User login
Anesthesia care team may be quicker for GI endoscopy
Gastrointestinal endoscopy takes less time when an anesthesiologist oversees the sedation, researchers say.
“We have increased patient access to our GI unit by making these modifications,” said Adeel Faruki, MD, a senior instructor of anesthesiology and fellow in operations at the University of Colorado at Denver, Aurora.
The finding was presented at the American Society of Anesthesiologists’ ADVANCE 2022, the Anesthesiology Business Event.
Sedation for endoscopy in the United States generally follows one of two models, Dr. Faruki told this news organization: nurse-administered sedation (NAS) or monitored anesthesia care (MAC). During NAS, a GI proceduralist monitors a registered nurse who sedates patients using medications such as fentanyl, midazolam, and diphenhydramine. This was the approach at the researchers’ GI unit until July 1, 2021.
After that date, the GI unit switched to the MAC model, in which an anesthesiologist supervises a certified registered nurse anesthesiologist or an anesthesiology assistant who administers propofol. Propofol is faster acting than the drug combination the GI unit previously used and causes deeper sedation. But it can also cause respiratory or cardiovascular depression or low blood pressure, Dr. Faruki said, so most institutions require an anesthesiologist to oversee its use.
NAS versus MAC: Seeking the superior model
To see which approach was faster, Dr. Faruki and colleagues recorded times for endoscopic procedures from Aug. 1, 2021, to Oct. 31, 2021, and compared them with the data they had logged in electronic medical records from Jan. 1, 2021, to June 30, 2021. They excluded the month of July to allow for a transition period between the two approaches.
After comparing results from 4,606 patients undergoing endoscopy with NAS to 1,034 undergoing it with MAC, they observed that switching to the latter model reduced the time from sedation start to scope-in by 2-2.5 minutes.
Because recovery is faster with propofol, the patients also spent 7 minutes less in the postanesthesia care unit for upper GI endoscopies and 2 minutes less for lower GI endoscopies. Patients also told the researchers they felt less groggy.
At the same time the unit was transitioning from NAS to MAC, they also began requiring patients to sign consent forms for both the anesthesia and GI procedures in the preoperative room rather than in the procedure room. That saved about 19 minutes.
Putting all these changes together, the researchers calculated that they increased the capacity of their GI unit by 25%.
“With a pandemic raging and capacity crises continuing, it becomes very relevant to the care we can provide patients,” Dr. Faruki said. “That’s something we’re actually really proud of.”
The university is now instituting similar procedures at its other ambulatory surgical centers, he added.
How efficient is your endoscopy center?
“Other factors can also affect the efficiency of endoscopy,” said Joseph Vicari, MD, MBA, a partner at Rockford (Ill.) Gastroenterology Associates, who was not involved in this study.
For example, the unit has to have enough endoscopes and enough techs to clean them so they’re always available, he said in an interview. There have to be enough nurses and other staff to turn the rooms over efficiently. There also have to be enough pre- and postoperative beds, so that no one is waiting for either one.
Dr. Vicari recommended that GI endoscopy centers compare their times with those of benchmarks provided by professional societies and in published papers.
Having sorted out these factors, the MAC and NAS approaches both have their pros and cons, said Dr. Vicari.
“I think it’s a good idea for units that are struggling with efficiency, especially hospital-based units, to consider new ways to upload patient information and maybe have a dedicated anesthesia team to improve efficiency,” he said. “Procedure time can be reduced because you generally have a much steadier state of sedation with MAC, and then the recovery is much faster with propofol. Your patients wake up faster.”
But Rockford Gastroenterology continues to use the NAS approach in at least 90% of its endoscopies, because it is already so efficient that it doesn’t believe that MAC would make a significant difference.
“Academic centers tend to be less efficient,” he said. “Units like ours, an ambulatory endoscopy center, are different.”
NAS is also less expensive, Dr. Vicari said. “We have leveraged our lower-cost ambulatory endoscopy center by providing fentanyl and Versed [midazolam], turning it into an advantage in developing bundled contracts. Payers can significantly reduce expenses.”
The involvement of an anesthesiologist could increase the cost, Dr. Faruki acknowledged, and he said the researchers are analyzing that question. But he added that anesthesiologists can also oversee four rooms at once.
Dr. Faruki and Dr. Vicari reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gastrointestinal endoscopy takes less time when an anesthesiologist oversees the sedation, researchers say.
“We have increased patient access to our GI unit by making these modifications,” said Adeel Faruki, MD, a senior instructor of anesthesiology and fellow in operations at the University of Colorado at Denver, Aurora.
The finding was presented at the American Society of Anesthesiologists’ ADVANCE 2022, the Anesthesiology Business Event.
Sedation for endoscopy in the United States generally follows one of two models, Dr. Faruki told this news organization: nurse-administered sedation (NAS) or monitored anesthesia care (MAC). During NAS, a GI proceduralist monitors a registered nurse who sedates patients using medications such as fentanyl, midazolam, and diphenhydramine. This was the approach at the researchers’ GI unit until July 1, 2021.
After that date, the GI unit switched to the MAC model, in which an anesthesiologist supervises a certified registered nurse anesthesiologist or an anesthesiology assistant who administers propofol. Propofol is faster acting than the drug combination the GI unit previously used and causes deeper sedation. But it can also cause respiratory or cardiovascular depression or low blood pressure, Dr. Faruki said, so most institutions require an anesthesiologist to oversee its use.
NAS versus MAC: Seeking the superior model
To see which approach was faster, Dr. Faruki and colleagues recorded times for endoscopic procedures from Aug. 1, 2021, to Oct. 31, 2021, and compared them with the data they had logged in electronic medical records from Jan. 1, 2021, to June 30, 2021. They excluded the month of July to allow for a transition period between the two approaches.
After comparing results from 4,606 patients undergoing endoscopy with NAS to 1,034 undergoing it with MAC, they observed that switching to the latter model reduced the time from sedation start to scope-in by 2-2.5 minutes.
Because recovery is faster with propofol, the patients also spent 7 minutes less in the postanesthesia care unit for upper GI endoscopies and 2 minutes less for lower GI endoscopies. Patients also told the researchers they felt less groggy.
At the same time the unit was transitioning from NAS to MAC, they also began requiring patients to sign consent forms for both the anesthesia and GI procedures in the preoperative room rather than in the procedure room. That saved about 19 minutes.
Putting all these changes together, the researchers calculated that they increased the capacity of their GI unit by 25%.
“With a pandemic raging and capacity crises continuing, it becomes very relevant to the care we can provide patients,” Dr. Faruki said. “That’s something we’re actually really proud of.”
The university is now instituting similar procedures at its other ambulatory surgical centers, he added.
How efficient is your endoscopy center?
“Other factors can also affect the efficiency of endoscopy,” said Joseph Vicari, MD, MBA, a partner at Rockford (Ill.) Gastroenterology Associates, who was not involved in this study.
For example, the unit has to have enough endoscopes and enough techs to clean them so they’re always available, he said in an interview. There have to be enough nurses and other staff to turn the rooms over efficiently. There also have to be enough pre- and postoperative beds, so that no one is waiting for either one.
Dr. Vicari recommended that GI endoscopy centers compare their times with those of benchmarks provided by professional societies and in published papers.
Having sorted out these factors, the MAC and NAS approaches both have their pros and cons, said Dr. Vicari.
“I think it’s a good idea for units that are struggling with efficiency, especially hospital-based units, to consider new ways to upload patient information and maybe have a dedicated anesthesia team to improve efficiency,” he said. “Procedure time can be reduced because you generally have a much steadier state of sedation with MAC, and then the recovery is much faster with propofol. Your patients wake up faster.”
But Rockford Gastroenterology continues to use the NAS approach in at least 90% of its endoscopies, because it is already so efficient that it doesn’t believe that MAC would make a significant difference.
“Academic centers tend to be less efficient,” he said. “Units like ours, an ambulatory endoscopy center, are different.”
NAS is also less expensive, Dr. Vicari said. “We have leveraged our lower-cost ambulatory endoscopy center by providing fentanyl and Versed [midazolam], turning it into an advantage in developing bundled contracts. Payers can significantly reduce expenses.”
The involvement of an anesthesiologist could increase the cost, Dr. Faruki acknowledged, and he said the researchers are analyzing that question. But he added that anesthesiologists can also oversee four rooms at once.
Dr. Faruki and Dr. Vicari reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gastrointestinal endoscopy takes less time when an anesthesiologist oversees the sedation, researchers say.
“We have increased patient access to our GI unit by making these modifications,” said Adeel Faruki, MD, a senior instructor of anesthesiology and fellow in operations at the University of Colorado at Denver, Aurora.
The finding was presented at the American Society of Anesthesiologists’ ADVANCE 2022, the Anesthesiology Business Event.
Sedation for endoscopy in the United States generally follows one of two models, Dr. Faruki told this news organization: nurse-administered sedation (NAS) or monitored anesthesia care (MAC). During NAS, a GI proceduralist monitors a registered nurse who sedates patients using medications such as fentanyl, midazolam, and diphenhydramine. This was the approach at the researchers’ GI unit until July 1, 2021.
After that date, the GI unit switched to the MAC model, in which an anesthesiologist supervises a certified registered nurse anesthesiologist or an anesthesiology assistant who administers propofol. Propofol is faster acting than the drug combination the GI unit previously used and causes deeper sedation. But it can also cause respiratory or cardiovascular depression or low blood pressure, Dr. Faruki said, so most institutions require an anesthesiologist to oversee its use.
NAS versus MAC: Seeking the superior model
To see which approach was faster, Dr. Faruki and colleagues recorded times for endoscopic procedures from Aug. 1, 2021, to Oct. 31, 2021, and compared them with the data they had logged in electronic medical records from Jan. 1, 2021, to June 30, 2021. They excluded the month of July to allow for a transition period between the two approaches.
After comparing results from 4,606 patients undergoing endoscopy with NAS to 1,034 undergoing it with MAC, they observed that switching to the latter model reduced the time from sedation start to scope-in by 2-2.5 minutes.
Because recovery is faster with propofol, the patients also spent 7 minutes less in the postanesthesia care unit for upper GI endoscopies and 2 minutes less for lower GI endoscopies. Patients also told the researchers they felt less groggy.
At the same time the unit was transitioning from NAS to MAC, they also began requiring patients to sign consent forms for both the anesthesia and GI procedures in the preoperative room rather than in the procedure room. That saved about 19 minutes.
Putting all these changes together, the researchers calculated that they increased the capacity of their GI unit by 25%.
“With a pandemic raging and capacity crises continuing, it becomes very relevant to the care we can provide patients,” Dr. Faruki said. “That’s something we’re actually really proud of.”
The university is now instituting similar procedures at its other ambulatory surgical centers, he added.
How efficient is your endoscopy center?
“Other factors can also affect the efficiency of endoscopy,” said Joseph Vicari, MD, MBA, a partner at Rockford (Ill.) Gastroenterology Associates, who was not involved in this study.
For example, the unit has to have enough endoscopes and enough techs to clean them so they’re always available, he said in an interview. There have to be enough nurses and other staff to turn the rooms over efficiently. There also have to be enough pre- and postoperative beds, so that no one is waiting for either one.
Dr. Vicari recommended that GI endoscopy centers compare their times with those of benchmarks provided by professional societies and in published papers.
Having sorted out these factors, the MAC and NAS approaches both have their pros and cons, said Dr. Vicari.
“I think it’s a good idea for units that are struggling with efficiency, especially hospital-based units, to consider new ways to upload patient information and maybe have a dedicated anesthesia team to improve efficiency,” he said. “Procedure time can be reduced because you generally have a much steadier state of sedation with MAC, and then the recovery is much faster with propofol. Your patients wake up faster.”
But Rockford Gastroenterology continues to use the NAS approach in at least 90% of its endoscopies, because it is already so efficient that it doesn’t believe that MAC would make a significant difference.
“Academic centers tend to be less efficient,” he said. “Units like ours, an ambulatory endoscopy center, are different.”
NAS is also less expensive, Dr. Vicari said. “We have leveraged our lower-cost ambulatory endoscopy center by providing fentanyl and Versed [midazolam], turning it into an advantage in developing bundled contracts. Payers can significantly reduce expenses.”
The involvement of an anesthesiologist could increase the cost, Dr. Faruki acknowledged, and he said the researchers are analyzing that question. But he added that anesthesiologists can also oversee four rooms at once.
Dr. Faruki and Dr. Vicari reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ADVANCE 2022
Docs react: NyQuil chicken and endless eye mucus
It’s the season of love. In that spirit, Lean in and get a whiff of the latest good, bad, and ugly videos making the rounds on the internet’s most perplexing platform. But don’t get too close; these videos are especially ripe.
The bad: NyQuil chicken
You know something bad has happened when your TikTok search ends with a warning from the app that says “Learn how to recognize harmful trends and hoaxes.” That’s what shows up now when you try to find out what the “NyQuil chicken” or “sleepy chicken” trend is (or was) all about.
TikTok videos, including this one from TikTok user @janelleandkate, show users trying out a trend meant to cook up a meal that will also cure your cold symptoms. The trend involves cooking chicken in a pan full of the cold and flu medicine NyQuil. The NyQuil chicken idea stems from a Twitter meme from 2017, so it is possible that some of the recent videos are fake (blue food coloring is easy to get, people).
However, in the instance that people believe the videos to be real and want to try the trend out, it is important to warn that this shouldn’t be attempted.
Aaron Hartman, MD, assistant clinical professor of family medicine at Virginia Commonwealth University, told the website Mic about the trend’s dangers: “When you cook cough medicine like NyQuil, however, you boil off the water and alcohol in it, leaving the chicken saturated with a super concentrated amount of drugs in the meat. If you ate one of those cutlets completely cooked, it’d be as if you’re actually consuming a quarter to half a bottle of NyQuil.”
And that’s not good for anyone. What ever happened to an old fashioned herb marinade?
The good: Can you fart yourself blind? Doc explains
It’s something we’ve all wondered about, right?
TikTok and YouTube’s mainstay plastic surgeon Anthony Youn, MD, took it upon himself to reply to a comment saying “I once farted so hard I went blind for 3 minutes.” This phenomenon, according to Dr. Youn, is very rare, but not impossible, though we wouldn’t exactly want to try it for ourselves.
In the humorous (but very informative!) video, Dr. Youn explains that particularly pungent flatulence can contain large amounts of hydrogen sulfide, a gas that is known for smelling like rotten eggs. According to the Occupational Safety and Health Administration, hydrogen sulfide is produced in a number of industries, like oil and gas refining, mining, and paper processing. Exposure to higher concentrations of hydrogen sulfide can be dangerous, with prolonged exposure at a 2-5 parts per million (ppm) concentration causing nausea, headaches, and airway problems in some asthma patients. At very high concentrations, it can be fatal.
Thankfully, a person’s gas is not at all that dangerous. When it comes to the commentor’s claim, Dr. Youn says that something else hydrogen sulfide can do is reduce blood pressure.
“If it reduces blood pressure to the central retinal artery,” Dr. Youn says, “your silent but deadly toot could theoretically make you go blind.”
Thank goodness we can lay that question to rest.
The ugly: Eye boogers from hell
Get a look at this!
This video from @mikaylaadiorr has amassed over 8 million likes and over 89,000 comments, and shows someone, who we can assume is Mikayla, pulling some sort of long string-like material out of the corner of her eye. It’s like a clown’s never-ending handkerchief, only goopy.
These mucus eye strings are caused by untreated eye conditions, like dry eye or pink eye (conjunctivitis), but pulling the mucus out is actually a symptom of what is called mucus fishing syndrome. As you know, our eyes are covered in layers of mucus and tears, which keeps our eyeballs lubricated and also protects us from bacteria and viruses. It’s possible to dry out the eyes by pulling some mucus off, but our eyes aren’t big fans of that, so they’ll create more mucus to keep from drying out.
A person who might get a bit addicted to pulling the strings out has likely developed mucus fishing syndrome, which is considered a body-focused repetitive behavior (BFRB); other BFRBs include skin-picking (dermatillomania) or picking hairs out (trichotillomania).
Popular TikToker and Oregon ophthalmologist Will Flanary, MD, aka Dr. Glaucomflecken, responded to the videos, which have been encouraging others to try it.
“This is called mucus fishing syndrome,” the ophthalmologist explained via text captions in his video. “The trauma from pulling mucus out of your eye causes more mucus to form. You get caught in a never-ending cycle that gets worse over time. So…stop it.”
Fingers off the mucus, people.
A version of this article first appeared on Medscape.com.
It’s the season of love. In that spirit, Lean in and get a whiff of the latest good, bad, and ugly videos making the rounds on the internet’s most perplexing platform. But don’t get too close; these videos are especially ripe.
The bad: NyQuil chicken
You know something bad has happened when your TikTok search ends with a warning from the app that says “Learn how to recognize harmful trends and hoaxes.” That’s what shows up now when you try to find out what the “NyQuil chicken” or “sleepy chicken” trend is (or was) all about.
TikTok videos, including this one from TikTok user @janelleandkate, show users trying out a trend meant to cook up a meal that will also cure your cold symptoms. The trend involves cooking chicken in a pan full of the cold and flu medicine NyQuil. The NyQuil chicken idea stems from a Twitter meme from 2017, so it is possible that some of the recent videos are fake (blue food coloring is easy to get, people).
However, in the instance that people believe the videos to be real and want to try the trend out, it is important to warn that this shouldn’t be attempted.
Aaron Hartman, MD, assistant clinical professor of family medicine at Virginia Commonwealth University, told the website Mic about the trend’s dangers: “When you cook cough medicine like NyQuil, however, you boil off the water and alcohol in it, leaving the chicken saturated with a super concentrated amount of drugs in the meat. If you ate one of those cutlets completely cooked, it’d be as if you’re actually consuming a quarter to half a bottle of NyQuil.”
And that’s not good for anyone. What ever happened to an old fashioned herb marinade?
The good: Can you fart yourself blind? Doc explains
It’s something we’ve all wondered about, right?
TikTok and YouTube’s mainstay plastic surgeon Anthony Youn, MD, took it upon himself to reply to a comment saying “I once farted so hard I went blind for 3 minutes.” This phenomenon, according to Dr. Youn, is very rare, but not impossible, though we wouldn’t exactly want to try it for ourselves.
In the humorous (but very informative!) video, Dr. Youn explains that particularly pungent flatulence can contain large amounts of hydrogen sulfide, a gas that is known for smelling like rotten eggs. According to the Occupational Safety and Health Administration, hydrogen sulfide is produced in a number of industries, like oil and gas refining, mining, and paper processing. Exposure to higher concentrations of hydrogen sulfide can be dangerous, with prolonged exposure at a 2-5 parts per million (ppm) concentration causing nausea, headaches, and airway problems in some asthma patients. At very high concentrations, it can be fatal.
Thankfully, a person’s gas is not at all that dangerous. When it comes to the commentor’s claim, Dr. Youn says that something else hydrogen sulfide can do is reduce blood pressure.
“If it reduces blood pressure to the central retinal artery,” Dr. Youn says, “your silent but deadly toot could theoretically make you go blind.”
Thank goodness we can lay that question to rest.
The ugly: Eye boogers from hell
Get a look at this!
This video from @mikaylaadiorr has amassed over 8 million likes and over 89,000 comments, and shows someone, who we can assume is Mikayla, pulling some sort of long string-like material out of the corner of her eye. It’s like a clown’s never-ending handkerchief, only goopy.
These mucus eye strings are caused by untreated eye conditions, like dry eye or pink eye (conjunctivitis), but pulling the mucus out is actually a symptom of what is called mucus fishing syndrome. As you know, our eyes are covered in layers of mucus and tears, which keeps our eyeballs lubricated and also protects us from bacteria and viruses. It’s possible to dry out the eyes by pulling some mucus off, but our eyes aren’t big fans of that, so they’ll create more mucus to keep from drying out.
A person who might get a bit addicted to pulling the strings out has likely developed mucus fishing syndrome, which is considered a body-focused repetitive behavior (BFRB); other BFRBs include skin-picking (dermatillomania) or picking hairs out (trichotillomania).
Popular TikToker and Oregon ophthalmologist Will Flanary, MD, aka Dr. Glaucomflecken, responded to the videos, which have been encouraging others to try it.
“This is called mucus fishing syndrome,” the ophthalmologist explained via text captions in his video. “The trauma from pulling mucus out of your eye causes more mucus to form. You get caught in a never-ending cycle that gets worse over time. So…stop it.”
Fingers off the mucus, people.
A version of this article first appeared on Medscape.com.
It’s the season of love. In that spirit, Lean in and get a whiff of the latest good, bad, and ugly videos making the rounds on the internet’s most perplexing platform. But don’t get too close; these videos are especially ripe.
The bad: NyQuil chicken
You know something bad has happened when your TikTok search ends with a warning from the app that says “Learn how to recognize harmful trends and hoaxes.” That’s what shows up now when you try to find out what the “NyQuil chicken” or “sleepy chicken” trend is (or was) all about.
TikTok videos, including this one from TikTok user @janelleandkate, show users trying out a trend meant to cook up a meal that will also cure your cold symptoms. The trend involves cooking chicken in a pan full of the cold and flu medicine NyQuil. The NyQuil chicken idea stems from a Twitter meme from 2017, so it is possible that some of the recent videos are fake (blue food coloring is easy to get, people).
However, in the instance that people believe the videos to be real and want to try the trend out, it is important to warn that this shouldn’t be attempted.
Aaron Hartman, MD, assistant clinical professor of family medicine at Virginia Commonwealth University, told the website Mic about the trend’s dangers: “When you cook cough medicine like NyQuil, however, you boil off the water and alcohol in it, leaving the chicken saturated with a super concentrated amount of drugs in the meat. If you ate one of those cutlets completely cooked, it’d be as if you’re actually consuming a quarter to half a bottle of NyQuil.”
And that’s not good for anyone. What ever happened to an old fashioned herb marinade?
The good: Can you fart yourself blind? Doc explains
It’s something we’ve all wondered about, right?
TikTok and YouTube’s mainstay plastic surgeon Anthony Youn, MD, took it upon himself to reply to a comment saying “I once farted so hard I went blind for 3 minutes.” This phenomenon, according to Dr. Youn, is very rare, but not impossible, though we wouldn’t exactly want to try it for ourselves.
In the humorous (but very informative!) video, Dr. Youn explains that particularly pungent flatulence can contain large amounts of hydrogen sulfide, a gas that is known for smelling like rotten eggs. According to the Occupational Safety and Health Administration, hydrogen sulfide is produced in a number of industries, like oil and gas refining, mining, and paper processing. Exposure to higher concentrations of hydrogen sulfide can be dangerous, with prolonged exposure at a 2-5 parts per million (ppm) concentration causing nausea, headaches, and airway problems in some asthma patients. At very high concentrations, it can be fatal.
Thankfully, a person’s gas is not at all that dangerous. When it comes to the commentor’s claim, Dr. Youn says that something else hydrogen sulfide can do is reduce blood pressure.
“If it reduces blood pressure to the central retinal artery,” Dr. Youn says, “your silent but deadly toot could theoretically make you go blind.”
Thank goodness we can lay that question to rest.
The ugly: Eye boogers from hell
Get a look at this!
This video from @mikaylaadiorr has amassed over 8 million likes and over 89,000 comments, and shows someone, who we can assume is Mikayla, pulling some sort of long string-like material out of the corner of her eye. It’s like a clown’s never-ending handkerchief, only goopy.
These mucus eye strings are caused by untreated eye conditions, like dry eye or pink eye (conjunctivitis), but pulling the mucus out is actually a symptom of what is called mucus fishing syndrome. As you know, our eyes are covered in layers of mucus and tears, which keeps our eyeballs lubricated and also protects us from bacteria and viruses. It’s possible to dry out the eyes by pulling some mucus off, but our eyes aren’t big fans of that, so they’ll create more mucus to keep from drying out.
A person who might get a bit addicted to pulling the strings out has likely developed mucus fishing syndrome, which is considered a body-focused repetitive behavior (BFRB); other BFRBs include skin-picking (dermatillomania) or picking hairs out (trichotillomania).
Popular TikToker and Oregon ophthalmologist Will Flanary, MD, aka Dr. Glaucomflecken, responded to the videos, which have been encouraging others to try it.
“This is called mucus fishing syndrome,” the ophthalmologist explained via text captions in his video. “The trauma from pulling mucus out of your eye causes more mucus to form. You get caught in a never-ending cycle that gets worse over time. So…stop it.”
Fingers off the mucus, people.
A version of this article first appeared on Medscape.com.
Endometriosis not linked with preterm birth, new study finds
These new findings, which were published online in JAMA Network Open, suggest that changing monitoring strategies to prevent preterm birth for women with the disease may not be necessary.
The research team, led by Louis Marcellin, MD, PhD, with the department of obstetrics and gynecology at Université de Paris, also found that disease phenotype or whether the preterm birth was induced or spontaneous did not appear to alter the result.
Those results differ from previous research. Data on the phenotypes and their link with preterm birth have been scarce, but previous studies have shown the risk for preterm birth is more pronounced in women who have deep endometriosis than in women with ovarian endometriosis.
Dr. Marcellin said in an interview that “little is known about the impact of endometriosis on obstetric outcomes. In contrast to previous studies, we reported no differences in the risk for preterm delivery between women with endometriosis (34 of 470 [7.2%]) and those without endometriosis (53 of 881 [6.0%]), even when adjusted for multiple factors.”
The authors accounted for mother’s age, body mass index before pregnancy, birth country, number of times the woman had given birth, previous cesarean delivery, and history of preterm birth. After adjusting for potential confounders, endometriosis was not associated with preterm birth (adjusted odds ratio, 1.07; 95% confidence interval, 0.64-1.77).
The researchers found no differences among preterm births based on a mother’s endometriosis phenotype. Those phenotypes include Isolated superficial peritoneal endometriosis, ovarian endometrioma, and deep endometriosis.
“Monitoring pregnancy beyond the normal protocols or changing management strategies may not be warranted in cases of endometriosis,” Dr. Marcellin said.
More research on endometriosis’ potential link to birth outcomes is needed.
An expert not involved with the study said the new paper highlights important new avenues of research but should not be seen as the final word on the connection between endometriosis and preterm birth.
Of the 1,351 study participants (mean age, 32.9 years) who had a singleton delivery after 22 weeks’ gestation, 470 were assigned to the endometriosis group, and 881 were assigned to the control group.
The authors concluded that “pregnant women with endometriosis should not be considered to have an exceptionally high risk for preterm birth. However, further studies are needed to examine the potential for other adverse perinatal outcomes or specific but rare complications.”
Daniela Carusi, MD, said the difficulty with the study’s design is that “premature birth is not one problem or one disease.”
Many very different problems can all end with premature birth. Sometimes it’s an infection or inflammation or bleeding in the uterus or hypertension in the mother, for example, and all those things can lead to a preterm birth, she explained.
“This study inherently lumps all those things together,” said Dr. Carusi, who is director of surgical obstetrics and placental abnormalities in the department of obstetrics and gynecology at Brigham and Women’s Hospital, Boston. “It’s quite possible endometriosis can have a big impact in one of those areas and no impact in the other areas, but the study design wouldn’t be able to pick that up.”
Editorialists: Results challenge findings of previous studies
In an accompanying commentary, Liisu Saavalainen, MD, PhD, and Oskari Heikinheimo, MD, PhD, both with the department of obstetrics and gynecology, Helsinki University Hospital, wrote that several previous studies have suggested that women with endometriosis have a slightly higher risk for preterm birth.
Those studies were mostly retrospective and differed in the way they classified endometriosis and the way they selected patients, the editorialists write. Also, most women in these studies typically had subfertility, they added.
The study by Dr. Marcellin and colleagues differs from previous related research in that was prospective and assessed the risk for preterm delivery in women both with endometriosis and those without endometriosis from several maternity centers in France. The women with endometriosis were classified according to the severity of their disease.
The editorialists wrote: “The novel results by Marcellin et al. challenge the findings of most previous studies on this topic. These results are valuable and comforting. However, they are also likely to trigger new studies on the pregnancy risks associated with different types of endometriosis. That is good news.”
Dr. Carusi said the study was well done and included a notably large size. Further complimenting the research, she said it’s important to talk about this little-discussed pregnancy complication. There’s been much more focus for women with endometriosis and their physicians on getting pregnant and on talking about the length of their term.
The study leaves some things unanswered.
The study was funded by research grants from the French Ministry of Health and was sponsored by the Département de la Recherche Clinique et du Développement de l’Assistance Publique–Hôpitaux de Paris. Dr. Carusi reported no relevant financial relationships. One study coauthor reported receiving personal fees from Bioserinity and Ferring outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
These new findings, which were published online in JAMA Network Open, suggest that changing monitoring strategies to prevent preterm birth for women with the disease may not be necessary.
The research team, led by Louis Marcellin, MD, PhD, with the department of obstetrics and gynecology at Université de Paris, also found that disease phenotype or whether the preterm birth was induced or spontaneous did not appear to alter the result.
Those results differ from previous research. Data on the phenotypes and their link with preterm birth have been scarce, but previous studies have shown the risk for preterm birth is more pronounced in women who have deep endometriosis than in women with ovarian endometriosis.
Dr. Marcellin said in an interview that “little is known about the impact of endometriosis on obstetric outcomes. In contrast to previous studies, we reported no differences in the risk for preterm delivery between women with endometriosis (34 of 470 [7.2%]) and those without endometriosis (53 of 881 [6.0%]), even when adjusted for multiple factors.”
The authors accounted for mother’s age, body mass index before pregnancy, birth country, number of times the woman had given birth, previous cesarean delivery, and history of preterm birth. After adjusting for potential confounders, endometriosis was not associated with preterm birth (adjusted odds ratio, 1.07; 95% confidence interval, 0.64-1.77).
The researchers found no differences among preterm births based on a mother’s endometriosis phenotype. Those phenotypes include Isolated superficial peritoneal endometriosis, ovarian endometrioma, and deep endometriosis.
“Monitoring pregnancy beyond the normal protocols or changing management strategies may not be warranted in cases of endometriosis,” Dr. Marcellin said.
More research on endometriosis’ potential link to birth outcomes is needed.
An expert not involved with the study said the new paper highlights important new avenues of research but should not be seen as the final word on the connection between endometriosis and preterm birth.
Of the 1,351 study participants (mean age, 32.9 years) who had a singleton delivery after 22 weeks’ gestation, 470 were assigned to the endometriosis group, and 881 were assigned to the control group.
The authors concluded that “pregnant women with endometriosis should not be considered to have an exceptionally high risk for preterm birth. However, further studies are needed to examine the potential for other adverse perinatal outcomes or specific but rare complications.”
Daniela Carusi, MD, said the difficulty with the study’s design is that “premature birth is not one problem or one disease.”
Many very different problems can all end with premature birth. Sometimes it’s an infection or inflammation or bleeding in the uterus or hypertension in the mother, for example, and all those things can lead to a preterm birth, she explained.
“This study inherently lumps all those things together,” said Dr. Carusi, who is director of surgical obstetrics and placental abnormalities in the department of obstetrics and gynecology at Brigham and Women’s Hospital, Boston. “It’s quite possible endometriosis can have a big impact in one of those areas and no impact in the other areas, but the study design wouldn’t be able to pick that up.”
Editorialists: Results challenge findings of previous studies
In an accompanying commentary, Liisu Saavalainen, MD, PhD, and Oskari Heikinheimo, MD, PhD, both with the department of obstetrics and gynecology, Helsinki University Hospital, wrote that several previous studies have suggested that women with endometriosis have a slightly higher risk for preterm birth.
Those studies were mostly retrospective and differed in the way they classified endometriosis and the way they selected patients, the editorialists write. Also, most women in these studies typically had subfertility, they added.
The study by Dr. Marcellin and colleagues differs from previous related research in that was prospective and assessed the risk for preterm delivery in women both with endometriosis and those without endometriosis from several maternity centers in France. The women with endometriosis were classified according to the severity of their disease.
The editorialists wrote: “The novel results by Marcellin et al. challenge the findings of most previous studies on this topic. These results are valuable and comforting. However, they are also likely to trigger new studies on the pregnancy risks associated with different types of endometriosis. That is good news.”
Dr. Carusi said the study was well done and included a notably large size. Further complimenting the research, she said it’s important to talk about this little-discussed pregnancy complication. There’s been much more focus for women with endometriosis and their physicians on getting pregnant and on talking about the length of their term.
The study leaves some things unanswered.
The study was funded by research grants from the French Ministry of Health and was sponsored by the Département de la Recherche Clinique et du Développement de l’Assistance Publique–Hôpitaux de Paris. Dr. Carusi reported no relevant financial relationships. One study coauthor reported receiving personal fees from Bioserinity and Ferring outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
These new findings, which were published online in JAMA Network Open, suggest that changing monitoring strategies to prevent preterm birth for women with the disease may not be necessary.
The research team, led by Louis Marcellin, MD, PhD, with the department of obstetrics and gynecology at Université de Paris, also found that disease phenotype or whether the preterm birth was induced or spontaneous did not appear to alter the result.
Those results differ from previous research. Data on the phenotypes and their link with preterm birth have been scarce, but previous studies have shown the risk for preterm birth is more pronounced in women who have deep endometriosis than in women with ovarian endometriosis.
Dr. Marcellin said in an interview that “little is known about the impact of endometriosis on obstetric outcomes. In contrast to previous studies, we reported no differences in the risk for preterm delivery between women with endometriosis (34 of 470 [7.2%]) and those without endometriosis (53 of 881 [6.0%]), even when adjusted for multiple factors.”
The authors accounted for mother’s age, body mass index before pregnancy, birth country, number of times the woman had given birth, previous cesarean delivery, and history of preterm birth. After adjusting for potential confounders, endometriosis was not associated with preterm birth (adjusted odds ratio, 1.07; 95% confidence interval, 0.64-1.77).
The researchers found no differences among preterm births based on a mother’s endometriosis phenotype. Those phenotypes include Isolated superficial peritoneal endometriosis, ovarian endometrioma, and deep endometriosis.
“Monitoring pregnancy beyond the normal protocols or changing management strategies may not be warranted in cases of endometriosis,” Dr. Marcellin said.
More research on endometriosis’ potential link to birth outcomes is needed.
An expert not involved with the study said the new paper highlights important new avenues of research but should not be seen as the final word on the connection between endometriosis and preterm birth.
Of the 1,351 study participants (mean age, 32.9 years) who had a singleton delivery after 22 weeks’ gestation, 470 were assigned to the endometriosis group, and 881 were assigned to the control group.
The authors concluded that “pregnant women with endometriosis should not be considered to have an exceptionally high risk for preterm birth. However, further studies are needed to examine the potential for other adverse perinatal outcomes or specific but rare complications.”
Daniela Carusi, MD, said the difficulty with the study’s design is that “premature birth is not one problem or one disease.”
Many very different problems can all end with premature birth. Sometimes it’s an infection or inflammation or bleeding in the uterus or hypertension in the mother, for example, and all those things can lead to a preterm birth, she explained.
“This study inherently lumps all those things together,” said Dr. Carusi, who is director of surgical obstetrics and placental abnormalities in the department of obstetrics and gynecology at Brigham and Women’s Hospital, Boston. “It’s quite possible endometriosis can have a big impact in one of those areas and no impact in the other areas, but the study design wouldn’t be able to pick that up.”
Editorialists: Results challenge findings of previous studies
In an accompanying commentary, Liisu Saavalainen, MD, PhD, and Oskari Heikinheimo, MD, PhD, both with the department of obstetrics and gynecology, Helsinki University Hospital, wrote that several previous studies have suggested that women with endometriosis have a slightly higher risk for preterm birth.
Those studies were mostly retrospective and differed in the way they classified endometriosis and the way they selected patients, the editorialists write. Also, most women in these studies typically had subfertility, they added.
The study by Dr. Marcellin and colleagues differs from previous related research in that was prospective and assessed the risk for preterm delivery in women both with endometriosis and those without endometriosis from several maternity centers in France. The women with endometriosis were classified according to the severity of their disease.
The editorialists wrote: “The novel results by Marcellin et al. challenge the findings of most previous studies on this topic. These results are valuable and comforting. However, they are also likely to trigger new studies on the pregnancy risks associated with different types of endometriosis. That is good news.”
Dr. Carusi said the study was well done and included a notably large size. Further complimenting the research, she said it’s important to talk about this little-discussed pregnancy complication. There’s been much more focus for women with endometriosis and their physicians on getting pregnant and on talking about the length of their term.
The study leaves some things unanswered.
The study was funded by research grants from the French Ministry of Health and was sponsored by the Département de la Recherche Clinique et du Développement de l’Assistance Publique–Hôpitaux de Paris. Dr. Carusi reported no relevant financial relationships. One study coauthor reported receiving personal fees from Bioserinity and Ferring outside the submitted work. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Guselkumab controls axial involvement in PsA through 2 years
Guselkumab (Tremfya) received Food and Drug Administration approval for the treatment of psoriatic arthritis (PsA) almost 2 years ago on the basis of a phase 3 trial, but a new substudy from that trial has now demonstrated long-term benefit in the subgroup of patients who entered the trial with axial involvement, according to data presented at the annual meeting of the Canadian Rheumatology Association.
“The symptom relief was clinically meaningful and durable through week 100,” reported Dafna D. Gladman, MD, professor of medicine and director of the psoriatic arthritis program at the University of Toronto.
In the previously published double-blind, placebo-controlled DISCOVER-2 trial, two dosing regimens of the interleukin-23 (IL-23) inhibitor guselkumab were compared with placebo in biologic-naive patients. The active regimens were similarly effective relative to placebo for the primary endpoint of 20% improvement in American College of Rheumatology response criteria (ACR20) at week 24.
In this new long-term subgroup analysis, outcomes at 2 years were evaluated in the 246 patients with axial involvement (33.3% of the total number of 739 evaluable patients). Baseline characteristics across treatment groups in this subset of the DISCOVER-2 trial were similar.
Guselkumab exhibits nearly twofold advantage
At 24 weeks relative to baseline, the improvement on multiple axial involvement outcome measures was approximately twofold greater with active therapy than with placebo. For example, the mean Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score fell 2.6 points in both active treatment arms versus 1.4 on placebo.
The same relative advantage was observed when the BASDAI spinal pain subscore was isolated. There were also comparable responses on a modified BASDAI that excluded the peripheral pain response, and the Ankylosing Spondylitis Disease Activity Score (ASDAS).
When evaluated at week 52 and again at week 100, all outcomes employed to evaluate change in axial involvement were sustained. Many were further improved. In patients who initiated therapy on placebo, all of whom were switched to guselkumab at the end of the 24-week double-blind period, at least the same degree of axial symptom control relative to baseline was achieved at both time periods.
Incremental improvement observed over time
“For most measures there was further improvement at 2 years, and there was generally consistent response across patient groups stratified by HLA [human leucocyte antigen] status,” Dr. Gladman reported.
Relative to the 2.6-point reduction in the BASDAI score in the two guselkumab arms at week 24, the reductions reached 3.0, 3.1, and 3.3 at 100 weeks in the every-4-week guselkumab group, every-8-week guselkumab group, and the crossed-over placebo group, respectively. For ASDAS, the reductions at week 24 were 1.4, 1.5, and 0.7 points and reached 1.6, 1.7, and 1.6 points at 100 weeks in the every-4-week, every-8-week, and placebo crossover groups, respectively.
The sustained improvement is consistent with a previous post hoc analysis in which data from the phase 3 DISCOVER-1 trial were pooled with those from DISCOVER-2. This analysis focused on the 312 patients in these studies with axial disease documented by imaging. Again, the study showed improvement at week 24 was sustained at week 52 independent of HLA-B27 status.
Need for MRI confirmation seen
The potential problem with this new analysis as well as the previous analysis is the absence of MRI to provide objective evidence of axial involvement, according to Walter P. Maksymowych, MD, professor in the division of rheumatology at the University of Alberta, Edmonton.
Noting that previous studies have indicated that axial involvement assessed by investigators is not reliable even when performed with x-rays, Dr. Maksymowych said these data would be much more reassuring with MRI controls.
“We have seen little correlation between clinical symptoms and MRI manifestations of disease,” he said.
Dr. Gladman conceded this point. Baseline MRI was performed in some of the patients in this subgroup analysis, but it was not mandated. As a result, the data support benefit from guselkumab for symptomatic axial involvement, but she indicated that better evidence of a disease-modifying effect is expected from a more rigorous placebo-controlled trial of guselkumab called STAR.
This trial is requiring MRI at baseline and at week 24 and is using the Spondyloarthritis Research Consortium of Canada (SPARCC) score to assess change. Dr. Gladman said the trial is enrolling “as we speak.”
Overall, Dr. Gladman agreed with Dr. Maksymowych that objective biomarkers are important for demonstrating that treatments are improving long-term outcomes, not just relieving symptoms.
Guselkumab manufacturer Janssen supported the post hoc analysis. Dr. Gladman reported financial relationships with AbbVie, Amgen, Bristol-Myers Squibb, Eli Lilly, Galapagos, Gilead Janssen, Novartis, Pfizer, and UCB. Dr. Maksymowych reported financial relationships with AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, and UCB.
Guselkumab (Tremfya) received Food and Drug Administration approval for the treatment of psoriatic arthritis (PsA) almost 2 years ago on the basis of a phase 3 trial, but a new substudy from that trial has now demonstrated long-term benefit in the subgroup of patients who entered the trial with axial involvement, according to data presented at the annual meeting of the Canadian Rheumatology Association.
“The symptom relief was clinically meaningful and durable through week 100,” reported Dafna D. Gladman, MD, professor of medicine and director of the psoriatic arthritis program at the University of Toronto.
In the previously published double-blind, placebo-controlled DISCOVER-2 trial, two dosing regimens of the interleukin-23 (IL-23) inhibitor guselkumab were compared with placebo in biologic-naive patients. The active regimens were similarly effective relative to placebo for the primary endpoint of 20% improvement in American College of Rheumatology response criteria (ACR20) at week 24.
In this new long-term subgroup analysis, outcomes at 2 years were evaluated in the 246 patients with axial involvement (33.3% of the total number of 739 evaluable patients). Baseline characteristics across treatment groups in this subset of the DISCOVER-2 trial were similar.
Guselkumab exhibits nearly twofold advantage
At 24 weeks relative to baseline, the improvement on multiple axial involvement outcome measures was approximately twofold greater with active therapy than with placebo. For example, the mean Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score fell 2.6 points in both active treatment arms versus 1.4 on placebo.
The same relative advantage was observed when the BASDAI spinal pain subscore was isolated. There were also comparable responses on a modified BASDAI that excluded the peripheral pain response, and the Ankylosing Spondylitis Disease Activity Score (ASDAS).
When evaluated at week 52 and again at week 100, all outcomes employed to evaluate change in axial involvement were sustained. Many were further improved. In patients who initiated therapy on placebo, all of whom were switched to guselkumab at the end of the 24-week double-blind period, at least the same degree of axial symptom control relative to baseline was achieved at both time periods.
Incremental improvement observed over time
“For most measures there was further improvement at 2 years, and there was generally consistent response across patient groups stratified by HLA [human leucocyte antigen] status,” Dr. Gladman reported.
Relative to the 2.6-point reduction in the BASDAI score in the two guselkumab arms at week 24, the reductions reached 3.0, 3.1, and 3.3 at 100 weeks in the every-4-week guselkumab group, every-8-week guselkumab group, and the crossed-over placebo group, respectively. For ASDAS, the reductions at week 24 were 1.4, 1.5, and 0.7 points and reached 1.6, 1.7, and 1.6 points at 100 weeks in the every-4-week, every-8-week, and placebo crossover groups, respectively.
The sustained improvement is consistent with a previous post hoc analysis in which data from the phase 3 DISCOVER-1 trial were pooled with those from DISCOVER-2. This analysis focused on the 312 patients in these studies with axial disease documented by imaging. Again, the study showed improvement at week 24 was sustained at week 52 independent of HLA-B27 status.
Need for MRI confirmation seen
The potential problem with this new analysis as well as the previous analysis is the absence of MRI to provide objective evidence of axial involvement, according to Walter P. Maksymowych, MD, professor in the division of rheumatology at the University of Alberta, Edmonton.
Noting that previous studies have indicated that axial involvement assessed by investigators is not reliable even when performed with x-rays, Dr. Maksymowych said these data would be much more reassuring with MRI controls.
“We have seen little correlation between clinical symptoms and MRI manifestations of disease,” he said.
Dr. Gladman conceded this point. Baseline MRI was performed in some of the patients in this subgroup analysis, but it was not mandated. As a result, the data support benefit from guselkumab for symptomatic axial involvement, but she indicated that better evidence of a disease-modifying effect is expected from a more rigorous placebo-controlled trial of guselkumab called STAR.
This trial is requiring MRI at baseline and at week 24 and is using the Spondyloarthritis Research Consortium of Canada (SPARCC) score to assess change. Dr. Gladman said the trial is enrolling “as we speak.”
Overall, Dr. Gladman agreed with Dr. Maksymowych that objective biomarkers are important for demonstrating that treatments are improving long-term outcomes, not just relieving symptoms.
Guselkumab manufacturer Janssen supported the post hoc analysis. Dr. Gladman reported financial relationships with AbbVie, Amgen, Bristol-Myers Squibb, Eli Lilly, Galapagos, Gilead Janssen, Novartis, Pfizer, and UCB. Dr. Maksymowych reported financial relationships with AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, and UCB.
Guselkumab (Tremfya) received Food and Drug Administration approval for the treatment of psoriatic arthritis (PsA) almost 2 years ago on the basis of a phase 3 trial, but a new substudy from that trial has now demonstrated long-term benefit in the subgroup of patients who entered the trial with axial involvement, according to data presented at the annual meeting of the Canadian Rheumatology Association.
“The symptom relief was clinically meaningful and durable through week 100,” reported Dafna D. Gladman, MD, professor of medicine and director of the psoriatic arthritis program at the University of Toronto.
In the previously published double-blind, placebo-controlled DISCOVER-2 trial, two dosing regimens of the interleukin-23 (IL-23) inhibitor guselkumab were compared with placebo in biologic-naive patients. The active regimens were similarly effective relative to placebo for the primary endpoint of 20% improvement in American College of Rheumatology response criteria (ACR20) at week 24.
In this new long-term subgroup analysis, outcomes at 2 years were evaluated in the 246 patients with axial involvement (33.3% of the total number of 739 evaluable patients). Baseline characteristics across treatment groups in this subset of the DISCOVER-2 trial were similar.
Guselkumab exhibits nearly twofold advantage
At 24 weeks relative to baseline, the improvement on multiple axial involvement outcome measures was approximately twofold greater with active therapy than with placebo. For example, the mean Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score fell 2.6 points in both active treatment arms versus 1.4 on placebo.
The same relative advantage was observed when the BASDAI spinal pain subscore was isolated. There were also comparable responses on a modified BASDAI that excluded the peripheral pain response, and the Ankylosing Spondylitis Disease Activity Score (ASDAS).
When evaluated at week 52 and again at week 100, all outcomes employed to evaluate change in axial involvement were sustained. Many were further improved. In patients who initiated therapy on placebo, all of whom were switched to guselkumab at the end of the 24-week double-blind period, at least the same degree of axial symptom control relative to baseline was achieved at both time periods.
Incremental improvement observed over time
“For most measures there was further improvement at 2 years, and there was generally consistent response across patient groups stratified by HLA [human leucocyte antigen] status,” Dr. Gladman reported.
Relative to the 2.6-point reduction in the BASDAI score in the two guselkumab arms at week 24, the reductions reached 3.0, 3.1, and 3.3 at 100 weeks in the every-4-week guselkumab group, every-8-week guselkumab group, and the crossed-over placebo group, respectively. For ASDAS, the reductions at week 24 were 1.4, 1.5, and 0.7 points and reached 1.6, 1.7, and 1.6 points at 100 weeks in the every-4-week, every-8-week, and placebo crossover groups, respectively.
The sustained improvement is consistent with a previous post hoc analysis in which data from the phase 3 DISCOVER-1 trial were pooled with those from DISCOVER-2. This analysis focused on the 312 patients in these studies with axial disease documented by imaging. Again, the study showed improvement at week 24 was sustained at week 52 independent of HLA-B27 status.
Need for MRI confirmation seen
The potential problem with this new analysis as well as the previous analysis is the absence of MRI to provide objective evidence of axial involvement, according to Walter P. Maksymowych, MD, professor in the division of rheumatology at the University of Alberta, Edmonton.
Noting that previous studies have indicated that axial involvement assessed by investigators is not reliable even when performed with x-rays, Dr. Maksymowych said these data would be much more reassuring with MRI controls.
“We have seen little correlation between clinical symptoms and MRI manifestations of disease,” he said.
Dr. Gladman conceded this point. Baseline MRI was performed in some of the patients in this subgroup analysis, but it was not mandated. As a result, the data support benefit from guselkumab for symptomatic axial involvement, but she indicated that better evidence of a disease-modifying effect is expected from a more rigorous placebo-controlled trial of guselkumab called STAR.
This trial is requiring MRI at baseline and at week 24 and is using the Spondyloarthritis Research Consortium of Canada (SPARCC) score to assess change. Dr. Gladman said the trial is enrolling “as we speak.”
Overall, Dr. Gladman agreed with Dr. Maksymowych that objective biomarkers are important for demonstrating that treatments are improving long-term outcomes, not just relieving symptoms.
Guselkumab manufacturer Janssen supported the post hoc analysis. Dr. Gladman reported financial relationships with AbbVie, Amgen, Bristol-Myers Squibb, Eli Lilly, Galapagos, Gilead Janssen, Novartis, Pfizer, and UCB. Dr. Maksymowych reported financial relationships with AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, and UCB.
FROM THE ANNUAL MEETING OF THE CANADIAN RHEUMATOLOGY ASSOCIATION
Chronic truncal rash
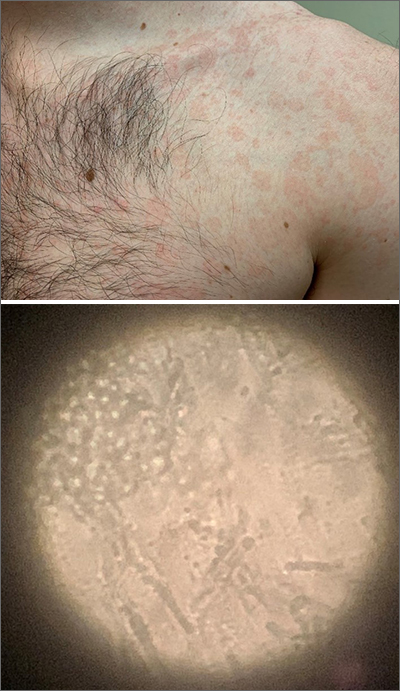
The patient was given a diagnosis of tinea versicolor (TV), also known as pityriasis versicolor, after a potassium hydroxide (KOH) prep test on a skin scraping confirmed the spaghetti and meatballs pattern of Malassezia Furfur (see image above). Note that in most cases, a KOH prep is not required for the diagnosis. Experienced clinicians will usually make the diagnosis based on the appearance of hyper- or hypopigmented macules or patches with fine scale on the trunk of adults. KOH prep is useful if the diagnosis is uncertain.
TV is a common fungal infection that’s seen more frequently in tropical climates and occurs equally in men and women.1 M. Furfur thrives on the lipids in the skin of sebum-rich areas, which explains its truncal distribution and rare occurrence in children (who have much lower sebum production).
Usually, topical antifungal medications are considered first-line treatment, but since large areas of skin are involved, adequate amounts need to be used. One of the most common and inexpensive treatments is to apply selenium sulfide shampoo (Selsun Blue) undiluted to the entire trunk, then allow to dry and remain in place overnight before showering. A repeat application should be done 1 week later. Topical terbinafine cream applied bid for 2 weeks is another option, as is oral itraconazole in a single 400 mg dose.
This patient declined the selenium sulfide topical treatment and requested systemic therapy, so he was prescribed itraconazole 400 mg orally as a single dose. He was advised that it might take a few weeks to clear up, and to use the selenium sulfide application if the itraconazole was not effective. Follow-up was not planned due to the high success rate of these therapies.
Image courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Saunte DML, Gaitanis G, Hay RJ. Malassezia-associated skin diseases, the use of diagnostics and treatment. Front Cell Infect Microbiol. 2020;10:112. doi: 10.3389/fcimb.2020.00112
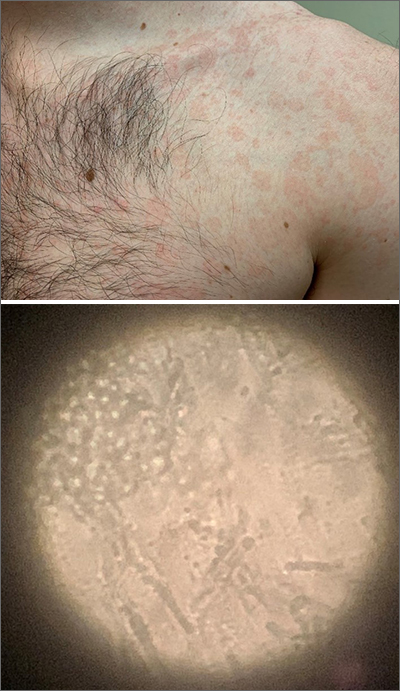
The patient was given a diagnosis of tinea versicolor (TV), also known as pityriasis versicolor, after a potassium hydroxide (KOH) prep test on a skin scraping confirmed the spaghetti and meatballs pattern of Malassezia Furfur (see image above). Note that in most cases, a KOH prep is not required for the diagnosis. Experienced clinicians will usually make the diagnosis based on the appearance of hyper- or hypopigmented macules or patches with fine scale on the trunk of adults. KOH prep is useful if the diagnosis is uncertain.
TV is a common fungal infection that’s seen more frequently in tropical climates and occurs equally in men and women.1 M. Furfur thrives on the lipids in the skin of sebum-rich areas, which explains its truncal distribution and rare occurrence in children (who have much lower sebum production).
Usually, topical antifungal medications are considered first-line treatment, but since large areas of skin are involved, adequate amounts need to be used. One of the most common and inexpensive treatments is to apply selenium sulfide shampoo (Selsun Blue) undiluted to the entire trunk, then allow to dry and remain in place overnight before showering. A repeat application should be done 1 week later. Topical terbinafine cream applied bid for 2 weeks is another option, as is oral itraconazole in a single 400 mg dose.
This patient declined the selenium sulfide topical treatment and requested systemic therapy, so he was prescribed itraconazole 400 mg orally as a single dose. He was advised that it might take a few weeks to clear up, and to use the selenium sulfide application if the itraconazole was not effective. Follow-up was not planned due to the high success rate of these therapies.
Image courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
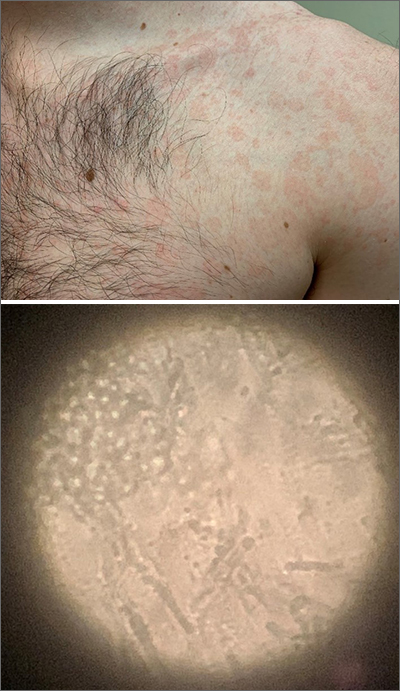
The patient was given a diagnosis of tinea versicolor (TV), also known as pityriasis versicolor, after a potassium hydroxide (KOH) prep test on a skin scraping confirmed the spaghetti and meatballs pattern of Malassezia Furfur (see image above). Note that in most cases, a KOH prep is not required for the diagnosis. Experienced clinicians will usually make the diagnosis based on the appearance of hyper- or hypopigmented macules or patches with fine scale on the trunk of adults. KOH prep is useful if the diagnosis is uncertain.
TV is a common fungal infection that’s seen more frequently in tropical climates and occurs equally in men and women.1 M. Furfur thrives on the lipids in the skin of sebum-rich areas, which explains its truncal distribution and rare occurrence in children (who have much lower sebum production).
Usually, topical antifungal medications are considered first-line treatment, but since large areas of skin are involved, adequate amounts need to be used. One of the most common and inexpensive treatments is to apply selenium sulfide shampoo (Selsun Blue) undiluted to the entire trunk, then allow to dry and remain in place overnight before showering. A repeat application should be done 1 week later. Topical terbinafine cream applied bid for 2 weeks is another option, as is oral itraconazole in a single 400 mg dose.
This patient declined the selenium sulfide topical treatment and requested systemic therapy, so he was prescribed itraconazole 400 mg orally as a single dose. He was advised that it might take a few weeks to clear up, and to use the selenium sulfide application if the itraconazole was not effective. Follow-up was not planned due to the high success rate of these therapies.
Image courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Saunte DML, Gaitanis G, Hay RJ. Malassezia-associated skin diseases, the use of diagnostics and treatment. Front Cell Infect Microbiol. 2020;10:112. doi: 10.3389/fcimb.2020.00112
1. Saunte DML, Gaitanis G, Hay RJ. Malassezia-associated skin diseases, the use of diagnostics and treatment. Front Cell Infect Microbiol. 2020;10:112. doi: 10.3389/fcimb.2020.00112
If you’ve got 3 seconds, then you’ve got time to work out
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
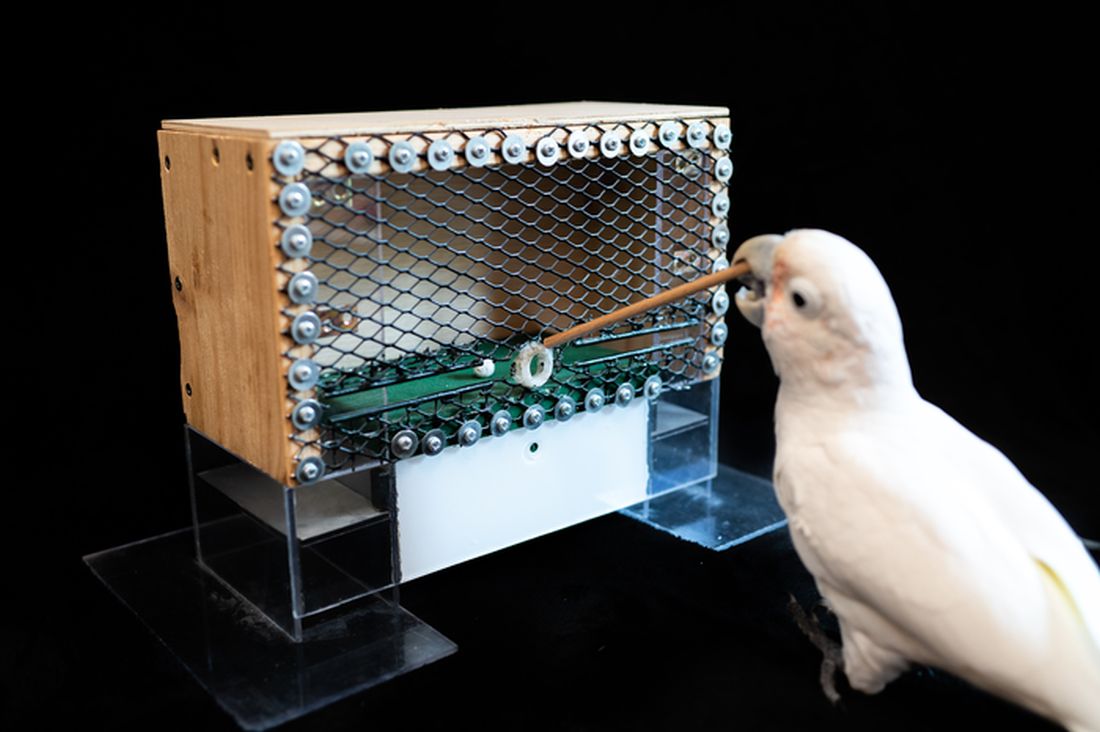
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Bullous Dermatoses and Quality of Life: A Summary of Tools to Assess Psychosocial Health
Autoimmune bullous dermatoses (ABDs) develop due to antibodies directed against antigens within the epidermis or at the dermoepidermal junction. They are categorized histologically by the location of acantholysis (separation of keratinocytes), clinical presentation, and presence of autoantibodies. The most common ABDs include pemphigus vulgaris, pemphigus foliaceus, and bullous pemphigoid (BP). These conditions present on a spectrum of symptoms and severity.1
Although multiple studies have evaluated the impact of bullous dermatoses on mental health, most were designed with a small sample size, thus limiting the generalizability of each study. Sebaratnam et al2 summarized several studies in 2012. In this review, we will analyze additional relevant literature and systematically combine the data to determine the psychological burden of disease of ABDs. We also will discuss the existing questionnaires frequently used in the dermatology setting to assess adverse psychosocial symptoms.
Methods
We searched PubMed, MEDLINE, and Google Scholar for articles published within the last 15 years using the terms bullous pemphigoid, pemphigus, quality of life, anxiety, and depression. We reviewed the citations in each article to further our search.
Criteria for Inclusion and Exclusion—Studies that utilized validated questionnaires to evaluate the effects of pemphigus vulgaris, pemphigus foliaceus, and/or BP on mental health were included. All research participants were 18 years and older. For the questionnaires administered, each study must have included numerical scores in the results. The studies all reported statistically significant results (P<.05), but no studies were excluded on the basis of statistical significance.
Studies were excluded if they did not use a validated questionnaire to examine quality of life (QOL) or psychological status. We also excluded database, retrospective, qualitative, and observational studies. We did not include studies with a sample size less than 20. Studies that administered questionnaires that were uncommon in this realm of research such as the Attitude to Appearance Scale or The Anxiety Questionnaire also were excluded. We did not exclude articles based on their primary language.
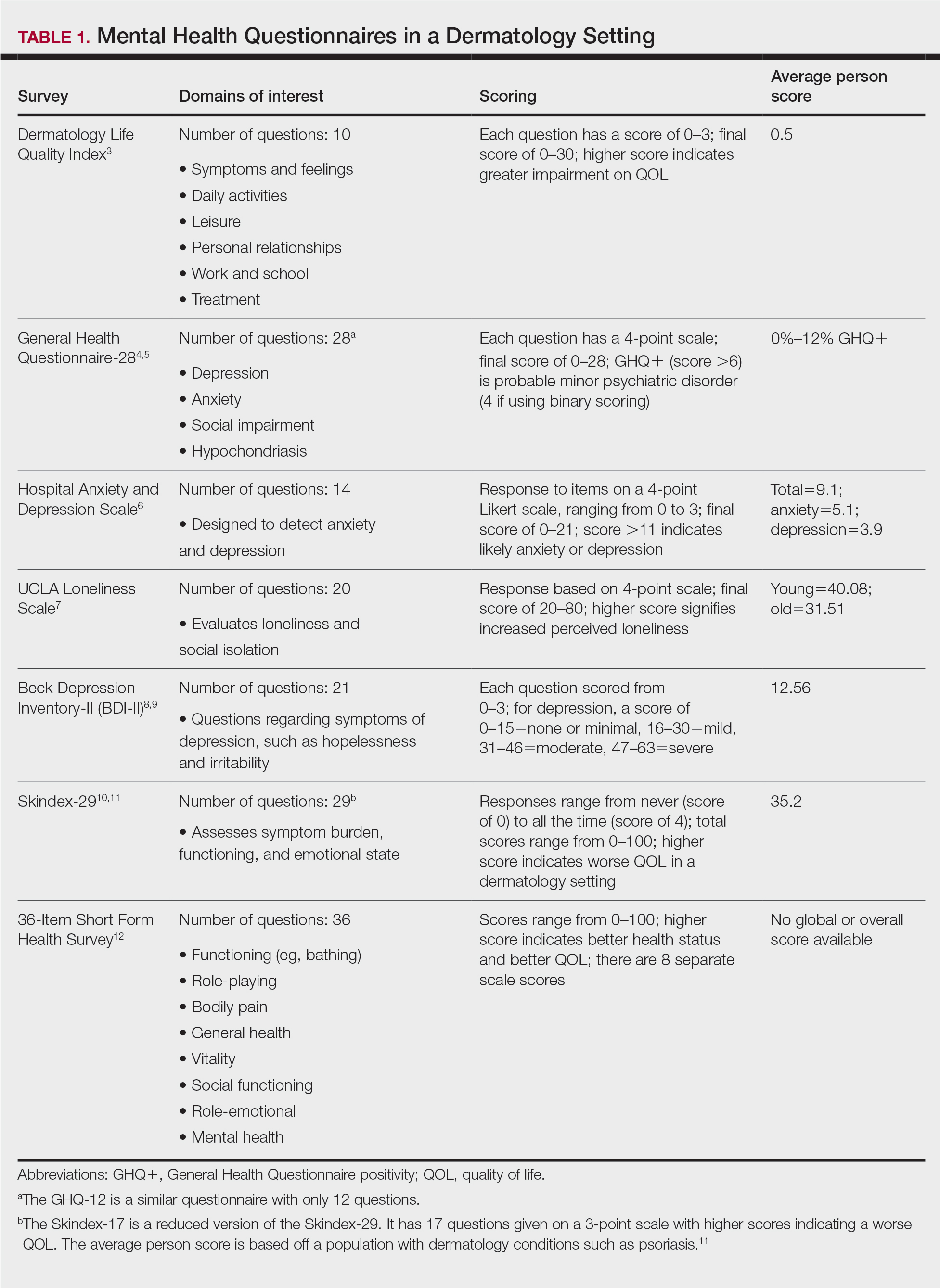
Results
A total of 13 studies met the inclusion criteria with a total of 1716 participants enrolled in the trials. The questionnaires most commonly used are summarized in Table 1. Tables 2 and 3 demonstrate the studies that evaluate QOL and psychological state in patients with bullous dermatoses, respectively.
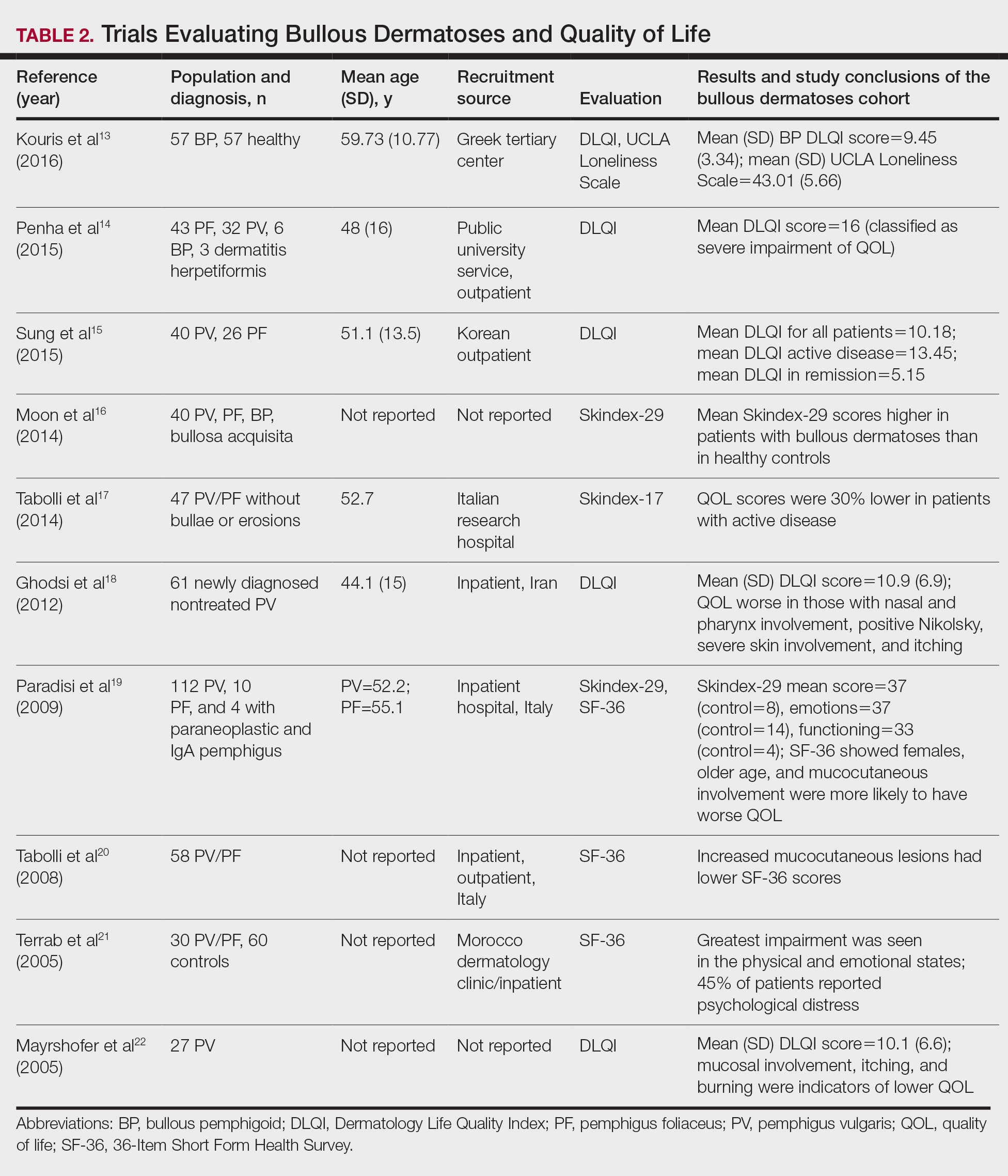
The Dermatology Life Quality Index (DLQI) was the most utilized method for analyzing QOL followed by the Skindex-17, Skindex-29, and 36-Item Short Form Health Survey. The DLQI is a skin-specific measurement tool with higher scores translating to greater impairment in QOL. Healthy patients have an average score of 0.5.3 The mean DLQI scores for ABD patients as seen in Table 2 were 9.45, 10.18, 16, 10.9, and 10.1.13-15,18,22 The most commonly reported concerns among patients included feelings about appearance and disturbances in daily activities.18 Symptoms of mucosal involvement, itching, and burning also were indicators of lower QOL.15,18,20,22 Furthermore, women consistently had lower scores than men.15,17,19,25 Multiple studies concluded that severity of the disease correlated with a lower QOL, though the subtype of pemphigus did not have an effect on QOL scores.15,19,20,21 Lastly, recent onset of symptoms was associated with a worse QOL score.15,18-20 Age, education level, and marital status did not have an effect on QOL.
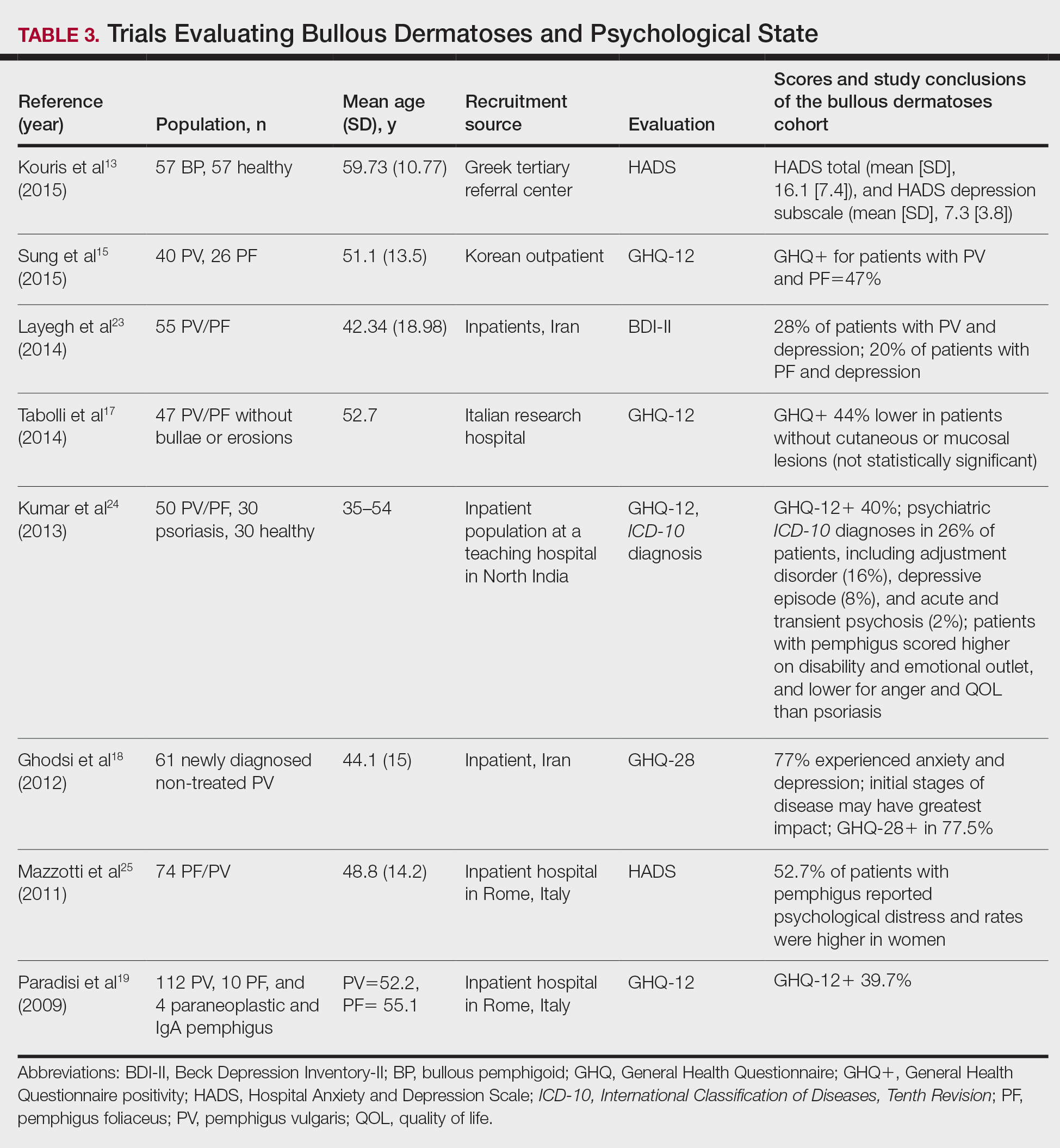
To evaluate psychological state, the General Health Questionnaire (GHQ)-28 and -12 primarily were used, in addition to the Hospital Anxiety and Depression Scale; the International Classification of Diseases, Tenth Revision; the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; and the Beck Depression Inventory-II. As seen in Table 3, GHQ-12 positivity, reflecting probable minor nonpsychotic psychiatric disorders such as depression and anxiety, was identified in 47%, 39.7%, and 40% of patients with pemphigus15,19,24; GHQ-28 positivity was seen in 77.5% of pemphigus patients.18 In the average population, GHQ positivity was found in up to 12% of patients.26,27 Similar to the QOL scores, no significant differences were seen based on subtype of pemphigus for symptoms of depression or anxiety.20,23
Comment
Mental Health of Patients With ABDs—Immunobullous diseases are painful, potentially lifelong conditions that have no definitive cure. These conditions are characterized by bullae and erosions of the skin and mucosae that physically are disabling and often create a stigma for patients. Across multiple different validated psychosocial assessments, the 13 studies included in this review consistently reported that ABDs have a negative effect on mental well-being of patients that is more pronounced in women and worse at the onset of symptoms.13-25
QOL Scores in Patients With ABDs—Quality of life is a broad term that encompasses a general sense of psychological and overall well-being. A score of approximately 10 on the DLQI most often was reported in patients with ABDs, which translates to a moderate impact on QOL. Incomparison, a large cohort study reported the mean (SD) DLQI scores for patients with atopic dermatitis and psoriasis as 7.31 (5.98) and 5.93 (5.66), respectively.28 In another study, Penha et al14 found that patients with psoriasis have a mean DLQI score of 10. Reasons for the similarly low QOL scores in patients with ABDs include long hospitalization periods, disease chronicity, social anxiety, inability to control symptoms, difficulty with activities of daily living, and the belief that the disease is incurable.17,19,23 Although there is a need for increased family and social support with performing necessary daily tasks, personal relationships often are negatively affected, resulting in social isolation, loneliness, and worsening of cutaneous symptoms.
Severity of cutaneous disease and recent onset of symptoms correlated with worse QOL scores. Tabolli et al20 proposed the reason for this relates to not having had enough time to find the best treatment regimen. We believe there also may be an element of habituation involved, whereby patients become accustomed to the appearance of the lesions over time and therefore they become less distressing. Interestingly, Tabolli et al17 determined that patients in the quiescent phase of the disease—without any mucosal or cutaneous lesions—still maintained lower QOL scores than the average population, particularly on the psychosocial section of the 36-Item Short Form Health Survey, which may be due to a concern of disease relapse or from adverse effects of treatment. Providers should monitor patients for mental health complications not only in the disease infancy but throughout the disease course.
Future Directions—Cause and effect of the relationship between the psychosocial variables and ABD disease state has yet to be determined. Most studies included in this review were cross-sectional in design. Although many studies concluded that bullous dermatoses were the cause of impaired QOL, Ren and colleagues29 proposed that medications used to treat neuropsychiatric disorders may trigger the autoimmune antigens of BP. Possible triggers for BP have been reported including hydrochlorothiazide, ciprofloxacin, and dipeptidyl peptidase-4 inhibitors.27,30-32 A longitudinal study design would better evaluate the causal relationship.
The effects of the medications were included in 2 cases, one in which the steroid dose was not found to have a significant impact on rates of depression23 and another in which patients treated with a higher dose of corticosteroids (>10 mg) had worse QOL scores.17 Sung et al15 suggested this may be because patients who took higher doses of steroids had worse symptoms and therefore also had a worse QOL. It also is possible that those patients taking higher doses had increased side effects.17 Further studies that evaluate treatment modalities and timing in relation to the disease onset would be helpful.
Study Limitations—There are potential barriers to combining these data. Multiple different questionnaires were used, and it was difficult to ascertain if all the participants were experiencing active disease. Additionally, questionnaires are not always the best proxy for what is happening in everyday life. Lastly, the sample size of each individual study was small, and the studies only included adults.
Conclusion
As demonstrated by the 13 studies in this review, patients with ABDs have lower QOL scores and higher numbers of psychological symptoms. Clinicians should be mindful of this at-risk population and create opportunities in clinic to discuss personal hardship associated with the disease process and recommend psychiatric intervention if indicated. Additionally, family members often are overburdened with the chronicity of ABDs, and they should not be forgotten. Using one of the aforementioned questionnaires is a practical way to screen patients for lower QOL scores. We agree with Paradisi and colleagues19 that although these questionnaires may be helpful, clinicians still need to determine if the use of a dermatologic QOL evaluation tool in clinical practice improves patient satisfaction.
- Baum S, Sakka N, Artsi O, et al. Diagnosis and classification of autoimmune blistering diseases. Autoimmun Rev. 2014;13:482-489. https://doi.org/10.1016/j.autrev.2014.01.047
- Sebaratnam DF, McMillan JR, Werth VP, et al. Quality of life in patients with bullous dermatoses. Clin Dermatol. 2012;30:103-107. doi:10.1016/j.clindermatol.2011.03.016
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
- Goldberg DP. The Detection of Psychiatric Illness by Questionnaire. Oxford University Press; 1972.
- Cano A, Sprafkin RP, Scaturo DJ, et al. Mental health screening in primary care: a comparison of 3 brief measures of psychological distress. Prim Care Companion J Clin Psychiatry. 2001;3:206-210.
- Zigmond A, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361-370.
- Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20-40. doi:10.1207/s15327752jpa6601_2
- Beck A, Alford B. Depression: Causes and Treatment. 2nd ed. Philadelphia University of Pennsylvania Press; 2009.
- Ghassemzadeh H, Mojtabai R, Karamghadiri N, et al. Psychometric properties of a Persian-language version of the Beck Depression Inventory—Second Edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21:185-192. doi:10.1002/da.20070
- Chren MM, Lasek RJ, Sahay AP, et al. Measurement properties of Skindex-16: a brief quality-of-life measure for patients with skin diseases. J Cutan Med Surg. 2001;5:105-110.
- Nijsten TEC, Sampogna F, Chren M, et al. Testing and reducing Skindex-29 using Rasch analysis: Skindex-17. J Invest Dermatol. 2006;126:1244-1250. https://doi.org/10.1038/sj.jid.5700212
- Ware JE Jr, Sherbourne C. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Med Care. 1992;30:473-483.
- Kouris A, Platsidaki E, Christodoulou C, et al. Quality of life, depression, anxiety and loneliness in patients with bullous pemphigoid: a case control study. An Bras Dermatol. 2016;91:601-603. doi:10.1590/abd1806-4841.2016493
- Penha MA, Farat JG, Miot HA, et al. Quality of life index in autoimmune bullous dermatosis patients. An Bras Dermatol. 2015;90:190-194. https://dx.doi.org/10.1590/abd1806-4841.20153372
- Sung JY, Roh MR, Kim SC. Quality of life assessment in Korean patients with pemphigus. Ann Dermatol. 2015;27:492-498.
- Moon SH, Kwon HI, Park HC, et al. Assessment of the quality of life in autoimmune blistering skin disease patients. Korean J Dermatol. 2014;52:402-409.
- Tabolli S, Pagliarello C, Paradisi A, et al. Burden of disease during quiescent periods in patients with pemphigus. Br J Dermatol. 2014;170:1087-1091. doi:10.1111/bjd.12836
- Ghodsi SZ, Chams-Davatchi C, Daneshpazhooh M, et al. Quality of life and psychological status of patients with pemphigus vulgaris using Dermatology Life Quality Index and general health questionnaires. J Dermatol. 2012;39:141-144. doi:10.1111/j.1346-8138.2011.01382
- Paradisi A, Sampogna F, Di Pietro C, et al. Quality-of-life assessment in patients with pemphigus using a minimum set of evaluation tools. J Am Acad Dermatol. 2009;60:261-269. doi:10.1016/j.jaad.2008.09.014
- Tabolli S, Mozzetta A, Antinone V, et al. The health impact of pemphigus vulgaris and pemphigus foliaceus assessed using the Medical Outcomes Study 36-item short form health survey questionnaire. Br J Dermatol. 2008;158:1029-1034. doi:10.1111/j.1365-2133.2008.08481.x
- Terrab Z, Benchikhi H, Maaroufi A, et al. Quality of life and pemphigus. Ann Dermatol Venereol. 2005;132:321-328.
- Mayrshofer F, Hertl M, Sinkgraven R, et al. Significant decrease in quality of life in patients with pemphigus vulgaris: results from the German Bullous Skin Disease (BSD) Study Group [in German]. J Dtsch Dermatol Ges. 2005;3:431-435. doi:10.1111/j.1610-0387.2005.05722.x
- Layegh P, Mokhber N, Javidi Z, et al. Depression in patients with pemphigus: is it a major concern? J Dermatol. 2014;40:434-437. doi:10.1111/1346-8138.12067
- Kumar V, Mattoo SK, Handa S. Psychiatric morbidity in pemphigus and psoriasis: a comparative study from India. Asian J Psychiatr. 2013;6:151-156. doi:10.1016/j.ajp.2012.10.005
- Mazzotti E, Mozzetta A, Antinone V, et al. Psychological distress and investment in one’s appearance in patients with pemphigus. J Eur Acad Dermatol Venereol. 2011;25:285-289. doi:10.1111/j.1468-3083.2010.03780.x
- Regier DA, Boyd JH, Burke JD, et al. One-month prevalence of mental disorders in the United States: based on five epidemiologic catchment area sites. Arch Gen Psychiatr. 1988;45:977-986. doi:10.1001/archpsyc.1988.01800350011002
- Cozzani E, Chinazzo C, Burlando M, et al. Ciprofloxacin as a trigger for bullous pemphigoid: the second case in the literature. Am J Ther. 2016;23:E1202-E1204. doi:10.1097/MJT.0000000000000283
- Lundberg L, Johannesson M, Silverdahl M, et al. Health-related quality of life in patients with psoriasis and atopic dermatitis measured with SF-36, DLQI and a subjective measure of disease activity. Acta Derm Venereol. 2000;80:430-434.
- Ren Z, Hsu DY, Brieva J, et al. Hospitalization, inpatient burden and comorbidities associated with bullous pemphigoid in the U.S.A. Br J Dermatol. 2017;176:87-99. doi:10.1111/bjd.14821
- Warner C, Kwak Y, Glover MH, et al. Bullous pemphigoid induced by hydrochlorothiazide therapy. J Drugs Dermatol. 2014;13:360-362.
- Mendonca FM, Martin-Gutierrez FJ, Rios-Martin JJ, et al. Three cases of bullous pemphigoid associated with dipeptidyl peptidase-4 inhibitors—one due to linagliptin. Dermatology. 2016;232:249-253. doi:10.1159/000443330
- Attaway A, Mersfelder TL, Vaishnav S, et al. Bullous pemphigoid associated with dipeptidyl peptidase IV inhibitors: a case report and review of literature. J Dermatol Case Rep. 2014;8:24-28.
Autoimmune bullous dermatoses (ABDs) develop due to antibodies directed against antigens within the epidermis or at the dermoepidermal junction. They are categorized histologically by the location of acantholysis (separation of keratinocytes), clinical presentation, and presence of autoantibodies. The most common ABDs include pemphigus vulgaris, pemphigus foliaceus, and bullous pemphigoid (BP). These conditions present on a spectrum of symptoms and severity.1
Although multiple studies have evaluated the impact of bullous dermatoses on mental health, most were designed with a small sample size, thus limiting the generalizability of each study. Sebaratnam et al2 summarized several studies in 2012. In this review, we will analyze additional relevant literature and systematically combine the data to determine the psychological burden of disease of ABDs. We also will discuss the existing questionnaires frequently used in the dermatology setting to assess adverse psychosocial symptoms.
Methods
We searched PubMed, MEDLINE, and Google Scholar for articles published within the last 15 years using the terms bullous pemphigoid, pemphigus, quality of life, anxiety, and depression. We reviewed the citations in each article to further our search.
Criteria for Inclusion and Exclusion—Studies that utilized validated questionnaires to evaluate the effects of pemphigus vulgaris, pemphigus foliaceus, and/or BP on mental health were included. All research participants were 18 years and older. For the questionnaires administered, each study must have included numerical scores in the results. The studies all reported statistically significant results (P<.05), but no studies were excluded on the basis of statistical significance.
Studies were excluded if they did not use a validated questionnaire to examine quality of life (QOL) or psychological status. We also excluded database, retrospective, qualitative, and observational studies. We did not include studies with a sample size less than 20. Studies that administered questionnaires that were uncommon in this realm of research such as the Attitude to Appearance Scale or The Anxiety Questionnaire also were excluded. We did not exclude articles based on their primary language.
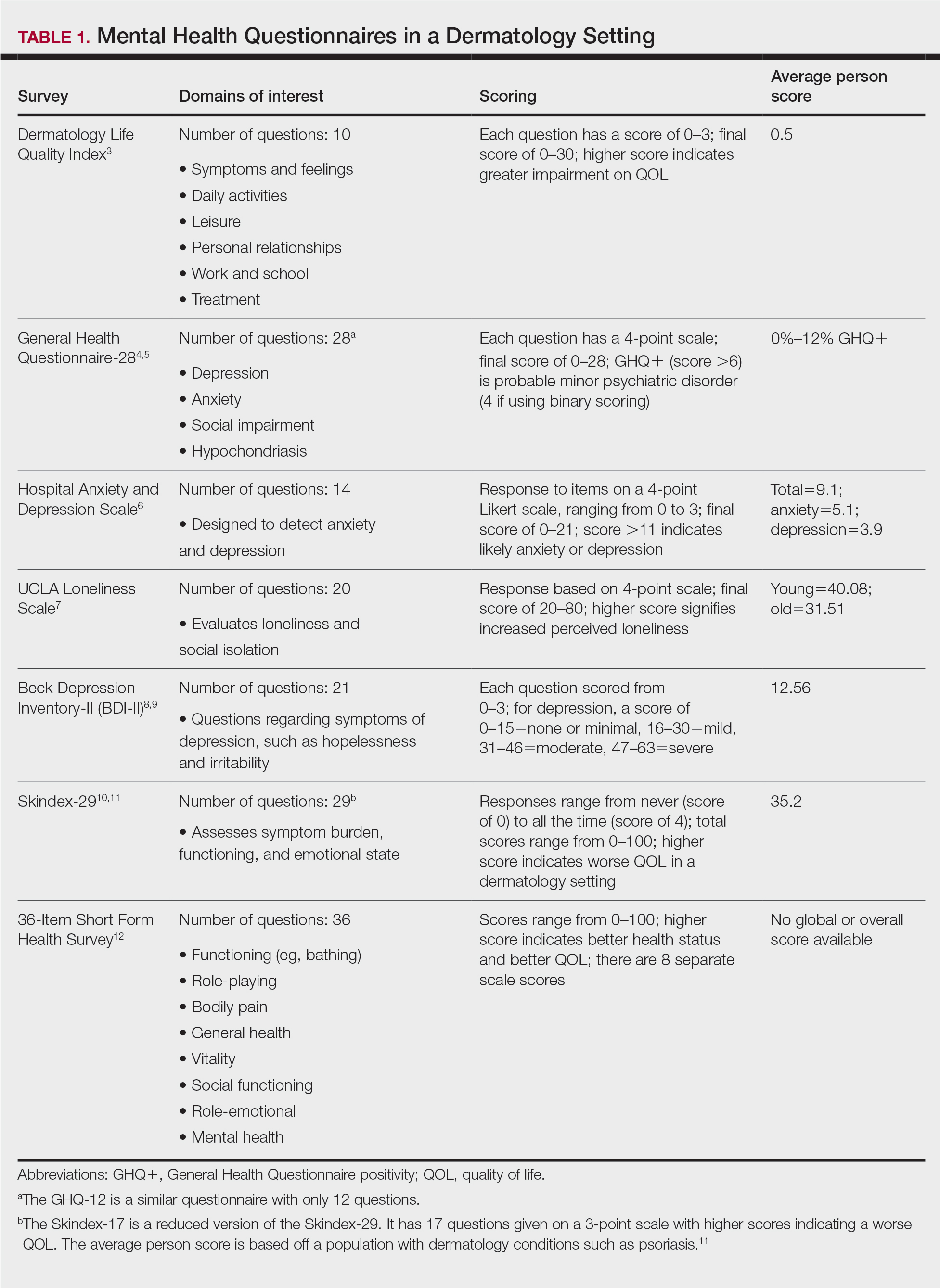
Results
A total of 13 studies met the inclusion criteria with a total of 1716 participants enrolled in the trials. The questionnaires most commonly used are summarized in Table 1. Tables 2 and 3 demonstrate the studies that evaluate QOL and psychological state in patients with bullous dermatoses, respectively.
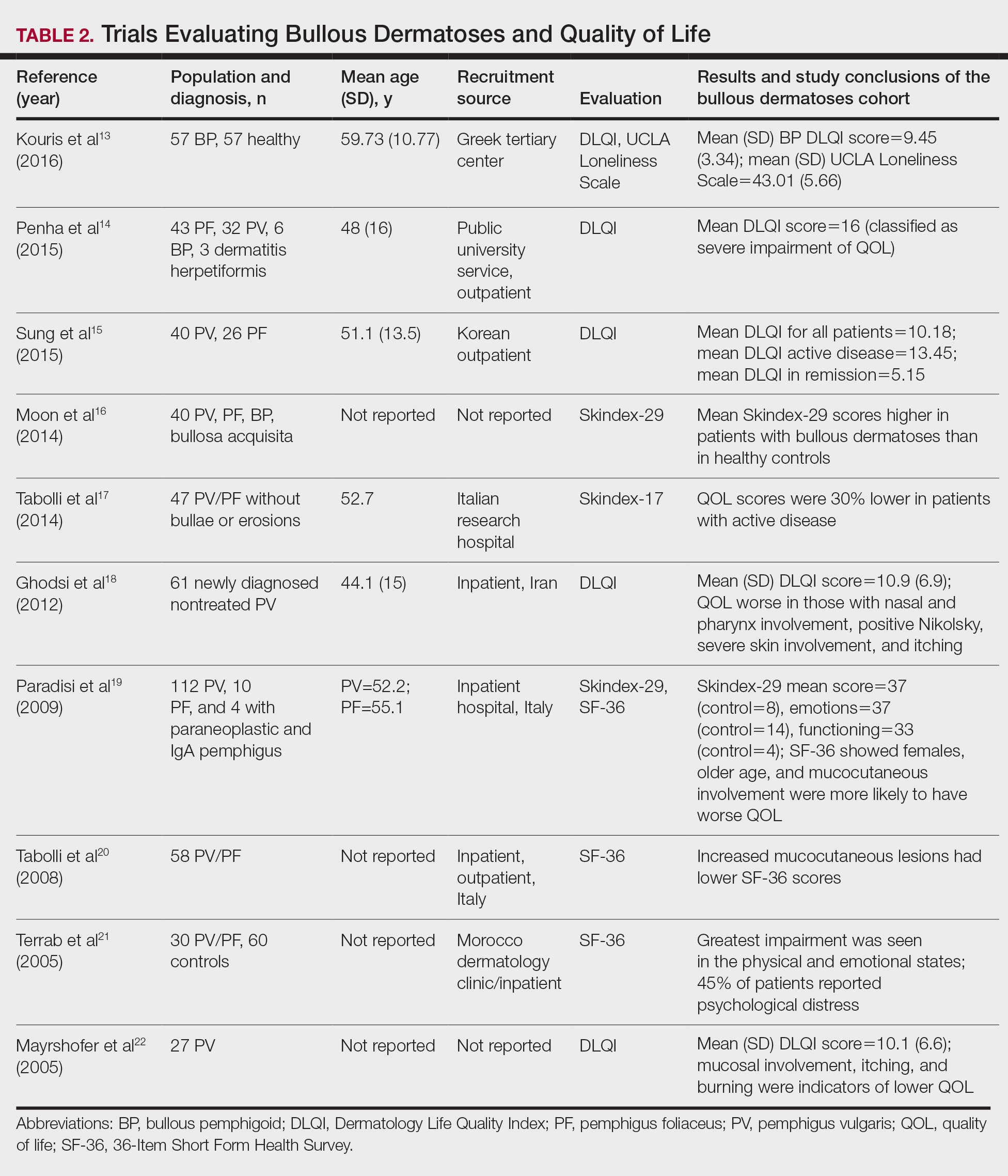
The Dermatology Life Quality Index (DLQI) was the most utilized method for analyzing QOL followed by the Skindex-17, Skindex-29, and 36-Item Short Form Health Survey. The DLQI is a skin-specific measurement tool with higher scores translating to greater impairment in QOL. Healthy patients have an average score of 0.5.3 The mean DLQI scores for ABD patients as seen in Table 2 were 9.45, 10.18, 16, 10.9, and 10.1.13-15,18,22 The most commonly reported concerns among patients included feelings about appearance and disturbances in daily activities.18 Symptoms of mucosal involvement, itching, and burning also were indicators of lower QOL.15,18,20,22 Furthermore, women consistently had lower scores than men.15,17,19,25 Multiple studies concluded that severity of the disease correlated with a lower QOL, though the subtype of pemphigus did not have an effect on QOL scores.15,19,20,21 Lastly, recent onset of symptoms was associated with a worse QOL score.15,18-20 Age, education level, and marital status did not have an effect on QOL.
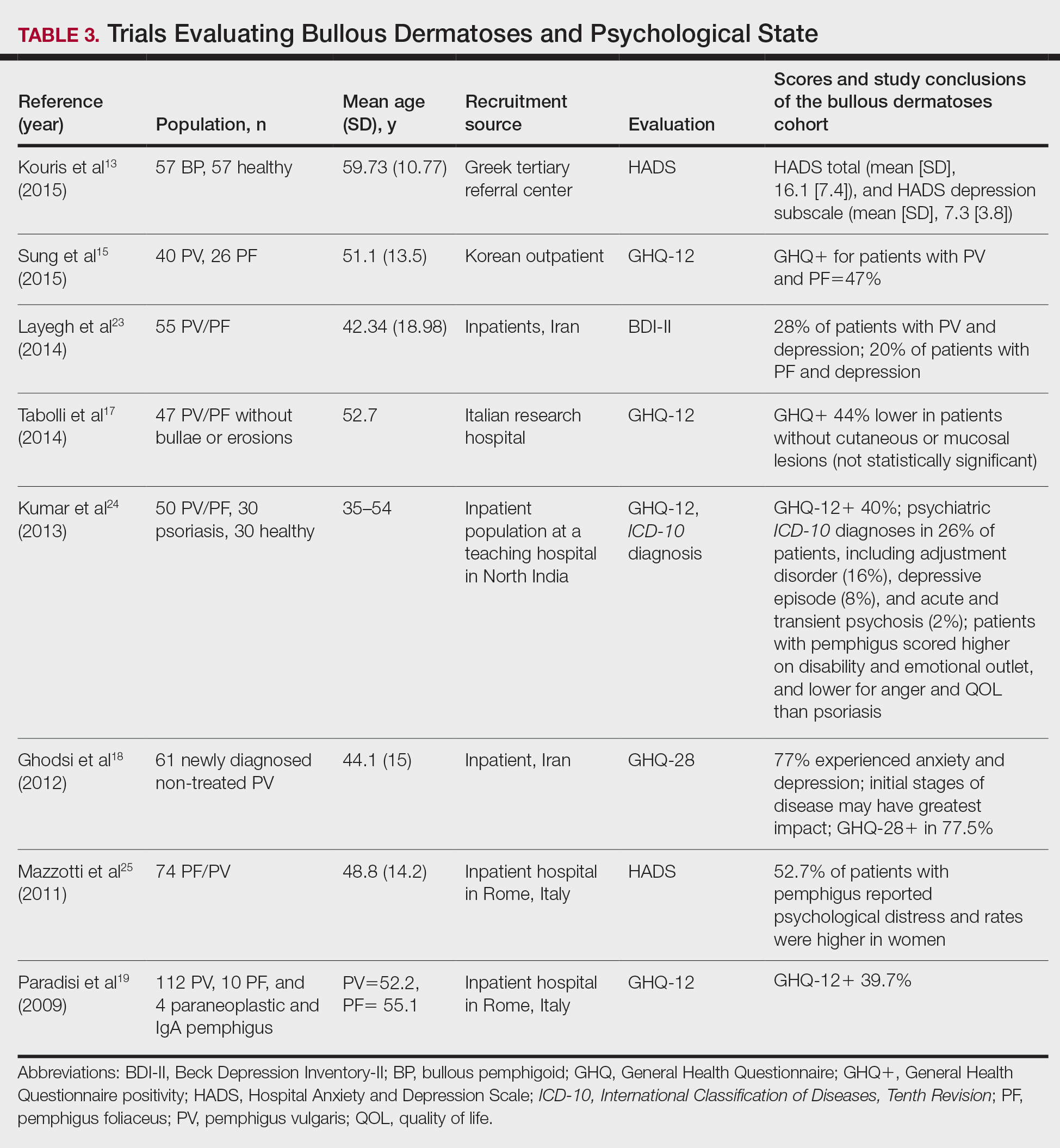
To evaluate psychological state, the General Health Questionnaire (GHQ)-28 and -12 primarily were used, in addition to the Hospital Anxiety and Depression Scale; the International Classification of Diseases, Tenth Revision; the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; and the Beck Depression Inventory-II. As seen in Table 3, GHQ-12 positivity, reflecting probable minor nonpsychotic psychiatric disorders such as depression and anxiety, was identified in 47%, 39.7%, and 40% of patients with pemphigus15,19,24; GHQ-28 positivity was seen in 77.5% of pemphigus patients.18 In the average population, GHQ positivity was found in up to 12% of patients.26,27 Similar to the QOL scores, no significant differences were seen based on subtype of pemphigus for symptoms of depression or anxiety.20,23
Comment
Mental Health of Patients With ABDs—Immunobullous diseases are painful, potentially lifelong conditions that have no definitive cure. These conditions are characterized by bullae and erosions of the skin and mucosae that physically are disabling and often create a stigma for patients. Across multiple different validated psychosocial assessments, the 13 studies included in this review consistently reported that ABDs have a negative effect on mental well-being of patients that is more pronounced in women and worse at the onset of symptoms.13-25
QOL Scores in Patients With ABDs—Quality of life is a broad term that encompasses a general sense of psychological and overall well-being. A score of approximately 10 on the DLQI most often was reported in patients with ABDs, which translates to a moderate impact on QOL. Incomparison, a large cohort study reported the mean (SD) DLQI scores for patients with atopic dermatitis and psoriasis as 7.31 (5.98) and 5.93 (5.66), respectively.28 In another study, Penha et al14 found that patients with psoriasis have a mean DLQI score of 10. Reasons for the similarly low QOL scores in patients with ABDs include long hospitalization periods, disease chronicity, social anxiety, inability to control symptoms, difficulty with activities of daily living, and the belief that the disease is incurable.17,19,23 Although there is a need for increased family and social support with performing necessary daily tasks, personal relationships often are negatively affected, resulting in social isolation, loneliness, and worsening of cutaneous symptoms.
Severity of cutaneous disease and recent onset of symptoms correlated with worse QOL scores. Tabolli et al20 proposed the reason for this relates to not having had enough time to find the best treatment regimen. We believe there also may be an element of habituation involved, whereby patients become accustomed to the appearance of the lesions over time and therefore they become less distressing. Interestingly, Tabolli et al17 determined that patients in the quiescent phase of the disease—without any mucosal or cutaneous lesions—still maintained lower QOL scores than the average population, particularly on the psychosocial section of the 36-Item Short Form Health Survey, which may be due to a concern of disease relapse or from adverse effects of treatment. Providers should monitor patients for mental health complications not only in the disease infancy but throughout the disease course.
Future Directions—Cause and effect of the relationship between the psychosocial variables and ABD disease state has yet to be determined. Most studies included in this review were cross-sectional in design. Although many studies concluded that bullous dermatoses were the cause of impaired QOL, Ren and colleagues29 proposed that medications used to treat neuropsychiatric disorders may trigger the autoimmune antigens of BP. Possible triggers for BP have been reported including hydrochlorothiazide, ciprofloxacin, and dipeptidyl peptidase-4 inhibitors.27,30-32 A longitudinal study design would better evaluate the causal relationship.
The effects of the medications were included in 2 cases, one in which the steroid dose was not found to have a significant impact on rates of depression23 and another in which patients treated with a higher dose of corticosteroids (>10 mg) had worse QOL scores.17 Sung et al15 suggested this may be because patients who took higher doses of steroids had worse symptoms and therefore also had a worse QOL. It also is possible that those patients taking higher doses had increased side effects.17 Further studies that evaluate treatment modalities and timing in relation to the disease onset would be helpful.
Study Limitations—There are potential barriers to combining these data. Multiple different questionnaires were used, and it was difficult to ascertain if all the participants were experiencing active disease. Additionally, questionnaires are not always the best proxy for what is happening in everyday life. Lastly, the sample size of each individual study was small, and the studies only included adults.
Conclusion
As demonstrated by the 13 studies in this review, patients with ABDs have lower QOL scores and higher numbers of psychological symptoms. Clinicians should be mindful of this at-risk population and create opportunities in clinic to discuss personal hardship associated with the disease process and recommend psychiatric intervention if indicated. Additionally, family members often are overburdened with the chronicity of ABDs, and they should not be forgotten. Using one of the aforementioned questionnaires is a practical way to screen patients for lower QOL scores. We agree with Paradisi and colleagues19 that although these questionnaires may be helpful, clinicians still need to determine if the use of a dermatologic QOL evaluation tool in clinical practice improves patient satisfaction.
Autoimmune bullous dermatoses (ABDs) develop due to antibodies directed against antigens within the epidermis or at the dermoepidermal junction. They are categorized histologically by the location of acantholysis (separation of keratinocytes), clinical presentation, and presence of autoantibodies. The most common ABDs include pemphigus vulgaris, pemphigus foliaceus, and bullous pemphigoid (BP). These conditions present on a spectrum of symptoms and severity.1
Although multiple studies have evaluated the impact of bullous dermatoses on mental health, most were designed with a small sample size, thus limiting the generalizability of each study. Sebaratnam et al2 summarized several studies in 2012. In this review, we will analyze additional relevant literature and systematically combine the data to determine the psychological burden of disease of ABDs. We also will discuss the existing questionnaires frequently used in the dermatology setting to assess adverse psychosocial symptoms.
Methods
We searched PubMed, MEDLINE, and Google Scholar for articles published within the last 15 years using the terms bullous pemphigoid, pemphigus, quality of life, anxiety, and depression. We reviewed the citations in each article to further our search.
Criteria for Inclusion and Exclusion—Studies that utilized validated questionnaires to evaluate the effects of pemphigus vulgaris, pemphigus foliaceus, and/or BP on mental health were included. All research participants were 18 years and older. For the questionnaires administered, each study must have included numerical scores in the results. The studies all reported statistically significant results (P<.05), but no studies were excluded on the basis of statistical significance.
Studies were excluded if they did not use a validated questionnaire to examine quality of life (QOL) or psychological status. We also excluded database, retrospective, qualitative, and observational studies. We did not include studies with a sample size less than 20. Studies that administered questionnaires that were uncommon in this realm of research such as the Attitude to Appearance Scale or The Anxiety Questionnaire also were excluded. We did not exclude articles based on their primary language.
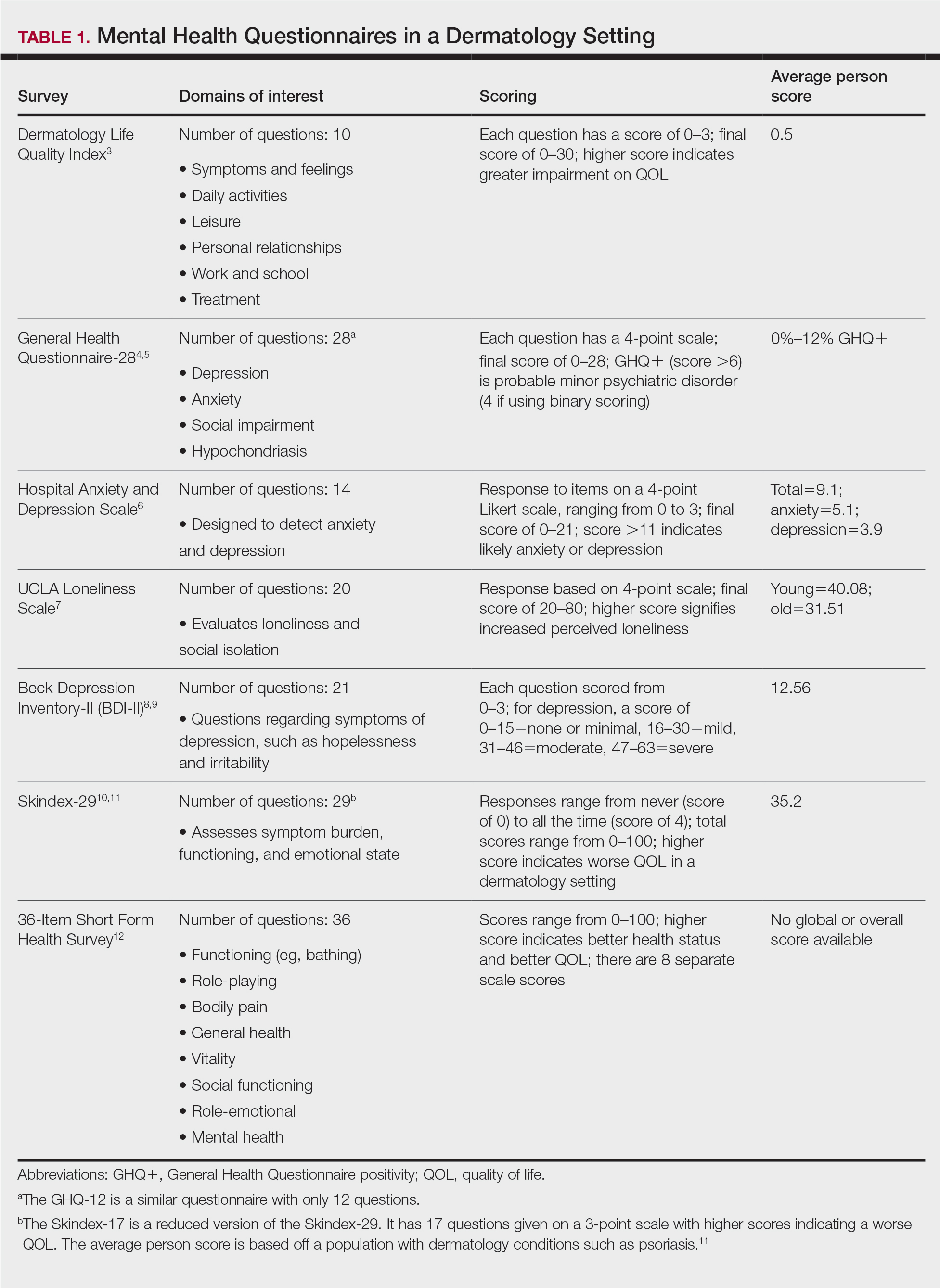
Results
A total of 13 studies met the inclusion criteria with a total of 1716 participants enrolled in the trials. The questionnaires most commonly used are summarized in Table 1. Tables 2 and 3 demonstrate the studies that evaluate QOL and psychological state in patients with bullous dermatoses, respectively.
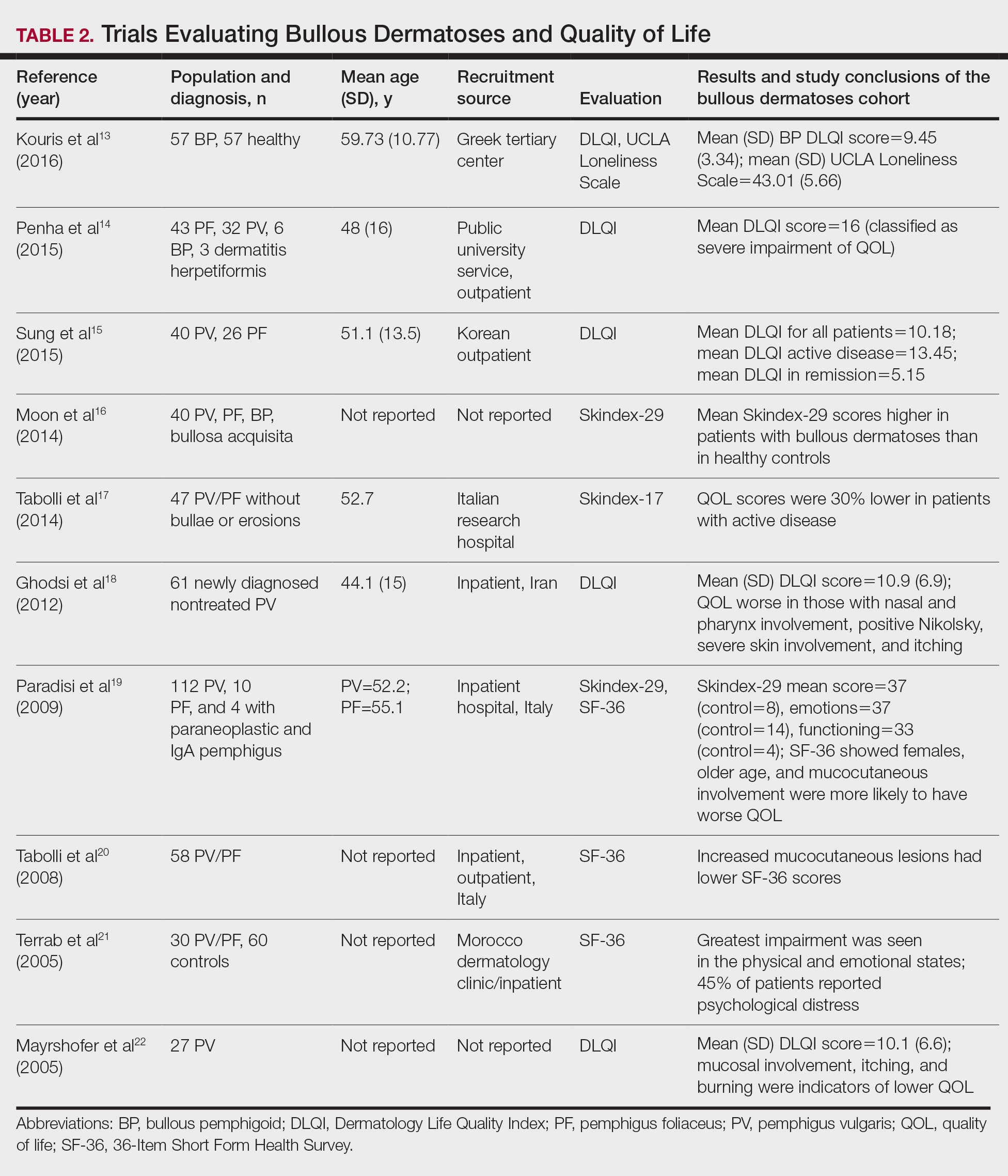
The Dermatology Life Quality Index (DLQI) was the most utilized method for analyzing QOL followed by the Skindex-17, Skindex-29, and 36-Item Short Form Health Survey. The DLQI is a skin-specific measurement tool with higher scores translating to greater impairment in QOL. Healthy patients have an average score of 0.5.3 The mean DLQI scores for ABD patients as seen in Table 2 were 9.45, 10.18, 16, 10.9, and 10.1.13-15,18,22 The most commonly reported concerns among patients included feelings about appearance and disturbances in daily activities.18 Symptoms of mucosal involvement, itching, and burning also were indicators of lower QOL.15,18,20,22 Furthermore, women consistently had lower scores than men.15,17,19,25 Multiple studies concluded that severity of the disease correlated with a lower QOL, though the subtype of pemphigus did not have an effect on QOL scores.15,19,20,21 Lastly, recent onset of symptoms was associated with a worse QOL score.15,18-20 Age, education level, and marital status did not have an effect on QOL.
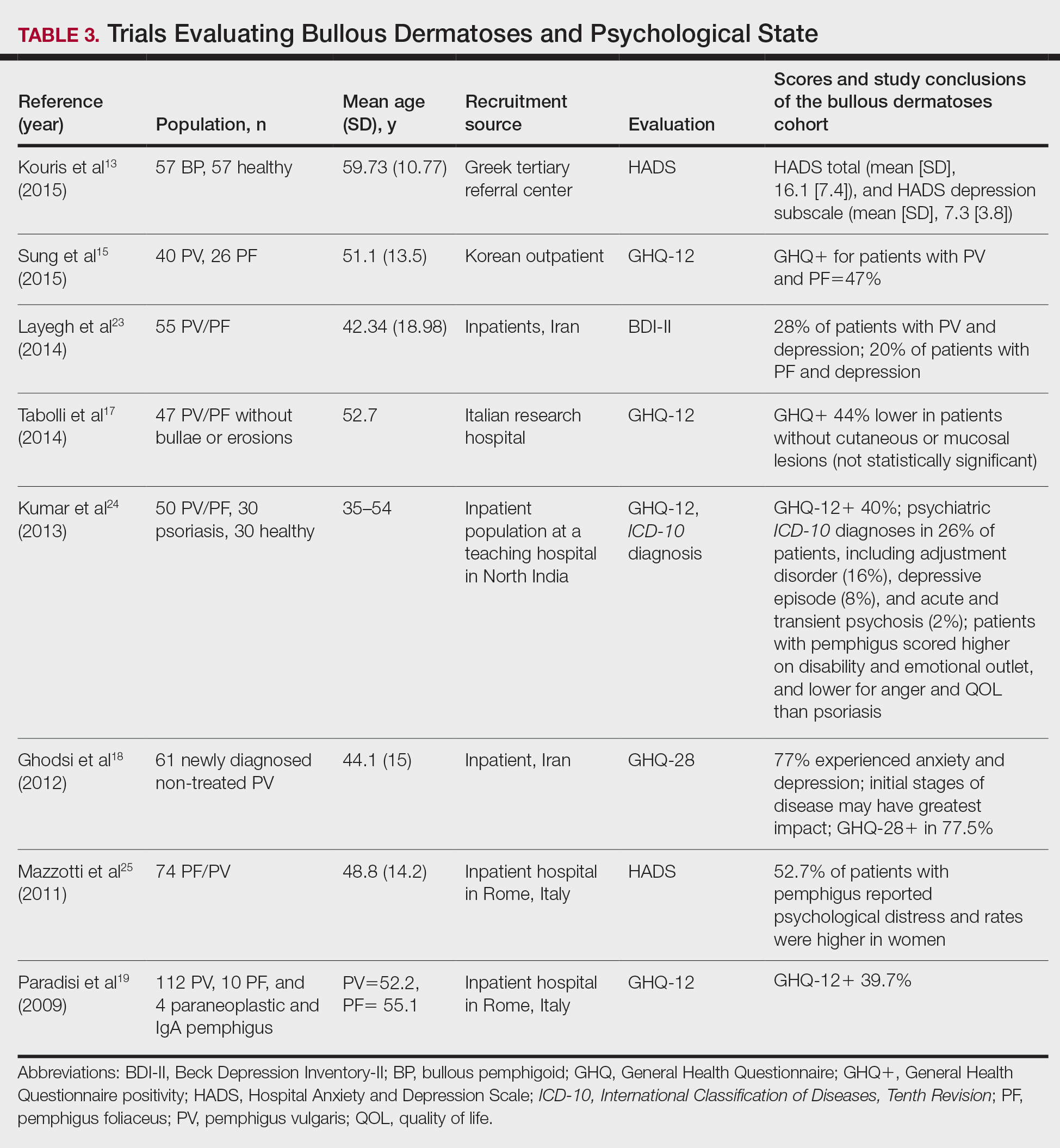
To evaluate psychological state, the General Health Questionnaire (GHQ)-28 and -12 primarily were used, in addition to the Hospital Anxiety and Depression Scale; the International Classification of Diseases, Tenth Revision; the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; and the Beck Depression Inventory-II. As seen in Table 3, GHQ-12 positivity, reflecting probable minor nonpsychotic psychiatric disorders such as depression and anxiety, was identified in 47%, 39.7%, and 40% of patients with pemphigus15,19,24; GHQ-28 positivity was seen in 77.5% of pemphigus patients.18 In the average population, GHQ positivity was found in up to 12% of patients.26,27 Similar to the QOL scores, no significant differences were seen based on subtype of pemphigus for symptoms of depression or anxiety.20,23
Comment
Mental Health of Patients With ABDs—Immunobullous diseases are painful, potentially lifelong conditions that have no definitive cure. These conditions are characterized by bullae and erosions of the skin and mucosae that physically are disabling and often create a stigma for patients. Across multiple different validated psychosocial assessments, the 13 studies included in this review consistently reported that ABDs have a negative effect on mental well-being of patients that is more pronounced in women and worse at the onset of symptoms.13-25
QOL Scores in Patients With ABDs—Quality of life is a broad term that encompasses a general sense of psychological and overall well-being. A score of approximately 10 on the DLQI most often was reported in patients with ABDs, which translates to a moderate impact on QOL. Incomparison, a large cohort study reported the mean (SD) DLQI scores for patients with atopic dermatitis and psoriasis as 7.31 (5.98) and 5.93 (5.66), respectively.28 In another study, Penha et al14 found that patients with psoriasis have a mean DLQI score of 10. Reasons for the similarly low QOL scores in patients with ABDs include long hospitalization periods, disease chronicity, social anxiety, inability to control symptoms, difficulty with activities of daily living, and the belief that the disease is incurable.17,19,23 Although there is a need for increased family and social support with performing necessary daily tasks, personal relationships often are negatively affected, resulting in social isolation, loneliness, and worsening of cutaneous symptoms.
Severity of cutaneous disease and recent onset of symptoms correlated with worse QOL scores. Tabolli et al20 proposed the reason for this relates to not having had enough time to find the best treatment regimen. We believe there also may be an element of habituation involved, whereby patients become accustomed to the appearance of the lesions over time and therefore they become less distressing. Interestingly, Tabolli et al17 determined that patients in the quiescent phase of the disease—without any mucosal or cutaneous lesions—still maintained lower QOL scores than the average population, particularly on the psychosocial section of the 36-Item Short Form Health Survey, which may be due to a concern of disease relapse or from adverse effects of treatment. Providers should monitor patients for mental health complications not only in the disease infancy but throughout the disease course.
Future Directions—Cause and effect of the relationship between the psychosocial variables and ABD disease state has yet to be determined. Most studies included in this review were cross-sectional in design. Although many studies concluded that bullous dermatoses were the cause of impaired QOL, Ren and colleagues29 proposed that medications used to treat neuropsychiatric disorders may trigger the autoimmune antigens of BP. Possible triggers for BP have been reported including hydrochlorothiazide, ciprofloxacin, and dipeptidyl peptidase-4 inhibitors.27,30-32 A longitudinal study design would better evaluate the causal relationship.
The effects of the medications were included in 2 cases, one in which the steroid dose was not found to have a significant impact on rates of depression23 and another in which patients treated with a higher dose of corticosteroids (>10 mg) had worse QOL scores.17 Sung et al15 suggested this may be because patients who took higher doses of steroids had worse symptoms and therefore also had a worse QOL. It also is possible that those patients taking higher doses had increased side effects.17 Further studies that evaluate treatment modalities and timing in relation to the disease onset would be helpful.
Study Limitations—There are potential barriers to combining these data. Multiple different questionnaires were used, and it was difficult to ascertain if all the participants were experiencing active disease. Additionally, questionnaires are not always the best proxy for what is happening in everyday life. Lastly, the sample size of each individual study was small, and the studies only included adults.
Conclusion
As demonstrated by the 13 studies in this review, patients with ABDs have lower QOL scores and higher numbers of psychological symptoms. Clinicians should be mindful of this at-risk population and create opportunities in clinic to discuss personal hardship associated with the disease process and recommend psychiatric intervention if indicated. Additionally, family members often are overburdened with the chronicity of ABDs, and they should not be forgotten. Using one of the aforementioned questionnaires is a practical way to screen patients for lower QOL scores. We agree with Paradisi and colleagues19 that although these questionnaires may be helpful, clinicians still need to determine if the use of a dermatologic QOL evaluation tool in clinical practice improves patient satisfaction.
- Baum S, Sakka N, Artsi O, et al. Diagnosis and classification of autoimmune blistering diseases. Autoimmun Rev. 2014;13:482-489. https://doi.org/10.1016/j.autrev.2014.01.047
- Sebaratnam DF, McMillan JR, Werth VP, et al. Quality of life in patients with bullous dermatoses. Clin Dermatol. 2012;30:103-107. doi:10.1016/j.clindermatol.2011.03.016
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
- Goldberg DP. The Detection of Psychiatric Illness by Questionnaire. Oxford University Press; 1972.
- Cano A, Sprafkin RP, Scaturo DJ, et al. Mental health screening in primary care: a comparison of 3 brief measures of psychological distress. Prim Care Companion J Clin Psychiatry. 2001;3:206-210.
- Zigmond A, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361-370.
- Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20-40. doi:10.1207/s15327752jpa6601_2
- Beck A, Alford B. Depression: Causes and Treatment. 2nd ed. Philadelphia University of Pennsylvania Press; 2009.
- Ghassemzadeh H, Mojtabai R, Karamghadiri N, et al. Psychometric properties of a Persian-language version of the Beck Depression Inventory—Second Edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21:185-192. doi:10.1002/da.20070
- Chren MM, Lasek RJ, Sahay AP, et al. Measurement properties of Skindex-16: a brief quality-of-life measure for patients with skin diseases. J Cutan Med Surg. 2001;5:105-110.
- Nijsten TEC, Sampogna F, Chren M, et al. Testing and reducing Skindex-29 using Rasch analysis: Skindex-17. J Invest Dermatol. 2006;126:1244-1250. https://doi.org/10.1038/sj.jid.5700212
- Ware JE Jr, Sherbourne C. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Med Care. 1992;30:473-483.
- Kouris A, Platsidaki E, Christodoulou C, et al. Quality of life, depression, anxiety and loneliness in patients with bullous pemphigoid: a case control study. An Bras Dermatol. 2016;91:601-603. doi:10.1590/abd1806-4841.2016493
- Penha MA, Farat JG, Miot HA, et al. Quality of life index in autoimmune bullous dermatosis patients. An Bras Dermatol. 2015;90:190-194. https://dx.doi.org/10.1590/abd1806-4841.20153372
- Sung JY, Roh MR, Kim SC. Quality of life assessment in Korean patients with pemphigus. Ann Dermatol. 2015;27:492-498.
- Moon SH, Kwon HI, Park HC, et al. Assessment of the quality of life in autoimmune blistering skin disease patients. Korean J Dermatol. 2014;52:402-409.
- Tabolli S, Pagliarello C, Paradisi A, et al. Burden of disease during quiescent periods in patients with pemphigus. Br J Dermatol. 2014;170:1087-1091. doi:10.1111/bjd.12836
- Ghodsi SZ, Chams-Davatchi C, Daneshpazhooh M, et al. Quality of life and psychological status of patients with pemphigus vulgaris using Dermatology Life Quality Index and general health questionnaires. J Dermatol. 2012;39:141-144. doi:10.1111/j.1346-8138.2011.01382
- Paradisi A, Sampogna F, Di Pietro C, et al. Quality-of-life assessment in patients with pemphigus using a minimum set of evaluation tools. J Am Acad Dermatol. 2009;60:261-269. doi:10.1016/j.jaad.2008.09.014
- Tabolli S, Mozzetta A, Antinone V, et al. The health impact of pemphigus vulgaris and pemphigus foliaceus assessed using the Medical Outcomes Study 36-item short form health survey questionnaire. Br J Dermatol. 2008;158:1029-1034. doi:10.1111/j.1365-2133.2008.08481.x
- Terrab Z, Benchikhi H, Maaroufi A, et al. Quality of life and pemphigus. Ann Dermatol Venereol. 2005;132:321-328.
- Mayrshofer F, Hertl M, Sinkgraven R, et al. Significant decrease in quality of life in patients with pemphigus vulgaris: results from the German Bullous Skin Disease (BSD) Study Group [in German]. J Dtsch Dermatol Ges. 2005;3:431-435. doi:10.1111/j.1610-0387.2005.05722.x
- Layegh P, Mokhber N, Javidi Z, et al. Depression in patients with pemphigus: is it a major concern? J Dermatol. 2014;40:434-437. doi:10.1111/1346-8138.12067
- Kumar V, Mattoo SK, Handa S. Psychiatric morbidity in pemphigus and psoriasis: a comparative study from India. Asian J Psychiatr. 2013;6:151-156. doi:10.1016/j.ajp.2012.10.005
- Mazzotti E, Mozzetta A, Antinone V, et al. Psychological distress and investment in one’s appearance in patients with pemphigus. J Eur Acad Dermatol Venereol. 2011;25:285-289. doi:10.1111/j.1468-3083.2010.03780.x
- Regier DA, Boyd JH, Burke JD, et al. One-month prevalence of mental disorders in the United States: based on five epidemiologic catchment area sites. Arch Gen Psychiatr. 1988;45:977-986. doi:10.1001/archpsyc.1988.01800350011002
- Cozzani E, Chinazzo C, Burlando M, et al. Ciprofloxacin as a trigger for bullous pemphigoid: the second case in the literature. Am J Ther. 2016;23:E1202-E1204. doi:10.1097/MJT.0000000000000283
- Lundberg L, Johannesson M, Silverdahl M, et al. Health-related quality of life in patients with psoriasis and atopic dermatitis measured with SF-36, DLQI and a subjective measure of disease activity. Acta Derm Venereol. 2000;80:430-434.
- Ren Z, Hsu DY, Brieva J, et al. Hospitalization, inpatient burden and comorbidities associated with bullous pemphigoid in the U.S.A. Br J Dermatol. 2017;176:87-99. doi:10.1111/bjd.14821
- Warner C, Kwak Y, Glover MH, et al. Bullous pemphigoid induced by hydrochlorothiazide therapy. J Drugs Dermatol. 2014;13:360-362.
- Mendonca FM, Martin-Gutierrez FJ, Rios-Martin JJ, et al. Three cases of bullous pemphigoid associated with dipeptidyl peptidase-4 inhibitors—one due to linagliptin. Dermatology. 2016;232:249-253. doi:10.1159/000443330
- Attaway A, Mersfelder TL, Vaishnav S, et al. Bullous pemphigoid associated with dipeptidyl peptidase IV inhibitors: a case report and review of literature. J Dermatol Case Rep. 2014;8:24-28.
- Baum S, Sakka N, Artsi O, et al. Diagnosis and classification of autoimmune blistering diseases. Autoimmun Rev. 2014;13:482-489. https://doi.org/10.1016/j.autrev.2014.01.047
- Sebaratnam DF, McMillan JR, Werth VP, et al. Quality of life in patients with bullous dermatoses. Clin Dermatol. 2012;30:103-107. doi:10.1016/j.clindermatol.2011.03.016
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)—a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
- Goldberg DP. The Detection of Psychiatric Illness by Questionnaire. Oxford University Press; 1972.
- Cano A, Sprafkin RP, Scaturo DJ, et al. Mental health screening in primary care: a comparison of 3 brief measures of psychological distress. Prim Care Companion J Clin Psychiatry. 2001;3:206-210.
- Zigmond A, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361-370.
- Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66:20-40. doi:10.1207/s15327752jpa6601_2
- Beck A, Alford B. Depression: Causes and Treatment. 2nd ed. Philadelphia University of Pennsylvania Press; 2009.
- Ghassemzadeh H, Mojtabai R, Karamghadiri N, et al. Psychometric properties of a Persian-language version of the Beck Depression Inventory—Second Edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21:185-192. doi:10.1002/da.20070
- Chren MM, Lasek RJ, Sahay AP, et al. Measurement properties of Skindex-16: a brief quality-of-life measure for patients with skin diseases. J Cutan Med Surg. 2001;5:105-110.
- Nijsten TEC, Sampogna F, Chren M, et al. Testing and reducing Skindex-29 using Rasch analysis: Skindex-17. J Invest Dermatol. 2006;126:1244-1250. https://doi.org/10.1038/sj.jid.5700212
- Ware JE Jr, Sherbourne C. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Med Care. 1992;30:473-483.
- Kouris A, Platsidaki E, Christodoulou C, et al. Quality of life, depression, anxiety and loneliness in patients with bullous pemphigoid: a case control study. An Bras Dermatol. 2016;91:601-603. doi:10.1590/abd1806-4841.2016493
- Penha MA, Farat JG, Miot HA, et al. Quality of life index in autoimmune bullous dermatosis patients. An Bras Dermatol. 2015;90:190-194. https://dx.doi.org/10.1590/abd1806-4841.20153372
- Sung JY, Roh MR, Kim SC. Quality of life assessment in Korean patients with pemphigus. Ann Dermatol. 2015;27:492-498.
- Moon SH, Kwon HI, Park HC, et al. Assessment of the quality of life in autoimmune blistering skin disease patients. Korean J Dermatol. 2014;52:402-409.
- Tabolli S, Pagliarello C, Paradisi A, et al. Burden of disease during quiescent periods in patients with pemphigus. Br J Dermatol. 2014;170:1087-1091. doi:10.1111/bjd.12836
- Ghodsi SZ, Chams-Davatchi C, Daneshpazhooh M, et al. Quality of life and psychological status of patients with pemphigus vulgaris using Dermatology Life Quality Index and general health questionnaires. J Dermatol. 2012;39:141-144. doi:10.1111/j.1346-8138.2011.01382
- Paradisi A, Sampogna F, Di Pietro C, et al. Quality-of-life assessment in patients with pemphigus using a minimum set of evaluation tools. J Am Acad Dermatol. 2009;60:261-269. doi:10.1016/j.jaad.2008.09.014
- Tabolli S, Mozzetta A, Antinone V, et al. The health impact of pemphigus vulgaris and pemphigus foliaceus assessed using the Medical Outcomes Study 36-item short form health survey questionnaire. Br J Dermatol. 2008;158:1029-1034. doi:10.1111/j.1365-2133.2008.08481.x
- Terrab Z, Benchikhi H, Maaroufi A, et al. Quality of life and pemphigus. Ann Dermatol Venereol. 2005;132:321-328.
- Mayrshofer F, Hertl M, Sinkgraven R, et al. Significant decrease in quality of life in patients with pemphigus vulgaris: results from the German Bullous Skin Disease (BSD) Study Group [in German]. J Dtsch Dermatol Ges. 2005;3:431-435. doi:10.1111/j.1610-0387.2005.05722.x
- Layegh P, Mokhber N, Javidi Z, et al. Depression in patients with pemphigus: is it a major concern? J Dermatol. 2014;40:434-437. doi:10.1111/1346-8138.12067
- Kumar V, Mattoo SK, Handa S. Psychiatric morbidity in pemphigus and psoriasis: a comparative study from India. Asian J Psychiatr. 2013;6:151-156. doi:10.1016/j.ajp.2012.10.005
- Mazzotti E, Mozzetta A, Antinone V, et al. Psychological distress and investment in one’s appearance in patients with pemphigus. J Eur Acad Dermatol Venereol. 2011;25:285-289. doi:10.1111/j.1468-3083.2010.03780.x
- Regier DA, Boyd JH, Burke JD, et al. One-month prevalence of mental disorders in the United States: based on five epidemiologic catchment area sites. Arch Gen Psychiatr. 1988;45:977-986. doi:10.1001/archpsyc.1988.01800350011002
- Cozzani E, Chinazzo C, Burlando M, et al. Ciprofloxacin as a trigger for bullous pemphigoid: the second case in the literature. Am J Ther. 2016;23:E1202-E1204. doi:10.1097/MJT.0000000000000283
- Lundberg L, Johannesson M, Silverdahl M, et al. Health-related quality of life in patients with psoriasis and atopic dermatitis measured with SF-36, DLQI and a subjective measure of disease activity. Acta Derm Venereol. 2000;80:430-434.
- Ren Z, Hsu DY, Brieva J, et al. Hospitalization, inpatient burden and comorbidities associated with bullous pemphigoid in the U.S.A. Br J Dermatol. 2017;176:87-99. doi:10.1111/bjd.14821
- Warner C, Kwak Y, Glover MH, et al. Bullous pemphigoid induced by hydrochlorothiazide therapy. J Drugs Dermatol. 2014;13:360-362.
- Mendonca FM, Martin-Gutierrez FJ, Rios-Martin JJ, et al. Three cases of bullous pemphigoid associated with dipeptidyl peptidase-4 inhibitors—one due to linagliptin. Dermatology. 2016;232:249-253. doi:10.1159/000443330
- Attaway A, Mersfelder TL, Vaishnav S, et al. Bullous pemphigoid associated with dipeptidyl peptidase IV inhibitors: a case report and review of literature. J Dermatol Case Rep. 2014;8:24-28.
Practice Points
- Autoimmune bullous dermatoses cause cutaneous lesions that are painful and disfiguring. These conditions affect a patient’s ability to perform everyday tasks, and individual lesions can take years to heal.
- Providers should take necessary steps to address patient well-being, especially at disease onset in patients with bullous dermatoses.
Malpractice suits against ob.gyns. continue downward trend
Nearly 80% of obstetrician-gynecologists report having been named in at least one malpractice claim, but the total number who report such suits has fallen steadily since 2017, according to the Medscape Ob/Gyn Malpractice Report 2021.
Ob.gyns. were the fifth most likely among practitioners in 29 specialties to be sued, and they are much more likely than are the typical physicians to be parties to a malpractice case (51%), according to the new report. However, the number of ob.gyns. who reported a malpractice suit has been dropping, from 85% in 2017 to 83% in 2019 to 79% in 2021. In most cases, multiple parties were named in the lawsuit (64%), although 27% of ob.gyns. reported having been sued individually.
The most common reasons for lawsuits were complications from treatment/surgery (39%), poor outcome/disease progression (30%), failure to diagnose/delayed diagnosis (25%), patients suffering an abnormal injury (17%), and failure to treat/delayed treatment (16%).
The 2021 report was compiled from an online survey that included more than 4,300 physicians representing 29 specialties; the survey was available from May 21 to Aug. 28, 2021. Respondents include 314 ob.gyns. Most respondents had been in practice at least 25 years (60%), and 55% were at least 60 years old.
Ob.gyns. carry higher malpractice insurance costs than nearly every other medical specialty, owing to the unique challenges and inherent risks of delivering newborn babies. In 2021, 33% of ob.gyns. reported paying at least $30,000 in annual premiums, and only 27% said they paid less than $20,000. Over half of all specialists (52%) paid less than $20,000 in annual insurance premiums.
More than 70% of ob.gyns. were “very” (32%) or “somewhat” surprised (40%) by their malpractice suits. A large majority said they believed the lawsuit was unwarranted (78%). One respondent wrote: “Feeling like I had done my best for the patient and she sued me anyway.”
Many cases settled before trial (40%), although some (12%) were still in process at the time of the survey. Other outcomes ranged from a judge or jury ruling on behalf of the physician (8%) or the lawsuit being dismissed within a few months of filing (8%). Ob.gyns. reported having lost 2% the suits.
The largest proportion of cases took less than 2 years (39%), although almost as many cases (33%) lasted between 3 and 5 years. Monetary awards to plaintiffs exceeded $1 million in 15% of cases that resulted in economic damages, with 8% of these awards exceeding $2 million. One in five awards were between $500,000 and $1 million.
Most ob.gyns. (67%) said the lawsuits did not negatively affect their careers. Roughly one in five ob.gyns. (21%) said they now trusted their patients less than they did before the suit, modestly fewer than specialists overall (24%).
The largest proportion of ob.gyns. (44%) said they would not have done anything differently, almost identical to the proportion of physicians overall (43%). Approximately 10% of ob.gyns. said they would never have taken the patient in the first place, while 9% said they should have developed better chart documentation, and 8% said they should have referred the patient to another physician.
A version of this article first appeared on Medscape.com.
Nearly 80% of obstetrician-gynecologists report having been named in at least one malpractice claim, but the total number who report such suits has fallen steadily since 2017, according to the Medscape Ob/Gyn Malpractice Report 2021.
Ob.gyns. were the fifth most likely among practitioners in 29 specialties to be sued, and they are much more likely than are the typical physicians to be parties to a malpractice case (51%), according to the new report. However, the number of ob.gyns. who reported a malpractice suit has been dropping, from 85% in 2017 to 83% in 2019 to 79% in 2021. In most cases, multiple parties were named in the lawsuit (64%), although 27% of ob.gyns. reported having been sued individually.
The most common reasons for lawsuits were complications from treatment/surgery (39%), poor outcome/disease progression (30%), failure to diagnose/delayed diagnosis (25%), patients suffering an abnormal injury (17%), and failure to treat/delayed treatment (16%).
The 2021 report was compiled from an online survey that included more than 4,300 physicians representing 29 specialties; the survey was available from May 21 to Aug. 28, 2021. Respondents include 314 ob.gyns. Most respondents had been in practice at least 25 years (60%), and 55% were at least 60 years old.
Ob.gyns. carry higher malpractice insurance costs than nearly every other medical specialty, owing to the unique challenges and inherent risks of delivering newborn babies. In 2021, 33% of ob.gyns. reported paying at least $30,000 in annual premiums, and only 27% said they paid less than $20,000. Over half of all specialists (52%) paid less than $20,000 in annual insurance premiums.
More than 70% of ob.gyns. were “very” (32%) or “somewhat” surprised (40%) by their malpractice suits. A large majority said they believed the lawsuit was unwarranted (78%). One respondent wrote: “Feeling like I had done my best for the patient and she sued me anyway.”
Many cases settled before trial (40%), although some (12%) were still in process at the time of the survey. Other outcomes ranged from a judge or jury ruling on behalf of the physician (8%) or the lawsuit being dismissed within a few months of filing (8%). Ob.gyns. reported having lost 2% the suits.
The largest proportion of cases took less than 2 years (39%), although almost as many cases (33%) lasted between 3 and 5 years. Monetary awards to plaintiffs exceeded $1 million in 15% of cases that resulted in economic damages, with 8% of these awards exceeding $2 million. One in five awards were between $500,000 and $1 million.
Most ob.gyns. (67%) said the lawsuits did not negatively affect their careers. Roughly one in five ob.gyns. (21%) said they now trusted their patients less than they did before the suit, modestly fewer than specialists overall (24%).
The largest proportion of ob.gyns. (44%) said they would not have done anything differently, almost identical to the proportion of physicians overall (43%). Approximately 10% of ob.gyns. said they would never have taken the patient in the first place, while 9% said they should have developed better chart documentation, and 8% said they should have referred the patient to another physician.
A version of this article first appeared on Medscape.com.
Nearly 80% of obstetrician-gynecologists report having been named in at least one malpractice claim, but the total number who report such suits has fallen steadily since 2017, according to the Medscape Ob/Gyn Malpractice Report 2021.
Ob.gyns. were the fifth most likely among practitioners in 29 specialties to be sued, and they are much more likely than are the typical physicians to be parties to a malpractice case (51%), according to the new report. However, the number of ob.gyns. who reported a malpractice suit has been dropping, from 85% in 2017 to 83% in 2019 to 79% in 2021. In most cases, multiple parties were named in the lawsuit (64%), although 27% of ob.gyns. reported having been sued individually.
The most common reasons for lawsuits were complications from treatment/surgery (39%), poor outcome/disease progression (30%), failure to diagnose/delayed diagnosis (25%), patients suffering an abnormal injury (17%), and failure to treat/delayed treatment (16%).
The 2021 report was compiled from an online survey that included more than 4,300 physicians representing 29 specialties; the survey was available from May 21 to Aug. 28, 2021. Respondents include 314 ob.gyns. Most respondents had been in practice at least 25 years (60%), and 55% were at least 60 years old.
Ob.gyns. carry higher malpractice insurance costs than nearly every other medical specialty, owing to the unique challenges and inherent risks of delivering newborn babies. In 2021, 33% of ob.gyns. reported paying at least $30,000 in annual premiums, and only 27% said they paid less than $20,000. Over half of all specialists (52%) paid less than $20,000 in annual insurance premiums.
More than 70% of ob.gyns. were “very” (32%) or “somewhat” surprised (40%) by their malpractice suits. A large majority said they believed the lawsuit was unwarranted (78%). One respondent wrote: “Feeling like I had done my best for the patient and she sued me anyway.”
Many cases settled before trial (40%), although some (12%) were still in process at the time of the survey. Other outcomes ranged from a judge or jury ruling on behalf of the physician (8%) or the lawsuit being dismissed within a few months of filing (8%). Ob.gyns. reported having lost 2% the suits.
The largest proportion of cases took less than 2 years (39%), although almost as many cases (33%) lasted between 3 and 5 years. Monetary awards to plaintiffs exceeded $1 million in 15% of cases that resulted in economic damages, with 8% of these awards exceeding $2 million. One in five awards were between $500,000 and $1 million.
Most ob.gyns. (67%) said the lawsuits did not negatively affect their careers. Roughly one in five ob.gyns. (21%) said they now trusted their patients less than they did before the suit, modestly fewer than specialists overall (24%).
The largest proportion of ob.gyns. (44%) said they would not have done anything differently, almost identical to the proportion of physicians overall (43%). Approximately 10% of ob.gyns. said they would never have taken the patient in the first place, while 9% said they should have developed better chart documentation, and 8% said they should have referred the patient to another physician.
A version of this article first appeared on Medscape.com.
Chronic marijuana use linked to recurrent stroke
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
, new observational research suggests. “Our analysis shows young marijuana users with a history of stroke or transient ischemic attack remain at significantly high risk for future strokes,” said lead study author Akhil Jain, MD, a resident physician at Mercy Fitzgerald Hospital in Darby, Pennsylvania.
“It’s essential to raise awareness among young adults about the impact of chronic habitual use of marijuana, especially if they have established cardiovascular risk factors or previous stroke.”
The study will be presented during the International Stroke Conference, presented by the American Stroke Association, a division of the American Heart Association.
An increasing number of jurisdictions are allowing marijuana use. To date, 18 states and the District of Columbia have legalized recreational cannabis use, the investigators noted.
Research suggests cannabis use disorder – defined as the chronic habitual use of cannabis – is more prevalent in the young adult population. But Dr. Jain said the population of marijuana users is “a changing dynamic.”
Cannabis use has been linked to an increased risk for first-time stroke or transient ischemic attack (TIA). Traditional stroke risk factors include hypertension, diabetes, and diseases related to blood vessels or blood circulation, including atherosclerosis.
Young adults might have additional stroke risk factors, such as behavioral habits like substance abuse, low physical activity, and smoking, oral contraceptives use among females, and brain infections, especially in the immunocompromised, said Dr. Jain.
Research from the American Heart Association shows stroke rates are increasing among adults 18 to 45 years of age. Each year, young adults account for up to 15% of strokes in the United States.
Prevalence and risk for recurrent stroke in patients with previous stroke or TIA in cannabis users have not been clearly established, the researchers pointed out.
A higher rate of recurrent stroke
For this new study, Dr. Jain and colleagues used data from the National Inpatient Sample from October 2015 to December 2017. They identified hospitalizations among young adults 18 to 45 years of age with a previous history of stroke or TIA.
They then grouped these patients into those with cannabis use disorder (4,690) and those without cannabis use disorder (156,700). The median age in both cohorts was 37 years.
The analysis did not include those who were considered in remission from cannabis use disorder.
Results showed that 6.9% of those with cannabis use disorder were hospitalized for a recurrent stroke, compared with 5.4% of those without cannabis use disorder (P < .001).
After adjustment for demographic factors (age, sex, race, household income), and pre-existing conditions, patients with cannabis use disorder were 48% more likely to be hospitalized for recurrent stroke than those without cannabis use disorder (odds ratio, 1.48; 95% confidence interval, 1.28-1.71; P < .001).
Compared with the group without cannabis use disorder, the cannabis use disorder group had more men (55.2% vs. 40.2%), more African American people (44.6% vs. 37.2%), and more use of tobacco (73.9% vs. 39.6%) and alcohol (16.5% vs. 3.6%). They also had a greater percentage of chronic obstructive pulmonary disease, depression, and psychoses.
But a smaller percentage of those with cannabis use disorder had hypertension (51.3% vs. 55.6%; P = .001) and diabetes (16.3% vs. 22.7%; P < .001), which is an “interesting” finding, said Dr. Jain.
“We observed that even with a lower rate of cardiovascular risk factors, after controlling for all the risk factors, we still found the cannabis users had a higher rate of recurrent stroke.”
He noted this was a retrospective study without a control group. “If both groups had comparable hypertension, then this risk might actually be more evident,” said Dr. Jain. “We need a prospective study with comparable groups.”
Living in low-income neighborhoods and in northeast and southern regions of the United States was also more common in the cannabis use disorder group.
Hypothesis-generating research
The study did not investigate the possible mechanisms by which marijuana use might increase stroke risk, but Dr. Jain speculated that these could include factors such as impaired blood vessel function, changes in blood supply, an increased tendency of blood clotting, impaired energy production in brain cells, and an imbalance between molecules that harm healthy tissue and the antioxidant defenses that neutralize them.
As cannabis use may pose a different risk for a new stroke, as opposed a previous stroke, Dr. Jain said it would be interesting to study the amount of “residual function deficit” experienced with the first stroke.
The new study represents “foundational research” upon which other research teams can build, said Dr. Jain. “Our study is hypothesis-generating research for a future prospective randomized controlled trial.”
A limitation of the study is that it did not consider the effect of various doses, duration, and forms of cannabis abuse, or use of medicinal cannabis or other drugs.
Robert L. Page II, PharmD, professor, departments of clinical pharmacy and physical medicine/rehabilitation, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora, provided a comment on this new research.
A cannabis use disorder diagnosis provides “specific criteria” with regard to chronicity of use and reflects “more of a physical and psychological dependence upon cannabis,” said Dr. Page, who chaired the writing group for the AHA 2020 cannabis and cardiovascular disease scientific statement.
He explained what sets people with cannabis use disorder apart from “run-of-the-mill” recreational cannabis users is that “these are individuals who use a cannabis product, whether it’s smoking it, vaping it, or consuming it via an edible, and are using it on a regular basis, in a chronic fashion.”
The study received no outside funding. The authors report no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ISC 2022
Substantial numbers of U.S. youth report vaping cannabis
Adolescents and young adults who use e-cigarettes reported vaping cannabis, according to selected data from the national Population Assessment of Tobacco and Health (PATH) study.
Ruoyan Sun, PhD, an assistant professor at the University of Alabama at Birmingham, and colleagues examined results of PATH’s wave5 survey conducted from December 2018 to November 2019. PATH is a National Institutes of Health–Food and Drug Administration collaboration begun in 2013.
Their analysis, published online Feb. 7, 2022, in JAMA Pediatrics, evaluated the frequency of cannabis vaping across several age groups: 164 respondents ages 12-14; 919 participants ages 15-17; and 3,038 participants ages 18-24. Respondents included for analysis reported electronic nicotine product consumption in the past 30 days. In response to the question “When you have used an electronic product, how often were you using it to smoke marijuana, marijuana concentrates, marijuana waxes, THC, or hash oils?” 35.0% (95% confidence interval, 29.3%-41.2%) of current e-smokers aged 12-14 years said they had done so, as did 51.3% (95% CI, 47.7%-54.9%) of those aged 15-17 years and 54.6% (95% CI, 52.5%-56.7%) of young adults aged 18-24.
The prevalence of those who reported vaping cannabis every time they vaped was 3.1% (95% CI, 1.3%-6.9%) of youths aged 12-14 years, 6.7% (95% CI, 5.3%-8.6%) of youths aged 15-17 years, and 10.3% (95% CI, 9.0%-11.6%) of young adults aged 18-24.
Among children ages 12-14, 65% said they never vaped cannabis, while 48.7% and 45.4%, respectively, in the two older groups said they did.
“This is a very important finding and it mirrors what some of us have already seen in practice,” said pediatric pulmonologist S. Christy Sadreameli, MD, MHS, an assistant professor of pediatrics at John Hopkins University, Baltimore. “It is important for pediatricians to realize that dual use of cannabis and nicotine vaping, and exclusive use of cannabis vaping, are not uncommon. It informs how we ask questions and how we counsel our patients.” Dr. Sadreameli was not involved in the PATH study.
Overall, the survey participants were 56% male, with 24% of respondents identifying as Hispanic, 8% as non-Hispanic Black, 58% as non-Hispanic White, and 10% as of other race/ethnicity. The weighted proportion of current e-cigarette use was 3.0% (95% CI, 2.6%-3.4%) in youths ages 12-14 years, 14.4% (95% CI, 13.5%-15.3%) in those 15-17 years, and 26.2% (95% CI, 25.3%-27.1%) in young adults.
Other recent national surveys such as the National Institute on Drug Abuses’s Monitoring the Future are reporting a growing prevalence of youth cannabis vaping, Dr. Sun said. For example, the prevalence of cannabis vaping in the past 12-month period among grade 12 students grew from 9.5% in 2017 to 22.1% in 2020. Vaping cannabis was more prevalent among Hispanic teens than other ethnicities.
Vaping devices such as e-cigarettes, vaping pens, e-cigars, and e-hookahs can be used to inhale multiple substances, including nicotine, cannabis, and opium, Dr. Sun noted in an interview. “So in addition to asking about the behavior of vaping itself, pediatricians could pay more attention to what is being vaped in these devices.”
According to Dr. Sadreameli, vaping more than one substance at a time could potentially work synergistically to cause more harm, compared with one product alone. “The other aspect to consider is that vaping multiple types of products may increase the chance of harm from other components of the mixture,” she said. For instance, a lot of the e-cigarette or vaping use-associated lung injury (EVALI) cases have been linked to vitamin E acetate, which was found in certain cannabis formulations. “Anecdotally, most EVALI patients I’ve met seemed to report use of multiple products, including cannabis-containing and nicotine-containing products.”
Dr. Sadreameli added that some cannabis vapers will have other issues. “For example, there is a severe vomiting syndrome I’ve seen, which is induced by cannabis and improved by cessation from cannabis,” she said. “It is important for pediatricians to ask the right questions of their patients in order to better understand what they may be experiencing, provide counseling, and to help them.”
A related issue is cessation, she said. “For those working to achieve cessation from nicotine-based products, sometimes nicotine replacement therapies are helpful. However, cessation from cannabis-containing products is going to look different.”
Although the study did not yield information on the prevalence simultaneous nicotine/cannabis vaping, the authors suggested that some vapers may be combining substances. Previous studies may have modestly overestimated the prevalence of nicotine vaping given their finding that some current e-cigarette users reported vaping cannabis every time they vaped and may be vaping cannabis exclusively. “However, if some current users vaped nicotine and cannabis simultaneously, then overestimation of nicotine vaping would be smaller,” they wrote.
Future surveys on this area should contain detailed questions on nicotine and cannabis vaping, including the substance being vaped and the frequency and intensity of use, Dr. Sun said. “In addition, these surveys could examine some other substances that are being vaped, such as opium and cocaine.”
The PATH study is supported by the NIH, National Institute on Drug Abuse, Department of Health & Human Services, and the FDA’s Center for Tobacco Products. The authors and Dr. Sadreameli had no competing interests to disclose.
Adolescents and young adults who use e-cigarettes reported vaping cannabis, according to selected data from the national Population Assessment of Tobacco and Health (PATH) study.
Ruoyan Sun, PhD, an assistant professor at the University of Alabama at Birmingham, and colleagues examined results of PATH’s wave5 survey conducted from December 2018 to November 2019. PATH is a National Institutes of Health–Food and Drug Administration collaboration begun in 2013.
Their analysis, published online Feb. 7, 2022, in JAMA Pediatrics, evaluated the frequency of cannabis vaping across several age groups: 164 respondents ages 12-14; 919 participants ages 15-17; and 3,038 participants ages 18-24. Respondents included for analysis reported electronic nicotine product consumption in the past 30 days. In response to the question “When you have used an electronic product, how often were you using it to smoke marijuana, marijuana concentrates, marijuana waxes, THC, or hash oils?” 35.0% (95% confidence interval, 29.3%-41.2%) of current e-smokers aged 12-14 years said they had done so, as did 51.3% (95% CI, 47.7%-54.9%) of those aged 15-17 years and 54.6% (95% CI, 52.5%-56.7%) of young adults aged 18-24.
The prevalence of those who reported vaping cannabis every time they vaped was 3.1% (95% CI, 1.3%-6.9%) of youths aged 12-14 years, 6.7% (95% CI, 5.3%-8.6%) of youths aged 15-17 years, and 10.3% (95% CI, 9.0%-11.6%) of young adults aged 18-24.
Among children ages 12-14, 65% said they never vaped cannabis, while 48.7% and 45.4%, respectively, in the two older groups said they did.
“This is a very important finding and it mirrors what some of us have already seen in practice,” said pediatric pulmonologist S. Christy Sadreameli, MD, MHS, an assistant professor of pediatrics at John Hopkins University, Baltimore. “It is important for pediatricians to realize that dual use of cannabis and nicotine vaping, and exclusive use of cannabis vaping, are not uncommon. It informs how we ask questions and how we counsel our patients.” Dr. Sadreameli was not involved in the PATH study.
Overall, the survey participants were 56% male, with 24% of respondents identifying as Hispanic, 8% as non-Hispanic Black, 58% as non-Hispanic White, and 10% as of other race/ethnicity. The weighted proportion of current e-cigarette use was 3.0% (95% CI, 2.6%-3.4%) in youths ages 12-14 years, 14.4% (95% CI, 13.5%-15.3%) in those 15-17 years, and 26.2% (95% CI, 25.3%-27.1%) in young adults.
Other recent national surveys such as the National Institute on Drug Abuses’s Monitoring the Future are reporting a growing prevalence of youth cannabis vaping, Dr. Sun said. For example, the prevalence of cannabis vaping in the past 12-month period among grade 12 students grew from 9.5% in 2017 to 22.1% in 2020. Vaping cannabis was more prevalent among Hispanic teens than other ethnicities.
Vaping devices such as e-cigarettes, vaping pens, e-cigars, and e-hookahs can be used to inhale multiple substances, including nicotine, cannabis, and opium, Dr. Sun noted in an interview. “So in addition to asking about the behavior of vaping itself, pediatricians could pay more attention to what is being vaped in these devices.”
According to Dr. Sadreameli, vaping more than one substance at a time could potentially work synergistically to cause more harm, compared with one product alone. “The other aspect to consider is that vaping multiple types of products may increase the chance of harm from other components of the mixture,” she said. For instance, a lot of the e-cigarette or vaping use-associated lung injury (EVALI) cases have been linked to vitamin E acetate, which was found in certain cannabis formulations. “Anecdotally, most EVALI patients I’ve met seemed to report use of multiple products, including cannabis-containing and nicotine-containing products.”
Dr. Sadreameli added that some cannabis vapers will have other issues. “For example, there is a severe vomiting syndrome I’ve seen, which is induced by cannabis and improved by cessation from cannabis,” she said. “It is important for pediatricians to ask the right questions of their patients in order to better understand what they may be experiencing, provide counseling, and to help them.”
A related issue is cessation, she said. “For those working to achieve cessation from nicotine-based products, sometimes nicotine replacement therapies are helpful. However, cessation from cannabis-containing products is going to look different.”
Although the study did not yield information on the prevalence simultaneous nicotine/cannabis vaping, the authors suggested that some vapers may be combining substances. Previous studies may have modestly overestimated the prevalence of nicotine vaping given their finding that some current e-cigarette users reported vaping cannabis every time they vaped and may be vaping cannabis exclusively. “However, if some current users vaped nicotine and cannabis simultaneously, then overestimation of nicotine vaping would be smaller,” they wrote.
Future surveys on this area should contain detailed questions on nicotine and cannabis vaping, including the substance being vaped and the frequency and intensity of use, Dr. Sun said. “In addition, these surveys could examine some other substances that are being vaped, such as opium and cocaine.”
The PATH study is supported by the NIH, National Institute on Drug Abuse, Department of Health & Human Services, and the FDA’s Center for Tobacco Products. The authors and Dr. Sadreameli had no competing interests to disclose.
Adolescents and young adults who use e-cigarettes reported vaping cannabis, according to selected data from the national Population Assessment of Tobacco and Health (PATH) study.
Ruoyan Sun, PhD, an assistant professor at the University of Alabama at Birmingham, and colleagues examined results of PATH’s wave5 survey conducted from December 2018 to November 2019. PATH is a National Institutes of Health–Food and Drug Administration collaboration begun in 2013.
Their analysis, published online Feb. 7, 2022, in JAMA Pediatrics, evaluated the frequency of cannabis vaping across several age groups: 164 respondents ages 12-14; 919 participants ages 15-17; and 3,038 participants ages 18-24. Respondents included for analysis reported electronic nicotine product consumption in the past 30 days. In response to the question “When you have used an electronic product, how often were you using it to smoke marijuana, marijuana concentrates, marijuana waxes, THC, or hash oils?” 35.0% (95% confidence interval, 29.3%-41.2%) of current e-smokers aged 12-14 years said they had done so, as did 51.3% (95% CI, 47.7%-54.9%) of those aged 15-17 years and 54.6% (95% CI, 52.5%-56.7%) of young adults aged 18-24.
The prevalence of those who reported vaping cannabis every time they vaped was 3.1% (95% CI, 1.3%-6.9%) of youths aged 12-14 years, 6.7% (95% CI, 5.3%-8.6%) of youths aged 15-17 years, and 10.3% (95% CI, 9.0%-11.6%) of young adults aged 18-24.
Among children ages 12-14, 65% said they never vaped cannabis, while 48.7% and 45.4%, respectively, in the two older groups said they did.
“This is a very important finding and it mirrors what some of us have already seen in practice,” said pediatric pulmonologist S. Christy Sadreameli, MD, MHS, an assistant professor of pediatrics at John Hopkins University, Baltimore. “It is important for pediatricians to realize that dual use of cannabis and nicotine vaping, and exclusive use of cannabis vaping, are not uncommon. It informs how we ask questions and how we counsel our patients.” Dr. Sadreameli was not involved in the PATH study.
Overall, the survey participants were 56% male, with 24% of respondents identifying as Hispanic, 8% as non-Hispanic Black, 58% as non-Hispanic White, and 10% as of other race/ethnicity. The weighted proportion of current e-cigarette use was 3.0% (95% CI, 2.6%-3.4%) in youths ages 12-14 years, 14.4% (95% CI, 13.5%-15.3%) in those 15-17 years, and 26.2% (95% CI, 25.3%-27.1%) in young adults.
Other recent national surveys such as the National Institute on Drug Abuses’s Monitoring the Future are reporting a growing prevalence of youth cannabis vaping, Dr. Sun said. For example, the prevalence of cannabis vaping in the past 12-month period among grade 12 students grew from 9.5% in 2017 to 22.1% in 2020. Vaping cannabis was more prevalent among Hispanic teens than other ethnicities.
Vaping devices such as e-cigarettes, vaping pens, e-cigars, and e-hookahs can be used to inhale multiple substances, including nicotine, cannabis, and opium, Dr. Sun noted in an interview. “So in addition to asking about the behavior of vaping itself, pediatricians could pay more attention to what is being vaped in these devices.”
According to Dr. Sadreameli, vaping more than one substance at a time could potentially work synergistically to cause more harm, compared with one product alone. “The other aspect to consider is that vaping multiple types of products may increase the chance of harm from other components of the mixture,” she said. For instance, a lot of the e-cigarette or vaping use-associated lung injury (EVALI) cases have been linked to vitamin E acetate, which was found in certain cannabis formulations. “Anecdotally, most EVALI patients I’ve met seemed to report use of multiple products, including cannabis-containing and nicotine-containing products.”
Dr. Sadreameli added that some cannabis vapers will have other issues. “For example, there is a severe vomiting syndrome I’ve seen, which is induced by cannabis and improved by cessation from cannabis,” she said. “It is important for pediatricians to ask the right questions of their patients in order to better understand what they may be experiencing, provide counseling, and to help them.”
A related issue is cessation, she said. “For those working to achieve cessation from nicotine-based products, sometimes nicotine replacement therapies are helpful. However, cessation from cannabis-containing products is going to look different.”
Although the study did not yield information on the prevalence simultaneous nicotine/cannabis vaping, the authors suggested that some vapers may be combining substances. Previous studies may have modestly overestimated the prevalence of nicotine vaping given their finding that some current e-cigarette users reported vaping cannabis every time they vaped and may be vaping cannabis exclusively. “However, if some current users vaped nicotine and cannabis simultaneously, then overestimation of nicotine vaping would be smaller,” they wrote.
Future surveys on this area should contain detailed questions on nicotine and cannabis vaping, including the substance being vaped and the frequency and intensity of use, Dr. Sun said. “In addition, these surveys could examine some other substances that are being vaped, such as opium and cocaine.”
The PATH study is supported by the NIH, National Institute on Drug Abuse, Department of Health & Human Services, and the FDA’s Center for Tobacco Products. The authors and Dr. Sadreameli had no competing interests to disclose.
FROM JAMA PEDIATRICS