User login
Infectious disease pop quiz: Clinical challenge #19 for the ObGyn
Should a postpartum patient with chronic hepatitis C infection be discouraged from breastfeeding her infant?
Continue to the answer...
Hepatitis C is not a contraindication to breastfeeding. Although the virus has been identified in breast milk, the risk of transmission to the infant is exceedingly low.
- Duff P. Maternal and perinatal infections: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021:1124-1146.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TJ, et al. Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
Should a postpartum patient with chronic hepatitis C infection be discouraged from breastfeeding her infant?
Continue to the answer...
Hepatitis C is not a contraindication to breastfeeding. Although the virus has been identified in breast milk, the risk of transmission to the infant is exceedingly low.
Should a postpartum patient with chronic hepatitis C infection be discouraged from breastfeeding her infant?
Continue to the answer...
Hepatitis C is not a contraindication to breastfeeding. Although the virus has been identified in breast milk, the risk of transmission to the infant is exceedingly low.
- Duff P. Maternal and perinatal infections: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021:1124-1146.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TJ, et al. Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
- Duff P. Maternal and perinatal infections: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021:1124-1146.
- Duff P. Maternal and fetal infections. In: Resnik R, Lockwood CJ, Moore TJ, et al. Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
Doctors have failed them, say those with transgender regret
In a unique Zoom conference,
The forum was convened on what was dubbed #DetransitionAwarenessDay by Genspect, a parent-based organization that seeks to put the brakes on medical transitions for children and adolescents. The group has doubts about the gender-affirming care model supported by the World Professional Association for Transgender Health, the American Medical Association, the American Academy of Pediatrics, and other medical groups.
“Affirmative” medical care is defined as treatment with puberty blockers and cross-sex hormones for those with gender dysphoria to transition to the opposite sex and is often followed by gender reassignment surgery. However, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed for those under aged 18, in particular, with several countries pulling back on medical treatment and instead emphasizing psychotherapy first.
The purpose of the second annual Genspect meeting was to shed light on the experiences of individuals who have detransitioned – those that identified as transgender and transitioned, but then decided to end their medical transition. People logged on from all over the United States, Canada, New Zealand, Australia, the United Kingdom, Germany, Spain, Chile, and Brazil, among other countries.
“This is a minority within a minority,” said Genspect advisor Stella O’Malley, adding that the first meeting in 2021 was held because “too many people were dismissing the stories of the detransitioners.” Ms. O’Malley is a psychotherapist, a clinical advisor to the Society for Evidence-Based Gender Medicine, and a founding member of the International Association of Therapists for Desisters and Detransitioners.
“It’s become blindingly obvious over the last year that ... ‘detrans’ is a huge part of the trans phenomenon,” said Ms. O’Malley, adding that detransitioners have been “undermined and dismissed.”
Laura Edwards-Leeper, PhD (@DrLauraEL), a prominent gender therapist who has recently expressed concern regarding adequate gatekeeping when treating youth with gender dysphoria, agreed.
She tweeted: “You simply can’t call yourself a legit gender provider if you don’t believe that detransitioners exist. As part of the informed consent process for transitioning, it is unethical to not discuss this possibility with young people.” Dr. Edwards-Leeper is professor emeritus at Pacific University in Hillsboro, Ore.
Speakers in the forum largely offered experiences, not data. They pointed out that there has been little to no study of detransition, but all testified that it was less rare than it has been portrayed by the transgender community.
Struggles with going back
“There are so many reasons why people detransition,” said Sinead Watson, aged 30, a Genspect advisor who transitioned from female to male, starting in 2015, and who decided to detransition in 2019. Citing a study by Lisa Littman, MD, MPH, published in 2021, Ms. Watson said the most common reasons for detransitioning were realizing that gender dysphoria was caused by other issues; internal homophobia; and the unbearable nature of transphobia.
Ms. Watson said the hardest part of detransitioning was admitting to herself that her transition had been a mistake. “It’s embarrassing and you feel ashamed and guilty,” she said, adding that it may mean losing friends who now regard you as a “bigot, while you’re also dealing with transition regret.”
“It’s a living hell, especially when none of your therapists or counselors will listen to you,” she said. “Detransitioning isn’t fun.”
Carol (@sourpatches2077) said she knew for a year that her transition had been a mistake.
“The biggest part was I couldn’t tell my family,” said Carol, who identifies as a lesbian. “I put them through so much. It seems ridiculous to go: ‘Oops, I made this huge [expletive] mistake,’ ” she said, describing the moment she did tell them as “devastating.”
Grace (@hormonehangover) said she remembers finally hitting a moment of “undeniability” some years after transitioning. “I accept it, I’ve ruined my life, this is wrong,” she remembers thinking. “It was devastating, but I couldn’t deny it anymore.”
Don’t trust therapists
People experiencing feelings of unease “need a therapist who will listen to them,” said Ms. Watson. When she first detransitioned, her therapists treated her badly. “They just didn’t want to speak about detransition,” she said, adding that “it was like a kick in the stomach.”
Ms. Watson said she’d like to see more training about detransition, but also on “preventative techniques,” adding that many people transition who should not. “I don’t want more detransitioners – I want less.
“In order for that to happen, we need to treat people with gender dysphoria properly,” said Ms. Watson, adding that the affirmative model is “disgusting, and that’s what needs to change.”
“I would tell somebody to not go to a therapist,” said Carol. Identifying as a butch lesbian, she felt like her therapists had pushed her into transitioning to male. “The No. 1 thing not understood by the mental health professionals is that the vast majority of homosexuals were gender-nonconforming children.” She added that this is especially true of butch lesbians.
Therapists – and doctors – also need to acknowledge both the trauma of transition and detransition, she said.
Kaiser, where she had transitioned, offered her breast reconstruction. Carol said it felt demeaning. “Like you’re Mr. Potatohead: ‘Here, we can just ... put on some new parts and you’re good to go.’ ”
“Doctors are concretizing transient obsessions,” said Helena Kerschner (@lacroicsz), quoting a chatroom user.
Ms. Kerschner gave a presentation on “fandom”: becoming obsessed with a movie, book, TV show, musician, or celebrity, spending every waking hour chatting online or writing fan fiction, or attempting to interact with the celebrity online. It’s a fantasy-dominated world and “the vast majority” of participants are teenage girls who are “identifying as trans,” in part, because they are fed a community-reinforced message that it’s better to be a boy.
Therapists and physicians who help them transition “are harming them for life based on something they would have grown out of or overcome without the permanent damage,” Ms. Kerschner added.
Doctors ‘gaslighting’ people into believing that transition is the answer
A pervasive theme during the webinar was that many people are being misdiagnosed with gender dysphoria, which may not be resolved by medical transition.
Allie, a 22-year-old who stopped taking testosterone after 1½ years, said she initially started the transition to male when she gave up trying to figure out why she could not identify with, or befriend, women, and after a childhood and adolescence spent mostly in the company of boys and being more interested in traditionally male activities.
She endured sexual abuse as a teenager and her parents divorced while she was in high school. Allie also had multiple suicide attempts and many incidents of self-harm. When she decided to transition, at age 18, she went to a private clinic and received cross-sex hormones within a few months of her first and only 30-minute consultation. “There was no explorative therapy,” she said, adding that she was never given a formal diagnosis of gender dysphoria.
For the first year, she said she was “over the freaking moon” because she felt like it was the answer. But things started to unravel while she attended university, and she attempted suicide attempt at age 20. A social worker at the school identified her symptoms – which had been the same since childhood – as autism. She then decided to cease her transition.
Another detransitioner, Laura Becker, said it took 5 years after her transition to recognize that she had undiagnosed PTSD from emotional and psychiatric abuse. Despite a history of substance abuse, self-harm, suicidal ideation, and other mental health issues, she was given testosterone and had a double mastectomy at age 20. She became fixated on gay men, which devolved into a methamphetamine- and crack-fueled relationship with a man she met on the gay dating platform Grindr.
“No one around me knew any better or knew how to help, including the medical professionals who performed the mastectomy and who casually signed off and administered my medical transition,” she said.
Once she was aware of her PTSD she started to detransition, which itself was traumatic, said Laura.
Limpida, aged 24, said he felt pushed into transitioning after seeking help at a Planned Parenthood clinic. He identified as trans at age 15 and spent years attempting to be a woman socially, but every step made him feel more miserable, he said. When he went to the clinic at age 21 to get estrogen, he said he felt like the staff was dismissive of his mental health concerns – including that he was suicidal, had substance abuse, and was severely depressed. He was told he was the “perfect candidate” for transitioning.
A year later, he said he felt worse. The nurse suggested he seek out surgery. After Limpida researched what was involved, he decided to detransition. He has since received an autism diagnosis.
Robin, also aged 24, said the idea of surgery had helped push him into detransitioning, which began in 2020 after 4 years of estrogen. He said he had always been gender nonconforming and knew he was gay at an early age. He believes that gender-nonconforming people are “gaslighted” into thinking that transitioning is the answer.
Lack of evidence-based, informed consent
Michelle Alleva, who stopped identifying as transgender in 2020 but had ceased testosterone 4 years earlier because of side effects, cited what she called a lack of evidence base for the effectiveness and safety of medical transitions.
“You need to have a really, really good evidence base in place if you’re going straight to an invasive treatment that is going to cause permanent changes to your body,” she said.
Access to medical transition used to involve more “gatekeeping” through mental health evaluations and other interventions, she said, but there has been a shift from treating what was considered a psychiatric issue to essentially affirming an identity.
“This shift was activist driven, not evidence based,” she emphasized.
Most studies showing satisfaction with transition only involve a few years of follow-up, she said. She added that the longest follow-up study of transition, published in 2011 and spanning 30 years, showed that the suicide rate 10-15 years post surgery was 20 times higher than the general population.
Studies of regret were primarily conducted before the rapid increase in the number of trans-identifying individuals, she said, which makes it hard to draw conclusions about pediatric transition. Getting estimates on this population is difficult because so many who detransition do not tell their clinicians, and many studies have short follow-up times or a high loss to follow-up.
Ms. Alleva also took issue with the notion that physicians were offering true informed consent, noting that it’s not possible to know if someone is psychologically sound if they haven’t had a thorough mental health evaluation and that there are so many unknowns with medical transition, including that many of the therapies are not approved for the uses being employed.
With regret on the rise, “we need professionals that are prepared for detransitioners,” said Ms. Alleva. “Some of us have lost trust in health care professionals as a result of our experience.”
“It’s a huge feeling of institutional betrayal,” said Grace.
A version of this article first appeared on Medscape.com.
In a unique Zoom conference,
The forum was convened on what was dubbed #DetransitionAwarenessDay by Genspect, a parent-based organization that seeks to put the brakes on medical transitions for children and adolescents. The group has doubts about the gender-affirming care model supported by the World Professional Association for Transgender Health, the American Medical Association, the American Academy of Pediatrics, and other medical groups.
“Affirmative” medical care is defined as treatment with puberty blockers and cross-sex hormones for those with gender dysphoria to transition to the opposite sex and is often followed by gender reassignment surgery. However, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed for those under aged 18, in particular, with several countries pulling back on medical treatment and instead emphasizing psychotherapy first.
The purpose of the second annual Genspect meeting was to shed light on the experiences of individuals who have detransitioned – those that identified as transgender and transitioned, but then decided to end their medical transition. People logged on from all over the United States, Canada, New Zealand, Australia, the United Kingdom, Germany, Spain, Chile, and Brazil, among other countries.
“This is a minority within a minority,” said Genspect advisor Stella O’Malley, adding that the first meeting in 2021 was held because “too many people were dismissing the stories of the detransitioners.” Ms. O’Malley is a psychotherapist, a clinical advisor to the Society for Evidence-Based Gender Medicine, and a founding member of the International Association of Therapists for Desisters and Detransitioners.
“It’s become blindingly obvious over the last year that ... ‘detrans’ is a huge part of the trans phenomenon,” said Ms. O’Malley, adding that detransitioners have been “undermined and dismissed.”
Laura Edwards-Leeper, PhD (@DrLauraEL), a prominent gender therapist who has recently expressed concern regarding adequate gatekeeping when treating youth with gender dysphoria, agreed.
She tweeted: “You simply can’t call yourself a legit gender provider if you don’t believe that detransitioners exist. As part of the informed consent process for transitioning, it is unethical to not discuss this possibility with young people.” Dr. Edwards-Leeper is professor emeritus at Pacific University in Hillsboro, Ore.
Speakers in the forum largely offered experiences, not data. They pointed out that there has been little to no study of detransition, but all testified that it was less rare than it has been portrayed by the transgender community.
Struggles with going back
“There are so many reasons why people detransition,” said Sinead Watson, aged 30, a Genspect advisor who transitioned from female to male, starting in 2015, and who decided to detransition in 2019. Citing a study by Lisa Littman, MD, MPH, published in 2021, Ms. Watson said the most common reasons for detransitioning were realizing that gender dysphoria was caused by other issues; internal homophobia; and the unbearable nature of transphobia.
Ms. Watson said the hardest part of detransitioning was admitting to herself that her transition had been a mistake. “It’s embarrassing and you feel ashamed and guilty,” she said, adding that it may mean losing friends who now regard you as a “bigot, while you’re also dealing with transition regret.”
“It’s a living hell, especially when none of your therapists or counselors will listen to you,” she said. “Detransitioning isn’t fun.”
Carol (@sourpatches2077) said she knew for a year that her transition had been a mistake.
“The biggest part was I couldn’t tell my family,” said Carol, who identifies as a lesbian. “I put them through so much. It seems ridiculous to go: ‘Oops, I made this huge [expletive] mistake,’ ” she said, describing the moment she did tell them as “devastating.”
Grace (@hormonehangover) said she remembers finally hitting a moment of “undeniability” some years after transitioning. “I accept it, I’ve ruined my life, this is wrong,” she remembers thinking. “It was devastating, but I couldn’t deny it anymore.”
Don’t trust therapists
People experiencing feelings of unease “need a therapist who will listen to them,” said Ms. Watson. When she first detransitioned, her therapists treated her badly. “They just didn’t want to speak about detransition,” she said, adding that “it was like a kick in the stomach.”
Ms. Watson said she’d like to see more training about detransition, but also on “preventative techniques,” adding that many people transition who should not. “I don’t want more detransitioners – I want less.
“In order for that to happen, we need to treat people with gender dysphoria properly,” said Ms. Watson, adding that the affirmative model is “disgusting, and that’s what needs to change.”
“I would tell somebody to not go to a therapist,” said Carol. Identifying as a butch lesbian, she felt like her therapists had pushed her into transitioning to male. “The No. 1 thing not understood by the mental health professionals is that the vast majority of homosexuals were gender-nonconforming children.” She added that this is especially true of butch lesbians.
Therapists – and doctors – also need to acknowledge both the trauma of transition and detransition, she said.
Kaiser, where she had transitioned, offered her breast reconstruction. Carol said it felt demeaning. “Like you’re Mr. Potatohead: ‘Here, we can just ... put on some new parts and you’re good to go.’ ”
“Doctors are concretizing transient obsessions,” said Helena Kerschner (@lacroicsz), quoting a chatroom user.
Ms. Kerschner gave a presentation on “fandom”: becoming obsessed with a movie, book, TV show, musician, or celebrity, spending every waking hour chatting online or writing fan fiction, or attempting to interact with the celebrity online. It’s a fantasy-dominated world and “the vast majority” of participants are teenage girls who are “identifying as trans,” in part, because they are fed a community-reinforced message that it’s better to be a boy.
Therapists and physicians who help them transition “are harming them for life based on something they would have grown out of or overcome without the permanent damage,” Ms. Kerschner added.
Doctors ‘gaslighting’ people into believing that transition is the answer
A pervasive theme during the webinar was that many people are being misdiagnosed with gender dysphoria, which may not be resolved by medical transition.
Allie, a 22-year-old who stopped taking testosterone after 1½ years, said she initially started the transition to male when she gave up trying to figure out why she could not identify with, or befriend, women, and after a childhood and adolescence spent mostly in the company of boys and being more interested in traditionally male activities.
She endured sexual abuse as a teenager and her parents divorced while she was in high school. Allie also had multiple suicide attempts and many incidents of self-harm. When she decided to transition, at age 18, she went to a private clinic and received cross-sex hormones within a few months of her first and only 30-minute consultation. “There was no explorative therapy,” she said, adding that she was never given a formal diagnosis of gender dysphoria.
For the first year, she said she was “over the freaking moon” because she felt like it was the answer. But things started to unravel while she attended university, and she attempted suicide attempt at age 20. A social worker at the school identified her symptoms – which had been the same since childhood – as autism. She then decided to cease her transition.
Another detransitioner, Laura Becker, said it took 5 years after her transition to recognize that she had undiagnosed PTSD from emotional and psychiatric abuse. Despite a history of substance abuse, self-harm, suicidal ideation, and other mental health issues, she was given testosterone and had a double mastectomy at age 20. She became fixated on gay men, which devolved into a methamphetamine- and crack-fueled relationship with a man she met on the gay dating platform Grindr.
“No one around me knew any better or knew how to help, including the medical professionals who performed the mastectomy and who casually signed off and administered my medical transition,” she said.
Once she was aware of her PTSD she started to detransition, which itself was traumatic, said Laura.
Limpida, aged 24, said he felt pushed into transitioning after seeking help at a Planned Parenthood clinic. He identified as trans at age 15 and spent years attempting to be a woman socially, but every step made him feel more miserable, he said. When he went to the clinic at age 21 to get estrogen, he said he felt like the staff was dismissive of his mental health concerns – including that he was suicidal, had substance abuse, and was severely depressed. He was told he was the “perfect candidate” for transitioning.
A year later, he said he felt worse. The nurse suggested he seek out surgery. After Limpida researched what was involved, he decided to detransition. He has since received an autism diagnosis.
Robin, also aged 24, said the idea of surgery had helped push him into detransitioning, which began in 2020 after 4 years of estrogen. He said he had always been gender nonconforming and knew he was gay at an early age. He believes that gender-nonconforming people are “gaslighted” into thinking that transitioning is the answer.
Lack of evidence-based, informed consent
Michelle Alleva, who stopped identifying as transgender in 2020 but had ceased testosterone 4 years earlier because of side effects, cited what she called a lack of evidence base for the effectiveness and safety of medical transitions.
“You need to have a really, really good evidence base in place if you’re going straight to an invasive treatment that is going to cause permanent changes to your body,” she said.
Access to medical transition used to involve more “gatekeeping” through mental health evaluations and other interventions, she said, but there has been a shift from treating what was considered a psychiatric issue to essentially affirming an identity.
“This shift was activist driven, not evidence based,” she emphasized.
Most studies showing satisfaction with transition only involve a few years of follow-up, she said. She added that the longest follow-up study of transition, published in 2011 and spanning 30 years, showed that the suicide rate 10-15 years post surgery was 20 times higher than the general population.
Studies of regret were primarily conducted before the rapid increase in the number of trans-identifying individuals, she said, which makes it hard to draw conclusions about pediatric transition. Getting estimates on this population is difficult because so many who detransition do not tell their clinicians, and many studies have short follow-up times or a high loss to follow-up.
Ms. Alleva also took issue with the notion that physicians were offering true informed consent, noting that it’s not possible to know if someone is psychologically sound if they haven’t had a thorough mental health evaluation and that there are so many unknowns with medical transition, including that many of the therapies are not approved for the uses being employed.
With regret on the rise, “we need professionals that are prepared for detransitioners,” said Ms. Alleva. “Some of us have lost trust in health care professionals as a result of our experience.”
“It’s a huge feeling of institutional betrayal,” said Grace.
A version of this article first appeared on Medscape.com.
In a unique Zoom conference,
The forum was convened on what was dubbed #DetransitionAwarenessDay by Genspect, a parent-based organization that seeks to put the brakes on medical transitions for children and adolescents. The group has doubts about the gender-affirming care model supported by the World Professional Association for Transgender Health, the American Medical Association, the American Academy of Pediatrics, and other medical groups.
“Affirmative” medical care is defined as treatment with puberty blockers and cross-sex hormones for those with gender dysphoria to transition to the opposite sex and is often followed by gender reassignment surgery. However, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed for those under aged 18, in particular, with several countries pulling back on medical treatment and instead emphasizing psychotherapy first.
The purpose of the second annual Genspect meeting was to shed light on the experiences of individuals who have detransitioned – those that identified as transgender and transitioned, but then decided to end their medical transition. People logged on from all over the United States, Canada, New Zealand, Australia, the United Kingdom, Germany, Spain, Chile, and Brazil, among other countries.
“This is a minority within a minority,” said Genspect advisor Stella O’Malley, adding that the first meeting in 2021 was held because “too many people were dismissing the stories of the detransitioners.” Ms. O’Malley is a psychotherapist, a clinical advisor to the Society for Evidence-Based Gender Medicine, and a founding member of the International Association of Therapists for Desisters and Detransitioners.
“It’s become blindingly obvious over the last year that ... ‘detrans’ is a huge part of the trans phenomenon,” said Ms. O’Malley, adding that detransitioners have been “undermined and dismissed.”
Laura Edwards-Leeper, PhD (@DrLauraEL), a prominent gender therapist who has recently expressed concern regarding adequate gatekeeping when treating youth with gender dysphoria, agreed.
She tweeted: “You simply can’t call yourself a legit gender provider if you don’t believe that detransitioners exist. As part of the informed consent process for transitioning, it is unethical to not discuss this possibility with young people.” Dr. Edwards-Leeper is professor emeritus at Pacific University in Hillsboro, Ore.
Speakers in the forum largely offered experiences, not data. They pointed out that there has been little to no study of detransition, but all testified that it was less rare than it has been portrayed by the transgender community.
Struggles with going back
“There are so many reasons why people detransition,” said Sinead Watson, aged 30, a Genspect advisor who transitioned from female to male, starting in 2015, and who decided to detransition in 2019. Citing a study by Lisa Littman, MD, MPH, published in 2021, Ms. Watson said the most common reasons for detransitioning were realizing that gender dysphoria was caused by other issues; internal homophobia; and the unbearable nature of transphobia.
Ms. Watson said the hardest part of detransitioning was admitting to herself that her transition had been a mistake. “It’s embarrassing and you feel ashamed and guilty,” she said, adding that it may mean losing friends who now regard you as a “bigot, while you’re also dealing with transition regret.”
“It’s a living hell, especially when none of your therapists or counselors will listen to you,” she said. “Detransitioning isn’t fun.”
Carol (@sourpatches2077) said she knew for a year that her transition had been a mistake.
“The biggest part was I couldn’t tell my family,” said Carol, who identifies as a lesbian. “I put them through so much. It seems ridiculous to go: ‘Oops, I made this huge [expletive] mistake,’ ” she said, describing the moment she did tell them as “devastating.”
Grace (@hormonehangover) said she remembers finally hitting a moment of “undeniability” some years after transitioning. “I accept it, I’ve ruined my life, this is wrong,” she remembers thinking. “It was devastating, but I couldn’t deny it anymore.”
Don’t trust therapists
People experiencing feelings of unease “need a therapist who will listen to them,” said Ms. Watson. When she first detransitioned, her therapists treated her badly. “They just didn’t want to speak about detransition,” she said, adding that “it was like a kick in the stomach.”
Ms. Watson said she’d like to see more training about detransition, but also on “preventative techniques,” adding that many people transition who should not. “I don’t want more detransitioners – I want less.
“In order for that to happen, we need to treat people with gender dysphoria properly,” said Ms. Watson, adding that the affirmative model is “disgusting, and that’s what needs to change.”
“I would tell somebody to not go to a therapist,” said Carol. Identifying as a butch lesbian, she felt like her therapists had pushed her into transitioning to male. “The No. 1 thing not understood by the mental health professionals is that the vast majority of homosexuals were gender-nonconforming children.” She added that this is especially true of butch lesbians.
Therapists – and doctors – also need to acknowledge both the trauma of transition and detransition, she said.
Kaiser, where she had transitioned, offered her breast reconstruction. Carol said it felt demeaning. “Like you’re Mr. Potatohead: ‘Here, we can just ... put on some new parts and you’re good to go.’ ”
“Doctors are concretizing transient obsessions,” said Helena Kerschner (@lacroicsz), quoting a chatroom user.
Ms. Kerschner gave a presentation on “fandom”: becoming obsessed with a movie, book, TV show, musician, or celebrity, spending every waking hour chatting online or writing fan fiction, or attempting to interact with the celebrity online. It’s a fantasy-dominated world and “the vast majority” of participants are teenage girls who are “identifying as trans,” in part, because they are fed a community-reinforced message that it’s better to be a boy.
Therapists and physicians who help them transition “are harming them for life based on something they would have grown out of or overcome without the permanent damage,” Ms. Kerschner added.
Doctors ‘gaslighting’ people into believing that transition is the answer
A pervasive theme during the webinar was that many people are being misdiagnosed with gender dysphoria, which may not be resolved by medical transition.
Allie, a 22-year-old who stopped taking testosterone after 1½ years, said she initially started the transition to male when she gave up trying to figure out why she could not identify with, or befriend, women, and after a childhood and adolescence spent mostly in the company of boys and being more interested in traditionally male activities.
She endured sexual abuse as a teenager and her parents divorced while she was in high school. Allie also had multiple suicide attempts and many incidents of self-harm. When she decided to transition, at age 18, she went to a private clinic and received cross-sex hormones within a few months of her first and only 30-minute consultation. “There was no explorative therapy,” she said, adding that she was never given a formal diagnosis of gender dysphoria.
For the first year, she said she was “over the freaking moon” because she felt like it was the answer. But things started to unravel while she attended university, and she attempted suicide attempt at age 20. A social worker at the school identified her symptoms – which had been the same since childhood – as autism. She then decided to cease her transition.
Another detransitioner, Laura Becker, said it took 5 years after her transition to recognize that she had undiagnosed PTSD from emotional and psychiatric abuse. Despite a history of substance abuse, self-harm, suicidal ideation, and other mental health issues, she was given testosterone and had a double mastectomy at age 20. She became fixated on gay men, which devolved into a methamphetamine- and crack-fueled relationship with a man she met on the gay dating platform Grindr.
“No one around me knew any better or knew how to help, including the medical professionals who performed the mastectomy and who casually signed off and administered my medical transition,” she said.
Once she was aware of her PTSD she started to detransition, which itself was traumatic, said Laura.
Limpida, aged 24, said he felt pushed into transitioning after seeking help at a Planned Parenthood clinic. He identified as trans at age 15 and spent years attempting to be a woman socially, but every step made him feel more miserable, he said. When he went to the clinic at age 21 to get estrogen, he said he felt like the staff was dismissive of his mental health concerns – including that he was suicidal, had substance abuse, and was severely depressed. He was told he was the “perfect candidate” for transitioning.
A year later, he said he felt worse. The nurse suggested he seek out surgery. After Limpida researched what was involved, he decided to detransition. He has since received an autism diagnosis.
Robin, also aged 24, said the idea of surgery had helped push him into detransitioning, which began in 2020 after 4 years of estrogen. He said he had always been gender nonconforming and knew he was gay at an early age. He believes that gender-nonconforming people are “gaslighted” into thinking that transitioning is the answer.
Lack of evidence-based, informed consent
Michelle Alleva, who stopped identifying as transgender in 2020 but had ceased testosterone 4 years earlier because of side effects, cited what she called a lack of evidence base for the effectiveness and safety of medical transitions.
“You need to have a really, really good evidence base in place if you’re going straight to an invasive treatment that is going to cause permanent changes to your body,” she said.
Access to medical transition used to involve more “gatekeeping” through mental health evaluations and other interventions, she said, but there has been a shift from treating what was considered a psychiatric issue to essentially affirming an identity.
“This shift was activist driven, not evidence based,” she emphasized.
Most studies showing satisfaction with transition only involve a few years of follow-up, she said. She added that the longest follow-up study of transition, published in 2011 and spanning 30 years, showed that the suicide rate 10-15 years post surgery was 20 times higher than the general population.
Studies of regret were primarily conducted before the rapid increase in the number of trans-identifying individuals, she said, which makes it hard to draw conclusions about pediatric transition. Getting estimates on this population is difficult because so many who detransition do not tell their clinicians, and many studies have short follow-up times or a high loss to follow-up.
Ms. Alleva also took issue with the notion that physicians were offering true informed consent, noting that it’s not possible to know if someone is psychologically sound if they haven’t had a thorough mental health evaluation and that there are so many unknowns with medical transition, including that many of the therapies are not approved for the uses being employed.
With regret on the rise, “we need professionals that are prepared for detransitioners,” said Ms. Alleva. “Some of us have lost trust in health care professionals as a result of our experience.”
“It’s a huge feeling of institutional betrayal,” said Grace.
A version of this article first appeared on Medscape.com.
FDA approves upadacitinib for ulcerative colitis
The Food and Drug Administration has approved upadacitinib (Rinvoq) for the treatment of adults with moderately to severely active ulcerative colitis (UC) who do not respond adequately to or can’t tolerate anti–tumor necrosis factor (TNF) agents.
It marks the first FDA approval for the selective Janus kinase (JAK) inhibitor in gastroenterology and is supported by efficacy and safety data from three phase 3 randomized, double-blind, placebo-controlled clinical studies.
In clinical trials, upadacitinib achieved the primary endpoints of clinical remission, per modified Mayo Score, at 8 and 52 weeks.
In addition, a greater proportion of patients who received upadacitinib achieved clinical response as early as the second week of treatment and steroid-free clinical remission at 1 year, as well as key endoscopic and histologic improvement endpoints at 8 and 52 weeks.
“Ulcerative colitis patients live with unpredictable symptoms such as increased stool frequency and bleeding, which can make daily activities difficult,” Maria T. Abreu, MD, director, Crohn’s and Colitis Center, University of Miami Health System, said in a news release issued by AbbVie.
Upadacitinib has been shown to “rapidly control symptoms,” said Dr. Abreu, adding, “I believe these types of improvements can make a positive difference for my patients.”
Upadacitinib is also approved in the United States to treat adults with moderate to severe rheumatoid arthritis, moderate to severe atopic dermatitis, and active psoriatic arthritis.
Overall, the safety profile observed in patients with UC who were treated with upadacitinib was generally similar to the safety profile in patients with rheumatoid arthritis and atopic dermatitis.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved upadacitinib (Rinvoq) for the treatment of adults with moderately to severely active ulcerative colitis (UC) who do not respond adequately to or can’t tolerate anti–tumor necrosis factor (TNF) agents.
It marks the first FDA approval for the selective Janus kinase (JAK) inhibitor in gastroenterology and is supported by efficacy and safety data from three phase 3 randomized, double-blind, placebo-controlled clinical studies.
In clinical trials, upadacitinib achieved the primary endpoints of clinical remission, per modified Mayo Score, at 8 and 52 weeks.
In addition, a greater proportion of patients who received upadacitinib achieved clinical response as early as the second week of treatment and steroid-free clinical remission at 1 year, as well as key endoscopic and histologic improvement endpoints at 8 and 52 weeks.
“Ulcerative colitis patients live with unpredictable symptoms such as increased stool frequency and bleeding, which can make daily activities difficult,” Maria T. Abreu, MD, director, Crohn’s and Colitis Center, University of Miami Health System, said in a news release issued by AbbVie.
Upadacitinib has been shown to “rapidly control symptoms,” said Dr. Abreu, adding, “I believe these types of improvements can make a positive difference for my patients.”
Upadacitinib is also approved in the United States to treat adults with moderate to severe rheumatoid arthritis, moderate to severe atopic dermatitis, and active psoriatic arthritis.
Overall, the safety profile observed in patients with UC who were treated with upadacitinib was generally similar to the safety profile in patients with rheumatoid arthritis and atopic dermatitis.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved upadacitinib (Rinvoq) for the treatment of adults with moderately to severely active ulcerative colitis (UC) who do not respond adequately to or can’t tolerate anti–tumor necrosis factor (TNF) agents.
It marks the first FDA approval for the selective Janus kinase (JAK) inhibitor in gastroenterology and is supported by efficacy and safety data from three phase 3 randomized, double-blind, placebo-controlled clinical studies.
In clinical trials, upadacitinib achieved the primary endpoints of clinical remission, per modified Mayo Score, at 8 and 52 weeks.
In addition, a greater proportion of patients who received upadacitinib achieved clinical response as early as the second week of treatment and steroid-free clinical remission at 1 year, as well as key endoscopic and histologic improvement endpoints at 8 and 52 weeks.
“Ulcerative colitis patients live with unpredictable symptoms such as increased stool frequency and bleeding, which can make daily activities difficult,” Maria T. Abreu, MD, director, Crohn’s and Colitis Center, University of Miami Health System, said in a news release issued by AbbVie.
Upadacitinib has been shown to “rapidly control symptoms,” said Dr. Abreu, adding, “I believe these types of improvements can make a positive difference for my patients.”
Upadacitinib is also approved in the United States to treat adults with moderate to severe rheumatoid arthritis, moderate to severe atopic dermatitis, and active psoriatic arthritis.
Overall, the safety profile observed in patients with UC who were treated with upadacitinib was generally similar to the safety profile in patients with rheumatoid arthritis and atopic dermatitis.
A version of this article first appeared on Medscape.com.
Don’t drink calories: Artificial sweeteners beat sugar in new analysis
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
When I counsel patients who are trying to lose weight, there is something I always discuss: “Don’t drink calories.” The idea is that it is so easy to consume sweetened beverages (and alcoholic ones, for that matter) and we don’t really get a sense of how many calories we’re taking in.
Some patients balk at the idea, saying they can’t stand the taste of water or just can’t bring themselves to drink it. While, as a nephrologist, this pains me deeply to hear, I often suggest going for low- or zero-calorie flavored drinks instead of the sugary stuff.
And yet ... I need to admit that recently I’ve been more nervous about that advice. A very nice study in Nature, for example, found that artificial sweeteners induce glucose intolerance and weight gain – in mice.
Several observational studies have suggested that the use of nonnutritive sweeteners – sucralose, aspartame, and so on – are associated with higher body weight and type 2 diabetes. Of course,
Randomized trials, as ever, are the key to deeper understanding, but most trials in this space are relatively small. That makes a good case for this study, appearing in JAMA Network Open, which combines data from 17 randomized trials to determine what effects substituting sugary drinks with low- and zero-calorie drinks truly has.
So, what’s the bottom line? Should I ditch the Splenda in my morning coffee and drop in some sugar cubes?
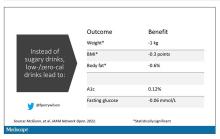
It turns out that the effects of drinking low- or zero-calorie drinks instead of sugary ones is modest, but overall beneficial, depending on the outcome you’re trying to achieve.
Randomized trials show that switching to low-cal drinks reduces body weight by about a kilogram, and BMI by 0.3 points. It also reduces body fat by about half a percent.
Effects on glucose homeostasis – hemoglobin A1c level and fasting glucose – were not that impressive, though.
The authors also compared sugar-sweetened beverages with plain old water. I expected this analysis to show more dramatic benefits. After all, we’re all just ugly, giant bags of mostly water. Interestingly, the effects of switching to water were not as dramatic and largely nonsignificant with respect to most outcomes evaluated.
So, what do we make of this? If someone is a habitual drinker of sugar-sweetened beverages, is it preferable to switch to a zero-calorie flavored drink, compared with plain water?
One possibility is that in the trials where people are randomized to switch to water, they aren’t as adherent. Just because we ask someone to drink water doesn’t mean they do it, and so there may be a tendency to “cheat” with sugar-sweetened beverages. However, if told that low- or zero-calorie flavored drinks are okay, maybe it’s easier to stick to the plan? This is essentially the argument you get from people who say that vaping is a good way to quit smoking. It may or may not be true.
It could also be that we just don’t have enough rigorous data to make a firm conclusion. Of the 17 trials examined, only three of them used water substitution as an intervention.
All in all, these data provide some reassurance that the zero-calorie sweeteners aren’t secretly exacerbating the obesity epidemic. I’d certainly rather my patients drink Diet Coke than regular Coke. That said, these studies are necessarily short term; the longer-term effects of sugar substitutes, while perhaps not as bad as the long-term effects of sugar, must necessarily be worse than the long-term effects of drinking water. Maybe this is the nephrologist in me talking again, but I doubt that there could possibly be a fluid better for the human body than good old H2O. Except coffee, of course.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
When I counsel patients who are trying to lose weight, there is something I always discuss: “Don’t drink calories.” The idea is that it is so easy to consume sweetened beverages (and alcoholic ones, for that matter) and we don’t really get a sense of how many calories we’re taking in.
Some patients balk at the idea, saying they can’t stand the taste of water or just can’t bring themselves to drink it. While, as a nephrologist, this pains me deeply to hear, I often suggest going for low- or zero-calorie flavored drinks instead of the sugary stuff.
And yet ... I need to admit that recently I’ve been more nervous about that advice. A very nice study in Nature, for example, found that artificial sweeteners induce glucose intolerance and weight gain – in mice.
Several observational studies have suggested that the use of nonnutritive sweeteners – sucralose, aspartame, and so on – are associated with higher body weight and type 2 diabetes. Of course,
Randomized trials, as ever, are the key to deeper understanding, but most trials in this space are relatively small. That makes a good case for this study, appearing in JAMA Network Open, which combines data from 17 randomized trials to determine what effects substituting sugary drinks with low- and zero-calorie drinks truly has.
So, what’s the bottom line? Should I ditch the Splenda in my morning coffee and drop in some sugar cubes?
It turns out that the effects of drinking low- or zero-calorie drinks instead of sugary ones is modest, but overall beneficial, depending on the outcome you’re trying to achieve.
Randomized trials show that switching to low-cal drinks reduces body weight by about a kilogram, and BMI by 0.3 points. It also reduces body fat by about half a percent.
Effects on glucose homeostasis – hemoglobin A1c level and fasting glucose – were not that impressive, though.
The authors also compared sugar-sweetened beverages with plain old water. I expected this analysis to show more dramatic benefits. After all, we’re all just ugly, giant bags of mostly water. Interestingly, the effects of switching to water were not as dramatic and largely nonsignificant with respect to most outcomes evaluated.
So, what do we make of this? If someone is a habitual drinker of sugar-sweetened beverages, is it preferable to switch to a zero-calorie flavored drink, compared with plain water?
One possibility is that in the trials where people are randomized to switch to water, they aren’t as adherent. Just because we ask someone to drink water doesn’t mean they do it, and so there may be a tendency to “cheat” with sugar-sweetened beverages. However, if told that low- or zero-calorie flavored drinks are okay, maybe it’s easier to stick to the plan? This is essentially the argument you get from people who say that vaping is a good way to quit smoking. It may or may not be true.
It could also be that we just don’t have enough rigorous data to make a firm conclusion. Of the 17 trials examined, only three of them used water substitution as an intervention.
All in all, these data provide some reassurance that the zero-calorie sweeteners aren’t secretly exacerbating the obesity epidemic. I’d certainly rather my patients drink Diet Coke than regular Coke. That said, these studies are necessarily short term; the longer-term effects of sugar substitutes, while perhaps not as bad as the long-term effects of sugar, must necessarily be worse than the long-term effects of drinking water. Maybe this is the nephrologist in me talking again, but I doubt that there could possibly be a fluid better for the human body than good old H2O. Except coffee, of course.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript of Impact Factor with F. Perry Wilson has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
When I counsel patients who are trying to lose weight, there is something I always discuss: “Don’t drink calories.” The idea is that it is so easy to consume sweetened beverages (and alcoholic ones, for that matter) and we don’t really get a sense of how many calories we’re taking in.
Some patients balk at the idea, saying they can’t stand the taste of water or just can’t bring themselves to drink it. While, as a nephrologist, this pains me deeply to hear, I often suggest going for low- or zero-calorie flavored drinks instead of the sugary stuff.
And yet ... I need to admit that recently I’ve been more nervous about that advice. A very nice study in Nature, for example, found that artificial sweeteners induce glucose intolerance and weight gain – in mice.
Several observational studies have suggested that the use of nonnutritive sweeteners – sucralose, aspartame, and so on – are associated with higher body weight and type 2 diabetes. Of course,
Randomized trials, as ever, are the key to deeper understanding, but most trials in this space are relatively small. That makes a good case for this study, appearing in JAMA Network Open, which combines data from 17 randomized trials to determine what effects substituting sugary drinks with low- and zero-calorie drinks truly has.
So, what’s the bottom line? Should I ditch the Splenda in my morning coffee and drop in some sugar cubes?
It turns out that the effects of drinking low- or zero-calorie drinks instead of sugary ones is modest, but overall beneficial, depending on the outcome you’re trying to achieve.
Randomized trials show that switching to low-cal drinks reduces body weight by about a kilogram, and BMI by 0.3 points. It also reduces body fat by about half a percent.
Effects on glucose homeostasis – hemoglobin A1c level and fasting glucose – were not that impressive, though.
The authors also compared sugar-sweetened beverages with plain old water. I expected this analysis to show more dramatic benefits. After all, we’re all just ugly, giant bags of mostly water. Interestingly, the effects of switching to water were not as dramatic and largely nonsignificant with respect to most outcomes evaluated.
So, what do we make of this? If someone is a habitual drinker of sugar-sweetened beverages, is it preferable to switch to a zero-calorie flavored drink, compared with plain water?
One possibility is that in the trials where people are randomized to switch to water, they aren’t as adherent. Just because we ask someone to drink water doesn’t mean they do it, and so there may be a tendency to “cheat” with sugar-sweetened beverages. However, if told that low- or zero-calorie flavored drinks are okay, maybe it’s easier to stick to the plan? This is essentially the argument you get from people who say that vaping is a good way to quit smoking. It may or may not be true.
It could also be that we just don’t have enough rigorous data to make a firm conclusion. Of the 17 trials examined, only three of them used water substitution as an intervention.
All in all, these data provide some reassurance that the zero-calorie sweeteners aren’t secretly exacerbating the obesity epidemic. I’d certainly rather my patients drink Diet Coke than regular Coke. That said, these studies are necessarily short term; the longer-term effects of sugar substitutes, while perhaps not as bad as the long-term effects of sugar, must necessarily be worse than the long-term effects of drinking water. Maybe this is the nephrologist in me talking again, but I doubt that there could possibly be a fluid better for the human body than good old H2O. Except coffee, of course.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale University’s Clinical and Translational Research Accelerator. He disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
French fries vs. almonds every day for a month: What changes?
Eat french fries every day for a month? Sure, as long as it’s for science.
That’s exactly what 107 people did in a scientific study, while 58 others ate a daily serving of almonds with the same number of calories.
At the end of the study, the researchers found no significant differences between the groups in people’s total amount of fat or their fasting glucose measures, according to the study, published Feb. 18 in the American Journal of Clinical Nutrition.
The french fry eaters gained a little more weight, but it was not statistically significant. The people who ate french fries gained 0.49 kilograms (just over a pound), vs. about a tenth of a kilogram (about one-fifth of a pound) in the group of people who ate almonds.
“The take-home is if you like almonds, eat some almonds. If you like potatoes, eat some potatoes, but don’t overeat either,” said study leader David B. Allison, PhD, a professor at Indiana University’s School of Public Health in Bloomington. ‘It’s probably good to have a little bit of each – each has some unique advantages in terms of nutrition.”
“This study confirms what registered dietitian nutritionists already know – all foods can fit. We can eat almonds, french fries, kale, and cookies,” said Melissa Majumdar, a registered dietitian and certified specialist in obesity and weight management at Emory University Hospital Midtown in Atlanta. ‘The consumption of one food or the avoidance of another does not make a healthy diet.”
At the same time, people should not interpret the results to mean it’s OK to eat french fries all day, every day. “We know that while potatoes are nutrient dense, the frying process reduces the nutritional value,” Ms. Majumdar said.
“Because french fries are often consumed alongside other nutrient-poor or high-fat foods, they should not be consumed daily but can fit into an overall balanced diet,” she added.
Would you like fries with that?
The researchers compared french fries to almonds because almonds are known for positive effects on energy balance, body composition, and low glycemic index. The research was partly funded by the Alliance for Potato Research and Education.
French fries are an incredibly popular food in the United States. According to an August 2021 post on the food website Mashed, Americans eat an average of 30 pounds of french fries each year.
Although consumption of almonds is increasing, Americans eat far less in volume each year than they do fries – an estimated 2.4 pounds of almonds per person, according to August 2021 figures from the Almond Board of California.
Dr. Allison and colleagues recruited 180 healthy adults for the study. Their average age was 30, and about two-thirds were women.
They randomly assigned 60 people to add about a medium serving of plain french fries (Tater Pals Ovenable Crinkle Cut Fries, Simplot Foods) to their diet. Another 60 people were assigned to the same amount of Tater Pals fries with herbs (oregano, basil, garlic, onion, and rosemary), and another 60 people ate Wonderful brand roasted and salted almonds.
Investigators told people to add either the potatoes or nuts to their diet every day for a month and gave no further instructions.
After some people dropped out of the study, results were based on 55 who ate regular french fries, 52 who ate french fries with herbs and spices, and 58 who ate the nuts.
The researchers scanned people to detect any changes in fat mass. They also measured changes in body weight, carbohydrate metabolism, and fasting blood glucose and insulin.
Key findings
Changes in total body fat mass and fat mass were not significantly different between the french fry groups and the almond group.
In terms of glycemic control, eating french fries for a month “is no better or worse than consuming a caloric equivalent of nuts,” the researchers noted.
Similarly, the change in total fat mass did not differ significantly among the three treatment groups.
Adding the herb and spice mix to the french fries did not make a significant difference on glycemic control, contrary to what the researchers thought might happen.
And fasting glucose, insulin, and HbA1c levels did not differ significantly between the combined french fry and almond groups. When comparisons were made among the three groups, the almond group had a lower insulin response, compared to the plain french fry group.
Many different things could be explored in future research, said study coauthor Rebecca Hanson, a registered dietitian nutritionist and research study coordinator at the University of Alabama at Birmingham. “People were not told to change their exercise or diet, so there are so many different variables,” she said. Repeating the research in people with diabetes is another possibility going forward.
The researchers acknowledged that 30 days may not have been long enough to show a significant difference. But they also noted that many previous studies were observational while they used a randomized controlled trial, considered a more robust study design.
Dr. Allison, the senior author, emphasized that this is just one study. “No one study has all the answers.
“I don’t want to tell you our results are the be all and end all or that we’ve now learned everything there is to learn about potatoes and almonds,” he said.
“Our study shows for the variables we looked at ... we did not see important, discernible differences,” he said. “That doesn’t mean if you ate 500 potatoes a day or 500 kilograms of almonds it would be the same. But at these modest levels, it doesn’t seem to make much difference.”
The study was funded by grants from the National Institutes of Health and from the Alliance for Potato Research and Education.
Asked if the industry support should be a concern, Ms. Majumdar said, “Funding from a specific food board does not necessarily dilute the results of a well-designed study. It’s not uncommon for a funding source to come from a food board that may benefit from the findings. Research money has to come from somewhere.
“This study has reputable researchers, some of the best in the field,” she said.
The U.S. produces the most almonds in the world, and California is the only state where almonds are grown commercially. Asked for the almond industry’s take on the findings, “We don’t have a comment,” said Rick Kushman, a spokesman for the Almond Board of California.
A version of this article first appeared on WebMD.com.
Eat french fries every day for a month? Sure, as long as it’s for science.
That’s exactly what 107 people did in a scientific study, while 58 others ate a daily serving of almonds with the same number of calories.
At the end of the study, the researchers found no significant differences between the groups in people’s total amount of fat or their fasting glucose measures, according to the study, published Feb. 18 in the American Journal of Clinical Nutrition.
The french fry eaters gained a little more weight, but it was not statistically significant. The people who ate french fries gained 0.49 kilograms (just over a pound), vs. about a tenth of a kilogram (about one-fifth of a pound) in the group of people who ate almonds.
“The take-home is if you like almonds, eat some almonds. If you like potatoes, eat some potatoes, but don’t overeat either,” said study leader David B. Allison, PhD, a professor at Indiana University’s School of Public Health in Bloomington. ‘It’s probably good to have a little bit of each – each has some unique advantages in terms of nutrition.”
“This study confirms what registered dietitian nutritionists already know – all foods can fit. We can eat almonds, french fries, kale, and cookies,” said Melissa Majumdar, a registered dietitian and certified specialist in obesity and weight management at Emory University Hospital Midtown in Atlanta. ‘The consumption of one food or the avoidance of another does not make a healthy diet.”
At the same time, people should not interpret the results to mean it’s OK to eat french fries all day, every day. “We know that while potatoes are nutrient dense, the frying process reduces the nutritional value,” Ms. Majumdar said.
“Because french fries are often consumed alongside other nutrient-poor or high-fat foods, they should not be consumed daily but can fit into an overall balanced diet,” she added.
Would you like fries with that?
The researchers compared french fries to almonds because almonds are known for positive effects on energy balance, body composition, and low glycemic index. The research was partly funded by the Alliance for Potato Research and Education.
French fries are an incredibly popular food in the United States. According to an August 2021 post on the food website Mashed, Americans eat an average of 30 pounds of french fries each year.
Although consumption of almonds is increasing, Americans eat far less in volume each year than they do fries – an estimated 2.4 pounds of almonds per person, according to August 2021 figures from the Almond Board of California.
Dr. Allison and colleagues recruited 180 healthy adults for the study. Their average age was 30, and about two-thirds were women.
They randomly assigned 60 people to add about a medium serving of plain french fries (Tater Pals Ovenable Crinkle Cut Fries, Simplot Foods) to their diet. Another 60 people were assigned to the same amount of Tater Pals fries with herbs (oregano, basil, garlic, onion, and rosemary), and another 60 people ate Wonderful brand roasted and salted almonds.
Investigators told people to add either the potatoes or nuts to their diet every day for a month and gave no further instructions.
After some people dropped out of the study, results were based on 55 who ate regular french fries, 52 who ate french fries with herbs and spices, and 58 who ate the nuts.
The researchers scanned people to detect any changes in fat mass. They also measured changes in body weight, carbohydrate metabolism, and fasting blood glucose and insulin.
Key findings
Changes in total body fat mass and fat mass were not significantly different between the french fry groups and the almond group.
In terms of glycemic control, eating french fries for a month “is no better or worse than consuming a caloric equivalent of nuts,” the researchers noted.
Similarly, the change in total fat mass did not differ significantly among the three treatment groups.
Adding the herb and spice mix to the french fries did not make a significant difference on glycemic control, contrary to what the researchers thought might happen.
And fasting glucose, insulin, and HbA1c levels did not differ significantly between the combined french fry and almond groups. When comparisons were made among the three groups, the almond group had a lower insulin response, compared to the plain french fry group.
Many different things could be explored in future research, said study coauthor Rebecca Hanson, a registered dietitian nutritionist and research study coordinator at the University of Alabama at Birmingham. “People were not told to change their exercise or diet, so there are so many different variables,” she said. Repeating the research in people with diabetes is another possibility going forward.
The researchers acknowledged that 30 days may not have been long enough to show a significant difference. But they also noted that many previous studies were observational while they used a randomized controlled trial, considered a more robust study design.
Dr. Allison, the senior author, emphasized that this is just one study. “No one study has all the answers.
“I don’t want to tell you our results are the be all and end all or that we’ve now learned everything there is to learn about potatoes and almonds,” he said.
“Our study shows for the variables we looked at ... we did not see important, discernible differences,” he said. “That doesn’t mean if you ate 500 potatoes a day or 500 kilograms of almonds it would be the same. But at these modest levels, it doesn’t seem to make much difference.”
The study was funded by grants from the National Institutes of Health and from the Alliance for Potato Research and Education.
Asked if the industry support should be a concern, Ms. Majumdar said, “Funding from a specific food board does not necessarily dilute the results of a well-designed study. It’s not uncommon for a funding source to come from a food board that may benefit from the findings. Research money has to come from somewhere.
“This study has reputable researchers, some of the best in the field,” she said.
The U.S. produces the most almonds in the world, and California is the only state where almonds are grown commercially. Asked for the almond industry’s take on the findings, “We don’t have a comment,” said Rick Kushman, a spokesman for the Almond Board of California.
A version of this article first appeared on WebMD.com.
Eat french fries every day for a month? Sure, as long as it’s for science.
That’s exactly what 107 people did in a scientific study, while 58 others ate a daily serving of almonds with the same number of calories.
At the end of the study, the researchers found no significant differences between the groups in people’s total amount of fat or their fasting glucose measures, according to the study, published Feb. 18 in the American Journal of Clinical Nutrition.
The french fry eaters gained a little more weight, but it was not statistically significant. The people who ate french fries gained 0.49 kilograms (just over a pound), vs. about a tenth of a kilogram (about one-fifth of a pound) in the group of people who ate almonds.
“The take-home is if you like almonds, eat some almonds. If you like potatoes, eat some potatoes, but don’t overeat either,” said study leader David B. Allison, PhD, a professor at Indiana University’s School of Public Health in Bloomington. ‘It’s probably good to have a little bit of each – each has some unique advantages in terms of nutrition.”
“This study confirms what registered dietitian nutritionists already know – all foods can fit. We can eat almonds, french fries, kale, and cookies,” said Melissa Majumdar, a registered dietitian and certified specialist in obesity and weight management at Emory University Hospital Midtown in Atlanta. ‘The consumption of one food or the avoidance of another does not make a healthy diet.”
At the same time, people should not interpret the results to mean it’s OK to eat french fries all day, every day. “We know that while potatoes are nutrient dense, the frying process reduces the nutritional value,” Ms. Majumdar said.
“Because french fries are often consumed alongside other nutrient-poor or high-fat foods, they should not be consumed daily but can fit into an overall balanced diet,” she added.
Would you like fries with that?
The researchers compared french fries to almonds because almonds are known for positive effects on energy balance, body composition, and low glycemic index. The research was partly funded by the Alliance for Potato Research and Education.
French fries are an incredibly popular food in the United States. According to an August 2021 post on the food website Mashed, Americans eat an average of 30 pounds of french fries each year.
Although consumption of almonds is increasing, Americans eat far less in volume each year than they do fries – an estimated 2.4 pounds of almonds per person, according to August 2021 figures from the Almond Board of California.
Dr. Allison and colleagues recruited 180 healthy adults for the study. Their average age was 30, and about two-thirds were women.
They randomly assigned 60 people to add about a medium serving of plain french fries (Tater Pals Ovenable Crinkle Cut Fries, Simplot Foods) to their diet. Another 60 people were assigned to the same amount of Tater Pals fries with herbs (oregano, basil, garlic, onion, and rosemary), and another 60 people ate Wonderful brand roasted and salted almonds.
Investigators told people to add either the potatoes or nuts to their diet every day for a month and gave no further instructions.
After some people dropped out of the study, results were based on 55 who ate regular french fries, 52 who ate french fries with herbs and spices, and 58 who ate the nuts.
The researchers scanned people to detect any changes in fat mass. They also measured changes in body weight, carbohydrate metabolism, and fasting blood glucose and insulin.
Key findings
Changes in total body fat mass and fat mass were not significantly different between the french fry groups and the almond group.
In terms of glycemic control, eating french fries for a month “is no better or worse than consuming a caloric equivalent of nuts,” the researchers noted.
Similarly, the change in total fat mass did not differ significantly among the three treatment groups.
Adding the herb and spice mix to the french fries did not make a significant difference on glycemic control, contrary to what the researchers thought might happen.
And fasting glucose, insulin, and HbA1c levels did not differ significantly between the combined french fry and almond groups. When comparisons were made among the three groups, the almond group had a lower insulin response, compared to the plain french fry group.
Many different things could be explored in future research, said study coauthor Rebecca Hanson, a registered dietitian nutritionist and research study coordinator at the University of Alabama at Birmingham. “People were not told to change their exercise or diet, so there are so many different variables,” she said. Repeating the research in people with diabetes is another possibility going forward.
The researchers acknowledged that 30 days may not have been long enough to show a significant difference. But they also noted that many previous studies were observational while they used a randomized controlled trial, considered a more robust study design.
Dr. Allison, the senior author, emphasized that this is just one study. “No one study has all the answers.
“I don’t want to tell you our results are the be all and end all or that we’ve now learned everything there is to learn about potatoes and almonds,” he said.
“Our study shows for the variables we looked at ... we did not see important, discernible differences,” he said. “That doesn’t mean if you ate 500 potatoes a day or 500 kilograms of almonds it would be the same. But at these modest levels, it doesn’t seem to make much difference.”
The study was funded by grants from the National Institutes of Health and from the Alliance for Potato Research and Education.
Asked if the industry support should be a concern, Ms. Majumdar said, “Funding from a specific food board does not necessarily dilute the results of a well-designed study. It’s not uncommon for a funding source to come from a food board that may benefit from the findings. Research money has to come from somewhere.
“This study has reputable researchers, some of the best in the field,” she said.
The U.S. produces the most almonds in the world, and California is the only state where almonds are grown commercially. Asked for the almond industry’s take on the findings, “We don’t have a comment,” said Rick Kushman, a spokesman for the Almond Board of California.
A version of this article first appeared on WebMD.com.
FROM AMERICAN JOURNAL OF CLINICAL NUTRITION
Physician loses right leg, sues podiatrist; more
, as a story in the Pennsylvania Record, among other news sites, reports.
In December 2020, Mario Adajar, MD, 59, an internist in Wyoming, Penn., sought treatment for his foot calluses and the chronic ulceration of his right foot.
Dr. Adajar consulted a podiatrist, who has surgical privileges at Wilkes-Barre Commonwealth Hospital. According to his complaint, Dr. Adajar made the podiatrist aware that he had type 2 diabetes and had recently undergone a kidney transplant.
Over the next several months, Adajar continued to be treated by the podiatrist who, among other things, debrided and cleaned his patient’s ulcerated right foot on multiple occasions. In June 2021, working out of the hospital’s Wound Healing Center, the podiatrist placed Dr. Adajar’s right leg in a total contact cast.
By the following day, the patient experienced what he later described as “excruciating” pain around the cast. He was also running a fever of 102.3. Taken to a local emergency department, Dr. Adajar soon went into septic shock, accompanied by both atrial fibrillation and acute hypoxic respiratory failure.
Doctors soon had a diagnosis: a gram-negative bacilli infection. Meanwhile, his right leg had become severely gangrenous, of the gas gangrene type. Nevertheless, after treatment, Dr. Adajar was discharged on June 15, 2021, and advised to continue with his follow-up, which included a referral to physical therapy. However, on July 27, 2021, doctors at Wilkes-Barre Commonwealth were forced to amputate Dr. Adajar’s right leg through the fibula and tibia.
In his suit, Dr. Adajar claims that the decision by the podiatrist and his associates to place him in a total contact cast was the direct and immediate cause of his injuries, most catastrophically the amputation of his right leg. He and his legal team are seeking damages “in excess of $50,000,” the standard language in Pennsylvania for cases likely to involve much larger awards.
Dr. Adajar, despite the loss of his right leg, continues to practice internal medicine.
Doctor wins forceps-delivery suit
Last month, a Virginia jury decided in favor of a physician accused of damaging a baby’s eye during delivery, a story in The Winchester Star reports.
In December 2015, Melissa Clements went to Winchester Medical Center, part of Valley Health, to have her baby delivered. Her doctor was ob.gyn. George F. Craft II, at the time a member of Winchester Women’s Specialists. At one point during the roughly 30-minute delivery, Dr. Craft used forceps to remove Ms. Clements’s baby, who in the process sustained facial fractures and left-eye damage.
At trial, Craft argued that a forceps delivery was justified because the baby was stuck and his patient had refused a C-section.
The attorney for the plaintiffs — which included Ms. Clements’s husband — claimed that the use of forceps was premature, as professional guidelines require that a woman in labor be allowed at least 3 hours to push on her own before forceps are employed. (The suit, initially filed in 2019, also accused Dr. Craft of failing to properly inform his patient about the risks of, and alternatives to, this form of delivery. That part of the complaint was dropped, however, prior to the recent trial.)
The jury debated just 50 minutes before deciding Dr. Craft wasn’t medically negligent in the birth of William, Ms. Clements’s now 6-year-old son, who will be forced to wear contact lenses or glasses for life, or undergo corrective surgery.
As Dr. Craft’s attorney explained at trial: “He [Dr. Craft] hoped to give her [Ms. Clements] what she wanted: a vaginal delivery. But forceps techniques can and will cause injuries, even when properly placed.”
Unsupervised PAs subject to med-mal cap, state says
The California Supreme Court ruled late last month that even unsupervised physician assistants (PAs) are protected under the state’s $250,000 cap on noneconomic damages, according to a posting on the website of the Claims Journal, among other news sites.
The ruling stems from a 2013 suit filed by Marisol Lopez, who claimed that a dermatologist, a plastic surgeon, and two PAs had misdiagnosed her child’s skin cancer. Ms. Lopez’s child, Olivia Sarinana, died in February 2014, causing her mother to amend her original claim to a wrongful-death suit.
A trial court found both the doctors and the PAs liable for negligence, awarding the plaintiff $11,200 in economic damages and $4.25 million in noneconomic damages. The court subsequently reduced that amount, however, referencing the state’s $250,000 limit on noneconomic damages, which is part of the Medical Injury Compensation Reform Act of 1975, known as MICRA.
Ms. Lopez appealed the decision, arguing that the cap shouldn’t apply to the two PAs, because neither was under a physician’s direct supervision and therefore not acting within the proper scope of practice, as defined by state law. Despite agreeing with the factual basis of Ms. Lopez’s claim — that neither PA was being supervised during the period in question — the trial court refused to wave the state cap. Ms. Lopez again appealed, and, in a split decision, the Second District Court of Appeal upheld the trial court’s decision.
At this point, attorneys for Ms. Lopez applied for, and obtained, a review before the state’s highest court. Last month, the justices weighed in, ruling that the PAs were still entitled to protection under MICRA because they “had valid delegation-of-service agreements in place.” In other words, while the two PAs had not been directly supervised by a physician, their services had been properly delegated by one.
Said Associate Justice Goodwin Liu, who wrote the opinion: “To be sure, there are reasonable policy arguments for excluding physician assistants who perform medical services without actual supervision from a cap on non-economic damages, and the Legislature is well equipped to weigh and reweigh the competing policy considerations. But our role is confined to interpreting the statute before us in the manner that comports most closely with the Legislature’s purpose in enacting MICRA.”
Despite the high-court ruling, voters may soon get a chance to amend the nearly 5-decades-old MICRA legislation. A November ballot initiative would not only adjust the cap for inflation, raising it to more than $1.2 million, but would also permit “judges and juries to waive the cap entirely for cases involving death and permanent disability.”
Medical groups have said that if either or both of these changes happen the cost of healthcare in the Golden State will surely go up.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
, as a story in the Pennsylvania Record, among other news sites, reports.
In December 2020, Mario Adajar, MD, 59, an internist in Wyoming, Penn., sought treatment for his foot calluses and the chronic ulceration of his right foot.
Dr. Adajar consulted a podiatrist, who has surgical privileges at Wilkes-Barre Commonwealth Hospital. According to his complaint, Dr. Adajar made the podiatrist aware that he had type 2 diabetes and had recently undergone a kidney transplant.
Over the next several months, Adajar continued to be treated by the podiatrist who, among other things, debrided and cleaned his patient’s ulcerated right foot on multiple occasions. In June 2021, working out of the hospital’s Wound Healing Center, the podiatrist placed Dr. Adajar’s right leg in a total contact cast.
By the following day, the patient experienced what he later described as “excruciating” pain around the cast. He was also running a fever of 102.3. Taken to a local emergency department, Dr. Adajar soon went into septic shock, accompanied by both atrial fibrillation and acute hypoxic respiratory failure.
Doctors soon had a diagnosis: a gram-negative bacilli infection. Meanwhile, his right leg had become severely gangrenous, of the gas gangrene type. Nevertheless, after treatment, Dr. Adajar was discharged on June 15, 2021, and advised to continue with his follow-up, which included a referral to physical therapy. However, on July 27, 2021, doctors at Wilkes-Barre Commonwealth were forced to amputate Dr. Adajar’s right leg through the fibula and tibia.
In his suit, Dr. Adajar claims that the decision by the podiatrist and his associates to place him in a total contact cast was the direct and immediate cause of his injuries, most catastrophically the amputation of his right leg. He and his legal team are seeking damages “in excess of $50,000,” the standard language in Pennsylvania for cases likely to involve much larger awards.
Dr. Adajar, despite the loss of his right leg, continues to practice internal medicine.
Doctor wins forceps-delivery suit
Last month, a Virginia jury decided in favor of a physician accused of damaging a baby’s eye during delivery, a story in The Winchester Star reports.
In December 2015, Melissa Clements went to Winchester Medical Center, part of Valley Health, to have her baby delivered. Her doctor was ob.gyn. George F. Craft II, at the time a member of Winchester Women’s Specialists. At one point during the roughly 30-minute delivery, Dr. Craft used forceps to remove Ms. Clements’s baby, who in the process sustained facial fractures and left-eye damage.
At trial, Craft argued that a forceps delivery was justified because the baby was stuck and his patient had refused a C-section.
The attorney for the plaintiffs — which included Ms. Clements’s husband — claimed that the use of forceps was premature, as professional guidelines require that a woman in labor be allowed at least 3 hours to push on her own before forceps are employed. (The suit, initially filed in 2019, also accused Dr. Craft of failing to properly inform his patient about the risks of, and alternatives to, this form of delivery. That part of the complaint was dropped, however, prior to the recent trial.)
The jury debated just 50 minutes before deciding Dr. Craft wasn’t medically negligent in the birth of William, Ms. Clements’s now 6-year-old son, who will be forced to wear contact lenses or glasses for life, or undergo corrective surgery.
As Dr. Craft’s attorney explained at trial: “He [Dr. Craft] hoped to give her [Ms. Clements] what she wanted: a vaginal delivery. But forceps techniques can and will cause injuries, even when properly placed.”
Unsupervised PAs subject to med-mal cap, state says
The California Supreme Court ruled late last month that even unsupervised physician assistants (PAs) are protected under the state’s $250,000 cap on noneconomic damages, according to a posting on the website of the Claims Journal, among other news sites.
The ruling stems from a 2013 suit filed by Marisol Lopez, who claimed that a dermatologist, a plastic surgeon, and two PAs had misdiagnosed her child’s skin cancer. Ms. Lopez’s child, Olivia Sarinana, died in February 2014, causing her mother to amend her original claim to a wrongful-death suit.
A trial court found both the doctors and the PAs liable for negligence, awarding the plaintiff $11,200 in economic damages and $4.25 million in noneconomic damages. The court subsequently reduced that amount, however, referencing the state’s $250,000 limit on noneconomic damages, which is part of the Medical Injury Compensation Reform Act of 1975, known as MICRA.
Ms. Lopez appealed the decision, arguing that the cap shouldn’t apply to the two PAs, because neither was under a physician’s direct supervision and therefore not acting within the proper scope of practice, as defined by state law. Despite agreeing with the factual basis of Ms. Lopez’s claim — that neither PA was being supervised during the period in question — the trial court refused to wave the state cap. Ms. Lopez again appealed, and, in a split decision, the Second District Court of Appeal upheld the trial court’s decision.
At this point, attorneys for Ms. Lopez applied for, and obtained, a review before the state’s highest court. Last month, the justices weighed in, ruling that the PAs were still entitled to protection under MICRA because they “had valid delegation-of-service agreements in place.” In other words, while the two PAs had not been directly supervised by a physician, their services had been properly delegated by one.
Said Associate Justice Goodwin Liu, who wrote the opinion: “To be sure, there are reasonable policy arguments for excluding physician assistants who perform medical services without actual supervision from a cap on non-economic damages, and the Legislature is well equipped to weigh and reweigh the competing policy considerations. But our role is confined to interpreting the statute before us in the manner that comports most closely with the Legislature’s purpose in enacting MICRA.”
Despite the high-court ruling, voters may soon get a chance to amend the nearly 5-decades-old MICRA legislation. A November ballot initiative would not only adjust the cap for inflation, raising it to more than $1.2 million, but would also permit “judges and juries to waive the cap entirely for cases involving death and permanent disability.”
Medical groups have said that if either or both of these changes happen the cost of healthcare in the Golden State will surely go up.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
, as a story in the Pennsylvania Record, among other news sites, reports.
In December 2020, Mario Adajar, MD, 59, an internist in Wyoming, Penn., sought treatment for his foot calluses and the chronic ulceration of his right foot.
Dr. Adajar consulted a podiatrist, who has surgical privileges at Wilkes-Barre Commonwealth Hospital. According to his complaint, Dr. Adajar made the podiatrist aware that he had type 2 diabetes and had recently undergone a kidney transplant.
Over the next several months, Adajar continued to be treated by the podiatrist who, among other things, debrided and cleaned his patient’s ulcerated right foot on multiple occasions. In June 2021, working out of the hospital’s Wound Healing Center, the podiatrist placed Dr. Adajar’s right leg in a total contact cast.
By the following day, the patient experienced what he later described as “excruciating” pain around the cast. He was also running a fever of 102.3. Taken to a local emergency department, Dr. Adajar soon went into septic shock, accompanied by both atrial fibrillation and acute hypoxic respiratory failure.
Doctors soon had a diagnosis: a gram-negative bacilli infection. Meanwhile, his right leg had become severely gangrenous, of the gas gangrene type. Nevertheless, after treatment, Dr. Adajar was discharged on June 15, 2021, and advised to continue with his follow-up, which included a referral to physical therapy. However, on July 27, 2021, doctors at Wilkes-Barre Commonwealth were forced to amputate Dr. Adajar’s right leg through the fibula and tibia.
In his suit, Dr. Adajar claims that the decision by the podiatrist and his associates to place him in a total contact cast was the direct and immediate cause of his injuries, most catastrophically the amputation of his right leg. He and his legal team are seeking damages “in excess of $50,000,” the standard language in Pennsylvania for cases likely to involve much larger awards.
Dr. Adajar, despite the loss of his right leg, continues to practice internal medicine.
Doctor wins forceps-delivery suit
Last month, a Virginia jury decided in favor of a physician accused of damaging a baby’s eye during delivery, a story in The Winchester Star reports.
In December 2015, Melissa Clements went to Winchester Medical Center, part of Valley Health, to have her baby delivered. Her doctor was ob.gyn. George F. Craft II, at the time a member of Winchester Women’s Specialists. At one point during the roughly 30-minute delivery, Dr. Craft used forceps to remove Ms. Clements’s baby, who in the process sustained facial fractures and left-eye damage.
At trial, Craft argued that a forceps delivery was justified because the baby was stuck and his patient had refused a C-section.
The attorney for the plaintiffs — which included Ms. Clements’s husband — claimed that the use of forceps was premature, as professional guidelines require that a woman in labor be allowed at least 3 hours to push on her own before forceps are employed. (The suit, initially filed in 2019, also accused Dr. Craft of failing to properly inform his patient about the risks of, and alternatives to, this form of delivery. That part of the complaint was dropped, however, prior to the recent trial.)
The jury debated just 50 minutes before deciding Dr. Craft wasn’t medically negligent in the birth of William, Ms. Clements’s now 6-year-old son, who will be forced to wear contact lenses or glasses for life, or undergo corrective surgery.
As Dr. Craft’s attorney explained at trial: “He [Dr. Craft] hoped to give her [Ms. Clements] what she wanted: a vaginal delivery. But forceps techniques can and will cause injuries, even when properly placed.”
Unsupervised PAs subject to med-mal cap, state says
The California Supreme Court ruled late last month that even unsupervised physician assistants (PAs) are protected under the state’s $250,000 cap on noneconomic damages, according to a posting on the website of the Claims Journal, among other news sites.
The ruling stems from a 2013 suit filed by Marisol Lopez, who claimed that a dermatologist, a plastic surgeon, and two PAs had misdiagnosed her child’s skin cancer. Ms. Lopez’s child, Olivia Sarinana, died in February 2014, causing her mother to amend her original claim to a wrongful-death suit.
A trial court found both the doctors and the PAs liable for negligence, awarding the plaintiff $11,200 in economic damages and $4.25 million in noneconomic damages. The court subsequently reduced that amount, however, referencing the state’s $250,000 limit on noneconomic damages, which is part of the Medical Injury Compensation Reform Act of 1975, known as MICRA.
Ms. Lopez appealed the decision, arguing that the cap shouldn’t apply to the two PAs, because neither was under a physician’s direct supervision and therefore not acting within the proper scope of practice, as defined by state law. Despite agreeing with the factual basis of Ms. Lopez’s claim — that neither PA was being supervised during the period in question — the trial court refused to wave the state cap. Ms. Lopez again appealed, and, in a split decision, the Second District Court of Appeal upheld the trial court’s decision.
At this point, attorneys for Ms. Lopez applied for, and obtained, a review before the state’s highest court. Last month, the justices weighed in, ruling that the PAs were still entitled to protection under MICRA because they “had valid delegation-of-service agreements in place.” In other words, while the two PAs had not been directly supervised by a physician, their services had been properly delegated by one.
Said Associate Justice Goodwin Liu, who wrote the opinion: “To be sure, there are reasonable policy arguments for excluding physician assistants who perform medical services without actual supervision from a cap on non-economic damages, and the Legislature is well equipped to weigh and reweigh the competing policy considerations. But our role is confined to interpreting the statute before us in the manner that comports most closely with the Legislature’s purpose in enacting MICRA.”
Despite the high-court ruling, voters may soon get a chance to amend the nearly 5-decades-old MICRA legislation. A November ballot initiative would not only adjust the cap for inflation, raising it to more than $1.2 million, but would also permit “judges and juries to waive the cap entirely for cases involving death and permanent disability.”
Medical groups have said that if either or both of these changes happen the cost of healthcare in the Golden State will surely go up.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
Standard of care in suicide prevention in pediatrics: A review of the Blueprint for Youth Suicide Prevention
In March, an unprecedented collaboration between the American Academy of Pediatrics (AAP), American Foundation for Suicide Prevention (AFSP), and National Institute of Mental Health (NIMH) resulted in the development of the Blueprint for Youth Suicide Prevention. The blueprint comprises a consensus summary of expert recommendations, educational resources, and specific and practical strategies for pediatricians and other health care providers to support youth at risk for suicide in pediatric primary care settings. It is ambitious and far-reaching in scope and speaks to the growing understanding that suicide care pathways offer a clear ray of hope toward a shared “zero suicide” goal.
Following the declaration of a national emergency for child and adolescent mental health, the blueprint represents a resource to help us move forward during this national emergency. It offers practically focused suggestions at the clinic site and individual level, in addition to community and school levels, to tackle the deeply concerning and alarming increasing rate of emergency department visits by 30% in the last 2 pandemic years for youth suicide attempts. A reflexive visit for an emergency mental health evaluation in an emergency department after a disclosure of suicidal ideation isn’t always the next best step in a pathway to care, nor a sustainable community solution with the dearth of mental health and crisis resources nationally.
With this new tool, let’s proceed through a case of how one would approach a patient in the office setting with a concerning disclosure.
Case
Emily is a 12-year-old girl who presents for a routine well-check in your practice. Her mother shared with you before your examination that she has wondered if Emily may need more support. Since the pandemic, Emily had increasingly spent time using social media and watching television. When you meet with Emily on her own, she says, “I know that life is getting back to normal, and I am supposed to be excited for that, but now I have some anxiety about doing what I used to do. I’ve had some thoughts that it would be better to sleep forever and not wake up ...”
Case discussion
The blueprint recommends universal screening for suicide in all youths aged 12 and over. Not all children, like Emily, will be as open about their inner thoughts. The blueprint provides a link to the ASQ, which comprises questions to ascertain suicide risk and takes 20 seconds to complete with a patient. It is recommended as a first-line screening tool by the NIMH: Suicide Risk Screening Tool. This tool can guide one’s clinical thinking beyond the question of whether or not a child feels “suicidal” after a disclosure such as Emily’s. The blueprint also provides a tip sheet on how to frame these screenings to ensure their thoroughness and interpersonal effectiveness.
Case continued
You go through the ASQ with Emily and she revealed that she has had thoughts about suicide but not currently and without further plans. According to the ASQ, this screening falls into the category of a “non-acute positive screen (potential risk identified),” and now the patient requires a brief suicide safety assessment to determine if an emergency mental health evaluation is needed.
Case discussion
An initial screen (ASQ) should be followed by a Brief Suicide Safety Assessment (BSSA). Two common ones are the ASQ-BSSA (created by the same group that created the ASQ) or the C-SSRS (Columbia suicide severity rating scale).
The blueprint suggests adding this level of depth to one’s investigation in a pediatrics office for a divulged concern with suicidal ideation and following the algorithm to ensure safety.
The complete screening process is also described, in detail, in this instructional video: Suicide Risk Screening Training: How to Manage Patients at Risk for Suicide.
Case continued
Following the ASQ-BSSA, you determine that a referral to more immediate mental health resources would be most helpful and discuss your concerns with Emily and her family. You connect her via a “warm handoff” to a therapist in the office available from the newly adopted primary care mental health integration model. Emily completes further screening for anxiety and depressive disorders and begins a course of cognitive-behavioral therapy. You feel reassured that the therapist can connect with the consulting psychiatrist in the model who can offer a comprehensive psychiatric evaluation if needed. A referral to the emergency department to complete this screening has been avoided. You also plan for a “caring contact” from the office in a day to check in on Emily and her family and, before they go, provide them with crisis services and resources.
The blueprint represents a thoughtful means to know when emergency department visits are necessary and when other forms of support such as robust safety planning, a connection to other nonemergency services, and “caring contacts” from the office within 24-48 hours are actually of more benefit. “Caring contacts,” in particular, have been lauded as having a significant impact in modifying the course of a patient with suicidal ideation. Data show that differences such as follow-up phone calls by any staff member or even postcards from the clinic over 6-12 months can affect suicide risk.
Beyond outlining suicide care pathways, the blueprint also shares clinical algorithms from the National Network of Child Psychiatry Access Programs (NNCPAP). These algorithms help clinicians assess common issues in pediatrics and reserve referrals to psychiatry and escalations of care to the emergency department for certain high-risk circumstances.
The blueprint seeks to provide a “one-stop-shop” for accessible and usable resources in the clinic workflow for suicide prevention. It is inspiring to see our professional organizations pursuing practical and practice-based solutions to our children’s mental health crisis in unison.
Dr. Pawlowski is a child and adolescent consulting psychiatrist. She is a division chief at the University of Vermont Medical Center where she focuses on primary care mental health integration within primary care pediatrics, internal medicine, and family medicine. Email her at [email protected].
In March, an unprecedented collaboration between the American Academy of Pediatrics (AAP), American Foundation for Suicide Prevention (AFSP), and National Institute of Mental Health (NIMH) resulted in the development of the Blueprint for Youth Suicide Prevention. The blueprint comprises a consensus summary of expert recommendations, educational resources, and specific and practical strategies for pediatricians and other health care providers to support youth at risk for suicide in pediatric primary care settings. It is ambitious and far-reaching in scope and speaks to the growing understanding that suicide care pathways offer a clear ray of hope toward a shared “zero suicide” goal.
Following the declaration of a national emergency for child and adolescent mental health, the blueprint represents a resource to help us move forward during this national emergency. It offers practically focused suggestions at the clinic site and individual level, in addition to community and school levels, to tackle the deeply concerning and alarming increasing rate of emergency department visits by 30% in the last 2 pandemic years for youth suicide attempts. A reflexive visit for an emergency mental health evaluation in an emergency department after a disclosure of suicidal ideation isn’t always the next best step in a pathway to care, nor a sustainable community solution with the dearth of mental health and crisis resources nationally.
With this new tool, let’s proceed through a case of how one would approach a patient in the office setting with a concerning disclosure.
Case
Emily is a 12-year-old girl who presents for a routine well-check in your practice. Her mother shared with you before your examination that she has wondered if Emily may need more support. Since the pandemic, Emily had increasingly spent time using social media and watching television. When you meet with Emily on her own, she says, “I know that life is getting back to normal, and I am supposed to be excited for that, but now I have some anxiety about doing what I used to do. I’ve had some thoughts that it would be better to sleep forever and not wake up ...”
Case discussion
The blueprint recommends universal screening for suicide in all youths aged 12 and over. Not all children, like Emily, will be as open about their inner thoughts. The blueprint provides a link to the ASQ, which comprises questions to ascertain suicide risk and takes 20 seconds to complete with a patient. It is recommended as a first-line screening tool by the NIMH: Suicide Risk Screening Tool. This tool can guide one’s clinical thinking beyond the question of whether or not a child feels “suicidal” after a disclosure such as Emily’s. The blueprint also provides a tip sheet on how to frame these screenings to ensure their thoroughness and interpersonal effectiveness.
Case continued
You go through the ASQ with Emily and she revealed that she has had thoughts about suicide but not currently and without further plans. According to the ASQ, this screening falls into the category of a “non-acute positive screen (potential risk identified),” and now the patient requires a brief suicide safety assessment to determine if an emergency mental health evaluation is needed.
Case discussion
An initial screen (ASQ) should be followed by a Brief Suicide Safety Assessment (BSSA). Two common ones are the ASQ-BSSA (created by the same group that created the ASQ) or the C-SSRS (Columbia suicide severity rating scale).
The blueprint suggests adding this level of depth to one’s investigation in a pediatrics office for a divulged concern with suicidal ideation and following the algorithm to ensure safety.
The complete screening process is also described, in detail, in this instructional video: Suicide Risk Screening Training: How to Manage Patients at Risk for Suicide.
Case continued
Following the ASQ-BSSA, you determine that a referral to more immediate mental health resources would be most helpful and discuss your concerns with Emily and her family. You connect her via a “warm handoff” to a therapist in the office available from the newly adopted primary care mental health integration model. Emily completes further screening for anxiety and depressive disorders and begins a course of cognitive-behavioral therapy. You feel reassured that the therapist can connect with the consulting psychiatrist in the model who can offer a comprehensive psychiatric evaluation if needed. A referral to the emergency department to complete this screening has been avoided. You also plan for a “caring contact” from the office in a day to check in on Emily and her family and, before they go, provide them with crisis services and resources.
The blueprint represents a thoughtful means to know when emergency department visits are necessary and when other forms of support such as robust safety planning, a connection to other nonemergency services, and “caring contacts” from the office within 24-48 hours are actually of more benefit. “Caring contacts,” in particular, have been lauded as having a significant impact in modifying the course of a patient with suicidal ideation. Data show that differences such as follow-up phone calls by any staff member or even postcards from the clinic over 6-12 months can affect suicide risk.
Beyond outlining suicide care pathways, the blueprint also shares clinical algorithms from the National Network of Child Psychiatry Access Programs (NNCPAP). These algorithms help clinicians assess common issues in pediatrics and reserve referrals to psychiatry and escalations of care to the emergency department for certain high-risk circumstances.
The blueprint seeks to provide a “one-stop-shop” for accessible and usable resources in the clinic workflow for suicide prevention. It is inspiring to see our professional organizations pursuing practical and practice-based solutions to our children’s mental health crisis in unison.
Dr. Pawlowski is a child and adolescent consulting psychiatrist. She is a division chief at the University of Vermont Medical Center where she focuses on primary care mental health integration within primary care pediatrics, internal medicine, and family medicine. Email her at [email protected].
In March, an unprecedented collaboration between the American Academy of Pediatrics (AAP), American Foundation for Suicide Prevention (AFSP), and National Institute of Mental Health (NIMH) resulted in the development of the Blueprint for Youth Suicide Prevention. The blueprint comprises a consensus summary of expert recommendations, educational resources, and specific and practical strategies for pediatricians and other health care providers to support youth at risk for suicide in pediatric primary care settings. It is ambitious and far-reaching in scope and speaks to the growing understanding that suicide care pathways offer a clear ray of hope toward a shared “zero suicide” goal.
Following the declaration of a national emergency for child and adolescent mental health, the blueprint represents a resource to help us move forward during this national emergency. It offers practically focused suggestions at the clinic site and individual level, in addition to community and school levels, to tackle the deeply concerning and alarming increasing rate of emergency department visits by 30% in the last 2 pandemic years for youth suicide attempts. A reflexive visit for an emergency mental health evaluation in an emergency department after a disclosure of suicidal ideation isn’t always the next best step in a pathway to care, nor a sustainable community solution with the dearth of mental health and crisis resources nationally.
With this new tool, let’s proceed through a case of how one would approach a patient in the office setting with a concerning disclosure.
Case
Emily is a 12-year-old girl who presents for a routine well-check in your practice. Her mother shared with you before your examination that she has wondered if Emily may need more support. Since the pandemic, Emily had increasingly spent time using social media and watching television. When you meet with Emily on her own, she says, “I know that life is getting back to normal, and I am supposed to be excited for that, but now I have some anxiety about doing what I used to do. I’ve had some thoughts that it would be better to sleep forever and not wake up ...”
Case discussion
The blueprint recommends universal screening for suicide in all youths aged 12 and over. Not all children, like Emily, will be as open about their inner thoughts. The blueprint provides a link to the ASQ, which comprises questions to ascertain suicide risk and takes 20 seconds to complete with a patient. It is recommended as a first-line screening tool by the NIMH: Suicide Risk Screening Tool. This tool can guide one’s clinical thinking beyond the question of whether or not a child feels “suicidal” after a disclosure such as Emily’s. The blueprint also provides a tip sheet on how to frame these screenings to ensure their thoroughness and interpersonal effectiveness.
Case continued
You go through the ASQ with Emily and she revealed that she has had thoughts about suicide but not currently and without further plans. According to the ASQ, this screening falls into the category of a “non-acute positive screen (potential risk identified),” and now the patient requires a brief suicide safety assessment to determine if an emergency mental health evaluation is needed.
Case discussion
An initial screen (ASQ) should be followed by a Brief Suicide Safety Assessment (BSSA). Two common ones are the ASQ-BSSA (created by the same group that created the ASQ) or the C-SSRS (Columbia suicide severity rating scale).
The blueprint suggests adding this level of depth to one’s investigation in a pediatrics office for a divulged concern with suicidal ideation and following the algorithm to ensure safety.
The complete screening process is also described, in detail, in this instructional video: Suicide Risk Screening Training: How to Manage Patients at Risk for Suicide.
Case continued
Following the ASQ-BSSA, you determine that a referral to more immediate mental health resources would be most helpful and discuss your concerns with Emily and her family. You connect her via a “warm handoff” to a therapist in the office available from the newly adopted primary care mental health integration model. Emily completes further screening for anxiety and depressive disorders and begins a course of cognitive-behavioral therapy. You feel reassured that the therapist can connect with the consulting psychiatrist in the model who can offer a comprehensive psychiatric evaluation if needed. A referral to the emergency department to complete this screening has been avoided. You also plan for a “caring contact” from the office in a day to check in on Emily and her family and, before they go, provide them with crisis services and resources.
The blueprint represents a thoughtful means to know when emergency department visits are necessary and when other forms of support such as robust safety planning, a connection to other nonemergency services, and “caring contacts” from the office within 24-48 hours are actually of more benefit. “Caring contacts,” in particular, have been lauded as having a significant impact in modifying the course of a patient with suicidal ideation. Data show that differences such as follow-up phone calls by any staff member or even postcards from the clinic over 6-12 months can affect suicide risk.
Beyond outlining suicide care pathways, the blueprint also shares clinical algorithms from the National Network of Child Psychiatry Access Programs (NNCPAP). These algorithms help clinicians assess common issues in pediatrics and reserve referrals to psychiatry and escalations of care to the emergency department for certain high-risk circumstances.
The blueprint seeks to provide a “one-stop-shop” for accessible and usable resources in the clinic workflow for suicide prevention. It is inspiring to see our professional organizations pursuing practical and practice-based solutions to our children’s mental health crisis in unison.
Dr. Pawlowski is a child and adolescent consulting psychiatrist. She is a division chief at the University of Vermont Medical Center where she focuses on primary care mental health integration within primary care pediatrics, internal medicine, and family medicine. Email her at [email protected].
Diagnosing adolescent ADHD
Pediatricians are increasingly expert in the assessment and treatment of attention-deficit/hyperactivity disorder. But what do you do when adolescents present to your office saying they think they have ADHD? While ADHD is a common and treatable disorder of youth, it is important to take special care when assessing an adolescent. Difficulties with attention and concentration are common symptoms for many different challenges of adolescence, and for ADHD to be the underlying cause, those symptoms must have started prior to adolescence (according to DSM-5, prior to the age of 12). When your adolescent patients or their parents come to your office complaining of inattention, it is important to consider the full range of possible explanations.
Sleep
We have written in this column previously about the challenges that adolescents face in getting adequate sleep consistently. Teenagers, on average, need more than 9 hours of sleep nightly and American teenagers get fewer than 6. This mismatch is because of physiologic shifts that move their natural sleep onset time significantly later, while school still starts early. It’s often compounded by other demands on their time, including homework, extracurricular activities, and the gravitational pull of social connections. Independent teenagers make their own decisions about how to manage their time and may feel sleep is optional, or manage their fatigue with naps and caffeine, both of which will further compromise the quality and efficiency of sleep.
Chronic sleep deprivation will present with difficulties with focus, attention, memory, and cognitive performance. Treatment of this problem with stimulants is likely to make the underlying poor sleep habits even worse. When your patient presents complaining of difficulty concentrating and worsening school performance, be sure to start with a thorough sleep history, and always provide guidance about the body’s need for sleep and healthy sleep habits.
Anxiety
Anxiety disorders are the most common psychiatric illnesses of youth, with estimates of as many as 30% of children and adolescents experiencing one. The true prevalence of ADHD is estimated to be about 4% of the population. Whether social phobia, generalized anxiety disorder, or even posttraumatic stress disorder, anxiety disorders interfere with attention as ruminative worry tends to distract those experiencing it. It can also affect attention and focus indirectly by interfering with restful sleep. Anxiety disorders can be difficult to identify, as the sufferers typically internalize their symptoms. But inquire about specific worries (such as speaking in front of others, meeting new people, or an illness or accident striking themselves or a loved one) and how much time they take up. Explore if worries fill their thoughts during quiet or downtime, and explore more about their worries. You may use a screening instrument such as the Pediatric Symptom Checklist or the SCARED, both of which will indicate a likely problem with anxiety. While it is possible to have comorbid ADHD with an anxiety disorder, the anxiety disorder will likely worsen with stimulants and should be treated first. These are usually curable illnesses and you may find that remission of anxiety symptoms resolves the attentional problems.
Depression
Mood disorders are less common than anxiety disorders in youth, but far more prevalent than ADHD. And depression is usually marked by serious difficulty concentrating across settings (including for things that were previously very interesting). A sullen teenager who is deeply self-critical about school performance would benefit from exploration of associated changes in mood, interests, energy, appetite, sleep, and for feelings of worthlessness, guilt, and suicidal thoughts. The PHQ9A is a simple, free screening instrument that is reasonable to use with every sick visit (and well-check) with your adolescent patients, given the risks of undetected and untreated depression. If your patient presents complaining of poor school performance, always screen for depression. As with anxiety disorders, comorbid ADHD is possible, but it is always recommended to treat the mood disorder first and then to assess for residual ADHD symptoms once the mood disorder is in remission.
Substance abuse
Adolescence is a time of exploration, and drug and alcohol use is common. While attentional impairment will happen with intoxication, occasional or rare use should not lead to consistent impairment in school. But when parents are more worried than their children about a significant change in school performance, it is important to screen for substance abuse. A child with a secret substance use disorder will often present with behavioral changes and deteriorating school performance and might deny any drug or alcohol use to parents. Indeed, stimulants have some street value and some patients may be seeking a stimulant prescription to sell or trade for other drugs. Regular marijuana use may present with only deteriorating school performance and no irritability or other noticeable behavioral changes. Marijuana is seen as safe and even healthy by many teenagers (and even many parents), and some youth may be using it recreationally or to manage difficulties with sleep, anxiety, or mood symptoms.
But there is compelling evidence that marijuana use causes cognitive impairment, including difficulty with sustaining attention, short-term memory, and processing speed, for as long as 24 hours after use. If a teenager is using marijuana daily after school, it is certainly going to interfere, in a dose-dependent manner, with attention and cognitive function. Sustained heavy use can lead to permanent cognitive deficits. It can also trigger or worsen anxiety or mood symptoms (contrary to much popular opinion).
Gathering a thorough substance use history is essential when assessing a teenager for difficulties with focus or attention, especially when these are accompanied by change in behavior and school performance. Remember, it is critical to interview these children without their parents present to invite them to be forthcoming with you.
History
While true ADHD should have been present throughout childhood, it is possible that the symptoms have become noticeable only in adolescence. For patients with very high intelligence and lower levels of impulsivity and hyperactivity, they might easily have “flown under the radar” during their elementary and even middle school years. Their difficulties with attention and focus might become apparent only when the volume and difficulty of schoolwork both are great enough that their intelligence is not enough to get good grades. That is, their problems with executive function, prioritizing, shifting sets, and completing tasks in a timely way make it impossible to keep up good grades when the work gets harder.
Your history should reveal a long history of dreaminess or distractibility, a tendency to lose and forget things, and the other symptoms of inattention. Did they often seem to not be listening when they were younger? Forget to hand in homework? Leave chores unfinished? Leave messes behind everywhere they went? These will not be definitive, but they do reassure that symptoms may have been present for a long time, even if school performance was considered fine until the workload got too large. If such problems were not present before puberty, consider whether a subtle learning disability could be impairing them as they face more challenging academic subjects.
If you have ruled out anxiety, mood, and substance use concerns, and helped them to address a sleep deficit, then you can proceed. It is worthwhile to get Vanderbilt Assessments as you would for a younger child. If they meet criteria, discuss the risks and benefits of medication, executive skills coaching, and environmental adjustments (extra time for tests, a less stimulating environment) that can help them explore academic challenges without the discouragement that ADHD can bring.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Pediatricians are increasingly expert in the assessment and treatment of attention-deficit/hyperactivity disorder. But what do you do when adolescents present to your office saying they think they have ADHD? While ADHD is a common and treatable disorder of youth, it is important to take special care when assessing an adolescent. Difficulties with attention and concentration are common symptoms for many different challenges of adolescence, and for ADHD to be the underlying cause, those symptoms must have started prior to adolescence (according to DSM-5, prior to the age of 12). When your adolescent patients or their parents come to your office complaining of inattention, it is important to consider the full range of possible explanations.
Sleep
We have written in this column previously about the challenges that adolescents face in getting adequate sleep consistently. Teenagers, on average, need more than 9 hours of sleep nightly and American teenagers get fewer than 6. This mismatch is because of physiologic shifts that move their natural sleep onset time significantly later, while school still starts early. It’s often compounded by other demands on their time, including homework, extracurricular activities, and the gravitational pull of social connections. Independent teenagers make their own decisions about how to manage their time and may feel sleep is optional, or manage their fatigue with naps and caffeine, both of which will further compromise the quality and efficiency of sleep.
Chronic sleep deprivation will present with difficulties with focus, attention, memory, and cognitive performance. Treatment of this problem with stimulants is likely to make the underlying poor sleep habits even worse. When your patient presents complaining of difficulty concentrating and worsening school performance, be sure to start with a thorough sleep history, and always provide guidance about the body’s need for sleep and healthy sleep habits.
Anxiety
Anxiety disorders are the most common psychiatric illnesses of youth, with estimates of as many as 30% of children and adolescents experiencing one. The true prevalence of ADHD is estimated to be about 4% of the population. Whether social phobia, generalized anxiety disorder, or even posttraumatic stress disorder, anxiety disorders interfere with attention as ruminative worry tends to distract those experiencing it. It can also affect attention and focus indirectly by interfering with restful sleep. Anxiety disorders can be difficult to identify, as the sufferers typically internalize their symptoms. But inquire about specific worries (such as speaking in front of others, meeting new people, or an illness or accident striking themselves or a loved one) and how much time they take up. Explore if worries fill their thoughts during quiet or downtime, and explore more about their worries. You may use a screening instrument such as the Pediatric Symptom Checklist or the SCARED, both of which will indicate a likely problem with anxiety. While it is possible to have comorbid ADHD with an anxiety disorder, the anxiety disorder will likely worsen with stimulants and should be treated first. These are usually curable illnesses and you may find that remission of anxiety symptoms resolves the attentional problems.
Depression
Mood disorders are less common than anxiety disorders in youth, but far more prevalent than ADHD. And depression is usually marked by serious difficulty concentrating across settings (including for things that were previously very interesting). A sullen teenager who is deeply self-critical about school performance would benefit from exploration of associated changes in mood, interests, energy, appetite, sleep, and for feelings of worthlessness, guilt, and suicidal thoughts. The PHQ9A is a simple, free screening instrument that is reasonable to use with every sick visit (and well-check) with your adolescent patients, given the risks of undetected and untreated depression. If your patient presents complaining of poor school performance, always screen for depression. As with anxiety disorders, comorbid ADHD is possible, but it is always recommended to treat the mood disorder first and then to assess for residual ADHD symptoms once the mood disorder is in remission.
Substance abuse
Adolescence is a time of exploration, and drug and alcohol use is common. While attentional impairment will happen with intoxication, occasional or rare use should not lead to consistent impairment in school. But when parents are more worried than their children about a significant change in school performance, it is important to screen for substance abuse. A child with a secret substance use disorder will often present with behavioral changes and deteriorating school performance and might deny any drug or alcohol use to parents. Indeed, stimulants have some street value and some patients may be seeking a stimulant prescription to sell or trade for other drugs. Regular marijuana use may present with only deteriorating school performance and no irritability or other noticeable behavioral changes. Marijuana is seen as safe and even healthy by many teenagers (and even many parents), and some youth may be using it recreationally or to manage difficulties with sleep, anxiety, or mood symptoms.
But there is compelling evidence that marijuana use causes cognitive impairment, including difficulty with sustaining attention, short-term memory, and processing speed, for as long as 24 hours after use. If a teenager is using marijuana daily after school, it is certainly going to interfere, in a dose-dependent manner, with attention and cognitive function. Sustained heavy use can lead to permanent cognitive deficits. It can also trigger or worsen anxiety or mood symptoms (contrary to much popular opinion).
Gathering a thorough substance use history is essential when assessing a teenager for difficulties with focus or attention, especially when these are accompanied by change in behavior and school performance. Remember, it is critical to interview these children without their parents present to invite them to be forthcoming with you.
History
While true ADHD should have been present throughout childhood, it is possible that the symptoms have become noticeable only in adolescence. For patients with very high intelligence and lower levels of impulsivity and hyperactivity, they might easily have “flown under the radar” during their elementary and even middle school years. Their difficulties with attention and focus might become apparent only when the volume and difficulty of schoolwork both are great enough that their intelligence is not enough to get good grades. That is, their problems with executive function, prioritizing, shifting sets, and completing tasks in a timely way make it impossible to keep up good grades when the work gets harder.
Your history should reveal a long history of dreaminess or distractibility, a tendency to lose and forget things, and the other symptoms of inattention. Did they often seem to not be listening when they were younger? Forget to hand in homework? Leave chores unfinished? Leave messes behind everywhere they went? These will not be definitive, but they do reassure that symptoms may have been present for a long time, even if school performance was considered fine until the workload got too large. If such problems were not present before puberty, consider whether a subtle learning disability could be impairing them as they face more challenging academic subjects.
If you have ruled out anxiety, mood, and substance use concerns, and helped them to address a sleep deficit, then you can proceed. It is worthwhile to get Vanderbilt Assessments as you would for a younger child. If they meet criteria, discuss the risks and benefits of medication, executive skills coaching, and environmental adjustments (extra time for tests, a less stimulating environment) that can help them explore academic challenges without the discouragement that ADHD can bring.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Pediatricians are increasingly expert in the assessment and treatment of attention-deficit/hyperactivity disorder. But what do you do when adolescents present to your office saying they think they have ADHD? While ADHD is a common and treatable disorder of youth, it is important to take special care when assessing an adolescent. Difficulties with attention and concentration are common symptoms for many different challenges of adolescence, and for ADHD to be the underlying cause, those symptoms must have started prior to adolescence (according to DSM-5, prior to the age of 12). When your adolescent patients or their parents come to your office complaining of inattention, it is important to consider the full range of possible explanations.
Sleep
We have written in this column previously about the challenges that adolescents face in getting adequate sleep consistently. Teenagers, on average, need more than 9 hours of sleep nightly and American teenagers get fewer than 6. This mismatch is because of physiologic shifts that move their natural sleep onset time significantly later, while school still starts early. It’s often compounded by other demands on their time, including homework, extracurricular activities, and the gravitational pull of social connections. Independent teenagers make their own decisions about how to manage their time and may feel sleep is optional, or manage their fatigue with naps and caffeine, both of which will further compromise the quality and efficiency of sleep.
Chronic sleep deprivation will present with difficulties with focus, attention, memory, and cognitive performance. Treatment of this problem with stimulants is likely to make the underlying poor sleep habits even worse. When your patient presents complaining of difficulty concentrating and worsening school performance, be sure to start with a thorough sleep history, and always provide guidance about the body’s need for sleep and healthy sleep habits.
Anxiety
Anxiety disorders are the most common psychiatric illnesses of youth, with estimates of as many as 30% of children and adolescents experiencing one. The true prevalence of ADHD is estimated to be about 4% of the population. Whether social phobia, generalized anxiety disorder, or even posttraumatic stress disorder, anxiety disorders interfere with attention as ruminative worry tends to distract those experiencing it. It can also affect attention and focus indirectly by interfering with restful sleep. Anxiety disorders can be difficult to identify, as the sufferers typically internalize their symptoms. But inquire about specific worries (such as speaking in front of others, meeting new people, or an illness or accident striking themselves or a loved one) and how much time they take up. Explore if worries fill their thoughts during quiet or downtime, and explore more about their worries. You may use a screening instrument such as the Pediatric Symptom Checklist or the SCARED, both of which will indicate a likely problem with anxiety. While it is possible to have comorbid ADHD with an anxiety disorder, the anxiety disorder will likely worsen with stimulants and should be treated first. These are usually curable illnesses and you may find that remission of anxiety symptoms resolves the attentional problems.
Depression
Mood disorders are less common than anxiety disorders in youth, but far more prevalent than ADHD. And depression is usually marked by serious difficulty concentrating across settings (including for things that were previously very interesting). A sullen teenager who is deeply self-critical about school performance would benefit from exploration of associated changes in mood, interests, energy, appetite, sleep, and for feelings of worthlessness, guilt, and suicidal thoughts. The PHQ9A is a simple, free screening instrument that is reasonable to use with every sick visit (and well-check) with your adolescent patients, given the risks of undetected and untreated depression. If your patient presents complaining of poor school performance, always screen for depression. As with anxiety disorders, comorbid ADHD is possible, but it is always recommended to treat the mood disorder first and then to assess for residual ADHD symptoms once the mood disorder is in remission.
Substance abuse
Adolescence is a time of exploration, and drug and alcohol use is common. While attentional impairment will happen with intoxication, occasional or rare use should not lead to consistent impairment in school. But when parents are more worried than their children about a significant change in school performance, it is important to screen for substance abuse. A child with a secret substance use disorder will often present with behavioral changes and deteriorating school performance and might deny any drug or alcohol use to parents. Indeed, stimulants have some street value and some patients may be seeking a stimulant prescription to sell or trade for other drugs. Regular marijuana use may present with only deteriorating school performance and no irritability or other noticeable behavioral changes. Marijuana is seen as safe and even healthy by many teenagers (and even many parents), and some youth may be using it recreationally or to manage difficulties with sleep, anxiety, or mood symptoms.
But there is compelling evidence that marijuana use causes cognitive impairment, including difficulty with sustaining attention, short-term memory, and processing speed, for as long as 24 hours after use. If a teenager is using marijuana daily after school, it is certainly going to interfere, in a dose-dependent manner, with attention and cognitive function. Sustained heavy use can lead to permanent cognitive deficits. It can also trigger or worsen anxiety or mood symptoms (contrary to much popular opinion).
Gathering a thorough substance use history is essential when assessing a teenager for difficulties with focus or attention, especially when these are accompanied by change in behavior and school performance. Remember, it is critical to interview these children without their parents present to invite them to be forthcoming with you.
History
While true ADHD should have been present throughout childhood, it is possible that the symptoms have become noticeable only in adolescence. For patients with very high intelligence and lower levels of impulsivity and hyperactivity, they might easily have “flown under the radar” during their elementary and even middle school years. Their difficulties with attention and focus might become apparent only when the volume and difficulty of schoolwork both are great enough that their intelligence is not enough to get good grades. That is, their problems with executive function, prioritizing, shifting sets, and completing tasks in a timely way make it impossible to keep up good grades when the work gets harder.
Your history should reveal a long history of dreaminess or distractibility, a tendency to lose and forget things, and the other symptoms of inattention. Did they often seem to not be listening when they were younger? Forget to hand in homework? Leave chores unfinished? Leave messes behind everywhere they went? These will not be definitive, but they do reassure that symptoms may have been present for a long time, even if school performance was considered fine until the workload got too large. If such problems were not present before puberty, consider whether a subtle learning disability could be impairing them as they face more challenging academic subjects.
If you have ruled out anxiety, mood, and substance use concerns, and helped them to address a sleep deficit, then you can proceed. It is worthwhile to get Vanderbilt Assessments as you would for a younger child. If they meet criteria, discuss the risks and benefits of medication, executive skills coaching, and environmental adjustments (extra time for tests, a less stimulating environment) that can help them explore academic challenges without the discouragement that ADHD can bring.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at [email protected].
Ways to lessen toxic effects of chemo in older adults
Age-related changes that potentiate adverse drug reactions include alterations in absorption, distribution, metabolism, and excretion. As such, older patients often require adjustments in medications to optimize safety and use. Medication adjustment is especially important for older patients on complex medication regimens for multiple conditions, such as those undergoing cancer treatment. Three recent high-quality randomized trials evaluated the use of geriatric assessment (GA) in older adults with cancer.1-3
Interdisciplinary GA can identify aging-related conditions associated with poor outcomes in older patients with cancer (e.g., toxic effects of chemotherapy) and provide recommendations aimed at improving health outcomes. The results of these trials suggest that interdisciplinary GA can improve care outcomes and oncologists’ communication for older adults with cancer, and should be considered an emerging standard of care.
Geriatric assessment and chemotherapy-related toxic effects
A cluster randomized trial1 at City of Hope National Medical Center conducted between August 2015 and February 2019 enrolled 613 participants and randomly assigned them to receive a GA-guided intervention or usual standard of care in a 2-to-1 ratio. Participants were eligible for the study if they were aged ≥65 years; had a diagnosis of solid malignant neoplasm of any stage; were starting a new chemotherapy regimen; and were fluent in English, Spanish, or Chinese.
The intervention included a GA at baseline followed by assessments focused on six common areas: sleep problems, problems with eating and feeding, incontinence, confusion, evidence of falls, and skin breakdown. An interdisciplinary team (oncologist, nurse practitioner, pharmacist, physical therapist, occupational therapist, social worker, and nutritionist) performed the assessment and developed a plan of care. Interventions were multifactorial and could include referral to specialists; recommendations for medication changes; symptom management; nutritional intervention with diet recommendations and supplementation; and interventions targeting social, spiritual, and functional well-being. Follow-up by a nurse practitioner continued until completion of chemotherapy or 6 months after starting chemotherapy, whichever was earlier.
The primary outcome was grade 3 or higher chemotherapy-related toxic effects using National Cancer Institute criteria, and secondary outcomes were advance directive completion, emergency room visits and unplanned hospitalizations, and survival up to 12 months. Results showed a 10% absolute reduction in the incidence of grade 3 or higher toxic effects (P = .02), with a number needed to treat of 10. Advance directive completion also increased by 15%, but no differences were observed for other outcomes. This study offers high-quality evidence that a GA-based intervention can reduce toxic effects of chemotherapy regimens for older adults with cancer.
Geriatric assessment in community oncology practices
A recent study by Supriya G. Mohile, MD, and colleagues2 is the first nationwide multicenter clinical trial to demonstrate the effects of GA and GA-guided management. This study was conducted in 40 oncology practices from the University of Rochester National Cancer Institute Community Oncology Research Program network. Centers were randomly assigned to intervention or usual care (362 patients treated by 68 oncologists in the intervention group and 371 patients treated by 91 oncologists in the usual-care group). Eligibility criteria were age ≥70 years; impairment in at least one GA domain other than polypharmacy; incurable advanced solid tumor or lymphoma with a plan to start new cancer treatment with a high risk for toxic effects within 4 weeks; and English language fluency. Both study groups underwent a baseline GA that assessed patients’ physical performance, functional status, comorbidity, cognition, nutrition, social support, polypharmacy, and psychological status. For the intervention group, a summary and management recommendations were provided to the treating oncologists.
The primary outcome was grade 3 or higher toxic effects within 3 months of starting a new regimen; secondary outcomes included treatment intensity and survival and GA outcomes within 3 months. A smaller proportion of patients in the intervention group experienced toxicity (51% vs. 71%), with an absolute risk reduction of 20%. Patients in the intervention group also had fewer falls and a greater reduction in medications used; there were no other differences in secondary outcomes. This study offers very strong and generalizable evidence that incorporating GA in the care of older adults with cancer at risk for toxicity can reduce toxicity as well as improve other outcomes, such as falls and polypharmacy.
Geriatric assessment and oncologist-patient communication
A secondary analysis3 of data from Dr. Mohile and colleagues2 evaluated the effect of GA-guided recommendations on oncologist-patient communication regarding comorbidities. Patients (n = 541) included in this analysis were 76.6 years of age on average and had 3.2 (standard deviation, 1.9) comorbid conditions. All patients underwent GA, but only oncologists in the intervention arm received GA-based recommendations. Clinical encounters between oncologist and patient immediately following the GA were audio recorded and analyzed to examine communication between oncologists and participants as it relates to chronic comorbid conditions.
In the intervention arm, more discussions regarding comorbidities took place, and more participants’ concerns about comorbidities were acknowledged. More importantly, participants in the intervention group were 2.4 times more likely to have their concerns about comorbidities addressed through referral or education, compared with the usual-care group (P = .004). Moreover, 41% of oncologists in the intervention arm modified dosage or cancer treatment schedule because of concern about tolerability or comorbidities. This study demonstrates beneficial effects of GA in increasing communication and perhaps consideration of comorbidities of older adults when planning cancer treatment.
Dr. Hung is professor of geriatrics and palliative care at Mount Sinai Hospital, New York. He disclosed no relevant conflicts of interest.
References
1. Li D et al. JAMA Oncol. 2021;7:e214158.
2. Mohile SG et al. Lancet. 2021;398:1894-1904.
3. Kleckner AS et al. JCO Oncol Pract. 2022;18:e9-19.
A version of this article first appeared on Medscape.com.
Age-related changes that potentiate adverse drug reactions include alterations in absorption, distribution, metabolism, and excretion. As such, older patients often require adjustments in medications to optimize safety and use. Medication adjustment is especially important for older patients on complex medication regimens for multiple conditions, such as those undergoing cancer treatment. Three recent high-quality randomized trials evaluated the use of geriatric assessment (GA) in older adults with cancer.1-3
Interdisciplinary GA can identify aging-related conditions associated with poor outcomes in older patients with cancer (e.g., toxic effects of chemotherapy) and provide recommendations aimed at improving health outcomes. The results of these trials suggest that interdisciplinary GA can improve care outcomes and oncologists’ communication for older adults with cancer, and should be considered an emerging standard of care.
Geriatric assessment and chemotherapy-related toxic effects
A cluster randomized trial1 at City of Hope National Medical Center conducted between August 2015 and February 2019 enrolled 613 participants and randomly assigned them to receive a GA-guided intervention or usual standard of care in a 2-to-1 ratio. Participants were eligible for the study if they were aged ≥65 years; had a diagnosis of solid malignant neoplasm of any stage; were starting a new chemotherapy regimen; and were fluent in English, Spanish, or Chinese.
The intervention included a GA at baseline followed by assessments focused on six common areas: sleep problems, problems with eating and feeding, incontinence, confusion, evidence of falls, and skin breakdown. An interdisciplinary team (oncologist, nurse practitioner, pharmacist, physical therapist, occupational therapist, social worker, and nutritionist) performed the assessment and developed a plan of care. Interventions were multifactorial and could include referral to specialists; recommendations for medication changes; symptom management; nutritional intervention with diet recommendations and supplementation; and interventions targeting social, spiritual, and functional well-being. Follow-up by a nurse practitioner continued until completion of chemotherapy or 6 months after starting chemotherapy, whichever was earlier.
The primary outcome was grade 3 or higher chemotherapy-related toxic effects using National Cancer Institute criteria, and secondary outcomes were advance directive completion, emergency room visits and unplanned hospitalizations, and survival up to 12 months. Results showed a 10% absolute reduction in the incidence of grade 3 or higher toxic effects (P = .02), with a number needed to treat of 10. Advance directive completion also increased by 15%, but no differences were observed for other outcomes. This study offers high-quality evidence that a GA-based intervention can reduce toxic effects of chemotherapy regimens for older adults with cancer.
Geriatric assessment in community oncology practices
A recent study by Supriya G. Mohile, MD, and colleagues2 is the first nationwide multicenter clinical trial to demonstrate the effects of GA and GA-guided management. This study was conducted in 40 oncology practices from the University of Rochester National Cancer Institute Community Oncology Research Program network. Centers were randomly assigned to intervention or usual care (362 patients treated by 68 oncologists in the intervention group and 371 patients treated by 91 oncologists in the usual-care group). Eligibility criteria were age ≥70 years; impairment in at least one GA domain other than polypharmacy; incurable advanced solid tumor or lymphoma with a plan to start new cancer treatment with a high risk for toxic effects within 4 weeks; and English language fluency. Both study groups underwent a baseline GA that assessed patients’ physical performance, functional status, comorbidity, cognition, nutrition, social support, polypharmacy, and psychological status. For the intervention group, a summary and management recommendations were provided to the treating oncologists.
The primary outcome was grade 3 or higher toxic effects within 3 months of starting a new regimen; secondary outcomes included treatment intensity and survival and GA outcomes within 3 months. A smaller proportion of patients in the intervention group experienced toxicity (51% vs. 71%), with an absolute risk reduction of 20%. Patients in the intervention group also had fewer falls and a greater reduction in medications used; there were no other differences in secondary outcomes. This study offers very strong and generalizable evidence that incorporating GA in the care of older adults with cancer at risk for toxicity can reduce toxicity as well as improve other outcomes, such as falls and polypharmacy.
Geriatric assessment and oncologist-patient communication
A secondary analysis3 of data from Dr. Mohile and colleagues2 evaluated the effect of GA-guided recommendations on oncologist-patient communication regarding comorbidities. Patients (n = 541) included in this analysis were 76.6 years of age on average and had 3.2 (standard deviation, 1.9) comorbid conditions. All patients underwent GA, but only oncologists in the intervention arm received GA-based recommendations. Clinical encounters between oncologist and patient immediately following the GA were audio recorded and analyzed to examine communication between oncologists and participants as it relates to chronic comorbid conditions.
In the intervention arm, more discussions regarding comorbidities took place, and more participants’ concerns about comorbidities were acknowledged. More importantly, participants in the intervention group were 2.4 times more likely to have their concerns about comorbidities addressed through referral or education, compared with the usual-care group (P = .004). Moreover, 41% of oncologists in the intervention arm modified dosage or cancer treatment schedule because of concern about tolerability or comorbidities. This study demonstrates beneficial effects of GA in increasing communication and perhaps consideration of comorbidities of older adults when planning cancer treatment.
Dr. Hung is professor of geriatrics and palliative care at Mount Sinai Hospital, New York. He disclosed no relevant conflicts of interest.
References
1. Li D et al. JAMA Oncol. 2021;7:e214158.
2. Mohile SG et al. Lancet. 2021;398:1894-1904.
3. Kleckner AS et al. JCO Oncol Pract. 2022;18:e9-19.
A version of this article first appeared on Medscape.com.
Age-related changes that potentiate adverse drug reactions include alterations in absorption, distribution, metabolism, and excretion. As such, older patients often require adjustments in medications to optimize safety and use. Medication adjustment is especially important for older patients on complex medication regimens for multiple conditions, such as those undergoing cancer treatment. Three recent high-quality randomized trials evaluated the use of geriatric assessment (GA) in older adults with cancer.1-3
Interdisciplinary GA can identify aging-related conditions associated with poor outcomes in older patients with cancer (e.g., toxic effects of chemotherapy) and provide recommendations aimed at improving health outcomes. The results of these trials suggest that interdisciplinary GA can improve care outcomes and oncologists’ communication for older adults with cancer, and should be considered an emerging standard of care.
Geriatric assessment and chemotherapy-related toxic effects
A cluster randomized trial1 at City of Hope National Medical Center conducted between August 2015 and February 2019 enrolled 613 participants and randomly assigned them to receive a GA-guided intervention or usual standard of care in a 2-to-1 ratio. Participants were eligible for the study if they were aged ≥65 years; had a diagnosis of solid malignant neoplasm of any stage; were starting a new chemotherapy regimen; and were fluent in English, Spanish, or Chinese.
The intervention included a GA at baseline followed by assessments focused on six common areas: sleep problems, problems with eating and feeding, incontinence, confusion, evidence of falls, and skin breakdown. An interdisciplinary team (oncologist, nurse practitioner, pharmacist, physical therapist, occupational therapist, social worker, and nutritionist) performed the assessment and developed a plan of care. Interventions were multifactorial and could include referral to specialists; recommendations for medication changes; symptom management; nutritional intervention with diet recommendations and supplementation; and interventions targeting social, spiritual, and functional well-being. Follow-up by a nurse practitioner continued until completion of chemotherapy or 6 months after starting chemotherapy, whichever was earlier.
The primary outcome was grade 3 or higher chemotherapy-related toxic effects using National Cancer Institute criteria, and secondary outcomes were advance directive completion, emergency room visits and unplanned hospitalizations, and survival up to 12 months. Results showed a 10% absolute reduction in the incidence of grade 3 or higher toxic effects (P = .02), with a number needed to treat of 10. Advance directive completion also increased by 15%, but no differences were observed for other outcomes. This study offers high-quality evidence that a GA-based intervention can reduce toxic effects of chemotherapy regimens for older adults with cancer.
Geriatric assessment in community oncology practices
A recent study by Supriya G. Mohile, MD, and colleagues2 is the first nationwide multicenter clinical trial to demonstrate the effects of GA and GA-guided management. This study was conducted in 40 oncology practices from the University of Rochester National Cancer Institute Community Oncology Research Program network. Centers were randomly assigned to intervention or usual care (362 patients treated by 68 oncologists in the intervention group and 371 patients treated by 91 oncologists in the usual-care group). Eligibility criteria were age ≥70 years; impairment in at least one GA domain other than polypharmacy; incurable advanced solid tumor or lymphoma with a plan to start new cancer treatment with a high risk for toxic effects within 4 weeks; and English language fluency. Both study groups underwent a baseline GA that assessed patients’ physical performance, functional status, comorbidity, cognition, nutrition, social support, polypharmacy, and psychological status. For the intervention group, a summary and management recommendations were provided to the treating oncologists.
The primary outcome was grade 3 or higher toxic effects within 3 months of starting a new regimen; secondary outcomes included treatment intensity and survival and GA outcomes within 3 months. A smaller proportion of patients in the intervention group experienced toxicity (51% vs. 71%), with an absolute risk reduction of 20%. Patients in the intervention group also had fewer falls and a greater reduction in medications used; there were no other differences in secondary outcomes. This study offers very strong and generalizable evidence that incorporating GA in the care of older adults with cancer at risk for toxicity can reduce toxicity as well as improve other outcomes, such as falls and polypharmacy.
Geriatric assessment and oncologist-patient communication
A secondary analysis3 of data from Dr. Mohile and colleagues2 evaluated the effect of GA-guided recommendations on oncologist-patient communication regarding comorbidities. Patients (n = 541) included in this analysis were 76.6 years of age on average and had 3.2 (standard deviation, 1.9) comorbid conditions. All patients underwent GA, but only oncologists in the intervention arm received GA-based recommendations. Clinical encounters between oncologist and patient immediately following the GA were audio recorded and analyzed to examine communication between oncologists and participants as it relates to chronic comorbid conditions.
In the intervention arm, more discussions regarding comorbidities took place, and more participants’ concerns about comorbidities were acknowledged. More importantly, participants in the intervention group were 2.4 times more likely to have their concerns about comorbidities addressed through referral or education, compared with the usual-care group (P = .004). Moreover, 41% of oncologists in the intervention arm modified dosage or cancer treatment schedule because of concern about tolerability or comorbidities. This study demonstrates beneficial effects of GA in increasing communication and perhaps consideration of comorbidities of older adults when planning cancer treatment.
Dr. Hung is professor of geriatrics and palliative care at Mount Sinai Hospital, New York. He disclosed no relevant conflicts of interest.
References
1. Li D et al. JAMA Oncol. 2021;7:e214158.
2. Mohile SG et al. Lancet. 2021;398:1894-1904.
3. Kleckner AS et al. JCO Oncol Pract. 2022;18:e9-19.
A version of this article first appeared on Medscape.com.
Is cancer testing going to the dogs? Nope, ants
The oncologist’s new best friend
We know that dogs have very sensitive noses. They can track criminals and missing persons and sniff out drugs and bombs. They can even detect cancer cells … after months of training.
And then there are ants.
Cancer cells produce volatile organic compounds (VOCs), which can be sniffed out by dogs and other animals with sufficiently sophisticated olfactory senses. A group of French investigators decided to find out if Formica fusca is such an animal.
First, they placed breast cancer cells and healthy cells in a petri dish. The sample of cancer cells, however, included a sugary treat. “Over successive trials, the ants got quicker and quicker at finding the treat, indicating that they had learned to recognize the VOCs produced by the cancerous cells, using these as a beacon to guide their way to the sugary delight,” according to IFL Science.
When the researchers removed the treat, the ants still went straight for the cancer cells. Then they removed the healthy cells and substituted another type of breast cancer cell, with just one type getting the treat. They went for the cancer cells with the treat, “indicating that they were capable of distinguishing between the different cancer types based on the unique pattern of VOCs emitted by each one,” IFL Science explained.
It’s just another chapter in the eternal struggle between dogs and ants. Dogs need months of training to learn to detect cancer cells; ants can do it in 30 minutes. Over the course of a dog’s training, Fido eats more food than 10,000 ants combined. (Okay, we’re guessing here, but it’s got to be a pretty big number, right?)
Then there’s the warm and fuzzy factor. Just look at that picture. Who wouldn’t want a cutie like that curling up in the bed next to you?
Console War II: Battle of the Twitter users
Video games can be a lot of fun, provided you’re not playing something like Rock Simulator. Or Surgeon Simulator. Or Surgeon Simulator 2. Yes, those are all real games. But calling yourself a video gamer invites a certain negative connotation, and nowhere can that be better exemplified than the increasingly ridiculous console war.
For those who don’t know their video game history, back in the early 90s Nintendo and Sega were the main video game console makers. Nintendo had Mario, Sega had Sonic, and everyone had an opinion on which was best. With Sega now but a shell of its former self and Nintendo viewed as too “casual” for the true gaming connoisseur, today’s battle pits Playstation against Xbox, and fans of both consoles spend their time trying to one-up each other in increasingly silly online arguments.
That brings us nicely to a Twitter user named “Shreeveera,” who is very vocal about his love of Playstation and hatred of the Xbox. Importantly, for LOTME purposes, Shreeveera identified himself as a doctor on his profile, and in the middle of an argument, Xbox enthusiasts called his credentials into question.
At this point, most people would recognize that there are very few noteworthy console-exclusive video games in today’s world and that any argument about consoles essentially comes down to which console design you like or which company you find less distasteful, and they would step away from the Twitter argument. Shreeveera is not most people, and he decided the next logical move was to post a video of himself and an anesthetized patient about to undergo a laparoscopic cholecystectomy.
This move did prove that he was indeed a doctor, but the ethics of posting such a video with a patient in the room is a bit dubious at best. Since Shreeveera also listed the hospital he worked at, numerous Twitter users review bombed the hospital with one-star reviews. Shreeveera’s fate is unknown, but he did take down the video and removed “doctor by profession” from his profile. He also made a second video asking Twitter to stop trying to ruin his life. We’re sure that’ll go well. Twitter is known for being completely fair and reasonable.
Use your words to gain power
We live in the age of the emoji. The use of emojis in texts and emails is basically the new shorthand. It’s a fun and easy way to chat with people close to us, but a new study shows that it doesn’t help in a business setting. In fact, it may do a little damage.
The use of images such as emojis in communication or logos can make a person seem less powerful than someone who opts for written words, according to Elinor Amit, PhD, of Tel Aviv University and associates.
Participants in their study were asked to imagine shopping with a person wearing a T-shirt. Half were then shown the logo of the Red Sox baseball team and half saw the words “Red Sox.” In another scenario, they were asked to imagine attending a retreat of a company called Lotus. Then half were shown an employee wearing a shirt with an image of lotus flower and half saw the verbal logo “Lotus.” In both scenarios, the individuals wearing shirts with images were seen as less powerful than the people who wore shirts with words on them.
Why is that? In a Eurekalert statement, Dr. Amit said that “visual messages are often interpreted as a signal for desire for social proximity.” In a world with COVID-19, that could give anyone pause.
That desire for more social proximity, in turn, equals a suggested loss of power because research shows that people who want to be around other people more are less powerful than people who don’t.
With the reduced social proximity we have these days, we may want to keep things cool and lighthearted, especially in work emails with people who we’ve never met. It may be, however, that using your words to say thank you in the multitude of emails you respond to on a regular basis is better than that thumbs-up emoji. Nobody will think less of you.
Should Daylight Savings Time still be a thing?
This past week, we just experienced the spring-forward portion of Daylight Savings Time, which took an hour of sleep away from us all. Some of us may still be struggling to find our footing with the time change, but at least it’s still sunny out at 7 pm. For those who don’t really see the point of changing the clocks twice a year, there are actually some good reasons to do so.
Sen. Marco Rubio, sponsor of a bill to make the time change permanent, put it simply: “If we can get this passed, we don’t have to do this stupidity anymore.” Message received, apparently, since the measure just passed unanimously in the Senate.
It’s not clear if President Biden will approve it, though, because there’s a lot that comes into play: economic needs, seasonal depression, and safety.
“I know this is not the most important issue confronting America, but it’s one of those issues where there’s a lot of agreement,” Sen. Rubio said.
Not total agreement, though. The National Association of Convenience Stores is opposed to the bill, and Reuters noted that one witness at a recent hearing said the time change “is like living in the wrong time zone for almost eight months out of the year.”
Many people, however, seem to be leaning toward the permanent spring-forward as it gives businesses a longer window to provide entertainment in the evenings and kids are able to play outside longer after school.
Honestly, we’re leaning toward whichever one can reduce seasonal depression.
The oncologist’s new best friend
We know that dogs have very sensitive noses. They can track criminals and missing persons and sniff out drugs and bombs. They can even detect cancer cells … after months of training.
And then there are ants.
Cancer cells produce volatile organic compounds (VOCs), which can be sniffed out by dogs and other animals with sufficiently sophisticated olfactory senses. A group of French investigators decided to find out if Formica fusca is such an animal.
First, they placed breast cancer cells and healthy cells in a petri dish. The sample of cancer cells, however, included a sugary treat. “Over successive trials, the ants got quicker and quicker at finding the treat, indicating that they had learned to recognize the VOCs produced by the cancerous cells, using these as a beacon to guide their way to the sugary delight,” according to IFL Science.
When the researchers removed the treat, the ants still went straight for the cancer cells. Then they removed the healthy cells and substituted another type of breast cancer cell, with just one type getting the treat. They went for the cancer cells with the treat, “indicating that they were capable of distinguishing between the different cancer types based on the unique pattern of VOCs emitted by each one,” IFL Science explained.
It’s just another chapter in the eternal struggle between dogs and ants. Dogs need months of training to learn to detect cancer cells; ants can do it in 30 minutes. Over the course of a dog’s training, Fido eats more food than 10,000 ants combined. (Okay, we’re guessing here, but it’s got to be a pretty big number, right?)
Then there’s the warm and fuzzy factor. Just look at that picture. Who wouldn’t want a cutie like that curling up in the bed next to you?
Console War II: Battle of the Twitter users
Video games can be a lot of fun, provided you’re not playing something like Rock Simulator. Or Surgeon Simulator. Or Surgeon Simulator 2. Yes, those are all real games. But calling yourself a video gamer invites a certain negative connotation, and nowhere can that be better exemplified than the increasingly ridiculous console war.
For those who don’t know their video game history, back in the early 90s Nintendo and Sega were the main video game console makers. Nintendo had Mario, Sega had Sonic, and everyone had an opinion on which was best. With Sega now but a shell of its former self and Nintendo viewed as too “casual” for the true gaming connoisseur, today’s battle pits Playstation against Xbox, and fans of both consoles spend their time trying to one-up each other in increasingly silly online arguments.
That brings us nicely to a Twitter user named “Shreeveera,” who is very vocal about his love of Playstation and hatred of the Xbox. Importantly, for LOTME purposes, Shreeveera identified himself as a doctor on his profile, and in the middle of an argument, Xbox enthusiasts called his credentials into question.
At this point, most people would recognize that there are very few noteworthy console-exclusive video games in today’s world and that any argument about consoles essentially comes down to which console design you like or which company you find less distasteful, and they would step away from the Twitter argument. Shreeveera is not most people, and he decided the next logical move was to post a video of himself and an anesthetized patient about to undergo a laparoscopic cholecystectomy.
This move did prove that he was indeed a doctor, but the ethics of posting such a video with a patient in the room is a bit dubious at best. Since Shreeveera also listed the hospital he worked at, numerous Twitter users review bombed the hospital with one-star reviews. Shreeveera’s fate is unknown, but he did take down the video and removed “doctor by profession” from his profile. He also made a second video asking Twitter to stop trying to ruin his life. We’re sure that’ll go well. Twitter is known for being completely fair and reasonable.
Use your words to gain power
We live in the age of the emoji. The use of emojis in texts and emails is basically the new shorthand. It’s a fun and easy way to chat with people close to us, but a new study shows that it doesn’t help in a business setting. In fact, it may do a little damage.
The use of images such as emojis in communication or logos can make a person seem less powerful than someone who opts for written words, according to Elinor Amit, PhD, of Tel Aviv University and associates.
Participants in their study were asked to imagine shopping with a person wearing a T-shirt. Half were then shown the logo of the Red Sox baseball team and half saw the words “Red Sox.” In another scenario, they were asked to imagine attending a retreat of a company called Lotus. Then half were shown an employee wearing a shirt with an image of lotus flower and half saw the verbal logo “Lotus.” In both scenarios, the individuals wearing shirts with images were seen as less powerful than the people who wore shirts with words on them.
Why is that? In a Eurekalert statement, Dr. Amit said that “visual messages are often interpreted as a signal for desire for social proximity.” In a world with COVID-19, that could give anyone pause.
That desire for more social proximity, in turn, equals a suggested loss of power because research shows that people who want to be around other people more are less powerful than people who don’t.
With the reduced social proximity we have these days, we may want to keep things cool and lighthearted, especially in work emails with people who we’ve never met. It may be, however, that using your words to say thank you in the multitude of emails you respond to on a regular basis is better than that thumbs-up emoji. Nobody will think less of you.
Should Daylight Savings Time still be a thing?
This past week, we just experienced the spring-forward portion of Daylight Savings Time, which took an hour of sleep away from us all. Some of us may still be struggling to find our footing with the time change, but at least it’s still sunny out at 7 pm. For those who don’t really see the point of changing the clocks twice a year, there are actually some good reasons to do so.
Sen. Marco Rubio, sponsor of a bill to make the time change permanent, put it simply: “If we can get this passed, we don’t have to do this stupidity anymore.” Message received, apparently, since the measure just passed unanimously in the Senate.
It’s not clear if President Biden will approve it, though, because there’s a lot that comes into play: economic needs, seasonal depression, and safety.
“I know this is not the most important issue confronting America, but it’s one of those issues where there’s a lot of agreement,” Sen. Rubio said.
Not total agreement, though. The National Association of Convenience Stores is opposed to the bill, and Reuters noted that one witness at a recent hearing said the time change “is like living in the wrong time zone for almost eight months out of the year.”
Many people, however, seem to be leaning toward the permanent spring-forward as it gives businesses a longer window to provide entertainment in the evenings and kids are able to play outside longer after school.
Honestly, we’re leaning toward whichever one can reduce seasonal depression.
The oncologist’s new best friend
We know that dogs have very sensitive noses. They can track criminals and missing persons and sniff out drugs and bombs. They can even detect cancer cells … after months of training.
And then there are ants.
Cancer cells produce volatile organic compounds (VOCs), which can be sniffed out by dogs and other animals with sufficiently sophisticated olfactory senses. A group of French investigators decided to find out if Formica fusca is such an animal.
First, they placed breast cancer cells and healthy cells in a petri dish. The sample of cancer cells, however, included a sugary treat. “Over successive trials, the ants got quicker and quicker at finding the treat, indicating that they had learned to recognize the VOCs produced by the cancerous cells, using these as a beacon to guide their way to the sugary delight,” according to IFL Science.
When the researchers removed the treat, the ants still went straight for the cancer cells. Then they removed the healthy cells and substituted another type of breast cancer cell, with just one type getting the treat. They went for the cancer cells with the treat, “indicating that they were capable of distinguishing between the different cancer types based on the unique pattern of VOCs emitted by each one,” IFL Science explained.
It’s just another chapter in the eternal struggle between dogs and ants. Dogs need months of training to learn to detect cancer cells; ants can do it in 30 minutes. Over the course of a dog’s training, Fido eats more food than 10,000 ants combined. (Okay, we’re guessing here, but it’s got to be a pretty big number, right?)
Then there’s the warm and fuzzy factor. Just look at that picture. Who wouldn’t want a cutie like that curling up in the bed next to you?
Console War II: Battle of the Twitter users
Video games can be a lot of fun, provided you’re not playing something like Rock Simulator. Or Surgeon Simulator. Or Surgeon Simulator 2. Yes, those are all real games. But calling yourself a video gamer invites a certain negative connotation, and nowhere can that be better exemplified than the increasingly ridiculous console war.
For those who don’t know their video game history, back in the early 90s Nintendo and Sega were the main video game console makers. Nintendo had Mario, Sega had Sonic, and everyone had an opinion on which was best. With Sega now but a shell of its former self and Nintendo viewed as too “casual” for the true gaming connoisseur, today’s battle pits Playstation against Xbox, and fans of both consoles spend their time trying to one-up each other in increasingly silly online arguments.
That brings us nicely to a Twitter user named “Shreeveera,” who is very vocal about his love of Playstation and hatred of the Xbox. Importantly, for LOTME purposes, Shreeveera identified himself as a doctor on his profile, and in the middle of an argument, Xbox enthusiasts called his credentials into question.
At this point, most people would recognize that there are very few noteworthy console-exclusive video games in today’s world and that any argument about consoles essentially comes down to which console design you like or which company you find less distasteful, and they would step away from the Twitter argument. Shreeveera is not most people, and he decided the next logical move was to post a video of himself and an anesthetized patient about to undergo a laparoscopic cholecystectomy.
This move did prove that he was indeed a doctor, but the ethics of posting such a video with a patient in the room is a bit dubious at best. Since Shreeveera also listed the hospital he worked at, numerous Twitter users review bombed the hospital with one-star reviews. Shreeveera’s fate is unknown, but he did take down the video and removed “doctor by profession” from his profile. He also made a second video asking Twitter to stop trying to ruin his life. We’re sure that’ll go well. Twitter is known for being completely fair and reasonable.
Use your words to gain power
We live in the age of the emoji. The use of emojis in texts and emails is basically the new shorthand. It’s a fun and easy way to chat with people close to us, but a new study shows that it doesn’t help in a business setting. In fact, it may do a little damage.
The use of images such as emojis in communication or logos can make a person seem less powerful than someone who opts for written words, according to Elinor Amit, PhD, of Tel Aviv University and associates.
Participants in their study were asked to imagine shopping with a person wearing a T-shirt. Half were then shown the logo of the Red Sox baseball team and half saw the words “Red Sox.” In another scenario, they were asked to imagine attending a retreat of a company called Lotus. Then half were shown an employee wearing a shirt with an image of lotus flower and half saw the verbal logo “Lotus.” In both scenarios, the individuals wearing shirts with images were seen as less powerful than the people who wore shirts with words on them.
Why is that? In a Eurekalert statement, Dr. Amit said that “visual messages are often interpreted as a signal for desire for social proximity.” In a world with COVID-19, that could give anyone pause.
That desire for more social proximity, in turn, equals a suggested loss of power because research shows that people who want to be around other people more are less powerful than people who don’t.
With the reduced social proximity we have these days, we may want to keep things cool and lighthearted, especially in work emails with people who we’ve never met. It may be, however, that using your words to say thank you in the multitude of emails you respond to on a regular basis is better than that thumbs-up emoji. Nobody will think less of you.
Should Daylight Savings Time still be a thing?
This past week, we just experienced the spring-forward portion of Daylight Savings Time, which took an hour of sleep away from us all. Some of us may still be struggling to find our footing with the time change, but at least it’s still sunny out at 7 pm. For those who don’t really see the point of changing the clocks twice a year, there are actually some good reasons to do so.
Sen. Marco Rubio, sponsor of a bill to make the time change permanent, put it simply: “If we can get this passed, we don’t have to do this stupidity anymore.” Message received, apparently, since the measure just passed unanimously in the Senate.
It’s not clear if President Biden will approve it, though, because there’s a lot that comes into play: economic needs, seasonal depression, and safety.
“I know this is not the most important issue confronting America, but it’s one of those issues where there’s a lot of agreement,” Sen. Rubio said.
Not total agreement, though. The National Association of Convenience Stores is opposed to the bill, and Reuters noted that one witness at a recent hearing said the time change “is like living in the wrong time zone for almost eight months out of the year.”
Many people, however, seem to be leaning toward the permanent spring-forward as it gives businesses a longer window to provide entertainment in the evenings and kids are able to play outside longer after school.
Honestly, we’re leaning toward whichever one can reduce seasonal depression.