User login
Does giving moms cash make babies smarter?
In his first State of the Union address in early March, President Joe Biden broached a tax policy question that neuroscientists and pediatricians also see as a scientific one.
President Biden urged lawmakers to extend the Child Tax Credit “so no one has to raise a family in poverty.”
Apart from the usual political and budgetary calculus, physicians and social scientists are actively examining the ramifications that such policies could have on child development and long-term health outcomes.
To do so, they have turned to brain scans and rigorous studies to better understand the effects of being raised in poverty and whether giving families more cash makes a difference.
Initial results from an ongoing study known as Baby’s First Years suggest that providing extra money to mothers may influence brain activity in infants in ways that reflect improvements in cognitive ability.
Researchers, doctors, and advocates say the findings cement the case for policies such as the expanded Child Tax Credit. Others argue that reducing child poverty is a social good on its own, regardless of what brain scans show.
The new findings were published Jan. 24 in Proceedings of the National Academy of Sciences (PNAS), as lawmakers were weighing whether to resume an expansion of the tax credit, which had temporarily provided monthly payments akin to the $333 a month looked at in the study.
The expiration of the expanded credit in December left some 3.6 million more children in poverty, bringing the total number to more than 12.5 million and pushing the child poverty rate to 17%.
Philanthropists and research teams have partnered to conduct other guaranteed income experiments around the United States, including one in New York called the Bridge Project, which is evaluating different levels of financial support for mothers with babies.
Some mothers are receiving $500 per month, others twice that amount.
Angelina Matos, 18, receives $1,000 a month, allowing her to attend college and pay for necessities like diapers, clothes, and toys for her nearly 1-year-old daughter.
As one of 600 mothers participating in the project, Ms. Matos periodically answers questions about her daughter’s progress, like whether she is eating solid foods.
Megha Agarwal, BS, executive director of the Bridge Project and its funder the Monarch Foundation, said she was thrilled to see the early results from Baby’s First Years. “We are looking for ways in which we can strengthen our future generations,” she said. “It is exciting to see that direct cash and a guaranteed income might be part of the solution.”
A scientific perspective
Growing up in poverty is well-known to increase the likelihood of lower academic achievement and chronic conditions such as asthma and obesity. Relative to higher income levels, poverty is associated with differences in the structure and function of the developing brain. But whether interventions to reduce poverty can influence how newborns develop is less clear.
“There would be plenty of people who would say, ‘Well, it’s not poverty. It’s all the things associated with poverty. It’s the choices you make that are actually leading to differences in outcomes,’” said Kimberly Noble, MD, PhD, a neuroscientist at Columbia University, New York, and a coauthor of the PNAS study. Regardless of ideology, she said, the best way to address that question from a scientific perspective is through a randomized controlled trial.
“You can’t, and wouldn’t want to, randomize kids to living in poverty or not, but you can take a group of families who are unfortunately living in poverty and randomize them to receive different levels of economic support,” Dr. Noble said.
$333 per month
Baby’s First Years has done just that. Researchers gave 1,000 low-income mothers with newborns a cash gift of $333 per month or a smaller gift of $20 per month, disbursed on debit cards, starting in 2018. Participants live in four metropolitan areas – New York City, greater New Orleans, Minneapolis-Saint Paul, and Omaha – and were recruited at the time of their child’s birth. Investigators currently have funding to continue the cash support until the children turn 4 years old.
When the infants were about 1 year old, investigators measured their resting brain activity using EEG.
The COVID-19 pandemic disrupted the ability to conduct in-person testing, so the number of children with EEG data was smaller than planned. Still, the researchers analyzed data from 251 kids in the group that received the smaller cash gift and 184 kids in the group that received the larger amount. Patterns of brain activity largely tracked those seen in earlier observational studies: more mid- and high-frequency activity (alpha-, beta-, and gamma-bands) and less low-frequency activity (theta-bands) among children in the households that received more money.
Faster brain activity is associated with better scores on measures of language, cognition, and social-emotional development. Slower activity has been linked to problems with behavior, attention, and learning.
“We predicted that our poverty reduction intervention would mitigate the neurobiological signal of poverty,” Dr. Noble said. “And that’s exactly what we report in this paper.”
The study builds on decades of work showing that poverty can harm child development, said Joan Luby, MD, with Washington University School of Medicine, St. Louis, who served as a peer reviewer for the PNAS paper.
More follow-up data and information about the babies’ cognitive function and behavior over time are needed, but the study shows a signal that cannot be ignored, Dr. Luby said.
Dr. Luby began exploring the effects of poverty on brain development in earnest while working on a study that was meant to focus on another variable altogether: early childhood depression. The investigators on that 2013 study found that poverty had a “very, very big effect in our sample, and we realized we had to learn more about it,” she said.
The American Academy of Pediatrics likewise has recognized poverty as an important determinant of health. A policy statement that the group published in 2016 and reaffirmed in 2021 outlines ways pediatricians and social programs can address poverty.
Benard Dreyer, MD, director of pediatrics at Bellevue Hospital, New York, was president of the AAP when it published this guidance.
One lingering question has been how much low income worsens educational outcomes, Dr. Dreyer said. Perhaps other issues, such as single motherhood, a lack of parental education, or living in neighborhoods with more crime may be the cause. If so, simply giving more money to parents might not overcome those barriers.
Natural experiments have hinted that money itself can influence child development. For example, families on an American Indian reservation in North Carolina started receiving a share of casino profits after a casino opened there.
The new infusion of funds arrived in the middle of a study in which researchers were examining the development of mental illness in children.
Among children who were no longer poor as a result of the casino payments, symptoms of conduct and oppositional defiant disorders decreased.
Guaranteeing income
How extra money affects families across different levels of income also interests researchers and policymakers.
“One of the policy debates in Washington is to what degree should it be to everyone,” Ajay Chaudry, PhD, a research scholar at New York University who is advising the Bridge Project, said.
Guaranteed income programs may need to be available to most of the population out of political necessity, even if the benefits turn out to be the most pronounced at lower income levels, added Dr. Chaudry, who served in the Obama administration as deputy assistant secretary for human services policy.
If giving moms money affects babies’ brains, Dr. Dreyer pointed to two pathways that could explain the link: more resources and less family stress.
Money helps families buy toys and books, which in turn could support a child’s cognitive development. Meanwhile, low-income mothers and fathers may experience worries about eviction, adequate food, and the loss of heat and electricity, which could detract from their ability to parent.
Of course, many ways to support a child’s development do not require money. Engaging with children in a warm and nurturing way, having conversations with them, and reading with them are all important.
If the pattern in the PNAS study holds, individual experiences and outcomes will still vary, Dr. Noble said. Many children in the group that received the smaller gift had fast-paced brain activity, whereas some babies in the group that received the larger gift showed slower brain activity. Knowing family income would not allow you to accurately predict anything about an individual child’s brain, Dr. Noble said.
“I certainly wouldn’t want the message to be that money is the only thing that matters,” Dr. Noble said. “Money is something that can be easily manipulated by policy, which is why I think this is important.”
For the 18-year-old new mom Ms. Matos, accepting assistance “makes me feel less of myself. But honestly, I feel like mothers shouldn’t be afraid to ask for help or reach out for help or apply to programs like these.”
The sources reported a variety of funders, including federal agencies and foundations and donors.
A version of this article first appeared on Medscape.com.
In his first State of the Union address in early March, President Joe Biden broached a tax policy question that neuroscientists and pediatricians also see as a scientific one.
President Biden urged lawmakers to extend the Child Tax Credit “so no one has to raise a family in poverty.”
Apart from the usual political and budgetary calculus, physicians and social scientists are actively examining the ramifications that such policies could have on child development and long-term health outcomes.
To do so, they have turned to brain scans and rigorous studies to better understand the effects of being raised in poverty and whether giving families more cash makes a difference.
Initial results from an ongoing study known as Baby’s First Years suggest that providing extra money to mothers may influence brain activity in infants in ways that reflect improvements in cognitive ability.
Researchers, doctors, and advocates say the findings cement the case for policies such as the expanded Child Tax Credit. Others argue that reducing child poverty is a social good on its own, regardless of what brain scans show.
The new findings were published Jan. 24 in Proceedings of the National Academy of Sciences (PNAS), as lawmakers were weighing whether to resume an expansion of the tax credit, which had temporarily provided monthly payments akin to the $333 a month looked at in the study.
The expiration of the expanded credit in December left some 3.6 million more children in poverty, bringing the total number to more than 12.5 million and pushing the child poverty rate to 17%.
Philanthropists and research teams have partnered to conduct other guaranteed income experiments around the United States, including one in New York called the Bridge Project, which is evaluating different levels of financial support for mothers with babies.
Some mothers are receiving $500 per month, others twice that amount.
Angelina Matos, 18, receives $1,000 a month, allowing her to attend college and pay for necessities like diapers, clothes, and toys for her nearly 1-year-old daughter.
As one of 600 mothers participating in the project, Ms. Matos periodically answers questions about her daughter’s progress, like whether she is eating solid foods.
Megha Agarwal, BS, executive director of the Bridge Project and its funder the Monarch Foundation, said she was thrilled to see the early results from Baby’s First Years. “We are looking for ways in which we can strengthen our future generations,” she said. “It is exciting to see that direct cash and a guaranteed income might be part of the solution.”
A scientific perspective
Growing up in poverty is well-known to increase the likelihood of lower academic achievement and chronic conditions such as asthma and obesity. Relative to higher income levels, poverty is associated with differences in the structure and function of the developing brain. But whether interventions to reduce poverty can influence how newborns develop is less clear.
“There would be plenty of people who would say, ‘Well, it’s not poverty. It’s all the things associated with poverty. It’s the choices you make that are actually leading to differences in outcomes,’” said Kimberly Noble, MD, PhD, a neuroscientist at Columbia University, New York, and a coauthor of the PNAS study. Regardless of ideology, she said, the best way to address that question from a scientific perspective is through a randomized controlled trial.
“You can’t, and wouldn’t want to, randomize kids to living in poverty or not, but you can take a group of families who are unfortunately living in poverty and randomize them to receive different levels of economic support,” Dr. Noble said.
$333 per month
Baby’s First Years has done just that. Researchers gave 1,000 low-income mothers with newborns a cash gift of $333 per month or a smaller gift of $20 per month, disbursed on debit cards, starting in 2018. Participants live in four metropolitan areas – New York City, greater New Orleans, Minneapolis-Saint Paul, and Omaha – and were recruited at the time of their child’s birth. Investigators currently have funding to continue the cash support until the children turn 4 years old.
When the infants were about 1 year old, investigators measured their resting brain activity using EEG.
The COVID-19 pandemic disrupted the ability to conduct in-person testing, so the number of children with EEG data was smaller than planned. Still, the researchers analyzed data from 251 kids in the group that received the smaller cash gift and 184 kids in the group that received the larger amount. Patterns of brain activity largely tracked those seen in earlier observational studies: more mid- and high-frequency activity (alpha-, beta-, and gamma-bands) and less low-frequency activity (theta-bands) among children in the households that received more money.
Faster brain activity is associated with better scores on measures of language, cognition, and social-emotional development. Slower activity has been linked to problems with behavior, attention, and learning.
“We predicted that our poverty reduction intervention would mitigate the neurobiological signal of poverty,” Dr. Noble said. “And that’s exactly what we report in this paper.”
The study builds on decades of work showing that poverty can harm child development, said Joan Luby, MD, with Washington University School of Medicine, St. Louis, who served as a peer reviewer for the PNAS paper.
More follow-up data and information about the babies’ cognitive function and behavior over time are needed, but the study shows a signal that cannot be ignored, Dr. Luby said.
Dr. Luby began exploring the effects of poverty on brain development in earnest while working on a study that was meant to focus on another variable altogether: early childhood depression. The investigators on that 2013 study found that poverty had a “very, very big effect in our sample, and we realized we had to learn more about it,” she said.
The American Academy of Pediatrics likewise has recognized poverty as an important determinant of health. A policy statement that the group published in 2016 and reaffirmed in 2021 outlines ways pediatricians and social programs can address poverty.
Benard Dreyer, MD, director of pediatrics at Bellevue Hospital, New York, was president of the AAP when it published this guidance.
One lingering question has been how much low income worsens educational outcomes, Dr. Dreyer said. Perhaps other issues, such as single motherhood, a lack of parental education, or living in neighborhoods with more crime may be the cause. If so, simply giving more money to parents might not overcome those barriers.
Natural experiments have hinted that money itself can influence child development. For example, families on an American Indian reservation in North Carolina started receiving a share of casino profits after a casino opened there.
The new infusion of funds arrived in the middle of a study in which researchers were examining the development of mental illness in children.
Among children who were no longer poor as a result of the casino payments, symptoms of conduct and oppositional defiant disorders decreased.
Guaranteeing income
How extra money affects families across different levels of income also interests researchers and policymakers.
“One of the policy debates in Washington is to what degree should it be to everyone,” Ajay Chaudry, PhD, a research scholar at New York University who is advising the Bridge Project, said.
Guaranteed income programs may need to be available to most of the population out of political necessity, even if the benefits turn out to be the most pronounced at lower income levels, added Dr. Chaudry, who served in the Obama administration as deputy assistant secretary for human services policy.
If giving moms money affects babies’ brains, Dr. Dreyer pointed to two pathways that could explain the link: more resources and less family stress.
Money helps families buy toys and books, which in turn could support a child’s cognitive development. Meanwhile, low-income mothers and fathers may experience worries about eviction, adequate food, and the loss of heat and electricity, which could detract from their ability to parent.
Of course, many ways to support a child’s development do not require money. Engaging with children in a warm and nurturing way, having conversations with them, and reading with them are all important.
If the pattern in the PNAS study holds, individual experiences and outcomes will still vary, Dr. Noble said. Many children in the group that received the smaller gift had fast-paced brain activity, whereas some babies in the group that received the larger gift showed slower brain activity. Knowing family income would not allow you to accurately predict anything about an individual child’s brain, Dr. Noble said.
“I certainly wouldn’t want the message to be that money is the only thing that matters,” Dr. Noble said. “Money is something that can be easily manipulated by policy, which is why I think this is important.”
For the 18-year-old new mom Ms. Matos, accepting assistance “makes me feel less of myself. But honestly, I feel like mothers shouldn’t be afraid to ask for help or reach out for help or apply to programs like these.”
The sources reported a variety of funders, including federal agencies and foundations and donors.
A version of this article first appeared on Medscape.com.
In his first State of the Union address in early March, President Joe Biden broached a tax policy question that neuroscientists and pediatricians also see as a scientific one.
President Biden urged lawmakers to extend the Child Tax Credit “so no one has to raise a family in poverty.”
Apart from the usual political and budgetary calculus, physicians and social scientists are actively examining the ramifications that such policies could have on child development and long-term health outcomes.
To do so, they have turned to brain scans and rigorous studies to better understand the effects of being raised in poverty and whether giving families more cash makes a difference.
Initial results from an ongoing study known as Baby’s First Years suggest that providing extra money to mothers may influence brain activity in infants in ways that reflect improvements in cognitive ability.
Researchers, doctors, and advocates say the findings cement the case for policies such as the expanded Child Tax Credit. Others argue that reducing child poverty is a social good on its own, regardless of what brain scans show.
The new findings were published Jan. 24 in Proceedings of the National Academy of Sciences (PNAS), as lawmakers were weighing whether to resume an expansion of the tax credit, which had temporarily provided monthly payments akin to the $333 a month looked at in the study.
The expiration of the expanded credit in December left some 3.6 million more children in poverty, bringing the total number to more than 12.5 million and pushing the child poverty rate to 17%.
Philanthropists and research teams have partnered to conduct other guaranteed income experiments around the United States, including one in New York called the Bridge Project, which is evaluating different levels of financial support for mothers with babies.
Some mothers are receiving $500 per month, others twice that amount.
Angelina Matos, 18, receives $1,000 a month, allowing her to attend college and pay for necessities like diapers, clothes, and toys for her nearly 1-year-old daughter.
As one of 600 mothers participating in the project, Ms. Matos periodically answers questions about her daughter’s progress, like whether she is eating solid foods.
Megha Agarwal, BS, executive director of the Bridge Project and its funder the Monarch Foundation, said she was thrilled to see the early results from Baby’s First Years. “We are looking for ways in which we can strengthen our future generations,” she said. “It is exciting to see that direct cash and a guaranteed income might be part of the solution.”
A scientific perspective
Growing up in poverty is well-known to increase the likelihood of lower academic achievement and chronic conditions such as asthma and obesity. Relative to higher income levels, poverty is associated with differences in the structure and function of the developing brain. But whether interventions to reduce poverty can influence how newborns develop is less clear.
“There would be plenty of people who would say, ‘Well, it’s not poverty. It’s all the things associated with poverty. It’s the choices you make that are actually leading to differences in outcomes,’” said Kimberly Noble, MD, PhD, a neuroscientist at Columbia University, New York, and a coauthor of the PNAS study. Regardless of ideology, she said, the best way to address that question from a scientific perspective is through a randomized controlled trial.
“You can’t, and wouldn’t want to, randomize kids to living in poverty or not, but you can take a group of families who are unfortunately living in poverty and randomize them to receive different levels of economic support,” Dr. Noble said.
$333 per month
Baby’s First Years has done just that. Researchers gave 1,000 low-income mothers with newborns a cash gift of $333 per month or a smaller gift of $20 per month, disbursed on debit cards, starting in 2018. Participants live in four metropolitan areas – New York City, greater New Orleans, Minneapolis-Saint Paul, and Omaha – and were recruited at the time of their child’s birth. Investigators currently have funding to continue the cash support until the children turn 4 years old.
When the infants were about 1 year old, investigators measured their resting brain activity using EEG.
The COVID-19 pandemic disrupted the ability to conduct in-person testing, so the number of children with EEG data was smaller than planned. Still, the researchers analyzed data from 251 kids in the group that received the smaller cash gift and 184 kids in the group that received the larger amount. Patterns of brain activity largely tracked those seen in earlier observational studies: more mid- and high-frequency activity (alpha-, beta-, and gamma-bands) and less low-frequency activity (theta-bands) among children in the households that received more money.
Faster brain activity is associated with better scores on measures of language, cognition, and social-emotional development. Slower activity has been linked to problems with behavior, attention, and learning.
“We predicted that our poverty reduction intervention would mitigate the neurobiological signal of poverty,” Dr. Noble said. “And that’s exactly what we report in this paper.”
The study builds on decades of work showing that poverty can harm child development, said Joan Luby, MD, with Washington University School of Medicine, St. Louis, who served as a peer reviewer for the PNAS paper.
More follow-up data and information about the babies’ cognitive function and behavior over time are needed, but the study shows a signal that cannot be ignored, Dr. Luby said.
Dr. Luby began exploring the effects of poverty on brain development in earnest while working on a study that was meant to focus on another variable altogether: early childhood depression. The investigators on that 2013 study found that poverty had a “very, very big effect in our sample, and we realized we had to learn more about it,” she said.
The American Academy of Pediatrics likewise has recognized poverty as an important determinant of health. A policy statement that the group published in 2016 and reaffirmed in 2021 outlines ways pediatricians and social programs can address poverty.
Benard Dreyer, MD, director of pediatrics at Bellevue Hospital, New York, was president of the AAP when it published this guidance.
One lingering question has been how much low income worsens educational outcomes, Dr. Dreyer said. Perhaps other issues, such as single motherhood, a lack of parental education, or living in neighborhoods with more crime may be the cause. If so, simply giving more money to parents might not overcome those barriers.
Natural experiments have hinted that money itself can influence child development. For example, families on an American Indian reservation in North Carolina started receiving a share of casino profits after a casino opened there.
The new infusion of funds arrived in the middle of a study in which researchers were examining the development of mental illness in children.
Among children who were no longer poor as a result of the casino payments, symptoms of conduct and oppositional defiant disorders decreased.
Guaranteeing income
How extra money affects families across different levels of income also interests researchers and policymakers.
“One of the policy debates in Washington is to what degree should it be to everyone,” Ajay Chaudry, PhD, a research scholar at New York University who is advising the Bridge Project, said.
Guaranteed income programs may need to be available to most of the population out of political necessity, even if the benefits turn out to be the most pronounced at lower income levels, added Dr. Chaudry, who served in the Obama administration as deputy assistant secretary for human services policy.
If giving moms money affects babies’ brains, Dr. Dreyer pointed to two pathways that could explain the link: more resources and less family stress.
Money helps families buy toys and books, which in turn could support a child’s cognitive development. Meanwhile, low-income mothers and fathers may experience worries about eviction, adequate food, and the loss of heat and electricity, which could detract from their ability to parent.
Of course, many ways to support a child’s development do not require money. Engaging with children in a warm and nurturing way, having conversations with them, and reading with them are all important.
If the pattern in the PNAS study holds, individual experiences and outcomes will still vary, Dr. Noble said. Many children in the group that received the smaller gift had fast-paced brain activity, whereas some babies in the group that received the larger gift showed slower brain activity. Knowing family income would not allow you to accurately predict anything about an individual child’s brain, Dr. Noble said.
“I certainly wouldn’t want the message to be that money is the only thing that matters,” Dr. Noble said. “Money is something that can be easily manipulated by policy, which is why I think this is important.”
For the 18-year-old new mom Ms. Matos, accepting assistance “makes me feel less of myself. But honestly, I feel like mothers shouldn’t be afraid to ask for help or reach out for help or apply to programs like these.”
The sources reported a variety of funders, including federal agencies and foundations and donors.
A version of this article first appeared on Medscape.com.
What’s the future of microbiome therapies in C. diff, cancer?
WASHINGTON – Research on standardized microbiome-based therapies designed to prevent the recurrence of Clostridioides difficile infection (CDI) is moving “with a lot of momentum,” according to one expert, and modulation of the gut microbiome may even enhance responses to immunotherapy and/or abrogate toxicity, according to another.
Several products for prevention of CDI recurrence are poised for either phase 3 trials or upcoming Food and Drug Administration approval, Sahil Khanna, MBBS, MS, professor of medicine, gastroenterology, and hepatology at the Mayo Clinic in Rochester, Minn., reported at the annual Gut Microbiota for Health World Summit.
Jennifer A. Wargo, MD, MMSc, of the University of Texas MD Anderson Cancer Center, Houston, described her investigations of microbiome modulation’s role in cancer treatment. “I used to say yes [we can do this] somewhat enthusiastically without data, but now we have data to support this,” she said at the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility. “The answer now is totally yes.”
New approaches for CDI
“Based on how the field is moving, we might be able to [offer our patients] earlier microbiome restoration” than is currently afforded with fecal microbiota transplantation (FMT), he said. “Right now the [Food and Drug Administration] and our clinical guidelines say we should do FMT after three or more episodes [of CDI] – that’s heartbreaking for patients.”
Several of the microbiome-based therapies under investigation – including two poised for phase 3 trials – have shown efficacy after a second episode of CDI, and one of these two has also had positive results after one episode of CDI in patients 65 at older, a group at particularly high risk of recurrence, said Dr. Khanna.
The value of standardized, mostly pill-form microbiome therapies has been heightened during the pandemic. “We’ve been doing conventional FMT for recurrent C. difficile for over a decade now, and it’s probably the most effective treatment we have,” said Colleen R. Kelly, MD, associate professor of medicine at Brown University, Providence, R.I., and moderator of the session on microbiota-based therapies.
Prepandemic “it got really hard, with issues of identifying donors, and quality control and safety ... And then when COVID hit the stool banks shut down,” she said in an interview after the meeting. With stool testing for SARS-CoV-2 now in place, some stool is again available, “but it made me realize how fragile our current system is,” Dr. Kelly said. “The fact that companies are putting these products through the FDA pipeline and investigating them in rigorous, scientific randomized controlled trials is really good for the field.”
The products vary in composition; some are live multi-strain biotherapeutics derived from donor stool, for instance, while others are defined live bacterial consortia not from stool. Most are oral formulations, given one or multiple times, that do not require any bowel preparation.
One of the products most advanced in the pipeline, RBX2660 (Rebiotix, Ferring Pharmaceuticals) is stool derived and rectally administered. In phase 3 research, 70.5% of patients who received one active enema after having had two or more CDI recurrences and standard-of-care antibiotic treatment had no additional recurrence at 8 weeks compared to 58.1% in the placebo group, Dr. Khanna said.
The other product with positive phase 3 results, SER-109 (Seres Therapeutics), is a donor stool-derived oral formulation of purified Firmicutes spores that is administered after bowel prep. In results published earlier this year, the percentage of patients with recurrence of CDI up to 8 weeks after standard antibiotic treatment was 12% in the SER-109 group and 40% in the placebo group.
Patients in this trial were required to have had three episodes of CDI, and interestingly, Dr. Khanna said, the diagnosis of CDI was made only by toxin enzyme immunoassay (EIA). Earlier phase 2 research, which allowed either toxin EIA or polymerase chain reaction testing for the diagnosis of CDI (as other trials have done), produced negative results, leading investigators to surmise that some of the included patients had been colonized with C. difficile rather than being actively infected, Dr. Khanna said.
Researchers of these trials are documenting not only resolution of CDI but what they believe are positive shifts in the gut microbiota after microbiome-based therapy, he said. For instance, a phase 1 trial he led of the product RBX7455 (Rebiotix, Ferring Pharmaceuticals) – an oral capsule of lyophilized stool-based bacteria that can be kept for several days at room temperature – showed increases in Bacteroidia and Clostridia.
And other trials’ analyses of microbiome engraftment have demonstrated that “you can restore [species] even when these bacteria aren’t [included in the therapy],” he noted. “As the milieu of the gut improves, species that were not detected start coming back up.”
Asked about rates of efficacy in the trials’ placebo arms, Dr. Khanna said that “we’ve become smarter with our antibiotic regimens ... the placebo response rate is the response to newer guideline-based therapies.”
In addition to CDI, microbiome-based therapies are being studied, mostly in phase 1 research, for indications such as Crohn’s disease, ulcerative colitis, autism spectrum disorder, hepatitis B, and hepatic encephalopathy, Dr. Khanna noted.
Dr. Kelly, whose own research has focused on FMT for CDI, said she anticipates an expansion of research into other indications once products to prevent CDI recurrence are on the market. “There have been a couple of promising ulcerative colitis trials that haven’t gone anywhere clinically yet,” she said in the interview. “But will we now identify patients with UC who may be more sensitive to microbial manipulation, for whom we can use these microbial therapies along with a biologic?”
Some of her patients with IBD and CDI who are treated with FMT have not only had their CDI eradicated but have subsequently seen improvements in their IBD, she noted.
The role of traditional FMT and of stool banks will likely change in the future with new standardized oral microbiome-based therapies that can be approved and regulated by the FDA, she said. However, “we think the stool banks will still have some value,” she said, certainly for clinical research and probably for some treatment purposes as well. Regarding new therapies, “I just really hope they’re affordable,” she said.
Gut microbiome manipulation for cancer
Dr. Wargo’s research at MD Anderson has focused on metastatic breast cancer and immunotherapeutic checkpoint blockade. By sequencing microbiota samples and performing immune profiling in hundreds of patients, her team found that responders to PD-1 blockage have a greater diversity of gut bacteria and that “favorable signatures in the gut microbiome” are associated with enhanced immune responses in the tumor microenvironment.
Studies published last year in Science from investigators in Israel (2021 Feb 5;371[6529]:602-9) and Pittsburgh (2021 Feb 5;371[6529]:595-602), demonstrated that FMT promotes response in immunotherapy-refractory melanoma patients. In one study, FMT provided clinical benefit in 6 of 15 patients whose cancer had progressed on prior anti-PD-1 therapy, “which is pretty remarkable,” Dr. Wargo said.
Both research groups, she noted, saw favorable changes in the gut microbiome and immune cell infiltrates both at the level of the colon and the tumor.
Current research on FMT and other microbiome modulation strategies for cancer is guided in part by knowledge that tumors have microbial signatures – these signatures are now being identified across all tumor types – and by findings of “cross talk” between the gut and tumor microbiomes, she explained.
“Researchers are working hard to identify optimal consortia to enhance immune responses in the cancer setting, with promising work in preclinical models,” she said, and clinical trials are in progress. The role of diet in modulating the microbiome and enhancing anti-tumor immunity, with a focus on high dietary fiber intake, is also being investigated, she said.
Dr. Wargo reported that she serves on the advisory boards and is a paid speaker of numerous pharmaceutical and biotechnology companies, and is the coinventor of a patent submitted by the Texas MD Anderson Cancer Center on modulating the microbiome to enhance response to checkpoint blockade, and another related patent. Dr. Khanna reported that he is involved in research with Ferring/Rebiotix, Finch, Seres, Pfizer and Vendata, and does consulting for Immuron and several other companies. Dr. Kelly said she serves as an unpaid adviser for OpenBiome, a nonprofit stool bank, and that her site has enrolled patients in two of the trials testing products for CDI.
WASHINGTON – Research on standardized microbiome-based therapies designed to prevent the recurrence of Clostridioides difficile infection (CDI) is moving “with a lot of momentum,” according to one expert, and modulation of the gut microbiome may even enhance responses to immunotherapy and/or abrogate toxicity, according to another.
Several products for prevention of CDI recurrence are poised for either phase 3 trials or upcoming Food and Drug Administration approval, Sahil Khanna, MBBS, MS, professor of medicine, gastroenterology, and hepatology at the Mayo Clinic in Rochester, Minn., reported at the annual Gut Microbiota for Health World Summit.
Jennifer A. Wargo, MD, MMSc, of the University of Texas MD Anderson Cancer Center, Houston, described her investigations of microbiome modulation’s role in cancer treatment. “I used to say yes [we can do this] somewhat enthusiastically without data, but now we have data to support this,” she said at the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility. “The answer now is totally yes.”
New approaches for CDI
“Based on how the field is moving, we might be able to [offer our patients] earlier microbiome restoration” than is currently afforded with fecal microbiota transplantation (FMT), he said. “Right now the [Food and Drug Administration] and our clinical guidelines say we should do FMT after three or more episodes [of CDI] – that’s heartbreaking for patients.”
Several of the microbiome-based therapies under investigation – including two poised for phase 3 trials – have shown efficacy after a second episode of CDI, and one of these two has also had positive results after one episode of CDI in patients 65 at older, a group at particularly high risk of recurrence, said Dr. Khanna.
The value of standardized, mostly pill-form microbiome therapies has been heightened during the pandemic. “We’ve been doing conventional FMT for recurrent C. difficile for over a decade now, and it’s probably the most effective treatment we have,” said Colleen R. Kelly, MD, associate professor of medicine at Brown University, Providence, R.I., and moderator of the session on microbiota-based therapies.
Prepandemic “it got really hard, with issues of identifying donors, and quality control and safety ... And then when COVID hit the stool banks shut down,” she said in an interview after the meeting. With stool testing for SARS-CoV-2 now in place, some stool is again available, “but it made me realize how fragile our current system is,” Dr. Kelly said. “The fact that companies are putting these products through the FDA pipeline and investigating them in rigorous, scientific randomized controlled trials is really good for the field.”
The products vary in composition; some are live multi-strain biotherapeutics derived from donor stool, for instance, while others are defined live bacterial consortia not from stool. Most are oral formulations, given one or multiple times, that do not require any bowel preparation.
One of the products most advanced in the pipeline, RBX2660 (Rebiotix, Ferring Pharmaceuticals) is stool derived and rectally administered. In phase 3 research, 70.5% of patients who received one active enema after having had two or more CDI recurrences and standard-of-care antibiotic treatment had no additional recurrence at 8 weeks compared to 58.1% in the placebo group, Dr. Khanna said.
The other product with positive phase 3 results, SER-109 (Seres Therapeutics), is a donor stool-derived oral formulation of purified Firmicutes spores that is administered after bowel prep. In results published earlier this year, the percentage of patients with recurrence of CDI up to 8 weeks after standard antibiotic treatment was 12% in the SER-109 group and 40% in the placebo group.
Patients in this trial were required to have had three episodes of CDI, and interestingly, Dr. Khanna said, the diagnosis of CDI was made only by toxin enzyme immunoassay (EIA). Earlier phase 2 research, which allowed either toxin EIA or polymerase chain reaction testing for the diagnosis of CDI (as other trials have done), produced negative results, leading investigators to surmise that some of the included patients had been colonized with C. difficile rather than being actively infected, Dr. Khanna said.
Researchers of these trials are documenting not only resolution of CDI but what they believe are positive shifts in the gut microbiota after microbiome-based therapy, he said. For instance, a phase 1 trial he led of the product RBX7455 (Rebiotix, Ferring Pharmaceuticals) – an oral capsule of lyophilized stool-based bacteria that can be kept for several days at room temperature – showed increases in Bacteroidia and Clostridia.
And other trials’ analyses of microbiome engraftment have demonstrated that “you can restore [species] even when these bacteria aren’t [included in the therapy],” he noted. “As the milieu of the gut improves, species that were not detected start coming back up.”
Asked about rates of efficacy in the trials’ placebo arms, Dr. Khanna said that “we’ve become smarter with our antibiotic regimens ... the placebo response rate is the response to newer guideline-based therapies.”
In addition to CDI, microbiome-based therapies are being studied, mostly in phase 1 research, for indications such as Crohn’s disease, ulcerative colitis, autism spectrum disorder, hepatitis B, and hepatic encephalopathy, Dr. Khanna noted.
Dr. Kelly, whose own research has focused on FMT for CDI, said she anticipates an expansion of research into other indications once products to prevent CDI recurrence are on the market. “There have been a couple of promising ulcerative colitis trials that haven’t gone anywhere clinically yet,” she said in the interview. “But will we now identify patients with UC who may be more sensitive to microbial manipulation, for whom we can use these microbial therapies along with a biologic?”
Some of her patients with IBD and CDI who are treated with FMT have not only had their CDI eradicated but have subsequently seen improvements in their IBD, she noted.
The role of traditional FMT and of stool banks will likely change in the future with new standardized oral microbiome-based therapies that can be approved and regulated by the FDA, she said. However, “we think the stool banks will still have some value,” she said, certainly for clinical research and probably for some treatment purposes as well. Regarding new therapies, “I just really hope they’re affordable,” she said.
Gut microbiome manipulation for cancer
Dr. Wargo’s research at MD Anderson has focused on metastatic breast cancer and immunotherapeutic checkpoint blockade. By sequencing microbiota samples and performing immune profiling in hundreds of patients, her team found that responders to PD-1 blockage have a greater diversity of gut bacteria and that “favorable signatures in the gut microbiome” are associated with enhanced immune responses in the tumor microenvironment.
Studies published last year in Science from investigators in Israel (2021 Feb 5;371[6529]:602-9) and Pittsburgh (2021 Feb 5;371[6529]:595-602), demonstrated that FMT promotes response in immunotherapy-refractory melanoma patients. In one study, FMT provided clinical benefit in 6 of 15 patients whose cancer had progressed on prior anti-PD-1 therapy, “which is pretty remarkable,” Dr. Wargo said.
Both research groups, she noted, saw favorable changes in the gut microbiome and immune cell infiltrates both at the level of the colon and the tumor.
Current research on FMT and other microbiome modulation strategies for cancer is guided in part by knowledge that tumors have microbial signatures – these signatures are now being identified across all tumor types – and by findings of “cross talk” between the gut and tumor microbiomes, she explained.
“Researchers are working hard to identify optimal consortia to enhance immune responses in the cancer setting, with promising work in preclinical models,” she said, and clinical trials are in progress. The role of diet in modulating the microbiome and enhancing anti-tumor immunity, with a focus on high dietary fiber intake, is also being investigated, she said.
Dr. Wargo reported that she serves on the advisory boards and is a paid speaker of numerous pharmaceutical and biotechnology companies, and is the coinventor of a patent submitted by the Texas MD Anderson Cancer Center on modulating the microbiome to enhance response to checkpoint blockade, and another related patent. Dr. Khanna reported that he is involved in research with Ferring/Rebiotix, Finch, Seres, Pfizer and Vendata, and does consulting for Immuron and several other companies. Dr. Kelly said she serves as an unpaid adviser for OpenBiome, a nonprofit stool bank, and that her site has enrolled patients in two of the trials testing products for CDI.
WASHINGTON – Research on standardized microbiome-based therapies designed to prevent the recurrence of Clostridioides difficile infection (CDI) is moving “with a lot of momentum,” according to one expert, and modulation of the gut microbiome may even enhance responses to immunotherapy and/or abrogate toxicity, according to another.
Several products for prevention of CDI recurrence are poised for either phase 3 trials or upcoming Food and Drug Administration approval, Sahil Khanna, MBBS, MS, professor of medicine, gastroenterology, and hepatology at the Mayo Clinic in Rochester, Minn., reported at the annual Gut Microbiota for Health World Summit.
Jennifer A. Wargo, MD, MMSc, of the University of Texas MD Anderson Cancer Center, Houston, described her investigations of microbiome modulation’s role in cancer treatment. “I used to say yes [we can do this] somewhat enthusiastically without data, but now we have data to support this,” she said at the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility. “The answer now is totally yes.”
New approaches for CDI
“Based on how the field is moving, we might be able to [offer our patients] earlier microbiome restoration” than is currently afforded with fecal microbiota transplantation (FMT), he said. “Right now the [Food and Drug Administration] and our clinical guidelines say we should do FMT after three or more episodes [of CDI] – that’s heartbreaking for patients.”
Several of the microbiome-based therapies under investigation – including two poised for phase 3 trials – have shown efficacy after a second episode of CDI, and one of these two has also had positive results after one episode of CDI in patients 65 at older, a group at particularly high risk of recurrence, said Dr. Khanna.
The value of standardized, mostly pill-form microbiome therapies has been heightened during the pandemic. “We’ve been doing conventional FMT for recurrent C. difficile for over a decade now, and it’s probably the most effective treatment we have,” said Colleen R. Kelly, MD, associate professor of medicine at Brown University, Providence, R.I., and moderator of the session on microbiota-based therapies.
Prepandemic “it got really hard, with issues of identifying donors, and quality control and safety ... And then when COVID hit the stool banks shut down,” she said in an interview after the meeting. With stool testing for SARS-CoV-2 now in place, some stool is again available, “but it made me realize how fragile our current system is,” Dr. Kelly said. “The fact that companies are putting these products through the FDA pipeline and investigating them in rigorous, scientific randomized controlled trials is really good for the field.”
The products vary in composition; some are live multi-strain biotherapeutics derived from donor stool, for instance, while others are defined live bacterial consortia not from stool. Most are oral formulations, given one or multiple times, that do not require any bowel preparation.
One of the products most advanced in the pipeline, RBX2660 (Rebiotix, Ferring Pharmaceuticals) is stool derived and rectally administered. In phase 3 research, 70.5% of patients who received one active enema after having had two or more CDI recurrences and standard-of-care antibiotic treatment had no additional recurrence at 8 weeks compared to 58.1% in the placebo group, Dr. Khanna said.
The other product with positive phase 3 results, SER-109 (Seres Therapeutics), is a donor stool-derived oral formulation of purified Firmicutes spores that is administered after bowel prep. In results published earlier this year, the percentage of patients with recurrence of CDI up to 8 weeks after standard antibiotic treatment was 12% in the SER-109 group and 40% in the placebo group.
Patients in this trial were required to have had three episodes of CDI, and interestingly, Dr. Khanna said, the diagnosis of CDI was made only by toxin enzyme immunoassay (EIA). Earlier phase 2 research, which allowed either toxin EIA or polymerase chain reaction testing for the diagnosis of CDI (as other trials have done), produced negative results, leading investigators to surmise that some of the included patients had been colonized with C. difficile rather than being actively infected, Dr. Khanna said.
Researchers of these trials are documenting not only resolution of CDI but what they believe are positive shifts in the gut microbiota after microbiome-based therapy, he said. For instance, a phase 1 trial he led of the product RBX7455 (Rebiotix, Ferring Pharmaceuticals) – an oral capsule of lyophilized stool-based bacteria that can be kept for several days at room temperature – showed increases in Bacteroidia and Clostridia.
And other trials’ analyses of microbiome engraftment have demonstrated that “you can restore [species] even when these bacteria aren’t [included in the therapy],” he noted. “As the milieu of the gut improves, species that were not detected start coming back up.”
Asked about rates of efficacy in the trials’ placebo arms, Dr. Khanna said that “we’ve become smarter with our antibiotic regimens ... the placebo response rate is the response to newer guideline-based therapies.”
In addition to CDI, microbiome-based therapies are being studied, mostly in phase 1 research, for indications such as Crohn’s disease, ulcerative colitis, autism spectrum disorder, hepatitis B, and hepatic encephalopathy, Dr. Khanna noted.
Dr. Kelly, whose own research has focused on FMT for CDI, said she anticipates an expansion of research into other indications once products to prevent CDI recurrence are on the market. “There have been a couple of promising ulcerative colitis trials that haven’t gone anywhere clinically yet,” she said in the interview. “But will we now identify patients with UC who may be more sensitive to microbial manipulation, for whom we can use these microbial therapies along with a biologic?”
Some of her patients with IBD and CDI who are treated with FMT have not only had their CDI eradicated but have subsequently seen improvements in their IBD, she noted.
The role of traditional FMT and of stool banks will likely change in the future with new standardized oral microbiome-based therapies that can be approved and regulated by the FDA, she said. However, “we think the stool banks will still have some value,” she said, certainly for clinical research and probably for some treatment purposes as well. Regarding new therapies, “I just really hope they’re affordable,” she said.
Gut microbiome manipulation for cancer
Dr. Wargo’s research at MD Anderson has focused on metastatic breast cancer and immunotherapeutic checkpoint blockade. By sequencing microbiota samples and performing immune profiling in hundreds of patients, her team found that responders to PD-1 blockage have a greater diversity of gut bacteria and that “favorable signatures in the gut microbiome” are associated with enhanced immune responses in the tumor microenvironment.
Studies published last year in Science from investigators in Israel (2021 Feb 5;371[6529]:602-9) and Pittsburgh (2021 Feb 5;371[6529]:595-602), demonstrated that FMT promotes response in immunotherapy-refractory melanoma patients. In one study, FMT provided clinical benefit in 6 of 15 patients whose cancer had progressed on prior anti-PD-1 therapy, “which is pretty remarkable,” Dr. Wargo said.
Both research groups, she noted, saw favorable changes in the gut microbiome and immune cell infiltrates both at the level of the colon and the tumor.
Current research on FMT and other microbiome modulation strategies for cancer is guided in part by knowledge that tumors have microbial signatures – these signatures are now being identified across all tumor types – and by findings of “cross talk” between the gut and tumor microbiomes, she explained.
“Researchers are working hard to identify optimal consortia to enhance immune responses in the cancer setting, with promising work in preclinical models,” she said, and clinical trials are in progress. The role of diet in modulating the microbiome and enhancing anti-tumor immunity, with a focus on high dietary fiber intake, is also being investigated, she said.
Dr. Wargo reported that she serves on the advisory boards and is a paid speaker of numerous pharmaceutical and biotechnology companies, and is the coinventor of a patent submitted by the Texas MD Anderson Cancer Center on modulating the microbiome to enhance response to checkpoint blockade, and another related patent. Dr. Khanna reported that he is involved in research with Ferring/Rebiotix, Finch, Seres, Pfizer and Vendata, and does consulting for Immuron and several other companies. Dr. Kelly said she serves as an unpaid adviser for OpenBiome, a nonprofit stool bank, and that her site has enrolled patients in two of the trials testing products for CDI.
REPORTING FROM GMFH 2022
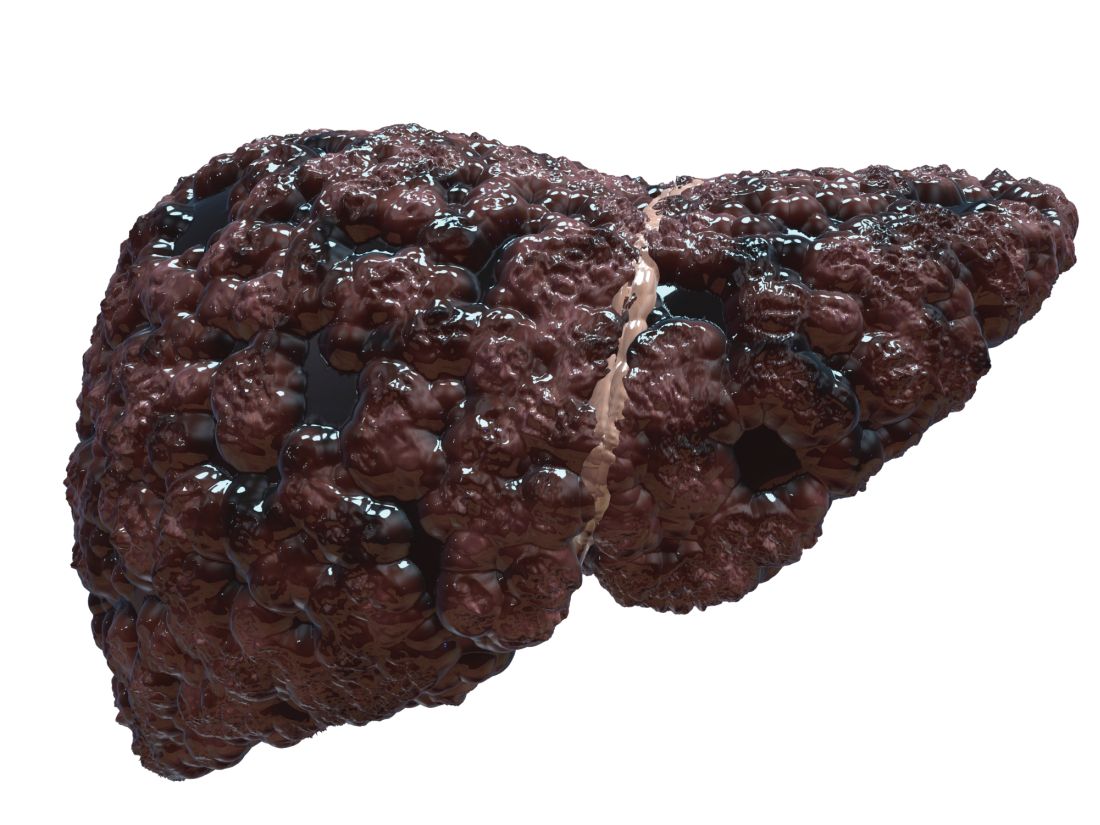
Shunt diameter predicts liver function after obliteration procedure
Patients with cirrhosis and larger spontaneous shunt diameters showed a significantly greater increase in hepatic venous pressure gradient (HVPG) following balloon-occluded retrograde transvenous obliteration compared to patients with smaller shunt diameters, based on data from 34 adults.
Portal hypertension remains a key source of complications that greatly impact quality of life in patients with cirrhosis, wrote Akihisa Tatsumi, MD, of the University of Yamanashi, Japan, and colleagues. These patients sometimes develop spontaneous portosystemic shunts (SPSS) to lower portal pressure, but these natural shunts are an incomplete solution – one that may contribute to liver dysfunction by reducing hepatic portal blood flow. However, the association of SPSS with liver functional reserve remains unclear, the researchers said.
Balloon-occluded retrograde transvenous obliteration (BRTO) is gaining popularity as a treatment for SPSS in patients with cirrhosis but determining the patients who will benefit from this procedure remains a challenge, the researchers wrote. “Apart from BRTO, some recent studies have reported the impact of the SPSS diameter on the future pathological state of the liver,” which prompted the question of whether SPSS diameter plays a role in predicting portal hypertension–related liver function at baseline and after BRTO, the researchers explained.
In their study, published in JGH Open, the researchers identified 34 cirrhotic patients with SPSS who underwent BRTO at a single center in Japan between 2006 and 2018; all of the patients were available for follow-up at least 6 months after the procedure.
The reasons for BRTO were intractable gastric varices in 18 patients and refractory hepatic encephalopathy with shunt in 16 patients; the mean observation period was 1,182 days (3.24 years). The median age of the patients was 66.5 years, and 53% were male. A majority (76%) of the patients had decompensated cirrhosis with Child-Pugh (CP) scores of B or C, and the maximum diameter of SPSS increased significantly with increased in CP scores (P < .001), the researchers noted.
Overall, at 6 months after BRTO, patients showed significant improvements in liver function from baseline. However, the improvement rate was lower in patients whose shunt diameter was 10 mm or less, and improvement was greatest when the shunt diameter was between 10 mm and 20 mm. “Because the CP score is a significant cofounding factor of the SPSS diameter, we next evaluated the changes in liver function classified by CP scores,” the researchers wrote. In this analysis, the post-BRTO changes in liver function in patients with CP scores of A or B still showed an association between improvement in liver function and larger shunt diameter, but this relationship did not extend to patients with CP scores of C, the researchers said.
A larger shunt diameter also was significantly associated with a greater increase in HVPG after balloon occlusion (P = .005).
“Considering that patients with large SPSS diameters might gain higher portal flow following elevation of HVPG after BRTO, it is natural that the larger the SPSS diameter, the greater the improvements in liver function,” the researchers wrote in their discussion of the findings. “However, such a clear correlation was evident only when the baseline CP scores were within A or B, and not in C, indicating that the improvement of liver function might not parallel HVPG increase in some CP C patients,” they noted.
The study was limited by several factors including the retrospective design from a single center and its small sample size, the researchers noted. Other limitations included selecting and measuring only the largest SPSS of each patient and lack of data on the impact of SPSS diameter on overall survival, they said.
However, the results suggest that SPSS diameter may serve not only as an indicator of portal hypertension involvement at baseline, but also as a useful clinical predictor of liver function after BRTO, they concluded.
Study supports potential benefits of BRTO
“While the association between SPSS and complications of portal hypertension such as variceal bleeding and hepatic encephalopathy have been known, data are lacking in regard to characteristics of SPSS that are most dysfunctional, and whether certain patients may benefit from BRTO to occlude these shunts,” Khashayar Farsad, MD, of Oregon Health & Science University, Portland, said in an interview.
“The results are in many ways expected based on anticipated impact of larger versus smaller SPSS in overall liver function,” Dr. Farsad noted. “The study, however, does show a nice correlation between several factors involved in liver function and their changes depending on shunt diameter, correlated with changes in the relative venous pressure gradient across the liver,” he said. “Furthermore, the finding that changes were most evident in those with relatively preserved liver function [Child-Turcotte-Pugh grades A and B] suggests less of a relationship between SPSS and liver function in those with more decompensated liver disease,” he added.
“The impact of the study is significantly limited by its retrospective design, small numbers with potential patient heterogeneity, and lack of a control cohort,” said Dr. Farsad. However, “The major take-home message for clinicians is a potential signal that the size of the SPSS at baseline may predict the impact of the SPSS on liver function, and therefore, the potential benefit of a procedure such as BRTO to positively influence this,” he said. “Additional research with larger cohorts and a prospective study design would be warranted, however, before this information would be meaningful in daily clinical decision making,” he emphasized.
The study was supported by the Research Program on Hepatitis of the Japanese Agency for Medical Research and Development. The researchers had no financial conflicts to disclose. Dr. Farsad disclosed research support from W.L. Gore & Associates, Guerbet LLC, Boston Scientific, and Exelixis; serving as a consultant for NeuWave Medical, Cook Medical, Guerbet LLC, and Eisai, and holding equity in Auxetics Inc.
Patients with cirrhosis and larger spontaneous shunt diameters showed a significantly greater increase in hepatic venous pressure gradient (HVPG) following balloon-occluded retrograde transvenous obliteration compared to patients with smaller shunt diameters, based on data from 34 adults.
Portal hypertension remains a key source of complications that greatly impact quality of life in patients with cirrhosis, wrote Akihisa Tatsumi, MD, of the University of Yamanashi, Japan, and colleagues. These patients sometimes develop spontaneous portosystemic shunts (SPSS) to lower portal pressure, but these natural shunts are an incomplete solution – one that may contribute to liver dysfunction by reducing hepatic portal blood flow. However, the association of SPSS with liver functional reserve remains unclear, the researchers said.
Balloon-occluded retrograde transvenous obliteration (BRTO) is gaining popularity as a treatment for SPSS in patients with cirrhosis but determining the patients who will benefit from this procedure remains a challenge, the researchers wrote. “Apart from BRTO, some recent studies have reported the impact of the SPSS diameter on the future pathological state of the liver,” which prompted the question of whether SPSS diameter plays a role in predicting portal hypertension–related liver function at baseline and after BRTO, the researchers explained.
In their study, published in JGH Open, the researchers identified 34 cirrhotic patients with SPSS who underwent BRTO at a single center in Japan between 2006 and 2018; all of the patients were available for follow-up at least 6 months after the procedure.
The reasons for BRTO were intractable gastric varices in 18 patients and refractory hepatic encephalopathy with shunt in 16 patients; the mean observation period was 1,182 days (3.24 years). The median age of the patients was 66.5 years, and 53% were male. A majority (76%) of the patients had decompensated cirrhosis with Child-Pugh (CP) scores of B or C, and the maximum diameter of SPSS increased significantly with increased in CP scores (P < .001), the researchers noted.
Overall, at 6 months after BRTO, patients showed significant improvements in liver function from baseline. However, the improvement rate was lower in patients whose shunt diameter was 10 mm or less, and improvement was greatest when the shunt diameter was between 10 mm and 20 mm. “Because the CP score is a significant cofounding factor of the SPSS diameter, we next evaluated the changes in liver function classified by CP scores,” the researchers wrote. In this analysis, the post-BRTO changes in liver function in patients with CP scores of A or B still showed an association between improvement in liver function and larger shunt diameter, but this relationship did not extend to patients with CP scores of C, the researchers said.
A larger shunt diameter also was significantly associated with a greater increase in HVPG after balloon occlusion (P = .005).
“Considering that patients with large SPSS diameters might gain higher portal flow following elevation of HVPG after BRTO, it is natural that the larger the SPSS diameter, the greater the improvements in liver function,” the researchers wrote in their discussion of the findings. “However, such a clear correlation was evident only when the baseline CP scores were within A or B, and not in C, indicating that the improvement of liver function might not parallel HVPG increase in some CP C patients,” they noted.
The study was limited by several factors including the retrospective design from a single center and its small sample size, the researchers noted. Other limitations included selecting and measuring only the largest SPSS of each patient and lack of data on the impact of SPSS diameter on overall survival, they said.
However, the results suggest that SPSS diameter may serve not only as an indicator of portal hypertension involvement at baseline, but also as a useful clinical predictor of liver function after BRTO, they concluded.
Study supports potential benefits of BRTO
“While the association between SPSS and complications of portal hypertension such as variceal bleeding and hepatic encephalopathy have been known, data are lacking in regard to characteristics of SPSS that are most dysfunctional, and whether certain patients may benefit from BRTO to occlude these shunts,” Khashayar Farsad, MD, of Oregon Health & Science University, Portland, said in an interview.
“The results are in many ways expected based on anticipated impact of larger versus smaller SPSS in overall liver function,” Dr. Farsad noted. “The study, however, does show a nice correlation between several factors involved in liver function and their changes depending on shunt diameter, correlated with changes in the relative venous pressure gradient across the liver,” he said. “Furthermore, the finding that changes were most evident in those with relatively preserved liver function [Child-Turcotte-Pugh grades A and B] suggests less of a relationship between SPSS and liver function in those with more decompensated liver disease,” he added.
“The impact of the study is significantly limited by its retrospective design, small numbers with potential patient heterogeneity, and lack of a control cohort,” said Dr. Farsad. However, “The major take-home message for clinicians is a potential signal that the size of the SPSS at baseline may predict the impact of the SPSS on liver function, and therefore, the potential benefit of a procedure such as BRTO to positively influence this,” he said. “Additional research with larger cohorts and a prospective study design would be warranted, however, before this information would be meaningful in daily clinical decision making,” he emphasized.
The study was supported by the Research Program on Hepatitis of the Japanese Agency for Medical Research and Development. The researchers had no financial conflicts to disclose. Dr. Farsad disclosed research support from W.L. Gore & Associates, Guerbet LLC, Boston Scientific, and Exelixis; serving as a consultant for NeuWave Medical, Cook Medical, Guerbet LLC, and Eisai, and holding equity in Auxetics Inc.
Patients with cirrhosis and larger spontaneous shunt diameters showed a significantly greater increase in hepatic venous pressure gradient (HVPG) following balloon-occluded retrograde transvenous obliteration compared to patients with smaller shunt diameters, based on data from 34 adults.
Portal hypertension remains a key source of complications that greatly impact quality of life in patients with cirrhosis, wrote Akihisa Tatsumi, MD, of the University of Yamanashi, Japan, and colleagues. These patients sometimes develop spontaneous portosystemic shunts (SPSS) to lower portal pressure, but these natural shunts are an incomplete solution – one that may contribute to liver dysfunction by reducing hepatic portal blood flow. However, the association of SPSS with liver functional reserve remains unclear, the researchers said.
Balloon-occluded retrograde transvenous obliteration (BRTO) is gaining popularity as a treatment for SPSS in patients with cirrhosis but determining the patients who will benefit from this procedure remains a challenge, the researchers wrote. “Apart from BRTO, some recent studies have reported the impact of the SPSS diameter on the future pathological state of the liver,” which prompted the question of whether SPSS diameter plays a role in predicting portal hypertension–related liver function at baseline and after BRTO, the researchers explained.
In their study, published in JGH Open, the researchers identified 34 cirrhotic patients with SPSS who underwent BRTO at a single center in Japan between 2006 and 2018; all of the patients were available for follow-up at least 6 months after the procedure.
The reasons for BRTO were intractable gastric varices in 18 patients and refractory hepatic encephalopathy with shunt in 16 patients; the mean observation period was 1,182 days (3.24 years). The median age of the patients was 66.5 years, and 53% were male. A majority (76%) of the patients had decompensated cirrhosis with Child-Pugh (CP) scores of B or C, and the maximum diameter of SPSS increased significantly with increased in CP scores (P < .001), the researchers noted.
Overall, at 6 months after BRTO, patients showed significant improvements in liver function from baseline. However, the improvement rate was lower in patients whose shunt diameter was 10 mm or less, and improvement was greatest when the shunt diameter was between 10 mm and 20 mm. “Because the CP score is a significant cofounding factor of the SPSS diameter, we next evaluated the changes in liver function classified by CP scores,” the researchers wrote. In this analysis, the post-BRTO changes in liver function in patients with CP scores of A or B still showed an association between improvement in liver function and larger shunt diameter, but this relationship did not extend to patients with CP scores of C, the researchers said.
A larger shunt diameter also was significantly associated with a greater increase in HVPG after balloon occlusion (P = .005).
“Considering that patients with large SPSS diameters might gain higher portal flow following elevation of HVPG after BRTO, it is natural that the larger the SPSS diameter, the greater the improvements in liver function,” the researchers wrote in their discussion of the findings. “However, such a clear correlation was evident only when the baseline CP scores were within A or B, and not in C, indicating that the improvement of liver function might not parallel HVPG increase in some CP C patients,” they noted.
The study was limited by several factors including the retrospective design from a single center and its small sample size, the researchers noted. Other limitations included selecting and measuring only the largest SPSS of each patient and lack of data on the impact of SPSS diameter on overall survival, they said.
However, the results suggest that SPSS diameter may serve not only as an indicator of portal hypertension involvement at baseline, but also as a useful clinical predictor of liver function after BRTO, they concluded.
Study supports potential benefits of BRTO
“While the association between SPSS and complications of portal hypertension such as variceal bleeding and hepatic encephalopathy have been known, data are lacking in regard to characteristics of SPSS that are most dysfunctional, and whether certain patients may benefit from BRTO to occlude these shunts,” Khashayar Farsad, MD, of Oregon Health & Science University, Portland, said in an interview.
“The results are in many ways expected based on anticipated impact of larger versus smaller SPSS in overall liver function,” Dr. Farsad noted. “The study, however, does show a nice correlation between several factors involved in liver function and their changes depending on shunt diameter, correlated with changes in the relative venous pressure gradient across the liver,” he said. “Furthermore, the finding that changes were most evident in those with relatively preserved liver function [Child-Turcotte-Pugh grades A and B] suggests less of a relationship between SPSS and liver function in those with more decompensated liver disease,” he added.
“The impact of the study is significantly limited by its retrospective design, small numbers with potential patient heterogeneity, and lack of a control cohort,” said Dr. Farsad. However, “The major take-home message for clinicians is a potential signal that the size of the SPSS at baseline may predict the impact of the SPSS on liver function, and therefore, the potential benefit of a procedure such as BRTO to positively influence this,” he said. “Additional research with larger cohorts and a prospective study design would be warranted, however, before this information would be meaningful in daily clinical decision making,” he emphasized.
The study was supported by the Research Program on Hepatitis of the Japanese Agency for Medical Research and Development. The researchers had no financial conflicts to disclose. Dr. Farsad disclosed research support from W.L. Gore & Associates, Guerbet LLC, Boston Scientific, and Exelixis; serving as a consultant for NeuWave Medical, Cook Medical, Guerbet LLC, and Eisai, and holding equity in Auxetics Inc.
FROM JGH OPEN
Kawasaki disease guideline highlights rheumatology angles
All Kawasaki disease (KD) patients should be treated first with intravenous immunoglobulin, according to an updated guideline issued jointly by the American College of Rheumatology and the Vasculitis Foundation.
KD has low mortality when treated appropriately, guideline first author Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, and colleagues wrote.
The update is important at this time because new evidence continues to emerge in the clinical management of KD, Dr. Gorelik said in an interview.
“In addition, this guideline approaches Kawasaki disease from a perspective of acting as an adjunct to the already existing and excellent American Heart Association guidelines by adding information in areas that rheumatologists may play a role,” Dr. Gorelik said. “This is specifically regarding patients who may require additional therapy beyond standard IVIg, such as patients who may be at higher risk of morbidity from disease and patients who have refractory disease,” he explained.
The guideline, published in Arthritis & Rheumatology, includes 11 recommendations, 1 good practice statement, and 1 ungraded position statement. The good practice statement emphasizes that all patients with KD should be initially treated with IVIg.
The position statement advises that either nonglucocorticoid immunosuppressive therapy or glucocorticoids may be used for patients with acute KD whose fever persists despite repeated IVIg treatment. No clinical evidence currently supports the superiority of either nonglucocorticoid immunosuppressive therapy or glucocorticoids; therefore, the authors support the use of either based on what is appropriate in any given clinical situation. Although optimal dosage and duration of glucocorticoids have yet to be determined in a U.S. population, the authors described a typical glucocorticoid dosage as starting prednisone at 2 mg/kg per day, with a maximum of 60 mg/day, and dose tapering over 15 days.
The 11 recommendations consist of 7 strong and 4 conditional recommendations. The strong recommendations focus on prompt treatment of incomplete KD, treatment with aspirin, and obtaining an echocardiogram in patients with unexplained macrophage activation syndrome or shock. The conditional recommendations support using established therapy promptly at disease onset, then identifying cases in which additional therapy is needed.
Dr. Gorelik highlighted four clinical takeaways from the guideline. First, “patients with higher risk for complications do exist in Kawasaki disease, and that these patients can be treated more aggressively,” he said. “Specifically, patients with aneurysms seen at first ultrasound, and patients who are under 6 months, are more likely to have progressive and/or refractory disease; these patients can be treated with an adjunctive short course of corticosteroids.”
Second, “the use of high-dose aspirin for patients with Kawasaki disease does not have strong basis in evidence. While aspirin itself of some dose is necessary for patients with Kawasaki disease, use of either high- or low-dose aspirin has the same outcome for patients, and a physician may choose either of these in practice,” he said.
Third, “we continue to recommend that refractory patients with Kawasaki disease be treated with a second dose of IVIg; however, there are many scenarios in which a physician may choose either corticosteroids [either a single high dose of >10 mg/kg, or a short moderate-dose course of 2 mg/kg per day for 5-7 days] or a biologic agent such as infliximab. ... These are valid choices for therapy in patients with refractory Kawasaki disease,” he emphasized.
Fourth, “physicians should discard the idea of treating before [and conversely, not treating after] 10 days of fever,” Dr. Gorelik said. “Patients with Kawasaki disease should be treated as soon as the diagnosis is made, regardless of whether this patient is on day 5, day 12, or day 20 of symptoms.”
Update incorporates emerging evidence
Potential barriers to implementing the guideline in practice include the challenge of weaning doctors from practices that are habitual in medicine, Dr. Gorelik said. “One of these is the use of high-dose aspirin for Kawasaki disease; a number of studies have shown over the past decade or more that high-dose aspirin has no greater effect than lower-dose aspirin for Kawasaki disease. Despite all of these studies, the use of high-dose aspirin continued. High-dose aspirin for Kawasaki disease was used in the era prior to use of IVIg as an anti-inflammatory agent. However, it has poor efficacy in this regard, and the true benefit for aspirin is for anticoagulation for patients at risk of a clot, and this is just as effective in lower doses. Expressing this in a guideline could help to change practices by helping physicians understand not only what they are guided to do, but why.”
Additional research is needed to better identify high-risk patients in non-Japanese populations, he noted. “While studies from Japan suggest that higher-risk patients can be identified based on various parameters, these have not been well replicated in non-Japanese populations. Good research that identifies which patients may be more at risk in other populations would be helpful to more precisely target high-risk therapy.”
Other research needs include a clearer understanding of the best therapies for refractory patients, Dr. Gorelik said. “One area of the most difficulty was determining whether patients with refractory disease should have repeated IVIg or a switch to glucocorticoids and biologic agents. Some of this research is underway, and some was published just as these guidelines were being drawn, and this particular area is one that is likely to change significantly. While currently we recommend a repeated dose of IVIg, it is likely that over the very near term, the use of repeated IVIg in KD will be curtailed” because of concerns such as the relatively high rate of hemolysis. Research to identify which therapy has a noninferior effect with a superior risk profile is needed; such research “will likely result in a future iteration of these guidelines specifically related to this question,” he concluded.
The KD guideline is the final companion to three additional ACR/VF vasculitis guidelines that were released in July 2021. The guideline research received no outside funding. The researchers had no financial conflicts to disclose.
All Kawasaki disease (KD) patients should be treated first with intravenous immunoglobulin, according to an updated guideline issued jointly by the American College of Rheumatology and the Vasculitis Foundation.
KD has low mortality when treated appropriately, guideline first author Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, and colleagues wrote.
The update is important at this time because new evidence continues to emerge in the clinical management of KD, Dr. Gorelik said in an interview.
“In addition, this guideline approaches Kawasaki disease from a perspective of acting as an adjunct to the already existing and excellent American Heart Association guidelines by adding information in areas that rheumatologists may play a role,” Dr. Gorelik said. “This is specifically regarding patients who may require additional therapy beyond standard IVIg, such as patients who may be at higher risk of morbidity from disease and patients who have refractory disease,” he explained.
The guideline, published in Arthritis & Rheumatology, includes 11 recommendations, 1 good practice statement, and 1 ungraded position statement. The good practice statement emphasizes that all patients with KD should be initially treated with IVIg.
The position statement advises that either nonglucocorticoid immunosuppressive therapy or glucocorticoids may be used for patients with acute KD whose fever persists despite repeated IVIg treatment. No clinical evidence currently supports the superiority of either nonglucocorticoid immunosuppressive therapy or glucocorticoids; therefore, the authors support the use of either based on what is appropriate in any given clinical situation. Although optimal dosage and duration of glucocorticoids have yet to be determined in a U.S. population, the authors described a typical glucocorticoid dosage as starting prednisone at 2 mg/kg per day, with a maximum of 60 mg/day, and dose tapering over 15 days.
The 11 recommendations consist of 7 strong and 4 conditional recommendations. The strong recommendations focus on prompt treatment of incomplete KD, treatment with aspirin, and obtaining an echocardiogram in patients with unexplained macrophage activation syndrome or shock. The conditional recommendations support using established therapy promptly at disease onset, then identifying cases in which additional therapy is needed.
Dr. Gorelik highlighted four clinical takeaways from the guideline. First, “patients with higher risk for complications do exist in Kawasaki disease, and that these patients can be treated more aggressively,” he said. “Specifically, patients with aneurysms seen at first ultrasound, and patients who are under 6 months, are more likely to have progressive and/or refractory disease; these patients can be treated with an adjunctive short course of corticosteroids.”
Second, “the use of high-dose aspirin for patients with Kawasaki disease does not have strong basis in evidence. While aspirin itself of some dose is necessary for patients with Kawasaki disease, use of either high- or low-dose aspirin has the same outcome for patients, and a physician may choose either of these in practice,” he said.
Third, “we continue to recommend that refractory patients with Kawasaki disease be treated with a second dose of IVIg; however, there are many scenarios in which a physician may choose either corticosteroids [either a single high dose of >10 mg/kg, or a short moderate-dose course of 2 mg/kg per day for 5-7 days] or a biologic agent such as infliximab. ... These are valid choices for therapy in patients with refractory Kawasaki disease,” he emphasized.
Fourth, “physicians should discard the idea of treating before [and conversely, not treating after] 10 days of fever,” Dr. Gorelik said. “Patients with Kawasaki disease should be treated as soon as the diagnosis is made, regardless of whether this patient is on day 5, day 12, or day 20 of symptoms.”
Update incorporates emerging evidence
Potential barriers to implementing the guideline in practice include the challenge of weaning doctors from practices that are habitual in medicine, Dr. Gorelik said. “One of these is the use of high-dose aspirin for Kawasaki disease; a number of studies have shown over the past decade or more that high-dose aspirin has no greater effect than lower-dose aspirin for Kawasaki disease. Despite all of these studies, the use of high-dose aspirin continued. High-dose aspirin for Kawasaki disease was used in the era prior to use of IVIg as an anti-inflammatory agent. However, it has poor efficacy in this regard, and the true benefit for aspirin is for anticoagulation for patients at risk of a clot, and this is just as effective in lower doses. Expressing this in a guideline could help to change practices by helping physicians understand not only what they are guided to do, but why.”
Additional research is needed to better identify high-risk patients in non-Japanese populations, he noted. “While studies from Japan suggest that higher-risk patients can be identified based on various parameters, these have not been well replicated in non-Japanese populations. Good research that identifies which patients may be more at risk in other populations would be helpful to more precisely target high-risk therapy.”
Other research needs include a clearer understanding of the best therapies for refractory patients, Dr. Gorelik said. “One area of the most difficulty was determining whether patients with refractory disease should have repeated IVIg or a switch to glucocorticoids and biologic agents. Some of this research is underway, and some was published just as these guidelines were being drawn, and this particular area is one that is likely to change significantly. While currently we recommend a repeated dose of IVIg, it is likely that over the very near term, the use of repeated IVIg in KD will be curtailed” because of concerns such as the relatively high rate of hemolysis. Research to identify which therapy has a noninferior effect with a superior risk profile is needed; such research “will likely result in a future iteration of these guidelines specifically related to this question,” he concluded.
The KD guideline is the final companion to three additional ACR/VF vasculitis guidelines that were released in July 2021. The guideline research received no outside funding. The researchers had no financial conflicts to disclose.
All Kawasaki disease (KD) patients should be treated first with intravenous immunoglobulin, according to an updated guideline issued jointly by the American College of Rheumatology and the Vasculitis Foundation.
KD has low mortality when treated appropriately, guideline first author Mark Gorelik, MD, assistant professor of pediatrics at Columbia University, New York, and colleagues wrote.
The update is important at this time because new evidence continues to emerge in the clinical management of KD, Dr. Gorelik said in an interview.
“In addition, this guideline approaches Kawasaki disease from a perspective of acting as an adjunct to the already existing and excellent American Heart Association guidelines by adding information in areas that rheumatologists may play a role,” Dr. Gorelik said. “This is specifically regarding patients who may require additional therapy beyond standard IVIg, such as patients who may be at higher risk of morbidity from disease and patients who have refractory disease,” he explained.
The guideline, published in Arthritis & Rheumatology, includes 11 recommendations, 1 good practice statement, and 1 ungraded position statement. The good practice statement emphasizes that all patients with KD should be initially treated with IVIg.
The position statement advises that either nonglucocorticoid immunosuppressive therapy or glucocorticoids may be used for patients with acute KD whose fever persists despite repeated IVIg treatment. No clinical evidence currently supports the superiority of either nonglucocorticoid immunosuppressive therapy or glucocorticoids; therefore, the authors support the use of either based on what is appropriate in any given clinical situation. Although optimal dosage and duration of glucocorticoids have yet to be determined in a U.S. population, the authors described a typical glucocorticoid dosage as starting prednisone at 2 mg/kg per day, with a maximum of 60 mg/day, and dose tapering over 15 days.
The 11 recommendations consist of 7 strong and 4 conditional recommendations. The strong recommendations focus on prompt treatment of incomplete KD, treatment with aspirin, and obtaining an echocardiogram in patients with unexplained macrophage activation syndrome or shock. The conditional recommendations support using established therapy promptly at disease onset, then identifying cases in which additional therapy is needed.
Dr. Gorelik highlighted four clinical takeaways from the guideline. First, “patients with higher risk for complications do exist in Kawasaki disease, and that these patients can be treated more aggressively,” he said. “Specifically, patients with aneurysms seen at first ultrasound, and patients who are under 6 months, are more likely to have progressive and/or refractory disease; these patients can be treated with an adjunctive short course of corticosteroids.”
Second, “the use of high-dose aspirin for patients with Kawasaki disease does not have strong basis in evidence. While aspirin itself of some dose is necessary for patients with Kawasaki disease, use of either high- or low-dose aspirin has the same outcome for patients, and a physician may choose either of these in practice,” he said.
Third, “we continue to recommend that refractory patients with Kawasaki disease be treated with a second dose of IVIg; however, there are many scenarios in which a physician may choose either corticosteroids [either a single high dose of >10 mg/kg, or a short moderate-dose course of 2 mg/kg per day for 5-7 days] or a biologic agent such as infliximab. ... These are valid choices for therapy in patients with refractory Kawasaki disease,” he emphasized.
Fourth, “physicians should discard the idea of treating before [and conversely, not treating after] 10 days of fever,” Dr. Gorelik said. “Patients with Kawasaki disease should be treated as soon as the diagnosis is made, regardless of whether this patient is on day 5, day 12, or day 20 of symptoms.”
Update incorporates emerging evidence
Potential barriers to implementing the guideline in practice include the challenge of weaning doctors from practices that are habitual in medicine, Dr. Gorelik said. “One of these is the use of high-dose aspirin for Kawasaki disease; a number of studies have shown over the past decade or more that high-dose aspirin has no greater effect than lower-dose aspirin for Kawasaki disease. Despite all of these studies, the use of high-dose aspirin continued. High-dose aspirin for Kawasaki disease was used in the era prior to use of IVIg as an anti-inflammatory agent. However, it has poor efficacy in this regard, and the true benefit for aspirin is for anticoagulation for patients at risk of a clot, and this is just as effective in lower doses. Expressing this in a guideline could help to change practices by helping physicians understand not only what they are guided to do, but why.”
Additional research is needed to better identify high-risk patients in non-Japanese populations, he noted. “While studies from Japan suggest that higher-risk patients can be identified based on various parameters, these have not been well replicated in non-Japanese populations. Good research that identifies which patients may be more at risk in other populations would be helpful to more precisely target high-risk therapy.”
Other research needs include a clearer understanding of the best therapies for refractory patients, Dr. Gorelik said. “One area of the most difficulty was determining whether patients with refractory disease should have repeated IVIg or a switch to glucocorticoids and biologic agents. Some of this research is underway, and some was published just as these guidelines were being drawn, and this particular area is one that is likely to change significantly. While currently we recommend a repeated dose of IVIg, it is likely that over the very near term, the use of repeated IVIg in KD will be curtailed” because of concerns such as the relatively high rate of hemolysis. Research to identify which therapy has a noninferior effect with a superior risk profile is needed; such research “will likely result in a future iteration of these guidelines specifically related to this question,” he concluded.
The KD guideline is the final companion to three additional ACR/VF vasculitis guidelines that were released in July 2021. The guideline research received no outside funding. The researchers had no financial conflicts to disclose.
FROM ARTHRITIS & RHEUMATOLOGY
Updates in DMTs and MS Economic Burden From ACTRIMS 2022
Dr Michael Wilson, associate professor at the University of California, San Francisco, School of Medicine, shares updates on disease-modifying therapies (DMTs) and health economics that were presented at the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) 2022 meeting.
First, Dr Wilson reports on a holistic review of the US economic burdens associated with MS and DMT use. The total burden of MS was estimated to be $85 billion in both direct and indirect costs, with the average annual DMT cost ranging between $57,000 and $90,000.
Another study looked at long-term outcomes for patients who were treated with autologous hematopoietic stem cell transplantation (aHSCT). With follow-up periods ranging from 8 months to 20 years, there were no reported relapses after aHSCT. In contrast, there were 1.1 relapses per patient year before aHSCT. Patients also saw improvement in Expanded Disability Status Scale scores during follow-up.
Finally, Dr Wilson reviews the 18-month results from a long-term extension study of tolebrutinib, which looked at MRI activity, efficacy, and safety. Investigators reported a significant decrease in the number of new or enhancing lesions and in annual relapse rates, while T2 lesion burden remained stable.
--
Michael Wilson, MD, Associate Professor, Department of Neurology, University of California, San Francisco, School of Medicine; Director, UCSF Center for Encephalitis and Meningitis, San Francisco, California
Michael Wilson, MD, has disclosed the following relevant financial relationships:
Received research grant from: Roche/Genentech
Received income in an amount equal to or greater than $250 from: Takeda; Genentech; Novartis
Dr Michael Wilson, associate professor at the University of California, San Francisco, School of Medicine, shares updates on disease-modifying therapies (DMTs) and health economics that were presented at the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) 2022 meeting.
First, Dr Wilson reports on a holistic review of the US economic burdens associated with MS and DMT use. The total burden of MS was estimated to be $85 billion in both direct and indirect costs, with the average annual DMT cost ranging between $57,000 and $90,000.
Another study looked at long-term outcomes for patients who were treated with autologous hematopoietic stem cell transplantation (aHSCT). With follow-up periods ranging from 8 months to 20 years, there were no reported relapses after aHSCT. In contrast, there were 1.1 relapses per patient year before aHSCT. Patients also saw improvement in Expanded Disability Status Scale scores during follow-up.
Finally, Dr Wilson reviews the 18-month results from a long-term extension study of tolebrutinib, which looked at MRI activity, efficacy, and safety. Investigators reported a significant decrease in the number of new or enhancing lesions and in annual relapse rates, while T2 lesion burden remained stable.
--
Michael Wilson, MD, Associate Professor, Department of Neurology, University of California, San Francisco, School of Medicine; Director, UCSF Center for Encephalitis and Meningitis, San Francisco, California
Michael Wilson, MD, has disclosed the following relevant financial relationships:
Received research grant from: Roche/Genentech
Received income in an amount equal to or greater than $250 from: Takeda; Genentech; Novartis
Dr Michael Wilson, associate professor at the University of California, San Francisco, School of Medicine, shares updates on disease-modifying therapies (DMTs) and health economics that were presented at the Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS) 2022 meeting.
First, Dr Wilson reports on a holistic review of the US economic burdens associated with MS and DMT use. The total burden of MS was estimated to be $85 billion in both direct and indirect costs, with the average annual DMT cost ranging between $57,000 and $90,000.
Another study looked at long-term outcomes for patients who were treated with autologous hematopoietic stem cell transplantation (aHSCT). With follow-up periods ranging from 8 months to 20 years, there were no reported relapses after aHSCT. In contrast, there were 1.1 relapses per patient year before aHSCT. Patients also saw improvement in Expanded Disability Status Scale scores during follow-up.
Finally, Dr Wilson reviews the 18-month results from a long-term extension study of tolebrutinib, which looked at MRI activity, efficacy, and safety. Investigators reported a significant decrease in the number of new or enhancing lesions and in annual relapse rates, while T2 lesion burden remained stable.
--
Michael Wilson, MD, Associate Professor, Department of Neurology, University of California, San Francisco, School of Medicine; Director, UCSF Center for Encephalitis and Meningitis, San Francisco, California
Michael Wilson, MD, has disclosed the following relevant financial relationships:
Received research grant from: Roche/Genentech
Received income in an amount equal to or greater than $250 from: Takeda; Genentech; Novartis

Excess weight over lifetime hikes risk for colorectal cancer
Excess weight over a lifetime may play a greater role in a person’s risk for colorectal cancer (CRC) than previously thought, according to new research.
In their paper published online March 17 in JAMA Oncology, the authors liken the cumulative effects of a lifetime with overweight or obesity to the increased risk of cancer the more people smoke over time.
This population-based, case-control study was led by Xiangwei Li, MSc, of the division of clinical epidemiology and aging research at the German Cancer Research Center in Heidelberg.
It looked at height and self-reported weight documented in 10-year increments starting at age 20 years up to the current age for 5,635 people with CRC compared with 4,515 people in a control group.
Odds for colorectal cancer increased substantially over the decades when people carried the excess weight long term compared with participants who remained within the normal weight range during the period.
Coauthor Hermann Brenner, MD, MPH, a colleague in Li’s division at the German Cancer Research Center, said in an interview that a key message in the research is that “overweight and obesity are likely to increase the risk of colorectal cancer more strongly than suggested by previous studies that typically had considered body weight only at a single point of time.”
The researchers used a measure of weighted number of years lived with overweight or obesity (WYOs) determined by multiplying excess body mass index by number of years the person carried the excess weight.
They found a link between WYOs and CRC risk, with adjusted odds ratios (ORs) increasing from 1.25 (95% confidence interval [CI], 1.09-1.44) to 2.54 (95% CI, 2.24-2.89) from the first to the fourth quartile of WYOs, compared with people who stayed within normal weight parameters.
The odds went up substantially the longer the time carrying the excess weight.
“Each SD increment in WYOs was associated with an increase of CRC risk by 55% (adjusted OR, 1.55; 95% CI, 1.46-1.64),” the authors wrote. “This OR was higher than the OR per SD increase of excess body mass index at any single point of time, which ranged from 1.04 (95% CI, 0.93-1.16) to 1.27 (95% CI 1.16-1.39).”
Dr. Brenner said that although this study focused on colorectal cancer, “the same is likely to apply for other cancers and other chronic diseases.”
Prevention of overweight and obesity to reduce burden of cancer and other chronic diseases “should become a public health priority,” he said.
Preventing overweight in childhood is important
Overweight and obesity increasingly are starting in childhood, he noted, and may be a lifelong burden.
Therefore, “efforts to prevent their development in childhood, adolescence, and young adulthood are particularly important,” Dr. Brenner said.
The average age of the patients was 68 years in both the CRC and control groups. There were more men than women in both groups: 59.7% were men in the CRC group and 61.1% were men in the control group.
“Our proposed concept of WYOs is comparable to the concept of pack-years in that WYOs can be considered a weighted measure of years lived with the exposure, with weights reflecting the intensity of exposure,” the authors wrote.
Study helps confirm what is becoming more clear to researchers
Kimmie Ng, MD, MPH, a professor at Harvard Medical School and oncologist at Dana-Farber Cancer Institute, both in Boston, said in an interview that the study helps confirm what is becoming more clear to researchers.
“We do think that exposures over the life course are the ones that will be most strongly contributing to a risk of colorectal cancer as an adult,” she said. “With obesity, what we think is happening is that it’s setting up this milieu of chronic inflammation and insulin resistance and we know those two factors can lead to higher rates of colorectal cancer development and increased tumor growth.”
She said the ideal, but impractical, way to do the study would be to follow healthy people from childhood and document their weight over a lifetime. In this case-control study, people were asked to recall their weight at different time periods, which is a limitation and could lead to recall bias.
But the study is important, Dr. Ng said, and it adds convincing evidence that addressing the link between excess weight and CRC and chronic diseases should be a public health priority. “With the recent rise in young-onset colorectal cancer since the 1990s there has been a lot of interest in looking at whether obesity is a major contributor to that rising trend,” Dr. Ng noted. “If obesity is truly linked to colorectal cancer, these rising rates of obesity are very worrisome for potentially leading to more colorectal cancers in young adulthood and beyond.“
The study authors and Dr. Ng report no relevant financial relationships.
The new research was funded by the German Research Council, the Interdisciplinary Research Program of the National Center for Tumor Diseases, Germany, and the German Federal Ministry of Education and Research.
Excess weight over a lifetime may play a greater role in a person’s risk for colorectal cancer (CRC) than previously thought, according to new research.
In their paper published online March 17 in JAMA Oncology, the authors liken the cumulative effects of a lifetime with overweight or obesity to the increased risk of cancer the more people smoke over time.
This population-based, case-control study was led by Xiangwei Li, MSc, of the division of clinical epidemiology and aging research at the German Cancer Research Center in Heidelberg.
It looked at height and self-reported weight documented in 10-year increments starting at age 20 years up to the current age for 5,635 people with CRC compared with 4,515 people in a control group.
Odds for colorectal cancer increased substantially over the decades when people carried the excess weight long term compared with participants who remained within the normal weight range during the period.
Coauthor Hermann Brenner, MD, MPH, a colleague in Li’s division at the German Cancer Research Center, said in an interview that a key message in the research is that “overweight and obesity are likely to increase the risk of colorectal cancer more strongly than suggested by previous studies that typically had considered body weight only at a single point of time.”
The researchers used a measure of weighted number of years lived with overweight or obesity (WYOs) determined by multiplying excess body mass index by number of years the person carried the excess weight.
They found a link between WYOs and CRC risk, with adjusted odds ratios (ORs) increasing from 1.25 (95% confidence interval [CI], 1.09-1.44) to 2.54 (95% CI, 2.24-2.89) from the first to the fourth quartile of WYOs, compared with people who stayed within normal weight parameters.
The odds went up substantially the longer the time carrying the excess weight.
“Each SD increment in WYOs was associated with an increase of CRC risk by 55% (adjusted OR, 1.55; 95% CI, 1.46-1.64),” the authors wrote. “This OR was higher than the OR per SD increase of excess body mass index at any single point of time, which ranged from 1.04 (95% CI, 0.93-1.16) to 1.27 (95% CI 1.16-1.39).”
Dr. Brenner said that although this study focused on colorectal cancer, “the same is likely to apply for other cancers and other chronic diseases.”
Prevention of overweight and obesity to reduce burden of cancer and other chronic diseases “should become a public health priority,” he said.
Preventing overweight in childhood is important
Overweight and obesity increasingly are starting in childhood, he noted, and may be a lifelong burden.
Therefore, “efforts to prevent their development in childhood, adolescence, and young adulthood are particularly important,” Dr. Brenner said.
The average age of the patients was 68 years in both the CRC and control groups. There were more men than women in both groups: 59.7% were men in the CRC group and 61.1% were men in the control group.
“Our proposed concept of WYOs is comparable to the concept of pack-years in that WYOs can be considered a weighted measure of years lived with the exposure, with weights reflecting the intensity of exposure,” the authors wrote.
Study helps confirm what is becoming more clear to researchers
Kimmie Ng, MD, MPH, a professor at Harvard Medical School and oncologist at Dana-Farber Cancer Institute, both in Boston, said in an interview that the study helps confirm what is becoming more clear to researchers.
“We do think that exposures over the life course are the ones that will be most strongly contributing to a risk of colorectal cancer as an adult,” she said. “With obesity, what we think is happening is that it’s setting up this milieu of chronic inflammation and insulin resistance and we know those two factors can lead to higher rates of colorectal cancer development and increased tumor growth.”
She said the ideal, but impractical, way to do the study would be to follow healthy people from childhood and document their weight over a lifetime. In this case-control study, people were asked to recall their weight at different time periods, which is a limitation and could lead to recall bias.
But the study is important, Dr. Ng said, and it adds convincing evidence that addressing the link between excess weight and CRC and chronic diseases should be a public health priority. “With the recent rise in young-onset colorectal cancer since the 1990s there has been a lot of interest in looking at whether obesity is a major contributor to that rising trend,” Dr. Ng noted. “If obesity is truly linked to colorectal cancer, these rising rates of obesity are very worrisome for potentially leading to more colorectal cancers in young adulthood and beyond.“
The study authors and Dr. Ng report no relevant financial relationships.
The new research was funded by the German Research Council, the Interdisciplinary Research Program of the National Center for Tumor Diseases, Germany, and the German Federal Ministry of Education and Research.
Excess weight over a lifetime may play a greater role in a person’s risk for colorectal cancer (CRC) than previously thought, according to new research.
In their paper published online March 17 in JAMA Oncology, the authors liken the cumulative effects of a lifetime with overweight or obesity to the increased risk of cancer the more people smoke over time.
This population-based, case-control study was led by Xiangwei Li, MSc, of the division of clinical epidemiology and aging research at the German Cancer Research Center in Heidelberg.
It looked at height and self-reported weight documented in 10-year increments starting at age 20 years up to the current age for 5,635 people with CRC compared with 4,515 people in a control group.
Odds for colorectal cancer increased substantially over the decades when people carried the excess weight long term compared with participants who remained within the normal weight range during the period.
Coauthor Hermann Brenner, MD, MPH, a colleague in Li’s division at the German Cancer Research Center, said in an interview that a key message in the research is that “overweight and obesity are likely to increase the risk of colorectal cancer more strongly than suggested by previous studies that typically had considered body weight only at a single point of time.”
The researchers used a measure of weighted number of years lived with overweight or obesity (WYOs) determined by multiplying excess body mass index by number of years the person carried the excess weight.
They found a link between WYOs and CRC risk, with adjusted odds ratios (ORs) increasing from 1.25 (95% confidence interval [CI], 1.09-1.44) to 2.54 (95% CI, 2.24-2.89) from the first to the fourth quartile of WYOs, compared with people who stayed within normal weight parameters.
The odds went up substantially the longer the time carrying the excess weight.
“Each SD increment in WYOs was associated with an increase of CRC risk by 55% (adjusted OR, 1.55; 95% CI, 1.46-1.64),” the authors wrote. “This OR was higher than the OR per SD increase of excess body mass index at any single point of time, which ranged from 1.04 (95% CI, 0.93-1.16) to 1.27 (95% CI 1.16-1.39).”
Dr. Brenner said that although this study focused on colorectal cancer, “the same is likely to apply for other cancers and other chronic diseases.”
Prevention of overweight and obesity to reduce burden of cancer and other chronic diseases “should become a public health priority,” he said.
Preventing overweight in childhood is important
Overweight and obesity increasingly are starting in childhood, he noted, and may be a lifelong burden.
Therefore, “efforts to prevent their development in childhood, adolescence, and young adulthood are particularly important,” Dr. Brenner said.
The average age of the patients was 68 years in both the CRC and control groups. There were more men than women in both groups: 59.7% were men in the CRC group and 61.1% were men in the control group.
“Our proposed concept of WYOs is comparable to the concept of pack-years in that WYOs can be considered a weighted measure of years lived with the exposure, with weights reflecting the intensity of exposure,” the authors wrote.
Study helps confirm what is becoming more clear to researchers
Kimmie Ng, MD, MPH, a professor at Harvard Medical School and oncologist at Dana-Farber Cancer Institute, both in Boston, said in an interview that the study helps confirm what is becoming more clear to researchers.
“We do think that exposures over the life course are the ones that will be most strongly contributing to a risk of colorectal cancer as an adult,” she said. “With obesity, what we think is happening is that it’s setting up this milieu of chronic inflammation and insulin resistance and we know those two factors can lead to higher rates of colorectal cancer development and increased tumor growth.”
She said the ideal, but impractical, way to do the study would be to follow healthy people from childhood and document their weight over a lifetime. In this case-control study, people were asked to recall their weight at different time periods, which is a limitation and could lead to recall bias.
But the study is important, Dr. Ng said, and it adds convincing evidence that addressing the link between excess weight and CRC and chronic diseases should be a public health priority. “With the recent rise in young-onset colorectal cancer since the 1990s there has been a lot of interest in looking at whether obesity is a major contributor to that rising trend,” Dr. Ng noted. “If obesity is truly linked to colorectal cancer, these rising rates of obesity are very worrisome for potentially leading to more colorectal cancers in young adulthood and beyond.“
The study authors and Dr. Ng report no relevant financial relationships.
The new research was funded by the German Research Council, the Interdisciplinary Research Program of the National Center for Tumor Diseases, Germany, and the German Federal Ministry of Education and Research.
FROM JAMA ONCOLOGY
Sleep experts recommend permanent standard time, rather than DST
Sleep experts tend to agree with U.S. lawmakers about getting rid of the twice-per-year time shift, with one exception: They typically call for standard time rather than daylight saving time.
After the Senate voted unanimously on March 15 to make daylight saving time permanent, the American Academy of Sleep Medicine issued a statement that urged caution about adopting a fixed, year-round time with potential health risks.
“We do applaud stopping the switching during the course of the year and settling on a permanent time,” Jocelyn Cheng, MD, a member of the association’s public safety committee, told The Washington Post.
But she said.
Now it’s up to the House of Representatives to decide what to do next. The legislation, which would take effect in 2023, must be passed by the House and signed by President Joe Biden before becoming a law.
Legislators and health experts have debated the shift in recent years. In 2020, the American Academy of Sleep Medicine released a position statement in the Journal of Clinical Sleep Medicine that recommended that the United States move to year-round standard time. Standard time is more aligned with humans’ circadian rhythms and natural light/dark cycles, the group wrote, and disrupting that rhythm has been linked to higher risks of heart disease, obesity, and depression.
At the same time, few studies have focused on the long-term effects of adopting daylight saving time. Most research has focused on the short-term risks of the seasonal shift, such as reduced sleep and increased car crashes, or circadian misalignment caused by other things. Some health experts have called for more research before deciding on a permanent time, the newspaper reported.
Still, the March 15 statement from sleep experts received support from more than 20 groups, including the National Safety Council, National Parent Teacher Association, and the World Sleep Society.
“We have all enjoyed those summer evenings with seemingly endless dusks,” David Neubauer, MD, an associate professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, told the Post.
But daylight saving time “does not ‘save’ evening light at all, it simply steals it from the morning, when it is necessary to maintain our healthy biological rhythms,” he said.
Permanent daylight saving time would lead to more dark mornings, which opponents have said could be dangerous for kids going to school, adults driving to work, and overall sleep cycles.
“With daylight saving time, we are perpetually out of synchronization with our internal clocks, and we often achieve less nighttime sleep, both circumstances having negative health impacts,” Dr. Neubauer said. “Extra evening light suppresses the melatonin that should be preparing us for falling asleep. The later dawn during daylight saving time deprives our biological clocks of the critical light signal.”
The pros and cons of daylight saving time and standard time were debated during a hearing held by a House Energy and Commerce subcommittee recently. Sleep experts argued in favor of standard time, while other industry experts argued for daylight saving time to reduce crime, save energy, and help businesses that benefit from more daylight in the evenings.
“Everybody advocates a permanent time, but this difference between 1 hour back or 1 hour forward is not so clear in everybody’s mind,” Dr. Cheng said. “I would like to see further debate and some due diligence done on these health consequences and public safety measures before anything else goes forward.”
A version of this article first appeared on WebMD.com.
Sleep experts tend to agree with U.S. lawmakers about getting rid of the twice-per-year time shift, with one exception: They typically call for standard time rather than daylight saving time.
After the Senate voted unanimously on March 15 to make daylight saving time permanent, the American Academy of Sleep Medicine issued a statement that urged caution about adopting a fixed, year-round time with potential health risks.
“We do applaud stopping the switching during the course of the year and settling on a permanent time,” Jocelyn Cheng, MD, a member of the association’s public safety committee, told The Washington Post.
But she said.
Now it’s up to the House of Representatives to decide what to do next. The legislation, which would take effect in 2023, must be passed by the House and signed by President Joe Biden before becoming a law.
Legislators and health experts have debated the shift in recent years. In 2020, the American Academy of Sleep Medicine released a position statement in the Journal of Clinical Sleep Medicine that recommended that the United States move to year-round standard time. Standard time is more aligned with humans’ circadian rhythms and natural light/dark cycles, the group wrote, and disrupting that rhythm has been linked to higher risks of heart disease, obesity, and depression.
At the same time, few studies have focused on the long-term effects of adopting daylight saving time. Most research has focused on the short-term risks of the seasonal shift, such as reduced sleep and increased car crashes, or circadian misalignment caused by other things. Some health experts have called for more research before deciding on a permanent time, the newspaper reported.
Still, the March 15 statement from sleep experts received support from more than 20 groups, including the National Safety Council, National Parent Teacher Association, and the World Sleep Society.
“We have all enjoyed those summer evenings with seemingly endless dusks,” David Neubauer, MD, an associate professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, told the Post.
But daylight saving time “does not ‘save’ evening light at all, it simply steals it from the morning, when it is necessary to maintain our healthy biological rhythms,” he said.
Permanent daylight saving time would lead to more dark mornings, which opponents have said could be dangerous for kids going to school, adults driving to work, and overall sleep cycles.
“With daylight saving time, we are perpetually out of synchronization with our internal clocks, and we often achieve less nighttime sleep, both circumstances having negative health impacts,” Dr. Neubauer said. “Extra evening light suppresses the melatonin that should be preparing us for falling asleep. The later dawn during daylight saving time deprives our biological clocks of the critical light signal.”
The pros and cons of daylight saving time and standard time were debated during a hearing held by a House Energy and Commerce subcommittee recently. Sleep experts argued in favor of standard time, while other industry experts argued for daylight saving time to reduce crime, save energy, and help businesses that benefit from more daylight in the evenings.
“Everybody advocates a permanent time, but this difference between 1 hour back or 1 hour forward is not so clear in everybody’s mind,” Dr. Cheng said. “I would like to see further debate and some due diligence done on these health consequences and public safety measures before anything else goes forward.”
A version of this article first appeared on WebMD.com.
Sleep experts tend to agree with U.S. lawmakers about getting rid of the twice-per-year time shift, with one exception: They typically call for standard time rather than daylight saving time.
After the Senate voted unanimously on March 15 to make daylight saving time permanent, the American Academy of Sleep Medicine issued a statement that urged caution about adopting a fixed, year-round time with potential health risks.
“We do applaud stopping the switching during the course of the year and settling on a permanent time,” Jocelyn Cheng, MD, a member of the association’s public safety committee, told The Washington Post.
But she said.
Now it’s up to the House of Representatives to decide what to do next. The legislation, which would take effect in 2023, must be passed by the House and signed by President Joe Biden before becoming a law.
Legislators and health experts have debated the shift in recent years. In 2020, the American Academy of Sleep Medicine released a position statement in the Journal of Clinical Sleep Medicine that recommended that the United States move to year-round standard time. Standard time is more aligned with humans’ circadian rhythms and natural light/dark cycles, the group wrote, and disrupting that rhythm has been linked to higher risks of heart disease, obesity, and depression.
At the same time, few studies have focused on the long-term effects of adopting daylight saving time. Most research has focused on the short-term risks of the seasonal shift, such as reduced sleep and increased car crashes, or circadian misalignment caused by other things. Some health experts have called for more research before deciding on a permanent time, the newspaper reported.
Still, the March 15 statement from sleep experts received support from more than 20 groups, including the National Safety Council, National Parent Teacher Association, and the World Sleep Society.
“We have all enjoyed those summer evenings with seemingly endless dusks,” David Neubauer, MD, an associate professor of psychiatry and behavioral sciences at Johns Hopkins University, Baltimore, told the Post.
But daylight saving time “does not ‘save’ evening light at all, it simply steals it from the morning, when it is necessary to maintain our healthy biological rhythms,” he said.
Permanent daylight saving time would lead to more dark mornings, which opponents have said could be dangerous for kids going to school, adults driving to work, and overall sleep cycles.
“With daylight saving time, we are perpetually out of synchronization with our internal clocks, and we often achieve less nighttime sleep, both circumstances having negative health impacts,” Dr. Neubauer said. “Extra evening light suppresses the melatonin that should be preparing us for falling asleep. The later dawn during daylight saving time deprives our biological clocks of the critical light signal.”
The pros and cons of daylight saving time and standard time were debated during a hearing held by a House Energy and Commerce subcommittee recently. Sleep experts argued in favor of standard time, while other industry experts argued for daylight saving time to reduce crime, save energy, and help businesses that benefit from more daylight in the evenings.
“Everybody advocates a permanent time, but this difference between 1 hour back or 1 hour forward is not so clear in everybody’s mind,” Dr. Cheng said. “I would like to see further debate and some due diligence done on these health consequences and public safety measures before anything else goes forward.”
A version of this article first appeared on WebMD.com.
COVID surge in Western Europe puts U.S. health experts on alert
, even as states and cities continue to lift restrictions amid low case numbers.
Infectious disease experts are watching BA.2, the Omicron subvariant that appears to be more transmissible than the original strain. BA.2 is fueling outbreaks across Europe and is growing in dominance across the United States.
“It’s picking up steam. It’s across at least 12 countries … from Finland to Greece,” Eric Topol, MD, director of the Scripps Research Translational Institute, told The Washington Post.
He has been following the surge and has posted recent charts of the outbreak on Twitter. Hospitalizations appear to be increasing in some places as well, he noted, despite the higher vaccination rates of many Western European countries.
“There’s no question there’s a significant wave there,” Dr. Topol said.
Germany recorded more than 260,000 new cases on March 15, according to the data tracker from the New York Times, but coronavirus restrictions are still being lifted this week. The U.K. is reporting more than 75,000 daily cases, and the Netherlands is reporting more than 60,000 daily cases, which are considered major numbers, compared to their population sizes. Meanwhile, France, Italy, and Switzerland are also reporting large increases in infections.
During the past 2 years, widespread outbreaks in Europe have been followed by similar surges in the U.S. weeks later. Most experts interviewed by the Post predicted that it’s likely to happen again.
In the United States, the BA.2 subvariant accounted for 23% of new COVID-19 cases for the week ending March 12, according to the latest estimate from the Centers for Disease Control and Prevention, while the original Omicron strain made up about 66% of cases. The BA.2 percentage is up from 13.7% of new cases for the week ending March 5, 7.1% the previous week, and 4.1% the week before that. In parts of the Northeast and New England, BA.2 makes up more than 38% of new cases.
At the same time, the 7 -day average of COVID-19 cases continues to drop in the United States, with about 31,000 daily cases currently, the New York Times data tracker shows. About 25,000 COVID-19 patients are hospitalized across the country, which has fallen 44% in the past 2 weeks, and about 1,200 deaths are being reported daily.
Several variables could affect the course of a future surge, the Post reported. Vaccination rates, coronavirus safety protocols, and access to antiviral medications could dictate how another wave unfolds across the country.
About 82% of the eligible U.S. population has received at least one vaccine dose, and 69% is fully vaccinated, according to the latest CDC data. About half of those who are eligible for booster doses have received one. In Germany, nearly 76% of people are fully vaccinated, the newspaper reported, and in the United Kingdom, about 74% are fully vaccinated.
Health experts are also considering how natural immunity from a previous infection could affect a BA.2 surge. Millions of Americans were infected with the original Omicron strain, BA.1, which could provide protection. That said, researchers aren’t quite sure whether BA.1 infection protects against BA.2.
“It’s like a weather alert. Right now, the skies are sunny and bright, and we hope they stay that way,” Michael Osterholm, PhD, director of the University of Minnesota’s Center for Infectious Disease Research and Policy, told CNN.
“But we could have some bad weather by evening,” he said. “We just don’t know.”
A version of this article first appeared on WebMD.com.
, even as states and cities continue to lift restrictions amid low case numbers.
Infectious disease experts are watching BA.2, the Omicron subvariant that appears to be more transmissible than the original strain. BA.2 is fueling outbreaks across Europe and is growing in dominance across the United States.
“It’s picking up steam. It’s across at least 12 countries … from Finland to Greece,” Eric Topol, MD, director of the Scripps Research Translational Institute, told The Washington Post.
He has been following the surge and has posted recent charts of the outbreak on Twitter. Hospitalizations appear to be increasing in some places as well, he noted, despite the higher vaccination rates of many Western European countries.
“There’s no question there’s a significant wave there,” Dr. Topol said.
Germany recorded more than 260,000 new cases on March 15, according to the data tracker from the New York Times, but coronavirus restrictions are still being lifted this week. The U.K. is reporting more than 75,000 daily cases, and the Netherlands is reporting more than 60,000 daily cases, which are considered major numbers, compared to their population sizes. Meanwhile, France, Italy, and Switzerland are also reporting large increases in infections.
During the past 2 years, widespread outbreaks in Europe have been followed by similar surges in the U.S. weeks later. Most experts interviewed by the Post predicted that it’s likely to happen again.
In the United States, the BA.2 subvariant accounted for 23% of new COVID-19 cases for the week ending March 12, according to the latest estimate from the Centers for Disease Control and Prevention, while the original Omicron strain made up about 66% of cases. The BA.2 percentage is up from 13.7% of new cases for the week ending March 5, 7.1% the previous week, and 4.1% the week before that. In parts of the Northeast and New England, BA.2 makes up more than 38% of new cases.
At the same time, the 7 -day average of COVID-19 cases continues to drop in the United States, with about 31,000 daily cases currently, the New York Times data tracker shows. About 25,000 COVID-19 patients are hospitalized across the country, which has fallen 44% in the past 2 weeks, and about 1,200 deaths are being reported daily.
Several variables could affect the course of a future surge, the Post reported. Vaccination rates, coronavirus safety protocols, and access to antiviral medications could dictate how another wave unfolds across the country.
About 82% of the eligible U.S. population has received at least one vaccine dose, and 69% is fully vaccinated, according to the latest CDC data. About half of those who are eligible for booster doses have received one. In Germany, nearly 76% of people are fully vaccinated, the newspaper reported, and in the United Kingdom, about 74% are fully vaccinated.
Health experts are also considering how natural immunity from a previous infection could affect a BA.2 surge. Millions of Americans were infected with the original Omicron strain, BA.1, which could provide protection. That said, researchers aren’t quite sure whether BA.1 infection protects against BA.2.
“It’s like a weather alert. Right now, the skies are sunny and bright, and we hope they stay that way,” Michael Osterholm, PhD, director of the University of Minnesota’s Center for Infectious Disease Research and Policy, told CNN.
“But we could have some bad weather by evening,” he said. “We just don’t know.”
A version of this article first appeared on WebMD.com.
, even as states and cities continue to lift restrictions amid low case numbers.
Infectious disease experts are watching BA.2, the Omicron subvariant that appears to be more transmissible than the original strain. BA.2 is fueling outbreaks across Europe and is growing in dominance across the United States.
“It’s picking up steam. It’s across at least 12 countries … from Finland to Greece,” Eric Topol, MD, director of the Scripps Research Translational Institute, told The Washington Post.
He has been following the surge and has posted recent charts of the outbreak on Twitter. Hospitalizations appear to be increasing in some places as well, he noted, despite the higher vaccination rates of many Western European countries.
“There’s no question there’s a significant wave there,” Dr. Topol said.
Germany recorded more than 260,000 new cases on March 15, according to the data tracker from the New York Times, but coronavirus restrictions are still being lifted this week. The U.K. is reporting more than 75,000 daily cases, and the Netherlands is reporting more than 60,000 daily cases, which are considered major numbers, compared to their population sizes. Meanwhile, France, Italy, and Switzerland are also reporting large increases in infections.
During the past 2 years, widespread outbreaks in Europe have been followed by similar surges in the U.S. weeks later. Most experts interviewed by the Post predicted that it’s likely to happen again.
In the United States, the BA.2 subvariant accounted for 23% of new COVID-19 cases for the week ending March 12, according to the latest estimate from the Centers for Disease Control and Prevention, while the original Omicron strain made up about 66% of cases. The BA.2 percentage is up from 13.7% of new cases for the week ending March 5, 7.1% the previous week, and 4.1% the week before that. In parts of the Northeast and New England, BA.2 makes up more than 38% of new cases.
At the same time, the 7 -day average of COVID-19 cases continues to drop in the United States, with about 31,000 daily cases currently, the New York Times data tracker shows. About 25,000 COVID-19 patients are hospitalized across the country, which has fallen 44% in the past 2 weeks, and about 1,200 deaths are being reported daily.
Several variables could affect the course of a future surge, the Post reported. Vaccination rates, coronavirus safety protocols, and access to antiviral medications could dictate how another wave unfolds across the country.
About 82% of the eligible U.S. population has received at least one vaccine dose, and 69% is fully vaccinated, according to the latest CDC data. About half of those who are eligible for booster doses have received one. In Germany, nearly 76% of people are fully vaccinated, the newspaper reported, and in the United Kingdom, about 74% are fully vaccinated.
Health experts are also considering how natural immunity from a previous infection could affect a BA.2 surge. Millions of Americans were infected with the original Omicron strain, BA.1, which could provide protection. That said, researchers aren’t quite sure whether BA.1 infection protects against BA.2.
“It’s like a weather alert. Right now, the skies are sunny and bright, and we hope they stay that way,” Michael Osterholm, PhD, director of the University of Minnesota’s Center for Infectious Disease Research and Policy, told CNN.
“But we could have some bad weather by evening,” he said. “We just don’t know.”
A version of this article first appeared on WebMD.com.
Waiting for the under-5 COVID-19 vaccine
In February, citing the need for more data, Pfizer and BioNTech announced that they were delaying the application for their COVID-19 vaccine for children under the age of 5. Earlier evidence suggests that two doses may not provide adequate protection in the 2- to 4-year old age group. With the larger number of infections and illness in the younger age group from the Omicron variant, Pfizer and BioNTech felt they needed more data on the effectiveness of a third dose.
This delay came as a disappointment to parents of children under 5 who have been eager to have them receive the vaccination. However, Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the Food and Drug Administration, told parents that this delay should be reassuring – that the companies were doing important due diligence before releasing a product that is both safe and effective. The American Academy of Pediatrics wisely released a similar statement of reassurance and support.
It is difficult to know how many parents will eventually immunize their young children once the vaccine is approved. Any survey done more than a few weeks ago must be viewed cautiously as “the COVID numbers” around the country continue to improve and parental attitudes are likely to change.
There will always remain subgroups of parents on either extreme of the bell-shaped curve. Some will reject the under-5 vaccine simply because it is a vaccine. Some parents are so anxious to vaccinate that they will want to be first in line even if waiting is the more prudent approach. In a recent opinion piece appearing in the New York Times, a statistician writes that he is so eager to have his young children immunized that he is encouraging the FDA to replace its traditional reliance on “statistical significance” with a less rigid and binary method such as one based on Bayesian theory (Aubrey Carlton, “I’m a parent and a statistician. There’s a smarter way to think about the under-5 vaccine.” The New York Times. 2022 Mar 1.). However, what this statistician misses in his haste to vaccinate his own children is that we are dealing with an entire population with varying levels of scientific sophistication and appetite for risk. While “statistical significance” may no longer be cutting edge to some statisticians, most of the rest of the country finds the term reassuring.
It will be interesting to see what happens if and when the vaccine is approved. Will the American Academy of Pediatrics come out with a strong recommendation? I hope they are careful and provide a sufficient number of caveats, otherwise we in the trenches will again be left to provide more nuanced advice to families who are both anxious and hesitant.
Despite the recent surge in cases among young children, apparently as a result of the Omicron variant, the disease continues to cause less and milder disease among young children than it does in adults. And the degree to which illness in the pediatric population contributes to the health of the general population appears to still be a matter of debate. This may be yet another instance of when the crafty COVID-19 has moved with a pace that will make an under–age-5 vaccine of relatively little value.
First, we must be careful to assure ourselves that any side effects the vaccine might generate are well within an even more restricted acceptable range. Second, we must be careful not to squander our persuasive currency by promoting a vaccine that in retrospect may turn out to be of relatively little value.
Although there is ample evidence that education often fails to convince the committed anti-vaxxers, pediatricians continue to be held in high regard by most parents, many of whom are understandably confused by the tsunami of health information of mixed quality generated by the pandemic. We must be cautious not to cast ourselves as a group whose knee-jerk reaction is to recommend every vaccine with equal vigor. All vaccines are not created equal. We must be patient and prepared to adjust the level of our enthusiasm. We must continue to tailor our advice based on the hard data. Otherwise, parents will stop asking for our advice because they will believe that they already know what we’re going to say.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In February, citing the need for more data, Pfizer and BioNTech announced that they were delaying the application for their COVID-19 vaccine for children under the age of 5. Earlier evidence suggests that two doses may not provide adequate protection in the 2- to 4-year old age group. With the larger number of infections and illness in the younger age group from the Omicron variant, Pfizer and BioNTech felt they needed more data on the effectiveness of a third dose.
This delay came as a disappointment to parents of children under 5 who have been eager to have them receive the vaccination. However, Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the Food and Drug Administration, told parents that this delay should be reassuring – that the companies were doing important due diligence before releasing a product that is both safe and effective. The American Academy of Pediatrics wisely released a similar statement of reassurance and support.
It is difficult to know how many parents will eventually immunize their young children once the vaccine is approved. Any survey done more than a few weeks ago must be viewed cautiously as “the COVID numbers” around the country continue to improve and parental attitudes are likely to change.
There will always remain subgroups of parents on either extreme of the bell-shaped curve. Some will reject the under-5 vaccine simply because it is a vaccine. Some parents are so anxious to vaccinate that they will want to be first in line even if waiting is the more prudent approach. In a recent opinion piece appearing in the New York Times, a statistician writes that he is so eager to have his young children immunized that he is encouraging the FDA to replace its traditional reliance on “statistical significance” with a less rigid and binary method such as one based on Bayesian theory (Aubrey Carlton, “I’m a parent and a statistician. There’s a smarter way to think about the under-5 vaccine.” The New York Times. 2022 Mar 1.). However, what this statistician misses in his haste to vaccinate his own children is that we are dealing with an entire population with varying levels of scientific sophistication and appetite for risk. While “statistical significance” may no longer be cutting edge to some statisticians, most of the rest of the country finds the term reassuring.
It will be interesting to see what happens if and when the vaccine is approved. Will the American Academy of Pediatrics come out with a strong recommendation? I hope they are careful and provide a sufficient number of caveats, otherwise we in the trenches will again be left to provide more nuanced advice to families who are both anxious and hesitant.
Despite the recent surge in cases among young children, apparently as a result of the Omicron variant, the disease continues to cause less and milder disease among young children than it does in adults. And the degree to which illness in the pediatric population contributes to the health of the general population appears to still be a matter of debate. This may be yet another instance of when the crafty COVID-19 has moved with a pace that will make an under–age-5 vaccine of relatively little value.
First, we must be careful to assure ourselves that any side effects the vaccine might generate are well within an even more restricted acceptable range. Second, we must be careful not to squander our persuasive currency by promoting a vaccine that in retrospect may turn out to be of relatively little value.
Although there is ample evidence that education often fails to convince the committed anti-vaxxers, pediatricians continue to be held in high regard by most parents, many of whom are understandably confused by the tsunami of health information of mixed quality generated by the pandemic. We must be cautious not to cast ourselves as a group whose knee-jerk reaction is to recommend every vaccine with equal vigor. All vaccines are not created equal. We must be patient and prepared to adjust the level of our enthusiasm. We must continue to tailor our advice based on the hard data. Otherwise, parents will stop asking for our advice because they will believe that they already know what we’re going to say.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In February, citing the need for more data, Pfizer and BioNTech announced that they were delaying the application for their COVID-19 vaccine for children under the age of 5. Earlier evidence suggests that two doses may not provide adequate protection in the 2- to 4-year old age group. With the larger number of infections and illness in the younger age group from the Omicron variant, Pfizer and BioNTech felt they needed more data on the effectiveness of a third dose.
This delay came as a disappointment to parents of children under 5 who have been eager to have them receive the vaccination. However, Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the Food and Drug Administration, told parents that this delay should be reassuring – that the companies were doing important due diligence before releasing a product that is both safe and effective. The American Academy of Pediatrics wisely released a similar statement of reassurance and support.
It is difficult to know how many parents will eventually immunize their young children once the vaccine is approved. Any survey done more than a few weeks ago must be viewed cautiously as “the COVID numbers” around the country continue to improve and parental attitudes are likely to change.
There will always remain subgroups of parents on either extreme of the bell-shaped curve. Some will reject the under-5 vaccine simply because it is a vaccine. Some parents are so anxious to vaccinate that they will want to be first in line even if waiting is the more prudent approach. In a recent opinion piece appearing in the New York Times, a statistician writes that he is so eager to have his young children immunized that he is encouraging the FDA to replace its traditional reliance on “statistical significance” with a less rigid and binary method such as one based on Bayesian theory (Aubrey Carlton, “I’m a parent and a statistician. There’s a smarter way to think about the under-5 vaccine.” The New York Times. 2022 Mar 1.). However, what this statistician misses in his haste to vaccinate his own children is that we are dealing with an entire population with varying levels of scientific sophistication and appetite for risk. While “statistical significance” may no longer be cutting edge to some statisticians, most of the rest of the country finds the term reassuring.
It will be interesting to see what happens if and when the vaccine is approved. Will the American Academy of Pediatrics come out with a strong recommendation? I hope they are careful and provide a sufficient number of caveats, otherwise we in the trenches will again be left to provide more nuanced advice to families who are both anxious and hesitant.
Despite the recent surge in cases among young children, apparently as a result of the Omicron variant, the disease continues to cause less and milder disease among young children than it does in adults. And the degree to which illness in the pediatric population contributes to the health of the general population appears to still be a matter of debate. This may be yet another instance of when the crafty COVID-19 has moved with a pace that will make an under–age-5 vaccine of relatively little value.
First, we must be careful to assure ourselves that any side effects the vaccine might generate are well within an even more restricted acceptable range. Second, we must be careful not to squander our persuasive currency by promoting a vaccine that in retrospect may turn out to be of relatively little value.
Although there is ample evidence that education often fails to convince the committed anti-vaxxers, pediatricians continue to be held in high regard by most parents, many of whom are understandably confused by the tsunami of health information of mixed quality generated by the pandemic. We must be cautious not to cast ourselves as a group whose knee-jerk reaction is to recommend every vaccine with equal vigor. All vaccines are not created equal. We must be patient and prepared to adjust the level of our enthusiasm. We must continue to tailor our advice based on the hard data. Otherwise, parents will stop asking for our advice because they will believe that they already know what we’re going to say.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Answering parents’ questions about Cronobacter and powdered formula
A 6-month-old boy presented with 2 days of looser-than-normal stools without blood or mucous. Before the onset of diarrhea, he had been fed at least two bottles of an infant formula identified in a national recall. His mom requested testing for Cronobacter sakazakii.
In mid-February, Abbott Nutrition recalled specific lots of powdered formula produced at one Michigan manufacturing facility because of possible Cronobacter contamination. To date, a public health investigation has identified four infants in three states who developed Cronobacter infection after consuming formula that was part of the recall. Two of the infants died.
As media reports urged families to search their kitchens for containers of the implicated formula and return them for a refund, worried parents reached out to pediatric care providers for advice.
Cronobacter sakazakii and other Cronobacter species are Gram-negative environmental organisms that occasionally cause bacteremia and meningitis in young infants. Although these infections are not subject to mandatory reporting in most states, laboratory-based surveillance suggests that 18 cases occur annually in the United States (0.49 cases/100,00 infants).
While early reports in the literature described cases in hospitalized, preterm infants, infections also occur in the community and in children born at or near term. A Centers for Disease Control and Prevention review of domestic and international cases identified 183 children <12 months of age between 1961 and 2018 described as diagnosed with Cronobacter bacteremia or meningitis.1 Of the 79 U.S. cases, 34 occurred in term infants and 50 were community onset. Most cases occurred in the first month of life; the oldest child was 35 days of age at the onset of symptoms. Meningitis was more likely in infants born close to term and who were not hospitalized at the time of infection. The majority of infants for whom a feeding history was available had consumed powdered formula.
Back in the exam room, the 6-month-old was examined and found to be vigorous and well-appearing with normal vital signs and no signs of dehydration. The infant’s pediatrician found no clinical indication to perform a blood culture or lumbar puncture, the tests used to diagnose invasive Cronobacter infection. She explained that stool cultures are not recommended, as Cronobacter does not usually cause diarrhea in infants and finding the bacteria in the stool may represent colonization rather than infection.
The pediatrician did take the opportunity to talk to the mom about her formula preparation practices and shared a handout. Powdered formula isn’t sterile, but it is safe for most infants when prepared according to manufacturer’s directions. Contamination of formula during or after preparation can also result in Cronobacter infection in vulnerable infants.
The mom was surprised – and unhappy – to learn that Cronobacter could be lurking in her kitchen. More than a decade ago, investigators visited 78 households in Tennessee and cultured multiple kitchen surfaces.2C. sakazakii was recovered from 21 homes. Most of the positive cultures were from sinks, counter tops, and used dishcloths. Cronobacter has also been cultured from a variety of dried food items, including powdered milk, herbal tea, and starches.
According to the CDC, liquid formula, a product that is sterile until opened, is a safer choice for formula-fed infants who are less than 3 months of age, were born prematurely, or have a compromised immune system. When these infants must be fed powdered formula, preparing it with water heated to at least 158°F or 70°C can kill Cronobacter organisms. Parents should be instructed to boil water and let it cool for about 5 minutes before using it to mix formula.
While most cases of Cronobacter in infants have been epidemiologically linked to consumption of powdered formula, sporadic case reports describe infection in infants fed expressed breast milk. In one report, identical bacterial isolates were recovered from expressed milk fed to an infected infant and the breast pump used to express the milk.3
Moms who express milk should be instructed in proper breast pump hygiene, including washing hands thoroughly before handling breast pumps; disassembling and cleaning breast pumps kits after each use, either in hot soapy water with a dedicated brush and basin or in the dishwasher; air drying on a clean surface; and sanitizing at least daily by boiling, steaming, or using a dishwasher’s sanitize cycle.
Health care providers are encouraged to report Cronobacter cases to their state or local health departments.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Strysko J et al. Emerg Infect Dis. 2020;26(5):857-65.
2. Kilonzo-Nthenge A et al. J Food Protect 2012;75(8):1512-7.
3. Bowen A et al. MMWR Morb Mortal Wkly Rep. 2017;66:761-2.
A 6-month-old boy presented with 2 days of looser-than-normal stools without blood or mucous. Before the onset of diarrhea, he had been fed at least two bottles of an infant formula identified in a national recall. His mom requested testing for Cronobacter sakazakii.
In mid-February, Abbott Nutrition recalled specific lots of powdered formula produced at one Michigan manufacturing facility because of possible Cronobacter contamination. To date, a public health investigation has identified four infants in three states who developed Cronobacter infection after consuming formula that was part of the recall. Two of the infants died.
As media reports urged families to search their kitchens for containers of the implicated formula and return them for a refund, worried parents reached out to pediatric care providers for advice.
Cronobacter sakazakii and other Cronobacter species are Gram-negative environmental organisms that occasionally cause bacteremia and meningitis in young infants. Although these infections are not subject to mandatory reporting in most states, laboratory-based surveillance suggests that 18 cases occur annually in the United States (0.49 cases/100,00 infants).
While early reports in the literature described cases in hospitalized, preterm infants, infections also occur in the community and in children born at or near term. A Centers for Disease Control and Prevention review of domestic and international cases identified 183 children <12 months of age between 1961 and 2018 described as diagnosed with Cronobacter bacteremia or meningitis.1 Of the 79 U.S. cases, 34 occurred in term infants and 50 were community onset. Most cases occurred in the first month of life; the oldest child was 35 days of age at the onset of symptoms. Meningitis was more likely in infants born close to term and who were not hospitalized at the time of infection. The majority of infants for whom a feeding history was available had consumed powdered formula.
Back in the exam room, the 6-month-old was examined and found to be vigorous and well-appearing with normal vital signs and no signs of dehydration. The infant’s pediatrician found no clinical indication to perform a blood culture or lumbar puncture, the tests used to diagnose invasive Cronobacter infection. She explained that stool cultures are not recommended, as Cronobacter does not usually cause diarrhea in infants and finding the bacteria in the stool may represent colonization rather than infection.
The pediatrician did take the opportunity to talk to the mom about her formula preparation practices and shared a handout. Powdered formula isn’t sterile, but it is safe for most infants when prepared according to manufacturer’s directions. Contamination of formula during or after preparation can also result in Cronobacter infection in vulnerable infants.
The mom was surprised – and unhappy – to learn that Cronobacter could be lurking in her kitchen. More than a decade ago, investigators visited 78 households in Tennessee and cultured multiple kitchen surfaces.2C. sakazakii was recovered from 21 homes. Most of the positive cultures were from sinks, counter tops, and used dishcloths. Cronobacter has also been cultured from a variety of dried food items, including powdered milk, herbal tea, and starches.
According to the CDC, liquid formula, a product that is sterile until opened, is a safer choice for formula-fed infants who are less than 3 months of age, were born prematurely, or have a compromised immune system. When these infants must be fed powdered formula, preparing it with water heated to at least 158°F or 70°C can kill Cronobacter organisms. Parents should be instructed to boil water and let it cool for about 5 minutes before using it to mix formula.
While most cases of Cronobacter in infants have been epidemiologically linked to consumption of powdered formula, sporadic case reports describe infection in infants fed expressed breast milk. In one report, identical bacterial isolates were recovered from expressed milk fed to an infected infant and the breast pump used to express the milk.3
Moms who express milk should be instructed in proper breast pump hygiene, including washing hands thoroughly before handling breast pumps; disassembling and cleaning breast pumps kits after each use, either in hot soapy water with a dedicated brush and basin or in the dishwasher; air drying on a clean surface; and sanitizing at least daily by boiling, steaming, or using a dishwasher’s sanitize cycle.
Health care providers are encouraged to report Cronobacter cases to their state or local health departments.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Strysko J et al. Emerg Infect Dis. 2020;26(5):857-65.
2. Kilonzo-Nthenge A et al. J Food Protect 2012;75(8):1512-7.
3. Bowen A et al. MMWR Morb Mortal Wkly Rep. 2017;66:761-2.
A 6-month-old boy presented with 2 days of looser-than-normal stools without blood or mucous. Before the onset of diarrhea, he had been fed at least two bottles of an infant formula identified in a national recall. His mom requested testing for Cronobacter sakazakii.
In mid-February, Abbott Nutrition recalled specific lots of powdered formula produced at one Michigan manufacturing facility because of possible Cronobacter contamination. To date, a public health investigation has identified four infants in three states who developed Cronobacter infection after consuming formula that was part of the recall. Two of the infants died.
As media reports urged families to search their kitchens for containers of the implicated formula and return them for a refund, worried parents reached out to pediatric care providers for advice.
Cronobacter sakazakii and other Cronobacter species are Gram-negative environmental organisms that occasionally cause bacteremia and meningitis in young infants. Although these infections are not subject to mandatory reporting in most states, laboratory-based surveillance suggests that 18 cases occur annually in the United States (0.49 cases/100,00 infants).
While early reports in the literature described cases in hospitalized, preterm infants, infections also occur in the community and in children born at or near term. A Centers for Disease Control and Prevention review of domestic and international cases identified 183 children <12 months of age between 1961 and 2018 described as diagnosed with Cronobacter bacteremia or meningitis.1 Of the 79 U.S. cases, 34 occurred in term infants and 50 were community onset. Most cases occurred in the first month of life; the oldest child was 35 days of age at the onset of symptoms. Meningitis was more likely in infants born close to term and who were not hospitalized at the time of infection. The majority of infants for whom a feeding history was available had consumed powdered formula.
Back in the exam room, the 6-month-old was examined and found to be vigorous and well-appearing with normal vital signs and no signs of dehydration. The infant’s pediatrician found no clinical indication to perform a blood culture or lumbar puncture, the tests used to diagnose invasive Cronobacter infection. She explained that stool cultures are not recommended, as Cronobacter does not usually cause diarrhea in infants and finding the bacteria in the stool may represent colonization rather than infection.
The pediatrician did take the opportunity to talk to the mom about her formula preparation practices and shared a handout. Powdered formula isn’t sterile, but it is safe for most infants when prepared according to manufacturer’s directions. Contamination of formula during or after preparation can also result in Cronobacter infection in vulnerable infants.
The mom was surprised – and unhappy – to learn that Cronobacter could be lurking in her kitchen. More than a decade ago, investigators visited 78 households in Tennessee and cultured multiple kitchen surfaces.2C. sakazakii was recovered from 21 homes. Most of the positive cultures were from sinks, counter tops, and used dishcloths. Cronobacter has also been cultured from a variety of dried food items, including powdered milk, herbal tea, and starches.
According to the CDC, liquid formula, a product that is sterile until opened, is a safer choice for formula-fed infants who are less than 3 months of age, were born prematurely, or have a compromised immune system. When these infants must be fed powdered formula, preparing it with water heated to at least 158°F or 70°C can kill Cronobacter organisms. Parents should be instructed to boil water and let it cool for about 5 minutes before using it to mix formula.
While most cases of Cronobacter in infants have been epidemiologically linked to consumption of powdered formula, sporadic case reports describe infection in infants fed expressed breast milk. In one report, identical bacterial isolates were recovered from expressed milk fed to an infected infant and the breast pump used to express the milk.3
Moms who express milk should be instructed in proper breast pump hygiene, including washing hands thoroughly before handling breast pumps; disassembling and cleaning breast pumps kits after each use, either in hot soapy water with a dedicated brush and basin or in the dishwasher; air drying on a clean surface; and sanitizing at least daily by boiling, steaming, or using a dishwasher’s sanitize cycle.
Health care providers are encouraged to report Cronobacter cases to their state or local health departments.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
References
1. Strysko J et al. Emerg Infect Dis. 2020;26(5):857-65.
2. Kilonzo-Nthenge A et al. J Food Protect 2012;75(8):1512-7.
3. Bowen A et al. MMWR Morb Mortal Wkly Rep. 2017;66:761-2.