User login
Is there a cure for aging?
Heart disease. Cancer. Diabetes. Dementia.
Researchers spend billions of dollars every year trying to eradicate these medical scourges.
Yet even if we discover cures to these and all other chronic conditions, it won’t change our ultimate prognosis: death.
“That’s because you haven’t stopped aging,” says Jay Olshansky, PhD, a professor of epidemiology and biostatistics at the University of Illinois at Chicago School of Public Health.
But what if we could?
Some scientists think so. Fueled in part by a billion dollars of investor money, they are attempting to reverse-engineer your molecular biological clock. Their goal? To eliminate not merely diseases that kill people, but to prevent death itself.
Hacking the code for immortality
Aubrey de Grey, PhD, a biomedical gerontologist, has drawn wide attention for his belief that the first person who will live to be 1,000 years old is already among us.
He believes there’s no cap on how long we can live, depending on what medicines we develop in the future.
“The whole idea is that there would not be a limit on how long we can keep people healthy,” Dr. de Grey says. He’s the chief science officer and co-founder of the SENS Research Foundation, which funds research on how to put the brakes on aging.
Dr. De Grey’s view, in theory, isn’t so far-fetched.
Scientists have studied the immortal jellyfish, Turritopsis dohrnii. It’s the only animal that can cheat death by reverting from adulthood back to its polyp stage when threatened with danger or starvation.
Other clues to possible eternal life also may exist underwater. Certain marine clams can live more than 500 years. And lobsters stock a seemingly limitless supply of a youthful enzyme that has some scientists wondering if the crustacean, under the best conditions, just might live forever.
Among humans, researchers have been studying “super-agers” – people who not only live exceptionally long, but also do so without many of the chronic diseases that plague their peers. That’s even though they share some of the same bad habits as everyone else.
“They are making it past the age of 80 with their minds completely intact. That’s what’s so unusual,” Dr. Olshansky says. The rest of their bodies are doing better than those of average 80-year-olds, too.
People who reached ages 95 to 112 got cancer, heart disease, diabetes, osteoporosis, and stroke up to 24 years later than those with average lifespans, data show. Figuring out why might pave the way for targeted gene therapy to mimic the DNA of these nonagenarians and centenarians.
“There’s likely to be secrets contained within their genome that are eventually discovered that will help us develop therapeutic interventions to mimic the effects of decelerated aging,” Dr. Olshansky says.
Treating aging this way may offer a bigger payoff than targeting individual diseases. That’s because even if you manage to dodge any illnesses, there’s ultimately no escaping old age.
“Longevity is a side effect of health,” Dr. de Grey says. “If we can keep people healthy, then their likelihood of dying is reduced.”
Aging as a preventable condition
In 2015, Michael Cantor was prescribed metformin for prediabetes. Once that was under control, his doctor said Mr. Cantor could quit the drug. But Mr. Cantor had heard about studies testing it as an anti-aging drug. The 62-year-old Connecticut-based attorney asked if he could stay on it. A year ago Cantor’s wife, Shari, who is mayor of West Hartford, Conn., started to take metformin, too.
“I read the articles, they made a lot of sense to me, and with the number of people that have been taking this drug worldwide for decades, I felt like there was nothing to lose,” he says.
The couple can’t say if their daily doses have led to any changes in how they look or feel. After all, they’re taking the pills not to treat current ailments but to prevent ones in the future.
They may have answers soon. Nir Barzilai, MD, director of the National Institutes of Health’s Nathan Shock Centers of Excellence in the Basic Biology of Aging, is leading a study that hopes to prove aging is a preventable health condition. The TAME (Targeting Aging with Metformin) study is designed to do this by demonstrating that metformin, a cheap and widely prescribed pill for diabetes, may also be an anti-aging elixir.
The TAME trial is currently in phase III – typically the final step of research into any treatment before drugmakers can apply for FDA approval.
Earlier studies found that people with type 2 diabetes who take metformin have lower death rates from any cause, compared to peers who don’t take the drug. Metformin also seems to help curb the incidence of age-related diseases, including heart disease, dementia, and Alzheimer›s. It also may lower the risk of many types of cancer as well as raise the chances of survival. Observations made since the beginning of the COVID-19 pandemic suggest that people who get the virus while taking metformin are less likely to land in the hospital or die from it.
It’s not clear exactly how metformin works to do all that. The compound was originally derived from Galega officinalis, also known as goat’s rue, a perennial plant used as medicine since medieval times.
Dr. Barzilai says he hopes to prove that aging is a preventable condition.
“If the results are what they think they will be, the whole world could go on metformin and extend life for everybody – extend your good quality of life,” Dr. Barzilai says. “That’s what we all want. Every extra year that we could get where we’re still vigorous and vital would be amazing.”
Long life versus healthy life
Some researchers argue that only the “healthspan” – the period of life free of illness – is worth extending. Of course, a healthy lifestyle can add years to most people’s lives and actually improve cellular aging. Some of the biggest payoffs come from quitting or never smoking, logging more than 5½ hours of physical activity per week, and keeping a normal weight.
Drugs may be able to do that as well by interrupting common markers of aging, including telomere length, inflammation, oxidative stress, and slower cell metabolism.
“You don’t have to target all of these hallmarks to get improvement” in healthspans, says Dr. Barzilai, who also is director of the Institute for Aging Research at the Albert Einstein College of Medicine in the Bronx and scientific director of the American Federation for Aging Research.
“If you target one, you show benefit in the others.”
The medical term for growing old is senescence. Buffeted by DNA damage and stresses, your cells deteriorate and eventually stop multiplying, but don’t die.
That slowdown may have big consequences for your health. Your genes become more likely to get mutations, which can pave the way for cancer. Mitochondria, which produce energy in the cell, struggle to fuel your body. That can damage cells and cause chronic inflammation, which plays a part in diabetes, arthritis, ulcerative colitis, and many other diseases.
One major hallmark of aging is the growing stockpile of these senescent cells. Damaged cells become deactivated as a way to protect your body from harmful or uncontrolled cell division. But like the rotten apple that spoils the whole bunch, senescent cells encourage their neighbors to turn dysfunctional, too. They also emit proteins that trigger inflammation. Your body naturally removes these dormant cells. But older immune systems have a harder time cleaning up, so the senescent cells are more likely to hang around.
Flushing out this accumulated debris may be one way to avert aging, some experts say.
Dr. De Grey also believes that could be done with drugs.
“These therapies would actually repair [cellular] damage,” he says. “They’ll eliminate damage from the body by resetting or turning back the clock.”
James Kirkland, MD, PhD, of the Mayo Clinic, is one researcher exploring this theory. He gave a mixture of the cancer drug dasatinib and a plant pigment called quercetin to people with diabetic kidney disease. Quercetin is an antioxidant that gives grapes, tomatoes, and other fruits and vegetables their flavor.
A small phase I clinical trial showed that the dasatinib-quercetin combination got rid of senescent cells in the tissues of people with the disease.
The researchers don’t know yet if the results will translate into prolonged youth. They also don’t know how high a dosage is needed and what long-term problems the treatment might cause. People with chronic leukemia take dasatinib for years with few serious ill effects.
In another recent study, scientists used oxygen therapy to tackle senescent cells. Thirty-five adults ages 64 and older received oxygen therapy in a pressurized chamber. After 60 daily sessions, they showed a decrease in senescent cells and improvement in the length of DNA segments called telomeres. Shortened segments of telomeres are thought to be another marker of aging.
Researchers are also looking to the gene-editing technology CRISPR for anti-aging treatments, but the testing is only in mice so far.
Dr. Barzilai hopes that if the metformin trial succeeds, it will open the floodgates to a wave of new drugs that can stop or reverse human aging. Some of the major players in this field include Juvenescence, AgeX Therapeutics, LyGenesis, and Life Biosciences, which Dr. Barzilai founded.
“Until aging is seen as preventable, health plans won’t have to pay for this type of treatment,” he says. And if health plans won’t cover aging, pharmaceutical companies have little incentive to invest in drug development.
That may be the only thing standing between humans and unprecedented lifespans. The Census Bureau projects that Americans born in 2060 should live an average of 85.6 years, up from 78.7 years in 2018. Dr. De Grey’s prediction tops that mark by a factor of about 50. He believes that the life expectancy for someone born in 2100 may well be 5,000 years.
Dr. Barzilai, for his part, has a prediction that’s seemingly more modest.
“We die at 80. Getting an additional 35 years is relatively low-hanging fruit,” he says. “But I don’t believe that is a fixed limit.”
A version of this article first appeared on WebMD.com.
Heart disease. Cancer. Diabetes. Dementia.
Researchers spend billions of dollars every year trying to eradicate these medical scourges.
Yet even if we discover cures to these and all other chronic conditions, it won’t change our ultimate prognosis: death.
“That’s because you haven’t stopped aging,” says Jay Olshansky, PhD, a professor of epidemiology and biostatistics at the University of Illinois at Chicago School of Public Health.
But what if we could?
Some scientists think so. Fueled in part by a billion dollars of investor money, they are attempting to reverse-engineer your molecular biological clock. Their goal? To eliminate not merely diseases that kill people, but to prevent death itself.
Hacking the code for immortality
Aubrey de Grey, PhD, a biomedical gerontologist, has drawn wide attention for his belief that the first person who will live to be 1,000 years old is already among us.
He believes there’s no cap on how long we can live, depending on what medicines we develop in the future.
“The whole idea is that there would not be a limit on how long we can keep people healthy,” Dr. de Grey says. He’s the chief science officer and co-founder of the SENS Research Foundation, which funds research on how to put the brakes on aging.
Dr. De Grey’s view, in theory, isn’t so far-fetched.
Scientists have studied the immortal jellyfish, Turritopsis dohrnii. It’s the only animal that can cheat death by reverting from adulthood back to its polyp stage when threatened with danger or starvation.
Other clues to possible eternal life also may exist underwater. Certain marine clams can live more than 500 years. And lobsters stock a seemingly limitless supply of a youthful enzyme that has some scientists wondering if the crustacean, under the best conditions, just might live forever.
Among humans, researchers have been studying “super-agers” – people who not only live exceptionally long, but also do so without many of the chronic diseases that plague their peers. That’s even though they share some of the same bad habits as everyone else.
“They are making it past the age of 80 with their minds completely intact. That’s what’s so unusual,” Dr. Olshansky says. The rest of their bodies are doing better than those of average 80-year-olds, too.
People who reached ages 95 to 112 got cancer, heart disease, diabetes, osteoporosis, and stroke up to 24 years later than those with average lifespans, data show. Figuring out why might pave the way for targeted gene therapy to mimic the DNA of these nonagenarians and centenarians.
“There’s likely to be secrets contained within their genome that are eventually discovered that will help us develop therapeutic interventions to mimic the effects of decelerated aging,” Dr. Olshansky says.
Treating aging this way may offer a bigger payoff than targeting individual diseases. That’s because even if you manage to dodge any illnesses, there’s ultimately no escaping old age.
“Longevity is a side effect of health,” Dr. de Grey says. “If we can keep people healthy, then their likelihood of dying is reduced.”
Aging as a preventable condition
In 2015, Michael Cantor was prescribed metformin for prediabetes. Once that was under control, his doctor said Mr. Cantor could quit the drug. But Mr. Cantor had heard about studies testing it as an anti-aging drug. The 62-year-old Connecticut-based attorney asked if he could stay on it. A year ago Cantor’s wife, Shari, who is mayor of West Hartford, Conn., started to take metformin, too.
“I read the articles, they made a lot of sense to me, and with the number of people that have been taking this drug worldwide for decades, I felt like there was nothing to lose,” he says.
The couple can’t say if their daily doses have led to any changes in how they look or feel. After all, they’re taking the pills not to treat current ailments but to prevent ones in the future.
They may have answers soon. Nir Barzilai, MD, director of the National Institutes of Health’s Nathan Shock Centers of Excellence in the Basic Biology of Aging, is leading a study that hopes to prove aging is a preventable health condition. The TAME (Targeting Aging with Metformin) study is designed to do this by demonstrating that metformin, a cheap and widely prescribed pill for diabetes, may also be an anti-aging elixir.
The TAME trial is currently in phase III – typically the final step of research into any treatment before drugmakers can apply for FDA approval.
Earlier studies found that people with type 2 diabetes who take metformin have lower death rates from any cause, compared to peers who don’t take the drug. Metformin also seems to help curb the incidence of age-related diseases, including heart disease, dementia, and Alzheimer›s. It also may lower the risk of many types of cancer as well as raise the chances of survival. Observations made since the beginning of the COVID-19 pandemic suggest that people who get the virus while taking metformin are less likely to land in the hospital or die from it.
It’s not clear exactly how metformin works to do all that. The compound was originally derived from Galega officinalis, also known as goat’s rue, a perennial plant used as medicine since medieval times.
Dr. Barzilai says he hopes to prove that aging is a preventable condition.
“If the results are what they think they will be, the whole world could go on metformin and extend life for everybody – extend your good quality of life,” Dr. Barzilai says. “That’s what we all want. Every extra year that we could get where we’re still vigorous and vital would be amazing.”
Long life versus healthy life
Some researchers argue that only the “healthspan” – the period of life free of illness – is worth extending. Of course, a healthy lifestyle can add years to most people’s lives and actually improve cellular aging. Some of the biggest payoffs come from quitting or never smoking, logging more than 5½ hours of physical activity per week, and keeping a normal weight.
Drugs may be able to do that as well by interrupting common markers of aging, including telomere length, inflammation, oxidative stress, and slower cell metabolism.
“You don’t have to target all of these hallmarks to get improvement” in healthspans, says Dr. Barzilai, who also is director of the Institute for Aging Research at the Albert Einstein College of Medicine in the Bronx and scientific director of the American Federation for Aging Research.
“If you target one, you show benefit in the others.”
The medical term for growing old is senescence. Buffeted by DNA damage and stresses, your cells deteriorate and eventually stop multiplying, but don’t die.
That slowdown may have big consequences for your health. Your genes become more likely to get mutations, which can pave the way for cancer. Mitochondria, which produce energy in the cell, struggle to fuel your body. That can damage cells and cause chronic inflammation, which plays a part in diabetes, arthritis, ulcerative colitis, and many other diseases.
One major hallmark of aging is the growing stockpile of these senescent cells. Damaged cells become deactivated as a way to protect your body from harmful or uncontrolled cell division. But like the rotten apple that spoils the whole bunch, senescent cells encourage their neighbors to turn dysfunctional, too. They also emit proteins that trigger inflammation. Your body naturally removes these dormant cells. But older immune systems have a harder time cleaning up, so the senescent cells are more likely to hang around.
Flushing out this accumulated debris may be one way to avert aging, some experts say.
Dr. De Grey also believes that could be done with drugs.
“These therapies would actually repair [cellular] damage,” he says. “They’ll eliminate damage from the body by resetting or turning back the clock.”
James Kirkland, MD, PhD, of the Mayo Clinic, is one researcher exploring this theory. He gave a mixture of the cancer drug dasatinib and a plant pigment called quercetin to people with diabetic kidney disease. Quercetin is an antioxidant that gives grapes, tomatoes, and other fruits and vegetables their flavor.
A small phase I clinical trial showed that the dasatinib-quercetin combination got rid of senescent cells in the tissues of people with the disease.
The researchers don’t know yet if the results will translate into prolonged youth. They also don’t know how high a dosage is needed and what long-term problems the treatment might cause. People with chronic leukemia take dasatinib for years with few serious ill effects.
In another recent study, scientists used oxygen therapy to tackle senescent cells. Thirty-five adults ages 64 and older received oxygen therapy in a pressurized chamber. After 60 daily sessions, they showed a decrease in senescent cells and improvement in the length of DNA segments called telomeres. Shortened segments of telomeres are thought to be another marker of aging.
Researchers are also looking to the gene-editing technology CRISPR for anti-aging treatments, but the testing is only in mice so far.
Dr. Barzilai hopes that if the metformin trial succeeds, it will open the floodgates to a wave of new drugs that can stop or reverse human aging. Some of the major players in this field include Juvenescence, AgeX Therapeutics, LyGenesis, and Life Biosciences, which Dr. Barzilai founded.
“Until aging is seen as preventable, health plans won’t have to pay for this type of treatment,” he says. And if health plans won’t cover aging, pharmaceutical companies have little incentive to invest in drug development.
That may be the only thing standing between humans and unprecedented lifespans. The Census Bureau projects that Americans born in 2060 should live an average of 85.6 years, up from 78.7 years in 2018. Dr. De Grey’s prediction tops that mark by a factor of about 50. He believes that the life expectancy for someone born in 2100 may well be 5,000 years.
Dr. Barzilai, for his part, has a prediction that’s seemingly more modest.
“We die at 80. Getting an additional 35 years is relatively low-hanging fruit,” he says. “But I don’t believe that is a fixed limit.”
A version of this article first appeared on WebMD.com.
Heart disease. Cancer. Diabetes. Dementia.
Researchers spend billions of dollars every year trying to eradicate these medical scourges.
Yet even if we discover cures to these and all other chronic conditions, it won’t change our ultimate prognosis: death.
“That’s because you haven’t stopped aging,” says Jay Olshansky, PhD, a professor of epidemiology and biostatistics at the University of Illinois at Chicago School of Public Health.
But what if we could?
Some scientists think so. Fueled in part by a billion dollars of investor money, they are attempting to reverse-engineer your molecular biological clock. Their goal? To eliminate not merely diseases that kill people, but to prevent death itself.
Hacking the code for immortality
Aubrey de Grey, PhD, a biomedical gerontologist, has drawn wide attention for his belief that the first person who will live to be 1,000 years old is already among us.
He believes there’s no cap on how long we can live, depending on what medicines we develop in the future.
“The whole idea is that there would not be a limit on how long we can keep people healthy,” Dr. de Grey says. He’s the chief science officer and co-founder of the SENS Research Foundation, which funds research on how to put the brakes on aging.
Dr. De Grey’s view, in theory, isn’t so far-fetched.
Scientists have studied the immortal jellyfish, Turritopsis dohrnii. It’s the only animal that can cheat death by reverting from adulthood back to its polyp stage when threatened with danger or starvation.
Other clues to possible eternal life also may exist underwater. Certain marine clams can live more than 500 years. And lobsters stock a seemingly limitless supply of a youthful enzyme that has some scientists wondering if the crustacean, under the best conditions, just might live forever.
Among humans, researchers have been studying “super-agers” – people who not only live exceptionally long, but also do so without many of the chronic diseases that plague their peers. That’s even though they share some of the same bad habits as everyone else.
“They are making it past the age of 80 with their minds completely intact. That’s what’s so unusual,” Dr. Olshansky says. The rest of their bodies are doing better than those of average 80-year-olds, too.
People who reached ages 95 to 112 got cancer, heart disease, diabetes, osteoporosis, and stroke up to 24 years later than those with average lifespans, data show. Figuring out why might pave the way for targeted gene therapy to mimic the DNA of these nonagenarians and centenarians.
“There’s likely to be secrets contained within their genome that are eventually discovered that will help us develop therapeutic interventions to mimic the effects of decelerated aging,” Dr. Olshansky says.
Treating aging this way may offer a bigger payoff than targeting individual diseases. That’s because even if you manage to dodge any illnesses, there’s ultimately no escaping old age.
“Longevity is a side effect of health,” Dr. de Grey says. “If we can keep people healthy, then their likelihood of dying is reduced.”
Aging as a preventable condition
In 2015, Michael Cantor was prescribed metformin for prediabetes. Once that was under control, his doctor said Mr. Cantor could quit the drug. But Mr. Cantor had heard about studies testing it as an anti-aging drug. The 62-year-old Connecticut-based attorney asked if he could stay on it. A year ago Cantor’s wife, Shari, who is mayor of West Hartford, Conn., started to take metformin, too.
“I read the articles, they made a lot of sense to me, and with the number of people that have been taking this drug worldwide for decades, I felt like there was nothing to lose,” he says.
The couple can’t say if their daily doses have led to any changes in how they look or feel. After all, they’re taking the pills not to treat current ailments but to prevent ones in the future.
They may have answers soon. Nir Barzilai, MD, director of the National Institutes of Health’s Nathan Shock Centers of Excellence in the Basic Biology of Aging, is leading a study that hopes to prove aging is a preventable health condition. The TAME (Targeting Aging with Metformin) study is designed to do this by demonstrating that metformin, a cheap and widely prescribed pill for diabetes, may also be an anti-aging elixir.
The TAME trial is currently in phase III – typically the final step of research into any treatment before drugmakers can apply for FDA approval.
Earlier studies found that people with type 2 diabetes who take metformin have lower death rates from any cause, compared to peers who don’t take the drug. Metformin also seems to help curb the incidence of age-related diseases, including heart disease, dementia, and Alzheimer›s. It also may lower the risk of many types of cancer as well as raise the chances of survival. Observations made since the beginning of the COVID-19 pandemic suggest that people who get the virus while taking metformin are less likely to land in the hospital or die from it.
It’s not clear exactly how metformin works to do all that. The compound was originally derived from Galega officinalis, also known as goat’s rue, a perennial plant used as medicine since medieval times.
Dr. Barzilai says he hopes to prove that aging is a preventable condition.
“If the results are what they think they will be, the whole world could go on metformin and extend life for everybody – extend your good quality of life,” Dr. Barzilai says. “That’s what we all want. Every extra year that we could get where we’re still vigorous and vital would be amazing.”
Long life versus healthy life
Some researchers argue that only the “healthspan” – the period of life free of illness – is worth extending. Of course, a healthy lifestyle can add years to most people’s lives and actually improve cellular aging. Some of the biggest payoffs come from quitting or never smoking, logging more than 5½ hours of physical activity per week, and keeping a normal weight.
Drugs may be able to do that as well by interrupting common markers of aging, including telomere length, inflammation, oxidative stress, and slower cell metabolism.
“You don’t have to target all of these hallmarks to get improvement” in healthspans, says Dr. Barzilai, who also is director of the Institute for Aging Research at the Albert Einstein College of Medicine in the Bronx and scientific director of the American Federation for Aging Research.
“If you target one, you show benefit in the others.”
The medical term for growing old is senescence. Buffeted by DNA damage and stresses, your cells deteriorate and eventually stop multiplying, but don’t die.
That slowdown may have big consequences for your health. Your genes become more likely to get mutations, which can pave the way for cancer. Mitochondria, which produce energy in the cell, struggle to fuel your body. That can damage cells and cause chronic inflammation, which plays a part in diabetes, arthritis, ulcerative colitis, and many other diseases.
One major hallmark of aging is the growing stockpile of these senescent cells. Damaged cells become deactivated as a way to protect your body from harmful or uncontrolled cell division. But like the rotten apple that spoils the whole bunch, senescent cells encourage their neighbors to turn dysfunctional, too. They also emit proteins that trigger inflammation. Your body naturally removes these dormant cells. But older immune systems have a harder time cleaning up, so the senescent cells are more likely to hang around.
Flushing out this accumulated debris may be one way to avert aging, some experts say.
Dr. De Grey also believes that could be done with drugs.
“These therapies would actually repair [cellular] damage,” he says. “They’ll eliminate damage from the body by resetting or turning back the clock.”
James Kirkland, MD, PhD, of the Mayo Clinic, is one researcher exploring this theory. He gave a mixture of the cancer drug dasatinib and a plant pigment called quercetin to people with diabetic kidney disease. Quercetin is an antioxidant that gives grapes, tomatoes, and other fruits and vegetables their flavor.
A small phase I clinical trial showed that the dasatinib-quercetin combination got rid of senescent cells in the tissues of people with the disease.
The researchers don’t know yet if the results will translate into prolonged youth. They also don’t know how high a dosage is needed and what long-term problems the treatment might cause. People with chronic leukemia take dasatinib for years with few serious ill effects.
In another recent study, scientists used oxygen therapy to tackle senescent cells. Thirty-five adults ages 64 and older received oxygen therapy in a pressurized chamber. After 60 daily sessions, they showed a decrease in senescent cells and improvement in the length of DNA segments called telomeres. Shortened segments of telomeres are thought to be another marker of aging.
Researchers are also looking to the gene-editing technology CRISPR for anti-aging treatments, but the testing is only in mice so far.
Dr. Barzilai hopes that if the metformin trial succeeds, it will open the floodgates to a wave of new drugs that can stop or reverse human aging. Some of the major players in this field include Juvenescence, AgeX Therapeutics, LyGenesis, and Life Biosciences, which Dr. Barzilai founded.
“Until aging is seen as preventable, health plans won’t have to pay for this type of treatment,” he says. And if health plans won’t cover aging, pharmaceutical companies have little incentive to invest in drug development.
That may be the only thing standing between humans and unprecedented lifespans. The Census Bureau projects that Americans born in 2060 should live an average of 85.6 years, up from 78.7 years in 2018. Dr. De Grey’s prediction tops that mark by a factor of about 50. He believes that the life expectancy for someone born in 2100 may well be 5,000 years.
Dr. Barzilai, for his part, has a prediction that’s seemingly more modest.
“We die at 80. Getting an additional 35 years is relatively low-hanging fruit,” he says. “But I don’t believe that is a fixed limit.”
A version of this article first appeared on WebMD.com.
Oncologists in malpractice suits: Less than other specialties
, notes the latest Medscape Malpractice Report.
Over a third (39%) of oncologists who were surveyed said that they had been named in at least one malpractice suit, according to the Medscape Oncologist Malpractice Report 2021.
This number is considerably lower than that reported by physicians across all specialties (51%), and it is also much lower than that reported by oncologists in past years. In the 2019 report, 54% of oncologists surveyed said they had been named in a malpractice suit, while in the 2017 report, the figure was 53%.
The dramatic decline in malpractice suits may have much to do with the COVID-19 pandemic, when oncology care was in a state of flux.
“Fewer people were seeking cancer care during the COVID pandemic, which might have impacted the number of lawsuits brought against oncologists,” says Paul Walker, a New York–based malpractice attorney at Walker Medical Law, who represents physicians and other healthcare professionals.
“Additionally, a fair number of people who died of COVID were also older,” he pointed out, and it is often older people who get cancer, so there were fewer older people who consulted an oncologist or were treated by one, he added.
However, the pandemic may be storing up trouble for future years. “Patient fears of contracting COVID-19 have led many to avoid seeking or resuming care, so delays in diagnosing new cancer cases could mean that more patients are diagnosed at a later stage of their disease, leading to potential adverse events and malpractice claims,” commented David L. Feldman, MD, MBA, chief medical officer of The Doctors Company Group.
This latest 2021 Medscape Malpractice Report was compiled from an online survey that included more than 4,300 physicians from 29 specialties. It included 106 oncologists. More than half of respondents (56%) had been in practice for more than 25 years, and 54% were aged 60 years or older. The survey was available from May 21 to August 28, 2021.
Similar to findings in previous years, complications from treatment/surgery were the most common reason for the lawsuits (31%). Failure to make a correct diagnosis or a delay in diagnosis was the second most common reason (23%), while 20% of patients sued because of a poor outcome or disease progression.
Surprise at being sued
Among the oncologists who reported involvement in a lawsuit in 2021, the majority (86%) said they were “very surprised” or “somewhat surprised” by the malpractice suit, which is similar to that of other physicians surveyed. However, fewer were surprised this year as compared to 2019 and 2017 (90% and 94%).
One reason for the surprise over the litigation was that it concerned a patient who had been treated a long time ago. One oncologist wrote that “the patient had not seen me for over 7 years and during that time, he did not call me with his new symptomatology. I was only named in the suit because I had previously been involved.”
Another common scenario reported by oncologists was being named in a lawsuit which was brought by another clinician’s patient. “I was the chairperson of the department, and one of the doctors in the practice was involved in the suit,” wrote one respondent. “I was named as an accomplice.”
More than half of surveyed oncologists said that they were able to identify the patient who bought the suit, and these figures are again comparable to those of other physicians. One oncologist commented that in the case he was involved with, the family did not understand or accept the nature of cancer and the different ways that a patient could die of complications. This patient had died of sepsis and pneumonia related to decubitus ulcers that were completely unrelated to her radiation therapy.
As in the case above, sometimes it is the family who filed the lawsuit, not the patient.
“The patient may even recognize that you did your best and be grateful for your skill and efforts, but the family can’t accept that grandma died of cancer and brings a lawsuit,” said Dennis Hursh, an attorney with Physicians Agreement Health Law in Pennsylvania.
When looking at outcomes of the lawsuit, 40% of oncologists were dismissed from the suit within the first few months, or the case was settled before going to trial. This trend is also consistent with the results from the 2019 and 2017 surveys. When the case did go to trial, 10% received a favorable verdict, which was the same in 2019.
“It seems that most of my clients end up being released from lawsuits, and many lawsuits are dismissed prior to proceeding to trial,” Mr. Hursh commented.
Murdering psychopath
Some oncologists weighed in on what they felt was the worst experience of being sued.
“Mental anguish, knowing that I did nothing wrong,” said one physician. Another reported that it was a feeling of being “inadequate and totally alone.”
Another oncologist commented that the “depositions from lawyers implied that I was worse than a murdering psychopath. My reputation was permanently damaged.”
However, the vast majority of oncologists (88%) did not believe that the lawsuit negatively affected their career, which was similar to physicians in general. That said, many did complain about the ongoing requirement to report the lawsuit to the credentialing committee, even if it was dismissed, and then having to pay increased malpractice premiums. “I still need to document this episode every single time I apply for any medical position, even more than 29 years after I was dismissed from the case,” said one respondent.
When asked if they would do anything differently, many oncologists (42%) said no, they would not have done anything differently. This is similar to the responses from physicians in general and with 2019 responses from oncologists. However, 15% of the respondents said that in retrospect, they would not have taken on that patient to begin with.
Some oncologists noted that they would have been more conscientious in relaying the information to the referring physician. Evan Lyman, an associate attorney at Voute, Lohrfink, McAndrew, Meisner & Roberts, LLP, in White Plains, N.Y., pointed out that a common reason for lawsuits is a slip-up of communication between the specialist and the referring physician.
Oncologists who had been sued have some insights to offer to colleagues, should they find themselves in a similar situation.
“Only answer with short and precise statements,” wrote one oncologist. “Attend all the depositions as much as you can; they are more likely to fabricate or exaggerate if you are not sitting in the room.”
Another physician said to base “everything on the medical record and do not answer hypothetical questions.”
“Document all interactions with patients as if a jury will be reading them, word by word,” said one respondent.
As for the public or patients, oncologists had this message: “malpractice suits should be rarely launched and only when gross errors can be absolutely proven.”
Another oncologist pointed out that communication is key. “Speak to the physicians against whom you have distrust. Lots of things could be cleared by good communication.”
A version of this article first appeared on Medscape.com.
, notes the latest Medscape Malpractice Report.
Over a third (39%) of oncologists who were surveyed said that they had been named in at least one malpractice suit, according to the Medscape Oncologist Malpractice Report 2021.
This number is considerably lower than that reported by physicians across all specialties (51%), and it is also much lower than that reported by oncologists in past years. In the 2019 report, 54% of oncologists surveyed said they had been named in a malpractice suit, while in the 2017 report, the figure was 53%.
The dramatic decline in malpractice suits may have much to do with the COVID-19 pandemic, when oncology care was in a state of flux.
“Fewer people were seeking cancer care during the COVID pandemic, which might have impacted the number of lawsuits brought against oncologists,” says Paul Walker, a New York–based malpractice attorney at Walker Medical Law, who represents physicians and other healthcare professionals.
“Additionally, a fair number of people who died of COVID were also older,” he pointed out, and it is often older people who get cancer, so there were fewer older people who consulted an oncologist or were treated by one, he added.
However, the pandemic may be storing up trouble for future years. “Patient fears of contracting COVID-19 have led many to avoid seeking or resuming care, so delays in diagnosing new cancer cases could mean that more patients are diagnosed at a later stage of their disease, leading to potential adverse events and malpractice claims,” commented David L. Feldman, MD, MBA, chief medical officer of The Doctors Company Group.
This latest 2021 Medscape Malpractice Report was compiled from an online survey that included more than 4,300 physicians from 29 specialties. It included 106 oncologists. More than half of respondents (56%) had been in practice for more than 25 years, and 54% were aged 60 years or older. The survey was available from May 21 to August 28, 2021.
Similar to findings in previous years, complications from treatment/surgery were the most common reason for the lawsuits (31%). Failure to make a correct diagnosis or a delay in diagnosis was the second most common reason (23%), while 20% of patients sued because of a poor outcome or disease progression.
Surprise at being sued
Among the oncologists who reported involvement in a lawsuit in 2021, the majority (86%) said they were “very surprised” or “somewhat surprised” by the malpractice suit, which is similar to that of other physicians surveyed. However, fewer were surprised this year as compared to 2019 and 2017 (90% and 94%).
One reason for the surprise over the litigation was that it concerned a patient who had been treated a long time ago. One oncologist wrote that “the patient had not seen me for over 7 years and during that time, he did not call me with his new symptomatology. I was only named in the suit because I had previously been involved.”
Another common scenario reported by oncologists was being named in a lawsuit which was brought by another clinician’s patient. “I was the chairperson of the department, and one of the doctors in the practice was involved in the suit,” wrote one respondent. “I was named as an accomplice.”
More than half of surveyed oncologists said that they were able to identify the patient who bought the suit, and these figures are again comparable to those of other physicians. One oncologist commented that in the case he was involved with, the family did not understand or accept the nature of cancer and the different ways that a patient could die of complications. This patient had died of sepsis and pneumonia related to decubitus ulcers that were completely unrelated to her radiation therapy.
As in the case above, sometimes it is the family who filed the lawsuit, not the patient.
“The patient may even recognize that you did your best and be grateful for your skill and efforts, but the family can’t accept that grandma died of cancer and brings a lawsuit,” said Dennis Hursh, an attorney with Physicians Agreement Health Law in Pennsylvania.
When looking at outcomes of the lawsuit, 40% of oncologists were dismissed from the suit within the first few months, or the case was settled before going to trial. This trend is also consistent with the results from the 2019 and 2017 surveys. When the case did go to trial, 10% received a favorable verdict, which was the same in 2019.
“It seems that most of my clients end up being released from lawsuits, and many lawsuits are dismissed prior to proceeding to trial,” Mr. Hursh commented.
Murdering psychopath
Some oncologists weighed in on what they felt was the worst experience of being sued.
“Mental anguish, knowing that I did nothing wrong,” said one physician. Another reported that it was a feeling of being “inadequate and totally alone.”
Another oncologist commented that the “depositions from lawyers implied that I was worse than a murdering psychopath. My reputation was permanently damaged.”
However, the vast majority of oncologists (88%) did not believe that the lawsuit negatively affected their career, which was similar to physicians in general. That said, many did complain about the ongoing requirement to report the lawsuit to the credentialing committee, even if it was dismissed, and then having to pay increased malpractice premiums. “I still need to document this episode every single time I apply for any medical position, even more than 29 years after I was dismissed from the case,” said one respondent.
When asked if they would do anything differently, many oncologists (42%) said no, they would not have done anything differently. This is similar to the responses from physicians in general and with 2019 responses from oncologists. However, 15% of the respondents said that in retrospect, they would not have taken on that patient to begin with.
Some oncologists noted that they would have been more conscientious in relaying the information to the referring physician. Evan Lyman, an associate attorney at Voute, Lohrfink, McAndrew, Meisner & Roberts, LLP, in White Plains, N.Y., pointed out that a common reason for lawsuits is a slip-up of communication between the specialist and the referring physician.
Oncologists who had been sued have some insights to offer to colleagues, should they find themselves in a similar situation.
“Only answer with short and precise statements,” wrote one oncologist. “Attend all the depositions as much as you can; they are more likely to fabricate or exaggerate if you are not sitting in the room.”
Another physician said to base “everything on the medical record and do not answer hypothetical questions.”
“Document all interactions with patients as if a jury will be reading them, word by word,” said one respondent.
As for the public or patients, oncologists had this message: “malpractice suits should be rarely launched and only when gross errors can be absolutely proven.”
Another oncologist pointed out that communication is key. “Speak to the physicians against whom you have distrust. Lots of things could be cleared by good communication.”
A version of this article first appeared on Medscape.com.
, notes the latest Medscape Malpractice Report.
Over a third (39%) of oncologists who were surveyed said that they had been named in at least one malpractice suit, according to the Medscape Oncologist Malpractice Report 2021.
This number is considerably lower than that reported by physicians across all specialties (51%), and it is also much lower than that reported by oncologists in past years. In the 2019 report, 54% of oncologists surveyed said they had been named in a malpractice suit, while in the 2017 report, the figure was 53%.
The dramatic decline in malpractice suits may have much to do with the COVID-19 pandemic, when oncology care was in a state of flux.
“Fewer people were seeking cancer care during the COVID pandemic, which might have impacted the number of lawsuits brought against oncologists,” says Paul Walker, a New York–based malpractice attorney at Walker Medical Law, who represents physicians and other healthcare professionals.
“Additionally, a fair number of people who died of COVID were also older,” he pointed out, and it is often older people who get cancer, so there were fewer older people who consulted an oncologist or were treated by one, he added.
However, the pandemic may be storing up trouble for future years. “Patient fears of contracting COVID-19 have led many to avoid seeking or resuming care, so delays in diagnosing new cancer cases could mean that more patients are diagnosed at a later stage of their disease, leading to potential adverse events and malpractice claims,” commented David L. Feldman, MD, MBA, chief medical officer of The Doctors Company Group.
This latest 2021 Medscape Malpractice Report was compiled from an online survey that included more than 4,300 physicians from 29 specialties. It included 106 oncologists. More than half of respondents (56%) had been in practice for more than 25 years, and 54% were aged 60 years or older. The survey was available from May 21 to August 28, 2021.
Similar to findings in previous years, complications from treatment/surgery were the most common reason for the lawsuits (31%). Failure to make a correct diagnosis or a delay in diagnosis was the second most common reason (23%), while 20% of patients sued because of a poor outcome or disease progression.
Surprise at being sued
Among the oncologists who reported involvement in a lawsuit in 2021, the majority (86%) said they were “very surprised” or “somewhat surprised” by the malpractice suit, which is similar to that of other physicians surveyed. However, fewer were surprised this year as compared to 2019 and 2017 (90% and 94%).
One reason for the surprise over the litigation was that it concerned a patient who had been treated a long time ago. One oncologist wrote that “the patient had not seen me for over 7 years and during that time, he did not call me with his new symptomatology. I was only named in the suit because I had previously been involved.”
Another common scenario reported by oncologists was being named in a lawsuit which was brought by another clinician’s patient. “I was the chairperson of the department, and one of the doctors in the practice was involved in the suit,” wrote one respondent. “I was named as an accomplice.”
More than half of surveyed oncologists said that they were able to identify the patient who bought the suit, and these figures are again comparable to those of other physicians. One oncologist commented that in the case he was involved with, the family did not understand or accept the nature of cancer and the different ways that a patient could die of complications. This patient had died of sepsis and pneumonia related to decubitus ulcers that were completely unrelated to her radiation therapy.
As in the case above, sometimes it is the family who filed the lawsuit, not the patient.
“The patient may even recognize that you did your best and be grateful for your skill and efforts, but the family can’t accept that grandma died of cancer and brings a lawsuit,” said Dennis Hursh, an attorney with Physicians Agreement Health Law in Pennsylvania.
When looking at outcomes of the lawsuit, 40% of oncologists were dismissed from the suit within the first few months, or the case was settled before going to trial. This trend is also consistent with the results from the 2019 and 2017 surveys. When the case did go to trial, 10% received a favorable verdict, which was the same in 2019.
“It seems that most of my clients end up being released from lawsuits, and many lawsuits are dismissed prior to proceeding to trial,” Mr. Hursh commented.
Murdering psychopath
Some oncologists weighed in on what they felt was the worst experience of being sued.
“Mental anguish, knowing that I did nothing wrong,” said one physician. Another reported that it was a feeling of being “inadequate and totally alone.”
Another oncologist commented that the “depositions from lawyers implied that I was worse than a murdering psychopath. My reputation was permanently damaged.”
However, the vast majority of oncologists (88%) did not believe that the lawsuit negatively affected their career, which was similar to physicians in general. That said, many did complain about the ongoing requirement to report the lawsuit to the credentialing committee, even if it was dismissed, and then having to pay increased malpractice premiums. “I still need to document this episode every single time I apply for any medical position, even more than 29 years after I was dismissed from the case,” said one respondent.
When asked if they would do anything differently, many oncologists (42%) said no, they would not have done anything differently. This is similar to the responses from physicians in general and with 2019 responses from oncologists. However, 15% of the respondents said that in retrospect, they would not have taken on that patient to begin with.
Some oncologists noted that they would have been more conscientious in relaying the information to the referring physician. Evan Lyman, an associate attorney at Voute, Lohrfink, McAndrew, Meisner & Roberts, LLP, in White Plains, N.Y., pointed out that a common reason for lawsuits is a slip-up of communication between the specialist and the referring physician.
Oncologists who had been sued have some insights to offer to colleagues, should they find themselves in a similar situation.
“Only answer with short and precise statements,” wrote one oncologist. “Attend all the depositions as much as you can; they are more likely to fabricate or exaggerate if you are not sitting in the room.”
Another physician said to base “everything on the medical record and do not answer hypothetical questions.”
“Document all interactions with patients as if a jury will be reading them, word by word,” said one respondent.
As for the public or patients, oncologists had this message: “malpractice suits should be rarely launched and only when gross errors can be absolutely proven.”
Another oncologist pointed out that communication is key. “Speak to the physicians against whom you have distrust. Lots of things could be cleared by good communication.”
A version of this article first appeared on Medscape.com.
Rapid Desensitization after a Type I Hypersensitivity Reaction to Ceftazidime/Avibactam
Cerebral palsy (CP) embodies a collection of disorders involving permanent but nonprogressive motor dysfunction secondary to one of a variety of abnormal disturbances that can occur in the developing fetal or infantile brain.1 The motor impairment of CP classically leads to irregularities in muscle tone, posture, and/or movement, resulting in limitations of functional abilities that vary in severity.1,2 Patients with CP commonly experience dysphagia, gastroesophageal reflux disease, impaired airway clearance, chest wall and spine deformities, restrictive lung disease, and/or recurrent aspiration.1 Consequently, pulmonary disease is the leading cause of morbidity and mortality in patients with severe CP, characterized by recurrent bacterial infections.3,4
Frequent antibiotic use increases the risk of multidrug-resistant pathogen formation and hypersensitivity to antibiotics. Life-threatening allergic reactions in a patient population with impaired lung function significantly complicates patient management, often leading to suboptimal treatment with second-line agents.5 This case study describes a previously penicillin-tolerant patient with CP who developed a type I hypersensitivity reaction to ceftazidime/avibactam and was treated successfully with the antibiotic after rapid induction of temporary tolerance.
Case Presentation
A 34-year-old male with a complex medical history of severe spastic CP and atonic seizures was recently diagnosed with adenocarcinoma of the colon and admitted for ileostomy and sigmoidectomy. The surgery was complicated by spillage of intestinal contents into the peritoneal cavity 3 days postoperation. The patient was urgently taken to the operating room for exploratory laparotomy, culminating in remaining colectomy, complete abdominal washout, and wound vacuum placement. He continued to deteriorate clinically over the next few weeks, beginning with the development of feculent peritonitis and septic shock. Respiratory distress ensued, and the patient required a tracheostomy with mechanical ventilation. A computed tomography of the chest was consistent with multifocal pneumonia, and a respiratory culture of bronchioalveolar lavage fluid cultivated Klebsiella pneumoniae, a carbapenem-resistant Enterobacteriaceae.
The infectious disease service was consulted and recommended ceftazidime/avibactam as the only acceptable antibiotic to treat this organism. The patient had no history of drug hypersensitivities. However, he developed diffuse, generalized urticaria and predominately right-sided flushing immediately following the onset of the antibiotic infusion. The urticaria was pruritic. The patient did not have angioedema, and he did not experience any adverse respiratory, cardiac, gastrointestinal, or neurologic symptoms. The infusion was ceased immediately, and the patient was treated with a combination of diphenhydramine 50 mg IV and ranitidine 50 mg IV. Resolution of his hypersensitivity symptoms occurred within an hour of treatment, and vital signs remained stable with no resurgence of symptoms. At the time of his reaction, the patient also was taking pantoprazole, valproate, metoprolol, risperidone, and oxycodone as needed for pain. A tryptase level was not measured.
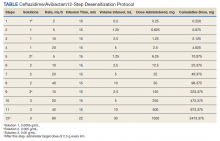
The allergy and immunology service was consulted for rapid desensitization to ceftazidime/avibactam as the culture and sensitivity test demonstrated the bacterium to be resistant to alternative antibiotics. Skin testing to ceftazidime/avibactam was deferred at the time due to the patient’s critical illness. The patient was premedicated with diphenhydramine and ranitidine 50 mg IV. Rapid IV desensitization was performed using a standard 12-step protocol developed for chemotherapeutic agents but demonstrated as safe and effective when applied to antibiotics in patients with cystic fibrosis.5 The antibiotic was administered in sequential 15-minute intervals for a total of 12 progressively doubled doses with continuous monitoring for the appearance of allergic reactions (Table). The target dose of 2.5 g was successfully achieved, and the patient tolerated a complete 14-day treatment regimen with no further adverse reactions to the medication. During the remainder of his hospital admission, the patient improved significantly without further complications.
Discussion
This is the first reported case in the literature to describe a type I hypersensitivity reaction with rapid IV induction of tolerance to ceftazidime/avibactam. We describe his reaction as type I hypersensitivity because the patient developed immediate generalized urticaria and flushing. Use of a safe desensitization protocol, demonstrated in this case report, is paramount to optimal management of infections in patient populations with severely decreased lung function, such as CP.5-7 It provides a safe and effective technique to maintain patients on first line, preferred therapy, despite their increased risk of potentially life-threatening allergic reactions.
Interestingly, this patient previously tolerated penicillins and cephalosporins without adverse reactions, suggesting the possibility of a non–IgE-mediated vs an IgE-mediated mechanism to the hypersensitivity reaction. The patient also was receiving oxycodone at the time of his reaction, and oxycodone can cause nonspecific mast cell degranulation. Additional information from skin testing to ceftazidime/avibactam could help determine whether the patient had an IgE-mediated hypersensitivity reaction. This information could help clarify the culprit agent and guide further avoidance recommendations.
Unfortunately, because the patient was critically ill, skin testing was not performed, and he underwent an urgent antibiotic desensitization with success. It was recommended that the patient follow up in the allergy and immunology clinic for further evaluation with skin testing to ceftazidime/avibactam as well as other β-lactams to determine his future risk of reaction. Unfortunately, he was lost to follow-up.
Frequent IV antibiotic use is a risk factor for the development of antibiotic allergies.8,9 This patient had received many prior courses of IV antibiotics, and this factor most likely contributed to his immediate hypersensitivity reaction to ceftazidime/avibactam. Fortunately, he tolerated a rapid induction of tolerance.
As life expectancies for patients with chronic medical conditions that involve recurrent infections increase, the associated emergence of multidrug-resistant pathogens and necessity for use of novel combination antibiotics should prompt further investigation of nonirritating doses of these drugs for skin testing in the case of drug hypersensitivities. This information would be essential for skin prick testing and determination of whether patients have a true IgE-mediated reaction to these antibiotics.
Conclusions
This is the first case report demonstrating a successful rapid induction of tolerance for the antibiotic ceftazidime/avibactam. Fortunately, the patient tolerated the desensitization procedure without further adverse reactions, and he had a resolution of his infection.
1. Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol. 2007;109:8-14.
2. Haak P, Lenski M, Hidecker MJ, et al. Cerebral palsy and aging. Dev Med Child Neurol. 2009;51(suppl 4):16-23. doi:10.1111/j.1469-8749.2009.03428.x
3. Duruflé-Tapin A, Colin A, Nicolas B, Lebreton C, Dauvergne F, Gallien P. Analysis of the medical causes of death in cerebral palsy. Ann Phys Rehabil Med. 2014;57(1):24-37. doi:10.1016/j.rehab.2013.11.002
4. Boel L, Pernet K, Toussaint M, et al. Respiratory morbidity in children with cerebral palsy: an overview. Dev Med Child Neurol. 2019;61(6):646-653. doi:10.1111/dmcn.14060
5. Legere HJ 3rd, Palis RI, Rodriguez Bouza T, Uluer AZ, Castells MC. A safe protocol for rapid desensitization in patients with cystic fibrosis and antibiotic hypersensitivity. J Cyst Fibros. 2009;8(6):418-424. doi:10.1016/j.jcf.2009.08.002
6. Castells M. Rapid desensitization for hypersensitivity reactions to medications. Immunol Allergy Clin North Am. 2009;29(3):585-606. doi:10.1016/j.iac.2009.04.012
7. Liu A, Fanning L, Chong H, et al. Desensitization regimens for drug allergy: state of the art in the 21st century. Clin Exp Allergy. 2011;41(12):1679-1689. doi:10.1111/j.1365-2222.2011.03825.x
8. Thong BY, Tan TC. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol. 2011;71(5):684-700. doi:10.1111/j.1365-2125.2010.03774.x
9. Adkinson NF Jr. Risk factors for drug allergy. J Allergy Clin Immunol. 1984;74(4, pt 2):567-572. doi:10.1016/0091-6749(84)90108-8
Cerebral palsy (CP) embodies a collection of disorders involving permanent but nonprogressive motor dysfunction secondary to one of a variety of abnormal disturbances that can occur in the developing fetal or infantile brain.1 The motor impairment of CP classically leads to irregularities in muscle tone, posture, and/or movement, resulting in limitations of functional abilities that vary in severity.1,2 Patients with CP commonly experience dysphagia, gastroesophageal reflux disease, impaired airway clearance, chest wall and spine deformities, restrictive lung disease, and/or recurrent aspiration.1 Consequently, pulmonary disease is the leading cause of morbidity and mortality in patients with severe CP, characterized by recurrent bacterial infections.3,4
Frequent antibiotic use increases the risk of multidrug-resistant pathogen formation and hypersensitivity to antibiotics. Life-threatening allergic reactions in a patient population with impaired lung function significantly complicates patient management, often leading to suboptimal treatment with second-line agents.5 This case study describes a previously penicillin-tolerant patient with CP who developed a type I hypersensitivity reaction to ceftazidime/avibactam and was treated successfully with the antibiotic after rapid induction of temporary tolerance.
Case Presentation
A 34-year-old male with a complex medical history of severe spastic CP and atonic seizures was recently diagnosed with adenocarcinoma of the colon and admitted for ileostomy and sigmoidectomy. The surgery was complicated by spillage of intestinal contents into the peritoneal cavity 3 days postoperation. The patient was urgently taken to the operating room for exploratory laparotomy, culminating in remaining colectomy, complete abdominal washout, and wound vacuum placement. He continued to deteriorate clinically over the next few weeks, beginning with the development of feculent peritonitis and septic shock. Respiratory distress ensued, and the patient required a tracheostomy with mechanical ventilation. A computed tomography of the chest was consistent with multifocal pneumonia, and a respiratory culture of bronchioalveolar lavage fluid cultivated Klebsiella pneumoniae, a carbapenem-resistant Enterobacteriaceae.
The infectious disease service was consulted and recommended ceftazidime/avibactam as the only acceptable antibiotic to treat this organism. The patient had no history of drug hypersensitivities. However, he developed diffuse, generalized urticaria and predominately right-sided flushing immediately following the onset of the antibiotic infusion. The urticaria was pruritic. The patient did not have angioedema, and he did not experience any adverse respiratory, cardiac, gastrointestinal, or neurologic symptoms. The infusion was ceased immediately, and the patient was treated with a combination of diphenhydramine 50 mg IV and ranitidine 50 mg IV. Resolution of his hypersensitivity symptoms occurred within an hour of treatment, and vital signs remained stable with no resurgence of symptoms. At the time of his reaction, the patient also was taking pantoprazole, valproate, metoprolol, risperidone, and oxycodone as needed for pain. A tryptase level was not measured.
The allergy and immunology service was consulted for rapid desensitization to ceftazidime/avibactam as the culture and sensitivity test demonstrated the bacterium to be resistant to alternative antibiotics. Skin testing to ceftazidime/avibactam was deferred at the time due to the patient’s critical illness. The patient was premedicated with diphenhydramine and ranitidine 50 mg IV. Rapid IV desensitization was performed using a standard 12-step protocol developed for chemotherapeutic agents but demonstrated as safe and effective when applied to antibiotics in patients with cystic fibrosis.5 The antibiotic was administered in sequential 15-minute intervals for a total of 12 progressively doubled doses with continuous monitoring for the appearance of allergic reactions (Table). The target dose of 2.5 g was successfully achieved, and the patient tolerated a complete 14-day treatment regimen with no further adverse reactions to the medication. During the remainder of his hospital admission, the patient improved significantly without further complications.
Discussion
This is the first reported case in the literature to describe a type I hypersensitivity reaction with rapid IV induction of tolerance to ceftazidime/avibactam. We describe his reaction as type I hypersensitivity because the patient developed immediate generalized urticaria and flushing. Use of a safe desensitization protocol, demonstrated in this case report, is paramount to optimal management of infections in patient populations with severely decreased lung function, such as CP.5-7 It provides a safe and effective technique to maintain patients on first line, preferred therapy, despite their increased risk of potentially life-threatening allergic reactions.
Interestingly, this patient previously tolerated penicillins and cephalosporins without adverse reactions, suggesting the possibility of a non–IgE-mediated vs an IgE-mediated mechanism to the hypersensitivity reaction. The patient also was receiving oxycodone at the time of his reaction, and oxycodone can cause nonspecific mast cell degranulation. Additional information from skin testing to ceftazidime/avibactam could help determine whether the patient had an IgE-mediated hypersensitivity reaction. This information could help clarify the culprit agent and guide further avoidance recommendations.
Unfortunately, because the patient was critically ill, skin testing was not performed, and he underwent an urgent antibiotic desensitization with success. It was recommended that the patient follow up in the allergy and immunology clinic for further evaluation with skin testing to ceftazidime/avibactam as well as other β-lactams to determine his future risk of reaction. Unfortunately, he was lost to follow-up.
Frequent IV antibiotic use is a risk factor for the development of antibiotic allergies.8,9 This patient had received many prior courses of IV antibiotics, and this factor most likely contributed to his immediate hypersensitivity reaction to ceftazidime/avibactam. Fortunately, he tolerated a rapid induction of tolerance.
As life expectancies for patients with chronic medical conditions that involve recurrent infections increase, the associated emergence of multidrug-resistant pathogens and necessity for use of novel combination antibiotics should prompt further investigation of nonirritating doses of these drugs for skin testing in the case of drug hypersensitivities. This information would be essential for skin prick testing and determination of whether patients have a true IgE-mediated reaction to these antibiotics.
Conclusions
This is the first case report demonstrating a successful rapid induction of tolerance for the antibiotic ceftazidime/avibactam. Fortunately, the patient tolerated the desensitization procedure without further adverse reactions, and he had a resolution of his infection.
Cerebral palsy (CP) embodies a collection of disorders involving permanent but nonprogressive motor dysfunction secondary to one of a variety of abnormal disturbances that can occur in the developing fetal or infantile brain.1 The motor impairment of CP classically leads to irregularities in muscle tone, posture, and/or movement, resulting in limitations of functional abilities that vary in severity.1,2 Patients with CP commonly experience dysphagia, gastroesophageal reflux disease, impaired airway clearance, chest wall and spine deformities, restrictive lung disease, and/or recurrent aspiration.1 Consequently, pulmonary disease is the leading cause of morbidity and mortality in patients with severe CP, characterized by recurrent bacterial infections.3,4
Frequent antibiotic use increases the risk of multidrug-resistant pathogen formation and hypersensitivity to antibiotics. Life-threatening allergic reactions in a patient population with impaired lung function significantly complicates patient management, often leading to suboptimal treatment with second-line agents.5 This case study describes a previously penicillin-tolerant patient with CP who developed a type I hypersensitivity reaction to ceftazidime/avibactam and was treated successfully with the antibiotic after rapid induction of temporary tolerance.
Case Presentation
A 34-year-old male with a complex medical history of severe spastic CP and atonic seizures was recently diagnosed with adenocarcinoma of the colon and admitted for ileostomy and sigmoidectomy. The surgery was complicated by spillage of intestinal contents into the peritoneal cavity 3 days postoperation. The patient was urgently taken to the operating room for exploratory laparotomy, culminating in remaining colectomy, complete abdominal washout, and wound vacuum placement. He continued to deteriorate clinically over the next few weeks, beginning with the development of feculent peritonitis and septic shock. Respiratory distress ensued, and the patient required a tracheostomy with mechanical ventilation. A computed tomography of the chest was consistent with multifocal pneumonia, and a respiratory culture of bronchioalveolar lavage fluid cultivated Klebsiella pneumoniae, a carbapenem-resistant Enterobacteriaceae.
The infectious disease service was consulted and recommended ceftazidime/avibactam as the only acceptable antibiotic to treat this organism. The patient had no history of drug hypersensitivities. However, he developed diffuse, generalized urticaria and predominately right-sided flushing immediately following the onset of the antibiotic infusion. The urticaria was pruritic. The patient did not have angioedema, and he did not experience any adverse respiratory, cardiac, gastrointestinal, or neurologic symptoms. The infusion was ceased immediately, and the patient was treated with a combination of diphenhydramine 50 mg IV and ranitidine 50 mg IV. Resolution of his hypersensitivity symptoms occurred within an hour of treatment, and vital signs remained stable with no resurgence of symptoms. At the time of his reaction, the patient also was taking pantoprazole, valproate, metoprolol, risperidone, and oxycodone as needed for pain. A tryptase level was not measured.
The allergy and immunology service was consulted for rapid desensitization to ceftazidime/avibactam as the culture and sensitivity test demonstrated the bacterium to be resistant to alternative antibiotics. Skin testing to ceftazidime/avibactam was deferred at the time due to the patient’s critical illness. The patient was premedicated with diphenhydramine and ranitidine 50 mg IV. Rapid IV desensitization was performed using a standard 12-step protocol developed for chemotherapeutic agents but demonstrated as safe and effective when applied to antibiotics in patients with cystic fibrosis.5 The antibiotic was administered in sequential 15-minute intervals for a total of 12 progressively doubled doses with continuous monitoring for the appearance of allergic reactions (Table). The target dose of 2.5 g was successfully achieved, and the patient tolerated a complete 14-day treatment regimen with no further adverse reactions to the medication. During the remainder of his hospital admission, the patient improved significantly without further complications.
Discussion
This is the first reported case in the literature to describe a type I hypersensitivity reaction with rapid IV induction of tolerance to ceftazidime/avibactam. We describe his reaction as type I hypersensitivity because the patient developed immediate generalized urticaria and flushing. Use of a safe desensitization protocol, demonstrated in this case report, is paramount to optimal management of infections in patient populations with severely decreased lung function, such as CP.5-7 It provides a safe and effective technique to maintain patients on first line, preferred therapy, despite their increased risk of potentially life-threatening allergic reactions.
Interestingly, this patient previously tolerated penicillins and cephalosporins without adverse reactions, suggesting the possibility of a non–IgE-mediated vs an IgE-mediated mechanism to the hypersensitivity reaction. The patient also was receiving oxycodone at the time of his reaction, and oxycodone can cause nonspecific mast cell degranulation. Additional information from skin testing to ceftazidime/avibactam could help determine whether the patient had an IgE-mediated hypersensitivity reaction. This information could help clarify the culprit agent and guide further avoidance recommendations.
Unfortunately, because the patient was critically ill, skin testing was not performed, and he underwent an urgent antibiotic desensitization with success. It was recommended that the patient follow up in the allergy and immunology clinic for further evaluation with skin testing to ceftazidime/avibactam as well as other β-lactams to determine his future risk of reaction. Unfortunately, he was lost to follow-up.
Frequent IV antibiotic use is a risk factor for the development of antibiotic allergies.8,9 This patient had received many prior courses of IV antibiotics, and this factor most likely contributed to his immediate hypersensitivity reaction to ceftazidime/avibactam. Fortunately, he tolerated a rapid induction of tolerance.
As life expectancies for patients with chronic medical conditions that involve recurrent infections increase, the associated emergence of multidrug-resistant pathogens and necessity for use of novel combination antibiotics should prompt further investigation of nonirritating doses of these drugs for skin testing in the case of drug hypersensitivities. This information would be essential for skin prick testing and determination of whether patients have a true IgE-mediated reaction to these antibiotics.
Conclusions
This is the first case report demonstrating a successful rapid induction of tolerance for the antibiotic ceftazidime/avibactam. Fortunately, the patient tolerated the desensitization procedure without further adverse reactions, and he had a resolution of his infection.
1. Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol. 2007;109:8-14.
2. Haak P, Lenski M, Hidecker MJ, et al. Cerebral palsy and aging. Dev Med Child Neurol. 2009;51(suppl 4):16-23. doi:10.1111/j.1469-8749.2009.03428.x
3. Duruflé-Tapin A, Colin A, Nicolas B, Lebreton C, Dauvergne F, Gallien P. Analysis of the medical causes of death in cerebral palsy. Ann Phys Rehabil Med. 2014;57(1):24-37. doi:10.1016/j.rehab.2013.11.002
4. Boel L, Pernet K, Toussaint M, et al. Respiratory morbidity in children with cerebral palsy: an overview. Dev Med Child Neurol. 2019;61(6):646-653. doi:10.1111/dmcn.14060
5. Legere HJ 3rd, Palis RI, Rodriguez Bouza T, Uluer AZ, Castells MC. A safe protocol for rapid desensitization in patients with cystic fibrosis and antibiotic hypersensitivity. J Cyst Fibros. 2009;8(6):418-424. doi:10.1016/j.jcf.2009.08.002
6. Castells M. Rapid desensitization for hypersensitivity reactions to medications. Immunol Allergy Clin North Am. 2009;29(3):585-606. doi:10.1016/j.iac.2009.04.012
7. Liu A, Fanning L, Chong H, et al. Desensitization regimens for drug allergy: state of the art in the 21st century. Clin Exp Allergy. 2011;41(12):1679-1689. doi:10.1111/j.1365-2222.2011.03825.x
8. Thong BY, Tan TC. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol. 2011;71(5):684-700. doi:10.1111/j.1365-2125.2010.03774.x
9. Adkinson NF Jr. Risk factors for drug allergy. J Allergy Clin Immunol. 1984;74(4, pt 2):567-572. doi:10.1016/0091-6749(84)90108-8
1. Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol. 2007;109:8-14.
2. Haak P, Lenski M, Hidecker MJ, et al. Cerebral palsy and aging. Dev Med Child Neurol. 2009;51(suppl 4):16-23. doi:10.1111/j.1469-8749.2009.03428.x
3. Duruflé-Tapin A, Colin A, Nicolas B, Lebreton C, Dauvergne F, Gallien P. Analysis of the medical causes of death in cerebral palsy. Ann Phys Rehabil Med. 2014;57(1):24-37. doi:10.1016/j.rehab.2013.11.002
4. Boel L, Pernet K, Toussaint M, et al. Respiratory morbidity in children with cerebral palsy: an overview. Dev Med Child Neurol. 2019;61(6):646-653. doi:10.1111/dmcn.14060
5. Legere HJ 3rd, Palis RI, Rodriguez Bouza T, Uluer AZ, Castells MC. A safe protocol for rapid desensitization in patients with cystic fibrosis and antibiotic hypersensitivity. J Cyst Fibros. 2009;8(6):418-424. doi:10.1016/j.jcf.2009.08.002
6. Castells M. Rapid desensitization for hypersensitivity reactions to medications. Immunol Allergy Clin North Am. 2009;29(3):585-606. doi:10.1016/j.iac.2009.04.012
7. Liu A, Fanning L, Chong H, et al. Desensitization regimens for drug allergy: state of the art in the 21st century. Clin Exp Allergy. 2011;41(12):1679-1689. doi:10.1111/j.1365-2222.2011.03825.x
8. Thong BY, Tan TC. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol. 2011;71(5):684-700. doi:10.1111/j.1365-2125.2010.03774.x
9. Adkinson NF Jr. Risk factors for drug allergy. J Allergy Clin Immunol. 1984;74(4, pt 2):567-572. doi:10.1016/0091-6749(84)90108-8
Updated guidance for COVID vaccination in rheumatology patients arrives amid continued hesitancy
As rheumatologists contend with vaccine hesitancy among certain subsets of patients, the American College of Rheumatology has released updated clinical guidelines on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases (RMDs), including new recommendations on supplemental and booster doses.
The revised guidance from this fifth version of the ACR guidelines includes strongly recommending that all RMD patients receive a booster after their primary vaccine series, regardless of whether they have been naturally infected with COVID-19. In addition, they strongly recommend third supplemental doses for patients with autoimmune inflammatory rheumatic diseases (AIIRDs) who likely mounted an inadequate vaccine response, which would then be followed by a fourth booster dose as advised by the Centers for Disease Control and Prevention for immunocompromised individuals.
Other recommendations include pre-exposure prophylaxis monoclonal antibody treatment for high-risk AIIRD patients, defined as those with moderate to severely compromised immune systems who may not mount an adequate immune response to COVID-19 vaccination, when it is available and authorized for emergency use by the Food and Drug Administration, as well as monoclonal antibody therapy for postexposure prophylaxis of asymptomatic, recently exposed high-risk AIIRD patients or as treatment for newly symptomatic, high-risk AIIRD patients. The ACR guidance notes that, currently, neither the monoclonal antibodies bamlanivimab and etesevimab (administered together) nor casirivimab and imdevimab (REGEN-COV), are licensed or available under an emergency use authorization given their lack of activity against the Omicron variant, the dominant strain of SARS-CoV-2 circulating in the United States.
Finally, the guidance clarified that the timing of intravenous immunoglobulin doses does not need to be modified around the administration of COVID vaccine doses, based on moderate consensus among task force members.
Vaccine hesitancy in community rheumatology practices
The revised guidelines were released just as Arthritis & Rheumatology published a new study that assessed vaccine hesitancy among rheumatology patients on immunomodulatory therapies. A three-item electronic survey was conducted at 101 offices within a community practice–based rheumatology research network and ultimately collected responses from 58,529 patients, 20,987 of whom had an AIIRD and were receiving targeted therapies like biologics or Janus kinase inhibitors.
Of the total respondents, 77% (n = 43,675) had been vaccinated, 16.9% were not vaccinated and did not plan to be, and 6.1% were not vaccinated but planned to be. However, AIIRD patients were 16% less likely to be vaccinated, compared with the other patients, such as those with osteoarthritis or osteoporosis who were not receiving disease-modifying antirheumatic drugs (76.9% vs. 87%; odds ratio, 0.84; 95% confidence interval, 0.77-0.92; P < .001). Multivariable analysis also found that older patients (OR, 1.49 per 10 years) and Asians (OR, 2.42; 95% CI, 1.77-3.33) were more likely to be vaccinated.
“Rheumatologists need to be asking their patients more than just: ‘Are you vaccinated?’ ” Jeffrey Curtis, MD, MPH, head of the ACR COVID-19 vaccine task force and a coauthor of the vaccine hesitancy study, said in an interview. “A year ago, that was a fine approach, but now they need to be asking whether you’ve been vaccinated, and with what, and how many times, and how recently. There are a whole lot of subtleties there; ‘vaccinated: yes or no’ is just the tip of the iceberg.”
His research into the vaccine hesitant includes recent anecdotal data from thousands of patients treated in local rheumatology community practices, many of whom cited long-term safety data and potential side effects as reasons why they were unwilling to get vaccinated. But despite their on-paper responses, he cautioned rheumatologists to think critically when determining which patients may truly be open to vaccination.
“If you’re designing strategies to affect vaccine hesitancy, you may be wasting your time with some people,” said Dr. Curtis, professor of medicine at the University of Alabama at Birmingham. “A critical need is to figure out who are the patients who may be amendable to more information or an intervention or a little bit more time and care, and who are the people where you know, this is a lost cause: You don’t get a flu shot, you haven’t been vaccinated for shingles, [and] you’re not going to get this one either.
“In terms of a research agenda, how do we develop efficient, simple, short screening tools?” he added. “Something with a few helpful questions, on a patient portal or an iPad, that will do a good job identifying your patients at risk who haven’t had vaccination but that you might be able to spend time with, intervene, and actually change their mind. If you spend gobs of time with everyone, you’ll help some people, but clinicians don’t have an infinite amount of time.”
One of the authors of the vaccine hesitancy study acknowledged being employed by the rheumatology research network that hosted the survey. Several others, including Dr. Curtis, reported receiving grants and consulting fees from various pharmaceutical companies.
As rheumatologists contend with vaccine hesitancy among certain subsets of patients, the American College of Rheumatology has released updated clinical guidelines on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases (RMDs), including new recommendations on supplemental and booster doses.
The revised guidance from this fifth version of the ACR guidelines includes strongly recommending that all RMD patients receive a booster after their primary vaccine series, regardless of whether they have been naturally infected with COVID-19. In addition, they strongly recommend third supplemental doses for patients with autoimmune inflammatory rheumatic diseases (AIIRDs) who likely mounted an inadequate vaccine response, which would then be followed by a fourth booster dose as advised by the Centers for Disease Control and Prevention for immunocompromised individuals.
Other recommendations include pre-exposure prophylaxis monoclonal antibody treatment for high-risk AIIRD patients, defined as those with moderate to severely compromised immune systems who may not mount an adequate immune response to COVID-19 vaccination, when it is available and authorized for emergency use by the Food and Drug Administration, as well as monoclonal antibody therapy for postexposure prophylaxis of asymptomatic, recently exposed high-risk AIIRD patients or as treatment for newly symptomatic, high-risk AIIRD patients. The ACR guidance notes that, currently, neither the monoclonal antibodies bamlanivimab and etesevimab (administered together) nor casirivimab and imdevimab (REGEN-COV), are licensed or available under an emergency use authorization given their lack of activity against the Omicron variant, the dominant strain of SARS-CoV-2 circulating in the United States.
Finally, the guidance clarified that the timing of intravenous immunoglobulin doses does not need to be modified around the administration of COVID vaccine doses, based on moderate consensus among task force members.
Vaccine hesitancy in community rheumatology practices
The revised guidelines were released just as Arthritis & Rheumatology published a new study that assessed vaccine hesitancy among rheumatology patients on immunomodulatory therapies. A three-item electronic survey was conducted at 101 offices within a community practice–based rheumatology research network and ultimately collected responses from 58,529 patients, 20,987 of whom had an AIIRD and were receiving targeted therapies like biologics or Janus kinase inhibitors.
Of the total respondents, 77% (n = 43,675) had been vaccinated, 16.9% were not vaccinated and did not plan to be, and 6.1% were not vaccinated but planned to be. However, AIIRD patients were 16% less likely to be vaccinated, compared with the other patients, such as those with osteoarthritis or osteoporosis who were not receiving disease-modifying antirheumatic drugs (76.9% vs. 87%; odds ratio, 0.84; 95% confidence interval, 0.77-0.92; P < .001). Multivariable analysis also found that older patients (OR, 1.49 per 10 years) and Asians (OR, 2.42; 95% CI, 1.77-3.33) were more likely to be vaccinated.
“Rheumatologists need to be asking their patients more than just: ‘Are you vaccinated?’ ” Jeffrey Curtis, MD, MPH, head of the ACR COVID-19 vaccine task force and a coauthor of the vaccine hesitancy study, said in an interview. “A year ago, that was a fine approach, but now they need to be asking whether you’ve been vaccinated, and with what, and how many times, and how recently. There are a whole lot of subtleties there; ‘vaccinated: yes or no’ is just the tip of the iceberg.”
His research into the vaccine hesitant includes recent anecdotal data from thousands of patients treated in local rheumatology community practices, many of whom cited long-term safety data and potential side effects as reasons why they were unwilling to get vaccinated. But despite their on-paper responses, he cautioned rheumatologists to think critically when determining which patients may truly be open to vaccination.
“If you’re designing strategies to affect vaccine hesitancy, you may be wasting your time with some people,” said Dr. Curtis, professor of medicine at the University of Alabama at Birmingham. “A critical need is to figure out who are the patients who may be amendable to more information or an intervention or a little bit more time and care, and who are the people where you know, this is a lost cause: You don’t get a flu shot, you haven’t been vaccinated for shingles, [and] you’re not going to get this one either.
“In terms of a research agenda, how do we develop efficient, simple, short screening tools?” he added. “Something with a few helpful questions, on a patient portal or an iPad, that will do a good job identifying your patients at risk who haven’t had vaccination but that you might be able to spend time with, intervene, and actually change their mind. If you spend gobs of time with everyone, you’ll help some people, but clinicians don’t have an infinite amount of time.”
One of the authors of the vaccine hesitancy study acknowledged being employed by the rheumatology research network that hosted the survey. Several others, including Dr. Curtis, reported receiving grants and consulting fees from various pharmaceutical companies.
As rheumatologists contend with vaccine hesitancy among certain subsets of patients, the American College of Rheumatology has released updated clinical guidelines on COVID-19 vaccination for patients with rheumatic and musculoskeletal diseases (RMDs), including new recommendations on supplemental and booster doses.
The revised guidance from this fifth version of the ACR guidelines includes strongly recommending that all RMD patients receive a booster after their primary vaccine series, regardless of whether they have been naturally infected with COVID-19. In addition, they strongly recommend third supplemental doses for patients with autoimmune inflammatory rheumatic diseases (AIIRDs) who likely mounted an inadequate vaccine response, which would then be followed by a fourth booster dose as advised by the Centers for Disease Control and Prevention for immunocompromised individuals.
Other recommendations include pre-exposure prophylaxis monoclonal antibody treatment for high-risk AIIRD patients, defined as those with moderate to severely compromised immune systems who may not mount an adequate immune response to COVID-19 vaccination, when it is available and authorized for emergency use by the Food and Drug Administration, as well as monoclonal antibody therapy for postexposure prophylaxis of asymptomatic, recently exposed high-risk AIIRD patients or as treatment for newly symptomatic, high-risk AIIRD patients. The ACR guidance notes that, currently, neither the monoclonal antibodies bamlanivimab and etesevimab (administered together) nor casirivimab and imdevimab (REGEN-COV), are licensed or available under an emergency use authorization given their lack of activity against the Omicron variant, the dominant strain of SARS-CoV-2 circulating in the United States.
Finally, the guidance clarified that the timing of intravenous immunoglobulin doses does not need to be modified around the administration of COVID vaccine doses, based on moderate consensus among task force members.
Vaccine hesitancy in community rheumatology practices
The revised guidelines were released just as Arthritis & Rheumatology published a new study that assessed vaccine hesitancy among rheumatology patients on immunomodulatory therapies. A three-item electronic survey was conducted at 101 offices within a community practice–based rheumatology research network and ultimately collected responses from 58,529 patients, 20,987 of whom had an AIIRD and were receiving targeted therapies like biologics or Janus kinase inhibitors.
Of the total respondents, 77% (n = 43,675) had been vaccinated, 16.9% were not vaccinated and did not plan to be, and 6.1% were not vaccinated but planned to be. However, AIIRD patients were 16% less likely to be vaccinated, compared with the other patients, such as those with osteoarthritis or osteoporosis who were not receiving disease-modifying antirheumatic drugs (76.9% vs. 87%; odds ratio, 0.84; 95% confidence interval, 0.77-0.92; P < .001). Multivariable analysis also found that older patients (OR, 1.49 per 10 years) and Asians (OR, 2.42; 95% CI, 1.77-3.33) were more likely to be vaccinated.
“Rheumatologists need to be asking their patients more than just: ‘Are you vaccinated?’ ” Jeffrey Curtis, MD, MPH, head of the ACR COVID-19 vaccine task force and a coauthor of the vaccine hesitancy study, said in an interview. “A year ago, that was a fine approach, but now they need to be asking whether you’ve been vaccinated, and with what, and how many times, and how recently. There are a whole lot of subtleties there; ‘vaccinated: yes or no’ is just the tip of the iceberg.”
His research into the vaccine hesitant includes recent anecdotal data from thousands of patients treated in local rheumatology community practices, many of whom cited long-term safety data and potential side effects as reasons why they were unwilling to get vaccinated. But despite their on-paper responses, he cautioned rheumatologists to think critically when determining which patients may truly be open to vaccination.
“If you’re designing strategies to affect vaccine hesitancy, you may be wasting your time with some people,” said Dr. Curtis, professor of medicine at the University of Alabama at Birmingham. “A critical need is to figure out who are the patients who may be amendable to more information or an intervention or a little bit more time and care, and who are the people where you know, this is a lost cause: You don’t get a flu shot, you haven’t been vaccinated for shingles, [and] you’re not going to get this one either.
“In terms of a research agenda, how do we develop efficient, simple, short screening tools?” he added. “Something with a few helpful questions, on a patient portal or an iPad, that will do a good job identifying your patients at risk who haven’t had vaccination but that you might be able to spend time with, intervene, and actually change their mind. If you spend gobs of time with everyone, you’ll help some people, but clinicians don’t have an infinite amount of time.”
One of the authors of the vaccine hesitancy study acknowledged being employed by the rheumatology research network that hosted the survey. Several others, including Dr. Curtis, reported receiving grants and consulting fees from various pharmaceutical companies.
FROM ARTHRITIS & RHEUMATOLOGY
FDA investigates possible increased risk of death with lymphoma drug
The FDA granted accelerated approval to umbralisib in February 2021 for patients with two types of lymphoma: Adults with relapsed or refractory marginal zone lymphoma who received at least one prior therapy, and those with relapsed or refractory follicular lymphoma who received at least three prior therapies.
According to the FDA, the possible increased risk of death arose from early findings in a phase 3 trial evaluating the drug in a related type of cancer: chronic lymphocytic leukemia.
“Because of the seriousness of this safety concern and the similarities between the two types of cancer for which this drug is approved and the type of cancer that was studied in the clinical trial, we are alerting patients and health care professionals that we are reevaluating this risk against the benefits of Ukoniq [umbralisib] for its approved uses,” the FDA safety communication states.
The FDA said it performed an initial review of data from the phase 3, randomized controlled UNITY trial, which is evaluating the efficacy of umbralisib plus a monoclonal antibody in patients with chronic lymphocytic leukemia.
“The results showed a possible increased risk of death in patients receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody compared to the control arm,” according to the FDA. “Those receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody also experienced more serious adverse events than those in the control arm.”
Although the drug has not been approved for patients with chronic lymphocytic leukemia, the FDA believes the findings could “have implications for its approved uses” in marginal zone lymphoma and follicular lymphoma.
However, the phase 2 trial that led to February 2021 approvals found the drug’s safety profile to be “manageable,” with serious adverse reactions reported in 18% of patients receiving the dual oral inhibitor of phosphoinositide 3 kinase delta and casein kinase 1 epsilon. These adverse reactions included diarrhea-colitis (4%), pneumonia (3%), sepsis (2%), and urinary tract infection (2%); however, no elevated risk of death was indicated in that analysis.
The FDA noted it will continue to evaluate the results from the phase 3 UNITY trial in chronic lymphocytic leukemia and has suspended enrollment of new patients in other ongoing clinical trials of the drug.
The FDA stated that it would communicate its “final conclusions and recommendations when we have completed our review.” In the meantime, the agency asks health care professionals to review how patients receiving umbralisib are faring and discuss “the risks and benefits of continuing” versus switching to other treatments.
The FDA also asks clinicians and patients to report side effects involving the drug to the FDA MedWatch program.
A version of this article first appeared on Medscape.com.
The FDA granted accelerated approval to umbralisib in February 2021 for patients with two types of lymphoma: Adults with relapsed or refractory marginal zone lymphoma who received at least one prior therapy, and those with relapsed or refractory follicular lymphoma who received at least three prior therapies.
According to the FDA, the possible increased risk of death arose from early findings in a phase 3 trial evaluating the drug in a related type of cancer: chronic lymphocytic leukemia.
“Because of the seriousness of this safety concern and the similarities between the two types of cancer for which this drug is approved and the type of cancer that was studied in the clinical trial, we are alerting patients and health care professionals that we are reevaluating this risk against the benefits of Ukoniq [umbralisib] for its approved uses,” the FDA safety communication states.
The FDA said it performed an initial review of data from the phase 3, randomized controlled UNITY trial, which is evaluating the efficacy of umbralisib plus a monoclonal antibody in patients with chronic lymphocytic leukemia.
“The results showed a possible increased risk of death in patients receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody compared to the control arm,” according to the FDA. “Those receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody also experienced more serious adverse events than those in the control arm.”
Although the drug has not been approved for patients with chronic lymphocytic leukemia, the FDA believes the findings could “have implications for its approved uses” in marginal zone lymphoma and follicular lymphoma.
However, the phase 2 trial that led to February 2021 approvals found the drug’s safety profile to be “manageable,” with serious adverse reactions reported in 18% of patients receiving the dual oral inhibitor of phosphoinositide 3 kinase delta and casein kinase 1 epsilon. These adverse reactions included diarrhea-colitis (4%), pneumonia (3%), sepsis (2%), and urinary tract infection (2%); however, no elevated risk of death was indicated in that analysis.
The FDA noted it will continue to evaluate the results from the phase 3 UNITY trial in chronic lymphocytic leukemia and has suspended enrollment of new patients in other ongoing clinical trials of the drug.
The FDA stated that it would communicate its “final conclusions and recommendations when we have completed our review.” In the meantime, the agency asks health care professionals to review how patients receiving umbralisib are faring and discuss “the risks and benefits of continuing” versus switching to other treatments.
The FDA also asks clinicians and patients to report side effects involving the drug to the FDA MedWatch program.
A version of this article first appeared on Medscape.com.
The FDA granted accelerated approval to umbralisib in February 2021 for patients with two types of lymphoma: Adults with relapsed or refractory marginal zone lymphoma who received at least one prior therapy, and those with relapsed or refractory follicular lymphoma who received at least three prior therapies.
According to the FDA, the possible increased risk of death arose from early findings in a phase 3 trial evaluating the drug in a related type of cancer: chronic lymphocytic leukemia.
“Because of the seriousness of this safety concern and the similarities between the two types of cancer for which this drug is approved and the type of cancer that was studied in the clinical trial, we are alerting patients and health care professionals that we are reevaluating this risk against the benefits of Ukoniq [umbralisib] for its approved uses,” the FDA safety communication states.
The FDA said it performed an initial review of data from the phase 3, randomized controlled UNITY trial, which is evaluating the efficacy of umbralisib plus a monoclonal antibody in patients with chronic lymphocytic leukemia.
“The results showed a possible increased risk of death in patients receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody compared to the control arm,” according to the FDA. “Those receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody also experienced more serious adverse events than those in the control arm.”
Although the drug has not been approved for patients with chronic lymphocytic leukemia, the FDA believes the findings could “have implications for its approved uses” in marginal zone lymphoma and follicular lymphoma.
However, the phase 2 trial that led to February 2021 approvals found the drug’s safety profile to be “manageable,” with serious adverse reactions reported in 18% of patients receiving the dual oral inhibitor of phosphoinositide 3 kinase delta and casein kinase 1 epsilon. These adverse reactions included diarrhea-colitis (4%), pneumonia (3%), sepsis (2%), and urinary tract infection (2%); however, no elevated risk of death was indicated in that analysis.
The FDA noted it will continue to evaluate the results from the phase 3 UNITY trial in chronic lymphocytic leukemia and has suspended enrollment of new patients in other ongoing clinical trials of the drug.
The FDA stated that it would communicate its “final conclusions and recommendations when we have completed our review.” In the meantime, the agency asks health care professionals to review how patients receiving umbralisib are faring and discuss “the risks and benefits of continuing” versus switching to other treatments.
The FDA also asks clinicians and patients to report side effects involving the drug to the FDA MedWatch program.
A version of this article first appeared on Medscape.com.
What Federal Practitioners Need to Know About the National Practitioner Data Bank
Not all federal practitioners know about the National Practitioner Data Bank (NPDB), a federal web-based repository of reports containing information on medical malpractice payments and certain adverse actions related to health care practitioners, providers, and suppliers. This article explains how NPDB statutes and regulations specifically affect federal health care practitioners, which may differ from how the rules affect practitioners in the private sector.1
National Practitioner Data Bank
Established by Congress in 1986, the NPDB contains information health care organizations need to make informed decisions about the health care practitionerss they license, credential, and hire. Federal regulations authorize eligible entities, including government agencies, to report to and query the NPDB. Individuals and organizations that are subjects of these reports have access to their own information. The reports are confidential and not available to the public. The NPDB currently contains > 1.6 million reports.2
Federal Agencies Queries
A query is a search for information in the NPDB regarding a health care practitioners or organization. Some federal agencies are permitted to query the NPDB, and all hospitals, including federal hospitals, are required to query. Agencies administering government health care programs (including private entities administering such programs under contract), federal law enforcement officials and agencies, and federal agencies responsible for the licensing or certification of health care practitioners, health care providers, or health care suppliers may query NPDB. Information received in response to queries includes, among other actions, licensure and certification actions taken by states, medical malpractice payment information, federal licensing and certification actions, and adverse privileging actions.3
Federal Reporting Requirements
Federal government agencies must report exclusions (described below), adjudicated actions, civil judgments, and criminal convictions concerning health care practitioners, providers, or suppliers. The following provides detailed information about the actions federal government agencies are required to report.
Adjudicated Actions or Decisions
Adjudicated actions or decisions are formal or official final actions.3 They include, but are not limited to, personnel-related actions such as suspensions without pay, reductions in pay, reductions in grade for cause, terminations, or other comparable actions. To be reportable, adjudicated actions or decisions must include due process mechanisms. Whether the subject of a report elects not to use the due process mechanism is immaterial as long as such a process is available to the subject before the adjudicated action or decision is made final. In general, if an adjudicated action or decision follows an agency’s established administrative procedures and those procedures ensure that due process is available to the subject, the due process requirement is satisfied. This definition specifically excludes clinical privileging actions taken by federal government agencies, which are described in appropriate memorandums of understanding.
Exclusions
An exclusion is a temporary or permanent debarment of an individual or organization from participation in a federal health-related program, such that items or services furnished by the individual or organization will not be reimbursed under the federal program.3
Civil Judgments and Criminal Convictions
Health care–related civil judgments and settlements must be reported.However, settlements in which no findings of liability have been made are not reportable.3 Health care–related criminal convictions prosecuted by federal government agencies in federal court must be reported to the NPDB. Pleas of guilt and nolo contendere, or no contest, by individuals or organizations also are reportable.3
In addition, final adverse licensure and certification actions are those taken against health care practitioners, providers, or suppliers, regardless of whether the final adverse action is the subject of a pending appeal.3 These must be reported.
Additional Reporting Requirements
Federal hospitals or federal government agencies administering health care services may have additional reporting requirements besides reporting adjudicated actions, exclusions, civil judgments, and criminal convictions. They may include submitting reports under a memorandum of understanding on clinical privileges actions and medical malpractice payments.3 The US Department of Health and Human Services (HHS) has entered into memorandums of understanding with the US Department of Defense and the US Department of Veteran Affairs to ensure their participation in the NPDB system. Federal hospitals should refer to applicable memorandums of understanding and agency-specific policies for guidance on carrying out their reporting responsibilities.4
Responding to a Report
The NPDB sends a letter to health care practitioners when an organization submits a report about the practitioner. The letter has the report number and a password is required to view the report.2 Health care practitioners also can order a self-query online to view any reports on them in the NPDB.
The subject of the report can also add a statement and dispute the report. The statement is an opportunity to provide additional information the subject would like to have included in the report. If the subject disagrees with the accuracy of a report or believes it does not meet NPDB reporting requirements, it can be disputed. The dispute will become part of the report. When the subject adds a statement or dispute, the NPDB notifies the reporting organization and all organizations that received the report within the previous 3 years of the report activity.
Health care practitioners must contact the reporting organization to try to resolve their dispute. If the subject of the report has contacted or tried to contact the reporting organization and could not resolve the dispute after 60 days, or if, within the 60-day period, the organization informs the subject that it will not modify the report, that individual may request dispute resolution.Requesting dispute resolution does not remove the report from the NPDB.
Dispute Resolution
Dispute resolution is a request for the HHS secretary to review the report. The secretary authorizes the Division of Practitioner Data Bank (DPDB) to conduct this review. The DPDB is responsible for oversight of the NPDB. The subject of the report will need to submit relevant supporting documentation to request dispute resolution. This documentation should show that the information in the report is not accurate or that the action is not reportable. Also, proof should be included that the subject contacted or attempted to contact the reporting organization. Submitting large volumes or extraneous documentation can delay the review process.
A dispute resolution manager will review the case and send the reporting organization a request for information if needed. The DPDB will send the subject of the report a courtesy copy of all correspondence. The dispute resolution timeline varies, as the DPDB reviews disputes in the order they are received. It completes a fair and thorough review based on the unique circumstances of each case and will review the case as soon as possible. Once the DPDB receives documentation from the subject and the reporting organization, it reviews the documentation to determine whether the report accurately reflects the record.
The DPDB decides to either maintain the report as is, correct it, or remove it from the NPDB. Once the process is complete, the dispute resolution manager sends a decision letter to the subject of the report and the reporting organization. The dispute resolution decision will appear in the report.
Regulations strictly limit the DPDB’s jurisdiction for reviewing disputed reports. It may only review the following: whether the report was submitted in accordance with reporting requirements, whether the reporting organization was eligible to report the information, and whether the report accurately depicts the action taken by the reporting organization and the basis for the action the reporting organization cited, as shown in the organization’s written record. The subject of the report must resolve any other issues with the reporting organization.
Under the dispute resolution review process, the DPDB cannot conduct an independent review of the merits of the action taken by the reporting organization, review the due process provided by the organization, or substitute its judgment for that of the reporting organization.2 The DPDB does not examine whether the subject of a report was informed of an ongoing investigation. The DPDB does not examine civil rights issues such as claims of discrimination or harassment in the work environment. Practitioners can find additional information at www.npdb.hrsa.gov.
1. US Department of Health and Human Services, National Practitioner Data Bank. NPDB guidebook. Updated October 2018. Accessed December 16, 2021. https://www.npdb.hrsa.gov/resources/aboutGuidebooks.jsp
2. US Department of Health and Human Services, National Practitioner Data Bank. A practitioner’s guide to the NPDB. Updated February 2021. Accessed December 16, 2021. https://www.npdb.hrsa.gov/pract/practGuide.jsp
3. US Department of Health and Human Services, National Practitioner Data Bank. Federal hospitals and federal government agencies. Accessed December 16, 2021. https://www.npdb.hrsa.gov/orgs/federalAgencies.jsp
4. US Department of Health and Human Services, National Practitioner Data Bank. Federal hospitals. Accessed December 16, 2021. https://www.npdb.hrsa.gov/orgs/federalHospitals.jsp
Not all federal practitioners know about the National Practitioner Data Bank (NPDB), a federal web-based repository of reports containing information on medical malpractice payments and certain adverse actions related to health care practitioners, providers, and suppliers. This article explains how NPDB statutes and regulations specifically affect federal health care practitioners, which may differ from how the rules affect practitioners in the private sector.1
National Practitioner Data Bank
Established by Congress in 1986, the NPDB contains information health care organizations need to make informed decisions about the health care practitionerss they license, credential, and hire. Federal regulations authorize eligible entities, including government agencies, to report to and query the NPDB. Individuals and organizations that are subjects of these reports have access to their own information. The reports are confidential and not available to the public. The NPDB currently contains > 1.6 million reports.2
Federal Agencies Queries
A query is a search for information in the NPDB regarding a health care practitioners or organization. Some federal agencies are permitted to query the NPDB, and all hospitals, including federal hospitals, are required to query. Agencies administering government health care programs (including private entities administering such programs under contract), federal law enforcement officials and agencies, and federal agencies responsible for the licensing or certification of health care practitioners, health care providers, or health care suppliers may query NPDB. Information received in response to queries includes, among other actions, licensure and certification actions taken by states, medical malpractice payment information, federal licensing and certification actions, and adverse privileging actions.3
Federal Reporting Requirements
Federal government agencies must report exclusions (described below), adjudicated actions, civil judgments, and criminal convictions concerning health care practitioners, providers, or suppliers. The following provides detailed information about the actions federal government agencies are required to report.
Adjudicated Actions or Decisions
Adjudicated actions or decisions are formal or official final actions.3 They include, but are not limited to, personnel-related actions such as suspensions without pay, reductions in pay, reductions in grade for cause, terminations, or other comparable actions. To be reportable, adjudicated actions or decisions must include due process mechanisms. Whether the subject of a report elects not to use the due process mechanism is immaterial as long as such a process is available to the subject before the adjudicated action or decision is made final. In general, if an adjudicated action or decision follows an agency’s established administrative procedures and those procedures ensure that due process is available to the subject, the due process requirement is satisfied. This definition specifically excludes clinical privileging actions taken by federal government agencies, which are described in appropriate memorandums of understanding.
Exclusions
An exclusion is a temporary or permanent debarment of an individual or organization from participation in a federal health-related program, such that items or services furnished by the individual or organization will not be reimbursed under the federal program.3
Civil Judgments and Criminal Convictions
Health care–related civil judgments and settlements must be reported.However, settlements in which no findings of liability have been made are not reportable.3 Health care–related criminal convictions prosecuted by federal government agencies in federal court must be reported to the NPDB. Pleas of guilt and nolo contendere, or no contest, by individuals or organizations also are reportable.3
In addition, final adverse licensure and certification actions are those taken against health care practitioners, providers, or suppliers, regardless of whether the final adverse action is the subject of a pending appeal.3 These must be reported.
Additional Reporting Requirements
Federal hospitals or federal government agencies administering health care services may have additional reporting requirements besides reporting adjudicated actions, exclusions, civil judgments, and criminal convictions. They may include submitting reports under a memorandum of understanding on clinical privileges actions and medical malpractice payments.3 The US Department of Health and Human Services (HHS) has entered into memorandums of understanding with the US Department of Defense and the US Department of Veteran Affairs to ensure their participation in the NPDB system. Federal hospitals should refer to applicable memorandums of understanding and agency-specific policies for guidance on carrying out their reporting responsibilities.4
Responding to a Report
The NPDB sends a letter to health care practitioners when an organization submits a report about the practitioner. The letter has the report number and a password is required to view the report.2 Health care practitioners also can order a self-query online to view any reports on them in the NPDB.
The subject of the report can also add a statement and dispute the report. The statement is an opportunity to provide additional information the subject would like to have included in the report. If the subject disagrees with the accuracy of a report or believes it does not meet NPDB reporting requirements, it can be disputed. The dispute will become part of the report. When the subject adds a statement or dispute, the NPDB notifies the reporting organization and all organizations that received the report within the previous 3 years of the report activity.
Health care practitioners must contact the reporting organization to try to resolve their dispute. If the subject of the report has contacted or tried to contact the reporting organization and could not resolve the dispute after 60 days, or if, within the 60-day period, the organization informs the subject that it will not modify the report, that individual may request dispute resolution.Requesting dispute resolution does not remove the report from the NPDB.
Dispute Resolution
Dispute resolution is a request for the HHS secretary to review the report. The secretary authorizes the Division of Practitioner Data Bank (DPDB) to conduct this review. The DPDB is responsible for oversight of the NPDB. The subject of the report will need to submit relevant supporting documentation to request dispute resolution. This documentation should show that the information in the report is not accurate or that the action is not reportable. Also, proof should be included that the subject contacted or attempted to contact the reporting organization. Submitting large volumes or extraneous documentation can delay the review process.
A dispute resolution manager will review the case and send the reporting organization a request for information if needed. The DPDB will send the subject of the report a courtesy copy of all correspondence. The dispute resolution timeline varies, as the DPDB reviews disputes in the order they are received. It completes a fair and thorough review based on the unique circumstances of each case and will review the case as soon as possible. Once the DPDB receives documentation from the subject and the reporting organization, it reviews the documentation to determine whether the report accurately reflects the record.
The DPDB decides to either maintain the report as is, correct it, or remove it from the NPDB. Once the process is complete, the dispute resolution manager sends a decision letter to the subject of the report and the reporting organization. The dispute resolution decision will appear in the report.
Regulations strictly limit the DPDB’s jurisdiction for reviewing disputed reports. It may only review the following: whether the report was submitted in accordance with reporting requirements, whether the reporting organization was eligible to report the information, and whether the report accurately depicts the action taken by the reporting organization and the basis for the action the reporting organization cited, as shown in the organization’s written record. The subject of the report must resolve any other issues with the reporting organization.
Under the dispute resolution review process, the DPDB cannot conduct an independent review of the merits of the action taken by the reporting organization, review the due process provided by the organization, or substitute its judgment for that of the reporting organization.2 The DPDB does not examine whether the subject of a report was informed of an ongoing investigation. The DPDB does not examine civil rights issues such as claims of discrimination or harassment in the work environment. Practitioners can find additional information at www.npdb.hrsa.gov.
Not all federal practitioners know about the National Practitioner Data Bank (NPDB), a federal web-based repository of reports containing information on medical malpractice payments and certain adverse actions related to health care practitioners, providers, and suppliers. This article explains how NPDB statutes and regulations specifically affect federal health care practitioners, which may differ from how the rules affect practitioners in the private sector.1
National Practitioner Data Bank
Established by Congress in 1986, the NPDB contains information health care organizations need to make informed decisions about the health care practitionerss they license, credential, and hire. Federal regulations authorize eligible entities, including government agencies, to report to and query the NPDB. Individuals and organizations that are subjects of these reports have access to their own information. The reports are confidential and not available to the public. The NPDB currently contains > 1.6 million reports.2
Federal Agencies Queries
A query is a search for information in the NPDB regarding a health care practitioners or organization. Some federal agencies are permitted to query the NPDB, and all hospitals, including federal hospitals, are required to query. Agencies administering government health care programs (including private entities administering such programs under contract), federal law enforcement officials and agencies, and federal agencies responsible for the licensing or certification of health care practitioners, health care providers, or health care suppliers may query NPDB. Information received in response to queries includes, among other actions, licensure and certification actions taken by states, medical malpractice payment information, federal licensing and certification actions, and adverse privileging actions.3
Federal Reporting Requirements
Federal government agencies must report exclusions (described below), adjudicated actions, civil judgments, and criminal convictions concerning health care practitioners, providers, or suppliers. The following provides detailed information about the actions federal government agencies are required to report.
Adjudicated Actions or Decisions
Adjudicated actions or decisions are formal or official final actions.3 They include, but are not limited to, personnel-related actions such as suspensions without pay, reductions in pay, reductions in grade for cause, terminations, or other comparable actions. To be reportable, adjudicated actions or decisions must include due process mechanisms. Whether the subject of a report elects not to use the due process mechanism is immaterial as long as such a process is available to the subject before the adjudicated action or decision is made final. In general, if an adjudicated action or decision follows an agency’s established administrative procedures and those procedures ensure that due process is available to the subject, the due process requirement is satisfied. This definition specifically excludes clinical privileging actions taken by federal government agencies, which are described in appropriate memorandums of understanding.
Exclusions
An exclusion is a temporary or permanent debarment of an individual or organization from participation in a federal health-related program, such that items or services furnished by the individual or organization will not be reimbursed under the federal program.3
Civil Judgments and Criminal Convictions
Health care–related civil judgments and settlements must be reported.However, settlements in which no findings of liability have been made are not reportable.3 Health care–related criminal convictions prosecuted by federal government agencies in federal court must be reported to the NPDB. Pleas of guilt and nolo contendere, or no contest, by individuals or organizations also are reportable.3
In addition, final adverse licensure and certification actions are those taken against health care practitioners, providers, or suppliers, regardless of whether the final adverse action is the subject of a pending appeal.3 These must be reported.
Additional Reporting Requirements
Federal hospitals or federal government agencies administering health care services may have additional reporting requirements besides reporting adjudicated actions, exclusions, civil judgments, and criminal convictions. They may include submitting reports under a memorandum of understanding on clinical privileges actions and medical malpractice payments.3 The US Department of Health and Human Services (HHS) has entered into memorandums of understanding with the US Department of Defense and the US Department of Veteran Affairs to ensure their participation in the NPDB system. Federal hospitals should refer to applicable memorandums of understanding and agency-specific policies for guidance on carrying out their reporting responsibilities.4
Responding to a Report
The NPDB sends a letter to health care practitioners when an organization submits a report about the practitioner. The letter has the report number and a password is required to view the report.2 Health care practitioners also can order a self-query online to view any reports on them in the NPDB.
The subject of the report can also add a statement and dispute the report. The statement is an opportunity to provide additional information the subject would like to have included in the report. If the subject disagrees with the accuracy of a report or believes it does not meet NPDB reporting requirements, it can be disputed. The dispute will become part of the report. When the subject adds a statement or dispute, the NPDB notifies the reporting organization and all organizations that received the report within the previous 3 years of the report activity.
Health care practitioners must contact the reporting organization to try to resolve their dispute. If the subject of the report has contacted or tried to contact the reporting organization and could not resolve the dispute after 60 days, or if, within the 60-day period, the organization informs the subject that it will not modify the report, that individual may request dispute resolution.Requesting dispute resolution does not remove the report from the NPDB.
Dispute Resolution
Dispute resolution is a request for the HHS secretary to review the report. The secretary authorizes the Division of Practitioner Data Bank (DPDB) to conduct this review. The DPDB is responsible for oversight of the NPDB. The subject of the report will need to submit relevant supporting documentation to request dispute resolution. This documentation should show that the information in the report is not accurate or that the action is not reportable. Also, proof should be included that the subject contacted or attempted to contact the reporting organization. Submitting large volumes or extraneous documentation can delay the review process.
A dispute resolution manager will review the case and send the reporting organization a request for information if needed. The DPDB will send the subject of the report a courtesy copy of all correspondence. The dispute resolution timeline varies, as the DPDB reviews disputes in the order they are received. It completes a fair and thorough review based on the unique circumstances of each case and will review the case as soon as possible. Once the DPDB receives documentation from the subject and the reporting organization, it reviews the documentation to determine whether the report accurately reflects the record.
The DPDB decides to either maintain the report as is, correct it, or remove it from the NPDB. Once the process is complete, the dispute resolution manager sends a decision letter to the subject of the report and the reporting organization. The dispute resolution decision will appear in the report.
Regulations strictly limit the DPDB’s jurisdiction for reviewing disputed reports. It may only review the following: whether the report was submitted in accordance with reporting requirements, whether the reporting organization was eligible to report the information, and whether the report accurately depicts the action taken by the reporting organization and the basis for the action the reporting organization cited, as shown in the organization’s written record. The subject of the report must resolve any other issues with the reporting organization.
Under the dispute resolution review process, the DPDB cannot conduct an independent review of the merits of the action taken by the reporting organization, review the due process provided by the organization, or substitute its judgment for that of the reporting organization.2 The DPDB does not examine whether the subject of a report was informed of an ongoing investigation. The DPDB does not examine civil rights issues such as claims of discrimination or harassment in the work environment. Practitioners can find additional information at www.npdb.hrsa.gov.
1. US Department of Health and Human Services, National Practitioner Data Bank. NPDB guidebook. Updated October 2018. Accessed December 16, 2021. https://www.npdb.hrsa.gov/resources/aboutGuidebooks.jsp
2. US Department of Health and Human Services, National Practitioner Data Bank. A practitioner’s guide to the NPDB. Updated February 2021. Accessed December 16, 2021. https://www.npdb.hrsa.gov/pract/practGuide.jsp
3. US Department of Health and Human Services, National Practitioner Data Bank. Federal hospitals and federal government agencies. Accessed December 16, 2021. https://www.npdb.hrsa.gov/orgs/federalAgencies.jsp
4. US Department of Health and Human Services, National Practitioner Data Bank. Federal hospitals. Accessed December 16, 2021. https://www.npdb.hrsa.gov/orgs/federalHospitals.jsp
1. US Department of Health and Human Services, National Practitioner Data Bank. NPDB guidebook. Updated October 2018. Accessed December 16, 2021. https://www.npdb.hrsa.gov/resources/aboutGuidebooks.jsp
2. US Department of Health and Human Services, National Practitioner Data Bank. A practitioner’s guide to the NPDB. Updated February 2021. Accessed December 16, 2021. https://www.npdb.hrsa.gov/pract/practGuide.jsp
3. US Department of Health and Human Services, National Practitioner Data Bank. Federal hospitals and federal government agencies. Accessed December 16, 2021. https://www.npdb.hrsa.gov/orgs/federalAgencies.jsp
4. US Department of Health and Human Services, National Practitioner Data Bank. Federal hospitals. Accessed December 16, 2021. https://www.npdb.hrsa.gov/orgs/federalHospitals.jsp
Naloxone Dispensing in Patients at Risk for Opioid Overdose After Total Knee Arthroplasty Within the Veterans Health Administration
Opioid overdose is a major public health challenge, with recent reports estimating 41 deaths per day in the United States from prescription opioid overdose.1,2 Prescribing naloxone has increasingly been advocated to reduce the risk of opioid overdose for patients identified as high risk. Naloxone distribution has been shown to decrease the incidence of opioid overdoses in the general population.3,4 The Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain recommends considering naloxone prescription for patients with a history of overdose or substance use disorder, opioid dosages ≥ 50 morphine equivalent daily dose (MEDD), and concurrent use of benzodiazepines.5
Although the CDC guidelines are intended for primary care clinicians in outpatient settings, naloxone prescribing is also relevant in the postsurgical setting.5 Many surgical patients are at risk for opioid overdose and data from the Veterans Health Administration (VHA) has shown that risk of opioid overdose is 11-fold higher in the 30 days following discharge from a surgical admission, when compared with the subsequent calendar year.6,7 This likely occurs due to new prescriptions or escalated doses of opioids following surgery. Overdose risk may be particularly relevant to orthopedic surgery as postoperative opioids are commonly prescribed.8 Patients undergoing total knee arthroplasty (TKA) may represent a vulnerable population to overdose as it is one of the most commonly performed surgeries for the treatment of chronic pain, and is frequently performed in older adults with medical comorbidities.9,10
Identifying patients at high risk for opioid overdose is important for targeted naloxone dispensing.5 A risk index for overdose or serious opioid-induced respiratory depression (RIOSORD) tool has been developed and validated in veteran and other populations to identify such patients.11 The RIOSORD tool classifies patients by risk level (1-10) and predicts probability of overdose or serious opioid-induced respiratory depression (OSORD). A patient’s level of risk is based on a weighted combination of the 15 independent risk factors most highly associated with OSORD, including comorbid conditions, prescription drug use, and health care utilization.12 Using the RIOSORD tool, the VHA Opioid Education and Naloxone Distribution (OEND) program is a risk mitigation initiative that aims to decrease opioid-related overdose morbidity and mortality. This is achieved via opioid overdose education for prevention, recognition, and response and includes outpatient naloxone prescription.13,14
Despite the comprehensive OEND program, there exists very little data to guide postsurgical naloxone prescribing. The prevalence of known risk factors for overdose in surgical patients remains unknown, as does the prevalence of perioperative naloxone distribution. Understanding overdose risk factors and naloxone prescribing patterns in surgical patients may identify potential targets for OEND efforts. This study retrospectively estimated RIOSORD scores for TKA patients between 2013 to 2016 and described naloxone distribution based on RIOSORD scores and risk factors.
Methods
We identified patients who had undergone primary TKA at VHA hospitals using Current Procedural Terminology (CPT), International Classification of Diseases, Ninth Revision (ICD-9) procedure codes, and data extracted from the VHA Corporate Data Warehouse (CDW) of electronic health records (EHRs). Our study was granted approval with exemption from informed consent by the Durham Veteran Affairs Healthcare System Institutional Review Board.
This retrospective cohort study included all veterans who underwent elective primary TKA from January 1, 2013 through December 31, 2016. We excluded patients who died before discharge.
Outcomes
Our primary outcome was being dispensed an outpatient naloxone prescription following TKA. Naloxone dispensing was identified by examining CDW outpatient pharmacy records with a final dispense date from 1 year before surgery through 7 days after discharge following TKA. To exclude naloxone administration that may have been given in a clinic, prescription data included only records with an outpatient prescription copay. Naloxone dispensing in the year before surgery was chosen to estimate likely preoperative possession of naloxone which could be available in the postoperative period. Naloxone dispensing until 7 days after discharge was chosen to identify any new dispensing that would be available in the postoperative period. These outcomes were examined over the study time frame on an annual basis.
Patient Factors
Demographic variables included age, sex, and race/ethnicity. Independent risk factors for overdose from RIOSORD were identified for each patient.15 These risk factors included comorbidities (opioid use disorder, schizophrenia, bipolar disorder, liver disease, chronic kidney disease, sleep apnea, or lung disease) and prescription drug use (use of opioids, benzodiazepines, long-acting opioids, ≥ 50 MEDD or ≥ 100 MEDD). ICD-9 and ICD-10 diagnosis codes were used to identify comorbidities. Risk classes on day of surgery were identified using a RIOSORD algorithm code. Consistent with the display of RIOSORD risk classes on the VHA Academic Detailing Service OEND risk report, patients were grouped into 3 groups based on their RIOSORD score: classes 1 to 4 (low risk), 5 to 7 (moderate risk), and 8 to 10 (high risk).
Descriptive statistics were used to summarize data on patient demographics, RIOSORD risk factors, overdose events, and naloxone dispensing over time.
Results
The study cohort included 38,011 veterans who underwent primary TKA in the VHA between January 1, 2013 and December 30, 2016. In this cohort, the mean age was 65 years, 93% were male, and 77% were White patients (Table 1). The most common comorbidities were lung disease in 9170 (24.1%) patients, sleep apnea in 6630 (17.4%) patients, chronic kidney disease in 4036 (10.6%) patients, liver disease in 2822 (7.4%) patients, and bipolar disorder in 1748 (4.6%) patients.
In 2013, 63.1% of patients presenting for surgery were actively prescribed opioids. By 2016, this decreased to 50.5%. Benzodiazepine use decreased from 13.2 to 8.8% and long-acting opioid use decreased from 8.5 to 5.8% over the same period. Patients taking ≥ 50 MEDD decreased from 8.0 to 5.3% and patients taking ≥ 100 MEDD decreased from 3.3 to 2.2%. The prevalence of moderate-risk patients decreased from 2.5 to 1.6% and high-risk patients decreased from 0.8 to 0.6% (Figure 1). Cumulatively, the prevalence of presenting with either moderate or high risk of overdose decreased from 3.3 to 2.2% between 2013 to 2016.
Naloxone Dispensing
In 2013, naloxone was not dispensed to any patients at moderate or high risk for overdose between 365 days prior to surgery until 7 days after discharge (Table 2 and Figure 2). Low-risk group naloxone dispensing increased to 2 (0.0%) in 2014, to 13 (0.1%), in 2015, and to 86 (0.9%) in 2016. Moderate-risk group naloxone dispensing remained at 0 (0.0%) in 2014, but increased to 8 (3.5%) in 2015, and to 18 (10.9%) in 2016. High-risk group naloxone dispensing remained at 0 (0.0%) in 2014, but increased to 5 (5.8%) in 2015, and to 8 (12.7%) in 2016 (Figure 3).
Discussion
Our data demonstrate that patients presenting for TKA between 2013 and 2016 routinely had individual risk factors for overdose related to either prescription drug use or comorbidities. We also show that, although the number of patients at moderate and high risk for opioid overdose is decreasing, 2.2% of TKA patients remain at moderate or high risk for opioid overdose based on a weighted combination of these individual risk factors using RIOSORD. As demand for primary TKA is projected to grow to 3.5 million procedures by 2030, using prevalence from 2016, we estimate that 76,560 patients may present for TKA across the US with moderate or high risk for opioid overdose.9 Following discharge, this risk may be even higher as this estimate does not yet account for postoperative opioid use. We demonstrate that through a VHA OEND initiative, naloxone distribution increased and appeared to be targeted to those most at risk using a simple validated tool like RIOSORD.
Presence of an individual risk factor for overdose was present in as many as 63.1% of patients presenting for TKA, as was seen in 2013 with preoperative opioid use. The 3 highest scoring prescription use–related risk factors in RIOSORD are use of opioids ≥ 100 MEDD (16 points), ≥ 50 MEDD (9 points), and long-acting formulations (9 points). All 3 decreased in prevalence over the study period but by 2016 were still seen in 2.2% for ≥ 100 MEDD, 5.3% for ≥ 50 MEDD, and 5.8% for long-acting opioids. This decrease was not surprising given implementation of a VHA-wide opioid safety initiative and the OEND program, but this could also be related to changes in patient selection for surgery in the context of increased awareness of the opioid epidemic. Despite the trend toward safer opioid prescribing, by 2016 over half of patients (50.5%) who presented for TKA were already taking opioids, with 10.6% (543 of 5127) on doses ≥ 50 MEDD.
We observed a decrease in RIOSORD risk each year, consistent with decreasing prescription-related risk factors over time. This was most obvious in the moderate-risk group. It is unclear why a similar decrease was not as obvious in the high-risk group, but this in part may be due to the already low numbers of patients in the high-risk group. This may also represent the high-risk group being somewhat resistant to the initiatives that shifted moderate-risk patients to the low-risk group. There were proportionately more patients in the moderate- and high-risk groups in the original RIOSORD population than in our surgical population, which may be attributed to the fewer comorbidities seen in our surgical population, as well as the higher opioid-prescribing patterns seen prior to the VA OEND initiative.12
Naloxone prescribing was rare prior to the OEND initiative and increased from 2013 to 2016. Increases were most marked in those in moderate- and high-risk groups, although naloxone prescribing also increased among the low-risk group. Integration of RIOSORD stratification into the OEND initiative likely played a role in targeting increased access to naloxone among those at highest risk of overdose. Naloxone dispensing increased for every group, although a significant proportion of moderate- and high-risk patients, 89.1% and 87.3%, respectively, were still not dispensed naloxone by 2016. Moreover, our estimates of perioperative naloxone access were likely an overestimate by including patients dispensed naloxone up to 1 year before surgery until 7 days after surgery. The aim was to include patients who may not have been prescribed naloxone postoperatively because of an existing naloxone prescription at home. Perioperative naloxone access estimates would have been even lower if a narrower window had been used to approximate perioperative access. This identifies an important gap between those who may benefit from naloxone dispensing and those who received naloxone. This in part may be because OEND has not been implemented as routinely in surgical settings as other settings (eg, primary care). OEND efforts may more effectively increase naloxone prescribing among surgical patients if these efforts were targeted at surgical and anesthesia departments. Given that the Comprehensive Addiction and Recovery Act of 2016 requires an assessment of patient risk prior to opioid prescribing and VHA efforts to increase utilization of tools like the Stratification Tool for Opioid Risk Mitigation (STORM), which estimates patient risk when initiating an opioid prescription and includes naloxone as one of many risk mitigation strategies, we anticipate that rates of naloxone prescribing will increase over time.
Limitations
Our study captures a large number of patients across VHA hospitals of varying size nationwide, including a mix of those with and without academic medical center affiliations. This veteran population may not represent the US commercially insured population (CIP). Zedler and colleagues highlighted the differences in prevalence of individual risk factors: notably, the CIP had a substantially higher proportion of females and younger patients.11 VHA had a greater prevalence of common chronic conditions associated with older age. The frequency of opioid dependence was similar among CIP and VHA. However, substance abuse and nonopioid substance dependence diagnoses were 4-fold more frequent among VHA controls as CIP controls. Prescribing of all opioids, except morphine and methadone, was substantially greater in CIP than in VHA.11 Despite a difference in individual risk factors, a CIP-specific RIOSORD has been validated and can be used outside of the VHA to obviate the limitations of the VHA-specific RIOSORD.11
Other limitations include our estimation of naloxone access. We do not know whether naloxone was administered or have a reliable estimate of overdose incidence in this postoperative TKA population. Also, it is important to note that RIOSORD was not developed for surgical patients. The use of RIOSORD in a postoperative population likely underestimates risk of opioid overdose due to the frequent prescriptions of new opioids or escalation of existing MEDD to the postoperative patient. Our study was also retrospective in nature and reliant on accurate coding of patient risk factors. It is possible that comorbidities were not accurately identified by EHR and therefore subject to inconsistency.
Conclusions
Veterans presenting for TKA routinely have risk factors for opioid overdose. We observed a trend toward decreasing overdose risk which coincided with the Opioid Safety and OEND initiatives within the VHA. We also observed an increase in naloxone prescription for moderate- and high-risk patients undergoing TKA, although most of these patients still did not receive naloxone as of 2016. More research is needed to refine and validate the RIOSORD score for surgical populations. Expanding initiatives such as OEND to include surgical patients presents an opportunity to improve access to naloxone for postoperative patients that may help reduce opioid overdose in this population.
1. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452. Published 2016 Dec 30. doi:10.15585/mmwr.mm655051e1
2. Wilson N, Kariisa M, Seth P, Smith H, Davis NL. Drug and opioid-involved overdose deaths - United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290-297. doi:10.15585/mmwr.mm6911a4
3. Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. Jan 30 2013;346:f174. doi:10.1136/bmj.f174
4. McClellan C, Lambdin BH, Ali MM, et al. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav. 2018;86:90-95. doi:10.1016/j.addbeh.2018.03.014
5. Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315(15):1624-1645. doi:10.1001/jama.2016.1464
6. Brat GA, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ. 2018;360:j5790. Published 2018 Jan 17. doi:10.1136/bmj.j5790
7. Mudumbai SC, Lewis ET, Oliva EM, et al. Overdose risk associated with opioid use upon hospital discharge in Veterans Health Administration surgical patients. Pain Med. 2019;20(5):1020-1031. doi:10.1093/pm/pny150
8. Hsia HL, Takemoto S, van de Ven T, et al. Acute pain is associated with chronic opioid use after total knee arthroplasty. Reg Anesth Pain Med. 2018;43(7):705-711. doi:10.1097/AAP.0000000000000831
9. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-785. doi:10.2106/JBJS.F.00222
10. Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96(8):624-630. doi:10.2106/JBJS.M.00285
11. Zedler BK, Saunders WB, Joyce AR, Vick CC, Murrelle EL. Validation of a screening risk index for serious prescription opioid-induced respiratory depression or overdose in a US commercial health plan claims database. Pain Med. 2018;19(1):68-78. doi:10.1093/pm/pnx009
12. Zedler B, Xie L, Wang L, et al. Development of a risk index for serious prescription opioid-induced respiratory depression or overdose in Veterans Health Administration patients. Pain Med. 2015;16(8):1566-79. doi:10.1111/pme.12777
13. Oliva EM, Bowe T, Tavakoli S, et al. Development and applications of the Veterans Health Administration’s Stratification Tool for Opioid Risk Mitigation (STORM) to improve opioid safety and prevent overdose and suicide. Psychol Serv. 2017;14(1):34-49. doi:10.1037/ser0000099
14. Oliva EM, Christopher MLD, Wells D, et al. Opioid overdose education and naloxone distribution: development of the Veterans Health Administration’s national program. J Am Pharm Assoc (2003). 2017;57(2S):S168-S179.e4. doi:10.1016/j.japh.2017.01.022
15. Noël PH, Copeland LA, Perrin RA, et al. VHA Corporate Data Warehouse height and weight data: opportunities and challenges for health services research. J Rehabil Res Dev. 2010;47(8):739-750. doi:10.1682/jrrd.2009.08.0110
Opioid overdose is a major public health challenge, with recent reports estimating 41 deaths per day in the United States from prescription opioid overdose.1,2 Prescribing naloxone has increasingly been advocated to reduce the risk of opioid overdose for patients identified as high risk. Naloxone distribution has been shown to decrease the incidence of opioid overdoses in the general population.3,4 The Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain recommends considering naloxone prescription for patients with a history of overdose or substance use disorder, opioid dosages ≥ 50 morphine equivalent daily dose (MEDD), and concurrent use of benzodiazepines.5
Although the CDC guidelines are intended for primary care clinicians in outpatient settings, naloxone prescribing is also relevant in the postsurgical setting.5 Many surgical patients are at risk for opioid overdose and data from the Veterans Health Administration (VHA) has shown that risk of opioid overdose is 11-fold higher in the 30 days following discharge from a surgical admission, when compared with the subsequent calendar year.6,7 This likely occurs due to new prescriptions or escalated doses of opioids following surgery. Overdose risk may be particularly relevant to orthopedic surgery as postoperative opioids are commonly prescribed.8 Patients undergoing total knee arthroplasty (TKA) may represent a vulnerable population to overdose as it is one of the most commonly performed surgeries for the treatment of chronic pain, and is frequently performed in older adults with medical comorbidities.9,10
Identifying patients at high risk for opioid overdose is important for targeted naloxone dispensing.5 A risk index for overdose or serious opioid-induced respiratory depression (RIOSORD) tool has been developed and validated in veteran and other populations to identify such patients.11 The RIOSORD tool classifies patients by risk level (1-10) and predicts probability of overdose or serious opioid-induced respiratory depression (OSORD). A patient’s level of risk is based on a weighted combination of the 15 independent risk factors most highly associated with OSORD, including comorbid conditions, prescription drug use, and health care utilization.12 Using the RIOSORD tool, the VHA Opioid Education and Naloxone Distribution (OEND) program is a risk mitigation initiative that aims to decrease opioid-related overdose morbidity and mortality. This is achieved via opioid overdose education for prevention, recognition, and response and includes outpatient naloxone prescription.13,14
Despite the comprehensive OEND program, there exists very little data to guide postsurgical naloxone prescribing. The prevalence of known risk factors for overdose in surgical patients remains unknown, as does the prevalence of perioperative naloxone distribution. Understanding overdose risk factors and naloxone prescribing patterns in surgical patients may identify potential targets for OEND efforts. This study retrospectively estimated RIOSORD scores for TKA patients between 2013 to 2016 and described naloxone distribution based on RIOSORD scores and risk factors.
Methods
We identified patients who had undergone primary TKA at VHA hospitals using Current Procedural Terminology (CPT), International Classification of Diseases, Ninth Revision (ICD-9) procedure codes, and data extracted from the VHA Corporate Data Warehouse (CDW) of electronic health records (EHRs). Our study was granted approval with exemption from informed consent by the Durham Veteran Affairs Healthcare System Institutional Review Board.
This retrospective cohort study included all veterans who underwent elective primary TKA from January 1, 2013 through December 31, 2016. We excluded patients who died before discharge.
Outcomes
Our primary outcome was being dispensed an outpatient naloxone prescription following TKA. Naloxone dispensing was identified by examining CDW outpatient pharmacy records with a final dispense date from 1 year before surgery through 7 days after discharge following TKA. To exclude naloxone administration that may have been given in a clinic, prescription data included only records with an outpatient prescription copay. Naloxone dispensing in the year before surgery was chosen to estimate likely preoperative possession of naloxone which could be available in the postoperative period. Naloxone dispensing until 7 days after discharge was chosen to identify any new dispensing that would be available in the postoperative period. These outcomes were examined over the study time frame on an annual basis.
Patient Factors
Demographic variables included age, sex, and race/ethnicity. Independent risk factors for overdose from RIOSORD were identified for each patient.15 These risk factors included comorbidities (opioid use disorder, schizophrenia, bipolar disorder, liver disease, chronic kidney disease, sleep apnea, or lung disease) and prescription drug use (use of opioids, benzodiazepines, long-acting opioids, ≥ 50 MEDD or ≥ 100 MEDD). ICD-9 and ICD-10 diagnosis codes were used to identify comorbidities. Risk classes on day of surgery were identified using a RIOSORD algorithm code. Consistent with the display of RIOSORD risk classes on the VHA Academic Detailing Service OEND risk report, patients were grouped into 3 groups based on their RIOSORD score: classes 1 to 4 (low risk), 5 to 7 (moderate risk), and 8 to 10 (high risk).
Descriptive statistics were used to summarize data on patient demographics, RIOSORD risk factors, overdose events, and naloxone dispensing over time.
Results
The study cohort included 38,011 veterans who underwent primary TKA in the VHA between January 1, 2013 and December 30, 2016. In this cohort, the mean age was 65 years, 93% were male, and 77% were White patients (Table 1). The most common comorbidities were lung disease in 9170 (24.1%) patients, sleep apnea in 6630 (17.4%) patients, chronic kidney disease in 4036 (10.6%) patients, liver disease in 2822 (7.4%) patients, and bipolar disorder in 1748 (4.6%) patients.
In 2013, 63.1% of patients presenting for surgery were actively prescribed opioids. By 2016, this decreased to 50.5%. Benzodiazepine use decreased from 13.2 to 8.8% and long-acting opioid use decreased from 8.5 to 5.8% over the same period. Patients taking ≥ 50 MEDD decreased from 8.0 to 5.3% and patients taking ≥ 100 MEDD decreased from 3.3 to 2.2%. The prevalence of moderate-risk patients decreased from 2.5 to 1.6% and high-risk patients decreased from 0.8 to 0.6% (Figure 1). Cumulatively, the prevalence of presenting with either moderate or high risk of overdose decreased from 3.3 to 2.2% between 2013 to 2016.
Naloxone Dispensing
In 2013, naloxone was not dispensed to any patients at moderate or high risk for overdose between 365 days prior to surgery until 7 days after discharge (Table 2 and Figure 2). Low-risk group naloxone dispensing increased to 2 (0.0%) in 2014, to 13 (0.1%), in 2015, and to 86 (0.9%) in 2016. Moderate-risk group naloxone dispensing remained at 0 (0.0%) in 2014, but increased to 8 (3.5%) in 2015, and to 18 (10.9%) in 2016. High-risk group naloxone dispensing remained at 0 (0.0%) in 2014, but increased to 5 (5.8%) in 2015, and to 8 (12.7%) in 2016 (Figure 3).
Discussion
Our data demonstrate that patients presenting for TKA between 2013 and 2016 routinely had individual risk factors for overdose related to either prescription drug use or comorbidities. We also show that, although the number of patients at moderate and high risk for opioid overdose is decreasing, 2.2% of TKA patients remain at moderate or high risk for opioid overdose based on a weighted combination of these individual risk factors using RIOSORD. As demand for primary TKA is projected to grow to 3.5 million procedures by 2030, using prevalence from 2016, we estimate that 76,560 patients may present for TKA across the US with moderate or high risk for opioid overdose.9 Following discharge, this risk may be even higher as this estimate does not yet account for postoperative opioid use. We demonstrate that through a VHA OEND initiative, naloxone distribution increased and appeared to be targeted to those most at risk using a simple validated tool like RIOSORD.
Presence of an individual risk factor for overdose was present in as many as 63.1% of patients presenting for TKA, as was seen in 2013 with preoperative opioid use. The 3 highest scoring prescription use–related risk factors in RIOSORD are use of opioids ≥ 100 MEDD (16 points), ≥ 50 MEDD (9 points), and long-acting formulations (9 points). All 3 decreased in prevalence over the study period but by 2016 were still seen in 2.2% for ≥ 100 MEDD, 5.3% for ≥ 50 MEDD, and 5.8% for long-acting opioids. This decrease was not surprising given implementation of a VHA-wide opioid safety initiative and the OEND program, but this could also be related to changes in patient selection for surgery in the context of increased awareness of the opioid epidemic. Despite the trend toward safer opioid prescribing, by 2016 over half of patients (50.5%) who presented for TKA were already taking opioids, with 10.6% (543 of 5127) on doses ≥ 50 MEDD.
We observed a decrease in RIOSORD risk each year, consistent with decreasing prescription-related risk factors over time. This was most obvious in the moderate-risk group. It is unclear why a similar decrease was not as obvious in the high-risk group, but this in part may be due to the already low numbers of patients in the high-risk group. This may also represent the high-risk group being somewhat resistant to the initiatives that shifted moderate-risk patients to the low-risk group. There were proportionately more patients in the moderate- and high-risk groups in the original RIOSORD population than in our surgical population, which may be attributed to the fewer comorbidities seen in our surgical population, as well as the higher opioid-prescribing patterns seen prior to the VA OEND initiative.12
Naloxone prescribing was rare prior to the OEND initiative and increased from 2013 to 2016. Increases were most marked in those in moderate- and high-risk groups, although naloxone prescribing also increased among the low-risk group. Integration of RIOSORD stratification into the OEND initiative likely played a role in targeting increased access to naloxone among those at highest risk of overdose. Naloxone dispensing increased for every group, although a significant proportion of moderate- and high-risk patients, 89.1% and 87.3%, respectively, were still not dispensed naloxone by 2016. Moreover, our estimates of perioperative naloxone access were likely an overestimate by including patients dispensed naloxone up to 1 year before surgery until 7 days after surgery. The aim was to include patients who may not have been prescribed naloxone postoperatively because of an existing naloxone prescription at home. Perioperative naloxone access estimates would have been even lower if a narrower window had been used to approximate perioperative access. This identifies an important gap between those who may benefit from naloxone dispensing and those who received naloxone. This in part may be because OEND has not been implemented as routinely in surgical settings as other settings (eg, primary care). OEND efforts may more effectively increase naloxone prescribing among surgical patients if these efforts were targeted at surgical and anesthesia departments. Given that the Comprehensive Addiction and Recovery Act of 2016 requires an assessment of patient risk prior to opioid prescribing and VHA efforts to increase utilization of tools like the Stratification Tool for Opioid Risk Mitigation (STORM), which estimates patient risk when initiating an opioid prescription and includes naloxone as one of many risk mitigation strategies, we anticipate that rates of naloxone prescribing will increase over time.
Limitations
Our study captures a large number of patients across VHA hospitals of varying size nationwide, including a mix of those with and without academic medical center affiliations. This veteran population may not represent the US commercially insured population (CIP). Zedler and colleagues highlighted the differences in prevalence of individual risk factors: notably, the CIP had a substantially higher proportion of females and younger patients.11 VHA had a greater prevalence of common chronic conditions associated with older age. The frequency of opioid dependence was similar among CIP and VHA. However, substance abuse and nonopioid substance dependence diagnoses were 4-fold more frequent among VHA controls as CIP controls. Prescribing of all opioids, except morphine and methadone, was substantially greater in CIP than in VHA.11 Despite a difference in individual risk factors, a CIP-specific RIOSORD has been validated and can be used outside of the VHA to obviate the limitations of the VHA-specific RIOSORD.11
Other limitations include our estimation of naloxone access. We do not know whether naloxone was administered or have a reliable estimate of overdose incidence in this postoperative TKA population. Also, it is important to note that RIOSORD was not developed for surgical patients. The use of RIOSORD in a postoperative population likely underestimates risk of opioid overdose due to the frequent prescriptions of new opioids or escalation of existing MEDD to the postoperative patient. Our study was also retrospective in nature and reliant on accurate coding of patient risk factors. It is possible that comorbidities were not accurately identified by EHR and therefore subject to inconsistency.
Conclusions
Veterans presenting for TKA routinely have risk factors for opioid overdose. We observed a trend toward decreasing overdose risk which coincided with the Opioid Safety and OEND initiatives within the VHA. We also observed an increase in naloxone prescription for moderate- and high-risk patients undergoing TKA, although most of these patients still did not receive naloxone as of 2016. More research is needed to refine and validate the RIOSORD score for surgical populations. Expanding initiatives such as OEND to include surgical patients presents an opportunity to improve access to naloxone for postoperative patients that may help reduce opioid overdose in this population.
Opioid overdose is a major public health challenge, with recent reports estimating 41 deaths per day in the United States from prescription opioid overdose.1,2 Prescribing naloxone has increasingly been advocated to reduce the risk of opioid overdose for patients identified as high risk. Naloxone distribution has been shown to decrease the incidence of opioid overdoses in the general population.3,4 The Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain recommends considering naloxone prescription for patients with a history of overdose or substance use disorder, opioid dosages ≥ 50 morphine equivalent daily dose (MEDD), and concurrent use of benzodiazepines.5
Although the CDC guidelines are intended for primary care clinicians in outpatient settings, naloxone prescribing is also relevant in the postsurgical setting.5 Many surgical patients are at risk for opioid overdose and data from the Veterans Health Administration (VHA) has shown that risk of opioid overdose is 11-fold higher in the 30 days following discharge from a surgical admission, when compared with the subsequent calendar year.6,7 This likely occurs due to new prescriptions or escalated doses of opioids following surgery. Overdose risk may be particularly relevant to orthopedic surgery as postoperative opioids are commonly prescribed.8 Patients undergoing total knee arthroplasty (TKA) may represent a vulnerable population to overdose as it is one of the most commonly performed surgeries for the treatment of chronic pain, and is frequently performed in older adults with medical comorbidities.9,10
Identifying patients at high risk for opioid overdose is important for targeted naloxone dispensing.5 A risk index for overdose or serious opioid-induced respiratory depression (RIOSORD) tool has been developed and validated in veteran and other populations to identify such patients.11 The RIOSORD tool classifies patients by risk level (1-10) and predicts probability of overdose or serious opioid-induced respiratory depression (OSORD). A patient’s level of risk is based on a weighted combination of the 15 independent risk factors most highly associated with OSORD, including comorbid conditions, prescription drug use, and health care utilization.12 Using the RIOSORD tool, the VHA Opioid Education and Naloxone Distribution (OEND) program is a risk mitigation initiative that aims to decrease opioid-related overdose morbidity and mortality. This is achieved via opioid overdose education for prevention, recognition, and response and includes outpatient naloxone prescription.13,14
Despite the comprehensive OEND program, there exists very little data to guide postsurgical naloxone prescribing. The prevalence of known risk factors for overdose in surgical patients remains unknown, as does the prevalence of perioperative naloxone distribution. Understanding overdose risk factors and naloxone prescribing patterns in surgical patients may identify potential targets for OEND efforts. This study retrospectively estimated RIOSORD scores for TKA patients between 2013 to 2016 and described naloxone distribution based on RIOSORD scores and risk factors.
Methods
We identified patients who had undergone primary TKA at VHA hospitals using Current Procedural Terminology (CPT), International Classification of Diseases, Ninth Revision (ICD-9) procedure codes, and data extracted from the VHA Corporate Data Warehouse (CDW) of electronic health records (EHRs). Our study was granted approval with exemption from informed consent by the Durham Veteran Affairs Healthcare System Institutional Review Board.
This retrospective cohort study included all veterans who underwent elective primary TKA from January 1, 2013 through December 31, 2016. We excluded patients who died before discharge.
Outcomes
Our primary outcome was being dispensed an outpatient naloxone prescription following TKA. Naloxone dispensing was identified by examining CDW outpatient pharmacy records with a final dispense date from 1 year before surgery through 7 days after discharge following TKA. To exclude naloxone administration that may have been given in a clinic, prescription data included only records with an outpatient prescription copay. Naloxone dispensing in the year before surgery was chosen to estimate likely preoperative possession of naloxone which could be available in the postoperative period. Naloxone dispensing until 7 days after discharge was chosen to identify any new dispensing that would be available in the postoperative period. These outcomes were examined over the study time frame on an annual basis.
Patient Factors
Demographic variables included age, sex, and race/ethnicity. Independent risk factors for overdose from RIOSORD were identified for each patient.15 These risk factors included comorbidities (opioid use disorder, schizophrenia, bipolar disorder, liver disease, chronic kidney disease, sleep apnea, or lung disease) and prescription drug use (use of opioids, benzodiazepines, long-acting opioids, ≥ 50 MEDD or ≥ 100 MEDD). ICD-9 and ICD-10 diagnosis codes were used to identify comorbidities. Risk classes on day of surgery were identified using a RIOSORD algorithm code. Consistent with the display of RIOSORD risk classes on the VHA Academic Detailing Service OEND risk report, patients were grouped into 3 groups based on their RIOSORD score: classes 1 to 4 (low risk), 5 to 7 (moderate risk), and 8 to 10 (high risk).
Descriptive statistics were used to summarize data on patient demographics, RIOSORD risk factors, overdose events, and naloxone dispensing over time.
Results
The study cohort included 38,011 veterans who underwent primary TKA in the VHA between January 1, 2013 and December 30, 2016. In this cohort, the mean age was 65 years, 93% were male, and 77% were White patients (Table 1). The most common comorbidities were lung disease in 9170 (24.1%) patients, sleep apnea in 6630 (17.4%) patients, chronic kidney disease in 4036 (10.6%) patients, liver disease in 2822 (7.4%) patients, and bipolar disorder in 1748 (4.6%) patients.
In 2013, 63.1% of patients presenting for surgery were actively prescribed opioids. By 2016, this decreased to 50.5%. Benzodiazepine use decreased from 13.2 to 8.8% and long-acting opioid use decreased from 8.5 to 5.8% over the same period. Patients taking ≥ 50 MEDD decreased from 8.0 to 5.3% and patients taking ≥ 100 MEDD decreased from 3.3 to 2.2%. The prevalence of moderate-risk patients decreased from 2.5 to 1.6% and high-risk patients decreased from 0.8 to 0.6% (Figure 1). Cumulatively, the prevalence of presenting with either moderate or high risk of overdose decreased from 3.3 to 2.2% between 2013 to 2016.
Naloxone Dispensing
In 2013, naloxone was not dispensed to any patients at moderate or high risk for overdose between 365 days prior to surgery until 7 days after discharge (Table 2 and Figure 2). Low-risk group naloxone dispensing increased to 2 (0.0%) in 2014, to 13 (0.1%), in 2015, and to 86 (0.9%) in 2016. Moderate-risk group naloxone dispensing remained at 0 (0.0%) in 2014, but increased to 8 (3.5%) in 2015, and to 18 (10.9%) in 2016. High-risk group naloxone dispensing remained at 0 (0.0%) in 2014, but increased to 5 (5.8%) in 2015, and to 8 (12.7%) in 2016 (Figure 3).
Discussion
Our data demonstrate that patients presenting for TKA between 2013 and 2016 routinely had individual risk factors for overdose related to either prescription drug use or comorbidities. We also show that, although the number of patients at moderate and high risk for opioid overdose is decreasing, 2.2% of TKA patients remain at moderate or high risk for opioid overdose based on a weighted combination of these individual risk factors using RIOSORD. As demand for primary TKA is projected to grow to 3.5 million procedures by 2030, using prevalence from 2016, we estimate that 76,560 patients may present for TKA across the US with moderate or high risk for opioid overdose.9 Following discharge, this risk may be even higher as this estimate does not yet account for postoperative opioid use. We demonstrate that through a VHA OEND initiative, naloxone distribution increased and appeared to be targeted to those most at risk using a simple validated tool like RIOSORD.
Presence of an individual risk factor for overdose was present in as many as 63.1% of patients presenting for TKA, as was seen in 2013 with preoperative opioid use. The 3 highest scoring prescription use–related risk factors in RIOSORD are use of opioids ≥ 100 MEDD (16 points), ≥ 50 MEDD (9 points), and long-acting formulations (9 points). All 3 decreased in prevalence over the study period but by 2016 were still seen in 2.2% for ≥ 100 MEDD, 5.3% for ≥ 50 MEDD, and 5.8% for long-acting opioids. This decrease was not surprising given implementation of a VHA-wide opioid safety initiative and the OEND program, but this could also be related to changes in patient selection for surgery in the context of increased awareness of the opioid epidemic. Despite the trend toward safer opioid prescribing, by 2016 over half of patients (50.5%) who presented for TKA were already taking opioids, with 10.6% (543 of 5127) on doses ≥ 50 MEDD.
We observed a decrease in RIOSORD risk each year, consistent with decreasing prescription-related risk factors over time. This was most obvious in the moderate-risk group. It is unclear why a similar decrease was not as obvious in the high-risk group, but this in part may be due to the already low numbers of patients in the high-risk group. This may also represent the high-risk group being somewhat resistant to the initiatives that shifted moderate-risk patients to the low-risk group. There were proportionately more patients in the moderate- and high-risk groups in the original RIOSORD population than in our surgical population, which may be attributed to the fewer comorbidities seen in our surgical population, as well as the higher opioid-prescribing patterns seen prior to the VA OEND initiative.12
Naloxone prescribing was rare prior to the OEND initiative and increased from 2013 to 2016. Increases were most marked in those in moderate- and high-risk groups, although naloxone prescribing also increased among the low-risk group. Integration of RIOSORD stratification into the OEND initiative likely played a role in targeting increased access to naloxone among those at highest risk of overdose. Naloxone dispensing increased for every group, although a significant proportion of moderate- and high-risk patients, 89.1% and 87.3%, respectively, were still not dispensed naloxone by 2016. Moreover, our estimates of perioperative naloxone access were likely an overestimate by including patients dispensed naloxone up to 1 year before surgery until 7 days after surgery. The aim was to include patients who may not have been prescribed naloxone postoperatively because of an existing naloxone prescription at home. Perioperative naloxone access estimates would have been even lower if a narrower window had been used to approximate perioperative access. This identifies an important gap between those who may benefit from naloxone dispensing and those who received naloxone. This in part may be because OEND has not been implemented as routinely in surgical settings as other settings (eg, primary care). OEND efforts may more effectively increase naloxone prescribing among surgical patients if these efforts were targeted at surgical and anesthesia departments. Given that the Comprehensive Addiction and Recovery Act of 2016 requires an assessment of patient risk prior to opioid prescribing and VHA efforts to increase utilization of tools like the Stratification Tool for Opioid Risk Mitigation (STORM), which estimates patient risk when initiating an opioid prescription and includes naloxone as one of many risk mitigation strategies, we anticipate that rates of naloxone prescribing will increase over time.
Limitations
Our study captures a large number of patients across VHA hospitals of varying size nationwide, including a mix of those with and without academic medical center affiliations. This veteran population may not represent the US commercially insured population (CIP). Zedler and colleagues highlighted the differences in prevalence of individual risk factors: notably, the CIP had a substantially higher proportion of females and younger patients.11 VHA had a greater prevalence of common chronic conditions associated with older age. The frequency of opioid dependence was similar among CIP and VHA. However, substance abuse and nonopioid substance dependence diagnoses were 4-fold more frequent among VHA controls as CIP controls. Prescribing of all opioids, except morphine and methadone, was substantially greater in CIP than in VHA.11 Despite a difference in individual risk factors, a CIP-specific RIOSORD has been validated and can be used outside of the VHA to obviate the limitations of the VHA-specific RIOSORD.11
Other limitations include our estimation of naloxone access. We do not know whether naloxone was administered or have a reliable estimate of overdose incidence in this postoperative TKA population. Also, it is important to note that RIOSORD was not developed for surgical patients. The use of RIOSORD in a postoperative population likely underestimates risk of opioid overdose due to the frequent prescriptions of new opioids or escalation of existing MEDD to the postoperative patient. Our study was also retrospective in nature and reliant on accurate coding of patient risk factors. It is possible that comorbidities were not accurately identified by EHR and therefore subject to inconsistency.
Conclusions
Veterans presenting for TKA routinely have risk factors for opioid overdose. We observed a trend toward decreasing overdose risk which coincided with the Opioid Safety and OEND initiatives within the VHA. We also observed an increase in naloxone prescription for moderate- and high-risk patients undergoing TKA, although most of these patients still did not receive naloxone as of 2016. More research is needed to refine and validate the RIOSORD score for surgical populations. Expanding initiatives such as OEND to include surgical patients presents an opportunity to improve access to naloxone for postoperative patients that may help reduce opioid overdose in this population.
1. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452. Published 2016 Dec 30. doi:10.15585/mmwr.mm655051e1
2. Wilson N, Kariisa M, Seth P, Smith H, Davis NL. Drug and opioid-involved overdose deaths - United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290-297. doi:10.15585/mmwr.mm6911a4
3. Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. Jan 30 2013;346:f174. doi:10.1136/bmj.f174
4. McClellan C, Lambdin BH, Ali MM, et al. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav. 2018;86:90-95. doi:10.1016/j.addbeh.2018.03.014
5. Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315(15):1624-1645. doi:10.1001/jama.2016.1464
6. Brat GA, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ. 2018;360:j5790. Published 2018 Jan 17. doi:10.1136/bmj.j5790
7. Mudumbai SC, Lewis ET, Oliva EM, et al. Overdose risk associated with opioid use upon hospital discharge in Veterans Health Administration surgical patients. Pain Med. 2019;20(5):1020-1031. doi:10.1093/pm/pny150
8. Hsia HL, Takemoto S, van de Ven T, et al. Acute pain is associated with chronic opioid use after total knee arthroplasty. Reg Anesth Pain Med. 2018;43(7):705-711. doi:10.1097/AAP.0000000000000831
9. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-785. doi:10.2106/JBJS.F.00222
10. Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96(8):624-630. doi:10.2106/JBJS.M.00285
11. Zedler BK, Saunders WB, Joyce AR, Vick CC, Murrelle EL. Validation of a screening risk index for serious prescription opioid-induced respiratory depression or overdose in a US commercial health plan claims database. Pain Med. 2018;19(1):68-78. doi:10.1093/pm/pnx009
12. Zedler B, Xie L, Wang L, et al. Development of a risk index for serious prescription opioid-induced respiratory depression or overdose in Veterans Health Administration patients. Pain Med. 2015;16(8):1566-79. doi:10.1111/pme.12777
13. Oliva EM, Bowe T, Tavakoli S, et al. Development and applications of the Veterans Health Administration’s Stratification Tool for Opioid Risk Mitigation (STORM) to improve opioid safety and prevent overdose and suicide. Psychol Serv. 2017;14(1):34-49. doi:10.1037/ser0000099
14. Oliva EM, Christopher MLD, Wells D, et al. Opioid overdose education and naloxone distribution: development of the Veterans Health Administration’s national program. J Am Pharm Assoc (2003). 2017;57(2S):S168-S179.e4. doi:10.1016/j.japh.2017.01.022
15. Noël PH, Copeland LA, Perrin RA, et al. VHA Corporate Data Warehouse height and weight data: opportunities and challenges for health services research. J Rehabil Res Dev. 2010;47(8):739-750. doi:10.1682/jrrd.2009.08.0110
1. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452. Published 2016 Dec 30. doi:10.15585/mmwr.mm655051e1
2. Wilson N, Kariisa M, Seth P, Smith H, Davis NL. Drug and opioid-involved overdose deaths - United States, 2017-2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290-297. doi:10.15585/mmwr.mm6911a4
3. Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. Jan 30 2013;346:f174. doi:10.1136/bmj.f174
4. McClellan C, Lambdin BH, Ali MM, et al. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav. 2018;86:90-95. doi:10.1016/j.addbeh.2018.03.014
5. Dowell D, Haegerich TM, Chou R. CDC Guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 2016;315(15):1624-1645. doi:10.1001/jama.2016.1464
6. Brat GA, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ. 2018;360:j5790. Published 2018 Jan 17. doi:10.1136/bmj.j5790
7. Mudumbai SC, Lewis ET, Oliva EM, et al. Overdose risk associated with opioid use upon hospital discharge in Veterans Health Administration surgical patients. Pain Med. 2019;20(5):1020-1031. doi:10.1093/pm/pny150
8. Hsia HL, Takemoto S, van de Ven T, et al. Acute pain is associated with chronic opioid use after total knee arthroplasty. Reg Anesth Pain Med. 2018;43(7):705-711. doi:10.1097/AAP.0000000000000831
9. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-785. doi:10.2106/JBJS.F.00222
10. Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96(8):624-630. doi:10.2106/JBJS.M.00285
11. Zedler BK, Saunders WB, Joyce AR, Vick CC, Murrelle EL. Validation of a screening risk index for serious prescription opioid-induced respiratory depression or overdose in a US commercial health plan claims database. Pain Med. 2018;19(1):68-78. doi:10.1093/pm/pnx009
12. Zedler B, Xie L, Wang L, et al. Development of a risk index for serious prescription opioid-induced respiratory depression or overdose in Veterans Health Administration patients. Pain Med. 2015;16(8):1566-79. doi:10.1111/pme.12777
13. Oliva EM, Bowe T, Tavakoli S, et al. Development and applications of the Veterans Health Administration’s Stratification Tool for Opioid Risk Mitigation (STORM) to improve opioid safety and prevent overdose and suicide. Psychol Serv. 2017;14(1):34-49. doi:10.1037/ser0000099
14. Oliva EM, Christopher MLD, Wells D, et al. Opioid overdose education and naloxone distribution: development of the Veterans Health Administration’s national program. J Am Pharm Assoc (2003). 2017;57(2S):S168-S179.e4. doi:10.1016/j.japh.2017.01.022
15. Noël PH, Copeland LA, Perrin RA, et al. VHA Corporate Data Warehouse height and weight data: opportunities and challenges for health services research. J Rehabil Res Dev. 2010;47(8):739-750. doi:10.1682/jrrd.2009.08.0110
Anxiety in men tied to risk factors for CVD, diabetes
Among healthy middle-aged men, those who were more anxious were more likely to develop high levels of multiple biomarkers of cardiometabolic risk over a 40-year follow-up in a new study.
“By middle adulthood, higher anxiety levels are associated with stable differences” in biomarkers of risk for coronary artery disease (CAD), stroke, and type 2 diabetes, which “are maintained into older ages,” the researchers wrote.
Anxious individuals “may experience deteriorations in cardiometabolic health earlier in life and remain on a stable trajectory of heightened risk into older ages,” they concluded.
The study, led by Lewina Lee, PhD, was published online Jan. 24, 2022, in the Journal of the American Heart Association.
“Men who had higher levels of anxiety at the beginning of the study had consistently higher biological risk for cardiometabolic disease than less anxious men from midlife into old age,” Dr. Lee, assistant professor of psychiatry, Boston University, summarized in an email.
Clinicians may not screen for heart disease and diabetes, and/or only discuss lifestyle modifications when patients are older or have the first signs of disease, she added.
However, the study findings “suggest that worries and anxiety are associated with preclinical pathophysiological processes that tend to culminate in cardiometabolic disease” and show “the importance of screening for mental health difficulties, such as worries and anxiety, in men as early as in their 30s and 40s,” she stressed.
Since most of the men were White (97%) and veterans (94%), “it would be important for future studies to evaluate if these associations exist among women, people from diverse racial and ethnic groups, and in more socioeconomically varying samples, and to consider how anxiety may relate to the development of cardiometabolic risk in much younger individuals than those in our study,” Dr. Lee said in a press release from the American Heart Association.
“This study adds to the growing body of research that link psychological health to cardiovascular risk,” Glenn N. Levine, MD, who was not involved with this research, told this news organization in an email.
“We know that factors such as depression and stress can increase cardiac risk; this study further supports that anxiety can as well,” added Dr. Levine, chief of cardiology, Michael E. DeBakey Veterans Affairs Medical Center, Houston.
“Everyone experiences some anxiety in their life,” he added. However, “if a provider senses that a patient’s anxiety is far beyond the ‘normal’ that we all have from time to time, and it is seemingly adversely impacting both their psychological and physical health, it would be reasonable to suggest to the patient that it might be useful to speak with a mental health professional, and if the patient is receptive, to then make a formal consultation or referral,” said Dr. Levine, who was writing group chair of a recent AHA Scientific Statement on mind-heart-body connection.
Neuroticism and worry
Several studies have linked anxiety to a greater risk of cardiometabolic disease onset, Dr. Lee and colleagues wrote, but it is unclear if anxious individuals have a steadily worsening risk as they age, or if they have a higher risk in middle age, which stays the same in older age.
To investigate this, they analyzed data from 1561 men who were seen at the VA Boston outpatient clinic and did not have CAD, type 2 diabetes, stroke, or cancer when they enrolled in the Normative Aging Study.
The men had a mean age of 53 years (range, 33-84) in 1975 and were followed until 2015 or until dropout from the study or death.
At baseline, the study participants filled in the Eysenck Personality Inventory, which assesses neuroticism, and also responded to a scale indicating how much they worry about 20 issues (excluding health).
“Neuroticism,” the researchers explained, “is a tendency to perceive experiences as threatening, feel that challenges are uncontrollable, and experience frequent and disproportionately intense negative emotions,” such as fear, anxiety, sadness, and anger, “across many situations.”
“Worry refers to attempts to solve a problem where future outcome is uncertain and potentially positive or negative,” Dr. Lee noted. Although worry can be healthy and lead to constructive solutions, “it may be unhealthy, especially when it becomes uncontrollable and interferes with day-to-day functioning.”
Of note, in 1980, the American Psychiatric Association removed the term neurosis from its diagnostic manual. What was previously called neurosis is included as part of generalized anxiety disorder; GAD also encompasses excessive worry.
Cardiometabolic risk from midlife to old age
The men in the current study had on-site physical examinations every 3-5 years.
The researchers calculated the men’s cardiometabolic risk score (from 0 to 7) by assigning 1 point each for the following: systolic blood pressure greater than 130 mm Hg, diastolic blood pressure greater than 85 mm Hg, total cholesterol of at least 240 mg/dL, triglycerides of at least 150 mg/dL, body mass index of at least 30 kg/m2, glucose of at least 100 mg/dL, and erythrocyte sedimentation rate of at least 14 mm/hour.
Alternatively, patients were assigned a point each for taking medication that could affect these markers (except for body mass index).
Overall, on average, at baseline, the men had a cardiometabolic risk score of 2.9. From age 33-65, this score increased to 3.8, and then it did not increase as much later on.
That is, the cardiometabolic risk score increased by 0.8 per decade until age 65, followed by a slower increase of 0.5 per decade.
At all ages, men with higher levels of neuroticism or worry had a higher cardiometabolic risk score
Each additional standard deviation of neuroticism was associated with a 13% increased risk of having six or more of the seven cardiometabolic risk markers during follow-up, after adjusting for age, demographics, and family history of CAD, but the relationship was attenuated after also adjusting for health behaviors (for example, smoking, alcohol consumption, physical activity, and past-year physician visit at baseline).
Similarly, each additional standard deviation of worry was associated with a 10% increased risk of having six or more of the seven cardiometabolic risk markers during follow-up after the same adjustments, and was also no longer significantly different after the same further adjustments.
The research was supported by grants from the National Institutes of Health and a Senior Research Career Scientist Award from the Office of Research and Development, Department of Veterans Affairs. The Normative Aging Study is a research component of the Massachusetts Veterans Epidemiology Research and Information Center and is supported by the VA Cooperative Studies Program/Epidemiological Research Centers. The study authors and Dr. Levine disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among healthy middle-aged men, those who were more anxious were more likely to develop high levels of multiple biomarkers of cardiometabolic risk over a 40-year follow-up in a new study.
“By middle adulthood, higher anxiety levels are associated with stable differences” in biomarkers of risk for coronary artery disease (CAD), stroke, and type 2 diabetes, which “are maintained into older ages,” the researchers wrote.
Anxious individuals “may experience deteriorations in cardiometabolic health earlier in life and remain on a stable trajectory of heightened risk into older ages,” they concluded.
The study, led by Lewina Lee, PhD, was published online Jan. 24, 2022, in the Journal of the American Heart Association.
“Men who had higher levels of anxiety at the beginning of the study had consistently higher biological risk for cardiometabolic disease than less anxious men from midlife into old age,” Dr. Lee, assistant professor of psychiatry, Boston University, summarized in an email.
Clinicians may not screen for heart disease and diabetes, and/or only discuss lifestyle modifications when patients are older or have the first signs of disease, she added.
However, the study findings “suggest that worries and anxiety are associated with preclinical pathophysiological processes that tend to culminate in cardiometabolic disease” and show “the importance of screening for mental health difficulties, such as worries and anxiety, in men as early as in their 30s and 40s,” she stressed.
Since most of the men were White (97%) and veterans (94%), “it would be important for future studies to evaluate if these associations exist among women, people from diverse racial and ethnic groups, and in more socioeconomically varying samples, and to consider how anxiety may relate to the development of cardiometabolic risk in much younger individuals than those in our study,” Dr. Lee said in a press release from the American Heart Association.
“This study adds to the growing body of research that link psychological health to cardiovascular risk,” Glenn N. Levine, MD, who was not involved with this research, told this news organization in an email.
“We know that factors such as depression and stress can increase cardiac risk; this study further supports that anxiety can as well,” added Dr. Levine, chief of cardiology, Michael E. DeBakey Veterans Affairs Medical Center, Houston.
“Everyone experiences some anxiety in their life,” he added. However, “if a provider senses that a patient’s anxiety is far beyond the ‘normal’ that we all have from time to time, and it is seemingly adversely impacting both their psychological and physical health, it would be reasonable to suggest to the patient that it might be useful to speak with a mental health professional, and if the patient is receptive, to then make a formal consultation or referral,” said Dr. Levine, who was writing group chair of a recent AHA Scientific Statement on mind-heart-body connection.
Neuroticism and worry
Several studies have linked anxiety to a greater risk of cardiometabolic disease onset, Dr. Lee and colleagues wrote, but it is unclear if anxious individuals have a steadily worsening risk as they age, or if they have a higher risk in middle age, which stays the same in older age.
To investigate this, they analyzed data from 1561 men who were seen at the VA Boston outpatient clinic and did not have CAD, type 2 diabetes, stroke, or cancer when they enrolled in the Normative Aging Study.
The men had a mean age of 53 years (range, 33-84) in 1975 and were followed until 2015 or until dropout from the study or death.
At baseline, the study participants filled in the Eysenck Personality Inventory, which assesses neuroticism, and also responded to a scale indicating how much they worry about 20 issues (excluding health).
“Neuroticism,” the researchers explained, “is a tendency to perceive experiences as threatening, feel that challenges are uncontrollable, and experience frequent and disproportionately intense negative emotions,” such as fear, anxiety, sadness, and anger, “across many situations.”
“Worry refers to attempts to solve a problem where future outcome is uncertain and potentially positive or negative,” Dr. Lee noted. Although worry can be healthy and lead to constructive solutions, “it may be unhealthy, especially when it becomes uncontrollable and interferes with day-to-day functioning.”
Of note, in 1980, the American Psychiatric Association removed the term neurosis from its diagnostic manual. What was previously called neurosis is included as part of generalized anxiety disorder; GAD also encompasses excessive worry.
Cardiometabolic risk from midlife to old age
The men in the current study had on-site physical examinations every 3-5 years.
The researchers calculated the men’s cardiometabolic risk score (from 0 to 7) by assigning 1 point each for the following: systolic blood pressure greater than 130 mm Hg, diastolic blood pressure greater than 85 mm Hg, total cholesterol of at least 240 mg/dL, triglycerides of at least 150 mg/dL, body mass index of at least 30 kg/m2, glucose of at least 100 mg/dL, and erythrocyte sedimentation rate of at least 14 mm/hour.
Alternatively, patients were assigned a point each for taking medication that could affect these markers (except for body mass index).
Overall, on average, at baseline, the men had a cardiometabolic risk score of 2.9. From age 33-65, this score increased to 3.8, and then it did not increase as much later on.
That is, the cardiometabolic risk score increased by 0.8 per decade until age 65, followed by a slower increase of 0.5 per decade.
At all ages, men with higher levels of neuroticism or worry had a higher cardiometabolic risk score
Each additional standard deviation of neuroticism was associated with a 13% increased risk of having six or more of the seven cardiometabolic risk markers during follow-up, after adjusting for age, demographics, and family history of CAD, but the relationship was attenuated after also adjusting for health behaviors (for example, smoking, alcohol consumption, physical activity, and past-year physician visit at baseline).
Similarly, each additional standard deviation of worry was associated with a 10% increased risk of having six or more of the seven cardiometabolic risk markers during follow-up after the same adjustments, and was also no longer significantly different after the same further adjustments.
The research was supported by grants from the National Institutes of Health and a Senior Research Career Scientist Award from the Office of Research and Development, Department of Veterans Affairs. The Normative Aging Study is a research component of the Massachusetts Veterans Epidemiology Research and Information Center and is supported by the VA Cooperative Studies Program/Epidemiological Research Centers. The study authors and Dr. Levine disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among healthy middle-aged men, those who were more anxious were more likely to develop high levels of multiple biomarkers of cardiometabolic risk over a 40-year follow-up in a new study.
“By middle adulthood, higher anxiety levels are associated with stable differences” in biomarkers of risk for coronary artery disease (CAD), stroke, and type 2 diabetes, which “are maintained into older ages,” the researchers wrote.
Anxious individuals “may experience deteriorations in cardiometabolic health earlier in life and remain on a stable trajectory of heightened risk into older ages,” they concluded.
The study, led by Lewina Lee, PhD, was published online Jan. 24, 2022, in the Journal of the American Heart Association.
“Men who had higher levels of anxiety at the beginning of the study had consistently higher biological risk for cardiometabolic disease than less anxious men from midlife into old age,” Dr. Lee, assistant professor of psychiatry, Boston University, summarized in an email.
Clinicians may not screen for heart disease and diabetes, and/or only discuss lifestyle modifications when patients are older or have the first signs of disease, she added.
However, the study findings “suggest that worries and anxiety are associated with preclinical pathophysiological processes that tend to culminate in cardiometabolic disease” and show “the importance of screening for mental health difficulties, such as worries and anxiety, in men as early as in their 30s and 40s,” she stressed.
Since most of the men were White (97%) and veterans (94%), “it would be important for future studies to evaluate if these associations exist among women, people from diverse racial and ethnic groups, and in more socioeconomically varying samples, and to consider how anxiety may relate to the development of cardiometabolic risk in much younger individuals than those in our study,” Dr. Lee said in a press release from the American Heart Association.
“This study adds to the growing body of research that link psychological health to cardiovascular risk,” Glenn N. Levine, MD, who was not involved with this research, told this news organization in an email.
“We know that factors such as depression and stress can increase cardiac risk; this study further supports that anxiety can as well,” added Dr. Levine, chief of cardiology, Michael E. DeBakey Veterans Affairs Medical Center, Houston.
“Everyone experiences some anxiety in their life,” he added. However, “if a provider senses that a patient’s anxiety is far beyond the ‘normal’ that we all have from time to time, and it is seemingly adversely impacting both their psychological and physical health, it would be reasonable to suggest to the patient that it might be useful to speak with a mental health professional, and if the patient is receptive, to then make a formal consultation or referral,” said Dr. Levine, who was writing group chair of a recent AHA Scientific Statement on mind-heart-body connection.
Neuroticism and worry
Several studies have linked anxiety to a greater risk of cardiometabolic disease onset, Dr. Lee and colleagues wrote, but it is unclear if anxious individuals have a steadily worsening risk as they age, or if they have a higher risk in middle age, which stays the same in older age.
To investigate this, they analyzed data from 1561 men who were seen at the VA Boston outpatient clinic and did not have CAD, type 2 diabetes, stroke, or cancer when they enrolled in the Normative Aging Study.
The men had a mean age of 53 years (range, 33-84) in 1975 and were followed until 2015 or until dropout from the study or death.
At baseline, the study participants filled in the Eysenck Personality Inventory, which assesses neuroticism, and also responded to a scale indicating how much they worry about 20 issues (excluding health).
“Neuroticism,” the researchers explained, “is a tendency to perceive experiences as threatening, feel that challenges are uncontrollable, and experience frequent and disproportionately intense negative emotions,” such as fear, anxiety, sadness, and anger, “across many situations.”
“Worry refers to attempts to solve a problem where future outcome is uncertain and potentially positive or negative,” Dr. Lee noted. Although worry can be healthy and lead to constructive solutions, “it may be unhealthy, especially when it becomes uncontrollable and interferes with day-to-day functioning.”
Of note, in 1980, the American Psychiatric Association removed the term neurosis from its diagnostic manual. What was previously called neurosis is included as part of generalized anxiety disorder; GAD also encompasses excessive worry.
Cardiometabolic risk from midlife to old age
The men in the current study had on-site physical examinations every 3-5 years.
The researchers calculated the men’s cardiometabolic risk score (from 0 to 7) by assigning 1 point each for the following: systolic blood pressure greater than 130 mm Hg, diastolic blood pressure greater than 85 mm Hg, total cholesterol of at least 240 mg/dL, triglycerides of at least 150 mg/dL, body mass index of at least 30 kg/m2, glucose of at least 100 mg/dL, and erythrocyte sedimentation rate of at least 14 mm/hour.
Alternatively, patients were assigned a point each for taking medication that could affect these markers (except for body mass index).
Overall, on average, at baseline, the men had a cardiometabolic risk score of 2.9. From age 33-65, this score increased to 3.8, and then it did not increase as much later on.
That is, the cardiometabolic risk score increased by 0.8 per decade until age 65, followed by a slower increase of 0.5 per decade.
At all ages, men with higher levels of neuroticism or worry had a higher cardiometabolic risk score
Each additional standard deviation of neuroticism was associated with a 13% increased risk of having six or more of the seven cardiometabolic risk markers during follow-up, after adjusting for age, demographics, and family history of CAD, but the relationship was attenuated after also adjusting for health behaviors (for example, smoking, alcohol consumption, physical activity, and past-year physician visit at baseline).
Similarly, each additional standard deviation of worry was associated with a 10% increased risk of having six or more of the seven cardiometabolic risk markers during follow-up after the same adjustments, and was also no longer significantly different after the same further adjustments.
The research was supported by grants from the National Institutes of Health and a Senior Research Career Scientist Award from the Office of Research and Development, Department of Veterans Affairs. The Normative Aging Study is a research component of the Massachusetts Veterans Epidemiology Research and Information Center and is supported by the VA Cooperative Studies Program/Epidemiological Research Centers. The study authors and Dr. Levine disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Integrating Massage Therapy Into the Health Care of Female Veterans
There are approximately 2 million female veterans in the United States, representing about 10% of the veteran population.1 In 2015, 456,000 female veterans used the US Department of Veterans Affairs (VA) health care services. The VA predicts an increase in utilization over the next 20 years.2
Female veterans are more likely to have musculoskeletal disorder multimorbidity compared with male veterans and have higher rates of depressive and bipolar disorders, anxiety, and posttraumatic stress disorder (PTSD).3,4 Compared with male veterans, female veterans are younger, more likely to be unmarried and to have served during the wars in Iraq and Afghanistan.3 Fifty-five percent of women veterans vs 41% of men veterans have a service-connected disability, and a greater percentage of women veterans have a service connection rating > 50%.5 The top service-connected disabilities for women veterans are PTSD, major depressive disorder, migraines, and lumbosacral or cervical strain.2 In addition, one-third of women veterans using VA health care report experiencing military sexual trauma (MST).6 Military service may impact the health of female veterans both physically and mentally. Providing treatments and programs to improve their health and their health care experience are current VA priorities.
The VA is changing the way health care is conceptualized and delivered by implementing a holistic model of care known as Whole Health, which seeks to empower and equip patients to take charge of their health, blending conventional medicine with self-care and complementary and integrative health (CIH) approaches, such as massage therapy, yoga, acupuncture, and meditation.7 CIH therapies can help improve physical and mental health with little to no adverse effects.8-10
As part of the Whole Health initiative at the VA Ann Arbor Healthcare System (VAAAHS) in Michigan, the massage program was expanded in 2017 to offer relaxation massages to female veterans attending the women’s health clinic, which provides gynecologic care. Patients visiting a gynecology clinic often experience anxiety and pain related to invasive procedures and examinations. This is especially true for female veterans who experienced MST.11
VAAAHS has 1 staff massage therapist (MT). To expand the program to the women’s health clinic, volunteer licensed MTs were recruited and trained in specific procedures by the staff MT.
Several studies have demonstrated the effect of therapeutic massage on pain and anxiety in predominantly male veteran study populations, including veterans needing postsurgical and palliative care as well as those experiencing chronic pain and knee osteoarthritis.12-16 Little is known about the effects of massage therapy on female veterans. The purpose of this pilot study was to examine the effects of massage therapy among female veterans participating in the women’s health massage program.
Methods
The setting for this pre-post intervention study was VAAAHS. Veterans were called in advance by clinic staff and scheduled for 60-minute appointments either before or after their clinic appointment, depending on availability. MTs were instructed to provide relaxation massage using Swedish massage techniques with moderate pressure, avoiding deep pressure techniques.
The volunteer MTs gave the participants a survey to provide comments and to rate baseline pain and other symptoms prior to and following the massage. The MT left the room to provide privacy while completing the survey. The staff included the symptom data in the massage note as clinical outcomes and entered them into the electronic health record. Massages were given from October 1, 2017 to June 30, 2018. Data including symptom scores, demographics, the presence of chronic pain, mental health diagnoses, patient comments, and opioid use were abstracted from the electronic health record by 2 members of the study team and entered into an Excel database. This study was approved by the VAAAHS Institutional Review Board.
Study Measures
Pain intensity, pain unpleasantness (the affective component of pain), anxiety, shortness of breath, relaxation, and inner peace were rated pre- and postmassage on a 0 to 10 scale. Shortness of breath was included due to the relationship between breathing and anxiety. Inner peace was assessed to measure the calming effects of massage therapy. Beck and colleagues found the concept of inner peace was an important outcome of massage therapy.17 The scale anchors for pain intensity were “no pain” and “severe pain”; and “not at all unpleasant” and “as unpleasant as it can be” for pain unpleasantness. For anxiety, the anchors were “no anxiety” and “as anxious as I can be.” Anchors for relaxation and inner peace were reversed so that a 0 indicated low relaxation and inner peace while a 10 indicated the highest state of relaxation and inner peace.
Chronic pain was defined as pain existing for > 3 months. A history of chronic pain was determined from a review and synthesis of primary care and specialty care recorded diagnoses, patient concerns, and service-connected disabilities. The diagnoses included lumbosacral or cervical strain, chronic low back, joint (knee, shoulder, hip, ankle), neck, or pelvic pain, fibromyalgia, headache, migraine, osteoarthritis, and myofascial pain syndrome. The presence of mental health conditions, including depression, anxiety, bipolar disorders, and PTSD, were similarly determined by a review of mental health clinical notes. Sex was determined from the gynecology note.
Statistical Analysis
Means and medians were calculated for short-term changes in symptom scores. Due to skewness in the short-term changes, significance was tested using a nonparametric sign test. Significance was adjusted using the Bonferroni correction to protect the overall type I error level at 5% from multiple testing. We also assessed for differences in symptom changes in 4 subgroups, using an unadjusted general linear model: those with (1) chronic pain vs without; (2) an anxiety diagnosis vs without; (3) depression vs without; and (4) a PTSD diagnosis vs without. Data were analyzed using SPSS 25 and SAS 9.4.
Results
Results are based on the first massage received by 96 unique individuals (Table 1). Fifty-one (53%) patients were aged 21 to 40 years, and 45 (47%) were aged ≥ 41 years. Most participants (80%) had had a previous massage. Seven (7%) participants were currently on prescription opioids; 76 (79%) participants had a history of one or more chronic pain diagnoses (eg, back pain, migraine headaches, fibromyalgia) and 78 (81%) had a history of a mental health diagnosis (eg, depression, anxiety, PTSD). Massage sessions ranged from 30 to 60 minutes; most patients received massage therapy for 50 minutes.
Prior to massage, mean scores were 3.9 pain intensity, 3.7 pain unpleasantness, 3.8 anxiety, 1.0 shortness of breath, 4.0 relaxation, and 4.2 inner peace. Short-term changes in symptom scores are shown in Table 2. The mean score for pain intensity decreased by 1.9 points, pain unpleasantness by 2.0 points, anxiety by 2.4 points. The greatest change occurred for relaxation, which increased by 4.3 points. All changes in symptoms were statistically significant (P < .001). For subgroup comparisons
Verbal feedback and written comments about the massage experience were all favorable: No adverse events were reported.
Discussion
Massage therapy may be a useful treatment for female veterans experiencing chronic pain, anxiety disorders, depression, or situational anxiety related to gynecologic procedures. After receiving a relaxation massage, female veterans reported decreased pain intensity, pain unpleasantness, and anxiety while reporting increased relaxation and feelings of inner peace. The effects of massage were consistent for all the symptoms or characteristics assessed, suggesting that massage may act on the body in multiple ways.
These changes parallel those seen in a palliative care population primarily composed of male veterans.14 However, the female veterans in this cohort experienced greater changes in relaxation and feelings of inner peace, which may be partly due to relief of tension related to an upcoming stressful appointment. The large mean decrease in anxiety level among female veterans with PTSD is notable as well as the larger increase in inner peace in those with chronic pain.
Many patients expressed their gratitude for the massage and interest in having access to more massage therapy. Female patients who have experienced sexual trauma or other trauma may especially benefit from massage prior to painful, invasive gynecologic procedures. Anecdotally, 2 nurse chaperones in the clinic mentioned separately to the massage program supervisor that the massages helped some very anxious women better tolerate an invasive procedure that would have been otherwise extremely difficult.
Female veterans are more likely to have musculoskeletal issues after deployment and have higher rates of anxiety, PTSD, and depression compared with those of male veterans.3,4,18,19 Determining relationships between and causes of chronic pain, depression, and PTSD is very challenging but the increased prevalence of chronic pain and comorbid mental health conditions in female veterans may be partially related to MST or other trauma experiences.20-22 Female veterans are most likely to have more than one source of chronic pain.23-25 Female patients with chronic musculoskeletal pain report more pain-related disability.26 Furthermore, greater disability in the context of depression is reported by women with pain compared with those of men.27 Most (78%) female veterans in a primary care population reported chronic pain.23 Similarly, 79% of the female veterans in this study population had chronic pain and 81% had a history of mental health disorders, including depression, anxiety, and PTSD.
Studies have shown that massage therapy improves pain in populations experiencing chronic low back, neck, and knee pain.28-32 A 2020 Agency for Healthcare Research and Quality review determined there is some evidence that massage therapy is helpful for chronic low back and neck pain and fibromyalgia.33 Research also has demonstrated that massage reduces anxiety and depression in several different population types.13,34,35 Li and colleagues showed that foot massage increased oxytocin levels in healthy males.36 Although further research is needed to determine the mechanisms of massage therapy, there are important physiologic effects. Unlike most medications, massage therapy is unique in that it can impact health and well-being through multiple mechanisms; for example, by reducing pain, improving mood, providing a sense of social connection and/or improving mobility.
Patients using CIH therapies report greater awareness of the need for ongoing engagement in their own care and health behavior changes.37,38
Driscoll and colleagues reported that women veterans are interested in conservative treatment for their chronic musculoskeletal pain and are open to using CIH therapies.39 Research suggests that veterans are interested in and, in some cases, already using massage therapy.23,40-43 Access to massage therapy and other CIH therapies offers patients choice and control over the types and timing of therapy they receive, exemplified by the 80% of patients in our study who previously received a massage and sought another before a potentially stressful situation.
Access to massage therapy or other CIH therapies may reduce the need for more expensive procedures. Although research on the cost-effectiveness of massage therapy is limited, Herman and colleagues did an economic evaluation of CIH therapies in a veteran population, finding that CIH users had lower annual health care costs and lower pain in the year after CIH started. Sensitivity analyses indicated similar results for acupuncture, chiropractic care, and massage but higher costs for those with 8 or more visits.44
The prevalence of comorbid mental health conditions with MSD suggests that female veterans may benefit from multidisciplinary treatment of pain and depression.3,26 Women-centered programs would be both encouraging and validating to women.39 Massage therapy can be combined with physical therapy, yoga, tai chi, and meditation programs to improve pain, anxiety, strength, and flexibility and can be incorporated into a multimodal treatment plan. Likewise, other subpopulations of female veterans with chronic pain, mental health conditions, or cancer could be targeted with multidisciplinary programs that include massage therapy.
Limitations
This study has several limitations including lack of a control group, a self-selected population, the lack of objective biochemical measurements, and possible respondent bias to please the MTs. Eighty percent had previously experienced massage therapy and may have been biased toward the effects of massage before receiving the intervention. The first report of the effects of massage therapy in an exclusively female veteran population is a major strength of this study.
Further research including randomized controlled trials is needed, especially in populations with coexisting chronic pain and mental health disorders, as is exploring the acceptability of massage therapy for female veterans with MST. Finding viable alternatives to medications has become even more important as the nation addresses the challenge of the opioid crisis.45,46
Conclusions
Female veterans are increasingly seeking VA health care.
Acknowledgments
The authors express our gratitude to the Women Veteran Program Manager, Cheryl Allen, RN; Massage Therapists Denise McGee and Kimberly Morro; Dara Ganoczy, MPH, for help with statistical analysis; and Mark Hausman, MD, for leadership support.
1. US Department of Veteran Affairs, National Center for Veterans Analysis and Statistics. Veteran population. Updated April 14, 2021. Accessed January 6, 2022. https://www.va.gov/vetdata/veteran_population.asp
2. US Department of Veteran Affairs. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed January 6, 2022. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Higgins DM, Fenton BT, Driscoll MA, et al. Gender differences in demographic and clinical correlates among veterans with musculoskeletal disorders. Womens Health Issues. 2017;27(4):463-470. doi:10.1016/j.whi.2017.01.008
4. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD?. Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953. doi:10.1007/s00127-018-1550-x
5. Levander XA, Overland MK. Care of women veterans. Med Clin North Am. 2015;99(3):651-662. doi:10.1016/j.mcna.2015.01.013
6. US Department of Veteran Affairs. Facts and statistics about women veterans. Updated May 28. 2020. Accessed January 6, 2022. https://www.womenshealth.va.gov/womenshealth/latestinformation/facts.asp
7. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12)(suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
8. Elwy AR, Taylor SL, Zhao S, et al. Participating in complementary and integrative health approaches is associated with veterans’ patient-reported outcomes over time. Med Care. 2020;58:S125-S132. doi:10.1097/MLR.0000000000001357
9. Smeeding SJ, Bradshaw DH, Kumpfer K, Trevithick S, Stoddard GJ. Outcome evaluation of the Veterans Affairs Salt Lake City Integrative Health Clinic for chronic pain and stress-related depression, anxiety, and post-traumatic stress disorder. J Altern Complement Med. 2010;16(8):823-835. doi:10.1089/acm.2009.0510
10. Hull A, Brooks Holliday S, Eickhoff C, et al. Veteran participation in the integrative health and wellness program: impact on self-reported mental and physical health outcomes. Psychol Serv. 2019;16(3):475-483. doi:10.1037/ser0000192
11. Zephyrin LC. Reproductive health management for the care of women veterans [published correction appears in Obstet Gynecol. 2016 Mar;127(3):605]. Obstet Gynecol. 2016;127(2):383-392. doi:10.1097/AOG.0000000000001252
12. Piotrowski MM, Paterson C, Mitchinson A, Kim HM, Kirsh M, Hinshaw DB. Massage as adjuvant therapy in the management of acute postoperative pain: a preliminary study in men. J Am Coll Surg. 2003;197(6):1037-1046. doi:10.1016/j.jamcollsurg.2003.07.020
13. Mitchinson AR, Kim HM, Rosenberg JM, et al. Acute postoperative pain management using massage as an adjuvant therapy: a randomized trial. Arch Surg. 2007;142(12):1158-1167. doi:10.1001/archsurg.142.12.1158
14. Mitchinson A, Fletcher CE, Kim HM, Montagnini M, Hinshaw DB. Integrating massage therapy within the palliative care of veterans with advanced illnesses: an outcome study. Am J Hosp Palliat Care. 2014;31(1):6-12. doi:10.1177/1049909113476568
15. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Perceptions of other integrative health therapies by veterans with pain who are receiving massage. J Rehabil Res Dev. 2016;53(1):117-126. doi:10.1682/JRRD.2015.01.0015
16. Juberg M, Jerger KK, Allen KD, Dmitrieva NO, Keever T, Perlman AI. Pilot study of massage in veterans with knee osteoarthritis. J Altern Complement Med. 2015;21(6):333-338. doi:10.1089/acm.2014.0254
17. Beck I, Runeson I, Blomqvist K. To find inner peace: soft massage as an established and integrated part of palliative care. Int J Palliate Nurse. 2009;15(11):541-545. doi: 10.12968/ijpn.2009.15.11.45493
18. Haskell SG, Ning Y, Krebs E, et al. Prevalence of painful musculoskeletal conditions in female and male veterans in 7 years after return from deployment in Operation Enduring Freedom/Operation Iraqi Freedom. Clin J Pain. 2012;28(2):163-167. doi:10.1097/AJP.0b013e318223d951
19. Maguen S, Ren L, Bosch JO, Marmar CR, Seal KH. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. Am J Public Health. 2010;100(12):2450-2456. doi:10.2105/AJPH.2009.166165
20. Outcalt SD, Kroenke K, Krebs EE, et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J Behav Med. 2015;38(3):535-543. doi:10.1007/s10865-015-9628-3
21. Gibson CJ, Maguen S, Xia F, Barnes DE, Peltz CB, Yaffe K. Military sexual trauma in older women veterans: prevalence and comorbidities. J Gen Intern Med. 2020;35(1):207-213. doi:10.1007/s11606-019-05342-7
22. Tan G, Teo I, Srivastava D, et al. Improving access to care for women veterans suffering from chronic pain and depression associated with trauma. Pain Med. 2013;14(7):1010-1020. doi:10.1111/pme.12131
23. Haskell SG, Heapy A, Reid MC, Papas RK, Kerns RD. The prevalence and age-related characteristics of pain in a sample of women veterans receiving primary care. J Womens Health (Larchmt). 2006;15(7):862-869. doi:10.1089/jwh.2006.15.862
24. Driscoll MA, Higgins D, Shamaskin-Garroway A, et al. Examining gender as a correlate of self-reported pain treatment use among recent service veterans with deployment-related musculoskeletal disorders. Pain Med. 2017;18(9):1767-1777. doi:10.1093/pm/pnx023
25. Weimer MB, Macey TA, Nicolaidis C, Dobscha SK, Duckart JP, Morasco BJ. Sex differences in the medical care of VA patients with chronic non-cancer pain. Pain Med. 2013;14(12):1839-1847. doi:10.1111/pme.12177
26. Stubbs D, Krebs E, Bair M, et al. Sex differences in pain and pain-related disability among primary care patients with chronic musculoskeletal pain. Pain Med. 2010;11(2):232-239. doi:10.1111/j.1526-4637.2009.00760.x
27. Keogh E, McCracken LM, Eccleston C. Gender moderates the association between depression and disability in chronic pain patients. Eur J Pain. 2006;10(5):413-422. doi:10.1016/j.ejpain.2005.05.007
28. Miake-Lye IM, Mak S, Lee J, et al. Massage for pain: an evidence map. J Altern Complement Med. 2019;25(5):475-502. doi:10.1089/acm.2018.0282
29. Cherkin DC, Sherman KJ, Kahn J, et al. A comparison of the effects of 2 types of massage and usual care on chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2011;155(1):1-9. doi:10.7326/0003-4819-155-1-201107050-00002
30. Sherman KJ, Cook AJ, Wellman RD, et al. Five-week outcomes from a dosing trial of therapeutic massage for chronic neck pain. Ann Fam Med. 2014;12(2):112-120. doi:10.1370/afm.1602
31. Perlman AI, Sabina A, Williams AL, Njike VY, Katz DL. Massage therapy for osteoarthritis of the knee: a randomized controlled trial. Arch Intern Med. 2006;166(22):2533-2538. doi:10.1001/archinte.166.22.2533
32. Perlman A, Fogerite SG, Glass O, et al. Efficacy and safety of massage for osteoarthritis of the knee: a randomized clinical trial. J Gen Intern Med. 2019;34(3):379-386. doi:10.1007/s11606-018-4763-5
33. Skelly AC, Chou R, Dettori JR, et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. Comparative Effectiveness Review. No. 227. Agency for Healthcare Research and Quality; 2020. doi:10.23970/AHRQEPCCER227
34. Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol Bull. 2004;130(1):3-18. doi:10.1037/0033-2909.130.1.3
35. Field T, Hernandez-Reif M, Diego M, Schanberg S, Kuhn C. Cortisol decreases and serotonin and dopamine increase following massage therapy. Int J Neurosci. 2005;115(10):1397-1413. doi:10.1080/ 00207450590956459
36. Li Q, Becker B, Wernicke J, et al. Foot massage evokes oxytocin release and activation of orbitofrontal cortex and superior temporal sulcus. Psychoneuroendocrinology. 2019;101:193-203. doi:10.1016/j.psyneuen.2018.11.016
37. Eaves ER, Sherman KJ, Ritenbaugh C, et al. A qualitative study of changes in expectations over time among patients with chronic low back pain seeking four CAM therapies. BMC Complement Altern Med. 2015;15:12. Published 2015 Feb 5. doi:10.1186/s12906-015-0531-9
38. Bishop FL, Lauche R, Cramer H, et al. Health behavior change and complementary medicine use: National Health Interview Survey 2012. Medicina (Kaunas). 2019;55(10):632. Published 2019 Sep 24. doi:10.3390/medicina55100632
39. Driscoll MA, Knobf MT, Higgins DM, Heapy A, Lee A, Haskell S. Patient experiences navigating chronic pain management in an integrated health care system: a qualitative investigation of women and men. Pain Med. 2018;19(suppl 1):S19-S29. doi:10.1093/pm/pny139
40. Denneson LM, Corson K, Dobscha SK. Complementary and alternative medicine use among veterans with chronic noncancer pain. J Rehabil Res Dev. 2011;48(9):1119-1128. doi:10.1682/jrrd.2010.12.0243
41. Taylor SL, Herman PM, Marshall NJ, et al. Use of complementary and integrated health: a retrospective analysis of U.S. veterans with chronic musculoskeletal pain nationally. J Altern Complement Med. 2019;25(1):32-39. doi:10.1089/acm.2018.0276
42. Evans EA, Herman PM, Washington DL, et al. Gender differences in use of complementary and integrative health by U.S. military veterans with chronic musculoskeletal pain. Womens Health Issues. 2018;28(5):379-386. doi:10.1016/j.whi.2018.07.003
43. Reinhard MJ, Nassif TH, Bloeser K, et al. CAM utilization among OEF/OIF veterans: findings from the National Health Study for a New Generation of US Veterans. Med Care. 2014;52(12)(suppl 5):S45-S49. doi:10.1097/MLR.0000000000000229
44. Herman PM, Yuan AH, Cefalu MS, et al. The use of complementary and integrative health approaches for chronic musculoskeletal pain in younger US Veterans: An economic evaluation. PLoS One. 2019;14(6):e0217831. Published 2019 Jun 5. doi:10.1371/journal.pone.0217831
45. Jonas WB, Schoomaker EB. Pain and opioids in the military: we must do better. JAMA Intern Med. 2014;174(8):1402-1403. doi:10.1001/jamainternmed.2014.2114
46. Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293-301. doi:10.7326/M17-0865
There are approximately 2 million female veterans in the United States, representing about 10% of the veteran population.1 In 2015, 456,000 female veterans used the US Department of Veterans Affairs (VA) health care services. The VA predicts an increase in utilization over the next 20 years.2
Female veterans are more likely to have musculoskeletal disorder multimorbidity compared with male veterans and have higher rates of depressive and bipolar disorders, anxiety, and posttraumatic stress disorder (PTSD).3,4 Compared with male veterans, female veterans are younger, more likely to be unmarried and to have served during the wars in Iraq and Afghanistan.3 Fifty-five percent of women veterans vs 41% of men veterans have a service-connected disability, and a greater percentage of women veterans have a service connection rating > 50%.5 The top service-connected disabilities for women veterans are PTSD, major depressive disorder, migraines, and lumbosacral or cervical strain.2 In addition, one-third of women veterans using VA health care report experiencing military sexual trauma (MST).6 Military service may impact the health of female veterans both physically and mentally. Providing treatments and programs to improve their health and their health care experience are current VA priorities.
The VA is changing the way health care is conceptualized and delivered by implementing a holistic model of care known as Whole Health, which seeks to empower and equip patients to take charge of their health, blending conventional medicine with self-care and complementary and integrative health (CIH) approaches, such as massage therapy, yoga, acupuncture, and meditation.7 CIH therapies can help improve physical and mental health with little to no adverse effects.8-10
As part of the Whole Health initiative at the VA Ann Arbor Healthcare System (VAAAHS) in Michigan, the massage program was expanded in 2017 to offer relaxation massages to female veterans attending the women’s health clinic, which provides gynecologic care. Patients visiting a gynecology clinic often experience anxiety and pain related to invasive procedures and examinations. This is especially true for female veterans who experienced MST.11
VAAAHS has 1 staff massage therapist (MT). To expand the program to the women’s health clinic, volunteer licensed MTs were recruited and trained in specific procedures by the staff MT.
Several studies have demonstrated the effect of therapeutic massage on pain and anxiety in predominantly male veteran study populations, including veterans needing postsurgical and palliative care as well as those experiencing chronic pain and knee osteoarthritis.12-16 Little is known about the effects of massage therapy on female veterans. The purpose of this pilot study was to examine the effects of massage therapy among female veterans participating in the women’s health massage program.
Methods
The setting for this pre-post intervention study was VAAAHS. Veterans were called in advance by clinic staff and scheduled for 60-minute appointments either before or after their clinic appointment, depending on availability. MTs were instructed to provide relaxation massage using Swedish massage techniques with moderate pressure, avoiding deep pressure techniques.
The volunteer MTs gave the participants a survey to provide comments and to rate baseline pain and other symptoms prior to and following the massage. The MT left the room to provide privacy while completing the survey. The staff included the symptom data in the massage note as clinical outcomes and entered them into the electronic health record. Massages were given from October 1, 2017 to June 30, 2018. Data including symptom scores, demographics, the presence of chronic pain, mental health diagnoses, patient comments, and opioid use were abstracted from the electronic health record by 2 members of the study team and entered into an Excel database. This study was approved by the VAAAHS Institutional Review Board.
Study Measures
Pain intensity, pain unpleasantness (the affective component of pain), anxiety, shortness of breath, relaxation, and inner peace were rated pre- and postmassage on a 0 to 10 scale. Shortness of breath was included due to the relationship between breathing and anxiety. Inner peace was assessed to measure the calming effects of massage therapy. Beck and colleagues found the concept of inner peace was an important outcome of massage therapy.17 The scale anchors for pain intensity were “no pain” and “severe pain”; and “not at all unpleasant” and “as unpleasant as it can be” for pain unpleasantness. For anxiety, the anchors were “no anxiety” and “as anxious as I can be.” Anchors for relaxation and inner peace were reversed so that a 0 indicated low relaxation and inner peace while a 10 indicated the highest state of relaxation and inner peace.
Chronic pain was defined as pain existing for > 3 months. A history of chronic pain was determined from a review and synthesis of primary care and specialty care recorded diagnoses, patient concerns, and service-connected disabilities. The diagnoses included lumbosacral or cervical strain, chronic low back, joint (knee, shoulder, hip, ankle), neck, or pelvic pain, fibromyalgia, headache, migraine, osteoarthritis, and myofascial pain syndrome. The presence of mental health conditions, including depression, anxiety, bipolar disorders, and PTSD, were similarly determined by a review of mental health clinical notes. Sex was determined from the gynecology note.
Statistical Analysis
Means and medians were calculated for short-term changes in symptom scores. Due to skewness in the short-term changes, significance was tested using a nonparametric sign test. Significance was adjusted using the Bonferroni correction to protect the overall type I error level at 5% from multiple testing. We also assessed for differences in symptom changes in 4 subgroups, using an unadjusted general linear model: those with (1) chronic pain vs without; (2) an anxiety diagnosis vs without; (3) depression vs without; and (4) a PTSD diagnosis vs without. Data were analyzed using SPSS 25 and SAS 9.4.
Results
Results are based on the first massage received by 96 unique individuals (Table 1). Fifty-one (53%) patients were aged 21 to 40 years, and 45 (47%) were aged ≥ 41 years. Most participants (80%) had had a previous massage. Seven (7%) participants were currently on prescription opioids; 76 (79%) participants had a history of one or more chronic pain diagnoses (eg, back pain, migraine headaches, fibromyalgia) and 78 (81%) had a history of a mental health diagnosis (eg, depression, anxiety, PTSD). Massage sessions ranged from 30 to 60 minutes; most patients received massage therapy for 50 minutes.
Prior to massage, mean scores were 3.9 pain intensity, 3.7 pain unpleasantness, 3.8 anxiety, 1.0 shortness of breath, 4.0 relaxation, and 4.2 inner peace. Short-term changes in symptom scores are shown in Table 2. The mean score for pain intensity decreased by 1.9 points, pain unpleasantness by 2.0 points, anxiety by 2.4 points. The greatest change occurred for relaxation, which increased by 4.3 points. All changes in symptoms were statistically significant (P < .001). For subgroup comparisons
Verbal feedback and written comments about the massage experience were all favorable: No adverse events were reported.
Discussion
Massage therapy may be a useful treatment for female veterans experiencing chronic pain, anxiety disorders, depression, or situational anxiety related to gynecologic procedures. After receiving a relaxation massage, female veterans reported decreased pain intensity, pain unpleasantness, and anxiety while reporting increased relaxation and feelings of inner peace. The effects of massage were consistent for all the symptoms or characteristics assessed, suggesting that massage may act on the body in multiple ways.
These changes parallel those seen in a palliative care population primarily composed of male veterans.14 However, the female veterans in this cohort experienced greater changes in relaxation and feelings of inner peace, which may be partly due to relief of tension related to an upcoming stressful appointment. The large mean decrease in anxiety level among female veterans with PTSD is notable as well as the larger increase in inner peace in those with chronic pain.
Many patients expressed their gratitude for the massage and interest in having access to more massage therapy. Female patients who have experienced sexual trauma or other trauma may especially benefit from massage prior to painful, invasive gynecologic procedures. Anecdotally, 2 nurse chaperones in the clinic mentioned separately to the massage program supervisor that the massages helped some very anxious women better tolerate an invasive procedure that would have been otherwise extremely difficult.
Female veterans are more likely to have musculoskeletal issues after deployment and have higher rates of anxiety, PTSD, and depression compared with those of male veterans.3,4,18,19 Determining relationships between and causes of chronic pain, depression, and PTSD is very challenging but the increased prevalence of chronic pain and comorbid mental health conditions in female veterans may be partially related to MST or other trauma experiences.20-22 Female veterans are most likely to have more than one source of chronic pain.23-25 Female patients with chronic musculoskeletal pain report more pain-related disability.26 Furthermore, greater disability in the context of depression is reported by women with pain compared with those of men.27 Most (78%) female veterans in a primary care population reported chronic pain.23 Similarly, 79% of the female veterans in this study population had chronic pain and 81% had a history of mental health disorders, including depression, anxiety, and PTSD.
Studies have shown that massage therapy improves pain in populations experiencing chronic low back, neck, and knee pain.28-32 A 2020 Agency for Healthcare Research and Quality review determined there is some evidence that massage therapy is helpful for chronic low back and neck pain and fibromyalgia.33 Research also has demonstrated that massage reduces anxiety and depression in several different population types.13,34,35 Li and colleagues showed that foot massage increased oxytocin levels in healthy males.36 Although further research is needed to determine the mechanisms of massage therapy, there are important physiologic effects. Unlike most medications, massage therapy is unique in that it can impact health and well-being through multiple mechanisms; for example, by reducing pain, improving mood, providing a sense of social connection and/or improving mobility.
Patients using CIH therapies report greater awareness of the need for ongoing engagement in their own care and health behavior changes.37,38
Driscoll and colleagues reported that women veterans are interested in conservative treatment for their chronic musculoskeletal pain and are open to using CIH therapies.39 Research suggests that veterans are interested in and, in some cases, already using massage therapy.23,40-43 Access to massage therapy and other CIH therapies offers patients choice and control over the types and timing of therapy they receive, exemplified by the 80% of patients in our study who previously received a massage and sought another before a potentially stressful situation.
Access to massage therapy or other CIH therapies may reduce the need for more expensive procedures. Although research on the cost-effectiveness of massage therapy is limited, Herman and colleagues did an economic evaluation of CIH therapies in a veteran population, finding that CIH users had lower annual health care costs and lower pain in the year after CIH started. Sensitivity analyses indicated similar results for acupuncture, chiropractic care, and massage but higher costs for those with 8 or more visits.44
The prevalence of comorbid mental health conditions with MSD suggests that female veterans may benefit from multidisciplinary treatment of pain and depression.3,26 Women-centered programs would be both encouraging and validating to women.39 Massage therapy can be combined with physical therapy, yoga, tai chi, and meditation programs to improve pain, anxiety, strength, and flexibility and can be incorporated into a multimodal treatment plan. Likewise, other subpopulations of female veterans with chronic pain, mental health conditions, or cancer could be targeted with multidisciplinary programs that include massage therapy.
Limitations
This study has several limitations including lack of a control group, a self-selected population, the lack of objective biochemical measurements, and possible respondent bias to please the MTs. Eighty percent had previously experienced massage therapy and may have been biased toward the effects of massage before receiving the intervention. The first report of the effects of massage therapy in an exclusively female veteran population is a major strength of this study.
Further research including randomized controlled trials is needed, especially in populations with coexisting chronic pain and mental health disorders, as is exploring the acceptability of massage therapy for female veterans with MST. Finding viable alternatives to medications has become even more important as the nation addresses the challenge of the opioid crisis.45,46
Conclusions
Female veterans are increasingly seeking VA health care.
Acknowledgments
The authors express our gratitude to the Women Veteran Program Manager, Cheryl Allen, RN; Massage Therapists Denise McGee and Kimberly Morro; Dara Ganoczy, MPH, for help with statistical analysis; and Mark Hausman, MD, for leadership support.
There are approximately 2 million female veterans in the United States, representing about 10% of the veteran population.1 In 2015, 456,000 female veterans used the US Department of Veterans Affairs (VA) health care services. The VA predicts an increase in utilization over the next 20 years.2
Female veterans are more likely to have musculoskeletal disorder multimorbidity compared with male veterans and have higher rates of depressive and bipolar disorders, anxiety, and posttraumatic stress disorder (PTSD).3,4 Compared with male veterans, female veterans are younger, more likely to be unmarried and to have served during the wars in Iraq and Afghanistan.3 Fifty-five percent of women veterans vs 41% of men veterans have a service-connected disability, and a greater percentage of women veterans have a service connection rating > 50%.5 The top service-connected disabilities for women veterans are PTSD, major depressive disorder, migraines, and lumbosacral or cervical strain.2 In addition, one-third of women veterans using VA health care report experiencing military sexual trauma (MST).6 Military service may impact the health of female veterans both physically and mentally. Providing treatments and programs to improve their health and their health care experience are current VA priorities.
The VA is changing the way health care is conceptualized and delivered by implementing a holistic model of care known as Whole Health, which seeks to empower and equip patients to take charge of their health, blending conventional medicine with self-care and complementary and integrative health (CIH) approaches, such as massage therapy, yoga, acupuncture, and meditation.7 CIH therapies can help improve physical and mental health with little to no adverse effects.8-10
As part of the Whole Health initiative at the VA Ann Arbor Healthcare System (VAAAHS) in Michigan, the massage program was expanded in 2017 to offer relaxation massages to female veterans attending the women’s health clinic, which provides gynecologic care. Patients visiting a gynecology clinic often experience anxiety and pain related to invasive procedures and examinations. This is especially true for female veterans who experienced MST.11
VAAAHS has 1 staff massage therapist (MT). To expand the program to the women’s health clinic, volunteer licensed MTs were recruited and trained in specific procedures by the staff MT.
Several studies have demonstrated the effect of therapeutic massage on pain and anxiety in predominantly male veteran study populations, including veterans needing postsurgical and palliative care as well as those experiencing chronic pain and knee osteoarthritis.12-16 Little is known about the effects of massage therapy on female veterans. The purpose of this pilot study was to examine the effects of massage therapy among female veterans participating in the women’s health massage program.
Methods
The setting for this pre-post intervention study was VAAAHS. Veterans were called in advance by clinic staff and scheduled for 60-minute appointments either before or after their clinic appointment, depending on availability. MTs were instructed to provide relaxation massage using Swedish massage techniques with moderate pressure, avoiding deep pressure techniques.
The volunteer MTs gave the participants a survey to provide comments and to rate baseline pain and other symptoms prior to and following the massage. The MT left the room to provide privacy while completing the survey. The staff included the symptom data in the massage note as clinical outcomes and entered them into the electronic health record. Massages were given from October 1, 2017 to June 30, 2018. Data including symptom scores, demographics, the presence of chronic pain, mental health diagnoses, patient comments, and opioid use were abstracted from the electronic health record by 2 members of the study team and entered into an Excel database. This study was approved by the VAAAHS Institutional Review Board.
Study Measures
Pain intensity, pain unpleasantness (the affective component of pain), anxiety, shortness of breath, relaxation, and inner peace were rated pre- and postmassage on a 0 to 10 scale. Shortness of breath was included due to the relationship between breathing and anxiety. Inner peace was assessed to measure the calming effects of massage therapy. Beck and colleagues found the concept of inner peace was an important outcome of massage therapy.17 The scale anchors for pain intensity were “no pain” and “severe pain”; and “not at all unpleasant” and “as unpleasant as it can be” for pain unpleasantness. For anxiety, the anchors were “no anxiety” and “as anxious as I can be.” Anchors for relaxation and inner peace were reversed so that a 0 indicated low relaxation and inner peace while a 10 indicated the highest state of relaxation and inner peace.
Chronic pain was defined as pain existing for > 3 months. A history of chronic pain was determined from a review and synthesis of primary care and specialty care recorded diagnoses, patient concerns, and service-connected disabilities. The diagnoses included lumbosacral or cervical strain, chronic low back, joint (knee, shoulder, hip, ankle), neck, or pelvic pain, fibromyalgia, headache, migraine, osteoarthritis, and myofascial pain syndrome. The presence of mental health conditions, including depression, anxiety, bipolar disorders, and PTSD, were similarly determined by a review of mental health clinical notes. Sex was determined from the gynecology note.
Statistical Analysis
Means and medians were calculated for short-term changes in symptom scores. Due to skewness in the short-term changes, significance was tested using a nonparametric sign test. Significance was adjusted using the Bonferroni correction to protect the overall type I error level at 5% from multiple testing. We also assessed for differences in symptom changes in 4 subgroups, using an unadjusted general linear model: those with (1) chronic pain vs without; (2) an anxiety diagnosis vs without; (3) depression vs without; and (4) a PTSD diagnosis vs without. Data were analyzed using SPSS 25 and SAS 9.4.
Results
Results are based on the first massage received by 96 unique individuals (Table 1). Fifty-one (53%) patients were aged 21 to 40 years, and 45 (47%) were aged ≥ 41 years. Most participants (80%) had had a previous massage. Seven (7%) participants were currently on prescription opioids; 76 (79%) participants had a history of one or more chronic pain diagnoses (eg, back pain, migraine headaches, fibromyalgia) and 78 (81%) had a history of a mental health diagnosis (eg, depression, anxiety, PTSD). Massage sessions ranged from 30 to 60 minutes; most patients received massage therapy for 50 minutes.
Prior to massage, mean scores were 3.9 pain intensity, 3.7 pain unpleasantness, 3.8 anxiety, 1.0 shortness of breath, 4.0 relaxation, and 4.2 inner peace. Short-term changes in symptom scores are shown in Table 2. The mean score for pain intensity decreased by 1.9 points, pain unpleasantness by 2.0 points, anxiety by 2.4 points. The greatest change occurred for relaxation, which increased by 4.3 points. All changes in symptoms were statistically significant (P < .001). For subgroup comparisons
Verbal feedback and written comments about the massage experience were all favorable: No adverse events were reported.
Discussion
Massage therapy may be a useful treatment for female veterans experiencing chronic pain, anxiety disorders, depression, or situational anxiety related to gynecologic procedures. After receiving a relaxation massage, female veterans reported decreased pain intensity, pain unpleasantness, and anxiety while reporting increased relaxation and feelings of inner peace. The effects of massage were consistent for all the symptoms or characteristics assessed, suggesting that massage may act on the body in multiple ways.
These changes parallel those seen in a palliative care population primarily composed of male veterans.14 However, the female veterans in this cohort experienced greater changes in relaxation and feelings of inner peace, which may be partly due to relief of tension related to an upcoming stressful appointment. The large mean decrease in anxiety level among female veterans with PTSD is notable as well as the larger increase in inner peace in those with chronic pain.
Many patients expressed their gratitude for the massage and interest in having access to more massage therapy. Female patients who have experienced sexual trauma or other trauma may especially benefit from massage prior to painful, invasive gynecologic procedures. Anecdotally, 2 nurse chaperones in the clinic mentioned separately to the massage program supervisor that the massages helped some very anxious women better tolerate an invasive procedure that would have been otherwise extremely difficult.
Female veterans are more likely to have musculoskeletal issues after deployment and have higher rates of anxiety, PTSD, and depression compared with those of male veterans.3,4,18,19 Determining relationships between and causes of chronic pain, depression, and PTSD is very challenging but the increased prevalence of chronic pain and comorbid mental health conditions in female veterans may be partially related to MST or other trauma experiences.20-22 Female veterans are most likely to have more than one source of chronic pain.23-25 Female patients with chronic musculoskeletal pain report more pain-related disability.26 Furthermore, greater disability in the context of depression is reported by women with pain compared with those of men.27 Most (78%) female veterans in a primary care population reported chronic pain.23 Similarly, 79% of the female veterans in this study population had chronic pain and 81% had a history of mental health disorders, including depression, anxiety, and PTSD.
Studies have shown that massage therapy improves pain in populations experiencing chronic low back, neck, and knee pain.28-32 A 2020 Agency for Healthcare Research and Quality review determined there is some evidence that massage therapy is helpful for chronic low back and neck pain and fibromyalgia.33 Research also has demonstrated that massage reduces anxiety and depression in several different population types.13,34,35 Li and colleagues showed that foot massage increased oxytocin levels in healthy males.36 Although further research is needed to determine the mechanisms of massage therapy, there are important physiologic effects. Unlike most medications, massage therapy is unique in that it can impact health and well-being through multiple mechanisms; for example, by reducing pain, improving mood, providing a sense of social connection and/or improving mobility.
Patients using CIH therapies report greater awareness of the need for ongoing engagement in their own care and health behavior changes.37,38
Driscoll and colleagues reported that women veterans are interested in conservative treatment for their chronic musculoskeletal pain and are open to using CIH therapies.39 Research suggests that veterans are interested in and, in some cases, already using massage therapy.23,40-43 Access to massage therapy and other CIH therapies offers patients choice and control over the types and timing of therapy they receive, exemplified by the 80% of patients in our study who previously received a massage and sought another before a potentially stressful situation.
Access to massage therapy or other CIH therapies may reduce the need for more expensive procedures. Although research on the cost-effectiveness of massage therapy is limited, Herman and colleagues did an economic evaluation of CIH therapies in a veteran population, finding that CIH users had lower annual health care costs and lower pain in the year after CIH started. Sensitivity analyses indicated similar results for acupuncture, chiropractic care, and massage but higher costs for those with 8 or more visits.44
The prevalence of comorbid mental health conditions with MSD suggests that female veterans may benefit from multidisciplinary treatment of pain and depression.3,26 Women-centered programs would be both encouraging and validating to women.39 Massage therapy can be combined with physical therapy, yoga, tai chi, and meditation programs to improve pain, anxiety, strength, and flexibility and can be incorporated into a multimodal treatment plan. Likewise, other subpopulations of female veterans with chronic pain, mental health conditions, or cancer could be targeted with multidisciplinary programs that include massage therapy.
Limitations
This study has several limitations including lack of a control group, a self-selected population, the lack of objective biochemical measurements, and possible respondent bias to please the MTs. Eighty percent had previously experienced massage therapy and may have been biased toward the effects of massage before receiving the intervention. The first report of the effects of massage therapy in an exclusively female veteran population is a major strength of this study.
Further research including randomized controlled trials is needed, especially in populations with coexisting chronic pain and mental health disorders, as is exploring the acceptability of massage therapy for female veterans with MST. Finding viable alternatives to medications has become even more important as the nation addresses the challenge of the opioid crisis.45,46
Conclusions
Female veterans are increasingly seeking VA health care.
Acknowledgments
The authors express our gratitude to the Women Veteran Program Manager, Cheryl Allen, RN; Massage Therapists Denise McGee and Kimberly Morro; Dara Ganoczy, MPH, for help with statistical analysis; and Mark Hausman, MD, for leadership support.
1. US Department of Veteran Affairs, National Center for Veterans Analysis and Statistics. Veteran population. Updated April 14, 2021. Accessed January 6, 2022. https://www.va.gov/vetdata/veteran_population.asp
2. US Department of Veteran Affairs. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed January 6, 2022. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Higgins DM, Fenton BT, Driscoll MA, et al. Gender differences in demographic and clinical correlates among veterans with musculoskeletal disorders. Womens Health Issues. 2017;27(4):463-470. doi:10.1016/j.whi.2017.01.008
4. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD?. Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953. doi:10.1007/s00127-018-1550-x
5. Levander XA, Overland MK. Care of women veterans. Med Clin North Am. 2015;99(3):651-662. doi:10.1016/j.mcna.2015.01.013
6. US Department of Veteran Affairs. Facts and statistics about women veterans. Updated May 28. 2020. Accessed January 6, 2022. https://www.womenshealth.va.gov/womenshealth/latestinformation/facts.asp
7. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12)(suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
8. Elwy AR, Taylor SL, Zhao S, et al. Participating in complementary and integrative health approaches is associated with veterans’ patient-reported outcomes over time. Med Care. 2020;58:S125-S132. doi:10.1097/MLR.0000000000001357
9. Smeeding SJ, Bradshaw DH, Kumpfer K, Trevithick S, Stoddard GJ. Outcome evaluation of the Veterans Affairs Salt Lake City Integrative Health Clinic for chronic pain and stress-related depression, anxiety, and post-traumatic stress disorder. J Altern Complement Med. 2010;16(8):823-835. doi:10.1089/acm.2009.0510
10. Hull A, Brooks Holliday S, Eickhoff C, et al. Veteran participation in the integrative health and wellness program: impact on self-reported mental and physical health outcomes. Psychol Serv. 2019;16(3):475-483. doi:10.1037/ser0000192
11. Zephyrin LC. Reproductive health management for the care of women veterans [published correction appears in Obstet Gynecol. 2016 Mar;127(3):605]. Obstet Gynecol. 2016;127(2):383-392. doi:10.1097/AOG.0000000000001252
12. Piotrowski MM, Paterson C, Mitchinson A, Kim HM, Kirsh M, Hinshaw DB. Massage as adjuvant therapy in the management of acute postoperative pain: a preliminary study in men. J Am Coll Surg. 2003;197(6):1037-1046. doi:10.1016/j.jamcollsurg.2003.07.020
13. Mitchinson AR, Kim HM, Rosenberg JM, et al. Acute postoperative pain management using massage as an adjuvant therapy: a randomized trial. Arch Surg. 2007;142(12):1158-1167. doi:10.1001/archsurg.142.12.1158
14. Mitchinson A, Fletcher CE, Kim HM, Montagnini M, Hinshaw DB. Integrating massage therapy within the palliative care of veterans with advanced illnesses: an outcome study. Am J Hosp Palliat Care. 2014;31(1):6-12. doi:10.1177/1049909113476568
15. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Perceptions of other integrative health therapies by veterans with pain who are receiving massage. J Rehabil Res Dev. 2016;53(1):117-126. doi:10.1682/JRRD.2015.01.0015
16. Juberg M, Jerger KK, Allen KD, Dmitrieva NO, Keever T, Perlman AI. Pilot study of massage in veterans with knee osteoarthritis. J Altern Complement Med. 2015;21(6):333-338. doi:10.1089/acm.2014.0254
17. Beck I, Runeson I, Blomqvist K. To find inner peace: soft massage as an established and integrated part of palliative care. Int J Palliate Nurse. 2009;15(11):541-545. doi: 10.12968/ijpn.2009.15.11.45493
18. Haskell SG, Ning Y, Krebs E, et al. Prevalence of painful musculoskeletal conditions in female and male veterans in 7 years after return from deployment in Operation Enduring Freedom/Operation Iraqi Freedom. Clin J Pain. 2012;28(2):163-167. doi:10.1097/AJP.0b013e318223d951
19. Maguen S, Ren L, Bosch JO, Marmar CR, Seal KH. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. Am J Public Health. 2010;100(12):2450-2456. doi:10.2105/AJPH.2009.166165
20. Outcalt SD, Kroenke K, Krebs EE, et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J Behav Med. 2015;38(3):535-543. doi:10.1007/s10865-015-9628-3
21. Gibson CJ, Maguen S, Xia F, Barnes DE, Peltz CB, Yaffe K. Military sexual trauma in older women veterans: prevalence and comorbidities. J Gen Intern Med. 2020;35(1):207-213. doi:10.1007/s11606-019-05342-7
22. Tan G, Teo I, Srivastava D, et al. Improving access to care for women veterans suffering from chronic pain and depression associated with trauma. Pain Med. 2013;14(7):1010-1020. doi:10.1111/pme.12131
23. Haskell SG, Heapy A, Reid MC, Papas RK, Kerns RD. The prevalence and age-related characteristics of pain in a sample of women veterans receiving primary care. J Womens Health (Larchmt). 2006;15(7):862-869. doi:10.1089/jwh.2006.15.862
24. Driscoll MA, Higgins D, Shamaskin-Garroway A, et al. Examining gender as a correlate of self-reported pain treatment use among recent service veterans with deployment-related musculoskeletal disorders. Pain Med. 2017;18(9):1767-1777. doi:10.1093/pm/pnx023
25. Weimer MB, Macey TA, Nicolaidis C, Dobscha SK, Duckart JP, Morasco BJ. Sex differences in the medical care of VA patients with chronic non-cancer pain. Pain Med. 2013;14(12):1839-1847. doi:10.1111/pme.12177
26. Stubbs D, Krebs E, Bair M, et al. Sex differences in pain and pain-related disability among primary care patients with chronic musculoskeletal pain. Pain Med. 2010;11(2):232-239. doi:10.1111/j.1526-4637.2009.00760.x
27. Keogh E, McCracken LM, Eccleston C. Gender moderates the association between depression and disability in chronic pain patients. Eur J Pain. 2006;10(5):413-422. doi:10.1016/j.ejpain.2005.05.007
28. Miake-Lye IM, Mak S, Lee J, et al. Massage for pain: an evidence map. J Altern Complement Med. 2019;25(5):475-502. doi:10.1089/acm.2018.0282
29. Cherkin DC, Sherman KJ, Kahn J, et al. A comparison of the effects of 2 types of massage and usual care on chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2011;155(1):1-9. doi:10.7326/0003-4819-155-1-201107050-00002
30. Sherman KJ, Cook AJ, Wellman RD, et al. Five-week outcomes from a dosing trial of therapeutic massage for chronic neck pain. Ann Fam Med. 2014;12(2):112-120. doi:10.1370/afm.1602
31. Perlman AI, Sabina A, Williams AL, Njike VY, Katz DL. Massage therapy for osteoarthritis of the knee: a randomized controlled trial. Arch Intern Med. 2006;166(22):2533-2538. doi:10.1001/archinte.166.22.2533
32. Perlman A, Fogerite SG, Glass O, et al. Efficacy and safety of massage for osteoarthritis of the knee: a randomized clinical trial. J Gen Intern Med. 2019;34(3):379-386. doi:10.1007/s11606-018-4763-5
33. Skelly AC, Chou R, Dettori JR, et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. Comparative Effectiveness Review. No. 227. Agency for Healthcare Research and Quality; 2020. doi:10.23970/AHRQEPCCER227
34. Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol Bull. 2004;130(1):3-18. doi:10.1037/0033-2909.130.1.3
35. Field T, Hernandez-Reif M, Diego M, Schanberg S, Kuhn C. Cortisol decreases and serotonin and dopamine increase following massage therapy. Int J Neurosci. 2005;115(10):1397-1413. doi:10.1080/ 00207450590956459
36. Li Q, Becker B, Wernicke J, et al. Foot massage evokes oxytocin release and activation of orbitofrontal cortex and superior temporal sulcus. Psychoneuroendocrinology. 2019;101:193-203. doi:10.1016/j.psyneuen.2018.11.016
37. Eaves ER, Sherman KJ, Ritenbaugh C, et al. A qualitative study of changes in expectations over time among patients with chronic low back pain seeking four CAM therapies. BMC Complement Altern Med. 2015;15:12. Published 2015 Feb 5. doi:10.1186/s12906-015-0531-9
38. Bishop FL, Lauche R, Cramer H, et al. Health behavior change and complementary medicine use: National Health Interview Survey 2012. Medicina (Kaunas). 2019;55(10):632. Published 2019 Sep 24. doi:10.3390/medicina55100632
39. Driscoll MA, Knobf MT, Higgins DM, Heapy A, Lee A, Haskell S. Patient experiences navigating chronic pain management in an integrated health care system: a qualitative investigation of women and men. Pain Med. 2018;19(suppl 1):S19-S29. doi:10.1093/pm/pny139
40. Denneson LM, Corson K, Dobscha SK. Complementary and alternative medicine use among veterans with chronic noncancer pain. J Rehabil Res Dev. 2011;48(9):1119-1128. doi:10.1682/jrrd.2010.12.0243
41. Taylor SL, Herman PM, Marshall NJ, et al. Use of complementary and integrated health: a retrospective analysis of U.S. veterans with chronic musculoskeletal pain nationally. J Altern Complement Med. 2019;25(1):32-39. doi:10.1089/acm.2018.0276
42. Evans EA, Herman PM, Washington DL, et al. Gender differences in use of complementary and integrative health by U.S. military veterans with chronic musculoskeletal pain. Womens Health Issues. 2018;28(5):379-386. doi:10.1016/j.whi.2018.07.003
43. Reinhard MJ, Nassif TH, Bloeser K, et al. CAM utilization among OEF/OIF veterans: findings from the National Health Study for a New Generation of US Veterans. Med Care. 2014;52(12)(suppl 5):S45-S49. doi:10.1097/MLR.0000000000000229
44. Herman PM, Yuan AH, Cefalu MS, et al. The use of complementary and integrative health approaches for chronic musculoskeletal pain in younger US Veterans: An economic evaluation. PLoS One. 2019;14(6):e0217831. Published 2019 Jun 5. doi:10.1371/journal.pone.0217831
45. Jonas WB, Schoomaker EB. Pain and opioids in the military: we must do better. JAMA Intern Med. 2014;174(8):1402-1403. doi:10.1001/jamainternmed.2014.2114
46. Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293-301. doi:10.7326/M17-0865
1. US Department of Veteran Affairs, National Center for Veterans Analysis and Statistics. Veteran population. Updated April 14, 2021. Accessed January 6, 2022. https://www.va.gov/vetdata/veteran_population.asp
2. US Department of Veteran Affairs. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed January 6, 2022. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Higgins DM, Fenton BT, Driscoll MA, et al. Gender differences in demographic and clinical correlates among veterans with musculoskeletal disorders. Womens Health Issues. 2017;27(4):463-470. doi:10.1016/j.whi.2017.01.008
4. Lehavot K, Goldberg SB, Chen JA, et al. Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD?. Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):943-953. doi:10.1007/s00127-018-1550-x
5. Levander XA, Overland MK. Care of women veterans. Med Clin North Am. 2015;99(3):651-662. doi:10.1016/j.mcna.2015.01.013
6. US Department of Veteran Affairs. Facts and statistics about women veterans. Updated May 28. 2020. Accessed January 6, 2022. https://www.womenshealth.va.gov/womenshealth/latestinformation/facts.asp
7. Krejci LP, Carter K, Gaudet T. Whole health: the vision and implementation of personalized, proactive, patient-driven health care for veterans. Med Care. 2014;52(12)(suppl 5):S5-S8. doi:10.1097/MLR.0000000000000226
8. Elwy AR, Taylor SL, Zhao S, et al. Participating in complementary and integrative health approaches is associated with veterans’ patient-reported outcomes over time. Med Care. 2020;58:S125-S132. doi:10.1097/MLR.0000000000001357
9. Smeeding SJ, Bradshaw DH, Kumpfer K, Trevithick S, Stoddard GJ. Outcome evaluation of the Veterans Affairs Salt Lake City Integrative Health Clinic for chronic pain and stress-related depression, anxiety, and post-traumatic stress disorder. J Altern Complement Med. 2010;16(8):823-835. doi:10.1089/acm.2009.0510
10. Hull A, Brooks Holliday S, Eickhoff C, et al. Veteran participation in the integrative health and wellness program: impact on self-reported mental and physical health outcomes. Psychol Serv. 2019;16(3):475-483. doi:10.1037/ser0000192
11. Zephyrin LC. Reproductive health management for the care of women veterans [published correction appears in Obstet Gynecol. 2016 Mar;127(3):605]. Obstet Gynecol. 2016;127(2):383-392. doi:10.1097/AOG.0000000000001252
12. Piotrowski MM, Paterson C, Mitchinson A, Kim HM, Kirsh M, Hinshaw DB. Massage as adjuvant therapy in the management of acute postoperative pain: a preliminary study in men. J Am Coll Surg. 2003;197(6):1037-1046. doi:10.1016/j.jamcollsurg.2003.07.020
13. Mitchinson AR, Kim HM, Rosenberg JM, et al. Acute postoperative pain management using massage as an adjuvant therapy: a randomized trial. Arch Surg. 2007;142(12):1158-1167. doi:10.1001/archsurg.142.12.1158
14. Mitchinson A, Fletcher CE, Kim HM, Montagnini M, Hinshaw DB. Integrating massage therapy within the palliative care of veterans with advanced illnesses: an outcome study. Am J Hosp Palliat Care. 2014;31(1):6-12. doi:10.1177/1049909113476568
15. Fletcher CE, Mitchinson AR, Trumble EL, Hinshaw DB, Dusek JA. Perceptions of other integrative health therapies by veterans with pain who are receiving massage. J Rehabil Res Dev. 2016;53(1):117-126. doi:10.1682/JRRD.2015.01.0015
16. Juberg M, Jerger KK, Allen KD, Dmitrieva NO, Keever T, Perlman AI. Pilot study of massage in veterans with knee osteoarthritis. J Altern Complement Med. 2015;21(6):333-338. doi:10.1089/acm.2014.0254
17. Beck I, Runeson I, Blomqvist K. To find inner peace: soft massage as an established and integrated part of palliative care. Int J Palliate Nurse. 2009;15(11):541-545. doi: 10.12968/ijpn.2009.15.11.45493
18. Haskell SG, Ning Y, Krebs E, et al. Prevalence of painful musculoskeletal conditions in female and male veterans in 7 years after return from deployment in Operation Enduring Freedom/Operation Iraqi Freedom. Clin J Pain. 2012;28(2):163-167. doi:10.1097/AJP.0b013e318223d951
19. Maguen S, Ren L, Bosch JO, Marmar CR, Seal KH. Gender differences in mental health diagnoses among Iraq and Afghanistan veterans enrolled in veterans affairs health care. Am J Public Health. 2010;100(12):2450-2456. doi:10.2105/AJPH.2009.166165
20. Outcalt SD, Kroenke K, Krebs EE, et al. Chronic pain and comorbid mental health conditions: independent associations of posttraumatic stress disorder and depression with pain, disability, and quality of life. J Behav Med. 2015;38(3):535-543. doi:10.1007/s10865-015-9628-3
21. Gibson CJ, Maguen S, Xia F, Barnes DE, Peltz CB, Yaffe K. Military sexual trauma in older women veterans: prevalence and comorbidities. J Gen Intern Med. 2020;35(1):207-213. doi:10.1007/s11606-019-05342-7
22. Tan G, Teo I, Srivastava D, et al. Improving access to care for women veterans suffering from chronic pain and depression associated with trauma. Pain Med. 2013;14(7):1010-1020. doi:10.1111/pme.12131
23. Haskell SG, Heapy A, Reid MC, Papas RK, Kerns RD. The prevalence and age-related characteristics of pain in a sample of women veterans receiving primary care. J Womens Health (Larchmt). 2006;15(7):862-869. doi:10.1089/jwh.2006.15.862
24. Driscoll MA, Higgins D, Shamaskin-Garroway A, et al. Examining gender as a correlate of self-reported pain treatment use among recent service veterans with deployment-related musculoskeletal disorders. Pain Med. 2017;18(9):1767-1777. doi:10.1093/pm/pnx023
25. Weimer MB, Macey TA, Nicolaidis C, Dobscha SK, Duckart JP, Morasco BJ. Sex differences in the medical care of VA patients with chronic non-cancer pain. Pain Med. 2013;14(12):1839-1847. doi:10.1111/pme.12177
26. Stubbs D, Krebs E, Bair M, et al. Sex differences in pain and pain-related disability among primary care patients with chronic musculoskeletal pain. Pain Med. 2010;11(2):232-239. doi:10.1111/j.1526-4637.2009.00760.x
27. Keogh E, McCracken LM, Eccleston C. Gender moderates the association between depression and disability in chronic pain patients. Eur J Pain. 2006;10(5):413-422. doi:10.1016/j.ejpain.2005.05.007
28. Miake-Lye IM, Mak S, Lee J, et al. Massage for pain: an evidence map. J Altern Complement Med. 2019;25(5):475-502. doi:10.1089/acm.2018.0282
29. Cherkin DC, Sherman KJ, Kahn J, et al. A comparison of the effects of 2 types of massage and usual care on chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2011;155(1):1-9. doi:10.7326/0003-4819-155-1-201107050-00002
30. Sherman KJ, Cook AJ, Wellman RD, et al. Five-week outcomes from a dosing trial of therapeutic massage for chronic neck pain. Ann Fam Med. 2014;12(2):112-120. doi:10.1370/afm.1602
31. Perlman AI, Sabina A, Williams AL, Njike VY, Katz DL. Massage therapy for osteoarthritis of the knee: a randomized controlled trial. Arch Intern Med. 2006;166(22):2533-2538. doi:10.1001/archinte.166.22.2533
32. Perlman A, Fogerite SG, Glass O, et al. Efficacy and safety of massage for osteoarthritis of the knee: a randomized clinical trial. J Gen Intern Med. 2019;34(3):379-386. doi:10.1007/s11606-018-4763-5
33. Skelly AC, Chou R, Dettori JR, et al. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. Comparative Effectiveness Review. No. 227. Agency for Healthcare Research and Quality; 2020. doi:10.23970/AHRQEPCCER227
34. Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol Bull. 2004;130(1):3-18. doi:10.1037/0033-2909.130.1.3
35. Field T, Hernandez-Reif M, Diego M, Schanberg S, Kuhn C. Cortisol decreases and serotonin and dopamine increase following massage therapy. Int J Neurosci. 2005;115(10):1397-1413. doi:10.1080/ 00207450590956459
36. Li Q, Becker B, Wernicke J, et al. Foot massage evokes oxytocin release and activation of orbitofrontal cortex and superior temporal sulcus. Psychoneuroendocrinology. 2019;101:193-203. doi:10.1016/j.psyneuen.2018.11.016
37. Eaves ER, Sherman KJ, Ritenbaugh C, et al. A qualitative study of changes in expectations over time among patients with chronic low back pain seeking four CAM therapies. BMC Complement Altern Med. 2015;15:12. Published 2015 Feb 5. doi:10.1186/s12906-015-0531-9
38. Bishop FL, Lauche R, Cramer H, et al. Health behavior change and complementary medicine use: National Health Interview Survey 2012. Medicina (Kaunas). 2019;55(10):632. Published 2019 Sep 24. doi:10.3390/medicina55100632
39. Driscoll MA, Knobf MT, Higgins DM, Heapy A, Lee A, Haskell S. Patient experiences navigating chronic pain management in an integrated health care system: a qualitative investigation of women and men. Pain Med. 2018;19(suppl 1):S19-S29. doi:10.1093/pm/pny139
40. Denneson LM, Corson K, Dobscha SK. Complementary and alternative medicine use among veterans with chronic noncancer pain. J Rehabil Res Dev. 2011;48(9):1119-1128. doi:10.1682/jrrd.2010.12.0243
41. Taylor SL, Herman PM, Marshall NJ, et al. Use of complementary and integrated health: a retrospective analysis of U.S. veterans with chronic musculoskeletal pain nationally. J Altern Complement Med. 2019;25(1):32-39. doi:10.1089/acm.2018.0276
42. Evans EA, Herman PM, Washington DL, et al. Gender differences in use of complementary and integrative health by U.S. military veterans with chronic musculoskeletal pain. Womens Health Issues. 2018;28(5):379-386. doi:10.1016/j.whi.2018.07.003
43. Reinhard MJ, Nassif TH, Bloeser K, et al. CAM utilization among OEF/OIF veterans: findings from the National Health Study for a New Generation of US Veterans. Med Care. 2014;52(12)(suppl 5):S45-S49. doi:10.1097/MLR.0000000000000229
44. Herman PM, Yuan AH, Cefalu MS, et al. The use of complementary and integrative health approaches for chronic musculoskeletal pain in younger US Veterans: An economic evaluation. PLoS One. 2019;14(6):e0217831. Published 2019 Jun 5. doi:10.1371/journal.pone.0217831
45. Jonas WB, Schoomaker EB. Pain and opioids in the military: we must do better. JAMA Intern Med. 2014;174(8):1402-1403. doi:10.1001/jamainternmed.2014.2114
46. Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293-301. doi:10.7326/M17-0865
PTSD Disability Examination Reports: A Comparison of Veterans Health Administration and Contract Examiners
Updated June 17, 2022
The US Department of Veterans Affairs (VA) provides health care for > 9 million military veterans, nearly half of all former service members.1 Over the past 15 years, there has been a steady and substantial increase in the frequency of disability awards for veterans with post-9/11 military service. Recent data from the Bureau of Labor Statistics indicate that 41% of veterans who served after 9/11 receive service-connected disability benefits compared with 28% of veterans overall.2 More than 5 million veterans receive VA service-related disability benefits.2,3 More than half of the VA $243 billion budget for fiscal year (FY) 2021 ($135.5 billion) was allocated to the Veterans Benefits Administration (VBA), of which $115.7 billion (85%) was allocated specifically for service-related compensation claims payments.4
The VA predicted that VBA will have completed 1.4 million ratings for disability claims in 2021.5 A substantial percentage of these claims will be for mental disorders, specifically posttraumatic stress disorder (PTSD). VA officials testifying before Congress in 2017 noted that the number of PTSD claims had nearly tripled in the previous 10 years.6 As far back as 2013, McNally and Frueh analyzed “the skyrocketing of disability claims,” particularly for PTSD, among veterans who served in Iraq and Afghanistan.7
This large increase has placed an unprecedented burden on the VBA to expand its capacity to conduct initial PTSD disability evaluations that by regulations are completed by psychologists or psychiatrists. This need has led the VBA to make significant changes in the compensation and pension (C&P) process, including a reduced role for Veterans Health Administration (VHA) examiners and increased reliance on non-VA (contract) examiners through the Contract Medical Disability Examination (MDE) program. In 2019, the MDE budget was $1.23 billion; in 2020, it was increased to $1.79 billion, and for 2021, it was $2.23 billion, reflecting the increasing investment of resources in non-VA examiners, ostensibly to both increase capacity and save costs.5
Anecdotally, concerns have been raised regarding inadequate training of contract examiners as well as inadequate reports by these examiners. A 2018 Government Accountability Office (GAO) report concluded that VA lacked the data to determine whether contract examiners were meeting standards for quality, timeliness, and accuracy.8 The GAO report noted that VA required 92% of contractor reports contained no obvious errors, a relatively low target; however, in the first half of 2017, only 1 contractor group met that target. The report noted further that “VBA does not verify if examiners have completed training nor does it collect information to assess training effectiveness in preparing examiners.”8 A subsequent analysis of contract examinations completed by the VA Office of the Inspector General (OIG) in 2019 concluded that the MDE program was “hampered in their ability to provide oversight because of limitations with VBA’s electronic examination management systems, the lack of reliable data, and inadequate staffing of the program.”9
These reports have focused almost exclusively on simple performance metrics, such as timeliness of examination completion. However, the 2018 GAO report referenced isolated “focused reviews” of complaints about the quality of examinations by contract examiners and gave as an example an isolated “review of one contracted examiner who had high rates of diagnosing severe posttraumatic stress disorder.”8 After review indicated the examiner’s reports were of poor quality, the VBA discontinued the examiner’s contract.
Unfortunately, despite such anecdotal reports and isolated actions, to date there are no published reports examining and comparing the quality of PTSD examination reports completed by VHA and contract examiners or the subsequent disability determinations made by the VBA as a result of these evaluations. In a November 2020 letter to the VA Secretary, 11 US Senators expressed “grave concerns” regarding the VA decision to privatize C&P programs noting, among other concerns, that there were “no clinical quality measurement for, or evaluation of, contractor examinations.”10 The letter cited anecdotal evidence of contract examiners not reviewing veteran’s medical records and diagnosing conditions “without supporting evidence.”10
The purpose of the present evaluation was to provide a systematic comparison of the content and quality of initial PTSD disability examinations conducted by VHA and non-VA contract examiners. In addition, this study compared the disability rating decisions resulting from VHA and contract examinations.
Methods
A random sample of 100 Initial PTSD Disability Benefits Questionnaires (DBQs)—structured forms completed by all examiners—were obtained from a list supplied by the VA Office of Performance Analysis and Integrity. All examinations were from the Veterans Integrated Service Network (VISN) 1, encompassing the New England region and were conducted in 2019 and 2020. Two of the 100 cases were excluded for technical reasons, resulting in 98 examination reports. However, the final pool yielded 62 contract examinations and only 36 VHA examinations. To make the sample sizes more comparable, an additional 15 examinations were randomly selected from the local examination database (also VISN 1) to complement the original examination pool.
Once DBQs were retrieved, all identifying information was deleted, and cases were analyzed using assigned record numbers. All coding was completed by the 2 principal investigators, both VA psychologists with extensive training and experience in C&P evaluation and treatment of veterans with PTSD. Due to inherent structural differences between the forms used for VA and contract examinations, raters could not be masked/blinded to the source of the report.
A number of measures were taken to reduce bias and enhance objectivity of rating. First, objectively coded variables (eg, age and sex of veteran, period of service, trauma type, diagnoses rendered by the examiner, impairment category endorsed, number and type of symptoms) were transcribed directly from the DBQ as recorded by the examiner. Second, to rate report quality, an initial categorical rating scale was developed based on predetermined elements of examination quality that were considered essential. After refinement and preliminary analysis of interrater reliabilities, 3 quality-related indices were identified: (1) level of detail in description of key content areas (history before service, service trauma, after service social and vocational history, mental health history, substance use); (2) synthesis of history and findings in explaining opinion rendered; and (3) clarity of opinion regarding causation required “at least as likely as not” degree of confidence. The first 2 quality ratings were based on a 3-point scale (poor, fair, good), and the third variable was coded as yes or no. (eAppendix available at doi:10.12788/fp.0225). Interrater reliabilities calculated based on a subsample of 18 cases, randomly selected and rated by both raters, yielded Cohen κ in the acceptable range (.61, .72, and .89 for detail, synthesis, and clarity, respectively). Finally, for information regarding VBA decision making, rating decision documents contained in the Veterans Benefit Management System database were reviewed to determine whether the veteran was granted service connection for PTSD or another mental disorder based on the examination report in question and, if so, the disability rating percentage awarded. These were recorded independently after all other coding had been completed.
Results
Comparison of VHA and contract examinations revealed no significant differences between groups on relevant sociodemographic and other measures (Table). Missing data were not obtained from other records or sources, and for this study, reflect only what is recorded in the examination reports except for age, which was calculated using veteran’s date of birth and the date of examination.
To examine differences between VHA and contract examinations, the groups were first compared on a set of predetermined objectively coded variables taken directly from the DBQ. The frequency of PTSD diagnoses by VHA (57%) and contract (71%) examiners was not significantly different nor were rates of non-PTSD diagnoses by VHA (51%) and contract (73%) examiners. There also was no difference in the mean number of PTSD symptoms endorsed across PTSD diagnostic criteria B, C, D, and E (maximum of 20) recorded by VHA (9.4) and contract (10.9) examiners.
Contract examiners recorded a significantly greater mean number of “other symptoms” on a checklist of 31 possible symptoms as compared to VHA examiners: 7.3 vs 5.8, respectively (t[104] = 2.27, P < .05). An initial analysis of overall social/vocational impairment ratings coded by examiners did not reveal significant differences between examiner groups. However, when the 2 most severe impairment categories were combined to create a pooled “severe” category, 31% of contract examiners rated veterans as severely impaired compared with only 12% of VHA examiners (χ2 = 5.79, 1 df, P < .05) (Figure 1).
VHA and contract examinations were compared on 3 measures of report quality. Significant differences were found for both level of detail (χ2 = 16.44, 2 df, P < .01) and synthesis (χ2 = 6.68, 2 df, P < .05). Contract examinations were more likely to be rated as poor and less likely to be rated good, with a similar proportion of fair ratings for the 2 examination types (Figures 2 and 3). There was no significant difference in the proportion of VHA and contract examinations providing clear statement of opinion regarding causation (ie, whether or not the diagnosed condition was service related), with the majority rendering an adequate opinion in both examiner groups (VHA, 78%; contract, 79%).
Qualitative review revealed examples of markedly deficient examinations among contract examinations, including several reports that contained no review of records, no report of relevant background, and no mention or assessment of social and vocational function needed to inform opinions about diagnosis and impairment.
Finally, the VBA database was used to compare the resulting disability award decisions made by VBA based on the examination reports in question. Examination by contractors resulted in significantly higher mean service-connected disability ratings for examinees compared with VHA examiners (46.8 vs 33.5, respectively; t[108] = 2.3, P < .05).
Discussion
The present study provides the first reported systematic comparison of VA disability examinations for PTSD completed by examiners employed by the VHA and those hired as contract examiners through the MDE program. Although the frequency of PTSD diagnoses by contract examiners was higher than that of VHA examiners (71% vs 57%, respectively), the difference was not statistically significant. However, contract examiners recorded significantly more symptoms for examinees and rated them as severely impaired more frequently than did their VHA counterparts. In keeping with rating guidelines used by the VBA, these differences in examination content resulted in higher disability ratings for veterans seen by contract examiners.
Along with these elevated reports in symptom and severity ratings, contract examiners were less likely to provide adequate detail in the narrative sections of their reports and less frequently provided a satisfactory explanation and synthesis of relevant history and findings in support of their conclusions. Although not reflected in the statistical analysis, case-by-case review revealed some startlingly inadequate examination reports by contract examiners, several of which contained no review of records, no report or discussion of relevant background, and no discussion or analysis of social and vocational function to inform and support their opinion about level of impairment. None of the VHA examination reports reviewed lacked information to that degree.
Such deficiencies in detail and synthesis run counter to accepted guidelines for the adequate assessment of psychological injury in general and in VA disability claims specifically.11,12 For example, Watson and colleagues proposed that a minimum of 3 hours was required to conduct an initial PTSD examination, with more complex cases possibly taking longer.11 There is no information available about how long contract examiners take to complete their examinations and how that compares with the time taken by VA examiners. The VBA failure to monitor whether or not examiners follow accepted guidelines for PTSD examination has not previously been evaluated. Historically, a large number of clinicians, researchers, and policy critics have raised concerns about the potential for exaggeration or malingering among VA PTSD disability claimants and have urged the need to adequately assess for unreliable reporting and presentation.13,14 However, the possibility of systematic examiner deficiency and/or bias increasing the frequency of false or inflated claims being approved has received little empirical attention.
Although contract examiners did not diagnose PTSD significantly more frequently than VHA examiners (71% vs 57%, respectively), the overall frequency of PTSD diagnosis across both groups (65%) was substantially higher than previous figures that have, on average, estimated the lifetime prevalence of PTSD in trauma-exposed veterans to be about 31%.15 A re-analysis of the same National Vietnam Veterans Readjustment Survey data, but applying more conservative diagnostic criteria, reduced the lifetime prevalence to just under 19%, with point prevalence estimates even lower.15,16
In a study of concordance rates between service connection for PTSD and both current and lifetime diagnosis by independent, structured assessment, Marx and colleagues found that a “significant minority” of veterans who were already receiving service-connected disability for PTSD did not meet lifetime and/or current diagnostic criteria.17 Although it is possible that the group of veterans who were applying for disability benefits in our study had a higher rate of PTSD, it also is possible if not likely that the PTSD examination process overall yields inflated rates of diagnosis and levels of impairment. This speaks to the concern raised by Marx and colleagues who found that veterans with service connection for PTSD who received related benefits “may not have the disorder.”17
Limitations
A methodological limitation of the present study was that, due to structural differences in the DBQ forms used for VHA and contract examinations, the reports could not be de-identified as to examiner type and thus raters could not be masked/blinded. To mitigate bias, a predetermined, piloted, and refined coding and rating plan for report quality metrics was adhered to strictly, and interrater reliabilities were acceptable. Future study is suggested in which all report content is standardized for coding using the same format, which at present would require a complete rewriting of the entire report; this problem could be resolved by having the VBA adopt a more coherent system in which all reports, regardless of examiner type, use a single, standardized template. Further study using larger data sets and expanding to other VA regions also is needed.
Conclusions
The present study suggests that poor examination and report quality—by contract examiners and to a lesser degree VHA examiners—are not uncommon. The findings confirm and extend previous anecdotal reports of deficiencies in PTSD examinations performed by contract examiners and provide empirical support for concerns raised of global deficiencies in the VBA oversight of the MDE program. Such deficiencies have significant implications for the quality and integrity of the VA disability determination process for veterans claiming PTSD related to military service.
The current findings support and strengthen the call for development and management of a structured and enforced training and quality assurance/improvement program for VA PTSD disability examinations. Such training and oversight will be critical to improve the quality and integrity of these examinations, reduce error and waste in VBA’s Compensation and Pension process, and in doing so optimize VA financial resources to best serve veterans’ benefits and health care needs.
1. US Department of Veterans Affairs, Veterans Health Adminstration. About VHA. Updated April 23, 2021. Accessed January 6, 2022. www.va.gov/health/aboutvha.asp
2. US Department of Labor, Bureau of Labor Statistics. News release. Employment situation of veterans—2020. Published March 18, 2020. Accessed January 6, 2022. https://www.bls.gov/news.release/pdf/vet.pdf
3. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Department of Veterans Affairs statistics at a glance. Updated December 31, 2020. Accessed January 6, 2022. https://www.va.gov/vetdata/docs/Quickfacts/Stats_at_a_glance_12_31_20.PDF
4. US Department of Veterans Affairs. FY 2021 Budget submission: budget in brief. Published February 2020. Accessed January 6, 2022. https://www.va.gov/budget/docs/summary/archive/FY-2021-VA-BudgetSubmission.zip
5. US Department of Veterans Affairs. FY 2021 budget submission: benefits and burial programs and Departmental Administration volume 3 of 4:178. Published February 2020. Accessed January 6, 2022. https://www.va.gov/budget/docs/summary/archive/FY-2021-VA-BudgetSubmission.zip
6. Statement of Ronald Burke, assistant deputy under secretary, office of field operations Veterans Benefits Administration before the Subcommittee on Disability And Memorial Affairs of the House Committee on Veterans’ Affairs. Published July 25, 2017. Accessed January 6, 2022. https://www.congress.gov/115/meeting/house/106322/witnesses/HHRG-115-VR09-Wstate-BurkeR-20170725.pdf
7. McNally RJ, Frueh BC. Why are Iraq and Afghanistan War veterans seeking PTSD disability compensation at unprecedented rates? J Anxiety Disord. 2013;27(5):520-526. doi:10.1016/j.janxdis.2013.07.002
8. US Government Accountability Office. VA disability exams: improved performance analysis and training oversight needed for contracted exams. GAO-19-13. Published October 2018. Accessed January 6, 2022. https://www.gao.gov/assets/gao-19-13.pdf
9. US Department of Veterans Affairs, Office of Inspector General. Inadequate oversight of contracted disability exam cancellations. Report #18-04266-115. Published June 10, 2019. Accessed January 6, 2022. https://www.va.gov/oig/pubs/VAOIG-18-04266-115.pdf
10. Letter to VA Secretary Wilkie. Published November 11, 2020. Accessed January 6, 2022. https://www.veterans.senate.gov/download/candp-exam-va-letter
11. Watson PW, McFall M, McBrine C, Schnurr PP, Friedman MJ, Keane TM, Hamblen JL (2005). Best practice manual for posttraumatic stress disorder (PTSD) compensation and pension examinations. Portland, OR: Northwest Network Mental Illness Research, Education, and Clinical Center, VA Puget Sound Healthcare System.
12. Worthen MD, Moering RG. A practical guide to conducting VA compensation and pension exams for PTSD and other mental disorders. Psychol Inj and Law. 2011;4:187-216. doi:10.1007/s12207-011-9115-2
13. DeViva JC, Bloem WD. Symptom exaggeration and compensation seeking among combat veterans with posttraumatic stress disorder. J Trauma Stress. 2003;16(5):503-507. doi:10.1023/A:1025766713188
14. Ray CL. Feigning screeners in VA PTSD compensation and pension examinations. Psychol Inj and Law. 2014;7:370-387. doi:10.1007/s12207-014-9210-2
15. Kulka RA, Schlenger WE, Fairbank JA, et al. Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. Brunner Mazel Publishers; 1990.
16. Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313(5789):979-982. doi:10.1126/science.1128944
17. Marx BP, Bovin MJ, Szafranski DD, et al. Validity of posttraumatic stress disorder service connection status in Veterans Affairs electronic records of Iraq and Afghanistan Veterans. J Clin Psychiatry. 2016;77(4):517-522. doi:10.4088/JCP.14m09666
Updated June 17, 2022
The US Department of Veterans Affairs (VA) provides health care for > 9 million military veterans, nearly half of all former service members.1 Over the past 15 years, there has been a steady and substantial increase in the frequency of disability awards for veterans with post-9/11 military service. Recent data from the Bureau of Labor Statistics indicate that 41% of veterans who served after 9/11 receive service-connected disability benefits compared with 28% of veterans overall.2 More than 5 million veterans receive VA service-related disability benefits.2,3 More than half of the VA $243 billion budget for fiscal year (FY) 2021 ($135.5 billion) was allocated to the Veterans Benefits Administration (VBA), of which $115.7 billion (85%) was allocated specifically for service-related compensation claims payments.4
The VA predicted that VBA will have completed 1.4 million ratings for disability claims in 2021.5 A substantial percentage of these claims will be for mental disorders, specifically posttraumatic stress disorder (PTSD). VA officials testifying before Congress in 2017 noted that the number of PTSD claims had nearly tripled in the previous 10 years.6 As far back as 2013, McNally and Frueh analyzed “the skyrocketing of disability claims,” particularly for PTSD, among veterans who served in Iraq and Afghanistan.7
This large increase has placed an unprecedented burden on the VBA to expand its capacity to conduct initial PTSD disability evaluations that by regulations are completed by psychologists or psychiatrists. This need has led the VBA to make significant changes in the compensation and pension (C&P) process, including a reduced role for Veterans Health Administration (VHA) examiners and increased reliance on non-VA (contract) examiners through the Contract Medical Disability Examination (MDE) program. In 2019, the MDE budget was $1.23 billion; in 2020, it was increased to $1.79 billion, and for 2021, it was $2.23 billion, reflecting the increasing investment of resources in non-VA examiners, ostensibly to both increase capacity and save costs.5
Anecdotally, concerns have been raised regarding inadequate training of contract examiners as well as inadequate reports by these examiners. A 2018 Government Accountability Office (GAO) report concluded that VA lacked the data to determine whether contract examiners were meeting standards for quality, timeliness, and accuracy.8 The GAO report noted that VA required 92% of contractor reports contained no obvious errors, a relatively low target; however, in the first half of 2017, only 1 contractor group met that target. The report noted further that “VBA does not verify if examiners have completed training nor does it collect information to assess training effectiveness in preparing examiners.”8 A subsequent analysis of contract examinations completed by the VA Office of the Inspector General (OIG) in 2019 concluded that the MDE program was “hampered in their ability to provide oversight because of limitations with VBA’s electronic examination management systems, the lack of reliable data, and inadequate staffing of the program.”9
These reports have focused almost exclusively on simple performance metrics, such as timeliness of examination completion. However, the 2018 GAO report referenced isolated “focused reviews” of complaints about the quality of examinations by contract examiners and gave as an example an isolated “review of one contracted examiner who had high rates of diagnosing severe posttraumatic stress disorder.”8 After review indicated the examiner’s reports were of poor quality, the VBA discontinued the examiner’s contract.
Unfortunately, despite such anecdotal reports and isolated actions, to date there are no published reports examining and comparing the quality of PTSD examination reports completed by VHA and contract examiners or the subsequent disability determinations made by the VBA as a result of these evaluations. In a November 2020 letter to the VA Secretary, 11 US Senators expressed “grave concerns” regarding the VA decision to privatize C&P programs noting, among other concerns, that there were “no clinical quality measurement for, or evaluation of, contractor examinations.”10 The letter cited anecdotal evidence of contract examiners not reviewing veteran’s medical records and diagnosing conditions “without supporting evidence.”10
The purpose of the present evaluation was to provide a systematic comparison of the content and quality of initial PTSD disability examinations conducted by VHA and non-VA contract examiners. In addition, this study compared the disability rating decisions resulting from VHA and contract examinations.
Methods
A random sample of 100 Initial PTSD Disability Benefits Questionnaires (DBQs)—structured forms completed by all examiners—were obtained from a list supplied by the VA Office of Performance Analysis and Integrity. All examinations were from the Veterans Integrated Service Network (VISN) 1, encompassing the New England region and were conducted in 2019 and 2020. Two of the 100 cases were excluded for technical reasons, resulting in 98 examination reports. However, the final pool yielded 62 contract examinations and only 36 VHA examinations. To make the sample sizes more comparable, an additional 15 examinations were randomly selected from the local examination database (also VISN 1) to complement the original examination pool.
Once DBQs were retrieved, all identifying information was deleted, and cases were analyzed using assigned record numbers. All coding was completed by the 2 principal investigators, both VA psychologists with extensive training and experience in C&P evaluation and treatment of veterans with PTSD. Due to inherent structural differences between the forms used for VA and contract examinations, raters could not be masked/blinded to the source of the report.
A number of measures were taken to reduce bias and enhance objectivity of rating. First, objectively coded variables (eg, age and sex of veteran, period of service, trauma type, diagnoses rendered by the examiner, impairment category endorsed, number and type of symptoms) were transcribed directly from the DBQ as recorded by the examiner. Second, to rate report quality, an initial categorical rating scale was developed based on predetermined elements of examination quality that were considered essential. After refinement and preliminary analysis of interrater reliabilities, 3 quality-related indices were identified: (1) level of detail in description of key content areas (history before service, service trauma, after service social and vocational history, mental health history, substance use); (2) synthesis of history and findings in explaining opinion rendered; and (3) clarity of opinion regarding causation required “at least as likely as not” degree of confidence. The first 2 quality ratings were based on a 3-point scale (poor, fair, good), and the third variable was coded as yes or no. (eAppendix available at doi:10.12788/fp.0225). Interrater reliabilities calculated based on a subsample of 18 cases, randomly selected and rated by both raters, yielded Cohen κ in the acceptable range (.61, .72, and .89 for detail, synthesis, and clarity, respectively). Finally, for information regarding VBA decision making, rating decision documents contained in the Veterans Benefit Management System database were reviewed to determine whether the veteran was granted service connection for PTSD or another mental disorder based on the examination report in question and, if so, the disability rating percentage awarded. These were recorded independently after all other coding had been completed.
Results
Comparison of VHA and contract examinations revealed no significant differences between groups on relevant sociodemographic and other measures (Table). Missing data were not obtained from other records or sources, and for this study, reflect only what is recorded in the examination reports except for age, which was calculated using veteran’s date of birth and the date of examination.
To examine differences between VHA and contract examinations, the groups were first compared on a set of predetermined objectively coded variables taken directly from the DBQ. The frequency of PTSD diagnoses by VHA (57%) and contract (71%) examiners was not significantly different nor were rates of non-PTSD diagnoses by VHA (51%) and contract (73%) examiners. There also was no difference in the mean number of PTSD symptoms endorsed across PTSD diagnostic criteria B, C, D, and E (maximum of 20) recorded by VHA (9.4) and contract (10.9) examiners.
Contract examiners recorded a significantly greater mean number of “other symptoms” on a checklist of 31 possible symptoms as compared to VHA examiners: 7.3 vs 5.8, respectively (t[104] = 2.27, P < .05). An initial analysis of overall social/vocational impairment ratings coded by examiners did not reveal significant differences between examiner groups. However, when the 2 most severe impairment categories were combined to create a pooled “severe” category, 31% of contract examiners rated veterans as severely impaired compared with only 12% of VHA examiners (χ2 = 5.79, 1 df, P < .05) (Figure 1).
VHA and contract examinations were compared on 3 measures of report quality. Significant differences were found for both level of detail (χ2 = 16.44, 2 df, P < .01) and synthesis (χ2 = 6.68, 2 df, P < .05). Contract examinations were more likely to be rated as poor and less likely to be rated good, with a similar proportion of fair ratings for the 2 examination types (Figures 2 and 3). There was no significant difference in the proportion of VHA and contract examinations providing clear statement of opinion regarding causation (ie, whether or not the diagnosed condition was service related), with the majority rendering an adequate opinion in both examiner groups (VHA, 78%; contract, 79%).
Qualitative review revealed examples of markedly deficient examinations among contract examinations, including several reports that contained no review of records, no report of relevant background, and no mention or assessment of social and vocational function needed to inform opinions about diagnosis and impairment.
Finally, the VBA database was used to compare the resulting disability award decisions made by VBA based on the examination reports in question. Examination by contractors resulted in significantly higher mean service-connected disability ratings for examinees compared with VHA examiners (46.8 vs 33.5, respectively; t[108] = 2.3, P < .05).
Discussion
The present study provides the first reported systematic comparison of VA disability examinations for PTSD completed by examiners employed by the VHA and those hired as contract examiners through the MDE program. Although the frequency of PTSD diagnoses by contract examiners was higher than that of VHA examiners (71% vs 57%, respectively), the difference was not statistically significant. However, contract examiners recorded significantly more symptoms for examinees and rated them as severely impaired more frequently than did their VHA counterparts. In keeping with rating guidelines used by the VBA, these differences in examination content resulted in higher disability ratings for veterans seen by contract examiners.
Along with these elevated reports in symptom and severity ratings, contract examiners were less likely to provide adequate detail in the narrative sections of their reports and less frequently provided a satisfactory explanation and synthesis of relevant history and findings in support of their conclusions. Although not reflected in the statistical analysis, case-by-case review revealed some startlingly inadequate examination reports by contract examiners, several of which contained no review of records, no report or discussion of relevant background, and no discussion or analysis of social and vocational function to inform and support their opinion about level of impairment. None of the VHA examination reports reviewed lacked information to that degree.
Such deficiencies in detail and synthesis run counter to accepted guidelines for the adequate assessment of psychological injury in general and in VA disability claims specifically.11,12 For example, Watson and colleagues proposed that a minimum of 3 hours was required to conduct an initial PTSD examination, with more complex cases possibly taking longer.11 There is no information available about how long contract examiners take to complete their examinations and how that compares with the time taken by VA examiners. The VBA failure to monitor whether or not examiners follow accepted guidelines for PTSD examination has not previously been evaluated. Historically, a large number of clinicians, researchers, and policy critics have raised concerns about the potential for exaggeration or malingering among VA PTSD disability claimants and have urged the need to adequately assess for unreliable reporting and presentation.13,14 However, the possibility of systematic examiner deficiency and/or bias increasing the frequency of false or inflated claims being approved has received little empirical attention.
Although contract examiners did not diagnose PTSD significantly more frequently than VHA examiners (71% vs 57%, respectively), the overall frequency of PTSD diagnosis across both groups (65%) was substantially higher than previous figures that have, on average, estimated the lifetime prevalence of PTSD in trauma-exposed veterans to be about 31%.15 A re-analysis of the same National Vietnam Veterans Readjustment Survey data, but applying more conservative diagnostic criteria, reduced the lifetime prevalence to just under 19%, with point prevalence estimates even lower.15,16
In a study of concordance rates between service connection for PTSD and both current and lifetime diagnosis by independent, structured assessment, Marx and colleagues found that a “significant minority” of veterans who were already receiving service-connected disability for PTSD did not meet lifetime and/or current diagnostic criteria.17 Although it is possible that the group of veterans who were applying for disability benefits in our study had a higher rate of PTSD, it also is possible if not likely that the PTSD examination process overall yields inflated rates of diagnosis and levels of impairment. This speaks to the concern raised by Marx and colleagues who found that veterans with service connection for PTSD who received related benefits “may not have the disorder.”17
Limitations
A methodological limitation of the present study was that, due to structural differences in the DBQ forms used for VHA and contract examinations, the reports could not be de-identified as to examiner type and thus raters could not be masked/blinded. To mitigate bias, a predetermined, piloted, and refined coding and rating plan for report quality metrics was adhered to strictly, and interrater reliabilities were acceptable. Future study is suggested in which all report content is standardized for coding using the same format, which at present would require a complete rewriting of the entire report; this problem could be resolved by having the VBA adopt a more coherent system in which all reports, regardless of examiner type, use a single, standardized template. Further study using larger data sets and expanding to other VA regions also is needed.
Conclusions
The present study suggests that poor examination and report quality—by contract examiners and to a lesser degree VHA examiners—are not uncommon. The findings confirm and extend previous anecdotal reports of deficiencies in PTSD examinations performed by contract examiners and provide empirical support for concerns raised of global deficiencies in the VBA oversight of the MDE program. Such deficiencies have significant implications for the quality and integrity of the VA disability determination process for veterans claiming PTSD related to military service.
The current findings support and strengthen the call for development and management of a structured and enforced training and quality assurance/improvement program for VA PTSD disability examinations. Such training and oversight will be critical to improve the quality and integrity of these examinations, reduce error and waste in VBA’s Compensation and Pension process, and in doing so optimize VA financial resources to best serve veterans’ benefits and health care needs.
Updated June 17, 2022
The US Department of Veterans Affairs (VA) provides health care for > 9 million military veterans, nearly half of all former service members.1 Over the past 15 years, there has been a steady and substantial increase in the frequency of disability awards for veterans with post-9/11 military service. Recent data from the Bureau of Labor Statistics indicate that 41% of veterans who served after 9/11 receive service-connected disability benefits compared with 28% of veterans overall.2 More than 5 million veterans receive VA service-related disability benefits.2,3 More than half of the VA $243 billion budget for fiscal year (FY) 2021 ($135.5 billion) was allocated to the Veterans Benefits Administration (VBA), of which $115.7 billion (85%) was allocated specifically for service-related compensation claims payments.4
The VA predicted that VBA will have completed 1.4 million ratings for disability claims in 2021.5 A substantial percentage of these claims will be for mental disorders, specifically posttraumatic stress disorder (PTSD). VA officials testifying before Congress in 2017 noted that the number of PTSD claims had nearly tripled in the previous 10 years.6 As far back as 2013, McNally and Frueh analyzed “the skyrocketing of disability claims,” particularly for PTSD, among veterans who served in Iraq and Afghanistan.7
This large increase has placed an unprecedented burden on the VBA to expand its capacity to conduct initial PTSD disability evaluations that by regulations are completed by psychologists or psychiatrists. This need has led the VBA to make significant changes in the compensation and pension (C&P) process, including a reduced role for Veterans Health Administration (VHA) examiners and increased reliance on non-VA (contract) examiners through the Contract Medical Disability Examination (MDE) program. In 2019, the MDE budget was $1.23 billion; in 2020, it was increased to $1.79 billion, and for 2021, it was $2.23 billion, reflecting the increasing investment of resources in non-VA examiners, ostensibly to both increase capacity and save costs.5
Anecdotally, concerns have been raised regarding inadequate training of contract examiners as well as inadequate reports by these examiners. A 2018 Government Accountability Office (GAO) report concluded that VA lacked the data to determine whether contract examiners were meeting standards for quality, timeliness, and accuracy.8 The GAO report noted that VA required 92% of contractor reports contained no obvious errors, a relatively low target; however, in the first half of 2017, only 1 contractor group met that target. The report noted further that “VBA does not verify if examiners have completed training nor does it collect information to assess training effectiveness in preparing examiners.”8 A subsequent analysis of contract examinations completed by the VA Office of the Inspector General (OIG) in 2019 concluded that the MDE program was “hampered in their ability to provide oversight because of limitations with VBA’s electronic examination management systems, the lack of reliable data, and inadequate staffing of the program.”9
These reports have focused almost exclusively on simple performance metrics, such as timeliness of examination completion. However, the 2018 GAO report referenced isolated “focused reviews” of complaints about the quality of examinations by contract examiners and gave as an example an isolated “review of one contracted examiner who had high rates of diagnosing severe posttraumatic stress disorder.”8 After review indicated the examiner’s reports were of poor quality, the VBA discontinued the examiner’s contract.
Unfortunately, despite such anecdotal reports and isolated actions, to date there are no published reports examining and comparing the quality of PTSD examination reports completed by VHA and contract examiners or the subsequent disability determinations made by the VBA as a result of these evaluations. In a November 2020 letter to the VA Secretary, 11 US Senators expressed “grave concerns” regarding the VA decision to privatize C&P programs noting, among other concerns, that there were “no clinical quality measurement for, or evaluation of, contractor examinations.”10 The letter cited anecdotal evidence of contract examiners not reviewing veteran’s medical records and diagnosing conditions “without supporting evidence.”10
The purpose of the present evaluation was to provide a systematic comparison of the content and quality of initial PTSD disability examinations conducted by VHA and non-VA contract examiners. In addition, this study compared the disability rating decisions resulting from VHA and contract examinations.
Methods
A random sample of 100 Initial PTSD Disability Benefits Questionnaires (DBQs)—structured forms completed by all examiners—were obtained from a list supplied by the VA Office of Performance Analysis and Integrity. All examinations were from the Veterans Integrated Service Network (VISN) 1, encompassing the New England region and were conducted in 2019 and 2020. Two of the 100 cases were excluded for technical reasons, resulting in 98 examination reports. However, the final pool yielded 62 contract examinations and only 36 VHA examinations. To make the sample sizes more comparable, an additional 15 examinations were randomly selected from the local examination database (also VISN 1) to complement the original examination pool.
Once DBQs were retrieved, all identifying information was deleted, and cases were analyzed using assigned record numbers. All coding was completed by the 2 principal investigators, both VA psychologists with extensive training and experience in C&P evaluation and treatment of veterans with PTSD. Due to inherent structural differences between the forms used for VA and contract examinations, raters could not be masked/blinded to the source of the report.
A number of measures were taken to reduce bias and enhance objectivity of rating. First, objectively coded variables (eg, age and sex of veteran, period of service, trauma type, diagnoses rendered by the examiner, impairment category endorsed, number and type of symptoms) were transcribed directly from the DBQ as recorded by the examiner. Second, to rate report quality, an initial categorical rating scale was developed based on predetermined elements of examination quality that were considered essential. After refinement and preliminary analysis of interrater reliabilities, 3 quality-related indices were identified: (1) level of detail in description of key content areas (history before service, service trauma, after service social and vocational history, mental health history, substance use); (2) synthesis of history and findings in explaining opinion rendered; and (3) clarity of opinion regarding causation required “at least as likely as not” degree of confidence. The first 2 quality ratings were based on a 3-point scale (poor, fair, good), and the third variable was coded as yes or no. (eAppendix available at doi:10.12788/fp.0225). Interrater reliabilities calculated based on a subsample of 18 cases, randomly selected and rated by both raters, yielded Cohen κ in the acceptable range (.61, .72, and .89 for detail, synthesis, and clarity, respectively). Finally, for information regarding VBA decision making, rating decision documents contained in the Veterans Benefit Management System database were reviewed to determine whether the veteran was granted service connection for PTSD or another mental disorder based on the examination report in question and, if so, the disability rating percentage awarded. These were recorded independently after all other coding had been completed.
Results
Comparison of VHA and contract examinations revealed no significant differences between groups on relevant sociodemographic and other measures (Table). Missing data were not obtained from other records or sources, and for this study, reflect only what is recorded in the examination reports except for age, which was calculated using veteran’s date of birth and the date of examination.
To examine differences between VHA and contract examinations, the groups were first compared on a set of predetermined objectively coded variables taken directly from the DBQ. The frequency of PTSD diagnoses by VHA (57%) and contract (71%) examiners was not significantly different nor were rates of non-PTSD diagnoses by VHA (51%) and contract (73%) examiners. There also was no difference in the mean number of PTSD symptoms endorsed across PTSD diagnostic criteria B, C, D, and E (maximum of 20) recorded by VHA (9.4) and contract (10.9) examiners.
Contract examiners recorded a significantly greater mean number of “other symptoms” on a checklist of 31 possible symptoms as compared to VHA examiners: 7.3 vs 5.8, respectively (t[104] = 2.27, P < .05). An initial analysis of overall social/vocational impairment ratings coded by examiners did not reveal significant differences between examiner groups. However, when the 2 most severe impairment categories were combined to create a pooled “severe” category, 31% of contract examiners rated veterans as severely impaired compared with only 12% of VHA examiners (χ2 = 5.79, 1 df, P < .05) (Figure 1).
VHA and contract examinations were compared on 3 measures of report quality. Significant differences were found for both level of detail (χ2 = 16.44, 2 df, P < .01) and synthesis (χ2 = 6.68, 2 df, P < .05). Contract examinations were more likely to be rated as poor and less likely to be rated good, with a similar proportion of fair ratings for the 2 examination types (Figures 2 and 3). There was no significant difference in the proportion of VHA and contract examinations providing clear statement of opinion regarding causation (ie, whether or not the diagnosed condition was service related), with the majority rendering an adequate opinion in both examiner groups (VHA, 78%; contract, 79%).
Qualitative review revealed examples of markedly deficient examinations among contract examinations, including several reports that contained no review of records, no report of relevant background, and no mention or assessment of social and vocational function needed to inform opinions about diagnosis and impairment.
Finally, the VBA database was used to compare the resulting disability award decisions made by VBA based on the examination reports in question. Examination by contractors resulted in significantly higher mean service-connected disability ratings for examinees compared with VHA examiners (46.8 vs 33.5, respectively; t[108] = 2.3, P < .05).
Discussion
The present study provides the first reported systematic comparison of VA disability examinations for PTSD completed by examiners employed by the VHA and those hired as contract examiners through the MDE program. Although the frequency of PTSD diagnoses by contract examiners was higher than that of VHA examiners (71% vs 57%, respectively), the difference was not statistically significant. However, contract examiners recorded significantly more symptoms for examinees and rated them as severely impaired more frequently than did their VHA counterparts. In keeping with rating guidelines used by the VBA, these differences in examination content resulted in higher disability ratings for veterans seen by contract examiners.
Along with these elevated reports in symptom and severity ratings, contract examiners were less likely to provide adequate detail in the narrative sections of their reports and less frequently provided a satisfactory explanation and synthesis of relevant history and findings in support of their conclusions. Although not reflected in the statistical analysis, case-by-case review revealed some startlingly inadequate examination reports by contract examiners, several of which contained no review of records, no report or discussion of relevant background, and no discussion or analysis of social and vocational function to inform and support their opinion about level of impairment. None of the VHA examination reports reviewed lacked information to that degree.
Such deficiencies in detail and synthesis run counter to accepted guidelines for the adequate assessment of psychological injury in general and in VA disability claims specifically.11,12 For example, Watson and colleagues proposed that a minimum of 3 hours was required to conduct an initial PTSD examination, with more complex cases possibly taking longer.11 There is no information available about how long contract examiners take to complete their examinations and how that compares with the time taken by VA examiners. The VBA failure to monitor whether or not examiners follow accepted guidelines for PTSD examination has not previously been evaluated. Historically, a large number of clinicians, researchers, and policy critics have raised concerns about the potential for exaggeration or malingering among VA PTSD disability claimants and have urged the need to adequately assess for unreliable reporting and presentation.13,14 However, the possibility of systematic examiner deficiency and/or bias increasing the frequency of false or inflated claims being approved has received little empirical attention.
Although contract examiners did not diagnose PTSD significantly more frequently than VHA examiners (71% vs 57%, respectively), the overall frequency of PTSD diagnosis across both groups (65%) was substantially higher than previous figures that have, on average, estimated the lifetime prevalence of PTSD in trauma-exposed veterans to be about 31%.15 A re-analysis of the same National Vietnam Veterans Readjustment Survey data, but applying more conservative diagnostic criteria, reduced the lifetime prevalence to just under 19%, with point prevalence estimates even lower.15,16
In a study of concordance rates between service connection for PTSD and both current and lifetime diagnosis by independent, structured assessment, Marx and colleagues found that a “significant minority” of veterans who were already receiving service-connected disability for PTSD did not meet lifetime and/or current diagnostic criteria.17 Although it is possible that the group of veterans who were applying for disability benefits in our study had a higher rate of PTSD, it also is possible if not likely that the PTSD examination process overall yields inflated rates of diagnosis and levels of impairment. This speaks to the concern raised by Marx and colleagues who found that veterans with service connection for PTSD who received related benefits “may not have the disorder.”17
Limitations
A methodological limitation of the present study was that, due to structural differences in the DBQ forms used for VHA and contract examinations, the reports could not be de-identified as to examiner type and thus raters could not be masked/blinded. To mitigate bias, a predetermined, piloted, and refined coding and rating plan for report quality metrics was adhered to strictly, and interrater reliabilities were acceptable. Future study is suggested in which all report content is standardized for coding using the same format, which at present would require a complete rewriting of the entire report; this problem could be resolved by having the VBA adopt a more coherent system in which all reports, regardless of examiner type, use a single, standardized template. Further study using larger data sets and expanding to other VA regions also is needed.
Conclusions
The present study suggests that poor examination and report quality—by contract examiners and to a lesser degree VHA examiners—are not uncommon. The findings confirm and extend previous anecdotal reports of deficiencies in PTSD examinations performed by contract examiners and provide empirical support for concerns raised of global deficiencies in the VBA oversight of the MDE program. Such deficiencies have significant implications for the quality and integrity of the VA disability determination process for veterans claiming PTSD related to military service.
The current findings support and strengthen the call for development and management of a structured and enforced training and quality assurance/improvement program for VA PTSD disability examinations. Such training and oversight will be critical to improve the quality and integrity of these examinations, reduce error and waste in VBA’s Compensation and Pension process, and in doing so optimize VA financial resources to best serve veterans’ benefits and health care needs.
1. US Department of Veterans Affairs, Veterans Health Adminstration. About VHA. Updated April 23, 2021. Accessed January 6, 2022. www.va.gov/health/aboutvha.asp
2. US Department of Labor, Bureau of Labor Statistics. News release. Employment situation of veterans—2020. Published March 18, 2020. Accessed January 6, 2022. https://www.bls.gov/news.release/pdf/vet.pdf
3. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Department of Veterans Affairs statistics at a glance. Updated December 31, 2020. Accessed January 6, 2022. https://www.va.gov/vetdata/docs/Quickfacts/Stats_at_a_glance_12_31_20.PDF
4. US Department of Veterans Affairs. FY 2021 Budget submission: budget in brief. Published February 2020. Accessed January 6, 2022. https://www.va.gov/budget/docs/summary/archive/FY-2021-VA-BudgetSubmission.zip
5. US Department of Veterans Affairs. FY 2021 budget submission: benefits and burial programs and Departmental Administration volume 3 of 4:178. Published February 2020. Accessed January 6, 2022. https://www.va.gov/budget/docs/summary/archive/FY-2021-VA-BudgetSubmission.zip
6. Statement of Ronald Burke, assistant deputy under secretary, office of field operations Veterans Benefits Administration before the Subcommittee on Disability And Memorial Affairs of the House Committee on Veterans’ Affairs. Published July 25, 2017. Accessed January 6, 2022. https://www.congress.gov/115/meeting/house/106322/witnesses/HHRG-115-VR09-Wstate-BurkeR-20170725.pdf
7. McNally RJ, Frueh BC. Why are Iraq and Afghanistan War veterans seeking PTSD disability compensation at unprecedented rates? J Anxiety Disord. 2013;27(5):520-526. doi:10.1016/j.janxdis.2013.07.002
8. US Government Accountability Office. VA disability exams: improved performance analysis and training oversight needed for contracted exams. GAO-19-13. Published October 2018. Accessed January 6, 2022. https://www.gao.gov/assets/gao-19-13.pdf
9. US Department of Veterans Affairs, Office of Inspector General. Inadequate oversight of contracted disability exam cancellations. Report #18-04266-115. Published June 10, 2019. Accessed January 6, 2022. https://www.va.gov/oig/pubs/VAOIG-18-04266-115.pdf
10. Letter to VA Secretary Wilkie. Published November 11, 2020. Accessed January 6, 2022. https://www.veterans.senate.gov/download/candp-exam-va-letter
11. Watson PW, McFall M, McBrine C, Schnurr PP, Friedman MJ, Keane TM, Hamblen JL (2005). Best practice manual for posttraumatic stress disorder (PTSD) compensation and pension examinations. Portland, OR: Northwest Network Mental Illness Research, Education, and Clinical Center, VA Puget Sound Healthcare System.
12. Worthen MD, Moering RG. A practical guide to conducting VA compensation and pension exams for PTSD and other mental disorders. Psychol Inj and Law. 2011;4:187-216. doi:10.1007/s12207-011-9115-2
13. DeViva JC, Bloem WD. Symptom exaggeration and compensation seeking among combat veterans with posttraumatic stress disorder. J Trauma Stress. 2003;16(5):503-507. doi:10.1023/A:1025766713188
14. Ray CL. Feigning screeners in VA PTSD compensation and pension examinations. Psychol Inj and Law. 2014;7:370-387. doi:10.1007/s12207-014-9210-2
15. Kulka RA, Schlenger WE, Fairbank JA, et al. Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. Brunner Mazel Publishers; 1990.
16. Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313(5789):979-982. doi:10.1126/science.1128944
17. Marx BP, Bovin MJ, Szafranski DD, et al. Validity of posttraumatic stress disorder service connection status in Veterans Affairs electronic records of Iraq and Afghanistan Veterans. J Clin Psychiatry. 2016;77(4):517-522. doi:10.4088/JCP.14m09666
1. US Department of Veterans Affairs, Veterans Health Adminstration. About VHA. Updated April 23, 2021. Accessed January 6, 2022. www.va.gov/health/aboutvha.asp
2. US Department of Labor, Bureau of Labor Statistics. News release. Employment situation of veterans—2020. Published March 18, 2020. Accessed January 6, 2022. https://www.bls.gov/news.release/pdf/vet.pdf
3. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Department of Veterans Affairs statistics at a glance. Updated December 31, 2020. Accessed January 6, 2022. https://www.va.gov/vetdata/docs/Quickfacts/Stats_at_a_glance_12_31_20.PDF
4. US Department of Veterans Affairs. FY 2021 Budget submission: budget in brief. Published February 2020. Accessed January 6, 2022. https://www.va.gov/budget/docs/summary/archive/FY-2021-VA-BudgetSubmission.zip
5. US Department of Veterans Affairs. FY 2021 budget submission: benefits and burial programs and Departmental Administration volume 3 of 4:178. Published February 2020. Accessed January 6, 2022. https://www.va.gov/budget/docs/summary/archive/FY-2021-VA-BudgetSubmission.zip
6. Statement of Ronald Burke, assistant deputy under secretary, office of field operations Veterans Benefits Administration before the Subcommittee on Disability And Memorial Affairs of the House Committee on Veterans’ Affairs. Published July 25, 2017. Accessed January 6, 2022. https://www.congress.gov/115/meeting/house/106322/witnesses/HHRG-115-VR09-Wstate-BurkeR-20170725.pdf
7. McNally RJ, Frueh BC. Why are Iraq and Afghanistan War veterans seeking PTSD disability compensation at unprecedented rates? J Anxiety Disord. 2013;27(5):520-526. doi:10.1016/j.janxdis.2013.07.002
8. US Government Accountability Office. VA disability exams: improved performance analysis and training oversight needed for contracted exams. GAO-19-13. Published October 2018. Accessed January 6, 2022. https://www.gao.gov/assets/gao-19-13.pdf
9. US Department of Veterans Affairs, Office of Inspector General. Inadequate oversight of contracted disability exam cancellations. Report #18-04266-115. Published June 10, 2019. Accessed January 6, 2022. https://www.va.gov/oig/pubs/VAOIG-18-04266-115.pdf
10. Letter to VA Secretary Wilkie. Published November 11, 2020. Accessed January 6, 2022. https://www.veterans.senate.gov/download/candp-exam-va-letter
11. Watson PW, McFall M, McBrine C, Schnurr PP, Friedman MJ, Keane TM, Hamblen JL (2005). Best practice manual for posttraumatic stress disorder (PTSD) compensation and pension examinations. Portland, OR: Northwest Network Mental Illness Research, Education, and Clinical Center, VA Puget Sound Healthcare System.
12. Worthen MD, Moering RG. A practical guide to conducting VA compensation and pension exams for PTSD and other mental disorders. Psychol Inj and Law. 2011;4:187-216. doi:10.1007/s12207-011-9115-2
13. DeViva JC, Bloem WD. Symptom exaggeration and compensation seeking among combat veterans with posttraumatic stress disorder. J Trauma Stress. 2003;16(5):503-507. doi:10.1023/A:1025766713188
14. Ray CL. Feigning screeners in VA PTSD compensation and pension examinations. Psychol Inj and Law. 2014;7:370-387. doi:10.1007/s12207-014-9210-2
15. Kulka RA, Schlenger WE, Fairbank JA, et al. Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. Brunner Mazel Publishers; 1990.
16. Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313(5789):979-982. doi:10.1126/science.1128944
17. Marx BP, Bovin MJ, Szafranski DD, et al. Validity of posttraumatic stress disorder service connection status in Veterans Affairs electronic records of Iraq and Afghanistan Veterans. J Clin Psychiatry. 2016;77(4):517-522. doi:10.4088/JCP.14m09666