in Endometriosis Is Promoted by Hepatic Metabolic Gene Dysregulation in Mice. Biol Reprod. 2016;95(6):115.
Li T, et al. Endometriosis alters brain electrophysiology, gene expression and increases pain sensitization, anxiety, and depression in female mice. Biol Reprod. 2018;99(2):349-359.
Moustafa S, Burn M, Mamillapalli R, Nematian S, Flores V, Taylor HS. Accurate diagnosis of endometriosis using serum microRNAs. Am J Obstet Gynecol. 2020;223(4):557.e1-557.e11.
Nematian SE, et al. Systemic Inflammation Induced by microRNAs: Endometriosis-Derived Alterations in Circulating microRNA 125b-5p and Let-7b-5p Regulate Macrophage Cytokine Production. J Clin Endocrinol Metab. 2018;103(1):64-74.
Nnoaham KE, Hummelshoj L, Webster P, et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2011;96(2):366-373.e8.
Rogers PA, D'Hooghe TM, Fazleabas A, et al. Defining future directions for endometriosis research: workshop report from the 2011 World Congress of Endometriosis In Montpellier, France. Reprod Sci. 2013;20(5):483-499.
Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations. Lancet. 2021 Feb 27
Zolbin MM, et al. Adipocyte alterations in endometriosis: reduced numbers of stem cells and microRNA induced alterations in adipocyte metabolic gene expression. Reprod Biol Endocrinol. 2019;17(1):36.
Absolute increase in Kawasaki CV risk remains small in long-term follow-up
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
Vasculitis of the coronary arteries is a well-recognized acute complication of Kawasaki disease, but the long-term risk of cardiovascular (CV) sequelae does not appear to be clinically meaningful for most patients, according to results from an analysis of data presented at the annual meeting of the Canadian Rheumatology Association.
For patients and parents, these data provide “a message of reassurance,” according to Jennifer J.Y. Lee, MD, a pediatric rheumatologist affiliated with the Hospital for Sick Children, Toronto.
The long-term outcomes were characterized as reassuring even though rates of hypertension, major adverse cardiac events (MACE), and death from CV events were higher in patients with Kawasaki disease relative to controls in a retrospective data-linkage study. In fact, these differences were highly statistically significant, but the absolute differences were extremely small.
For this analysis, the 1,174 patients diagnosed with Kawasaki disease at Dr. Lee’s institution between 1991 and 2008 were compared in a 10:1 ratio to 11,740 controls matched for factors such as age, sex, ethnicity, and geographic region. The median follow-up period was 20 years, and the maximum was 28 years.
Adjusted CV risks are significant
In an adjusted Cox proportional hazard ratio model, patients in the Kawasaki group had a more than twofold increase in risk for hypertension (aHR, 2.3; P < .0001) and all-cause mortality (aHR, 2.5; P = .009). They also had more than a 10-fold increase in risk for MACE (aHR, 10.3; P < .0001).
These statistics belie the clinical relevance, according to Dr. Lee. Because of the very low rates of all the measured events in both groups, there was just one more case of hypertension per 1,250 patient-years of follow-up, one more case of MACE per 833 patient-years of follow-up, and one more death for 3,846 patient years of follow-up.
Moreover, when these outcomes were graphed over time, most events occurred during the acute period or in the initial years of follow-up.
“There was not a constant increase in risk of these outcomes over time for patients with Kawasaki disease relative to the controls,” Dr. Lee reported. “The long-term prognosis for Kawasaki patients remains favorable.”
European group reports similar results
Similar results from a single-center experience were published 3 years ago. In that study, 207 Kawasaki patients treated at the University of Lausanne (Switzerland) were followed for 30 years. Complications after the acute phase were characterized as “rare.”
For example, only three patients (1.4%) had a subsequent episode of myocardial ischemia. All three had developed a coronary aneurysm during the acute phase of Kawasaki disease. The authors of that study reported that children who had not received immunoglobulins during the acute phase or who developed Kawasaki disease outside of the usual age range were more likely to have subsequent events, such as disease recurrence.
Other studies of long-term CV outcomes in patients with Kawasaki disease generally show similar data, according to James T. Gaensbauer, MD, a pediatric infectious disease specialist at the Mayo Clinic, Rochester, Minn.
“I generally agree with the premise that major complications are rare when you compare a cohort of patients with Kawasaki disease with the general population,” Dr. Gaensbauer said. However, he added, “I do not think you can say no one needs to worry.”
Severity of acute disease might matter
During the acute phase of Kawasaki disease, the arterial damage varies. As suggested in the University of Lausanne follow-up, patients with significant coronary aneurysms do appear to be at greater risk of long-term complications. Dr. Gaensbauer cited a statement from the American Heart Association that noted a higher risk of CV sequelae from Kawasaki disease with a greater or more severe coronary aneurysm or in the face of other evidence of damage to the arterial tree.
“The clinical course within the first 2 years of Kawasaki disease appears to be important for risk of CV complications after this time,” Dr. Gaensbauer said.
The absolute risk of CV events in patients with a more complicated acute course of Kawasaki disease remains incompletely understood, but Dr. Gaensbauer said that there are several sets of data, including these new data from the Hospital for Sick Children, that suggest that the overall prognosis is good. However, he cautioned that this reassurance does not necessarily apply to children with a difficult acute course.
According to the 2017 AHA statement on Kawasaki disease, risk stratification based on echocardiography and other measures after the acute phase of Kawasaki disease are reasonable to determine if long-term follow-up is needed. In those without abnormalities, it is reasonable to forgo further cardiology assessment.
Dr. Lee and Dr. Gaensbauer reported having no potential conflicts of interest.
FROM THE ANNUAL MEETING OF THE CANADIAN RHEUMATOLOGY ASSOCIATION
Q&A: Long COVID symptoms, management, and where we’re headed
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Long COVID continues to be a moving target – continuously evolving and still surprising doctors and patients who have sometimes incapacitating long-term symptoms.
Little about the disorder seems predictable at this point. People can have long COVID after asymptomatic, mild, or severe COVID-19, for example. And when a person gets long COVID – also known as long-haul COVID – symptoms can vary widely.
To address all the uncertainty, the New York State Department of Health gathered experts in primary care, pediatrics, physical medicine, rehabilitation, and pulmonology to answer some pressing questions.
New York in 2020 was the first epicenter of the pandemic in the United States, making it also the center of the long COVID epidemic, says Emily Lutterloh, MD, director of the Division of Epidemiology at the New York State Department of Health.
What do you do when you’re seeing a patient with long COVID for the first time?
The first exam varies because there are so many different ways long COVID presents itself, says Benjamin Abramoff, MD, a physical medicine and rehabilitation specialist at Penn Medicine in Philadelphia.
I’ve now been seriously ill with #LongCovid for 11 months. I was never hospitalized. I didn’t even have a “mild” covid case. Instead, I developed Long Covid from an asymptomatic infection.
I’m far from unique. Up to 1/5 of asymptomatic patients go on to have long-term symptoms.
— Ravi Veriah Jacques (@RaviHVJ) February 3, 2022
Assessing their previous and current care also helps to direct their ongoing management, says Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai Health System in New York.
Can vaccination help people with long COVID?
Anything that we can do to help prevent people from being critically ill or being hospitalized with COVID-19 is helpful to prevent long COVID, says Dr. Abramoff, who is also director of the long COVID clinic at the University of Pennsylvania, Philadelphia.
“So that’s something I always discuss with patients. In some research, sometimes patients do feel better after the vaccine,” he says.
What kind of therapies do you find helpful for your patients?
Rehabilitation is a key part of recovery from long COVID, Dr. Abramoff says. “It is very important to make this very patient-specific.”
“We have patients that are working. They’re already going to the gym in some cases but don’t feel like they have the same endurance,” he says. “And then we have patients who are so crippled by their fatigue that they can’t get out of bed.”
1/ What is #LongCOVID?!
A disabling malady from ongoing inflammation, autoimmunity, & potential viral reservoirs (GI, brain?)
NEW DATA: The Lungs “light up” on special MRI Scans 3 to 9 months later in patients never hospitalized for COVID.https://t.co/I2kyZ4cK5F pic.twitter.com/dL1P67L2DK
— WesElyMD (@WesElyMD) February 2, 2022
An exercise program can help people who have long COVID.
“There’s a big role for therapy services in the recovery of these patients,” says John Baratta, MD, of the department of physical medicine and rehabilitation at the University of North Carolina at Chapel Hill.
But the limited number of long COVID clinics can mean some people are unable to get to therapists trained on the needs of patients with lingering COVID symptoms. Educating community physical and occupational therapists is one solution.
How long does it take for people with long COVID to recover and get back to 100% if they can?
Specific numbers aren’t really available, Dr. Baratta says.
“But I can tell you the general trend that I see is that a lot of patients have a gradual improvement of symptoms. The slow but steady improvement with time may be the body’s natural healing process, a result of medical interventions, or both.”
It can help to reassure people with long COVID that they will not be discharged from care until they feel they’ve maximized their health, says Sharagim Kemp, DO, medical director of the COVID Recovery Program for Nuvance Health, a health system in New York and Connecticut.
It’s essential to set realistic recovery expectations and tell patients that not everyone will return to 100% of their pre-COVID functioning, she says.
“Once we are able to help them reset their expectations, there’s almost an accelerated recovery because they are not putting that pressure on themselves anymore,” Dr. Kemp says.
What are the most common symptoms you’re seeing in long COVID?
It’s helpful to think of long COVID as a very broad umbrella term, Dr. Abramoff says.
Echoing what many others have observed, fatigue, cognitive dysfunction or “brain fog,“ and shortness of breath or troubled breathing appear to be the most common symptoms, he says.
Some reported vague symptoms, Dr. Kemp says.
People may go to the doctor “not even realizing that they had COVID. That’s one of the important points here – to have a high index of suspicion for patients who come in with multiple symptoms,” she says.
For this reason, patients can report symptoms that don’t necessarily fit into any specialty, says Sarah J. Ryan, MD, an internal medicine doctor at Columbia University Irving Medical Center in New York. People say they are “just not themselves” or they are tired after their COVID-19 recovery.
Is there a connection between severe COVID cases and severe long COVID?
“It’s not like that at all. I would say that more than 80% of the patients that we see had mild to moderate illness and they were not hospitalized,” Dr. Baratta says.
Long COVID is a bit different in children and teenagers, says Ixsy Ramirez, MD, a pediatric pulmonologist at University of Michigan Health, Ann Arbor. Most patients in the long COVID clinic at the University of Michigan were previously healthy, and not children with asthma or other lung conditions as one might expect. In fact, many are student athletes, or were before they had long COVID.
In this population, shortness of breath is most common, followed by chest pain and fatigue. Unfortunately, the symptoms are so serious for many kids that their performance is limited, even if they can return to competitive play.
Are there defined criteria you use to diagnose long COVID? How do you give someone a diagnosis?
That’s an ever-evolving question, Dr. Kemp says. The generally accepted definition centers on persistent or new symptoms 4 weeks or more after the original COVID-19 illness, but there are exceptions.
Researchers are working on lab tests to help confirm the diagnosis. But without a definitive blood biomarker, getting to the diagnosis requires “some thorough detective work,” Dr. Ryan says.
Do you bring in mental health providers to help with treatment?
“We focus on mental health quite a bit actually,” says, Dr. Chen, cofounder of his institution’s COVID recovery clinic. Mount Sinai offers one-on-one and group mental health services, for example.
“Personally, I’ve seen patients that I did not expect to have such severe mental health changes” with long COVID.
One of the most powerful accounts and testimonies I have seen on what most #LongCovid patients experience when interacting with their doctors.
“I did not fit in a box, so they chose not to see me, even worse they made me feel like it was my fault for not fitting in their box” pic.twitter.com/7GQLBucuO5
— charlos (@loscharlos) February 3, 2022
Examples include severe depression, cases of acute psychosis, hallucinations, and other problems “that are really unexpected after a viral illness.”
Stony Brook University Hospital in New York has a long COVID clinic staffed by multiple primary care doctors who do exams and refer patients to services. A bonus of offering psychological services to all post-COVID patients is doctors get a more complete picture of each person and a better understanding of what they are going through, says Abigail Chua, MD, a pulmonologist at Stony Brook.
Some empathy is essential, Dr. Baratta says. “It’s important to recognize that a lot of these patients present with a sense of grief or loss for their prior life.”
What does the future hold?
A simple test to diagnose long COVID, combined with an effective treatment that helps people feel better within a week, would be ideal, Dr. Abramoff says.
“That would be lovely. But you know, we’re just not at that point.”
And it would be helpful to start identifying subtypes of long COVID so diagnosis and treatment can be more targeted, Dr. Abramoff says. Otherwise, “It’s going to be a very challenging approach to try to treat all of our patients with long COVID symptoms the same way.”
Good clinical trials likewise are needed to address all the subtleties of long COVID.
A number of long COVID centers are collaborating on research to find out more, Dr. Chen says. Actions include setting up a bank of tissue samples from people with long COVID so researchers can continue to figure out the condition.
One goal, Dr. Chen says, would be the ability to treat long COVID rather than just its symptoms.
Long COVID emphasizes the need to prevent people from getting COVID in the first place, Dr. Ramirez says. This will continue to be important, particularly when some people dismiss the seriousness of COVID, comparing it to a cold if they get it. That attitude discounts the large number of people who unfortunately go on to develop long-term, often debilitating, symptoms.
A version of this article first appeared on WebMD.com.
Enjoy the ride
She was a 20-year-old barista when we first met, working her way through college.
I was a newly minted attending physician. I’d stopped at the place she worked for coffee on the way to my office. When I got up to the front she was wearing sunglasses and apologized for them. She said she was having bad headaches, and couldn’t get into a doctor she’d been referred to. Feeling bad for her, and needing patients, I handed her my card.
She showed up a few days later, a little nervous as she’d never met a “regular” outside the coffee place before, and had brought her sister along for support.
She was back last week. Now she’s head of human resources for the same chain of local coffee shops. She’s married, with kids, a mortgage, and a minivan.
We were talking about our chance meeting and reminiscing. Her migraines had taken a few medication trials to control, but after a year or 2 we’d found the right one for her and she’s been on it since.
Like many of my longtime patients, she moved past calling me “doctor” long ago. Our one to two visits a year are now more social than medical, chatting about our kids, dogs, and lives.
The same passage of time that brings us from grade school, to medical school, to medical practice takes others along with it. We may not see the changes of days, but when they drop by only once a year it’s obvious. Just like the way we don’t see daily changes in family and friends, but when we look at old pictures we’re shocked by how different they (not to mention ourselves) look.
We all follow the same course around the sun, usually facing the same milestones and similar memories on the trip. Our long-term patients, like distant relatives, may only come by infrequently, so the changes are greater. I’m sure they say the same things about me. “I saw Dr. Block today; boy, he’s really gone gray.”
I don’t mind that (too much) anymore. My thinning, graying, hair (I hope) makes me look a little more distinguished, although my complete lack of fashion sense more than goes the other way.
The river only goes in one direction, carrying us, our patients, and our families, all along with it. We often lose track of time’s effects on us until we see the changes it has brought to another.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
She was a 20-year-old barista when we first met, working her way through college.
I was a newly minted attending physician. I’d stopped at the place she worked for coffee on the way to my office. When I got up to the front she was wearing sunglasses and apologized for them. She said she was having bad headaches, and couldn’t get into a doctor she’d been referred to. Feeling bad for her, and needing patients, I handed her my card.
She showed up a few days later, a little nervous as she’d never met a “regular” outside the coffee place before, and had brought her sister along for support.
She was back last week. Now she’s head of human resources for the same chain of local coffee shops. She’s married, with kids, a mortgage, and a minivan.
We were talking about our chance meeting and reminiscing. Her migraines had taken a few medication trials to control, but after a year or 2 we’d found the right one for her and she’s been on it since.
Like many of my longtime patients, she moved past calling me “doctor” long ago. Our one to two visits a year are now more social than medical, chatting about our kids, dogs, and lives.
The same passage of time that brings us from grade school, to medical school, to medical practice takes others along with it. We may not see the changes of days, but when they drop by only once a year it’s obvious. Just like the way we don’t see daily changes in family and friends, but when we look at old pictures we’re shocked by how different they (not to mention ourselves) look.
We all follow the same course around the sun, usually facing the same milestones and similar memories on the trip. Our long-term patients, like distant relatives, may only come by infrequently, so the changes are greater. I’m sure they say the same things about me. “I saw Dr. Block today; boy, he’s really gone gray.”
I don’t mind that (too much) anymore. My thinning, graying, hair (I hope) makes me look a little more distinguished, although my complete lack of fashion sense more than goes the other way.
The river only goes in one direction, carrying us, our patients, and our families, all along with it. We often lose track of time’s effects on us until we see the changes it has brought to another.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
She was a 20-year-old barista when we first met, working her way through college.
I was a newly minted attending physician. I’d stopped at the place she worked for coffee on the way to my office. When I got up to the front she was wearing sunglasses and apologized for them. She said she was having bad headaches, and couldn’t get into a doctor she’d been referred to. Feeling bad for her, and needing patients, I handed her my card.
She showed up a few days later, a little nervous as she’d never met a “regular” outside the coffee place before, and had brought her sister along for support.
She was back last week. Now she’s head of human resources for the same chain of local coffee shops. She’s married, with kids, a mortgage, and a minivan.
We were talking about our chance meeting and reminiscing. Her migraines had taken a few medication trials to control, but after a year or 2 we’d found the right one for her and she’s been on it since.
Like many of my longtime patients, she moved past calling me “doctor” long ago. Our one to two visits a year are now more social than medical, chatting about our kids, dogs, and lives.
The same passage of time that brings us from grade school, to medical school, to medical practice takes others along with it. We may not see the changes of days, but when they drop by only once a year it’s obvious. Just like the way we don’t see daily changes in family and friends, but when we look at old pictures we’re shocked by how different they (not to mention ourselves) look.
We all follow the same course around the sun, usually facing the same milestones and similar memories on the trip. Our long-term patients, like distant relatives, may only come by infrequently, so the changes are greater. I’m sure they say the same things about me. “I saw Dr. Block today; boy, he’s really gone gray.”
I don’t mind that (too much) anymore. My thinning, graying, hair (I hope) makes me look a little more distinguished, although my complete lack of fashion sense more than goes the other way.
The river only goes in one direction, carrying us, our patients, and our families, all along with it. We often lose track of time’s effects on us until we see the changes it has brought to another.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Two emerging drugs exacerbating opioid crisis
Two illicit drugs are contributing to a sharp rise in fentanyl-related deaths, a new study from the Centers for Disease Control and Prevention shows.
Para-fluorofentanyl, a schedule I substance often found in heroin packets and counterfeit pills, is making a comeback on the illicit drug market, Jordan Trecki, PhD, and associates reported in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report (2022 Jan 28;71[4]:153-5). U.S. medical examiner reports and national law enforcement seizure data point to a rise in encounters of this drug along with metonitazene, a benzimidazole-opioid, in combination with fentanyl.
On their own, para-fluorofentanyl and metonitazene can kill the user through respiratory depression. Combinations of these substances and other opioids, including fentanyl-related compounds or adulterants, “pose an even greater potential harm to the patient than previously observed,” reported Dr. Trecki, a pharmacologist affiliated with the Drug Enforcement Administration, and colleagues.
Opioids contribute to about 75% of all U.S. drug overdose deaths, which rose by 28.5% during 2020-2021, according to the National Center for Health Statistics. And fentanyl is replacing heroin as the primary drug of use, said addiction specialist Brian Fuehrlein, MD, PhD, in an interview.
“For patients with stimulant use disorder and even cannabis use disorder, fentanyl is becoming more and more common as an adulterant in those substances, often resulting in inadvertent use. Hence, fentanyl and fentanyl-like drugs and fentanyl analogues are becoming increasingly common and important,” said Dr. Fuehrlein, director of the psychiatric emergency room at the VA Connecticut Healthcare System. He was not involved with the MMWR study.
Tennessee data reflect national problem
Recent data from a medical examiner in Knoxville, Tenn., illustrate what might be happening nationwide with those two emerging substances.
Over the last 2 years, the Knox County Regional Forensic Center has identified para-fluorofentanyl in the toxicology results of drug overdose victims, and metonitazene – either on its own or in combination with fentanyl and para-fluorofentanyl. Fentanyl appeared in 562 or 73% of 770 unintentional drug overdose deaths from November 2020 to August 2021. Forty-eight of these cases involved para-fluorofentanyl, and 26 involved metonitazene.
“Although the percentage of law enforcement encounters with these substances in Tennessee decreased relative to the national total percentage within this time frame, the increase in encounters both within Tennessee and nationally reflect an increased distribution of para-fluorofentanyl and metonitazene throughout the United States,” the authors reported.
How to identify substances, manage overdoses
The authors encouraged physicians, labs, and medical examiners to be on the lookout for these two substances either in the emergency department or when identifying the cause of drug overdose deaths.
They also advised that stronger opioids, such as fentanyl, para-fluorofentanyl, metonitazene, or other benzimidazoles may warrant additional doses of the opioid-reversal drug naloxone.
While he hasn’t personally seen any of these drugs in his practice, “I would assume that these are on the rise due to inexpensive cost to manufacture and potency of effect,” said Dr. Fuehrlein, also an associate professor of psychiatry at Yale University, New Haven, Conn.
The need for additional naloxone to manage acute overdoses is a key takeaway of the MMWR paper, he added. Clinicians should also educate patients about harm reduction strategies to avoid overdose death when using potentially powerful and unknown drugs. “Things like start low and go slow, buy from the same supplier, do not use opioids with alcohol or benzos, have Narcan available, do not use alone, etc.”
Dr. Fuehrlein had no disclosures.
Two illicit drugs are contributing to a sharp rise in fentanyl-related deaths, a new study from the Centers for Disease Control and Prevention shows.
Para-fluorofentanyl, a schedule I substance often found in heroin packets and counterfeit pills, is making a comeback on the illicit drug market, Jordan Trecki, PhD, and associates reported in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report (2022 Jan 28;71[4]:153-5). U.S. medical examiner reports and national law enforcement seizure data point to a rise in encounters of this drug along with metonitazene, a benzimidazole-opioid, in combination with fentanyl.
On their own, para-fluorofentanyl and metonitazene can kill the user through respiratory depression. Combinations of these substances and other opioids, including fentanyl-related compounds or adulterants, “pose an even greater potential harm to the patient than previously observed,” reported Dr. Trecki, a pharmacologist affiliated with the Drug Enforcement Administration, and colleagues.
Opioids contribute to about 75% of all U.S. drug overdose deaths, which rose by 28.5% during 2020-2021, according to the National Center for Health Statistics. And fentanyl is replacing heroin as the primary drug of use, said addiction specialist Brian Fuehrlein, MD, PhD, in an interview.
“For patients with stimulant use disorder and even cannabis use disorder, fentanyl is becoming more and more common as an adulterant in those substances, often resulting in inadvertent use. Hence, fentanyl and fentanyl-like drugs and fentanyl analogues are becoming increasingly common and important,” said Dr. Fuehrlein, director of the psychiatric emergency room at the VA Connecticut Healthcare System. He was not involved with the MMWR study.
Tennessee data reflect national problem
Recent data from a medical examiner in Knoxville, Tenn., illustrate what might be happening nationwide with those two emerging substances.
Over the last 2 years, the Knox County Regional Forensic Center has identified para-fluorofentanyl in the toxicology results of drug overdose victims, and metonitazene – either on its own or in combination with fentanyl and para-fluorofentanyl. Fentanyl appeared in 562 or 73% of 770 unintentional drug overdose deaths from November 2020 to August 2021. Forty-eight of these cases involved para-fluorofentanyl, and 26 involved metonitazene.
“Although the percentage of law enforcement encounters with these substances in Tennessee decreased relative to the national total percentage within this time frame, the increase in encounters both within Tennessee and nationally reflect an increased distribution of para-fluorofentanyl and metonitazene throughout the United States,” the authors reported.
How to identify substances, manage overdoses
The authors encouraged physicians, labs, and medical examiners to be on the lookout for these two substances either in the emergency department or when identifying the cause of drug overdose deaths.
They also advised that stronger opioids, such as fentanyl, para-fluorofentanyl, metonitazene, or other benzimidazoles may warrant additional doses of the opioid-reversal drug naloxone.
While he hasn’t personally seen any of these drugs in his practice, “I would assume that these are on the rise due to inexpensive cost to manufacture and potency of effect,” said Dr. Fuehrlein, also an associate professor of psychiatry at Yale University, New Haven, Conn.
The need for additional naloxone to manage acute overdoses is a key takeaway of the MMWR paper, he added. Clinicians should also educate patients about harm reduction strategies to avoid overdose death when using potentially powerful and unknown drugs. “Things like start low and go slow, buy from the same supplier, do not use opioids with alcohol or benzos, have Narcan available, do not use alone, etc.”
Dr. Fuehrlein had no disclosures.
Two illicit drugs are contributing to a sharp rise in fentanyl-related deaths, a new study from the Centers for Disease Control and Prevention shows.
Para-fluorofentanyl, a schedule I substance often found in heroin packets and counterfeit pills, is making a comeback on the illicit drug market, Jordan Trecki, PhD, and associates reported in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report (2022 Jan 28;71[4]:153-5). U.S. medical examiner reports and national law enforcement seizure data point to a rise in encounters of this drug along with metonitazene, a benzimidazole-opioid, in combination with fentanyl.
On their own, para-fluorofentanyl and metonitazene can kill the user through respiratory depression. Combinations of these substances and other opioids, including fentanyl-related compounds or adulterants, “pose an even greater potential harm to the patient than previously observed,” reported Dr. Trecki, a pharmacologist affiliated with the Drug Enforcement Administration, and colleagues.
Opioids contribute to about 75% of all U.S. drug overdose deaths, which rose by 28.5% during 2020-2021, according to the National Center for Health Statistics. And fentanyl is replacing heroin as the primary drug of use, said addiction specialist Brian Fuehrlein, MD, PhD, in an interview.
“For patients with stimulant use disorder and even cannabis use disorder, fentanyl is becoming more and more common as an adulterant in those substances, often resulting in inadvertent use. Hence, fentanyl and fentanyl-like drugs and fentanyl analogues are becoming increasingly common and important,” said Dr. Fuehrlein, director of the psychiatric emergency room at the VA Connecticut Healthcare System. He was not involved with the MMWR study.
Tennessee data reflect national problem
Recent data from a medical examiner in Knoxville, Tenn., illustrate what might be happening nationwide with those two emerging substances.
Over the last 2 years, the Knox County Regional Forensic Center has identified para-fluorofentanyl in the toxicology results of drug overdose victims, and metonitazene – either on its own or in combination with fentanyl and para-fluorofentanyl. Fentanyl appeared in 562 or 73% of 770 unintentional drug overdose deaths from November 2020 to August 2021. Forty-eight of these cases involved para-fluorofentanyl, and 26 involved metonitazene.
“Although the percentage of law enforcement encounters with these substances in Tennessee decreased relative to the national total percentage within this time frame, the increase in encounters both within Tennessee and nationally reflect an increased distribution of para-fluorofentanyl and metonitazene throughout the United States,” the authors reported.
How to identify substances, manage overdoses
The authors encouraged physicians, labs, and medical examiners to be on the lookout for these two substances either in the emergency department or when identifying the cause of drug overdose deaths.
They also advised that stronger opioids, such as fentanyl, para-fluorofentanyl, metonitazene, or other benzimidazoles may warrant additional doses of the opioid-reversal drug naloxone.
While he hasn’t personally seen any of these drugs in his practice, “I would assume that these are on the rise due to inexpensive cost to manufacture and potency of effect,” said Dr. Fuehrlein, also an associate professor of psychiatry at Yale University, New Haven, Conn.
The need for additional naloxone to manage acute overdoses is a key takeaway of the MMWR paper, he added. Clinicians should also educate patients about harm reduction strategies to avoid overdose death when using potentially powerful and unknown drugs. “Things like start low and go slow, buy from the same supplier, do not use opioids with alcohol or benzos, have Narcan available, do not use alone, etc.”
Dr. Fuehrlein had no disclosures.
Bowel prep: Electrolyte disturbances remain rare but serious
Patients undergoing bowel prep for colonoscopy had significantly greater decreases in potassium after prep with sodium phosphate, compared with those whose prep involved polyethylene glycol, based on data from a meta-analysis of more than 2,000 patients.
Electrolyte disturbances, though rare, represent a serious adverse event associated with bowel preparation, and the prevalence remains unclear, Atsushi Sakuraba, MD, of the University of Chicago said in an interview. Dr. Sakuraba, who was not involved in the study, said he was surprised by some of the study findings. “The incidence and degree of hypokalemia associated with sodium phosphate bowel preparation was greater than what I would have thought.”
Authors of the current analysis, led by Ankie Reumkens, MD, of Maastricht (the Netherlands) University Medical Center, noted in Digestive Endoscopy that the severity of adverse events is not directly related to the degree of electrolyte disturbance. “Electrolyte disturbances may vary from asymptomatic via mild and moderate symptoms (i.e., muscle weakness, constipation, nausea, and vomiting), to severe symptoms (i.e., paralysis, seizures, cardiac arrhythmias, coma, and death).” Although current guidelines do not include recommendations for electrolyte measurement, the European Society of Gastrointestinal Endoscopy recommends against routine use of sodium phosphate (NaP) despite a low level of evidence. Although polyethylene glycol (PEG) is the preferred choice for older patients and in patients with renal impairment, heart failure, and inflammatory bowel disease, the investigators noted that NaP and picosulfate with magnesium titrate (SPMC) have been associated with higher patient tolerance and compliance.
Bowel preparation solutions are available in high-volume versions that include high-volume PEG, while low-volume options include low-volume PEG, NaP, and SPMC; despite the variety of choices, bowel preparations of any type may cause electrolyte disturbances, and their extent, magnitude, and risk factors have not been well studied.
In their systemic review and meta-analysis, the researchers examined the pooled prevalence of electrolyte disturbances; the primary endpoint was the pooled prevalence of hypokalemia, hyponatremia, hyperphosphatemia, and hypocalcemia after bowel preparation, and the changes in mean potassium values. The review was based on 13 studies published between Jan. 1, 1995, and July 1, 2021, with a total of 2,386 patients.
Overall, hypokalemia occurred in 17.2 % of patients who underwent NaP for bowel preparation versus 4.8% of those who underwent PEG. Hyponatremia occurred in 0.9% of NaP patients versus3.3% of PEG patients; hyperphosphatemia occurred in 37.3% and 0.65% of NaP and PEG patients, respectively; and hypocalcemia occurred in 15.6% and 8.1% of NaP and PEG patients, respectively.
Pharmacokinetics may explain the increased disturbances in electrolyte balance with NaP, the researchers noted.
“PEG is iso-osmotic with plasma, causing no net absorption or excretion of water or ions,” they said, but “NaP is highly osmotic and therefore results in fluid shifts from the systemic compartment to the gastrointestinal tract.”
The study findings were limited by several factors including the potential underreporting of the prevalence of electrolyte disturbances, the exclusion of patients with renal insufficiency, heart failure, and bowel problems, and the incomplete data on bowel cleansing scores and adverse events, the researchers noted. More data on the prevalences of electrolyte disturbances after low-volume bowel preparations are needed to inform evidence-based recommendations, especially in light of the increased numbers of colonoscopies and increasing numbers of older patients and patients with comorbidities.
From a clinical practice perspective, Dr. Sakuraba agreed with the authors’ conclusion that the results support the recommendations of some current guidelines against the routine use of sodium phosphate for bowel preparation, even if the number of included studies was small.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Sakuraba had no financial conflicts to disclose.
Patients undergoing bowel prep for colonoscopy had significantly greater decreases in potassium after prep with sodium phosphate, compared with those whose prep involved polyethylene glycol, based on data from a meta-analysis of more than 2,000 patients.
Electrolyte disturbances, though rare, represent a serious adverse event associated with bowel preparation, and the prevalence remains unclear, Atsushi Sakuraba, MD, of the University of Chicago said in an interview. Dr. Sakuraba, who was not involved in the study, said he was surprised by some of the study findings. “The incidence and degree of hypokalemia associated with sodium phosphate bowel preparation was greater than what I would have thought.”
Authors of the current analysis, led by Ankie Reumkens, MD, of Maastricht (the Netherlands) University Medical Center, noted in Digestive Endoscopy that the severity of adverse events is not directly related to the degree of electrolyte disturbance. “Electrolyte disturbances may vary from asymptomatic via mild and moderate symptoms (i.e., muscle weakness, constipation, nausea, and vomiting), to severe symptoms (i.e., paralysis, seizures, cardiac arrhythmias, coma, and death).” Although current guidelines do not include recommendations for electrolyte measurement, the European Society of Gastrointestinal Endoscopy recommends against routine use of sodium phosphate (NaP) despite a low level of evidence. Although polyethylene glycol (PEG) is the preferred choice for older patients and in patients with renal impairment, heart failure, and inflammatory bowel disease, the investigators noted that NaP and picosulfate with magnesium titrate (SPMC) have been associated with higher patient tolerance and compliance.
Bowel preparation solutions are available in high-volume versions that include high-volume PEG, while low-volume options include low-volume PEG, NaP, and SPMC; despite the variety of choices, bowel preparations of any type may cause electrolyte disturbances, and their extent, magnitude, and risk factors have not been well studied.
In their systemic review and meta-analysis, the researchers examined the pooled prevalence of electrolyte disturbances; the primary endpoint was the pooled prevalence of hypokalemia, hyponatremia, hyperphosphatemia, and hypocalcemia after bowel preparation, and the changes in mean potassium values. The review was based on 13 studies published between Jan. 1, 1995, and July 1, 2021, with a total of 2,386 patients.
Overall, hypokalemia occurred in 17.2 % of patients who underwent NaP for bowel preparation versus 4.8% of those who underwent PEG. Hyponatremia occurred in 0.9% of NaP patients versus3.3% of PEG patients; hyperphosphatemia occurred in 37.3% and 0.65% of NaP and PEG patients, respectively; and hypocalcemia occurred in 15.6% and 8.1% of NaP and PEG patients, respectively.
Pharmacokinetics may explain the increased disturbances in electrolyte balance with NaP, the researchers noted.
“PEG is iso-osmotic with plasma, causing no net absorption or excretion of water or ions,” they said, but “NaP is highly osmotic and therefore results in fluid shifts from the systemic compartment to the gastrointestinal tract.”
The study findings were limited by several factors including the potential underreporting of the prevalence of electrolyte disturbances, the exclusion of patients with renal insufficiency, heart failure, and bowel problems, and the incomplete data on bowel cleansing scores and adverse events, the researchers noted. More data on the prevalences of electrolyte disturbances after low-volume bowel preparations are needed to inform evidence-based recommendations, especially in light of the increased numbers of colonoscopies and increasing numbers of older patients and patients with comorbidities.
From a clinical practice perspective, Dr. Sakuraba agreed with the authors’ conclusion that the results support the recommendations of some current guidelines against the routine use of sodium phosphate for bowel preparation, even if the number of included studies was small.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Sakuraba had no financial conflicts to disclose.
Patients undergoing bowel prep for colonoscopy had significantly greater decreases in potassium after prep with sodium phosphate, compared with those whose prep involved polyethylene glycol, based on data from a meta-analysis of more than 2,000 patients.
Electrolyte disturbances, though rare, represent a serious adverse event associated with bowel preparation, and the prevalence remains unclear, Atsushi Sakuraba, MD, of the University of Chicago said in an interview. Dr. Sakuraba, who was not involved in the study, said he was surprised by some of the study findings. “The incidence and degree of hypokalemia associated with sodium phosphate bowel preparation was greater than what I would have thought.”
Authors of the current analysis, led by Ankie Reumkens, MD, of Maastricht (the Netherlands) University Medical Center, noted in Digestive Endoscopy that the severity of adverse events is not directly related to the degree of electrolyte disturbance. “Electrolyte disturbances may vary from asymptomatic via mild and moderate symptoms (i.e., muscle weakness, constipation, nausea, and vomiting), to severe symptoms (i.e., paralysis, seizures, cardiac arrhythmias, coma, and death).” Although current guidelines do not include recommendations for electrolyte measurement, the European Society of Gastrointestinal Endoscopy recommends against routine use of sodium phosphate (NaP) despite a low level of evidence. Although polyethylene glycol (PEG) is the preferred choice for older patients and in patients with renal impairment, heart failure, and inflammatory bowel disease, the investigators noted that NaP and picosulfate with magnesium titrate (SPMC) have been associated with higher patient tolerance and compliance.
Bowel preparation solutions are available in high-volume versions that include high-volume PEG, while low-volume options include low-volume PEG, NaP, and SPMC; despite the variety of choices, bowel preparations of any type may cause electrolyte disturbances, and their extent, magnitude, and risk factors have not been well studied.
In their systemic review and meta-analysis, the researchers examined the pooled prevalence of electrolyte disturbances; the primary endpoint was the pooled prevalence of hypokalemia, hyponatremia, hyperphosphatemia, and hypocalcemia after bowel preparation, and the changes in mean potassium values. The review was based on 13 studies published between Jan. 1, 1995, and July 1, 2021, with a total of 2,386 patients.
Overall, hypokalemia occurred in 17.2 % of patients who underwent NaP for bowel preparation versus 4.8% of those who underwent PEG. Hyponatremia occurred in 0.9% of NaP patients versus3.3% of PEG patients; hyperphosphatemia occurred in 37.3% and 0.65% of NaP and PEG patients, respectively; and hypocalcemia occurred in 15.6% and 8.1% of NaP and PEG patients, respectively.
Pharmacokinetics may explain the increased disturbances in electrolyte balance with NaP, the researchers noted.
“PEG is iso-osmotic with plasma, causing no net absorption or excretion of water or ions,” they said, but “NaP is highly osmotic and therefore results in fluid shifts from the systemic compartment to the gastrointestinal tract.”
The study findings were limited by several factors including the potential underreporting of the prevalence of electrolyte disturbances, the exclusion of patients with renal insufficiency, heart failure, and bowel problems, and the incomplete data on bowel cleansing scores and adverse events, the researchers noted. More data on the prevalences of electrolyte disturbances after low-volume bowel preparations are needed to inform evidence-based recommendations, especially in light of the increased numbers of colonoscopies and increasing numbers of older patients and patients with comorbidities.
From a clinical practice perspective, Dr. Sakuraba agreed with the authors’ conclusion that the results support the recommendations of some current guidelines against the routine use of sodium phosphate for bowel preparation, even if the number of included studies was small.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Sakuraba had no financial conflicts to disclose.
FROM DIGESTIVE ENDOSCOPY
Teaching Evidence-Based Dermatology Using a Web-Based Journal Club: A Pilot Study and Survey
To the Editor:
With a steady increase in dermatology publications over recent decades, there is an expanding pool of evidence to address clinical questions.1 Residency training is the time when appraising the medical literature and practicing evidence-based medicine is most honed. Evidence-based medicine is an essential component of Practice-based Learning and Improvement, a required core competency of the Accreditation Council for Graduate Medical Education.2 Assimilation of new research evidence is traditionally taught through didactics and journal club discussions in residency.
However, at a time when the demand for information overwhelms safeguards that exist to evaluate its quality, it is more important than ever to be equipped with the proper tools to critically appraise novel literature. Beyond accepting a scientific article at face value, physicians must learn to ask targeted questions of the study design, results, and clinical relevance. These questions change based on the type of study, and organizations such as the Oxford Centre for Evidence-Based Medicine provide guidance through critical appraisal worksheets.3
To investigate the utility of using guided questions to evaluate the reliability, significance, and applicability of clinical evidence, we beta tested a novel web-based application in an academic dermatology setting to design and run a journal club for residents. Six dermatology residents participated in this institutional review board–approved study comprised of 3 phases: (1) independent article appraisal through the web-based application, (2) group discussion, and (3) anonymous postsurvey.
Using this platform, we uploaded a recent article into the interactive reader, which contained an integrated tool for appraisal based on specific questions. Because the article described the results of a randomized clinical trial, we used questions from the Centre for Evidence-Based Medicine’s Randomised Controlled Trials Critical Appraisal Worksheet, which has a series of questions to evaluate internal validity, results, and external validity and applicability.3
Residents used the platform to independently read the article, highlight areas of the text that corresponded to 8 critical appraisal questions, and answer yes or no to these questions. Based on residents’ answers, a final appraisal score (on a scale of 1% to 100%) was generated. Simultaneously, the attending dermatologist leading the journal club (C.W.) also completed the assignment to establish an expert score.
Scores from the residents’ independent appraisal ranged from 75% to 100% (mean, 85.4%). Upon discussing the article in a group setting, the residents established a consensus score of 75%. This consensus score matched the expert score, which suggested to us that both independently reviewing the article using guided questions and conducting a group debriefing were necessary to match the expert level of critical appraisal.
Of note, the residents’ average independent appraisal score was higher than both the consensus and expert scores, indicating that the residents evaluated the article less critically on their own. With more practice using this method, it is possible that the precision and accuracy of the residents’ critical appraisal of scientific articles will improve.
In the postsurvey, we asked residents about the critical appraisal of the medical literature. All residents agreed that evaluating the quality of evidence when reading a scientific article was somewhat important or very important to them; however, only 2 of 6 evaluated the quality of evidence all the time, and the other 4 did so half of the time or less than half of the time.
When critically appraising articles, 2 of 6 residents used specific rubrics half of the time; 4 of 6 less than half of the time. Most important, 5 of 6 residents agreed that the quality of evidence affected their management decisions more than half of the time or all of the time. Although it is clear that residents value evidence-based medicine and understand the importance of evaluating the quality of evidence, doing so currently might not be simple or practical.
An organized framework for appraising articles would streamline the process. Five of 6 residents agreed that the use of specific questions as a guide made it easier to appraise an article for the quality of its evidence. Four of 6 residents found that juxtaposing specific questions with the interactive reader was helpful; 5 of 6 agreed that they would use a web-based journal club platform if given the option.
Lastly, 5 of 6 residents agreed that if such a tool were available, a platform containing all major dermatology publications in an interactive reader format, along with relevant appraisal questions on the side, would be useful.
This pilot study augmented the typical journal club experience by emphasizing goal-directed reading and the importance of analyzing the quality of evidence. The combination of independent appraisal of an article using targeted questions and a group debrief led to better understanding of the evidence and its clinical applicability. The COVID-19 pandemic may be a better time than ever to explore innovative ways to teach evidence-based medicine in residency training.
- Mimouni D, Pavlovsky L, Akerman L, et al. Trends in dermatology publications over the past 15 years. Am J Clin Dermatol. 2010;11:55-58. doi:10.2165/11530190-000000000-00000.
- NEJM Knowledge+ Team. Exploring the ACGME Core Competencies: Practice-Based Learning and Improvement (part 2 of 7). Massachusetts Medical Society. NEJM Knowledge+ website. Published July 28, 2016. Accessed January 15, 2022. https://knowledgeplus.nejm.org/blog/practice-based-learning-and-improvement/
- University of Oxford. Critical appraisal tools. Centre for Evidence-Based Medicine website. Accessed January 2, 2022. www.cebm.ox.ac.uk/resources/ebm-tools/critical-appraisal-tools
To the Editor:
With a steady increase in dermatology publications over recent decades, there is an expanding pool of evidence to address clinical questions.1 Residency training is the time when appraising the medical literature and practicing evidence-based medicine is most honed. Evidence-based medicine is an essential component of Practice-based Learning and Improvement, a required core competency of the Accreditation Council for Graduate Medical Education.2 Assimilation of new research evidence is traditionally taught through didactics and journal club discussions in residency.
However, at a time when the demand for information overwhelms safeguards that exist to evaluate its quality, it is more important than ever to be equipped with the proper tools to critically appraise novel literature. Beyond accepting a scientific article at face value, physicians must learn to ask targeted questions of the study design, results, and clinical relevance. These questions change based on the type of study, and organizations such as the Oxford Centre for Evidence-Based Medicine provide guidance through critical appraisal worksheets.3
To investigate the utility of using guided questions to evaluate the reliability, significance, and applicability of clinical evidence, we beta tested a novel web-based application in an academic dermatology setting to design and run a journal club for residents. Six dermatology residents participated in this institutional review board–approved study comprised of 3 phases: (1) independent article appraisal through the web-based application, (2) group discussion, and (3) anonymous postsurvey.
Using this platform, we uploaded a recent article into the interactive reader, which contained an integrated tool for appraisal based on specific questions. Because the article described the results of a randomized clinical trial, we used questions from the Centre for Evidence-Based Medicine’s Randomised Controlled Trials Critical Appraisal Worksheet, which has a series of questions to evaluate internal validity, results, and external validity and applicability.3
Residents used the platform to independently read the article, highlight areas of the text that corresponded to 8 critical appraisal questions, and answer yes or no to these questions. Based on residents’ answers, a final appraisal score (on a scale of 1% to 100%) was generated. Simultaneously, the attending dermatologist leading the journal club (C.W.) also completed the assignment to establish an expert score.
Scores from the residents’ independent appraisal ranged from 75% to 100% (mean, 85.4%). Upon discussing the article in a group setting, the residents established a consensus score of 75%. This consensus score matched the expert score, which suggested to us that both independently reviewing the article using guided questions and conducting a group debriefing were necessary to match the expert level of critical appraisal.
Of note, the residents’ average independent appraisal score was higher than both the consensus and expert scores, indicating that the residents evaluated the article less critically on their own. With more practice using this method, it is possible that the precision and accuracy of the residents’ critical appraisal of scientific articles will improve.
In the postsurvey, we asked residents about the critical appraisal of the medical literature. All residents agreed that evaluating the quality of evidence when reading a scientific article was somewhat important or very important to them; however, only 2 of 6 evaluated the quality of evidence all the time, and the other 4 did so half of the time or less than half of the time.
When critically appraising articles, 2 of 6 residents used specific rubrics half of the time; 4 of 6 less than half of the time. Most important, 5 of 6 residents agreed that the quality of evidence affected their management decisions more than half of the time or all of the time. Although it is clear that residents value evidence-based medicine and understand the importance of evaluating the quality of evidence, doing so currently might not be simple or practical.
An organized framework for appraising articles would streamline the process. Five of 6 residents agreed that the use of specific questions as a guide made it easier to appraise an article for the quality of its evidence. Four of 6 residents found that juxtaposing specific questions with the interactive reader was helpful; 5 of 6 agreed that they would use a web-based journal club platform if given the option.
Lastly, 5 of 6 residents agreed that if such a tool were available, a platform containing all major dermatology publications in an interactive reader format, along with relevant appraisal questions on the side, would be useful.
This pilot study augmented the typical journal club experience by emphasizing goal-directed reading and the importance of analyzing the quality of evidence. The combination of independent appraisal of an article using targeted questions and a group debrief led to better understanding of the evidence and its clinical applicability. The COVID-19 pandemic may be a better time than ever to explore innovative ways to teach evidence-based medicine in residency training.
To the Editor:
With a steady increase in dermatology publications over recent decades, there is an expanding pool of evidence to address clinical questions.1 Residency training is the time when appraising the medical literature and practicing evidence-based medicine is most honed. Evidence-based medicine is an essential component of Practice-based Learning and Improvement, a required core competency of the Accreditation Council for Graduate Medical Education.2 Assimilation of new research evidence is traditionally taught through didactics and journal club discussions in residency.
However, at a time when the demand for information overwhelms safeguards that exist to evaluate its quality, it is more important than ever to be equipped with the proper tools to critically appraise novel literature. Beyond accepting a scientific article at face value, physicians must learn to ask targeted questions of the study design, results, and clinical relevance. These questions change based on the type of study, and organizations such as the Oxford Centre for Evidence-Based Medicine provide guidance through critical appraisal worksheets.3
To investigate the utility of using guided questions to evaluate the reliability, significance, and applicability of clinical evidence, we beta tested a novel web-based application in an academic dermatology setting to design and run a journal club for residents. Six dermatology residents participated in this institutional review board–approved study comprised of 3 phases: (1) independent article appraisal through the web-based application, (2) group discussion, and (3) anonymous postsurvey.
Using this platform, we uploaded a recent article into the interactive reader, which contained an integrated tool for appraisal based on specific questions. Because the article described the results of a randomized clinical trial, we used questions from the Centre for Evidence-Based Medicine’s Randomised Controlled Trials Critical Appraisal Worksheet, which has a series of questions to evaluate internal validity, results, and external validity and applicability.3
Residents used the platform to independently read the article, highlight areas of the text that corresponded to 8 critical appraisal questions, and answer yes or no to these questions. Based on residents’ answers, a final appraisal score (on a scale of 1% to 100%) was generated. Simultaneously, the attending dermatologist leading the journal club (C.W.) also completed the assignment to establish an expert score.
Scores from the residents’ independent appraisal ranged from 75% to 100% (mean, 85.4%). Upon discussing the article in a group setting, the residents established a consensus score of 75%. This consensus score matched the expert score, which suggested to us that both independently reviewing the article using guided questions and conducting a group debriefing were necessary to match the expert level of critical appraisal.
Of note, the residents’ average independent appraisal score was higher than both the consensus and expert scores, indicating that the residents evaluated the article less critically on their own. With more practice using this method, it is possible that the precision and accuracy of the residents’ critical appraisal of scientific articles will improve.
In the postsurvey, we asked residents about the critical appraisal of the medical literature. All residents agreed that evaluating the quality of evidence when reading a scientific article was somewhat important or very important to them; however, only 2 of 6 evaluated the quality of evidence all the time, and the other 4 did so half of the time or less than half of the time.
When critically appraising articles, 2 of 6 residents used specific rubrics half of the time; 4 of 6 less than half of the time. Most important, 5 of 6 residents agreed that the quality of evidence affected their management decisions more than half of the time or all of the time. Although it is clear that residents value evidence-based medicine and understand the importance of evaluating the quality of evidence, doing so currently might not be simple or practical.
An organized framework for appraising articles would streamline the process. Five of 6 residents agreed that the use of specific questions as a guide made it easier to appraise an article for the quality of its evidence. Four of 6 residents found that juxtaposing specific questions with the interactive reader was helpful; 5 of 6 agreed that they would use a web-based journal club platform if given the option.
Lastly, 5 of 6 residents agreed that if such a tool were available, a platform containing all major dermatology publications in an interactive reader format, along with relevant appraisal questions on the side, would be useful.
This pilot study augmented the typical journal club experience by emphasizing goal-directed reading and the importance of analyzing the quality of evidence. The combination of independent appraisal of an article using targeted questions and a group debrief led to better understanding of the evidence and its clinical applicability. The COVID-19 pandemic may be a better time than ever to explore innovative ways to teach evidence-based medicine in residency training.
- Mimouni D, Pavlovsky L, Akerman L, et al. Trends in dermatology publications over the past 15 years. Am J Clin Dermatol. 2010;11:55-58. doi:10.2165/11530190-000000000-00000.
- NEJM Knowledge+ Team. Exploring the ACGME Core Competencies: Practice-Based Learning and Improvement (part 2 of 7). Massachusetts Medical Society. NEJM Knowledge+ website. Published July 28, 2016. Accessed January 15, 2022. https://knowledgeplus.nejm.org/blog/practice-based-learning-and-improvement/
- University of Oxford. Critical appraisal tools. Centre for Evidence-Based Medicine website. Accessed January 2, 2022. www.cebm.ox.ac.uk/resources/ebm-tools/critical-appraisal-tools
- Mimouni D, Pavlovsky L, Akerman L, et al. Trends in dermatology publications over the past 15 years. Am J Clin Dermatol. 2010;11:55-58. doi:10.2165/11530190-000000000-00000.
- NEJM Knowledge+ Team. Exploring the ACGME Core Competencies: Practice-Based Learning and Improvement (part 2 of 7). Massachusetts Medical Society. NEJM Knowledge+ website. Published July 28, 2016. Accessed January 15, 2022. https://knowledgeplus.nejm.org/blog/practice-based-learning-and-improvement/
- University of Oxford. Critical appraisal tools. Centre for Evidence-Based Medicine website. Accessed January 2, 2022. www.cebm.ox.ac.uk/resources/ebm-tools/critical-appraisal-tools
Practice Points
- A novel web-based application was beta tested in an academic dermatology setting to design and run a journal club for residents.
- Goal-directed reading was emphasized by using guided questions to critically appraise literature based on reliability, significance, and applicability.
- The combination of independent appraisal of an article using targeted questions and a group debrief led to better understanding of the evidence and its clinical applicability.
Referrals to gender clinics in Sweden drop after media coverage
Media coverage of transgender health care judged to be “negative” was associated with a drop of around 30% in referral rates to gender identity clinics in Sweden among young people under age 19, a new study indicates.
Malin Indremo, MS, from the department of neuroscience, Uppsala (Sweden) University, and colleagues explored the effect of the documentaries, “The Trans Train and Teenage Girls,” which they explain was a “Swedish public service television show” representing “investigative journalism.” The two-part documentary series was aired in Sweden in April 2019 and October 2019, respectively, and is now available in English on YouTube.
In their article, published online in JAMA Network Open, the authors said they consider “The Trans Train” programs to be “negative” media coverage because the “documentaries addressed the distinct increase among adolescents referred to gender identity clinics in recent years. Two young adults who regretted their transition and parents of transgender individuals who questioned the clinics’ assessments of their children were interviewed, and concerns were raised about whether gender-confirming treatments are based on sufficient scientific evidence.”
The programs, they suggest, may have influenced and jeopardized young transgender individuals’ access to transgender-specific health care.
Stella O’Malley, a U.K.-based psychotherapist specializing in transgender care and executive director of Genspect, an international organization that provides support to the parents of young people who are questioning their gender, expressed her disappointment with the study’s conclusions.
“I’m really surprised and disappointed that the researchers believe that negative coverage is the reason for a drop in referrals when it is more accurate to say that the information provided by ‘The Trans Train’ documentaries was concerning and suggests that further critical analysis and a review needs to be carried out on the clinics in question,” she said in an interview.
Ms. O’Malley herself made a documentary for Channel 4 in the United Kingdom, broadcast in 2018, called: “Trans Kids: It’s Time to Talk.”
Rapidly increasing numbers of youth, especially girls, question gender
As Ms. Indremo and coauthors explained – and as has been widely reported by this news organization – “the number of referrals to gender identity clinics have rapidly increased worldwide” in recent years, and this “has been especially prominent in adolescents and young adults.”
In addition, they acknowledged, “there has been a shift in gender ratio, with a preponderance toward individuals who were assigned female at birth (AFAB).”
This was the topic of “The Trans Train” programs, and in fact, following their broadcast, Ms. Indremo and colleagues noted that “an intense debate in national media [in Sweden] arose from the documentaries.”
Their research aimed to explore the association between both “positive” and “negative” media coverage and the number of referrals to gender identity clinics for young people (under aged 19) respectively. Data from the six gender clinics in Sweden were included between January 2017 and December 2019.
In the period studied, the clinics received 1,784 referrals, including 613 referrals in 2017, 663 referrals in 2018, and 508 referrals in 2019.
From the age-specific data that included 1,674 referrals, 359 individuals (21.4%) were younger than 13 years and 1,315 individuals (78.6%) were aged 13-18 years. From the assigned sex-specific data that included 1,435 referrals, 1,034 individuals (72.1%) were AFAB and 401 individuals (27.9%) were assigned male at birth (AMAB). Information on sex assigned at birth was lacking from one clinic, which was excluded from the analysis.
When they examined data for the 3 months following the airing of the first part of “The Trans Train” documentary series (in April 2019), they found that referrals to gender clinics fell by 25.4% overall, compared with the 3 months before part 1 was screened. Specifically, they fell by 25.3% for young people aged 13-18 years and by 32.2% for those born female.
In the extended analyses of 6 months following part 1, a decrease of total referrals by 30.7% was observed, while referrals for AFAB individuals decreased by 37.4% and referrals for individuals aged 13-18 years decreased by 27.7%. A decrease of referrals by 41.7% for children aged younger than 13 years was observed in the 6-month analysis, as well as a decrease of 8.2% among AMAB individuals.
“The Trans Train” documentaries, Ms. Indremo and colleagues said, “were criticized for being negatively biased and giving an oversimplified picture of transgender health care.”
Did the nature of the trans train documentaries influence referrals?
In an invited commentary published in JAMA Network Open, Ken C. Pang, PhD, from the Murdoch Children’s Research Institute, Melbourne, and colleagues noted: “Although the mechanisms underlying this decrease [in referrals] were not formally explored in their study, the authors reasonably speculated that both parents and referring health professionals may have been less likely to support a child or adolescent’s attendance at a specialist pediatric gender clinic following the documentaries.”
Dr. Pang and colleagues went on to say it is “the ... responsibility of media organizations in ensuring that stories depicting health care for transgender and gender diverse (TGD) young people are fair, balanced, nuanced, and accurate.”
Often, media reports have “fallen short of these standards and lacked the voices of TGD young people who have benefited from gender-affirming care or the perspectives of health professionals with expertise in providing such care,” they added.
“For example, some [media reports] have suggested that the growing number of referrals to such clinics is not owing to greater awareness of gender diversity and empowerment of TGD young people but is instead being driven by other factors such as peer influence, while others have warned that the use of gender-affirming hormonal interventions in TGD young people represents an undue risk,” they continue.
Ms. Indremo and colleagues didn’t see any drop-in referrals after the second part of the series, aired in October 2019, but they say this was likely because referrals were “already lowered” by the airing of the first part of the documentaries.
Nor did they see an increase in referrals following what they say was a “positive” media event in the form of a story about a professional Swedish handball player who announced the decision to quit his career to seek care for gender dysphoria.
“One may assume that a single news event is not significant enough to influence referral counts,” they suggested, noting also that Sweden represents “a society where there is already a relatively high level of awareness of gender identity issues.”
“Our results point to a differential association of media attention depending on the tone of the media content,” they observed.
Dr. Pang and coauthors noted it would be “helpful to examine whether similar media coverage in other countries has been associated with similar decreases in referral numbers and whether particular types of media stories are more prone to having this association.”
Parents and doctors debate treatment of gender dysphoria
In Sweden, custodians’ permission as well as custodians’ help is needed for minors to access care for gender dysphoria, said Ms. Indremo and coauthors. “It is possible that the content of the documentaries contributed to a higher custodian barrier to having their children referred for assessment, believing it may not be in the best interest of their child. This would highly impact young transgender individuals’ possibilities to access care.”
They also acknowledge that health care practitioners who refer young people to specialist clinics might also have been influenced by the documentaries, noting “some commentators argued that all treatments for gender dysphoria be stopped, and that ‘all health care given at the gender identity clinics was an experiment lacking scientific basis.’ ”
In April 2021, Angela Sämfjord, MD, child and adolescent psychiatrist at Sahlgrenska University Hospital, Gothenburg, Sweden, who started a child and adolescent clinic – the Lundstrom Gender Clinic – told this news organization she had reevaluated her approach even prior to “The Trans Train” documentaries and had resigned in 2018 because of her own fears about the lack of evidence for hormonal and surgical treatments of youth with gender dysphoria.
Following the debate that ensued after the airing of “The Trans Train” programs, the Swedish National Board of Health and Welfare published new recommendations in March 2021, which reflected a significant change in direction for the evaluation of gender dysphoria in minors, emphasizing the requirement for a thorough mental health assessment.
And in May 2021, Karolinska Children’s Hospital, which houses one of the leading gender identity clinics in Sweden, announced it would stop the routine medical treatment of children with gender dysphoria under the age of 18, which meant a total ban on the prescribing of puberty blockers and cross-sex hormones to minors. Such treatment could henceforth only be carried out within the setting of a clinical trial approved by the EPM (Ethical Review Agency/Swedish Institutional Review Board), it said.
The remaining five gender identity clinics in Sweden decided upon their own rules, but in general, they have become much more cautious regarding medical treatment of minors within the past year. Also, there is a desire in Sweden to reduce the number of gender identity clinics for minors from the current six to perhaps a maximum of three nationwide.
However, neither Ms. Indremo and colleagues nor Dr. Pang and colleagues mentioned the subsequent change to the Swedish NBHW recommendations on evaluation of gender dysphoria in minors in JAMA articles.
New NBHW recommendations about medical treatment of gender dysphoria with puberty blockers and cross-sex hormones for minors were due to be issued in 2021 but have been delayed.
Debate in other countries
Sweden is not alone in discussing this issue. In 2020, Finland became the first country in the world to issue new guidelines that concluded there is a lack of quality evidence to support the use of hormonal interventions in adolescents with gender dysphoria.
This issue has been hotly debated in the United Kingdom – not least with the Keira Bell court case and two National Institute for Health and Clinical Excellence evidence reviews concluding there is a lack of data to support the use of puberty-blocking agents and “cross-sex” hormones in youth with gender dysphoria.
And a number of U.S. states are attempting to outlaw the medical and surgical treatment of gender dysphoria in minors. Even health care professionals who have been treating young people with gender dysphoria for years – some of whom are transgender themselves – have started to speak out and are questioning what they call “sloppy care” given to many such youth.
Indeed, a recent survey shows that detransitioners – individuals who suffer from gender dysphoria, transition to the opposite sex but then regret their decision and detransition – are getting short shrift when it comes to care, with over half of the 100 surveyed saying they feel they did not receive adequate evaluation from a doctor or mental health professional before starting to transition.
And new draft standards of care for treating people with gender dysphoria by the World Professional Association for Transgender Health have drawn criticism from experts.
‘First do no harm’
In their conclusion, Dr. Pang and coauthors said that, with respect to the media coverage of young people with gender dysphoria, “who are, after all, one of the most vulnerable subgroups within our society, perhaps our media should recall one of the core tenets of health care and ensure their stories ‘first, do no harm.’”
However, in a commentary recently published in Child and Adolescent Mental Health, Alison Clayton, MBBS, from the University of Melbourne, and coauthors again pointed out that evidence reviews of the use of puberty blockers in young people with gender dysphoria show “there is very low certainty of the benefits of puberty blockers, an unknown risk of harm, and there is need for more rigorous research.”
“The clinically prudent thing to do, if we aim to ‘first, do no harm,’ is to proceed with extreme caution, especially given the rapidly rising case numbers and novel gender dysphoria presentations,” Clayton and colleagues concluded.
Ms. Indremo and coauthors reported no relevant financial relationships. Dr. Pang reported being a member of the Australian Professional Association for Trans Health and its research committee. One commentary coauthor has reported being a member of WPATH.
A version of this article first appeared on Medscape.com.
Media coverage of transgender health care judged to be “negative” was associated with a drop of around 30% in referral rates to gender identity clinics in Sweden among young people under age 19, a new study indicates.
Malin Indremo, MS, from the department of neuroscience, Uppsala (Sweden) University, and colleagues explored the effect of the documentaries, “The Trans Train and Teenage Girls,” which they explain was a “Swedish public service television show” representing “investigative journalism.” The two-part documentary series was aired in Sweden in April 2019 and October 2019, respectively, and is now available in English on YouTube.
In their article, published online in JAMA Network Open, the authors said they consider “The Trans Train” programs to be “negative” media coverage because the “documentaries addressed the distinct increase among adolescents referred to gender identity clinics in recent years. Two young adults who regretted their transition and parents of transgender individuals who questioned the clinics’ assessments of their children were interviewed, and concerns were raised about whether gender-confirming treatments are based on sufficient scientific evidence.”
The programs, they suggest, may have influenced and jeopardized young transgender individuals’ access to transgender-specific health care.
Stella O’Malley, a U.K.-based psychotherapist specializing in transgender care and executive director of Genspect, an international organization that provides support to the parents of young people who are questioning their gender, expressed her disappointment with the study’s conclusions.
“I’m really surprised and disappointed that the researchers believe that negative coverage is the reason for a drop in referrals when it is more accurate to say that the information provided by ‘The Trans Train’ documentaries was concerning and suggests that further critical analysis and a review needs to be carried out on the clinics in question,” she said in an interview.
Ms. O’Malley herself made a documentary for Channel 4 in the United Kingdom, broadcast in 2018, called: “Trans Kids: It’s Time to Talk.”
Rapidly increasing numbers of youth, especially girls, question gender
As Ms. Indremo and coauthors explained – and as has been widely reported by this news organization – “the number of referrals to gender identity clinics have rapidly increased worldwide” in recent years, and this “has been especially prominent in adolescents and young adults.”
In addition, they acknowledged, “there has been a shift in gender ratio, with a preponderance toward individuals who were assigned female at birth (AFAB).”
This was the topic of “The Trans Train” programs, and in fact, following their broadcast, Ms. Indremo and colleagues noted that “an intense debate in national media [in Sweden] arose from the documentaries.”
Their research aimed to explore the association between both “positive” and “negative” media coverage and the number of referrals to gender identity clinics for young people (under aged 19) respectively. Data from the six gender clinics in Sweden were included between January 2017 and December 2019.
In the period studied, the clinics received 1,784 referrals, including 613 referrals in 2017, 663 referrals in 2018, and 508 referrals in 2019.
From the age-specific data that included 1,674 referrals, 359 individuals (21.4%) were younger than 13 years and 1,315 individuals (78.6%) were aged 13-18 years. From the assigned sex-specific data that included 1,435 referrals, 1,034 individuals (72.1%) were AFAB and 401 individuals (27.9%) were assigned male at birth (AMAB). Information on sex assigned at birth was lacking from one clinic, which was excluded from the analysis.
When they examined data for the 3 months following the airing of the first part of “The Trans Train” documentary series (in April 2019), they found that referrals to gender clinics fell by 25.4% overall, compared with the 3 months before part 1 was screened. Specifically, they fell by 25.3% for young people aged 13-18 years and by 32.2% for those born female.
In the extended analyses of 6 months following part 1, a decrease of total referrals by 30.7% was observed, while referrals for AFAB individuals decreased by 37.4% and referrals for individuals aged 13-18 years decreased by 27.7%. A decrease of referrals by 41.7% for children aged younger than 13 years was observed in the 6-month analysis, as well as a decrease of 8.2% among AMAB individuals.
“The Trans Train” documentaries, Ms. Indremo and colleagues said, “were criticized for being negatively biased and giving an oversimplified picture of transgender health care.”
Did the nature of the trans train documentaries influence referrals?
In an invited commentary published in JAMA Network Open, Ken C. Pang, PhD, from the Murdoch Children’s Research Institute, Melbourne, and colleagues noted: “Although the mechanisms underlying this decrease [in referrals] were not formally explored in their study, the authors reasonably speculated that both parents and referring health professionals may have been less likely to support a child or adolescent’s attendance at a specialist pediatric gender clinic following the documentaries.”
Dr. Pang and colleagues went on to say it is “the ... responsibility of media organizations in ensuring that stories depicting health care for transgender and gender diverse (TGD) young people are fair, balanced, nuanced, and accurate.”
Often, media reports have “fallen short of these standards and lacked the voices of TGD young people who have benefited from gender-affirming care or the perspectives of health professionals with expertise in providing such care,” they added.
“For example, some [media reports] have suggested that the growing number of referrals to such clinics is not owing to greater awareness of gender diversity and empowerment of TGD young people but is instead being driven by other factors such as peer influence, while others have warned that the use of gender-affirming hormonal interventions in TGD young people represents an undue risk,” they continue.
Ms. Indremo and colleagues didn’t see any drop-in referrals after the second part of the series, aired in October 2019, but they say this was likely because referrals were “already lowered” by the airing of the first part of the documentaries.
Nor did they see an increase in referrals following what they say was a “positive” media event in the form of a story about a professional Swedish handball player who announced the decision to quit his career to seek care for gender dysphoria.
“One may assume that a single news event is not significant enough to influence referral counts,” they suggested, noting also that Sweden represents “a society where there is already a relatively high level of awareness of gender identity issues.”
“Our results point to a differential association of media attention depending on the tone of the media content,” they observed.
Dr. Pang and coauthors noted it would be “helpful to examine whether similar media coverage in other countries has been associated with similar decreases in referral numbers and whether particular types of media stories are more prone to having this association.”
Parents and doctors debate treatment of gender dysphoria
In Sweden, custodians’ permission as well as custodians’ help is needed for minors to access care for gender dysphoria, said Ms. Indremo and coauthors. “It is possible that the content of the documentaries contributed to a higher custodian barrier to having their children referred for assessment, believing it may not be in the best interest of their child. This would highly impact young transgender individuals’ possibilities to access care.”
They also acknowledge that health care practitioners who refer young people to specialist clinics might also have been influenced by the documentaries, noting “some commentators argued that all treatments for gender dysphoria be stopped, and that ‘all health care given at the gender identity clinics was an experiment lacking scientific basis.’ ”
In April 2021, Angela Sämfjord, MD, child and adolescent psychiatrist at Sahlgrenska University Hospital, Gothenburg, Sweden, who started a child and adolescent clinic – the Lundstrom Gender Clinic – told this news organization she had reevaluated her approach even prior to “The Trans Train” documentaries and had resigned in 2018 because of her own fears about the lack of evidence for hormonal and surgical treatments of youth with gender dysphoria.
Following the debate that ensued after the airing of “The Trans Train” programs, the Swedish National Board of Health and Welfare published new recommendations in March 2021, which reflected a significant change in direction for the evaluation of gender dysphoria in minors, emphasizing the requirement for a thorough mental health assessment.
And in May 2021, Karolinska Children’s Hospital, which houses one of the leading gender identity clinics in Sweden, announced it would stop the routine medical treatment of children with gender dysphoria under the age of 18, which meant a total ban on the prescribing of puberty blockers and cross-sex hormones to minors. Such treatment could henceforth only be carried out within the setting of a clinical trial approved by the EPM (Ethical Review Agency/Swedish Institutional Review Board), it said.
The remaining five gender identity clinics in Sweden decided upon their own rules, but in general, they have become much more cautious regarding medical treatment of minors within the past year. Also, there is a desire in Sweden to reduce the number of gender identity clinics for minors from the current six to perhaps a maximum of three nationwide.
However, neither Ms. Indremo and colleagues nor Dr. Pang and colleagues mentioned the subsequent change to the Swedish NBHW recommendations on evaluation of gender dysphoria in minors in JAMA articles.
New NBHW recommendations about medical treatment of gender dysphoria with puberty blockers and cross-sex hormones for minors were due to be issued in 2021 but have been delayed.
Debate in other countries
Sweden is not alone in discussing this issue. In 2020, Finland became the first country in the world to issue new guidelines that concluded there is a lack of quality evidence to support the use of hormonal interventions in adolescents with gender dysphoria.
This issue has been hotly debated in the United Kingdom – not least with the Keira Bell court case and two National Institute for Health and Clinical Excellence evidence reviews concluding there is a lack of data to support the use of puberty-blocking agents and “cross-sex” hormones in youth with gender dysphoria.
And a number of U.S. states are attempting to outlaw the medical and surgical treatment of gender dysphoria in minors. Even health care professionals who have been treating young people with gender dysphoria for years – some of whom are transgender themselves – have started to speak out and are questioning what they call “sloppy care” given to many such youth.
Indeed, a recent survey shows that detransitioners – individuals who suffer from gender dysphoria, transition to the opposite sex but then regret their decision and detransition – are getting short shrift when it comes to care, with over half of the 100 surveyed saying they feel they did not receive adequate evaluation from a doctor or mental health professional before starting to transition.
And new draft standards of care for treating people with gender dysphoria by the World Professional Association for Transgender Health have drawn criticism from experts.
‘First do no harm’
In their conclusion, Dr. Pang and coauthors said that, with respect to the media coverage of young people with gender dysphoria, “who are, after all, one of the most vulnerable subgroups within our society, perhaps our media should recall one of the core tenets of health care and ensure their stories ‘first, do no harm.’”
However, in a commentary recently published in Child and Adolescent Mental Health, Alison Clayton, MBBS, from the University of Melbourne, and coauthors again pointed out that evidence reviews of the use of puberty blockers in young people with gender dysphoria show “there is very low certainty of the benefits of puberty blockers, an unknown risk of harm, and there is need for more rigorous research.”
“The clinically prudent thing to do, if we aim to ‘first, do no harm,’ is to proceed with extreme caution, especially given the rapidly rising case numbers and novel gender dysphoria presentations,” Clayton and colleagues concluded.
Ms. Indremo and coauthors reported no relevant financial relationships. Dr. Pang reported being a member of the Australian Professional Association for Trans Health and its research committee. One commentary coauthor has reported being a member of WPATH.
A version of this article first appeared on Medscape.com.
Media coverage of transgender health care judged to be “negative” was associated with a drop of around 30% in referral rates to gender identity clinics in Sweden among young people under age 19, a new study indicates.
Malin Indremo, MS, from the department of neuroscience, Uppsala (Sweden) University, and colleagues explored the effect of the documentaries, “The Trans Train and Teenage Girls,” which they explain was a “Swedish public service television show” representing “investigative journalism.” The two-part documentary series was aired in Sweden in April 2019 and October 2019, respectively, and is now available in English on YouTube.
In their article, published online in JAMA Network Open, the authors said they consider “The Trans Train” programs to be “negative” media coverage because the “documentaries addressed the distinct increase among adolescents referred to gender identity clinics in recent years. Two young adults who regretted their transition and parents of transgender individuals who questioned the clinics’ assessments of their children were interviewed, and concerns were raised about whether gender-confirming treatments are based on sufficient scientific evidence.”
The programs, they suggest, may have influenced and jeopardized young transgender individuals’ access to transgender-specific health care.
Stella O’Malley, a U.K.-based psychotherapist specializing in transgender care and executive director of Genspect, an international organization that provides support to the parents of young people who are questioning their gender, expressed her disappointment with the study’s conclusions.
“I’m really surprised and disappointed that the researchers believe that negative coverage is the reason for a drop in referrals when it is more accurate to say that the information provided by ‘The Trans Train’ documentaries was concerning and suggests that further critical analysis and a review needs to be carried out on the clinics in question,” she said in an interview.
Ms. O’Malley herself made a documentary for Channel 4 in the United Kingdom, broadcast in 2018, called: “Trans Kids: It’s Time to Talk.”
Rapidly increasing numbers of youth, especially girls, question gender
As Ms. Indremo and coauthors explained – and as has been widely reported by this news organization – “the number of referrals to gender identity clinics have rapidly increased worldwide” in recent years, and this “has been especially prominent in adolescents and young adults.”
In addition, they acknowledged, “there has been a shift in gender ratio, with a preponderance toward individuals who were assigned female at birth (AFAB).”
This was the topic of “The Trans Train” programs, and in fact, following their broadcast, Ms. Indremo and colleagues noted that “an intense debate in national media [in Sweden] arose from the documentaries.”
Their research aimed to explore the association between both “positive” and “negative” media coverage and the number of referrals to gender identity clinics for young people (under aged 19) respectively. Data from the six gender clinics in Sweden were included between January 2017 and December 2019.
In the period studied, the clinics received 1,784 referrals, including 613 referrals in 2017, 663 referrals in 2018, and 508 referrals in 2019.
From the age-specific data that included 1,674 referrals, 359 individuals (21.4%) were younger than 13 years and 1,315 individuals (78.6%) were aged 13-18 years. From the assigned sex-specific data that included 1,435 referrals, 1,034 individuals (72.1%) were AFAB and 401 individuals (27.9%) were assigned male at birth (AMAB). Information on sex assigned at birth was lacking from one clinic, which was excluded from the analysis.
When they examined data for the 3 months following the airing of the first part of “The Trans Train” documentary series (in April 2019), they found that referrals to gender clinics fell by 25.4% overall, compared with the 3 months before part 1 was screened. Specifically, they fell by 25.3% for young people aged 13-18 years and by 32.2% for those born female.
In the extended analyses of 6 months following part 1, a decrease of total referrals by 30.7% was observed, while referrals for AFAB individuals decreased by 37.4% and referrals for individuals aged 13-18 years decreased by 27.7%. A decrease of referrals by 41.7% for children aged younger than 13 years was observed in the 6-month analysis, as well as a decrease of 8.2% among AMAB individuals.
“The Trans Train” documentaries, Ms. Indremo and colleagues said, “were criticized for being negatively biased and giving an oversimplified picture of transgender health care.”
Did the nature of the trans train documentaries influence referrals?
In an invited commentary published in JAMA Network Open, Ken C. Pang, PhD, from the Murdoch Children’s Research Institute, Melbourne, and colleagues noted: “Although the mechanisms underlying this decrease [in referrals] were not formally explored in their study, the authors reasonably speculated that both parents and referring health professionals may have been less likely to support a child or adolescent’s attendance at a specialist pediatric gender clinic following the documentaries.”
Dr. Pang and colleagues went on to say it is “the ... responsibility of media organizations in ensuring that stories depicting health care for transgender and gender diverse (TGD) young people are fair, balanced, nuanced, and accurate.”
Often, media reports have “fallen short of these standards and lacked the voices of TGD young people who have benefited from gender-affirming care or the perspectives of health professionals with expertise in providing such care,” they added.
“For example, some [media reports] have suggested that the growing number of referrals to such clinics is not owing to greater awareness of gender diversity and empowerment of TGD young people but is instead being driven by other factors such as peer influence, while others have warned that the use of gender-affirming hormonal interventions in TGD young people represents an undue risk,” they continue.
Ms. Indremo and colleagues didn’t see any drop-in referrals after the second part of the series, aired in October 2019, but they say this was likely because referrals were “already lowered” by the airing of the first part of the documentaries.
Nor did they see an increase in referrals following what they say was a “positive” media event in the form of a story about a professional Swedish handball player who announced the decision to quit his career to seek care for gender dysphoria.
“One may assume that a single news event is not significant enough to influence referral counts,” they suggested, noting also that Sweden represents “a society where there is already a relatively high level of awareness of gender identity issues.”
“Our results point to a differential association of media attention depending on the tone of the media content,” they observed.
Dr. Pang and coauthors noted it would be “helpful to examine whether similar media coverage in other countries has been associated with similar decreases in referral numbers and whether particular types of media stories are more prone to having this association.”
Parents and doctors debate treatment of gender dysphoria
In Sweden, custodians’ permission as well as custodians’ help is needed for minors to access care for gender dysphoria, said Ms. Indremo and coauthors. “It is possible that the content of the documentaries contributed to a higher custodian barrier to having their children referred for assessment, believing it may not be in the best interest of their child. This would highly impact young transgender individuals’ possibilities to access care.”
They also acknowledge that health care practitioners who refer young people to specialist clinics might also have been influenced by the documentaries, noting “some commentators argued that all treatments for gender dysphoria be stopped, and that ‘all health care given at the gender identity clinics was an experiment lacking scientific basis.’ ”
In April 2021, Angela Sämfjord, MD, child and adolescent psychiatrist at Sahlgrenska University Hospital, Gothenburg, Sweden, who started a child and adolescent clinic – the Lundstrom Gender Clinic – told this news organization she had reevaluated her approach even prior to “The Trans Train” documentaries and had resigned in 2018 because of her own fears about the lack of evidence for hormonal and surgical treatments of youth with gender dysphoria.
Following the debate that ensued after the airing of “The Trans Train” programs, the Swedish National Board of Health and Welfare published new recommendations in March 2021, which reflected a significant change in direction for the evaluation of gender dysphoria in minors, emphasizing the requirement for a thorough mental health assessment.
And in May 2021, Karolinska Children’s Hospital, which houses one of the leading gender identity clinics in Sweden, announced it would stop the routine medical treatment of children with gender dysphoria under the age of 18, which meant a total ban on the prescribing of puberty blockers and cross-sex hormones to minors. Such treatment could henceforth only be carried out within the setting of a clinical trial approved by the EPM (Ethical Review Agency/Swedish Institutional Review Board), it said.
The remaining five gender identity clinics in Sweden decided upon their own rules, but in general, they have become much more cautious regarding medical treatment of minors within the past year. Also, there is a desire in Sweden to reduce the number of gender identity clinics for minors from the current six to perhaps a maximum of three nationwide.
However, neither Ms. Indremo and colleagues nor Dr. Pang and colleagues mentioned the subsequent change to the Swedish NBHW recommendations on evaluation of gender dysphoria in minors in JAMA articles.
New NBHW recommendations about medical treatment of gender dysphoria with puberty blockers and cross-sex hormones for minors were due to be issued in 2021 but have been delayed.
Debate in other countries
Sweden is not alone in discussing this issue. In 2020, Finland became the first country in the world to issue new guidelines that concluded there is a lack of quality evidence to support the use of hormonal interventions in adolescents with gender dysphoria.
This issue has been hotly debated in the United Kingdom – not least with the Keira Bell court case and two National Institute for Health and Clinical Excellence evidence reviews concluding there is a lack of data to support the use of puberty-blocking agents and “cross-sex” hormones in youth with gender dysphoria.
And a number of U.S. states are attempting to outlaw the medical and surgical treatment of gender dysphoria in minors. Even health care professionals who have been treating young people with gender dysphoria for years – some of whom are transgender themselves – have started to speak out and are questioning what they call “sloppy care” given to many such youth.
Indeed, a recent survey shows that detransitioners – individuals who suffer from gender dysphoria, transition to the opposite sex but then regret their decision and detransition – are getting short shrift when it comes to care, with over half of the 100 surveyed saying they feel they did not receive adequate evaluation from a doctor or mental health professional before starting to transition.
And new draft standards of care for treating people with gender dysphoria by the World Professional Association for Transgender Health have drawn criticism from experts.
‘First do no harm’
In their conclusion, Dr. Pang and coauthors said that, with respect to the media coverage of young people with gender dysphoria, “who are, after all, one of the most vulnerable subgroups within our society, perhaps our media should recall one of the core tenets of health care and ensure their stories ‘first, do no harm.’”
However, in a commentary recently published in Child and Adolescent Mental Health, Alison Clayton, MBBS, from the University of Melbourne, and coauthors again pointed out that evidence reviews of the use of puberty blockers in young people with gender dysphoria show “there is very low certainty of the benefits of puberty blockers, an unknown risk of harm, and there is need for more rigorous research.”
“The clinically prudent thing to do, if we aim to ‘first, do no harm,’ is to proceed with extreme caution, especially given the rapidly rising case numbers and novel gender dysphoria presentations,” Clayton and colleagues concluded.
Ms. Indremo and coauthors reported no relevant financial relationships. Dr. Pang reported being a member of the Australian Professional Association for Trans Health and its research committee. One commentary coauthor has reported being a member of WPATH.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN